User login
NICE publishes guideline for multiple myeloma

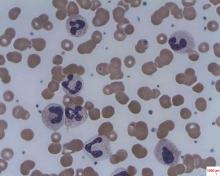
Photo courtesy of NIH
The National Institute for Health and Care Excellence (NICE) has published a guideline containing recommendations for diagnosing, treating, and monitoring patients with multiple myeloma (MM).
The aim of the guideline is to help the National Health Service provide optimal care for MM patients over the age of 16 in England.
The guideline complements existing NICE guidance on the treatment of MM.
“Although there is no cure for myeloma, several novel drug treatments have been licensed in the past 10 years that have led to substantial improvements in the quality and length of time it is possible to live with the disease,” said Mark Baker, clinical practice director for NICE.
“However, there is still variation across the country in terms of providing a coherent and consistent approach to the management of myeloma. Myeloma is also a difficult condition to diagnose because many of the symptoms are non-specific. Our guideline sets out best-practice care to ensure people live as normal a life as possible for as long as possible.”
Some of the recommendations in the guideline include:
Communication and support: Offer prompt psychological assessment and support to MM patients at diagnosis and, as appropriate, at the beginning and end of each treatment, whenever the disease progresses, and when patients require end-of-life care.
Laboratory investigations to provide prognostic information: Use the same sample for all diagnostic and prognostic tests on bone marrow so patients only have to have one bone marrow aspirate and trephine biopsy.
Imaging for people with suspected MM: Offer imaging to all people with a plasma cell disorder suspected to be myeloma. Doctors should consider whole-body MRI as the first imaging procedure.
Service organizations: Each hospital treating MM patients should provide regional access through its network to facilities for intensive inpatient chemotherapy or transplantation, renal support, spinal disease management, specialized pain management, therapeutic apheresis, radiotherapy, restorative dentistry and oral surgery, and clinical trials, in particular early phase trials.
Managing relapsed MM: Offer a second autologous stem cell transplant to people with relapsed MM who are suitable and who have completed re-induction therapy without disease progression and had a response duration of more than 24 months after their first transplant. A second autologous stem cell transplant should be considered in people who have had a response duration of between 12 and 24 months after their first transplant. ![]()

Photo courtesy of NIH
The National Institute for Health and Care Excellence (NICE) has published a guideline containing recommendations for diagnosing, treating, and monitoring patients with multiple myeloma (MM).
The aim of the guideline is to help the National Health Service provide optimal care for MM patients over the age of 16 in England.
The guideline complements existing NICE guidance on the treatment of MM.
“Although there is no cure for myeloma, several novel drug treatments have been licensed in the past 10 years that have led to substantial improvements in the quality and length of time it is possible to live with the disease,” said Mark Baker, clinical practice director for NICE.
“However, there is still variation across the country in terms of providing a coherent and consistent approach to the management of myeloma. Myeloma is also a difficult condition to diagnose because many of the symptoms are non-specific. Our guideline sets out best-practice care to ensure people live as normal a life as possible for as long as possible.”
Some of the recommendations in the guideline include:
Communication and support: Offer prompt psychological assessment and support to MM patients at diagnosis and, as appropriate, at the beginning and end of each treatment, whenever the disease progresses, and when patients require end-of-life care.
Laboratory investigations to provide prognostic information: Use the same sample for all diagnostic and prognostic tests on bone marrow so patients only have to have one bone marrow aspirate and trephine biopsy.
Imaging for people with suspected MM: Offer imaging to all people with a plasma cell disorder suspected to be myeloma. Doctors should consider whole-body MRI as the first imaging procedure.
Service organizations: Each hospital treating MM patients should provide regional access through its network to facilities for intensive inpatient chemotherapy or transplantation, renal support, spinal disease management, specialized pain management, therapeutic apheresis, radiotherapy, restorative dentistry and oral surgery, and clinical trials, in particular early phase trials.
Managing relapsed MM: Offer a second autologous stem cell transplant to people with relapsed MM who are suitable and who have completed re-induction therapy without disease progression and had a response duration of more than 24 months after their first transplant. A second autologous stem cell transplant should be considered in people who have had a response duration of between 12 and 24 months after their first transplant. ![]()

Photo courtesy of NIH
The National Institute for Health and Care Excellence (NICE) has published a guideline containing recommendations for diagnosing, treating, and monitoring patients with multiple myeloma (MM).
The aim of the guideline is to help the National Health Service provide optimal care for MM patients over the age of 16 in England.
The guideline complements existing NICE guidance on the treatment of MM.
“Although there is no cure for myeloma, several novel drug treatments have been licensed in the past 10 years that have led to substantial improvements in the quality and length of time it is possible to live with the disease,” said Mark Baker, clinical practice director for NICE.
“However, there is still variation across the country in terms of providing a coherent and consistent approach to the management of myeloma. Myeloma is also a difficult condition to diagnose because many of the symptoms are non-specific. Our guideline sets out best-practice care to ensure people live as normal a life as possible for as long as possible.”
Some of the recommendations in the guideline include:
Communication and support: Offer prompt psychological assessment and support to MM patients at diagnosis and, as appropriate, at the beginning and end of each treatment, whenever the disease progresses, and when patients require end-of-life care.
Laboratory investigations to provide prognostic information: Use the same sample for all diagnostic and prognostic tests on bone marrow so patients only have to have one bone marrow aspirate and trephine biopsy.
Imaging for people with suspected MM: Offer imaging to all people with a plasma cell disorder suspected to be myeloma. Doctors should consider whole-body MRI as the first imaging procedure.
Service organizations: Each hospital treating MM patients should provide regional access through its network to facilities for intensive inpatient chemotherapy or transplantation, renal support, spinal disease management, specialized pain management, therapeutic apheresis, radiotherapy, restorative dentistry and oral surgery, and clinical trials, in particular early phase trials.
Managing relapsed MM: Offer a second autologous stem cell transplant to people with relapsed MM who are suitable and who have completed re-induction therapy without disease progression and had a response duration of more than 24 months after their first transplant. A second autologous stem cell transplant should be considered in people who have had a response duration of between 12 and 24 months after their first transplant. ![]()
Method may reduce toxicity of anticancer agents

Researchers believe they have found a way to make certain anticancer agents safer without compromising their efficacy.
The team noted that Aurora B kinase inhibitors and other agents targeting the cell cycle have proven effective but highly toxic in clinical trials.
In an attempt to solve this problem, the researchers turned to nanotechnology. They encapsulated the Aurora B kinase inhibitor AZD2811 in polymeric nanoparticles called Accurins.
Susan Ashton, of AstraZeneca in Macclesfield, Cheshire, UK, and her colleagues developed the Accurins and described the work in Science Translational Medicine. The work was funded by AstraZeneca.
The Accurins consist of block copolymers of poly-D,L-lactide and poly(ethylene glycol). The researchers used an ion pairing approach to efficiently encapsulate AZD2811 and control release of the drug.
They found the Accurins could release AZD2811 continuously for more than 1 week in vitro. The nanoparticles also reduced tumor phosphorylated histone H3 levels in vivo for up to 96 hours after a single administration.
The researchers tested the AZD2811 Accurins in mice with diffuse large B-cell lymphoma and rats with colorectal tumors. The nanoparticles accumulated specifically in tumors, where they slowly released AZD2811 to cancer cells.
Compared to AZD1152 (a water-soluble prodrug of AZD2811), the AZD2811 Accurins blocked tumor growth more effectively at one-half the drug dose and caused fewer side effects in the rodents.
Based on these results, the researchers said Accurins could provide efficacy and tolerability using a more convenient dosing regimen, which may extend the utility of Aurora B kinase inhibition to a broader range of hematologic and solid tumor malignancies.
A phase 1 study (NCT02579226) testing AZD2811 Accurins in advanced solid tumors is currently recruiting patients.
A related Focus article published in Science Translational Medicine offers more insights on how Accurin nanoparticles may help enhance the safety and antitumor activity of Aurora kinase inhibitors and other molecularly targeted drugs. ![]()

Researchers believe they have found a way to make certain anticancer agents safer without compromising their efficacy.
The team noted that Aurora B kinase inhibitors and other agents targeting the cell cycle have proven effective but highly toxic in clinical trials.
In an attempt to solve this problem, the researchers turned to nanotechnology. They encapsulated the Aurora B kinase inhibitor AZD2811 in polymeric nanoparticles called Accurins.
Susan Ashton, of AstraZeneca in Macclesfield, Cheshire, UK, and her colleagues developed the Accurins and described the work in Science Translational Medicine. The work was funded by AstraZeneca.
The Accurins consist of block copolymers of poly-D,L-lactide and poly(ethylene glycol). The researchers used an ion pairing approach to efficiently encapsulate AZD2811 and control release of the drug.
They found the Accurins could release AZD2811 continuously for more than 1 week in vitro. The nanoparticles also reduced tumor phosphorylated histone H3 levels in vivo for up to 96 hours after a single administration.
The researchers tested the AZD2811 Accurins in mice with diffuse large B-cell lymphoma and rats with colorectal tumors. The nanoparticles accumulated specifically in tumors, where they slowly released AZD2811 to cancer cells.
Compared to AZD1152 (a water-soluble prodrug of AZD2811), the AZD2811 Accurins blocked tumor growth more effectively at one-half the drug dose and caused fewer side effects in the rodents.
Based on these results, the researchers said Accurins could provide efficacy and tolerability using a more convenient dosing regimen, which may extend the utility of Aurora B kinase inhibition to a broader range of hematologic and solid tumor malignancies.
A phase 1 study (NCT02579226) testing AZD2811 Accurins in advanced solid tumors is currently recruiting patients.
A related Focus article published in Science Translational Medicine offers more insights on how Accurin nanoparticles may help enhance the safety and antitumor activity of Aurora kinase inhibitors and other molecularly targeted drugs. ![]()

Researchers believe they have found a way to make certain anticancer agents safer without compromising their efficacy.
The team noted that Aurora B kinase inhibitors and other agents targeting the cell cycle have proven effective but highly toxic in clinical trials.
