User login
Adherence to Topical Treatment Can Improve Treatment-Resistant Moderate Psoriasis
High-potency topical corticosteroids are first-line treatments for psoriasis, but many patients report that they are ineffective or lose effectiveness over time.1-5 The mechanism underlying the lack or loss of activity is not well characterized but may be due to poor adherence to treatment. Adherence to topical treatment is poor in the short run and even worse in the long run.6,7 We evaluated 12 patients with psoriasis resistant to topical corticosteroids to determine if they would respond to topical corticosteroids under conditions designed to promote adherence to treatment.
Methods
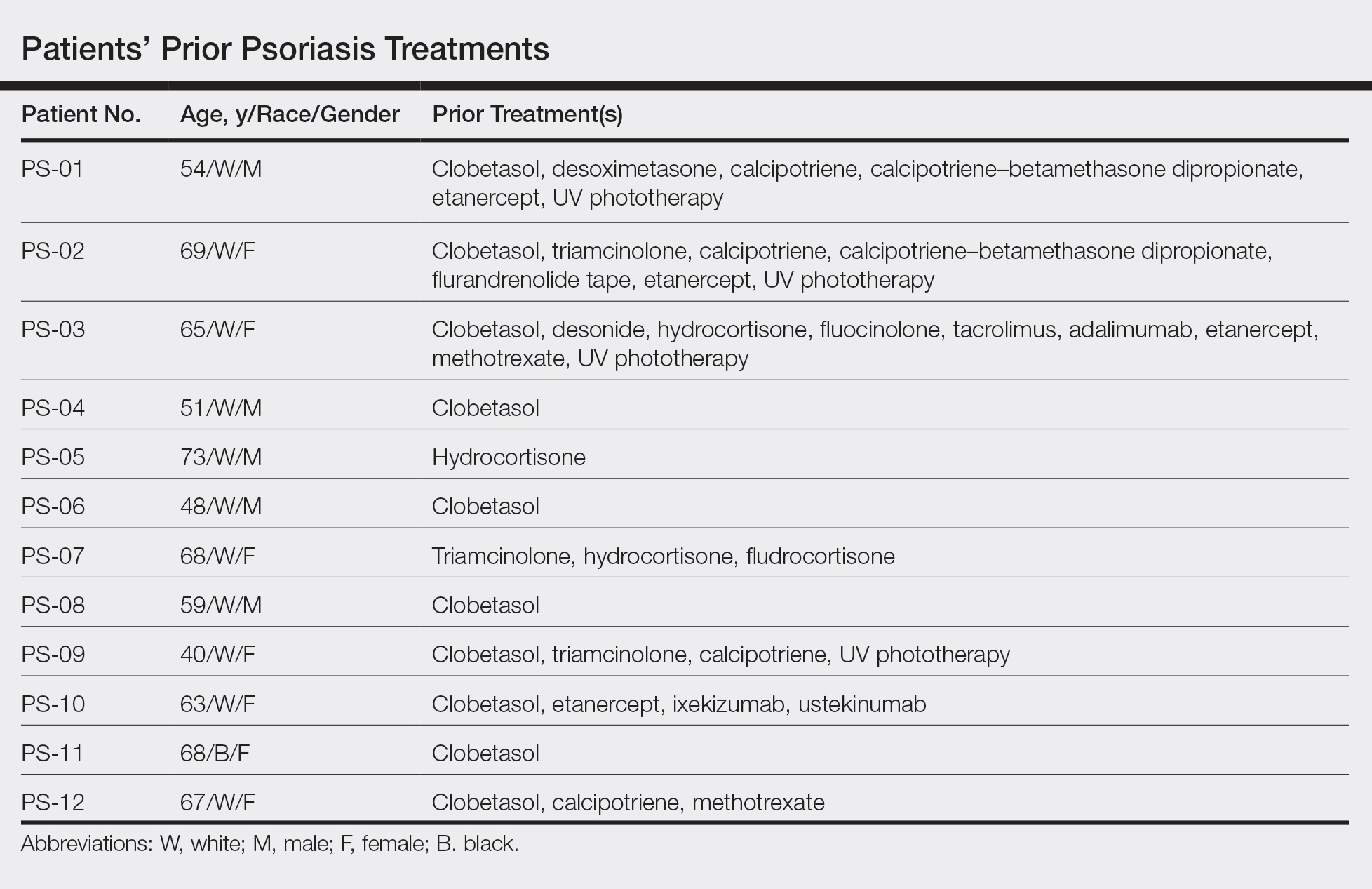
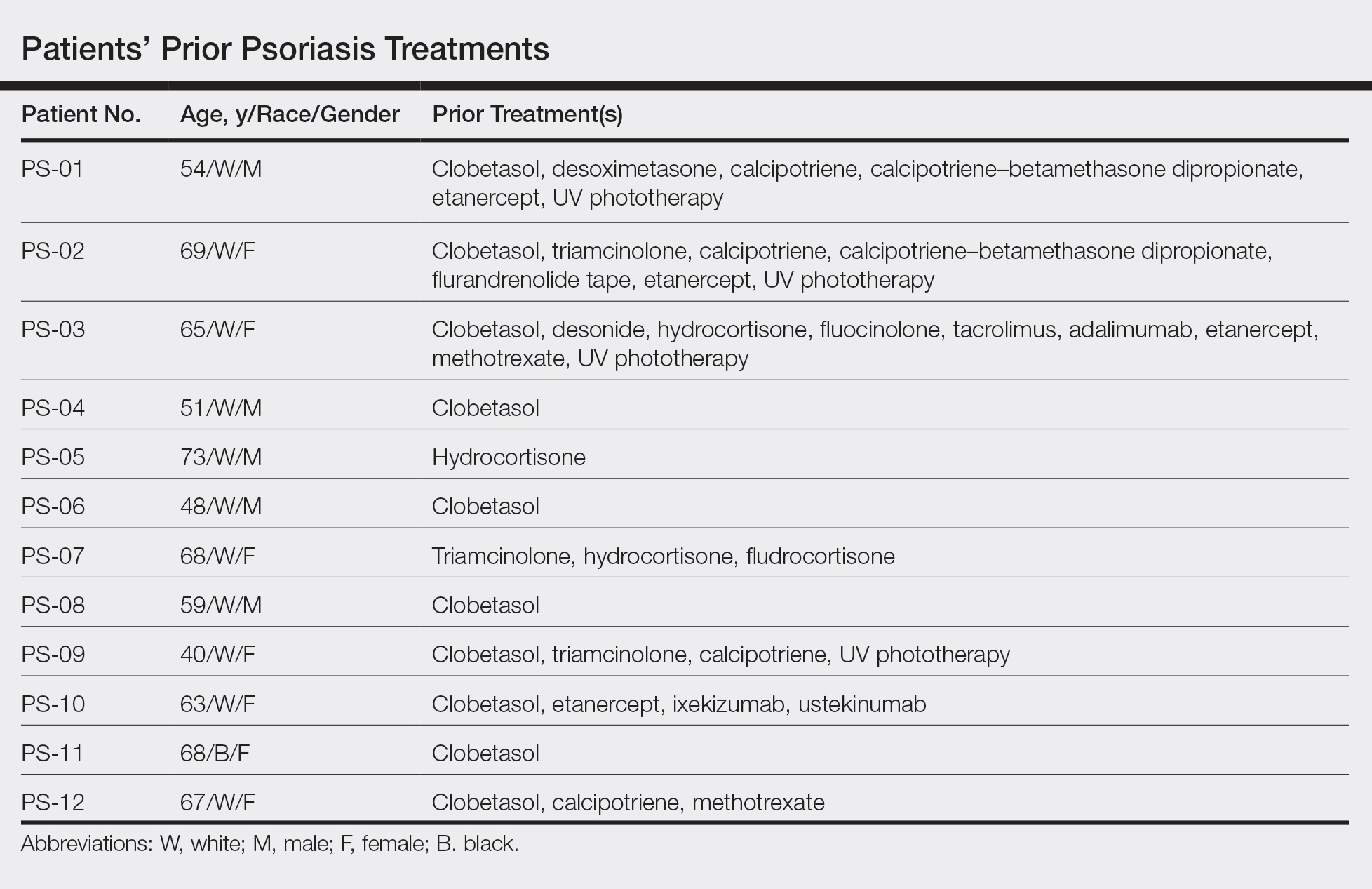
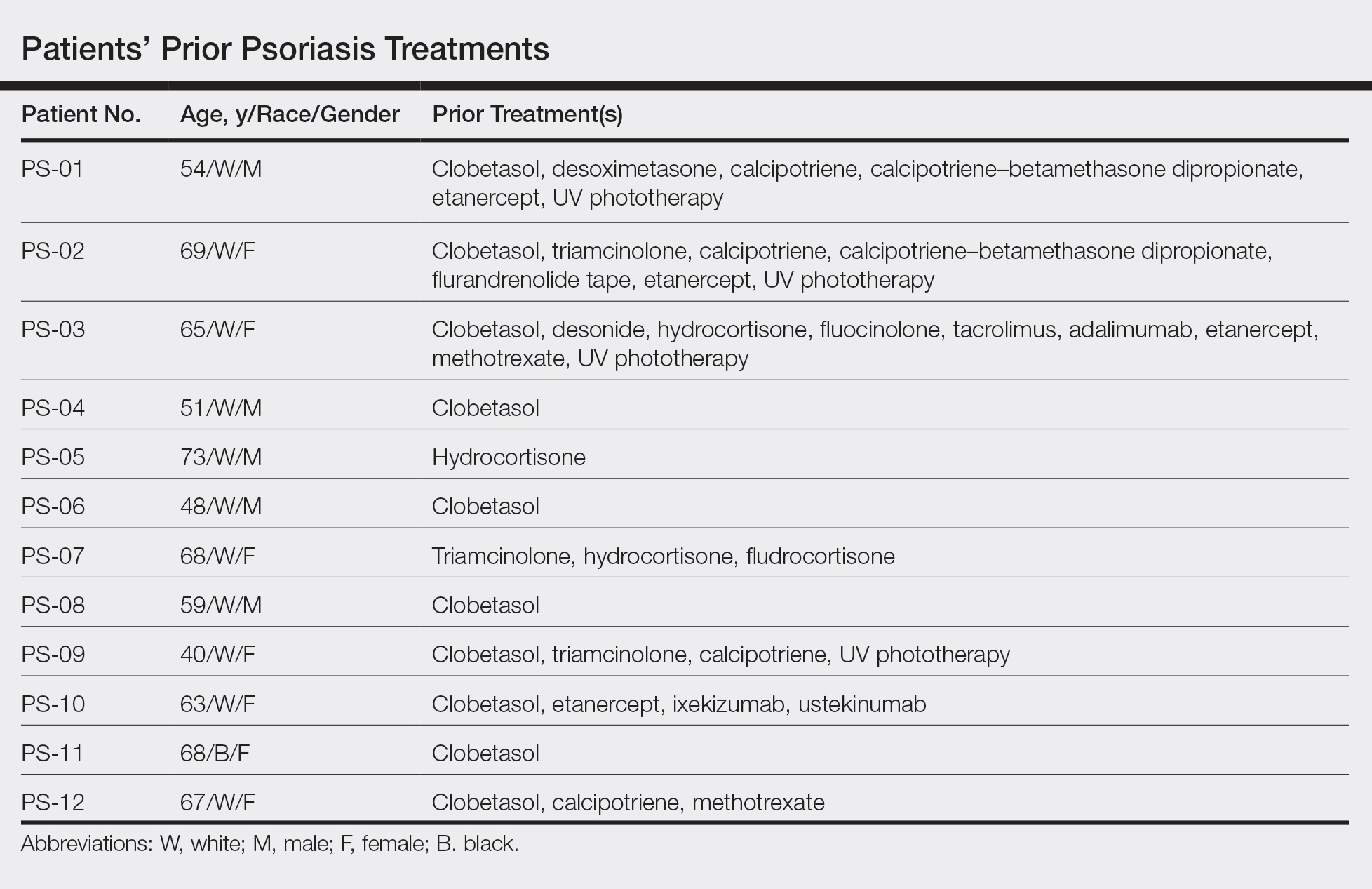
This open-label, randomized, single-center clinical study recruited 12 patients with plaque psoriasis that previously failed treatment with topical corticosteroids and other therapies (Table). We stratified disease by body surface area: mild (<3%), moderate (3%–10%), and severe (>10%). Inclusion criteria included adult patients with plaque psoriasis amenable to topical corticosteroid therapy, ability to comply with requirements of the study, and a history of failed topical corticosteroid treatment (Figure). Patients were excluded if they were pregnant, breastfeeding, had conditions that would affect adherence or potentially bias results (eg, dementia, Alzheimer disease), had a history of allergy or sensitivity to corticosteroids, and had a history of drug hypersensitivity.

All patients received desoximetasone spray 0.25% twice daily for 14 days. At the baseline visit, 6 patients were randomly selected to also receive a twice-daily reminder telephone call. Study visits occurred frequently—at baseline and on days 3, 7, and 14—to further assure good adherence to the treatment regimen.
During visits, disease severity was scored using the visual analog scale for pruritus, psoriasis area and severity index (PASI), total lesion severity score (TLSS), and investigator global assessment (IGA). Descriptive statistics were used to report the outcomes for each patient.
The study was designed to assess the number of topical treatment–resistant patients who would improve with topical treatment but was not designed or powered to test if the telephone call reminders increased adherence.
Results
All patients completed the study; 10 of 12 patients (83.3%) had previously used topical clobetasol and it failed (Table). At the 2-week end-of-study visit, most patients improved on all measures. Patients who received telephone call reminders improved more than patients who did not. All 12 patients (100%) reported relief of itching; 11 of 12 (91.7%) had an improved PASI; 10 of 12 (83.3%) had an improved TLSS; and 7 of 12 (58.3%) had an improved IGA (eTables 1 and 2).
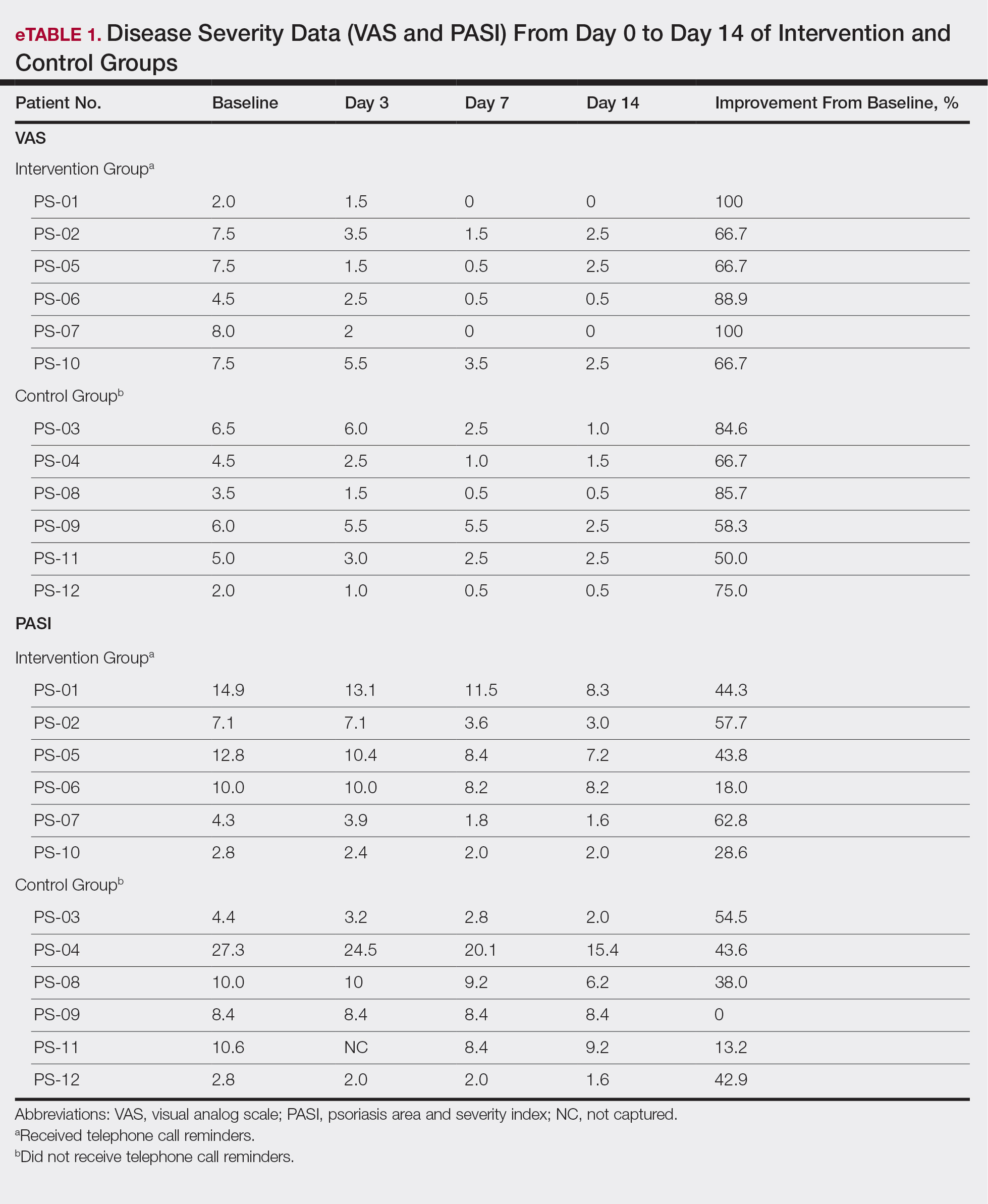
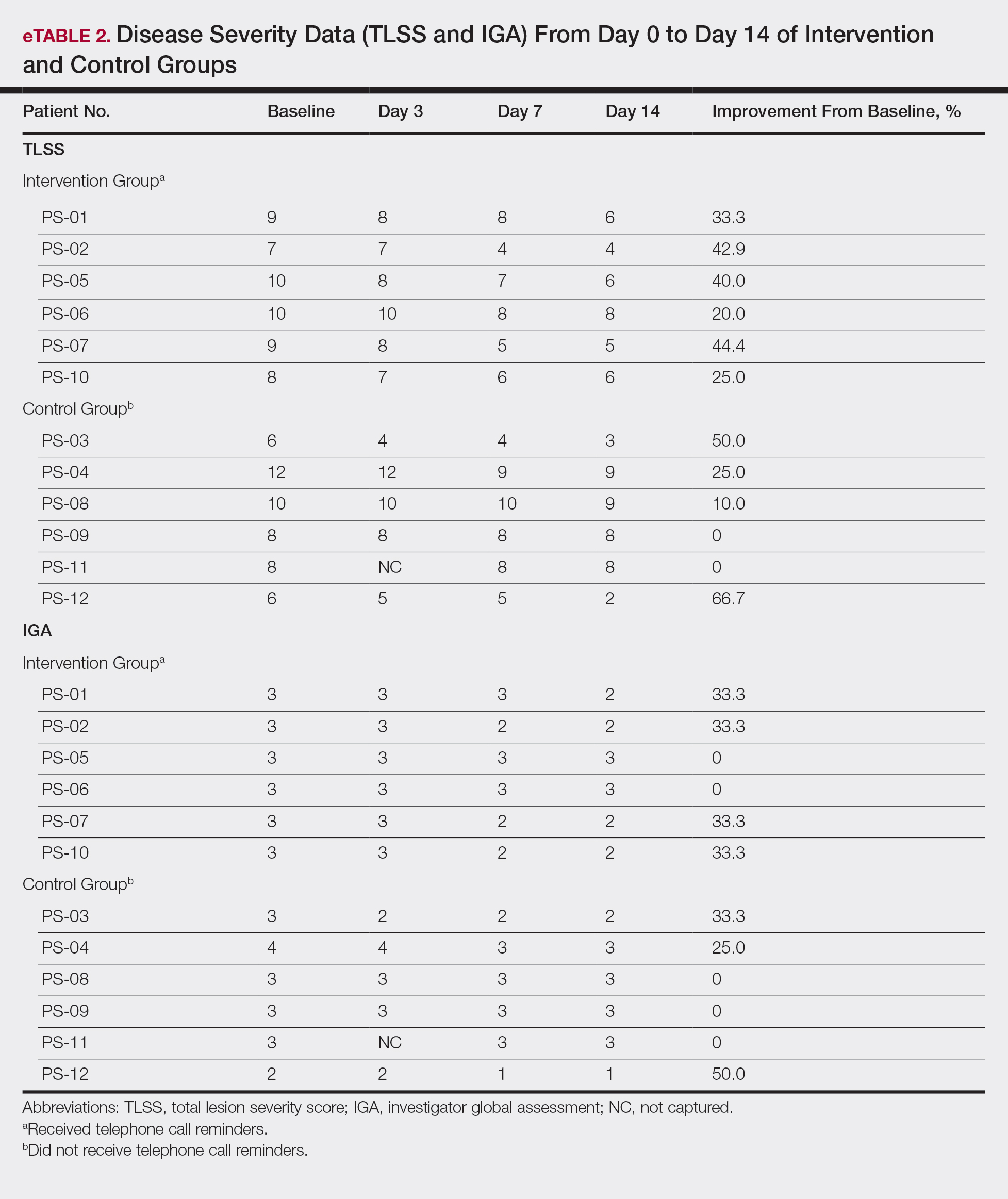
The percentage reduction in pruritus ranged from 66.7% to 100% and 50.0% to 85.7% with and without telephone call reminders, respectively. Improvement in PASI ranged from 18.0% to 62.8% and 0% to 54.5% with and without telephone call reminders, respectively. Improvement in TLSS and IGA was of lower magnitude but showed a similar pattern, with numerically greater improvement in the telephone call reminders group compared to the group that was not called (eTable 2). No patients showed a worse score for pruritus on the visual analog scale, PASI, TLSS, or IGA.
Discussion
Topical corticosteroids are highly effective for psoriasis in clinical trials, with clearance in 2 to 4 weeks in 60% to 80% of patients, a rapidity of response not matched by even the most potent biologic treatments.8,9 However, topical corticosteroids are not always effective in clinical practice. There may be primary inefficacy (they do not work at first) or secondary inefficacy (a previously effective treatment loses efficacy over time).10 Poor adherence can explain both phenomena. Primary adherence occurs when patients fill their prescription; secondary adherence occurs when patients follow the medication recommendations.11 Primary nonadherence is common in patients with psoriasis; in one study, 50% of psoriasis prescriptions were not filled.12 Secondary adherence also is poor and declines over time; electronic monitoring revealed adherence to topical treatments in psoriasis patients decreased from 85% initially to 51% at the end of 8 weeks.7 Given the high efficacy of topical corticosteroids in clinical trials and the poor adherence to topical treatment in patients with psoriasis, we anticipated that psoriasis that is resistant to topical corticosteroids would improve rapidly under conditions designed to promote adherence.
As expected, disease improved in almost every patient in this small cohort when they were given a potent topical corticosteroid, even though they previously reported that their psoriasis was resistant to potent topical corticosteroids. Although this study enrolled only a small cohort, it appears that the majority of patients with limited psoriasis that was reported to be resistant to topical treatment can see a response to topical treatment under conditions designed to encourage good adherence.
We believe that the good outcomes seen in our study were a result of good adherence. Although the desoximetasone spray 0.25% used in this study is a superpotent topical corticosteroid,8 the response to treatment was unlikely due to changing corticosteroid potency because 10 of 12 patients had tried another superpotent topical corticosteroid (clobetasol) and it failed. We chose a spray product for this study rather than an ointment to promote adherence; however, this choice limited the ability to assess adherence directly, as adherence-monitoring devices for spray delivery systems are not readily available.
Our study was limited by the small sample size and brief duration of treatment. However, the effect size is so large (ie, the topical treatment was so effective) that only a small sample size and brief treatment duration were needed to show that a high percentage of patients with psoriasis that had previously failed treatment with topical corticosteroids can in fact respond to this treatment.
We used telephone calls as reminders in 50% of patients to further encourage adherence. The study was not designed or powered to assess the effect of the telephone call reminders, but patients receiving those calls appeared to have slightly greater reduction in disease severity. Nonetheless, twice-daily telephone call reminders are unlikely to be a wanted or practical intervention; other approaches to encourage adherence are needed.
Frequent follow-up visits were incorporated in our study design to maximize adherence. Although it might not be feasible for clinical practices to schedule follow-up visits as often as in our study, other approaches such as virtual visits and electronic interaction might provide a practical alternative. Multifaceted approaches to increasing adherence include encouraging patients to participate in the treatment plan, prescribing therapy consistent with a patient’s preferred vehicle, and extensive patient education.13 If patients do not respond as expected, poor adherence can be considered. Other potential causes of poor outcomes include error in diagnosis; resistance to the prescribed treatment; concomitant infection; irritant exposure; and, in the case of biologics, antidrug antibody formation.14,15
- Feldman SR, Fleischer AB Jr, Cooper JZ. New topical treatments change the pattern of treatment of psoriasis: dermatologists remain the primary providers of this care. Int J Dermatol. 2000;39:41-44.
- Menter A. Topical monotherapy with clobetasol propionate spray 0.05% in the COBRA trial. Cutis. 2007;80(suppl 5):12-19.
- Saleem MD, Negus D, Feldman SR. Topical 0.25% desoximetasone spray efficacy for moderate to severe plaque psoriasis: a randomized clinical trial. J Dermatolog Treat. 2018;29:32-35.
- Mraz S, Leonardi C, Colón LE, et al. Different treatment outcomes with different formulations of clobetasol propionate 0.05% for the treatment of plaque psoriasis. J Dermatolog Treat. 2008;19:354-359.
- Chiricozzi A, Pimpinelli N, Ricceri F, et al. Treatment of psoriasis with topical agents: recommendations from a Tuscany Consensus. Dermatol Ther. 2017;30:e12549.
- Carroll CL, Feldman SR, Camacho FT, et al. Adherence to topical therapy decreases during the course of an 8-week psoriasis clinical trial: commonly used methods of measuring adherence to topical therapy overestimate actual use. J Am Acad Dermatol. 2004;51:212-216.
- Alinia H, Moradi Tuchayi S, Smith JA, et al. Long-term adherence to topical psoriasis treatment can be abysmal: a 1-year randomized intervention study using objective electronic adherence monitoring. Br J Dermatol. 2017;176:759-764.
- Keegan BR. Desoximetasone 0.25% spray for the relief of scaling in adults with plaque psoriasis. J Drugs Dermatol. 2015;14:835-840.
- Beutner K, Chakrabarty A, Lemke S, et al. An intra-individual randomized safety and efficacy comparison of clobetasol propionate 0.05% spray and its vehicle in the treatment of plaque psoriasis. J Drugs Dermatol. 2006;5:357-360.
- Mehta AB, Nadkarni NJ, Patil SP, et al. Topical corticosteroids in dermatology. Indian J Dermatol Venereol Leprol. 2016;82:371-378.
- Blais L, Kettani FZ, Forget A, et al. Assessing adherence to inhaled corticosteroids in asthma patients using an integrated measure based on primary and secondary adherence. Eur J Clin Pharmacol. 2016;73:91-97.
- Storm A, Andersen SE, Benfeldt E, et al. One in 3 prescriptions are never redeemed: primary nonadherence in an outpatient clinic. J Am Acad Dermatol. 2008;59:27-33.
- Zschocke I, Mrowietz U, Karakasili E, et al. Non-adherence and measures to improve adherence in the topical treatment of psoriasis. J Eur Acad Dermatol Venereol. 2014;28(Suppl 2):4-9.
- Mooney E, Rademaker M, Dailey R, et al. Adverse effects of topical corticosteroids in paediatric eczema: Australasian consensus statement. Australas J Dermatol. 2015;56:241-251.
- Varada S, Tintle SJ, Gottlieb AB. Apremilast for the treatment of psoriatic arthritis. Expert Rev Clin Pharmacol. 2014;7:239-250.
High-potency topical corticosteroids are first-line treatments for psoriasis, but many patients report that they are ineffective or lose effectiveness over time.1-5 The mechanism underlying the lack or loss of activity is not well characterized but may be due to poor adherence to treatment. Adherence to topical treatment is poor in the short run and even worse in the long run.6,7 We evaluated 12 patients with psoriasis resistant to topical corticosteroids to determine if they would respond to topical corticosteroids under conditions designed to promote adherence to treatment.
Methods
This open-label, randomized, single-center clinical study recruited 12 patients with plaque psoriasis that previously failed treatment with topical corticosteroids and other therapies (Table). We stratified disease by body surface area: mild (<3%), moderate (3%–10%), and severe (>10%). Inclusion criteria included adult patients with plaque psoriasis amenable to topical corticosteroid therapy, ability to comply with requirements of the study, and a history of failed topical corticosteroid treatment (Figure). Patients were excluded if they were pregnant, breastfeeding, had conditions that would affect adherence or potentially bias results (eg, dementia, Alzheimer disease), had a history of allergy or sensitivity to corticosteroids, and had a history of drug hypersensitivity.

All patients received desoximetasone spray 0.25% twice daily for 14 days. At the baseline visit, 6 patients were randomly selected to also receive a twice-daily reminder telephone call. Study visits occurred frequently—at baseline and on days 3, 7, and 14—to further assure good adherence to the treatment regimen.
During visits, disease severity was scored using the visual analog scale for pruritus, psoriasis area and severity index (PASI), total lesion severity score (TLSS), and investigator global assessment (IGA). Descriptive statistics were used to report the outcomes for each patient.
The study was designed to assess the number of topical treatment–resistant patients who would improve with topical treatment but was not designed or powered to test if the telephone call reminders increased adherence.
Results
All patients completed the study; 10 of 12 patients (83.3%) had previously used topical clobetasol and it failed (Table). At the 2-week end-of-study visit, most patients improved on all measures. Patients who received telephone call reminders improved more than patients who did not. All 12 patients (100%) reported relief of itching; 11 of 12 (91.7%) had an improved PASI; 10 of 12 (83.3%) had an improved TLSS; and 7 of 12 (58.3%) had an improved IGA (eTables 1 and 2).
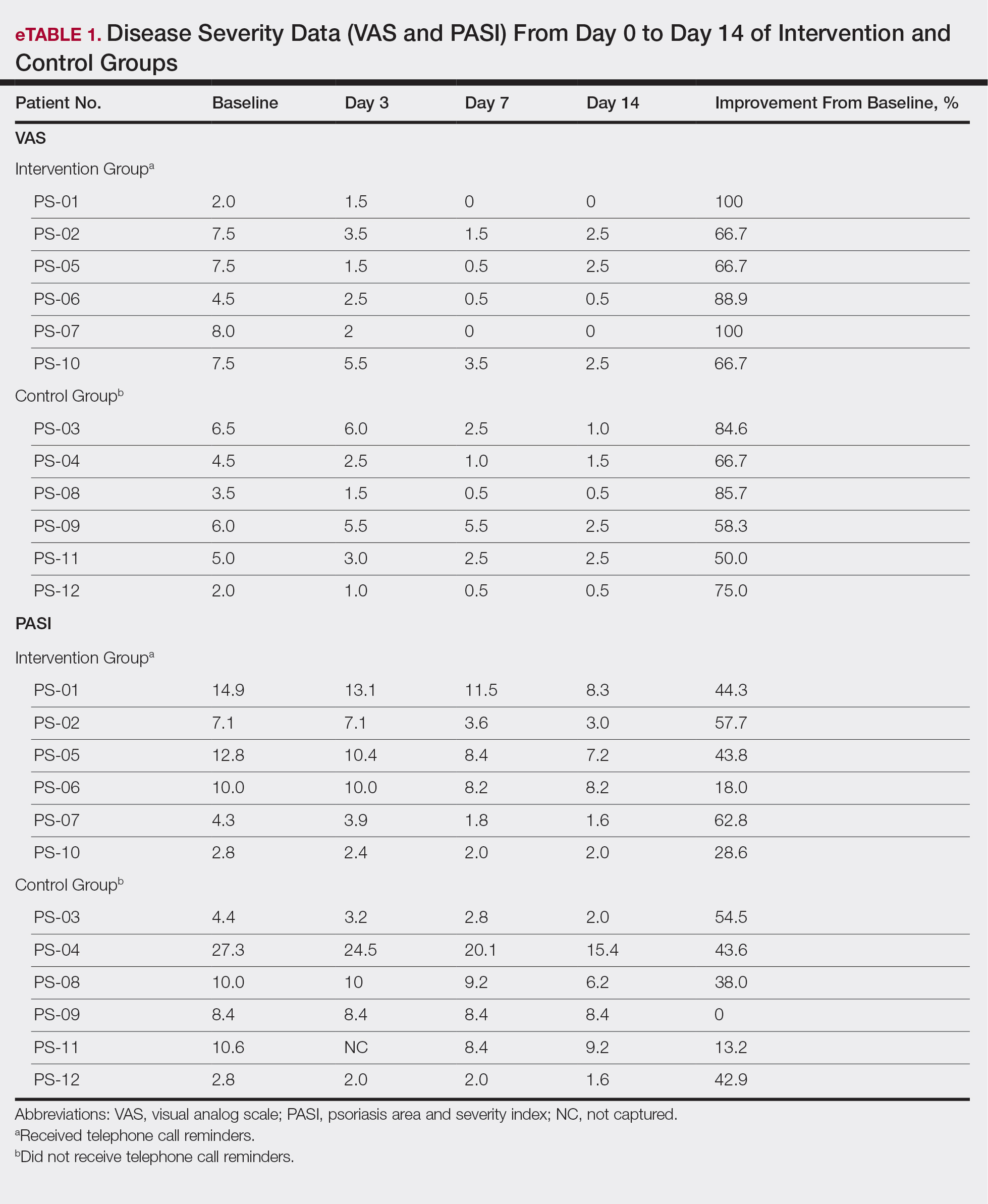
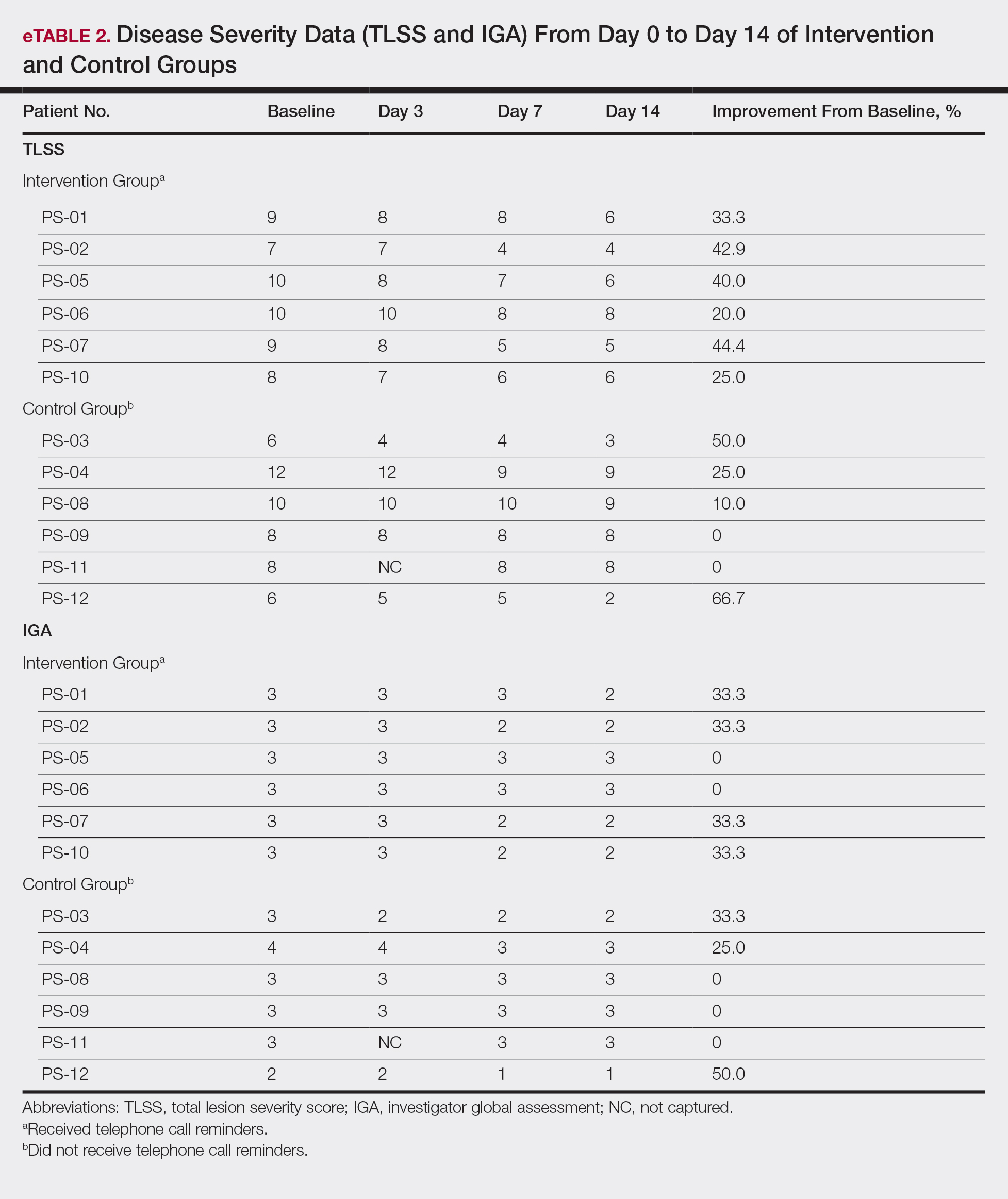
The percentage reduction in pruritus ranged from 66.7% to 100% and 50.0% to 85.7% with and without telephone call reminders, respectively. Improvement in PASI ranged from 18.0% to 62.8% and 0% to 54.5% with and without telephone call reminders, respectively. Improvement in TLSS and IGA was of lower magnitude but showed a similar pattern, with numerically greater improvement in the telephone call reminders group compared to the group that was not called (eTable 2). No patients showed a worse score for pruritus on the visual analog scale, PASI, TLSS, or IGA.
Discussion
Topical corticosteroids are highly effective for psoriasis in clinical trials, with clearance in 2 to 4 weeks in 60% to 80% of patients, a rapidity of response not matched by even the most potent biologic treatments.8,9 However, topical corticosteroids are not always effective in clinical practice. There may be primary inefficacy (they do not work at first) or secondary inefficacy (a previously effective treatment loses efficacy over time).10 Poor adherence can explain both phenomena. Primary adherence occurs when patients fill their prescription; secondary adherence occurs when patients follow the medication recommendations.11 Primary nonadherence is common in patients with psoriasis; in one study, 50% of psoriasis prescriptions were not filled.12 Secondary adherence also is poor and declines over time; electronic monitoring revealed adherence to topical treatments in psoriasis patients decreased from 85% initially to 51% at the end of 8 weeks.7 Given the high efficacy of topical corticosteroids in clinical trials and the poor adherence to topical treatment in patients with psoriasis, we anticipated that psoriasis that is resistant to topical corticosteroids would improve rapidly under conditions designed to promote adherence.
As expected, disease improved in almost every patient in this small cohort when they were given a potent topical corticosteroid, even though they previously reported that their psoriasis was resistant to potent topical corticosteroids. Although this study enrolled only a small cohort, it appears that the majority of patients with limited psoriasis that was reported to be resistant to topical treatment can see a response to topical treatment under conditions designed to encourage good adherence.
We believe that the good outcomes seen in our study were a result of good adherence. Although the desoximetasone spray 0.25% used in this study is a superpotent topical corticosteroid,8 the response to treatment was unlikely due to changing corticosteroid potency because 10 of 12 patients had tried another superpotent topical corticosteroid (clobetasol) and it failed. We chose a spray product for this study rather than an ointment to promote adherence; however, this choice limited the ability to assess adherence directly, as adherence-monitoring devices for spray delivery systems are not readily available.
Our study was limited by the small sample size and brief duration of treatment. However, the effect size is so large (ie, the topical treatment was so effective) that only a small sample size and brief treatment duration were needed to show that a high percentage of patients with psoriasis that had previously failed treatment with topical corticosteroids can in fact respond to this treatment.
We used telephone calls as reminders in 50% of patients to further encourage adherence. The study was not designed or powered to assess the effect of the telephone call reminders, but patients receiving those calls appeared to have slightly greater reduction in disease severity. Nonetheless, twice-daily telephone call reminders are unlikely to be a wanted or practical intervention; other approaches to encourage adherence are needed.
Frequent follow-up visits were incorporated in our study design to maximize adherence. Although it might not be feasible for clinical practices to schedule follow-up visits as often as in our study, other approaches such as virtual visits and electronic interaction might provide a practical alternative. Multifaceted approaches to increasing adherence include encouraging patients to participate in the treatment plan, prescribing therapy consistent with a patient’s preferred vehicle, and extensive patient education.13 If patients do not respond as expected, poor adherence can be considered. Other potential causes of poor outcomes include error in diagnosis; resistance to the prescribed treatment; concomitant infection; irritant exposure; and, in the case of biologics, antidrug antibody formation.14,15
High-potency topical corticosteroids are first-line treatments for psoriasis, but many patients report that they are ineffective or lose effectiveness over time.1-5 The mechanism underlying the lack or loss of activity is not well characterized but may be due to poor adherence to treatment. Adherence to topical treatment is poor in the short run and even worse in the long run.6,7 We evaluated 12 patients with psoriasis resistant to topical corticosteroids to determine if they would respond to topical corticosteroids under conditions designed to promote adherence to treatment.
Methods
This open-label, randomized, single-center clinical study recruited 12 patients with plaque psoriasis that previously failed treatment with topical corticosteroids and other therapies (Table). We stratified disease by body surface area: mild (<3%), moderate (3%–10%), and severe (>10%). Inclusion criteria included adult patients with plaque psoriasis amenable to topical corticosteroid therapy, ability to comply with requirements of the study, and a history of failed topical corticosteroid treatment (Figure). Patients were excluded if they were pregnant, breastfeeding, had conditions that would affect adherence or potentially bias results (eg, dementia, Alzheimer disease), had a history of allergy or sensitivity to corticosteroids, and had a history of drug hypersensitivity.

All patients received desoximetasone spray 0.25% twice daily for 14 days. At the baseline visit, 6 patients were randomly selected to also receive a twice-daily reminder telephone call. Study visits occurred frequently—at baseline and on days 3, 7, and 14—to further assure good adherence to the treatment regimen.
During visits, disease severity was scored using the visual analog scale for pruritus, psoriasis area and severity index (PASI), total lesion severity score (TLSS), and investigator global assessment (IGA). Descriptive statistics were used to report the outcomes for each patient.
The study was designed to assess the number of topical treatment–resistant patients who would improve with topical treatment but was not designed or powered to test if the telephone call reminders increased adherence.
Results
All patients completed the study; 10 of 12 patients (83.3%) had previously used topical clobetasol and it failed (Table). At the 2-week end-of-study visit, most patients improved on all measures. Patients who received telephone call reminders improved more than patients who did not. All 12 patients (100%) reported relief of itching; 11 of 12 (91.7%) had an improved PASI; 10 of 12 (83.3%) had an improved TLSS; and 7 of 12 (58.3%) had an improved IGA (eTables 1 and 2).
