User login
Influenza linked to atrial fibrillation in large observational study
A diagnosis of influenza increased the risk of subsequent atrial fibrillation by about 18%, investigators reported online in Heart Rhythm.
Clinicians therefore should consider atrial fibrillation (AF) in patients with influenza-like symptoms who report palpitations or experience an ischemic stroke, said Dr. Ting-Yung Chang of Taipei Veterans General Hospital in Taiwan and his associates. Influenza vaccination might help prevent AF, and high-risk patients should be encouraged to receive the vaccination annually, they said. However, a large prospective study is needed to clarify whether influenza vaccination reduces the risk of AF and subsequent ischemic stroke and systemic thromboembolic events, they added.
Atrial fibrillation increases the risk of stroke about fivefold, triples the risk of heart failure, and doubles the chances of dementia and death, the researchers noted. Mounting evidence implicates inflammation and sympathetic nervous system dysregulation in the pathogenesis of AF, raising questions about whether influenza might underlie or contribute to some cases of AF. To explore relationships among AF, influenza, and influenza vaccination, the investigators analyzed data for 11,374 patients with AF who were enrolled in the Taiwan National Health Insurance Research Database between 2000 and 2010. They matched each patient with AF to four controls based on age, sex, enrollment date, and the Charlson comorbidity index (
Heart Rhythm. 2016 Feb. doi: 10.1016/j.hrthm.2016.01.026
).
Unvaccinated patients with influenza were 18% more likely to develop AF than unvaccinated patients without influenza (odds ratio, 1.18; 95% confidence interval, 1.01-1.38; P = .032), even after adjusting for demographic factors, medical history, and use of relevant health care services, the researchers reported. In contrast, vaccinated patients who later developed influenza were about as likely to develop AF as unvaccinated patients who did not develop influenza, both in the overall analysis and in subgroups stratified by age, sex, and comorbidities. Moreover, vaccinated patients without influenza were even less likely to develop AF than unvaccinated patients without influenza (OR, 0.88; 95% CI, 0.84-0.93; P less than .001).
The registry database excluded relevant data on smoking history, body mass index, and physical activity level, the researchers said. “Influenza infection was diagnosed using ICD-9 codes with concomitant use of antiviral agents, and was not further confirmed based on the results of viral culture with throat swab,” they added. “The diagnostic accuracy of influenza infection cannot be fully ascertained.”
The National Science Council and the Taipei Veterans General Hospital funded the study. The researchers had no disclosures.
The authors readily acknowledge the limitations of [this] large, observational study using an insurance database. Despite these admitted limitations, the authors should be commended on adding to the literature regarding modifiable risk factor reduction for the prevention of AF. Recently, a growing body of literature has examined this topic with several straightforward yet promising interventions identified. Weight loss, moderate exercise, and treatment for underlying obstructive sleep apnea have all been shown to reduce the risk of atrial fibrillation incidence or recurrence. Influenza vaccination could represent another simple, cost‐effective intervention to prevent AF. Although the flu vaccine is already recommended for many patient groups, this study suggests that there are even more potential public health benefits of the vaccine.
Dr. Bradley P. Knight is with the division of cardiology, department of medicine, at Northwestern University, Chicago. He had no disclosures. These comments were adapted from his editorial (Heart Rhythm. 2016 Feb. doi: 10.1016/j.hrthm.2016.01.025).
The authors readily acknowledge the limitations of [this] large, observational study using an insurance database. Despite these admitted limitations, the authors should be commended on adding to the literature regarding modifiable risk factor reduction for the prevention of AF. Recently, a growing body of literature has examined this topic with several straightforward yet promising interventions identified. Weight loss, moderate exercise, and treatment for underlying obstructive sleep apnea have all been shown to reduce the risk of atrial fibrillation incidence or recurrence. Influenza vaccination could represent another simple, cost‐effective intervention to prevent AF. Although the flu vaccine is already recommended for many patient groups, this study suggests that there are even more potential public health benefits of the vaccine.
Dr. Bradley P. Knight is with the division of cardiology, department of medicine, at Northwestern University, Chicago. He had no disclosures. These comments were adapted from his editorial (Heart Rhythm. 2016 Feb. doi: 10.1016/j.hrthm.2016.01.025).
The authors readily acknowledge the limitations of [this] large, observational study using an insurance database. Despite these admitted limitations, the authors should be commended on adding to the literature regarding modifiable risk factor reduction for the prevention of AF. Recently, a growing body of literature has examined this topic with several straightforward yet promising interventions identified. Weight loss, moderate exercise, and treatment for underlying obstructive sleep apnea have all been shown to reduce the risk of atrial fibrillation incidence or recurrence. Influenza vaccination could represent another simple, cost‐effective intervention to prevent AF. Although the flu vaccine is already recommended for many patient groups, this study suggests that there are even more potential public health benefits of the vaccine.
Dr. Bradley P. Knight is with the division of cardiology, department of medicine, at Northwestern University, Chicago. He had no disclosures. These comments were adapted from his editorial (Heart Rhythm. 2016 Feb. doi: 10.1016/j.hrthm.2016.01.025).
A diagnosis of influenza increased the risk of subsequent atrial fibrillation by about 18%, investigators reported online in Heart Rhythm.
Clinicians therefore should consider atrial fibrillation (AF) in patients with influenza-like symptoms who report palpitations or experience an ischemic stroke, said Dr. Ting-Yung Chang of Taipei Veterans General Hospital in Taiwan and his associates. Influenza vaccination might help prevent AF, and high-risk patients should be encouraged to receive the vaccination annually, they said. However, a large prospective study is needed to clarify whether influenza vaccination reduces the risk of AF and subsequent ischemic stroke and systemic thromboembolic events, they added.
Atrial fibrillation increases the risk of stroke about fivefold, triples the risk of heart failure, and doubles the chances of dementia and death, the researchers noted. Mounting evidence implicates inflammation and sympathetic nervous system dysregulation in the pathogenesis of AF, raising questions about whether influenza might underlie or contribute to some cases of AF. To explore relationships among AF, influenza, and influenza vaccination, the investigators analyzed data for 11,374 patients with AF who were enrolled in the Taiwan National Health Insurance Research Database between 2000 and 2010. They matched each patient with AF to four controls based on age, sex, enrollment date, and the Charlson comorbidity index (
Heart Rhythm. 2016 Feb. doi: 10.1016/j.hrthm.2016.01.026
).
Unvaccinated patients with influenza were 18% more likely to develop AF than unvaccinated patients without influenza (odds ratio, 1.18; 95% confidence interval, 1.01-1.38; P = .032), even after adjusting for demographic factors, medical history, and use of relevant health care services, the researchers reported. In contrast, vaccinated patients who later developed influenza were about as likely to develop AF as unvaccinated patients who did not develop influenza, both in the overall analysis and in subgroups stratified by age, sex, and comorbidities. Moreover, vaccinated patients without influenza were even less likely to develop AF than unvaccinated patients without influenza (OR, 0.88; 95% CI, 0.84-0.93; P less than .001).
The registry database excluded relevant data on smoking history, body mass index, and physical activity level, the researchers said. “Influenza infection was diagnosed using ICD-9 codes with concomitant use of antiviral agents, and was not further confirmed based on the results of viral culture with throat swab,” they added. “The diagnostic accuracy of influenza infection cannot be fully ascertained.”
The National Science Council and the Taipei Veterans General Hospital funded the study. The researchers had no disclosures.
A diagnosis of influenza increased the risk of subsequent atrial fibrillation by about 18%, investigators reported online in Heart Rhythm.
Clinicians therefore should consider atrial fibrillation (AF) in patients with influenza-like symptoms who report palpitations or experience an ischemic stroke, said Dr. Ting-Yung Chang of Taipei Veterans General Hospital in Taiwan and his associates. Influenza vaccination might help prevent AF, and high-risk patients should be encouraged to receive the vaccination annually, they said. However, a large prospective study is needed to clarify whether influenza vaccination reduces the risk of AF and subsequent ischemic stroke and systemic thromboembolic events, they added.
Atrial fibrillation increases the risk of stroke about fivefold, triples the risk of heart failure, and doubles the chances of dementia and death, the researchers noted. Mounting evidence implicates inflammation and sympathetic nervous system dysregulation in the pathogenesis of AF, raising questions about whether influenza might underlie or contribute to some cases of AF. To explore relationships among AF, influenza, and influenza vaccination, the investigators analyzed data for 11,374 patients with AF who were enrolled in the Taiwan National Health Insurance Research Database between 2000 and 2010. They matched each patient with AF to four controls based on age, sex, enrollment date, and the Charlson comorbidity index (
Heart Rhythm. 2016 Feb. doi: 10.1016/j.hrthm.2016.01.026
).
Unvaccinated patients with influenza were 18% more likely to develop AF than unvaccinated patients without influenza (odds ratio, 1.18; 95% confidence interval, 1.01-1.38; P = .032), even after adjusting for demographic factors, medical history, and use of relevant health care services, the researchers reported. In contrast, vaccinated patients who later developed influenza were about as likely to develop AF as unvaccinated patients who did not develop influenza, both in the overall analysis and in subgroups stratified by age, sex, and comorbidities. Moreover, vaccinated patients without influenza were even less likely to develop AF than unvaccinated patients without influenza (OR, 0.88; 95% CI, 0.84-0.93; P less than .001).
The registry database excluded relevant data on smoking history, body mass index, and physical activity level, the researchers said. “Influenza infection was diagnosed using ICD-9 codes with concomitant use of antiviral agents, and was not further confirmed based on the results of viral culture with throat swab,” they added. “The diagnostic accuracy of influenza infection cannot be fully ascertained.”
The National Science Council and the Taipei Veterans General Hospital funded the study. The researchers had no disclosures.
Key clinical point: Influenza might underlie some cases of atrial fibrillation.
Major finding: Among unvaccinated patients, an influenza diagnosis increased the odds of atrial fibrillation by 18% (OR, 1.18; P = .03).
Data source: An observational registry study of 11,374 patients with atrial fibrillation and 45,496 healthy controls.
Disclosures: The National Science Council and the Taipei Veterans General Hospital funded the study. The researchers had no disclosures.
Designer drug symptoms can mimic schizophrenia, anxiety, depression
LAS VEGAS – People who use spice, bath salts, and other so-called designer drugs may present with symptoms that resemble numerous psychiatric conditions, including schizophrenia, anxiety disorders, and depression.
“Given the recent emergence of designer drugs, the long-term consequences of their use have not been extensively studied and are relatively unknown,” Dr. William M. Sauve said at the annual psychopharmacology update held by the Nevada Psychiatric Association.
Dr. Sauve, medical director of TMS NeuroHealth Centers of Richmond and Charlottesville, both in Virginia, said designer drugs have grown in popularity in recent years because they are perceived as legal alternatives to illicit substances. In addition, their detection by standard drug toxicology screens is limited.
In October 2011, components of designer drugs, including synthetic cannabinoids and the major constituents of bath salts, were categorized as emergency Schedule I substances. In July 2012, President Obama signed the Synthetic Drug Abuse Prevention Act, which doubled the time that a substance may be temporarily assigned to Schedule I, from 18 months to 36 months.
“Under federal law, any chemical that is similar to a classified drug and is meant to be used for the same purposes is considered to be classified,” Dr. Sauve said. However, designer drugs “get labeled ‘not for human consumption’ and can be sold out in the open and camouflaged under names such as ‘stain remover,’ ‘research chemicals,’ and even ‘insect repellent.’ That’s why it’s very difficult for the law to catch up with these things. Active ingredients are also a moving target.”
He discussed three types of these designer drugs: synthetic cannabinoids, bath salts, and krokodil.
Synthetic cannabinoids mimic THC
Also known as spice, K2, and incense, these substances began to appear in the United States in 2008 and are mostly used by males. Primarily inhaled, these substances are meant to mimic the effects of tetrahydrocannabinol (THC). They work by decreasing levels of gamma-aminobutyric acid (GABA) and by increasing levels of glutamate and dopamine. “Serotonin levels can also be affected indirectly by endocannabinoid control of GABA and glutamate release,” he added.
Unlike marijuana, which is a partial agonist at the cannabinoid 1 (CB-1) receptor, synthetics are full agonists at the CB-1 receptor, “so as you use it, it will hit every receptor until you have maximal stimulation, and it may have 800 times greater affinity than THC,” he said. Signs and symptoms of acute intoxication can be wide ranging, from agitation and dysphoria to paranoia and tachycardia, and can last up to 6 hours. While commercial tests are available to detect synthetic cannabinoid metabolites, formulations change so often that “most tests quickly become obsolete,” Dr. Sauve said. He noted that intoxication with spice should be suspected in patients who present with bizarre behavior, anxiety, agitation, and/or psychosis in those with no known psychiatric history. Intravaneous benzodiazepines can be used for agitation and seizures. While knowledge of their long-term impact is lacking, synthetic cannabinoids may increase the risk of subsequent psychosis by threefold, he said, and kidney failure has been reported in several cases.
Bath salts widely available
Also labeled as “plant food,” “pond water cleaner,” “novelty collector’s items,” and “not for human consumption,” these stimulants began to be used in the United States in 2010, and are widely available online and in smoke shops. Users have a median age of 26 years, Dr. Sauve said, and are mostly male.
Bath salts may be comprised of methcathinones, especially synthetic cathinones. Natural cathinones are found in khat, a root from a shrub that is chewed upon primarily by people in North Africa. Bath salts also may contain methamphetamine analogues, which can be synthesized from ephedrine and pseudoephedrine. These include methylone (similar to MDMA, or ecstasy), mephedrone (similar to methamphetamine), and methylenedioxypyrovalerone (similar to cocaine). Bath salts can be inhaled, injected, snorted, swallowed, or inserted into the rectum or vagina, and effects occur in doses of 2-5 mg. Pharmacological effects vary and may include increased plasma norepinephrine, sympathetic effects, serotonin syndrome, and increased dopamine. He also noted that the transition from recreational to addictive use “may occur in a matter of days.”
Signs of toxicity with bath salts, Dr. Sauve continued, include the following: disorientation and agitation; dilated pupils with involuntary eye movements; lockjaw and teeth grinding; rapid, inappropriate, incoherent speech; being emotionally, verbally, or physically abusive, and having elevated liver enzymes and/or liver failure.
Treatment is primarily supportive and may include sedatives for anxiety, agitation, aggression, tremors, seizures, and psychosis. Physical restraints may be necessary.
Krokodil not seen much in U.S.
Formally known as desomorphine, this substance is synthesized from codeine and became popular in Russia after a crackdown on heroin there in 2010, Dr. Sauve said. The ingredients for krokodil synthesis include tablets containing codeine, caustic soda, gasoline, hydrochloric acid, iodine from disinfectants, and red phosphorus from matchboxes. While desomorphine is believed to be highly addictive, “all the other sequelae of krokodil are generally thought to be a result of phosphorus” and other substances. No good data exist in the prevalence of its use, he said. “We’re not really seeing this much in the United States, because it’s way too easy to get Oxycontin and heroin [here].”
Dr. Sauve reported that he is a consultant to Avanir Pharmaceuticals and Otsuka Pharmaceutical. He also reported being a member of the speakers bureau or receiving honoraria from Avanir Pharmaceuticals, Otsuka Pharmaceutical, and Sunovion Pharmaceuticals.
LAS VEGAS – People who use spice, bath salts, and other so-called designer drugs may present with symptoms that resemble numerous psychiatric conditions, including schizophrenia, anxiety disorders, and depression.
“Given the recent emergence of designer drugs, the long-term consequences of their use have not been extensively studied and are relatively unknown,” Dr. William M. Sauve said at the annual psychopharmacology update held by the Nevada Psychiatric Association.
Dr. Sauve, medical director of TMS NeuroHealth Centers of Richmond and Charlottesville, both in Virginia, said designer drugs have grown in popularity in recent years because they are perceived as legal alternatives to illicit substances. In addition, their detection by standard drug toxicology screens is limited.
In October 2011, components of designer drugs, including synthetic cannabinoids and the major constituents of bath salts, were categorized as emergency Schedule I substances. In July 2012, President Obama signed the Synthetic Drug Abuse Prevention Act, which doubled the time that a substance may be temporarily assigned to Schedule I, from 18 months to 36 months.
“Under federal law, any chemical that is similar to a classified drug and is meant to be used for the same purposes is considered to be classified,” Dr. Sauve said. However, designer drugs “get labeled ‘not for human consumption’ and can be sold out in the open and camouflaged under names such as ‘stain remover,’ ‘research chemicals,’ and even ‘insect repellent.’ That’s why it’s very difficult for the law to catch up with these things. Active ingredients are also a moving target.”
He discussed three types of these designer drugs: synthetic cannabinoids, bath salts, and krokodil.
Synthetic cannabinoids mimic THC
Also known as spice, K2, and incense, these substances began to appear in the United States in 2008 and are mostly used by males. Primarily inhaled, these substances are meant to mimic the effects of tetrahydrocannabinol (THC). They work by decreasing levels of gamma-aminobutyric acid (GABA) and by increasing levels of glutamate and dopamine. “Serotonin levels can also be affected indirectly by endocannabinoid control of GABA and glutamate release,” he added.
Unlike marijuana, which is a partial agonist at the cannabinoid 1 (CB-1) receptor, synthetics are full agonists at the CB-1 receptor, “so as you use it, it will hit every receptor until you have maximal stimulation, and it may have 800 times greater affinity than THC,” he said. Signs and symptoms of acute intoxication can be wide ranging, from agitation and dysphoria to paranoia and tachycardia, and can last up to 6 hours. While commercial tests are available to detect synthetic cannabinoid metabolites, formulations change so often that “most tests quickly become obsolete,” Dr. Sauve said. He noted that intoxication with spice should be suspected in patients who present with bizarre behavior, anxiety, agitation, and/or psychosis in those with no known psychiatric history. Intravaneous benzodiazepines can be used for agitation and seizures. While knowledge of their long-term impact is lacking, synthetic cannabinoids may increase the risk of subsequent psychosis by threefold, he said, and kidney failure has been reported in several cases.
