User login
In atopic dermatitis trial, abrocitinib offers faster itch relief than dupilumab
), in a multicenter randomized trial presented as a late breaker at the annual meeting of the European Academy of Dermatology and Venereology.
The earlier onset of action with the JAK inhibitor was achieved even though most patients in both arms were on topical corticosteroids, a design element that “is clinically relevant” for a practical comparison of these two agents, according to Kristian Reich, MD, PhD, Center for Translational Research in Inflammatory Skin Diseases, University Medical Center, Hamburg-Eppendorf, Germany.
The goal of this phase 3b trial, called JADE DARE, was to compare relative safety and efficacy of these strategies over the early course of treatment, he said.
Over 700 patients randomized
JADE DARE enrolled 727 patients over age 18 years who previously had an inadequate response to conventional topical therapies. All had moderate to severe AD defined by criteria such as body surface area greater than or equal to 10% and Eczema Area Severity Index (EASI) greater than or equal to 16. They were randomly assigned to 200 mg oral abrocitinib once daily or 300 mg subcutaneous dupilumab (after a loading dose of 600 mg) every 2 weeks. A double-dummy design preserved blinding.
The coprimary endpoints were at least a 4-point improvement in pruritus as measured with the Peak Pruritus Numerical Rating Scale (PP-NRS) score at week 2 and at least a 90% improvement in the EASI (EASI 90) at week 4.
The primary endpoint for pruritus at 2 weeks was reached by nearly twice as many patients randomly assigned to abrocitinib (46.2% vs. 25.5%; P < .001). The proportion of those meeting the EASI 90 endpoint at week 4 was also superior on abrocitinib (28.5% vs. 14.6%; P < .001)
Advantage for pruritus control dissipates
For the pruritus endpoint, the advantage of abrocitinib slowly diminished over time after the peak difference observed at 2 weeks. Although the advantage at week 4 (58.1% vs. 40.8%) and week 8 (65.8% vs. 52.7%) remained sizable, there were very small differences thereafter. However, Dr. Reich pointed out that the percentages continued to favor abrocitinib at least numerically through the 26 weeks of follow-up completed so far.
The pattern of response on EASI 90 was not the same. After demonstrating superiority at the 4-week timepoint, the advantage of abrocitinib persisted. When compared at week 16, which was a secondary endpoint of the JADE DARE trial, the advantage of abrocitinib remained significant (54.3% vs. 41.9%; P < .001). The advantage of abrocitinib narrowed but remained numerically superior at 26 weeks (54.6% vs. 47.6%).
Based on the data collected to date, “abrocitinib is clearly superior early on,” Dr. Reich said. Moreover, he reiterated that topical corticosteroids were allowed as background therapy in both arms.
“It is difficult to show an advantage for one active therapy over the other in patients on background corticosteroids,” Dr. Reich maintained.
Both drugs are well tolerated
The drugs were similarly well tolerated. Serious adverse events were uncommon in either arm. The rate of study dropouts due to an adverse event potentially related to treatment assignment was 3% in each group.
Nausea (19% vs. 2%), acne (13.5% vs. 2%), and headache (13% vs. 7.5%) were all more common in patients randomly assigned to abrocitinib. Conjunctivitis was more common in the group randomly assigned to dupilumab (10% vs. 2%).
The two deaths that occurred during this study were in the abrocitinib arm, but one was the result of COVID-19 infection and the other was a cardiovascular event in a patient with risk factors. Neither was considered to be treatment-related.
Abrocitinib’s relative selectivity for the JAK1 inhibitor is a potential differentiator from other currently available JAK inhibitors, although direct comparisons of these therapies for clinical activity in AD as well as most other diseases remains limited.
The relatively rapid relief of pruritus with the JAK inhibitor relative to the monoclonal antibody in the JADE DARE trial is likely to be perceived as clinically significant by patients with AD, according to Sonja Ständer, MD, professor of dermatology and neurodermatology at the University Hospital Münster, Germany.
“One of the highest needs of patients with atopic dermatitis is a rapid and profound relief of itch,” Dr. Ständer, who wrote a review article on AD earlier this year, said in an interview.
Although several current therapies are effective against pruritus, Dr. Ständer believes that the higher proportion of patients achieving itch control at 2 weeks on abrocitinib “will attract the attention of affected patients.”
However, she added that patients need to take both benefits and risks into account, indicating that clinical utility cannot be judged on a single outcome. In selecting one drug over the others, she advised “a balanced use of therapies.”
Abrocitinib was first approved in the United Kingdom in early September, followed by Japan last Thursday, for the treatment of moderate to severe AD in patients ages 12 and older. It is under review elsewhere, including in the United States and the European Union for AD.
In September, the FDA approved the first JAK inhibitor for treating AD – a topical JAK inhibitor, ruxolitinib.
Dr. Reich reports financial relationships with 20 pharmaceutical companies, including Pfizer, which provided funding for the JADE DARE trial. Dr. Ständer reports financial relationships with Beiersdorf AG, Galderma, Kliniska, Lilly, Pfizer, and Sanofi.
A version of this article first appeared on Medscape.com.
), in a multicenter randomized trial presented as a late breaker at the annual meeting of the European Academy of Dermatology and Venereology.
The earlier onset of action with the JAK inhibitor was achieved even though most patients in both arms were on topical corticosteroids, a design element that “is clinically relevant” for a practical comparison of these two agents, according to Kristian Reich, MD, PhD, Center for Translational Research in Inflammatory Skin Diseases, University Medical Center, Hamburg-Eppendorf, Germany.
The goal of this phase 3b trial, called JADE DARE, was to compare relative safety and efficacy of these strategies over the early course of treatment, he said.
Over 700 patients randomized
JADE DARE enrolled 727 patients over age 18 years who previously had an inadequate response to conventional topical therapies. All had moderate to severe AD defined by criteria such as body surface area greater than or equal to 10% and Eczema Area Severity Index (EASI) greater than or equal to 16. They were randomly assigned to 200 mg oral abrocitinib once daily or 300 mg subcutaneous dupilumab (after a loading dose of 600 mg) every 2 weeks. A double-dummy design preserved blinding.
The coprimary endpoints were at least a 4-point improvement in pruritus as measured with the Peak Pruritus Numerical Rating Scale (PP-NRS) score at week 2 and at least a 90% improvement in the EASI (EASI 90) at week 4.
The primary endpoint for pruritus at 2 weeks was reached by nearly twice as many patients randomly assigned to abrocitinib (46.2% vs. 25.5%; P < .001). The proportion of those meeting the EASI 90 endpoint at week 4 was also superior on abrocitinib (28.5% vs. 14.6%; P < .001)
Advantage for pruritus control dissipates
For the pruritus endpoint, the advantage of abrocitinib slowly diminished over time after the peak difference observed at 2 weeks. Although the advantage at week 4 (58.1% vs. 40.8%) and week 8 (65.8% vs. 52.7%) remained sizable, there were very small differences thereafter. However, Dr. Reich pointed out that the percentages continued to favor abrocitinib at least numerically through the 26 weeks of follow-up completed so far.
The pattern of response on EASI 90 was not the same. After demonstrating superiority at the 4-week timepoint, the advantage of abrocitinib persisted. When compared at week 16, which was a secondary endpoint of the JADE DARE trial, the advantage of abrocitinib remained significant (54.3% vs. 41.9%; P < .001). The advantage of abrocitinib narrowed but remained numerically superior at 26 weeks (54.6% vs. 47.6%).
Based on the data collected to date, “abrocitinib is clearly superior early on,” Dr. Reich said. Moreover, he reiterated that topical corticosteroids were allowed as background therapy in both arms.
“It is difficult to show an advantage for one active therapy over the other in patients on background corticosteroids,” Dr. Reich maintained.
Both drugs are well tolerated
The drugs were similarly well tolerated. Serious adverse events were uncommon in either arm. The rate of study dropouts due to an adverse event potentially related to treatment assignment was 3% in each group.
Nausea (19% vs. 2%), acne (13.5% vs. 2%), and headache (13% vs. 7.5%) were all more common in patients randomly assigned to abrocitinib. Conjunctivitis was more common in the group randomly assigned to dupilumab (10% vs. 2%).
The two deaths that occurred during this study were in the abrocitinib arm, but one was the result of COVID-19 infection and the other was a cardiovascular event in a patient with risk factors. Neither was considered to be treatment-related.
Abrocitinib’s relative selectivity for the JAK1 inhibitor is a potential differentiator from other currently available JAK inhibitors, although direct comparisons of these therapies for clinical activity in AD as well as most other diseases remains limited.
The relatively rapid relief of pruritus with the JAK inhibitor relative to the monoclonal antibody in the JADE DARE trial is likely to be perceived as clinically significant by patients with AD, according to Sonja Ständer, MD, professor of dermatology and neurodermatology at the University Hospital Münster, Germany.
“One of the highest needs of patients with atopic dermatitis is a rapid and profound relief of itch,” Dr. Ständer, who wrote a review article on AD earlier this year, said in an interview.
Although several current therapies are effective against pruritus, Dr. Ständer believes that the higher proportion of patients achieving itch control at 2 weeks on abrocitinib “will attract the attention of affected patients.”
However, she added that patients need to take both benefits and risks into account, indicating that clinical utility cannot be judged on a single outcome. In selecting one drug over the others, she advised “a balanced use of therapies.”
Abrocitinib was first approved in the United Kingdom in early September, followed by Japan last Thursday, for the treatment of moderate to severe AD in patients ages 12 and older. It is under review elsewhere, including in the United States and the European Union for AD.
In September, the FDA approved the first JAK inhibitor for treating AD – a topical JAK inhibitor, ruxolitinib.
Dr. Reich reports financial relationships with 20 pharmaceutical companies, including Pfizer, which provided funding for the JADE DARE trial. Dr. Ständer reports financial relationships with Beiersdorf AG, Galderma, Kliniska, Lilly, Pfizer, and Sanofi.
A version of this article first appeared on Medscape.com.
), in a multicenter randomized trial presented as a late breaker at the annual meeting of the European Academy of Dermatology and Venereology.
The earlier onset of action with the JAK inhibitor was achieved even though most patients in both arms were on topical corticosteroids, a design element that “is clinically relevant” for a practical comparison of these two agents, according to Kristian Reich, MD, PhD, Center for Translational Research in Inflammatory Skin Diseases, University Medical Center, Hamburg-Eppendorf, Germany.
The goal of this phase 3b trial, called JADE DARE, was to compare relative safety and efficacy of these strategies over the early course of treatment, he said.
Over 700 patients randomized
JADE DARE enrolled 727 patients over age 18 years who previously had an inadequate response to conventional topical therapies. All had moderate to severe AD defined by criteria such as body surface area greater than or equal to 10% and Eczema Area Severity Index (EASI) greater than or equal to 16. They were randomly assigned to 200 mg oral abrocitinib once daily or 300 mg subcutaneous dupilumab (after a loading dose of 600 mg) every 2 weeks. A double-dummy design preserved blinding.
The coprimary endpoints were at least a 4-point improvement in pruritus as measured with the Peak Pruritus Numerical Rating Scale (PP-NRS) score at week 2 and at least a 90% improvement in the EASI (EASI 90) at week 4.
The primary endpoint for pruritus at 2 weeks was reached by nearly twice as many patients randomly assigned to abrocitinib (46.2% vs. 25.5%; P < .001). The proportion of those meeting the EASI 90 endpoint at week 4 was also superior on abrocitinib (28.5% vs. 14.6%; P < .001)
Advantage for pruritus control dissipates
For the pruritus endpoint, the advantage of abrocitinib slowly diminished over time after the peak difference observed at 2 weeks. Although the advantage at week 4 (58.1% vs. 40.8%) and week 8 (65.8% vs. 52.7%) remained sizable, there were very small differences thereafter. However, Dr. Reich pointed out that the percentages continued to favor abrocitinib at least numerically through the 26 weeks of follow-up completed so far.
The pattern of response on EASI 90 was not the same. After demonstrating superiority at the 4-week timepoint, the advantage of abrocitinib persisted. When compared at week 16, which was a secondary endpoint of the JADE DARE trial, the advantage of abrocitinib remained significant (54.3% vs. 41.9%; P < .001). The advantage of abrocitinib narrowed but remained numerically superior at 26 weeks (54.6% vs. 47.6%).
Based on the data collected to date, “abrocitinib is clearly superior early on,” Dr. Reich said. Moreover, he reiterated that topical corticosteroids were allowed as background therapy in both arms.
“It is difficult to show an advantage for one active therapy over the other in patients on background corticosteroids,” Dr. Reich maintained.
Both drugs are well tolerated
The drugs were similarly well tolerated. Serious adverse events were uncommon in either arm. The rate of study dropouts due to an adverse event potentially related to treatment assignment was 3% in each group.
Nausea (19% vs. 2%), acne (13.5% vs. 2%), and headache (13% vs. 7.5%) were all more common in patients randomly assigned to abrocitinib. Conjunctivitis was more common in the group randomly assigned to dupilumab (10% vs. 2%).
The two deaths that occurred during this study were in the abrocitinib arm, but one was the result of COVID-19 infection and the other was a cardiovascular event in a patient with risk factors. Neither was considered to be treatment-related.
Abrocitinib’s relative selectivity for the JAK1 inhibitor is a potential differentiator from other currently available JAK inhibitors, although direct comparisons of these therapies for clinical activity in AD as well as most other diseases remains limited.
The relatively rapid relief of pruritus with the JAK inhibitor relative to the monoclonal antibody in the JADE DARE trial is likely to be perceived as clinically significant by patients with AD, according to Sonja Ständer, MD, professor of dermatology and neurodermatology at the University Hospital Münster, Germany.
“One of the highest needs of patients with atopic dermatitis is a rapid and profound relief of itch,” Dr. Ständer, who wrote a review article on AD earlier this year, said in an interview.
Although several current therapies are effective against pruritus, Dr. Ständer believes that the higher proportion of patients achieving itch control at 2 weeks on abrocitinib “will attract the attention of affected patients.”
However, she added that patients need to take both benefits and risks into account, indicating that clinical utility cannot be judged on a single outcome. In selecting one drug over the others, she advised “a balanced use of therapies.”
Abrocitinib was first approved in the United Kingdom in early September, followed by Japan last Thursday, for the treatment of moderate to severe AD in patients ages 12 and older. It is under review elsewhere, including in the United States and the European Union for AD.
In September, the FDA approved the first JAK inhibitor for treating AD – a topical JAK inhibitor, ruxolitinib.
Dr. Reich reports financial relationships with 20 pharmaceutical companies, including Pfizer, which provided funding for the JADE DARE trial. Dr. Ständer reports financial relationships with Beiersdorf AG, Galderma, Kliniska, Lilly, Pfizer, and Sanofi.
A version of this article first appeared on Medscape.com.
Case reports underscore risk of cerebral edema, AFCE in children with COVID-19
according to pediatric neurologists who are urging colleagues to watch out for similar cases.
At least one other child in the United States has died after becoming infected with the virus and developing cerebral edema. “The rapid and devastating clinical course in both of these cases highlights the need for early recognition of a cerebral edema and AFCE as potential complications of COVID-19 in pediatric patients,” the neurologists wrote.
The case was highlighted in a poster presented at the annual meeting of the Child Neurology Society and in a report published earlier this year in Child Neurology Open.
According to pediatric neurologist Timothy Gershon, MD, PhD , of the University of North Carolina at Chapel Hill, the child appeared in clinic in July 2020. She had been healthy but was suffering from 1 day of fever, seizure-like activity (generalized convulsions and drooling), anorexia, and lethargy.
The girl, who was subsequently diagnosed with COVID-19, deteriorated in the hospital. “She received IV dexamethasone in attempts to reduce cerebral edema,” the neurologists wrote. “Regarding immunomodulatory therapy, she received intravenous immunoglobulin (2 g/kg), anakinra, and hydrocortisone; despite approval for remdesivir and COVID-19 convalescent plasma, these were ultimately withheld due to poor prognosis.”
Brain death examinations at 24 and 48 hours after cardiac arrest were consistent with brain death, they reported.
Neurologists believe the patient suffered from AFCE, “an often fatal pediatric clinical entity consisting of fever, encephalopathy, and new-onset seizures followed by rapid, diffuse, and medically-refractory cerebral edema.” They add that “AFCE occurs as a rare complication of a variety of common pediatric infections, and a CNS [central nervous system] pathogen is identified in only a minority of cases, suggesting a para-infectious mechanism of edema.”
Neurologists offered a case definition of the “recently recognized” AFCE earlier this year.
“This was an extremely rare rapid progression to cerebral edema. I think it was related to the patient’s COVID infection, but why this patient got it and others don’t is unknown,” Dr. Gershon said in an interview. “The full spectrum of neurological complications of COVID were not yet known [at the time]. We didn’t know, and still don’t know, what the causative links are between COVID and suddenly having seizures and brain swelling.”
He said he’d treat a similar patient differently now and give dexamethasone earlier in the clinical course, although “there is no data to tell us if any therapy could have reversed it.” Specifically, he said, “I’d give dexamethasone at the first sign of brain involvement, using the dosing recommended for cerebral edema, and try to get the MRI earlier in the course.”
Dr. Gershon and colleagues noted another case of fatal cerebral edema in a child, a 7-year-old boy who was treated in New York state. That case “shows that fatal cerebral edema may complicate pediatric multisystem inflammatory syndrome,” they wrote.
Pediatric critical care specialist Preetha Krishnan, MD, of Randall Children’s Hospital at Legacy Emanuel in Portland, Ore., helped develop the new definition of AFCE. In an interview, she said AFCE is difficult to diagnose because the signs/symptoms – such as fever, altered sensorium, and seizures – are found in other conditions such as febrile status epilepticus with a viral illness.
“The key to recognition of AFCE is that unlike other disease processes, these children have rapid neurologic progression,” she said. “In addition, many of our AFCE patients also had vomiting and/or headache, which in retrospect was likely an indication of elevated ICP [intracranial pressure] rather than viral infection.”
She added that “if a child with fever, seizures, and encephalopathy has cerebral edema on imaging and/or has neurologic progression, AFCE should be considered. Most of our cases of AFCE had fulminant progression within the first 3 days of their head imaging noting cerebral edema. There are other neurologic diseases, such as acute necrotizing encephalopathy of childhood, that also have progressive signs/symptoms, but head imaging and lab work should help differentiate many of these etiologies.”
In regard to treatment, she said, “our unit would likely err on the side of providing as much neuroprotective measures as is reasonable, such as maintaining normothermia, consideration of hyperosmolar therapy, maintaining normocarbia and normoxemia, managing seizures, etc. I would recommend getting the entire neurocritical care team involved in the management discussion. This varies by center, but will likely include neurology, ID [infectious disease], possibly neurosurgery, and PICU.”
As for the new case report, Krishnan said COVID-19 has been linked to neurologic complications, “so it does not surprise me that AFCE is part of the neurologic spectrum of disease.”
No funding was reported, and the authors report no relevant disclosures. Dr. Krishnan has no disclosures.
according to pediatric neurologists who are urging colleagues to watch out for similar cases.
At least one other child in the United States has died after becoming infected with the virus and developing cerebral edema. “The rapid and devastating clinical course in both of these cases highlights the need for early recognition of a cerebral edema and AFCE as potential complications of COVID-19 in pediatric patients,” the neurologists wrote.
The case was highlighted in a poster presented at the annual meeting of the Child Neurology Society and in a report published earlier this year in Child Neurology Open.
According to pediatric neurologist Timothy Gershon, MD, PhD , of the University of North Carolina at Chapel Hill, the child appeared in clinic in July 2020. She had been healthy but was suffering from 1 day of fever, seizure-like activity (generalized convulsions and drooling), anorexia, and lethargy.
The girl, who was subsequently diagnosed with COVID-19, deteriorated in the hospital. “She received IV dexamethasone in attempts to reduce cerebral edema,” the neurologists wrote. “Regarding immunomodulatory therapy, she received intravenous immunoglobulin (2 g/kg), anakinra, and hydrocortisone; despite approval for remdesivir and COVID-19 convalescent plasma, these were ultimately withheld due to poor prognosis.”
Brain death examinations at 24 and 48 hours after cardiac arrest were consistent with brain death, they reported.
Neurologists believe the patient suffered from AFCE, “an often fatal pediatric clinical entity consisting of fever, encephalopathy, and new-onset seizures followed by rapid, diffuse, and medically-refractory cerebral edema.” They add that “AFCE occurs as a rare complication of a variety of common pediatric infections, and a CNS [central nervous system] pathogen is identified in only a minority of cases, suggesting a para-infectious mechanism of edema.”
