User login
Denosumab effective against osteoporosis in TDT patients
Denosumab can be effective against osteoporosis caused by transfusion-dependent thalassemia (TDT), according to new research.
The study authors found that patients who received twice-yearly injections of denosumab experienced a significant increase in bone density and reduction in bone pain. Their findings were published in Blood Advances.
“Not only is denosumab associated with improved bone health and reduced pain, but its ease of administration may very well make this drug superior to bisphosphonates for the treatment of osteoporosis in patients with TDT and osteoporosis,” senior study author Evangelos Terpos, MD, of the National and Kapodistrian University of Athens, said in a statement.
For this phase 2b study, Dr. Terpos and his colleagues evaluated 63 patients with TDT and osteoporosis, randomized to receive 60 mg of denosumab (n = 32) or placebo (n = 31) on days 0 and 180 of a 12-month period. Patients in both arms also received daily supplements of calcium and vitamin D.
Baseline characteristics were largely similar between the treatment arms. However, the mean value of bone-specific alkaline phosphatase (bALP) was significantly lower in the placebo arm than the denosumab arm – 68.48 IU/L versus 85.45 IU/L (P = .013). And the mean value of the tartrate-resistant acid phosphatase isoform–5b (TRACP-5b) marker was significantly higher in the denosumab arm than in the placebo arm – 0.42 IU/L versus 0.16 IU/L (P = .026).
The researchers measured bone mineral density in the L1-L4 lumbar spine, wrist, and femoral neck. At 12 months, the mean increase in L1-L4 bone mineral density was 5.92% in the denosumab arm and 2.92% in the placebo arm (P = .043). The mean decrease in wrist bone mineral density was –0.26% and –3.92%, respectively (P = .035).
Femoral neck bone mineral density was increased in the denosumab arm (4.08%), compared with the placebo arm (1.96%), but the difference between the two groups was not statistically significant.
Patients in the denosumab arm had a significant reduction in bone pain at 12 months, according to the McGill-Melzack scoring system and the Huskisson visual analog scale (P less than .001 for both). There was no significant change in pain for patients in the placebo arm on either scale.
At 12 months, patients in the denosumab arm had experienced a significant reduction from baseline in several markers of bone remodeling, including soluble receptor activator of nuclear factor–kappa B ligand (sRANKL), osteoprotegerin (OPG), sRANKL/OPG ratio, C-terminal telopeptide of type I collagen (CTx), TRACP-5b, and bALP.
There were no significant changes in dickkopf-1, sclerostin, or osteocalcin in the denosumab arm.
In the placebo arm, patients had a significant increase from baseline in several markers of bone remodeling, including sRANKL, OPG, dickkopf-1, sclerostin, CTx, TRACP-5b, and bALP. There was no significant change from baseline in the sRANKL/OPG ratio or osteocalcin.
In all, there were 17 adverse events in 14 patients. There were three serious adverse events in the denosumab arm – pleural effusion (grade 3), atrial fibrillation (grade 3), and supraventricular tachycardia (grade 4). All three of these adverse events were considered unrelated to denosumab.
The study was funded by Amgen, which markets denosumab. The authors reported that they had no competing financial interests.
SOURCE: Terpos E et al. Blood Adv. 2018;2:2837-47.
Denosumab can be effective against osteoporosis caused by transfusion-dependent thalassemia (TDT), according to new research.
The study authors found that patients who received twice-yearly injections of denosumab experienced a significant increase in bone density and reduction in bone pain. Their findings were published in Blood Advances.
“Not only is denosumab associated with improved bone health and reduced pain, but its ease of administration may very well make this drug superior to bisphosphonates for the treatment of osteoporosis in patients with TDT and osteoporosis,” senior study author Evangelos Terpos, MD, of the National and Kapodistrian University of Athens, said in a statement.
For this phase 2b study, Dr. Terpos and his colleagues evaluated 63 patients with TDT and osteoporosis, randomized to receive 60 mg of denosumab (n = 32) or placebo (n = 31) on days 0 and 180 of a 12-month period. Patients in both arms also received daily supplements of calcium and vitamin D.
Baseline characteristics were largely similar between the treatment arms. However, the mean value of bone-specific alkaline phosphatase (bALP) was significantly lower in the placebo arm than the denosumab arm – 68.48 IU/L versus 85.45 IU/L (P = .013). And the mean value of the tartrate-resistant acid phosphatase isoform–5b (TRACP-5b) marker was significantly higher in the denosumab arm than in the placebo arm – 0.42 IU/L versus 0.16 IU/L (P = .026).
The researchers measured bone mineral density in the L1-L4 lumbar spine, wrist, and femoral neck. At 12 months, the mean increase in L1-L4 bone mineral density was 5.92% in the denosumab arm and 2.92% in the placebo arm (P = .043). The mean decrease in wrist bone mineral density was –0.26% and –3.92%, respectively (P = .035).
Femoral neck bone mineral density was increased in the denosumab arm (4.08%), compared with the placebo arm (1.96%), but the difference between the two groups was not statistically significant.
Patients in the denosumab arm had a significant reduction in bone pain at 12 months, according to the McGill-Melzack scoring system and the Huskisson visual analog scale (P less than .001 for both). There was no significant change in pain for patients in the placebo arm on either scale.
At 12 months, patients in the denosumab arm had experienced a significant reduction from baseline in several markers of bone remodeling, including soluble receptor activator of nuclear factor–kappa B ligand (sRANKL), osteoprotegerin (OPG), sRANKL/OPG ratio, C-terminal telopeptide of type I collagen (CTx), TRACP-5b, and bALP.
There were no significant changes in dickkopf-1, sclerostin, or osteocalcin in the denosumab arm.
In the placebo arm, patients had a significant increase from baseline in several markers of bone remodeling, including sRANKL, OPG, dickkopf-1, sclerostin, CTx, TRACP-5b, and bALP. There was no significant change from baseline in the sRANKL/OPG ratio or osteocalcin.
In all, there were 17 adverse events in 14 patients. There were three serious adverse events in the denosumab arm – pleural effusion (grade 3), atrial fibrillation (grade 3), and supraventricular tachycardia (grade 4). All three of these adverse events were considered unrelated to denosumab.
The study was funded by Amgen, which markets denosumab. The authors reported that they had no competing financial interests.
SOURCE: Terpos E et al. Blood Adv. 2018;2:2837-47.
Denosumab can be effective against osteoporosis caused by transfusion-dependent thalassemia (TDT), according to new research.
The study authors found that patients who received twice-yearly injections of denosumab experienced a significant increase in bone density and reduction in bone pain. Their findings were published in Blood Advances.
“Not only is denosumab associated with improved bone health and reduced pain, but its ease of administration may very well make this drug superior to bisphosphonates for the treatment of osteoporosis in patients with TDT and osteoporosis,” senior study author Evangelos Terpos, MD, of the National and Kapodistrian University of Athens, said in a statement.
For this phase 2b study, Dr. Terpos and his colleagues evaluated 63 patients with TDT and osteoporosis, randomized to receive 60 mg of denosumab (n = 32) or placebo (n = 31) on days 0 and 180 of a 12-month period. Patients in both arms also received daily supplements of calcium and vitamin D.
Baseline characteristics were largely similar between the treatment arms. However, the mean value of bone-specific alkaline phosphatase (bALP) was significantly lower in the placebo arm than the denosumab arm – 68.48 IU/L versus 85.45 IU/L (P = .013). And the mean value of the tartrate-resistant acid phosphatase isoform–5b (TRACP-5b) marker was significantly higher in the denosumab arm than in the placebo arm – 0.42 IU/L versus 0.16 IU/L (P = .026).
The researchers measured bone mineral density in the L1-L4 lumbar spine, wrist, and femoral neck. At 12 months, the mean increase in L1-L4 bone mineral density was 5.92% in the denosumab arm and 2.92% in the placebo arm (P = .043). The mean decrease in wrist bone mineral density was –0.26% and –3.92%, respectively (P = .035).
Femoral neck bone mineral density was increased in the denosumab arm (4.08%), compared with the placebo arm (1.96%), but the difference between the two groups was not statistically significant.
Patients in the denosumab arm had a significant reduction in bone pain at 12 months, according to the McGill-Melzack scoring system and the Huskisson visual analog scale (P less than .001 for both). There was no significant change in pain for patients in the placebo arm on either scale.
At 12 months, patients in the denosumab arm had experienced a significant reduction from baseline in several markers of bone remodeling, including soluble receptor activator of nuclear factor–kappa B ligand (sRANKL), osteoprotegerin (OPG), sRANKL/OPG ratio, C-terminal telopeptide of type I collagen (CTx), TRACP-5b, and bALP.
There were no significant changes in dickkopf-1, sclerostin, or osteocalcin in the denosumab arm.
In the placebo arm, patients had a significant increase from baseline in several markers of bone remodeling, including sRANKL, OPG, dickkopf-1, sclerostin, CTx, TRACP-5b, and bALP. There was no significant change from baseline in the sRANKL/OPG ratio or osteocalcin.
In all, there were 17 adverse events in 14 patients. There were three serious adverse events in the denosumab arm – pleural effusion (grade 3), atrial fibrillation (grade 3), and supraventricular tachycardia (grade 4). All three of these adverse events were considered unrelated to denosumab.
The study was funded by Amgen, which markets denosumab. The authors reported that they had no competing financial interests.
SOURCE: Terpos E et al. Blood Adv. 2018;2:2837-47.
FROM BLOOD ADVANCES
Key clinical point:
Major finding: The mean increase in L1-L4 bone mineral density was 5.92% in patients treated with denosumab, compared with 2.92% in patients who received placebo (P = .043).
Study details: A phase 2b study that included 63 patients.
Disclosures: The research was funded by Amgen. The authors reported having no competing financial interests.
Source: Terpos E et al. Blood Adv. 2018;2:2837-47.
Pediatric migraine linked to multiple comorbidities
Pediatric headache and migraine are associated with a variety of conditions including respiratory, gastrointestinal, neurologic, and mood disorders, according to findings published in the Journal of Pediatrics.
