User login
Migraineurs’ Initiation of Behavioral Treatment
Less than one-third of eligible migraineurs were referred for behavioral treatment and only about half initiated behavioral migraine treatment in a recent prospective cohort study. Researchers compared patients who initiated behavioral migraine treatment following a provider recommendation with those who did not (demographics, migraine characteristics, and locus of control) with analysis of variance and chi-square tests. They found:
- Of the 234 eligible patients, 69 (29.5%) were referred for behavioral treatment.
- 53 (76.8%) patients referred for behavioral treatment were reached by phone.
- The mean duration from time of referral to follow-up was 76 (median 76, SD=45) days.
- 30 (56.6%) patients initiated behavioral migraine treatment.
- There was no difference in initiation of behavioral migraine treatment with regard to sex, age, age of diagnosis, years suffered with headaches, health care utilization visits, Migraine Disability Assessment Screen, and locus of control.
- Patients who had previously seen a psychologist for migraine were more likely to initiate behavioral migraine treatment than patients who had not.
- Time constraints were the most common barrier cited for not initiating behavioral migraine treatment.
Factors related to migraine patients’ decisions to initiate behavioral migraine treatment following a headache specialist’s recommendation: A prospective observational study. [Published online ahead of print June 5, 2018]. Pain Medicine. doi:10.1093/pm/pny028.
Less than one-third of eligible migraineurs were referred for behavioral treatment and only about half initiated behavioral migraine treatment in a recent prospective cohort study. Researchers compared patients who initiated behavioral migraine treatment following a provider recommendation with those who did not (demographics, migraine characteristics, and locus of control) with analysis of variance and chi-square tests. They found:
- Of the 234 eligible patients, 69 (29.5%) were referred for behavioral treatment.
- 53 (76.8%) patients referred for behavioral treatment were reached by phone.
- The mean duration from time of referral to follow-up was 76 (median 76, SD=45) days.
- 30 (56.6%) patients initiated behavioral migraine treatment.
- There was no difference in initiation of behavioral migraine treatment with regard to sex, age, age of diagnosis, years suffered with headaches, health care utilization visits, Migraine Disability Assessment Screen, and locus of control.
- Patients who had previously seen a psychologist for migraine were more likely to initiate behavioral migraine treatment than patients who had not.
- Time constraints were the most common barrier cited for not initiating behavioral migraine treatment.
Factors related to migraine patients’ decisions to initiate behavioral migraine treatment following a headache specialist’s recommendation: A prospective observational study. [Published online ahead of print June 5, 2018]. Pain Medicine. doi:10.1093/pm/pny028.
Less than one-third of eligible migraineurs were referred for behavioral treatment and only about half initiated behavioral migraine treatment in a recent prospective cohort study. Researchers compared patients who initiated behavioral migraine treatment following a provider recommendation with those who did not (demographics, migraine characteristics, and locus of control) with analysis of variance and chi-square tests. They found:
- Of the 234 eligible patients, 69 (29.5%) were referred for behavioral treatment.
- 53 (76.8%) patients referred for behavioral treatment were reached by phone.
- The mean duration from time of referral to follow-up was 76 (median 76, SD=45) days.
- 30 (56.6%) patients initiated behavioral migraine treatment.
- There was no difference in initiation of behavioral migraine treatment with regard to sex, age, age of diagnosis, years suffered with headaches, health care utilization visits, Migraine Disability Assessment Screen, and locus of control.
- Patients who had previously seen a psychologist for migraine were more likely to initiate behavioral migraine treatment than patients who had not.
- Time constraints were the most common barrier cited for not initiating behavioral migraine treatment.
Factors related to migraine patients’ decisions to initiate behavioral migraine treatment following a headache specialist’s recommendation: A prospective observational study. [Published online ahead of print June 5, 2018]. Pain Medicine. doi:10.1093/pm/pny028.
Dismantling the sports-betting ban: A mental health gamble
The Supreme Court decision to overturn the federal law that prohibited state-sanctioned college and professional sports betting is bad news for clinicians who treat patients with addictions.
On May 14, the high court ruled 7-2 that the 1992 law, called the Professional and Amateur Sports Protection Act (PASPA), was unconstitutional. Now every state is free to operate, sponsor, promote, license, advertise, or authorize gambling for any college or professional sport–based event.
Optimistic outlooks on the death of PASPA include the foreseen opportunity by the states to tax and generate revenue on such gambling. Proponents of the ruling also argue that illegal activity that thrived on sports betting will now end.
But to what extent will either of those scenarios benefit the public?
If passage of various state marijuana laws is any example, assumptions that legal avenues will usurp illegal enterprises are flawed. Also, taxation likely will generate a large sum of revenue for each state. But those revenues might be offset by subsequent changes that will be needed in mental health, addiction, and wellness programs – a difficult proposition given the opioid epidemic already overburdening the country. Remember the tobacco cases and promise of state support for education, treatment, and other noble activities? Addiction medicine specialists worry that taxes collected by the states, and promises to prevent and treat gambling problems – and prevent addiction – will not end up in those coffers.
As clinicians, perhaps our most important contribution to the debates on this ruling lies in raising awareness of pathological gambling as an addiction disorder.
Redefining the act of gambling
Breaking down previous barriers to access and increasing convenience to gambling undoubtedly will be associated with increased pathological engagement in gambling. This conclusion is clear, based on past national experiments with substances of addiction (such as alcohol prohibition).
Since the cocaine epidemic of the 1980s, and our increased understanding that addictions need not have prominent withdrawal syndromes, we have focused on addiction as a fatal attraction. Psychiatrists and other clinicians made the case – in some quarters, at least – for sugar, sex, and Internet compulsivity as addictions. Compared with those addictions, the evidence was clearest and most compelling for pathological gambling as an addiction disorder. Indeed, gambling disorder was introduced in 2013 to the DSM-5 as the very first non–substance-based addictive disorder. This was a decisive change, as it recognizes that gambling is more than an environmental hazard for those suffering from dopamine-driven obsessive-compulsive-like dysfunction (the DSM section where it had lived previously). Instead, gambling acts as an agent that can initiate a usurpation of the brain’s reward circuitry. (In addition, this change has reopened the door for other increasingly recognized non–substance-based disorder categories such as video game and pornography addiction, and others.)
Gambling disorder certainly fits well into what many experts view as the essential phenotype of any addiction: Continued use despite harm, waning self-control over engagement, a craving state, and compulsive use. Current research is expanding rapidly and filling in the theoretical framework, strongly supporting gambling disorder based on biological evidence. Much of what we now know about the biology of addiction has been through the efforts of the Yale University–based research group, led by psychiatrist Marc N. Potenza. Dr. Potenza and his colleagues have been investigating gambling disorder in a thorough manner (Harv Rev Psychiatry. 2015 Mar-Apr;23[2]:134-46) and (Curr Treat Options Psychiatry. 2014 Jun 1;1[2]:189-203). Indeed, gambling disorder is much like the other substance-use disorders in which it is grouped, in that it has been found to share some similarities/pathways common to all addictions while also carrying its own specific nuances.
Twin studies have unearthed a wealth of information, such as knowledge that environmental factors seem to be the predominant source of the comorbid development of gambling disorder with the more socially acceptable substances as associated use disorders (alcohol, tobacco, and marijuana) through mechanisms such as peer association and place preference conditioning. Similarly, genetic influences also might be meaningful to treatment. For example, one finding showed that patients with gambling disorder and a family history of alcoholism were found to more preferentially respond to opioid-receptor antagonists as treatment for gambling disorder, compared with individuals without such family history (Psychopharmacology [Berl]. 2008;200[4]:521-7).
Explorations of neurotransmitter involvement and brain connectivity also have been conducted for gambling behaviors. Dopaminergic underpinnings of addiction have been particularly indicated in imaging studies focused on the ventral striatum and other components of reward circuitry. In addition, functional MRI studies have identified both overlapping and discordant brain imaging findings between gambling and many other substance use disorders such as cocaine. All these indicate that gambling seems, like its use-disorder counterparts, to follow a similar but distinct course of hijacking reward systems and priming the brain to seek out further gambling in a pathological manner.
Vulnerable populations
Another key finding of recent research exploring the biological foundations of gambling disorder is gender dimorphism. In numerous studies, women have been found to experience a “telescoping effect” from gambling, compared with their male counterparts, where they seem to more quickly advance from first exposure to problematic use. This phenomenon also is seen in women who use cocaine. Also, functional MRI studies also have found that women appear to have alternative signal changes in regions germane to addiction, compared with their male counterparts. One such example was greater activity in the hippocampus and middle temporal gyrus in women, suggestive of stronger activation of regions key for memory retrieval used in craving/urge-related emotions. These data highlight the need for not only understanding how gambling and other addictions diverge between men and women, but also for how prevention and treatment of these disorders might differ based on sex.
Adolescents also get special consideration: How will they be affected by this expected growth in gambling avenues? Adolescence and young adulthood are periods of development defined by increased impulsivity and risk taking, making this population particularly vulnerable to addiction that can then persist into adulthood. It is expected that age laws will persist and prevent the legal access adults might enjoy, but shifts in opinions of harm and ease of access are likely to contribute to increased gambling exposure. To use another addictive phenomena as an example, data from the Substance Abuse and Mental Health Services Administration show a clear correlation between marijuana use, marijuana legal status, and perceptions of risk. Specifically, areas with unfettered/loosened marijuana regulation have much lower levels of perceived risk among youth and much higher levels of use. Gambling could follow a similar course.
Perhaps the most crucial observation is that the most severe pathological gamblers began gambling before adulthood. Many factors have been identified that seem to increase rates of gambling in youth: Receiving scratch-off lotto cards as gifts, gambling on school grounds, and even smoking status (quite significant given the advent of e-cigarettes now common to many high school students). All of these essentially boil down to the common pathway of proximity and social referencing. As such, the notion that an increased social presence of (what will likely be) large scale, polished, mass televised sports gambling events will be associated with increased gambling behavior (and other mental health comorbidities) among youth is not far-fetched. What also is known for gambling, as well as for other addictive disorders, is that earlier age of onset is correlated to a worse prognosis of gambling disorder in adulthood. In other words, the earlier an addiction strikes, the deeper and more severe it is in the individual – further highlighting the impetus to focus concerns about the PASPA ruling toward the impact on youth.
Prevention and treatment
Lastly, it is important to consider the ground gained in preventing and treating gambling addiction. Many groups focused on treating and preventing gambling already are well established, such as Gamblers Anonymous, and these groups have produced favorable results. More targeted interventions such as cognitive-behavioral therapy adjusted for addiction disorders also have proved effective, as they often not only tackle the gambling disorder but also the collection of conditions it is so often comorbid with (affective illnesses, anxiety disorders).
Pharmacotherapy also has a role, further justifying the view of gambling disorder, and indeed all addiction disorders, as biological processes with biological solutions. Examinations into opiate antagonism and glutamatergic modulation (N-acetylcysteine) also have shown some promise. Prevention programs offer perhaps the best cost-effective ratio in reducing the societal burden of gambling, which is about $7 billion annually, according to 2013 estimates by the National Council on Problem Gambling). These programs have been conducted in schools through parent-teacher groups as well as publicly through distribution of informative psychoeducation via TV and advertising channels.
All available research conducted on treatment shows that further research and validation are needed. We should not pretend that increasing access to sports betting and normalizing the activity will not have an effect on gambling prevalence and problems. Prevention, even simple cautionary public warnings, requires time, money, and planning for effective execution.
Dr. Wenzinger is a clinical fellow, PGY-4, in the department of child and adolescent psychiatry at St. Louis Children’s Hospital. Dr. Gold is the 17th Distinguished Alumni Professor at the University of Florida, Gainesville, and professor of psychiatry (adjunct) at Washington University in St. Louis. He also serves as chairman of the scientific advisory boards for RiverMend Health.
The Supreme Court decision to overturn the federal law that prohibited state-sanctioned college and professional sports betting is bad news for clinicians who treat patients with addictions.
On May 14, the high court ruled 7-2 that the 1992 law, called the Professional and Amateur Sports Protection Act (PASPA), was unconstitutional. Now every state is free to operate, sponsor, promote, license, advertise, or authorize gambling for any college or professional sport–based event.
Optimistic outlooks on the death of PASPA include the foreseen opportunity by the states to tax and generate revenue on such gambling. Proponents of the ruling also argue that illegal activity that thrived on sports betting will now end.
But to what extent will either of those scenarios benefit the public?
