User login
Course Takes Aim at Innovative Approaches to Rare Congenital Heart Disease
One of the noteworthy courses to be held on Saturday will focus exclusively on congenital heart disease and the skills necessary to treat some of its most unusual and difficult complications.
“We looked at previous years to see what are some good areas that are either complicated or controversial, that have not been covered in recent years, and that will bring something new to practitioners or to present various views of controversies,” explained session chair David P. Bichell, MD, of Vanderbilt University. “And it’s really centered on techniques.”
Repairing and replacing atrioventricular valves will also be discussed at length. Special attention will be paid to Ebstein’s tricuspid valve – something that comes up very rarely for most surgeons, which will be presented by Joseph A. Dearani, MD, of the Mayo Clinic – along with a way to reconstruct a tricuspid valve called the Cone Technique. Dr. Bichell noted that too many surgeons are unaware of the Cone Technique.
“Replacing valves in infants is a really special problem because the infants grow, because prosthetic knobs are too small, [and] because anticoagulation is a headache,” explained Dr. Bichell. “There are various options for replacing a valve, creating a valve out of a cylinder of material, and putting in a valve that is balloon deployed. We depend on those colleagues who see these rare things to share their experiences.
“There will be some profusion talks on miniaturizing the circuit, bloodless surgery, and other topics that are of interest to everyone, but few have good answers for,” said Dr. Bichell. “But those who have put more thought and experience into it are going to share what they know.”
The sessions will run about 15 minutes each and will feature a video of the technique being demonstrated while the speaker discusses the procedure. The overarching goal of the session is to give attendees the confidence to go into their practice the next day and, should they see a patient with a presentation they’ve never seen before, have the confidence to perform the necessary procedure. “We want to focus on the rare but relevant end of what people would be interested in,” said Dr. Bichell.
One of the noteworthy courses to be held on Saturday will focus exclusively on congenital heart disease and the skills necessary to treat some of its most unusual and difficult complications.
“We looked at previous years to see what are some good areas that are either complicated or controversial, that have not been covered in recent years, and that will bring something new to practitioners or to present various views of controversies,” explained session chair David P. Bichell, MD, of Vanderbilt University. “And it’s really centered on techniques.”
Repairing and replacing atrioventricular valves will also be discussed at length. Special attention will be paid to Ebstein’s tricuspid valve – something that comes up very rarely for most surgeons, which will be presented by Joseph A. Dearani, MD, of the Mayo Clinic – along with a way to reconstruct a tricuspid valve called the Cone Technique. Dr. Bichell noted that too many surgeons are unaware of the Cone Technique.
“Replacing valves in infants is a really special problem because the infants grow, because prosthetic knobs are too small, [and] because anticoagulation is a headache,” explained Dr. Bichell. “There are various options for replacing a valve, creating a valve out of a cylinder of material, and putting in a valve that is balloon deployed. We depend on those colleagues who see these rare things to share their experiences.
“There will be some profusion talks on miniaturizing the circuit, bloodless surgery, and other topics that are of interest to everyone, but few have good answers for,” said Dr. Bichell. “But those who have put more thought and experience into it are going to share what they know.”
The sessions will run about 15 minutes each and will feature a video of the technique being demonstrated while the speaker discusses the procedure. The overarching goal of the session is to give attendees the confidence to go into their practice the next day and, should they see a patient with a presentation they’ve never seen before, have the confidence to perform the necessary procedure. “We want to focus on the rare but relevant end of what people would be interested in,” said Dr. Bichell.
One of the noteworthy courses to be held on Saturday will focus exclusively on congenital heart disease and the skills necessary to treat some of its most unusual and difficult complications.
“We looked at previous years to see what are some good areas that are either complicated or controversial, that have not been covered in recent years, and that will bring something new to practitioners or to present various views of controversies,” explained session chair David P. Bichell, MD, of Vanderbilt University. “And it’s really centered on techniques.”
Repairing and replacing atrioventricular valves will also be discussed at length. Special attention will be paid to Ebstein’s tricuspid valve – something that comes up very rarely for most surgeons, which will be presented by Joseph A. Dearani, MD, of the Mayo Clinic – along with a way to reconstruct a tricuspid valve called the Cone Technique. Dr. Bichell noted that too many surgeons are unaware of the Cone Technique.
“Replacing valves in infants is a really special problem because the infants grow, because prosthetic knobs are too small, [and] because anticoagulation is a headache,” explained Dr. Bichell. “There are various options for replacing a valve, creating a valve out of a cylinder of material, and putting in a valve that is balloon deployed. We depend on those colleagues who see these rare things to share their experiences.
“There will be some profusion talks on miniaturizing the circuit, bloodless surgery, and other topics that are of interest to everyone, but few have good answers for,” said Dr. Bichell. “But those who have put more thought and experience into it are going to share what they know.”
The sessions will run about 15 minutes each and will feature a video of the technique being demonstrated while the speaker discusses the procedure. The overarching goal of the session is to give attendees the confidence to go into their practice the next day and, should they see a patient with a presentation they’ve never seen before, have the confidence to perform the necessary procedure. “We want to focus on the rare but relevant end of what people would be interested in,” said Dr. Bichell.
NCCN myelofibrosis guideline: Patient voice is key
ORLANDO – Referral to a specialized center with expertise in the management of myeloproliferative neoplasms is strongly recommended for all patients diagnosed with myelofibrosis, according to a new treatment guideline from the National Comprehensive Cancer Network.
The guideline is the first in a series addressing myeloproliferative neoplasms (MPNs), and it focuses on the diagnostic work-up of MPNs, as well as the treatment of myelofibrosis. The guideline panel, led by panel chair Ruben A. Mesa, MD, is working next on guidelines for the other two “core classic” Philadelphia chromosome–negative MPNs: polycythemia vera, and essential thrombocythemia.
Nearly two-thirds of myelofibrosis patients have intermediate-risk 2 or high-risk disease, and treatment decisions in these patients are complex and require patient input – particularly in candidates for allogeneic hematopoietic stem cell transplantation, he said.
“These diseases can be a little different than other malignant diseases,” Dr. Mesa said, explaining that while there is a clear risk of progression to acute myeloid leukemia, and from polycythemia vera and essential thrombocythemia to myelofibrosis, and while the diseases can be fatal, the burden patients face is not solely related to mortality.
There are implications in terms of health that are independent of that, such as the risk of thrombosis and bleeding, the potential for cytopenia, and severe splenomegaly that results in significant symptoms, he said.
Further, while molecular mutations and their implications for prognosis are a “rapidly moving part of the discussion,” the care of patients with MPNs involves far more than a molecular understanding of the disease.
In fact, the role of molecular changes in these patients is speculative, he said.
While such changes can be assessed and used for patient stratification, their role in myelofibrosis – unlike in other diseases such as chronic myeloid leukemia where the level of change in a target gene is highly relevant and prognostic, is not yet clear.
Thus, a core aspect of the guideline is inclusion of the voice of the patient in individualizing care, he said, noting that many factors should be considered, including how well the patient metabolizes drugs, and the symptom profile, psychosocial circumstances, support structure, and personal beliefs.
“It’s not solely about the tumor,” he stressed.
In fact, the answer to the question of whether a patient can be symptomatic enough to require a specific treatment is “no,” because of the potential for side effects, risk, expense, and other considerations.
“So the voice of the patient is always a key part [of the decision],” he said, noting also that as with all NCCN guidelines, this guideline is a partnership with the treating physician; deciding who is a transplant candidate is a nuanced issue for which the panel provides “discussion and guidance.”
“But clearly, these guidelines are the most useful and helpful in the setting of experienced providers bringing all of their experiences to bear,” he said.
In general, however, the guidelines call for allogeneic hematopoietic stem cell transplantation (HCT) in those with intermediate-risk 2 or high-risk disease who are transplant candidates, and treatment based on assessment of symptom burden (using the MPN–Symptom Assessment Form Total Symptom Score–10 Items) in those who are not HCT candidates. Those with platelets at 50,000 or below should be considered for clinical trial enrollment, and those with platelets above 50,000 should be considered for a clinical trial or treatment with the oral JAK1 and JAK2 inhibitor ruxolitinib, which has been shown to have beneficial effects on both symptoms and survival and which is approved for patients with platelets above 50,000. .
Treated patients should be monitored for response and for signs and symptoms of disease progression every 3-6 months. Treatment should continue in those who respond, as well as in those who do not – as long as there is no disease progression.
Those with progressive disease include patients who are moving toward acute leukemia, and those with overt acute leukemia.
“Here is where the key decision occurs. Are they or are they not a transplant candidate? If they are a candidate, we have a potentially curative track which would include cytoreduction followed by transplant,” Dr. Mesa said.
Cytoreduction can involve hypomethylating agents if the patient doesn’t have excess blast cells or too high a burden of disease.
Acute myeloid leukemia–like induction chemotherapy followed by allogeneic HCT is also an option in these patients.
As for treatment of low-risk myelofibrosis, the guideline states that asymptomatic patients can be observed or enrolled in a clinical trial and monitored for progression every 3-6 months, and that symptomatic patients should receive ruxolitinib or interferons (which are used off label), or be enrolled in a clinical trial. Treatment is important for patients with particularly difficult symptoms, he said, noting that some patients have had pruritus so severe that they have committed suicide. Treatment should continue unless monitoring shows signs of progression to intermediate risk 1, intermediate risk 2/high-risk, or advanced stage disease.
For those with intermediate risk 1 disease, the guideline calls for observation or ruxolitinib in those who are symptomatic, or clinical trial enrollment or allogeneic HCT. Treatment should continue unless monitoring shows disease progression, in which case the appropriate algorithm should be considered.
The guideline also addresses several special circumstances, including the management of anemia in myelofibrosis patients, which can be a difficult issue, he said.
Since the guideline was first published in December, two updates have been incorporated, and Dr. Mesa said that he anticipates regular updates given the rapidly evolving understanding of MPNs and new findings with respect to potential treatment strategies.
He noted that a number of drugs are currently in clinical trials involving patients with myelofibrosis, including the JAK2/FLT3 inhibitor pacritinib, the JAK1/JAK2 inhibitor momelotinib, the active antifibrosing agent PRM-151, and the telomerase inhibitor imetelstat, as well as numerous drug combinations.
Going forward, the guideline panel will be focusing on four different areas of assessment, including new therapies and new genetic therapies, improving transplant outcomes, MPN symptom and quality of life assessment, and nonpharmacologic interventions such as yoga.
“We certainly hope to complement things over time, to look not only at pharmacologic interventions, but others that patients may be able to utilize from a toolkit of resources,” he said.
COMFORT-1 update: ruxolitinib responses durable in myelofibrosis
To date, ruxolitinib is the only Food and Drug Administration–approved drug for the treatment of myelofibrosis.
The randomized controlled phase III COMFORT I and II trials conducted in the United States and Europe, respectively, demonstrated that the oral JAK1/JAK2 inhibitor has a rapid, beneficial impact on both survival and disease-associated enlargement of the spleen and improvement in related symptoms, Dr. Mesa said.
A 5-year update on data from 309 patients in the COMFORT-1 trial, as reported at the annual meeting of the American Society of Clinical Oncology in 2016, confirmed the durability of treatment responses to ruxolitinib in patients initially randomized to receive the drug, he said.
“We were able to demonstrate a continued survival advantage for those individuals receiving ruxolitinib,” he added.
At weeks 24 and 264, the mean spleen volume reduction was 31.6% and 37.6%, respectively, in those originally randomized to ruxolitinib. The median duration of at least 35% spleen volume reduction was 168.3 weeks.
Overall survival favored ruxolitinib (hazard ratio, 0.69). Median overall survival in the ruxolitinib group had not yet been reached.
“But we realize our work is not done. The survival curve does not plateau; we are not curing these patients. We’re having meaningful impact, but we have room to continue to improve,” he said.
Also, there is an initial drop in platelet counts that tends to stabilize, but not improve, and there is worsening of anemia (new onset grade 3 or 4 anemia was 25.2% with ruxolitinib, and 26.1% in 111 of 154 patients who crossed over from the placebo group), and although this tends to improve, these are among areas of unmet need, he added.
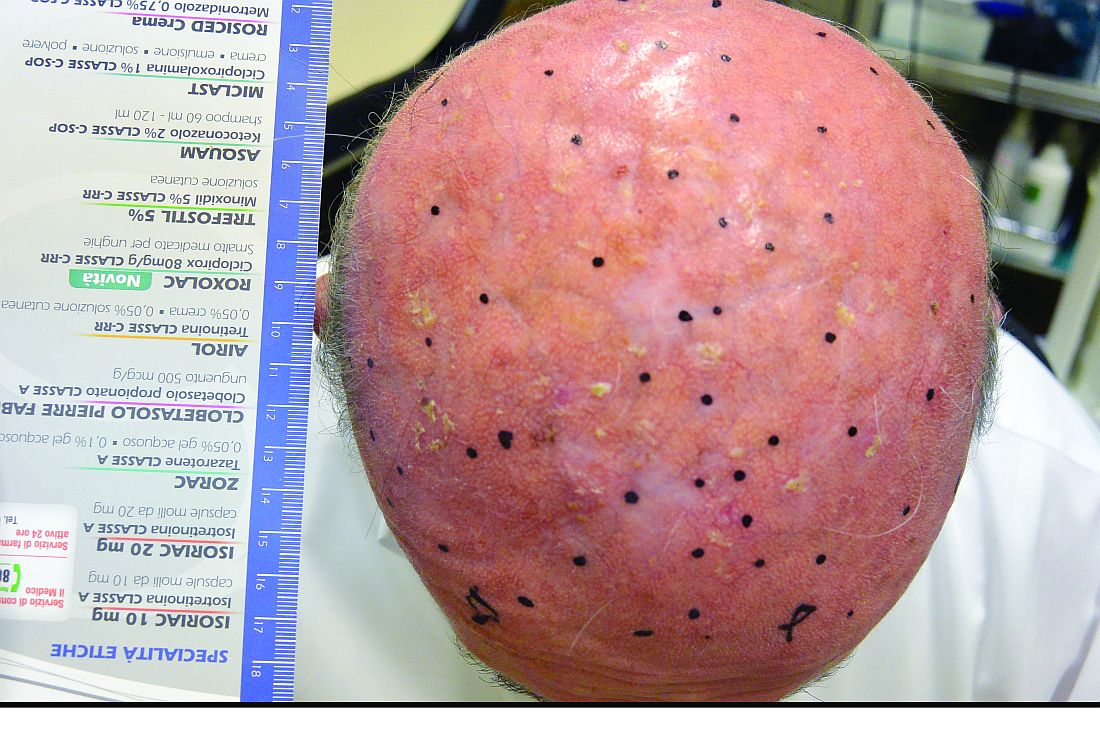
Further, long-term risks of treatment include cutaneous malignancies (basal cell carcinoma occurred in 7.7% and 9.0% of treatment and crossover patients, respectively), which are difficult to separate from baseline hydroxyurea use, and increased risk of herpes zoster (which occurred in 10.3% and 13.5% of treated and crossover patients).
However, there appears to be no increased risk – and there may be a slight decreased risk – of progression to acute leukemia, Dr. Mesa said.
Dr. Mesa disclosed that he has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals, Celgene, CTI BioPharma, Galena Biopharma, Gilead Sciences, Incyte, Novartis Pharmaceuticals, and Promedior.
A step toward harmonizing treatment
Myelofibrosis is a rare chronic leukemia with a complex biology. Disease heterogeneity poses several challenges in the appropriate selection and timing of treatments in this disorder. The NCCN Practice Guidelines in Myelofibrosis is an important step towards harmonizing clinical practice for treating this disease and improving the care of patients.
Vikas Gupta, MD, FRCP, FRCPath, is Director of The Elizabeth and Tony Comper MPN Program at Princess Margaret Cancer Centre in Toronto and a member of the editorial advisory board of Hematology News.
