User login
Take precautions as cancer picture in MS remains hazy
NASHVILLE, TENN. – With much unknown about the risks of cancer and vaccination associated with immunosuppressants used in multiple sclerosis treatment, a neurologist advised colleagues to be aware of the potential dangers and take appropriate precautions.
For example, Eric Williamson, MD, of the University of Pennsylvania and Philadelphia Veterans Administration Hospital, said he goes a step further than recommending that adult female patients with MS who take ocrelizumab (Ocrevus) get regular mammograms. Per policy, he also double-checks to make sure that patients actually get screened.
“I know two women who were diagnosed with breast cancer before they began on their treatment because we asked about mammograms,” said Dr. Williamson, who spoke in a presentation about the risks of immunosuppressants in MS at the annual meeting of the Consortium of Multiple Sclerosis Centers.
In regard to cancer as a whole, he said, “it’s unclear if there is any true increased risk in MS patients.” But this doesn’t mean there is no danger, he said, since research into immunosuppressants in other contexts show that they can boost the risk of cancer by three times to as much as several hundred times.
In transplant patients, he said, immunosuppressants are linked to higher rates of lymphoproliferative tumors (such as those linked to Epstein-Barr virus), Kaposi sarcoma, and cutaneous, renal, hepatobiliary, and anogenital tumors.
Research is also hazy in regard to specific immunosuppressants used to treat MS. Two reports published about a decade ago raised the possibility that natalizumab (Tysabri) may have sparked a slightly higher risk cancer in patients taking the drug for Crohn’s disease and MS, respectively; the latter report hinted at a higher risk of melanoma specifically. However, Dr. Williamson said postmarketing surveillance has not detected any further sign of trouble (N Engl J Med. 2006;354:899‐910; N Engl J Med. 2008;358;647‐8).
Another drug, ocrelizumab (Ocrevus), has sparked questions about a possible breast cancer risk. As Genentech, its manufacturer, notes: “breast cancer occurred in 6 of 781 females treated with Ocrevus and none of 668 females treated with Rebif [interferon beta-1a] or placebo.”
However, a researcher reported ocrelizumab open-label extension study data at the 2017 CMSC annual meeting and said, “incidence rates of malignancies and breast cancer observed with ocrelizumab treatment in MS remain within the range of epidemiologic background data.”
For now, Dr. Williamson, said, it may take decades to understand if there’s actually an increased breast cancer risk with ocrelizumab.
Skin cancer is a concern for fingolimod (Gilenya), Dr. Williamson said, specifically basal cell carcinoma and melanoma. It’s debatable whether patients should be required to see a dermatologist or make annual visits, he said. Per policy, his VA employer requires these patients to visit a dermatologist.
Whatever the case, it’s important to keep in mind that skin cancer screenings are advisable in general, he said.
Guidance on vaccinations
On the vaccination front, Dr. Williamson said vaccines are a good idea for MS patients – as long as they’re “relatively safe” – because some infectious diseases appear to be more severe in this population.
Flu is a special danger, Dr. Williamson said. He recommends the flu vaccine to patients “because people with MS are at higher risk of influenza-related complications or hospitalizations.”
With guidance from a report led by Dr. Williamson, the National Multiple Sclerosis Society offers recommendations about whether patients with MS should use various vaccines (Curr Neurol Neurosci Rep. 2016;16:36).
Dr. Williamson cautioned that patients with MS who take dimethyl fumarate (Tecfidera), ocrelizumab (Ocrevus), and fingolimod (Gilenya) should not use live vaccines. The drugs can pose issues in regard to other vaccines, too, he said (Plos ONE 2013; 8:e78532; Neurol Res 2012;34:730-3; Neurology. 2013;81:552-8).
Autoimmune risk with alemtuzumab
Alemtuzumab (Lemtrada) has been linked to autoimmune thyroid disorders, especially Graves’ disease, Dr. Williamson said. It’s estimated to affect 17%-41% of patients (Front Endocrinol [Lausanne]. 2017;8:254).
Potentially life-threatening idiopathic thrombocytopenic purpura occurs in 2% of patients on Lemtrada, he said, and anti-GMB nephropathy/Goodpasture’s syndrome has been reported in 0.1%.
Dr. Williamson also noted case reports of autoimmune hemolytic anemia and hepatitis. Earlier this year, three reports in Neurology noted acute coronary syndrome in one patient, hemophagocytic lymphohistiocytosis (HLH) in two patients, and acute acalculous cholecystitis in eight patients (Neurology. 2018 Mar 30. doi: 10.1212/WNL.0000000000005422, doi: 10.1212/WNL.0000000000005420, doi: 10.1212/WNL.0000000000005417).
Dr. Williamson disclosed past consulting for Bayer, Biogen, Celgene, Genentech, EMD Serono, Teva, and Novartis, and current research support from Actelion and Alexion.
NASHVILLE, TENN. – With much unknown about the risks of cancer and vaccination associated with immunosuppressants used in multiple sclerosis treatment, a neurologist advised colleagues to be aware of the potential dangers and take appropriate precautions.
For example, Eric Williamson, MD, of the University of Pennsylvania and Philadelphia Veterans Administration Hospital, said he goes a step further than recommending that adult female patients with MS who take ocrelizumab (Ocrevus) get regular mammograms. Per policy, he also double-checks to make sure that patients actually get screened.
“I know two women who were diagnosed with breast cancer before they began on their treatment because we asked about mammograms,” said Dr. Williamson, who spoke in a presentation about the risks of immunosuppressants in MS at the annual meeting of the Consortium of Multiple Sclerosis Centers.
In regard to cancer as a whole, he said, “it’s unclear if there is any true increased risk in MS patients.” But this doesn’t mean there is no danger, he said, since research into immunosuppressants in other contexts show that they can boost the risk of cancer by three times to as much as several hundred times.
In transplant patients, he said, immunosuppressants are linked to higher rates of lymphoproliferative tumors (such as those linked to Epstein-Barr virus), Kaposi sarcoma, and cutaneous, renal, hepatobiliary, and anogenital tumors.
Research is also hazy in regard to specific immunosuppressants used to treat MS. Two reports published about a decade ago raised the possibility that natalizumab (Tysabri) may have sparked a slightly higher risk cancer in patients taking the drug for Crohn’s disease and MS, respectively; the latter report hinted at a higher risk of melanoma specifically. However, Dr. Williamson said postmarketing surveillance has not detected any further sign of trouble (N Engl J Med. 2006;354:899‐910; N Engl J Med. 2008;358;647‐8).
Another drug, ocrelizumab (Ocrevus), has sparked questions about a possible breast cancer risk. As Genentech, its manufacturer, notes: “breast cancer occurred in 6 of 781 females treated with Ocrevus and none of 668 females treated with Rebif [interferon beta-1a] or placebo.”
However, a researcher reported ocrelizumab open-label extension study data at the 2017 CMSC annual meeting and said, “incidence rates of malignancies and breast cancer observed with ocrelizumab treatment in MS remain within the range of epidemiologic background data.”
For now, Dr. Williamson, said, it may take decades to understand if there’s actually an increased breast cancer risk with ocrelizumab.
Skin cancer is a concern for fingolimod (Gilenya), Dr. Williamson said, specifically basal cell carcinoma and melanoma. It’s debatable whether patients should be required to see a dermatologist or make annual visits, he said. Per policy, his VA employer requires these patients to visit a dermatologist.
Whatever the case, it’s important to keep in mind that skin cancer screenings are advisable in general, he said.
Guidance on vaccinations
On the vaccination front, Dr. Williamson said vaccines are a good idea for MS patients – as long as they’re “relatively safe” – because some infectious diseases appear to be more severe in this population.
Flu is a special danger, Dr. Williamson said. He recommends the flu vaccine to patients “because people with MS are at higher risk of influenza-related complications or hospitalizations.”
With guidance from a report led by Dr. Williamson, the National Multiple Sclerosis Society offers recommendations about whether patients with MS should use various vaccines (Curr Neurol Neurosci Rep. 2016;16:36).
Dr. Williamson cautioned that patients with MS who take dimethyl fumarate (Tecfidera), ocrelizumab (Ocrevus), and fingolimod (Gilenya) should not use live vaccines. The drugs can pose issues in regard to other vaccines, too, he said (Plos ONE 2013; 8:e78532; Neurol Res 2012;34:730-3; Neurology. 2013;81:552-8).
Autoimmune risk with alemtuzumab
Alemtuzumab (Lemtrada) has been linked to autoimmune thyroid disorders, especially Graves’ disease, Dr. Williamson said. It’s estimated to affect 17%-41% of patients (Front Endocrinol [Lausanne]. 2017;8:254).
Potentially life-threatening idiopathic thrombocytopenic purpura occurs in 2% of patients on Lemtrada, he said, and anti-GMB nephropathy/Goodpasture’s syndrome has been reported in 0.1%.
Dr. Williamson also noted case reports of autoimmune hemolytic anemia and hepatitis. Earlier this year, three reports in Neurology noted acute coronary syndrome in one patient, hemophagocytic lymphohistiocytosis (HLH) in two patients, and acute acalculous cholecystitis in eight patients (Neurology. 2018 Mar 30. doi: 10.1212/WNL.0000000000005422, doi: 10.1212/WNL.0000000000005420, doi: 10.1212/WNL.0000000000005417).
Dr. Williamson disclosed past consulting for Bayer, Biogen, Celgene, Genentech, EMD Serono, Teva, and Novartis, and current research support from Actelion and Alexion.
NASHVILLE, TENN. – With much unknown about the risks of cancer and vaccination associated with immunosuppressants used in multiple sclerosis treatment, a neurologist advised colleagues to be aware of the potential dangers and take appropriate precautions.
For example, Eric Williamson, MD, of the University of Pennsylvania and Philadelphia Veterans Administration Hospital, said he goes a step further than recommending that adult female patients with MS who take ocrelizumab (Ocrevus) get regular mammograms. Per policy, he also double-checks to make sure that patients actually get screened.
“I know two women who were diagnosed with breast cancer before they began on their treatment because we asked about mammograms,” said Dr. Williamson, who spoke in a presentation about the risks of immunosuppressants in MS at the annual meeting of the Consortium of Multiple Sclerosis Centers.
In regard to cancer as a whole, he said, “it’s unclear if there is any true increased risk in MS patients.” But this doesn’t mean there is no danger, he said, since research into immunosuppressants in other contexts show that they can boost the risk of cancer by three times to as much as several hundred times.
In transplant patients, he said, immunosuppressants are linked to higher rates of lymphoproliferative tumors (such as those linked to Epstein-Barr virus), Kaposi sarcoma, and cutaneous, renal, hepatobiliary, and anogenital tumors.
Research is also hazy in regard to specific immunosuppressants used to treat MS. Two reports published about a decade ago raised the possibility that natalizumab (Tysabri) may have sparked a slightly higher risk cancer in patients taking the drug for Crohn’s disease and MS, respectively; the latter report hinted at a higher risk of melanoma specifically. However, Dr. Williamson said postmarketing surveillance has not detected any further sign of trouble (N Engl J Med. 2006;354:899‐910; N Engl J Med. 2008;358;647‐8).
Another drug, ocrelizumab (Ocrevus), has sparked questions about a possible breast cancer risk. As Genentech, its manufacturer, notes: “breast cancer occurred in 6 of 781 females treated with Ocrevus and none of 668 females treated with Rebif [interferon beta-1a] or placebo.”
However, a researcher reported ocrelizumab open-label extension study data at the 2017 CMSC annual meeting and said, “incidence rates of malignancies and breast cancer observed with ocrelizumab treatment in MS remain within the range of epidemiologic background data.”
For now, Dr. Williamson, said, it may take decades to understand if there’s actually an increased breast cancer risk with ocrelizumab.
Skin cancer is a concern for fingolimod (Gilenya), Dr. Williamson said, specifically basal cell carcinoma and melanoma. It’s debatable whether patients should be required to see a dermatologist or make annual visits, he said. Per policy, his VA employer requires these patients to visit a dermatologist.
Whatever the case, it’s important to keep in mind that skin cancer screenings are advisable in general, he said.
Guidance on vaccinations
On the vaccination front, Dr. Williamson said vaccines are a good idea for MS patients – as long as they’re “relatively safe” – because some infectious diseases appear to be more severe in this population.
Flu is a special danger, Dr. Williamson said. He recommends the flu vaccine to patients “because people with MS are at higher risk of influenza-related complications or hospitalizations.”
With guidance from a report led by Dr. Williamson, the National Multiple Sclerosis Society offers recommendations about whether patients with MS should use various vaccines (Curr Neurol Neurosci Rep. 2016;16:36).
Dr. Williamson cautioned that patients with MS who take dimethyl fumarate (Tecfidera), ocrelizumab (Ocrevus), and fingolimod (Gilenya) should not use live vaccines. The drugs can pose issues in regard to other vaccines, too, he said (Plos ONE 2013; 8:e78532; Neurol Res 2012;34:730-3; Neurology. 2013;81:552-8).
Autoimmune risk with alemtuzumab
Alemtuzumab (Lemtrada) has been linked to autoimmune thyroid disorders, especially Graves’ disease, Dr. Williamson said. It’s estimated to affect 17%-41% of patients (Front Endocrinol [Lausanne]. 2017;8:254).
Potentially life-threatening idiopathic thrombocytopenic purpura occurs in 2% of patients on Lemtrada, he said, and anti-GMB nephropathy/Goodpasture’s syndrome has been reported in 0.1%.
Dr. Williamson also noted case reports of autoimmune hemolytic anemia and hepatitis. Earlier this year, three reports in Neurology noted acute coronary syndrome in one patient, hemophagocytic lymphohistiocytosis (HLH) in two patients, and acute acalculous cholecystitis in eight patients (Neurology. 2018 Mar 30. doi: 10.1212/WNL.0000000000005422, doi: 10.1212/WNL.0000000000005420, doi: 10.1212/WNL.0000000000005417).
Dr. Williamson disclosed past consulting for Bayer, Biogen, Celgene, Genentech, EMD Serono, Teva, and Novartis, and current research support from Actelion and Alexion.
REPORTING FROM THE CMSC ANNUAL MEETING
Open vs Percutaneous vs Arthroscopic Surgical Treatment of Lateral Epicondylitis: An Updated Systematic Review
ABSTRACT
This study was performed to compare outcomes of open, arthroscopic, and percutaneous surgical techniques for lateral epicondylitis. We searched PubMed (MEDLINE) for literature published between January 1, 2004 and May 23, 2015 using these key words: lateral epicondylitis AND (surgery OR operative OR surgical OR open OR arthroscopic OR percutaneous). Meta-analyses were performed for outcomes reported in 3 studies using 2-sample and 2-proportion Z-tests. Thirty-five studies including 1640 elbows (1055 open, 401 arthroscopic, 184 percutaneous) met the inclusion criteria. There were no differences between groups regarding duration to return to work, complication rate, or patient satisfaction. A greater proportion of patients were pain free in the open group than in the arthroscopic group (70% vs 60%). Despite the absence of a difference among techniques regarding return to work and subjective function, we recommend open débridement as the technique most likely to achieve a pain-free outcome.
Continue to: Lateral epicondylitis affects...
Lateral epicondylitis affects 1% to 3% of adults each year. Although common, symptoms of lateral epicondylitis resolve spontaneously within a year of symptom onset in 80% of cases, and only 3% of patients who seek medical treatment ultimately require surgical intervention within 2 years of symptom onset.1 Despite a relatively low percentage of patients who require surgery, Sanders and colleagues1 noted a significant increase in the rate of surgical intervention from 1.1% to 3.2% of cases in the last 15 years. Surgical intervention is generally indicated when pain and functional disability persist after 6 to 12 months of nonsurgical treatment. Traditional surgical treatment involves open release/débridement of the extensor carpi radialis (ECRB) origin; however, with the increasing prevalence of surgical intervention, surgeons have demonstrated a rising interest in less invasive techniques like arthroscopic release/débridement and percutaneous tenotomy as alternatives to traditional open débridement. While favorable results have been reported for all 3 techniques, there is no current consensus regarding the optimal surgical technique. In 2007, Lo and Safran2 reported no difference in the results of open, percutaneous, and arthroscopic techniques regarding any outcome measure in a systematic review of 33 papers. We conducted a repeat systematic review of the current literature to update Lo and Safran’s2 review and to ascertain if more recent literature demonstrates superiority of 1 technique regarding pain relief, subjective questionnaire data, subjective satisfaction, restoration of strength, and return to work. We hypothesized that return to work would be accelerated, pain decreased, and function improved in the early postoperative period in the arthroscopic and percutaneous groups, but there would be no difference in ultimate pain, functional outcome, or subjective satisfaction.
METHODS
SEARCH STRATEGY AND STUDY SELECTION
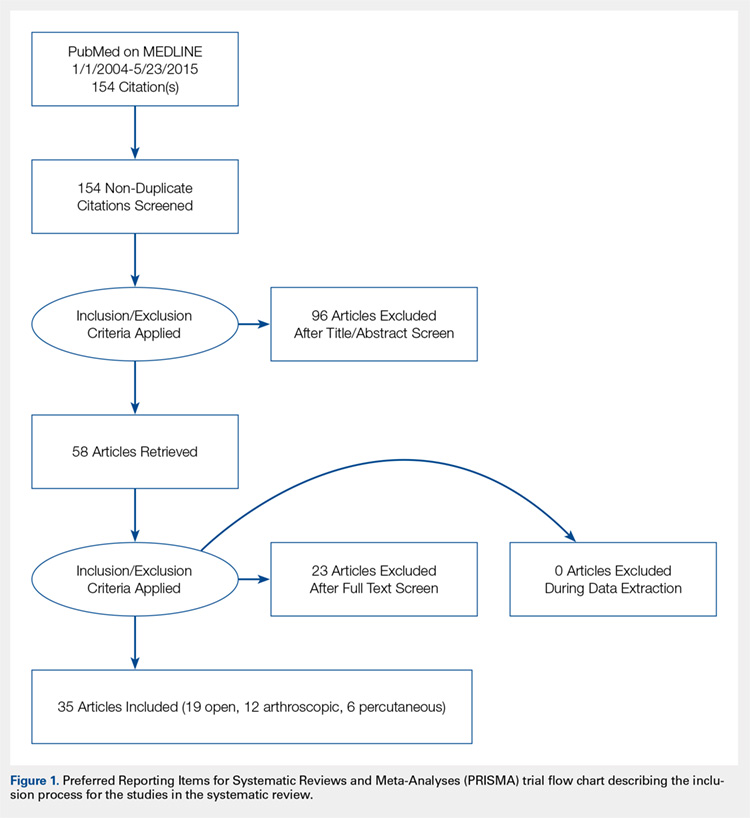
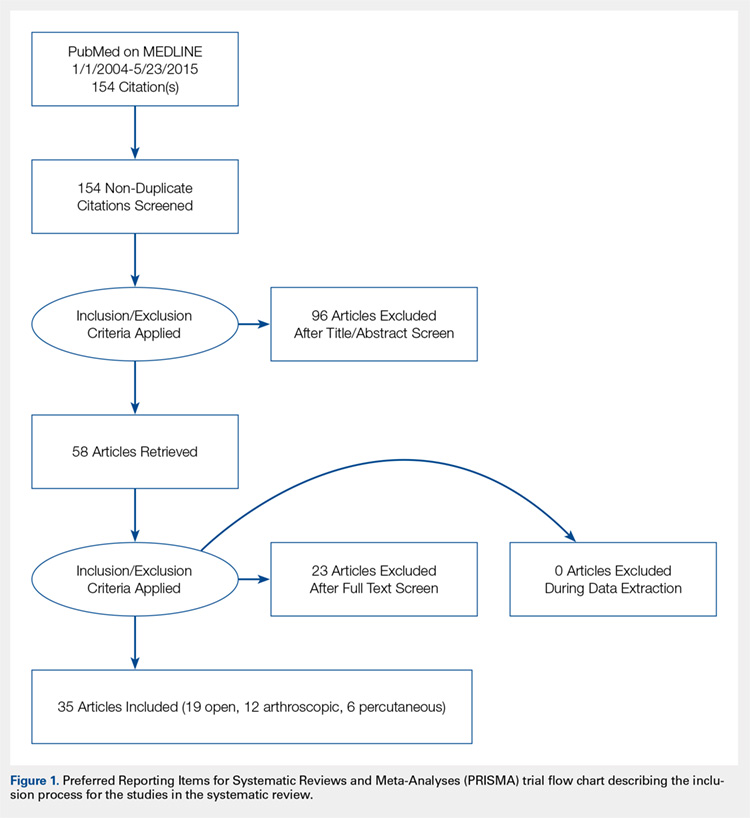
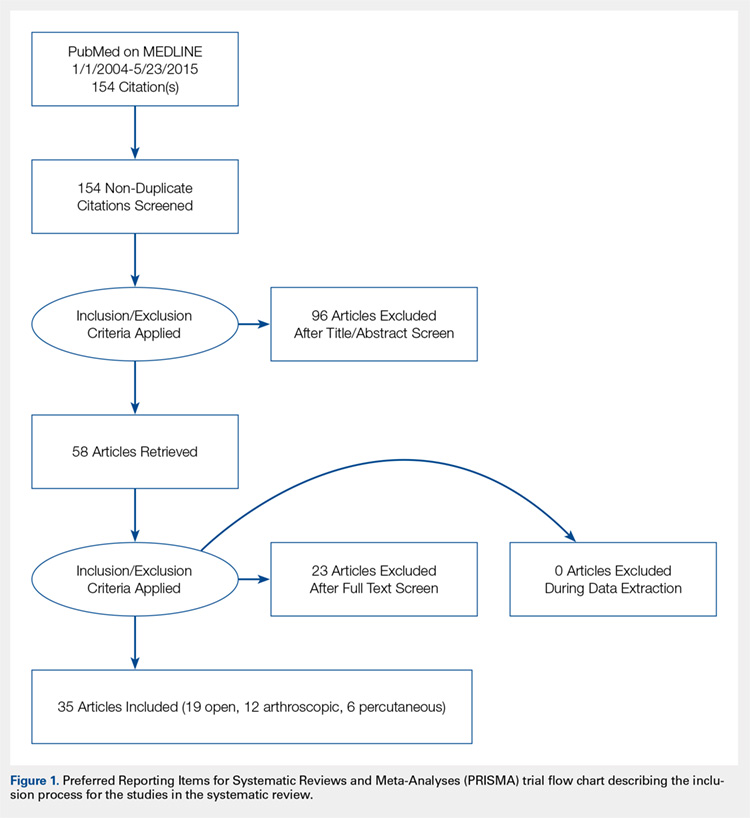
We conducted a systematic review of the literature to update the topic of surgical intervention with lateral epicondylitis since the publication of the most recent review by Lo and Safran2 in 2007, which included all relevant studies published up to 2004. To include all relevant studies published since that time, we searched PubMed (MEDLINE) for all literature published from January 1, 2004 to May 23, 2015 using the following key words: lateral epicondylitis AND (surgery OR operative OR surgical OR open OR arthroscopic OR percutaneous). General search terms were utilized to avoid unintentional exclusion of relevant studies. Two authors reviewed the abstracts of all resultant citations. Table 1 outlines the inclusion and exclusion criteria for the search. References from all included studies were reviewed for applicable articles that were not captured by the initial broad search strategy. A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) trial flow chart shows the study selection algorithm (Figure 1).
Table 1. Inclusion and Exclusion Criteria for the Analyzed Studies
Inclusion Criteria | Exclusion Criteria |
|
|
DATA EXTRACTION AND ANALYSIS
Data were extracted from the included studies by 2 reviewers using data abstraction forms. All study, subject, and surgery parameters were collected. The study and subject demographic parameters analyzed included year of publication, level of evidence, presence of study financial conflict of interest, number of subjects and elbows, gender, age, proportion in whom the dominant extremity was involved, proportion who were laborers, proportion who had a workman’s compensation claim, duration of symptoms prior to surgical intervention, and surgical technique employed (open, arthroscopic, or percutaneous). We recorded the following clinical outcomes: proportion of patients with complete pain relief, proportion who were partially or completely satisfied, proportion who were improved, duration to return to work, grip strength, Disabilities of the Arm, Shoulder, and Hand (DASH) score, visual analog scale (VAS) pain score, and complication rate.
Continue to: Statistical analysis...
STATISTICAL ANALYSIS
Data from all studies were pooled and descriptive statistics were reported as weighted mean ± weighted standard deviation for continuous variables and frequency with percentage for categorical variables. A meta-analysis was performed for all outcome measures that were reported in 3 or more studies within a specific treatment cohort. Data were analyzed using 2-sample and 2-proportion Z-tests. Results were considered statistically significant at P < .05.
RESULTS
LITERATURE RESEARCH
Using the aforementioned search strategy, 154 studies were identified. Following application of the inclusion and exclusion criteria, 35 studies were included in the analysis (Figure 1). One study compared open and percutaneous techniques, and another compared arthroscopic and percutaneous techniques, rendering a total of 19 studies examining open surgical techniques for treatment of lateral epicondylitis,3-21 12 studies examining arthroscopic techniques,14,22-32 and 6 studies reporting percutaneous surgical treatment of lateral epicondylitis29,33-37 (Table 2). There was1 level I study (3%), 6 level III studies (17%), and 28 level IV studies (80%).