If passage of various state marijuana laws is any example, assumptions that legal avenues will usurp illegal enterprises are flawed. Also, taxation likely will generate a large sum of revenue for each state. But those revenues might be offset by subsequent changes that will be needed in mental health, addiction, and wellness programs – a difficult proposition given the opioid epidemic already overburdening the country. Remember the tobacco cases and promise of state support for education, treatment, and other noble activities? Addiction medicine specialists worry that taxes collected by the states, and promises to prevent and treat gambling problems – and prevent addiction – will not end up in those coffers.
As clinicians, perhaps our most important contribution to the debates on this ruling lies in raising awareness of pathological gambling as an addiction disorder.
Redefining the act of gambling
Breaking down previous barriers to access and increasing convenience to gambling undoubtedly will be associated with increased pathological engagement in gambling. This conclusion is clear, based on past national experiments with substances of addiction (such as alcohol prohibition).
Since the cocaine epidemic of the 1980s, and our increased understanding that addictions need not have prominent withdrawal syndromes, we have focused on addiction as a fatal attraction. Psychiatrists and other clinicians made the case – in some quarters, at least – for sugar, sex, and Internet compulsivity as addictions. Compared with those addictions, the evidence was clearest and most compelling for pathological gambling as an addiction disorder. Indeed, gambling disorder was introduced in 2013 to the DSM-5 as the very first non–substance-based addictive disorder. This was a decisive change, as it recognizes that gambling is more than an environmental hazard for those suffering from dopamine-driven obsessive-compulsive-like dysfunction (the DSM section where it had lived previously). Instead, gambling acts as an agent that can initiate a usurpation of the brain’s reward circuitry. (In addition, this change has reopened the door for other increasingly recognized non–substance-based disorder categories such as video game and pornography addiction, and others.)
Gambling disorder certainly fits well into what many experts view as the essential phenotype of any addiction: Continued use despite harm, waning self-control over engagement, a craving state, and compulsive use. Current research is expanding rapidly and filling in the theoretical framework, strongly supporting gambling disorder based on biological evidence. Much of what we now know about the biology of addiction has been through the efforts of the Yale University–based research group, led by psychiatrist Marc N. Potenza. Dr. Potenza and his colleagues have been investigating gambling disorder in a thorough manner (Harv Rev Psychiatry. 2015 Mar-Apr;23[2]:134-46) and (Curr Treat Options Psychiatry. 2014 Jun 1;1[2]:189-203). Indeed, gambling disorder is much like the other substance-use disorders in which it is grouped, in that it has been found to share some similarities/pathways common to all addictions while also carrying its own specific nuances.
Twin studies have unearthed a wealth of information, such as knowledge that environmental factors seem to be the predominant source of the comorbid development of gambling disorder with the more socially acceptable substances as associated use disorders (alcohol, tobacco, and marijuana) through mechanisms such as peer association and place preference conditioning. Similarly, genetic influences also might be meaningful to treatment. For example, one finding showed that patients with gambling disorder and a family history of alcoholism were found to more preferentially respond to opioid-receptor antagonists as treatment for gambling disorder, compared with individuals without such family history (Psychopharmacology [Berl]. 2008;200[4]:521-7).
Explorations of neurotransmitter involvement and brain connectivity also have been conducted for gambling behaviors. Dopaminergic underpinnings of addiction have been particularly indicated in imaging studies focused on the ventral striatum and other components of reward circuitry. In addition, functional MRI studies have identified both overlapping and discordant brain imaging findings between gambling and many other substance use disorders such as cocaine. All these indicate that gambling seems, like its use-disorder counterparts, to follow a similar but distinct course of hijacking reward systems and priming the brain to seek out further gambling in a pathological manner.
Vulnerable populations
Another key finding of recent research exploring the biological foundations of gambling disorder is gender dimorphism. In numerous studies, women have been found to experience a “telescoping effect” from gambling, compared with their male counterparts, where they seem to more quickly advance from first exposure to problematic use. This phenomenon also is seen in women who use cocaine. Also, functional MRI studies also have found that women appear to have alternative signal changes in regions germane to addiction, compared with their male counterparts. One such example was greater activity in the hippocampus and middle temporal gyrus in women, suggestive of stronger activation of regions key for memory retrieval used in craving/urge-related emotions. These data highlight the need for not only understanding how gambling and other addictions diverge between men and women, but also for how prevention and treatment of these disorders might differ based on sex.
Adolescents also get special consideration: How will they be affected by this expected growth in gambling avenues? Adolescence and young adulthood are periods of development defined by increased impulsivity and risk taking, making this population particularly vulnerable to addiction that can then persist into adulthood. It is expected that age laws will persist and prevent the legal access adults might enjoy, but shifts in opinions of harm and ease of access are likely to contribute to increased gambling exposure. To use another addictive phenomena as an example, data from the Substance Abuse and Mental Health Services Administration show a clear correlation between marijuana use, marijuana legal status, and perceptions of risk. Specifically, areas with unfettered/loosened marijuana regulation have much lower levels of perceived risk among youth and much higher levels of use. Gambling could follow a similar course.
Perhaps the most crucial observation is that the most severe pathological gamblers began gambling before adulthood. Many factors have been identified that seem to increase rates of gambling in youth: Receiving scratch-off lotto cards as gifts, gambling on school grounds, and even smoking status (quite significant given the advent of e-cigarettes now common to many high school students). All of these essentially boil down to the common pathway of proximity and social referencing. As such, the notion that an increased social presence of (what will likely be) large scale, polished, mass televised sports gambling events will be associated with increased gambling behavior (and other mental health comorbidities) among youth is not far-fetched. What also is known for gambling, as well as for other addictive disorders, is that earlier age of onset is correlated to a worse prognosis of gambling disorder in adulthood. In other words, the earlier an addiction strikes, the deeper and more severe it is in the individual – further highlighting the impetus to focus concerns about the PASPA ruling toward the impact on youth.
Prevention and treatment
Lastly, it is important to consider the ground gained in preventing and treating gambling addiction. Many groups focused on treating and preventing gambling already are well established, such as Gamblers Anonymous, and these groups have produced favorable results. More targeted interventions such as cognitive-behavioral therapy adjusted for addiction disorders also have proved effective, as they often not only tackle the gambling disorder but also the collection of conditions it is so often comorbid with (affective illnesses, anxiety disorders).
Pharmacotherapy also has a role, further justifying the view of gambling disorder, and indeed all addiction disorders, as biological processes with biological solutions. Examinations into opiate antagonism and glutamatergic modulation (N-acetylcysteine) also have shown some promise. Prevention programs offer perhaps the best cost-effective ratio in reducing the societal burden of gambling, which is about $7 billion annually, according to 2013 estimates by the National Council on Problem Gambling). These programs have been conducted in schools through parent-teacher groups as well as publicly through distribution of informative psychoeducation via TV and advertising channels.
All available research conducted on treatment shows that further research and validation are needed. We should not pretend that increasing access to sports betting and normalizing the activity will not have an effect on gambling prevalence and problems. Prevention, even simple cautionary public warnings, requires time, money, and planning for effective execution.
Dr. Wenzinger is a clinical fellow, PGY-4, in the department of child and adolescent psychiatry at St. Louis Children’s Hospital. Dr. Gold is the 17th Distinguished Alumni Professor at the University of Florida, Gainesville, and professor of psychiatry (adjunct) at Washington University in St. Louis. He also serves as chairman of the scientific advisory boards for RiverMend Health.
The Supreme Court decision to overturn the federal law that prohibited state-sanctioned college and professional sports betting is bad news for clinicians who treat patients with addictions.
On May 14, the high court ruled 7-2 that the 1992 law, called the Professional and Amateur Sports Protection Act (PASPA), was unconstitutional. Now every state is free to operate, sponsor, promote, license, advertise, or authorize gambling for any college or professional sport–based event.
Optimistic outlooks on the death of PASPA include the foreseen opportunity by the states to tax and generate revenue on such gambling. Proponents of the ruling also argue that illegal activity that thrived on sports betting will now end.
But to what extent will either of those scenarios benefit the public?
If passage of various state marijuana laws is any example, assumptions that legal avenues will usurp illegal enterprises are flawed. Also, taxation likely will generate a large sum of revenue for each state. But those revenues might be offset by subsequent changes that will be needed in mental health, addiction, and wellness programs – a difficult proposition given the opioid epidemic already overburdening the country. Remember the tobacco cases and promise of state support for education, treatment, and other noble activities? Addiction medicine specialists worry that taxes collected by the states, and promises to prevent and treat gambling problems – and prevent addiction – will not end up in those coffers.
As clinicians, perhaps our most important contribution to the debates on this ruling lies in raising awareness of pathological gambling as an addiction disorder.
Redefining the act of gambling
Breaking down previous barriers to access and increasing convenience to gambling undoubtedly will be associated with increased pathological engagement in gambling. This conclusion is clear, based on past national experiments with substances of addiction (such as alcohol prohibition).
Since the cocaine epidemic of the 1980s, and our increased understanding that addictions need not have prominent withdrawal syndromes, we have focused on addiction as a fatal attraction. Psychiatrists and other clinicians made the case – in some quarters, at least – for sugar, sex, and Internet compulsivity as addictions. Compared with those addictions, the evidence was clearest and most compelling for pathological gambling as an addiction disorder. Indeed, gambling disorder was introduced in 2013 to the DSM-5 as the very first non–substance-based addictive disorder. This was a decisive change, as it recognizes that gambling is more than an environmental hazard for those suffering from dopamine-driven obsessive-compulsive-like dysfunction (the DSM section where it had lived previously). Instead, gambling acts as an agent that can initiate a usurpation of the brain’s reward circuitry. (In addition, this change has reopened the door for other increasingly recognized non–substance-based disorder categories such as video game and pornography addiction, and others.)
Gambling disorder certainly fits well into what many experts view as the essential phenotype of any addiction: Continued use despite harm, waning self-control over engagement, a craving state, and compulsive use. Current research is expanding rapidly and filling in the theoretical framework, strongly supporting gambling disorder based on biological evidence. Much of what we now know about the biology of addiction has been through the efforts of the Yale University–based research group, led by psychiatrist Marc N. Potenza. Dr. Potenza and his colleagues have been investigating gambling disorder in a thorough manner (Harv Rev Psychiatry. 2015 Mar-Apr;23[2]:134-46) and (Curr Treat Options Psychiatry. 2014 Jun 1;1[2]:189-203). Indeed, gambling disorder is much like the other substance-use disorders in which it is grouped, in that it has been found to share some similarities/pathways common to all addictions while also carrying its own specific nuances.
Twin studies have unearthed a wealth of information, such as knowledge that environmental factors seem to be the predominant source of the comorbid development of gambling disorder with the more socially acceptable substances as associated use disorders (alcohol, tobacco, and marijuana) through mechanisms such as peer association and place preference conditioning. Similarly, genetic influences also might be meaningful to treatment. For example, one finding showed that patients with gambling disorder and a family history of alcoholism were found to more preferentially respond to opioid-receptor antagonists as treatment for gambling disorder, compared with individuals without such family history (Psychopharmacology [Berl]. 2008;200[4]:521-7).
Explorations of neurotransmitter involvement and brain connectivity also have been conducted for gambling behaviors. Dopaminergic underpinnings of addiction have been particularly indicated in imaging studies focused on the ventral striatum and other components of reward circuitry. In addition, functional MRI studies have identified both overlapping and discordant brain imaging findings between gambling and many other substance use disorders such as cocaine. All these indicate that gambling seems, like its use-disorder counterparts, to follow a similar but distinct course of hijacking reward systems and priming the brain to seek out further gambling in a pathological manner.
Vulnerable populations
Another key finding of recent research exploring the biological foundations of gambling disorder is gender dimorphism. In numerous studies, women have been found to experience a “telescoping effect” from gambling, compared with their male counterparts, where they seem to more quickly advance from first exposure to problematic use. This phenomenon also is seen in women who use cocaine. Also, functional MRI studies also have found that women appear to have alternative signal changes in regions germane to addiction, compared with their male counterparts. One such example was greater activity in the hippocampus and middle temporal gyrus in women, suggestive of stronger activation of regions key for memory retrieval used in craving/urge-related emotions. These data highlight the need for not only understanding how gambling and other addictions diverge between men and women, but also for how prevention and treatment of these disorders might differ based on sex.
Adolescents also get special consideration: How will they be affected by this expected growth in gambling avenues? Adolescence and young adulthood are periods of development defined by increased impulsivity and risk taking, making this population particularly vulnerable to addiction that can then persist into adulthood. It is expected that age laws will persist and prevent the legal access adults might enjoy, but shifts in opinions of harm and ease of access are likely to contribute to increased gambling exposure. To use another addictive phenomena as an example, data from the Substance Abuse and Mental Health Services Administration show a clear correlation between marijuana use, marijuana legal status, and perceptions of risk. Specifically, areas with unfettered/loosened marijuana regulation have much lower levels of perceived risk among youth and much higher levels of use. Gambling could follow a similar course.