Bath salts widely available
Also labeled as “plant food,” “pond water cleaner,” “novelty collector’s items,” and “not for human consumption,” these stimulants began to be used in the United States in 2010, and are widely available online and in smoke shops. Users have a median age of 26 years, Dr. Sauve said, and are mostly male.
Bath salts may be comprised of methcathinones, especially synthetic cathinones. Natural cathinones are found in khat, a root from a shrub that is chewed upon primarily by people in North Africa. Bath salts also may contain methamphetamine analogues, which can be synthesized from ephedrine and pseudoephedrine. These include methylone (similar to MDMA, or ecstasy), mephedrone (similar to methamphetamine), and methylenedioxypyrovalerone (similar to cocaine). Bath salts can be inhaled, injected, snorted, swallowed, or inserted into the rectum or vagina, and effects occur in doses of 2-5 mg. Pharmacological effects vary and may include increased plasma norepinephrine, sympathetic effects, serotonin syndrome, and increased dopamine. He also noted that the transition from recreational to addictive use “may occur in a matter of days.”
Signs of toxicity with bath salts, Dr. Sauve continued, include the following: disorientation and agitation; dilated pupils with involuntary eye movements; lockjaw and teeth grinding; rapid, inappropriate, incoherent speech; being emotionally, verbally, or physically abusive, and having elevated liver enzymes and/or liver failure.
Treatment is primarily supportive and may include sedatives for anxiety, agitation, aggression, tremors, seizures, and psychosis. Physical restraints may be necessary.
Krokodil not seen much in U.S.
Formally known as desomorphine, this substance is synthesized from codeine and became popular in Russia after a crackdown on heroin there in 2010, Dr. Sauve said. The ingredients for krokodil synthesis include tablets containing codeine, caustic soda, gasoline, hydrochloric acid, iodine from disinfectants, and red phosphorus from matchboxes. While desomorphine is believed to be highly addictive, “all the other sequelae of krokodil are generally thought to be a result of phosphorus” and other substances. No good data exist in the prevalence of its use, he said. “We’re not really seeing this much in the United States, because it’s way too easy to get Oxycontin and heroin [here].”
Dr. Sauve reported that he is a consultant to Avanir Pharmaceuticals and Otsuka Pharmaceutical. He also reported being a member of the speakers bureau or receiving honoraria from Avanir Pharmaceuticals, Otsuka Pharmaceutical, and Sunovion Pharmaceuticals.
LAS VEGAS – People who use spice, bath salts, and other so-called designer drugs may present with symptoms that resemble numerous psychiatric conditions, including schizophrenia, anxiety disorders, and depression.
“Given the recent emergence of designer drugs, the long-term consequences of their use have not been extensively studied and are relatively unknown,” Dr. William M. Sauve said at the annual psychopharmacology update held by the Nevada Psychiatric Association.
Dr. Sauve, medical director of TMS NeuroHealth Centers of Richmond and Charlottesville, both in Virginia, said designer drugs have grown in popularity in recent years because they are perceived as legal alternatives to illicit substances. In addition, their detection by standard drug toxicology screens is limited.
In October 2011, components of designer drugs, including synthetic cannabinoids and the major constituents of bath salts, were categorized as emergency Schedule I substances. In July 2012, President Obama signed the Synthetic Drug Abuse Prevention Act, which doubled the time that a substance may be temporarily assigned to Schedule I, from 18 months to 36 months.
“Under federal law, any chemical that is similar to a classified drug and is meant to be used for the same purposes is considered to be classified,” Dr. Sauve said. However, designer drugs “get labeled ‘not for human consumption’ and can be sold out in the open and camouflaged under names such as ‘stain remover,’ ‘research chemicals,’ and even ‘insect repellent.’ That’s why it’s very difficult for the law to catch up with these things. Active ingredients are also a moving target.”
He discussed three types of these designer drugs: synthetic cannabinoids, bath salts, and krokodil.
Synthetic cannabinoids mimic THC
Also known as spice, K2, and incense, these substances began to appear in the United States in 2008 and are mostly used by males. Primarily inhaled, these substances are meant to mimic the effects of tetrahydrocannabinol (THC). They work by decreasing levels of gamma-aminobutyric acid (GABA) and by increasing levels of glutamate and dopamine. “Serotonin levels can also be affected indirectly by endocannabinoid control of GABA and glutamate release,” he added.
Unlike marijuana, which is a partial agonist at the cannabinoid 1 (CB-1) receptor, synthetics are full agonists at the CB-1 receptor, “so as you use it, it will hit every receptor until you have maximal stimulation, and it may have 800 times greater affinity than THC,” he said. Signs and symptoms of acute intoxication can be wide ranging, from agitation and dysphoria to paranoia and tachycardia, and can last up to 6 hours. While commercial tests are available to detect synthetic cannabinoid metabolites, formulations change so often that “most tests quickly become obsolete,” Dr. Sauve said. He noted that intoxication with spice should be suspected in patients who present with bizarre behavior, anxiety, agitation, and/or psychosis in those with no known psychiatric history. Intravaneous benzodiazepines can be used for agitation and seizures. While knowledge of their long-term impact is lacking, synthetic cannabinoids may increase the risk of subsequent psychosis by threefold, he said, and kidney failure has been reported in several cases.
Bath salts widely available
Also labeled as “plant food,” “pond water cleaner,” “novelty collector’s items,” and “not for human consumption,” these stimulants began to be used in the United States in 2010, and are widely available online and in smoke shops. Users have a median age of 26 years, Dr. Sauve said, and are mostly male.
Bath salts may be comprised of methcathinones, especially synthetic cathinones. Natural cathinones are found in khat, a root from a shrub that is chewed upon primarily by people in North Africa. Bath salts also may contain methamphetamine analogues, which can be synthesized from ephedrine and pseudoephedrine. These include methylone (similar to MDMA, or ecstasy), mephedrone (similar to methamphetamine), and methylenedioxypyrovalerone (similar to cocaine). Bath salts can be inhaled, injected, snorted, swallowed, or inserted into the rectum or vagina, and effects occur in doses of 2-5 mg. Pharmacological effects vary and may include increased plasma norepinephrine, sympathetic effects, serotonin syndrome, and increased dopamine. He also noted that the transition from recreational to addictive use “may occur in a matter of days.”
Signs of toxicity with bath salts, Dr. Sauve continued, include the following: disorientation and agitation; dilated pupils with involuntary eye movements; lockjaw and teeth grinding; rapid, inappropriate, incoherent speech; being emotionally, verbally, or physically abusive, and having elevated liver enzymes and/or liver failure.
Treatment is primarily supportive and may include sedatives for anxiety, agitation, aggression, tremors, seizures, and psychosis. Physical restraints may be necessary.
Krokodil not seen much in U.S.
Formally known as desomorphine, this substance is synthesized from codeine and became popular in Russia after a crackdown on heroin there in 2010, Dr. Sauve said. The ingredients for krokodil synthesis include tablets containing codeine, caustic soda, gasoline, hydrochloric acid, iodine from disinfectants, and red phosphorus from matchboxes. While desomorphine is believed to be highly addictive, “all the other sequelae of krokodil are generally thought to be a result of phosphorus” and other substances. No good data exist in the prevalence of its use, he said. “We’re not really seeing this much in the United States, because it’s way too easy to get Oxycontin and heroin [here].”
Dr. Sauve reported that he is a consultant to Avanir Pharmaceuticals and Otsuka Pharmaceutical. He also reported being a member of the speakers bureau or receiving honoraria from Avanir Pharmaceuticals, Otsuka Pharmaceutical, and Sunovion Pharmaceuticals.
EXPERT ANALYSIS AT THE NPA PSYCHOPHARMACOLOGY UPDATE
Project aims to improve care in the ‘4th trimester’
The way Sarah Verbiest, Dr.P.H., sees it, postpartum care for new moms could use a little more respect.
“We see [childbirth] in movies all the time: It’s so exciting when a woman gives birth, and then the next thing you see is that she’s fitting back into her jeans and she looks fabulous and rested,” said Dr. Verbiest, executive director of the center for maternal and infant health at the University of North Carolina (UNC) at Chapel Hill.
“We perpetuate this myth that you’re supposed to feel great. It’s not true,” she said. “It’s a huge physical event that has been unattended and kind of downplayed for a long time, and I think a lot of women suffer because we don’t have the best advice to give them or we don’t talk about it.”
Dr. Verbiest and her colleagues at UNC are hoping to shake up the postpartum paradigm by better defining the gaps in care that occur in those first 12 weeks after childbirth or as they are calling this time, the “4th trimester.”
Defining postpartum care
The goal of the 4th Trimester Project is to bring together about 100 mothers, clinicians, researchers, and other stakeholders to identify ways to improve outcomes for mothers, infants, and families. Participants will gather in Chapel Hill, following the Breastfeeding and Feminism International Conference in March. There, experts will deliver state-of-the-art talks on what’s currently known about the six domains of postpartum care, and make recommendations for future research projects.
The six domains of postpartum care are:
• Physical recovery from childbirth.
• Mood.
• Infant feeding.
• Medications, substances, and environmental exposures.
• Sexuality, contraception, and birth spacing.
• Sleep and fatigue.
“The first step is connecting moms and researchers, coming to some agreement and enthusiasm about what needs to be studied,” Dr. Verbiest said. “We’re going to have a nice diversity of opinions around the table. It will be interesting to see what clinicians think is important and what moms think is important, and how those match up.”
A national survey of new mothers sheds light on some of the postpartum health issues. In a survey from the Childbirth Connection, released in 2008, more than 15 specific health problems were cited as new problems by 25% or more of the mothers during the first 2 months after delivery. At 6 months, many women continued to experience these issues, including stress (43%), weight control (40%), sleep loss (34%), lack of sexual desire (26%), physical exhaustion (25%), and backache (24%).
Drop-off in care
Although national efforts to promote breastfeeding and increase awareness of the potential for postpartum depression have emerged in recent years, many gaps exist in today’s postpartum care landscape, Dr. Verbiest said, including what she described as a “precipitous drop-off” in basic follow-up care during the first 3 months after giving birth.
New mothers are discharged from the hospital, and they don’t necessarily come back to see anybody for another 6 weeks. “Some women never come back for a visit. So they’ve had all this care, and we care about them so much when they’re carrying a baby, but once they have the baby, the focus is all on that baby, and not on mom,” she said.
Some clinicians and researchers may not view postpartum sleep and fatigue as an important issue to explore, but it’s something that affects quality of life for the mother and the family, as well as overall health and wellness, Dr. Verbiest said.
“It’s exhausting having your body completely change from a hormonal standpoint and being dedicated to this little being that doesn’t sleep very well,” she said. “But have we done a lot of research so we can provide moms with the best coping strategies?”
Dr. Alison Stuebe, who is also part of the interdisciplinary research team working on the 4th Trimester Project, saw this firsthand with one of her friends.
About a year ago, a longtime friend had her first baby, and required a cesarean for arrest of descent. “She said, ‘I cannot believe someone would cut me open and they’re not even going to see me in 6 weeks,’” recalled Dr. Stuebe of the department of obstetrics and gynecology at UNC.
“There’s a sense that it’s customary to see the women at 6 weeks, make sure they have birth control, and their partners are hoping that means they’re cleared to come home and have sex again,” Dr. Stuebe said. “That’s what the extent is for a lot of women, but there are a lot of things moms need in that time period. I do a lot of work with moms who are struggling with breastfeeding. It’s usually not purely an issue of how the baby is attaching.”
Moving research forward
Dr. Stuebe, who is a distinguished scholar of infant and young child feeding in the Gillings School of Global Public Health at UNC, described the 4th Trimester Project as “not a be all and end all,” but rather as an opportunity to “specifically engage moms to tell us what we’re not telling them or what they wish we would tell them in the postpartum period.”
After the first in-person meeting of the project participants in March 2016, the investigators will stage a series of webinars and discussion groups aimed at refining specific research projects before the participants reconvene in person in March 2017.
The project recently got a boost when the Patient-Centered Outcomes Research Institute (PCORI) approved $248,594 in funding for the research.
“This will hopefully launch a whole series of research projects, whether funded through PCORI or through other research mechanisms, to drive the work forward,” Dr. Verbiest said.
One such project, for example, could compare the effectiveness of a postpartum doula coming to a mother’s house versus offering her postpartum support by phone.
“Part of what we hope in the long term from this PCORI work is to ask, ‘If moms felt really supported during the postpartum period, what questions would we need to ask to show that we’re doing it well?’” Dr. Stuebe said. “If there were a quality of postpartum care questionnaire, what would we want moms to check?”
The way Sarah Verbiest, Dr.P.H., sees it, postpartum care for new moms could use a little more respect.
“We see [childbirth] in movies all the time: It’s so exciting when a woman gives birth, and then the next thing you see is that she’s fitting back into her jeans and she looks fabulous and rested,” said Dr. Verbiest, executive director of the center for maternal and infant health at the University of North Carolina (UNC) at Chapel Hill.
“We perpetuate this myth that you’re supposed to feel great. It’s not true,” she said. “It’s a huge physical event that has been unattended and kind of downplayed for a long time, and I think a lot of women suffer because we don’t have the best advice to give them or we don’t talk about it.”
Dr. Verbiest and her colleagues at UNC are hoping to shake up the postpartum paradigm by better defining the gaps in care that occur in those first 12 weeks after childbirth or as they are calling this time, the “4th trimester.”
Defining postpartum care
The goal of the 4th Trimester Project is to bring together about 100 mothers, clinicians, researchers, and other stakeholders to identify ways to improve outcomes for mothers, infants, and families. Participants will gather in Chapel Hill, following the Breastfeeding and Feminism International Conference in March. There, experts will deliver state-of-the-art talks on what’s currently known about the six domains of postpartum care, and make recommendations for future research projects.
The six domains of postpartum care are:
• Physical recovery from childbirth.
• Mood.
• Infant feeding.
• Medications, substances, and environmental exposures.
• Sexuality, contraception, and birth spacing.
• Sleep and fatigue.
“The first step is connecting moms and researchers, coming to some agreement and enthusiasm about what needs to be studied,” Dr. Verbiest said. “We’re going to have a nice diversity of opinions around the table. It will be interesting to see what clinicians think is important and what moms think is important, and how those match up.”
A national survey of new mothers sheds light on some of the postpartum health issues. In a survey from the Childbirth Connection, released in 2008, more than 15 specific health problems were cited as new problems by 25% or more of the mothers during the first 2 months after delivery. At 6 months, many women continued to experience these issues, including stress (43%), weight control (40%), sleep loss (34%), lack of sexual desire (26%), physical exhaustion (25%), and backache (24%).
Drop-off in care
Although national efforts to promote breastfeeding and increase awareness of the potential for postpartum depression have emerged in recent years, many gaps exist in today’s postpartum care landscape, Dr. Verbiest said, including what she described as a “precipitous drop-off” in basic follow-up care during the first 3 months after giving birth.
New mothers are discharged from the hospital, and they don’t necessarily come back to see anybody for another 6 weeks. “Some women never come back for a visit. So they’ve had all this care, and we care about them so much when they’re carrying a baby, but once they have the baby, the focus is all on that baby, and not on mom,” she said.
Some clinicians and researchers may not view postpartum sleep and fatigue as an important issue to explore, but it’s something that affects quality of life for the mother and the family, as well as overall health and wellness, Dr. Verbiest said.
“It’s exhausting having your body completely change from a hormonal standpoint and being dedicated to this little being that doesn’t sleep very well,” she said. “But have we done a lot of research so we can provide moms with the best coping strategies?”
Dr. Alison Stuebe, who is also part of the interdisciplinary research team working on the 4th Trimester Project, saw this firsthand with one of her friends.
About a year ago, a longtime friend had her first baby, and required a cesarean for arrest of descent. “She said, ‘I cannot believe someone would cut me open and they’re not even going to see me in 6 weeks,’” recalled Dr. Stuebe of the department of obstetrics and gynecology at UNC.
“There’s a sense that it’s customary to see the women at 6 weeks, make sure they have birth control, and their partners are hoping that means they’re cleared to come home and have sex again,” Dr. Stuebe said. “That’s what the extent is for a lot of women, but there are a lot of things moms need in that time period. I do a lot of work with moms who are struggling with breastfeeding. It’s usually not purely an issue of how the baby is attaching.”
Moving research forward
Dr. Stuebe, who is a distinguished scholar of infant and young child feeding in the Gillings School of Global Public Health at UNC, described the 4th Trimester Project as “not a be all and end all,” but rather as an opportunity to “specifically engage moms to tell us what we’re not telling them or what they wish we would tell them in the postpartum period.”
After the first in-person meeting of the project participants in March 2016, the investigators will stage a series of webinars and discussion groups aimed at refining specific research projects before the participants reconvene in person in March 2017.
The project recently got a boost when the Patient-Centered Outcomes Research Institute (PCORI) approved $248,594 in funding for the research.
“This will hopefully launch a whole series of research projects, whether funded through PCORI or through other research mechanisms, to drive the work forward,” Dr. Verbiest said.
One such project, for example, could compare the effectiveness of a postpartum doula coming to a mother’s house versus offering her postpartum support by phone.
“Part of what we hope in the long term from this PCORI work is to ask, ‘If moms felt really supported during the postpartum period, what questions would we need to ask to show that we’re doing it well?’” Dr. Stuebe said. “If there were a quality of postpartum care questionnaire, what would we want moms to check?”
The way Sarah Verbiest, Dr.P.H., sees it, postpartum care for new moms could use a little more respect.
“We see [childbirth] in movies all the time: It’s so exciting when a woman gives birth, and then the next thing you see is that she’s fitting back into her jeans and she looks fabulous and rested,” said Dr. Verbiest, executive director of the center for maternal and infant health at the University of North Carolina (UNC) at Chapel Hill.
“We perpetuate this myth that you’re supposed to feel great. It’s not true,” she said. “It’s a huge physical event that has been unattended and kind of downplayed for a long time, and I think a lot of women suffer because we don’t have the best advice to give them or we don’t talk about it.”