Table 2. Study Demographic Data for Open, Arthroscopic, and Percutaneous Lateral Epicondylectomy
| Open | Arthroscopic | Percutaneous | Total |
Number of studies | 19 | 12 | 6 | 35 |
Level of evidence |
|
|
|
|
I | 1 (5%) | 0 | 0 | 1 (3%) |
II | 0 | 0 | 0 | 0 |
III | 3 (16%) | 4 (33%) | 1 (17%) | 6 (17%) |
IV | 15 (79%) | 8 (67%) | 5 (83%) | 28 (80%) |
US: International | 8:12 | 3:9 | 1:5 | 12:24 |
Journals of publication |
|
|
|
|
AJSM | 3 | 1 | 1 | 5 |
JSES | 2 | 2 | 1 | 5 |
Arthroscopy | 2 | 2 | 0 | 3 |
KSSTA | 1 | 2 | 0 | 3 |
CORR | 0 | 2 | 0 | 2 |
JHS | 0 | 1 | 0 | 1 |
JOS | 1 | 1 | 0 | 2 |
AJO | 2 | 0 | 0 | 2 |
Other | 8 | 1 | 4 | 12 |
Abbreviations: AJO, The American Journal of Orthopedics; AJSM, American Journal of Sports Medicine; Arthroscopy, The Journal of Arthroscopy and Related Surgery; CORR, Clinical Orthopaedics & Related Research; JHS, Journal of Hand Surgery; JOS, Journal of Orthopaedic Surgery; JSES, Journal of Shoulder and Elbow Surgery; KSSTA, Knee Surgery, Sports Traumatology, and Arthroscopy.
SUBJECT DEMOGRAPHICS
The 35 included studies comprised 1579 patients and 1640 elbows. Among these, 1055 (64%) elbows underwent open (O), 401 (25%) underwent arthroscopic (A), and 184 (11%) underwent percutaneous (P) treatment. The average age was 45.7 years, 47% of the patients were male, 43% were laborers, 31% had worker’s compensation claims, and the dominant extremity was involved in 62% of patients. The percutaneous cohort was older than the open cohort (P = 46.9, O = 45.4, A = 45.8; P = .036). The duration of symptoms was shorter in the percutaneous cohort than in the other 2 groups and shorter in the arthroscopic cohort than in the open cohort (P = 8 months, O = 23 months, A = 18 months; P < .001). There were no significant differences between groups regarding gender, occupation, worker’s compensation status, or involvement of the dominant extremity (Table 3).
Table 3. Subject Demographics for Open, Arthroscopic, and Percutaneous Groups
| Open | Arthroscopic | Percutaneous |
Subjects (N) | 999 | 397 | 183 |
Elbows (N) | 1055 | 401 | 184 |
Elbows with follow-up (%) | 915 (87%) | 350 (87%) | 181 (98%) |
Males (%) | 427 (47%) | 173 (49%) | 78 (43%) |
Females (%) | 488 (53%) | 177 (51%) | 103 (57%) |
Mean age (years) | 45.4 | 45.8 | 46.9 |
Dominant elbow (%) | 70% | 69% | 53% |
Laborer (%) | 56% | 53% | 48% |
Work comp (%) | 36% | 30% | NR |
Symptoms to operation (months) | 23 | 18 | 8 |
Min. symptoms to operation (months) | 6 | 6 | 3 |
Mean follow-up (months) | 60 | 44 | 11 |
MATA-ANALYSIS CLINICAL OUTCOMES
Clinical outcome results were pooled for all studies reporting the same outcome measure for the same technique (open, arthroscopic, or percutaneous). A meta-analysis was performed for all outcome measures that were reported in a minimum of 3 studies utilizing the same surgical technique (Table 4).
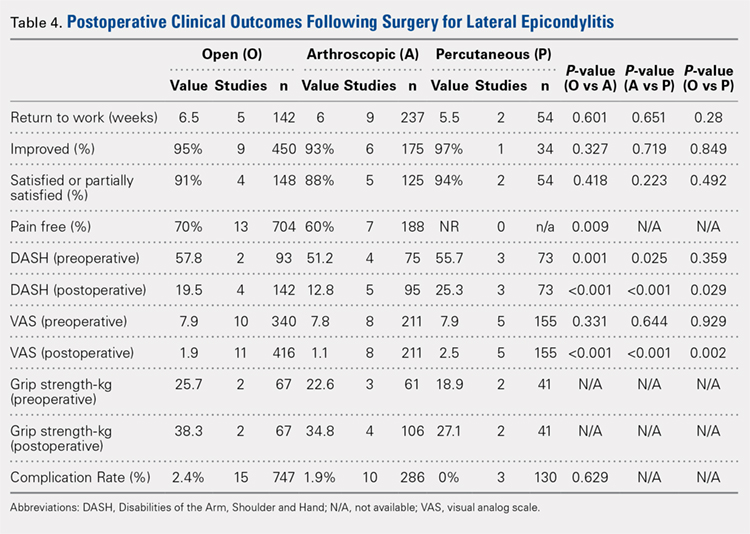
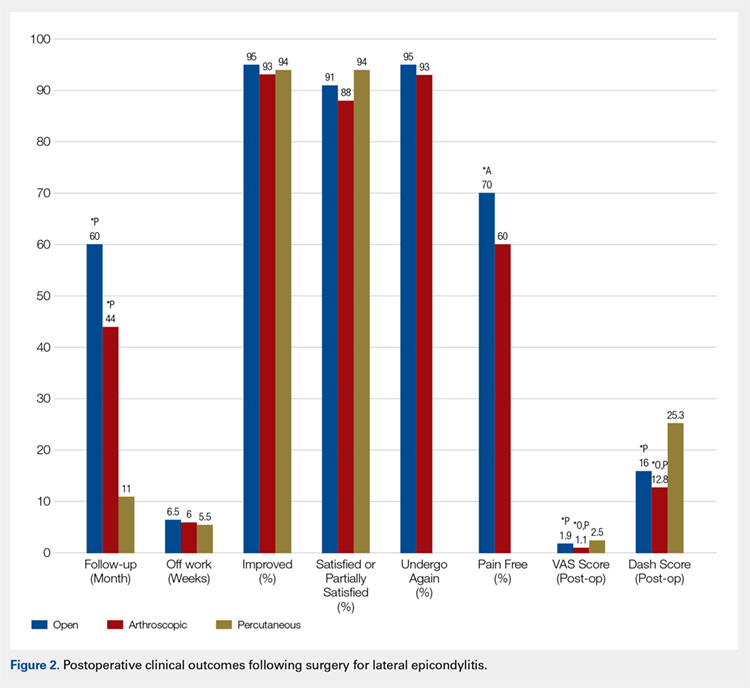
PAIN RELIEF
Thirteen open studies,3,5,7,8,11-16,18,19,21 7 arthroscopic studies14,22-24,26,27,31 and 0 percutaneous studies reported the proportion of patients who were pain free at final follow-up. The proportion of patients who were pain free following open débridement was greater than that in the arthroscopic cohort (O = 70%, A = 60%; P = .009) (Table 4).
Continue to: Subjective improvement and satisfaction...
SUBJECTIVE IMPROVEMENT AND SATISFACTION
Nine open studies, 6 arthroscopic studies, and 1 percutaneous study reported the proportion of patients who felt that their condition had been improved as a result of surgery. There was no difference in the proportion of patients who experienced improvement between the open and arthroscopic cohorts. Four open studies,3,11,12 5 arthroscopic studies,22,26,28,29,32 and 2 percutaneous studies29,36 reported the proportion of patients who were satisfied or partially satisfied with the results of the procedure. There was no difference between the open and arthroscopic groups in the proportion of patients who were satisfied or partially satisfied (Table 4).
RETURN TO WORK
The duration to return to work following surgery was reported in 5 open studies,4,5,10,13,14 9 arthroscopic studies,14,23-29,32 and 2 percutaneous studies.29,36 There was no statistically significant difference between the open and arthroscopic groups with regard to duration to return to work (O = 6.5 weeks, A = 6 weeks; P = .601). The percutaneous technique could not be included in the meta-analysis due to the presence of only 2 studies, but the pooled mean duration to return to work in these 2 studies was 5.5 weeks (Table 4).
GRIP STRENGTH
Postoperative grip strength was reported in 2 open studies,10,19 4 arthroscopic studies,28,30,32 and 2 percutaneous studies.35-36 A meta-analysis could not be performed on all the groups due to the presence of only 2 open and 2 percutaneous studies reporting grip strength. The pooled averages were O = 38.3 kg, A = 34.8 kg, and P = 27.1 kg (Table 4).
DASH SCORE
The postoperative DASH score was reported in 4 open studies,4,15,17,19,20 5 arthroscopic studies,28-31 and 3 percutaneous studies.29,33,36 At final follow-up, the mean DASH score was higher in the arthroscopic group than in the open and percutaneous groups (A = 12.8, O = 19.5, P = 25.3; P < .001 for both comparisons), and the mean DASH score was significantly higher in the open group than in the percutaneous group (P = .029). The reporting of DASH scores in the early postoperative period was not sufficiently consistent to allow us to test our hypothesis that there would be early differences in function between groups (Table 4).
VAS PAIN SCORE
Postoperative VAS pain scores were reported in 11 open studies,6,8-10,12,15,19-21 8 arthroscopic studies,24-26,29-32 and 5 percutaneous studies.29,33,35-37 At final follow-up, there was a lower mean VAS score in the arthroscopic group than in the open and percutaneous groups (A = 1.1, O = 1.9, and P = 2.5; P < .001 for both comparisons) and a lower mean VAS score in the open group than in the percutaneous group (P = .002) (Table 4). Reporting of VAS scores in the early postoperative period in the included studies wan not sufficiently consistent to allow us to test our hypothesis that there would be early differences in pain between groups.
COMPLICATIONS
The complication rate was reported in 15 open studies, 10 arthroscopic studies, and 3 percutaneous studies. There was no difference in the complication rate between the open and arthroscopic techniques (O = 2.4%, A = 1.9%; P = .629) (Table 4). Complications noted in the open cohort included superficial wound infection (6), hematoma (5), synovial fistula (2), seroma (2), and posterior interosseous nerve palsy (1). Complications noted in the arthroscopic cohort included superficial infection (3), hematoma (1), and transient paresthesia (1). Of note, there were no complications in the percutaneous group.
Continue to: Discussion...
DISCUSSION
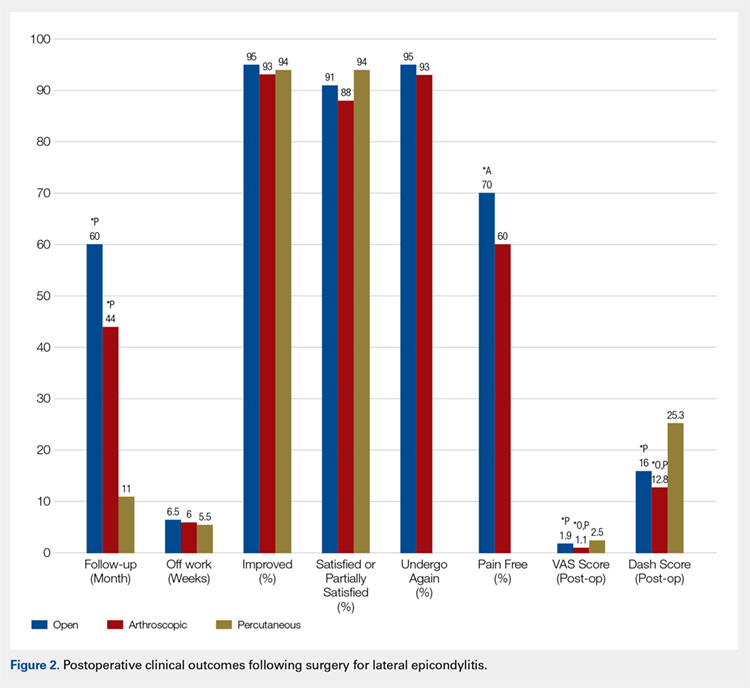
The primary purpose of this review was to determine if definitive evidence suggests that any 1 of open, percutaneous, or arthroscopic surgical treatment is superior to the other 2 for relieving pain, improving functionality, restoring strength, or accelerating return to work. The most striking finding of this study was a significantly higher proportion of patients who were pain free at final follow-up in the open group than in the arthroscopic group (70% vs 60%, P = .009) (Table 4). At final follow-up, there were no significant differences between groups regarding duration to return to work, proportion who were improved, proportion who were satisfied or partially satisfied, and complication rate. Average VAS and DASH scores at final follow-up were lower in the arthroscopic group than in the open and percutaneous groups (Figure 2). However, although the difference between mean DASH scores in the arthroscopic and open groups (6.7 points) was statistically significant, it is likely not clinically significant, as the minimal clinically important difference (MCID) for the DASH score is 10 points, as demonstrated by Sorensen and colleagues.38 Although it has not been specifically defined for lateral epicondylitis, the MCID for VAS pain has been reported in the literature to range from 1.0 to 1.4.39-40 Therefore, as for the DASH score, the difference witnessed between the open and arthroscopic groups (0.8) is likely not clinically significant. Of note, the differences between values for arthroscopic and percutaneous techniques are greater than the MCID.
In light of a recent increase in the prevalence of surgical intervention for lateral epicondylitis, many authors have promoted arthroscopic and percutaneous techniques as alternatives to traditional open débridement with the goal of achieving the same results with decreased morbidity and accelerated return to work. Given the increased proportion of patients who were pain free at final follow-up in the open cohort, it is our contention that open release/débridement of the common extensor/ECRB origin allows the surgeon to fully appreciate the extent of tendinotic tissue that is contributing to the patient’s symptoms and to address the pathology in its entirety. Other authors have also questioned whether the full extent of extra-articular tendinosis can be accurately identified arthroscopically. Cummins41 demonstrated, in a series of 18 patients who underwent arthroscopic ECRB débridement, that 6 patients had residual tendinosis upon open evaluation and 10 had residual tendinosis on histologic assessment. Additionally, in the same series, residual tendinopathy was associated with poorer clinical outcomes.
The improved visualization associated with an open technique comes at minimal expense, as the incision was only 1.5 cm to 5 cm in 13 of 15 papers reporting incision length.3,4,6,8-11,13,15,18-20 This increased exposure may not translate into increased morbidity, as there was no increase in the duration to return to work nor the complication rate. As a result of the extensive instrumentation necessary for arthroscopic techniques, open techniques also appear to be less expensive. Analyses in the literature have suggested increased expenditures associated with arthroscopic treatment ranging from 23%42 to 100%43 greater than those of open treatment.
Although obvious, it should be noted that a percutaneous tenotomy does not permit assessment of the extent of pathologic tendinosis. As a result of an inability to visualize and débride pathologic tissue, percutaneous tenotomy rendered inferior outcomes to open and arthroscopic techniques in terms of both postoperative VAS pain score and DASH score. Nonetheless, it is a relatively rapid and simple technique and resulted in zero complications in 184 elbows. Overall, percutaneous tenotomy appears to be an inferior technique to open and arthroscopic techniques in terms of achieving complete pain relief and optimal functional recovery; however, it may be useful in those who wish to avoid a more invasive intervention.
LIMITATIONS
The most significant limitation of this study was the heterogeneity in the techniques utilized in each group. Among the 19 papers in the open cohort, 11 used techniques aimed at lengthening or release of the extensor origin, 7 performed débridement of tendinotic tissue at the ECRB origin, and 1 compared these approaches. Exposures ranged from 1.5 cm to 8 cm in length, 3 techniques added tendon repair following débridement, and 2 utilized a radiofrequency device.
Among the 12 papers in the arthroscopic cohort, 8 performed arthroscopic (inside-out) débridement of the tendinotic tissue at the ECRB origin, 3 performed arthroscopic release of the ECRB tendon, and 1 performed endoscopic ECRB release in an outside-in fashion. Four techniques added posterior synovial plica excision and 4 added decortication of the lateral epicondyle débridement or release. Some authors advocate for arthroscopic intervention on the grounds that it permits evaluation and correction of other intra-articular pathology. With this in mind, some authors have suggested that a synovial fold (plica) adjacent to the radiocapitellar joint may contribute to lateral elbow pain.27,44 Nevertheless, in the only comparative trial in the literature, Rhyou and Kim30 demonstrated that excision of posterior synovial fold failed to enhance pain relief or function in a retrospective cohort study comparing arthroscopic débridement with and without plica excision.
Continue to: Some authors advocate...
Some authors advocate decorticating the non-articular, lateral epicondyle with a shaver to stimulate bleeding and promote a healing response. However, 1 study in our review compared arthroscopic ECRB release with and without decortication and found that decortication significantly increased pain up to 4 weeks postoperatively, increased duration to return to work, and did not improve the ultimate clinical result.25 Of note, others have used a similar rationale to advocate drilling the lateral epicondyle when utilizing an open technique. However, Dunn and colleagues8 note that they have modified the Nirschl technique to eliminate drilling because they feel it increases postoperative pain and may damage the extensor digitorum communis origin.
Among the 6 papers in the percutaneous tenotomy cohort, 2 performed tenotomy with a hypodermic needle, 2 with a scalpel through a limited incision (0.5 cm-1 cm), 1 using a TX1 tissue removal system (Tenex Health), and 1 with a percutaneous radiofrequency probe. In 3 techniques, ultrasound was used to direct the tenotomy.
The quality of this review is also limited by the studies included for analysis, as with any systematic review. Because 28 of the 35 included studies were classified as evidence level IV, the likelihood of methodological bias is increased. The majority of studies contained ≥1 demonstrable biases, including selection, detection, attrition biases, or a combination. Selection bias is prevalent among predominantly level IV studies, in which the authors have selected their preferred surgical technique. There was heterogeneity in the reporting of preoperative variables and the outcome measures that were utilized. Scoring systems, such as the Nirschl Tennis Elbow Score and the Mayo Elbow Performance Index, would have been valuable in comparing the groups had they been more consistently reported. The heterogeneity in clinical outcome tools and the lack of reported outcome variance or standard deviations prevented a formal meta-analysis of some of these outcome measures. Due to inconsistent reporting, we were also unable to test our hypothesis that there would be less pain and improved function in the arthroscopic and/or percutaneous cohorts in the early postoperative period compared to the open cohort due to the less invasive techniques used. Although the differences in DASH and VAS scores at final follow-up likely did not meet the MCID threshold, these differences may have been greater and more clinically relevant in the early postoperative period.
CONCLUSION
We hypothesized that the arthroscopic and percutaneous groups would experience accelerated return to work and reduced pain in the early postoperative period but no difference in ultimate pain, functional outcome, or subjective satisfaction. There is no difference between open, arthroscopic, and percutaneous surgical treatment for lateral epicondylitis regarding return to work and subjective satisfaction; however, open treatment led to a greater percentage of patients being pain free at final follow-up. While arthroscopic treatment led to better pain and functional scores at final follow-up, the absolute differences were quite small and likely not clinically significant. In light of the available evidence, we recommend open débridement as the best means of minimizing cost and achieving a pain-free outcome in the long term. For future investigators, it would be useful to perform a randomized clinical study directly comparing open, arthroscopic, and percutaneous techniques, including assessment of pain and functional scores in the early postoperative period, and to further evaluate differences in cost among the various techniques.
This paper will be judged for the Resident Writer’s Award.
- Sanders TL Jr, Maradit Kremers H, Bryan AJ, Ransom JE, Smith J, Morrey BF. The epidemiology and health care burden of tennis elbow: a population-based study. Am J Sports Med. 2015;43(5):1066-1071. doi:10.1177/0363546514568087.
- Lo MY, Safran MR. Surgical treatment of lateral epicondylitis: a systematic review. Clin Orthop Relat Res. 2007;463:98-106. doi:10.1097/BLO.0b013e3181483dc4.
- Balk ML, Hagberg WC, Buterbaugh GA, Imbriglia JE. Outcome of surgery for lateral epicondylitis (tennis elbow): effect of worker’s compensation. Am J Orthop. 2005;34(3):122-126; discussion 126.
- Barth J, Mahieu P, Hollevoet N. Extensor tendon and fascia sectioning of extensors at the musculotendinous unit in lateral epicondylitis. Acta Orthop Belg. 2013;79(3):266-270.
- Bigorre N, Raimbeau G, Fouque PA, Cast YS, Rabarin F, Cesari B. Lateral epicondylitis treatment by extensor carpi radialis fasciotomy and radial nerve decompression: is outcome influenced by the occupational disease compensation aspect? Orthop Traumatol Surg Res. 2011;97(2):159-163. doi:10.1016/j.otsr.2010.11.007.
- Cho BK, Kim YM, Kim DS, et al. Mini-open muscle resection procedure under local anesthesia for lateral and medial epicondylitis. Clin Orthop Surg. 2009;1(3):123-127. doi:10.4055/cios.2009.1.3.123.
- Coleman B, Quinlan JF, Matheson JA. Surgical treatment for lateral epicondylitis: a long-term follow-up of results. J Shoulder Elbow Surg. 2010;19(3):363-367. doi:10.1016/j.jse.2009.09.008.
- Dunn JH, Kim JJ, Davis L, Nirschl RP. Ten- to 14-year follow-up of the Nirschl surgical technique for lateral epicondylitis. Am J Sports Med. 2008;36(2):261-266. doi:10.1177/0363546507308932.
- Manon-Matos Y, Oron A, Wolff TW. Combined common extensor and supinator aponeurotomy for the treatment of lateral epicondylitis. Tech Hand Up Extrem Surg. 2013;17(3):179-181. doi:10.1097/BTH.0b013e31829e0eeb.
- Meknas K, Odden-Miland A, Mercer JB, Castillejo M, Johansen O. Radiofrequency microtenotomy: a promising method for treatment of recalcitrant lateral epicondylitis. Am J Sports Med. 2008;36(10):1960-1965. doi:10.1177/0363546508318045.
- Pruzansky ME, Gantsoudes GD, Watters N. Late surgical results of reattachment to bone in repair of chronic lateral epicondylitis. Am J Orthop. 2009;38(6):295-299.
- Rayan F, Rao V Sr, Purushothamdas S, Mukundan C, Shafqat SO. Common extensor origin release in recalcitrant lateral epicondylitis – role justified? J Orthop Surg Res. 2010;5:31. doi:10.1186/1749-799X-5-31.
- Reddy VR, Satheesan KS, Bayliss N. Outcome of Boyd-McLeod procedure for recalcitrant lateral epicondylitis of elbow. Rheumatol Int. 2011;31(8):1081-1084. doi:10.1007/s00296-010-1450-1.
- Rubenthaler F, Wiese M, Senge A, Keller L, Wittenberg RH. Long-term follow-up of open and endoscopic Hohmann procedures for lateral epicondylitis. Arthroscopy. 2005;21(6):684-690. doi:10.1016/j.arthro.2005.03.017.
- Ruch DS, Orr SB, Richard MJ, Leversedge FJ, Mithani SK, Laino DK. A comparison of debridement with and without anconeus muscle flap for treatment of refractory lateral epicondylitis. J Shoulder Elbow Surg. 2015;24(2):236-241. doi:10.1016/j.jse.2014.09.035.
- Siddiqui MA, Koh J, Kua J, Cheung T, Chang P. Functional outcome assessment after open tennis elbow release: what are the predictor parameters? Singapore Med J. 2011;52(2):73-76.
- Solheim E, Hegna J, Øyen J. Extensor tendon release in tennis elbow: results and prognostic factors in 80 elbows. Knee Surg Sports Traumatol Arthrosc. 2011;19(6):1023-1027. doi:10.1007/s00167-011-1477-1.
- Svernlöv B, Adolfsson L. Outcome of release of the lateral extensor muscle origin for epicondylitis. Scand J Plast Reconstr Surg Hand Surg. 2006;40(3):161-165. doi:10.1080/02844310500491492.
- Tasto JP, Cummings J, Medlock V, Hardesty R, Amiel D. Microtenotomy using a radiofrequency probe to treat lateral epicondylitis. Arthroscopy. 2005;21(7):851-860. doi:10.1016/j.arthro.2005.03.019.
- Thornton SJ, Rogers JR, Prickett WD, Dunn WR, Allen AA, Hannafin JA. Treatment of recalcitrant lateral epicondylitis with suture anchor repair. Am J Sports Med. 2005;33(10):1558-1564. doi:10.1177/0363546505276758.
- Wang AW, Erak S. Fractional lengthening of forearm extensors for resistant lateral epicondylitis. ANZ J Surg. 2007;77(11):981-984. doi:10.1111/j.1445-2197.2007.04294.x.
- Baker CL Jr, Baker CL 3rd. Long-term follow-up of arthroscopic treatment of lateral epicondylitis. Am J Sports Med. 2008;36(2):254-260. doi:10.1177/0363546507311599.
- Grewal R, MacDermid JC, Shah P, King GJ. Functional outcome of arthroscopic extensor carpi radialis brevis tendon release in chronic lateral epicondylitis. J Hand Surg Am. 2009;34(5):849-857. doi:10.1016/j.jhsa.2009.02.006.
- Jerosch J, Schunck J. Arthroscopic treatment of lateral epicondylitis: indication, technique and early results. Knee Surg Sports Traumatol Arthrosc. 2006;14(4):379-382. doi:10.1007/s00167-005-0662-5.
- Kim JW, Chun CH, Shim DM, et al. Arthroscopic treatment of lateral epicondylitis: comparison of the outcome of ECRB release with and without decortication. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1178-1183. doi:10.1007/s00167-011-1507-z.
- Lattermann C, Romeo AA, Anbari A, et al. Arthroscopic debridement of the extensor carpi radialis brevis for recalcitrant lateral epicondylitis. J Shoulder Elbow Surg. 2010;19(5):651-656. doi:10.1016/j.jse.2010.02.008.
- Mullett H, Sprague M, Brown G, Hausman M. Arthroscopic treatment of lateral epicondylitis: clinical and cadaveric studies. Clin Orthop Relat Res. 2005;439:123-128. doi:10.1097/01.blo.0000176143.08886.fe.
