User login
Dual inhibitor could treat ATLL

Photo by Larry Young
SAN FRANCISCO—Preclinical research suggests a compound that inhibits both EZH1 and EZH2 could be effective against adult T-cell leukemia/lymphoma (ATLL).
The compound, known as OR-S1, has demonstrated activity against ATLL in vitro and in vivo.
Researchers said OR-S1 reversed epigenetic disruption in ATLL cells, selectively eliminated both ATLL cells and cells infected with human T-cell leukemia virus type I (HTLV-1), and inhibited tumor growth in mouse models of ATLL.
Based on these results, the researchers are planning a phase 1 study of the compound.
Makoto Yamagishi, PhD, of The University of Tokyo in Japan, described the preclinical research with OR-S1 and discussed the rationale for developing the compound at the 8th Annual T-cell Lymphoma Forum. The work was carried out in collaboration with Daiichi Sankyo Co., Ltd.
“We do not precisely understand the molecular mechanism of ATLL development, including genetic and epigenetic abnormalities,” Dr Yamagishi noted.
To gain some insight, he and his colleagues performed microRNA profiling, gene expression profiling, and histone methylation/epigenetic factor profiling on cells from ATLL patients and CD4+ T cells from healthy donors.
The team found that PRC2 factors were significantly upregulated in ATLL. EZH2 was the most upregulated histone methyltransferase, but ATLL cells did not have active mutations in the EZH2 gene. Dr Yamagishi said this suggests EZH2 upregulation is critical for the ATLL-specific epigenome.
“At long last, we determined the epigenetic pattern of ATLL,” he said. “ATLL cells showed specific and significant reprogramming of the epigenome, especially H3K27me3 gain. We found abnormal H3K27me3 change in half of genes, and gain was dominant.”
“But, interestingly, the methylated genes are specific in ATLL and do not overlap with other EZH2-dependent cell types, such as embryonic stem cells and diffuse large B-cell lymphoma cells. So ATLL has a very unique epigenome.”
Further investigation revealed that both EZH1 and EZH2 contribute to ATLL-specific epigenetic deregulation. More than 80% of H3K27me3 accumulated genes are occupied by EZH1 and/or EZH2.
So the researchers decided to examine the effects of knocking down EZH1 and EZH2 in ATLL cells.
Compared with knockdown of either gene alone, double knockdown synergistically influenced target gene expression. It led to complete dysfunction of the Polycomb family and had a significant impact on ATLL cell survival.
The researchers also found that EZH1 depletion enhanced ATLL cells’ sensitivity to the EZH2 inhibitor GSK126.
So the team decided to develop a dual EZH1/EZH2 inhibitor. They created OR-S1, which showed “strong activity” against EZH1 and EZH2 but none of the other histone methyltransferases tested.
In in vitro experiments, OR-S1 completely removed H3K27me3 and significantly reduced cell growth in the ATLL-derived cell line TL-Om1.
The drug also reduced cell viability in primary ATLL cells. All 15 samples tested proved sensitive to OR-S1. In addition, OR-S1 treatment selectively removed HTLV-1-infected cells from samples taken from 16 asymptomatic carriers.
Finally, OR-S1 proved active in mice. The drug prevented engraftment of ATLL cells in immunocompromised mice. All 6 OR-S1-treated mice were alive and tumor-free at 49 days, whereas 5 of 6 control mice had died (P=0.0041).
In mice treated after ATLL cell engraftment, OR-S1 reduced tumor growth without causing notable weight loss.
“Synthetic lethality by targeting EZH1 and EZH2 is promising [for ATLL],” Dr Yamagishi said. “Toxicity tests suggest the EZH1/2 dual inhibitor may be sufficient for clinical use, so we are now planning a phase 1 study.” ![]()

Photo by Larry Young
SAN FRANCISCO—Preclinical research suggests a compound that inhibits both EZH1 and EZH2 could be effective against adult T-cell leukemia/lymphoma (ATLL).
The compound, known as OR-S1, has demonstrated activity against ATLL in vitro and in vivo.
Researchers said OR-S1 reversed epigenetic disruption in ATLL cells, selectively eliminated both ATLL cells and cells infected with human T-cell leukemia virus type I (HTLV-1), and inhibited tumor growth in mouse models of ATLL.
Based on these results, the researchers are planning a phase 1 study of the compound.
Makoto Yamagishi, PhD, of The University of Tokyo in Japan, described the preclinical research with OR-S1 and discussed the rationale for developing the compound at the 8th Annual T-cell Lymphoma Forum. The work was carried out in collaboration with Daiichi Sankyo Co., Ltd.
“We do not precisely understand the molecular mechanism of ATLL development, including genetic and epigenetic abnormalities,” Dr Yamagishi noted.
To gain some insight, he and his colleagues performed microRNA profiling, gene expression profiling, and histone methylation/epigenetic factor profiling on cells from ATLL patients and CD4+ T cells from healthy donors.
The team found that PRC2 factors were significantly upregulated in ATLL. EZH2 was the most upregulated histone methyltransferase, but ATLL cells did not have active mutations in the EZH2 gene. Dr Yamagishi said this suggests EZH2 upregulation is critical for the ATLL-specific epigenome.
“At long last, we determined the epigenetic pattern of ATLL,” he said. “ATLL cells showed specific and significant reprogramming of the epigenome, especially H3K27me3 gain. We found abnormal H3K27me3 change in half of genes, and gain was dominant.”
“But, interestingly, the methylated genes are specific in ATLL and do not overlap with other EZH2-dependent cell types, such as embryonic stem cells and diffuse large B-cell lymphoma cells. So ATLL has a very unique epigenome.”
Further investigation revealed that both EZH1 and EZH2 contribute to ATLL-specific epigenetic deregulation. More than 80% of H3K27me3 accumulated genes are occupied by EZH1 and/or EZH2.
So the researchers decided to examine the effects of knocking down EZH1 and EZH2 in ATLL cells.
Compared with knockdown of either gene alone, double knockdown synergistically influenced target gene expression. It led to complete dysfunction of the Polycomb family and had a significant impact on ATLL cell survival.
The researchers also found that EZH1 depletion enhanced ATLL cells’ sensitivity to the EZH2 inhibitor GSK126.
So the team decided to develop a dual EZH1/EZH2 inhibitor. They created OR-S1, which showed “strong activity” against EZH1 and EZH2 but none of the other histone methyltransferases tested.
In in vitro experiments, OR-S1 completely removed H3K27me3 and significantly reduced cell growth in the ATLL-derived cell line TL-Om1.
The drug also reduced cell viability in primary ATLL cells. All 15 samples tested proved sensitive to OR-S1. In addition, OR-S1 treatment selectively removed HTLV-1-infected cells from samples taken from 16 asymptomatic carriers.
Finally, OR-S1 proved active in mice. The drug prevented engraftment of ATLL cells in immunocompromised mice. All 6 OR-S1-treated mice were alive and tumor-free at 49 days, whereas 5 of 6 control mice had died (P=0.0041).
In mice treated after ATLL cell engraftment, OR-S1 reduced tumor growth without causing notable weight loss.
“Synthetic lethality by targeting EZH1 and EZH2 is promising [for ATLL],” Dr Yamagishi said. “Toxicity tests suggest the EZH1/2 dual inhibitor may be sufficient for clinical use, so we are now planning a phase 1 study.” ![]()

Photo by Larry Young
SAN FRANCISCO—Preclinical research suggests a compound that inhibits both EZH1 and EZH2 could be effective against adult T-cell leukemia/lymphoma (ATLL).
The compound, known as OR-S1, has demonstrated activity against ATLL in vitro and in vivo.
Researchers said OR-S1 reversed epigenetic disruption in ATLL cells, selectively eliminated both ATLL cells and cells infected with human T-cell leukemia virus type I (HTLV-1), and inhibited tumor growth in mouse models of ATLL.
Based on these results, the researchers are planning a phase 1 study of the compound.
Makoto Yamagishi, PhD, of The University of Tokyo in Japan, described the preclinical research with OR-S1 and discussed the rationale for developing the compound at the 8th Annual T-cell Lymphoma Forum. The work was carried out in collaboration with Daiichi Sankyo Co., Ltd.
“We do not precisely understand the molecular mechanism of ATLL development, including genetic and epigenetic abnormalities,” Dr Yamagishi noted.
To gain some insight, he and his colleagues performed microRNA profiling, gene expression profiling, and histone methylation/epigenetic factor profiling on cells from ATLL patients and CD4+ T cells from healthy donors.
The team found that PRC2 factors were significantly upregulated in ATLL. EZH2 was the most upregulated histone methyltransferase, but ATLL cells did not have active mutations in the EZH2 gene. Dr Yamagishi said this suggests EZH2 upregulation is critical for the ATLL-specific epigenome.
“At long last, we determined the epigenetic pattern of ATLL,” he said. “ATLL cells showed specific and significant reprogramming of the epigenome, especially H3K27me3 gain. We found abnormal H3K27me3 change in half of genes, and gain was dominant.”
“But, interestingly, the methylated genes are specific in ATLL and do not overlap with other EZH2-dependent cell types, such as embryonic stem cells and diffuse large B-cell lymphoma cells. So ATLL has a very unique epigenome.”
Further investigation revealed that both EZH1 and EZH2 contribute to ATLL-specific epigenetic deregulation. More than 80% of H3K27me3 accumulated genes are occupied by EZH1 and/or EZH2.
So the researchers decided to examine the effects of knocking down EZH1 and EZH2 in ATLL cells.
Compared with knockdown of either gene alone, double knockdown synergistically influenced target gene expression. It led to complete dysfunction of the Polycomb family and had a significant impact on ATLL cell survival.
The researchers also found that EZH1 depletion enhanced ATLL cells’ sensitivity to the EZH2 inhibitor GSK126.