Dr. Verbiest and her colleagues at UNC are hoping to shake up the postpartum paradigm by better defining the gaps in care that occur in those first 12 weeks after childbirth or as they are calling this time, the “4th trimester.”
Defining postpartum care
The goal of the 4th Trimester Project is to bring together about 100 mothers, clinicians, researchers, and other stakeholders to identify ways to improve outcomes for mothers, infants, and families. Participants will gather in Chapel Hill, following the Breastfeeding and Feminism International Conference in March. There, experts will deliver state-of-the-art talks on what’s currently known about the six domains of postpartum care, and make recommendations for future research projects.
The six domains of postpartum care are:
• Physical recovery from childbirth.
• Mood.
• Infant feeding.
• Medications, substances, and environmental exposures.
• Sexuality, contraception, and birth spacing.
• Sleep and fatigue.
“The first step is connecting moms and researchers, coming to some agreement and enthusiasm about what needs to be studied,” Dr. Verbiest said. “We’re going to have a nice diversity of opinions around the table. It will be interesting to see what clinicians think is important and what moms think is important, and how those match up.”
A national survey of new mothers sheds light on some of the postpartum health issues. In a survey from the Childbirth Connection, released in 2008, more than 15 specific health problems were cited as new problems by 25% or more of the mothers during the first 2 months after delivery. At 6 months, many women continued to experience these issues, including stress (43%), weight control (40%), sleep loss (34%), lack of sexual desire (26%), physical exhaustion (25%), and backache (24%).
Drop-off in care
Although national efforts to promote breastfeeding and increase awareness of the potential for postpartum depression have emerged in recent years, many gaps exist in today’s postpartum care landscape, Dr. Verbiest said, including what she described as a “precipitous drop-off” in basic follow-up care during the first 3 months after giving birth.
New mothers are discharged from the hospital, and they don’t necessarily come back to see anybody for another 6 weeks. “Some women never come back for a visit. So they’ve had all this care, and we care about them so much when they’re carrying a baby, but once they have the baby, the focus is all on that baby, and not on mom,” she said.
Some clinicians and researchers may not view postpartum sleep and fatigue as an important issue to explore, but it’s something that affects quality of life for the mother and the family, as well as overall health and wellness, Dr. Verbiest said.
“It’s exhausting having your body completely change from a hormonal standpoint and being dedicated to this little being that doesn’t sleep very well,” she said. “But have we done a lot of research so we can provide moms with the best coping strategies?”
Dr. Alison Stuebe, who is also part of the interdisciplinary research team working on the 4th Trimester Project, saw this firsthand with one of her friends.
About a year ago, a longtime friend had her first baby, and required a cesarean for arrest of descent. “She said, ‘I cannot believe someone would cut me open and they’re not even going to see me in 6 weeks,’” recalled Dr. Stuebe of the department of obstetrics and gynecology at UNC.
“There’s a sense that it’s customary to see the women at 6 weeks, make sure they have birth control, and their partners are hoping that means they’re cleared to come home and have sex again,” Dr. Stuebe said. “That’s what the extent is for a lot of women, but there are a lot of things moms need in that time period. I do a lot of work with moms who are struggling with breastfeeding. It’s usually not purely an issue of how the baby is attaching.”
Moving research forward
Dr. Stuebe, who is a distinguished scholar of infant and young child feeding in the Gillings School of Global Public Health at UNC, described the 4th Trimester Project as “not a be all and end all,” but rather as an opportunity to “specifically engage moms to tell us what we’re not telling them or what they wish we would tell them in the postpartum period.”
After the first in-person meeting of the project participants in March 2016, the investigators will stage a series of webinars and discussion groups aimed at refining specific research projects before the participants reconvene in person in March 2017.
The project recently got a boost when the Patient-Centered Outcomes Research Institute (PCORI) approved $248,594 in funding for the research.
“This will hopefully launch a whole series of research projects, whether funded through PCORI or through other research mechanisms, to drive the work forward,” Dr. Verbiest said.
One such project, for example, could compare the effectiveness of a postpartum doula coming to a mother’s house versus offering her postpartum support by phone.
“Part of what we hope in the long term from this PCORI work is to ask, ‘If moms felt really supported during the postpartum period, what questions would we need to ask to show that we’re doing it well?’” Dr. Stuebe said. “If there were a quality of postpartum care questionnaire, what would we want moms to check?”
Human gene editing consensus study underway
A consensus study of the scientific underpinnings of human gene editing technologies is underway, and the committee of experts behind the effort will independently review potential applications for those technologies, as well as the clinical, ethical, legal, and social implications of their use.
The multidisciplinary committee met Feb. 11 to receive input from select stakeholders as it launches its review, the results of which will represent the official views of the National Academy of Sciences and the National Academy of Medicine.
Among those stakeholders were representatives from several companies commercializing gene editing, a representative from the National Institutes of Health, and patient advocacy groups.
With some caveats, participants lobbied to maintain the existing regulatory framework related to gene therapy.
Michael Werner, cofounder and executive director of the Alliance for Regenerative Medicine, which advocates globally for regenerative medicine and advanced therapies, said his organization believes “the existing regulatory framework overall works for these technologies.”
“We don’t believe the [Food and Drug Administration], for example, needs to create a whole separate oversight process in addition to the process we already have now for gene therapy,” he said, adding that “the ultimate goal here is not to have regulatory action or legislative action that will hinder or delay the development of these technologies.”
The consensus study follows an International Summit on Human Gene Editing held in December, and is the next component of the Human Gene Editing Initiative. The committee will study the potential for gene editing in biomedical research and medicine – including human germline editing – although representatives from each of the companies represented at the meeting noted that they are not currently focused on germline applications.
Rather, the commercial focus is on other areas, such as correcting genes in somatic cells.
“We start with medical need. We want to work on things where there is not currently a therapy that addresses adequately the medical need, and we need the ability to generate a differentiated product,” said Vic Myer, Ph.D., of Editas Medicine in Cambridge, Mass.
The company has projects underway for opthalmologic applications, sickle cell anemia, beta-thalassemia, Duchenne muscular dystrophy, cystic fibrosis, alpha1-antitrypsin deficiency in the liver, and others.
“We are working on a number of different types of edits in a number of different tissues with a number of delivery modalities,” Dr. Myer said, noting that some programs will move quickly, while others will not.
Similarly, Intellia Therapeutics, also of Cambridge, Mass., is “focusing very much on what we hope will be curative products for somatic gene-based disorders,” said Dr. John Leonard, the company’s chief medical officer.
“We limit our work to somatic cells. We thought very carefully about that and that is what we do,” he added, noting that a recently launched division of Intellia is focused on autoimmune oncology opportunities (ex vivo), and on liver disease (in vivo).
The committee of experts conducting the consensus study, which began its information-gathering process in December at the International Summit on Human Gene Editing, will take these and other views expressed at the meeting into consideration during its work over the next year. The study will include a literature review and data gathering via meetings in the United States and abroad. The committee will continue to seek input from researchers, clinicians, policy makers, and the public.
“The committee will also monitor in real time the latest scientific achievements of importance in this rapidly developing field,” according to information from the National Academies.
The field has enormous potential, according to Mr. Werner, who explained that combined, the various types of gene editing technology available are “pretty powerful” in terms of an approach for targeting and changing DNA sequences in human cells.
“We’re talking about the potential to durably treat and potentially even cure diseases that currently represent unmet medical needs,” he said. “We could, in theory, be talking about millions of patients worldwide.”
A consensus study of the scientific underpinnings of human gene editing technologies is underway, and the committee of experts behind the effort will independently review potential applications for those technologies, as well as the clinical, ethical, legal, and social implications of their use.
The multidisciplinary committee met Feb. 11 to receive input from select stakeholders as it launches its review, the results of which will represent the official views of the National Academy of Sciences and the National Academy of Medicine.
Among those stakeholders were representatives from several companies commercializing gene editing, a representative from the National Institutes of Health, and patient advocacy groups.
With some caveats, participants lobbied to maintain the existing regulatory framework related to gene therapy.
Michael Werner, cofounder and executive director of the Alliance for Regenerative Medicine, which advocates globally for regenerative medicine and advanced therapies, said his organization believes “the existing regulatory framework overall works for these technologies.”
“We don’t believe the [Food and Drug Administration], for example, needs to create a whole separate oversight process in addition to the process we already have now for gene therapy,” he said, adding that “the ultimate goal here is not to have regulatory action or legislative action that will hinder or delay the development of these technologies.”
The consensus study follows an International Summit on Human Gene Editing held in December, and is the next component of the Human Gene Editing Initiative. The committee will study the potential for gene editing in biomedical research and medicine – including human germline editing – although representatives from each of the companies represented at the meeting noted that they are not currently focused on germline applications.
Rather, the commercial focus is on other areas, such as correcting genes in somatic cells.
“We start with medical need. We want to work on things where there is not currently a therapy that addresses adequately the medical need, and we need the ability to generate a differentiated product,” said Vic Myer, Ph.D., of Editas Medicine in Cambridge, Mass.
The company has projects underway for opthalmologic applications, sickle cell anemia, beta-thalassemia, Duchenne muscular dystrophy, cystic fibrosis, alpha1-antitrypsin deficiency in the liver, and others.
“We are working on a number of different types of edits in a number of different tissues with a number of delivery modalities,” Dr. Myer said, noting that some programs will move quickly, while others will not.
Similarly, Intellia Therapeutics, also of Cambridge, Mass., is “focusing very much on what we hope will be curative products for somatic gene-based disorders,” said Dr. John Leonard, the company’s chief medical officer.
“We limit our work to somatic cells. We thought very carefully about that and that is what we do,” he added, noting that a recently launched division of Intellia is focused on autoimmune oncology opportunities (ex vivo), and on liver disease (in vivo).
The committee of experts conducting the consensus study, which began its information-gathering process in December at the International Summit on Human Gene Editing, will take these and other views expressed at the meeting into consideration during its work over the next year. The study will include a literature review and data gathering via meetings in the United States and abroad. The committee will continue to seek input from researchers, clinicians, policy makers, and the public.
“The committee will also monitor in real time the latest scientific achievements of importance in this rapidly developing field,” according to information from the National Academies.
The field has enormous potential, according to Mr. Werner, who explained that combined, the various types of gene editing technology available are “pretty powerful” in terms of an approach for targeting and changing DNA sequences in human cells.
“We’re talking about the potential to durably treat and potentially even cure diseases that currently represent unmet medical needs,” he said. “We could, in theory, be talking about millions of patients worldwide.”
A consensus study of the scientific underpinnings of human gene editing technologies is underway, and the committee of experts behind the effort will independently review potential applications for those technologies, as well as the clinical, ethical, legal, and social implications of their use.
The multidisciplinary committee met Feb. 11 to receive input from select stakeholders as it launches its review, the results of which will represent the official views of the National Academy of Sciences and the National Academy of Medicine.
Among those stakeholders were representatives from several companies commercializing gene editing, a representative from the National Institutes of Health, and patient advocacy groups.
With some caveats, participants lobbied to maintain the existing regulatory framework related to gene therapy.
Michael Werner, cofounder and executive director of the Alliance for Regenerative Medicine, which advocates globally for regenerative medicine and advanced therapies, said his organization believes “the existing regulatory framework overall works for these technologies.”
“We don’t believe the [Food and Drug Administration], for example, needs to create a whole separate oversight process in addition to the process we already have now for gene therapy,” he said, adding that “the ultimate goal here is not to have regulatory action or legislative action that will hinder or delay the development of these technologies.”
The consensus study follows an International Summit on Human Gene Editing held in December, and is the next component of the Human Gene Editing Initiative. The committee will study the potential for gene editing in biomedical research and medicine – including human germline editing – although representatives from each of the companies represented at the meeting noted that they are not currently focused on germline applications.
Rather, the commercial focus is on other areas, such as correcting genes in somatic cells.
“We start with medical need. We want to work on things where there is not currently a therapy that addresses adequately the medical need, and we need the ability to generate a differentiated product,” said Vic Myer, Ph.D., of Editas Medicine in Cambridge, Mass.
The company has projects underway for opthalmologic applications, sickle cell anemia, beta-thalassemia, Duchenne muscular dystrophy, cystic fibrosis, alpha1-antitrypsin deficiency in the liver, and others.
“We are working on a number of different types of edits in a number of different tissues with a number of delivery modalities,” Dr. Myer said, noting that some programs will move quickly, while others will not.
Similarly, Intellia Therapeutics, also of Cambridge, Mass., is “focusing very much on what we hope will be curative products for somatic gene-based disorders,” said Dr. John Leonard, the company’s chief medical officer.
“We limit our work to somatic cells. We thought very carefully about that and that is what we do,” he added, noting that a recently launched division of Intellia is focused on autoimmune oncology opportunities (ex vivo), and on liver disease (in vivo).
The committee of experts conducting the consensus study, which began its information-gathering process in December at the International Summit on Human Gene Editing, will take these and other views expressed at the meeting into consideration during its work over the next year. The study will include a literature review and data gathering via meetings in the United States and abroad. The committee will continue to seek input from researchers, clinicians, policy makers, and the public.
“The committee will also monitor in real time the latest scientific achievements of importance in this rapidly developing field,” according to information from the National Academies.
The field has enormous potential, according to Mr. Werner, who explained that combined, the various types of gene editing technology available are “pretty powerful” in terms of an approach for targeting and changing DNA sequences in human cells.
“We’re talking about the potential to durably treat and potentially even cure diseases that currently represent unmet medical needs,” he said. “We could, in theory, be talking about millions of patients worldwide.”
Psychiatry can promote growth amid chronic illness
Promoting resilience, benefit finding, and post-traumatic growth help patients and families cope well with chronic illness. A resilient family has good problem-solving skills and communication, and a shared belief system (Fam Process. 2003; 42:1-18). Benefit finding coexists with feelings of burden, grief, and loss, and post-traumatic growth can occur despite grief and loss. Convening family meetings, for example, is a way to provide a therapeutic space for families and an opportunity to reflect on ways that chronic illness has affected the family, both negatively and positively.
What is coping well?
Resilient families cope well by identifying and solving illness-related problems, communicating about symptoms, negotiating role changes, and developing new interests as a family and new ways of emotionally being together. In addition, resilient families are able to adapt or change their life goals or health behaviors, such as improving diet, increasing exercise, and stopping smoking. A family member may work fewer hours, for example, and older children may give up some childhood activities to take on caregiving responsibilities.
Families do not usually think about how they cope; they just get along the best they can. Families may not consider how each family member’s individual coping style meshes with the coping styles of other family members. Illness management often is punctuated by crises where change happens quickly, without the family having time to deliberate on what coping styles might work best. Family changes can become fixed, therefore, not by choice, but by happenstance.
The initial stage of coping is “assimilative.” This is when the impact of the illness is being understood and absorbed. Emotional coping occurs when distress is highest, for example, at the beginning of an illness – when uncertainty exists about the diagnosis. Another characteristic of emotional coping is that it is characterized by attempts to regulate negative emotions. For example, family members may blame themselves or others, engage in wishful thinking, or become avoidant.
At later stages of illness, coping becomes “accommodative” after attempts to change or cure the illness have been found to be ineffective. Emotional coping can then be replaced with a problem-based coping style, allowing a stressor to be discussed and a solution chosen from several alternatives. Reflective coping, a related concept, is the ability to generate and consider coping options, and to recognize the usefulness of a particular coping strategy in a particular situation.
Psychiatric imperatives
While providing psychotherapy with these couples, it is helpful to:
• Help families differentiate between emotional difficulties such as “I am the primary caregiver, and I feel overburdened,” and more general practical problems, such as “I am happy to be the primary caregiver, but I need some extra help.”
• Describe coping to the family. Coping is a dynamic process, and coping styles change over time. Each person copes in their own way, depending on their experiences of illness and expectations of living with illness. In a family, the experiences and behaviors of all the individuals influence the way the family unit functions as a whole.
• Promote a balance between acceptance and change.
• Encourage the family to talk about their experience with others who are experiencing the same stressors.
• Give the family a handout that outlines different coping styles to get the discussion started.
• Provide a therapeutic space for family members to think together about how they want to cope and what coping well means to their family.
Developing dyadic coping
When dyadic coping takes place, couples cope as a single entity. Dyadic coping research is relatively new; most studies have been conducted in the past 15 years. Couples who use positive dyadic coping employ joint problem solving, joint information seeking, sharing of feelings, mutual commitment, and relaxing together. Meanwhile, couples who use negative dyadic coping hide concerns from each other and avoid shared discussion. A systemic review of dyadic coping in couples with cancer found that couples using positive dyadic coping styles experienced higher relationship functioning (Br J Health Psychol. 2015 Feb;20[1]:85-114).
Couples with good dyadic coping view the illness as “our problem.” This approach necessitates a shared understanding of the illness. The couple usually has prior experience working together as a team, for example, parenting and dividing roles within the house. They are able to relax together and provide emotional support, such as mutual calming and expressions of solidarity. Talking together about one’s worries and needs allows couples to share the experience more adequately. Dyadic coping is reflected in the amount of “we” talk.
The person in the family who copes “best” may provide the model for developing the family coping style. In a study of 66 couples faced with the stress of forced relocation, nearly all the couples adapted to the stress “as a couple,” rather than “as individuals” (Fam Process. 1991 Sep;30[3]:347-61). At the 2-year follow-up, each husband and wife developed similar coping styles, with one individual’s coping ability driving the adjustment of his or her partner. The need to adjust together or to adapt as a couple lessened the stress of relocation. Adaptation occurred through the development of shared meaning of the relocation that emerged from conversation within the couples. In other words, the couple developed a shared worldview. The coping style of the person who coped best was the strongest predictor of adjustment for both members of the couple. For most couples, the style of the person who coped best dominated.
Questions to ask during therapy
While working with these couples, assess their motivation to develop dyadic coping, by asking:
• “Do either of you feel that the patient should do this alone?” If the answer is yes, it will be difficult, if not impossible, to move the couple to a dyadic coping style.
• “Do your efforts to work together result in greater conflict?”
• “How much do you want this to change?” This questions clarifies their motivation to work together.