- Oki G, Iba K, Sasaki K, Yamashita T, Wada T. Time to functional recovery after arthroscopic surgery for tennis elbow. J Shoulder Elbow Surg. 2014;23(10):1527-1531. doi:10.1016/j.jse.2014.05.010.
- Othman AM. Arthroscopic versus percutaneous release of common extensor origin for treatment of chronic tennis elbow. Arch Orthop Trauma Surg. 2011;131(3):383-388. doi:10.1007/s00402-011-1260-2.
- Rhyou IH, Kim KW. Is posterior synovial plica excision necessary for refractory lateral epicondylitis of the elbow? Clin Orthop Relat Res. 2013;471(1):284-290. doi:10.1007/s11999-012-2585-z.
- Wada T, Moriya T, Iba K, et al. Functional outcomes after arthroscopic treatment of lateral epicondylitis. J Orthop Sci. 2009;14(2):167-174. doi:10.1007/s00776-008-1304-9.
- Yoon JP, Chung SW, Yi JH, et al. Prognostic factors of arthroscopic extensor carpi radialis brevis release for lateral epicondylitis. Arthroscopy. 2015;31(7):1232-1237. doi:10.1016/j.arthro.2015.02.006.
- Barnes DE, Beckley JM, Smith J. Percutaneous ultrasonic tenotomy for chronic elbow tendinosis: a prospective study. J Shoulder Elbow Surg. 2015;24(1):67-73. doi:10.1016/j.jse.2014.07.017.
- Kaleli T, Ozturk C, Temiz A, Tirelioglu O. Surgical treatment of tennis elbow: percutaneous release of the common extensor origin. Acta Orthop Belg. 2004;70(2):131-133.
- Lin MT, Chou LW, Chen HS, Kao MJ. Percutaneous soft tissue release for treating chronic recurrent myofascial pain associated with lateral epicondylitis: 6 case studies. Evid Based Complement Alternat Med. 2012;2012:142941. doi:10.1155/2012/142941.
- Lin CL, Lee JS, Su WR, Kuo LC, Tai TW, Jou IM. Clinical and ultrasonographic results of ultrasonographically guided percutaneous radiofrequency lesioning in the treatment of recalcitrant lateral epicondylitis. Am J Sports Med. 2011;39(11):2429-2435. doi:10.1177/0363546511417096.
- Zhu J, Hu B, Xing C, Li J. Ultrasound-guided, minimally invasive, percutaneous needle puncture treatment for tennis elbow. Adv Ther. 2008;25(10):1031-1036. doi:10.1007/s12325-008-0099-6.
- Sorensen AA, Howard D, Tan WH, Ketchersid J, Calfee RP. Minimal clinically important differences of 3 patient-related outcomes instruments. J Hand Surg Am. 2013;38(4):641-649. doi:10.1016/j.jhsa.2012.12.032.
- Kelly AM. The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J. 2001;18(3):205-207. doi:10.1136/emj.18.3.205.
- Tashjian RZ, Deloach J, Porucznik CA, Powell AP. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg. 2009;18(6):927-932. doi:10.1016/j.jse.2009.03.021.
- Cummins CA. Lateral epicondylitis: in vivo assessment of arthroscopic debridement and correlation with patient outcomes. Am J Sports Med. 2006;34(9):1486-1491. doi:10.1177/0363546506288016.
- Stapleton TR, Baker CL. Arthroscopic treatment of lateral epicondylitis: a clinical study. Arthroscopy. 1996;1:365-366.
- Hastings H. Open treatment for lateral tennis elbow good for certain indications. Orthop Today. 2009;2:1-2.
- Duparc F, Putz R, Michot C, Muller JM, Fréger P. The synovial fold of the humeroradial joint: anatomical and histological features, and clinical relevance in lateral epicondylalgia of the elbow. Surg Radiol Anat. 2002;24(5):302-307. doi:10.1007/s00276-002-0055-0.
ABSTRACT
This study was performed to compare outcomes of open, arthroscopic, and percutaneous surgical techniques for lateral epicondylitis. We searched PubMed (MEDLINE) for literature published between January 1, 2004 and May 23, 2015 using these key words: lateral epicondylitis AND (surgery OR operative OR surgical OR open OR arthroscopic OR percutaneous). Meta-analyses were performed for outcomes reported in 3 studies using 2-sample and 2-proportion Z-tests. Thirty-five studies including 1640 elbows (1055 open, 401 arthroscopic, 184 percutaneous) met the inclusion criteria. There were no differences between groups regarding duration to return to work, complication rate, or patient satisfaction. A greater proportion of patients were pain free in the open group than in the arthroscopic group (70% vs 60%). Despite the absence of a difference among techniques regarding return to work and subjective function, we recommend open débridement as the technique most likely to achieve a pain-free outcome.
Continue to: Lateral epicondylitis affects...
Lateral epicondylitis affects 1% to 3% of adults each year. Although common, symptoms of lateral epicondylitis resolve spontaneously within a year of symptom onset in 80% of cases, and only 3% of patients who seek medical treatment ultimately require surgical intervention within 2 years of symptom onset.1 Despite a relatively low percentage of patients who require surgery, Sanders and colleagues1 noted a significant increase in the rate of surgical intervention from 1.1% to 3.2% of cases in the last 15 years. Surgical intervention is generally indicated when pain and functional disability persist after 6 to 12 months of nonsurgical treatment. Traditional surgical treatment involves open release/débridement of the extensor carpi radialis (ECRB) origin; however, with the increasing prevalence of surgical intervention, surgeons have demonstrated a rising interest in less invasive techniques like arthroscopic release/débridement and percutaneous tenotomy as alternatives to traditional open débridement. While favorable results have been reported for all 3 techniques, there is no current consensus regarding the optimal surgical technique. In 2007, Lo and Safran2 reported no difference in the results of open, percutaneous, and arthroscopic techniques regarding any outcome measure in a systematic review of 33 papers. We conducted a repeat systematic review of the current literature to update Lo and Safran’s2 review and to ascertain if more recent literature demonstrates superiority of 1 technique regarding pain relief, subjective questionnaire data, subjective satisfaction, restoration of strength, and return to work. We hypothesized that return to work would be accelerated, pain decreased, and function improved in the early postoperative period in the arthroscopic and percutaneous groups, but there would be no difference in ultimate pain, functional outcome, or subjective satisfaction.
METHODS
SEARCH STRATEGY AND STUDY SELECTION
We conducted a systematic review of the literature to update the topic of surgical intervention with lateral epicondylitis since the publication of the most recent review by Lo and Safran2 in 2007, which included all relevant studies published up to 2004. To include all relevant studies published since that time, we searched PubMed (MEDLINE) for all literature published from January 1, 2004 to May 23, 2015 using the following key words: lateral epicondylitis AND (surgery OR operative OR surgical OR open OR arthroscopic OR percutaneous). General search terms were utilized to avoid unintentional exclusion of relevant studies. Two authors reviewed the abstracts of all resultant citations. Table 1 outlines the inclusion and exclusion criteria for the search. References from all included studies were reviewed for applicable articles that were not captured by the initial broad search strategy. A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) trial flow chart shows the study selection algorithm (Figure 1).
Table 1. Inclusion and Exclusion Criteria for the Analyzed Studies
Inclusion Criteria | Exclusion Criteria |
|
|
DATA EXTRACTION AND ANALYSIS
Data were extracted from the included studies by 2 reviewers using data abstraction forms. All study, subject, and surgery parameters were collected. The study and subject demographic parameters analyzed included year of publication, level of evidence, presence of study financial conflict of interest, number of subjects and elbows, gender, age, proportion in whom the dominant extremity was involved, proportion who were laborers, proportion who had a workman’s compensation claim, duration of symptoms prior to surgical intervention, and surgical technique employed (open, arthroscopic, or percutaneous). We recorded the following clinical outcomes: proportion of patients with complete pain relief, proportion who were partially or completely satisfied, proportion who were improved, duration to return to work, grip strength, Disabilities of the Arm, Shoulder, and Hand (DASH) score, visual analog scale (VAS) pain score, and complication rate.
Continue to: Statistical analysis...
STATISTICAL ANALYSIS
Data from all studies were pooled and descriptive statistics were reported as weighted mean ± weighted standard deviation for continuous variables and frequency with percentage for categorical variables. A meta-analysis was performed for all outcome measures that were reported in 3 or more studies within a specific treatment cohort. Data were analyzed using 2-sample and 2-proportion Z-tests. Results were considered statistically significant at P < .05.
RESULTS
LITERATURE RESEARCH
Using the aforementioned search strategy, 154 studies were identified. Following application of the inclusion and exclusion criteria, 35 studies were included in the analysis (Figure 1). One study compared open and percutaneous techniques, and another compared arthroscopic and percutaneous techniques, rendering a total of 19 studies examining open surgical techniques for treatment of lateral epicondylitis,3-21 12 studies examining arthroscopic techniques,14,22-32 and 6 studies reporting percutaneous surgical treatment of lateral epicondylitis29,33-37 (Table 2). There was1 level I study (3%), 6 level III studies (17%), and 28 level IV studies (80%).
Table 2. Study Demographic Data for Open, Arthroscopic, and Percutaneous Lateral Epicondylectomy
| Open | Arthroscopic | Percutaneous | Total |
Number of studies | 19 | 12 | 6 | 35 |
Level of evidence |
|
|
|
|
I | 1 (5%) | 0 | 0 | 1 (3%) |
II | 0 | 0 | 0 | 0 |
III | 3 (16%) | 4 (33%) | 1 (17%) | 6 (17%) |
IV | 15 (79%) | 8 (67%) | 5 (83%) | 28 (80%) |
US: International | 8:12 | 3:9 | 1:5 | 12:24 |
Journals of publication |
|
|
|
|
AJSM | 3 | 1 | 1 | 5 |
JSES | 2 | 2 | 1 | 5 |
Arthroscopy | 2 | 2 | 0 | 3 |
KSSTA | 1 | 2 | 0 | 3 |
CORR | 0 | 2 | 0 | 2 |
JHS | 0 | 1 | 0 | 1 |
JOS | 1 | 1 | 0 | 2 |
AJO | 2 | 0 | 0 | 2 |
Other | 8 | 1 | 4 | 12 |
Abbreviations: AJO, The American Journal of Orthopedics; AJSM, American Journal of Sports Medicine; Arthroscopy, The Journal of Arthroscopy and Related Surgery; CORR, Clinical Orthopaedics & Related Research; JHS, Journal of Hand Surgery; JOS, Journal of Orthopaedic Surgery; JSES, Journal of Shoulder and Elbow Surgery; KSSTA, Knee Surgery, Sports Traumatology, and Arthroscopy.
SUBJECT DEMOGRAPHICS
The 35 included studies comprised 1579 patients and 1640 elbows. Among these, 1055 (64%) elbows underwent open (O), 401 (25%) underwent arthroscopic (A), and 184 (11%) underwent percutaneous (P) treatment. The average age was 45.7 years, 47% of the patients were male, 43% were laborers, 31% had worker’s compensation claims, and the dominant extremity was involved in 62% of patients. The percutaneous cohort was older than the open cohort (P = 46.9, O = 45.4, A = 45.8; P = .036). The duration of symptoms was shorter in the percutaneous cohort than in the other 2 groups and shorter in the arthroscopic cohort than in the open cohort (P = 8 months, O = 23 months, A = 18 months; P < .001). There were no significant differences between groups regarding gender, occupation, worker’s compensation status, or involvement of the dominant extremity (Table 3).
Table 3. Subject Demographics for Open, Arthroscopic, and Percutaneous Groups
| Open | Arthroscopic | Percutaneous |
Subjects (N) | 999 | 397 | 183 |
Elbows (N) | 1055 | 401 | 184 |
Elbows with follow-up (%) | 915 (87%) | 350 (87%) | 181 (98%) |
Males (%) | 427 (47%) | 173 (49%) | 78 (43%) |
Females (%) | 488 (53%) | 177 (51%) | 103 (57%) |
Mean age (years) | 45.4 | 45.8 | 46.9 |
Dominant elbow (%) | 70% | 69% | 53% |
Laborer (%) | 56% | 53% | 48% |
Work comp (%) | 36% | 30% | NR |
Symptoms to operation (months) | 23 | 18 | 8 |
Min. symptoms to operation (months) | 6 | 6 | 3 |
Mean follow-up (months) | 60 | 44 | 11 |
MATA-ANALYSIS CLINICAL OUTCOMES
Clinical outcome results were pooled for all studies reporting the same outcome measure for the same technique (open, arthroscopic, or percutaneous). A meta-analysis was performed for all outcome measures that were reported in a minimum of 3 studies utilizing the same surgical technique (Table 4).
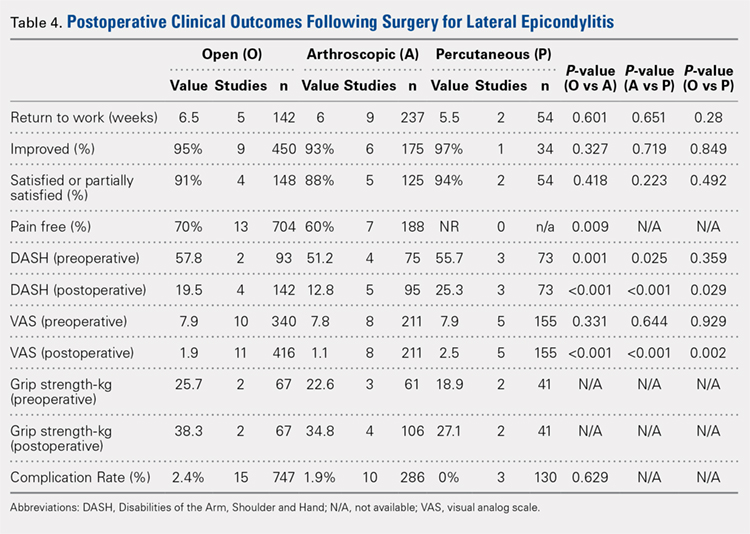
PAIN RELIEF
Thirteen open studies,3,5,7,8,11-16,18,19,21 7 arthroscopic studies14,22-24,26,27,31 and 0 percutaneous studies reported the proportion of patients who were pain free at final follow-up. The proportion of patients who were pain free following open débridement was greater than that in the arthroscopic cohort (O = 70%, A = 60%; P = .009) (Table 4).
Continue to: Subjective improvement and satisfaction...
SUBJECTIVE IMPROVEMENT AND SATISFACTION
Nine open studies, 6 arthroscopic studies, and 1 percutaneous study reported the proportion of patients who felt that their condition had been improved as a result of surgery. There was no difference in the proportion of patients who experienced improvement between the open and arthroscopic cohorts. Four open studies,3,11,12 5 arthroscopic studies,22,26,28,29,32 and 2 percutaneous studies29,36 reported the proportion of patients who were satisfied or partially satisfied with the results of the procedure. There was no difference between the open and arthroscopic groups in the proportion of patients who were satisfied or partially satisfied (Table 4).
RETURN TO WORK
The duration to return to work following surgery was reported in 5 open studies,4,5,10,13,14 9 arthroscopic studies,14,23-29,32 and 2 percutaneous studies.29,36 There was no statistically significant difference between the open and arthroscopic groups with regard to duration to return to work (O = 6.5 weeks, A = 6 weeks; P = .601). The percutaneous technique could not be included in the meta-analysis due to the presence of only 2 studies, but the pooled mean duration to return to work in these 2 studies was 5.5 weeks (Table 4).
GRIP STRENGTH
Postoperative grip strength was reported in 2 open studies,10,19 4 arthroscopic studies,28,30,32 and 2 percutaneous studies.35-36 A meta-analysis could not be performed on all the groups due to the presence of only 2 open and 2 percutaneous studies reporting grip strength. The pooled averages were O = 38.3 kg, A = 34.8 kg, and P = 27.1 kg (Table 4).
DASH SCORE
The postoperative DASH score was reported in 4 open studies,4,15,17,19,20 5 arthroscopic studies,28-31 and 3 percutaneous studies.29,33,36 At final follow-up, the mean DASH score was higher in the arthroscopic group than in the open and percutaneous groups (A = 12.8, O = 19.5, P = 25.3; P < .001 for both comparisons), and the mean DASH score was significantly higher in the open group than in the percutaneous group (P = .029). The reporting of DASH scores in the early postoperative period was not sufficiently consistent to allow us to test our hypothesis that there would be early differences in function between groups (Table 4).
VAS PAIN SCORE
Postoperative VAS pain scores were reported in 11 open studies,6,8-10,12,15,19-21 8 arthroscopic studies,24-26,29-32 and 5 percutaneous studies.29,33,35-37 At final follow-up, there was a lower mean VAS score in the arthroscopic group than in the open and percutaneous groups (A = 1.1, O = 1.9, and P = 2.5; P < .001 for both comparisons) and a lower mean VAS score in the open group than in the percutaneous group (P = .002) (Table 4). Reporting of VAS scores in the early postoperative period in the included studies wan not sufficiently consistent to allow us to test our hypothesis that there would be early differences in pain between groups.
COMPLICATIONS
The complication rate was reported in 15 open studies, 10 arthroscopic studies, and 3 percutaneous studies. There was no difference in the complication rate between the open and arthroscopic techniques (O = 2.4%, A = 1.9%; P = .629) (Table 4). Complications noted in the open cohort included superficial wound infection (6), hematoma (5), synovial fistula (2), seroma (2), and posterior interosseous nerve palsy (1). Complications noted in the arthroscopic cohort included superficial infection (3), hematoma (1), and transient paresthesia (1). Of note, there were no complications in the percutaneous group.
Continue to: Discussion...
DISCUSSION
The primary purpose of this review was to determine if definitive evidence suggests that any 1 of open, percutaneous, or arthroscopic surgical treatment is superior to the other 2 for relieving pain, improving functionality, restoring strength, or accelerating return to work. The most striking finding of this study was a significantly higher proportion of patients who were pain free at final follow-up in the open group than in the arthroscopic group (70% vs 60%, P = .009) (Table 4). At final follow-up, there were no significant differences between groups regarding duration to return to work, proportion who were improved, proportion who were satisfied or partially satisfied, and complication rate. Average VAS and DASH scores at final follow-up were lower in the arthroscopic group than in the open and percutaneous groups (Figure 2). However, although the difference between mean DASH scores in the arthroscopic and open groups (6.7 points) was statistically significant, it is likely not clinically significant, as the minimal clinically important difference (MCID) for the DASH score is 10 points, as demonstrated by Sorensen and colleagues.38 Although it has not been specifically defined for lateral epicondylitis, the MCID for VAS pain has been reported in the literature to range from 1.0 to 1.4.39-40 Therefore, as for the DASH score, the difference witnessed between the open and arthroscopic groups (0.8) is likely not clinically significant. Of note, the differences between values for arthroscopic and percutaneous techniques are greater than the MCID.
In light of a recent increase in the prevalence of surgical intervention for lateral epicondylitis, many authors have promoted arthroscopic and percutaneous techniques as alternatives to traditional open débridement with the goal of achieving the same results with decreased morbidity and accelerated return to work. Given the increased proportion of patients who were pain free at final follow-up in the open cohort, it is our contention that open release/débridement of the common extensor/ECRB origin allows the surgeon to fully appreciate the extent of tendinotic tissue that is contributing to the patient’s symptoms and to address the pathology in its entirety. Other authors have also questioned whether the full extent of extra-articular tendinosis can be accurately identified arthroscopically. Cummins41 demonstrated, in a series of 18 patients who underwent arthroscopic ECRB débridement, that 6 patients had residual tendinosis upon open evaluation and 10 had residual tendinosis on histologic assessment. Additionally, in the same series, residual tendinopathy was associated with poorer clinical outcomes.
The improved visualization associated with an open technique comes at minimal expense, as the incision was only 1.5 cm to 5 cm in 13 of 15 papers reporting incision length.3,4,6,8-11,13,15,18-20 This increased exposure may not translate into increased morbidity, as there was no increase in the duration to return to work nor the complication rate. As a result of the extensive instrumentation necessary for arthroscopic techniques, open techniques also appear to be less expensive. Analyses in the literature have suggested increased expenditures associated with arthroscopic treatment ranging from 23%42 to 100%43 greater than those of open treatment.
Although obvious, it should be noted that a percutaneous tenotomy does not permit assessment of the extent of pathologic tendinosis. As a result of an inability to visualize and débride pathologic tissue, percutaneous tenotomy rendered inferior outcomes to open and arthroscopic techniques in terms of both postoperative VAS pain score and DASH score. Nonetheless, it is a relatively rapid and simple technique and resulted in zero complications in 184 elbows. Overall, percutaneous tenotomy appears to be an inferior technique to open and arthroscopic techniques in terms of achieving complete pain relief and optimal functional recovery; however, it may be useful in those who wish to avoid a more invasive intervention.
LIMITATIONS
The most significant limitation of this study was the heterogeneity in the techniques utilized in each group. Among the 19 papers in the open cohort, 11 used techniques aimed at lengthening or release of the extensor origin, 7 performed débridement of tendinotic tissue at the ECRB origin, and 1 compared these approaches. Exposures ranged from 1.5 cm to 8 cm in length, 3 techniques added tendon repair following débridement, and 2 utilized a radiofrequency device.
Among the 12 papers in the arthroscopic cohort, 8 performed arthroscopic (inside-out) débridement of the tendinotic tissue at the ECRB origin, 3 performed arthroscopic release of the ECRB tendon, and 1 performed endoscopic ECRB release in an outside-in fashion. Four techniques added posterior synovial plica excision and 4 added decortication of the lateral epicondyle débridement or release. Some authors advocate for arthroscopic intervention on the grounds that it permits evaluation and correction of other intra-articular pathology. With this in mind, some authors have suggested that a synovial fold (plica) adjacent to the radiocapitellar joint may contribute to lateral elbow pain.27,44 Nevertheless, in the only comparative trial in the literature, Rhyou and Kim30 demonstrated that excision of posterior synovial fold failed to enhance pain relief or function in a retrospective cohort study comparing arthroscopic débridement with and without plica excision.
Continue to: Some authors advocate...
Some authors advocate decorticating the non-articular, lateral epicondyle with a shaver to stimulate bleeding and promote a healing response. However, 1 study in our review compared arthroscopic ECRB release with and without decortication and found that decortication significantly increased pain up to 4 weeks postoperatively, increased duration to return to work, and did not improve the ultimate clinical result.25 Of note, others have used a similar rationale to advocate drilling the lateral epicondyle when utilizing an open technique. However, Dunn and colleagues8 note that they have modified the Nirschl technique to eliminate drilling because they feel it increases postoperative pain and may damage the extensor digitorum communis origin.
Among the 6 papers in the percutaneous tenotomy cohort, 2 performed tenotomy with a hypodermic needle, 2 with a scalpel through a limited incision (0.5 cm-1 cm), 1 using a TX1 tissue removal system (Tenex Health), and 1 with a percutaneous radiofrequency probe. In 3 techniques, ultrasound was used to direct the tenotomy.
The quality of this review is also limited by the studies included for analysis, as with any systematic review. Because 28 of the 35 included studies were classified as evidence level IV, the likelihood of methodological bias is increased. The majority of studies contained ≥1 demonstrable biases, including selection, detection, attrition biases, or a combination. Selection bias is prevalent among predominantly level IV studies, in which the authors have selected their preferred surgical technique. There was heterogeneity in the reporting of preoperative variables and the outcome measures that were utilized. Scoring systems, such as the Nirschl Tennis Elbow Score and the Mayo Elbow Performance Index, would have been valuable in comparing the groups had they been more consistently reported. The heterogeneity in clinical outcome tools and the lack of reported outcome variance or standard deviations prevented a formal meta-analysis of some of these outcome measures. Due to inconsistent reporting, we were also unable to test our hypothesis that there would be less pain and improved function in the arthroscopic and/or percutaneous cohorts in the early postoperative period compared to the open cohort due to the less invasive techniques used. Although the differences in DASH and VAS scores at final follow-up likely did not meet the MCID threshold, these differences may have been greater and more clinically relevant in the early postoperative period.
CONCLUSION
We hypothesized that the arthroscopic and percutaneous groups would experience accelerated return to work and reduced pain in the early postoperative period but no difference in ultimate pain, functional outcome, or subjective satisfaction. There is no difference between open, arthroscopic, and percutaneous surgical treatment for lateral epicondylitis regarding return to work and subjective satisfaction; however, open treatment led to a greater percentage of patients being pain free at final follow-up. While arthroscopic treatment led to better pain and functional scores at final follow-up, the absolute differences were quite small and likely not clinically significant. In light of the available evidence, we recommend open débridement as the best means of minimizing cost and achieving a pain-free outcome in the long term. For future investigators, it would be useful to perform a randomized clinical study directly comparing open, arthroscopic, and percutaneous techniques, including assessment of pain and functional scores in the early postoperative period, and to further evaluate differences in cost among the various techniques.
This paper will be judged for the Resident Writer’s Award.
ABSTRACT
This study was performed to compare outcomes of open, arthroscopic, and percutaneous surgical techniques for lateral epicondylitis. We searched PubMed (MEDLINE) for literature published between January 1, 2004 and May 23, 2015 using these key words: lateral epicondylitis AND (surgery OR operative OR surgical OR open OR arthroscopic OR percutaneous). Meta-analyses were performed for outcomes reported in 3 studies using 2-sample and 2-proportion Z-tests. Thirty-five studies including 1640 elbows (1055 open, 401 arthroscopic, 184 percutaneous) met the inclusion criteria. There were no differences between groups regarding duration to return to work, complication rate, or patient satisfaction. A greater proportion of patients were pain free in the open group than in the arthroscopic group (70% vs 60%). Despite the absence of a difference among techniques regarding return to work and subjective function, we recommend open débridement as the technique most likely to achieve a pain-free outcome.