So the team decided to develop a dual EZH1/EZH2 inhibitor. They created OR-S1, which showed “strong activity” against EZH1 and EZH2 but none of the other histone methyltransferases tested.
In in vitro experiments, OR-S1 completely removed H3K27me3 and significantly reduced cell growth in the ATLL-derived cell line TL-Om1.
The drug also reduced cell viability in primary ATLL cells. All 15 samples tested proved sensitive to OR-S1. In addition, OR-S1 treatment selectively removed HTLV-1-infected cells from samples taken from 16 asymptomatic carriers.
Finally, OR-S1 proved active in mice. The drug prevented engraftment of ATLL cells in immunocompromised mice. All 6 OR-S1-treated mice were alive and tumor-free at 49 days, whereas 5 of 6 control mice had died (P=0.0041).
In mice treated after ATLL cell engraftment, OR-S1 reduced tumor growth without causing notable weight loss.
“Synthetic lethality by targeting EZH1 and EZH2 is promising [for ATLL],” Dr Yamagishi said. “Toxicity tests suggest the EZH1/2 dual inhibitor may be sufficient for clinical use, so we are now planning a phase 1 study.” ![]()
New insight into Ph-like ALL could lead to new treatment

Photo courtesy of St. Jude
Children’s Research Hospital
Research published in Cancer Cell appears to explain how the abnormal breakage and rearrangement of chromosomes in white blood cells triggers Philadelphia chromosome-like (Ph-like) acute lymphoblastic leukemia (ALL).
Genomic analysis revealed 4 chromosomal rearrangements that all resulted in a truncated version of the erythropoietin receptor (EPOR) gene and drove white blood cells to proliferate out of control.
“To our knowledge, this is a previously unknown mechanism for leukemia,” said study author Charles Mullighan, MBBS, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“Our search of cancer genomic data has shown that there are many other examples of chromosomal rearrangements that alter genes’ structure, but this type—where a truncating rearrangement leads to activation—is new.”
Although Dr Mullighan and his colleagues had previously identified an abnormal chromosome rearrangement in Ph-like ALL, little was known about the biological effects of that rearrangement. So they set out to pinpoint those effects by studying human leukemic cells and mouse cells engineered to mimic Ph-like ALL.
The investigators discovered the 4 rearrangements of EPOR, all of which resulted in truncation of the cytoplasmic tail of EPOR at residues similar to those mutated in primary familial congenital polycythemia. The proximal tyrosine essential for receptor activation was preserved, but distal regulatory residues were lost.
The team said these rearrangements resulted in deregulated EPOR expression, hypersensitivity to erythropoietin stimulation, and heightened JAK-STAT activation.
The investigators noted that the rearrangements were present in all of the leukemic cells from patients, which suggests these changes were fundamental to Ph-like ALL development. The team also showed that introducing truncated EPOR in mouse B-cell progenitors gave rise to ALL in mice.
Further investigation revealed that EPOR rearrangements arise early in the development of Ph-like ALL and persist as the disease progresses.
“That finding was important because it suggests that treatments for this leukemia targeting this receptor won’t just impact a subset of the leukemia cells, allowing others to keep proliferating,” said study author Ilaria Iacobucci, PhD, of St. Jude Children’s Research Hospital.
The investigators then found that human leukemic cells with EPOR rearrangements were sensitive to JAK-STAT inhibition via treatment with ruxolitinib.
The team also cited the case of an adult patient treated at MD Anderson Cancer Research Center in Houston, Texas, whose genetic analysis revealed EPOR-rearranged ALL. That patient had not responded significantly to other chemotherapy drugs. But, when given ruxolitinib, the patient showed a major drop in leukemia cells.
In experiments with leukemic cells, the investigators found that ruxolitinib worked synergistically with 3 chemotherapeutic agents—dexamethasone, vincristine, and daunorubicin.
“We think these findings provide a useful road map for planning more accurate testing of combination chemotherapies,” Dr Mullighan said.
“These findings expand the number of ALL patients who should be amenable to precision medicine therapies that add targeted inhibitors to chemotherapy for ALL patents with specific genetic changes in the leukemia cells,” added study author Stephen Hunger, MD, of Children’s Hospital of Philadelphia in Pennsylvania.
Dr Hunger said the Children’s Oncology Group has developed a clinical trial testing this strategy with ruxolitinib, which will begin treating patients in mid-2016. Based on the results of the Cancer Cell research, the trial will include children with ALL and EPOR rearrangements. ![]()

Photo courtesy of St. Jude
Children’s Research Hospital
Research published in Cancer Cell appears to explain how the abnormal breakage and rearrangement of chromosomes in white blood cells triggers Philadelphia chromosome-like (Ph-like) acute lymphoblastic leukemia (ALL).
Genomic analysis revealed 4 chromosomal rearrangements that all resulted in a truncated version of the erythropoietin receptor (EPOR) gene and drove white blood cells to proliferate out of control.
“To our knowledge, this is a previously unknown mechanism for leukemia,” said study author Charles Mullighan, MBBS, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“Our search of cancer genomic data has shown that there are many other examples of chromosomal rearrangements that alter genes’ structure, but this type—where a truncating rearrangement leads to activation—is new.”
Although Dr Mullighan and his colleagues had previously identified an abnormal chromosome rearrangement in Ph-like ALL, little was known about the biological effects of that rearrangement. So they set out to pinpoint those effects by studying human leukemic cells and mouse cells engineered to mimic Ph-like ALL.
The investigators discovered the 4 rearrangements of EPOR, all of which resulted in truncation of the cytoplasmic tail of EPOR at residues similar to those mutated in primary familial congenital polycythemia. The proximal tyrosine essential for receptor activation was preserved, but distal regulatory residues were lost.
The team said these rearrangements resulted in deregulated EPOR expression, hypersensitivity to erythropoietin stimulation, and heightened JAK-STAT activation.
The investigators noted that the rearrangements were present in all of the leukemic cells from patients, which suggests these changes were fundamental to Ph-like ALL development. The team also showed that introducing truncated EPOR in mouse B-cell progenitors gave rise to ALL in mice.
Further investigation revealed that EPOR rearrangements arise early in the development of Ph-like ALL and persist as the disease progresses.
“That finding was important because it suggests that treatments for this leukemia targeting this receptor won’t just impact a subset of the leukemia cells, allowing others to keep proliferating,” said study author Ilaria Iacobucci, PhD, of St. Jude Children’s Research Hospital.
The investigators then found that human leukemic cells with EPOR rearrangements were sensitive to JAK-STAT inhibition via treatment with ruxolitinib.
The team also cited the case of an adult patient treated at MD Anderson Cancer Research Center in Houston, Texas, whose genetic analysis revealed EPOR-rearranged ALL. That patient had not responded significantly to other chemotherapy drugs. But, when given ruxolitinib, the patient showed a major drop in leukemia cells.
In experiments with leukemic cells, the investigators found that ruxolitinib worked synergistically with 3 chemotherapeutic agents—dexamethasone, vincristine, and daunorubicin.
“We think these findings provide a useful road map for planning more accurate testing of combination chemotherapies,” Dr Mullighan said.
“These findings expand the number of ALL patients who should be amenable to precision medicine therapies that add targeted inhibitors to chemotherapy for ALL patents with specific genetic changes in the leukemia cells,” added study author Stephen Hunger, MD, of Children’s Hospital of Philadelphia in Pennsylvania.
Dr Hunger said the Children’s Oncology Group has developed a clinical trial testing this strategy with ruxolitinib, which will begin treating patients in mid-2016. Based on the results of the Cancer Cell research, the trial will include children with ALL and EPOR rearrangements. ![]()

Photo courtesy of St. Jude
Children’s Research Hospital
Research published in Cancer Cell appears to explain how the abnormal breakage and rearrangement of chromosomes in white blood cells triggers Philadelphia chromosome-like (Ph-like) acute lymphoblastic leukemia (ALL).
Genomic analysis revealed 4 chromosomal rearrangements that all resulted in a truncated version of the erythropoietin receptor (EPOR) gene and drove white blood cells to proliferate out of control.
“To our knowledge, this is a previously unknown mechanism for leukemia,” said study author Charles Mullighan, MBBS, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“Our search of cancer genomic data has shown that there are many other examples of chromosomal rearrangements that alter genes’ structure, but this type—where a truncating rearrangement leads to activation—is new.”
Although Dr Mullighan and his colleagues had previously identified an abnormal chromosome rearrangement in Ph-like ALL, little was known about the biological effects of that rearrangement. So they set out to pinpoint those effects by studying human leukemic cells and mouse cells engineered to mimic Ph-like ALL.
The investigators discovered the 4 rearrangements of EPOR, all of which resulted in truncation of the cytoplasmic tail of EPOR at residues similar to those mutated in primary familial congenital polycythemia. The proximal tyrosine essential for receptor activation was preserved, but distal regulatory residues were lost.
The team said these rearrangements resulted in deregulated EPOR expression, hypersensitivity to erythropoietin stimulation, and heightened JAK-STAT activation.
The investigators noted that the rearrangements were present in all of the leukemic cells from patients, which suggests these changes were fundamental to Ph-like ALL development. The team also showed that introducing truncated EPOR in mouse B-cell progenitors gave rise to ALL in mice.
Further investigation revealed that EPOR rearrangements arise early in the development of Ph-like ALL and persist as the disease progresses.
“That finding was important because it suggests that treatments for this leukemia targeting this receptor won’t just impact a subset of the leukemia cells, allowing others to keep proliferating,” said study author Ilaria Iacobucci, PhD, of St. Jude Children’s Research Hospital.
The investigators then found that human leukemic cells with EPOR rearrangements were sensitive to JAK-STAT inhibition via treatment with ruxolitinib.
