User login
Fibromyalgia found in 20% with spondyloarthritis; could affect management decisions
The presence of fibromyalgia in patients who are undergoing treatment of spondyloarthritis (SpA) is associated with higher measures of disease activity and shorter duration of first-time treatment with tumor necrosis factor inhibitors, according to results of a study measuring the impact and prevalence of fibromyalgia coexisting with SpA.
The results confirm “that the existence of concomitant FM [fibromyalgia] in SpA might complicate the evaluation of treatment response and [suggest] that coexistence of FM should be carefully screened when initiating a TNFi [tumor necrosis factor inhibitor] and/or evaluating its treatment effect, especially in the presence of peripheral and/or enthesitic symptoms and in the presence of very severe disease activity and patient-reported scores,” wrote Dr. Natalia Bello and her colleagues at Cochin Hospital, Paris (Arthritis Res Ther. 2016 Feb 9;18:42. doi: 10.1186/s13075-016-0943-z).
They recruited patients from Cochin Hospital, a tertiary care facility, and its rheumatology department’s outpatient clinic. Rather than use the 1990 American College of Rheumatology (ACR) classification criteria of FM or the 2010 ACR or modified 2010 ACR diagnostic criteria, which were developed for research and classification purposes, the investigators diagnosed FM based on a score of 5 or 6 on the six-question, self-reported Fibromyalgia Rapid Screening Tool (FiRST), which has 90.5% sensitivity and 85.7% specificity for FM. Patients’ SpA diagnoses were made by their rheumatologists. Overall, 30% of the cohort was female and had a mean age of 43 years.
The overall FM prevalence in the cohort was 21.4% (42 of 196 patients) and did not differ significantly according to whether the patients met either the clinical or imaging ASAS (Assessment of Spondyloarthritis International Society) criteria (21.3% vs. 18.8%, respectively) or whether they did or did not fulfill the ASAS criteria (21.1% vs. 30.0%, respectively).
Previous studies have shown the prevalence of FM at 12.6%-15.0% in SpA patients. Classifying axial SpA based on the clinical arm criteria alone has been controversial, the investigators said, mainly because it does not require an objective sign of inflammation (abnormal C-reactive protein or presence of inflammatory lesions seen on MRI of the sacroiliac joint) or structural damage in the sacroiliac joint seen on pelvic radiographs. But at least in this study there was no difference in FM prevalence in regard to whether patients met either the imaging and clinical arms of the ASAS classification criteria for axial SpA or both.
The study, according to the best knowledge of the investigators, is the first “to evaluate the prevalence of FM in a population of patients with SpA with regard to the fulfillment of the ASAS classification criteria.”
FM patients had as expected a significantly higher rate of either history of depression, or use of psychotropic drugs or strong opioids, compared with patients without FM (67% vs. 35%; P less than .01). Rates of exposure to treatment with different drug types (nonsteroidal anti-inflammatory drugs or conventional antirheumatic disease-modifying drugs) did not differ between those with and without FM, but FM patients switched significantly more often from their first TNFi (15.2% vs. 4.0%) and used it for a significantly shorter mean duration (1.7 vs. 3.5 years). The percentage of patients still taking their first TNFi after 2 years also was significantly lower among FM patients (28.1% vs. 41.7%).
Within the entire cohort, FM patients more often had enthesitis (59.5% vs. 39.0%, P = .01), a higher total Bath Ankylosing Spondylitis Disease Activity Index (4.7 vs. 2.6; P less than .01), higher global visual analog scale (5.9 vs. 3.0; P less than .01), and higher Bath Ankylosing Spondylitis Functional Index (4.8 vs. 2.0; P less than .01).
The authors suggested that FM patients’ higher rates of peripheral symptoms and enthesitis may warrant the use of the FiRST questionnaire in clinical practice before starting a TNFi in SpA patients to detect potentially coexisting FM.
The authors had no conflicts of interest to declare.
The presence of fibromyalgia in patients who are undergoing treatment of spondyloarthritis (SpA) is associated with higher measures of disease activity and shorter duration of first-time treatment with tumor necrosis factor inhibitors, according to results of a study measuring the impact and prevalence of fibromyalgia coexisting with SpA.
The results confirm “that the existence of concomitant FM [fibromyalgia] in SpA might complicate the evaluation of treatment response and [suggest] that coexistence of FM should be carefully screened when initiating a TNFi [tumor necrosis factor inhibitor] and/or evaluating its treatment effect, especially in the presence of peripheral and/or enthesitic symptoms and in the presence of very severe disease activity and patient-reported scores,” wrote Dr. Natalia Bello and her colleagues at Cochin Hospital, Paris (Arthritis Res Ther. 2016 Feb 9;18:42. doi: 10.1186/s13075-016-0943-z).
They recruited patients from Cochin Hospital, a tertiary care facility, and its rheumatology department’s outpatient clinic. Rather than use the 1990 American College of Rheumatology (ACR) classification criteria of FM or the 2010 ACR or modified 2010 ACR diagnostic criteria, which were developed for research and classification purposes, the investigators diagnosed FM based on a score of 5 or 6 on the six-question, self-reported Fibromyalgia Rapid Screening Tool (FiRST), which has 90.5% sensitivity and 85.7% specificity for FM. Patients’ SpA diagnoses were made by their rheumatologists. Overall, 30% of the cohort was female and had a mean age of 43 years.
The overall FM prevalence in the cohort was 21.4% (42 of 196 patients) and did not differ significantly according to whether the patients met either the clinical or imaging ASAS (Assessment of Spondyloarthritis International Society) criteria (21.3% vs. 18.8%, respectively) or whether they did or did not fulfill the ASAS criteria (21.1% vs. 30.0%, respectively).
Previous studies have shown the prevalence of FM at 12.6%-15.0% in SpA patients. Classifying axial SpA based on the clinical arm criteria alone has been controversial, the investigators said, mainly because it does not require an objective sign of inflammation (abnormal C-reactive protein or presence of inflammatory lesions seen on MRI of the sacroiliac joint) or structural damage in the sacroiliac joint seen on pelvic radiographs. But at least in this study there was no difference in FM prevalence in regard to whether patients met either the imaging and clinical arms of the ASAS classification criteria for axial SpA or both.
The study, according to the best knowledge of the investigators, is the first “to evaluate the prevalence of FM in a population of patients with SpA with regard to the fulfillment of the ASAS classification criteria.”
FM patients had as expected a significantly higher rate of either history of depression, or use of psychotropic drugs or strong opioids, compared with patients without FM (67% vs. 35%; P less than .01). Rates of exposure to treatment with different drug types (nonsteroidal anti-inflammatory drugs or conventional antirheumatic disease-modifying drugs) did not differ between those with and without FM, but FM patients switched significantly more often from their first TNFi (15.2% vs. 4.0%) and used it for a significantly shorter mean duration (1.7 vs. 3.5 years). The percentage of patients still taking their first TNFi after 2 years also was significantly lower among FM patients (28.1% vs. 41.7%).
Within the entire cohort, FM patients more often had enthesitis (59.5% vs. 39.0%, P = .01), a higher total Bath Ankylosing Spondylitis Disease Activity Index (4.7 vs. 2.6; P less than .01), higher global visual analog scale (5.9 vs. 3.0; P less than .01), and higher Bath Ankylosing Spondylitis Functional Index (4.8 vs. 2.0; P less than .01).
The authors suggested that FM patients’ higher rates of peripheral symptoms and enthesitis may warrant the use of the FiRST questionnaire in clinical practice before starting a TNFi in SpA patients to detect potentially coexisting FM.
The authors had no conflicts of interest to declare.
The presence of fibromyalgia in patients who are undergoing treatment of spondyloarthritis (SpA) is associated with higher measures of disease activity and shorter duration of first-time treatment with tumor necrosis factor inhibitors, according to results of a study measuring the impact and prevalence of fibromyalgia coexisting with SpA.
The results confirm “that the existence of concomitant FM [fibromyalgia] in SpA might complicate the evaluation of treatment response and [suggest] that coexistence of FM should be carefully screened when initiating a TNFi [tumor necrosis factor inhibitor] and/or evaluating its treatment effect, especially in the presence of peripheral and/or enthesitic symptoms and in the presence of very severe disease activity and patient-reported scores,” wrote Dr. Natalia Bello and her colleagues at Cochin Hospital, Paris (Arthritis Res Ther. 2016 Feb 9;18:42. doi: 10.1186/s13075-016-0943-z).
They recruited patients from Cochin Hospital, a tertiary care facility, and its rheumatology department’s outpatient clinic. Rather than use the 1990 American College of Rheumatology (ACR) classification criteria of FM or the 2010 ACR or modified 2010 ACR diagnostic criteria, which were developed for research and classification purposes, the investigators diagnosed FM based on a score of 5 or 6 on the six-question, self-reported Fibromyalgia Rapid Screening Tool (FiRST), which has 90.5% sensitivity and 85.7% specificity for FM. Patients’ SpA diagnoses were made by their rheumatologists. Overall, 30% of the cohort was female and had a mean age of 43 years.
