User login
About 13% of liver transplant recipients affected by PTSD
SAN FRANCISCO –
“Serving the emotional and mental health of these patients is just as important as [improving] liver function and their immunosuppression,” study author Meg O’Meara, NP, said in an interview at the annual meeting of the American Association for the Study of Liver Diseases.
Recent data suggests that patients who undergo significant medical events like solid organ transplantation face a risk of developing PTSD, but limited information exists regarding the psychological effects following adult liver transplantation, said Ms. O’Meara, a nurse practitioner in the division of gastroenterology and hepatology at the University of Colorado at Denver, Aurora. In an effort to determine the prevalence of and risk factors for PTSD in adult liver transplant recipients, she and her associates used the PCL-5 to screen 71 patients seen at the university’s posttransplant clinic from Dec. 1, 2017, to May 31, 2018. The PCL-5 is a validated 20-item questionnaire that corresponds to the DSM-5 symptom criteria for PTSD.
The researchers also collected clinical and demographic information including pretransplant disease severity, history of psychiatric disease, duration of transplant hospitalization, and need for rehospitalization. They used a multivariable regression model to evaluate associations between clinical and demographic variables and a positive screen for PTSD.
The median age of the 71 patients was 58 years; 61% were male. A preexisting diagnosis of depression was present in 25 patients (35%), their mean Model for End-Stage Liver Disease (MELD) score at time of transplant was 31, and their median time from transplant was 1,163 days. In all, nine patients (12.7%) tested positive for PTSD on the PCL-5, and all met criteria for a provisional diagnosis of PTSD based on the DSM-5 criteria. This prevalence is about two times higher than the prevalence of PTSD in the general population (6.7%), comparable with that reported for heart transplant recipients (10.8%) and coronary artery disease (9%), but lower than that reported for ICU patients (38%), HIV patients (35.3%), and in those with Crohn’s disease (19.1%).
On multivariable logistic regression, only three factors were found to be significantly associated with the development of PTSD: younger age at transplant (P = .019), history of depression (P = .008), and a history of PTSD (P less than .001). “What I found surprising was that the MELD score at the time of transplant and the number of readmissions or complications around the time of transplant were not predictive of PTSD,” Ms. O’Meara said.
One possible explanation for the finding of younger age being a predictor of PTSD, she continued, is that younger liver transplant patients may lack certain coping skills, compared with their older counterparts. “Maybe patients who have had more years to deal with their disease are more accepting of it and they learn how to use productive tools to manage it.”
In their abstract, the researchers acknowledged certain limitations of the study, including its cross-sectional design, small sample size, and lack of corresponding pretransplant data.
The researchers reported having no financial disclosures.
SAN FRANCISCO –
“Serving the emotional and mental health of these patients is just as important as [improving] liver function and their immunosuppression,” study author Meg O’Meara, NP, said in an interview at the annual meeting of the American Association for the Study of Liver Diseases.
Recent data suggests that patients who undergo significant medical events like solid organ transplantation face a risk of developing PTSD, but limited information exists regarding the psychological effects following adult liver transplantation, said Ms. O’Meara, a nurse practitioner in the division of gastroenterology and hepatology at the University of Colorado at Denver, Aurora. In an effort to determine the prevalence of and risk factors for PTSD in adult liver transplant recipients, she and her associates used the PCL-5 to screen 71 patients seen at the university’s posttransplant clinic from Dec. 1, 2017, to May 31, 2018. The PCL-5 is a validated 20-item questionnaire that corresponds to the DSM-5 symptom criteria for PTSD.
The researchers also collected clinical and demographic information including pretransplant disease severity, history of psychiatric disease, duration of transplant hospitalization, and need for rehospitalization. They used a multivariable regression model to evaluate associations between clinical and demographic variables and a positive screen for PTSD.
The median age of the 71 patients was 58 years; 61% were male. A preexisting diagnosis of depression was present in 25 patients (35%), their mean Model for End-Stage Liver Disease (MELD) score at time of transplant was 31, and their median time from transplant was 1,163 days. In all, nine patients (12.7%) tested positive for PTSD on the PCL-5, and all met criteria for a provisional diagnosis of PTSD based on the DSM-5 criteria. This prevalence is about two times higher than the prevalence of PTSD in the general population (6.7%), comparable with that reported for heart transplant recipients (10.8%) and coronary artery disease (9%), but lower than that reported for ICU patients (38%), HIV patients (35.3%), and in those with Crohn’s disease (19.1%).
On multivariable logistic regression, only three factors were found to be significantly associated with the development of PTSD: younger age at transplant (P = .019), history of depression (P = .008), and a history of PTSD (P less than .001). “What I found surprising was that the MELD score at the time of transplant and the number of readmissions or complications around the time of transplant were not predictive of PTSD,” Ms. O’Meara said.
One possible explanation for the finding of younger age being a predictor of PTSD, she continued, is that younger liver transplant patients may lack certain coping skills, compared with their older counterparts. “Maybe patients who have had more years to deal with their disease are more accepting of it and they learn how to use productive tools to manage it.”
In their abstract, the researchers acknowledged certain limitations of the study, including its cross-sectional design, small sample size, and lack of corresponding pretransplant data.
The researchers reported having no financial disclosures.
SAN FRANCISCO –
“Serving the emotional and mental health of these patients is just as important as [improving] liver function and their immunosuppression,” study author Meg O’Meara, NP, said in an interview at the annual meeting of the American Association for the Study of Liver Diseases.
Recent data suggests that patients who undergo significant medical events like solid organ transplantation face a risk of developing PTSD, but limited information exists regarding the psychological effects following adult liver transplantation, said Ms. O’Meara, a nurse practitioner in the division of gastroenterology and hepatology at the University of Colorado at Denver, Aurora. In an effort to determine the prevalence of and risk factors for PTSD in adult liver transplant recipients, she and her associates used the PCL-5 to screen 71 patients seen at the university’s posttransplant clinic from Dec. 1, 2017, to May 31, 2018. The PCL-5 is a validated 20-item questionnaire that corresponds to the DSM-5 symptom criteria for PTSD.
The researchers also collected clinical and demographic information including pretransplant disease severity, history of psychiatric disease, duration of transplant hospitalization, and need for rehospitalization. They used a multivariable regression model to evaluate associations between clinical and demographic variables and a positive screen for PTSD.
The median age of the 71 patients was 58 years; 61% were male. A preexisting diagnosis of depression was present in 25 patients (35%), their mean Model for End-Stage Liver Disease (MELD) score at time of transplant was 31, and their median time from transplant was 1,163 days. In all, nine patients (12.7%) tested positive for PTSD on the PCL-5, and all met criteria for a provisional diagnosis of PTSD based on the DSM-5 criteria. This prevalence is about two times higher than the prevalence of PTSD in the general population (6.7%), comparable with that reported for heart transplant recipients (10.8%) and coronary artery disease (9%), but lower than that reported for ICU patients (38%), HIV patients (35.3%), and in those with Crohn’s disease (19.1%).
On multivariable logistic regression, only three factors were found to be significantly associated with the development of PTSD: younger age at transplant (P = .019), history of depression (P = .008), and a history of PTSD (P less than .001). “What I found surprising was that the MELD score at the time of transplant and the number of readmissions or complications around the time of transplant were not predictive of PTSD,” Ms. O’Meara said.
One possible explanation for the finding of younger age being a predictor of PTSD, she continued, is that younger liver transplant patients may lack certain coping skills, compared with their older counterparts. “Maybe patients who have had more years to deal with their disease are more accepting of it and they learn how to use productive tools to manage it.”
In their abstract, the researchers acknowledged certain limitations of the study, including its cross-sectional design, small sample size, and lack of corresponding pretransplant data.
The researchers reported having no financial disclosures.
REPORTING FROM THE LIVER MEETING 2018
Key clinical point: Liver transplant recipients have a higher rate of PTSD than the general population and younger patients may be at a higher risk.
Major finding: In all, nine liver transplant patients (12.7%) tested positive for PTSD, which is about two times higher than the prevalence of PTSD in the general population (6.7%).
Study details: A cross-sectional analysis of 71 liver transplant recipients.
Disclosures: The researchers reported having no financial disclosures.
Adding pembrolizumab to cisplatin-based CRT shows promise in HPV+ head and neck cancers
WASHINGTON – according to Steven F. Powell, MD.
Of 34 patients with a mean age of 59 years and stage III-IVb disease enrolled as part of an expansion cohort following a prior study demonstrating the safety of the regimen, 85% had a complete response (CR) at a median follow-up of 21 months based on imaging or salvage surgery, and an additional 2 patients had no clinical evidence of disease, Dr. Powell reported in a late-breaking oral abstract session at the annual meeting of the Society for Immunotherapy of Cancer.
About 80% of the patients had intermediate-risk disease, which is “higher risk than your standard HPV-related cancers,” said Dr. Powell of Sanford Cancer Center, Sioux Falls, S.D.
“On posttreatment imaging ... we showed a 62% complete response rate based on [RECIST 1.1 CT criteria], with 11 patients having a partial response and 2 felt to have a partial response based on CT imaging. Looking at Hopkins criteria [for PET scans] alone – 78% of our patients had a complete response,” he said.
Of the patients with a partial response based on either criteria, 11 were negative for disease on PET and 1 that was positive based on Hopkins criteria underwent neck dissection and had only inflammatory tissue; these 12 patients were also considered to have had a CR.
Additionally, of the two patients with progressive disease, one had a positive PET scan, but all biopsies were negative for ongoing disease, thus that patient was also considered to have a CR, for the overall CR rate of 85%, Dr. Powell said.
Two of the four other patients with a partial response were found at surgery to have “nothing to biopsy or resect,” so it was felt that they had a complete response clinically, and the remaining two had partial responses locoregionally and had residual disease, including residual disease at the primary site in one patient, and nodal disease in one patient.
It is important to consider the challenges of PET imaging in this study, he noted, explaining that in one patient with progressive disease, a posttreatment PET appeared to show bone and dermal metastases, but biopsies of all the areas showed that those were granulomatous disease – most likely sarcoidosis that was not present prior to the treatment.
“This ended up resolving over a year and the PET scan became negative, so I think this highlights that as we move into the curative intent setting we need to be very careful that with PET scanning we need to confirm with biopsy [in patients treated with immuno-oncology] therapies,” Dr. Powell said.
As for survival, the early data are “very encouraging,” with only one patient progressing to date (progression-free survival, 97.1%), but he cautioned that follow-up is “still only 23 months.”
The patient who progressed developed distant metastases and died from their disease, he said.
Treatment in this study included 40 mg/m2 of cisplatin weekly (six planned doses), 200 mg of pembrolizumab every 3 weeks (eight planned doses) and radiation therapy at 2 Gy once daily for 35 fractions (total of 70 Gy). The primary efficacy endpoint was complete response at 100 days after completion of chemoradiotherapy (CRT).
“Looking at safety ... we did not see any new safety signals. We had two dose discontinuations due to immune-related adverse events, which resolved on their own without therapy. Two patients stopped early due to protocol reasons,” Dr. Powell said, noting that the discontinuation rate was comparable with that seen in pembrolizumab monotherapy studies.
Standard therapy compliance was also good, with the chemotherapy goal dose reached in 88% of patients. The CRT dose was reached in all patients with no major delays in treatment.
“So adding CRT did not impact the safety of giving standard therapy,” he said.
Enrollment in this ongoing study was completed as of August, and data for the HPV-negative cohort should be available sometime in 2019. Several correlative research projects are also underway, he said.
The findings thus far show that pembrolizumab can be safely given with CRT in both HPV-positive and HPV-negative disease, with “encouraging response and progression-free survival in predominantly higher-risk patients,” Dr. Powell said.
“It is important to know that PET may pose challenges as we move into big phase 3, randomized trials, and I would strongly recommend biopsy to confirm PET findings,” he said, adding that it will be “interesting to see how this pans out in high-risk disease.
“I’m hopeful that our correlative research will help guide how we time therapy and how we move ahead in this field,” he said.
The Merck Investigator Studies Program provided grant support for this study. Dr. Powell has received research funding (to his institution) from Bristol-Myers Squibb, Genentech, Incyte, Merck, Novartis, and Pfizer.
WASHINGTON – according to Steven F. Powell, MD.
Of 34 patients with a mean age of 59 years and stage III-IVb disease enrolled as part of an expansion cohort following a prior study demonstrating the safety of the regimen, 85% had a complete response (CR) at a median follow-up of 21 months based on imaging or salvage surgery, and an additional 2 patients had no clinical evidence of disease, Dr. Powell reported in a late-breaking oral abstract session at the annual meeting of the Society for Immunotherapy of Cancer.
About 80% of the patients had intermediate-risk disease, which is “higher risk than your standard HPV-related cancers,” said Dr. Powell of Sanford Cancer Center, Sioux Falls, S.D.
“On posttreatment imaging ... we showed a 62% complete response rate based on [RECIST 1.1 CT criteria], with 11 patients having a partial response and 2 felt to have a partial response based on CT imaging. Looking at Hopkins criteria [for PET scans] alone – 78% of our patients had a complete response,” he said.
Of the patients with a partial response based on either criteria, 11 were negative for disease on PET and 1 that was positive based on Hopkins criteria underwent neck dissection and had only inflammatory tissue; these 12 patients were also considered to have had a CR.
Additionally, of the two patients with progressive disease, one had a positive PET scan, but all biopsies were negative for ongoing disease, thus that patient was also considered to have a CR, for the overall CR rate of 85%, Dr. Powell said.
Two of the four other patients with a partial response were found at surgery to have “nothing to biopsy or resect,” so it was felt that they had a complete response clinically, and the remaining two had partial responses locoregionally and had residual disease, including residual disease at the primary site in one patient, and nodal disease in one patient.
It is important to consider the challenges of PET imaging in this study, he noted, explaining that in one patient with progressive disease, a posttreatment PET appeared to show bone and dermal metastases, but biopsies of all the areas showed that those were granulomatous disease – most likely sarcoidosis that was not present prior to the treatment.
“This ended up resolving over a year and the PET scan became negative, so I think this highlights that as we move into the curative intent setting we need to be very careful that with PET scanning we need to confirm with biopsy [in patients treated with immuno-oncology] therapies,” Dr. Powell said.
As for survival, the early data are “very encouraging,” with only one patient progressing to date (progression-free survival, 97.1%), but he cautioned that follow-up is “still only 23 months.”
The patient who progressed developed distant metastases and died from their disease, he said.
Treatment in this study included 40 mg/m2 of cisplatin weekly (six planned doses), 200 mg of pembrolizumab every 3 weeks (eight planned doses) and radiation therapy at 2 Gy once daily for 35 fractions (total of 70 Gy). The primary efficacy endpoint was complete response at 100 days after completion of chemoradiotherapy (CRT).
