User login
VIDEO: Why Weijen Chang, MD, SFHM, and Shawn Ralston, MD, Chose Hospital Medicine Careers
University of California-San Diego med-peds hospitalist Weijen Chang, MD, SFHM, and Shawn Ralson, MD, vice chair of clinical affairs, Children's Hospital at Dartmouth-Hitchcock in Lebanon, N.H., discuss the factors that went into their hospital medicine career choices, and why they find hospitalist careers so fascinating.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
University of California-San Diego med-peds hospitalist Weijen Chang, MD, SFHM, and Shawn Ralson, MD, vice chair of clinical affairs, Children's Hospital at Dartmouth-Hitchcock in Lebanon, N.H., discuss the factors that went into their hospital medicine career choices, and why they find hospitalist careers so fascinating.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
University of California-San Diego med-peds hospitalist Weijen Chang, MD, SFHM, and Shawn Ralson, MD, vice chair of clinical affairs, Children's Hospital at Dartmouth-Hitchcock in Lebanon, N.H., discuss the factors that went into their hospital medicine career choices, and why they find hospitalist careers so fascinating.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Law & Medicine: Which doctors get sued?
Question: Doctors are more prone to lawsuits if they:
A. Have been sued before.
B. Spend fewer dollars per hospitalized patient.
C. Show poor communication skills.
D. A and C only.
E. A, B, and C.
Answer: E. Two very recent studies, one by David M. Studdert and the other by Dr. Anupam B. Jena, offer fresh insights into factors linked to the likelihood of a malpractice lawsuit.
The Studdert study concluded that doctors with prior paid claims are at increased risk of incurring yet another lawsuit.1 Instead of simply relying on data from a single insurer or state, the researchers accessed the National Practitioner Data Bank (NPDB) from 2005 through 2014 and identified 66,426 claims paid against 54,099 physicians.
Over that 10-year period, only 1% of physicians accounted for 32% of paid claims. Of all the physicians, 84% incurred only one paid claim during the study period, and 16% had at least two. Four percent of the physicians had at least three. In adjusted analyses, the risk of recurrence increased with the number of previous paid claims.
For example, compared with physicians with a single claim, the 2,160 physicians who had three paid claims had three times the risk of incurring another (hazard ratio, 3.11); this corresponded in absolute terms to a 24% risk within 2 years.
Likelihood of recurrence also varied widely according to specialty. For example, the risk among neurosurgeons was four times greater than that of psychiatrists. As for internists, the risk of recurrence was approximately double that of neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, or obstetrician-gynecologists. The lowest risks of recurrence were seen among psychiatrists (HR, 0.60) and pediatricians (HR, 0.71).
Male physicians had a 38% higher risk of recurrence than did female physicians, and the risk among physicians younger than 35 years was approximately one-third that of their older colleagues (after adjustment for age). Residents had a lower risk of recurrence than did nonresidents, and MDs had a lower risk than did DOs.
Using all 915,564 active physicians in the United States as a denominator, the authors calculated that over the 10-year study period, only 6% of physicians had a paid claim. Note that the 6% figure refers to paid claims reported to the NPDB, which can be expected to be lower than statistics derived from published surveys. These latter studies typically feature self-reported malpractice claims made over a given time period; but it is well known that the majority of such claims are dropped or decided in favor of the doctor, and so will not be reported to the NPDB.
For example, in 2010, the American Medical Association found that 42.2% of 5,825 physicians who responded to its Physician Practice Information survey reported having been sued, with 22.4% sued twice or more.2 The report headlined that by mid career, 61% of doctor have been sued.
Rates varied by specialty, with general surgeons and obstetrician-gynecologists being most likely to be sued (69.2%). Family physicians and general internists had similar rates (38.9% and 34%), and pediatricians and psychiatrists were sued the least.
In that report, male doctors were twice as likely to be sued as were their female counterparts, and physicians in solo and specialty practices were sued more often than those in multispecialty practices. Physicians who had an ownership interest in a practice were also at greater risk, with 47.5% reporting being sued, compared with 33.4% for those with no ownership interest.
The second recent study, reported by Dr. Jena of Harvard Medical School, Boston, and his colleagues, analyzed Florida hospital admissions data covering some 24,000 physicians.3 They found that higher spending by physicians was associated with reduced malpractice claims made the following year.
This pattern held true for physicians in all specialties but one (family practice). For example, among internists, the malpractice risk probability was 1.5% in the bottom spending fifth ($19,725 per admission) and 0.3% in the top fifth ($39,379 per admission). Among obstetricians, the comparable figures were 1.9% and 0.4% respectively.
In addition, a separate subgroup analysis of cesarean-section rates revealed that malpractice claims were approximately halved among obstetricians with rates in the highest fifth, compared with the lowest fifth.
Unfortunately, the Jena study lacked information on illness severity and past malpractice history, and it remains speculative whether increased resource utilization could be attributed entirely to defensive medical practice.4
As interesting as these new reports may be, it is worth remembering that what prompts a lawsuit are poor communication and patient perception that the physician is uncaring and at fault for the bad result.
It is well known that quality of medical care correlates poorly with the filing of malpractice lawsuits, as illustrated in the conclusion of the landmark Harvard study that “medical malpractice litigation infrequently compensates patients injured by medical negligence and rarely identifies, and holds providers accountable for, substandard care.”5 The authors estimated that there was only 1 malpractice claim for every 7.6 adverse events caused by negligence.
In another retrospective chart review study, the quality of treatment as judged by independent peer review was no different in frequently sued versus never-sued obstetricians.6
Communication problems exist in more than 70% of malpractice cases, centering around four themes: 1) deserting the patient; 2) devaluing patient/family views; 3) delivering information poorly; and 4) failing to understand the patient/family perspective.7
Anger, either from the adverse result itself or perceived lack of caring, turns an injured patient into a plaintiff, and lies at the root of all malpractice claims. The patients may not even have a serious injury or a meritorious claim, but they are so frustrated with their physician or the hospital that they contact an attorney to vent their anger.
One experienced attorney volunteered that close to half his malpractice cases could have been avoided through disclosure or apology, noting: “What the patients really wanted was simply an honest explanation of what happened, and, if appropriate, an apology. Unfortunately, when they were not only offered neither, but were rejected as well, they felt doubly wronged and then sought legal counsel.”8
Communicating well begins with active listening. Patients want their doctors to listen to them and to explain their conditions and treatment plans in simple, understandable language. The physician should give them ample opportunity to tell their story and to ask questions.
In one well-publicized study, only 23% of patients were able to complete their opening statement before the doctor interrupted, which occurred, on the average, 18 seconds after the patient began to speak!9
References
1. N Engl J Med. 2016 Jan 28;374(4):354-62.
2. “Medical liability: By late career, 61% of doctors have been sued,” Aug. 16, 2010, American Medical News.
4. “Law & Medicine: Health care costs and defensive medicine,” Jan. 19, 2016, Internal Medicine News.
5. N Engl J Med. 1991 Jul 25;325(4):245-51.
6. JAMA. 1994 Nov 23-30;272(20):1588-91.
7. Arch Intern Med. 1994 Jun 27;154(12):1365-70.
8. Ann Intern Med. 1999 Dec 21;131(12):970-2.
9. Ann Intern Med. 1984 Nov;101(5):692-6.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected]
Question: Doctors are more prone to lawsuits if they:
A. Have been sued before.
B. Spend fewer dollars per hospitalized patient.
C. Show poor communication skills.
D. A and C only.
E. A, B, and C.
Answer: E. Two very recent studies, one by David M. Studdert and the other by Dr. Anupam B. Jena, offer fresh insights into factors linked to the likelihood of a malpractice lawsuit.
The Studdert study concluded that doctors with prior paid claims are at increased risk of incurring yet another lawsuit.1 Instead of simply relying on data from a single insurer or state, the researchers accessed the National Practitioner Data Bank (NPDB) from 2005 through 2014 and identified 66,426 claims paid against 54,099 physicians.
Over that 10-year period, only 1% of physicians accounted for 32% of paid claims. Of all the physicians, 84% incurred only one paid claim during the study period, and 16% had at least two. Four percent of the physicians had at least three. In adjusted analyses, the risk of recurrence increased with the number of previous paid claims.
For example, compared with physicians with a single claim, the 2,160 physicians who had three paid claims had three times the risk of incurring another (hazard ratio, 3.11); this corresponded in absolute terms to a 24% risk within 2 years.
Likelihood of recurrence also varied widely according to specialty. For example, the risk among neurosurgeons was four times greater than that of psychiatrists. As for internists, the risk of recurrence was approximately double that of neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, or obstetrician-gynecologists. The lowest risks of recurrence were seen among psychiatrists (HR, 0.60) and pediatricians (HR, 0.71).
Male physicians had a 38% higher risk of recurrence than did female physicians, and the risk among physicians younger than 35 years was approximately one-third that of their older colleagues (after adjustment for age). Residents had a lower risk of recurrence than did nonresidents, and MDs had a lower risk than did DOs.
Using all 915,564 active physicians in the United States as a denominator, the authors calculated that over the 10-year study period, only 6% of physicians had a paid claim. Note that the 6% figure refers to paid claims reported to the NPDB, which can be expected to be lower than statistics derived from published surveys. These latter studies typically feature self-reported malpractice claims made over a given time period; but it is well known that the majority of such claims are dropped or decided in favor of the doctor, and so will not be reported to the NPDB.
For example, in 2010, the American Medical Association found that 42.2% of 5,825 physicians who responded to its Physician Practice Information survey reported having been sued, with 22.4% sued twice or more.2 The report headlined that by mid career, 61% of doctor have been sued.
Rates varied by specialty, with general surgeons and obstetrician-gynecologists being most likely to be sued (69.2%). Family physicians and general internists had similar rates (38.9% and 34%), and pediatricians and psychiatrists were sued the least.
In that report, male doctors were twice as likely to be sued as were their female counterparts, and physicians in solo and specialty practices were sued more often than those in multispecialty practices. Physicians who had an ownership interest in a practice were also at greater risk, with 47.5% reporting being sued, compared with 33.4% for those with no ownership interest.
The second recent study, reported by Dr. Jena of Harvard Medical School, Boston, and his colleagues, analyzed Florida hospital admissions data covering some 24,000 physicians.3 They found that higher spending by physicians was associated with reduced malpractice claims made the following year.
This pattern held true for physicians in all specialties but one (family practice). For example, among internists, the malpractice risk probability was 1.5% in the bottom spending fifth ($19,725 per admission) and 0.3% in the top fifth ($39,379 per admission). Among obstetricians, the comparable figures were 1.9% and 0.4% respectively.
In addition, a separate subgroup analysis of cesarean-section rates revealed that malpractice claims were approximately halved among obstetricians with rates in the highest fifth, compared with the lowest fifth.
Unfortunately, the Jena study lacked information on illness severity and past malpractice history, and it remains speculative whether increased resource utilization could be attributed entirely to defensive medical practice.4
As interesting as these new reports may be, it is worth remembering that what prompts a lawsuit are poor communication and patient perception that the physician is uncaring and at fault for the bad result.
It is well known that quality of medical care correlates poorly with the filing of malpractice lawsuits, as illustrated in the conclusion of the landmark Harvard study that “medical malpractice litigation infrequently compensates patients injured by medical negligence and rarely identifies, and holds providers accountable for, substandard care.”5 The authors estimated that there was only 1 malpractice claim for every 7.6 adverse events caused by negligence.
In another retrospective chart review study, the quality of treatment as judged by independent peer review was no different in frequently sued versus never-sued obstetricians.6
Communication problems exist in more than 70% of malpractice cases, centering around four themes: 1) deserting the patient; 2) devaluing patient/family views; 3) delivering information poorly; and 4) failing to understand the patient/family perspective.7
Anger, either from the adverse result itself or perceived lack of caring, turns an injured patient into a plaintiff, and lies at the root of all malpractice claims. The patients may not even have a serious injury or a meritorious claim, but they are so frustrated with their physician or the hospital that they contact an attorney to vent their anger.
One experienced attorney volunteered that close to half his malpractice cases could have been avoided through disclosure or apology, noting: “What the patients really wanted was simply an honest explanation of what happened, and, if appropriate, an apology. Unfortunately, when they were not only offered neither, but were rejected as well, they felt doubly wronged and then sought legal counsel.”8
Communicating well begins with active listening. Patients want their doctors to listen to them and to explain their conditions and treatment plans in simple, understandable language. The physician should give them ample opportunity to tell their story and to ask questions.
