User login
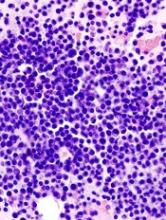
Triplet improves PFS in relapsed/refractory MM
Adding elotuzumab to pomalidomide and low-dose dexamethasone can improve progression-free survival (PFS) in patients with relapsed/refractory multiple myeloma (MM), according to the ELOQUENT-3 trial.
These results support the recent U.S. approval of elotuzumab, pomalidomide, and dexamethasone in adults with MM who have received at least two prior therapies, including lenalidomide and a proteasome inhibitor.
Results from ELOQUENT-3 were recently published in The New England Journal of Medicine and previously presented at the 23rd Congress of the European Hematology Association in June.
The phase 2 trial included patients with refractory or relapsed and refractory MM who had received lenalidomide and a proteasome inhibitor.
The patients were randomized to receive elotuzumab plus pomalidomide and low-dose dexamethasone (EPd, n=60) or pomalidomide and low-dose dexamethasone (Pd, n=57) in 28-day cycles until disease progression or unacceptable toxicity.
The overall response rate was 53% in the EPd arm and 26% in the Pd arm (odds ratio=3.25; P=0.0029).
There were two stringent complete responses (CRs) and three CRs in the EPd arm, and there was one CR in the Pd arm.
The median duration of response was 8.3 months in the Pd arm and was not reached in the EPd arm.
The median PFS was 10.3 months with EPd and 4.7 months with Pd (hazard ratio=0.54, P=0.008).
Overall survival data were not mature at the time of analysis, but there was a trend favoring EPd over Pd (hazard ratio=0.62). There were 13 deaths in the EPd arm and 18 in the Pd arm.
The most common treatment-related adverse events (in the EPd and Pd arms, respectively) were neutropenia (18% and 20%), hyperglycemia (18% and 11%), and anemia (10% and 15%).
This trial was supported by Bristol-Myers Squibb and AbbVie Biotherapeutics, and researchers reported relationships with several other companies.
Adding elotuzumab to pomalidomide and low-dose dexamethasone can improve progression-free survival (PFS) in patients with relapsed/refractory multiple myeloma (MM), according to the ELOQUENT-3 trial.
These results support the recent U.S. approval of elotuzumab, pomalidomide, and dexamethasone in adults with MM who have received at least two prior therapies, including lenalidomide and a proteasome inhibitor.
Results from ELOQUENT-3 were recently published in The New England Journal of Medicine and previously presented at the 23rd Congress of the European Hematology Association in June.
The phase 2 trial included patients with refractory or relapsed and refractory MM who had received lenalidomide and a proteasome inhibitor.
The patients were randomized to receive elotuzumab plus pomalidomide and low-dose dexamethasone (EPd, n=60) or pomalidomide and low-dose dexamethasone (Pd, n=57) in 28-day cycles until disease progression or unacceptable toxicity.
The overall response rate was 53% in the EPd arm and 26% in the Pd arm (odds ratio=3.25; P=0.0029).
There were two stringent complete responses (CRs) and three CRs in the EPd arm, and there was one CR in the Pd arm.
The median duration of response was 8.3 months in the Pd arm and was not reached in the EPd arm.
The median PFS was 10.3 months with EPd and 4.7 months with Pd (hazard ratio=0.54, P=0.008).
Overall survival data were not mature at the time of analysis, but there was a trend favoring EPd over Pd (hazard ratio=0.62). There were 13 deaths in the EPd arm and 18 in the Pd arm.
The most common treatment-related adverse events (in the EPd and Pd arms, respectively) were neutropenia (18% and 20%), hyperglycemia (18% and 11%), and anemia (10% and 15%).
This trial was supported by Bristol-Myers Squibb and AbbVie Biotherapeutics, and researchers reported relationships with several other companies.
Adding elotuzumab to pomalidomide and low-dose dexamethasone can improve progression-free survival (PFS) in patients with relapsed/refractory multiple myeloma (MM), according to the ELOQUENT-3 trial.
These results support the recent U.S. approval of elotuzumab, pomalidomide, and dexamethasone in adults with MM who have received at least two prior therapies, including lenalidomide and a proteasome inhibitor.
Results from ELOQUENT-3 were recently published in The New England Journal of Medicine and previously presented at the 23rd Congress of the European Hematology Association in June.
The phase 2 trial included patients with refractory or relapsed and refractory MM who had received lenalidomide and a proteasome inhibitor.
The patients were randomized to receive elotuzumab plus pomalidomide and low-dose dexamethasone (EPd, n=60) or pomalidomide and low-dose dexamethasone (Pd, n=57) in 28-day cycles until disease progression or unacceptable toxicity.
The overall response rate was 53% in the EPd arm and 26% in the Pd arm (odds ratio=3.25; P=0.0029).
There were two stringent complete responses (CRs) and three CRs in the EPd arm, and there was one CR in the Pd arm.
The median duration of response was 8.3 months in the Pd arm and was not reached in the EPd arm.
The median PFS was 10.3 months with EPd and 4.7 months with Pd (hazard ratio=0.54, P=0.008).
Overall survival data were not mature at the time of analysis, but there was a trend favoring EPd over Pd (hazard ratio=0.62). There were 13 deaths in the EPd arm and 18 in the Pd arm.
The most common treatment-related adverse events (in the EPd and Pd arms, respectively) were neutropenia (18% and 20%), hyperglycemia (18% and 11%), and anemia (10% and 15%).
This trial was supported by Bristol-Myers Squibb and AbbVie Biotherapeutics, and researchers reported relationships with several other companies.
Quality tool tied to improved adherence
CHICAGO – A multifaceted quality initiative that consists of staff education, patient reminders and a feedback loop may help to improve therapy adherence and encourage lifestyle changes of at-risk cardiovascular patients in settings with limited resources, according to results of a clinical trial from Brazil presented at the American Heart Association scientific sessions 2018.
“In patients at high cardiovascular risk – in this case patients with established cardiovascular disease – a multifaceted quality-improvement intervention resulted in significant improvement in the use of evidence-based therapies,” said Otavio Berwanger, MD, PhD, of the Heart Hospital in Sao Paolo. He reported results of the BRIDGE Cardiovascular Prevention Cluster Randomized Trial. “The tools used in our trial can become the basis for developing quality-improvement programs to maximize the use of evidence-based therapies for the management of these high-risk patients with, especially in limited-resource settings.”
BRIDGE-CV included 1,619 patients from 40 care settings. Institutions that adopted the multifaceted intervention adhered to 73.5% of the evidence-based therapies (antiplatelet agents, statins and ACE inhibitors) while those in the control group adhered to 58.7% of the performance measures, Dr. Berwanger said. That represents a gain of 25%. The study employed an “all-or-none” model. That is, participating sites were required to adopt all components of the quality-improvement initiative or none.
He noted that although the evidence supporting the use of platelet therapies, statins, and ACE inhibitors is strong, “translation of these findings in practice is clearly suboptimal.” He added, “It seems to be an even larger problem in settings like mine in Brazil, so quality-improvement interventions, especially in lower-resource settings such as low- and middle-income countries, are definitely needed.”
The quality-improvement model the trial evaluated involved two levels of intervention. The first level comprised three steps: a case manager evaluating the patient’s treatment needs with the aid of a checklist; then an evaluation by the physician; and then providing physicians with what Dr. Berwanger described as “a physician support tool” – a one-page summary of major guideline recommendations. The second level comprised monthly audit and feedback reports to the providers and patient education about lifestyle modification. Staff education and training was also provided to sites that adopted the model. “Our intervention was sort of based on behavioral marketing,” Dr. Berwanger said.
The trial also identified a number of trends among secondary endpoints, although the populations were too small to reach statistical significance. For example, Dr. Berwanger noted that intervention sites had higher use of high-dose statins and more than double the rate of smoking cessation. He also noted a 24% relative risk reduction in major cardiovascular events in the intervention group vs. controls. Among the intervention sites, teaching institutions seems to have a notable improvement in adherence outcomes than other settings, Dr. Berwanger said, but the study did not fully analyze that trend.
“We see this study not as the final word but as the first step,” he said. “More studies are needed.”
Dr. Berwanger reported receiving research support and/or honoraria from Astra Zeneca, Amgen, Bayer, Eurofarma, Servier, Novartis and NovoNordisk. Amgen sponsored the investigator-initiated trial.
SOURCE: Berwanger O, et al. AHA 2018 Abstr.19360.
CHICAGO – A multifaceted quality initiative that consists of staff education, patient reminders and a feedback loop may help to improve therapy adherence and encourage lifestyle changes of at-risk cardiovascular patients in settings with limited resources, according to results of a clinical trial from Brazil presented at the American Heart Association scientific sessions 2018.
“In patients at high cardiovascular risk – in this case patients with established cardiovascular disease – a multifaceted quality-improvement intervention resulted in significant improvement in the use of evidence-based therapies,” said Otavio Berwanger, MD, PhD, of the Heart Hospital in Sao Paolo. He reported results of the BRIDGE Cardiovascular Prevention Cluster Randomized Trial. “The tools used in our trial can become the basis for developing quality-improvement programs to maximize the use of evidence-based therapies for the management of these high-risk patients with, especially in limited-resource settings.”
BRIDGE-CV included 1,619 patients from 40 care settings. Institutions that adopted the multifaceted intervention adhered to 73.5% of the evidence-based therapies (antiplatelet agents, statins and ACE inhibitors) while those in the control group adhered to 58.7% of the performance measures, Dr. Berwanger said. That represents a gain of 25%. The study employed an “all-or-none” model. That is, participating sites were required to adopt all components of the quality-improvement initiative or none.
He noted that although the evidence supporting the use of platelet therapies, statins, and ACE inhibitors is strong, “translation of these findings in practice is clearly suboptimal.” He added, “It seems to be an even larger problem in settings like mine in Brazil, so quality-improvement interventions, especially in lower-resource settings such as low- and middle-income countries, are definitely needed.”
The quality-improvement model the trial evaluated involved two levels of intervention. The first level comprised three steps: a case manager evaluating the patient’s treatment needs with the aid of a checklist; then an evaluation by the physician; and then providing physicians with what Dr. Berwanger described as “a physician support tool” – a one-page summary of major guideline recommendations. The second level comprised monthly audit and feedback reports to the providers and patient education about lifestyle modification. Staff education and training was also provided to sites that adopted the model. “Our intervention was sort of based on behavioral marketing,” Dr. Berwanger said.
The trial also identified a number of trends among secondary endpoints, although the populations were too small to reach statistical significance. For example, Dr. Berwanger noted that intervention sites had higher use of high-dose statins and more than double the rate of smoking cessation. He also noted a 24% relative risk reduction in major cardiovascular events in the intervention group vs. controls. Among the intervention sites, teaching institutions seems to have a notable improvement in adherence outcomes than other settings, Dr. Berwanger said, but the study did not fully analyze that trend.
“We see this study not as the final word but as the first step,” he said. “More studies are needed.”
Dr. Berwanger reported receiving research support and/or honoraria from Astra Zeneca, Amgen, Bayer, Eurofarma, Servier, Novartis and NovoNordisk. Amgen sponsored the investigator-initiated trial.
SOURCE: Berwanger O, et al. AHA 2018 Abstr.19360.
CHICAGO – A multifaceted quality initiative that consists of staff education, patient reminders and a feedback loop may help to improve therapy adherence and encourage lifestyle changes of at-risk cardiovascular patients in settings with limited resources, according to results of a clinical trial from Brazil presented at the American Heart Association scientific sessions 2018.