In an attempt to solve this problem, the researchers turned to nanotechnology. They encapsulated the Aurora B kinase inhibitor AZD2811 in polymeric nanoparticles called Accurins.
Susan Ashton, of AstraZeneca in Macclesfield, Cheshire, UK, and her colleagues developed the Accurins and described the work in Science Translational Medicine. The work was funded by AstraZeneca.
The Accurins consist of block copolymers of poly-D,L-lactide and poly(ethylene glycol). The researchers used an ion pairing approach to efficiently encapsulate AZD2811 and control release of the drug.
They found the Accurins could release AZD2811 continuously for more than 1 week in vitro. The nanoparticles also reduced tumor phosphorylated histone H3 levels in vivo for up to 96 hours after a single administration.
The researchers tested the AZD2811 Accurins in mice with diffuse large B-cell lymphoma and rats with colorectal tumors. The nanoparticles accumulated specifically in tumors, where they slowly released AZD2811 to cancer cells.
Compared to AZD1152 (a water-soluble prodrug of AZD2811), the AZD2811 Accurins blocked tumor growth more effectively at one-half the drug dose and caused fewer side effects in the rodents.
Based on these results, the researchers said Accurins could provide efficacy and tolerability using a more convenient dosing regimen, which may extend the utility of Aurora B kinase inhibition to a broader range of hematologic and solid tumor malignancies.
A phase 1 study (NCT02579226) testing AZD2811 Accurins in advanced solid tumors is currently recruiting patients.
A related Focus article published in Science Translational Medicine offers more insights on how Accurin nanoparticles may help enhance the safety and antitumor activity of Aurora kinase inhibitors and other molecularly targeted drugs. ![]()
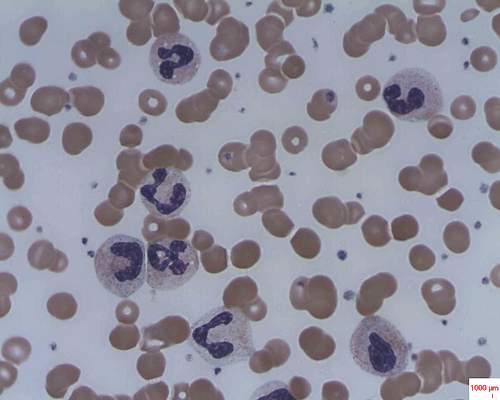
Dendritic cells appear to promote T-ALL

Dendritic cells may play a key role in T-cell acute lymphoblastic leukemia (T-ALL), according to research published in PNAS.
Investigators identified tumor-associated dendritic cells that appeared to promote T-ALL growth and survival at primary and metastatic tumor sites in mice.
Analyses of samples from patients with T-ALL suggested dendritic cells are positioned to support T-ALL growth in humans as well.
“It’s only more recently that people have really appreciated that tumors are complex organs in and of themselves, with all of the heterogenous cell types that can talk to each other and promote each other’s survival and proliferation,” said study author Lauren Ehrlich, PhD, of the University of Texas at Austin.
Dr Ehrlich and her colleagues first found that primary T-ALL cells required tumor stroma for survival ex vivo. When T-ALL cells were cultured alone or in wild-type thymic stroma, the cells died off. Only T-ALL cells cultured with tumor-associated stroma survived.
Subsequent experiments suggested it was tumor-associated dendritic cells that spurred T-ALL growth, both for newly developing T-ALL cells and tumors that had spread to distant organs in mouse models. Tissue samples from pediatric T-ALL patients had similar growth environments with abundant dendritic cells.
To determine the mechanism by which dendritic cells support T-ALL, the investigators performed gene expression profiling. They found upregulation of PDGFRB and IGF1R on T-ALL cells, with concomitant expression of their ligands by tumor-associated dendritic cells.
The team said PDGFRB and IGF1R were activated in T-ALL cells ex vivo. And when they cocultured T-ALL cells with tumor-associated dendritic cells, they observed sustained IGF1R activation. However, they did not see this activation when they cocultured T-ALL cells with normal thymic dendritic cells.
Finally, the investigators found that IGF1R signaling was necessary for dendritic cell-mediated T-ALL survival.
The team said this is the first evidence that endogenous tumor-associated dendritic cells supply signals driving T-ALL growth.
“We hope this study will be a catalyst to spur other research groups to further elucidate the roles of dendritic cells in supporting T-ALL,” said study author Todd Triplett, PhD, also of the University of Texas at Austin.
“[T]hat could ultimately lead to the discovery of novel therapeutic targets that are more effective and less toxic than current treatment regimens.” ![]()

Dendritic cells may play a key role in T-cell acute lymphoblastic leukemia (T-ALL), according to research published in PNAS.
Investigators identified tumor-associated dendritic cells that appeared to promote T-ALL growth and survival at primary and metastatic tumor sites in mice.
Analyses of samples from patients with T-ALL suggested dendritic cells are positioned to support T-ALL growth in humans as well.
“It’s only more recently that people have really appreciated that tumors are complex organs in and of themselves, with all of the heterogenous cell types that can talk to each other and promote each other’s survival and proliferation,” said study author Lauren Ehrlich, PhD, of the University of Texas at Austin.
Dr Ehrlich and her colleagues first found that primary T-ALL cells required tumor stroma for survival ex vivo. When T-ALL cells were cultured alone or in wild-type thymic stroma, the cells died off. Only T-ALL cells cultured with tumor-associated stroma survived.
Subsequent experiments suggested it was tumor-associated dendritic cells that spurred T-ALL growth, both for newly developing T-ALL cells and tumors that had spread to distant organs in mouse models. Tissue samples from pediatric T-ALL patients had similar growth environments with abundant dendritic cells.
To determine the mechanism by which dendritic cells support T-ALL, the investigators performed gene expression profiling. They found upregulation of PDGFRB and IGF1R on T-ALL cells, with concomitant expression of their ligands by tumor-associated dendritic cells.
The team said PDGFRB and IGF1R were activated in T-ALL cells ex vivo. And when they cocultured T-ALL cells with tumor-associated dendritic cells, they observed sustained IGF1R activation. However, they did not see this activation when they cocultured T-ALL cells with normal thymic dendritic cells.
Finally, the investigators found that IGF1R signaling was necessary for dendritic cell-mediated T-ALL survival.
The team said this is the first evidence that endogenous tumor-associated dendritic cells supply signals driving T-ALL growth.
“We hope this study will be a catalyst to spur other research groups to further elucidate the roles of dendritic cells in supporting T-ALL,” said study author Todd Triplett, PhD, also of the University of Texas at Austin.
“[T]hat could ultimately lead to the discovery of novel therapeutic targets that are more effective and less toxic than current treatment regimens.” ![]()

Dendritic cells may play a key role in T-cell acute lymphoblastic leukemia (T-ALL), according to research published in PNAS.
Investigators identified tumor-associated dendritic cells that appeared to promote T-ALL growth and survival at primary and metastatic tumor sites in mice.
Analyses of samples from patients with T-ALL suggested dendritic cells are positioned to support T-ALL growth in humans as well.
“It’s only more recently that people have really appreciated that tumors are complex organs in and of themselves, with all of the heterogenous cell types that can talk to each other and promote each other’s survival and proliferation,” said study author Lauren Ehrlich, PhD, of the University of Texas at Austin.
Dr Ehrlich and her colleagues first found that primary T-ALL cells required tumor stroma for survival ex vivo. When T-ALL cells were cultured alone or in wild-type thymic stroma, the cells died off. Only T-ALL cells cultured with tumor-associated stroma survived.
Subsequent experiments suggested it was tumor-associated dendritic cells that spurred T-ALL growth, both for newly developing T-ALL cells and tumors that had spread to distant organs in mouse models. Tissue samples from pediatric T-ALL patients had similar growth environments with abundant dendritic cells.
To determine the mechanism by which dendritic cells support T-ALL, the investigators performed gene expression profiling. They found upregulation of PDGFRB and IGF1R on T-ALL cells, with concomitant expression of their ligands by tumor-associated dendritic cells.
The team said PDGFRB and IGF1R were activated in T-ALL cells ex vivo. And when they cocultured T-ALL cells with tumor-associated dendritic cells, they observed sustained IGF1R activation. However, they did not see this activation when they cocultured T-ALL cells with normal thymic dendritic cells.
Finally, the investigators found that IGF1R signaling was necessary for dendritic cell-mediated T-ALL survival.
The team said this is the first evidence that endogenous tumor-associated dendritic cells supply signals driving T-ALL growth.
“We hope this study will be a catalyst to spur other research groups to further elucidate the roles of dendritic cells in supporting T-ALL,” said study author Todd Triplett, PhD, also of the University of Texas at Austin.
“[T]hat could ultimately lead to the discovery of novel therapeutic targets that are more effective and less toxic than current treatment regimens.” ![]()
Development of myelofibrosis drug on hold

The US Food and Drug Administration (FDA) has placed a full clinical hold on trials conducted under the investigational new drug application for pacritinib, a JAK2/FLT3 inhibitor being developed by CTI BioPharma for the treatment of myelofibrosis (MF).
The hold means all patients currently on pacritinib must stop taking the drug immediately, and no patients can be enrolled on a pacritinib trial or start pacritinib as initial or crossover treatment.
In addition, CTI BioPharma has withdrawn the new drug application for pacritinib while the company reviews data from the phase 3 PERSIST-2 trial.
The FDA’s decision to place a full clinical hold on pacritinib trials was due to interim results from PERSIST-2. The aim of this trial was to compare pacritinib to best available therapy in patients with thrombocytopenia and primary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF.
The overall survival results from PERSIST-2 indicate that pacritinib had a detrimental effect on survival, which is consistent with results from the PERSIST-1 trial. The deaths in pacritinib-treated patients on PERSIST-2 include intracranial hemorrhage, cardiac failure, and cardiac arrest.
Based on these results, the FDA has made recommendations for CTI BioPharma that supersede the agency’s previous recommendations.
On February 4, 2016, the FDA placed a partial clinical hold on pacritinib trials and made related recommendations for CTI BioPharma, advising that the company modify trial protocols and take other actions in compliance with the partial clinical hold.