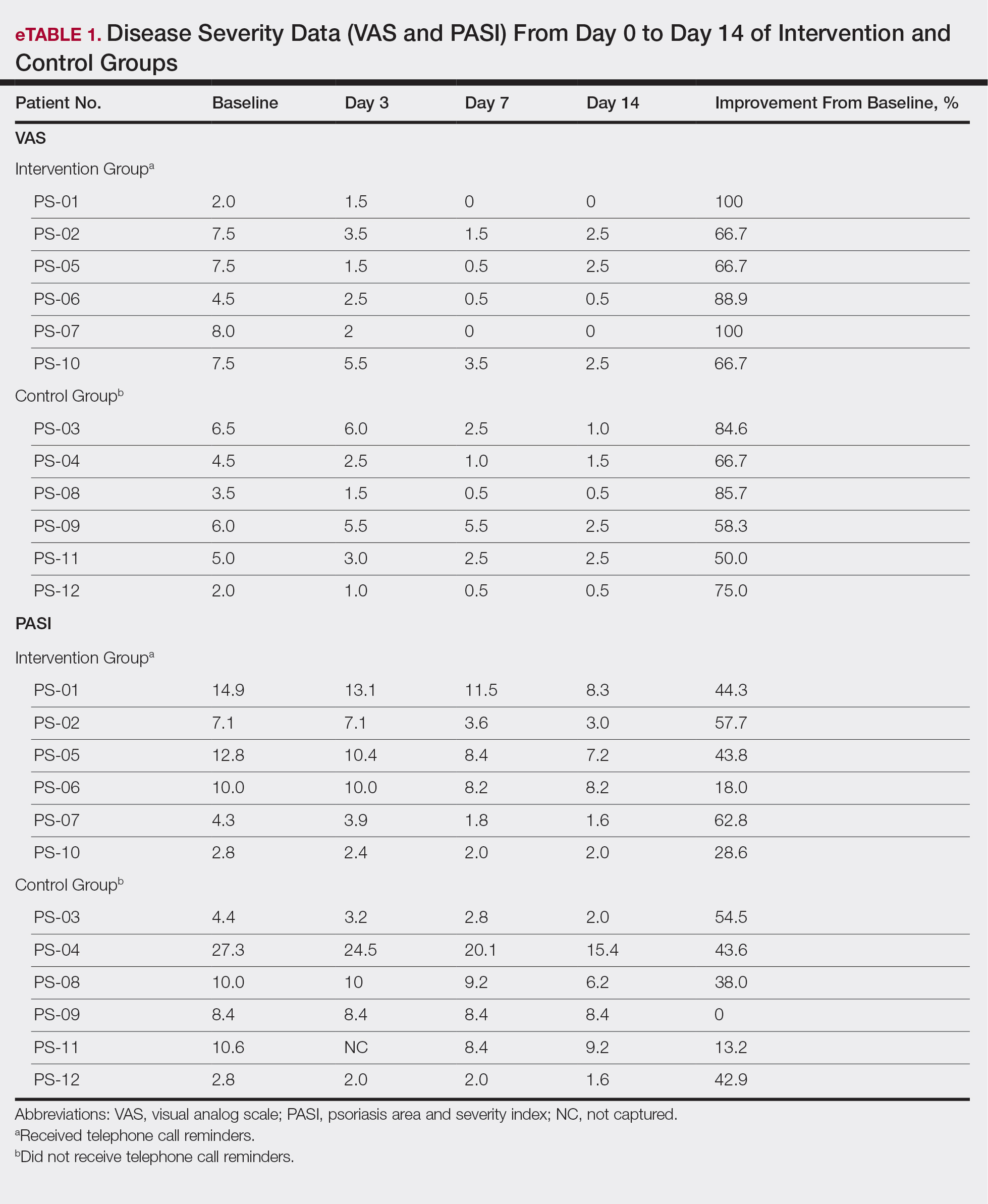
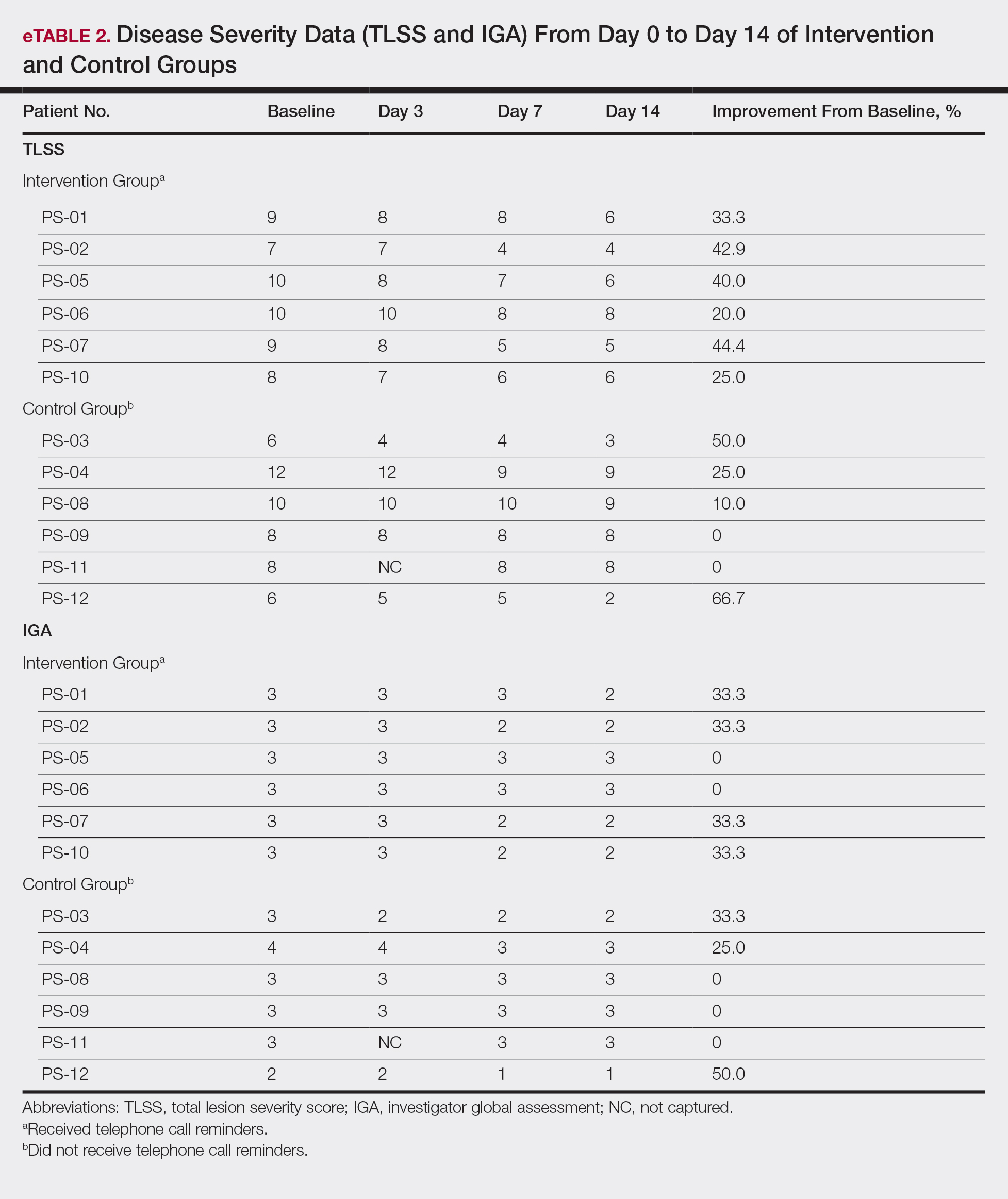
The percentage reduction in pruritus ranged from 66.7% to 100% and 50.0% to 85.7% with and without telephone call reminders, respectively. Improvement in PASI ranged from 18.0% to 62.8% and 0% to 54.5% with and without telephone call reminders, respectively. Improvement in TLSS and IGA was of lower magnitude but showed a similar pattern, with numerically greater improvement in the telephone call reminders group compared to the group that was not called (eTable 2). No patients showed a worse score for pruritus on the visual analog scale, PASI, TLSS, or IGA.
Discussion
Topical corticosteroids are highly effective for psoriasis in clinical trials, with clearance in 2 to 4 weeks in 60% to 80% of patients, a rapidity of response not matched by even the most potent biologic treatments.8,9 However, topical corticosteroids are not always effective in clinical practice. There may be primary inefficacy (they do not work at first) or secondary inefficacy (a previously effective treatment loses efficacy over time).10 Poor adherence can explain both phenomena. Primary adherence occurs when patients fill their prescription; secondary adherence occurs when patients follow the medication recommendations.11 Primary nonadherence is common in patients with psoriasis; in one study, 50% of psoriasis prescriptions were not filled.12 Secondary adherence also is poor and declines over time; electronic monitoring revealed adherence to topical treatments in psoriasis patients decreased from 85% initially to 51% at the end of 8 weeks.7 Given the high efficacy of topical corticosteroids in clinical trials and the poor adherence to topical treatment in patients with psoriasis, we anticipated that psoriasis that is resistant to topical corticosteroids would improve rapidly under conditions designed to promote adherence.
As expected, disease improved in almost every patient in this small cohort when they were given a potent topical corticosteroid, even though they previously reported that their psoriasis was resistant to potent topical corticosteroids. Although this study enrolled only a small cohort, it appears that the majority of patients with limited psoriasis that was reported to be resistant to topical treatment can see a response to topical treatment under conditions designed to encourage good adherence.
We believe that the good outcomes seen in our study were a result of good adherence. Although the desoximetasone spray 0.25% used in this study is a superpotent topical corticosteroid,8 the response to treatment was unlikely due to changing corticosteroid potency because 10 of 12 patients had tried another superpotent topical corticosteroid (clobetasol) and it failed. We chose a spray product for this study rather than an ointment to promote adherence; however, this choice limited the ability to assess adherence directly, as adherence-monitoring devices for spray delivery systems are not readily available.
Our study was limited by the small sample size and brief duration of treatment. However, the effect size is so large (ie, the topical treatment was so effective) that only a small sample size and brief treatment duration were needed to show that a high percentage of patients with psoriasis that had previously failed treatment with topical corticosteroids can in fact respond to this treatment.
We used telephone calls as reminders in 50% of patients to further encourage adherence. The study was not designed or powered to assess the effect of the telephone call reminders, but patients receiving those calls appeared to have slightly greater reduction in disease severity. Nonetheless, twice-daily telephone call reminders are unlikely to be a wanted or practical intervention; other approaches to encourage adherence are needed.
Frequent follow-up visits were incorporated in our study design to maximize adherence. Although it might not be feasible for clinical practices to schedule follow-up visits as often as in our study, other approaches such as virtual visits and electronic interaction might provide a practical alternative. Multifaceted approaches to increasing adherence include encouraging patients to participate in the treatment plan, prescribing therapy consistent with a patient’s preferred vehicle, and extensive patient education.13 If patients do not respond as expected, poor adherence can be considered. Other potential causes of poor outcomes include error in diagnosis; resistance to the prescribed treatment; concomitant infection; irritant exposure; and, in the case of biologics, antidrug antibody formation.14,15
- Feldman SR, Fleischer AB Jr, Cooper JZ. New topical treatments change the pattern of treatment of psoriasis: dermatologists remain the primary providers of this care. Int J Dermatol. 2000;39:41-44.
- Menter A. Topical monotherapy with clobetasol propionate spray 0.05% in the COBRA trial. Cutis. 2007;80(suppl 5):12-19.
- Saleem MD, Negus D, Feldman SR. Topical 0.25% desoximetasone spray efficacy for moderate to severe plaque psoriasis: a randomized clinical trial. J Dermatolog Treat. 2018;29:32-35.
- Mraz S, Leonardi C, Colón LE, et al. Different treatment outcomes with different formulations of clobetasol propionate 0.05% for the treatment of plaque psoriasis. J Dermatolog Treat. 2008;19:354-359.
- Chiricozzi A, Pimpinelli N, Ricceri F, et al. Treatment of psoriasis with topical agents: recommendations from a Tuscany Consensus. Dermatol Ther. 2017;30:e12549.
- Carroll CL, Feldman SR, Camacho FT, et al. Adherence to topical therapy decreases during the course of an 8-week psoriasis clinical trial: commonly used methods of measuring adherence to topical therapy overestimate actual use. J Am Acad Dermatol. 2004;51:212-216.
- Alinia H, Moradi Tuchayi S, Smith JA, et al. Long-term adherence to topical psoriasis treatment can be abysmal: a 1-year randomized intervention study using objective electronic adherence monitoring. Br J Dermatol. 2017;176:759-764.
- Keegan BR. Desoximetasone 0.25% spray for the relief of scaling in adults with plaque psoriasis. J Drugs Dermatol. 2015;14:835-840.
- Beutner K, Chakrabarty A, Lemke S, et al. An intra-individual randomized safety and efficacy comparison of clobetasol propionate 0.05% spray and its vehicle in the treatment of plaque psoriasis. J Drugs Dermatol. 2006;5:357-360.
- Mehta AB, Nadkarni NJ, Patil SP, et al. Topical corticosteroids in dermatology. Indian J Dermatol Venereol Leprol. 2016;82:371-378.
- Blais L, Kettani FZ, Forget A, et al. Assessing adherence to inhaled corticosteroids in asthma patients using an integrated measure based on primary and secondary adherence. Eur J Clin Pharmacol. 2016;73:91-97.
- Storm A, Andersen SE, Benfeldt E, et al. One in 3 prescriptions are never redeemed: primary nonadherence in an outpatient clinic. J Am Acad Dermatol. 2008;59:27-33.
- Zschocke I, Mrowietz U, Karakasili E, et al. Non-adherence and measures to improve adherence in the topical treatment of psoriasis. J Eur Acad Dermatol Venereol. 2014;28(Suppl 2):4-9.
- Mooney E, Rademaker M, Dailey R, et al. Adverse effects of topical corticosteroids in paediatric eczema: Australasian consensus statement. Australas J Dermatol. 2015;56:241-251.
- Varada S, Tintle SJ, Gottlieb AB. Apremilast for the treatment of psoriatic arthritis. Expert Rev Clin Pharmacol. 2014;7:239-250.
- Feldman SR, Fleischer AB Jr, Cooper JZ. New topical treatments change the pattern of treatment of psoriasis: dermatologists remain the primary providers of this care. Int J Dermatol. 2000;39:41-44.
- Menter A. Topical monotherapy with clobetasol propionate spray 0.05% in the COBRA trial. Cutis. 2007;80(suppl 5):12-19.
- Saleem MD, Negus D, Feldman SR. Topical 0.25% desoximetasone spray efficacy for moderate to severe plaque psoriasis: a randomized clinical trial. J Dermatolog Treat. 2018;29:32-35.
- Mraz S, Leonardi C, Colón LE, et al. Different treatment outcomes with different formulations of clobetasol propionate 0.05% for the treatment of plaque psoriasis. J Dermatolog Treat. 2008;19:354-359.
- Chiricozzi A, Pimpinelli N, Ricceri F, et al. Treatment of psoriasis with topical agents: recommendations from a Tuscany Consensus. Dermatol Ther. 2017;30:e12549.
- Carroll CL, Feldman SR, Camacho FT, et al. Adherence to topical therapy decreases during the course of an 8-week psoriasis clinical trial: commonly used methods of measuring adherence to topical therapy overestimate actual use. J Am Acad Dermatol. 2004;51:212-216.
- Alinia H, Moradi Tuchayi S, Smith JA, et al. Long-term adherence to topical psoriasis treatment can be abysmal: a 1-year randomized intervention study using objective electronic adherence monitoring. Br J Dermatol. 2017;176:759-764.
- Keegan BR. Desoximetasone 0.25% spray for the relief of scaling in adults with plaque psoriasis. J Drugs Dermatol. 2015;14:835-840.
- Beutner K, Chakrabarty A, Lemke S, et al. An intra-individual randomized safety and efficacy comparison of clobetasol propionate 0.05% spray and its vehicle in the treatment of plaque psoriasis. J Drugs Dermatol. 2006;5:357-360.
- Mehta AB, Nadkarni NJ, Patil SP, et al. Topical corticosteroids in dermatology. Indian J Dermatol Venereol Leprol. 2016;82:371-378.
- Blais L, Kettani FZ, Forget A, et al. Assessing adherence to inhaled corticosteroids in asthma patients using an integrated measure based on primary and secondary adherence. Eur J Clin Pharmacol. 2016;73:91-97.
- Storm A, Andersen SE, Benfeldt E, et al. One in 3 prescriptions are never redeemed: primary nonadherence in an outpatient clinic. J Am Acad Dermatol. 2008;59:27-33.
- Zschocke I, Mrowietz U, Karakasili E, et al. Non-adherence and measures to improve adherence in the topical treatment of psoriasis. J Eur Acad Dermatol Venereol. 2014;28(Suppl 2):4-9.
- Mooney E, Rademaker M, Dailey R, et al. Adverse effects of topical corticosteroids in paediatric eczema: Australasian consensus statement. Australas J Dermatol. 2015;56:241-251.
- Varada S, Tintle SJ, Gottlieb AB. Apremilast for the treatment of psoriatic arthritis. Expert Rev Clin Pharmacol. 2014;7:239-250.
Practice Points
- Most patients with psoriasis are good candidates for topical treatment.
- Topical treatment of psoriasis often is ineffective.
- Topical treatment of psoriasis can be rapidly effective, even in patients who reported disease that was resistant to topical treatment.
Betamethasone Dipropionate Spray 0.05% Alleviates Troublesome Symptoms of Plaque Psoriasis
Psoriasis affects approximately 2% to 3% of the US population and is characterized by plaques that are red, scaly, and elevated.1 Cutaneous symptoms of the disease are described by patients as itching, burning, and stinging sensations. Large multinational and US surveys have reported pruritus as patients’ most bothersome symptom, with scaling/flaking reported as the second most bothersome.2,3 Reported incidence rates for itching range from 60.4% to 98.3%, with at least half of these patients reporting daily or constant pruritus.2,4-7 Consequent effects on quality of life include impaired sleep,6 difficulty concentrating, lower sex drive, and depression.7 Despite these findings, pruritus is rarely included in the efficacy assessments of psoriasis treatments. In addition, 2 of the most commonly reported but difficult-to-treat locations for plaques are the outside of the elbows (45%) and the knees (32%),1,2,8 areas where the stratum corneum typically is thicker, less hydrated, and less likely to absorb topical products.9-11 Clinical studies have not focused specifically on these areas when assessing treatments.
Topical corticosteroids have been the mainstay of psoriasis therapy for decades because of their anti-inflammatory and antiproliferative properties.7 One large multinational physician survey indicated that 75% of patients are prescribed topical steroids,12 which are important for first-line treatment and are often maintained as adjunctive therapy in combination with other treatments for patients with extensive disease or recalcitrant lesions.13 Topical corticosteroids are ranked into different classes based on their vasoconstrictor assay (VCA), a measure of skin blanching used as a marker for vasoconstriction. Topical agents with VCA ratings of mid-potency or superpotency are generally recommended for initial therapy, with superpotent agents required for the treatment of thick chronic plaques. However, longer durations of use may contribute to systemic absorption and adverse events.13 The vehicle composition is important for corticosteroid delivery and retention at the site of pathology, contributing to the efficacy of the steroid.13,14 Selecting the appropriate steroid and vehicle is important to maximize efficacy and minimize adverse events.
Betamethasone dipropionate (BD) spray 0.05% is an emollient formulation of 0.05% BD that can be sprayed onto psoriatic plaques. The BD spray formulation was designed to penetrate the stratum corneum and be retained within the dermis and epidermis, the site of T-cell activity that drives the psoriatic disease process.14 In 2 phase 3 studies, BD spray demonstrated the ability to reduce the signs of plaque psoriasis with indication of improvement by day 4.15,16 These studies also showed improvement in the local cutaneous symptoms of itching, burning and stinging, and pain. As a mid-potent steroid, BD spray displays less systemic absorption but similar efficacy compared to a superpotent augmented BD (AugBD) lotion in relieving the signs and symptoms of plaque psoriasis.15-17
The objective of the current investigation was to assess the ability of BD spray to relieve itching and to clear plaque psoriasis on the knees and elbows utilizing post hoc analyses of the 2 phase 3 trials. The goal of these analyses was to demonstrate BD spray as effective at relieving the most troublesome signs and symptoms affecting patients with plaque psoriasis.
Methods
Two phase 3 studies were conducted to demonstrate the efficacy and safety of BD spray.15,16 The design of the studies was similar15,16 to allow the data to be pooled for post hoc analyses.
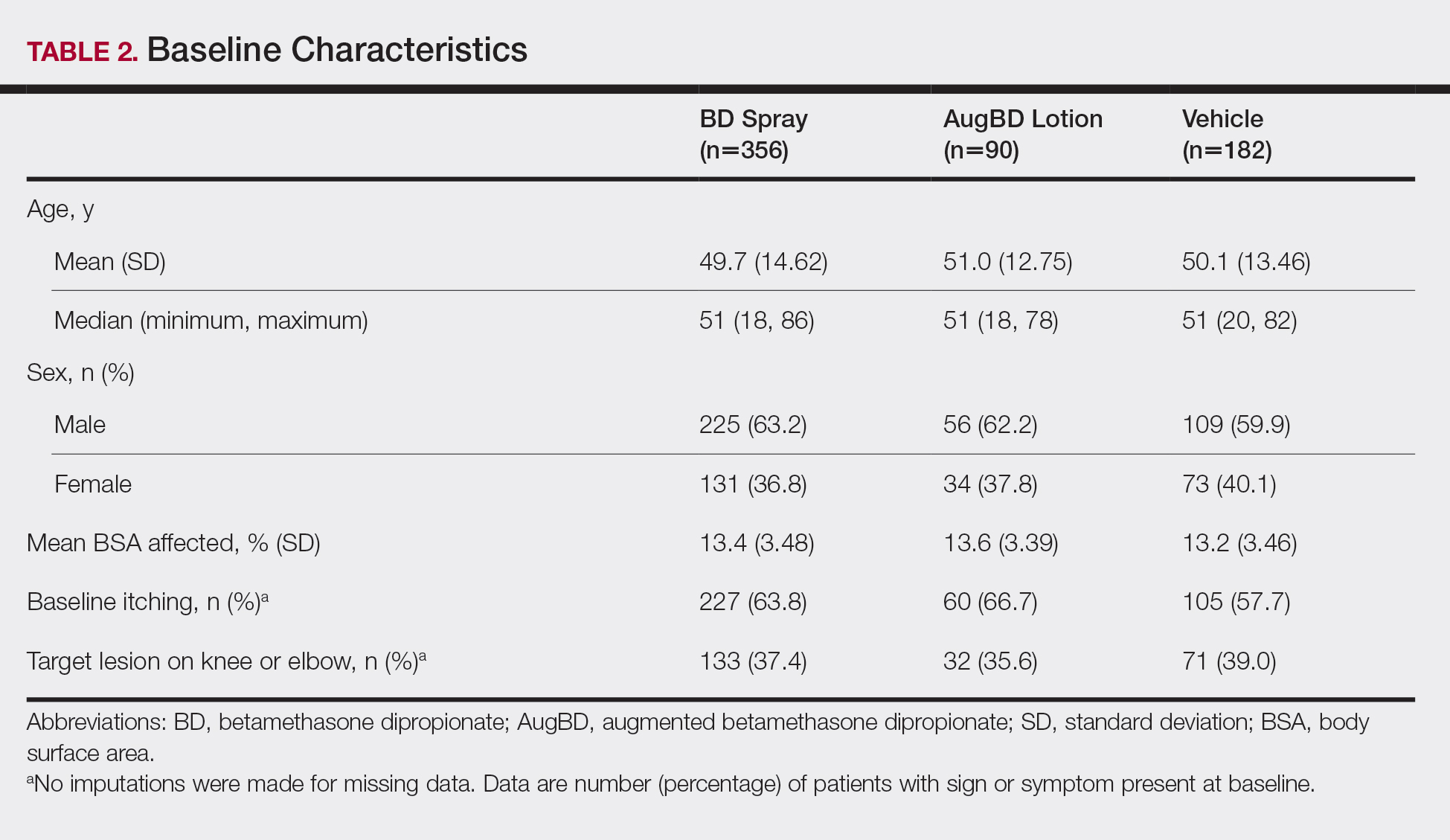
Both were US multicenter, randomized, vehicle-controlled, double-blind, parallel-group studies comparing the safety and efficacy of BD spray 0.05% (Sernivo, Promius Pharma) with its vehicle formulation spray (identical to BD spray, but lacking the active steroid component).15,16 One of the studies also compared BD spray with an AugBD lotion 0.05% (Diprolene,Merck & Co). Adults with moderate plaque psoriasis (investigator global assessment of 3; 10%–20% body surface area) were randomized to apply BD spray, vehicle spray, or AugBD lotion (1 study only) twice daily to all affected areas, excluding the face, scalp, and intertriginous areas for 28 days (BD spray and vehicle) or 14 days (AugBD lotion, per product label).15
Assessments
Two post hoc analyses were conducted on data pooled from the 2 phase 3 trials: (1) incidence of itching, and (2) total sign score (TSS) for lesions located on the knees and elbows.
Itching
Itching was assessed proactively by asking patients if they were experiencing itching (yes/no) at each visit (baseline and days 4, 8, 15, and 29) or had experienced itching since their last visit. As itching could be an adverse event of topical application, application-site pruritus was also recorded.
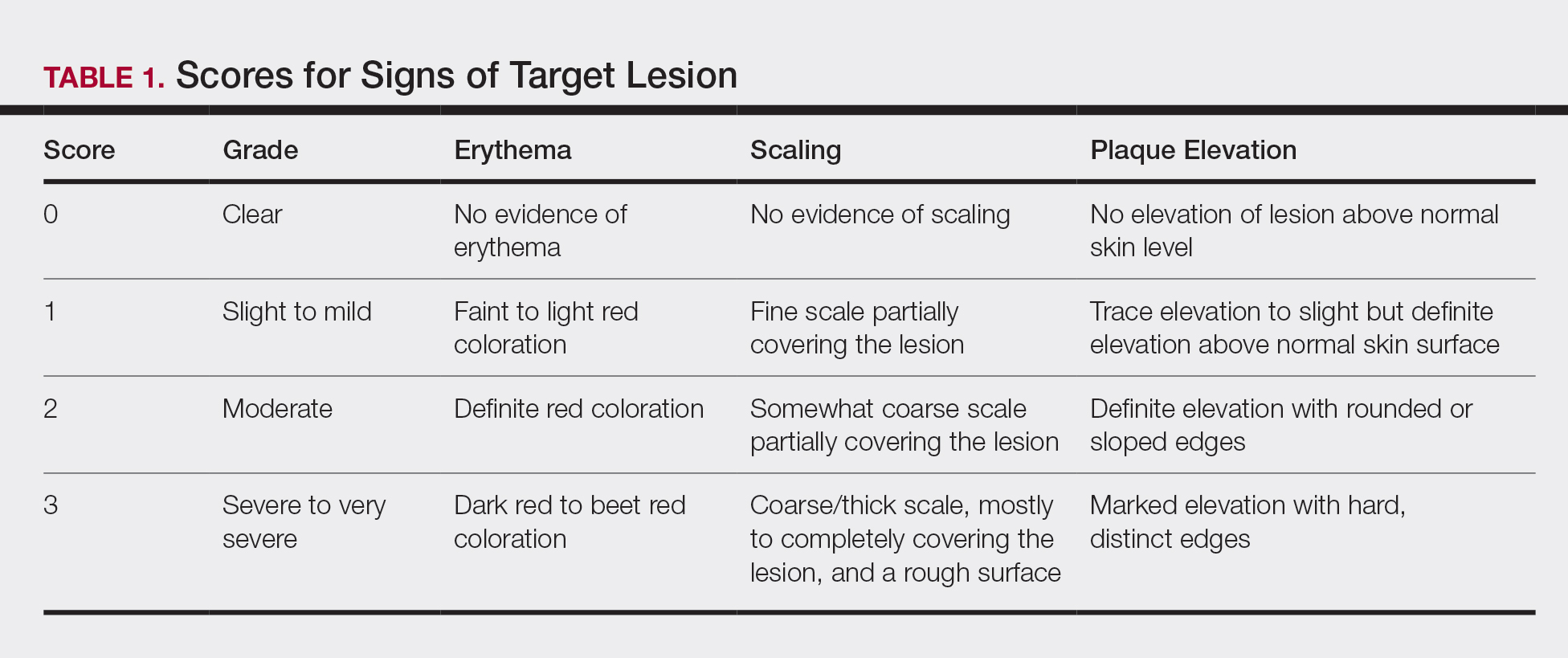
Total Sign Score
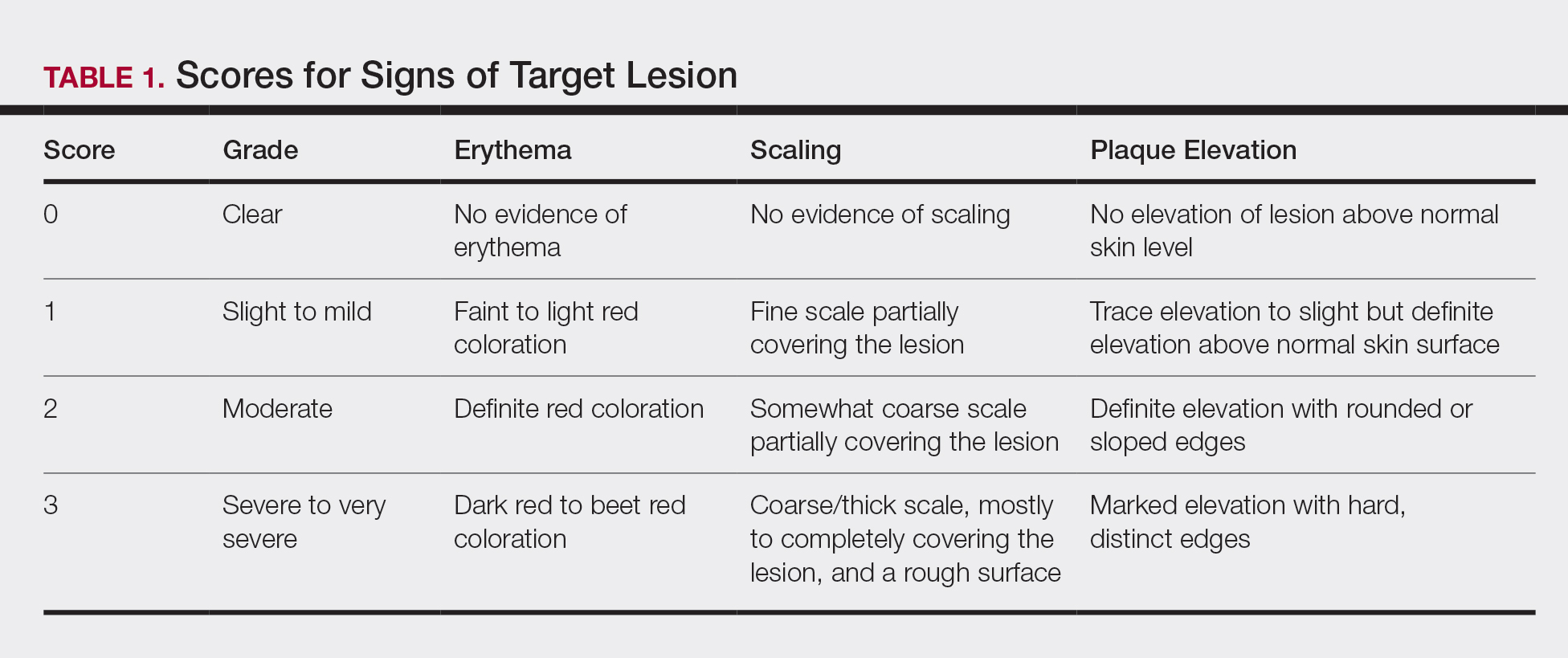
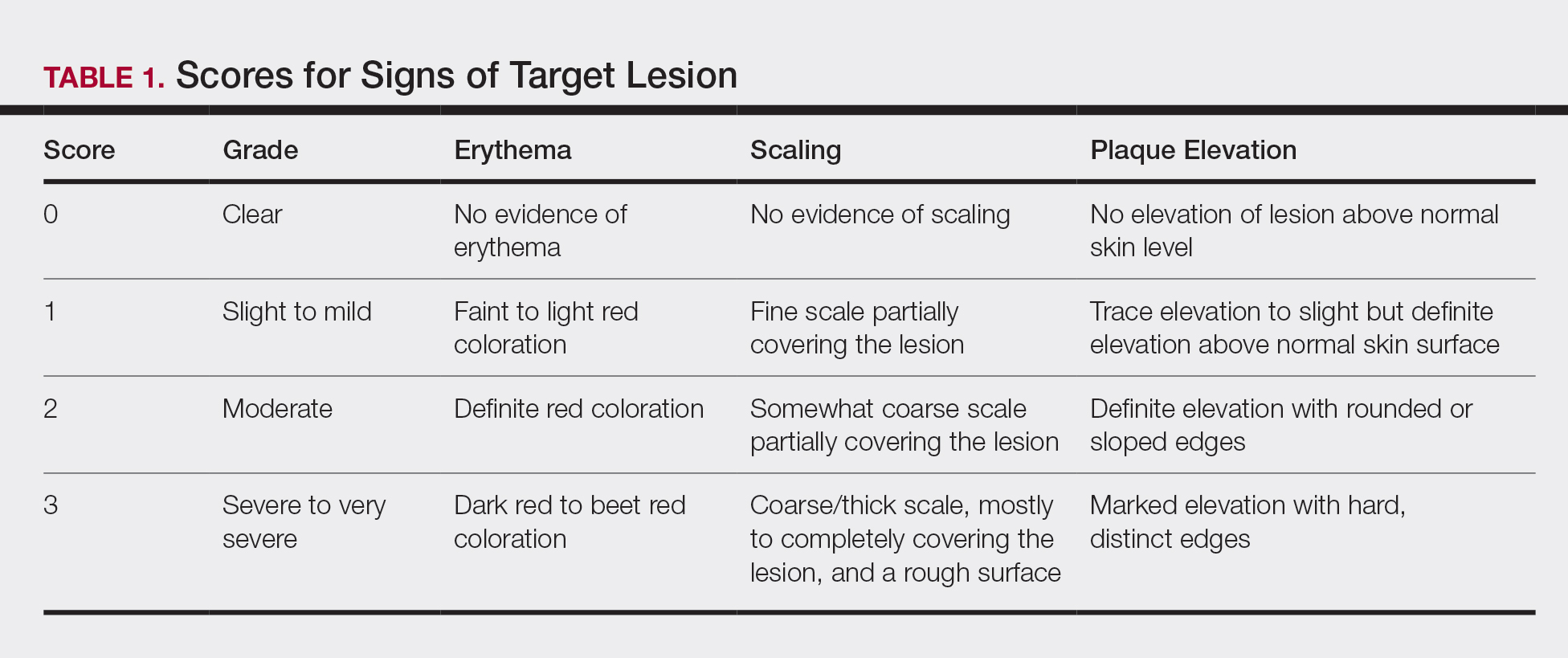
For each patient, a target plaque was selected that was representative of their psoriasis. The plaque was assessed on a 3-point grading scale for each of 3 key signs of plaque psoriasis: erythema, scaling, and plaque elevation (Table 1) at baseline and days 4, 8, 15, and 29. Total sign score was calculated by summing the scores for these 3 signs, resulting in a score ranging from 0 to 9. Treatment success was measured as (1) achieving a score of 0 or 1 (ie, reducing the plaque to clear or slight to mild) for the individual signs of erythema, scaling, and plaque elevation; and (2) achieving a TSS of 0 or 1 for all 3 signs—erythema, scaling, and plaque elevation—for each target lesion. Total sign score was assessed proactively for all patients.15,16 The post hoc analysis reported here examined patients whose target lesion was located on either the knee or the elbow.
Statistical Analyses
Because both study protocols were identical, data were pooled from the 2 phase 3 trials. All statistical analyses were performed using SAS software (SAS Institute). Two-sided hypothesis testing was conducted for all analyses using a significance level of P=.05. Post hoc analyses used Fisher exact test. No imputations were made for missing data.
Statistical analyses of itching compared the incidence of itching at each assessment time point (baseline and days 4, 8, 15, and 29) between BD spray and vehicle and between BD spray and AugBD lotion. Additional analysis included a statistical test on the incidence of itching in the subgroup of patients who reported itching at baseline.
Statistical analyses for the knees and elbows included only patients with their target lesion located on either the knee or the elbow. Analyses compared BD spray with vehicle and BD spray with AugBD lotion at days 4, 8, 15, and 29. Comparison with AugBD lotion treatment was up to day 14 only, consistent with application time limits in the AugBD lotion product label.18
Results
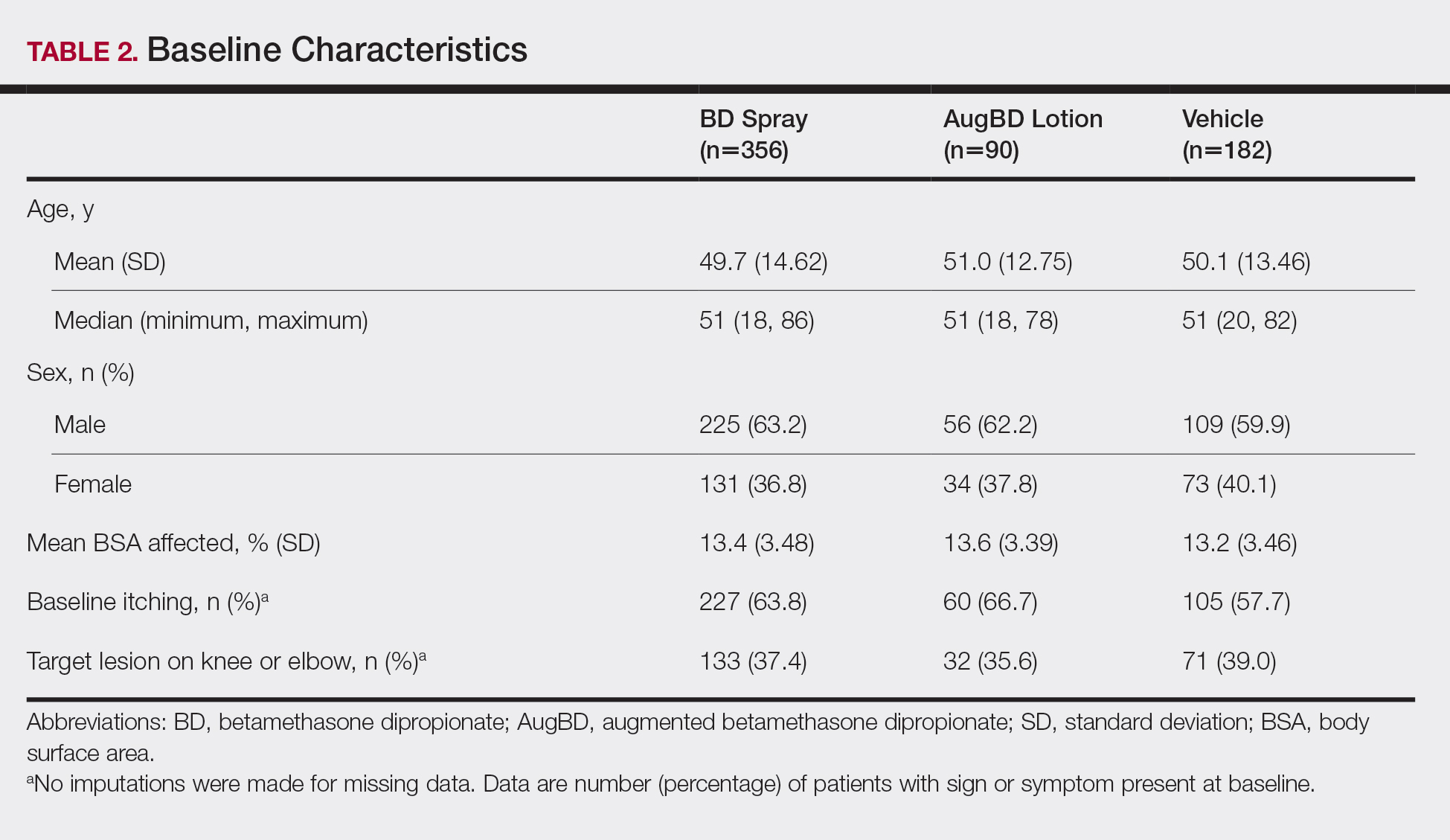
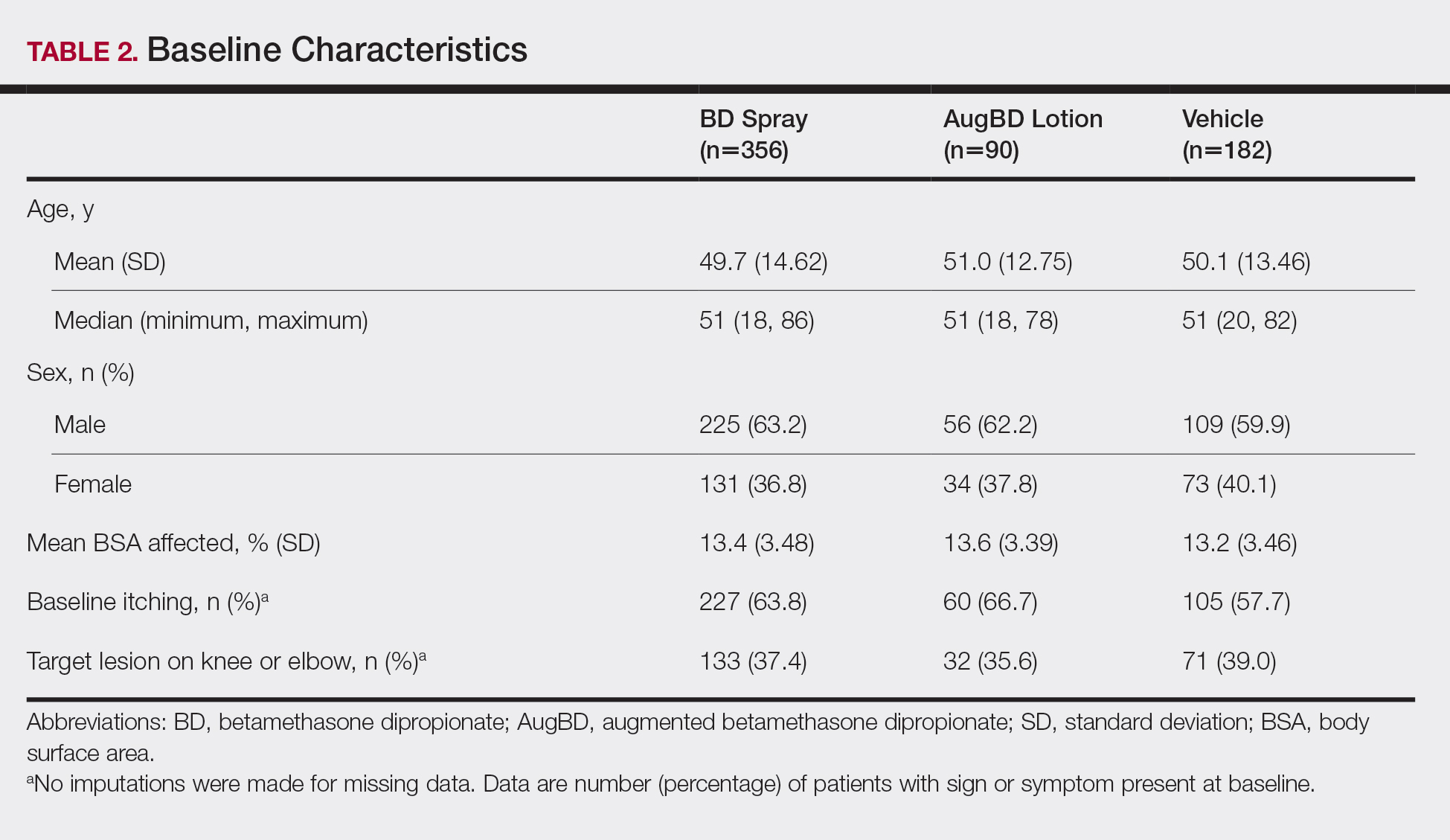
These analyses included data from the 628 patients enrolled in the 2 phase 3 trials. Patients had similar baseline characteristics across treatment groups (Table 2). Itching was the most common cutaneous symptom at baseline, reported by almost two-thirds (n=392, 62.4%) of patients. Of the 628 patients, 236 (37.6%) had a target lesion located on the elbow or knee selected for assessment. The mean baseline body surface area was 13% to 14% across groups.