In a study of 9,329 pediatric patients from the Philadelphia Neurodevelopmental Cohort, at the University of Pennsylvania, children with any headache type were more likely to have cardiovascular (odds ratio, 1.4; 95% confidence interval, 1.1-1.7) and gastrointestinal (OR, 1.2; 95% CI, 1.1-1.4) problems than did those without headache. In addition, they were more likely to have attention deficit hyperactivity disorder (OR, 1.2; 95% CI, 1.1-1.4), wrote Tarannum M. Lateef, MD, MPH, of the Center for Neuroscience and Behavioral Medicine at Children’s National Medical Center in Washington, and her coauthors.
Study participants were aged 8-21 years and were enrolled in the cohort from November 2009 to November 2011. Physical conditions were identified using EMRs and interviews and were later grouped together by general category.
Patients were asked about lifetime headache and migraine symptoms including sensitivity to light and noise, gastrointestinal symptoms, unilateral pain, throbbing and pulsation, and interference at school or work. Migraine was defined as headache accompanied by any three of these symptoms. Mental disorders were identified using an abbreviated version of the Kiddie-Schedule for Affective Disorders and Schizophrenia, reported Dr. Lateef and her associates.
Lifetime prevalence of any headache was 45.5%, and 22.6% for migraine. Migraine was more common in female patients (25.5%) than in male patients (19.4%).
Compared with nonmigraine headache patients, those with migraine more frequently had neurologic/central nervous system disorders (OR, 1.7; 95% CI, 1.4-2.0), developmental disorders (OR, 1.3; 95% CI, 1.1-1.6), respiratory problems (OR, 1.3; 95% CI, 1.1-1.6), anxiety (OR, 1.6; 95% CI, 1.3-2), mood disorders (OR, 2; 95% CI, 1.6-2.3), and behavioral disorders (OR, 1.3; 95% CI, 1.1-1.6).
The results suggest that “headache, particularly migraine, is associated with respiratory and other neurologic and developmental disorders, as well as with anxiety and mood disorders,” the authors wrote.
“Comorbidity may be an important index of heterogeneity … that can guide clinical management, genetic investigation, and future research on shared pathophysiology” with other disorders, they concluded.
No disclosures were reported.
SOURCE: Lateef T et al. J Pediatr. 2018 Oct 29. doi: 10.1016/j.jpeds.2018.09.033.
Pediatric headache and migraine are associated with a variety of conditions including respiratory, gastrointestinal, neurologic, and mood disorders, according to findings published in the Journal of Pediatrics.
In a study of 9,329 pediatric patients from the Philadelphia Neurodevelopmental Cohort, at the University of Pennsylvania, children with any headache type were more likely to have cardiovascular (odds ratio, 1.4; 95% confidence interval, 1.1-1.7) and gastrointestinal (OR, 1.2; 95% CI, 1.1-1.4) problems than did those without headache. In addition, they were more likely to have attention deficit hyperactivity disorder (OR, 1.2; 95% CI, 1.1-1.4), wrote Tarannum M. Lateef, MD, MPH, of the Center for Neuroscience and Behavioral Medicine at Children’s National Medical Center in Washington, and her coauthors.
Study participants were aged 8-21 years and were enrolled in the cohort from November 2009 to November 2011. Physical conditions were identified using EMRs and interviews and were later grouped together by general category.
Patients were asked about lifetime headache and migraine symptoms including sensitivity to light and noise, gastrointestinal symptoms, unilateral pain, throbbing and pulsation, and interference at school or work. Migraine was defined as headache accompanied by any three of these symptoms. Mental disorders were identified using an abbreviated version of the Kiddie-Schedule for Affective Disorders and Schizophrenia, reported Dr. Lateef and her associates.
Lifetime prevalence of any headache was 45.5%, and 22.6% for migraine. Migraine was more common in female patients (25.5%) than in male patients (19.4%).
Compared with nonmigraine headache patients, those with migraine more frequently had neurologic/central nervous system disorders (OR, 1.7; 95% CI, 1.4-2.0), developmental disorders (OR, 1.3; 95% CI, 1.1-1.6), respiratory problems (OR, 1.3; 95% CI, 1.1-1.6), anxiety (OR, 1.6; 95% CI, 1.3-2), mood disorders (OR, 2; 95% CI, 1.6-2.3), and behavioral disorders (OR, 1.3; 95% CI, 1.1-1.6).
The results suggest that “headache, particularly migraine, is associated with respiratory and other neurologic and developmental disorders, as well as with anxiety and mood disorders,” the authors wrote.
“Comorbidity may be an important index of heterogeneity … that can guide clinical management, genetic investigation, and future research on shared pathophysiology” with other disorders, they concluded.
No disclosures were reported.
SOURCE: Lateef T et al. J Pediatr. 2018 Oct 29. doi: 10.1016/j.jpeds.2018.09.033.
Pediatric headache and migraine are associated with a variety of conditions including respiratory, gastrointestinal, neurologic, and mood disorders, according to findings published in the Journal of Pediatrics.
In a study of 9,329 pediatric patients from the Philadelphia Neurodevelopmental Cohort, at the University of Pennsylvania, children with any headache type were more likely to have cardiovascular (odds ratio, 1.4; 95% confidence interval, 1.1-1.7) and gastrointestinal (OR, 1.2; 95% CI, 1.1-1.4) problems than did those without headache. In addition, they were more likely to have attention deficit hyperactivity disorder (OR, 1.2; 95% CI, 1.1-1.4), wrote Tarannum M. Lateef, MD, MPH, of the Center for Neuroscience and Behavioral Medicine at Children’s National Medical Center in Washington, and her coauthors.
Study participants were aged 8-21 years and were enrolled in the cohort from November 2009 to November 2011. Physical conditions were identified using EMRs and interviews and were later grouped together by general category.
Patients were asked about lifetime headache and migraine symptoms including sensitivity to light and noise, gastrointestinal symptoms, unilateral pain, throbbing and pulsation, and interference at school or work. Migraine was defined as headache accompanied by any three of these symptoms. Mental disorders were identified using an abbreviated version of the Kiddie-Schedule for Affective Disorders and Schizophrenia, reported Dr. Lateef and her associates.
Lifetime prevalence of any headache was 45.5%, and 22.6% for migraine. Migraine was more common in female patients (25.5%) than in male patients (19.4%).
Compared with nonmigraine headache patients, those with migraine more frequently had neurologic/central nervous system disorders (OR, 1.7; 95% CI, 1.4-2.0), developmental disorders (OR, 1.3; 95% CI, 1.1-1.6), respiratory problems (OR, 1.3; 95% CI, 1.1-1.6), anxiety (OR, 1.6; 95% CI, 1.3-2), mood disorders (OR, 2; 95% CI, 1.6-2.3), and behavioral disorders (OR, 1.3; 95% CI, 1.1-1.6).
The results suggest that “headache, particularly migraine, is associated with respiratory and other neurologic and developmental disorders, as well as with anxiety and mood disorders,” the authors wrote.
“Comorbidity may be an important index of heterogeneity … that can guide clinical management, genetic investigation, and future research on shared pathophysiology” with other disorders, they concluded.
No disclosures were reported.
SOURCE: Lateef T et al. J Pediatr. 2018 Oct 29. doi: 10.1016/j.jpeds.2018.09.033.
FROM THE JOURNAL OF PEDIATRICS
Key clinical point: Pediatric headache and migraine are associated with respiratory, neurologic, developmental, anxiety, and mood disorders.
Major finding: Patients with migraine more frequently had neurologic/central nervous system disorders (odds ratio, 1.7; 95% confidence interval, 1.4-2), developmental disorders (OR, 1.3; 95% CI, 1.1-1.6), respiratory problems (OR, 1.3; 95% CI, 1.1-1.6), anxiety (OR, 1.6; 95% CI, 1.3-2), mood disorders (OR, 2; 95% CI, 1.6-2.3), and behavioral disorders (OR, 1.3; 95% CI, 1.1-1.6).
Study details: A study of 9,329 patients aged 8-21 years from the Philadelphia Neurodevelopmental Cohort.
Disclosures: No disclosures were reported.
Source: Lateef T et al. J Pediatr. 2018 Oct 29. doi: 10.1016/j.jpeds.2018.09.033.
Samuel Shem: Part II
Mr. Shem is the author of the satirical novel The House of God, which examined medical residency in the United States in the 1970s.
Mr. Shem is the author of the satirical novel The House of God, which examined medical residency in the United States in the 1970s.
Mr. Shem is the author of the satirical novel The House of God, which examined medical residency in the United States in the 1970s.
U.S. death rates from chronic liver disease continue to rise
SAN FRANCISCO –
“I believe it’s all related to a big increase in obesity and type 2 diabetes in this country,” lead study author Zobair M. Younossi, MD, MPH, said in an interview in advance of the annual meeting of the American Association for the Study of Liver Diseases. “Those two risk factors drive NAFLD and its progressive type, nonalcoholic steatohepatitis (NASH). That accounts for at least part of the increase in mortality related to liver disease.”
In an effort to evaluate recent mortality trends in chronic liver disease in the United States, Dr. Younossi and his colleagues drew from National Vital Statistics Data during 2007-2016. They used ICD-10 codes to select mortality data for alcoholic liver disease, chronic hepatitis B and C, iron overload, NAFLD, cirrhosis, and hepatocellular carcinoma. NAFLD cases were defined as those having an ICD-10 code for NAFLD/NASH or an ICD-10 code for “cirrhosis of unknown etiology.” Next, the researchers adjusted age-standardized death rates to the 2000 U.S. Census population and used logistic regression and propensity scores to estimate predictors of chronic liver disease-related deaths.
Dr. Younossi, who chairs the department of medicine at Inova Fairfax Medical Campus, in Falls Church, Va., and his colleagues reported findings from 838,809 chronic liver disease–related deaths during the study period. They found that the age-standardized death rate for chronic liver disease increased from 21.9/100,000 population in 2007 to 24.9/100,000 population in 2016, which translated into an annual percentage change of 1.3% for males and 2.5% for females. Chronic liver disease–related deaths increased with age and were highest among those aged 55-64 years, followed by those aged 65-74 years – an average annual percentage change of 3.4% and 3.1% in each group.