A step toward harmonizing treatment
Myelofibrosis is a rare chronic leukemia with a complex biology. Disease heterogeneity poses several challenges in the appropriate selection and timing of treatments in this disorder. The NCCN Practice Guidelines in Myelofibrosis is an important step towards harmonizing clinical practice for treating this disease and improving the care of patients.
Vikas Gupta, MD, FRCP, FRCPath, is Director of The Elizabeth and Tony Comper MPN Program at Princess Margaret Cancer Centre in Toronto and a member of the editorial advisory board of Hematology News.
A step toward harmonizing treatment
Myelofibrosis is a rare chronic leukemia with a complex biology. Disease heterogeneity poses several challenges in the appropriate selection and timing of treatments in this disorder. The NCCN Practice Guidelines in Myelofibrosis is an important step towards harmonizing clinical practice for treating this disease and improving the care of patients.
Vikas Gupta, MD, FRCP, FRCPath, is Director of The Elizabeth and Tony Comper MPN Program at Princess Margaret Cancer Centre in Toronto and a member of the editorial advisory board of Hematology News.
ORLANDO – Referral to a specialized center with expertise in the management of myeloproliferative neoplasms is strongly recommended for all patients diagnosed with myelofibrosis, according to a new treatment guideline from the National Comprehensive Cancer Network.
The guideline is the first in a series addressing myeloproliferative neoplasms (MPNs), and it focuses on the diagnostic work-up of MPNs, as well as the treatment of myelofibrosis. The guideline panel, led by panel chair Ruben A. Mesa, MD, is working next on guidelines for the other two “core classic” Philadelphia chromosome–negative MPNs: polycythemia vera, and essential thrombocythemia.
Nearly two-thirds of myelofibrosis patients have intermediate-risk 2 or high-risk disease, and treatment decisions in these patients are complex and require patient input – particularly in candidates for allogeneic hematopoietic stem cell transplantation, he said.
“These diseases can be a little different than other malignant diseases,” Dr. Mesa said, explaining that while there is a clear risk of progression to acute myeloid leukemia, and from polycythemia vera and essential thrombocythemia to myelofibrosis, and while the diseases can be fatal, the burden patients face is not solely related to mortality.
There are implications in terms of health that are independent of that, such as the risk of thrombosis and bleeding, the potential for cytopenia, and severe splenomegaly that results in significant symptoms, he said.
Further, while molecular mutations and their implications for prognosis are a “rapidly moving part of the discussion,” the care of patients with MPNs involves far more than a molecular understanding of the disease.
In fact, the role of molecular changes in these patients is speculative, he said.
While such changes can be assessed and used for patient stratification, their role in myelofibrosis – unlike in other diseases such as chronic myeloid leukemia where the level of change in a target gene is highly relevant and prognostic, is not yet clear.
Thus, a core aspect of the guideline is inclusion of the voice of the patient in individualizing care, he said, noting that many factors should be considered, including how well the patient metabolizes drugs, and the symptom profile, psychosocial circumstances, support structure, and personal beliefs.
“It’s not solely about the tumor,” he stressed.
In fact, the answer to the question of whether a patient can be symptomatic enough to require a specific treatment is “no,” because of the potential for side effects, risk, expense, and other considerations.
“So the voice of the patient is always a key part [of the decision],” he said, noting also that as with all NCCN guidelines, this guideline is a partnership with the treating physician; deciding who is a transplant candidate is a nuanced issue for which the panel provides “discussion and guidance.”
“But clearly, these guidelines are the most useful and helpful in the setting of experienced providers bringing all of their experiences to bear,” he said.
In general, however, the guidelines call for allogeneic hematopoietic stem cell transplantation (HCT) in those with intermediate-risk 2 or high-risk disease who are transplant candidates, and treatment based on assessment of symptom burden (using the MPN–Symptom Assessment Form Total Symptom Score–10 Items) in those who are not HCT candidates. Those with platelets at 50,000 or below should be considered for clinical trial enrollment, and those with platelets above 50,000 should be considered for a clinical trial or treatment with the oral JAK1 and JAK2 inhibitor ruxolitinib, which has been shown to have beneficial effects on both symptoms and survival and which is approved for patients with platelets above 50,000. .
Treated patients should be monitored for response and for signs and symptoms of disease progression every 3-6 months. Treatment should continue in those who respond, as well as in those who do not – as long as there is no disease progression.
Those with progressive disease include patients who are moving toward acute leukemia, and those with overt acute leukemia.
“Here is where the key decision occurs. Are they or are they not a transplant candidate? If they are a candidate, we have a potentially curative track which would include cytoreduction followed by transplant,” Dr. Mesa said.
Cytoreduction can involve hypomethylating agents if the patient doesn’t have excess blast cells or too high a burden of disease.
Acute myeloid leukemia–like induction chemotherapy followed by allogeneic HCT is also an option in these patients.
As for treatment of low-risk myelofibrosis, the guideline states that asymptomatic patients can be observed or enrolled in a clinical trial and monitored for progression every 3-6 months, and that symptomatic patients should receive ruxolitinib or interferons (which are used off label), or be enrolled in a clinical trial. Treatment is important for patients with particularly difficult symptoms, he said, noting that some patients have had pruritus so severe that they have committed suicide. Treatment should continue unless monitoring shows signs of progression to intermediate risk 1, intermediate risk 2/high-risk, or advanced stage disease.
For those with intermediate risk 1 disease, the guideline calls for observation or ruxolitinib in those who are symptomatic, or clinical trial enrollment or allogeneic HCT. Treatment should continue unless monitoring shows disease progression, in which case the appropriate algorithm should be considered.
The guideline also addresses several special circumstances, including the management of anemia in myelofibrosis patients, which can be a difficult issue, he said.
Since the guideline was first published in December, two updates have been incorporated, and Dr. Mesa said that he anticipates regular updates given the rapidly evolving understanding of MPNs and new findings with respect to potential treatment strategies.
He noted that a number of drugs are currently in clinical trials involving patients with myelofibrosis, including the JAK2/FLT3 inhibitor pacritinib, the JAK1/JAK2 inhibitor momelotinib, the active antifibrosing agent PRM-151, and the telomerase inhibitor imetelstat, as well as numerous drug combinations.
Going forward, the guideline panel will be focusing on four different areas of assessment, including new therapies and new genetic therapies, improving transplant outcomes, MPN symptom and quality of life assessment, and nonpharmacologic interventions such as yoga.
“We certainly hope to complement things over time, to look not only at pharmacologic interventions, but others that patients may be able to utilize from a toolkit of resources,” he said.
COMFORT-1 update: ruxolitinib responses durable in myelofibrosis
To date, ruxolitinib is the only Food and Drug Administration–approved drug for the treatment of myelofibrosis.
The randomized controlled phase III COMFORT I and II trials conducted in the United States and Europe, respectively, demonstrated that the oral JAK1/JAK2 inhibitor has a rapid, beneficial impact on both survival and disease-associated enlargement of the spleen and improvement in related symptoms, Dr. Mesa said.
A 5-year update on data from 309 patients in the COMFORT-1 trial, as reported at the annual meeting of the American Society of Clinical Oncology in 2016, confirmed the durability of treatment responses to ruxolitinib in patients initially randomized to receive the drug, he said.
“We were able to demonstrate a continued survival advantage for those individuals receiving ruxolitinib,” he added.
At weeks 24 and 264, the mean spleen volume reduction was 31.6% and 37.6%, respectively, in those originally randomized to ruxolitinib. The median duration of at least 35% spleen volume reduction was 168.3 weeks.
Overall survival favored ruxolitinib (hazard ratio, 0.69). Median overall survival in the ruxolitinib group had not yet been reached.
“But we realize our work is not done. The survival curve does not plateau; we are not curing these patients. We’re having meaningful impact, but we have room to continue to improve,” he said.
Also, there is an initial drop in platelet counts that tends to stabilize, but not improve, and there is worsening of anemia (new onset grade 3 or 4 anemia was 25.2% with ruxolitinib, and 26.1% in 111 of 154 patients who crossed over from the placebo group), and although this tends to improve, these are among areas of unmet need, he added.
Further, long-term risks of treatment include cutaneous malignancies (basal cell carcinoma occurred in 7.7% and 9.0% of treatment and crossover patients, respectively), which are difficult to separate from baseline hydroxyurea use, and increased risk of herpes zoster (which occurred in 10.3% and 13.5% of treated and crossover patients).
However, there appears to be no increased risk – and there may be a slight decreased risk – of progression to acute leukemia, Dr. Mesa said.
Dr. Mesa disclosed that he has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals, Celgene, CTI BioPharma, Galena Biopharma, Gilead Sciences, Incyte, Novartis Pharmaceuticals, and Promedior.
ORLANDO – Referral to a specialized center with expertise in the management of myeloproliferative neoplasms is strongly recommended for all patients diagnosed with myelofibrosis, according to a new treatment guideline from the National Comprehensive Cancer Network.
The guideline is the first in a series addressing myeloproliferative neoplasms (MPNs), and it focuses on the diagnostic work-up of MPNs, as well as the treatment of myelofibrosis. The guideline panel, led by panel chair Ruben A. Mesa, MD, is working next on guidelines for the other two “core classic” Philadelphia chromosome–negative MPNs: polycythemia vera, and essential thrombocythemia.
Nearly two-thirds of myelofibrosis patients have intermediate-risk 2 or high-risk disease, and treatment decisions in these patients are complex and require patient input – particularly in candidates for allogeneic hematopoietic stem cell transplantation, he said.
“These diseases can be a little different than other malignant diseases,” Dr. Mesa said, explaining that while there is a clear risk of progression to acute myeloid leukemia, and from polycythemia vera and essential thrombocythemia to myelofibrosis, and while the diseases can be fatal, the burden patients face is not solely related to mortality.
There are implications in terms of health that are independent of that, such as the risk of thrombosis and bleeding, the potential for cytopenia, and severe splenomegaly that results in significant symptoms, he said.
Further, while molecular mutations and their implications for prognosis are a “rapidly moving part of the discussion,” the care of patients with MPNs involves far more than a molecular understanding of the disease.
In fact, the role of molecular changes in these patients is speculative, he said.
While such changes can be assessed and used for patient stratification, their role in myelofibrosis – unlike in other diseases such as chronic myeloid leukemia where the level of change in a target gene is highly relevant and prognostic, is not yet clear.
Thus, a core aspect of the guideline is inclusion of the voice of the patient in individualizing care, he said, noting that many factors should be considered, including how well the patient metabolizes drugs, and the symptom profile, psychosocial circumstances, support structure, and personal beliefs.
“It’s not solely about the tumor,” he stressed.
In fact, the answer to the question of whether a patient can be symptomatic enough to require a specific treatment is “no,” because of the potential for side effects, risk, expense, and other considerations.
“So the voice of the patient is always a key part [of the decision],” he said, noting also that as with all NCCN guidelines, this guideline is a partnership with the treating physician; deciding who is a transplant candidate is a nuanced issue for which the panel provides “discussion and guidance.”
“But clearly, these guidelines are the most useful and helpful in the setting of experienced providers bringing all of their experiences to bear,” he said.
In general, however, the guidelines call for allogeneic hematopoietic stem cell transplantation (HCT) in those with intermediate-risk 2 or high-risk disease who are transplant candidates, and treatment based on assessment of symptom burden (using the MPN–Symptom Assessment Form Total Symptom Score–10 Items) in those who are not HCT candidates. Those with platelets at 50,000 or below should be considered for clinical trial enrollment, and those with platelets above 50,000 should be considered for a clinical trial or treatment with the oral JAK1 and JAK2 inhibitor ruxolitinib, which has been shown to have beneficial effects on both symptoms and survival and which is approved for patients with platelets above 50,000. .
Treated patients should be monitored for response and for signs and symptoms of disease progression every 3-6 months. Treatment should continue in those who respond, as well as in those who do not – as long as there is no disease progression.
Those with progressive disease include patients who are moving toward acute leukemia, and those with overt acute leukemia.
“Here is where the key decision occurs. Are they or are they not a transplant candidate? If they are a candidate, we have a potentially curative track which would include cytoreduction followed by transplant,” Dr. Mesa said.
Cytoreduction can involve hypomethylating agents if the patient doesn’t have excess blast cells or too high a burden of disease.
Acute myeloid leukemia–like induction chemotherapy followed by allogeneic HCT is also an option in these patients.
As for treatment of low-risk myelofibrosis, the guideline states that asymptomatic patients can be observed or enrolled in a clinical trial and monitored for progression every 3-6 months, and that symptomatic patients should receive ruxolitinib or interferons (which are used off label), or be enrolled in a clinical trial. Treatment is important for patients with particularly difficult symptoms, he said, noting that some patients have had pruritus so severe that they have committed suicide. Treatment should continue unless monitoring shows signs of progression to intermediate risk 1, intermediate risk 2/high-risk, or advanced stage disease.
For those with intermediate risk 1 disease, the guideline calls for observation or ruxolitinib in those who are symptomatic, or clinical trial enrollment or allogeneic HCT. Treatment should continue unless monitoring shows disease progression, in which case the appropriate algorithm should be considered.
The guideline also addresses several special circumstances, including the management of anemia in myelofibrosis patients, which can be a difficult issue, he said.
Since the guideline was first published in December, two updates have been incorporated, and Dr. Mesa said that he anticipates regular updates given the rapidly evolving understanding of MPNs and new findings with respect to potential treatment strategies.
He noted that a number of drugs are currently in clinical trials involving patients with myelofibrosis, including the JAK2/FLT3 inhibitor pacritinib, the JAK1/JAK2 inhibitor momelotinib, the active antifibrosing agent PRM-151, and the telomerase inhibitor imetelstat, as well as numerous drug combinations.
Going forward, the guideline panel will be focusing on four different areas of assessment, including new therapies and new genetic therapies, improving transplant outcomes, MPN symptom and quality of life assessment, and nonpharmacologic interventions such as yoga.
“We certainly hope to complement things over time, to look not only at pharmacologic interventions, but others that patients may be able to utilize from a toolkit of resources,” he said.
COMFORT-1 update: ruxolitinib responses durable in myelofibrosis
To date, ruxolitinib is the only Food and Drug Administration–approved drug for the treatment of myelofibrosis.
The randomized controlled phase III COMFORT I and II trials conducted in the United States and Europe, respectively, demonstrated that the oral JAK1/JAK2 inhibitor has a rapid, beneficial impact on both survival and disease-associated enlargement of the spleen and improvement in related symptoms, Dr. Mesa said.
A 5-year update on data from 309 patients in the COMFORT-1 trial, as reported at the annual meeting of the American Society of Clinical Oncology in 2016, confirmed the durability of treatment responses to ruxolitinib in patients initially randomized to receive the drug, he said.
“We were able to demonstrate a continued survival advantage for those individuals receiving ruxolitinib,” he added.
At weeks 24 and 264, the mean spleen volume reduction was 31.6% and 37.6%, respectively, in those originally randomized to ruxolitinib. The median duration of at least 35% spleen volume reduction was 168.3 weeks.
Overall survival favored ruxolitinib (hazard ratio, 0.69). Median overall survival in the ruxolitinib group had not yet been reached.
“But we realize our work is not done. The survival curve does not plateau; we are not curing these patients. We’re having meaningful impact, but we have room to continue to improve,” he said.
Also, there is an initial drop in platelet counts that tends to stabilize, but not improve, and there is worsening of anemia (new onset grade 3 or 4 anemia was 25.2% with ruxolitinib, and 26.1% in 111 of 154 patients who crossed over from the placebo group), and although this tends to improve, these are among areas of unmet need, he added.