Now that pacritinib trials are on full clinical hold, the FDA is recommending that CTI BioPharma conduct dose exploration studies for pacritinib in patients with MF and submit final study reports and datasets for PERSIST-1 and PERSIST-2.
The FDA is also recommending that CTI BioPharma provide certain notifications, revise relevant statements in the related investigator’s brochure and informed consent documents, make certain modifications to protocols, and request a meeting with the FDA prior to submitting a response to the full clinical hold.
CTI BioPharma said all clinical investigators worldwide have been notified of the hold. ![]()

The US Food and Drug Administration (FDA) has placed a full clinical hold on trials conducted under the investigational new drug application for pacritinib, a JAK2/FLT3 inhibitor being developed by CTI BioPharma for the treatment of myelofibrosis (MF).
The hold means all patients currently on pacritinib must stop taking the drug immediately, and no patients can be enrolled on a pacritinib trial or start pacritinib as initial or crossover treatment.
In addition, CTI BioPharma has withdrawn the new drug application for pacritinib while the company reviews data from the phase 3 PERSIST-2 trial.
The FDA’s decision to place a full clinical hold on pacritinib trials was due to interim results from PERSIST-2. The aim of this trial was to compare pacritinib to best available therapy in patients with thrombocytopenia and primary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF.
The overall survival results from PERSIST-2 indicate that pacritinib had a detrimental effect on survival, which is consistent with results from the PERSIST-1 trial. The deaths in pacritinib-treated patients on PERSIST-2 include intracranial hemorrhage, cardiac failure, and cardiac arrest.
Based on these results, the FDA has made recommendations for CTI BioPharma that supersede the agency’s previous recommendations.
On February 4, 2016, the FDA placed a partial clinical hold on pacritinib trials and made related recommendations for CTI BioPharma, advising that the company modify trial protocols and take other actions in compliance with the partial clinical hold.
Now that pacritinib trials are on full clinical hold, the FDA is recommending that CTI BioPharma conduct dose exploration studies for pacritinib in patients with MF and submit final study reports and datasets for PERSIST-1 and PERSIST-2.
The FDA is also recommending that CTI BioPharma provide certain notifications, revise relevant statements in the related investigator’s brochure and informed consent documents, make certain modifications to protocols, and request a meeting with the FDA prior to submitting a response to the full clinical hold.
CTI BioPharma said all clinical investigators worldwide have been notified of the hold. ![]()

The US Food and Drug Administration (FDA) has placed a full clinical hold on trials conducted under the investigational new drug application for pacritinib, a JAK2/FLT3 inhibitor being developed by CTI BioPharma for the treatment of myelofibrosis (MF).
The hold means all patients currently on pacritinib must stop taking the drug immediately, and no patients can be enrolled on a pacritinib trial or start pacritinib as initial or crossover treatment.
In addition, CTI BioPharma has withdrawn the new drug application for pacritinib while the company reviews data from the phase 3 PERSIST-2 trial.
The FDA’s decision to place a full clinical hold on pacritinib trials was due to interim results from PERSIST-2. The aim of this trial was to compare pacritinib to best available therapy in patients with thrombocytopenia and primary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF.
The overall survival results from PERSIST-2 indicate that pacritinib had a detrimental effect on survival, which is consistent with results from the PERSIST-1 trial. The deaths in pacritinib-treated patients on PERSIST-2 include intracranial hemorrhage, cardiac failure, and cardiac arrest.
Based on these results, the FDA has made recommendations for CTI BioPharma that supersede the agency’s previous recommendations.
On February 4, 2016, the FDA placed a partial clinical hold on pacritinib trials and made related recommendations for CTI BioPharma, advising that the company modify trial protocols and take other actions in compliance with the partial clinical hold.
Now that pacritinib trials are on full clinical hold, the FDA is recommending that CTI BioPharma conduct dose exploration studies for pacritinib in patients with MF and submit final study reports and datasets for PERSIST-1 and PERSIST-2.
The FDA is also recommending that CTI BioPharma provide certain notifications, revise relevant statements in the related investigator’s brochure and informed consent documents, make certain modifications to protocols, and request a meeting with the FDA prior to submitting a response to the full clinical hold.
CTI BioPharma said all clinical investigators worldwide have been notified of the hold. ![]()
ERAS eliminated racial disparities in postop hospital stay
JACKSONVILLE, FLA. – An enhanced recovery protocol after colorectal surgery nearly eliminated differences in hospital stays between black and white patients, according to a study based on data from the University of Alabama at Birmingham.
Dr. Tyler S. Wahl, a resident at UAB reported on the institution’s experience with the Enhanced Recovery After Surgery (ERAS) pathway at the Association of Academic Surgery/Society of University Surgeons Academic Surgical Congress. “ERAS has been shown to reduce length of stay, cost, and perioperative complications without compromising readmission or mortality rates,” Dr. Wahl said. Dr. Daniel Chu was senior author.
Surgical literature has increasingly demonstrated disparities among black patients undergoing major surgery: longer lengths of stay, more readmissions, increased postoperative mortality and lower survival rates after colorectal cancer resections, Dr. Wahl said. The UAB investigators set out to determine whether the ERAS pathway would reduce disparities in length of stay among black and white patients when compared to the traditional pathway.
Before UAB started using ERAS for colorectal patients, the average length of stay for patients undergoing colorectal surgery was 6.7 days with significant differences between black and white patients: 8 days vs. 6.1 days, respectively. However, after implementation of the ERAS pathway in January 2015, average length of stay declined to 4.7 days overall. Black patients had dramatic reductions in length of stay, compared with white patients, with stays of 3.9 days vs. 5 days, respectively.
“Not only were patients leaving much earlier, but their length of stay was also shorter than predicted using the American College of Surgeons Risk Calculator,” Dr. Wahl said.
The UAB study was a retrospective, matched cohort analysis of 258 patients – 129 patients from pre-ERAS years were compared with 129 ERAS patients from January to October 2015.
Study subjects were similar in many patient- and procedure-specific factors; however, differences in operative approach, indication, ostomy formation, and operative time did not change the predicted length of stay among races, Dr. Wahl said.
Dr. Wahl said the racial makeup of the study differs from most ERAS literature in colorectal patients. “The overall percentage of the African American population was 30% within our study, as most ERAS literature has 10% or less,” he added.
“Further work needs to be pursued to find what’s driving these dramatic results among the black population,” he said.
Dr. Wahl and coauthors had no disclosures.
JACKSONVILLE, FLA. – An enhanced recovery protocol after colorectal surgery nearly eliminated differences in hospital stays between black and white patients, according to a study based on data from the University of Alabama at Birmingham.
Dr. Tyler S. Wahl, a resident at UAB reported on the institution’s experience with the Enhanced Recovery After Surgery (ERAS) pathway at the Association of Academic Surgery/Society of University Surgeons Academic Surgical Congress. “ERAS has been shown to reduce length of stay, cost, and perioperative complications without compromising readmission or mortality rates,” Dr. Wahl said. Dr. Daniel Chu was senior author.
Surgical literature has increasingly demonstrated disparities among black patients undergoing major surgery: longer lengths of stay, more readmissions, increased postoperative mortality and lower survival rates after colorectal cancer resections, Dr. Wahl said. The UAB investigators set out to determine whether the ERAS pathway would reduce disparities in length of stay among black and white patients when compared to the traditional pathway.
Before UAB started using ERAS for colorectal patients, the average length of stay for patients undergoing colorectal surgery was 6.7 days with significant differences between black and white patients: 8 days vs. 6.1 days, respectively. However, after implementation of the ERAS pathway in January 2015, average length of stay declined to 4.7 days overall. Black patients had dramatic reductions in length of stay, compared with white patients, with stays of 3.9 days vs. 5 days, respectively.
“Not only were patients leaving much earlier, but their length of stay was also shorter than predicted using the American College of Surgeons Risk Calculator,” Dr. Wahl said.
The UAB study was a retrospective, matched cohort analysis of 258 patients – 129 patients from pre-ERAS years were compared with 129 ERAS patients from January to October 2015.
Study subjects were similar in many patient- and procedure-specific factors; however, differences in operative approach, indication, ostomy formation, and operative time did not change the predicted length of stay among races, Dr. Wahl said.
Dr. Wahl said the racial makeup of the study differs from most ERAS literature in colorectal patients. “The overall percentage of the African American population was 30% within our study, as most ERAS literature has 10% or less,” he added.
“Further work needs to be pursued to find what’s driving these dramatic results among the black population,” he said.
Dr. Wahl and coauthors had no disclosures.
JACKSONVILLE, FLA. – An enhanced recovery protocol after colorectal surgery nearly eliminated differences in hospital stays between black and white patients, according to a study based on data from the University of Alabama at Birmingham.
Dr. Tyler S. Wahl, a resident at UAB reported on the institution’s experience with the Enhanced Recovery After Surgery (ERAS) pathway at the Association of Academic Surgery/Society of University Surgeons Academic Surgical Congress. “ERAS has been shown to reduce length of stay, cost, and perioperative complications without compromising readmission or mortality rates,” Dr. Wahl said. Dr. Daniel Chu was senior author.
Surgical literature has increasingly demonstrated disparities among black patients undergoing major surgery: longer lengths of stay, more readmissions, increased postoperative mortality and lower survival rates after colorectal cancer resections, Dr. Wahl said. The UAB investigators set out to determine whether the ERAS pathway would reduce disparities in length of stay among black and white patients when compared to the traditional pathway.
Before UAB started using ERAS for colorectal patients, the average length of stay for patients undergoing colorectal surgery was 6.7 days with significant differences between black and white patients: 8 days vs. 6.1 days, respectively. However, after implementation of the ERAS pathway in January 2015, average length of stay declined to 4.7 days overall. Black patients had dramatic reductions in length of stay, compared with white patients, with stays of 3.9 days vs. 5 days, respectively.
“Not only were patients leaving much earlier, but their length of stay was also shorter than predicted using the American College of Surgeons Risk Calculator,” Dr. Wahl said.