The overall FM prevalence in the cohort was 21.4% (42 of 196 patients) and did not differ significantly according to whether the patients met either the clinical or imaging ASAS (Assessment of Spondyloarthritis International Society) criteria (21.3% vs. 18.8%, respectively) or whether they did or did not fulfill the ASAS criteria (21.1% vs. 30.0%, respectively).
Previous studies have shown the prevalence of FM at 12.6%-15.0% in SpA patients. Classifying axial SpA based on the clinical arm criteria alone has been controversial, the investigators said, mainly because it does not require an objective sign of inflammation (abnormal C-reactive protein or presence of inflammatory lesions seen on MRI of the sacroiliac joint) or structural damage in the sacroiliac joint seen on pelvic radiographs. But at least in this study there was no difference in FM prevalence in regard to whether patients met either the imaging and clinical arms of the ASAS classification criteria for axial SpA or both.
The study, according to the best knowledge of the investigators, is the first “to evaluate the prevalence of FM in a population of patients with SpA with regard to the fulfillment of the ASAS classification criteria.”
FM patients had as expected a significantly higher rate of either history of depression, or use of psychotropic drugs or strong opioids, compared with patients without FM (67% vs. 35%; P less than .01). Rates of exposure to treatment with different drug types (nonsteroidal anti-inflammatory drugs or conventional antirheumatic disease-modifying drugs) did not differ between those with and without FM, but FM patients switched significantly more often from their first TNFi (15.2% vs. 4.0%) and used it for a significantly shorter mean duration (1.7 vs. 3.5 years). The percentage of patients still taking their first TNFi after 2 years also was significantly lower among FM patients (28.1% vs. 41.7%).
Within the entire cohort, FM patients more often had enthesitis (59.5% vs. 39.0%, P = .01), a higher total Bath Ankylosing Spondylitis Disease Activity Index (4.7 vs. 2.6; P less than .01), higher global visual analog scale (5.9 vs. 3.0; P less than .01), and higher Bath Ankylosing Spondylitis Functional Index (4.8 vs. 2.0; P less than .01).
The authors suggested that FM patients’ higher rates of peripheral symptoms and enthesitis may warrant the use of the FiRST questionnaire in clinical practice before starting a TNFi in SpA patients to detect potentially coexisting FM.
The authors had no conflicts of interest to declare.
FROM ARTHRITIS RESEARCH & THERAPY
Key clinical point: Coexistence of fibromyalgia in patients diagnosed with spondyloarthritis might be slightly more frequent than previously reported and does not differ according to whether SpA was classified based on imaging or clinical criteria.
Major finding: The overall FM prevalence in the cohort was 21.4% (42 of 196 patients) and did not differ significantly according to whether the patients met either the clinical or imaging ASAS criteria (21.3% vs. 18.8%, respectively).
Data source: A cohort study of 196 patients diagnosed with spondyloarthritis.
Disclosures: The authors had no conflicts of interest to declare.
Gretchen Tietjen, MD
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dronabinol: A Controversial Acute Leukemia Treatment
Researchers from University Hospital Tübingen, Germany, say that although the data for treating acute leukemia with dronabinol (THC), a cannabinoid derivative, are “controversial,” it has been shown to have antitumor potential for several cancers. When the researchers tested THC in several leukemia cell lines and native leukemia blasts cultured ex vivo, they found “meaningful” antiproliferative and proapoptotic effects.
Related: Lawmakers Urge VA to Reform Medical Marijuana Rules
From the data, they also found cannabinoid receptor agonists may be useful as low-toxic agents, especially for patients who are “heavily pretreated,” elderly, or have refractory disease. Evidence was cited that THC retained antileukemic activity in a sample from a patient with otherwise chemotherapy- and steroid-refractory acute lymphocytic leukemia (ALL).
Related: Veterans’ Use of Designer Cathinones and Cannabinoids
Due to the excellent safety profile of THC, the researchers say, effective doses are achievable in vivo, although tolerable doses may vary widely. They suggest starting with a subeffective dose and increasing gradually, which will help the patient build tolerance to the well-known psychoactive effects, which have been a drawback to widespread use of THC for patients with cancer.
They add that, due to sparse densities of cannabinoid receptors in lower brain stem areas, severe intoxications with THC rarely have been reported.
Related: Surgeon General Murthy Discusses Marijuana Efficacy
In addition to the direct antileukemic effects, the researchers suggest that therapeutic use of THC has many desirable adverse effects, such as general physical well-being, cachexia control, and relief of pain, anxiety and stress—which, they note, should “facilitate the decision process.”
Source:
Kampa-Schittenhelm KM, Salitzky O, Akmut F, et al. BMC Cancer. 2016;16(25)1-12.
doi: 10.1186/s12885-015-2029.
Researchers from University Hospital Tübingen, Germany, say that although the data for treating acute leukemia with dronabinol (THC), a cannabinoid derivative, are “controversial,” it has been shown to have antitumor potential for several cancers. When the researchers tested THC in several leukemia cell lines and native leukemia blasts cultured ex vivo, they found “meaningful” antiproliferative and proapoptotic effects.
Related: Lawmakers Urge VA to Reform Medical Marijuana Rules
From the data, they also found cannabinoid receptor agonists may be useful as low-toxic agents, especially for patients who are “heavily pretreated,” elderly, or have refractory disease. Evidence was cited that THC retained antileukemic activity in a sample from a patient with otherwise chemotherapy- and steroid-refractory acute lymphocytic leukemia (ALL).
Related: Veterans’ Use of Designer Cathinones and Cannabinoids
Due to the excellent safety profile of THC, the researchers say, effective doses are achievable in vivo, although tolerable doses may vary widely. They suggest starting with a subeffective dose and increasing gradually, which will help the patient build tolerance to the well-known psychoactive effects, which have been a drawback to widespread use of THC for patients with cancer.
They add that, due to sparse densities of cannabinoid receptors in lower brain stem areas, severe intoxications with THC rarely have been reported.
Related: Surgeon General Murthy Discusses Marijuana Efficacy
In addition to the direct antileukemic effects, the researchers suggest that therapeutic use of THC has many desirable adverse effects, such as general physical well-being, cachexia control, and relief of pain, anxiety and stress—which, they note, should “facilitate the decision process.”
Source:
Kampa-Schittenhelm KM, Salitzky O, Akmut F, et al. BMC Cancer. 2016;16(25)1-12.
doi: 10.1186/s12885-015-2029.
Researchers from University Hospital Tübingen, Germany, say that although the data for treating acute leukemia with dronabinol (THC), a cannabinoid derivative, are “controversial,” it has been shown to have antitumor potential for several cancers. When the researchers tested THC in several leukemia cell lines and native leukemia blasts cultured ex vivo, they found “meaningful” antiproliferative and proapoptotic effects.
Related: Lawmakers Urge VA to Reform Medical Marijuana Rules
From the data, they also found cannabinoid receptor agonists may be useful as low-toxic agents, especially for patients who are “heavily pretreated,” elderly, or have refractory disease. Evidence was cited that THC retained antileukemic activity in a sample from a patient with otherwise chemotherapy- and steroid-refractory acute lymphocytic leukemia (ALL).
Related: Veterans’ Use of Designer Cathinones and Cannabinoids
Due to the excellent safety profile of THC, the researchers say, effective doses are achievable in vivo, although tolerable doses may vary widely. They suggest starting with a subeffective dose and increasing gradually, which will help the patient build tolerance to the well-known psychoactive effects, which have been a drawback to widespread use of THC for patients with cancer.
They add that, due to sparse densities of cannabinoid receptors in lower brain stem areas, severe intoxications with THC rarely have been reported.
Related: Surgeon General Murthy Discusses Marijuana Efficacy
In addition to the direct antileukemic effects, the researchers suggest that therapeutic use of THC has many desirable adverse effects, such as general physical well-being, cachexia control, and relief of pain, anxiety and stress—which, they note, should “facilitate the decision process.”
Source:
Kampa-Schittenhelm KM, Salitzky O, Akmut F, et al. BMC Cancer. 2016;16(25)1-12.
doi: 10.1186/s12885-015-2029.
Bert Vargas, MD
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Early elective colon resection common in diverticulitis
A significant number of elective colon resections for uncomplicated diverticulitis are done in individuals who have experienced fewer than three episodes.
Researchers analyzed nationwide data from 87,461 immunocompetent patients with at least one claim for diverticulitis, of whom 5,604 (6.4%) underwent a resection.
According to a paper published online Feb. 10 in JAMA Surgery, 94.9% of resections, in a final cohort of 3,054 patients, occurred in individuals with fewer than three episodes of diverticulitis, if only inpatient claims were counted (doi:10.1001/jamasurg.2015.5478).
If both inpatient and outpatient claims for diverticulitis were counted, 80.5% of patients who underwent resection had experienced fewer than three episodes, and if all types of claims (including antibiotic prescription claims for diverticulitis) were counted, that figure dropped to 56.3%.
Individuals who underwent early resection were slightly more likely to be male (risk ratio [RR], 1.07; 95% confidence interval [CI], 1.02-1.13; P = .004) but were of a similar age to those who underwent resection after three or more episodes of diverticulitis.
The mean time between the last two episodes of diverticulitis was longer in individuals who underwent early surgery compared to those who delayed surgery (157 days vs. 96 days; P less than .001).