Further, long-term risks of treatment include cutaneous malignancies (basal cell carcinoma occurred in 7.7% and 9.0% of treatment and crossover patients, respectively), which are difficult to separate from baseline hydroxyurea use, and increased risk of herpes zoster (which occurred in 10.3% and 13.5% of treated and crossover patients).
However, there appears to be no increased risk – and there may be a slight decreased risk – of progression to acute leukemia, Dr. Mesa said.
Dr. Mesa disclosed that he has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals, Celgene, CTI BioPharma, Galena Biopharma, Gilead Sciences, Incyte, Novartis Pharmaceuticals, and Promedior.
EXPERT ANALYSIS AT THE NCCN ANNUAL CONFERENCE
Is this psychotherapy?
“Create a safe zone where anything can gain expression.”
– Carl Rogers, PhD
The patient
“I have no purpose,” Audrey said. She sat immobile, a woman of 45 who looked 10 years older. Audrey hated New York, the crowds, the weather. Her husband, a successful sales executive, supported her; a month earlier, they had moved from California to New York. Her depression and panic attacks dated back to childhood. She also suffered from arthritis, asthma, and lupus. Audrey told me that her parents, long dead, were dreadful. “My mother was the most abusive person. She put out cigarettes on my arm; beat the s*** out of me, my brother, and sister.” She said that in New York, she stayed in her apartment on her couch or shopped for clothes that, ultimately, remained in the closet.
According to Audrey, nothing helped. She was on psychoactive medications prescribed by her Beverly Hills psychiatrist – Cymbalta and Wellbutrin for depression, Klonopin for anxiety, Abilify for agitation. She also took Neurontin for nerve pain and opioids for arthritis, prescribed by a pain specialist.
The process
In residency and beyond, psychiatrists learn to develop a treatment plan based on the patient’s history and symptoms. Some individuals want to understand the origin of their suffering with a thrust toward recovery and independence. Others lack that capacity and need to shore up their defenses through supportive intervention. The direction of how to proceed is often a compromise between what the doctor sees as ideal and what the patient desires.
Outcome
All seemed stagnant for 2 years. Then, Audrey’s demeanor changed dramatically. She enjoyed walking her dog in Central Park; she reflected on her devoted husband, who encouraged her. Audrey’s transformation progressed.
Three months later, her husband took a position in Montreal. On a visit to New York, she told me that she no longer disliked the city, even the noise and the cold weather. I questioned what made the difference. “You saved my life,” Audrey said. I asked what she meant. “You were always there for me,” she said. “You made an effort to try to help me get better. ... You can be funny, witty.” She ventured that she had been through “a change of life, maybe a midlife crisis.” She made new friends in Montreal. “I’m getting rid of the negative people.” Audrey planned to continue psychiatric care in Montreal. In part, Audrey credited improvement to our sessions, and I told her I was grateful to be of help.
Another case
Arthur was a seriously ill, 88-year-old retired pulmonologist, so weak that he was being spoon-fed when I entered his room. He had a “fear of dying or living with disability” from diffuse lymphoma, complicated by tumor lysis syndrome after chemotherapy. “I don’t want to give up, for myself and my family,” he said.
Arthur told me about his struggles to achieve despite poverty in childhood. He needed a scholarship to attend a local college. There were trials at a medical school that failed out less capable students. He commuted and studied at the kitchen table until 3 a.m. Arthur’s mother-in-law had disapproved of him and wanted her daughter to marry a wealthy businessman. During their courtship, Arthur gave his girlfriend a gold bracelet, which he said she should keep it regardless of whether they broke up.
Arthur had a modest evaluation of his capabilities despite a good practice. Meanwhile, his home life progressed: Two of his three children became doctors; the third succeeded as an accountant. His marriage thrived.
At the end of our session, I expressed surprise that his mother-in-law had taken such a dim view of a suitor with determination, impressive credentials, and a future that would be a source of pride. I also assured him that he had chosen fine doctors for his care.
The next time I visited Arthur, he heaped praise on me for turning his life around. I had restored his hope. His daughter, who was visiting later, told me that, no matter how much the family and medical staff encouraged Arthur, “nothing happened until he met you.” I, of course, thanked Arthur for his gratitude and experienced amazement at the success of the talking cure.
Lessons learned
These examples fail to prove that the unraveling of psychodynamics has lost its place. And there is value in the variety of treatment and medications psychiatrists that can offer. But exceptions occur. Do they show there is magic in transference? Is there an ideal way for a therapist to behave? Should we influence the patient by giving advice or wait until he reaches conclusions? Psychiatrists try to free the patient from his suffering, enhancing his perspective, ultimately his independence. How often do we fail to understand how that happens when it does occur?
The flight into health
The early or sudden disappearance of symptoms is referred to as a flight into health, a perhaps-outdated concept that presents “a defense against the anxiety engendered by the prospect of further psychoanalytic exploration of the patient’s conflict” (Farlex Partner Medical Dictionary, 2012). Some patients settle for less. Either they reach their own conclusions, as did Audrey, or they unburden themselves to a compassionate listener, as did Arthur.
What to conclude
The methodical sometimes exists in psychiatric treatment but often not. The practice of medicine is based on science. As described by writer Lisa Randall in a review of the book “Reality Is Not What It Seems: The Journey to Quantum Gravity” (New York: Riverhead Books, 2017): “Science provides a systematic method of building up from the measured and tested … to realms that we don’t yet understand because measurements are not yet sufficiently precise or are too outside our limited perspective” (New York Times Book Review, March 5, 2017, p. 15). The author was describing physics, but her insight applies to medical specialties as well. It is alluring to try to understand our patients. The complexity of mental illness challenges psychiatrists to use science, compassion, and intuition.
Dr. Cohen is in private practice and is a clinical assistant professor of psychiatry at Weill Cornell Medical Center of New York-Presbyterian Hospital, and psychiatric consultant at the Hospital for Special Surgery, also in New York. She made changes to the patient narratives to protect their identities.
“Create a safe zone where anything can gain expression.”
– Carl Rogers, PhD
The patient
“I have no purpose,” Audrey said. She sat immobile, a woman of 45 who looked 10 years older. Audrey hated New York, the crowds, the weather. Her husband, a successful sales executive, supported her; a month earlier, they had moved from California to New York. Her depression and panic attacks dated back to childhood. She also suffered from arthritis, asthma, and lupus. Audrey told me that her parents, long dead, were dreadful. “My mother was the most abusive person. She put out cigarettes on my arm; beat the s*** out of me, my brother, and sister.” She said that in New York, she stayed in her apartment on her couch or shopped for clothes that, ultimately, remained in the closet.
According to Audrey, nothing helped. She was on psychoactive medications prescribed by her Beverly Hills psychiatrist – Cymbalta and Wellbutrin for depression, Klonopin for anxiety, Abilify for agitation. She also took Neurontin for nerve pain and opioids for arthritis, prescribed by a pain specialist.
The process
In residency and beyond, psychiatrists learn to develop a treatment plan based on the patient’s history and symptoms. Some individuals want to understand the origin of their suffering with a thrust toward recovery and independence. Others lack that capacity and need to shore up their defenses through supportive intervention. The direction of how to proceed is often a compromise between what the doctor sees as ideal and what the patient desires.
Outcome
All seemed stagnant for 2 years. Then, Audrey’s demeanor changed dramatically. She enjoyed walking her dog in Central Park; she reflected on her devoted husband, who encouraged her. Audrey’s transformation progressed.
Three months later, her husband took a position in Montreal. On a visit to New York, she told me that she no longer disliked the city, even the noise and the cold weather. I questioned what made the difference. “You saved my life,” Audrey said. I asked what she meant. “You were always there for me,” she said. “You made an effort to try to help me get better. ... You can be funny, witty.” She ventured that she had been through “a change of life, maybe a midlife crisis.” She made new friends in Montreal. “I’m getting rid of the negative people.” Audrey planned to continue psychiatric care in Montreal. In part, Audrey credited improvement to our sessions, and I told her I was grateful to be of help.
Another case
Arthur was a seriously ill, 88-year-old retired pulmonologist, so weak that he was being spoon-fed when I entered his room. He had a “fear of dying or living with disability” from diffuse lymphoma, complicated by tumor lysis syndrome after chemotherapy. “I don’t want to give up, for myself and my family,” he said.
Arthur told me about his struggles to achieve despite poverty in childhood. He needed a scholarship to attend a local college. There were trials at a medical school that failed out less capable students. He commuted and studied at the kitchen table until 3 a.m. Arthur’s mother-in-law had disapproved of him and wanted her daughter to marry a wealthy businessman. During their courtship, Arthur gave his girlfriend a gold bracelet, which he said she should keep it regardless of whether they broke up.
Arthur had a modest evaluation of his capabilities despite a good practice. Meanwhile, his home life progressed: Two of his three children became doctors; the third succeeded as an accountant. His marriage thrived.
At the end of our session, I expressed surprise that his mother-in-law had taken such a dim view of a suitor with determination, impressive credentials, and a future that would be a source of pride. I also assured him that he had chosen fine doctors for his care.
The next time I visited Arthur, he heaped praise on me for turning his life around. I had restored his hope. His daughter, who was visiting later, told me that, no matter how much the family and medical staff encouraged Arthur, “nothing happened until he met you.” I, of course, thanked Arthur for his gratitude and experienced amazement at the success of the talking cure.
Lessons learned
These examples fail to prove that the unraveling of psychodynamics has lost its place. And there is value in the variety of treatment and medications psychiatrists that can offer. But exceptions occur. Do they show there is magic in transference? Is there an ideal way for a therapist to behave? Should we influence the patient by giving advice or wait until he reaches conclusions? Psychiatrists try to free the patient from his suffering, enhancing his perspective, ultimately his independence. How often do we fail to understand how that happens when it does occur?
The flight into health
The early or sudden disappearance of symptoms is referred to as a flight into health, a perhaps-outdated concept that presents “a defense against the anxiety engendered by the prospect of further psychoanalytic exploration of the patient’s conflict” (Farlex Partner Medical Dictionary, 2012). Some patients settle for less. Either they reach their own conclusions, as did Audrey, or they unburden themselves to a compassionate listener, as did Arthur.
What to conclude
The methodical sometimes exists in psychiatric treatment but often not. The practice of medicine is based on science. As described by writer Lisa Randall in a review of the book “Reality Is Not What It Seems: The Journey to Quantum Gravity” (New York: Riverhead Books, 2017): “Science provides a systematic method of building up from the measured and tested … to realms that we don’t yet understand because measurements are not yet sufficiently precise or are too outside our limited perspective” (New York Times Book Review, March 5, 2017, p. 15). The author was describing physics, but her insight applies to medical specialties as well. It is alluring to try to understand our patients. The complexity of mental illness challenges psychiatrists to use science, compassion, and intuition.
Dr. Cohen is in private practice and is a clinical assistant professor of psychiatry at Weill Cornell Medical Center of New York-Presbyterian Hospital, and psychiatric consultant at the Hospital for Special Surgery, also in New York. She made changes to the patient narratives to protect their identities.
“Create a safe zone where anything can gain expression.”
– Carl Rogers, PhD
The patient
“I have no purpose,” Audrey said. She sat immobile, a woman of 45 who looked 10 years older. Audrey hated New York, the crowds, the weather. Her husband, a successful sales executive, supported her; a month earlier, they had moved from California to New York. Her depression and panic attacks dated back to childhood. She also suffered from arthritis, asthma, and lupus. Audrey told me that her parents, long dead, were dreadful. “My mother was the most abusive person. She put out cigarettes on my arm; beat the s*** out of me, my brother, and sister.” She said that in New York, she stayed in her apartment on her couch or shopped for clothes that, ultimately, remained in the closet.
According to Audrey, nothing helped. She was on psychoactive medications prescribed by her Beverly Hills psychiatrist – Cymbalta and Wellbutrin for depression, Klonopin for anxiety, Abilify for agitation. She also took Neurontin for nerve pain and opioids for arthritis, prescribed by a pain specialist.
The process
In residency and beyond, psychiatrists learn to develop a treatment plan based on the patient’s history and symptoms. Some individuals want to understand the origin of their suffering with a thrust toward recovery and independence. Others lack that capacity and need to shore up their defenses through supportive intervention. The direction of how to proceed is often a compromise between what the doctor sees as ideal and what the patient desires.
Outcome
All seemed stagnant for 2 years. Then, Audrey’s demeanor changed dramatically. She enjoyed walking her dog in Central Park; she reflected on her devoted husband, who encouraged her. Audrey’s transformation progressed.
Three months later, her husband took a position in Montreal. On a visit to New York, she told me that she no longer disliked the city, even the noise and the cold weather. I questioned what made the difference. “You saved my life,” Audrey said. I asked what she meant. “You were always there for me,” she said. “You made an effort to try to help me get better. ... You can be funny, witty.” She ventured that she had been through “a change of life, maybe a midlife crisis.” She made new friends in Montreal. “I’m getting rid of the negative people.” Audrey planned to continue psychiatric care in Montreal. In part, Audrey credited improvement to our sessions, and I told her I was grateful to be of help.
Another case
Arthur was a seriously ill, 88-year-old retired pulmonologist, so weak that he was being spoon-fed when I entered his room. He had a “fear of dying or living with disability” from diffuse lymphoma, complicated by tumor lysis syndrome after chemotherapy. “I don’t want to give up, for myself and my family,” he said.
Arthur told me about his struggles to achieve despite poverty in childhood. He needed a scholarship to attend a local college. There were trials at a medical school that failed out less capable students. He commuted and studied at the kitchen table until 3 a.m. Arthur’s mother-in-law had disapproved of him and wanted her daughter to marry a wealthy businessman. During their courtship, Arthur gave his girlfriend a gold bracelet, which he said she should keep it regardless of whether they broke up.
Arthur had a modest evaluation of his capabilities despite a good practice. Meanwhile, his home life progressed: Two of his three children became doctors; the third succeeded as an accountant. His marriage thrived.
At the end of our session, I expressed surprise that his mother-in-law had taken such a dim view of a suitor with determination, impressive credentials, and a future that would be a source of pride. I also assured him that he had chosen fine doctors for his care.
The next time I visited Arthur, he heaped praise on me for turning his life around. I had restored his hope. His daughter, who was visiting later, told me that, no matter how much the family and medical staff encouraged Arthur, “nothing happened until he met you.” I, of course, thanked Arthur for his gratitude and experienced amazement at the success of the talking cure.
Lessons learned
These examples fail to prove that the unraveling of psychodynamics has lost its place. And there is value in the variety of treatment and medications psychiatrists that can offer. But exceptions occur. Do they show there is magic in transference? Is there an ideal way for a therapist to behave? Should we influence the patient by giving advice or wait until he reaches conclusions? Psychiatrists try to free the patient from his suffering, enhancing his perspective, ultimately his independence. How often do we fail to understand how that happens when it does occur?
The flight into health
The early or sudden disappearance of symptoms is referred to as a flight into health, a perhaps-outdated concept that presents “a defense against the anxiety engendered by the prospect of further psychoanalytic exploration of the patient’s conflict” (Farlex Partner Medical Dictionary, 2012). Some patients settle for less. Either they reach their own conclusions, as did Audrey, or they unburden themselves to a compassionate listener, as did Arthur.
What to conclude
The methodical sometimes exists in psychiatric treatment but often not. The practice of medicine is based on science. As described by writer Lisa Randall in a review of the book “Reality Is Not What It Seems: The Journey to Quantum Gravity” (New York: Riverhead Books, 2017): “Science provides a systematic method of building up from the measured and tested … to realms that we don’t yet understand because measurements are not yet sufficiently precise or are too outside our limited perspective” (New York Times Book Review, March 5, 2017, p. 15). The author was describing physics, but her insight applies to medical specialties as well. It is alluring to try to understand our patients. The complexity of mental illness challenges psychiatrists to use science, compassion, and intuition.
