User login
Do sleep interventions prevent atrial fibrillation?
WASHINGTON – If patients have sleep disordered breathing with obstructive sleep apnea, will its treatment have cardiovascular disease benefits, especially in terms of the incidence or severity of atrial fibrillation?
Observational evidence suggests that apnea interventions may help these patients, but no clear case yet exists to prove that a breathing intervention works, experts say, and, as a result, U.S. practice is mixed when it comes to using treatment for obstructive sleep apnea (OSA), specifically continuous positive airway pressure (CPAP), to prevent or treat atrial fibrillation.
“Only a very small number of patients with atrial fibrillation undergo a sleep study,” he said in an interview. “Before I’d send my mother for atrial fibrillation ablation, I would first look for sleep disordered breathing [SDB],” but this generally isn’t happening routinely. Patients with other types of cardiovascular disease who could potentially benefit from sleep disordered breathing diagnosis and treatment are those with hypertension, especially patients who don’t fully respond to three or more antihypertensive drugs and patients with heart failure with preserved ejection fraction, he added.
Dr. Oldenburg also echoed Dr. Mehra in saying that the evidence supporting this approach for managing atrial fibrillation is less than conclusive.
“We need more precise phenotyping of patients” to better focus on patients with cardiovascular disease and sleep disordered breathing who clearly benefit from CPAP intervention, he said.
Results from the Sleep Apnea Cardiovascular Endpoints (SAVE) trial, reported in September 2016, especially tarnished the notion that treating sleep disordered breathing in patients with various cardiovascular diseases can help avoid future cardiovascular events. The multicenter trial enrolled 2,717 adults with moderate to severe obstructive sleep apnea and cardiovascular disease to receive either CPAP plus optimal routine care or optimal routine care only. After an average follow-up of close to 4 years, the patients treated with CPAP showed no benefit in terms of reduced cardiovascular events (N Engl J Med. 2016 Sept 8;375[10]:919-31).
An editorial that ran with this report suggested that the neutral outcome may have occurred because the average nightly duration of CPAP that patients in the trial self administered was just over 3 hours, arguably an inadequate dose. Other possible reasons for the lack of benefit include the time during their sleep cycle when patients administered CPAP (at the start of sleep rather than later) and that CPAP may have a reduced ability to avert new cardiovascular events in patients with established cardiovascular disease (N Engl J Med. 2016 Sept 8;375[8]:994-6).
Regardless of the reasons, the SAVE results, coupled with the neutral results and suggestion of harm from using adaptive servo-ventilation in patients with heart failure with reduced ejection fraction and central sleep apnea in the SERVE-HF trial (N Engl J Med. 2015 Sept 17;373[12]:1095-105), have thrust the management of SDB in patients with cardiovascular disease back to the point where SDB interventions have no well-proven indications for cardiovascular disease patients.
“With the SERVE-HF and SAVE trials not showing benefit, we now have equipoise” for using or not using SDB interventions in these patients, Dr. Mehra said. “It’s not clear that treating OSA improves outcomes. That allows us to randomize patients to a control placebo arm” in future trials.
An important issue in the failure to clearly establish a role for treating OSA in patients with atrial fibrillation or other cardiovascular diseases may have been over reliance on the apnea-hypopnea index (AHI) as the arbiter of OSA severity, Dr. Oldenburg said. “Maybe there are parameters to look at aside from AHI, perhaps hypoxemia burden or desaturation time. AHI is not the whole truth; we need to look at other parameters. AHI may not be the correct metric to look at in patients with various cardiovascular diseases.”
Her analysis also showed that patients with at least 10 minutes of sleep time with an oxygen saturation rate of 90% or less had a 64% increased rate of later atrial fibrillation hospitalizations, compared with those with fewer than 10 minutes spent in this state. Nearly a quarter of the patients studied fell into this category.
“Nocturnal oxygen desaturation may be stronger than AHI for predicting atrial fibrillation development,” Dr. Kendzerska concluded. “The severity of OSA-related intermittent hypoxia may be more important than sleep fragmentation in the development of atrial fibrillation. These findings support a relationship between OSA, chronic nocturnal hypoxemia, and new onset atrial fibrillation.”
However, using oxygen desaturation instead of AHI to gauge the severity of OSA won’t solve all the challenges that sleep researchers currently face in trying to determine the efficacy of breathing interventions to prevent or treat cardiovascular disease. In the neutral SAVE trial, researchers used nocturnal oxygen saturation levels to select patients with clinically meaningful OSA.
Dr. Mehra and Dr. Kendzerska had no disclosures. Dr. Oldenburg has received consultant fees, honoraria, and/or research support from ResMed, Respicardia, and Weinmann.
[email protected]
On Twitter @mitchelzoler
This article was updated on 7/10/17.
WASHINGTON – If patients have sleep disordered breathing with obstructive sleep apnea, will its treatment have cardiovascular disease benefits, especially in terms of the incidence or severity of atrial fibrillation?
Observational evidence suggests that apnea interventions may help these patients, but no clear case yet exists to prove that a breathing intervention works, experts say, and, as a result, U.S. practice is mixed when it comes to using treatment for obstructive sleep apnea (OSA), specifically continuous positive airway pressure (CPAP), to prevent or treat atrial fibrillation.
“Only a very small number of patients with atrial fibrillation undergo a sleep study,” he said in an interview. “Before I’d send my mother for atrial fibrillation ablation, I would first look for sleep disordered breathing [SDB],” but this generally isn’t happening routinely. Patients with other types of cardiovascular disease who could potentially benefit from sleep disordered breathing diagnosis and treatment are those with hypertension, especially patients who don’t fully respond to three or more antihypertensive drugs and patients with heart failure with preserved ejection fraction, he added.
Dr. Oldenburg also echoed Dr. Mehra in saying that the evidence supporting this approach for managing atrial fibrillation is less than conclusive.
“We need more precise phenotyping of patients” to better focus on patients with cardiovascular disease and sleep disordered breathing who clearly benefit from CPAP intervention, he said.
Results from the Sleep Apnea Cardiovascular Endpoints (SAVE) trial, reported in September 2016, especially tarnished the notion that treating sleep disordered breathing in patients with various cardiovascular diseases can help avoid future cardiovascular events. The multicenter trial enrolled 2,717 adults with moderate to severe obstructive sleep apnea and cardiovascular disease to receive either CPAP plus optimal routine care or optimal routine care only. After an average follow-up of close to 4 years, the patients treated with CPAP showed no benefit in terms of reduced cardiovascular events (N Engl J Med. 2016 Sept 8;375[10]:919-31).
An editorial that ran with this report suggested that the neutral outcome may have occurred because the average nightly duration of CPAP that patients in the trial self administered was just over 3 hours, arguably an inadequate dose. Other possible reasons for the lack of benefit include the time during their sleep cycle when patients administered CPAP (at the start of sleep rather than later) and that CPAP may have a reduced ability to avert new cardiovascular events in patients with established cardiovascular disease (N Engl J Med. 2016 Sept 8;375[8]:994-6).
Regardless of the reasons, the SAVE results, coupled with the neutral results and suggestion of harm from using adaptive servo-ventilation in patients with heart failure with reduced ejection fraction and central sleep apnea in the SERVE-HF trial (N Engl J Med. 2015 Sept 17;373[12]:1095-105), have thrust the management of SDB in patients with cardiovascular disease back to the point where SDB interventions have no well-proven indications for cardiovascular disease patients.
“With the SERVE-HF and SAVE trials not showing benefit, we now have equipoise” for using or not using SDB interventions in these patients, Dr. Mehra said. “It’s not clear that treating OSA improves outcomes. That allows us to randomize patients to a control placebo arm” in future trials.
An important issue in the failure to clearly establish a role for treating OSA in patients with atrial fibrillation or other cardiovascular diseases may have been over reliance on the apnea-hypopnea index (AHI) as the arbiter of OSA severity, Dr. Oldenburg said. “Maybe there are parameters to look at aside from AHI, perhaps hypoxemia burden or desaturation time. AHI is not the whole truth; we need to look at other parameters. AHI may not be the correct metric to look at in patients with various cardiovascular diseases.”
Her analysis also showed that patients with at least 10 minutes of sleep time with an oxygen saturation rate of 90% or less had a 64% increased rate of later atrial fibrillation hospitalizations, compared with those with fewer than 10 minutes spent in this state. Nearly a quarter of the patients studied fell into this category.
“Nocturnal oxygen desaturation may be stronger than AHI for predicting atrial fibrillation development,” Dr. Kendzerska concluded. “The severity of OSA-related intermittent hypoxia may be more important than sleep fragmentation in the development of atrial fibrillation. These findings support a relationship between OSA, chronic nocturnal hypoxemia, and new onset atrial fibrillation.”
However, using oxygen desaturation instead of AHI to gauge the severity of OSA won’t solve all the challenges that sleep researchers currently face in trying to determine the efficacy of breathing interventions to prevent or treat cardiovascular disease. In the neutral SAVE trial, researchers used nocturnal oxygen saturation levels to select patients with clinically meaningful OSA.
Dr. Mehra and Dr. Kendzerska had no disclosures. Dr. Oldenburg has received consultant fees, honoraria, and/or research support from ResMed, Respicardia, and Weinmann.
[email protected]
On Twitter @mitchelzoler
This article was updated on 7/10/17.
WASHINGTON – If patients have sleep disordered breathing with obstructive sleep apnea, will its treatment have cardiovascular disease benefits, especially in terms of the incidence or severity of atrial fibrillation?
Observational evidence suggests that apnea interventions may help these patients, but no clear case yet exists to prove that a breathing intervention works, experts say, and, as a result, U.S. practice is mixed when it comes to using treatment for obstructive sleep apnea (OSA), specifically continuous positive airway pressure (CPAP), to prevent or treat atrial fibrillation.
“Only a very small number of patients with atrial fibrillation undergo a sleep study,” he said in an interview. “Before I’d send my mother for atrial fibrillation ablation, I would first look for sleep disordered breathing [SDB],” but this generally isn’t happening routinely. Patients with other types of cardiovascular disease who could potentially benefit from sleep disordered breathing diagnosis and treatment are those with hypertension, especially patients who don’t fully respond to three or more antihypertensive drugs and patients with heart failure with preserved ejection fraction, he added.
Dr. Oldenburg also echoed Dr. Mehra in saying that the evidence supporting this approach for managing atrial fibrillation is less than conclusive.
“We need more precise phenotyping of patients” to better focus on patients with cardiovascular disease and sleep disordered breathing who clearly benefit from CPAP intervention, he said.
Results from the Sleep Apnea Cardiovascular Endpoints (SAVE) trial, reported in September 2016, especially tarnished the notion that treating sleep disordered breathing in patients with various cardiovascular diseases can help avoid future cardiovascular events. The multicenter trial enrolled 2,717 adults with moderate to severe obstructive sleep apnea and cardiovascular disease to receive either CPAP plus optimal routine care or optimal routine care only. After an average follow-up of close to 4 years, the patients treated with CPAP showed no benefit in terms of reduced cardiovascular events (N Engl J Med. 2016 Sept 8;375[10]:919-31).
An editorial that ran with this report suggested that the neutral outcome may have occurred because the average nightly duration of CPAP that patients in the trial self administered was just over 3 hours, arguably an inadequate dose. Other possible reasons for the lack of benefit include the time during their sleep cycle when patients administered CPAP (at the start of sleep rather than later) and that CPAP may have a reduced ability to avert new cardiovascular events in patients with established cardiovascular disease (N Engl J Med. 2016 Sept 8;375[8]:994-6).
Regardless of the reasons, the SAVE results, coupled with the neutral results and suggestion of harm from using adaptive servo-ventilation in patients with heart failure with reduced ejection fraction and central sleep apnea in the SERVE-HF trial (N Engl J Med. 2015 Sept 17;373[12]:1095-105), have thrust the management of SDB in patients with cardiovascular disease back to the point where SDB interventions have no well-proven indications for cardiovascular disease patients.
“With the SERVE-HF and SAVE trials not showing benefit, we now have equipoise” for using or not using SDB interventions in these patients, Dr. Mehra said. “It’s not clear that treating OSA improves outcomes. That allows us to randomize patients to a control placebo arm” in future trials.
An important issue in the failure to clearly establish a role for treating OSA in patients with atrial fibrillation or other cardiovascular diseases may have been over reliance on the apnea-hypopnea index (AHI) as the arbiter of OSA severity, Dr. Oldenburg said. “Maybe there are parameters to look at aside from AHI, perhaps hypoxemia burden or desaturation time. AHI is not the whole truth; we need to look at other parameters. AHI may not be the correct metric to look at in patients with various cardiovascular diseases.”
Her analysis also showed that patients with at least 10 minutes of sleep time with an oxygen saturation rate of 90% or less had a 64% increased rate of later atrial fibrillation hospitalizations, compared with those with fewer than 10 minutes spent in this state. Nearly a quarter of the patients studied fell into this category.
“Nocturnal oxygen desaturation may be stronger than AHI for predicting atrial fibrillation development,” Dr. Kendzerska concluded. “The severity of OSA-related intermittent hypoxia may be more important than sleep fragmentation in the development of atrial fibrillation. These findings support a relationship between OSA, chronic nocturnal hypoxemia, and new onset atrial fibrillation.”
However, using oxygen desaturation instead of AHI to gauge the severity of OSA won’t solve all the challenges that sleep researchers currently face in trying to determine the efficacy of breathing interventions to prevent or treat cardiovascular disease. In the neutral SAVE trial, researchers used nocturnal oxygen saturation levels to select patients with clinically meaningful OSA.
Dr. Mehra and Dr. Kendzerska had no disclosures. Dr. Oldenburg has received consultant fees, honoraria, and/or research support from ResMed, Respicardia, and Weinmann.
[email protected]
On Twitter @mitchelzoler
This article was updated on 7/10/17.
EXPERT ANALYSIS FROM ATS 2017
Vascular Injury Following a Fall Onto an Outstretched Hand
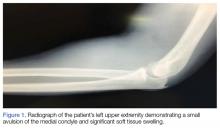
A 46-year-old man with a remote history of general tonic-clonic seizures, for which he was taking phenytoin, presented to the ED 30 minutes after sustaining a witnessed mechanical fall. The patient had fallen onto his nondominant left hand, which resulted in an injury to his elbow. He reported neither losing consciousness nor experiencing any seizures following the incident. He denied dislocating the joint or sustaining any other injuries from the fall. He also denied a history of past left elbow injury.
The patient was alert, oriented, and provided a full history of the incident. Regarding medical history, he stated that his last seizure had occurred 10 years prior. Except for the left elbow pain, a review of his systems was negative. The patient appeared in no acute distress, and supported his left upper extremity with a bandana and his right hand.
The patient’s vital signs were normal. The physical examination was negative except for the left elbow, which had significant swelling and limited range of motion without skin break, leading to suspicion for a prehospital dislocation with self-reduction. The joints above, below, and at the injury site were assessed for neurovascular injury.
Computed tomography angiography of the left upper extremity showed a brachial artery occlusion above the elbow, with reconstitution below the joint (Figure 2).
Discussion
There is a paucity of information on vascular injury from elbow dislocation in the emergency medicine literature. A recent literature search referenced orthopedic pitfalls in the ED,1 but most data appear in the orthopedic and vascular literature. A case report from the orthopedic literature in Brazil cites a vascular injury after ED relocation of a dislocated elbow following an assault.2
The elbow is the second most commonly dislocated joint (not including the patella) after the shoulder.3 Posterior dislocations make up the majority of these injuries. Simple versus complex injuries can be differentiated by the presence or absence of fracture.4 Simple complications include stiffness; loss of mobility, especially with full extension; neurovascular injuries; and compartment syndrome. Complex injuries involve fractures and potential neurovascular injuries, stiffness, pain, and loss of mobility.
Soft tissue injuries, fractures, and neurovascular complaints represent the majority of ED encounters, and are commonly related to falls. The elbow is the articulation of the humerus, ulna, and radius bones. Range of motion includes, but is not limited to, flexion, extension, supination, and pronation. Tears in the lateral ulnar ligament, joint capsule, and medial collateral ligament lead to instability of the joint and increase risk of dislocation.
Fractures make up to 20% of injuries to the elbow. These include fractures of the radial head and neck (most common), olecranon, and distal humerus.5 Open elbow fractures are rare, as are vascular injuries (5%-13% of cases).6 When present, vascular elbow injuries usually involve the brachial artery, and display abnormal palpable and Doppler assessment of the brachial and radial arteries.6
Nerve injuries may include injury to the radial nerve. Manifestations of radial nerve injury include abnormal sensation to the dorsum of the hand, trouble straightening the arm, and wrist-drop. Ulnar nerve injury typically presents with abnormal sensation to the fourth and fifth digits and decreased grip strength.
Conclusion
Vascular abnormalities are rare complications following elbow injuries. Our patient sustained a lacerated brachial artery, which was repaired via saphenous graft; brachial and basilic vein lacerations, which were ligated; and an avulsion fracture with an unstable joint, which was stabilized with external fixation and stabilization. He was discharged the following day with full neurovascular function.
A methodical approach to assessing patients presenting with elbow injury is essential to making the correct diagnosis. This should include a careful evaluation of the joints above and below the area of injury, as well as attention to the neurovascular examination, with a heightened suspicion for a vascular abnormality in complex injuries. Doppler and ultrasound evaluation with multiple rechecks can assist with the diagnosis. Our patient was rapidly assessed with a concern for a vascular injury, and was emergently referred to vascular surgery for repair of the brachial artery and stabilization of the joint.
1. Carter SJ, Germann CA, Dacus AA, Sweeney TW, Perron AD. Orthopedic pitfalls in the ED: neurovascular injury associated with posterior elbow dislocations. Am J Emerg Med. 2010;28(8):960-965. doi:10.1016/j.ajem.2009.05.024.
2. Miyazaki AN, Fregoneze M, Santos PD, do Val Sella G, Checchia CS, Checchia SL. Brachial artery injury due to closed posterior elbow dislocation: case report. Rev Bras Ortop. 2016;51(2):239-243. doi:10.1016/j.rboe.2016.02.007.
3. Beingessner J, Pollock W, King GJW. Elbow fractures and dislocations. In: Court-Brown CM, Heckman JD, McQueen MM, Ricci WM, Tornetta P, eds. Rockwood and Green’s Fractures in Adults. Vol 1. 8th ed. Philadelphia, PA: Wolters Kluwer Health; 2015:1179-1228.
4. McCabe MP, Savoie FH 3rd. Simple elbow dislocations: evaluation, management, and outcomes. Phys Sportsmed. 2012;40(1):62-71. doi:10.3810/psm.2012.02.1952.
5. Jungbluth P, Hakimi M, Linhart W, Windolf J. Current concepts: simple and complex elbow dislocations—acute and definitive treatment. Eur J Trauma Emerg Surg. 2008;34(2):120-130. doi:10.1007/s00068-008-8033-9.
6. Marcheix B, Chaufour X, Ayel J, et al. Transection of the brachial artery after closed posterior elbow dislocation. J Vasc Surg. 2005;42(6):1230-1232. doi:10.1016/j.jvs.2005.07.046.
A 46-year-old man with a remote history of general tonic-clonic seizures, for which he was taking phenytoin, presented to the ED 30 minutes after sustaining a witnessed mechanical fall. The patient had fallen onto his nondominant left hand, which resulted in an injury to his elbow. He reported neither losing consciousness nor experiencing any seizures following the incident. He denied dislocating the joint or sustaining any other injuries from the fall. He also denied a history of past left elbow injury.
The patient was alert, oriented, and provided a full history of the incident. Regarding medical history, he stated that his last seizure had occurred 10 years prior. Except for the left elbow pain, a review of his systems was negative. The patient appeared in no acute distress, and supported his left upper extremity with a bandana and his right hand.
The patient’s vital signs were normal. The physical examination was negative except for the left elbow, which had significant swelling and limited range of motion without skin break, leading to suspicion for a prehospital dislocation with self-reduction. The joints above, below, and at the injury site were assessed for neurovascular injury.
Computed tomography angiography of the left upper extremity showed a brachial artery occlusion above the elbow, with reconstitution below the joint (Figure 2).
Discussion
There is a paucity of information on vascular injury from elbow dislocation in the emergency medicine literature. A recent literature search referenced orthopedic pitfalls in the ED,1 but most data appear in the orthopedic and vascular literature. A case report from the orthopedic literature in Brazil cites a vascular injury after ED relocation of a dislocated elbow following an assault.2
The elbow is the second most commonly dislocated joint (not including the patella) after the shoulder.3 Posterior dislocations make up the majority of these injuries. Simple versus complex injuries can be differentiated by the presence or absence of fracture.4 Simple complications include stiffness; loss of mobility, especially with full extension; neurovascular injuries; and compartment syndrome. Complex injuries involve fractures and potential neurovascular injuries, stiffness, pain, and loss of mobility.
Soft tissue injuries, fractures, and neurovascular complaints represent the majority of ED encounters, and are commonly related to falls. The elbow is the articulation of the humerus, ulna, and radius bones. Range of motion includes, but is not limited to, flexion, extension, supination, and pronation. Tears in the lateral ulnar ligament, joint capsule, and medial collateral ligament lead to instability of the joint and increase risk of dislocation.
Fractures make up to 20% of injuries to the elbow. These include fractures of the radial head and neck (most common), olecranon, and distal humerus.5 Open elbow fractures are rare, as are vascular injuries (5%-13% of cases).6 When present, vascular elbow injuries usually involve the brachial artery, and display abnormal palpable and Doppler assessment of the brachial and radial arteries.6
Nerve injuries may include injury to the radial nerve. Manifestations of radial nerve injury include abnormal sensation to the dorsum of the hand, trouble straightening the arm, and wrist-drop. Ulnar nerve injury typically presents with abnormal sensation to the fourth and fifth digits and decreased grip strength.
Conclusion
Vascular abnormalities are rare complications following elbow injuries. Our patient sustained a lacerated brachial artery, which was repaired via saphenous graft; brachial and basilic vein lacerations, which were ligated; and an avulsion fracture with an unstable joint, which was stabilized with external fixation and stabilization. He was discharged the following day with full neurovascular function.
A methodical approach to assessing patients presenting with elbow injury is essential to making the correct diagnosis. This should include a careful evaluation of the joints above and below the area of injury, as well as attention to the neurovascular examination, with a heightened suspicion for a vascular abnormality in complex injuries. Doppler and ultrasound evaluation with multiple rechecks can assist with the diagnosis. Our patient was rapidly assessed with a concern for a vascular injury, and was emergently referred to vascular surgery for repair of the brachial artery and stabilization of the joint.
A 46-year-old man with a remote history of general tonic-clonic seizures, for which he was taking phenytoin, presented to the ED 30 minutes after sustaining a witnessed mechanical fall. The patient had fallen onto his nondominant left hand, which resulted in an injury to his elbow. He reported neither losing consciousness nor experiencing any seizures following the incident. He denied dislocating the joint or sustaining any other injuries from the fall. He also denied a history of past left elbow injury.
The patient was alert, oriented, and provided a full history of the incident. Regarding medical history, he stated that his last seizure had occurred 10 years prior. Except for the left elbow pain, a review of his systems was negative. The patient appeared in no acute distress, and supported his left upper extremity with a bandana and his right hand.
The patient’s vital signs were normal. The physical examination was negative except for the left elbow, which had significant swelling and limited range of motion without skin break, leading to suspicion for a prehospital dislocation with self-reduction. The joints above, below, and at the injury site were assessed for neurovascular injury.
Computed tomography angiography of the left upper extremity showed a brachial artery occlusion above the elbow, with reconstitution below the joint (Figure 2).
Discussion
There is a paucity of information on vascular injury from elbow dislocation in the emergency medicine literature. A recent literature search referenced orthopedic pitfalls in the ED,1 but most data appear in the orthopedic and vascular literature. A case report from the orthopedic literature in Brazil cites a vascular injury after ED relocation of a dislocated elbow following an assault.2
The elbow is the second most commonly dislocated joint (not including the patella) after the shoulder.3 Posterior dislocations make up the majority of these injuries. Simple versus complex injuries can be differentiated by the presence or absence of fracture.4 Simple complications include stiffness; loss of mobility, especially with full extension; neurovascular injuries; and compartment syndrome. Complex injuries involve fractures and potential neurovascular injuries, stiffness, pain, and loss of mobility.
Soft tissue injuries, fractures, and neurovascular complaints represent the majority of ED encounters, and are commonly related to falls. The elbow is the articulation of the humerus, ulna, and radius bones. Range of motion includes, but is not limited to, flexion, extension, supination, and pronation. Tears in the lateral ulnar ligament, joint capsule, and medial collateral ligament lead to instability of the joint and increase risk of dislocation.
Fractures make up to 20% of injuries to the elbow. These include fractures of the radial head and neck (most common), olecranon, and distal humerus.5 Open elbow fractures are rare, as are vascular injuries (5%-13% of cases).6 When present, vascular elbow injuries usually involve the brachial artery, and display abnormal palpable and Doppler assessment of the brachial and radial arteries.6
Nerve injuries may include injury to the radial nerve. Manifestations of radial nerve injury include abnormal sensation to the dorsum of the hand, trouble straightening the arm, and wrist-drop. Ulnar nerve injury typically presents with abnormal sensation to the fourth and fifth digits and decreased grip strength.