Patients residing in the South were also significantly more likely to undergo early surgery than were those residing in an other regions, with 60.5% of policy holders there undergoing early surgery compared to 50.7% in the West.
Insurance status also influenced the likelihood of early surgery, as patients with HMO or capitated insurance plans were less likely to undergo early surgery than were patients with other plan types.
In the last decade, professional guidelines have moved toward recommending elective surgery for diverticulitis after three or more episodes, but at the same time, the incidence of elective resection has more than doubled, reported Dr. Vlad V. Simianu of the University of Washington, Seattle, and coauthors.
This study covered a period of data in which guidelines on elective resection have remained in a relatively steady state, offering an opportunity to assess guideline adherence.
“Within this context, the suspected drivers of early elective surgery (younger age, laparoscopy, more frequent episodes, and personal financial risk) were not found to be associated with earlier operations for diverticulitis,” the authors wrote.
The analysis found laparoscopy was not associated with early surgery, which the authors said challenged the hypothesis that the threshold for early surgical resection might be lowered by the availability of laparoscopy.
The lack of an age difference between those undergoing early resection also challenged the notion that younger patients may experience more severe diverticulitis and suffer a greater impact on their quality of life and that this may drive physicians to operate earlier.
The authors noted that patient factors such as quality of life and anxiety about future episodes of diverticulitis, and surgeon-related factors such as training, local practice, and referral patterns were not tested, and that these may account for some of decisions about early surgery.
The National Institute of Diabetes and Digestive and Kidney Diseases and the University of Washington supported the study. No conflicts of interest were declared.
A significant number of elective colon resections for uncomplicated diverticulitis are done in individuals who have experienced fewer than three episodes.
Researchers analyzed nationwide data from 87,461 immunocompetent patients with at least one claim for diverticulitis, of whom 5,604 (6.4%) underwent a resection.
According to a paper published online Feb. 10 in JAMA Surgery, 94.9% of resections, in a final cohort of 3,054 patients, occurred in individuals with fewer than three episodes of diverticulitis, if only inpatient claims were counted (doi:10.1001/jamasurg.2015.5478).
If both inpatient and outpatient claims for diverticulitis were counted, 80.5% of patients who underwent resection had experienced fewer than three episodes, and if all types of claims (including antibiotic prescription claims for diverticulitis) were counted, that figure dropped to 56.3%.
Individuals who underwent early resection were slightly more likely to be male (risk ratio [RR], 1.07; 95% confidence interval [CI], 1.02-1.13; P = .004) but were of a similar age to those who underwent resection after three or more episodes of diverticulitis.
The mean time between the last two episodes of diverticulitis was longer in individuals who underwent early surgery compared to those who delayed surgery (157 days vs. 96 days; P less than .001).
Patients residing in the South were also significantly more likely to undergo early surgery than were those residing in an other regions, with 60.5% of policy holders there undergoing early surgery compared to 50.7% in the West.
Insurance status also influenced the likelihood of early surgery, as patients with HMO or capitated insurance plans were less likely to undergo early surgery than were patients with other plan types.
In the last decade, professional guidelines have moved toward recommending elective surgery for diverticulitis after three or more episodes, but at the same time, the incidence of elective resection has more than doubled, reported Dr. Vlad V. Simianu of the University of Washington, Seattle, and coauthors.
This study covered a period of data in which guidelines on elective resection have remained in a relatively steady state, offering an opportunity to assess guideline adherence.
“Within this context, the suspected drivers of early elective surgery (younger age, laparoscopy, more frequent episodes, and personal financial risk) were not found to be associated with earlier operations for diverticulitis,” the authors wrote.
The analysis found laparoscopy was not associated with early surgery, which the authors said challenged the hypothesis that the threshold for early surgical resection might be lowered by the availability of laparoscopy.
The lack of an age difference between those undergoing early resection also challenged the notion that younger patients may experience more severe diverticulitis and suffer a greater impact on their quality of life and that this may drive physicians to operate earlier.
The authors noted that patient factors such as quality of life and anxiety about future episodes of diverticulitis, and surgeon-related factors such as training, local practice, and referral patterns were not tested, and that these may account for some of decisions about early surgery.
The National Institute of Diabetes and Digestive and Kidney Diseases and the University of Washington supported the study. No conflicts of interest were declared.
A significant number of elective colon resections for uncomplicated diverticulitis are done in individuals who have experienced fewer than three episodes.
Researchers analyzed nationwide data from 87,461 immunocompetent patients with at least one claim for diverticulitis, of whom 5,604 (6.4%) underwent a resection.
According to a paper published online Feb. 10 in JAMA Surgery, 94.9% of resections, in a final cohort of 3,054 patients, occurred in individuals with fewer than three episodes of diverticulitis, if only inpatient claims were counted (doi:10.1001/jamasurg.2015.5478).
If both inpatient and outpatient claims for diverticulitis were counted, 80.5% of patients who underwent resection had experienced fewer than three episodes, and if all types of claims (including antibiotic prescription claims for diverticulitis) were counted, that figure dropped to 56.3%.
Individuals who underwent early resection were slightly more likely to be male (risk ratio [RR], 1.07; 95% confidence interval [CI], 1.02-1.13; P = .004) but were of a similar age to those who underwent resection after three or more episodes of diverticulitis.
The mean time between the last two episodes of diverticulitis was longer in individuals who underwent early surgery compared to those who delayed surgery (157 days vs. 96 days; P less than .001).
Patients residing in the South were also significantly more likely to undergo early surgery than were those residing in an other regions, with 60.5% of policy holders there undergoing early surgery compared to 50.7% in the West.
Insurance status also influenced the likelihood of early surgery, as patients with HMO or capitated insurance plans were less likely to undergo early surgery than were patients with other plan types.
In the last decade, professional guidelines have moved toward recommending elective surgery for diverticulitis after three or more episodes, but at the same time, the incidence of elective resection has more than doubled, reported Dr. Vlad V. Simianu of the University of Washington, Seattle, and coauthors.
This study covered a period of data in which guidelines on elective resection have remained in a relatively steady state, offering an opportunity to assess guideline adherence.
“Within this context, the suspected drivers of early elective surgery (younger age, laparoscopy, more frequent episodes, and personal financial risk) were not found to be associated with earlier operations for diverticulitis,” the authors wrote.
The analysis found laparoscopy was not associated with early surgery, which the authors said challenged the hypothesis that the threshold for early surgical resection might be lowered by the availability of laparoscopy.
The lack of an age difference between those undergoing early resection also challenged the notion that younger patients may experience more severe diverticulitis and suffer a greater impact on their quality of life and that this may drive physicians to operate earlier.
The authors noted that patient factors such as quality of life and anxiety about future episodes of diverticulitis, and surgeon-related factors such as training, local practice, and referral patterns were not tested, and that these may account for some of decisions about early surgery.
The National Institute of Diabetes and Digestive and Kidney Diseases and the University of Washington supported the study. No conflicts of interest were declared.
FROM JAMA SURGERY
Key clinical point: A majority of elective colon resections for uncomplicated diverticulitis are done in individuals who have experienced fewer than three episodes.
Major finding: More than 90% of elective resections occur in patients who have experienced fewer than three inpatient-managed episodes of diverticulitis.
Data source: Retrospective cohort study of 87,461 patients who underwent surgical resection.
Disclosures: The National Institute of Diabetes and Digestive and Kidney Diseases and the University of Washington supported the study. No conflicts of interest were declared.
Aortic aneurysms pose unique challenges in transplant recipients
CHICAGO – Surgeons can expect to see more abdominal organ transplant recipients presenting with aortic aneurysms, as transplant survival rates increase along with the age of organ donors and recipients.
“The consensus is that abdominal aortic aneurysms (AAAs) have a more aggressive course post-transplant and within that context, probably need to be managed more aggressively,” Dr. Michael J. Englesbe of the University of Michigan, Ann Arbor said at the annual Northwestern Vascular Symposium.
Some 270,000 Americans are living with a functioning liver or kidney graft, and their average age has risen from 47 years to 57 years over the last decade.
Though the data isn’t great, it’s hypothesized that the immunosuppression prerequisite for successful organ transplantation promotes the progression of atherosclerosis and aneurysm growth in transplant patients, he said.
New-onset diabetes, hyperlipidemia, and hypertension are all common post-transplant due to immunosuppression therapy. Aortic aneurysms are also reported to rupture at smaller sizes in transplant recipients.
Intriguingly, the opposite effect has been observed in experimental animal models, where immunosuppression with calcineurin inhibitors and mammalian target of rapamycin (mTOR) inhibitors has been shown to stabilize atherosclerotic lesions and inhibit aneurysm expansion.
The reason for this disparity is unclear, but immunosuppressants likely augment other cardiovascular comorbidities such as hypertension and atherosclerosis and this may trump their anti-inflammatory effects and lead to worse aneurysm disease and faster expansion in humans, Dr. Englesbe speculated in an interview.
As for when aneurysms should be fixed, kidney transplant candidates should undergo AAA repair prior to transplantation since the risk of renal complications after aneurysm repair puts the allograft at risk, Dr. Englesbe advised. Either an open or endovascular approach can be used.
