User login
Rivaroxaban’s single daily dose may lead to higher bleeding risk than other DOACs
The results, which were published in the Annals of Internal Medicine, could help guide DOAC selection for high-risk groups with a prior history of peptic ulcer disease or major GI bleeding, said lead study authors Arnar Bragi Ingason, MD and Einar S. Björnsson, MD, PhD, in an email.
DOACs treat conditions such as atrial fibrillation, venous thromboembolism, and ischemic stroke and are known to cause GI bleeding. Previous studies have suggested that rivaroxaban poses a higher GI-bleeding risk than other DOACs.
These studies, which used large administrative databases, “had an inherent risk of selection bias due to insurance status, age, and comorbidities due to their origin from insurance/administrative databases. In addition, they lacked phenotypic details on GI bleeding events,” said Dr. Björnsson and Dr. Ingason, who are both of Landspitali University Hospital, Reykjavik, Iceland,
Daily dosage may exacerbate risk
Rivaroxaban is administered as a single daily dose, compared with apixaban’s and dabigatran’s twice-daily regimens. “We hypothesized that this may lead to a greater variance in drug plasma concentration, making these patients more susceptible to GI bleeding,” the lead authors said.
Using data from the Icelandic Medicine Registry, a national database of outpatient prescription information, they compared rates of GI bleeding among new users of apixaban, dabigatran, and rivaroxaban from 2014 to 2019. Overall, 5,868 patients receiving one of the DOACs took part in the study. Among these participants, 3,217 received rivaroxaban, 2,157 received apixaban, and 494 received dabigatran. The researchers used inverse probability weighting, Kaplan–Meier survival estimates, and Cox regression to compare GI bleeding.
Compared with dabigatran, rivaroxaban was associated with a 63%-104% higher overall risk for GI bleeding and 39%-95% higher risk for major GI bleeding. Rivaroxaban also had a 40%-42% higher overall risk for GI bleeding and 49%-50% higher risk for major GI bleeding, compared with apixaban.
The investigators were surprised by the low rate of upper GI bleeding for dabigatran, compared with the other two drugs. “However, these results must be interpreted in the context that the dabigatran group was relatively small,” said Dr. Björnsson and Dr. Ingason via email.
Overall, the study cohort was small, compared with previous registry studies.
Investigators also did not account for account for socioeconomic status or lifestyle factors, such as alcohol consumption or smoking. “However, because the cost of all DOACs is similar in Iceland, selection bias due to socioeconomic status is unlikely,” the investigators reported in their paper. “We are currently working on comparing the rates of thromboembolisms and overall major bleeding events between the drugs,” the lead authors said.
Clinicians should consider location of bleeding
Though retrospective, the study by Ingason et. al. “is likely as close as is feasible to a randomized trial as is possible,” said Don C. Rockey, MD, a professor of medicine at the Medical University of South Carolina, Charleston, in an interview.
“From the clinician’s perspective, it is important to take away that there may be differences among the DOACs in terms of where in the GI tract the bleeding occurs,” said Dr. Rockey. In the study, the greatest differences appeared to be in the upper GI tract, with rivaroxaban outpacing apixaban and dabigatran. In patients who are at risk for upper GI bleeding, it may be reasonable to consider use of dabigatran or apixaban, he suggested.
“A limitation of the study is that it is likely underpowered overall,” said Dr. Rockey. It also wasn’t clear how many deaths occurred either directly from GI bleeding or as a complication of GI bleeding, he said.The study also didn’t differentiate major bleeding among DOACs specifically in the upper or lower GI tract, Dr. Rockey added.
Other studies yield similar results
Dr. Ingason and Dr. Björnsson said their work complements previous studies, and Neena S. Abraham, MD, MSc , who has conducted a similar investigation to the new study, agreed with that statement.
Data from the last 4 years overwhelmingly show that rivaroxaban is most likely to cause GI bleeding, said Dr. Abraham, professor of medicine and a consultant with Mayo Clinic’s division of gastroenterology and hepatology, in an interview.
A comparative safety study Dr. Abraham coauthored in 2017 of rivaroxaban, apixaban, and dabigatran in a much larger U.S. cohort of 372,380 patients revealed that rivaroxaban had the worst GI bleeding profile. Apixaban was 66% safer than rivaroxaban and 64% safer than dabigatran to prevent gastrointestinal bleeding.
“I believe our group was the first to conduct this study and show clinically significant differences in GI safety of the available direct oral anticoagulants,” she said. Other investigators have since published similar results, and the topic of the new study needs no further investigation, according to Dr. Abraham.
“It is time for physicians to choose a better choice when prescribing a direct oral anticoagulant to their atrial fibrillation patients, and that choice is not rivaroxaban,” she said.
The Icelandic Centre for Research and the Landspítali University Hospital Research Fund provided funds for this study. Dr. Ingason, Dr. Björnsson, Dr. Rockey, and Dr. Abraham reported no disclosures.
The results, which were published in the Annals of Internal Medicine, could help guide DOAC selection for high-risk groups with a prior history of peptic ulcer disease or major GI bleeding, said lead study authors Arnar Bragi Ingason, MD and Einar S. Björnsson, MD, PhD, in an email.
DOACs treat conditions such as atrial fibrillation, venous thromboembolism, and ischemic stroke and are known to cause GI bleeding. Previous studies have suggested that rivaroxaban poses a higher GI-bleeding risk than other DOACs.
These studies, which used large administrative databases, “had an inherent risk of selection bias due to insurance status, age, and comorbidities due to their origin from insurance/administrative databases. In addition, they lacked phenotypic details on GI bleeding events,” said Dr. Björnsson and Dr. Ingason, who are both of Landspitali University Hospital, Reykjavik, Iceland,
Daily dosage may exacerbate risk
Rivaroxaban is administered as a single daily dose, compared with apixaban’s and dabigatran’s twice-daily regimens. “We hypothesized that this may lead to a greater variance in drug plasma concentration, making these patients more susceptible to GI bleeding,” the lead authors said.
Using data from the Icelandic Medicine Registry, a national database of outpatient prescription information, they compared rates of GI bleeding among new users of apixaban, dabigatran, and rivaroxaban from 2014 to 2019. Overall, 5,868 patients receiving one of the DOACs took part in the study. Among these participants, 3,217 received rivaroxaban, 2,157 received apixaban, and 494 received dabigatran. The researchers used inverse probability weighting, Kaplan–Meier survival estimates, and Cox regression to compare GI bleeding.
Compared with dabigatran, rivaroxaban was associated with a 63%-104% higher overall risk for GI bleeding and 39%-95% higher risk for major GI bleeding. Rivaroxaban also had a 40%-42% higher overall risk for GI bleeding and 49%-50% higher risk for major GI bleeding, compared with apixaban.
The investigators were surprised by the low rate of upper GI bleeding for dabigatran, compared with the other two drugs. “However, these results must be interpreted in the context that the dabigatran group was relatively small,” said Dr. Björnsson and Dr. Ingason via email.
Overall, the study cohort was small, compared with previous registry studies.
Investigators also did not account for account for socioeconomic status or lifestyle factors, such as alcohol consumption or smoking. “However, because the cost of all DOACs is similar in Iceland, selection bias due to socioeconomic status is unlikely,” the investigators reported in their paper. “We are currently working on comparing the rates of thromboembolisms and overall major bleeding events between the drugs,” the lead authors said.
Clinicians should consider location of bleeding
Though retrospective, the study by Ingason et. al. “is likely as close as is feasible to a randomized trial as is possible,” said Don C. Rockey, MD, a professor of medicine at the Medical University of South Carolina, Charleston, in an interview.
“From the clinician’s perspective, it is important to take away that there may be differences among the DOACs in terms of where in the GI tract the bleeding occurs,” said Dr. Rockey. In the study, the greatest differences appeared to be in the upper GI tract, with rivaroxaban outpacing apixaban and dabigatran. In patients who are at risk for upper GI bleeding, it may be reasonable to consider use of dabigatran or apixaban, he suggested.
“A limitation of the study is that it is likely underpowered overall,” said Dr. Rockey. It also wasn’t clear how many deaths occurred either directly from GI bleeding or as a complication of GI bleeding, he said.The study also didn’t differentiate major bleeding among DOACs specifically in the upper or lower GI tract, Dr. Rockey added.
Other studies yield similar results
Dr. Ingason and Dr. Björnsson said their work complements previous studies, and Neena S. Abraham, MD, MSc , who has conducted a similar investigation to the new study, agreed with that statement.
Data from the last 4 years overwhelmingly show that rivaroxaban is most likely to cause GI bleeding, said Dr. Abraham, professor of medicine and a consultant with Mayo Clinic’s division of gastroenterology and hepatology, in an interview.
A comparative safety study Dr. Abraham coauthored in 2017 of rivaroxaban, apixaban, and dabigatran in a much larger U.S. cohort of 372,380 patients revealed that rivaroxaban had the worst GI bleeding profile. Apixaban was 66% safer than rivaroxaban and 64% safer than dabigatran to prevent gastrointestinal bleeding.
“I believe our group was the first to conduct this study and show clinically significant differences in GI safety of the available direct oral anticoagulants,” she said. Other investigators have since published similar results, and the topic of the new study needs no further investigation, according to Dr. Abraham.
“It is time for physicians to choose a better choice when prescribing a direct oral anticoagulant to their atrial fibrillation patients, and that choice is not rivaroxaban,” she said.
The Icelandic Centre for Research and the Landspítali University Hospital Research Fund provided funds for this study. Dr. Ingason, Dr. Björnsson, Dr. Rockey, and Dr. Abraham reported no disclosures.
The results, which were published in the Annals of Internal Medicine, could help guide DOAC selection for high-risk groups with a prior history of peptic ulcer disease or major GI bleeding, said lead study authors Arnar Bragi Ingason, MD and Einar S. Björnsson, MD, PhD, in an email.
DOACs treat conditions such as atrial fibrillation, venous thromboembolism, and ischemic stroke and are known to cause GI bleeding. Previous studies have suggested that rivaroxaban poses a higher GI-bleeding risk than other DOACs.
These studies, which used large administrative databases, “had an inherent risk of selection bias due to insurance status, age, and comorbidities due to their origin from insurance/administrative databases. In addition, they lacked phenotypic details on GI bleeding events,” said Dr. Björnsson and Dr. Ingason, who are both of Landspitali University Hospital, Reykjavik, Iceland,
Daily dosage may exacerbate risk
Rivaroxaban is administered as a single daily dose, compared with apixaban’s and dabigatran’s twice-daily regimens. “We hypothesized that this may lead to a greater variance in drug plasma concentration, making these patients more susceptible to GI bleeding,” the lead authors said.
Using data from the Icelandic Medicine Registry, a national database of outpatient prescription information, they compared rates of GI bleeding among new users of apixaban, dabigatran, and rivaroxaban from 2014 to 2019. Overall, 5,868 patients receiving one of the DOACs took part in the study. Among these participants, 3,217 received rivaroxaban, 2,157 received apixaban, and 494 received dabigatran. The researchers used inverse probability weighting, Kaplan–Meier survival estimates, and Cox regression to compare GI bleeding.
Compared with dabigatran, rivaroxaban was associated with a 63%-104% higher overall risk for GI bleeding and 39%-95% higher risk for major GI bleeding. Rivaroxaban also had a 40%-42% higher overall risk for GI bleeding and 49%-50% higher risk for major GI bleeding, compared with apixaban.
The investigators were surprised by the low rate of upper GI bleeding for dabigatran, compared with the other two drugs. “However, these results must be interpreted in the context that the dabigatran group was relatively small,” said Dr. Björnsson and Dr. Ingason via email.
Overall, the study cohort was small, compared with previous registry studies.
Investigators also did not account for account for socioeconomic status or lifestyle factors, such as alcohol consumption or smoking. “However, because the cost of all DOACs is similar in Iceland, selection bias due to socioeconomic status is unlikely,” the investigators reported in their paper. “We are currently working on comparing the rates of thromboembolisms and overall major bleeding events between the drugs,” the lead authors said.
Clinicians should consider location of bleeding
Though retrospective, the study by Ingason et. al. “is likely as close as is feasible to a randomized trial as is possible,” said Don C. Rockey, MD, a professor of medicine at the Medical University of South Carolina, Charleston, in an interview.
“From the clinician’s perspective, it is important to take away that there may be differences among the DOACs in terms of where in the GI tract the bleeding occurs,” said Dr. Rockey. In the study, the greatest differences appeared to be in the upper GI tract, with rivaroxaban outpacing apixaban and dabigatran. In patients who are at risk for upper GI bleeding, it may be reasonable to consider use of dabigatran or apixaban, he suggested.
“A limitation of the study is that it is likely underpowered overall,” said Dr. Rockey. It also wasn’t clear how many deaths occurred either directly from GI bleeding or as a complication of GI bleeding, he said.The study also didn’t differentiate major bleeding among DOACs specifically in the upper or lower GI tract, Dr. Rockey added.
Other studies yield similar results
Dr. Ingason and Dr. Björnsson said their work complements previous studies, and Neena S. Abraham, MD, MSc , who has conducted a similar investigation to the new study, agreed with that statement.
Data from the last 4 years overwhelmingly show that rivaroxaban is most likely to cause GI bleeding, said Dr. Abraham, professor of medicine and a consultant with Mayo Clinic’s division of gastroenterology and hepatology, in an interview.
A comparative safety study Dr. Abraham coauthored in 2017 of rivaroxaban, apixaban, and dabigatran in a much larger U.S. cohort of 372,380 patients revealed that rivaroxaban had the worst GI bleeding profile. Apixaban was 66% safer than rivaroxaban and 64% safer than dabigatran to prevent gastrointestinal bleeding.
“I believe our group was the first to conduct this study and show clinically significant differences in GI safety of the available direct oral anticoagulants,” she said. Other investigators have since published similar results, and the topic of the new study needs no further investigation, according to Dr. Abraham.
“It is time for physicians to choose a better choice when prescribing a direct oral anticoagulant to their atrial fibrillation patients, and that choice is not rivaroxaban,” she said.
The Icelandic Centre for Research and the Landspítali University Hospital Research Fund provided funds for this study. Dr. Ingason, Dr. Björnsson, Dr. Rockey, and Dr. Abraham reported no disclosures.
FROM ANNALS OF INTERNAL MEDICINE
Family violence patterns change during pandemic
Among adolescents treated for injuries caused by family-member violence, the proportion of incidents that involved illegal drugs or weapons more than doubled during the pandemic, and incidents that involved alcohol nearly doubled, according to data presented October 10 at the American Academy of Pediatrics 2021 National Conference.
“The COVID-19 pandemic amplified risk factors known to increase family interpersonal violence, such as increased need for parental supervision, parental stress, financial hardship, poor mental health, and isolation,” said investigator Mattea Miller, an MD candidate at the Johns Hopkins University School of Medicine, Baltimore.
To examine the issue, she and her colleagues “sought to characterize the prevalence and circumstances of adolescent injuries resulting from family interpersonal violence,” Ms. Miller told this news organization.
Their retrospective analysis involved children 10 to 15 years of age seen before or during the pandemic in the emergency department at Johns Hopkins Children’s Center for injuries that resulted from a violent incident with a family member.
Of the 819 incidents of violence-related injuries seen during the study period – the prepandemic ran from Jan. 1, 2019 to March 29, 2020, and the pandemic period ran from March 30, 2020, the date a stay-at-home order was first issued in Maryland, to Dec. 31, 2020 – 448 (54.7%) involved a family member. The proportion of such injuries was similar before and during the pandemic (54.6% vs. 54.9%; P = .99).
Most (83.9%) of these incidents occurred at home, 76.6% involved a parent or guardian, and 66.7% involved the youth being transported to the hospital by police.
It is surprising that families accounted for such a high level of violence involving adolescents, said Christopher S. Greeley, MD, MS, chief of the division of public health pediatrics at Texas Children’s Hospital and professor of pediatrics at Baylor College of Medicine, Houston, who was not involved in the research.
“The most common source of child physical abuse in younger children – infants and toddlers – [is the] parents,” who account for about 75% of cases, “but to see that amount of violence in adolescents was unexpected,” he told this news organization.
Patients in the study cohort were more likely to be Black than the hospital’s overall emergency-department population (84.4% vs. 60.0%), and more likely to be covered by public insurance (71.2% vs. 60.0%).
In the study cohort, 54.0% of the patients were female.
“We were surprised to see that 8% of visits did not have a referral to a social worker” – 92% of patients in the study cohort received a social work consult during their visit to the emergency department – and that number “did not vary during the COVID-19 pandemic,” Ms. Miller said. The pandemic exacerbated the types of stresses that social workers can help address, so “this potentially represents a gap in care that is important to address,” she added.
Increase in use of alcohol, drugs, weapons
The most significant increases from the prepandemic period to the pandemic period were in incidents that involved alcohol (10.0% vs. 18.8%; P ≤ .001), illegal drugs (6.5% vs. 14.9%; P ≤ .001), and weapons, most often a knife (10.7% vs. 23.8%; P ≤ .001).
“An obvious potential explanation for the increase in alcohol, drug, and weapons [involvement] would be the mental health impact of the pandemic in conjunction with the economic stressors that some families may be feeling,” Dr. Greeley said. Teachers are the most common reporters of child abuse, so it’s possible that reports of violence decreased when schools switched to remote learning. But with most schools back to in-person learning, data have not yet shown a surge in reporting, he noted.
The “epidemiology of family violence may be impacted by increased time at home, disruptions in school and family routines, exacerbations in mental health conditions, and financial stresses common during the pandemic,” said senior study investigator Leticia Ryan, MD, MPH, director of research in pediatrics at Johns Hopkins Medicine.
And research has shown increases in the use of alcohol and illegal drugs during the pandemic, she noted.