Continue to: Lateral epicondylitis affects...
Lateral epicondylitis affects 1% to 3% of adults each year. Although common, symptoms of lateral epicondylitis resolve spontaneously within a year of symptom onset in 80% of cases, and only 3% of patients who seek medical treatment ultimately require surgical intervention within 2 years of symptom onset.1 Despite a relatively low percentage of patients who require surgery, Sanders and colleagues1 noted a significant increase in the rate of surgical intervention from 1.1% to 3.2% of cases in the last 15 years. Surgical intervention is generally indicated when pain and functional disability persist after 6 to 12 months of nonsurgical treatment. Traditional surgical treatment involves open release/débridement of the extensor carpi radialis (ECRB) origin; however, with the increasing prevalence of surgical intervention, surgeons have demonstrated a rising interest in less invasive techniques like arthroscopic release/débridement and percutaneous tenotomy as alternatives to traditional open débridement. While favorable results have been reported for all 3 techniques, there is no current consensus regarding the optimal surgical technique. In 2007, Lo and Safran2 reported no difference in the results of open, percutaneous, and arthroscopic techniques regarding any outcome measure in a systematic review of 33 papers. We conducted a repeat systematic review of the current literature to update Lo and Safran’s2 review and to ascertain if more recent literature demonstrates superiority of 1 technique regarding pain relief, subjective questionnaire data, subjective satisfaction, restoration of strength, and return to work. We hypothesized that return to work would be accelerated, pain decreased, and function improved in the early postoperative period in the arthroscopic and percutaneous groups, but there would be no difference in ultimate pain, functional outcome, or subjective satisfaction.
METHODS
SEARCH STRATEGY AND STUDY SELECTION
We conducted a systematic review of the literature to update the topic of surgical intervention with lateral epicondylitis since the publication of the most recent review by Lo and Safran2 in 2007, which included all relevant studies published up to 2004. To include all relevant studies published since that time, we searched PubMed (MEDLINE) for all literature published from January 1, 2004 to May 23, 2015 using the following key words: lateral epicondylitis AND (surgery OR operative OR surgical OR open OR arthroscopic OR percutaneous). General search terms were utilized to avoid unintentional exclusion of relevant studies. Two authors reviewed the abstracts of all resultant citations. Table 1 outlines the inclusion and exclusion criteria for the search. References from all included studies were reviewed for applicable articles that were not captured by the initial broad search strategy. A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) trial flow chart shows the study selection algorithm (Figure 1).
Table 1. Inclusion and Exclusion Criteria for the Analyzed Studies
Inclusion Criteria | Exclusion Criteria |
|
|
DATA EXTRACTION AND ANALYSIS
Data were extracted from the included studies by 2 reviewers using data abstraction forms. All study, subject, and surgery parameters were collected. The study and subject demographic parameters analyzed included year of publication, level of evidence, presence of study financial conflict of interest, number of subjects and elbows, gender, age, proportion in whom the dominant extremity was involved, proportion who were laborers, proportion who had a workman’s compensation claim, duration of symptoms prior to surgical intervention, and surgical technique employed (open, arthroscopic, or percutaneous). We recorded the following clinical outcomes: proportion of patients with complete pain relief, proportion who were partially or completely satisfied, proportion who were improved, duration to return to work, grip strength, Disabilities of the Arm, Shoulder, and Hand (DASH) score, visual analog scale (VAS) pain score, and complication rate.
Continue to: Statistical analysis...
STATISTICAL ANALYSIS
Data from all studies were pooled and descriptive statistics were reported as weighted mean ± weighted standard deviation for continuous variables and frequency with percentage for categorical variables. A meta-analysis was performed for all outcome measures that were reported in 3 or more studies within a specific treatment cohort. Data were analyzed using 2-sample and 2-proportion Z-tests. Results were considered statistically significant at P < .05.
RESULTS
LITERATURE RESEARCH
Using the aforementioned search strategy, 154 studies were identified. Following application of the inclusion and exclusion criteria, 35 studies were included in the analysis (Figure 1). One study compared open and percutaneous techniques, and another compared arthroscopic and percutaneous techniques, rendering a total of 19 studies examining open surgical techniques for treatment of lateral epicondylitis,3-21 12 studies examining arthroscopic techniques,14,22-32 and 6 studies reporting percutaneous surgical treatment of lateral epicondylitis29,33-37 (Table 2). There was1 level I study (3%), 6 level III studies (17%), and 28 level IV studies (80%).
Table 2. Study Demographic Data for Open, Arthroscopic, and Percutaneous Lateral Epicondylectomy
| Open | Arthroscopic | Percutaneous | Total |
Number of studies | 19 | 12 | 6 | 35 |
Level of evidence |
|
|
|
|
I | 1 (5%) | 0 | 0 | 1 (3%) |
II | 0 | 0 | 0 | 0 |
III | 3 (16%) | 4 (33%) | 1 (17%) | 6 (17%) |
IV | 15 (79%) | 8 (67%) | 5 (83%) | 28 (80%) |
US: International | 8:12 | 3:9 | 1:5 | 12:24 |
Journals of publication |
|
|
|
|
AJSM | 3 | 1 | 1 | 5 |
JSES | 2 | 2 | 1 | 5 |
Arthroscopy | 2 | 2 | 0 | 3 |
KSSTA | 1 | 2 | 0 | 3 |
CORR | 0 | 2 | 0 | 2 |
JHS | 0 | 1 | 0 | 1 |
JOS | 1 | 1 | 0 | 2 |
AJO | 2 | 0 | 0 | 2 |
Other | 8 | 1 | 4 | 12 |
Abbreviations: AJO, The American Journal of Orthopedics; AJSM, American Journal of Sports Medicine; Arthroscopy, The Journal of Arthroscopy and Related Surgery; CORR, Clinical Orthopaedics & Related Research; JHS, Journal of Hand Surgery; JOS, Journal of Orthopaedic Surgery; JSES, Journal of Shoulder and Elbow Surgery; KSSTA, Knee Surgery, Sports Traumatology, and Arthroscopy.
SUBJECT DEMOGRAPHICS
The 35 included studies comprised 1579 patients and 1640 elbows. Among these, 1055 (64%) elbows underwent open (O), 401 (25%) underwent arthroscopic (A), and 184 (11%) underwent percutaneous (P) treatment. The average age was 45.7 years, 47% of the patients were male, 43% were laborers, 31% had worker’s compensation claims, and the dominant extremity was involved in 62% of patients. The percutaneous cohort was older than the open cohort (P = 46.9, O = 45.4, A = 45.8; P = .036). The duration of symptoms was shorter in the percutaneous cohort than in the other 2 groups and shorter in the arthroscopic cohort than in the open cohort (P = 8 months, O = 23 months, A = 18 months; P < .001). There were no significant differences between groups regarding gender, occupation, worker’s compensation status, or involvement of the dominant extremity (Table 3).
Table 3. Subject Demographics for Open, Arthroscopic, and Percutaneous Groups
| Open | Arthroscopic | Percutaneous |
Subjects (N) | 999 | 397 | 183 |
Elbows (N) | 1055 | 401 | 184 |
Elbows with follow-up (%) | 915 (87%) | 350 (87%) | 181 (98%) |
Males (%) | 427 (47%) | 173 (49%) | 78 (43%) |
Females (%) | 488 (53%) | 177 (51%) | 103 (57%) |
Mean age (years) | 45.4 | 45.8 | 46.9 |
Dominant elbow (%) | 70% | 69% | 53% |
Laborer (%) | 56% | 53% | 48% |
Work comp (%) | 36% | 30% | NR |
Symptoms to operation (months) | 23 | 18 | 8 |
Min. symptoms to operation (months) | 6 | 6 | 3 |
Mean follow-up (months) | 60 | 44 | 11 |
MATA-ANALYSIS CLINICAL OUTCOMES
Clinical outcome results were pooled for all studies reporting the same outcome measure for the same technique (open, arthroscopic, or percutaneous). A meta-analysis was performed for all outcome measures that were reported in a minimum of 3 studies utilizing the same surgical technique (Table 4).
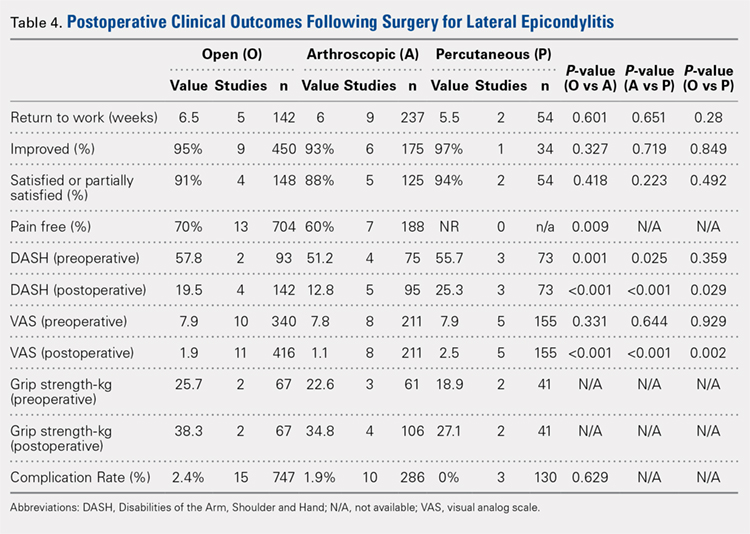
PAIN RELIEF
Thirteen open studies,3,5,7,8,11-16,18,19,21 7 arthroscopic studies14,22-24,26,27,31 and 0 percutaneous studies reported the proportion of patients who were pain free at final follow-up. The proportion of patients who were pain free following open débridement was greater than that in the arthroscopic cohort (O = 70%, A = 60%; P = .009) (Table 4).
Continue to: Subjective improvement and satisfaction...
SUBJECTIVE IMPROVEMENT AND SATISFACTION
Nine open studies, 6 arthroscopic studies, and 1 percutaneous study reported the proportion of patients who felt that their condition had been improved as a result of surgery. There was no difference in the proportion of patients who experienced improvement between the open and arthroscopic cohorts. Four open studies,3,11,12 5 arthroscopic studies,22,26,28,29,32 and 2 percutaneous studies29,36 reported the proportion of patients who were satisfied or partially satisfied with the results of the procedure. There was no difference between the open and arthroscopic groups in the proportion of patients who were satisfied or partially satisfied (Table 4).
RETURN TO WORK
The duration to return to work following surgery was reported in 5 open studies,4,5,10,13,14 9 arthroscopic studies,14,23-29,32 and 2 percutaneous studies.29,36 There was no statistically significant difference between the open and arthroscopic groups with regard to duration to return to work (O = 6.5 weeks, A = 6 weeks; P = .601). The percutaneous technique could not be included in the meta-analysis due to the presence of only 2 studies, but the pooled mean duration to return to work in these 2 studies was 5.5 weeks (Table 4).
GRIP STRENGTH
Postoperative grip strength was reported in 2 open studies,10,19 4 arthroscopic studies,28,30,32 and 2 percutaneous studies.35-36 A meta-analysis could not be performed on all the groups due to the presence of only 2 open and 2 percutaneous studies reporting grip strength. The pooled averages were O = 38.3 kg, A = 34.8 kg, and P = 27.1 kg (Table 4).
DASH SCORE
The postoperative DASH score was reported in 4 open studies,4,15,17,19,20 5 arthroscopic studies,28-31 and 3 percutaneous studies.29,33,36 At final follow-up, the mean DASH score was higher in the arthroscopic group than in the open and percutaneous groups (A = 12.8, O = 19.5, P = 25.3; P < .001 for both comparisons), and the mean DASH score was significantly higher in the open group than in the percutaneous group (P = .029). The reporting of DASH scores in the early postoperative period was not sufficiently consistent to allow us to test our hypothesis that there would be early differences in function between groups (Table 4).
VAS PAIN SCORE
Postoperative VAS pain scores were reported in 11 open studies,6,8-10,12,15,19-21 8 arthroscopic studies,24-26,29-32 and 5 percutaneous studies.29,33,35-37 At final follow-up, there was a lower mean VAS score in the arthroscopic group than in the open and percutaneous groups (A = 1.1, O = 1.9, and P = 2.5; P < .001 for both comparisons) and a lower mean VAS score in the open group than in the percutaneous group (P = .002) (Table 4). Reporting of VAS scores in the early postoperative period in the included studies wan not sufficiently consistent to allow us to test our hypothesis that there would be early differences in pain between groups.
COMPLICATIONS
The complication rate was reported in 15 open studies, 10 arthroscopic studies, and 3 percutaneous studies. There was no difference in the complication rate between the open and arthroscopic techniques (O = 2.4%, A = 1.9%; P = .629) (Table 4). Complications noted in the open cohort included superficial wound infection (6), hematoma (5), synovial fistula (2), seroma (2), and posterior interosseous nerve palsy (1). Complications noted in the arthroscopic cohort included superficial infection (3), hematoma (1), and transient paresthesia (1). Of note, there were no complications in the percutaneous group.
Continue to: Discussion...
DISCUSSION
The primary purpose of this review was to determine if definitive evidence suggests that any 1 of open, percutaneous, or arthroscopic surgical treatment is superior to the other 2 for relieving pain, improving functionality, restoring strength, or accelerating return to work. The most striking finding of this study was a significantly higher proportion of patients who were pain free at final follow-up in the open group than in the arthroscopic group (70% vs 60%, P = .009) (Table 4). At final follow-up, there were no significant differences between groups regarding duration to return to work, proportion who were improved, proportion who were satisfied or partially satisfied, and complication rate. Average VAS and DASH scores at final follow-up were lower in the arthroscopic group than in the open and percutaneous groups (Figure 2). However, although the difference between mean DASH scores in the arthroscopic and open groups (6.7 points) was statistically significant, it is likely not clinically significant, as the minimal clinically important difference (MCID) for the DASH score is 10 points, as demonstrated by Sorensen and colleagues.38 Although it has not been specifically defined for lateral epicondylitis, the MCID for VAS pain has been reported in the literature to range from 1.0 to 1.4.39-40 Therefore, as for the DASH score, the difference witnessed between the open and arthroscopic groups (0.8) is likely not clinically significant. Of note, the differences between values for arthroscopic and percutaneous techniques are greater than the MCID.
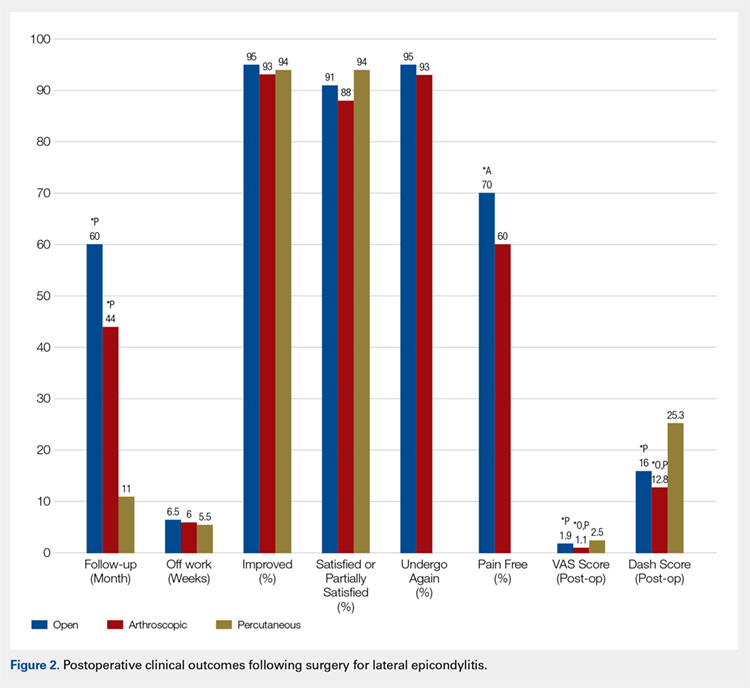
In light of a recent increase in the prevalence of surgical intervention for lateral epicondylitis, many authors have promoted arthroscopic and percutaneous techniques as alternatives to traditional open débridement with the goal of achieving the same results with decreased morbidity and accelerated return to work. Given the increased proportion of patients who were pain free at final follow-up in the open cohort, it is our contention that open release/débridement of the common extensor/ECRB origin allows the surgeon to fully appreciate the extent of tendinotic tissue that is contributing to the patient’s symptoms and to address the pathology in its entirety. Other authors have also questioned whether the full extent of extra-articular tendinosis can be accurately identified arthroscopically. Cummins41 demonstrated, in a series of 18 patients who underwent arthroscopic ECRB débridement, that 6 patients had residual tendinosis upon open evaluation and 10 had residual tendinosis on histologic assessment. Additionally, in the same series, residual tendinopathy was associated with poorer clinical outcomes.
The improved visualization associated with an open technique comes at minimal expense, as the incision was only 1.5 cm to 5 cm in 13 of 15 papers reporting incision length.3,4,6,8-11,13,15,18-20 This increased exposure may not translate into increased morbidity, as there was no increase in the duration to return to work nor the complication rate. As a result of the extensive instrumentation necessary for arthroscopic techniques, open techniques also appear to be less expensive. Analyses in the literature have suggested increased expenditures associated with arthroscopic treatment ranging from 23%42 to 100%43 greater than those of open treatment.
Although obvious, it should be noted that a percutaneous tenotomy does not permit assessment of the extent of pathologic tendinosis. As a result of an inability to visualize and débride pathologic tissue, percutaneous tenotomy rendered inferior outcomes to open and arthroscopic techniques in terms of both postoperative VAS pain score and DASH score. Nonetheless, it is a relatively rapid and simple technique and resulted in zero complications in 184 elbows. Overall, percutaneous tenotomy appears to be an inferior technique to open and arthroscopic techniques in terms of achieving complete pain relief and optimal functional recovery; however, it may be useful in those who wish to avoid a more invasive intervention.
LIMITATIONS
The most significant limitation of this study was the heterogeneity in the techniques utilized in each group. Among the 19 papers in the open cohort, 11 used techniques aimed at lengthening or release of the extensor origin, 7 performed débridement of tendinotic tissue at the ECRB origin, and 1 compared these approaches. Exposures ranged from 1.5 cm to 8 cm in length, 3 techniques added tendon repair following débridement, and 2 utilized a radiofrequency device.
Among the 12 papers in the arthroscopic cohort, 8 performed arthroscopic (inside-out) débridement of the tendinotic tissue at the ECRB origin, 3 performed arthroscopic release of the ECRB tendon, and 1 performed endoscopic ECRB release in an outside-in fashion. Four techniques added posterior synovial plica excision and 4 added decortication of the lateral epicondyle débridement or release. Some authors advocate for arthroscopic intervention on the grounds that it permits evaluation and correction of other intra-articular pathology. With this in mind, some authors have suggested that a synovial fold (plica) adjacent to the radiocapitellar joint may contribute to lateral elbow pain.27,44 Nevertheless, in the only comparative trial in the literature, Rhyou and Kim30 demonstrated that excision of posterior synovial fold failed to enhance pain relief or function in a retrospective cohort study comparing arthroscopic débridement with and without plica excision.
Continue to: Some authors advocate...
Some authors advocate decorticating the non-articular, lateral epicondyle with a shaver to stimulate bleeding and promote a healing response. However, 1 study in our review compared arthroscopic ECRB release with and without decortication and found that decortication significantly increased pain up to 4 weeks postoperatively, increased duration to return to work, and did not improve the ultimate clinical result.25 Of note, others have used a similar rationale to advocate drilling the lateral epicondyle when utilizing an open technique. However, Dunn and colleagues8 note that they have modified the Nirschl technique to eliminate drilling because they feel it increases postoperative pain and may damage the extensor digitorum communis origin.
Among the 6 papers in the percutaneous tenotomy cohort, 2 performed tenotomy with a hypodermic needle, 2 with a scalpel through a limited incision (0.5 cm-1 cm), 1 using a TX1 tissue removal system (Tenex Health), and 1 with a percutaneous radiofrequency probe. In 3 techniques, ultrasound was used to direct the tenotomy.
The quality of this review is also limited by the studies included for analysis, as with any systematic review. Because 28 of the 35 included studies were classified as evidence level IV, the likelihood of methodological bias is increased. The majority of studies contained ≥1 demonstrable biases, including selection, detection, attrition biases, or a combination. Selection bias is prevalent among predominantly level IV studies, in which the authors have selected their preferred surgical technique. There was heterogeneity in the reporting of preoperative variables and the outcome measures that were utilized. Scoring systems, such as the Nirschl Tennis Elbow Score and the Mayo Elbow Performance Index, would have been valuable in comparing the groups had they been more consistently reported. The heterogeneity in clinical outcome tools and the lack of reported outcome variance or standard deviations prevented a formal meta-analysis of some of these outcome measures. Due to inconsistent reporting, we were also unable to test our hypothesis that there would be less pain and improved function in the arthroscopic and/or percutaneous cohorts in the early postoperative period compared to the open cohort due to the less invasive techniques used. Although the differences in DASH and VAS scores at final follow-up likely did not meet the MCID threshold, these differences may have been greater and more clinically relevant in the early postoperative period.
CONCLUSION
We hypothesized that the arthroscopic and percutaneous groups would experience accelerated return to work and reduced pain in the early postoperative period but no difference in ultimate pain, functional outcome, or subjective satisfaction. There is no difference between open, arthroscopic, and percutaneous surgical treatment for lateral epicondylitis regarding return to work and subjective satisfaction; however, open treatment led to a greater percentage of patients being pain free at final follow-up. While arthroscopic treatment led to better pain and functional scores at final follow-up, the absolute differences were quite small and likely not clinically significant. In light of the available evidence, we recommend open débridement as the best means of minimizing cost and achieving a pain-free outcome in the long term. For future investigators, it would be useful to perform a randomized clinical study directly comparing open, arthroscopic, and percutaneous techniques, including assessment of pain and functional scores in the early postoperative period, and to further evaluate differences in cost among the various techniques.
This paper will be judged for the Resident Writer’s Award.
- Sanders TL Jr, Maradit Kremers H, Bryan AJ, Ransom JE, Smith J, Morrey BF. The epidemiology and health care burden of tennis elbow: a population-based study. Am J Sports Med. 2015;43(5):1066-1071. doi:10.1177/0363546514568087.
- Lo MY, Safran MR. Surgical treatment of lateral epicondylitis: a systematic review. Clin Orthop Relat Res. 2007;463:98-106. doi:10.1097/BLO.0b013e3181483dc4.
- Balk ML, Hagberg WC, Buterbaugh GA, Imbriglia JE. Outcome of surgery for lateral epicondylitis (tennis elbow): effect of worker’s compensation. Am J Orthop. 2005;34(3):122-126; discussion 126.
- Barth J, Mahieu P, Hollevoet N. Extensor tendon and fascia sectioning of extensors at the musculotendinous unit in lateral epicondylitis. Acta Orthop Belg. 2013;79(3):266-270.
- Bigorre N, Raimbeau G, Fouque PA, Cast YS, Rabarin F, Cesari B. Lateral epicondylitis treatment by extensor carpi radialis fasciotomy and radial nerve decompression: is outcome influenced by the occupational disease compensation aspect? Orthop Traumatol Surg Res. 2011;97(2):159-163. doi:10.1016/j.otsr.2010.11.007.
- Cho BK, Kim YM, Kim DS, et al. Mini-open muscle resection procedure under local anesthesia for lateral and medial epicondylitis. Clin Orthop Surg. 2009;1(3):123-127. doi:10.4055/cios.2009.1.3.123.
- Coleman B, Quinlan JF, Matheson JA. Surgical treatment for lateral epicondylitis: a long-term follow-up of results. J Shoulder Elbow Surg. 2010;19(3):363-367. doi:10.1016/j.jse.2009.09.008.
- Dunn JH, Kim JJ, Davis L, Nirschl RP. Ten- to 14-year follow-up of the Nirschl surgical technique for lateral epicondylitis. Am J Sports Med. 2008;36(2):261-266. doi:10.1177/0363546507308932.
- Manon-Matos Y, Oron A, Wolff TW. Combined common extensor and supinator aponeurotomy for the treatment of lateral epicondylitis. Tech Hand Up Extrem Surg. 2013;17(3):179-181. doi:10.1097/BTH.0b013e31829e0eeb.
- Meknas K, Odden-Miland A, Mercer JB, Castillejo M, Johansen O. Radiofrequency microtenotomy: a promising method for treatment of recalcitrant lateral epicondylitis. Am J Sports Med. 2008;36(10):1960-1965. doi:10.1177/0363546508318045.
- Pruzansky ME, Gantsoudes GD, Watters N. Late surgical results of reattachment to bone in repair of chronic lateral epicondylitis. Am J Orthop. 2009;38(6):295-299.
- Rayan F, Rao V Sr, Purushothamdas S, Mukundan C, Shafqat SO. Common extensor origin release in recalcitrant lateral epicondylitis – role justified? J Orthop Surg Res. 2010;5:31. doi:10.1186/1749-799X-5-31.
- Reddy VR, Satheesan KS, Bayliss N. Outcome of Boyd-McLeod procedure for recalcitrant lateral epicondylitis of elbow. Rheumatol Int. 2011;31(8):1081-1084. doi:10.1007/s00296-010-1450-1.
- Rubenthaler F, Wiese M, Senge A, Keller L, Wittenberg RH. Long-term follow-up of open and endoscopic Hohmann procedures for lateral epicondylitis. Arthroscopy. 2005;21(6):684-690. doi:10.1016/j.arthro.2005.03.017.