The UAB study was a retrospective, matched cohort analysis of 258 patients – 129 patients from pre-ERAS years were compared with 129 ERAS patients from January to October 2015.
Study subjects were similar in many patient- and procedure-specific factors; however, differences in operative approach, indication, ostomy formation, and operative time did not change the predicted length of stay among races, Dr. Wahl said.
Dr. Wahl said the racial makeup of the study differs from most ERAS literature in colorectal patients. “The overall percentage of the African American population was 30% within our study, as most ERAS literature has 10% or less,” he added.
“Further work needs to be pursued to find what’s driving these dramatic results among the black population,” he said.
Dr. Wahl and coauthors had no disclosures.
FROM THE ACADEMIC SURGICAL CONGRESS
Key clinical point: Use of the ERAS pathway reduced hospital stays for all patients after colorectal surgery, with results most dramatic in black patients.
Major finding: Hospital stays declined from 6.7 days before ERAS to 4.7 days afterward, with stays for blacks declining from 8 days before ERAS to 3.9 days afterward.
Data source: Retrospective, matched cohort analysis of 258 patients – 129 patients from pre-ERAS years were compared to 129 ERAS patients from January to October 2015.
Disclosures: The study authors reported having no financial disclosures.
Do we give too much iron?
A 69-year-old man is evaluated for fatigue. He undergoes a colonoscopy and is found to have a right-sided colon cancer. His hematocrit is 33 with an MCV of 72. His ferritin level is 3. What do you recommend to help with his iron deficiency?
A. Ferrous sulfate 325 mg daily.
B. Ferrous sulfate 325 mg b.i.d.
C. Ferrous sulfate 325 mg t.i.d.
Treatment of iron deficiency with oral iron has traditionally been done by giving 150-200 mg of elemental iron (which is equal to three 325 mg tablets of iron sulfate).1 This dosing regimen has considerable gastrointestinal side effects. Recent research into iron absorption suggests that the higher the dose of iron given, the more absorption may be hindered. In a study of 54 women who had low ferritin levels, lower daily doses of iron – and not giving it multiple times a day – led to better iron absorption.2
In a study of elderly patients with iron deficiency, 90 hospitalized elderly patients older than 80 years with iron deficiency anemia were randomized to receive elemental iron as 15 mg or 50 mg of liquid ferrous gluconate, or 150 mg of ferrous calcium citrate for 60 days.3 Two months of iron treatment raised hemoglobin and ferritin levels to a similar degree in all groups, with no significant differences between the 15-mg, 50-mg, and 150-mg groups.
There was a significant difference in abdominal discomfort, with much less (20%) in the patients who received 15 mg of ferrous gluconate, compared with 60% in those who received 50 mg and 70% in those receiving 150 mg (P less than .05 comparing 15 mg with 50 mg and 150 mg). Statistically significant differences were also seen for nausea/vomiting, constipation, and dropout, with much lower rates seen in the low-dose (15-mg) group.
In a study of iron supplementation in individuals undergoing blood donation, a single daily dose of iron was used (37.5 mg of elemental iron) in half of the subjects, with the rest of the subjects receiving no iron.4 The mean age of the participants was 48 years.
Subjects who received the once-daily low-dose iron recovered much more quickly toward predonation hematocrit than did those who did not receive the low-dose iron (time to 80% hemoglobin recovery, 32 days vs. 92 days in the non–iron treated patients, P = .02). The effect was more dramatic in subjects who started with a low ferritin level (defined as less than 26), where time to 80% hemoglobin recovery was 36 days in the iron-treated patients vs. 153 days for the no-iron group.
The results of this study are in line with what we know about avid iron absorption in iron deficient patients, and the success of low doses in a younger patient population is encouraging.
In a small study looking at two different doses of elemental iron for the treatment of iron deficiency, 24 women (ages 18-35 years) with iron deficiency were randomized to 60 mg or 80 mg of elemental iron or placebo for 16 weeks.5 There was no difference in normalization of ferritin levels in the women who received either dose of iron. There was also no difference in side effects between the groups.
This study is small and had minimal difference in iron dose. In addition, the dosing was given once a day for both groups. I suspect that the lack of difference in side effects was due to both the small size of the study and the minimal difference in iron dose.
What does this all mean? I think that the most appropriate dosing for oral iron replacement is a single daily low-dose iron preparation. Whether that dose is 15 mg of elemental iron to 68 mg of elemental iron (the amount in a 325-mg ferrous sulfate tablet) isn’t clear. Low doses appear to be effective, and avoiding high doses likely decreases side effects without sacrificing efficacy.
References
1. Fairbanks V.F., Beutler E. Iron deficiency, in “Williams Textbook of Hematology, 6th ed. Beutler E., Coller B.S., Lichtman M.A., Kipps T.J., eds. (New York: McGraw-Hill; 2001, pp. 460-2).
2. Blood. 2015 Oct 22;126(17):1981-9.
3. Am J Med. 2005 Oct;118(10):1142-7.
4. JAMA. 2015 Feb 10;313(6):575-83.
5. Nutrients. 2014 Apr 4;6(4):1394-405.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
A 69-year-old man is evaluated for fatigue. He undergoes a colonoscopy and is found to have a right-sided colon cancer. His hematocrit is 33 with an MCV of 72. His ferritin level is 3. What do you recommend to help with his iron deficiency?
A. Ferrous sulfate 325 mg daily.
B. Ferrous sulfate 325 mg b.i.d.
C. Ferrous sulfate 325 mg t.i.d.
Treatment of iron deficiency with oral iron has traditionally been done by giving 150-200 mg of elemental iron (which is equal to three 325 mg tablets of iron sulfate).1 This dosing regimen has considerable gastrointestinal side effects. Recent research into iron absorption suggests that the higher the dose of iron given, the more absorption may be hindered. In a study of 54 women who had low ferritin levels, lower daily doses of iron – and not giving it multiple times a day – led to better iron absorption.2
In a study of elderly patients with iron deficiency, 90 hospitalized elderly patients older than 80 years with iron deficiency anemia were randomized to receive elemental iron as 15 mg or 50 mg of liquid ferrous gluconate, or 150 mg of ferrous calcium citrate for 60 days.3 Two months of iron treatment raised hemoglobin and ferritin levels to a similar degree in all groups, with no significant differences between the 15-mg, 50-mg, and 150-mg groups.
There was a significant difference in abdominal discomfort, with much less (20%) in the patients who received 15 mg of ferrous gluconate, compared with 60% in those who received 50 mg and 70% in those receiving 150 mg (P less than .05 comparing 15 mg with 50 mg and 150 mg). Statistically significant differences were also seen for nausea/vomiting, constipation, and dropout, with much lower rates seen in the low-dose (15-mg) group.
In a study of iron supplementation in individuals undergoing blood donation, a single daily dose of iron was used (37.5 mg of elemental iron) in half of the subjects, with the rest of the subjects receiving no iron.4 The mean age of the participants was 48 years.
Subjects who received the once-daily low-dose iron recovered much more quickly toward predonation hematocrit than did those who did not receive the low-dose iron (time to 80% hemoglobin recovery, 32 days vs. 92 days in the non–iron treated patients, P = .02). The effect was more dramatic in subjects who started with a low ferritin level (defined as less than 26), where time to 80% hemoglobin recovery was 36 days in the iron-treated patients vs. 153 days for the no-iron group.
The results of this study are in line with what we know about avid iron absorption in iron deficient patients, and the success of low doses in a younger patient population is encouraging.
In a small study looking at two different doses of elemental iron for the treatment of iron deficiency, 24 women (ages 18-35 years) with iron deficiency were randomized to 60 mg or 80 mg of elemental iron or placebo for 16 weeks.5 There was no difference in normalization of ferritin levels in the women who received either dose of iron. There was also no difference in side effects between the groups.
This study is small and had minimal difference in iron dose. In addition, the dosing was given once a day for both groups. I suspect that the lack of difference in side effects was due to both the small size of the study and the minimal difference in iron dose.
What does this all mean? I think that the most appropriate dosing for oral iron replacement is a single daily low-dose iron preparation. Whether that dose is 15 mg of elemental iron to 68 mg of elemental iron (the amount in a 325-mg ferrous sulfate tablet) isn’t clear. Low doses appear to be effective, and avoiding high doses likely decreases side effects without sacrificing efficacy.
References
1. Fairbanks V.F., Beutler E. Iron deficiency, in “Williams Textbook of Hematology, 6th ed. Beutler E., Coller B.S., Lichtman M.A., Kipps T.J., eds. (New York: McGraw-Hill; 2001, pp. 460-2).
2. Blood. 2015 Oct 22;126(17):1981-9.
3. Am J Med. 2005 Oct;118(10):1142-7.
4. JAMA. 2015 Feb 10;313(6):575-83.
5. Nutrients. 2014 Apr 4;6(4):1394-405.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
A 69-year-old man is evaluated for fatigue. He undergoes a colonoscopy and is found to have a right-sided colon cancer. His hematocrit is 33 with an MCV of 72. His ferritin level is 3. What do you recommend to help with his iron deficiency?
A. Ferrous sulfate 325 mg daily.
B. Ferrous sulfate 325 mg b.i.d.
C. Ferrous sulfate 325 mg t.i.d.
Treatment of iron deficiency with oral iron has traditionally been done by giving 150-200 mg of elemental iron (which is equal to three 325 mg tablets of iron sulfate).1 This dosing regimen has considerable gastrointestinal side effects. Recent research into iron absorption suggests that the higher the dose of iron given, the more absorption may be hindered. In a study of 54 women who had low ferritin levels, lower daily doses of iron – and not giving it multiple times a day – led to better iron absorption.2
In a study of elderly patients with iron deficiency, 90 hospitalized elderly patients older than 80 years with iron deficiency anemia were randomized to receive elemental iron as 15 mg or 50 mg of liquid ferrous gluconate, or 150 mg of ferrous calcium citrate for 60 days.3 Two months of iron treatment raised hemoglobin and ferritin levels to a similar degree in all groups, with no significant differences between the 15-mg, 50-mg, and 150-mg groups.