• “When you think about problems related to your heart condition, to what extent do you view those as ‘our problem’ [shared by the patient and the spouse equally] or mainly as ‘your own problem?’ ”
• “When a problem related to your heart condition arises, to what extent do you and your partner work together to solve it?”
• “When you both talk about the illness, how much do you use ‘we-talk’?”
• “It is important that you both agree about what is causing the illness. Can I answer any questions that might help you reach this understanding?”
• “Are there times in the past where you have successfully solved difficult problems? How did you do that?”
• “How do you respond when your spouse becomes ill?”
• “What can your spouse do that will help you get better?”
• “Can you ask your spouse for help and support?”
• “Can you work on your spouse’s health problem together?”
‘Benefit finding’ and PTG
Benefit finding emerges later in the adjustment to chronic illness. For example, caregivers may develop a greater appreciation of their own health and ability to enjoy their own pursuits. Family connectedness is a frequent source of meaning, and a critical aspect of well-being and benefit finding. Seven factors make up benefit finding: compassion/empathy, spiritual growth, mindfulness, family relations growth, lifestyle gains, personal growth, and new opportunities (Psychol Health. 2009 Apr;24[4]:373-93). Benefit finding is associated with higher marital adjustment, improved life satisfaction, and a more positive affect, especially at high levels of stress.
Post-traumatic growth, or PTG, refers to positive changes that occur after traumatic life events. People who experience PTG are transformed by their struggles with adversity. It is the struggle after the trauma, not the trauma itself, that produces PTG. In contrast to resilience, PTG refers to changes that go beyond pretrauma levels of adaptation and beyond benefit finding. Relational benefits in the aftermath of a cancer diagnosis are well recognized. An instrument used to assess these outcomes is called the Post-traumatic Growth Inventory, or PTGI (J Trauma Stress. 1996 Jul;9:455-71).
Interventions for couples coping with cancer resulted in improvements in communication, dyadic coping, quality of life, psychosocial distress, sexual functioning, and marital satisfaction (Psychooncology. 2014 Apr;23[7]:731-9). PTG may, however, be more apparent in patients than spouses.
Potential interventions
Promoting dyadic coping is effective if the couple wants to engage in intervention. According to one study, a partner-assisted emotional disclosure improved relationship functioning and intimacy (J Marital Fam Ther. 2012 Jun;38 Suppl 1:284-95). Couples therapy improves relational functioning in couples coping with cancer, at 1-year follow-up (Psychooncology. 2009 Mar;18[3]:276-83). Most important, as a first step, the couple must agree that they want to develop dyadic coping. The concept of individual versus dyadic coping may be novel for couples, and it is worth spending time on this review before offering couples intervention.
A psychoeducational program also can teach dyadic coping. The Resilient Partners discussion group developed in collaboration with the Multiple Sclerosis Society focused on developing couples’ strengths in coping with multiple sclerosis (Rolland, J., McPheters, J., and Carbonell, E., 2008). This multifamily group program is based on the Family Systems Illness Model, which integrates the demands of multiple sclerosis over time within a family developmental framework. In a comparison of a couple skills intervention with a psychoeducation program, women in the couple skills intervention benefited more in terms of their relationship functioning (Ann Behav Med. 2012 Apr;43[2]:239-52).
Dr. John S. Rolland’s Family Systems Illness (FSI) model provides a framework for the psychoeducation, assessment, and intervention with families dealing with chronic illness. This model, developed in clinical experience with more than 1,000 families, views families as valued partners and resources, and emphasizes resilience and growth. The FSI model takes into account the interaction of an illness with the individual’s development and the family’s development, the multigenerational ways of coping with illness, the family’s health/illness belief system, available resources, and relationships between health care providers.
The PTGI includes five domains: improved relationships, new possibilities for one’s life, a greater appreciation for life, a greater sense of personal strength, and spiritual development. Several family oriented themes within the PTGI can be used by the psychiatrist to inquire about positive change. These themes are:
• Knowing that I can count on people in times of trouble.
• A sense of closeness with others.
• Having compassion for others.
• Putting effort into my relationships.
• I learned a great deal about how wonderful people are.
• I accept needing others.
To promote PTG, the psychiatrists can listen for accounts of the experience of growth, label the experience, decide when the patient is ready for more focused questioning, and recognize that a life narrative including the aftermath of a trauma has value. In order to get the patient to recognize PTG, the psychiatrist can state and ask: “You may have heard people say that they have found some benefit in their struggle with trauma. Given what has happened to you, do you think that is possible?” Another exchange might flow like this: “You mentioned last time that you noticed that you and your wife have grown closer since this happened. Can you tell me more about this closeness. What is it about this struggle that has produced this closeness?”
Conclusion
Strengths, resilience, and post-traumatic growth are distinct constructs that share conceptual overlap. Using these constructs, the psychiatrist can help the patients and their families move forward. At the time of diagnosis/trauma/bereavement, family and couple interventions provide support, education, and symptom management. Specific psychoeducational interventions or family therapy can be used if needed. As the illness progresses and the family moves from an assimilative stance to an accommodative stance, and as problem-solving moves from emotional problem solving to reflective problem solving, the possibility of benefit finding and PTG emerge. Most importantly, the psychiatrist can provide the family with a therapeutic space to consider their coping styles, and offer the family a path forward through discussion of dyadic coping and family growth.
Further reading
1. Tedeschi and Kilmer, “Assessing Strengths, Resilience, and Growth to Guide Clinical Interventions,” Professional Psychology: Research and Practice. 2005;36(3), p. 230-7.
2. Heru A.M., “Working With Families in Medical Settings,” (New York: Routledge), 2013.
3. Rolland J.S. “Families, Illness, & Disability: An Integrative Treatment Model,” (New York: Basic Books), 1994. New edition in press.
Thank you to Dr. Jennifer Caspari for assisting with resources for this article.
Dr. Heru is with the department of psychiatry at the University of Denver, Aurora. She has no conflicts of interest to disclose.
Promoting resilience, benefit finding, and post-traumatic growth help patients and families cope well with chronic illness. A resilient family has good problem-solving skills and communication, and a shared belief system (Fam Process. 2003; 42:1-18). Benefit finding coexists with feelings of burden, grief, and loss, and post-traumatic growth can occur despite grief and loss. Convening family meetings, for example, is a way to provide a therapeutic space for families and an opportunity to reflect on ways that chronic illness has affected the family, both negatively and positively.
What is coping well?
Resilient families cope well by identifying and solving illness-related problems, communicating about symptoms, negotiating role changes, and developing new interests as a family and new ways of emotionally being together. In addition, resilient families are able to adapt or change their life goals or health behaviors, such as improving diet, increasing exercise, and stopping smoking. A family member may work fewer hours, for example, and older children may give up some childhood activities to take on caregiving responsibilities.
Families do not usually think about how they cope; they just get along the best they can. Families may not consider how each family member’s individual coping style meshes with the coping styles of other family members. Illness management often is punctuated by crises where change happens quickly, without the family having time to deliberate on what coping styles might work best. Family changes can become fixed, therefore, not by choice, but by happenstance.
The initial stage of coping is “assimilative.” This is when the impact of the illness is being understood and absorbed. Emotional coping occurs when distress is highest, for example, at the beginning of an illness – when uncertainty exists about the diagnosis. Another characteristic of emotional coping is that it is characterized by attempts to regulate negative emotions. For example, family members may blame themselves or others, engage in wishful thinking, or become avoidant.
At later stages of illness, coping becomes “accommodative” after attempts to change or cure the illness have been found to be ineffective. Emotional coping can then be replaced with a problem-based coping style, allowing a stressor to be discussed and a solution chosen from several alternatives. Reflective coping, a related concept, is the ability to generate and consider coping options, and to recognize the usefulness of a particular coping strategy in a particular situation.
Psychiatric imperatives
While providing psychotherapy with these couples, it is helpful to:
• Help families differentiate between emotional difficulties such as “I am the primary caregiver, and I feel overburdened,” and more general practical problems, such as “I am happy to be the primary caregiver, but I need some extra help.”
• Describe coping to the family. Coping is a dynamic process, and coping styles change over time. Each person copes in their own way, depending on their experiences of illness and expectations of living with illness. In a family, the experiences and behaviors of all the individuals influence the way the family unit functions as a whole.
• Promote a balance between acceptance and change.
• Encourage the family to talk about their experience with others who are experiencing the same stressors.
• Give the family a handout that outlines different coping styles to get the discussion started.
• Provide a therapeutic space for family members to think together about how they want to cope and what coping well means to their family.
Developing dyadic coping
When dyadic coping takes place, couples cope as a single entity. Dyadic coping research is relatively new; most studies have been conducted in the past 15 years. Couples who use positive dyadic coping employ joint problem solving, joint information seeking, sharing of feelings, mutual commitment, and relaxing together. Meanwhile, couples who use negative dyadic coping hide concerns from each other and avoid shared discussion. A systemic review of dyadic coping in couples with cancer found that couples using positive dyadic coping styles experienced higher relationship functioning (Br J Health Psychol. 2015 Feb;20[1]:85-114).
Couples with good dyadic coping view the illness as “our problem.” This approach necessitates a shared understanding of the illness. The couple usually has prior experience working together as a team, for example, parenting and dividing roles within the house. They are able to relax together and provide emotional support, such as mutual calming and expressions of solidarity. Talking together about one’s worries and needs allows couples to share the experience more adequately. Dyadic coping is reflected in the amount of “we” talk.
The person in the family who copes “best” may provide the model for developing the family coping style. In a study of 66 couples faced with the stress of forced relocation, nearly all the couples adapted to the stress “as a couple,” rather than “as individuals” (Fam Process. 1991 Sep;30[3]:347-61). At the 2-year follow-up, each husband and wife developed similar coping styles, with one individual’s coping ability driving the adjustment of his or her partner. The need to adjust together or to adapt as a couple lessened the stress of relocation. Adaptation occurred through the development of shared meaning of the relocation that emerged from conversation within the couples. In other words, the couple developed a shared worldview. The coping style of the person who coped best was the strongest predictor of adjustment for both members of the couple. For most couples, the style of the person who coped best dominated.
Questions to ask during therapy
While working with these couples, assess their motivation to develop dyadic coping, by asking:
• “Do either of you feel that the patient should do this alone?” If the answer is yes, it will be difficult, if not impossible, to move the couple to a dyadic coping style.
• “Do your efforts to work together result in greater conflict?”
• “How much do you want this to change?” This questions clarifies their motivation to work together.
• “When you think about problems related to your heart condition, to what extent do you view those as ‘our problem’ [shared by the patient and the spouse equally] or mainly as ‘your own problem?’ ”
• “When a problem related to your heart condition arises, to what extent do you and your partner work together to solve it?”
• “When you both talk about the illness, how much do you use ‘we-talk’?”
• “It is important that you both agree about what is causing the illness. Can I answer any questions that might help you reach this understanding?”
• “Are there times in the past where you have successfully solved difficult problems? How did you do that?”
• “How do you respond when your spouse becomes ill?”
• “What can your spouse do that will help you get better?”
• “Can you ask your spouse for help and support?”
• “Can you work on your spouse’s health problem together?”
‘Benefit finding’ and PTG
Benefit finding emerges later in the adjustment to chronic illness. For example, caregivers may develop a greater appreciation of their own health and ability to enjoy their own pursuits. Family connectedness is a frequent source of meaning, and a critical aspect of well-being and benefit finding. Seven factors make up benefit finding: compassion/empathy, spiritual growth, mindfulness, family relations growth, lifestyle gains, personal growth, and new opportunities (Psychol Health. 2009 Apr;24[4]:373-93). Benefit finding is associated with higher marital adjustment, improved life satisfaction, and a more positive affect, especially at high levels of stress.
Post-traumatic growth, or PTG, refers to positive changes that occur after traumatic life events. People who experience PTG are transformed by their struggles with adversity. It is the struggle after the trauma, not the trauma itself, that produces PTG. In contrast to resilience, PTG refers to changes that go beyond pretrauma levels of adaptation and beyond benefit finding. Relational benefits in the aftermath of a cancer diagnosis are well recognized. An instrument used to assess these outcomes is called the Post-traumatic Growth Inventory, or PTGI (J Trauma Stress. 1996 Jul;9:455-71).
Interventions for couples coping with cancer resulted in improvements in communication, dyadic coping, quality of life, psychosocial distress, sexual functioning, and marital satisfaction (Psychooncology. 2014 Apr;23[7]:731-9). PTG may, however, be more apparent in patients than spouses.
Potential interventions
Promoting dyadic coping is effective if the couple wants to engage in intervention. According to one study, a partner-assisted emotional disclosure improved relationship functioning and intimacy (J Marital Fam Ther. 2012 Jun;38 Suppl 1:284-95). Couples therapy improves relational functioning in couples coping with cancer, at 1-year follow-up (Psychooncology. 2009 Mar;18[3]:276-83). Most important, as a first step, the couple must agree that they want to develop dyadic coping. The concept of individual versus dyadic coping may be novel for couples, and it is worth spending time on this review before offering couples intervention.
A psychoeducational program also can teach dyadic coping. The Resilient Partners discussion group developed in collaboration with the Multiple Sclerosis Society focused on developing couples’ strengths in coping with multiple sclerosis (Rolland, J., McPheters, J., and Carbonell, E., 2008). This multifamily group program is based on the Family Systems Illness Model, which integrates the demands of multiple sclerosis over time within a family developmental framework. In a comparison of a couple skills intervention with a psychoeducation program, women in the couple skills intervention benefited more in terms of their relationship functioning (Ann Behav Med. 2012 Apr;43[2]:239-52).
Dr. John S. Rolland’s Family Systems Illness (FSI) model provides a framework for the psychoeducation, assessment, and intervention with families dealing with chronic illness. This model, developed in clinical experience with more than 1,000 families, views families as valued partners and resources, and emphasizes resilience and growth. The FSI model takes into account the interaction of an illness with the individual’s development and the family’s development, the multigenerational ways of coping with illness, the family’s health/illness belief system, available resources, and relationships between health care providers.
The PTGI includes five domains: improved relationships, new possibilities for one’s life, a greater appreciation for life, a greater sense of personal strength, and spiritual development. Several family oriented themes within the PTGI can be used by the psychiatrist to inquire about positive change. These themes are:
• Knowing that I can count on people in times of trouble.
• A sense of closeness with others.
• Having compassion for others.
• Putting effort into my relationships.
• I learned a great deal about how wonderful people are.
• I accept needing others.
To promote PTG, the psychiatrists can listen for accounts of the experience of growth, label the experience, decide when the patient is ready for more focused questioning, and recognize that a life narrative including the aftermath of a trauma has value. In order to get the patient to recognize PTG, the psychiatrist can state and ask: “You may have heard people say that they have found some benefit in their struggle with trauma. Given what has happened to you, do you think that is possible?” Another exchange might flow like this: “You mentioned last time that you noticed that you and your wife have grown closer since this happened. Can you tell me more about this closeness. What is it about this struggle that has produced this closeness?”
Conclusion
Strengths, resilience, and post-traumatic growth are distinct constructs that share conceptual overlap. Using these constructs, the psychiatrist can help the patients and their families move forward. At the time of diagnosis/trauma/bereavement, family and couple interventions provide support, education, and symptom management. Specific psychoeducational interventions or family therapy can be used if needed. As the illness progresses and the family moves from an assimilative stance to an accommodative stance, and as problem-solving moves from emotional problem solving to reflective problem solving, the possibility of benefit finding and PTG emerge. Most importantly, the psychiatrist can provide the family with a therapeutic space to consider their coping styles, and offer the family a path forward through discussion of dyadic coping and family growth.
Further reading
1. Tedeschi and Kilmer, “Assessing Strengths, Resilience, and Growth to Guide Clinical Interventions,” Professional Psychology: Research and Practice. 2005;36(3), p. 230-7.
2. Heru A.M., “Working With Families in Medical Settings,” (New York: Routledge), 2013.
3. Rolland J.S. “Families, Illness, & Disability: An Integrative Treatment Model,” (New York: Basic Books), 1994. New edition in press.
Thank you to Dr. Jennifer Caspari for assisting with resources for this article.
Dr. Heru is with the department of psychiatry at the University of Denver, Aurora. She has no conflicts of interest to disclose.
Promoting resilience, benefit finding, and post-traumatic growth help patients and families cope well with chronic illness. A resilient family has good problem-solving skills and communication, and a shared belief system (Fam Process. 2003; 42:1-18). Benefit finding coexists with feelings of burden, grief, and loss, and post-traumatic growth can occur despite grief and loss. Convening family meetings, for example, is a way to provide a therapeutic space for families and an opportunity to reflect on ways that chronic illness has affected the family, both negatively and positively.
What is coping well?
Resilient families cope well by identifying and solving illness-related problems, communicating about symptoms, negotiating role changes, and developing new interests as a family and new ways of emotionally being together. In addition, resilient families are able to adapt or change their life goals or health behaviors, such as improving diet, increasing exercise, and stopping smoking. A family member may work fewer hours, for example, and older children may give up some childhood activities to take on caregiving responsibilities.
Families do not usually think about how they cope; they just get along the best they can. Families may not consider how each family member’s individual coping style meshes with the coping styles of other family members. Illness management often is punctuated by crises where change happens quickly, without the family having time to deliberate on what coping styles might work best. Family changes can become fixed, therefore, not by choice, but by happenstance.
The initial stage of coping is “assimilative.” This is when the impact of the illness is being understood and absorbed. Emotional coping occurs when distress is highest, for example, at the beginning of an illness – when uncertainty exists about the diagnosis. Another characteristic of emotional coping is that it is characterized by attempts to regulate negative emotions. For example, family members may blame themselves or others, engage in wishful thinking, or become avoidant.
At later stages of illness, coping becomes “accommodative” after attempts to change or cure the illness have been found to be ineffective. Emotional coping can then be replaced with a problem-based coping style, allowing a stressor to be discussed and a solution chosen from several alternatives. Reflective coping, a related concept, is the ability to generate and consider coping options, and to recognize the usefulness of a particular coping strategy in a particular situation.