“As we transition to postpandemic life, it will be important to identify at-risk adolescents and families and provide supports,” Dr. Ryan told this news organization. “The emergency department is an appropriate setting to intervene with youth who have experienced family violence and initiate preventive strategies to avoid future violence.”
Among the strategies to identify and intervene for at-risk patients is the CRAFFT substance use screening tool. Furthermore, “case management, involvement of child protection services, and linkage with relevant support services may all be appropriate, depending on circumstances,” Ms. Miller added.
“Exposure to family violence at a young age increases the likelihood that a child will be exposed to additional violence or become a perpetrator of violence in the future, continuing a cycle of violence,” Ms. Miller explained. “Given that studies of adolescent violence often focus on peer violence, a better understanding of the epidemiology of violence-related injuries resulting from family violence is needed to better inform the development of more comprehensive prevention strategies.”
This study did not note any external funding. Ms. Miller, Dr. Greeley, and Dr. Ryan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Among adolescents treated for injuries caused by family-member violence, the proportion of incidents that involved illegal drugs or weapons more than doubled during the pandemic, and incidents that involved alcohol nearly doubled, according to data presented October 10 at the American Academy of Pediatrics 2021 National Conference.
“The COVID-19 pandemic amplified risk factors known to increase family interpersonal violence, such as increased need for parental supervision, parental stress, financial hardship, poor mental health, and isolation,” said investigator Mattea Miller, an MD candidate at the Johns Hopkins University School of Medicine, Baltimore.
To examine the issue, she and her colleagues “sought to characterize the prevalence and circumstances of adolescent injuries resulting from family interpersonal violence,” Ms. Miller told this news organization.
Their retrospective analysis involved children 10 to 15 years of age seen before or during the pandemic in the emergency department at Johns Hopkins Children’s Center for injuries that resulted from a violent incident with a family member.
Of the 819 incidents of violence-related injuries seen during the study period – the prepandemic ran from Jan. 1, 2019 to March 29, 2020, and the pandemic period ran from March 30, 2020, the date a stay-at-home order was first issued in Maryland, to Dec. 31, 2020 – 448 (54.7%) involved a family member. The proportion of such injuries was similar before and during the pandemic (54.6% vs. 54.9%; P = .99).
Most (83.9%) of these incidents occurred at home, 76.6% involved a parent or guardian, and 66.7% involved the youth being transported to the hospital by police.
It is surprising that families accounted for such a high level of violence involving adolescents, said Christopher S. Greeley, MD, MS, chief of the division of public health pediatrics at Texas Children’s Hospital and professor of pediatrics at Baylor College of Medicine, Houston, who was not involved in the research.
“The most common source of child physical abuse in younger children – infants and toddlers – [is the] parents,” who account for about 75% of cases, “but to see that amount of violence in adolescents was unexpected,” he told this news organization.
Patients in the study cohort were more likely to be Black than the hospital’s overall emergency-department population (84.4% vs. 60.0%), and more likely to be covered by public insurance (71.2% vs. 60.0%).
In the study cohort, 54.0% of the patients were female.
“We were surprised to see that 8% of visits did not have a referral to a social worker” – 92% of patients in the study cohort received a social work consult during their visit to the emergency department – and that number “did not vary during the COVID-19 pandemic,” Ms. Miller said. The pandemic exacerbated the types of stresses that social workers can help address, so “this potentially represents a gap in care that is important to address,” she added.
Increase in use of alcohol, drugs, weapons
The most significant increases from the prepandemic period to the pandemic period were in incidents that involved alcohol (10.0% vs. 18.8%; P ≤ .001), illegal drugs (6.5% vs. 14.9%; P ≤ .001), and weapons, most often a knife (10.7% vs. 23.8%; P ≤ .001).
“An obvious potential explanation for the increase in alcohol, drug, and weapons [involvement] would be the mental health impact of the pandemic in conjunction with the economic stressors that some families may be feeling,” Dr. Greeley said. Teachers are the most common reporters of child abuse, so it’s possible that reports of violence decreased when schools switched to remote learning. But with most schools back to in-person learning, data have not yet shown a surge in reporting, he noted.
The “epidemiology of family violence may be impacted by increased time at home, disruptions in school and family routines, exacerbations in mental health conditions, and financial stresses common during the pandemic,” said senior study investigator Leticia Ryan, MD, MPH, director of research in pediatrics at Johns Hopkins Medicine.
And research has shown increases in the use of alcohol and illegal drugs during the pandemic, she noted.
“As we transition to postpandemic life, it will be important to identify at-risk adolescents and families and provide supports,” Dr. Ryan told this news organization. “The emergency department is an appropriate setting to intervene with youth who have experienced family violence and initiate preventive strategies to avoid future violence.”
Among the strategies to identify and intervene for at-risk patients is the CRAFFT substance use screening tool. Furthermore, “case management, involvement of child protection services, and linkage with relevant support services may all be appropriate, depending on circumstances,” Ms. Miller added.
“Exposure to family violence at a young age increases the likelihood that a child will be exposed to additional violence or become a perpetrator of violence in the future, continuing a cycle of violence,” Ms. Miller explained. “Given that studies of adolescent violence often focus on peer violence, a better understanding of the epidemiology of violence-related injuries resulting from family violence is needed to better inform the development of more comprehensive prevention strategies.”
This study did not note any external funding. Ms. Miller, Dr. Greeley, and Dr. Ryan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Among adolescents treated for injuries caused by family-member violence, the proportion of incidents that involved illegal drugs or weapons more than doubled during the pandemic, and incidents that involved alcohol nearly doubled, according to data presented October 10 at the American Academy of Pediatrics 2021 National Conference.
“The COVID-19 pandemic amplified risk factors known to increase family interpersonal violence, such as increased need for parental supervision, parental stress, financial hardship, poor mental health, and isolation,” said investigator Mattea Miller, an MD candidate at the Johns Hopkins University School of Medicine, Baltimore.
To examine the issue, she and her colleagues “sought to characterize the prevalence and circumstances of adolescent injuries resulting from family interpersonal violence,” Ms. Miller told this news organization.
Their retrospective analysis involved children 10 to 15 years of age seen before or during the pandemic in the emergency department at Johns Hopkins Children’s Center for injuries that resulted from a violent incident with a family member.
Of the 819 incidents of violence-related injuries seen during the study period – the prepandemic ran from Jan. 1, 2019 to March 29, 2020, and the pandemic period ran from March 30, 2020, the date a stay-at-home order was first issued in Maryland, to Dec. 31, 2020 – 448 (54.7%) involved a family member. The proportion of such injuries was similar before and during the pandemic (54.6% vs. 54.9%; P = .99).
Most (83.9%) of these incidents occurred at home, 76.6% involved a parent or guardian, and 66.7% involved the youth being transported to the hospital by police.
It is surprising that families accounted for such a high level of violence involving adolescents, said Christopher S. Greeley, MD, MS, chief of the division of public health pediatrics at Texas Children’s Hospital and professor of pediatrics at Baylor College of Medicine, Houston, who was not involved in the research.
“The most common source of child physical abuse in younger children – infants and toddlers – [is the] parents,” who account for about 75% of cases, “but to see that amount of violence in adolescents was unexpected,” he told this news organization.
Patients in the study cohort were more likely to be Black than the hospital’s overall emergency-department population (84.4% vs. 60.0%), and more likely to be covered by public insurance (71.2% vs. 60.0%).
In the study cohort, 54.0% of the patients were female.
“We were surprised to see that 8% of visits did not have a referral to a social worker” – 92% of patients in the study cohort received a social work consult during their visit to the emergency department – and that number “did not vary during the COVID-19 pandemic,” Ms. Miller said. The pandemic exacerbated the types of stresses that social workers can help address, so “this potentially represents a gap in care that is important to address,” she added.
Increase in use of alcohol, drugs, weapons
The most significant increases from the prepandemic period to the pandemic period were in incidents that involved alcohol (10.0% vs. 18.8%; P ≤ .001), illegal drugs (6.5% vs. 14.9%; P ≤ .001), and weapons, most often a knife (10.7% vs. 23.8%; P ≤ .001).
“An obvious potential explanation for the increase in alcohol, drug, and weapons [involvement] would be the mental health impact of the pandemic in conjunction with the economic stressors that some families may be feeling,” Dr. Greeley said. Teachers are the most common reporters of child abuse, so it’s possible that reports of violence decreased when schools switched to remote learning. But with most schools back to in-person learning, data have not yet shown a surge in reporting, he noted.
The “epidemiology of family violence may be impacted by increased time at home, disruptions in school and family routines, exacerbations in mental health conditions, and financial stresses common during the pandemic,” said senior study investigator Leticia Ryan, MD, MPH, director of research in pediatrics at Johns Hopkins Medicine.
And research has shown increases in the use of alcohol and illegal drugs during the pandemic, she noted.
“As we transition to postpandemic life, it will be important to identify at-risk adolescents and families and provide supports,” Dr. Ryan told this news organization. “The emergency department is an appropriate setting to intervene with youth who have experienced family violence and initiate preventive strategies to avoid future violence.”
Among the strategies to identify and intervene for at-risk patients is the CRAFFT substance use screening tool. Furthermore, “case management, involvement of child protection services, and linkage with relevant support services may all be appropriate, depending on circumstances,” Ms. Miller added.
“Exposure to family violence at a young age increases the likelihood that a child will be exposed to additional violence or become a perpetrator of violence in the future, continuing a cycle of violence,” Ms. Miller explained. “Given that studies of adolescent violence often focus on peer violence, a better understanding of the epidemiology of violence-related injuries resulting from family violence is needed to better inform the development of more comprehensive prevention strategies.”
This study did not note any external funding. Ms. Miller, Dr. Greeley, and Dr. Ryan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New reports help nail down myocarditis risk with COVID-19 vaccine
Recent literature features new descriptions of myocarditis linked to the two available mRNA vaccines against SARS-CoV-2. They tell a story largely consistent with experience to date, and support what might be its most useful public health message: The associated myocarditis is usually mild and self-limiting, and is far less likely to occur than myocarditis or death in unvaccinated people with COVID-19.
In line with previous research, the new analyses suggest the myocarditis – with onset usually a few days to a week after injection – has an overall incidence that ranges from less than 1 to perhaps 3 per 100,000 people who received at least one of the full mRNA-vaccine regimen’s two injections. Also, as in earlier studies, the incidence climbed higher – sometimes sharply – in certain groups by age and sex, particularly in young men and older male teens.
The new studies “are confirmatory, in terms of the risk being low,” but underscore that clinicians still must be wary of myocarditis as a potential complication of the mRNA vaccines, Biykem Bozkurt, MD, PhD, Baylor College of Medicine, Houston, told this news organization.
Dr. Bozkurt, a leading heart failure specialist and researcher, did not contribute to any of the new reports but does study the myocarditis of COVID-19 and was lead author on a recent review of the potential vaccine complication’s features and possible mechanisms.
In the new myocarditis reports, she observed, more than 90% of the cases were mild and “resolved on their own without a major adverse outcome.” Dr. Bozkurt emphasized the need for perspective regarding the risk. For example, the myocarditis associated with SARS-CoV-2 infection is not only more likely than the vaccine-related myocarditis, but it’s also usually far more severe.
Dr. Bozkurt pointed to a recent study in which the mRNA vaccines, compared with no vaccination, appeared to escalate the myocarditis risk by a factor of 3, whereas the risk for myocarditis in SARS-CoV-2 infection was increased 18 times.
In contrast, she observed, the new myocarditis cases reported this week feature a few that are novel or are at least very rare, including the case of a patient who developed cardiogenic shock and another with fulminant myocarditis who died.
The Centers for Disease Control and Prevention in May publicly described the apparent link between myocarditis and the two available mRNA vaccines against SARS-CoV-2: BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna). The next month, the Food and Drug Administration added a warning about the risk to the labeling.
Less than 1 case per 100,000
Fifteen confirmed cases of myocarditis were identified among about 2.4 million members of Kaiser Permanente Southern California aged 18 or older who received at least one injection of the Pfizer or Moderna mRNA vaccines between December 2020 and July 2021, in a report published in JAMA Internal Medicine. The study counted cases up to 10 days after the first or second injection, of which there were 2 and 13, respectively.
All eight patients who received the Pfizer BNT162b2 vaccine and the eight given the Moderna mRNA-1273 vaccine were male with a median age of 25 years (interquartile range, 20-32 years).
“The main takeaway messages from our study are that the incidence of myocarditis after COVID-19 mRNA vaccinations is very low, that this condition is primarily observed in young men within a few days after the second dose, and that most patients recover quickly,” senior author Mingsum Lee, MD, PhD, Kaiser Permanente Los Angeles Medical Center, told this news organization.
“The incidence of vaccine-related myocarditis was significantly lower than rates of COVID-19 hospitalization during the same period and population area,” she added.
The group saw a per-million incidence of 0.8 and 5.8 myocarditis cases in the 10 days after first and second injections, respectively. That made for an incidence of 0.58 per 100,000, or 1 case per 172,414 fully vaccinated adults.
The group also considered a cohort of 1,577,741 unvaccinated people with a median age of 39 years (interquartile range, 28-53 years) during the same period. Of the 75 cases of myocarditis, 52% were in men, they reported.
Comparing the vaccinated and unvaccinated cohorts, they saw a 10-day vaccine-associated myocarditis incidence rate ratio of 0.38 (95% confidence interval, 0.05-1.40; P = .15) after the first dose, and 2.7 (95% CI, 1.4-4.8; P = .004) after the second dose.
In a comparison of the vaccinated group with itself using data from a 10-day period in the previous year, the corresponding myocarditis IRRs were 1.0 (P > .99) and 3.3 (P = .03), respectively.
Dr. Lee said none of the 15 patients required admission to an intensive care unit. “All patients with myocarditis responded well to treatment and felt better quickly,” she noted.
Myocarditis after an mRNA vaccine injection is rare and, Dr. Lee said emphatically, and “the benefits of the COVID-19 vaccine greatly outweigh the risks.”
Sex- and age-stratified rates
In a separate analysis of 5,442,696 people given a first dose of the Pfizer BNT162b2 vaccine and 5,125,635 given a second dose, there were 142 cases of myocarditis with onset 21 days after dose 1 and 30 days after dose 2. Of those cases, 136 were documented as “definite or probable” in an Israeli Ministry of Health database that covered up to the end of May 2021.
There were also 40 cases among vaccinated people seen after the 30-day window, which were considered not related to the vaccination, and 101 cases among unvaccinated people; of the latter, 29 had confirmed diagnoses of COVID-19.
Of the 136 people with definite or probable cases, the myocarditis was “generally mild” in 129 and usually resolved on its own, notes the report on the study, published in the New England Journal of Medicine, with lead author Dror Mevorach, MD, Hadassah-Hebrew University Medical Center, Jerusalem.
The estimated myocarditis incidence after a second such vaccine dose across the entire Israeli population, based on the current study, was about one per 26,000 males and one per 218,000 females, the group writes. Those figures compare with one case per 10,857 among “the general unvaccinated population.”
Again, the risk was concentrated among younger men and male adolescents. In an analysis limited to vaccinated people aged 16-19 years, myocarditis in the 21 days after a second mRNA injection was seen in about one of 6,637 males and one of 99,853 females, the group reported.
The standardized incidence ratio of 5.34 (95% CI, 4.48-6.40) after a second injection, across all groups, “was driven mostly by the diagnosis of myocarditis in younger male recipients.” Among that male subgroup, the ratios by age group were 13.60 (95% CI, 9.30-19.20) for 16-19 years, 8.53 (95% CI, 5.57-12.50) for 20-24 years, and 6.96 (95% CI, 4.25-10.75) for 25-29 years.
Among people who received a second injection, compared with unvaccinated people, the 30-day rate ratio was 2.35 (95% CI, 1.10-5.02). Again, the effect was concentrated in males aged 16-19 years. Among them, the myocarditis rate ratios in the 30 days after a second mRNA vaccine injection were 8.96 (95% CI, 4.50-17.83) for the 16-19 years group, 6.13 (95% CI, 3.16-11.88) for the 20-24 group, and 3.58 (95% CI, 1.82-7.01) for 25-29 years.
Most of the patients with myocarditis showed “significant clinical improvement,” with a mean hospitalization time of only 3-4 days, the report notes. Treatment consisted of nonsteroidal anti-inflammatory drugs “with or without colchicine for presumed pericardial inflammation.”
However, seven patients (4.9%) developed important complications, including left-ventricular dysfunction, ventricular arrhythmias, and heart failure. Among them was a 22-year-old patient who died of fulminant myocarditis within 24 hours of diagnosis, the group wrote.
From an Israeli health care organization
Published by the same journal as the study by Dr. Menvorach and associates, an analysis of a separate database showed largely consistent findings among patients in the largest of Israel’s four health care organizations charged by the government to administer health services.
The report, with authors led by Guy Witberg, MD, Rabin Medical Center, Petah Tikva, Israel, focused on members of the health care organization aged 16 years or older who had received at least one Pfizer mRNA vaccine dose by the end of May 2021.
The cohorts from the two separate reports surely overlap substantially, as the Ministry of Health analysis from Dr. Mevorach and colleagues derived from a nationwide database, and – as Dr. Witberg and associates wrote – the health care organization providing their data covers 52% of the Israeli population.
Of 2,558,421 vaccinated people in the analysis, of whom 94% received two doses, 54 developed confirmed myocarditis in the 42 days after the first dose. Their median age was 27 years (interquartile range, 21-35 years) and all but three (94%) were male. Of those 54 cases, 41 were considered mild and 12 intermediate in severity, and one was fulminant with the patient in cardiogenic shock, the group writes. In addition, nonsustained ventricular tachycardia and atrial fibrillation developed in 5% and 3% of cases, respectively.
The estimated myocarditis incidence in the 42 days after administration of at least one mRNA vaccine dose was 2.13 per 100,000 vaccinated people. In that group, Dr. Witberg and colleagues note, the corresponding incidences per 100,000 were 4.12 and 0.23 for males and females, respectively.