Conclusion
Vascular abnormalities are rare complications following elbow injuries. Our patient sustained a lacerated brachial artery, which was repaired via saphenous graft; brachial and basilic vein lacerations, which were ligated; and an avulsion fracture with an unstable joint, which was stabilized with external fixation and stabilization. He was discharged the following day with full neurovascular function.
A methodical approach to assessing patients presenting with elbow injury is essential to making the correct diagnosis. This should include a careful evaluation of the joints above and below the area of injury, as well as attention to the neurovascular examination, with a heightened suspicion for a vascular abnormality in complex injuries. Doppler and ultrasound evaluation with multiple rechecks can assist with the diagnosis. Our patient was rapidly assessed with a concern for a vascular injury, and was emergently referred to vascular surgery for repair of the brachial artery and stabilization of the joint.
1. Carter SJ, Germann CA, Dacus AA, Sweeney TW, Perron AD. Orthopedic pitfalls in the ED: neurovascular injury associated with posterior elbow dislocations. Am J Emerg Med. 2010;28(8):960-965. doi:10.1016/j.ajem.2009.05.024.
2. Miyazaki AN, Fregoneze M, Santos PD, do Val Sella G, Checchia CS, Checchia SL. Brachial artery injury due to closed posterior elbow dislocation: case report. Rev Bras Ortop. 2016;51(2):239-243. doi:10.1016/j.rboe.2016.02.007.
3. Beingessner J, Pollock W, King GJW. Elbow fractures and dislocations. In: Court-Brown CM, Heckman JD, McQueen MM, Ricci WM, Tornetta P, eds. Rockwood and Green’s Fractures in Adults. Vol 1. 8th ed. Philadelphia, PA: Wolters Kluwer Health; 2015:1179-1228.
4. McCabe MP, Savoie FH 3rd. Simple elbow dislocations: evaluation, management, and outcomes. Phys Sportsmed. 2012;40(1):62-71. doi:10.3810/psm.2012.02.1952.
5. Jungbluth P, Hakimi M, Linhart W, Windolf J. Current concepts: simple and complex elbow dislocations—acute and definitive treatment. Eur J Trauma Emerg Surg. 2008;34(2):120-130. doi:10.1007/s00068-008-8033-9.
6. Marcheix B, Chaufour X, Ayel J, et al. Transection of the brachial artery after closed posterior elbow dislocation. J Vasc Surg. 2005;42(6):1230-1232. doi:10.1016/j.jvs.2005.07.046.
1. Carter SJ, Germann CA, Dacus AA, Sweeney TW, Perron AD. Orthopedic pitfalls in the ED: neurovascular injury associated with posterior elbow dislocations. Am J Emerg Med. 2010;28(8):960-965. doi:10.1016/j.ajem.2009.05.024.
2. Miyazaki AN, Fregoneze M, Santos PD, do Val Sella G, Checchia CS, Checchia SL. Brachial artery injury due to closed posterior elbow dislocation: case report. Rev Bras Ortop. 2016;51(2):239-243. doi:10.1016/j.rboe.2016.02.007.
3. Beingessner J, Pollock W, King GJW. Elbow fractures and dislocations. In: Court-Brown CM, Heckman JD, McQueen MM, Ricci WM, Tornetta P, eds. Rockwood and Green’s Fractures in Adults. Vol 1. 8th ed. Philadelphia, PA: Wolters Kluwer Health; 2015:1179-1228.
4. McCabe MP, Savoie FH 3rd. Simple elbow dislocations: evaluation, management, and outcomes. Phys Sportsmed. 2012;40(1):62-71. doi:10.3810/psm.2012.02.1952.
5. Jungbluth P, Hakimi M, Linhart W, Windolf J. Current concepts: simple and complex elbow dislocations—acute and definitive treatment. Eur J Trauma Emerg Surg. 2008;34(2):120-130. doi:10.1007/s00068-008-8033-9.
6. Marcheix B, Chaufour X, Ayel J, et al. Transection of the brachial artery after closed posterior elbow dislocation. J Vasc Surg. 2005;42(6):1230-1232. doi:10.1016/j.jvs.2005.07.046.
What's Eating You? Sticktight Flea Revisited
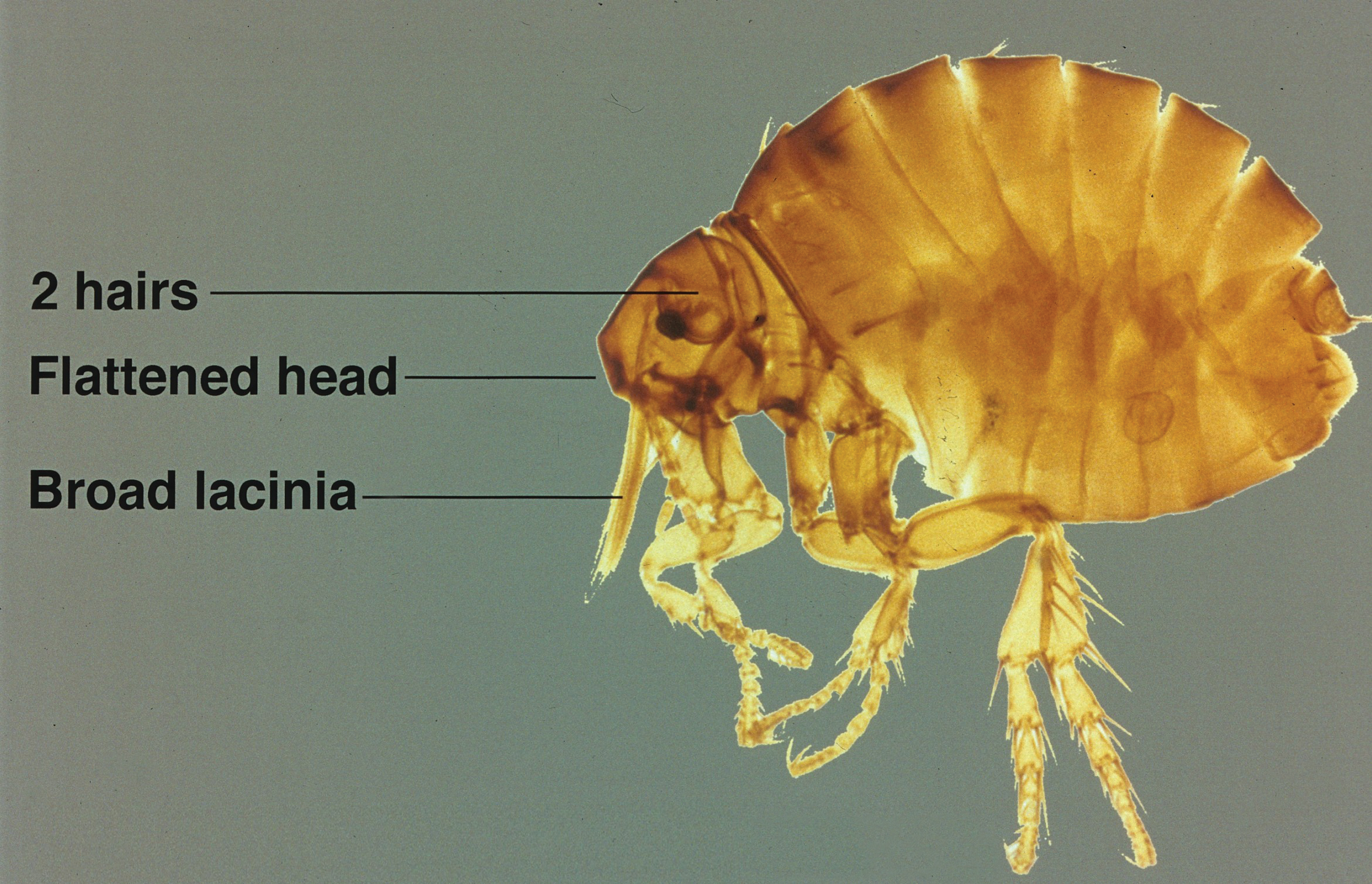
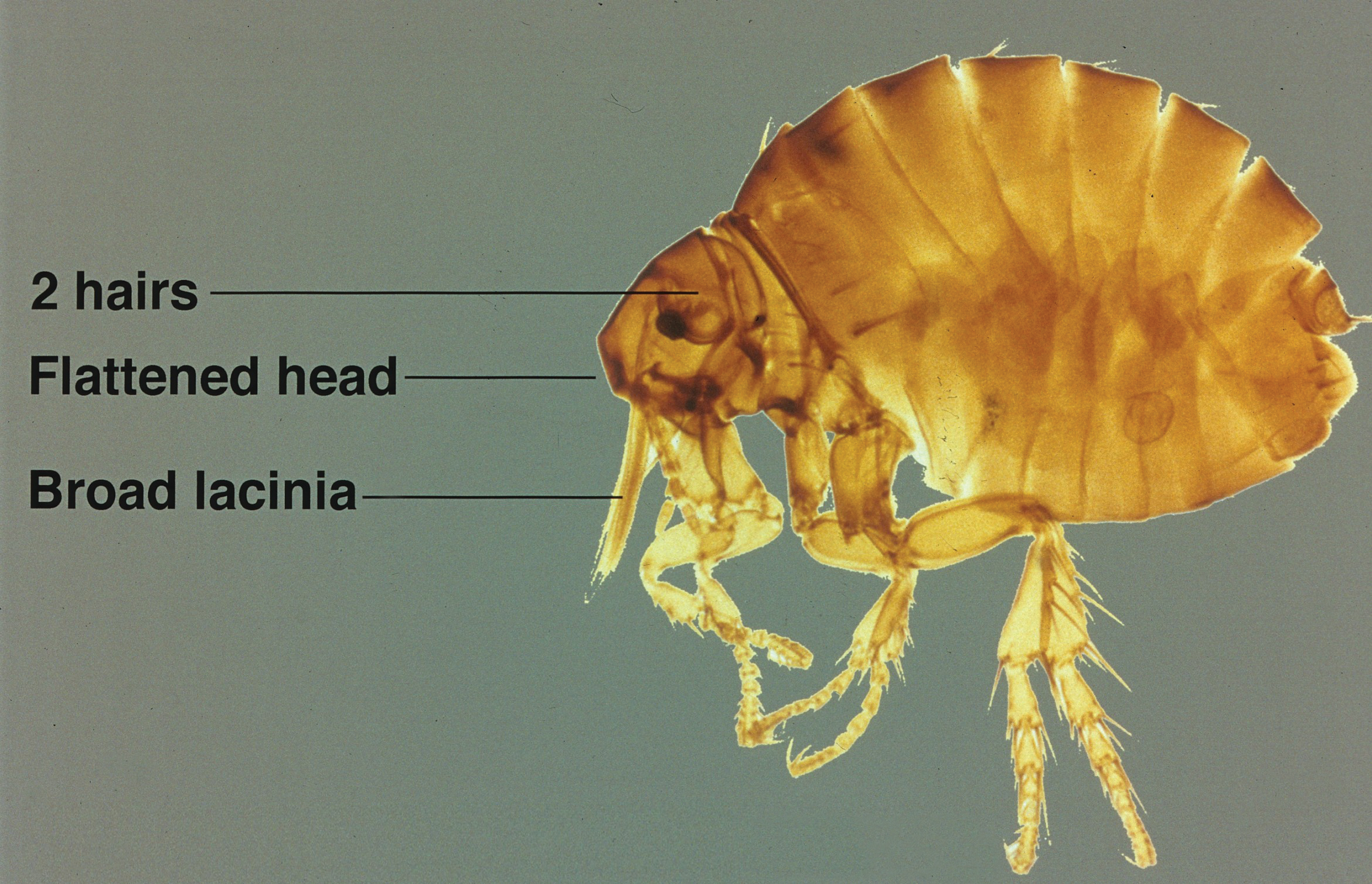
Identifying Characteristics
The sticktight flea (Echidnophaga gallinacea) earns its name by embedding its head in the host's skin using broad and serrated laciniae and can feed at one site for up to 19 days.1 It differs in morphology from dog (Ctenocephalides canis) and cat (Ctenocephalides felis) fleas, lacking genal (mustache area) and promotal (back of the head) ctenidia (combs), and is half the size of the cat flea. It has 2 pairs of setae (hairs) behind the antennae with an anteriorly flattened head (Figure).
Disease Transmission
Although its primary host is poultry and it also is known as the stickfast or chicken flea, the sticktight flea has been found in many species of birds and mammals, including humans. It is becoming more common in dogs in many parts of the world, including the United States,2-5 and has been found to be the most common flea on dogs in areas of South Africa.6 Other noted hosts of E gallinacea are rodents, cottontail rabbits, cats, ground squirrels, and pigs.7-14 Human infestation occurs from exposure to affected animals.15 As blood feeders, fleas have long been known to serve as vectors for many diseases, including bubonic plague, typhus, and tularemia, as well as an intermediate host of the dog tapeworm (Dipylidium caninum).5 Rickettsia felis, belonging to the spotted fever group, is an emerging infectious disease in humans commonly found in the cat flea (C felis) but also has been detected in E gallinacea.7 Echidnophaga gallinacea is found worldwide in the tropics, subtropics, and temperate zones, and it is the only representative of the genus found in the United States.1 Given the wide range of wild and domestic animal hosts and wide geographic distribution for E gallinacea, it represents an increasing risk for humans.
Echidnophaga gallinacea favors feeding from fleshy areas without thick fur or plumage. In birds, the area around the eyes, comb, and wattles is included; in dogs, it can be the eyes, in between the toes, and in the genital area.1 Flea bites cause irritation and itching for hosts including humans, typically resulting in clusters of firm, pruritic, erythematous papules with a central punctum.15 Severe bites also may lead to bullous lesions. In birds, symptoms can be extreme, with infestation around the eyes leading to swelling and blindness, a decline in egg production, weight loss, and death in young birds.1 Similar to other fleas, E gallinacea is wingless and depends on jumping onto a host for transmission, which can be from the ground, carpeting and flooring, furniture, or another host. Fleas are champion jumpers (relative to body size) and can jump 100 times their length.16
Management
Treating sticktight fleas can be tricky, as they embed tightly into the host's skin. Animals should be treated by a qualified veterinarian. Removal of attached fleas in humans requires grasping the flea firmly with tweezers and pulling from the skin. If the infestation is considerable, malathion 5% liquid or gel can be applied. Patients can treat itching with topical steroids and antipruritic creams, and oral antihistamines can be used to relieve symptoms and reduce the likelihood of damaged skin as well as the potential for secondary infection. The flea-infested environment should be treated with insecticides. For treatment of hard surfaces, dichlorvos and propetamphos are effective. Organophosphates work well on fabric and carpeting. Domestic pets and livestock may be treated by a veterinarian with agents such as fipronil, selamectin, imidacloprid, metaflumizone, nitenpyram, lufenuron, methoprene, and pyriproxyfen.
- Gyimesi ZS, Hayden ER, Greiner EC. Sticktight flea (Echidnophaga gallinacea) infestation in a Victoria crowned pigeon (Goura victoria). J Zoo Wildl Med. 2007;38:594-596.
- Kalkofen UP, Greenberg J. Echidnophaga gallinacea infestation in dogs. J Am Vet Med Assoc. 1974;165:447-448.
- Harman DW, Halliwell RE, Greiner EC. Flea species from dogs and cats in north-central Florida. Vet Parasitol. 1987;23:135-140.
- Boughton RK, Atwell JW, Schoech SJ. An introduced generalist parasite, the sticktight flea (Echidnophaga gallinacea), and its pathology in the threatened Florida scrub-jay (Aphelocoma coerulescens). J Parasitol. 2006;92:941-948.
- Durden LA, Judy TN, Martin JE, et al. Fleas parasitizing domestic dogs in Georgia, USA: species composition and seasonal abundance. Vet Parasitol. 2005;130:157-162.
- Rautenbach GH, Boomker J, de Villiers IL. A descriptive study of the canine population in a rural town in southern Africa. J S Afr Vet Assoc. 1991;62:158-162.
- Leulmi H, Socolovschi C, Laudisoit A, et al. Detection of Rickettsia felis, Rickettsia typhi, Bartonella species and Yersinia pestis in fleas (Siphonaptera) from Africa. PLoS Negl Trop Dis. 2014;8:e3152.
- Guernier V, Lagadec E, LeMinter G, et al. Fleas of small mammals on Reunion Island: diversity, distribution and epidemiological consequences. PLoS Negl Trop Dis. 2014;8:e3129.
- Cantó GJ, Guerrero RI, Olvera-Ramírez AM, et al. Prevalence of fleas and gastrointestinal parasites in free-roaming cats in central Mexico [published online April 3, 2013]. PLoS One. 2013;8:e60744.
- Akucewich LH, Philman K, Clark A, et al. Prevalence of ectoparasites in a population of feral cats from north central Florida during the summer. Vet Parasitol. 2002;109:129-139.
- Linardi PM, Gomes AF, Botelho JR, et al. Some ectoparasites of commensal rodents from Huambo, Angola. J Med Entomol. 1994;31:754-756.
- Pfaffenberger GS, Valencia VB. Ectoparasites of sympatric cottontails (Sylvilagus audubonii Nelson) and jack rabbits (Lepus californicus Mearns) from the high plains of eastern New Mexico. J Parasitol. 1988;74:842-846.
- Hubbart JA, Jachowski DS, Eads DA. Seasonal and among-site variation in the occurrence and abundance of fleas on California ground squirrels (Otospermophilus beecheyi). J Vector Ecol. 2011;36:117-123.
- Braae UC, Ngowi HA, Johansen MV. Smallholder pig production: prevalence and risk factors of ectoparasites. Vet Parasitol. 2013;196:241-244.
- Carlson JC, Fox MS. A sticktight flea removed from the cheek of a two-year-old boy from Los Angeles. Dermatol Online J. 2009;15:4.
- Rothschild M, Schlein Y, Parker K, et al. The flying leap of the flea. Scientific American. 1973;229:92.
Identifying Characteristics
The sticktight flea (Echidnophaga gallinacea) earns its name by embedding its head in the host's skin using broad and serrated laciniae and can feed at one site for up to 19 days.1 It differs in morphology from dog (Ctenocephalides canis) and cat (Ctenocephalides felis) fleas, lacking genal (mustache area) and promotal (back of the head) ctenidia (combs), and is half the size of the cat flea. It has 2 pairs of setae (hairs) behind the antennae with an anteriorly flattened head (Figure).
Disease Transmission
Although its primary host is poultry and it also is known as the stickfast or chicken flea, the sticktight flea has been found in many species of birds and mammals, including humans. It is becoming more common in dogs in many parts of the world, including the United States,2-5 and has been found to be the most common flea on dogs in areas of South Africa.6 Other noted hosts of E gallinacea are rodents, cottontail rabbits, cats, ground squirrels, and pigs.7-14 Human infestation occurs from exposure to affected animals.15 As blood feeders, fleas have long been known to serve as vectors for many diseases, including bubonic plague, typhus, and tularemia, as well as an intermediate host of the dog tapeworm (Dipylidium caninum).5 Rickettsia felis, belonging to the spotted fever group, is an emerging infectious disease in humans commonly found in the cat flea (C felis) but also has been detected in E gallinacea.7 Echidnophaga gallinacea is found worldwide in the tropics, subtropics, and temperate zones, and it is the only representative of the genus found in the United States.1 Given the wide range of wild and domestic animal hosts and wide geographic distribution for E gallinacea, it represents an increasing risk for humans.
Echidnophaga gallinacea favors feeding from fleshy areas without thick fur or plumage. In birds, the area around the eyes, comb, and wattles is included; in dogs, it can be the eyes, in between the toes, and in the genital area.1 Flea bites cause irritation and itching for hosts including humans, typically resulting in clusters of firm, pruritic, erythematous papules with a central punctum.15 Severe bites also may lead to bullous lesions. In birds, symptoms can be extreme, with infestation around the eyes leading to swelling and blindness, a decline in egg production, weight loss, and death in young birds.1 Similar to other fleas, E gallinacea is wingless and depends on jumping onto a host for transmission, which can be from the ground, carpeting and flooring, furniture, or another host. Fleas are champion jumpers (relative to body size) and can jump 100 times their length.16
Management
Treating sticktight fleas can be tricky, as they embed tightly into the host's skin. Animals should be treated by a qualified veterinarian. Removal of attached fleas in humans requires grasping the flea firmly with tweezers and pulling from the skin. If the infestation is considerable, malathion 5% liquid or gel can be applied. Patients can treat itching with topical steroids and antipruritic creams, and oral antihistamines can be used to relieve symptoms and reduce the likelihood of damaged skin as well as the potential for secondary infection. The flea-infested environment should be treated with insecticides. For treatment of hard surfaces, dichlorvos and propetamphos are effective. Organophosphates work well on fabric and carpeting. Domestic pets and livestock may be treated by a veterinarian with agents such as fipronil, selamectin, imidacloprid, metaflumizone, nitenpyram, lufenuron, methoprene, and pyriproxyfen.
Identifying Characteristics
The sticktight flea (Echidnophaga gallinacea) earns its name by embedding its head in the host's skin using broad and serrated laciniae and can feed at one site for up to 19 days.1 It differs in morphology from dog (Ctenocephalides canis) and cat (Ctenocephalides felis) fleas, lacking genal (mustache area) and promotal (back of the head) ctenidia (combs), and is half the size of the cat flea. It has 2 pairs of setae (hairs) behind the antennae with an anteriorly flattened head (Figure).
Disease Transmission
Although its primary host is poultry and it also is known as the stickfast or chicken flea, the sticktight flea has been found in many species of birds and mammals, including humans. It is becoming more common in dogs in many parts of the world, including the United States,2-5 and has been found to be the most common flea on dogs in areas of South Africa.6 Other noted hosts of E gallinacea are rodents, cottontail rabbits, cats, ground squirrels, and pigs.7-14 Human infestation occurs from exposure to affected animals.15 As blood feeders, fleas have long been known to serve as vectors for many diseases, including bubonic plague, typhus, and tularemia, as well as an intermediate host of the dog tapeworm (Dipylidium caninum).5 Rickettsia felis, belonging to the spotted fever group, is an emerging infectious disease in humans commonly found in the cat flea (C felis) but also has been detected in E gallinacea.7 Echidnophaga gallinacea is found worldwide in the tropics, subtropics, and temperate zones, and it is the only representative of the genus found in the United States.1 Given the wide range of wild and domestic animal hosts and wide geographic distribution for E gallinacea, it represents an increasing risk for humans.
Echidnophaga gallinacea favors feeding from fleshy areas without thick fur or plumage. In birds, the area around the eyes, comb, and wattles is included; in dogs, it can be the eyes, in between the toes, and in the genital area.1 Flea bites cause irritation and itching for hosts including humans, typically resulting in clusters of firm, pruritic, erythematous papules with a central punctum.15 Severe bites also may lead to bullous lesions. In birds, symptoms can be extreme, with infestation around the eyes leading to swelling and blindness, a decline in egg production, weight loss, and death in young birds.1 Similar to other fleas, E gallinacea is wingless and depends on jumping onto a host for transmission, which can be from the ground, carpeting and flooring, furniture, or another host. Fleas are champion jumpers (relative to body size) and can jump 100 times their length.16
Management
Treating sticktight fleas can be tricky, as they embed tightly into the host's skin. Animals should be treated by a qualified veterinarian. Removal of attached fleas in humans requires grasping the flea firmly with tweezers and pulling from the skin. If the infestation is considerable, malathion 5% liquid or gel can be applied. Patients can treat itching with topical steroids and antipruritic creams, and oral antihistamines can be used to relieve symptoms and reduce the likelihood of damaged skin as well as the potential for secondary infection. The flea-infested environment should be treated with insecticides. For treatment of hard surfaces, dichlorvos and propetamphos are effective. Organophosphates work well on fabric and carpeting. Domestic pets and livestock may be treated by a veterinarian with agents such as fipronil, selamectin, imidacloprid, metaflumizone, nitenpyram, lufenuron, methoprene, and pyriproxyfen.
- Gyimesi ZS, Hayden ER, Greiner EC. Sticktight flea (Echidnophaga gallinacea) infestation in a Victoria crowned pigeon (Goura victoria). J Zoo Wildl Med. 2007;38:594-596.
- Kalkofen UP, Greenberg J. Echidnophaga gallinacea infestation in dogs. J Am Vet Med Assoc. 1974;165:447-448.
- Harman DW, Halliwell RE, Greiner EC. Flea species from dogs and cats in north-central Florida. Vet Parasitol. 1987;23:135-140.
- Boughton RK, Atwell JW, Schoech SJ. An introduced generalist parasite, the sticktight flea (Echidnophaga gallinacea), and its pathology in the threatened Florida scrub-jay (Aphelocoma coerulescens). J Parasitol. 2006;92:941-948.
- Durden LA, Judy TN, Martin JE, et al. Fleas parasitizing domestic dogs in Georgia, USA: species composition and seasonal abundance. Vet Parasitol. 2005;130:157-162.
- Rautenbach GH, Boomker J, de Villiers IL. A descriptive study of the canine population in a rural town in southern Africa. J S Afr Vet Assoc. 1991;62:158-162.
- Leulmi H, Socolovschi C, Laudisoit A, et al. Detection of Rickettsia felis, Rickettsia typhi, Bartonella species and Yersinia pestis in fleas (Siphonaptera) from Africa. PLoS Negl Trop Dis. 2014;8:e3152.