The team also cited the case of an adult patient treated at MD Anderson Cancer Research Center in Houston, Texas, whose genetic analysis revealed EPOR-rearranged ALL. That patient had not responded significantly to other chemotherapy drugs. But, when given ruxolitinib, the patient showed a major drop in leukemia cells.
In experiments with leukemic cells, the investigators found that ruxolitinib worked synergistically with 3 chemotherapeutic agents—dexamethasone, vincristine, and daunorubicin.
“We think these findings provide a useful road map for planning more accurate testing of combination chemotherapies,” Dr Mullighan said.
“These findings expand the number of ALL patients who should be amenable to precision medicine therapies that add targeted inhibitors to chemotherapy for ALL patents with specific genetic changes in the leukemia cells,” added study author Stephen Hunger, MD, of Children’s Hospital of Philadelphia in Pennsylvania.
Dr Hunger said the Children’s Oncology Group has developed a clinical trial testing this strategy with ruxolitinib, which will begin treating patients in mid-2016. Based on the results of the Cancer Cell research, the trial will include children with ALL and EPOR rearrangements. ![]()
Study reveals delays in emergency blood transfusions

Photo courtesy of UAB Hospital
A new study suggests that as few as 2% of patients with life-threatening bleeding after serious injury receive optimal blood transfusion therapy in England and Wales.
Researchers estimate that nearly 5000 trauma patients sustain a major hemorrhage in England and Wales each year, and one-third of those patients die.
The current study, published in the British Journal of Surgery, highlights how delays in transfusions may contribute to this death rate.
“The rapid and consistent delivery of blood, plasma, platelets, and other clotting products to trauma patients is essential to maintain clotting during hemorrhage and has been shown to halve mortality,” said study author Karim Brohi, MBBS, of Queen Mary University of London in the UK.
“However, we found that only 2% of patients with massive hemorrhage received the optimal type of blood transfusion for their resuscitation. There is a clear opportunity for clinicians to improve the delivery of blood and clotting products during resuscitation for major hemorrhage.”
Dr Brohi and his colleagues analyzed 442 patients treated at 22 hospitals in England and Wales. The patients had experienced major hemorrhage as a result of injuries and received at least 4 units of packed red blood cells (PRBCs) in the first 24 hours of admission.
The patients’ median age was 38 (range, 24-54), and 74% were men. Thirty-three percent of patients (n=146) had massive hemorrhage.
Mortality from bleeding tended to occur early in these patients. Twenty-seven percent of patients (n=117) died in hospital—18% (n=79) within the first 24 hours. The 30-day mortality rate was about 27% (n=119), and 33% of evaluable patients had died at 1 year (127/383).
All 442 patients received PRBCs. The median number of PRBC units transfused within 24 hours was 7 (range, 5-11), and the median number of PRBC units given in 30 days was 9 (range, 6-15).
The average time to transfusion of PRBCs was longer than expected, at 41 minutes (range, 1-122).
Similarly, the researchers found the administration of blood components such as plasma and platelets to be significantly delayed, occurring, on average, 2 to 3 hours after admission.
Three-quarters of patients (n=330) received fresh-frozen plasma (FFP). The median number of FFP units given within 24 hours was 4 (range, 0-7), and the time to first FFP transfusion was 87 minutes (range, 42.5-229).
About 45% of patients (n=197) received platelets. The median dose was 0 (range, 0-1), and the time to first platelet transfusion was 146 minutes (range, 72.5-364).
About 28% of patients (n=122) received cryoprecipitate. The median dose was 0 (range, 0-1), and the time to first cryoprecipitate infusion was 179.5 minutes (range, 84.5-333.5).
“The rapid delivery of the right mix of blood components in an emergency environment is extremely challenging,” Dr Brohi said.
“Some transfusion components have to be thawed and, at present, aren’t always available for the patient quickly enough. More research is also needed into techniques and devices to control bleeding earlier, even at the scene of injury.”
The researchers noted that this study had its limitations, such as incomplete data for some patients. ![]()

Photo courtesy of UAB Hospital
A new study suggests that as few as 2% of patients with life-threatening bleeding after serious injury receive optimal blood transfusion therapy in England and Wales.
Researchers estimate that nearly 5000 trauma patients sustain a major hemorrhage in England and Wales each year, and one-third of those patients die.
The current study, published in the British Journal of Surgery, highlights how delays in transfusions may contribute to this death rate.
“The rapid and consistent delivery of blood, plasma, platelets, and other clotting products to trauma patients is essential to maintain clotting during hemorrhage and has been shown to halve mortality,” said study author Karim Brohi, MBBS, of Queen Mary University of London in the UK.
“However, we found that only 2% of patients with massive hemorrhage received the optimal type of blood transfusion for their resuscitation. There is a clear opportunity for clinicians to improve the delivery of blood and clotting products during resuscitation for major hemorrhage.”
Dr Brohi and his colleagues analyzed 442 patients treated at 22 hospitals in England and Wales. The patients had experienced major hemorrhage as a result of injuries and received at least 4 units of packed red blood cells (PRBCs) in the first 24 hours of admission.
The patients’ median age was 38 (range, 24-54), and 74% were men. Thirty-three percent of patients (n=146) had massive hemorrhage.
Mortality from bleeding tended to occur early in these patients. Twenty-seven percent of patients (n=117) died in hospital—18% (n=79) within the first 24 hours. The 30-day mortality rate was about 27% (n=119), and 33% of evaluable patients had died at 1 year (127/383).
All 442 patients received PRBCs. The median number of PRBC units transfused within 24 hours was 7 (range, 5-11), and the median number of PRBC units given in 30 days was 9 (range, 6-15).
The average time to transfusion of PRBCs was longer than expected, at 41 minutes (range, 1-122).
Similarly, the researchers found the administration of blood components such as plasma and platelets to be significantly delayed, occurring, on average, 2 to 3 hours after admission.
Three-quarters of patients (n=330) received fresh-frozen plasma (FFP). The median number of FFP units given within 24 hours was 4 (range, 0-7), and the time to first FFP transfusion was 87 minutes (range, 42.5-229).
About 45% of patients (n=197) received platelets. The median dose was 0 (range, 0-1), and the time to first platelet transfusion was 146 minutes (range, 72.5-364).
About 28% of patients (n=122) received cryoprecipitate. The median dose was 0 (range, 0-1), and the time to first cryoprecipitate infusion was 179.5 minutes (range, 84.5-333.5).
“The rapid delivery of the right mix of blood components in an emergency environment is extremely challenging,” Dr Brohi said.
“Some transfusion components have to be thawed and, at present, aren’t always available for the patient quickly enough. More research is also needed into techniques and devices to control bleeding earlier, even at the scene of injury.”
The researchers noted that this study had its limitations, such as incomplete data for some patients. ![]()

Photo courtesy of UAB Hospital
A new study suggests that as few as 2% of patients with life-threatening bleeding after serious injury receive optimal blood transfusion therapy in England and Wales.
Researchers estimate that nearly 5000 trauma patients sustain a major hemorrhage in England and Wales each year, and one-third of those patients die.
The current study, published in the British Journal of Surgery, highlights how delays in transfusions may contribute to this death rate.
“The rapid and consistent delivery of blood, plasma, platelets, and other clotting products to trauma patients is essential to maintain clotting during hemorrhage and has been shown to halve mortality,” said study author Karim Brohi, MBBS, of Queen Mary University of London in the UK.
“However, we found that only 2% of patients with massive hemorrhage received the optimal type of blood transfusion for their resuscitation. There is a clear opportunity for clinicians to improve the delivery of blood and clotting products during resuscitation for major hemorrhage.”
Dr Brohi and his colleagues analyzed 442 patients treated at 22 hospitals in England and Wales. The patients had experienced major hemorrhage as a result of injuries and received at least 4 units of packed red blood cells (PRBCs) in the first 24 hours of admission.
The patients’ median age was 38 (range, 24-54), and 74% were men. Thirty-three percent of patients (n=146) had massive hemorrhage.
Mortality from bleeding tended to occur early in these patients. Twenty-seven percent of patients (n=117) died in hospital—18% (n=79) within the first 24 hours. The 30-day mortality rate was about 27% (n=119), and 33% of evaluable patients had died at 1 year (127/383).
All 442 patients received PRBCs. The median number of PRBC units transfused within 24 hours was 7 (range, 5-11), and the median number of PRBC units given in 30 days was 9 (range, 6-15).
The average time to transfusion of PRBCs was longer than expected, at 41 minutes (range, 1-122).
Similarly, the researchers found the administration of blood components such as plasma and platelets to be significantly delayed, occurring, on average, 2 to 3 hours after admission.
Three-quarters of patients (n=330) received fresh-frozen plasma (FFP). The median number of FFP units given within 24 hours was 4 (range, 0-7), and the time to first FFP transfusion was 87 minutes (range, 42.5-229).
About 45% of patients (n=197) received platelets. The median dose was 0 (range, 0-1), and the time to first platelet transfusion was 146 minutes (range, 72.5-364).
About 28% of patients (n=122) received cryoprecipitate. The median dose was 0 (range, 0-1), and the time to first cryoprecipitate infusion was 179.5 minutes (range, 84.5-333.5).
“The rapid delivery of the right mix of blood components in an emergency environment is extremely challenging,” Dr Brohi said.
“Some transfusion components have to be thawed and, at present, aren’t always available for the patient quickly enough. More research is also needed into techniques and devices to control bleeding earlier, even at the scene of injury.”
The researchers noted that this study had its limitations, such as incomplete data for some patients. ![]()
MF drug trials placed on partial clinical hold

The US Food and Drug Administration (FDA) has placed a partial clinical hold on trials conducted under the investigational new drug
(IND) application for pacritinib.
Pacritinib is a JAK2/FLT3 inhibitor being developed by CTI BioPharma for the treatment of myelofibrosis (MF).