Also in the current report, incidences per 100,000 vaccinated people aged 16-29 years, by sex, included 5.49 (95% CI, 3.59-7.39) overall, and 10.69 (95% CI, 6.93-14.46) for males (the highest rate in the report).
There was only one case in a female aged 16-29 years, and two cases in females 30 years or older.
Of note, some authors of the current study are also authors on the high-profile report from Noam Barda, MD, and colleagues published in the New England Journal of Medicine, that used the same database to arrive at an mRNA-vaccine-related incidence of myocarditis of 2.7 per 100,000. Eligibility criteria and follow-up time were different in that report, as were case ascertainment criteria.
The myocarditis risk associated with the two mRNA vaccines is small compared with “the morbidity and mortality of COVID-19 infection, in which up to 28% of hospitalized patients showed signs of myocardial injury,” wrote Vinay Guduguntla, MD, University of California, San Francisco, and Mitchell H. Katz, MD, NYC Health + Hospitals, New York, in an editorial accompanying the report from Dr. Lee and associates.
“Randomized clinical trials show that COVID-19 mRNA vaccines represent a safe and effective method of preventing infection,” they stated. “The identification of rare myocarditis does not change clinical decision-making.”
Dr. Bozkurt, who is immediate past president of the Heart Failure Society of America, has disclosed consulting for Bayer and scPharmaceuticals and serving on a clinical events committee for a trial supported by Abbott Pharmaceuticals and on a data and safety monitoring board for a trial supported by Liva Nova Pharmaceuticals. Dr. Lee and the report’s other authors had no disclosures. Dr. Mevorach discloses consulting for Enlivex Therapeutics; disclosures for the other authors are available at NEJM.org. Dr. Witberg said he has no interests to disclose; disclosures for the other authors are available at NEJM.org. Dr. Guduguntla is an editorial fellow and Dr. Katz a deputy editor at JAMA Internal Medicine; neither had disclosures.
A version of this article first appeared on Medscape.com.
Recent literature features new descriptions of myocarditis linked to the two available mRNA vaccines against SARS-CoV-2. They tell a story largely consistent with experience to date, and support what might be its most useful public health message: The associated myocarditis is usually mild and self-limiting, and is far less likely to occur than myocarditis or death in unvaccinated people with COVID-19.
In line with previous research, the new analyses suggest the myocarditis – with onset usually a few days to a week after injection – has an overall incidence that ranges from less than 1 to perhaps 3 per 100,000 people who received at least one of the full mRNA-vaccine regimen’s two injections. Also, as in earlier studies, the incidence climbed higher – sometimes sharply – in certain groups by age and sex, particularly in young men and older male teens.
The new studies “are confirmatory, in terms of the risk being low,” but underscore that clinicians still must be wary of myocarditis as a potential complication of the mRNA vaccines, Biykem Bozkurt, MD, PhD, Baylor College of Medicine, Houston, told this news organization.
Dr. Bozkurt, a leading heart failure specialist and researcher, did not contribute to any of the new reports but does study the myocarditis of COVID-19 and was lead author on a recent review of the potential vaccine complication’s features and possible mechanisms.
In the new myocarditis reports, she observed, more than 90% of the cases were mild and “resolved on their own without a major adverse outcome.” Dr. Bozkurt emphasized the need for perspective regarding the risk. For example, the myocarditis associated with SARS-CoV-2 infection is not only more likely than the vaccine-related myocarditis, but it’s also usually far more severe.
Dr. Bozkurt pointed to a recent study in which the mRNA vaccines, compared with no vaccination, appeared to escalate the myocarditis risk by a factor of 3, whereas the risk for myocarditis in SARS-CoV-2 infection was increased 18 times.
In contrast, she observed, the new myocarditis cases reported this week feature a few that are novel or are at least very rare, including the case of a patient who developed cardiogenic shock and another with fulminant myocarditis who died.
The Centers for Disease Control and Prevention in May publicly described the apparent link between myocarditis and the two available mRNA vaccines against SARS-CoV-2: BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna). The next month, the Food and Drug Administration added a warning about the risk to the labeling.
Less than 1 case per 100,000
Fifteen confirmed cases of myocarditis were identified among about 2.4 million members of Kaiser Permanente Southern California aged 18 or older who received at least one injection of the Pfizer or Moderna mRNA vaccines between December 2020 and July 2021, in a report published in JAMA Internal Medicine. The study counted cases up to 10 days after the first or second injection, of which there were 2 and 13, respectively.
All eight patients who received the Pfizer BNT162b2 vaccine and the eight given the Moderna mRNA-1273 vaccine were male with a median age of 25 years (interquartile range, 20-32 years).
“The main takeaway messages from our study are that the incidence of myocarditis after COVID-19 mRNA vaccinations is very low, that this condition is primarily observed in young men within a few days after the second dose, and that most patients recover quickly,” senior author Mingsum Lee, MD, PhD, Kaiser Permanente Los Angeles Medical Center, told this news organization.
“The incidence of vaccine-related myocarditis was significantly lower than rates of COVID-19 hospitalization during the same period and population area,” she added.
The group saw a per-million incidence of 0.8 and 5.8 myocarditis cases in the 10 days after first and second injections, respectively. That made for an incidence of 0.58 per 100,000, or 1 case per 172,414 fully vaccinated adults.
The group also considered a cohort of 1,577,741 unvaccinated people with a median age of 39 years (interquartile range, 28-53 years) during the same period. Of the 75 cases of myocarditis, 52% were in men, they reported.
Comparing the vaccinated and unvaccinated cohorts, they saw a 10-day vaccine-associated myocarditis incidence rate ratio of 0.38 (95% confidence interval, 0.05-1.40; P = .15) after the first dose, and 2.7 (95% CI, 1.4-4.8; P = .004) after the second dose.
In a comparison of the vaccinated group with itself using data from a 10-day period in the previous year, the corresponding myocarditis IRRs were 1.0 (P > .99) and 3.3 (P = .03), respectively.
Dr. Lee said none of the 15 patients required admission to an intensive care unit. “All patients with myocarditis responded well to treatment and felt better quickly,” she noted.
Myocarditis after an mRNA vaccine injection is rare and, Dr. Lee said emphatically, and “the benefits of the COVID-19 vaccine greatly outweigh the risks.”
Sex- and age-stratified rates
In a separate analysis of 5,442,696 people given a first dose of the Pfizer BNT162b2 vaccine and 5,125,635 given a second dose, there were 142 cases of myocarditis with onset 21 days after dose 1 and 30 days after dose 2. Of those cases, 136 were documented as “definite or probable” in an Israeli Ministry of Health database that covered up to the end of May 2021.
There were also 40 cases among vaccinated people seen after the 30-day window, which were considered not related to the vaccination, and 101 cases among unvaccinated people; of the latter, 29 had confirmed diagnoses of COVID-19.
Of the 136 people with definite or probable cases, the myocarditis was “generally mild” in 129 and usually resolved on its own, notes the report on the study, published in the New England Journal of Medicine, with lead author Dror Mevorach, MD, Hadassah-Hebrew University Medical Center, Jerusalem.
The estimated myocarditis incidence after a second such vaccine dose across the entire Israeli population, based on the current study, was about one per 26,000 males and one per 218,000 females, the group writes. Those figures compare with one case per 10,857 among “the general unvaccinated population.”
Again, the risk was concentrated among younger men and male adolescents. In an analysis limited to vaccinated people aged 16-19 years, myocarditis in the 21 days after a second mRNA injection was seen in about one of 6,637 males and one of 99,853 females, the group reported.
The standardized incidence ratio of 5.34 (95% CI, 4.48-6.40) after a second injection, across all groups, “was driven mostly by the diagnosis of myocarditis in younger male recipients.” Among that male subgroup, the ratios by age group were 13.60 (95% CI, 9.30-19.20) for 16-19 years, 8.53 (95% CI, 5.57-12.50) for 20-24 years, and 6.96 (95% CI, 4.25-10.75) for 25-29 years.
Among people who received a second injection, compared with unvaccinated people, the 30-day rate ratio was 2.35 (95% CI, 1.10-5.02). Again, the effect was concentrated in males aged 16-19 years. Among them, the myocarditis rate ratios in the 30 days after a second mRNA vaccine injection were 8.96 (95% CI, 4.50-17.83) for the 16-19 years group, 6.13 (95% CI, 3.16-11.88) for the 20-24 group, and 3.58 (95% CI, 1.82-7.01) for 25-29 years.
Most of the patients with myocarditis showed “significant clinical improvement,” with a mean hospitalization time of only 3-4 days, the report notes. Treatment consisted of nonsteroidal anti-inflammatory drugs “with or without colchicine for presumed pericardial inflammation.”
However, seven patients (4.9%) developed important complications, including left-ventricular dysfunction, ventricular arrhythmias, and heart failure. Among them was a 22-year-old patient who died of fulminant myocarditis within 24 hours of diagnosis, the group wrote.
From an Israeli health care organization
Published by the same journal as the study by Dr. Menvorach and associates, an analysis of a separate database showed largely consistent findings among patients in the largest of Israel’s four health care organizations charged by the government to administer health services.
The report, with authors led by Guy Witberg, MD, Rabin Medical Center, Petah Tikva, Israel, focused on members of the health care organization aged 16 years or older who had received at least one Pfizer mRNA vaccine dose by the end of May 2021.
The cohorts from the two separate reports surely overlap substantially, as the Ministry of Health analysis from Dr. Mevorach and colleagues derived from a nationwide database, and – as Dr. Witberg and associates wrote – the health care organization providing their data covers 52% of the Israeli population.
Of 2,558,421 vaccinated people in the analysis, of whom 94% received two doses, 54 developed confirmed myocarditis in the 42 days after the first dose. Their median age was 27 years (interquartile range, 21-35 years) and all but three (94%) were male. Of those 54 cases, 41 were considered mild and 12 intermediate in severity, and one was fulminant with the patient in cardiogenic shock, the group writes. In addition, nonsustained ventricular tachycardia and atrial fibrillation developed in 5% and 3% of cases, respectively.
The estimated myocarditis incidence in the 42 days after administration of at least one mRNA vaccine dose was 2.13 per 100,000 vaccinated people. In that group, Dr. Witberg and colleagues note, the corresponding incidences per 100,000 were 4.12 and 0.23 for males and females, respectively.
Also in the current report, incidences per 100,000 vaccinated people aged 16-29 years, by sex, included 5.49 (95% CI, 3.59-7.39) overall, and 10.69 (95% CI, 6.93-14.46) for males (the highest rate in the report).
There was only one case in a female aged 16-29 years, and two cases in females 30 years or older.
Of note, some authors of the current study are also authors on the high-profile report from Noam Barda, MD, and colleagues published in the New England Journal of Medicine, that used the same database to arrive at an mRNA-vaccine-related incidence of myocarditis of 2.7 per 100,000. Eligibility criteria and follow-up time were different in that report, as were case ascertainment criteria.
The myocarditis risk associated with the two mRNA vaccines is small compared with “the morbidity and mortality of COVID-19 infection, in which up to 28% of hospitalized patients showed signs of myocardial injury,” wrote Vinay Guduguntla, MD, University of California, San Francisco, and Mitchell H. Katz, MD, NYC Health + Hospitals, New York, in an editorial accompanying the report from Dr. Lee and associates.
“Randomized clinical trials show that COVID-19 mRNA vaccines represent a safe and effective method of preventing infection,” they stated. “The identification of rare myocarditis does not change clinical decision-making.”
Dr. Bozkurt, who is immediate past president of the Heart Failure Society of America, has disclosed consulting for Bayer and scPharmaceuticals and serving on a clinical events committee for a trial supported by Abbott Pharmaceuticals and on a data and safety monitoring board for a trial supported by Liva Nova Pharmaceuticals. Dr. Lee and the report’s other authors had no disclosures. Dr. Mevorach discloses consulting for Enlivex Therapeutics; disclosures for the other authors are available at NEJM.org. Dr. Witberg said he has no interests to disclose; disclosures for the other authors are available at NEJM.org. Dr. Guduguntla is an editorial fellow and Dr. Katz a deputy editor at JAMA Internal Medicine; neither had disclosures.
A version of this article first appeared on Medscape.com.
Recent literature features new descriptions of myocarditis linked to the two available mRNA vaccines against SARS-CoV-2. They tell a story largely consistent with experience to date, and support what might be its most useful public health message: The associated myocarditis is usually mild and self-limiting, and is far less likely to occur than myocarditis or death in unvaccinated people with COVID-19.
In line with previous research, the new analyses suggest the myocarditis – with onset usually a few days to a week after injection – has an overall incidence that ranges from less than 1 to perhaps 3 per 100,000 people who received at least one of the full mRNA-vaccine regimen’s two injections. Also, as in earlier studies, the incidence climbed higher – sometimes sharply – in certain groups by age and sex, particularly in young men and older male teens.
The new studies “are confirmatory, in terms of the risk being low,” but underscore that clinicians still must be wary of myocarditis as a potential complication of the mRNA vaccines, Biykem Bozkurt, MD, PhD, Baylor College of Medicine, Houston, told this news organization.
Dr. Bozkurt, a leading heart failure specialist and researcher, did not contribute to any of the new reports but does study the myocarditis of COVID-19 and was lead author on a recent review of the potential vaccine complication’s features and possible mechanisms.
In the new myocarditis reports, she observed, more than 90% of the cases were mild and “resolved on their own without a major adverse outcome.” Dr. Bozkurt emphasized the need for perspective regarding the risk. For example, the myocarditis associated with SARS-CoV-2 infection is not only more likely than the vaccine-related myocarditis, but it’s also usually far more severe.
Dr. Bozkurt pointed to a recent study in which the mRNA vaccines, compared with no vaccination, appeared to escalate the myocarditis risk by a factor of 3, whereas the risk for myocarditis in SARS-CoV-2 infection was increased 18 times.
In contrast, she observed, the new myocarditis cases reported this week feature a few that are novel or are at least very rare, including the case of a patient who developed cardiogenic shock and another with fulminant myocarditis who died.
The Centers for Disease Control and Prevention in May publicly described the apparent link between myocarditis and the two available mRNA vaccines against SARS-CoV-2: BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna). The next month, the Food and Drug Administration added a warning about the risk to the labeling.
Less than 1 case per 100,000
Fifteen confirmed cases of myocarditis were identified among about 2.4 million members of Kaiser Permanente Southern California aged 18 or older who received at least one injection of the Pfizer or Moderna mRNA vaccines between December 2020 and July 2021, in a report published in JAMA Internal Medicine. The study counted cases up to 10 days after the first or second injection, of which there were 2 and 13, respectively.
All eight patients who received the Pfizer BNT162b2 vaccine and the eight given the Moderna mRNA-1273 vaccine were male with a median age of 25 years (interquartile range, 20-32 years).
“The main takeaway messages from our study are that the incidence of myocarditis after COVID-19 mRNA vaccinations is very low, that this condition is primarily observed in young men within a few days after the second dose, and that most patients recover quickly,” senior author Mingsum Lee, MD, PhD, Kaiser Permanente Los Angeles Medical Center, told this news organization.
“The incidence of vaccine-related myocarditis was significantly lower than rates of COVID-19 hospitalization during the same period and population area,” she added.
The group saw a per-million incidence of 0.8 and 5.8 myocarditis cases in the 10 days after first and second injections, respectively. That made for an incidence of 0.58 per 100,000, or 1 case per 172,414 fully vaccinated adults.
The group also considered a cohort of 1,577,741 unvaccinated people with a median age of 39 years (interquartile range, 28-53 years) during the same period. Of the 75 cases of myocarditis, 52% were in men, they reported.
Comparing the vaccinated and unvaccinated cohorts, they saw a 10-day vaccine-associated myocarditis incidence rate ratio of 0.38 (95% confidence interval, 0.05-1.40; P = .15) after the first dose, and 2.7 (95% CI, 1.4-4.8; P = .004) after the second dose.
In a comparison of the vaccinated group with itself using data from a 10-day period in the previous year, the corresponding myocarditis IRRs were 1.0 (P > .99) and 3.3 (P = .03), respectively.
Dr. Lee said none of the 15 patients required admission to an intensive care unit. “All patients with myocarditis responded well to treatment and felt better quickly,” she noted.
Myocarditis after an mRNA vaccine injection is rare and, Dr. Lee said emphatically, and “the benefits of the COVID-19 vaccine greatly outweigh the risks.”
Sex- and age-stratified rates
In a separate analysis of 5,442,696 people given a first dose of the Pfizer BNT162b2 vaccine and 5,125,635 given a second dose, there were 142 cases of myocarditis with onset 21 days after dose 1 and 30 days after dose 2. Of those cases, 136 were documented as “definite or probable” in an Israeli Ministry of Health database that covered up to the end of May 2021.
There were also 40 cases among vaccinated people seen after the 30-day window, which were considered not related to the vaccination, and 101 cases among unvaccinated people; of the latter, 29 had confirmed diagnoses of COVID-19.
Of the 136 people with definite or probable cases, the myocarditis was “generally mild” in 129 and usually resolved on its own, notes the report on the study, published in the New England Journal of Medicine, with lead author Dror Mevorach, MD, Hadassah-Hebrew University Medical Center, Jerusalem.
The estimated myocarditis incidence after a second such vaccine dose across the entire Israeli population, based on the current study, was about one per 26,000 males and one per 218,000 females, the group writes. Those figures compare with one case per 10,857 among “the general unvaccinated population.”
Again, the risk was concentrated among younger men and male adolescents. In an analysis limited to vaccinated people aged 16-19 years, myocarditis in the 21 days after a second mRNA injection was seen in about one of 6,637 males and one of 99,853 females, the group reported.