“In patients at high cardiovascular risk – in this case patients with established cardiovascular disease – a multifaceted quality-improvement intervention resulted in significant improvement in the use of evidence-based therapies,” said Otavio Berwanger, MD, PhD, of the Heart Hospital in Sao Paolo. He reported results of the BRIDGE Cardiovascular Prevention Cluster Randomized Trial. “The tools used in our trial can become the basis for developing quality-improvement programs to maximize the use of evidence-based therapies for the management of these high-risk patients with, especially in limited-resource settings.”
BRIDGE-CV included 1,619 patients from 40 care settings. Institutions that adopted the multifaceted intervention adhered to 73.5% of the evidence-based therapies (antiplatelet agents, statins and ACE inhibitors) while those in the control group adhered to 58.7% of the performance measures, Dr. Berwanger said. That represents a gain of 25%. The study employed an “all-or-none” model. That is, participating sites were required to adopt all components of the quality-improvement initiative or none.
He noted that although the evidence supporting the use of platelet therapies, statins, and ACE inhibitors is strong, “translation of these findings in practice is clearly suboptimal.” He added, “It seems to be an even larger problem in settings like mine in Brazil, so quality-improvement interventions, especially in lower-resource settings such as low- and middle-income countries, are definitely needed.”
The quality-improvement model the trial evaluated involved two levels of intervention. The first level comprised three steps: a case manager evaluating the patient’s treatment needs with the aid of a checklist; then an evaluation by the physician; and then providing physicians with what Dr. Berwanger described as “a physician support tool” – a one-page summary of major guideline recommendations. The second level comprised monthly audit and feedback reports to the providers and patient education about lifestyle modification. Staff education and training was also provided to sites that adopted the model. “Our intervention was sort of based on behavioral marketing,” Dr. Berwanger said.
The trial also identified a number of trends among secondary endpoints, although the populations were too small to reach statistical significance. For example, Dr. Berwanger noted that intervention sites had higher use of high-dose statins and more than double the rate of smoking cessation. He also noted a 24% relative risk reduction in major cardiovascular events in the intervention group vs. controls. Among the intervention sites, teaching institutions seems to have a notable improvement in adherence outcomes than other settings, Dr. Berwanger said, but the study did not fully analyze that trend.
“We see this study not as the final word but as the first step,” he said. “More studies are needed.”
Dr. Berwanger reported receiving research support and/or honoraria from Astra Zeneca, Amgen, Bayer, Eurofarma, Servier, Novartis and NovoNordisk. Amgen sponsored the investigator-initiated trial.
SOURCE: Berwanger O, et al. AHA 2018 Abstr.19360.
REPORTING FROM AMERICAN HEART ASSOCIATION SCIENTIFIC SESSIONS 2018
Key clinical point: A multifaceted quality-improvement initiative led to improved adherence to evidence-based therapies.
Major finding: Sites that adopted the intervention had adherence rates 25% higher than control sites.
Study details: Two-arm, cluster-randomized, controlled trial of 1,619 high-risk, stable patients with established CVD from 40 sites.
Disclosures: Dr. Berwanger disclosed receiving research support and/or honoraria from AstraZeneca, Amgen, Bayer, Eurofarma, Servier, Novartis and NovoNordisk. Amgen sponsored the investigator-initiated trial.
Source: Berwanger O, et al. 2018-LBCT-19360-AHA.
High rates of prescription opioid, benzodiazepine use observed in chronic liver disease
SAN FRANCISCO – .
“Middle-aged individuals and those with a background of substance abuse and mental health conditions appear to have highest rates of use and represent populations for which targeted interventions to curb use could be highest yield,” lead study author Monica Konerman, MD, said in an interview in advance of the annual meeting of the American Association for the Study of Liver Diseases.
In an effort to better understand the rates of prescription opioid and benzodiazepine use in chronic liver disease, Dr. Konerman, director of the Michigan Medicine NAFLD Clinic at the University of Michigan, Ann Arbor, and her colleagues drew from the Truven Health Analytics Marketscan databases from 2009 to 2015. They limited the analysis to individuals with drug coverage who had chronic hepatitis C (HCV) without cirrhosis, cirrhosis, congestive heart failure (CHF), or chronic obstructive pulmonary disease (COPD), and examined pharmacy files for outpatient prescriptions.
Dr. Konerman reported data from 210,191 patients with HCV, 79,332 with cirrhosis, 766,840 with CHF, and 1,438,798 with COPD. Their median age was 59 years, and 51% were female. In per person-years, the prevalence of prescription opioid use was 25% among patients with chronic HCV, 53% among patients with cirrhosis, 26% among those with CHF, and 24% among those with COPD. At the same time, in per person-years, the prevalence of benzodiazepine use was 12% among patients with chronic HCV, 21% among patients with cirrhosis, 12% among those with CHF, and 13% among those with COPD. Use of opioids was greatest in adults 40-59 years of age (P less than .001). High-dose opioid use, defined as 100 opioid morphine equivalents per day or greater, occurred in 23% of those with cirrhosis and in 22% of those with HCV.
“The significant increase in rates of use in chronic liver disease, compared to other chronic conditions was remarkable, particularly given that patients with liver disease are at higher risk for adverse consequences of use due to hepatic metabolism of these medications,” Dr. Konerman said.
She went on to acknowledge “inherent limitations to studies that are secondary database analyses that rely on diagnosis codes for categorization of disease with potential for both over and under classification. We also did not capture inpatient prescriptions,” she said.
Dr. Konerman reported having no financial disclosures.
SAN FRANCISCO – .
“Middle-aged individuals and those with a background of substance abuse and mental health conditions appear to have highest rates of use and represent populations for which targeted interventions to curb use could be highest yield,” lead study author Monica Konerman, MD, said in an interview in advance of the annual meeting of the American Association for the Study of Liver Diseases.
In an effort to better understand the rates of prescription opioid and benzodiazepine use in chronic liver disease, Dr. Konerman, director of the Michigan Medicine NAFLD Clinic at the University of Michigan, Ann Arbor, and her colleagues drew from the Truven Health Analytics Marketscan databases from 2009 to 2015. They limited the analysis to individuals with drug coverage who had chronic hepatitis C (HCV) without cirrhosis, cirrhosis, congestive heart failure (CHF), or chronic obstructive pulmonary disease (COPD), and examined pharmacy files for outpatient prescriptions.
Dr. Konerman reported data from 210,191 patients with HCV, 79,332 with cirrhosis, 766,840 with CHF, and 1,438,798 with COPD. Their median age was 59 years, and 51% were female. In per person-years, the prevalence of prescription opioid use was 25% among patients with chronic HCV, 53% among patients with cirrhosis, 26% among those with CHF, and 24% among those with COPD. At the same time, in per person-years, the prevalence of benzodiazepine use was 12% among patients with chronic HCV, 21% among patients with cirrhosis, 12% among those with CHF, and 13% among those with COPD. Use of opioids was greatest in adults 40-59 years of age (P less than .001). High-dose opioid use, defined as 100 opioid morphine equivalents per day or greater, occurred in 23% of those with cirrhosis and in 22% of those with HCV.
“The significant increase in rates of use in chronic liver disease, compared to other chronic conditions was remarkable, particularly given that patients with liver disease are at higher risk for adverse consequences of use due to hepatic metabolism of these medications,” Dr. Konerman said.
She went on to acknowledge “inherent limitations to studies that are secondary database analyses that rely on diagnosis codes for categorization of disease with potential for both over and under classification. We also did not capture inpatient prescriptions,” she said.
Dr. Konerman reported having no financial disclosures.
SAN FRANCISCO – .
“Middle-aged individuals and those with a background of substance abuse and mental health conditions appear to have highest rates of use and represent populations for which targeted interventions to curb use could be highest yield,” lead study author Monica Konerman, MD, said in an interview in advance of the annual meeting of the American Association for the Study of Liver Diseases.
In an effort to better understand the rates of prescription opioid and benzodiazepine use in chronic liver disease, Dr. Konerman, director of the Michigan Medicine NAFLD Clinic at the University of Michigan, Ann Arbor, and her colleagues drew from the Truven Health Analytics Marketscan databases from 2009 to 2015. They limited the analysis to individuals with drug coverage who had chronic hepatitis C (HCV) without cirrhosis, cirrhosis, congestive heart failure (CHF), or chronic obstructive pulmonary disease (COPD), and examined pharmacy files for outpatient prescriptions.
Dr. Konerman reported data from 210,191 patients with HCV, 79,332 with cirrhosis, 766,840 with CHF, and 1,438,798 with COPD. Their median age was 59 years, and 51% were female. In per person-years, the prevalence of prescription opioid use was 25% among patients with chronic HCV, 53% among patients with cirrhosis, 26% among those with CHF, and 24% among those with COPD. At the same time, in per person-years, the prevalence of benzodiazepine use was 12% among patients with chronic HCV, 21% among patients with cirrhosis, 12% among those with CHF, and 13% among those with COPD. Use of opioids was greatest in adults 40-59 years of age (P less than .001). High-dose opioid use, defined as 100 opioid morphine equivalents per day or greater, occurred in 23% of those with cirrhosis and in 22% of those with HCV.
“The significant increase in rates of use in chronic liver disease, compared to other chronic conditions was remarkable, particularly given that patients with liver disease are at higher risk for adverse consequences of use due to hepatic metabolism of these medications,” Dr. Konerman said.
She went on to acknowledge “inherent limitations to studies that are secondary database analyses that rely on diagnosis codes for categorization of disease with potential for both over and under classification. We also did not capture inpatient prescriptions,” she said.
Dr. Konerman reported having no financial disclosures.
REPORTING FROM THE LIVER MEETING 2018
Key clinical point: About one-fourth of patients with chronic hepatitis C use prescription opioids.
Major finding: In per person-years, the prevalence of prescription opioid use was 25% among patients with chronic HCV, 53% among patients with cirrhosis, 26% among those with congestive heart failure, and 24% among those with chronic obstructive pulmonary disease.
Study details: An analysis of 210,191 patients who had chronic hepatitis C.
Disclosures: Dr. Konerman reported having no financial disclosures.
No difference for blacks vs. whites in precancerous colorectal neoplasm prevalence: A meta-analysis
, prompting investigators to suggest that the age at which screening starts need not differ based on race.
There was also no difference in advanced neoplasia in the proximal colon between black and white screen-eligible individuals in the most rigorous of the studies included in the meta-analysis, investigators reported.
Those findings support eliminating the age difference at which to begin screening of average-risk individuals, as is currently recommended in some guidelines, said Thomas F. Imperiale, MD, the Lawrence Lumeng Professor of Gastroenterology and Hepatology at Indiana University, Indianapolis, and his coinvestigators.
In areas with no disparities in screening access, average-risk screening could begin at age 50 years, regardless of race, at least based on results of this meta-analysis, Dr. Imperiale and his colleagues said in their report.
“To the extent that advanced adenoma is the precursor lesion for colorectal cancer, tailoring the age at which to begin screening and how to screen based on race is not supported by our findings,” they said in the report, which appears in the journal Gastroenterology.
Dr. Imperiale and his coinvestigators scanned the medical literature and identified nine studies looking at the prevalence of advanced adenomas or advanced precancerous colorectal neoplasms in both black and white individuals of average risk who had undergone screening colonoscopy.
Those nine cross-sectional studies, all published during 2010-2017, represented a total of 302,128 participants. Six studies were of high methodologic quality and had a low risk of bias, while the remaining three failed to adjust for age and sex, authors of the meta-analysis said in their report.
Prevalence of advanced adenomas or advanced precancerous colorectal neoplasms ranged from 2% to 10% for whites and from 5% to 12% for blacks in the nine studies, with only one study, which had no histology results available, showing a higher prevalence in blacks, investigators found.