Neurologists offered a case definition of the “recently recognized” AFCE earlier this year.
“This was an extremely rare rapid progression to cerebral edema. I think it was related to the patient’s COVID infection, but why this patient got it and others don’t is unknown,” Dr. Gershon said in an interview. “The full spectrum of neurological complications of COVID were not yet known [at the time]. We didn’t know, and still don’t know, what the causative links are between COVID and suddenly having seizures and brain swelling.”
He said he’d treat a similar patient differently now and give dexamethasone earlier in the clinical course, although “there is no data to tell us if any therapy could have reversed it.” Specifically, he said, “I’d give dexamethasone at the first sign of brain involvement, using the dosing recommended for cerebral edema, and try to get the MRI earlier in the course.”
Dr. Gershon and colleagues noted another case of fatal cerebral edema in a child, a 7-year-old boy who was treated in New York state. That case “shows that fatal cerebral edema may complicate pediatric multisystem inflammatory syndrome,” they wrote.
Pediatric critical care specialist Preetha Krishnan, MD, of Randall Children’s Hospital at Legacy Emanuel in Portland, Ore., helped develop the new definition of AFCE. In an interview, she said AFCE is difficult to diagnose because the signs/symptoms – such as fever, altered sensorium, and seizures – are found in other conditions such as febrile status epilepticus with a viral illness.
“The key to recognition of AFCE is that unlike other disease processes, these children have rapid neurologic progression,” she said. “In addition, many of our AFCE patients also had vomiting and/or headache, which in retrospect was likely an indication of elevated ICP [intracranial pressure] rather than viral infection.”
She added that “if a child with fever, seizures, and encephalopathy has cerebral edema on imaging and/or has neurologic progression, AFCE should be considered. Most of our cases of AFCE had fulminant progression within the first 3 days of their head imaging noting cerebral edema. There are other neurologic diseases, such as acute necrotizing encephalopathy of childhood, that also have progressive signs/symptoms, but head imaging and lab work should help differentiate many of these etiologies.”
In regard to treatment, she said, “our unit would likely err on the side of providing as much neuroprotective measures as is reasonable, such as maintaining normothermia, consideration of hyperosmolar therapy, maintaining normocarbia and normoxemia, managing seizures, etc. I would recommend getting the entire neurocritical care team involved in the management discussion. This varies by center, but will likely include neurology, ID [infectious disease], possibly neurosurgery, and PICU.”
As for the new case report, Krishnan said COVID-19 has been linked to neurologic complications, “so it does not surprise me that AFCE is part of the neurologic spectrum of disease.”
No funding was reported, and the authors report no relevant disclosures. Dr. Krishnan has no disclosures.
according to pediatric neurologists who are urging colleagues to watch out for similar cases.
At least one other child in the United States has died after becoming infected with the virus and developing cerebral edema. “The rapid and devastating clinical course in both of these cases highlights the need for early recognition of a cerebral edema and AFCE as potential complications of COVID-19 in pediatric patients,” the neurologists wrote.
The case was highlighted in a poster presented at the annual meeting of the Child Neurology Society and in a report published earlier this year in Child Neurology Open.
According to pediatric neurologist Timothy Gershon, MD, PhD , of the University of North Carolina at Chapel Hill, the child appeared in clinic in July 2020. She had been healthy but was suffering from 1 day of fever, seizure-like activity (generalized convulsions and drooling), anorexia, and lethargy.
The girl, who was subsequently diagnosed with COVID-19, deteriorated in the hospital. “She received IV dexamethasone in attempts to reduce cerebral edema,” the neurologists wrote. “Regarding immunomodulatory therapy, she received intravenous immunoglobulin (2 g/kg), anakinra, and hydrocortisone; despite approval for remdesivir and COVID-19 convalescent plasma, these were ultimately withheld due to poor prognosis.”
Brain death examinations at 24 and 48 hours after cardiac arrest were consistent with brain death, they reported.
Neurologists believe the patient suffered from AFCE, “an often fatal pediatric clinical entity consisting of fever, encephalopathy, and new-onset seizures followed by rapid, diffuse, and medically-refractory cerebral edema.” They add that “AFCE occurs as a rare complication of a variety of common pediatric infections, and a CNS [central nervous system] pathogen is identified in only a minority of cases, suggesting a para-infectious mechanism of edema.”
Neurologists offered a case definition of the “recently recognized” AFCE earlier this year.
“This was an extremely rare rapid progression to cerebral edema. I think it was related to the patient’s COVID infection, but why this patient got it and others don’t is unknown,” Dr. Gershon said in an interview. “The full spectrum of neurological complications of COVID were not yet known [at the time]. We didn’t know, and still don’t know, what the causative links are between COVID and suddenly having seizures and brain swelling.”
He said he’d treat a similar patient differently now and give dexamethasone earlier in the clinical course, although “there is no data to tell us if any therapy could have reversed it.” Specifically, he said, “I’d give dexamethasone at the first sign of brain involvement, using the dosing recommended for cerebral edema, and try to get the MRI earlier in the course.”
Dr. Gershon and colleagues noted another case of fatal cerebral edema in a child, a 7-year-old boy who was treated in New York state. That case “shows that fatal cerebral edema may complicate pediatric multisystem inflammatory syndrome,” they wrote.
Pediatric critical care specialist Preetha Krishnan, MD, of Randall Children’s Hospital at Legacy Emanuel in Portland, Ore., helped develop the new definition of AFCE. In an interview, she said AFCE is difficult to diagnose because the signs/symptoms – such as fever, altered sensorium, and seizures – are found in other conditions such as febrile status epilepticus with a viral illness.
“The key to recognition of AFCE is that unlike other disease processes, these children have rapid neurologic progression,” she said. “In addition, many of our AFCE patients also had vomiting and/or headache, which in retrospect was likely an indication of elevated ICP [intracranial pressure] rather than viral infection.”
She added that “if a child with fever, seizures, and encephalopathy has cerebral edema on imaging and/or has neurologic progression, AFCE should be considered. Most of our cases of AFCE had fulminant progression within the first 3 days of their head imaging noting cerebral edema. There are other neurologic diseases, such as acute necrotizing encephalopathy of childhood, that also have progressive signs/symptoms, but head imaging and lab work should help differentiate many of these etiologies.”
In regard to treatment, she said, “our unit would likely err on the side of providing as much neuroprotective measures as is reasonable, such as maintaining normothermia, consideration of hyperosmolar therapy, maintaining normocarbia and normoxemia, managing seizures, etc. I would recommend getting the entire neurocritical care team involved in the management discussion. This varies by center, but will likely include neurology, ID [infectious disease], possibly neurosurgery, and PICU.”
As for the new case report, Krishnan said COVID-19 has been linked to neurologic complications, “so it does not surprise me that AFCE is part of the neurologic spectrum of disease.”
No funding was reported, and the authors report no relevant disclosures. Dr. Krishnan has no disclosures.
FROM CNS 2021
Diminishing number of clerkship sites poses threat to psychiatry training
Medical school clinical rotations are a rite of passage as students emerge from their basic science courses and first board exam to the clinical world where the patients vaguely resemble the question stem descriptions. Finally, intangible theory can be put into practice. Yet, it is becoming increasingly difficult for 3rd-year medical student clerkship directors to find enough clinical sites to support the growing number of medical students as enrollment numbers steadily increase and outpace the current clinical resources.
In a 2019 Association of American Medical Colleges report, 84% of medical school deans were concerned about the diminishing number of clerkship sites, and there was additional worry about lack of qualified specialty preceptors. This lack of clerkship availability is especially true for psychiatry sites.
Psychiatry clerkship directors are in need of more clinical sites to address the educational needs of medical students, and psychiatrists in the broader clinical community are positioned to help medical schools expand their clinical sites.
Inpatient psychiatric units and consult services continue to be popular sites for medical student rotations, but it has been hard to expand into other settings, where psychiatric treatment is seen as more private and intimate than other specialties. Reasons for falling site availability are varied and include 1) financial disincentive to take students – because they can be seen as a burden on supervisors who must meet revenue-generating patient quotas; 2) competition with other learners, including residents, PA students, NPs, and NP students; and 3) the general financial and operational obstacles to clinical practice inflicted by the pandemic. COVID-19 affected medical education – for better and worse (JAMA. 2020;324[11]:1033-4). Psychiatry clerkships particularly suffered from restricted patient access as inpatient units reduced their census to comply with COVID-19 safety protocols, and during the height of the pandemic inpatient units provided psychiatric care to COVID-19–positive patients, which precluded student involvement. On the other hand, many more students were introduced to telepsychiatry and witnessed creative forms of mental health intervention as clinicians adapted their practices to the pandemic.
When rotations began
Clinical rotations entered the American medical school curriculum in the 1890s when Sir William Osler brought the European standard of medical education with him as Physician in Chief at the newly opened Johns Hopkins University Hospital. He formalized the traditional apprenticeship model by standardizing 3rd- and 4th-year clerkships as rotations in which medical students worked in clinics and on the wards, learning from residents and attendings.
Clinical rotations, their location, the supervisors, and the patients and their ailments all go in to influence a student’s specialty choice. Some students enter medical school knowing they want to be a surgeon, a pediatrician, or a psychiatrist. And some are compelled by a specific rotation, when they realize that it’s not at all what they expected and maybe they could dedicate their professional life to this area of medicine.
High-quality clinical clerkship sites are essential to the future of psychiatry. At clerkship sites, undecided students interested in psychiatry may affirm their commitment to psychiatry. Other students will have their only dedicated exposure to psychiatrically ill patients. This represents students’ only opportunity to learn the skills to treat comorbid psychiatric and medical illness. Regardless of specialty, nearly every physician will have to treat patients with some psychiatric illnesses.
What constitutes a “high-quality clinical site” is difficult to measure and define. Some measures of quality include a safe learning environment, a reasonable ratio of students to supervisors (including residents, fellows, and attendings), and an adequate number and diversity of patients. Many medical schools may prefer an affiliated academic medical center or Veterans’ Affairs hospitals for their rotating students. Private psychiatric hospitals are proliferating, and if these are to be sites for medical students, the following standards are suggested: Private psychiatric hospitals must follow standard safety precautions with sufficient staff presence, ensure willing preceptors who can provide adequate student supervision, and adjust their expectations to students who can carry a few patients of diverse background, but are not to be treated merely as scribes.
Psychiatrists, whether they consider themselves “academic” or not, have a role to play in expanding access to clinical sites. Students are eager to learn in any setting. Inpatient settings have long been seen as the norm for clinical education in psychiatry. Yet inpatient settings perpetuate the idea that those with severe mental illness or individuals with psychosocial stressors or disabling, comorbid substance use disorders are the only people who seek help from a psychiatrist. without an academic affiliation to explore the possibility of creating space for a medical student in their clinical practice.
We cannot deny the demands on psychiatrists’ time – every minute is counted by the patient and doctor, and every encounter is accounted for in some revenue stream. However, the academic world is running out of space for its students, and there’s a serious question as to whether an academic center is the only place for students. If you are a psychiatrist who still loves to learn and prides themselves on high-quality patient care, then you have an essential role in shaping the students who will one day be your peers in psychiatry, or the physicians treating your patients’ comorbid medical illnesses.
There are upfront challenges to teaching 3rd-year medical students, including teaching the psychiatric interview, note writing, persuading patients to allow students into their care, and setting time aside at the end of the workday to provide feedback on performance. Yet, after learning the ropes of psychiatric patient care, medical students can provide help in writing notes, calling collateral, contacting patients with their laboratory results, and even helping with the tedious but necessary administrative tasks like prior authorizations. In exchange for training students, some medical schools may offer perks, such as a volunteer faculty position that comes with access to usually expensive library resources, such as medical databases.
You can help expand clinical sites in psychiatry rotations by contacting your alma mater or the medical school closest to your community and asking about their need for clerkship sites. Many medical schools are branching out by sending students to stay near the clinical sites and immerse themselves in the community where their site director practices. Even one-half day a week in an outpatient setting provides patient and setting diversity to students and helps spread out students to different sites, easing the burden on inpatient supervisors while providing students more individualized supervision.
The practice of medicine is built on apprenticeship and teaching wisdom through patient care. Just because we leave residency doesn’t mean we leave academics. Taking students into your practice is an invaluable service to the medical education community and future physicians.
Dr. Posada is assistant clinical professor in the department of psychiatry and behavioral sciences at George Washington University in Washington, and staff physician at George Washington Medical Faculty Associates, also in Washington. She has no conflicts of interest. Dr. Ortiz is assistant professor and clerkship director in the department of psychiatry at Texas Tech University Health Sciences Center – El Paso. She has no conflicts of interest.
Medical school clinical rotations are a rite of passage as students emerge from their basic science courses and first board exam to the clinical world where the patients vaguely resemble the question stem descriptions. Finally, intangible theory can be put into practice. Yet, it is becoming increasingly difficult for 3rd-year medical student clerkship directors to find enough clinical sites to support the growing number of medical students as enrollment numbers steadily increase and outpace the current clinical resources.
In a 2019 Association of American Medical Colleges report, 84% of medical school deans were concerned about the diminishing number of clerkship sites, and there was additional worry about lack of qualified specialty preceptors. This lack of clerkship availability is especially true for psychiatry sites.
Psychiatry clerkship directors are in need of more clinical sites to address the educational needs of medical students, and psychiatrists in the broader clinical community are positioned to help medical schools expand their clinical sites.
Inpatient psychiatric units and consult services continue to be popular sites for medical student rotations, but it has been hard to expand into other settings, where psychiatric treatment is seen as more private and intimate than other specialties. Reasons for falling site availability are varied and include 1) financial disincentive to take students – because they can be seen as a burden on supervisors who must meet revenue-generating patient quotas; 2) competition with other learners, including residents, PA students, NPs, and NP students; and 3) the general financial and operational obstacles to clinical practice inflicted by the pandemic. COVID-19 affected medical education – for better and worse (JAMA. 2020;324[11]:1033-4). Psychiatry clerkships particularly suffered from restricted patient access as inpatient units reduced their census to comply with COVID-19 safety protocols, and during the height of the pandemic inpatient units provided psychiatric care to COVID-19–positive patients, which precluded student involvement. On the other hand, many more students were introduced to telepsychiatry and witnessed creative forms of mental health intervention as clinicians adapted their practices to the pandemic.
When rotations began
Clinical rotations entered the American medical school curriculum in the 1890s when Sir William Osler brought the European standard of medical education with him as Physician in Chief at the newly opened Johns Hopkins University Hospital. He formalized the traditional apprenticeship model by standardizing 3rd- and 4th-year clerkships as rotations in which medical students worked in clinics and on the wards, learning from residents and attendings.
Clinical rotations, their location, the supervisors, and the patients and their ailments all go in to influence a student’s specialty choice. Some students enter medical school knowing they want to be a surgeon, a pediatrician, or a psychiatrist. And some are compelled by a specific rotation, when they realize that it’s not at all what they expected and maybe they could dedicate their professional life to this area of medicine.
High-quality clinical clerkship sites are essential to the future of psychiatry. At clerkship sites, undecided students interested in psychiatry may affirm their commitment to psychiatry. Other students will have their only dedicated exposure to psychiatrically ill patients. This represents students’ only opportunity to learn the skills to treat comorbid psychiatric and medical illness. Regardless of specialty, nearly every physician will have to treat patients with some psychiatric illnesses.
What constitutes a “high-quality clinical site” is difficult to measure and define. Some measures of quality include a safe learning environment, a reasonable ratio of students to supervisors (including residents, fellows, and attendings), and an adequate number and diversity of patients. Many medical schools may prefer an affiliated academic medical center or Veterans’ Affairs hospitals for their rotating students. Private psychiatric hospitals are proliferating, and if these are to be sites for medical students, the following standards are suggested: Private psychiatric hospitals must follow standard safety precautions with sufficient staff presence, ensure willing preceptors who can provide adequate student supervision, and adjust their expectations to students who can carry a few patients of diverse background, but are not to be treated merely as scribes.
Psychiatrists, whether they consider themselves “academic” or not, have a role to play in expanding access to clinical sites. Students are eager to learn in any setting. Inpatient settings have long been seen as the norm for clinical education in psychiatry. Yet inpatient settings perpetuate the idea that those with severe mental illness or individuals with psychosocial stressors or disabling, comorbid substance use disorders are the only people who seek help from a psychiatrist. without an academic affiliation to explore the possibility of creating space for a medical student in their clinical practice.
We cannot deny the demands on psychiatrists’ time – every minute is counted by the patient and doctor, and every encounter is accounted for in some revenue stream. However, the academic world is running out of space for its students, and there’s a serious question as to whether an academic center is the only place for students. If you are a psychiatrist who still loves to learn and prides themselves on high-quality patient care, then you have an essential role in shaping the students who will one day be your peers in psychiatry, or the physicians treating your patients’ comorbid medical illnesses.
There are upfront challenges to teaching 3rd-year medical students, including teaching the psychiatric interview, note writing, persuading patients to allow students into their care, and setting time aside at the end of the workday to provide feedback on performance. Yet, after learning the ropes of psychiatric patient care, medical students can provide help in writing notes, calling collateral, contacting patients with their laboratory results, and even helping with the tedious but necessary administrative tasks like prior authorizations. In exchange for training students, some medical schools may offer perks, such as a volunteer faculty position that comes with access to usually expensive library resources, such as medical databases.
You can help expand clinical sites in psychiatry rotations by contacting your alma mater or the medical school closest to your community and asking about their need for clerkship sites. Many medical schools are branching out by sending students to stay near the clinical sites and immerse themselves in the community where their site director practices. Even one-half day a week in an outpatient setting provides patient and setting diversity to students and helps spread out students to different sites, easing the burden on inpatient supervisors while providing students more individualized supervision.
The practice of medicine is built on apprenticeship and teaching wisdom through patient care. Just because we leave residency doesn’t mean we leave academics. Taking students into your practice is an invaluable service to the medical education community and future physicians.
Dr. Posada is assistant clinical professor in the department of psychiatry and behavioral sciences at George Washington University in Washington, and staff physician at George Washington Medical Faculty Associates, also in Washington. She has no conflicts of interest. Dr. Ortiz is assistant professor and clerkship director in the department of psychiatry at Texas Tech University Health Sciences Center – El Paso. She has no conflicts of interest.
Medical school clinical rotations are a rite of passage as students emerge from their basic science courses and first board exam to the clinical world where the patients vaguely resemble the question stem descriptions. Finally, intangible theory can be put into practice. Yet, it is becoming increasingly difficult for 3rd-year medical student clerkship directors to find enough clinical sites to support the growing number of medical students as enrollment numbers steadily increase and outpace the current clinical resources.
In a 2019 Association of American Medical Colleges report, 84% of medical school deans were concerned about the diminishing number of clerkship sites, and there was additional worry about lack of qualified specialty preceptors. This lack of clerkship availability is especially true for psychiatry sites.
Psychiatry clerkship directors are in need of more clinical sites to address the educational needs of medical students, and psychiatrists in the broader clinical community are positioned to help medical schools expand their clinical sites.
Inpatient psychiatric units and consult services continue to be popular sites for medical student rotations, but it has been hard to expand into other settings, where psychiatric treatment is seen as more private and intimate than other specialties. Reasons for falling site availability are varied and include 1) financial disincentive to take students – because they can be seen as a burden on supervisors who must meet revenue-generating patient quotas; 2) competition with other learners, including residents, PA students, NPs, and NP students; and 3) the general financial and operational obstacles to clinical practice inflicted by the pandemic. COVID-19 affected medical education – for better and worse (JAMA. 2020;324[11]:1033-4). Psychiatry clerkships particularly suffered from restricted patient access as inpatient units reduced their census to comply with COVID-19 safety protocols, and during the height of the pandemic inpatient units provided psychiatric care to COVID-19–positive patients, which precluded student involvement. On the other hand, many more students were introduced to telepsychiatry and witnessed creative forms of mental health intervention as clinicians adapted their practices to the pandemic.
When rotations began
Clinical rotations entered the American medical school curriculum in the 1890s when Sir William Osler brought the European standard of medical education with him as Physician in Chief at the newly opened Johns Hopkins University Hospital. He formalized the traditional apprenticeship model by standardizing 3rd- and 4th-year clerkships as rotations in which medical students worked in clinics and on the wards, learning from residents and attendings.
Clinical rotations, their location, the supervisors, and the patients and their ailments all go in to influence a student’s specialty choice. Some students enter medical school knowing they want to be a surgeon, a pediatrician, or a psychiatrist. And some are compelled by a specific rotation, when they realize that it’s not at all what they expected and maybe they could dedicate their professional life to this area of medicine.