Among chronic liver disease–related deaths, the most common diagnostic etiology was NAFLD (34.7%), followed by alcoholic liver disease (28.8%) and chronic hepatitis C (21.1%). Between 2007 and 2016, death rates increased from 7.6 to 9.0 per 100,000 population for NAFLD (an average annual percentage change of 2.1%) and from 6.1 to 7.9 per 100,000 population for alcoholic liver disease (an average annual percentage change of 3.1%). “What surprised me was that, despite highly effective treatment for HCV, we still have a burden of hepatitis C in this country,” Dr. Younossi said. “It’s still the most common cause of liver disease in the U.S. But it seems like hepatitis C–related liver disease is being replaced quickly by liver disease from nonalcoholic steatohepatitis. This transition between hepatitis C as the most important cause of liver disease and liver mortality to NASH or obesity-related NASH is becoming more rapid than I expected.”
On multivariate analysis, three factors were independently associated with an increased risk of death in NAFLD: the presence of type 2 diabetes (odds ratio, 1.78), cardiovascular disease (OR, 1.07), and renal failure (OR, 1.08).
“One important message from this study is that NASH is very common in the U.S. population,” said Dr. Younossi, who is also a professor of medicine at Virginia Commonwealth University, Richmond. “These patients are underrecognized and underdiagnosed because they are asymptomatic. The second message is that there is a subtype of patients with fatty liver disease – even a subtype of NASH – that can progress to cirrhosis and its complications. We have to pay attention to this silent disease to identify patients who are at risk for progressive liver disease and try to address some of the risk issues, such as tight control of diabetes, obesity, and control of hypertension and hyperlipidemia. Short of that, right now we have very few medical treatments such as vitamin E and pioglitazone recommended for a very selected group. In contrast, there are plenty of new medications that are being developed. The first step in tackling this disease is to identify who the patients are with fatty liver disease who are at risk for bad outcomes and make sure they’re linked to care by a knowledgeable caregiver [who] understands the importance of NASH.”
Dr. Younossi acknowledged certain limitations of the study, including the fact that liver disease diagnoses were based on ICD-10 coding. He disclosed that he is a consultant for Gilead, Intercept, Novo Nordisk, BMS, AbbVie, Viking, Term Quest Diagnostics, Echosens,and Shionogi. He has also received grant/research support from Gilead, Intercept, and BMS.
Source: Hepatol. 2018;68[S1], Abstract 763.
SAN FRANCISCO –
“I believe it’s all related to a big increase in obesity and type 2 diabetes in this country,” lead study author Zobair M. Younossi, MD, MPH, said in an interview in advance of the annual meeting of the American Association for the Study of Liver Diseases. “Those two risk factors drive NAFLD and its progressive type, nonalcoholic steatohepatitis (NASH). That accounts for at least part of the increase in mortality related to liver disease.”
In an effort to evaluate recent mortality trends in chronic liver disease in the United States, Dr. Younossi and his colleagues drew from National Vital Statistics Data during 2007-2016. They used ICD-10 codes to select mortality data for alcoholic liver disease, chronic hepatitis B and C, iron overload, NAFLD, cirrhosis, and hepatocellular carcinoma. NAFLD cases were defined as those having an ICD-10 code for NAFLD/NASH or an ICD-10 code for “cirrhosis of unknown etiology.” Next, the researchers adjusted age-standardized death rates to the 2000 U.S. Census population and used logistic regression and propensity scores to estimate predictors of chronic liver disease-related deaths.
Dr. Younossi, who chairs the department of medicine at Inova Fairfax Medical Campus, in Falls Church, Va., and his colleagues reported findings from 838,809 chronic liver disease–related deaths during the study period. They found that the age-standardized death rate for chronic liver disease increased from 21.9/100,000 population in 2007 to 24.9/100,000 population in 2016, which translated into an annual percentage change of 1.3% for males and 2.5% for females. Chronic liver disease–related deaths increased with age and were highest among those aged 55-64 years, followed by those aged 65-74 years – an average annual percentage change of 3.4% and 3.1% in each group.
Among chronic liver disease–related deaths, the most common diagnostic etiology was NAFLD (34.7%), followed by alcoholic liver disease (28.8%) and chronic hepatitis C (21.1%). Between 2007 and 2016, death rates increased from 7.6 to 9.0 per 100,000 population for NAFLD (an average annual percentage change of 2.1%) and from 6.1 to 7.9 per 100,000 population for alcoholic liver disease (an average annual percentage change of 3.1%). “What surprised me was that, despite highly effective treatment for HCV, we still have a burden of hepatitis C in this country,” Dr. Younossi said. “It’s still the most common cause of liver disease in the U.S. But it seems like hepatitis C–related liver disease is being replaced quickly by liver disease from nonalcoholic steatohepatitis. This transition between hepatitis C as the most important cause of liver disease and liver mortality to NASH or obesity-related NASH is becoming more rapid than I expected.”
On multivariate analysis, three factors were independently associated with an increased risk of death in NAFLD: the presence of type 2 diabetes (odds ratio, 1.78), cardiovascular disease (OR, 1.07), and renal failure (OR, 1.08).
“One important message from this study is that NASH is very common in the U.S. population,” said Dr. Younossi, who is also a professor of medicine at Virginia Commonwealth University, Richmond. “These patients are underrecognized and underdiagnosed because they are asymptomatic. The second message is that there is a subtype of patients with fatty liver disease – even a subtype of NASH – that can progress to cirrhosis and its complications. We have to pay attention to this silent disease to identify patients who are at risk for progressive liver disease and try to address some of the risk issues, such as tight control of diabetes, obesity, and control of hypertension and hyperlipidemia. Short of that, right now we have very few medical treatments such as vitamin E and pioglitazone recommended for a very selected group. In contrast, there are plenty of new medications that are being developed. The first step in tackling this disease is to identify who the patients are with fatty liver disease who are at risk for bad outcomes and make sure they’re linked to care by a knowledgeable caregiver [who] understands the importance of NASH.”
Dr. Younossi acknowledged certain limitations of the study, including the fact that liver disease diagnoses were based on ICD-10 coding. He disclosed that he is a consultant for Gilead, Intercept, Novo Nordisk, BMS, AbbVie, Viking, Term Quest Diagnostics, Echosens,and Shionogi. He has also received grant/research support from Gilead, Intercept, and BMS.
Source: Hepatol. 2018;68[S1], Abstract 763.
SAN FRANCISCO –
“I believe it’s all related to a big increase in obesity and type 2 diabetes in this country,” lead study author Zobair M. Younossi, MD, MPH, said in an interview in advance of the annual meeting of the American Association for the Study of Liver Diseases. “Those two risk factors drive NAFLD and its progressive type, nonalcoholic steatohepatitis (NASH). That accounts for at least part of the increase in mortality related to liver disease.”
In an effort to evaluate recent mortality trends in chronic liver disease in the United States, Dr. Younossi and his colleagues drew from National Vital Statistics Data during 2007-2016. They used ICD-10 codes to select mortality data for alcoholic liver disease, chronic hepatitis B and C, iron overload, NAFLD, cirrhosis, and hepatocellular carcinoma. NAFLD cases were defined as those having an ICD-10 code for NAFLD/NASH or an ICD-10 code for “cirrhosis of unknown etiology.” Next, the researchers adjusted age-standardized death rates to the 2000 U.S. Census population and used logistic regression and propensity scores to estimate predictors of chronic liver disease-related deaths.
Dr. Younossi, who chairs the department of medicine at Inova Fairfax Medical Campus, in Falls Church, Va., and his colleagues reported findings from 838,809 chronic liver disease–related deaths during the study period. They found that the age-standardized death rate for chronic liver disease increased from 21.9/100,000 population in 2007 to 24.9/100,000 population in 2016, which translated into an annual percentage change of 1.3% for males and 2.5% for females. Chronic liver disease–related deaths increased with age and were highest among those aged 55-64 years, followed by those aged 65-74 years – an average annual percentage change of 3.4% and 3.1% in each group.
Among chronic liver disease–related deaths, the most common diagnostic etiology was NAFLD (34.7%), followed by alcoholic liver disease (28.8%) and chronic hepatitis C (21.1%). Between 2007 and 2016, death rates increased from 7.6 to 9.0 per 100,000 population for NAFLD (an average annual percentage change of 2.1%) and from 6.1 to 7.9 per 100,000 population for alcoholic liver disease (an average annual percentage change of 3.1%). “What surprised me was that, despite highly effective treatment for HCV, we still have a burden of hepatitis C in this country,” Dr. Younossi said. “It’s still the most common cause of liver disease in the U.S. But it seems like hepatitis C–related liver disease is being replaced quickly by liver disease from nonalcoholic steatohepatitis. This transition between hepatitis C as the most important cause of liver disease and liver mortality to NASH or obesity-related NASH is becoming more rapid than I expected.”
On multivariate analysis, three factors were independently associated with an increased risk of death in NAFLD: the presence of type 2 diabetes (odds ratio, 1.78), cardiovascular disease (OR, 1.07), and renal failure (OR, 1.08).
“One important message from this study is that NASH is very common in the U.S. population,” said Dr. Younossi, who is also a professor of medicine at Virginia Commonwealth University, Richmond. “These patients are underrecognized and underdiagnosed because they are asymptomatic. The second message is that there is a subtype of patients with fatty liver disease – even a subtype of NASH – that can progress to cirrhosis and its complications. We have to pay attention to this silent disease to identify patients who are at risk for progressive liver disease and try to address some of the risk issues, such as tight control of diabetes, obesity, and control of hypertension and hyperlipidemia. Short of that, right now we have very few medical treatments such as vitamin E and pioglitazone recommended for a very selected group. In contrast, there are plenty of new medications that are being developed. The first step in tackling this disease is to identify who the patients are with fatty liver disease who are at risk for bad outcomes and make sure they’re linked to care by a knowledgeable caregiver [who] understands the importance of NASH.”
Dr. Younossi acknowledged certain limitations of the study, including the fact that liver disease diagnoses were based on ICD-10 coding. He disclosed that he is a consultant for Gilead, Intercept, Novo Nordisk, BMS, AbbVie, Viking, Term Quest Diagnostics, Echosens,and Shionogi. He has also received grant/research support from Gilead, Intercept, and BMS.