“Looking at safety ... we did not see any new safety signals. We had two dose discontinuations due to immune-related adverse events, which resolved on their own without therapy. Two patients stopped early due to protocol reasons,” Dr. Powell said, noting that the discontinuation rate was comparable with that seen in pembrolizumab monotherapy studies.
Standard therapy compliance was also good, with the chemotherapy goal dose reached in 88% of patients. The CRT dose was reached in all patients with no major delays in treatment.
“So adding CRT did not impact the safety of giving standard therapy,” he said.
Enrollment in this ongoing study was completed as of August, and data for the HPV-negative cohort should be available sometime in 2019. Several correlative research projects are also underway, he said.
The findings thus far show that pembrolizumab can be safely given with CRT in both HPV-positive and HPV-negative disease, with “encouraging response and progression-free survival in predominantly higher-risk patients,” Dr. Powell said.
“It is important to know that PET may pose challenges as we move into big phase 3, randomized trials, and I would strongly recommend biopsy to confirm PET findings,” he said, adding that it will be “interesting to see how this pans out in high-risk disease.
“I’m hopeful that our correlative research will help guide how we time therapy and how we move ahead in this field,” he said.
The Merck Investigator Studies Program provided grant support for this study. Dr. Powell has received research funding (to his institution) from Bristol-Myers Squibb, Genentech, Incyte, Merck, Novartis, and Pfizer.
WASHINGTON – according to Steven F. Powell, MD.
Of 34 patients with a mean age of 59 years and stage III-IVb disease enrolled as part of an expansion cohort following a prior study demonstrating the safety of the regimen, 85% had a complete response (CR) at a median follow-up of 21 months based on imaging or salvage surgery, and an additional 2 patients had no clinical evidence of disease, Dr. Powell reported in a late-breaking oral abstract session at the annual meeting of the Society for Immunotherapy of Cancer.
About 80% of the patients had intermediate-risk disease, which is “higher risk than your standard HPV-related cancers,” said Dr. Powell of Sanford Cancer Center, Sioux Falls, S.D.
“On posttreatment imaging ... we showed a 62% complete response rate based on [RECIST 1.1 CT criteria], with 11 patients having a partial response and 2 felt to have a partial response based on CT imaging. Looking at Hopkins criteria [for PET scans] alone – 78% of our patients had a complete response,” he said.
Of the patients with a partial response based on either criteria, 11 were negative for disease on PET and 1 that was positive based on Hopkins criteria underwent neck dissection and had only inflammatory tissue; these 12 patients were also considered to have had a CR.
Additionally, of the two patients with progressive disease, one had a positive PET scan, but all biopsies were negative for ongoing disease, thus that patient was also considered to have a CR, for the overall CR rate of 85%, Dr. Powell said.
Two of the four other patients with a partial response were found at surgery to have “nothing to biopsy or resect,” so it was felt that they had a complete response clinically, and the remaining two had partial responses locoregionally and had residual disease, including residual disease at the primary site in one patient, and nodal disease in one patient.
It is important to consider the challenges of PET imaging in this study, he noted, explaining that in one patient with progressive disease, a posttreatment PET appeared to show bone and dermal metastases, but biopsies of all the areas showed that those were granulomatous disease – most likely sarcoidosis that was not present prior to the treatment.
“This ended up resolving over a year and the PET scan became negative, so I think this highlights that as we move into the curative intent setting we need to be very careful that with PET scanning we need to confirm with biopsy [in patients treated with immuno-oncology] therapies,” Dr. Powell said.
As for survival, the early data are “very encouraging,” with only one patient progressing to date (progression-free survival, 97.1%), but he cautioned that follow-up is “still only 23 months.”
The patient who progressed developed distant metastases and died from their disease, he said.
Treatment in this study included 40 mg/m2 of cisplatin weekly (six planned doses), 200 mg of pembrolizumab every 3 weeks (eight planned doses) and radiation therapy at 2 Gy once daily for 35 fractions (total of 70 Gy). The primary efficacy endpoint was complete response at 100 days after completion of chemoradiotherapy (CRT).
“Looking at safety ... we did not see any new safety signals. We had two dose discontinuations due to immune-related adverse events, which resolved on their own without therapy. Two patients stopped early due to protocol reasons,” Dr. Powell said, noting that the discontinuation rate was comparable with that seen in pembrolizumab monotherapy studies.
Standard therapy compliance was also good, with the chemotherapy goal dose reached in 88% of patients. The CRT dose was reached in all patients with no major delays in treatment.
“So adding CRT did not impact the safety of giving standard therapy,” he said.
Enrollment in this ongoing study was completed as of August, and data for the HPV-negative cohort should be available sometime in 2019. Several correlative research projects are also underway, he said.
The findings thus far show that pembrolizumab can be safely given with CRT in both HPV-positive and HPV-negative disease, with “encouraging response and progression-free survival in predominantly higher-risk patients,” Dr. Powell said.
“It is important to know that PET may pose challenges as we move into big phase 3, randomized trials, and I would strongly recommend biopsy to confirm PET findings,” he said, adding that it will be “interesting to see how this pans out in high-risk disease.
“I’m hopeful that our correlative research will help guide how we time therapy and how we move ahead in this field,” he said.
The Merck Investigator Studies Program provided grant support for this study. Dr. Powell has received research funding (to his institution) from Bristol-Myers Squibb, Genentech, Incyte, Merck, Novartis, and Pfizer.
REPORTING FROM SITC 2018
Key clinical point: Adding pembrolizumab to weekly low-dose cisplatin-based chemoradiotherapy shows promise in human papillomavirus–associated head and neck squamous cell carcinoma.
Major finding: A total of 85% of patients had a complete response at the 21-month follow-up; progression-free survival was 97.1%.
Study details: An expansion cohort of 34 patients.
Disclosures: The Merck Investigator Studies Program provided grant support for this study. Dr. Powell has received research funding (to his institution) from Bristol-Myers Squibb, Genentech, Incyte, Merck, Novartis, and Pfizer.
Reprocessed bronchoscopes found to harbor microbial growth
even when done in accordance with endoscope reprocessing standards, according to results of a prospective, multisite investigation.
All clinically used bronchoscopes evaluated in the study had residual contamination after reprocessing, and more than half showed microbial growth, the researchers reported in the journal CHEST.
These findings suggest that systematic changes are needed to improve cleaning and disinfection and to avoid the retention of bioburden, said researcher Cori L. Ofstead, MSPH, and her coinvestigators (Chest 2018 Nov;154[5]:1024-34).
“Evidence-based, bronchoscope-specific reprocessing and maintenance guidelines are needed, along with quality management programs to ensure that these complex processes are carried out effectively,” Ms. Ofstead and her colleagues said in their report.
Institutions also should consider shifting from high-level disinfection (HLD) to sterilization to reduce patient exposure to contaminated bronchoscopes, they added.
The study was conducted in three large, tertiary hospitals that contributed a total of 24 clinically used devices. That total comprised nine therapeutic, nine pediatric, and six endobronchial ultrasound (EBUS) bronchoscopes that were all reprocessed in accordance with each institution’s standard practices.
Proteins were detected in 100% of the bronchoscopes after HLD, according to researchers.
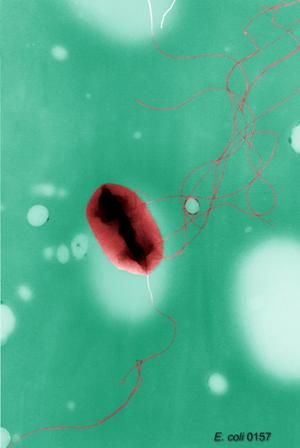
Looking at 20 paired postcleaning and post-HLD samples, the researchers found microbial growth in 11 of 20 (55%) manually-cleaned bronchoscopes and 14 of 24 (58%) bronchoscopes after HLD. The post-HLD samples included mold and recognized pathogens such as Escherichia coli, as well as normal flora and environmental bacteria, they said.
All 24 of the bronchoscopes had visible irregularities, including brown, red, or oily residue, retained fluid, debris in channels, scratches, or damage at insertion tubes and distal ends, they added.
Substandard reprocessing practices were found at two of the three participating institutions, according to the investigators. At one site, technicians reused syringes to flush channels with alcohol stored in an uncovered bowl during the day, according to the report, and bronchoscopes at that site were dried with reused towels and stored in a cabinet without active ventilation.
“Nursing staff were observed handling patient-ready bronchoscopes with bare hands,” the investigators reported.
Although clinical outcomes were not measured, the contamination, microbial growth, and defects observed in this study are “worrisome,” according to authors, because of the high infection risk in many patients undergoing bronchoscopy, and because of the infectious outbreaks and patient deaths linked to contaminated bronchoscopes in previous investigations.
Research funding for the study was provided by 3M Company. Study materials were provided by 3M Company and Healthmark Industries. Ms. Ofstead and several coauthors reported employment with Ofstead & Associates, which has received research funding and speaking fees related to infection prevention from 3M Company, Healthmark Industries, Advanced Sterilization Products (Johnson & Johnson), and others.
The senior author of the study was J. Scott Ferguson, MD, of the division of pulmonary and critical care medicine at the University of Wisconsin School of Medicine and Public Health, Madison. Dr. Ferguson provided disclosures related to NewWave Medical, Pharmaceutical Product Development, Oncocyte, Concordia, and PneumRx.
SOURCE: Ofstead C et al. Chest. 2018 Nov;154(5):1024-34.
Results of this study, which document biological contamination of inadequately reprocessed bronchoscopes, are provocative and “alarming,” warranting attention from physicians, paramedical staff, administrators, and manufacturers, Atul C. Mehta, MBBS, and Thomas Gildea, MD, wrote in an editorial (Chest 2018 Nov;154[5]:1001-3).
A breach in the disinfection protocol is the “most common culprit” behind the spread of infection during bronchoscopy, they noted.
“In our opinion, the interventional pulmonology community has buried its head in the sand regarding this issue,” they wrote.
While cases of true infection related to bronchoscopy “can seldom be differentiated” in the literature, it is nevertheless “mandatory” that biologic contamination from one patient to another be avoided, they wrote.
One dismaying observation in the present study is that human proteins were detected in the working channels of all of bronchoscopes after high-level disinfection (HLD), Dr. Mehta and Dr. Gildea stated.
“It is critical that if HLD remains the standard of care and is sufficient, it must be done properly,” they wrote. “This study raises concerns that HLD itself may not be sufficient, and we have no options for disposable specialty bronchoscopes.”
Unfortunately, requiring sterilized bronchoscopes is time-consuming and impractical for a busy bronchoscopy practice, according to the authors, while disposable bronchoscopes need to be established as clinically effective and cost effective.
In the meantime, the authors recommended that clinicians proactively consider initiatives to ensure patient safety, including formally assessing HLD processes, examining all bronchoscopes for visible damage, and ensuring that HLD guidelines are met or exceeded.
Dr. Mehta and Dr. Gildea are with the department of pulmonary medicine at Cleveland Clinic. Neither author reported conflicts of interest related to the editorial, which was published in Chest.
Results of this study, which document biological contamination of inadequately reprocessed bronchoscopes, are provocative and “alarming,” warranting attention from physicians, paramedical staff, administrators, and manufacturers, Atul C. Mehta, MBBS, and Thomas Gildea, MD, wrote in an editorial (Chest 2018 Nov;154[5]:1001-3).
A breach in the disinfection protocol is the “most common culprit” behind the spread of infection during bronchoscopy, they noted.
“In our opinion, the interventional pulmonology community has buried its head in the sand regarding this issue,” they wrote.
While cases of true infection related to bronchoscopy “can seldom be differentiated” in the literature, it is nevertheless “mandatory” that biologic contamination from one patient to another be avoided, they wrote.
One dismaying observation in the present study is that human proteins were detected in the working channels of all of bronchoscopes after high-level disinfection (HLD), Dr. Mehta and Dr. Gildea stated.
“It is critical that if HLD remains the standard of care and is sufficient, it must be done properly,” they wrote. “This study raises concerns that HLD itself may not be sufficient, and we have no options for disposable specialty bronchoscopes.”
Unfortunately, requiring sterilized bronchoscopes is time-consuming and impractical for a busy bronchoscopy practice, according to the authors, while disposable bronchoscopes need to be established as clinically effective and cost effective.
In the meantime, the authors recommended that clinicians proactively consider initiatives to ensure patient safety, including formally assessing HLD processes, examining all bronchoscopes for visible damage, and ensuring that HLD guidelines are met or exceeded.
Dr. Mehta and Dr. Gildea are with the department of pulmonary medicine at Cleveland Clinic. Neither author reported conflicts of interest related to the editorial, which was published in Chest.
Results of this study, which document biological contamination of inadequately reprocessed bronchoscopes, are provocative and “alarming,” warranting attention from physicians, paramedical staff, administrators, and manufacturers, Atul C. Mehta, MBBS, and Thomas Gildea, MD, wrote in an editorial (Chest 2018 Nov;154[5]:1001-3).
A breach in the disinfection protocol is the “most common culprit” behind the spread of infection during bronchoscopy, they noted.
“In our opinion, the interventional pulmonology community has buried its head in the sand regarding this issue,” they wrote.
While cases of true infection related to bronchoscopy “can seldom be differentiated” in the literature, it is nevertheless “mandatory” that biologic contamination from one patient to another be avoided, they wrote.
One dismaying observation in the present study is that human proteins were detected in the working channels of all of bronchoscopes after high-level disinfection (HLD), Dr. Mehta and Dr. Gildea stated.
“It is critical that if HLD remains the standard of care and is sufficient, it must be done properly,” they wrote. “This study raises concerns that HLD itself may not be sufficient, and we have no options for disposable specialty bronchoscopes.”
Unfortunately, requiring sterilized bronchoscopes is time-consuming and impractical for a busy bronchoscopy practice, according to the authors, while disposable bronchoscopes need to be established as clinically effective and cost effective.
In the meantime, the authors recommended that clinicians proactively consider initiatives to ensure patient safety, including formally assessing HLD processes, examining all bronchoscopes for visible damage, and ensuring that HLD guidelines are met or exceeded.
Dr. Mehta and Dr. Gildea are with the department of pulmonary medicine at Cleveland Clinic. Neither author reported conflicts of interest related to the editorial, which was published in Chest.
even when done in accordance with endoscope reprocessing standards, according to results of a prospective, multisite investigation.
All clinically used bronchoscopes evaluated in the study had residual contamination after reprocessing, and more than half showed microbial growth, the researchers reported in the journal CHEST.
These findings suggest that systematic changes are needed to improve cleaning and disinfection and to avoid the retention of bioburden, said researcher Cori L. Ofstead, MSPH, and her coinvestigators (Chest 2018 Nov;154[5]:1024-34).
“Evidence-based, bronchoscope-specific reprocessing and maintenance guidelines are needed, along with quality management programs to ensure that these complex processes are carried out effectively,” Ms. Ofstead and her colleagues said in their report.