- Ruch DS, Orr SB, Richard MJ, Leversedge FJ, Mithani SK, Laino DK. A comparison of debridement with and without anconeus muscle flap for treatment of refractory lateral epicondylitis. J Shoulder Elbow Surg. 2015;24(2):236-241. doi:10.1016/j.jse.2014.09.035.
- Siddiqui MA, Koh J, Kua J, Cheung T, Chang P. Functional outcome assessment after open tennis elbow release: what are the predictor parameters? Singapore Med J. 2011;52(2):73-76.
- Solheim E, Hegna J, Øyen J. Extensor tendon release in tennis elbow: results and prognostic factors in 80 elbows. Knee Surg Sports Traumatol Arthrosc. 2011;19(6):1023-1027. doi:10.1007/s00167-011-1477-1.
- Svernlöv B, Adolfsson L. Outcome of release of the lateral extensor muscle origin for epicondylitis. Scand J Plast Reconstr Surg Hand Surg. 2006;40(3):161-165. doi:10.1080/02844310500491492.
- Tasto JP, Cummings J, Medlock V, Hardesty R, Amiel D. Microtenotomy using a radiofrequency probe to treat lateral epicondylitis. Arthroscopy. 2005;21(7):851-860. doi:10.1016/j.arthro.2005.03.019.
- Thornton SJ, Rogers JR, Prickett WD, Dunn WR, Allen AA, Hannafin JA. Treatment of recalcitrant lateral epicondylitis with suture anchor repair. Am J Sports Med. 2005;33(10):1558-1564. doi:10.1177/0363546505276758.
- Wang AW, Erak S. Fractional lengthening of forearm extensors for resistant lateral epicondylitis. ANZ J Surg. 2007;77(11):981-984. doi:10.1111/j.1445-2197.2007.04294.x.
- Baker CL Jr, Baker CL 3rd. Long-term follow-up of arthroscopic treatment of lateral epicondylitis. Am J Sports Med. 2008;36(2):254-260. doi:10.1177/0363546507311599.
- Grewal R, MacDermid JC, Shah P, King GJ. Functional outcome of arthroscopic extensor carpi radialis brevis tendon release in chronic lateral epicondylitis. J Hand Surg Am. 2009;34(5):849-857. doi:10.1016/j.jhsa.2009.02.006.
- Jerosch J, Schunck J. Arthroscopic treatment of lateral epicondylitis: indication, technique and early results. Knee Surg Sports Traumatol Arthrosc. 2006;14(4):379-382. doi:10.1007/s00167-005-0662-5.
- Kim JW, Chun CH, Shim DM, et al. Arthroscopic treatment of lateral epicondylitis: comparison of the outcome of ECRB release with and without decortication. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1178-1183. doi:10.1007/s00167-011-1507-z.
- Lattermann C, Romeo AA, Anbari A, et al. Arthroscopic debridement of the extensor carpi radialis brevis for recalcitrant lateral epicondylitis. J Shoulder Elbow Surg. 2010;19(5):651-656. doi:10.1016/j.jse.2010.02.008.
- Mullett H, Sprague M, Brown G, Hausman M. Arthroscopic treatment of lateral epicondylitis: clinical and cadaveric studies. Clin Orthop Relat Res. 2005;439:123-128. doi:10.1097/01.blo.0000176143.08886.fe.
- Oki G, Iba K, Sasaki K, Yamashita T, Wada T. Time to functional recovery after arthroscopic surgery for tennis elbow. J Shoulder Elbow Surg. 2014;23(10):1527-1531. doi:10.1016/j.jse.2014.05.010.
- Othman AM. Arthroscopic versus percutaneous release of common extensor origin for treatment of chronic tennis elbow. Arch Orthop Trauma Surg. 2011;131(3):383-388. doi:10.1007/s00402-011-1260-2.
- Rhyou IH, Kim KW. Is posterior synovial plica excision necessary for refractory lateral epicondylitis of the elbow? Clin Orthop Relat Res. 2013;471(1):284-290. doi:10.1007/s11999-012-2585-z.
- Wada T, Moriya T, Iba K, et al. Functional outcomes after arthroscopic treatment of lateral epicondylitis. J Orthop Sci. 2009;14(2):167-174. doi:10.1007/s00776-008-1304-9.
- Yoon JP, Chung SW, Yi JH, et al. Prognostic factors of arthroscopic extensor carpi radialis brevis release for lateral epicondylitis. Arthroscopy. 2015;31(7):1232-1237. doi:10.1016/j.arthro.2015.02.006.
- Barnes DE, Beckley JM, Smith J. Percutaneous ultrasonic tenotomy for chronic elbow tendinosis: a prospective study. J Shoulder Elbow Surg. 2015;24(1):67-73. doi:10.1016/j.jse.2014.07.017.
- Kaleli T, Ozturk C, Temiz A, Tirelioglu O. Surgical treatment of tennis elbow: percutaneous release of the common extensor origin. Acta Orthop Belg. 2004;70(2):131-133.
- Lin MT, Chou LW, Chen HS, Kao MJ. Percutaneous soft tissue release for treating chronic recurrent myofascial pain associated with lateral epicondylitis: 6 case studies. Evid Based Complement Alternat Med. 2012;2012:142941. doi:10.1155/2012/142941.
- Lin CL, Lee JS, Su WR, Kuo LC, Tai TW, Jou IM. Clinical and ultrasonographic results of ultrasonographically guided percutaneous radiofrequency lesioning in the treatment of recalcitrant lateral epicondylitis. Am J Sports Med. 2011;39(11):2429-2435. doi:10.1177/0363546511417096.
- Zhu J, Hu B, Xing C, Li J. Ultrasound-guided, minimally invasive, percutaneous needle puncture treatment for tennis elbow. Adv Ther. 2008;25(10):1031-1036. doi:10.1007/s12325-008-0099-6.
- Sorensen AA, Howard D, Tan WH, Ketchersid J, Calfee RP. Minimal clinically important differences of 3 patient-related outcomes instruments. J Hand Surg Am. 2013;38(4):641-649. doi:10.1016/j.jhsa.2012.12.032.
- Kelly AM. The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J. 2001;18(3):205-207. doi:10.1136/emj.18.3.205.
- Tashjian RZ, Deloach J, Porucznik CA, Powell AP. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg. 2009;18(6):927-932. doi:10.1016/j.jse.2009.03.021.
- Cummins CA. Lateral epicondylitis: in vivo assessment of arthroscopic debridement and correlation with patient outcomes. Am J Sports Med. 2006;34(9):1486-1491. doi:10.1177/0363546506288016.
- Stapleton TR, Baker CL. Arthroscopic treatment of lateral epicondylitis: a clinical study. Arthroscopy. 1996;1:365-366.
- Hastings H. Open treatment for lateral tennis elbow good for certain indications. Orthop Today. 2009;2:1-2.
- Duparc F, Putz R, Michot C, Muller JM, Fréger P. The synovial fold of the humeroradial joint: anatomical and histological features, and clinical relevance in lateral epicondylalgia of the elbow. Surg Radiol Anat. 2002;24(5):302-307. doi:10.1007/s00276-002-0055-0.
- Sanders TL Jr, Maradit Kremers H, Bryan AJ, Ransom JE, Smith J, Morrey BF. The epidemiology and health care burden of tennis elbow: a population-based study. Am J Sports Med. 2015;43(5):1066-1071. doi:10.1177/0363546514568087.
- Lo MY, Safran MR. Surgical treatment of lateral epicondylitis: a systematic review. Clin Orthop Relat Res. 2007;463:98-106. doi:10.1097/BLO.0b013e3181483dc4.
- Balk ML, Hagberg WC, Buterbaugh GA, Imbriglia JE. Outcome of surgery for lateral epicondylitis (tennis elbow): effect of worker’s compensation. Am J Orthop. 2005;34(3):122-126; discussion 126.
- Barth J, Mahieu P, Hollevoet N. Extensor tendon and fascia sectioning of extensors at the musculotendinous unit in lateral epicondylitis. Acta Orthop Belg. 2013;79(3):266-270.
- Bigorre N, Raimbeau G, Fouque PA, Cast YS, Rabarin F, Cesari B. Lateral epicondylitis treatment by extensor carpi radialis fasciotomy and radial nerve decompression: is outcome influenced by the occupational disease compensation aspect? Orthop Traumatol Surg Res. 2011;97(2):159-163. doi:10.1016/j.otsr.2010.11.007.
- Cho BK, Kim YM, Kim DS, et al. Mini-open muscle resection procedure under local anesthesia for lateral and medial epicondylitis. Clin Orthop Surg. 2009;1(3):123-127. doi:10.4055/cios.2009.1.3.123.
- Coleman B, Quinlan JF, Matheson JA. Surgical treatment for lateral epicondylitis: a long-term follow-up of results. J Shoulder Elbow Surg. 2010;19(3):363-367. doi:10.1016/j.jse.2009.09.008.
- Dunn JH, Kim JJ, Davis L, Nirschl RP. Ten- to 14-year follow-up of the Nirschl surgical technique for lateral epicondylitis. Am J Sports Med. 2008;36(2):261-266. doi:10.1177/0363546507308932.
- Manon-Matos Y, Oron A, Wolff TW. Combined common extensor and supinator aponeurotomy for the treatment of lateral epicondylitis. Tech Hand Up Extrem Surg. 2013;17(3):179-181. doi:10.1097/BTH.0b013e31829e0eeb.
- Meknas K, Odden-Miland A, Mercer JB, Castillejo M, Johansen O. Radiofrequency microtenotomy: a promising method for treatment of recalcitrant lateral epicondylitis. Am J Sports Med. 2008;36(10):1960-1965. doi:10.1177/0363546508318045.
- Pruzansky ME, Gantsoudes GD, Watters N. Late surgical results of reattachment to bone in repair of chronic lateral epicondylitis. Am J Orthop. 2009;38(6):295-299.
- Rayan F, Rao V Sr, Purushothamdas S, Mukundan C, Shafqat SO. Common extensor origin release in recalcitrant lateral epicondylitis – role justified? J Orthop Surg Res. 2010;5:31. doi:10.1186/1749-799X-5-31.
- Reddy VR, Satheesan KS, Bayliss N. Outcome of Boyd-McLeod procedure for recalcitrant lateral epicondylitis of elbow. Rheumatol Int. 2011;31(8):1081-1084. doi:10.1007/s00296-010-1450-1.
- Rubenthaler F, Wiese M, Senge A, Keller L, Wittenberg RH. Long-term follow-up of open and endoscopic Hohmann procedures for lateral epicondylitis. Arthroscopy. 2005;21(6):684-690. doi:10.1016/j.arthro.2005.03.017.
- Ruch DS, Orr SB, Richard MJ, Leversedge FJ, Mithani SK, Laino DK. A comparison of debridement with and without anconeus muscle flap for treatment of refractory lateral epicondylitis. J Shoulder Elbow Surg. 2015;24(2):236-241. doi:10.1016/j.jse.2014.09.035.
- Siddiqui MA, Koh J, Kua J, Cheung T, Chang P. Functional outcome assessment after open tennis elbow release: what are the predictor parameters? Singapore Med J. 2011;52(2):73-76.
- Solheim E, Hegna J, Øyen J. Extensor tendon release in tennis elbow: results and prognostic factors in 80 elbows. Knee Surg Sports Traumatol Arthrosc. 2011;19(6):1023-1027. doi:10.1007/s00167-011-1477-1.
- Svernlöv B, Adolfsson L. Outcome of release of the lateral extensor muscle origin for epicondylitis. Scand J Plast Reconstr Surg Hand Surg. 2006;40(3):161-165. doi:10.1080/02844310500491492.
- Tasto JP, Cummings J, Medlock V, Hardesty R, Amiel D. Microtenotomy using a radiofrequency probe to treat lateral epicondylitis. Arthroscopy. 2005;21(7):851-860. doi:10.1016/j.arthro.2005.03.019.
- Thornton SJ, Rogers JR, Prickett WD, Dunn WR, Allen AA, Hannafin JA. Treatment of recalcitrant lateral epicondylitis with suture anchor repair. Am J Sports Med. 2005;33(10):1558-1564. doi:10.1177/0363546505276758.
- Wang AW, Erak S. Fractional lengthening of forearm extensors for resistant lateral epicondylitis. ANZ J Surg. 2007;77(11):981-984. doi:10.1111/j.1445-2197.2007.04294.x.
- Baker CL Jr, Baker CL 3rd. Long-term follow-up of arthroscopic treatment of lateral epicondylitis. Am J Sports Med. 2008;36(2):254-260. doi:10.1177/0363546507311599.
- Grewal R, MacDermid JC, Shah P, King GJ. Functional outcome of arthroscopic extensor carpi radialis brevis tendon release in chronic lateral epicondylitis. J Hand Surg Am. 2009;34(5):849-857. doi:10.1016/j.jhsa.2009.02.006.
- Jerosch J, Schunck J. Arthroscopic treatment of lateral epicondylitis: indication, technique and early results. Knee Surg Sports Traumatol Arthrosc. 2006;14(4):379-382. doi:10.1007/s00167-005-0662-5.
- Kim JW, Chun CH, Shim DM, et al. Arthroscopic treatment of lateral epicondylitis: comparison of the outcome of ECRB release with and without decortication. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1178-1183. doi:10.1007/s00167-011-1507-z.
- Lattermann C, Romeo AA, Anbari A, et al. Arthroscopic debridement of the extensor carpi radialis brevis for recalcitrant lateral epicondylitis. J Shoulder Elbow Surg. 2010;19(5):651-656. doi:10.1016/j.jse.2010.02.008.
- Mullett H, Sprague M, Brown G, Hausman M. Arthroscopic treatment of lateral epicondylitis: clinical and cadaveric studies. Clin Orthop Relat Res. 2005;439:123-128. doi:10.1097/01.blo.0000176143.08886.fe.
- Oki G, Iba K, Sasaki K, Yamashita T, Wada T. Time to functional recovery after arthroscopic surgery for tennis elbow. J Shoulder Elbow Surg. 2014;23(10):1527-1531. doi:10.1016/j.jse.2014.05.010.
- Othman AM. Arthroscopic versus percutaneous release of common extensor origin for treatment of chronic tennis elbow. Arch Orthop Trauma Surg. 2011;131(3):383-388. doi:10.1007/s00402-011-1260-2.
- Rhyou IH, Kim KW. Is posterior synovial plica excision necessary for refractory lateral epicondylitis of the elbow? Clin Orthop Relat Res. 2013;471(1):284-290. doi:10.1007/s11999-012-2585-z.
- Wada T, Moriya T, Iba K, et al. Functional outcomes after arthroscopic treatment of lateral epicondylitis. J Orthop Sci. 2009;14(2):167-174. doi:10.1007/s00776-008-1304-9.
- Yoon JP, Chung SW, Yi JH, et al. Prognostic factors of arthroscopic extensor carpi radialis brevis release for lateral epicondylitis. Arthroscopy. 2015;31(7):1232-1237. doi:10.1016/j.arthro.2015.02.006.
- Barnes DE, Beckley JM, Smith J. Percutaneous ultrasonic tenotomy for chronic elbow tendinosis: a prospective study. J Shoulder Elbow Surg. 2015;24(1):67-73. doi:10.1016/j.jse.2014.07.017.
- Kaleli T, Ozturk C, Temiz A, Tirelioglu O. Surgical treatment of tennis elbow: percutaneous release of the common extensor origin. Acta Orthop Belg. 2004;70(2):131-133.
- Lin MT, Chou LW, Chen HS, Kao MJ. Percutaneous soft tissue release for treating chronic recurrent myofascial pain associated with lateral epicondylitis: 6 case studies. Evid Based Complement Alternat Med. 2012;2012:142941. doi:10.1155/2012/142941.
- Lin CL, Lee JS, Su WR, Kuo LC, Tai TW, Jou IM. Clinical and ultrasonographic results of ultrasonographically guided percutaneous radiofrequency lesioning in the treatment of recalcitrant lateral epicondylitis. Am J Sports Med. 2011;39(11):2429-2435. doi:10.1177/0363546511417096.
- Zhu J, Hu B, Xing C, Li J. Ultrasound-guided, minimally invasive, percutaneous needle puncture treatment for tennis elbow. Adv Ther. 2008;25(10):1031-1036. doi:10.1007/s12325-008-0099-6.
- Sorensen AA, Howard D, Tan WH, Ketchersid J, Calfee RP. Minimal clinically important differences of 3 patient-related outcomes instruments. J Hand Surg Am. 2013;38(4):641-649. doi:10.1016/j.jhsa.2012.12.032.
- Kelly AM. The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J. 2001;18(3):205-207. doi:10.1136/emj.18.3.205.
- Tashjian RZ, Deloach J, Porucznik CA, Powell AP. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg. 2009;18(6):927-932. doi:10.1016/j.jse.2009.03.021.
- Cummins CA. Lateral epicondylitis: in vivo assessment of arthroscopic debridement and correlation with patient outcomes. Am J Sports Med. 2006;34(9):1486-1491. doi:10.1177/0363546506288016.
- Stapleton TR, Baker CL. Arthroscopic treatment of lateral epicondylitis: a clinical study. Arthroscopy. 1996;1:365-366.
- Hastings H. Open treatment for lateral tennis elbow good for certain indications. Orthop Today. 2009;2:1-2.
- Duparc F, Putz R, Michot C, Muller JM, Fréger P. The synovial fold of the humeroradial joint: anatomical and histological features, and clinical relevance in lateral epicondylalgia of the elbow. Surg Radiol Anat. 2002;24(5):302-307. doi:10.1007/s00276-002-0055-0.
TAKE-HOME POINTS
- While favorable results have been reported for open, arthroscopic, and percutaneous surgical techniques, there is no current consensus regarding the optimal technique for lateral epicondylitis.
- There is no difference between open, arthroscopic, and percutaneous surgical treatment for lateral epicondylitis regarding return to work and subjective satisfaction.
- Open treatment led to a greater percentage of patients being pain free at final follow-up.
- While arthroscopic treatment led to better pain and functional scores at final follow-up, the absolute differences were quite small and likely not clinically significant.
- We recommend open débridement as the best means of minimizing cost and achieving a pain-free outcome in the long-term.
Youth with rhabdomyosarcoma see better survival with maintenance chemo
CHICAGO – , finds a phase 3 randomized controlled trial of the European Paediatric Soft Tissue Sarcoma Study Group (EpSSG).
Rhabdomyosarcoma is a rare but very aggressive tumor, lead study author Gianni Bisogno, MD, PhD, a professor at the University Hospital of Padova, Italy, and chair of the EpSSG, noted in a press briefing at the annual meeting of the American Society of Clinical Oncology, where the findings were reported. Among pediatric patients who achieve complete response to standard therapy, “we know that after 1 or 2 years, one-third of these children relapse, and most of them die,” he said.
The EpSSG trial, which took about 10 years to conduct, enrolled 371 patients aged 0-21 years with high-risk rhabdomyosarcoma who had had a complete response to standard intensive therapy. They were randomized evenly to stop treatment or to receive 6 months of maintenance treatment consisting of low-dose vinorelbine and cyclophosphamide.
Results reported in the meeting’s plenary session showed that giving maintenance chemotherapy improved the 5-year overall survival rate by an absolute 12.8%, which translated to a near halving of the risk of death. And the maintenance regimen used was generally well tolerated.
“At the end of this long, not-easy study, we concluded that maintenance chemotherapy is an effective and well tolerated treatment for children with high-risk rhabdomyosarcoma,” Dr. Bisogno said.
There are three possibilities for its efficacy, he speculated. “It may be the duration, the type of drugs used, or the metronomic approach. Maybe altogether, these three different actions have a benefit to increase survival.
“Our group has decided this is the new standard treatment for patients. At least in Europe, we give standard intensive therapy and then we continue with 6 more months of low-dose chemotherapy,” Dr. Bisogno concluded. “We think that this approach – a new way of using old drugs – can be of interest also for other pediatric tumors.”
The trial is noteworthy in that it shows “how to successfully conduct large and important trials in rare diseases,” said ASCO Expert Warren Chow, MD.
The standard therapy for rhabdomyosarcomas is somewhat different in the United States, typically a regimen containing vincristine, actinomycin D, cyclophosphamide, and (more recently) irinotecan, he noted. “We have not been traditionally using maintenance chemo for any of the pediatric sarcomas, so this is a paradigm shift. These results will need to be tested with U.S.-based protocols before becoming standard of care in the United States. Also, we will need to determine if these results are applicable to patients older than 21 years of age who are considered high risk based solely on their age.
“Even with these caveats, this is the first significant treatment advance in this rare cancer in more than 30 years,” concluded Dr. Chow, a medical oncologist and clinical professor at City of Hope, Duarte, Calif. “No doubt, this trial was a home run.”
Study details
Patients enrolled in the EpSSG trial had had a complete response to the standard intensive therapy used in Europe: high-dose chemotherapy (ifosfamide, vincristine, and actinomycin D, with or without doxorubicin), radiation therapy, and surgery.
The maintenance chemotherapy consisted of a combination of low-dose intravenous vinorelbine given weekly and oral cyclophosphamide given daily. The 6-month duration was somewhat arbitrary, according to Dr. Bisogno. “We had to start somewhere. So when we started, we decided to use 6 months because there was some evidence in the past for regimens that long. In our next European trial, we are going to test different kinds and durations of maintenance because this is very important.”
The maintenance regimen was well tolerated compared with the regimen given during standard intensive therapy, with, for example, lower rates of grade 3 and 4 anemia (8.9% vs. 48.9%), neutropenia (80.6% vs. 91.6%), and thrombocytopenia (0.6% vs. 26.0%), which translated to less need for transfusions, and a lower rate of grade 3 or 4 infection (29.4% vs. 56.4%), Dr. Bisogno reported. There were no cases of grade 3 or 4 cardiac, hepatobiliary/pancreatic, or renal toxicity.
Relative to peers who stopped treatment after standard intensive therapy, patients who received maintenance treatment tended to have better disease-free survival (77.6% vs. 69.8%; hazard ratio, 0.68; P = .0613) and had significantly better overall survival (86.5% vs. 73.7%; hazard ratio, 0.52; P = .0111).
Dr. Bisogno disclosed that he has a consulting or advisory role with Clinigen Group, and receives travel, accommodations, and/or expenses from Jazz Pharmaceuticals. The study received funding from Fondazione Città della Speranza, Italy.
SOURCE: Bisogno et al. ASCO 2018 Abstract LBA2.
CHICAGO – , finds a phase 3 randomized controlled trial of the European Paediatric Soft Tissue Sarcoma Study Group (EpSSG).
Rhabdomyosarcoma is a rare but very aggressive tumor, lead study author Gianni Bisogno, MD, PhD, a professor at the University Hospital of Padova, Italy, and chair of the EpSSG, noted in a press briefing at the annual meeting of the American Society of Clinical Oncology, where the findings were reported. Among pediatric patients who achieve complete response to standard therapy, “we know that after 1 or 2 years, one-third of these children relapse, and most of them die,” he said.
The EpSSG trial, which took about 10 years to conduct, enrolled 371 patients aged 0-21 years with high-risk rhabdomyosarcoma who had had a complete response to standard intensive therapy. They were randomized evenly to stop treatment or to receive 6 months of maintenance treatment consisting of low-dose vinorelbine and cyclophosphamide.
Results reported in the meeting’s plenary session showed that giving maintenance chemotherapy improved the 5-year overall survival rate by an absolute 12.8%, which translated to a near halving of the risk of death. And the maintenance regimen used was generally well tolerated.
“At the end of this long, not-easy study, we concluded that maintenance chemotherapy is an effective and well tolerated treatment for children with high-risk rhabdomyosarcoma,” Dr. Bisogno said.
There are three possibilities for its efficacy, he speculated. “It may be the duration, the type of drugs used, or the metronomic approach. Maybe altogether, these three different actions have a benefit to increase survival.
“Our group has decided this is the new standard treatment for patients. At least in Europe, we give standard intensive therapy and then we continue with 6 more months of low-dose chemotherapy,” Dr. Bisogno concluded. “We think that this approach – a new way of using old drugs – can be of interest also for other pediatric tumors.”
The trial is noteworthy in that it shows “how to successfully conduct large and important trials in rare diseases,” said ASCO Expert Warren Chow, MD.
The standard therapy for rhabdomyosarcomas is somewhat different in the United States, typically a regimen containing vincristine, actinomycin D, cyclophosphamide, and (more recently) irinotecan, he noted. “We have not been traditionally using maintenance chemo for any of the pediatric sarcomas, so this is a paradigm shift. These results will need to be tested with U.S.-based protocols before becoming standard of care in the United States. Also, we will need to determine if these results are applicable to patients older than 21 years of age who are considered high risk based solely on their age.
“Even with these caveats, this is the first significant treatment advance in this rare cancer in more than 30 years,” concluded Dr. Chow, a medical oncologist and clinical professor at City of Hope, Duarte, Calif. “No doubt, this trial was a home run.”
Study details
Patients enrolled in the EpSSG trial had had a complete response to the standard intensive therapy used in Europe: high-dose chemotherapy (ifosfamide, vincristine, and actinomycin D, with or without doxorubicin), radiation therapy, and surgery.
The maintenance chemotherapy consisted of a combination of low-dose intravenous vinorelbine given weekly and oral cyclophosphamide given daily. The 6-month duration was somewhat arbitrary, according to Dr. Bisogno. “We had to start somewhere. So when we started, we decided to use 6 months because there was some evidence in the past for regimens that long. In our next European trial, we are going to test different kinds and durations of maintenance because this is very important.”