The partial clinical hold impacts part of the clinical work currently being conducted under the pacritinib IND and will also affect planned clinical trials.
The FDA said the reasons for the partial clinical hold are excess mortality and other adverse events in pacritinib-treated patients (compared to the control arm) in the PERSIST-1 trial.
The excess mortality was most evident during the non-randomized crossover period following the initial 24 weeks of randomized treatment, during which patients in the control arm could switch to pacritinib treatment.
Under the partial clinical hold, investigators may not enroll new patients or start pacritinib as initial or crossover treatment, and patients not deriving benefit after 30 weeks of pacritinib treatment must stop using pacritinib.
In addition, the FDA has recommended that CTI BioPharma make certain modifications to protocols, provide certain notifications, revise relevant statements in the related investigator’s brochure and informed consent documents, and take certain other actions.
CTI BioPharma said it intends to implement the FDA’s recommendations, and all clinical investigators worldwide have been notified of the partial clinical hold.
Just before the FDA notified CTI BioPharma of the partial clinical hold, the company completed enrollment in the phase 3 PERSIST-2 trial.
In PERSIST-2, researchers are comparing the efficacy and safety of pacritinib and best available therapy in patients with thrombocytopenia and primary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF.
Under the partial clinical hold, patients on this trial who are currently receiving pacritinib may continue to do so unless they are not deriving benefit after 30 weeks of pacritinib treatment, and crossover of patients from the control arm to the pacritinib arm will not be allowed. ![]()

The US Food and Drug Administration (FDA) has placed a partial clinical hold on trials conducted under the investigational new drug
(IND) application for pacritinib.
Pacritinib is a JAK2/FLT3 inhibitor being developed by CTI BioPharma for the treatment of myelofibrosis (MF).
The partial clinical hold impacts part of the clinical work currently being conducted under the pacritinib IND and will also affect planned clinical trials.
The FDA said the reasons for the partial clinical hold are excess mortality and other adverse events in pacritinib-treated patients (compared to the control arm) in the PERSIST-1 trial.
The excess mortality was most evident during the non-randomized crossover period following the initial 24 weeks of randomized treatment, during which patients in the control arm could switch to pacritinib treatment.
Under the partial clinical hold, investigators may not enroll new patients or start pacritinib as initial or crossover treatment, and patients not deriving benefit after 30 weeks of pacritinib treatment must stop using pacritinib.
In addition, the FDA has recommended that CTI BioPharma make certain modifications to protocols, provide certain notifications, revise relevant statements in the related investigator’s brochure and informed consent documents, and take certain other actions.
CTI BioPharma said it intends to implement the FDA’s recommendations, and all clinical investigators worldwide have been notified of the partial clinical hold.
Just before the FDA notified CTI BioPharma of the partial clinical hold, the company completed enrollment in the phase 3 PERSIST-2 trial.
In PERSIST-2, researchers are comparing the efficacy and safety of pacritinib and best available therapy in patients with thrombocytopenia and primary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF.
Under the partial clinical hold, patients on this trial who are currently receiving pacritinib may continue to do so unless they are not deriving benefit after 30 weeks of pacritinib treatment, and crossover of patients from the control arm to the pacritinib arm will not be allowed. ![]()

The US Food and Drug Administration (FDA) has placed a partial clinical hold on trials conducted under the investigational new drug
(IND) application for pacritinib.
Pacritinib is a JAK2/FLT3 inhibitor being developed by CTI BioPharma for the treatment of myelofibrosis (MF).
The partial clinical hold impacts part of the clinical work currently being conducted under the pacritinib IND and will also affect planned clinical trials.
The FDA said the reasons for the partial clinical hold are excess mortality and other adverse events in pacritinib-treated patients (compared to the control arm) in the PERSIST-1 trial.
The excess mortality was most evident during the non-randomized crossover period following the initial 24 weeks of randomized treatment, during which patients in the control arm could switch to pacritinib treatment.
Under the partial clinical hold, investigators may not enroll new patients or start pacritinib as initial or crossover treatment, and patients not deriving benefit after 30 weeks of pacritinib treatment must stop using pacritinib.
In addition, the FDA has recommended that CTI BioPharma make certain modifications to protocols, provide certain notifications, revise relevant statements in the related investigator’s brochure and informed consent documents, and take certain other actions.
CTI BioPharma said it intends to implement the FDA’s recommendations, and all clinical investigators worldwide have been notified of the partial clinical hold.
Just before the FDA notified CTI BioPharma of the partial clinical hold, the company completed enrollment in the phase 3 PERSIST-2 trial.
In PERSIST-2, researchers are comparing the efficacy and safety of pacritinib and best available therapy in patients with thrombocytopenia and primary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF.
Under the partial clinical hold, patients on this trial who are currently receiving pacritinib may continue to do so unless they are not deriving benefit after 30 weeks of pacritinib treatment, and crossover of patients from the control arm to the pacritinib arm will not be allowed. ![]()
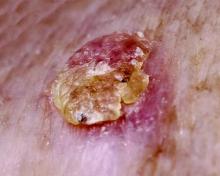
Average person with atopic dermatitis has no increased risk of actinic keratosis or nonmelanoma skin cancer
People with atopic dermatitis do not appear to be at greater risk for actinic keratosis or basal cell and squamous cell cancer, according to a recent population-based, cross-sectional study.
“This is the first study to examine the association between atopic dermatitis and actinic keratosis [AK]. Our findings suggest that within a population-based sample, atopic dermatitis patients do not have more AKs than the rest of the population. Patients with atopic dermatitis were not found to have more AKs or keratotic cancers [basal or squamous cell cancers]. Moreover, individuals with atopic dermatitis seem to be less likely to develop multiple AKs,” said Dr. Enes Hajdarbegovic and his associates of the Erasmus Medical Centre, Rotterdam, the Netherlands.
The study is part of an ongoing, prospective, Dutch population-based cohort study that follows people in a district of Rotterdam since 1990. There are now 14,926 participants in the database. The current study included 4,375 participants who had undergone full body skin examinations; 56% of patients were female, and the mean age was 68 years (Br J Dermatol. 2016 Jan 29. doi: 10.1111/bjd.14423).
Twenty-four percent had 1 or more AKs; 57% had 1-3 of these lesions; 23% had 4-9, and 20% had more than 10. The mean age of participants with AK was significantly higher, compared with those without AK (73 years vs. 66 years; P less than .01).
Of the 4,375 participants screened, 6.3% met the diagnostic criteria for atopic dermatitis. A lower proportion of those with atopic dermatitis had AK: 16% vs. 24%, respectively (P = .002). In a multinomial model, atopic dermatitis patients were 78% less likely to have 10 or more AKs than were those without atopic dermatitis. No effect of atopic dermatitis was found on basal cell cancer (adjusted odds ratio, 0.71) and squamous cell cancer (adjusted OR, 1.54).
The authors explained that it is already known that patients with severe atopic dermatitis exposed to ultraviolet light and immunosuppressants are at increased risk of keratinocyte malignancies. This study shows that a community-dwelling person with moderate atopic dermatitis does not develop more AKs or keratinocyte cancers.
The investigators said they had no relevant financial disclosures.
People with atopic dermatitis do not appear to be at greater risk for actinic keratosis or basal cell and squamous cell cancer, according to a recent population-based, cross-sectional study.
“This is the first study to examine the association between atopic dermatitis and actinic keratosis [AK]. Our findings suggest that within a population-based sample, atopic dermatitis patients do not have more AKs than the rest of the population. Patients with atopic dermatitis were not found to have more AKs or keratotic cancers [basal or squamous cell cancers]. Moreover, individuals with atopic dermatitis seem to be less likely to develop multiple AKs,” said Dr. Enes Hajdarbegovic and his associates of the Erasmus Medical Centre, Rotterdam, the Netherlands.
The study is part of an ongoing, prospective, Dutch population-based cohort study that follows people in a district of Rotterdam since 1990. There are now 14,926 participants in the database. The current study included 4,375 participants who had undergone full body skin examinations; 56% of patients were female, and the mean age was 68 years (Br J Dermatol. 2016 Jan 29. doi: 10.1111/bjd.14423).
Twenty-four percent had 1 or more AKs; 57% had 1-3 of these lesions; 23% had 4-9, and 20% had more than 10. The mean age of participants with AK was significantly higher, compared with those without AK (73 years vs. 66 years; P less than .01).
Of the 4,375 participants screened, 6.3% met the diagnostic criteria for atopic dermatitis. A lower proportion of those with atopic dermatitis had AK: 16% vs. 24%, respectively (P = .002). In a multinomial model, atopic dermatitis patients were 78% less likely to have 10 or more AKs than were those without atopic dermatitis. No effect of atopic dermatitis was found on basal cell cancer (adjusted odds ratio, 0.71) and squamous cell cancer (adjusted OR, 1.54).
The authors explained that it is already known that patients with severe atopic dermatitis exposed to ultraviolet light and immunosuppressants are at increased risk of keratinocyte malignancies. This study shows that a community-dwelling person with moderate atopic dermatitis does not develop more AKs or keratinocyte cancers.
The investigators said they had no relevant financial disclosures.
People with atopic dermatitis do not appear to be at greater risk for actinic keratosis or basal cell and squamous cell cancer, according to a recent population-based, cross-sectional study.
“This is the first study to examine the association between atopic dermatitis and actinic keratosis [AK]. Our findings suggest that within a population-based sample, atopic dermatitis patients do not have more AKs than the rest of the population. Patients with atopic dermatitis were not found to have more AKs or keratotic cancers [basal or squamous cell cancers]. Moreover, individuals with atopic dermatitis seem to be less likely to develop multiple AKs,” said Dr. Enes Hajdarbegovic and his associates of the Erasmus Medical Centre, Rotterdam, the Netherlands.