Institutions also should consider shifting from high-level disinfection (HLD) to sterilization to reduce patient exposure to contaminated bronchoscopes, they added.
The study was conducted in three large, tertiary hospitals that contributed a total of 24 clinically used devices. That total comprised nine therapeutic, nine pediatric, and six endobronchial ultrasound (EBUS) bronchoscopes that were all reprocessed in accordance with each institution’s standard practices.
Proteins were detected in 100% of the bronchoscopes after HLD, according to researchers.
Looking at 20 paired postcleaning and post-HLD samples, the researchers found microbial growth in 11 of 20 (55%) manually-cleaned bronchoscopes and 14 of 24 (58%) bronchoscopes after HLD. The post-HLD samples included mold and recognized pathogens such as Escherichia coli, as well as normal flora and environmental bacteria, they said.
All 24 of the bronchoscopes had visible irregularities, including brown, red, or oily residue, retained fluid, debris in channels, scratches, or damage at insertion tubes and distal ends, they added.
Substandard reprocessing practices were found at two of the three participating institutions, according to the investigators. At one site, technicians reused syringes to flush channels with alcohol stored in an uncovered bowl during the day, according to the report, and bronchoscopes at that site were dried with reused towels and stored in a cabinet without active ventilation.
“Nursing staff were observed handling patient-ready bronchoscopes with bare hands,” the investigators reported.
Although clinical outcomes were not measured, the contamination, microbial growth, and defects observed in this study are “worrisome,” according to authors, because of the high infection risk in many patients undergoing bronchoscopy, and because of the infectious outbreaks and patient deaths linked to contaminated bronchoscopes in previous investigations.
Research funding for the study was provided by 3M Company. Study materials were provided by 3M Company and Healthmark Industries. Ms. Ofstead and several coauthors reported employment with Ofstead & Associates, which has received research funding and speaking fees related to infection prevention from 3M Company, Healthmark Industries, Advanced Sterilization Products (Johnson & Johnson), and others.
The senior author of the study was J. Scott Ferguson, MD, of the division of pulmonary and critical care medicine at the University of Wisconsin School of Medicine and Public Health, Madison. Dr. Ferguson provided disclosures related to NewWave Medical, Pharmaceutical Product Development, Oncocyte, Concordia, and PneumRx.
SOURCE: Ofstead C et al. Chest. 2018 Nov;154(5):1024-34.
even when done in accordance with endoscope reprocessing standards, according to results of a prospective, multisite investigation.
All clinically used bronchoscopes evaluated in the study had residual contamination after reprocessing, and more than half showed microbial growth, the researchers reported in the journal CHEST.
These findings suggest that systematic changes are needed to improve cleaning and disinfection and to avoid the retention of bioburden, said researcher Cori L. Ofstead, MSPH, and her coinvestigators (Chest 2018 Nov;154[5]:1024-34).
“Evidence-based, bronchoscope-specific reprocessing and maintenance guidelines are needed, along with quality management programs to ensure that these complex processes are carried out effectively,” Ms. Ofstead and her colleagues said in their report.
Institutions also should consider shifting from high-level disinfection (HLD) to sterilization to reduce patient exposure to contaminated bronchoscopes, they added.
The study was conducted in three large, tertiary hospitals that contributed a total of 24 clinically used devices. That total comprised nine therapeutic, nine pediatric, and six endobronchial ultrasound (EBUS) bronchoscopes that were all reprocessed in accordance with each institution’s standard practices.
Proteins were detected in 100% of the bronchoscopes after HLD, according to researchers.
Looking at 20 paired postcleaning and post-HLD samples, the researchers found microbial growth in 11 of 20 (55%) manually-cleaned bronchoscopes and 14 of 24 (58%) bronchoscopes after HLD. The post-HLD samples included mold and recognized pathogens such as Escherichia coli, as well as normal flora and environmental bacteria, they said.
All 24 of the bronchoscopes had visible irregularities, including brown, red, or oily residue, retained fluid, debris in channels, scratches, or damage at insertion tubes and distal ends, they added.
Substandard reprocessing practices were found at two of the three participating institutions, according to the investigators. At one site, technicians reused syringes to flush channels with alcohol stored in an uncovered bowl during the day, according to the report, and bronchoscopes at that site were dried with reused towels and stored in a cabinet without active ventilation.
“Nursing staff were observed handling patient-ready bronchoscopes with bare hands,” the investigators reported.
Although clinical outcomes were not measured, the contamination, microbial growth, and defects observed in this study are “worrisome,” according to authors, because of the high infection risk in many patients undergoing bronchoscopy, and because of the infectious outbreaks and patient deaths linked to contaminated bronchoscopes in previous investigations.
Research funding for the study was provided by 3M Company. Study materials were provided by 3M Company and Healthmark Industries. Ms. Ofstead and several coauthors reported employment with Ofstead & Associates, which has received research funding and speaking fees related to infection prevention from 3M Company, Healthmark Industries, Advanced Sterilization Products (Johnson & Johnson), and others.
The senior author of the study was J. Scott Ferguson, MD, of the division of pulmonary and critical care medicine at the University of Wisconsin School of Medicine and Public Health, Madison. Dr. Ferguson provided disclosures related to NewWave Medical, Pharmaceutical Product Development, Oncocyte, Concordia, and PneumRx.
SOURCE: Ofstead C et al. Chest. 2018 Nov;154(5):1024-34.
FROM CHEST
Key clinical point: Bronchoscope reprocessing was ineffective, even when performed in accordance with endoscope reprocessing standards.
Major finding: After high-level disinfection, residual contamination was found in 100% of bronchoscopes, while microbial growth was seen in 58%.
Study details: Observation and testing of 24 bronchoscopes contributed by three tertiary care hospitals.
Disclosures: 3M Company and Healthmark Industries provided study materials. Ms. Ofstead and several coauthors reported employment with Ofstead & Associates, which has received funding related to infection prevention from these two companies, among others. The senior study author disclosed ties to NewWave Medical, Pharmaceutical Product Development, Oncocyte, Concordia, and PneumRx.
Source: Ofstead C et al. Chest. 2018 Nov;154(5):1024-34.
DBT can help traumatized, suicidal youth manage emotions
SEATTLE – Children who are suicidal and victims of trauma, especially those with PTSD, pose an especially difficult challenge for psychiatrists. Trauma, suicidality, and self-harm often present together, and they might heighten the risk of treatment.
“It becomes a dilemma to know in what order to treat those symptoms, because sometimes it feels like one will not get better without treating the other,” said Michele Berk, PhD. “But there’s also some question around when it’s safe to do exposure-based treatments – which are the key ingredient to resolving PTSD symptoms,” Dr. Berk said during a session focused on trauma and suicidality in youth at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
Dialectical behavior therapy, or DBT, is an option. DBT was developed by Marsha M. Linehan, PhD, to treat chronic suicidality comorbid with borderline personality disorder. In addition to PTSD, newer work has shown DBT as efficacious for treating substance use disorders, depression, and eating disorders.
DBT is based on the idea that self-harm occurs, at least in some cases, because the patient is predisposed to experiencing heightened emotional reactions. When the patient is exposed to an invalidating environment, such as when a parent or caregiver tells them to “just get over it; you’re overreacting,” this can lead patients to question their emotions. Most importantly, patients never learn effective strategies to that manage their emotions, according to Dr. Berk, assistant professor of psychiatry and behavioral sciences at Stanford (Calif.) University.
In addition, Dr. Berk said, traumatized youth sometimes present with the most extreme form of invalidation, in which the patient’s entire being is violated through physical violence.
“So you have people who have these really intense negative emotions but don’t know how to help themselves manage them, and that is where DBT believes suicidal and self-harm behavior comes in,” Dr. Berk said. “We know that self-harm, though not suicidal self-injury, does in fact reduce emotion.”
DBT aims to counter suicidality by assisting the patient to build a life worth living. It encompasses five modes, including skills training, individual psychotherapy, in-the-moment coaching, case management, and a DBT consultation team to support the therapist.
The program prioritizes life-threatening behaviors in stage I and saving any exposure or PTSD therapy for stage II, which might begin up to 12 months later.
Also in stage I, after life-threatening behaviors have been resolved, the therapist addresses symptoms or factors that potentially interfere with further therapy. That’s important, because patients usually have comorbid symptoms and might be acutely distressed. “DBT has developed a clear hierarchy of how to target those things so that the sessions don’t get chaotic or off track,” Dr. Berk said.
Trauma symptoms might be tackled in stage I if they’re directly linked to suicidality or interfere with treatment, through reluctance to share information or because they might lead to dissociation during a session. After that, the program addresses quality of life, since its goal is to help patients create lives they deem worth living.
The skills training component of DBT includes mindfulness to help ground patients in the present moment. It also fosters skills that can be used to address trauma, including distress tolerance. Distress tolerance incorporates actions such as distraction and self-soothing. Emotional regulation seeks to help patients alter their emotions when possible. Interpersonal relationship skills help the patients ask for what they want and how to say “no” effectively.
Exposure therapy does not begin until patients have gone at least 2 months without any self-harming behavior, and it is interrupted if the patients exhibit self-harming behavior after it starts.
DBT remains a subject of continuing research. One avenue would be to more directly integrate exposure therapy with DBT in adolescents, but a protocol has not yet been developed. Prolonged exposure is typically used in adult PTSD patients, but trauma-focused cognitive-behavioral therapy more often is the choice for adolescents.
Whatever the choice, involvement of caring adults would be key. “In adolescents, there’s a need to involve parents and caregivers in whatever the trauma treatment is going to be,” Dr. Berk said.
Dr. Berk disclosed no conflicts of interest.
SEATTLE – Children who are suicidal and victims of trauma, especially those with PTSD, pose an especially difficult challenge for psychiatrists. Trauma, suicidality, and self-harm often present together, and they might heighten the risk of treatment.
“It becomes a dilemma to know in what order to treat those symptoms, because sometimes it feels like one will not get better without treating the other,” said Michele Berk, PhD. “But there’s also some question around when it’s safe to do exposure-based treatments – which are the key ingredient to resolving PTSD symptoms,” Dr. Berk said during a session focused on trauma and suicidality in youth at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
Dialectical behavior therapy, or DBT, is an option. DBT was developed by Marsha M. Linehan, PhD, to treat chronic suicidality comorbid with borderline personality disorder. In addition to PTSD, newer work has shown DBT as efficacious for treating substance use disorders, depression, and eating disorders.
DBT is based on the idea that self-harm occurs, at least in some cases, because the patient is predisposed to experiencing heightened emotional reactions. When the patient is exposed to an invalidating environment, such as when a parent or caregiver tells them to “just get over it; you’re overreacting,” this can lead patients to question their emotions. Most importantly, patients never learn effective strategies to that manage their emotions, according to Dr. Berk, assistant professor of psychiatry and behavioral sciences at Stanford (Calif.) University.
In addition, Dr. Berk said, traumatized youth sometimes present with the most extreme form of invalidation, in which the patient’s entire being is violated through physical violence.
“So you have people who have these really intense negative emotions but don’t know how to help themselves manage them, and that is where DBT believes suicidal and self-harm behavior comes in,” Dr. Berk said. “We know that self-harm, though not suicidal self-injury, does in fact reduce emotion.”
DBT aims to counter suicidality by assisting the patient to build a life worth living. It encompasses five modes, including skills training, individual psychotherapy, in-the-moment coaching, case management, and a DBT consultation team to support the therapist.
The program prioritizes life-threatening behaviors in stage I and saving any exposure or PTSD therapy for stage II, which might begin up to 12 months later.
Also in stage I, after life-threatening behaviors have been resolved, the therapist addresses symptoms or factors that potentially interfere with further therapy. That’s important, because patients usually have comorbid symptoms and might be acutely distressed. “DBT has developed a clear hierarchy of how to target those things so that the sessions don’t get chaotic or off track,” Dr. Berk said.
Trauma symptoms might be tackled in stage I if they’re directly linked to suicidality or interfere with treatment, through reluctance to share information or because they might lead to dissociation during a session. After that, the program addresses quality of life, since its goal is to help patients create lives they deem worth living.
The skills training component of DBT includes mindfulness to help ground patients in the present moment. It also fosters skills that can be used to address trauma, including distress tolerance. Distress tolerance incorporates actions such as distraction and self-soothing. Emotional regulation seeks to help patients alter their emotions when possible. Interpersonal relationship skills help the patients ask for what they want and how to say “no” effectively.
Exposure therapy does not begin until patients have gone at least 2 months without any self-harming behavior, and it is interrupted if the patients exhibit self-harming behavior after it starts.
DBT remains a subject of continuing research. One avenue would be to more directly integrate exposure therapy with DBT in adolescents, but a protocol has not yet been developed. Prolonged exposure is typically used in adult PTSD patients, but trauma-focused cognitive-behavioral therapy more often is the choice for adolescents.
Whatever the choice, involvement of caring adults would be key. “In adolescents, there’s a need to involve parents and caregivers in whatever the trauma treatment is going to be,” Dr. Berk said.
Dr. Berk disclosed no conflicts of interest.
SEATTLE – Children who are suicidal and victims of trauma, especially those with PTSD, pose an especially difficult challenge for psychiatrists. Trauma, suicidality, and self-harm often present together, and they might heighten the risk of treatment.
“It becomes a dilemma to know in what order to treat those symptoms, because sometimes it feels like one will not get better without treating the other,” said Michele Berk, PhD. “But there’s also some question around when it’s safe to do exposure-based treatments – which are the key ingredient to resolving PTSD symptoms,” Dr. Berk said during a session focused on trauma and suicidality in youth at the annual meeting of the American Academy of Child and Adolescent Psychiatry.
Dialectical behavior therapy, or DBT, is an option. DBT was developed by Marsha M. Linehan, PhD, to treat chronic suicidality comorbid with borderline personality disorder. In addition to PTSD, newer work has shown DBT as efficacious for treating substance use disorders, depression, and eating disorders.
DBT is based on the idea that self-harm occurs, at least in some cases, because the patient is predisposed to experiencing heightened emotional reactions. When the patient is exposed to an invalidating environment, such as when a parent or caregiver tells them to “just get over it; you’re overreacting,” this can lead patients to question their emotions. Most importantly, patients never learn effective strategies to that manage their emotions, according to Dr. Berk, assistant professor of psychiatry and behavioral sciences at Stanford (Calif.) University.
In addition, Dr. Berk said, traumatized youth sometimes present with the most extreme form of invalidation, in which the patient’s entire being is violated through physical violence.
“So you have people who have these really intense negative emotions but don’t know how to help themselves manage them, and that is where DBT believes suicidal and self-harm behavior comes in,” Dr. Berk said. “We know that self-harm, though not suicidal self-injury, does in fact reduce emotion.”
DBT aims to counter suicidality by assisting the patient to build a life worth living. It encompasses five modes, including skills training, individual psychotherapy, in-the-moment coaching, case management, and a DBT consultation team to support the therapist.