There was a significant difference in abdominal discomfort, with much less (20%) in the patients who received 15 mg of ferrous gluconate, compared with 60% in those who received 50 mg and 70% in those receiving 150 mg (P less than .05 comparing 15 mg with 50 mg and 150 mg). Statistically significant differences were also seen for nausea/vomiting, constipation, and dropout, with much lower rates seen in the low-dose (15-mg) group.
In a study of iron supplementation in individuals undergoing blood donation, a single daily dose of iron was used (37.5 mg of elemental iron) in half of the subjects, with the rest of the subjects receiving no iron.4 The mean age of the participants was 48 years.
Subjects who received the once-daily low-dose iron recovered much more quickly toward predonation hematocrit than did those who did not receive the low-dose iron (time to 80% hemoglobin recovery, 32 days vs. 92 days in the non–iron treated patients, P = .02). The effect was more dramatic in subjects who started with a low ferritin level (defined as less than 26), where time to 80% hemoglobin recovery was 36 days in the iron-treated patients vs. 153 days for the no-iron group.
The results of this study are in line with what we know about avid iron absorption in iron deficient patients, and the success of low doses in a younger patient population is encouraging.
In a small study looking at two different doses of elemental iron for the treatment of iron deficiency, 24 women (ages 18-35 years) with iron deficiency were randomized to 60 mg or 80 mg of elemental iron or placebo for 16 weeks.5 There was no difference in normalization of ferritin levels in the women who received either dose of iron. There was also no difference in side effects between the groups.
This study is small and had minimal difference in iron dose. In addition, the dosing was given once a day for both groups. I suspect that the lack of difference in side effects was due to both the small size of the study and the minimal difference in iron dose.
What does this all mean? I think that the most appropriate dosing for oral iron replacement is a single daily low-dose iron preparation. Whether that dose is 15 mg of elemental iron to 68 mg of elemental iron (the amount in a 325-mg ferrous sulfate tablet) isn’t clear. Low doses appear to be effective, and avoiding high doses likely decreases side effects without sacrificing efficacy.
References
1. Fairbanks V.F., Beutler E. Iron deficiency, in “Williams Textbook of Hematology, 6th ed. Beutler E., Coller B.S., Lichtman M.A., Kipps T.J., eds. (New York: McGraw-Hill; 2001, pp. 460-2).
2. Blood. 2015 Oct 22;126(17):1981-9.
3. Am J Med. 2005 Oct;118(10):1142-7.
4. JAMA. 2015 Feb 10;313(6):575-83.
5. Nutrients. 2014 Apr 4;6(4):1394-405.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Cadaveric allograft system used to reconstruct anterior chest wall
PHOENIX – Cadaveric allograft sternal replacement has proven to be safe, providing optimal stability to the chest wall and protection of surrounding organs, an analysis of 18 cases demonstrated.
“The allograft was biologically well tolerated, allowing a perfect integration into the host,” Dr. Giuseppe Marulli said at the annual meeting of the Society of Thoracic Surgeons. “Donor cryopreserved sternochondral allograft may become the ideal way for anterior chest wall reconstruction, particularly for wide resections.”
Dr. Marulli, a thoracic surgeon at the University of Padova, Italy, noted that prior experimental studies have demonstrated that cryopreserved bone allografts preserve osteoconduction and osteoinduction capacity (Eur Spine J. 2001 Oct;10:S96-101). “Therefore, they form the basis for new bone tissue formation, allowing for the capillary and perivascular blood supply,” he said.
Limitations of current materials used for sternal reconstruction include “excessive rigidity with risk of erosion and insufficient support for large chest wall defects,” he said. Perceived advantages of using cadaveric bone allograft include easy incorporation, no risk of rejection, and a low risk of infection. For each procedure used in the current analysis, cadaveric allograft sternums with costal cartilages were harvested with an aseptic method and treated with an antibiotic solution for 72 hours. Next, they were cryopreserved at –80º C and underwent microbiologic testing for at least 1 month to ensure sterility and absence of immunogenic capacity.
Dr. Marulli reported results from 18 patients who underwent the procedure between January 2009 and January 2015, 13 of whom were female. Their median age was 59 years, their median tumor diameter was 4.75 cm, most (88%) had undergone preoperative needle biopsy, and 50% had undergone induction therapy. The main indication for sternectomy was a single-site sternal metastasis (nine patients), primary chondrosarcoma (four cases), sternal dehiscence after cardiac surgery (two cases), malignant fibrous tumor (one case), radioinduced soft-tissue sarcoma (one case), and a thymic carcinoma invading the sternum (one case).
All patients were extubated in the OR, and one patient died in the hospital from a pulmonary embolism. Two patients (11%) developed postoperative complications: one case of Candida urinary infection and one case of bleeding at the site of the muscle flap. The median postoperative length of stay was 11 days.
To date, no infections or rejections of the grafts have occurred, Dr. Marulli said. After a median of 36 months, 13 patients are alive and 4 are dead (3 from a metastatic recurrence and 1 from an unrelated cause). One patient required removal of a clavicular screw for dislocation 4 months after the operation.
Dr. Marulli reported having no financial disclosures.
PHOENIX – Cadaveric allograft sternal replacement has proven to be safe, providing optimal stability to the chest wall and protection of surrounding organs, an analysis of 18 cases demonstrated.
“The allograft was biologically well tolerated, allowing a perfect integration into the host,” Dr. Giuseppe Marulli said at the annual meeting of the Society of Thoracic Surgeons. “Donor cryopreserved sternochondral allograft may become the ideal way for anterior chest wall reconstruction, particularly for wide resections.”
Dr. Marulli, a thoracic surgeon at the University of Padova, Italy, noted that prior experimental studies have demonstrated that cryopreserved bone allografts preserve osteoconduction and osteoinduction capacity (Eur Spine J. 2001 Oct;10:S96-101). “Therefore, they form the basis for new bone tissue formation, allowing for the capillary and perivascular blood supply,” he said.
Limitations of current materials used for sternal reconstruction include “excessive rigidity with risk of erosion and insufficient support for large chest wall defects,” he said. Perceived advantages of using cadaveric bone allograft include easy incorporation, no risk of rejection, and a low risk of infection. For each procedure used in the current analysis, cadaveric allograft sternums with costal cartilages were harvested with an aseptic method and treated with an antibiotic solution for 72 hours. Next, they were cryopreserved at –80º C and underwent microbiologic testing for at least 1 month to ensure sterility and absence of immunogenic capacity.
Dr. Marulli reported results from 18 patients who underwent the procedure between January 2009 and January 2015, 13 of whom were female. Their median age was 59 years, their median tumor diameter was 4.75 cm, most (88%) had undergone preoperative needle biopsy, and 50% had undergone induction therapy. The main indication for sternectomy was a single-site sternal metastasis (nine patients), primary chondrosarcoma (four cases), sternal dehiscence after cardiac surgery (two cases), malignant fibrous tumor (one case), radioinduced soft-tissue sarcoma (one case), and a thymic carcinoma invading the sternum (one case).
All patients were extubated in the OR, and one patient died in the hospital from a pulmonary embolism. Two patients (11%) developed postoperative complications: one case of Candida urinary infection and one case of bleeding at the site of the muscle flap. The median postoperative length of stay was 11 days.
To date, no infections or rejections of the grafts have occurred, Dr. Marulli said. After a median of 36 months, 13 patients are alive and 4 are dead (3 from a metastatic recurrence and 1 from an unrelated cause). One patient required removal of a clavicular screw for dislocation 4 months after the operation.
Dr. Marulli reported having no financial disclosures.
PHOENIX – Cadaveric allograft sternal replacement has proven to be safe, providing optimal stability to the chest wall and protection of surrounding organs, an analysis of 18 cases demonstrated.
“The allograft was biologically well tolerated, allowing a perfect integration into the host,” Dr. Giuseppe Marulli said at the annual meeting of the Society of Thoracic Surgeons. “Donor cryopreserved sternochondral allograft may become the ideal way for anterior chest wall reconstruction, particularly for wide resections.”
Dr. Marulli, a thoracic surgeon at the University of Padova, Italy, noted that prior experimental studies have demonstrated that cryopreserved bone allografts preserve osteoconduction and osteoinduction capacity (Eur Spine J. 2001 Oct;10:S96-101). “Therefore, they form the basis for new bone tissue formation, allowing for the capillary and perivascular blood supply,” he said.
Limitations of current materials used for sternal reconstruction include “excessive rigidity with risk of erosion and insufficient support for large chest wall defects,” he said. Perceived advantages of using cadaveric bone allograft include easy incorporation, no risk of rejection, and a low risk of infection. For each procedure used in the current analysis, cadaveric allograft sternums with costal cartilages were harvested with an aseptic method and treated with an antibiotic solution for 72 hours. Next, they were cryopreserved at –80º C and underwent microbiologic testing for at least 1 month to ensure sterility and absence of immunogenic capacity.
Dr. Marulli reported results from 18 patients who underwent the procedure between January 2009 and January 2015, 13 of whom were female. Their median age was 59 years, their median tumor diameter was 4.75 cm, most (88%) had undergone preoperative needle biopsy, and 50% had undergone induction therapy. The main indication for sternectomy was a single-site sternal metastasis (nine patients), primary chondrosarcoma (four cases), sternal dehiscence after cardiac surgery (two cases), malignant fibrous tumor (one case), radioinduced soft-tissue sarcoma (one case), and a thymic carcinoma invading the sternum (one case).
All patients were extubated in the OR, and one patient died in the hospital from a pulmonary embolism. Two patients (11%) developed postoperative complications: one case of Candida urinary infection and one case of bleeding at the site of the muscle flap. The median postoperative length of stay was 11 days.
To date, no infections or rejections of the grafts have occurred, Dr. Marulli said. After a median of 36 months, 13 patients are alive and 4 are dead (3 from a metastatic recurrence and 1 from an unrelated cause). One patient required removal of a clavicular screw for dislocation 4 months after the operation.
Dr. Marulli reported having no financial disclosures.