- Guernier V, Lagadec E, LeMinter G, et al. Fleas of small mammals on Reunion Island: diversity, distribution and epidemiological consequences. PLoS Negl Trop Dis. 2014;8:e3129.
- Cantó GJ, Guerrero RI, Olvera-Ramírez AM, et al. Prevalence of fleas and gastrointestinal parasites in free-roaming cats in central Mexico [published online April 3, 2013]. PLoS One. 2013;8:e60744.
- Akucewich LH, Philman K, Clark A, et al. Prevalence of ectoparasites in a population of feral cats from north central Florida during the summer. Vet Parasitol. 2002;109:129-139.
- Linardi PM, Gomes AF, Botelho JR, et al. Some ectoparasites of commensal rodents from Huambo, Angola. J Med Entomol. 1994;31:754-756.
- Pfaffenberger GS, Valencia VB. Ectoparasites of sympatric cottontails (Sylvilagus audubonii Nelson) and jack rabbits (Lepus californicus Mearns) from the high plains of eastern New Mexico. J Parasitol. 1988;74:842-846.
- Hubbart JA, Jachowski DS, Eads DA. Seasonal and among-site variation in the occurrence and abundance of fleas on California ground squirrels (Otospermophilus beecheyi). J Vector Ecol. 2011;36:117-123.
- Braae UC, Ngowi HA, Johansen MV. Smallholder pig production: prevalence and risk factors of ectoparasites. Vet Parasitol. 2013;196:241-244.
- Carlson JC, Fox MS. A sticktight flea removed from the cheek of a two-year-old boy from Los Angeles. Dermatol Online J. 2009;15:4.
- Rothschild M, Schlein Y, Parker K, et al. The flying leap of the flea. Scientific American. 1973;229:92.
- Gyimesi ZS, Hayden ER, Greiner EC. Sticktight flea (Echidnophaga gallinacea) infestation in a Victoria crowned pigeon (Goura victoria). J Zoo Wildl Med. 2007;38:594-596.
- Kalkofen UP, Greenberg J. Echidnophaga gallinacea infestation in dogs. J Am Vet Med Assoc. 1974;165:447-448.
- Harman DW, Halliwell RE, Greiner EC. Flea species from dogs and cats in north-central Florida. Vet Parasitol. 1987;23:135-140.
- Boughton RK, Atwell JW, Schoech SJ. An introduced generalist parasite, the sticktight flea (Echidnophaga gallinacea), and its pathology in the threatened Florida scrub-jay (Aphelocoma coerulescens). J Parasitol. 2006;92:941-948.
- Durden LA, Judy TN, Martin JE, et al. Fleas parasitizing domestic dogs in Georgia, USA: species composition and seasonal abundance. Vet Parasitol. 2005;130:157-162.
- Rautenbach GH, Boomker J, de Villiers IL. A descriptive study of the canine population in a rural town in southern Africa. J S Afr Vet Assoc. 1991;62:158-162.
- Leulmi H, Socolovschi C, Laudisoit A, et al. Detection of Rickettsia felis, Rickettsia typhi, Bartonella species and Yersinia pestis in fleas (Siphonaptera) from Africa. PLoS Negl Trop Dis. 2014;8:e3152.
- Guernier V, Lagadec E, LeMinter G, et al. Fleas of small mammals on Reunion Island: diversity, distribution and epidemiological consequences. PLoS Negl Trop Dis. 2014;8:e3129.
- Cantó GJ, Guerrero RI, Olvera-Ramírez AM, et al. Prevalence of fleas and gastrointestinal parasites in free-roaming cats in central Mexico [published online April 3, 2013]. PLoS One. 2013;8:e60744.
- Akucewich LH, Philman K, Clark A, et al. Prevalence of ectoparasites in a population of feral cats from north central Florida during the summer. Vet Parasitol. 2002;109:129-139.
- Linardi PM, Gomes AF, Botelho JR, et al. Some ectoparasites of commensal rodents from Huambo, Angola. J Med Entomol. 1994;31:754-756.
- Pfaffenberger GS, Valencia VB. Ectoparasites of sympatric cottontails (Sylvilagus audubonii Nelson) and jack rabbits (Lepus californicus Mearns) from the high plains of eastern New Mexico. J Parasitol. 1988;74:842-846.
- Hubbart JA, Jachowski DS, Eads DA. Seasonal and among-site variation in the occurrence and abundance of fleas on California ground squirrels (Otospermophilus beecheyi). J Vector Ecol. 2011;36:117-123.
- Braae UC, Ngowi HA, Johansen MV. Smallholder pig production: prevalence and risk factors of ectoparasites. Vet Parasitol. 2013;196:241-244.
- Carlson JC, Fox MS. A sticktight flea removed from the cheek of a two-year-old boy from Los Angeles. Dermatol Online J. 2009;15:4.
- Rothschild M, Schlein Y, Parker K, et al. The flying leap of the flea. Scientific American. 1973;229:92.
Practice Points
- Although the primary host of the sticktight flea is poultry, it has been found in many species of birds and mammals, including humans.
- Flea bites cause irritation and itching for hosts, typically resulting in clusters of firm, pruritic, erythematous papules with a central punctum.
- Removal of attached fleas in humans requires grasping the flea firmly with tweezers and pulling from the skin.
Some adjuvant endocrine therapies better than others for young breast cancer patients
Young women treated for early hormone receptor–positive, HER2-negative breast cancer fare better if their adjuvant endocrine therapy includes ovarian function suppression (OFS), according to a new analysis published online.
Senior author Gini F. Fleming, MD, director of the medical oncology breast program at the University of Chicago Medical Center, and her colleagues analyzed data from a pair of international phase III randomized adjuvant trials: the Suppression of Ovarian Function Trial (SOFT) and the Tamoxifen and Exemestane Trial (TEXT).
Main analyses were based on a respective 240 and 145 women younger than 35 years who had undergone surgery for early hormone receptor–positive, HER2-negative early breast cancer, received chemotherapy, and were randomly assigned to 5 years of various adjuvant endocrine therapies.
In SOFT, the 5-year breast cancer–free interval was 67.1% (95% CI, 54.6%-76.9%) with tamoxifen (Nolvadex) alone, 75.9% (64.0%-84.4%) with tamoxifen plus OFS, and 83.2% (72.7%-90.0%) with exemestane (Aromasin) plus OFS (J Clin Oncol. 2017 June 27 doi: 10.1200/JCO.2016.72.0946). In TEXT, it was 79.2% (66.2%-87.7%) with tamoxifen plus OFS and 81.6% (69.8%-89.2%) with exemestane plus OFS.
In a quality of life analysis among women receiving OFS, vasomotor symptoms (hot flushes and sweats) showed greatest increase from baseline (roughly 30-40 points) in the first 6 months of therapy. Loss of sexual interest and difficulties in becoming aroused were also noteworthy (8 points or greater). However, scores for global quality of life (physical well-being, mood, coping effort, and health perception) showed little change from baseline and were essentially the same as those seen among premenopausal women aged 35 or older in the same trials.
Overall, 19.8% of the young women in SOFT and TEXT stopped all protocol-assigned endocrine therapy early. The proportion rose with time and was higher than that among the older premenopausal group.
“There was a meaningful clinical benefit in breast cancer outcomes with the addition of OFS to tamoxifen and some additional benefit from use of an aromatase inhibitor with OFS. Longer follow-up is critical to clarify potential survival benefits,” the investigators wrote. “There were substantial adverse effects from these combined endocrine treatments, but they were not different in the younger and older than 35 years populations. Despite this, rates of nonadherence were slightly higher in women younger than 35 years.
“Availability of these age-specific data regarding risks and benefits of combined endocrine therapy will support shared decision making regarding OFS among young women at high risk for recurrence and death from breast cancer and, it is hoped, improve adherence among those who select OFS,” they concluded.
Young women treated for early hormone receptor–positive, HER2-negative breast cancer fare better if their adjuvant endocrine therapy includes ovarian function suppression (OFS), according to a new analysis published online.
Senior author Gini F. Fleming, MD, director of the medical oncology breast program at the University of Chicago Medical Center, and her colleagues analyzed data from a pair of international phase III randomized adjuvant trials: the Suppression of Ovarian Function Trial (SOFT) and the Tamoxifen and Exemestane Trial (TEXT).
Main analyses were based on a respective 240 and 145 women younger than 35 years who had undergone surgery for early hormone receptor–positive, HER2-negative early breast cancer, received chemotherapy, and were randomly assigned to 5 years of various adjuvant endocrine therapies.
In SOFT, the 5-year breast cancer–free interval was 67.1% (95% CI, 54.6%-76.9%) with tamoxifen (Nolvadex) alone, 75.9% (64.0%-84.4%) with tamoxifen plus OFS, and 83.2% (72.7%-90.0%) with exemestane (Aromasin) plus OFS (J Clin Oncol. 2017 June 27 doi: 10.1200/JCO.2016.72.0946). In TEXT, it was 79.2% (66.2%-87.7%) with tamoxifen plus OFS and 81.6% (69.8%-89.2%) with exemestane plus OFS.
In a quality of life analysis among women receiving OFS, vasomotor symptoms (hot flushes and sweats) showed greatest increase from baseline (roughly 30-40 points) in the first 6 months of therapy. Loss of sexual interest and difficulties in becoming aroused were also noteworthy (8 points or greater). However, scores for global quality of life (physical well-being, mood, coping effort, and health perception) showed little change from baseline and were essentially the same as those seen among premenopausal women aged 35 or older in the same trials.
Overall, 19.8% of the young women in SOFT and TEXT stopped all protocol-assigned endocrine therapy early. The proportion rose with time and was higher than that among the older premenopausal group.
“There was a meaningful clinical benefit in breast cancer outcomes with the addition of OFS to tamoxifen and some additional benefit from use of an aromatase inhibitor with OFS. Longer follow-up is critical to clarify potential survival benefits,” the investigators wrote. “There were substantial adverse effects from these combined endocrine treatments, but they were not different in the younger and older than 35 years populations. Despite this, rates of nonadherence were slightly higher in women younger than 35 years.
“Availability of these age-specific data regarding risks and benefits of combined endocrine therapy will support shared decision making regarding OFS among young women at high risk for recurrence and death from breast cancer and, it is hoped, improve adherence among those who select OFS,” they concluded.
Young women treated for early hormone receptor–positive, HER2-negative breast cancer fare better if their adjuvant endocrine therapy includes ovarian function suppression (OFS), according to a new analysis published online.
Senior author Gini F. Fleming, MD, director of the medical oncology breast program at the University of Chicago Medical Center, and her colleagues analyzed data from a pair of international phase III randomized adjuvant trials: the Suppression of Ovarian Function Trial (SOFT) and the Tamoxifen and Exemestane Trial (TEXT).
Main analyses were based on a respective 240 and 145 women younger than 35 years who had undergone surgery for early hormone receptor–positive, HER2-negative early breast cancer, received chemotherapy, and were randomly assigned to 5 years of various adjuvant endocrine therapies.
In SOFT, the 5-year breast cancer–free interval was 67.1% (95% CI, 54.6%-76.9%) with tamoxifen (Nolvadex) alone, 75.9% (64.0%-84.4%) with tamoxifen plus OFS, and 83.2% (72.7%-90.0%) with exemestane (Aromasin) plus OFS (J Clin Oncol. 2017 June 27 doi: 10.1200/JCO.2016.72.0946). In TEXT, it was 79.2% (66.2%-87.7%) with tamoxifen plus OFS and 81.6% (69.8%-89.2%) with exemestane plus OFS.
In a quality of life analysis among women receiving OFS, vasomotor symptoms (hot flushes and sweats) showed greatest increase from baseline (roughly 30-40 points) in the first 6 months of therapy. Loss of sexual interest and difficulties in becoming aroused were also noteworthy (8 points or greater). However, scores for global quality of life (physical well-being, mood, coping effort, and health perception) showed little change from baseline and were essentially the same as those seen among premenopausal women aged 35 or older in the same trials.
Overall, 19.8% of the young women in SOFT and TEXT stopped all protocol-assigned endocrine therapy early. The proportion rose with time and was higher than that among the older premenopausal group.
“There was a meaningful clinical benefit in breast cancer outcomes with the addition of OFS to tamoxifen and some additional benefit from use of an aromatase inhibitor with OFS. Longer follow-up is critical to clarify potential survival benefits,” the investigators wrote. “There were substantial adverse effects from these combined endocrine treatments, but they were not different in the younger and older than 35 years populations. Despite this, rates of nonadherence were slightly higher in women younger than 35 years.
“Availability of these age-specific data regarding risks and benefits of combined endocrine therapy will support shared decision making regarding OFS among young women at high risk for recurrence and death from breast cancer and, it is hoped, improve adherence among those who select OFS,” they concluded.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point:
Major finding: In SOFT, the 5-year breast cancer–free interval was 67.1% with tamoxifen alone, 75.9% with tamoxifen plus OFS, and 83.2% with exemestane plus OFS. In TEXT, it was 79.2% with tamoxifen plus OFS and 81.6% with exemestane plus OFS.
Data source: An analysis of women younger than 35 years treated for early hormone receptor–positive, HER2-negative breast cancer and given adjuvant endocrine therapy in the phase III randomized SOFT trial (240 women) or TEXT trial (145 women).
Disclosures: Dr. Fleming disclosed that she receives research funding from Corcept Therapeutics (institutional) and has a relationship with Aeterna Zentaris.
Cognitive declines tied to stress in older African Americans
Higher levels of perceived stress appear to be associated with faster declines in two cognitive domains – episodic memory and visuospatial ability – among older African Americans without dementia, results from a longitudinal study of 467 participants suggest.
“To our knowledge, this is the first study to examine the relationship between perceived stress and cognition in specific cognitive domains in general and in a minority population in particular,” reported Arlener D. Turner, PhD, of the Rush Alzheimer’s Disease Center and the department of behavioral sciences at Rush University, Chicago, and her associates.
Each participant took a battery of neuropsychological tests, including the MMSE, annually for up to 9 years. The participants’ stress levels were assessed using a 4-item version of Cohen’s Perceived Stress Scale (PSS), “an index of the degree to which a person finds their lives unpredictable, uncontrollable, and overloading – characteristics central to the evaluation of stress” (Am J Geriatr Psychiatry. 2017;25[1]:25-34).
Dr. Turner and her associates found that participants with a mean age and education level, and a PSS score 1 point above the mean experienced annual declines in episodic memory of 0.022 points (P = .047) and in visuospatial ability of 0.021 points (P = .017). No such associations were found for semantic or working memory or for perceptual speed.
The investigators said that the study did not pinpoint the mechanisms that link stress to cognition. “The well-established mechanism of hypothalamic-pituitary-adrenal-axis dysregulation in chronic stress may play a role,” they wrote. Another contributing factor could be inflammation, they said, citing research showing that discrimination is “a persistent stressor in African Americans and that perceived discrimination is associated with elevated levels of C-reactive protein.” Future studies are needed, they said, to test which mechanisms might be pathways between perceived stress and cognitive decline.
They cited several limitations. For example, because less educational attainment is associated with higher levels of stress and this cohort had achieved educational levels that were relatively high, this cohort’s reports of perceived stress might have been modest. In addition, “perception of stress is, by nature, a self-report measure,” the investigators wrote.
The National Institute on Aging and the Illinois Department of Public Health funded the study. Neither Dr. Turner nor her associates had any conflicts of interest.
[email protected]
On Twitter @ginahenderson
Higher levels of perceived stress appear to be associated with faster declines in two cognitive domains – episodic memory and visuospatial ability – among older African Americans without dementia, results from a longitudinal study of 467 participants suggest.
“To our knowledge, this is the first study to examine the relationship between perceived stress and cognition in specific cognitive domains in general and in a minority population in particular,” reported Arlener D. Turner, PhD, of the Rush Alzheimer’s Disease Center and the department of behavioral sciences at Rush University, Chicago, and her associates.
Each participant took a battery of neuropsychological tests, including the MMSE, annually for up to 9 years. The participants’ stress levels were assessed using a 4-item version of Cohen’s Perceived Stress Scale (PSS), “an index of the degree to which a person finds their lives unpredictable, uncontrollable, and overloading – characteristics central to the evaluation of stress” (Am J Geriatr Psychiatry. 2017;25[1]:25-34).
Dr. Turner and her associates found that participants with a mean age and education level, and a PSS score 1 point above the mean experienced annual declines in episodic memory of 0.022 points (P = .047) and in visuospatial ability of 0.021 points (P = .017). No such associations were found for semantic or working memory or for perceptual speed.
The investigators said that the study did not pinpoint the mechanisms that link stress to cognition. “The well-established mechanism of hypothalamic-pituitary-adrenal-axis dysregulation in chronic stress may play a role,” they wrote. Another contributing factor could be inflammation, they said, citing research showing that discrimination is “a persistent stressor in African Americans and that perceived discrimination is associated with elevated levels of C-reactive protein.” Future studies are needed, they said, to test which mechanisms might be pathways between perceived stress and cognitive decline.
They cited several limitations. For example, because less educational attainment is associated with higher levels of stress and this cohort had achieved educational levels that were relatively high, this cohort’s reports of perceived stress might have been modest. In addition, “perception of stress is, by nature, a self-report measure,” the investigators wrote.
The National Institute on Aging and the Illinois Department of Public Health funded the study. Neither Dr. Turner nor her associates had any conflicts of interest.
[email protected]
On Twitter @ginahenderson
Higher levels of perceived stress appear to be associated with faster declines in two cognitive domains – episodic memory and visuospatial ability – among older African Americans without dementia, results from a longitudinal study of 467 participants suggest.
“To our knowledge, this is the first study to examine the relationship between perceived stress and cognition in specific cognitive domains in general and in a minority population in particular,” reported Arlener D. Turner, PhD, of the Rush Alzheimer’s Disease Center and the department of behavioral sciences at Rush University, Chicago, and her associates.
Each participant took a battery of neuropsychological tests, including the MMSE, annually for up to 9 years. The participants’ stress levels were assessed using a 4-item version of Cohen’s Perceived Stress Scale (PSS), “an index of the degree to which a person finds their lives unpredictable, uncontrollable, and overloading – characteristics central to the evaluation of stress” (Am J Geriatr Psychiatry. 2017;25[1]:25-34).
Dr. Turner and her associates found that participants with a mean age and education level, and a PSS score 1 point above the mean experienced annual declines in episodic memory of 0.022 points (P = .047) and in visuospatial ability of 0.021 points (P = .017). No such associations were found for semantic or working memory or for perceptual speed.
The investigators said that the study did not pinpoint the mechanisms that link stress to cognition. “The well-established mechanism of hypothalamic-pituitary-adrenal-axis dysregulation in chronic stress may play a role,” they wrote. Another contributing factor could be inflammation, they said, citing research showing that discrimination is “a persistent stressor in African Americans and that perceived discrimination is associated with elevated levels of C-reactive protein.” Future studies are needed, they said, to test which mechanisms might be pathways between perceived stress and cognitive decline.
They cited several limitations. For example, because less educational attainment is associated with higher levels of stress and this cohort had achieved educational levels that were relatively high, this cohort’s reports of perceived stress might have been modest. In addition, “perception of stress is, by nature, a self-report measure,” the investigators wrote.
The National Institute on Aging and the Illinois Department of Public Health funded the study. Neither Dr. Turner nor her associates had any conflicts of interest.
[email protected]
On Twitter @ginahenderson
FROM THE AMERICAN JOURNAL OF GERIATRIC PSYCHIATRY
Key clinical point:
Major finding: Participants with a mean age of 73.4 years and education level of 15 years and a score 1 point above the mean on Cohen’s Perceived Stress Scale experienced annual declines in episodic memory of 0.022 points (P = .047) and in visuospatial ability of 0.021 points (P = .017).
Data source: An analysis of 467 African Americans enrolled in the longitudinal Minority Aging Research Study.
Disclosures: The National Institute on Aging and the Illinois Department of Public Health funded the study. Neither Dr. Turner nor her associates had any conflicts of interest.
Low-fat diet reduces risk of death if breast cancer is diagnosed
Women can reduce their risk of dying should they receive a breast cancer diagnosis by following a low-fat diet, suggests an analysis from the phase III multicenter randomized Women’s Health Initiative Dietary Modification trial.
Investigators led by Rowan T. Chlebowski, MD, PhD, formerly of the Los Angeles Biomedical Research Institute at Harbor-UCLA Medical Center, Torrance, California, and now at City of Hope National Medical Center, Duarte, California, analyzed data from 48,835 postmenopausal women who had never had breast cancer and had normal mammograms. The women were randomly assigned 2:3 to a diet aimed at reducing fat intake to 20% of energy and increasing intake of fruits, vegetables, and grains or to a usual diet.
However, the rate of deaths after breast cancer from any cause was 0.025% per year in the former group and 0.038% per year in the latter group, a difference that translated to a more than one-third reduction in risk (hazard ratio, 0.65; P = .02).
Similarly, during the median 16.1-year total follow-up, the rate of deaths attributed to breast cancer was 0.035% per year in the low-fat diet group and 0.039% per year in the usual diet group, a difference that was not significant (P =. 41). However, the rate of deaths after breast cancer from any cause was 0.085% per year in the former group and 0.11% per year in the latter group, a difference that translated to a nearly one-fifth reduction in the risk of death (HR, 0.82; P = .01).
In subgroup analyses, there were significant interactions whereby benefit was greater for women who had a baseline waist circumference of at least 88 cm and increased with the baseline percentage of total energy from fat.
“The lower risk of poor prognosis, ER+, PR– breast cancers … in the dietary group contributed to the favorable dietary effect on death after breast cancer,” the investigators noted. “An additional factor that potentially influenced deaths after breast cancer could be a favorable dietary influence on mortality as a result of other causes, including cardiovascular disease.”
“Future studies of other lifestyle interventions on breast cancer incidence and outcome could incorporate some form of a low-fat dietary pattern as a base,” they concluded.
Women can reduce their risk of dying should they receive a breast cancer diagnosis by following a low-fat diet, suggests an analysis from the phase III multicenter randomized Women’s Health Initiative Dietary Modification trial.
Investigators led by Rowan T. Chlebowski, MD, PhD, formerly of the Los Angeles Biomedical Research Institute at Harbor-UCLA Medical Center, Torrance, California, and now at City of Hope National Medical Center, Duarte, California, analyzed data from 48,835 postmenopausal women who had never had breast cancer and had normal mammograms. The women were randomly assigned 2:3 to a diet aimed at reducing fat intake to 20% of energy and increasing intake of fruits, vegetables, and grains or to a usual diet.
However, the rate of deaths after breast cancer from any cause was 0.025% per year in the former group and 0.038% per year in the latter group, a difference that translated to a more than one-third reduction in risk (hazard ratio, 0.65; P = .02).
Similarly, during the median 16.1-year total follow-up, the rate of deaths attributed to breast cancer was 0.035% per year in the low-fat diet group and 0.039% per year in the usual diet group, a difference that was not significant (P =. 41). However, the rate of deaths after breast cancer from any cause was 0.085% per year in the former group and 0.11% per year in the latter group, a difference that translated to a nearly one-fifth reduction in the risk of death (HR, 0.82; P = .01).
In subgroup analyses, there were significant interactions whereby benefit was greater for women who had a baseline waist circumference of at least 88 cm and increased with the baseline percentage of total energy from fat.
“The lower risk of poor prognosis, ER+, PR– breast cancers … in the dietary group contributed to the favorable dietary effect on death after breast cancer,” the investigators noted. “An additional factor that potentially influenced deaths after breast cancer could be a favorable dietary influence on mortality as a result of other causes, including cardiovascular disease.”
“Future studies of other lifestyle interventions on breast cancer incidence and outcome could incorporate some form of a low-fat dietary pattern as a base,” they concluded.
Women can reduce their risk of dying should they receive a breast cancer diagnosis by following a low-fat diet, suggests an analysis from the phase III multicenter randomized Women’s Health Initiative Dietary Modification trial.
Investigators led by Rowan T. Chlebowski, MD, PhD, formerly of the Los Angeles Biomedical Research Institute at Harbor-UCLA Medical Center, Torrance, California, and now at City of Hope National Medical Center, Duarte, California, analyzed data from 48,835 postmenopausal women who had never had breast cancer and had normal mammograms. The women were randomly assigned 2:3 to a diet aimed at reducing fat intake to 20% of energy and increasing intake of fruits, vegetables, and grains or to a usual diet.
However, the rate of deaths after breast cancer from any cause was 0.025% per year in the former group and 0.038% per year in the latter group, a difference that translated to a more than one-third reduction in risk (hazard ratio, 0.65; P = .02).
Similarly, during the median 16.1-year total follow-up, the rate of deaths attributed to breast cancer was 0.035% per year in the low-fat diet group and 0.039% per year in the usual diet group, a difference that was not significant (P =. 41). However, the rate of deaths after breast cancer from any cause was 0.085% per year in the former group and 0.11% per year in the latter group, a difference that translated to a nearly one-fifth reduction in the risk of death (HR, 0.82; P = .01).
In subgroup analyses, there were significant interactions whereby benefit was greater for women who had a baseline waist circumference of at least 88 cm and increased with the baseline percentage of total energy from fat.
“The lower risk of poor prognosis, ER+, PR– breast cancers … in the dietary group contributed to the favorable dietary effect on death after breast cancer,” the investigators noted. “An additional factor that potentially influenced deaths after breast cancer could be a favorable dietary influence on mortality as a result of other causes, including cardiovascular disease.”