In liver transplant candidates, elective AAA repair should be avoided if possible and is contraindicated if any signs of hepatic decompensation are present such as muscle wasting, ascites, platelet count less than 50 x 109/L, or encephalopathy. For well-compensated cirrhotic patients, endovascular repair is best.
One of the most important considerations for any solid-organ transplant patient undergoing aneurysm repair is perioperative management of immunosuppression, Dr. Englesbe stressed.
Transplant patients are maintained on oral calcineurin inhibitors such as cyclosporine and tacrolimus (Prograf) throughout the perioperative period to prevent organ rejection, but these drugs have nephrotoxic effects. About 10% of recipients, typically the sicker patients, will be switched to mTOR inhibitors such as everolimus (Afinitor) and sirolumus (Rapamune) as a kidney-sparing alternative.
“Part of the mechanism of these [mTOR] drugs is that they really affect fibroblast functioning, so patients that are on these medications, their wound will fall apart and they will invariably get a hernia,” Dr. Englesbe said. “You have to stop them upwards of about 6 weeks before surgical intervention, and I think this is also true for many endografts.”
He highlighted a case in which an mTOR inhibitor was started three months after liver transplant due to renal dysfunction in a patient who was fully healed, but within three weeks, “her wound fell apart, completely fell apart.” She developed several seromas underneath her incision, one of which became infected and took months to close.
“The transplant professionals – your nephrologists, your cardiologists – aren’t going to know this fact, but as a transplant surgeon it’s usually the first question we’re going to ask with respect to any post-transplant patient we’re going to operate on, so it’s something to keep in mind,” Dr. Englesbe said.
Another take-home message was the importance of maintaining kidney function in kidney recipients presenting with aortic aneurysm, as mortality in these patients is about 10-fold higher once the kidney fails, he said. A recent study reported that AAAs are significantly more common in kidney than liver transplant recipients (29.6% vs. 11.4%; P = .02), despite a similar prevalence for any aneurysm (4%) in both groups (J Vasc Surg. 2014 Mar;59;594-8).
When kidney recipients present, preoperative imaging of the aorta from the aneurysm to the kidney allograft is mandatory, he said. Endovascular repair is preferred, whenever possible.
The renal graft is typically sewn to the external iliac artery 3 cm to 10 cm from the bifurcation of the external and internal iliac arteries. Because of this, repair is challenging when aneurysmal disease involves the iliac artery, Dr. Englesbe observed. Aneurysmal dilation is less common in the external iliac, but stenting an iliac aneurysm can still compromise inflow to the transplanted kidney.
Several surgical techniques including axillofemoral bypass, aortofemoral shunt, or extracorporeal circuit have been reported to preserve renal function during open AAA repair in renal transplant recipients. These techniques are not without their own risk of complications and should be avoided in patients with low creatinine, but are appropriate in patients with marginal or impaired renal function, according to Dr. Englesbe, who reported having no relevant disclosures.
CHICAGO – Surgeons can expect to see more abdominal organ transplant recipients presenting with aortic aneurysms, as transplant survival rates increase along with the age of organ donors and recipients.
“The consensus is that abdominal aortic aneurysms (AAAs) have a more aggressive course post-transplant and within that context, probably need to be managed more aggressively,” Dr. Michael J. Englesbe of the University of Michigan, Ann Arbor said at the annual Northwestern Vascular Symposium.
Some 270,000 Americans are living with a functioning liver or kidney graft, and their average age has risen from 47 years to 57 years over the last decade.
Though the data isn’t great, it’s hypothesized that the immunosuppression prerequisite for successful organ transplantation promotes the progression of atherosclerosis and aneurysm growth in transplant patients, he said.
New-onset diabetes, hyperlipidemia, and hypertension are all common post-transplant due to immunosuppression therapy. Aortic aneurysms are also reported to rupture at smaller sizes in transplant recipients.
Intriguingly, the opposite effect has been observed in experimental animal models, where immunosuppression with calcineurin inhibitors and mammalian target of rapamycin (mTOR) inhibitors has been shown to stabilize atherosclerotic lesions and inhibit aneurysm expansion.
The reason for this disparity is unclear, but immunosuppressants likely augment other cardiovascular comorbidities such as hypertension and atherosclerosis and this may trump their anti-inflammatory effects and lead to worse aneurysm disease and faster expansion in humans, Dr. Englesbe speculated in an interview.
As for when aneurysms should be fixed, kidney transplant candidates should undergo AAA repair prior to transplantation since the risk of renal complications after aneurysm repair puts the allograft at risk, Dr. Englesbe advised. Either an open or endovascular approach can be used.
In liver transplant candidates, elective AAA repair should be avoided if possible and is contraindicated if any signs of hepatic decompensation are present such as muscle wasting, ascites, platelet count less than 50 x 109/L, or encephalopathy. For well-compensated cirrhotic patients, endovascular repair is best.
One of the most important considerations for any solid-organ transplant patient undergoing aneurysm repair is perioperative management of immunosuppression, Dr. Englesbe stressed.
Transplant patients are maintained on oral calcineurin inhibitors such as cyclosporine and tacrolimus (Prograf) throughout the perioperative period to prevent organ rejection, but these drugs have nephrotoxic effects. About 10% of recipients, typically the sicker patients, will be switched to mTOR inhibitors such as everolimus (Afinitor) and sirolumus (Rapamune) as a kidney-sparing alternative.
“Part of the mechanism of these [mTOR] drugs is that they really affect fibroblast functioning, so patients that are on these medications, their wound will fall apart and they will invariably get a hernia,” Dr. Englesbe said. “You have to stop them upwards of about 6 weeks before surgical intervention, and I think this is also true for many endografts.”
He highlighted a case in which an mTOR inhibitor was started three months after liver transplant due to renal dysfunction in a patient who was fully healed, but within three weeks, “her wound fell apart, completely fell apart.” She developed several seromas underneath her incision, one of which became infected and took months to close.
“The transplant professionals – your nephrologists, your cardiologists – aren’t going to know this fact, but as a transplant surgeon it’s usually the first question we’re going to ask with respect to any post-transplant patient we’re going to operate on, so it’s something to keep in mind,” Dr. Englesbe said.
Another take-home message was the importance of maintaining kidney function in kidney recipients presenting with aortic aneurysm, as mortality in these patients is about 10-fold higher once the kidney fails, he said. A recent study reported that AAAs are significantly more common in kidney than liver transplant recipients (29.6% vs. 11.4%; P = .02), despite a similar prevalence for any aneurysm (4%) in both groups (J Vasc Surg. 2014 Mar;59;594-8).
When kidney recipients present, preoperative imaging of the aorta from the aneurysm to the kidney allograft is mandatory, he said. Endovascular repair is preferred, whenever possible.
The renal graft is typically sewn to the external iliac artery 3 cm to 10 cm from the bifurcation of the external and internal iliac arteries. Because of this, repair is challenging when aneurysmal disease involves the iliac artery, Dr. Englesbe observed. Aneurysmal dilation is less common in the external iliac, but stenting an iliac aneurysm can still compromise inflow to the transplanted kidney.
Several surgical techniques including axillofemoral bypass, aortofemoral shunt, or extracorporeal circuit have been reported to preserve renal function during open AAA repair in renal transplant recipients. These techniques are not without their own risk of complications and should be avoided in patients with low creatinine, but are appropriate in patients with marginal or impaired renal function, according to Dr. Englesbe, who reported having no relevant disclosures.
CHICAGO – Surgeons can expect to see more abdominal organ transplant recipients presenting with aortic aneurysms, as transplant survival rates increase along with the age of organ donors and recipients.
“The consensus is that abdominal aortic aneurysms (AAAs) have a more aggressive course post-transplant and within that context, probably need to be managed more aggressively,” Dr. Michael J. Englesbe of the University of Michigan, Ann Arbor said at the annual Northwestern Vascular Symposium.
Some 270,000 Americans are living with a functioning liver or kidney graft, and their average age has risen from 47 years to 57 years over the last decade.
Though the data isn’t great, it’s hypothesized that the immunosuppression prerequisite for successful organ transplantation promotes the progression of atherosclerosis and aneurysm growth in transplant patients, he said.
New-onset diabetes, hyperlipidemia, and hypertension are all common post-transplant due to immunosuppression therapy. Aortic aneurysms are also reported to rupture at smaller sizes in transplant recipients.
Intriguingly, the opposite effect has been observed in experimental animal models, where immunosuppression with calcineurin inhibitors and mammalian target of rapamycin (mTOR) inhibitors has been shown to stabilize atherosclerotic lesions and inhibit aneurysm expansion.
The reason for this disparity is unclear, but immunosuppressants likely augment other cardiovascular comorbidities such as hypertension and atherosclerosis and this may trump their anti-inflammatory effects and lead to worse aneurysm disease and faster expansion in humans, Dr. Englesbe speculated in an interview.
As for when aneurysms should be fixed, kidney transplant candidates should undergo AAA repair prior to transplantation since the risk of renal complications after aneurysm repair puts the allograft at risk, Dr. Englesbe advised. Either an open or endovascular approach can be used.