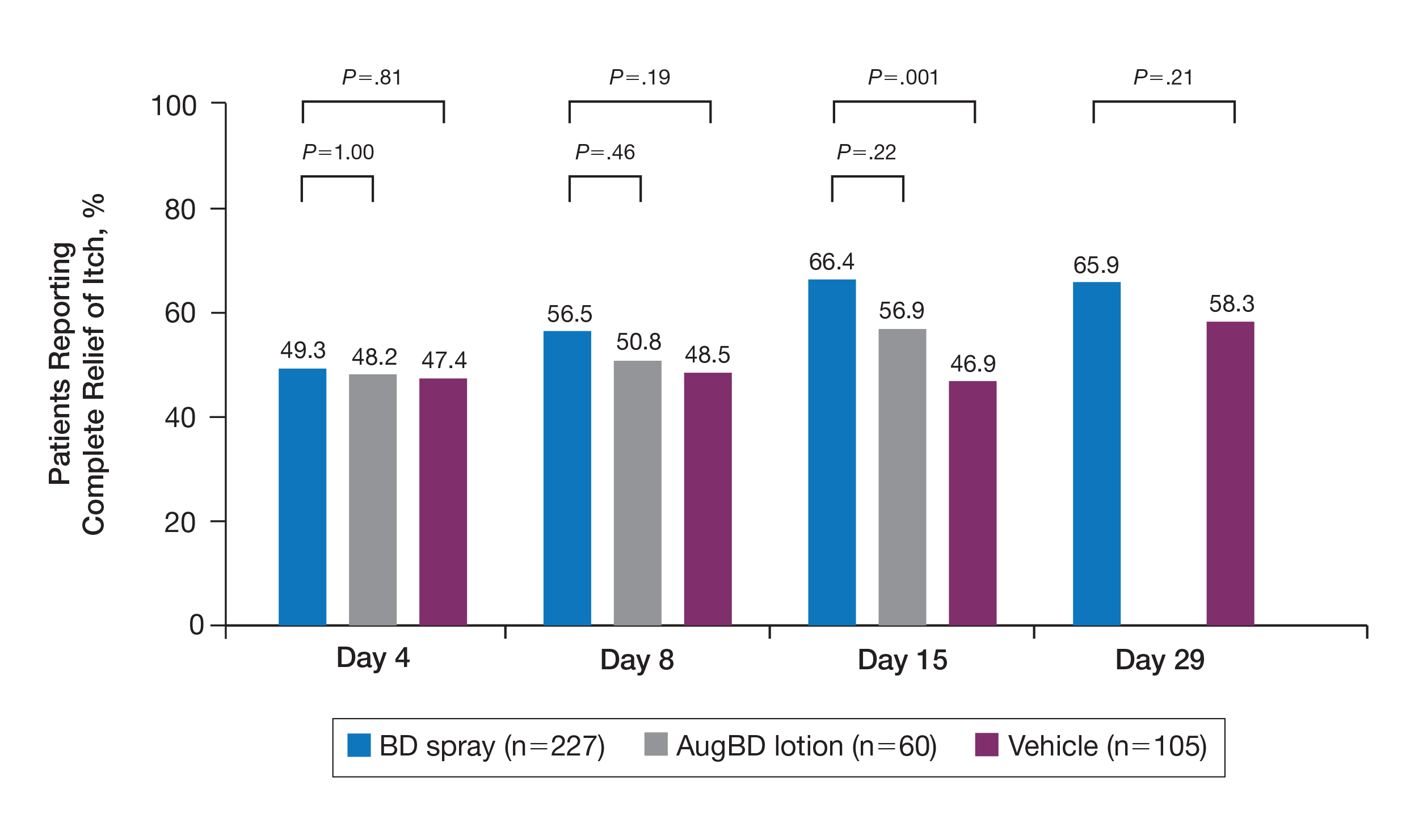
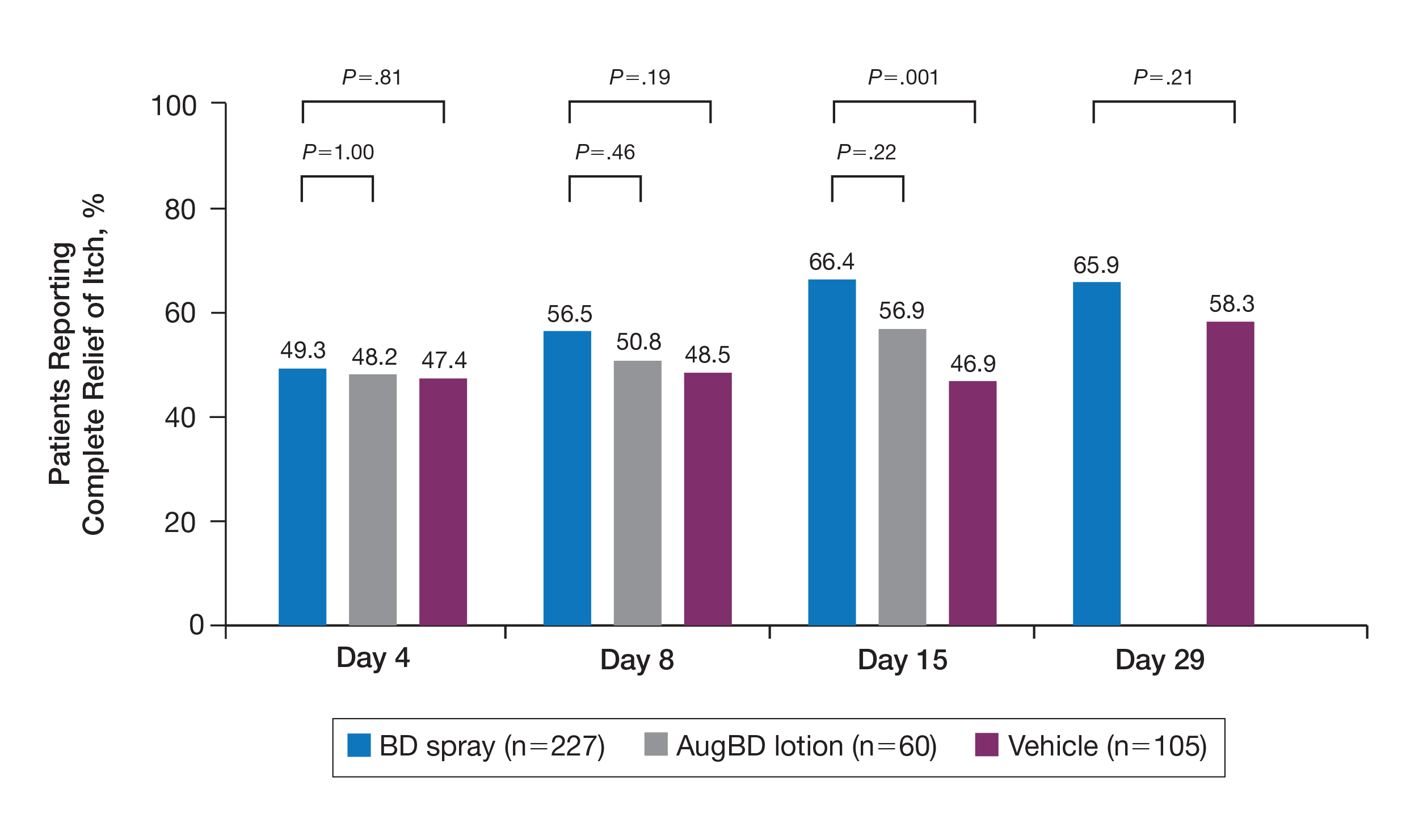
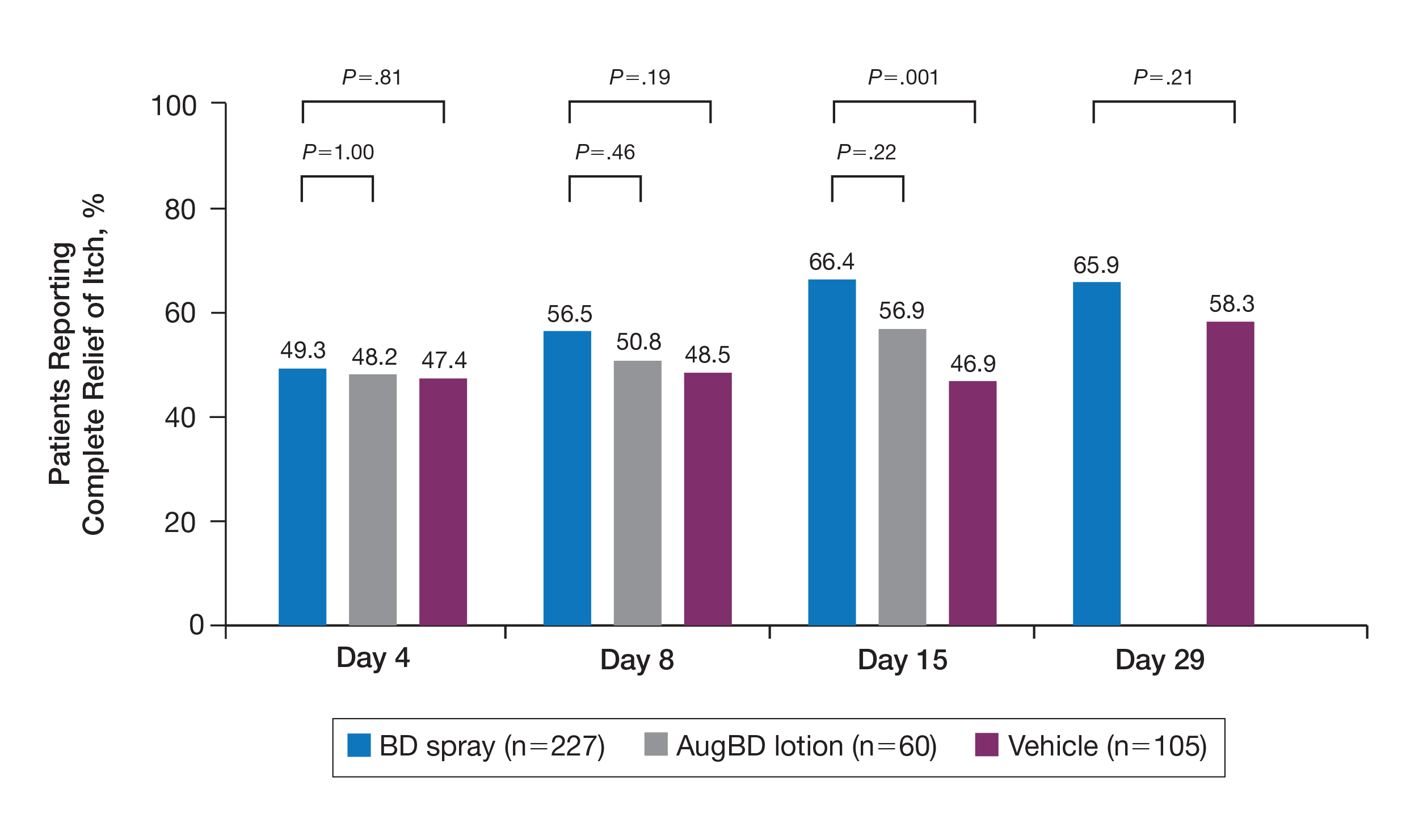
A post hoc analysis was performed on the subgroup of patients who reported itching at baseline (N=392)(eFigure 1). For these patients, almost half were itch free by day 4 across all groups (49.3% BD spray, 48.2% AugBD lotion, and 47.4% vehicle). By the end of treatment, 65.9% of patients using BD spray and 58.3% of patients using vehicle were itch free at day 29, with 56.9% of AugBD lotion patients itch free at day 15.
Application-site pruritus recorded as a treatment-emergent adverse event was seen in low numbers and was similar in proportion between the 2 steroid treatments (7.7% BD spray, 6.7% AugBD lotion, and 14.4% vehicle).
Psoriasis Individual Sign Scores for Knee and Elbow Plaques
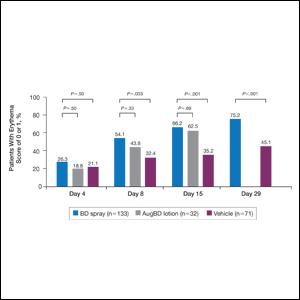
Target lesions located on the knee or elbow represented 37.6% of all target lesions assessed. Efficacy analysis of the pooled data on knee and elbow lesions revealed that BD spray was similar to AugBD lotion in reducing sign scores to 0 or 1 (Figures 1 and 2).
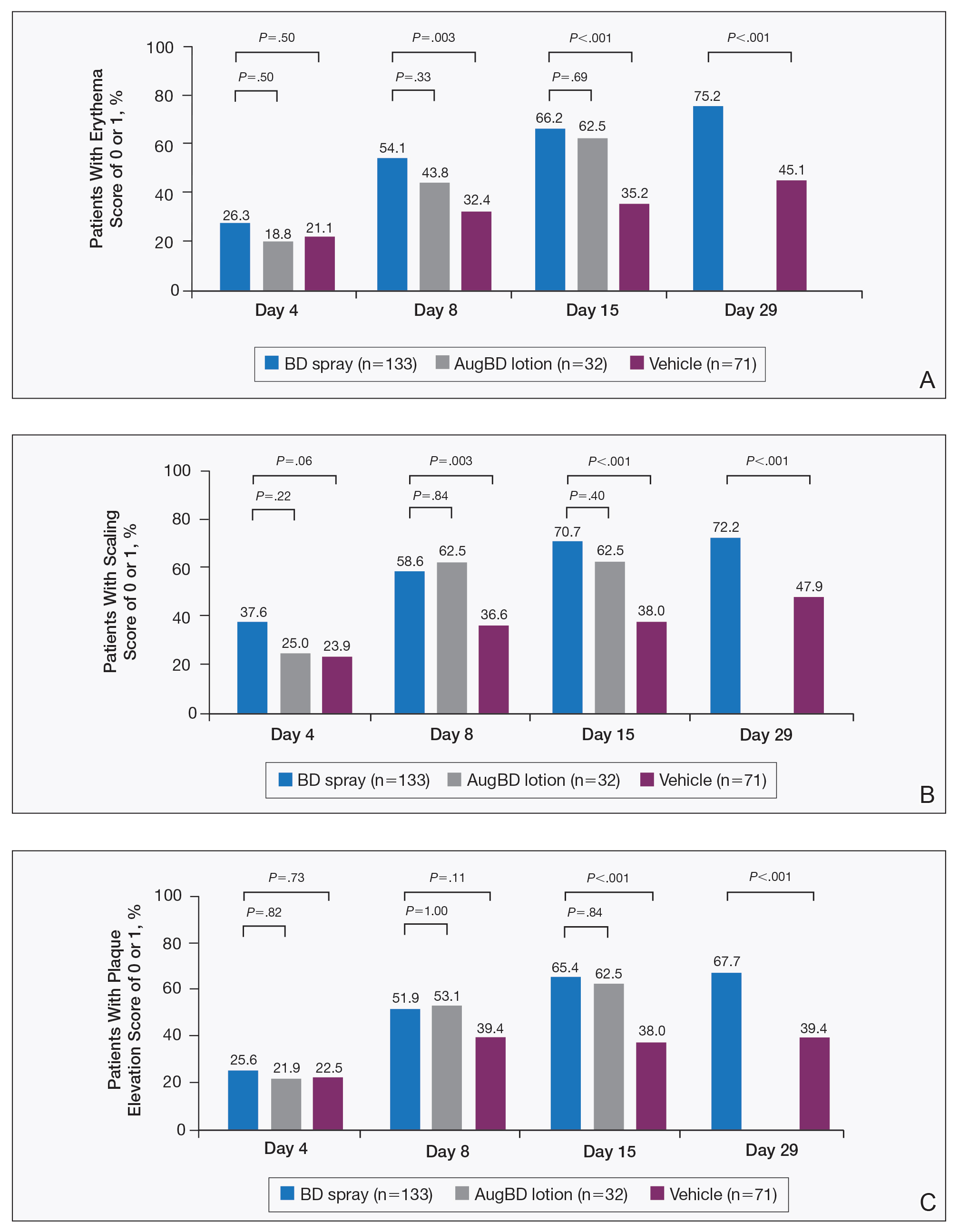
The percentage of patients reporting improvements in erythema, scaling, and plaque elevation scores at day 4
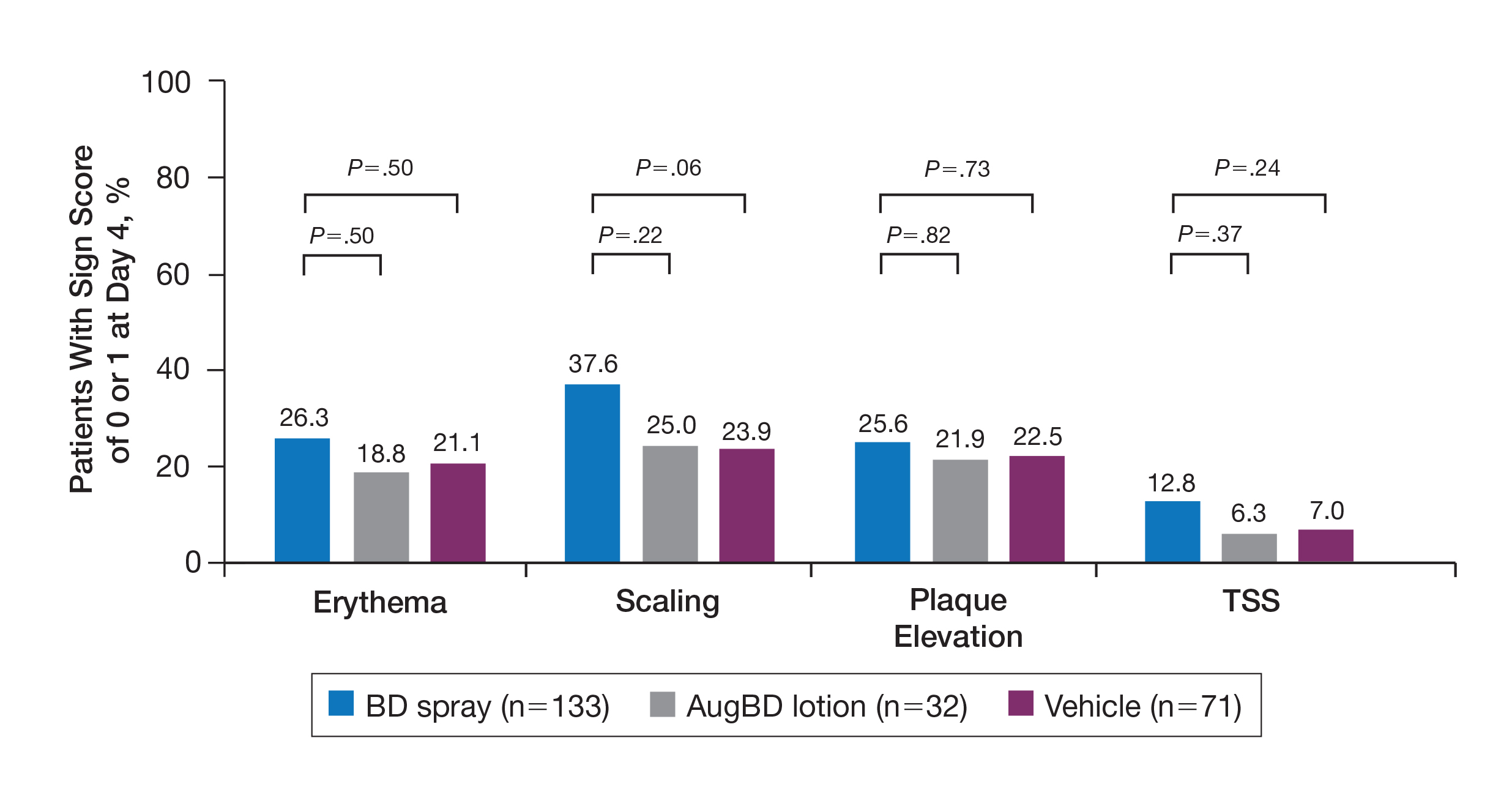
The proportion of patients achieving treatment success (defined as a score of 0 or 1) was comparable for the2 products on day 15 for erythema (66.2% BD spray vs 62.5% AugBD lotion), scaling (70.7% BD spray vs 62.5% AugBD lotion), and plaque elevation (65.4% BD spray vs 62.5% AugBD lotion)(Figure 1). From day 8, BD spray reduced erythema and scaling in significantly more patients than vehicle (P=.003 for both), and BD spray reduced erythema, scaling, and plaque elevation in more patients than vehicle from day 15 (P<.001 for all). No statistically significant difference was found between BD spray and AugBD lotion on erythema, scaling, and plaque elevation scores.
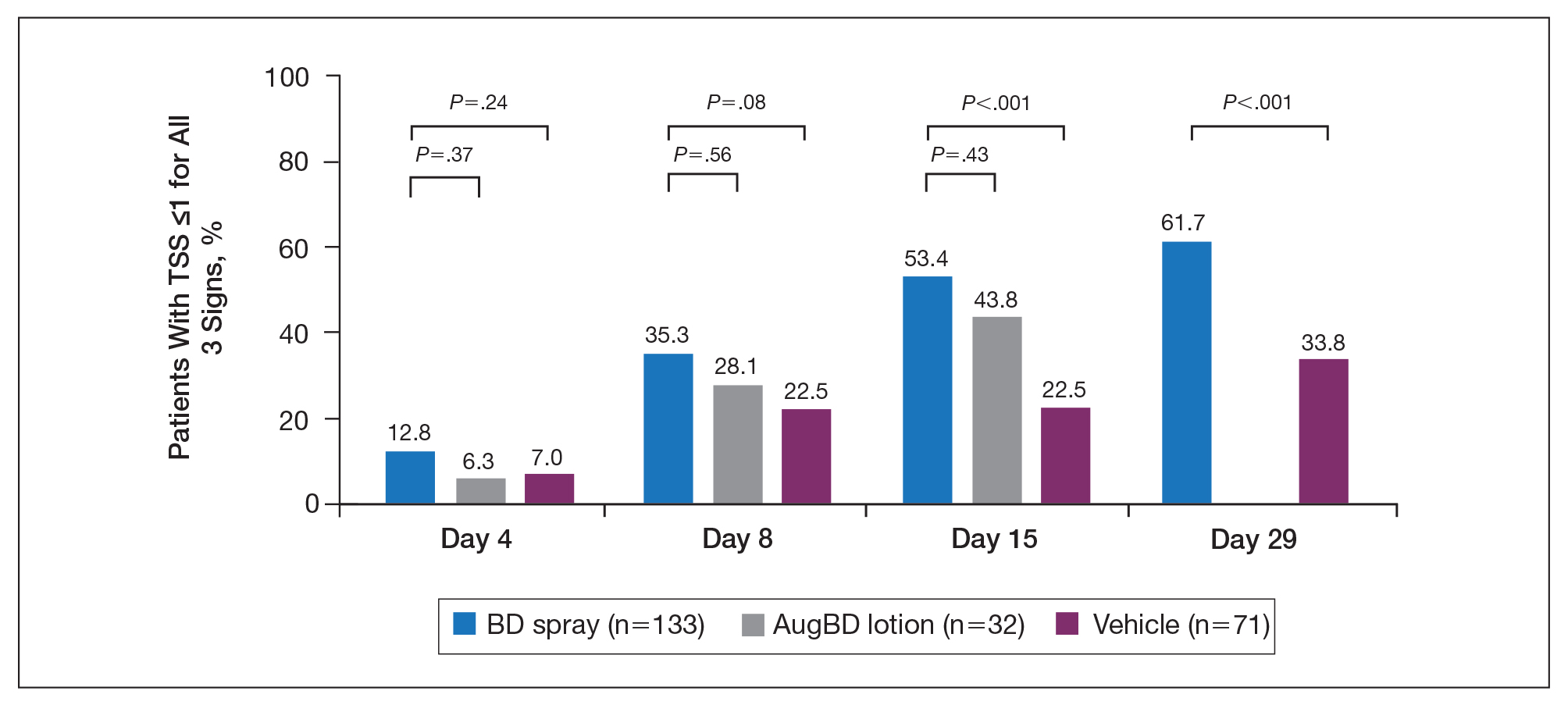
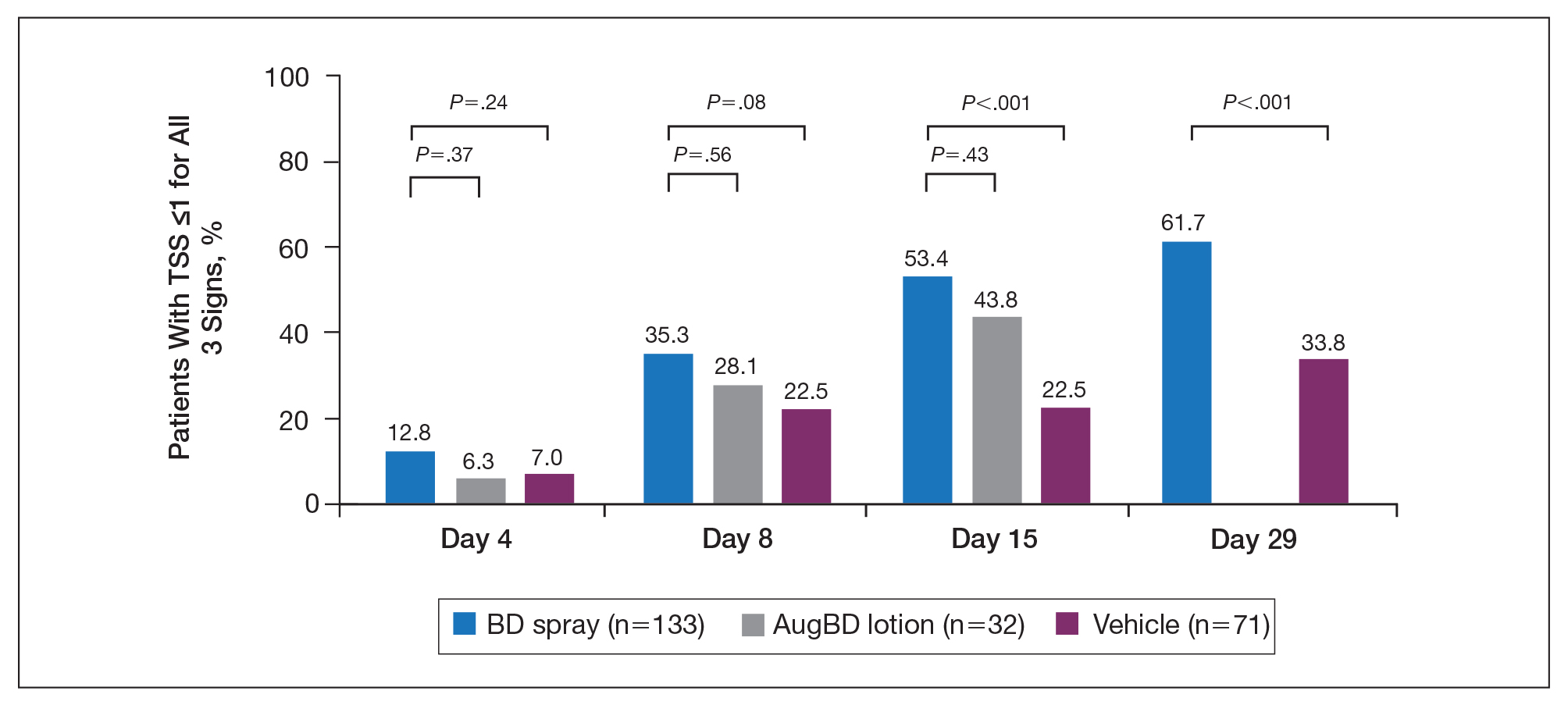
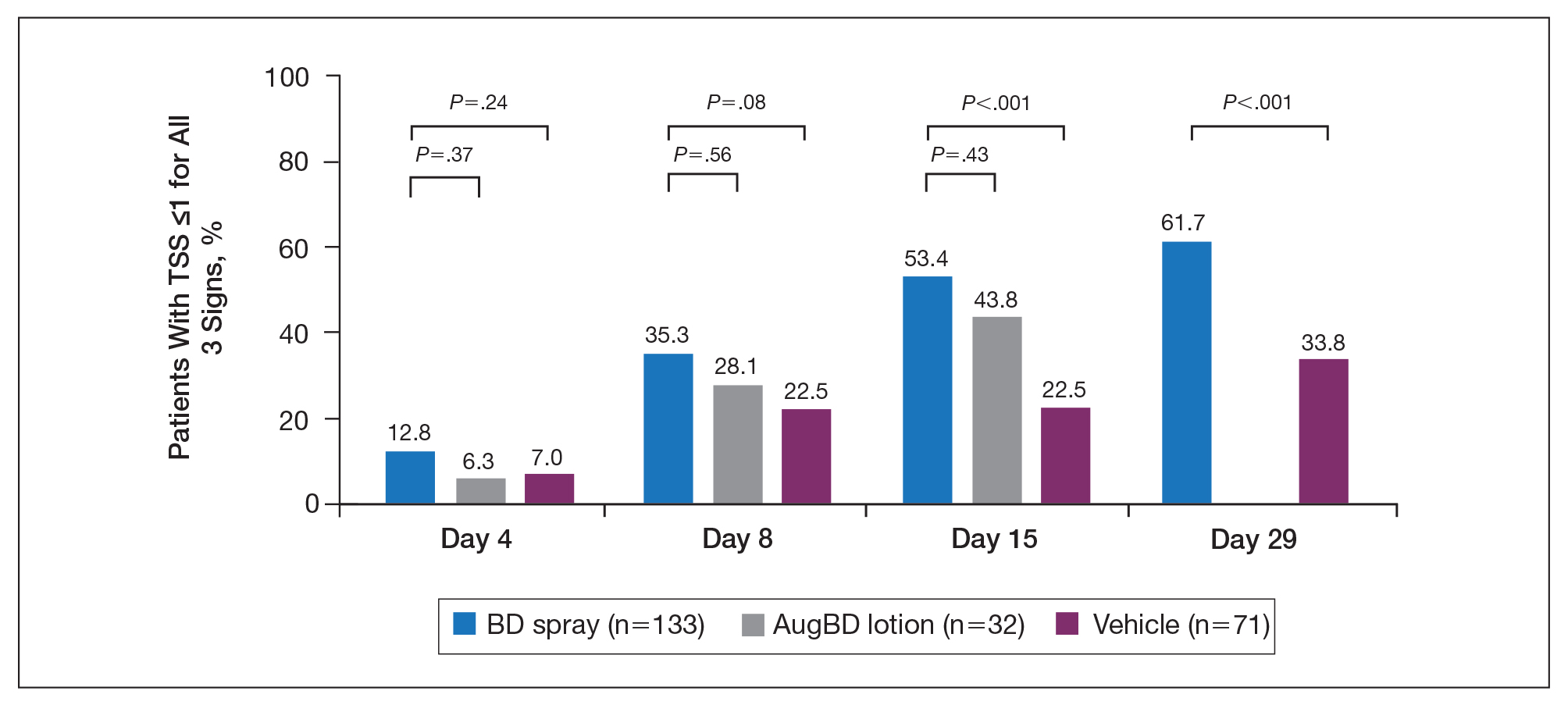
Total Sign Score
Total sign score results showed that the mean percentage of patients achieving a TSS of 0 or 1 for all signs for lesions located on the knees or elbows was numerically higher for BD spray vs AugBD lotion at day 4, but this difference was not statistically significant (Figure 2). Day 15 outcomes for TSS also showed a numerically greater success rate for BD spray, but again this difference was not statistically significant (53.4% BD spray vs 43.8% AugBD lotion). At days 15 and 29, significantly more patients treated with BD spray achieved TSS of 0 or 1 for all 3 signs compared to those treated with vehicle (P<.001). Improvement in TSS with BD spray continued through to day 29 of the study.
Comment
In these post hoc analyses, mid-potency BD spray demonstrated early relief of itching and early efficacy in the treatment of psoriasis plaques on the elbows and knees with minimal systemic absorption and a low rate of adverse events.
Betamethasone dipropionate spray and its vehicle formulation relieved psoriatic itching with similar efficacy to the superpotent AugBD steroid lotion. Notably, relief was rapid, with approximately half of responding patients reporting relief of itching by day 4. The results seen with vehicle suggest that the emollient formulation of BD spray is responsible for hydrating dry skin, contributing to the relief of this cutaneous symptom. Dry skin can exacerbate itching, and emollients are recognized as being able to alleviate itching by hydrating and soothing the skin.7
The second set of post hoc analyses reported here demonstrated that BD spray was efficacious in clearing the signs of psoriatic lesions on the difficult-to-treat areas of the knees and elbows. Efficacy with BD spray was similar to the superpotent steroid AugBD lotion, with no statistical difference between the 2 products at any time point. Betamethasone dipropionate spray was significantly more effective than its vehicle in reducing the signs of erythema and scaling from day 8 and plaque elevation from day 15.
Rapid relief of symptoms is important for patient comfort and to improve treatment adherence. These analyses showed that by day 4, BD spray resulted in numerically higher percentages of patients achieving a score of 0 or 1 for the individual signs of erythema, scaling, and plaque elevation compared to AugBD lotion. Of particular note, 37.6% of patients treated with BD spray had scaling scores of clear or almost clear by day 4 compared to 25.0% of patients treated with AugBD lotion. Scaling has been consistently reported as the second most bothersome symptom experienced by patients2,3 and has been shown to be associated with decreased quality of life and work productivity.19
Betamethasone dipropionate spray has a rationally designed vehicle, with the formulation selected specifically to maximize penetration of the product through the stratum corneum and retention of BD steroid in the epidermis and upper dermis while reducing absorption into the systemic circulation.14 The reduced absorption into the systemic circulation leads to less vasoconstriction; fewer adverse events; and a “medium potent” VCA designation compared to the “superpotent” designation of the AugBD formulation, despite containing the same active ingredient.
These analyses demonstrate that BD spray is effective at addressing 2 symptoms that patients with psoriasis consider most bothersome: itching and scaling. Notably, BD spray was able to achieve these results rapidly, with many patients experiencing improvements in 4 days. In these analyses, mid-potent BD spray demonstrated similar efficacy to AugBD lotion, a superpotent steroid formulation.
This analysis is limited by being post hoc. Although the statistical methodology is valid, the AugBD lotion arm of the analyses was relatively small compared with the BD spray and vehicle arms, as it was only included in 1 of 2 studies pooled.
Conclusion
Mid-potency BD spray effectively improved the symptom of itching and cleared hard-to-treat lesions on knees and elbows with efficacy similar to a superpotent AugBD formulation but with less systemic absorption. Improvements were seen in erythema, scaling, and plaque elevation. Reductions in psoriatic signs were observed as early as day 4, with continued improvement seen throughout the study period. These findings provide evidence that BD spray can rapidly relieve 2 of the most troublesome symptoms affecting patients with psoriasis (itching and scaling), potentially improving quality of life.
Acknowledgments
The authors wish to thank Alix Bennett, PhD, formerly of Promius Pharma, a subsidiary of Dr. Reddy’s Laboratories, Inc (Princeton, New Jersey), and Jodie Macoun, PhD, of CUBE Information (Katonah, New York), for their review and assistance with the preparation of this manuscript. Manuscript preparation was supported by Promius Pharma (Princeton, New Jersey)(DRL #866).
- About psoriasis. National Psoriasis Foundation website. https://www.psoriasis.org/about-psoriasis. Accessed October 1, 2019.
- Lebwohl MG, Bachelez H, Barker J, et al. Patient perspectives in the management of psoriasis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis Survey. J Am Acad Dermatol. 2014;70:871-881.e1-30.
- Pariser D, Schenkel B, Carter C, et al; Psoriasis Patient Interview Study Group. A multicenter, non-interventional study to evaluate patient-reported experiences of living with psoriasis. J Dermatolog Treat. 2016;27:19-26.
- Dickison P, Swain G, Peek JJ, et al. Itching for answers: prevalence and severity of pruritus in psoriasis. Australas J Dermatol. 2018;59:206-209.
- Bahali AG, Onsun N, Su O, et al. The relationship between pruritus and clinical variables in patients with psoriasis. An Bras Dermatol. 2017;92:470-473.
- Prignano F, Ricceri F, Pescitelli L, et al. Itch in psoriasis: epidemiology, clinical aspects and treatment options. Clin Cosmet Investig Dermatol. 2009;2:9-13.
- Dawn A, Yosipovitch G. Treating itch in psoriasis. Dermatol Nurs. 2006;18:227-233.
- Queille-Roussel C, Rosen M, Clonier F, et al. Efficacy and safety of calcipotriol plus betamethasone dipropionate aerosol foam compared with betamethasone 17-valerate-medicated plaster for the treatment of psoriasis. Clin Drug Investig. 2017;37:355-361.
- Betesil [package insert]. Lodi, Italy: IBSA Pharmaceutici Italia S.r.I; 2013.
- Cannavò SP, Guarneri F, Giuffrida R, et al. Evaluation of cutaneous surface parameters in psoriatic patients. Skin Res Technol. 2017;23:41-47.
- Egawa M, Arimoto H, Hirao T, et al. Regional difference of water content in human skin studied by diffuse-reflectance near-infrared spectroscopy: consideration of measurement depth. Appl Spectrosc. 2006;60:24-28.
- van de Kerkhof PC, Reich K, Kavanaugh A, et al. Physician perspectives in the management of psoriasis and psoriatic arthritis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis survey. J Eur Acad Dermatol Venereol. 2015;29:2002-2010.
- Menter A, Korman NJ, Elmets CA, et al; American Academy of Dermatology. Guidelines of care for the management of psoriasis and psoriatic arthritis. section 3. guidelines of care for the management and treatment of psoriasis with topical therapies. J Am Acad Dermatol. 2009;60:643-659.
- Kircik L, Okumu F, Kandavilli S, et al. Rational vehicle design ensures targeted cutaneous steroid delivery. J Clin Aesthet Dermatol. 2017;10:12-19.
- Fowler JF Jr, Herbert AA, Sugarman J. DFD-01, a novel medium potency betamethasone dipropionate 0.05% emollient spray, demonstrates similar efficacy to augmented betamethasone dipropionate 0.05% lotion for the treatment of moderate plaque psoriasis. J Drugs Dermatol. 2016;15:154-162.
- Stein Gold L, Jackson JM, Knuckles ML, et al. Improvement in extensive moderate plaque psoriasis with a novel emollient spray formulation of betamethasone dipropionate 0.05. J Drugs Dermatol. 2016;15:334-342.
- Sidgiddi S, Pakunlu RI, Allenby K. Efficacy, safety, and potency of betamethasone dipropionate spray 0.05%: a treatment for adults with mild-to-moderate plaque psoriasis. J Clin Aesthet Dermatol. 2018;11:14-22.
- Diprolene Lotion (augmented betamethasone dipropionate 0.05%) [package insert]. Kenilworth, NJ: Schering Corporation; 1999.
- Korman NJ, Zhao Y, Pike J, et al. Increased severity of itching, pain, and scaling in psoriasis patients is associated with increased disease severity, reduced quality of life, and reduced work productivity. Dermatol Online J. 2015;21. pii:13030/qt1x16v3dg.
Psoriasis affects approximately 2% to 3% of the US population and is characterized by plaques that are red, scaly, and elevated.1 Cutaneous symptoms of the disease are described by patients as itching, burning, and stinging sensations. Large multinational and US surveys have reported pruritus as patients’ most bothersome symptom, with scaling/flaking reported as the second most bothersome.2,3 Reported incidence rates for itching range from 60.4% to 98.3%, with at least half of these patients reporting daily or constant pruritus.2,4-7 Consequent effects on quality of life include impaired sleep,6 difficulty concentrating, lower sex drive, and depression.7 Despite these findings, pruritus is rarely included in the efficacy assessments of psoriasis treatments. In addition, 2 of the most commonly reported but difficult-to-treat locations for plaques are the outside of the elbows (45%) and the knees (32%),1,2,8 areas where the stratum corneum typically is thicker, less hydrated, and less likely to absorb topical products.9-11 Clinical studies have not focused specifically on these areas when assessing treatments.
Topical corticosteroids have been the mainstay of psoriasis therapy for decades because of their anti-inflammatory and antiproliferative properties.7 One large multinational physician survey indicated that 75% of patients are prescribed topical steroids,12 which are important for first-line treatment and are often maintained as adjunctive therapy in combination with other treatments for patients with extensive disease or recalcitrant lesions.13 Topical corticosteroids are ranked into different classes based on their vasoconstrictor assay (VCA), a measure of skin blanching used as a marker for vasoconstriction. Topical agents with VCA ratings of mid-potency or superpotency are generally recommended for initial therapy, with superpotent agents required for the treatment of thick chronic plaques. However, longer durations of use may contribute to systemic absorption and adverse events.13 The vehicle composition is important for corticosteroid delivery and retention at the site of pathology, contributing to the efficacy of the steroid.13,14 Selecting the appropriate steroid and vehicle is important to maximize efficacy and minimize adverse events.
Betamethasone dipropionate (BD) spray 0.05% is an emollient formulation of 0.05% BD that can be sprayed onto psoriatic plaques. The BD spray formulation was designed to penetrate the stratum corneum and be retained within the dermis and epidermis, the site of T-cell activity that drives the psoriatic disease process.14 In 2 phase 3 studies, BD spray demonstrated the ability to reduce the signs of plaque psoriasis with indication of improvement by day 4.15,16 These studies also showed improvement in the local cutaneous symptoms of itching, burning and stinging, and pain. As a mid-potent steroid, BD spray displays less systemic absorption but similar efficacy compared to a superpotent augmented BD (AugBD) lotion in relieving the signs and symptoms of plaque psoriasis.15-17
The objective of the current investigation was to assess the ability of BD spray to relieve itching and to clear plaque psoriasis on the knees and elbows utilizing post hoc analyses of the 2 phase 3 trials. The goal of these analyses was to demonstrate BD spray as effective at relieving the most troublesome signs and symptoms affecting patients with plaque psoriasis.
Methods
Two phase 3 studies were conducted to demonstrate the efficacy and safety of BD spray.15,16 The design of the studies was similar15,16 to allow the data to be pooled for post hoc analyses.
Both were US multicenter, randomized, vehicle-controlled, double-blind, parallel-group studies comparing the safety and efficacy of BD spray 0.05% (Sernivo, Promius Pharma) with its vehicle formulation spray (identical to BD spray, but lacking the active steroid component).15,16 One of the studies also compared BD spray with an AugBD lotion 0.05% (Diprolene,Merck & Co). Adults with moderate plaque psoriasis (investigator global assessment of 3; 10%–20% body surface area) were randomized to apply BD spray, vehicle spray, or AugBD lotion (1 study only) twice daily to all affected areas, excluding the face, scalp, and intertriginous areas for 28 days (BD spray and vehicle) or 14 days (AugBD lotion, per product label).15
Assessments
Two post hoc analyses were conducted on data pooled from the 2 phase 3 trials: (1) incidence of itching, and (2) total sign score (TSS) for lesions located on the knees and elbows.
Itching
Itching was assessed proactively by asking patients if they were experiencing itching (yes/no) at each visit (baseline and days 4, 8, 15, and 29) or had experienced itching since their last visit. As itching could be an adverse event of topical application, application-site pruritus was also recorded.
Total Sign Score
For each patient, a target plaque was selected that was representative of their psoriasis. The plaque was assessed on a 3-point grading scale for each of 3 key signs of plaque psoriasis: erythema, scaling, and plaque elevation (Table 1) at baseline and days 4, 8, 15, and 29. Total sign score was calculated by summing the scores for these 3 signs, resulting in a score ranging from 0 to 9. Treatment success was measured as (1) achieving a score of 0 or 1 (ie, reducing the plaque to clear or slight to mild) for the individual signs of erythema, scaling, and plaque elevation; and (2) achieving a TSS of 0 or 1 for all 3 signs—erythema, scaling, and plaque elevation—for each target lesion. Total sign score was assessed proactively for all patients.15,16 The post hoc analysis reported here examined patients whose target lesion was located on either the knee or the elbow.