Dr. Cohen is in private practice and is a clinical assistant professor of psychiatry at Weill Cornell Medical Center of New York-Presbyterian Hospital, and psychiatric consultant at the Hospital for Special Surgery, also in New York. She made changes to the patient narratives to protect their identities.
Safety of N9-GP for hemophilia B needs further study, FDA committee agrees
Concerns about a possible safety issue with the investigational glycoPEGylated factor IX product nonacog beta pegol (N9-GP) for the treatment of hemophilia B left members of the Blood Products Advisory Committee of the Food and Drug Administration divided during an April 4 committee meeting about whether additional study should take place prior to FDA approval of a Biologics Licensing Application or in the postmarketing setting.
The committee was not asked to vote on a recommendation for approval of N9-GP. Committee members agreed that if N9-GP is approved, standardized postmarketing monitoring would be needed, particularly in very young and very old patients.
As a result, the FDA asked the advisory committee to consider the clinical significance of the preclinical findings, the nature and level of any safety concerns in various populations, the sufficiency of evidence from toxicology and clinical studies for intermittent and chronic use, clinical or laboratory assessments that might help ensure patient safety, and recommendations for additional studies to support the safety of the product.
Novo Nordisk is specifically seeking FDA marketing approval of N9-GP, which is administered weekly, for control and prevention of bleeding episodes, perioperative management, and routine prophylaxis in adults and children. The company submitted evidence for these indications from three phase III trials and a phase III extension study in adults and children.
“The Office of Tissues and Advanced Therapies – OTAT – appreciates that hemophilia B is a serious disease and we need improved therapies to benefit patients. We also appreciate that this is a rare disease, which limits the availability of data to address issues of safety and effectiveness,” Wilson Bryan, MD, director of OTAT, which is part of the FDA’s Center for Biologics Evaluation and Research, told the advisory committee.
The committee then heard from Novo Nordisk representatives who spoke about the unmet public health need for hemophilia B treatments, and N9-GP clinical efficacy, long-term safety, and risk/benefit analyses.
Shawn Hoskin, senior director of regulatory affairs for Novo Nordisk, noted that with weekly dosing of N9-GP, no adverse effects were seen in preclinical studies at doses up to 42 times the human dose. Further, no adverse effects were reported in clinical studies, in which high levels of factor IX were achieved.
“Our trials demonstrated that the higher factor IX levels achieved with N9-GP lead to better outcomes for patients, including reduced annual bleed rate, reduction in the number of spontaneous bleeds, and resolution of target joints,” he said.
Stephanie Seremetis, MD, chief medical officer and corporate vice president for hemophilia at Novo Nordisk, said the company has proposed a postapproval monitoring plan and safety study.
The advisory committee also heard from patients invited by Novo Nordisk to share their experiences, and from Maria Lehtinen, PhD, of Boston Children’s Hospital, who was invited to speak about choroid plexus biology.
The patients agreed that there is an urgent need and desire for effective, long-acting treatments. Ben Shuldiner, for example, said he was part of the clinical trials for N9-GP, has never had as much success sticking to a treatment regimen, and “is in much better shape, much less pain.”
“The [hemophilia] community needs choice,” said Mr. Shuldiner, a professor at Hunter College in New York, and an activist. He stressed that what works for one patient doesn’t necessarily work for another.
Committee members didn’t question the efficacy or value of the long-acting product, but did express concern about the unknown effects of PEG accumulation. One member questioned whether it might be feasible to restrict licensing to children over age 6 years and to adults under age 65 years pending additional study. Other members said that approach would restrict treatment for patients who might benefit the most from N9-GP.
Meera B. Chitlur, MD, noted that most children with hemophilia B are treated prophylactically by age 1, or at least by the time they are walking, and suggested it might be better to allow use of the product in those who need it, while collecting data going forward.
“Only over the last couple years have our patients finally had the opportunity to have something that has substantially changed how they are managed or what they can do. This class of drugs is one that has made it possible for these patients to lead a better life, so I think it is really important for us,” said Dr. Chitlur of Wayne State University and Children’s Hospital of Michigan, Detroit.
“The youngest children will probably benefit the most. Yes, there are concerns ... but at the same time I think I haven’t heard anything today, or read anything, that has made me want to say it is not safe for the patients that I’m going to take care of,” she added, noting that informed consent is possible and important.
Dr. Chitlur said she completely agrees with the need for systematic data collection, and feels there are already mechanisms in place to achieve that goal.
“I feel comfortable taking this to my patients and saying that here is another option for you,” she said.
Laura Manuelidis, MD, of Yale University, New Haven, Conn., a temporary voting member of the committee, said she was “less sanguine,” about immediate approval. Additional studies of the effects of PEG accumulation in animals are feasible, she said, and could be performed rapidly before approving treatment in children under age 2 years.
Michael Dobbs, MD, of the University of Kentucky, Lexington, also a temporary voting member, agreed it would be valuable to test available cerebrospinal fluid of animals from the preclinical studies. He had no recommendation for additional studies, but agreed on the importance of extensive postmarketing surveillance. He added that patients who undergo CSF testing or magnetic resonance imaging for other clinical reasons should be evaluated for the possible effects of PEG accumulation.
“I think we should follow cognitive outcomes in the postmarket data, probably requiring more neurocognitive data in pediatrics with some validated, standardized tests. It would be reasonable to require a full neurological exam pre- and post-[treatment], especially in those at fixed developmental states,” he said.
It would also be reasonable to monitor children for signs and symptoms of hydrocephalus and for papilledema and other visual disturbances, he added.
“But again, most of all ... whatever we really do recommend, we need standardization, validation – to do this the same [way] for all of the patients,” he said.
Dr. Bryan, of OTAT, said the input from members and guests will be considered as the FDA proceeds with its review of the Biologics Licensing Application for N9-GP. The FDA is not bound by the committee’s guidance.
All members of the advisory committee have been screened and found to be in compliance with respect to potential conflicts of interest. No conflict of interest waivers were issued. Patients who spoke in favor of N9-GP received travel and/or other support from Novo Nordisk.
Concerns about a possible safety issue with the investigational glycoPEGylated factor IX product nonacog beta pegol (N9-GP) for the treatment of hemophilia B left members of the Blood Products Advisory Committee of the Food and Drug Administration divided during an April 4 committee meeting about whether additional study should take place prior to FDA approval of a Biologics Licensing Application or in the postmarketing setting.
The committee was not asked to vote on a recommendation for approval of N9-GP. Committee members agreed that if N9-GP is approved, standardized postmarketing monitoring would be needed, particularly in very young and very old patients.
As a result, the FDA asked the advisory committee to consider the clinical significance of the preclinical findings, the nature and level of any safety concerns in various populations, the sufficiency of evidence from toxicology and clinical studies for intermittent and chronic use, clinical or laboratory assessments that might help ensure patient safety, and recommendations for additional studies to support the safety of the product.
Novo Nordisk is specifically seeking FDA marketing approval of N9-GP, which is administered weekly, for control and prevention of bleeding episodes, perioperative management, and routine prophylaxis in adults and children. The company submitted evidence for these indications from three phase III trials and a phase III extension study in adults and children.
“The Office of Tissues and Advanced Therapies – OTAT – appreciates that hemophilia B is a serious disease and we need improved therapies to benefit patients. We also appreciate that this is a rare disease, which limits the availability of data to address issues of safety and effectiveness,” Wilson Bryan, MD, director of OTAT, which is part of the FDA’s Center for Biologics Evaluation and Research, told the advisory committee.
The committee then heard from Novo Nordisk representatives who spoke about the unmet public health need for hemophilia B treatments, and N9-GP clinical efficacy, long-term safety, and risk/benefit analyses.
Shawn Hoskin, senior director of regulatory affairs for Novo Nordisk, noted that with weekly dosing of N9-GP, no adverse effects were seen in preclinical studies at doses up to 42 times the human dose. Further, no adverse effects were reported in clinical studies, in which high levels of factor IX were achieved.
“Our trials demonstrated that the higher factor IX levels achieved with N9-GP lead to better outcomes for patients, including reduced annual bleed rate, reduction in the number of spontaneous bleeds, and resolution of target joints,” he said.
Stephanie Seremetis, MD, chief medical officer and corporate vice president for hemophilia at Novo Nordisk, said the company has proposed a postapproval monitoring plan and safety study.
The advisory committee also heard from patients invited by Novo Nordisk to share their experiences, and from Maria Lehtinen, PhD, of Boston Children’s Hospital, who was invited to speak about choroid plexus biology.
The patients agreed that there is an urgent need and desire for effective, long-acting treatments. Ben Shuldiner, for example, said he was part of the clinical trials for N9-GP, has never had as much success sticking to a treatment regimen, and “is in much better shape, much less pain.”
“The [hemophilia] community needs choice,” said Mr. Shuldiner, a professor at Hunter College in New York, and an activist. He stressed that what works for one patient doesn’t necessarily work for another.
Committee members didn’t question the efficacy or value of the long-acting product, but did express concern about the unknown effects of PEG accumulation. One member questioned whether it might be feasible to restrict licensing to children over age 6 years and to adults under age 65 years pending additional study. Other members said that approach would restrict treatment for patients who might benefit the most from N9-GP.
Meera B. Chitlur, MD, noted that most children with hemophilia B are treated prophylactically by age 1, or at least by the time they are walking, and suggested it might be better to allow use of the product in those who need it, while collecting data going forward.
“Only over the last couple years have our patients finally had the opportunity to have something that has substantially changed how they are managed or what they can do. This class of drugs is one that has made it possible for these patients to lead a better life, so I think it is really important for us,” said Dr. Chitlur of Wayne State University and Children’s Hospital of Michigan, Detroit.
“The youngest children will probably benefit the most. Yes, there are concerns ... but at the same time I think I haven’t heard anything today, or read anything, that has made me want to say it is not safe for the patients that I’m going to take care of,” she added, noting that informed consent is possible and important.
Dr. Chitlur said she completely agrees with the need for systematic data collection, and feels there are already mechanisms in place to achieve that goal.
“I feel comfortable taking this to my patients and saying that here is another option for you,” she said.
Laura Manuelidis, MD, of Yale University, New Haven, Conn., a temporary voting member of the committee, said she was “less sanguine,” about immediate approval. Additional studies of the effects of PEG accumulation in animals are feasible, she said, and could be performed rapidly before approving treatment in children under age 2 years.
Michael Dobbs, MD, of the University of Kentucky, Lexington, also a temporary voting member, agreed it would be valuable to test available cerebrospinal fluid of animals from the preclinical studies. He had no recommendation for additional studies, but agreed on the importance of extensive postmarketing surveillance. He added that patients who undergo CSF testing or magnetic resonance imaging for other clinical reasons should be evaluated for the possible effects of PEG accumulation.
“I think we should follow cognitive outcomes in the postmarket data, probably requiring more neurocognitive data in pediatrics with some validated, standardized tests. It would be reasonable to require a full neurological exam pre- and post-[treatment], especially in those at fixed developmental states,” he said.
It would also be reasonable to monitor children for signs and symptoms of hydrocephalus and for papilledema and other visual disturbances, he added.
“But again, most of all ... whatever we really do recommend, we need standardization, validation – to do this the same [way] for all of the patients,” he said.
Dr. Bryan, of OTAT, said the input from members and guests will be considered as the FDA proceeds with its review of the Biologics Licensing Application for N9-GP. The FDA is not bound by the committee’s guidance.
All members of the advisory committee have been screened and found to be in compliance with respect to potential conflicts of interest. No conflict of interest waivers were issued. Patients who spoke in favor of N9-GP received travel and/or other support from Novo Nordisk.
Concerns about a possible safety issue with the investigational glycoPEGylated factor IX product nonacog beta pegol (N9-GP) for the treatment of hemophilia B left members of the Blood Products Advisory Committee of the Food and Drug Administration divided during an April 4 committee meeting about whether additional study should take place prior to FDA approval of a Biologics Licensing Application or in the postmarketing setting.
The committee was not asked to vote on a recommendation for approval of N9-GP. Committee members agreed that if N9-GP is approved, standardized postmarketing monitoring would be needed, particularly in very young and very old patients.
As a result, the FDA asked the advisory committee to consider the clinical significance of the preclinical findings, the nature and level of any safety concerns in various populations, the sufficiency of evidence from toxicology and clinical studies for intermittent and chronic use, clinical or laboratory assessments that might help ensure patient safety, and recommendations for additional studies to support the safety of the product.
Novo Nordisk is specifically seeking FDA marketing approval of N9-GP, which is administered weekly, for control and prevention of bleeding episodes, perioperative management, and routine prophylaxis in adults and children. The company submitted evidence for these indications from three phase III trials and a phase III extension study in adults and children.
“The Office of Tissues and Advanced Therapies – OTAT – appreciates that hemophilia B is a serious disease and we need improved therapies to benefit patients. We also appreciate that this is a rare disease, which limits the availability of data to address issues of safety and effectiveness,” Wilson Bryan, MD, director of OTAT, which is part of the FDA’s Center for Biologics Evaluation and Research, told the advisory committee.
The committee then heard from Novo Nordisk representatives who spoke about the unmet public health need for hemophilia B treatments, and N9-GP clinical efficacy, long-term safety, and risk/benefit analyses.
Shawn Hoskin, senior director of regulatory affairs for Novo Nordisk, noted that with weekly dosing of N9-GP, no adverse effects were seen in preclinical studies at doses up to 42 times the human dose. Further, no adverse effects were reported in clinical studies, in which high levels of factor IX were achieved.
“Our trials demonstrated that the higher factor IX levels achieved with N9-GP lead to better outcomes for patients, including reduced annual bleed rate, reduction in the number of spontaneous bleeds, and resolution of target joints,” he said.
Stephanie Seremetis, MD, chief medical officer and corporate vice president for hemophilia at Novo Nordisk, said the company has proposed a postapproval monitoring plan and safety study.
The advisory committee also heard from patients invited by Novo Nordisk to share their experiences, and from Maria Lehtinen, PhD, of Boston Children’s Hospital, who was invited to speak about choroid plexus biology.
The patients agreed that there is an urgent need and desire for effective, long-acting treatments. Ben Shuldiner, for example, said he was part of the clinical trials for N9-GP, has never had as much success sticking to a treatment regimen, and “is in much better shape, much less pain.”
“The [hemophilia] community needs choice,” said Mr. Shuldiner, a professor at Hunter College in New York, and an activist. He stressed that what works for one patient doesn’t necessarily work for another.
Committee members didn’t question the efficacy or value of the long-acting product, but did express concern about the unknown effects of PEG accumulation. One member questioned whether it might be feasible to restrict licensing to children over age 6 years and to adults under age 65 years pending additional study. Other members said that approach would restrict treatment for patients who might benefit the most from N9-GP.
Meera B. Chitlur, MD, noted that most children with hemophilia B are treated prophylactically by age 1, or at least by the time they are walking, and suggested it might be better to allow use of the product in those who need it, while collecting data going forward.
“Only over the last couple years have our patients finally had the opportunity to have something that has substantially changed how they are managed or what they can do. This class of drugs is one that has made it possible for these patients to lead a better life, so I think it is really important for us,” said Dr. Chitlur of Wayne State University and Children’s Hospital of Michigan, Detroit.
“The youngest children will probably benefit the most. Yes, there are concerns ... but at the same time I think I haven’t heard anything today, or read anything, that has made me want to say it is not safe for the patients that I’m going to take care of,” she added, noting that informed consent is possible and important.
Dr. Chitlur said she completely agrees with the need for systematic data collection, and feels there are already mechanisms in place to achieve that goal.
“I feel comfortable taking this to my patients and saying that here is another option for you,” she said.
Laura Manuelidis, MD, of Yale University, New Haven, Conn., a temporary voting member of the committee, said she was “less sanguine,” about immediate approval. Additional studies of the effects of PEG accumulation in animals are feasible, she said, and could be performed rapidly before approving treatment in children under age 2 years.