Perhaps the most crucial observation is that the most severe pathological gamblers began gambling before adulthood. Many factors have been identified that seem to increase rates of gambling in youth: Receiving scratch-off lotto cards as gifts, gambling on school grounds, and even smoking status (quite significant given the advent of e-cigarettes now common to many high school students). All of these essentially boil down to the common pathway of proximity and social referencing. As such, the notion that an increased social presence of (what will likely be) large scale, polished, mass televised sports gambling events will be associated with increased gambling behavior (and other mental health comorbidities) among youth is not far-fetched. What also is known for gambling, as well as for other addictive disorders, is that earlier age of onset is correlated to a worse prognosis of gambling disorder in adulthood. In other words, the earlier an addiction strikes, the deeper and more severe it is in the individual – further highlighting the impetus to focus concerns about the PASPA ruling toward the impact on youth.
Prevention and treatment
Lastly, it is important to consider the ground gained in preventing and treating gambling addiction. Many groups focused on treating and preventing gambling already are well established, such as Gamblers Anonymous, and these groups have produced favorable results. More targeted interventions such as cognitive-behavioral therapy adjusted for addiction disorders also have proved effective, as they often not only tackle the gambling disorder but also the collection of conditions it is so often comorbid with (affective illnesses, anxiety disorders).
Pharmacotherapy also has a role, further justifying the view of gambling disorder, and indeed all addiction disorders, as biological processes with biological solutions. Examinations into opiate antagonism and glutamatergic modulation (N-acetylcysteine) also have shown some promise. Prevention programs offer perhaps the best cost-effective ratio in reducing the societal burden of gambling, which is about $7 billion annually, according to 2013 estimates by the National Council on Problem Gambling). These programs have been conducted in schools through parent-teacher groups as well as publicly through distribution of informative psychoeducation via TV and advertising channels.
All available research conducted on treatment shows that further research and validation are needed. We should not pretend that increasing access to sports betting and normalizing the activity will not have an effect on gambling prevalence and problems. Prevention, even simple cautionary public warnings, requires time, money, and planning for effective execution.
Dr. Wenzinger is a clinical fellow, PGY-4, in the department of child and adolescent psychiatry at St. Louis Children’s Hospital. Dr. Gold is the 17th Distinguished Alumni Professor at the University of Florida, Gainesville, and professor of psychiatry (adjunct) at Washington University in St. Louis. He also serves as chairman of the scientific advisory boards for RiverMend Health.
Debunking Atopic Dermatitis Myths: Should You Use Systemic Therapy?
Myth: Because atopic dermatitis is skin-deep, systemic therapy is unnecessary.
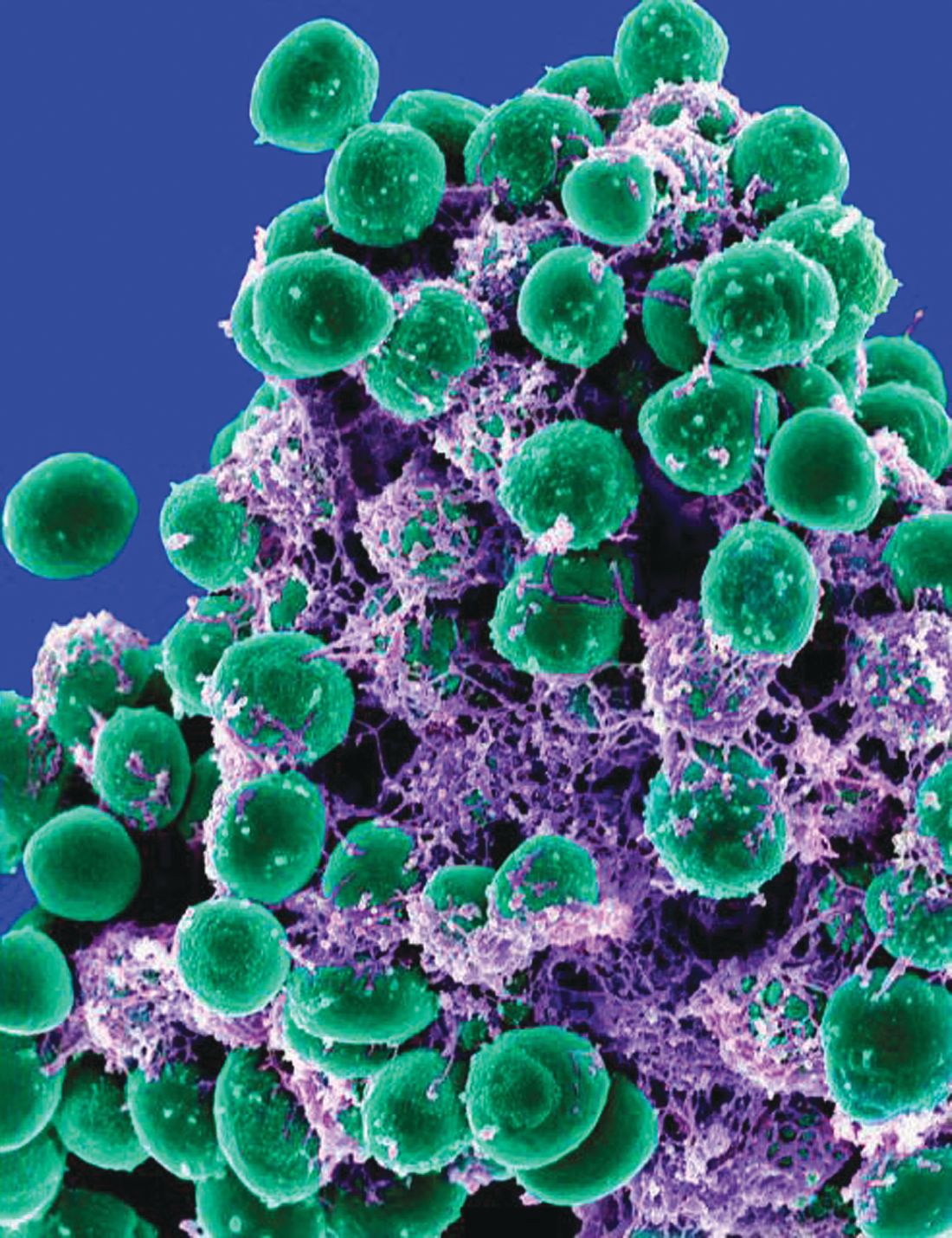
Although atopic dermatitis (AD) primarily is known as a skin condition, recent research has indicated that it may be the start of the “atopic march” leading to the development of 1 or more other atopic conditions with multiorgan involvement. In infancy AD can progress to asthma and allergic rhinitis. Adult AD can be accompanied by systemic diseases such as inflammatory bowel disease, nephritic syndrome, and others. There also is a link between impairment of epidermal barrier function and disturbed skin microbiome in patients with AD. Therefore, systemic therapy may be warranted; the question is when should you use systemic therapy?
Most AD patients have mild to moderate disease that responds well to emollients and avoidance of disease triggers and other skin irritants. However, many AD patients experience a more severe disease course that does not respond adequately to topical therapy. For these patients, systemic therapy is a viable treatment option to improve quality of life (QOL), prevent flares, and control skin inflammation and other AD symptoms.
In 2017 an expert panel of the International Eczema Council proposed an algorithm to be used to determine if systemic therapy is warranted in patients with AD. Dermatologists must consider disease severity, impact on QOL, and risks and benefits of systemic therapies. Before starting systemic therapy, the panel recommends the following:
- Consider alternate or concomitant diagnoses
- Avoid triggers
- Optimize topical therapy
- Ensure adequate patient/caregiver education
- Treat coexistent infection
- Assess QOL
- Consider phototherapy
The American Academy of Dermatology established Guidelines of Care for the Management of AD in 2014, which provide recommendations for the most efficacious systemic agents.
Armed with these guidelines, dermatologists can work with patients to determine the most appropriate treatment course for this condition that is more than skin-deep.
Expert Commentary
Atopic dermatitis is a skin barrier abnormality that causes inflammatory skin disease and an inflammatory disorder triggering abnormal barrier. Whether we choose the outside-in or inside-out approach, it is clear that there is a systemic inflammation associated with skin disease. It is true that children respond well to barrier repair and topical therapy in many settings, as do many adults. However, chronic skin inflammation is not in isolation, triggering mucosal barrier changes allowing for more sensitization to foods and respiratory allergens as well as systemic inflammation in adults. Despite the utility of systemic steroids, the side effects generally outweigh benefit. On the other hand, phototherapy and systemic agents can clear skin and induce remissions and improved QOL. The AAD guidelines were reported before US Food and Drug Administration approval of newer agents such as dupilumab, leaving it up to the dermatologist to find the niche for this first biologic agent for AD.
—Nanette B. Silverberg, MD
Suggested Readings
Darlenski R, Kazandjieva J, Hristakieva E, et al. Atopic dermatitis as a systemic disease [published online November 22, 2013]. Clin Dermatol. 2014;32:409-413.
Sidbury R, Davis DM, Cohen DE, et al; American Academy of Dermatology. Guidelines of care for the management of atopic dermatitis: section 3. management and treatment with phototherapy and systemic agents [published online May 9, 2014]. J Am Acad Dermatol. 2014;71:327-349.
Simpson EL, Bruin-Weller M, Flohr C, et al. When does atopic dermatitis warrant systemic therapy? recommendations from an expert panel of the International Eczema Council [published online August 10, 2017]. J Am Acad Dermatol. 2017;77:623-633.
Thomas CL, Fernández-Peñas P. The microbiome and atopic eczema: more than skin deep [published online January 28, 2016]. Australas J Dermatol. 2017;58:18-24.
Myth: Because atopic dermatitis is skin-deep, systemic therapy is unnecessary.
Although atopic dermatitis (AD) primarily is known as a skin condition, recent research has indicated that it may be the start of the “atopic march” leading to the development of 1 or more other atopic conditions with multiorgan involvement. In infancy AD can progress to asthma and allergic rhinitis. Adult AD can be accompanied by systemic diseases such as inflammatory bowel disease, nephritic syndrome, and others. There also is a link between impairment of epidermal barrier function and disturbed skin microbiome in patients with AD. Therefore, systemic therapy may be warranted; the question is when should you use systemic therapy?
Most AD patients have mild to moderate disease that responds well to emollients and avoidance of disease triggers and other skin irritants. However, many AD patients experience a more severe disease course that does not respond adequately to topical therapy. For these patients, systemic therapy is a viable treatment option to improve quality of life (QOL), prevent flares, and control skin inflammation and other AD symptoms.
In 2017 an expert panel of the International Eczema Council proposed an algorithm to be used to determine if systemic therapy is warranted in patients with AD. Dermatologists must consider disease severity, impact on QOL, and risks and benefits of systemic therapies. Before starting systemic therapy, the panel recommends the following:
- Consider alternate or concomitant diagnoses
- Avoid triggers
- Optimize topical therapy
- Ensure adequate patient/caregiver education
- Treat coexistent infection
- Assess QOL
- Consider phototherapy
The American Academy of Dermatology established Guidelines of Care for the Management of AD in 2014, which provide recommendations for the most efficacious systemic agents.
Armed with these guidelines, dermatologists can work with patients to determine the most appropriate treatment course for this condition that is more than skin-deep.
Expert Commentary
Atopic dermatitis is a skin barrier abnormality that causes inflammatory skin disease and an inflammatory disorder triggering abnormal barrier. Whether we choose the outside-in or inside-out approach, it is clear that there is a systemic inflammation associated with skin disease. It is true that children respond well to barrier repair and topical therapy in many settings, as do many adults. However, chronic skin inflammation is not in isolation, triggering mucosal barrier changes allowing for more sensitization to foods and respiratory allergens as well as systemic inflammation in adults. Despite the utility of systemic steroids, the side effects generally outweigh benefit. On the other hand, phototherapy and systemic agents can clear skin and induce remissions and improved QOL. The AAD guidelines were reported before US Food and Drug Administration approval of newer agents such as dupilumab, leaving it up to the dermatologist to find the niche for this first biologic agent for AD.
—Nanette B. Silverberg, MD
Suggested Readings
Darlenski R, Kazandjieva J, Hristakieva E, et al. Atopic dermatitis as a systemic disease [published online November 22, 2013]. Clin Dermatol. 2014;32:409-413.
Sidbury R, Davis DM, Cohen DE, et al; American Academy of Dermatology. Guidelines of care for the management of atopic dermatitis: section 3. management and treatment with phototherapy and systemic agents [published online May 9, 2014]. J Am Acad Dermatol. 2014;71:327-349.