“Future studies of other lifestyle interventions on breast cancer incidence and outcome could incorporate some form of a low-fat dietary pattern as a base,” they concluded.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point:
Major finding: Compared with peers assigned to a usual diet, women assigned to a low-fat diet were less likely to die after breast cancer diagnosis from any cause during both the 8.5-year intervention (HR 0.65) and the 16.1-year total follow-up (HR, 0.82).
Data source: A posthoc analysis of a phase III randomized controlled trial among 48,835 postmenopausal women who had never had breast cancer and had normal mammograms (Women’s Health Initiative Dietary Modification trial).
Disclosures: Dr. Chlebowski disclosed consulting or advisory roles with Novartis, Genentech, Amgen, Pfizer, and AstraZeneca. He is also on the Speakers’ Bureau for Novartis and Genentech.
Phototherapy Coding and Documentation in the Time of Biologics
In this era of biologics for psoriasis with ever-increasing effectiveness and safety as well as patients who have less and less time to visit the physician's office, it would seem that the days of in-office UV treatments would be numbered. However, rumors of the demise of phototherapy may be greatly exaggerated. Phototherapy is still one of the safest and most cost-effective treatments for psoriasis and other dermatoses.1 Its use often is a prerequisite for biologic therapy, and it may be the only therapeutic option for certain subsets of patients, such as children, pregnant women, and immunosuppressed patients. Moreover, narrowband UVB technology has breathed new life into phototherapy, with better efficacy and less long-term risk. Although the utilization of psoralen plus UVA (PUVA) light therapy has indeed decreased over the last 2 decades, the use of UVB therapies continues to increase dramatically.2
Phototherapy Codes
There are 4 chief Current Procedural Terminology (CPT) codes for reporting phototherapy services: (1) 96900: actinotherapy (UV light treatment); (2) 96910: photochemotherapy, tar, and UVB (Goeckerman treatment) or petrolatum and UVB; (3) 96912: photochemotherapy and PUVA; and (4) 96913: photochemotherapy (Goeckerman and/or PUVA) for severe photoresponsive dermatoses requiring at least 4 to 8 hours of care under direct supervision of the physician.3
There is lack of specificity of the CPT code descriptions for phototherapy. Moreover, insurer guidance for documentation for phototherapy is vague to nonexistent, and of course whenever the use of any medical service increases, insurer scrutiny is sure to follow. Therefore, it is not surprising that dermatology practices have reported that private insurers as well as Medicare are auditing medical records for phototherapy treatments.4 In fact, recently we have seen a Midwest private insurer demand payment from dermatologists for hundreds of 96910 phototherapy services, which the insurer asserted should have been coded as 96900 because topical therapies were not applied by the dermatology staff. The insurer did not just evaluate medical records but also contacted patients directly and asked how services had been provided. Clearly, more detailed guidance for dermatologists and insurers on documentation and performance standards for each phototherapy service is needed.
Existing coding guidance for phototherapy indicates that actinotherapy (96900) defines the basic service of treating a patient with a UV light unit.5 Actinotherapy does not involve application of topical medications while the patient is in the office.
In contrast, photochemotherapy (96910) implies addition of a chemo agent to phototherapy. Despite the somewhat nonspecific nature of the code descriptor, it is apparent that application of photoenhancing agents such as tar, petrolatum, or distillates of petrolatum meet the requirements of 96910. The Coder's Desk Reference for Procedures 2017 describes 96910 as "the physician uses photosensitizing chemicals and light rays to treat skin ailments."6 Application of light-enhancing topical products should occur within the office by either staff or the patient. In fact, examination of practice expense data from the Centers for Medicare & Medicaid Services indicated that the 96910 code includes payment for clinical staff time to apply topical products as well as the cost of the topical agent(s).7
The PUVA code 96912 is defined by the use of photosensitizing psoralen medication, which can be administered topically or orally, followed by UVA treatment. In my experience, PUVA has similar performance standards with in-office application of psoralen, if applicable. If application of topical photoenhancing products occurs outside the office, the requirements of photochemotherapy are not met, and 96900 should be reported.
The 96913 code defines prolonged phototherapy service with intensive topical therapy requirements and multiple phototherapy sessions per day.3 This code is rarely reported (average of fewer than 100 times in the Medicare population per year), and most insurers do not reimburse this service.
Protecting Yourself From an Audit
In my experience, review of private insurer audits of phototherapy services has yielded important lessons. First, having a written standard operating procedure in place regarding the performance of phototherapy services and how application of topicals will be handled has been helpful in audit defense. The other key to beating audits for phototherapy services is to have detailed documentation or a flowchart in the medical record regarding the topical agent and the light administration. The medical record should include what topical agent was applied, if any; whether the topical agent was applied in the office; where the topical product was applied; and who applied the topical product. Sometimes topical product application by a physician or staff is not feasible because of patient preference or the site of application. If the patient applied the topical, document that assistance was offered and refused, along with what type of UV light was used and the dosage. Inclusion of these elements in the medical record provides a clear picture of the delivery of the phototherapy service and will aid in responding to medical record audit.
Final Thoughts
Phototherapy is a critical treatment modality that continues to be utilized frequently in the expanding armamentarium of treatments for dermatoses. Phototherapy is performed almost exclusively by dermatologists and allows dermatologists to offer a unique level of care and value in the treatment of skin disease. Careful documentation, a written standard operating procedure, and adherence to proper performance standards will allow dermatologists to be compensated fairly for this important treatment modality and pass audits that are likely to occur.
- Lapolla W, Yentzer BA, Bagel J, et al. A review of phototherapy protocols for psoriasis treatment. J Am Acad Dermatol. 2011;64:936-949.
- Simpson GL, Yelverton CB, Rittenberg S, et al. Do utilization management controls for phototherapy increase the prescription of biologics? J Dermatolog Treat. 2006;17:359-361.
- Current Procedural Terminology 2017, Professional Edition. Chicago IL: American Medical Association; 2016.
- American Academy of Dermatology Association. Insurers review billing for photochemotherapy (CPT 96910). Derm Coding Consult. Spring 2009;13:4.
- American Academy of Dermatology Association. Coding Q&A's. Derm Coding Consult. Spring 2007;11:5, 7, 8.
- Coders' Desk Reference for Procedures 2017. Chicago, IL: Optum360; 2017.
- Relative Value Scale Update Committee Database. Chicago, IL: American Medical Association; 2016.
In this era of biologics for psoriasis with ever-increasing effectiveness and safety as well as patients who have less and less time to visit the physician's office, it would seem that the days of in-office UV treatments would be numbered. However, rumors of the demise of phototherapy may be greatly exaggerated. Phototherapy is still one of the safest and most cost-effective treatments for psoriasis and other dermatoses.1 Its use often is a prerequisite for biologic therapy, and it may be the only therapeutic option for certain subsets of patients, such as children, pregnant women, and immunosuppressed patients. Moreover, narrowband UVB technology has breathed new life into phototherapy, with better efficacy and less long-term risk. Although the utilization of psoralen plus UVA (PUVA) light therapy has indeed decreased over the last 2 decades, the use of UVB therapies continues to increase dramatically.2
Phototherapy Codes
There are 4 chief Current Procedural Terminology (CPT) codes for reporting phototherapy services: (1) 96900: actinotherapy (UV light treatment); (2) 96910: photochemotherapy, tar, and UVB (Goeckerman treatment) or petrolatum and UVB; (3) 96912: photochemotherapy and PUVA; and (4) 96913: photochemotherapy (Goeckerman and/or PUVA) for severe photoresponsive dermatoses requiring at least 4 to 8 hours of care under direct supervision of the physician.3
There is lack of specificity of the CPT code descriptions for phototherapy. Moreover, insurer guidance for documentation for phototherapy is vague to nonexistent, and of course whenever the use of any medical service increases, insurer scrutiny is sure to follow. Therefore, it is not surprising that dermatology practices have reported that private insurers as well as Medicare are auditing medical records for phototherapy treatments.4 In fact, recently we have seen a Midwest private insurer demand payment from dermatologists for hundreds of 96910 phototherapy services, which the insurer asserted should have been coded as 96900 because topical therapies were not applied by the dermatology staff. The insurer did not just evaluate medical records but also contacted patients directly and asked how services had been provided. Clearly, more detailed guidance for dermatologists and insurers on documentation and performance standards for each phototherapy service is needed.
Existing coding guidance for phototherapy indicates that actinotherapy (96900) defines the basic service of treating a patient with a UV light unit.5 Actinotherapy does not involve application of topical medications while the patient is in the office.
In contrast, photochemotherapy (96910) implies addition of a chemo agent to phototherapy. Despite the somewhat nonspecific nature of the code descriptor, it is apparent that application of photoenhancing agents such as tar, petrolatum, or distillates of petrolatum meet the requirements of 96910. The Coder's Desk Reference for Procedures 2017 describes 96910 as "the physician uses photosensitizing chemicals and light rays to treat skin ailments."6 Application of light-enhancing topical products should occur within the office by either staff or the patient. In fact, examination of practice expense data from the Centers for Medicare & Medicaid Services indicated that the 96910 code includes payment for clinical staff time to apply topical products as well as the cost of the topical agent(s).7
The PUVA code 96912 is defined by the use of photosensitizing psoralen medication, which can be administered topically or orally, followed by UVA treatment. In my experience, PUVA has similar performance standards with in-office application of psoralen, if applicable. If application of topical photoenhancing products occurs outside the office, the requirements of photochemotherapy are not met, and 96900 should be reported.
The 96913 code defines prolonged phototherapy service with intensive topical therapy requirements and multiple phototherapy sessions per day.3 This code is rarely reported (average of fewer than 100 times in the Medicare population per year), and most insurers do not reimburse this service.
Protecting Yourself From an Audit
In my experience, review of private insurer audits of phototherapy services has yielded important lessons. First, having a written standard operating procedure in place regarding the performance of phototherapy services and how application of topicals will be handled has been helpful in audit defense. The other key to beating audits for phototherapy services is to have detailed documentation or a flowchart in the medical record regarding the topical agent and the light administration. The medical record should include what topical agent was applied, if any; whether the topical agent was applied in the office; where the topical product was applied; and who applied the topical product. Sometimes topical product application by a physician or staff is not feasible because of patient preference or the site of application. If the patient applied the topical, document that assistance was offered and refused, along with what type of UV light was used and the dosage. Inclusion of these elements in the medical record provides a clear picture of the delivery of the phototherapy service and will aid in responding to medical record audit.
Final Thoughts
Phototherapy is a critical treatment modality that continues to be utilized frequently in the expanding armamentarium of treatments for dermatoses. Phototherapy is performed almost exclusively by dermatologists and allows dermatologists to offer a unique level of care and value in the treatment of skin disease. Careful documentation, a written standard operating procedure, and adherence to proper performance standards will allow dermatologists to be compensated fairly for this important treatment modality and pass audits that are likely to occur.
In this era of biologics for psoriasis with ever-increasing effectiveness and safety as well as patients who have less and less time to visit the physician's office, it would seem that the days of in-office UV treatments would be numbered. However, rumors of the demise of phototherapy may be greatly exaggerated. Phototherapy is still one of the safest and most cost-effective treatments for psoriasis and other dermatoses.1 Its use often is a prerequisite for biologic therapy, and it may be the only therapeutic option for certain subsets of patients, such as children, pregnant women, and immunosuppressed patients. Moreover, narrowband UVB technology has breathed new life into phototherapy, with better efficacy and less long-term risk. Although the utilization of psoralen plus UVA (PUVA) light therapy has indeed decreased over the last 2 decades, the use of UVB therapies continues to increase dramatically.2
Phototherapy Codes
There are 4 chief Current Procedural Terminology (CPT) codes for reporting phototherapy services: (1) 96900: actinotherapy (UV light treatment); (2) 96910: photochemotherapy, tar, and UVB (Goeckerman treatment) or petrolatum and UVB; (3) 96912: photochemotherapy and PUVA; and (4) 96913: photochemotherapy (Goeckerman and/or PUVA) for severe photoresponsive dermatoses requiring at least 4 to 8 hours of care under direct supervision of the physician.3
There is lack of specificity of the CPT code descriptions for phototherapy. Moreover, insurer guidance for documentation for phototherapy is vague to nonexistent, and of course whenever the use of any medical service increases, insurer scrutiny is sure to follow. Therefore, it is not surprising that dermatology practices have reported that private insurers as well as Medicare are auditing medical records for phototherapy treatments.4 In fact, recently we have seen a Midwest private insurer demand payment from dermatologists for hundreds of 96910 phototherapy services, which the insurer asserted should have been coded as 96900 because topical therapies were not applied by the dermatology staff. The insurer did not just evaluate medical records but also contacted patients directly and asked how services had been provided. Clearly, more detailed guidance for dermatologists and insurers on documentation and performance standards for each phototherapy service is needed.
Existing coding guidance for phototherapy indicates that actinotherapy (96900) defines the basic service of treating a patient with a UV light unit.5 Actinotherapy does not involve application of topical medications while the patient is in the office.
In contrast, photochemotherapy (96910) implies addition of a chemo agent to phototherapy. Despite the somewhat nonspecific nature of the code descriptor, it is apparent that application of photoenhancing agents such as tar, petrolatum, or distillates of petrolatum meet the requirements of 96910. The Coder's Desk Reference for Procedures 2017 describes 96910 as "the physician uses photosensitizing chemicals and light rays to treat skin ailments."6 Application of light-enhancing topical products should occur within the office by either staff or the patient. In fact, examination of practice expense data from the Centers for Medicare & Medicaid Services indicated that the 96910 code includes payment for clinical staff time to apply topical products as well as the cost of the topical agent(s).7
The PUVA code 96912 is defined by the use of photosensitizing psoralen medication, which can be administered topically or orally, followed by UVA treatment. In my experience, PUVA has similar performance standards with in-office application of psoralen, if applicable. If application of topical photoenhancing products occurs outside the office, the requirements of photochemotherapy are not met, and 96900 should be reported.
The 96913 code defines prolonged phototherapy service with intensive topical therapy requirements and multiple phototherapy sessions per day.3 This code is rarely reported (average of fewer than 100 times in the Medicare population per year), and most insurers do not reimburse this service.
Protecting Yourself From an Audit
In my experience, review of private insurer audits of phototherapy services has yielded important lessons. First, having a written standard operating procedure in place regarding the performance of phototherapy services and how application of topicals will be handled has been helpful in audit defense. The other key to beating audits for phototherapy services is to have detailed documentation or a flowchart in the medical record regarding the topical agent and the light administration. The medical record should include what topical agent was applied, if any; whether the topical agent was applied in the office; where the topical product was applied; and who applied the topical product. Sometimes topical product application by a physician or staff is not feasible because of patient preference or the site of application. If the patient applied the topical, document that assistance was offered and refused, along with what type of UV light was used and the dosage. Inclusion of these elements in the medical record provides a clear picture of the delivery of the phototherapy service and will aid in responding to medical record audit.
Final Thoughts
Phototherapy is a critical treatment modality that continues to be utilized frequently in the expanding armamentarium of treatments for dermatoses. Phototherapy is performed almost exclusively by dermatologists and allows dermatologists to offer a unique level of care and value in the treatment of skin disease. Careful documentation, a written standard operating procedure, and adherence to proper performance standards will allow dermatologists to be compensated fairly for this important treatment modality and pass audits that are likely to occur.
- Lapolla W, Yentzer BA, Bagel J, et al. A review of phototherapy protocols for psoriasis treatment. J Am Acad Dermatol. 2011;64:936-949.
- Simpson GL, Yelverton CB, Rittenberg S, et al. Do utilization management controls for phototherapy increase the prescription of biologics? J Dermatolog Treat. 2006;17:359-361.
- Current Procedural Terminology 2017, Professional Edition. Chicago IL: American Medical Association; 2016.
- American Academy of Dermatology Association. Insurers review billing for photochemotherapy (CPT 96910). Derm Coding Consult. Spring 2009;13:4.
- American Academy of Dermatology Association. Coding Q&A's. Derm Coding Consult. Spring 2007;11:5, 7, 8.
- Coders' Desk Reference for Procedures 2017. Chicago, IL: Optum360; 2017.
- Relative Value Scale Update Committee Database. Chicago, IL: American Medical Association; 2016.
- Lapolla W, Yentzer BA, Bagel J, et al. A review of phototherapy protocols for psoriasis treatment. J Am Acad Dermatol. 2011;64:936-949.
- Simpson GL, Yelverton CB, Rittenberg S, et al. Do utilization management controls for phototherapy increase the prescription of biologics? J Dermatolog Treat. 2006;17:359-361.
- Current Procedural Terminology 2017, Professional Edition. Chicago IL: American Medical Association; 2016.
- American Academy of Dermatology Association. Insurers review billing for photochemotherapy (CPT 96910). Derm Coding Consult. Spring 2009;13:4.
- American Academy of Dermatology Association. Coding Q&A's. Derm Coding Consult. Spring 2007;11:5, 7, 8.
- Coders' Desk Reference for Procedures 2017. Chicago, IL: Optum360; 2017.
- Relative Value Scale Update Committee Database. Chicago, IL: American Medical Association; 2016.
How to raise HPV vaccine rates: Work together
Despite widespread availability of the human papillomavirus vaccine over the last 11 years, vaccination rates continue to lag behind national targets and are far behind other vaccines routinely administered in adolescence, such as the meningococcal and tetanus vaccines.
Better collaboration among pediatricians and obstetrician-gynecologists to promote the HPV vaccine may be one answer to turning the tide, said David W. Kimberlin, MD, codirector of the division of pediatric infectious diseases at the University of Alabama at Birmingham and president of the Pediatric Infectious Diseases Society.
As of 2015, just 63% of eligible U.S. girls completed the first dose of the HPV vaccination, 52% completed two doses, and 42% finished the three-dose series, according to a recent “Call to Action” paper in the American Journal of Obstetrics and Gynecology (doi: 10.1016/j.ajog.2017.02.026). Although the HPV vaccine has been recommended for boys since 2011, just half of eligible boys completed the first dose, 39% completed two doses, and 28% finished the full series. By contrast, 86% of adolescents received the tetanus, diphtheria, and acellular pertussis vaccine, and 81% received the first dose of the meningococcal vaccine. The federal government’s Office of Disease Prevention and Health Promotion aims for an 80% HPV vaccination completion rate for girls and boys aged 13-15 years by 2020.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/how-to-raise-hpv-vaccine-rates?iframe=1"}]The CDC now recommends that 11- to 12-year-olds get two doses of the HPV vaccine, rather than three, with the second dose given 6-12 months after the first (MMWR. 2016;65:1405-8).
The common ways in which the HPV vaccine is introduced to parents likely contributes to the low vaccination rates, said Beth Auslander, PhD, a clinical psychologist and associate professor in the department of pediatrics at the University of Texas Medical Branch in Galveston. Some pediatricians may tell parents about school-mandated vaccines first and then as a side note, mention the HPV vaccine.
“The way it’s presented at times is being separate from the other vaccines,” Dr. Auslander said. “Sometimes it sounds optional.”
Parents often are uncertain about the safety and efficacy of the HPV vaccine, she added, and some wrongly assume the vaccine will lead to sexual activity among their children.
“Sometimes it can take a little longer to talk about,” Dr. Yoost said in an interview. “A lot of times, parents will bring up questions or concerns about the HPV vaccine. If physicians aren’t comfortable talking about those topics, they may not give the best recommendation. Pediatricians are not dealing with cervical cancer, so they may have a harder time recommending a vaccine based on outcomes they don’t deal with.”
Ob.gyns. are in a unique position to reach out to their pediatric counterparts and discuss strategies for catching more patients eligible for the HPV vaccine, said Sarah Dilley, MD, a gynecologic oncology fellow at the University of Alabama at Birmingham and the lead author of the recent Call to Action paper.
“We offer a unique perspective in that we are treating the conditions that the HPV vaccine is preventing, so we have more of a sense of urgency and an understanding of why that is so important,” Dr. Dilley said in an interview. “Obviously, pediatricians understand this as well, but it’s not something they see every day in their practice. We, as ob.gyns., have the opportunity to talk to our pediatric colleagues about the importance and really how devastating these conditions can be and how important it is to prevent them.”
In the recent paper, Dr. Dilley and her colleagues recommend that ob.gyns. speak to pediatricians and primary care physicians in their community to promote the vaccine and encourage them to view the Centers for Disease Control and Prevention’s You Are the Key presentation. The CDC resources include tips for how to discuss the burden of HPV-related diseases and effective communication with parents, an update on state vaccination rates, and the latest HPV vaccination recommendations.
Dr. Dilley encourages ob.gyns. and pediatricians to find different opportunities and venues to discuss the HPV vaccine. Ask about the pediatrician’s current approach to the vaccine, the doctor’s communication with parents, and how such practices could be improved, she said.
“People like to hear from their colleagues,” Dr. Dilley said. “Hearing from ob.gyns. [about] their experiences could be really helpful, whether it’s doing lunch and learns, formal education, grand rounds, or even more informal talks at the hospital.”
Ob.gyns. and pediatricians also need to better coordinate their messaging so that there is more consistent emphasis during each patient encounter about the need of the HPV vaccination, Dr. Kimberlin said. There needs to be a renewed focus on the vaccine as a cancer vaccination, he said.
“The nuances of HPV and the way that HPV is acquired, namely sexually transmitted, has taken too much of a front row consideration in the conversations that parents sometimes want to have with their child’s health care providers,” Dr. Kimberlin said. “We have to stress this is a cancer vaccine. This is a vaccine that prevents the deaths of thousands of women and men. We simply need to get that message out more forcefully.”
In addition, there’s a need for joint action to debunk myths about the vaccine and work toward eliminating the stigma surrounding it, Dr. Dilley said.
“I talk to a lot parents about the HPV vaccine and there’s so much misinformation online,” she said. “But a lot of patients do look at websites of their ob.gyn. or their pediatrician, [and] if they see something reputable coming from one of those sites, they might listen. We have a lot of patients who are mothers or grandmothers of kids; that’s also an opportunity for us to say, ‘Hey while we’re screening you for cervical cancer, let’s talk about the HPV vaccine.’ That’s a really good opportunity to help our [pediatric] colleagues out.”
5 steps to increase HPV vaccination
Melissa Kottke, MD, director of the Jane Fonda Center for Adolescent Reproductive Health at Emory University offered her practice steps for increased HPV vaccination rates.
1. Be clear about your recommendation. For example, “I recommend the HPV vaccine. It can help prevent cancer.”
3. Educate the entire clinical team (front desk staff, nursing, medical assistants, etc.) about the HPV vaccine so there is consistent messaging and delivery.
4. Establish streamlined systems. The vaccine recommendation, order, and follow-up should be streamlined and automated, if possible. Systems should also ensure documentation of vaccine receipt.
5. Make time for conversations with patients who are mothers and grandmothers. Recommend the HPV vaccine for males and females aged 9-26 years old. Encourage parents/grandparents to follow-up with the child’s doctor or offer to provide the vaccine in your office.
*This story was updated 8/22/2017.
[email protected]
On Twitter @legal_med
Despite widespread availability of the human papillomavirus vaccine over the last 11 years, vaccination rates continue to lag behind national targets and are far behind other vaccines routinely administered in adolescence, such as the meningococcal and tetanus vaccines.
Better collaboration among pediatricians and obstetrician-gynecologists to promote the HPV vaccine may be one answer to turning the tide, said David W. Kimberlin, MD, codirector of the division of pediatric infectious diseases at the University of Alabama at Birmingham and president of the Pediatric Infectious Diseases Society.
As of 2015, just 63% of eligible U.S. girls completed the first dose of the HPV vaccination, 52% completed two doses, and 42% finished the three-dose series, according to a recent “Call to Action” paper in the American Journal of Obstetrics and Gynecology (doi: 10.1016/j.ajog.2017.02.026). Although the HPV vaccine has been recommended for boys since 2011, just half of eligible boys completed the first dose, 39% completed two doses, and 28% finished the full series. By contrast, 86% of adolescents received the tetanus, diphtheria, and acellular pertussis vaccine, and 81% received the first dose of the meningococcal vaccine. The federal government’s Office of Disease Prevention and Health Promotion aims for an 80% HPV vaccination completion rate for girls and boys aged 13-15 years by 2020.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/how-to-raise-hpv-vaccine-rates?iframe=1"}]The CDC now recommends that 11- to 12-year-olds get two doses of the HPV vaccine, rather than three, with the second dose given 6-12 months after the first (MMWR. 2016;65:1405-8).
The common ways in which the HPV vaccine is introduced to parents likely contributes to the low vaccination rates, said Beth Auslander, PhD, a clinical psychologist and associate professor in the department of pediatrics at the University of Texas Medical Branch in Galveston. Some pediatricians may tell parents about school-mandated vaccines first and then as a side note, mention the HPV vaccine.
“The way it’s presented at times is being separate from the other vaccines,” Dr. Auslander said. “Sometimes it sounds optional.”
Parents often are uncertain about the safety and efficacy of the HPV vaccine, she added, and some wrongly assume the vaccine will lead to sexual activity among their children.
“Sometimes it can take a little longer to talk about,” Dr. Yoost said in an interview. “A lot of times, parents will bring up questions or concerns about the HPV vaccine. If physicians aren’t comfortable talking about those topics, they may not give the best recommendation. Pediatricians are not dealing with cervical cancer, so they may have a harder time recommending a vaccine based on outcomes they don’t deal with.”