Source: Hepatol. 2018;68[S1], Abstract 763.
AT THE LIVER MEETING 2018
Key clinical point: Nonalcoholic steatohepatitis is very common in the U.S. population.
Major finding: Between 2007 and 2016, the age-standardized death rate for chronic liver disease increased from 21.9/100,000 population to 24.9/100,000 population.
Study details: An analysis of 838,809 chronic liver disease–related deaths from 2007 to 2016.
Disclosures: Dr. Younossi disclosed that he is a consultant for Gilead, Intercept, Novo Nordisk, Bristol-Myers Squibb, AbbVie, Viking, Term Quest Diagnostics, Echosens, and Shionogi. He has also received grant/research support from Gilead, Intercept, and Bristol-Myers Squibb.
Source: Hepatol. 2018;68[S1], Abstract 763.
Biomarkers and concussions
A novel theory explains the variable efficacy of SSRIs, single-dose zoliflodacin is successful for uncomplicated urogenital gonorrhea, and drinking regular, caffeinated coffee is linked with a decreased risk of rosacea.
Amazon Alexa
Apple Podcasts
Spotify
A novel theory explains the variable efficacy of SSRIs, single-dose zoliflodacin is successful for uncomplicated urogenital gonorrhea, and drinking regular, caffeinated coffee is linked with a decreased risk of rosacea.
Amazon Alexa
Apple Podcasts
Spotify
A novel theory explains the variable efficacy of SSRIs, single-dose zoliflodacin is successful for uncomplicated urogenital gonorrhea, and drinking regular, caffeinated coffee is linked with a decreased risk of rosacea.
Amazon Alexa
Apple Podcasts
Spotify
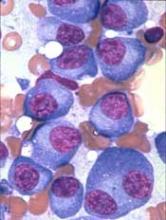
‘Encouraging’ phase 2 results in rel/ref AML
The combination of azacitidine and nivolumab produced “encouraging” results in a phase 2 trial of patients with relapsed or refractory acute myeloid leukemia (AML), according to researchers.
The overall response rate was 33%, and the median overall survival (OS) was 6.3 months.
However, the researchers identified factors associated with improved response and survival that they believe could be used to select patients for this treatment.
A quarter of patients on this trial had immune-related adverse events (AEs) that were considered related to treatment, and two patients died of AEs that may have been treatment-related.
Naval Daver, MD, of The University of Texas MD Anderson Cancer Center in Houston, and his colleagues reported these results in Cancer Discovery.
The trial included 70 patients with a median age of 70 (range, 22-90). Fifty-six percent had de novo AML, and 44% had secondary AML.
The median number of prior therapies was 2 (range, 1 to 7). Sixty-four percent of patients had received hypomethylating agents, 47% had received targeted therapies, and 19% had received allogeneic stem cell transplant (SCT).
For this trial, patients received azacitidine at 75 mg/m2 on days 1 to 7 and nivolumab at 3 mg/kg on days 1 and 14 of each cycle. The median number of cycles was 3 (range, 1 to 25).
Patients had a median time on study of 3.5 months (range, 0.3 to 26.3 months). Reasons for discontinuation included primary refractory disease (n=27), relapse after initial response (n=19), death (n=16), proceeding to SCT (n=3), and patient preference (n=3).
Safety
The most common treatment-related, non-hematologic AEs were constipation (26%), diarrhea (20%), pneumonitis (13%), nausea (11%), and lung infection (11%).
The rate of immune-related AEs was 25% (n=18), with grade 2-4 immune-related AEs occurring in 16 patients (8 with grade 3-4). Fourteen of these patients responded to steroids and were safely re-challenged with nivolumab, according to the researchers.
Nine patients (13%) discontinued nivolumab (but continued with azacitidine) due to AEs—pneumonitis (n=7), cytokine release syndrome (n=1), and immune nephritis (n=1).
Two patients died of AEs that were considered possibly related to treatment. One death was due to progressive pneumonia/pneumonitis, and one was due to hemophagocytosis lymphohistiocytosis.
Response
The overall response rate was 33% (n=23). Four patients had a complete response (CR), and 11 had a CR with incomplete count recovery (CRi).
One patient had a partial response, and seven had hematologic improvement in one or more parameter maintained for more than 6 months. Six patients had stable disease lasting more than 6 months.
The researchers noted that the response rate was higher among patients who had not received prior treatment with hypomethylating agents. In addition, a higher frequency of pre-therapy CD3 and CD8 cells in the bone marrow or peripheral blood appeared to predict response.
“In particular, CD3 appeared to have a high sensitivity and specificity rate for predicting response, indicating it might serve as a reliable biomarker for selecting patients for this combination therapy,” Dr. Daver said.
Survival
At a median follow-up of 21.4 months, 81% of patients (n=57) had died. Sixteen patients died on study treatment, and 41 died after discontinuation.
The median OS was 6.3 months, and the median event-free survival was 4.5 months.
The median OS was 16.1 months in patients with CR/CRi, partial response, hematologic improvement, or stable disease and 4.1 months in non-responders (P<0.0001). This difference was still significant after the researchers censored the three patients who had gone on to SCT in CR/CRi (P<0.001).
The researchers also found that being in first salvage was associated with improved OS in a univariate analysis and in a comparison with historical controls.
Dr. Daver and his colleagues concluded that azacitidine and nivolumab “produced an encouraging response rate and overall survival” in patients with relapsed/refractory AML.
“We believe that implementation of clinical and immune biomarkers to select patients are likely to yield further improved outcomes with these types of therapies in AML,” Dr. Daver noted.
This research was supported by Bristol-Myers Squibb, MD Anderson, and the Dick Clark Immunotherapy Research Fund. In addition, individual researchers reported financial relationships with Bristol-Myers Squibb.
The combination of azacitidine and nivolumab produced “encouraging” results in a phase 2 trial of patients with relapsed or refractory acute myeloid leukemia (AML), according to researchers.
The overall response rate was 33%, and the median overall survival (OS) was 6.3 months.
However, the researchers identified factors associated with improved response and survival that they believe could be used to select patients for this treatment.
A quarter of patients on this trial had immune-related adverse events (AEs) that were considered related to treatment, and two patients died of AEs that may have been treatment-related.
Naval Daver, MD, of The University of Texas MD Anderson Cancer Center in Houston, and his colleagues reported these results in Cancer Discovery.
The trial included 70 patients with a median age of 70 (range, 22-90). Fifty-six percent had de novo AML, and 44% had secondary AML.
The median number of prior therapies was 2 (range, 1 to 7). Sixty-four percent of patients had received hypomethylating agents, 47% had received targeted therapies, and 19% had received allogeneic stem cell transplant (SCT).
For this trial, patients received azacitidine at 75 mg/m2 on days 1 to 7 and nivolumab at 3 mg/kg on days 1 and 14 of each cycle. The median number of cycles was 3 (range, 1 to 25).
Patients had a median time on study of 3.5 months (range, 0.3 to 26.3 months). Reasons for discontinuation included primary refractory disease (n=27), relapse after initial response (n=19), death (n=16), proceeding to SCT (n=3), and patient preference (n=3).
Safety
The most common treatment-related, non-hematologic AEs were constipation (26%), diarrhea (20%), pneumonitis (13%), nausea (11%), and lung infection (11%).
The rate of immune-related AEs was 25% (n=18), with grade 2-4 immune-related AEs occurring in 16 patients (8 with grade 3-4). Fourteen of these patients responded to steroids and were safely re-challenged with nivolumab, according to the researchers.
Nine patients (13%) discontinued nivolumab (but continued with azacitidine) due to AEs—pneumonitis (n=7), cytokine release syndrome (n=1), and immune nephritis (n=1).
Two patients died of AEs that were considered possibly related to treatment. One death was due to progressive pneumonia/pneumonitis, and one was due to hemophagocytosis lymphohistiocytosis.
Response
The overall response rate was 33% (n=23). Four patients had a complete response (CR), and 11 had a CR with incomplete count recovery (CRi).
One patient had a partial response, and seven had hematologic improvement in one or more parameter maintained for more than 6 months. Six patients had stable disease lasting more than 6 months.
The researchers noted that the response rate was higher among patients who had not received prior treatment with hypomethylating agents. In addition, a higher frequency of pre-therapy CD3 and CD8 cells in the bone marrow or peripheral blood appeared to predict response.
“In particular, CD3 appeared to have a high sensitivity and specificity rate for predicting response, indicating it might serve as a reliable biomarker for selecting patients for this combination therapy,” Dr. Daver said.
Survival
At a median follow-up of 21.4 months, 81% of patients (n=57) had died. Sixteen patients died on study treatment, and 41 died after discontinuation.
The median OS was 6.3 months, and the median event-free survival was 4.5 months.
The median OS was 16.1 months in patients with CR/CRi, partial response, hematologic improvement, or stable disease and 4.1 months in non-responders (P<0.0001). This difference was still significant after the researchers censored the three patients who had gone on to SCT in CR/CRi (P<0.001).
The researchers also found that being in first salvage was associated with improved OS in a univariate analysis and in a comparison with historical controls.
Dr. Daver and his colleagues concluded that azacitidine and nivolumab “produced an encouraging response rate and overall survival” in patients with relapsed/refractory AML.
“We believe that implementation of clinical and immune biomarkers to select patients are likely to yield further improved outcomes with these types of therapies in AML,” Dr. Daver noted.
This research was supported by Bristol-Myers Squibb, MD Anderson, and the Dick Clark Immunotherapy Research Fund. In addition, individual researchers reported financial relationships with Bristol-Myers Squibb.
The combination of azacitidine and nivolumab produced “encouraging” results in a phase 2 trial of patients with relapsed or refractory acute myeloid leukemia (AML), according to researchers.
The overall response rate was 33%, and the median overall survival (OS) was 6.3 months.
However, the researchers identified factors associated with improved response and survival that they believe could be used to select patients for this treatment.
A quarter of patients on this trial had immune-related adverse events (AEs) that were considered related to treatment, and two patients died of AEs that may have been treatment-related.
