User login
Revised U.S. cholesterol guidelines promote personalized risk assessment
CHICAGO – The latest cholesterol management guideline for U.S. practice has a core treatment principal that propels the field from its long-held focus on “know your cholesterol number,” that then became “know your risk” with the 2013 guideline, to what is now “personalize your risk.”
“The new guideline put special focus not just on risk, but on risk assessment that uses ‘enhancing factors’ to help patients understand their risk in a personal way and decide whether statin treatment is right for them” Neil J. Stone, MD, said at the American Heart Association scientific sessions.
Other novel features of the 2018 edition of the cholesterol management guideline included: specification of the role for two types of drugs other than statins – ezetimibe and PCSK9 inhibitors (including mention of the cost-value consideration when prescribing an expensive PCSK9 inhibitor); inclusion of coronary artery calcium (CAC) score assessment for patients with intermediate risk who are unsure whether statin treatment is right for them; and acknowledgment that nonfasting measurement of blood cholesterol levels is fine for most screening circumstances.
“Nonfasting is okay for many situations,” said Dr. Stone, a professor of medicine at Northwestern University here, and vice-chair of the writing panel for the guidelines, released by the American College of Cardiology, the American Heart Association, and 10 additional endorsing societies (J Am Coll Cardiol. 2018;doi:10.1016/j.jacc.2018.11.003)
But among the changes in the 2018 guideline that distinguish it from the preceding, 2013 version (Circulation. 2014 June 24;129[25, suppl 2]:S1-S45), the expanded approach to risk assessment in the primary-prevention setting stood out as the biggest shift.
“In 2013 we said calculate a person’s risk” for atherosclerotic cardiovascular disease. “Now that is much more fleshed out,” said Donald M. Lloyd-Jones, MD, a member of the guideline-writing group who helped develop the risk assessment tools used by the guideline.*
“The risk equations now are the same as we introduced in 2013,” he noted, and research done by Dr. Lloyd-Jones and others since that introduction showed that the “pooled cohort equations” are “well calibrated” for estimating a person’s 10-year risk for a cardiovascular event, especially at a risk level around 7.5%, which serves as the threshold for identifying a person with enough risk to warrant statin treatment. “But there are subgroups where the risk calculator clearly over- or under-estimates risk,” and that’s why the new guideline introduced the concept of risk enhancers--additional features not included in the basic risk calculation that enhance risk: family history; metabolic syndrome; chronic kidney disease; chronic inflammatory diseases such as psoriasis, rheumatoid arthritis, or HIV infection; a history of premature menopause or preeclampsia, certain ethnicity, or high levels of Lp(a) or apolipoprotein B.
“We didn’t need new risk scores; we needed to understand how to use the scores better, and the new guideline goes a long way toward helping clinicians do that,” Dr. Lloyd-Jones said in an interview.
Another aspect of this new, more nuanced approach to individualized risk assessment is the introduction of the CAC score as a possible tie breaker when a person who is otherwise a candidate for statin treatment for primary prevention is unsure about committing to possibly decades of daily statin treatment.
The guideline does not endorse obtaining a person’s CAC score for everyone as screening, stressed Dr. Stone, but this score, obtained by noncontrast CT with a radiation dose of about 1 mSv – comparable to a mammography exam, received a IIa rating” – is reasonable” for helping patients decide. Dr. Stone and others cited the importance of a CAC score of zero for patients on the fence for statin treatment as a strong indicator for many people that they can safely defer treatment.
As a result of this new endorsement for selectively obtaining CAC scores, “I think the number of tests will increase, probably fairly substantially,” said Dr. Lloyd-Jones, professor and chair of preventive medicine at Northwestern University here. He also expressed hope that this acknowledgment of an evidenced-based role for selected CAC score imaging may prompt health insurers to start coving this expense, something they don’t now do. Patients generally pay out-of-pocket from $50 to $300 for CAC score imaging. “I hope they will start paying for this,” Dr. Lloyd-Jones said.
The guidelines also deal, at least in passing, with another financial issue that has loomed large for cholesterol treatment, the role of the notoriously expensive PCSK9 inhibitors, alirocumab (Praluent) and evolocumab (Repatha). For secondary prevention patients or for patients with familial hypercholesterolemia who do not reach their LDL cholesterol goal on statin treatment alone, the guideline recommended treatment first with generic ezetimibe. If the goal remains elusive, the next step is prescribing a PCSK9 inhibitor. The guideline also noted the poor cost-benefit ratio for the PCSK9 inhibitors at the U.S. list prices that existed in mid-2018, about $14,000 a year.
The guideline writers noted that this is one of the first times that cost considerations found their way into cardiology guidelines. Clinicians “need to be attuned to prescribing PCSK9 inhibitors only in those settings when it provides good value to patients,” explained Mark A. Hlatky, MD, a professor of medicine, cardiologist, and health policy specialist at Stanford (Calif.) University. The guideline “focuses on patient selection for PCSK9 inhibitors, limiting it to patients who get the most benefit,” said Dr. Hlatky, another member of the writing panel.
Although 10 medical groups joined the American College of Cardiology and American Heart Association in endorsing the guideline, conspicuously absent were the two largest U.S. societies representing primary care physicians, the American College of Physicians and American Academy of Family Practitioners. The guideline’s organizers invited both these societies to participate in the process and they declined, said Sidney C. Smith, Jr., MD, a member of the guideline committee.
Dr. Stone and Dr. Lloyd-Jones had no financial disclosures. The writing committee members’ disclosures can be found at jaccjacc.acc.org/Clinical_Document/Cholesterol_GL_Au_Comp_RWI.pdf.
*Correction, 11/13/18: An earlier version of this article misstated the name of Dr. Donald M. Lloyd-Jones.
SOURCE: AHA 2018 and Grundy S et al. J Am Coll Cardiol. 2018;doi:10.1016/j.jacc.2018.11.003.
CHICAGO – The latest cholesterol management guideline for U.S. practice has a core treatment principal that propels the field from its long-held focus on “know your cholesterol number,” that then became “know your risk” with the 2013 guideline, to what is now “personalize your risk.”
“The new guideline put special focus not just on risk, but on risk assessment that uses ‘enhancing factors’ to help patients understand their risk in a personal way and decide whether statin treatment is right for them” Neil J. Stone, MD, said at the American Heart Association scientific sessions.
Other novel features of the 2018 edition of the cholesterol management guideline included: specification of the role for two types of drugs other than statins – ezetimibe and PCSK9 inhibitors (including mention of the cost-value consideration when prescribing an expensive PCSK9 inhibitor); inclusion of coronary artery calcium (CAC) score assessment for patients with intermediate risk who are unsure whether statin treatment is right for them; and acknowledgment that nonfasting measurement of blood cholesterol levels is fine for most screening circumstances.
“Nonfasting is okay for many situations,” said Dr. Stone, a professor of medicine at Northwestern University here, and vice-chair of the writing panel for the guidelines, released by the American College of Cardiology, the American Heart Association, and 10 additional endorsing societies (J Am Coll Cardiol. 2018;doi:10.1016/j.jacc.2018.11.003)
But among the changes in the 2018 guideline that distinguish it from the preceding, 2013 version (Circulation. 2014 June 24;129[25, suppl 2]:S1-S45), the expanded approach to risk assessment in the primary-prevention setting stood out as the biggest shift.
“In 2013 we said calculate a person’s risk” for atherosclerotic cardiovascular disease. “Now that is much more fleshed out,” said Donald M. Lloyd-Jones, MD, a member of the guideline-writing group who helped develop the risk assessment tools used by the guideline.*
“The risk equations now are the same as we introduced in 2013,” he noted, and research done by Dr. Lloyd-Jones and others since that introduction showed that the “pooled cohort equations” are “well calibrated” for estimating a person’s 10-year risk for a cardiovascular event, especially at a risk level around 7.5%, which serves as the threshold for identifying a person with enough risk to warrant statin treatment. “But there are subgroups where the risk calculator clearly over- or under-estimates risk,” and that’s why the new guideline introduced the concept of risk enhancers--additional features not included in the basic risk calculation that enhance risk: family history; metabolic syndrome; chronic kidney disease; chronic inflammatory diseases such as psoriasis, rheumatoid arthritis, or HIV infection; a history of premature menopause or preeclampsia, certain ethnicity, or high levels of Lp(a) or apolipoprotein B.
“We didn’t need new risk scores; we needed to understand how to use the scores better, and the new guideline goes a long way toward helping clinicians do that,” Dr. Lloyd-Jones said in an interview.
Another aspect of this new, more nuanced approach to individualized risk assessment is the introduction of the CAC score as a possible tie breaker when a person who is otherwise a candidate for statin treatment for primary prevention is unsure about committing to possibly decades of daily statin treatment.
The guideline does not endorse obtaining a person’s CAC score for everyone as screening, stressed Dr. Stone, but this score, obtained by noncontrast CT with a radiation dose of about 1 mSv – comparable to a mammography exam, received a IIa rating” – is reasonable” for helping patients decide. Dr. Stone and others cited the importance of a CAC score of zero for patients on the fence for statin treatment as a strong indicator for many people that they can safely defer treatment.
As a result of this new endorsement for selectively obtaining CAC scores, “I think the number of tests will increase, probably fairly substantially,” said Dr. Lloyd-Jones, professor and chair of preventive medicine at Northwestern University here. He also expressed hope that this acknowledgment of an evidenced-based role for selected CAC score imaging may prompt health insurers to start coving this expense, something they don’t now do. Patients generally pay out-of-pocket from $50 to $300 for CAC score imaging. “I hope they will start paying for this,” Dr. Lloyd-Jones said.
The guidelines also deal, at least in passing, with another financial issue that has loomed large for cholesterol treatment, the role of the notoriously expensive PCSK9 inhibitors, alirocumab (Praluent) and evolocumab (Repatha). For secondary prevention patients or for patients with familial hypercholesterolemia who do not reach their LDL cholesterol goal on statin treatment alone, the guideline recommended treatment first with generic ezetimibe. If the goal remains elusive, the next step is prescribing a PCSK9 inhibitor. The guideline also noted the poor cost-benefit ratio for the PCSK9 inhibitors at the U.S. list prices that existed in mid-2018, about $14,000 a year.
The guideline writers noted that this is one of the first times that cost considerations found their way into cardiology guidelines. Clinicians “need to be attuned to prescribing PCSK9 inhibitors only in those settings when it provides good value to patients,” explained Mark A. Hlatky, MD, a professor of medicine, cardiologist, and health policy specialist at Stanford (Calif.) University. The guideline “focuses on patient selection for PCSK9 inhibitors, limiting it to patients who get the most benefit,” said Dr. Hlatky, another member of the writing panel.
Although 10 medical groups joined the American College of Cardiology and American Heart Association in endorsing the guideline, conspicuously absent were the two largest U.S. societies representing primary care physicians, the American College of Physicians and American Academy of Family Practitioners. The guideline’s organizers invited both these societies to participate in the process and they declined, said Sidney C. Smith, Jr., MD, a member of the guideline committee.
Dr. Stone and Dr. Lloyd-Jones had no financial disclosures. The writing committee members’ disclosures can be found at jaccjacc.acc.org/Clinical_Document/Cholesterol_GL_Au_Comp_RWI.pdf.
*Correction, 11/13/18: An earlier version of this article misstated the name of Dr. Donald M. Lloyd-Jones.
SOURCE: AHA 2018 and Grundy S et al. J Am Coll Cardiol. 2018;doi:10.1016/j.jacc.2018.11.003.
CHICAGO – The latest cholesterol management guideline for U.S. practice has a core treatment principal that propels the field from its long-held focus on “know your cholesterol number,” that then became “know your risk” with the 2013 guideline, to what is now “personalize your risk.”
“The new guideline put special focus not just on risk, but on risk assessment that uses ‘enhancing factors’ to help patients understand their risk in a personal way and decide whether statin treatment is right for them” Neil J. Stone, MD, said at the American Heart Association scientific sessions.
Other novel features of the 2018 edition of the cholesterol management guideline included: specification of the role for two types of drugs other than statins – ezetimibe and PCSK9 inhibitors (including mention of the cost-value consideration when prescribing an expensive PCSK9 inhibitor); inclusion of coronary artery calcium (CAC) score assessment for patients with intermediate risk who are unsure whether statin treatment is right for them; and acknowledgment that nonfasting measurement of blood cholesterol levels is fine for most screening circumstances.
“Nonfasting is okay for many situations,” said Dr. Stone, a professor of medicine at Northwestern University here, and vice-chair of the writing panel for the guidelines, released by the American College of Cardiology, the American Heart Association, and 10 additional endorsing societies (J Am Coll Cardiol. 2018;doi:10.1016/j.jacc.2018.11.003)
But among the changes in the 2018 guideline that distinguish it from the preceding, 2013 version (Circulation. 2014 June 24;129[25, suppl 2]:S1-S45), the expanded approach to risk assessment in the primary-prevention setting stood out as the biggest shift.