Simpson EL, Bruin-Weller M, Flohr C, et al. When does atopic dermatitis warrant systemic therapy? recommendations from an expert panel of the International Eczema Council [published online August 10, 2017]. J Am Acad Dermatol. 2017;77:623-633.
Thomas CL, Fernández-Peñas P. The microbiome and atopic eczema: more than skin deep [published online January 28, 2016]. Australas J Dermatol. 2017;58:18-24.
Myth: Because atopic dermatitis is skin-deep, systemic therapy is unnecessary.
Although atopic dermatitis (AD) primarily is known as a skin condition, recent research has indicated that it may be the start of the “atopic march” leading to the development of 1 or more other atopic conditions with multiorgan involvement. In infancy AD can progress to asthma and allergic rhinitis. Adult AD can be accompanied by systemic diseases such as inflammatory bowel disease, nephritic syndrome, and others. There also is a link between impairment of epidermal barrier function and disturbed skin microbiome in patients with AD. Therefore, systemic therapy may be warranted; the question is when should you use systemic therapy?
Most AD patients have mild to moderate disease that responds well to emollients and avoidance of disease triggers and other skin irritants. However, many AD patients experience a more severe disease course that does not respond adequately to topical therapy. For these patients, systemic therapy is a viable treatment option to improve quality of life (QOL), prevent flares, and control skin inflammation and other AD symptoms.
In 2017 an expert panel of the International Eczema Council proposed an algorithm to be used to determine if systemic therapy is warranted in patients with AD. Dermatologists must consider disease severity, impact on QOL, and risks and benefits of systemic therapies. Before starting systemic therapy, the panel recommends the following:
- Consider alternate or concomitant diagnoses
- Avoid triggers
- Optimize topical therapy
- Ensure adequate patient/caregiver education
- Treat coexistent infection
- Assess QOL
- Consider phototherapy
The American Academy of Dermatology established Guidelines of Care for the Management of AD in 2014, which provide recommendations for the most efficacious systemic agents.
Armed with these guidelines, dermatologists can work with patients to determine the most appropriate treatment course for this condition that is more than skin-deep.
Expert Commentary
Atopic dermatitis is a skin barrier abnormality that causes inflammatory skin disease and an inflammatory disorder triggering abnormal barrier. Whether we choose the outside-in or inside-out approach, it is clear that there is a systemic inflammation associated with skin disease. It is true that children respond well to barrier repair and topical therapy in many settings, as do many adults. However, chronic skin inflammation is not in isolation, triggering mucosal barrier changes allowing for more sensitization to foods and respiratory allergens as well as systemic inflammation in adults. Despite the utility of systemic steroids, the side effects generally outweigh benefit. On the other hand, phototherapy and systemic agents can clear skin and induce remissions and improved QOL. The AAD guidelines were reported before US Food and Drug Administration approval of newer agents such as dupilumab, leaving it up to the dermatologist to find the niche for this first biologic agent for AD.
—Nanette B. Silverberg, MD
Suggested Readings
Darlenski R, Kazandjieva J, Hristakieva E, et al. Atopic dermatitis as a systemic disease [published online November 22, 2013]. Clin Dermatol. 2014;32:409-413.
Sidbury R, Davis DM, Cohen DE, et al; American Academy of Dermatology. Guidelines of care for the management of atopic dermatitis: section 3. management and treatment with phototherapy and systemic agents [published online May 9, 2014]. J Am Acad Dermatol. 2014;71:327-349.
Simpson EL, Bruin-Weller M, Flohr C, et al. When does atopic dermatitis warrant systemic therapy? recommendations from an expert panel of the International Eczema Council [published online August 10, 2017]. J Am Acad Dermatol. 2017;77:623-633.
Thomas CL, Fernández-Peñas P. The microbiome and atopic eczema: more than skin deep [published online January 28, 2016]. Australas J Dermatol. 2017;58:18-24.
The demise of family dinners may play role in picky eating
My wife and I have dinner together almost every evening. There is a candle on the table regardless of the menu. And the meal begins with a toast, usually “To this chance to be together.” I can hear you muttering to yourself, “They must be one of those sappy, sweet hand-holding couples that appear to be joined at the hip.” Far from it, we lead very busy, active, but separate lives that only rarely intersect. But we make it a priority that one of those intersections occurs at a meal. For us, an evening dinner works best.
Listening to our friends, we have learned that an increasing number of them have drifted away from sharing a meal together. This phenomenon is surprising because most of them are retired, and time is not an issue. Of course, it is no secret that, for young overscheduled families, sitting down for a shared dining experience is becoming increasingly less frequent. Like some of you, I would like to claim that a return to family meal times would solve all of society’s ills. But some of the literature supporting this claim suggests shared family experiences in general, not particularly those associated with eating, may be just as important in supporting emotional health. But because everyone needs to eat, meals seem to me to be the easy target, low-hanging fruit if you will.
It is interesting that parents’ reports of their children’s eating patterns were validated by the behaviors videotaped by the researchers. But what is really interesting is that children who grew up in households where mealtimes followed a routine were more likely to be in the low–picky eating group. Routines included things like having a specific place times for eating, a habitual way of serving food, and other rituals such as saying grace.
Unfortunately, because this Michigan study began at age 4 years it doesn’t tell us if the worst picky eaters were that way from the beginning. I suspect that some were. But my hunch is that picky eaters who are managed in a home environment that includes mealtime rituals and puts dining together as a high priority are more likely to outgrow their pickiness.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater: A Guide for the Perplexed Parent.” Email him at [email protected].
My wife and I have dinner together almost every evening. There is a candle on the table regardless of the menu. And the meal begins with a toast, usually “To this chance to be together.” I can hear you muttering to yourself, “They must be one of those sappy, sweet hand-holding couples that appear to be joined at the hip.” Far from it, we lead very busy, active, but separate lives that only rarely intersect. But we make it a priority that one of those intersections occurs at a meal. For us, an evening dinner works best.
Listening to our friends, we have learned that an increasing number of them have drifted away from sharing a meal together. This phenomenon is surprising because most of them are retired, and time is not an issue. Of course, it is no secret that, for young overscheduled families, sitting down for a shared dining experience is becoming increasingly less frequent. Like some of you, I would like to claim that a return to family meal times would solve all of society’s ills. But some of the literature supporting this claim suggests shared family experiences in general, not particularly those associated with eating, may be just as important in supporting emotional health. But because everyone needs to eat, meals seem to me to be the easy target, low-hanging fruit if you will.
It is interesting that parents’ reports of their children’s eating patterns were validated by the behaviors videotaped by the researchers. But what is really interesting is that children who grew up in households where mealtimes followed a routine were more likely to be in the low–picky eating group. Routines included things like having a specific place times for eating, a habitual way of serving food, and other rituals such as saying grace.
Unfortunately, because this Michigan study began at age 4 years it doesn’t tell us if the worst picky eaters were that way from the beginning. I suspect that some were. But my hunch is that picky eaters who are managed in a home environment that includes mealtime rituals and puts dining together as a high priority are more likely to outgrow their pickiness.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater: A Guide for the Perplexed Parent.” Email him at [email protected].
My wife and I have dinner together almost every evening. There is a candle on the table regardless of the menu. And the meal begins with a toast, usually “To this chance to be together.” I can hear you muttering to yourself, “They must be one of those sappy, sweet hand-holding couples that appear to be joined at the hip.” Far from it, we lead very busy, active, but separate lives that only rarely intersect. But we make it a priority that one of those intersections occurs at a meal. For us, an evening dinner works best.
Listening to our friends, we have learned that an increasing number of them have drifted away from sharing a meal together. This phenomenon is surprising because most of them are retired, and time is not an issue. Of course, it is no secret that, for young overscheduled families, sitting down for a shared dining experience is becoming increasingly less frequent. Like some of you, I would like to claim that a return to family meal times would solve all of society’s ills. But some of the literature supporting this claim suggests shared family experiences in general, not particularly those associated with eating, may be just as important in supporting emotional health. But because everyone needs to eat, meals seem to me to be the easy target, low-hanging fruit if you will.
It is interesting that parents’ reports of their children’s eating patterns were validated by the behaviors videotaped by the researchers. But what is really interesting is that children who grew up in households where mealtimes followed a routine were more likely to be in the low–picky eating group. Routines included things like having a specific place times for eating, a habitual way of serving food, and other rituals such as saying grace.
Unfortunately, because this Michigan study began at age 4 years it doesn’t tell us if the worst picky eaters were that way from the beginning. I suspect that some were. But my hunch is that picky eaters who are managed in a home environment that includes mealtime rituals and puts dining together as a high priority are more likely to outgrow their pickiness.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater: A Guide for the Perplexed Parent.” Email him at [email protected].
The work schedule that prevents burnout
The schedule is easier to change than the work itself
Burnout is influenced by a seemingly infinite combination of variables. An optimal schedule alone isn’t the key to preventing it, but maybe a good schedule can reduce your risk you’ll suffer from it.
Smart people who have spent years as hospitalists, working multiple different schedules, have formed a variety of conclusions about which work schedules best reduce the risk of burnout. There’s no meaningful research to settle the question, so everyone will have to reach their own conclusions, as I’ve done here.
Scheduling flexibility: Often overlooked?
Someone who typically works the same number of consecutive day shifts, each of which is the same duration, might suffer from the monotony and inexorable predictability. Schedules that vary the number of consecutive day shifts, the intensity or length of shifts, and the number of consecutive days off might result in lower rates of burnout. This is especially likely to be the case if each provider has some flexibility to control how her schedule varies over time.
Personal time goes on the calendar first
Those who have a regularly repeating work schedule tend to work hard arranging such important things as family vacations on days the schedule dictates. In other words, the first thing that goes on the personal calendar are the weeks of work; they’re “X-ed” out and personal events filled into the remaining days.
That’s fine for many personal activities, but it means the hospitalist might tend to set a pretty high bar for activities that are worth negotiating alterations to the usual schedule. For example, you might want to see U2 but decide to skip their concert in your town since it falls in the middle of your regularly scheduled week of work. Maybe that’s not a big deal (Isn’t U2 overplayed and out of date anyway?), but an accumulation of small sacrifices like this might increase resentment of work.
It’s possible to organize a hospitalist group schedule in which each provider’s personally requested days off, like the U2 concert, go on the work calendar first, and the clinical schedule is built around them. It can get pretty time consuming to manage, but might be a worthwhile investment to reduce burnout risk.
A paradox: Fewer shifts could increase burnout risk
I’m convinced many hospitalists make the mistake of seeking to maximize their number of days off with the idea that it will be good for happiness, career longevity, burnout, etc. While having more days off provides more time for nonwork activities and rest/recovery from work, it usually means the average workday is busier and more stressful to maintain expected levels of productivity. The net effect for some seems to be increased burnout.
Consider someone who has been working 182 hospitalist shifts and generating a total of 2,114 billed encounters annually (both are the most recent national medians available from surveys). This hospitalist successfully negotiates a reduction to 161 annual shifts. This would probably feel good to anyone at first, but keep in mind that it means the average number of daily encounters to maintain median annual productivity would increase 13% (from 11.6 to 13.1 in this example). That is, each day of work just got 13% busier.
I regularly encounter career hospitalists with more than 10 years of experience who say they still appreciate – or even are addicted to – having lots of days off. But the worked days often are so busy they don’t know how long they can keep doing it. It is possible some of them might be happier and less burned out if they work more shifts annually, and the average shift is meaningfully less busy.
The “right” number of shifts depends on a combination of personal and economic factors. Rather than focusing almost exclusively on the number of shifts worked annually, it may be better to think about the total amount of annual work measured in billed encounters, or wRVUs [work relative value units], and how it is titrated out on the calendar.
Other scheduling attributes and burnout
I think it’s really important to ensure the hospitalist group always has the target number of providers working each day. Many groups have experienced staffing deficits for so long that they’ve essentially given up on this goal, and staffing levels vary day to day. This means each provider has uncertainty regarding how often he will be scheduled on days with fewer than the targeted numbers of providers working.
All hospitalist groups should ensure their schedule has day-shift providers work a meaningful series of shifts consecutively to support good patient-provider continuity. I think “continuity is king” and influences efficiency, quality of care, and provider burnout. Of course, there is tension between working many consecutive day shifts and still having a reasonable lifestyle; you’ll have to make up your own mind about the sweet spot between these to competing needs.
Schedule and number of shifts are only part of the burnout picture. The nature of hospitalist work, including EHR frustrations and distressing conversations regarding observation status, etc., probably has more significant influence on burnout and job satisfaction than does the work schedule itself.
But there is still lots of value in thinking carefully about your group’s work schedule and making adjustments where needed. The schedule is a lot easier to change than the nature of the work itself.