AT THE STS ANNUAL MEETING
Key clinical point: Cadaveric allograft sternal replacement appears to be an effective option for reconstructing the anterior chest wall.
Major finding: To date, no infections or rejections of the grafts have occurred in patients who underwent cadaveric allograft sternal replacement.
Data source: An analysis of 18 patients who underwent the procedure between January 2009 and January 2015.
Disclosures: Dr. Marulli reported having no financial disclosures.
Dexamethasone harmful for patients with HIV-associated cryptococcal meningitis
Adjunctive dexamethasone not only failed to decrease mortality, it actually induced more disability and adverse events than placebo in patients with HIV-associated cryptococcal meningitis, according to a report published online Feb. 11 in the New England Journal of Medicine.
Glucocorticoids are inexpensive, readily available, and relatively safe for patients with central nervous system infections, and they are widely used for HIV-associated cryptococcal meningitis in regions where the burden of the infection is highest. Glucocorticoids are even recommended for this indication in some international guidelines, as they are thought to reduce intracranial pressure and inflammatory complications. But evidence of their usefulness from randomized controlled trials is sparse, said Dr. Jeremy Day of Oxford University Clinical Research Unit, Wellcome Trust Major Overseas Programme Vietnam, Ho Chi Minh City, and his associates.
They performed a double-blind, randomized trial to compare the effectiveness and safety of adjunctive dexamethasone against placebo, which involved 451 patients treated for 6 weeks at 13 hospitals in Indonesia, Laos, Thailand, Vietnam, Malawi, and Uganda. The study participants also received standard antifungal therapy including amphotericin B and fluconazole, as well as antiretroviral therapy and Pneumocystis prophylaxis with trimethoprim-sulfamethoxazole.
The trial was stopped prematurely when the safety committee found “dexamethasone was causing harm across key outcomes, including fungal clearance, adverse events, and disability outcomes.” Consequently, the study didn’t have the statistical power to show an effect of dexamethasone on the primary outcome measure – mortality at 10 weeks after randomization (4 weeks after study treatment ended).
Dexamethasone did reduce intracranial pressure more rapidly than placebo, but this effect didn’t translate into improved survival. Mortality at 10 weeks was 47% for the 224 patients assigned to dexamethasone and 41% for the 226 patients assigned to placebo, a nonsignificant difference. However, the drug’s effects changed over time: Hazard ratios for death were 0.77 at days 1-22 but rose to 1.94 at days 23-43 and to 2.50 at days 44-71. By 6-month follow-up, mortality risk showed a trend toward harm with dexamethasone, and was 9% higher in the intention-to-treat population and 11% higher in the per-protocol population analyses, Dr. Day and his associates said (N. Engl J Med. 2016 Feb 11;374[6]: doi:10.1056/NEJMoa1509024). The rate of disability or death was significantly higher with dexamethasone than with placebo at both 10 weeks and 6 months, with odds ratios for a good outcome of only 0.42 and 0.49, respectively. Infections or infestations developed in 48 patients (21%) taking dexamethasone but only 25 (11%) of those taking placebo. Gastrointestinal disorders (13% vs. 7%), renal or urinary disorders (10% vs. 3%), and cardiac disorders (4% vs. 0%) also were significantly more frequent with dexamethasone, as were episodes of hyperglycemia, hypercreatinemia, hyperkalemia, and hyponatremia.
This study was supported by the United Kingdom Department for International Development, the Wellcome Trust, and the U.K. Medical Research Council through the Joint Global Health Trials Program. Dr. Day and his associates reported having no relevant financial disclosures.
Adjunctive dexamethasone not only failed to decrease mortality, it actually induced more disability and adverse events than placebo in patients with HIV-associated cryptococcal meningitis, according to a report published online Feb. 11 in the New England Journal of Medicine.
Glucocorticoids are inexpensive, readily available, and relatively safe for patients with central nervous system infections, and they are widely used for HIV-associated cryptococcal meningitis in regions where the burden of the infection is highest. Glucocorticoids are even recommended for this indication in some international guidelines, as they are thought to reduce intracranial pressure and inflammatory complications. But evidence of their usefulness from randomized controlled trials is sparse, said Dr. Jeremy Day of Oxford University Clinical Research Unit, Wellcome Trust Major Overseas Programme Vietnam, Ho Chi Minh City, and his associates.
They performed a double-blind, randomized trial to compare the effectiveness and safety of adjunctive dexamethasone against placebo, which involved 451 patients treated for 6 weeks at 13 hospitals in Indonesia, Laos, Thailand, Vietnam, Malawi, and Uganda. The study participants also received standard antifungal therapy including amphotericin B and fluconazole, as well as antiretroviral therapy and Pneumocystis prophylaxis with trimethoprim-sulfamethoxazole.
The trial was stopped prematurely when the safety committee found “dexamethasone was causing harm across key outcomes, including fungal clearance, adverse events, and disability outcomes.” Consequently, the study didn’t have the statistical power to show an effect of dexamethasone on the primary outcome measure – mortality at 10 weeks after randomization (4 weeks after study treatment ended).
Dexamethasone did reduce intracranial pressure more rapidly than placebo, but this effect didn’t translate into improved survival. Mortality at 10 weeks was 47% for the 224 patients assigned to dexamethasone and 41% for the 226 patients assigned to placebo, a nonsignificant difference. However, the drug’s effects changed over time: Hazard ratios for death were 0.77 at days 1-22 but rose to 1.94 at days 23-43 and to 2.50 at days 44-71. By 6-month follow-up, mortality risk showed a trend toward harm with dexamethasone, and was 9% higher in the intention-to-treat population and 11% higher in the per-protocol population analyses, Dr. Day and his associates said (N. Engl J Med. 2016 Feb 11;374[6]: doi:10.1056/NEJMoa1509024). The rate of disability or death was significantly higher with dexamethasone than with placebo at both 10 weeks and 6 months, with odds ratios for a good outcome of only 0.42 and 0.49, respectively. Infections or infestations developed in 48 patients (21%) taking dexamethasone but only 25 (11%) of those taking placebo. Gastrointestinal disorders (13% vs. 7%), renal or urinary disorders (10% vs. 3%), and cardiac disorders (4% vs. 0%) also were significantly more frequent with dexamethasone, as were episodes of hyperglycemia, hypercreatinemia, hyperkalemia, and hyponatremia.
This study was supported by the United Kingdom Department for International Development, the Wellcome Trust, and the U.K. Medical Research Council through the Joint Global Health Trials Program. Dr. Day and his associates reported having no relevant financial disclosures.
Adjunctive dexamethasone not only failed to decrease mortality, it actually induced more disability and adverse events than placebo in patients with HIV-associated cryptococcal meningitis, according to a report published online Feb. 11 in the New England Journal of Medicine.
Glucocorticoids are inexpensive, readily available, and relatively safe for patients with central nervous system infections, and they are widely used for HIV-associated cryptococcal meningitis in regions where the burden of the infection is highest. Glucocorticoids are even recommended for this indication in some international guidelines, as they are thought to reduce intracranial pressure and inflammatory complications. But evidence of their usefulness from randomized controlled trials is sparse, said Dr. Jeremy Day of Oxford University Clinical Research Unit, Wellcome Trust Major Overseas Programme Vietnam, Ho Chi Minh City, and his associates.
They performed a double-blind, randomized trial to compare the effectiveness and safety of adjunctive dexamethasone against placebo, which involved 451 patients treated for 6 weeks at 13 hospitals in Indonesia, Laos, Thailand, Vietnam, Malawi, and Uganda. The study participants also received standard antifungal therapy including amphotericin B and fluconazole, as well as antiretroviral therapy and Pneumocystis prophylaxis with trimethoprim-sulfamethoxazole.
The trial was stopped prematurely when the safety committee found “dexamethasone was causing harm across key outcomes, including fungal clearance, adverse events, and disability outcomes.” Consequently, the study didn’t have the statistical power to show an effect of dexamethasone on the primary outcome measure – mortality at 10 weeks after randomization (4 weeks after study treatment ended).
Dexamethasone did reduce intracranial pressure more rapidly than placebo, but this effect didn’t translate into improved survival. Mortality at 10 weeks was 47% for the 224 patients assigned to dexamethasone and 41% for the 226 patients assigned to placebo, a nonsignificant difference. However, the drug’s effects changed over time: Hazard ratios for death were 0.77 at days 1-22 but rose to 1.94 at days 23-43 and to 2.50 at days 44-71. By 6-month follow-up, mortality risk showed a trend toward harm with dexamethasone, and was 9% higher in the intention-to-treat population and 11% higher in the per-protocol population analyses, Dr. Day and his associates said (N. Engl J Med. 2016 Feb 11;374[6]: doi:10.1056/NEJMoa1509024). The rate of disability or death was significantly higher with dexamethasone than with placebo at both 10 weeks and 6 months, with odds ratios for a good outcome of only 0.42 and 0.49, respectively. Infections or infestations developed in 48 patients (21%) taking dexamethasone but only 25 (11%) of those taking placebo. Gastrointestinal disorders (13% vs. 7%), renal or urinary disorders (10% vs. 3%), and cardiac disorders (4% vs. 0%) also were significantly more frequent with dexamethasone, as were episodes of hyperglycemia, hypercreatinemia, hyperkalemia, and hyponatremia.
This study was supported by the United Kingdom Department for International Development, the Wellcome Trust, and the U.K. Medical Research Council through the Joint Global Health Trials Program. Dr. Day and his associates reported having no relevant financial disclosures.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Dexamethasone failed to decrease mortality and induced more disability and adverse events than placebo in patients with HIV-associated cryptococcal meningitis.
Major finding: The hazard ratio for death in the dexamethasone group relative to the placebo group was 0.77 at days 1-22 but rose to 1.94 at days 23-43, and to 2.50 at days 44-71.
Data source: An international, randomized, double-blind, placebo-controlled trial involving 451 patients treated for 6 weeks and followed for a further 4 weeks.
Disclosures: This study was supported by the United Kingdom Department for International Development, the Wellcome Trust, and the U.K. Medical Research Council through the Joint Global Health Trials Program. Dr. Day and his associates reported having no relevant financial disclosures.