“In 2013 we said calculate a person’s risk” for atherosclerotic cardiovascular disease. “Now that is much more fleshed out,” said Donald M. Lloyd-Jones, MD, a member of the guideline-writing group who helped develop the risk assessment tools used by the guideline.*
“The risk equations now are the same as we introduced in 2013,” he noted, and research done by Dr. Lloyd-Jones and others since that introduction showed that the “pooled cohort equations” are “well calibrated” for estimating a person’s 10-year risk for a cardiovascular event, especially at a risk level around 7.5%, which serves as the threshold for identifying a person with enough risk to warrant statin treatment. “But there are subgroups where the risk calculator clearly over- or under-estimates risk,” and that’s why the new guideline introduced the concept of risk enhancers--additional features not included in the basic risk calculation that enhance risk: family history; metabolic syndrome; chronic kidney disease; chronic inflammatory diseases such as psoriasis, rheumatoid arthritis, or HIV infection; a history of premature menopause or preeclampsia, certain ethnicity, or high levels of Lp(a) or apolipoprotein B.
“We didn’t need new risk scores; we needed to understand how to use the scores better, and the new guideline goes a long way toward helping clinicians do that,” Dr. Lloyd-Jones said in an interview.
Another aspect of this new, more nuanced approach to individualized risk assessment is the introduction of the CAC score as a possible tie breaker when a person who is otherwise a candidate for statin treatment for primary prevention is unsure about committing to possibly decades of daily statin treatment.
The guideline does not endorse obtaining a person’s CAC score for everyone as screening, stressed Dr. Stone, but this score, obtained by noncontrast CT with a radiation dose of about 1 mSv – comparable to a mammography exam, received a IIa rating” – is reasonable” for helping patients decide. Dr. Stone and others cited the importance of a CAC score of zero for patients on the fence for statin treatment as a strong indicator for many people that they can safely defer treatment.
As a result of this new endorsement for selectively obtaining CAC scores, “I think the number of tests will increase, probably fairly substantially,” said Dr. Lloyd-Jones, professor and chair of preventive medicine at Northwestern University here. He also expressed hope that this acknowledgment of an evidenced-based role for selected CAC score imaging may prompt health insurers to start coving this expense, something they don’t now do. Patients generally pay out-of-pocket from $50 to $300 for CAC score imaging. “I hope they will start paying for this,” Dr. Lloyd-Jones said.
The guidelines also deal, at least in passing, with another financial issue that has loomed large for cholesterol treatment, the role of the notoriously expensive PCSK9 inhibitors, alirocumab (Praluent) and evolocumab (Repatha). For secondary prevention patients or for patients with familial hypercholesterolemia who do not reach their LDL cholesterol goal on statin treatment alone, the guideline recommended treatment first with generic ezetimibe. If the goal remains elusive, the next step is prescribing a PCSK9 inhibitor. The guideline also noted the poor cost-benefit ratio for the PCSK9 inhibitors at the U.S. list prices that existed in mid-2018, about $14,000 a year.
The guideline writers noted that this is one of the first times that cost considerations found their way into cardiology guidelines. Clinicians “need to be attuned to prescribing PCSK9 inhibitors only in those settings when it provides good value to patients,” explained Mark A. Hlatky, MD, a professor of medicine, cardiologist, and health policy specialist at Stanford (Calif.) University. The guideline “focuses on patient selection for PCSK9 inhibitors, limiting it to patients who get the most benefit,” said Dr. Hlatky, another member of the writing panel.
Although 10 medical groups joined the American College of Cardiology and American Heart Association in endorsing the guideline, conspicuously absent were the two largest U.S. societies representing primary care physicians, the American College of Physicians and American Academy of Family Practitioners. The guideline’s organizers invited both these societies to participate in the process and they declined, said Sidney C. Smith, Jr., MD, a member of the guideline committee.
Dr. Stone and Dr. Lloyd-Jones had no financial disclosures. The writing committee members’ disclosures can be found at jaccjacc.acc.org/Clinical_Document/Cholesterol_GL_Au_Comp_RWI.pdf.
*Correction, 11/13/18: An earlier version of this article misstated the name of Dr. Donald M. Lloyd-Jones.
SOURCE: AHA 2018 and Grundy S et al. J Am Coll Cardiol. 2018;doi:10.1016/j.jacc.2018.11.003.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Vitamin D, fish oil circling the drain for primary prevention
CHICAGO – In what will surely come as a major disappointment to many millions of nutritional supplement enthusiasts, the daily use of vitamin D3 and/or omega-3 fatty acid capsules for a median of 5.3 years did not result in a lower incidence of invasive cancers or cardiovascular events than placebo in nearly 26,000 average-risk Americans who participated in the VITAL trial, JoAnn E. Manson, MD, reported at the American Heart Association scientific sessions.
VITAL (the Vitamin D and Omega-3 Trial) featured a 2x2 factorial design in which 25,871 subjects, including 5,016 black participants, were randomized in double-blind fashion to either vitamin D3, also known as cholecalciferol, at 2,000 IU/day and/or 1 g/day of omega-3 fatty acid, or placebo. The men had to be at least 50 years old, the women 55, and none had a baseline history of cardiovascular disease or invasive cancer. Their mean age was 67. Study pill adherence exceeded 83% over the course of 5.3 years.
This major study, funded by the National Institutes of Health, was designed to answer the question of whether two relatively inexpensive supplements with plausible mechanisms of potential benefit could be harnessed as effective agents for primary prevention of the two leading causes of death in the United States.
The simple answer turned out to be no. Invasive cancer of any type occurred in 793 patients in the vitamin D group and 824 placebo-treated controls, for a nonsignificant hazard ratio of 0.96. Major cardiovascular events – a composite of MI, stroke, or cardiovascular mortality – occurred in 396 and 409 patients, respectively, for a hazard ratio of 0.97.
Similarly, invasive cancer was diagnosed in 820 subjects in the omega-3 fatty acid group and 797 controls, while major cardiovascular events occurred in 386 patients taking fish oil and 419 on placebo. Again, the between-group differences were nonsignificant, noted Dr. Manson, chief of the division of preventive medicine and Brigham and Women’s Hospital and professor of medicine and women’s health at Harvard Medical School, Boston.
Buried within this vast data set were a few intriguing bright spots. For example, the prespecified secondary endpoint of total MIs was significantly reduced by 28% in patients using omega-3 fatty acid compared with placebo. In nonprespecified exploratory analyses, the risk of PCI was decreased by 22% in the omega-3 fatty acid group and total coronary heart disease events - a composite of MI, revascularization, or death due to coronary heart disease – was reduced by 17%. In black subjects, the use of omega-3 fatty acids reduced the risk of MIs by 77%.
Dietary fish consumption interacted with the effects of omega-3 supplementation. Subjects in the omega-3 group who ate less than the median 1.5 servings of fish per week had a statistically significant 19% relative risk reduction in major cardiovascular events and 40% fewer MIs than with placebo. In contrast, subjects who ate 1.5 or more fish servings derived no benefit from omega-3 supplements.
The most noteworthy finding in the vitamin D group was that, after excluding the first 2 years of follow-up, they had a 25% reduction in cancer mortality compared with controls.
However, Dr. Manson cautioned that these subgroup analyses should be interpreted with caution.
Discussant Jane Armitage, MD, went further, emphasizing that the primary study endpoints of invasive cancer and major cardiovascular events were negative for both vitamin D and fish oil.
“To drill down into the secondary endpoints is of some concern because I think there is often the risk of getting spurious results,” said Dr. Armitage, professor of clinical trials and epidemiology at the University of Oxford (England).
“I think the primary result that universal supplementation with vitamin D in a primary prevention population has not been shown to be beneficial is a robust result, and these other results need to be seen as hypothesis-generating,” according to Dr. Armitage.
She added that she thinks the VITAL trial is practice-changing.
“I think the general recommendation to take vitamin D is not supported by this paper,” she said.
The same holds true for omega-3 fatty acid supplementation based on the VITAL results, Dr. Armitage continued. She noted that the VITAL findings are consistent with a recent meta-analysis of 10 large trials of omega-3 which found no benefit in nearly 78,000 high-cardiovascular-risk subjects (JAMA Cardiol. 2018 Mar 1;3[3]:225-234).
VITAL vs. REDUCE-IT
The negative results in VITAL stood in sharp contrast to the findings of the REDUCE-IT trial, presented at the same late-breaker session by Deepak Bhatt, MD, of Harvard Medical School. In REDUCE-IT, icosapent ethyl, another fish-derived product, reduced major cardiovascular events by 25% in a study of more than 8,000 high-cardiovascular-risk patients with elevated triglycerides.
Why the difference in outcomes? Among the proposed explanations were that participants in VITAL got 1 g/day of omega-3 while those in REDUCE-IT got a much higher dose of 4 g/day of iscosapent ethyl, the REDUCE-IT population was at much higher cardiovascular risk, and icosapent ethyl has a mechanism of action that’s distinct from that of conventional fish oil products.
Dr. Manson said numerous ancillary studies from VITAL are underway and will begin appearing soon. These will look at the impact of vitamin D and fish oil supplementation on cognitive function, hypertension, atrial fibrillation, autoimmune disorders, bone health, depression, kidney disease, and other issues.
Simultaneously with her presentation at the AHA scientific sessions, the VITAL results were published online (N Engl J Med. 2018 Nov 10; doi: 10.1056/NEJMoa1809944 and 10.1056/NEJMoa1811403).
The study was sponsored by the National Institutes of Health. The presenter reported having no financial conflicts.
SOURCE: Manson JE. AHA Abstr. #19539
CHICAGO – In what will surely come as a major disappointment to many millions of nutritional supplement enthusiasts, the daily use of vitamin D3 and/or omega-3 fatty acid capsules for a median of 5.3 years did not result in a lower incidence of invasive cancers or cardiovascular events than placebo in nearly 26,000 average-risk Americans who participated in the VITAL trial, JoAnn E. Manson, MD, reported at the American Heart Association scientific sessions.
VITAL (the Vitamin D and Omega-3 Trial) featured a 2x2 factorial design in which 25,871 subjects, including 5,016 black participants, were randomized in double-blind fashion to either vitamin D3, also known as cholecalciferol, at 2,000 IU/day and/or 1 g/day of omega-3 fatty acid, or placebo. The men had to be at least 50 years old, the women 55, and none had a baseline history of cardiovascular disease or invasive cancer. Their mean age was 67. Study pill adherence exceeded 83% over the course of 5.3 years.
This major study, funded by the National Institutes of Health, was designed to answer the question of whether two relatively inexpensive supplements with plausible mechanisms of potential benefit could be harnessed as effective agents for primary prevention of the two leading causes of death in the United States.
The simple answer turned out to be no. Invasive cancer of any type occurred in 793 patients in the vitamin D group and 824 placebo-treated controls, for a nonsignificant hazard ratio of 0.96. Major cardiovascular events – a composite of MI, stroke, or cardiovascular mortality – occurred in 396 and 409 patients, respectively, for a hazard ratio of 0.97.
Similarly, invasive cancer was diagnosed in 820 subjects in the omega-3 fatty acid group and 797 controls, while major cardiovascular events occurred in 386 patients taking fish oil and 419 on placebo. Again, the between-group differences were nonsignificant, noted Dr. Manson, chief of the division of preventive medicine and Brigham and Women’s Hospital and professor of medicine and women’s health at Harvard Medical School, Boston.
Buried within this vast data set were a few intriguing bright spots. For example, the prespecified secondary endpoint of total MIs was significantly reduced by 28% in patients using omega-3 fatty acid compared with placebo. In nonprespecified exploratory analyses, the risk of PCI was decreased by 22% in the omega-3 fatty acid group and total coronary heart disease events - a composite of MI, revascularization, or death due to coronary heart disease – was reduced by 17%. In black subjects, the use of omega-3 fatty acids reduced the risk of MIs by 77%.
Dietary fish consumption interacted with the effects of omega-3 supplementation. Subjects in the omega-3 group who ate less than the median 1.5 servings of fish per week had a statistically significant 19% relative risk reduction in major cardiovascular events and 40% fewer MIs than with placebo. In contrast, subjects who ate 1.5 or more fish servings derived no benefit from omega-3 supplements.
The most noteworthy finding in the vitamin D group was that, after excluding the first 2 years of follow-up, they had a 25% reduction in cancer mortality compared with controls.
However, Dr. Manson cautioned that these subgroup analyses should be interpreted with caution.
Discussant Jane Armitage, MD, went further, emphasizing that the primary study endpoints of invasive cancer and major cardiovascular events were negative for both vitamin D and fish oil.
“To drill down into the secondary endpoints is of some concern because I think there is often the risk of getting spurious results,” said Dr. Armitage, professor of clinical trials and epidemiology at the University of Oxford (England).
“I think the primary result that universal supplementation with vitamin D in a primary prevention population has not been shown to be beneficial is a robust result, and these other results need to be seen as hypothesis-generating,” according to Dr. Armitage.
She added that she thinks the VITAL trial is practice-changing.
“I think the general recommendation to take vitamin D is not supported by this paper,” she said.