Dr. Nelson has had a career in clinical practice as a hospitalist starting in 1988. He is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses. Contact him at [email protected].
The schedule is easier to change than the work itself
The schedule is easier to change than the work itself
Burnout is influenced by a seemingly infinite combination of variables. An optimal schedule alone isn’t the key to preventing it, but maybe a good schedule can reduce your risk you’ll suffer from it.
Smart people who have spent years as hospitalists, working multiple different schedules, have formed a variety of conclusions about which work schedules best reduce the risk of burnout. There’s no meaningful research to settle the question, so everyone will have to reach their own conclusions, as I’ve done here.
Scheduling flexibility: Often overlooked?
Someone who typically works the same number of consecutive day shifts, each of which is the same duration, might suffer from the monotony and inexorable predictability. Schedules that vary the number of consecutive day shifts, the intensity or length of shifts, and the number of consecutive days off might result in lower rates of burnout. This is especially likely to be the case if each provider has some flexibility to control how her schedule varies over time.
Personal time goes on the calendar first
Those who have a regularly repeating work schedule tend to work hard arranging such important things as family vacations on days the schedule dictates. In other words, the first thing that goes on the personal calendar are the weeks of work; they’re “X-ed” out and personal events filled into the remaining days.
That’s fine for many personal activities, but it means the hospitalist might tend to set a pretty high bar for activities that are worth negotiating alterations to the usual schedule. For example, you might want to see U2 but decide to skip their concert in your town since it falls in the middle of your regularly scheduled week of work. Maybe that’s not a big deal (Isn’t U2 overplayed and out of date anyway?), but an accumulation of small sacrifices like this might increase resentment of work.
It’s possible to organize a hospitalist group schedule in which each provider’s personally requested days off, like the U2 concert, go on the work calendar first, and the clinical schedule is built around them. It can get pretty time consuming to manage, but might be a worthwhile investment to reduce burnout risk.
A paradox: Fewer shifts could increase burnout risk
I’m convinced many hospitalists make the mistake of seeking to maximize their number of days off with the idea that it will be good for happiness, career longevity, burnout, etc. While having more days off provides more time for nonwork activities and rest/recovery from work, it usually means the average workday is busier and more stressful to maintain expected levels of productivity. The net effect for some seems to be increased burnout.
Consider someone who has been working 182 hospitalist shifts and generating a total of 2,114 billed encounters annually (both are the most recent national medians available from surveys). This hospitalist successfully negotiates a reduction to 161 annual shifts. This would probably feel good to anyone at first, but keep in mind that it means the average number of daily encounters to maintain median annual productivity would increase 13% (from 11.6 to 13.1 in this example). That is, each day of work just got 13% busier.
I regularly encounter career hospitalists with more than 10 years of experience who say they still appreciate – or even are addicted to – having lots of days off. But the worked days often are so busy they don’t know how long they can keep doing it. It is possible some of them might be happier and less burned out if they work more shifts annually, and the average shift is meaningfully less busy.
The “right” number of shifts depends on a combination of personal and economic factors. Rather than focusing almost exclusively on the number of shifts worked annually, it may be better to think about the total amount of annual work measured in billed encounters, or wRVUs [work relative value units], and how it is titrated out on the calendar.
Other scheduling attributes and burnout
I think it’s really important to ensure the hospitalist group always has the target number of providers working each day. Many groups have experienced staffing deficits for so long that they’ve essentially given up on this goal, and staffing levels vary day to day. This means each provider has uncertainty regarding how often he will be scheduled on days with fewer than the targeted numbers of providers working.
All hospitalist groups should ensure their schedule has day-shift providers work a meaningful series of shifts consecutively to support good patient-provider continuity. I think “continuity is king” and influences efficiency, quality of care, and provider burnout. Of course, there is tension between working many consecutive day shifts and still having a reasonable lifestyle; you’ll have to make up your own mind about the sweet spot between these to competing needs.
Schedule and number of shifts are only part of the burnout picture. The nature of hospitalist work, including EHR frustrations and distressing conversations regarding observation status, etc., probably has more significant influence on burnout and job satisfaction than does the work schedule itself.
But there is still lots of value in thinking carefully about your group’s work schedule and making adjustments where needed. The schedule is a lot easier to change than the nature of the work itself.
Dr. Nelson has had a career in clinical practice as a hospitalist starting in 1988. He is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses. Contact him at [email protected].
Burnout is influenced by a seemingly infinite combination of variables. An optimal schedule alone isn’t the key to preventing it, but maybe a good schedule can reduce your risk you’ll suffer from it.
Smart people who have spent years as hospitalists, working multiple different schedules, have formed a variety of conclusions about which work schedules best reduce the risk of burnout. There’s no meaningful research to settle the question, so everyone will have to reach their own conclusions, as I’ve done here.
Scheduling flexibility: Often overlooked?
Someone who typically works the same number of consecutive day shifts, each of which is the same duration, might suffer from the monotony and inexorable predictability. Schedules that vary the number of consecutive day shifts, the intensity or length of shifts, and the number of consecutive days off might result in lower rates of burnout. This is especially likely to be the case if each provider has some flexibility to control how her schedule varies over time.
Personal time goes on the calendar first
Those who have a regularly repeating work schedule tend to work hard arranging such important things as family vacations on days the schedule dictates. In other words, the first thing that goes on the personal calendar are the weeks of work; they’re “X-ed” out and personal events filled into the remaining days.
That’s fine for many personal activities, but it means the hospitalist might tend to set a pretty high bar for activities that are worth negotiating alterations to the usual schedule. For example, you might want to see U2 but decide to skip their concert in your town since it falls in the middle of your regularly scheduled week of work. Maybe that’s not a big deal (Isn’t U2 overplayed and out of date anyway?), but an accumulation of small sacrifices like this might increase resentment of work.
It’s possible to organize a hospitalist group schedule in which each provider’s personally requested days off, like the U2 concert, go on the work calendar first, and the clinical schedule is built around them. It can get pretty time consuming to manage, but might be a worthwhile investment to reduce burnout risk.
A paradox: Fewer shifts could increase burnout risk
I’m convinced many hospitalists make the mistake of seeking to maximize their number of days off with the idea that it will be good for happiness, career longevity, burnout, etc. While having more days off provides more time for nonwork activities and rest/recovery from work, it usually means the average workday is busier and more stressful to maintain expected levels of productivity. The net effect for some seems to be increased burnout.
Consider someone who has been working 182 hospitalist shifts and generating a total of 2,114 billed encounters annually (both are the most recent national medians available from surveys). This hospitalist successfully negotiates a reduction to 161 annual shifts. This would probably feel good to anyone at first, but keep in mind that it means the average number of daily encounters to maintain median annual productivity would increase 13% (from 11.6 to 13.1 in this example). That is, each day of work just got 13% busier.
I regularly encounter career hospitalists with more than 10 years of experience who say they still appreciate – or even are addicted to – having lots of days off. But the worked days often are so busy they don’t know how long they can keep doing it. It is possible some of them might be happier and less burned out if they work more shifts annually, and the average shift is meaningfully less busy.
The “right” number of shifts depends on a combination of personal and economic factors. Rather than focusing almost exclusively on the number of shifts worked annually, it may be better to think about the total amount of annual work measured in billed encounters, or wRVUs [work relative value units], and how it is titrated out on the calendar.
Other scheduling attributes and burnout
I think it’s really important to ensure the hospitalist group always has the target number of providers working each day. Many groups have experienced staffing deficits for so long that they’ve essentially given up on this goal, and staffing levels vary day to day. This means each provider has uncertainty regarding how often he will be scheduled on days with fewer than the targeted numbers of providers working.
All hospitalist groups should ensure their schedule has day-shift providers work a meaningful series of shifts consecutively to support good patient-provider continuity. I think “continuity is king” and influences efficiency, quality of care, and provider burnout. Of course, there is tension between working many consecutive day shifts and still having a reasonable lifestyle; you’ll have to make up your own mind about the sweet spot between these to competing needs.
Schedule and number of shifts are only part of the burnout picture. The nature of hospitalist work, including EHR frustrations and distressing conversations regarding observation status, etc., probably has more significant influence on burnout and job satisfaction than does the work schedule itself.
But there is still lots of value in thinking carefully about your group’s work schedule and making adjustments where needed. The schedule is a lot easier to change than the nature of the work itself.
Dr. Nelson has had a career in clinical practice as a hospitalist starting in 1988. He is cofounder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is codirector for SHM’s practice management courses. Contact him at [email protected].
Thyroid markers linked to risk of gestational diabetes
Thyroid dysfunction early in pregnancy may increase risk of gestational diabetes, results of a longitudinal study suggest.
Increased levels of free triiodothyronine (fT3) and the ratio of fT3 to free thyroxine (fT4) were associated with increased risk of this common metabolic complication of pregnancy, study authors reported in the Journal of Clinical Endocrinology & Metabolism.
“To our knowledge, this is the first study to identify fT3 and the fT3:fT4 ratio measured early in pregnancy as independent risk factors of gestational diabetes,” wrote Shristi Rawal, PhD, of the National Institute of Child Health and Human Development (NICHD) , and her colleagues.
Although routine thyroid function screening during pregnancy remains controversial, Dr. Rawal and colleagues said their results support the “potential benefits” of the practice, particularly in light of other recent evidence suggesting thyroid-related adverse pregnancy outcomes.
The current case control study by Dr. Rawal and her coinvestigators included 107 women with gestational diabetes and 214 nongestational diabetes controls selected from a 12-center pregnancy cohort, which included 2,802 women aged between 18 and 40 years. The thyroid markers fT3, fT4, and thyroid-stimulating hormone (TSH) were measured at four pregnancy visits, including first trimester (weeks 10-14) and second trimester (weeks 15-26).
The fT3:fT4 ratio had the strongest association with gestational diabetes. In the second trimester measurement, women in the highest quartile had an almost 14-fold increase in risk when compared to the lowest quartile, after adjusting for potential confounders including prepregnancy body mass index and diabetes family history (adjusted odds ratio, 13.60; 95% confidence interval, 3.97-46.30), Dr. Rawal and her colleagues reported. The ratio of fT3:fT4 at the first trimester was also associated with increased risk (aOR, 8.63; 95% CI, 2.87-26.00).
Similarly, fT3 was positively associated with gestational diabetes at the first trimester (aOR, 4.25; 95% CI, 1.67-10.80) and second trimester (aOR, 3.89; 95% CI, 1.50-10.10), investigators reported.
By contrast, there was no association between fT4 or TSH and gestational diabetes, they found.
“These findings, in combination with previous evidence of thyroid-related adverse pregnancy outcomes, support the benefits of thyroid screening among pregnant women in early to mid pregnancy,” senior author Cuilin Zhang, MD, MPH, PhD, of the NICHD, said in a press statement.
Thyroid function abnormalities are relatively common in pregnant women and have been associated with obstetric complications such as pregnancy loss and premature delivery, investigators noted.
Previous evidence is sparse regarding a potential link between thyroid dysfunction and gestational diabetes. There are some prospective studies that show women with hypothyroidism have an increased incidence of gestational diabetes, Dr. Rawal and her colleagues wrote. Isolated hypothyroxinema, or normal TSH and low fT4, has also been linked to increased risk in some studies, but not in others, they added.
Support for the study came from NICHD and the American Recovery and Reinvestment Act research grants. The authors reported no conflicts of interest.
SOURCE: Rawal S et al. J Clin Endocrinol Metab. 2018 Jun 7. doi: 10.1210/jc.2017-024421.
Thyroid dysfunction early in pregnancy may increase risk of gestational diabetes, results of a longitudinal study suggest.
Increased levels of free triiodothyronine (fT3) and the ratio of fT3 to free thyroxine (fT4) were associated with increased risk of this common metabolic complication of pregnancy, study authors reported in the Journal of Clinical Endocrinology & Metabolism.
“To our knowledge, this is the first study to identify fT3 and the fT3:fT4 ratio measured early in pregnancy as independent risk factors of gestational diabetes,” wrote Shristi Rawal, PhD, of the National Institute of Child Health and Human Development (NICHD) , and her colleagues.
Although routine thyroid function screening during pregnancy remains controversial, Dr. Rawal and colleagues said their results support the “potential benefits” of the practice, particularly in light of other recent evidence suggesting thyroid-related adverse pregnancy outcomes.
The current case control study by Dr. Rawal and her coinvestigators included 107 women with gestational diabetes and 214 nongestational diabetes controls selected from a 12-center pregnancy cohort, which included 2,802 women aged between 18 and 40 years. The thyroid markers fT3, fT4, and thyroid-stimulating hormone (TSH) were measured at four pregnancy visits, including first trimester (weeks 10-14) and second trimester (weeks 15-26).