Ob.gyns. are in a unique position to reach out to their pediatric counterparts and discuss strategies for catching more patients eligible for the HPV vaccine, said Sarah Dilley, MD, a gynecologic oncology fellow at the University of Alabama at Birmingham and the lead author of the recent Call to Action paper.
“We offer a unique perspective in that we are treating the conditions that the HPV vaccine is preventing, so we have more of a sense of urgency and an understanding of why that is so important,” Dr. Dilley said in an interview. “Obviously, pediatricians understand this as well, but it’s not something they see every day in their practice. We, as ob.gyns., have the opportunity to talk to our pediatric colleagues about the importance and really how devastating these conditions can be and how important it is to prevent them.”
In the recent paper, Dr. Dilley and her colleagues recommend that ob.gyns. speak to pediatricians and primary care physicians in their community to promote the vaccine and encourage them to view the Centers for Disease Control and Prevention’s You Are the Key presentation. The CDC resources include tips for how to discuss the burden of HPV-related diseases and effective communication with parents, an update on state vaccination rates, and the latest HPV vaccination recommendations.
Dr. Dilley encourages ob.gyns. and pediatricians to find different opportunities and venues to discuss the HPV vaccine. Ask about the pediatrician’s current approach to the vaccine, the doctor’s communication with parents, and how such practices could be improved, she said.
“People like to hear from their colleagues,” Dr. Dilley said. “Hearing from ob.gyns. [about] their experiences could be really helpful, whether it’s doing lunch and learns, formal education, grand rounds, or even more informal talks at the hospital.”
Ob.gyns. and pediatricians also need to better coordinate their messaging so that there is more consistent emphasis during each patient encounter about the need of the HPV vaccination, Dr. Kimberlin said. There needs to be a renewed focus on the vaccine as a cancer vaccination, he said.
“The nuances of HPV and the way that HPV is acquired, namely sexually transmitted, has taken too much of a front row consideration in the conversations that parents sometimes want to have with their child’s health care providers,” Dr. Kimberlin said. “We have to stress this is a cancer vaccine. This is a vaccine that prevents the deaths of thousands of women and men. We simply need to get that message out more forcefully.”
In addition, there’s a need for joint action to debunk myths about the vaccine and work toward eliminating the stigma surrounding it, Dr. Dilley said.
“I talk to a lot parents about the HPV vaccine and there’s so much misinformation online,” she said. “But a lot of patients do look at websites of their ob.gyn. or their pediatrician, [and] if they see something reputable coming from one of those sites, they might listen. We have a lot of patients who are mothers or grandmothers of kids; that’s also an opportunity for us to say, ‘Hey while we’re screening you for cervical cancer, let’s talk about the HPV vaccine.’ That’s a really good opportunity to help our [pediatric] colleagues out.”
5 steps to increase HPV vaccination
Melissa Kottke, MD, director of the Jane Fonda Center for Adolescent Reproductive Health at Emory University offered her practice steps for increased HPV vaccination rates.
1. Be clear about your recommendation. For example, “I recommend the HPV vaccine. It can help prevent cancer.”
3. Educate the entire clinical team (front desk staff, nursing, medical assistants, etc.) about the HPV vaccine so there is consistent messaging and delivery.
4. Establish streamlined systems. The vaccine recommendation, order, and follow-up should be streamlined and automated, if possible. Systems should also ensure documentation of vaccine receipt.
5. Make time for conversations with patients who are mothers and grandmothers. Recommend the HPV vaccine for males and females aged 9-26 years old. Encourage parents/grandparents to follow-up with the child’s doctor or offer to provide the vaccine in your office.
*This story was updated 8/22/2017.
[email protected]
On Twitter @legal_med
Despite widespread availability of the human papillomavirus vaccine over the last 11 years, vaccination rates continue to lag behind national targets and are far behind other vaccines routinely administered in adolescence, such as the meningococcal and tetanus vaccines.
Better collaboration among pediatricians and obstetrician-gynecologists to promote the HPV vaccine may be one answer to turning the tide, said David W. Kimberlin, MD, codirector of the division of pediatric infectious diseases at the University of Alabama at Birmingham and president of the Pediatric Infectious Diseases Society.
As of 2015, just 63% of eligible U.S. girls completed the first dose of the HPV vaccination, 52% completed two doses, and 42% finished the three-dose series, according to a recent “Call to Action” paper in the American Journal of Obstetrics and Gynecology (doi: 10.1016/j.ajog.2017.02.026). Although the HPV vaccine has been recommended for boys since 2011, just half of eligible boys completed the first dose, 39% completed two doses, and 28% finished the full series. By contrast, 86% of adolescents received the tetanus, diphtheria, and acellular pertussis vaccine, and 81% received the first dose of the meningococcal vaccine. The federal government’s Office of Disease Prevention and Health Promotion aims for an 80% HPV vaccination completion rate for girls and boys aged 13-15 years by 2020.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/how-to-raise-hpv-vaccine-rates?iframe=1"}]The CDC now recommends that 11- to 12-year-olds get two doses of the HPV vaccine, rather than three, with the second dose given 6-12 months after the first (MMWR. 2016;65:1405-8).
The common ways in which the HPV vaccine is introduced to parents likely contributes to the low vaccination rates, said Beth Auslander, PhD, a clinical psychologist and associate professor in the department of pediatrics at the University of Texas Medical Branch in Galveston. Some pediatricians may tell parents about school-mandated vaccines first and then as a side note, mention the HPV vaccine.
“The way it’s presented at times is being separate from the other vaccines,” Dr. Auslander said. “Sometimes it sounds optional.”
Parents often are uncertain about the safety and efficacy of the HPV vaccine, she added, and some wrongly assume the vaccine will lead to sexual activity among their children.
“Sometimes it can take a little longer to talk about,” Dr. Yoost said in an interview. “A lot of times, parents will bring up questions or concerns about the HPV vaccine. If physicians aren’t comfortable talking about those topics, they may not give the best recommendation. Pediatricians are not dealing with cervical cancer, so they may have a harder time recommending a vaccine based on outcomes they don’t deal with.”
Ob.gyns. are in a unique position to reach out to their pediatric counterparts and discuss strategies for catching more patients eligible for the HPV vaccine, said Sarah Dilley, MD, a gynecologic oncology fellow at the University of Alabama at Birmingham and the lead author of the recent Call to Action paper.
“We offer a unique perspective in that we are treating the conditions that the HPV vaccine is preventing, so we have more of a sense of urgency and an understanding of why that is so important,” Dr. Dilley said in an interview. “Obviously, pediatricians understand this as well, but it’s not something they see every day in their practice. We, as ob.gyns., have the opportunity to talk to our pediatric colleagues about the importance and really how devastating these conditions can be and how important it is to prevent them.”
In the recent paper, Dr. Dilley and her colleagues recommend that ob.gyns. speak to pediatricians and primary care physicians in their community to promote the vaccine and encourage them to view the Centers for Disease Control and Prevention’s You Are the Key presentation. The CDC resources include tips for how to discuss the burden of HPV-related diseases and effective communication with parents, an update on state vaccination rates, and the latest HPV vaccination recommendations.
Dr. Dilley encourages ob.gyns. and pediatricians to find different opportunities and venues to discuss the HPV vaccine. Ask about the pediatrician’s current approach to the vaccine, the doctor’s communication with parents, and how such practices could be improved, she said.
“People like to hear from their colleagues,” Dr. Dilley said. “Hearing from ob.gyns. [about] their experiences could be really helpful, whether it’s doing lunch and learns, formal education, grand rounds, or even more informal talks at the hospital.”
Ob.gyns. and pediatricians also need to better coordinate their messaging so that there is more consistent emphasis during each patient encounter about the need of the HPV vaccination, Dr. Kimberlin said. There needs to be a renewed focus on the vaccine as a cancer vaccination, he said.
“The nuances of HPV and the way that HPV is acquired, namely sexually transmitted, has taken too much of a front row consideration in the conversations that parents sometimes want to have with their child’s health care providers,” Dr. Kimberlin said. “We have to stress this is a cancer vaccine. This is a vaccine that prevents the deaths of thousands of women and men. We simply need to get that message out more forcefully.”
In addition, there’s a need for joint action to debunk myths about the vaccine and work toward eliminating the stigma surrounding it, Dr. Dilley said.
“I talk to a lot parents about the HPV vaccine and there’s so much misinformation online,” she said. “But a lot of patients do look at websites of their ob.gyn. or their pediatrician, [and] if they see something reputable coming from one of those sites, they might listen. We have a lot of patients who are mothers or grandmothers of kids; that’s also an opportunity for us to say, ‘Hey while we’re screening you for cervical cancer, let’s talk about the HPV vaccine.’ That’s a really good opportunity to help our [pediatric] colleagues out.”
5 steps to increase HPV vaccination
Melissa Kottke, MD, director of the Jane Fonda Center for Adolescent Reproductive Health at Emory University offered her practice steps for increased HPV vaccination rates.
1. Be clear about your recommendation. For example, “I recommend the HPV vaccine. It can help prevent cancer.”
3. Educate the entire clinical team (front desk staff, nursing, medical assistants, etc.) about the HPV vaccine so there is consistent messaging and delivery.
4. Establish streamlined systems. The vaccine recommendation, order, and follow-up should be streamlined and automated, if possible. Systems should also ensure documentation of vaccine receipt.
5. Make time for conversations with patients who are mothers and grandmothers. Recommend the HPV vaccine for males and females aged 9-26 years old. Encourage parents/grandparents to follow-up with the child’s doctor or offer to provide the vaccine in your office.
*This story was updated 8/22/2017.
[email protected]
On Twitter @legal_med
Start ART in first 3 months in infants with perinatal HIV
MADRID – Infants with perinatal HIV infection are significantly more likely to achieve viral suppression by age 12 months if they start antiretroviral therapy (ART) before age 3 months than if physicians wait until 3-6 months of age, Paolo Palma, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
He presented a study of the factors associated with time to virologic sup
The purpose of this study was to identify the key factors involved in attaining early virologic control of perinatally acquired HIV. This information is necessary to lay the groundwork for planned future investigations of immunotherapeutic strategies designed to achieve sustained ART-free remission. Such strategies are most likely to be successful in very young children who have not yet built up a massive viral load, explained Dr. Palma of Bambino Gesù Children’s Hospital in Rome.
“A major obstacle to curing HIV infection is persistence of virus as integrated proviral DNA in long-lived cells even after many years on ART. ART-free HIV remission is more likely to occur if viral suppression is achieved very early in infection,” he said.
The median age of the 420 subjects at the time ART was initiated was 2.9 months. Their CD4 cell percentage was 34%, with a median CD4 cell count of 1,780 and an average viral load at baseline of 316,228 copies/mL.
At 12 months of age, 84% of patients had achieved viral suppression. In multivariate analyses adjusted for initial ART regimen and geographic location, three factors were associated with this outcome: younger age at ART onset, a lower baseline viral load, and a higher per
Indeed, for each 1-month increase in age at onset of ART, the likelihood of virologic response at age 12 months decreased by 16%. Similarly, the rate of virologic response at 1 year of age decreased by 15% for each 10 copies/mL increase in viral load at the start of ART. In contrast, the likelihood of virologic suppression at age 12 months increased by 10% for each 10% increase in CD4 cell percentage at the start of treatment.
Among the variables that proved unrelated to virologic suppression at 1 year of age were gender, AIDS status, feeding style (breastfed versus bottle-fed), and ethnicity.
Dr. Palma reported having no relevant financial disclosures.
MADRID – Infants with perinatal HIV infection are significantly more likely to achieve viral suppression by age 12 months if they start antiretroviral therapy (ART) before age 3 months than if physicians wait until 3-6 months of age, Paolo Palma, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
He presented a study of the factors associated with time to virologic sup
The purpose of this study was to identify the key factors involved in attaining early virologic control of perinatally acquired HIV. This information is necessary to lay the groundwork for planned future investigations of immunotherapeutic strategies designed to achieve sustained ART-free remission. Such strategies are most likely to be successful in very young children who have not yet built up a massive viral load, explained Dr. Palma of Bambino Gesù Children’s Hospital in Rome.
“A major obstacle to curing HIV infection is persistence of virus as integrated proviral DNA in long-lived cells even after many years on ART. ART-free HIV remission is more likely to occur if viral suppression is achieved very early in infection,” he said.
The median age of the 420 subjects at the time ART was initiated was 2.9 months. Their CD4 cell percentage was 34%, with a median CD4 cell count of 1,780 and an average viral load at baseline of 316,228 copies/mL.
At 12 months of age, 84% of patients had achieved viral suppression. In multivariate analyses adjusted for initial ART regimen and geographic location, three factors were associated with this outcome: younger age at ART onset, a lower baseline viral load, and a higher per
Indeed, for each 1-month increase in age at onset of ART, the likelihood of virologic response at age 12 months decreased by 16%. Similarly, the rate of virologic response at 1 year of age decreased by 15% for each 10 copies/mL increase in viral load at the start of ART. In contrast, the likelihood of virologic suppression at age 12 months increased by 10% for each 10% increase in CD4 cell percentage at the start of treatment.
Among the variables that proved unrelated to virologic suppression at 1 year of age were gender, AIDS status, feeding style (breastfed versus bottle-fed), and ethnicity.
Dr. Palma reported having no relevant financial disclosures.
MADRID – Infants with perinatal HIV infection are significantly more likely to achieve viral suppression by age 12 months if they start antiretroviral therapy (ART) before age 3 months than if physicians wait until 3-6 months of age, Paolo Palma, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
He presented a study of the factors associated with time to virologic sup
The purpose of this study was to identify the key factors involved in attaining early virologic control of perinatally acquired HIV. This information is necessary to lay the groundwork for planned future investigations of immunotherapeutic strategies designed to achieve sustained ART-free remission. Such strategies are most likely to be successful in very young children who have not yet built up a massive viral load, explained Dr. Palma of Bambino Gesù Children’s Hospital in Rome.
“A major obstacle to curing HIV infection is persistence of virus as integrated proviral DNA in long-lived cells even after many years on ART. ART-free HIV remission is more likely to occur if viral suppression is achieved very early in infection,” he said.
The median age of the 420 subjects at the time ART was initiated was 2.9 months. Their CD4 cell percentage was 34%, with a median CD4 cell count of 1,780 and an average viral load at baseline of 316,228 copies/mL.
At 12 months of age, 84% of patients had achieved viral suppression. In multivariate analyses adjusted for initial ART regimen and geographic location, three factors were associated with this outcome: younger age at ART onset, a lower baseline viral load, and a higher per
Indeed, for each 1-month increase in age at onset of ART, the likelihood of virologic response at age 12 months decreased by 16%. Similarly, the rate of virologic response at 1 year of age decreased by 15% for each 10 copies/mL increase in viral load at the start of ART. In contrast, the likelihood of virologic suppression at age 12 months increased by 10% for each 10% increase in CD4 cell percentage at the start of treatment.
Among the variables that proved unrelated to virologic suppression at 1 year of age were gender, AIDS status, feeding style (breastfed versus bottle-fed), and ethnicity.
Dr. Palma reported having no relevant financial disclosures.
AT ESPID 2017
Key clinical point:
Major finding: With each 1-month delay in starting antiretroviral therapy, the likelihood of attaining viral suppression by age 12 months drops by 16%.
Data source: This observational study included 420 infants with perinatally acquired HIV infection who began antiretroviral therapy prior to age 6 months.
Disclosures: Dr. Palma reported having no relevant financial disclosures.
Lack of Significant Anti-inflammatory Activity With Clindamycin in the Treatment of Rosacea: Results of 2 Randomized, Vehicle-Controlled Trials
Rosacea is a chronic inflammatory skin disease characterized by central facial erythema with or without intermittent papules and pustules (described as the inflammatory lesions of rosacea). Although twice-daily clindamycin 1% solution or gel has been used in the treatment of acne, few studies have investigated the use of clindamycin in rosacea.1,2 In one study comparing twice-daily clindamycin lotion 1% with oral tetracycline in 43 rosacea patients, clindamycin was found to be superior in the eradication of pustules.3 A combination therapy of clindamycin 1% and benzoyl peroxide 5% was found to be more effective than the vehicle in inflammatory lesions and erythema of rosacea in a 12-week randomized controlled trial; however, a definitive advantage over US Food and Drug Administration-approved topical agents used to treat papulopustular rosacea was not established.4,5 Two further studies evaluated clindamycin phosphate 1.2%-tretinoin 0.025% combination gel in the treatment of rosacea, but only 1 showed any effect on papulopustular lesions.6-8 The objective of the studies reported here was to evaluate the efficacy and safety of clindamycin in the treatment of patients with moderate to severe rosacea.
Methods
Study Design
Two multicenter (study A, 20 centers; study B, 10 centers), randomized, investigator-blinded, vehicle-controlled studies were conducted in the United States between 1999 and 2002 in accordance with the Declaration of Helsinki, International Conference on Harmonisation Good Clinical Practice guidelines, and local regulatory requirements. The studies were reviewed and approved by the respective institutional review boards, and all participants provided written informed consent.
In study A, moderate to severe rosacea patients with erythema, telangiectasia, and at least 8 inflammatory lesions were randomized to receive clindamycin cream 1% or vehicle cream once (in the evening) or twice daily (in the morning and evening) or clindamycin cream 0.3% once daily (in the evening) for 12 weeks (1:1:1:1:1 ratio). All study treatments were supplied in identical tubes with blinded labels.
In study B, patients with moderate to severe rosacea and at least 8 inflammatory lesions were randomized in a 1:1 ratio with instructions to apply clindamycin gel 1% or vehicle gel to the affected areas twice daily (morning and evening) for 12 weeks.
Efficacy Evaluation
Evaluations were performed at baseline and weeks 2, 4, 8, and 12 on the intention-to-treat population with the last observation carried forward.
Efficacy assessments in both studies included inflammatory lesion counts (papules and pustules) of 5 facial regions--forehead, chin, nose, right cheek, left cheek--counted separately and then combined to give the total inflammatory lesion count (both studies), as well as improvement in the investigator global rosacea severity score (0=none/clear; 1=mild, detectable erythema with ≤7 papules/pustules; 2=moderate, prominent erythema with ≥8 papules/pustules; 3=severe, intense erythema with ≥10 to <50 papules/pustules; 3.5 [study A] or 4 [study B]=very severe, intense erythema with >50 papules/pustules). In study B, the proportion of participants dichotomized to success (a score of 0 [none/clear] or 1 [mild/almost clear]) or failure (a score of ≥2) on the 5-point investigator global rosacea severity scale at week 12 was evaluated. In study A, investigator global improvement assessment at week 12, based on photographs taken at baseline, was graded on a 7-point scale (from -1 [worse], 0 [no change], and 1 [minimal improvement] to 5 [clear]). In both studies, erythema severity was graded on a 7-point scale in increments of 0.5 (from 0=no erythema to 3.5=very severe redness, very intense redness). Skin irritation also was graded as none, mild, moderate, or severe.
Safety Evaluation
Safety was assessed by the incidence of adverse events (AEs).
Statistical Analysis
Studies were powered assuming 60% reduction in inflammatory lesion counts with active and 40% with vehicle, based on historical data from a prior study with metronidazole cream 0.75% versus vehicle; 64 participants were required in each treatment group to detect this effect using a 2-sided t test (α=.017). Pairwise comparisons (clindamycin vs respective vehicle) were performed using the Cochran-Mantel-Haenszel test for combined lesion count percentage change.
Results
Participant Disposition and Baseline Characteristics
Overall, a total of 629 participants were randomized across both studies. In study A, a total of 416 participants were randomized into 5 treatment arms, with 369 participants (88.7%) completing the study; 47 (11.3%) participants discontinued study A, mainly due to participant request (19/47 [40.4%]) or lost to follow-up (11/47 [23.4%]). In study B, a total of 213 participants were randomized to receive either clindamycin gel 1% (n=109 [51.2%]) twice daily or vehicle gel (n=104 [48.8%]) twice daily, with 193 participants (90.6%) completing the study; 20 (9.4%) participants discontinued study B, mainly due to participant request (6/20 [30%]) or lost to follow-up (4/20 [20%]). Participants in studies A and B were similar in demographics and baseline disease characteristics (Table). The majority of participants were white females.
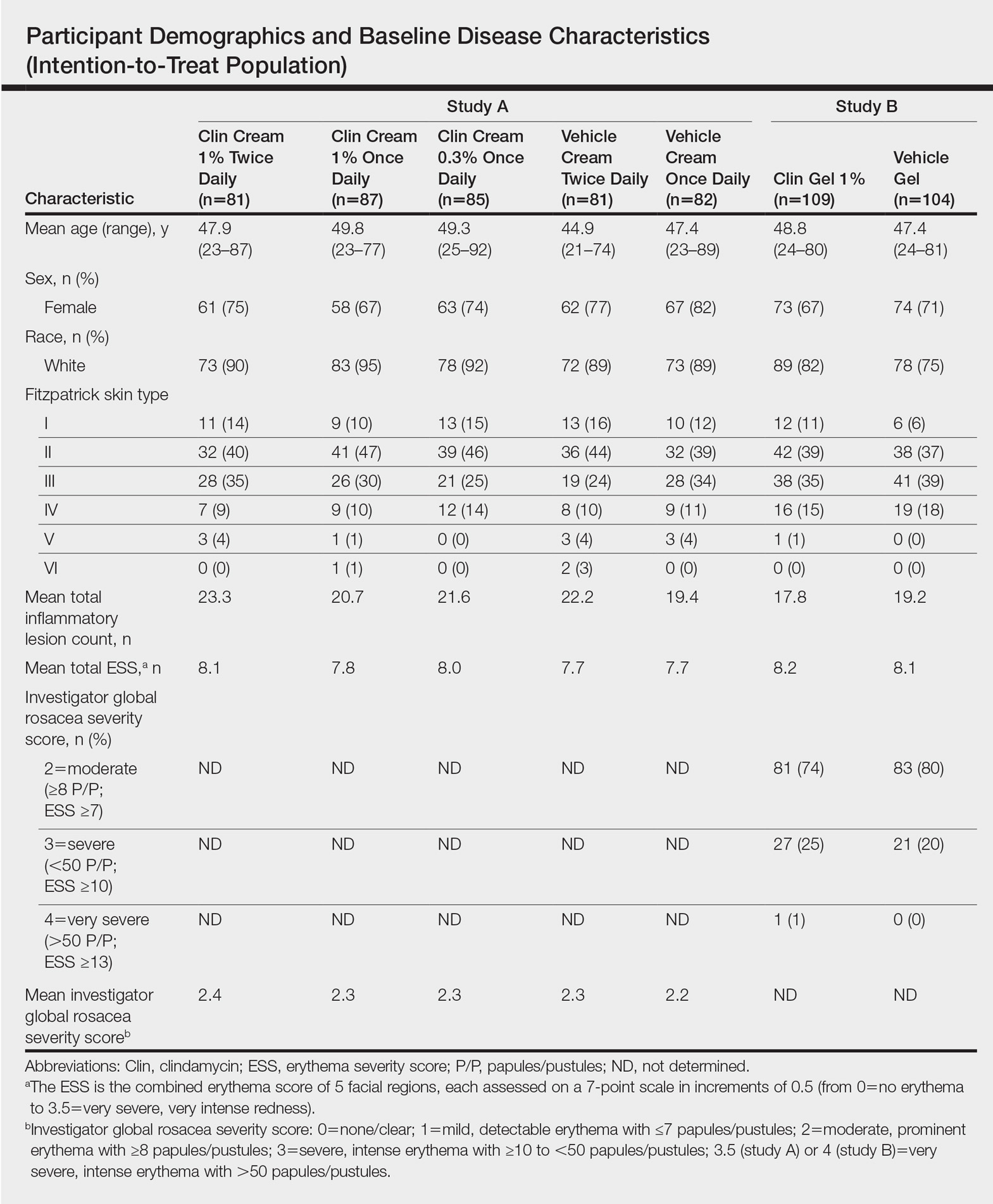
Efficacy
No statistically significant difference was observed in all pairwise comparisons (clindamycin cream twice daily vs vehicle twice daily, clindamycin cream once daily vs vehicle once daily, clindamycin gel vs vehicle gel) for the primary end point of mean percentage change from baseline in inflammatory lesion counts at week 12 (Figure 1; P>.5 for all pairwise comparisons).