Statistical Analyses
Because both study protocols were identical, data were pooled from the 2 phase 3 trials. All statistical analyses were performed using SAS software (SAS Institute). Two-sided hypothesis testing was conducted for all analyses using a significance level of P=.05. Post hoc analyses used Fisher exact test. No imputations were made for missing data.
Statistical analyses of itching compared the incidence of itching at each assessment time point (baseline and days 4, 8, 15, and 29) between BD spray and vehicle and between BD spray and AugBD lotion. Additional analysis included a statistical test on the incidence of itching in the subgroup of patients who reported itching at baseline.
Statistical analyses for the knees and elbows included only patients with their target lesion located on either the knee or the elbow. Analyses compared BD spray with vehicle and BD spray with AugBD lotion at days 4, 8, 15, and 29. Comparison with AugBD lotion treatment was up to day 14 only, consistent with application time limits in the AugBD lotion product label.18
Results
These analyses included data from the 628 patients enrolled in the 2 phase 3 trials. Patients had similar baseline characteristics across treatment groups (Table 2). Itching was the most common cutaneous symptom at baseline, reported by almost two-thirds (n=392, 62.4%) of patients. Of the 628 patients, 236 (37.6%) had a target lesion located on the elbow or knee selected for assessment. The mean baseline body surface area was 13% to 14% across groups.
A post hoc analysis was performed on the subgroup of patients who reported itching at baseline (N=392)(eFigure 1). For these patients, almost half were itch free by day 4 across all groups (49.3% BD spray, 48.2% AugBD lotion, and 47.4% vehicle). By the end of treatment, 65.9% of patients using BD spray and 58.3% of patients using vehicle were itch free at day 29, with 56.9% of AugBD lotion patients itch free at day 15.
Application-site pruritus recorded as a treatment-emergent adverse event was seen in low numbers and was similar in proportion between the 2 steroid treatments (7.7% BD spray, 6.7% AugBD lotion, and 14.4% vehicle).
Psoriasis Individual Sign Scores for Knee and Elbow Plaques
Target lesions located on the knee or elbow represented 37.6% of all target lesions assessed. Efficacy analysis of the pooled data on knee and elbow lesions revealed that BD spray was similar to AugBD lotion in reducing sign scores to 0 or 1 (Figures 1 and 2).
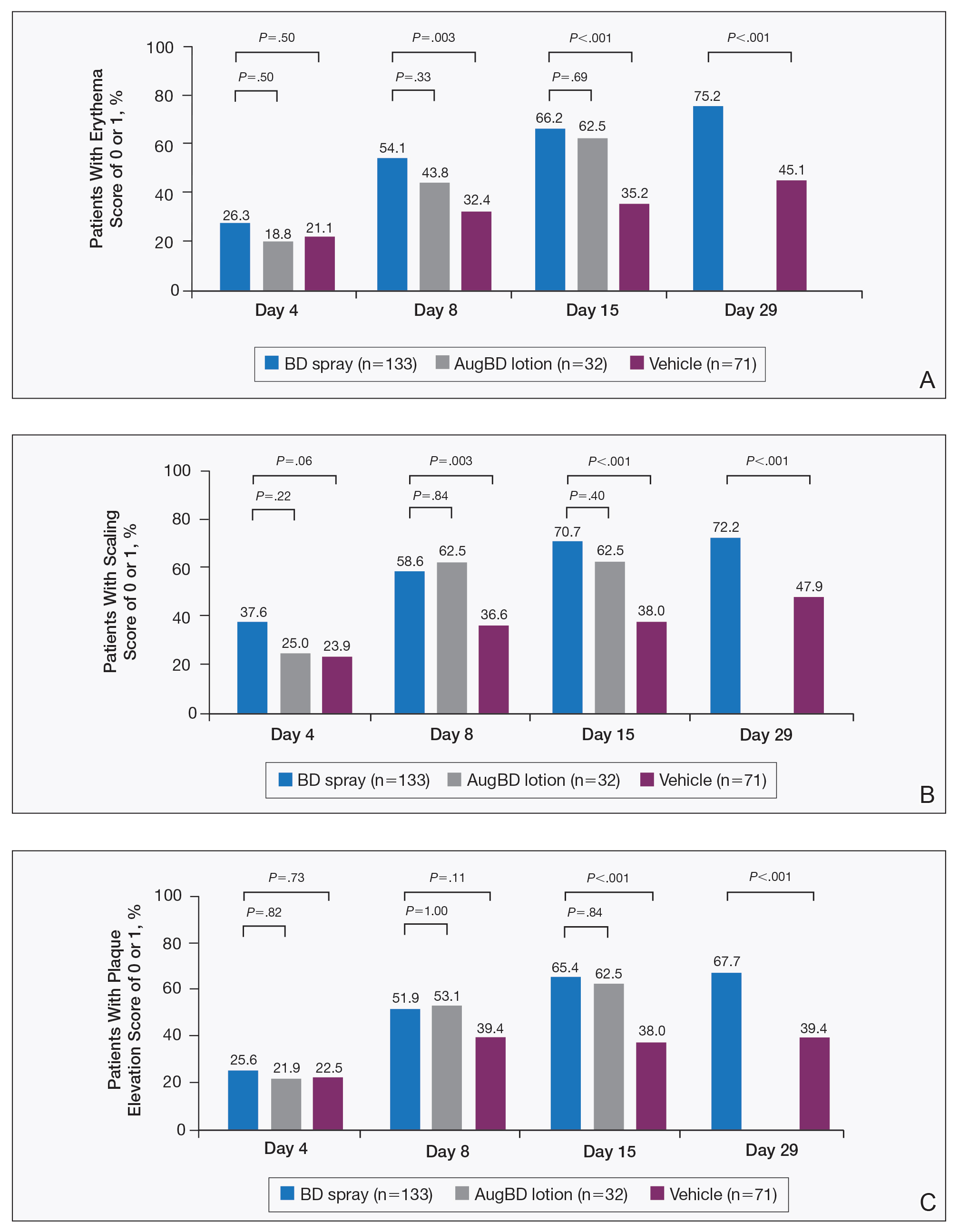
The percentage of patients reporting improvements in erythema, scaling, and plaque elevation scores at day 4
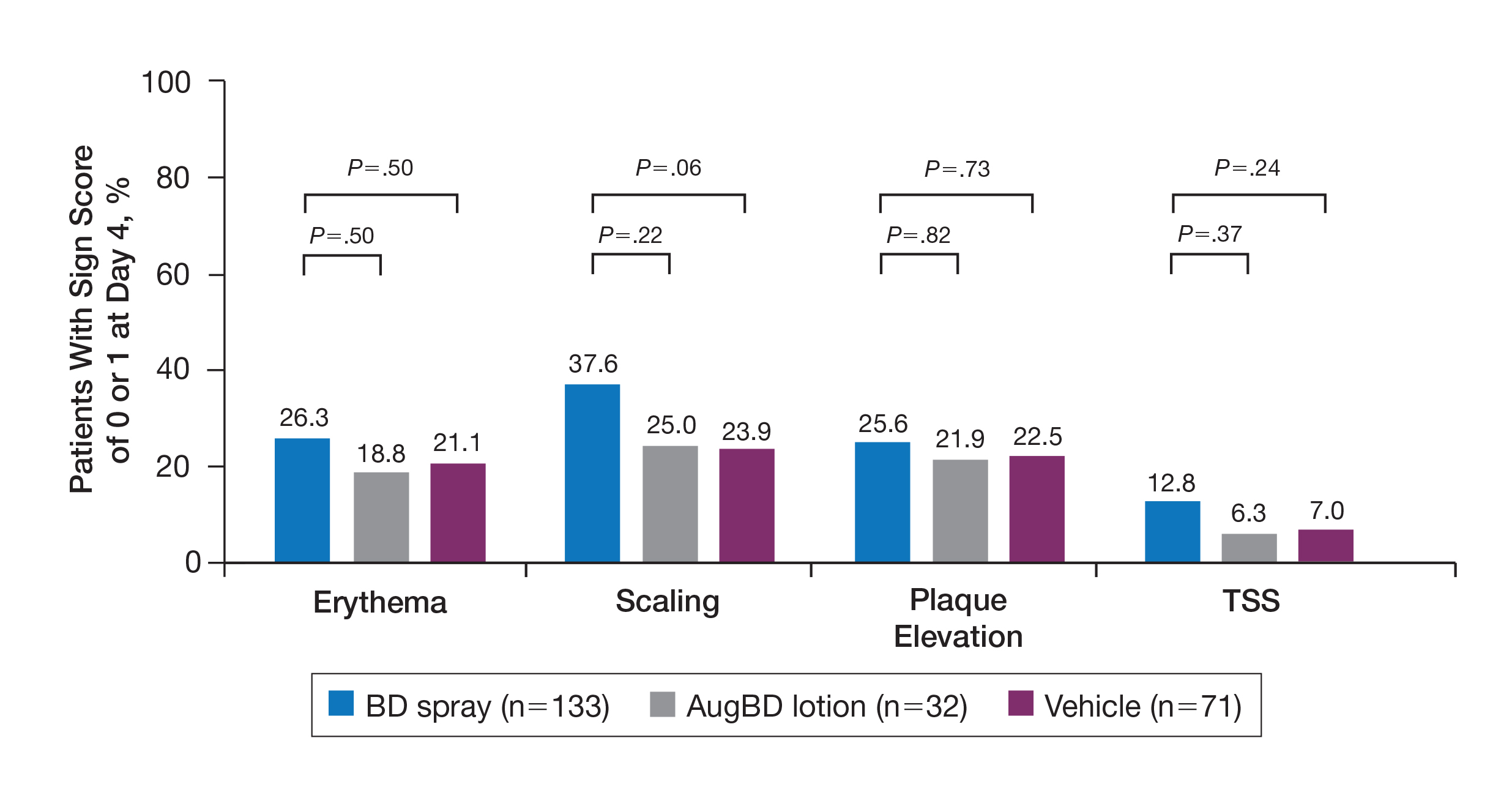
The proportion of patients achieving treatment success (defined as a score of 0 or 1) was comparable for the2 products on day 15 for erythema (66.2% BD spray vs 62.5% AugBD lotion), scaling (70.7% BD spray vs 62.5% AugBD lotion), and plaque elevation (65.4% BD spray vs 62.5% AugBD lotion)(Figure 1). From day 8, BD spray reduced erythema and scaling in significantly more patients than vehicle (P=.003 for both), and BD spray reduced erythema, scaling, and plaque elevation in more patients than vehicle from day 15 (P<.001 for all). No statistically significant difference was found between BD spray and AugBD lotion on erythema, scaling, and plaque elevation scores.
Total Sign Score
Total sign score results showed that the mean percentage of patients achieving a TSS of 0 or 1 for all signs for lesions located on the knees or elbows was numerically higher for BD spray vs AugBD lotion at day 4, but this difference was not statistically significant (Figure 2). Day 15 outcomes for TSS also showed a numerically greater success rate for BD spray, but again this difference was not statistically significant (53.4% BD spray vs 43.8% AugBD lotion). At days 15 and 29, significantly more patients treated with BD spray achieved TSS of 0 or 1 for all 3 signs compared to those treated with vehicle (P<.001). Improvement in TSS with BD spray continued through to day 29 of the study.
Comment
In these post hoc analyses, mid-potency BD spray demonstrated early relief of itching and early efficacy in the treatment of psoriasis plaques on the elbows and knees with minimal systemic absorption and a low rate of adverse events.
Betamethasone dipropionate spray and its vehicle formulation relieved psoriatic itching with similar efficacy to the superpotent AugBD steroid lotion. Notably, relief was rapid, with approximately half of responding patients reporting relief of itching by day 4. The results seen with vehicle suggest that the emollient formulation of BD spray is responsible for hydrating dry skin, contributing to the relief of this cutaneous symptom. Dry skin can exacerbate itching, and emollients are recognized as being able to alleviate itching by hydrating and soothing the skin.7
The second set of post hoc analyses reported here demonstrated that BD spray was efficacious in clearing the signs of psoriatic lesions on the difficult-to-treat areas of the knees and elbows. Efficacy with BD spray was similar to the superpotent steroid AugBD lotion, with no statistical difference between the 2 products at any time point. Betamethasone dipropionate spray was significantly more effective than its vehicle in reducing the signs of erythema and scaling from day 8 and plaque elevation from day 15.
Rapid relief of symptoms is important for patient comfort and to improve treatment adherence. These analyses showed that by day 4, BD spray resulted in numerically higher percentages of patients achieving a score of 0 or 1 for the individual signs of erythema, scaling, and plaque elevation compared to AugBD lotion. Of particular note, 37.6% of patients treated with BD spray had scaling scores of clear or almost clear by day 4 compared to 25.0% of patients treated with AugBD lotion. Scaling has been consistently reported as the second most bothersome symptom experienced by patients2,3 and has been shown to be associated with decreased quality of life and work productivity.19
Betamethasone dipropionate spray has a rationally designed vehicle, with the formulation selected specifically to maximize penetration of the product through the stratum corneum and retention of BD steroid in the epidermis and upper dermis while reducing absorption into the systemic circulation.14 The reduced absorption into the systemic circulation leads to less vasoconstriction; fewer adverse events; and a “medium potent” VCA designation compared to the “superpotent” designation of the AugBD formulation, despite containing the same active ingredient.
These analyses demonstrate that BD spray is effective at addressing 2 symptoms that patients with psoriasis consider most bothersome: itching and scaling. Notably, BD spray was able to achieve these results rapidly, with many patients experiencing improvements in 4 days. In these analyses, mid-potent BD spray demonstrated similar efficacy to AugBD lotion, a superpotent steroid formulation.
This analysis is limited by being post hoc. Although the statistical methodology is valid, the AugBD lotion arm of the analyses was relatively small compared with the BD spray and vehicle arms, as it was only included in 1 of 2 studies pooled.
Conclusion
Mid-potency BD spray effectively improved the symptom of itching and cleared hard-to-treat lesions on knees and elbows with efficacy similar to a superpotent AugBD formulation but with less systemic absorption. Improvements were seen in erythema, scaling, and plaque elevation. Reductions in psoriatic signs were observed as early as day 4, with continued improvement seen throughout the study period. These findings provide evidence that BD spray can rapidly relieve 2 of the most troublesome symptoms affecting patients with psoriasis (itching and scaling), potentially improving quality of life.
Acknowledgments
The authors wish to thank Alix Bennett, PhD, formerly of Promius Pharma, a subsidiary of Dr. Reddy’s Laboratories, Inc (Princeton, New Jersey), and Jodie Macoun, PhD, of CUBE Information (Katonah, New York), for their review and assistance with the preparation of this manuscript. Manuscript preparation was supported by Promius Pharma (Princeton, New Jersey)(DRL #866).
Psoriasis affects approximately 2% to 3% of the US population and is characterized by plaques that are red, scaly, and elevated.1 Cutaneous symptoms of the disease are described by patients as itching, burning, and stinging sensations. Large multinational and US surveys have reported pruritus as patients’ most bothersome symptom, with scaling/flaking reported as the second most bothersome.2,3 Reported incidence rates for itching range from 60.4% to 98.3%, with at least half of these patients reporting daily or constant pruritus.2,4-7 Consequent effects on quality of life include impaired sleep,6 difficulty concentrating, lower sex drive, and depression.7 Despite these findings, pruritus is rarely included in the efficacy assessments of psoriasis treatments. In addition, 2 of the most commonly reported but difficult-to-treat locations for plaques are the outside of the elbows (45%) and the knees (32%),1,2,8 areas where the stratum corneum typically is thicker, less hydrated, and less likely to absorb topical products.9-11 Clinical studies have not focused specifically on these areas when assessing treatments.
Topical corticosteroids have been the mainstay of psoriasis therapy for decades because of their anti-inflammatory and antiproliferative properties.7 One large multinational physician survey indicated that 75% of patients are prescribed topical steroids,12 which are important for first-line treatment and are often maintained as adjunctive therapy in combination with other treatments for patients with extensive disease or recalcitrant lesions.13 Topical corticosteroids are ranked into different classes based on their vasoconstrictor assay (VCA), a measure of skin blanching used as a marker for vasoconstriction. Topical agents with VCA ratings of mid-potency or superpotency are generally recommended for initial therapy, with superpotent agents required for the treatment of thick chronic plaques. However, longer durations of use may contribute to systemic absorption and adverse events.13 The vehicle composition is important for corticosteroid delivery and retention at the site of pathology, contributing to the efficacy of the steroid.13,14 Selecting the appropriate steroid and vehicle is important to maximize efficacy and minimize adverse events.
Betamethasone dipropionate (BD) spray 0.05% is an emollient formulation of 0.05% BD that can be sprayed onto psoriatic plaques. The BD spray formulation was designed to penetrate the stratum corneum and be retained within the dermis and epidermis, the site of T-cell activity that drives the psoriatic disease process.14 In 2 phase 3 studies, BD spray demonstrated the ability to reduce the signs of plaque psoriasis with indication of improvement by day 4.15,16 These studies also showed improvement in the local cutaneous symptoms of itching, burning and stinging, and pain. As a mid-potent steroid, BD spray displays less systemic absorption but similar efficacy compared to a superpotent augmented BD (AugBD) lotion in relieving the signs and symptoms of plaque psoriasis.15-17
The objective of the current investigation was to assess the ability of BD spray to relieve itching and to clear plaque psoriasis on the knees and elbows utilizing post hoc analyses of the 2 phase 3 trials. The goal of these analyses was to demonstrate BD spray as effective at relieving the most troublesome signs and symptoms affecting patients with plaque psoriasis.
Methods
Two phase 3 studies were conducted to demonstrate the efficacy and safety of BD spray.15,16 The design of the studies was similar15,16 to allow the data to be pooled for post hoc analyses.
Both were US multicenter, randomized, vehicle-controlled, double-blind, parallel-group studies comparing the safety and efficacy of BD spray 0.05% (Sernivo, Promius Pharma) with its vehicle formulation spray (identical to BD spray, but lacking the active steroid component).15,16 One of the studies also compared BD spray with an AugBD lotion 0.05% (Diprolene,Merck & Co). Adults with moderate plaque psoriasis (investigator global assessment of 3; 10%–20% body surface area) were randomized to apply BD spray, vehicle spray, or AugBD lotion (1 study only) twice daily to all affected areas, excluding the face, scalp, and intertriginous areas for 28 days (BD spray and vehicle) or 14 days (AugBD lotion, per product label).15
Assessments
Two post hoc analyses were conducted on data pooled from the 2 phase 3 trials: (1) incidence of itching, and (2) total sign score (TSS) for lesions located on the knees and elbows.
Itching
Itching was assessed proactively by asking patients if they were experiencing itching (yes/no) at each visit (baseline and days 4, 8, 15, and 29) or had experienced itching since their last visit. As itching could be an adverse event of topical application, application-site pruritus was also recorded.
Total Sign Score
For each patient, a target plaque was selected that was representative of their psoriasis. The plaque was assessed on a 3-point grading scale for each of 3 key signs of plaque psoriasis: erythema, scaling, and plaque elevation (Table 1) at baseline and days 4, 8, 15, and 29. Total sign score was calculated by summing the scores for these 3 signs, resulting in a score ranging from 0 to 9. Treatment success was measured as (1) achieving a score of 0 or 1 (ie, reducing the plaque to clear or slight to mild) for the individual signs of erythema, scaling, and plaque elevation; and (2) achieving a TSS of 0 or 1 for all 3 signs—erythema, scaling, and plaque elevation—for each target lesion. Total sign score was assessed proactively for all patients.15,16 The post hoc analysis reported here examined patients whose target lesion was located on either the knee or the elbow.
Statistical Analyses
Because both study protocols were identical, data were pooled from the 2 phase 3 trials. All statistical analyses were performed using SAS software (SAS Institute). Two-sided hypothesis testing was conducted for all analyses using a significance level of P=.05. Post hoc analyses used Fisher exact test. No imputations were made for missing data.
Statistical analyses of itching compared the incidence of itching at each assessment time point (baseline and days 4, 8, 15, and 29) between BD spray and vehicle and between BD spray and AugBD lotion. Additional analysis included a statistical test on the incidence of itching in the subgroup of patients who reported itching at baseline.
Statistical analyses for the knees and elbows included only patients with their target lesion located on either the knee or the elbow. Analyses compared BD spray with vehicle and BD spray with AugBD lotion at days 4, 8, 15, and 29. Comparison with AugBD lotion treatment was up to day 14 only, consistent with application time limits in the AugBD lotion product label.18
Results
These analyses included data from the 628 patients enrolled in the 2 phase 3 trials. Patients had similar baseline characteristics across treatment groups (Table 2). Itching was the most common cutaneous symptom at baseline, reported by almost two-thirds (n=392, 62.4%) of patients. Of the 628 patients, 236 (37.6%) had a target lesion located on the elbow or knee selected for assessment. The mean baseline body surface area was 13% to 14% across groups.
A post hoc analysis was performed on the subgroup of patients who reported itching at baseline (N=392)(eFigure 1). For these patients, almost half were itch free by day 4 across all groups (49.3% BD spray, 48.2% AugBD lotion, and 47.4% vehicle). By the end of treatment, 65.9% of patients using BD spray and 58.3% of patients using vehicle were itch free at day 29, with 56.9% of AugBD lotion patients itch free at day 15.
Application-site pruritus recorded as a treatment-emergent adverse event was seen in low numbers and was similar in proportion between the 2 steroid treatments (7.7% BD spray, 6.7% AugBD lotion, and 14.4% vehicle).
Psoriasis Individual Sign Scores for Knee and Elbow Plaques
Target lesions located on the knee or elbow represented 37.6% of all target lesions assessed. Efficacy analysis of the pooled data on knee and elbow lesions revealed that BD spray was similar to AugBD lotion in reducing sign scores to 0 or 1 (Figures 1 and 2).
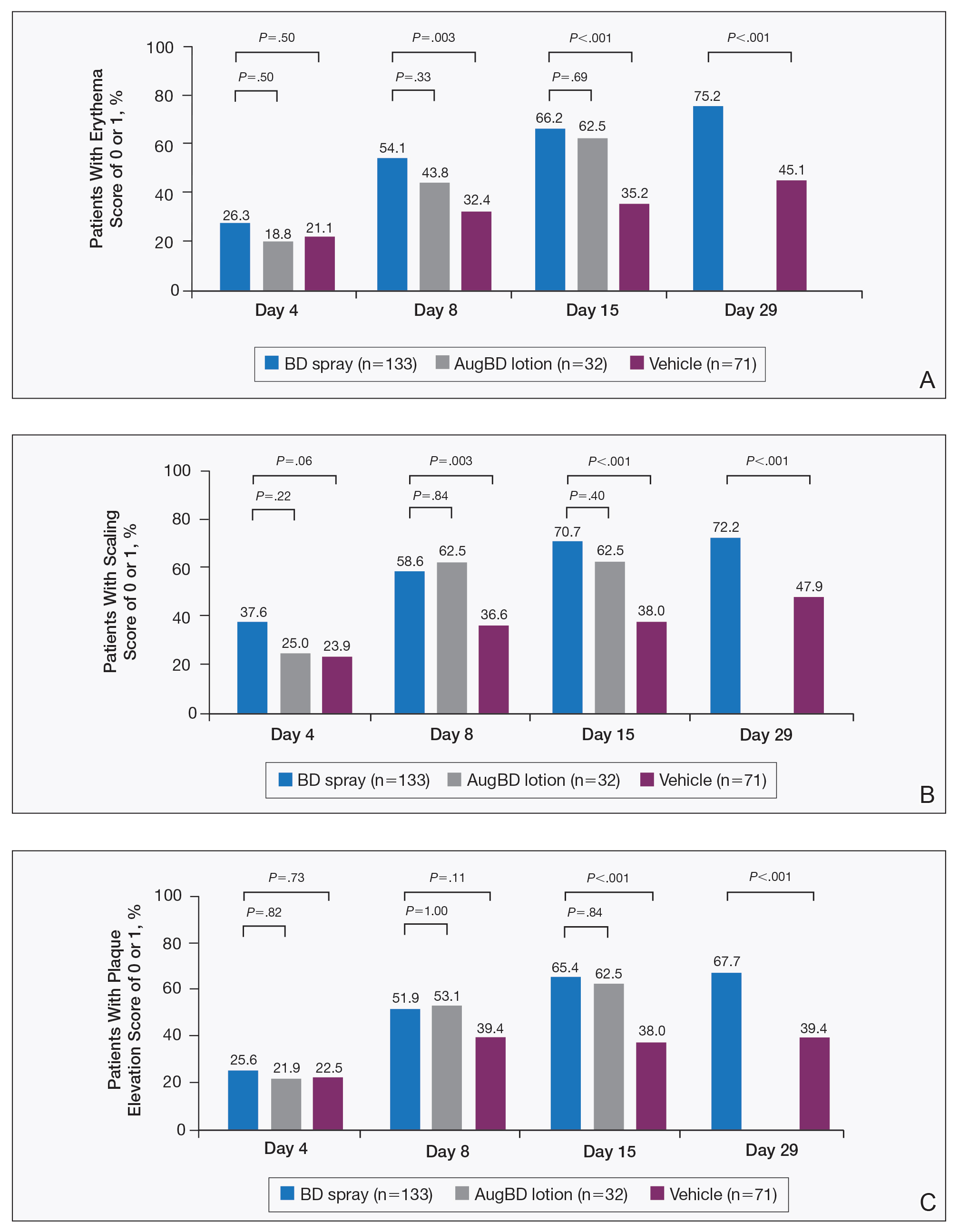
The percentage of patients reporting improvements in erythema, scaling, and plaque elevation scores at day 4
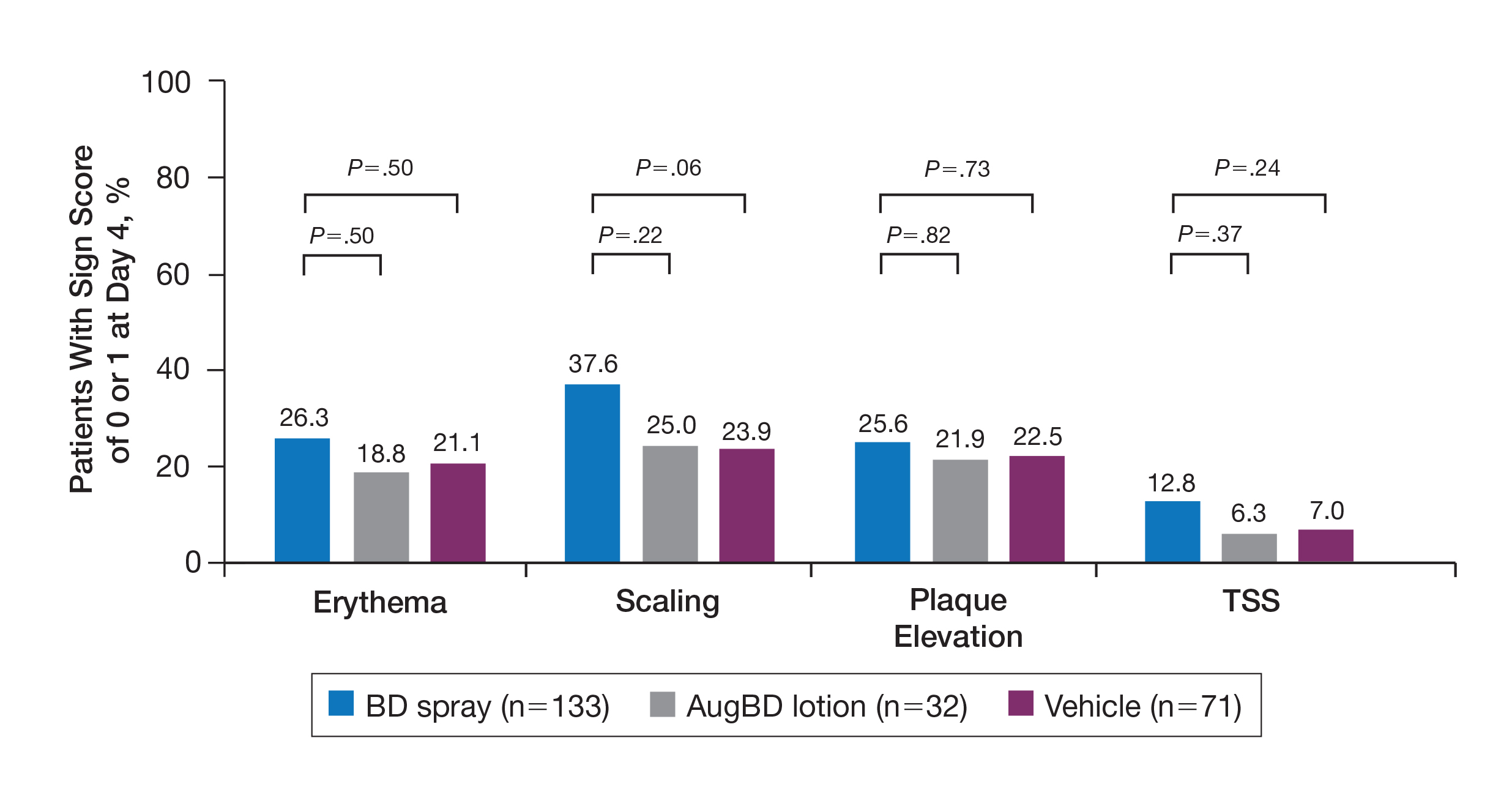
The proportion of patients achieving treatment success (defined as a score of 0 or 1) was comparable for the2 products on day 15 for erythema (66.2% BD spray vs 62.5% AugBD lotion), scaling (70.7% BD spray vs 62.5% AugBD lotion), and plaque elevation (65.4% BD spray vs 62.5% AugBD lotion)(Figure 1). From day 8, BD spray reduced erythema and scaling in significantly more patients than vehicle (P=.003 for both), and BD spray reduced erythema, scaling, and plaque elevation in more patients than vehicle from day 15 (P<.001 for all). No statistically significant difference was found between BD spray and AugBD lotion on erythema, scaling, and plaque elevation scores.
Total Sign Score
Total sign score results showed that the mean percentage of patients achieving a TSS of 0 or 1 for all signs for lesions located on the knees or elbows was numerically higher for BD spray vs AugBD lotion at day 4, but this difference was not statistically significant (Figure 2). Day 15 outcomes for TSS also showed a numerically greater success rate for BD spray, but again this difference was not statistically significant (53.4% BD spray vs 43.8% AugBD lotion). At days 15 and 29, significantly more patients treated with BD spray achieved TSS of 0 or 1 for all 3 signs compared to those treated with vehicle (P<.001). Improvement in TSS with BD spray continued through to day 29 of the study.
Comment
In these post hoc analyses, mid-potency BD spray demonstrated early relief of itching and early efficacy in the treatment of psoriasis plaques on the elbows and knees with minimal systemic absorption and a low rate of adverse events.
Betamethasone dipropionate spray and its vehicle formulation relieved psoriatic itching with similar efficacy to the superpotent AugBD steroid lotion. Notably, relief was rapid, with approximately half of responding patients reporting relief of itching by day 4. The results seen with vehicle suggest that the emollient formulation of BD spray is responsible for hydrating dry skin, contributing to the relief of this cutaneous symptom. Dry skin can exacerbate itching, and emollients are recognized as being able to alleviate itching by hydrating and soothing the skin.7
The second set of post hoc analyses reported here demonstrated that BD spray was efficacious in clearing the signs of psoriatic lesions on the difficult-to-treat areas of the knees and elbows. Efficacy with BD spray was similar to the superpotent steroid AugBD lotion, with no statistical difference between the 2 products at any time point. Betamethasone dipropionate spray was significantly more effective than its vehicle in reducing the signs of erythema and scaling from day 8 and plaque elevation from day 15.
Rapid relief of symptoms is important for patient comfort and to improve treatment adherence. These analyses showed that by day 4, BD spray resulted in numerically higher percentages of patients achieving a score of 0 or 1 for the individual signs of erythema, scaling, and plaque elevation compared to AugBD lotion. Of particular note, 37.6% of patients treated with BD spray had scaling scores of clear or almost clear by day 4 compared to 25.0% of patients treated with AugBD lotion. Scaling has been consistently reported as the second most bothersome symptom experienced by patients2,3 and has been shown to be associated with decreased quality of life and work productivity.19
Betamethasone dipropionate spray has a rationally designed vehicle, with the formulation selected specifically to maximize penetration of the product through the stratum corneum and retention of BD steroid in the epidermis and upper dermis while reducing absorption into the systemic circulation.14 The reduced absorption into the systemic circulation leads to less vasoconstriction; fewer adverse events; and a “medium potent” VCA designation compared to the “superpotent” designation of the AugBD formulation, despite containing the same active ingredient.
These analyses demonstrate that BD spray is effective at addressing 2 symptoms that patients with psoriasis consider most bothersome: itching and scaling. Notably, BD spray was able to achieve these results rapidly, with many patients experiencing improvements in 4 days. In these analyses, mid-potent BD spray demonstrated similar efficacy to AugBD lotion, a superpotent steroid formulation.
This analysis is limited by being post hoc. Although the statistical methodology is valid, the AugBD lotion arm of the analyses was relatively small compared with the BD spray and vehicle arms, as it was only included in 1 of 2 studies pooled.
Conclusion
Mid-potency BD spray effectively improved the symptom of itching and cleared hard-to-treat lesions on knees and elbows with efficacy similar to a superpotent AugBD formulation but with less systemic absorption. Improvements were seen in erythema, scaling, and plaque elevation. Reductions in psoriatic signs were observed as early as day 4, with continued improvement seen throughout the study period. These findings provide evidence that BD spray can rapidly relieve 2 of the most troublesome symptoms affecting patients with psoriasis (itching and scaling), potentially improving quality of life.
Acknowledgments
The authors wish to thank Alix Bennett, PhD, formerly of Promius Pharma, a subsidiary of Dr. Reddy’s Laboratories, Inc (Princeton, New Jersey), and Jodie Macoun, PhD, of CUBE Information (Katonah, New York), for their review and assistance with the preparation of this manuscript. Manuscript preparation was supported by Promius Pharma (Princeton, New Jersey)(DRL #866).
- About psoriasis. National Psoriasis Foundation website. https://www.psoriasis.org/about-psoriasis. Accessed October 1, 2019.
- Lebwohl MG, Bachelez H, Barker J, et al. Patient perspectives in the management of psoriasis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis Survey. J Am Acad Dermatol. 2014;70:871-881.e1-30.
- Pariser D, Schenkel B, Carter C, et al; Psoriasis Patient Interview Study Group. A multicenter, non-interventional study to evaluate patient-reported experiences of living with psoriasis. J Dermatolog Treat. 2016;27:19-26.
- Dickison P, Swain G, Peek JJ, et al. Itching for answers: prevalence and severity of pruritus in psoriasis. Australas J Dermatol. 2018;59:206-209.
- Bahali AG, Onsun N, Su O, et al. The relationship between pruritus and clinical variables in patients with psoriasis. An Bras Dermatol. 2017;92:470-473.
- Prignano F, Ricceri F, Pescitelli L, et al. Itch in psoriasis: epidemiology, clinical aspects and treatment options. Clin Cosmet Investig Dermatol. 2009;2:9-13.
- Dawn A, Yosipovitch G. Treating itch in psoriasis. Dermatol Nurs. 2006;18:227-233.
- Queille-Roussel C, Rosen M, Clonier F, et al. Efficacy and safety of calcipotriol plus betamethasone dipropionate aerosol foam compared with betamethasone 17-valerate-medicated plaster for the treatment of psoriasis. Clin Drug Investig. 2017;37:355-361.
- Betesil [package insert]. Lodi, Italy: IBSA Pharmaceutici Italia S.r.I; 2013.
- Cannavò SP, Guarneri F, Giuffrida R, et al. Evaluation of cutaneous surface parameters in psoriatic patients. Skin Res Technol. 2017;23:41-47.
- Egawa M, Arimoto H, Hirao T, et al. Regional difference of water content in human skin studied by diffuse-reflectance near-infrared spectroscopy: consideration of measurement depth. Appl Spectrosc. 2006;60:24-28.
- van de Kerkhof PC, Reich K, Kavanaugh A, et al. Physician perspectives in the management of psoriasis and psoriatic arthritis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis survey. J Eur Acad Dermatol Venereol. 2015;29:2002-2010.
- Menter A, Korman NJ, Elmets CA, et al; American Academy of Dermatology. Guidelines of care for the management of psoriasis and psoriatic arthritis. section 3. guidelines of care for the management and treatment of psoriasis with topical therapies. J Am Acad Dermatol. 2009;60:643-659.
- Kircik L, Okumu F, Kandavilli S, et al. Rational vehicle design ensures targeted cutaneous steroid delivery. J Clin Aesthet Dermatol. 2017;10:12-19.
- Fowler JF Jr, Herbert AA, Sugarman J. DFD-01, a novel medium potency betamethasone dipropionate 0.05% emollient spray, demonstrates similar efficacy to augmented betamethasone dipropionate 0.05% lotion for the treatment of moderate plaque psoriasis. J Drugs Dermatol. 2016;15:154-162.
- Stein Gold L, Jackson JM, Knuckles ML, et al. Improvement in extensive moderate plaque psoriasis with a novel emollient spray formulation of betamethasone dipropionate 0.05. J Drugs Dermatol. 2016;15:334-342.
- Sidgiddi S, Pakunlu RI, Allenby K. Efficacy, safety, and potency of betamethasone dipropionate spray 0.05%: a treatment for adults with mild-to-moderate plaque psoriasis. J Clin Aesthet Dermatol. 2018;11:14-22.
- Diprolene Lotion (augmented betamethasone dipropionate 0.05%) [package insert]. Kenilworth, NJ: Schering Corporation; 1999.
- Korman NJ, Zhao Y, Pike J, et al. Increased severity of itching, pain, and scaling in psoriasis patients is associated with increased disease severity, reduced quality of life, and reduced work productivity. Dermatol Online J. 2015;21. pii:13030/qt1x16v3dg.
- About psoriasis. National Psoriasis Foundation website. https://www.psoriasis.org/about-psoriasis. Accessed October 1, 2019.
- Lebwohl MG, Bachelez H, Barker J, et al. Patient perspectives in the management of psoriasis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis Survey. J Am Acad Dermatol. 2014;70:871-881.e1-30.
- Pariser D, Schenkel B, Carter C, et al; Psoriasis Patient Interview Study Group. A multicenter, non-interventional study to evaluate patient-reported experiences of living with psoriasis. J Dermatolog Treat. 2016;27:19-26.
- Dickison P, Swain G, Peek JJ, et al. Itching for answers: prevalence and severity of pruritus in psoriasis. Australas J Dermatol. 2018;59:206-209.
- Bahali AG, Onsun N, Su O, et al. The relationship between pruritus and clinical variables in patients with psoriasis. An Bras Dermatol. 2017;92:470-473.
- Prignano F, Ricceri F, Pescitelli L, et al. Itch in psoriasis: epidemiology, clinical aspects and treatment options. Clin Cosmet Investig Dermatol. 2009;2:9-13.
- Dawn A, Yosipovitch G. Treating itch in psoriasis. Dermatol Nurs. 2006;18:227-233.
- Queille-Roussel C, Rosen M, Clonier F, et al. Efficacy and safety of calcipotriol plus betamethasone dipropionate aerosol foam compared with betamethasone 17-valerate-medicated plaster for the treatment of psoriasis. Clin Drug Investig. 2017;37:355-361.
- Betesil [package insert]. Lodi, Italy: IBSA Pharmaceutici Italia S.r.I; 2013.
- Cannavò SP, Guarneri F, Giuffrida R, et al. Evaluation of cutaneous surface parameters in psoriatic patients. Skin Res Technol. 2017;23:41-47.
- Egawa M, Arimoto H, Hirao T, et al. Regional difference of water content in human skin studied by diffuse-reflectance near-infrared spectroscopy: consideration of measurement depth. Appl Spectrosc. 2006;60:24-28.
- van de Kerkhof PC, Reich K, Kavanaugh A, et al. Physician perspectives in the management of psoriasis and psoriatic arthritis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis survey. J Eur Acad Dermatol Venereol. 2015;29:2002-2010.
- Menter A, Korman NJ, Elmets CA, et al; American Academy of Dermatology. Guidelines of care for the management of psoriasis and psoriatic arthritis. section 3. guidelines of care for the management and treatment of psoriasis with topical therapies. J Am Acad Dermatol. 2009;60:643-659.
- Kircik L, Okumu F, Kandavilli S, et al. Rational vehicle design ensures targeted cutaneous steroid delivery. J Clin Aesthet Dermatol. 2017;10:12-19.
- Fowler JF Jr, Herbert AA, Sugarman J. DFD-01, a novel medium potency betamethasone dipropionate 0.05% emollient spray, demonstrates similar efficacy to augmented betamethasone dipropionate 0.05% lotion for the treatment of moderate plaque psoriasis. J Drugs Dermatol. 2016;15:154-162.
- Stein Gold L, Jackson JM, Knuckles ML, et al. Improvement in extensive moderate plaque psoriasis with a novel emollient spray formulation of betamethasone dipropionate 0.05. J Drugs Dermatol. 2016;15:334-342.
- Sidgiddi S, Pakunlu RI, Allenby K. Efficacy, safety, and potency of betamethasone dipropionate spray 0.05%: a treatment for adults with mild-to-moderate plaque psoriasis. J Clin Aesthet Dermatol. 2018;11:14-22.
- Diprolene Lotion (augmented betamethasone dipropionate 0.05%) [package insert]. Kenilworth, NJ: Schering Corporation; 1999.
- Korman NJ, Zhao Y, Pike J, et al. Increased severity of itching, pain, and scaling in psoriasis patients is associated with increased disease severity, reduced quality of life, and reduced work productivity. Dermatol Online J. 2015;21. pii:13030/qt1x16v3dg.
Practice Points
- Pruritus is one of the most bothersome symptoms of psoriasis; plaques located on the knees and elbows remain hard to treat.
- Topical corticosteroids are the initial form of treatment of localized plaque psoriasis.
- The choice of vehicle can change the penetration of the medication, alter the efficacy, and minimize side effects of the drug.
- Betamethasone dipropionate spray 0.05% is a mid-potent corticosteroid that provides fast symptom relief and early efficacy in clearing plaques, similar to a high-potency topical corticosteroid but with less potential for systemic absorption and adverse events.
Dermatology Residency Applications: Correlation of Applicant Personal Statement Content With Match Result
The personal statement is a narrative written by an applicant to residency programs to discuss his/her interests. It is one of the few places in the residency application process where applicants can express their personalities.1 Applicants believe the personal statement is an important opportunity to distinguish themselves from others, thus increasing their chances of successful matching, particularly in competitive specialties.1,2
Dermatology is a highly competitive specialty, with 614 medical students applying for 440 total dermatology positions in 2016.3 According to the results of the 2016 National Resident Matching program director survey, 82% (27/33) of dermatology program directors reported that the personal statement was a factor in selecting applicants to interview. Furthermore, dermatology program directors, on average, rated personal statements as more important than the Medical Student Performance Evaluation/Dean’s Letter, US Medical Licensing Examination (USMLE) Step 2 scores, and class ranking/quartile.4
Prior studies have sought to evaluate the impact of personal statements on the application process. A 2014 study of personal statements submitted by dermatology residency applicants found that the prevalence of certain themes differed according to match outcome.5 However, some of the conclusions drawn in this study were not supported by the reported results or were based on low numbers of participants. The purpose of our study was to examine personal statements from applications to a dermatology program at a major academic institution. This study identified common themes in personal statements, allowing for an analysis of their association with successful matching into dermatology.