The program prioritizes life-threatening behaviors in stage I and saving any exposure or PTSD therapy for stage II, which might begin up to 12 months later.
Also in stage I, after life-threatening behaviors have been resolved, the therapist addresses symptoms or factors that potentially interfere with further therapy. That’s important, because patients usually have comorbid symptoms and might be acutely distressed. “DBT has developed a clear hierarchy of how to target those things so that the sessions don’t get chaotic or off track,” Dr. Berk said.
Trauma symptoms might be tackled in stage I if they’re directly linked to suicidality or interfere with treatment, through reluctance to share information or because they might lead to dissociation during a session. After that, the program addresses quality of life, since its goal is to help patients create lives they deem worth living.
The skills training component of DBT includes mindfulness to help ground patients in the present moment. It also fosters skills that can be used to address trauma, including distress tolerance. Distress tolerance incorporates actions such as distraction and self-soothing. Emotional regulation seeks to help patients alter their emotions when possible. Interpersonal relationship skills help the patients ask for what they want and how to say “no” effectively.
Exposure therapy does not begin until patients have gone at least 2 months without any self-harming behavior, and it is interrupted if the patients exhibit self-harming behavior after it starts.
DBT remains a subject of continuing research. One avenue would be to more directly integrate exposure therapy with DBT in adolescents, but a protocol has not yet been developed. Prolonged exposure is typically used in adult PTSD patients, but trauma-focused cognitive-behavioral therapy more often is the choice for adolescents.
Whatever the choice, involvement of caring adults would be key. “In adolescents, there’s a need to involve parents and caregivers in whatever the trauma treatment is going to be,” Dr. Berk said.
Dr. Berk disclosed no conflicts of interest.
REPORTING FROM AACAP 2018
Novel acetaminophen hepatotoxicity strategy curbs inflammation
SAN FRANCISCO – A novel therapeutic strategy shows initial promise in dampening hepatic cell injury in mice caused by overexposure to acetaminophen. The approach relies on a synthetic version of heparan sulfate, which is believed to interfere with recruitment of neutrophils to the site of hepatic injury. That reduces harm caused by inflammation and may offer a longer therapeutic window than N-acetyl cysteine, which is the current standard therapy but is only effective if given within 8 hours of the injury.
The endogenous syndecan-1, which is a heparan sulfate, is also known to act as a native defense mechanism against inflammatory injury to hepatocytes. “It looks like heparan sulfate attenuates inflammatory responses,” said Jian Liu, PhD, during a presentation of his research at the annual meeting of the American Association for the Study of Liver Diseases. Dr. Liu is a professor of chemical biology and medicinal chemistry at the University of North Carolina at Chapel Hill.
The heparan sulfate analogue heparin has long been used as an anticoagulant, of course, which suggests that a novel heparan sulfate has a good chance of also being safe.
Dr. Liu’s team had to identify a heparan sulfate that had a hepatoprotective effect, but a heparan sulfate’s unique biological activity depends on the specific pattern of sulfation on the heparan molecule. Heparans isolated from natural sources are generally a complex mixture, which makes them difficult to study and produce in large enough quantities to be therapeutically useful.
Dr. Liu’s team used a combinatory approach, harnessing various enzymes to produce hundreds of different heparan sulfate variants, and then screened them for hepatoprotective activity. That process identified an 18-chain heparan sulfate with hepatoprotective activity. With an active formula in hand, they could employ the enzymes to create enough of the pure compound to further the research. “It’s probably two to three hundred times more efficient than the traditional chemical synthesis,” said Dr. Liu.
In mice, researchers injected the 18-mer 30 minutes after a hepatotoxic dose of acetaminophen and again after 12 hours. Tissue staining showed less migration of neutrophils, as well as lower concentrations of tumor necrosis factor–alpha. The animals also had lower alanine transferase levels than did the untreated animals, as well as greater survival after 4 days.
The pathological process surrounding acetaminophen overdose involves release of the high mobility group box 1 (HMGB1) protein from necrotic hepatocytes, which in turn binds to the receptor for advanced glycation end-products (RAGE). The HMGB1/RAGE complex then binds to neutrophils, recruiting them to the site of the injury and initiating inflammation.
To better understand the molecule’s role in the pathological process, the researchers studied RAGE knockout mice, and found that the 18-mer had no protective effect in these animals, suggesting that it relies on RAGE for its biological activity.
Heparan sulfates are widely present in the body, which prompted the researchers to investigate their endogenous effect. In the liver, the primary heparan sulfate is syndecan-1. The researchers demonstrated that the molecule is shed from cell surfaces in response to acetaminophen toxicity and that the levels correlate with HMGB1 release.
Dr. Liu believes that syndecan-1 acts as a natural buffer to inflammation, helping to neutralize HMGB1 and limit damage. “The problem is that when the damage is massive, the shed of syndecan-1 is not enough,” said Dr. Liu. He hopes that something like his team’s heparan sulfate 18-mer can be used therapeutically to bolster these endogenous controls and prevent further damage.
The research was funded by Glycan Therapeutics. Dr. Liu founded Glycan, which offers custom-synthesized heparan sulfates and chondroitin sulfates for research purposes.
SOURCE: Liu J. AASLD 2018, Abstract 0040.
SAN FRANCISCO – A novel therapeutic strategy shows initial promise in dampening hepatic cell injury in mice caused by overexposure to acetaminophen. The approach relies on a synthetic version of heparan sulfate, which is believed to interfere with recruitment of neutrophils to the site of hepatic injury. That reduces harm caused by inflammation and may offer a longer therapeutic window than N-acetyl cysteine, which is the current standard therapy but is only effective if given within 8 hours of the injury.
The endogenous syndecan-1, which is a heparan sulfate, is also known to act as a native defense mechanism against inflammatory injury to hepatocytes. “It looks like heparan sulfate attenuates inflammatory responses,” said Jian Liu, PhD, during a presentation of his research at the annual meeting of the American Association for the Study of Liver Diseases. Dr. Liu is a professor of chemical biology and medicinal chemistry at the University of North Carolina at Chapel Hill.
The heparan sulfate analogue heparin has long been used as an anticoagulant, of course, which suggests that a novel heparan sulfate has a good chance of also being safe.
Dr. Liu’s team had to identify a heparan sulfate that had a hepatoprotective effect, but a heparan sulfate’s unique biological activity depends on the specific pattern of sulfation on the heparan molecule. Heparans isolated from natural sources are generally a complex mixture, which makes them difficult to study and produce in large enough quantities to be therapeutically useful.
Dr. Liu’s team used a combinatory approach, harnessing various enzymes to produce hundreds of different heparan sulfate variants, and then screened them for hepatoprotective activity. That process identified an 18-chain heparan sulfate with hepatoprotective activity. With an active formula in hand, they could employ the enzymes to create enough of the pure compound to further the research. “It’s probably two to three hundred times more efficient than the traditional chemical synthesis,” said Dr. Liu.
In mice, researchers injected the 18-mer 30 minutes after a hepatotoxic dose of acetaminophen and again after 12 hours. Tissue staining showed less migration of neutrophils, as well as lower concentrations of tumor necrosis factor–alpha. The animals also had lower alanine transferase levels than did the untreated animals, as well as greater survival after 4 days.
The pathological process surrounding acetaminophen overdose involves release of the high mobility group box 1 (HMGB1) protein from necrotic hepatocytes, which in turn binds to the receptor for advanced glycation end-products (RAGE). The HMGB1/RAGE complex then binds to neutrophils, recruiting them to the site of the injury and initiating inflammation.
To better understand the molecule’s role in the pathological process, the researchers studied RAGE knockout mice, and found that the 18-mer had no protective effect in these animals, suggesting that it relies on RAGE for its biological activity.
Heparan sulfates are widely present in the body, which prompted the researchers to investigate their endogenous effect. In the liver, the primary heparan sulfate is syndecan-1. The researchers demonstrated that the molecule is shed from cell surfaces in response to acetaminophen toxicity and that the levels correlate with HMGB1 release.
Dr. Liu believes that syndecan-1 acts as a natural buffer to inflammation, helping to neutralize HMGB1 and limit damage. “The problem is that when the damage is massive, the shed of syndecan-1 is not enough,” said Dr. Liu. He hopes that something like his team’s heparan sulfate 18-mer can be used therapeutically to bolster these endogenous controls and prevent further damage.
The research was funded by Glycan Therapeutics. Dr. Liu founded Glycan, which offers custom-synthesized heparan sulfates and chondroitin sulfates for research purposes.
SOURCE: Liu J. AASLD 2018, Abstract 0040.
SAN FRANCISCO – A novel therapeutic strategy shows initial promise in dampening hepatic cell injury in mice caused by overexposure to acetaminophen. The approach relies on a synthetic version of heparan sulfate, which is believed to interfere with recruitment of neutrophils to the site of hepatic injury. That reduces harm caused by inflammation and may offer a longer therapeutic window than N-acetyl cysteine, which is the current standard therapy but is only effective if given within 8 hours of the injury.
The endogenous syndecan-1, which is a heparan sulfate, is also known to act as a native defense mechanism against inflammatory injury to hepatocytes. “It looks like heparan sulfate attenuates inflammatory responses,” said Jian Liu, PhD, during a presentation of his research at the annual meeting of the American Association for the Study of Liver Diseases. Dr. Liu is a professor of chemical biology and medicinal chemistry at the University of North Carolina at Chapel Hill.
The heparan sulfate analogue heparin has long been used as an anticoagulant, of course, which suggests that a novel heparan sulfate has a good chance of also being safe.
Dr. Liu’s team had to identify a heparan sulfate that had a hepatoprotective effect, but a heparan sulfate’s unique biological activity depends on the specific pattern of sulfation on the heparan molecule. Heparans isolated from natural sources are generally a complex mixture, which makes them difficult to study and produce in large enough quantities to be therapeutically useful.
Dr. Liu’s team used a combinatory approach, harnessing various enzymes to produce hundreds of different heparan sulfate variants, and then screened them for hepatoprotective activity. That process identified an 18-chain heparan sulfate with hepatoprotective activity. With an active formula in hand, they could employ the enzymes to create enough of the pure compound to further the research. “It’s probably two to three hundred times more efficient than the traditional chemical synthesis,” said Dr. Liu.
In mice, researchers injected the 18-mer 30 minutes after a hepatotoxic dose of acetaminophen and again after 12 hours. Tissue staining showed less migration of neutrophils, as well as lower concentrations of tumor necrosis factor–alpha. The animals also had lower alanine transferase levels than did the untreated animals, as well as greater survival after 4 days.
The pathological process surrounding acetaminophen overdose involves release of the high mobility group box 1 (HMGB1) protein from necrotic hepatocytes, which in turn binds to the receptor for advanced glycation end-products (RAGE). The HMGB1/RAGE complex then binds to neutrophils, recruiting them to the site of the injury and initiating inflammation.
To better understand the molecule’s role in the pathological process, the researchers studied RAGE knockout mice, and found that the 18-mer had no protective effect in these animals, suggesting that it relies on RAGE for its biological activity.
Heparan sulfates are widely present in the body, which prompted the researchers to investigate their endogenous effect. In the liver, the primary heparan sulfate is syndecan-1. The researchers demonstrated that the molecule is shed from cell surfaces in response to acetaminophen toxicity and that the levels correlate with HMGB1 release.
Dr. Liu believes that syndecan-1 acts as a natural buffer to inflammation, helping to neutralize HMGB1 and limit damage. “The problem is that when the damage is massive, the shed of syndecan-1 is not enough,” said Dr. Liu. He hopes that something like his team’s heparan sulfate 18-mer can be used therapeutically to bolster these endogenous controls and prevent further damage.
The research was funded by Glycan Therapeutics. Dr. Liu founded Glycan, which offers custom-synthesized heparan sulfates and chondroitin sulfates for research purposes.
SOURCE: Liu J. AASLD 2018, Abstract 0040.
REPORTING FROM AASLD 2018
Refractory immune-mediated colitis: Fecal transplant may be the answer
WASHINGTON – , according to Yinghong Wang, MD.
In two patients who developed severe, refractory, immune-mediated colitis (IMC), FMT led to recovery, Dr. Wang of M.D. Anderson Cancer Center, Houston, reported at the annual meeting of the Society for Immunotherapy of Cancer.
Patient 1 was a woman with renal cell cancer who developed grade 2+ IMC within 1 month of initiation of treatment with combined ipilimumab and nivolumab. Infectious etiology was ruled out, and her symptoms and ulcers persisted despite 3 months of treatment with corticosteroids, two doses of infliximab, and one dose of vedolizumab.
A single FMT delivered via colonoscopy led to complete symptom resolution within 10 days, and a repeat colonoscopy showed “very nice healing of inflammation and ulcers,” Dr. Wang said.
Patient 2 was a man with prostate cancer who developed grade 2+ IMC 3 months after receiving two doses of ipilimumab. Infectious etiologies were ruled out, and like patient 1, his symptoms and mucosal ulcerations persisted despite 5 months of immunosuppression with corticosteroids, two doses of infliximab, and three doses of vedolizumab. He underwent two FMTs via colonoscopy.
“The first fecal transplant achieved partial response, and the second fecal transplant achieved complete clinical response, and this remission was sustained for a total of 8 months,” Dr. Wang said.
Immune checkpoint inhibitor–related IMC is typically treated with immunosuppressive therapy that is associated with significant morbidity, including a possible adverse impact on the antitumor effects of checkpoint inhibitors, Dr. Wang said.
However, studies have suggested that “the microbiome in healthy people potentially plays a very important and synergistic role for tumor regression in combination with immunotherapy,” and animal models also suggest that patients who develop IMC have differential bacterial signatures in their gut microbiome, she said.
“Based on that preliminary information, we performed fecal transplant as a compassionate treatment for cases refractory to all immunosuppression in June 2017 at M.D. Anderson,” she said.
Stool microbiome analyses showed successful engraftment of donor microbiome in recipient stool samples, and microbiome taxonomy showed increases in specific Escherichia species that “we think potentially play a role in this colitis recovery,” she said.
“Fecal transplant is safe and effective based on our preliminary study,” she said, adding that restoration of a healthy microbiome seems to reverse IMC. “Future large-scale studies are needed to evaluate this finding.”
Dr. Wang reported having no disclosures.
SOURCE: Wang Y et al. SITC 2018, Abstract P194.
WASHINGTON – , according to Yinghong Wang, MD.
In two patients who developed severe, refractory, immune-mediated colitis (IMC), FMT led to recovery, Dr. Wang of M.D. Anderson Cancer Center, Houston, reported at the annual meeting of the Society for Immunotherapy of Cancer.
Patient 1 was a woman with renal cell cancer who developed grade 2+ IMC within 1 month of initiation of treatment with combined ipilimumab and nivolumab. Infectious etiology was ruled out, and her symptoms and ulcers persisted despite 3 months of treatment with corticosteroids, two doses of infliximab, and one dose of vedolizumab.