Michael Dobbs, MD, of the University of Kentucky, Lexington, also a temporary voting member, agreed it would be valuable to test available cerebrospinal fluid of animals from the preclinical studies. He had no recommendation for additional studies, but agreed on the importance of extensive postmarketing surveillance. He added that patients who undergo CSF testing or magnetic resonance imaging for other clinical reasons should be evaluated for the possible effects of PEG accumulation.
“I think we should follow cognitive outcomes in the postmarket data, probably requiring more neurocognitive data in pediatrics with some validated, standardized tests. It would be reasonable to require a full neurological exam pre- and post-[treatment], especially in those at fixed developmental states,” he said.
It would also be reasonable to monitor children for signs and symptoms of hydrocephalus and for papilledema and other visual disturbances, he added.
“But again, most of all ... whatever we really do recommend, we need standardization, validation – to do this the same [way] for all of the patients,” he said.
Dr. Bryan, of OTAT, said the input from members and guests will be considered as the FDA proceeds with its review of the Biologics Licensing Application for N9-GP. The FDA is not bound by the committee’s guidance.
All members of the advisory committee have been screened and found to be in compliance with respect to potential conflicts of interest. No conflict of interest waivers were issued. Patients who spoke in favor of N9-GP received travel and/or other support from Novo Nordisk.
Stroke hospitals owe all patients rapid thrombolysis
The best way to minimize death and disability in most patients having an acute ischemic stroke is rapid thrombolysis by infusion of tissue plasminogen activator. Mechanical clot removal – thrombectomy – has recently been shown even better, but it’s applicable to just a fraction of these stroke patients, and even for them thrombolysis remains, for the time being, the recommended first step, with thrombectomy following soon after.
The good news is that more eligible U.S. stroke patients than ever before get this effective treatment. As I reported recently from the International Stroke Conference, as of mid-2016, 68% of U.S. acute ischemic stroke patients treated at about 2,000 of the largest and most focused U.S. stroke hospitals received thrombolytic treatment within 60 minutes of their hospital arrival. That’s up from 30% in late 2009. Hooray! The sad news is that many eligible stroke patients seen at these hospitals don’t get treated this way. Simple math puts that figure at 32%. In other words, last year, nearly a third of U.S. stroke patients who should have received quick thrombolysis didn’t, even though they were taken to the country’s top stroke hospitals.
How do I know that more universal rapid thrombolysis is possible? The 2016 numbers reported from the Get With the Guidelines (GWTG)–Stroke hospitals showed that roughly 2% of the 788 hospitals included in this analysis treated 90% or more of their eligible stroke patients with thrombolysis within an hour. That’s about 16 hospitals. Another 8%, upward of 60 hospitals, treated 80%-89% of their eligible stroke patients within this window. So a high level of thrombolysis treatment is possible. It just isn’t being done everywhere. About 20% of the hospitals in the program treated 40% or fewer of eligible patients they saw within the 60-minute window.
I have no idea why some hospitals do so well while others don’t, despite being in the GWTG-Stroke program that promotes excellence in stroke care delivery. In the most recent iteration of the GWTG–Stroke Target Stroke program, phase II, the organization promoted 11 steps for hospitals to take to optimize rapid delivery of thrombolysis. The obvious inference is that some hospitals are doing all 11 steps very well and consistently, and many others aren’t. Underperforming hospitals owe it to their patients to do a much better job; the top-performing hospitals show it’s possible.
I have heard a lot recently at meetings about how research has established that a range of medical treatments, if used diligently by patients as directed, will substantially improve and prolong their life. Patient compliance then becomes a big issue, and so now I’m hearing more about new approaches to improve compliance. But what about hospital compliance?
Treating acute ischemic stroke as well as possible is different from most disorders – it’s not about patient compliance. It’s about the ambulance that picks up the patient and the hospital where the patient gets taken. The success or failure of the acute treatment that the roughly 700,000 annual U.S. acute ischemic stroke patients receive lies entirely in the hands of the hospital staff. Fewer than 10% of U.S. stroke hospitals offer the vast majority of these patients the best care currently available. Many others don’t do as well, and a huge fraction remain woefully slow, even though everyone knows the pathway to doing better. Underperforming hospitals owe it to patients to up their game, and they need to start doing it now.
[email protected]
On Twitter @mitchelzoler
The best way to minimize death and disability in most patients having an acute ischemic stroke is rapid thrombolysis by infusion of tissue plasminogen activator. Mechanical clot removal – thrombectomy – has recently been shown even better, but it’s applicable to just a fraction of these stroke patients, and even for them thrombolysis remains, for the time being, the recommended first step, with thrombectomy following soon after.
The good news is that more eligible U.S. stroke patients than ever before get this effective treatment. As I reported recently from the International Stroke Conference, as of mid-2016, 68% of U.S. acute ischemic stroke patients treated at about 2,000 of the largest and most focused U.S. stroke hospitals received thrombolytic treatment within 60 minutes of their hospital arrival. That’s up from 30% in late 2009. Hooray! The sad news is that many eligible stroke patients seen at these hospitals don’t get treated this way. Simple math puts that figure at 32%. In other words, last year, nearly a third of U.S. stroke patients who should have received quick thrombolysis didn’t, even though they were taken to the country’s top stroke hospitals.
How do I know that more universal rapid thrombolysis is possible? The 2016 numbers reported from the Get With the Guidelines (GWTG)–Stroke hospitals showed that roughly 2% of the 788 hospitals included in this analysis treated 90% or more of their eligible stroke patients with thrombolysis within an hour. That’s about 16 hospitals. Another 8%, upward of 60 hospitals, treated 80%-89% of their eligible stroke patients within this window. So a high level of thrombolysis treatment is possible. It just isn’t being done everywhere. About 20% of the hospitals in the program treated 40% or fewer of eligible patients they saw within the 60-minute window.
I have no idea why some hospitals do so well while others don’t, despite being in the GWTG-Stroke program that promotes excellence in stroke care delivery. In the most recent iteration of the GWTG–Stroke Target Stroke program, phase II, the organization promoted 11 steps for hospitals to take to optimize rapid delivery of thrombolysis. The obvious inference is that some hospitals are doing all 11 steps very well and consistently, and many others aren’t. Underperforming hospitals owe it to their patients to do a much better job; the top-performing hospitals show it’s possible.
I have heard a lot recently at meetings about how research has established that a range of medical treatments, if used diligently by patients as directed, will substantially improve and prolong their life. Patient compliance then becomes a big issue, and so now I’m hearing more about new approaches to improve compliance. But what about hospital compliance?
Treating acute ischemic stroke as well as possible is different from most disorders – it’s not about patient compliance. It’s about the ambulance that picks up the patient and the hospital where the patient gets taken. The success or failure of the acute treatment that the roughly 700,000 annual U.S. acute ischemic stroke patients receive lies entirely in the hands of the hospital staff. Fewer than 10% of U.S. stroke hospitals offer the vast majority of these patients the best care currently available. Many others don’t do as well, and a huge fraction remain woefully slow, even though everyone knows the pathway to doing better. Underperforming hospitals owe it to patients to up their game, and they need to start doing it now.
[email protected]
On Twitter @mitchelzoler
The best way to minimize death and disability in most patients having an acute ischemic stroke is rapid thrombolysis by infusion of tissue plasminogen activator. Mechanical clot removal – thrombectomy – has recently been shown even better, but it’s applicable to just a fraction of these stroke patients, and even for them thrombolysis remains, for the time being, the recommended first step, with thrombectomy following soon after.
The good news is that more eligible U.S. stroke patients than ever before get this effective treatment. As I reported recently from the International Stroke Conference, as of mid-2016, 68% of U.S. acute ischemic stroke patients treated at about 2,000 of the largest and most focused U.S. stroke hospitals received thrombolytic treatment within 60 minutes of their hospital arrival. That’s up from 30% in late 2009. Hooray! The sad news is that many eligible stroke patients seen at these hospitals don’t get treated this way. Simple math puts that figure at 32%. In other words, last year, nearly a third of U.S. stroke patients who should have received quick thrombolysis didn’t, even though they were taken to the country’s top stroke hospitals.
How do I know that more universal rapid thrombolysis is possible? The 2016 numbers reported from the Get With the Guidelines (GWTG)–Stroke hospitals showed that roughly 2% of the 788 hospitals included in this analysis treated 90% or more of their eligible stroke patients with thrombolysis within an hour. That’s about 16 hospitals. Another 8%, upward of 60 hospitals, treated 80%-89% of their eligible stroke patients within this window. So a high level of thrombolysis treatment is possible. It just isn’t being done everywhere. About 20% of the hospitals in the program treated 40% or fewer of eligible patients they saw within the 60-minute window.
I have no idea why some hospitals do so well while others don’t, despite being in the GWTG-Stroke program that promotes excellence in stroke care delivery. In the most recent iteration of the GWTG–Stroke Target Stroke program, phase II, the organization promoted 11 steps for hospitals to take to optimize rapid delivery of thrombolysis. The obvious inference is that some hospitals are doing all 11 steps very well and consistently, and many others aren’t. Underperforming hospitals owe it to their patients to do a much better job; the top-performing hospitals show it’s possible.
I have heard a lot recently at meetings about how research has established that a range of medical treatments, if used diligently by patients as directed, will substantially improve and prolong their life. Patient compliance then becomes a big issue, and so now I’m hearing more about new approaches to improve compliance. But what about hospital compliance?
Treating acute ischemic stroke as well as possible is different from most disorders – it’s not about patient compliance. It’s about the ambulance that picks up the patient and the hospital where the patient gets taken. The success or failure of the acute treatment that the roughly 700,000 annual U.S. acute ischemic stroke patients receive lies entirely in the hands of the hospital staff. Fewer than 10% of U.S. stroke hospitals offer the vast majority of these patients the best care currently available. Many others don’t do as well, and a huge fraction remain woefully slow, even though everyone knows the pathway to doing better. Underperforming hospitals owe it to patients to up their game, and they need to start doing it now.
[email protected]
On Twitter @mitchelzoler
Belimumab response at 2 years achieved by two-thirds of lupus patients
MELBOURNE – Two-thirds of patients with active systemic lupus erythematosus responded to treatment with belimumab at 2 years in a clinical practice setting, particularly those with higher disease activity or polyarthritis, according to data presented at an international conference on systemic lupus erythematosus.
In a multicenter prospective study of 188 patients with active systemic lupus erythematosus (SLE), Maddalena Larosa, MD, of the University of Padova (Italy) and her colleagues reported a 71.3% response rate with belimumab (Benlysta) at 12 months based on achieving SLE Responder Index (SRI-4) criteria. SRI-4 is a composite endpoint requiring at least a 4-point reduction in SLE Disease Activity Index 2000 (SLEDAI-2K) score, no worsening (less than 10-mm increase) from baseline in the Physician’s Global Assessment of Disease Activity score (PGA), and no new British Isles Lupus Assessment Group (BILAG) Domain A and no more than 1 new BILAG Domain B scores.
Patients were treated with belimumab as an add-on to standard care, with a treatment regimen of 10 mg/kg at day 0, 14, 28, and then every 28 days. The mean SLEDAI-2K score among patients was 8.3, all were positive for double-stranded DNA autoantibodies, and the mean Systemic Lupus International Collaborative Clinics (SLICC) Damage Index was 0.84. Nearly two-thirds of patients were also being treated with immunosuppressants.
Patients with a SLEDAI-2K score of 10 or above were 25 times more likely to respond by 12 months and 12 times more likely to respond by 24 months, both of which were statistically significant.
Similarly, patients with polyarthritis – who constituted nearly half of all patients in the study – were 8 times more likely to respond at 12 months, and 32 times more likely to respond at 24 months. Patients on a prednisone dose of 7.5 mg/day or greater were also significantly more likely to respond at 24 months.
“What was surprising in these patients who respond better are patients with higher disease activity,” Dr. Larosa said in an interview, noting that many patients had also had refractory disease.
Belimumab treatment was also associated with a plateauing of damage accrual, as measured by the SLICC Damage Index, she said.
“In the 5 years before belimumab initiation, we observed an increase of damage accrual related to SLE, but after the first belimumab infusion we did not observe any increase of damage accrual related to the disease,” Dr. Larosa told the audience.
The median duration of treatment was 12 months, but 58 patients (30.9%) discontinued belimumab, mainly because of adverse events. Eight patients also discontinued because of pregnancy, and two because of remission.
In response to a question on the effect of treatment on flare, Dr. Larosa said the treatment was also associated with a reduction in the number of patients who experienced flares, and a significant reduction in renal flares in patients with renal involvement.
No conflicts of interest were declared.
MELBOURNE – Two-thirds of patients with active systemic lupus erythematosus responded to treatment with belimumab at 2 years in a clinical practice setting, particularly those with higher disease activity or polyarthritis, according to data presented at an international conference on systemic lupus erythematosus.
In a multicenter prospective study of 188 patients with active systemic lupus erythematosus (SLE), Maddalena Larosa, MD, of the University of Padova (Italy) and her colleagues reported a 71.3% response rate with belimumab (Benlysta) at 12 months based on achieving SLE Responder Index (SRI-4) criteria. SRI-4 is a composite endpoint requiring at least a 4-point reduction in SLE Disease Activity Index 2000 (SLEDAI-2K) score, no worsening (less than 10-mm increase) from baseline in the Physician’s Global Assessment of Disease Activity score (PGA), and no new British Isles Lupus Assessment Group (BILAG) Domain A and no more than 1 new BILAG Domain B scores.
Patients were treated with belimumab as an add-on to standard care, with a treatment regimen of 10 mg/kg at day 0, 14, 28, and then every 28 days. The mean SLEDAI-2K score among patients was 8.3, all were positive for double-stranded DNA autoantibodies, and the mean Systemic Lupus International Collaborative Clinics (SLICC) Damage Index was 0.84. Nearly two-thirds of patients were also being treated with immunosuppressants.
Patients with a SLEDAI-2K score of 10 or above were 25 times more likely to respond by 12 months and 12 times more likely to respond by 24 months, both of which were statistically significant.
Similarly, patients with polyarthritis – who constituted nearly half of all patients in the study – were 8 times more likely to respond at 12 months, and 32 times more likely to respond at 24 months. Patients on a prednisone dose of 7.5 mg/day or greater were also significantly more likely to respond at 24 months.
“What was surprising in these patients who respond better are patients with higher disease activity,” Dr. Larosa said in an interview, noting that many patients had also had refractory disease.
Belimumab treatment was also associated with a plateauing of damage accrual, as measured by the SLICC Damage Index, she said.
“In the 5 years before belimumab initiation, we observed an increase of damage accrual related to SLE, but after the first belimumab infusion we did not observe any increase of damage accrual related to the disease,” Dr. Larosa told the audience.
The median duration of treatment was 12 months, but 58 patients (30.9%) discontinued belimumab, mainly because of adverse events. Eight patients also discontinued because of pregnancy, and two because of remission.
In response to a question on the effect of treatment on flare, Dr. Larosa said the treatment was also associated with a reduction in the number of patients who experienced flares, and a significant reduction in renal flares in patients with renal involvement.
No conflicts of interest were declared.
MELBOURNE – Two-thirds of patients with active systemic lupus erythematosus responded to treatment with belimumab at 2 years in a clinical practice setting, particularly those with higher disease activity or polyarthritis, according to data presented at an international conference on systemic lupus erythematosus.
In a multicenter prospective study of 188 patients with active systemic lupus erythematosus (SLE), Maddalena Larosa, MD, of the University of Padova (Italy) and her colleagues reported a 71.3% response rate with belimumab (Benlysta) at 12 months based on achieving SLE Responder Index (SRI-4) criteria. SRI-4 is a composite endpoint requiring at least a 4-point reduction in SLE Disease Activity Index 2000 (SLEDAI-2K) score, no worsening (less than 10-mm increase) from baseline in the Physician’s Global Assessment of Disease Activity score (PGA), and no new British Isles Lupus Assessment Group (BILAG) Domain A and no more than 1 new BILAG Domain B scores.