The standardized incidence ratio of 5.34 (95% CI, 4.48-6.40) after a second injection, across all groups, “was driven mostly by the diagnosis of myocarditis in younger male recipients.” Among that male subgroup, the ratios by age group were 13.60 (95% CI, 9.30-19.20) for 16-19 years, 8.53 (95% CI, 5.57-12.50) for 20-24 years, and 6.96 (95% CI, 4.25-10.75) for 25-29 years.
Among people who received a second injection, compared with unvaccinated people, the 30-day rate ratio was 2.35 (95% CI, 1.10-5.02). Again, the effect was concentrated in males aged 16-19 years. Among them, the myocarditis rate ratios in the 30 days after a second mRNA vaccine injection were 8.96 (95% CI, 4.50-17.83) for the 16-19 years group, 6.13 (95% CI, 3.16-11.88) for the 20-24 group, and 3.58 (95% CI, 1.82-7.01) for 25-29 years.
Most of the patients with myocarditis showed “significant clinical improvement,” with a mean hospitalization time of only 3-4 days, the report notes. Treatment consisted of nonsteroidal anti-inflammatory drugs “with or without colchicine for presumed pericardial inflammation.”
However, seven patients (4.9%) developed important complications, including left-ventricular dysfunction, ventricular arrhythmias, and heart failure. Among them was a 22-year-old patient who died of fulminant myocarditis within 24 hours of diagnosis, the group wrote.
From an Israeli health care organization
Published by the same journal as the study by Dr. Menvorach and associates, an analysis of a separate database showed largely consistent findings among patients in the largest of Israel’s four health care organizations charged by the government to administer health services.
The report, with authors led by Guy Witberg, MD, Rabin Medical Center, Petah Tikva, Israel, focused on members of the health care organization aged 16 years or older who had received at least one Pfizer mRNA vaccine dose by the end of May 2021.
The cohorts from the two separate reports surely overlap substantially, as the Ministry of Health analysis from Dr. Mevorach and colleagues derived from a nationwide database, and – as Dr. Witberg and associates wrote – the health care organization providing their data covers 52% of the Israeli population.
Of 2,558,421 vaccinated people in the analysis, of whom 94% received two doses, 54 developed confirmed myocarditis in the 42 days after the first dose. Their median age was 27 years (interquartile range, 21-35 years) and all but three (94%) were male. Of those 54 cases, 41 were considered mild and 12 intermediate in severity, and one was fulminant with the patient in cardiogenic shock, the group writes. In addition, nonsustained ventricular tachycardia and atrial fibrillation developed in 5% and 3% of cases, respectively.
The estimated myocarditis incidence in the 42 days after administration of at least one mRNA vaccine dose was 2.13 per 100,000 vaccinated people. In that group, Dr. Witberg and colleagues note, the corresponding incidences per 100,000 were 4.12 and 0.23 for males and females, respectively.
Also in the current report, incidences per 100,000 vaccinated people aged 16-29 years, by sex, included 5.49 (95% CI, 3.59-7.39) overall, and 10.69 (95% CI, 6.93-14.46) for males (the highest rate in the report).
There was only one case in a female aged 16-29 years, and two cases in females 30 years or older.
Of note, some authors of the current study are also authors on the high-profile report from Noam Barda, MD, and colleagues published in the New England Journal of Medicine, that used the same database to arrive at an mRNA-vaccine-related incidence of myocarditis of 2.7 per 100,000. Eligibility criteria and follow-up time were different in that report, as were case ascertainment criteria.
The myocarditis risk associated with the two mRNA vaccines is small compared with “the morbidity and mortality of COVID-19 infection, in which up to 28% of hospitalized patients showed signs of myocardial injury,” wrote Vinay Guduguntla, MD, University of California, San Francisco, and Mitchell H. Katz, MD, NYC Health + Hospitals, New York, in an editorial accompanying the report from Dr. Lee and associates.
“Randomized clinical trials show that COVID-19 mRNA vaccines represent a safe and effective method of preventing infection,” they stated. “The identification of rare myocarditis does not change clinical decision-making.”
Dr. Bozkurt, who is immediate past president of the Heart Failure Society of America, has disclosed consulting for Bayer and scPharmaceuticals and serving on a clinical events committee for a trial supported by Abbott Pharmaceuticals and on a data and safety monitoring board for a trial supported by Liva Nova Pharmaceuticals. Dr. Lee and the report’s other authors had no disclosures. Dr. Mevorach discloses consulting for Enlivex Therapeutics; disclosures for the other authors are available at NEJM.org. Dr. Witberg said he has no interests to disclose; disclosures for the other authors are available at NEJM.org. Dr. Guduguntla is an editorial fellow and Dr. Katz a deputy editor at JAMA Internal Medicine; neither had disclosures.
A version of this article first appeared on Medscape.com.
Merck seeks FDA authorization for antiviral COVID-19 pill
, an experimental antiviral COVID-19 treatment.
If the FDA grants authorization, the drug would be the first oral antiviral treatment for COVID-19. The capsule, made by Merck and Ridgeback Biotherapeutics, is intended to treat mild to moderate COVID-19 in adults who are at risk of having severe COVID-19 or hospitalization.
“The extraordinary impact of this pandemic demands that we move with unprecedented urgency, and that is what our teams have done by submitting this application for molnupiravir to the FDA within 10 days of receiving the data,” Robert Davis, CEO and president of Merck, said in a statement. On Oct. 1, Merck and Ridgeback released interim data from its phase III clinical trial, which showed that molnupiravir reduced the risk of hospitalization or death by about 50%. About 7% of patients who received the drug were hospitalized within 30 days in the study, as compared with 14% of patients who took a placebo, the company said.
No deaths were reported in the group that received the drug, as compared with eight deaths in the group that received the placebo. None of the trial participants had been vaccinated.
“Medicines and vaccines are both essential to our collective efforts,” Mr. Davis said. “We look forward to working with the FDA on its review of our application, and to working with other regulatory agencies as we do everything we can to bring molnupiravir to patients around the world as quickly as possible.”
Merck has been producing molnupiravir in anticipation of the clinical trial results and FDA authorization. The company expects to produce 10 million courses of treatment by the end of the year, with more expected for 2022.
In June, Merck signed an agreement with the United States to supply 1.7 million courses of molnupiravir once the FDA authorizes the drug. The company has agreed to advance purchase agreements with other countries as well.
Earlier in the year, Merck also announced voluntary licensing agreements with several generics manufacturers in India to provide molnupiravir to more than 100 low- and middle-income countries after approval from local regulatory agencies.
Data from the company’s late-stage clinical trial has not yet been peer-reviewed or published.
Last week, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said the clinical trial results were “very encouraging” but noted that the FDA should closely scrutinize the drug, CNN reported.
“It is very important that this now must go through the usual process of careful examination of the data by the Food and Drug Administration, both for effectiveness but also for safety, because whenever you introduce a new compound, safety is very important,” Dr. Fauci said, adding that vaccines remain “our best tools against COVID-19.”
A version of this article firsts appeared on WebMD.com.
, an experimental antiviral COVID-19 treatment.
If the FDA grants authorization, the drug would be the first oral antiviral treatment for COVID-19. The capsule, made by Merck and Ridgeback Biotherapeutics, is intended to treat mild to moderate COVID-19 in adults who are at risk of having severe COVID-19 or hospitalization.
“The extraordinary impact of this pandemic demands that we move with unprecedented urgency, and that is what our teams have done by submitting this application for molnupiravir to the FDA within 10 days of receiving the data,” Robert Davis, CEO and president of Merck, said in a statement. On Oct. 1, Merck and Ridgeback released interim data from its phase III clinical trial, which showed that molnupiravir reduced the risk of hospitalization or death by about 50%. About 7% of patients who received the drug were hospitalized within 30 days in the study, as compared with 14% of patients who took a placebo, the company said.
No deaths were reported in the group that received the drug, as compared with eight deaths in the group that received the placebo. None of the trial participants had been vaccinated.
“Medicines and vaccines are both essential to our collective efforts,” Mr. Davis said. “We look forward to working with the FDA on its review of our application, and to working with other regulatory agencies as we do everything we can to bring molnupiravir to patients around the world as quickly as possible.”
Merck has been producing molnupiravir in anticipation of the clinical trial results and FDA authorization. The company expects to produce 10 million courses of treatment by the end of the year, with more expected for 2022.
In June, Merck signed an agreement with the United States to supply 1.7 million courses of molnupiravir once the FDA authorizes the drug. The company has agreed to advance purchase agreements with other countries as well.
Earlier in the year, Merck also announced voluntary licensing agreements with several generics manufacturers in India to provide molnupiravir to more than 100 low- and middle-income countries after approval from local regulatory agencies.
Data from the company’s late-stage clinical trial has not yet been peer-reviewed or published.
Last week, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said the clinical trial results were “very encouraging” but noted that the FDA should closely scrutinize the drug, CNN reported.
“It is very important that this now must go through the usual process of careful examination of the data by the Food and Drug Administration, both for effectiveness but also for safety, because whenever you introduce a new compound, safety is very important,” Dr. Fauci said, adding that vaccines remain “our best tools against COVID-19.”
A version of this article firsts appeared on WebMD.com.
, an experimental antiviral COVID-19 treatment.
If the FDA grants authorization, the drug would be the first oral antiviral treatment for COVID-19. The capsule, made by Merck and Ridgeback Biotherapeutics, is intended to treat mild to moderate COVID-19 in adults who are at risk of having severe COVID-19 or hospitalization.
“The extraordinary impact of this pandemic demands that we move with unprecedented urgency, and that is what our teams have done by submitting this application for molnupiravir to the FDA within 10 days of receiving the data,” Robert Davis, CEO and president of Merck, said in a statement. On Oct. 1, Merck and Ridgeback released interim data from its phase III clinical trial, which showed that molnupiravir reduced the risk of hospitalization or death by about 50%. About 7% of patients who received the drug were hospitalized within 30 days in the study, as compared with 14% of patients who took a placebo, the company said.
No deaths were reported in the group that received the drug, as compared with eight deaths in the group that received the placebo. None of the trial participants had been vaccinated.
“Medicines and vaccines are both essential to our collective efforts,” Mr. Davis said. “We look forward to working with the FDA on its review of our application, and to working with other regulatory agencies as we do everything we can to bring molnupiravir to patients around the world as quickly as possible.”
Merck has been producing molnupiravir in anticipation of the clinical trial results and FDA authorization. The company expects to produce 10 million courses of treatment by the end of the year, with more expected for 2022.
In June, Merck signed an agreement with the United States to supply 1.7 million courses of molnupiravir once the FDA authorizes the drug. The company has agreed to advance purchase agreements with other countries as well.
Earlier in the year, Merck also announced voluntary licensing agreements with several generics manufacturers in India to provide molnupiravir to more than 100 low- and middle-income countries after approval from local regulatory agencies.
Data from the company’s late-stage clinical trial has not yet been peer-reviewed or published.
Last week, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said the clinical trial results were “very encouraging” but noted that the FDA should closely scrutinize the drug, CNN reported.
“It is very important that this now must go through the usual process of careful examination of the data by the Food and Drug Administration, both for effectiveness but also for safety, because whenever you introduce a new compound, safety is very important,” Dr. Fauci said, adding that vaccines remain “our best tools against COVID-19.”
A version of this article firsts appeared on WebMD.com.
High-dose omega-3s tied to higher AFib risk
Taking high-doses of marine omega-3 fatty acids, more than 1 gram daily, may raise the risk for atrial fibrillation (AFib), according to a meta-analysis of relevant research.
However, the risk of developing AFib appears to be “relatively small” for those taking 1 gram or less of fish oil per day, Christine M. Albert, MD, chair of the department of cardiology at the Smidt Heart Institute at Cedars-Sinai, Los Angeles, told this news organization.
The study was published online Oct. 6 in the journal Circulation.
It’s estimated that 7.8% of U.S. adults – almost 19 million in all – take fish oil supplements, often unbeknownst to their health care providers, the researchers noted. Yet, the literature on the effects of omega-3 fatty acid supplementation on cardiovascular outcomes are mixed.
“Some, but not all” large-scale randomized controlled trials investigating the effects of marine omega-3 fatty acid supplements on cardiovascular outcomes have reported increased risks for AFib. The potential reasons for differing findings may be dose related, the authors note in their paper.
The goal of this meta-analysis was to “bring clarity, answers, and actionable information” to doctors and patients, said Dr. Albert. The results suggest, however, that there may not be a “straightforward answer” to whether fish oil is good or bad for AFib. Instead, the answer may depend on the dose, she added.
Pooled data
After screening 4,049 articles and abstracts, the researchers included in their analysis seven large-scale randomized controlled trials reporting cardiovascular outcomes of marine omega-3 fatty acids.
The trials reported results for AFib, either as prespecified outcome, adverse event, or a reason for hospitalization. Each had a minimum of 500 patients and a median follow-up of at least 1 year.
Trials examining the effects of omega-3 fatty acids on recurrent AFib in patients with established AFib or postoperative AFib were excluded.
The seven trials enrolled a total of 81,210 patients (mean age, 65 years; 39% women); 72.6% of participants were enrolled in clinical trials testing ≤1 gram of marine omega-3 fatty acids per day and 27.4% were enrolled in clinical trials testing >1 gram of the supplement per day. The weighted average follow-up was 4.9 years.
Overall, use of omega-3 fatty acids was associated with a 25% increased risk for AFib (hazard ratio, 1.25; 95% confidence interval, 1.07-1.46; P = .013).
In analyses stratified by dose, the risk for AFib was “significantly more pronounced” in trials testing high doses of marine omega-3 fatty acid supplements (>1 gram per day: HR, 1.49; 95% CI, 1.04-2.15; P = .042) compared with those testing lower doses (≤1 gram per day: HR, 1.12; 95% CI, 1.03-1.22; P = .024; P for interaction < .001).
In meta-regression, the HR for AFib increased per 1 gram increase in daily omega-3 fatty acid dose (HR. 1.11; 95% CI, 1.06-1.15; P = .001).
Risk-benefit balance
“This meta-analysis adds new evidence regarding the risk of AFib in patients taking marine omega-3 fatty acid supplements,” wrote Dr. Albert and colleagues.
“Since the benefit of omega-3 fatty acids also appears to be dose dependent, the associated risk of AFib should be balanced against the benefit on atherosclerotic cardiovascular outcomes,” they suggested.
They cautioned that the meta-analysis pooled aggregate-level trial data, not individual patient data. Therefore, subgroup analyses by age or other patient level characteristics were not possible.
The risk of developing AFib increases with advancing age and is more common in men than in women. Additional risk factors include elevated blood pressure, coronary artery disease, heart failure, heart valve defects, obesity, and diabetes.
The authors said the potential risk of developing AFib with high doses of omega-3 fatty acid supplements should be discussed with patients and they should know the signs and symptoms of the condition.
The study had no specific funding. Dr. Albert has received grants from St. Jude Medical, Abbott, and Roche Diagnostics.
A version of this article first appeared on Medscape.com.
Taking high-doses of marine omega-3 fatty acids, more than 1 gram daily, may raise the risk for atrial fibrillation (AFib), according to a meta-analysis of relevant research.
However, the risk of developing AFib appears to be “relatively small” for those taking 1 gram or less of fish oil per day, Christine M. Albert, MD, chair of the department of cardiology at the Smidt Heart Institute at Cedars-Sinai, Los Angeles, told this news organization.
The study was published online Oct. 6 in the journal Circulation.
It’s estimated that 7.8% of U.S. adults – almost 19 million in all – take fish oil supplements, often unbeknownst to their health care providers, the researchers noted. Yet, the literature on the effects of omega-3 fatty acid supplementation on cardiovascular outcomes are mixed.
“Some, but not all” large-scale randomized controlled trials investigating the effects of marine omega-3 fatty acid supplements on cardiovascular outcomes have reported increased risks for AFib. The potential reasons for differing findings may be dose related, the authors note in their paper.
The goal of this meta-analysis was to “bring clarity, answers, and actionable information” to doctors and patients, said Dr. Albert. The results suggest, however, that there may not be a “straightforward answer” to whether fish oil is good or bad for AFib. Instead, the answer may depend on the dose, she added.
Pooled data
After screening 4,049 articles and abstracts, the researchers included in their analysis seven large-scale randomized controlled trials reporting cardiovascular outcomes of marine omega-3 fatty acids.
The trials reported results for AFib, either as prespecified outcome, adverse event, or a reason for hospitalization. Each had a minimum of 500 patients and a median follow-up of at least 1 year.
Trials examining the effects of omega-3 fatty acids on recurrent AFib in patients with established AFib or postoperative AFib were excluded.
The seven trials enrolled a total of 81,210 patients (mean age, 65 years; 39% women); 72.6% of participants were enrolled in clinical trials testing ≤1 gram of marine omega-3 fatty acids per day and 27.4% were enrolled in clinical trials testing >1 gram of the supplement per day. The weighted average follow-up was 4.9 years.
Overall, use of omega-3 fatty acids was associated with a 25% increased risk for AFib (hazard ratio, 1.25; 95% confidence interval, 1.07-1.46; P = .013).
In analyses stratified by dose, the risk for AFib was “significantly more pronounced” in trials testing high doses of marine omega-3 fatty acid supplements (>1 gram per day: HR, 1.49; 95% CI, 1.04-2.15; P = .042) compared with those testing lower doses (≤1 gram per day: HR, 1.12; 95% CI, 1.03-1.22; P = .024; P for interaction < .001).
In meta-regression, the HR for AFib increased per 1 gram increase in daily omega-3 fatty acid dose (HR. 1.11; 95% CI, 1.06-1.15; P = .001).
Risk-benefit balance
“This meta-analysis adds new evidence regarding the risk of AFib in patients taking marine omega-3 fatty acid supplements,” wrote Dr. Albert and colleagues.
“Since the benefit of omega-3 fatty acids also appears to be dose dependent, the associated risk of AFib should be balanced against the benefit on atherosclerotic cardiovascular outcomes,” they suggested.