In liver transplant candidates, elective AAA repair should be avoided if possible and is contraindicated if any signs of hepatic decompensation are present such as muscle wasting, ascites, platelet count less than 50 x 109/L, or encephalopathy. For well-compensated cirrhotic patients, endovascular repair is best.
One of the most important considerations for any solid-organ transplant patient undergoing aneurysm repair is perioperative management of immunosuppression, Dr. Englesbe stressed.
Transplant patients are maintained on oral calcineurin inhibitors such as cyclosporine and tacrolimus (Prograf) throughout the perioperative period to prevent organ rejection, but these drugs have nephrotoxic effects. About 10% of recipients, typically the sicker patients, will be switched to mTOR inhibitors such as everolimus (Afinitor) and sirolumus (Rapamune) as a kidney-sparing alternative.
“Part of the mechanism of these [mTOR] drugs is that they really affect fibroblast functioning, so patients that are on these medications, their wound will fall apart and they will invariably get a hernia,” Dr. Englesbe said. “You have to stop them upwards of about 6 weeks before surgical intervention, and I think this is also true for many endografts.”
He highlighted a case in which an mTOR inhibitor was started three months after liver transplant due to renal dysfunction in a patient who was fully healed, but within three weeks, “her wound fell apart, completely fell apart.” She developed several seromas underneath her incision, one of which became infected and took months to close.
“The transplant professionals – your nephrologists, your cardiologists – aren’t going to know this fact, but as a transplant surgeon it’s usually the first question we’re going to ask with respect to any post-transplant patient we’re going to operate on, so it’s something to keep in mind,” Dr. Englesbe said.
Another take-home message was the importance of maintaining kidney function in kidney recipients presenting with aortic aneurysm, as mortality in these patients is about 10-fold higher once the kidney fails, he said. A recent study reported that AAAs are significantly more common in kidney than liver transplant recipients (29.6% vs. 11.4%; P = .02), despite a similar prevalence for any aneurysm (4%) in both groups (J Vasc Surg. 2014 Mar;59;594-8).
When kidney recipients present, preoperative imaging of the aorta from the aneurysm to the kidney allograft is mandatory, he said. Endovascular repair is preferred, whenever possible.
The renal graft is typically sewn to the external iliac artery 3 cm to 10 cm from the bifurcation of the external and internal iliac arteries. Because of this, repair is challenging when aneurysmal disease involves the iliac artery, Dr. Englesbe observed. Aneurysmal dilation is less common in the external iliac, but stenting an iliac aneurysm can still compromise inflow to the transplanted kidney.
Several surgical techniques including axillofemoral bypass, aortofemoral shunt, or extracorporeal circuit have been reported to preserve renal function during open AAA repair in renal transplant recipients. These techniques are not without their own risk of complications and should be avoided in patients with low creatinine, but are appropriate in patients with marginal or impaired renal function, according to Dr. Englesbe, who reported having no relevant disclosures.
EXPERT ANALYSIS FROM THE NORTHWESTERN VASCULAR SYMPOSIUM
Why Are You Still Prescribing a 66-Year-Old Drug?
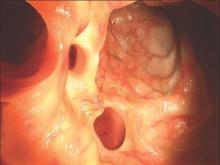
Several weeks ago, this 14-year-old boy developed an itchy spot on his neck. Concerned that the problem was “ringworm,” the boy’s grandfather took him to the primary care provider, who prescribed nystatin cream. This produced modest improvement in the appearance of the lesion but had no effect on the associated itching. At that point, they were referred to dermatology for further evaluation.
The patient denies any other skin problems. The only animal he has been exposed to is his own dog, who has been part of the household for years. The boy is not involved in contact sports (eg, football, wrestling), and he reports that none of his siblings or friends have any skin complaints.
He is otherwise healthy and does not take any prescription medications.
EXAMINATION
The “rash” consists of a single, 2-cm lesion on the patient’s anterolateral neck. It is perfectly round and slightly erythematous, with a cleared center and scaly advancing margin. Palpable adenopathy is evident just above the lesion. There are no other lesions elsewhere, and the patient’s skin is otherwise unremarkable.
What is the diagnosis?
DISCUSSION
A KOH prep revealed abundant fungal elements, confirming the diagnosis of tinea corporis. This conclusion had already been reached empirically by the primary care provider, who chose nystatin cream for treatment. When that drug faltered, diagnostic doubt reared its head. The KOH settled the question once and for all—a crucial step, since nystatin is often prescribed for conditions that have no likelihood of responding to it (eg, eczema, psoriasis, granuloma annulare).
Nystatin, a polyene antifungal, was discovered and brought to market in 1950—that’s nearly 66 years ago! At that time, very few antifungal agents were available, so nystatin gained instant acceptance practically overnight. Since then, although dozens of newer and better antifungals have come on the market, nystatin continues to be prescribed out of sheer habit. A lot of water has gone down the river since 1950!
Nystatin was first isolated and developed by two scientists (Brown and Fuller) who worked in the lab at the New York State Health Department in the ’40s and ’50s. A popular practice at the time was to collect soil samples from local farmers to see what bacteria could be isolated. Brown and Fuller found a unique species of Streptomyces that they named S noursei after the dairy farmer whose soil they sampled.
They noted that this organism exuded a substance that inhibited yeast, mold, and fungi in vitro; when this substance was isolated and purified, it worked topically as well. They named this substance nystatin in honor of their employer, the New York State Health Department.
As charming as this history is, in the intervening 60+ years, better antifungals have been introduced and organisms have become less responsive to nystatin. In my opinion, except for unusual selective instances, there is no reason to prescribe nystatin instead of imidazole and allylamine (eg, miconazole, terbinafine, or naftifine).
For this patient, I prescribed oxiconazole lotion for twice-daily application to this small and limited lesion. With more extensive disease, I might add an oral antifungal, such as terbinafine. The patient’s lesion should resolve in two weeks or less.
One final note: In dermatology, we discourage the use of the term ringworm because it contributes to the “ick” factor associated with “worms”—which are not even involved in tinea corporis.
TAKE-HOME LEARNING POINTS
• Nystatin is a 66-year-old relic that has no place in treating ordinary dermatophytosis.
• “Newer” antifungals are more effective and kill a wider range of organisms, including yeast and fungi.
• In my experience, most nystatin is prescribed for conditions that have no chance of responding to it (eg, eczema, psoriasis, or granuloma annulare), because a differential was not considered.
• Primary care offices that are comfortable doing wet preps for clue cells and trichomonas feel no such need to perform KOHs to confirm fungal infection, and so diagnostic confusion results.
• There is no medical entity called ringworm. This is lay terminology based on the misbelief that worms are somehow involved in tinea.
Several weeks ago, this 14-year-old boy developed an itchy spot on his neck. Concerned that the problem was “ringworm,” the boy’s grandfather took him to the primary care provider, who prescribed nystatin cream. This produced modest improvement in the appearance of the lesion but had no effect on the associated itching. At that point, they were referred to dermatology for further evaluation.
The patient denies any other skin problems. The only animal he has been exposed to is his own dog, who has been part of the household for years. The boy is not involved in contact sports (eg, football, wrestling), and he reports that none of his siblings or friends have any skin complaints.
He is otherwise healthy and does not take any prescription medications.
EXAMINATION
The “rash” consists of a single, 2-cm lesion on the patient’s anterolateral neck. It is perfectly round and slightly erythematous, with a cleared center and scaly advancing margin. Palpable adenopathy is evident just above the lesion. There are no other lesions elsewhere, and the patient’s skin is otherwise unremarkable.
What is the diagnosis?
DISCUSSION
A KOH prep revealed abundant fungal elements, confirming the diagnosis of tinea corporis. This conclusion had already been reached empirically by the primary care provider, who chose nystatin cream for treatment. When that drug faltered, diagnostic doubt reared its head. The KOH settled the question once and for all—a crucial step, since nystatin is often prescribed for conditions that have no likelihood of responding to it (eg, eczema, psoriasis, granuloma annulare).
Nystatin, a polyene antifungal, was discovered and brought to market in 1950—that’s nearly 66 years ago! At that time, very few antifungal agents were available, so nystatin gained instant acceptance practically overnight. Since then, although dozens of newer and better antifungals have come on the market, nystatin continues to be prescribed out of sheer habit. A lot of water has gone down the river since 1950!
Nystatin was first isolated and developed by two scientists (Brown and Fuller) who worked in the lab at the New York State Health Department in the ’40s and ’50s. A popular practice at the time was to collect soil samples from local farmers to see what bacteria could be isolated. Brown and Fuller found a unique species of Streptomyces that they named S noursei after the dairy farmer whose soil they sampled.
They noted that this organism exuded a substance that inhibited yeast, mold, and fungi in vitro; when this substance was isolated and purified, it worked topically as well. They named this substance nystatin in honor of their employer, the New York State Health Department.
As charming as this history is, in the intervening 60+ years, better antifungals have been introduced and organisms have become less responsive to nystatin. In my opinion, except for unusual selective instances, there is no reason to prescribe nystatin instead of imidazole and allylamine (eg, miconazole, terbinafine, or naftifine).
For this patient, I prescribed oxiconazole lotion for twice-daily application to this small and limited lesion. With more extensive disease, I might add an oral antifungal, such as terbinafine. The patient’s lesion should resolve in two weeks or less.