Naval Daver, MD, of The University of Texas MD Anderson Cancer Center in Houston, and his colleagues reported these results in Cancer Discovery.
The trial included 70 patients with a median age of 70 (range, 22-90). Fifty-six percent had de novo AML, and 44% had secondary AML.
The median number of prior therapies was 2 (range, 1 to 7). Sixty-four percent of patients had received hypomethylating agents, 47% had received targeted therapies, and 19% had received allogeneic stem cell transplant (SCT).
For this trial, patients received azacitidine at 75 mg/m2 on days 1 to 7 and nivolumab at 3 mg/kg on days 1 and 14 of each cycle. The median number of cycles was 3 (range, 1 to 25).
Patients had a median time on study of 3.5 months (range, 0.3 to 26.3 months). Reasons for discontinuation included primary refractory disease (n=27), relapse after initial response (n=19), death (n=16), proceeding to SCT (n=3), and patient preference (n=3).
Safety
The most common treatment-related, non-hematologic AEs were constipation (26%), diarrhea (20%), pneumonitis (13%), nausea (11%), and lung infection (11%).
The rate of immune-related AEs was 25% (n=18), with grade 2-4 immune-related AEs occurring in 16 patients (8 with grade 3-4). Fourteen of these patients responded to steroids and were safely re-challenged with nivolumab, according to the researchers.
Nine patients (13%) discontinued nivolumab (but continued with azacitidine) due to AEs—pneumonitis (n=7), cytokine release syndrome (n=1), and immune nephritis (n=1).
Two patients died of AEs that were considered possibly related to treatment. One death was due to progressive pneumonia/pneumonitis, and one was due to hemophagocytosis lymphohistiocytosis.
Response
The overall response rate was 33% (n=23). Four patients had a complete response (CR), and 11 had a CR with incomplete count recovery (CRi).
One patient had a partial response, and seven had hematologic improvement in one or more parameter maintained for more than 6 months. Six patients had stable disease lasting more than 6 months.
The researchers noted that the response rate was higher among patients who had not received prior treatment with hypomethylating agents. In addition, a higher frequency of pre-therapy CD3 and CD8 cells in the bone marrow or peripheral blood appeared to predict response.
“In particular, CD3 appeared to have a high sensitivity and specificity rate for predicting response, indicating it might serve as a reliable biomarker for selecting patients for this combination therapy,” Dr. Daver said.
Survival
At a median follow-up of 21.4 months, 81% of patients (n=57) had died. Sixteen patients died on study treatment, and 41 died after discontinuation.
The median OS was 6.3 months, and the median event-free survival was 4.5 months.
The median OS was 16.1 months in patients with CR/CRi, partial response, hematologic improvement, or stable disease and 4.1 months in non-responders (P<0.0001). This difference was still significant after the researchers censored the three patients who had gone on to SCT in CR/CRi (P<0.001).
The researchers also found that being in first salvage was associated with improved OS in a univariate analysis and in a comparison with historical controls.
Dr. Daver and his colleagues concluded that azacitidine and nivolumab “produced an encouraging response rate and overall survival” in patients with relapsed/refractory AML.
“We believe that implementation of clinical and immune biomarkers to select patients are likely to yield further improved outcomes with these types of therapies in AML,” Dr. Daver noted.
This research was supported by Bristol-Myers Squibb, MD Anderson, and the Dick Clark Immunotherapy Research Fund. In addition, individual researchers reported financial relationships with Bristol-Myers Squibb.
CAR T therapy for MM receives RMAT designation
P-BCMA-101, an autologous chimeric antigen receptor (CAR) T-cell therapy being developed to treat patients with relapsed/refractory multiple myeloma (MM), has received regenerative medicine advanced therapy (RMAT) designation from the U.S. Food and Drug Administration (FDA).
RMAT designation is intended to expedite the development and review of regenerative medicines that are intended to treat, modify, reverse, or cure a serious or life-threatening disease or condition.
For a therapy to receive RMAT designation, preliminary evidence must indicate the therapy has the potential to address unmet medical needs for the disease or condition.
RMAT designation provides all the benefits of fast track and breakthrough therapy designations, including early interactions with the FDA.
About P-BCMA-101
To create P-BCMA-101, patients’ T cells are modified using a non-viral DNA modification system known as piggyBac™. The modified T cells target cells expressing B-cell maturation antigen (BCMA), which is expressed on essentially all MM cells.
Early results from the phase 1 trial (NCT03288493) of P-BCMA-101 were recently reported at the 2018 CAR-TCR Summit by Eric Ostertag, MD, PhD, chief executive officer of Poseida Therapeutics Inc., the company developing P-BCMA-101.
The presentation included data on 11 patients with heavily pretreated MM. Patients were a median age of 60, and 73% were high risk. They had a median of six prior therapies.
Patients received conditioning with fludarabine and cyclophosphamide for 3 days prior to receiving P-BCMA-101. They then received one of three doses of CAR T cells—51×106 (n=3), 152×106 (n=7), or 430×106 (n=1).
The investigators observed no dose-limiting toxicities. Adverse events included neutropenia in eight patients and thrombocytopenia in five.
One patient may have had cytokine release syndrome, but the condition resolved without drug intervention. And investigators observed no neurotoxicity.
Seven of ten patients evaluable for response by International Myeloma Working Group criteria achieved at least a partial response, including very good partial responses and stringent complete response.
The eleventh patient has oligosecretory disease and was only evaluable by PET, which indicated a near complete response.
Additional results from this trial are scheduled to be presented at the 2018 ASH Annual Meeting (abstract 1012).
The study is funded by the California Institute for Regenerative Medicine and Poseida Therapeutics.
P-BCMA-101, an autologous chimeric antigen receptor (CAR) T-cell therapy being developed to treat patients with relapsed/refractory multiple myeloma (MM), has received regenerative medicine advanced therapy (RMAT) designation from the U.S. Food and Drug Administration (FDA).
RMAT designation is intended to expedite the development and review of regenerative medicines that are intended to treat, modify, reverse, or cure a serious or life-threatening disease or condition.
For a therapy to receive RMAT designation, preliminary evidence must indicate the therapy has the potential to address unmet medical needs for the disease or condition.
RMAT designation provides all the benefits of fast track and breakthrough therapy designations, including early interactions with the FDA.
About P-BCMA-101
To create P-BCMA-101, patients’ T cells are modified using a non-viral DNA modification system known as piggyBac™. The modified T cells target cells expressing B-cell maturation antigen (BCMA), which is expressed on essentially all MM cells.
Early results from the phase 1 trial (NCT03288493) of P-BCMA-101 were recently reported at the 2018 CAR-TCR Summit by Eric Ostertag, MD, PhD, chief executive officer of Poseida Therapeutics Inc., the company developing P-BCMA-101.
The presentation included data on 11 patients with heavily pretreated MM. Patients were a median age of 60, and 73% were high risk. They had a median of six prior therapies.
Patients received conditioning with fludarabine and cyclophosphamide for 3 days prior to receiving P-BCMA-101. They then received one of three doses of CAR T cells—51×106 (n=3), 152×106 (n=7), or 430×106 (n=1).
The investigators observed no dose-limiting toxicities. Adverse events included neutropenia in eight patients and thrombocytopenia in five.
One patient may have had cytokine release syndrome, but the condition resolved without drug intervention. And investigators observed no neurotoxicity.
Seven of ten patients evaluable for response by International Myeloma Working Group criteria achieved at least a partial response, including very good partial responses and stringent complete response.
The eleventh patient has oligosecretory disease and was only evaluable by PET, which indicated a near complete response.
Additional results from this trial are scheduled to be presented at the 2018 ASH Annual Meeting (abstract 1012).
The study is funded by the California Institute for Regenerative Medicine and Poseida Therapeutics.
P-BCMA-101, an autologous chimeric antigen receptor (CAR) T-cell therapy being developed to treat patients with relapsed/refractory multiple myeloma (MM), has received regenerative medicine advanced therapy (RMAT) designation from the U.S. Food and Drug Administration (FDA).
RMAT designation is intended to expedite the development and review of regenerative medicines that are intended to treat, modify, reverse, or cure a serious or life-threatening disease or condition.
For a therapy to receive RMAT designation, preliminary evidence must indicate the therapy has the potential to address unmet medical needs for the disease or condition.
RMAT designation provides all the benefits of fast track and breakthrough therapy designations, including early interactions with the FDA.
About P-BCMA-101
To create P-BCMA-101, patients’ T cells are modified using a non-viral DNA modification system known as piggyBac™. The modified T cells target cells expressing B-cell maturation antigen (BCMA), which is expressed on essentially all MM cells.
Early results from the phase 1 trial (NCT03288493) of P-BCMA-101 were recently reported at the 2018 CAR-TCR Summit by Eric Ostertag, MD, PhD, chief executive officer of Poseida Therapeutics Inc., the company developing P-BCMA-101.
The presentation included data on 11 patients with heavily pretreated MM. Patients were a median age of 60, and 73% were high risk. They had a median of six prior therapies.
Patients received conditioning with fludarabine and cyclophosphamide for 3 days prior to receiving P-BCMA-101. They then received one of three doses of CAR T cells—51×106 (n=3), 152×106 (n=7), or 430×106 (n=1).
The investigators observed no dose-limiting toxicities. Adverse events included neutropenia in eight patients and thrombocytopenia in five.
One patient may have had cytokine release syndrome, but the condition resolved without drug intervention. And investigators observed no neurotoxicity.
Seven of ten patients evaluable for response by International Myeloma Working Group criteria achieved at least a partial response, including very good partial responses and stringent complete response.
The eleventh patient has oligosecretory disease and was only evaluable by PET, which indicated a near complete response.
Additional results from this trial are scheduled to be presented at the 2018 ASH Annual Meeting (abstract 1012).
The study is funded by the California Institute for Regenerative Medicine and Poseida Therapeutics.
Vaccine inhibits thrombus formation in mice
Investigators designed an antiplatelet vaccine they say could be a novel therapy to prevent recurrent ischemic stroke.