Methods
All applications to the dermatology residency program at UNC School of Medicine (Chapel Hill, North Carolina) during the 2012 application cycle (N=422) were eligible. All submitted personal statements (N=422) were included with all personal identifiers removed prior to analysis. The investigator (D.S.M.) was blinded to other Electronic Residency Application Service data and match outcome.
The investigator initially reviewed a small, randomly selected subset of 20 personal statements to identify characteristics and common themes. The investigator then analyzed each of the personal statements to quantify the frequency of each theme. All personal statements submitted to the dermatology residency program at UNC School of Medicine were analyzed in this manner. Dermatology match outcomes for each applicant were confirmed later using dermatology program websites.
Differences in the prevalence of common themes between matched and unmatched applicants were calculated. Analysis of variance tests were used to determine if the differences in prevalence were statistically significant (P≤.05).
Results
All 422 submitted personal statements were evaluated, with 308 personal statements from applicants who matched and 114 personal statements from unmatched applicants. The screening of the initial subset of 20 personal statements resulted in a total of 9 content themes. The prevalence of each theme among matched and unmatched applicants is shown in the Table.
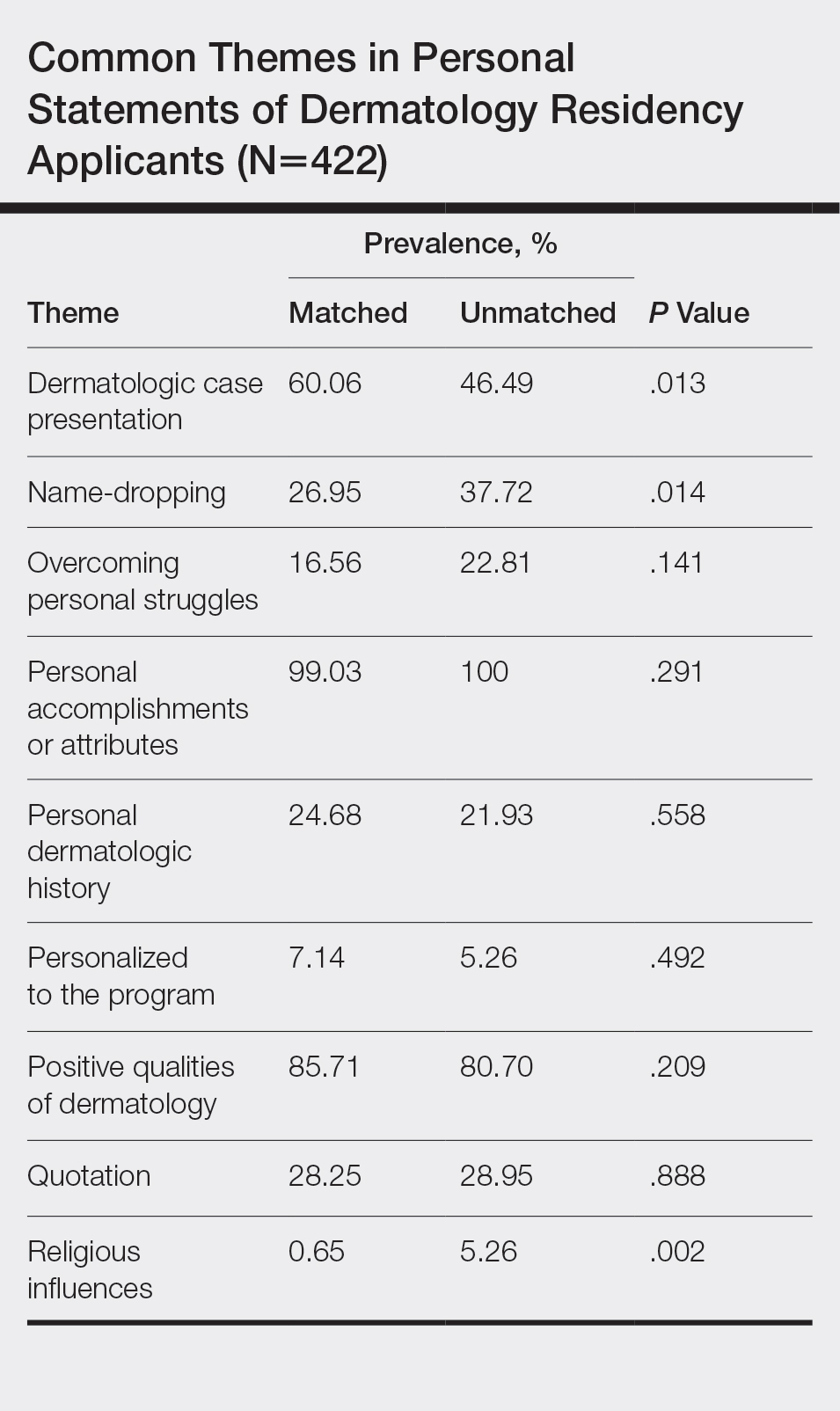
The most common themes among both matched and unmatched groups were personal accomplishments or attributes and positive qualities of dermatology. The prevalence of certain themes varied between matched and unmatched groups. Dermatologic cases were discussed significantly more frequently in the matched group compared to the unmatched group (60.06% vs 46.49%, P=.013). Name-dropping was more prevalent in the unmatched group (37.72%) compared to the matched group (26.95%). This difference in prevalence reached statistical significance (P=.014). Religious influences also were discussed more frequently in the unmatched group (5.26%) vs the matched group (0.65%) with statistical significance (P=.002).
Comment
This study of 422 personal statements submitted to a major academic institution showed that certain themes were common in personal statements among both matched and unmatched applicants. These themes included personal accomplishments/attributes and positive qualities of dermatology. This finding is consistent with prior studies that show common themes in the personal statements of applicants across a wide variety of specialties, including dermatology, anesthesiology, pediatrics, general surgery, internal medicine, and radiology.5-10 Most commonly, applicants feel the need to justify why they chose their particular specialty, with Olazagasti et al5 (N=332) reporting that 70% of submitted dermatology personal statements explained why the applicant chose dermatology.
Certain themes, however, varied in prevalence between matched and unmatched groups in our study. Discussion of dermatologic cases was significantly more prevalent in the matched group compared to the unmatched group (P=.013), possibly because dermatology faculty enjoy hearing about cases and how the applicant responds and interacts with the cases. These data suggest that matched applicants focus more on characteristics specific to the clinical aspects of dermatology.
Conversely, name-dropping was significantly more prevalent in the unmatched group (P=.014). Dermatology is a highly competitive specialty. In 2016, applicants who matched into dermatology had a mean USMLE Step 1 score of 249 with a mean number of 4.7 research experiences and 11.7 abstracts, presentations, or publications, which is higher than the average USMLE Step 1 score of 239 with a mean number of 3.8 research experiences and 8.7 abstracts, presentations, or publications for unmatched applicants.3 It is possible that residency selection committees may view name-dropping negatively if applicants choose to name-drop to strengthen their applications in comparison to more competitive candidates. Religious influences also were significantly more prevalent in the unmatched group (P=.002), but the overall frequency of religious influences was low (approximately 2% of all applicants).
The 422 personal statements examined in our study represent 83.1% of the total pool of applicants to postgraduate year 2 dermatology positions in 2012 (N=508).11 Our data differed somewhat from an analysis of same-year dermatology personal statements of 65% of the national applicant pool.5 Olazagasti et al5 found that themes of a family member in medicine (more in unmatched), a desire to contribute to decreasing literature gap (more in matched), and a desire to better understand dermatologic pathophysiology (more in matched) to be statistically significant (P≤.05 for all). Unfortunately, these themes were found in a small number of applicants, with each being reported in less than 7%.5 Our study included 23% more unmatched candidates and likely better estimated potential significant differences between matched and unmatched applicants.
In the Results section, Olazagasti et al5 reported that matched applicants emphasized the study of cutaneous manifestations of systemic disease significantly more frequently than unmatched applicants. However, the P value in their report did not support this statement (P=.054). In addition, their Conclusion section discussed matched candidates including themes of “why dermatology” and unmatched candidates including a “personal story” as differences between groups. Again, their results did not show any statistical significance to support these recommendations.5 When providing medical student mentorship in a field as competitive as dermatology, faculty must be careful in giving accurate advice that, if at all possible, is supported by objective data rather than personal preference or anecdotes.
Our study was limited in that only personal statements of applicants to a single program in a specific specialty were analyzed. Applicants may have submitted personalized versions of their personal statements to specific schools, which may have biased the themes present in this subset of personal statements. Given these limitations, we are unable to determine if these results are generalizable to all dermatology residency applicants. Further limitation is that the analysis of personal statements is in itself a subjective process.
This study included a larger number of personal statements representing a larger proportion of the total pool of applicants in 2012 than prior studies examining personal statements of dermatology residency applicants. In addition, this study examined the ultimate dermatology match outcome for each applicant during the 2012 application cycle. Future investigations could explore the role of other factors in the residency selection process such as USMLE Step scores, community service, research experiences, and Alpha Omega Alpha Honor Medical Society status.
Conclusion
There are common themes in the personal statements of dermatology residency applicants, including personal accomplishments/attributes and positive qualities of dermatology. In addition, discussion of dermatologic cases was statistically more prevalent in applicants who ultimately matched, whereas name-dropping and religious influences were more prevalent in applicants who did not match. This information may be useful to effectively mentor medical students about the writing process for the personal statement. Further investigation is needed to explore these associations and the role of other aspects of the application in the residency selection process.
- Arbelaez C, Ganguli I. The personal statement for residency application: review and guidance. J Natl Med Assoc. 2011;103:439-442.
- White BA, Sadoski M, Thomas S, et al. Is the evaluation of the personal statement a reliable component of the general surgery residency application? J Surg Educ. 2012;69:340-343.
- Charting Outcomes in the Match for U.S. Allopathic Seniors: Characteristics of US Allopathic Seniors Who Matched to Their Preferred Specialty in the 2016 Main Residency Match. Washington, DC: National Resident Matching Program; September 2016. https://www.nrmp.org/wp-content/uploads/2016/09/Charting-Outcomes-US-Allopathic-Seniors-2016.pdf. Accessed January 21, 2020.
- Results of the 2016 NRMP Program Director Survey. Washington, DC: National Resident Matching Program; June 2016. https://www.nrmp.org/wp-content/uploads/2016/09/NRMP-2016-Program-Director-Survey.pdf. Accessed January 21, 2020.
- Olazagasti J, Gorouhi F, Fazel N. A critical review of personal statements submitted by dermatology residency applicants. Dermatol Res Pract. 2014;2014:934874.
- Max BA, Gelfand B, Brooks MR, et al. Have personal statements become impersonal? an evaluation of personal statements in anesthesiology residency applications. J Clin Anesth. 2010;22:346-351.
- Nield LS, Nease EK, Mitra S, et al. Major themes in the personal statements of pediatric resident applicants. Clin Pediatr (Phila). 2016;55:671-672.
- Ostapenko L, Schonhardt-Bailey C, Sublette JW, et al. Textual analysis of general surgery residency personal statements: topics and gender differences. J Surg Educ. 2018;75:573-581.
- Osman NY, Schonhardt-Bailey C, Walling JL, et al. Textual analysis of internal medicine residency personal statements: themes and gender differences. Med Educ. 2015;49:93-102.
- Smith EA, Weyhing B, Mody Y, et al. A critical analysis of personal statements submitted by radiology residency applicants. Acad Radiol. 2005;12:1024-1028.
- Results and Data: 2012 Main Residency Match. Washington, DC: National Resident Matching Program; April 2012. http://www.nrmp.org/wp-content/uploads/2013/08/resultsanddata20121.pdf. Accessed January 21, 2020.
The personal statement is a narrative written by an applicant to residency programs to discuss his/her interests. It is one of the few places in the residency application process where applicants can express their personalities.1 Applicants believe the personal statement is an important opportunity to distinguish themselves from others, thus increasing their chances of successful matching, particularly in competitive specialties.1,2
Dermatology is a highly competitive specialty, with 614 medical students applying for 440 total dermatology positions in 2016.3 According to the results of the 2016 National Resident Matching program director survey, 82% (27/33) of dermatology program directors reported that the personal statement was a factor in selecting applicants to interview. Furthermore, dermatology program directors, on average, rated personal statements as more important than the Medical Student Performance Evaluation/Dean’s Letter, US Medical Licensing Examination (USMLE) Step 2 scores, and class ranking/quartile.4
Prior studies have sought to evaluate the impact of personal statements on the application process. A 2014 study of personal statements submitted by dermatology residency applicants found that the prevalence of certain themes differed according to match outcome.5 However, some of the conclusions drawn in this study were not supported by the reported results or were based on low numbers of participants. The purpose of our study was to examine personal statements from applications to a dermatology program at a major academic institution. This study identified common themes in personal statements, allowing for an analysis of their association with successful matching into dermatology.
Methods
All applications to the dermatology residency program at UNC School of Medicine (Chapel Hill, North Carolina) during the 2012 application cycle (N=422) were eligible. All submitted personal statements (N=422) were included with all personal identifiers removed prior to analysis. The investigator (D.S.M.) was blinded to other Electronic Residency Application Service data and match outcome.
The investigator initially reviewed a small, randomly selected subset of 20 personal statements to identify characteristics and common themes. The investigator then analyzed each of the personal statements to quantify the frequency of each theme. All personal statements submitted to the dermatology residency program at UNC School of Medicine were analyzed in this manner. Dermatology match outcomes for each applicant were confirmed later using dermatology program websites.
Differences in the prevalence of common themes between matched and unmatched applicants were calculated. Analysis of variance tests were used to determine if the differences in prevalence were statistically significant (P≤.05).
Results
All 422 submitted personal statements were evaluated, with 308 personal statements from applicants who matched and 114 personal statements from unmatched applicants. The screening of the initial subset of 20 personal statements resulted in a total of 9 content themes. The prevalence of each theme among matched and unmatched applicants is shown in the Table.
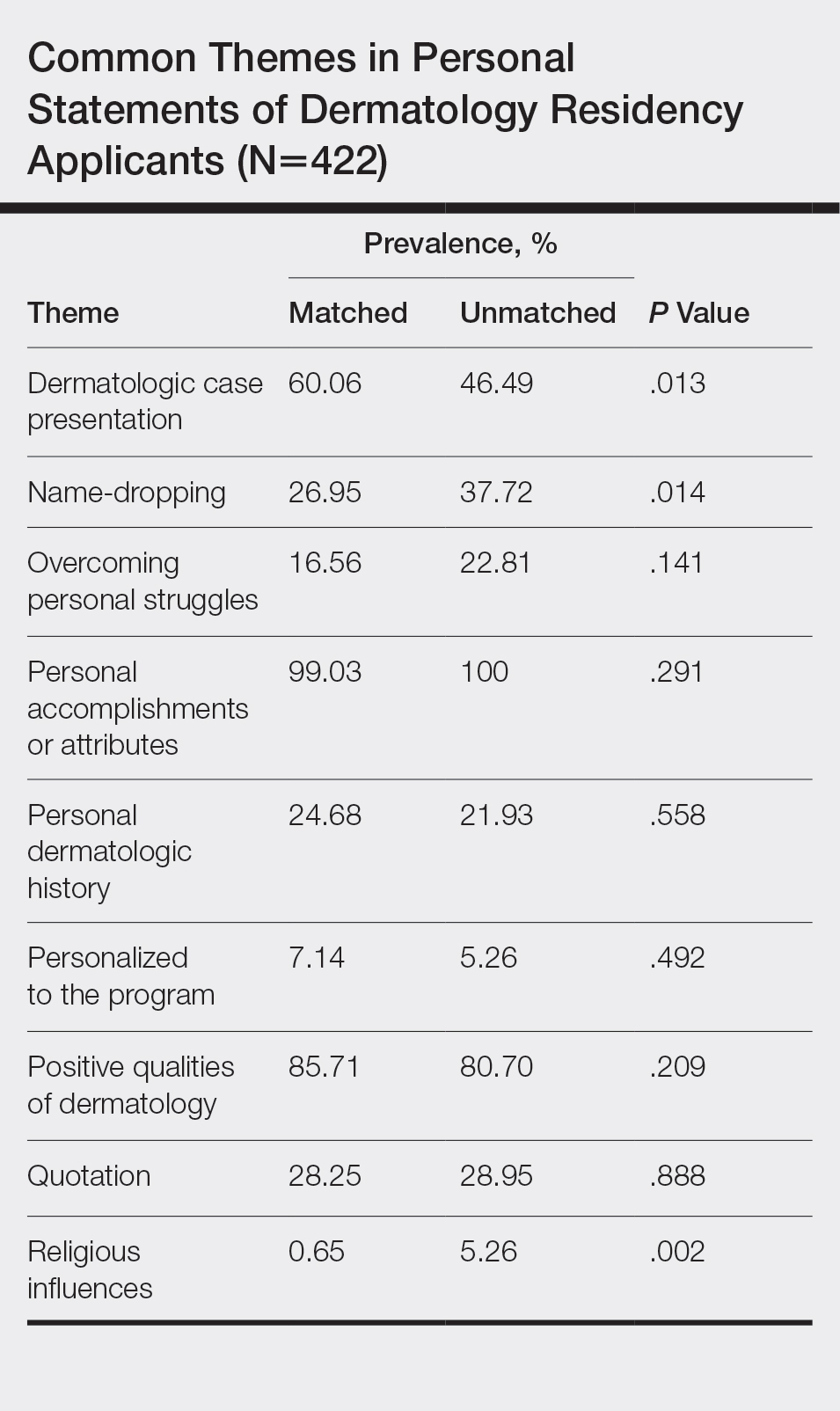
The most common themes among both matched and unmatched groups were personal accomplishments or attributes and positive qualities of dermatology. The prevalence of certain themes varied between matched and unmatched groups. Dermatologic cases were discussed significantly more frequently in the matched group compared to the unmatched group (60.06% vs 46.49%, P=.013). Name-dropping was more prevalent in the unmatched group (37.72%) compared to the matched group (26.95%). This difference in prevalence reached statistical significance (P=.014). Religious influences also were discussed more frequently in the unmatched group (5.26%) vs the matched group (0.65%) with statistical significance (P=.002).
Comment
This study of 422 personal statements submitted to a major academic institution showed that certain themes were common in personal statements among both matched and unmatched applicants. These themes included personal accomplishments/attributes and positive qualities of dermatology. This finding is consistent with prior studies that show common themes in the personal statements of applicants across a wide variety of specialties, including dermatology, anesthesiology, pediatrics, general surgery, internal medicine, and radiology.5-10 Most commonly, applicants feel the need to justify why they chose their particular specialty, with Olazagasti et al5 (N=332) reporting that 70% of submitted dermatology personal statements explained why the applicant chose dermatology.
Certain themes, however, varied in prevalence between matched and unmatched groups in our study. Discussion of dermatologic cases was significantly more prevalent in the matched group compared to the unmatched group (P=.013), possibly because dermatology faculty enjoy hearing about cases and how the applicant responds and interacts with the cases. These data suggest that matched applicants focus more on characteristics specific to the clinical aspects of dermatology.
Conversely, name-dropping was significantly more prevalent in the unmatched group (P=.014). Dermatology is a highly competitive specialty. In 2016, applicants who matched into dermatology had a mean USMLE Step 1 score of 249 with a mean number of 4.7 research experiences and 11.7 abstracts, presentations, or publications, which is higher than the average USMLE Step 1 score of 239 with a mean number of 3.8 research experiences and 8.7 abstracts, presentations, or publications for unmatched applicants.3 It is possible that residency selection committees may view name-dropping negatively if applicants choose to name-drop to strengthen their applications in comparison to more competitive candidates. Religious influences also were significantly more prevalent in the unmatched group (P=.002), but the overall frequency of religious influences was low (approximately 2% of all applicants).
The 422 personal statements examined in our study represent 83.1% of the total pool of applicants to postgraduate year 2 dermatology positions in 2012 (N=508).11 Our data differed somewhat from an analysis of same-year dermatology personal statements of 65% of the national applicant pool.5 Olazagasti et al5 found that themes of a family member in medicine (more in unmatched), a desire to contribute to decreasing literature gap (more in matched), and a desire to better understand dermatologic pathophysiology (more in matched) to be statistically significant (P≤.05 for all). Unfortunately, these themes were found in a small number of applicants, with each being reported in less than 7%.5 Our study included 23% more unmatched candidates and likely better estimated potential significant differences between matched and unmatched applicants.
In the Results section, Olazagasti et al5 reported that matched applicants emphasized the study of cutaneous manifestations of systemic disease significantly more frequently than unmatched applicants. However, the P value in their report did not support this statement (P=.054). In addition, their Conclusion section discussed matched candidates including themes of “why dermatology” and unmatched candidates including a “personal story” as differences between groups. Again, their results did not show any statistical significance to support these recommendations.5 When providing medical student mentorship in a field as competitive as dermatology, faculty must be careful in giving accurate advice that, if at all possible, is supported by objective data rather than personal preference or anecdotes.
Our study was limited in that only personal statements of applicants to a single program in a specific specialty were analyzed. Applicants may have submitted personalized versions of their personal statements to specific schools, which may have biased the themes present in this subset of personal statements. Given these limitations, we are unable to determine if these results are generalizable to all dermatology residency applicants. Further limitation is that the analysis of personal statements is in itself a subjective process.
This study included a larger number of personal statements representing a larger proportion of the total pool of applicants in 2012 than prior studies examining personal statements of dermatology residency applicants. In addition, this study examined the ultimate dermatology match outcome for each applicant during the 2012 application cycle. Future investigations could explore the role of other factors in the residency selection process such as USMLE Step scores, community service, research experiences, and Alpha Omega Alpha Honor Medical Society status.
Conclusion
There are common themes in the personal statements of dermatology residency applicants, including personal accomplishments/attributes and positive qualities of dermatology. In addition, discussion of dermatologic cases was statistically more prevalent in applicants who ultimately matched, whereas name-dropping and religious influences were more prevalent in applicants who did not match. This information may be useful to effectively mentor medical students about the writing process for the personal statement. Further investigation is needed to explore these associations and the role of other aspects of the application in the residency selection process.
The personal statement is a narrative written by an applicant to residency programs to discuss his/her interests. It is one of the few places in the residency application process where applicants can express their personalities.1 Applicants believe the personal statement is an important opportunity to distinguish themselves from others, thus increasing their chances of successful matching, particularly in competitive specialties.1,2
Dermatology is a highly competitive specialty, with 614 medical students applying for 440 total dermatology positions in 2016.3 According to the results of the 2016 National Resident Matching program director survey, 82% (27/33) of dermatology program directors reported that the personal statement was a factor in selecting applicants to interview. Furthermore, dermatology program directors, on average, rated personal statements as more important than the Medical Student Performance Evaluation/Dean’s Letter, US Medical Licensing Examination (USMLE) Step 2 scores, and class ranking/quartile.4
Prior studies have sought to evaluate the impact of personal statements on the application process. A 2014 study of personal statements submitted by dermatology residency applicants found that the prevalence of certain themes differed according to match outcome.5 However, some of the conclusions drawn in this study were not supported by the reported results or were based on low numbers of participants. The purpose of our study was to examine personal statements from applications to a dermatology program at a major academic institution. This study identified common themes in personal statements, allowing for an analysis of their association with successful matching into dermatology.
Methods
All applications to the dermatology residency program at UNC School of Medicine (Chapel Hill, North Carolina) during the 2012 application cycle (N=422) were eligible. All submitted personal statements (N=422) were included with all personal identifiers removed prior to analysis. The investigator (D.S.M.) was blinded to other Electronic Residency Application Service data and match outcome.
The investigator initially reviewed a small, randomly selected subset of 20 personal statements to identify characteristics and common themes. The investigator then analyzed each of the personal statements to quantify the frequency of each theme. All personal statements submitted to the dermatology residency program at UNC School of Medicine were analyzed in this manner. Dermatology match outcomes for each applicant were confirmed later using dermatology program websites.
Differences in the prevalence of common themes between matched and unmatched applicants were calculated. Analysis of variance tests were used to determine if the differences in prevalence were statistically significant (P≤.05).
Results
All 422 submitted personal statements were evaluated, with 308 personal statements from applicants who matched and 114 personal statements from unmatched applicants. The screening of the initial subset of 20 personal statements resulted in a total of 9 content themes. The prevalence of each theme among matched and unmatched applicants is shown in the Table.
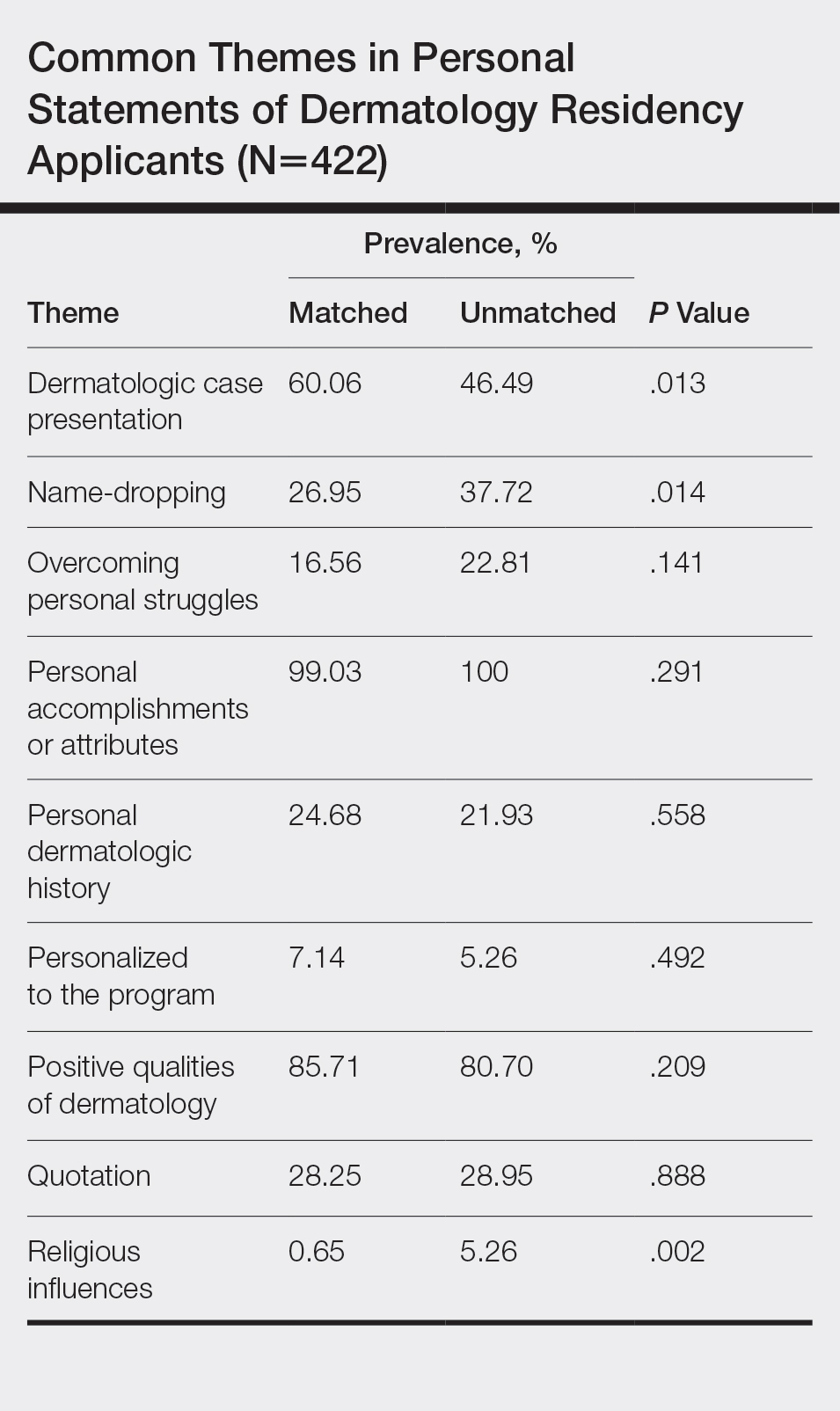
The most common themes among both matched and unmatched groups were personal accomplishments or attributes and positive qualities of dermatology. The prevalence of certain themes varied between matched and unmatched groups. Dermatologic cases were discussed significantly more frequently in the matched group compared to the unmatched group (60.06% vs 46.49%, P=.013). Name-dropping was more prevalent in the unmatched group (37.72%) compared to the matched group (26.95%). This difference in prevalence reached statistical significance (P=.014). Religious influences also were discussed more frequently in the unmatched group (5.26%) vs the matched group (0.65%) with statistical significance (P=.002).
Comment
This study of 422 personal statements submitted to a major academic institution showed that certain themes were common in personal statements among both matched and unmatched applicants. These themes included personal accomplishments/attributes and positive qualities of dermatology. This finding is consistent with prior studies that show common themes in the personal statements of applicants across a wide variety of specialties, including dermatology, anesthesiology, pediatrics, general surgery, internal medicine, and radiology.5-10 Most commonly, applicants feel the need to justify why they chose their particular specialty, with Olazagasti et al5 (N=332) reporting that 70% of submitted dermatology personal statements explained why the applicant chose dermatology.
Certain themes, however, varied in prevalence between matched and unmatched groups in our study. Discussion of dermatologic cases was significantly more prevalent in the matched group compared to the unmatched group (P=.013), possibly because dermatology faculty enjoy hearing about cases and how the applicant responds and interacts with the cases. These data suggest that matched applicants focus more on characteristics specific to the clinical aspects of dermatology.
Conversely, name-dropping was significantly more prevalent in the unmatched group (P=.014). Dermatology is a highly competitive specialty. In 2016, applicants who matched into dermatology had a mean USMLE Step 1 score of 249 with a mean number of 4.7 research experiences and 11.7 abstracts, presentations, or publications, which is higher than the average USMLE Step 1 score of 239 with a mean number of 3.8 research experiences and 8.7 abstracts, presentations, or publications for unmatched applicants.3 It is possible that residency selection committees may view name-dropping negatively if applicants choose to name-drop to strengthen their applications in comparison to more competitive candidates. Religious influences also were significantly more prevalent in the unmatched group (P=.002), but the overall frequency of religious influences was low (approximately 2% of all applicants).
The 422 personal statements examined in our study represent 83.1% of the total pool of applicants to postgraduate year 2 dermatology positions in 2012 (N=508).11 Our data differed somewhat from an analysis of same-year dermatology personal statements of 65% of the national applicant pool.5 Olazagasti et al5 found that themes of a family member in medicine (more in unmatched), a desire to contribute to decreasing literature gap (more in matched), and a desire to better understand dermatologic pathophysiology (more in matched) to be statistically significant (P≤.05 for all). Unfortunately, these themes were found in a small number of applicants, with each being reported in less than 7%.5 Our study included 23% more unmatched candidates and likely better estimated potential significant differences between matched and unmatched applicants.
In the Results section, Olazagasti et al5 reported that matched applicants emphasized the study of cutaneous manifestations of systemic disease significantly more frequently than unmatched applicants. However, the P value in their report did not support this statement (P=.054). In addition, their Conclusion section discussed matched candidates including themes of “why dermatology” and unmatched candidates including a “personal story” as differences between groups. Again, their results did not show any statistical significance to support these recommendations.5 When providing medical student mentorship in a field as competitive as dermatology, faculty must be careful in giving accurate advice that, if at all possible, is supported by objective data rather than personal preference or anecdotes.
Our study was limited in that only personal statements of applicants to a single program in a specific specialty were analyzed. Applicants may have submitted personalized versions of their personal statements to specific schools, which may have biased the themes present in this subset of personal statements. Given these limitations, we are unable to determine if these results are generalizable to all dermatology residency applicants. Further limitation is that the analysis of personal statements is in itself a subjective process.
This study included a larger number of personal statements representing a larger proportion of the total pool of applicants in 2012 than prior studies examining personal statements of dermatology residency applicants. In addition, this study examined the ultimate dermatology match outcome for each applicant during the 2012 application cycle. Future investigations could explore the role of other factors in the residency selection process such as USMLE Step scores, community service, research experiences, and Alpha Omega Alpha Honor Medical Society status.
Conclusion
There are common themes in the personal statements of dermatology residency applicants, including personal accomplishments/attributes and positive qualities of dermatology. In addition, discussion of dermatologic cases was statistically more prevalent in applicants who ultimately matched, whereas name-dropping and religious influences were more prevalent in applicants who did not match. This information may be useful to effectively mentor medical students about the writing process for the personal statement. Further investigation is needed to explore these associations and the role of other aspects of the application in the residency selection process.
- Arbelaez C, Ganguli I. The personal statement for residency application: review and guidance. J Natl Med Assoc. 2011;103:439-442.
- White BA, Sadoski M, Thomas S, et al. Is the evaluation of the personal statement a reliable component of the general surgery residency application? J Surg Educ. 2012;69:340-343.
- Charting Outcomes in the Match for U.S. Allopathic Seniors: Characteristics of US Allopathic Seniors Who Matched to Their Preferred Specialty in the 2016 Main Residency Match. Washington, DC: National Resident Matching Program; September 2016. https://www.nrmp.org/wp-content/uploads/2016/09/Charting-Outcomes-US-Allopathic-Seniors-2016.pdf. Accessed January 21, 2020.
- Results of the 2016 NRMP Program Director Survey. Washington, DC: National Resident Matching Program; June 2016. https://www.nrmp.org/wp-content/uploads/2016/09/NRMP-2016-Program-Director-Survey.pdf. Accessed January 21, 2020.
- Olazagasti J, Gorouhi F, Fazel N. A critical review of personal statements submitted by dermatology residency applicants. Dermatol Res Pract. 2014;2014:934874.
- Max BA, Gelfand B, Brooks MR, et al. Have personal statements become impersonal? an evaluation of personal statements in anesthesiology residency applications. J Clin Anesth. 2010;22:346-351.
- Nield LS, Nease EK, Mitra S, et al. Major themes in the personal statements of pediatric resident applicants. Clin Pediatr (Phila). 2016;55:671-672.
- Ostapenko L, Schonhardt-Bailey C, Sublette JW, et al. Textual analysis of general surgery residency personal statements: topics and gender differences. J Surg Educ. 2018;75:573-581.
- Osman NY, Schonhardt-Bailey C, Walling JL, et al. Textual analysis of internal medicine residency personal statements: themes and gender differences. Med Educ. 2015;49:93-102.
- Smith EA, Weyhing B, Mody Y, et al. A critical analysis of personal statements submitted by radiology residency applicants. Acad Radiol. 2005;12:1024-1028.
- Results and Data: 2012 Main Residency Match. Washington, DC: National Resident Matching Program; April 2012. http://www.nrmp.org/wp-content/uploads/2013/08/resultsanddata20121.pdf. Accessed January 21, 2020.
- Arbelaez C, Ganguli I. The personal statement for residency application: review and guidance. J Natl Med Assoc. 2011;103:439-442.
- White BA, Sadoski M, Thomas S, et al. Is the evaluation of the personal statement a reliable component of the general surgery residency application? J Surg Educ. 2012;69:340-343.
- Charting Outcomes in the Match for U.S. Allopathic Seniors: Characteristics of US Allopathic Seniors Who Matched to Their Preferred Specialty in the 2016 Main Residency Match. Washington, DC: National Resident Matching Program; September 2016. https://www.nrmp.org/wp-content/uploads/2016/09/Charting-Outcomes-US-Allopathic-Seniors-2016.pdf. Accessed January 21, 2020.
- Results of the 2016 NRMP Program Director Survey. Washington, DC: National Resident Matching Program; June 2016. https://www.nrmp.org/wp-content/uploads/2016/09/NRMP-2016-Program-Director-Survey.pdf. Accessed January 21, 2020.
- Olazagasti J, Gorouhi F, Fazel N. A critical review of personal statements submitted by dermatology residency applicants. Dermatol Res Pract. 2014;2014:934874.
- Max BA, Gelfand B, Brooks MR, et al. Have personal statements become impersonal? an evaluation of personal statements in anesthesiology residency applications. J Clin Anesth. 2010;22:346-351.
- Nield LS, Nease EK, Mitra S, et al. Major themes in the personal statements of pediatric resident applicants. Clin Pediatr (Phila). 2016;55:671-672.
- Ostapenko L, Schonhardt-Bailey C, Sublette JW, et al. Textual analysis of general surgery residency personal statements: topics and gender differences. J Surg Educ. 2018;75:573-581.
- Osman NY, Schonhardt-Bailey C, Walling JL, et al. Textual analysis of internal medicine residency personal statements: themes and gender differences. Med Educ. 2015;49:93-102.
- Smith EA, Weyhing B, Mody Y, et al. A critical analysis of personal statements submitted by radiology residency applicants. Acad Radiol. 2005;12:1024-1028.
- Results and Data: 2012 Main Residency Match. Washington, DC: National Resident Matching Program; April 2012. http://www.nrmp.org/wp-content/uploads/2013/08/resultsanddata20121.pdf. Accessed January 21, 2020.
Practice Points
- The most common themes discussed in applicant personal statements include personal accomplishments/attributes and positive qualities of dermatology.
- Presentation of dermatologic cases was more prevalent in personal statements of matched applicants.
- Name-dropping was more common among unmatched applicants.
Transillumination for Improved Diagnosis of Digital Myxoid Cysts
Practice Gap
Myxoid cysts are among the most common space-occupying lesions involving the nail unit. Their etiology has not been fully elucidated, but these cysts likely form due to leakage of synovial fluid following trauma or chronic wear and tear. They are highly associated with osteoarthritis and typically are found in close proximity to the distal interphalangeal joints.1 Myxoid cysts often extend into the eponychium, where mechanical stress on the nail matrix may lead to nail dystrophy, most commonly resulting in a longitudinal groove in the nail plate (Figure, A). The presence of multiple myxoid cysts is not uncommon. Differentiation of this lesion from other nodules of the digits, including epidermoid cysts, acquired digital fibrokeratomas, and giant cell tendon sheath tumors often is challenging without a biopsy.

Technique
The normal nail unit transmits light to some extent, and masses may be identified by how easily they transmit light relative to the adjacent skin. Solid tumors of the nail unit, such as acquired digital fibrokeratomas and giant cell tendon sheath tumors, will not transmit light, while myxoid cysts transmit light easily. A dermatoscope can be used to project light from the dorsal digit through the nail unit. The area occupied by the myxoid cyst will appear bright compared to the surrounding skin (Figure, B). Drainage of the lesion using an 18-gauge needle yielded a clear jellylike fluid that was consistent with a myxoid cyst. This technique aids in localizing and characterizing the myxoid cyst for treatment or drainage. Physician assessment of transillumination has been shown to demonstrate clinical accuracy and high intraobserver reliability in differentiating between cystic and solid tumors.2
Practice Implications
Transillumination is a valuable technique that may aid dermatologists in both the diagnosis and subsequent treatment of myxoid cysts. Location is important to consider when choosing a treatment option. Although lower recurrence rates are achieved with nail surgery, permanent nail dystrophy is likely when cysts are in close proximity to the nail matrix.3 When multiple cysts are present, only the largest may be apparent. Transillumination can guide the physician in achieving more accurate and thorough drainage of the cyst contents, negating the need for more costly imaging modalities. Dermatologists may utilize transillumination as a rapid and economical diagnostic method for space-occupying lesions involving the nail unit.
- Dermatol Surg. 2008;34:364-369.
- Erne HC, Gardner TR, Strauch RJ. Transillumination of hand tumors: a cadaver study to evaluate accuracy and intraobserver reliability. Hand (N Y). 2011;6:390-393.
- Fritz GR, Stern PJ, Dickey M. Complications following mucous cyst excision. J Hand Surg Br. 1997;22:222-225.
Practice Gap
Myxoid cysts are among the most common space-occupying lesions involving the nail unit. Their etiology has not been fully elucidated, but these cysts likely form due to leakage of synovial fluid following trauma or chronic wear and tear. They are highly associated with osteoarthritis and typically are found in close proximity to the distal interphalangeal joints.1 Myxoid cysts often extend into the eponychium, where mechanical stress on the nail matrix may lead to nail dystrophy, most commonly resulting in a longitudinal groove in the nail plate (Figure, A). The presence of multiple myxoid cysts is not uncommon. Differentiation of this lesion from other nodules of the digits, including epidermoid cysts, acquired digital fibrokeratomas, and giant cell tendon sheath tumors often is challenging without a biopsy.

Technique
The normal nail unit transmits light to some extent, and masses may be identified by how easily they transmit light relative to the adjacent skin. Solid tumors of the nail unit, such as acquired digital fibrokeratomas and giant cell tendon sheath tumors, will not transmit light, while myxoid cysts transmit light easily. A dermatoscope can be used to project light from the dorsal digit through the nail unit. The area occupied by the myxoid cyst will appear bright compared to the surrounding skin (Figure, B). Drainage of the lesion using an 18-gauge needle yielded a clear jellylike fluid that was consistent with a myxoid cyst. This technique aids in localizing and characterizing the myxoid cyst for treatment or drainage. Physician assessment of transillumination has been shown to demonstrate clinical accuracy and high intraobserver reliability in differentiating between cystic and solid tumors.2
Practice Implications
Transillumination is a valuable technique that may aid dermatologists in both the diagnosis and subsequent treatment of myxoid cysts. Location is important to consider when choosing a treatment option. Although lower recurrence rates are achieved with nail surgery, permanent nail dystrophy is likely when cysts are in close proximity to the nail matrix.3 When multiple cysts are present, only the largest may be apparent. Transillumination can guide the physician in achieving more accurate and thorough drainage of the cyst contents, negating the need for more costly imaging modalities. Dermatologists may utilize transillumination as a rapid and economical diagnostic method for space-occupying lesions involving the nail unit.
Practice Gap
Myxoid cysts are among the most common space-occupying lesions involving the nail unit. Their etiology has not been fully elucidated, but these cysts likely form due to leakage of synovial fluid following trauma or chronic wear and tear. They are highly associated with osteoarthritis and typically are found in close proximity to the distal interphalangeal joints.1 Myxoid cysts often extend into the eponychium, where mechanical stress on the nail matrix may lead to nail dystrophy, most commonly resulting in a longitudinal groove in the nail plate (Figure, A). The presence of multiple myxoid cysts is not uncommon. Differentiation of this lesion from other nodules of the digits, including epidermoid cysts, acquired digital fibrokeratomas, and giant cell tendon sheath tumors often is challenging without a biopsy.

Technique
The normal nail unit transmits light to some extent, and masses may be identified by how easily they transmit light relative to the adjacent skin. Solid tumors of the nail unit, such as acquired digital fibrokeratomas and giant cell tendon sheath tumors, will not transmit light, while myxoid cysts transmit light easily. A dermatoscope can be used to project light from the dorsal digit through the nail unit. The area occupied by the myxoid cyst will appear bright compared to the surrounding skin (Figure, B). Drainage of the lesion using an 18-gauge needle yielded a clear jellylike fluid that was consistent with a myxoid cyst. This technique aids in localizing and characterizing the myxoid cyst for treatment or drainage. Physician assessment of transillumination has been shown to demonstrate clinical accuracy and high intraobserver reliability in differentiating between cystic and solid tumors.2
Practice Implications
Transillumination is a valuable technique that may aid dermatologists in both the diagnosis and subsequent treatment of myxoid cysts. Location is important to consider when choosing a treatment option. Although lower recurrence rates are achieved with nail surgery, permanent nail dystrophy is likely when cysts are in close proximity to the nail matrix.3 When multiple cysts are present, only the largest may be apparent. Transillumination can guide the physician in achieving more accurate and thorough drainage of the cyst contents, negating the need for more costly imaging modalities. Dermatologists may utilize transillumination as a rapid and economical diagnostic method for space-occupying lesions involving the nail unit.
- Dermatol Surg. 2008;34:364-369.
- Erne HC, Gardner TR, Strauch RJ. Transillumination of hand tumors: a cadaver study to evaluate accuracy and intraobserver reliability. Hand (N Y). 2011;6:390-393.
- Fritz GR, Stern PJ, Dickey M. Complications following mucous cyst excision. J Hand Surg Br. 1997;22:222-225.