The same holds true for omega-3 fatty acid supplementation based on the VITAL results, Dr. Armitage continued. She noted that the VITAL findings are consistent with a recent meta-analysis of 10 large trials of omega-3 which found no benefit in nearly 78,000 high-cardiovascular-risk subjects (JAMA Cardiol. 2018 Mar 1;3[3]:225-234).
VITAL vs. REDUCE-IT
The negative results in VITAL stood in sharp contrast to the findings of the REDUCE-IT trial, presented at the same late-breaker session by Deepak Bhatt, MD, of Harvard Medical School. In REDUCE-IT, icosapent ethyl, another fish-derived product, reduced major cardiovascular events by 25% in a study of more than 8,000 high-cardiovascular-risk patients with elevated triglycerides.
Why the difference in outcomes? Among the proposed explanations were that participants in VITAL got 1 g/day of omega-3 while those in REDUCE-IT got a much higher dose of 4 g/day of iscosapent ethyl, the REDUCE-IT population was at much higher cardiovascular risk, and icosapent ethyl has a mechanism of action that’s distinct from that of conventional fish oil products.
Dr. Manson said numerous ancillary studies from VITAL are underway and will begin appearing soon. These will look at the impact of vitamin D and fish oil supplementation on cognitive function, hypertension, atrial fibrillation, autoimmune disorders, bone health, depression, kidney disease, and other issues.
Simultaneously with her presentation at the AHA scientific sessions, the VITAL results were published online (N Engl J Med. 2018 Nov 10; doi: 10.1056/NEJMoa1809944 and 10.1056/NEJMoa1811403).
The study was sponsored by the National Institutes of Health. The presenter reported having no financial conflicts.
SOURCE: Manson JE. AHA Abstr. #19539
CHICAGO – In what will surely come as a major disappointment to many millions of nutritional supplement enthusiasts, the daily use of vitamin D3 and/or omega-3 fatty acid capsules for a median of 5.3 years did not result in a lower incidence of invasive cancers or cardiovascular events than placebo in nearly 26,000 average-risk Americans who participated in the VITAL trial, JoAnn E. Manson, MD, reported at the American Heart Association scientific sessions.
VITAL (the Vitamin D and Omega-3 Trial) featured a 2x2 factorial design in which 25,871 subjects, including 5,016 black participants, were randomized in double-blind fashion to either vitamin D3, also known as cholecalciferol, at 2,000 IU/day and/or 1 g/day of omega-3 fatty acid, or placebo. The men had to be at least 50 years old, the women 55, and none had a baseline history of cardiovascular disease or invasive cancer. Their mean age was 67. Study pill adherence exceeded 83% over the course of 5.3 years.
This major study, funded by the National Institutes of Health, was designed to answer the question of whether two relatively inexpensive supplements with plausible mechanisms of potential benefit could be harnessed as effective agents for primary prevention of the two leading causes of death in the United States.
The simple answer turned out to be no. Invasive cancer of any type occurred in 793 patients in the vitamin D group and 824 placebo-treated controls, for a nonsignificant hazard ratio of 0.96. Major cardiovascular events – a composite of MI, stroke, or cardiovascular mortality – occurred in 396 and 409 patients, respectively, for a hazard ratio of 0.97.
Similarly, invasive cancer was diagnosed in 820 subjects in the omega-3 fatty acid group and 797 controls, while major cardiovascular events occurred in 386 patients taking fish oil and 419 on placebo. Again, the between-group differences were nonsignificant, noted Dr. Manson, chief of the division of preventive medicine and Brigham and Women’s Hospital and professor of medicine and women’s health at Harvard Medical School, Boston.
Buried within this vast data set were a few intriguing bright spots. For example, the prespecified secondary endpoint of total MIs was significantly reduced by 28% in patients using omega-3 fatty acid compared with placebo. In nonprespecified exploratory analyses, the risk of PCI was decreased by 22% in the omega-3 fatty acid group and total coronary heart disease events - a composite of MI, revascularization, or death due to coronary heart disease – was reduced by 17%. In black subjects, the use of omega-3 fatty acids reduced the risk of MIs by 77%.
Dietary fish consumption interacted with the effects of omega-3 supplementation. Subjects in the omega-3 group who ate less than the median 1.5 servings of fish per week had a statistically significant 19% relative risk reduction in major cardiovascular events and 40% fewer MIs than with placebo. In contrast, subjects who ate 1.5 or more fish servings derived no benefit from omega-3 supplements.
The most noteworthy finding in the vitamin D group was that, after excluding the first 2 years of follow-up, they had a 25% reduction in cancer mortality compared with controls.
However, Dr. Manson cautioned that these subgroup analyses should be interpreted with caution.
Discussant Jane Armitage, MD, went further, emphasizing that the primary study endpoints of invasive cancer and major cardiovascular events were negative for both vitamin D and fish oil.
“To drill down into the secondary endpoints is of some concern because I think there is often the risk of getting spurious results,” said Dr. Armitage, professor of clinical trials and epidemiology at the University of Oxford (England).
“I think the primary result that universal supplementation with vitamin D in a primary prevention population has not been shown to be beneficial is a robust result, and these other results need to be seen as hypothesis-generating,” according to Dr. Armitage.
She added that she thinks the VITAL trial is practice-changing.
“I think the general recommendation to take vitamin D is not supported by this paper,” she said.
The same holds true for omega-3 fatty acid supplementation based on the VITAL results, Dr. Armitage continued. She noted that the VITAL findings are consistent with a recent meta-analysis of 10 large trials of omega-3 which found no benefit in nearly 78,000 high-cardiovascular-risk subjects (JAMA Cardiol. 2018 Mar 1;3[3]:225-234).
VITAL vs. REDUCE-IT
The negative results in VITAL stood in sharp contrast to the findings of the REDUCE-IT trial, presented at the same late-breaker session by Deepak Bhatt, MD, of Harvard Medical School. In REDUCE-IT, icosapent ethyl, another fish-derived product, reduced major cardiovascular events by 25% in a study of more than 8,000 high-cardiovascular-risk patients with elevated triglycerides.
Why the difference in outcomes? Among the proposed explanations were that participants in VITAL got 1 g/day of omega-3 while those in REDUCE-IT got a much higher dose of 4 g/day of iscosapent ethyl, the REDUCE-IT population was at much higher cardiovascular risk, and icosapent ethyl has a mechanism of action that’s distinct from that of conventional fish oil products.
Dr. Manson said numerous ancillary studies from VITAL are underway and will begin appearing soon. These will look at the impact of vitamin D and fish oil supplementation on cognitive function, hypertension, atrial fibrillation, autoimmune disorders, bone health, depression, kidney disease, and other issues.
Simultaneously with her presentation at the AHA scientific sessions, the VITAL results were published online (N Engl J Med. 2018 Nov 10; doi: 10.1056/NEJMoa1809944 and 10.1056/NEJMoa1811403).
The study was sponsored by the National Institutes of Health. The presenter reported having no financial conflicts.
SOURCE: Manson JE. AHA Abstr. #19539
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: The primary cancer and cardiovascular outcomes were unaffected by either supplement in the VITAL study.
Study details: VITAL was a randomized, double-blind trial in which nearly 26,000 middle-age or older Americans at average cardiovascular risk were assigned to vitamin D3, omega-3 fatty acid, and placebo in a 2x2 factorial design and followed prospectively for a median of 5.3 years.
Disclosures: The study was sponsored by the National Institutes of Health. The presenter reported having no financial conflicts.
Source: Manson JE. AHA 2018 Abst. #19539.
New private online community for SVS members
The Society for Vascular Surgery is creating a private online community, SVSConnect, with a number of resources for SVS members and their peers. This new collaborative online community will let members connect and engage with, and learn from, fellow members and peers on an infinite number of topics. It is expected to launch by late 2018. Users will enjoy a member directory search, forums, mentor match programs and resource sharing. More information will be communicated to members soon via Pulse newsletters, emails and the SVS Website.
The Society for Vascular Surgery is creating a private online community, SVSConnect, with a number of resources for SVS members and their peers. This new collaborative online community will let members connect and engage with, and learn from, fellow members and peers on an infinite number of topics. It is expected to launch by late 2018. Users will enjoy a member directory search, forums, mentor match programs and resource sharing. More information will be communicated to members soon via Pulse newsletters, emails and the SVS Website.
The Society for Vascular Surgery is creating a private online community, SVSConnect, with a number of resources for SVS members and their peers. This new collaborative online community will let members connect and engage with, and learn from, fellow members and peers on an infinite number of topics. It is expected to launch by late 2018. Users will enjoy a member directory search, forums, mentor match programs and resource sharing. More information will be communicated to members soon via Pulse newsletters, emails and the SVS Website.
‘Compelling’ new target found for monocytic AML
Efforts to determine why immune checkpoint blockade is not successful in treating leukemia have resulted in a “compelling” new target to treat monocytic acute myeloid leukemia (AML), according to researchers.
They discovered that leukocyte immunoglobulin-like receptor B4 (LILRB4), a marker of monocytic leukemia, creates an immunosuppressive microenvironment by mediating T-cell suppression.
Using a mouse model and human cells, the research team showed that LILRB4 supports tumor infiltration into tissues and suppresses T-cell activity through a signaling pathway involving APOE, LILRB4, SHP-2, uPAR, and ARG1.
Senior author Chengcheng “Alec” Zhang, PhD, of the University of Texas Southwestern Medical Center in Dallas, and his colleagues reported their findings in Nature.
The team first compared surface expression of LILRB4 on normal monocytes and neoplastic monocytes from 105 AML patient samples. They observed that LILRB4 levels were higher on monocytic AML cells than on normal monocytes.
The researchers then tested whether LILRB4 expressed on AML cells suppressed T cells. They cultured LILRB4-positive leukemia cells, LILRB4-negative leukemia cells, and normal hematopoietic cells with either autologous T cells or T cells from healthy donors. The team determined that only LILRB4-positive monocytic AML cells substantially suppressed T-cell proliferation.
When the researchers knocked out LILRB4, the ability of AML cells to suppress T cells was reduced and could be restored with forced expression of wild-type LILRB4. Additionally, LILRB4-mediated T-cell inhibition could be reversed by LILRB4-blocking antibodies.
The team then used a humanized mouse xenograft model and an immunocompetent mouse model to investigate LILRB4 function in immune checkpoint blockade. Blocking LILRB4 lowered tumor burden and prolonged survival in the mice.
The researchers performed numerous in vitro and in vivo experiments and observed that antibody blockade of LILRB4 shrank tumors and decreased leukemic infiltration into internal organs, including the bone marrow, liver, and brain.
And so the team hypothesized that LILRB4 promotes leukemia infiltration in addition to inhibiting T cells.
To test the hypothesis, they performed transendothelial migration and homing assays and monitored leukemia infiltration relative to LILRB4 expression on leukemia cells. They observed that LILRB4-mediated migration enhanced extramedullary infiltration of monocytic AML cells, thus contributing to immune evasion.
The researchers also found that APOE protein activated the immune inhibitory receptor LILRB4.
To ascertain whether suppression of T cells by LILRB4 depends on APOE, the team co-cultured T cells with control or human AML cells with APOE knocked out.
Through a series of experiments, they determined that APOE is an extracellular binding protein of LILRB4 and that APOE activates LILRB4 to support T-cell proliferation and AML cell migration.
The researchers believe that targeting LILRB4 may have minimal toxicity. This is because LILRB4 expression on normal monocytic cells is limited, LILRB4 signaling may differ in leukemia cells, and LILRB4 blockade did not significantly interfere with normal hematopoietic function.
Dr. Zhang anticipates that if the preclinical studies go well, clinical trials could begin as early as next year.
The University of Texas System has exclusively licensed LILRB4-related patent applications to California-based Immune-Onc Therapeutics Inc., which contributed to the research and is conducting preclinical studies.
Dr. Zhang and another author are scientific advisory board members with Immune-Onc Therapeutics. Two other authors are employees of and hold equities in Immune-Onc Therapeutics.
The researchers received additional funding for this work from the National Cancer Institute, Leukemia & Lymphoma Society, the March of Dimes, the Cancer Prevention and Research Institute of Texas, the Robert A. Welch Foundation, the National Natural Science Foundation of China, the National Basic Research Program of China, and the China Scholarship Council.
Efforts to determine why immune checkpoint blockade is not successful in treating leukemia have resulted in a “compelling” new target to treat monocytic acute myeloid leukemia (AML), according to researchers.
They discovered that leukocyte immunoglobulin-like receptor B4 (LILRB4), a marker of monocytic leukemia, creates an immunosuppressive microenvironment by mediating T-cell suppression.
Using a mouse model and human cells, the research team showed that LILRB4 supports tumor infiltration into tissues and suppresses T-cell activity through a signaling pathway involving APOE, LILRB4, SHP-2, uPAR, and ARG1.
Senior author Chengcheng “Alec” Zhang, PhD, of the University of Texas Southwestern Medical Center in Dallas, and his colleagues reported their findings in Nature.
The team first compared surface expression of LILRB4 on normal monocytes and neoplastic monocytes from 105 AML patient samples. They observed that LILRB4 levels were higher on monocytic AML cells than on normal monocytes.