A single FMT delivered via colonoscopy led to complete symptom resolution within 10 days, and a repeat colonoscopy showed “very nice healing of inflammation and ulcers,” Dr. Wang said.
Patient 2 was a man with prostate cancer who developed grade 2+ IMC 3 months after receiving two doses of ipilimumab. Infectious etiologies were ruled out, and like patient 1, his symptoms and mucosal ulcerations persisted despite 5 months of immunosuppression with corticosteroids, two doses of infliximab, and three doses of vedolizumab. He underwent two FMTs via colonoscopy.
“The first fecal transplant achieved partial response, and the second fecal transplant achieved complete clinical response, and this remission was sustained for a total of 8 months,” Dr. Wang said.
Immune checkpoint inhibitor–related IMC is typically treated with immunosuppressive therapy that is associated with significant morbidity, including a possible adverse impact on the antitumor effects of checkpoint inhibitors, Dr. Wang said.
However, studies have suggested that “the microbiome in healthy people potentially plays a very important and synergistic role for tumor regression in combination with immunotherapy,” and animal models also suggest that patients who develop IMC have differential bacterial signatures in their gut microbiome, she said.
“Based on that preliminary information, we performed fecal transplant as a compassionate treatment for cases refractory to all immunosuppression in June 2017 at M.D. Anderson,” she said.
Stool microbiome analyses showed successful engraftment of donor microbiome in recipient stool samples, and microbiome taxonomy showed increases in specific Escherichia species that “we think potentially play a role in this colitis recovery,” she said.
“Fecal transplant is safe and effective based on our preliminary study,” she said, adding that restoration of a healthy microbiome seems to reverse IMC. “Future large-scale studies are needed to evaluate this finding.”
Dr. Wang reported having no disclosures.
SOURCE: Wang Y et al. SITC 2018, Abstract P194.
WASHINGTON – , according to Yinghong Wang, MD.
In two patients who developed severe, refractory, immune-mediated colitis (IMC), FMT led to recovery, Dr. Wang of M.D. Anderson Cancer Center, Houston, reported at the annual meeting of the Society for Immunotherapy of Cancer.
Patient 1 was a woman with renal cell cancer who developed grade 2+ IMC within 1 month of initiation of treatment with combined ipilimumab and nivolumab. Infectious etiology was ruled out, and her symptoms and ulcers persisted despite 3 months of treatment with corticosteroids, two doses of infliximab, and one dose of vedolizumab.
A single FMT delivered via colonoscopy led to complete symptom resolution within 10 days, and a repeat colonoscopy showed “very nice healing of inflammation and ulcers,” Dr. Wang said.
Patient 2 was a man with prostate cancer who developed grade 2+ IMC 3 months after receiving two doses of ipilimumab. Infectious etiologies were ruled out, and like patient 1, his symptoms and mucosal ulcerations persisted despite 5 months of immunosuppression with corticosteroids, two doses of infliximab, and three doses of vedolizumab. He underwent two FMTs via colonoscopy.
“The first fecal transplant achieved partial response, and the second fecal transplant achieved complete clinical response, and this remission was sustained for a total of 8 months,” Dr. Wang said.
Immune checkpoint inhibitor–related IMC is typically treated with immunosuppressive therapy that is associated with significant morbidity, including a possible adverse impact on the antitumor effects of checkpoint inhibitors, Dr. Wang said.
However, studies have suggested that “the microbiome in healthy people potentially plays a very important and synergistic role for tumor regression in combination with immunotherapy,” and animal models also suggest that patients who develop IMC have differential bacterial signatures in their gut microbiome, she said.
“Based on that preliminary information, we performed fecal transplant as a compassionate treatment for cases refractory to all immunosuppression in June 2017 at M.D. Anderson,” she said.
Stool microbiome analyses showed successful engraftment of donor microbiome in recipient stool samples, and microbiome taxonomy showed increases in specific Escherichia species that “we think potentially play a role in this colitis recovery,” she said.
“Fecal transplant is safe and effective based on our preliminary study,” she said, adding that restoration of a healthy microbiome seems to reverse IMC. “Future large-scale studies are needed to evaluate this finding.”
Dr. Wang reported having no disclosures.
SOURCE: Wang Y et al. SITC 2018, Abstract P194.
REPORTING FROM SITC 2018
Key clinical point: FMT lead to recovery in two patients with refractory IMC.
Major finding: FMT was effective for the treatment of IMC in two patients.
Study details: Two case reports.
Disclosures: Dr. Wang reported having no disclosures.
Source: Wang Y et al. SITC 2018, Abstract P194.
PIONEER-HF called “practice changing” for acute decompensated heart failure
CHICAGO – Initiation of angiotensin-neprilysin inhibition using sacubitril/valsartan during hospitalization for acute decompensated heart failure, instead of relying upon enalapril, resulted in a substantially greater reduction in N-terminal of the prohormone brain natriuretic peptide concentration and a markedly lower rate of rehospitalization with no safety downside in the PIONEER-HF trial, Eric J. Velazquez, MD, reported at the American Heart Association scientific sessions.
“We believe these results have clinical implications that support the in-hospital initiation of sacubitril/valsartan in stabilized patients with acute decompensated heart failure and reduced ejection fraction irrespective of prior ACE inhibitor or ARB [angiotensin II receptor blocker] use or prior diagnosis of heart failure,” said Dr. Velazquez, a professor of medicine and chief of the section of cardiovascular medicine at Yale University, New Haven, Conn., and physician in chief of the Heart and Vascular Center for the Yale-New Haven Health System.
Sacubitril/valsartan (Entresto) has a class I indication for treatment of symptomatic heart failure with reduced ejection fraction (HFrEF) in the AHA/American College of Cardiology guidelines. This strong recommendation is based largely upon the impressive results of the PARADIGM-HF trial, which in ambulatory outpatients demonstrated a lower risk of cardiovascular mortality or hospitalization for heart failure than enalapril (N Engl J Med. 2014 Sep 11;371[11]:993-1004).
However, since patients with acute decompensated heart failure (ADHF) were excluded from PARADIGM-HF, the safety and effectiveness of starting such patients on the drug while hospitalized for acute decompensation was unknown.
PIONEER-HF was carried out to shed light on that issue and thereby address a major unmet need for better treatments for ADHF. Even though this condition accounts for more than 1 million hospitalizations annually in the United States, short-term rehospitalization and mortality rates in affected patients remain unacceptably high at 21% and 12%, respectively. And the standard-of-care treatment – decongestion with intravenous diuretics and hemodynamic support with inotropes and vasodilators – hasn’t changed in nearly half a century, Dr. Velazquez noted.
The trial included 881 patients hospitalized for acute decompensated HFrEF at 129 U.S. centers. The study population was diverse: 36% of participants were black and one-third of subjects had no diagnosis of heart failure prior to their hospitalization. After achieving hemodynamic stabilization, patients were randomized to receive sacubitril/valsartan or enalapril.
Key outcomes
The primary endpoint was change in N-terminal of the prohormone brain natriuretic peptide concentration from baseline to week 8. There was a 25% reduction in the enalapril group and a 45% reduction with sacubitril/valsartan. This translated to a highly significant 29% greater relative risk reduction with sacubitril/valsartan.
More eye opening was the between-group difference in the prespecified composite clinical endpoint comprising death, rehospitalization for heart failure, implantation of a left ventricular assist device, or listing for heart transplant during the 8-week study.
The rate was 16.8% in the enalapril group and 9.3% with sacubitril/valsartan. This worked out to a 46% relative risk reduction, with a number needed to treat of 13.
The composite result was driven by a 44% reduction in risk of heart failure rehospitalization in the sacubitril/valsartan group: 8.0% versus 13.8%. The sacubitril/valsartan group also had a numerically lower mortality rate: 2.3% versus 3.4%, although the number of fatalities was small and this 34% relative risk reduction didn’t achieve statistical significance.
Rates of the key safety outcomes – symptomatic hypotension, worsening renal function, hyperkalemia, and angioedema – didn’t differ between the two study arms. Of interest, however, all six cases of angioedema in the enalapril group occurred in black patients, while the only case in the sacubitril/valsartan group was in a white patient.
PIONEER-HF treatment strategy
Hemodynamic stabilization as a prelude to randomization to sacubitril/valsartan or enalapril required maintaining a systolic blood pressure of at least 100 mm Hg in the previous 6 hours, with no symptomatic hypotension, intensification of intravenous diuretics, or use of intravenous vasodilators during that time period, and no intravenous inotropes in the previous 24 hours.
Enalapril was titrated to a target dose of 10 mg twice daily. Sacubitril/valsartan was titrated to a target dose of 97/103 mg twice daily. Titration was carried out using an algorithm based upon systolic BP. If the SBP was at least 100 and less than 120 mm Hg at baseline, sacubitril/valsartan was initiated at 24/26 mg twice daily, enalapril at 2.5 mg b.i.d. If the SBP at randomization was 120 mm Hg or higher, the initial dosing was sacubitril/valsartan at 49/51 mm Hg b.i.d. or enalapril at 5 mg b.i.d. Up-titration occurred after 1 week, then biweekly through week 8.
PIONEER in perspective
Discussant Larry A. Allen, MD, a heart failure specialist at the University of Colorado at Denver, Aurora, predicted that this will be a practice-changing study.
“There has been a need for a study like PIONEER in heart failure,” he observed. While multiple randomized trials have advanced the treatment of ambulatory HFrEF patients, demonstrating benefit for initiation and intensification of treatment with ACE inhibitors, angiotensin II receptor blockers, beta-blockers, and mineralocorticoid receptor antagonists, the treatment of patients with ADHF has remained relatively static, marked by failed trials of once-promising novel agents including tolvaptan, nesiritide, and serelaxin.
“All the data is in ambulatory patients, but the action for the care of heart failure patients actually occurs largely in the hospital. Seventy percent of care provided in the U.S. to patients with heart failure occurs in the hospital setting. These patients are a captive audience at that time, and the transitions from inpatient to outpatient care are fragile,” Dr. Allen said.
He noted that the use of sacubitril/valsartan in routine practice as reflected in national registries has been “extremely low” – less than 15% among eligible patients – despite the drug having been approved more than 3 years ago. One major reason for the low uptake, in his view, is clinical inertia. That should melt away in what he termed “the post-PIONEER world.”
“I think one of the great things about this study is it keeps it simple. We now have a simpler algorithm for inpatient and subsequent outpatient management of heart failure with reduced ejection fraction. It’s easier for us to start with the treatment we want patients to be on, and it’s better for patients, too. Most importantly, this study reinforces the importance and safety of aggressive guideline-directed medical therapy starting from the beginning in most patients,” Dr. Allen said.
The study findings were published simultaneously in the New England Journal of Medicine (2018 Nov 11. doi: 10.1056/NEJMoa1812851).
PIONEER-HF was sponsored by Novartis. Dr. Velazquez reported receiving research grants from and serving as a consultant to that company and others. Dr. Allen reported having no financial conflicts.
CHICAGO – Initiation of angiotensin-neprilysin inhibition using sacubitril/valsartan during hospitalization for acute decompensated heart failure, instead of relying upon enalapril, resulted in a substantially greater reduction in N-terminal of the prohormone brain natriuretic peptide concentration and a markedly lower rate of rehospitalization with no safety downside in the PIONEER-HF trial, Eric J. Velazquez, MD, reported at the American Heart Association scientific sessions.
“We believe these results have clinical implications that support the in-hospital initiation of sacubitril/valsartan in stabilized patients with acute decompensated heart failure and reduced ejection fraction irrespective of prior ACE inhibitor or ARB [angiotensin II receptor blocker] use or prior diagnosis of heart failure,” said Dr. Velazquez, a professor of medicine and chief of the section of cardiovascular medicine at Yale University, New Haven, Conn., and physician in chief of the Heart and Vascular Center for the Yale-New Haven Health System.
Sacubitril/valsartan (Entresto) has a class I indication for treatment of symptomatic heart failure with reduced ejection fraction (HFrEF) in the AHA/American College of Cardiology guidelines. This strong recommendation is based largely upon the impressive results of the PARADIGM-HF trial, which in ambulatory outpatients demonstrated a lower risk of cardiovascular mortality or hospitalization for heart failure than enalapril (N Engl J Med. 2014 Sep 11;371[11]:993-1004).
However, since patients with acute decompensated heart failure (ADHF) were excluded from PARADIGM-HF, the safety and effectiveness of starting such patients on the drug while hospitalized for acute decompensation was unknown.
PIONEER-HF was carried out to shed light on that issue and thereby address a major unmet need for better treatments for ADHF. Even though this condition accounts for more than 1 million hospitalizations annually in the United States, short-term rehospitalization and mortality rates in affected patients remain unacceptably high at 21% and 12%, respectively. And the standard-of-care treatment – decongestion with intravenous diuretics and hemodynamic support with inotropes and vasodilators – hasn’t changed in nearly half a century, Dr. Velazquez noted.
The trial included 881 patients hospitalized for acute decompensated HFrEF at 129 U.S. centers. The study population was diverse: 36% of participants were black and one-third of subjects had no diagnosis of heart failure prior to their hospitalization. After achieving hemodynamic stabilization, patients were randomized to receive sacubitril/valsartan or enalapril.
Key outcomes
The primary endpoint was change in N-terminal of the prohormone brain natriuretic peptide concentration from baseline to week 8. There was a 25% reduction in the enalapril group and a 45% reduction with sacubitril/valsartan. This translated to a highly significant 29% greater relative risk reduction with sacubitril/valsartan.
More eye opening was the between-group difference in the prespecified composite clinical endpoint comprising death, rehospitalization for heart failure, implantation of a left ventricular assist device, or listing for heart transplant during the 8-week study.
The rate was 16.8% in the enalapril group and 9.3% with sacubitril/valsartan. This worked out to a 46% relative risk reduction, with a number needed to treat of 13.
The composite result was driven by a 44% reduction in risk of heart failure rehospitalization in the sacubitril/valsartan group: 8.0% versus 13.8%. The sacubitril/valsartan group also had a numerically lower mortality rate: 2.3% versus 3.4%, although the number of fatalities was small and this 34% relative risk reduction didn’t achieve statistical significance.
Rates of the key safety outcomes – symptomatic hypotension, worsening renal function, hyperkalemia, and angioedema – didn’t differ between the two study arms. Of interest, however, all six cases of angioedema in the enalapril group occurred in black patients, while the only case in the sacubitril/valsartan group was in a white patient.
PIONEER-HF treatment strategy
Hemodynamic stabilization as a prelude to randomization to sacubitril/valsartan or enalapril required maintaining a systolic blood pressure of at least 100 mm Hg in the previous 6 hours, with no symptomatic hypotension, intensification of intravenous diuretics, or use of intravenous vasodilators during that time period, and no intravenous inotropes in the previous 24 hours.