High-quality clinical clerkship sites are essential to the future of psychiatry. At clerkship sites, undecided students interested in psychiatry may affirm their commitment to psychiatry. Other students will have their only dedicated exposure to psychiatrically ill patients. This represents students’ only opportunity to learn the skills to treat comorbid psychiatric and medical illness. Regardless of specialty, nearly every physician will have to treat patients with some psychiatric illnesses.
What constitutes a “high-quality clinical site” is difficult to measure and define. Some measures of quality include a safe learning environment, a reasonable ratio of students to supervisors (including residents, fellows, and attendings), and an adequate number and diversity of patients. Many medical schools may prefer an affiliated academic medical center or Veterans’ Affairs hospitals for their rotating students. Private psychiatric hospitals are proliferating, and if these are to be sites for medical students, the following standards are suggested: Private psychiatric hospitals must follow standard safety precautions with sufficient staff presence, ensure willing preceptors who can provide adequate student supervision, and adjust their expectations to students who can carry a few patients of diverse background, but are not to be treated merely as scribes.
Psychiatrists, whether they consider themselves “academic” or not, have a role to play in expanding access to clinical sites. Students are eager to learn in any setting. Inpatient settings have long been seen as the norm for clinical education in psychiatry. Yet inpatient settings perpetuate the idea that those with severe mental illness or individuals with psychosocial stressors or disabling, comorbid substance use disorders are the only people who seek help from a psychiatrist. without an academic affiliation to explore the possibility of creating space for a medical student in their clinical practice.
We cannot deny the demands on psychiatrists’ time – every minute is counted by the patient and doctor, and every encounter is accounted for in some revenue stream. However, the academic world is running out of space for its students, and there’s a serious question as to whether an academic center is the only place for students. If you are a psychiatrist who still loves to learn and prides themselves on high-quality patient care, then you have an essential role in shaping the students who will one day be your peers in psychiatry, or the physicians treating your patients’ comorbid medical illnesses.
There are upfront challenges to teaching 3rd-year medical students, including teaching the psychiatric interview, note writing, persuading patients to allow students into their care, and setting time aside at the end of the workday to provide feedback on performance. Yet, after learning the ropes of psychiatric patient care, medical students can provide help in writing notes, calling collateral, contacting patients with their laboratory results, and even helping with the tedious but necessary administrative tasks like prior authorizations. In exchange for training students, some medical schools may offer perks, such as a volunteer faculty position that comes with access to usually expensive library resources, such as medical databases.
You can help expand clinical sites in psychiatry rotations by contacting your alma mater or the medical school closest to your community and asking about their need for clerkship sites. Many medical schools are branching out by sending students to stay near the clinical sites and immerse themselves in the community where their site director practices. Even one-half day a week in an outpatient setting provides patient and setting diversity to students and helps spread out students to different sites, easing the burden on inpatient supervisors while providing students more individualized supervision.
The practice of medicine is built on apprenticeship and teaching wisdom through patient care. Just because we leave residency doesn’t mean we leave academics. Taking students into your practice is an invaluable service to the medical education community and future physicians.
Dr. Posada is assistant clinical professor in the department of psychiatry and behavioral sciences at George Washington University in Washington, and staff physician at George Washington Medical Faculty Associates, also in Washington. She has no conflicts of interest. Dr. Ortiz is assistant professor and clerkship director in the department of psychiatry at Texas Tech University Health Sciences Center – El Paso. She has no conflicts of interest.
Maternal SSRI use linked to more encephalopathy in newborns, risk still small
, although the overall risk remains extremely low, a new study finds.
The findings were presented in a poster at the 50th annual meeting of the Child Neurology Society.
“Our work showed that neonates exposed to SSRI in utero had higher risks of neonatal encephalopathy even when adjusting for confounders such as maternal mental health disorders and age. SSRIs could cause side effects such as encephalopathy in neonates, and these risks need to be balanced carefully with the potential benefits of treatment to the mother,” study lead author Marie Cornet, MD, a neonatology fellow with Benioff Children’s Hospital at the University of California, San Francisco, said in an interview.
According to Dr. Cornet, “we know that SSRI exposure in utero is associated with increased risks of respiratory distress at birth, need for positive-pressure ventilation, and an abnormal neurologic exam.” The researchers launched the new study to determine if the estimated 4%-8% of pregnant women who take SSRIs may be putting their newborns at greater risk of NE.
The researchers retrospectively tracked 305,426 infants who were born in the Kaiser Permanente Northern California health system (≥35 weeks) from 2011 to 2019. The mothers had an average age of 31 years, and approximately 34.7% were White, 34.7% of unknown race, 23.3% Asian, and 6.2% Black.
The researchers defined NE as a “5-minute APGAR score <7 and abnormal level of consciousness, activity, tone, or reflexes.”
A total of 8,024 infants (2.6%) had mothers who used SSRIs in the third trimester, and 510 (0.17%) were determined to have had NE.
After adjustment for maternal depression or anxiety, maternal age, race, and hospital, exposed neonates had 2.7 times higher odds of NE (odds ratio, 2.7).
Each 25 mg per day increase in the dose of SSRIs, as equalized to doses of sertraline (Zoloft), was linked to a significant 31% increase in the odds of developing NE (OR, 1.31).
The study doesn’t examine the benefits of SSRI treatment in pregnancy. Those taking SSRIs were much more likely to have depression during pregnancy (76.5% vs. 13.5%) and anxiety (56.7% vs. 6.9%), compared with those who did not take the drug.
The possible connection between SSRIs and NE is unclear. “SSRIs may contribute to NE by a withdrawal mechanism or by a toxicity mechanism. It is also possible that SSRIs themselves are not responsible for encephalopathy, or that the severity of maternal mental health is itself responsible for increased neonatal encephalopathy,” Dr. Cornet said. “However, we believe we adjusted our results thoroughly for that. Furthermore, in this cohort, neonates born from mothers with untreated depression were not at higher risk of encephalopathy than neonates born to mothers without depression.”
She added: “When infants have acidosis or require prolonged resuscitation after birth, they get treated with therapeutic hypothermia. This invasive treatment was shown to decrease mortality and morbidity in neonates with hypoxic-ischemic encephalopathy. However, therapeutic hypothermia may not be helpful in infants with encephalopathy due to other causes than acute hypoxia-ischemia, such as infection, inflammation, genetic conditions, or exposure to toxins. In the case of SSRIs, our results show that, while neonates often have encephalopathy, this encephalopathy is often mild and self-resolved. We did not see a statistically significant increase in acidosis or treatment with therapeutic hypothermia.”
In the future neurologists should consider SSRI use as a potential cause in cases of NE, Dr. Cornet said. “If there are no signs of hypoxic-ischemic encephalopathy – no evidence of acidosis, acute perinatal event – treatment with therapeutic hypothermia may not be indicated.”
Dr. Cornet said more research is in the works. “Studying the long-term side effect of SSRIs on neonatal brain development and injury is essential,” she said. “We plan to compare brain injury in neonates exposed and unexposed to SSRIs and examine long-term outcomes to assess if the effect of SSRI exposure is transient or has a lasting impact.”
This study was funded by the Thrasher Early Career Research Grant and by the Newborn Brain Research Innovation Award at UCSF. The authors have no relevant disclosures.
, although the overall risk remains extremely low, a new study finds.
The findings were presented in a poster at the 50th annual meeting of the Child Neurology Society.
“Our work showed that neonates exposed to SSRI in utero had higher risks of neonatal encephalopathy even when adjusting for confounders such as maternal mental health disorders and age. SSRIs could cause side effects such as encephalopathy in neonates, and these risks need to be balanced carefully with the potential benefits of treatment to the mother,” study lead author Marie Cornet, MD, a neonatology fellow with Benioff Children’s Hospital at the University of California, San Francisco, said in an interview.
According to Dr. Cornet, “we know that SSRI exposure in utero is associated with increased risks of respiratory distress at birth, need for positive-pressure ventilation, and an abnormal neurologic exam.” The researchers launched the new study to determine if the estimated 4%-8% of pregnant women who take SSRIs may be putting their newborns at greater risk of NE.
The researchers retrospectively tracked 305,426 infants who were born in the Kaiser Permanente Northern California health system (≥35 weeks) from 2011 to 2019. The mothers had an average age of 31 years, and approximately 34.7% were White, 34.7% of unknown race, 23.3% Asian, and 6.2% Black.
The researchers defined NE as a “5-minute APGAR score <7 and abnormal level of consciousness, activity, tone, or reflexes.”
A total of 8,024 infants (2.6%) had mothers who used SSRIs in the third trimester, and 510 (0.17%) were determined to have had NE.
After adjustment for maternal depression or anxiety, maternal age, race, and hospital, exposed neonates had 2.7 times higher odds of NE (odds ratio, 2.7).
Each 25 mg per day increase in the dose of SSRIs, as equalized to doses of sertraline (Zoloft), was linked to a significant 31% increase in the odds of developing NE (OR, 1.31).
The study doesn’t examine the benefits of SSRI treatment in pregnancy. Those taking SSRIs were much more likely to have depression during pregnancy (76.5% vs. 13.5%) and anxiety (56.7% vs. 6.9%), compared with those who did not take the drug.
The possible connection between SSRIs and NE is unclear. “SSRIs may contribute to NE by a withdrawal mechanism or by a toxicity mechanism. It is also possible that SSRIs themselves are not responsible for encephalopathy, or that the severity of maternal mental health is itself responsible for increased neonatal encephalopathy,” Dr. Cornet said. “However, we believe we adjusted our results thoroughly for that. Furthermore, in this cohort, neonates born from mothers with untreated depression were not at higher risk of encephalopathy than neonates born to mothers without depression.”
She added: “When infants have acidosis or require prolonged resuscitation after birth, they get treated with therapeutic hypothermia. This invasive treatment was shown to decrease mortality and morbidity in neonates with hypoxic-ischemic encephalopathy. However, therapeutic hypothermia may not be helpful in infants with encephalopathy due to other causes than acute hypoxia-ischemia, such as infection, inflammation, genetic conditions, or exposure to toxins. In the case of SSRIs, our results show that, while neonates often have encephalopathy, this encephalopathy is often mild and self-resolved. We did not see a statistically significant increase in acidosis or treatment with therapeutic hypothermia.”
In the future neurologists should consider SSRI use as a potential cause in cases of NE, Dr. Cornet said. “If there are no signs of hypoxic-ischemic encephalopathy – no evidence of acidosis, acute perinatal event – treatment with therapeutic hypothermia may not be indicated.”
Dr. Cornet said more research is in the works. “Studying the long-term side effect of SSRIs on neonatal brain development and injury is essential,” she said. “We plan to compare brain injury in neonates exposed and unexposed to SSRIs and examine long-term outcomes to assess if the effect of SSRI exposure is transient or has a lasting impact.”
This study was funded by the Thrasher Early Career Research Grant and by the Newborn Brain Research Innovation Award at UCSF. The authors have no relevant disclosures.
, although the overall risk remains extremely low, a new study finds.
The findings were presented in a poster at the 50th annual meeting of the Child Neurology Society.
“Our work showed that neonates exposed to SSRI in utero had higher risks of neonatal encephalopathy even when adjusting for confounders such as maternal mental health disorders and age. SSRIs could cause side effects such as encephalopathy in neonates, and these risks need to be balanced carefully with the potential benefits of treatment to the mother,” study lead author Marie Cornet, MD, a neonatology fellow with Benioff Children’s Hospital at the University of California, San Francisco, said in an interview.
According to Dr. Cornet, “we know that SSRI exposure in utero is associated with increased risks of respiratory distress at birth, need for positive-pressure ventilation, and an abnormal neurologic exam.” The researchers launched the new study to determine if the estimated 4%-8% of pregnant women who take SSRIs may be putting their newborns at greater risk of NE.
The researchers retrospectively tracked 305,426 infants who were born in the Kaiser Permanente Northern California health system (≥35 weeks) from 2011 to 2019. The mothers had an average age of 31 years, and approximately 34.7% were White, 34.7% of unknown race, 23.3% Asian, and 6.2% Black.
The researchers defined NE as a “5-minute APGAR score <7 and abnormal level of consciousness, activity, tone, or reflexes.”
A total of 8,024 infants (2.6%) had mothers who used SSRIs in the third trimester, and 510 (0.17%) were determined to have had NE.
After adjustment for maternal depression or anxiety, maternal age, race, and hospital, exposed neonates had 2.7 times higher odds of NE (odds ratio, 2.7).
Each 25 mg per day increase in the dose of SSRIs, as equalized to doses of sertraline (Zoloft), was linked to a significant 31% increase in the odds of developing NE (OR, 1.31).
The study doesn’t examine the benefits of SSRI treatment in pregnancy. Those taking SSRIs were much more likely to have depression during pregnancy (76.5% vs. 13.5%) and anxiety (56.7% vs. 6.9%), compared with those who did not take the drug.
The possible connection between SSRIs and NE is unclear. “SSRIs may contribute to NE by a withdrawal mechanism or by a toxicity mechanism. It is also possible that SSRIs themselves are not responsible for encephalopathy, or that the severity of maternal mental health is itself responsible for increased neonatal encephalopathy,” Dr. Cornet said. “However, we believe we adjusted our results thoroughly for that. Furthermore, in this cohort, neonates born from mothers with untreated depression were not at higher risk of encephalopathy than neonates born to mothers without depression.”
She added: “When infants have acidosis or require prolonged resuscitation after birth, they get treated with therapeutic hypothermia. This invasive treatment was shown to decrease mortality and morbidity in neonates with hypoxic-ischemic encephalopathy. However, therapeutic hypothermia may not be helpful in infants with encephalopathy due to other causes than acute hypoxia-ischemia, such as infection, inflammation, genetic conditions, or exposure to toxins. In the case of SSRIs, our results show that, while neonates often have encephalopathy, this encephalopathy is often mild and self-resolved. We did not see a statistically significant increase in acidosis or treatment with therapeutic hypothermia.”
In the future neurologists should consider SSRI use as a potential cause in cases of NE, Dr. Cornet said. “If there are no signs of hypoxic-ischemic encephalopathy – no evidence of acidosis, acute perinatal event – treatment with therapeutic hypothermia may not be indicated.”
Dr. Cornet said more research is in the works. “Studying the long-term side effect of SSRIs on neonatal brain development and injury is essential,” she said. “We plan to compare brain injury in neonates exposed and unexposed to SSRIs and examine long-term outcomes to assess if the effect of SSRI exposure is transient or has a lasting impact.”
This study was funded by the Thrasher Early Career Research Grant and by the Newborn Brain Research Innovation Award at UCSF. The authors have no relevant disclosures.
FROM CNS 2021
Taper, withdrawal of RA meds tested in real-life randomized trial setting
About half of patients with rheumatoid arthritis who taper or stop disease-modifying antirheumatic drugs (DMARDs) retain stable remission after 12 months, and a majority of those who do relapse regain remission when back on their original treatments, according to data from the open-label, randomized Rheumatoid Arthritis in Ongoing Remission (RETRO) study.
“Currently, 40%-50% of patients with rheumatoid arthritis reach stable remission,” as a result of factors including earlier diagnosis and a wider range of treatments, Koray Tascilar, MD, of Friedrich Alexander University Erlangen-Nuremberg (Germany) and colleagues wrote in their publication of the RETRO trial results in Lancet Rheumatology.
Previous studies have suggested that patients with RA in sustained remission may be able to taper or withdraw treatment, but data from randomized trials are limited, the researchers said.
In the RETRO trial, researchers compared three strategies for RA patients in remission, which was defined as <2.6 on the 28-joint Disease Activity Score with erythrocyte sedimentation rate (DAS28-ESR). They randomized 100 adults to continue DMARDs and glucocorticoids, 102 to taper DMARDs and glucocorticoids to half their prior doses, and 101 to reduce the doses to half for 6 months and then stop DMARDs. Patients were enrolled between May 26, 2010, and May 29, 2018, from 14 treatment centers in Germany. The final analysis included 282 patients; 92 in the continuation group, 93 in the taper group, and 96 in the stop group. The mean age of the patients was 56.5 years, and 59% were women. The mean duration of RA was 7.4 years, and the mean duration of remission was 20 months.
Overall, at 12 months, 61% of the patients remained in remission without relapse; 81.2% of the continuation group, 58.6% of the taper group, and 43.3% of the stop group. Relapses occurred in 17%, 43%, and 55% of patients in the continuation, taper, and stop groups, respectively. The median times to relapse in the three groups were 30.6 weeks, 24.3 weeks, and 26.1 weeks, respectively.
Most of the relapses occurred between weeks 24 and 36 after stopping treatment, the researchers wrote. Corresponding hazard ratios for relapse were 3.02 for the taper group and 4.34 for the stop group, compared with the continuation group. In comparison to continuing treatment, the number needed to treat for one more relapse to occur during the 12-month observation period was four for tapering and three for stopping, they noted.
The study protocol called for a return to baseline treatment for any patients who relapsed in the taper and stop groups, and most patients who relapsed regained remission after restarting their baseline treatments. Among patients who had a follow-up visit after a relapse, 10 (63%) of 16 patients in the continuation group reachieved remission before the end of the study, as did 21 (62%) of 34 in the taper group and 35 (76%) of 46 in the stop group.
The most common treatments at baseline were methotrexate (76%) and tumor necrosis factor (TNF) inhibitors (32%).
The researchers also identified several baseline characteristics associated with relapse. Overall, relapse occurred more often in biologic DMARD users than in participants treated with other drugs, more often in women than men, and more often in those with a longer disease duration, higher baseline DAS28-ESR and Health Assessment Questionnaire scores, and in those who were positive for rheumatoid factor or anti–citrullinated protein antibodies.
A total of 38 serious adverse events occurred in 29 participants during the study period, but none were deemed treatment related, and none led to study withdrawal.
The study findings were limited by several factors including the lack of masking of patients and assessors and potential underestimation of disease activity, the researchers noted. Also, the study did not include radiographic data that might have been used to confirm progression; however, such data could have produced a null result and were not feasible in the study population, they wrote.
“If RETRO had been a trial to test the superiority of 100% dose continuation, compared with tapering plus rescue treatment or stopping plus rescue treatment, we would not be able to show that continuation is superior to tapering or stopping,” the researchers noted.
The study results support “an increasingly dynamic management approach in patients with rheumatoid arthritis in stable remission,” given the changing nature of RA management, that may help reduce overtreatment in many RA patients, the researchers concluded. “Furthermore, the observation that most of the patients regained remission after reintroduction of antirheumatic treatments is helpful with regard to the benefit-risk aspect of treatment reduction.”
Real-world setting serves as starting point
The RETRO study is unique in that it tried to reflect a real-life setting by enrolling patients on baseline treatment with combinations of conventional synthetic DMARDs and biologic DMARDs seen in clinical practice rather than only patients taking biologic DMARDs – primarily TNF inhibitors – as done in previous studies of tapering and stopping DMARDs, wrote Catherine L. Hill, MD, of the University of Adelaide (Australia), in an accompanying editorial. It is also “used a simple, pragmatic one-size-fits-all treatment-tapering strategy,” she wrote.
However, she emphasized that answers are needed to questions about what relapse rates are acceptable, what duration of treatment-free time is ideal, and whether benefits to the patient outweigh risks.
Dr. Hill also highlighted the issue of identifying patients who are appropriate candidates for tapering or withdrawal. Stricter remission criteria may not be feasible in routine practice, and so “the development of algorithms to guide patient selection is likely to be the most practical way forward for clinicians and patients,” she wrote.
“Contemplation of treatment tapering or discontinuation in some patients with rheumatoid arthritis is remarkable and a measure of how far treatments have advanced,” Dr. Hill wrote. “However, further work to address outstanding questions on who should taper and how best to do it is still required,” she concluded.
The study received no outside funding. Lead author Dr. Tascilar disclosed lecture fees from Gilead and Union Chimique Belge; several coauthors disclosed relationships with multiple companies outside the current study. Dr. Hill had no financial conflicts to disclose.
About half of patients with rheumatoid arthritis who taper or stop disease-modifying antirheumatic drugs (DMARDs) retain stable remission after 12 months, and a majority of those who do relapse regain remission when back on their original treatments, according to data from the open-label, randomized Rheumatoid Arthritis in Ongoing Remission (RETRO) study.
“Currently, 40%-50% of patients with rheumatoid arthritis reach stable remission,” as a result of factors including earlier diagnosis and a wider range of treatments, Koray Tascilar, MD, of Friedrich Alexander University Erlangen-Nuremberg (Germany) and colleagues wrote in their publication of the RETRO trial results in Lancet Rheumatology.