They cautioned that the meta-analysis pooled aggregate-level trial data, not individual patient data. Therefore, subgroup analyses by age or other patient level characteristics were not possible.
The risk of developing AFib increases with advancing age and is more common in men than in women. Additional risk factors include elevated blood pressure, coronary artery disease, heart failure, heart valve defects, obesity, and diabetes.
The authors said the potential risk of developing AFib with high doses of omega-3 fatty acid supplements should be discussed with patients and they should know the signs and symptoms of the condition.
The study had no specific funding. Dr. Albert has received grants from St. Jude Medical, Abbott, and Roche Diagnostics.
A version of this article first appeared on Medscape.com.
Taking high-doses of marine omega-3 fatty acids, more than 1 gram daily, may raise the risk for atrial fibrillation (AFib), according to a meta-analysis of relevant research.
However, the risk of developing AFib appears to be “relatively small” for those taking 1 gram or less of fish oil per day, Christine M. Albert, MD, chair of the department of cardiology at the Smidt Heart Institute at Cedars-Sinai, Los Angeles, told this news organization.
The study was published online Oct. 6 in the journal Circulation.
It’s estimated that 7.8% of U.S. adults – almost 19 million in all – take fish oil supplements, often unbeknownst to their health care providers, the researchers noted. Yet, the literature on the effects of omega-3 fatty acid supplementation on cardiovascular outcomes are mixed.
“Some, but not all” large-scale randomized controlled trials investigating the effects of marine omega-3 fatty acid supplements on cardiovascular outcomes have reported increased risks for AFib. The potential reasons for differing findings may be dose related, the authors note in their paper.
The goal of this meta-analysis was to “bring clarity, answers, and actionable information” to doctors and patients, said Dr. Albert. The results suggest, however, that there may not be a “straightforward answer” to whether fish oil is good or bad for AFib. Instead, the answer may depend on the dose, she added.
Pooled data
After screening 4,049 articles and abstracts, the researchers included in their analysis seven large-scale randomized controlled trials reporting cardiovascular outcomes of marine omega-3 fatty acids.
The trials reported results for AFib, either as prespecified outcome, adverse event, or a reason for hospitalization. Each had a minimum of 500 patients and a median follow-up of at least 1 year.
Trials examining the effects of omega-3 fatty acids on recurrent AFib in patients with established AFib or postoperative AFib were excluded.
The seven trials enrolled a total of 81,210 patients (mean age, 65 years; 39% women); 72.6% of participants were enrolled in clinical trials testing ≤1 gram of marine omega-3 fatty acids per day and 27.4% were enrolled in clinical trials testing >1 gram of the supplement per day. The weighted average follow-up was 4.9 years.
Overall, use of omega-3 fatty acids was associated with a 25% increased risk for AFib (hazard ratio, 1.25; 95% confidence interval, 1.07-1.46; P = .013).
In analyses stratified by dose, the risk for AFib was “significantly more pronounced” in trials testing high doses of marine omega-3 fatty acid supplements (>1 gram per day: HR, 1.49; 95% CI, 1.04-2.15; P = .042) compared with those testing lower doses (≤1 gram per day: HR, 1.12; 95% CI, 1.03-1.22; P = .024; P for interaction < .001).
In meta-regression, the HR for AFib increased per 1 gram increase in daily omega-3 fatty acid dose (HR. 1.11; 95% CI, 1.06-1.15; P = .001).
Risk-benefit balance
“This meta-analysis adds new evidence regarding the risk of AFib in patients taking marine omega-3 fatty acid supplements,” wrote Dr. Albert and colleagues.
“Since the benefit of omega-3 fatty acids also appears to be dose dependent, the associated risk of AFib should be balanced against the benefit on atherosclerotic cardiovascular outcomes,” they suggested.
They cautioned that the meta-analysis pooled aggregate-level trial data, not individual patient data. Therefore, subgroup analyses by age or other patient level characteristics were not possible.
The risk of developing AFib increases with advancing age and is more common in men than in women. Additional risk factors include elevated blood pressure, coronary artery disease, heart failure, heart valve defects, obesity, and diabetes.
The authors said the potential risk of developing AFib with high doses of omega-3 fatty acid supplements should be discussed with patients and they should know the signs and symptoms of the condition.
The study had no specific funding. Dr. Albert has received grants from St. Jude Medical, Abbott, and Roche Diagnostics.
A version of this article first appeared on Medscape.com.
PDT for actinic keratoses continues to be refined
.

“We have conventional PDT, daylight PDT; we can combine with a range of topicals, and we can combine a range of different physical treatment procedures in order to provide better and individualized treatment regimens for our patients,” Merete Haedersdal, MD, PhD, DMSc, professor of dermatology at the University of Copenhagen, said during a course on laser and aesthetic skin therapy.
In Europe, PDT consists of a three-step procedure: curettage of AKs, application of photosensitizer on the skin (typically methyl aminolevulinate, versus aminolevulinic acid, used more often in the United States), and illumination with red light (versus blue light, used more often in the United States), which causes a photochemical reaction.
“It’s a photochemical-reaction concept with which we can achieve up to 90% cure rates of AKs at 3 months,” Dr. Haedersdal said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine.
PDT is also used in Europe for select patients with Bowen’s disease (yielding a 90% cure rate at 3 months, 70% at 2 years); superficial basal cell carcinoma (yielding a 90% cure rate at 3 months, 75% at 5 years), and nodular BCC (yielding a 90% cure rate at 3 months, 75% at 5 years.
“With conventional PDT, whether it’s blue light, red light, MAL, or ALA, we have beautiful cosmesis, but we also have a challenge, which is pain,” she said. This is behind the motivation to look at other ways to provide PDT.
Daylight PDT, which was pioneered by Dr. Haedersdal’s mentor, Hans Christian Wulf, MD, DMSc, PharmD, professor of dermatology at the University of Copenhagen, provides 80%-90% clearance of thin AKs, lower clearance of thick AKs – and is a nearly pain-free procedure because of continuous photoactivation of protoporphyrin IX, with a Visual Analog Scale in the range of 1-3. “Globally, thousands of patients have been treated [with daylight PDT], which is backed up in the literature with more than 150 publications,” she said.
According to Dr. Haedersdal, MAL cream with daylight activation for treatment of AK was approved in Colombia and Mexico in 2013; in Australia, Brazil, and Costa Rica in 2014; and in Chile, Europe, and New Zealand in 2015. “I do hope that one day you will have daylight PDT approved in the United States,” she said.
The suggested protocol for daylight PDT starts by applying a sunscreen with an organic filter. After about 15 minutes, the lesion or lesions are prepared, and MAL is applied with no occlusion. Patients should start their exposure to daylight within 30 minutes of application, remaining outdoors for 2 hours of continuous exposure, either at a dedicated space located on the ground of the hospital or clinic or at their home. After 2 hours, patients wipe off the remaining cream and are advised to stay indoors for the rest of the day.
“Ideal candidates are those who have large skin areas that can be easily exposed to sunlight,” such as the scalp and lower legs, said Dr. Haedersdal, who is also a visiting scientist at the Wellman Center for Photomedicine, Boston. “If patients are treated in areas covered by clothing, it can be greasy and sticky with the cream. In these cases, you can cover the area with Tegaderm, which allows for 99% light transmission. Daylight can shine through and the Tegaderm can be removed after the procedure.”
On rainy days between April 1 and October 1 in Copenhagen, she said, daylight PDT is provided in a greenhouse in the hospital garden, with a heater and blankets for patients when the temperature falls below 10° C.
The amount of light required for a treatment effect is 5,000-10,000 lux, and the number of lux on a sunny day in Denmark is about 100,000, she said. “That means that all year round in countries south of latitude 45 degrees N, patients can be treated with daylight PDT.”
To intensify the treatment efficacy of conventional PDT and daylight PDT, especially in those with severely photodamaged skin, combining treatment with a physical pretreatment technique such as curettage, ablative fractional laser, microdermabrasion, microneedling, and nonablative fractional laser is another strategy. A small randomized controlled trial found that ablative fractional laser treatment extended notable relative effectiveness, compared with other physical enhancement techniques.
Dr. Haedersdal and colleagues published a study that compared pretreatment with ablative fractional laser and microdermabrasion pads before daylight PDT for AKs in field-cancerized skin. They found that with a single treatment, combination therapy with ablative fractional laser before daylight PDT led to significantly greater efficacious AK clearance and skin rejuvenation, compared with treatment with microdermabrasion.
“We don’t know why this is, but we believe it may be due to the fact that with the laser, we have a photothermal response, which in combination with the photochemical response from the photodynamic therapy induces a synergistic effect,” she said.
A range of topical treatments can also be given in combination with PDT. In a meta-analysis of 10 randomized controlled trials, German researchers evaluated the efficacy of PDT combined with imiquimod cream, 5-fluorouracil cream, tazarotene gel, and calcipotriol ointment. They concluded that the combination of PDT with another topical drug intervention improves AK clearance rates, compared with monotherapy.
More recently, the same authors summarized the current knowledge on the efficacy and safety of local combination therapies for the treatment of patients with AK in a review article, which Dr. Haedersdal said provides a nice overview of this topic.
Dr. Haedersdal disclosed that she has received equipment from Cherry Imaging, Cynosure-Hologic, MiraDry, and PerfAction Technologies. She has also received research grants from Leo Pharma, Lutronic, Mirai Medical, Novoxel, and Venus Concept.
.

“We have conventional PDT, daylight PDT; we can combine with a range of topicals, and we can combine a range of different physical treatment procedures in order to provide better and individualized treatment regimens for our patients,” Merete Haedersdal, MD, PhD, DMSc, professor of dermatology at the University of Copenhagen, said during a course on laser and aesthetic skin therapy.
In Europe, PDT consists of a three-step procedure: curettage of AKs, application of photosensitizer on the skin (typically methyl aminolevulinate, versus aminolevulinic acid, used more often in the United States), and illumination with red light (versus blue light, used more often in the United States), which causes a photochemical reaction.
“It’s a photochemical-reaction concept with which we can achieve up to 90% cure rates of AKs at 3 months,” Dr. Haedersdal said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine.
PDT is also used in Europe for select patients with Bowen’s disease (yielding a 90% cure rate at 3 months, 70% at 2 years); superficial basal cell carcinoma (yielding a 90% cure rate at 3 months, 75% at 5 years), and nodular BCC (yielding a 90% cure rate at 3 months, 75% at 5 years.
“With conventional PDT, whether it’s blue light, red light, MAL, or ALA, we have beautiful cosmesis, but we also have a challenge, which is pain,” she said. This is behind the motivation to look at other ways to provide PDT.
Daylight PDT, which was pioneered by Dr. Haedersdal’s mentor, Hans Christian Wulf, MD, DMSc, PharmD, professor of dermatology at the University of Copenhagen, provides 80%-90% clearance of thin AKs, lower clearance of thick AKs – and is a nearly pain-free procedure because of continuous photoactivation of protoporphyrin IX, with a Visual Analog Scale in the range of 1-3. “Globally, thousands of patients have been treated [with daylight PDT], which is backed up in the literature with more than 150 publications,” she said.
According to Dr. Haedersdal, MAL cream with daylight activation for treatment of AK was approved in Colombia and Mexico in 2013; in Australia, Brazil, and Costa Rica in 2014; and in Chile, Europe, and New Zealand in 2015. “I do hope that one day you will have daylight PDT approved in the United States,” she said.
The suggested protocol for daylight PDT starts by applying a sunscreen with an organic filter. After about 15 minutes, the lesion or lesions are prepared, and MAL is applied with no occlusion. Patients should start their exposure to daylight within 30 minutes of application, remaining outdoors for 2 hours of continuous exposure, either at a dedicated space located on the ground of the hospital or clinic or at their home. After 2 hours, patients wipe off the remaining cream and are advised to stay indoors for the rest of the day.
“Ideal candidates are those who have large skin areas that can be easily exposed to sunlight,” such as the scalp and lower legs, said Dr. Haedersdal, who is also a visiting scientist at the Wellman Center for Photomedicine, Boston. “If patients are treated in areas covered by clothing, it can be greasy and sticky with the cream. In these cases, you can cover the area with Tegaderm, which allows for 99% light transmission. Daylight can shine through and the Tegaderm can be removed after the procedure.”
On rainy days between April 1 and October 1 in Copenhagen, she said, daylight PDT is provided in a greenhouse in the hospital garden, with a heater and blankets for patients when the temperature falls below 10° C.
The amount of light required for a treatment effect is 5,000-10,000 lux, and the number of lux on a sunny day in Denmark is about 100,000, she said. “That means that all year round in countries south of latitude 45 degrees N, patients can be treated with daylight PDT.”
To intensify the treatment efficacy of conventional PDT and daylight PDT, especially in those with severely photodamaged skin, combining treatment with a physical pretreatment technique such as curettage, ablative fractional laser, microdermabrasion, microneedling, and nonablative fractional laser is another strategy. A small randomized controlled trial found that ablative fractional laser treatment extended notable relative effectiveness, compared with other physical enhancement techniques.
Dr. Haedersdal and colleagues published a study that compared pretreatment with ablative fractional laser and microdermabrasion pads before daylight PDT for AKs in field-cancerized skin. They found that with a single treatment, combination therapy with ablative fractional laser before daylight PDT led to significantly greater efficacious AK clearance and skin rejuvenation, compared with treatment with microdermabrasion.
“We don’t know why this is, but we believe it may be due to the fact that with the laser, we have a photothermal response, which in combination with the photochemical response from the photodynamic therapy induces a synergistic effect,” she said.
A range of topical treatments can also be given in combination with PDT. In a meta-analysis of 10 randomized controlled trials, German researchers evaluated the efficacy of PDT combined with imiquimod cream, 5-fluorouracil cream, tazarotene gel, and calcipotriol ointment. They concluded that the combination of PDT with another topical drug intervention improves AK clearance rates, compared with monotherapy.
More recently, the same authors summarized the current knowledge on the efficacy and safety of local combination therapies for the treatment of patients with AK in a review article, which Dr. Haedersdal said provides a nice overview of this topic.
Dr. Haedersdal disclosed that she has received equipment from Cherry Imaging, Cynosure-Hologic, MiraDry, and PerfAction Technologies. She has also received research grants from Leo Pharma, Lutronic, Mirai Medical, Novoxel, and Venus Concept.
.

“We have conventional PDT, daylight PDT; we can combine with a range of topicals, and we can combine a range of different physical treatment procedures in order to provide better and individualized treatment regimens for our patients,” Merete Haedersdal, MD, PhD, DMSc, professor of dermatology at the University of Copenhagen, said during a course on laser and aesthetic skin therapy.
In Europe, PDT consists of a three-step procedure: curettage of AKs, application of photosensitizer on the skin (typically methyl aminolevulinate, versus aminolevulinic acid, used more often in the United States), and illumination with red light (versus blue light, used more often in the United States), which causes a photochemical reaction.
“It’s a photochemical-reaction concept with which we can achieve up to 90% cure rates of AKs at 3 months,” Dr. Haedersdal said during the meeting, which was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine.
PDT is also used in Europe for select patients with Bowen’s disease (yielding a 90% cure rate at 3 months, 70% at 2 years); superficial basal cell carcinoma (yielding a 90% cure rate at 3 months, 75% at 5 years), and nodular BCC (yielding a 90% cure rate at 3 months, 75% at 5 years.
“With conventional PDT, whether it’s blue light, red light, MAL, or ALA, we have beautiful cosmesis, but we also have a challenge, which is pain,” she said. This is behind the motivation to look at other ways to provide PDT.
Daylight PDT, which was pioneered by Dr. Haedersdal’s mentor, Hans Christian Wulf, MD, DMSc, PharmD, professor of dermatology at the University of Copenhagen, provides 80%-90% clearance of thin AKs, lower clearance of thick AKs – and is a nearly pain-free procedure because of continuous photoactivation of protoporphyrin IX, with a Visual Analog Scale in the range of 1-3. “Globally, thousands of patients have been treated [with daylight PDT], which is backed up in the literature with more than 150 publications,” she said.
According to Dr. Haedersdal, MAL cream with daylight activation for treatment of AK was approved in Colombia and Mexico in 2013; in Australia, Brazil, and Costa Rica in 2014; and in Chile, Europe, and New Zealand in 2015. “I do hope that one day you will have daylight PDT approved in the United States,” she said.
The suggested protocol for daylight PDT starts by applying a sunscreen with an organic filter. After about 15 minutes, the lesion or lesions are prepared, and MAL is applied with no occlusion. Patients should start their exposure to daylight within 30 minutes of application, remaining outdoors for 2 hours of continuous exposure, either at a dedicated space located on the ground of the hospital or clinic or at their home. After 2 hours, patients wipe off the remaining cream and are advised to stay indoors for the rest of the day.
“Ideal candidates are those who have large skin areas that can be easily exposed to sunlight,” such as the scalp and lower legs, said Dr. Haedersdal, who is also a visiting scientist at the Wellman Center for Photomedicine, Boston. “If patients are treated in areas covered by clothing, it can be greasy and sticky with the cream. In these cases, you can cover the area with Tegaderm, which allows for 99% light transmission. Daylight can shine through and the Tegaderm can be removed after the procedure.”
On rainy days between April 1 and October 1 in Copenhagen, she said, daylight PDT is provided in a greenhouse in the hospital garden, with a heater and blankets for patients when the temperature falls below 10° C.
The amount of light required for a treatment effect is 5,000-10,000 lux, and the number of lux on a sunny day in Denmark is about 100,000, she said. “That means that all year round in countries south of latitude 45 degrees N, patients can be treated with daylight PDT.”
To intensify the treatment efficacy of conventional PDT and daylight PDT, especially in those with severely photodamaged skin, combining treatment with a physical pretreatment technique such as curettage, ablative fractional laser, microdermabrasion, microneedling, and nonablative fractional laser is another strategy. A small randomized controlled trial found that ablative fractional laser treatment extended notable relative effectiveness, compared with other physical enhancement techniques.