Enalapril was titrated to a target dose of 10 mg twice daily. Sacubitril/valsartan was titrated to a target dose of 97/103 mg twice daily. Titration was carried out using an algorithm based upon systolic BP. If the SBP was at least 100 and less than 120 mm Hg at baseline, sacubitril/valsartan was initiated at 24/26 mg twice daily, enalapril at 2.5 mg b.i.d. If the SBP at randomization was 120 mm Hg or higher, the initial dosing was sacubitril/valsartan at 49/51 mm Hg b.i.d. or enalapril at 5 mg b.i.d. Up-titration occurred after 1 week, then biweekly through week 8.
PIONEER in perspective
Discussant Larry A. Allen, MD, a heart failure specialist at the University of Colorado at Denver, Aurora, predicted that this will be a practice-changing study.
“There has been a need for a study like PIONEER in heart failure,” he observed. While multiple randomized trials have advanced the treatment of ambulatory HFrEF patients, demonstrating benefit for initiation and intensification of treatment with ACE inhibitors, angiotensin II receptor blockers, beta-blockers, and mineralocorticoid receptor antagonists, the treatment of patients with ADHF has remained relatively static, marked by failed trials of once-promising novel agents including tolvaptan, nesiritide, and serelaxin.
“All the data is in ambulatory patients, but the action for the care of heart failure patients actually occurs largely in the hospital. Seventy percent of care provided in the U.S. to patients with heart failure occurs in the hospital setting. These patients are a captive audience at that time, and the transitions from inpatient to outpatient care are fragile,” Dr. Allen said.
He noted that the use of sacubitril/valsartan in routine practice as reflected in national registries has been “extremely low” – less than 15% among eligible patients – despite the drug having been approved more than 3 years ago. One major reason for the low uptake, in his view, is clinical inertia. That should melt away in what he termed “the post-PIONEER world.”
“I think one of the great things about this study is it keeps it simple. We now have a simpler algorithm for inpatient and subsequent outpatient management of heart failure with reduced ejection fraction. It’s easier for us to start with the treatment we want patients to be on, and it’s better for patients, too. Most importantly, this study reinforces the importance and safety of aggressive guideline-directed medical therapy starting from the beginning in most patients,” Dr. Allen said.
The study findings were published simultaneously in the New England Journal of Medicine (2018 Nov 11. doi: 10.1056/NEJMoa1812851).
PIONEER-HF was sponsored by Novartis. Dr. Velazquez reported receiving research grants from and serving as a consultant to that company and others. Dr. Allen reported having no financial conflicts.
CHICAGO – Initiation of angiotensin-neprilysin inhibition using sacubitril/valsartan during hospitalization for acute decompensated heart failure, instead of relying upon enalapril, resulted in a substantially greater reduction in N-terminal of the prohormone brain natriuretic peptide concentration and a markedly lower rate of rehospitalization with no safety downside in the PIONEER-HF trial, Eric J. Velazquez, MD, reported at the American Heart Association scientific sessions.
“We believe these results have clinical implications that support the in-hospital initiation of sacubitril/valsartan in stabilized patients with acute decompensated heart failure and reduced ejection fraction irrespective of prior ACE inhibitor or ARB [angiotensin II receptor blocker] use or prior diagnosis of heart failure,” said Dr. Velazquez, a professor of medicine and chief of the section of cardiovascular medicine at Yale University, New Haven, Conn., and physician in chief of the Heart and Vascular Center for the Yale-New Haven Health System.
Sacubitril/valsartan (Entresto) has a class I indication for treatment of symptomatic heart failure with reduced ejection fraction (HFrEF) in the AHA/American College of Cardiology guidelines. This strong recommendation is based largely upon the impressive results of the PARADIGM-HF trial, which in ambulatory outpatients demonstrated a lower risk of cardiovascular mortality or hospitalization for heart failure than enalapril (N Engl J Med. 2014 Sep 11;371[11]:993-1004).
However, since patients with acute decompensated heart failure (ADHF) were excluded from PARADIGM-HF, the safety and effectiveness of starting such patients on the drug while hospitalized for acute decompensation was unknown.
PIONEER-HF was carried out to shed light on that issue and thereby address a major unmet need for better treatments for ADHF. Even though this condition accounts for more than 1 million hospitalizations annually in the United States, short-term rehospitalization and mortality rates in affected patients remain unacceptably high at 21% and 12%, respectively. And the standard-of-care treatment – decongestion with intravenous diuretics and hemodynamic support with inotropes and vasodilators – hasn’t changed in nearly half a century, Dr. Velazquez noted.
The trial included 881 patients hospitalized for acute decompensated HFrEF at 129 U.S. centers. The study population was diverse: 36% of participants were black and one-third of subjects had no diagnosis of heart failure prior to their hospitalization. After achieving hemodynamic stabilization, patients were randomized to receive sacubitril/valsartan or enalapril.
Key outcomes
The primary endpoint was change in N-terminal of the prohormone brain natriuretic peptide concentration from baseline to week 8. There was a 25% reduction in the enalapril group and a 45% reduction with sacubitril/valsartan. This translated to a highly significant 29% greater relative risk reduction with sacubitril/valsartan.
More eye opening was the between-group difference in the prespecified composite clinical endpoint comprising death, rehospitalization for heart failure, implantation of a left ventricular assist device, or listing for heart transplant during the 8-week study.
The rate was 16.8% in the enalapril group and 9.3% with sacubitril/valsartan. This worked out to a 46% relative risk reduction, with a number needed to treat of 13.
The composite result was driven by a 44% reduction in risk of heart failure rehospitalization in the sacubitril/valsartan group: 8.0% versus 13.8%. The sacubitril/valsartan group also had a numerically lower mortality rate: 2.3% versus 3.4%, although the number of fatalities was small and this 34% relative risk reduction didn’t achieve statistical significance.
Rates of the key safety outcomes – symptomatic hypotension, worsening renal function, hyperkalemia, and angioedema – didn’t differ between the two study arms. Of interest, however, all six cases of angioedema in the enalapril group occurred in black patients, while the only case in the sacubitril/valsartan group was in a white patient.
PIONEER-HF treatment strategy
Hemodynamic stabilization as a prelude to randomization to sacubitril/valsartan or enalapril required maintaining a systolic blood pressure of at least 100 mm Hg in the previous 6 hours, with no symptomatic hypotension, intensification of intravenous diuretics, or use of intravenous vasodilators during that time period, and no intravenous inotropes in the previous 24 hours.
Enalapril was titrated to a target dose of 10 mg twice daily. Sacubitril/valsartan was titrated to a target dose of 97/103 mg twice daily. Titration was carried out using an algorithm based upon systolic BP. If the SBP was at least 100 and less than 120 mm Hg at baseline, sacubitril/valsartan was initiated at 24/26 mg twice daily, enalapril at 2.5 mg b.i.d. If the SBP at randomization was 120 mm Hg or higher, the initial dosing was sacubitril/valsartan at 49/51 mm Hg b.i.d. or enalapril at 5 mg b.i.d. Up-titration occurred after 1 week, then biweekly through week 8.
PIONEER in perspective
Discussant Larry A. Allen, MD, a heart failure specialist at the University of Colorado at Denver, Aurora, predicted that this will be a practice-changing study.
“There has been a need for a study like PIONEER in heart failure,” he observed. While multiple randomized trials have advanced the treatment of ambulatory HFrEF patients, demonstrating benefit for initiation and intensification of treatment with ACE inhibitors, angiotensin II receptor blockers, beta-blockers, and mineralocorticoid receptor antagonists, the treatment of patients with ADHF has remained relatively static, marked by failed trials of once-promising novel agents including tolvaptan, nesiritide, and serelaxin.
“All the data is in ambulatory patients, but the action for the care of heart failure patients actually occurs largely in the hospital. Seventy percent of care provided in the U.S. to patients with heart failure occurs in the hospital setting. These patients are a captive audience at that time, and the transitions from inpatient to outpatient care are fragile,” Dr. Allen said.
He noted that the use of sacubitril/valsartan in routine practice as reflected in national registries has been “extremely low” – less than 15% among eligible patients – despite the drug having been approved more than 3 years ago. One major reason for the low uptake, in his view, is clinical inertia. That should melt away in what he termed “the post-PIONEER world.”
“I think one of the great things about this study is it keeps it simple. We now have a simpler algorithm for inpatient and subsequent outpatient management of heart failure with reduced ejection fraction. It’s easier for us to start with the treatment we want patients to be on, and it’s better for patients, too. Most importantly, this study reinforces the importance and safety of aggressive guideline-directed medical therapy starting from the beginning in most patients,” Dr. Allen said.
The study findings were published simultaneously in the New England Journal of Medicine (2018 Nov 11. doi: 10.1056/NEJMoa1812851).
PIONEER-HF was sponsored by Novartis. Dr. Velazquez reported receiving research grants from and serving as a consultant to that company and others. Dr. Allen reported having no financial conflicts.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: The rate of rehospitalization for heart failure during the next 2 months after initiation of sacubitril/valsartan during hospitalization for acute decompensated heart failure was 44% lower than with enalapril.
Study details: A randomized, multicenter trial involving 881 patients hospitalized for acute decompensated heart failure.
Disclosures: The PIONEER-HF trial was sponsored by Novartis. The presenter reported receiving research grants from and serving as a consultant to that company and others.
‘Organoid technology’ poised to transform cancer care
BOSTON– Imagine being able to .
The implications are nearly endless. To start, chemotherapy and radiation options could be screened in vitro, much like culture and sensitivity testing of bacteria, to find a patient’s best option. Tumor cultures could be banked for mass screening of new cytotoxic candidates.
It’s already beginning to happen in a few research labs around the world, and it might foretell a breakthrough in cancer treatment.
After decades of failure, the trick to growing tumor cells in culture has finally been figured out. When stem cells are fished out of healthy tissue – from the crypts of the gastrointestinal lining, for instance – and put into a three-dimensional matrix culture with growth factors, they grow into little replications of the organs they came from, called “organoids;” when stem cells are pulled from cancers, they replicate the primary tumor, growing into “tumoroids” ready to be tested against cytotoxic drugs and radiation.
Philip B. Paty, MD, FACS, a colorectal surgeon and organoid researcher at Memorial Sloan Kettering Cancer Center, New York, said he is certain that the person who led the team that figured out the right culture condition – Hans Clevers, MD, PhD, a molecular genetics professor at the University of Utrecht (the Netherlands) – is destined for a Nobel Prize.
Dr. Paty took a few minutes at the annual clinical congress of the American College of Surgeons to explain in an interview why, and what ‘organoid technology’ will likely mean for cancer treatment in a few years.
“The ability to grow and sustain cancer means that we now can start doing real science on human tissues. We could never do this before. We’ve been treating cancer without being able to grow tumors and study them.” The breakthrough opens the door to “clinical trials in a dish,” and will likely take personalized cancer treatment to a new level, he said.
“It remains to be proven that “organoid technology “can change outcomes for patients, but those studies are likely coming,” said Dr. Paty, who investigates tumoroid response to radiation in his own lab work.
BOSTON– Imagine being able to .
The implications are nearly endless. To start, chemotherapy and radiation options could be screened in vitro, much like culture and sensitivity testing of bacteria, to find a patient’s best option. Tumor cultures could be banked for mass screening of new cytotoxic candidates.
It’s already beginning to happen in a few research labs around the world, and it might foretell a breakthrough in cancer treatment.
After decades of failure, the trick to growing tumor cells in culture has finally been figured out. When stem cells are fished out of healthy tissue – from the crypts of the gastrointestinal lining, for instance – and put into a three-dimensional matrix culture with growth factors, they grow into little replications of the organs they came from, called “organoids;” when stem cells are pulled from cancers, they replicate the primary tumor, growing into “tumoroids” ready to be tested against cytotoxic drugs and radiation.
Philip B. Paty, MD, FACS, a colorectal surgeon and organoid researcher at Memorial Sloan Kettering Cancer Center, New York, said he is certain that the person who led the team that figured out the right culture condition – Hans Clevers, MD, PhD, a molecular genetics professor at the University of Utrecht (the Netherlands) – is destined for a Nobel Prize.
Dr. Paty took a few minutes at the annual clinical congress of the American College of Surgeons to explain in an interview why, and what ‘organoid technology’ will likely mean for cancer treatment in a few years.
“The ability to grow and sustain cancer means that we now can start doing real science on human tissues. We could never do this before. We’ve been treating cancer without being able to grow tumors and study them.” The breakthrough opens the door to “clinical trials in a dish,” and will likely take personalized cancer treatment to a new level, he said.
“It remains to be proven that “organoid technology “can change outcomes for patients, but those studies are likely coming,” said Dr. Paty, who investigates tumoroid response to radiation in his own lab work.
BOSTON– Imagine being able to .
The implications are nearly endless. To start, chemotherapy and radiation options could be screened in vitro, much like culture and sensitivity testing of bacteria, to find a patient’s best option. Tumor cultures could be banked for mass screening of new cytotoxic candidates.
It’s already beginning to happen in a few research labs around the world, and it might foretell a breakthrough in cancer treatment.
After decades of failure, the trick to growing tumor cells in culture has finally been figured out. When stem cells are fished out of healthy tissue – from the crypts of the gastrointestinal lining, for instance – and put into a three-dimensional matrix culture with growth factors, they grow into little replications of the organs they came from, called “organoids;” when stem cells are pulled from cancers, they replicate the primary tumor, growing into “tumoroids” ready to be tested against cytotoxic drugs and radiation.
Philip B. Paty, MD, FACS, a colorectal surgeon and organoid researcher at Memorial Sloan Kettering Cancer Center, New York, said he is certain that the person who led the team that figured out the right culture condition – Hans Clevers, MD, PhD, a molecular genetics professor at the University of Utrecht (the Netherlands) – is destined for a Nobel Prize.
Dr. Paty took a few minutes at the annual clinical congress of the American College of Surgeons to explain in an interview why, and what ‘organoid technology’ will likely mean for cancer treatment in a few years.
“The ability to grow and sustain cancer means that we now can start doing real science on human tissues. We could never do this before. We’ve been treating cancer without being able to grow tumors and study them.” The breakthrough opens the door to “clinical trials in a dish,” and will likely take personalized cancer treatment to a new level, he said.
“It remains to be proven that “organoid technology “can change outcomes for patients, but those studies are likely coming,” said Dr. Paty, who investigates tumoroid response to radiation in his own lab work.
REPORTING FROM THE ACS CLINICAL CONGRESS
MIS for cervical cancer: Is it not for anyone or not for everyone?
Shock waves moved through the gynecologic oncology world on Oct. 31, 2018, when the New England Journal of Medicine published two papers on survival outcomes for women undergoing surgery for early stage cervical cancer.