Previous studies have suggested that patients with RA in sustained remission may be able to taper or withdraw treatment, but data from randomized trials are limited, the researchers said.
In the RETRO trial, researchers compared three strategies for RA patients in remission, which was defined as <2.6 on the 28-joint Disease Activity Score with erythrocyte sedimentation rate (DAS28-ESR). They randomized 100 adults to continue DMARDs and glucocorticoids, 102 to taper DMARDs and glucocorticoids to half their prior doses, and 101 to reduce the doses to half for 6 months and then stop DMARDs. Patients were enrolled between May 26, 2010, and May 29, 2018, from 14 treatment centers in Germany. The final analysis included 282 patients; 92 in the continuation group, 93 in the taper group, and 96 in the stop group. The mean age of the patients was 56.5 years, and 59% were women. The mean duration of RA was 7.4 years, and the mean duration of remission was 20 months.
Overall, at 12 months, 61% of the patients remained in remission without relapse; 81.2% of the continuation group, 58.6% of the taper group, and 43.3% of the stop group. Relapses occurred in 17%, 43%, and 55% of patients in the continuation, taper, and stop groups, respectively. The median times to relapse in the three groups were 30.6 weeks, 24.3 weeks, and 26.1 weeks, respectively.
Most of the relapses occurred between weeks 24 and 36 after stopping treatment, the researchers wrote. Corresponding hazard ratios for relapse were 3.02 for the taper group and 4.34 for the stop group, compared with the continuation group. In comparison to continuing treatment, the number needed to treat for one more relapse to occur during the 12-month observation period was four for tapering and three for stopping, they noted.
The study protocol called for a return to baseline treatment for any patients who relapsed in the taper and stop groups, and most patients who relapsed regained remission after restarting their baseline treatments. Among patients who had a follow-up visit after a relapse, 10 (63%) of 16 patients in the continuation group reachieved remission before the end of the study, as did 21 (62%) of 34 in the taper group and 35 (76%) of 46 in the stop group.
The most common treatments at baseline were methotrexate (76%) and tumor necrosis factor (TNF) inhibitors (32%).
The researchers also identified several baseline characteristics associated with relapse. Overall, relapse occurred more often in biologic DMARD users than in participants treated with other drugs, more often in women than men, and more often in those with a longer disease duration, higher baseline DAS28-ESR and Health Assessment Questionnaire scores, and in those who were positive for rheumatoid factor or anti–citrullinated protein antibodies.
A total of 38 serious adverse events occurred in 29 participants during the study period, but none were deemed treatment related, and none led to study withdrawal.
The study findings were limited by several factors including the lack of masking of patients and assessors and potential underestimation of disease activity, the researchers noted. Also, the study did not include radiographic data that might have been used to confirm progression; however, such data could have produced a null result and were not feasible in the study population, they wrote.
“If RETRO had been a trial to test the superiority of 100% dose continuation, compared with tapering plus rescue treatment or stopping plus rescue treatment, we would not be able to show that continuation is superior to tapering or stopping,” the researchers noted.
The study results support “an increasingly dynamic management approach in patients with rheumatoid arthritis in stable remission,” given the changing nature of RA management, that may help reduce overtreatment in many RA patients, the researchers concluded. “Furthermore, the observation that most of the patients regained remission after reintroduction of antirheumatic treatments is helpful with regard to the benefit-risk aspect of treatment reduction.”
Real-world setting serves as starting point
The RETRO study is unique in that it tried to reflect a real-life setting by enrolling patients on baseline treatment with combinations of conventional synthetic DMARDs and biologic DMARDs seen in clinical practice rather than only patients taking biologic DMARDs – primarily TNF inhibitors – as done in previous studies of tapering and stopping DMARDs, wrote Catherine L. Hill, MD, of the University of Adelaide (Australia), in an accompanying editorial. It is also “used a simple, pragmatic one-size-fits-all treatment-tapering strategy,” she wrote.
However, she emphasized that answers are needed to questions about what relapse rates are acceptable, what duration of treatment-free time is ideal, and whether benefits to the patient outweigh risks.
Dr. Hill also highlighted the issue of identifying patients who are appropriate candidates for tapering or withdrawal. Stricter remission criteria may not be feasible in routine practice, and so “the development of algorithms to guide patient selection is likely to be the most practical way forward for clinicians and patients,” she wrote.
“Contemplation of treatment tapering or discontinuation in some patients with rheumatoid arthritis is remarkable and a measure of how far treatments have advanced,” Dr. Hill wrote. “However, further work to address outstanding questions on who should taper and how best to do it is still required,” she concluded.
The study received no outside funding. Lead author Dr. Tascilar disclosed lecture fees from Gilead and Union Chimique Belge; several coauthors disclosed relationships with multiple companies outside the current study. Dr. Hill had no financial conflicts to disclose.
About half of patients with rheumatoid arthritis who taper or stop disease-modifying antirheumatic drugs (DMARDs) retain stable remission after 12 months, and a majority of those who do relapse regain remission when back on their original treatments, according to data from the open-label, randomized Rheumatoid Arthritis in Ongoing Remission (RETRO) study.
“Currently, 40%-50% of patients with rheumatoid arthritis reach stable remission,” as a result of factors including earlier diagnosis and a wider range of treatments, Koray Tascilar, MD, of Friedrich Alexander University Erlangen-Nuremberg (Germany) and colleagues wrote in their publication of the RETRO trial results in Lancet Rheumatology.
Previous studies have suggested that patients with RA in sustained remission may be able to taper or withdraw treatment, but data from randomized trials are limited, the researchers said.
In the RETRO trial, researchers compared three strategies for RA patients in remission, which was defined as <2.6 on the 28-joint Disease Activity Score with erythrocyte sedimentation rate (DAS28-ESR). They randomized 100 adults to continue DMARDs and glucocorticoids, 102 to taper DMARDs and glucocorticoids to half their prior doses, and 101 to reduce the doses to half for 6 months and then stop DMARDs. Patients were enrolled between May 26, 2010, and May 29, 2018, from 14 treatment centers in Germany. The final analysis included 282 patients; 92 in the continuation group, 93 in the taper group, and 96 in the stop group. The mean age of the patients was 56.5 years, and 59% were women. The mean duration of RA was 7.4 years, and the mean duration of remission was 20 months.
Overall, at 12 months, 61% of the patients remained in remission without relapse; 81.2% of the continuation group, 58.6% of the taper group, and 43.3% of the stop group. Relapses occurred in 17%, 43%, and 55% of patients in the continuation, taper, and stop groups, respectively. The median times to relapse in the three groups were 30.6 weeks, 24.3 weeks, and 26.1 weeks, respectively.
Most of the relapses occurred between weeks 24 and 36 after stopping treatment, the researchers wrote. Corresponding hazard ratios for relapse were 3.02 for the taper group and 4.34 for the stop group, compared with the continuation group. In comparison to continuing treatment, the number needed to treat for one more relapse to occur during the 12-month observation period was four for tapering and three for stopping, they noted.
The study protocol called for a return to baseline treatment for any patients who relapsed in the taper and stop groups, and most patients who relapsed regained remission after restarting their baseline treatments. Among patients who had a follow-up visit after a relapse, 10 (63%) of 16 patients in the continuation group reachieved remission before the end of the study, as did 21 (62%) of 34 in the taper group and 35 (76%) of 46 in the stop group.
The most common treatments at baseline were methotrexate (76%) and tumor necrosis factor (TNF) inhibitors (32%).
The researchers also identified several baseline characteristics associated with relapse. Overall, relapse occurred more often in biologic DMARD users than in participants treated with other drugs, more often in women than men, and more often in those with a longer disease duration, higher baseline DAS28-ESR and Health Assessment Questionnaire scores, and in those who were positive for rheumatoid factor or anti–citrullinated protein antibodies.
A total of 38 serious adverse events occurred in 29 participants during the study period, but none were deemed treatment related, and none led to study withdrawal.
The study findings were limited by several factors including the lack of masking of patients and assessors and potential underestimation of disease activity, the researchers noted. Also, the study did not include radiographic data that might have been used to confirm progression; however, such data could have produced a null result and were not feasible in the study population, they wrote.
“If RETRO had been a trial to test the superiority of 100% dose continuation, compared with tapering plus rescue treatment or stopping plus rescue treatment, we would not be able to show that continuation is superior to tapering or stopping,” the researchers noted.
The study results support “an increasingly dynamic management approach in patients with rheumatoid arthritis in stable remission,” given the changing nature of RA management, that may help reduce overtreatment in many RA patients, the researchers concluded. “Furthermore, the observation that most of the patients regained remission after reintroduction of antirheumatic treatments is helpful with regard to the benefit-risk aspect of treatment reduction.”
Real-world setting serves as starting point
The RETRO study is unique in that it tried to reflect a real-life setting by enrolling patients on baseline treatment with combinations of conventional synthetic DMARDs and biologic DMARDs seen in clinical practice rather than only patients taking biologic DMARDs – primarily TNF inhibitors – as done in previous studies of tapering and stopping DMARDs, wrote Catherine L. Hill, MD, of the University of Adelaide (Australia), in an accompanying editorial. It is also “used a simple, pragmatic one-size-fits-all treatment-tapering strategy,” she wrote.
However, she emphasized that answers are needed to questions about what relapse rates are acceptable, what duration of treatment-free time is ideal, and whether benefits to the patient outweigh risks.
Dr. Hill also highlighted the issue of identifying patients who are appropriate candidates for tapering or withdrawal. Stricter remission criteria may not be feasible in routine practice, and so “the development of algorithms to guide patient selection is likely to be the most practical way forward for clinicians and patients,” she wrote.
“Contemplation of treatment tapering or discontinuation in some patients with rheumatoid arthritis is remarkable and a measure of how far treatments have advanced,” Dr. Hill wrote. “However, further work to address outstanding questions on who should taper and how best to do it is still required,” she concluded.
The study received no outside funding. Lead author Dr. Tascilar disclosed lecture fees from Gilead and Union Chimique Belge; several coauthors disclosed relationships with multiple companies outside the current study. Dr. Hill had no financial conflicts to disclose.
FROM LANCET RHEUMATOLOGY
Atypical Presentation of Pityriasis Rubra Pilaris: Challenges in Diagnosis and Management
To the Editor:
Pityriasis rubra pilaris (PRP) is a rare inflammatory dermatosis of unknown etiology characterized by erythematosquamous salmon-colored plaques with well-demarcated islands of unaffected skin and hyperkeratotic follicles.1 In the United States, an incidence of 1 in 3500to 5000 patients presenting to dermatology clinics has been reported.2 Pityriasis rubra pilaris has several subtypes and variability in presentation that can make accurate and timely diagnosis challenging.3-5 Herein, we present a case of PRP with complex diagnostic and therapeutic challenges.
A 22-year-old woman presented with symmetrical, well-demarcated, hyperkeratotic, erythematous plaques with a carnauba wax–like appearance on the palms (Figure 1), soles, elbows, and trunk covering approximately 5% of the body surface area. Two weeks prior to presentation, she experienced an upper respiratory tract infection without any treatment and subsequently developed redness on the palms, which became very hard and scaly. The redness then spread to the elbows, soles, and trunk. She reported itching as well as pain in areas of fissuring. Hand mobility became restricted due to thick scale.
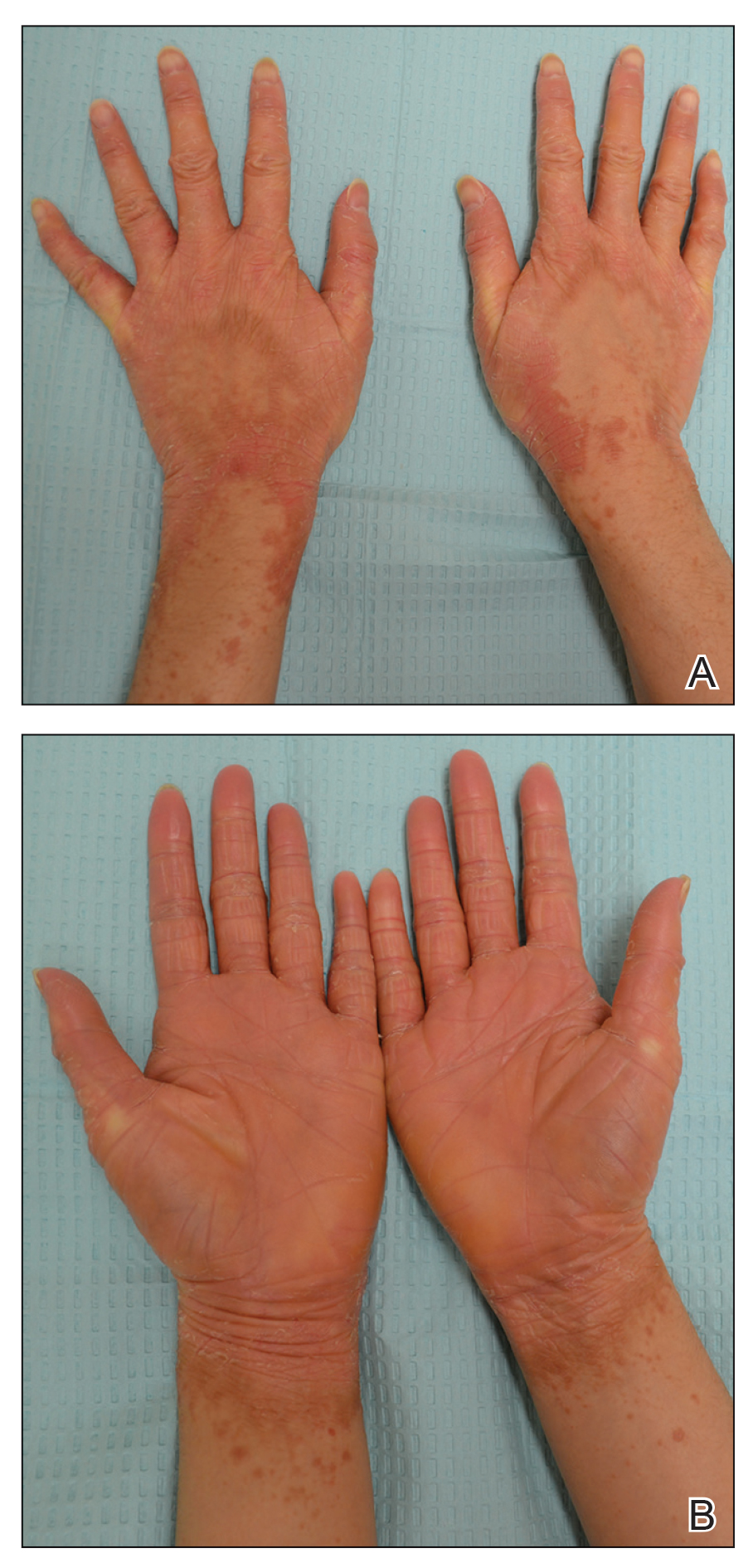
The patient’s medical history was notable for suspected psoriasis 9 years prior, but there were no records or biopsy reports that could be obtained to confirm the diagnosis. She also reported a similar skin condition in her father, which also was diagnosed as psoriasis, but this diagnosis could not be verified.
Although the morphology of the lesions was most consistent with localized PRP, atypical psoriasis, palmoplantar keratoderma (PPK), and erythroderma progressive symmetrica (EPS) also were considered given the personal and family history of suspected psoriasis. A biopsy could not be obtained due to an insurance issue. She was started on clobetasol cream 0.05% and ointment. At 2-week follow-up, her condition remained unchanged. Empiric systemic treatment was discussed, which would potentially work for diagnoses of both PRP and psoriasis. Due to the history of psoriasis and level of discomfort, cyclosporine 300 mg once daily was started to gain rapid control of the disease. Methotrexate also was considered due to its efficacy and economic considerations but was not selected due to patient concerns about the medication.
After 10 weeks of cyclosporine treatment, our patient showed some improvement of the skin with decreased scale and flattening of plaques but not complete resolution. At this point, a biopsy was able to be obtained with prior authorization. A 4-mm punch biopsy of the right flank demonstrated a psoriasiform and papillated epidermis with multifocally capped, compact parakeratosis and minimal lymphocytic infiltrate consistent with PRP. Although EPS also was on the histologic differential, clinical history was more consistent with a diagnosis of PRP. There was some minimal improvement with cyclosporine, but with the diagnosis of PRP confirmed, a systemic retinoid became the treatment of choice. Although acitretin is the preferred treatment for PRP, given that pregnancy would be contraindicated during and for 3 years following acitretin therapy, a trial of isotretinoin 40 mg once daily was started due to its shorter half-life compared to acitretin and was continued for 3 months (Figure 2).6,7
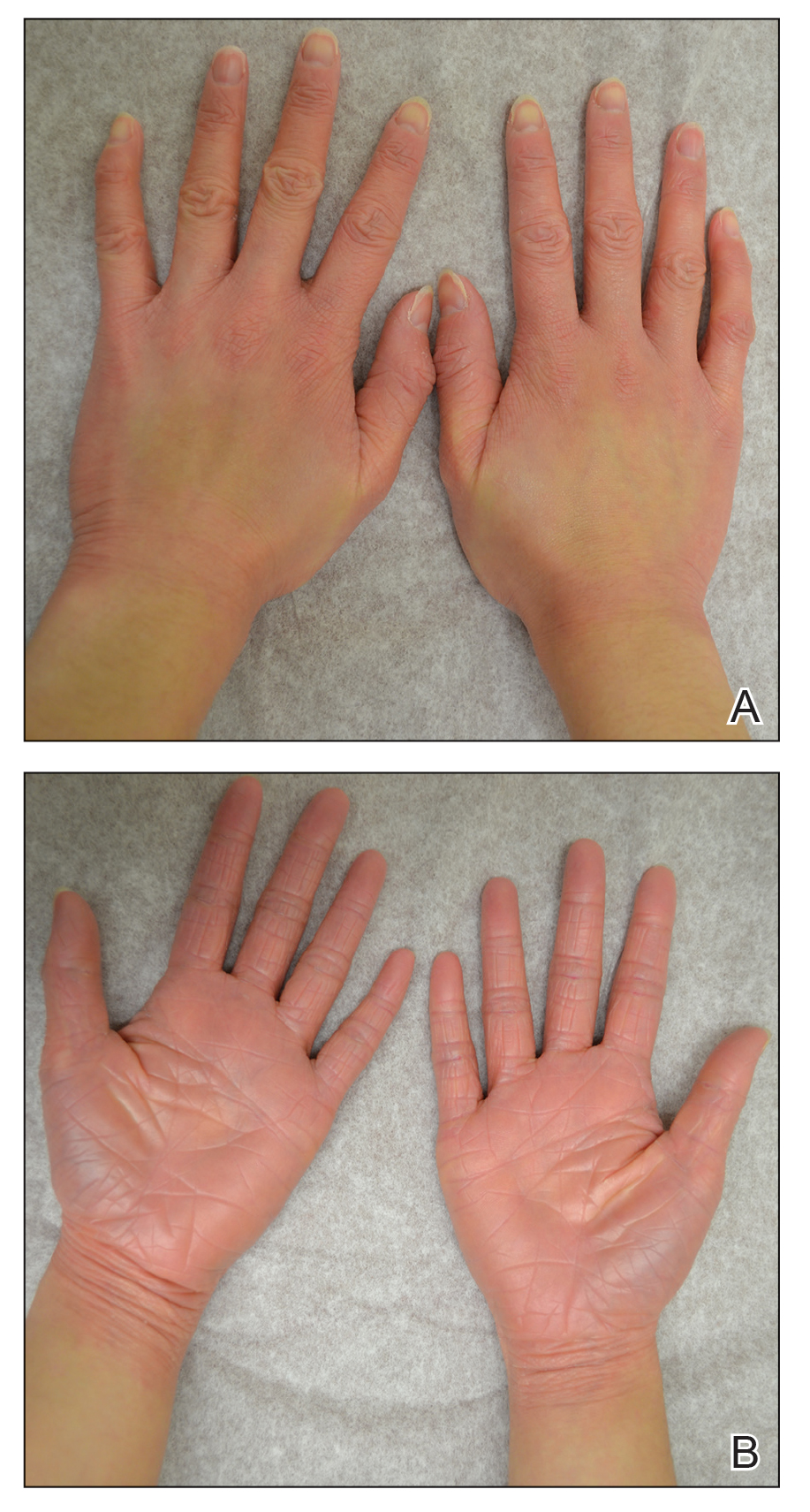
The diagnosis of PRP often can be challenging given the variety of clinical presentations. This case was an atypical presentation of PRP with several learning points, as our patient’s condition did not fit perfectly into any of the 6 types of PRP. The age of onset was atypical at 22 years old. Pityriasis rubra pilaris typically presents with a bimodal age distribution, appearing either in the first decade or the fifth to sixth decades of life.3,8 Her clinical presentation was atypical for adult-onset types I and II, which typically present with cephalocaudal progression or ichthyosiform dermatitis, respectively. Her presentation also was atypical for juvenile onset in types III, IV, and V, which tend to present in younger children and with different physical examination findings.3,8
The morphology of our patient’s lesions also was atypical for PRP, PPK, EPS, and psoriasis. The clinical presentation had features of these entities with erythema, fissuring, xerosis, carnauba wax–like appearance, symmetric scale, and well-demarcated plaques. Although these findings are not mutually exclusive, their combined presentation is atypical. Coupled with the ambiguous family history of similar skin disease in the patient’s father, the discussion of genodermatoses, particularly PPK, further confounded the diagnosis.4,9 When evaluating for PRP, especially with any family history of skin conditions, genodermatoses should be considered. Furthermore, our patient’s remote and unverifiable history of psoriasis serves as a cautionary reminder that prior diagnoses and medical history always should be reasonably scrutinized. Additionally, a drug-induced PRP eruption also should be considered. Although our patient received no medical treatment for the upper respiratory tract infection prior to the onset of PRP, there have been several reports of drug-induced PRP.10-12
The therapeutic challenge in this case is one that often is encountered in clinical practice. The health care system often may pose a barrier to diagnosis by inhibiting particular services required for adequate patient care. For our patient, diagnosis was delayed by several weeks due to difficulties obtaining a diagnostic skin biopsy. When faced with challenges from health care infrastructure, creativity with treatment options, such as finding an empiric treatment option (cyclosporine in this case), must be considered.