Patients were treated with belimumab as an add-on to standard care, with a treatment regimen of 10 mg/kg at day 0, 14, 28, and then every 28 days. The mean SLEDAI-2K score among patients was 8.3, all were positive for double-stranded DNA autoantibodies, and the mean Systemic Lupus International Collaborative Clinics (SLICC) Damage Index was 0.84. Nearly two-thirds of patients were also being treated with immunosuppressants.
Patients with a SLEDAI-2K score of 10 or above were 25 times more likely to respond by 12 months and 12 times more likely to respond by 24 months, both of which were statistically significant.
Similarly, patients with polyarthritis – who constituted nearly half of all patients in the study – were 8 times more likely to respond at 12 months, and 32 times more likely to respond at 24 months. Patients on a prednisone dose of 7.5 mg/day or greater were also significantly more likely to respond at 24 months.
“What was surprising in these patients who respond better are patients with higher disease activity,” Dr. Larosa said in an interview, noting that many patients had also had refractory disease.
Belimumab treatment was also associated with a plateauing of damage accrual, as measured by the SLICC Damage Index, she said.
“In the 5 years before belimumab initiation, we observed an increase of damage accrual related to SLE, but after the first belimumab infusion we did not observe any increase of damage accrual related to the disease,” Dr. Larosa told the audience.
The median duration of treatment was 12 months, but 58 patients (30.9%) discontinued belimumab, mainly because of adverse events. Eight patients also discontinued because of pregnancy, and two because of remission.
In response to a question on the effect of treatment on flare, Dr. Larosa said the treatment was also associated with a reduction in the number of patients who experienced flares, and a significant reduction in renal flares in patients with renal involvement.
No conflicts of interest were declared.
AT LUPUS 2017
Key clinical point:
Major finding: Belimumab as an add-on therapy in systemic lupus erythematosus was associated with a 71.3% response rate at 12 months and 68.7% response rate at 24 months.
Data source: Prospective, multicenter cohort study of 188 patients with systemic lupus erythematosus.
Disclosures: No conflicts of interest were declared.
A new form of photodynamic therapy remains controversial
A new approach to photodynamic therapy (PDT) – where patients expose their skin to daylight after application of a photosensitizing agent – is gaining traction in Europe, and dermatologists in the United States could soon see more patients inquiring about daylight PDT.
While proponents of daylight PDT point to less pain and greater convenience for patients who have when acne or precancerous actinic keratosis (AK) lesions or are trying to improve the appearance of their skin, not everyone is convinced this approach is safe.
The European experience
Italy is among the European countries where daylight PDT has been evaluated in quality studies. In one Italian study, a split-face study of 35 patients with multiple grade 1 AKs of the face and scalp, no statistically significant difference in the complete response rate of grade 1 AKs at 3 months emerged between the side of the face treated with daylight PDT (87%) and the side treated with conventional PDT (91%). Most of the patients preferred the treatment with daylight PDT, reported the investigators, from the University of L’Aquila (Italy) and the University of Milan (J Eur Acad Dermatol Venereol. 2015 Oct;29[10]:1926-32).
Another advantage of daylight PDT is the ability to treat a larger surface area, he said, pointing out that it is possible to treat half of the face (200 cm2) in only one session. “The drawback is the cost, but, if you compare this with Picato [ingenol mebutate] and Aldara [imiquimod], you must calculate that they are approved for 25 cm2. Therefore, if you need to treat 200 cm2, you need eight packages,” added Dr. Calzavara-Pinton, who is also the president of the Italian Society of Dermatology.
“Daylight PDT with methyl aminolevulinate ... has proven to be efficacious in the treatment of mild to moderate actinic keratoses on the face and scalp,” agreed Rolf-Markus Szeimies, MD, PhD, head of the department of dermatology and allergology at Klinikum Vest, Recklinghausen, Germany.
He cited two randomized, controlled, split-face studies conducted in Australia and Europe, the COMET-1 and COMET-2 trials in patients with mild to moderate AKs of the face and scalp, which found that cure rates with daylight PDT “were not statistically inferior to conventional PDT with red light.” The biggest advantages “are the single-treatment setting, the possibility to treat large areas in one step, the excellent cosmesis, and the almost total lack of pain during the procedure,” he said in an interview.
While it is not approved by the Food and Drug Administration for use in the United States, daylight PDT is a registered treatment modality in Europe, Australia, and South America, said Dr. Szeimies, who presented an update on daylight PDT during a session on PDT at the 2017 annual meeting of the American Academy of Dermatology in Orlando.
U.S. dermatologists urge caution
The potential benefits of daylight PDT for patients mentioned in the published studies are less pain and fewer office visits, “so it’s more convenient,” said Dr. Spencer, a dermatologist and dermatologic surgeon in private practice in St. Petersburg, Fla. “I don’t think those benefits are strong [enough] to outweigh the potential risks.”
He added that most of the studies are from Norway and other Northern European countries where residents generally are exposed to less intense sun, so the generalizability of the findings could be an issue.
Nevertheless, Dr. Spencer predicted there will be more attention to daylight PDT in the United States soon. “This has certainly caught on in Europe. This is out there, and you’re definitely going to hear more about this.”
Some wavelengths of ultraviolet light are harmful to the skin, “and we don’t want to increase the sensitivity. If anything, you want to protect against it,” she noted. In her practice, when she treats patients with conventional PDT, using ALA (with the Levulan Kerastick) most often combined with blue light therapy, she said she cautions patients to avoid exposure to light for up to 24 hour post procedure.
“If you’re going to photosensitize someone, you need to control the amount of energy they are exposed to until that photosensitizer is deactivated, and sunlight is too broad and, in my view, causes more potential harm than good,” Dr. Day commented.
When administered in a controlled fashion, conventional PDT can improve patient outcomes and appearance, she said. “We use it for acne [and] for precancerous actinic keratoses, and, depending on what we do it with – different chromophores or different color light – you can have benefits for photorejuvenation as well.”
Patient adherence to instructions is paramount
“The idea of taking this and applying it to a much broader population, because acne is so common, is interesting but a little bit scary in the sense that it’s such a poorly controlled experiment,” said Samantha B. Conrad, MD, a dermatologist at Northwestern Medicine in Chicago. “Every day, the sun is different, people’s habits are different, and, if people have irritated skin, they’re going to take up a lot more of the ALA. If people have thicker, more oily skin, they may not take as much up. It also depends on the climate – it would be different in Chicago than it would be in LA.”
“I always have patients stay indoors with the blinds closed for 24 hours after [therapy]. I try to schedule the treatments in the wintertime here in New York when the daytime is shorter,” Dr. Day said. “We do the treatment in the afternoon, they leave when it’s dark or almost dark, and then they stay indoors the next day.”
Exposure to sunlight after ALA is applied to the skin “will just increase the specific D-dimers and specific [matrix metalloproteinases] uptake that breaks down collagen, accelerates the aging of the skin, and increases your risk of skin cancer,” she pointed out.
“We’ve all had patients who received their Levulan but then didn’t follow instructions and, the day after, got significant burns from something that would not normally precipitate a severe sunburn,” Dr. Conrad added.
She cited a study recently published from South Korea in which 46 patients with facial acne applied a much lower concentration of ALA, a new variant of 5-aminolevulinate ester (1.5% 3-butenyl ALA-bu gel), compared with the 20% concentration in the Levulan Kerastick available in the United States. (J Dermatol. 2016 May;43[5]:515-21). “With this very low concentration, it’s something of a different ball game,” she said.
“Patients applied that gel every other day and then just basically went about their business, getting daily, normal amounts of sun,” she said. After 12 weeks, the researchers reported a 58% reduction in inflammatory acne lesions and a 34% decrease in noninflammatory acne lesions among those who applied the ALA-bu gel to acne lesions every other day and used daylight as the only light source. “There was very little pain involved, and it was relatively easy to do,” Dr. Conrad said.
“You know people are always looking for the next big thing for acne. The idea is interesting but very rough.”
Dr. Spencer, Dr. Day, and Dr. Conrad had no relevant financial disclosures. Dr. Calzavara-Pinton is a consultant for Leo Pharma, Galderma, Almirall, and Meda AB. Dr. Szeimies is an adviser for Almirall, Biofrontera, Galderma, and Pierre Fabre Dermo Cosmetique, France and is a member of the speakers bureau for Almirall, Desitin, Galderma, Janssen, Pierre Fabre Dermo Cosmetique, France.
A new approach to photodynamic therapy (PDT) – where patients expose their skin to daylight after application of a photosensitizing agent – is gaining traction in Europe, and dermatologists in the United States could soon see more patients inquiring about daylight PDT.
While proponents of daylight PDT point to less pain and greater convenience for patients who have when acne or precancerous actinic keratosis (AK) lesions or are trying to improve the appearance of their skin, not everyone is convinced this approach is safe.
The European experience
Italy is among the European countries where daylight PDT has been evaluated in quality studies. In one Italian study, a split-face study of 35 patients with multiple grade 1 AKs of the face and scalp, no statistically significant difference in the complete response rate of grade 1 AKs at 3 months emerged between the side of the face treated with daylight PDT (87%) and the side treated with conventional PDT (91%). Most of the patients preferred the treatment with daylight PDT, reported the investigators, from the University of L’Aquila (Italy) and the University of Milan (J Eur Acad Dermatol Venereol. 2015 Oct;29[10]:1926-32).
Another advantage of daylight PDT is the ability to treat a larger surface area, he said, pointing out that it is possible to treat half of the face (200 cm2) in only one session. “The drawback is the cost, but, if you compare this with Picato [ingenol mebutate] and Aldara [imiquimod], you must calculate that they are approved for 25 cm2. Therefore, if you need to treat 200 cm2, you need eight packages,” added Dr. Calzavara-Pinton, who is also the president of the Italian Society of Dermatology.
“Daylight PDT with methyl aminolevulinate ... has proven to be efficacious in the treatment of mild to moderate actinic keratoses on the face and scalp,” agreed Rolf-Markus Szeimies, MD, PhD, head of the department of dermatology and allergology at Klinikum Vest, Recklinghausen, Germany.
He cited two randomized, controlled, split-face studies conducted in Australia and Europe, the COMET-1 and COMET-2 trials in patients with mild to moderate AKs of the face and scalp, which found that cure rates with daylight PDT “were not statistically inferior to conventional PDT with red light.” The biggest advantages “are the single-treatment setting, the possibility to treat large areas in one step, the excellent cosmesis, and the almost total lack of pain during the procedure,” he said in an interview.
While it is not approved by the Food and Drug Administration for use in the United States, daylight PDT is a registered treatment modality in Europe, Australia, and South America, said Dr. Szeimies, who presented an update on daylight PDT during a session on PDT at the 2017 annual meeting of the American Academy of Dermatology in Orlando.
U.S. dermatologists urge caution
The potential benefits of daylight PDT for patients mentioned in the published studies are less pain and fewer office visits, “so it’s more convenient,” said Dr. Spencer, a dermatologist and dermatologic surgeon in private practice in St. Petersburg, Fla. “I don’t think those benefits are strong [enough] to outweigh the potential risks.”
He added that most of the studies are from Norway and other Northern European countries where residents generally are exposed to less intense sun, so the generalizability of the findings could be an issue.
Nevertheless, Dr. Spencer predicted there will be more attention to daylight PDT in the United States soon. “This has certainly caught on in Europe. This is out there, and you’re definitely going to hear more about this.”
Some wavelengths of ultraviolet light are harmful to the skin, “and we don’t want to increase the sensitivity. If anything, you want to protect against it,” she noted. In her practice, when she treats patients with conventional PDT, using ALA (with the Levulan Kerastick) most often combined with blue light therapy, she said she cautions patients to avoid exposure to light for up to 24 hour post procedure.
“If you’re going to photosensitize someone, you need to control the amount of energy they are exposed to until that photosensitizer is deactivated, and sunlight is too broad and, in my view, causes more potential harm than good,” Dr. Day commented.
When administered in a controlled fashion, conventional PDT can improve patient outcomes and appearance, she said. “We use it for acne [and] for precancerous actinic keratoses, and, depending on what we do it with – different chromophores or different color light – you can have benefits for photorejuvenation as well.”
Patient adherence to instructions is paramount
“The idea of taking this and applying it to a much broader population, because acne is so common, is interesting but a little bit scary in the sense that it’s such a poorly controlled experiment,” said Samantha B. Conrad, MD, a dermatologist at Northwestern Medicine in Chicago. “Every day, the sun is different, people’s habits are different, and, if people have irritated skin, they’re going to take up a lot more of the ALA. If people have thicker, more oily skin, they may not take as much up. It also depends on the climate – it would be different in Chicago than it would be in LA.”
“I always have patients stay indoors with the blinds closed for 24 hours after [therapy]. I try to schedule the treatments in the wintertime here in New York when the daytime is shorter,” Dr. Day said. “We do the treatment in the afternoon, they leave when it’s dark or almost dark, and then they stay indoors the next day.”
Exposure to sunlight after ALA is applied to the skin “will just increase the specific D-dimers and specific [matrix metalloproteinases] uptake that breaks down collagen, accelerates the aging of the skin, and increases your risk of skin cancer,” she pointed out.
“We’ve all had patients who received their Levulan but then didn’t follow instructions and, the day after, got significant burns from something that would not normally precipitate a severe sunburn,” Dr. Conrad added.
She cited a study recently published from South Korea in which 46 patients with facial acne applied a much lower concentration of ALA, a new variant of 5-aminolevulinate ester (1.5% 3-butenyl ALA-bu gel), compared with the 20% concentration in the Levulan Kerastick available in the United States. (J Dermatol. 2016 May;43[5]:515-21). “With this very low concentration, it’s something of a different ball game,” she said.
“Patients applied that gel every other day and then just basically went about their business, getting daily, normal amounts of sun,” she said. After 12 weeks, the researchers reported a 58% reduction in inflammatory acne lesions and a 34% decrease in noninflammatory acne lesions among those who applied the ALA-bu gel to acne lesions every other day and used daylight as the only light source. “There was very little pain involved, and it was relatively easy to do,” Dr. Conrad said.
“You know people are always looking for the next big thing for acne. The idea is interesting but very rough.”
Dr. Spencer, Dr. Day, and Dr. Conrad had no relevant financial disclosures. Dr. Calzavara-Pinton is a consultant for Leo Pharma, Galderma, Almirall, and Meda AB. Dr. Szeimies is an adviser for Almirall, Biofrontera, Galderma, and Pierre Fabre Dermo Cosmetique, France and is a member of the speakers bureau for Almirall, Desitin, Galderma, Janssen, Pierre Fabre Dermo Cosmetique, France.
A new approach to photodynamic therapy (PDT) – where patients expose their skin to daylight after application of a photosensitizing agent – is gaining traction in Europe, and dermatologists in the United States could soon see more patients inquiring about daylight PDT.
While proponents of daylight PDT point to less pain and greater convenience for patients who have when acne or precancerous actinic keratosis (AK) lesions or are trying to improve the appearance of their skin, not everyone is convinced this approach is safe.
The European experience
Italy is among the European countries where daylight PDT has been evaluated in quality studies. In one Italian study, a split-face study of 35 patients with multiple grade 1 AKs of the face and scalp, no statistically significant difference in the complete response rate of grade 1 AKs at 3 months emerged between the side of the face treated with daylight PDT (87%) and the side treated with conventional PDT (91%). Most of the patients preferred the treatment with daylight PDT, reported the investigators, from the University of L’Aquila (Italy) and the University of Milan (J Eur Acad Dermatol Venereol. 2015 Oct;29[10]:1926-32).