Taken together, there was no difference between racial groups, with a point prevalence of 6.57% for blacks and 6.20% for whites (odds ratio, 1.03; 95% confidence interval, 0.81-1.30) and an absolute risk difference of zero, according to the statistical analysis.
Of five studies that included data on proximal advanced adenomas or advanced precancerous colorectal neoplasms, two showed a greater prevalence in blacks versus whites, with point prevalences of 3.30% and 2.42%, respectively. However, there was no difference in prevalence for the “best subset” of three studies with a moderate degree of heterogeneity, investigators said.
Given these findings, the higher colorectal cancer incidence and mortality seen in black adults is less likely because of biology, and more likely from differences in symptom recognition, diagnostic evaluation, or acceptance of preventive services, Dr. Imperiale and his coauthors said in a discussion of the results.
Some current guidelines suggest starting colorectal cancer screening at age 40 years for average-risk blacks, which is 5-10 years earlier than for nonblacks, investigators said, though of note, the most recent American Cancer Society recommendations recommend screening starting at age 45 years for all average-risk individuals.
“If this recommendation is followed broadly, it would lessen the clinical and policy implications of our findings,” they wrote. “However, the uptake of this recommendation is yet to be determined, as it differs from those of all other professional organizations.”
The study was supported by Indiana CTSI Collaboration in Translational Research Grants. Dr. Imperiale and hiscoauthors reported no conflicts of interest.
SOURCE: Imperiale TF et al. Gastroenterology. 2018 Aug 21. doi: 10.1053/j.gastro.2018.08.020.
, prompting investigators to suggest that the age at which screening starts need not differ based on race.
There was also no difference in advanced neoplasia in the proximal colon between black and white screen-eligible individuals in the most rigorous of the studies included in the meta-analysis, investigators reported.
Those findings support eliminating the age difference at which to begin screening of average-risk individuals, as is currently recommended in some guidelines, said Thomas F. Imperiale, MD, the Lawrence Lumeng Professor of Gastroenterology and Hepatology at Indiana University, Indianapolis, and his coinvestigators.
In areas with no disparities in screening access, average-risk screening could begin at age 50 years, regardless of race, at least based on results of this meta-analysis, Dr. Imperiale and his colleagues said in their report.
“To the extent that advanced adenoma is the precursor lesion for colorectal cancer, tailoring the age at which to begin screening and how to screen based on race is not supported by our findings,” they said in the report, which appears in the journal Gastroenterology.
Dr. Imperiale and his coinvestigators scanned the medical literature and identified nine studies looking at the prevalence of advanced adenomas or advanced precancerous colorectal neoplasms in both black and white individuals of average risk who had undergone screening colonoscopy.
Those nine cross-sectional studies, all published during 2010-2017, represented a total of 302,128 participants. Six studies were of high methodologic quality and had a low risk of bias, while the remaining three failed to adjust for age and sex, authors of the meta-analysis said in their report.
Prevalence of advanced adenomas or advanced precancerous colorectal neoplasms ranged from 2% to 10% for whites and from 5% to 12% for blacks in the nine studies, with only one study, which had no histology results available, showing a higher prevalence in blacks, investigators found.
Taken together, there was no difference between racial groups, with a point prevalence of 6.57% for blacks and 6.20% for whites (odds ratio, 1.03; 95% confidence interval, 0.81-1.30) and an absolute risk difference of zero, according to the statistical analysis.
Of five studies that included data on proximal advanced adenomas or advanced precancerous colorectal neoplasms, two showed a greater prevalence in blacks versus whites, with point prevalences of 3.30% and 2.42%, respectively. However, there was no difference in prevalence for the “best subset” of three studies with a moderate degree of heterogeneity, investigators said.
Given these findings, the higher colorectal cancer incidence and mortality seen in black adults is less likely because of biology, and more likely from differences in symptom recognition, diagnostic evaluation, or acceptance of preventive services, Dr. Imperiale and his coauthors said in a discussion of the results.
Some current guidelines suggest starting colorectal cancer screening at age 40 years for average-risk blacks, which is 5-10 years earlier than for nonblacks, investigators said, though of note, the most recent American Cancer Society recommendations recommend screening starting at age 45 years for all average-risk individuals.
“If this recommendation is followed broadly, it would lessen the clinical and policy implications of our findings,” they wrote. “However, the uptake of this recommendation is yet to be determined, as it differs from those of all other professional organizations.”
The study was supported by Indiana CTSI Collaboration in Translational Research Grants. Dr. Imperiale and hiscoauthors reported no conflicts of interest.
SOURCE: Imperiale TF et al. Gastroenterology. 2018 Aug 21. doi: 10.1053/j.gastro.2018.08.020.
, prompting investigators to suggest that the age at which screening starts need not differ based on race.
There was also no difference in advanced neoplasia in the proximal colon between black and white screen-eligible individuals in the most rigorous of the studies included in the meta-analysis, investigators reported.
Those findings support eliminating the age difference at which to begin screening of average-risk individuals, as is currently recommended in some guidelines, said Thomas F. Imperiale, MD, the Lawrence Lumeng Professor of Gastroenterology and Hepatology at Indiana University, Indianapolis, and his coinvestigators.
In areas with no disparities in screening access, average-risk screening could begin at age 50 years, regardless of race, at least based on results of this meta-analysis, Dr. Imperiale and his colleagues said in their report.
“To the extent that advanced adenoma is the precursor lesion for colorectal cancer, tailoring the age at which to begin screening and how to screen based on race is not supported by our findings,” they said in the report, which appears in the journal Gastroenterology.
Dr. Imperiale and his coinvestigators scanned the medical literature and identified nine studies looking at the prevalence of advanced adenomas or advanced precancerous colorectal neoplasms in both black and white individuals of average risk who had undergone screening colonoscopy.
Those nine cross-sectional studies, all published during 2010-2017, represented a total of 302,128 participants. Six studies were of high methodologic quality and had a low risk of bias, while the remaining three failed to adjust for age and sex, authors of the meta-analysis said in their report.
Prevalence of advanced adenomas or advanced precancerous colorectal neoplasms ranged from 2% to 10% for whites and from 5% to 12% for blacks in the nine studies, with only one study, which had no histology results available, showing a higher prevalence in blacks, investigators found.
Taken together, there was no difference between racial groups, with a point prevalence of 6.57% for blacks and 6.20% for whites (odds ratio, 1.03; 95% confidence interval, 0.81-1.30) and an absolute risk difference of zero, according to the statistical analysis.
Of five studies that included data on proximal advanced adenomas or advanced precancerous colorectal neoplasms, two showed a greater prevalence in blacks versus whites, with point prevalences of 3.30% and 2.42%, respectively. However, there was no difference in prevalence for the “best subset” of three studies with a moderate degree of heterogeneity, investigators said.
Given these findings, the higher colorectal cancer incidence and mortality seen in black adults is less likely because of biology, and more likely from differences in symptom recognition, diagnostic evaluation, or acceptance of preventive services, Dr. Imperiale and his coauthors said in a discussion of the results.
Some current guidelines suggest starting colorectal cancer screening at age 40 years for average-risk blacks, which is 5-10 years earlier than for nonblacks, investigators said, though of note, the most recent American Cancer Society recommendations recommend screening starting at age 45 years for all average-risk individuals.
“If this recommendation is followed broadly, it would lessen the clinical and policy implications of our findings,” they wrote. “However, the uptake of this recommendation is yet to be determined, as it differs from those of all other professional organizations.”
The study was supported by Indiana CTSI Collaboration in Translational Research Grants. Dr. Imperiale and hiscoauthors reported no conflicts of interest.
SOURCE: Imperiale TF et al. Gastroenterology. 2018 Aug 21. doi: 10.1053/j.gastro.2018.08.020.
FROM GASTROENTEROLOGY
Key clinical point: Rates of advanced precancerous neoplasia did not differ between average-risk black and white individuals who underwent screening colonoscopy; starting age for screening may need not differ based on race.
Major finding: There was no difference between racial groups, with a point prevalence of 6.57% for blacks and 6.20% for whites (odds ratio, 1.03; 95% confidence interval, 0.81-1.30).
Study details: A meta-analysis of nine cross-sectional studies published during 2010-2017 and representing 302,128 individuals.
Disclosures: The study was supported by Indiana CTSI Collaboration in Translational Research Grants. Dr. Imperiale and coauthors reported no conflicts of interest.
Source: Imperiale TF et al. Gastroenterology. 2018 Aug 21. doi: 10.1053/j.gastro.2018.08.020.
Ask depressed patients about hypersomnia to screen for mixicity
BARCELONA – Hypersomnia is a novel, previously unappreciated factor useful in tipping the balance in favor of an underlying bipolar predisposition in patients with an acute major depressive episode, Andrea Murru, MD, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
“This may help us in clinical practice. It’s an effective, costless, and highly objective clinical measure. It’s one question, and it takes a second. It’s simply asking the patient: ‘Are you sleeping more hours at night than usual?’ It’s a very simple clinical question that could really change the focus of treatment for a patient,” said Dr. Murru, a clinical psychiatrist in the bipolar disorders program of the University of Barcelona.
He presented a post hoc analysis of 2,514 acutely depressed individuals who participated in the BRIDGE-II-MIX (Bipolar Disorders: Improving Diagnosis, Guidance and Education) study, an international, multicenter, cross-sectional, observational study aimed at better characterizing clinically valid mixed features of depression indicative of concurrent manic symptoms.
“This is one of a whole series of hypothesis-generating studies from BRIDGE-II-MIX that are trying to deal with the struggle of understanding whether all the elements that favor mixicity and an underpinning bipolar diathesis are fairly represented in the diagnostic criteria in DSM-5. And what we are basically finding is the DSM-5 criteria are leaving out important symptoms that really do play a role,” the psychiatrist said in an interview.
One of those missing factors, he continued, is hypersomnia. It was present in 16.8% of the study population, and he and his coinvestigators compared them in terms of clinical variables, current and past psychiatric symptoms, and sociodemographics with the 83.2% of patients with insomnia. That is, patients who got fewer hours of sleep than normal and felt fatigued during the next day were compared with those who felt a reduced need to sleep.
The two groups differed in important ways. Hypersomnia showed a powerful correlation with a physician diagnosis of major depressive episode with atypical features, being present in 32.2% of such patients, while a mere 1.8% had insomnia. Moreover, among patients diagnosed with bipolar disorder I or II, 20.6% reported hypersomnia, a significantly higher proportion than the 16% who had insomnia.
The finding that only 5% of BRIDGE-II-MIX participants with hypersomnia met DSM-5 criteria for a mixed-state specifier, a rate not significantly different from the 8.3% figure in those with insomnia, underscores the drawbacks of the DSM-5 criteria, according to Dr. Murru. He noted that, in contrast to the DSM-5 criteria, 32.9% of the hypersomniac patients with a major depressive episode met Research Diagnostic Criteria (RDC) for a mixed-state specifier, a rate significantly higher than the 27.6% figure in patients with insomnia.
Specifically, the individual RDC mixed-state specifiers that stood out as significantly more frequent among depressed patients with hypersomnia than insomnia were racing thoughts, by a margin of 15.1% to 10.6%; impulsivity, 16.8% versus 13.2%; distractibility, 29.6% versus 23.4%; hypersexuality, which was present in 4% of patients with hypersomnia but only 2.3% with insomnia; irritable mood, 33.1% versus 24.8%; and a history of insufficient response to previous antidepressant therapy, 34.3%, compared with 27.1% in insomniacs.