The fT3:fT4 ratio had the strongest association with gestational diabetes. In the second trimester measurement, women in the highest quartile had an almost 14-fold increase in risk when compared to the lowest quartile, after adjusting for potential confounders including prepregnancy body mass index and diabetes family history (adjusted odds ratio, 13.60; 95% confidence interval, 3.97-46.30), Dr. Rawal and her colleagues reported. The ratio of fT3:fT4 at the first trimester was also associated with increased risk (aOR, 8.63; 95% CI, 2.87-26.00).
Similarly, fT3 was positively associated with gestational diabetes at the first trimester (aOR, 4.25; 95% CI, 1.67-10.80) and second trimester (aOR, 3.89; 95% CI, 1.50-10.10), investigators reported.
By contrast, there was no association between fT4 or TSH and gestational diabetes, they found.
“These findings, in combination with previous evidence of thyroid-related adverse pregnancy outcomes, support the benefits of thyroid screening among pregnant women in early to mid pregnancy,” senior author Cuilin Zhang, MD, MPH, PhD, of the NICHD, said in a press statement.
Thyroid function abnormalities are relatively common in pregnant women and have been associated with obstetric complications such as pregnancy loss and premature delivery, investigators noted.
Previous evidence is sparse regarding a potential link between thyroid dysfunction and gestational diabetes. There are some prospective studies that show women with hypothyroidism have an increased incidence of gestational diabetes, Dr. Rawal and her colleagues wrote. Isolated hypothyroxinema, or normal TSH and low fT4, has also been linked to increased risk in some studies, but not in others, they added.
Support for the study came from NICHD and the American Recovery and Reinvestment Act research grants. The authors reported no conflicts of interest.
SOURCE: Rawal S et al. J Clin Endocrinol Metab. 2018 Jun 7. doi: 10.1210/jc.2017-024421.
Thyroid dysfunction early in pregnancy may increase risk of gestational diabetes, results of a longitudinal study suggest.
Increased levels of free triiodothyronine (fT3) and the ratio of fT3 to free thyroxine (fT4) were associated with increased risk of this common metabolic complication of pregnancy, study authors reported in the Journal of Clinical Endocrinology & Metabolism.
“To our knowledge, this is the first study to identify fT3 and the fT3:fT4 ratio measured early in pregnancy as independent risk factors of gestational diabetes,” wrote Shristi Rawal, PhD, of the National Institute of Child Health and Human Development (NICHD) , and her colleagues.
Although routine thyroid function screening during pregnancy remains controversial, Dr. Rawal and colleagues said their results support the “potential benefits” of the practice, particularly in light of other recent evidence suggesting thyroid-related adverse pregnancy outcomes.
The current case control study by Dr. Rawal and her coinvestigators included 107 women with gestational diabetes and 214 nongestational diabetes controls selected from a 12-center pregnancy cohort, which included 2,802 women aged between 18 and 40 years. The thyroid markers fT3, fT4, and thyroid-stimulating hormone (TSH) were measured at four pregnancy visits, including first trimester (weeks 10-14) and second trimester (weeks 15-26).
The fT3:fT4 ratio had the strongest association with gestational diabetes. In the second trimester measurement, women in the highest quartile had an almost 14-fold increase in risk when compared to the lowest quartile, after adjusting for potential confounders including prepregnancy body mass index and diabetes family history (adjusted odds ratio, 13.60; 95% confidence interval, 3.97-46.30), Dr. Rawal and her colleagues reported. The ratio of fT3:fT4 at the first trimester was also associated with increased risk (aOR, 8.63; 95% CI, 2.87-26.00).
Similarly, fT3 was positively associated with gestational diabetes at the first trimester (aOR, 4.25; 95% CI, 1.67-10.80) and second trimester (aOR, 3.89; 95% CI, 1.50-10.10), investigators reported.
By contrast, there was no association between fT4 or TSH and gestational diabetes, they found.
“These findings, in combination with previous evidence of thyroid-related adverse pregnancy outcomes, support the benefits of thyroid screening among pregnant women in early to mid pregnancy,” senior author Cuilin Zhang, MD, MPH, PhD, of the NICHD, said in a press statement.
Thyroid function abnormalities are relatively common in pregnant women and have been associated with obstetric complications such as pregnancy loss and premature delivery, investigators noted.
Previous evidence is sparse regarding a potential link between thyroid dysfunction and gestational diabetes. There are some prospective studies that show women with hypothyroidism have an increased incidence of gestational diabetes, Dr. Rawal and her colleagues wrote. Isolated hypothyroxinema, or normal TSH and low fT4, has also been linked to increased risk in some studies, but not in others, they added.
Support for the study came from NICHD and the American Recovery and Reinvestment Act research grants. The authors reported no conflicts of interest.
SOURCE: Rawal S et al. J Clin Endocrinol Metab. 2018 Jun 7. doi: 10.1210/jc.2017-024421.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM.
Key clinical point: Thyroid dysfunction early in pregnancy may increase risk of gestational diabetes.
Major finding: The triiodothyronine to thyroxine ratio in the second trimester had the strongest association with gestational diabetes (adjusted odds ratio, 13.60; 95% confidence interval, 3.97-46.30).
Study details: A case control study including 107 gestational diabetes cases and 214 nongestational diabetes controls.
Disclosures: The authors had no disclosures. Support for the study came from the National Institute of Child Health and Human Development and the American Recovery and Reinvestment Act research grants.
Source: Rawal S et al. J Clin Endocrinol Metab. 2018 Jun 7. doi: 10.1210/jc.2017-024421.
'Systemic changes' needed for bronchoscope disinfection
as researchers found all reprocessed bronchoscopes they observed had residual contamination and over half showed microbial growth, according to results from a recent study in CHEST.
“Evidence-based, bronchoscope-specific reprocessing and maintenance guidelines are needed, along with quality management programs to ensure that these complex processes are carried out effectively,” Cori L. Ofstead, MSPH, president and CEO of Ofstead & Associates, and her colleagues wrote in their study. “Shifting toward using sterilized or single-use bronchoscopes could reduce the risk of infection transmission among vulnerable pulmonary patient populations.”
The researchers inspected 24 reprocessed bronchoscopes used clinically (9 pediatric, 9 therapeutic, 6 endobronchial ultrasound) at three U.S. tertiary care centers in 2017 and compared them with two bronchoscopes that had not been used. Of the bronchoscopes observed, all had residual contamination after manual cleaning and high-level disinfection (HLD). Manually cleaned bronchoscopes had microbial growth in 11 of 20 (55%) samples, while 14 of 24 (58%) of HLD samples contained microbial growth. Upon inspection, the researchers said they discovered “oily residue; dried fluid spots; brown, red, and white residue; scratches; insertion tube buckling; and damaged distal ends,” while internal inspections yielded “fluid, discoloration, scratches, filamentous debris, and dented channels.”
Ms. Ofstead and colleagues noted that, while the first site exceeded national guidelines, sites B and C contained technicians who did not wear personal protective equipment and the sites did not follow national or manufacturer use guidelines, such as passing bronchoscopes “through a window to a clean room for automated cleaning and HLD with peracetic acid in automated endoscope reprocessor,” flushing the bronchoscopes with alcohol, drying them with medical-grade forced air pressure, and storing them in a dedicated clean and dry area. Site A had microbial growth in 20% and 50% of manually cleaned and HLD bronchoscopes, respectively, site B had microbial growth in 100% and 75% of manually cleaned and HLD bronchoscopes, respectively, and site C had microbial growth in 83% and 50% of manually cleaned and HLD bronchoscopes, respectively. Among the microbial species identified were “environmental bacteria and normal flora” such as Bacillus spp and Staphylococcus epidermidis, molds such as Lecanicillium lecanii and Verticillium dahliae, and pathogens such as Stenotrophomonas maltophilia and Escherichia coli/Shigella spp.
“The clinical implications for patients are unknown as the study did not involve assessing patients or reviewing medical records,” Ms. Ofstead and her colleagues wrote. “However, the results are worrisome as patients undergoing bronchoscopy are commonly at high risk for infection due to transplant status, critical illness, or immune suppression due to malignancy or chronic disease.”
Ms. Ofstead and three authors are employees of Ofstead & Associates, which received research funding and speaking honoraria from 3M, Advanced Sterilization Products (Johnson & Johnson), Ambu, Auris Health, Boston Scientific, Cogentix, ConvergAscent, Healthmark Industries, Invendo Medical, Medivators, Nanosonics, and STERIS. Dr. Ferguson has received fees from NeuWave Medical and PPD, research grants and personal fees from OncoCyte, and research grants from Concordia and PneumRx. Dr. Sonetti reported no relevant financial disclosures.
SOURCE: Ofstead CL et al. Chest. 2018 May 30. doi: 10.1016/j.chest.2018.04.045.
as researchers found all reprocessed bronchoscopes they observed had residual contamination and over half showed microbial growth, according to results from a recent study in CHEST.
“Evidence-based, bronchoscope-specific reprocessing and maintenance guidelines are needed, along with quality management programs to ensure that these complex processes are carried out effectively,” Cori L. Ofstead, MSPH, president and CEO of Ofstead & Associates, and her colleagues wrote in their study. “Shifting toward using sterilized or single-use bronchoscopes could reduce the risk of infection transmission among vulnerable pulmonary patient populations.”
The researchers inspected 24 reprocessed bronchoscopes used clinically (9 pediatric, 9 therapeutic, 6 endobronchial ultrasound) at three U.S. tertiary care centers in 2017 and compared them with two bronchoscopes that had not been used. Of the bronchoscopes observed, all had residual contamination after manual cleaning and high-level disinfection (HLD). Manually cleaned bronchoscopes had microbial growth in 11 of 20 (55%) samples, while 14 of 24 (58%) of HLD samples contained microbial growth. Upon inspection, the researchers said they discovered “oily residue; dried fluid spots; brown, red, and white residue; scratches; insertion tube buckling; and damaged distal ends,” while internal inspections yielded “fluid, discoloration, scratches, filamentous debris, and dented channels.”
Ms. Ofstead and colleagues noted that, while the first site exceeded national guidelines, sites B and C contained technicians who did not wear personal protective equipment and the sites did not follow national or manufacturer use guidelines, such as passing bronchoscopes “through a window to a clean room for automated cleaning and HLD with peracetic acid in automated endoscope reprocessor,” flushing the bronchoscopes with alcohol, drying them with medical-grade forced air pressure, and storing them in a dedicated clean and dry area. Site A had microbial growth in 20% and 50% of manually cleaned and HLD bronchoscopes, respectively, site B had microbial growth in 100% and 75% of manually cleaned and HLD bronchoscopes, respectively, and site C had microbial growth in 83% and 50% of manually cleaned and HLD bronchoscopes, respectively. Among the microbial species identified were “environmental bacteria and normal flora” such as Bacillus spp and Staphylococcus epidermidis, molds such as Lecanicillium lecanii and Verticillium dahliae, and pathogens such as Stenotrophomonas maltophilia and Escherichia coli/Shigella spp.
“The clinical implications for patients are unknown as the study did not involve assessing patients or reviewing medical records,” Ms. Ofstead and her colleagues wrote. “However, the results are worrisome as patients undergoing bronchoscopy are commonly at high risk for infection due to transplant status, critical illness, or immune suppression due to malignancy or chronic disease.”
Ms. Ofstead and three authors are employees of Ofstead & Associates, which received research funding and speaking honoraria from 3M, Advanced Sterilization Products (Johnson & Johnson), Ambu, Auris Health, Boston Scientific, Cogentix, ConvergAscent, Healthmark Industries, Invendo Medical, Medivators, Nanosonics, and STERIS. Dr. Ferguson has received fees from NeuWave Medical and PPD, research grants and personal fees from OncoCyte, and research grants from Concordia and PneumRx. Dr. Sonetti reported no relevant financial disclosures.
SOURCE: Ofstead CL et al. Chest. 2018 May 30. doi: 10.1016/j.chest.2018.04.045.
as researchers found all reprocessed bronchoscopes they observed had residual contamination and over half showed microbial growth, according to results from a recent study in CHEST.
“Evidence-based, bronchoscope-specific reprocessing and maintenance guidelines are needed, along with quality management programs to ensure that these complex processes are carried out effectively,” Cori L. Ofstead, MSPH, president and CEO of Ofstead & Associates, and her colleagues wrote in their study. “Shifting toward using sterilized or single-use bronchoscopes could reduce the risk of infection transmission among vulnerable pulmonary patient populations.”