Another advantage of daylight PDT is the ability to treat a larger surface area, he said, pointing out that it is possible to treat half of the face (200 cm2) in only one session. “The drawback is the cost, but, if you compare this with Picato [ingenol mebutate] and Aldara [imiquimod], you must calculate that they are approved for 25 cm2. Therefore, if you need to treat 200 cm2, you need eight packages,” added Dr. Calzavara-Pinton, who is also the president of the Italian Society of Dermatology.
“Daylight PDT with methyl aminolevulinate ... has proven to be efficacious in the treatment of mild to moderate actinic keratoses on the face and scalp,” agreed Rolf-Markus Szeimies, MD, PhD, head of the department of dermatology and allergology at Klinikum Vest, Recklinghausen, Germany.
He cited two randomized, controlled, split-face studies conducted in Australia and Europe, the COMET-1 and COMET-2 trials in patients with mild to moderate AKs of the face and scalp, which found that cure rates with daylight PDT “were not statistically inferior to conventional PDT with red light.” The biggest advantages “are the single-treatment setting, the possibility to treat large areas in one step, the excellent cosmesis, and the almost total lack of pain during the procedure,” he said in an interview.
While it is not approved by the Food and Drug Administration for use in the United States, daylight PDT is a registered treatment modality in Europe, Australia, and South America, said Dr. Szeimies, who presented an update on daylight PDT during a session on PDT at the 2017 annual meeting of the American Academy of Dermatology in Orlando.
U.S. dermatologists urge caution
The potential benefits of daylight PDT for patients mentioned in the published studies are less pain and fewer office visits, “so it’s more convenient,” said Dr. Spencer, a dermatologist and dermatologic surgeon in private practice in St. Petersburg, Fla. “I don’t think those benefits are strong [enough] to outweigh the potential risks.”
He added that most of the studies are from Norway and other Northern European countries where residents generally are exposed to less intense sun, so the generalizability of the findings could be an issue.
Nevertheless, Dr. Spencer predicted there will be more attention to daylight PDT in the United States soon. “This has certainly caught on in Europe. This is out there, and you’re definitely going to hear more about this.”
Some wavelengths of ultraviolet light are harmful to the skin, “and we don’t want to increase the sensitivity. If anything, you want to protect against it,” she noted. In her practice, when she treats patients with conventional PDT, using ALA (with the Levulan Kerastick) most often combined with blue light therapy, she said she cautions patients to avoid exposure to light for up to 24 hour post procedure.
“If you’re going to photosensitize someone, you need to control the amount of energy they are exposed to until that photosensitizer is deactivated, and sunlight is too broad and, in my view, causes more potential harm than good,” Dr. Day commented.
When administered in a controlled fashion, conventional PDT can improve patient outcomes and appearance, she said. “We use it for acne [and] for precancerous actinic keratoses, and, depending on what we do it with – different chromophores or different color light – you can have benefits for photorejuvenation as well.”
Patient adherence to instructions is paramount
“The idea of taking this and applying it to a much broader population, because acne is so common, is interesting but a little bit scary in the sense that it’s such a poorly controlled experiment,” said Samantha B. Conrad, MD, a dermatologist at Northwestern Medicine in Chicago. “Every day, the sun is different, people’s habits are different, and, if people have irritated skin, they’re going to take up a lot more of the ALA. If people have thicker, more oily skin, they may not take as much up. It also depends on the climate – it would be different in Chicago than it would be in LA.”
“I always have patients stay indoors with the blinds closed for 24 hours after [therapy]. I try to schedule the treatments in the wintertime here in New York when the daytime is shorter,” Dr. Day said. “We do the treatment in the afternoon, they leave when it’s dark or almost dark, and then they stay indoors the next day.”
Exposure to sunlight after ALA is applied to the skin “will just increase the specific D-dimers and specific [matrix metalloproteinases] uptake that breaks down collagen, accelerates the aging of the skin, and increases your risk of skin cancer,” she pointed out.
“We’ve all had patients who received their Levulan but then didn’t follow instructions and, the day after, got significant burns from something that would not normally precipitate a severe sunburn,” Dr. Conrad added.
She cited a study recently published from South Korea in which 46 patients with facial acne applied a much lower concentration of ALA, a new variant of 5-aminolevulinate ester (1.5% 3-butenyl ALA-bu gel), compared with the 20% concentration in the Levulan Kerastick available in the United States. (J Dermatol. 2016 May;43[5]:515-21). “With this very low concentration, it’s something of a different ball game,” she said.
“Patients applied that gel every other day and then just basically went about their business, getting daily, normal amounts of sun,” she said. After 12 weeks, the researchers reported a 58% reduction in inflammatory acne lesions and a 34% decrease in noninflammatory acne lesions among those who applied the ALA-bu gel to acne lesions every other day and used daylight as the only light source. “There was very little pain involved, and it was relatively easy to do,” Dr. Conrad said.
“You know people are always looking for the next big thing for acne. The idea is interesting but very rough.”
Dr. Spencer, Dr. Day, and Dr. Conrad had no relevant financial disclosures. Dr. Calzavara-Pinton is a consultant for Leo Pharma, Galderma, Almirall, and Meda AB. Dr. Szeimies is an adviser for Almirall, Biofrontera, Galderma, and Pierre Fabre Dermo Cosmetique, France and is a member of the speakers bureau for Almirall, Desitin, Galderma, Janssen, Pierre Fabre Dermo Cosmetique, France.
Perfluorodecalin-spiked patch improves tattoo removal results
Laser tattoo removal with use of a perfluorodecalin (PFD)-infused patch allowed significantly more passes during a 5-minute treatment session, in a randomized trial of 30 adults.
In the study, published online in Lasers in Surgery and Medicine, an average of 3.7 laser treatment passes (range 2-4) were used when the laser was combined with a PFD-infused patch during a 5-minute session, compared with an average of 1.4 passes (range 1-3) with the laser alone (P less than .0001).
“Laser-assisted tattoo removal is generally regarded as safe and effective, but the procedure is subject to several important limitations,” wrote Brian S. Biesman, MD, and Cara Costner, RN, FNP, who practice in Nashville, Tenn. These limitations include the need to wait for epidermal whitening to dissipate between laser passes, but “one strategy for improving the efficiency of laser-assisted tattoo removal involves the topical use of an optical clearing agent to reduce the epidermal whitening effect,” they explained.
“Topical use of PFD reduces optical scattering at the skin surface, which helps to improve energy delivery to the tattoo ink in deeper layers of the skin and may reduce the potential of epidermal injury and treatment-related AEs,” they added (Lasers Surg Med. 2017 March 20. doi: 10.1002/lsm.22659).
They enrolled 16 women and 14 men seeking tattoo removal in the randomized, split-area study. The mean age of the subjects was 37 years; most were Fitzpatrick skin type II or III. One side of each tattoo was treated with the 755-nm Q-Switched Alexandrite nanosecond laser alone, and the other half was treated with the same laser through the PFD patch.
Patients’ reports of pain based on the Visual Analog Scale were approximately one point lower on the areas treated with the laser and the patch compared with the laser alone. Compared with the laser-only areas, a lower proportion of the areas treated with the patch were affected by edema (36.7% vs. 63.3%) or erythema (33.3% vs. 70%). None of the patients had hypopigmentation or hyperpigmentation. “All AEs [adverse events] were transient and had resolved by the 1-month follow-up visit,” at which time all 30 patients said they preferred to continue their tattoo removal using the PFD patch, the investigators wrote.
The findings were limited by several factors, including the use of a single laser and the predominance of black or dark blue tattoos, as well as the lack of patients with darker skin types. However, “incorporation of the PFD patch into laser tattoo removal procedures may afford multiple benefits to the patient and provider, including increased efficiency, improved patient safety, fewer AEs associated with epidermal injury, and protection of the patient and provider from tissue splatter and laser plume,” the authors concluded.
Dr. Biesman disclosed grant support, honoraria, or consulting fees from Allergan, Cutera, Cytrellis, Evolus Galderma, Intraderm, Merz, ON Light Sciences, Revance, Sienna, Suneva, Syneron-Candela, Valeant, and Zeltiq. The study was sponsored by ON Light Sciences.
Laser tattoo removal with use of a perfluorodecalin (PFD)-infused patch allowed significantly more passes during a 5-minute treatment session, in a randomized trial of 30 adults.
In the study, published online in Lasers in Surgery and Medicine, an average of 3.7 laser treatment passes (range 2-4) were used when the laser was combined with a PFD-infused patch during a 5-minute session, compared with an average of 1.4 passes (range 1-3) with the laser alone (P less than .0001).
“Laser-assisted tattoo removal is generally regarded as safe and effective, but the procedure is subject to several important limitations,” wrote Brian S. Biesman, MD, and Cara Costner, RN, FNP, who practice in Nashville, Tenn. These limitations include the need to wait for epidermal whitening to dissipate between laser passes, but “one strategy for improving the efficiency of laser-assisted tattoo removal involves the topical use of an optical clearing agent to reduce the epidermal whitening effect,” they explained.
“Topical use of PFD reduces optical scattering at the skin surface, which helps to improve energy delivery to the tattoo ink in deeper layers of the skin and may reduce the potential of epidermal injury and treatment-related AEs,” they added (Lasers Surg Med. 2017 March 20. doi: 10.1002/lsm.22659).
They enrolled 16 women and 14 men seeking tattoo removal in the randomized, split-area study. The mean age of the subjects was 37 years; most were Fitzpatrick skin type II or III. One side of each tattoo was treated with the 755-nm Q-Switched Alexandrite nanosecond laser alone, and the other half was treated with the same laser through the PFD patch.
Patients’ reports of pain based on the Visual Analog Scale were approximately one point lower on the areas treated with the laser and the patch compared with the laser alone. Compared with the laser-only areas, a lower proportion of the areas treated with the patch were affected by edema (36.7% vs. 63.3%) or erythema (33.3% vs. 70%). None of the patients had hypopigmentation or hyperpigmentation. “All AEs [adverse events] were transient and had resolved by the 1-month follow-up visit,” at which time all 30 patients said they preferred to continue their tattoo removal using the PFD patch, the investigators wrote.
The findings were limited by several factors, including the use of a single laser and the predominance of black or dark blue tattoos, as well as the lack of patients with darker skin types. However, “incorporation of the PFD patch into laser tattoo removal procedures may afford multiple benefits to the patient and provider, including increased efficiency, improved patient safety, fewer AEs associated with epidermal injury, and protection of the patient and provider from tissue splatter and laser plume,” the authors concluded.
Dr. Biesman disclosed grant support, honoraria, or consulting fees from Allergan, Cutera, Cytrellis, Evolus Galderma, Intraderm, Merz, ON Light Sciences, Revance, Sienna, Suneva, Syneron-Candela, Valeant, and Zeltiq. The study was sponsored by ON Light Sciences.
Laser tattoo removal with use of a perfluorodecalin (PFD)-infused patch allowed significantly more passes during a 5-minute treatment session, in a randomized trial of 30 adults.
In the study, published online in Lasers in Surgery and Medicine, an average of 3.7 laser treatment passes (range 2-4) were used when the laser was combined with a PFD-infused patch during a 5-minute session, compared with an average of 1.4 passes (range 1-3) with the laser alone (P less than .0001).
“Laser-assisted tattoo removal is generally regarded as safe and effective, but the procedure is subject to several important limitations,” wrote Brian S. Biesman, MD, and Cara Costner, RN, FNP, who practice in Nashville, Tenn. These limitations include the need to wait for epidermal whitening to dissipate between laser passes, but “one strategy for improving the efficiency of laser-assisted tattoo removal involves the topical use of an optical clearing agent to reduce the epidermal whitening effect,” they explained.
“Topical use of PFD reduces optical scattering at the skin surface, which helps to improve energy delivery to the tattoo ink in deeper layers of the skin and may reduce the potential of epidermal injury and treatment-related AEs,” they added (Lasers Surg Med. 2017 March 20. doi: 10.1002/lsm.22659).
They enrolled 16 women and 14 men seeking tattoo removal in the randomized, split-area study. The mean age of the subjects was 37 years; most were Fitzpatrick skin type II or III. One side of each tattoo was treated with the 755-nm Q-Switched Alexandrite nanosecond laser alone, and the other half was treated with the same laser through the PFD patch.
Patients’ reports of pain based on the Visual Analog Scale were approximately one point lower on the areas treated with the laser and the patch compared with the laser alone. Compared with the laser-only areas, a lower proportion of the areas treated with the patch were affected by edema (36.7% vs. 63.3%) or erythema (33.3% vs. 70%). None of the patients had hypopigmentation or hyperpigmentation. “All AEs [adverse events] were transient and had resolved by the 1-month follow-up visit,” at which time all 30 patients said they preferred to continue their tattoo removal using the PFD patch, the investigators wrote.
The findings were limited by several factors, including the use of a single laser and the predominance of black or dark blue tattoos, as well as the lack of patients with darker skin types. However, “incorporation of the PFD patch into laser tattoo removal procedures may afford multiple benefits to the patient and provider, including increased efficiency, improved patient safety, fewer AEs associated with epidermal injury, and protection of the patient and provider from tissue splatter and laser plume,” the authors concluded.
Dr. Biesman disclosed grant support, honoraria, or consulting fees from Allergan, Cutera, Cytrellis, Evolus Galderma, Intraderm, Merz, ON Light Sciences, Revance, Sienna, Suneva, Syneron-Candela, Valeant, and Zeltiq. The study was sponsored by ON Light Sciences.
Key clinical point: Addition of a perfluorodecalin-infused patch to a laser treatment protocol allowed significantly more laser passes with no difference in adverse events.
Major finding: More laser treatment passes for tattoo removal were possible when the laser was combined with a perfluorodecalin patch vs. laser alone (an average of 3.7 vs. 1.4 passes in a 5-minute session, a significant difference).
Data source: A prospective, randomized study of 30 adults seeking removal of tattoos.
Disclosures: Dr. Biesman disclosed grant support, honoraria, or consulting fees from Allergan, Cutera, Cytrellis, Evolus Galderma, Intraderm, Merz, ON Light Sciences, Revance, Sienna, Suneva, Syneron-Candela, Valeant, and Zeltiq. The study was sponsored by ON Light Sciences.
Update on the False Claims Act
Question: Which of the following is correct?
A. The False Claims Act dates back to the Civil War era.
B. The FCA covers only patently false statements.
C. Material misrepresentation is insufficient.
D. Negligence constitutes a violation.
E. A qui tam lawsuit under FCA refers to a third party who has suffered personal harm.
Answer: A. The False Claims Act (FCA) is an old law, enacted by Congress in 1863 to impose liability for submitting a payment demand to the federal government when there is actual or constructive knowledge that the claim is false.1 Many states now have their own versions of FCA.
Intent to defraud is not a required element, but knowing or reckless disregard of the truth or material misrepresentation are – whereas negligence is insufficient to constitute a violation.
In the health care field, FCA most commonly involves false claims made to Medicare or Medicaid. Pitfalls include billing for noncovered services such as experimental treatments, double billing, unnecessary services, billing the government as the primary payer when inappropriate, or regularly waiving deductibles and copayments.
Other activities that constitute wrongdoing in this context include knowingly using another patient’s name for purposes of federal drug coverage, billing for no-shows, and misrepresenting the diagnosis to justify services.
The electronic medical record enables easy check-offs as documentation of actual work done, and fraud is implicated if the information is deliberately misleading, as in the example of upcoding.
Importantly, physicians are liable for the actions of their office staff, so it is prudent to oversee and supervise all billing activities. Aggrieved or disgruntled employees or contractors, popularly known as whistle-blowers, can file a qui tam action. They stand to collect a substantial bounty, up to 30% of the proceeds. They do not have to show legal standing and need not sustain any personal injury.