When Dr. Murru and his coinvestigators performed a stepwise linear regression analysis to identify significant predictors of hypersomnia in patients with a major depressive episode, they found that the sleep abnormality keeps some interesting company. Patients with current bulimia were 4.21-fold more likely to have hypersomnia than those without the eating disorder. Current social phobia was associated with a 1.77-fold increased risk of hypersomnia; mood lability on prior antidepressant therapy carried a 1.37-fold risk, as did current mood lability; prior attempted suicide was associated with a 1.31-fold increased risk; being overweight or obese was associated with a 1.42-fold risk; currently being on a mood stabilizer carried a 1.33-fold increased risk of hypersomnia; and currently being on an atypical antipsychotic agent had a 1.36-fold greater risk.
Dr. Murru concluded that the take-home message of this study – “Of course, conceding it’s highly exploratory nature intrinsic to a post hoc analysis,” he noted – is that hypersomnia should be included among the symptoms that trigger the “with mixed features” specifier in patients with a major depressive episode.
The BRIDGE-II-MIX study was sponsored by Sanofi-Aventis. Dr. Murru reported having no financial conflicts of interest regarding the study.
BARCELONA – Hypersomnia is a novel, previously unappreciated factor useful in tipping the balance in favor of an underlying bipolar predisposition in patients with an acute major depressive episode, Andrea Murru, MD, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
“This may help us in clinical practice. It’s an effective, costless, and highly objective clinical measure. It’s one question, and it takes a second. It’s simply asking the patient: ‘Are you sleeping more hours at night than usual?’ It’s a very simple clinical question that could really change the focus of treatment for a patient,” said Dr. Murru, a clinical psychiatrist in the bipolar disorders program of the University of Barcelona.
He presented a post hoc analysis of 2,514 acutely depressed individuals who participated in the BRIDGE-II-MIX (Bipolar Disorders: Improving Diagnosis, Guidance and Education) study, an international, multicenter, cross-sectional, observational study aimed at better characterizing clinically valid mixed features of depression indicative of concurrent manic symptoms.
“This is one of a whole series of hypothesis-generating studies from BRIDGE-II-MIX that are trying to deal with the struggle of understanding whether all the elements that favor mixicity and an underpinning bipolar diathesis are fairly represented in the diagnostic criteria in DSM-5. And what we are basically finding is the DSM-5 criteria are leaving out important symptoms that really do play a role,” the psychiatrist said in an interview.
One of those missing factors, he continued, is hypersomnia. It was present in 16.8% of the study population, and he and his coinvestigators compared them in terms of clinical variables, current and past psychiatric symptoms, and sociodemographics with the 83.2% of patients with insomnia. That is, patients who got fewer hours of sleep than normal and felt fatigued during the next day were compared with those who felt a reduced need to sleep.
The two groups differed in important ways. Hypersomnia showed a powerful correlation with a physician diagnosis of major depressive episode with atypical features, being present in 32.2% of such patients, while a mere 1.8% had insomnia. Moreover, among patients diagnosed with bipolar disorder I or II, 20.6% reported hypersomnia, a significantly higher proportion than the 16% who had insomnia.
The finding that only 5% of BRIDGE-II-MIX participants with hypersomnia met DSM-5 criteria for a mixed-state specifier, a rate not significantly different from the 8.3% figure in those with insomnia, underscores the drawbacks of the DSM-5 criteria, according to Dr. Murru. He noted that, in contrast to the DSM-5 criteria, 32.9% of the hypersomniac patients with a major depressive episode met Research Diagnostic Criteria (RDC) for a mixed-state specifier, a rate significantly higher than the 27.6% figure in patients with insomnia.
Specifically, the individual RDC mixed-state specifiers that stood out as significantly more frequent among depressed patients with hypersomnia than insomnia were racing thoughts, by a margin of 15.1% to 10.6%; impulsivity, 16.8% versus 13.2%; distractibility, 29.6% versus 23.4%; hypersexuality, which was present in 4% of patients with hypersomnia but only 2.3% with insomnia; irritable mood, 33.1% versus 24.8%; and a history of insufficient response to previous antidepressant therapy, 34.3%, compared with 27.1% in insomniacs.
When Dr. Murru and his coinvestigators performed a stepwise linear regression analysis to identify significant predictors of hypersomnia in patients with a major depressive episode, they found that the sleep abnormality keeps some interesting company. Patients with current bulimia were 4.21-fold more likely to have hypersomnia than those without the eating disorder. Current social phobia was associated with a 1.77-fold increased risk of hypersomnia; mood lability on prior antidepressant therapy carried a 1.37-fold risk, as did current mood lability; prior attempted suicide was associated with a 1.31-fold increased risk; being overweight or obese was associated with a 1.42-fold risk; currently being on a mood stabilizer carried a 1.33-fold increased risk of hypersomnia; and currently being on an atypical antipsychotic agent had a 1.36-fold greater risk.
Dr. Murru concluded that the take-home message of this study – “Of course, conceding it’s highly exploratory nature intrinsic to a post hoc analysis,” he noted – is that hypersomnia should be included among the symptoms that trigger the “with mixed features” specifier in patients with a major depressive episode.
The BRIDGE-II-MIX study was sponsored by Sanofi-Aventis. Dr. Murru reported having no financial conflicts of interest regarding the study.
BARCELONA – Hypersomnia is a novel, previously unappreciated factor useful in tipping the balance in favor of an underlying bipolar predisposition in patients with an acute major depressive episode, Andrea Murru, MD, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
“This may help us in clinical practice. It’s an effective, costless, and highly objective clinical measure. It’s one question, and it takes a second. It’s simply asking the patient: ‘Are you sleeping more hours at night than usual?’ It’s a very simple clinical question that could really change the focus of treatment for a patient,” said Dr. Murru, a clinical psychiatrist in the bipolar disorders program of the University of Barcelona.
He presented a post hoc analysis of 2,514 acutely depressed individuals who participated in the BRIDGE-II-MIX (Bipolar Disorders: Improving Diagnosis, Guidance and Education) study, an international, multicenter, cross-sectional, observational study aimed at better characterizing clinically valid mixed features of depression indicative of concurrent manic symptoms.
“This is one of a whole series of hypothesis-generating studies from BRIDGE-II-MIX that are trying to deal with the struggle of understanding whether all the elements that favor mixicity and an underpinning bipolar diathesis are fairly represented in the diagnostic criteria in DSM-5. And what we are basically finding is the DSM-5 criteria are leaving out important symptoms that really do play a role,” the psychiatrist said in an interview.
One of those missing factors, he continued, is hypersomnia. It was present in 16.8% of the study population, and he and his coinvestigators compared them in terms of clinical variables, current and past psychiatric symptoms, and sociodemographics with the 83.2% of patients with insomnia. That is, patients who got fewer hours of sleep than normal and felt fatigued during the next day were compared with those who felt a reduced need to sleep.
The two groups differed in important ways. Hypersomnia showed a powerful correlation with a physician diagnosis of major depressive episode with atypical features, being present in 32.2% of such patients, while a mere 1.8% had insomnia. Moreover, among patients diagnosed with bipolar disorder I or II, 20.6% reported hypersomnia, a significantly higher proportion than the 16% who had insomnia.
The finding that only 5% of BRIDGE-II-MIX participants with hypersomnia met DSM-5 criteria for a mixed-state specifier, a rate not significantly different from the 8.3% figure in those with insomnia, underscores the drawbacks of the DSM-5 criteria, according to Dr. Murru. He noted that, in contrast to the DSM-5 criteria, 32.9% of the hypersomniac patients with a major depressive episode met Research Diagnostic Criteria (RDC) for a mixed-state specifier, a rate significantly higher than the 27.6% figure in patients with insomnia.
Specifically, the individual RDC mixed-state specifiers that stood out as significantly more frequent among depressed patients with hypersomnia than insomnia were racing thoughts, by a margin of 15.1% to 10.6%; impulsivity, 16.8% versus 13.2%; distractibility, 29.6% versus 23.4%; hypersexuality, which was present in 4% of patients with hypersomnia but only 2.3% with insomnia; irritable mood, 33.1% versus 24.8%; and a history of insufficient response to previous antidepressant therapy, 34.3%, compared with 27.1% in insomniacs.
When Dr. Murru and his coinvestigators performed a stepwise linear regression analysis to identify significant predictors of hypersomnia in patients with a major depressive episode, they found that the sleep abnormality keeps some interesting company. Patients with current bulimia were 4.21-fold more likely to have hypersomnia than those without the eating disorder. Current social phobia was associated with a 1.77-fold increased risk of hypersomnia; mood lability on prior antidepressant therapy carried a 1.37-fold risk, as did current mood lability; prior attempted suicide was associated with a 1.31-fold increased risk; being overweight or obese was associated with a 1.42-fold risk; currently being on a mood stabilizer carried a 1.33-fold increased risk of hypersomnia; and currently being on an atypical antipsychotic agent had a 1.36-fold greater risk.
Dr. Murru concluded that the take-home message of this study – “Of course, conceding it’s highly exploratory nature intrinsic to a post hoc analysis,” he noted – is that hypersomnia should be included among the symptoms that trigger the “with mixed features” specifier in patients with a major depressive episode.
The BRIDGE-II-MIX study was sponsored by Sanofi-Aventis. Dr. Murru reported having no financial conflicts of interest regarding the study.
REPORTING FROM THE ECNP CONGRESS
Key clinical point: Ask patients with a major depressive episode about hypersomnia.
Major finding: Hypersomnia in patients with an acute major depressive episode clusters with numerous elements of a bipolar diathesis.
Study details: This was a post hoc analysis of 2,514 acutely depressed individuals who participated in an international, multicenter, cross-sectional, observational study.
Disclosures: The BRIDGE-II-MIX study was sponsored by Sanofi-Aventis. The presenter reported having no financial conflicts of interest regarding the study.
Higher prenatal exposure to daylight tied to lower depression risk
Prenatal programming of the circadian and limbic systems might play a role in the odds of developing lifetime depression, a longitudinal study of almost 161,000 women shows.
“Our results could add support to an emerging hypothesis that perinatal photoperiod may influence depression risk,” wrote Elizabeth E. Devore of Brigham and Women’s Hospital, Boston, and her associates. “If replicated, ... these results could translate into safe and inexpensive light-related interventions for mothers and babies.”
In the study, which was published in the Journal of Psychiatric Research, Ms. Devore and her associates examined the influence of daylight exposure during maternal pregnancy and lifetime depression risk in the resulting offspring. They found that increased exposure to daylight during maternal pregnancy correlated with reduced lifetime risk of depression. wrote Ms. Devore, who also is affiliated with Harvard Medical School, Boston, and her associates.
The effects of daylight exposure were considered modest within the study population, but the authors emphasized that the finding would have much “larger effects at the population level,” given the occurrence of depression in the general population. They added that their findings reinforce a growing consensus that perinatal exposure to daylight could have the ability to influence the risk of developing a mood disorder.
The investigators accessed the Nurses’ Health Study (NHS) and the NHS II, established in 1976 and 1989, respectively, to assess risk factors for chronic conditions in female nurses. Both studies biennially surveyed demographic data on health, lifestyle, and medication use through mailed questionnaires. The first group was composed of 121,701 women aged 30-55 years; the second included 116,430 women aged 25-42 years. Altogether, 160,737 women born full-term were included in the study; 20,912 were excluded from the original survey group for not reporting depression status, as well as an additional 43,325 for not reporting their state of birth.
From data collected regarding participants’ day and state of birth, the researchers were able to estimate total length of daylight exposure during pregnancy using mathematical equations published by the National Oceanic and Atmospheric Administration.
Longitudinal coordinates pinpointing the center of population density for a participant’s birth state were used to identify the location of each participant during gestation. Using those assumptions, the authors were able to establish the two key data points evaluated for the study: total daylight exposure during pregnancy gestation, which was calculated by adding the lengths of all 280 days of the pregnancy, and extreme differences in daylight exposure that might have occurred throughout the pregnancy, which was measured by subtracting the longest and shortest day lengths during gestation.