The researchers inspected 24 reprocessed bronchoscopes used clinically (9 pediatric, 9 therapeutic, 6 endobronchial ultrasound) at three U.S. tertiary care centers in 2017 and compared them with two bronchoscopes that had not been used. Of the bronchoscopes observed, all had residual contamination after manual cleaning and high-level disinfection (HLD). Manually cleaned bronchoscopes had microbial growth in 11 of 20 (55%) samples, while 14 of 24 (58%) of HLD samples contained microbial growth. Upon inspection, the researchers said they discovered “oily residue; dried fluid spots; brown, red, and white residue; scratches; insertion tube buckling; and damaged distal ends,” while internal inspections yielded “fluid, discoloration, scratches, filamentous debris, and dented channels.”
Ms. Ofstead and colleagues noted that, while the first site exceeded national guidelines, sites B and C contained technicians who did not wear personal protective equipment and the sites did not follow national or manufacturer use guidelines, such as passing bronchoscopes “through a window to a clean room for automated cleaning and HLD with peracetic acid in automated endoscope reprocessor,” flushing the bronchoscopes with alcohol, drying them with medical-grade forced air pressure, and storing them in a dedicated clean and dry area. Site A had microbial growth in 20% and 50% of manually cleaned and HLD bronchoscopes, respectively, site B had microbial growth in 100% and 75% of manually cleaned and HLD bronchoscopes, respectively, and site C had microbial growth in 83% and 50% of manually cleaned and HLD bronchoscopes, respectively. Among the microbial species identified were “environmental bacteria and normal flora” such as Bacillus spp and Staphylococcus epidermidis, molds such as Lecanicillium lecanii and Verticillium dahliae, and pathogens such as Stenotrophomonas maltophilia and Escherichia coli/Shigella spp.
“The clinical implications for patients are unknown as the study did not involve assessing patients or reviewing medical records,” Ms. Ofstead and her colleagues wrote. “However, the results are worrisome as patients undergoing bronchoscopy are commonly at high risk for infection due to transplant status, critical illness, or immune suppression due to malignancy or chronic disease.”
Ms. Ofstead and three authors are employees of Ofstead & Associates, which received research funding and speaking honoraria from 3M, Advanced Sterilization Products (Johnson & Johnson), Ambu, Auris Health, Boston Scientific, Cogentix, ConvergAscent, Healthmark Industries, Invendo Medical, Medivators, Nanosonics, and STERIS. Dr. Ferguson has received fees from NeuWave Medical and PPD, research grants and personal fees from OncoCyte, and research grants from Concordia and PneumRx. Dr. Sonetti reported no relevant financial disclosures.
SOURCE: Ofstead CL et al. Chest. 2018 May 30. doi: 10.1016/j.chest.2018.04.045.
FROM CHEST
Key clinical point: Despite following disinfection guidelines, damaged or contaminated reprocessed bronchoscopes were being used at all study sites.
Major finding: All reprocessed bronchoscopes observed had residual contamination, while 58% that underwent high-level disinfection contained microbial growth.
Data source: A prospective study of 24 bronchoscopes from three large U.S. tertiary care hospitals in 2017.
Disclosures: Ms. Ofstead and three authors are employees of Ofstead & Associates, which received research funding and speaking honoraria from 3M, Advanced Sterilization Products (Johnson & Johnson), Ambu, Auris Health, Boston Scientific, Cogentix, ConvergAscent, Healthmark Industries, Invendo Medical, Medivators, Nanosonics, and STERIS. Dr. Ferguson has received fees from NeuWave Medical and PPD, research grants and personal fees from OncoCyte, and research grants from Concordia and PneumRx. Dr. Sonetti reported no relevant financial disclosures.
Source: Ofstead CL et al. Chest. 2018 May 30. doi: 10.1016/j.chest.2018.04.045.
Study finds widespread use of medications with depression as side effect
About one-third of U.S. adults may be using prescription medications that have depression as a possible side effect, results of a cross-sectional survey study suggest.
Use of multiple medications with depression as a possible side effect was associated with greater likelihood of concurrent depression, authors of the study reported in JAMA.
“The results suggest that physicians should consider discussing these associations with their patients who are prescribed medications that have depression as a potential adverse effect,” said authors, including Dima Mazen Qato, PharmD, MPH, PhD, Department of Pharmacy Systems, Outcomes and Policy, University of Illinois at Chicago.
The study included data from 26,192 adults who participated in the National Health and Nutrition Examination Survey between 2005 and 2014. The mean age of participants was 46.2 years, 51.1% were women, and 7.6% reported depression.
Overall, 37.2% of participants reported using medications that had depression as an adverse effect. Use of those medications has increased over time, from 35.0% in 2005-2006 to 38.4% in 2013-2014 (P = .03 for the trend), investigators reported.
Likewise, the proportion of people using at least three medications with depression as a potential side effect, increased from 6.9% to 9.5% from the 2005-2006 to 2013-2014 time period (P = .001), they added.
The prevalence of depression increased with the number of medications with depression as a side effect, in an analysis that excluded antidepressant users. Prevalence was just 4.7% for people who did not use them, up to 15% for those using three or more, a 10.7 percentage point difference, authors noted.
In all, U.S. adults reported more than 200 different medications associated with depression or suicidal symptoms as adverse effects, said Dr. Qato and co-authors.
The most common, aside from antidepressants, which as a class have a black-box warning for risk of depression, were antihypertensive medications, analgesics, hormonal contraceptives, and proton pump inhibitors. Some are over-the-counter medications that are not labeled indicating depression risk: “Many patients may therefore not be aware of the greater likelihood of concurrent depression associated with these commonly used medications,” Dr. Qato and co-authors wrote.
Dr. Qato reported serving as a consultant for Public Citizen’s Health Research Group, and said she is supported in part by the Robert Wood Johnson Foundation. One co-author reported a grant from Janssen Scientific Affairs, LLC, to Columbia University Medical Center.
SOURCE: Qato DM, et al. JAMA
About one-third of U.S. adults may be using prescription medications that have depression as a possible side effect, results of a cross-sectional survey study suggest.
Use of multiple medications with depression as a possible side effect was associated with greater likelihood of concurrent depression, authors of the study reported in JAMA.
“The results suggest that physicians should consider discussing these associations with their patients who are prescribed medications that have depression as a potential adverse effect,” said authors, including Dima Mazen Qato, PharmD, MPH, PhD, Department of Pharmacy Systems, Outcomes and Policy, University of Illinois at Chicago.
The study included data from 26,192 adults who participated in the National Health and Nutrition Examination Survey between 2005 and 2014. The mean age of participants was 46.2 years, 51.1% were women, and 7.6% reported depression.
Overall, 37.2% of participants reported using medications that had depression as an adverse effect. Use of those medications has increased over time, from 35.0% in 2005-2006 to 38.4% in 2013-2014 (P = .03 for the trend), investigators reported.
Likewise, the proportion of people using at least three medications with depression as a potential side effect, increased from 6.9% to 9.5% from the 2005-2006 to 2013-2014 time period (P = .001), they added.
The prevalence of depression increased with the number of medications with depression as a side effect, in an analysis that excluded antidepressant users. Prevalence was just 4.7% for people who did not use them, up to 15% for those using three or more, a 10.7 percentage point difference, authors noted.
In all, U.S. adults reported more than 200 different medications associated with depression or suicidal symptoms as adverse effects, said Dr. Qato and co-authors.
The most common, aside from antidepressants, which as a class have a black-box warning for risk of depression, were antihypertensive medications, analgesics, hormonal contraceptives, and proton pump inhibitors. Some are over-the-counter medications that are not labeled indicating depression risk: “Many patients may therefore not be aware of the greater likelihood of concurrent depression associated with these commonly used medications,” Dr. Qato and co-authors wrote.
Dr. Qato reported serving as a consultant for Public Citizen’s Health Research Group, and said she is supported in part by the Robert Wood Johnson Foundation. One co-author reported a grant from Janssen Scientific Affairs, LLC, to Columbia University Medical Center.
SOURCE: Qato DM, et al. JAMA
About one-third of U.S. adults may be using prescription medications that have depression as a possible side effect, results of a cross-sectional survey study suggest.
Use of multiple medications with depression as a possible side effect was associated with greater likelihood of concurrent depression, authors of the study reported in JAMA.
“The results suggest that physicians should consider discussing these associations with their patients who are prescribed medications that have depression as a potential adverse effect,” said authors, including Dima Mazen Qato, PharmD, MPH, PhD, Department of Pharmacy Systems, Outcomes and Policy, University of Illinois at Chicago.
The study included data from 26,192 adults who participated in the National Health and Nutrition Examination Survey between 2005 and 2014. The mean age of participants was 46.2 years, 51.1% were women, and 7.6% reported depression.
Overall, 37.2% of participants reported using medications that had depression as an adverse effect. Use of those medications has increased over time, from 35.0% in 2005-2006 to 38.4% in 2013-2014 (P = .03 for the trend), investigators reported.
Likewise, the proportion of people using at least three medications with depression as a potential side effect, increased from 6.9% to 9.5% from the 2005-2006 to 2013-2014 time period (P = .001), they added.
The prevalence of depression increased with the number of medications with depression as a side effect, in an analysis that excluded antidepressant users. Prevalence was just 4.7% for people who did not use them, up to 15% for those using three or more, a 10.7 percentage point difference, authors noted.
In all, U.S. adults reported more than 200 different medications associated with depression or suicidal symptoms as adverse effects, said Dr. Qato and co-authors.
The most common, aside from antidepressants, which as a class have a black-box warning for risk of depression, were antihypertensive medications, analgesics, hormonal contraceptives, and proton pump inhibitors. Some are over-the-counter medications that are not labeled indicating depression risk: “Many patients may therefore not be aware of the greater likelihood of concurrent depression associated with these commonly used medications,” Dr. Qato and co-authors wrote.
Dr. Qato reported serving as a consultant for Public Citizen’s Health Research Group, and said she is supported in part by the Robert Wood Johnson Foundation. One co-author reported a grant from Janssen Scientific Affairs, LLC, to Columbia University Medical Center.
SOURCE: Qato DM, et al. JAMA
No link found between fluconazole use and neonatal death risk
Use of oral fluconazole during pregnancy is not associated with an increase in risk of stillbirth or neonatal death, results of a large European cohort study suggest.
The rate of stillbirths was 2.7 per 1,000 fluconazole-exposed pregnancies, versus 3.6 per 1,000 unexposed pregnancies (hazard ratio, 0.76, 95% confidence interval, 0.52-1.10), investigators reported based on an analysis of national registry data including nearly 1.5 million recent pregnancies in Sweden and Norway.
Neonatal deaths occurred in 1.2 per 1,000 exposed pregnancies and 1.7 per 1,000 unexposed pregnancies, investigators added in the report, which appeared in JAMA.
Results were not different for doses of 300 mg or less versus more than 300 mg, said senior researcher Björn Pasternak, MD, PhD, of Karolinska Institutet, Stockholm, and his co-authors.
“Although the data on fluconazole use in pregnancy suggest no increased risk of stillbirth, additional studies should be conducted and the collective body of data scrutinized by drug authorities before recommendations to guide clinical decision making are made, and weighed against the benefits of therapy,” the investigators wrote.
About 4% of pregnant women in the United States take oral fluconazole, even though it is generally discouraged during pregnancy due to concerns that its use may be associated with stillbirth in a previous Danish nationwide register-based study, published in JAMA.
In 2016, investigators similarly found no increased risk of stillbirth in 2,215 fluconazole-exposed women, though they noted the outcome was “relatively rare and the results therefore imprecise.” In a sensitivity analysis, they did find an association between higher doses of fluconazole (i.e., above 300 mg) and stillbirth, with a hazard ratio of 4.10 (95% CI, 1.89-8.90).
The stillbirth analysis in the present study included 10,669 fluconazole-exposed pregnancies from Sweden and Norway, though the number exposed to higher doses was small, Dr. Pasterak and co-authors said in their report.
Although more research and deliberation is needed, this new study does add one novel endpoint to the literature: “The outcome of neonatal death has not been reported previously, to our knowledge.”
Their study was supported by the Thrasher Research Fund, the Magnus Bergvall Foundation, and the Karolinska Institutet Research Foundation. Dr. Pasternak and co-authors reported no conflicts of interest.
SOURCE: Pasternak B, et al. JAMA. 2018 Jun 12;319:22.
Use of oral fluconazole during pregnancy is not associated with an increase in risk of stillbirth or neonatal death, results of a large European cohort study suggest.
The rate of stillbirths was 2.7 per 1,000 fluconazole-exposed pregnancies, versus 3.6 per 1,000 unexposed pregnancies (hazard ratio, 0.76, 95% confidence interval, 0.52-1.10), investigators reported based on an analysis of national registry data including nearly 1.5 million recent pregnancies in Sweden and Norway.