Systemic retinoids have been found to be efficacious treatment options for PRP, but when dealing with a woman of reproductive age, reproductive preferences must be discussed before identifying an appropriate treatment regimen.1,13-15 The half-life of acitretin compared to isotretinoin is 2 days vs 22 hours.6,16 With alcohol consumption, acitretin can be metabolized to etretinate, which has a half-life of 120 days.17 In our patient, isotretinoin was a more manageable option to allow for greater reproductive freedom upon treatment completion.
- Klein A, Landthaler M, Karrer S. Pityriasis rubra pilaris: a review of diagnosis and treatment. Am J Clin Dermatol. 2010;11:157-170.
- Shenefelt PD. Pityriasis rubra pilaris. Medscape website. Updated September 11, 2020. Accessed September 28, 2021. https://reference.medscape.com/article/1107742-overview
- Griffiths WA. Pityriasis rubra pilaris. Clin Exp Dermatol. 1980;5:105-112.
- Itin PH, Lautenschlager S. Palmoplantar keratoderma and associated syndromes. Semin Dermatol. 1995;14:152-161.
- Guidelines of care for psoriasis. Committee on Guidelines of Care. Task Force on Psoriasis. J Am Acad Dermatol. 1993;28:632-637.
- Larsen FG, Jakobsen P, Eriksen H, et al. The pharmacokinetics of acitretin and its 13-cis-metabolite in psoriatic patients. J Clin Pharmacol. 1991;31:477-483.
- Layton A. The use of isotretinoin in acne. Dermatoendocrinol. 2009;1:162-169.
- Sørensen KB, Thestrup-Pedersen K. Pityriasis rubra pilaris: a retrospective analysis of 43 patients. Acta Derm Venereol. 1999;79:405-406.
- Lucker GP, Van de Kerkhof PC, Steijlen PM. The hereditary palmoplantar keratoses: an updated review and classification. Br J Dermatol. 1994;131:1-14.
- Cutaneous reactions to labetalol. Br Med J. 1978;1:987.
- Plana A, Carrascosa JM, Vilavella M. Pityriasis rubra pilaris‐like reaction induced by imatinib. Clin Exp Dermatol. 2013;38:520-522.
- Gajinov ZT, Matc´ MB, Duran VD, et al. Drug-related pityriasis rubra pilaris with acantholysis. Vojnosanit Pregl. 2013;70:871-873.
- Clayton BD, Jorizzo JL, Hitchcock MG, et al. Adult pityriasis rubra pilaris: a 10-year case series. J Am Acad Dermatol. 1997;36:959-964.
- Cohen PR, Prystowsky JH. Pityriasis rubra pilaris: a review of diagnosis and treatment. J Am Acad Dermatol. 1989;20:801-807.
- Dicken CH. Isotretinoin treatment of pityriasis rubra pilaris. J Am Acad Dermatol. 1987;16(2 pt 1):297-301.
- Layton A. The use of isotretinoin in acne. Dermatoendocrinol. 2009;1:162-169.
- Grønhøj Larsen F, Steinkjer B, Jakobsen P, et al. Acitretin is converted to etretinate only during concomitant alcohol intake. Br J Dermatol. 2000;143:1164-1169.
To the Editor:
Pityriasis rubra pilaris (PRP) is a rare inflammatory dermatosis of unknown etiology characterized by erythematosquamous salmon-colored plaques with well-demarcated islands of unaffected skin and hyperkeratotic follicles.1 In the United States, an incidence of 1 in 3500to 5000 patients presenting to dermatology clinics has been reported.2 Pityriasis rubra pilaris has several subtypes and variability in presentation that can make accurate and timely diagnosis challenging.3-5 Herein, we present a case of PRP with complex diagnostic and therapeutic challenges.
A 22-year-old woman presented with symmetrical, well-demarcated, hyperkeratotic, erythematous plaques with a carnauba wax–like appearance on the palms (Figure 1), soles, elbows, and trunk covering approximately 5% of the body surface area. Two weeks prior to presentation, she experienced an upper respiratory tract infection without any treatment and subsequently developed redness on the palms, which became very hard and scaly. The redness then spread to the elbows, soles, and trunk. She reported itching as well as pain in areas of fissuring. Hand mobility became restricted due to thick scale.
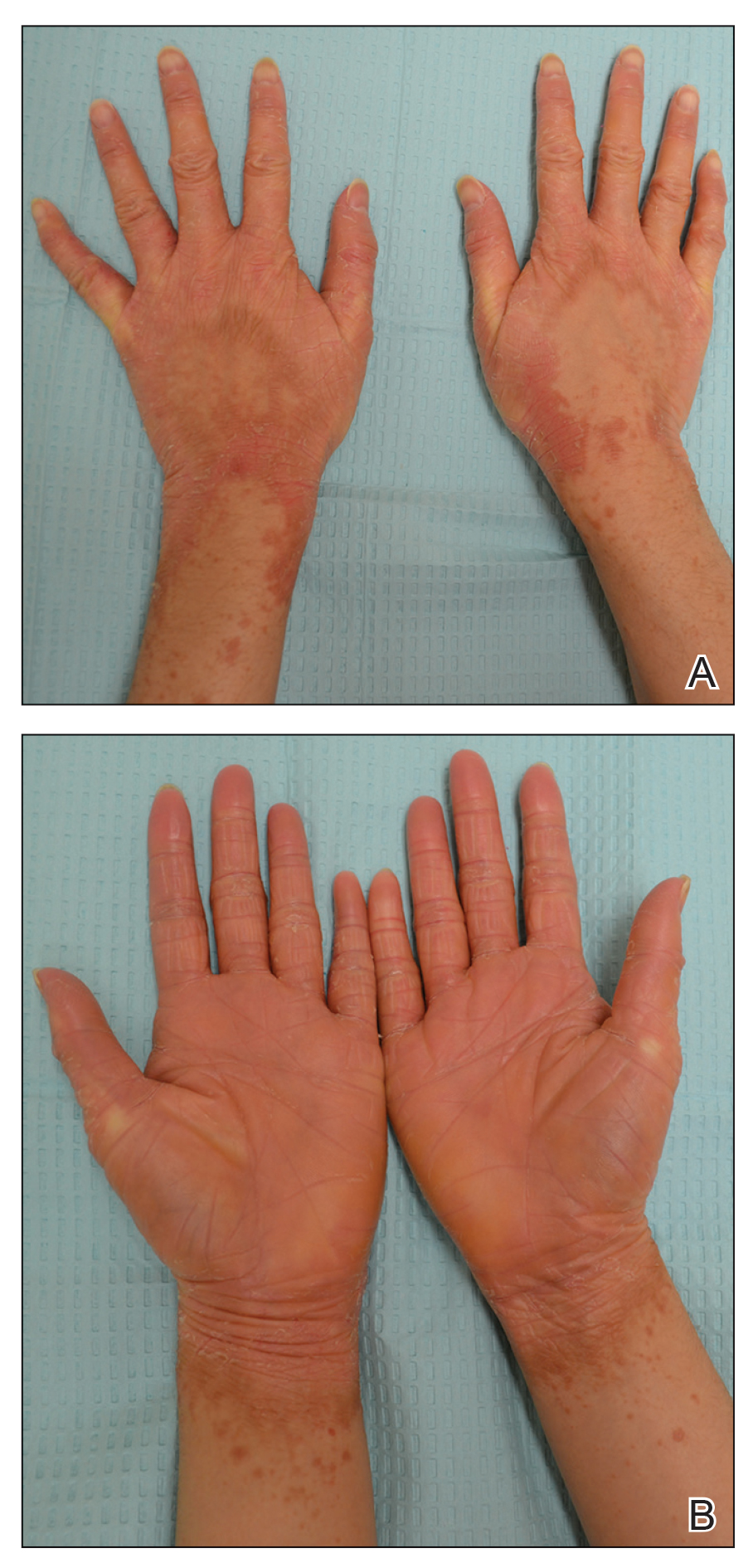
The patient’s medical history was notable for suspected psoriasis 9 years prior, but there were no records or biopsy reports that could be obtained to confirm the diagnosis. She also reported a similar skin condition in her father, which also was diagnosed as psoriasis, but this diagnosis could not be verified.
Although the morphology of the lesions was most consistent with localized PRP, atypical psoriasis, palmoplantar keratoderma (PPK), and erythroderma progressive symmetrica (EPS) also were considered given the personal and family history of suspected psoriasis. A biopsy could not be obtained due to an insurance issue. She was started on clobetasol cream 0.05% and ointment. At 2-week follow-up, her condition remained unchanged. Empiric systemic treatment was discussed, which would potentially work for diagnoses of both PRP and psoriasis. Due to the history of psoriasis and level of discomfort, cyclosporine 300 mg once daily was started to gain rapid control of the disease. Methotrexate also was considered due to its efficacy and economic considerations but was not selected due to patient concerns about the medication.
After 10 weeks of cyclosporine treatment, our patient showed some improvement of the skin with decreased scale and flattening of plaques but not complete resolution. At this point, a biopsy was able to be obtained with prior authorization. A 4-mm punch biopsy of the right flank demonstrated a psoriasiform and papillated epidermis with multifocally capped, compact parakeratosis and minimal lymphocytic infiltrate consistent with PRP. Although EPS also was on the histologic differential, clinical history was more consistent with a diagnosis of PRP. There was some minimal improvement with cyclosporine, but with the diagnosis of PRP confirmed, a systemic retinoid became the treatment of choice. Although acitretin is the preferred treatment for PRP, given that pregnancy would be contraindicated during and for 3 years following acitretin therapy, a trial of isotretinoin 40 mg once daily was started due to its shorter half-life compared to acitretin and was continued for 3 months (Figure 2).6,7
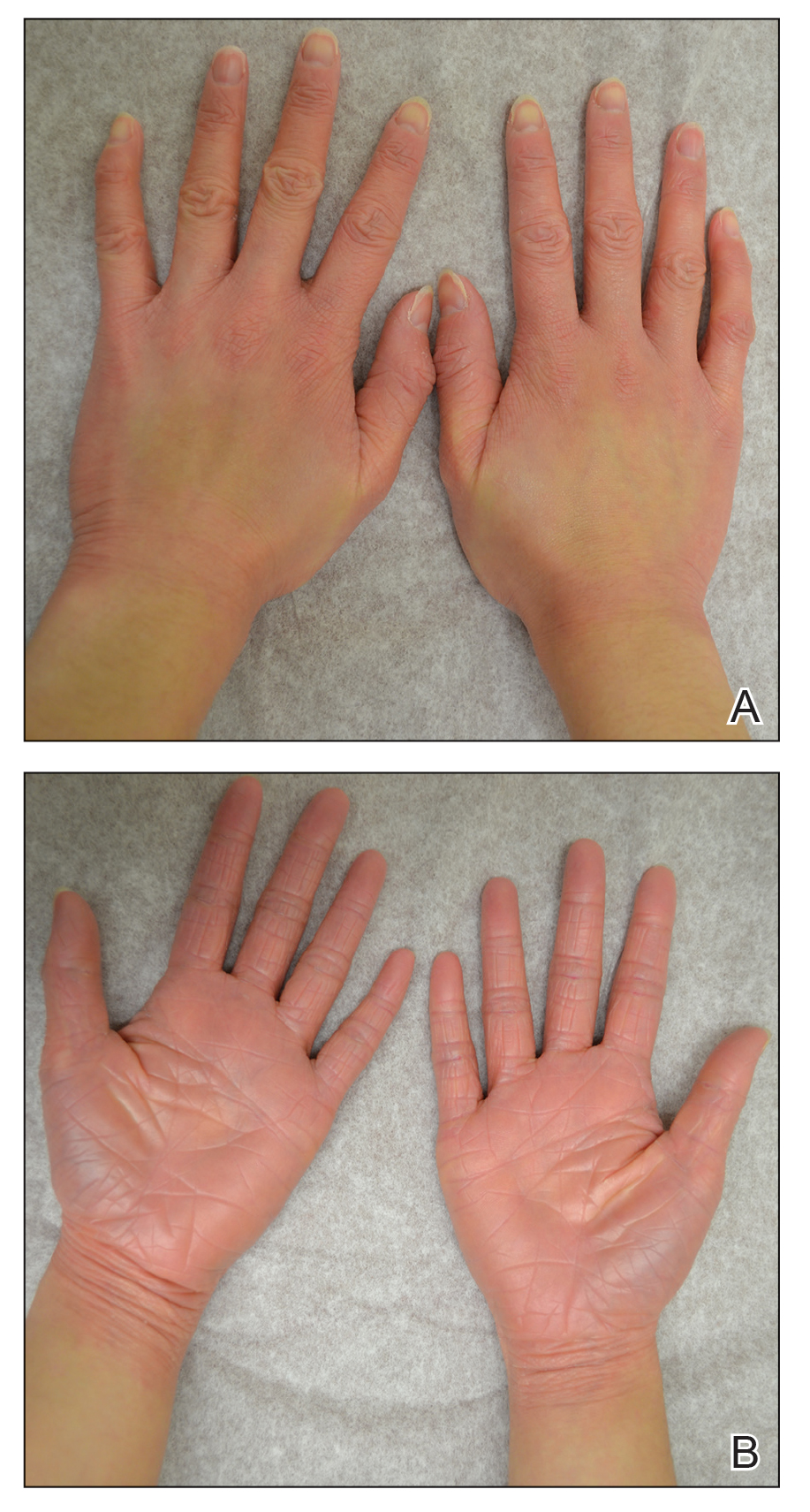
The diagnosis of PRP often can be challenging given the variety of clinical presentations. This case was an atypical presentation of PRP with several learning points, as our patient’s condition did not fit perfectly into any of the 6 types of PRP. The age of onset was atypical at 22 years old. Pityriasis rubra pilaris typically presents with a bimodal age distribution, appearing either in the first decade or the fifth to sixth decades of life.3,8 Her clinical presentation was atypical for adult-onset types I and II, which typically present with cephalocaudal progression or ichthyosiform dermatitis, respectively. Her presentation also was atypical for juvenile onset in types III, IV, and V, which tend to present in younger children and with different physical examination findings.3,8
The morphology of our patient’s lesions also was atypical for PRP, PPK, EPS, and psoriasis. The clinical presentation had features of these entities with erythema, fissuring, xerosis, carnauba wax–like appearance, symmetric scale, and well-demarcated plaques. Although these findings are not mutually exclusive, their combined presentation is atypical. Coupled with the ambiguous family history of similar skin disease in the patient’s father, the discussion of genodermatoses, particularly PPK, further confounded the diagnosis.4,9 When evaluating for PRP, especially with any family history of skin conditions, genodermatoses should be considered. Furthermore, our patient’s remote and unverifiable history of psoriasis serves as a cautionary reminder that prior diagnoses and medical history always should be reasonably scrutinized. Additionally, a drug-induced PRP eruption also should be considered. Although our patient received no medical treatment for the upper respiratory tract infection prior to the onset of PRP, there have been several reports of drug-induced PRP.10-12
The therapeutic challenge in this case is one that often is encountered in clinical practice. The health care system often may pose a barrier to diagnosis by inhibiting particular services required for adequate patient care. For our patient, diagnosis was delayed by several weeks due to difficulties obtaining a diagnostic skin biopsy. When faced with challenges from health care infrastructure, creativity with treatment options, such as finding an empiric treatment option (cyclosporine in this case), must be considered.
Systemic retinoids have been found to be efficacious treatment options for PRP, but when dealing with a woman of reproductive age, reproductive preferences must be discussed before identifying an appropriate treatment regimen.1,13-15 The half-life of acitretin compared to isotretinoin is 2 days vs 22 hours.6,16 With alcohol consumption, acitretin can be metabolized to etretinate, which has a half-life of 120 days.17 In our patient, isotretinoin was a more manageable option to allow for greater reproductive freedom upon treatment completion.
To the Editor:
Pityriasis rubra pilaris (PRP) is a rare inflammatory dermatosis of unknown etiology characterized by erythematosquamous salmon-colored plaques with well-demarcated islands of unaffected skin and hyperkeratotic follicles.1 In the United States, an incidence of 1 in 3500to 5000 patients presenting to dermatology clinics has been reported.2 Pityriasis rubra pilaris has several subtypes and variability in presentation that can make accurate and timely diagnosis challenging.3-5 Herein, we present a case of PRP with complex diagnostic and therapeutic challenges.
A 22-year-old woman presented with symmetrical, well-demarcated, hyperkeratotic, erythematous plaques with a carnauba wax–like appearance on the palms (Figure 1), soles, elbows, and trunk covering approximately 5% of the body surface area. Two weeks prior to presentation, she experienced an upper respiratory tract infection without any treatment and subsequently developed redness on the palms, which became very hard and scaly. The redness then spread to the elbows, soles, and trunk. She reported itching as well as pain in areas of fissuring. Hand mobility became restricted due to thick scale.