In one well-publicized study, only 23% of patients were able to complete their opening statement before the doctor interrupted, which occurred, on the average, 18 seconds after the patient began to speak!9
References
1. N Engl J Med. 2016 Jan 28;374(4):354-62.
2. “Medical liability: By late career, 61% of doctors have been sued,” Aug. 16, 2010, American Medical News.
4. “Law & Medicine: Health care costs and defensive medicine,” Jan. 19, 2016, Internal Medicine News.
5. N Engl J Med. 1991 Jul 25;325(4):245-51.
6. JAMA. 1994 Nov 23-30;272(20):1588-91.
7. Arch Intern Med. 1994 Jun 27;154(12):1365-70.
8. Ann Intern Med. 1999 Dec 21;131(12):970-2.
9. Ann Intern Med. 1984 Nov;101(5):692-6.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected]
Question: Doctors are more prone to lawsuits if they:
A. Have been sued before.
B. Spend fewer dollars per hospitalized patient.
C. Show poor communication skills.
D. A and C only.
E. A, B, and C.
Answer: E. Two very recent studies, one by David M. Studdert and the other by Dr. Anupam B. Jena, offer fresh insights into factors linked to the likelihood of a malpractice lawsuit.
The Studdert study concluded that doctors with prior paid claims are at increased risk of incurring yet another lawsuit.1 Instead of simply relying on data from a single insurer or state, the researchers accessed the National Practitioner Data Bank (NPDB) from 2005 through 2014 and identified 66,426 claims paid against 54,099 physicians.
Over that 10-year period, only 1% of physicians accounted for 32% of paid claims. Of all the physicians, 84% incurred only one paid claim during the study period, and 16% had at least two. Four percent of the physicians had at least three. In adjusted analyses, the risk of recurrence increased with the number of previous paid claims.
For example, compared with physicians with a single claim, the 2,160 physicians who had three paid claims had three times the risk of incurring another (hazard ratio, 3.11); this corresponded in absolute terms to a 24% risk within 2 years.
Likelihood of recurrence also varied widely according to specialty. For example, the risk among neurosurgeons was four times greater than that of psychiatrists. As for internists, the risk of recurrence was approximately double that of neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, or obstetrician-gynecologists. The lowest risks of recurrence were seen among psychiatrists (HR, 0.60) and pediatricians (HR, 0.71).
Male physicians had a 38% higher risk of recurrence than did female physicians, and the risk among physicians younger than 35 years was approximately one-third that of their older colleagues (after adjustment for age). Residents had a lower risk of recurrence than did nonresidents, and MDs had a lower risk than did DOs.
Using all 915,564 active physicians in the United States as a denominator, the authors calculated that over the 10-year study period, only 6% of physicians had a paid claim. Note that the 6% figure refers to paid claims reported to the NPDB, which can be expected to be lower than statistics derived from published surveys. These latter studies typically feature self-reported malpractice claims made over a given time period; but it is well known that the majority of such claims are dropped or decided in favor of the doctor, and so will not be reported to the NPDB.
For example, in 2010, the American Medical Association found that 42.2% of 5,825 physicians who responded to its Physician Practice Information survey reported having been sued, with 22.4% sued twice or more.2 The report headlined that by mid career, 61% of doctor have been sued.
Rates varied by specialty, with general surgeons and obstetrician-gynecologists being most likely to be sued (69.2%). Family physicians and general internists had similar rates (38.9% and 34%), and pediatricians and psychiatrists were sued the least.
In that report, male doctors were twice as likely to be sued as were their female counterparts, and physicians in solo and specialty practices were sued more often than those in multispecialty practices. Physicians who had an ownership interest in a practice were also at greater risk, with 47.5% reporting being sued, compared with 33.4% for those with no ownership interest.
The second recent study, reported by Dr. Jena of Harvard Medical School, Boston, and his colleagues, analyzed Florida hospital admissions data covering some 24,000 physicians.3 They found that higher spending by physicians was associated with reduced malpractice claims made the following year.
This pattern held true for physicians in all specialties but one (family practice). For example, among internists, the malpractice risk probability was 1.5% in the bottom spending fifth ($19,725 per admission) and 0.3% in the top fifth ($39,379 per admission). Among obstetricians, the comparable figures were 1.9% and 0.4% respectively.
In addition, a separate subgroup analysis of cesarean-section rates revealed that malpractice claims were approximately halved among obstetricians with rates in the highest fifth, compared with the lowest fifth.
Unfortunately, the Jena study lacked information on illness severity and past malpractice history, and it remains speculative whether increased resource utilization could be attributed entirely to defensive medical practice.4
As interesting as these new reports may be, it is worth remembering that what prompts a lawsuit are poor communication and patient perception that the physician is uncaring and at fault for the bad result.
It is well known that quality of medical care correlates poorly with the filing of malpractice lawsuits, as illustrated in the conclusion of the landmark Harvard study that “medical malpractice litigation infrequently compensates patients injured by medical negligence and rarely identifies, and holds providers accountable for, substandard care.”5 The authors estimated that there was only 1 malpractice claim for every 7.6 adverse events caused by negligence.
In another retrospective chart review study, the quality of treatment as judged by independent peer review was no different in frequently sued versus never-sued obstetricians.6
Communication problems exist in more than 70% of malpractice cases, centering around four themes: 1) deserting the patient; 2) devaluing patient/family views; 3) delivering information poorly; and 4) failing to understand the patient/family perspective.7
Anger, either from the adverse result itself or perceived lack of caring, turns an injured patient into a plaintiff, and lies at the root of all malpractice claims. The patients may not even have a serious injury or a meritorious claim, but they are so frustrated with their physician or the hospital that they contact an attorney to vent their anger.
One experienced attorney volunteered that close to half his malpractice cases could have been avoided through disclosure or apology, noting: “What the patients really wanted was simply an honest explanation of what happened, and, if appropriate, an apology. Unfortunately, when they were not only offered neither, but were rejected as well, they felt doubly wronged and then sought legal counsel.”8
Communicating well begins with active listening. Patients want their doctors to listen to them and to explain their conditions and treatment plans in simple, understandable language. The physician should give them ample opportunity to tell their story and to ask questions.
In one well-publicized study, only 23% of patients were able to complete their opening statement before the doctor interrupted, which occurred, on the average, 18 seconds after the patient began to speak!9
References
1. N Engl J Med. 2016 Jan 28;374(4):354-62.
2. “Medical liability: By late career, 61% of doctors have been sued,” Aug. 16, 2010, American Medical News.
4. “Law & Medicine: Health care costs and defensive medicine,” Jan. 19, 2016, Internal Medicine News.
5. N Engl J Med. 1991 Jul 25;325(4):245-51.
6. JAMA. 1994 Nov 23-30;272(20):1588-91.
7. Arch Intern Med. 1994 Jun 27;154(12):1365-70.
8. Ann Intern Med. 1999 Dec 21;131(12):970-2.
9. Ann Intern Med. 1984 Nov;101(5):692-6.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected]
A mind full of what?
I hope I am correct, but it seems to me that the “holistic” label is fading into the sunset. I never quite got what a holistic physician was doing that I wasn’t. Was I ignoring the fact that my patient came from a certain ethnic group and that his family had a particular set of religious beliefs? I may not have understood or agreed with those customs or beliefs. But I knew that I had better take them into account as I tried to find what was troubling the patient and help him search for a solution.
When the patient with frequent abdominal pains asked me for advice, did I fail to ask a social history because I didn’t think that the fact that her father had just lost his job or that her favorite grandmother was dying of cancer was important? Did I simply write prescriptions and avoid making recommendations about bedtimes, diet, exercise, and relaxation strategies? Did I stop my exam at the clavicles when the patient’s chief complaint was headache?
I’m sure that most physicians who marketed themselves as being holistic passionately believed that a good doctor must consider the whole patient. But what troubled me was the implication that the rest of us didn’t. I suspect that the fading popularity of the label reflects that patients began to realize that it was meaningless.
However, another buzzword has begun to flutter across the medical landscape. Every few days I open a magazine or journal in which someone is suggesting that I need to be more mindful. And they are more than willing to show me or sell me a technique for achieving mindfulness.
Is this just another packaging ploy, or should I begin paddling out to catch this new wave? The more I began to see mindfulness offered and promoted in a wider variety of settings, the more confused I became. So I did what anyone with a WiFi connection would do. I Googled “mindfulness” and discovered that I had good reason to feel confused.
It turns out that in some form or another mindfulness has been a practice in the Buddhist tradition with a history dating back hundreds of years. The first definition I found in Wikipedia read: “being aware moment-to-moment of one’s subjective conscious experience from a first-person perspective.” However, as I read further I discovered a reference to no fewer than 13 disparate definitions across a spectrum from attention and awareness on one end to retention and remindfulness on the other.
Some advocates feel that meditation should be used to prepare oneself to be mindful or that meditation is integral to mindfulness. Other folks don’t seem to see meditation as particularly necessary.
There is a growing body of literature reporting that something labeled mindfulness has helped patients and practitioners improve one or more aspects of wellness. Although the quality of these reports varies widely, it suggests along with the long Buddhist tradition that there is something out there called mindfulness worth investigating.
However, I wonder why it is becoming so widely ballyhooed. It seems to me that at its core, being mindful is simply just trying to do a better job of paying attention to the world around us and our fellow inhabitants. Is it simply the flip side of an attention deficiency? Or, is it an attempt to give a more exotic and mysterious Asian-influenced label to cognitive-behavioral therapy? Could it just be a less judgmental way of asking ourselves, “What were (are) you thinking?”
“Mindfulness” appears to have considerably more substance than “holistic,” but I fear that its indiscriminant use is going to damage its credibility. The overexposure has certainly triggered my skepticism.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
I hope I am correct, but it seems to me that the “holistic” label is fading into the sunset. I never quite got what a holistic physician was doing that I wasn’t. Was I ignoring the fact that my patient came from a certain ethnic group and that his family had a particular set of religious beliefs? I may not have understood or agreed with those customs or beliefs. But I knew that I had better take them into account as I tried to find what was troubling the patient and help him search for a solution.
When the patient with frequent abdominal pains asked me for advice, did I fail to ask a social history because I didn’t think that the fact that her father had just lost his job or that her favorite grandmother was dying of cancer was important? Did I simply write prescriptions and avoid making recommendations about bedtimes, diet, exercise, and relaxation strategies? Did I stop my exam at the clavicles when the patient’s chief complaint was headache?
I’m sure that most physicians who marketed themselves as being holistic passionately believed that a good doctor must consider the whole patient. But what troubled me was the implication that the rest of us didn’t. I suspect that the fading popularity of the label reflects that patients began to realize that it was meaningless.
However, another buzzword has begun to flutter across the medical landscape. Every few days I open a magazine or journal in which someone is suggesting that I need to be more mindful. And they are more than willing to show me or sell me a technique for achieving mindfulness.
Is this just another packaging ploy, or should I begin paddling out to catch this new wave? The more I began to see mindfulness offered and promoted in a wider variety of settings, the more confused I became. So I did what anyone with a WiFi connection would do. I Googled “mindfulness” and discovered that I had good reason to feel confused.
It turns out that in some form or another mindfulness has been a practice in the Buddhist tradition with a history dating back hundreds of years. The first definition I found in Wikipedia read: “being aware moment-to-moment of one’s subjective conscious experience from a first-person perspective.” However, as I read further I discovered a reference to no fewer than 13 disparate definitions across a spectrum from attention and awareness on one end to retention and remindfulness on the other.
Some advocates feel that meditation should be used to prepare oneself to be mindful or that meditation is integral to mindfulness. Other folks don’t seem to see meditation as particularly necessary.
There is a growing body of literature reporting that something labeled mindfulness has helped patients and practitioners improve one or more aspects of wellness. Although the quality of these reports varies widely, it suggests along with the long Buddhist tradition that there is something out there called mindfulness worth investigating.
However, I wonder why it is becoming so widely ballyhooed. It seems to me that at its core, being mindful is simply just trying to do a better job of paying attention to the world around us and our fellow inhabitants. Is it simply the flip side of an attention deficiency? Or, is it an attempt to give a more exotic and mysterious Asian-influenced label to cognitive-behavioral therapy? Could it just be a less judgmental way of asking ourselves, “What were (are) you thinking?”