The vaccine inhibits S100A9 (S100 calcium-binding protein A9)/CD36 (cluster of differentiation 36) signaling in platelets, which is a key signal in arterial thrombosis but not hemostasis.
Mice immunized with the vaccine experienced an antithrombotic effect that lasted 84 days.
The vaccine inhibited thrombus formation without the risk of bleeding or adverse autoimmune responses.
The researchers say the vaccine worked as well as clopidogrel.
“Many stroke patients don’t take their blood thinning drugs as prescribed, which makes it more likely they will have another stroke,” said Hironori Nakagami, MD, of Osaka University Graduate School of Medicine in Japan.
“This vaccine might one day help solve this issue since it would only need to be injected periodically.”
Dr. Nakagami and his colleagues described the vaccine in Hypertension.
S100A9 had previously been reported to be a key molecule in the regulation of thrombus formation. The investigators therefore hypothesized that neutralizing S100A9 with a vaccine would provide sustained antithrombotic effects without increasing the risk of bleeding.
First, the researchers selected a region in S100A9 as a candidate target for the vaccine and conjugated it to keyhole limpet hemocyanin (KLH) as a carrier protein.
They also designed a S100A8 peptide vaccine. S100A8 forms a heterodimer with S100A9 but was not known to play a key role in thrombus formation.
The investigators then randomly assigned male C57BL/6J mice to receive either vaccine or KLH only as control.
The researchers vaccinated mice with S100A9 on days 0, 14, 28, and 126 with either 20 µg or 50 µg of S100A9 peptide. Other mice were vaccinated with S100A8 at a dose of 20 µg on days 0 and 14.
The vaccinated mice developed antibodies against either S100A8 or S100A9, the latter at the 50 µg dose of vaccine. The antibodies recognized the recombinant S100A8 and S100A9 without cross reactivity, which suggested specific binding of each induced antibody.
Assessing thrombus formation
The researchers examined the antithrombotic effects of S100A8 or S100A9 in mouse models of thrombotic middle cerebral artery (MCA) occlusion.
Twenty-one days after the final vaccination, mice immunized with S100A9 had significantly delayed MCA occlusion, with a greater antithrombotic effect in the 50 µg group.
This antithrombotic effect, the investigators said, was comparable to that observed in mice treated with clopidogrel at a dose of 6 mg/kg for 2 days.
The S100A8 vaccine did not prevent MCA occlusion, so the researchers focused on the S100A9 vaccine in subsequent experiments.
They studied the vaccine’s antithrombotic effects in a model of common carotid artery (CCA) occlusion and observed results similar to those seen in the MCA model.
Specifically, there was no significant difference in the CCA occlusion time between mice vaccinated with S100A9 and mice treated with clopidogrel.
The investigators also found the antithrombotic effect of the S100A9 vaccine lasted more than 2 months.
Post-stroke model
Dr. Nakagami and his colleagues then examined the antithrombotic effect of S100A9 in mice after a transient MCA stroke.
The researchers administered the S100A9 vaccine every 2 weeks, starting 1 week after the stroke, for a total of three times.
The vaccine induced anti-S100A9 antibodies, and the mice had significantly prolonged CCA occlusion times compared to KLH control mice. (The investigators said they assessed CCA occlusion because it was impossible to measure the regional cerebral blood flow after a transient MCA occlusion due to post-surgical cranial skin adhesions.)
This result suggested that S100A9 could prevent thrombus formation in mice that had already had a stroke.
Hemostatic parameters and safety
Additional experiments indicated that the S100A9 vaccine had no effect on hemostatic parameters as indicated by tail bleeding time, platelet count, activated partial thromboplastin time, and prothrombin time.
The researchers also evaluated the vaccine’s safety by examining immunologic responses.
Histological analysis at day 147 after the first immunization revealed no pathological changes, such as CD4+ T-cell infiltration or activation of F4/80+ microglia/macrophages.
The immunized mice had predominantly IgG1 responses. This indicated that the S100A9 vaccine selectively induced primary T helper 2 responses.
“We are continuing our research in hopes of being able to start clinical trials between 5 and 10 years from now, but there are differences between mice and humans in how the vaccine will be recognized by the immune system,” Dr. Nakagami explained.
“We should be able to overcome such problems and believe this vaccine provides a very promising strategy in secondary prevention of stroke.”
This research was funded by the Mochida Memorial Foundation for Medical and Pharmaceutical Research, the Japan Cardiovascular Research Foundation, the SENSHIN Medical Research Foundation, and the Japan Agency for Medical Research and Development.
Dr. Nakagami and five of the eleven authors have applied for a patent for the S100A9 vaccine.
Dr. Nakagami and five other authors are affiliated with departments at Osaka University that receive financial support from AnGes, DAICEL, FunPep, Novartis, Shionogi, Boehringer, and Rohto. One author is a founder, stockholder, and former board member of AnGes.
Investigators designed an antiplatelet vaccine they say could be a novel therapy to prevent recurrent ischemic stroke.
The vaccine inhibits S100A9 (S100 calcium-binding protein A9)/CD36 (cluster of differentiation 36) signaling in platelets, which is a key signal in arterial thrombosis but not hemostasis.
Mice immunized with the vaccine experienced an antithrombotic effect that lasted 84 days.
The vaccine inhibited thrombus formation without the risk of bleeding or adverse autoimmune responses.
The researchers say the vaccine worked as well as clopidogrel.
“Many stroke patients don’t take their blood thinning drugs as prescribed, which makes it more likely they will have another stroke,” said Hironori Nakagami, MD, of Osaka University Graduate School of Medicine in Japan.
“This vaccine might one day help solve this issue since it would only need to be injected periodically.”
Dr. Nakagami and his colleagues described the vaccine in Hypertension.
S100A9 had previously been reported to be a key molecule in the regulation of thrombus formation. The investigators therefore hypothesized that neutralizing S100A9 with a vaccine would provide sustained antithrombotic effects without increasing the risk of bleeding.
First, the researchers selected a region in S100A9 as a candidate target for the vaccine and conjugated it to keyhole limpet hemocyanin (KLH) as a carrier protein.
They also designed a S100A8 peptide vaccine. S100A8 forms a heterodimer with S100A9 but was not known to play a key role in thrombus formation.
The investigators then randomly assigned male C57BL/6J mice to receive either vaccine or KLH only as control.
The researchers vaccinated mice with S100A9 on days 0, 14, 28, and 126 with either 20 µg or 50 µg of S100A9 peptide. Other mice were vaccinated with S100A8 at a dose of 20 µg on days 0 and 14.
The vaccinated mice developed antibodies against either S100A8 or S100A9, the latter at the 50 µg dose of vaccine. The antibodies recognized the recombinant S100A8 and S100A9 without cross reactivity, which suggested specific binding of each induced antibody.
Assessing thrombus formation
The researchers examined the antithrombotic effects of S100A8 or S100A9 in mouse models of thrombotic middle cerebral artery (MCA) occlusion.
Twenty-one days after the final vaccination, mice immunized with S100A9 had significantly delayed MCA occlusion, with a greater antithrombotic effect in the 50 µg group.
This antithrombotic effect, the investigators said, was comparable to that observed in mice treated with clopidogrel at a dose of 6 mg/kg for 2 days.
The S100A8 vaccine did not prevent MCA occlusion, so the researchers focused on the S100A9 vaccine in subsequent experiments.
They studied the vaccine’s antithrombotic effects in a model of common carotid artery (CCA) occlusion and observed results similar to those seen in the MCA model.
Specifically, there was no significant difference in the CCA occlusion time between mice vaccinated with S100A9 and mice treated with clopidogrel.
The investigators also found the antithrombotic effect of the S100A9 vaccine lasted more than 2 months.
Post-stroke model
Dr. Nakagami and his colleagues then examined the antithrombotic effect of S100A9 in mice after a transient MCA stroke.
The researchers administered the S100A9 vaccine every 2 weeks, starting 1 week after the stroke, for a total of three times.
The vaccine induced anti-S100A9 antibodies, and the mice had significantly prolonged CCA occlusion times compared to KLH control mice. (The investigators said they assessed CCA occlusion because it was impossible to measure the regional cerebral blood flow after a transient MCA occlusion due to post-surgical cranial skin adhesions.)
This result suggested that S100A9 could prevent thrombus formation in mice that had already had a stroke.
Hemostatic parameters and safety
Additional experiments indicated that the S100A9 vaccine had no effect on hemostatic parameters as indicated by tail bleeding time, platelet count, activated partial thromboplastin time, and prothrombin time.
The researchers also evaluated the vaccine’s safety by examining immunologic responses.
Histological analysis at day 147 after the first immunization revealed no pathological changes, such as CD4+ T-cell infiltration or activation of F4/80+ microglia/macrophages.
The immunized mice had predominantly IgG1 responses. This indicated that the S100A9 vaccine selectively induced primary T helper 2 responses.
“We are continuing our research in hopes of being able to start clinical trials between 5 and 10 years from now, but there are differences between mice and humans in how the vaccine will be recognized by the immune system,” Dr. Nakagami explained.
“We should be able to overcome such problems and believe this vaccine provides a very promising strategy in secondary prevention of stroke.”
This research was funded by the Mochida Memorial Foundation for Medical and Pharmaceutical Research, the Japan Cardiovascular Research Foundation, the SENSHIN Medical Research Foundation, and the Japan Agency for Medical Research and Development.
Dr. Nakagami and five of the eleven authors have applied for a patent for the S100A9 vaccine.
Dr. Nakagami and five other authors are affiliated with departments at Osaka University that receive financial support from AnGes, DAICEL, FunPep, Novartis, Shionogi, Boehringer, and Rohto. One author is a founder, stockholder, and former board member of AnGes.
Investigators designed an antiplatelet vaccine they say could be a novel therapy to prevent recurrent ischemic stroke.
The vaccine inhibits S100A9 (S100 calcium-binding protein A9)/CD36 (cluster of differentiation 36) signaling in platelets, which is a key signal in arterial thrombosis but not hemostasis.
Mice immunized with the vaccine experienced an antithrombotic effect that lasted 84 days.
The vaccine inhibited thrombus formation without the risk of bleeding or adverse autoimmune responses.