Psychiatric imperatives
While providing psychotherapy with these couples, it is helpful to:
• Help families differentiate between emotional difficulties such as “I am the primary caregiver, and I feel overburdened,” and more general practical problems, such as “I am happy to be the primary caregiver, but I need some extra help.”
• Describe coping to the family. Coping is a dynamic process, and coping styles change over time. Each person copes in their own way, depending on their experiences of illness and expectations of living with illness. In a family, the experiences and behaviors of all the individuals influence the way the family unit functions as a whole.
• Promote a balance between acceptance and change.
• Encourage the family to talk about their experience with others who are experiencing the same stressors.
• Give the family a handout that outlines different coping styles to get the discussion started.
• Provide a therapeutic space for family members to think together about how they want to cope and what coping well means to their family.
Developing dyadic coping
When dyadic coping takes place, couples cope as a single entity. Dyadic coping research is relatively new; most studies have been conducted in the past 15 years. Couples who use positive dyadic coping employ joint problem solving, joint information seeking, sharing of feelings, mutual commitment, and relaxing together. Meanwhile, couples who use negative dyadic coping hide concerns from each other and avoid shared discussion. A systemic review of dyadic coping in couples with cancer found that couples using positive dyadic coping styles experienced higher relationship functioning (Br J Health Psychol. 2015 Feb;20[1]:85-114).
Couples with good dyadic coping view the illness as “our problem.” This approach necessitates a shared understanding of the illness. The couple usually has prior experience working together as a team, for example, parenting and dividing roles within the house. They are able to relax together and provide emotional support, such as mutual calming and expressions of solidarity. Talking together about one’s worries and needs allows couples to share the experience more adequately. Dyadic coping is reflected in the amount of “we” talk.
The person in the family who copes “best” may provide the model for developing the family coping style. In a study of 66 couples faced with the stress of forced relocation, nearly all the couples adapted to the stress “as a couple,” rather than “as individuals” (Fam Process. 1991 Sep;30[3]:347-61). At the 2-year follow-up, each husband and wife developed similar coping styles, with one individual’s coping ability driving the adjustment of his or her partner. The need to adjust together or to adapt as a couple lessened the stress of relocation. Adaptation occurred through the development of shared meaning of the relocation that emerged from conversation within the couples. In other words, the couple developed a shared worldview. The coping style of the person who coped best was the strongest predictor of adjustment for both members of the couple. For most couples, the style of the person who coped best dominated.
Questions to ask during therapy
While working with these couples, assess their motivation to develop dyadic coping, by asking:
• “Do either of you feel that the patient should do this alone?” If the answer is yes, it will be difficult, if not impossible, to move the couple to a dyadic coping style.
• “Do your efforts to work together result in greater conflict?”
• “How much do you want this to change?” This questions clarifies their motivation to work together.
• “When you think about problems related to your heart condition, to what extent do you view those as ‘our problem’ [shared by the patient and the spouse equally] or mainly as ‘your own problem?’ ”
• “When a problem related to your heart condition arises, to what extent do you and your partner work together to solve it?”
• “When you both talk about the illness, how much do you use ‘we-talk’?”
• “It is important that you both agree about what is causing the illness. Can I answer any questions that might help you reach this understanding?”
• “Are there times in the past where you have successfully solved difficult problems? How did you do that?”
• “How do you respond when your spouse becomes ill?”
• “What can your spouse do that will help you get better?”
• “Can you ask your spouse for help and support?”
• “Can you work on your spouse’s health problem together?”
‘Benefit finding’ and PTG
Benefit finding emerges later in the adjustment to chronic illness. For example, caregivers may develop a greater appreciation of their own health and ability to enjoy their own pursuits. Family connectedness is a frequent source of meaning, and a critical aspect of well-being and benefit finding. Seven factors make up benefit finding: compassion/empathy, spiritual growth, mindfulness, family relations growth, lifestyle gains, personal growth, and new opportunities (Psychol Health. 2009 Apr;24[4]:373-93). Benefit finding is associated with higher marital adjustment, improved life satisfaction, and a more positive affect, especially at high levels of stress.
Post-traumatic growth, or PTG, refers to positive changes that occur after traumatic life events. People who experience PTG are transformed by their struggles with adversity. It is the struggle after the trauma, not the trauma itself, that produces PTG. In contrast to resilience, PTG refers to changes that go beyond pretrauma levels of adaptation and beyond benefit finding. Relational benefits in the aftermath of a cancer diagnosis are well recognized. An instrument used to assess these outcomes is called the Post-traumatic Growth Inventory, or PTGI (J Trauma Stress. 1996 Jul;9:455-71).
Interventions for couples coping with cancer resulted in improvements in communication, dyadic coping, quality of life, psychosocial distress, sexual functioning, and marital satisfaction (Psychooncology. 2014 Apr;23[7]:731-9). PTG may, however, be more apparent in patients than spouses.
Potential interventions
Promoting dyadic coping is effective if the couple wants to engage in intervention. According to one study, a partner-assisted emotional disclosure improved relationship functioning and intimacy (J Marital Fam Ther. 2012 Jun;38 Suppl 1:284-95). Couples therapy improves relational functioning in couples coping with cancer, at 1-year follow-up (Psychooncology. 2009 Mar;18[3]:276-83). Most important, as a first step, the couple must agree that they want to develop dyadic coping. The concept of individual versus dyadic coping may be novel for couples, and it is worth spending time on this review before offering couples intervention.
A psychoeducational program also can teach dyadic coping. The Resilient Partners discussion group developed in collaboration with the Multiple Sclerosis Society focused on developing couples’ strengths in coping with multiple sclerosis (Rolland, J., McPheters, J., and Carbonell, E., 2008). This multifamily group program is based on the Family Systems Illness Model, which integrates the demands of multiple sclerosis over time within a family developmental framework. In a comparison of a couple skills intervention with a psychoeducation program, women in the couple skills intervention benefited more in terms of their relationship functioning (Ann Behav Med. 2012 Apr;43[2]:239-52).
Dr. John S. Rolland’s Family Systems Illness (FSI) model provides a framework for the psychoeducation, assessment, and intervention with families dealing with chronic illness. This model, developed in clinical experience with more than 1,000 families, views families as valued partners and resources, and emphasizes resilience and growth. The FSI model takes into account the interaction of an illness with the individual’s development and the family’s development, the multigenerational ways of coping with illness, the family’s health/illness belief system, available resources, and relationships between health care providers.
The PTGI includes five domains: improved relationships, new possibilities for one’s life, a greater appreciation for life, a greater sense of personal strength, and spiritual development. Several family oriented themes within the PTGI can be used by the psychiatrist to inquire about positive change. These themes are:
• Knowing that I can count on people in times of trouble.
• A sense of closeness with others.
• Having compassion for others.
• Putting effort into my relationships.
• I learned a great deal about how wonderful people are.
• I accept needing others.
To promote PTG, the psychiatrists can listen for accounts of the experience of growth, label the experience, decide when the patient is ready for more focused questioning, and recognize that a life narrative including the aftermath of a trauma has value. In order to get the patient to recognize PTG, the psychiatrist can state and ask: “You may have heard people say that they have found some benefit in their struggle with trauma. Given what has happened to you, do you think that is possible?” Another exchange might flow like this: “You mentioned last time that you noticed that you and your wife have grown closer since this happened. Can you tell me more about this closeness. What is it about this struggle that has produced this closeness?”
Conclusion
Strengths, resilience, and post-traumatic growth are distinct constructs that share conceptual overlap. Using these constructs, the psychiatrist can help the patients and their families move forward. At the time of diagnosis/trauma/bereavement, family and couple interventions provide support, education, and symptom management. Specific psychoeducational interventions or family therapy can be used if needed. As the illness progresses and the family moves from an assimilative stance to an accommodative stance, and as problem-solving moves from emotional problem solving to reflective problem solving, the possibility of benefit finding and PTG emerge. Most importantly, the psychiatrist can provide the family with a therapeutic space to consider their coping styles, and offer the family a path forward through discussion of dyadic coping and family growth.
Further reading
1. Tedeschi and Kilmer, “Assessing Strengths, Resilience, and Growth to Guide Clinical Interventions,” Professional Psychology: Research and Practice. 2005;36(3), p. 230-7.
2. Heru A.M., “Working With Families in Medical Settings,” (New York: Routledge), 2013.
3. Rolland J.S. “Families, Illness, & Disability: An Integrative Treatment Model,” (New York: Basic Books), 1994. New edition in press.
Thank you to Dr. Jennifer Caspari for assisting with resources for this article.
Dr. Heru is with the department of psychiatry at the University of Denver, Aurora. She has no conflicts of interest to disclose.
Lichen Striatus
Lichen striatus (LS) is a benign, uncommon, self-limited, linear inflammatory skin disorder that primarily affects children up to 15 years of age, most commonly around 2 to 3 years of age, and is seen more frequently in girls.1 It presents with a sudden eruption of asymptomatic small, flat-topped, lichenoid, scaly papules in a linear array on a single extremity. The lesions may be erythematous, flesh colored, or hypopigmented.1,2 Multiple lesions appear over days to weeks and coalesce into linear plaques in a continuous or interrupted pattern along the lines of Blaschko, indicating possible somatic mosaicism.1 Although typically asymptomatic, it may be pruritic. Most cases spontaneously resolve within 1 year.3 Recurrences are unusual. Digital involvement may result in onycholysis, longitudinal ridging, splitting, and nail loss.1 The underlying cause of LS may be an abnormal immunologic reaction or genetic predisposition that is precipitated by some trigger such as a viral infection, trauma, hypersensitivity reaction, vaccine, seasonal variation, medication, or pregnancy.1,2 An association with atopy has been described. Treatment is not necessary but options include topical steroids, topical retinoids, and topical calcineurin inhibitors.2
Histologically, findings in LS are somewhat variable but typically show a combination of spongiotic and lichenoid interface dermatitis with a perivascular and periadnexal lymphocytic infiltrate (Figure 1). Epidermal changes include intercellular and intracellular edema, focal spongiosis, lymphocytic exocytosis, parakeratosis, patchy hyperkeratosis, and keratinocyte necrosis (Figure 2A).1,3 The epidermis is normal or slightly acanthotic, and dyskeratotic keratinocytes can be found in the granular and horny layers or at the dermoepidermal junction.2 The lymphohistiocytic infiltrate in the superficial and deep dermis surrounds vascular plexuses and cutaneous adnexa such as eccrine glands and hair follicles.1 Perivascular lymphoid aggregates and eccrine coil involvement are particularly distinctive of LS (Figure 2B).4 Pigment incontinence also may be seen.
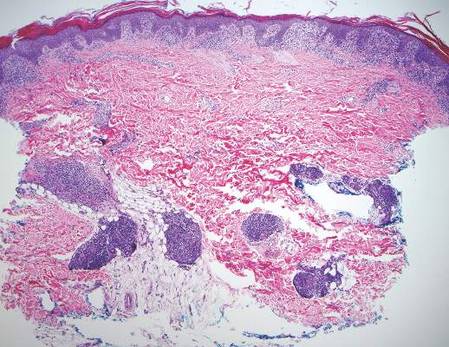
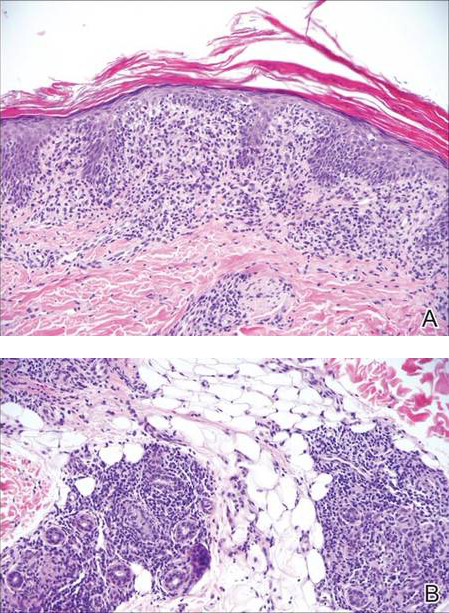
Another condition that distributes linearly along the lines of Blaschko is linear epidermolytic hyperkeratosis (EHK). Similar to LS, histology shows hyperkeratosis, focal parakeratosis, and acanthosis of the epidermis.5 However, EHK shows epidermolysis, acantholysis, and perinuclear vacuolization in spinous and granular layers (Figure 3).5 The lack of perivascular and periadnexal inflammation also can help differentiate EHK from LS.
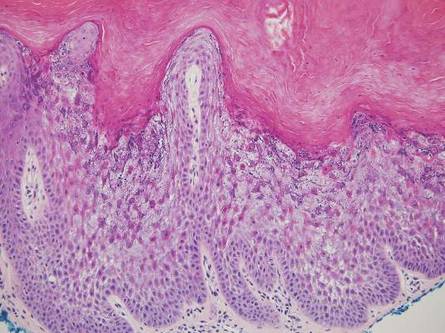
Linear lichen planus (LLP), similar to LS, histologically shows a lichenoid lymphocytic bandlike infiltrate obscuring the dermoepidermal junction, vacuolization of the basal cell layer, and pigment incontinence.1,2 Although LS and LLP can have histologic overlap, the absence of adnexal or perieccrine lymphocytic inflammation can help distinguish the two.3 The histopathologic changes of intercellular edema or mild spongiosis, exocytosis, and parakeratosis present in LS also are typically absent in LLP. Linear lichen planus characteristically consists of wedge-shaped hypergranulosis and irregular acanthosis with saw-toothed rete ridges (Figure 4).2 In addition, lobular eosinophilic deposits known as cytoid or Civatte bodies representing degenerated keratinocytes can be visualized at the dermoepidermal junction in LLP.2 Immunofluorescence will highlight Civatte bodies with IgM, IgG, and C3, also helping to differentiate these 2 conditions.1
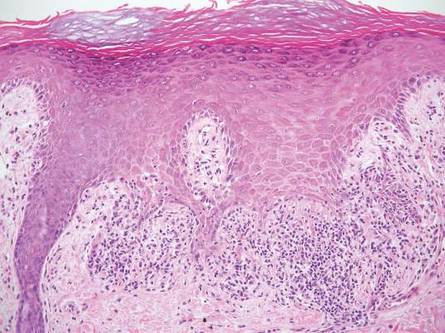
Linear porokeratosis can be mistaken for the linear lesion of LS. Both entities may reveal perivascular lymphocytes in the dermis, and porokeratosis can be lichenoid in the central portion of the lesion.6 However, porokeratosis is unique in that it contains a cornoid lamella, characterized by a thin column of tightly packed parakeratotic cells extending from an invagination of the epidermis through the adjacent stratum corneum (Figure 5).6 Beneath the cornoid lamella, the granular layer is either absent or markedly attenuated, and pyknotic keratinocytes with perinuclear edema are present in the spinous layer.6 The epidermis in the central portion of the porokeratotic lesion may be normal, hyperplastic, or atrophic with effacement of rete ridges.
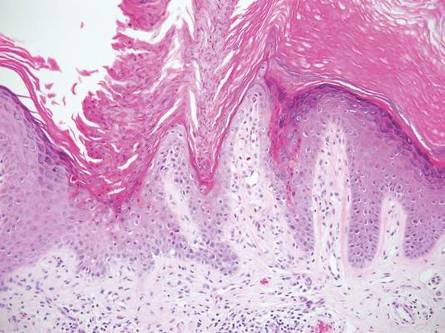
Similar to LS, linear psoriasis follows lines of Blaschko clinically. However, it is distinguished by its characteristic psoriatic epidermal changes as well as its lack of lichenoid or perieccrine inflammation.3 Typical findings in linear psoriasis include hyperkeratosis, confluent parakeratosis with entrapped neutrophilic microabscesses, acanthosis with regular elongation of rete ridges, intraepidermal neutrophils, thinned suprapapillary plates, dilated capillaries in the tips of the dermal papillae, and a chronic dermal inflammatory infiltrate (Figure 6).4
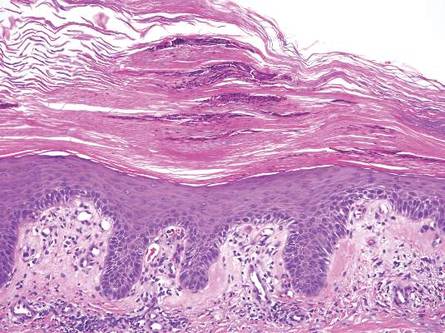
- Wang WL, Lazar A. Lichenoid and interface dermatitis. In: Calonje E, Brenn T, Lazar A, et al, eds. McKee’s Pathology of the Skin. 4th ed. London, England: Elsevier/Saunders; 2011:219-258.
- Shiohara T, Kano Y. Lichen planus and lichenoid dermatoses. In: Bolognia J, Jorizzo J, Schaffer J, eds. Dermatology. 3rd ed. Philadelphia, PA: Elsevier/Saunders; 2012:183-202.
- Zhang Y, McNutt NS. Lichen striatus. histological, immunohistochemical, and ultrastructural study of 37 cases. J Cutan Pathol. 2001;28:65-71.
- Johnson M, Walker D, Galloway W, et al. Interface dermatitis along Blaschko’s lines. J Cutan Pathol. 2014;41:950-954.
- Kumar P, Kumar R, Kumar Mandal RK, et al. Systematized linear epidermolytic hyperkeratosis. Dermatol Online J. 2014;20:21248.
- Requena L, Requena C, Cockerell C. Benign epidermal tumors and proliferations. In: Bolognia J, Jorizzo J, Schaffer J. Dermatology. 3rd ed. Philadelphia, PA: Elsevier/Saunders; 2012:1795-1815.