“Mindfulness” appears to have considerably more substance than “holistic,” but I fear that its indiscriminant use is going to damage its credibility. The overexposure has certainly triggered my skepticism.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
I hope I am correct, but it seems to me that the “holistic” label is fading into the sunset. I never quite got what a holistic physician was doing that I wasn’t. Was I ignoring the fact that my patient came from a certain ethnic group and that his family had a particular set of religious beliefs? I may not have understood or agreed with those customs or beliefs. But I knew that I had better take them into account as I tried to find what was troubling the patient and help him search for a solution.
When the patient with frequent abdominal pains asked me for advice, did I fail to ask a social history because I didn’t think that the fact that her father had just lost his job or that her favorite grandmother was dying of cancer was important? Did I simply write prescriptions and avoid making recommendations about bedtimes, diet, exercise, and relaxation strategies? Did I stop my exam at the clavicles when the patient’s chief complaint was headache?
I’m sure that most physicians who marketed themselves as being holistic passionately believed that a good doctor must consider the whole patient. But what troubled me was the implication that the rest of us didn’t. I suspect that the fading popularity of the label reflects that patients began to realize that it was meaningless.
However, another buzzword has begun to flutter across the medical landscape. Every few days I open a magazine or journal in which someone is suggesting that I need to be more mindful. And they are more than willing to show me or sell me a technique for achieving mindfulness.
Is this just another packaging ploy, or should I begin paddling out to catch this new wave? The more I began to see mindfulness offered and promoted in a wider variety of settings, the more confused I became. So I did what anyone with a WiFi connection would do. I Googled “mindfulness” and discovered that I had good reason to feel confused.
It turns out that in some form or another mindfulness has been a practice in the Buddhist tradition with a history dating back hundreds of years. The first definition I found in Wikipedia read: “being aware moment-to-moment of one’s subjective conscious experience from a first-person perspective.” However, as I read further I discovered a reference to no fewer than 13 disparate definitions across a spectrum from attention and awareness on one end to retention and remindfulness on the other.
Some advocates feel that meditation should be used to prepare oneself to be mindful or that meditation is integral to mindfulness. Other folks don’t seem to see meditation as particularly necessary.
There is a growing body of literature reporting that something labeled mindfulness has helped patients and practitioners improve one or more aspects of wellness. Although the quality of these reports varies widely, it suggests along with the long Buddhist tradition that there is something out there called mindfulness worth investigating.
However, I wonder why it is becoming so widely ballyhooed. It seems to me that at its core, being mindful is simply just trying to do a better job of paying attention to the world around us and our fellow inhabitants. Is it simply the flip side of an attention deficiency? Or, is it an attempt to give a more exotic and mysterious Asian-influenced label to cognitive-behavioral therapy? Could it just be a less judgmental way of asking ourselves, “What were (are) you thinking?”
“Mindfulness” appears to have considerably more substance than “holistic,” but I fear that its indiscriminant use is going to damage its credibility. The overexposure has certainly triggered my skepticism.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including “How to Say No to Your Toddler.”
Greater myocardial inflammation found in RA patients after heart attack
The presence of rheumatoid arthritis in individuals who died from a myocardial infarction was associated with greater inflammatory burden at different levels of myocardial tissue than in those without the disease in a small, retrospective, case-control autopsy study.
“These findings support the hypothesis that RA [rheumatoid arthritis] patients are prone to develop more vulnerable plaques due to more inflammation in the coronary arteries, but also develop increased intramyocardial inflammation indicative of a higher risk of myocardial tissue damage post MI. This might not only explain the higher incidence of cardiovascular events in this population, but also the higher fatality rate after myocardial infarction,” wrote Dr. Inge A.M. van den Oever of the Amsterdam Rheumatology and Immunology Center and colleagues (Int J Cardiol. 2016 Feb 3. doi: 10.1016/j.ijcard.2016.02.065).
The investigators took tissue samples from the infarcted left ventricle and microscopically determined infarct border area of five patients with RA and MI and five controls with MI but without RA. They found that RA patients had a greater burden of inflammatory cells in the adventitia of infarct-related epicardial coronary arteries, the intramyocardial vasculature, and the border area of the infarcted heart, compared with controls matched for age, sex, year of death, grade of stenosis, and infarct phase.
Specifically, the adventitial layer of the infarct-related epicardial coronary artery of RA patients had significantly more lymphocytes and mast cells. Intramyocardial arteries in infarct and infarct border areas of RA patients, compared with controls, showed significantly greater staining for advanced glycation end product N-epsilon-(carboxymethyl) lysine (CML), which is thought to reflect oxidative damage to cells, as well as noninfarcted tissues taken from the right ventricle.
The researchers included cases and controls from a postmortem tissue database of subjects who underwent autopsy within 24 hours after death at the VU University Medical Centre, Amsterdam, between January 1990 and December 2010.
The research was partly funded by a grant from the Dutch Society for Rheumatology. The authors had no conflicts of interest to declare.
The presence of rheumatoid arthritis in individuals who died from a myocardial infarction was associated with greater inflammatory burden at different levels of myocardial tissue than in those without the disease in a small, retrospective, case-control autopsy study.
“These findings support the hypothesis that RA [rheumatoid arthritis] patients are prone to develop more vulnerable plaques due to more inflammation in the coronary arteries, but also develop increased intramyocardial inflammation indicative of a higher risk of myocardial tissue damage post MI. This might not only explain the higher incidence of cardiovascular events in this population, but also the higher fatality rate after myocardial infarction,” wrote Dr. Inge A.M. van den Oever of the Amsterdam Rheumatology and Immunology Center and colleagues (Int J Cardiol. 2016 Feb 3. doi: 10.1016/j.ijcard.2016.02.065).
The investigators took tissue samples from the infarcted left ventricle and microscopically determined infarct border area of five patients with RA and MI and five controls with MI but without RA. They found that RA patients had a greater burden of inflammatory cells in the adventitia of infarct-related epicardial coronary arteries, the intramyocardial vasculature, and the border area of the infarcted heart, compared with controls matched for age, sex, year of death, grade of stenosis, and infarct phase.
Specifically, the adventitial layer of the infarct-related epicardial coronary artery of RA patients had significantly more lymphocytes and mast cells. Intramyocardial arteries in infarct and infarct border areas of RA patients, compared with controls, showed significantly greater staining for advanced glycation end product N-epsilon-(carboxymethyl) lysine (CML), which is thought to reflect oxidative damage to cells, as well as noninfarcted tissues taken from the right ventricle.
The researchers included cases and controls from a postmortem tissue database of subjects who underwent autopsy within 24 hours after death at the VU University Medical Centre, Amsterdam, between January 1990 and December 2010.
The research was partly funded by a grant from the Dutch Society for Rheumatology. The authors had no conflicts of interest to declare.
The presence of rheumatoid arthritis in individuals who died from a myocardial infarction was associated with greater inflammatory burden at different levels of myocardial tissue than in those without the disease in a small, retrospective, case-control autopsy study.
“These findings support the hypothesis that RA [rheumatoid arthritis] patients are prone to develop more vulnerable plaques due to more inflammation in the coronary arteries, but also develop increased intramyocardial inflammation indicative of a higher risk of myocardial tissue damage post MI. This might not only explain the higher incidence of cardiovascular events in this population, but also the higher fatality rate after myocardial infarction,” wrote Dr. Inge A.M. van den Oever of the Amsterdam Rheumatology and Immunology Center and colleagues (Int J Cardiol. 2016 Feb 3. doi: 10.1016/j.ijcard.2016.02.065).
The investigators took tissue samples from the infarcted left ventricle and microscopically determined infarct border area of five patients with RA and MI and five controls with MI but without RA. They found that RA patients had a greater burden of inflammatory cells in the adventitia of infarct-related epicardial coronary arteries, the intramyocardial vasculature, and the border area of the infarcted heart, compared with controls matched for age, sex, year of death, grade of stenosis, and infarct phase.
Specifically, the adventitial layer of the infarct-related epicardial coronary artery of RA patients had significantly more lymphocytes and mast cells. Intramyocardial arteries in infarct and infarct border areas of RA patients, compared with controls, showed significantly greater staining for advanced glycation end product N-epsilon-(carboxymethyl) lysine (CML), which is thought to reflect oxidative damage to cells, as well as noninfarcted tissues taken from the right ventricle.
The researchers included cases and controls from a postmortem tissue database of subjects who underwent autopsy within 24 hours after death at the VU University Medical Centre, Amsterdam, between January 1990 and December 2010.
The research was partly funded by a grant from the Dutch Society for Rheumatology. The authors had no conflicts of interest to declare.
FROM THE INTERNATIONAL JOURNAL OF CARDIOLOGY
Key clinical point:Post-MI autopsy data support the view that RA patients have greater intramyocardial inflammatory burden than do patients without the disease.
Major finding: The adventitial layer of the infarct-related epicardial coronary artery of RA patients had significantly more lymphocytes and mast cells than did controls.
Data source: A retrospective, case-control, autopsy study of five patients with RA and MI and five controls with MI but without RA.
Disclosures: The research was partly funded by a grant from the Dutch Society for Rheumatology. The authors had no conflicts of interest to declare.
Chemo regimen can be ‘highly effective’ against ENKTL

Photo by Larry Young
SAN FRANCISCO—A 3-agent chemotherapy regimen can be “highly effective” in patients with extranodal natural killer/T-cell lymphoma (ENKTL), according to researchers.
In a single-center study, this regimen—pegaspargase, gemcitabine, and oxaliplatin (P-GEMOX)—followed by extensive involved-field radiotherapy (EIFRT) produced high rates of long-term overall survival (OS) and progression-free survival (PFS) in newly diagnosed patients with stage I/II ENKTL.
P-GEMOX also proved effective—though to a much lesser degree—in advanced, relapsed, or refractory ENKTL, and these patients appeared to benefit from autologous stem cell transplant (auto-SCT) as consolidation.
Toxicity associated with P-GEMOX was mild to moderate and tolerable, according to Hui-Qiang Huang, MD, PhD, of State Key Laboratory of Oncology in Southern China, Guangzhou, China.
Dr Huang presented these results at the 8th Annual T-cell Lymphoma Forum.
Newly diagnosed patients
Dr Huang and his colleagues studied 56 patients newly diagnosed with stage I/II, nasal-type ENKTL. Most patients were younger than 60 years of age (80.4%, n=45).
About 79% (n=44) had an ECOG status of 0, and 21.4% (n=12) had a status of 1. About 61% (n=34) had stage I disease, and 39.3% (n=22) had stage II.
All patients received P-GEMOX—gemcitabine at 1000 mg/m2 on days 1 and 8, oxaliplatin at 150 mg/m2 on day 1, and pegaspargase at 2000 U/m2 on day 1. Doses could be adjusted in the event of toxicity.
The regimen was repeated every 3 weeks for a maximum of 4 cycles. Patients then underwent EIFRT—56 Gy in 28 fractions over 4 weeks.
The overall response rate (ORR) after P-GEMOX was 89.3% (50/56). Thirty-five patients achieved a complete response (CR), 15 had a partial response (PR), and 4 had stable disease (SD).
After EIFRT, the ORR increased to 94.6% (53/56). Fifty patients had a CR, 3 had a PR, and 1 had SD.
The median follow-up was 35.2 months (range, 10.6-51.4). Six patients relapsed, and the median time to relapse was 6.2 months.
Five patients died of disease progression. The median time to death was 10.9 months after the completion of EIFRT.
The 4-year OS rate was 90.7±4.0%, and the 4-year PFS rate was 89.1±4.2%.
OS and PFS were superior in patients with stage I disease as compared to stage II (P=0.056 and 0.023, respectively). And OS and PFS were superior in patients who responded to P-GEMOX (P=0.004 and 0.001, respectively).
There were no treatment-related deaths. The most common toxicities (occurring in more than 50% of patients) after P-GEMOX were neutropenia (80.3%), thrombocytopenia (55.3%), and hypoproteinemia (75.0%).
The most common grade 3/4 toxicities (occurring in more than 10% of patients) were granulocytosis (23.2%), thrombocytopenia (19.6%), and hypoproteinemia (10.7%).
Advanced & relapsed/refractory patients
Dr Huang and his colleagues also studied 60 patients with newly diagnosed, stage III/IV ENKTL (25%, n=15), relapsed ENKTL (21.7%, n=19), or refractory disease (43.3%, n=26). Seventy percent of these patients (n=42) had nasal-type ENKTL.