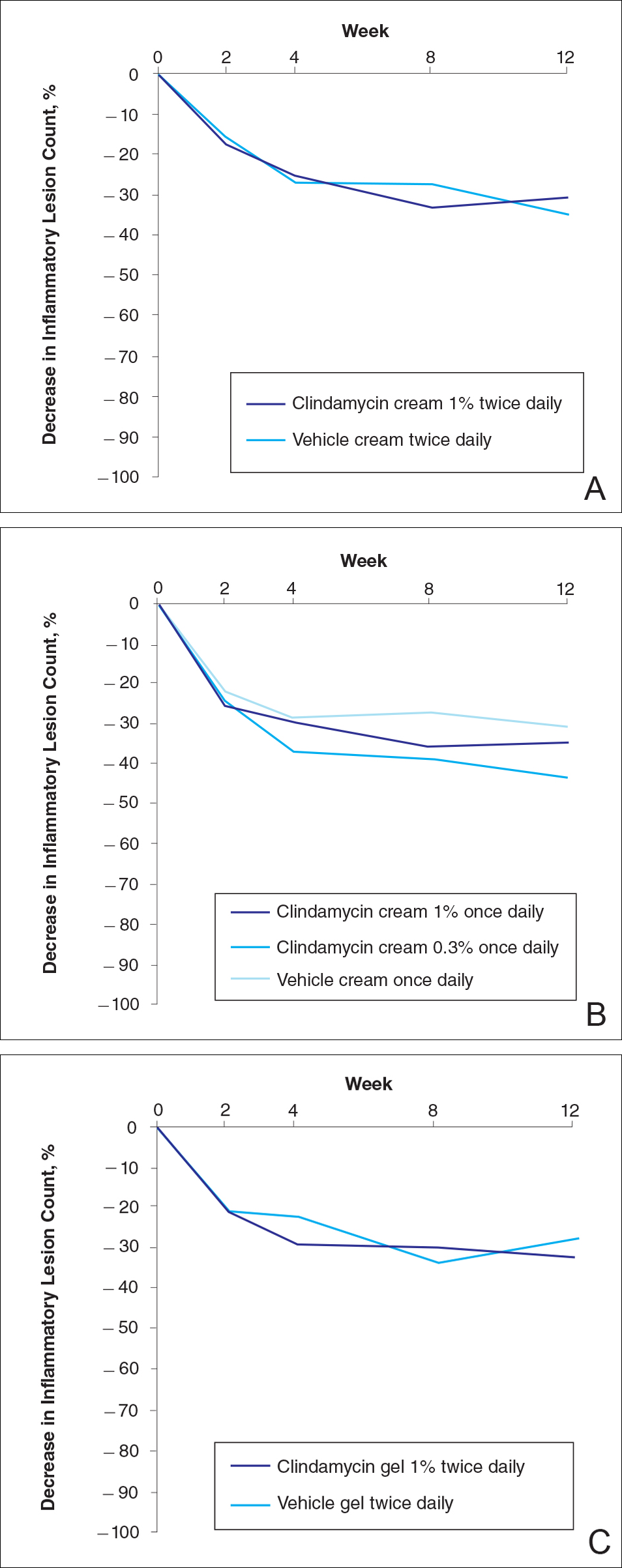
At week 12, the proportion of participants in study B deemed as a success (none/clear or mild/almost clear [investigator global rosacea severity score of 0 or 1]) in the clindamycin gel 1% and vehicle gel groups were 45% versus 38%, respectively (P=.347) (Figure 2).
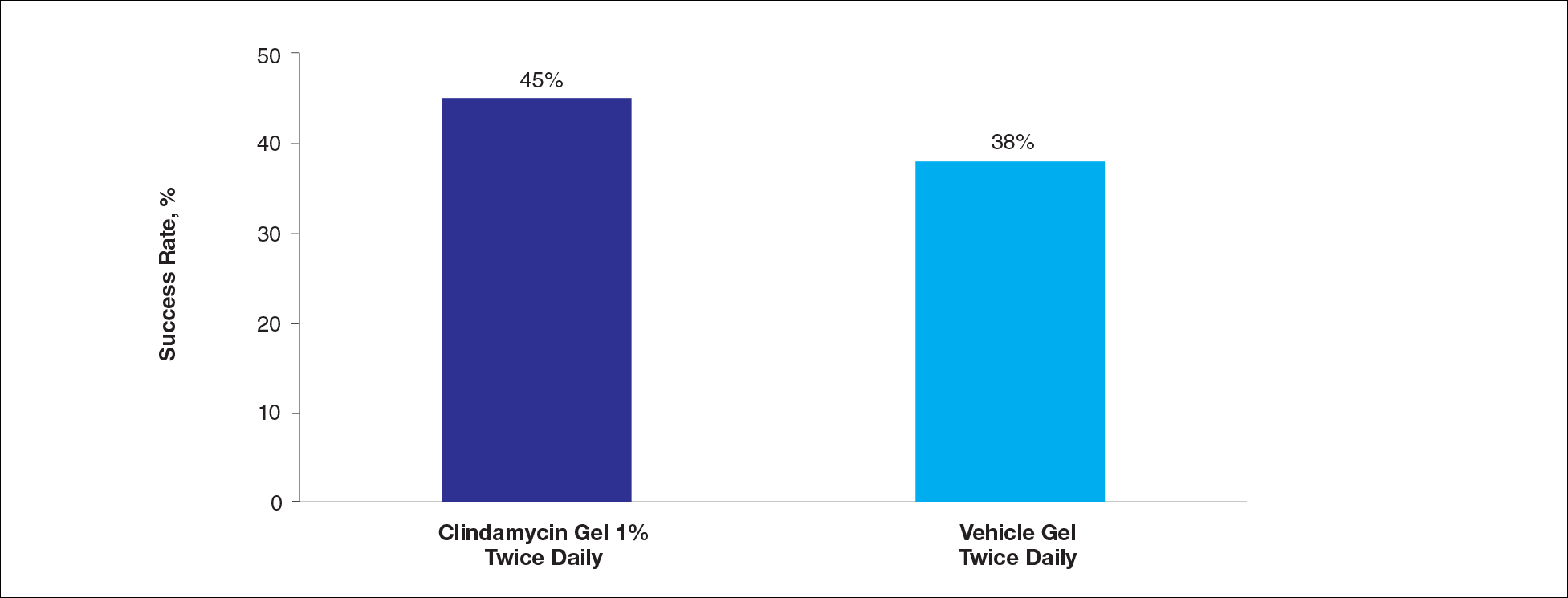
For the secondary end point of mean investigator global rosacea severity assessment at week 12 (study A), there were no significant differences between the active and vehicle control groups (P>.5 for all pairwise comparisons)(Figure 3). Also, the proportion of participants with at least a moderate investigator global improvement assessment from baseline to week 12 ranged from 45% for clindamycin cream 1% twice daily to 56% for clindamycin cream 0.3% cream once daily and from 45% for vehicle cream once daily to 51% for vehicle cream twice daily (P>.5 for all pairwise comparisons).
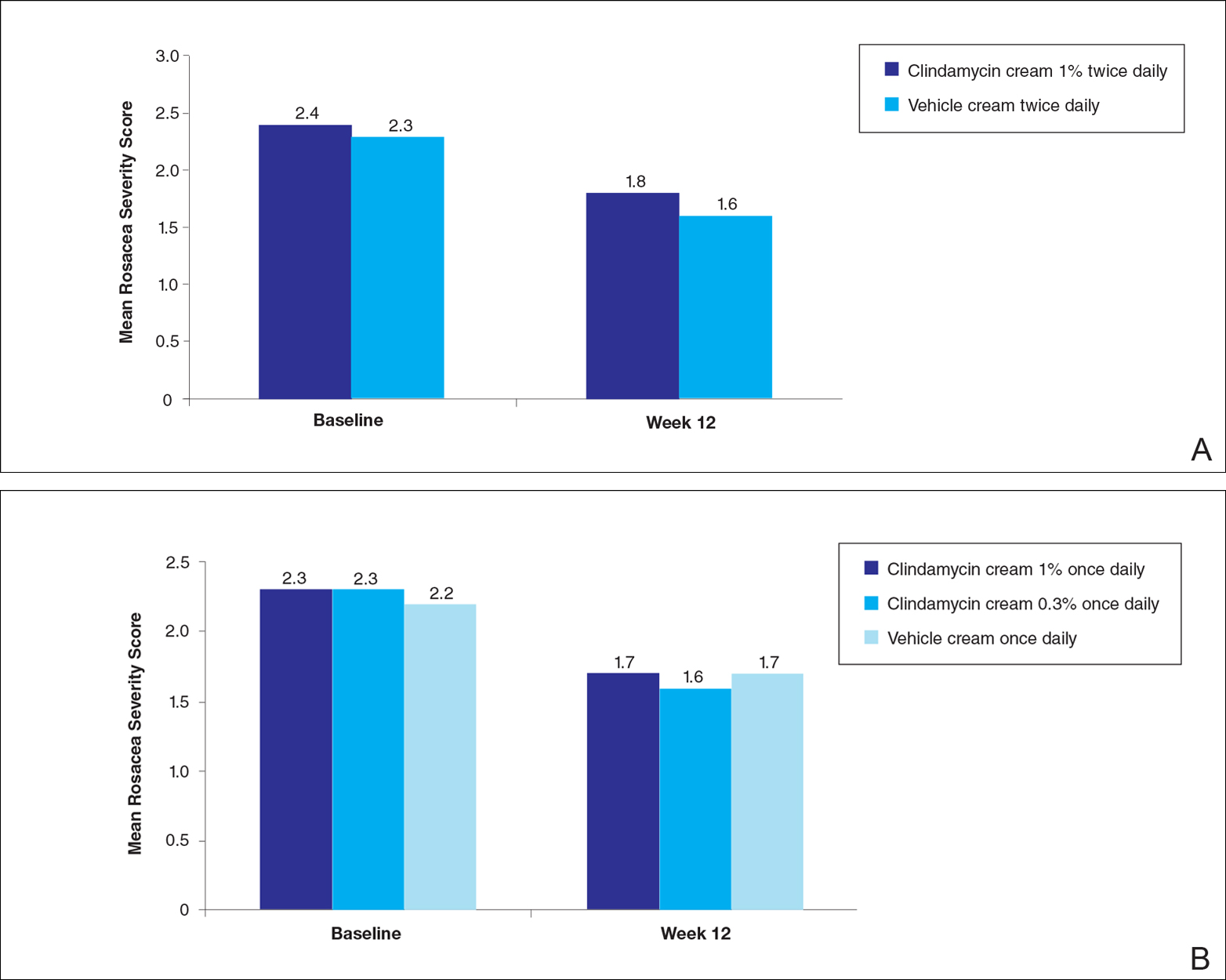
There were no significant differences in the mean total erythema severity scores at week 12 for clindamycin cream 1% twice daily versus vehicle cream twice daily (6.3 vs 6.0; P>.5), clindamycin cream 1% once daily versus vehicle cream once daily (6.2 vs 6.0; P>.5), clindamycin cream 0.3% once daily versus vehicle cream once daily (5.9 vs 6.0; P>.5), and clindamycin gel 1% twice daily versus vehicle gel twice daily (6.7 vs 6.2; P>.5).
There were no relevant differences between any of the clindamycin cream groups and their respective vehicle group at week 12 for skin irritation, including desquamation, edema, dryness, pruritus, and stinging/burning.
Safety
In study A, the majority of AEs in all 5 treatment arms were nondermatologic, mild in intensity, and not considered to be related to the study treatment by the investigator. Overall, 12 participants had AEs considered by the investigator as possibly or probably related to the study treatment: 4.9% in the clindamycin cream 1% twice daily group, 4.6% in the clindamycin cream 1% once daily group, 3.7% in the vehicle cream twice daily group, 1.2% in the clindamycin cream 0.3% once daily group, and 0% in the vehicle cream once daily group. Two treatment-related AEs led to treatment discontinuation, including dermatitis in 1 participant from the clindamycin cream 1% once daily group and contact dermatitis in 1 participant from the clindamycin cream 1% twice daily group.
Comment
No evidence of increased efficacy over the respective vehicles was observed with clindamycin cream or gel, whatever the regimen, in the treatment of rosacea patients in either of these well-designed and well-powered, blinded studies. Slight improvements in the various efficacy criteria were observed, even in the vehicle groups, highlighting the importance of using a good basic skin care regimen in the management of rosacea.9 In contrast to our observations of lack of efficacy in the treatment of rosacea, clinical efficacy of clindamycin has been demonstrated in acne,10-12 albeit with low efficacy for clindamycin monotherapy.13 It is noteworthy that oral or topical antibiotics are no longer recommended as monotherapy for acne to prevent and minimize antibiotic resistance and to preserve the therapeutic value of antibiotics.14
Acne and rosacea are both chronic inflammatory disorders of the skin associated with papules and pustules, and they share some common inflammatory patterns.15-19 Furthermore, the intrinsic anti-inflammatory activity of clindamycin in addition to its antibiotic effects has been suggested by some authors as the main reason for treating acne with clindamycin.20 However, the relative contributions of antibacterial and/or anti-inflammatory properties remain to be fully elucidated, and evidence for direct anti-inflammatory effects of clindamycin remains heterogeneous.21,22 Several pathophysiological factors have been implicated in acne, including hormonal effects, abnormal keratinocyte function, increased sebum production, and microbial components (eg, hypercolonization of the skin follicles by Propionibacterium acnes).23,24 The antibiotic activity of clindamycin against P acnes may be the key factor responsible for the clinical effects in acne.25,26 Although clindamycin may have anti-inflammatory effects in acne via a different inflammatory pathway not shared by rosacea, a purely antibiotic mechanism of action of clindamycin also could explain why we observed no evidence of efficacy in the treatment of rosacea, as no causative bacterial component has been clearly demonstrated in rosacea.27
Conclusion
In these studies, clindamycin cream 0.3% once daily, clindamycin cream 1% once or twice daily, and clindamycin gel 1% twice daily were all well tolerated; however, they were no more effective than the vehicles in the treatment of moderate to severe rosacea.
Acknowledgment
The authors would like to thank Helen Simpson, PhD, of Galderma R&D (Sophia Antipolis, France), for editorial and medical writing assistance.
- Whitney KM, Ditre CM. Anti-inflammatory properties of clindamycin: a review of its use in the treatment of acne vulgaris. Clinical Medicine Insights: Dermatology. 2011;4:27-41.
- Mays RM, Gordon RA, Wilson JM, et al. New antibiotic therapies for acne and rosacea. Dermatol Ther. 2012;25:23-37.
- Wilkin JK, DeWitt S. Treatment of rosacea: topical clindamycin versus oral tetracycline. Int J Dermatol. 1993;32:65-67.
- Breneman D, Savin R, VandePol C, et al. Double-blind, randomized, vehicle-controlled clinical trial of once-daily benzoyl peroxide/clindamycin topical gel in the treatment of patients with moderate to severe rosacea. Int J Dermatol. 2004;43:381-387.
- Leyden JJ, Thiboutot D, Shalita A. Photographic review of results from a clinical study comparing benzoyl peroxide 5%/clindamycin 1% topical gel with vehicle in the treatment of rosacea. Cutis. 2004;73(6 suppl):11-17.
- Chang AL, Alora-Palli M, Lima XT, et al. A randomized, double-blind, placebo-controlled, pilot study to assess the efficacy and safety of clindamycin 1.2% and tretinoin 0.025% combination gel for the treatment of acne rosacea over 12 weeks. J Drugs Dermatol. 2012;11:333-339.
- Freeman SA, Moon SD, Spencer JM. Clindamycin phosphate 1.2% and tretinoin 0.025% gel for rosacea: summary of a placebo-controlled, double-blind trial. J Drugs Dermatol. 2012;11:1410-1414.
- van Zuuren EJ, Fedorowicz Z, Carter B, et al. Interventions for rosacea. Cochrane Database Syst Rev. 2015;4:CD003262.
- Laquieze S, Czernielewski J, Baltas E. Beneficial use of Cetaphil moisturizing cream as part of a daily skin care regimen for individuals with rosacea. J Dermatolog Treat. 2007;18:158-162.
- Lookingbill DP, Chalker DK, Lindholm JS, et al. Treatment of acne with a combination clindamycin/benzoyl peroxide gel compared with clindamycin gel, benzoyl peroxide gel and vehicle gel: combined results of two double-blind investigations. J Am Acad Dermatol. 1997;37:590-595.
- Alirezaï M, Gerlach B, Horvath A, et al. Results of a randomised, multicentre study comparing a new water-based gel of clindamycin 1% versus clindamycin 1% topical solution in the treatment of acne vulgaris. Eur J Dermatol. 2005;15:274-278.
- Jarratt MT, Brundage T. Efficacy and safety of clindamycin-tretinoin gel versus clindamycin or tretinoin alone in acne vulgaris: a randomized, double-blind, vehicle-controlled study. J Drugs Dermatol. 2012;11:318-326.
- Benzaclin. Med Library website. http://medlibrary.org/lib/rx/meds/benzaclin-3. Updated May 8, 2013. Accessed January 24, 2017.
- Walsh TR, Efthimiou J, Dréno B. Systematic review of antibiotic resistance in acne: an increasing topical and oral threat. Lancet Infect Dis. 2016;16:E23-E33.
- Jeremy AH, Holland DB, Roberts SG, et al. Inflammatory events are involved in acne lesion initiation. J Invest Dermatol. 2003;121:20-27.
- Kircik LH. Re-evaluating treatment targets in acne vulgaris: adapting to a new understanding of pathophysiology. J Drugs Dermatol. 2014;13:S57-S60.
- Salzer S, Kresse S, Hirai Y, et al. Cathelicidin peptide LL-37 increases UVB-triggered inflammasome activation: possible implications for rosacea. J Dermatol Sci. 2014;76:173-179.
- Buhl T, Sulk M, Nowak P, et al. Molecular and morphological characterization of inflammatory infiltrate in rosacea reveals activation of Th1/Th17 pathways. J Invest Dermatol. 2015;135:2198-2208.
- Kistowska M, Meier B, Proust T, et al. Propionibacterium acnes promotes Th17 and Th17/Th1 responses in acne patients. J Invest Dermatol. 2015;135:110-118.
- Zeichner JA. Inflammatory acne treatment: review of current and new topical therapeutic options. J Drugs Dermatol. 2016;15(1 suppl 1):S11-S16.
- Nakano T, Hiramatsu K, Kishi K, et al. Clindamycin modulates inflammatory-cytokine induction in lipopolysaccharide-stimulated mouse peritoneal macrophages. Antimicrob Agents Chemother. 2003;47:363-367.
- Orman KL, English BK. Effects of antibiotic class on the macrophage inflammatory response to Streptococcus pneumoniae. J Infect Dis. 2000;182:1561-1565.
- Taylor M, Gonzalez M, Porter R. Pathways to inflammation: acne pathophysiology. Eur J Dermatol. 2011;21:323-333.
- Del Rosso JQ, Kircik LH. The sequence of inflammation, relevant biomarkers, and the pathogenesis of acne vulgaris: what does recent research show and what does it mean to the clinician? J Drugs Dermatol. 2013;12(8 suppl):S109-S115.
- Leyden J, Kaidbey K, Levy SF. The combination formulation of clindamycin 1% plus benzoyl peroxide 5% versus 3 different formulations of topical clindamycin alone in the reduction of Propionibacterium acnes. an in vivo comparative study. Am J Clin Dermatol. 2001;2:263-266.
- Wang WL, Everett ED, Johnson M, et al. Susceptibility of Propionibacterium acnes to seventeen antibiotics. Antimicrob Agents Chemother. 1977;11:171-173.
- Steinhoff M, Schauber J, Leyden JJ. New insights into rosacea pathophysiology: a review of recent findings. J Am Acad Dermatol. 2013;69(6 suppl 1):S15-S26.
Rosacea is a chronic inflammatory skin disease characterized by central facial erythema with or without intermittent papules and pustules (described as the inflammatory lesions of rosacea). Although twice-daily clindamycin 1% solution or gel has been used in the treatment of acne, few studies have investigated the use of clindamycin in rosacea.1,2 In one study comparing twice-daily clindamycin lotion 1% with oral tetracycline in 43 rosacea patients, clindamycin was found to be superior in the eradication of pustules.3 A combination therapy of clindamycin 1% and benzoyl peroxide 5% was found to be more effective than the vehicle in inflammatory lesions and erythema of rosacea in a 12-week randomized controlled trial; however, a definitive advantage over US Food and Drug Administration-approved topical agents used to treat papulopustular rosacea was not established.4,5 Two further studies evaluated clindamycin phosphate 1.2%-tretinoin 0.025% combination gel in the treatment of rosacea, but only 1 showed any effect on papulopustular lesions.6-8 The objective of the studies reported here was to evaluate the efficacy and safety of clindamycin in the treatment of patients with moderate to severe rosacea.
Methods
Study Design
Two multicenter (study A, 20 centers; study B, 10 centers), randomized, investigator-blinded, vehicle-controlled studies were conducted in the United States between 1999 and 2002 in accordance with the Declaration of Helsinki, International Conference on Harmonisation Good Clinical Practice guidelines, and local regulatory requirements. The studies were reviewed and approved by the respective institutional review boards, and all participants provided written informed consent.
In study A, moderate to severe rosacea patients with erythema, telangiectasia, and at least 8 inflammatory lesions were randomized to receive clindamycin cream 1% or vehicle cream once (in the evening) or twice daily (in the morning and evening) or clindamycin cream 0.3% once daily (in the evening) for 12 weeks (1:1:1:1:1 ratio). All study treatments were supplied in identical tubes with blinded labels.
In study B, patients with moderate to severe rosacea and at least 8 inflammatory lesions were randomized in a 1:1 ratio with instructions to apply clindamycin gel 1% or vehicle gel to the affected areas twice daily (morning and evening) for 12 weeks.
Efficacy Evaluation
Evaluations were performed at baseline and weeks 2, 4, 8, and 12 on the intention-to-treat population with the last observation carried forward.
Efficacy assessments in both studies included inflammatory lesion counts (papules and pustules) of 5 facial regions--forehead, chin, nose, right cheek, left cheek--counted separately and then combined to give the total inflammatory lesion count (both studies), as well as improvement in the investigator global rosacea severity score (0=none/clear; 1=mild, detectable erythema with ≤7 papules/pustules; 2=moderate, prominent erythema with ≥8 papules/pustules; 3=severe, intense erythema with ≥10 to <50 papules/pustules; 3.5 [study A] or 4 [study B]=very severe, intense erythema with >50 papules/pustules). In study B, the proportion of participants dichotomized to success (a score of 0 [none/clear] or 1 [mild/almost clear]) or failure (a score of ≥2) on the 5-point investigator global rosacea severity scale at week 12 was evaluated. In study A, investigator global improvement assessment at week 12, based on photographs taken at baseline, was graded on a 7-point scale (from -1 [worse], 0 [no change], and 1 [minimal improvement] to 5 [clear]). In both studies, erythema severity was graded on a 7-point scale in increments of 0.5 (from 0=no erythema to 3.5=very severe redness, very intense redness). Skin irritation also was graded as none, mild, moderate, or severe.
Safety Evaluation
Safety was assessed by the incidence of adverse events (AEs).
Statistical Analysis
Studies were powered assuming 60% reduction in inflammatory lesion counts with active and 40% with vehicle, based on historical data from a prior study with metronidazole cream 0.75% versus vehicle; 64 participants were required in each treatment group to detect this effect using a 2-sided t test (α=.017). Pairwise comparisons (clindamycin vs respective vehicle) were performed using the Cochran-Mantel-Haenszel test for combined lesion count percentage change.
Results
Participant Disposition and Baseline Characteristics
Overall, a total of 629 participants were randomized across both studies. In study A, a total of 416 participants were randomized into 5 treatment arms, with 369 participants (88.7%) completing the study; 47 (11.3%) participants discontinued study A, mainly due to participant request (19/47 [40.4%]) or lost to follow-up (11/47 [23.4%]). In study B, a total of 213 participants were randomized to receive either clindamycin gel 1% (n=109 [51.2%]) twice daily or vehicle gel (n=104 [48.8%]) twice daily, with 193 participants (90.6%) completing the study; 20 (9.4%) participants discontinued study B, mainly due to participant request (6/20 [30%]) or lost to follow-up (4/20 [20%]). Participants in studies A and B were similar in demographics and baseline disease characteristics (Table). The majority of participants were white females.