The researchers then tested whether LILRB4 expressed on AML cells suppressed T cells. They cultured LILRB4-positive leukemia cells, LILRB4-negative leukemia cells, and normal hematopoietic cells with either autologous T cells or T cells from healthy donors. The team determined that only LILRB4-positive monocytic AML cells substantially suppressed T-cell proliferation.
When the researchers knocked out LILRB4, the ability of AML cells to suppress T cells was reduced and could be restored with forced expression of wild-type LILRB4. Additionally, LILRB4-mediated T-cell inhibition could be reversed by LILRB4-blocking antibodies.
The team then used a humanized mouse xenograft model and an immunocompetent mouse model to investigate LILRB4 function in immune checkpoint blockade. Blocking LILRB4 lowered tumor burden and prolonged survival in the mice.
The researchers performed numerous in vitro and in vivo experiments and observed that antibody blockade of LILRB4 shrank tumors and decreased leukemic infiltration into internal organs, including the bone marrow, liver, and brain.
And so the team hypothesized that LILRB4 promotes leukemia infiltration in addition to inhibiting T cells.
To test the hypothesis, they performed transendothelial migration and homing assays and monitored leukemia infiltration relative to LILRB4 expression on leukemia cells. They observed that LILRB4-mediated migration enhanced extramedullary infiltration of monocytic AML cells, thus contributing to immune evasion.
The researchers also found that APOE protein activated the immune inhibitory receptor LILRB4.
To ascertain whether suppression of T cells by LILRB4 depends on APOE, the team co-cultured T cells with control or human AML cells with APOE knocked out.
Through a series of experiments, they determined that APOE is an extracellular binding protein of LILRB4 and that APOE activates LILRB4 to support T-cell proliferation and AML cell migration.
The researchers believe that targeting LILRB4 may have minimal toxicity. This is because LILRB4 expression on normal monocytic cells is limited, LILRB4 signaling may differ in leukemia cells, and LILRB4 blockade did not significantly interfere with normal hematopoietic function.
Dr. Zhang anticipates that if the preclinical studies go well, clinical trials could begin as early as next year.
The University of Texas System has exclusively licensed LILRB4-related patent applications to California-based Immune-Onc Therapeutics Inc., which contributed to the research and is conducting preclinical studies.
Dr. Zhang and another author are scientific advisory board members with Immune-Onc Therapeutics. Two other authors are employees of and hold equities in Immune-Onc Therapeutics.
The researchers received additional funding for this work from the National Cancer Institute, Leukemia & Lymphoma Society, the March of Dimes, the Cancer Prevention and Research Institute of Texas, the Robert A. Welch Foundation, the National Natural Science Foundation of China, the National Basic Research Program of China, and the China Scholarship Council.
Efforts to determine why immune checkpoint blockade is not successful in treating leukemia have resulted in a “compelling” new target to treat monocytic acute myeloid leukemia (AML), according to researchers.
They discovered that leukocyte immunoglobulin-like receptor B4 (LILRB4), a marker of monocytic leukemia, creates an immunosuppressive microenvironment by mediating T-cell suppression.
Using a mouse model and human cells, the research team showed that LILRB4 supports tumor infiltration into tissues and suppresses T-cell activity through a signaling pathway involving APOE, LILRB4, SHP-2, uPAR, and ARG1.
Senior author Chengcheng “Alec” Zhang, PhD, of the University of Texas Southwestern Medical Center in Dallas, and his colleagues reported their findings in Nature.
The team first compared surface expression of LILRB4 on normal monocytes and neoplastic monocytes from 105 AML patient samples. They observed that LILRB4 levels were higher on monocytic AML cells than on normal monocytes.
The researchers then tested whether LILRB4 expressed on AML cells suppressed T cells. They cultured LILRB4-positive leukemia cells, LILRB4-negative leukemia cells, and normal hematopoietic cells with either autologous T cells or T cells from healthy donors. The team determined that only LILRB4-positive monocytic AML cells substantially suppressed T-cell proliferation.
When the researchers knocked out LILRB4, the ability of AML cells to suppress T cells was reduced and could be restored with forced expression of wild-type LILRB4. Additionally, LILRB4-mediated T-cell inhibition could be reversed by LILRB4-blocking antibodies.
The team then used a humanized mouse xenograft model and an immunocompetent mouse model to investigate LILRB4 function in immune checkpoint blockade. Blocking LILRB4 lowered tumor burden and prolonged survival in the mice.
The researchers performed numerous in vitro and in vivo experiments and observed that antibody blockade of LILRB4 shrank tumors and decreased leukemic infiltration into internal organs, including the bone marrow, liver, and brain.
And so the team hypothesized that LILRB4 promotes leukemia infiltration in addition to inhibiting T cells.
To test the hypothesis, they performed transendothelial migration and homing assays and monitored leukemia infiltration relative to LILRB4 expression on leukemia cells. They observed that LILRB4-mediated migration enhanced extramedullary infiltration of monocytic AML cells, thus contributing to immune evasion.
The researchers also found that APOE protein activated the immune inhibitory receptor LILRB4.
To ascertain whether suppression of T cells by LILRB4 depends on APOE, the team co-cultured T cells with control or human AML cells with APOE knocked out.
Through a series of experiments, they determined that APOE is an extracellular binding protein of LILRB4 and that APOE activates LILRB4 to support T-cell proliferation and AML cell migration.
The researchers believe that targeting LILRB4 may have minimal toxicity. This is because LILRB4 expression on normal monocytic cells is limited, LILRB4 signaling may differ in leukemia cells, and LILRB4 blockade did not significantly interfere with normal hematopoietic function.
Dr. Zhang anticipates that if the preclinical studies go well, clinical trials could begin as early as next year.
The University of Texas System has exclusively licensed LILRB4-related patent applications to California-based Immune-Onc Therapeutics Inc., which contributed to the research and is conducting preclinical studies.
Dr. Zhang and another author are scientific advisory board members with Immune-Onc Therapeutics. Two other authors are employees of and hold equities in Immune-Onc Therapeutics.
The researchers received additional funding for this work from the National Cancer Institute, Leukemia & Lymphoma Society, the March of Dimes, the Cancer Prevention and Research Institute of Texas, the Robert A. Welch Foundation, the National Natural Science Foundation of China, the National Basic Research Program of China, and the China Scholarship Council.
New cholesterol guidelines expand options for primary care
CHICAGO – New U.S. cholesterol guidelines spell out the role for ezetimibe and PCSK9 inhibitors, expand the scope of individualized risk assessment, and cite the potential value of a coronary artery calcium score as an additional risk determinant.
Neil J. Stone MD, vice chair of the of the 2018 Cholesterol Guidelines Committee, sat down for an interview and detailed the research behind the guidelines and how new features can help guide treatment decisions for patients at risk for a cardiovascular event.
CHICAGO – New U.S. cholesterol guidelines spell out the role for ezetimibe and PCSK9 inhibitors, expand the scope of individualized risk assessment, and cite the potential value of a coronary artery calcium score as an additional risk determinant.
Neil J. Stone MD, vice chair of the of the 2018 Cholesterol Guidelines Committee, sat down for an interview and detailed the research behind the guidelines and how new features can help guide treatment decisions for patients at risk for a cardiovascular event.
CHICAGO – New U.S. cholesterol guidelines spell out the role for ezetimibe and PCSK9 inhibitors, expand the scope of individualized risk assessment, and cite the potential value of a coronary artery calcium score as an additional risk determinant.
Neil J. Stone MD, vice chair of the of the 2018 Cholesterol Guidelines Committee, sat down for an interview and detailed the research behind the guidelines and how new features can help guide treatment decisions for patients at risk for a cardiovascular event.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
DECLARE: Dapagliflozin improves some cardiovascular, renal outcomes
For patients with type 2 diabetes who have or are at risk for atherosclerotic cardiovascular disease, do, according to investigators.
A composite measure of major adverse cardiovascular events (MACE), including cardiovascular death, ischemic stroke, or myocardial infarction, was comparable between dapagliflozin and placebo; in contrast, diabetic ketoacidosis occurred more frequently with dapagliflozin, reported lead author Stephen D. Wiviott, MD at the American Heart Association scientific sessions.
“As a result of [the] intersection of diabetes, atherosclerotic cardiovascular disease, and heart failure, the importance of determining diabetes therapies that are not only safe but also effective in reducing cardiovascular risk is paramount,” Dr. Wiviott and colleagues wrote in an article published simultaneously in the New England Journal of Medicine.
“Dapagliflozin is a selective inhibitor of sodium–glucose cotransporter (SGLT2) that blocks glucose resorption in the proximal tubule of the kidney and promotes glucosuria,” the investigators wrote. “Other SGLT2 inhibitors have shown favorable cardiovascular effects, including a reduction in the risk of hospitalization for heart failure, predominantly in patients with type 2 diabetes and established cardiovascular disease; they have also been shown to delay the progression of kidney disease.”
The goal of the Dapagliflozin Effect on Cardiovascular Events–Thrombolysis in Myocardial Infarction 58 (DECLARE–TIMI 58) trial was to determine what impact, if any, dapagliflozin has on renal and cardiovascular outcomes in a diverse array of patients with or at risk for atherosclerotic cardiovascular disease. The phase III, double-blind, placebo-controlled, randomized study involved 17,160 adults with type 2 diabetes from 33 countries. Of these, nearly 7,000 patients had atherosclerotic cardiovascular disease and the remaining 10,000 or so patients had multiple risk factors for atherosclerotic cardiovascular disease. Patients were at least 40 years of age, had a creatinine clearance of at least 60 mL/minute, and a HbA1c level between 6.5% and 12.0%. They were randomly assigned to receive either dapagliflozin 10 mg daily or placebo. Every 6 months, patients had laboratory testing with in-person follow-up for safety, clinical response, and adherence; patients were contacted via telephone at the halfway point between appointments (3 months).
The primary safety outcome of the study was major adverse cardiovascular outcomes (MACE: ischemic stroke, myocardial infarction, or cardiovascular death). The trial began with MACE as the sole primary safety outcome, as guided by the Food and Drug Administration, but this changed before completion. “During the trial,” the investigators explained, “compelling external scientific information from the EMPA-REG OUTCOME trial, which evaluated another SGLT2 inhibitor, showed greater benefit with respect to cardiovascular death and hospitalization for heart failure than with respect to MACE.” Therefore, before data were known, the investigators added a second primary outcome: a composite of cardiovascular death or hospitalization for heart failure. The two secondary outcomes were a renal composite (new end-stage renal disease, estimated glomerular filtration rate decrease by at least 40% to less than 60 m/min per 1.73 m2 of body-surface area, or death from renal or cardiovascular disease), and death from any cause.
The primary safety outcome (MACE rate) showed that dapagliflozin was noninferior to placebo (upper boundary of the 95% confidence interval, less than 1.3; P less than .001 for noninferiority). Although the MACE rate was similar between treatment groups (8.8% for dapagliflozin vs 9.4% for placebo; P = .017), the composite rate of cardiovascular death or hospitalization for heart failure was 17% lower for patients receiving dapagliflozin, compared with those who received placebo (4.9% vs 5.8%); this latter finding was attributable mostly to a 27% lower risk of hospitalization, instead of the 2% reduction in cardiovascular death. Seven percent fewer deaths of any kind were observed in the dapagliflozin group (6.2%) than in the placebo group (6.6%). Renal events saw a bigger difference, of 23% (4.3% vs 5.6%).
Statistically significant adverse events seen in more dapagliflozin than placebo patients included diabetic ketoacidosis and genital infection. Dr. Wiviott noted that adverse events favoring hypoglycemia included major hypoglycemia and bladder cancer..
“We did not find that SGLT2 inhibition with dapagliflozin resulted in a lower rate of cardiovascular death or death from any cause than placebo, a finding that contrasts with that in the EMPA-REG OUTCOME trial,” the investigators noted. Apart from possible differences in drugs within the same class, the investigators pointed to more restrictive renal criteria in the DECLARE trial and possible inherent differences between patient populations, among other possible factors.
“…in a broad population of patients with type 2 diabetes [dapagliflozin] did result in a significantly lower rate of cardiovascular death or hospitalization for heart failure than placebo, with additional findings supporting a possible lower rate of adverse renal outcomes,” the investigators concluded.
The DECLARE-TIMI 58 trial was sponsored by AstraZeneca and Bristol-Myers Squibb. Authors reported various financial affiliations with Eisai, Medtronic, Sanofi Aventis, Abbott, Regeneron, and others.
SOURCE: Wiviott et al. N Engl J Med. 2018 Nov 10. doi: 10.1056/NEJMoa1812389
For patients with type 2 diabetes who have or are at risk for atherosclerotic cardiovascular disease, do, according to investigators.
A composite measure of major adverse cardiovascular events (MACE), including cardiovascular death, ischemic stroke, or myocardial infarction, was comparable between dapagliflozin and placebo; in contrast, diabetic ketoacidosis occurred more frequently with dapagliflozin, reported lead author Stephen D. Wiviott, MD at the American Heart Association scientific sessions.