The first was a randomized controlled trial of laparotomy and minimally invasive surgery (MIS) for radical hysterectomy called the LACC trial.1 In the multicenter, international trial of 631 women, the primary objective was disease-specific survival (cervical cancer–related deaths) and was powered to detect noninferiority of the MIS approach when compared with laparotomy. The trial was closed early when investigators noted a lower than expected rate of 3-year, disease-free survival (91% vs. 97%) from cervical cancer in the MIS group, which was made up of 84% laparoscopic and 16% robotic approaches, versus laparotomy. There were 19 deaths in the MIS group observed versus three in the laparotomy group. The conclusions of the trial were that MIS surgery is associated with inferior cervical cancer survival.
In the second study, authors analyzed data from large U.S. databases – the National Cancer Database (NCDB) and the Surveillance, Epidemiology, and End Results (SEER) Program – to collect all-cause mortality for patients with early-stage cervical cancer who had undergone radical hysterectomy during 2010-2013.2 Among 2,461 observed results, 1,225 had undergone MIS surgery with the majority (79.8%) via robotic-assistance. Women undergoing MIS approaches had smaller, lower grade tumors; were more likely to be white, privately insured, and of a higher income; and had surgery later in the cohort and by nonacademic centers. The researchers adjusted for risk factors with an analytic process called propensity-score weighting, which matched the groups more closely in an attempt to minimize confounders. They identified higher all-cause mortality among women who were treated with an MIS approach, compared with those treated with laparotomy (hazard ratio, 1.65). They also observed a significant decline in the survival from cervical cancer annually that corresponded to the uptake of MIS radical hysterectomies.
In the wake of these publications, many concluded that gynecologic oncologists should no longer offer a minimally invasive approach for radical hysterectomy. Certainly level I evidence published in a highly influential journal is compelling, and the consistency in findings over two studies adds further weight to the results. However, was this the correct conclusion to draw from these results? Surgeons who had been performing MIS radical hysterectomies for many years with favorable outcomes are challenging this and are raising questions about external generalizability and whether these findings were driven by the surgery itself or by the surgeon.
The studies’ authors proposed hypotheses for their results that implicate the surgical route rather than the surgeon; however, these seem ad hoc and not well supported by data, including the authors’ own data. The first was the hypothesis that cervical tumors were being disrupted and disseminated through the use of uterine manipulators in MIS approaches. However, cervical cancers are fairly routinely “disrupted” by preoperative cone biopsies, loop electrosurgical excision procedures (LEEP), and sharp biopsies, which are arguably more invasive than placement of a manipulator. Uterine manipulators routinely are used in endometrial cancer surgeries, in which the manipulator is embedded within the tumor, without an associated negative survival effect in randomized trials.3 Additionally, not all surgeons utilize manipulators for radical hysterectomies, and these studies did not measure or report on their use; therefore, it is impossible to know whether, and by what magnitude, manipulators played a role. Finally, if uterine manipulators are the explanation for inferior survival, surely the recommendation should be to discourage their use, rather than abandon the MIS approach all together.
The other explanation offered was exposure of the tumor to CO2 gas. This seems an even less plausible explanation because CO2 gas is routinely used in MIS cancer surgeries for endometrial, prostate, gastric, and colorectal surgeries and is used as insufflation for malignant interventional endoscopies without a significant deleterious effect. Additionally, the cervix is not exposed to CO2 until colpotomy at the procedure’s end – and only briefly. The in vitro studies implicating a negative effect of simulated CO2 pneumoperitoneum are neither compelling nor consistent.4,5
I would like to propose another hypothesis for the results: surgical proficiency. Surgery, unlike medical interventions, is not a simple variable that is dichotomous – performed or not. Surgeons do not randomly select operative approaches for patients. We select surgical approaches based on patients’ circumstances and surgeon factors, including our own mastery of the various techniques. and any surgeon recognizes this if he or she has observed more than one surgeon or has attempted a procedure via different routes. While some procedures, such as extrafascial hysterectomy for endometrial cancer, are relatively straightforward and surgeon capabilities are more equitable across different approaches, cervical cancer surgery is quite different.
Early-stage cervical cancer primarily exerts radial growth into the cervical stroma and parametria. Curative surgical excision requires broadly negative margins through this tissue, a so called “radical hysterectomy.” The radicality of hysterectomy has been categorized in stages, acknowledging that different sized lesions require different volumes of parametrial resection to achieve adequate clearance from the tumor.6 In doing so, the surgeon must skeletonize and mobilize the distal ureters, cardinal ligament webs, and uterosacral ligaments. These structures are in close proximity to major vascular and neural structures. Hence, the radical hysterectomy is, without dispute, a technically challenging procedure.
Minimally invasive surgery further handicaps the surgeon by eliminating manual contact with tissue, and relying on complex instrumentation, electrosurgical modalities, and loss of haptics. The learning curve for MIS radical hysterectomy is further attenuated by their relative infrequency. Therefore, it makes sense that, when the MIS approach is randomly assigned to surgeons (such as in the LACC trial) or broadly and independently applied (as in the retrospective series), one might see variations in skill, quality, and outcomes, including oncologic outcomes.
The retrospective study by Melamed et al. acknowledged that surgeon skill and volume may contribute to their findings but stated that, because of the nature of their source data, they were unable to explain why they observed their results. The LACC trial attempted to overcome the issue of surgeon skill by ensuring all surgeons were from high-volume sites and had videos reviewed of their cases. However, the videos were chosen by the surgeons themselves and not available for audit in the study’s supplemental material. The LACC trial was conducted over a 9-year period across 33 sites and enrolled a total of 631 subjects. This equates to an enrollment of approximately two patients per site per year and either reflects extremely low-volume sites or highly selective patient enrollment. If the latter, what was different about the unenrolled patients and what was the preferred chosen route of surgery for them?
All 34 recurrences occurred in patients from just 14 of the 33 sites in the LACC trial. That means that less than half of the sites contributed to all of the recurrences. The authors provided no details on the specific sites, surgeons, or accrual rates in their manuscript or supplemental materials. Therefore, readers are unable to know what was different about those sites; whether they contributed the most patients and, therefore, the most recurrences; or whether they were low-volume sites with lower quality.
While margin status, positive or negative, was reported, there was no data captured regarding volume of resected parametrial tissue, or relative distance from tumor to margin, both of which might provide the reader with a better appraisal of surgeon proficiency and consistency in radicality of the two approaches. The incidence of locoregional (pelvic) recurrences were higher in the MIS arm, which is expected if there were inadequate margins around the laparoscopically resected tumors.
Finally, the authors of the LACC trial observed equivalent rates of postoperative complications between the laparotomy and MIS groups. The main virtue for MIS approaches is the reduction in perioperative morbidity. To observe no perioperative morbidity benefit in the MIS group is a red flag suggesting that these surgeons may not have achieved proficiency with the MIS approach.
Despite these arguments, the results of these studies should be taken seriously. Clearly, it is apparent that preservation of oncologic outcomes is not guaranteed with MIS radical hysterectomy, and it should not be the chosen approach for all patients and all surgeons. However, rather than entirely abandoning this less morbid approach, I would argue that it is a call to arms for gynecologic oncologists to self-evaluate. We should know our own data with respect to case volumes, perioperative complications, and cancer-related recurrence and death.
Perhaps MIS radical hysterectomies should be consolidated among high-volume surgeons with demonstrated good outcomes? Just as has been done for rectal cancer surgery with positive effect, we should establish accredited centers of excellence.7 We also need to improve the training of surgeons in novel, difficult techniques, as well as enhance the sophistication of MIS equipment such as improved instrumentation, haptics, and vision-guided surgery (for example, real-time intraoperative assessment of the tumor margins).
Let’s not take a wholesale step backwards to the surgical approaches of a 100 years ago just because they are more straightforward. Let’s do a better job of advancing the quality of what we do for our patients in the future.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She said she had no conflicts of interest. Email Dr. Rossi at [email protected].
References
1. N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1806395.
2. N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1804923.
3. J Clin Oncol. 2012 Mar 1;30(7):695-700.
4. Med Sci Monit. 2014 Dec 1;20:2497-503.
5. Surg Endosc. 2006 Oct;20(10):1556-9.
6. Gynecol Oncol. 2011 Aug;122(2):264-8.
7. Surgery. 2016 Mar;159(3):736-48.
Shock waves moved through the gynecologic oncology world on Oct. 31, 2018, when the New England Journal of Medicine published two papers on survival outcomes for women undergoing surgery for early stage cervical cancer.
The first was a randomized controlled trial of laparotomy and minimally invasive surgery (MIS) for radical hysterectomy called the LACC trial.1 In the multicenter, international trial of 631 women, the primary objective was disease-specific survival (cervical cancer–related deaths) and was powered to detect noninferiority of the MIS approach when compared with laparotomy. The trial was closed early when investigators noted a lower than expected rate of 3-year, disease-free survival (91% vs. 97%) from cervical cancer in the MIS group, which was made up of 84% laparoscopic and 16% robotic approaches, versus laparotomy. There were 19 deaths in the MIS group observed versus three in the laparotomy group. The conclusions of the trial were that MIS surgery is associated with inferior cervical cancer survival.
In the second study, authors analyzed data from large U.S. databases – the National Cancer Database (NCDB) and the Surveillance, Epidemiology, and End Results (SEER) Program – to collect all-cause mortality for patients with early-stage cervical cancer who had undergone radical hysterectomy during 2010-2013.2 Among 2,461 observed results, 1,225 had undergone MIS surgery with the majority (79.8%) via robotic-assistance. Women undergoing MIS approaches had smaller, lower grade tumors; were more likely to be white, privately insured, and of a higher income; and had surgery later in the cohort and by nonacademic centers. The researchers adjusted for risk factors with an analytic process called propensity-score weighting, which matched the groups more closely in an attempt to minimize confounders. They identified higher all-cause mortality among women who were treated with an MIS approach, compared with those treated with laparotomy (hazard ratio, 1.65). They also observed a significant decline in the survival from cervical cancer annually that corresponded to the uptake of MIS radical hysterectomies.
In the wake of these publications, many concluded that gynecologic oncologists should no longer offer a minimally invasive approach for radical hysterectomy. Certainly level I evidence published in a highly influential journal is compelling, and the consistency in findings over two studies adds further weight to the results. However, was this the correct conclusion to draw from these results? Surgeons who had been performing MIS radical hysterectomies for many years with favorable outcomes are challenging this and are raising questions about external generalizability and whether these findings were driven by the surgery itself or by the surgeon.
The studies’ authors proposed hypotheses for their results that implicate the surgical route rather than the surgeon; however, these seem ad hoc and not well supported by data, including the authors’ own data. The first was the hypothesis that cervical tumors were being disrupted and disseminated through the use of uterine manipulators in MIS approaches. However, cervical cancers are fairly routinely “disrupted” by preoperative cone biopsies, loop electrosurgical excision procedures (LEEP), and sharp biopsies, which are arguably more invasive than placement of a manipulator. Uterine manipulators routinely are used in endometrial cancer surgeries, in which the manipulator is embedded within the tumor, without an associated negative survival effect in randomized trials.3 Additionally, not all surgeons utilize manipulators for radical hysterectomies, and these studies did not measure or report on their use; therefore, it is impossible to know whether, and by what magnitude, manipulators played a role. Finally, if uterine manipulators are the explanation for inferior survival, surely the recommendation should be to discourage their use, rather than abandon the MIS approach all together.
The other explanation offered was exposure of the tumor to CO2 gas. This seems an even less plausible explanation because CO2 gas is routinely used in MIS cancer surgeries for endometrial, prostate, gastric, and colorectal surgeries and is used as insufflation for malignant interventional endoscopies without a significant deleterious effect. Additionally, the cervix is not exposed to CO2 until colpotomy at the procedure’s end – and only briefly. The in vitro studies implicating a negative effect of simulated CO2 pneumoperitoneum are neither compelling nor consistent.4,5
I would like to propose another hypothesis for the results: surgical proficiency. Surgery, unlike medical interventions, is not a simple variable that is dichotomous – performed or not. Surgeons do not randomly select operative approaches for patients. We select surgical approaches based on patients’ circumstances and surgeon factors, including our own mastery of the various techniques. and any surgeon recognizes this if he or she has observed more than one surgeon or has attempted a procedure via different routes. While some procedures, such as extrafascial hysterectomy for endometrial cancer, are relatively straightforward and surgeon capabilities are more equitable across different approaches, cervical cancer surgery is quite different.
Early-stage cervical cancer primarily exerts radial growth into the cervical stroma and parametria. Curative surgical excision requires broadly negative margins through this tissue, a so called “radical hysterectomy.” The radicality of hysterectomy has been categorized in stages, acknowledging that different sized lesions require different volumes of parametrial resection to achieve adequate clearance from the tumor.6 In doing so, the surgeon must skeletonize and mobilize the distal ureters, cardinal ligament webs, and uterosacral ligaments. These structures are in close proximity to major vascular and neural structures. Hence, the radical hysterectomy is, without dispute, a technically challenging procedure.
Minimally invasive surgery further handicaps the surgeon by eliminating manual contact with tissue, and relying on complex instrumentation, electrosurgical modalities, and loss of haptics. The learning curve for MIS radical hysterectomy is further attenuated by their relative infrequency. Therefore, it makes sense that, when the MIS approach is randomly assigned to surgeons (such as in the LACC trial) or broadly and independently applied (as in the retrospective series), one might see variations in skill, quality, and outcomes, including oncologic outcomes.
The retrospective study by Melamed et al. acknowledged that surgeon skill and volume may contribute to their findings but stated that, because of the nature of their source data, they were unable to explain why they observed their results. The LACC trial attempted to overcome the issue of surgeon skill by ensuring all surgeons were from high-volume sites and had videos reviewed of their cases. However, the videos were chosen by the surgeons themselves and not available for audit in the study’s supplemental material. The LACC trial was conducted over a 9-year period across 33 sites and enrolled a total of 631 subjects. This equates to an enrollment of approximately two patients per site per year and either reflects extremely low-volume sites or highly selective patient enrollment. If the latter, what was different about the unenrolled patients and what was the preferred chosen route of surgery for them?
All 34 recurrences occurred in patients from just 14 of the 33 sites in the LACC trial. That means that less than half of the sites contributed to all of the recurrences. The authors provided no details on the specific sites, surgeons, or accrual rates in their manuscript or supplemental materials. Therefore, readers are unable to know what was different about those sites; whether they contributed the most patients and, therefore, the most recurrences; or whether they were low-volume sites with lower quality.
While margin status, positive or negative, was reported, there was no data captured regarding volume of resected parametrial tissue, or relative distance from tumor to margin, both of which might provide the reader with a better appraisal of surgeon proficiency and consistency in radicality of the two approaches. The incidence of locoregional (pelvic) recurrences were higher in the MIS arm, which is expected if there were inadequate margins around the laparoscopically resected tumors.