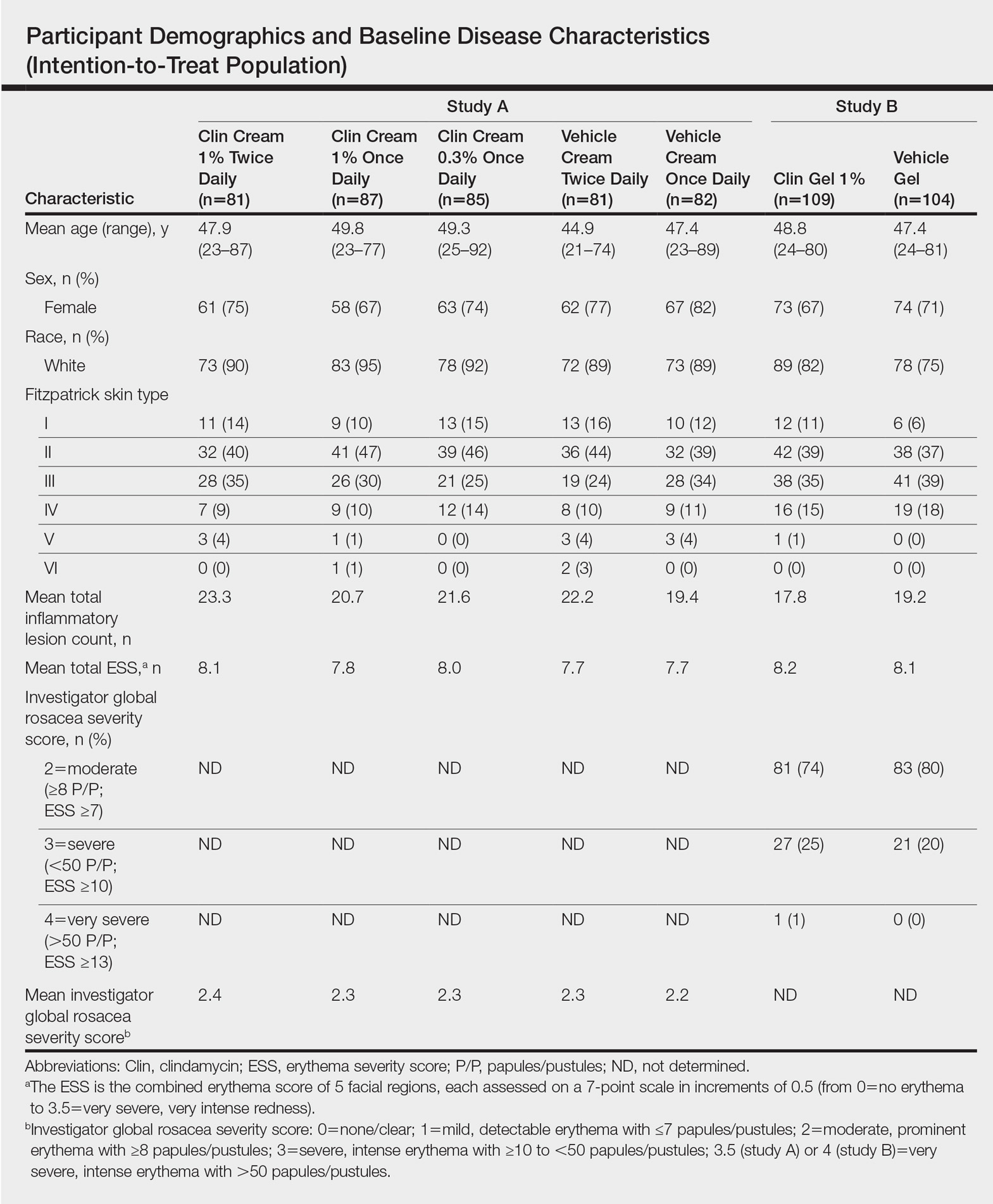
Efficacy
No statistically significant difference was observed in all pairwise comparisons (clindamycin cream twice daily vs vehicle twice daily, clindamycin cream once daily vs vehicle once daily, clindamycin gel vs vehicle gel) for the primary end point of mean percentage change from baseline in inflammatory lesion counts at week 12 (Figure 1; P>.5 for all pairwise comparisons).
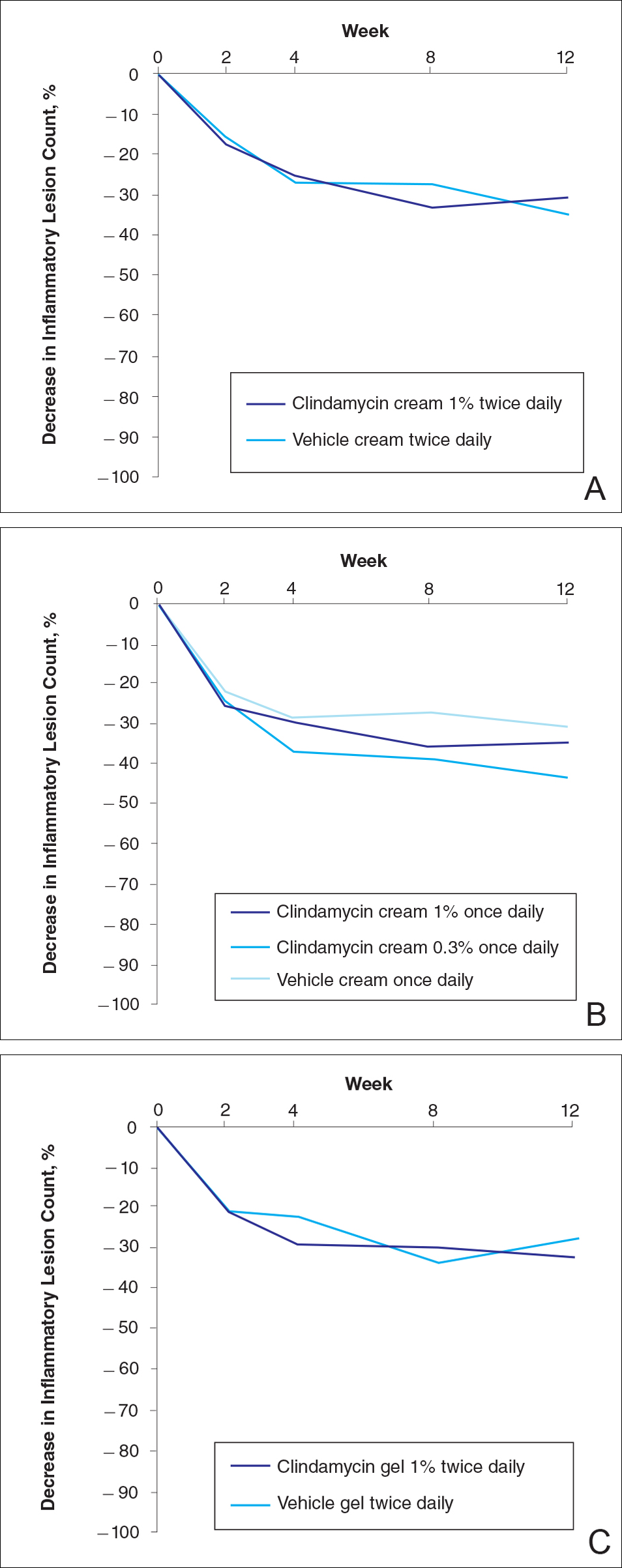
At week 12, the proportion of participants in study B deemed as a success (none/clear or mild/almost clear [investigator global rosacea severity score of 0 or 1]) in the clindamycin gel 1% and vehicle gel groups were 45% versus 38%, respectively (P=.347) (Figure 2).
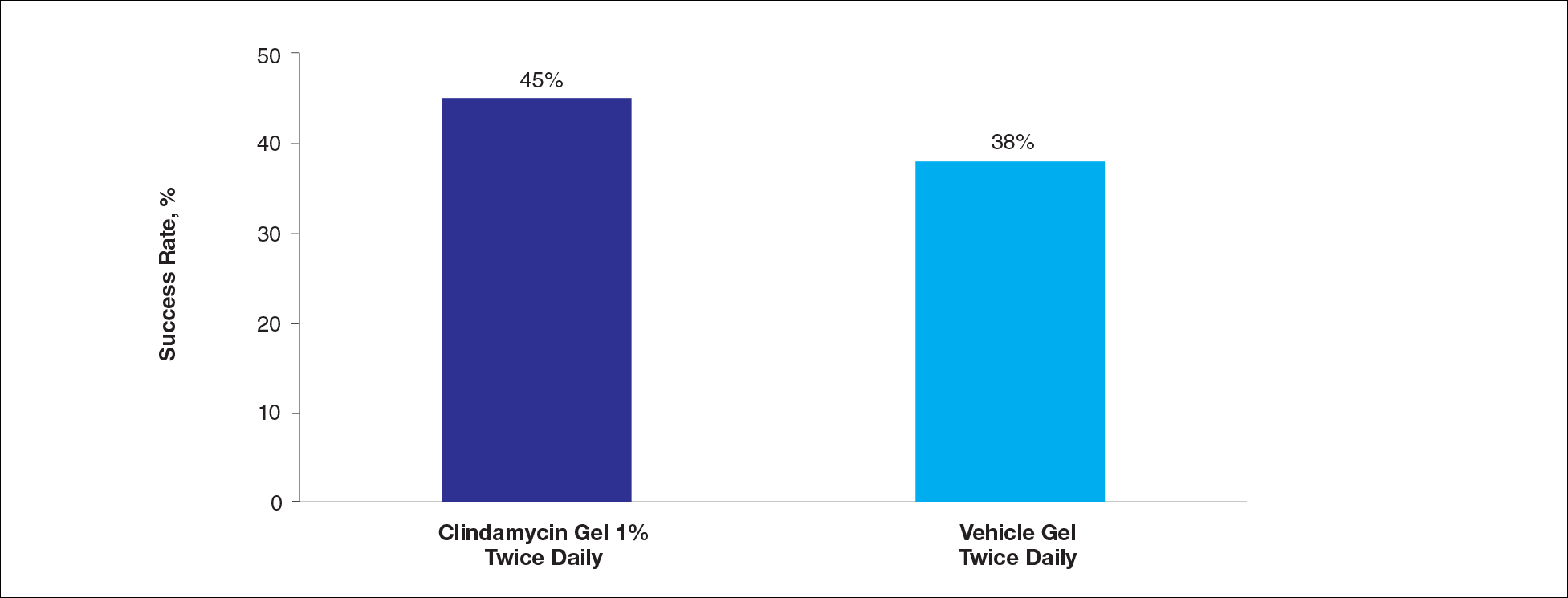
For the secondary end point of mean investigator global rosacea severity assessment at week 12 (study A), there were no significant differences between the active and vehicle control groups (P>.5 for all pairwise comparisons)(Figure 3). Also, the proportion of participants with at least a moderate investigator global improvement assessment from baseline to week 12 ranged from 45% for clindamycin cream 1% twice daily to 56% for clindamycin cream 0.3% cream once daily and from 45% for vehicle cream once daily to 51% for vehicle cream twice daily (P>.5 for all pairwise comparisons).
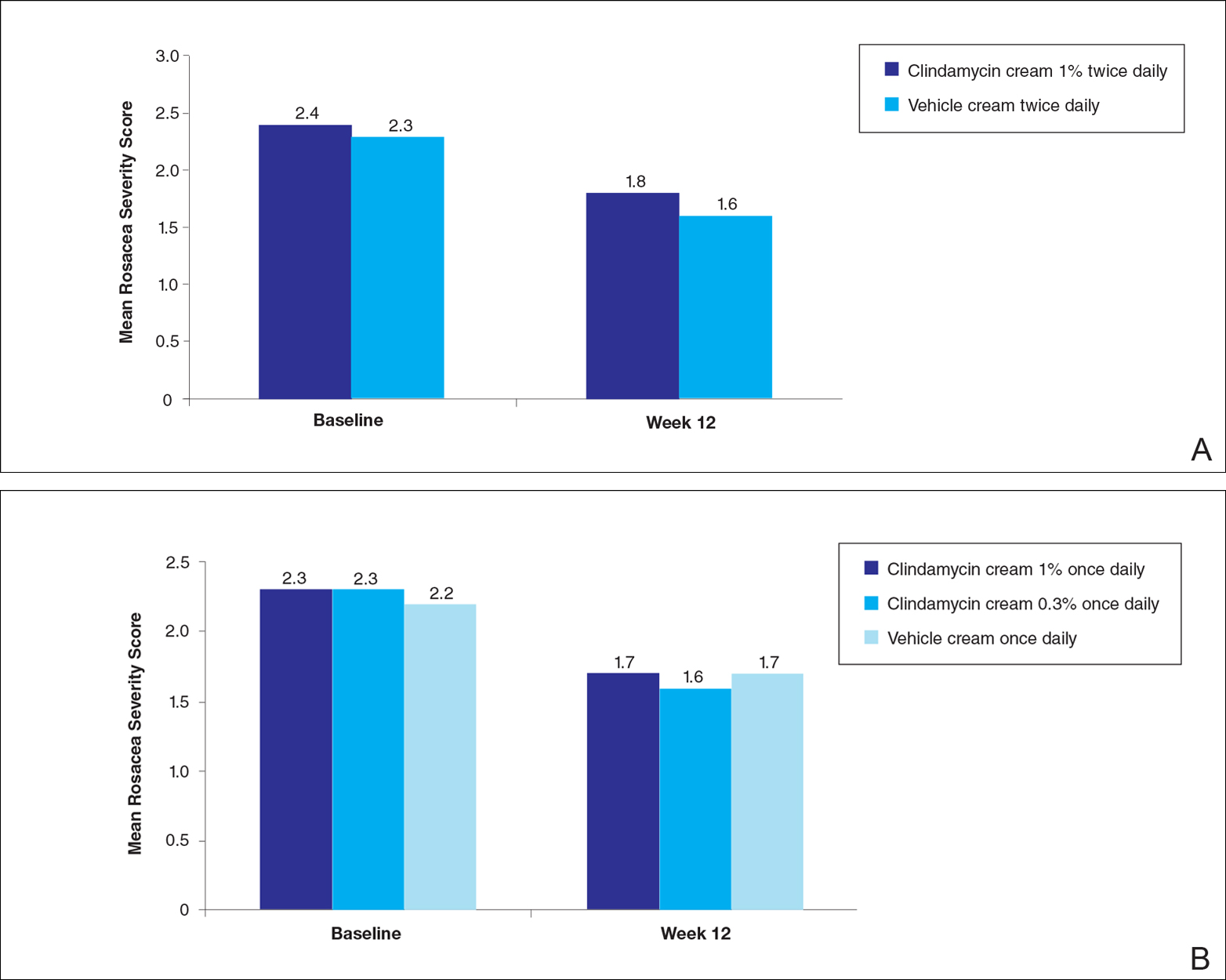
There were no significant differences in the mean total erythema severity scores at week 12 for clindamycin cream 1% twice daily versus vehicle cream twice daily (6.3 vs 6.0; P>.5), clindamycin cream 1% once daily versus vehicle cream once daily (6.2 vs 6.0; P>.5), clindamycin cream 0.3% once daily versus vehicle cream once daily (5.9 vs 6.0; P>.5), and clindamycin gel 1% twice daily versus vehicle gel twice daily (6.7 vs 6.2; P>.5).
There were no relevant differences between any of the clindamycin cream groups and their respective vehicle group at week 12 for skin irritation, including desquamation, edema, dryness, pruritus, and stinging/burning.
Safety
In study A, the majority of AEs in all 5 treatment arms were nondermatologic, mild in intensity, and not considered to be related to the study treatment by the investigator. Overall, 12 participants had AEs considered by the investigator as possibly or probably related to the study treatment: 4.9% in the clindamycin cream 1% twice daily group, 4.6% in the clindamycin cream 1% once daily group, 3.7% in the vehicle cream twice daily group, 1.2% in the clindamycin cream 0.3% once daily group, and 0% in the vehicle cream once daily group. Two treatment-related AEs led to treatment discontinuation, including dermatitis in 1 participant from the clindamycin cream 1% once daily group and contact dermatitis in 1 participant from the clindamycin cream 1% twice daily group.
Comment
No evidence of increased efficacy over the respective vehicles was observed with clindamycin cream or gel, whatever the regimen, in the treatment of rosacea patients in either of these well-designed and well-powered, blinded studies. Slight improvements in the various efficacy criteria were observed, even in the vehicle groups, highlighting the importance of using a good basic skin care regimen in the management of rosacea.9 In contrast to our observations of lack of efficacy in the treatment of rosacea, clinical efficacy of clindamycin has been demonstrated in acne,10-12 albeit with low efficacy for clindamycin monotherapy.13 It is noteworthy that oral or topical antibiotics are no longer recommended as monotherapy for acne to prevent and minimize antibiotic resistance and to preserve the therapeutic value of antibiotics.14
Acne and rosacea are both chronic inflammatory disorders of the skin associated with papules and pustules, and they share some common inflammatory patterns.15-19 Furthermore, the intrinsic anti-inflammatory activity of clindamycin in addition to its antibiotic effects has been suggested by some authors as the main reason for treating acne with clindamycin.20 However, the relative contributions of antibacterial and/or anti-inflammatory properties remain to be fully elucidated, and evidence for direct anti-inflammatory effects of clindamycin remains heterogeneous.21,22 Several pathophysiological factors have been implicated in acne, including hormonal effects, abnormal keratinocyte function, increased sebum production, and microbial components (eg, hypercolonization of the skin follicles by Propionibacterium acnes).23,24 The antibiotic activity of clindamycin against P acnes may be the key factor responsible for the clinical effects in acne.25,26 Although clindamycin may have anti-inflammatory effects in acne via a different inflammatory pathway not shared by rosacea, a purely antibiotic mechanism of action of clindamycin also could explain why we observed no evidence of efficacy in the treatment of rosacea, as no causative bacterial component has been clearly demonstrated in rosacea.27
Conclusion
In these studies, clindamycin cream 0.3% once daily, clindamycin cream 1% once or twice daily, and clindamycin gel 1% twice daily were all well tolerated; however, they were no more effective than the vehicles in the treatment of moderate to severe rosacea.
Acknowledgment
The authors would like to thank Helen Simpson, PhD, of Galderma R&D (Sophia Antipolis, France), for editorial and medical writing assistance.
Rosacea is a chronic inflammatory skin disease characterized by central facial erythema with or without intermittent papules and pustules (described as the inflammatory lesions of rosacea). Although twice-daily clindamycin 1% solution or gel has been used in the treatment of acne, few studies have investigated the use of clindamycin in rosacea.1,2 In one study comparing twice-daily clindamycin lotion 1% with oral tetracycline in 43 rosacea patients, clindamycin was found to be superior in the eradication of pustules.3 A combination therapy of clindamycin 1% and benzoyl peroxide 5% was found to be more effective than the vehicle in inflammatory lesions and erythema of rosacea in a 12-week randomized controlled trial; however, a definitive advantage over US Food and Drug Administration-approved topical agents used to treat papulopustular rosacea was not established.4,5 Two further studies evaluated clindamycin phosphate 1.2%-tretinoin 0.025% combination gel in the treatment of rosacea, but only 1 showed any effect on papulopustular lesions.6-8 The objective of the studies reported here was to evaluate the efficacy and safety of clindamycin in the treatment of patients with moderate to severe rosacea.
Methods
Study Design
Two multicenter (study A, 20 centers; study B, 10 centers), randomized, investigator-blinded, vehicle-controlled studies were conducted in the United States between 1999 and 2002 in accordance with the Declaration of Helsinki, International Conference on Harmonisation Good Clinical Practice guidelines, and local regulatory requirements. The studies were reviewed and approved by the respective institutional review boards, and all participants provided written informed consent.
In study A, moderate to severe rosacea patients with erythema, telangiectasia, and at least 8 inflammatory lesions were randomized to receive clindamycin cream 1% or vehicle cream once (in the evening) or twice daily (in the morning and evening) or clindamycin cream 0.3% once daily (in the evening) for 12 weeks (1:1:1:1:1 ratio). All study treatments were supplied in identical tubes with blinded labels.
In study B, patients with moderate to severe rosacea and at least 8 inflammatory lesions were randomized in a 1:1 ratio with instructions to apply clindamycin gel 1% or vehicle gel to the affected areas twice daily (morning and evening) for 12 weeks.
Efficacy Evaluation
Evaluations were performed at baseline and weeks 2, 4, 8, and 12 on the intention-to-treat population with the last observation carried forward.
Efficacy assessments in both studies included inflammatory lesion counts (papules and pustules) of 5 facial regions--forehead, chin, nose, right cheek, left cheek--counted separately and then combined to give the total inflammatory lesion count (both studies), as well as improvement in the investigator global rosacea severity score (0=none/clear; 1=mild, detectable erythema with ≤7 papules/pustules; 2=moderate, prominent erythema with ≥8 papules/pustules; 3=severe, intense erythema with ≥10 to <50 papules/pustules; 3.5 [study A] or 4 [study B]=very severe, intense erythema with >50 papules/pustules). In study B, the proportion of participants dichotomized to success (a score of 0 [none/clear] or 1 [mild/almost clear]) or failure (a score of ≥2) on the 5-point investigator global rosacea severity scale at week 12 was evaluated. In study A, investigator global improvement assessment at week 12, based on photographs taken at baseline, was graded on a 7-point scale (from -1 [worse], 0 [no change], and 1 [minimal improvement] to 5 [clear]). In both studies, erythema severity was graded on a 7-point scale in increments of 0.5 (from 0=no erythema to 3.5=very severe redness, very intense redness). Skin irritation also was graded as none, mild, moderate, or severe.
Safety Evaluation
Safety was assessed by the incidence of adverse events (AEs).
Statistical Analysis
Studies were powered assuming 60% reduction in inflammatory lesion counts with active and 40% with vehicle, based on historical data from a prior study with metronidazole cream 0.75% versus vehicle; 64 participants were required in each treatment group to detect this effect using a 2-sided t test (α=.017). Pairwise comparisons (clindamycin vs respective vehicle) were performed using the Cochran-Mantel-Haenszel test for combined lesion count percentage change.
Results
Participant Disposition and Baseline Characteristics
Overall, a total of 629 participants were randomized across both studies. In study A, a total of 416 participants were randomized into 5 treatment arms, with 369 participants (88.7%) completing the study; 47 (11.3%) participants discontinued study A, mainly due to participant request (19/47 [40.4%]) or lost to follow-up (11/47 [23.4%]). In study B, a total of 213 participants were randomized to receive either clindamycin gel 1% (n=109 [51.2%]) twice daily or vehicle gel (n=104 [48.8%]) twice daily, with 193 participants (90.6%) completing the study; 20 (9.4%) participants discontinued study B, mainly due to participant request (6/20 [30%]) or lost to follow-up (4/20 [20%]). Participants in studies A and B were similar in demographics and baseline disease characteristics (Table). The majority of participants were white females.
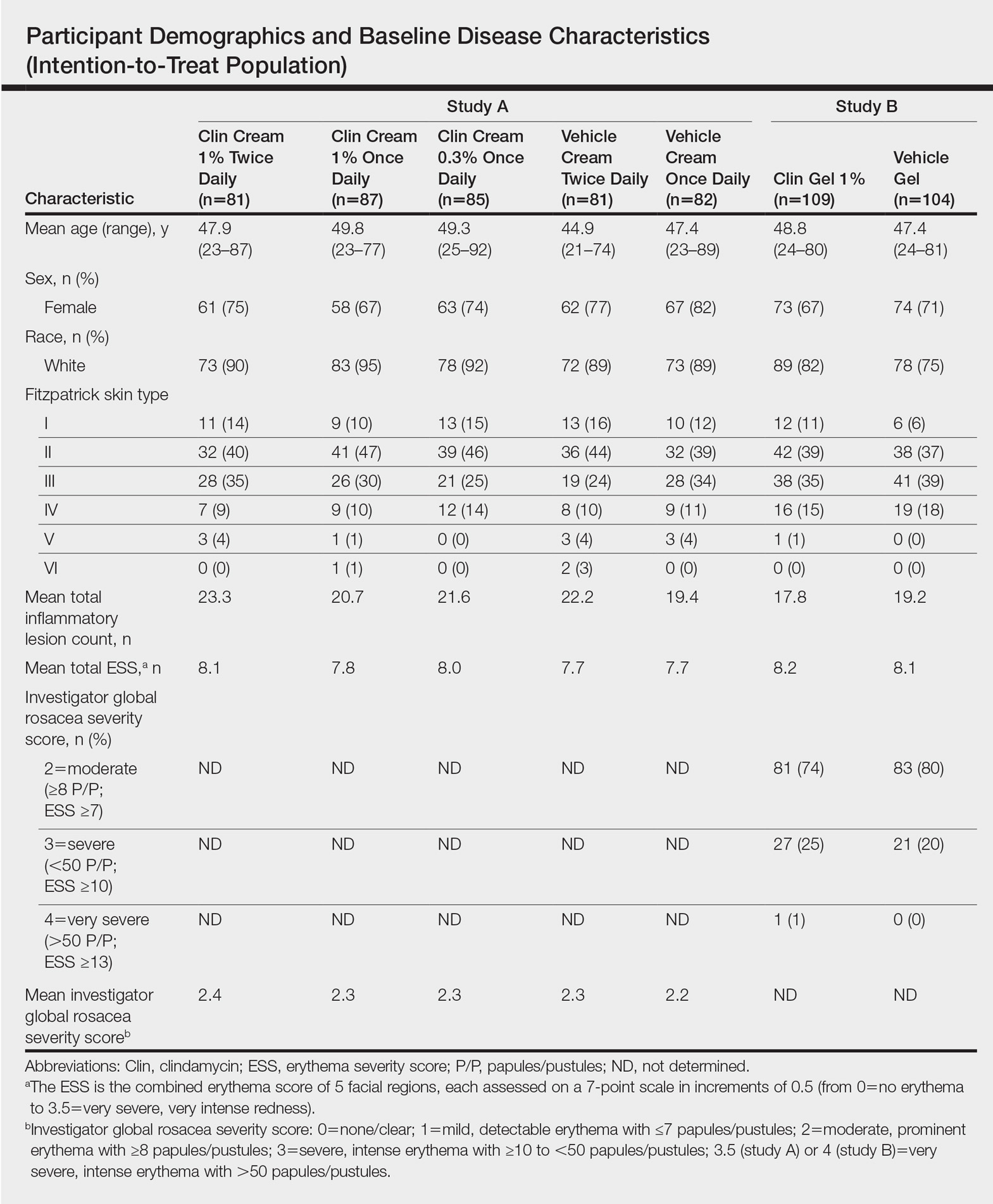
Efficacy
No statistically significant difference was observed in all pairwise comparisons (clindamycin cream twice daily vs vehicle twice daily, clindamycin cream once daily vs vehicle once daily, clindamycin gel vs vehicle gel) for the primary end point of mean percentage change from baseline in inflammatory lesion counts at week 12 (Figure 1; P>.5 for all pairwise comparisons).