Most patients were younger than 60 years of age (91.7%, n=55). About 73% (n=44) had an ECOG status of 0-1, and 26.7% (n=16) had a status of 2. Fifteen percent of patients (n=9) had stage I disease, 16.7% (n=10) had stage II, 35% (n=21) had stage III, and 33.3% (n=20) had stage IV.
The patients received the same P-GEMOX regimen as the newly diagnosed, stage I/II patients, but they did not receive EIFRT, and responders could undergo auto-SCT.
For the whole cohort, the ORR after P-GEMOX was 70% (42/60). Twenty-one patients had a CR, 21 had a PR, and 9 had SD.
In the newly diagnosed patients, the ORR was 80% (12/15). Four patients had a CR, 8 had a PR, and 2 had SD. In the relapsed/refractory patients, the ORR was 66.7% (30/45). Seventeen patients had a CR, 13 had a PR, and 7 had SD.
The 4-year OS was 43.0±7.3%, and the 4-year PFS was 36.5±6.9%.
There was no significant difference in OS or PFS between the newly diagnosed and relapsed/refractory patients (P=0.653 and 0.825, respectively). However, there was a significant difference in PFS and OS between responders and non-responders (P<0.001 for both).
There was a difference in 3-year OS between patients who went on to auto-SCT and those did not, although it did not reach statistical significance (P=0.08). Eleven patients who achieved a CR went on to auto-SCT.
There were no treatment-related deaths. The most common toxicities (occurring in more than 50% of patients) after P-GEMOX were neutropenia (85%), hypoproteinemia (88.3%), anemia (71.6%), fibrinogen decrease (68.3%), and anorexia (53.3%).
The most common grade 3/4 toxicities (occurring in more than 10% of patients) were neutropenia (31.6%), hypoproteinemia (13.3%), and thrombocytopenia (11.7%).
Dr Huang said this research suggests P-GEMOX can be effective for patients with newly diagnosed or previously treated ENKTL. The next step is to investigate which novel agents could be added to the regimen to improve its efficacy. ![]()

Photo by Larry Young
SAN FRANCISCO—A 3-agent chemotherapy regimen can be “highly effective” in patients with extranodal natural killer/T-cell lymphoma (ENKTL), according to researchers.
In a single-center study, this regimen—pegaspargase, gemcitabine, and oxaliplatin (P-GEMOX)—followed by extensive involved-field radiotherapy (EIFRT) produced high rates of long-term overall survival (OS) and progression-free survival (PFS) in newly diagnosed patients with stage I/II ENKTL.
P-GEMOX also proved effective—though to a much lesser degree—in advanced, relapsed, or refractory ENKTL, and these patients appeared to benefit from autologous stem cell transplant (auto-SCT) as consolidation.
Toxicity associated with P-GEMOX was mild to moderate and tolerable, according to Hui-Qiang Huang, MD, PhD, of State Key Laboratory of Oncology in Southern China, Guangzhou, China.
Dr Huang presented these results at the 8th Annual T-cell Lymphoma Forum.
Newly diagnosed patients
Dr Huang and his colleagues studied 56 patients newly diagnosed with stage I/II, nasal-type ENKTL. Most patients were younger than 60 years of age (80.4%, n=45).
About 79% (n=44) had an ECOG status of 0, and 21.4% (n=12) had a status of 1. About 61% (n=34) had stage I disease, and 39.3% (n=22) had stage II.
All patients received P-GEMOX—gemcitabine at 1000 mg/m2 on days 1 and 8, oxaliplatin at 150 mg/m2 on day 1, and pegaspargase at 2000 U/m2 on day 1. Doses could be adjusted in the event of toxicity.
The regimen was repeated every 3 weeks for a maximum of 4 cycles. Patients then underwent EIFRT—56 Gy in 28 fractions over 4 weeks.
The overall response rate (ORR) after P-GEMOX was 89.3% (50/56). Thirty-five patients achieved a complete response (CR), 15 had a partial response (PR), and 4 had stable disease (SD).
After EIFRT, the ORR increased to 94.6% (53/56). Fifty patients had a CR, 3 had a PR, and 1 had SD.
The median follow-up was 35.2 months (range, 10.6-51.4). Six patients relapsed, and the median time to relapse was 6.2 months.
Five patients died of disease progression. The median time to death was 10.9 months after the completion of EIFRT.
The 4-year OS rate was 90.7±4.0%, and the 4-year PFS rate was 89.1±4.2%.
OS and PFS were superior in patients with stage I disease as compared to stage II (P=0.056 and 0.023, respectively). And OS and PFS were superior in patients who responded to P-GEMOX (P=0.004 and 0.001, respectively).
There were no treatment-related deaths. The most common toxicities (occurring in more than 50% of patients) after P-GEMOX were neutropenia (80.3%), thrombocytopenia (55.3%), and hypoproteinemia (75.0%).
The most common grade 3/4 toxicities (occurring in more than 10% of patients) were granulocytosis (23.2%), thrombocytopenia (19.6%), and hypoproteinemia (10.7%).
Advanced & relapsed/refractory patients
Dr Huang and his colleagues also studied 60 patients with newly diagnosed, stage III/IV ENKTL (25%, n=15), relapsed ENKTL (21.7%, n=19), or refractory disease (43.3%, n=26). Seventy percent of these patients (n=42) had nasal-type ENKTL.
Most patients were younger than 60 years of age (91.7%, n=55). About 73% (n=44) had an ECOG status of 0-1, and 26.7% (n=16) had a status of 2. Fifteen percent of patients (n=9) had stage I disease, 16.7% (n=10) had stage II, 35% (n=21) had stage III, and 33.3% (n=20) had stage IV.
The patients received the same P-GEMOX regimen as the newly diagnosed, stage I/II patients, but they did not receive EIFRT, and responders could undergo auto-SCT.
For the whole cohort, the ORR after P-GEMOX was 70% (42/60). Twenty-one patients had a CR, 21 had a PR, and 9 had SD.
In the newly diagnosed patients, the ORR was 80% (12/15). Four patients had a CR, 8 had a PR, and 2 had SD. In the relapsed/refractory patients, the ORR was 66.7% (30/45). Seventeen patients had a CR, 13 had a PR, and 7 had SD.
The 4-year OS was 43.0±7.3%, and the 4-year PFS was 36.5±6.9%.
There was no significant difference in OS or PFS between the newly diagnosed and relapsed/refractory patients (P=0.653 and 0.825, respectively). However, there was a significant difference in PFS and OS between responders and non-responders (P<0.001 for both).
There was a difference in 3-year OS between patients who went on to auto-SCT and those did not, although it did not reach statistical significance (P=0.08). Eleven patients who achieved a CR went on to auto-SCT.
There were no treatment-related deaths. The most common toxicities (occurring in more than 50% of patients) after P-GEMOX were neutropenia (85%), hypoproteinemia (88.3%), anemia (71.6%), fibrinogen decrease (68.3%), and anorexia (53.3%).
The most common grade 3/4 toxicities (occurring in more than 10% of patients) were neutropenia (31.6%), hypoproteinemia (13.3%), and thrombocytopenia (11.7%).
Dr Huang said this research suggests P-GEMOX can be effective for patients with newly diagnosed or previously treated ENKTL. The next step is to investigate which novel agents could be added to the regimen to improve its efficacy. ![]()

Photo by Larry Young
SAN FRANCISCO—A 3-agent chemotherapy regimen can be “highly effective” in patients with extranodal natural killer/T-cell lymphoma (ENKTL), according to researchers.
In a single-center study, this regimen—pegaspargase, gemcitabine, and oxaliplatin (P-GEMOX)—followed by extensive involved-field radiotherapy (EIFRT) produced high rates of long-term overall survival (OS) and progression-free survival (PFS) in newly diagnosed patients with stage I/II ENKTL.
P-GEMOX also proved effective—though to a much lesser degree—in advanced, relapsed, or refractory ENKTL, and these patients appeared to benefit from autologous stem cell transplant (auto-SCT) as consolidation.
Toxicity associated with P-GEMOX was mild to moderate and tolerable, according to Hui-Qiang Huang, MD, PhD, of State Key Laboratory of Oncology in Southern China, Guangzhou, China.
Dr Huang presented these results at the 8th Annual T-cell Lymphoma Forum.
Newly diagnosed patients
Dr Huang and his colleagues studied 56 patients newly diagnosed with stage I/II, nasal-type ENKTL. Most patients were younger than 60 years of age (80.4%, n=45).
About 79% (n=44) had an ECOG status of 0, and 21.4% (n=12) had a status of 1. About 61% (n=34) had stage I disease, and 39.3% (n=22) had stage II.
All patients received P-GEMOX—gemcitabine at 1000 mg/m2 on days 1 and 8, oxaliplatin at 150 mg/m2 on day 1, and pegaspargase at 2000 U/m2 on day 1. Doses could be adjusted in the event of toxicity.
The regimen was repeated every 3 weeks for a maximum of 4 cycles. Patients then underwent EIFRT—56 Gy in 28 fractions over 4 weeks.
The overall response rate (ORR) after P-GEMOX was 89.3% (50/56). Thirty-five patients achieved a complete response (CR), 15 had a partial response (PR), and 4 had stable disease (SD).
After EIFRT, the ORR increased to 94.6% (53/56). Fifty patients had a CR, 3 had a PR, and 1 had SD.
The median follow-up was 35.2 months (range, 10.6-51.4). Six patients relapsed, and the median time to relapse was 6.2 months.
Five patients died of disease progression. The median time to death was 10.9 months after the completion of EIFRT.
The 4-year OS rate was 90.7±4.0%, and the 4-year PFS rate was 89.1±4.2%.
OS and PFS were superior in patients with stage I disease as compared to stage II (P=0.056 and 0.023, respectively). And OS and PFS were superior in patients who responded to P-GEMOX (P=0.004 and 0.001, respectively).
There were no treatment-related deaths. The most common toxicities (occurring in more than 50% of patients) after P-GEMOX were neutropenia (80.3%), thrombocytopenia (55.3%), and hypoproteinemia (75.0%).
The most common grade 3/4 toxicities (occurring in more than 10% of patients) were granulocytosis (23.2%), thrombocytopenia (19.6%), and hypoproteinemia (10.7%).
Advanced & relapsed/refractory patients
Dr Huang and his colleagues also studied 60 patients with newly diagnosed, stage III/IV ENKTL (25%, n=15), relapsed ENKTL (21.7%, n=19), or refractory disease (43.3%, n=26). Seventy percent of these patients (n=42) had nasal-type ENKTL.
Most patients were younger than 60 years of age (91.7%, n=55). About 73% (n=44) had an ECOG status of 0-1, and 26.7% (n=16) had a status of 2. Fifteen percent of patients (n=9) had stage I disease, 16.7% (n=10) had stage II, 35% (n=21) had stage III, and 33.3% (n=20) had stage IV.
The patients received the same P-GEMOX regimen as the newly diagnosed, stage I/II patients, but they did not receive EIFRT, and responders could undergo auto-SCT.
For the whole cohort, the ORR after P-GEMOX was 70% (42/60). Twenty-one patients had a CR, 21 had a PR, and 9 had SD.
In the newly diagnosed patients, the ORR was 80% (12/15). Four patients had a CR, 8 had a PR, and 2 had SD. In the relapsed/refractory patients, the ORR was 66.7% (30/45). Seventeen patients had a CR, 13 had a PR, and 7 had SD.
The 4-year OS was 43.0±7.3%, and the 4-year PFS was 36.5±6.9%.
There was no significant difference in OS or PFS between the newly diagnosed and relapsed/refractory patients (P=0.653 and 0.825, respectively). However, there was a significant difference in PFS and OS between responders and non-responders (P<0.001 for both).
There was a difference in 3-year OS between patients who went on to auto-SCT and those did not, although it did not reach statistical significance (P=0.08). Eleven patients who achieved a CR went on to auto-SCT.
There were no treatment-related deaths. The most common toxicities (occurring in more than 50% of patients) after P-GEMOX were neutropenia (85%), hypoproteinemia (88.3%), anemia (71.6%), fibrinogen decrease (68.3%), and anorexia (53.3%).
The most common grade 3/4 toxicities (occurring in more than 10% of patients) were neutropenia (31.6%), hypoproteinemia (13.3%), and thrombocytopenia (11.7%).