FCA prosecutions are daily affairs, with egregious examples regularly making the news headlines. A few random pickings might give you an idea of the problem:
In 2015, in its largest case of health care fraud, the federal Department of Justice filed criminal charges against 243 individuals across the nation. Some of the violations included billings for intensive psychotherapy sessions for noncommunicative dementia patients, simply moving patients to different locations, and fraudulent prescriptions under Medicare Part D.
In 2016, a pain management clinic used “ill-equipped, desperate doctors in dire need of work” to write faked prescriptions for narcotics. The clinic owner, a doctor, was sentenced to 144 months in prison for running what was described as a “pill-mill zoo.”
Arguably, the most dramatic physician case occurred in 2017 and involved a Florida dermatologist who settled with the government for $18 million for treating patients for skin cancer they did not have. The action came from a qui tam lawsuit filed by another dermatologist.
A major development in the false claims law came with last year’s U.S. Supreme Court decision in Universal Health Services v. Escobar.2
This landmark case dealt with claims made by Arbour Counseling Services to the Massachusetts’ Medicaid program for mental health counseling and prescriptions, a satellite mental health facility of Universal Health Services. It turned out that relatively few Arbour employees were actually licensed to provide mental health counseling or authorized to prescribe medications. A death resulted from a reaction to an unlicensed prescription.
In a unanimous decision, the Supreme Court held that there can be FCA liability when a defendant submitting a claim makes specific representations about the goods or services provided but fails to disclose noncompliance with material statutory, regulatory, or contractual requirements. Technically referred to as “implied false certification,” such material omissions may amount to a misrepresentation and may be deemed fraudulent, even if the requirements were not expressly designated as conditions of payment.
In the words of the court, “Today’s decision holds that the claims at issue may be actionable because they do more than merely demand payment; they fall squarely within the rule that representations that state the truth only so far as it goes, while omitting critical qualifying information, can be actionable misrepresentations.”
The implied false certification, or implied fraud, ruling has widespread implications, as it does not require a patently false statement. A material misrepresentation or omission may suffice.
There is concern that this ruling will open the floodgates of FCA prosecution. However, the federal Ninth Circuit Court of Appeals has recently quashed an attempt to invoke the implied certification claim in an FCA suit against DJO Global and Biomet, brought by a medical device salesman and his private investigator. Their rejected whistle-blower suit alleged that the defendants were providing their spinal bone growth stimulation devices for use on the cervical spine, even though Food and Drug Administration approval was for use only on the lumbar spine.
Another concern is, can an alleged wrong prognosis regarding life expectancy amount to a false claim?
Under Medicare rules, a physician certifying that a patient is eligible for hospice care must attest that the condition is terminal, with death expected within 6 months.
AseraCare, a hospice company, was accused of knowingly submitting false claims to Medicare by certifying patients as eligible for hospice who did not have a life expectancy of 6 months or less. The government claimed that the medical records of the 123 patients at issue did not contain clinical information and other documentation that supported the medical prognosis. Thus, AseraCare’s claims for those patients were false.
The case brought out the conflicting views of physicians: Did the medical records supported AseraCare’s certifications that the patients were eligible? The defendants argued that, when hospice-certifying physicians and government medical experts look at the very same medical records and disagree about eligibility, the opinion of one medical expert alone cannot prove falsity without further evidence of an objective falsehood.
AseraCare won a summary judgment defending against the $200 million lawsuit in the U.S. District Court for the Northern District of Alabama.3 In a memorandum opinion, the court began with Blaise Pascal’s axiom that “Contradiction is not a sign of falsity, nor the lack of contradiction the sign of truth.” Federal prosecutors have appealed to the federal 11th Circuit Court of Appeals, which recently heard oral arguments. Its decision is pending.
In support of the hospice center physicians, the American Medical Association and other organizations have filed an amicus brief asserting that a physician’s opinion may be deemed false only if no reasonable physician could hold that opinion.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the materials have been taken from earlier columns in Internal Medicine News. For additional information, readers may contact the author at [email protected].
References
1. 31 U.S. Code, Section 3729(a)(1)(A).
2. Universal Health Services v. United States ex rel. Escobar, 579 U.S. ____ (2016).
3. U.S. ex rel. Paradies et al. v. AseraCare Inc. et al., Case number 2:12-CV-245-KOB, in the U.S. District Court for the Northern District of Alabama.
Question: Which of the following is correct?
A. The False Claims Act dates back to the Civil War era.
B. The FCA covers only patently false statements.
C. Material misrepresentation is insufficient.
D. Negligence constitutes a violation.
E. A qui tam lawsuit under FCA refers to a third party who has suffered personal harm.
Answer: A. The False Claims Act (FCA) is an old law, enacted by Congress in 1863 to impose liability for submitting a payment demand to the federal government when there is actual or constructive knowledge that the claim is false.1 Many states now have their own versions of FCA.
Intent to defraud is not a required element, but knowing or reckless disregard of the truth or material misrepresentation are – whereas negligence is insufficient to constitute a violation.
In the health care field, FCA most commonly involves false claims made to Medicare or Medicaid. Pitfalls include billing for noncovered services such as experimental treatments, double billing, unnecessary services, billing the government as the primary payer when inappropriate, or regularly waiving deductibles and copayments.
Other activities that constitute wrongdoing in this context include knowingly using another patient’s name for purposes of federal drug coverage, billing for no-shows, and misrepresenting the diagnosis to justify services.
The electronic medical record enables easy check-offs as documentation of actual work done, and fraud is implicated if the information is deliberately misleading, as in the example of upcoding.
Importantly, physicians are liable for the actions of their office staff, so it is prudent to oversee and supervise all billing activities. Aggrieved or disgruntled employees or contractors, popularly known as whistle-blowers, can file a qui tam action. They stand to collect a substantial bounty, up to 30% of the proceeds. They do not have to show legal standing and need not sustain any personal injury.
FCA prosecutions are daily affairs, with egregious examples regularly making the news headlines. A few random pickings might give you an idea of the problem:
In 2015, in its largest case of health care fraud, the federal Department of Justice filed criminal charges against 243 individuals across the nation. Some of the violations included billings for intensive psychotherapy sessions for noncommunicative dementia patients, simply moving patients to different locations, and fraudulent prescriptions under Medicare Part D.
In 2016, a pain management clinic used “ill-equipped, desperate doctors in dire need of work” to write faked prescriptions for narcotics. The clinic owner, a doctor, was sentenced to 144 months in prison for running what was described as a “pill-mill zoo.”
Arguably, the most dramatic physician case occurred in 2017 and involved a Florida dermatologist who settled with the government for $18 million for treating patients for skin cancer they did not have. The action came from a qui tam lawsuit filed by another dermatologist.
A major development in the false claims law came with last year’s U.S. Supreme Court decision in Universal Health Services v. Escobar.2
This landmark case dealt with claims made by Arbour Counseling Services to the Massachusetts’ Medicaid program for mental health counseling and prescriptions, a satellite mental health facility of Universal Health Services. It turned out that relatively few Arbour employees were actually licensed to provide mental health counseling or authorized to prescribe medications. A death resulted from a reaction to an unlicensed prescription.
In a unanimous decision, the Supreme Court held that there can be FCA liability when a defendant submitting a claim makes specific representations about the goods or services provided but fails to disclose noncompliance with material statutory, regulatory, or contractual requirements. Technically referred to as “implied false certification,” such material omissions may amount to a misrepresentation and may be deemed fraudulent, even if the requirements were not expressly designated as conditions of payment.
In the words of the court, “Today’s decision holds that the claims at issue may be actionable because they do more than merely demand payment; they fall squarely within the rule that representations that state the truth only so far as it goes, while omitting critical qualifying information, can be actionable misrepresentations.”
The implied false certification, or implied fraud, ruling has widespread implications, as it does not require a patently false statement. A material misrepresentation or omission may suffice.
There is concern that this ruling will open the floodgates of FCA prosecution. However, the federal Ninth Circuit Court of Appeals has recently quashed an attempt to invoke the implied certification claim in an FCA suit against DJO Global and Biomet, brought by a medical device salesman and his private investigator. Their rejected whistle-blower suit alleged that the defendants were providing their spinal bone growth stimulation devices for use on the cervical spine, even though Food and Drug Administration approval was for use only on the lumbar spine.
Another concern is, can an alleged wrong prognosis regarding life expectancy amount to a false claim?
Under Medicare rules, a physician certifying that a patient is eligible for hospice care must attest that the condition is terminal, with death expected within 6 months.
AseraCare, a hospice company, was accused of knowingly submitting false claims to Medicare by certifying patients as eligible for hospice who did not have a life expectancy of 6 months or less. The government claimed that the medical records of the 123 patients at issue did not contain clinical information and other documentation that supported the medical prognosis. Thus, AseraCare’s claims for those patients were false.
The case brought out the conflicting views of physicians: Did the medical records supported AseraCare’s certifications that the patients were eligible? The defendants argued that, when hospice-certifying physicians and government medical experts look at the very same medical records and disagree about eligibility, the opinion of one medical expert alone cannot prove falsity without further evidence of an objective falsehood.
AseraCare won a summary judgment defending against the $200 million lawsuit in the U.S. District Court for the Northern District of Alabama.3 In a memorandum opinion, the court began with Blaise Pascal’s axiom that “Contradiction is not a sign of falsity, nor the lack of contradiction the sign of truth.” Federal prosecutors have appealed to the federal 11th Circuit Court of Appeals, which recently heard oral arguments. Its decision is pending.
In support of the hospice center physicians, the American Medical Association and other organizations have filed an amicus brief asserting that a physician’s opinion may be deemed false only if no reasonable physician could hold that opinion.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the materials have been taken from earlier columns in Internal Medicine News. For additional information, readers may contact the author at [email protected].
References
1. 31 U.S. Code, Section 3729(a)(1)(A).
2. Universal Health Services v. United States ex rel. Escobar, 579 U.S. ____ (2016).
3. U.S. ex rel. Paradies et al. v. AseraCare Inc. et al., Case number 2:12-CV-245-KOB, in the U.S. District Court for the Northern District of Alabama.
Question: Which of the following is correct?
A. The False Claims Act dates back to the Civil War era.
B. The FCA covers only patently false statements.
C. Material misrepresentation is insufficient.
D. Negligence constitutes a violation.
E. A qui tam lawsuit under FCA refers to a third party who has suffered personal harm.
Answer: A. The False Claims Act (FCA) is an old law, enacted by Congress in 1863 to impose liability for submitting a payment demand to the federal government when there is actual or constructive knowledge that the claim is false.1 Many states now have their own versions of FCA.
Intent to defraud is not a required element, but knowing or reckless disregard of the truth or material misrepresentation are – whereas negligence is insufficient to constitute a violation.
In the health care field, FCA most commonly involves false claims made to Medicare or Medicaid. Pitfalls include billing for noncovered services such as experimental treatments, double billing, unnecessary services, billing the government as the primary payer when inappropriate, or regularly waiving deductibles and copayments.
Other activities that constitute wrongdoing in this context include knowingly using another patient’s name for purposes of federal drug coverage, billing for no-shows, and misrepresenting the diagnosis to justify services.
The electronic medical record enables easy check-offs as documentation of actual work done, and fraud is implicated if the information is deliberately misleading, as in the example of upcoding.
Importantly, physicians are liable for the actions of their office staff, so it is prudent to oversee and supervise all billing activities. Aggrieved or disgruntled employees or contractors, popularly known as whistle-blowers, can file a qui tam action. They stand to collect a substantial bounty, up to 30% of the proceeds. They do not have to show legal standing and need not sustain any personal injury.
FCA prosecutions are daily affairs, with egregious examples regularly making the news headlines. A few random pickings might give you an idea of the problem:
In 2015, in its largest case of health care fraud, the federal Department of Justice filed criminal charges against 243 individuals across the nation. Some of the violations included billings for intensive psychotherapy sessions for noncommunicative dementia patients, simply moving patients to different locations, and fraudulent prescriptions under Medicare Part D.
In 2016, a pain management clinic used “ill-equipped, desperate doctors in dire need of work” to write faked prescriptions for narcotics. The clinic owner, a doctor, was sentenced to 144 months in prison for running what was described as a “pill-mill zoo.”
Arguably, the most dramatic physician case occurred in 2017 and involved a Florida dermatologist who settled with the government for $18 million for treating patients for skin cancer they did not have. The action came from a qui tam lawsuit filed by another dermatologist.
A major development in the false claims law came with last year’s U.S. Supreme Court decision in Universal Health Services v. Escobar.2
This landmark case dealt with claims made by Arbour Counseling Services to the Massachusetts’ Medicaid program for mental health counseling and prescriptions, a satellite mental health facility of Universal Health Services. It turned out that relatively few Arbour employees were actually licensed to provide mental health counseling or authorized to prescribe medications. A death resulted from a reaction to an unlicensed prescription.
In a unanimous decision, the Supreme Court held that there can be FCA liability when a defendant submitting a claim makes specific representations about the goods or services provided but fails to disclose noncompliance with material statutory, regulatory, or contractual requirements. Technically referred to as “implied false certification,” such material omissions may amount to a misrepresentation and may be deemed fraudulent, even if the requirements were not expressly designated as conditions of payment.
In the words of the court, “Today’s decision holds that the claims at issue may be actionable because they do more than merely demand payment; they fall squarely within the rule that representations that state the truth only so far as it goes, while omitting critical qualifying information, can be actionable misrepresentations.”
The implied false certification, or implied fraud, ruling has widespread implications, as it does not require a patently false statement. A material misrepresentation or omission may suffice.
There is concern that this ruling will open the floodgates of FCA prosecution. However, the federal Ninth Circuit Court of Appeals has recently quashed an attempt to invoke the implied certification claim in an FCA suit against DJO Global and Biomet, brought by a medical device salesman and his private investigator. Their rejected whistle-blower suit alleged that the defendants were providing their spinal bone growth stimulation devices for use on the cervical spine, even though Food and Drug Administration approval was for use only on the lumbar spine.
Another concern is, can an alleged wrong prognosis regarding life expectancy amount to a false claim?
Under Medicare rules, a physician certifying that a patient is eligible for hospice care must attest that the condition is terminal, with death expected within 6 months.
AseraCare, a hospice company, was accused of knowingly submitting false claims to Medicare by certifying patients as eligible for hospice who did not have a life expectancy of 6 months or less. The government claimed that the medical records of the 123 patients at issue did not contain clinical information and other documentation that supported the medical prognosis. Thus, AseraCare’s claims for those patients were false.
The case brought out the conflicting views of physicians: Did the medical records supported AseraCare’s certifications that the patients were eligible? The defendants argued that, when hospice-certifying physicians and government medical experts look at the very same medical records and disagree about eligibility, the opinion of one medical expert alone cannot prove falsity without further evidence of an objective falsehood.
AseraCare won a summary judgment defending against the $200 million lawsuit in the U.S. District Court for the Northern District of Alabama.3 In a memorandum opinion, the court began with Blaise Pascal’s axiom that “Contradiction is not a sign of falsity, nor the lack of contradiction the sign of truth.” Federal prosecutors have appealed to the federal 11th Circuit Court of Appeals, which recently heard oral arguments. Its decision is pending.
In support of the hospice center physicians, the American Medical Association and other organizations have filed an amicus brief asserting that a physician’s opinion may be deemed false only if no reasonable physician could hold that opinion.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the materials have been taken from earlier columns in Internal Medicine News. For additional information, readers may contact the author at [email protected].
References
1. 31 U.S. Code, Section 3729(a)(1)(A).
2. Universal Health Services v. United States ex rel. Escobar, 579 U.S. ____ (2016).
3. U.S. ex rel. Paradies et al. v. AseraCare Inc. et al., Case number 2:12-CV-245-KOB, in the U.S. District Court for the Northern District of Alabama.