- Dermatol Surg. 2008;34:364-369.
- Erne HC, Gardner TR, Strauch RJ. Transillumination of hand tumors: a cadaver study to evaluate accuracy and intraobserver reliability. Hand (N Y). 2011;6:390-393.
- Fritz GR, Stern PJ, Dickey M. Complications following mucous cyst excision. J Hand Surg Br. 1997;22:222-225.
Racial Limitations of Fitzpatrick Skin Type
Fitzpatrick skin type (FST) is the most commonly used classification system in dermatologic practice. It was developed by Thomas B. Fitzpatrick, MD, PhD, in 1975 to assess the propensity of the skin to burn during phototherapy.1 Fitzpatrick skin type also can be used to assess the clinical benefits and efficacy of cosmetic procedures, including laser hair removal, chemical peel and dermabrasion, tattoo removal, spray tanning, and laser resurfacing for acne scarring.2 The original FST classifications included skin types I through IV; skin types V and VI were later added to include individuals of Asian, Indian, and African origin.1 As a result, FST often is used by providers as a means of describing constitutive skin color and ethnicity.3
How did FST transition from describing the propensity of the skin to burn from UV light exposure to categorizing skin color, thereby becoming a proxy for race? It most likely occurred because there has not been another widely adopted classification system for describing skin color that can be applied to all skin types. Even when the FST classification scale is used as intended, there are inconsistencies with its accuracy; for example, self-reported FSTs have correlated poorly with sunburn risk as well as physician-reported FSTs.4,5 Although physician-reported FSTs have been demonstrated to correlate with race, race does not consistently correlate with objective measures of pigmentation or self-reported FSTs.5 For example, Japanese women often self-identify as FST type II, but Asian skin generally is considered to be nonwhite.1 Fitzpatrick himself acknowledged that race and ethnicity are cultural and political terms with no scientific basis.6 Fitzpatrick skin type also has been demonstrated to correlate poorly with constitutive skin color and minimal erythema dose values.7
We conducted an anonymous survey of dermatologists and dermatology trainees to evaluate how providers use FST in their clinical practice as well as how it is used to describe race and ethnicity.
Methods
The survey was distributed electronically to dermatologists and dermatology trainees from March 13 to March 28, 2019, using the Association of Professors of Dermatology listserv, as well as in person at the annual Skin of Color Society meeting in Washington, DC, on February 28, 2019. The 8-item survey included questions about physician demographics (ie, primary practice setting, board certification, and geographic location); whether the respondent identified as an individual with skin of color; and how the respondent utilized FST in clinical notes (ie, describing race/ethnicity, skin cancer risk, and constitutive [baseline] skin color; determining initial phototherapy dosage and suitability for laser treatments, and likelihood of skin burning). A t test was used to determine whether dermatologists who identified as having skin of color utilized FST differently.
Results
A total of 141 surveys were returned, and 140 respondents were included in the final analysis. Given the methods used to distribute the survey, a response rate could not be calculated. The respondents included more board-certified dermatologists (70%) than dermatology trainees (30%). Ninety-three percent of respondents indicated an academic institution as their primary practice location. Notably, 26% of respondents self-identified as having skin of color.
Forty-one percent of all respondents agreed that FST should be included in their clinical documentation. In response to the question “In what scenarios would you refer to FST in a clinical note?” 31% said they used FST to describe patients’ race or ethnicity, 47% used it to describe patients’ constitutive skin color, and 22% utilized it in both scenarios. Respondents who did not identify as having skin of color were more likely to use FST to describe constitutive skin color, though this finding was not statistically significant (P=.063). Anecdotally, providers also included FST in clinical notes on postinflammatory hyperpigmentation, melasma, and treatment with cryotherapy.
Comment
The US Census Bureau has estimated that half of the US population will be of non-European descent by 2050.8 As racial and ethnic distinctions continue to be blurred, attempts to include all nonwhite skin types under the umbrella term skin of color becomes increasingly problematic. The true number of skin colors is unknown but likely is infinite, as Brazilian artist Angélica Dass has demonstrated with her photographic project “Humanae” (Figure). Given this shift in demographics and the limitations of the FST, alternative methods of describing skin color must be developed.

© Angélica Dass | Humanae Work in Progress (Courtesy of the artist).
The results of our survey suggest that approximately one-third to half of academic dermatologists/dermatology trainees use FST to describe race/ethnicity and/or constitutive skin color. This misuse of FST may occur more frequently among physicians who do not identify as having skin of color. Additionally, misuse of FST in academic settings may be problematic and confusing for medical students who may learn to use this common dermatologic tool outside of its original intent.
We acknowledge that the conundrum of how to classify individuals with nonwhite skin or skin of color is not simply answered. Several alternative skin classification models have been proposed to improve the sensitivity and specificity of identifying patients with skin of color (Table). Refining FST classification is one approach. Employing terms such as skin irritation, tenderness, itching, or skin becoming darker from sun exposure rather than painful burn or tanning may result in better identification.1,4 A study conducted in India modified the FST questionnaire to acknowledge cultural behaviors.15 Because lighter skin is culturally valued in this population, patient experience with purposeful sun exposure was limited; thus, the questionnaire was modified to remove questions on the use of tanning booths and/or creams as well as sun exposure and instead included more objective questions regarding dark brown eye color, black and dark brown hair color, and dark brown skin color.15 Other studies have suggested that patient-reported photosensitivity assessed via a questionnaire is a valid measure for assessing FST but is associated with an overestimation of skin color, known as “the dark shift.”20

Sharma et al15 utilized reflectance spectrophotometry as an objective measure of melanin and skin erythema. The melanin index consistently showed a positive correlation with FSTs as opposed to the erythema index, which correlated poorly.15 Although reflectance spectrometry accurately identifies skin color in patients with nonwhite skin,21,22 it is an impractical and cost-prohibitive tool for daily practice. A more practical tool for the clinical setting would be a visual color scale with skin hues spanning FST types I to VI, including bands of increasingly darker gradations that would be particularly useful in assessing skin of color. Once such tool is the Taylor Hyperpigmentation Scale.17 Although currently not widely available, this tool could be further refined with additional skin hues.
Conclusion
Other investigators have criticized the various limitations of FST, including physician vs patient assessment, interview vs questionnaire, and phrasing of questions on skin type.23 Our findings suggest that medical providers should be cognizant of conflating race and ethnicity with FST. Two authors of this report (O.R.W. and J.E.D.) are medical students with skin of color and frequently have observed the addition of FST to the medical records of patients who were not receiving phototherapy as a proxy for race. We believe that more culturally appropriate and clinically relevant methods for describing skin of color need to be developed and, in the interim, the original intent of FST should be emphasized and incorporated in medical school and resident education.
Acknowledgment
The authors thank Adewole Adamson, MD (Austin, Texas), for discussion and feedback.
- Goldsmith LA, Katz SI, Gilchrest BA, et al, eds. Fitzpatrick’s Dermatology in General Medicine. 8th ed. New York, NY: The McGraw-Hill Companies; 2012.
- Sachdeva S. Fitzpatrick skin typing: applications in dermatology. Indian J Dermatol Venereol Leprol. 2009;75:93-96.
- Everett JS, Budescu M, Sommers MS. Making sense of skin color in clinical care. Clin Nurs Res. 2012;21:495-516.
- Eilers S, Bach DQ, Gaber R, et al. Accuracy of self-report in assessingFitzpatrick skin phototypes I through VI. JAMA Dermatol. 2013;149:1289-1294.
- He SY, McCulloch CE, Boscardin WJ, et al. Self-reported pigmentary phenotypes and race are significant but incomplete predictors of Fitzpatrick skin phototype in an ethnically diverse population. J Am Acad Dermatol. 2014;71:731-737.
- Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869-871.
- Leenutaphong V. Relationship between skin color and cutaneous response to ultraviolet radiation in Thai. Photodermatol Photoimmunol Photomed. 1996;11:198-203.
- Colby SL, Ortman JM. Projections of the Size and Composition of the US Population: 2014 to 2060. Washington, DC: US Census Bureau; 2015.
- Baumann L. Understanding and treating various skin types: the Baumann Skin Type Indicator. Dermatol Clin. 2008;26:359-373.
- Fanous N. A new patient classification for laser resurfacing and peels: predicting responses, risks, and results. Aesthetic Plast Surg. 2002;26:99-104.
- Glogau RG. Chemical peeling and aging skin. J Geriatric Dermatol. 1994;2:30-35.
- Goldman M. Universal classification of skin type. In: Shiffman M, Mirrafati S, Lam S, et al, eds. Simplified Facial Rejuvenation. Berlin, Heidelberg, Germany: Springer; 2008:47-50.
- Kawada A. UVB-induced erythema, delayed tanning, and UVA-induced immediate tanning in Japanese skin. Photodermatol. 1986;3:327-333.
- Lancer HA. Lancer Ethnicity Scale (LES). Lasers Surg Med. 1998;22:9.
- Sharma VK, Gupta V, Jangid BL, et al. Modification of the Fitzpatrick system of skin phototype classification for the Indian population, and its correlation with narrowband diffuse reflectance spectrophotometry. Clin Exp Dermatol. 2018;43:274-280.
- Roberts WE. The Roberts Skin Type Classification System. J Drugs Dermatol. 2008;7:452-456.
- Taylor SC, Arsonnaud S, Czernielewski J. The Taylor hyperpigmentation scale: a new visual assessment tool for the evaluation of skin color and pigmentation. Cutis. 2005;76:270-274.
- Treesirichod A, Chansakulporn S, Wattanapan P. Correlation between skin color evaluation by skin color scale chart and narrowband reflectance spectrophotometer. Indian J Dermatol. 2014;59:339-342.
- Willis I, Earles RM. A new classification system relevant to people of African descent. J Cosmet Dermatol. 2005;18:209-216.
- Reeder AI, Hammond VA, Gray AR. Questionnaire items to assess skin color and erythemal sensitivity: reliability, validity, and “the dark shift.” Cancer Epidemiol Biomarkers Prev. 2010;19:1167-1173.
- Dwyer T, Muller HK, Blizzard L, et al. The use of spectrophotometry to estimate melanin density in Caucasians. Cancer Epidemiol Biomarkers Prev. 1998;7:203-206.
- Pershing LK, Tirumala VP, Nelson JL, et al. Reflectance spectrophotometer: the dermatologists’ sphygmomanometer for skin phototyping? J Invest Dermatol. 2008;128:1633-1640.
- Trakatelli M, Bylaite-Bucinskiene M, Correia O, et al. Clinical assessment of skin phototypes: watch your words! Eur J Dermatol. 2017;27:615-619.
Fitzpatrick skin type (FST) is the most commonly used classification system in dermatologic practice. It was developed by Thomas B. Fitzpatrick, MD, PhD, in 1975 to assess the propensity of the skin to burn during phototherapy.1 Fitzpatrick skin type also can be used to assess the clinical benefits and efficacy of cosmetic procedures, including laser hair removal, chemical peel and dermabrasion, tattoo removal, spray tanning, and laser resurfacing for acne scarring.2 The original FST classifications included skin types I through IV; skin types V and VI were later added to include individuals of Asian, Indian, and African origin.1 As a result, FST often is used by providers as a means of describing constitutive skin color and ethnicity.3
How did FST transition from describing the propensity of the skin to burn from UV light exposure to categorizing skin color, thereby becoming a proxy for race? It most likely occurred because there has not been another widely adopted classification system for describing skin color that can be applied to all skin types. Even when the FST classification scale is used as intended, there are inconsistencies with its accuracy; for example, self-reported FSTs have correlated poorly with sunburn risk as well as physician-reported FSTs.4,5 Although physician-reported FSTs have been demonstrated to correlate with race, race does not consistently correlate with objective measures of pigmentation or self-reported FSTs.5 For example, Japanese women often self-identify as FST type II, but Asian skin generally is considered to be nonwhite.1 Fitzpatrick himself acknowledged that race and ethnicity are cultural and political terms with no scientific basis.6 Fitzpatrick skin type also has been demonstrated to correlate poorly with constitutive skin color and minimal erythema dose values.7
We conducted an anonymous survey of dermatologists and dermatology trainees to evaluate how providers use FST in their clinical practice as well as how it is used to describe race and ethnicity.
Methods
The survey was distributed electronically to dermatologists and dermatology trainees from March 13 to March 28, 2019, using the Association of Professors of Dermatology listserv, as well as in person at the annual Skin of Color Society meeting in Washington, DC, on February 28, 2019. The 8-item survey included questions about physician demographics (ie, primary practice setting, board certification, and geographic location); whether the respondent identified as an individual with skin of color; and how the respondent utilized FST in clinical notes (ie, describing race/ethnicity, skin cancer risk, and constitutive [baseline] skin color; determining initial phototherapy dosage and suitability for laser treatments, and likelihood of skin burning). A t test was used to determine whether dermatologists who identified as having skin of color utilized FST differently.
Results
A total of 141 surveys were returned, and 140 respondents were included in the final analysis. Given the methods used to distribute the survey, a response rate could not be calculated. The respondents included more board-certified dermatologists (70%) than dermatology trainees (30%). Ninety-three percent of respondents indicated an academic institution as their primary practice location. Notably, 26% of respondents self-identified as having skin of color.
Forty-one percent of all respondents agreed that FST should be included in their clinical documentation. In response to the question “In what scenarios would you refer to FST in a clinical note?” 31% said they used FST to describe patients’ race or ethnicity, 47% used it to describe patients’ constitutive skin color, and 22% utilized it in both scenarios. Respondents who did not identify as having skin of color were more likely to use FST to describe constitutive skin color, though this finding was not statistically significant (P=.063). Anecdotally, providers also included FST in clinical notes on postinflammatory hyperpigmentation, melasma, and treatment with cryotherapy.
Comment
The US Census Bureau has estimated that half of the US population will be of non-European descent by 2050.8 As racial and ethnic distinctions continue to be blurred, attempts to include all nonwhite skin types under the umbrella term skin of color becomes increasingly problematic. The true number of skin colors is unknown but likely is infinite, as Brazilian artist Angélica Dass has demonstrated with her photographic project “Humanae” (Figure). Given this shift in demographics and the limitations of the FST, alternative methods of describing skin color must be developed.

© Angélica Dass | Humanae Work in Progress (Courtesy of the artist).
The results of our survey suggest that approximately one-third to half of academic dermatologists/dermatology trainees use FST to describe race/ethnicity and/or constitutive skin color. This misuse of FST may occur more frequently among physicians who do not identify as having skin of color. Additionally, misuse of FST in academic settings may be problematic and confusing for medical students who may learn to use this common dermatologic tool outside of its original intent.
We acknowledge that the conundrum of how to classify individuals with nonwhite skin or skin of color is not simply answered. Several alternative skin classification models have been proposed to improve the sensitivity and specificity of identifying patients with skin of color (Table). Refining FST classification is one approach. Employing terms such as skin irritation, tenderness, itching, or skin becoming darker from sun exposure rather than painful burn or tanning may result in better identification.1,4 A study conducted in India modified the FST questionnaire to acknowledge cultural behaviors.15 Because lighter skin is culturally valued in this population, patient experience with purposeful sun exposure was limited; thus, the questionnaire was modified to remove questions on the use of tanning booths and/or creams as well as sun exposure and instead included more objective questions regarding dark brown eye color, black and dark brown hair color, and dark brown skin color.15 Other studies have suggested that patient-reported photosensitivity assessed via a questionnaire is a valid measure for assessing FST but is associated with an overestimation of skin color, known as “the dark shift.”20

Sharma et al15 utilized reflectance spectrophotometry as an objective measure of melanin and skin erythema. The melanin index consistently showed a positive correlation with FSTs as opposed to the erythema index, which correlated poorly.15 Although reflectance spectrometry accurately identifies skin color in patients with nonwhite skin,21,22 it is an impractical and cost-prohibitive tool for daily practice. A more practical tool for the clinical setting would be a visual color scale with skin hues spanning FST types I to VI, including bands of increasingly darker gradations that would be particularly useful in assessing skin of color. Once such tool is the Taylor Hyperpigmentation Scale.17 Although currently not widely available, this tool could be further refined with additional skin hues.
Conclusion
Other investigators have criticized the various limitations of FST, including physician vs patient assessment, interview vs questionnaire, and phrasing of questions on skin type.23 Our findings suggest that medical providers should be cognizant of conflating race and ethnicity with FST. Two authors of this report (O.R.W. and J.E.D.) are medical students with skin of color and frequently have observed the addition of FST to the medical records of patients who were not receiving phototherapy as a proxy for race. We believe that more culturally appropriate and clinically relevant methods for describing skin of color need to be developed and, in the interim, the original intent of FST should be emphasized and incorporated in medical school and resident education.
Acknowledgment
The authors thank Adewole Adamson, MD (Austin, Texas), for discussion and feedback.
Fitzpatrick skin type (FST) is the most commonly used classification system in dermatologic practice. It was developed by Thomas B. Fitzpatrick, MD, PhD, in 1975 to assess the propensity of the skin to burn during phototherapy.1 Fitzpatrick skin type also can be used to assess the clinical benefits and efficacy of cosmetic procedures, including laser hair removal, chemical peel and dermabrasion, tattoo removal, spray tanning, and laser resurfacing for acne scarring.2 The original FST classifications included skin types I through IV; skin types V and VI were later added to include individuals of Asian, Indian, and African origin.1 As a result, FST often is used by providers as a means of describing constitutive skin color and ethnicity.3
How did FST transition from describing the propensity of the skin to burn from UV light exposure to categorizing skin color, thereby becoming a proxy for race? It most likely occurred because there has not been another widely adopted classification system for describing skin color that can be applied to all skin types. Even when the FST classification scale is used as intended, there are inconsistencies with its accuracy; for example, self-reported FSTs have correlated poorly with sunburn risk as well as physician-reported FSTs.4,5 Although physician-reported FSTs have been demonstrated to correlate with race, race does not consistently correlate with objective measures of pigmentation or self-reported FSTs.5 For example, Japanese women often self-identify as FST type II, but Asian skin generally is considered to be nonwhite.1 Fitzpatrick himself acknowledged that race and ethnicity are cultural and political terms with no scientific basis.6 Fitzpatrick skin type also has been demonstrated to correlate poorly with constitutive skin color and minimal erythema dose values.7
We conducted an anonymous survey of dermatologists and dermatology trainees to evaluate how providers use FST in their clinical practice as well as how it is used to describe race and ethnicity.
Methods
The survey was distributed electronically to dermatologists and dermatology trainees from March 13 to March 28, 2019, using the Association of Professors of Dermatology listserv, as well as in person at the annual Skin of Color Society meeting in Washington, DC, on February 28, 2019. The 8-item survey included questions about physician demographics (ie, primary practice setting, board certification, and geographic location); whether the respondent identified as an individual with skin of color; and how the respondent utilized FST in clinical notes (ie, describing race/ethnicity, skin cancer risk, and constitutive [baseline] skin color; determining initial phototherapy dosage and suitability for laser treatments, and likelihood of skin burning). A t test was used to determine whether dermatologists who identified as having skin of color utilized FST differently.
Results
A total of 141 surveys were returned, and 140 respondents were included in the final analysis. Given the methods used to distribute the survey, a response rate could not be calculated. The respondents included more board-certified dermatologists (70%) than dermatology trainees (30%). Ninety-three percent of respondents indicated an academic institution as their primary practice location. Notably, 26% of respondents self-identified as having skin of color.
Forty-one percent of all respondents agreed that FST should be included in their clinical documentation. In response to the question “In what scenarios would you refer to FST in a clinical note?” 31% said they used FST to describe patients’ race or ethnicity, 47% used it to describe patients’ constitutive skin color, and 22% utilized it in both scenarios. Respondents who did not identify as having skin of color were more likely to use FST to describe constitutive skin color, though this finding was not statistically significant (P=.063). Anecdotally, providers also included FST in clinical notes on postinflammatory hyperpigmentation, melasma, and treatment with cryotherapy.
Comment
The US Census Bureau has estimated that half of the US population will be of non-European descent by 2050.8 As racial and ethnic distinctions continue to be blurred, attempts to include all nonwhite skin types under the umbrella term skin of color becomes increasingly problematic. The true number of skin colors is unknown but likely is infinite, as Brazilian artist Angélica Dass has demonstrated with her photographic project “Humanae” (Figure). Given this shift in demographics and the limitations of the FST, alternative methods of describing skin color must be developed.

© Angélica Dass | Humanae Work in Progress (Courtesy of the artist).
The results of our survey suggest that approximately one-third to half of academic dermatologists/dermatology trainees use FST to describe race/ethnicity and/or constitutive skin color. This misuse of FST may occur more frequently among physicians who do not identify as having skin of color. Additionally, misuse of FST in academic settings may be problematic and confusing for medical students who may learn to use this common dermatologic tool outside of its original intent.
We acknowledge that the conundrum of how to classify individuals with nonwhite skin or skin of color is not simply answered. Several alternative skin classification models have been proposed to improve the sensitivity and specificity of identifying patients with skin of color (Table). Refining FST classification is one approach. Employing terms such as skin irritation, tenderness, itching, or skin becoming darker from sun exposure rather than painful burn or tanning may result in better identification.1,4 A study conducted in India modified the FST questionnaire to acknowledge cultural behaviors.15 Because lighter skin is culturally valued in this population, patient experience with purposeful sun exposure was limited; thus, the questionnaire was modified to remove questions on the use of tanning booths and/or creams as well as sun exposure and instead included more objective questions regarding dark brown eye color, black and dark brown hair color, and dark brown skin color.15 Other studies have suggested that patient-reported photosensitivity assessed via a questionnaire is a valid measure for assessing FST but is associated with an overestimation of skin color, known as “the dark shift.”20

Sharma et al15 utilized reflectance spectrophotometry as an objective measure of melanin and skin erythema. The melanin index consistently showed a positive correlation with FSTs as opposed to the erythema index, which correlated poorly.15 Although reflectance spectrometry accurately identifies skin color in patients with nonwhite skin,21,22 it is an impractical and cost-prohibitive tool for daily practice. A more practical tool for the clinical setting would be a visual color scale with skin hues spanning FST types I to VI, including bands of increasingly darker gradations that would be particularly useful in assessing skin of color. Once such tool is the Taylor Hyperpigmentation Scale.17 Although currently not widely available, this tool could be further refined with additional skin hues.
Conclusion
Other investigators have criticized the various limitations of FST, including physician vs patient assessment, interview vs questionnaire, and phrasing of questions on skin type.23 Our findings suggest that medical providers should be cognizant of conflating race and ethnicity with FST. Two authors of this report (O.R.W. and J.E.D.) are medical students with skin of color and frequently have observed the addition of FST to the medical records of patients who were not receiving phototherapy as a proxy for race. We believe that more culturally appropriate and clinically relevant methods for describing skin of color need to be developed and, in the interim, the original intent of FST should be emphasized and incorporated in medical school and resident education.
Acknowledgment
The authors thank Adewole Adamson, MD (Austin, Texas), for discussion and feedback.
- Goldsmith LA, Katz SI, Gilchrest BA, et al, eds. Fitzpatrick’s Dermatology in General Medicine. 8th ed. New York, NY: The McGraw-Hill Companies; 2012.
- Sachdeva S. Fitzpatrick skin typing: applications in dermatology. Indian J Dermatol Venereol Leprol. 2009;75:93-96.
- Everett JS, Budescu M, Sommers MS. Making sense of skin color in clinical care. Clin Nurs Res. 2012;21:495-516.
- Eilers S, Bach DQ, Gaber R, et al. Accuracy of self-report in assessingFitzpatrick skin phototypes I through VI. JAMA Dermatol. 2013;149:1289-1294.
- He SY, McCulloch CE, Boscardin WJ, et al. Self-reported pigmentary phenotypes and race are significant but incomplete predictors of Fitzpatrick skin phototype in an ethnically diverse population. J Am Acad Dermatol. 2014;71:731-737.
- Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869-871.
- Leenutaphong V. Relationship between skin color and cutaneous response to ultraviolet radiation in Thai. Photodermatol Photoimmunol Photomed. 1996;11:198-203.
- Colby SL, Ortman JM. Projections of the Size and Composition of the US Population: 2014 to 2060. Washington, DC: US Census Bureau; 2015.
- Baumann L. Understanding and treating various skin types: the Baumann Skin Type Indicator. Dermatol Clin. 2008;26:359-373.
- Fanous N. A new patient classification for laser resurfacing and peels: predicting responses, risks, and results. Aesthetic Plast Surg. 2002;26:99-104.
- Glogau RG. Chemical peeling and aging skin. J Geriatric Dermatol. 1994;2:30-35.
- Goldman M. Universal classification of skin type. In: Shiffman M, Mirrafati S, Lam S, et al, eds. Simplified Facial Rejuvenation. Berlin, Heidelberg, Germany: Springer; 2008:47-50.
- Kawada A. UVB-induced erythema, delayed tanning, and UVA-induced immediate tanning in Japanese skin. Photodermatol. 1986;3:327-333.
- Lancer HA. Lancer Ethnicity Scale (LES). Lasers Surg Med. 1998;22:9.
- Sharma VK, Gupta V, Jangid BL, et al. Modification of the Fitzpatrick system of skin phototype classification for the Indian population, and its correlation with narrowband diffuse reflectance spectrophotometry. Clin Exp Dermatol. 2018;43:274-280.
- Roberts WE. The Roberts Skin Type Classification System. J Drugs Dermatol. 2008;7:452-456.
- Taylor SC, Arsonnaud S, Czernielewski J. The Taylor hyperpigmentation scale: a new visual assessment tool for the evaluation of skin color and pigmentation. Cutis. 2005;76:270-274.
- Treesirichod A, Chansakulporn S, Wattanapan P. Correlation between skin color evaluation by skin color scale chart and narrowband reflectance spectrophotometer. Indian J Dermatol. 2014;59:339-342.
- Willis I, Earles RM. A new classification system relevant to people of African descent. J Cosmet Dermatol. 2005;18:209-216.
- Reeder AI, Hammond VA, Gray AR. Questionnaire items to assess skin color and erythemal sensitivity: reliability, validity, and “the dark shift.” Cancer Epidemiol Biomarkers Prev. 2010;19:1167-1173.
- Dwyer T, Muller HK, Blizzard L, et al. The use of spectrophotometry to estimate melanin density in Caucasians. Cancer Epidemiol Biomarkers Prev. 1998;7:203-206.
- Pershing LK, Tirumala VP, Nelson JL, et al. Reflectance spectrophotometer: the dermatologists’ sphygmomanometer for skin phototyping? J Invest Dermatol. 2008;128:1633-1640.
- Trakatelli M, Bylaite-Bucinskiene M, Correia O, et al. Clinical assessment of skin phototypes: watch your words! Eur J Dermatol. 2017;27:615-619.
- Goldsmith LA, Katz SI, Gilchrest BA, et al, eds. Fitzpatrick’s Dermatology in General Medicine. 8th ed. New York, NY: The McGraw-Hill Companies; 2012.
- Sachdeva S. Fitzpatrick skin typing: applications in dermatology. Indian J Dermatol Venereol Leprol. 2009;75:93-96.
- Everett JS, Budescu M, Sommers MS. Making sense of skin color in clinical care. Clin Nurs Res. 2012;21:495-516.
- Eilers S, Bach DQ, Gaber R, et al. Accuracy of self-report in assessingFitzpatrick skin phototypes I through VI. JAMA Dermatol. 2013;149:1289-1294.
- He SY, McCulloch CE, Boscardin WJ, et al. Self-reported pigmentary phenotypes and race are significant but incomplete predictors of Fitzpatrick skin phototype in an ethnically diverse population. J Am Acad Dermatol. 2014;71:731-737.
- Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869-871.
- Leenutaphong V. Relationship between skin color and cutaneous response to ultraviolet radiation in Thai. Photodermatol Photoimmunol Photomed. 1996;11:198-203.
- Colby SL, Ortman JM. Projections of the Size and Composition of the US Population: 2014 to 2060. Washington, DC: US Census Bureau; 2015.
- Baumann L. Understanding and treating various skin types: the Baumann Skin Type Indicator. Dermatol Clin. 2008;26:359-373.
- Fanous N. A new patient classification for laser resurfacing and peels: predicting responses, risks, and results. Aesthetic Plast Surg. 2002;26:99-104.
- Glogau RG. Chemical peeling and aging skin. J Geriatric Dermatol. 1994;2:30-35.
- Goldman M. Universal classification of skin type. In: Shiffman M, Mirrafati S, Lam S, et al, eds. Simplified Facial Rejuvenation. Berlin, Heidelberg, Germany: Springer; 2008:47-50.
- Kawada A. UVB-induced erythema, delayed tanning, and UVA-induced immediate tanning in Japanese skin. Photodermatol. 1986;3:327-333.
- Lancer HA. Lancer Ethnicity Scale (LES). Lasers Surg Med. 1998;22:9.
- Sharma VK, Gupta V, Jangid BL, et al. Modification of the Fitzpatrick system of skin phototype classification for the Indian population, and its correlation with narrowband diffuse reflectance spectrophotometry. Clin Exp Dermatol. 2018;43:274-280.
- Roberts WE. The Roberts Skin Type Classification System. J Drugs Dermatol. 2008;7:452-456.
- Taylor SC, Arsonnaud S, Czernielewski J. The Taylor hyperpigmentation scale: a new visual assessment tool for the evaluation of skin color and pigmentation. Cutis. 2005;76:270-274.
- Treesirichod A, Chansakulporn S, Wattanapan P. Correlation between skin color evaluation by skin color scale chart and narrowband reflectance spectrophotometer. Indian J Dermatol. 2014;59:339-342.
- Willis I, Earles RM. A new classification system relevant to people of African descent. J Cosmet Dermatol. 2005;18:209-216.
- Reeder AI, Hammond VA, Gray AR. Questionnaire items to assess skin color and erythemal sensitivity: reliability, validity, and “the dark shift.” Cancer Epidemiol Biomarkers Prev. 2010;19:1167-1173.
- Dwyer T, Muller HK, Blizzard L, et al. The use of spectrophotometry to estimate melanin density in Caucasians. Cancer Epidemiol Biomarkers Prev. 1998;7:203-206.
- Pershing LK, Tirumala VP, Nelson JL, et al. Reflectance spectrophotometer: the dermatologists’ sphygmomanometer for skin phototyping? J Invest Dermatol. 2008;128:1633-1640.
- Trakatelli M, Bylaite-Bucinskiene M, Correia O, et al. Clinical assessment of skin phototypes: watch your words! Eur J Dermatol. 2017;27:615-619.
Practice Points
- Medical providers should be cognizant of conflating race and ethnicity with Fitzpatrick skin type (FST).
- Misuse of FST may occur more frequently among physicians who do not identify as having skin of color.
- Although alternative skin type classification systems have been proposed, more clinically relevant methods for describing skin of color need to be developed.
Hypersensitivity Reactions to Orthopedic Implants: What’s All the Hype?
Hypersensitivity to metal implants remains a controversial field in contact dermatitis and patch testing. With positive reactions to nickel hovering around 20% in patch-tested populations,1 the question remains whether metal-allergic patients can safely receive metal implants. Unfortunately, large controlled studies are lacking, in part due to ethical concerns of knowingly placing a metal implant in a metal-allergic patient. Much of the focus of implant hypersensitivity reactions (IHRs) has been on orthopedic joints including hips, knees, and shoulders, as well as fixed orthopedic implanted materials such as screws and plates. However, there have been reports of IHRs to cardiac devices including defibrillators, pacemakers, and intracardiac devices; dental hardware including implants, crowns, dentures, and braces; and neurologic and gynecologic devices. For the purposes of this review, we will focus on IHRs to orthopedic implants.
Making the Case for IHRs
There are multiple case reports and series documenting likely orthopedic IHRs in the literature2-5; however, large prospective studies are lacking. Some of the largest series are from Danish registry studies. In 2009, Thyssen et al6 reviewed356 patients who had undergone both total hip arthroplasty and patch testing. Metal allergy frequencies were similar between patch-tested registry patients and patch test controls, showing no increase in positive patch tests to metals after receiving implants. Additionally, implant revision rates were comparable between registry patients with and without patch testing. The group concluded that the risk for revision after hip implantation in metal-allergic patients and the risk for development of metal allergy after implantation were both low.6 In 2015, Münch et al7 compared 327 patients who had undergone both total knee arthroplasty and patch testing and found that prevalence of allergy to nickel, cobalt, and chromium was similar between patients who had undergone revision surgery and those who had not; however, for patients who had 2 or more knee revisions, there was a higher prevalence of postimplant metal allergy. This study also showed that metal allergy identified before implantation did not increase the risk for postimplantation knee revision surgery or implant failure.7 These larger studies suggest that although individual cases of IHR exist, it is likely quite rare.
Patients have been found to have increased levels of chromium (serum and urine) and titanium (serum) following total hip arthroplasty.8 Additionally, metal wear particles have been identified in postmortem livers and spleens, which was more prevalent in patients with a history of failed hip arthroplasty.9 It is difficult to determine the meaning of this data, as the presence of metal ions does not necessarily indicate allergy or IHR. In 2001, Hallab et al10 pooled data from several implant cohort studies and concluded that in comparison to a baseline metal sensitivity prevalence of approximately 10%, patients with well-functioning implants had a metal sensitivity–weighted average of 25%, and those with poorly functioning implants had a weighted average of 60%. Again, positive patch testing to metals does not necessarily implicate allergy as the cause of implant failure.
Some small studies have shown that patients with evidence of metal hypersensitivity improve with revision. Zondervan et al11 reviewed results of 46 orthopedic revisions following painful total knee arthroplasty. Patients with knee pain and lymphocyte transformation testing (LTT) positive for metals received hypoallergenic revisions, and those with LTT negative for metals received standard revisions. The group who received hypoallergenic revisions had more pain reduction compared to the standard revision group (37.8% reduction in pain vs 27%). However, this study was limited in that the diagnosis of metal allergy was made entirely on results of LTT.11 In 2012, Atanaskova Mesinkovska et al12 described 41 patients who underwent orthopedic patch testing following implantation for symptoms including pain, dermatitis, pruritus, joint loosening, edema, and impaired wound healing. Fifteen (37%) patients had positive patch test reactions to metals, and 10 (67%) of them had reactions to metals that were present in their implants. Six (60%) of these patients had their implants removed and their symptoms resolved; the remaining 4 continued to experience implant symptoms.12 These studies support the existence of rare metal-related orthopedic IHRs and support the concept of proceeding with orthopedic implant revision when indicated, safe, and agreed upon by the surgeon and patient. However, as noted in the series by Zondervan et al,11 not every patient with confirmed metal allergy who undergoes revision improves, so an informed conversation between the patient and surgeon is mandatory.
Types of Orthopedic Implants
Orthopedic implanted materials consist of either dynamic (knees, hips) or static (screws, plates) components. Several generations of hip implants have evolved since the 1960s. First-generation implanted hips were metal-on-metal and had high rates of metal release and sensitization. Metal-on-plastic implants may be less likely to release metal but instead release large polyethylene wear particles. Second-generation metal-on-metal implants reportedly have lower wear rates. With these implants, wear particles are generated but are reportedly smaller than first-generation particles.13
Allergens in IHRs
Metals
Metals are the most commonly implicated allergens in orthopedic IHRs. Potentially relevant metal alloys include 316L stainless steel, cobalt-chromium-molybdenum steel, Vitallium alloy, titanium alloy, titanium-tantalum-niobium alloy, and Oxinium (Smith & Nephew).14,15 Each alloy contains several metals, which can include nickel, chromium, cobalt, manganese, molybdenum, iron, titanium, aluminum, vanadium, niobium, tantalum, and zirconium, among others. For example, 316L stainless steel contains iron, nickel, chromium, manganese, molybdenum, nitrogen, carbon, sulfur, silicon, and phosphorus, whereas Oxinium contains only oxidized zirconium and niobium.
Bone Cement
Bone cement also has been reported in cases of orthopedic IHRs and can contain several chemicals, including methyl methacrylate, N,N-dimethyl-p-toluidine, benzoyl peroxide, hydroquinone, and gentamicin.14 Other potential exposures include adhesives (cyanoacrylates) and topical antibiotics.
Clinical Presentation
Several clinical presentations of orthopedic IHRs have been described. Perhaps the most commonly recognized is a localized cutaneous eczematous eruption, with dermatitis typically overlying the site of the implanted material.1,2,16 Generalized cutaneous eczematous IHRs also have been reported, including diffuse generalized dermatitis from a stainless steel orthopedic screw4 and nummular dermatitis attributed to vanadium in an orthopedic plate.5 Urticaria, vasculitis, and bullous cutaneous reactions, as well as extracutaneous complications, also have been reported.14,15 Pain, edema, joint loosening or failure, and poor wound healing have been reported,12 but it remains unclear whether these symptoms represent IHR.
Patch Testing for IHR
Several groups have published recommended patch test series for IHR.12,14,15 Common components of implant patch testing panels include metals, adhesives (acrylates, epoxy resins) and antibiotics. Importantly, obtaining product information from the manufacturer of the suspected implant can guide which allergens to include in patch testing. Implant and metal panels also are available for commercial purchase.
Other Diagnostic Tests
We rarely (almost never) order LTTs in the workup for potential IHRs. This is an in vitro test that includes lymphocytes, metal ions, and the radioactive marker methyl-3H-thymidine. The goal of the test is to evaluate if patient lymphocytes are reactive or responsive to metal ions. A positive LTT suggests that lymphocytes can respond to the presence of metal ions but does not confirm allergy or the presence of IHR.
Typically, skin or tissue biopsies are not required to make a diagnosis of IHR; however, if performed, histopathology suggestive of IHR can support a suspected diagnosis. Typical findings include but are not limited to spongiotic dermatitis. Eosinophils may or may not be present. Metal disc testing has been utilized for orthopedic IHR but is not currently recommended due to low diagnostic yield. Prick testing rarely is used and also is not a primary method for diagnosis of IHR.17
Preimplantation Patch Testing
Expert opinion guidelines published by the American Contact Dermatitis Society (ACDS) state that routine preimplantation patch testing is not necessary; however, for those patients with a clear history of contact reactions to metal, preimplantation patch testing can be considered.17
Patch test results can influence the orthopedic surgeon’s choice of implant material. In one study, when preimplantation patch testing showed a positive patch test reaction to metals, the results influenced the surgeon’s decision-making in all cases.12
Postimplantation Patch Testing: Diagnostic Criteria for Metal IHR After Implantation
From 2012 to 2013, Schalock and Thyssen18 surveyed expert attendees at meetings of the European Society of Contact Dermatitis and the ACDS for their opinions on proposed diagnostic criteria for metal IHRs. Based on these results (N=119), the authors stratified 4 major and 5 minor diagnostic criteria, which were defined based on overall responses of meeting attendees. Major criteria included (1) chronic dermatitis beginning weeks to months after metallic implantation, (2) complete recovery after removal of the offending implant, (3) eruption overlying the metal implant, and (4) positive patch test reaction to a metal used in the implant. Minor criteria included (1) histology consistent with allergic contact dermatitis, (2) morphology consistent with dermatitis (ie, erythema, induration, papules, vesicles), (3) positive in vitro test to metals (eg, lymphocyte transformation test), (4) systemic allergic dermatitis reaction, and (5) therapy-resistant dermatitis reaction. The authors did not describe a scoring system for evaluation and confirmation of a diagnosis of IHR. Instead, the criteria should be used as general guidelines when evaluating patients for possible IHRs. From a standpoint of available diagnostic tests for metal IHR, 86.1% of experts agreed that a positive patch test reaction to a metal used in the implant was suggestive of a diagnosis, whereas a positive in vitro test to metals (LTT) was suggestive of a diagnosis for only 32.2% of respondents. This study was designed specifically for metal IHRs and therefore is not necessarily generalizable for nonmetal IHRs.18
Final Interpretation
We follow the 2016 ACDS guidelines17 and complete preimplantation patch testing only in the setting of suspected metal allergy and postimplantation patch testing based on the guidelines described by Schalock and Thyssen.18 However, an extended conversation is warranted prior to patch testing to ensure the patient fully understands the limitations of the test. Although we have both ordered the LTT, interpretation remains murky, and until this test is standardized, routine use is unlikely to benefit the patient. Until we are more reliably able to predict who will develop hypersensitivity to implanted metals, the decision to remove or revise an implant is one that should be made by a multidisciplinary team that includes the surgeon and the patient.
- Dekoven JG, Warshaw EM, Zug KA, et al. North American Contact Dermatitis Group patch test results: 2015-2016. Dermatitis. 2018;29:297-309.
- Gao X, He RX, Yan SG, et al. Dermatitis associated with chromium following total knee arthroplasty. J Arthroplasty. 2011;26:665.E613-665.E616.
- Treudler R, Simon JC. Benzoyl peroxide: is it a relevant bone cement allergen in patients with orthopaedic implants? Contact Dermatitis. 2007;57:177-180.
- Barranco VP, Soloman H. Eczematous dermatitis from nickel. JAMA. 1972;220:1244.
- Engelhart S, Segal RJ. Allergic reaction to vanadium causes a diffuse eczematous eruption and titanium alloy orthopedic implant failure. Cutis. 2017;99:245-249.
- Thyssen JP, Jakobsen SS, Engkilde K, et al. The association between metal allergy, total hip arthroplasty, and revision. Acta Orthop. 2009;80:646-652.
- Münch HJ, Jacobsen SS, Olesen JT, et al. The association between metal allergy, total knee arthroplasty, and revision: study based on the Danish Knee Arthroplasty Register. Acta Orthop. 2015;86:378-383.
- Jacobs JJ, Skipor AK, Patterson LM, et al. Metal release in patients who have had a primary total hip arthroplasty. a prospective, controlled, longitudinal study. J Bone Joint Surg Am. 1998;80:1447-1458.
- Urban RM, Jacobs JJ, Tomlinson MJ, et al. Dissemination of wear particles to the liver, spleen, and abdominal lymph nodes of patients with hip or knee replacement. J Bone Joint Surg Am. 2000;82:457-476.
- Hallab N, Merritt K, Jacobs JJ. Metal sensitivity in patients with orthopaedic implants. J Bone Joint Surg Am. 2001;83:428-436.
- Zondervan RL, Vaux JJ, Blackmer MJ, et al. Improved outcomes in patients with positive metal sensitivity following revision total knee arthroplasty. J Orthop Surg Res. 2019;14:182.
- Atanaskova Mesinkovska N, Tellez A, Molina L, et al. The effect of patch testing on surgical practices and outcomes in orthopedic patients with metal implants. Arch Dermatol. 2012;148:687-693.
- Kovochich M, Fung ES, Donovan E, et al. Characterization of wear debris from metal-on-metal hip implants during normal wear versus edge-loading conditions. J Biomed Mater Res B Appl Biomater. 2018;106:986-996.
- Basko-Plluska JL, Thyssen JP, Schalock PC. Cutaneous and systemic hypersensitivity reactions to metallic implants. Dermatitis. 2011;22:65-79.
- Schalock PC, Menné T, Johansen JD, et al. Hypersensitivity reactions to metallic implants—diagnostic algorithm and suggested patch test series for clinical use. Contact Dermatitis. 2012;66:4-19.
- Thomas P, Gollwitzer H, Maier S, et al. Osteosynthesis associated contact dermatitis with unusual perpetuation of hyperreactivity in a nickel allergic patient. Contact Dermatitis. 2006;54:222-225.
- Schalock PC, Crawford G, Nedorost S, et al. Patch testing for evaluation of hypersensitivity to implanted metal devices: a perspective from the American Contact Dermatitis Society. Dermatitis. 2016;27:241-247.
- Schalock PC, Thyssen JP. Patch testers’ opinions regarding diagnostic criteria for metal hypersensitivity reactions to metallic implants. Dermatitis. 2013;24:183-185.