The maintenance regimen was well tolerated compared with the regimen given during standard intensive therapy, with, for example, lower rates of grade 3 and 4 anemia (8.9% vs. 48.9%), neutropenia (80.6% vs. 91.6%), and thrombocytopenia (0.6% vs. 26.0%), which translated to less need for transfusions, and a lower rate of grade 3 or 4 infection (29.4% vs. 56.4%), Dr. Bisogno reported. There were no cases of grade 3 or 4 cardiac, hepatobiliary/pancreatic, or renal toxicity.
Relative to peers who stopped treatment after standard intensive therapy, patients who received maintenance treatment tended to have better disease-free survival (77.6% vs. 69.8%; hazard ratio, 0.68; P = .0613) and had significantly better overall survival (86.5% vs. 73.7%; hazard ratio, 0.52; P = .0111).
Dr. Bisogno disclosed that he has a consulting or advisory role with Clinigen Group, and receives travel, accommodations, and/or expenses from Jazz Pharmaceuticals. The study received funding from Fondazione Città della Speranza, Italy.
SOURCE: Bisogno et al. ASCO 2018 Abstract LBA2.
CHICAGO – , finds a phase 3 randomized controlled trial of the European Paediatric Soft Tissue Sarcoma Study Group (EpSSG).
Rhabdomyosarcoma is a rare but very aggressive tumor, lead study author Gianni Bisogno, MD, PhD, a professor at the University Hospital of Padova, Italy, and chair of the EpSSG, noted in a press briefing at the annual meeting of the American Society of Clinical Oncology, where the findings were reported. Among pediatric patients who achieve complete response to standard therapy, “we know that after 1 or 2 years, one-third of these children relapse, and most of them die,” he said.
The EpSSG trial, which took about 10 years to conduct, enrolled 371 patients aged 0-21 years with high-risk rhabdomyosarcoma who had had a complete response to standard intensive therapy. They were randomized evenly to stop treatment or to receive 6 months of maintenance treatment consisting of low-dose vinorelbine and cyclophosphamide.
Results reported in the meeting’s plenary session showed that giving maintenance chemotherapy improved the 5-year overall survival rate by an absolute 12.8%, which translated to a near halving of the risk of death. And the maintenance regimen used was generally well tolerated.
“At the end of this long, not-easy study, we concluded that maintenance chemotherapy is an effective and well tolerated treatment for children with high-risk rhabdomyosarcoma,” Dr. Bisogno said.
There are three possibilities for its efficacy, he speculated. “It may be the duration, the type of drugs used, or the metronomic approach. Maybe altogether, these three different actions have a benefit to increase survival.
“Our group has decided this is the new standard treatment for patients. At least in Europe, we give standard intensive therapy and then we continue with 6 more months of low-dose chemotherapy,” Dr. Bisogno concluded. “We think that this approach – a new way of using old drugs – can be of interest also for other pediatric tumors.”
The trial is noteworthy in that it shows “how to successfully conduct large and important trials in rare diseases,” said ASCO Expert Warren Chow, MD.
The standard therapy for rhabdomyosarcomas is somewhat different in the United States, typically a regimen containing vincristine, actinomycin D, cyclophosphamide, and (more recently) irinotecan, he noted. “We have not been traditionally using maintenance chemo for any of the pediatric sarcomas, so this is a paradigm shift. These results will need to be tested with U.S.-based protocols before becoming standard of care in the United States. Also, we will need to determine if these results are applicable to patients older than 21 years of age who are considered high risk based solely on their age.
“Even with these caveats, this is the first significant treatment advance in this rare cancer in more than 30 years,” concluded Dr. Chow, a medical oncologist and clinical professor at City of Hope, Duarte, Calif. “No doubt, this trial was a home run.”
Study details
Patients enrolled in the EpSSG trial had had a complete response to the standard intensive therapy used in Europe: high-dose chemotherapy (ifosfamide, vincristine, and actinomycin D, with or without doxorubicin), radiation therapy, and surgery.
The maintenance chemotherapy consisted of a combination of low-dose intravenous vinorelbine given weekly and oral cyclophosphamide given daily. The 6-month duration was somewhat arbitrary, according to Dr. Bisogno. “We had to start somewhere. So when we started, we decided to use 6 months because there was some evidence in the past for regimens that long. In our next European trial, we are going to test different kinds and durations of maintenance because this is very important.”
The maintenance regimen was well tolerated compared with the regimen given during standard intensive therapy, with, for example, lower rates of grade 3 and 4 anemia (8.9% vs. 48.9%), neutropenia (80.6% vs. 91.6%), and thrombocytopenia (0.6% vs. 26.0%), which translated to less need for transfusions, and a lower rate of grade 3 or 4 infection (29.4% vs. 56.4%), Dr. Bisogno reported. There were no cases of grade 3 or 4 cardiac, hepatobiliary/pancreatic, or renal toxicity.
Relative to peers who stopped treatment after standard intensive therapy, patients who received maintenance treatment tended to have better disease-free survival (77.6% vs. 69.8%; hazard ratio, 0.68; P = .0613) and had significantly better overall survival (86.5% vs. 73.7%; hazard ratio, 0.52; P = .0111).
Dr. Bisogno disclosed that he has a consulting or advisory role with Clinigen Group, and receives travel, accommodations, and/or expenses from Jazz Pharmaceuticals. The study received funding from Fondazione Città della Speranza, Italy.
SOURCE: Bisogno et al. ASCO 2018 Abstract LBA2.
REPORTING FROM ASCO 2018
Key clinical point: Six months of maintenance chemotherapy improves survival in youth with high-risk rhabdomyosarcoma.
Major finding: Compared with counterparts not receiving any additional treatment, patients given maintenance low-dose vinorelbine and cyclophosphamide had better 5-year overall survival (86.5% vs. 73.7%; hazard ratio, 0.52).
Study details: A phase 3 randomized controlled trial among 371 patients aged 0-21 years with high-risk rhabdomyosarcoma who had had a complete response to standard intensive therapy.
Disclosures: Dr. Bisogno disclosed that he has a consulting or advisory role with Clinigen Group, and receives travel, accommodations, and/or expenses from Jazz Pharmaceuticals. The study received funding from Fondazione Città della Speranza, Italy.
Source: Bisogno et al. ASCO 2018, Abstract LBA2.
CMS sepsis measure a challenge to report
Hospitalists can champion sepsis-improvement efforts
In October 2015, the Centers for Medicare & Medicaid Services implemented its first meaningful policy to attempt for addressing sepsis.
The condition – one of the leading causes of mortality among hospitalized patients – afflicts more than a million people each year in the United States, and between 15% and 30% of them die. Sepsis is one of the leading drivers of hospital readmissions, sending more patients back to the hospital than heart failure, pneumonia, and chronic obstructive pulmonary disease.1
However, while providers seem to agree that time to address sepsis is past due, not everyone has embraced the Sepsis CMS Core Measure program, or SEP-1, as the means to best achieve it. This is, in part, because of discrepancies in how sepsis is defined, the burden of reporting, and what some consider to be arbitrary clinical requirements that may not correlate with better patient outcomes.
“Sepsis is indeed a critical public health problem, and it’s appropriate and valuable that Medicare and other policy makers are focusing on sepsis,” said Jeremy Kahn, MD, professor of critical care medicine and health policy and management at the University of Pittsburgh. “This was really the first approach at that … but at 85-pages long, it really is an enormous effort for hospitals to adhere to this measure.”
This is because of the tension between the “intense desire to improve sepsis outcomes” and the “incredible burden” of keeping up with the necessary documentation while also providing quality care, Dr. Kahn said.
In December 2017, Dr. Kahn helped lead a study published in the Journal of Hospital Medicine aimed at trying to understand hospital perceptions of SEP-1. Over the course of 29 interviews with randomly selected hospital quality leaders across the United States, including physicians and nurses, the results came as a surprise.2
“Generally, hospitals were very supportive of the concept, and there was no pushback on the idea that we should be measuring and reporting sepsis quality to CMS,” he said.
However, the research team found that respondents believed the program’s requirements with respect to treatment and documentation were complex and not always linked to patient-centered outcomes. Meeting the SEP-1 bundles consistently required hospitals to dedicate resources that not all may have, especially those in small, rural communities and those serving as urban safety nets.
Some, like emergency medicine physician Annahieta Kalantari, DO (who did not participate in the survey), feel that SEP-1 forces providers to practice “check-box” medicine and undermines successful efforts that don’t necessarily align with the CMS policy.
She arrived at her institution, Aria-Jefferson Health in Philadelphia, before CMS adopted SEP-1; at that time, she took note of the fact that the rate of sepsis mortalities in her hospital was, in her words, not great when compared with that at similar institutions. And then she helped do something about it.
“I thought, ‘We’re a Premier reporting hospital,’ so we did a gap analysis as to why and put together protocols for the hospital to follow with our sepsis patients, including a sepsis alert and a lot of education,” said Dr. Kalantari, associate program director for the emergency medicine residency program at Aria-Jefferson and a former chair of its sepsis management committee. “Before you knew it, mortalities were below benchmark.”
But once SEP-1 began, she said, the hospital was unable to check all of the boxes all of the time.
“We kept track, but we weren’t hitting all the bundles exactly within the periods of time recommended, but our mortalities were still amazing,” she said. “CMS basically picked definitions [for sepsis], and most of us don’t know what they’re basing them on because no one can agree on a definition anyway. Now they’re penalizing hospitals if they don’t hit the check marks in time, but we’d already demonstrated that our mortality and patient care was exceptional.”
She added: “I am extremely dissatisfied, as someone who provides frontline patient care, with how CMS is choosing to measure us.”
Dr. Kalantari wrote a piece in the Western Journal of Emergency Medicine in July 2017 in which she and coauthors outline the issues they take with SEP-1. They lay out the tension among the varied definitions of what sepsis is – and isn’t – and they also illuminate the apparent conflict between what CMS has officially defined and what evidence-based studies conducted since 2001 have suggested.3
In particular, CMS defines severe sepsis as an initial lactate above 2 mmol/L and septic shock as an initial lactate presentation of greater than 4 mmol/L. However, Dr. Kalantari and here coauthors argue in the paper that there is no standard definition of sepsis and that decades of attempts to achieve one have failed to reach consensus among providers. CMS, she said, fails to acknowledge this.
Defining sepsis
In fact, in 2016, another new definition of sepsis emerged by way of a 19-member task-force of experts: The Third International Consensus Definitions for Sepsis and Septic Shock, also called Sepsis-3.4 In March 2017, the Surviving Sepsis Campaign adopted this definition, which defined sepsis as a “life-threatening organ dysfunction caused by a dysregulated host response to infection.”5
“I think the definition has always been a challenging part of sepsis,” said Kencee Graves, MD, a hospitalist at the University of Utah, Salt Lake City. “The definitions came about for research purposes, so … they are not perfectly sensitive nor specific.”
However, Dr. Graves believes SEP-1 is a step in the right direction in that it brings awareness to sepsis and holds providers accountable. Several years ago, she and her colleague Devin Horton, MD, also a hospitalist at the University of Utah, embarked on a massive undertaking to address sepsis in their hospital. It was, at the time, lacking in “sepsis culture,” Dr. Horton said.
“One of the big things that motivated both of us was that we started doing chart review together and – it’s always easier with 20/20 hindsight – we were noticing that residents were missing the signs of sepsis,” Dr. Horton explained. “The clinical criteria would be there, but no one would say the word.” This is important, he said, because sepsis is time critical.
So the pair set out to create a cultural change by sharing data and collecting input from each service and unit, which relied heavily on nursing staff to perpetuate change. They created an early warning system in the medical record and worked with units to achieve flexibility in their criteria.
While the early warning system seemed helpful on the floor, SEP-1 adherence rates changed little in the emergency department. So Dr. Graves and Dr. Horton worked out an ED-specific process map that started at triage and was modeled after myocardial infarction STEMI protocols. From April through December 2016, the ED achieved between 29.5% adherence to the SEP-1 bundles, they said according to CMS abstractor data. After the change, between January and March 2017, the ED saw 52.2% adherence.
Dr. Kalantari would like to see CMS allow hospitals to evaluate and alter their processes more individually, with the required result being lower sepsis mortality. Hospitalists, said Dr. Kahn, are well poised to champion these sepsis improvement efforts.
“Hospitalists are uniquely positioned to lead in this area because they are a visible presence and a link between providers doing multidisciplinary acute care,” he said. “The other thing hospitalists can do is insist on rolling out approaches that are evidence based and not likely to cause harm by leading to over resuscitation, or ensuring patients are receiving central-line insertions only when needed.”
This is currently a moment for hospitals to innovate and provide meaningful feedback to CMS, which, he said, is listening.
“It’s a myth that CMS rolls out policy without listening to the clinical community, but what they want is constructive criticism, not just to hear ‘We’re not ready and we have to push this down the road,’ ” Dr. Kahn said. “The time is now in the era of accountability in health care.”
References
1. Sepsis. National Institute of General Medical Sciences. https://www.nigms.nih.gov/education/pages/factsheet_sepsis.aspx. Updated Sept 2017. Accessed Jan 4, 2018.
2. Barbash I et al. Hospital perceptions of Medicare’s sepsis quality reporting initiative. J Hosp Med. 2017;12;963-8.
3. Kalantari A et al. Sepsis Definitions: The search for gold and what CMS got wrong. West J Emerg Med. 2017 Aug;18(5):951-6.
4. Singer M et. al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016 Feb 23;315(8):801-10.
5. Rhodes A et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43:304.
Hospitalists can champion sepsis-improvement efforts
Hospitalists can champion sepsis-improvement efforts
In October 2015, the Centers for Medicare & Medicaid Services implemented its first meaningful policy to attempt for addressing sepsis.
The condition – one of the leading causes of mortality among hospitalized patients – afflicts more than a million people each year in the United States, and between 15% and 30% of them die. Sepsis is one of the leading drivers of hospital readmissions, sending more patients back to the hospital than heart failure, pneumonia, and chronic obstructive pulmonary disease.1
However, while providers seem to agree that time to address sepsis is past due, not everyone has embraced the Sepsis CMS Core Measure program, or SEP-1, as the means to best achieve it. This is, in part, because of discrepancies in how sepsis is defined, the burden of reporting, and what some consider to be arbitrary clinical requirements that may not correlate with better patient outcomes.
“Sepsis is indeed a critical public health problem, and it’s appropriate and valuable that Medicare and other policy makers are focusing on sepsis,” said Jeremy Kahn, MD, professor of critical care medicine and health policy and management at the University of Pittsburgh. “This was really the first approach at that … but at 85-pages long, it really is an enormous effort for hospitals to adhere to this measure.”
This is because of the tension between the “intense desire to improve sepsis outcomes” and the “incredible burden” of keeping up with the necessary documentation while also providing quality care, Dr. Kahn said.
In December 2017, Dr. Kahn helped lead a study published in the Journal of Hospital Medicine aimed at trying to understand hospital perceptions of SEP-1. Over the course of 29 interviews with randomly selected hospital quality leaders across the United States, including physicians and nurses, the results came as a surprise.2
“Generally, hospitals were very supportive of the concept, and there was no pushback on the idea that we should be measuring and reporting sepsis quality to CMS,” he said.
However, the research team found that respondents believed the program’s requirements with respect to treatment and documentation were complex and not always linked to patient-centered outcomes. Meeting the SEP-1 bundles consistently required hospitals to dedicate resources that not all may have, especially those in small, rural communities and those serving as urban safety nets.
Some, like emergency medicine physician Annahieta Kalantari, DO (who did not participate in the survey), feel that SEP-1 forces providers to practice “check-box” medicine and undermines successful efforts that don’t necessarily align with the CMS policy.
She arrived at her institution, Aria-Jefferson Health in Philadelphia, before CMS adopted SEP-1; at that time, she took note of the fact that the rate of sepsis mortalities in her hospital was, in her words, not great when compared with that at similar institutions. And then she helped do something about it.
“I thought, ‘We’re a Premier reporting hospital,’ so we did a gap analysis as to why and put together protocols for the hospital to follow with our sepsis patients, including a sepsis alert and a lot of education,” said Dr. Kalantari, associate program director for the emergency medicine residency program at Aria-Jefferson and a former chair of its sepsis management committee. “Before you knew it, mortalities were below benchmark.”
But once SEP-1 began, she said, the hospital was unable to check all of the boxes all of the time.
“We kept track, but we weren’t hitting all the bundles exactly within the periods of time recommended, but our mortalities were still amazing,” she said. “CMS basically picked definitions [for sepsis], and most of us don’t know what they’re basing them on because no one can agree on a definition anyway. Now they’re penalizing hospitals if they don’t hit the check marks in time, but we’d already demonstrated that our mortality and patient care was exceptional.”
She added: “I am extremely dissatisfied, as someone who provides frontline patient care, with how CMS is choosing to measure us.”
Dr. Kalantari wrote a piece in the Western Journal of Emergency Medicine in July 2017 in which she and coauthors outline the issues they take with SEP-1. They lay out the tension among the varied definitions of what sepsis is – and isn’t – and they also illuminate the apparent conflict between what CMS has officially defined and what evidence-based studies conducted since 2001 have suggested.3
In particular, CMS defines severe sepsis as an initial lactate above 2 mmol/L and septic shock as an initial lactate presentation of greater than 4 mmol/L. However, Dr. Kalantari and here coauthors argue in the paper that there is no standard definition of sepsis and that decades of attempts to achieve one have failed to reach consensus among providers. CMS, she said, fails to acknowledge this.
Defining sepsis
In fact, in 2016, another new definition of sepsis emerged by way of a 19-member task-force of experts: The Third International Consensus Definitions for Sepsis and Septic Shock, also called Sepsis-3.4 In March 2017, the Surviving Sepsis Campaign adopted this definition, which defined sepsis as a “life-threatening organ dysfunction caused by a dysregulated host response to infection.”5
“I think the definition has always been a challenging part of sepsis,” said Kencee Graves, MD, a hospitalist at the University of Utah, Salt Lake City. “The definitions came about for research purposes, so … they are not perfectly sensitive nor specific.”
However, Dr. Graves believes SEP-1 is a step in the right direction in that it brings awareness to sepsis and holds providers accountable. Several years ago, she and her colleague Devin Horton, MD, also a hospitalist at the University of Utah, embarked on a massive undertaking to address sepsis in their hospital. It was, at the time, lacking in “sepsis culture,” Dr. Horton said.
“One of the big things that motivated both of us was that we started doing chart review together and – it’s always easier with 20/20 hindsight – we were noticing that residents were missing the signs of sepsis,” Dr. Horton explained. “The clinical criteria would be there, but no one would say the word.” This is important, he said, because sepsis is time critical.
So the pair set out to create a cultural change by sharing data and collecting input from each service and unit, which relied heavily on nursing staff to perpetuate change. They created an early warning system in the medical record and worked with units to achieve flexibility in their criteria.
While the early warning system seemed helpful on the floor, SEP-1 adherence rates changed little in the emergency department. So Dr. Graves and Dr. Horton worked out an ED-specific process map that started at triage and was modeled after myocardial infarction STEMI protocols. From April through December 2016, the ED achieved between 29.5% adherence to the SEP-1 bundles, they said according to CMS abstractor data. After the change, between January and March 2017, the ED saw 52.2% adherence.
Dr. Kalantari would like to see CMS allow hospitals to evaluate and alter their processes more individually, with the required result being lower sepsis mortality. Hospitalists, said Dr. Kahn, are well poised to champion these sepsis improvement efforts.
“Hospitalists are uniquely positioned to lead in this area because they are a visible presence and a link between providers doing multidisciplinary acute care,” he said. “The other thing hospitalists can do is insist on rolling out approaches that are evidence based and not likely to cause harm by leading to over resuscitation, or ensuring patients are receiving central-line insertions only when needed.”
This is currently a moment for hospitals to innovate and provide meaningful feedback to CMS, which, he said, is listening.
“It’s a myth that CMS rolls out policy without listening to the clinical community, but what they want is constructive criticism, not just to hear ‘We’re not ready and we have to push this down the road,’ ” Dr. Kahn said. “The time is now in the era of accountability in health care.”
References
1. Sepsis. National Institute of General Medical Sciences. https://www.nigms.nih.gov/education/pages/factsheet_sepsis.aspx. Updated Sept 2017. Accessed Jan 4, 2018.
2. Barbash I et al. Hospital perceptions of Medicare’s sepsis quality reporting initiative. J Hosp Med. 2017;12;963-8.
3. Kalantari A et al. Sepsis Definitions: The search for gold and what CMS got wrong. West J Emerg Med. 2017 Aug;18(5):951-6.
4. Singer M et. al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016 Feb 23;315(8):801-10.
5. Rhodes A et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43:304.
In October 2015, the Centers for Medicare & Medicaid Services implemented its first meaningful policy to attempt for addressing sepsis.
The condition – one of the leading causes of mortality among hospitalized patients – afflicts more than a million people each year in the United States, and between 15% and 30% of them die. Sepsis is one of the leading drivers of hospital readmissions, sending more patients back to the hospital than heart failure, pneumonia, and chronic obstructive pulmonary disease.1
However, while providers seem to agree that time to address sepsis is past due, not everyone has embraced the Sepsis CMS Core Measure program, or SEP-1, as the means to best achieve it. This is, in part, because of discrepancies in how sepsis is defined, the burden of reporting, and what some consider to be arbitrary clinical requirements that may not correlate with better patient outcomes.
“Sepsis is indeed a critical public health problem, and it’s appropriate and valuable that Medicare and other policy makers are focusing on sepsis,” said Jeremy Kahn, MD, professor of critical care medicine and health policy and management at the University of Pittsburgh. “This was really the first approach at that … but at 85-pages long, it really is an enormous effort for hospitals to adhere to this measure.”
This is because of the tension between the “intense desire to improve sepsis outcomes” and the “incredible burden” of keeping up with the necessary documentation while also providing quality care, Dr. Kahn said.
In December 2017, Dr. Kahn helped lead a study published in the Journal of Hospital Medicine aimed at trying to understand hospital perceptions of SEP-1. Over the course of 29 interviews with randomly selected hospital quality leaders across the United States, including physicians and nurses, the results came as a surprise.2
“Generally, hospitals were very supportive of the concept, and there was no pushback on the idea that we should be measuring and reporting sepsis quality to CMS,” he said.
However, the research team found that respondents believed the program’s requirements with respect to treatment and documentation were complex and not always linked to patient-centered outcomes. Meeting the SEP-1 bundles consistently required hospitals to dedicate resources that not all may have, especially those in small, rural communities and those serving as urban safety nets.
Some, like emergency medicine physician Annahieta Kalantari, DO (who did not participate in the survey), feel that SEP-1 forces providers to practice “check-box” medicine and undermines successful efforts that don’t necessarily align with the CMS policy.
She arrived at her institution, Aria-Jefferson Health in Philadelphia, before CMS adopted SEP-1; at that time, she took note of the fact that the rate of sepsis mortalities in her hospital was, in her words, not great when compared with that at similar institutions. And then she helped do something about it.
“I thought, ‘We’re a Premier reporting hospital,’ so we did a gap analysis as to why and put together protocols for the hospital to follow with our sepsis patients, including a sepsis alert and a lot of education,” said Dr. Kalantari, associate program director for the emergency medicine residency program at Aria-Jefferson and a former chair of its sepsis management committee. “Before you knew it, mortalities were below benchmark.”
But once SEP-1 began, she said, the hospital was unable to check all of the boxes all of the time.
“We kept track, but we weren’t hitting all the bundles exactly within the periods of time recommended, but our mortalities were still amazing,” she said. “CMS basically picked definitions [for sepsis], and most of us don’t know what they’re basing them on because no one can agree on a definition anyway. Now they’re penalizing hospitals if they don’t hit the check marks in time, but we’d already demonstrated that our mortality and patient care was exceptional.”
She added: “I am extremely dissatisfied, as someone who provides frontline patient care, with how CMS is choosing to measure us.”
Dr. Kalantari wrote a piece in the Western Journal of Emergency Medicine in July 2017 in which she and coauthors outline the issues they take with SEP-1. They lay out the tension among the varied definitions of what sepsis is – and isn’t – and they also illuminate the apparent conflict between what CMS has officially defined and what evidence-based studies conducted since 2001 have suggested.3
In particular, CMS defines severe sepsis as an initial lactate above 2 mmol/L and septic shock as an initial lactate presentation of greater than 4 mmol/L. However, Dr. Kalantari and here coauthors argue in the paper that there is no standard definition of sepsis and that decades of attempts to achieve one have failed to reach consensus among providers. CMS, she said, fails to acknowledge this.
Defining sepsis
In fact, in 2016, another new definition of sepsis emerged by way of a 19-member task-force of experts: The Third International Consensus Definitions for Sepsis and Septic Shock, also called Sepsis-3.4 In March 2017, the Surviving Sepsis Campaign adopted this definition, which defined sepsis as a “life-threatening organ dysfunction caused by a dysregulated host response to infection.”5
“I think the definition has always been a challenging part of sepsis,” said Kencee Graves, MD, a hospitalist at the University of Utah, Salt Lake City. “The definitions came about for research purposes, so … they are not perfectly sensitive nor specific.”
However, Dr. Graves believes SEP-1 is a step in the right direction in that it brings awareness to sepsis and holds providers accountable. Several years ago, she and her colleague Devin Horton, MD, also a hospitalist at the University of Utah, embarked on a massive undertaking to address sepsis in their hospital. It was, at the time, lacking in “sepsis culture,” Dr. Horton said.
“One of the big things that motivated both of us was that we started doing chart review together and – it’s always easier with 20/20 hindsight – we were noticing that residents were missing the signs of sepsis,” Dr. Horton explained. “The clinical criteria would be there, but no one would say the word.” This is important, he said, because sepsis is time critical.