“As a result of [the] intersection of diabetes, atherosclerotic cardiovascular disease, and heart failure, the importance of determining diabetes therapies that are not only safe but also effective in reducing cardiovascular risk is paramount,” Dr. Wiviott and colleagues wrote in an article published simultaneously in the New England Journal of Medicine.
“Dapagliflozin is a selective inhibitor of sodium–glucose cotransporter (SGLT2) that blocks glucose resorption in the proximal tubule of the kidney and promotes glucosuria,” the investigators wrote. “Other SGLT2 inhibitors have shown favorable cardiovascular effects, including a reduction in the risk of hospitalization for heart failure, predominantly in patients with type 2 diabetes and established cardiovascular disease; they have also been shown to delay the progression of kidney disease.”
The goal of the Dapagliflozin Effect on Cardiovascular Events–Thrombolysis in Myocardial Infarction 58 (DECLARE–TIMI 58) trial was to determine what impact, if any, dapagliflozin has on renal and cardiovascular outcomes in a diverse array of patients with or at risk for atherosclerotic cardiovascular disease. The phase III, double-blind, placebo-controlled, randomized study involved 17,160 adults with type 2 diabetes from 33 countries. Of these, nearly 7,000 patients had atherosclerotic cardiovascular disease and the remaining 10,000 or so patients had multiple risk factors for atherosclerotic cardiovascular disease. Patients were at least 40 years of age, had a creatinine clearance of at least 60 mL/minute, and a HbA1c level between 6.5% and 12.0%. They were randomly assigned to receive either dapagliflozin 10 mg daily or placebo. Every 6 months, patients had laboratory testing with in-person follow-up for safety, clinical response, and adherence; patients were contacted via telephone at the halfway point between appointments (3 months).
The primary safety outcome of the study was major adverse cardiovascular outcomes (MACE: ischemic stroke, myocardial infarction, or cardiovascular death). The trial began with MACE as the sole primary safety outcome, as guided by the Food and Drug Administration, but this changed before completion. “During the trial,” the investigators explained, “compelling external scientific information from the EMPA-REG OUTCOME trial, which evaluated another SGLT2 inhibitor, showed greater benefit with respect to cardiovascular death and hospitalization for heart failure than with respect to MACE.” Therefore, before data were known, the investigators added a second primary outcome: a composite of cardiovascular death or hospitalization for heart failure. The two secondary outcomes were a renal composite (new end-stage renal disease, estimated glomerular filtration rate decrease by at least 40% to less than 60 m/min per 1.73 m2 of body-surface area, or death from renal or cardiovascular disease), and death from any cause.
The primary safety outcome (MACE rate) showed that dapagliflozin was noninferior to placebo (upper boundary of the 95% confidence interval, less than 1.3; P less than .001 for noninferiority). Although the MACE rate was similar between treatment groups (8.8% for dapagliflozin vs 9.4% for placebo; P = .017), the composite rate of cardiovascular death or hospitalization for heart failure was 17% lower for patients receiving dapagliflozin, compared with those who received placebo (4.9% vs 5.8%); this latter finding was attributable mostly to a 27% lower risk of hospitalization, instead of the 2% reduction in cardiovascular death. Seven percent fewer deaths of any kind were observed in the dapagliflozin group (6.2%) than in the placebo group (6.6%). Renal events saw a bigger difference, of 23% (4.3% vs 5.6%).
Statistically significant adverse events seen in more dapagliflozin than placebo patients included diabetic ketoacidosis and genital infection. Dr. Wiviott noted that adverse events favoring hypoglycemia included major hypoglycemia and bladder cancer..
“We did not find that SGLT2 inhibition with dapagliflozin resulted in a lower rate of cardiovascular death or death from any cause than placebo, a finding that contrasts with that in the EMPA-REG OUTCOME trial,” the investigators noted. Apart from possible differences in drugs within the same class, the investigators pointed to more restrictive renal criteria in the DECLARE trial and possible inherent differences between patient populations, among other possible factors.
“…in a broad population of patients with type 2 diabetes [dapagliflozin] did result in a significantly lower rate of cardiovascular death or hospitalization for heart failure than placebo, with additional findings supporting a possible lower rate of adverse renal outcomes,” the investigators concluded.
The DECLARE-TIMI 58 trial was sponsored by AstraZeneca and Bristol-Myers Squibb. Authors reported various financial affiliations with Eisai, Medtronic, Sanofi Aventis, Abbott, Regeneron, and others.
SOURCE: Wiviott et al. N Engl J Med. 2018 Nov 10. doi: 10.1056/NEJMoa1812389
For patients with type 2 diabetes who have or are at risk for atherosclerotic cardiovascular disease, do, according to investigators.
A composite measure of major adverse cardiovascular events (MACE), including cardiovascular death, ischemic stroke, or myocardial infarction, was comparable between dapagliflozin and placebo; in contrast, diabetic ketoacidosis occurred more frequently with dapagliflozin, reported lead author Stephen D. Wiviott, MD at the American Heart Association scientific sessions.
“As a result of [the] intersection of diabetes, atherosclerotic cardiovascular disease, and heart failure, the importance of determining diabetes therapies that are not only safe but also effective in reducing cardiovascular risk is paramount,” Dr. Wiviott and colleagues wrote in an article published simultaneously in the New England Journal of Medicine.
“Dapagliflozin is a selective inhibitor of sodium–glucose cotransporter (SGLT2) that blocks glucose resorption in the proximal tubule of the kidney and promotes glucosuria,” the investigators wrote. “Other SGLT2 inhibitors have shown favorable cardiovascular effects, including a reduction in the risk of hospitalization for heart failure, predominantly in patients with type 2 diabetes and established cardiovascular disease; they have also been shown to delay the progression of kidney disease.”
The goal of the Dapagliflozin Effect on Cardiovascular Events–Thrombolysis in Myocardial Infarction 58 (DECLARE–TIMI 58) trial was to determine what impact, if any, dapagliflozin has on renal and cardiovascular outcomes in a diverse array of patients with or at risk for atherosclerotic cardiovascular disease. The phase III, double-blind, placebo-controlled, randomized study involved 17,160 adults with type 2 diabetes from 33 countries. Of these, nearly 7,000 patients had atherosclerotic cardiovascular disease and the remaining 10,000 or so patients had multiple risk factors for atherosclerotic cardiovascular disease. Patients were at least 40 years of age, had a creatinine clearance of at least 60 mL/minute, and a HbA1c level between 6.5% and 12.0%. They were randomly assigned to receive either dapagliflozin 10 mg daily or placebo. Every 6 months, patients had laboratory testing with in-person follow-up for safety, clinical response, and adherence; patients were contacted via telephone at the halfway point between appointments (3 months).
The primary safety outcome of the study was major adverse cardiovascular outcomes (MACE: ischemic stroke, myocardial infarction, or cardiovascular death). The trial began with MACE as the sole primary safety outcome, as guided by the Food and Drug Administration, but this changed before completion. “During the trial,” the investigators explained, “compelling external scientific information from the EMPA-REG OUTCOME trial, which evaluated another SGLT2 inhibitor, showed greater benefit with respect to cardiovascular death and hospitalization for heart failure than with respect to MACE.” Therefore, before data were known, the investigators added a second primary outcome: a composite of cardiovascular death or hospitalization for heart failure. The two secondary outcomes were a renal composite (new end-stage renal disease, estimated glomerular filtration rate decrease by at least 40% to less than 60 m/min per 1.73 m2 of body-surface area, or death from renal or cardiovascular disease), and death from any cause.
The primary safety outcome (MACE rate) showed that dapagliflozin was noninferior to placebo (upper boundary of the 95% confidence interval, less than 1.3; P less than .001 for noninferiority). Although the MACE rate was similar between treatment groups (8.8% for dapagliflozin vs 9.4% for placebo; P = .017), the composite rate of cardiovascular death or hospitalization for heart failure was 17% lower for patients receiving dapagliflozin, compared with those who received placebo (4.9% vs 5.8%); this latter finding was attributable mostly to a 27% lower risk of hospitalization, instead of the 2% reduction in cardiovascular death. Seven percent fewer deaths of any kind were observed in the dapagliflozin group (6.2%) than in the placebo group (6.6%). Renal events saw a bigger difference, of 23% (4.3% vs 5.6%).
Statistically significant adverse events seen in more dapagliflozin than placebo patients included diabetic ketoacidosis and genital infection. Dr. Wiviott noted that adverse events favoring hypoglycemia included major hypoglycemia and bladder cancer..
“We did not find that SGLT2 inhibition with dapagliflozin resulted in a lower rate of cardiovascular death or death from any cause than placebo, a finding that contrasts with that in the EMPA-REG OUTCOME trial,” the investigators noted. Apart from possible differences in drugs within the same class, the investigators pointed to more restrictive renal criteria in the DECLARE trial and possible inherent differences between patient populations, among other possible factors.
“…in a broad population of patients with type 2 diabetes [dapagliflozin] did result in a significantly lower rate of cardiovascular death or hospitalization for heart failure than placebo, with additional findings supporting a possible lower rate of adverse renal outcomes,” the investigators concluded.
The DECLARE-TIMI 58 trial was sponsored by AstraZeneca and Bristol-Myers Squibb. Authors reported various financial affiliations with Eisai, Medtronic, Sanofi Aventis, Abbott, Regeneron, and others.
SOURCE: Wiviott et al. N Engl J Med. 2018 Nov 10. doi: 10.1056/NEJMoa1812389
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: For patients with type 2 diabetes who have or are at risk for atherosclerotic cardiovascular disease, dapagliflozin is associated with a lower composite rate of cardiovascular death or hospitalization for heart failure, compared with placebo.
Major finding: Of patients taking dapagliflozin, 4.9% died of cardiovascular disease or were hospitalized for heart failure, compared with 5.8% of patients receiving placebo (P = .005).
Study details: The phase III DECLARE–TIMI 58 trial was a double-blind, placebo-controlled, randomized study that involved 17,160 patients with type 2 diabetes who had or were at risk for atherosclerotic cardiovascular disease.
Disclosures: DECLARE–TIMI 58 was sponsored by AstraZeneca and Bristol-Myers Squibb. Authors reported various financial affiliations with Eisai, Medtronic, Sanofi Aventis, Abbott, Regeneron, and others.
Source: Wiviott et al. N Engl J Med. 2018 Nov 10. doi: ___________
REDUCE-IT: Fish-derived agent cut CV events 25%
CHICAGO – Detailed results of the REDUCE-IT trial have confirmed earlier-reported top line results that showed a 25% reduction in the risk of cardiovascular death or nonfatal cardiovascular event with the fish-derived, triglyceride-reducing agent icosapent acid in combination with statin.
But they should not be interpreted as validation of the cardiovascular benefits of fish-oil supplements, according to Deepak L. Bhatt, MD, principal investigator and steering committee chair for REDUCE-IT, who presented the results at the American Heart Association scientific sessions.
He reported the results from 8,179 patients followed for a median of 4.9 years. The treatment group received 4 g/day of icosapent ethyl (Vascepa, Amarin), a single-molecule agent consisting of the omega-3 acid known as eicosapentaeonoic acid (EPA) in ethyl-ester form, which Dr. Bhatt called “a highly purified” formulation. Vascepa is derived from fish but it is not fish oil, a company press release states. Amarin, sponsor of the study, released top line results in September.
To qualify for the trial, patients had to have a diagnosis of cardiovascular disease or diabetes and other risk factors, had been on statin therapy and had above normal triglyceride (135-499 mg/dL) and optimal LDL (41-100 mg/dL) levels. Patients were randomly assigned to receive 4 g/day of icosapent ethyl or placebo.
Dr. Bhatt stressed that the REDUCE-IT results do not necessarily validate the use of fish oil to lower cardiovascular risk. “It would be mistake if patients and physicians” to interpret the results that way, and that classifying the purified formulation of icosapent ethyl used in REDUCE-IT as fish oil is a “misnomer.” He added, “Really, what we’re talking about is prescription therapy icosapent ethyl vs. over-the-counter supplements.” Icosapent ethyl is approved in the United States for patients with triglyceride levels of more than 500 mg/dL.
Dr. Bhatt and the study coauthors acknowledged that the results of REDUCE-IT deviate from other trials of triglyceride-lowering agents, including other n-3 fatty acids. They noted two potential explanations: a high dose; or higher ratios of EPA to docosahexaenoic acid in the REDUCE-IT formulation vs. agents used in the other studies. For example, the ASCEND study, presented at the European Society of Cardiology in September, reported no cardiovascular benefit from a 1-g/day dose of omega-3 fatty acids and low-dose aspirin in patients with diabetes.
The primary endpoint of REDUCE-IT was a composite of cardiovascular death, nonfatal MI or stroke, coronary revascularization or unstable angina, which occurred in 17.2% of the patients taking icosapent ethyl, compared with 22% of the controls, for a risk reduction of 25% (P less than .001). The key secondary endpoint was composite of cardiovascular death and nonfatal MI or stroke, which occurred in 11.2% and 14.8% of the treated and placebo groups, respectively, for a risk reduction of 26% (P less than .001).