Hypersensitivity to metal implants remains a controversial field in contact dermatitis and patch testing. With positive reactions to nickel hovering around 20% in patch-tested populations,1 the question remains whether metal-allergic patients can safely receive metal implants. Unfortunately, large controlled studies are lacking, in part due to ethical concerns of knowingly placing a metal implant in a metal-allergic patient. Much of the focus of implant hypersensitivity reactions (IHRs) has been on orthopedic joints including hips, knees, and shoulders, as well as fixed orthopedic implanted materials such as screws and plates. However, there have been reports of IHRs to cardiac devices including defibrillators, pacemakers, and intracardiac devices; dental hardware including implants, crowns, dentures, and braces; and neurologic and gynecologic devices. For the purposes of this review, we will focus on IHRs to orthopedic implants.
Making the Case for IHRs
There are multiple case reports and series documenting likely orthopedic IHRs in the literature2-5; however, large prospective studies are lacking. Some of the largest series are from Danish registry studies. In 2009, Thyssen et al6 reviewed356 patients who had undergone both total hip arthroplasty and patch testing. Metal allergy frequencies were similar between patch-tested registry patients and patch test controls, showing no increase in positive patch tests to metals after receiving implants. Additionally, implant revision rates were comparable between registry patients with and without patch testing. The group concluded that the risk for revision after hip implantation in metal-allergic patients and the risk for development of metal allergy after implantation were both low.6 In 2015, Münch et al7 compared 327 patients who had undergone both total knee arthroplasty and patch testing and found that prevalence of allergy to nickel, cobalt, and chromium was similar between patients who had undergone revision surgery and those who had not; however, for patients who had 2 or more knee revisions, there was a higher prevalence of postimplant metal allergy. This study also showed that metal allergy identified before implantation did not increase the risk for postimplantation knee revision surgery or implant failure.7 These larger studies suggest that although individual cases of IHR exist, it is likely quite rare.
Patients have been found to have increased levels of chromium (serum and urine) and titanium (serum) following total hip arthroplasty.8 Additionally, metal wear particles have been identified in postmortem livers and spleens, which was more prevalent in patients with a history of failed hip arthroplasty.9 It is difficult to determine the meaning of this data, as the presence of metal ions does not necessarily indicate allergy or IHR. In 2001, Hallab et al10 pooled data from several implant cohort studies and concluded that in comparison to a baseline metal sensitivity prevalence of approximately 10%, patients with well-functioning implants had a metal sensitivity–weighted average of 25%, and those with poorly functioning implants had a weighted average of 60%. Again, positive patch testing to metals does not necessarily implicate allergy as the cause of implant failure.
Some small studies have shown that patients with evidence of metal hypersensitivity improve with revision. Zondervan et al11 reviewed results of 46 orthopedic revisions following painful total knee arthroplasty. Patients with knee pain and lymphocyte transformation testing (LTT) positive for metals received hypoallergenic revisions, and those with LTT negative for metals received standard revisions. The group who received hypoallergenic revisions had more pain reduction compared to the standard revision group (37.8% reduction in pain vs 27%). However, this study was limited in that the diagnosis of metal allergy was made entirely on results of LTT.11 In 2012, Atanaskova Mesinkovska et al12 described 41 patients who underwent orthopedic patch testing following implantation for symptoms including pain, dermatitis, pruritus, joint loosening, edema, and impaired wound healing. Fifteen (37%) patients had positive patch test reactions to metals, and 10 (67%) of them had reactions to metals that were present in their implants. Six (60%) of these patients had their implants removed and their symptoms resolved; the remaining 4 continued to experience implant symptoms.12 These studies support the existence of rare metal-related orthopedic IHRs and support the concept of proceeding with orthopedic implant revision when indicated, safe, and agreed upon by the surgeon and patient. However, as noted in the series by Zondervan et al,11 not every patient with confirmed metal allergy who undergoes revision improves, so an informed conversation between the patient and surgeon is mandatory.
Types of Orthopedic Implants
Orthopedic implanted materials consist of either dynamic (knees, hips) or static (screws, plates) components. Several generations of hip implants have evolved since the 1960s. First-generation implanted hips were metal-on-metal and had high rates of metal release and sensitization. Metal-on-plastic implants may be less likely to release metal but instead release large polyethylene wear particles. Second-generation metal-on-metal implants reportedly have lower wear rates. With these implants, wear particles are generated but are reportedly smaller than first-generation particles.13
Allergens in IHRs
Metals
Metals are the most commonly implicated allergens in orthopedic IHRs. Potentially relevant metal alloys include 316L stainless steel, cobalt-chromium-molybdenum steel, Vitallium alloy, titanium alloy, titanium-tantalum-niobium alloy, and Oxinium (Smith & Nephew).14,15 Each alloy contains several metals, which can include nickel, chromium, cobalt, manganese, molybdenum, iron, titanium, aluminum, vanadium, niobium, tantalum, and zirconium, among others. For example, 316L stainless steel contains iron, nickel, chromium, manganese, molybdenum, nitrogen, carbon, sulfur, silicon, and phosphorus, whereas Oxinium contains only oxidized zirconium and niobium.
Bone Cement
Bone cement also has been reported in cases of orthopedic IHRs and can contain several chemicals, including methyl methacrylate, N,N-dimethyl-p-toluidine, benzoyl peroxide, hydroquinone, and gentamicin.14 Other potential exposures include adhesives (cyanoacrylates) and topical antibiotics.
Clinical Presentation
Several clinical presentations of orthopedic IHRs have been described. Perhaps the most commonly recognized is a localized cutaneous eczematous eruption, with dermatitis typically overlying the site of the implanted material.1,2,16 Generalized cutaneous eczematous IHRs also have been reported, including diffuse generalized dermatitis from a stainless steel orthopedic screw4 and nummular dermatitis attributed to vanadium in an orthopedic plate.5 Urticaria, vasculitis, and bullous cutaneous reactions, as well as extracutaneous complications, also have been reported.14,15 Pain, edema, joint loosening or failure, and poor wound healing have been reported,12 but it remains unclear whether these symptoms represent IHR.
Patch Testing for IHR
Several groups have published recommended patch test series for IHR.12,14,15 Common components of implant patch testing panels include metals, adhesives (acrylates, epoxy resins) and antibiotics. Importantly, obtaining product information from the manufacturer of the suspected implant can guide which allergens to include in patch testing. Implant and metal panels also are available for commercial purchase.
Other Diagnostic Tests
We rarely (almost never) order LTTs in the workup for potential IHRs. This is an in vitro test that includes lymphocytes, metal ions, and the radioactive marker methyl-3H-thymidine. The goal of the test is to evaluate if patient lymphocytes are reactive or responsive to metal ions. A positive LTT suggests that lymphocytes can respond to the presence of metal ions but does not confirm allergy or the presence of IHR.
Typically, skin or tissue biopsies are not required to make a diagnosis of IHR; however, if performed, histopathology suggestive of IHR can support a suspected diagnosis. Typical findings include but are not limited to spongiotic dermatitis. Eosinophils may or may not be present. Metal disc testing has been utilized for orthopedic IHR but is not currently recommended due to low diagnostic yield. Prick testing rarely is used and also is not a primary method for diagnosis of IHR.17
Preimplantation Patch Testing
Expert opinion guidelines published by the American Contact Dermatitis Society (ACDS) state that routine preimplantation patch testing is not necessary; however, for those patients with a clear history of contact reactions to metal, preimplantation patch testing can be considered.17
Patch test results can influence the orthopedic surgeon’s choice of implant material. In one study, when preimplantation patch testing showed a positive patch test reaction to metals, the results influenced the surgeon’s decision-making in all cases.12
Postimplantation Patch Testing: Diagnostic Criteria for Metal IHR After Implantation
From 2012 to 2013, Schalock and Thyssen18 surveyed expert attendees at meetings of the European Society of Contact Dermatitis and the ACDS for their opinions on proposed diagnostic criteria for metal IHRs. Based on these results (N=119), the authors stratified 4 major and 5 minor diagnostic criteria, which were defined based on overall responses of meeting attendees. Major criteria included (1) chronic dermatitis beginning weeks to months after metallic implantation, (2) complete recovery after removal of the offending implant, (3) eruption overlying the metal implant, and (4) positive patch test reaction to a metal used in the implant. Minor criteria included (1) histology consistent with allergic contact dermatitis, (2) morphology consistent with dermatitis (ie, erythema, induration, papules, vesicles), (3) positive in vitro test to metals (eg, lymphocyte transformation test), (4) systemic allergic dermatitis reaction, and (5) therapy-resistant dermatitis reaction. The authors did not describe a scoring system for evaluation and confirmation of a diagnosis of IHR. Instead, the criteria should be used as general guidelines when evaluating patients for possible IHRs. From a standpoint of available diagnostic tests for metal IHR, 86.1% of experts agreed that a positive patch test reaction to a metal used in the implant was suggestive of a diagnosis, whereas a positive in vitro test to metals (LTT) was suggestive of a diagnosis for only 32.2% of respondents. This study was designed specifically for metal IHRs and therefore is not necessarily generalizable for nonmetal IHRs.18
Final Interpretation
We follow the 2016 ACDS guidelines17 and complete preimplantation patch testing only in the setting of suspected metal allergy and postimplantation patch testing based on the guidelines described by Schalock and Thyssen.18 However, an extended conversation is warranted prior to patch testing to ensure the patient fully understands the limitations of the test. Although we have both ordered the LTT, interpretation remains murky, and until this test is standardized, routine use is unlikely to benefit the patient. Until we are more reliably able to predict who will develop hypersensitivity to implanted metals, the decision to remove or revise an implant is one that should be made by a multidisciplinary team that includes the surgeon and the patient.
Hypersensitivity to metal implants remains a controversial field in contact dermatitis and patch testing. With positive reactions to nickel hovering around 20% in patch-tested populations,1 the question remains whether metal-allergic patients can safely receive metal implants. Unfortunately, large controlled studies are lacking, in part due to ethical concerns of knowingly placing a metal implant in a metal-allergic patient. Much of the focus of implant hypersensitivity reactions (IHRs) has been on orthopedic joints including hips, knees, and shoulders, as well as fixed orthopedic implanted materials such as screws and plates. However, there have been reports of IHRs to cardiac devices including defibrillators, pacemakers, and intracardiac devices; dental hardware including implants, crowns, dentures, and braces; and neurologic and gynecologic devices. For the purposes of this review, we will focus on IHRs to orthopedic implants.
Making the Case for IHRs
There are multiple case reports and series documenting likely orthopedic IHRs in the literature2-5; however, large prospective studies are lacking. Some of the largest series are from Danish registry studies. In 2009, Thyssen et al6 reviewed356 patients who had undergone both total hip arthroplasty and patch testing. Metal allergy frequencies were similar between patch-tested registry patients and patch test controls, showing no increase in positive patch tests to metals after receiving implants. Additionally, implant revision rates were comparable between registry patients with and without patch testing. The group concluded that the risk for revision after hip implantation in metal-allergic patients and the risk for development of metal allergy after implantation were both low.6 In 2015, Münch et al7 compared 327 patients who had undergone both total knee arthroplasty and patch testing and found that prevalence of allergy to nickel, cobalt, and chromium was similar between patients who had undergone revision surgery and those who had not; however, for patients who had 2 or more knee revisions, there was a higher prevalence of postimplant metal allergy. This study also showed that metal allergy identified before implantation did not increase the risk for postimplantation knee revision surgery or implant failure.7 These larger studies suggest that although individual cases of IHR exist, it is likely quite rare.
Patients have been found to have increased levels of chromium (serum and urine) and titanium (serum) following total hip arthroplasty.8 Additionally, metal wear particles have been identified in postmortem livers and spleens, which was more prevalent in patients with a history of failed hip arthroplasty.9 It is difficult to determine the meaning of this data, as the presence of metal ions does not necessarily indicate allergy or IHR. In 2001, Hallab et al10 pooled data from several implant cohort studies and concluded that in comparison to a baseline metal sensitivity prevalence of approximately 10%, patients with well-functioning implants had a metal sensitivity–weighted average of 25%, and those with poorly functioning implants had a weighted average of 60%. Again, positive patch testing to metals does not necessarily implicate allergy as the cause of implant failure.
Some small studies have shown that patients with evidence of metal hypersensitivity improve with revision. Zondervan et al11 reviewed results of 46 orthopedic revisions following painful total knee arthroplasty. Patients with knee pain and lymphocyte transformation testing (LTT) positive for metals received hypoallergenic revisions, and those with LTT negative for metals received standard revisions. The group who received hypoallergenic revisions had more pain reduction compared to the standard revision group (37.8% reduction in pain vs 27%). However, this study was limited in that the diagnosis of metal allergy was made entirely on results of LTT.11 In 2012, Atanaskova Mesinkovska et al12 described 41 patients who underwent orthopedic patch testing following implantation for symptoms including pain, dermatitis, pruritus, joint loosening, edema, and impaired wound healing. Fifteen (37%) patients had positive patch test reactions to metals, and 10 (67%) of them had reactions to metals that were present in their implants. Six (60%) of these patients had their implants removed and their symptoms resolved; the remaining 4 continued to experience implant symptoms.12 These studies support the existence of rare metal-related orthopedic IHRs and support the concept of proceeding with orthopedic implant revision when indicated, safe, and agreed upon by the surgeon and patient. However, as noted in the series by Zondervan et al,11 not every patient with confirmed metal allergy who undergoes revision improves, so an informed conversation between the patient and surgeon is mandatory.
Types of Orthopedic Implants
Orthopedic implanted materials consist of either dynamic (knees, hips) or static (screws, plates) components. Several generations of hip implants have evolved since the 1960s. First-generation implanted hips were metal-on-metal and had high rates of metal release and sensitization. Metal-on-plastic implants may be less likely to release metal but instead release large polyethylene wear particles. Second-generation metal-on-metal implants reportedly have lower wear rates. With these implants, wear particles are generated but are reportedly smaller than first-generation particles.13
Allergens in IHRs
Metals
Metals are the most commonly implicated allergens in orthopedic IHRs. Potentially relevant metal alloys include 316L stainless steel, cobalt-chromium-molybdenum steel, Vitallium alloy, titanium alloy, titanium-tantalum-niobium alloy, and Oxinium (Smith & Nephew).14,15 Each alloy contains several metals, which can include nickel, chromium, cobalt, manganese, molybdenum, iron, titanium, aluminum, vanadium, niobium, tantalum, and zirconium, among others. For example, 316L stainless steel contains iron, nickel, chromium, manganese, molybdenum, nitrogen, carbon, sulfur, silicon, and phosphorus, whereas Oxinium contains only oxidized zirconium and niobium.
Bone Cement
Bone cement also has been reported in cases of orthopedic IHRs and can contain several chemicals, including methyl methacrylate, N,N-dimethyl-p-toluidine, benzoyl peroxide, hydroquinone, and gentamicin.14 Other potential exposures include adhesives (cyanoacrylates) and topical antibiotics.
Clinical Presentation
Several clinical presentations of orthopedic IHRs have been described. Perhaps the most commonly recognized is a localized cutaneous eczematous eruption, with dermatitis typically overlying the site of the implanted material.1,2,16 Generalized cutaneous eczematous IHRs also have been reported, including diffuse generalized dermatitis from a stainless steel orthopedic screw4 and nummular dermatitis attributed to vanadium in an orthopedic plate.5 Urticaria, vasculitis, and bullous cutaneous reactions, as well as extracutaneous complications, also have been reported.14,15 Pain, edema, joint loosening or failure, and poor wound healing have been reported,12 but it remains unclear whether these symptoms represent IHR.
Patch Testing for IHR
Several groups have published recommended patch test series for IHR.12,14,15 Common components of implant patch testing panels include metals, adhesives (acrylates, epoxy resins) and antibiotics. Importantly, obtaining product information from the manufacturer of the suspected implant can guide which allergens to include in patch testing. Implant and metal panels also are available for commercial purchase.
Other Diagnostic Tests
We rarely (almost never) order LTTs in the workup for potential IHRs. This is an in vitro test that includes lymphocytes, metal ions, and the radioactive marker methyl-3H-thymidine. The goal of the test is to evaluate if patient lymphocytes are reactive or responsive to metal ions. A positive LTT suggests that lymphocytes can respond to the presence of metal ions but does not confirm allergy or the presence of IHR.
Typically, skin or tissue biopsies are not required to make a diagnosis of IHR; however, if performed, histopathology suggestive of IHR can support a suspected diagnosis. Typical findings include but are not limited to spongiotic dermatitis. Eosinophils may or may not be present. Metal disc testing has been utilized for orthopedic IHR but is not currently recommended due to low diagnostic yield. Prick testing rarely is used and also is not a primary method for diagnosis of IHR.17
Preimplantation Patch Testing
Expert opinion guidelines published by the American Contact Dermatitis Society (ACDS) state that routine preimplantation patch testing is not necessary; however, for those patients with a clear history of contact reactions to metal, preimplantation patch testing can be considered.17
Patch test results can influence the orthopedic surgeon’s choice of implant material. In one study, when preimplantation patch testing showed a positive patch test reaction to metals, the results influenced the surgeon’s decision-making in all cases.12
Postimplantation Patch Testing: Diagnostic Criteria for Metal IHR After Implantation
From 2012 to 2013, Schalock and Thyssen18 surveyed expert attendees at meetings of the European Society of Contact Dermatitis and the ACDS for their opinions on proposed diagnostic criteria for metal IHRs. Based on these results (N=119), the authors stratified 4 major and 5 minor diagnostic criteria, which were defined based on overall responses of meeting attendees. Major criteria included (1) chronic dermatitis beginning weeks to months after metallic implantation, (2) complete recovery after removal of the offending implant, (3) eruption overlying the metal implant, and (4) positive patch test reaction to a metal used in the implant. Minor criteria included (1) histology consistent with allergic contact dermatitis, (2) morphology consistent with dermatitis (ie, erythema, induration, papules, vesicles), (3) positive in vitro test to metals (eg, lymphocyte transformation test), (4) systemic allergic dermatitis reaction, and (5) therapy-resistant dermatitis reaction. The authors did not describe a scoring system for evaluation and confirmation of a diagnosis of IHR. Instead, the criteria should be used as general guidelines when evaluating patients for possible IHRs. From a standpoint of available diagnostic tests for metal IHR, 86.1% of experts agreed that a positive patch test reaction to a metal used in the implant was suggestive of a diagnosis, whereas a positive in vitro test to metals (LTT) was suggestive of a diagnosis for only 32.2% of respondents. This study was designed specifically for metal IHRs and therefore is not necessarily generalizable for nonmetal IHRs.18
Final Interpretation
We follow the 2016 ACDS guidelines17 and complete preimplantation patch testing only in the setting of suspected metal allergy and postimplantation patch testing based on the guidelines described by Schalock and Thyssen.18 However, an extended conversation is warranted prior to patch testing to ensure the patient fully understands the limitations of the test. Although we have both ordered the LTT, interpretation remains murky, and until this test is standardized, routine use is unlikely to benefit the patient. Until we are more reliably able to predict who will develop hypersensitivity to implanted metals, the decision to remove or revise an implant is one that should be made by a multidisciplinary team that includes the surgeon and the patient.
- Dekoven JG, Warshaw EM, Zug KA, et al. North American Contact Dermatitis Group patch test results: 2015-2016. Dermatitis. 2018;29:297-309.
- Gao X, He RX, Yan SG, et al. Dermatitis associated with chromium following total knee arthroplasty. J Arthroplasty. 2011;26:665.E613-665.E616.
- Treudler R, Simon JC. Benzoyl peroxide: is it a relevant bone cement allergen in patients with orthopaedic implants? Contact Dermatitis. 2007;57:177-180.
- Barranco VP, Soloman H. Eczematous dermatitis from nickel. JAMA. 1972;220:1244.
- Engelhart S, Segal RJ. Allergic reaction to vanadium causes a diffuse eczematous eruption and titanium alloy orthopedic implant failure. Cutis. 2017;99:245-249.
- Thyssen JP, Jakobsen SS, Engkilde K, et al. The association between metal allergy, total hip arthroplasty, and revision. Acta Orthop. 2009;80:646-652.
- Münch HJ, Jacobsen SS, Olesen JT, et al. The association between metal allergy, total knee arthroplasty, and revision: study based on the Danish Knee Arthroplasty Register. Acta Orthop. 2015;86:378-383.
- Jacobs JJ, Skipor AK, Patterson LM, et al. Metal release in patients who have had a primary total hip arthroplasty. a prospective, controlled, longitudinal study. J Bone Joint Surg Am. 1998;80:1447-1458.
- Urban RM, Jacobs JJ, Tomlinson MJ, et al. Dissemination of wear particles to the liver, spleen, and abdominal lymph nodes of patients with hip or knee replacement. J Bone Joint Surg Am. 2000;82:457-476.
- Hallab N, Merritt K, Jacobs JJ. Metal sensitivity in patients with orthopaedic implants. J Bone Joint Surg Am. 2001;83:428-436.
- Zondervan RL, Vaux JJ, Blackmer MJ, et al. Improved outcomes in patients with positive metal sensitivity following revision total knee arthroplasty. J Orthop Surg Res. 2019;14:182.
- Atanaskova Mesinkovska N, Tellez A, Molina L, et al. The effect of patch testing on surgical practices and outcomes in orthopedic patients with metal implants. Arch Dermatol. 2012;148:687-693.
- Kovochich M, Fung ES, Donovan E, et al. Characterization of wear debris from metal-on-metal hip implants during normal wear versus edge-loading conditions. J Biomed Mater Res B Appl Biomater. 2018;106:986-996.
- Basko-Plluska JL, Thyssen JP, Schalock PC. Cutaneous and systemic hypersensitivity reactions to metallic implants. Dermatitis. 2011;22:65-79.
- Schalock PC, Menné T, Johansen JD, et al. Hypersensitivity reactions to metallic implants—diagnostic algorithm and suggested patch test series for clinical use. Contact Dermatitis. 2012;66:4-19.
- Thomas P, Gollwitzer H, Maier S, et al. Osteosynthesis associated contact dermatitis with unusual perpetuation of hyperreactivity in a nickel allergic patient. Contact Dermatitis. 2006;54:222-225.
- Schalock PC, Crawford G, Nedorost S, et al. Patch testing for evaluation of hypersensitivity to implanted metal devices: a perspective from the American Contact Dermatitis Society. Dermatitis. 2016;27:241-247.
- Schalock PC, Thyssen JP. Patch testers’ opinions regarding diagnostic criteria for metal hypersensitivity reactions to metallic implants. Dermatitis. 2013;24:183-185.
- Dekoven JG, Warshaw EM, Zug KA, et al. North American Contact Dermatitis Group patch test results: 2015-2016. Dermatitis. 2018;29:297-309.
- Gao X, He RX, Yan SG, et al. Dermatitis associated with chromium following total knee arthroplasty. J Arthroplasty. 2011;26:665.E613-665.E616.
- Treudler R, Simon JC. Benzoyl peroxide: is it a relevant bone cement allergen in patients with orthopaedic implants? Contact Dermatitis. 2007;57:177-180.
- Barranco VP, Soloman H. Eczematous dermatitis from nickel. JAMA. 1972;220:1244.
- Engelhart S, Segal RJ. Allergic reaction to vanadium causes a diffuse eczematous eruption and titanium alloy orthopedic implant failure. Cutis. 2017;99:245-249.
- Thyssen JP, Jakobsen SS, Engkilde K, et al. The association between metal allergy, total hip arthroplasty, and revision. Acta Orthop. 2009;80:646-652.
- Münch HJ, Jacobsen SS, Olesen JT, et al. The association between metal allergy, total knee arthroplasty, and revision: study based on the Danish Knee Arthroplasty Register. Acta Orthop. 2015;86:378-383.
- Jacobs JJ, Skipor AK, Patterson LM, et al. Metal release in patients who have had a primary total hip arthroplasty. a prospective, controlled, longitudinal study. J Bone Joint Surg Am. 1998;80:1447-1458.
- Urban RM, Jacobs JJ, Tomlinson MJ, et al. Dissemination of wear particles to the liver, spleen, and abdominal lymph nodes of patients with hip or knee replacement. J Bone Joint Surg Am. 2000;82:457-476.
- Hallab N, Merritt K, Jacobs JJ. Metal sensitivity in patients with orthopaedic implants. J Bone Joint Surg Am. 2001;83:428-436.
- Zondervan RL, Vaux JJ, Blackmer MJ, et al. Improved outcomes in patients with positive metal sensitivity following revision total knee arthroplasty. J Orthop Surg Res. 2019;14:182.
- Atanaskova Mesinkovska N, Tellez A, Molina L, et al. The effect of patch testing on surgical practices and outcomes in orthopedic patients with metal implants. Arch Dermatol. 2012;148:687-693.
- Kovochich M, Fung ES, Donovan E, et al. Characterization of wear debris from metal-on-metal hip implants during normal wear versus edge-loading conditions. J Biomed Mater Res B Appl Biomater. 2018;106:986-996.
- Basko-Plluska JL, Thyssen JP, Schalock PC. Cutaneous and systemic hypersensitivity reactions to metallic implants. Dermatitis. 2011;22:65-79.
- Schalock PC, Menné T, Johansen JD, et al. Hypersensitivity reactions to metallic implants—diagnostic algorithm and suggested patch test series for clinical use. Contact Dermatitis. 2012;66:4-19.
- Thomas P, Gollwitzer H, Maier S, et al. Osteosynthesis associated contact dermatitis with unusual perpetuation of hyperreactivity in a nickel allergic patient. Contact Dermatitis. 2006;54:222-225.
- Schalock PC, Crawford G, Nedorost S, et al. Patch testing for evaluation of hypersensitivity to implanted metal devices: a perspective from the American Contact Dermatitis Society. Dermatitis. 2016;27:241-247.
- Schalock PC, Thyssen JP. Patch testers’ opinions regarding diagnostic criteria for metal hypersensitivity reactions to metallic implants. Dermatitis. 2013;24:183-185.
Practice Points
- Common clinical presentations of orthopedic implant hypersensitivity reactions include localized cutaneous eruptions, generalized cutaneous eruptions, and noncutaneous reactions.
- Allergens implicated in orthopedic implant hypersensitivity reactions include metals and bone cement components.
- Routine preimplant patch testing for orthopedic hypersensitivity reactions is not recommended but can be performed when there is strong concern for metal allergy.
- Postimplant patch testing should be performed when symptoms are consistent with potential orthopedic implant hypersensitivity reactions.
Tumor Necrosis Factor Inhibitors May Reduce Cardiovascular Morbidity in Patients With Psoriasis
The connection between psoriasis and increased major adverse cardiovascular events (MACEs) has been well studied. 1,2 Although treatment of psoriasis can improve skin and joint symptoms, it is less clear whether therapies may mitigate the increased risk for cardiovascular comorbidities. Tumor necrosis factor (TNF) inhibitors in particular have been studied with great interest given the role of TNF in vascular and metabolic functions. 3 Using a retrospective cohort design, Wu and colleagues 4 examined if treatment with TNF inhibitors in patients with psoriasis would be associated with a lower risk for MACEs compared to phototherapy. Results suggested a significantly lower hazard of MACEs in patients using TNF inhibitors vs patients treated with phototherapy (adjusted hazard ratio, 0.77; P = .046). Moreover, based on these findings, they calculated that treating approximately 161 patients with TNF inhibitors rather than phototherapy would result in 1 less MACE per year overall. 4
Patients with psoriasis have been shown to have a greater noncalcified coronary plaque burden and prevalence of high-risk plaque compared to healthy patients.5 Lerman and colleagues5 measured the coronary plaque burden of 105 patients with psoriasis and 25 healthy volunteers using coronary computed tomography angiography. Although the patients were on average 10 years younger and had lower cardiovascular risk as measured by traditional risk scores, patients with psoriasis were found to have a greater noncalcified coronary plaque burden compared to 100 patients with hyperlipidemia. This burden was associated with an increased prevalence of high-risk plaques. Furthermore, in patients followed for 1 year, improvements in psoriasis severity were associated with reductions in noncalcified coronary plaque burden, though this finding was across all treatment modalities. However, there was no significant difference in calcified coronary plaque burden associated with reduced psoriasis severity.5
Moreover, Pina et al6 conducted a prospective study evaluating the use of the TNF inhibitor adalimumab to improve endothelial function and arterial stiffness in patients with moderate to severe psoriasis. Among 29 patients, they found a significant improvement in endothelial function as measured by flow-mediated dilatation after 6 months of adalimumab therapy, with a mean increase from 6.19% to 7.46% (P=.008). They also reported decreases in arterial stiffness by pulse wave velocity (P=.03). Despite a small sample size, these findings provide 2 potential mechanisms by which TNF inhibitor therapy may reduce the risk for cardiovascular events.6
A retrospective cohort study evaluating data from the Kaiser Permanente Southern California health plan assessed whether TNF inhibitor therapy was associated with a lower risk for MACE in patients with psoriasis.7 A total of 18,194 patients were included; of these, 1463 received TNF inhibitor therapy for at least 2 months. After controlling for other variables, including age at psoriasis diagnosis, sex, race/ethnicity, and other cardiovascular risk factors (eg, history of smoking or alcohol use; use of clopidogrel, antihypertensive agents, antihyperlipidemics, or anticoagulants), patients in the TNF inhibitor cohort demonstrated a significantly lower MACE hazard ratio compared to patients treated with topicals (hazard ratio, 0.80; 95% confidence interval, 0.66-0.98; P<.05).7
Conversely, a randomized, placebo-controlled trial of 107 patients found no difference in vascular inflammation of the ascending aorta and the carotids after 16 weeks of adalimumab treatment vs placebo. In this study, however, most patients had only moderate psoriasis based on a mean psoriasis area and severity index score of 9.8.8 Given studies finding higher risk burden in patients with more severe skin disease,2 it is possible that the effect of TNF inhibitor therapy may not be as pronounced in patients with less skin involvement. There was a significant effect on C-reactive protein levels in patients receiving TNF inhibitor therapy compared to placebo at 16 weeks (P=.012), suggesting TNF does play some role in systemic inflammation, and it is possible it may exert cardiovascular effects through a mechanism other than vascular inflammation.8
A second double-blind, randomized trial reported similar results.9 Among 97 patients randomized to receive adalimumab, placebo, or phototherapy, no significant difference in vascular inflammation was found after 12 weeks of therapy. In contrast, levels of C-reactive protein, IL-6, and glycoprotein acetylation were markedly reduced. The authors also reported adverse effects of adalimumab therapy on lipid metabolism with reduced cholesterol efflux capacity, a marker of ability of high-density-lipoprotein particles to perform reverse cholesterol transport, and high-density-lipoprotein particles, suggesting these effects may counteract some of the anti-inflammatory effects of TNF inhibitors.9
A growing body of data regarding the effect of TNF inhibitors on cardiovascular morbidity in patients with psoriasis is being collected, but no strong conclusions can be made. Given the disconnect of findings across these studies, it is possible that we have yet to elucidate the full mechanism by which TNF inhibitors may affect cardiovascular health. However, there may be additional confounding factors or patient characteristics at play. More large, prospective, randomized, controlled studies are needed to further understand this relationship.
- Ogdie A, Yu Y, Haynes K, et al. Risk of major cardiovascular events in patients with psoriatic arthritis, psoriasis and rheumatoid arthritis: a population-based cohort study. Ann Rheum Dis. 2015;74:326-332.
- Ahlehoff O, Gislason GH, Charlot M, et al. Psoriasis is associated with clinically significant cardiovascular risk: a Danish nationwide cohort study. J Intern Med. 2011;270:147-157.
- Kölliker Frers RA, Bisoendial RJ, Montoya SF, et al. Psoriasis and cardiovascular risk: immune-mediated crosstalk between metabolic, vascular, and autoimmune inflammation. Int J Cardiol Metab Endocr. 2015;6:43-54.
- Wu JJ, Sundaram M, Cloutier M, et al. The risk of cardiovascular events in psoriasis patients treated with tumor necrosis factor-α inhibitors versus phototherapy: an observational cohort study. J Am Acad Dermatol. 2018;79:60-68.
- Lerman JB, Joshi AA, Chaturvedi A, et al. Coronary plaque characterization in psoriasis reveals high-risk features that improve after treatment in a prospective observational study. Circulation. 2017;136:263-276.
- Pina T, Corrales A, Lopez-Mejias R, et al. Anti-tumor necrosis factor-α therapy improves endothelial function and arterial stiffness in patients with moderate to severe psoriasis: a 6 month prospective study. J Dermatol. 2016;43:1267-1272.
- Wu JJ, Joshi AA, Reddy SP, et al. Anti-inflammatory therapy with tumor necrosis factor inhibitors is associated with reduced risk of major adverse cardiovascular events in psoriasis [published online March 24, 2018]. J Eur Acad Dermatol Venereol. doi:10.1111/jdv.14951.
- Bissonnette R, Harel F, Krueger JG, et al. TNF-α antagonist and vascular inflammation patients with psoriasis vulgaris: a randomized placebo-controlled study. J Invest Dermatol. 2017;137:1638-1645 .
- Mehta NN, Shin DB, Joshi AA, et al. Effect of 2 psoriasis treatments on vascular inflammation and novel inflammatory cardiovascular biomarkers: a randomized placebo-controlled trial. Circ Cardiovasc Imaging. 2018;11:e007394.
The connection between psoriasis and increased major adverse cardiovascular events (MACEs) has been well studied. 1,2 Although treatment of psoriasis can improve skin and joint symptoms, it is less clear whether therapies may mitigate the increased risk for cardiovascular comorbidities. Tumor necrosis factor (TNF) inhibitors in particular have been studied with great interest given the role of TNF in vascular and metabolic functions. 3 Using a retrospective cohort design, Wu and colleagues 4 examined if treatment with TNF inhibitors in patients with psoriasis would be associated with a lower risk for MACEs compared to phototherapy. Results suggested a significantly lower hazard of MACEs in patients using TNF inhibitors vs patients treated with phototherapy (adjusted hazard ratio, 0.77; P = .046). Moreover, based on these findings, they calculated that treating approximately 161 patients with TNF inhibitors rather than phototherapy would result in 1 less MACE per year overall. 4
Patients with psoriasis have been shown to have a greater noncalcified coronary plaque burden and prevalence of high-risk plaque compared to healthy patients.5 Lerman and colleagues5 measured the coronary plaque burden of 105 patients with psoriasis and 25 healthy volunteers using coronary computed tomography angiography. Although the patients were on average 10 years younger and had lower cardiovascular risk as measured by traditional risk scores, patients with psoriasis were found to have a greater noncalcified coronary plaque burden compared to 100 patients with hyperlipidemia. This burden was associated with an increased prevalence of high-risk plaques. Furthermore, in patients followed for 1 year, improvements in psoriasis severity were associated with reductions in noncalcified coronary plaque burden, though this finding was across all treatment modalities. However, there was no significant difference in calcified coronary plaque burden associated with reduced psoriasis severity.5
Moreover, Pina et al6 conducted a prospective study evaluating the use of the TNF inhibitor adalimumab to improve endothelial function and arterial stiffness in patients with moderate to severe psoriasis. Among 29 patients, they found a significant improvement in endothelial function as measured by flow-mediated dilatation after 6 months of adalimumab therapy, with a mean increase from 6.19% to 7.46% (P=.008). They also reported decreases in arterial stiffness by pulse wave velocity (P=.03). Despite a small sample size, these findings provide 2 potential mechanisms by which TNF inhibitor therapy may reduce the risk for cardiovascular events.6
A retrospective cohort study evaluating data from the Kaiser Permanente Southern California health plan assessed whether TNF inhibitor therapy was associated with a lower risk for MACE in patients with psoriasis.7 A total of 18,194 patients were included; of these, 1463 received TNF inhibitor therapy for at least 2 months. After controlling for other variables, including age at psoriasis diagnosis, sex, race/ethnicity, and other cardiovascular risk factors (eg, history of smoking or alcohol use; use of clopidogrel, antihypertensive agents, antihyperlipidemics, or anticoagulants), patients in the TNF inhibitor cohort demonstrated a significantly lower MACE hazard ratio compared to patients treated with topicals (hazard ratio, 0.80; 95% confidence interval, 0.66-0.98; P<.05).7
Conversely, a randomized, placebo-controlled trial of 107 patients found no difference in vascular inflammation of the ascending aorta and the carotids after 16 weeks of adalimumab treatment vs placebo. In this study, however, most patients had only moderate psoriasis based on a mean psoriasis area and severity index score of 9.8.8 Given studies finding higher risk burden in patients with more severe skin disease,2 it is possible that the effect of TNF inhibitor therapy may not be as pronounced in patients with less skin involvement. There was a significant effect on C-reactive protein levels in patients receiving TNF inhibitor therapy compared to placebo at 16 weeks (P=.012), suggesting TNF does play some role in systemic inflammation, and it is possible it may exert cardiovascular effects through a mechanism other than vascular inflammation.8
A second double-blind, randomized trial reported similar results.9 Among 97 patients randomized to receive adalimumab, placebo, or phototherapy, no significant difference in vascular inflammation was found after 12 weeks of therapy. In contrast, levels of C-reactive protein, IL-6, and glycoprotein acetylation were markedly reduced. The authors also reported adverse effects of adalimumab therapy on lipid metabolism with reduced cholesterol efflux capacity, a marker of ability of high-density-lipoprotein particles to perform reverse cholesterol transport, and high-density-lipoprotein particles, suggesting these effects may counteract some of the anti-inflammatory effects of TNF inhibitors.9
A growing body of data regarding the effect of TNF inhibitors on cardiovascular morbidity in patients with psoriasis is being collected, but no strong conclusions can be made. Given the disconnect of findings across these studies, it is possible that we have yet to elucidate the full mechanism by which TNF inhibitors may affect cardiovascular health. However, there may be additional confounding factors or patient characteristics at play. More large, prospective, randomized, controlled studies are needed to further understand this relationship.
The connection between psoriasis and increased major adverse cardiovascular events (MACEs) has been well studied. 1,2 Although treatment of psoriasis can improve skin and joint symptoms, it is less clear whether therapies may mitigate the increased risk for cardiovascular comorbidities. Tumor necrosis factor (TNF) inhibitors in particular have been studied with great interest given the role of TNF in vascular and metabolic functions. 3 Using a retrospective cohort design, Wu and colleagues 4 examined if treatment with TNF inhibitors in patients with psoriasis would be associated with a lower risk for MACEs compared to phototherapy. Results suggested a significantly lower hazard of MACEs in patients using TNF inhibitors vs patients treated with phototherapy (adjusted hazard ratio, 0.77; P = .046). Moreover, based on these findings, they calculated that treating approximately 161 patients with TNF inhibitors rather than phototherapy would result in 1 less MACE per year overall. 4
Patients with psoriasis have been shown to have a greater noncalcified coronary plaque burden and prevalence of high-risk plaque compared to healthy patients.5 Lerman and colleagues5 measured the coronary plaque burden of 105 patients with psoriasis and 25 healthy volunteers using coronary computed tomography angiography. Although the patients were on average 10 years younger and had lower cardiovascular risk as measured by traditional risk scores, patients with psoriasis were found to have a greater noncalcified coronary plaque burden compared to 100 patients with hyperlipidemia. This burden was associated with an increased prevalence of high-risk plaques. Furthermore, in patients followed for 1 year, improvements in psoriasis severity were associated with reductions in noncalcified coronary plaque burden, though this finding was across all treatment modalities. However, there was no significant difference in calcified coronary plaque burden associated with reduced psoriasis severity.5
Moreover, Pina et al6 conducted a prospective study evaluating the use of the TNF inhibitor adalimumab to improve endothelial function and arterial stiffness in patients with moderate to severe psoriasis. Among 29 patients, they found a significant improvement in endothelial function as measured by flow-mediated dilatation after 6 months of adalimumab therapy, with a mean increase from 6.19% to 7.46% (P=.008). They also reported decreases in arterial stiffness by pulse wave velocity (P=.03). Despite a small sample size, these findings provide 2 potential mechanisms by which TNF inhibitor therapy may reduce the risk for cardiovascular events.6
A retrospective cohort study evaluating data from the Kaiser Permanente Southern California health plan assessed whether TNF inhibitor therapy was associated with a lower risk for MACE in patients with psoriasis.7 A total of 18,194 patients were included; of these, 1463 received TNF inhibitor therapy for at least 2 months. After controlling for other variables, including age at psoriasis diagnosis, sex, race/ethnicity, and other cardiovascular risk factors (eg, history of smoking or alcohol use; use of clopidogrel, antihypertensive agents, antihyperlipidemics, or anticoagulants), patients in the TNF inhibitor cohort demonstrated a significantly lower MACE hazard ratio compared to patients treated with topicals (hazard ratio, 0.80; 95% confidence interval, 0.66-0.98; P<.05).7
Conversely, a randomized, placebo-controlled trial of 107 patients found no difference in vascular inflammation of the ascending aorta and the carotids after 16 weeks of adalimumab treatment vs placebo. In this study, however, most patients had only moderate psoriasis based on a mean psoriasis area and severity index score of 9.8.8 Given studies finding higher risk burden in patients with more severe skin disease,2 it is possible that the effect of TNF inhibitor therapy may not be as pronounced in patients with less skin involvement. There was a significant effect on C-reactive protein levels in patients receiving TNF inhibitor therapy compared to placebo at 16 weeks (P=.012), suggesting TNF does play some role in systemic inflammation, and it is possible it may exert cardiovascular effects through a mechanism other than vascular inflammation.8
A second double-blind, randomized trial reported similar results.9 Among 97 patients randomized to receive adalimumab, placebo, or phototherapy, no significant difference in vascular inflammation was found after 12 weeks of therapy. In contrast, levels of C-reactive protein, IL-6, and glycoprotein acetylation were markedly reduced. The authors also reported adverse effects of adalimumab therapy on lipid metabolism with reduced cholesterol efflux capacity, a marker of ability of high-density-lipoprotein particles to perform reverse cholesterol transport, and high-density-lipoprotein particles, suggesting these effects may counteract some of the anti-inflammatory effects of TNF inhibitors.9
A growing body of data regarding the effect of TNF inhibitors on cardiovascular morbidity in patients with psoriasis is being collected, but no strong conclusions can be made. Given the disconnect of findings across these studies, it is possible that we have yet to elucidate the full mechanism by which TNF inhibitors may affect cardiovascular health. However, there may be additional confounding factors or patient characteristics at play. More large, prospective, randomized, controlled studies are needed to further understand this relationship.
- Ogdie A, Yu Y, Haynes K, et al. Risk of major cardiovascular events in patients with psoriatic arthritis, psoriasis and rheumatoid arthritis: a population-based cohort study. Ann Rheum Dis. 2015;74:326-332.
- Ahlehoff O, Gislason GH, Charlot M, et al. Psoriasis is associated with clinically significant cardiovascular risk: a Danish nationwide cohort study. J Intern Med. 2011;270:147-157.
- Kölliker Frers RA, Bisoendial RJ, Montoya SF, et al. Psoriasis and cardiovascular risk: immune-mediated crosstalk between metabolic, vascular, and autoimmune inflammation. Int J Cardiol Metab Endocr. 2015;6:43-54.
- Wu JJ, Sundaram M, Cloutier M, et al. The risk of cardiovascular events in psoriasis patients treated with tumor necrosis factor-α inhibitors versus phototherapy: an observational cohort study. J Am Acad Dermatol. 2018;79:60-68.
- Lerman JB, Joshi AA, Chaturvedi A, et al. Coronary plaque characterization in psoriasis reveals high-risk features that improve after treatment in a prospective observational study. Circulation. 2017;136:263-276.
- Pina T, Corrales A, Lopez-Mejias R, et al. Anti-tumor necrosis factor-α therapy improves endothelial function and arterial stiffness in patients with moderate to severe psoriasis: a 6 month prospective study. J Dermatol. 2016;43:1267-1272.
- Wu JJ, Joshi AA, Reddy SP, et al. Anti-inflammatory therapy with tumor necrosis factor inhibitors is associated with reduced risk of major adverse cardiovascular events in psoriasis [published online March 24, 2018]. J Eur Acad Dermatol Venereol. doi:10.1111/jdv.14951.