The study is part of an ongoing, prospective, Dutch population-based cohort study that follows people in a district of Rotterdam since 1990. There are now 14,926 participants in the database. The current study included 4,375 participants who had undergone full body skin examinations; 56% of patients were female, and the mean age was 68 years (Br J Dermatol. 2016 Jan 29. doi: 10.1111/bjd.14423).
Twenty-four percent had 1 or more AKs; 57% had 1-3 of these lesions; 23% had 4-9, and 20% had more than 10. The mean age of participants with AK was significantly higher, compared with those without AK (73 years vs. 66 years; P less than .01).
Of the 4,375 participants screened, 6.3% met the diagnostic criteria for atopic dermatitis. A lower proportion of those with atopic dermatitis had AK: 16% vs. 24%, respectively (P = .002). In a multinomial model, atopic dermatitis patients were 78% less likely to have 10 or more AKs than were those without atopic dermatitis. No effect of atopic dermatitis was found on basal cell cancer (adjusted odds ratio, 0.71) and squamous cell cancer (adjusted OR, 1.54).
The authors explained that it is already known that patients with severe atopic dermatitis exposed to ultraviolet light and immunosuppressants are at increased risk of keratinocyte malignancies. This study shows that a community-dwelling person with moderate atopic dermatitis does not develop more AKs or keratinocyte cancers.
The investigators said they had no relevant financial disclosures.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Key clinical point: People with atopic dermatitis do not appear to be at greater risk for actinic keratosis or basal cell and squamous cell cancer.
Major finding: In a multinomial model, atopic dermatitis patients were 78% less likely to have 10 or more actinic keratoses than were those without atopic dermatitis. No effect of atopic dermatitis was found on basal cell cancer (adjusted OR, 0.71) and squamous cell cancer (adjusted OR, 1.54).
Data source: A prospective, Dutch population-based cohort study of 4,375 participants who had undergone full body skin examinations.
Disclosures: The investigators said they had no relevant financial disclosures.
USPSTF: Screen all adults for depression
All adults, including pregnant and postpartum women, should be screened for depression, according to new recommendations of the U.S. Preventive Services Task Force.
The recommendation also calls for screening to be coupled with “adequate systems” to ensure diagnosis, treatment, and follow-up (JAMA. 2016 Jan 26;315[4]:380-7).
The depression screening recommendation, authored by Dr. Albert L. Siu and the other members of the USPSTF, is a level B recommendation, meaning that it has either high certainty of moderate net benefit, or moderate certainty of moderate to substantial net benefit.
The new guidance in screening for depression helps address a disorder that is “the leading cause of disability among adults in high-income countries,” said Dr. Siu and his coauthors. Lost productivity attributable to depression cost $23 billion in the United States in 2011, and $22.8 billion was spent on treatments for depression in 2009, the last year for which figures are available.
Dr. Siu, chair of geriatrics and palliative medicine at Icahn School of Medicine at Mount Sinai, New York, and his coauthors cited “convincing evidence that screening improves the accurate identification of adult patients with depression in primary care settings, including pregnant and postpartum women.”
In addition, the task force found convincing evidence that for older adults as well as the general adult population, treatment of “depression identified through screening in primary care settings with antidepressants, psychotherapy, or both decreases clinical morbidity.”
For pregnant and postpartum women with depression, Dr. Siu and his coauthors found “adequate” evidence that cognitive behavioral therapy (CBT) improves outcomes.
The recommendation does not identify optimal timing and intervals for depression screening, citing a need for more research in this area. However, “a pragmatic approach might include screening all adults who have not been screened previously and using clinical judgment in consideration of risk factors, comorbid conditions, and life events to determine if additional screening of high-risk patients is warranted,” explained Dr. Siu and his coauthors.
The new depression screening recommendation from USPSTF updates the 2009 recommendation, which recommended universal screening if “staff-assisted depression care supports” were in place, and targeted screening based on clinical judgment and patient preference if such support were unavailable.
The rationale for the current recommendation of universal screening for those 18 years and older is the “recognition that such support is now much more widely available and accepted as part of mental health care,” the task force members said.
Any potential harms of screening, said Dr. Siu and his coauthors, were minimal to nonexistent.
Overall, the USPSTF assigned a small to moderate risk to the use of medication in depression. However, the use of “second-generation” antidepressants – mostly SSRIs – was associated with some harms, including increased risk of suicidal behavior in young adults and of gastrointestinal bleeding in older adults, as well as potential fetal harms in pregnant women taking antidepressants.
Using CBT to treat depression in pregnant and postpartum women was also associated with minimal to no harm.
The USPSTF screening recommendation is aligned with the American Academy of Family Physicians’ recommendation to screen the general adult population for depression, and with the American Academy of Pediatrics’ recommendation that pediatricians screen mothers for depression at their babies’ 1-, 2-, and 4-month office visits.
Released in draft form in July 2015, the depression screening recommendation was available for public comment for a period of 4 weeks. In response to public input, the final recommendation’s implementation section clarifies and characterizes an “adequate system” of screening, and gives more resources for evidence-based depression screening and treatment.
The Agency for Healthcare Research and Quality supports the operations of the USPSTF, but the task force’s recommendations are independent of the federal government. Dr. Siu and the other task force members reported no conflicts of interest.
On Twitter @karioakes
Arthritis affects one in five adults and is one of the most frequent reasons for ambulatory visits to the primary care physician. Arthritis affects patients both physically and psychologically and often leads to depressed mood with subsequent worse health outcomes, including increased mortality. Specifically, depression in patients with arthritis is an independent risk factor for cardiovascular disease, myocardial infarction, and suicide. Patients with arthritis and associated depression have increased health service utilization and are less likely to be adherent with their medications. In addition to these negative health consequences, depression may contribute to unemployment, loss of work productivity, and increased healthcare costs in persons with arthritis.
Depression screening guidelines for adults with chronic musculoskeletal diseases such as arthritis have been endorsed by the U.K. National Institute of Clinical Excellence. The U.S. Preventive Service Task Force and the Canadian Task Force for Preventive Health Care recommend depression screening in all adults. However, before screening for depression in specific patient groups can be recommended, well-established criteria should be met. Generally, screening is reasonable if the condition, depression in this case, is important and prevalent, can be effectively treated, and cannot be readily detected without screening. Comorbid depression in patients with arthritis meets these criteria. It is highly prevalent with rates ranging from 18%-42%. Depression with inflammatory arthritis, such as rheumatoid arthritis (RA), occurs more frequently than with osteoarthritis but even though it is more prevalent, depression with RA is often unrecognized and/or untreated.
Performing depression screening should not unduly burden physicians because, on average, depression screening adds less than 3 minutes to a visit. Asking two simple questions about mood and anhedonia (“Over the past 2 weeks, have you felt down, depressed, or hopeless?” and “Over the past 2 weeks, have you felt little interest or pleasure in doing things?”) is as effective as using more formal instruments. Implicit in the use of depression screening is the assumption that screening will increase recognition of depression and that recognized patients would benefit from treatment. It has been shown that patients who screen positive but were not in treatment had high rates of depression and overall poor mental health outcomes. Thus, provision of or referral to treatment is a necessary follow-up to screening.
It has been shown that there is no difference in depression screening rates in patients with arthritis, compared with the general population, despite patients with arthritis being considered “high risk.” Given the endorsement of national guidelines for depression screening, quality improvement initiatives should target physicians and non-physicians to increase the recognition of depression in high-risk groups and the use of appropriate interventions, such as mental health referrals and/or treatment with antidepressants.
Dr. Mary Margaretten is an associate professor of medicine in the division of rheumatology at the University of California, San Francisco. She has no relevant disclosures.
Arthritis affects one in five adults and is one of the most frequent reasons for ambulatory visits to the primary care physician. Arthritis affects patients both physically and psychologically and often leads to depressed mood with subsequent worse health outcomes, including increased mortality. Specifically, depression in patients with arthritis is an independent risk factor for cardiovascular disease, myocardial infarction, and suicide. Patients with arthritis and associated depression have increased health service utilization and are less likely to be adherent with their medications. In addition to these negative health consequences, depression may contribute to unemployment, loss of work productivity, and increased healthcare costs in persons with arthritis.
Depression screening guidelines for adults with chronic musculoskeletal diseases such as arthritis have been endorsed by the U.K. National Institute of Clinical Excellence. The U.S. Preventive Service Task Force and the Canadian Task Force for Preventive Health Care recommend depression screening in all adults. However, before screening for depression in specific patient groups can be recommended, well-established criteria should be met. Generally, screening is reasonable if the condition, depression in this case, is important and prevalent, can be effectively treated, and cannot be readily detected without screening. Comorbid depression in patients with arthritis meets these criteria. It is highly prevalent with rates ranging from 18%-42%. Depression with inflammatory arthritis, such as rheumatoid arthritis (RA), occurs more frequently than with osteoarthritis but even though it is more prevalent, depression with RA is often unrecognized and/or untreated.
Performing depression screening should not unduly burden physicians because, on average, depression screening adds less than 3 minutes to a visit. Asking two simple questions about mood and anhedonia (“Over the past 2 weeks, have you felt down, depressed, or hopeless?” and “Over the past 2 weeks, have you felt little interest or pleasure in doing things?”) is as effective as using more formal instruments. Implicit in the use of depression screening is the assumption that screening will increase recognition of depression and that recognized patients would benefit from treatment. It has been shown that patients who screen positive but were not in treatment had high rates of depression and overall poor mental health outcomes. Thus, provision of or referral to treatment is a necessary follow-up to screening.
It has been shown that there is no difference in depression screening rates in patients with arthritis, compared with the general population, despite patients with arthritis being considered “high risk.” Given the endorsement of national guidelines for depression screening, quality improvement initiatives should target physicians and non-physicians to increase the recognition of depression in high-risk groups and the use of appropriate interventions, such as mental health referrals and/or treatment with antidepressants.