The study investigators also zeroed in on specific ischemic endpoints. Cardiovascular death rates were 20% lower in the treated patients (4.2% vs. 5.2%, P less than .03).
The study also evaluated lipid levels. The median change in triglyceride levels after a year of treatment was a decrease of 18.3%, or 39 mg/dL, in the treatment group while triglyceride levels rose 2.2% in the placebo patients (P less than .001). LDL levels increased in the treated patients by 3.1%, or 2 mg/dL (median) vs. 10.2%, or 7 mg/dL, in controls (P less than .001).
The trial also reported a 33% greater risk of hospitalization for atrial fibrillation or flutter and about a 30% heightened risk of serious bleeding among patients taking icosapent ethyl. Dr. Bhatt pointed out that, while the high rate of atrial fibrillation among treated patients was statistically significant, “the most feared complication of atrial fibrillation is stroke, but in this study we saw a 28% reduction in stroke.”
Likewise the nonsignificantly higher rate of bleeding in the treatment group was inconsequential. “When we looked at specific types of serious bleeding – GI or stomach bleeding, CNS or bleeding into the brain or fatal bleeding – there were no significant differences,” he said.
Discussant Carl Orringer, MD, of the University of Miami, said, “My perspective of this is that the likelihood of atrial fibrillation, although statistically higher, is something that should not prevent physicians from prescribing the drug because of the tremendous benefit that we’ve seen in those appropriate patients on high intensity statin.” However, he said, it does merit further investigation. He also pointed out that one limitation of the study was that the population was 90% white. “Thus the potential benefits of icosapent ethyl in patients of other ethnicities remains unclear,” he said.
The results were published simultaneously online in the New England Journal of Medicine.
Dr. Bhatt receives funding from Amarin, which sponsored the REDUCE-IT trial.
SOURCE: Bhatt DL, et al. N Engl J Med. 2018 Nov 10; doi: 10.1056/NEJMoa181279.
CHICAGO – Detailed results of the REDUCE-IT trial have confirmed earlier-reported top line results that showed a 25% reduction in the risk of cardiovascular death or nonfatal cardiovascular event with the fish-derived, triglyceride-reducing agent icosapent acid in combination with statin.
But they should not be interpreted as validation of the cardiovascular benefits of fish-oil supplements, according to Deepak L. Bhatt, MD, principal investigator and steering committee chair for REDUCE-IT, who presented the results at the American Heart Association scientific sessions.
He reported the results from 8,179 patients followed for a median of 4.9 years. The treatment group received 4 g/day of icosapent ethyl (Vascepa, Amarin), a single-molecule agent consisting of the omega-3 acid known as eicosapentaeonoic acid (EPA) in ethyl-ester form, which Dr. Bhatt called “a highly purified” formulation. Vascepa is derived from fish but it is not fish oil, a company press release states. Amarin, sponsor of the study, released top line results in September.
To qualify for the trial, patients had to have a diagnosis of cardiovascular disease or diabetes and other risk factors, had been on statin therapy and had above normal triglyceride (135-499 mg/dL) and optimal LDL (41-100 mg/dL) levels. Patients were randomly assigned to receive 4 g/day of icosapent ethyl or placebo.
Dr. Bhatt stressed that the REDUCE-IT results do not necessarily validate the use of fish oil to lower cardiovascular risk. “It would be mistake if patients and physicians” to interpret the results that way, and that classifying the purified formulation of icosapent ethyl used in REDUCE-IT as fish oil is a “misnomer.” He added, “Really, what we’re talking about is prescription therapy icosapent ethyl vs. over-the-counter supplements.” Icosapent ethyl is approved in the United States for patients with triglyceride levels of more than 500 mg/dL.
Dr. Bhatt and the study coauthors acknowledged that the results of REDUCE-IT deviate from other trials of triglyceride-lowering agents, including other n-3 fatty acids. They noted two potential explanations: a high dose; or higher ratios of EPA to docosahexaenoic acid in the REDUCE-IT formulation vs. agents used in the other studies. For example, the ASCEND study, presented at the European Society of Cardiology in September, reported no cardiovascular benefit from a 1-g/day dose of omega-3 fatty acids and low-dose aspirin in patients with diabetes.
The primary endpoint of REDUCE-IT was a composite of cardiovascular death, nonfatal MI or stroke, coronary revascularization or unstable angina, which occurred in 17.2% of the patients taking icosapent ethyl, compared with 22% of the controls, for a risk reduction of 25% (P less than .001). The key secondary endpoint was composite of cardiovascular death and nonfatal MI or stroke, which occurred in 11.2% and 14.8% of the treated and placebo groups, respectively, for a risk reduction of 26% (P less than .001).
The study investigators also zeroed in on specific ischemic endpoints. Cardiovascular death rates were 20% lower in the treated patients (4.2% vs. 5.2%, P less than .03).
The study also evaluated lipid levels. The median change in triglyceride levels after a year of treatment was a decrease of 18.3%, or 39 mg/dL, in the treatment group while triglyceride levels rose 2.2% in the placebo patients (P less than .001). LDL levels increased in the treated patients by 3.1%, or 2 mg/dL (median) vs. 10.2%, or 7 mg/dL, in controls (P less than .001).
The trial also reported a 33% greater risk of hospitalization for atrial fibrillation or flutter and about a 30% heightened risk of serious bleeding among patients taking icosapent ethyl. Dr. Bhatt pointed out that, while the high rate of atrial fibrillation among treated patients was statistically significant, “the most feared complication of atrial fibrillation is stroke, but in this study we saw a 28% reduction in stroke.”
Likewise the nonsignificantly higher rate of bleeding in the treatment group was inconsequential. “When we looked at specific types of serious bleeding – GI or stomach bleeding, CNS or bleeding into the brain or fatal bleeding – there were no significant differences,” he said.
Discussant Carl Orringer, MD, of the University of Miami, said, “My perspective of this is that the likelihood of atrial fibrillation, although statistically higher, is something that should not prevent physicians from prescribing the drug because of the tremendous benefit that we’ve seen in those appropriate patients on high intensity statin.” However, he said, it does merit further investigation. He also pointed out that one limitation of the study was that the population was 90% white. “Thus the potential benefits of icosapent ethyl in patients of other ethnicities remains unclear,” he said.
The results were published simultaneously online in the New England Journal of Medicine.
Dr. Bhatt receives funding from Amarin, which sponsored the REDUCE-IT trial.
SOURCE: Bhatt DL, et al. N Engl J Med. 2018 Nov 10; doi: 10.1056/NEJMoa181279.
CHICAGO – Detailed results of the REDUCE-IT trial have confirmed earlier-reported top line results that showed a 25% reduction in the risk of cardiovascular death or nonfatal cardiovascular event with the fish-derived, triglyceride-reducing agent icosapent acid in combination with statin.
But they should not be interpreted as validation of the cardiovascular benefits of fish-oil supplements, according to Deepak L. Bhatt, MD, principal investigator and steering committee chair for REDUCE-IT, who presented the results at the American Heart Association scientific sessions.
He reported the results from 8,179 patients followed for a median of 4.9 years. The treatment group received 4 g/day of icosapent ethyl (Vascepa, Amarin), a single-molecule agent consisting of the omega-3 acid known as eicosapentaeonoic acid (EPA) in ethyl-ester form, which Dr. Bhatt called “a highly purified” formulation. Vascepa is derived from fish but it is not fish oil, a company press release states. Amarin, sponsor of the study, released top line results in September.
To qualify for the trial, patients had to have a diagnosis of cardiovascular disease or diabetes and other risk factors, had been on statin therapy and had above normal triglyceride (135-499 mg/dL) and optimal LDL (41-100 mg/dL) levels. Patients were randomly assigned to receive 4 g/day of icosapent ethyl or placebo.
Dr. Bhatt stressed that the REDUCE-IT results do not necessarily validate the use of fish oil to lower cardiovascular risk. “It would be mistake if patients and physicians” to interpret the results that way, and that classifying the purified formulation of icosapent ethyl used in REDUCE-IT as fish oil is a “misnomer.” He added, “Really, what we’re talking about is prescription therapy icosapent ethyl vs. over-the-counter supplements.” Icosapent ethyl is approved in the United States for patients with triglyceride levels of more than 500 mg/dL.
Dr. Bhatt and the study coauthors acknowledged that the results of REDUCE-IT deviate from other trials of triglyceride-lowering agents, including other n-3 fatty acids. They noted two potential explanations: a high dose; or higher ratios of EPA to docosahexaenoic acid in the REDUCE-IT formulation vs. agents used in the other studies. For example, the ASCEND study, presented at the European Society of Cardiology in September, reported no cardiovascular benefit from a 1-g/day dose of omega-3 fatty acids and low-dose aspirin in patients with diabetes.
The primary endpoint of REDUCE-IT was a composite of cardiovascular death, nonfatal MI or stroke, coronary revascularization or unstable angina, which occurred in 17.2% of the patients taking icosapent ethyl, compared with 22% of the controls, for a risk reduction of 25% (P less than .001). The key secondary endpoint was composite of cardiovascular death and nonfatal MI or stroke, which occurred in 11.2% and 14.8% of the treated and placebo groups, respectively, for a risk reduction of 26% (P less than .001).
The study investigators also zeroed in on specific ischemic endpoints. Cardiovascular death rates were 20% lower in the treated patients (4.2% vs. 5.2%, P less than .03).
The study also evaluated lipid levels. The median change in triglyceride levels after a year of treatment was a decrease of 18.3%, or 39 mg/dL, in the treatment group while triglyceride levels rose 2.2% in the placebo patients (P less than .001). LDL levels increased in the treated patients by 3.1%, or 2 mg/dL (median) vs. 10.2%, or 7 mg/dL, in controls (P less than .001).
The trial also reported a 33% greater risk of hospitalization for atrial fibrillation or flutter and about a 30% heightened risk of serious bleeding among patients taking icosapent ethyl. Dr. Bhatt pointed out that, while the high rate of atrial fibrillation among treated patients was statistically significant, “the most feared complication of atrial fibrillation is stroke, but in this study we saw a 28% reduction in stroke.”
Likewise the nonsignificantly higher rate of bleeding in the treatment group was inconsequential. “When we looked at specific types of serious bleeding – GI or stomach bleeding, CNS or bleeding into the brain or fatal bleeding – there were no significant differences,” he said.
Discussant Carl Orringer, MD, of the University of Miami, said, “My perspective of this is that the likelihood of atrial fibrillation, although statistically higher, is something that should not prevent physicians from prescribing the drug because of the tremendous benefit that we’ve seen in those appropriate patients on high intensity statin.” However, he said, it does merit further investigation. He also pointed out that one limitation of the study was that the population was 90% white. “Thus the potential benefits of icosapent ethyl in patients of other ethnicities remains unclear,” he said.
The results were published simultaneously online in the New England Journal of Medicine.
Dr. Bhatt receives funding from Amarin, which sponsored the REDUCE-IT trial.
SOURCE: Bhatt DL, et al. N Engl J Med. 2018 Nov 10; doi: 10.1056/NEJMoa181279.
REPORTING FROM AMERICAN HEART ASSOCIATION SCIENTIFIC SESSIONS 2018
Key Clinical point: .
Major finding: Cardiovascular death or nonfatal cardiovascular event occurred in 17.7% of treated patients vs. 22% of controls.
Study details: Multicenter, randomized, double-blind, placebo-controlled clinical trial of 8,179 patients with established cardiovascular disease or diabetes and other risk factors.
Disclosures: Dr. Bhatt disclosed having a significant research relationship with Amarin Corp., which funded the trial.
Source: N Engl J Med. 2018; doi: 10.1056/NEJMoa181279.
Brain stimulation device improved fluency in persons who stutter
ATLANTA – After undergoing 10 days of noninvasive magnetic brain stimulation with a novel device, eight of nine persons who stutter experienced improvements in speech fluency.
“This is the first step in what we believe is a major breakthrough in treatment,” lead study author David B. Rosenfield, MD, said in an interview at the annual meeting of the American Neurological Association.
In previously published work, Dr. Rosenfield, Director of the Speech and Language Center at Houston Methodist Neurological Institute, and his colleagues showed significant reduction in functional connectivity between Broca’s and Wernicke’s areas in persons who stutter, compared with normal speakers, by performing resting-state functional MRI of the brain. In the current open-label pilot trial, they tested the hypothesis that using direct noninvasive synchronous bifocal stimulation to potentiate the strength of connectivity between Broca’s and Wernicke’s areas in persons who stutter should improve their fluency.
Researchers enrolled nine persons who stutter who ranged in age from 18 to 80 years. For 40 minutes each consecutive weekday over the course of 2 weeks, the participants wore a compact, portable device known as a Transcranial Rotating Permanent Magnetic Stimulator (TRPMS) to deliver highly focal stimuli to Broca’s and Wernicke’s area locations specified by 10-20 international electroencephalographic electrode sites on the left side. Magnetic stimuli were 100 milliseconds in duration and delivered at 0.2 Hz. Next, a certified speech-language pathologist viewed video recordings of the study subjects both speaking spontaneously and reading a passage aloud on day 1 (before stimulation), day 5 (after stimulation), and day 10 (after stimulation), to assess fluency using the Stuttering Speech Severity Instrument version 4 (SSI-4).