- Bissonnette R, Harel F, Krueger JG, et al. TNF-α antagonist and vascular inflammation patients with psoriasis vulgaris: a randomized placebo-controlled study. J Invest Dermatol. 2017;137:1638-1645 .
- Mehta NN, Shin DB, Joshi AA, et al. Effect of 2 psoriasis treatments on vascular inflammation and novel inflammatory cardiovascular biomarkers: a randomized placebo-controlled trial. Circ Cardiovasc Imaging. 2018;11:e007394.
- Ogdie A, Yu Y, Haynes K, et al. Risk of major cardiovascular events in patients with psoriatic arthritis, psoriasis and rheumatoid arthritis: a population-based cohort study. Ann Rheum Dis. 2015;74:326-332.
- Ahlehoff O, Gislason GH, Charlot M, et al. Psoriasis is associated with clinically significant cardiovascular risk: a Danish nationwide cohort study. J Intern Med. 2011;270:147-157.
- Kölliker Frers RA, Bisoendial RJ, Montoya SF, et al. Psoriasis and cardiovascular risk: immune-mediated crosstalk between metabolic, vascular, and autoimmune inflammation. Int J Cardiol Metab Endocr. 2015;6:43-54.
- Wu JJ, Sundaram M, Cloutier M, et al. The risk of cardiovascular events in psoriasis patients treated with tumor necrosis factor-α inhibitors versus phototherapy: an observational cohort study. J Am Acad Dermatol. 2018;79:60-68.
- Lerman JB, Joshi AA, Chaturvedi A, et al. Coronary plaque characterization in psoriasis reveals high-risk features that improve after treatment in a prospective observational study. Circulation. 2017;136:263-276.
- Pina T, Corrales A, Lopez-Mejias R, et al. Anti-tumor necrosis factor-α therapy improves endothelial function and arterial stiffness in patients with moderate to severe psoriasis: a 6 month prospective study. J Dermatol. 2016;43:1267-1272.
- Wu JJ, Joshi AA, Reddy SP, et al. Anti-inflammatory therapy with tumor necrosis factor inhibitors is associated with reduced risk of major adverse cardiovascular events in psoriasis [published online March 24, 2018]. J Eur Acad Dermatol Venereol. doi:10.1111/jdv.14951.
- Bissonnette R, Harel F, Krueger JG, et al. TNF-α antagonist and vascular inflammation patients with psoriasis vulgaris: a randomized placebo-controlled study. J Invest Dermatol. 2017;137:1638-1645 .
- Mehta NN, Shin DB, Joshi AA, et al. Effect of 2 psoriasis treatments on vascular inflammation and novel inflammatory cardiovascular biomarkers: a randomized placebo-controlled trial. Circ Cardiovasc Imaging. 2018;11:e007394.
Chronic cough in COPD linked to more severe disease
, according to research published in CHEST.
The results indicate “that chronic cough in individuals with COPD is associated with a more severe disease phenotype, which could be helpful for stratifying management of COPD in the future,” wrote Eskild Landt, PhD, a research assistant at Zealand University Hospital in Køge, Denmark, and colleagues.
A study by published in the Journal of Allergy and Clinical Immunology: In Practice (2019;7[6]:1783-92.e8) indicated that in patients with asthma, chronic cough was associated with worse respiratory symptoms, more health care utilization, decreased lung function, and increased inflammatory markers in blood. Dr. Landt and colleagues hypothesized that patients with COPD and chronic cough had a similar pattern of disease severity.
To test their hypothesis, they identified individuals with COPD and chronic cough among 43,271 participants in the Copenhagen General Population Study, a population-based cohort study. The researchers defined COPD as a ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) of less than 0.70 in individuals without asthma. Consecutive individuals answered questions about chronic cough, which was defined as a cough lasting more than 8 weeks, and responded to the Leicester Cough Questionnaire. They also underwent a physical health examination, including prebronchodilatory spirometry, and gave blood for biochemical analyses. The blood was analyzed for high-sensitive C-reactive protein, fibrinogen, leukocytes, eosinophils, neutrophils, and immunoglobulin E (i.e., inflammatory biomarkers).
Dr. Landt and colleagues identified 8,181 patients (19% of the population) with COPD, 796 (10%) of whom had chronic cough. Of the 33,364 participants without COPD, 1,585 (5%) had chronic cough. For patients with COPD and chronic cough, median total Leicester Cough Questionnaire score was 17.7, corresponding to 5.9 for the physical domain, 5.6 for the psychological domain, and 6.3 for the social domain.
Among participants with COPD, those with chronic cough had higher rates of sputum production (60% versus 8%), wheezing (46% versus 14%), dyspnea (66% versus 38%), chest pain or tightness (9% versus 4%), nighttime dyspnea (8% versus 3%), episodes of acute bronchitis or pneumonias in the past 10 years (45% versus 25%), and general practitioner visits in the past 12 months (53% versus 37%). In addition, these participants had lower FEV1% of predicted (81% versus 89%), lower ratio of FEV1 to FVC (0.64 versus 0.66), and higher levels of high-sensitive C-reactive protein, fibrinogen, leukocytes, neutrophils, eosinophils, and immunoglobulin E in blood.
“To our knowledge, this is the first study reporting Leicester Cough Questionnaire score for randomly selected individuals with COPD from a general population setting,” wrote Dr. Landt and colleagues. The study’s strengths include its randomly chosen population-based sample and investigator blinding to disease status and clinical outcome, they added. Some patients with the most severe types of COPD and chronic cough may not have attended the physical examination and participated in the study, however, and this factor could have biased the results. Furthermore, nearly the entire sample was white, so the results may not be generalizable to other ethnicities. “That said, we are not aware of results to suggest that our findings should not be relevant to individuals of all races,” wrote the investigators.
The study was funded by the private Lundbeck Foundation, as well as by the Danish Lung Association and the Danish Cancer Society. Several authors reported receiving grants and fees from AstraZeneca, GlaxoSmithKline, and Novartis that were unrelated to the study.
SOURCE: Landt E et al. CHEST. 2020 Jan 24. doi: 10.1016/j.chest.2019.12.038.
, according to research published in CHEST.
The results indicate “that chronic cough in individuals with COPD is associated with a more severe disease phenotype, which could be helpful for stratifying management of COPD in the future,” wrote Eskild Landt, PhD, a research assistant at Zealand University Hospital in Køge, Denmark, and colleagues.
A study by published in the Journal of Allergy and Clinical Immunology: In Practice (2019;7[6]:1783-92.e8) indicated that in patients with asthma, chronic cough was associated with worse respiratory symptoms, more health care utilization, decreased lung function, and increased inflammatory markers in blood. Dr. Landt and colleagues hypothesized that patients with COPD and chronic cough had a similar pattern of disease severity.
To test their hypothesis, they identified individuals with COPD and chronic cough among 43,271 participants in the Copenhagen General Population Study, a population-based cohort study. The researchers defined COPD as a ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) of less than 0.70 in individuals without asthma. Consecutive individuals answered questions about chronic cough, which was defined as a cough lasting more than 8 weeks, and responded to the Leicester Cough Questionnaire. They also underwent a physical health examination, including prebronchodilatory spirometry, and gave blood for biochemical analyses. The blood was analyzed for high-sensitive C-reactive protein, fibrinogen, leukocytes, eosinophils, neutrophils, and immunoglobulin E (i.e., inflammatory biomarkers).
Dr. Landt and colleagues identified 8,181 patients (19% of the population) with COPD, 796 (10%) of whom had chronic cough. Of the 33,364 participants without COPD, 1,585 (5%) had chronic cough. For patients with COPD and chronic cough, median total Leicester Cough Questionnaire score was 17.7, corresponding to 5.9 for the physical domain, 5.6 for the psychological domain, and 6.3 for the social domain.
Among participants with COPD, those with chronic cough had higher rates of sputum production (60% versus 8%), wheezing (46% versus 14%), dyspnea (66% versus 38%), chest pain or tightness (9% versus 4%), nighttime dyspnea (8% versus 3%), episodes of acute bronchitis or pneumonias in the past 10 years (45% versus 25%), and general practitioner visits in the past 12 months (53% versus 37%). In addition, these participants had lower FEV1% of predicted (81% versus 89%), lower ratio of FEV1 to FVC (0.64 versus 0.66), and higher levels of high-sensitive C-reactive protein, fibrinogen, leukocytes, neutrophils, eosinophils, and immunoglobulin E in blood.
“To our knowledge, this is the first study reporting Leicester Cough Questionnaire score for randomly selected individuals with COPD from a general population setting,” wrote Dr. Landt and colleagues. The study’s strengths include its randomly chosen population-based sample and investigator blinding to disease status and clinical outcome, they added. Some patients with the most severe types of COPD and chronic cough may not have attended the physical examination and participated in the study, however, and this factor could have biased the results. Furthermore, nearly the entire sample was white, so the results may not be generalizable to other ethnicities. “That said, we are not aware of results to suggest that our findings should not be relevant to individuals of all races,” wrote the investigators.
The study was funded by the private Lundbeck Foundation, as well as by the Danish Lung Association and the Danish Cancer Society. Several authors reported receiving grants and fees from AstraZeneca, GlaxoSmithKline, and Novartis that were unrelated to the study.
SOURCE: Landt E et al. CHEST. 2020 Jan 24. doi: 10.1016/j.chest.2019.12.038.
, according to research published in CHEST.
The results indicate “that chronic cough in individuals with COPD is associated with a more severe disease phenotype, which could be helpful for stratifying management of COPD in the future,” wrote Eskild Landt, PhD, a research assistant at Zealand University Hospital in Køge, Denmark, and colleagues.
A study by published in the Journal of Allergy and Clinical Immunology: In Practice (2019;7[6]:1783-92.e8) indicated that in patients with asthma, chronic cough was associated with worse respiratory symptoms, more health care utilization, decreased lung function, and increased inflammatory markers in blood. Dr. Landt and colleagues hypothesized that patients with COPD and chronic cough had a similar pattern of disease severity.
To test their hypothesis, they identified individuals with COPD and chronic cough among 43,271 participants in the Copenhagen General Population Study, a population-based cohort study. The researchers defined COPD as a ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) of less than 0.70 in individuals without asthma. Consecutive individuals answered questions about chronic cough, which was defined as a cough lasting more than 8 weeks, and responded to the Leicester Cough Questionnaire. They also underwent a physical health examination, including prebronchodilatory spirometry, and gave blood for biochemical analyses. The blood was analyzed for high-sensitive C-reactive protein, fibrinogen, leukocytes, eosinophils, neutrophils, and immunoglobulin E (i.e., inflammatory biomarkers).
Dr. Landt and colleagues identified 8,181 patients (19% of the population) with COPD, 796 (10%) of whom had chronic cough. Of the 33,364 participants without COPD, 1,585 (5%) had chronic cough. For patients with COPD and chronic cough, median total Leicester Cough Questionnaire score was 17.7, corresponding to 5.9 for the physical domain, 5.6 for the psychological domain, and 6.3 for the social domain.
Among participants with COPD, those with chronic cough had higher rates of sputum production (60% versus 8%), wheezing (46% versus 14%), dyspnea (66% versus 38%), chest pain or tightness (9% versus 4%), nighttime dyspnea (8% versus 3%), episodes of acute bronchitis or pneumonias in the past 10 years (45% versus 25%), and general practitioner visits in the past 12 months (53% versus 37%). In addition, these participants had lower FEV1% of predicted (81% versus 89%), lower ratio of FEV1 to FVC (0.64 versus 0.66), and higher levels of high-sensitive C-reactive protein, fibrinogen, leukocytes, neutrophils, eosinophils, and immunoglobulin E in blood.
“To our knowledge, this is the first study reporting Leicester Cough Questionnaire score for randomly selected individuals with COPD from a general population setting,” wrote Dr. Landt and colleagues. The study’s strengths include its randomly chosen population-based sample and investigator blinding to disease status and clinical outcome, they added. Some patients with the most severe types of COPD and chronic cough may not have attended the physical examination and participated in the study, however, and this factor could have biased the results. Furthermore, nearly the entire sample was white, so the results may not be generalizable to other ethnicities. “That said, we are not aware of results to suggest that our findings should not be relevant to individuals of all races,” wrote the investigators.
The study was funded by the private Lundbeck Foundation, as well as by the Danish Lung Association and the Danish Cancer Society. Several authors reported receiving grants and fees from AstraZeneca, GlaxoSmithKline, and Novartis that were unrelated to the study.
SOURCE: Landt E et al. CHEST. 2020 Jan 24. doi: 10.1016/j.chest.2019.12.038.
FROM CHEST
Documentation matters
Quality over quantity
Documentation has always been part of a physician’s job. Historically, in the days of paper records, physicians saw a patient on rounds and immediately following, while still on the unit, wrote a daily note detailing the events, test results, and plans since the last note. Addenda were written over the course of the day and night as needed.
The medical record was a chronological itemization of the encounter. The chart told the patient’s story, hopefully legibly and without excessive rehashing of previous material. The discharge summary then encapsulated the hospitalization in several coherent paragraphs.
In the current electronic records environment, we are inundated with excessive and repetitious information, data without interpretation, differentials without diagnoses. Prepopulation of templated notes, defaults without edit, and dictation without revision have degraded our documentation to the point of unintelligibility. The chronological storytelling and trustworthiness of the medical record has become suspect.
The Centers for Medicare & Medicaid Services is touting its “Patients over Paperwork” initiative. The solution is flawed (that is, future relaxation of documentation requirements for professional billing) because the premise is delusive. Documentation isn’t fundamentally the problem. Having clinicians jump through regulatory hoops which do not advance patients’ care, and providers misunderstanding the requirements for level-of-service billing are the essential issues. Getting no training on how to properly document in medical school/residency and receiving no formative feedback on documentation throughout one’s career compounds the problem. Having clinical documentation serve too many masters, including compliance, quality, medicolegal, utilization review, and reimbursement, is also to blame. The advent of the electronic medical record was just the straw that broke the camel’s back.
Many hospitals now have a clinical documentation integrity (CDI) team which is tasked with querying the provider when the health record documentation is conflicting, imprecise, incomplete, illegible, ambiguous, or inconsistent. They are charged with getting practitioners to associate clinical indicators with diagnoses and to consider removal of diagnoses which do not seem clinically valid from the existing documentation. From this explanation, you might well conclude that the CDI specialist could generate a query on every patient if they were so inclined, and you would be correct. But the goal isn’t to torture the physician – it is to ensure that the medical record is accurately depicting the encounter.
You are not being asked for more documentation by the CDI team; they are entreating you for higher-quality documentation. Let me give you some pointers to ward off queries.
- Tell the story. The most important goal of documentation is to clinically communicate to other caregivers. Think to yourself: “What would a fellow clinician need to know about this patient to understand why I drew those conclusions or to pick up where I left off?” At 2 a.m., that information, or lack thereof, could literally be a matter of life or death.
- Tell the truth. Embellishing the record or including invalid diagnoses with the intent to increase the severity of illness resulting in a more favorable diagnosis-related group – the inpatient risk-adjustment system – is considered fraud.
- You may like the convenience of copy forward, but do you relish reading other people’s copy and paste? Consider doing a documentation time-out. Before you copy and paste yesterday’s assessment and plan, stop and think: “Why is the patient still here? Why are we doing what we are doing?” If you choose to copy and paste, be certain to do mindful editing so the documentation represents the current situation and avoids redundancy. Appropriately editing copy and pasted documentation may prove more time consuming than generating a note de novo.
- Translate findings into diagnoses using your best medical judgment. One man’s hypotension may be another health care provider’s shock. Coders are not clinical and are not permitted to make inferences. A potassium of 6.7 may be hyperkalemia or it may be spurious – only a clinician may make that determination using their clinical expertise and experience. The coder is not allowed to read your mind. You must explicitly draw the conclusion that a febrile patient with bacteremia, encephalopathy, hypoxemia, and a blood pressure of 85/60 is in septic shock.
- Uncertain diagnoses (heralded by words such as: likely, possible, probable, suspected, rule out, etc.) which are not ruled out prior to discharge or demise are coded as if they were definitively present, for the inpatient technical side of hospital billing. This is distinctly different than the professional fee where you can only code definitive diagnoses. If you have a strong suspicion (not wild speculation) that a condition is present, best practice is to offer an uncertain diagnosis. Associate signs and symptoms with your most likely diagnosis: “Shortness of breath, pleuritic chest pain, and hypoxemia in the setting of cancer, probable pulmonary embolism.”
- Evolve, resolve, remove, and recap. If an uncertain diagnosis is ruled in, take away the uncertainty. If it is ruled out, don’t have 4 days of copy and pasted: “Possible eosinophilic pneumonia.” You do not have to maintain a resolved diagnosis ad infinitum. It can drop off the diagnosis list but be sure to have it reappear in the discharge summary.
- I know it can be a hASSLe to do excellent documentation, but it is critical for many reasons, most importantly for superlative patient care. More accurate coding and billing is an intended consequence. A: Acuity; S: Severity; S: Specificity (may affect the coding and the risk-adjustment implications. Acute systolic heart failure does not equal heart failure; type 2 diabetes mellitus with diabetic chronic kidney disease, stage 4 does not equal chronic kidney disease); and L: Linkage (of diagnosis with underlying cause or manifestation [e.g., because of, associated with, as a result of, secondary to, or from diabetic nephropathy, hypertensive encephalopathy]).
- If you have the capability to keep a running summary throughout the hospital stay, do so and keep it updated. A few moments of daily careful editing and composing can save time and effort at the back end creating the discharge summary. The follow-up care provider can reconstruct the hospital course and it is your last chance to spin the narrative for the lawyers.
- Read your documentation over. Ensure that it is clear, accurate, concise, and tells the story and the plans for the patient. Make sure that someone reading the note will know what you were thinking.
- Set up a program to self-audit documentation where monthly or quarterly, you and your partners mutually review a certain number of records and give each other feedback. Design an assessment tool which rates the quality of documentation elements which your hospital/network/service line values (clarity, copy and paste, complete and specific diagnoses, etc.). You know who the best documenters are. Why do you think their documentation is superior? How can you emulate them?
Finally, answer CDI queries. The CDI specialist is your ally, not your enemy. They want you to get credit for taking care of sick and complex patients. They are not permitted to lead the provider, so don’t ask them what they want you to write. But, if you don’t understand the query or issue, have a conversation and get it clarified. It is in everyone’s best interest to get this right.
Documentation improves patient care and demonstrates that you provided excellent patient care. Put mentation back into documentation.
Dr. Remer was a practicing emergency physician for 25 years and a physician advisor for 4 years. She is on the board of directors of the American College of Physician Advisors and the advisory board of the Association of Clinical Documentation Improvement Specialists. She currently provides consulting services for provider education on documentation, CDI, and ICD-10 coding. Dr. Remer can be reached at [email protected]
Quality over quantity
Quality over quantity
Documentation has always been part of a physician’s job. Historically, in the days of paper records, physicians saw a patient on rounds and immediately following, while still on the unit, wrote a daily note detailing the events, test results, and plans since the last note. Addenda were written over the course of the day and night as needed.
The medical record was a chronological itemization of the encounter. The chart told the patient’s story, hopefully legibly and without excessive rehashing of previous material. The discharge summary then encapsulated the hospitalization in several coherent paragraphs.
In the current electronic records environment, we are inundated with excessive and repetitious information, data without interpretation, differentials without diagnoses. Prepopulation of templated notes, defaults without edit, and dictation without revision have degraded our documentation to the point of unintelligibility. The chronological storytelling and trustworthiness of the medical record has become suspect.
The Centers for Medicare & Medicaid Services is touting its “Patients over Paperwork” initiative. The solution is flawed (that is, future relaxation of documentation requirements for professional billing) because the premise is delusive. Documentation isn’t fundamentally the problem. Having clinicians jump through regulatory hoops which do not advance patients’ care, and providers misunderstanding the requirements for level-of-service billing are the essential issues. Getting no training on how to properly document in medical school/residency and receiving no formative feedback on documentation throughout one’s career compounds the problem. Having clinical documentation serve too many masters, including compliance, quality, medicolegal, utilization review, and reimbursement, is also to blame. The advent of the electronic medical record was just the straw that broke the camel’s back.
Many hospitals now have a clinical documentation integrity (CDI) team which is tasked with querying the provider when the health record documentation is conflicting, imprecise, incomplete, illegible, ambiguous, or inconsistent. They are charged with getting practitioners to associate clinical indicators with diagnoses and to consider removal of diagnoses which do not seem clinically valid from the existing documentation. From this explanation, you might well conclude that the CDI specialist could generate a query on every patient if they were so inclined, and you would be correct. But the goal isn’t to torture the physician – it is to ensure that the medical record is accurately depicting the encounter.
You are not being asked for more documentation by the CDI team; they are entreating you for higher-quality documentation. Let me give you some pointers to ward off queries.
- Tell the story. The most important goal of documentation is to clinically communicate to other caregivers. Think to yourself: “What would a fellow clinician need to know about this patient to understand why I drew those conclusions or to pick up where I left off?” At 2 a.m., that information, or lack thereof, could literally be a matter of life or death.
- Tell the truth. Embellishing the record or including invalid diagnoses with the intent to increase the severity of illness resulting in a more favorable diagnosis-related group – the inpatient risk-adjustment system – is considered fraud.
- You may like the convenience of copy forward, but do you relish reading other people’s copy and paste? Consider doing a documentation time-out. Before you copy and paste yesterday’s assessment and plan, stop and think: “Why is the patient still here? Why are we doing what we are doing?” If you choose to copy and paste, be certain to do mindful editing so the documentation represents the current situation and avoids redundancy. Appropriately editing copy and pasted documentation may prove more time consuming than generating a note de novo.
- Translate findings into diagnoses using your best medical judgment. One man’s hypotension may be another health care provider’s shock. Coders are not clinical and are not permitted to make inferences. A potassium of 6.7 may be hyperkalemia or it may be spurious – only a clinician may make that determination using their clinical expertise and experience. The coder is not allowed to read your mind. You must explicitly draw the conclusion that a febrile patient with bacteremia, encephalopathy, hypoxemia, and a blood pressure of 85/60 is in septic shock.
- Uncertain diagnoses (heralded by words such as: likely, possible, probable, suspected, rule out, etc.) which are not ruled out prior to discharge or demise are coded as if they were definitively present, for the inpatient technical side of hospital billing. This is distinctly different than the professional fee where you can only code definitive diagnoses. If you have a strong suspicion (not wild speculation) that a condition is present, best practice is to offer an uncertain diagnosis. Associate signs and symptoms with your most likely diagnosis: “Shortness of breath, pleuritic chest pain, and hypoxemia in the setting of cancer, probable pulmonary embolism.”
- Evolve, resolve, remove, and recap. If an uncertain diagnosis is ruled in, take away the uncertainty. If it is ruled out, don’t have 4 days of copy and pasted: “Possible eosinophilic pneumonia.” You do not have to maintain a resolved diagnosis ad infinitum. It can drop off the diagnosis list but be sure to have it reappear in the discharge summary.
- I know it can be a hASSLe to do excellent documentation, but it is critical for many reasons, most importantly for superlative patient care. More accurate coding and billing is an intended consequence. A: Acuity; S: Severity; S: Specificity (may affect the coding and the risk-adjustment implications. Acute systolic heart failure does not equal heart failure; type 2 diabetes mellitus with diabetic chronic kidney disease, stage 4 does not equal chronic kidney disease); and L: Linkage (of diagnosis with underlying cause or manifestation [e.g., because of, associated with, as a result of, secondary to, or from diabetic nephropathy, hypertensive encephalopathy]).
- If you have the capability to keep a running summary throughout the hospital stay, do so and keep it updated. A few moments of daily careful editing and composing can save time and effort at the back end creating the discharge summary. The follow-up care provider can reconstruct the hospital course and it is your last chance to spin the narrative for the lawyers.
- Read your documentation over. Ensure that it is clear, accurate, concise, and tells the story and the plans for the patient. Make sure that someone reading the note will know what you were thinking.
- Set up a program to self-audit documentation where monthly or quarterly, you and your partners mutually review a certain number of records and give each other feedback. Design an assessment tool which rates the quality of documentation elements which your hospital/network/service line values (clarity, copy and paste, complete and specific diagnoses, etc.). You know who the best documenters are. Why do you think their documentation is superior? How can you emulate them?
Finally, answer CDI queries. The CDI specialist is your ally, not your enemy. They want you to get credit for taking care of sick and complex patients. They are not permitted to lead the provider, so don’t ask them what they want you to write. But, if you don’t understand the query or issue, have a conversation and get it clarified. It is in everyone’s best interest to get this right.
Documentation improves patient care and demonstrates that you provided excellent patient care. Put mentation back into documentation.
Dr. Remer was a practicing emergency physician for 25 years and a physician advisor for 4 years. She is on the board of directors of the American College of Physician Advisors and the advisory board of the Association of Clinical Documentation Improvement Specialists. She currently provides consulting services for provider education on documentation, CDI, and ICD-10 coding. Dr. Remer can be reached at [email protected]
Documentation has always been part of a physician’s job. Historically, in the days of paper records, physicians saw a patient on rounds and immediately following, while still on the unit, wrote a daily note detailing the events, test results, and plans since the last note. Addenda were written over the course of the day and night as needed.
The medical record was a chronological itemization of the encounter. The chart told the patient’s story, hopefully legibly and without excessive rehashing of previous material. The discharge summary then encapsulated the hospitalization in several coherent paragraphs.
In the current electronic records environment, we are inundated with excessive and repetitious information, data without interpretation, differentials without diagnoses. Prepopulation of templated notes, defaults without edit, and dictation without revision have degraded our documentation to the point of unintelligibility. The chronological storytelling and trustworthiness of the medical record has become suspect.
The Centers for Medicare & Medicaid Services is touting its “Patients over Paperwork” initiative. The solution is flawed (that is, future relaxation of documentation requirements for professional billing) because the premise is delusive. Documentation isn’t fundamentally the problem. Having clinicians jump through regulatory hoops which do not advance patients’ care, and providers misunderstanding the requirements for level-of-service billing are the essential issues. Getting no training on how to properly document in medical school/residency and receiving no formative feedback on documentation throughout one’s career compounds the problem. Having clinical documentation serve too many masters, including compliance, quality, medicolegal, utilization review, and reimbursement, is also to blame. The advent of the electronic medical record was just the straw that broke the camel’s back.
Many hospitals now have a clinical documentation integrity (CDI) team which is tasked with querying the provider when the health record documentation is conflicting, imprecise, incomplete, illegible, ambiguous, or inconsistent. They are charged with getting practitioners to associate clinical indicators with diagnoses and to consider removal of diagnoses which do not seem clinically valid from the existing documentation. From this explanation, you might well conclude that the CDI specialist could generate a query on every patient if they were so inclined, and you would be correct. But the goal isn’t to torture the physician – it is to ensure that the medical record is accurately depicting the encounter.
You are not being asked for more documentation by the CDI team; they are entreating you for higher-quality documentation. Let me give you some pointers to ward off queries.
- Tell the story. The most important goal of documentation is to clinically communicate to other caregivers. Think to yourself: “What would a fellow clinician need to know about this patient to understand why I drew those conclusions or to pick up where I left off?” At 2 a.m., that information, or lack thereof, could literally be a matter of life or death.
- Tell the truth. Embellishing the record or including invalid diagnoses with the intent to increase the severity of illness resulting in a more favorable diagnosis-related group – the inpatient risk-adjustment system – is considered fraud.
- You may like the convenience of copy forward, but do you relish reading other people’s copy and paste? Consider doing a documentation time-out. Before you copy and paste yesterday’s assessment and plan, stop and think: “Why is the patient still here? Why are we doing what we are doing?” If you choose to copy and paste, be certain to do mindful editing so the documentation represents the current situation and avoids redundancy. Appropriately editing copy and pasted documentation may prove more time consuming than generating a note de novo.
- Translate findings into diagnoses using your best medical judgment. One man’s hypotension may be another health care provider’s shock. Coders are not clinical and are not permitted to make inferences. A potassium of 6.7 may be hyperkalemia or it may be spurious – only a clinician may make that determination using their clinical expertise and experience. The coder is not allowed to read your mind. You must explicitly draw the conclusion that a febrile patient with bacteremia, encephalopathy, hypoxemia, and a blood pressure of 85/60 is in septic shock.
- Uncertain diagnoses (heralded by words such as: likely, possible, probable, suspected, rule out, etc.) which are not ruled out prior to discharge or demise are coded as if they were definitively present, for the inpatient technical side of hospital billing. This is distinctly different than the professional fee where you can only code definitive diagnoses. If you have a strong suspicion (not wild speculation) that a condition is present, best practice is to offer an uncertain diagnosis. Associate signs and symptoms with your most likely diagnosis: “Shortness of breath, pleuritic chest pain, and hypoxemia in the setting of cancer, probable pulmonary embolism.”
- Evolve, resolve, remove, and recap. If an uncertain diagnosis is ruled in, take away the uncertainty. If it is ruled out, don’t have 4 days of copy and pasted: “Possible eosinophilic pneumonia.” You do not have to maintain a resolved diagnosis ad infinitum. It can drop off the diagnosis list but be sure to have it reappear in the discharge summary.
- I know it can be a hASSLe to do excellent documentation, but it is critical for many reasons, most importantly for superlative patient care. More accurate coding and billing is an intended consequence. A: Acuity; S: Severity; S: Specificity (may affect the coding and the risk-adjustment implications. Acute systolic heart failure does not equal heart failure; type 2 diabetes mellitus with diabetic chronic kidney disease, stage 4 does not equal chronic kidney disease); and L: Linkage (of diagnosis with underlying cause or manifestation [e.g., because of, associated with, as a result of, secondary to, or from diabetic nephropathy, hypertensive encephalopathy]).
- If you have the capability to keep a running summary throughout the hospital stay, do so and keep it updated. A few moments of daily careful editing and composing can save time and effort at the back end creating the discharge summary. The follow-up care provider can reconstruct the hospital course and it is your last chance to spin the narrative for the lawyers.
- Read your documentation over. Ensure that it is clear, accurate, concise, and tells the story and the plans for the patient. Make sure that someone reading the note will know what you were thinking.
- Set up a program to self-audit documentation where monthly or quarterly, you and your partners mutually review a certain number of records and give each other feedback. Design an assessment tool which rates the quality of documentation elements which your hospital/network/service line values (clarity, copy and paste, complete and specific diagnoses, etc.). You know who the best documenters are. Why do you think their documentation is superior? How can you emulate them?
Finally, answer CDI queries. The CDI specialist is your ally, not your enemy. They want you to get credit for taking care of sick and complex patients. They are not permitted to lead the provider, so don’t ask them what they want you to write. But, if you don’t understand the query or issue, have a conversation and get it clarified. It is in everyone’s best interest to get this right.
Documentation improves patient care and demonstrates that you provided excellent patient care. Put mentation back into documentation.
Dr. Remer was a practicing emergency physician for 25 years and a physician advisor for 4 years. She is on the board of directors of the American College of Physician Advisors and the advisory board of the Association of Clinical Documentation Improvement Specialists. She currently provides consulting services for provider education on documentation, CDI, and ICD-10 coding. Dr. Remer can be reached at [email protected]
Value of very early etanercept plus methotrexate not confirmed in real-world RA trial
, investigators say.
A remission rate of 52% was seen with first-line etanercept plus methotrexate, compared with 38% for a strategy of methotrexate escalated to add etanercept in patients not in remission at 24 weeks in the study, known as VEDERA (Very Early Versus Delayed Etanercept in Patients With RA).
Investigators said a difference of 14 percentage points between remission rates was comparable to what was seen among patients with early RA in an earlier randomized trial of etanercept plus methotrexate versus methotrexate monotherapy.
However, the difference was not on par with the “larger than standard” effect of about 30% seen in an exploratory analysis of the very early RA subset in that previous study, according to VEDERA study authors, led by Paul Emery, MD, of the University of Leeds (England).
Taken together, the results highlight a “ceiling effect” in achieving remission in this real-life, treatment-naive cohort, Dr. Emery and coauthors noted in their report, which appears in Annals of the Rheumatic Diseases.
The study population aligned with real-world clinical practice, according to the investigators, who noted that half the cohort had at least one comorbidity.
“This may have partly driven the generally poorer than expected performance, the exact mechanisms for which are unclear,” they wrote in their discussion of results.
Delaying etanercept until failure of methotrexate, instead of giving both drugs up front, was linked to poorer etanercept response in an exploratory analysis of VEDERA. However, Dr. Emery and coinvestigators noted that this finding “requires validation and further investigation.”
While first-line etanercept plus methotrexate is a “clinically appropriate approach” in early RA, results of the VEDERA study don’t help to inform clinicians as to when it would be prudent to select that therapeutic approach, said Daniel E. Furst, MD, professor of medicine (emeritus) at the University of California, Los Angeles.
“Whether you’re treating with methotrexate or methotrexate plus etanercept, they do pretty well,” Dr. Furst said in an interview. “What that says to me is when you have patients with very early RA and the disease is moderately active, you should really try methotrexate before you add expensive other drugs.”
The phase 4, open-label, randomized VEDERA trial included 120 adult patients with new-onset early RA with symptom duration of less than 12 months. All patients in VEDERA had a 28-joint disease activity score based on erythrocyte sedimentation rate (DAS28-ESR) of 3.2 or greater and clinical evidence of synovitis. They were all positive for anti-citrullinated peptide antibody or rheumatoid factor, or had evidence of disease activity in at least one joint by power Doppler ultrasonography.
The patients were randomized to 48 weeks of treatment with either first-line etanercept plus methotrexate, or with methotrexate in a treat-to-target strategy that called for the addition of etanercept if the DAS28-ESR was still 2.6 or greater at 24 weeks.
Based on results of the earlier trial, known as COMET, a confirmatory remission rate in the etanercept plus methotrexate arm was anticipated to be 70%, versus 40% for the methotrexate treat-to-target arm, investigators said in a discussion of their statistical methods.
Study results did not confirm a large effect size, according to the investigators. By week 48, DAS28-ESR remission was achieved in 52% of patients in the first-line etanercept plus methotrexate arm, versus 38% in the methotrexate treat-to-target arm, for an absolute difference of 14 percentage points (odds ratio, 1.73; 95% confidence interval, 0.81-3.70; P = .160).
In early, new-onset RA, remission is the goal, Dr. Emery and coauthors said. The proportions of patients in remission in both arms are “suboptimal rates for the contemporary era,” they wrote.
The escalation to etanercept at week 24 did not improve remission rates appreciably, with about 60% still failing to achieve that endpoint. However, an exploratory analysis suggested the subsequent 24 weeks of etanercept exposure in those escalated patients was associated with a lower rate of remission, compared with 24 weeks of etanercept in the front-line approach, investigators said.
In that analysis, the adjusted odds ratio of achieving DAS28-ESR remission was 2.84 (95% CI, 0.84-9.60) in favor of the first-line etanercept approach.
Dr. Furst said in the interview that the VEDERA results are subject to the inherent biases of an open-label study. He also suggested that further investigations could compare the two first-line treatment approaches specifically in very early RA patients with markers of more severe disease.
“That’s the only way I would think we might gain a little bit more, but so far, these data don’t support getting terribly aggressive,” he said.
The study was funded through an investigator-sponsored research grant provided by Pfizer. Three authors disclosed financial relationships with multiple pharmaceutical companies that market drugs for RA, including Pfizer.
SOURCE: Emery P et al. Ann Rheum Dis. 2020 Jan 29. doi: 10.1136/annrheumdis-2019-216539.
, investigators say.
A remission rate of 52% was seen with first-line etanercept plus methotrexate, compared with 38% for a strategy of methotrexate escalated to add etanercept in patients not in remission at 24 weeks in the study, known as VEDERA (Very Early Versus Delayed Etanercept in Patients With RA).
Investigators said a difference of 14 percentage points between remission rates was comparable to what was seen among patients with early RA in an earlier randomized trial of etanercept plus methotrexate versus methotrexate monotherapy.
However, the difference was not on par with the “larger than standard” effect of about 30% seen in an exploratory analysis of the very early RA subset in that previous study, according to VEDERA study authors, led by Paul Emery, MD, of the University of Leeds (England).
Taken together, the results highlight a “ceiling effect” in achieving remission in this real-life, treatment-naive cohort, Dr. Emery and coauthors noted in their report, which appears in Annals of the Rheumatic Diseases.
The study population aligned with real-world clinical practice, according to the investigators, who noted that half the cohort had at least one comorbidity.
“This may have partly driven the generally poorer than expected performance, the exact mechanisms for which are unclear,” they wrote in their discussion of results.
Delaying etanercept until failure of methotrexate, instead of giving both drugs up front, was linked to poorer etanercept response in an exploratory analysis of VEDERA. However, Dr. Emery and coinvestigators noted that this finding “requires validation and further investigation.”
While first-line etanercept plus methotrexate is a “clinically appropriate approach” in early RA, results of the VEDERA study don’t help to inform clinicians as to when it would be prudent to select that therapeutic approach, said Daniel E. Furst, MD, professor of medicine (emeritus) at the University of California, Los Angeles.
“Whether you’re treating with methotrexate or methotrexate plus etanercept, they do pretty well,” Dr. Furst said in an interview. “What that says to me is when you have patients with very early RA and the disease is moderately active, you should really try methotrexate before you add expensive other drugs.”
The phase 4, open-label, randomized VEDERA trial included 120 adult patients with new-onset early RA with symptom duration of less than 12 months. All patients in VEDERA had a 28-joint disease activity score based on erythrocyte sedimentation rate (DAS28-ESR) of 3.2 or greater and clinical evidence of synovitis. They were all positive for anti-citrullinated peptide antibody or rheumatoid factor, or had evidence of disease activity in at least one joint by power Doppler ultrasonography.
The patients were randomized to 48 weeks of treatment with either first-line etanercept plus methotrexate, or with methotrexate in a treat-to-target strategy that called for the addition of etanercept if the DAS28-ESR was still 2.6 or greater at 24 weeks.
Based on results of the earlier trial, known as COMET, a confirmatory remission rate in the etanercept plus methotrexate arm was anticipated to be 70%, versus 40% for the methotrexate treat-to-target arm, investigators said in a discussion of their statistical methods.
Study results did not confirm a large effect size, according to the investigators. By week 48, DAS28-ESR remission was achieved in 52% of patients in the first-line etanercept plus methotrexate arm, versus 38% in the methotrexate treat-to-target arm, for an absolute difference of 14 percentage points (odds ratio, 1.73; 95% confidence interval, 0.81-3.70; P = .160).
In early, new-onset RA, remission is the goal, Dr. Emery and coauthors said. The proportions of patients in remission in both arms are “suboptimal rates for the contemporary era,” they wrote.
The escalation to etanercept at week 24 did not improve remission rates appreciably, with about 60% still failing to achieve that endpoint. However, an exploratory analysis suggested the subsequent 24 weeks of etanercept exposure in those escalated patients was associated with a lower rate of remission, compared with 24 weeks of etanercept in the front-line approach, investigators said.
In that analysis, the adjusted odds ratio of achieving DAS28-ESR remission was 2.84 (95% CI, 0.84-9.60) in favor of the first-line etanercept approach.
Dr. Furst said in the interview that the VEDERA results are subject to the inherent biases of an open-label study. He also suggested that further investigations could compare the two first-line treatment approaches specifically in very early RA patients with markers of more severe disease.
“That’s the only way I would think we might gain a little bit more, but so far, these data don’t support getting terribly aggressive,” he said.
The study was funded through an investigator-sponsored research grant provided by Pfizer. Three authors disclosed financial relationships with multiple pharmaceutical companies that market drugs for RA, including Pfizer.
SOURCE: Emery P et al. Ann Rheum Dis. 2020 Jan 29. doi: 10.1136/annrheumdis-2019-216539.
, investigators say.
A remission rate of 52% was seen with first-line etanercept plus methotrexate, compared with 38% for a strategy of methotrexate escalated to add etanercept in patients not in remission at 24 weeks in the study, known as VEDERA (Very Early Versus Delayed Etanercept in Patients With RA).
Investigators said a difference of 14 percentage points between remission rates was comparable to what was seen among patients with early RA in an earlier randomized trial of etanercept plus methotrexate versus methotrexate monotherapy.
However, the difference was not on par with the “larger than standard” effect of about 30% seen in an exploratory analysis of the very early RA subset in that previous study, according to VEDERA study authors, led by Paul Emery, MD, of the University of Leeds (England).
Taken together, the results highlight a “ceiling effect” in achieving remission in this real-life, treatment-naive cohort, Dr. Emery and coauthors noted in their report, which appears in Annals of the Rheumatic Diseases.
The study population aligned with real-world clinical practice, according to the investigators, who noted that half the cohort had at least one comorbidity.
“This may have partly driven the generally poorer than expected performance, the exact mechanisms for which are unclear,” they wrote in their discussion of results.
Delaying etanercept until failure of methotrexate, instead of giving both drugs up front, was linked to poorer etanercept response in an exploratory analysis of VEDERA. However, Dr. Emery and coinvestigators noted that this finding “requires validation and further investigation.”
While first-line etanercept plus methotrexate is a “clinically appropriate approach” in early RA, results of the VEDERA study don’t help to inform clinicians as to when it would be prudent to select that therapeutic approach, said Daniel E. Furst, MD, professor of medicine (emeritus) at the University of California, Los Angeles.
“Whether you’re treating with methotrexate or methotrexate plus etanercept, they do pretty well,” Dr. Furst said in an interview. “What that says to me is when you have patients with very early RA and the disease is moderately active, you should really try methotrexate before you add expensive other drugs.”
The phase 4, open-label, randomized VEDERA trial included 120 adult patients with new-onset early RA with symptom duration of less than 12 months. All patients in VEDERA had a 28-joint disease activity score based on erythrocyte sedimentation rate (DAS28-ESR) of 3.2 or greater and clinical evidence of synovitis. They were all positive for anti-citrullinated peptide antibody or rheumatoid factor, or had evidence of disease activity in at least one joint by power Doppler ultrasonography.
The patients were randomized to 48 weeks of treatment with either first-line etanercept plus methotrexate, or with methotrexate in a treat-to-target strategy that called for the addition of etanercept if the DAS28-ESR was still 2.6 or greater at 24 weeks.
Based on results of the earlier trial, known as COMET, a confirmatory remission rate in the etanercept plus methotrexate arm was anticipated to be 70%, versus 40% for the methotrexate treat-to-target arm, investigators said in a discussion of their statistical methods.
Study results did not confirm a large effect size, according to the investigators. By week 48, DAS28-ESR remission was achieved in 52% of patients in the first-line etanercept plus methotrexate arm, versus 38% in the methotrexate treat-to-target arm, for an absolute difference of 14 percentage points (odds ratio, 1.73; 95% confidence interval, 0.81-3.70; P = .160).
In early, new-onset RA, remission is the goal, Dr. Emery and coauthors said. The proportions of patients in remission in both arms are “suboptimal rates for the contemporary era,” they wrote.
The escalation to etanercept at week 24 did not improve remission rates appreciably, with about 60% still failing to achieve that endpoint. However, an exploratory analysis suggested the subsequent 24 weeks of etanercept exposure in those escalated patients was associated with a lower rate of remission, compared with 24 weeks of etanercept in the front-line approach, investigators said.
In that analysis, the adjusted odds ratio of achieving DAS28-ESR remission was 2.84 (95% CI, 0.84-9.60) in favor of the first-line etanercept approach.
Dr. Furst said in the interview that the VEDERA results are subject to the inherent biases of an open-label study. He also suggested that further investigations could compare the two first-line treatment approaches specifically in very early RA patients with markers of more severe disease.
“That’s the only way I would think we might gain a little bit more, but so far, these data don’t support getting terribly aggressive,” he said.
The study was funded through an investigator-sponsored research grant provided by Pfizer. Three authors disclosed financial relationships with multiple pharmaceutical companies that market drugs for RA, including Pfizer.
SOURCE: Emery P et al. Ann Rheum Dis. 2020 Jan 29. doi: 10.1136/annrheumdis-2019-216539.
FROM ANNALS OF THE RHEUMATIC DISEASES