The researchers say the vaccine worked as well as clopidogrel.
“Many stroke patients don’t take their blood thinning drugs as prescribed, which makes it more likely they will have another stroke,” said Hironori Nakagami, MD, of Osaka University Graduate School of Medicine in Japan.
“This vaccine might one day help solve this issue since it would only need to be injected periodically.”
Dr. Nakagami and his colleagues described the vaccine in Hypertension.
S100A9 had previously been reported to be a key molecule in the regulation of thrombus formation. The investigators therefore hypothesized that neutralizing S100A9 with a vaccine would provide sustained antithrombotic effects without increasing the risk of bleeding.
First, the researchers selected a region in S100A9 as a candidate target for the vaccine and conjugated it to keyhole limpet hemocyanin (KLH) as a carrier protein.
They also designed a S100A8 peptide vaccine. S100A8 forms a heterodimer with S100A9 but was not known to play a key role in thrombus formation.
The investigators then randomly assigned male C57BL/6J mice to receive either vaccine or KLH only as control.
The researchers vaccinated mice with S100A9 on days 0, 14, 28, and 126 with either 20 µg or 50 µg of S100A9 peptide. Other mice were vaccinated with S100A8 at a dose of 20 µg on days 0 and 14.
The vaccinated mice developed antibodies against either S100A8 or S100A9, the latter at the 50 µg dose of vaccine. The antibodies recognized the recombinant S100A8 and S100A9 without cross reactivity, which suggested specific binding of each induced antibody.
Assessing thrombus formation
The researchers examined the antithrombotic effects of S100A8 or S100A9 in mouse models of thrombotic middle cerebral artery (MCA) occlusion.
Twenty-one days after the final vaccination, mice immunized with S100A9 had significantly delayed MCA occlusion, with a greater antithrombotic effect in the 50 µg group.
This antithrombotic effect, the investigators said, was comparable to that observed in mice treated with clopidogrel at a dose of 6 mg/kg for 2 days.
The S100A8 vaccine did not prevent MCA occlusion, so the researchers focused on the S100A9 vaccine in subsequent experiments.
They studied the vaccine’s antithrombotic effects in a model of common carotid artery (CCA) occlusion and observed results similar to those seen in the MCA model.
Specifically, there was no significant difference in the CCA occlusion time between mice vaccinated with S100A9 and mice treated with clopidogrel.
The investigators also found the antithrombotic effect of the S100A9 vaccine lasted more than 2 months.
Post-stroke model
Dr. Nakagami and his colleagues then examined the antithrombotic effect of S100A9 in mice after a transient MCA stroke.
The researchers administered the S100A9 vaccine every 2 weeks, starting 1 week after the stroke, for a total of three times.
The vaccine induced anti-S100A9 antibodies, and the mice had significantly prolonged CCA occlusion times compared to KLH control mice. (The investigators said they assessed CCA occlusion because it was impossible to measure the regional cerebral blood flow after a transient MCA occlusion due to post-surgical cranial skin adhesions.)
This result suggested that S100A9 could prevent thrombus formation in mice that had already had a stroke.
Hemostatic parameters and safety
Additional experiments indicated that the S100A9 vaccine had no effect on hemostatic parameters as indicated by tail bleeding time, platelet count, activated partial thromboplastin time, and prothrombin time.
The researchers also evaluated the vaccine’s safety by examining immunologic responses.
Histological analysis at day 147 after the first immunization revealed no pathological changes, such as CD4+ T-cell infiltration or activation of F4/80+ microglia/macrophages.
The immunized mice had predominantly IgG1 responses. This indicated that the S100A9 vaccine selectively induced primary T helper 2 responses.
“We are continuing our research in hopes of being able to start clinical trials between 5 and 10 years from now, but there are differences between mice and humans in how the vaccine will be recognized by the immune system,” Dr. Nakagami explained.
“We should be able to overcome such problems and believe this vaccine provides a very promising strategy in secondary prevention of stroke.”
This research was funded by the Mochida Memorial Foundation for Medical and Pharmaceutical Research, the Japan Cardiovascular Research Foundation, the SENSHIN Medical Research Foundation, and the Japan Agency for Medical Research and Development.
Dr. Nakagami and five of the eleven authors have applied for a patent for the S100A9 vaccine.
Dr. Nakagami and five other authors are affiliated with departments at Osaka University that receive financial support from AnGes, DAICEL, FunPep, Novartis, Shionogi, Boehringer, and Rohto. One author is a founder, stockholder, and former board member of AnGes.
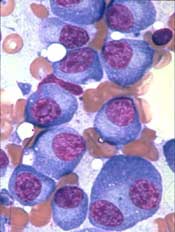
Aberrant RNA editing linked to aggressive myeloma
Overly zealous editing of messenger RNA in multiple myeloma cells appears to contribute to myeloma pathogenesis, and is prognostic of poor outcomes, investigators contend.
Over-expression of RNA editing enzymes in the adenosine deaminases acting on RNA (ADAR) family, specifically ADAR1, lead to hyperediting of the multiple myeloma (MM) transcriptome that in turn appears related to a drug-resistant disease phenotype and worse prognosis, reported Phaik Ju Teoh, PhD, of the Cancer Science Institute of Singapore, and colleagues.
The investigators implicate aberrant editing of adenosine to inosine (A-to-I) in malignant plasma cells, and its effects on NEIL1, a gene that encodes proteins involved in base excision repair of DNA, as important mechanisms in multiple myeloma pathogenesis.
“To the best of our knowledge, this is the first report of ADAR1-mediated hypereditome being an independent prognostic factor. The compromised integrity of MM transcriptome drives oncogenic phenotypes, likely contributing to the disease pathogenesis. Our current work, therefore, recognizes the clear biological and clinical importance of A-to-I editing at both the whole-transcriptome and gene-specific level (NEIL1) in MM,” they wrote in Blood.
A-to-I editing is the most prevalent form of RNA editing in humans, and aberrant editing mediated by ADAR1 has recently been linked to the development of several different cancer types, the investigators noted.
To see whether this process may also be involved in multiple myeloma, the investigators examined whole blood or bone marrow samples from healthy volunteers and patients with multiple myeloma.
They first looked at gene-expression profiling in the control and multiple myeloma samples and found that ADAR1 was overexpressed in the multiple myeloma cells, compared with nonmalignant plasma cells. Additionally, they saw that, at the protein level, ADAR1 was expressed at higher levels in patients with newly diagnosed or relapsed disease, compared with patients with smoldering myeloma or monoclonal gammopathy of undetermined significance.
They next determined that ADAR1 directly regulates hyperediting of the MM transcriptome, evidenced by the observation of a significant increase in A-to-G editing in the newly diagnosed and relapsed myeloma samples, compared with normal plasma cells. They confirmed this finding by observing the effects of ADAR1 levels on editing events across the transcriptome.
The authors followed this observation with experiments to see whether RNA editing by ADAR1 contributes to oncogenesis in myeloma cells. They silenced its expression and found that growth rate slowed and that ADAR1 wild-type protein introduced into cells promoted growth and proliferation.
“As the rescue with mutant ADAR1 is incomplete, we do not discount potential nonediting effects in ADAR1-induced oncogenesis in vivo. Nevertheless, taking into consideration the collective results from both the in vitro and in vivo studies, the RNA editing function of ADAR1 is important for its oncogenic effects in myeloma,” they wrote.
In the final steps, they identified NEIL1 as an important target for editing in multiple myeloma and observed that the editing compromised the ability of the proteins produced by the gene to accurately repair DNA damage.
“Further demonstrating its vital contribution to disease aggressiveness, patients with high ADAR1 expression showed less responsiveness toward standard and novel therapies. Therefore, our findings implied that a disturbed editome mediated by ADAR1 overexpression is both clinically and functionally crucial in our disease setting, and that ADAR1 confers oncogenic properties in myeloma in an editing-dependent manner,” they wrote.
The study was supported by the National Research Foundation Singapore, the Singapore Ministry of Education, and the National University of Singapore. The authors reported having no competing financial interests.
SOURCE: Teoh PJ et al. Blood. 2018;132(12):1304-17.
Overly zealous editing of messenger RNA in multiple myeloma cells appears to contribute to myeloma pathogenesis, and is prognostic of poor outcomes, investigators contend.
Over-expression of RNA editing enzymes in the adenosine deaminases acting on RNA (ADAR) family, specifically ADAR1, lead to hyperediting of the multiple myeloma (MM) transcriptome that in turn appears related to a drug-resistant disease phenotype and worse prognosis, reported Phaik Ju Teoh, PhD, of the Cancer Science Institute of Singapore, and colleagues.
The investigators implicate aberrant editing of adenosine to inosine (A-to-I) in malignant plasma cells, and its effects on NEIL1, a gene that encodes proteins involved in base excision repair of DNA, as important mechanisms in multiple myeloma pathogenesis.
“To the best of our knowledge, this is the first report of ADAR1-mediated hypereditome being an independent prognostic factor. The compromised integrity of MM transcriptome drives oncogenic phenotypes, likely contributing to the disease pathogenesis. Our current work, therefore, recognizes the clear biological and clinical importance of A-to-I editing at both the whole-transcriptome and gene-specific level (NEIL1) in MM,” they wrote in Blood.
A-to-I editing is the most prevalent form of RNA editing in humans, and aberrant editing mediated by ADAR1 has recently been linked to the development of several different cancer types, the investigators noted.
To see whether this process may also be involved in multiple myeloma, the investigators examined whole blood or bone marrow samples from healthy volunteers and patients with multiple myeloma.
They first looked at gene-expression profiling in the control and multiple myeloma samples and found that ADAR1 was overexpressed in the multiple myeloma cells, compared with nonmalignant plasma cells. Additionally, they saw that, at the protein level, ADAR1 was expressed at higher levels in patients with newly diagnosed or relapsed disease, compared with patients with smoldering myeloma or monoclonal gammopathy of undetermined significance.
They next determined that ADAR1 directly regulates hyperediting of the MM transcriptome, evidenced by the observation of a significant increase in A-to-G editing in the newly diagnosed and relapsed myeloma samples, compared with normal plasma cells. They confirmed this finding by observing the effects of ADAR1 levels on editing events across the transcriptome.