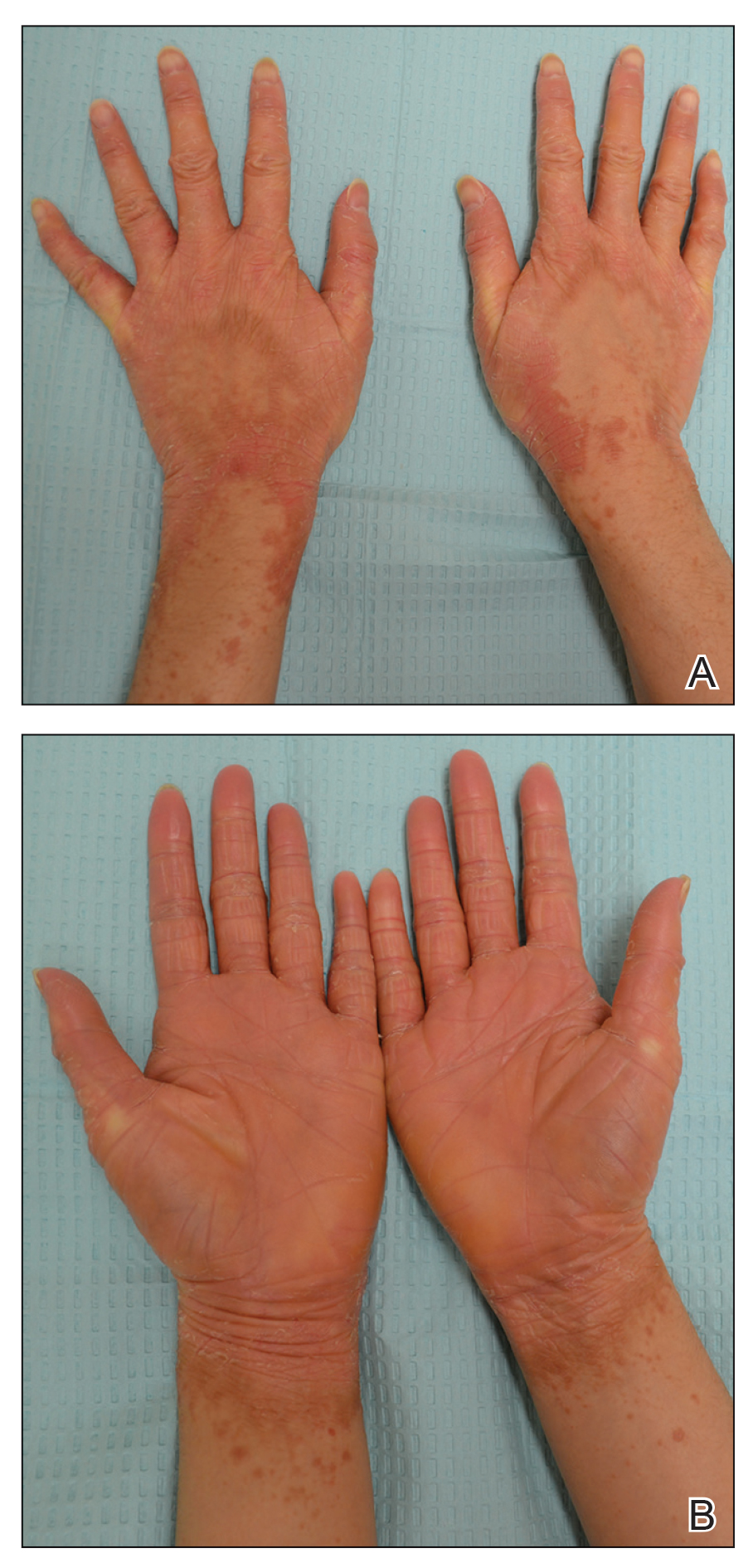
The patient’s medical history was notable for suspected psoriasis 9 years prior, but there were no records or biopsy reports that could be obtained to confirm the diagnosis. She also reported a similar skin condition in her father, which also was diagnosed as psoriasis, but this diagnosis could not be verified.
Although the morphology of the lesions was most consistent with localized PRP, atypical psoriasis, palmoplantar keratoderma (PPK), and erythroderma progressive symmetrica (EPS) also were considered given the personal and family history of suspected psoriasis. A biopsy could not be obtained due to an insurance issue. She was started on clobetasol cream 0.05% and ointment. At 2-week follow-up, her condition remained unchanged. Empiric systemic treatment was discussed, which would potentially work for diagnoses of both PRP and psoriasis. Due to the history of psoriasis and level of discomfort, cyclosporine 300 mg once daily was started to gain rapid control of the disease. Methotrexate also was considered due to its efficacy and economic considerations but was not selected due to patient concerns about the medication.
After 10 weeks of cyclosporine treatment, our patient showed some improvement of the skin with decreased scale and flattening of plaques but not complete resolution. At this point, a biopsy was able to be obtained with prior authorization. A 4-mm punch biopsy of the right flank demonstrated a psoriasiform and papillated epidermis with multifocally capped, compact parakeratosis and minimal lymphocytic infiltrate consistent with PRP. Although EPS also was on the histologic differential, clinical history was more consistent with a diagnosis of PRP. There was some minimal improvement with cyclosporine, but with the diagnosis of PRP confirmed, a systemic retinoid became the treatment of choice. Although acitretin is the preferred treatment for PRP, given that pregnancy would be contraindicated during and for 3 years following acitretin therapy, a trial of isotretinoin 40 mg once daily was started due to its shorter half-life compared to acitretin and was continued for 3 months (Figure 2).6,7
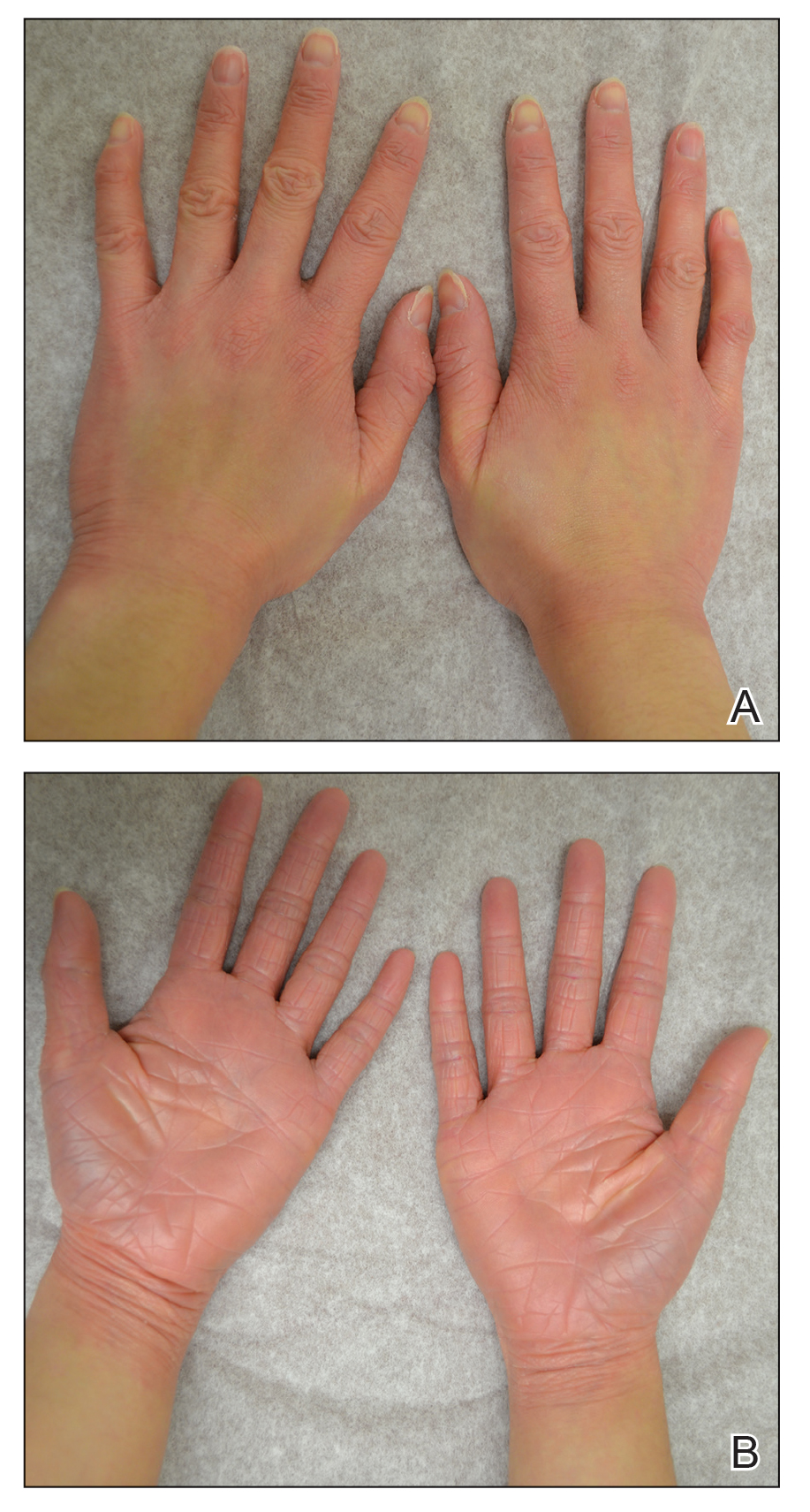
The diagnosis of PRP often can be challenging given the variety of clinical presentations. This case was an atypical presentation of PRP with several learning points, as our patient’s condition did not fit perfectly into any of the 6 types of PRP. The age of onset was atypical at 22 years old. Pityriasis rubra pilaris typically presents with a bimodal age distribution, appearing either in the first decade or the fifth to sixth decades of life.3,8 Her clinical presentation was atypical for adult-onset types I and II, which typically present with cephalocaudal progression or ichthyosiform dermatitis, respectively. Her presentation also was atypical for juvenile onset in types III, IV, and V, which tend to present in younger children and with different physical examination findings.3,8
The morphology of our patient’s lesions also was atypical for PRP, PPK, EPS, and psoriasis. The clinical presentation had features of these entities with erythema, fissuring, xerosis, carnauba wax–like appearance, symmetric scale, and well-demarcated plaques. Although these findings are not mutually exclusive, their combined presentation is atypical. Coupled with the ambiguous family history of similar skin disease in the patient’s father, the discussion of genodermatoses, particularly PPK, further confounded the diagnosis.4,9 When evaluating for PRP, especially with any family history of skin conditions, genodermatoses should be considered. Furthermore, our patient’s remote and unverifiable history of psoriasis serves as a cautionary reminder that prior diagnoses and medical history always should be reasonably scrutinized. Additionally, a drug-induced PRP eruption also should be considered. Although our patient received no medical treatment for the upper respiratory tract infection prior to the onset of PRP, there have been several reports of drug-induced PRP.10-12
The therapeutic challenge in this case is one that often is encountered in clinical practice. The health care system often may pose a barrier to diagnosis by inhibiting particular services required for adequate patient care. For our patient, diagnosis was delayed by several weeks due to difficulties obtaining a diagnostic skin biopsy. When faced with challenges from health care infrastructure, creativity with treatment options, such as finding an empiric treatment option (cyclosporine in this case), must be considered.
Systemic retinoids have been found to be efficacious treatment options for PRP, but when dealing with a woman of reproductive age, reproductive preferences must be discussed before identifying an appropriate treatment regimen.1,13-15 The half-life of acitretin compared to isotretinoin is 2 days vs 22 hours.6,16 With alcohol consumption, acitretin can be metabolized to etretinate, which has a half-life of 120 days.17 In our patient, isotretinoin was a more manageable option to allow for greater reproductive freedom upon treatment completion.
- Klein A, Landthaler M, Karrer S. Pityriasis rubra pilaris: a review of diagnosis and treatment. Am J Clin Dermatol. 2010;11:157-170.
- Shenefelt PD. Pityriasis rubra pilaris. Medscape website. Updated September 11, 2020. Accessed September 28, 2021. https://reference.medscape.com/article/1107742-overview
- Griffiths WA. Pityriasis rubra pilaris. Clin Exp Dermatol. 1980;5:105-112.
- Itin PH, Lautenschlager S. Palmoplantar keratoderma and associated syndromes. Semin Dermatol. 1995;14:152-161.
- Guidelines of care for psoriasis. Committee on Guidelines of Care. Task Force on Psoriasis. J Am Acad Dermatol. 1993;28:632-637.
- Larsen FG, Jakobsen P, Eriksen H, et al. The pharmacokinetics of acitretin and its 13-cis-metabolite in psoriatic patients. J Clin Pharmacol. 1991;31:477-483.
- Layton A. The use of isotretinoin in acne. Dermatoendocrinol. 2009;1:162-169.
- Sørensen KB, Thestrup-Pedersen K. Pityriasis rubra pilaris: a retrospective analysis of 43 patients. Acta Derm Venereol. 1999;79:405-406.
- Lucker GP, Van de Kerkhof PC, Steijlen PM. The hereditary palmoplantar keratoses: an updated review and classification. Br J Dermatol. 1994;131:1-14.
- Cutaneous reactions to labetalol. Br Med J. 1978;1:987.
- Plana A, Carrascosa JM, Vilavella M. Pityriasis rubra pilaris‐like reaction induced by imatinib. Clin Exp Dermatol. 2013;38:520-522.
- Gajinov ZT, Matc´ MB, Duran VD, et al. Drug-related pityriasis rubra pilaris with acantholysis. Vojnosanit Pregl. 2013;70:871-873.
- Clayton BD, Jorizzo JL, Hitchcock MG, et al. Adult pityriasis rubra pilaris: a 10-year case series. J Am Acad Dermatol. 1997;36:959-964.
- Cohen PR, Prystowsky JH. Pityriasis rubra pilaris: a review of diagnosis and treatment. J Am Acad Dermatol. 1989;20:801-807.
- Dicken CH. Isotretinoin treatment of pityriasis rubra pilaris. J Am Acad Dermatol. 1987;16(2 pt 1):297-301.
- Layton A. The use of isotretinoin in acne. Dermatoendocrinol. 2009;1:162-169.
- Grønhøj Larsen F, Steinkjer B, Jakobsen P, et al. Acitretin is converted to etretinate only during concomitant alcohol intake. Br J Dermatol. 2000;143:1164-1169.
- Klein A, Landthaler M, Karrer S. Pityriasis rubra pilaris: a review of diagnosis and treatment. Am J Clin Dermatol. 2010;11:157-170.
- Shenefelt PD. Pityriasis rubra pilaris. Medscape website. Updated September 11, 2020. Accessed September 28, 2021. https://reference.medscape.com/article/1107742-overview
- Griffiths WA. Pityriasis rubra pilaris. Clin Exp Dermatol. 1980;5:105-112.
- Itin PH, Lautenschlager S. Palmoplantar keratoderma and associated syndromes. Semin Dermatol. 1995;14:152-161.
- Guidelines of care for psoriasis. Committee on Guidelines of Care. Task Force on Psoriasis. J Am Acad Dermatol. 1993;28:632-637.
- Larsen FG, Jakobsen P, Eriksen H, et al. The pharmacokinetics of acitretin and its 13-cis-metabolite in psoriatic patients. J Clin Pharmacol. 1991;31:477-483.
- Layton A. The use of isotretinoin in acne. Dermatoendocrinol. 2009;1:162-169.
- Sørensen KB, Thestrup-Pedersen K. Pityriasis rubra pilaris: a retrospective analysis of 43 patients. Acta Derm Venereol. 1999;79:405-406.
- Lucker GP, Van de Kerkhof PC, Steijlen PM. The hereditary palmoplantar keratoses: an updated review and classification. Br J Dermatol. 1994;131:1-14.
- Cutaneous reactions to labetalol. Br Med J. 1978;1:987.
- Plana A, Carrascosa JM, Vilavella M. Pityriasis rubra pilaris‐like reaction induced by imatinib. Clin Exp Dermatol. 2013;38:520-522.
- Gajinov ZT, Matc´ MB, Duran VD, et al. Drug-related pityriasis rubra pilaris with acantholysis. Vojnosanit Pregl. 2013;70:871-873.
- Clayton BD, Jorizzo JL, Hitchcock MG, et al. Adult pityriasis rubra pilaris: a 10-year case series. J Am Acad Dermatol. 1997;36:959-964.
- Cohen PR, Prystowsky JH. Pityriasis rubra pilaris: a review of diagnosis and treatment. J Am Acad Dermatol. 1989;20:801-807.
- Dicken CH. Isotretinoin treatment of pityriasis rubra pilaris. J Am Acad Dermatol. 1987;16(2 pt 1):297-301.
- Layton A. The use of isotretinoin in acne. Dermatoendocrinol. 2009;1:162-169.
- Grønhøj Larsen F, Steinkjer B, Jakobsen P, et al. Acitretin is converted to etretinate only during concomitant alcohol intake. Br J Dermatol. 2000;143:1164-1169.
Practice Points
- Pityriasis rubra pilaris (PRP) is a rare inflammatory dermatosis of unknown etiology characterized by erythematosquamous salmon-colored plaques with well-demarcated islands of unaffected skin and hyperkeratotic follicles.
- The diagnosis of PRP often can be challenging given the variety of clinical presentations.
Why this round of COVID-19 feels worse
Exhaustion. Defeat. Hopelessness. Physicians, nurses, physician assistants, and nurse practitioners are overwhelmed with burnout.
The recent round of COVID-19 is more frustrating than the first, with scientific evidence supporting ways we can prevent disease and disease progression. The health care team is no longer viewed as heroes but as the enemy, fraudulently proposing a vaccine and painting a fictional story of death, though it’s all true. The daily educational battle with patients and family members creates a challenging environment that cultivates hopelessness.
Clinicians are physically exhausted from the numerous COVID cases. Gone are the medical patients we trained for, who either remain home and risk their health or lack access to medical providers because of excessive wait times. Empathy for COVID patients is being tested even more with this new surge, and without the two-way bond of trust, clinicians are running out of fuel. Anger and distrust regarding vaccination guidance dominate the interaction when patients present demanding urgent intervention, while clinicians know that more than 95% of hospitalized patients are unvaccinated.
The struggle to find the commitment to medicine and serving patients is made worse by the pandemic fog and loss of trust from patients. Every day, health care teams risk their personal well-being to provide medical care and intervention. Not by choice do we gown up, mask up, and glove up. Each time we enter a COVID patient’s room, we expose ourselves and risk our own lives and the lives of our families for the patients who have elected to ignore medical guidance.
This national wave of resistance to vaccination is spurring an exodus from health care. Physicians are retiring early and physician assistants and nurse practitioners are seeking non–patient-facing positions to improve their own wellness and balance. A national nursing shortage is impacting patients seeking care in every medical discipline. The underlying wave of exhaustion and frustration has not completely destroyed their empathy but has depleted their drive.
How can we regain this drive amid exhausting work hours and angry patients?
As much as we have heard it, we need to protect our time to recharge. The demand to pick up extra shifts and support our colleagues has affected our personal health. Setting boundaries and building time for exercise, meditation, and connecting with family is essential for survival. Mental health is key to retaining empathy and finding hope. Education is one path to reigniting the fires of critical thinking and commitment to patient care – consider precepting students to support the growth of health care teams. Memories of patient care before this pandemic give us the hope that there is light at the end of this tunnel.
Dr. Gadalla is a hospitalist at Treasure Coast Hospitalists in Port St. Lucie, Fla. She is a member of the Hospitalist’s editorial advisory board and also serves as a physician assistant program director at South University in West Palm Beach, Fla. She disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
Exhaustion. Defeat. Hopelessness. Physicians, nurses, physician assistants, and nurse practitioners are overwhelmed with burnout.
The recent round of COVID-19 is more frustrating than the first, with scientific evidence supporting ways we can prevent disease and disease progression. The health care team is no longer viewed as heroes but as the enemy, fraudulently proposing a vaccine and painting a fictional story of death, though it’s all true. The daily educational battle with patients and family members creates a challenging environment that cultivates hopelessness.
Clinicians are physically exhausted from the numerous COVID cases. Gone are the medical patients we trained for, who either remain home and risk their health or lack access to medical providers because of excessive wait times. Empathy for COVID patients is being tested even more with this new surge, and without the two-way bond of trust, clinicians are running out of fuel. Anger and distrust regarding vaccination guidance dominate the interaction when patients present demanding urgent intervention, while clinicians know that more than 95% of hospitalized patients are unvaccinated.
The struggle to find the commitment to medicine and serving patients is made worse by the pandemic fog and loss of trust from patients. Every day, health care teams risk their personal well-being to provide medical care and intervention. Not by choice do we gown up, mask up, and glove up. Each time we enter a COVID patient’s room, we expose ourselves and risk our own lives and the lives of our families for the patients who have elected to ignore medical guidance.
This national wave of resistance to vaccination is spurring an exodus from health care. Physicians are retiring early and physician assistants and nurse practitioners are seeking non–patient-facing positions to improve their own wellness and balance. A national nursing shortage is impacting patients seeking care in every medical discipline. The underlying wave of exhaustion and frustration has not completely destroyed their empathy but has depleted their drive.
How can we regain this drive amid exhausting work hours and angry patients?
As much as we have heard it, we need to protect our time to recharge. The demand to pick up extra shifts and support our colleagues has affected our personal health. Setting boundaries and building time for exercise, meditation, and connecting with family is essential for survival. Mental health is key to retaining empathy and finding hope. Education is one path to reigniting the fires of critical thinking and commitment to patient care – consider precepting students to support the growth of health care teams. Memories of patient care before this pandemic give us the hope that there is light at the end of this tunnel.
Dr. Gadalla is a hospitalist at Treasure Coast Hospitalists in Port St. Lucie, Fla. She is a member of the Hospitalist’s editorial advisory board and also serves as a physician assistant program director at South University in West Palm Beach, Fla. She disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
Exhaustion. Defeat. Hopelessness. Physicians, nurses, physician assistants, and nurse practitioners are overwhelmed with burnout.
The recent round of COVID-19 is more frustrating than the first, with scientific evidence supporting ways we can prevent disease and disease progression. The health care team is no longer viewed as heroes but as the enemy, fraudulently proposing a vaccine and painting a fictional story of death, though it’s all true. The daily educational battle with patients and family members creates a challenging environment that cultivates hopelessness.