Dr. Mary Margaretten is an associate professor of medicine in the division of rheumatology at the University of California, San Francisco. She has no relevant disclosures.
Arthritis affects one in five adults and is one of the most frequent reasons for ambulatory visits to the primary care physician. Arthritis affects patients both physically and psychologically and often leads to depressed mood with subsequent worse health outcomes, including increased mortality. Specifically, depression in patients with arthritis is an independent risk factor for cardiovascular disease, myocardial infarction, and suicide. Patients with arthritis and associated depression have increased health service utilization and are less likely to be adherent with their medications. In addition to these negative health consequences, depression may contribute to unemployment, loss of work productivity, and increased healthcare costs in persons with arthritis.
Depression screening guidelines for adults with chronic musculoskeletal diseases such as arthritis have been endorsed by the U.K. National Institute of Clinical Excellence. The U.S. Preventive Service Task Force and the Canadian Task Force for Preventive Health Care recommend depression screening in all adults. However, before screening for depression in specific patient groups can be recommended, well-established criteria should be met. Generally, screening is reasonable if the condition, depression in this case, is important and prevalent, can be effectively treated, and cannot be readily detected without screening. Comorbid depression in patients with arthritis meets these criteria. It is highly prevalent with rates ranging from 18%-42%. Depression with inflammatory arthritis, such as rheumatoid arthritis (RA), occurs more frequently than with osteoarthritis but even though it is more prevalent, depression with RA is often unrecognized and/or untreated.
Performing depression screening should not unduly burden physicians because, on average, depression screening adds less than 3 minutes to a visit. Asking two simple questions about mood and anhedonia (“Over the past 2 weeks, have you felt down, depressed, or hopeless?” and “Over the past 2 weeks, have you felt little interest or pleasure in doing things?”) is as effective as using more formal instruments. Implicit in the use of depression screening is the assumption that screening will increase recognition of depression and that recognized patients would benefit from treatment. It has been shown that patients who screen positive but were not in treatment had high rates of depression and overall poor mental health outcomes. Thus, provision of or referral to treatment is a necessary follow-up to screening.
It has been shown that there is no difference in depression screening rates in patients with arthritis, compared with the general population, despite patients with arthritis being considered “high risk.” Given the endorsement of national guidelines for depression screening, quality improvement initiatives should target physicians and non-physicians to increase the recognition of depression in high-risk groups and the use of appropriate interventions, such as mental health referrals and/or treatment with antidepressants.
Dr. Mary Margaretten is an associate professor of medicine in the division of rheumatology at the University of California, San Francisco. She has no relevant disclosures.
All adults, including pregnant and postpartum women, should be screened for depression, according to new recommendations of the U.S. Preventive Services Task Force.
The recommendation also calls for screening to be coupled with “adequate systems” to ensure diagnosis, treatment, and follow-up (JAMA. 2016 Jan 26;315[4]:380-7).
The depression screening recommendation, authored by Dr. Albert L. Siu and the other members of the USPSTF, is a level B recommendation, meaning that it has either high certainty of moderate net benefit, or moderate certainty of moderate to substantial net benefit.
The new guidance in screening for depression helps address a disorder that is “the leading cause of disability among adults in high-income countries,” said Dr. Siu and his coauthors. Lost productivity attributable to depression cost $23 billion in the United States in 2011, and $22.8 billion was spent on treatments for depression in 2009, the last year for which figures are available.
Dr. Siu, chair of geriatrics and palliative medicine at Icahn School of Medicine at Mount Sinai, New York, and his coauthors cited “convincing evidence that screening improves the accurate identification of adult patients with depression in primary care settings, including pregnant and postpartum women.”
In addition, the task force found convincing evidence that for older adults as well as the general adult population, treatment of “depression identified through screening in primary care settings with antidepressants, psychotherapy, or both decreases clinical morbidity.”
For pregnant and postpartum women with depression, Dr. Siu and his coauthors found “adequate” evidence that cognitive behavioral therapy (CBT) improves outcomes.
The recommendation does not identify optimal timing and intervals for depression screening, citing a need for more research in this area. However, “a pragmatic approach might include screening all adults who have not been screened previously and using clinical judgment in consideration of risk factors, comorbid conditions, and life events to determine if additional screening of high-risk patients is warranted,” explained Dr. Siu and his coauthors.
The new depression screening recommendation from USPSTF updates the 2009 recommendation, which recommended universal screening if “staff-assisted depression care supports” were in place, and targeted screening based on clinical judgment and patient preference if such support were unavailable.
The rationale for the current recommendation of universal screening for those 18 years and older is the “recognition that such support is now much more widely available and accepted as part of mental health care,” the task force members said.
Any potential harms of screening, said Dr. Siu and his coauthors, were minimal to nonexistent.
Overall, the USPSTF assigned a small to moderate risk to the use of medication in depression. However, the use of “second-generation” antidepressants – mostly SSRIs – was associated with some harms, including increased risk of suicidal behavior in young adults and of gastrointestinal bleeding in older adults, as well as potential fetal harms in pregnant women taking antidepressants.
Using CBT to treat depression in pregnant and postpartum women was also associated with minimal to no harm.
The USPSTF screening recommendation is aligned with the American Academy of Family Physicians’ recommendation to screen the general adult population for depression, and with the American Academy of Pediatrics’ recommendation that pediatricians screen mothers for depression at their babies’ 1-, 2-, and 4-month office visits.
Released in draft form in July 2015, the depression screening recommendation was available for public comment for a period of 4 weeks. In response to public input, the final recommendation’s implementation section clarifies and characterizes an “adequate system” of screening, and gives more resources for evidence-based depression screening and treatment.
The Agency for Healthcare Research and Quality supports the operations of the USPSTF, but the task force’s recommendations are independent of the federal government. Dr. Siu and the other task force members reported no conflicts of interest.
On Twitter @karioakes
All adults, including pregnant and postpartum women, should be screened for depression, according to new recommendations of the U.S. Preventive Services Task Force.
The recommendation also calls for screening to be coupled with “adequate systems” to ensure diagnosis, treatment, and follow-up (JAMA. 2016 Jan 26;315[4]:380-7).
The depression screening recommendation, authored by Dr. Albert L. Siu and the other members of the USPSTF, is a level B recommendation, meaning that it has either high certainty of moderate net benefit, or moderate certainty of moderate to substantial net benefit.
The new guidance in screening for depression helps address a disorder that is “the leading cause of disability among adults in high-income countries,” said Dr. Siu and his coauthors. Lost productivity attributable to depression cost $23 billion in the United States in 2011, and $22.8 billion was spent on treatments for depression in 2009, the last year for which figures are available.
Dr. Siu, chair of geriatrics and palliative medicine at Icahn School of Medicine at Mount Sinai, New York, and his coauthors cited “convincing evidence that screening improves the accurate identification of adult patients with depression in primary care settings, including pregnant and postpartum women.”
In addition, the task force found convincing evidence that for older adults as well as the general adult population, treatment of “depression identified through screening in primary care settings with antidepressants, psychotherapy, or both decreases clinical morbidity.”
For pregnant and postpartum women with depression, Dr. Siu and his coauthors found “adequate” evidence that cognitive behavioral therapy (CBT) improves outcomes.
The recommendation does not identify optimal timing and intervals for depression screening, citing a need for more research in this area. However, “a pragmatic approach might include screening all adults who have not been screened previously and using clinical judgment in consideration of risk factors, comorbid conditions, and life events to determine if additional screening of high-risk patients is warranted,” explained Dr. Siu and his coauthors.
The new depression screening recommendation from USPSTF updates the 2009 recommendation, which recommended universal screening if “staff-assisted depression care supports” were in place, and targeted screening based on clinical judgment and patient preference if such support were unavailable.
The rationale for the current recommendation of universal screening for those 18 years and older is the “recognition that such support is now much more widely available and accepted as part of mental health care,” the task force members said.
Any potential harms of screening, said Dr. Siu and his coauthors, were minimal to nonexistent.
Overall, the USPSTF assigned a small to moderate risk to the use of medication in depression. However, the use of “second-generation” antidepressants – mostly SSRIs – was associated with some harms, including increased risk of suicidal behavior in young adults and of gastrointestinal bleeding in older adults, as well as potential fetal harms in pregnant women taking antidepressants.
Using CBT to treat depression in pregnant and postpartum women was also associated with minimal to no harm.
The USPSTF screening recommendation is aligned with the American Academy of Family Physicians’ recommendation to screen the general adult population for depression, and with the American Academy of Pediatrics’ recommendation that pediatricians screen mothers for depression at their babies’ 1-, 2-, and 4-month office visits.
Released in draft form in July 2015, the depression screening recommendation was available for public comment for a period of 4 weeks. In response to public input, the final recommendation’s implementation section clarifies and characterizes an “adequate system” of screening, and gives more resources for evidence-based depression screening and treatment.
The Agency for Healthcare Research and Quality supports the operations of the USPSTF, but the task force’s recommendations are independent of the federal government. Dr. Siu and the other task force members reported no conflicts of interest.
On Twitter @karioakes
FROM JAMA
Survivors of childhood ALL show significant attention problems
Survivors of childhood acute lymphoblastic leukemia (ALL) who underwent CNS-directed chemotherapy show significant attention problems that impair their functioning 2 years later, according to a report published online Feb. 8 in the Journal of Clinical Oncology.
The attention problems were isolated from intelligence and academic performance, but they still “significantly and negatively impact real-world functioning,” said Lisa M. Jacola, Ph.D. of the department of psychology and her associates at St. Jude Children’s Research Hospital, Memphis (J Clin Oncol. 2016 Feb 8. [doi: 10.1200/JCO.2015.64.3205]).