One final note: In dermatology, we discourage the use of the term ringworm because it contributes to the “ick” factor associated with “worms”—which are not even involved in tinea corporis.
TAKE-HOME LEARNING POINTS
• Nystatin is a 66-year-old relic that has no place in treating ordinary dermatophytosis.
• “Newer” antifungals are more effective and kill a wider range of organisms, including yeast and fungi.
• In my experience, most nystatin is prescribed for conditions that have no chance of responding to it (eg, eczema, psoriasis, or granuloma annulare), because a differential was not considered.
• Primary care offices that are comfortable doing wet preps for clue cells and trichomonas feel no such need to perform KOHs to confirm fungal infection, and so diagnostic confusion results.
• There is no medical entity called ringworm. This is lay terminology based on the misbelief that worms are somehow involved in tinea.
Several weeks ago, this 14-year-old boy developed an itchy spot on his neck. Concerned that the problem was “ringworm,” the boy’s grandfather took him to the primary care provider, who prescribed nystatin cream. This produced modest improvement in the appearance of the lesion but had no effect on the associated itching. At that point, they were referred to dermatology for further evaluation.
The patient denies any other skin problems. The only animal he has been exposed to is his own dog, who has been part of the household for years. The boy is not involved in contact sports (eg, football, wrestling), and he reports that none of his siblings or friends have any skin complaints.
He is otherwise healthy and does not take any prescription medications.
EXAMINATION
The “rash” consists of a single, 2-cm lesion on the patient’s anterolateral neck. It is perfectly round and slightly erythematous, with a cleared center and scaly advancing margin. Palpable adenopathy is evident just above the lesion. There are no other lesions elsewhere, and the patient’s skin is otherwise unremarkable.
What is the diagnosis?
DISCUSSION
A KOH prep revealed abundant fungal elements, confirming the diagnosis of tinea corporis. This conclusion had already been reached empirically by the primary care provider, who chose nystatin cream for treatment. When that drug faltered, diagnostic doubt reared its head. The KOH settled the question once and for all—a crucial step, since nystatin is often prescribed for conditions that have no likelihood of responding to it (eg, eczema, psoriasis, granuloma annulare).
Nystatin, a polyene antifungal, was discovered and brought to market in 1950—that’s nearly 66 years ago! At that time, very few antifungal agents were available, so nystatin gained instant acceptance practically overnight. Since then, although dozens of newer and better antifungals have come on the market, nystatin continues to be prescribed out of sheer habit. A lot of water has gone down the river since 1950!
Nystatin was first isolated and developed by two scientists (Brown and Fuller) who worked in the lab at the New York State Health Department in the ’40s and ’50s. A popular practice at the time was to collect soil samples from local farmers to see what bacteria could be isolated. Brown and Fuller found a unique species of Streptomyces that they named S noursei after the dairy farmer whose soil they sampled.
They noted that this organism exuded a substance that inhibited yeast, mold, and fungi in vitro; when this substance was isolated and purified, it worked topically as well. They named this substance nystatin in honor of their employer, the New York State Health Department.
As charming as this history is, in the intervening 60+ years, better antifungals have been introduced and organisms have become less responsive to nystatin. In my opinion, except for unusual selective instances, there is no reason to prescribe nystatin instead of imidazole and allylamine (eg, miconazole, terbinafine, or naftifine).
For this patient, I prescribed oxiconazole lotion for twice-daily application to this small and limited lesion. With more extensive disease, I might add an oral antifungal, such as terbinafine. The patient’s lesion should resolve in two weeks or less.
One final note: In dermatology, we discourage the use of the term ringworm because it contributes to the “ick” factor associated with “worms”—which are not even involved in tinea corporis.
TAKE-HOME LEARNING POINTS
• Nystatin is a 66-year-old relic that has no place in treating ordinary dermatophytosis.
• “Newer” antifungals are more effective and kill a wider range of organisms, including yeast and fungi.
• In my experience, most nystatin is prescribed for conditions that have no chance of responding to it (eg, eczema, psoriasis, or granuloma annulare), because a differential was not considered.
• Primary care offices that are comfortable doing wet preps for clue cells and trichomonas feel no such need to perform KOHs to confirm fungal infection, and so diagnostic confusion results.
• There is no medical entity called ringworm. This is lay terminology based on the misbelief that worms are somehow involved in tinea.
An interview with film director Paul Dalio: Touched With Fire
In early December, I was fortunate to be invited to a film screening of “Touched With Fire,” starring Katie Holmes and Luke Kirby. The movie is about two young poets with bipolar disorder who meet and fall in love while on a psychiatric unit. It opens in theaters on Feb.12.
The screening was introduced by Johns Hopkins Hospital’s psychiatrist in chief Ray DePaulo and following the movie, director Paul Dalio and psychologist Kay Redfield Jamison, Ph.D., both gave short talks and answered questions. The movie was inspired by Dalio’s personal experience with bipolar disorder. Jamison, author of Touched With Fire: Manic-Depressive Illness and the Artistic Temperament (New York: Free Press, 1996) had offered hope to Dalio during a difficult moment with his illness. Numbed by the medications that made his moods tolerable, she had assured him that his creativity would reemerge, as indeed it did. Jamison’s book lent its name to the movie title, and she had a cameo role in the film. In the movie, Jamison, playing herself, tells the couple that it took a while for her moods to calibrate, but that medicines were a godsend and they helped her to become both happier and more productive.
“You’re concerned about losing your art and losing your passion,” Jamison says to Marco, the character played by Kirby. “Medication’s not going to take your personality away; it’s not going to take away your own gift. It’s a fire when it’s out of control, and what medication can do is tamp that down a bit without losing that gift.”
While this insight was helpful to the real-life Dalio, the character Marco struggles deeply as tries to hang on enough to love, work, and strive toward a future he longs for, all while mourning what he sees as the loss of himself. “I want the mania!” he tells Carla, played by Holmes, in one of the more poignant scenes.
Enough plot spoilers. The love story is emotional, and the portrayal of bipolar disorder is the best I have ever seen in the popular media. The characters are three-dimensional and about so much more than their illnesses, and many of the scenes ring so true. This is bipolar disorder with all its raw passion and pain laid out for an audience. No one has odd mannerisms and no one walks around dressed in plastic bags; instead, these are beautiful people ravaged by psychosis and the extremes of their moods, and when it’s not horrible, it’s absolutely wonderful.
In the question-and-answer session after the movie, a member of the audience asked Paul Dalio how to get treatment for someone who is manic. Dalio’s answer was swift: “You have to force them. There is no other way.” As someone who has been interested in patient responses to involuntary psychiatric care, I was a bit surprised to hear that answer from someone who has suffered with the condition and whom I presumed had been treated against his will. When I was asked a few weeks later if I’d like to interview Mr. Dalio, my answer was also swift: Yes, I would.
Dalio talked openly with me about his own psychiatric history, and he was quick to say that he shared Marco’s struggles. The love story that unfolded with Carla was fictional, but when I asked about several of the scenes, Dalio said, “Yes, that happened to me!”
Dalio has been admitted to the hospital four times, twice as an involuntary patient. “I know that in a manic state, no one is going to convince you to go into a hospital,” he said. “My experience was not good at all – it was horrific and frustrating – but it was the lesser of two evils. As difficult as it was, it doesn’t hold a candle to the pain. There is no way I can communicate the pain of bipolar depression.”
Like his character, Marco, Paul Dalio spent years ravaged by his illness. He worked in a warehouse, and he says that during those years he was not very likable. He credits his family with keeping him alive; his father would spend hours on the phone talking him out of committing suicide. The family researched treatment options, and eventually, Dalio began to travel from New York City to see a bipolar disorder expert in Baltimore. His treatment at Hopkins enabled his meeting with Kay Jamison.
“You can’t lie about this disorder,” Dalio said, “and you can’t sugarcoat it.”
Dalio’s life has done a turnaround from his days of being psychotic, suicidal, and unable to function. He holds a degree in screenwriting from New York University and has attended the NYU graduate program in filmmaking. He is married and has two small children.
I asked what helped.
“I resolved to stay on meds,” he said, “even if I felt numb. I don’t drink, not even a toast to the movie. I go to bed at 10 every night, drink green juices all day, use a light box, and take walks. Transcendental meditation helps. And patience – it took 3-5 years before I was really able to feel emotion again. I’ve been stable since 2007, but thriving since 2010, with rich emotions. I have a severe form of the condition.”
Dalio experiences symptoms if he misses even a couple of doses of medication, and with two toddlers, it can be difficult for his wife that he can’t help with the children in the middle of the night. It’s not all hard, though. “My wife is Eastern European, and she has a connection to the darkness. She was always attracted to crazy people and artists, and she finds a lot of pleasure in our lives.” Like Dalio, she is screenwriter, and they collaborate on their work.
Dalio is clear about his agenda for this movie. He sees his bipolar disorder as a gift that fuels creative pursuits, and he wants others to understand how people with this disorder struggle. He used the word “beautiful” to describe the intensity of emotions that Carla and Marco experience in the film, but tragedy and torment are also screaming on the big screen. His second agenda is a plug for mainstream psychiatry and a billboard for hope: take the medications, tolerate the downside, be patient; things will work out.