Lichen striatus (LS) is a benign, uncommon, self-limited, linear inflammatory skin disorder that primarily affects children up to 15 years of age, most commonly around 2 to 3 years of age, and is seen more frequently in girls.1 It presents with a sudden eruption of asymptomatic small, flat-topped, lichenoid, scaly papules in a linear array on a single extremity. The lesions may be erythematous, flesh colored, or hypopigmented.1,2 Multiple lesions appear over days to weeks and coalesce into linear plaques in a continuous or interrupted pattern along the lines of Blaschko, indicating possible somatic mosaicism.1 Although typically asymptomatic, it may be pruritic. Most cases spontaneously resolve within 1 year.3 Recurrences are unusual. Digital involvement may result in onycholysis, longitudinal ridging, splitting, and nail loss.1 The underlying cause of LS may be an abnormal immunologic reaction or genetic predisposition that is precipitated by some trigger such as a viral infection, trauma, hypersensitivity reaction, vaccine, seasonal variation, medication, or pregnancy.1,2 An association with atopy has been described. Treatment is not necessary but options include topical steroids, topical retinoids, and topical calcineurin inhibitors.2
Histologically, findings in LS are somewhat variable but typically show a combination of spongiotic and lichenoid interface dermatitis with a perivascular and periadnexal lymphocytic infiltrate (Figure 1). Epidermal changes include intercellular and intracellular edema, focal spongiosis, lymphocytic exocytosis, parakeratosis, patchy hyperkeratosis, and keratinocyte necrosis (Figure 2A).1,3 The epidermis is normal or slightly acanthotic, and dyskeratotic keratinocytes can be found in the granular and horny layers or at the dermoepidermal junction.2 The lymphohistiocytic infiltrate in the superficial and deep dermis surrounds vascular plexuses and cutaneous adnexa such as eccrine glands and hair follicles.1 Perivascular lymphoid aggregates and eccrine coil involvement are particularly distinctive of LS (Figure 2B).4 Pigment incontinence also may be seen.
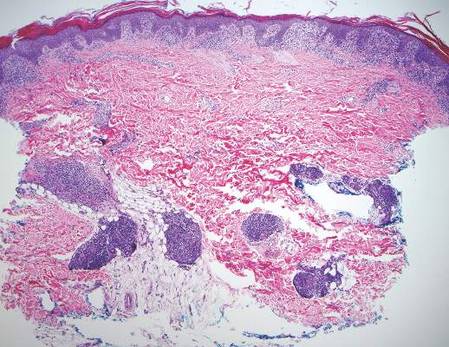
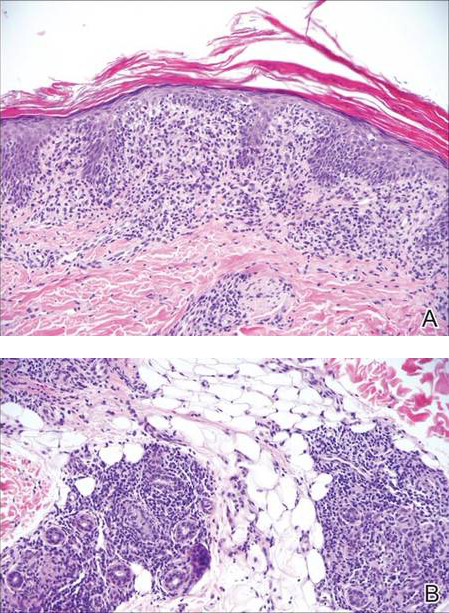
Another condition that distributes linearly along the lines of Blaschko is linear epidermolytic hyperkeratosis (EHK). Similar to LS, histology shows hyperkeratosis, focal parakeratosis, and acanthosis of the epidermis.5 However, EHK shows epidermolysis, acantholysis, and perinuclear vacuolization in spinous and granular layers (Figure 3).5 The lack of perivascular and periadnexal inflammation also can help differentiate EHK from LS.
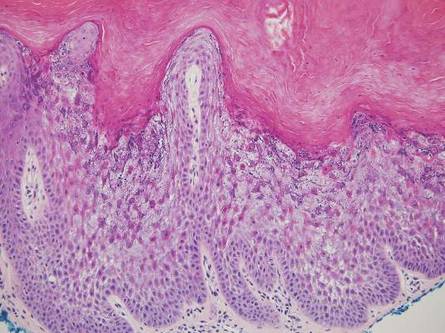
Linear lichen planus (LLP), similar to LS, histologically shows a lichenoid lymphocytic bandlike infiltrate obscuring the dermoepidermal junction, vacuolization of the basal cell layer, and pigment incontinence.1,2 Although LS and LLP can have histologic overlap, the absence of adnexal or perieccrine lymphocytic inflammation can help distinguish the two.3 The histopathologic changes of intercellular edema or mild spongiosis, exocytosis, and parakeratosis present in LS also are typically absent in LLP. Linear lichen planus characteristically consists of wedge-shaped hypergranulosis and irregular acanthosis with saw-toothed rete ridges (Figure 4).2 In addition, lobular eosinophilic deposits known as cytoid or Civatte bodies representing degenerated keratinocytes can be visualized at the dermoepidermal junction in LLP.2 Immunofluorescence will highlight Civatte bodies with IgM, IgG, and C3, also helping to differentiate these 2 conditions.1
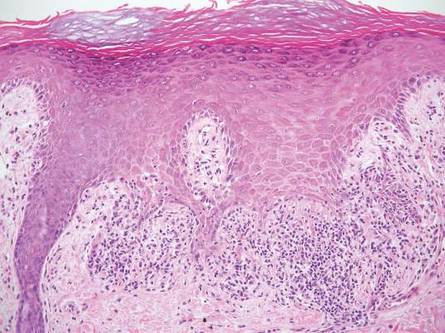
Linear porokeratosis can be mistaken for the linear lesion of LS. Both entities may reveal perivascular lymphocytes in the dermis, and porokeratosis can be lichenoid in the central portion of the lesion.6 However, porokeratosis is unique in that it contains a cornoid lamella, characterized by a thin column of tightly packed parakeratotic cells extending from an invagination of the epidermis through the adjacent stratum corneum (Figure 5).6 Beneath the cornoid lamella, the granular layer is either absent or markedly attenuated, and pyknotic keratinocytes with perinuclear edema are present in the spinous layer.6 The epidermis in the central portion of the porokeratotic lesion may be normal, hyperplastic, or atrophic with effacement of rete ridges.
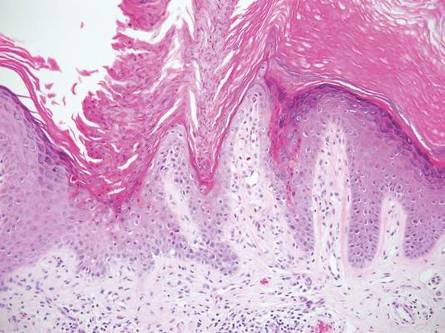
Similar to LS, linear psoriasis follows lines of Blaschko clinically. However, it is distinguished by its characteristic psoriatic epidermal changes as well as its lack of lichenoid or perieccrine inflammation.3 Typical findings in linear psoriasis include hyperkeratosis, confluent parakeratosis with entrapped neutrophilic microabscesses, acanthosis with regular elongation of rete ridges, intraepidermal neutrophils, thinned suprapapillary plates, dilated capillaries in the tips of the dermal papillae, and a chronic dermal inflammatory infiltrate (Figure 6).4
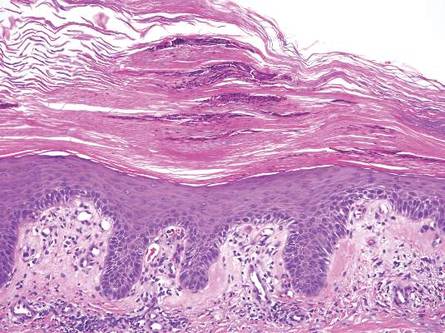
Lichen striatus (LS) is a benign, uncommon, self-limited, linear inflammatory skin disorder that primarily affects children up to 15 years of age, most commonly around 2 to 3 years of age, and is seen more frequently in girls.1 It presents with a sudden eruption of asymptomatic small, flat-topped, lichenoid, scaly papules in a linear array on a single extremity. The lesions may be erythematous, flesh colored, or hypopigmented.1,2 Multiple lesions appear over days to weeks and coalesce into linear plaques in a continuous or interrupted pattern along the lines of Blaschko, indicating possible somatic mosaicism.1 Although typically asymptomatic, it may be pruritic. Most cases spontaneously resolve within 1 year.3 Recurrences are unusual. Digital involvement may result in onycholysis, longitudinal ridging, splitting, and nail loss.1 The underlying cause of LS may be an abnormal immunologic reaction or genetic predisposition that is precipitated by some trigger such as a viral infection, trauma, hypersensitivity reaction, vaccine, seasonal variation, medication, or pregnancy.1,2 An association with atopy has been described. Treatment is not necessary but options include topical steroids, topical retinoids, and topical calcineurin inhibitors.2
Histologically, findings in LS are somewhat variable but typically show a combination of spongiotic and lichenoid interface dermatitis with a perivascular and periadnexal lymphocytic infiltrate (Figure 1). Epidermal changes include intercellular and intracellular edema, focal spongiosis, lymphocytic exocytosis, parakeratosis, patchy hyperkeratosis, and keratinocyte necrosis (Figure 2A).1,3 The epidermis is normal or slightly acanthotic, and dyskeratotic keratinocytes can be found in the granular and horny layers or at the dermoepidermal junction.2 The lymphohistiocytic infiltrate in the superficial and deep dermis surrounds vascular plexuses and cutaneous adnexa such as eccrine glands and hair follicles.1 Perivascular lymphoid aggregates and eccrine coil involvement are particularly distinctive of LS (Figure 2B).4 Pigment incontinence also may be seen.
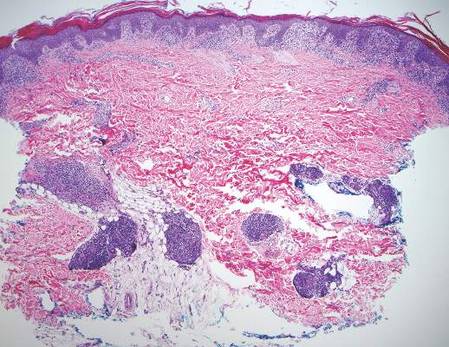
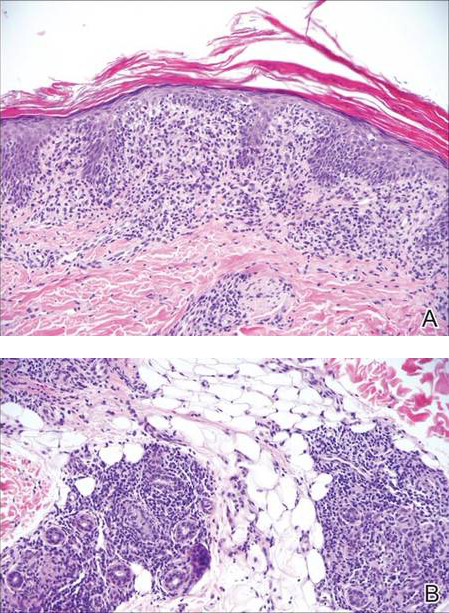
Another condition that distributes linearly along the lines of Blaschko is linear epidermolytic hyperkeratosis (EHK). Similar to LS, histology shows hyperkeratosis, focal parakeratosis, and acanthosis of the epidermis.5 However, EHK shows epidermolysis, acantholysis, and perinuclear vacuolization in spinous and granular layers (Figure 3).5 The lack of perivascular and periadnexal inflammation also can help differentiate EHK from LS.
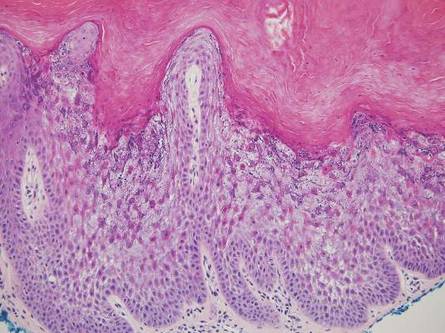
Linear lichen planus (LLP), similar to LS, histologically shows a lichenoid lymphocytic bandlike infiltrate obscuring the dermoepidermal junction, vacuolization of the basal cell layer, and pigment incontinence.1,2 Although LS and LLP can have histologic overlap, the absence of adnexal or perieccrine lymphocytic inflammation can help distinguish the two.3 The histopathologic changes of intercellular edema or mild spongiosis, exocytosis, and parakeratosis present in LS also are typically absent in LLP. Linear lichen planus characteristically consists of wedge-shaped hypergranulosis and irregular acanthosis with saw-toothed rete ridges (Figure 4).2 In addition, lobular eosinophilic deposits known as cytoid or Civatte bodies representing degenerated keratinocytes can be visualized at the dermoepidermal junction in LLP.2 Immunofluorescence will highlight Civatte bodies with IgM, IgG, and C3, also helping to differentiate these 2 conditions.1
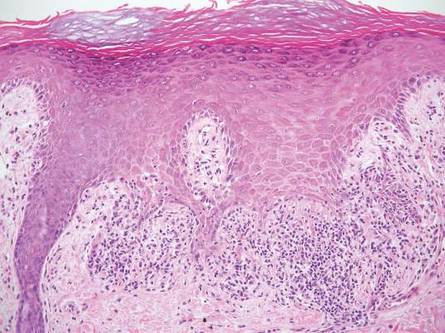
Linear porokeratosis can be mistaken for the linear lesion of LS. Both entities may reveal perivascular lymphocytes in the dermis, and porokeratosis can be lichenoid in the central portion of the lesion.6 However, porokeratosis is unique in that it contains a cornoid lamella, characterized by a thin column of tightly packed parakeratotic cells extending from an invagination of the epidermis through the adjacent stratum corneum (Figure 5).6 Beneath the cornoid lamella, the granular layer is either absent or markedly attenuated, and pyknotic keratinocytes with perinuclear edema are present in the spinous layer.6 The epidermis in the central portion of the porokeratotic lesion may be normal, hyperplastic, or atrophic with effacement of rete ridges.
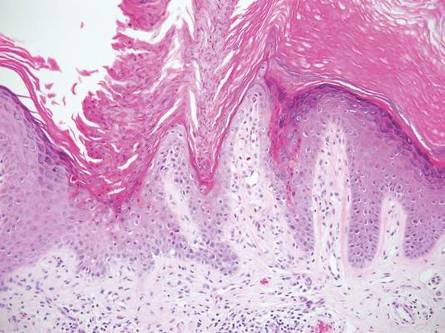
Similar to LS, linear psoriasis follows lines of Blaschko clinically. However, it is distinguished by its characteristic psoriatic epidermal changes as well as its lack of lichenoid or perieccrine inflammation.3 Typical findings in linear psoriasis include hyperkeratosis, confluent parakeratosis with entrapped neutrophilic microabscesses, acanthosis with regular elongation of rete ridges, intraepidermal neutrophils, thinned suprapapillary plates, dilated capillaries in the tips of the dermal papillae, and a chronic dermal inflammatory infiltrate (Figure 6).4
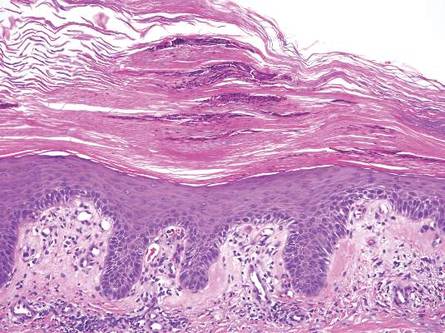
- Wang WL, Lazar A. Lichenoid and interface dermatitis. In: Calonje E, Brenn T, Lazar A, et al, eds. McKee’s Pathology of the Skin. 4th ed. London, England: Elsevier/Saunders; 2011:219-258.
- Shiohara T, Kano Y. Lichen planus and lichenoid dermatoses. In: Bolognia J, Jorizzo J, Schaffer J, eds. Dermatology. 3rd ed. Philadelphia, PA: Elsevier/Saunders; 2012:183-202.
- Zhang Y, McNutt NS. Lichen striatus. histological, immunohistochemical, and ultrastructural study of 37 cases. J Cutan Pathol. 2001;28:65-71.
- Johnson M, Walker D, Galloway W, et al. Interface dermatitis along Blaschko’s lines. J Cutan Pathol. 2014;41:950-954.
- Kumar P, Kumar R, Kumar Mandal RK, et al. Systematized linear epidermolytic hyperkeratosis. Dermatol Online J. 2014;20:21248.
- Requena L, Requena C, Cockerell C. Benign epidermal tumors and proliferations. In: Bolognia J, Jorizzo J, Schaffer J. Dermatology. 3rd ed. Philadelphia, PA: Elsevier/Saunders; 2012:1795-1815.
- Wang WL, Lazar A. Lichenoid and interface dermatitis. In: Calonje E, Brenn T, Lazar A, et al, eds. McKee’s Pathology of the Skin. 4th ed. London, England: Elsevier/Saunders; 2011:219-258.
- Shiohara T, Kano Y. Lichen planus and lichenoid dermatoses. In: Bolognia J, Jorizzo J, Schaffer J, eds. Dermatology. 3rd ed. Philadelphia, PA: Elsevier/Saunders; 2012:183-202.
- Zhang Y, McNutt NS. Lichen striatus. histological, immunohistochemical, and ultrastructural study of 37 cases. J Cutan Pathol. 2001;28:65-71.
- Johnson M, Walker D, Galloway W, et al. Interface dermatitis along Blaschko’s lines. J Cutan Pathol. 2014;41:950-954.
- Kumar P, Kumar R, Kumar Mandal RK, et al. Systematized linear epidermolytic hyperkeratosis. Dermatol Online J. 2014;20:21248.
- Requena L, Requena C, Cockerell C. Benign epidermal tumors and proliferations. In: Bolognia J, Jorizzo J, Schaffer J. Dermatology. 3rd ed. Philadelphia, PA: Elsevier/Saunders; 2012:1795-1815.
Subcision: The benefits of a classic technique
We’re always working toward medical breakthroughs so we can provide the most effective treatments for our patients with cutting-edge technology; however, there is a lot to be said about the techniques that have paved the way for new medical devices.
For certain conditions, the efficacy of classic procedures often cannot be matched by their modern successors. Subcision for treatment of deep depressed scars, for example, is often a more effective option than microneedling and can produce results with less healing time and fewer treatments, and at a more cost-effective price.