Dr. Haedersdal and colleagues published a study that compared pretreatment with ablative fractional laser and microdermabrasion pads before daylight PDT for AKs in field-cancerized skin. They found that with a single treatment, combination therapy with ablative fractional laser before daylight PDT led to significantly greater efficacious AK clearance and skin rejuvenation, compared with treatment with microdermabrasion.
“We don’t know why this is, but we believe it may be due to the fact that with the laser, we have a photothermal response, which in combination with the photochemical response from the photodynamic therapy induces a synergistic effect,” she said.
A range of topical treatments can also be given in combination with PDT. In a meta-analysis of 10 randomized controlled trials, German researchers evaluated the efficacy of PDT combined with imiquimod cream, 5-fluorouracil cream, tazarotene gel, and calcipotriol ointment. They concluded that the combination of PDT with another topical drug intervention improves AK clearance rates, compared with monotherapy.
More recently, the same authors summarized the current knowledge on the efficacy and safety of local combination therapies for the treatment of patients with AK in a review article, which Dr. Haedersdal said provides a nice overview of this topic.
Dr. Haedersdal disclosed that she has received equipment from Cherry Imaging, Cynosure-Hologic, MiraDry, and PerfAction Technologies. She has also received research grants from Leo Pharma, Lutronic, Mirai Medical, Novoxel, and Venus Concept.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
Adding statins to steroids in thyroid eye disease improves outcomes
Treatment of Graves’ orbitopathy with statins in combination with glucocorticoids shows benefits among people with – and even without – high cholesterol, results from a new randomized clinical trial show.
“Our results [indicate] that adding atorvastatin to intravenous glucocorticoids seems to potentiate the effects of glucocorticoids,” senior author Michelle Marino, MD, associate professor of endocrinology in the department of clinical and experimental medicine at the University of Pisa, Italy, told this news organization.
“At least in hypercholesterolemic patients with moderate to severe and active Graves’ orbitopathy, atorvastatin should be considered in addition to intravenous glucocorticoids,” Dr. Marino said.
The study was presented by first author Giulia Lanzolla, MD, also of the University of Pisa and University Hospital of Pisa, at the virtual annual meeting of the American Thyroid Association.
Hypercholesterolemia, well known to promote systemic inflammation, has been previously linked to Graves’ orbitopathy, and the use of statins has also been shown to possibly provide a protective effect in the risk of developing the thyroid eye disease.
Furthermore, patients with Graves’ orbitopathy and high cholesterol levels, compared with those with normal cholesterol, have been shown to have poorer responses to treatment with glucocorticoids, which have long been the first line of treatment.
Asked for comment on the findings, Marius Stan, MD, a consultant in the division of endocrinology, diabetes, metabolism, and nutrition, Mayo Clinic, Rochester, Minn., said he didn’t think the outcome measure used – a composite of a variety of measures of thyroid eye disease – was best to truly understand the benefits.
Statins for Graves’ orbitopathy (STAGO) study details
For a better understanding of the effects with and without the addition of statins in a randomized trial, Dr. Lanzolla and colleagues enrolled 88 patients with high cholesterol and moderate to severe active Graves’ orbitopathy in the phase 2 STAGO trial.
Patients were randomized to two groups of 44 patients each to receive treatment either with intravenous (IV) methylprednisolone at 500 mg per week for 6 weeks, followed by 250 mg per week for another 6 weeks, in combination with atorvastatin 20 mg daily for 12 weeks, or methylprednisolone alone for 12 weeks.
The primary endpoint was a composite of Graves orbitopathy outcomes and included measures of exophthalmos, clinical activity score, eyelid aperture, diplopia, and visual acuity, as assessed in the modified intention-to-treat population.
The trial met the primary composite endpoint, with 51.2% of those treated with statins achieving the outcome (21 of 41) versus 28.2% (11 of 39) of those treated with glucocorticoids alone (odds ratio, 2.76; P = .03).
The study also achieved secondary outcomes, with 43.9% in the statin group having a response to treatment at 12 weeks versus 23% in the glucocorticoid group (OR 2.60; P = .05). The statin group also had a greater improvement in quality of life measures (P = .03).
The glucocorticoid-only group meanwhile had a significantly greater rate of Graves orbitopathy relapse at 24 weeks, with six relapses versus none in the statin group (15.3% vs. 0.0%; OR 0.06; P = .01).
There were no significant differences in low-density lipoprotein (LDL) cholesterol between those who did and did not respond to treatment in the statin group.
The most likely explanation for those findings is that “atorvastatin acts through its pleiotropic action, resulting in an anti-inflammatory effect,” Dr. Marino said.
“In addition, the effect may be related to the capability of statins to inhibit fibroblast proliferation,” Dr. Marino added.
“Total cholesterol had a behavior similar to LDL cholesterol, [while] HDL cholesterol did not change across the study.”
There were no major adverse events related to atorvastatin, with one patient in each group requiring treatment discontinuation.
In the rapidly evolving landscape of treatments for Graves’ orbitopathy, including the recent Food and Drug Administration approval for teprotumumab in thyroid eye disease, the potential role of statins remains to be seen, Dr. Marino noted.
“Graves’ orbitopathy is a rather complex disease, and in its mild to moderate forms it is very rare for a patient to require only a single treatment,” Dr. Marino explained. “Rehabilitative surgery is needed quite often once the disease is inactive.”
The authors noted that a composite overall Graves’ orbitopathy outcome was used as the primary endpoint because the alternative of a change in single eye features may not reflect a true modification of Graves’ orbitopathy and could be affected by a number of unrelated factors.
“By contrast, the composite evaluation offers a more realistic picture,” the authors wrote in the article, which was published in The Lancet Diabetes and Endocrinology.
Composite outcome not best way of assessing effects of statins
Dr. Stan extrapolated on his criticism of the trial.
“The study has interesting results but fails to show that any particular eye feature is benefited by the combination therapy, showing only the composite outcome to be improved,” he told this news organization.
“Unfortunately, that is hard to extrapolate to patient care, where one or another of Graves’ orbitopathy features are present and are the intended target of therapy,” he said.
Dr. Stan added that IV glucocorticoids are meanwhile also changing the landscape of treatment of thyroid eye disease.
“This ... current plan is to recommend a more individualized approach, depending on what is the main problem for that thyroid eye disease case,” he explained.
Dr. Marino noted that the authors are planning a double-blind, placebo-controlled phase 3 clinical trial of the statin/glucocorticoid combination to include patients regardless of their cholesterol levels.
The study received funding from Associazione Allievi Endocrinologia Pisana. The authors have reported no relevant financial relationships. Dr. Stan is on the advisory board for Horizon Pharma/Immunovant and provides general consulting for VasaraGen/Septerna and ValenzaBio/Medicxi.
A version of this article first appeared on Medscape.com.
Treatment of Graves’ orbitopathy with statins in combination with glucocorticoids shows benefits among people with – and even without – high cholesterol, results from a new randomized clinical trial show.
“Our results [indicate] that adding atorvastatin to intravenous glucocorticoids seems to potentiate the effects of glucocorticoids,” senior author Michelle Marino, MD, associate professor of endocrinology in the department of clinical and experimental medicine at the University of Pisa, Italy, told this news organization.
“At least in hypercholesterolemic patients with moderate to severe and active Graves’ orbitopathy, atorvastatin should be considered in addition to intravenous glucocorticoids,” Dr. Marino said.
The study was presented by first author Giulia Lanzolla, MD, also of the University of Pisa and University Hospital of Pisa, at the virtual annual meeting of the American Thyroid Association.
Hypercholesterolemia, well known to promote systemic inflammation, has been previously linked to Graves’ orbitopathy, and the use of statins has also been shown to possibly provide a protective effect in the risk of developing the thyroid eye disease.
Furthermore, patients with Graves’ orbitopathy and high cholesterol levels, compared with those with normal cholesterol, have been shown to have poorer responses to treatment with glucocorticoids, which have long been the first line of treatment.
Asked for comment on the findings, Marius Stan, MD, a consultant in the division of endocrinology, diabetes, metabolism, and nutrition, Mayo Clinic, Rochester, Minn., said he didn’t think the outcome measure used – a composite of a variety of measures of thyroid eye disease – was best to truly understand the benefits.
Statins for Graves’ orbitopathy (STAGO) study details
For a better understanding of the effects with and without the addition of statins in a randomized trial, Dr. Lanzolla and colleagues enrolled 88 patients with high cholesterol and moderate to severe active Graves’ orbitopathy in the phase 2 STAGO trial.
Patients were randomized to two groups of 44 patients each to receive treatment either with intravenous (IV) methylprednisolone at 500 mg per week for 6 weeks, followed by 250 mg per week for another 6 weeks, in combination with atorvastatin 20 mg daily for 12 weeks, or methylprednisolone alone for 12 weeks.
The primary endpoint was a composite of Graves orbitopathy outcomes and included measures of exophthalmos, clinical activity score, eyelid aperture, diplopia, and visual acuity, as assessed in the modified intention-to-treat population.
The trial met the primary composite endpoint, with 51.2% of those treated with statins achieving the outcome (21 of 41) versus 28.2% (11 of 39) of those treated with glucocorticoids alone (odds ratio, 2.76; P = .03).
The study also achieved secondary outcomes, with 43.9% in the statin group having a response to treatment at 12 weeks versus 23% in the glucocorticoid group (OR 2.60; P = .05). The statin group also had a greater improvement in quality of life measures (P = .03).
The glucocorticoid-only group meanwhile had a significantly greater rate of Graves orbitopathy relapse at 24 weeks, with six relapses versus none in the statin group (15.3% vs. 0.0%; OR 0.06; P = .01).
There were no significant differences in low-density lipoprotein (LDL) cholesterol between those who did and did not respond to treatment in the statin group.
The most likely explanation for those findings is that “atorvastatin acts through its pleiotropic action, resulting in an anti-inflammatory effect,” Dr. Marino said.
“In addition, the effect may be related to the capability of statins to inhibit fibroblast proliferation,” Dr. Marino added.
“Total cholesterol had a behavior similar to LDL cholesterol, [while] HDL cholesterol did not change across the study.”
There were no major adverse events related to atorvastatin, with one patient in each group requiring treatment discontinuation.
In the rapidly evolving landscape of treatments for Graves’ orbitopathy, including the recent Food and Drug Administration approval for teprotumumab in thyroid eye disease, the potential role of statins remains to be seen, Dr. Marino noted.
“Graves’ orbitopathy is a rather complex disease, and in its mild to moderate forms it is very rare for a patient to require only a single treatment,” Dr. Marino explained. “Rehabilitative surgery is needed quite often once the disease is inactive.”
The authors noted that a composite overall Graves’ orbitopathy outcome was used as the primary endpoint because the alternative of a change in single eye features may not reflect a true modification of Graves’ orbitopathy and could be affected by a number of unrelated factors.
“By contrast, the composite evaluation offers a more realistic picture,” the authors wrote in the article, which was published in The Lancet Diabetes and Endocrinology.
Composite outcome not best way of assessing effects of statins
Dr. Stan extrapolated on his criticism of the trial.
“The study has interesting results but fails to show that any particular eye feature is benefited by the combination therapy, showing only the composite outcome to be improved,” he told this news organization.
“Unfortunately, that is hard to extrapolate to patient care, where one or another of Graves’ orbitopathy features are present and are the intended target of therapy,” he said.
Dr. Stan added that IV glucocorticoids are meanwhile also changing the landscape of treatment of thyroid eye disease.
“This ... current plan is to recommend a more individualized approach, depending on what is the main problem for that thyroid eye disease case,” he explained.
Dr. Marino noted that the authors are planning a double-blind, placebo-controlled phase 3 clinical trial of the statin/glucocorticoid combination to include patients regardless of their cholesterol levels.
The study received funding from Associazione Allievi Endocrinologia Pisana. The authors have reported no relevant financial relationships. Dr. Stan is on the advisory board for Horizon Pharma/Immunovant and provides general consulting for VasaraGen/Septerna and ValenzaBio/Medicxi.
A version of this article first appeared on Medscape.com.
Treatment of Graves’ orbitopathy with statins in combination with glucocorticoids shows benefits among people with – and even without – high cholesterol, results from a new randomized clinical trial show.
“Our results [indicate] that adding atorvastatin to intravenous glucocorticoids seems to potentiate the effects of glucocorticoids,” senior author Michelle Marino, MD, associate professor of endocrinology in the department of clinical and experimental medicine at the University of Pisa, Italy, told this news organization.
“At least in hypercholesterolemic patients with moderate to severe and active Graves’ orbitopathy, atorvastatin should be considered in addition to intravenous glucocorticoids,” Dr. Marino said.
The study was presented by first author Giulia Lanzolla, MD, also of the University of Pisa and University Hospital of Pisa, at the virtual annual meeting of the American Thyroid Association.
Hypercholesterolemia, well known to promote systemic inflammation, has been previously linked to Graves’ orbitopathy, and the use of statins has also been shown to possibly provide a protective effect in the risk of developing the thyroid eye disease.
Furthermore, patients with Graves’ orbitopathy and high cholesterol levels, compared with those with normal cholesterol, have been shown to have poorer responses to treatment with glucocorticoids, which have long been the first line of treatment.
Asked for comment on the findings, Marius Stan, MD, a consultant in the division of endocrinology, diabetes, metabolism, and nutrition, Mayo Clinic, Rochester, Minn., said he didn’t think the outcome measure used – a composite of a variety of measures of thyroid eye disease – was best to truly understand the benefits.
Statins for Graves’ orbitopathy (STAGO) study details
For a better understanding of the effects with and without the addition of statins in a randomized trial, Dr. Lanzolla and colleagues enrolled 88 patients with high cholesterol and moderate to severe active Graves’ orbitopathy in the phase 2 STAGO trial.
Patients were randomized to two groups of 44 patients each to receive treatment either with intravenous (IV) methylprednisolone at 500 mg per week for 6 weeks, followed by 250 mg per week for another 6 weeks, in combination with atorvastatin 20 mg daily for 12 weeks, or methylprednisolone alone for 12 weeks.
The primary endpoint was a composite of Graves orbitopathy outcomes and included measures of exophthalmos, clinical activity score, eyelid aperture, diplopia, and visual acuity, as assessed in the modified intention-to-treat population.
The trial met the primary composite endpoint, with 51.2% of those treated with statins achieving the outcome (21 of 41) versus 28.2% (11 of 39) of those treated with glucocorticoids alone (odds ratio, 2.76; P = .03).
The study also achieved secondary outcomes, with 43.9% in the statin group having a response to treatment at 12 weeks versus 23% in the glucocorticoid group (OR 2.60; P = .05). The statin group also had a greater improvement in quality of life measures (P = .03).
The glucocorticoid-only group meanwhile had a significantly greater rate of Graves orbitopathy relapse at 24 weeks, with six relapses versus none in the statin group (15.3% vs. 0.0%; OR 0.06; P = .01).
There were no significant differences in low-density lipoprotein (LDL) cholesterol between those who did and did not respond to treatment in the statin group.
The most likely explanation for those findings is that “atorvastatin acts through its pleiotropic action, resulting in an anti-inflammatory effect,” Dr. Marino said.
“In addition, the effect may be related to the capability of statins to inhibit fibroblast proliferation,” Dr. Marino added.
“Total cholesterol had a behavior similar to LDL cholesterol, [while] HDL cholesterol did not change across the study.”
There were no major adverse events related to atorvastatin, with one patient in each group requiring treatment discontinuation.
In the rapidly evolving landscape of treatments for Graves’ orbitopathy, including the recent Food and Drug Administration approval for teprotumumab in thyroid eye disease, the potential role of statins remains to be seen, Dr. Marino noted.
“Graves’ orbitopathy is a rather complex disease, and in its mild to moderate forms it is very rare for a patient to require only a single treatment,” Dr. Marino explained. “Rehabilitative surgery is needed quite often once the disease is inactive.”
The authors noted that a composite overall Graves’ orbitopathy outcome was used as the primary endpoint because the alternative of a change in single eye features may not reflect a true modification of Graves’ orbitopathy and could be affected by a number of unrelated factors.
“By contrast, the composite evaluation offers a more realistic picture,” the authors wrote in the article, which was published in The Lancet Diabetes and Endocrinology.
Composite outcome not best way of assessing effects of statins
Dr. Stan extrapolated on his criticism of the trial.
“The study has interesting results but fails to show that any particular eye feature is benefited by the combination therapy, showing only the composite outcome to be improved,” he told this news organization.
“Unfortunately, that is hard to extrapolate to patient care, where one or another of Graves’ orbitopathy features are present and are the intended target of therapy,” he said.
Dr. Stan added that IV glucocorticoids are meanwhile also changing the landscape of treatment of thyroid eye disease.
“This ... current plan is to recommend a more individualized approach, depending on what is the main problem for that thyroid eye disease case,” he explained.
Dr. Marino noted that the authors are planning a double-blind, placebo-controlled phase 3 clinical trial of the statin/glucocorticoid combination to include patients regardless of their cholesterol levels.
The study received funding from Associazione Allievi Endocrinologia Pisana. The authors have reported no relevant financial relationships. Dr. Stan is on the advisory board for Horizon Pharma/Immunovant and provides general consulting for VasaraGen/Septerna and ValenzaBio/Medicxi.
A version of this article first appeared on Medscape.com.
FROM ATA 2021
UC relapse associated with impaired luminal control of macrophage maturation
Patients with ulcerative colitis (UC) who are in remission from their disease lack luminal signals capable of inducing macrophage hyporesponsiveness, which may contribute to a patient’s persistent vulnerability to relapse, according to a new study.