So the pair set out to create a cultural change by sharing data and collecting input from each service and unit, which relied heavily on nursing staff to perpetuate change. They created an early warning system in the medical record and worked with units to achieve flexibility in their criteria.
While the early warning system seemed helpful on the floor, SEP-1 adherence rates changed little in the emergency department. So Dr. Graves and Dr. Horton worked out an ED-specific process map that started at triage and was modeled after myocardial infarction STEMI protocols. From April through December 2016, the ED achieved between 29.5% adherence to the SEP-1 bundles, they said according to CMS abstractor data. After the change, between January and March 2017, the ED saw 52.2% adherence.
Dr. Kalantari would like to see CMS allow hospitals to evaluate and alter their processes more individually, with the required result being lower sepsis mortality. Hospitalists, said Dr. Kahn, are well poised to champion these sepsis improvement efforts.
“Hospitalists are uniquely positioned to lead in this area because they are a visible presence and a link between providers doing multidisciplinary acute care,” he said. “The other thing hospitalists can do is insist on rolling out approaches that are evidence based and not likely to cause harm by leading to over resuscitation, or ensuring patients are receiving central-line insertions only when needed.”
This is currently a moment for hospitals to innovate and provide meaningful feedback to CMS, which, he said, is listening.
“It’s a myth that CMS rolls out policy without listening to the clinical community, but what they want is constructive criticism, not just to hear ‘We’re not ready and we have to push this down the road,’ ” Dr. Kahn said. “The time is now in the era of accountability in health care.”
References
1. Sepsis. National Institute of General Medical Sciences. https://www.nigms.nih.gov/education/pages/factsheet_sepsis.aspx. Updated Sept 2017. Accessed Jan 4, 2018.
2. Barbash I et al. Hospital perceptions of Medicare’s sepsis quality reporting initiative. J Hosp Med. 2017;12;963-8.
3. Kalantari A et al. Sepsis Definitions: The search for gold and what CMS got wrong. West J Emerg Med. 2017 Aug;18(5):951-6.
4. Singer M et. al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016 Feb 23;315(8):801-10.
5. Rhodes A et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43:304.
CDC warns of hepatitis A outbreaks in injection drug users
From January 2017 to April 2018, more than 2,500 cases of hepatitis A infection associated with person-to-person transmission were reported to the CDC; of the 1,900 cases where risk factors are known, 68% were related to drug use, homelessness, or both. Various state responses caused a shortage in hepatitis A vaccine during this time, however, because of improvements in controlling outbreaks and an increased vaccine supply, the vaccine has become more available.
Usage of contaminated needles or other injection paraphernalia increase risk of hepatitis A infection, and transience, economic instability, limited health care access, distrust of public officials and public messages, and frequent lack of follow-up contact information in the population who regularly inject drugs make them difficult to reach with preventative services, such as vaccination, use of sterile injection equipment, and case management and contact tracing.
“These challenges make outbreaks among these groups difficult to control,” the CDC said in a statement.
The CDC recommends health departments ensure people who report drug use are vaccinated for hepatitis A, and consider programs to educate at-risk populations, as well as to provide vaccinations in places where at-risk populations may seek treatment. Health care providers should encourage patients who report drug use to be vaccinated for the disease.
For health care professionals, the CDC recommends considering a diagnosis of hepatitis A in any patient with jaundice and clinically compatible symptoms. The agency also recommends one dose of single-antigen hepatitis A vaccine or immune globulin within 2 weeks of exposure for unvaccinated patients who have been exposed to hepatitis A virus.
Find the full Health Advisory on the CDC website.
From January 2017 to April 2018, more than 2,500 cases of hepatitis A infection associated with person-to-person transmission were reported to the CDC; of the 1,900 cases where risk factors are known, 68% were related to drug use, homelessness, or both. Various state responses caused a shortage in hepatitis A vaccine during this time, however, because of improvements in controlling outbreaks and an increased vaccine supply, the vaccine has become more available.
Usage of contaminated needles or other injection paraphernalia increase risk of hepatitis A infection, and transience, economic instability, limited health care access, distrust of public officials and public messages, and frequent lack of follow-up contact information in the population who regularly inject drugs make them difficult to reach with preventative services, such as vaccination, use of sterile injection equipment, and case management and contact tracing.
“These challenges make outbreaks among these groups difficult to control,” the CDC said in a statement.
The CDC recommends health departments ensure people who report drug use are vaccinated for hepatitis A, and consider programs to educate at-risk populations, as well as to provide vaccinations in places where at-risk populations may seek treatment. Health care providers should encourage patients who report drug use to be vaccinated for the disease.
For health care professionals, the CDC recommends considering a diagnosis of hepatitis A in any patient with jaundice and clinically compatible symptoms. The agency also recommends one dose of single-antigen hepatitis A vaccine or immune globulin within 2 weeks of exposure for unvaccinated patients who have been exposed to hepatitis A virus.
Find the full Health Advisory on the CDC website.
From January 2017 to April 2018, more than 2,500 cases of hepatitis A infection associated with person-to-person transmission were reported to the CDC; of the 1,900 cases where risk factors are known, 68% were related to drug use, homelessness, or both. Various state responses caused a shortage in hepatitis A vaccine during this time, however, because of improvements in controlling outbreaks and an increased vaccine supply, the vaccine has become more available.
Usage of contaminated needles or other injection paraphernalia increase risk of hepatitis A infection, and transience, economic instability, limited health care access, distrust of public officials and public messages, and frequent lack of follow-up contact information in the population who regularly inject drugs make them difficult to reach with preventative services, such as vaccination, use of sterile injection equipment, and case management and contact tracing.
“These challenges make outbreaks among these groups difficult to control,” the CDC said in a statement.
The CDC recommends health departments ensure people who report drug use are vaccinated for hepatitis A, and consider programs to educate at-risk populations, as well as to provide vaccinations in places where at-risk populations may seek treatment. Health care providers should encourage patients who report drug use to be vaccinated for the disease.
For health care professionals, the CDC recommends considering a diagnosis of hepatitis A in any patient with jaundice and clinically compatible symptoms. The agency also recommends one dose of single-antigen hepatitis A vaccine or immune globulin within 2 weeks of exposure for unvaccinated patients who have been exposed to hepatitis A virus.
Find the full Health Advisory on the CDC website.
EULAR scientific program highlights spectrum of translational research
EULAR 2018’s scientific program in Amsterdam is packed with lectures, clinical and basic science symposia, workshops, and special interest sessions covering the full spectrum of rheumatic diseases, said Dr. Robert Landewé, chair of the Scientific Program Committee.
“More than 5,000 scientific abstracts were submitted, which is an absolute, all-time record,” Dr. Landewé said. Four experts scored each abstract, and only the top 7% were invited for oral presentation during abstract sessions or symposia, he explained in an interview.
Wednesday, June 13
A high point of the 2018 scientific program is Wednesday’s opening plenary session, which will feature abstracts that were handpicked by Dr. Landewé and Dr. Thomas Dörner, professor of rheumatology at Charite Universitätsmedizin, Berlin. “This session includes highly scored abstracts, including late-breakers, on current advances in therapeutics and disease classification,” said Dr. Dörner, who chaired this year’s Abstract Selection Committee.
The plenary abstract session will cover new findings on gout and cardiovascular disease from CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study), long-term mortality in patients with early RA from the COBRA (Combinatietherapie Bij Reumatoide Artritis) study, the use of zoledronic acid to treat knee osteoarthritis with bone lesions, and the relationship between bisphosphonate drug holidays and hip fracture risk. Researchers also will discuss baricitinib in systemic lupus erythematosus (SLE), the value of MRI when treating remitted RA to target, the validation of SLE classification criteria, and draft classification criteria for ANCA-associated vasculitides.
A notable clinical science session on Wednesday will cover cancer and inflammation, Dr. Landewé said. “This is a topic of increasing interest because cancer and inflammation share mutual pathways.”
Novel cancer therapies such as immune checkpoint inhibitors have improved outcomes across a range of tumor types, but also can induce rheumatic disease, he added. Accordingly, presenters will discuss inflammation as “friend” versus “foe” in cancer treatment, the role of tumor necrosis factor in cancer, and risk of malignancy among patients with RA.
Also on Wednesday, a session will tackle the relationship between psychological distress and pain in immune-mediated disease. “Pain is the major symptom of rheumatic diseases, and the role of the psyche remains poorly understood,” Dr. Landewé said. “But we know one thing for sure: There is an association, and speakers from outside the field of rheumatology will help explain.”
Attendees at this bench-to-bedside session will learn how distress appears to exacerbate arthritis pain and how managing psychological stress can help optimize outcomes in arthritis pain. Experts also will describe research on integrated brain pathways in pain and distress, as well as risk factors for cognitive impairment in RA.
Thursday, June 14
Topics in this session will include the use of estrogens and other hormonal therapies in patients with rheumatic disease, registry studies of rheumatologic conditions during pregnancy, and how clinicians can best discuss sexual concerns with their rheumatology patients.
Another clinical science session scheduled for Thursday afternoon will delve into structural damage progression in patients with axial spondyloarthritis, Dr. Landewé said. “Can we inhibit this structural progression? Can we show it? Does it make sense? And which drug company will win the battle to have the precedent?”
He hopes that Dr. Désirée van der Heijde of the Netherlands and Dr. Xenofon Baraliakos of Germany will help answer these questions when they discuss the latest evidence on identifying and treating clinically relevant structural progression. Also in this session, researchers will describe the combined effects of tumor necrosis factor inhibitors and NSAIDs on radiographic progression in ankylosing spondylitis, and MRI evidence supporting treating early axial spondyloarthritis to target with the goal of achieving sustained remission of inflammation.
Also on Thursday afternoon, a case-based session will take a deep dive into giant cell arteritis (GCA), Dr. Landewé noted. Attendees will learn about diagnosing and managing vision loss and stroke and the latest on corticosteroid therapy in GCA. The session also will cover biologics. “Giant cell arteritis has entered the field of biologicals!” said Dr. Landewé. “This has major implications for this disease and the clinical choices to be made.”
The past 5 decades have seen marked progress in the diagnosis and treatment of SLE, with corresponding improvements in survival and quality of life. “Still, lupus is awfully difficult,” Dr. Landewé said. “Therefore, we have planned a classical bench-to-bedside symposium to provide an all-inclusive look at current thinking and future developments.”
Talks during this Thursday afternoon session will cover the latest findings on the pathogenesis of SLE, the clinical significance of autoantibodies, distinguishing early SLE from mimics, and the role of blood-brain barrier permeability and neuropsychiatric manifestations of SLE and progressive systemic sclerosis.
Friday, June 15
For the first time, the scientific program also will include a clinical science session held jointly with the European Society of Musculoskeletal Radiology (ESSR). Dr. Joachim Sieper of Germany and ESSR President Dr. Monique Reijnierse of the Netherlands will cochair the Friday afternoon session on the role of MRI in rheumatology. Attendees from both organizations will learn when to use MRI in early and established RA and spondyloarthritis, and how to interpret the results, with abundant time built in for questions and answers. Dr. Landewé called the joint session “a test case” for exciting web-based interactions between EULAR and ESSR.
Another clinical science session on Friday afternoon will dive into the diagnosis of spondyloarthritis, which Dr. Landewé called “a matter of recognizing patterns, not ticking boxes on a list of criteria. This symposium leads you through the art of pattern recognition.”
Later on Friday afternoon, a session will explore advances in biologic therapy of small-vessel vasculitis, he added. “Biologic disease-modifying antirheumatic drugs [bDMARDs] are becoming more and more important in this area of expanding interest.” Experts will address complement inhibition in ANCA-associated vasculitis (AAV), the use of induction and maintenance rituximab in AAV, the evolving role of mepolizumab in eosinophilic granulomatosis with polyangiitis, survival in AAV, and the use of rituximab for treating children with granulomatosis with polyangiitis and microscopic polyangiitis.
Saturday, June 16
On Saturday, a bench-to-bedside session will cover gout and kidney function. “This is an area with important new insights,” Dr. Dörner said. Presenters will discuss the genetics of hyperuricemia, renal urate transporters, and the pros and cons of using xanthine oxidase inhibitors to treat chronic kidney disease. Researchers will also cover studies of impaired neutrophil chemotaxis in patients with chronic kidney disease and hyperuricemia, and the relationship between renal medullar hyperechogenicity and gout severity.
Also on Saturday, a clinical science session titled, “Rheumatoid arthritis: Is it all in your head?” will explore emerging data on the relationship between inflammation and depression. Patients with RA often face both clinical depression and social isolation, and these complex psychosocial conditions can worsen one another. “In addition to proper drug choice, treating RA effectively depends on how concomitant problems, such as nonspecific pain, depression, and social isolation, are coped with in a broad context,” Dr. Landewé said. “When it comes to optimal management, rheumatologists need to communicate and prescribe, not just prescribe.”
Christian Apfelbacher, PhD, of Germany will discuss prevention and treatment strategies and Dr. Jonathan Cavanagh of the United Kingdom will cover neuroimaging in RA. Researchers also will discuss new findings on pain, depression, and anxiety in patients recently diagnosed with RA.
Also on Saturday, a special session will cover EULAR’s initiatives to improve clinical approaches (ESSCA), Dr. Dörner noted. This effort has produced new or updated recommendations on topics such as vaccination, Sjögren’s syndrome, glucocorticoid therapy, and management of hand osteoarthritis, he said. “These recommendations follow a number of others and are expected to impact clinical science as well as clinical practice.”
EULAR 2018’s scientific program in Amsterdam is packed with lectures, clinical and basic science symposia, workshops, and special interest sessions covering the full spectrum of rheumatic diseases, said Dr. Robert Landewé, chair of the Scientific Program Committee.
“More than 5,000 scientific abstracts were submitted, which is an absolute, all-time record,” Dr. Landewé said. Four experts scored each abstract, and only the top 7% were invited for oral presentation during abstract sessions or symposia, he explained in an interview.
Wednesday, June 13
A high point of the 2018 scientific program is Wednesday’s opening plenary session, which will feature abstracts that were handpicked by Dr. Landewé and Dr. Thomas Dörner, professor of rheumatology at Charite Universitätsmedizin, Berlin. “This session includes highly scored abstracts, including late-breakers, on current advances in therapeutics and disease classification,” said Dr. Dörner, who chaired this year’s Abstract Selection Committee.
The plenary abstract session will cover new findings on gout and cardiovascular disease from CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study), long-term mortality in patients with early RA from the COBRA (Combinatietherapie Bij Reumatoide Artritis) study, the use of zoledronic acid to treat knee osteoarthritis with bone lesions, and the relationship between bisphosphonate drug holidays and hip fracture risk. Researchers also will discuss baricitinib in systemic lupus erythematosus (SLE), the value of MRI when treating remitted RA to target, the validation of SLE classification criteria, and draft classification criteria for ANCA-associated vasculitides.
A notable clinical science session on Wednesday will cover cancer and inflammation, Dr. Landewé said. “This is a topic of increasing interest because cancer and inflammation share mutual pathways.”
Novel cancer therapies such as immune checkpoint inhibitors have improved outcomes across a range of tumor types, but also can induce rheumatic disease, he added. Accordingly, presenters will discuss inflammation as “friend” versus “foe” in cancer treatment, the role of tumor necrosis factor in cancer, and risk of malignancy among patients with RA.
Also on Wednesday, a session will tackle the relationship between psychological distress and pain in immune-mediated disease. “Pain is the major symptom of rheumatic diseases, and the role of the psyche remains poorly understood,” Dr. Landewé said. “But we know one thing for sure: There is an association, and speakers from outside the field of rheumatology will help explain.”
Attendees at this bench-to-bedside session will learn how distress appears to exacerbate arthritis pain and how managing psychological stress can help optimize outcomes in arthritis pain. Experts also will describe research on integrated brain pathways in pain and distress, as well as risk factors for cognitive impairment in RA.
Thursday, June 14
Topics in this session will include the use of estrogens and other hormonal therapies in patients with rheumatic disease, registry studies of rheumatologic conditions during pregnancy, and how clinicians can best discuss sexual concerns with their rheumatology patients.
Another clinical science session scheduled for Thursday afternoon will delve into structural damage progression in patients with axial spondyloarthritis, Dr. Landewé said. “Can we inhibit this structural progression? Can we show it? Does it make sense? And which drug company will win the battle to have the precedent?”
He hopes that Dr. Désirée van der Heijde of the Netherlands and Dr. Xenofon Baraliakos of Germany will help answer these questions when they discuss the latest evidence on identifying and treating clinically relevant structural progression. Also in this session, researchers will describe the combined effects of tumor necrosis factor inhibitors and NSAIDs on radiographic progression in ankylosing spondylitis, and MRI evidence supporting treating early axial spondyloarthritis to target with the goal of achieving sustained remission of inflammation.
Also on Thursday afternoon, a case-based session will take a deep dive into giant cell arteritis (GCA), Dr. Landewé noted. Attendees will learn about diagnosing and managing vision loss and stroke and the latest on corticosteroid therapy in GCA. The session also will cover biologics. “Giant cell arteritis has entered the field of biologicals!” said Dr. Landewé. “This has major implications for this disease and the clinical choices to be made.”
The past 5 decades have seen marked progress in the diagnosis and treatment of SLE, with corresponding improvements in survival and quality of life. “Still, lupus is awfully difficult,” Dr. Landewé said. “Therefore, we have planned a classical bench-to-bedside symposium to provide an all-inclusive look at current thinking and future developments.”
Talks during this Thursday afternoon session will cover the latest findings on the pathogenesis of SLE, the clinical significance of autoantibodies, distinguishing early SLE from mimics, and the role of blood-brain barrier permeability and neuropsychiatric manifestations of SLE and progressive systemic sclerosis.
Friday, June 15
For the first time, the scientific program also will include a clinical science session held jointly with the European Society of Musculoskeletal Radiology (ESSR). Dr. Joachim Sieper of Germany and ESSR President Dr. Monique Reijnierse of the Netherlands will cochair the Friday afternoon session on the role of MRI in rheumatology. Attendees from both organizations will learn when to use MRI in early and established RA and spondyloarthritis, and how to interpret the results, with abundant time built in for questions and answers. Dr. Landewé called the joint session “a test case” for exciting web-based interactions between EULAR and ESSR.
Another clinical science session on Friday afternoon will dive into the diagnosis of spondyloarthritis, which Dr. Landewé called “a matter of recognizing patterns, not ticking boxes on a list of criteria. This symposium leads you through the art of pattern recognition.”
Later on Friday afternoon, a session will explore advances in biologic therapy of small-vessel vasculitis, he added. “Biologic disease-modifying antirheumatic drugs [bDMARDs] are becoming more and more important in this area of expanding interest.” Experts will address complement inhibition in ANCA-associated vasculitis (AAV), the use of induction and maintenance rituximab in AAV, the evolving role of mepolizumab in eosinophilic granulomatosis with polyangiitis, survival in AAV, and the use of rituximab for treating children with granulomatosis with polyangiitis and microscopic polyangiitis.
Saturday, June 16
On Saturday, a bench-to-bedside session will cover gout and kidney function. “This is an area with important new insights,” Dr. Dörner said. Presenters will discuss the genetics of hyperuricemia, renal urate transporters, and the pros and cons of using xanthine oxidase inhibitors to treat chronic kidney disease. Researchers will also cover studies of impaired neutrophil chemotaxis in patients with chronic kidney disease and hyperuricemia, and the relationship between renal medullar hyperechogenicity and gout severity.
Also on Saturday, a clinical science session titled, “Rheumatoid arthritis: Is it all in your head?” will explore emerging data on the relationship between inflammation and depression. Patients with RA often face both clinical depression and social isolation, and these complex psychosocial conditions can worsen one another. “In addition to proper drug choice, treating RA effectively depends on how concomitant problems, such as nonspecific pain, depression, and social isolation, are coped with in a broad context,” Dr. Landewé said. “When it comes to optimal management, rheumatologists need to communicate and prescribe, not just prescribe.”
Christian Apfelbacher, PhD, of Germany will discuss prevention and treatment strategies and Dr. Jonathan Cavanagh of the United Kingdom will cover neuroimaging in RA. Researchers also will discuss new findings on pain, depression, and anxiety in patients recently diagnosed with RA.
Also on Saturday, a special session will cover EULAR’s initiatives to improve clinical approaches (ESSCA), Dr. Dörner noted. This effort has produced new or updated recommendations on topics such as vaccination, Sjögren’s syndrome, glucocorticoid therapy, and management of hand osteoarthritis, he said. “These recommendations follow a number of others and are expected to impact clinical science as well as clinical practice.”
EULAR 2018’s scientific program in Amsterdam is packed with lectures, clinical and basic science symposia, workshops, and special interest sessions covering the full spectrum of rheumatic diseases, said Dr. Robert Landewé, chair of the Scientific Program Committee.
“More than 5,000 scientific abstracts were submitted, which is an absolute, all-time record,” Dr. Landewé said. Four experts scored each abstract, and only the top 7% were invited for oral presentation during abstract sessions or symposia, he explained in an interview.
Wednesday, June 13
A high point of the 2018 scientific program is Wednesday’s opening plenary session, which will feature abstracts that were handpicked by Dr. Landewé and Dr. Thomas Dörner, professor of rheumatology at Charite Universitätsmedizin, Berlin. “This session includes highly scored abstracts, including late-breakers, on current advances in therapeutics and disease classification,” said Dr. Dörner, who chaired this year’s Abstract Selection Committee.
The plenary abstract session will cover new findings on gout and cardiovascular disease from CANTOS (Canakinumab Anti-inflammatory Thrombosis Outcome Study), long-term mortality in patients with early RA from the COBRA (Combinatietherapie Bij Reumatoide Artritis) study, the use of zoledronic acid to treat knee osteoarthritis with bone lesions, and the relationship between bisphosphonate drug holidays and hip fracture risk. Researchers also will discuss baricitinib in systemic lupus erythematosus (SLE), the value of MRI when treating remitted RA to target, the validation of SLE classification criteria, and draft classification criteria for ANCA-associated vasculitides.
A notable clinical science session on Wednesday will cover cancer and inflammation, Dr. Landewé said. “This is a topic of increasing interest because cancer and inflammation share mutual pathways.”
Novel cancer therapies such as immune checkpoint inhibitors have improved outcomes across a range of tumor types, but also can induce rheumatic disease, he added. Accordingly, presenters will discuss inflammation as “friend” versus “foe” in cancer treatment, the role of tumor necrosis factor in cancer, and risk of malignancy among patients with RA.
Also on Wednesday, a session will tackle the relationship between psychological distress and pain in immune-mediated disease. “Pain is the major symptom of rheumatic diseases, and the role of the psyche remains poorly understood,” Dr. Landewé said. “But we know one thing for sure: There is an association, and speakers from outside the field of rheumatology will help explain.”
Attendees at this bench-to-bedside session will learn how distress appears to exacerbate arthritis pain and how managing psychological stress can help optimize outcomes in arthritis pain. Experts also will describe research on integrated brain pathways in pain and distress, as well as risk factors for cognitive impairment in RA.
Thursday, June 14
Topics in this session will include the use of estrogens and other hormonal therapies in patients with rheumatic disease, registry studies of rheumatologic conditions during pregnancy, and how clinicians can best discuss sexual concerns with their rheumatology patients.
Another clinical science session scheduled for Thursday afternoon will delve into structural damage progression in patients with axial spondyloarthritis, Dr. Landewé said. “Can we inhibit this structural progression? Can we show it? Does it make sense? And which drug company will win the battle to have the precedent?”
He hopes that Dr. Désirée van der Heijde of the Netherlands and Dr. Xenofon Baraliakos of Germany will help answer these questions when they discuss the latest evidence on identifying and treating clinically relevant structural progression. Also in this session, researchers will describe the combined effects of tumor necrosis factor inhibitors and NSAIDs on radiographic progression in ankylosing spondylitis, and MRI evidence supporting treating early axial spondyloarthritis to target with the goal of achieving sustained remission of inflammation.
Also on Thursday afternoon, a case-based session will take a deep dive into giant cell arteritis (GCA), Dr. Landewé noted. Attendees will learn about diagnosing and managing vision loss and stroke and the latest on corticosteroid therapy in GCA. The session also will cover biologics. “Giant cell arteritis has entered the field of biologicals!” said Dr. Landewé. “This has major implications for this disease and the clinical choices to be made.”
The past 5 decades have seen marked progress in the diagnosis and treatment of SLE, with corresponding improvements in survival and quality of life. “Still, lupus is awfully difficult,” Dr. Landewé said. “Therefore, we have planned a classical bench-to-bedside symposium to provide an all-inclusive look at current thinking and future developments.”
Talks during this Thursday afternoon session will cover the latest findings on the pathogenesis of SLE, the clinical significance of autoantibodies, distinguishing early SLE from mimics, and the role of blood-brain barrier permeability and neuropsychiatric manifestations of SLE and progressive systemic sclerosis.
Friday, June 15
For the first time, the scientific program also will include a clinical science session held jointly with the European Society of Musculoskeletal Radiology (ESSR). Dr. Joachim Sieper of Germany and ESSR President Dr. Monique Reijnierse of the Netherlands will cochair the Friday afternoon session on the role of MRI in rheumatology. Attendees from both organizations will learn when to use MRI in early and established RA and spondyloarthritis, and how to interpret the results, with abundant time built in for questions and answers. Dr. Landewé called the joint session “a test case” for exciting web-based interactions between EULAR and ESSR.