Intrathecal chemotherapy has largely replaced cranial radiation therapy to protect the CNS in childhood ALL, but most research concerning neurocognitive outcomes after this treatment has been retrospective and has involved small sample sizes. So investigators performed a prospective study using data from an ongoing trial involving a representative cohort of more than 400 patients aged 1-18 years who were treated at a single center during a 7-year period.
These patients were classified as low- or high-risk based on comprehensive biologic and clinical factors, such as blast cell immunophenotype and genotype, presenting clinical features, and early treatment response. They then received intrathecal methotrexate, cytarabine, and hydrocortisone in doses appropriate to their risk status, as well as standardized leucovorin followed by mercaptopurine and vincristine plus dexamethasone.
The researchers focused on the 211 patients who underwent comprehensive neurocognitive assessment 2 years after diagnosis and treatment. “The overall group did not significantly differ from normative expectations on measures of global intelligence (estimated IQ), academic skills (reading, math, or spelling), and learning and memory.” However, half of them were rated as below average on several measures of attention. In addition, caregivers reported a significantly greater than expected frequency of hyperactivity, impulsivity, and learning problems in the children.
This adverse effect was strongest among children who were younger than age 5 at diagnosis and among those at high risk who received more aggressive treatment.
“Our findings ... emphasize the importance of routine neurocognitive monitoring of all survivors treated with contemporary therapy.” But early detection will only be helpful if effective interventions are developed to remediate these attention and behavior problems. Research has shown that pharmacologic therapies “have reduced acceptability among survivors of childhood cancer,” so nonpharmacologic approaches would be especially useful, the researchers added.
Survivors of childhood acute lymphoblastic leukemia (ALL) who underwent CNS-directed chemotherapy show significant attention problems that impair their functioning 2 years later, according to a report published online Feb. 8 in the Journal of Clinical Oncology.
The attention problems were isolated from intelligence and academic performance, but they still “significantly and negatively impact real-world functioning,” said Lisa M. Jacola, Ph.D. of the department of psychology and her associates at St. Jude Children’s Research Hospital, Memphis (J Clin Oncol. 2016 Feb 8. [doi: 10.1200/JCO.2015.64.3205]).
Intrathecal chemotherapy has largely replaced cranial radiation therapy to protect the CNS in childhood ALL, but most research concerning neurocognitive outcomes after this treatment has been retrospective and has involved small sample sizes. So investigators performed a prospective study using data from an ongoing trial involving a representative cohort of more than 400 patients aged 1-18 years who were treated at a single center during a 7-year period.
These patients were classified as low- or high-risk based on comprehensive biologic and clinical factors, such as blast cell immunophenotype and genotype, presenting clinical features, and early treatment response. They then received intrathecal methotrexate, cytarabine, and hydrocortisone in doses appropriate to their risk status, as well as standardized leucovorin followed by mercaptopurine and vincristine plus dexamethasone.
The researchers focused on the 211 patients who underwent comprehensive neurocognitive assessment 2 years after diagnosis and treatment. “The overall group did not significantly differ from normative expectations on measures of global intelligence (estimated IQ), academic skills (reading, math, or spelling), and learning and memory.” However, half of them were rated as below average on several measures of attention. In addition, caregivers reported a significantly greater than expected frequency of hyperactivity, impulsivity, and learning problems in the children.
This adverse effect was strongest among children who were younger than age 5 at diagnosis and among those at high risk who received more aggressive treatment.
“Our findings ... emphasize the importance of routine neurocognitive monitoring of all survivors treated with contemporary therapy.” But early detection will only be helpful if effective interventions are developed to remediate these attention and behavior problems. Research has shown that pharmacologic therapies “have reduced acceptability among survivors of childhood cancer,” so nonpharmacologic approaches would be especially useful, the researchers added.
Survivors of childhood acute lymphoblastic leukemia (ALL) who underwent CNS-directed chemotherapy show significant attention problems that impair their functioning 2 years later, according to a report published online Feb. 8 in the Journal of Clinical Oncology.
The attention problems were isolated from intelligence and academic performance, but they still “significantly and negatively impact real-world functioning,” said Lisa M. Jacola, Ph.D. of the department of psychology and her associates at St. Jude Children’s Research Hospital, Memphis (J Clin Oncol. 2016 Feb 8. [doi: 10.1200/JCO.2015.64.3205]).
Intrathecal chemotherapy has largely replaced cranial radiation therapy to protect the CNS in childhood ALL, but most research concerning neurocognitive outcomes after this treatment has been retrospective and has involved small sample sizes. So investigators performed a prospective study using data from an ongoing trial involving a representative cohort of more than 400 patients aged 1-18 years who were treated at a single center during a 7-year period.
These patients were classified as low- or high-risk based on comprehensive biologic and clinical factors, such as blast cell immunophenotype and genotype, presenting clinical features, and early treatment response. They then received intrathecal methotrexate, cytarabine, and hydrocortisone in doses appropriate to their risk status, as well as standardized leucovorin followed by mercaptopurine and vincristine plus dexamethasone.
The researchers focused on the 211 patients who underwent comprehensive neurocognitive assessment 2 years after diagnosis and treatment. “The overall group did not significantly differ from normative expectations on measures of global intelligence (estimated IQ), academic skills (reading, math, or spelling), and learning and memory.” However, half of them were rated as below average on several measures of attention. In addition, caregivers reported a significantly greater than expected frequency of hyperactivity, impulsivity, and learning problems in the children.
This adverse effect was strongest among children who were younger than age 5 at diagnosis and among those at high risk who received more aggressive treatment.
“Our findings ... emphasize the importance of routine neurocognitive monitoring of all survivors treated with contemporary therapy.” But early detection will only be helpful if effective interventions are developed to remediate these attention and behavior problems. Research has shown that pharmacologic therapies “have reduced acceptability among survivors of childhood cancer,” so nonpharmacologic approaches would be especially useful, the researchers added.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Survivors of childhood ALL who underwent CNS-directed chemotherapy show significant attention problems that impair their functioning 2 years later.
Major finding: 50% of the study participants were rated as below average on several measures of attention, and caregivers reported a significantly greater than expected frequency of hyperactivity, impulsivity, and learning problems.
Data source: A prospective longitudinal analysis of neurocognitive function in 211 ALL survivors assessed 2 years after diagnosis and treatment.
Disclosures: This study was supported by the National Cancer Institute and American Lebanese Syrian Associated Charities. Dr. Jacola reported having no relevant financial disclosures; one of her associates reported receiving research funding from Sigma Tau Pharmaceuticals.
Don’t Miss AATS Week
AATS Week 2016 Registration & Housing Open!
AATS Week 2016 includes Two Terrific Events
Aortic Symposium
May 12–13, 2016
New York, NY
96th Annual Meeting
May 14-18, 2016
Baltimore, MD
Register for AATS Week 2016 today & receive a $100 discount off the AATS Aortic Symposium registration fee
Registration & Housing Now Open: Register online or via phone or mail/fax.
Online
Phone: Customer Service Desk: (US) 800- 424-5249; (International) 847-996-5829
Mail/fax: Get the registration form online. By mail: AATS/Experient, 5202 Presidents Court, Frederick, MD 21705 with check and credit card information. By fax: 301-694-5124.
Take Advantage of These AATS Annual Meeting Opportunities
Annual Meeting Registration Packages
Health Care Professional Package: Includes registration for the Saturday Courses, Sunday Symposium and the 96th Annual Meeting (Monday-Wednesday). Register before March 25, 2016 for only $400, after which the fee goes up to $500 — a savings of $300.
Resident/Fellow and Medical Student Package: Includes registration for the Saturday Courses, Sunday Symposium and the 96th Annual Meeting (Monday-Wednesday). Register before March 25, 2016 and attend for no charge. After that date, the fee is $300 — a savings of $300.
Saturday Courses and Sunday Symposium Registration: Register for a Saturday course and/or a Sunday symposium and have access to all other courses/symposia taking place that same day. Note: Registration for the Saturday courses and/or Sunday symposium is separate from the Annual Meeting fee.
AATS Aortic Symposium
May 12–13, 2016
New York, NY
Course Directors
Joseph S. Coselli
Steven L. Lansman
The 2016 AATS Aortic Symposium is a two-day symposium focused on the pathophysiology, diagnosis and treatment of aortic aneurysms and dissections. The conference is designed for cardiovascular and thoracic surgeons, residents, perfusionists, ICU and OR nurses and others involved in aortic disease patient care. Faculty members include world leaders in the field who will share their experiences treating difficult aortic disease cases.
View Preliminary Program, Speakers, Presentations & Full Abstracts
AATS 96th Annual Meeting
May 14-18, 2016
Baltimore, MD
President & Annual Meeting ChaiR
Joseph S. Coselli
Annual Meeting Co-Chairs
Charles D. Fraser
David R. Jones
View Preliminary Program, Speakers, Presentations and Full Abstracts
The 96th Annual Meeting is a five-day program of state-of-the-art presentations by renowned experts. Attendees will enhance their knowledge and skills in a wide-range of subjects including general and specialized cardiac surgery, emerging technologies, congenital heart disease, critical care and aortic/endovascular surgery.
Don’t miss this year’s exciting program including:
Saturday Skills Courses featuring Combined Luncheon Speaker: Denton A. Cooley, followed by Hands-On Sessions
Sunday Postgraduate Symposia with Legends Luncheons featuring Joel D. Cooper and John L. Ochsner
New: Survival Guide for the Cardiothoracic Surgical Team course following by a Hands-On Session (Available to Residents, Fellows and Health Care Professionals Only)
Presidential Address: Competition: Perspiration to Inspiration “Aut viam inveniam aut faciam”, Joseph S. Coselli, Baylor College of Medicine
Basic Science Lecture: Stopping Incurable Cancers through Eliminating their Anti-Oxidative Defenses, James D. Watson, a Nobel Prize-winning biophysicist and researcher who is credited with co-discovering the double-helix structure of DNA.