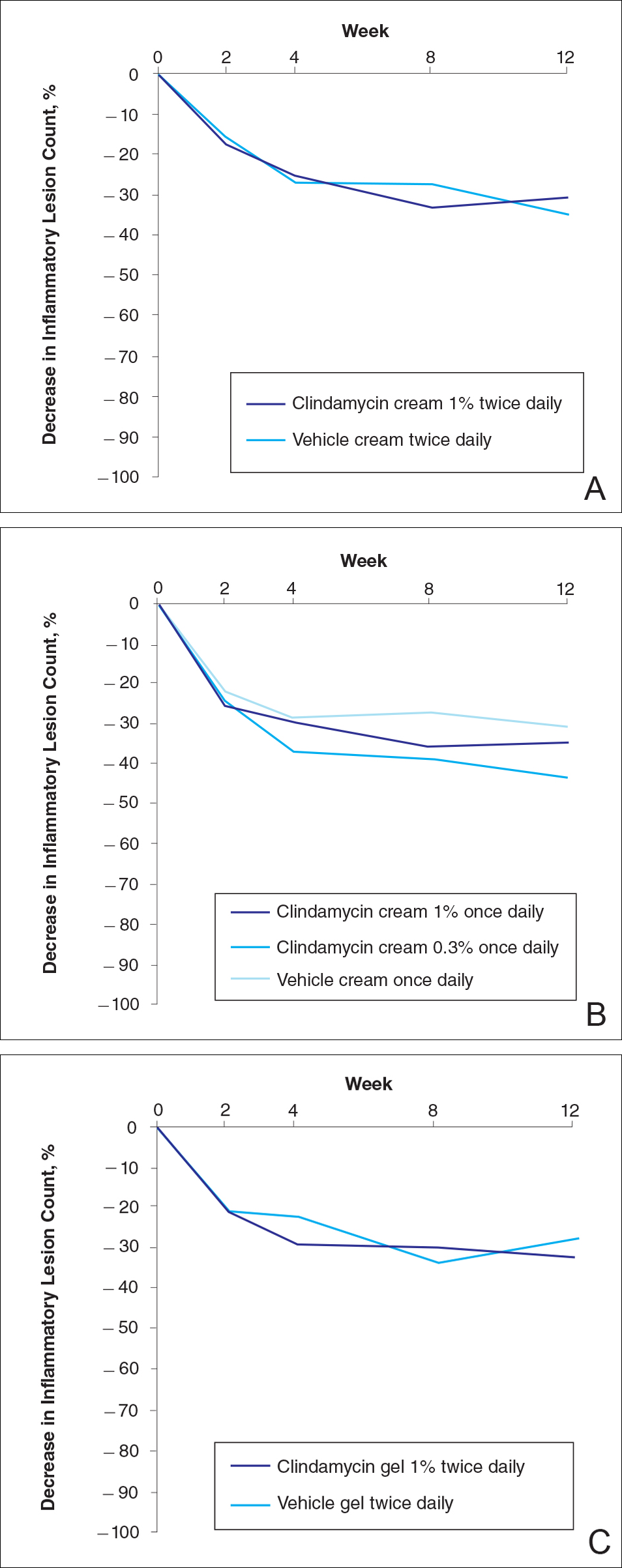
At week 12, the proportion of participants in study B deemed as a success (none/clear or mild/almost clear [investigator global rosacea severity score of 0 or 1]) in the clindamycin gel 1% and vehicle gel groups were 45% versus 38%, respectively (P=.347) (Figure 2).
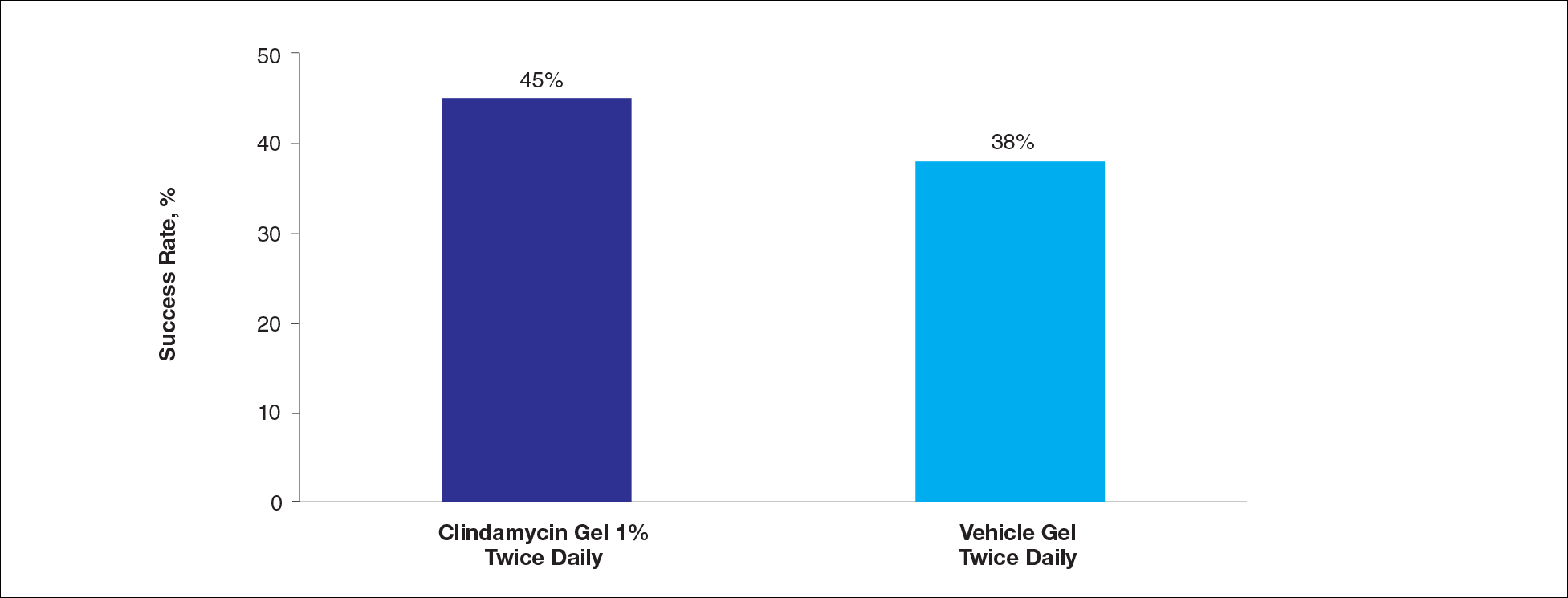
For the secondary end point of mean investigator global rosacea severity assessment at week 12 (study A), there were no significant differences between the active and vehicle control groups (P>.5 for all pairwise comparisons)(Figure 3). Also, the proportion of participants with at least a moderate investigator global improvement assessment from baseline to week 12 ranged from 45% for clindamycin cream 1% twice daily to 56% for clindamycin cream 0.3% cream once daily and from 45% for vehicle cream once daily to 51% for vehicle cream twice daily (P>.5 for all pairwise comparisons).
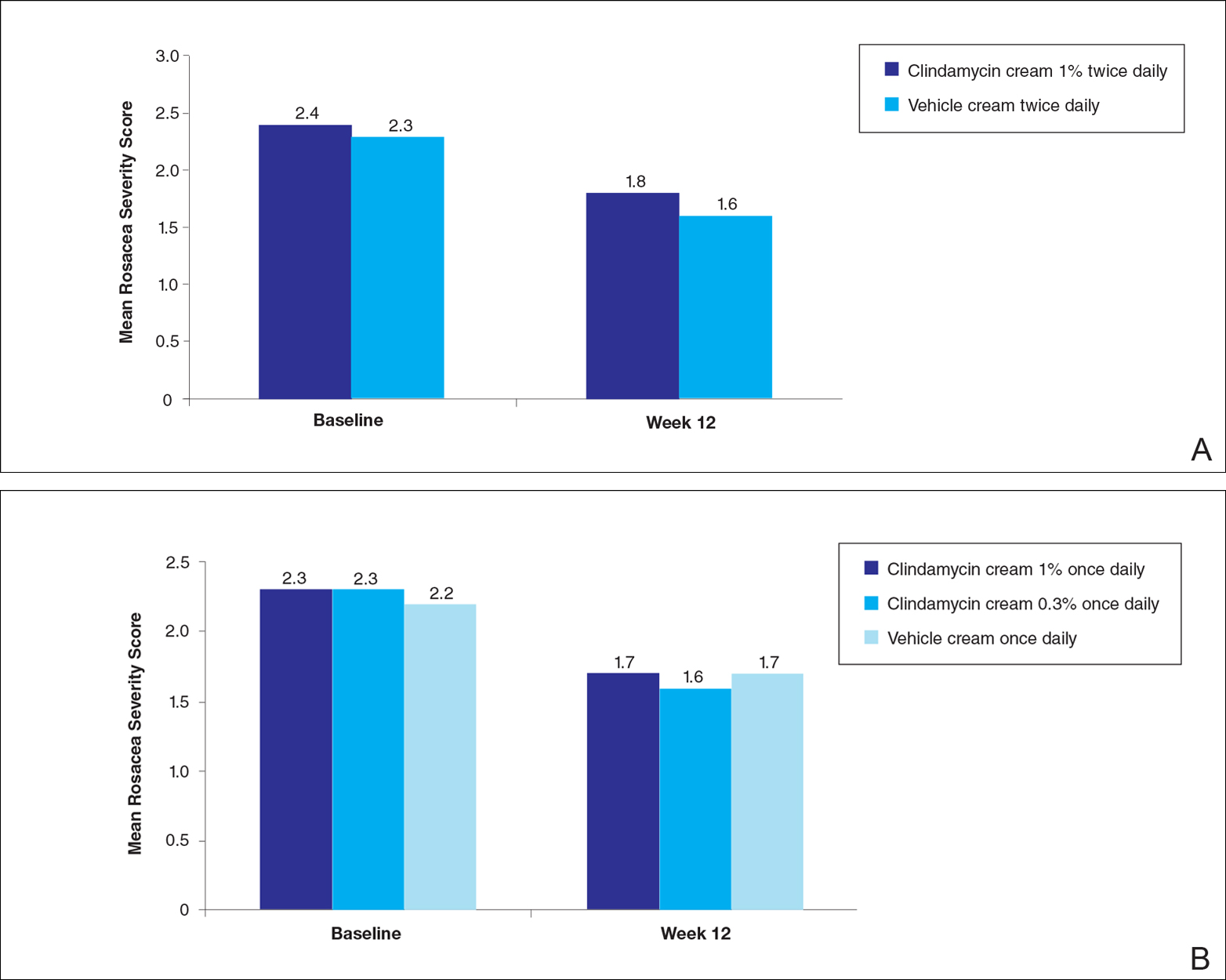
There were no significant differences in the mean total erythema severity scores at week 12 for clindamycin cream 1% twice daily versus vehicle cream twice daily (6.3 vs 6.0; P>.5), clindamycin cream 1% once daily versus vehicle cream once daily (6.2 vs 6.0; P>.5), clindamycin cream 0.3% once daily versus vehicle cream once daily (5.9 vs 6.0; P>.5), and clindamycin gel 1% twice daily versus vehicle gel twice daily (6.7 vs 6.2; P>.5).
There were no relevant differences between any of the clindamycin cream groups and their respective vehicle group at week 12 for skin irritation, including desquamation, edema, dryness, pruritus, and stinging/burning.
Safety
In study A, the majority of AEs in all 5 treatment arms were nondermatologic, mild in intensity, and not considered to be related to the study treatment by the investigator. Overall, 12 participants had AEs considered by the investigator as possibly or probably related to the study treatment: 4.9% in the clindamycin cream 1% twice daily group, 4.6% in the clindamycin cream 1% once daily group, 3.7% in the vehicle cream twice daily group, 1.2% in the clindamycin cream 0.3% once daily group, and 0% in the vehicle cream once daily group. Two treatment-related AEs led to treatment discontinuation, including dermatitis in 1 participant from the clindamycin cream 1% once daily group and contact dermatitis in 1 participant from the clindamycin cream 1% twice daily group.
Comment
No evidence of increased efficacy over the respective vehicles was observed with clindamycin cream or gel, whatever the regimen, in the treatment of rosacea patients in either of these well-designed and well-powered, blinded studies. Slight improvements in the various efficacy criteria were observed, even in the vehicle groups, highlighting the importance of using a good basic skin care regimen in the management of rosacea.9 In contrast to our observations of lack of efficacy in the treatment of rosacea, clinical efficacy of clindamycin has been demonstrated in acne,10-12 albeit with low efficacy for clindamycin monotherapy.13 It is noteworthy that oral or topical antibiotics are no longer recommended as monotherapy for acne to prevent and minimize antibiotic resistance and to preserve the therapeutic value of antibiotics.14
Acne and rosacea are both chronic inflammatory disorders of the skin associated with papules and pustules, and they share some common inflammatory patterns.15-19 Furthermore, the intrinsic anti-inflammatory activity of clindamycin in addition to its antibiotic effects has been suggested by some authors as the main reason for treating acne with clindamycin.20 However, the relative contributions of antibacterial and/or anti-inflammatory properties remain to be fully elucidated, and evidence for direct anti-inflammatory effects of clindamycin remains heterogeneous.21,22 Several pathophysiological factors have been implicated in acne, including hormonal effects, abnormal keratinocyte function, increased sebum production, and microbial components (eg, hypercolonization of the skin follicles by Propionibacterium acnes).23,24 The antibiotic activity of clindamycin against P acnes may be the key factor responsible for the clinical effects in acne.25,26 Although clindamycin may have anti-inflammatory effects in acne via a different inflammatory pathway not shared by rosacea, a purely antibiotic mechanism of action of clindamycin also could explain why we observed no evidence of efficacy in the treatment of rosacea, as no causative bacterial component has been clearly demonstrated in rosacea.27
Conclusion
In these studies, clindamycin cream 0.3% once daily, clindamycin cream 1% once or twice daily, and clindamycin gel 1% twice daily were all well tolerated; however, they were no more effective than the vehicles in the treatment of moderate to severe rosacea.
Acknowledgment
The authors would like to thank Helen Simpson, PhD, of Galderma R&D (Sophia Antipolis, France), for editorial and medical writing assistance.
- Whitney KM, Ditre CM. Anti-inflammatory properties of clindamycin: a review of its use in the treatment of acne vulgaris. Clinical Medicine Insights: Dermatology. 2011;4:27-41.
- Mays RM, Gordon RA, Wilson JM, et al. New antibiotic therapies for acne and rosacea. Dermatol Ther. 2012;25:23-37.
- Wilkin JK, DeWitt S. Treatment of rosacea: topical clindamycin versus oral tetracycline. Int J Dermatol. 1993;32:65-67.
- Breneman D, Savin R, VandePol C, et al. Double-blind, randomized, vehicle-controlled clinical trial of once-daily benzoyl peroxide/clindamycin topical gel in the treatment of patients with moderate to severe rosacea. Int J Dermatol. 2004;43:381-387.
- Leyden JJ, Thiboutot D, Shalita A. Photographic review of results from a clinical study comparing benzoyl peroxide 5%/clindamycin 1% topical gel with vehicle in the treatment of rosacea. Cutis. 2004;73(6 suppl):11-17.
- Chang AL, Alora-Palli M, Lima XT, et al. A randomized, double-blind, placebo-controlled, pilot study to assess the efficacy and safety of clindamycin 1.2% and tretinoin 0.025% combination gel for the treatment of acne rosacea over 12 weeks. J Drugs Dermatol. 2012;11:333-339.
- Freeman SA, Moon SD, Spencer JM. Clindamycin phosphate 1.2% and tretinoin 0.025% gel for rosacea: summary of a placebo-controlled, double-blind trial. J Drugs Dermatol. 2012;11:1410-1414.
- van Zuuren EJ, Fedorowicz Z, Carter B, et al. Interventions for rosacea. Cochrane Database Syst Rev. 2015;4:CD003262.
- Laquieze S, Czernielewski J, Baltas E. Beneficial use of Cetaphil moisturizing cream as part of a daily skin care regimen for individuals with rosacea. J Dermatolog Treat. 2007;18:158-162.
- Lookingbill DP, Chalker DK, Lindholm JS, et al. Treatment of acne with a combination clindamycin/benzoyl peroxide gel compared with clindamycin gel, benzoyl peroxide gel and vehicle gel: combined results of two double-blind investigations. J Am Acad Dermatol. 1997;37:590-595.
- Alirezaï M, Gerlach B, Horvath A, et al. Results of a randomised, multicentre study comparing a new water-based gel of clindamycin 1% versus clindamycin 1% topical solution in the treatment of acne vulgaris. Eur J Dermatol. 2005;15:274-278.
- Jarratt MT, Brundage T. Efficacy and safety of clindamycin-tretinoin gel versus clindamycin or tretinoin alone in acne vulgaris: a randomized, double-blind, vehicle-controlled study. J Drugs Dermatol. 2012;11:318-326.
- Benzaclin. Med Library website. http://medlibrary.org/lib/rx/meds/benzaclin-3. Updated May 8, 2013. Accessed January 24, 2017.
- Walsh TR, Efthimiou J, Dréno B. Systematic review of antibiotic resistance in acne: an increasing topical and oral threat. Lancet Infect Dis. 2016;16:E23-E33.
- Jeremy AH, Holland DB, Roberts SG, et al. Inflammatory events are involved in acne lesion initiation. J Invest Dermatol. 2003;121:20-27.
- Kircik LH. Re-evaluating treatment targets in acne vulgaris: adapting to a new understanding of pathophysiology. J Drugs Dermatol. 2014;13:S57-S60.
- Salzer S, Kresse S, Hirai Y, et al. Cathelicidin peptide LL-37 increases UVB-triggered inflammasome activation: possible implications for rosacea. J Dermatol Sci. 2014;76:173-179.
- Buhl T, Sulk M, Nowak P, et al. Molecular and morphological characterization of inflammatory infiltrate in rosacea reveals activation of Th1/Th17 pathways. J Invest Dermatol. 2015;135:2198-2208.
- Kistowska M, Meier B, Proust T, et al. Propionibacterium acnes promotes Th17 and Th17/Th1 responses in acne patients. J Invest Dermatol. 2015;135:110-118.
- Zeichner JA. Inflammatory acne treatment: review of current and new topical therapeutic options. J Drugs Dermatol. 2016;15(1 suppl 1):S11-S16.
- Nakano T, Hiramatsu K, Kishi K, et al. Clindamycin modulates inflammatory-cytokine induction in lipopolysaccharide-stimulated mouse peritoneal macrophages. Antimicrob Agents Chemother. 2003;47:363-367.
- Orman KL, English BK. Effects of antibiotic class on the macrophage inflammatory response to Streptococcus pneumoniae. J Infect Dis. 2000;182:1561-1565.
- Taylor M, Gonzalez M, Porter R. Pathways to inflammation: acne pathophysiology. Eur J Dermatol. 2011;21:323-333.
- Del Rosso JQ, Kircik LH. The sequence of inflammation, relevant biomarkers, and the pathogenesis of acne vulgaris: what does recent research show and what does it mean to the clinician? J Drugs Dermatol. 2013;12(8 suppl):S109-S115.
- Leyden J, Kaidbey K, Levy SF. The combination formulation of clindamycin 1% plus benzoyl peroxide 5% versus 3 different formulations of topical clindamycin alone in the reduction of Propionibacterium acnes. an in vivo comparative study. Am J Clin Dermatol. 2001;2:263-266.
- Wang WL, Everett ED, Johnson M, et al. Susceptibility of Propionibacterium acnes to seventeen antibiotics. Antimicrob Agents Chemother. 1977;11:171-173.
- Steinhoff M, Schauber J, Leyden JJ. New insights into rosacea pathophysiology: a review of recent findings. J Am Acad Dermatol. 2013;69(6 suppl 1):S15-S26.
- Whitney KM, Ditre CM. Anti-inflammatory properties of clindamycin: a review of its use in the treatment of acne vulgaris. Clinical Medicine Insights: Dermatology. 2011;4:27-41.
- Mays RM, Gordon RA, Wilson JM, et al. New antibiotic therapies for acne and rosacea. Dermatol Ther. 2012;25:23-37.
- Wilkin JK, DeWitt S. Treatment of rosacea: topical clindamycin versus oral tetracycline. Int J Dermatol. 1993;32:65-67.
- Breneman D, Savin R, VandePol C, et al. Double-blind, randomized, vehicle-controlled clinical trial of once-daily benzoyl peroxide/clindamycin topical gel in the treatment of patients with moderate to severe rosacea. Int J Dermatol. 2004;43:381-387.
- Leyden JJ, Thiboutot D, Shalita A. Photographic review of results from a clinical study comparing benzoyl peroxide 5%/clindamycin 1% topical gel with vehicle in the treatment of rosacea. Cutis. 2004;73(6 suppl):11-17.
- Chang AL, Alora-Palli M, Lima XT, et al. A randomized, double-blind, placebo-controlled, pilot study to assess the efficacy and safety of clindamycin 1.2% and tretinoin 0.025% combination gel for the treatment of acne rosacea over 12 weeks. J Drugs Dermatol. 2012;11:333-339.
- Freeman SA, Moon SD, Spencer JM. Clindamycin phosphate 1.2% and tretinoin 0.025% gel for rosacea: summary of a placebo-controlled, double-blind trial. J Drugs Dermatol. 2012;11:1410-1414.
- van Zuuren EJ, Fedorowicz Z, Carter B, et al. Interventions for rosacea. Cochrane Database Syst Rev. 2015;4:CD003262.
- Laquieze S, Czernielewski J, Baltas E. Beneficial use of Cetaphil moisturizing cream as part of a daily skin care regimen for individuals with rosacea. J Dermatolog Treat. 2007;18:158-162.
- Lookingbill DP, Chalker DK, Lindholm JS, et al. Treatment of acne with a combination clindamycin/benzoyl peroxide gel compared with clindamycin gel, benzoyl peroxide gel and vehicle gel: combined results of two double-blind investigations. J Am Acad Dermatol. 1997;37:590-595.
- Alirezaï M, Gerlach B, Horvath A, et al. Results of a randomised, multicentre study comparing a new water-based gel of clindamycin 1% versus clindamycin 1% topical solution in the treatment of acne vulgaris. Eur J Dermatol. 2005;15:274-278.
- Jarratt MT, Brundage T. Efficacy and safety of clindamycin-tretinoin gel versus clindamycin or tretinoin alone in acne vulgaris: a randomized, double-blind, vehicle-controlled study. J Drugs Dermatol. 2012;11:318-326.
- Benzaclin. Med Library website. http://medlibrary.org/lib/rx/meds/benzaclin-3. Updated May 8, 2013. Accessed January 24, 2017.
- Walsh TR, Efthimiou J, Dréno B. Systematic review of antibiotic resistance in acne: an increasing topical and oral threat. Lancet Infect Dis. 2016;16:E23-E33.
- Jeremy AH, Holland DB, Roberts SG, et al. Inflammatory events are involved in acne lesion initiation. J Invest Dermatol. 2003;121:20-27.
- Kircik LH. Re-evaluating treatment targets in acne vulgaris: adapting to a new understanding of pathophysiology. J Drugs Dermatol. 2014;13:S57-S60.
- Salzer S, Kresse S, Hirai Y, et al. Cathelicidin peptide LL-37 increases UVB-triggered inflammasome activation: possible implications for rosacea. J Dermatol Sci. 2014;76:173-179.
- Buhl T, Sulk M, Nowak P, et al. Molecular and morphological characterization of inflammatory infiltrate in rosacea reveals activation of Th1/Th17 pathways. J Invest Dermatol. 2015;135:2198-2208.
- Kistowska M, Meier B, Proust T, et al. Propionibacterium acnes promotes Th17 and Th17/Th1 responses in acne patients. J Invest Dermatol. 2015;135:110-118.
- Zeichner JA. Inflammatory acne treatment: review of current and new topical therapeutic options. J Drugs Dermatol. 2016;15(1 suppl 1):S11-S16.
- Nakano T, Hiramatsu K, Kishi K, et al. Clindamycin modulates inflammatory-cytokine induction in lipopolysaccharide-stimulated mouse peritoneal macrophages. Antimicrob Agents Chemother. 2003;47:363-367.
- Orman KL, English BK. Effects of antibiotic class on the macrophage inflammatory response to Streptococcus pneumoniae. J Infect Dis. 2000;182:1561-1565.
- Taylor M, Gonzalez M, Porter R. Pathways to inflammation: acne pathophysiology. Eur J Dermatol. 2011;21:323-333.
- Del Rosso JQ, Kircik LH. The sequence of inflammation, relevant biomarkers, and the pathogenesis of acne vulgaris: what does recent research show and what does it mean to the clinician? J Drugs Dermatol. 2013;12(8 suppl):S109-S115.
- Leyden J, Kaidbey K, Levy SF. The combination formulation of clindamycin 1% plus benzoyl peroxide 5% versus 3 different formulations of topical clindamycin alone in the reduction of Propionibacterium acnes. an in vivo comparative study. Am J Clin Dermatol. 2001;2:263-266.
- Wang WL, Everett ED, Johnson M, et al. Susceptibility of Propionibacterium acnes to seventeen antibiotics. Antimicrob Agents Chemother. 1977;11:171-173.
- Steinhoff M, Schauber J, Leyden JJ. New insights into rosacea pathophysiology: a review of recent findings. J Am Acad Dermatol. 2013;69(6 suppl 1):S15-S26.
Practice Points
- Clindamycin cream 0.3% and 1% and clindamycin gel 1% were no more effective than their respective vehicles in the treatment of moderate to severe rosacea.
- Clindamycin may have no intrinsic anti-inflammatory activity in rosacea.