Neonatal deaths occurred in 1.2 per 1,000 exposed pregnancies and 1.7 per 1,000 unexposed pregnancies, investigators added in the report, which appeared in JAMA.
Results were not different for doses of 300 mg or less versus more than 300 mg, said senior researcher Björn Pasternak, MD, PhD, of Karolinska Institutet, Stockholm, and his co-authors.
“Although the data on fluconazole use in pregnancy suggest no increased risk of stillbirth, additional studies should be conducted and the collective body of data scrutinized by drug authorities before recommendations to guide clinical decision making are made, and weighed against the benefits of therapy,” the investigators wrote.
About 4% of pregnant women in the United States take oral fluconazole, even though it is generally discouraged during pregnancy due to concerns that its use may be associated with stillbirth in a previous Danish nationwide register-based study, published in JAMA.
In 2016, investigators similarly found no increased risk of stillbirth in 2,215 fluconazole-exposed women, though they noted the outcome was “relatively rare and the results therefore imprecise.” In a sensitivity analysis, they did find an association between higher doses of fluconazole (i.e., above 300 mg) and stillbirth, with a hazard ratio of 4.10 (95% CI, 1.89-8.90).
The stillbirth analysis in the present study included 10,669 fluconazole-exposed pregnancies from Sweden and Norway, though the number exposed to higher doses was small, Dr. Pasterak and co-authors said in their report.
Although more research and deliberation is needed, this new study does add one novel endpoint to the literature: “The outcome of neonatal death has not been reported previously, to our knowledge.”
Their study was supported by the Thrasher Research Fund, the Magnus Bergvall Foundation, and the Karolinska Institutet Research Foundation. Dr. Pasternak and co-authors reported no conflicts of interest.
SOURCE: Pasternak B, et al. JAMA. 2018 Jun 12;319:22.
Use of oral fluconazole during pregnancy is not associated with an increase in risk of stillbirth or neonatal death, results of a large European cohort study suggest.
The rate of stillbirths was 2.7 per 1,000 fluconazole-exposed pregnancies, versus 3.6 per 1,000 unexposed pregnancies (hazard ratio, 0.76, 95% confidence interval, 0.52-1.10), investigators reported based on an analysis of national registry data including nearly 1.5 million recent pregnancies in Sweden and Norway.
Neonatal deaths occurred in 1.2 per 1,000 exposed pregnancies and 1.7 per 1,000 unexposed pregnancies, investigators added in the report, which appeared in JAMA.
Results were not different for doses of 300 mg or less versus more than 300 mg, said senior researcher Björn Pasternak, MD, PhD, of Karolinska Institutet, Stockholm, and his co-authors.
“Although the data on fluconazole use in pregnancy suggest no increased risk of stillbirth, additional studies should be conducted and the collective body of data scrutinized by drug authorities before recommendations to guide clinical decision making are made, and weighed against the benefits of therapy,” the investigators wrote.
About 4% of pregnant women in the United States take oral fluconazole, even though it is generally discouraged during pregnancy due to concerns that its use may be associated with stillbirth in a previous Danish nationwide register-based study, published in JAMA.
In 2016, investigators similarly found no increased risk of stillbirth in 2,215 fluconazole-exposed women, though they noted the outcome was “relatively rare and the results therefore imprecise.” In a sensitivity analysis, they did find an association between higher doses of fluconazole (i.e., above 300 mg) and stillbirth, with a hazard ratio of 4.10 (95% CI, 1.89-8.90).
The stillbirth analysis in the present study included 10,669 fluconazole-exposed pregnancies from Sweden and Norway, though the number exposed to higher doses was small, Dr. Pasterak and co-authors said in their report.
Although more research and deliberation is needed, this new study does add one novel endpoint to the literature: “The outcome of neonatal death has not been reported previously, to our knowledge.”
Their study was supported by the Thrasher Research Fund, the Magnus Bergvall Foundation, and the Karolinska Institutet Research Foundation. Dr. Pasternak and co-authors reported no conflicts of interest.
SOURCE: Pasternak B, et al. JAMA. 2018 Jun 12;319:22.
What Is the Impact of Adverse Childhood Experiences on Sleep in Adulthood?
Adults with three or more adverse childhood experiences are twice as likely to report insufficient sleep.
LOS ANGELES—Adverse childhood experiences increase the likelihood of chronic insufficient sleep in adulthood, according to data presented at the 70th Annual Meeting of the American Academy of Neurology. This study emphasizes the importance of childhood health and a need to identify psychologic challenges in adults with sleep difficulties, particularly given the established importance of sleep dysregulation for cognitive and physical health, said Kelly Sullivan, PhD, MSPH, Assistant Professor of Epidemiology at Jiann-Ping Hsu College of Public Health at Georgia Southern University in Statesboro, Georgia.
Long-term prospective studies have suggested that adverse childhood experiences such as abuse, neglect, and household challenges (ie, divorced or separated parents, or living with someone who served time in a prison, jail, or other correctional facility) are associated with mental health challenges and unhealthy behaviors (ie, smoking, alcohol or drug use)
Analyzing Data From a Nationwide Survey
To assess the association of adverse childhood experiences and subsequent insufficient sleep among a large group of adults in the United States, Dr. Sullivan and colleagues analyzed data from the 2011 Behavioral Risk Factor Surveillance System, a nationwide survey conducted by the Centers for Disease Control and Prevention.
Study participants were age 18 or older, were US residents, and were not incarcerated or institutionalized. For this study, participants completed standardized questionnaires to report childhood experiences of abuse, neglect, household challenges, and sleep time. Researchers calculated the total adverse childhood experiences score by summing the number of different experiences that patients reported, regardless of their severity or frequency.
The sleep questionnaire asked participants to provide an estimate of how many hours of sleep they get in a 24-hour period, not including naps. These questionnaires were categorized based on whether participants reported having optimum sleep (seven to nine hours of sleep per night), or insufficient sleep (less than six hours of sleep per night). Finally, the investigators adjusted for standard demographic covariates (age, sex, race, education and income) and stratified the analysis by decade of age.
Adverse Childhood Experiences Increased Odds of Insufficient Sleep
Data were available for 22,403 adults (mean age, 46.66). In all, 14,587 (65%) study participants reported optimum sleep duration, 2,069 (9%) participants reported insufficient sleep duration, and 216 (1%) participants reported sleep durations of 10 or more hours. The total number of adverse childhood experiences was associated with the odds of insufficient sleep. Each adverse childhood experience increased the odds of insufficient sleep by more than 20%.
The association held for each decade of age through the 60s. The magnitude of this association, however, lessened with age. Participants who were in their 20s at the time of their survey had the strongest association between their adverse experiences and their likelihood of insufficient sleep.
Adults with three or more adverse childhood experiences were twice as likely to report insufficient sleep versus normal sleep duration, as were those with five or more adverse childhood experiences. Long sleep duration was not associated with total adverse childhood experiences.
“Longitudinal studies would help us to have a better idea of the individual impact over the life course,” Dr. Sullivan concluded.
—Erica Tricarico
Adults with three or more adverse childhood experiences are twice as likely to report insufficient sleep.
Adults with three or more adverse childhood experiences are twice as likely to report insufficient sleep.
LOS ANGELES—Adverse childhood experiences increase the likelihood of chronic insufficient sleep in adulthood, according to data presented at the 70th Annual Meeting of the American Academy of Neurology. This study emphasizes the importance of childhood health and a need to identify psychologic challenges in adults with sleep difficulties, particularly given the established importance of sleep dysregulation for cognitive and physical health, said Kelly Sullivan, PhD, MSPH, Assistant Professor of Epidemiology at Jiann-Ping Hsu College of Public Health at Georgia Southern University in Statesboro, Georgia.
Long-term prospective studies have suggested that adverse childhood experiences such as abuse, neglect, and household challenges (ie, divorced or separated parents, or living with someone who served time in a prison, jail, or other correctional facility) are associated with mental health challenges and unhealthy behaviors (ie, smoking, alcohol or drug use)
Analyzing Data From a Nationwide Survey
To assess the association of adverse childhood experiences and subsequent insufficient sleep among a large group of adults in the United States, Dr. Sullivan and colleagues analyzed data from the 2011 Behavioral Risk Factor Surveillance System, a nationwide survey conducted by the Centers for Disease Control and Prevention.
Study participants were age 18 or older, were US residents, and were not incarcerated or institutionalized. For this study, participants completed standardized questionnaires to report childhood experiences of abuse, neglect, household challenges, and sleep time. Researchers calculated the total adverse childhood experiences score by summing the number of different experiences that patients reported, regardless of their severity or frequency.
The sleep questionnaire asked participants to provide an estimate of how many hours of sleep they get in a 24-hour period, not including naps. These questionnaires were categorized based on whether participants reported having optimum sleep (seven to nine hours of sleep per night), or insufficient sleep (less than six hours of sleep per night). Finally, the investigators adjusted for standard demographic covariates (age, sex, race, education and income) and stratified the analysis by decade of age.
Adverse Childhood Experiences Increased Odds of Insufficient Sleep
Data were available for 22,403 adults (mean age, 46.66). In all, 14,587 (65%) study participants reported optimum sleep duration, 2,069 (9%) participants reported insufficient sleep duration, and 216 (1%) participants reported sleep durations of 10 or more hours. The total number of adverse childhood experiences was associated with the odds of insufficient sleep. Each adverse childhood experience increased the odds of insufficient sleep by more than 20%.
The association held for each decade of age through the 60s. The magnitude of this association, however, lessened with age. Participants who were in their 20s at the time of their survey had the strongest association between their adverse experiences and their likelihood of insufficient sleep.
Adults with three or more adverse childhood experiences were twice as likely to report insufficient sleep versus normal sleep duration, as were those with five or more adverse childhood experiences. Long sleep duration was not associated with total adverse childhood experiences.
“Longitudinal studies would help us to have a better idea of the individual impact over the life course,” Dr. Sullivan concluded.
—Erica Tricarico
LOS ANGELES—Adverse childhood experiences increase the likelihood of chronic insufficient sleep in adulthood, according to data presented at the 70th Annual Meeting of the American Academy of Neurology. This study emphasizes the importance of childhood health and a need to identify psychologic challenges in adults with sleep difficulties, particularly given the established importance of sleep dysregulation for cognitive and physical health, said Kelly Sullivan, PhD, MSPH, Assistant Professor of Epidemiology at Jiann-Ping Hsu College of Public Health at Georgia Southern University in Statesboro, Georgia.
Long-term prospective studies have suggested that adverse childhood experiences such as abuse, neglect, and household challenges (ie, divorced or separated parents, or living with someone who served time in a prison, jail, or other correctional facility) are associated with mental health challenges and unhealthy behaviors (ie, smoking, alcohol or drug use)
Analyzing Data From a Nationwide Survey
To assess the association of adverse childhood experiences and subsequent insufficient sleep among a large group of adults in the United States, Dr. Sullivan and colleagues analyzed data from the 2011 Behavioral Risk Factor Surveillance System, a nationwide survey conducted by the Centers for Disease Control and Prevention.
Study participants were age 18 or older, were US residents, and were not incarcerated or institutionalized. For this study, participants completed standardized questionnaires to report childhood experiences of abuse, neglect, household challenges, and sleep time. Researchers calculated the total adverse childhood experiences score by summing the number of different experiences that patients reported, regardless of their severity or frequency.
The sleep questionnaire asked participants to provide an estimate of how many hours of sleep they get in a 24-hour period, not including naps. These questionnaires were categorized based on whether participants reported having optimum sleep (seven to nine hours of sleep per night), or insufficient sleep (less than six hours of sleep per night). Finally, the investigators adjusted for standard demographic covariates (age, sex, race, education and income) and stratified the analysis by decade of age.
Adverse Childhood Experiences Increased Odds of Insufficient Sleep
Data were available for 22,403 adults (mean age, 46.66). In all, 14,587 (65%) study participants reported optimum sleep duration, 2,069 (9%) participants reported insufficient sleep duration, and 216 (1%) participants reported sleep durations of 10 or more hours. The total number of adverse childhood experiences was associated with the odds of insufficient sleep. Each adverse childhood experience increased the odds of insufficient sleep by more than 20%.
The association held for each decade of age through the 60s. The magnitude of this association, however, lessened with age. Participants who were in their 20s at the time of their survey had the strongest association between their adverse experiences and their likelihood of insufficient sleep.
Adults with three or more adverse childhood experiences were twice as likely to report insufficient sleep versus normal sleep duration, as were those with five or more adverse childhood experiences. Long sleep duration was not associated with total adverse childhood experiences.
“Longitudinal studies would help us to have a better idea of the individual impact over the life course,” Dr. Sullivan concluded.
—Erica Tricarico