Both subcision and microneedling improve the appearance of scars by creating wounds in an effort to break up scar tissue and trigger collagen regrowth. Microneedling involves the use of a microneedling pen with several small needles that glide across the skin at different depths and speeds. Subcision is achieved with one larger gauge needle that is injected into scars at different angles and depths to break up scar tissue. Microneedling needles yield more epidermal damage than does subcision, causing more bleeding and ultimately lengthening the healing time.
The mechanism of subcising deeper scar tissue also seems to be more effective than that of microneedling. It often takes fewer subcision treatments than microneedling treatments to achieve comparable improvement of depressed scars. Microneedling needles are limited to penetrating at best 2.5 mm beneath the skin surface, while subcision allows the freedom to penetrate deeper into the dermis to reach deeper dermal scars. Subcising also creates larger channels within the scar tissue, which create more space for collagen regrowth, while microneedling does not.
A technique that has shown to improve treatment outcomes is the use of a 26- or 30-gauge needle, moving back and forth in a fanning pattern under the scar tissue while simultaneously injecting lidocaine or saline in those channels. The injection of a fluid component, particularly that of lidocaine, can both decrease the pain as well as inflate the scar in question, allowing more collagen regrowth and wound growth factors to fill the “gaps” created.
Unless scars have a significant epidermal component in addition to their dermal component, subcising the scar is a more effective and has faster healing times. Both procedures can cause bruising , edema, and erythema. However, the epidermal damage that can occur in microneedling has significantly more downtime.
In addition, subcision is a more cost-effective treatment than microneedling. The required materials for subcision are limited to materials that are readily used within practices: needles, syringes, saline, and lidocaine. Microneedling, on the other hand, requires purchase of expensive tools, including microneedling pens, sterile single-use microneedling tips, and protective sleeves for the device, in addition to topical skin care products to apply after the treatment to promote safe healing.
While microneedling is remarkably effective for treatment of superficial scars, fine lines, and hypopigmentation, subcision tends to be more effective for the treatment of deeper scars such as box-car acne scars.
We love new technology in our practices; however, sometimes our tried and true procedures may prove to be a better option in the appropriate patient.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
We’re always working toward medical breakthroughs so we can provide the most effective treatments for our patients with cutting-edge technology; however, there is a lot to be said about the techniques that have paved the way for new medical devices.
For certain conditions, the efficacy of classic procedures often cannot be matched by their modern successors. Subcision for treatment of deep depressed scars, for example, is often a more effective option than microneedling and can produce results with less healing time and fewer treatments, and at a more cost-effective price.
Both subcision and microneedling improve the appearance of scars by creating wounds in an effort to break up scar tissue and trigger collagen regrowth. Microneedling involves the use of a microneedling pen with several small needles that glide across the skin at different depths and speeds. Subcision is achieved with one larger gauge needle that is injected into scars at different angles and depths to break up scar tissue. Microneedling needles yield more epidermal damage than does subcision, causing more bleeding and ultimately lengthening the healing time.
The mechanism of subcising deeper scar tissue also seems to be more effective than that of microneedling. It often takes fewer subcision treatments than microneedling treatments to achieve comparable improvement of depressed scars. Microneedling needles are limited to penetrating at best 2.5 mm beneath the skin surface, while subcision allows the freedom to penetrate deeper into the dermis to reach deeper dermal scars. Subcising also creates larger channels within the scar tissue, which create more space for collagen regrowth, while microneedling does not.
A technique that has shown to improve treatment outcomes is the use of a 26- or 30-gauge needle, moving back and forth in a fanning pattern under the scar tissue while simultaneously injecting lidocaine or saline in those channels. The injection of a fluid component, particularly that of lidocaine, can both decrease the pain as well as inflate the scar in question, allowing more collagen regrowth and wound growth factors to fill the “gaps” created.
Unless scars have a significant epidermal component in addition to their dermal component, subcising the scar is a more effective and has faster healing times. Both procedures can cause bruising , edema, and erythema. However, the epidermal damage that can occur in microneedling has significantly more downtime.
In addition, subcision is a more cost-effective treatment than microneedling. The required materials for subcision are limited to materials that are readily used within practices: needles, syringes, saline, and lidocaine. Microneedling, on the other hand, requires purchase of expensive tools, including microneedling pens, sterile single-use microneedling tips, and protective sleeves for the device, in addition to topical skin care products to apply after the treatment to promote safe healing.
While microneedling is remarkably effective for treatment of superficial scars, fine lines, and hypopigmentation, subcision tends to be more effective for the treatment of deeper scars such as box-car acne scars.
We love new technology in our practices; however, sometimes our tried and true procedures may prove to be a better option in the appropriate patient.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
We’re always working toward medical breakthroughs so we can provide the most effective treatments for our patients with cutting-edge technology; however, there is a lot to be said about the techniques that have paved the way for new medical devices.
For certain conditions, the efficacy of classic procedures often cannot be matched by their modern successors. Subcision for treatment of deep depressed scars, for example, is often a more effective option than microneedling and can produce results with less healing time and fewer treatments, and at a more cost-effective price.
Both subcision and microneedling improve the appearance of scars by creating wounds in an effort to break up scar tissue and trigger collagen regrowth. Microneedling involves the use of a microneedling pen with several small needles that glide across the skin at different depths and speeds. Subcision is achieved with one larger gauge needle that is injected into scars at different angles and depths to break up scar tissue. Microneedling needles yield more epidermal damage than does subcision, causing more bleeding and ultimately lengthening the healing time.
The mechanism of subcising deeper scar tissue also seems to be more effective than that of microneedling. It often takes fewer subcision treatments than microneedling treatments to achieve comparable improvement of depressed scars. Microneedling needles are limited to penetrating at best 2.5 mm beneath the skin surface, while subcision allows the freedom to penetrate deeper into the dermis to reach deeper dermal scars. Subcising also creates larger channels within the scar tissue, which create more space for collagen regrowth, while microneedling does not.
A technique that has shown to improve treatment outcomes is the use of a 26- or 30-gauge needle, moving back and forth in a fanning pattern under the scar tissue while simultaneously injecting lidocaine or saline in those channels. The injection of a fluid component, particularly that of lidocaine, can both decrease the pain as well as inflate the scar in question, allowing more collagen regrowth and wound growth factors to fill the “gaps” created.
Unless scars have a significant epidermal component in addition to their dermal component, subcising the scar is a more effective and has faster healing times. Both procedures can cause bruising , edema, and erythema. However, the epidermal damage that can occur in microneedling has significantly more downtime.
In addition, subcision is a more cost-effective treatment than microneedling. The required materials for subcision are limited to materials that are readily used within practices: needles, syringes, saline, and lidocaine. Microneedling, on the other hand, requires purchase of expensive tools, including microneedling pens, sterile single-use microneedling tips, and protective sleeves for the device, in addition to topical skin care products to apply after the treatment to promote safe healing.
While microneedling is remarkably effective for treatment of superficial scars, fine lines, and hypopigmentation, subcision tends to be more effective for the treatment of deeper scars such as box-car acne scars.
We love new technology in our practices; however, sometimes our tried and true procedures may prove to be a better option in the appropriate patient.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
Nanoparticles deliver Aurora kinase inhibitor with increased safety and efficacy
Using nanoparticles to encapsulate an Aurora B kinase inhibitor improved the efficacy and tolerability of the drug and allowed less frequent dosing in preclinical models, according to researchers.
“The AZD2811 nanoparticles identified in this study have the potential to increase efficacy at tolerable doses using a more convenient dosing regimen, which may in turn extend the utility of Aurora B kinase inhibition to a broader range of hematological and solid tumor cancer indications,” wrote Susan Ashton of AstraZeneca, and her colleagues (Sci Transl Med. 2016 Feb 10. doi: 10.1126/scitranslmed.aad2355).
“The improved bone marrow profile observed with slow-releasing nanoparticles may enable efficacious combination treatments” with chemotherapy, radiotherapy, or poly(adenosine diphosphate–ribose) polymerase (PARP) inhibitors.
The study was undertaken because a free-drug version of the agent, known as AZD1152, had led to a significant improvement in the complete response rate of acute myeloid leukemia compared to standard of care in a phase II trial. Efficacy, however, was associated with major toxicities, including myelosuppression. Further, AZD1152 had to be administered as a 7-day continuous intravenous infusion.
By using the Accurin nanoparticle platform to vary drug release kinetics, the researchers devised a formulation to maximize the therapeutic effect of the kinase inhibitor while sparing healthy tissue. AZD1152 is a water-soluble prodrug of AZD2811, which the researchers used to develop their the nanoparticle formulation.
AZD2811 was encapsulated in polymeric nanoparticles termed Accurins, which are composed of block copolymers of poly-D,L-lactide (PLA) and poly(ethylene glycol) (PEG). Accurins accumulate in tumors, increasing the drug’s concentration and duration of exposure to the cancer cells. Organic acid counterions were used to increase encapsulation efficiency and decrease the release rate of AZD2811.
“We identified a formulation profile that could deliver active drug for more than 1 week, resulting in prolonged target inhibition in tumor tissue together with improved preclinical efficacy and therapeutic index over the AZD1152 prodrug in several animal models,” they wrote.
In nude rats bearing human colorectal adenocarcinoma SW620 xenografts, the nanoparticles inhibited kinase over a 96-hour time course, while the free drug resulted in complete enzyme recovery at 24 hours. Nanoparticles inhibited tumor growth by over 90%, compared with 58% for the free drug at twice the dose, and showed little toxicity as evidenced by stable body weight. Nanoparticles were retained in the tumor xenografts for up to 6 days, while the free drug was undetected in tumors 24 hours after administration.
“Although we selected a lead formulation using a tumor model (SW620) that supported the AZD1152 program – and, as such, we had extensive comparator data from which to benchmark the tolerability, PD, and efficacy of candidate nanoparticles – the model is subject to the known limitations of xenografted human tumor cell lines in assessing therapeutic candidates in oncology. Moreover, although rat bone marrow is commonly used to model myelotoxicity in humans, interrogation of the nanoparticle dose and schedule in patients may be required to achieve optimal clinical results,” they concluded.
AstraZeneca funded the study. Dr. Ashton and several coauthors are current or former employees and shareholders of AstraZeneca or BIND. The companies are developing the drug and technologies.
By encapsulating an Aurora B kinase inhibitor in Accurin particles, the researchers appear to have succeeded in enhancing the drug’s therapeutic activity and safety in mouse xenograft models. It remains to be seen how widely applicable this technology will be, and whether these results will be replicated in patients as the AZD1151-hQPA Accurin formulation heads toward first-in-human clinical trials. If the Accurin technology can solve the pharmacokinetic and toxicity issues for Aurora kinase inhibitors, it will likely also be applicable to other compounds that have encountered similar difficulties in clinical development and will add a formulation approach to address very meaningful and challenging issues that face many new molecules during clinical development.
David J. Bearss, Ph.D., is the chief executive officer of Tolero Pharmaceutical, Lehi, Utah. His remarks were part of an editorial accompanying the report in Science Translational Medicine (2016 Feb 10. doi: 10.1126/scitranslmed.aaf1417).
By encapsulating an Aurora B kinase inhibitor in Accurin particles, the researchers appear to have succeeded in enhancing the drug’s therapeutic activity and safety in mouse xenograft models. It remains to be seen how widely applicable this technology will be, and whether these results will be replicated in patients as the AZD1151-hQPA Accurin formulation heads toward first-in-human clinical trials. If the Accurin technology can solve the pharmacokinetic and toxicity issues for Aurora kinase inhibitors, it will likely also be applicable to other compounds that have encountered similar difficulties in clinical development and will add a formulation approach to address very meaningful and challenging issues that face many new molecules during clinical development.
David J. Bearss, Ph.D., is the chief executive officer of Tolero Pharmaceutical, Lehi, Utah. His remarks were part of an editorial accompanying the report in Science Translational Medicine (2016 Feb 10. doi: 10.1126/scitranslmed.aaf1417).
By encapsulating an Aurora B kinase inhibitor in Accurin particles, the researchers appear to have succeeded in enhancing the drug’s therapeutic activity and safety in mouse xenograft models. It remains to be seen how widely applicable this technology will be, and whether these results will be replicated in patients as the AZD1151-hQPA Accurin formulation heads toward first-in-human clinical trials. If the Accurin technology can solve the pharmacokinetic and toxicity issues for Aurora kinase inhibitors, it will likely also be applicable to other compounds that have encountered similar difficulties in clinical development and will add a formulation approach to address very meaningful and challenging issues that face many new molecules during clinical development.
David J. Bearss, Ph.D., is the chief executive officer of Tolero Pharmaceutical, Lehi, Utah. His remarks were part of an editorial accompanying the report in Science Translational Medicine (2016 Feb 10. doi: 10.1126/scitranslmed.aaf1417).
Using nanoparticles to encapsulate an Aurora B kinase inhibitor improved the efficacy and tolerability of the drug and allowed less frequent dosing in preclinical models, according to researchers.
“The AZD2811 nanoparticles identified in this study have the potential to increase efficacy at tolerable doses using a more convenient dosing regimen, which may in turn extend the utility of Aurora B kinase inhibition to a broader range of hematological and solid tumor cancer indications,” wrote Susan Ashton of AstraZeneca, and her colleagues (Sci Transl Med. 2016 Feb 10. doi: 10.1126/scitranslmed.aad2355).
“The improved bone marrow profile observed with slow-releasing nanoparticles may enable efficacious combination treatments” with chemotherapy, radiotherapy, or poly(adenosine diphosphate–ribose) polymerase (PARP) inhibitors.
The study was undertaken because a free-drug version of the agent, known as AZD1152, had led to a significant improvement in the complete response rate of acute myeloid leukemia compared to standard of care in a phase II trial. Efficacy, however, was associated with major toxicities, including myelosuppression. Further, AZD1152 had to be administered as a 7-day continuous intravenous infusion.
By using the Accurin nanoparticle platform to vary drug release kinetics, the researchers devised a formulation to maximize the therapeutic effect of the kinase inhibitor while sparing healthy tissue. AZD1152 is a water-soluble prodrug of AZD2811, which the researchers used to develop their the nanoparticle formulation.
AZD2811 was encapsulated in polymeric nanoparticles termed Accurins, which are composed of block copolymers of poly-D,L-lactide (PLA) and poly(ethylene glycol) (PEG). Accurins accumulate in tumors, increasing the drug’s concentration and duration of exposure to the cancer cells. Organic acid counterions were used to increase encapsulation efficiency and decrease the release rate of AZD2811.
“We identified a formulation profile that could deliver active drug for more than 1 week, resulting in prolonged target inhibition in tumor tissue together with improved preclinical efficacy and therapeutic index over the AZD1152 prodrug in several animal models,” they wrote.
In nude rats bearing human colorectal adenocarcinoma SW620 xenografts, the nanoparticles inhibited kinase over a 96-hour time course, while the free drug resulted in complete enzyme recovery at 24 hours. Nanoparticles inhibited tumor growth by over 90%, compared with 58% for the free drug at twice the dose, and showed little toxicity as evidenced by stable body weight. Nanoparticles were retained in the tumor xenografts for up to 6 days, while the free drug was undetected in tumors 24 hours after administration.
“Although we selected a lead formulation using a tumor model (SW620) that supported the AZD1152 program – and, as such, we had extensive comparator data from which to benchmark the tolerability, PD, and efficacy of candidate nanoparticles – the model is subject to the known limitations of xenografted human tumor cell lines in assessing therapeutic candidates in oncology. Moreover, although rat bone marrow is commonly used to model myelotoxicity in humans, interrogation of the nanoparticle dose and schedule in patients may be required to achieve optimal clinical results,” they concluded.
AstraZeneca funded the study. Dr. Ashton and several coauthors are current or former employees and shareholders of AstraZeneca or BIND. The companies are developing the drug and technologies.
Using nanoparticles to encapsulate an Aurora B kinase inhibitor improved the efficacy and tolerability of the drug and allowed less frequent dosing in preclinical models, according to researchers.
“The AZD2811 nanoparticles identified in this study have the potential to increase efficacy at tolerable doses using a more convenient dosing regimen, which may in turn extend the utility of Aurora B kinase inhibition to a broader range of hematological and solid tumor cancer indications,” wrote Susan Ashton of AstraZeneca, and her colleagues (Sci Transl Med. 2016 Feb 10. doi: 10.1126/scitranslmed.aad2355).
“The improved bone marrow profile observed with slow-releasing nanoparticles may enable efficacious combination treatments” with chemotherapy, radiotherapy, or poly(adenosine diphosphate–ribose) polymerase (PARP) inhibitors.
The study was undertaken because a free-drug version of the agent, known as AZD1152, had led to a significant improvement in the complete response rate of acute myeloid leukemia compared to standard of care in a phase II trial. Efficacy, however, was associated with major toxicities, including myelosuppression. Further, AZD1152 had to be administered as a 7-day continuous intravenous infusion.
By using the Accurin nanoparticle platform to vary drug release kinetics, the researchers devised a formulation to maximize the therapeutic effect of the kinase inhibitor while sparing healthy tissue. AZD1152 is a water-soluble prodrug of AZD2811, which the researchers used to develop their the nanoparticle formulation.
AZD2811 was encapsulated in polymeric nanoparticles termed Accurins, which are composed of block copolymers of poly-D,L-lactide (PLA) and poly(ethylene glycol) (PEG). Accurins accumulate in tumors, increasing the drug’s concentration and duration of exposure to the cancer cells. Organic acid counterions were used to increase encapsulation efficiency and decrease the release rate of AZD2811.
“We identified a formulation profile that could deliver active drug for more than 1 week, resulting in prolonged target inhibition in tumor tissue together with improved preclinical efficacy and therapeutic index over the AZD1152 prodrug in several animal models,” they wrote.
In nude rats bearing human colorectal adenocarcinoma SW620 xenografts, the nanoparticles inhibited kinase over a 96-hour time course, while the free drug resulted in complete enzyme recovery at 24 hours. Nanoparticles inhibited tumor growth by over 90%, compared with 58% for the free drug at twice the dose, and showed little toxicity as evidenced by stable body weight. Nanoparticles were retained in the tumor xenografts for up to 6 days, while the free drug was undetected in tumors 24 hours after administration.