“Together with the distinct fecal metabolomic profile of UC patients in remission, our data suggest that UC patients may lack the signals required for proper macrophage education, rendering them vulnerable to relapse,” wrote study authors Lujain Maasfeh, PhD, of the University of Gothenburg (Sweden) and colleagues in Cellular and Molecular Gastroenterology and Hepatology.
Macrophages found in the lamina propria play a role in sustaining intestinal homeostasis. Through education by local signals, intestinal macrophages adopt a hyporesponsive phenotype and tolerogenic nature and are replenished constantly from monocytes. In patients with UC who are in remission, however, the lack of proper macrophage maturation may result in gut inflammation.
Current evidence has yet to define fully the immunomodulating determinants in the education of intestinal macrophages; however, Dr. Maasfeh and associates wrote that “intestinal microbiota and microbiota-derived metabolites increasingly are recognized for their role in imprinting tissue-specific features of intestinal macrophages.”
The researchers added that previous evidence has established that patients with UC demonstrate dysbiosis, which may impact maturation of intestinal macrophages. As such, the hyporesponsive state of intestinal lamina propria macrophages induced by the microbiota may be lost in patients with UC who are in remission, ultimately resulting in disease relapse.
To gauge the effects of fecal luminal factors on macrophage phenotype and function, the researchers extracted fecal supernatants (FS) from the fecal samples of 10 healthy volunteers and 17 patients with UC who were in remission. Following maturation of monocytes to macrophages in the presence of granulocyte-macrophage colony-stimulating factor without and with FS, the researchers assessed macrophage phenotype and function. The investigators also used gas chromatography and mass spectrometry to analyze fecal metabolomic profiles.
In healthy donors, fecal luminal factors effectively downregulated Toll-like receptor signaling, cytokine signaling, as well as antigen presentation in macrophages. In contrast, the fecal luminal factors in patients with UC demonstrated less potency in their ability to induce lipopolysaccharide hyporesponsiveness. An immune pathway scoring analysis also showed a consistently higher reaction potential among UC remission FS-treated macrophages vs. healthy FS-treated macrophages.
While FS treatment did not seem to affect the phagocytic and bactericidal abilities of macrophages, the researchers observed that the healthy FS-treated macrophages better suppressed a cluster of differentiation 4+ T-cell activation as well as interferon gamma secretion vs. FS-treated macrophages from patients with UC in remission. The FS-treated macrophages in the UC remission population also featured less potency in their ability to suppress CD4+ T-cell activation and cytokine secretion.
The authors acknowledged a few limitations, including the small sample size and the effects from using in vitro system.
“Identification of the factors involved in intestinal macrophage education is important to maintain/reestablish gut homeostasis in patients with UC,” they concluded.
The study received financial support from Swedish Research Council-Medicine, in addition to funding from a Region Västra Götaland ALF-agreement, the Knut och Alice Wallenberg Foundation Wallenberg Centre for Molecular and Translational Medicine at the University of Gothenburg, Ruth and Richard Julin’s foundation, Adlerbertska Foundation, Wilhelm and Martina Lundgren Foundation, and Apotekare Hedberg’s Foundation. The authors disclose no conflicts.
Patients with ulcerative colitis (UC) who are in remission from their disease lack luminal signals capable of inducing macrophage hyporesponsiveness, which may contribute to a patient’s persistent vulnerability to relapse, according to a new study.
“Together with the distinct fecal metabolomic profile of UC patients in remission, our data suggest that UC patients may lack the signals required for proper macrophage education, rendering them vulnerable to relapse,” wrote study authors Lujain Maasfeh, PhD, of the University of Gothenburg (Sweden) and colleagues in Cellular and Molecular Gastroenterology and Hepatology.
Macrophages found in the lamina propria play a role in sustaining intestinal homeostasis. Through education by local signals, intestinal macrophages adopt a hyporesponsive phenotype and tolerogenic nature and are replenished constantly from monocytes. In patients with UC who are in remission, however, the lack of proper macrophage maturation may result in gut inflammation.
Current evidence has yet to define fully the immunomodulating determinants in the education of intestinal macrophages; however, Dr. Maasfeh and associates wrote that “intestinal microbiota and microbiota-derived metabolites increasingly are recognized for their role in imprinting tissue-specific features of intestinal macrophages.”
The researchers added that previous evidence has established that patients with UC demonstrate dysbiosis, which may impact maturation of intestinal macrophages. As such, the hyporesponsive state of intestinal lamina propria macrophages induced by the microbiota may be lost in patients with UC who are in remission, ultimately resulting in disease relapse.
To gauge the effects of fecal luminal factors on macrophage phenotype and function, the researchers extracted fecal supernatants (FS) from the fecal samples of 10 healthy volunteers and 17 patients with UC who were in remission. Following maturation of monocytes to macrophages in the presence of granulocyte-macrophage colony-stimulating factor without and with FS, the researchers assessed macrophage phenotype and function. The investigators also used gas chromatography and mass spectrometry to analyze fecal metabolomic profiles.
In healthy donors, fecal luminal factors effectively downregulated Toll-like receptor signaling, cytokine signaling, as well as antigen presentation in macrophages. In contrast, the fecal luminal factors in patients with UC demonstrated less potency in their ability to induce lipopolysaccharide hyporesponsiveness. An immune pathway scoring analysis also showed a consistently higher reaction potential among UC remission FS-treated macrophages vs. healthy FS-treated macrophages.
While FS treatment did not seem to affect the phagocytic and bactericidal abilities of macrophages, the researchers observed that the healthy FS-treated macrophages better suppressed a cluster of differentiation 4+ T-cell activation as well as interferon gamma secretion vs. FS-treated macrophages from patients with UC in remission. The FS-treated macrophages in the UC remission population also featured less potency in their ability to suppress CD4+ T-cell activation and cytokine secretion.
The authors acknowledged a few limitations, including the small sample size and the effects from using in vitro system.
“Identification of the factors involved in intestinal macrophage education is important to maintain/reestablish gut homeostasis in patients with UC,” they concluded.
The study received financial support from Swedish Research Council-Medicine, in addition to funding from a Region Västra Götaland ALF-agreement, the Knut och Alice Wallenberg Foundation Wallenberg Centre for Molecular and Translational Medicine at the University of Gothenburg, Ruth and Richard Julin’s foundation, Adlerbertska Foundation, Wilhelm and Martina Lundgren Foundation, and Apotekare Hedberg’s Foundation. The authors disclose no conflicts.
Patients with ulcerative colitis (UC) who are in remission from their disease lack luminal signals capable of inducing macrophage hyporesponsiveness, which may contribute to a patient’s persistent vulnerability to relapse, according to a new study.
“Together with the distinct fecal metabolomic profile of UC patients in remission, our data suggest that UC patients may lack the signals required for proper macrophage education, rendering them vulnerable to relapse,” wrote study authors Lujain Maasfeh, PhD, of the University of Gothenburg (Sweden) and colleagues in Cellular and Molecular Gastroenterology and Hepatology.
Macrophages found in the lamina propria play a role in sustaining intestinal homeostasis. Through education by local signals, intestinal macrophages adopt a hyporesponsive phenotype and tolerogenic nature and are replenished constantly from monocytes. In patients with UC who are in remission, however, the lack of proper macrophage maturation may result in gut inflammation.
Current evidence has yet to define fully the immunomodulating determinants in the education of intestinal macrophages; however, Dr. Maasfeh and associates wrote that “intestinal microbiota and microbiota-derived metabolites increasingly are recognized for their role in imprinting tissue-specific features of intestinal macrophages.”
The researchers added that previous evidence has established that patients with UC demonstrate dysbiosis, which may impact maturation of intestinal macrophages. As such, the hyporesponsive state of intestinal lamina propria macrophages induced by the microbiota may be lost in patients with UC who are in remission, ultimately resulting in disease relapse.
To gauge the effects of fecal luminal factors on macrophage phenotype and function, the researchers extracted fecal supernatants (FS) from the fecal samples of 10 healthy volunteers and 17 patients with UC who were in remission. Following maturation of monocytes to macrophages in the presence of granulocyte-macrophage colony-stimulating factor without and with FS, the researchers assessed macrophage phenotype and function. The investigators also used gas chromatography and mass spectrometry to analyze fecal metabolomic profiles.
In healthy donors, fecal luminal factors effectively downregulated Toll-like receptor signaling, cytokine signaling, as well as antigen presentation in macrophages. In contrast, the fecal luminal factors in patients with UC demonstrated less potency in their ability to induce lipopolysaccharide hyporesponsiveness. An immune pathway scoring analysis also showed a consistently higher reaction potential among UC remission FS-treated macrophages vs. healthy FS-treated macrophages.
While FS treatment did not seem to affect the phagocytic and bactericidal abilities of macrophages, the researchers observed that the healthy FS-treated macrophages better suppressed a cluster of differentiation 4+ T-cell activation as well as interferon gamma secretion vs. FS-treated macrophages from patients with UC in remission. The FS-treated macrophages in the UC remission population also featured less potency in their ability to suppress CD4+ T-cell activation and cytokine secretion.
The authors acknowledged a few limitations, including the small sample size and the effects from using in vitro system.
“Identification of the factors involved in intestinal macrophage education is important to maintain/reestablish gut homeostasis in patients with UC,” they concluded.
The study received financial support from Swedish Research Council-Medicine, in addition to funding from a Region Västra Götaland ALF-agreement, the Knut och Alice Wallenberg Foundation Wallenberg Centre for Molecular and Translational Medicine at the University of Gothenburg, Ruth and Richard Julin’s foundation, Adlerbertska Foundation, Wilhelm and Martina Lundgren Foundation, and Apotekare Hedberg’s Foundation. The authors disclose no conflicts.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
HEPA filters may clean SARS-CoV-2 from the air: Study
, researchers report in the preprint server medRxiv.
The journal Nature reported Oct. 6 that the research, which has not been peer-reviewed, suggests the filters may help reduce the risk of hospital-acquired SARS-CoV-2.
Researchers, led by intensivist Andrew Conway-Morris, MBChB, PhD, with the division of anaesthesia in the school of clinical medicine at University of Cambridge, United Kingdom, write that earlier experiments assessed air filters’ ability to remove inactive particles in carefully controlled environments, but it was unknown how they would work in a real-world setting.
Co-author Vilas Navapurkar, MBChB, an ICU physician at Addenbrooke’s Hospital in Cambridge, United Kingdom, said that hospitals have used portable air filters when their isolation facilities are full, but evidence was needed as to whether such filters are effective or whether they provide a false sense of security.
The researchers installed the filters in two fully occupied COVID-19 wards — a general ward and an ICU. They chose HEPA filters because they can catch extremely small particles.
The team collected air samples from the wards during a week when the air filters were on and 2 weeks when they were turned off, then compared results.
According to the study, “airborne SARS-CoV-2 was detected in the ward on all five days before activation of air/UV filtration, but on none of the five days when the air/UV filter was operational; SARS-CoV-2 was again detected on four out of five days when the filter was off.”
Airborne SARS-CoV-2 was not frequently detected in the ICU, even when the filters were off.
Cheap and easy
According to the Nature article, the authors suggest several potential explanations for this, “including slower viral replication at later stages of the disease.” Therefore, the authors say, filtering the virus from the air might be more important in general wards than in ICUs.
The filters significantly reduced the other microbial bioaerosols in both the ward (48 pathogens detected before filtration, 2 after, P = .05) and the ICU (45 pathogens detected before filtration, 5 after P = .05).
National Institute for Occupational Safety and Health (NIOSH) cyclonic aerosol samplers and PCR tests were used to detect airborne SARS-CoV-2 and other microbial bioaerosol.
David Fisman, MD, an epidemiologist at the University of Toronto, who was not involved in the research, said in the Nature article, “This study suggests that HEPA air cleaners, which remain little-used in Canadian hospitals, are a cheap and easy way to reduce risk from airborne pathogens.”This work was supported by a Wellcome senior research fellowship to co-author Stephen Baker. Conway Morris is supported by a Clinician Scientist Fellowship from the Medical Research Council. Dr. Navapurkar is the founder, director, and shareholder of Cambridge Infection Diagnostics Ltd. Dr. Conway-Morris and several co-authors are members of the Scientific Advisory Board of Cambridge Infection Diagnostics Ltd. Co-author Theodore Gouliouris has received a research grant from Shionogi and co-author R. Andres Floto has received research grants and/or consultancy payments from GSK, AstraZeneca, Chiesi, Shionogi, Insmed, and Thirty Technology.
A version of this article first appeared on Medscape.com.
, researchers report in the preprint server medRxiv.
The journal Nature reported Oct. 6 that the research, which has not been peer-reviewed, suggests the filters may help reduce the risk of hospital-acquired SARS-CoV-2.
Researchers, led by intensivist Andrew Conway-Morris, MBChB, PhD, with the division of anaesthesia in the school of clinical medicine at University of Cambridge, United Kingdom, write that earlier experiments assessed air filters’ ability to remove inactive particles in carefully controlled environments, but it was unknown how they would work in a real-world setting.
Co-author Vilas Navapurkar, MBChB, an ICU physician at Addenbrooke’s Hospital in Cambridge, United Kingdom, said that hospitals have used portable air filters when their isolation facilities are full, but evidence was needed as to whether such filters are effective or whether they provide a false sense of security.
The researchers installed the filters in two fully occupied COVID-19 wards — a general ward and an ICU. They chose HEPA filters because they can catch extremely small particles.
The team collected air samples from the wards during a week when the air filters were on and 2 weeks when they were turned off, then compared results.
According to the study, “airborne SARS-CoV-2 was detected in the ward on all five days before activation of air/UV filtration, but on none of the five days when the air/UV filter was operational; SARS-CoV-2 was again detected on four out of five days when the filter was off.”
Airborne SARS-CoV-2 was not frequently detected in the ICU, even when the filters were off.
Cheap and easy
According to the Nature article, the authors suggest several potential explanations for this, “including slower viral replication at later stages of the disease.” Therefore, the authors say, filtering the virus from the air might be more important in general wards than in ICUs.
The filters significantly reduced the other microbial bioaerosols in both the ward (48 pathogens detected before filtration, 2 after, P = .05) and the ICU (45 pathogens detected before filtration, 5 after P = .05).
National Institute for Occupational Safety and Health (NIOSH) cyclonic aerosol samplers and PCR tests were used to detect airborne SARS-CoV-2 and other microbial bioaerosol.
David Fisman, MD, an epidemiologist at the University of Toronto, who was not involved in the research, said in the Nature article, “This study suggests that HEPA air cleaners, which remain little-used in Canadian hospitals, are a cheap and easy way to reduce risk from airborne pathogens.”This work was supported by a Wellcome senior research fellowship to co-author Stephen Baker. Conway Morris is supported by a Clinician Scientist Fellowship from the Medical Research Council. Dr. Navapurkar is the founder, director, and shareholder of Cambridge Infection Diagnostics Ltd. Dr. Conway-Morris and several co-authors are members of the Scientific Advisory Board of Cambridge Infection Diagnostics Ltd. Co-author Theodore Gouliouris has received a research grant from Shionogi and co-author R. Andres Floto has received research grants and/or consultancy payments from GSK, AstraZeneca, Chiesi, Shionogi, Insmed, and Thirty Technology.
A version of this article first appeared on Medscape.com.
, researchers report in the preprint server medRxiv.
The journal Nature reported Oct. 6 that the research, which has not been peer-reviewed, suggests the filters may help reduce the risk of hospital-acquired SARS-CoV-2.
Researchers, led by intensivist Andrew Conway-Morris, MBChB, PhD, with the division of anaesthesia in the school of clinical medicine at University of Cambridge, United Kingdom, write that earlier experiments assessed air filters’ ability to remove inactive particles in carefully controlled environments, but it was unknown how they would work in a real-world setting.
Co-author Vilas Navapurkar, MBChB, an ICU physician at Addenbrooke’s Hospital in Cambridge, United Kingdom, said that hospitals have used portable air filters when their isolation facilities are full, but evidence was needed as to whether such filters are effective or whether they provide a false sense of security.
The researchers installed the filters in two fully occupied COVID-19 wards — a general ward and an ICU. They chose HEPA filters because they can catch extremely small particles.
The team collected air samples from the wards during a week when the air filters were on and 2 weeks when they were turned off, then compared results.
According to the study, “airborne SARS-CoV-2 was detected in the ward on all five days before activation of air/UV filtration, but on none of the five days when the air/UV filter was operational; SARS-CoV-2 was again detected on four out of five days when the filter was off.”
Airborne SARS-CoV-2 was not frequently detected in the ICU, even when the filters were off.
Cheap and easy
According to the Nature article, the authors suggest several potential explanations for this, “including slower viral replication at later stages of the disease.” Therefore, the authors say, filtering the virus from the air might be more important in general wards than in ICUs.
The filters significantly reduced the other microbial bioaerosols in both the ward (48 pathogens detected before filtration, 2 after, P = .05) and the ICU (45 pathogens detected before filtration, 5 after P = .05).
National Institute for Occupational Safety and Health (NIOSH) cyclonic aerosol samplers and PCR tests were used to detect airborne SARS-CoV-2 and other microbial bioaerosol.
David Fisman, MD, an epidemiologist at the University of Toronto, who was not involved in the research, said in the Nature article, “This study suggests that HEPA air cleaners, which remain little-used in Canadian hospitals, are a cheap and easy way to reduce risk from airborne pathogens.”This work was supported by a Wellcome senior research fellowship to co-author Stephen Baker. Conway Morris is supported by a Clinician Scientist Fellowship from the Medical Research Council. Dr. Navapurkar is the founder, director, and shareholder of Cambridge Infection Diagnostics Ltd. Dr. Conway-Morris and several co-authors are members of the Scientific Advisory Board of Cambridge Infection Diagnostics Ltd. Co-author Theodore Gouliouris has received a research grant from Shionogi and co-author R. Andres Floto has received research grants and/or consultancy payments from GSK, AstraZeneca, Chiesi, Shionogi, Insmed, and Thirty Technology.