The investigators paid particular attention to reported levels of depression, evidence of suicide, and personal characteristics and lifestyle factors, such as race, hair color, and early-life socioeconomic factors, including parents’ homeownership at the time of offspring birth; birth weight; history of having been breastfed; and parental occupation throughout the participant’s childhood.
Participants did not begin reporting antidepressant use for the first time until 1996; history of clinician-reported diagnoses of depression began in 2000, Ms. Devore and her associates reported.
Total daylight exposure during pregnancy was found to have “a borderline significant association with odds of lifetime depression,” but the trend was not convincing qualitatively, “and individual estimates across quintiles of exposure” were not considered to be statistically significant. In fact, the authors found that a larger difference between minimum and maximum daylight exposure throughout pregnancy significantly lowered lifetime risk of depression. Women with the largest differences in minimum/maximum daylight exposure during gestation had a 12% lower risk of depression in the NHS population. That reduced risk increased to 15% with the NHS II group. When both cohorts were combined, the reduced risk of depression was 13%.
When evaluating the role that daylight exposure plays with regard to trimester of pregnancy, the authors did note an association for the first trimester, but the association was much stronger for the second trimester; no association was found for the third trimester.
In terms of the effects of daylight exposure on incidence of suicide, no significant associations were found.
Because birth latitude and birth season were of key interest in this study, their relative contribution to total daylight exposure and extreme differences in exposure were considered. Citing observations from the National Health and Nutrition Examination Survey (NHANES), In this study, the authors found that women born in northern latitudes were found to have a 7% risk for lifetime depression, compared with women born in middle latitudes. Conversely, women born in southern latitudes had a 15% risk of depression. No association was found between birth season and incidence of depression, regardless of how season was defined.
The investigators cited several limitations. One is that they did not collect behavioral factors such as the time women spent outdoors. “Our method of exposure calculation relied on the assumption that participants’ mothers were exposed to sunlight from sunrise to sunset,” Ms. Devore and her associates wrote. This way of assessing exposure might have biased their results.
Nevertheless, they said, more studies are needed to examine the role that birth latitude and birth season might play with regard to depression.
The research for this study was supported by the National Institute of Mental Health and the Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health. Additional infrastructure support for the Nurses’ Health Studies was provided by the National Cancer Institute.
The authors declared no conflicts of interest. Ms. Devore has reported receiving consulting fees from Epi Excellence and Bohn Epidemiology.
SOURCE: Devore EE et al. J. Psychiatric Res. 2018. 104(08):e20180225.
Prenatal programming of the circadian and limbic systems might play a role in the odds of developing lifetime depression, a longitudinal study of almost 161,000 women shows.
“Our results could add support to an emerging hypothesis that perinatal photoperiod may influence depression risk,” wrote Elizabeth E. Devore of Brigham and Women’s Hospital, Boston, and her associates. “If replicated, ... these results could translate into safe and inexpensive light-related interventions for mothers and babies.”
In the study, which was published in the Journal of Psychiatric Research, Ms. Devore and her associates examined the influence of daylight exposure during maternal pregnancy and lifetime depression risk in the resulting offspring. They found that increased exposure to daylight during maternal pregnancy correlated with reduced lifetime risk of depression. wrote Ms. Devore, who also is affiliated with Harvard Medical School, Boston, and her associates.
The effects of daylight exposure were considered modest within the study population, but the authors emphasized that the finding would have much “larger effects at the population level,” given the occurrence of depression in the general population. They added that their findings reinforce a growing consensus that perinatal exposure to daylight could have the ability to influence the risk of developing a mood disorder.
The investigators accessed the Nurses’ Health Study (NHS) and the NHS II, established in 1976 and 1989, respectively, to assess risk factors for chronic conditions in female nurses. Both studies biennially surveyed demographic data on health, lifestyle, and medication use through mailed questionnaires. The first group was composed of 121,701 women aged 30-55 years; the second included 116,430 women aged 25-42 years. Altogether, 160,737 women born full-term were included in the study; 20,912 were excluded from the original survey group for not reporting depression status, as well as an additional 43,325 for not reporting their state of birth.
From data collected regarding participants’ day and state of birth, the researchers were able to estimate total length of daylight exposure during pregnancy using mathematical equations published by the National Oceanic and Atmospheric Administration.
Longitudinal coordinates pinpointing the center of population density for a participant’s birth state were used to identify the location of each participant during gestation. Using those assumptions, the authors were able to establish the two key data points evaluated for the study: total daylight exposure during pregnancy gestation, which was calculated by adding the lengths of all 280 days of the pregnancy, and extreme differences in daylight exposure that might have occurred throughout the pregnancy, which was measured by subtracting the longest and shortest day lengths during gestation.
The investigators paid particular attention to reported levels of depression, evidence of suicide, and personal characteristics and lifestyle factors, such as race, hair color, and early-life socioeconomic factors, including parents’ homeownership at the time of offspring birth; birth weight; history of having been breastfed; and parental occupation throughout the participant’s childhood.
Participants did not begin reporting antidepressant use for the first time until 1996; history of clinician-reported diagnoses of depression began in 2000, Ms. Devore and her associates reported.
Total daylight exposure during pregnancy was found to have “a borderline significant association with odds of lifetime depression,” but the trend was not convincing qualitatively, “and individual estimates across quintiles of exposure” were not considered to be statistically significant. In fact, the authors found that a larger difference between minimum and maximum daylight exposure throughout pregnancy significantly lowered lifetime risk of depression. Women with the largest differences in minimum/maximum daylight exposure during gestation had a 12% lower risk of depression in the NHS population. That reduced risk increased to 15% with the NHS II group. When both cohorts were combined, the reduced risk of depression was 13%.
When evaluating the role that daylight exposure plays with regard to trimester of pregnancy, the authors did note an association for the first trimester, but the association was much stronger for the second trimester; no association was found for the third trimester.
In terms of the effects of daylight exposure on incidence of suicide, no significant associations were found.
Because birth latitude and birth season were of key interest in this study, their relative contribution to total daylight exposure and extreme differences in exposure were considered. Citing observations from the National Health and Nutrition Examination Survey (NHANES), In this study, the authors found that women born in northern latitudes were found to have a 7% risk for lifetime depression, compared with women born in middle latitudes. Conversely, women born in southern latitudes had a 15% risk of depression. No association was found between birth season and incidence of depression, regardless of how season was defined.
The investigators cited several limitations. One is that they did not collect behavioral factors such as the time women spent outdoors. “Our method of exposure calculation relied on the assumption that participants’ mothers were exposed to sunlight from sunrise to sunset,” Ms. Devore and her associates wrote. This way of assessing exposure might have biased their results.
Nevertheless, they said, more studies are needed to examine the role that birth latitude and birth season might play with regard to depression.
The research for this study was supported by the National Institute of Mental Health and the Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health. Additional infrastructure support for the Nurses’ Health Studies was provided by the National Cancer Institute.
The authors declared no conflicts of interest. Ms. Devore has reported receiving consulting fees from Epi Excellence and Bohn Epidemiology.
SOURCE: Devore EE et al. J. Psychiatric Res. 2018. 104(08):e20180225.
Prenatal programming of the circadian and limbic systems might play a role in the odds of developing lifetime depression, a longitudinal study of almost 161,000 women shows.
“Our results could add support to an emerging hypothesis that perinatal photoperiod may influence depression risk,” wrote Elizabeth E. Devore of Brigham and Women’s Hospital, Boston, and her associates. “If replicated, ... these results could translate into safe and inexpensive light-related interventions for mothers and babies.”
In the study, which was published in the Journal of Psychiatric Research, Ms. Devore and her associates examined the influence of daylight exposure during maternal pregnancy and lifetime depression risk in the resulting offspring. They found that increased exposure to daylight during maternal pregnancy correlated with reduced lifetime risk of depression. wrote Ms. Devore, who also is affiliated with Harvard Medical School, Boston, and her associates.
The effects of daylight exposure were considered modest within the study population, but the authors emphasized that the finding would have much “larger effects at the population level,” given the occurrence of depression in the general population. They added that their findings reinforce a growing consensus that perinatal exposure to daylight could have the ability to influence the risk of developing a mood disorder.
The investigators accessed the Nurses’ Health Study (NHS) and the NHS II, established in 1976 and 1989, respectively, to assess risk factors for chronic conditions in female nurses. Both studies biennially surveyed demographic data on health, lifestyle, and medication use through mailed questionnaires. The first group was composed of 121,701 women aged 30-55 years; the second included 116,430 women aged 25-42 years. Altogether, 160,737 women born full-term were included in the study; 20,912 were excluded from the original survey group for not reporting depression status, as well as an additional 43,325 for not reporting their state of birth.
From data collected regarding participants’ day and state of birth, the researchers were able to estimate total length of daylight exposure during pregnancy using mathematical equations published by the National Oceanic and Atmospheric Administration.
Longitudinal coordinates pinpointing the center of population density for a participant’s birth state were used to identify the location of each participant during gestation. Using those assumptions, the authors were able to establish the two key data points evaluated for the study: total daylight exposure during pregnancy gestation, which was calculated by adding the lengths of all 280 days of the pregnancy, and extreme differences in daylight exposure that might have occurred throughout the pregnancy, which was measured by subtracting the longest and shortest day lengths during gestation.
The investigators paid particular attention to reported levels of depression, evidence of suicide, and personal characteristics and lifestyle factors, such as race, hair color, and early-life socioeconomic factors, including parents’ homeownership at the time of offspring birth; birth weight; history of having been breastfed; and parental occupation throughout the participant’s childhood.
Participants did not begin reporting antidepressant use for the first time until 1996; history of clinician-reported diagnoses of depression began in 2000, Ms. Devore and her associates reported.
Total daylight exposure during pregnancy was found to have “a borderline significant association with odds of lifetime depression,” but the trend was not convincing qualitatively, “and individual estimates across quintiles of exposure” were not considered to be statistically significant. In fact, the authors found that a larger difference between minimum and maximum daylight exposure throughout pregnancy significantly lowered lifetime risk of depression. Women with the largest differences in minimum/maximum daylight exposure during gestation had a 12% lower risk of depression in the NHS population. That reduced risk increased to 15% with the NHS II group. When both cohorts were combined, the reduced risk of depression was 13%.
When evaluating the role that daylight exposure plays with regard to trimester of pregnancy, the authors did note an association for the first trimester, but the association was much stronger for the second trimester; no association was found for the third trimester.
In terms of the effects of daylight exposure on incidence of suicide, no significant associations were found.
Because birth latitude and birth season were of key interest in this study, their relative contribution to total daylight exposure and extreme differences in exposure were considered. Citing observations from the National Health and Nutrition Examination Survey (NHANES), In this study, the authors found that women born in northern latitudes were found to have a 7% risk for lifetime depression, compared with women born in middle latitudes. Conversely, women born in southern latitudes had a 15% risk of depression. No association was found between birth season and incidence of depression, regardless of how season was defined.
The investigators cited several limitations. One is that they did not collect behavioral factors such as the time women spent outdoors. “Our method of exposure calculation relied on the assumption that participants’ mothers were exposed to sunlight from sunrise to sunset,” Ms. Devore and her associates wrote. This way of assessing exposure might have biased their results.
Nevertheless, they said, more studies are needed to examine the role that birth latitude and birth season might play with regard to depression.
The research for this study was supported by the National Institute of Mental Health and the Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health. Additional infrastructure support for the Nurses’ Health Studies was provided by the National Cancer Institute.