Honored Guest Lecture: Brian Kelly, Notre Dame Head Football Coach and a veteran of 23 seasons as a collegiate head coach. Brian Kelly brings a championship tradition to his fifth year as the 29th head football coach at the University of Notre Dame.
Emerging Technologies & Techniques Fora: Adult Cardiac and General Thoracic
VAD/ECMO Session
Masters of Surgery: Video Sessions
AATS Learning Center: Featuring cutting-edge case videos of novel procedures and surgical techniques.
AATS Week 2016 Registration & Housing Open!
AATS Week 2016 includes Two Terrific Events
Aortic Symposium
May 12–13, 2016
New York, NY
96th Annual Meeting
May 14-18, 2016
Baltimore, MD
Register for AATS Week 2016 today & receive a $100 discount off the AATS Aortic Symposium registration fee
Registration & Housing Now Open: Register online or via phone or mail/fax.
Online
Phone: Customer Service Desk: (US) 800- 424-5249; (International) 847-996-5829
Mail/fax: Get the registration form online. By mail: AATS/Experient, 5202 Presidents Court, Frederick, MD 21705 with check and credit card information. By fax: 301-694-5124.
Take Advantage of These AATS Annual Meeting Opportunities
Annual Meeting Registration Packages
Health Care Professional Package: Includes registration for the Saturday Courses, Sunday Symposium and the 96th Annual Meeting (Monday-Wednesday). Register before March 25, 2016 for only $400, after which the fee goes up to $500 — a savings of $300.
Resident/Fellow and Medical Student Package: Includes registration for the Saturday Courses, Sunday Symposium and the 96th Annual Meeting (Monday-Wednesday). Register before March 25, 2016 and attend for no charge. After that date, the fee is $300 — a savings of $300.
Saturday Courses and Sunday Symposium Registration: Register for a Saturday course and/or a Sunday symposium and have access to all other courses/symposia taking place that same day. Note: Registration for the Saturday courses and/or Sunday symposium is separate from the Annual Meeting fee.
AATS Aortic Symposium
May 12–13, 2016
New York, NY
Course Directors
Joseph S. Coselli
Steven L. Lansman
The 2016 AATS Aortic Symposium is a two-day symposium focused on the pathophysiology, diagnosis and treatment of aortic aneurysms and dissections. The conference is designed for cardiovascular and thoracic surgeons, residents, perfusionists, ICU and OR nurses and others involved in aortic disease patient care. Faculty members include world leaders in the field who will share their experiences treating difficult aortic disease cases.
View Preliminary Program, Speakers, Presentations & Full Abstracts
AATS 96th Annual Meeting
May 14-18, 2016
Baltimore, MD
President & Annual Meeting ChaiR
Joseph S. Coselli
Annual Meeting Co-Chairs
Charles D. Fraser
David R. Jones
View Preliminary Program, Speakers, Presentations and Full Abstracts
The 96th Annual Meeting is a five-day program of state-of-the-art presentations by renowned experts. Attendees will enhance their knowledge and skills in a wide-range of subjects including general and specialized cardiac surgery, emerging technologies, congenital heart disease, critical care and aortic/endovascular surgery.
Don’t miss this year’s exciting program including:
Saturday Skills Courses featuring Combined Luncheon Speaker: Denton A. Cooley, followed by Hands-On Sessions
Sunday Postgraduate Symposia with Legends Luncheons featuring Joel D. Cooper and John L. Ochsner
New: Survival Guide for the Cardiothoracic Surgical Team course following by a Hands-On Session (Available to Residents, Fellows and Health Care Professionals Only)
Presidential Address: Competition: Perspiration to Inspiration “Aut viam inveniam aut faciam”, Joseph S. Coselli, Baylor College of Medicine
Basic Science Lecture: Stopping Incurable Cancers through Eliminating their Anti-Oxidative Defenses, James D. Watson, a Nobel Prize-winning biophysicist and researcher who is credited with co-discovering the double-helix structure of DNA.
Honored Guest Lecture: Brian Kelly, Notre Dame Head Football Coach and a veteran of 23 seasons as a collegiate head coach. Brian Kelly brings a championship tradition to his fifth year as the 29th head football coach at the University of Notre Dame.
Emerging Technologies & Techniques Fora: Adult Cardiac and General Thoracic
VAD/ECMO Session
Masters of Surgery: Video Sessions
AATS Learning Center: Featuring cutting-edge case videos of novel procedures and surgical techniques.
AATS Week 2016 Registration & Housing Open!
AATS Week 2016 includes Two Terrific Events
Aortic Symposium
May 12–13, 2016
New York, NY
96th Annual Meeting
May 14-18, 2016
Baltimore, MD
Register for AATS Week 2016 today & receive a $100 discount off the AATS Aortic Symposium registration fee
Registration & Housing Now Open: Register online or via phone or mail/fax.
Online
Phone: Customer Service Desk: (US) 800- 424-5249; (International) 847-996-5829
Mail/fax: Get the registration form online. By mail: AATS/Experient, 5202 Presidents Court, Frederick, MD 21705 with check and credit card information. By fax: 301-694-5124.
Take Advantage of These AATS Annual Meeting Opportunities
Annual Meeting Registration Packages
Health Care Professional Package: Includes registration for the Saturday Courses, Sunday Symposium and the 96th Annual Meeting (Monday-Wednesday). Register before March 25, 2016 for only $400, after which the fee goes up to $500 — a savings of $300.
Resident/Fellow and Medical Student Package: Includes registration for the Saturday Courses, Sunday Symposium and the 96th Annual Meeting (Monday-Wednesday). Register before March 25, 2016 and attend for no charge. After that date, the fee is $300 — a savings of $300.
Saturday Courses and Sunday Symposium Registration: Register for a Saturday course and/or a Sunday symposium and have access to all other courses/symposia taking place that same day. Note: Registration for the Saturday courses and/or Sunday symposium is separate from the Annual Meeting fee.
AATS Aortic Symposium
May 12–13, 2016
New York, NY
Course Directors
Joseph S. Coselli
Steven L. Lansman
The 2016 AATS Aortic Symposium is a two-day symposium focused on the pathophysiology, diagnosis and treatment of aortic aneurysms and dissections. The conference is designed for cardiovascular and thoracic surgeons, residents, perfusionists, ICU and OR nurses and others involved in aortic disease patient care. Faculty members include world leaders in the field who will share their experiences treating difficult aortic disease cases.
View Preliminary Program, Speakers, Presentations & Full Abstracts
AATS 96th Annual Meeting
May 14-18, 2016
Baltimore, MD
President & Annual Meeting ChaiR
Joseph S. Coselli
Annual Meeting Co-Chairs
Charles D. Fraser
David R. Jones
View Preliminary Program, Speakers, Presentations and Full Abstracts
The 96th Annual Meeting is a five-day program of state-of-the-art presentations by renowned experts. Attendees will enhance their knowledge and skills in a wide-range of subjects including general and specialized cardiac surgery, emerging technologies, congenital heart disease, critical care and aortic/endovascular surgery.
Don’t miss this year’s exciting program including:
Saturday Skills Courses featuring Combined Luncheon Speaker: Denton A. Cooley, followed by Hands-On Sessions
Sunday Postgraduate Symposia with Legends Luncheons featuring Joel D. Cooper and John L. Ochsner
New: Survival Guide for the Cardiothoracic Surgical Team course following by a Hands-On Session (Available to Residents, Fellows and Health Care Professionals Only)
Presidential Address: Competition: Perspiration to Inspiration “Aut viam inveniam aut faciam”, Joseph S. Coselli, Baylor College of Medicine
Basic Science Lecture: Stopping Incurable Cancers through Eliminating their Anti-Oxidative Defenses, James D. Watson, a Nobel Prize-winning biophysicist and researcher who is credited with co-discovering the double-helix structure of DNA.
Honored Guest Lecture: Brian Kelly, Notre Dame Head Football Coach and a veteran of 23 seasons as a collegiate head coach. Brian Kelly brings a championship tradition to his fifth year as the 29th head football coach at the University of Notre Dame.
Emerging Technologies & Techniques Fora: Adult Cardiac and General Thoracic
VAD/ECMO Session
Masters of Surgery: Video Sessions
AATS Learning Center: Featuring cutting-edge case videos of novel procedures and surgical techniques.
LISTEN NOW: Harvard Health Policy Professor Robert Blendon Discusses Democratic Presidential Candidate Stances
Listen to more of our interview with Robert Blendon, professor of health policy and political analysis at the Harvard T.H. Chan School of Public Health and Harvard Kennedy School of Government.
Listen to more of our interview with Robert Blendon, professor of health policy and political analysis at the Harvard T.H. Chan School of Public Health and Harvard Kennedy School of Government.
Listen to more of our interview with Robert Blendon, professor of health policy and political analysis at the Harvard T.H. Chan School of Public Health and Harvard Kennedy School of Government.
LISTEN NOW: Kendall Rogers, MD, SFHM, Discusses Hm16's New Health IT Track
Kendall Rogers, MD, SFHM, chair of SHM’s Health IT Committee, discusses HM16 having a separate track for health IT, to whom the track is geared, and translating tech-savviness into actually being effective in helping to develop practical health IT.
Kendall Rogers, MD, SFHM, chair of SHM’s Health IT Committee, discusses HM16 having a separate track for health IT, to whom the track is geared, and translating tech-savviness into actually being effective in helping to develop practical health IT.
Kendall Rogers, MD, SFHM, chair of SHM’s Health IT Committee, discusses HM16 having a separate track for health IT, to whom the track is geared, and translating tech-savviness into actually being effective in helping to develop practical health IT.