Clinicians are physically exhausted from the numerous COVID cases. Gone are the medical patients we trained for, who either remain home and risk their health or lack access to medical providers because of excessive wait times. Empathy for COVID patients is being tested even more with this new surge, and without the two-way bond of trust, clinicians are running out of fuel. Anger and distrust regarding vaccination guidance dominate the interaction when patients present demanding urgent intervention, while clinicians know that more than 95% of hospitalized patients are unvaccinated.
The struggle to find the commitment to medicine and serving patients is made worse by the pandemic fog and loss of trust from patients. Every day, health care teams risk their personal well-being to provide medical care and intervention. Not by choice do we gown up, mask up, and glove up. Each time we enter a COVID patient’s room, we expose ourselves and risk our own lives and the lives of our families for the patients who have elected to ignore medical guidance.
This national wave of resistance to vaccination is spurring an exodus from health care. Physicians are retiring early and physician assistants and nurse practitioners are seeking non–patient-facing positions to improve their own wellness and balance. A national nursing shortage is impacting patients seeking care in every medical discipline. The underlying wave of exhaustion and frustration has not completely destroyed their empathy but has depleted their drive.
How can we regain this drive amid exhausting work hours and angry patients?
As much as we have heard it, we need to protect our time to recharge. The demand to pick up extra shifts and support our colleagues has affected our personal health. Setting boundaries and building time for exercise, meditation, and connecting with family is essential for survival. Mental health is key to retaining empathy and finding hope. Education is one path to reigniting the fires of critical thinking and commitment to patient care – consider precepting students to support the growth of health care teams. Memories of patient care before this pandemic give us the hope that there is light at the end of this tunnel.
Dr. Gadalla is a hospitalist at Treasure Coast Hospitalists in Port St. Lucie, Fla. She is a member of the Hospitalist’s editorial advisory board and also serves as a physician assistant program director at South University in West Palm Beach, Fla. She disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
Clinical Edge Journal Scan Commentary: CRC October 2021
Emerging data have helped to elucidate the real world experience of regorafenib vs trifluridine/tipiracil in the third-line setting. In a single-institution retrospective study, Patel and colleagues evaluated 126 patients who received trifluridine/tipiracil and 95 patients who received regorafenib. There were higher response and disease control rates seen with trifluridine/tipiracil, although median overall survival was similar (7.5 vs 7.1 months). These findings are limited by the single-institution, retrospective and non-randomized nature of the study. Also, the better-tolerated ReDOS dose-escalation schema for regorafenib was not utilized in this study, and it would be interesting to see how this novel dosing strategy compares to trifluridine/tipiracil in the real world setting.
Immunotherapy with anti-programmed death 1 (PD-1) or anti-programmed death ligand 1 (PD-L1) monoclonal antibodies has proven to be very effective in the rare group of patients with mCRC harboring deficiencies in mismatch repair, but has unfortunately largely fallen short for the vast majority of patients with mismatch repair proficient cancers. Martinelli et al. looked at adding avelumab, and anti-PD-L1 antibody, to cetuximab in an effort to rechallenge patients with RAS wild-type disease to anti-EGFR therapy in the single-arm phase 2 CAVE trial. 77 patients were treated and the median overall survival was an impressive 11.6 months, increasing to 17.3 months in patients with circulating tumor DNA (ctDNA) that was wild-type for both RAS and BRAF. This study suggests that rechallenging with anti-EGFR therapy can be effective in a ctDNA-selected population and that immunotherapy may have a role to play in this setting, although these findings would need to be confirmed in a larger, randomized phase 3 trial.
Finally, the COVID-19 pandemic has upended medical care, including oncology care. Thierry and co-workers evaluated the effect on the pandemic lockdown in France by looking at the baseline levels of ctDNA in 80 patients with newly diagnosed mCRC presenting pre-lockdown vs. post-lockdown. They showed that median ctDNA was much higher post-lockdown (119.2 vs 17.3 ng/mL), implying that delays in diagnosis related to the pandemic led to more advanced mCRC, at least in terms of ctDNA level. This study adds to the growing literature demonstrating that COVID-19 will continue to have effects on cancer care and cancer-related mortality for years to come.
Emerging data have helped to elucidate the real world experience of regorafenib vs trifluridine/tipiracil in the third-line setting. In a single-institution retrospective study, Patel and colleagues evaluated 126 patients who received trifluridine/tipiracil and 95 patients who received regorafenib. There were higher response and disease control rates seen with trifluridine/tipiracil, although median overall survival was similar (7.5 vs 7.1 months). These findings are limited by the single-institution, retrospective and non-randomized nature of the study. Also, the better-tolerated ReDOS dose-escalation schema for regorafenib was not utilized in this study, and it would be interesting to see how this novel dosing strategy compares to trifluridine/tipiracil in the real world setting.
Immunotherapy with anti-programmed death 1 (PD-1) or anti-programmed death ligand 1 (PD-L1) monoclonal antibodies has proven to be very effective in the rare group of patients with mCRC harboring deficiencies in mismatch repair, but has unfortunately largely fallen short for the vast majority of patients with mismatch repair proficient cancers. Martinelli et al. looked at adding avelumab, and anti-PD-L1 antibody, to cetuximab in an effort to rechallenge patients with RAS wild-type disease to anti-EGFR therapy in the single-arm phase 2 CAVE trial. 77 patients were treated and the median overall survival was an impressive 11.6 months, increasing to 17.3 months in patients with circulating tumor DNA (ctDNA) that was wild-type for both RAS and BRAF. This study suggests that rechallenging with anti-EGFR therapy can be effective in a ctDNA-selected population and that immunotherapy may have a role to play in this setting, although these findings would need to be confirmed in a larger, randomized phase 3 trial.
Finally, the COVID-19 pandemic has upended medical care, including oncology care. Thierry and co-workers evaluated the effect on the pandemic lockdown in France by looking at the baseline levels of ctDNA in 80 patients with newly diagnosed mCRC presenting pre-lockdown vs. post-lockdown. They showed that median ctDNA was much higher post-lockdown (119.2 vs 17.3 ng/mL), implying that delays in diagnosis related to the pandemic led to more advanced mCRC, at least in terms of ctDNA level. This study adds to the growing literature demonstrating that COVID-19 will continue to have effects on cancer care and cancer-related mortality for years to come.
Emerging data have helped to elucidate the real world experience of regorafenib vs trifluridine/tipiracil in the third-line setting. In a single-institution retrospective study, Patel and colleagues evaluated 126 patients who received trifluridine/tipiracil and 95 patients who received regorafenib. There were higher response and disease control rates seen with trifluridine/tipiracil, although median overall survival was similar (7.5 vs 7.1 months). These findings are limited by the single-institution, retrospective and non-randomized nature of the study. Also, the better-tolerated ReDOS dose-escalation schema for regorafenib was not utilized in this study, and it would be interesting to see how this novel dosing strategy compares to trifluridine/tipiracil in the real world setting.
Immunotherapy with anti-programmed death 1 (PD-1) or anti-programmed death ligand 1 (PD-L1) monoclonal antibodies has proven to be very effective in the rare group of patients with mCRC harboring deficiencies in mismatch repair, but has unfortunately largely fallen short for the vast majority of patients with mismatch repair proficient cancers. Martinelli et al. looked at adding avelumab, and anti-PD-L1 antibody, to cetuximab in an effort to rechallenge patients with RAS wild-type disease to anti-EGFR therapy in the single-arm phase 2 CAVE trial. 77 patients were treated and the median overall survival was an impressive 11.6 months, increasing to 17.3 months in patients with circulating tumor DNA (ctDNA) that was wild-type for both RAS and BRAF. This study suggests that rechallenging with anti-EGFR therapy can be effective in a ctDNA-selected population and that immunotherapy may have a role to play in this setting, although these findings would need to be confirmed in a larger, randomized phase 3 trial.
Finally, the COVID-19 pandemic has upended medical care, including oncology care. Thierry and co-workers evaluated the effect on the pandemic lockdown in France by looking at the baseline levels of ctDNA in 80 patients with newly diagnosed mCRC presenting pre-lockdown vs. post-lockdown. They showed that median ctDNA was much higher post-lockdown (119.2 vs 17.3 ng/mL), implying that delays in diagnosis related to the pandemic led to more advanced mCRC, at least in terms of ctDNA level. This study adds to the growing literature demonstrating that COVID-19 will continue to have effects on cancer care and cancer-related mortality for years to come.
A safer way to use Botox to treat challenging dystonia type?
, new research suggests.
Oromandibular dystonia causes an involuntary opening of the mouth, which can be disabling and disfiguring. Although injection of the lateral pterygoid muscle with botulinum toxin is the preferred treatment for oromandibular dystonia, a potential complication concerns the maxillary artery, which can run either lateral or medial to the lateral pterygoid muscle.
In a study of 200 Turkish patients, researchers documented significant variations between men and women in the anatomical location of the maxillary artery – and even found lateral versus medial differences on the left and right side in the same individual.
“The results showed that the maxillary artery runs lateral to the muscle in 67% of the Turkish patients,” Rezzak Yilmaz, MD, department of neurology, University of Ankara Medical School, Turkey, reported at the International Congress of Parkinson’s Disease and Movement Disorders.
Given this high rate, there is a high risk for injury “that may result in pain and hematoma” when using preauricular extraoral injections, Dr. Yilmaz and colleagues noted. Instead, they recommend an intraoral injection approach to the lateral pterygoid muscle. “However, this critical anatomical variation is still unrecognized by most clinicians performing [botulinum toxin] injections,” they wrote.
Significant gender differences
The maxillary artery is the largest branch of the external carotid artery.
In the current study, the researchers used magnetic resonance angiography to assess the relevant anatomy in a cohort of 200 individuals (mean age, 56.4 years; 64% women) without a history of facial trauma or movement disorders.
Results showed that the maxillary artery ran lateral to the lateral pterygoid muscle in 67% of the study population.
“This result was also more frequent in females compared with males. Also, there was a considerable variability between the left and the right side in 20% of the participants,” Dr. Yilmaz reported.
Statistically significant gender differences were found for the artery running lateral to the lateral pterygoid muscle on both sides (71.1% in women vs. 58.5% in men; P = .007) and for the artery running lateral to the lateral pterygoid muscle on just the left side (69.8% in women vs. 53.5% in men; P = .02).
In an email exchange, Dr. Yilmaz said if medical personnel are not trained to perform an intraoral approach, “imaging to visualize the path of the maxillary artery before an extraoral/transcutaneous injection can be recommended.”
“If the imaging reveals that the maxillary artery passes lateral to the muscle, then the patient needs to be referred to another center for an intraoral injection,” unless the clinician is trained for an intraoral approach, he added.
Useful education
Commenting on the study, Michele Tagliati, MD, director of the Movement Disorders Program at Cedars-Sinai Medical Center, Los Angeles, said the results were educational. “I didn’t know about all this variability. I was working under the assumption that the artery was medial,” said Dr. Tagliati, who was not involved with the research.
Among his large practice of about 2,000 patients, Dr. Tagliati estimated having five patients for whom he provides this type of injection – and has never encountered a problem with them.
“Maybe all my patients are medial, but now that I’m aware I’ll probably pay more attention,” Dr. Tagliati said. He does not currently perform magnetic resonance angiography before injecting them, “although maybe I should,” he said.
When asked if it is worth the time and expense to perform magnetic resonance angiography on every patient who comes in for lateral pterygoid muscle injections, Dr. Tagliati said that although he has done the injections without problems in his current patients, he may “start obtaining imaging studies to make sure that we’re not taking unnecessary risk” if the maxillary artery is lateral to the lateral pterygoid muscle in new patients.
If there is a risk, he’ll then consider talking with colleagues in oral or facial surgery. Dr. Tagliati added that the number of patients he sees with oromandibular dystonia is rather small, so this extra step would not add a lot of additional imaging.
Overall, Dr. Tagliati noted that the study outcome was significant enough to want to use it for professional education. “I can definitely tell you that I’m going to bring it to the attention of my Fellows. [Every year] I teach one or two Fellows to inject Botox,” he said.
There was no funding for the study. Dr. Yilmaz and Dr. Tagliati have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
Oromandibular dystonia causes an involuntary opening of the mouth, which can be disabling and disfiguring. Although injection of the lateral pterygoid muscle with botulinum toxin is the preferred treatment for oromandibular dystonia, a potential complication concerns the maxillary artery, which can run either lateral or medial to the lateral pterygoid muscle.
In a study of 200 Turkish patients, researchers documented significant variations between men and women in the anatomical location of the maxillary artery – and even found lateral versus medial differences on the left and right side in the same individual.
“The results showed that the maxillary artery runs lateral to the muscle in 67% of the Turkish patients,” Rezzak Yilmaz, MD, department of neurology, University of Ankara Medical School, Turkey, reported at the International Congress of Parkinson’s Disease and Movement Disorders.
Given this high rate, there is a high risk for injury “that may result in pain and hematoma” when using preauricular extraoral injections, Dr. Yilmaz and colleagues noted. Instead, they recommend an intraoral injection approach to the lateral pterygoid muscle. “However, this critical anatomical variation is still unrecognized by most clinicians performing [botulinum toxin] injections,” they wrote.
Significant gender differences
The maxillary artery is the largest branch of the external carotid artery.
In the current study, the researchers used magnetic resonance angiography to assess the relevant anatomy in a cohort of 200 individuals (mean age, 56.4 years; 64% women) without a history of facial trauma or movement disorders.
Results showed that the maxillary artery ran lateral to the lateral pterygoid muscle in 67% of the study population.
“This result was also more frequent in females compared with males. Also, there was a considerable variability between the left and the right side in 20% of the participants,” Dr. Yilmaz reported.
Statistically significant gender differences were found for the artery running lateral to the lateral pterygoid muscle on both sides (71.1% in women vs. 58.5% in men; P = .007) and for the artery running lateral to the lateral pterygoid muscle on just the left side (69.8% in women vs. 53.5% in men; P = .02).
In an email exchange, Dr. Yilmaz said if medical personnel are not trained to perform an intraoral approach, “imaging to visualize the path of the maxillary artery before an extraoral/transcutaneous injection can be recommended.”
“If the imaging reveals that the maxillary artery passes lateral to the muscle, then the patient needs to be referred to another center for an intraoral injection,” unless the clinician is trained for an intraoral approach, he added.
Useful education
Commenting on the study, Michele Tagliati, MD, director of the Movement Disorders Program at Cedars-Sinai Medical Center, Los Angeles, said the results were educational. “I didn’t know about all this variability. I was working under the assumption that the artery was medial,” said Dr. Tagliati, who was not involved with the research.
Among his large practice of about 2,000 patients, Dr. Tagliati estimated having five patients for whom he provides this type of injection – and has never encountered a problem with them.
“Maybe all my patients are medial, but now that I’m aware I’ll probably pay more attention,” Dr. Tagliati said. He does not currently perform magnetic resonance angiography before injecting them, “although maybe I should,” he said.
When asked if it is worth the time and expense to perform magnetic resonance angiography on every patient who comes in for lateral pterygoid muscle injections, Dr. Tagliati said that although he has done the injections without problems in his current patients, he may “start obtaining imaging studies to make sure that we’re not taking unnecessary risk” if the maxillary artery is lateral to the lateral pterygoid muscle in new patients.
If there is a risk, he’ll then consider talking with colleagues in oral or facial surgery. Dr. Tagliati added that the number of patients he sees with oromandibular dystonia is rather small, so this extra step would not add a lot of additional imaging.
Overall, Dr. Tagliati noted that the study outcome was significant enough to want to use it for professional education. “I can definitely tell you that I’m going to bring it to the attention of my Fellows. [Every year] I teach one or two Fellows to inject Botox,” he said.
There was no funding for the study. Dr. Yilmaz and Dr. Tagliati have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
Oromandibular dystonia causes an involuntary opening of the mouth, which can be disabling and disfiguring. Although injection of the lateral pterygoid muscle with botulinum toxin is the preferred treatment for oromandibular dystonia, a potential complication concerns the maxillary artery, which can run either lateral or medial to the lateral pterygoid muscle.
In a study of 200 Turkish patients, researchers documented significant variations between men and women in the anatomical location of the maxillary artery – and even found lateral versus medial differences on the left and right side in the same individual.
“The results showed that the maxillary artery runs lateral to the muscle in 67% of the Turkish patients,” Rezzak Yilmaz, MD, department of neurology, University of Ankara Medical School, Turkey, reported at the International Congress of Parkinson’s Disease and Movement Disorders.
Given this high rate, there is a high risk for injury “that may result in pain and hematoma” when using preauricular extraoral injections, Dr. Yilmaz and colleagues noted. Instead, they recommend an intraoral injection approach to the lateral pterygoid muscle. “However, this critical anatomical variation is still unrecognized by most clinicians performing [botulinum toxin] injections,” they wrote.
Significant gender differences
The maxillary artery is the largest branch of the external carotid artery.
In the current study, the researchers used magnetic resonance angiography to assess the relevant anatomy in a cohort of 200 individuals (mean age, 56.4 years; 64% women) without a history of facial trauma or movement disorders.
Results showed that the maxillary artery ran lateral to the lateral pterygoid muscle in 67% of the study population.
“This result was also more frequent in females compared with males. Also, there was a considerable variability between the left and the right side in 20% of the participants,” Dr. Yilmaz reported.
Statistically significant gender differences were found for the artery running lateral to the lateral pterygoid muscle on both sides (71.1% in women vs. 58.5% in men; P = .007) and for the artery running lateral to the lateral pterygoid muscle on just the left side (69.8% in women vs. 53.5% in men; P = .02).
In an email exchange, Dr. Yilmaz said if medical personnel are not trained to perform an intraoral approach, “imaging to visualize the path of the maxillary artery before an extraoral/transcutaneous injection can be recommended.”
“If the imaging reveals that the maxillary artery passes lateral to the muscle, then the patient needs to be referred to another center for an intraoral injection,” unless the clinician is trained for an intraoral approach, he added.
Useful education
Commenting on the study, Michele Tagliati, MD, director of the Movement Disorders Program at Cedars-Sinai Medical Center, Los Angeles, said the results were educational. “I didn’t know about all this variability. I was working under the assumption that the artery was medial,” said Dr. Tagliati, who was not involved with the research.
Among his large practice of about 2,000 patients, Dr. Tagliati estimated having five patients for whom he provides this type of injection – and has never encountered a problem with them.
“Maybe all my patients are medial, but now that I’m aware I’ll probably pay more attention,” Dr. Tagliati said. He does not currently perform magnetic resonance angiography before injecting them, “although maybe I should,” he said.
When asked if it is worth the time and expense to perform magnetic resonance angiography on every patient who comes in for lateral pterygoid muscle injections, Dr. Tagliati said that although he has done the injections without problems in his current patients, he may “start obtaining imaging studies to make sure that we’re not taking unnecessary risk” if the maxillary artery is lateral to the lateral pterygoid muscle in new patients.
If there is a risk, he’ll then consider talking with colleagues in oral or facial surgery. Dr. Tagliati added that the number of patients he sees with oromandibular dystonia is rather small, so this extra step would not add a lot of additional imaging.
Overall, Dr. Tagliati noted that the study outcome was significant enough to want to use it for professional education. “I can definitely tell you that I’m going to bring it to the attention of my Fellows. [Every year] I teach one or two Fellows to inject Botox,” he said.
There was no funding for the study. Dr. Yilmaz and Dr. Tagliati have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM MDS VIRTUAL CONGRESS 2021
Merck’s new COVID-19 pill: ‘Game changer’ or just one more tool?
Soon after Merck announced on Oct. 1 that it would ask federal regulators for emergency use authorization (EUA) for its auspicious new COVID-19 pill, the accolades began.
Former Food and Drug Administration chief Scott Gottlieb, MD, told CNBC the drug was “a profound game changer.” Top infectious disease expert Anthony S. Fauci, MD, called the early data “impressive.” The World Health Organization termed it “certainly good news,” while saying it awaits more data.
Merck, partnering with Ridgeback Biotherapeutics on the investigational oral antiviral medicine molnupiravir, plans to submit applications to regulatory agencies worldwide, hoping to deliver the first oral antiviral medication for COVID-19.
Interim clinical trial results show that the drug may slash the risk for hospitalization or death by 50% in those with mild to moderate COVID-19.
When the results were found to be so favorable, the study was halted at the recommendation of an independent data-monitoring committee and in consultation with the FDA.
“This anticipated drug has gotten a little more hype than it deserves,” said William Schaffner, MD, professor of preventive medicine and infectious disease specialist at Vanderbilt University Medical Center in Nashville, Tenn. He and others suggest a reality check.
“It’s not exactly a home run, like penicillin for strep throat,” agreed Carl Fichtenbaum, MD, professor of infectious diseases at the University of Cincinnati, who is investigating a similar pill for a rival company, Atea, partnering with Roche.