The authors declared no conflicts of interest. Ms. Devore has reported receiving consulting fees from Epi Excellence and Bohn Epidemiology.
SOURCE: Devore EE et al. J. Psychiatric Res. 2018. 104(08):e20180225.
FROM THE JOURNAL OF PSYCHIATRIC RESEARCH
Key clinical point: Future studies that are able to replicate findings have the potential to offer safe, inexpensive light-based treatments for both mothers and babies.
Major finding: Benefits of daytime light exposure are highest with second-trimester exposure.
Study details: Longitudinal cohort study of almost 161,000 women who were born full term.
Disclosures: The authors declared no conflicts of interest. Ms. Devore reported receiving consulting fees from Epi Excellence and Bohn Epidemiology.
Source: Devore EE et al. J Psychiatric Res. 2018.104(08):e20180225.
Facial exercises hastened the effects of botulinum toxin in small study
Performing of the injections by 1 day, a small, randomized study has shown.
The study addressed the lack of data regarding whether exercising treated muscles for several hours after injections helped “to enhance uptake” of botulinum toxin, said Murad Alam, MD, chief of cutaneous and aesthetic surgery and a professor of dermatology at Northwestern University, Chicago, and his coauthors.
“The results of this study suggest that a postinjection facial exercise regimen is a safe and effective method for achieving an earlier onset of clinical effect of botulinum toxin injections,” he and his coauthors concluded. The results were reported in the Journal of the American Academy of Dermatology.
The study enrolled 22 women, aged 27-66 years (mean age, 47 years) who received botulinum toxin injections for forehead and glabella dynamic rhytids. Following the injections, half of the women did the exercises for 4 hours and the other half avoided facial contractions for 4 hours. Exercises included raised motions of the forehead and scowls – such as knitting the brows – in three sets of 40 repetitions separated by 10 minutes, according to a Northwestern University press release. At 7 months, the women came back for treatment, and switched groups.
Two blinded dermatologists rated photos of forehead and glabella dynamic creases at baseline and on days 1,2,3,4,7, and 14 with the 5-point Carruthers’ Forehead Lines Grading Scale and the 4-point Gladys study group rating scale for glabellar frown lines. The women also assessed their own dynamic creases using a 7-point Subject Self-Evaluation Improvement Scale.
By day 3, ratings by dermatologists and patients of glabellar and forehead wrinkles were statistically significantly better for patients who had performed the exercises after the injections. When facial exercises followed the injections, women said they saw noticeable glabellar improvement by day 2 or 3, compared with day 3 or 4 among those who did not do facial exercises after the injections (P = .02).
“A significant advantage in the exercise group was detectable as early as day 3, at which point patients’ self-evaluation wrinkle scores increased by approximately twice as much in exercisers compared to non-exercisers,” the study authors noted.
But by 2 weeks, the effects of treatment were similar in both groups, and the effects of treatment lasted for a similar period of time with or without exercises.
“Expediting the time to noticeable benefit, even by one day, may be clinically significant for some patients,” the authors wrote. Exercises could be recommended only to those patients who need faster results “to avoid needless inconvenience,” they added.
The study was supported by research funds from the department of dermatology at Northwestern University. The authors had no relevant disclosures.
SOURCE: Alam M et al. J Am Acad Dermatol. 2018. doi: 10.1016/j.jaad.2018.10.013.
Performing of the injections by 1 day, a small, randomized study has shown.
The study addressed the lack of data regarding whether exercising treated muscles for several hours after injections helped “to enhance uptake” of botulinum toxin, said Murad Alam, MD, chief of cutaneous and aesthetic surgery and a professor of dermatology at Northwestern University, Chicago, and his coauthors.
“The results of this study suggest that a postinjection facial exercise regimen is a safe and effective method for achieving an earlier onset of clinical effect of botulinum toxin injections,” he and his coauthors concluded. The results were reported in the Journal of the American Academy of Dermatology.
The study enrolled 22 women, aged 27-66 years (mean age, 47 years) who received botulinum toxin injections for forehead and glabella dynamic rhytids. Following the injections, half of the women did the exercises for 4 hours and the other half avoided facial contractions for 4 hours. Exercises included raised motions of the forehead and scowls – such as knitting the brows – in three sets of 40 repetitions separated by 10 minutes, according to a Northwestern University press release. At 7 months, the women came back for treatment, and switched groups.
Two blinded dermatologists rated photos of forehead and glabella dynamic creases at baseline and on days 1,2,3,4,7, and 14 with the 5-point Carruthers’ Forehead Lines Grading Scale and the 4-point Gladys study group rating scale for glabellar frown lines. The women also assessed their own dynamic creases using a 7-point Subject Self-Evaluation Improvement Scale.
By day 3, ratings by dermatologists and patients of glabellar and forehead wrinkles were statistically significantly better for patients who had performed the exercises after the injections. When facial exercises followed the injections, women said they saw noticeable glabellar improvement by day 2 or 3, compared with day 3 or 4 among those who did not do facial exercises after the injections (P = .02).
“A significant advantage in the exercise group was detectable as early as day 3, at which point patients’ self-evaluation wrinkle scores increased by approximately twice as much in exercisers compared to non-exercisers,” the study authors noted.
But by 2 weeks, the effects of treatment were similar in both groups, and the effects of treatment lasted for a similar period of time with or without exercises.
“Expediting the time to noticeable benefit, even by one day, may be clinically significant for some patients,” the authors wrote. Exercises could be recommended only to those patients who need faster results “to avoid needless inconvenience,” they added.
The study was supported by research funds from the department of dermatology at Northwestern University. The authors had no relevant disclosures.
SOURCE: Alam M et al. J Am Acad Dermatol. 2018. doi: 10.1016/j.jaad.2018.10.013.
Performing of the injections by 1 day, a small, randomized study has shown.
The study addressed the lack of data regarding whether exercising treated muscles for several hours after injections helped “to enhance uptake” of botulinum toxin, said Murad Alam, MD, chief of cutaneous and aesthetic surgery and a professor of dermatology at Northwestern University, Chicago, and his coauthors.
“The results of this study suggest that a postinjection facial exercise regimen is a safe and effective method for achieving an earlier onset of clinical effect of botulinum toxin injections,” he and his coauthors concluded. The results were reported in the Journal of the American Academy of Dermatology.
The study enrolled 22 women, aged 27-66 years (mean age, 47 years) who received botulinum toxin injections for forehead and glabella dynamic rhytids. Following the injections, half of the women did the exercises for 4 hours and the other half avoided facial contractions for 4 hours. Exercises included raised motions of the forehead and scowls – such as knitting the brows – in three sets of 40 repetitions separated by 10 minutes, according to a Northwestern University press release. At 7 months, the women came back for treatment, and switched groups.
Two blinded dermatologists rated photos of forehead and glabella dynamic creases at baseline and on days 1,2,3,4,7, and 14 with the 5-point Carruthers’ Forehead Lines Grading Scale and the 4-point Gladys study group rating scale for glabellar frown lines. The women also assessed their own dynamic creases using a 7-point Subject Self-Evaluation Improvement Scale.
By day 3, ratings by dermatologists and patients of glabellar and forehead wrinkles were statistically significantly better for patients who had performed the exercises after the injections. When facial exercises followed the injections, women said they saw noticeable glabellar improvement by day 2 or 3, compared with day 3 or 4 among those who did not do facial exercises after the injections (P = .02).
“A significant advantage in the exercise group was detectable as early as day 3, at which point patients’ self-evaluation wrinkle scores increased by approximately twice as much in exercisers compared to non-exercisers,” the study authors noted.
But by 2 weeks, the effects of treatment were similar in both groups, and the effects of treatment lasted for a similar period of time with or without exercises.
“Expediting the time to noticeable benefit, even by one day, may be clinically significant for some patients,” the authors wrote. Exercises could be recommended only to those patients who need faster results “to avoid needless inconvenience,” they added.
The study was supported by research funds from the department of dermatology at Northwestern University. The authors had no relevant disclosures.
SOURCE: Alam M et al. J Am Acad Dermatol. 2018. doi: 10.1016/j.jaad.2018.10.013.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Key clinical point: Recommending facial muscle exercises after botulinum toxin injections to the forehead is now evidence based.
Major finding: Posttreatment facial exercise after botulinum toxin injections reduced the appearance of forehead wrinkles one day earlier.
Study details: A randomized, crossover clinical trial of 22 women treated with botulinum toxin for dynamic rhytids of the forehead and glabella.
Disclosures: The study was supported by research funds from the department of dermatology at Northwestern University. The authors had no relevant disclosures.
Source: Alam M et al. J Am Acad Dermatol. 2018. doi: 10.1016/j.jaad.2018.10.013.
Good news, bad news about HCV in kidney disease
SAN DIEGO – There’s good news and bad news about hepatitis C virus (HCV) in patients with chronic kidney disease (CKD): The new generation of drugs that cures HCV is effective in this population, but outbreaks of infection are still plaguing the nation’s dialysis clinics.
These perspectives came in a presentation about infections in CKD at Kidney Week 2018, sponsored by the American Society of Nephrology.
First, the good news about HCV. “Treatment is now feasible for all stages of chronic kidney disease,” said gastroenterologist Paul Martin, MD, of the University of Miami. “It was possible to achieve biological cure in 99% of patients, which is truly remarkable considering what a problem kidney patients were for hepatitis C until very recently.”
The key is to treat HCV with drug combinations that lower the risk of viral resistance. “These drugs are extremely well tolerated. They’re not like interferon or ribavirin,” he said, referring to a drug combo that was formerly used to treat HCV. “We can anticipate curing hepatitis C with a finite amount of therapy in virtually every patient we see, including those with kidney disease.”
In patients with CKD, all the new drugs are approved for glomerular filtration rates greater than 30 mL/min. Sofosbuvir (Sovaldi) is not approved for patients with a filtration rate under 30 mL/min, he said, but other options are available.
Ribavirin, he added, is no longer needed with current regimens.
Dr. Martin pointed to two studies that reveal the power of the new regimens against HCV in patients with CKD. One of the studies, a 2015 industry-funded report in the Lancet, found that “once-daily grazoprevir and elbasvir for 12 weeks had a low rate of adverse events and was effective in patients infected with HCV genotype 1 and stage 4-5 chronic kidney disease.” The other study, also funded by industry and published in 2017 in the New England Journal of Medicine, found that “treatment with glecaprevir and pibrentasvir for 12 weeks resulted in a high rate of sustained virologic response in patients with stage 4 or 5 chronic kidney disease and HCV infection.”
Meanwhile, there are signs that HCV treatment may boost survival in CKD patients on dialysis, Dr. Martin said.
In terms of bad news, Priti R. Patel, MD, MPH, a medical officer with the Centers for Disease Control and Prevention, warned that dialysis clinics are still seeing HCV outbreaks. “It’s a continuing problem,” she said. “What we hear about at the CDC is the tip of the iceberg.”
The CDC says it received word of 21 HCV outbreaks of two or more cases in dialysis clinics during 2008-2017. These affected 102 patients, and more than 3,000 patients were notified that they were at risk and should be screened.
One dialysis clinic in Philadelphia had 18 cases of HCV during 2008-2013; they were blamed on “multiple lapses in infection control ... including hand hygiene and glove use, vascular access care, medication preparation, cleaning, and disinfection.”
“There should be no more than one case that has to happen for a facility to detect that it has a problem and identify a solution,” Dr. Patel said.
Since acute HCV can appear without symptoms, every dialysis patients should be tested for HCV antibodies, she added. “If it’s positive, confirm it. If confirmed, they should be informed of their infection status and have an evaluation for treatment.”