“Although we selected a lead formulation using a tumor model (SW620) that supported the AZD1152 program – and, as such, we had extensive comparator data from which to benchmark the tolerability, PD, and efficacy of candidate nanoparticles – the model is subject to the known limitations of xenografted human tumor cell lines in assessing therapeutic candidates in oncology. Moreover, although rat bone marrow is commonly used to model myelotoxicity in humans, interrogation of the nanoparticle dose and schedule in patients may be required to achieve optimal clinical results,” they concluded.
AstraZeneca funded the study. Dr. Ashton and several coauthors are current or former employees and shareholders of AstraZeneca or BIND. The companies are developing the drug and technologies.
Key clinical point: Aurora B kinase inhibitor nanoparticles displayed accumulation and retention in tumors with improved efficacy and minimal bone marrow pathology in animal models.
Major finding: Nanoparticles inhibited tumor growth by over 90%, compared with 58% for the free drug at twice the dose, and showed little toxicity; the free drug was undetected in tumors 24 hours after administration, and nanoparticle-delivered drug was detectable up to 6 days.
Data sources: Nude rats and nude mice bearing human colorectal adenocarcinoma SW620 xenografts.
Disclosures: AstraZeneca funded the study. Dr. Ashton and several coauthors are current or former employees and shareholders of AstraZeneca or BIND. The companies are developing the drug and technologies.
Women with AF have a Higher Risk of Death and CVD
NEW YORK (Reuters Health) - Women with atrial fibrillation (AF) are at somewhat higher risk of death and cardiovascular disease (CVD) than men with the condition, a new systematic review and meta-analysis confirms.
"Physicians should be aware of this and they should also make sure they treat women as aggressively as men," Connor Emdin, a doctoral student at The George Institute for Global Health at the University of Oxford, U.K., told Reuters Health. "On average, women should probably be treated moreaggressively."
Smoking and diabetes are known to increase coronary heart disease risk more sharply for women than for men, Emdin and his team write in their report, online January 19 in The BMJ. Some studies have found that AF is more strongly associated with stroke and death in women than in men, but other studies have not, they add.
To better understand the relationship, the researchers looked at 30 studies including more than 4.3 million individuals. The ratio of relative risk for women compared to men with AF for all-cause mortality was 1.12. For stroke, the ratio was 1.99, while it was 1.93 for cardiovascular mortality, 1.55 for cardiac events, and 1.16 for heart failure. All increases were statistically significant.
While the CHADS2 score for estimating stroke risk in AF does not include female sex as a risk factor for stroke, Emdin noted, a more recent version, the CHA2DS2-VASc score, does. "Our results would support using risk scores which include female sex," he said.
AF is less prevalent among women than men, but thefindings confirm that it is more severe for them as well, Dr. Elsayed Soliman, director of the Epidemiological Cardiology Research Center at Wake Forest Baptist Medical Center in Wake Forest, North Carolina, told Reuters Health. Dr. Soliman was not involved in the new study.
"The article adds to this evidence that really women are different from men when it comes to cardiovascular disease and they need to be managed differently," Dr. Soliman said. He added that "we need to do more work to see what could bridge the gap in outcomes associated with atrial fibrillation."
NEW YORK (Reuters Health) - Women with atrial fibrillation (AF) are at somewhat higher risk of death and cardiovascular disease (CVD) than men with the condition, a new systematic review and meta-analysis confirms.
"Physicians should be aware of this and they should also make sure they treat women as aggressively as men," Connor Emdin, a doctoral student at The George Institute for Global Health at the University of Oxford, U.K., told Reuters Health. "On average, women should probably be treated moreaggressively."
Smoking and diabetes are known to increase coronary heart disease risk more sharply for women than for men, Emdin and his team write in their report, online January 19 in The BMJ. Some studies have found that AF is more strongly associated with stroke and death in women than in men, but other studies have not, they add.
To better understand the relationship, the researchers looked at 30 studies including more than 4.3 million individuals. The ratio of relative risk for women compared to men with AF for all-cause mortality was 1.12. For stroke, the ratio was 1.99, while it was 1.93 for cardiovascular mortality, 1.55 for cardiac events, and 1.16 for heart failure. All increases were statistically significant.
While the CHADS2 score for estimating stroke risk in AF does not include female sex as a risk factor for stroke, Emdin noted, a more recent version, the CHA2DS2-VASc score, does. "Our results would support using risk scores which include female sex," he said.
AF is less prevalent among women than men, but thefindings confirm that it is more severe for them as well, Dr. Elsayed Soliman, director of the Epidemiological Cardiology Research Center at Wake Forest Baptist Medical Center in Wake Forest, North Carolina, told Reuters Health. Dr. Soliman was not involved in the new study.
"The article adds to this evidence that really women are different from men when it comes to cardiovascular disease and they need to be managed differently," Dr. Soliman said. He added that "we need to do more work to see what could bridge the gap in outcomes associated with atrial fibrillation."
NEW YORK (Reuters Health) - Women with atrial fibrillation (AF) are at somewhat higher risk of death and cardiovascular disease (CVD) than men with the condition, a new systematic review and meta-analysis confirms.
"Physicians should be aware of this and they should also make sure they treat women as aggressively as men," Connor Emdin, a doctoral student at The George Institute for Global Health at the University of Oxford, U.K., told Reuters Health. "On average, women should probably be treated moreaggressively."
Smoking and diabetes are known to increase coronary heart disease risk more sharply for women than for men, Emdin and his team write in their report, online January 19 in The BMJ. Some studies have found that AF is more strongly associated with stroke and death in women than in men, but other studies have not, they add.
To better understand the relationship, the researchers looked at 30 studies including more than 4.3 million individuals. The ratio of relative risk for women compared to men with AF for all-cause mortality was 1.12. For stroke, the ratio was 1.99, while it was 1.93 for cardiovascular mortality, 1.55 for cardiac events, and 1.16 for heart failure. All increases were statistically significant.
While the CHADS2 score for estimating stroke risk in AF does not include female sex as a risk factor for stroke, Emdin noted, a more recent version, the CHA2DS2-VASc score, does. "Our results would support using risk scores which include female sex," he said.
AF is less prevalent among women than men, but thefindings confirm that it is more severe for them as well, Dr. Elsayed Soliman, director of the Epidemiological Cardiology Research Center at Wake Forest Baptist Medical Center in Wake Forest, North Carolina, told Reuters Health. Dr. Soliman was not involved in the new study.
"The article adds to this evidence that really women are different from men when it comes to cardiovascular disease and they need to be managed differently," Dr. Soliman said. He added that "we need to do more work to see what could bridge the gap in outcomes associated with atrial fibrillation."
Combo can produce durable remissions in PTCL

Photo by Larry Young
SAN FRANCISCO—A combination treatment regimen can produce durable remissions in patients newly diagnosed with peripheral T-cell lymphoma (PTCL), results of a phase 1 study suggest.
The patients received brentuximab vedotin plus cyclophosphamide, doxorubicin, and prednisolone (BV+CHP). In some cases, this was followed by BV monotherapy.
The estimated 3-year progression-free survival (PFS) for these patients was 52%, and the overall survival (OS) was 80%.
There was a high rate of peripheral neuropathy (73%), but most cases resolved or improved over time.
Steven Horwitz, MD, of Memorial Sloan Kettering Cancer Center in New York, New York, and his colleagues presented these data as a poster at the 8th Annual T-cell Lymphoma Forum. The study was supported by Seattle Genetics and Millennium Pharmaceuticals.
The researchers presented data on 26 patients newly diagnosed with PTCL. Nineteen patients had systemic anaplastic large-cell lymphoma (ALCL; 16 ALK- and 3 ALK+), 2 had PTCL not otherwise specified, 2 had angioimmunoblastic T-cell lymphoma, 2 had adult T-cell leukemia/lymphoma, and 1 had enteropathy-associated T-cell lymphoma.
The patients’ median age was 56 (range, 21-82). Sixty-nine percent of patients had an IPI score of 2 or higher, and 73% had stage III/IV disease.
Treatment
The patients received BV+CHP every 3 weeks for 6 cycles. Those who achieved at least a partial remission could go on to receive up to 10 additional cycles of single-agent BV at 1.8 mg/kg every 3 weeks.
Twenty-three patients (88%) completed all 6 cycles of BV+CHP, and 21 patients (81%) went on to receive BV monotherapy, 11 of whom (42%) received all 10 cycles.
Fifteen patients (58%) discontinued treatment, 3 due to progressive disease, 3 due to investigator decision, 6 due to adverse events, and 3 due to patient decision.
After a median observation period of 38.7 months (range, 4.6 to 44.3), 77% of patients (n=20) remained on study.
Toxicity
The most common adverse events (occurring in at least 30% of patients) were nausea (69%), peripheral sensory neuropathy (69%), diarrhea (62%), fatigue (58%), alopecia (54%), dyspnea (46%), constipation (35%), myalgia (31%), peripheral edema (31%), chills (31%), anemia (31%), insomnia (31%), and febrile neutropenia.
The most common grade 3 or higher adverse events (occurring in at least 10% of patients) were febrile neutropenia (31%), neutropenia (23%), anemia (15%), and pulmonary embolism (12%).
There were 6 adverse events resulting in treatment discontinuation—peripheral sensory neuropathy (n=3), abdominal pain (n=1), asthenia (n=1), and peripheral motor neuropathy (n=1).
Seventy-three percent of patients (19/26) experienced peripheral neuropathy. Thirty-seven percent (n=7) had a complete resolution of neuropathy, and 58% (n=11) had some improvement. The median time to resolution was 1.3 months. Twelve patients (63%) had ongoing neuropathy at last follow-up, but most had grade 1 (n=10).
Response and survival
The objective response rate was 100%, and the complete response rate was 88% (n=23). One patient who had a partial response at the end of combination therapy achieved a complete response after going on to single-agent BV.
Twenty-one of the 26 patients are still alive—15 with ALCL and 6 with other PTCLs. Sixteen patients have not progressed—9 with ALCL and 5 with other PTCLs.
After progression, 5 patients received BV again, and 3 received stem cell transplants (2 allogeneic and 1 autologous).
The estimated 3-year PFS was 52%, and the estimated OS was 80%. The researchers noted that these rates compare favorably with the historical 3-year PFS and OS rates of 30% and 40%, respectively.
Researchers are currently conducting a phase 3 trial comparing BV+CHP with CHOP as frontline treatment of CD30+ mature T-cell lymphomas (ECHELON-2, NCT01777152). ![]()

Photo by Larry Young
SAN FRANCISCO—A combination treatment regimen can produce durable remissions in patients newly diagnosed with peripheral T-cell lymphoma (PTCL), results of a phase 1 study suggest.
The patients received brentuximab vedotin plus cyclophosphamide, doxorubicin, and prednisolone (BV+CHP). In some cases, this was followed by BV monotherapy.
The estimated 3-year progression-free survival (PFS) for these patients was 52%, and the overall survival (OS) was 80%.
There was a high rate of peripheral neuropathy (73%), but most cases resolved or improved over time.
Steven Horwitz, MD, of Memorial Sloan Kettering Cancer Center in New York, New York, and his colleagues presented these data as a poster at the 8th Annual T-cell Lymphoma Forum. The study was supported by Seattle Genetics and Millennium Pharmaceuticals.
The researchers presented data on 26 patients newly diagnosed with PTCL. Nineteen patients had systemic anaplastic large-cell lymphoma (ALCL; 16 ALK- and 3 ALK+), 2 had PTCL not otherwise specified, 2 had angioimmunoblastic T-cell lymphoma, 2 had adult T-cell leukemia/lymphoma, and 1 had enteropathy-associated T-cell lymphoma.
The patients’ median age was 56 (range, 21-82). Sixty-nine percent of patients had an IPI score of 2 or higher, and 73% had stage III/IV disease.
Treatment
The patients received BV+CHP every 3 weeks for 6 cycles. Those who achieved at least a partial remission could go on to receive up to 10 additional cycles of single-agent BV at 1.8 mg/kg every 3 weeks.
Twenty-three patients (88%) completed all 6 cycles of BV+CHP, and 21 patients (81%) went on to receive BV monotherapy, 11 of whom (42%) received all 10 cycles.
Fifteen patients (58%) discontinued treatment, 3 due to progressive disease, 3 due to investigator decision, 6 due to adverse events, and 3 due to patient decision.
After a median observation period of 38.7 months (range, 4.6 to 44.3), 77% of patients (n=20) remained on study.
Toxicity
The most common adverse events (occurring in at least 30% of patients) were nausea (69%), peripheral sensory neuropathy (69%), diarrhea (62%), fatigue (58%), alopecia (54%), dyspnea (46%), constipation (35%), myalgia (31%), peripheral edema (31%), chills (31%), anemia (31%), insomnia (31%), and febrile neutropenia.
The most common grade 3 or higher adverse events (occurring in at least 10% of patients) were febrile neutropenia (31%), neutropenia (23%), anemia (15%), and pulmonary embolism (12%).
There were 6 adverse events resulting in treatment discontinuation—peripheral sensory neuropathy (n=3), abdominal pain (n=1), asthenia (n=1), and peripheral motor neuropathy (n=1).
Seventy-three percent of patients (19/26) experienced peripheral neuropathy. Thirty-seven percent (n=7) had a complete resolution of neuropathy, and 58% (n=11) had some improvement. The median time to resolution was 1.3 months. Twelve patients (63%) had ongoing neuropathy at last follow-up, but most had grade 1 (n=10).
Response and survival
The objective response rate was 100%, and the complete response rate was 88% (n=23). One patient who had a partial response at the end of combination therapy achieved a complete response after going on to single-agent BV.
Twenty-one of the 26 patients are still alive—15 with ALCL and 6 with other PTCLs. Sixteen patients have not progressed—9 with ALCL and 5 with other PTCLs.
After progression, 5 patients received BV again, and 3 received stem cell transplants (2 allogeneic and 1 autologous).
The estimated 3-year PFS was 52%, and the estimated OS was 80%. The researchers noted that these rates compare favorably with the historical 3-year PFS and OS rates of 30% and 40%, respectively.
Researchers are currently conducting a phase 3 trial comparing BV+CHP with CHOP as frontline treatment of CD30+ mature T-cell lymphomas (ECHELON-2, NCT01777152). ![]()

Photo by Larry Young
SAN FRANCISCO—A combination treatment regimen can produce durable remissions in patients newly diagnosed with peripheral T-cell lymphoma (PTCL), results of a phase 1 study suggest.
The patients received brentuximab vedotin plus cyclophosphamide, doxorubicin, and prednisolone (BV+CHP). In some cases, this was followed by BV monotherapy.
The estimated 3-year progression-free survival (PFS) for these patients was 52%, and the overall survival (OS) was 80%.
There was a high rate of peripheral neuropathy (73%), but most cases resolved or improved over time.
Steven Horwitz, MD, of Memorial Sloan Kettering Cancer Center in New York, New York, and his colleagues presented these data as a poster at the 8th Annual T-cell Lymphoma Forum. The study was supported by Seattle Genetics and Millennium Pharmaceuticals.
The researchers presented data on 26 patients newly diagnosed with PTCL. Nineteen patients had systemic anaplastic large-cell lymphoma (ALCL; 16 ALK- and 3 ALK+), 2 had PTCL not otherwise specified, 2 had angioimmunoblastic T-cell lymphoma, 2 had adult T-cell leukemia/lymphoma, and 1 had enteropathy-associated T-cell lymphoma.
The patients’ median age was 56 (range, 21-82). Sixty-nine percent of patients had an IPI score of 2 or higher, and 73% had stage III/IV disease.
Treatment
The patients received BV+CHP every 3 weeks for 6 cycles. Those who achieved at least a partial remission could go on to receive up to 10 additional cycles of single-agent BV at 1.8 mg/kg every 3 weeks.
Twenty-three patients (88%) completed all 6 cycles of BV+CHP, and 21 patients (81%) went on to receive BV monotherapy, 11 of whom (42%) received all 10 cycles.
Fifteen patients (58%) discontinued treatment, 3 due to progressive disease, 3 due to investigator decision, 6 due to adverse events, and 3 due to patient decision.
After a median observation period of 38.7 months (range, 4.6 to 44.3), 77% of patients (n=20) remained on study.
Toxicity
The most common adverse events (occurring in at least 30% of patients) were nausea (69%), peripheral sensory neuropathy (69%), diarrhea (62%), fatigue (58%), alopecia (54%), dyspnea (46%), constipation (35%), myalgia (31%), peripheral edema (31%), chills (31%), anemia (31%), insomnia (31%), and febrile neutropenia.
The most common grade 3 or higher adverse events (occurring in at least 10% of patients) were febrile neutropenia (31%), neutropenia (23%), anemia (15%), and pulmonary embolism (12%).
There were 6 adverse events resulting in treatment discontinuation—peripheral sensory neuropathy (n=3), abdominal pain (n=1), asthenia (n=1), and peripheral motor neuropathy (n=1).
Seventy-three percent of patients (19/26) experienced peripheral neuropathy. Thirty-seven percent (n=7) had a complete resolution of neuropathy, and 58% (n=11) had some improvement. The median time to resolution was 1.3 months. Twelve patients (63%) had ongoing neuropathy at last follow-up, but most had grade 1 (n=10).
Response and survival
The objective response rate was 100%, and the complete response rate was 88% (n=23). One patient who had a partial response at the end of combination therapy achieved a complete response after going on to single-agent BV.
Twenty-one of the 26 patients are still alive—15 with ALCL and 6 with other PTCLs. Sixteen patients have not progressed—9 with ALCL and 5 with other PTCLs.
After progression, 5 patients received BV again, and 3 received stem cell transplants (2 allogeneic and 1 autologous).
The estimated 3-year PFS was 52%, and the estimated OS was 80%. The researchers noted that these rates compare favorably with the historical 3-year PFS and OS rates of 30% and 40%, respectively.
Researchers are currently conducting a phase 3 trial comparing BV+CHP with CHOP as frontline treatment of CD30+ mature T-cell lymphomas (ECHELON-2, NCT01777152). ![]()