“But it is encouraging,” he said. “It will probably be an incremental improvement on what we have.” The fact that it can be taken at home is a plus: “Anything we can do to keep people from getting sicker is a good thing.”
“The data show in this higher risk group [those who were studied had at least one risk factor for severe COVID-19, such as age or a medical condition], it reduces the risk of advancing to severe disease by 50%,” Dr. Schaffner said. While that’s a clear benefit for half, it of course leaves the other half without benefit, he said.
Others critiqued the predicted cost of the drug. The U.S. government has already agreed to pay about $700 per patient, according to a new report from Harvard T. H. Chan School of Public Health, Boston, and King’s College Hospital, London. That analysis concluded that the actual cost of production for the 5-day course is $17.74.
“We fully expect that having an oral treatment that reduces the risk of hospitalizations will be significantly cost effective for society,” Melissa Moody, a Merck spokesperson, told this news organization. “We are optimistic that molnupiravir can become an important medicine as part of the global effort to fight the pandemic.”
Merck expects to produce 10 million courses of treatment by the end of the year, with additional doses expected to be produced in 2022, according to a company press release. Earlier in 2021, Merck finalized its agreement with the U.S. government to supply about 1.7 million courses of the drug at the $700 price, once an EUA or FDA approval is given.
Merck also has supply and purchase agreements with other governments worldwide, pending regulatory approval.
Study details
Details about the study findings came from a Merck press release. In the planned interim analysis, Merck and Ridgeback evaluated data from 775 patients initially enrolled in the phase 3 MOVe-OUT trial.
All adults had lab-confirmed mild to moderate COVID-19, and reported onset of symptoms within 5 days of being randomly assigned to the drug or placebo. All had at least one risk factor linked with poor disease outcome (such as older age or obesity).
The drug is a ribonucleoside and works by creating mutations in the virus’s genome, halting the ability of the virus to replicate.
Through day 29 of the study, the drug reduced the risk or hospitalization or death by about 50%. While 7.3% of those who received the drug either died or were hospitalized by day 29, 14.1% of those on placebo did, a statistically significant difference (P = .0012).
Side effects were similar in both groups, with 35% of the drug-treated and 40% of the placebo group reporting some side effect, Merck reported. Adverse drug-related events were 12% in the drug group and 11% in the placebo group. While 1.3% of the drug-treated group quit the study because of an adverse event, 3.4% of the placebo group quit.
Pros, cons, and unknowns
The ability to take the drug orally, and at home, is a definite plus, Dr. Schaffner said, compared with the monoclonal antibody treatment currently approved that must be given intravenously or subcutaneously and in certain locations.
More people could be reached and helped with the option of an at-home, oral medicine, he and others agreed.
The regimen for molnupiravir is four pills, two times daily, for 5 days, even if symptoms are mild. As with other prescription drugs, “there will always be folks who don’t comply completely” with the prescribed regimen, Dr. Schaffner said. With this pill, that might be especially true if the symptoms are very mild.
The 50% reduction is not as effective as the benefit often quoted for monoclonal antibody treatment. In clinical trials of Regeneron’s monoclonal antibody treatment, the regimen reduced COVID-19–related hospitalization or death in high-risk patients by 70%.
Even so, the new pill could change the pandemic’s course, others say. “I think molnupiravir has the potential to change how we take care of people who have COVID and risk factors for developing severe disease,” Rajesh Tim Gandhi, MD, an infectious disease physician at Massachusetts General Hospital and Harvard Medical School in Boston, told this news organization.
“What we’ll need to do, however, is make sure that people get tested quickly after they develop symptoms and, if they’re confirmed to have COVID, start on the pills within 5 days of developing symptoms,” he said, while warning that more data are needed about the drug and the trial results.
Another concern is that the promise of a pill will stall vaccination rates, with some people figuring why get vaccinated when they can obtain the pill if they do get sick.
Relying on treatment alone won’t work, Dr. Schaffner said. “Let’s [also] focus on prevention, which is the vaccine. We have to keep working both sides of the street.”
Dr. Gandhi added: “It’s important to remember that even though molnupiravir reduced the likelihood of hospitalization and death, a number of people who received the drug still got sick enough to end up in the hospital.”
Also unknown, he said, is how severe their disease was and whether they will develop long COVID.
The Merck study included only unvaccinated people. Might it work for those vaccinated people who get a breakthrough infection? “From a purely scientific perspective, there is no reason to believe molnupiravir would not work in people who are vaccinated, but the overall efficacy on top of the vaccine is likely dependent on how well they were able to mount a protective immune response to the vaccine,” Ms. Moody said. Still, Merck believes the pill could be of benefit for these infections too, she added.
As for the expected cost, Ms. Moody said that the company takes into account a number of factors in setting pricing, “but fundamentally we look at the impact of the disease, the benefits that the drug delivers to patients and to society, and at supporting ongoing drug development.”
On Merck’s heels: Pfizer, Roche, Atea
Pfizer is studying an antiviral pill, PF-07321332, a protease inhibitor that blocks the protease enzymes and halts replication of the virus.
In addition to studying the drug in infected patients at high risk of severe illness and in those at typical risk, Pfizer launched a phase 2-3 study in late September that will enroll people who live in the same household as a person with a confirmed, symptomatic COVID-19 infection to see if the drug can prevent disease in those who have been exposed.
Atea and Roche’s COVID pill, AT527, is in phase 3 trials as well. AT527 is an inhibitor of polymerase, an enzyme many viruses have, to stop replications. Atea is evaluating the drug to reduce disease “burden” and for both pre- and postexposure prevention.
Big picture: Role of COVID-19 pills
It may be necessary to target the coronavirus with more than one antiviral agent, said Dr. Fichtenbaum, a principal investigator for the AT527 trials.
“Sometimes viruses require two or three active agents to control their replication,” he said, citing information gleaned from other viral research, such as HIV. For control of HIV infection, a cocktail or combination of antivirals is often recommended.
That may well be the case for COVID-19, Dr. Fichtenbaum said. The goal would be to attack the virus at more than one pathway.
A version of this article first appeared on Medscape.com.
Soon after Merck announced on Oct. 1 that it would ask federal regulators for emergency use authorization (EUA) for its auspicious new COVID-19 pill, the accolades began.
Former Food and Drug Administration chief Scott Gottlieb, MD, told CNBC the drug was “a profound game changer.” Top infectious disease expert Anthony S. Fauci, MD, called the early data “impressive.” The World Health Organization termed it “certainly good news,” while saying it awaits more data.
Merck, partnering with Ridgeback Biotherapeutics on the investigational oral antiviral medicine molnupiravir, plans to submit applications to regulatory agencies worldwide, hoping to deliver the first oral antiviral medication for COVID-19.
Interim clinical trial results show that the drug may slash the risk for hospitalization or death by 50% in those with mild to moderate COVID-19.
When the results were found to be so favorable, the study was halted at the recommendation of an independent data-monitoring committee and in consultation with the FDA.
“This anticipated drug has gotten a little more hype than it deserves,” said William Schaffner, MD, professor of preventive medicine and infectious disease specialist at Vanderbilt University Medical Center in Nashville, Tenn. He and others suggest a reality check.
“It’s not exactly a home run, like penicillin for strep throat,” agreed Carl Fichtenbaum, MD, professor of infectious diseases at the University of Cincinnati, who is investigating a similar pill for a rival company, Atea, partnering with Roche.
“But it is encouraging,” he said. “It will probably be an incremental improvement on what we have.” The fact that it can be taken at home is a plus: “Anything we can do to keep people from getting sicker is a good thing.”
“The data show in this higher risk group [those who were studied had at least one risk factor for severe COVID-19, such as age or a medical condition], it reduces the risk of advancing to severe disease by 50%,” Dr. Schaffner said. While that’s a clear benefit for half, it of course leaves the other half without benefit, he said.
Others critiqued the predicted cost of the drug. The U.S. government has already agreed to pay about $700 per patient, according to a new report from Harvard T. H. Chan School of Public Health, Boston, and King’s College Hospital, London. That analysis concluded that the actual cost of production for the 5-day course is $17.74.
“We fully expect that having an oral treatment that reduces the risk of hospitalizations will be significantly cost effective for society,” Melissa Moody, a Merck spokesperson, told this news organization. “We are optimistic that molnupiravir can become an important medicine as part of the global effort to fight the pandemic.”
Merck expects to produce 10 million courses of treatment by the end of the year, with additional doses expected to be produced in 2022, according to a company press release. Earlier in 2021, Merck finalized its agreement with the U.S. government to supply about 1.7 million courses of the drug at the $700 price, once an EUA or FDA approval is given.
Merck also has supply and purchase agreements with other governments worldwide, pending regulatory approval.
Study details
Details about the study findings came from a Merck press release. In the planned interim analysis, Merck and Ridgeback evaluated data from 775 patients initially enrolled in the phase 3 MOVe-OUT trial.
All adults had lab-confirmed mild to moderate COVID-19, and reported onset of symptoms within 5 days of being randomly assigned to the drug or placebo. All had at least one risk factor linked with poor disease outcome (such as older age or obesity).
The drug is a ribonucleoside and works by creating mutations in the virus’s genome, halting the ability of the virus to replicate.
Through day 29 of the study, the drug reduced the risk or hospitalization or death by about 50%. While 7.3% of those who received the drug either died or were hospitalized by day 29, 14.1% of those on placebo did, a statistically significant difference (P = .0012).
Side effects were similar in both groups, with 35% of the drug-treated and 40% of the placebo group reporting some side effect, Merck reported. Adverse drug-related events were 12% in the drug group and 11% in the placebo group. While 1.3% of the drug-treated group quit the study because of an adverse event, 3.4% of the placebo group quit.
Pros, cons, and unknowns
The ability to take the drug orally, and at home, is a definite plus, Dr. Schaffner said, compared with the monoclonal antibody treatment currently approved that must be given intravenously or subcutaneously and in certain locations.
More people could be reached and helped with the option of an at-home, oral medicine, he and others agreed.
The regimen for molnupiravir is four pills, two times daily, for 5 days, even if symptoms are mild. As with other prescription drugs, “there will always be folks who don’t comply completely” with the prescribed regimen, Dr. Schaffner said. With this pill, that might be especially true if the symptoms are very mild.
The 50% reduction is not as effective as the benefit often quoted for monoclonal antibody treatment. In clinical trials of Regeneron’s monoclonal antibody treatment, the regimen reduced COVID-19–related hospitalization or death in high-risk patients by 70%.
Even so, the new pill could change the pandemic’s course, others say. “I think molnupiravir has the potential to change how we take care of people who have COVID and risk factors for developing severe disease,” Rajesh Tim Gandhi, MD, an infectious disease physician at Massachusetts General Hospital and Harvard Medical School in Boston, told this news organization.
“What we’ll need to do, however, is make sure that people get tested quickly after they develop symptoms and, if they’re confirmed to have COVID, start on the pills within 5 days of developing symptoms,” he said, while warning that more data are needed about the drug and the trial results.
Another concern is that the promise of a pill will stall vaccination rates, with some people figuring why get vaccinated when they can obtain the pill if they do get sick.
Relying on treatment alone won’t work, Dr. Schaffner said. “Let’s [also] focus on prevention, which is the vaccine. We have to keep working both sides of the street.”
Dr. Gandhi added: “It’s important to remember that even though molnupiravir reduced the likelihood of hospitalization and death, a number of people who received the drug still got sick enough to end up in the hospital.”
Also unknown, he said, is how severe their disease was and whether they will develop long COVID.
The Merck study included only unvaccinated people. Might it work for those vaccinated people who get a breakthrough infection? “From a purely scientific perspective, there is no reason to believe molnupiravir would not work in people who are vaccinated, but the overall efficacy on top of the vaccine is likely dependent on how well they were able to mount a protective immune response to the vaccine,” Ms. Moody said. Still, Merck believes the pill could be of benefit for these infections too, she added.
As for the expected cost, Ms. Moody said that the company takes into account a number of factors in setting pricing, “but fundamentally we look at the impact of the disease, the benefits that the drug delivers to patients and to society, and at supporting ongoing drug development.”
On Merck’s heels: Pfizer, Roche, Atea
Pfizer is studying an antiviral pill, PF-07321332, a protease inhibitor that blocks the protease enzymes and halts replication of the virus.
In addition to studying the drug in infected patients at high risk of severe illness and in those at typical risk, Pfizer launched a phase 2-3 study in late September that will enroll people who live in the same household as a person with a confirmed, symptomatic COVID-19 infection to see if the drug can prevent disease in those who have been exposed.
Atea and Roche’s COVID pill, AT527, is in phase 3 trials as well. AT527 is an inhibitor of polymerase, an enzyme many viruses have, to stop replications. Atea is evaluating the drug to reduce disease “burden” and for both pre- and postexposure prevention.
Big picture: Role of COVID-19 pills
It may be necessary to target the coronavirus with more than one antiviral agent, said Dr. Fichtenbaum, a principal investigator for the AT527 trials.
“Sometimes viruses require two or three active agents to control their replication,” he said, citing information gleaned from other viral research, such as HIV. For control of HIV infection, a cocktail or combination of antivirals is often recommended.
That may well be the case for COVID-19, Dr. Fichtenbaum said. The goal would be to attack the virus at more than one pathway.
A version of this article first appeared on Medscape.com.
Soon after Merck announced on Oct. 1 that it would ask federal regulators for emergency use authorization (EUA) for its auspicious new COVID-19 pill, the accolades began.
Former Food and Drug Administration chief Scott Gottlieb, MD, told CNBC the drug was “a profound game changer.” Top infectious disease expert Anthony S. Fauci, MD, called the early data “impressive.” The World Health Organization termed it “certainly good news,” while saying it awaits more data.
Merck, partnering with Ridgeback Biotherapeutics on the investigational oral antiviral medicine molnupiravir, plans to submit applications to regulatory agencies worldwide, hoping to deliver the first oral antiviral medication for COVID-19.
Interim clinical trial results show that the drug may slash the risk for hospitalization or death by 50% in those with mild to moderate COVID-19.
When the results were found to be so favorable, the study was halted at the recommendation of an independent data-monitoring committee and in consultation with the FDA.
“This anticipated drug has gotten a little more hype than it deserves,” said William Schaffner, MD, professor of preventive medicine and infectious disease specialist at Vanderbilt University Medical Center in Nashville, Tenn. He and others suggest a reality check.
“It’s not exactly a home run, like penicillin for strep throat,” agreed Carl Fichtenbaum, MD, professor of infectious diseases at the University of Cincinnati, who is investigating a similar pill for a rival company, Atea, partnering with Roche.
“But it is encouraging,” he said. “It will probably be an incremental improvement on what we have.” The fact that it can be taken at home is a plus: “Anything we can do to keep people from getting sicker is a good thing.”
“The data show in this higher risk group [those who were studied had at least one risk factor for severe COVID-19, such as age or a medical condition], it reduces the risk of advancing to severe disease by 50%,” Dr. Schaffner said. While that’s a clear benefit for half, it of course leaves the other half without benefit, he said.
Others critiqued the predicted cost of the drug. The U.S. government has already agreed to pay about $700 per patient, according to a new report from Harvard T. H. Chan School of Public Health, Boston, and King’s College Hospital, London. That analysis concluded that the actual cost of production for the 5-day course is $17.74.
“We fully expect that having an oral treatment that reduces the risk of hospitalizations will be significantly cost effective for society,” Melissa Moody, a Merck spokesperson, told this news organization. “We are optimistic that molnupiravir can become an important medicine as part of the global effort to fight the pandemic.”
Merck expects to produce 10 million courses of treatment by the end of the year, with additional doses expected to be produced in 2022, according to a company press release. Earlier in 2021, Merck finalized its agreement with the U.S. government to supply about 1.7 million courses of the drug at the $700 price, once an EUA or FDA approval is given.
Merck also has supply and purchase agreements with other governments worldwide, pending regulatory approval.
Study details
Details about the study findings came from a Merck press release. In the planned interim analysis, Merck and Ridgeback evaluated data from 775 patients initially enrolled in the phase 3 MOVe-OUT trial.
All adults had lab-confirmed mild to moderate COVID-19, and reported onset of symptoms within 5 days of being randomly assigned to the drug or placebo. All had at least one risk factor linked with poor disease outcome (such as older age or obesity).
The drug is a ribonucleoside and works by creating mutations in the virus’s genome, halting the ability of the virus to replicate.
Through day 29 of the study, the drug reduced the risk or hospitalization or death by about 50%. While 7.3% of those who received the drug either died or were hospitalized by day 29, 14.1% of those on placebo did, a statistically significant difference (P = .0012).
Side effects were similar in both groups, with 35% of the drug-treated and 40% of the placebo group reporting some side effect, Merck reported. Adverse drug-related events were 12% in the drug group and 11% in the placebo group. While 1.3% of the drug-treated group quit the study because of an adverse event, 3.4% of the placebo group quit.
Pros, cons, and unknowns
The ability to take the drug orally, and at home, is a definite plus, Dr. Schaffner said, compared with the monoclonal antibody treatment currently approved that must be given intravenously or subcutaneously and in certain locations.
More people could be reached and helped with the option of an at-home, oral medicine, he and others agreed.
The regimen for molnupiravir is four pills, two times daily, for 5 days, even if symptoms are mild. As with other prescription drugs, “there will always be folks who don’t comply completely” with the prescribed regimen, Dr. Schaffner said. With this pill, that might be especially true if the symptoms are very mild.
The 50% reduction is not as effective as the benefit often quoted for monoclonal antibody treatment. In clinical trials of Regeneron’s monoclonal antibody treatment, the regimen reduced COVID-19–related hospitalization or death in high-risk patients by 70%.
Even so, the new pill could change the pandemic’s course, others say. “I think molnupiravir has the potential to change how we take care of people who have COVID and risk factors for developing severe disease,” Rajesh Tim Gandhi, MD, an infectious disease physician at Massachusetts General Hospital and Harvard Medical School in Boston, told this news organization.
“What we’ll need to do, however, is make sure that people get tested quickly after they develop symptoms and, if they’re confirmed to have COVID, start on the pills within 5 days of developing symptoms,” he said, while warning that more data are needed about the drug and the trial results.
Another concern is that the promise of a pill will stall vaccination rates, with some people figuring why get vaccinated when they can obtain the pill if they do get sick.
Relying on treatment alone won’t work, Dr. Schaffner said. “Let’s [also] focus on prevention, which is the vaccine. We have to keep working both sides of the street.”
Dr. Gandhi added: “It’s important to remember that even though molnupiravir reduced the likelihood of hospitalization and death, a number of people who received the drug still got sick enough to end up in the hospital.”
Also unknown, he said, is how severe their disease was and whether they will develop long COVID.
The Merck study included only unvaccinated people. Might it work for those vaccinated people who get a breakthrough infection? “From a purely scientific perspective, there is no reason to believe molnupiravir would not work in people who are vaccinated, but the overall efficacy on top of the vaccine is likely dependent on how well they were able to mount a protective immune response to the vaccine,” Ms. Moody said. Still, Merck believes the pill could be of benefit for these infections too, she added.
As for the expected cost, Ms. Moody said that the company takes into account a number of factors in setting pricing, “but fundamentally we look at the impact of the disease, the benefits that the drug delivers to patients and to society, and at supporting ongoing drug development.”
On Merck’s heels: Pfizer, Roche, Atea
Pfizer is studying an antiviral pill, PF-07321332, a protease inhibitor that blocks the protease enzymes and halts replication of the virus.
In addition to studying the drug in infected patients at high risk of severe illness and in those at typical risk, Pfizer launched a phase 2-3 study in late September that will enroll people who live in the same household as a person with a confirmed, symptomatic COVID-19 infection to see if the drug can prevent disease in those who have been exposed.
Atea and Roche’s COVID pill, AT527, is in phase 3 trials as well. AT527 is an inhibitor of polymerase, an enzyme many viruses have, to stop replications. Atea is evaluating the drug to reduce disease “burden” and for both pre- and postexposure prevention.
Big picture: Role of COVID-19 pills
It may be necessary to target the coronavirus with more than one antiviral agent, said Dr. Fichtenbaum, a principal investigator for the AT527 trials.
“Sometimes viruses require two or three active agents to control their replication,” he said, citing information gleaned from other viral research, such as HIV. For control of HIV infection, a cocktail or combination of antivirals is often recommended.
That may well be the case for COVID-19, Dr. Fichtenbaum said. The goal would be to attack the virus at more than one pathway.
A version of this article first appeared on Medscape.com.