Dr. Martin reported consulting for Bristol-Myers Squibb and AbbVie and receiving research funding from Gilead, Bristol-Myers Squibb, AbbVie, and Merck. Dr. Patel reported no disclosures.
SAN DIEGO – There’s good news and bad news about hepatitis C virus (HCV) in patients with chronic kidney disease (CKD): The new generation of drugs that cures HCV is effective in this population, but outbreaks of infection are still plaguing the nation’s dialysis clinics.
These perspectives came in a presentation about infections in CKD at Kidney Week 2018, sponsored by the American Society of Nephrology.
First, the good news about HCV. “Treatment is now feasible for all stages of chronic kidney disease,” said gastroenterologist Paul Martin, MD, of the University of Miami. “It was possible to achieve biological cure in 99% of patients, which is truly remarkable considering what a problem kidney patients were for hepatitis C until very recently.”
The key is to treat HCV with drug combinations that lower the risk of viral resistance. “These drugs are extremely well tolerated. They’re not like interferon or ribavirin,” he said, referring to a drug combo that was formerly used to treat HCV. “We can anticipate curing hepatitis C with a finite amount of therapy in virtually every patient we see, including those with kidney disease.”
In patients with CKD, all the new drugs are approved for glomerular filtration rates greater than 30 mL/min. Sofosbuvir (Sovaldi) is not approved for patients with a filtration rate under 30 mL/min, he said, but other options are available.
Ribavirin, he added, is no longer needed with current regimens.
Dr. Martin pointed to two studies that reveal the power of the new regimens against HCV in patients with CKD. One of the studies, a 2015 industry-funded report in the Lancet, found that “once-daily grazoprevir and elbasvir for 12 weeks had a low rate of adverse events and was effective in patients infected with HCV genotype 1 and stage 4-5 chronic kidney disease.” The other study, also funded by industry and published in 2017 in the New England Journal of Medicine, found that “treatment with glecaprevir and pibrentasvir for 12 weeks resulted in a high rate of sustained virologic response in patients with stage 4 or 5 chronic kidney disease and HCV infection.”
Meanwhile, there are signs that HCV treatment may boost survival in CKD patients on dialysis, Dr. Martin said.
In terms of bad news, Priti R. Patel, MD, MPH, a medical officer with the Centers for Disease Control and Prevention, warned that dialysis clinics are still seeing HCV outbreaks. “It’s a continuing problem,” she said. “What we hear about at the CDC is the tip of the iceberg.”
The CDC says it received word of 21 HCV outbreaks of two or more cases in dialysis clinics during 2008-2017. These affected 102 patients, and more than 3,000 patients were notified that they were at risk and should be screened.
One dialysis clinic in Philadelphia had 18 cases of HCV during 2008-2013; they were blamed on “multiple lapses in infection control ... including hand hygiene and glove use, vascular access care, medication preparation, cleaning, and disinfection.”
“There should be no more than one case that has to happen for a facility to detect that it has a problem and identify a solution,” Dr. Patel said.
Since acute HCV can appear without symptoms, every dialysis patients should be tested for HCV antibodies, she added. “If it’s positive, confirm it. If confirmed, they should be informed of their infection status and have an evaluation for treatment.”
Dr. Martin reported consulting for Bristol-Myers Squibb and AbbVie and receiving research funding from Gilead, Bristol-Myers Squibb, AbbVie, and Merck. Dr. Patel reported no disclosures.
SAN DIEGO – There’s good news and bad news about hepatitis C virus (HCV) in patients with chronic kidney disease (CKD): The new generation of drugs that cures HCV is effective in this population, but outbreaks of infection are still plaguing the nation’s dialysis clinics.
These perspectives came in a presentation about infections in CKD at Kidney Week 2018, sponsored by the American Society of Nephrology.
First, the good news about HCV. “Treatment is now feasible for all stages of chronic kidney disease,” said gastroenterologist Paul Martin, MD, of the University of Miami. “It was possible to achieve biological cure in 99% of patients, which is truly remarkable considering what a problem kidney patients were for hepatitis C until very recently.”
The key is to treat HCV with drug combinations that lower the risk of viral resistance. “These drugs are extremely well tolerated. They’re not like interferon or ribavirin,” he said, referring to a drug combo that was formerly used to treat HCV. “We can anticipate curing hepatitis C with a finite amount of therapy in virtually every patient we see, including those with kidney disease.”
In patients with CKD, all the new drugs are approved for glomerular filtration rates greater than 30 mL/min. Sofosbuvir (Sovaldi) is not approved for patients with a filtration rate under 30 mL/min, he said, but other options are available.
Ribavirin, he added, is no longer needed with current regimens.
Dr. Martin pointed to two studies that reveal the power of the new regimens against HCV in patients with CKD. One of the studies, a 2015 industry-funded report in the Lancet, found that “once-daily grazoprevir and elbasvir for 12 weeks had a low rate of adverse events and was effective in patients infected with HCV genotype 1 and stage 4-5 chronic kidney disease.” The other study, also funded by industry and published in 2017 in the New England Journal of Medicine, found that “treatment with glecaprevir and pibrentasvir for 12 weeks resulted in a high rate of sustained virologic response in patients with stage 4 or 5 chronic kidney disease and HCV infection.”
Meanwhile, there are signs that HCV treatment may boost survival in CKD patients on dialysis, Dr. Martin said.
In terms of bad news, Priti R. Patel, MD, MPH, a medical officer with the Centers for Disease Control and Prevention, warned that dialysis clinics are still seeing HCV outbreaks. “It’s a continuing problem,” she said. “What we hear about at the CDC is the tip of the iceberg.”
The CDC says it received word of 21 HCV outbreaks of two or more cases in dialysis clinics during 2008-2017. These affected 102 patients, and more than 3,000 patients were notified that they were at risk and should be screened.
One dialysis clinic in Philadelphia had 18 cases of HCV during 2008-2013; they were blamed on “multiple lapses in infection control ... including hand hygiene and glove use, vascular access care, medication preparation, cleaning, and disinfection.”
“There should be no more than one case that has to happen for a facility to detect that it has a problem and identify a solution,” Dr. Patel said.
Since acute HCV can appear without symptoms, every dialysis patients should be tested for HCV antibodies, she added. “If it’s positive, confirm it. If confirmed, they should be informed of their infection status and have an evaluation for treatment.”
Dr. Martin reported consulting for Bristol-Myers Squibb and AbbVie and receiving research funding from Gilead, Bristol-Myers Squibb, AbbVie, and Merck. Dr. Patel reported no disclosures.
EXPERT ANALYSIS FROM KIDNEY WEEK 2018
FDA approves Yupelri for COPD maintenance therapy
The Food and Drug Administration has approved Yupelri (revefenacin) for maintenance therapy of patients with chronic obstructive pulmonary disease (COPD).
Revefenacin is a long-acting muscarinic antagonist aimed at improving the lung function of patients with COPD. Yupelri is an inhalation solution administered once daily through a standard jet nebulizer.
The most common adverse events associated with Yupelri are cough, nasopharyngitis, upper respiratory tract infection, headache, and back pain. Patients receiving other anticholinergic-containing drugs or OATP1B1 and OATP1B3 inhibitors should not receive Yupelri.
“Patients should also be alert for signs and symptoms of acute narrow-angle glaucoma [e.g., eye pain or discomfort, blurred vision, visual changes]. Patients should consult a healthcare professional immediately if any of these signs or symptoms develop,” the FDA said in the press release.
The expanded label for Yupelri can be found on the FDA website.
The Food and Drug Administration has approved Yupelri (revefenacin) for maintenance therapy of patients with chronic obstructive pulmonary disease (COPD).
Revefenacin is a long-acting muscarinic antagonist aimed at improving the lung function of patients with COPD. Yupelri is an inhalation solution administered once daily through a standard jet nebulizer.
The most common adverse events associated with Yupelri are cough, nasopharyngitis, upper respiratory tract infection, headache, and back pain. Patients receiving other anticholinergic-containing drugs or OATP1B1 and OATP1B3 inhibitors should not receive Yupelri.
“Patients should also be alert for signs and symptoms of acute narrow-angle glaucoma [e.g., eye pain or discomfort, blurred vision, visual changes]. Patients should consult a healthcare professional immediately if any of these signs or symptoms develop,” the FDA said in the press release.
The expanded label for Yupelri can be found on the FDA website.
The Food and Drug Administration has approved Yupelri (revefenacin) for maintenance therapy of patients with chronic obstructive pulmonary disease (COPD).
Revefenacin is a long-acting muscarinic antagonist aimed at improving the lung function of patients with COPD. Yupelri is an inhalation solution administered once daily through a standard jet nebulizer.
The most common adverse events associated with Yupelri are cough, nasopharyngitis, upper respiratory tract infection, headache, and back pain. Patients receiving other anticholinergic-containing drugs or OATP1B1 and OATP1B3 inhibitors should not receive Yupelri.
“Patients should also be alert for signs and symptoms of acute narrow-angle glaucoma [e.g., eye pain or discomfort, blurred vision, visual changes]. Patients should consult a healthcare professional immediately if any of these signs or symptoms develop,” the FDA said in the press release.
The expanded label for Yupelri can be found on the FDA website.
Lower glucose targets show improved mortality in cardiac patients
Tighter glucose control while minimizing the risk of severe hypoglycemia is associated with lower mortality among critically ill cardiac patents, new research suggests.
Researchers reported in CHEST on the outcomes of a multicenter retrospective cohort study in 1,809 adults in cardiac ICUs. Patients were treated either to a blood glucose target of 80-110 mg/dL or 90-140 mg/dL, based on the clinician’s preference, but using a computerized ICU insulin infusion protocol that the authors said had resulted in low rates of severe hypoglycemia.
The study found patients treated to the 80-110 mg/dL blood glucose target had a significantly lower unadjusted 30-day mortality compared to patients treated to the 90-140 mg/dL target (4.3% vs. 9.2%; P less than .001). The lower mortality in the lower target group was evident among both diabetic (4.7% vs. 12.9%; P less than .001) and nondiabetic patients (4.1% vs. 7.4%; P = .02).
Researchers also saw that unadjusted 30-day mortality increased with increasing median glucose levels; 5.5% in patients with a blood glucose of 70-110 mg/dL, 8.3% mortality in those with blood glucose levels of 141-180 mg/dL, and 25% in those with a blood glucose level higher than 180 mg/dL.
Patients treated to the 80-110 mg/dL blood glucose target were more likely to experience an episode of moderate hypoglycemia, compared with those in the higher target group (18.6% vs. 8.3%; P less than .001). However, the rates of severe hypoglycemia were low in both groups, and the difference between the low and high target groups did not reach statistical significance (1.16% vs. 0.35%; P = .051).
The authors did note that patients whose blood glucose dropped below 60 mg/dL showed increased mortality, regardless of what target they was set for them. The 30-day unadjusted mortality in these patients was 15%, compared with 5.2% for patients in either group who did not experience a blood glucose level below 60 mg/dL.
“Our results further the discussion about the appropriate BG [blood glucose] target in the critically ill because they suggest that the BG target and severe hypoglycemia effects can be separated,” wrote Andrew M. Hersh, MD, of the division of pulmonary and critical care at San Antonio Military Medical Center, and his coauthors.
But they said the large differences in mortality seen between the two treatment targets should be interpreted with caution, as it was difficult to attribute that difference solely to an 18 mg/dL difference in blood glucose treatment targets.
“While we attempted to capture factors that influenced clinician choice, and while our model successfully achieved balance, suggesting that residual confounding was minimized, we suspect that some of the mortality signal may be attributable to residual confounding,” they wrote.