Dr Huang said this research suggests P-GEMOX can be effective for patients with newly diagnosed or previously treated ENKTL. The next step is to investigate which novel agents could be added to the regimen to improve its efficacy. ![]()
More ob.gyns. find their niche as subspecialists
After 12 years as a private practice ob.gyn., Dr. Brigid McCue was beginning to feel overwhelmed. She loved her work, but keeping up with the kaleidoscope of care components and ever-changing clinical developments was daunting.
“I felt like it was hard to stay really good at all the different aspects of care,” Dr. McCue said. “I was doing fine with obstetrics, and I felt like I was managing my office well, but it’s hard to stay on top of the latest developments, especially in surgical areas. The other thing that was really hard to keep up with was the business aspect of medicine and running a private practice.”
So when an opportunity presented itself, Dr. McCue leaped at the chance to narrow her expertise to obstetrical hospital medicine. She helped establish the ob.gyn. hospitalist program at Beth Israel Deaconess Hospital-Plymouth in Massachusetts, and now serves as chief of ob.gyn. and midwifery for the hospital.
“I love the fact that I now have the time to get really good at [what] I really like, [such as] labor and delivery,” said Dr. McCue, who is president of the Society of OB/GYN Hospitalists. “Since I made this change, I feel like I’m so much more on top of things. I do simulations here on my unit over things like shoulder dystocia. When I was in private practice, I would go to one meeting a year and pray that I never had a shoulder dystocia [case]. Now I really understand the whole process and I take the time to run through that with my midwives and my other nurses and doctors.”
Dr. McCue is one of a growing number of ob.gyns. who have chosen to target their expertise to a single subspecialty or concentrated practice area. Data show subspecialization is on the rise in ob.gyn.
From 1985 to 2015, certificates issued by the American Board of Obstetrics and Gynecology (ABOG) for gynecologic oncology nearly tripled, and certificates issued for reproductive endocrinology and infertility more than doubled, according to data provided by the American Board of Medical Specialties (ABMS). Certificates issued for maternal-fetal medicine rose from 35 in 1985 to 100 in 2015.

Opportunities for ob.gyns. to subspecialize have steadily increased over the last 50 years. The subspecialties of maternal-fetal medicine, gynecologic oncology, and reproductive endocrinology and infertility were first approved for certification by ABOG in 1973. In 1983, ABMS approved a certificate of “added qualification” for ob.gyns. who complete fellowships in critical care. In 1995, ABOG and the American Board of Urology started the subspecialty of female pelvic medicine and reconstructive surgery, which was approved for certification by ABMS in 2011.
ABMS also approved a certificate of “added qualification” for ob.gyns. who complete a fellowship in hospice and palliative medicine in 2008. And fellowships now exist for minimally invasive gynecologic surgery and ob.gyn. hospital medicine.
The reasons that ob.gyns. choose to subspecialize are multifold, said Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill., and one of the medical editors of the Ob.Gyn. News column, Master Class.
“Physicians subspecialize so that they can provide more medical and surgical expertise for a given population,” he said. “Secondly, physicians may be driven to subspecialize for lifestyle reasons. Generalists refer to subspecialists when technical expertise is desired to help with a clinical situation and potentially reduce medical legal risk.”
Ultimately, it’s patients who benefit from the increased care provided by subspecialists, noted Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology, and women’s health at Rutgers, the State University of New Jersey, Newark. Generalist ob.gyns. are tremendously knowledgeable and experienced, he said, but there’s no way for them to know every area, he said. It’s the difference between someone who might be doing a complicated surgery one or twice a year versus someone who is doing that surgery once or twice a week, he added.
“That is ultimately helpful for patients,” Dr. Einstein said. “It’s really about outcomes. This is all better for the patient. That’s the most important thing.”
Not every consequence of subspecialization is positive, however.
“As with everything, subspecialization has both positive and negative effects,” said Dr. Sandra Ann Carson, vice president for education at the American College of Obstetricians and Gynecologists. “The more time one has to focus on a small area, the better that area becomes. However, if all you have is a hammer, everything looks like a nail. The larger population may not need the care that someone with a rare disease may need.”
Dr. Miller refers to this challenge as “losing the forest.” He explains that subspecialists sometimes become so focused on their area of expertise, that they may overlook suitable treatment plans with which they are unfamiliar. An infertility specialist, for example, who neglects to consider a minimally invasive surgical procedure that could allow a patient to become pregnant naturally and instead recommends in vitro fertilization treatment.
“The infertility specialist does not have that particular skill and therefore directs that patient to IVF,” Dr. Miller said. “In the process of subspecializing, we have a tendency to lose the forest and look only at the trees.”
Finding a job is another challenge for the growing number of subspecialists. In many cases, fellowship-trained minimally invasive gynecologic surgeons may have to go back to practicing general gynecology because of a lack of positions, Dr. Miller said.
“We have to be careful that we do not “oversubspecialize” so that we are oversaturating the field,” he said.
In the future, the number of ob.gyn subspecialists will likely continue to grow and become more refined, said Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center in Phoenix.
“I think subspecialists will continue to become more and more developed,” Dr. Chase said. “Perhaps, some areas like family planning or minimally invasive surgery may grow further and become board certified.”
Dr. Carson foresees subspecialization becoming more focused on centralized teaching hospitals, with patients who need special care being sent to these hubs.
“Telemedicine and long-distance communication with a local obstetrician-gynecologist managing the whole patient will allow the best of both worlds,” she said.
Regardless of how subspecialist growth evolves, general ob.gyns. and other primary care physicians will always be needed, said Dr. Mary E. Norton, a maternal-fetal medicine specialist and clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“With increasing complexity, experts are needed to interpret advances,” Dr. Norton said. “However, patients also need a ‘medical home’ and primary provider who sees the big picture, and provides ongoing care beyond a single pregnancy or pregnancy complication.”
Why I chose to subspecialize
“I went to medical school with a particular interest in obstetrics. Once there, I was exposed to pediatrics and to high-risk OB, which I found to be fascinating. I particularly enjoyed my exposure to genetics during my pediatrics rotation and cared for a few children with genetic diseases that had a big impact and made a substantial impression on me. I ultimately decided to pursue an ob.gyn. residency and loved the OB part, particularly the prenatal genetics and high-risk OB. I found the balance of maternal and fetal medicine to be an exciting opportunity to care for two patients. I did an elective in prenatal diagnosis during my third year, including a bit of research, and was hooked.”
Dr. Mary E. Norton, a maternal-fetal medicine specialist and a clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“In my second year of residency, I became really interested in [gynecology-oncology] because I was fascinated by the surgery and interested in the chemotherapy practice, which is interesting because there’s always new research and new agents and interesting changes in how you treat the various cancers. It’s a very comprehensive, research-based field and that was fascinating to me. It’s a very busy subspecialty with very complex cases on multiple levels. You do these radical surgeries but then you have to be really involved in the choice for which chemotherapy agent to use, what type of radiation to give, and you also get really involved with the families ... Every case is so different and you treat women who are 16 years old, but you also treat women who are 96 years old. You see women from all walks of life with all sorts of different issues. The ability to really get involved with cancer research is a great part of the field.”
Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center, Phoenix.
“I took the opportunity to come to a new program where they were looking for an ob.gyn. hospitalist. That was exciting for me because I got to help establish the program... I feel like we’re a better department because I’m here monitoring labor, but I’m also writing protocols and making sure everyone is up to date. And I still get to do what I love the most, which is birth and babies.”
Dr. Brigid McCue, an ob.gyn. hospitalist and chief of ob.gyn. and midwifery, Beth Israel Deaconess Hospital-Plymouth, Massachusetts.
“I never considered delivering babies for the rest of my life. I was always focused on treating infertile couples. I completed my fellowship in reproductive endocrinology-infertility at the University of Pennsylvania, Philadelphia, at a time when in vitro fertilization was in its infancy and the laparoscope and hysteroscope were virtually diagnostic tools ... As IVF became more successful, I felt it was essential to add this expertise to my armamentarium ... It is truly gratifying to be part of a subspecialty that has advanced so far that the majority of our patients are able to achieve pregnancy via IVF.”
Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill.
“During medical school, I was very interested in the surgical aspects of patient care. When I rotated in gyn-oncology – now knowing that I rotated with some of the best gyn-oncologists who ever practiced – I found myself drawn to the complexity of surgery, acuity of the patients, and the close relationships gyn-oncologists have with their patients. It hit me like a brick that this was the specialty for me. During my residency and fellowship, I was particularly drawn to the multiple modalities we use to treat cancers. I relished the idea that through clinical trials, gyn-oncologists keep pushing the bar to solve the cancer problem. What we do now is different than what we did 5 years ago. It keeps us professionally challenged all the time.”
Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology and women’s health at Rutgers, the State University of New Jersey, Newark.
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
On Twitter @legal_med
After 12 years as a private practice ob.gyn., Dr. Brigid McCue was beginning to feel overwhelmed. She loved her work, but keeping up with the kaleidoscope of care components and ever-changing clinical developments was daunting.
“I felt like it was hard to stay really good at all the different aspects of care,” Dr. McCue said. “I was doing fine with obstetrics, and I felt like I was managing my office well, but it’s hard to stay on top of the latest developments, especially in surgical areas. The other thing that was really hard to keep up with was the business aspect of medicine and running a private practice.”
So when an opportunity presented itself, Dr. McCue leaped at the chance to narrow her expertise to obstetrical hospital medicine. She helped establish the ob.gyn. hospitalist program at Beth Israel Deaconess Hospital-Plymouth in Massachusetts, and now serves as chief of ob.gyn. and midwifery for the hospital.
“I love the fact that I now have the time to get really good at [what] I really like, [such as] labor and delivery,” said Dr. McCue, who is president of the Society of OB/GYN Hospitalists. “Since I made this change, I feel like I’m so much more on top of things. I do simulations here on my unit over things like shoulder dystocia. When I was in private practice, I would go to one meeting a year and pray that I never had a shoulder dystocia [case]. Now I really understand the whole process and I take the time to run through that with my midwives and my other nurses and doctors.”
Dr. McCue is one of a growing number of ob.gyns. who have chosen to target their expertise to a single subspecialty or concentrated practice area. Data show subspecialization is on the rise in ob.gyn.
From 1985 to 2015, certificates issued by the American Board of Obstetrics and Gynecology (ABOG) for gynecologic oncology nearly tripled, and certificates issued for reproductive endocrinology and infertility more than doubled, according to data provided by the American Board of Medical Specialties (ABMS). Certificates issued for maternal-fetal medicine rose from 35 in 1985 to 100 in 2015.

Opportunities for ob.gyns. to subspecialize have steadily increased over the last 50 years. The subspecialties of maternal-fetal medicine, gynecologic oncology, and reproductive endocrinology and infertility were first approved for certification by ABOG in 1973. In 1983, ABMS approved a certificate of “added qualification” for ob.gyns. who complete fellowships in critical care. In 1995, ABOG and the American Board of Urology started the subspecialty of female pelvic medicine and reconstructive surgery, which was approved for certification by ABMS in 2011.
ABMS also approved a certificate of “added qualification” for ob.gyns. who complete a fellowship in hospice and palliative medicine in 2008. And fellowships now exist for minimally invasive gynecologic surgery and ob.gyn. hospital medicine.
The reasons that ob.gyns. choose to subspecialize are multifold, said Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill., and one of the medical editors of the Ob.Gyn. News column, Master Class.
“Physicians subspecialize so that they can provide more medical and surgical expertise for a given population,” he said. “Secondly, physicians may be driven to subspecialize for lifestyle reasons. Generalists refer to subspecialists when technical expertise is desired to help with a clinical situation and potentially reduce medical legal risk.”
Ultimately, it’s patients who benefit from the increased care provided by subspecialists, noted Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology, and women’s health at Rutgers, the State University of New Jersey, Newark. Generalist ob.gyns. are tremendously knowledgeable and experienced, he said, but there’s no way for them to know every area, he said. It’s the difference between someone who might be doing a complicated surgery one or twice a year versus someone who is doing that surgery once or twice a week, he added.
“That is ultimately helpful for patients,” Dr. Einstein said. “It’s really about outcomes. This is all better for the patient. That’s the most important thing.”
Not every consequence of subspecialization is positive, however.
“As with everything, subspecialization has both positive and negative effects,” said Dr. Sandra Ann Carson, vice president for education at the American College of Obstetricians and Gynecologists. “The more time one has to focus on a small area, the better that area becomes. However, if all you have is a hammer, everything looks like a nail. The larger population may not need the care that someone with a rare disease may need.”