The researchers found that all study participants significantly improved in fluency on either day 5 (P = 0.01) or day 10 (P = 0.02). Only one subject failed to show improvement on day 10 compared with day 1 after showing it on day 5. “This wasn’t meant to be a 10-day treatment that would last forever; this was meant to be a 10-day treatment to see whether the magnetic stimulation would work,” Dr. Rosenfield said. “It might well be that patients need treatment every day, once a week, or once a month. All we can say is that we have an input and an output. We gave them the treatment and they improved. One patient was so happy with it that he begged us to come back for additional treatment. It seems as though it’s a robust therapy.”
Going forward, the researchers plan to study fMRI brain imaging before and following external magnetic treatments to speech and language areas to confirm the efficacy of this therapy in a randomized, double-blind, sham treatment-controlled trial.
The TRPMS device was coinvented by Santosh A. Helekar, MD, PhD, and Henning Voss, PhD, both at Weill Cornell Medical College. The study received funding support from The Houston Methodist Hospital System Physicians Organization. Dr. Rosenfield reported having no financial disclosures. He noted that commercialization of the patented technology underlying the TRPMS device used in this study and in other diseases is currently being advanced by Seraya Medical Systems LLC.
[email protected]
Source: Ann Neurol. 2018;84[S22]:S45-6. Abstract S115.
ATLANTA – After undergoing 10 days of noninvasive magnetic brain stimulation with a novel device, eight of nine persons who stutter experienced improvements in speech fluency.
“This is the first step in what we believe is a major breakthrough in treatment,” lead study author David B. Rosenfield, MD, said in an interview at the annual meeting of the American Neurological Association.
In previously published work, Dr. Rosenfield, Director of the Speech and Language Center at Houston Methodist Neurological Institute, and his colleagues showed significant reduction in functional connectivity between Broca’s and Wernicke’s areas in persons who stutter, compared with normal speakers, by performing resting-state functional MRI of the brain. In the current open-label pilot trial, they tested the hypothesis that using direct noninvasive synchronous bifocal stimulation to potentiate the strength of connectivity between Broca’s and Wernicke’s areas in persons who stutter should improve their fluency.
Researchers enrolled nine persons who stutter who ranged in age from 18 to 80 years. For 40 minutes each consecutive weekday over the course of 2 weeks, the participants wore a compact, portable device known as a Transcranial Rotating Permanent Magnetic Stimulator (TRPMS) to deliver highly focal stimuli to Broca’s and Wernicke’s area locations specified by 10-20 international electroencephalographic electrode sites on the left side. Magnetic stimuli were 100 milliseconds in duration and delivered at 0.2 Hz. Next, a certified speech-language pathologist viewed video recordings of the study subjects both speaking spontaneously and reading a passage aloud on day 1 (before stimulation), day 5 (after stimulation), and day 10 (after stimulation), to assess fluency using the Stuttering Speech Severity Instrument version 4 (SSI-4).
The researchers found that all study participants significantly improved in fluency on either day 5 (P = 0.01) or day 10 (P = 0.02). Only one subject failed to show improvement on day 10 compared with day 1 after showing it on day 5. “This wasn’t meant to be a 10-day treatment that would last forever; this was meant to be a 10-day treatment to see whether the magnetic stimulation would work,” Dr. Rosenfield said. “It might well be that patients need treatment every day, once a week, or once a month. All we can say is that we have an input and an output. We gave them the treatment and they improved. One patient was so happy with it that he begged us to come back for additional treatment. It seems as though it’s a robust therapy.”
Going forward, the researchers plan to study fMRI brain imaging before and following external magnetic treatments to speech and language areas to confirm the efficacy of this therapy in a randomized, double-blind, sham treatment-controlled trial.
The TRPMS device was coinvented by Santosh A. Helekar, MD, PhD, and Henning Voss, PhD, both at Weill Cornell Medical College. The study received funding support from The Houston Methodist Hospital System Physicians Organization. Dr. Rosenfield reported having no financial disclosures. He noted that commercialization of the patented technology underlying the TRPMS device used in this study and in other diseases is currently being advanced by Seraya Medical Systems LLC.
[email protected]
Source: Ann Neurol. 2018;84[S22]:S45-6. Abstract S115.
ATLANTA – After undergoing 10 days of noninvasive magnetic brain stimulation with a novel device, eight of nine persons who stutter experienced improvements in speech fluency.
“This is the first step in what we believe is a major breakthrough in treatment,” lead study author David B. Rosenfield, MD, said in an interview at the annual meeting of the American Neurological Association.
In previously published work, Dr. Rosenfield, Director of the Speech and Language Center at Houston Methodist Neurological Institute, and his colleagues showed significant reduction in functional connectivity between Broca’s and Wernicke’s areas in persons who stutter, compared with normal speakers, by performing resting-state functional MRI of the brain. In the current open-label pilot trial, they tested the hypothesis that using direct noninvasive synchronous bifocal stimulation to potentiate the strength of connectivity between Broca’s and Wernicke’s areas in persons who stutter should improve their fluency.
Researchers enrolled nine persons who stutter who ranged in age from 18 to 80 years. For 40 minutes each consecutive weekday over the course of 2 weeks, the participants wore a compact, portable device known as a Transcranial Rotating Permanent Magnetic Stimulator (TRPMS) to deliver highly focal stimuli to Broca’s and Wernicke’s area locations specified by 10-20 international electroencephalographic electrode sites on the left side. Magnetic stimuli were 100 milliseconds in duration and delivered at 0.2 Hz. Next, a certified speech-language pathologist viewed video recordings of the study subjects both speaking spontaneously and reading a passage aloud on day 1 (before stimulation), day 5 (after stimulation), and day 10 (after stimulation), to assess fluency using the Stuttering Speech Severity Instrument version 4 (SSI-4).
The researchers found that all study participants significantly improved in fluency on either day 5 (P = 0.01) or day 10 (P = 0.02). Only one subject failed to show improvement on day 10 compared with day 1 after showing it on day 5. “This wasn’t meant to be a 10-day treatment that would last forever; this was meant to be a 10-day treatment to see whether the magnetic stimulation would work,” Dr. Rosenfield said. “It might well be that patients need treatment every day, once a week, or once a month. All we can say is that we have an input and an output. We gave them the treatment and they improved. One patient was so happy with it that he begged us to come back for additional treatment. It seems as though it’s a robust therapy.”
Going forward, the researchers plan to study fMRI brain imaging before and following external magnetic treatments to speech and language areas to confirm the efficacy of this therapy in a randomized, double-blind, sham treatment-controlled trial.
The TRPMS device was coinvented by Santosh A. Helekar, MD, PhD, and Henning Voss, PhD, both at Weill Cornell Medical College. The study received funding support from The Houston Methodist Hospital System Physicians Organization. Dr. Rosenfield reported having no financial disclosures. He noted that commercialization of the patented technology underlying the TRPMS device used in this study and in other diseases is currently being advanced by Seraya Medical Systems LLC.
[email protected]
Source: Ann Neurol. 2018;84[S22]:S45-6. Abstract S115.
AT ANA 2018
Key clinical point: .
Major finding: All study participants significantly improved in speech fluency on either day 5 of treatment or on day 10.
Study details: An open-label pilot trial of a novel devices used in nine persons who stutter.
Disclosures: The study received funding support from The Houston Methodist Hospital System Physicians Organization. Dr. Rosenfield reported having no financial disclosures. He noted that commercialization of the patented technology underlying the TRPMS device used in this study and in other diseases is currently being advanced by Seraya Medical Systems LLC.
Source: Ann Neurol. 2018;84[S22]:S45-6. Abstract S115.
Atopic dermatitis hits mental health, quality of life
Atopic dermatitis (AD) places a considerable burden on mental health and quality of life for patients with disease of even moderate severity, according to a cross-sectional study of data from the Atopic Dermatitis in America survey.
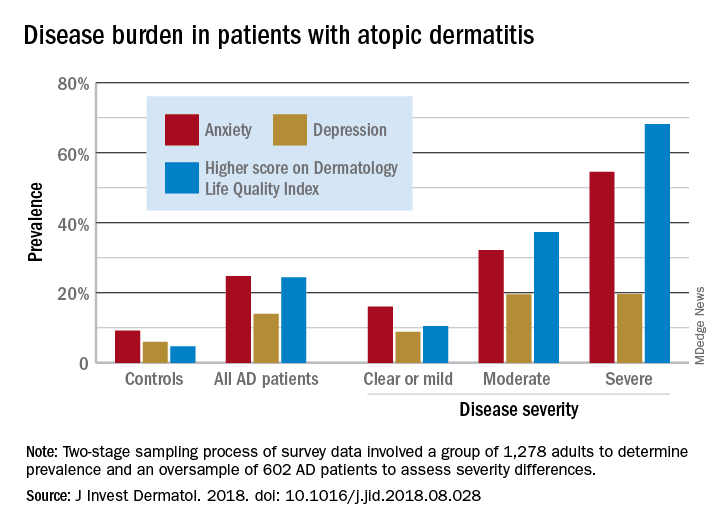
Among adults with severe AD, the mean score on the Dermatology Life Quality Index was 11.4, with a score of 6-30 representing a moderate to large effect on quality of life. The mean for those with moderate disease, 5.9, was just below that range, but 37% of that group did have scores between 6 and 30, Zelma C. Chiesa Fuxench, MD, of the University of Pennsylvania, Philadelphia, and her associates said in the Journal of Investigative Dermatology.
The mean on the Dermatology Life Quality Index for all AD patients was 4.1, with 24% falling into the moderate to large effect range, compared with 1% and 5% for controls. Results were similar on the mental health measure used, the Hospital Anxiety and Depression Scale (HADS). Mean HADS-anxiety scores were 7.0 for all AD patients and 4.7 for controls, and HADS-depression means were 5.8 for AD patients and 3.6 for controls, the investigators reported.
Analysis by disease severity found that 32% of those with moderate AD and almost 56% with severe AD had clinical anxiety (HADS-A score of 11-21), while somewhat lower prevalences were seen for clinical depression (HADS-D score of 11-21): 19.5% for those with moderate AD and 19.7% for patients with severe AD, Dr. Chiesa Fuxench and her associates said.
“An increasing number of studies provide evidence that AD is associated with marked [quality of life] impairment and increased health care costs with higher burden and costs in those with more severe disease. Additional studies should center on exploring those factors associated with AD, and AD disease severity, which lead to increased disease burden in this population,” they wrote.
Respondents to the Atopic Dermatitis in America survey were part of the GfK Knowledge Panel. The study involved a two-stage sampling process: one group of 1,278 adults determined prevalence ,and an oversample of 602 AD patients assessed severity differences.
Dr. Chiesa Fuxench has received research grants from Regeneron, Sanofi, Tioga, and Vanda for work related to atopic dermatitis and has received honoraria for CME work in atopic dermatitis sponsored by educational grants from Regeneron and Sanofi.
SOURCE: J Invest Dermatol. 2018. doi: 10.1016/j.jid.2018.08.028.
Atopic dermatitis (AD) places a considerable burden on mental health and quality of life for patients with disease of even moderate severity, according to a cross-sectional study of data from the Atopic Dermatitis in America survey.
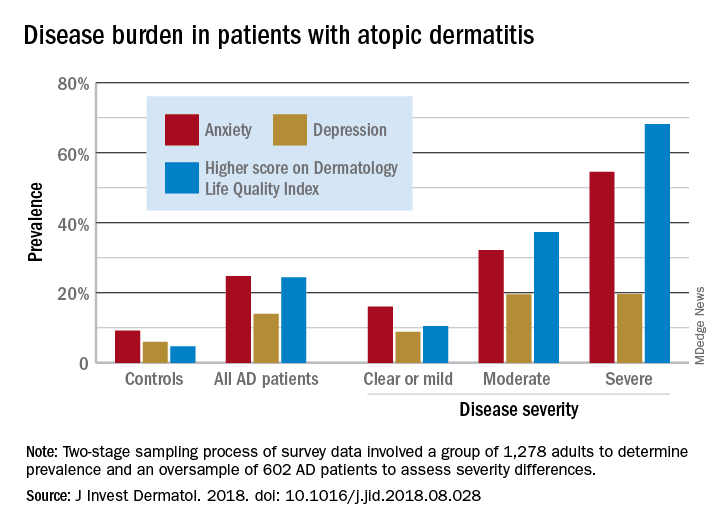
Among adults with severe AD, the mean score on the Dermatology Life Quality Index was 11.4, with a score of 6-30 representing a moderate to large effect on quality of life. The mean for those with moderate disease, 5.9, was just below that range, but 37% of that group did have scores between 6 and 30, Zelma C. Chiesa Fuxench, MD, of the University of Pennsylvania, Philadelphia, and her associates said in the Journal of Investigative Dermatology.