Lysolipid antigens prominent in MGUS and myeloma
Clonal immunoglobulin reactive to lyso-glucosylceramide (LGL1), which is elevated in Gaucher disease, was found in patients with Gaucher disease as well as in one third of patients with sporadic monoclonal gammopathies.
Antigen-specific immunoblots showed that 17 of 20 patients with Gaucher disease had clonal immunoglobulin against LGL1, researchers reported (N Engl J Med. 2016 Feb 10).
Analysis of immunoglobulin gene mutations has provided evidence for antigen-driven clonal expansion of plasma cells in multiple myeloma and monoclonal gammopathy of undetermined significance (MGUS), but the underlying antigens remained unknown. Myeloma risk is increased with lipid disorders such as Gaucher disease and obesity, suggesting lipid involvement in pathogenesis.
“These studies set the stage for newer approaches to lower the levels of these lipids in patients with Gaucher disease and others with precursors for myeloma. Potentially, this could be achieved with drugs or lifestyle changes to reduce the levels of lipids to lower the risk of cancer,” senior author Dr. Madhav Dhodapkar, chief of hematology at Yale Cancer Center, New Haven, Conn., said in a press release.
All six mouse models with Gaucher-like disease had clonal immunoglobulin against LGL1. Gaucher disease–associated gammopathy in mouse models can be targeted by the reduction of the underlying antigen. Feeding eliglustat to the mice with clonal immunoglobulins reduced anti-LGL1 antibodies detected by immunoblot and reduced clonal immunoglobulin in vivo.
Dysregulated lipids are sometimes present in sporadic myeloma, and M spikes on LGL1-specific blotting were LGL1-reactive in 22 of 66 patients (33%). These clonal immunoglobulins also were cross reactive to lysophosphatidylcholine. Patients with polyclonal gammopathies not associated with Gaucher disease did not react to the lysolipids.
“Understanding the antigenic reactivity of clonal immunoglobulin not only has direct implications for antigenic origins of myeloma but also may lead to new strategies to prevent or treat clinical cancer by targeting the underlying antigen,” wrote Shiny Nair, Ph.D., of Yale University and colleagues.
Clonal immunoglobulin reactive to lyso-glucosylceramide (LGL1), which is elevated in Gaucher disease, was found in patients with Gaucher disease as well as in one third of patients with sporadic monoclonal gammopathies.
Antigen-specific immunoblots showed that 17 of 20 patients with Gaucher disease had clonal immunoglobulin against LGL1, researchers reported (N Engl J Med. 2016 Feb 10).
Analysis of immunoglobulin gene mutations has provided evidence for antigen-driven clonal expansion of plasma cells in multiple myeloma and monoclonal gammopathy of undetermined significance (MGUS), but the underlying antigens remained unknown. Myeloma risk is increased with lipid disorders such as Gaucher disease and obesity, suggesting lipid involvement in pathogenesis.
“These studies set the stage for newer approaches to lower the levels of these lipids in patients with Gaucher disease and others with precursors for myeloma. Potentially, this could be achieved with drugs or lifestyle changes to reduce the levels of lipids to lower the risk of cancer,” senior author Dr. Madhav Dhodapkar, chief of hematology at Yale Cancer Center, New Haven, Conn., said in a press release.
All six mouse models with Gaucher-like disease had clonal immunoglobulin against LGL1. Gaucher disease–associated gammopathy in mouse models can be targeted by the reduction of the underlying antigen. Feeding eliglustat to the mice with clonal immunoglobulins reduced anti-LGL1 antibodies detected by immunoblot and reduced clonal immunoglobulin in vivo.
Dysregulated lipids are sometimes present in sporadic myeloma, and M spikes on LGL1-specific blotting were LGL1-reactive in 22 of 66 patients (33%). These clonal immunoglobulins also were cross reactive to lysophosphatidylcholine. Patients with polyclonal gammopathies not associated with Gaucher disease did not react to the lysolipids.
“Understanding the antigenic reactivity of clonal immunoglobulin not only has direct implications for antigenic origins of myeloma but also may lead to new strategies to prevent or treat clinical cancer by targeting the underlying antigen,” wrote Shiny Nair, Ph.D., of Yale University and colleagues.
Clonal immunoglobulin reactive to lyso-glucosylceramide (LGL1), which is elevated in Gaucher disease, was found in patients with Gaucher disease as well as in one third of patients with sporadic monoclonal gammopathies.
Antigen-specific immunoblots showed that 17 of 20 patients with Gaucher disease had clonal immunoglobulin against LGL1, researchers reported (N Engl J Med. 2016 Feb 10).
Analysis of immunoglobulin gene mutations has provided evidence for antigen-driven clonal expansion of plasma cells in multiple myeloma and monoclonal gammopathy of undetermined significance (MGUS), but the underlying antigens remained unknown. Myeloma risk is increased with lipid disorders such as Gaucher disease and obesity, suggesting lipid involvement in pathogenesis.
“These studies set the stage for newer approaches to lower the levels of these lipids in patients with Gaucher disease and others with precursors for myeloma. Potentially, this could be achieved with drugs or lifestyle changes to reduce the levels of lipids to lower the risk of cancer,” senior author Dr. Madhav Dhodapkar, chief of hematology at Yale Cancer Center, New Haven, Conn., said in a press release.
All six mouse models with Gaucher-like disease had clonal immunoglobulin against LGL1. Gaucher disease–associated gammopathy in mouse models can be targeted by the reduction of the underlying antigen. Feeding eliglustat to the mice with clonal immunoglobulins reduced anti-LGL1 antibodies detected by immunoblot and reduced clonal immunoglobulin in vivo.
Dysregulated lipids are sometimes present in sporadic myeloma, and M spikes on LGL1-specific blotting were LGL1-reactive in 22 of 66 patients (33%). These clonal immunoglobulins also were cross reactive to lysophosphatidylcholine. Patients with polyclonal gammopathies not associated with Gaucher disease did not react to the lysolipids.
“Understanding the antigenic reactivity of clonal immunoglobulin not only has direct implications for antigenic origins of myeloma but also may lead to new strategies to prevent or treat clinical cancer by targeting the underlying antigen,” wrote Shiny Nair, Ph.D., of Yale University and colleagues.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: In patients with Gaucher disease and in nearly one-third of patients with MGUS or myeloma, clonal immunoglobulins reacted with lysolipid antigens.
Major finding: Clonal immunoglobulin from 17 of 20 patients with Gaucher disease and from 22 of 66 patients with sporadic myeloma were reactive to lyso-glucosylceramide.
Data source: Peripheral blood or bone marrow samples from 25 healthy donors, 20 patients with Gaucher disease, and 66 patients with sporadic monoclonal gammopathy.
Disclosures: Dr. Nair reported having no disclosures. One of her coauthors reported ties to industry.
Caplacizumab induces rapid resolution of acute TTP
Caplacizumab induces faster resolution of acute episodes of acquired thrombotic thrombocytopenic purpura than does conventional therapy by blocking further platelet aggregation mediated by von Willebrand factor, according to a report published online Feb. 11 in the New England Journal of Medicine.
Faster normalization of the platelet count “prevents further consumption of platelets into microthrombi, and the consequent progression of tissue ischemia.” This in turn should prevent further ischemic injury to the brain, heart, and kidneys in both the short and the long term, said Dr. Flora Peyvandi of the Angelo Bianchi Bonomi Hemophilia and Thrombosis Center, Ospedale Maggiore Policlinico, Milan, and her associates.
The investigators assessed caplacizumab, an anti–von Willebrand factor immunoglobulin, as a potential treatment for acquired TTP in a manufacturer-sponsored phase II trial involving 75 patients treated at 56 medical centers worldwide. All the study participants received standard treatment – daily plasma exchange and immunosuppressive therapy. In addition, they were randomly assigned to receive daily caplacizumab (36 patients) or placebo injections (39 patients) after each plasma exchange procedure and for 30 days following the final procedure, for a maximum of 90 days.
“Caplacizumab rapidly neutralized its target as indicated by suppression of von Willebrand factor–ristocetin cofactor activity to a mean of less than 20% by day 1 and throughout the treatment period,” Dr. Peyvandi and her associates said. These values returned to baseline levels within 1 week of treatment cessation.
The primary endpoint of the study, median time to normalization of the platelet count, was significantly reduced by 39% with caplacizumab compared with placebo. Among the 69 patients who had not undergone an initial plasma-exchange session before study enrollment, the median time to response was 3.0 days with caplacizumab and 4.9 days with placebo. And among the six patients who had undergone an initial plasma-exchange session before enrollment, the median time to response was 2.4 days with caplacizumab and 4.3 days with placebo, Dr. Peyvandi and her associates said (N Engl J Med. 2016 Feb 11;374[6]. doi:10.1056/NEJMoa1505533).
At 1-month follow-up, 81% of the caplacizumab group showed complete remission, compared with 46% of the placebo group. Three patients in the caplacizumab group had TTP exacerbations, compared with 11 in the placebo group. Post hoc analyses showed that the mean number of plasma-exchange days (5.9 vs. 7.9) and the mean volume of plasma administered (19.9 liters vs. 28.3 liters) were lower with caplacizumab than with placebo. And post hoc analyses of markers of end-organ damage, such as lactate dehydrogenase, troponin T, troponin 1, and creatinine levels, showed more rapid normalization with caplacizumab.
As expected, the number of patients who had bleeding-related adverse events was higher with the active treatment (19 patients) than with placebo (14 patients), but these events “were generally mild” and didn’t require treatment. Serious bleeding events occurred in 2 patients in each study group and included subarachnoid hemorrhage, retinal hemorrhage, and metrorrhagia in the caplacizumab group and cerebral hemorrhage and hematuria in the placebo group.
The study was supported by Ablynx, maker of caplacizumab, which also designed and conducted the study, analyzed the data, and prepared the manuscript. Dr. Peyvandi reported ties to Ablynx, Alexion, Biotest, Kedrion Biopharma, Novo Nordisk, Baxter, Bayer, CSL Behring, Grifols, LFB, Roche, and Sobi; her associates’ financial disclosures are available at NEJM.org.