Another explanation could be that hypoglycemia was an ‘epiphenomenon’ of multiorgan failure, as some studies have found that both spontaneous and iatrogenic hypoglycemia were independently associated with mortality. “However, given the very-low rates of severe hypoglycemia found in both groups it is unlikely that this was a main driver of the mortality difference found,” the investigators wrote.
The majority of patients in the study had been admitted to the hospital for chest pain or acute coronary syndrome (43.3%), while 31.9% were admitted for cardiothoracic surgery, 6.8% for heart failure including cardiogenic shock, and 6% for vascular surgery.
The authors commented that a safe and reliable protocol for intensive insulin therapy, with high clinician compliance, could be the key to realizing its benefits, and could be aided by recent advances such as closed-loop insulin delivery systems.
They also stressed that their results did not support a rejection of current guidelines and instead called for large randomized, clinical trials to find a balance between benefits and harms of intensive insulin therapy.
“Instead our analysis suggests that trials such as NICE-SUGAR, and the conclusion they drew, may have been accurate only in the setting of technologies, which led to high rates of severe hypoglycemia.”
No conflicts of interest were declared.
After the multicenter NICE-SUGAR trial showed higher 90-day mortality in patients treated with intensive insulin therapy to lower blood glucose targets, compared with more moderate targets, enthusiasm has waned for tighter blood glucose control, James S. Krinsley, MD, argued in an editorial accompanying the study (CHEST 2018; 154[5]:1004-5). But the assumption of a “one-size-fits-all” approach to glucose control in the critically ill is a potential flaw of randomized clinical trials, he noted, and some patients may be better suited to tighter control than others. This study has shown that standardized protocols, including frequent measurement of blood glucose, can safely achieve tight blood glucose control in the ICU with low rates of hypoglycemia. If these findings are confirmed in larger multicenter clinical trials, it should prompt a rethink of blood glucose targets in the critically ill, he concluded.
Dr. Krinsley is director of critical care at Stamford (Conn.) Hospital and clinical professor of medicine at the Columbia University College of Physicians and Surgeons, New York. He declared consultancies or advisory board positions with Edwards Life Sciences, Medtronic, OptiScan Biomedical, and Roche Diagnostics.
After the multicenter NICE-SUGAR trial showed higher 90-day mortality in patients treated with intensive insulin therapy to lower blood glucose targets, compared with more moderate targets, enthusiasm has waned for tighter blood glucose control, James S. Krinsley, MD, argued in an editorial accompanying the study (CHEST 2018; 154[5]:1004-5). But the assumption of a “one-size-fits-all” approach to glucose control in the critically ill is a potential flaw of randomized clinical trials, he noted, and some patients may be better suited to tighter control than others. This study has shown that standardized protocols, including frequent measurement of blood glucose, can safely achieve tight blood glucose control in the ICU with low rates of hypoglycemia. If these findings are confirmed in larger multicenter clinical trials, it should prompt a rethink of blood glucose targets in the critically ill, he concluded.
Dr. Krinsley is director of critical care at Stamford (Conn.) Hospital and clinical professor of medicine at the Columbia University College of Physicians and Surgeons, New York. He declared consultancies or advisory board positions with Edwards Life Sciences, Medtronic, OptiScan Biomedical, and Roche Diagnostics.
After the multicenter NICE-SUGAR trial showed higher 90-day mortality in patients treated with intensive insulin therapy to lower blood glucose targets, compared with more moderate targets, enthusiasm has waned for tighter blood glucose control, James S. Krinsley, MD, argued in an editorial accompanying the study (CHEST 2018; 154[5]:1004-5). But the assumption of a “one-size-fits-all” approach to glucose control in the critically ill is a potential flaw of randomized clinical trials, he noted, and some patients may be better suited to tighter control than others. This study has shown that standardized protocols, including frequent measurement of blood glucose, can safely achieve tight blood glucose control in the ICU with low rates of hypoglycemia. If these findings are confirmed in larger multicenter clinical trials, it should prompt a rethink of blood glucose targets in the critically ill, he concluded.
Dr. Krinsley is director of critical care at Stamford (Conn.) Hospital and clinical professor of medicine at the Columbia University College of Physicians and Surgeons, New York. He declared consultancies or advisory board positions with Edwards Life Sciences, Medtronic, OptiScan Biomedical, and Roche Diagnostics.
Tighter glucose control while minimizing the risk of severe hypoglycemia is associated with lower mortality among critically ill cardiac patents, new research suggests.
Researchers reported in CHEST on the outcomes of a multicenter retrospective cohort study in 1,809 adults in cardiac ICUs. Patients were treated either to a blood glucose target of 80-110 mg/dL or 90-140 mg/dL, based on the clinician’s preference, but using a computerized ICU insulin infusion protocol that the authors said had resulted in low rates of severe hypoglycemia.
The study found patients treated to the 80-110 mg/dL blood glucose target had a significantly lower unadjusted 30-day mortality compared to patients treated to the 90-140 mg/dL target (4.3% vs. 9.2%; P less than .001). The lower mortality in the lower target group was evident among both diabetic (4.7% vs. 12.9%; P less than .001) and nondiabetic patients (4.1% vs. 7.4%; P = .02).
Researchers also saw that unadjusted 30-day mortality increased with increasing median glucose levels; 5.5% in patients with a blood glucose of 70-110 mg/dL, 8.3% mortality in those with blood glucose levels of 141-180 mg/dL, and 25% in those with a blood glucose level higher than 180 mg/dL.
Patients treated to the 80-110 mg/dL blood glucose target were more likely to experience an episode of moderate hypoglycemia, compared with those in the higher target group (18.6% vs. 8.3%; P less than .001). However, the rates of severe hypoglycemia were low in both groups, and the difference between the low and high target groups did not reach statistical significance (1.16% vs. 0.35%; P = .051).
The authors did note that patients whose blood glucose dropped below 60 mg/dL showed increased mortality, regardless of what target they was set for them. The 30-day unadjusted mortality in these patients was 15%, compared with 5.2% for patients in either group who did not experience a blood glucose level below 60 mg/dL.
“Our results further the discussion about the appropriate BG [blood glucose] target in the critically ill because they suggest that the BG target and severe hypoglycemia effects can be separated,” wrote Andrew M. Hersh, MD, of the division of pulmonary and critical care at San Antonio Military Medical Center, and his coauthors.
But they said the large differences in mortality seen between the two treatment targets should be interpreted with caution, as it was difficult to attribute that difference solely to an 18 mg/dL difference in blood glucose treatment targets.
“While we attempted to capture factors that influenced clinician choice, and while our model successfully achieved balance, suggesting that residual confounding was minimized, we suspect that some of the mortality signal may be attributable to residual confounding,” they wrote.
Another explanation could be that hypoglycemia was an ‘epiphenomenon’ of multiorgan failure, as some studies have found that both spontaneous and iatrogenic hypoglycemia were independently associated with mortality. “However, given the very-low rates of severe hypoglycemia found in both groups it is unlikely that this was a main driver of the mortality difference found,” the investigators wrote.
The majority of patients in the study had been admitted to the hospital for chest pain or acute coronary syndrome (43.3%), while 31.9% were admitted for cardiothoracic surgery, 6.8% for heart failure including cardiogenic shock, and 6% for vascular surgery.
The authors commented that a safe and reliable protocol for intensive insulin therapy, with high clinician compliance, could be the key to realizing its benefits, and could be aided by recent advances such as closed-loop insulin delivery systems.
They also stressed that their results did not support a rejection of current guidelines and instead called for large randomized, clinical trials to find a balance between benefits and harms of intensive insulin therapy.
“Instead our analysis suggests that trials such as NICE-SUGAR, and the conclusion they drew, may have been accurate only in the setting of technologies, which led to high rates of severe hypoglycemia.”
No conflicts of interest were declared.
Tighter glucose control while minimizing the risk of severe hypoglycemia is associated with lower mortality among critically ill cardiac patents, new research suggests.
Researchers reported in CHEST on the outcomes of a multicenter retrospective cohort study in 1,809 adults in cardiac ICUs. Patients were treated either to a blood glucose target of 80-110 mg/dL or 90-140 mg/dL, based on the clinician’s preference, but using a computerized ICU insulin infusion protocol that the authors said had resulted in low rates of severe hypoglycemia.
The study found patients treated to the 80-110 mg/dL blood glucose target had a significantly lower unadjusted 30-day mortality compared to patients treated to the 90-140 mg/dL target (4.3% vs. 9.2%; P less than .001). The lower mortality in the lower target group was evident among both diabetic (4.7% vs. 12.9%; P less than .001) and nondiabetic patients (4.1% vs. 7.4%; P = .02).
Researchers also saw that unadjusted 30-day mortality increased with increasing median glucose levels; 5.5% in patients with a blood glucose of 70-110 mg/dL, 8.3% mortality in those with blood glucose levels of 141-180 mg/dL, and 25% in those with a blood glucose level higher than 180 mg/dL.
Patients treated to the 80-110 mg/dL blood glucose target were more likely to experience an episode of moderate hypoglycemia, compared with those in the higher target group (18.6% vs. 8.3%; P less than .001). However, the rates of severe hypoglycemia were low in both groups, and the difference between the low and high target groups did not reach statistical significance (1.16% vs. 0.35%; P = .051).
The authors did note that patients whose blood glucose dropped below 60 mg/dL showed increased mortality, regardless of what target they was set for them. The 30-day unadjusted mortality in these patients was 15%, compared with 5.2% for patients in either group who did not experience a blood glucose level below 60 mg/dL.
“Our results further the discussion about the appropriate BG [blood glucose] target in the critically ill because they suggest that the BG target and severe hypoglycemia effects can be separated,” wrote Andrew M. Hersh, MD, of the division of pulmonary and critical care at San Antonio Military Medical Center, and his coauthors.
But they said the large differences in mortality seen between the two treatment targets should be interpreted with caution, as it was difficult to attribute that difference solely to an 18 mg/dL difference in blood glucose treatment targets.
“While we attempted to capture factors that influenced clinician choice, and while our model successfully achieved balance, suggesting that residual confounding was minimized, we suspect that some of the mortality signal may be attributable to residual confounding,” they wrote.
Another explanation could be that hypoglycemia was an ‘epiphenomenon’ of multiorgan failure, as some studies have found that both spontaneous and iatrogenic hypoglycemia were independently associated with mortality. “However, given the very-low rates of severe hypoglycemia found in both groups it is unlikely that this was a main driver of the mortality difference found,” the investigators wrote.
The majority of patients in the study had been admitted to the hospital for chest pain or acute coronary syndrome (43.3%), while 31.9% were admitted for cardiothoracic surgery, 6.8% for heart failure including cardiogenic shock, and 6% for vascular surgery.
The authors commented that a safe and reliable protocol for intensive insulin therapy, with high clinician compliance, could be the key to realizing its benefits, and could be aided by recent advances such as closed-loop insulin delivery systems.
They also stressed that their results did not support a rejection of current guidelines and instead called for large randomized, clinical trials to find a balance between benefits and harms of intensive insulin therapy.
“Instead our analysis suggests that trials such as NICE-SUGAR, and the conclusion they drew, may have been accurate only in the setting of technologies, which led to high rates of severe hypoglycemia.”
No conflicts of interest were declared.
FROM CHEST
Key clinical point: Tighter blood glucose control may reduce 30-day mortality in critically ill cardiac patients.
Major finding: Unadjusted 30-day mortality increased with increasing median glucose levels; 5.5% in patients with a blood glucose between 70 and 110 mg/dL, and 25% in those above 180 mg/dL.
Study details: A retrospective cohort study in 1,809 adults in cardiac intensive care units.
Disclosures: No conflicts of interest were declared.
Source: Hersh AM et al. Chest. 2018 Nov;154(5):1044-51.