A version of this article first appeared on Medscape.com.
Abaloparatide significantly reduced fractures, increased BMD in women at high fracture risk
Postmenopausal women at high or very high risk of fracture gained significantly more bone mineral density and were significantly less likely to experience a fracture when taking abaloparatide for 18 months, according to new research presented at the hybrid annual meeting of the North American Menopause Society.
“The findings showed that abaloparatide was better than teriparatide in a number of parameters important in osteoporosis treatment, and similar in others, in high-risk and very-high-risk postmenopausal women with osteoporosis,” Bart Clarke, MD, a professor of medicine at Mayo Clinic in Rochester, Minn., said in an interview. “Abaloparatide is safe and effective for use in high-risk or very-high-risk postmenopausal women,” as defined by the new American Association of Clinical Endocrinology/American College of Endocrinology osteoporosis guidelines.
Ricardo R. Correa, MD, of the department of endocrinology and director of diversity for graduate medical education at the University of Arizona, Phoenix, said that the study demonstrates that abaloparatide and teriparatide have a very similar effect with abaloparatide providing a slightly better absolute risk reduction in fracture. Dr. Correa was not involved in the research.
“What will drive my decision in what to prescribe will be the cost and insurance coverage,” Dr. Correa said. “At the Veterans Administration hospital, the option that we have is abaloparatide, so this is the option that we use.”
Among women at least 65 years old who have already had one fracture, 1 in 10 will experience another fracture within the next year, and 30% will have another fracture within the next 5 years, the authors noted in their background material. Since phase 3 ACTIVE study data in 2016 showed that abaloparatide reduces fracture risk while increasing bone mineral density, compared with placebo, the researchers reanalyzed that data to assess the drug’s efficacy in patients at high or very high risk for fracture.
The study involved 2,463 postmenopausal women with osteoporosis who received one of three interventions: 80 mcg abaloparatide daily, placebo, or 20 mcg subcutaneous teriparatide daily. Only the abaloparatide and placebo groups were double blinded.
“Teriparatide was used as the comparator drug because teriparatide was previously approved as the first anabolic drug for osteoporosis,” Dr. Clarke said in an interview. “The hope was to show that abaloparatide was a better anabolic drug.”
Women were considered at high or very high risk of fracture if they met at least one of the following four criteria from the 2020 American Association of Clinical Endocrinology guidelines:
- Fracture within the past 12 months or prevalent vertebral fracture.
- Very low T-score (less than –3.0) at baseline at any site.
- Multiple fractures at baseline since age 45.
- Very high fracture risk based on the Fracture Risk Assessment Tool (FRAX) (at least 30% for major osteoporotic fracture or at least 4.5% for hip fracture).
Among the 2,026 patients who met at least one of these criteria, 664 received abaloparatide, 685 received teriparatide, and 677 received placebo. Both the abaloparatide and teriparatide significantly reduced new vertebral fracture risk, compared with placebo. In the abaloparatide group, 0.72% of women had a new vertebral fracture, compared with 0.99% in the teriparatide group and 4.77% in the placebo group (P < .0001).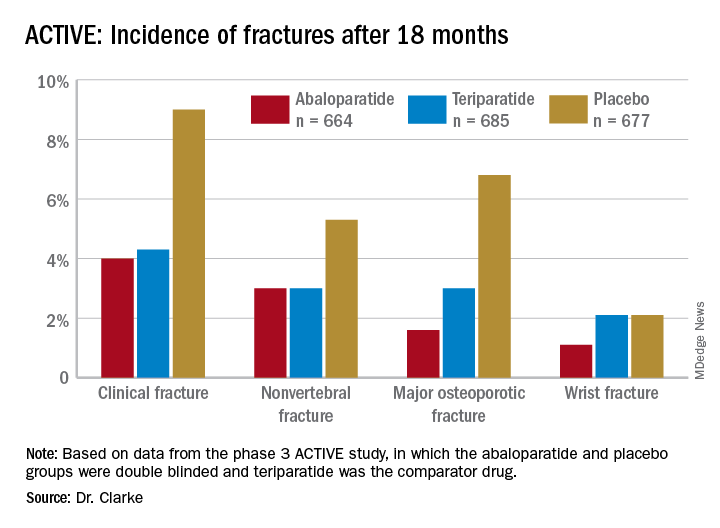
Abaloparatide and teriparatide also led to significant increases in lumbar spine, total hip, and femoral neck bone mineral density, compared with placebo (P < .0001).
The study was limited by its duration of 18 months and the Food and Drug Administration’s restriction on using abaloparatide for more than 2 years because of the theoretical risk of increasing osteosarcoma, although that risk has never been demonstrated in humans, Dr. Correa said. ”We need more data with abaloparitide in more than 2 years,” he added.
In determining which medication clinicians should first prescribe to manage osteoporosis, Dr. Correa said practitioners should consider the type of osteoporosis women have, their preferences, and their labs on kidney function.
With mild to moderate osteoporosis, bisphosphonates will be the first option while denosumab will be preferred for moderate to severe osteoporosis. Teriparatide and abaloparitide are the first-line options for severe osteoporosis, he said.
“If the glomerular filtration rate is low, we cannot use bisphosphonate and we will have to limit our use to denosumab,” he said. Route and frequency of delivery plays a role in patient preferences.
“If the patient prefers an infusion once a year or a pill, then bisphosphonate,” he said, but “if the patient is fine with an injection every 6 months, then denosumab.” Patients who need and can do an injection every day can take abaloparitide or teriparatide.
Failure of previous treatments also guide clinical decisions, he added. ”If the patient has been on one medication and has a fracture or the bone mineral density decreases, then we need to switch to another medication, usually teriparatide or abaloparitide, to build new bone.”
Contraindications for abaloparatide include a high serum calcium before therapy or prior allergic reactions to components in abaloparatide, Dr. Clarke said. No new safety signals showed up in the data analysis.
The research was funded by Radius Health. Dr. Clarke is an advisory board member of Amgen, and another author consults and speaks for Amgen and is a Radius Health Advisory Board member. Two other authors are Radius Health employees who own stock in the company. Dr Correa has no disclosures.
Postmenopausal women at high or very high risk of fracture gained significantly more bone mineral density and were significantly less likely to experience a fracture when taking abaloparatide for 18 months, according to new research presented at the hybrid annual meeting of the North American Menopause Society.
“The findings showed that abaloparatide was better than teriparatide in a number of parameters important in osteoporosis treatment, and similar in others, in high-risk and very-high-risk postmenopausal women with osteoporosis,” Bart Clarke, MD, a professor of medicine at Mayo Clinic in Rochester, Minn., said in an interview. “Abaloparatide is safe and effective for use in high-risk or very-high-risk postmenopausal women,” as defined by the new American Association of Clinical Endocrinology/American College of Endocrinology osteoporosis guidelines.
Ricardo R. Correa, MD, of the department of endocrinology and director of diversity for graduate medical education at the University of Arizona, Phoenix, said that the study demonstrates that abaloparatide and teriparatide have a very similar effect with abaloparatide providing a slightly better absolute risk reduction in fracture. Dr. Correa was not involved in the research.
“What will drive my decision in what to prescribe will be the cost and insurance coverage,” Dr. Correa said. “At the Veterans Administration hospital, the option that we have is abaloparatide, so this is the option that we use.”
Among women at least 65 years old who have already had one fracture, 1 in 10 will experience another fracture within the next year, and 30% will have another fracture within the next 5 years, the authors noted in their background material. Since phase 3 ACTIVE study data in 2016 showed that abaloparatide reduces fracture risk while increasing bone mineral density, compared with placebo, the researchers reanalyzed that data to assess the drug’s efficacy in patients at high or very high risk for fracture.
The study involved 2,463 postmenopausal women with osteoporosis who received one of three interventions: 80 mcg abaloparatide daily, placebo, or 20 mcg subcutaneous teriparatide daily. Only the abaloparatide and placebo groups were double blinded.
“Teriparatide was used as the comparator drug because teriparatide was previously approved as the first anabolic drug for osteoporosis,” Dr. Clarke said in an interview. “The hope was to show that abaloparatide was a better anabolic drug.”
Women were considered at high or very high risk of fracture if they met at least one of the following four criteria from the 2020 American Association of Clinical Endocrinology guidelines:
- Fracture within the past 12 months or prevalent vertebral fracture.
- Very low T-score (less than –3.0) at baseline at any site.
- Multiple fractures at baseline since age 45.
- Very high fracture risk based on the Fracture Risk Assessment Tool (FRAX) (at least 30% for major osteoporotic fracture or at least 4.5% for hip fracture).
Among the 2,026 patients who met at least one of these criteria, 664 received abaloparatide, 685 received teriparatide, and 677 received placebo. Both the abaloparatide and teriparatide significantly reduced new vertebral fracture risk, compared with placebo. In the abaloparatide group, 0.72% of women had a new vertebral fracture, compared with 0.99% in the teriparatide group and 4.77% in the placebo group (P < .0001).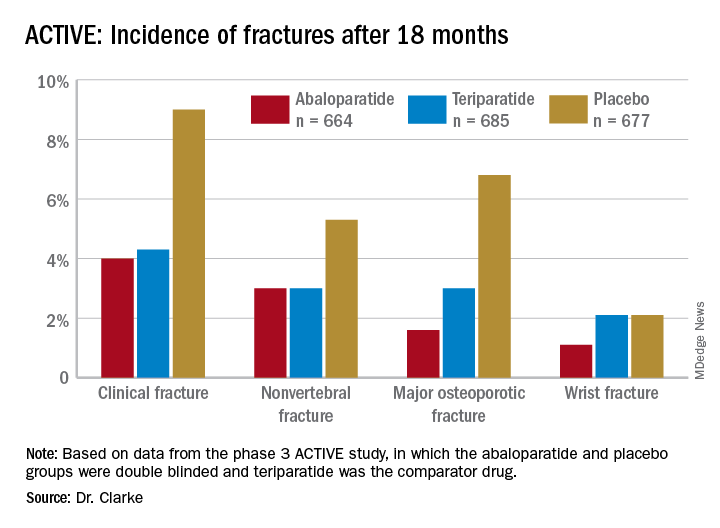
Abaloparatide and teriparatide also led to significant increases in lumbar spine, total hip, and femoral neck bone mineral density, compared with placebo (P < .0001).
The study was limited by its duration of 18 months and the Food and Drug Administration’s restriction on using abaloparatide for more than 2 years because of the theoretical risk of increasing osteosarcoma, although that risk has never been demonstrated in humans, Dr. Correa said. ”We need more data with abaloparitide in more than 2 years,” he added.
In determining which medication clinicians should first prescribe to manage osteoporosis, Dr. Correa said practitioners should consider the type of osteoporosis women have, their preferences, and their labs on kidney function.
With mild to moderate osteoporosis, bisphosphonates will be the first option while denosumab will be preferred for moderate to severe osteoporosis. Teriparatide and abaloparitide are the first-line options for severe osteoporosis, he said.
“If the glomerular filtration rate is low, we cannot use bisphosphonate and we will have to limit our use to denosumab,” he said. Route and frequency of delivery plays a role in patient preferences.
“If the patient prefers an infusion once a year or a pill, then bisphosphonate,” he said, but “if the patient is fine with an injection every 6 months, then denosumab.” Patients who need and can do an injection every day can take abaloparitide or teriparatide.
Failure of previous treatments also guide clinical decisions, he added. ”If the patient has been on one medication and has a fracture or the bone mineral density decreases, then we need to switch to another medication, usually teriparatide or abaloparitide, to build new bone.”
Contraindications for abaloparatide include a high serum calcium before therapy or prior allergic reactions to components in abaloparatide, Dr. Clarke said. No new safety signals showed up in the data analysis.
The research was funded by Radius Health. Dr. Clarke is an advisory board member of Amgen, and another author consults and speaks for Amgen and is a Radius Health Advisory Board member. Two other authors are Radius Health employees who own stock in the company. Dr Correa has no disclosures.
Postmenopausal women at high or very high risk of fracture gained significantly more bone mineral density and were significantly less likely to experience a fracture when taking abaloparatide for 18 months, according to new research presented at the hybrid annual meeting of the North American Menopause Society.
“The findings showed that abaloparatide was better than teriparatide in a number of parameters important in osteoporosis treatment, and similar in others, in high-risk and very-high-risk postmenopausal women with osteoporosis,” Bart Clarke, MD, a professor of medicine at Mayo Clinic in Rochester, Minn., said in an interview. “Abaloparatide is safe and effective for use in high-risk or very-high-risk postmenopausal women,” as defined by the new American Association of Clinical Endocrinology/American College of Endocrinology osteoporosis guidelines.
Ricardo R. Correa, MD, of the department of endocrinology and director of diversity for graduate medical education at the University of Arizona, Phoenix, said that the study demonstrates that abaloparatide and teriparatide have a very similar effect with abaloparatide providing a slightly better absolute risk reduction in fracture. Dr. Correa was not involved in the research.
“What will drive my decision in what to prescribe will be the cost and insurance coverage,” Dr. Correa said. “At the Veterans Administration hospital, the option that we have is abaloparatide, so this is the option that we use.”
Among women at least 65 years old who have already had one fracture, 1 in 10 will experience another fracture within the next year, and 30% will have another fracture within the next 5 years, the authors noted in their background material. Since phase 3 ACTIVE study data in 2016 showed that abaloparatide reduces fracture risk while increasing bone mineral density, compared with placebo, the researchers reanalyzed that data to assess the drug’s efficacy in patients at high or very high risk for fracture.
The study involved 2,463 postmenopausal women with osteoporosis who received one of three interventions: 80 mcg abaloparatide daily, placebo, or 20 mcg subcutaneous teriparatide daily. Only the abaloparatide and placebo groups were double blinded.
“Teriparatide was used as the comparator drug because teriparatide was previously approved as the first anabolic drug for osteoporosis,” Dr. Clarke said in an interview. “The hope was to show that abaloparatide was a better anabolic drug.”
Women were considered at high or very high risk of fracture if they met at least one of the following four criteria from the 2020 American Association of Clinical Endocrinology guidelines:
- Fracture within the past 12 months or prevalent vertebral fracture.
- Very low T-score (less than –3.0) at baseline at any site.
- Multiple fractures at baseline since age 45.
- Very high fracture risk based on the Fracture Risk Assessment Tool (FRAX) (at least 30% for major osteoporotic fracture or at least 4.5% for hip fracture).
Among the 2,026 patients who met at least one of these criteria, 664 received abaloparatide, 685 received teriparatide, and 677 received placebo. Both the abaloparatide and teriparatide significantly reduced new vertebral fracture risk, compared with placebo. In the abaloparatide group, 0.72% of women had a new vertebral fracture, compared with 0.99% in the teriparatide group and 4.77% in the placebo group (P < .0001).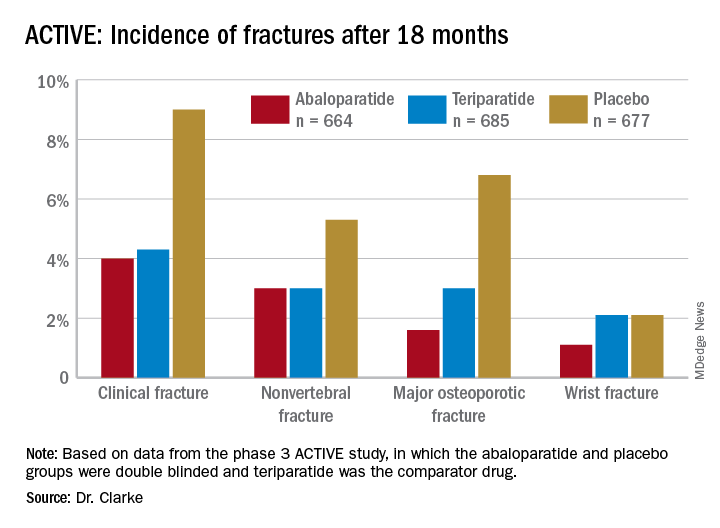
Abaloparatide and teriparatide also led to significant increases in lumbar spine, total hip, and femoral neck bone mineral density, compared with placebo (P < .0001).
The study was limited by its duration of 18 months and the Food and Drug Administration’s restriction on using abaloparatide for more than 2 years because of the theoretical risk of increasing osteosarcoma, although that risk has never been demonstrated in humans, Dr. Correa said. ”We need more data with abaloparitide in more than 2 years,” he added.
In determining which medication clinicians should first prescribe to manage osteoporosis, Dr. Correa said practitioners should consider the type of osteoporosis women have, their preferences, and their labs on kidney function.
With mild to moderate osteoporosis, bisphosphonates will be the first option while denosumab will be preferred for moderate to severe osteoporosis. Teriparatide and abaloparitide are the first-line options for severe osteoporosis, he said.
“If the glomerular filtration rate is low, we cannot use bisphosphonate and we will have to limit our use to denosumab,” he said. Route and frequency of delivery plays a role in patient preferences.
“If the patient prefers an infusion once a year or a pill, then bisphosphonate,” he said, but “if the patient is fine with an injection every 6 months, then denosumab.” Patients who need and can do an injection every day can take abaloparitide or teriparatide.
Failure of previous treatments also guide clinical decisions, he added. ”If the patient has been on one medication and has a fracture or the bone mineral density decreases, then we need to switch to another medication, usually teriparatide or abaloparitide, to build new bone.”
Contraindications for abaloparatide include a high serum calcium before therapy or prior allergic reactions to components in abaloparatide, Dr. Clarke said. No new safety signals showed up in the data analysis.
The research was funded by Radius Health. Dr. Clarke is an advisory board member of Amgen, and another author consults and speaks for Amgen and is a Radius Health Advisory Board member. Two other authors are Radius Health employees who own stock in the company. Dr Correa has no disclosures.
FROM NAMS 2021