These study findings prompt speculation that effective treatment of TTP will require a combination of interventions that target different aspects of the disorder’s pathophysiology.
First, using caplacizumab or similar agents to interfere with the binding of von Willebrand factor to platelets will prevent formation of new microthrombi. Second, replacing the specific cleaving metalloprotease ADAMTS13 using normal plasma will restore von Willebrand factor multimers to the appropriate size. And third, inducing disaggregation of platelet-rich thrombi will be the final step, but we haven’t yet found the means to accomplish that.
Dr. Agnes Veyradier is at the Institute of Hematology at the French Reference Center for Thrombotic Microangiopathies, Paris, and University Paris Diderot. Dr. Veyradier reported having no relevant financial disclosures and made these remarks in an editorial accompanying Dr. Peyvandi’s report (N Engl J Med. 2016 Feb 11;374[6]. doi:10.1056/NEJMe151876).
These study findings prompt speculation that effective treatment of TTP will require a combination of interventions that target different aspects of the disorder’s pathophysiology.
First, using caplacizumab or similar agents to interfere with the binding of von Willebrand factor to platelets will prevent formation of new microthrombi. Second, replacing the specific cleaving metalloprotease ADAMTS13 using normal plasma will restore von Willebrand factor multimers to the appropriate size. And third, inducing disaggregation of platelet-rich thrombi will be the final step, but we haven’t yet found the means to accomplish that.
Dr. Agnes Veyradier is at the Institute of Hematology at the French Reference Center for Thrombotic Microangiopathies, Paris, and University Paris Diderot. Dr. Veyradier reported having no relevant financial disclosures and made these remarks in an editorial accompanying Dr. Peyvandi’s report (N Engl J Med. 2016 Feb 11;374[6]. doi:10.1056/NEJMe151876).
These study findings prompt speculation that effective treatment of TTP will require a combination of interventions that target different aspects of the disorder’s pathophysiology.
First, using caplacizumab or similar agents to interfere with the binding of von Willebrand factor to platelets will prevent formation of new microthrombi. Second, replacing the specific cleaving metalloprotease ADAMTS13 using normal plasma will restore von Willebrand factor multimers to the appropriate size. And third, inducing disaggregation of platelet-rich thrombi will be the final step, but we haven’t yet found the means to accomplish that.
Dr. Agnes Veyradier is at the Institute of Hematology at the French Reference Center for Thrombotic Microangiopathies, Paris, and University Paris Diderot. Dr. Veyradier reported having no relevant financial disclosures and made these remarks in an editorial accompanying Dr. Peyvandi’s report (N Engl J Med. 2016 Feb 11;374[6]. doi:10.1056/NEJMe151876).
Caplacizumab induces faster resolution of acute episodes of acquired thrombotic thrombocytopenic purpura than does conventional therapy by blocking further platelet aggregation mediated by von Willebrand factor, according to a report published online Feb. 11 in the New England Journal of Medicine.
Faster normalization of the platelet count “prevents further consumption of platelets into microthrombi, and the consequent progression of tissue ischemia.” This in turn should prevent further ischemic injury to the brain, heart, and kidneys in both the short and the long term, said Dr. Flora Peyvandi of the Angelo Bianchi Bonomi Hemophilia and Thrombosis Center, Ospedale Maggiore Policlinico, Milan, and her associates.
The investigators assessed caplacizumab, an anti–von Willebrand factor immunoglobulin, as a potential treatment for acquired TTP in a manufacturer-sponsored phase II trial involving 75 patients treated at 56 medical centers worldwide. All the study participants received standard treatment – daily plasma exchange and immunosuppressive therapy. In addition, they were randomly assigned to receive daily caplacizumab (36 patients) or placebo injections (39 patients) after each plasma exchange procedure and for 30 days following the final procedure, for a maximum of 90 days.
“Caplacizumab rapidly neutralized its target as indicated by suppression of von Willebrand factor–ristocetin cofactor activity to a mean of less than 20% by day 1 and throughout the treatment period,” Dr. Peyvandi and her associates said. These values returned to baseline levels within 1 week of treatment cessation.
The primary endpoint of the study, median time to normalization of the platelet count, was significantly reduced by 39% with caplacizumab compared with placebo. Among the 69 patients who had not undergone an initial plasma-exchange session before study enrollment, the median time to response was 3.0 days with caplacizumab and 4.9 days with placebo. And among the six patients who had undergone an initial plasma-exchange session before enrollment, the median time to response was 2.4 days with caplacizumab and 4.3 days with placebo, Dr. Peyvandi and her associates said (N Engl J Med. 2016 Feb 11;374[6]. doi:10.1056/NEJMoa1505533).
At 1-month follow-up, 81% of the caplacizumab group showed complete remission, compared with 46% of the placebo group. Three patients in the caplacizumab group had TTP exacerbations, compared with 11 in the placebo group. Post hoc analyses showed that the mean number of plasma-exchange days (5.9 vs. 7.9) and the mean volume of plasma administered (19.9 liters vs. 28.3 liters) were lower with caplacizumab than with placebo. And post hoc analyses of markers of end-organ damage, such as lactate dehydrogenase, troponin T, troponin 1, and creatinine levels, showed more rapid normalization with caplacizumab.
As expected, the number of patients who had bleeding-related adverse events was higher with the active treatment (19 patients) than with placebo (14 patients), but these events “were generally mild” and didn’t require treatment. Serious bleeding events occurred in 2 patients in each study group and included subarachnoid hemorrhage, retinal hemorrhage, and metrorrhagia in the caplacizumab group and cerebral hemorrhage and hematuria in the placebo group.
The study was supported by Ablynx, maker of caplacizumab, which also designed and conducted the study, analyzed the data, and prepared the manuscript. Dr. Peyvandi reported ties to Ablynx, Alexion, Biotest, Kedrion Biopharma, Novo Nordisk, Baxter, Bayer, CSL Behring, Grifols, LFB, Roche, and Sobi; her associates’ financial disclosures are available at NEJM.org.
Caplacizumab induces faster resolution of acute episodes of acquired thrombotic thrombocytopenic purpura than does conventional therapy by blocking further platelet aggregation mediated by von Willebrand factor, according to a report published online Feb. 11 in the New England Journal of Medicine.
Faster normalization of the platelet count “prevents further consumption of platelets into microthrombi, and the consequent progression of tissue ischemia.” This in turn should prevent further ischemic injury to the brain, heart, and kidneys in both the short and the long term, said Dr. Flora Peyvandi of the Angelo Bianchi Bonomi Hemophilia and Thrombosis Center, Ospedale Maggiore Policlinico, Milan, and her associates.
The investigators assessed caplacizumab, an anti–von Willebrand factor immunoglobulin, as a potential treatment for acquired TTP in a manufacturer-sponsored phase II trial involving 75 patients treated at 56 medical centers worldwide. All the study participants received standard treatment – daily plasma exchange and immunosuppressive therapy. In addition, they were randomly assigned to receive daily caplacizumab (36 patients) or placebo injections (39 patients) after each plasma exchange procedure and for 30 days following the final procedure, for a maximum of 90 days.
“Caplacizumab rapidly neutralized its target as indicated by suppression of von Willebrand factor–ristocetin cofactor activity to a mean of less than 20% by day 1 and throughout the treatment period,” Dr. Peyvandi and her associates said. These values returned to baseline levels within 1 week of treatment cessation.
The primary endpoint of the study, median time to normalization of the platelet count, was significantly reduced by 39% with caplacizumab compared with placebo. Among the 69 patients who had not undergone an initial plasma-exchange session before study enrollment, the median time to response was 3.0 days with caplacizumab and 4.9 days with placebo. And among the six patients who had undergone an initial plasma-exchange session before enrollment, the median time to response was 2.4 days with caplacizumab and 4.3 days with placebo, Dr. Peyvandi and her associates said (N Engl J Med. 2016 Feb 11;374[6]. doi:10.1056/NEJMoa1505533).
At 1-month follow-up, 81% of the caplacizumab group showed complete remission, compared with 46% of the placebo group. Three patients in the caplacizumab group had TTP exacerbations, compared with 11 in the placebo group. Post hoc analyses showed that the mean number of plasma-exchange days (5.9 vs. 7.9) and the mean volume of plasma administered (19.9 liters vs. 28.3 liters) were lower with caplacizumab than with placebo. And post hoc analyses of markers of end-organ damage, such as lactate dehydrogenase, troponin T, troponin 1, and creatinine levels, showed more rapid normalization with caplacizumab.
As expected, the number of patients who had bleeding-related adverse events was higher with the active treatment (19 patients) than with placebo (14 patients), but these events “were generally mild” and didn’t require treatment. Serious bleeding events occurred in 2 patients in each study group and included subarachnoid hemorrhage, retinal hemorrhage, and metrorrhagia in the caplacizumab group and cerebral hemorrhage and hematuria in the placebo group.
The study was supported by Ablynx, maker of caplacizumab, which also designed and conducted the study, analyzed the data, and prepared the manuscript. Dr. Peyvandi reported ties to Ablynx, Alexion, Biotest, Kedrion Biopharma, Novo Nordisk, Baxter, Bayer, CSL Behring, Grifols, LFB, Roche, and Sobi; her associates’ financial disclosures are available at NEJM.org.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Caplacizumab induces more rapid resolution of an acute TTP episode than does conventional therapy.
Major finding: At 1-month follow-up, 81% of the caplacizumab group showed complete remission, compared with 46% of the placebo group.
Data source: An international single-blind placebo-controlled phase II trial involving 75 patients treated over a 3.5-year period.
Disclosures: This study was supported by Ablynx, maker of caplacizumab, which also designed and conducted the study, analyzed the data, and prepared the manuscript. Dr. Peyvandi reported ties to Ablynx, Alexion, Biotest, Kedrion Biopharma, Novo Nordisk, Baxter, Bayer, CSL Behring, Grifols, LFB, Roche, and Sobi; her associates’ financial disclosures are available at NEJM.org.