Finally, the authors of the LACC trial observed equivalent rates of postoperative complications between the laparotomy and MIS groups. The main virtue for MIS approaches is the reduction in perioperative morbidity. To observe no perioperative morbidity benefit in the MIS group is a red flag suggesting that these surgeons may not have achieved proficiency with the MIS approach.
Despite these arguments, the results of these studies should be taken seriously. Clearly, it is apparent that preservation of oncologic outcomes is not guaranteed with MIS radical hysterectomy, and it should not be the chosen approach for all patients and all surgeons. However, rather than entirely abandoning this less morbid approach, I would argue that it is a call to arms for gynecologic oncologists to self-evaluate. We should know our own data with respect to case volumes, perioperative complications, and cancer-related recurrence and death.
Perhaps MIS radical hysterectomies should be consolidated among high-volume surgeons with demonstrated good outcomes? Just as has been done for rectal cancer surgery with positive effect, we should establish accredited centers of excellence.7 We also need to improve the training of surgeons in novel, difficult techniques, as well as enhance the sophistication of MIS equipment such as improved instrumentation, haptics, and vision-guided surgery (for example, real-time intraoperative assessment of the tumor margins).
Let’s not take a wholesale step backwards to the surgical approaches of a 100 years ago just because they are more straightforward. Let’s do a better job of advancing the quality of what we do for our patients in the future.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She said she had no conflicts of interest. Email Dr. Rossi at [email protected].
References
1. N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1806395.
2. N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1804923.
3. J Clin Oncol. 2012 Mar 1;30(7):695-700.
4. Med Sci Monit. 2014 Dec 1;20:2497-503.
5. Surg Endosc. 2006 Oct;20(10):1556-9.
6. Gynecol Oncol. 2011 Aug;122(2):264-8.
7. Surgery. 2016 Mar;159(3):736-48.
Shock waves moved through the gynecologic oncology world on Oct. 31, 2018, when the New England Journal of Medicine published two papers on survival outcomes for women undergoing surgery for early stage cervical cancer.
The first was a randomized controlled trial of laparotomy and minimally invasive surgery (MIS) for radical hysterectomy called the LACC trial.1 In the multicenter, international trial of 631 women, the primary objective was disease-specific survival (cervical cancer–related deaths) and was powered to detect noninferiority of the MIS approach when compared with laparotomy. The trial was closed early when investigators noted a lower than expected rate of 3-year, disease-free survival (91% vs. 97%) from cervical cancer in the MIS group, which was made up of 84% laparoscopic and 16% robotic approaches, versus laparotomy. There were 19 deaths in the MIS group observed versus three in the laparotomy group. The conclusions of the trial were that MIS surgery is associated with inferior cervical cancer survival.
In the second study, authors analyzed data from large U.S. databases – the National Cancer Database (NCDB) and the Surveillance, Epidemiology, and End Results (SEER) Program – to collect all-cause mortality for patients with early-stage cervical cancer who had undergone radical hysterectomy during 2010-2013.2 Among 2,461 observed results, 1,225 had undergone MIS surgery with the majority (79.8%) via robotic-assistance. Women undergoing MIS approaches had smaller, lower grade tumors; were more likely to be white, privately insured, and of a higher income; and had surgery later in the cohort and by nonacademic centers. The researchers adjusted for risk factors with an analytic process called propensity-score weighting, which matched the groups more closely in an attempt to minimize confounders. They identified higher all-cause mortality among women who were treated with an MIS approach, compared with those treated with laparotomy (hazard ratio, 1.65). They also observed a significant decline in the survival from cervical cancer annually that corresponded to the uptake of MIS radical hysterectomies.
In the wake of these publications, many concluded that gynecologic oncologists should no longer offer a minimally invasive approach for radical hysterectomy. Certainly level I evidence published in a highly influential journal is compelling, and the consistency in findings over two studies adds further weight to the results. However, was this the correct conclusion to draw from these results? Surgeons who had been performing MIS radical hysterectomies for many years with favorable outcomes are challenging this and are raising questions about external generalizability and whether these findings were driven by the surgery itself or by the surgeon.
The studies’ authors proposed hypotheses for their results that implicate the surgical route rather than the surgeon; however, these seem ad hoc and not well supported by data, including the authors’ own data. The first was the hypothesis that cervical tumors were being disrupted and disseminated through the use of uterine manipulators in MIS approaches. However, cervical cancers are fairly routinely “disrupted” by preoperative cone biopsies, loop electrosurgical excision procedures (LEEP), and sharp biopsies, which are arguably more invasive than placement of a manipulator. Uterine manipulators routinely are used in endometrial cancer surgeries, in which the manipulator is embedded within the tumor, without an associated negative survival effect in randomized trials.3 Additionally, not all surgeons utilize manipulators for radical hysterectomies, and these studies did not measure or report on their use; therefore, it is impossible to know whether, and by what magnitude, manipulators played a role. Finally, if uterine manipulators are the explanation for inferior survival, surely the recommendation should be to discourage their use, rather than abandon the MIS approach all together.
The other explanation offered was exposure of the tumor to CO2 gas. This seems an even less plausible explanation because CO2 gas is routinely used in MIS cancer surgeries for endometrial, prostate, gastric, and colorectal surgeries and is used as insufflation for malignant interventional endoscopies without a significant deleterious effect. Additionally, the cervix is not exposed to CO2 until colpotomy at the procedure’s end – and only briefly. The in vitro studies implicating a negative effect of simulated CO2 pneumoperitoneum are neither compelling nor consistent.4,5
I would like to propose another hypothesis for the results: surgical proficiency. Surgery, unlike medical interventions, is not a simple variable that is dichotomous – performed or not. Surgeons do not randomly select operative approaches for patients. We select surgical approaches based on patients’ circumstances and surgeon factors, including our own mastery of the various techniques. and any surgeon recognizes this if he or she has observed more than one surgeon or has attempted a procedure via different routes. While some procedures, such as extrafascial hysterectomy for endometrial cancer, are relatively straightforward and surgeon capabilities are more equitable across different approaches, cervical cancer surgery is quite different.
Early-stage cervical cancer primarily exerts radial growth into the cervical stroma and parametria. Curative surgical excision requires broadly negative margins through this tissue, a so called “radical hysterectomy.” The radicality of hysterectomy has been categorized in stages, acknowledging that different sized lesions require different volumes of parametrial resection to achieve adequate clearance from the tumor.6 In doing so, the surgeon must skeletonize and mobilize the distal ureters, cardinal ligament webs, and uterosacral ligaments. These structures are in close proximity to major vascular and neural structures. Hence, the radical hysterectomy is, without dispute, a technically challenging procedure.
Minimally invasive surgery further handicaps the surgeon by eliminating manual contact with tissue, and relying on complex instrumentation, electrosurgical modalities, and loss of haptics. The learning curve for MIS radical hysterectomy is further attenuated by their relative infrequency. Therefore, it makes sense that, when the MIS approach is randomly assigned to surgeons (such as in the LACC trial) or broadly and independently applied (as in the retrospective series), one might see variations in skill, quality, and outcomes, including oncologic outcomes.
The retrospective study by Melamed et al. acknowledged that surgeon skill and volume may contribute to their findings but stated that, because of the nature of their source data, they were unable to explain why they observed their results. The LACC trial attempted to overcome the issue of surgeon skill by ensuring all surgeons were from high-volume sites and had videos reviewed of their cases. However, the videos were chosen by the surgeons themselves and not available for audit in the study’s supplemental material. The LACC trial was conducted over a 9-year period across 33 sites and enrolled a total of 631 subjects. This equates to an enrollment of approximately two patients per site per year and either reflects extremely low-volume sites or highly selective patient enrollment. If the latter, what was different about the unenrolled patients and what was the preferred chosen route of surgery for them?
All 34 recurrences occurred in patients from just 14 of the 33 sites in the LACC trial. That means that less than half of the sites contributed to all of the recurrences. The authors provided no details on the specific sites, surgeons, or accrual rates in their manuscript or supplemental materials. Therefore, readers are unable to know what was different about those sites; whether they contributed the most patients and, therefore, the most recurrences; or whether they were low-volume sites with lower quality.
While margin status, positive or negative, was reported, there was no data captured regarding volume of resected parametrial tissue, or relative distance from tumor to margin, both of which might provide the reader with a better appraisal of surgeon proficiency and consistency in radicality of the two approaches. The incidence of locoregional (pelvic) recurrences were higher in the MIS arm, which is expected if there were inadequate margins around the laparoscopically resected tumors.
Finally, the authors of the LACC trial observed equivalent rates of postoperative complications between the laparotomy and MIS groups. The main virtue for MIS approaches is the reduction in perioperative morbidity. To observe no perioperative morbidity benefit in the MIS group is a red flag suggesting that these surgeons may not have achieved proficiency with the MIS approach.
Despite these arguments, the results of these studies should be taken seriously. Clearly, it is apparent that preservation of oncologic outcomes is not guaranteed with MIS radical hysterectomy, and it should not be the chosen approach for all patients and all surgeons. However, rather than entirely abandoning this less morbid approach, I would argue that it is a call to arms for gynecologic oncologists to self-evaluate. We should know our own data with respect to case volumes, perioperative complications, and cancer-related recurrence and death.
Perhaps MIS radical hysterectomies should be consolidated among high-volume surgeons with demonstrated good outcomes? Just as has been done for rectal cancer surgery with positive effect, we should establish accredited centers of excellence.7 We also need to improve the training of surgeons in novel, difficult techniques, as well as enhance the sophistication of MIS equipment such as improved instrumentation, haptics, and vision-guided surgery (for example, real-time intraoperative assessment of the tumor margins).
Let’s not take a wholesale step backwards to the surgical approaches of a 100 years ago just because they are more straightforward. Let’s do a better job of advancing the quality of what we do for our patients in the future.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She said she had no conflicts of interest. Email Dr. Rossi at [email protected].
References
1. N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1806395.
2. N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1804923.
3. J Clin Oncol. 2012 Mar 1;30(7):695-700.
4. Med Sci Monit. 2014 Dec 1;20:2497-503.
5. Surg Endosc. 2006 Oct;20(10):1556-9.
6. Gynecol Oncol. 2011 Aug;122(2):264-8.
7. Surgery. 2016 Mar;159(3):736-48.
Burden of atrial fibrillation associated with stroke risk
Background: Atrial fibrillation (AF) is a well-known risk factor for ischemic stroke; however, it is unclear if atrial fibrillation burden in patients with PAF is correlated with increased stroke risk.
Study design: Retrospective cohort chart review study during October 2011–October 2016.
Setting: Outpatients in two Kaiser Permanente California health systems.
Synopsis: Among 1,965 adult patients with PAF not on anticoagulation therapy, PAF burden was defined as the percentage time spent in AF during 14-day ECG monitoring. Outcomes included hospitalization for ischemic stroke or arterial thromboembolism while not taking anticoagulants.
Patients in the highest tertile of PAF burden (less than 11%) had 215% higher risk of thromboembolic events, compared with those with lower PAF burden (less than 11%), yielding a hazard ratio of 3.15 (95% confidence interval, 1.51-6.61), even after adjustment.
This study was limited by short ECG monitoring period (14 days), low total number of events (29 total events, 17 in the highest tertile), and no minimum follow-up time. Further, with all patients insured in a single health care system, and excluded on disenrollment from the health plan, selection bias could have affected the results.
Bottom line: In patients with PAF, a larger AF burden (greater than 11%) is associated with increased risk of ischemic stroke. Assessment of AF burden may help determine the need for anticoagulation for stroke prevention.
Citation: Go AS et al. Association of burden of atrial fibrillation with risk of ischemic stroke in adults with paroxysmal atrial fibrillation: the KP-RHYTHM study. JAMA Cardiol. 2018 Jul 1;3(7):601-8.
Dr. Hanna is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Background: Atrial fibrillation (AF) is a well-known risk factor for ischemic stroke; however, it is unclear if atrial fibrillation burden in patients with PAF is correlated with increased stroke risk.
Study design: Retrospective cohort chart review study during October 2011–October 2016.
Setting: Outpatients in two Kaiser Permanente California health systems.
Synopsis: Among 1,965 adult patients with PAF not on anticoagulation therapy, PAF burden was defined as the percentage time spent in AF during 14-day ECG monitoring. Outcomes included hospitalization for ischemic stroke or arterial thromboembolism while not taking anticoagulants.
Patients in the highest tertile of PAF burden (less than 11%) had 215% higher risk of thromboembolic events, compared with those with lower PAF burden (less than 11%), yielding a hazard ratio of 3.15 (95% confidence interval, 1.51-6.61), even after adjustment.
This study was limited by short ECG monitoring period (14 days), low total number of events (29 total events, 17 in the highest tertile), and no minimum follow-up time. Further, with all patients insured in a single health care system, and excluded on disenrollment from the health plan, selection bias could have affected the results.
Bottom line: In patients with PAF, a larger AF burden (greater than 11%) is associated with increased risk of ischemic stroke. Assessment of AF burden may help determine the need for anticoagulation for stroke prevention.
Citation: Go AS et al. Association of burden of atrial fibrillation with risk of ischemic stroke in adults with paroxysmal atrial fibrillation: the KP-RHYTHM study. JAMA Cardiol. 2018 Jul 1;3(7):601-8.
Dr. Hanna is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Background: Atrial fibrillation (AF) is a well-known risk factor for ischemic stroke; however, it is unclear if atrial fibrillation burden in patients with PAF is correlated with increased stroke risk.
Study design: Retrospective cohort chart review study during October 2011–October 2016.
Setting: Outpatients in two Kaiser Permanente California health systems.
Synopsis: Among 1,965 adult patients with PAF not on anticoagulation therapy, PAF burden was defined as the percentage time spent in AF during 14-day ECG monitoring. Outcomes included hospitalization for ischemic stroke or arterial thromboembolism while not taking anticoagulants.
Patients in the highest tertile of PAF burden (less than 11%) had 215% higher risk of thromboembolic events, compared with those with lower PAF burden (less than 11%), yielding a hazard ratio of 3.15 (95% confidence interval, 1.51-6.61), even after adjustment.
This study was limited by short ECG monitoring period (14 days), low total number of events (29 total events, 17 in the highest tertile), and no minimum follow-up time. Further, with all patients insured in a single health care system, and excluded on disenrollment from the health plan, selection bias could have affected the results.
Bottom line: In patients with PAF, a larger AF burden (greater than 11%) is associated with increased risk of ischemic stroke. Assessment of AF burden may help determine the need for anticoagulation for stroke prevention.
Citation: Go AS et al. Association of burden of atrial fibrillation with risk of ischemic stroke in adults with paroxysmal atrial fibrillation: the KP-RHYTHM study. JAMA Cardiol. 2018 Jul 1;3(7):601-8.
Dr. Hanna is an assistant professor in the division of hospital medicine, University of Colorado, Denver.