The authors followed this observation with experiments to see whether RNA editing by ADAR1 contributes to oncogenesis in myeloma cells. They silenced its expression and found that growth rate slowed and that ADAR1 wild-type protein introduced into cells promoted growth and proliferation.
“As the rescue with mutant ADAR1 is incomplete, we do not discount potential nonediting effects in ADAR1-induced oncogenesis in vivo. Nevertheless, taking into consideration the collective results from both the in vitro and in vivo studies, the RNA editing function of ADAR1 is important for its oncogenic effects in myeloma,” they wrote.
In the final steps, they identified NEIL1 as an important target for editing in multiple myeloma and observed that the editing compromised the ability of the proteins produced by the gene to accurately repair DNA damage.
“Further demonstrating its vital contribution to disease aggressiveness, patients with high ADAR1 expression showed less responsiveness toward standard and novel therapies. Therefore, our findings implied that a disturbed editome mediated by ADAR1 overexpression is both clinically and functionally crucial in our disease setting, and that ADAR1 confers oncogenic properties in myeloma in an editing-dependent manner,” they wrote.
The study was supported by the National Research Foundation Singapore, the Singapore Ministry of Education, and the National University of Singapore. The authors reported having no competing financial interests.
SOURCE: Teoh PJ et al. Blood. 2018;132(12):1304-17.
Overly zealous editing of messenger RNA in multiple myeloma cells appears to contribute to myeloma pathogenesis, and is prognostic of poor outcomes, investigators contend.
Over-expression of RNA editing enzymes in the adenosine deaminases acting on RNA (ADAR) family, specifically ADAR1, lead to hyperediting of the multiple myeloma (MM) transcriptome that in turn appears related to a drug-resistant disease phenotype and worse prognosis, reported Phaik Ju Teoh, PhD, of the Cancer Science Institute of Singapore, and colleagues.
The investigators implicate aberrant editing of adenosine to inosine (A-to-I) in malignant plasma cells, and its effects on NEIL1, a gene that encodes proteins involved in base excision repair of DNA, as important mechanisms in multiple myeloma pathogenesis.
“To the best of our knowledge, this is the first report of ADAR1-mediated hypereditome being an independent prognostic factor. The compromised integrity of MM transcriptome drives oncogenic phenotypes, likely contributing to the disease pathogenesis. Our current work, therefore, recognizes the clear biological and clinical importance of A-to-I editing at both the whole-transcriptome and gene-specific level (NEIL1) in MM,” they wrote in Blood.
A-to-I editing is the most prevalent form of RNA editing in humans, and aberrant editing mediated by ADAR1 has recently been linked to the development of several different cancer types, the investigators noted.
To see whether this process may also be involved in multiple myeloma, the investigators examined whole blood or bone marrow samples from healthy volunteers and patients with multiple myeloma.
They first looked at gene-expression profiling in the control and multiple myeloma samples and found that ADAR1 was overexpressed in the multiple myeloma cells, compared with nonmalignant plasma cells. Additionally, they saw that, at the protein level, ADAR1 was expressed at higher levels in patients with newly diagnosed or relapsed disease, compared with patients with smoldering myeloma or monoclonal gammopathy of undetermined significance.
They next determined that ADAR1 directly regulates hyperediting of the MM transcriptome, evidenced by the observation of a significant increase in A-to-G editing in the newly diagnosed and relapsed myeloma samples, compared with normal plasma cells. They confirmed this finding by observing the effects of ADAR1 levels on editing events across the transcriptome.
The authors followed this observation with experiments to see whether RNA editing by ADAR1 contributes to oncogenesis in myeloma cells. They silenced its expression and found that growth rate slowed and that ADAR1 wild-type protein introduced into cells promoted growth and proliferation.
“As the rescue with mutant ADAR1 is incomplete, we do not discount potential nonediting effects in ADAR1-induced oncogenesis in vivo. Nevertheless, taking into consideration the collective results from both the in vitro and in vivo studies, the RNA editing function of ADAR1 is important for its oncogenic effects in myeloma,” they wrote.
In the final steps, they identified NEIL1 as an important target for editing in multiple myeloma and observed that the editing compromised the ability of the proteins produced by the gene to accurately repair DNA damage.
“Further demonstrating its vital contribution to disease aggressiveness, patients with high ADAR1 expression showed less responsiveness toward standard and novel therapies. Therefore, our findings implied that a disturbed editome mediated by ADAR1 overexpression is both clinically and functionally crucial in our disease setting, and that ADAR1 confers oncogenic properties in myeloma in an editing-dependent manner,” they wrote.
The study was supported by the National Research Foundation Singapore, the Singapore Ministry of Education, and the National University of Singapore. The authors reported having no competing financial interests.
SOURCE: Teoh PJ et al. Blood. 2018;132(12):1304-17.
FROM BLOOD
Key clinical point:
Major finding: ADAR1-mediated editing of NEIL1 leads to a weakened DNA base excision repair mechanism.
Study details: Experimental series using plasma samples from healthy volunteers and patients with multiple myeloma.
Disclosures: The study was supported by the National Research Foundation Singapore, the Singapore Ministry of Education, and the National University of Singapore. The authors reported having no competing financial interests.
Source: Teoh PJ et al. Blood. 2018;132(12):1304-17.
FDA puts selinexor on fast track for DLBCL
The Food and Drug Administration has granted fast track designation to selinexor for the treatment of diffuse large B-cell lymphoma (DLBCL).
The designation is for selinexor to treat DLBCL patients who have received at least two prior therapies and who are not eligible for high-dose chemotherapy with stem cell rescue or chimeric antigen receptor (CAR) T-cell therapy.
Selinexor is being studied in the phase 2b SADAL trial (NCT02227251), which is enrolling patients with relapsed or refractory DLBCL who have received two to five prior therapies and are not eligible for stem cell transplant.
Top-line results from this trial are scheduled to be presented at the 2018 ASH Annual Meeting (Abstract 1677).
Selinexor is an oral selective inhibitor of nuclear export compound being developed by Karyopharm Therapeutics.
The company previously received fast track designation for selinexor to treat patients with penta-refractory multiple myeloma who have received at least three prior lines of therapy.
The FDA’s fast track program is designed to facilitate the development and expedite the review of products that are intended to treat serious conditions and have the potential to address unmet medical needs. Fast track designation provides developers with greater access to the FDA as well as eligibility for accelerated approval, priority review, and rolling review.
“Pending positive results from the phase 2b SADAL study, we plan to submit a second NDA [new drug application] to the FDA in the first half of 2019, with a request for accelerated approval, for oral selinexor as a potential new treatment for patients with relapsed or refractory DLBCL,” Sharon Shacham, PhD, founder, president, and chief scientific officer of Karyopharm, said in a statement.
In October, the FDA accepted an NDA for selinexor as a treatment for penta-refractory multiple myeloma. The agency granted the application priority review and set an action date of April 6, 2019.
The Food and Drug Administration has granted fast track designation to selinexor for the treatment of diffuse large B-cell lymphoma (DLBCL).
The designation is for selinexor to treat DLBCL patients who have received at least two prior therapies and who are not eligible for high-dose chemotherapy with stem cell rescue or chimeric antigen receptor (CAR) T-cell therapy.
Selinexor is being studied in the phase 2b SADAL trial (NCT02227251), which is enrolling patients with relapsed or refractory DLBCL who have received two to five prior therapies and are not eligible for stem cell transplant.
Top-line results from this trial are scheduled to be presented at the 2018 ASH Annual Meeting (Abstract 1677).
Selinexor is an oral selective inhibitor of nuclear export compound being developed by Karyopharm Therapeutics.
The company previously received fast track designation for selinexor to treat patients with penta-refractory multiple myeloma who have received at least three prior lines of therapy.
The FDA’s fast track program is designed to facilitate the development and expedite the review of products that are intended to treat serious conditions and have the potential to address unmet medical needs. Fast track designation provides developers with greater access to the FDA as well as eligibility for accelerated approval, priority review, and rolling review.
“Pending positive results from the phase 2b SADAL study, we plan to submit a second NDA [new drug application] to the FDA in the first half of 2019, with a request for accelerated approval, for oral selinexor as a potential new treatment for patients with relapsed or refractory DLBCL,” Sharon Shacham, PhD, founder, president, and chief scientific officer of Karyopharm, said in a statement.
In October, the FDA accepted an NDA for selinexor as a treatment for penta-refractory multiple myeloma. The agency granted the application priority review and set an action date of April 6, 2019.
The Food and Drug Administration has granted fast track designation to selinexor for the treatment of diffuse large B-cell lymphoma (DLBCL).
The designation is for selinexor to treat DLBCL patients who have received at least two prior therapies and who are not eligible for high-dose chemotherapy with stem cell rescue or chimeric antigen receptor (CAR) T-cell therapy.
Selinexor is being studied in the phase 2b SADAL trial (NCT02227251), which is enrolling patients with relapsed or refractory DLBCL who have received two to five prior therapies and are not eligible for stem cell transplant.
Top-line results from this trial are scheduled to be presented at the 2018 ASH Annual Meeting (Abstract 1677).
Selinexor is an oral selective inhibitor of nuclear export compound being developed by Karyopharm Therapeutics.
The company previously received fast track designation for selinexor to treat patients with penta-refractory multiple myeloma who have received at least three prior lines of therapy.
The FDA’s fast track program is designed to facilitate the development and expedite the review of products that are intended to treat serious conditions and have the potential to address unmet medical needs. Fast track designation provides developers with greater access to the FDA as well as eligibility for accelerated approval, priority review, and rolling review.
“Pending positive results from the phase 2b SADAL study, we plan to submit a second NDA [new drug application] to the FDA in the first half of 2019, with a request for accelerated approval, for oral selinexor as a potential new treatment for patients with relapsed or refractory DLBCL,” Sharon Shacham, PhD, founder, president, and chief scientific officer of Karyopharm, said in a statement.
In October, the FDA accepted an NDA for selinexor as a treatment for penta-refractory multiple myeloma. The agency granted the application priority review and set an action date of April 6, 2019.