Another clinical science session on Friday afternoon will dive into the diagnosis of spondyloarthritis, which Dr. Landewé called “a matter of recognizing patterns, not ticking boxes on a list of criteria. This symposium leads you through the art of pattern recognition.”
Later on Friday afternoon, a session will explore advances in biologic therapy of small-vessel vasculitis, he added. “Biologic disease-modifying antirheumatic drugs [bDMARDs] are becoming more and more important in this area of expanding interest.” Experts will address complement inhibition in ANCA-associated vasculitis (AAV), the use of induction and maintenance rituximab in AAV, the evolving role of mepolizumab in eosinophilic granulomatosis with polyangiitis, survival in AAV, and the use of rituximab for treating children with granulomatosis with polyangiitis and microscopic polyangiitis.
Saturday, June 16
On Saturday, a bench-to-bedside session will cover gout and kidney function. “This is an area with important new insights,” Dr. Dörner said. Presenters will discuss the genetics of hyperuricemia, renal urate transporters, and the pros and cons of using xanthine oxidase inhibitors to treat chronic kidney disease. Researchers will also cover studies of impaired neutrophil chemotaxis in patients with chronic kidney disease and hyperuricemia, and the relationship between renal medullar hyperechogenicity and gout severity.
Also on Saturday, a clinical science session titled, “Rheumatoid arthritis: Is it all in your head?” will explore emerging data on the relationship between inflammation and depression. Patients with RA often face both clinical depression and social isolation, and these complex psychosocial conditions can worsen one another. “In addition to proper drug choice, treating RA effectively depends on how concomitant problems, such as nonspecific pain, depression, and social isolation, are coped with in a broad context,” Dr. Landewé said. “When it comes to optimal management, rheumatologists need to communicate and prescribe, not just prescribe.”
Christian Apfelbacher, PhD, of Germany will discuss prevention and treatment strategies and Dr. Jonathan Cavanagh of the United Kingdom will cover neuroimaging in RA. Researchers also will discuss new findings on pain, depression, and anxiety in patients recently diagnosed with RA.
Also on Saturday, a special session will cover EULAR’s initiatives to improve clinical approaches (ESSCA), Dr. Dörner noted. This effort has produced new or updated recommendations on topics such as vaccination, Sjögren’s syndrome, glucocorticoid therapy, and management of hand osteoarthritis, he said. “These recommendations follow a number of others and are expected to impact clinical science as well as clinical practice.”
Which IUD is right for me? Answering your patients’ questions about differences in LNG-IUDs
EULAR pediatric sessions to highlight big data, personalized medicine
Personalized medicine, big data, and monogenic inflammatory diseases are just a few of the high points of pediatric rheumatology sessions at this year’s EULAR Congress.
EULAR Standing Committee Chairperson for Paediatric Rheumatology Berent J. Prakken, MD, PhD, said that a bench-to-bedside session on Wednesday afternoon would highlight how EULAR projects are driving advances in pediatric rheumatology.
Attendees will learn from Vicki Seyfert-Margolis, PhD, an internationally recognized expert in personalized medicine, about how digital tools can facilitate cross-border partnerships in pediatric rheumatology, Dr. Prakken said in an interview.
“This talk will be groundbreaking because it’s not just about another useful app,” said Dr. Prakken, professor of pediatric rheumatology and vice dean of education at University Medical Center Utrecht (the Netherlands). “Dr. Seyfert-Margolis will show how the digital revolution will change the way we communicate with patients, monitor disease, and develop novel models for clinical trials.”
The session will also cover work by the Understanding Childhood Arthritis Network (UCAN), created to facilitate international translational research in pediatric rheumatology. Speakers will describe how UCAN is helping to spur personalized medicine and working with the Pediatric Rheumatology International Trials Organization (PRINTO) to align bench and bedside perspectives.
Another program highlight is a Thursday afternoon session on connections between monogenic autoinflammatory and pediatric rheumatic diseases. “Groundbreaking studies of these rare genetic inflammatory diseases have provided important new insights that, in turn, have led to new therapeutic options,” said Dr. Prakken.
During the session, Joost Swart, MD, of Utrecht, the Netherlands, will discuss promising research on the intravenous use of mesenchymal stromal cells derived from bone marrow for the treatment of refractory juvenile idiopathic arthritis (JIA).
Dr. Swart, who helped pioneer the approach, will discuss the first phase I/II trial of its use in children. “This is a truly innovative way to handle refractory inflammation,” Dr. Prakken said.
The session on monogenic autoinflammatory diseases also will cover their clinical presentation in children and adults, their pathogenesis as compared with adult-onset rheumatic diseases, and emerging treatment options, according to Dr. Prakken.
On Friday afternoon, a pediatric session will feature big data science in pediatric rheumatology, a lightning-paced field that is generating new research and treatment paradigms.
Of special note, Salvatore Albani, MD, PhD, will discuss how the human immunome is revolutionizing personalized treatment of paediatric inflammatory diseases, Dr. Prakken said. “This is the first application of big data to develop a completely new, personalized map of the human immune system,” he added. “This technology has the potential to revolutionize human clinical immunology, and it may be the key to true precision medicine in inflammatory diseases.”
Other talks in the session will cover signaling pathways in childhood systemic lupus erythematosus (SLE), galectin-9 as a biomarker in juvenile dermatomyositis, and evidence from the phase 3 PRINTO trial on how best to taper corticosteroids in patients with new-onset juvenile dermatomyositis.
Another crucial topic in pediatric rheumatology is systemic hyperinflammation, a potentially life-threatening situation requiring rapid detection and treatment.
A Saturday morning session will dive deeply into this topic. First, Sebastiaan Vastert, MD, PhD, will share a birds-eye view of systemic inflammation in JIA, setting the stage for a discussion by Angelo Ravelli, MD, of challenges in diagnosing macrophage activation syndrome, which disproportionately affects JIA patients.
Also during the session, Fabrizio de Benedetti, MD, PhD, will review new findings on the pathogenesis of hyperinflammation and how they can guide therapeutic development. Rounding off the session, Rebecca Davies will present research on first-onset uveitis in patients receiving etanercept or methotrexate to treat JIA. “Attendees will learn new insights about diagnosing and treating systemic inflammation in children,” Dr. Prakken said.
Once the dust has settled on the EULAR Congress in Amsterdam, delegates can look forward to the 2019 EULAR Congress in Madrid, which will be held jointly with the Paediatric Rheumatology European Society, further integrating the fields of pediatric and adult rheumatology.
Personalized medicine, big data, and monogenic inflammatory diseases are just a few of the high points of pediatric rheumatology sessions at this year’s EULAR Congress.
EULAR Standing Committee Chairperson for Paediatric Rheumatology Berent J. Prakken, MD, PhD, said that a bench-to-bedside session on Wednesday afternoon would highlight how EULAR projects are driving advances in pediatric rheumatology.
Attendees will learn from Vicki Seyfert-Margolis, PhD, an internationally recognized expert in personalized medicine, about how digital tools can facilitate cross-border partnerships in pediatric rheumatology, Dr. Prakken said in an interview.
“This talk will be groundbreaking because it’s not just about another useful app,” said Dr. Prakken, professor of pediatric rheumatology and vice dean of education at University Medical Center Utrecht (the Netherlands). “Dr. Seyfert-Margolis will show how the digital revolution will change the way we communicate with patients, monitor disease, and develop novel models for clinical trials.”
The session will also cover work by the Understanding Childhood Arthritis Network (UCAN), created to facilitate international translational research in pediatric rheumatology. Speakers will describe how UCAN is helping to spur personalized medicine and working with the Pediatric Rheumatology International Trials Organization (PRINTO) to align bench and bedside perspectives.
Another program highlight is a Thursday afternoon session on connections between monogenic autoinflammatory and pediatric rheumatic diseases. “Groundbreaking studies of these rare genetic inflammatory diseases have provided important new insights that, in turn, have led to new therapeutic options,” said Dr. Prakken.
During the session, Joost Swart, MD, of Utrecht, the Netherlands, will discuss promising research on the intravenous use of mesenchymal stromal cells derived from bone marrow for the treatment of refractory juvenile idiopathic arthritis (JIA).
Dr. Swart, who helped pioneer the approach, will discuss the first phase I/II trial of its use in children. “This is a truly innovative way to handle refractory inflammation,” Dr. Prakken said.
The session on monogenic autoinflammatory diseases also will cover their clinical presentation in children and adults, their pathogenesis as compared with adult-onset rheumatic diseases, and emerging treatment options, according to Dr. Prakken.
On Friday afternoon, a pediatric session will feature big data science in pediatric rheumatology, a lightning-paced field that is generating new research and treatment paradigms.
Of special note, Salvatore Albani, MD, PhD, will discuss how the human immunome is revolutionizing personalized treatment of paediatric inflammatory diseases, Dr. Prakken said. “This is the first application of big data to develop a completely new, personalized map of the human immune system,” he added. “This technology has the potential to revolutionize human clinical immunology, and it may be the key to true precision medicine in inflammatory diseases.”
Other talks in the session will cover signaling pathways in childhood systemic lupus erythematosus (SLE), galectin-9 as a biomarker in juvenile dermatomyositis, and evidence from the phase 3 PRINTO trial on how best to taper corticosteroids in patients with new-onset juvenile dermatomyositis.
Another crucial topic in pediatric rheumatology is systemic hyperinflammation, a potentially life-threatening situation requiring rapid detection and treatment.
A Saturday morning session will dive deeply into this topic. First, Sebastiaan Vastert, MD, PhD, will share a birds-eye view of systemic inflammation in JIA, setting the stage for a discussion by Angelo Ravelli, MD, of challenges in diagnosing macrophage activation syndrome, which disproportionately affects JIA patients.
Also during the session, Fabrizio de Benedetti, MD, PhD, will review new findings on the pathogenesis of hyperinflammation and how they can guide therapeutic development. Rounding off the session, Rebecca Davies will present research on first-onset uveitis in patients receiving etanercept or methotrexate to treat JIA. “Attendees will learn new insights about diagnosing and treating systemic inflammation in children,” Dr. Prakken said.
Once the dust has settled on the EULAR Congress in Amsterdam, delegates can look forward to the 2019 EULAR Congress in Madrid, which will be held jointly with the Paediatric Rheumatology European Society, further integrating the fields of pediatric and adult rheumatology.
Personalized medicine, big data, and monogenic inflammatory diseases are just a few of the high points of pediatric rheumatology sessions at this year’s EULAR Congress.
EULAR Standing Committee Chairperson for Paediatric Rheumatology Berent J. Prakken, MD, PhD, said that a bench-to-bedside session on Wednesday afternoon would highlight how EULAR projects are driving advances in pediatric rheumatology.
Attendees will learn from Vicki Seyfert-Margolis, PhD, an internationally recognized expert in personalized medicine, about how digital tools can facilitate cross-border partnerships in pediatric rheumatology, Dr. Prakken said in an interview.
“This talk will be groundbreaking because it’s not just about another useful app,” said Dr. Prakken, professor of pediatric rheumatology and vice dean of education at University Medical Center Utrecht (the Netherlands). “Dr. Seyfert-Margolis will show how the digital revolution will change the way we communicate with patients, monitor disease, and develop novel models for clinical trials.”
The session will also cover work by the Understanding Childhood Arthritis Network (UCAN), created to facilitate international translational research in pediatric rheumatology. Speakers will describe how UCAN is helping to spur personalized medicine and working with the Pediatric Rheumatology International Trials Organization (PRINTO) to align bench and bedside perspectives.
Another program highlight is a Thursday afternoon session on connections between monogenic autoinflammatory and pediatric rheumatic diseases. “Groundbreaking studies of these rare genetic inflammatory diseases have provided important new insights that, in turn, have led to new therapeutic options,” said Dr. Prakken.
During the session, Joost Swart, MD, of Utrecht, the Netherlands, will discuss promising research on the intravenous use of mesenchymal stromal cells derived from bone marrow for the treatment of refractory juvenile idiopathic arthritis (JIA).
Dr. Swart, who helped pioneer the approach, will discuss the first phase I/II trial of its use in children. “This is a truly innovative way to handle refractory inflammation,” Dr. Prakken said.
The session on monogenic autoinflammatory diseases also will cover their clinical presentation in children and adults, their pathogenesis as compared with adult-onset rheumatic diseases, and emerging treatment options, according to Dr. Prakken.
On Friday afternoon, a pediatric session will feature big data science in pediatric rheumatology, a lightning-paced field that is generating new research and treatment paradigms.
Of special note, Salvatore Albani, MD, PhD, will discuss how the human immunome is revolutionizing personalized treatment of paediatric inflammatory diseases, Dr. Prakken said. “This is the first application of big data to develop a completely new, personalized map of the human immune system,” he added. “This technology has the potential to revolutionize human clinical immunology, and it may be the key to true precision medicine in inflammatory diseases.”
Other talks in the session will cover signaling pathways in childhood systemic lupus erythematosus (SLE), galectin-9 as a biomarker in juvenile dermatomyositis, and evidence from the phase 3 PRINTO trial on how best to taper corticosteroids in patients with new-onset juvenile dermatomyositis.
Another crucial topic in pediatric rheumatology is systemic hyperinflammation, a potentially life-threatening situation requiring rapid detection and treatment.
A Saturday morning session will dive deeply into this topic. First, Sebastiaan Vastert, MD, PhD, will share a birds-eye view of systemic inflammation in JIA, setting the stage for a discussion by Angelo Ravelli, MD, of challenges in diagnosing macrophage activation syndrome, which disproportionately affects JIA patients.
Also during the session, Fabrizio de Benedetti, MD, PhD, will review new findings on the pathogenesis of hyperinflammation and how they can guide therapeutic development. Rounding off the session, Rebecca Davies will present research on first-onset uveitis in patients receiving etanercept or methotrexate to treat JIA. “Attendees will learn new insights about diagnosing and treating systemic inflammation in children,” Dr. Prakken said.
Once the dust has settled on the EULAR Congress in Amsterdam, delegates can look forward to the 2019 EULAR Congress in Madrid, which will be held jointly with the Paediatric Rheumatology European Society, further integrating the fields of pediatric and adult rheumatology.
EMEUNET network of young rheumatologists keeps moving forward
As the largest network of young rheumatologists in the world, the Emerging EULAR Network (EMEUNET) is looking forward to this year’s European Congress of Rheumatology to continue to build on what it set out to do as part of its mission – to give young rheumatologists and researchers an active say in education and research.
The rationale for the birth of EMEUNET in 2009 was to provide a network where European young rheumatologists and researchers, no matter where they were based, could access mentoring programs, research funding, and education initiatives, Alessia Alunno, MD, PhD, chair-elect and EMEUNET steering committee member, said in an interview.
Since its creation, EMEUNET has already achieved its goal several times over, but there’s certainly no intention for the network to rest on its laurels. One of its major achievements has been to secure a voice in the EULAR Strategy for the next 5 years.
“We are now able to sit at the table with the other EULAR pillars so that the educational offering of EULAR is tailored to meet the needs of young rheumatologists and researchers across Europe,” Dr. Alunno said.
And if the success of an organization can be measured by its membership numbers, then it’s clear that EMEUNET is on the right track.
Each year, membership continues to grow, and at 1,909 members, the 2,000 member milestone is tantalizingly close. This makes EMEUNET the largest network of rheumatologists and researchers, which Dr. Alunno said made the steering committee proud because it is a sign that what EMEUNET offers to members is suitable for more and more people.
So what is it that EULAR congress attendees can look forward to, apart from a bike tour around the canals of Amsterdam and an abundance of museums to visit?
“As always, we aim to foster collaboration, encourage educational activities and participation in them, to grow our network and increase our reach,” she said in an interview.
“It’s really an opportunity to attract as many young people as possible through our many educational initiatives, not just during the actual congress but also all year long.”
One of the congress highlights that’s been running successfully for a few years is the EMEUNET mentor/mentee meetings where young and upcoming clinicians and academics are given the opportunity to meet with a mentor, discuss their careers, and get some advice and coaching.
EMEUNET also will be bringing some crowd-pleasing initiatives to Amsterdam, such as its popular networking event that attracted more than 70 attendees in Madrid last year.
“We are very proud of our networking event. Opportunities for us to meet all together are very few, so we have the opportunity at EULAR to provide a platform where people can get together and create their own contacts that can be helpful in their everyday life,” Dr. Alunno said.
The networking event usually involves a relaxed local sightseeing tour followed by a chance to talk, network, and strengthen bonds.
The EULAR/EMEUNET ambassador program is also an important and popular initiative that has received positive feedback from past congress attendees. The program is set up to help first-time attendees who may need some support to get the most out of what can be an overwhelming scientific program.
Fellows are invited to apply for the program (for more information visit www.emeunet.eular.org) and successful applicants will receive congress mentorship from EMEUNET EULAR congress “veterans” on how to make the most of the 4 days.
It goes without saying that EMEUNET is also contributing to the congress’ scientific program.
EMEUNET also invites everyone to check out the Young Rheumatologists sessions in the scientific program, which will take place during the course of the congress.
These will include sessions on basic statistics; understanding the language of basic research, epidemiology, and health services articles; and conducting effective patient-physician communication in routine clinical settings.
“The Young Rheumatologist sessions may be a small grain in the large congress program, but they always gain a lot of interest,” Dr. Nikiphorou said.
As the largest network of young rheumatologists in the world, the Emerging EULAR Network (EMEUNET) is looking forward to this year’s European Congress of Rheumatology to continue to build on what it set out to do as part of its mission – to give young rheumatologists and researchers an active say in education and research.
The rationale for the birth of EMEUNET in 2009 was to provide a network where European young rheumatologists and researchers, no matter where they were based, could access mentoring programs, research funding, and education initiatives, Alessia Alunno, MD, PhD, chair-elect and EMEUNET steering committee member, said in an interview.
Since its creation, EMEUNET has already achieved its goal several times over, but there’s certainly no intention for the network to rest on its laurels. One of its major achievements has been to secure a voice in the EULAR Strategy for the next 5 years.
“We are now able to sit at the table with the other EULAR pillars so that the educational offering of EULAR is tailored to meet the needs of young rheumatologists and researchers across Europe,” Dr. Alunno said.
And if the success of an organization can be measured by its membership numbers, then it’s clear that EMEUNET is on the right track.
Each year, membership continues to grow, and at 1,909 members, the 2,000 member milestone is tantalizingly close. This makes EMEUNET the largest network of rheumatologists and researchers, which Dr. Alunno said made the steering committee proud because it is a sign that what EMEUNET offers to members is suitable for more and more people.
So what is it that EULAR congress attendees can look forward to, apart from a bike tour around the canals of Amsterdam and an abundance of museums to visit?
“As always, we aim to foster collaboration, encourage educational activities and participation in them, to grow our network and increase our reach,” she said in an interview.
“It’s really an opportunity to attract as many young people as possible through our many educational initiatives, not just during the actual congress but also all year long.”
One of the congress highlights that’s been running successfully for a few years is the EMEUNET mentor/mentee meetings where young and upcoming clinicians and academics are given the opportunity to meet with a mentor, discuss their careers, and get some advice and coaching.
EMEUNET also will be bringing some crowd-pleasing initiatives to Amsterdam, such as its popular networking event that attracted more than 70 attendees in Madrid last year.
“We are very proud of our networking event. Opportunities for us to meet all together are very few, so we have the opportunity at EULAR to provide a platform where people can get together and create their own contacts that can be helpful in their everyday life,” Dr. Alunno said.
The networking event usually involves a relaxed local sightseeing tour followed by a chance to talk, network, and strengthen bonds.
The EULAR/EMEUNET ambassador program is also an important and popular initiative that has received positive feedback from past congress attendees. The program is set up to help first-time attendees who may need some support to get the most out of what can be an overwhelming scientific program.
Fellows are invited to apply for the program (for more information visit www.emeunet.eular.org) and successful applicants will receive congress mentorship from EMEUNET EULAR congress “veterans” on how to make the most of the 4 days.
It goes without saying that EMEUNET is also contributing to the congress’ scientific program.
EMEUNET also invites everyone to check out the Young Rheumatologists sessions in the scientific program, which will take place during the course of the congress.
These will include sessions on basic statistics; understanding the language of basic research, epidemiology, and health services articles; and conducting effective patient-physician communication in routine clinical settings.
“The Young Rheumatologist sessions may be a small grain in the large congress program, but they always gain a lot of interest,” Dr. Nikiphorou said.
As the largest network of young rheumatologists in the world, the Emerging EULAR Network (EMEUNET) is looking forward to this year’s European Congress of Rheumatology to continue to build on what it set out to do as part of its mission – to give young rheumatologists and researchers an active say in education and research.
The rationale for the birth of EMEUNET in 2009 was to provide a network where European young rheumatologists and researchers, no matter where they were based, could access mentoring programs, research funding, and education initiatives, Alessia Alunno, MD, PhD, chair-elect and EMEUNET steering committee member, said in an interview.
Since its creation, EMEUNET has already achieved its goal several times over, but there’s certainly no intention for the network to rest on its laurels. One of its major achievements has been to secure a voice in the EULAR Strategy for the next 5 years.
“We are now able to sit at the table with the other EULAR pillars so that the educational offering of EULAR is tailored to meet the needs of young rheumatologists and researchers across Europe,” Dr. Alunno said.
And if the success of an organization can be measured by its membership numbers, then it’s clear that EMEUNET is on the right track.
Each year, membership continues to grow, and at 1,909 members, the 2,000 member milestone is tantalizingly close. This makes EMEUNET the largest network of rheumatologists and researchers, which Dr. Alunno said made the steering committee proud because it is a sign that what EMEUNET offers to members is suitable for more and more people.
So what is it that EULAR congress attendees can look forward to, apart from a bike tour around the canals of Amsterdam and an abundance of museums to visit?
“As always, we aim to foster collaboration, encourage educational activities and participation in them, to grow our network and increase our reach,” she said in an interview.
“It’s really an opportunity to attract as many young people as possible through our many educational initiatives, not just during the actual congress but also all year long.”
One of the congress highlights that’s been running successfully for a few years is the EMEUNET mentor/mentee meetings where young and upcoming clinicians and academics are given the opportunity to meet with a mentor, discuss their careers, and get some advice and coaching.
EMEUNET also will be bringing some crowd-pleasing initiatives to Amsterdam, such as its popular networking event that attracted more than 70 attendees in Madrid last year.
“We are very proud of our networking event. Opportunities for us to meet all together are very few, so we have the opportunity at EULAR to provide a platform where people can get together and create their own contacts that can be helpful in their everyday life,” Dr. Alunno said.
The networking event usually involves a relaxed local sightseeing tour followed by a chance to talk, network, and strengthen bonds.
The EULAR/EMEUNET ambassador program is also an important and popular initiative that has received positive feedback from past congress attendees. The program is set up to help first-time attendees who may need some support to get the most out of what can be an overwhelming scientific program.
Fellows are invited to apply for the program (for more information visit www.emeunet.eular.org) and successful applicants will receive congress mentorship from EMEUNET EULAR congress “veterans” on how to make the most of the 4 days.
It goes without saying that EMEUNET is also contributing to the congress’ scientific program.
EMEUNET also invites everyone to check out the Young Rheumatologists sessions in the scientific program, which will take place during the course of the congress.
These will include sessions on basic statistics; understanding the language of basic research, epidemiology, and health services articles; and conducting effective patient-physician communication in routine clinical settings.
“The Young Rheumatologist sessions may be a small grain in the large congress program, but they always gain a lot of interest,” Dr. Nikiphorou said.
Going to VAM? Download the VAM Mobile App
The mobile app for the 2018 Vascular Annual Meeting will be available Wednesday for both Apple and Android products. The app has been rebuilt from the ground up, for a very user-friendly experience. It’s interactive, comprehensive and searchable and includes many helpful features:
- My Schedule: Mark sessions as favorites on either the Planner or app, then see all of them in the My Schedule section.
- Educational Credits: Take self-assessment exams, via the app, and/or claim Continuing Medical Education credits.
- Scavenger Hunt: Participate in the big game in the Exhibit Hall; using your app, scan QR codes found in the booths of sponsors, then answer the question that pops up. The three people who earn the most points for correct answers win great prizes.
- Social Media – Let all your friends know what you’re up to by linking to social media
Download at Apple’s App Store and at Google Play.
The mobile app for the 2018 Vascular Annual Meeting will be available Wednesday for both Apple and Android products. The app has been rebuilt from the ground up, for a very user-friendly experience. It’s interactive, comprehensive and searchable and includes many helpful features:
- My Schedule: Mark sessions as favorites on either the Planner or app, then see all of them in the My Schedule section.
- Educational Credits: Take self-assessment exams, via the app, and/or claim Continuing Medical Education credits.
- Scavenger Hunt: Participate in the big game in the Exhibit Hall; using your app, scan QR codes found in the booths of sponsors, then answer the question that pops up. The three people who earn the most points for correct answers win great prizes.
- Social Media – Let all your friends know what you’re up to by linking to social media
Download at Apple’s App Store and at Google Play.
The mobile app for the 2018 Vascular Annual Meeting will be available Wednesday for both Apple and Android products. The app has been rebuilt from the ground up, for a very user-friendly experience. It’s interactive, comprehensive and searchable and includes many helpful features:
- My Schedule: Mark sessions as favorites on either the Planner or app, then see all of them in the My Schedule section.
- Educational Credits: Take self-assessment exams, via the app, and/or claim Continuing Medical Education credits.
- Scavenger Hunt: Participate in the big game in the Exhibit Hall; using your app, scan QR codes found in the booths of sponsors, then answer the question that pops up. The three people who earn the most points for correct answers win great prizes.
- Social Media – Let all your friends know what you’re up to by linking to social media
Download at Apple’s App Store and at Google Play.