Dr. Miller refers to this challenge as “losing the forest.” He explains that subspecialists sometimes become so focused on their area of expertise, that they may overlook suitable treatment plans with which they are unfamiliar. An infertility specialist, for example, who neglects to consider a minimally invasive surgical procedure that could allow a patient to become pregnant naturally and instead recommends in vitro fertilization treatment.
“The infertility specialist does not have that particular skill and therefore directs that patient to IVF,” Dr. Miller said. “In the process of subspecializing, we have a tendency to lose the forest and look only at the trees.”
Finding a job is another challenge for the growing number of subspecialists. In many cases, fellowship-trained minimally invasive gynecologic surgeons may have to go back to practicing general gynecology because of a lack of positions, Dr. Miller said.
“We have to be careful that we do not “oversubspecialize” so that we are oversaturating the field,” he said.
In the future, the number of ob.gyn subspecialists will likely continue to grow and become more refined, said Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center in Phoenix.
“I think subspecialists will continue to become more and more developed,” Dr. Chase said. “Perhaps, some areas like family planning or minimally invasive surgery may grow further and become board certified.”
Dr. Carson foresees subspecialization becoming more focused on centralized teaching hospitals, with patients who need special care being sent to these hubs.
“Telemedicine and long-distance communication with a local obstetrician-gynecologist managing the whole patient will allow the best of both worlds,” she said.
Regardless of how subspecialist growth evolves, general ob.gyns. and other primary care physicians will always be needed, said Dr. Mary E. Norton, a maternal-fetal medicine specialist and clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“With increasing complexity, experts are needed to interpret advances,” Dr. Norton said. “However, patients also need a ‘medical home’ and primary provider who sees the big picture, and provides ongoing care beyond a single pregnancy or pregnancy complication.”
Why I chose to subspecialize
“I went to medical school with a particular interest in obstetrics. Once there, I was exposed to pediatrics and to high-risk OB, which I found to be fascinating. I particularly enjoyed my exposure to genetics during my pediatrics rotation and cared for a few children with genetic diseases that had a big impact and made a substantial impression on me. I ultimately decided to pursue an ob.gyn. residency and loved the OB part, particularly the prenatal genetics and high-risk OB. I found the balance of maternal and fetal medicine to be an exciting opportunity to care for two patients. I did an elective in prenatal diagnosis during my third year, including a bit of research, and was hooked.”
Dr. Mary E. Norton, a maternal-fetal medicine specialist and a clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“In my second year of residency, I became really interested in [gynecology-oncology] because I was fascinated by the surgery and interested in the chemotherapy practice, which is interesting because there’s always new research and new agents and interesting changes in how you treat the various cancers. It’s a very comprehensive, research-based field and that was fascinating to me. It’s a very busy subspecialty with very complex cases on multiple levels. You do these radical surgeries but then you have to be really involved in the choice for which chemotherapy agent to use, what type of radiation to give, and you also get really involved with the families ... Every case is so different and you treat women who are 16 years old, but you also treat women who are 96 years old. You see women from all walks of life with all sorts of different issues. The ability to really get involved with cancer research is a great part of the field.”
Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center, Phoenix.
“I took the opportunity to come to a new program where they were looking for an ob.gyn. hospitalist. That was exciting for me because I got to help establish the program... I feel like we’re a better department because I’m here monitoring labor, but I’m also writing protocols and making sure everyone is up to date. And I still get to do what I love the most, which is birth and babies.”
Dr. Brigid McCue, an ob.gyn. hospitalist and chief of ob.gyn. and midwifery, Beth Israel Deaconess Hospital-Plymouth, Massachusetts.
“I never considered delivering babies for the rest of my life. I was always focused on treating infertile couples. I completed my fellowship in reproductive endocrinology-infertility at the University of Pennsylvania, Philadelphia, at a time when in vitro fertilization was in its infancy and the laparoscope and hysteroscope were virtually diagnostic tools ... As IVF became more successful, I felt it was essential to add this expertise to my armamentarium ... It is truly gratifying to be part of a subspecialty that has advanced so far that the majority of our patients are able to achieve pregnancy via IVF.”
Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill.
“During medical school, I was very interested in the surgical aspects of patient care. When I rotated in gyn-oncology – now knowing that I rotated with some of the best gyn-oncologists who ever practiced – I found myself drawn to the complexity of surgery, acuity of the patients, and the close relationships gyn-oncologists have with their patients. It hit me like a brick that this was the specialty for me. During my residency and fellowship, I was particularly drawn to the multiple modalities we use to treat cancers. I relished the idea that through clinical trials, gyn-oncologists keep pushing the bar to solve the cancer problem. What we do now is different than what we did 5 years ago. It keeps us professionally challenged all the time.”
Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology and women’s health at Rutgers, the State University of New Jersey, Newark.
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
On Twitter @legal_med
After 12 years as a private practice ob.gyn., Dr. Brigid McCue was beginning to feel overwhelmed. She loved her work, but keeping up with the kaleidoscope of care components and ever-changing clinical developments was daunting.
“I felt like it was hard to stay really good at all the different aspects of care,” Dr. McCue said. “I was doing fine with obstetrics, and I felt like I was managing my office well, but it’s hard to stay on top of the latest developments, especially in surgical areas. The other thing that was really hard to keep up with was the business aspect of medicine and running a private practice.”
So when an opportunity presented itself, Dr. McCue leaped at the chance to narrow her expertise to obstetrical hospital medicine. She helped establish the ob.gyn. hospitalist program at Beth Israel Deaconess Hospital-Plymouth in Massachusetts, and now serves as chief of ob.gyn. and midwifery for the hospital.
“I love the fact that I now have the time to get really good at [what] I really like, [such as] labor and delivery,” said Dr. McCue, who is president of the Society of OB/GYN Hospitalists. “Since I made this change, I feel like I’m so much more on top of things. I do simulations here on my unit over things like shoulder dystocia. When I was in private practice, I would go to one meeting a year and pray that I never had a shoulder dystocia [case]. Now I really understand the whole process and I take the time to run through that with my midwives and my other nurses and doctors.”
Dr. McCue is one of a growing number of ob.gyns. who have chosen to target their expertise to a single subspecialty or concentrated practice area. Data show subspecialization is on the rise in ob.gyn.
From 1985 to 2015, certificates issued by the American Board of Obstetrics and Gynecology (ABOG) for gynecologic oncology nearly tripled, and certificates issued for reproductive endocrinology and infertility more than doubled, according to data provided by the American Board of Medical Specialties (ABMS). Certificates issued for maternal-fetal medicine rose from 35 in 1985 to 100 in 2015.

Opportunities for ob.gyns. to subspecialize have steadily increased over the last 50 years. The subspecialties of maternal-fetal medicine, gynecologic oncology, and reproductive endocrinology and infertility were first approved for certification by ABOG in 1973. In 1983, ABMS approved a certificate of “added qualification” for ob.gyns. who complete fellowships in critical care. In 1995, ABOG and the American Board of Urology started the subspecialty of female pelvic medicine and reconstructive surgery, which was approved for certification by ABMS in 2011.
ABMS also approved a certificate of “added qualification” for ob.gyns. who complete a fellowship in hospice and palliative medicine in 2008. And fellowships now exist for minimally invasive gynecologic surgery and ob.gyn. hospital medicine.
The reasons that ob.gyns. choose to subspecialize are multifold, said Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill., and one of the medical editors of the Ob.Gyn. News column, Master Class.
“Physicians subspecialize so that they can provide more medical and surgical expertise for a given population,” he said. “Secondly, physicians may be driven to subspecialize for lifestyle reasons. Generalists refer to subspecialists when technical expertise is desired to help with a clinical situation and potentially reduce medical legal risk.”
Ultimately, it’s patients who benefit from the increased care provided by subspecialists, noted Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology, and women’s health at Rutgers, the State University of New Jersey, Newark. Generalist ob.gyns. are tremendously knowledgeable and experienced, he said, but there’s no way for them to know every area, he said. It’s the difference between someone who might be doing a complicated surgery one or twice a year versus someone who is doing that surgery once or twice a week, he added.
“That is ultimately helpful for patients,” Dr. Einstein said. “It’s really about outcomes. This is all better for the patient. That’s the most important thing.”
Not every consequence of subspecialization is positive, however.
“As with everything, subspecialization has both positive and negative effects,” said Dr. Sandra Ann Carson, vice president for education at the American College of Obstetricians and Gynecologists. “The more time one has to focus on a small area, the better that area becomes. However, if all you have is a hammer, everything looks like a nail. The larger population may not need the care that someone with a rare disease may need.”
Dr. Miller refers to this challenge as “losing the forest.” He explains that subspecialists sometimes become so focused on their area of expertise, that they may overlook suitable treatment plans with which they are unfamiliar. An infertility specialist, for example, who neglects to consider a minimally invasive surgical procedure that could allow a patient to become pregnant naturally and instead recommends in vitro fertilization treatment.
“The infertility specialist does not have that particular skill and therefore directs that patient to IVF,” Dr. Miller said. “In the process of subspecializing, we have a tendency to lose the forest and look only at the trees.”
Finding a job is another challenge for the growing number of subspecialists. In many cases, fellowship-trained minimally invasive gynecologic surgeons may have to go back to practicing general gynecology because of a lack of positions, Dr. Miller said.
“We have to be careful that we do not “oversubspecialize” so that we are oversaturating the field,” he said.
In the future, the number of ob.gyn subspecialists will likely continue to grow and become more refined, said Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center in Phoenix.
“I think subspecialists will continue to become more and more developed,” Dr. Chase said. “Perhaps, some areas like family planning or minimally invasive surgery may grow further and become board certified.”
Dr. Carson foresees subspecialization becoming more focused on centralized teaching hospitals, with patients who need special care being sent to these hubs.
“Telemedicine and long-distance communication with a local obstetrician-gynecologist managing the whole patient will allow the best of both worlds,” she said.
Regardless of how subspecialist growth evolves, general ob.gyns. and other primary care physicians will always be needed, said Dr. Mary E. Norton, a maternal-fetal medicine specialist and clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“With increasing complexity, experts are needed to interpret advances,” Dr. Norton said. “However, patients also need a ‘medical home’ and primary provider who sees the big picture, and provides ongoing care beyond a single pregnancy or pregnancy complication.”
Why I chose to subspecialize
“I went to medical school with a particular interest in obstetrics. Once there, I was exposed to pediatrics and to high-risk OB, which I found to be fascinating. I particularly enjoyed my exposure to genetics during my pediatrics rotation and cared for a few children with genetic diseases that had a big impact and made a substantial impression on me. I ultimately decided to pursue an ob.gyn. residency and loved the OB part, particularly the prenatal genetics and high-risk OB. I found the balance of maternal and fetal medicine to be an exciting opportunity to care for two patients. I did an elective in prenatal diagnosis during my third year, including a bit of research, and was hooked.”
Dr. Mary E. Norton, a maternal-fetal medicine specialist and a clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“In my second year of residency, I became really interested in [gynecology-oncology] because I was fascinated by the surgery and interested in the chemotherapy practice, which is interesting because there’s always new research and new agents and interesting changes in how you treat the various cancers. It’s a very comprehensive, research-based field and that was fascinating to me. It’s a very busy subspecialty with very complex cases on multiple levels. You do these radical surgeries but then you have to be really involved in the choice for which chemotherapy agent to use, what type of radiation to give, and you also get really involved with the families ... Every case is so different and you treat women who are 16 years old, but you also treat women who are 96 years old. You see women from all walks of life with all sorts of different issues. The ability to really get involved with cancer research is a great part of the field.”
Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center, Phoenix.
“I took the opportunity to come to a new program where they were looking for an ob.gyn. hospitalist. That was exciting for me because I got to help establish the program... I feel like we’re a better department because I’m here monitoring labor, but I’m also writing protocols and making sure everyone is up to date. And I still get to do what I love the most, which is birth and babies.”
Dr. Brigid McCue, an ob.gyn. hospitalist and chief of ob.gyn. and midwifery, Beth Israel Deaconess Hospital-Plymouth, Massachusetts.
“I never considered delivering babies for the rest of my life. I was always focused on treating infertile couples. I completed my fellowship in reproductive endocrinology-infertility at the University of Pennsylvania, Philadelphia, at a time when in vitro fertilization was in its infancy and the laparoscope and hysteroscope were virtually diagnostic tools ... As IVF became more successful, I felt it was essential to add this expertise to my armamentarium ... It is truly gratifying to be part of a subspecialty that has advanced so far that the majority of our patients are able to achieve pregnancy via IVF.”
Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill.
“During medical school, I was very interested in the surgical aspects of patient care. When I rotated in gyn-oncology – now knowing that I rotated with some of the best gyn-oncologists who ever practiced – I found myself drawn to the complexity of surgery, acuity of the patients, and the close relationships gyn-oncologists have with their patients. It hit me like a brick that this was the specialty for me. During my residency and fellowship, I was particularly drawn to the multiple modalities we use to treat cancers. I relished the idea that through clinical trials, gyn-oncologists keep pushing the bar to solve the cancer problem. What we do now is different than what we did 5 years ago. It keeps us professionally challenged all the time.”
Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology and women’s health at Rutgers, the State University of New Jersey, Newark.
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
On Twitter @legal_med
Method could improve diagnosis of platelet disorders
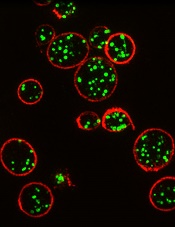
Courtesy of Dan Cutler
A proof-of-concept study suggests structured illumination microscopy (SIM) enables accurate diagnosis of Hermansky-Pudlak syndrome (HPS), an autosomal recessive disorder characterized by platelet dysfunction and prolonged bleeding.
Researchers therefore believe SIM could provide a more accessible and cost-effective method for diagnosing platelet disorders.
They also said SIM provides detailed data that may enable personalized treatments.
The researchers described their results with SIM in the Journal of Thrombosis and Haemostasis.
The team noted that electron microscopy can be used to diagnose HPS and other disorders characterized by platelet dysfunction. But the method is costly, requires fresh samples, gives limited information, and is not widely available.
“We’ve found that SIM has a lot of advantages over whole mount electron microscopy as a diagnosis method,” said study author David Westmoreland, of University College London in the UK.
“Samples don’t need to be analyzed live and can be reanalyzed, and automation means analysis is unbiased and less time-consuming. Given about 75% of patients with a bleeding disorder such as Hermansky-Pudlak syndrome are initially misdiagnosed, and 28% need to see between 4 to 6 specialists before receiving the correct diagnosis, there is a demand for a new method of analysis.”
For this proof-of-concept study, Westmoreland and his colleagues used SIM to image platelet granules in blood samples using a marker protein, CD63.
The imaging technology was custom-built by the team to automatically count the number of granules per platelet, thereby identifying patients with HPS, a rare disorder thought to affect 1 in 500,000 people.
The researchers distinguished the 3 patients with HPS from 7 normal controls with 99% confidence. Automated counting of granules showed that individuals with the disorder had a third as many granules as controls.
“Our limited analysis of this new method is extremely promising, and we hope to take it forward to test for multiple parameters with different markers,” said Dan Cutler, PhD, also of University College London.
“In this way, we could use a single super-resolution image to screen for many different platelet-based blood disorders.” ![]()
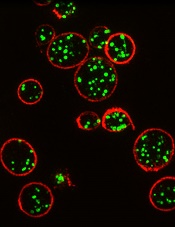
Courtesy of Dan Cutler
A proof-of-concept study suggests structured illumination microscopy (SIM) enables accurate diagnosis of Hermansky-Pudlak syndrome (HPS), an autosomal recessive disorder characterized by platelet dysfunction and prolonged bleeding.
Researchers therefore believe SIM could provide a more accessible and cost-effective method for diagnosing platelet disorders.
They also said SIM provides detailed data that may enable personalized treatments.
The researchers described their results with SIM in the Journal of Thrombosis and Haemostasis.
The team noted that electron microscopy can be used to diagnose HPS and other disorders characterized by platelet dysfunction. But the method is costly, requires fresh samples, gives limited information, and is not widely available.
“We’ve found that SIM has a lot of advantages over whole mount electron microscopy as a diagnosis method,” said study author David Westmoreland, of University College London in the UK.
“Samples don’t need to be analyzed live and can be reanalyzed, and automation means analysis is unbiased and less time-consuming. Given about 75% of patients with a bleeding disorder such as Hermansky-Pudlak syndrome are initially misdiagnosed, and 28% need to see between 4 to 6 specialists before receiving the correct diagnosis, there is a demand for a new method of analysis.”
For this proof-of-concept study, Westmoreland and his colleagues used SIM to image platelet granules in blood samples using a marker protein, CD63.
The imaging technology was custom-built by the team to automatically count the number of granules per platelet, thereby identifying patients with HPS, a rare disorder thought to affect 1 in 500,000 people.
The researchers distinguished the 3 patients with HPS from 7 normal controls with 99% confidence. Automated counting of granules showed that individuals with the disorder had a third as many granules as controls.
“Our limited analysis of this new method is extremely promising, and we hope to take it forward to test for multiple parameters with different markers,” said Dan Cutler, PhD, also of University College London.
“In this way, we could use a single super-resolution image to screen for many different platelet-based blood disorders.” ![]()
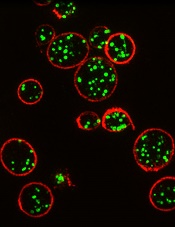
Courtesy of Dan Cutler
A proof-of-concept study suggests structured illumination microscopy (SIM) enables accurate diagnosis of Hermansky-Pudlak syndrome (HPS), an autosomal recessive disorder characterized by platelet dysfunction and prolonged bleeding.
Researchers therefore believe SIM could provide a more accessible and cost-effective method for diagnosing platelet disorders.
They also said SIM provides detailed data that may enable personalized treatments.
The researchers described their results with SIM in the Journal of Thrombosis and Haemostasis.
The team noted that electron microscopy can be used to diagnose HPS and other disorders characterized by platelet dysfunction. But the method is costly, requires fresh samples, gives limited information, and is not widely available.
“We’ve found that SIM has a lot of advantages over whole mount electron microscopy as a diagnosis method,” said study author David Westmoreland, of University College London in the UK.
“Samples don’t need to be analyzed live and can be reanalyzed, and automation means analysis is unbiased and less time-consuming. Given about 75% of patients with a bleeding disorder such as Hermansky-Pudlak syndrome are initially misdiagnosed, and 28% need to see between 4 to 6 specialists before receiving the correct diagnosis, there is a demand for a new method of analysis.”
For this proof-of-concept study, Westmoreland and his colleagues used SIM to image platelet granules in blood samples using a marker protein, CD63.
The imaging technology was custom-built by the team to automatically count the number of granules per platelet, thereby identifying patients with HPS, a rare disorder thought to affect 1 in 500,000 people.
The researchers distinguished the 3 patients with HPS from 7 normal controls with 99% confidence. Automated counting of granules showed that individuals with the disorder had a third as many granules as controls.
“Our limited analysis of this new method is extremely promising, and we hope to take it forward to test for multiple parameters with different markers,” said Dan Cutler, PhD, also of University College London.
“In this way, we could use a single super-resolution image to screen for many different platelet-based blood disorders.” ![]()
Research Shows Inpatient Dermatology Improves Diagnostic Accuracy and Intervention
NEW YORK (Reuters Health) - Inpatient dermatology consultations for skin disorders are associated with improved diagnostic accuracy and faster intervention, researchers have
found.
Information about the impact of hospitalist dermatology consultative services is limited, Dr. Daniela Kroshinsky from Massachusetts General Hospital in Boston and colleagues note in JAMA Dermatology, online January 13.
To learn more, the team conducted a cross-sectional study of data from dermatology consult teams at four academic medical centers in the U.S. Full-time inpatient dermatologists with resident teams performed a total of 1,661 inpatient dermatology consultations within 24 to 48 hours of request over 12 months from 2008 to 2009.
All final diagnoses were based on clinical history, examination findings, and laboratory testing. Each service (primary team) that asked for a dermatology consult provided its presumptive diagnosis at the time of its request.
The most common primary teams were Medicine (47%), followed by Surgery (15%), Intensive Care Units (12%), and Hematology-Oncology (9%). The most commonly undiagnosed or misdiagnosed conditions by the primary teams were cellulitis, leg ulcerations, and viral infections. The majority of primary team preliminary diagnoses included rash/unknown (n=814), followed by cellulitis/abscess (n=115), and drug rash (n=111). The majority of primary diagnoses by dermatologists included drug rash (n=292; 18%), psoriasis/eczema (n=170; 10%), and benign neoplasm (n=168; 10%).
The dermatologists identified additional cutaneous issues in 298 (18%) of consults; diagnosis was confirmed by biopsy in 667 (40%) patients. Overall, dermatology consultation changed the final diagnosis in 71% of consultation requests.
Just under a third of the patients were admitted to the hospitals because of their skin conditions. In the remaining cases, the dermatologic issues were found incidentally or developed during hospitalization.
In 40% of cases, dermatology-specific evaluation and treatment recommendations were carried out in a single visit; 29% required one follow-up evaluation and 16% required two.
"This is the first multicenter national study to define the nature of dermatologic issues presenting to academic medical centers and to demonstrate the impact dermatologists have on improving the correct diagnosis of patients with skin issues,"Dr. Kroshinsky told Reuters Health by email.
Hospitalist dermatology is an important and effective subset of dermatology and hospital medicine, she said.
"Ideally," Dr. Kroshinsky added, "hospitals would have access to a dermatologist in real-time or via teledermatology."
NEW YORK (Reuters Health) - Inpatient dermatology consultations for skin disorders are associated with improved diagnostic accuracy and faster intervention, researchers have
found.
Information about the impact of hospitalist dermatology consultative services is limited, Dr. Daniela Kroshinsky from Massachusetts General Hospital in Boston and colleagues note in JAMA Dermatology, online January 13.
To learn more, the team conducted a cross-sectional study of data from dermatology consult teams at four academic medical centers in the U.S. Full-time inpatient dermatologists with resident teams performed a total of 1,661 inpatient dermatology consultations within 24 to 48 hours of request over 12 months from 2008 to 2009.
All final diagnoses were based on clinical history, examination findings, and laboratory testing. Each service (primary team) that asked for a dermatology consult provided its presumptive diagnosis at the time of its request.
The most common primary teams were Medicine (47%), followed by Surgery (15%), Intensive Care Units (12%), and Hematology-Oncology (9%). The most commonly undiagnosed or misdiagnosed conditions by the primary teams were cellulitis, leg ulcerations, and viral infections. The majority of primary team preliminary diagnoses included rash/unknown (n=814), followed by cellulitis/abscess (n=115), and drug rash (n=111). The majority of primary diagnoses by dermatologists included drug rash (n=292; 18%), psoriasis/eczema (n=170; 10%), and benign neoplasm (n=168; 10%).
The dermatologists identified additional cutaneous issues in 298 (18%) of consults; diagnosis was confirmed by biopsy in 667 (40%) patients. Overall, dermatology consultation changed the final diagnosis in 71% of consultation requests.
Just under a third of the patients were admitted to the hospitals because of their skin conditions. In the remaining cases, the dermatologic issues were found incidentally or developed during hospitalization.
In 40% of cases, dermatology-specific evaluation and treatment recommendations were carried out in a single visit; 29% required one follow-up evaluation and 16% required two.
"This is the first multicenter national study to define the nature of dermatologic issues presenting to academic medical centers and to demonstrate the impact dermatologists have on improving the correct diagnosis of patients with skin issues,"Dr. Kroshinsky told Reuters Health by email.
Hospitalist dermatology is an important and effective subset of dermatology and hospital medicine, she said.
"Ideally," Dr. Kroshinsky added, "hospitals would have access to a dermatologist in real-time or via teledermatology."
NEW YORK (Reuters Health) - Inpatient dermatology consultations for skin disorders are associated with improved diagnostic accuracy and faster intervention, researchers have
found.
Information about the impact of hospitalist dermatology consultative services is limited, Dr. Daniela Kroshinsky from Massachusetts General Hospital in Boston and colleagues note in JAMA Dermatology, online January 13.
To learn more, the team conducted a cross-sectional study of data from dermatology consult teams at four academic medical centers in the U.S. Full-time inpatient dermatologists with resident teams performed a total of 1,661 inpatient dermatology consultations within 24 to 48 hours of request over 12 months from 2008 to 2009.
All final diagnoses were based on clinical history, examination findings, and laboratory testing. Each service (primary team) that asked for a dermatology consult provided its presumptive diagnosis at the time of its request.