Well worth seeing.
Dr. Miller is a psychiatrist who practices in Baltimore.
In early December, I was fortunate to be invited to a film screening of “Touched With Fire,” starring Katie Holmes and Luke Kirby. The movie is about two young poets with bipolar disorder who meet and fall in love while on a psychiatric unit. It opens in theaters on Feb.12.
The screening was introduced by Johns Hopkins Hospital’s psychiatrist in chief Ray DePaulo and following the movie, director Paul Dalio and psychologist Kay Redfield Jamison, Ph.D., both gave short talks and answered questions. The movie was inspired by Dalio’s personal experience with bipolar disorder. Jamison, author of Touched With Fire: Manic-Depressive Illness and the Artistic Temperament (New York: Free Press, 1996) had offered hope to Dalio during a difficult moment with his illness. Numbed by the medications that made his moods tolerable, she had assured him that his creativity would reemerge, as indeed it did. Jamison’s book lent its name to the movie title, and she had a cameo role in the film. In the movie, Jamison, playing herself, tells the couple that it took a while for her moods to calibrate, but that medicines were a godsend and they helped her to become both happier and more productive.
“You’re concerned about losing your art and losing your passion,” Jamison says to Marco, the character played by Kirby. “Medication’s not going to take your personality away; it’s not going to take away your own gift. It’s a fire when it’s out of control, and what medication can do is tamp that down a bit without losing that gift.”
While this insight was helpful to the real-life Dalio, the character Marco struggles deeply as tries to hang on enough to love, work, and strive toward a future he longs for, all while mourning what he sees as the loss of himself. “I want the mania!” he tells Carla, played by Holmes, in one of the more poignant scenes.
Enough plot spoilers. The love story is emotional, and the portrayal of bipolar disorder is the best I have ever seen in the popular media. The characters are three-dimensional and about so much more than their illnesses, and many of the scenes ring so true. This is bipolar disorder with all its raw passion and pain laid out for an audience. No one has odd mannerisms and no one walks around dressed in plastic bags; instead, these are beautiful people ravaged by psychosis and the extremes of their moods, and when it’s not horrible, it’s absolutely wonderful.
In the question-and-answer session after the movie, a member of the audience asked Paul Dalio how to get treatment for someone who is manic. Dalio’s answer was swift: “You have to force them. There is no other way.” As someone who has been interested in patient responses to involuntary psychiatric care, I was a bit surprised to hear that answer from someone who has suffered with the condition and whom I presumed had been treated against his will. When I was asked a few weeks later if I’d like to interview Mr. Dalio, my answer was also swift: Yes, I would.
Dalio talked openly with me about his own psychiatric history, and he was quick to say that he shared Marco’s struggles. The love story that unfolded with Carla was fictional, but when I asked about several of the scenes, Dalio said, “Yes, that happened to me!”
Dalio has been admitted to the hospital four times, twice as an involuntary patient. “I know that in a manic state, no one is going to convince you to go into a hospital,” he said. “My experience was not good at all – it was horrific and frustrating – but it was the lesser of two evils. As difficult as it was, it doesn’t hold a candle to the pain. There is no way I can communicate the pain of bipolar depression.”
Like his character, Marco, Paul Dalio spent years ravaged by his illness. He worked in a warehouse, and he says that during those years he was not very likable. He credits his family with keeping him alive; his father would spend hours on the phone talking him out of committing suicide. The family researched treatment options, and eventually, Dalio began to travel from New York City to see a bipolar disorder expert in Baltimore. His treatment at Hopkins enabled his meeting with Kay Jamison.
“You can’t lie about this disorder,” Dalio said, “and you can’t sugarcoat it.”
Dalio’s life has done a turnaround from his days of being psychotic, suicidal, and unable to function. He holds a degree in screenwriting from New York University and has attended the NYU graduate program in filmmaking. He is married and has two small children.
I asked what helped.
“I resolved to stay on meds,” he said, “even if I felt numb. I don’t drink, not even a toast to the movie. I go to bed at 10 every night, drink green juices all day, use a light box, and take walks. Transcendental meditation helps. And patience – it took 3-5 years before I was really able to feel emotion again. I’ve been stable since 2007, but thriving since 2010, with rich emotions. I have a severe form of the condition.”
Dalio experiences symptoms if he misses even a couple of doses of medication, and with two toddlers, it can be difficult for his wife that he can’t help with the children in the middle of the night. It’s not all hard, though. “My wife is Eastern European, and she has a connection to the darkness. She was always attracted to crazy people and artists, and she finds a lot of pleasure in our lives.” Like Dalio, she is screenwriter, and they collaborate on their work.
Dalio is clear about his agenda for this movie. He sees his bipolar disorder as a gift that fuels creative pursuits, and he wants others to understand how people with this disorder struggle. He used the word “beautiful” to describe the intensity of emotions that Carla and Marco experience in the film, but tragedy and torment are also screaming on the big screen. His second agenda is a plug for mainstream psychiatry and a billboard for hope: take the medications, tolerate the downside, be patient; things will work out.
Well worth seeing.
Dr. Miller is a psychiatrist who practices in Baltimore.
In early December, I was fortunate to be invited to a film screening of “Touched With Fire,” starring Katie Holmes and Luke Kirby. The movie is about two young poets with bipolar disorder who meet and fall in love while on a psychiatric unit. It opens in theaters on Feb.12.
The screening was introduced by Johns Hopkins Hospital’s psychiatrist in chief Ray DePaulo and following the movie, director Paul Dalio and psychologist Kay Redfield Jamison, Ph.D., both gave short talks and answered questions. The movie was inspired by Dalio’s personal experience with bipolar disorder. Jamison, author of Touched With Fire: Manic-Depressive Illness and the Artistic Temperament (New York: Free Press, 1996) had offered hope to Dalio during a difficult moment with his illness. Numbed by the medications that made his moods tolerable, she had assured him that his creativity would reemerge, as indeed it did. Jamison’s book lent its name to the movie title, and she had a cameo role in the film. In the movie, Jamison, playing herself, tells the couple that it took a while for her moods to calibrate, but that medicines were a godsend and they helped her to become both happier and more productive.
“You’re concerned about losing your art and losing your passion,” Jamison says to Marco, the character played by Kirby. “Medication’s not going to take your personality away; it’s not going to take away your own gift. It’s a fire when it’s out of control, and what medication can do is tamp that down a bit without losing that gift.”
While this insight was helpful to the real-life Dalio, the character Marco struggles deeply as tries to hang on enough to love, work, and strive toward a future he longs for, all while mourning what he sees as the loss of himself. “I want the mania!” he tells Carla, played by Holmes, in one of the more poignant scenes.
Enough plot spoilers. The love story is emotional, and the portrayal of bipolar disorder is the best I have ever seen in the popular media. The characters are three-dimensional and about so much more than their illnesses, and many of the scenes ring so true. This is bipolar disorder with all its raw passion and pain laid out for an audience. No one has odd mannerisms and no one walks around dressed in plastic bags; instead, these are beautiful people ravaged by psychosis and the extremes of their moods, and when it’s not horrible, it’s absolutely wonderful.
In the question-and-answer session after the movie, a member of the audience asked Paul Dalio how to get treatment for someone who is manic. Dalio’s answer was swift: “You have to force them. There is no other way.” As someone who has been interested in patient responses to involuntary psychiatric care, I was a bit surprised to hear that answer from someone who has suffered with the condition and whom I presumed had been treated against his will. When I was asked a few weeks later if I’d like to interview Mr. Dalio, my answer was also swift: Yes, I would.
Dalio talked openly with me about his own psychiatric history, and he was quick to say that he shared Marco’s struggles. The love story that unfolded with Carla was fictional, but when I asked about several of the scenes, Dalio said, “Yes, that happened to me!”
Dalio has been admitted to the hospital four times, twice as an involuntary patient. “I know that in a manic state, no one is going to convince you to go into a hospital,” he said. “My experience was not good at all – it was horrific and frustrating – but it was the lesser of two evils. As difficult as it was, it doesn’t hold a candle to the pain. There is no way I can communicate the pain of bipolar depression.”
Like his character, Marco, Paul Dalio spent years ravaged by his illness. He worked in a warehouse, and he says that during those years he was not very likable. He credits his family with keeping him alive; his father would spend hours on the phone talking him out of committing suicide. The family researched treatment options, and eventually, Dalio began to travel from New York City to see a bipolar disorder expert in Baltimore. His treatment at Hopkins enabled his meeting with Kay Jamison.
“You can’t lie about this disorder,” Dalio said, “and you can’t sugarcoat it.”
Dalio’s life has done a turnaround from his days of being psychotic, suicidal, and unable to function. He holds a degree in screenwriting from New York University and has attended the NYU graduate program in filmmaking. He is married and has two small children.
I asked what helped.
“I resolved to stay on meds,” he said, “even if I felt numb. I don’t drink, not even a toast to the movie. I go to bed at 10 every night, drink green juices all day, use a light box, and take walks. Transcendental meditation helps. And patience – it took 3-5 years before I was really able to feel emotion again. I’ve been stable since 2007, but thriving since 2010, with rich emotions. I have a severe form of the condition.”