The mean on the Dermatology Life Quality Index for all AD patients was 4.1, with 24% falling into the moderate to large effect range, compared with 1% and 5% for controls. Results were similar on the mental health measure used, the Hospital Anxiety and Depression Scale (HADS). Mean HADS-anxiety scores were 7.0 for all AD patients and 4.7 for controls, and HADS-depression means were 5.8 for AD patients and 3.6 for controls, the investigators reported.
Analysis by disease severity found that 32% of those with moderate AD and almost 56% with severe AD had clinical anxiety (HADS-A score of 11-21), while somewhat lower prevalences were seen for clinical depression (HADS-D score of 11-21): 19.5% for those with moderate AD and 19.7% for patients with severe AD, Dr. Chiesa Fuxench and her associates said.
“An increasing number of studies provide evidence that AD is associated with marked [quality of life] impairment and increased health care costs with higher burden and costs in those with more severe disease. Additional studies should center on exploring those factors associated with AD, and AD disease severity, which lead to increased disease burden in this population,” they wrote.
Respondents to the Atopic Dermatitis in America survey were part of the GfK Knowledge Panel. The study involved a two-stage sampling process: one group of 1,278 adults determined prevalence ,and an oversample of 602 AD patients assessed severity differences.
Dr. Chiesa Fuxench has received research grants from Regeneron, Sanofi, Tioga, and Vanda for work related to atopic dermatitis and has received honoraria for CME work in atopic dermatitis sponsored by educational grants from Regeneron and Sanofi.
SOURCE: J Invest Dermatol. 2018. doi: 10.1016/j.jid.2018.08.028.
Atopic dermatitis (AD) places a considerable burden on mental health and quality of life for patients with disease of even moderate severity, according to a cross-sectional study of data from the Atopic Dermatitis in America survey.
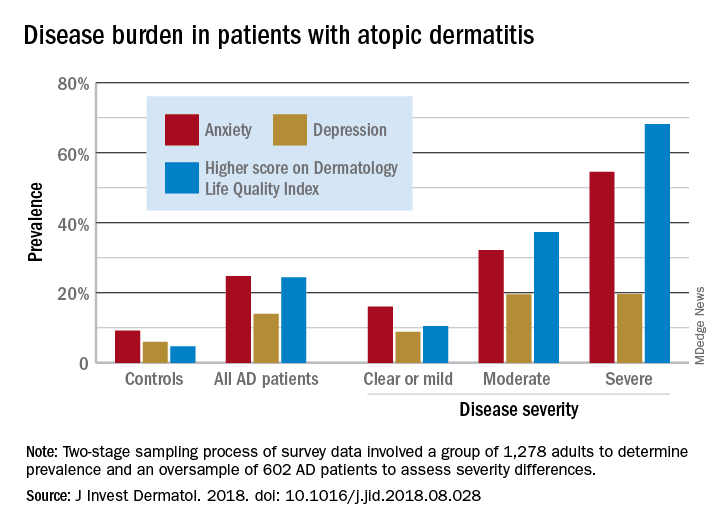
Among adults with severe AD, the mean score on the Dermatology Life Quality Index was 11.4, with a score of 6-30 representing a moderate to large effect on quality of life. The mean for those with moderate disease, 5.9, was just below that range, but 37% of that group did have scores between 6 and 30, Zelma C. Chiesa Fuxench, MD, of the University of Pennsylvania, Philadelphia, and her associates said in the Journal of Investigative Dermatology.
The mean on the Dermatology Life Quality Index for all AD patients was 4.1, with 24% falling into the moderate to large effect range, compared with 1% and 5% for controls. Results were similar on the mental health measure used, the Hospital Anxiety and Depression Scale (HADS). Mean HADS-anxiety scores were 7.0 for all AD patients and 4.7 for controls, and HADS-depression means were 5.8 for AD patients and 3.6 for controls, the investigators reported.
Analysis by disease severity found that 32% of those with moderate AD and almost 56% with severe AD had clinical anxiety (HADS-A score of 11-21), while somewhat lower prevalences were seen for clinical depression (HADS-D score of 11-21): 19.5% for those with moderate AD and 19.7% for patients with severe AD, Dr. Chiesa Fuxench and her associates said.
“An increasing number of studies provide evidence that AD is associated with marked [quality of life] impairment and increased health care costs with higher burden and costs in those with more severe disease. Additional studies should center on exploring those factors associated with AD, and AD disease severity, which lead to increased disease burden in this population,” they wrote.
Respondents to the Atopic Dermatitis in America survey were part of the GfK Knowledge Panel. The study involved a two-stage sampling process: one group of 1,278 adults determined prevalence ,and an oversample of 602 AD patients assessed severity differences.
Dr. Chiesa Fuxench has received research grants from Regeneron, Sanofi, Tioga, and Vanda for work related to atopic dermatitis and has received honoraria for CME work in atopic dermatitis sponsored by educational grants from Regeneron and Sanofi.
SOURCE: J Invest Dermatol. 2018. doi: 10.1016/j.jid.2018.08.028.
FROM THE JOURNAL OF INVESTIGATIVE DERMATOLOGY
Apixaban is safest effective DOAC for stroke prevention in Afib, per AHRQ report
, according to results of an updated comparative effectiveness review.
Dabigatran (Pradaxa), by contrast, has shown reductions in stroke events but a similar rate of bleeding events compared to warfarin, according to the report from the Duke Evidence-based Practice Center, Durham, N.C.
Rivaroxaban (Xarelto), meanwhile, is “similar in both benefits and harms with warfarin” in evidence to date, investigators wrote in the report, which was prepared for the Agency for Healthcare Research and Quality (AHRQ) and the Patient-Centered Outcomes Research Institute (PCORI).
Finally, edoxaban (Savaysa) is “most likely similar” to warfarin with respect to preventing stroke or systemic embolism, with less risk for major bleeding and hemorrhagic stroke, investigators wrote in a summary of their findings on the AHRQ website.
“Effectiveness of these direct oral anticoagulants as compared to one another however is limited by the lack of randomized studies directly comparing their safety and effectiveness,” concluded investigators, led by Gillian D. Sanders, PhD, of Duke University.
The 612-page report details a systematic review based on 320 articles representing 185 unique studies. The review was designed to update a 2013 AHRQ report that evaluated evidence not only for treatment options to prevent stroke in patients with atrial fibrillation, but also for tools used to predict risk of stroke or bleeding.
In the 2013 report, investigators concluded that the newer anticoagulants showed “early promise” in reducing stroke and bleeding events compared with warfarin.
That earlier report said that CHA2 and CHA2DS2-VASc had the best evidence to support prediction of stroke events, while HAS-BLED provided the best discrimination of bleeding risk.
The updated report adds the ABC stroke risk score as a tool that, along with CHADS2 and CHA2DS2-VASc, has the “best evidence” predicting thromboembolic risk, authors said.
Imaging tools, on the other hand, still need more evidence supporting their use to predict thromboembolic risk, Dr. Sanders and colleagues said in their report.
The literature review, which covered the January 2000 through February 2018, turned up 61 studies relevant to predicting thromboembolic risk, 38 on bleeding risk, and 117 on preventing thromboembolic events with anticoagulation therapies, antiplatelet therapies, or procedures.
Direct oral anticoagulants were evaluated in randomized clinical trials that were “often very large, of good quality, and considered definitive in the field,” Dr. Sanders and colleagues wrote in their report.
However, these trials were constrained to comparing direct oral anticoagulants with warfarin or aspirin, and have not involved head-to-head comparison among the newer agents, they added.
“Based on these trials though, clinical leaders and professional societies have determined that these newer agents are better than the prior lone treatment of warfarin in terms of stroke prevention, side effects, and risk of bleeding,” they said in the published report.
SOURCE: Sanders GD, et al. 2018 Oct 30. AHRQ Publication No. 18(19)-EHC018-EF.
, according to results of an updated comparative effectiveness review.
Dabigatran (Pradaxa), by contrast, has shown reductions in stroke events but a similar rate of bleeding events compared to warfarin, according to the report from the Duke Evidence-based Practice Center, Durham, N.C.
Rivaroxaban (Xarelto), meanwhile, is “similar in both benefits and harms with warfarin” in evidence to date, investigators wrote in the report, which was prepared for the Agency for Healthcare Research and Quality (AHRQ) and the Patient-Centered Outcomes Research Institute (PCORI).
Finally, edoxaban (Savaysa) is “most likely similar” to warfarin with respect to preventing stroke or systemic embolism, with less risk for major bleeding and hemorrhagic stroke, investigators wrote in a summary of their findings on the AHRQ website.
“Effectiveness of these direct oral anticoagulants as compared to one another however is limited by the lack of randomized studies directly comparing their safety and effectiveness,” concluded investigators, led by Gillian D. Sanders, PhD, of Duke University.
The 612-page report details a systematic review based on 320 articles representing 185 unique studies. The review was designed to update a 2013 AHRQ report that evaluated evidence not only for treatment options to prevent stroke in patients with atrial fibrillation, but also for tools used to predict risk of stroke or bleeding.
In the 2013 report, investigators concluded that the newer anticoagulants showed “early promise” in reducing stroke and bleeding events compared with warfarin.
That earlier report said that CHA2 and CHA2DS2-VASc had the best evidence to support prediction of stroke events, while HAS-BLED provided the best discrimination of bleeding risk.
The updated report adds the ABC stroke risk score as a tool that, along with CHADS2 and CHA2DS2-VASc, has the “best evidence” predicting thromboembolic risk, authors said.
Imaging tools, on the other hand, still need more evidence supporting their use to predict thromboembolic risk, Dr. Sanders and colleagues said in their report.
The literature review, which covered the January 2000 through February 2018, turned up 61 studies relevant to predicting thromboembolic risk, 38 on bleeding risk, and 117 on preventing thromboembolic events with anticoagulation therapies, antiplatelet therapies, or procedures.
Direct oral anticoagulants were evaluated in randomized clinical trials that were “often very large, of good quality, and considered definitive in the field,” Dr. Sanders and colleagues wrote in their report.
However, these trials were constrained to comparing direct oral anticoagulants with warfarin or aspirin, and have not involved head-to-head comparison among the newer agents, they added.
“Based on these trials though, clinical leaders and professional societies have determined that these newer agents are better than the prior lone treatment of warfarin in terms of stroke prevention, side effects, and risk of bleeding,” they said in the published report.
SOURCE: Sanders GD, et al. 2018 Oct 30. AHRQ Publication No. 18(19)-EHC018-EF.
, according to results of an updated comparative effectiveness review.
Dabigatran (Pradaxa), by contrast, has shown reductions in stroke events but a similar rate of bleeding events compared to warfarin, according to the report from the Duke Evidence-based Practice Center, Durham, N.C.
Rivaroxaban (Xarelto), meanwhile, is “similar in both benefits and harms with warfarin” in evidence to date, investigators wrote in the report, which was prepared for the Agency for Healthcare Research and Quality (AHRQ) and the Patient-Centered Outcomes Research Institute (PCORI).
Finally, edoxaban (Savaysa) is “most likely similar” to warfarin with respect to preventing stroke or systemic embolism, with less risk for major bleeding and hemorrhagic stroke, investigators wrote in a summary of their findings on the AHRQ website.
“Effectiveness of these direct oral anticoagulants as compared to one another however is limited by the lack of randomized studies directly comparing their safety and effectiveness,” concluded investigators, led by Gillian D. Sanders, PhD, of Duke University.
The 612-page report details a systematic review based on 320 articles representing 185 unique studies. The review was designed to update a 2013 AHRQ report that evaluated evidence not only for treatment options to prevent stroke in patients with atrial fibrillation, but also for tools used to predict risk of stroke or bleeding.
In the 2013 report, investigators concluded that the newer anticoagulants showed “early promise” in reducing stroke and bleeding events compared with warfarin.
That earlier report said that CHA2 and CHA2DS2-VASc had the best evidence to support prediction of stroke events, while HAS-BLED provided the best discrimination of bleeding risk.
The updated report adds the ABC stroke risk score as a tool that, along with CHADS2 and CHA2DS2-VASc, has the “best evidence” predicting thromboembolic risk, authors said.
Imaging tools, on the other hand, still need more evidence supporting their use to predict thromboembolic risk, Dr. Sanders and colleagues said in their report.
The literature review, which covered the January 2000 through February 2018, turned up 61 studies relevant to predicting thromboembolic risk, 38 on bleeding risk, and 117 on preventing thromboembolic events with anticoagulation therapies, antiplatelet therapies, or procedures.
Direct oral anticoagulants were evaluated in randomized clinical trials that were “often very large, of good quality, and considered definitive in the field,” Dr. Sanders and colleagues wrote in their report.
However, these trials were constrained to comparing direct oral anticoagulants with warfarin or aspirin, and have not involved head-to-head comparison among the newer agents, they added.
“Based on these trials though, clinical leaders and professional societies have determined that these newer agents are better than the prior lone treatment of warfarin in terms of stroke prevention, side effects, and risk of bleeding,” they said in the published report.
SOURCE: Sanders GD, et al. 2018 Oct 30. AHRQ Publication No. 18(19)-EHC018-EF.