The most common primary teams were Medicine (47%), followed by Surgery (15%), Intensive Care Units (12%), and Hematology-Oncology (9%). The most commonly undiagnosed or misdiagnosed conditions by the primary teams were cellulitis, leg ulcerations, and viral infections. The majority of primary team preliminary diagnoses included rash/unknown (n=814), followed by cellulitis/abscess (n=115), and drug rash (n=111). The majority of primary diagnoses by dermatologists included drug rash (n=292; 18%), psoriasis/eczema (n=170; 10%), and benign neoplasm (n=168; 10%).
The dermatologists identified additional cutaneous issues in 298 (18%) of consults; diagnosis was confirmed by biopsy in 667 (40%) patients. Overall, dermatology consultation changed the final diagnosis in 71% of consultation requests.
Just under a third of the patients were admitted to the hospitals because of their skin conditions. In the remaining cases, the dermatologic issues were found incidentally or developed during hospitalization.
In 40% of cases, dermatology-specific evaluation and treatment recommendations were carried out in a single visit; 29% required one follow-up evaluation and 16% required two.
"This is the first multicenter national study to define the nature of dermatologic issues presenting to academic medical centers and to demonstrate the impact dermatologists have on improving the correct diagnosis of patients with skin issues,"Dr. Kroshinsky told Reuters Health by email.
Hospitalist dermatology is an important and effective subset of dermatology and hospital medicine, she said.
"Ideally," Dr. Kroshinsky added, "hospitals would have access to a dermatologist in real-time or via teledermatology."
EBV-CTLs get orphan designation for EBV-PTLD

among uninfected cells (blue)
Image courtesy of
Benjamin Chaigne-Delalande
The US Food and Drug Administration (FDA) has granted orphan designation for cytotoxic T lymphocytes activated against Epstein-Barr virus (EBV-CTLs) to treat EBV post-transplant lymphoproliferative disorder (EBV-PTLD) occurring after solid organ or hematopoietic stem cell transplant.
The FDA grants orphan designation to products intended to treat, diagnose, or prevent disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases, which may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and a 7-year period of marketing exclusivity if the product is approved.
The EBV-CTL product is under development by Atara Biotherapeutics, Inc. It is produced by collecting T cells from third-party donors and exposing the cells to EBV antigens.
The activated T cells are then expanded, characterized, and stored for future use in a partially HLA-matched patient, providing an “off-the-shelf,” allogeneic, cellular therapeutic option for patients.
In the context of EBV-PTLD, Atara’s EBV-CTLs find the cancer cells expressing EBV and kill them. EBV-CTLs are currently being studied in phase 2 trials.
Results of a phase 1/2 study were presented at the APHON 37th Annual Conference and Exhibit and at the 2015 ASCO Annual Meeting.
The FDA previously granted EBV-CTLs breakthrough designation to treat EBV-PTLD. This designation is intended to expedite the development and review of new drugs for serious or life-threatening conditions.
To qualify for breakthrough designation, a drug must show credible evidence of a substantial improvement on a clinically significant endpoint over available therapies, or over placebo if there is no available therapy, or in a study that compares the new treatment plus the standard of care to the standard alone.
The designation confers several benefits, including intensive FDA guidance and eligibility for submission of a rolling biologic license application. ![]()

among uninfected cells (blue)
Image courtesy of
Benjamin Chaigne-Delalande
The US Food and Drug Administration (FDA) has granted orphan designation for cytotoxic T lymphocytes activated against Epstein-Barr virus (EBV-CTLs) to treat EBV post-transplant lymphoproliferative disorder (EBV-PTLD) occurring after solid organ or hematopoietic stem cell transplant.
The FDA grants orphan designation to products intended to treat, diagnose, or prevent disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases, which may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and a 7-year period of marketing exclusivity if the product is approved.
The EBV-CTL product is under development by Atara Biotherapeutics, Inc. It is produced by collecting T cells from third-party donors and exposing the cells to EBV antigens.
The activated T cells are then expanded, characterized, and stored for future use in a partially HLA-matched patient, providing an “off-the-shelf,” allogeneic, cellular therapeutic option for patients.
In the context of EBV-PTLD, Atara’s EBV-CTLs find the cancer cells expressing EBV and kill them. EBV-CTLs are currently being studied in phase 2 trials.
Results of a phase 1/2 study were presented at the APHON 37th Annual Conference and Exhibit and at the 2015 ASCO Annual Meeting.
The FDA previously granted EBV-CTLs breakthrough designation to treat EBV-PTLD. This designation is intended to expedite the development and review of new drugs for serious or life-threatening conditions.
To qualify for breakthrough designation, a drug must show credible evidence of a substantial improvement on a clinically significant endpoint over available therapies, or over placebo if there is no available therapy, or in a study that compares the new treatment plus the standard of care to the standard alone.
The designation confers several benefits, including intensive FDA guidance and eligibility for submission of a rolling biologic license application. ![]()

among uninfected cells (blue)
Image courtesy of
Benjamin Chaigne-Delalande
The US Food and Drug Administration (FDA) has granted orphan designation for cytotoxic T lymphocytes activated against Epstein-Barr virus (EBV-CTLs) to treat EBV post-transplant lymphoproliferative disorder (EBV-PTLD) occurring after solid organ or hematopoietic stem cell transplant.
The FDA grants orphan designation to products intended to treat, diagnose, or prevent disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases, which may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and a 7-year period of marketing exclusivity if the product is approved.
The EBV-CTL product is under development by Atara Biotherapeutics, Inc. It is produced by collecting T cells from third-party donors and exposing the cells to EBV antigens.
The activated T cells are then expanded, characterized, and stored for future use in a partially HLA-matched patient, providing an “off-the-shelf,” allogeneic, cellular therapeutic option for patients.
In the context of EBV-PTLD, Atara’s EBV-CTLs find the cancer cells expressing EBV and kill them. EBV-CTLs are currently being studied in phase 2 trials.
Results of a phase 1/2 study were presented at the APHON 37th Annual Conference and Exhibit and at the 2015 ASCO Annual Meeting.
The FDA previously granted EBV-CTLs breakthrough designation to treat EBV-PTLD. This designation is intended to expedite the development and review of new drugs for serious or life-threatening conditions.
To qualify for breakthrough designation, a drug must show credible evidence of a substantial improvement on a clinically significant endpoint over available therapies, or over placebo if there is no available therapy, or in a study that compares the new treatment plus the standard of care to the standard alone.
The designation confers several benefits, including intensive FDA guidance and eligibility for submission of a rolling biologic license application. ![]()
Gut microbiota linked to severity of malaria

Microorganisms in the gut play a role in the severity of malaria, according to a study published in PNAS.
Investigators examined the gut microbiomes of mice and found evidence to suggest that malaria severity is not only a function of the parasite or the host. It is also influenced by the microbes in the infected organism.
And 2 types of bacteria—Bifidobacterium and Lactobacillus—were associated with reduced malaria severity.
“The research provides a potential new avenue to investigate factors that control the severity of malaria,” said study author Steven Wilhelm, PhD, of the University of Tennessee at Knoxville.
“With 1 million people dying [of malaria] each year, many of whom are young children, any approach that may save even a few lives is worth following up on.”
With this study, Dr Wilhelm and his colleagues found that genetically similar mice acquired from different vendors had differences in pathology after malaria infection. There were significant differences in both parasite burden and mortality after infection with multiple Plasmodium species.
The investigators measured gut microbiomes in the mice by sequencing bacteria in the digestive tract and noted significant differences within the different mouse populations.
So the team transferred cecal content from the first set of mice into germ-free mice and found that differences in malaria severity were transferred.
The mice that received transplants from donors that were more resistant to malaria had low parasite burdens. And mice that received transplants from donors that were more susceptible to malaria had high parasite burdens.
The investigators also observed an increased abundance of Bifidobacterium and Lactobacillus bacteria in the mice that exhibited reduced malaria pathology.
So the team took mice that were more susceptible to malaria, treated them with antibiotics, and fed them yogurt containing Bifidobacterium and Lactobacillus. As expected, the severity of malaria in these mice decreased.
“These results demonstrate the possibility of modifying the gut microbiome to prevent severe malaria,” said study author Nathan Schmidt, PhD, of the University of Louisville in Kentucky.
Dr Wilhelm noted that, although the research interventions lessened the severity of malaria in mice, it did not prevent or cure it. And the investigators are a long way from perfecting similar treatments in humans but are working on understanding the mechanism.
“A way to help people who are infected—and especially a simple and cheap way, as much of the infection occurs in the developing world—would be a great service to society,” Dr Wilhelm said. ![]()

Microorganisms in the gut play a role in the severity of malaria, according to a study published in PNAS.
Investigators examined the gut microbiomes of mice and found evidence to suggest that malaria severity is not only a function of the parasite or the host. It is also influenced by the microbes in the infected organism.
And 2 types of bacteria—Bifidobacterium and Lactobacillus—were associated with reduced malaria severity.
“The research provides a potential new avenue to investigate factors that control the severity of malaria,” said study author Steven Wilhelm, PhD, of the University of Tennessee at Knoxville.
“With 1 million people dying [of malaria] each year, many of whom are young children, any approach that may save even a few lives is worth following up on.”
With this study, Dr Wilhelm and his colleagues found that genetically similar mice acquired from different vendors had differences in pathology after malaria infection. There were significant differences in both parasite burden and mortality after infection with multiple Plasmodium species.
The investigators measured gut microbiomes in the mice by sequencing bacteria in the digestive tract and noted significant differences within the different mouse populations.
So the team transferred cecal content from the first set of mice into germ-free mice and found that differences in malaria severity were transferred.
The mice that received transplants from donors that were more resistant to malaria had low parasite burdens. And mice that received transplants from donors that were more susceptible to malaria had high parasite burdens.
The investigators also observed an increased abundance of Bifidobacterium and Lactobacillus bacteria in the mice that exhibited reduced malaria pathology.
So the team took mice that were more susceptible to malaria, treated them with antibiotics, and fed them yogurt containing Bifidobacterium and Lactobacillus. As expected, the severity of malaria in these mice decreased.
“These results demonstrate the possibility of modifying the gut microbiome to prevent severe malaria,” said study author Nathan Schmidt, PhD, of the University of Louisville in Kentucky.
Dr Wilhelm noted that, although the research interventions lessened the severity of malaria in mice, it did not prevent or cure it. And the investigators are a long way from perfecting similar treatments in humans but are working on understanding the mechanism.
“A way to help people who are infected—and especially a simple and cheap way, as much of the infection occurs in the developing world—would be a great service to society,” Dr Wilhelm said. ![]()

Microorganisms in the gut play a role in the severity of malaria, according to a study published in PNAS.
Investigators examined the gut microbiomes of mice and found evidence to suggest that malaria severity is not only a function of the parasite or the host. It is also influenced by the microbes in the infected organism.
And 2 types of bacteria—Bifidobacterium and Lactobacillus—were associated with reduced malaria severity.
“The research provides a potential new avenue to investigate factors that control the severity of malaria,” said study author Steven Wilhelm, PhD, of the University of Tennessee at Knoxville.
“With 1 million people dying [of malaria] each year, many of whom are young children, any approach that may save even a few lives is worth following up on.”
With this study, Dr Wilhelm and his colleagues found that genetically similar mice acquired from different vendors had differences in pathology after malaria infection. There were significant differences in both parasite burden and mortality after infection with multiple Plasmodium species.
The investigators measured gut microbiomes in the mice by sequencing bacteria in the digestive tract and noted significant differences within the different mouse populations.
So the team transferred cecal content from the first set of mice into germ-free mice and found that differences in malaria severity were transferred.
The mice that received transplants from donors that were more resistant to malaria had low parasite burdens. And mice that received transplants from donors that were more susceptible to malaria had high parasite burdens.
The investigators also observed an increased abundance of Bifidobacterium and Lactobacillus bacteria in the mice that exhibited reduced malaria pathology.
So the team took mice that were more susceptible to malaria, treated them with antibiotics, and fed them yogurt containing Bifidobacterium and Lactobacillus. As expected, the severity of malaria in these mice decreased.
“These results demonstrate the possibility of modifying the gut microbiome to prevent severe malaria,” said study author Nathan Schmidt, PhD, of the University of Louisville in Kentucky.
Dr Wilhelm noted that, although the research interventions lessened the severity of malaria in mice, it did not prevent or cure it. And the investigators are a long way from perfecting similar treatments in humans but are working on understanding the mechanism.
“A way to help people who are infected—and especially a simple and cheap way, as much of the infection occurs in the developing world—would be a great service to society,” Dr Wilhelm said. ![]()