Dalio experiences symptoms if he misses even a couple of doses of medication, and with two toddlers, it can be difficult for his wife that he can’t help with the children in the middle of the night. It’s not all hard, though. “My wife is Eastern European, and she has a connection to the darkness. She was always attracted to crazy people and artists, and she finds a lot of pleasure in our lives.” Like Dalio, she is screenwriter, and they collaborate on their work.
Dalio is clear about his agenda for this movie. He sees his bipolar disorder as a gift that fuels creative pursuits, and he wants others to understand how people with this disorder struggle. He used the word “beautiful” to describe the intensity of emotions that Carla and Marco experience in the film, but tragedy and torment are also screaming on the big screen. His second agenda is a plug for mainstream psychiatry and a billboard for hope: take the medications, tolerate the downside, be patient; things will work out.
Well worth seeing.
Dr. Miller is a psychiatrist who practices in Baltimore.
Brian McGeeney, MD, MPH
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Cause and Warning Symptoms of MI Differentiate Among Men and Women
(Reuters Health) - The causes of acute myocardial infarction(MI) and the warning symptoms that can signal the need for immediate medical attention are different in women than in men, according to a scientific statement issued today by the American Heart Association.
When women don't recognize this, they may suffer worse outcomes, a fate that is even more likely in black and Hispanic women, according to the AHA.
The AHA published its first comprehensive statement on gender differences in acute MI patients in Circulation, January 25.
"Women seem to do worse for several reasons," said Dr. Laxmi Mehta, the lead author of the recommendations and the director of women's cardiovascular health at Ohio State University in Columbus.
Importantly, people don't realize that while both sexes may experience chest pain before or during a heart attack, women maybe more likely to have unusual symptoms instead, such as shortness of breath, nausea or vomiting, and back or neck pain.
Then, when they do get to a hospital, women may be less likely than men to receive medications that help to prevent clots, decrease the heart's workload and lower blood pressure or cholesterol.
"There is a lot at stake for women when there is a delay in treatment or lack of adherence to recommended therapies," Mehta added by email. "Women face higher rates of being readmitted to the hospital, heart failure and death."
Biology is also part of the problem. Even though both women and men suffer MI caused by blockages in the main arteries leading to the heart, the way the clots develop may differ, according to the scientific statement.
Men tend to have a more "classic" type of blockage where plaque ruptures off the artery wall, forms a blood clot and causes a complete halt of blood flow through the artery to the heart, said Dr. Sheila Sahni, chief fellow in cardiovascular disease at the David Geffen School of Medicine at the University of California Los Angeles.
"Women, more often, tend to have a plaque erosion where smaller pieces of plaque break off, become exposed and cause the formation of smaller blood clots which may or may not cause total occlusions all at once, leading to a more subtle presentation," Sahni, who wasn't involved in the study, said by email.
In addition, women tend to be about a decade older than men when they suffer acute MI, potentially making them frailer and more likely to suffer from other health problems such as diabetes that can make their treatment more complicated, Sahni added.
Risk factors also differ by gender, with hypertension more strongly associated with MI in women than in men. For young women with diabetes, the risk for heart disease is four to five times higher than it would be for a similar young man.
Race, too, is an issue. Compared to white women, black women have a higher incidence of MI in all age categories and young black women have greater odds of dying before they leave the hospital. Black and Hispanic women are also more likely to have
heart-related risk factors such as diabetes, obesity and hypertension at the time of their MI.
Once a heart attack begins, the best way for women to minimize damage is to get help quickly, said Dr. Leslie Cho, director of the women's cardiovascular center at the Cleveland Clinic and Clinic in Ohio.
"Time is muscle," Cho, who wasn't involved in the study, said by email. "If women are diagnosed and treated later in the course of the heart attack, they can suffer from irreversible heart damage."
(Reuters Health) - The causes of acute myocardial infarction(MI) and the warning symptoms that can signal the need for immediate medical attention are different in women than in men, according to a scientific statement issued today by the American Heart Association.
When women don't recognize this, they may suffer worse outcomes, a fate that is even more likely in black and Hispanic women, according to the AHA.
The AHA published its first comprehensive statement on gender differences in acute MI patients in Circulation, January 25.
"Women seem to do worse for several reasons," said Dr. Laxmi Mehta, the lead author of the recommendations and the director of women's cardiovascular health at Ohio State University in Columbus.
Importantly, people don't realize that while both sexes may experience chest pain before or during a heart attack, women maybe more likely to have unusual symptoms instead, such as shortness of breath, nausea or vomiting, and back or neck pain.
Then, when they do get to a hospital, women may be less likely than men to receive medications that help to prevent clots, decrease the heart's workload and lower blood pressure or cholesterol.
"There is a lot at stake for women when there is a delay in treatment or lack of adherence to recommended therapies," Mehta added by email. "Women face higher rates of being readmitted to the hospital, heart failure and death."
Biology is also part of the problem. Even though both women and men suffer MI caused by blockages in the main arteries leading to the heart, the way the clots develop may differ, according to the scientific statement.
Men tend to have a more "classic" type of blockage where plaque ruptures off the artery wall, forms a blood clot and causes a complete halt of blood flow through the artery to the heart, said Dr. Sheila Sahni, chief fellow in cardiovascular disease at the David Geffen School of Medicine at the University of California Los Angeles.
"Women, more often, tend to have a plaque erosion where smaller pieces of plaque break off, become exposed and cause the formation of smaller blood clots which may or may not cause total occlusions all at once, leading to a more subtle presentation," Sahni, who wasn't involved in the study, said by email.
In addition, women tend to be about a decade older than men when they suffer acute MI, potentially making them frailer and more likely to suffer from other health problems such as diabetes that can make their treatment more complicated, Sahni added.
Risk factors also differ by gender, with hypertension more strongly associated with MI in women than in men. For young women with diabetes, the risk for heart disease is four to five times higher than it would be for a similar young man.
Race, too, is an issue. Compared to white women, black women have a higher incidence of MI in all age categories and young black women have greater odds of dying before they leave the hospital. Black and Hispanic women are also more likely to have
heart-related risk factors such as diabetes, obesity and hypertension at the time of their MI.
Once a heart attack begins, the best way for women to minimize damage is to get help quickly, said Dr. Leslie Cho, director of the women's cardiovascular center at the Cleveland Clinic and Clinic in Ohio.
"Time is muscle," Cho, who wasn't involved in the study, said by email. "If women are diagnosed and treated later in the course of the heart attack, they can suffer from irreversible heart damage."
(Reuters Health) - The causes of acute myocardial infarction(MI) and the warning symptoms that can signal the need for immediate medical attention are different in women than in men, according to a scientific statement issued today by the American Heart Association.
When women don't recognize this, they may suffer worse outcomes, a fate that is even more likely in black and Hispanic women, according to the AHA.
The AHA published its first comprehensive statement on gender differences in acute MI patients in Circulation, January 25.
"Women seem to do worse for several reasons," said Dr. Laxmi Mehta, the lead author of the recommendations and the director of women's cardiovascular health at Ohio State University in Columbus.
Importantly, people don't realize that while both sexes may experience chest pain before or during a heart attack, women maybe more likely to have unusual symptoms instead, such as shortness of breath, nausea or vomiting, and back or neck pain.
Then, when they do get to a hospital, women may be less likely than men to receive medications that help to prevent clots, decrease the heart's workload and lower blood pressure or cholesterol.
"There is a lot at stake for women when there is a delay in treatment or lack of adherence to recommended therapies," Mehta added by email. "Women face higher rates of being readmitted to the hospital, heart failure and death."
Biology is also part of the problem. Even though both women and men suffer MI caused by blockages in the main arteries leading to the heart, the way the clots develop may differ, according to the scientific statement.
Men tend to have a more "classic" type of blockage where plaque ruptures off the artery wall, forms a blood clot and causes a complete halt of blood flow through the artery to the heart, said Dr. Sheila Sahni, chief fellow in cardiovascular disease at the David Geffen School of Medicine at the University of California Los Angeles.
"Women, more often, tend to have a plaque erosion where smaller pieces of plaque break off, become exposed and cause the formation of smaller blood clots which may or may not cause total occlusions all at once, leading to a more subtle presentation," Sahni, who wasn't involved in the study, said by email.
In addition, women tend to be about a decade older than men when they suffer acute MI, potentially making them frailer and more likely to suffer from other health problems such as diabetes that can make their treatment more complicated, Sahni added.
Risk factors also differ by gender, with hypertension more strongly associated with MI in women than in men. For young women with diabetes, the risk for heart disease is four to five times higher than it would be for a similar young man.
Race, too, is an issue. Compared to white women, black women have a higher incidence of MI in all age categories and young black women have greater odds of dying before they leave the hospital. Black and Hispanic women are also more likely to have
heart-related risk factors such as diabetes, obesity and hypertension at the time of their MI.
Once a heart attack begins, the best way for women to minimize damage is to get help quickly, said Dr. Leslie Cho, director of the women's cardiovascular center at the Cleveland Clinic and Clinic in Ohio.
"Time is muscle," Cho, who wasn't involved in the study, said by email. "If women are diagnosed and treated later in the course of the heart attack, they can suffer from irreversible heart damage."