User login
AAP approves 2023 child and adolescent immunization schedule
The American Academy of Pediatrics said it supports the Recommended Childhood and Adolescent Immunization Schedule: United States, 2023.
In a policy statement published online in the journal Pediatrics, the AAP said the updated recommendations do not include major changes from those released in 2022 by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
In one small shift, COVID-19 is now addressed in the main text instead of being relegated to the notes section.
“And a new vaccine – Priorix [GlaxoSmithKline] – has been added for MMR [measles, mumps, rubella], so now there are two available,” Sean T. O’Leary, MD, MPH, chair of the AAP’s Committee on Infectious Diseases, told this news organization. “There’s also a second pneumococcal conjugate vaccine listed, PCV15, and this and PCV13 can essentially be used interchangeably.”
Minor updates to the schedule, reflected on the cover page, relate to vaccines for COVID-19, dengue fever, and pneumococcal disease, added Dr. O’Leary, a professor of pediatrics at the University of Colorado Anschutz Medical Campus and Children’s Hospital Colorado, Aurora.
The committee also changed layouts to improve the usability of the schedule. Updated annually, the guidance provides a table on recommended pediatric immunizations from birth to age 18 years, and catch-up recommendations for children aged 4 months to 18 years who start their vaccinations late or are more than 1 month behind the recommended age for vaccine administration.
“We hope this annual update will encourage clinicians to make sure all their patients are up to date on their routine vaccinations,” Dr. O’Leary said. “It’s an opportunity to develop strategies to improve vaccination rates.”
The 2023 schedule follows news from the CDC that kindergarten vaccination rates declined during the 2021-2022 school year. Only 93% of kindergarteners obtained full vaccinations, representing a drop of 1 percentage point from the year before and 2 percentage points from the 2019-2020 school year.
The dip in coverage has been attributed to disruptions caused by the COVID-19 pandemic. AAP advises health care professionals to urge families to make sure their child’s vaccines are current.
Among other additions:
In Table 1
- MMR: Second vaccine added (Priorix, GlaxoSmithKline Biologicals)
- Pneumococcal disease: second conjugate vaccine, PCV15, added (Vaxneuvance, Merck Sharp & Dohme).
- COVID-19: New row added.
- Dengue: Text changed from “Seropositive in endemic areas only” to “Seropositive in endemic dengue areas.”
- Inactivated polio vaccine: “See Notes” added to the column for children aged 18 years.
In Table 2
- PCV: Dose 3 to dose 4 interval revised to align with ACIP’s recommendation for dose 4. This dose is necessary only for children ages 12-59 months regardless of risk, or age 60-71 months with any risk who received three doses before age 12 months.
A parent-friendly vaccine schedule for children and adolescents is available on the CDC’s website.
“Vaccines are essential for the health of our whole society, including children and adolescents,” Dr. O’Leary said in a press release from AAP. “These schedules provide a road map [that] parents and pediatricians can follow to help children get the vaccines they need so their immune systems will be ready to recognize and resist diseases.”
As previously, the 2023 schedule was adjusted to ensure consistency between the formats of the childhood/adolescent and adult immunization guidance. A meeting of stakeholder organizations in October 2022 harmonized the two formats.
A version of this article first appeared on Medscape.com.
The American Academy of Pediatrics said it supports the Recommended Childhood and Adolescent Immunization Schedule: United States, 2023.
In a policy statement published online in the journal Pediatrics, the AAP said the updated recommendations do not include major changes from those released in 2022 by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
In one small shift, COVID-19 is now addressed in the main text instead of being relegated to the notes section.
“And a new vaccine – Priorix [GlaxoSmithKline] – has been added for MMR [measles, mumps, rubella], so now there are two available,” Sean T. O’Leary, MD, MPH, chair of the AAP’s Committee on Infectious Diseases, told this news organization. “There’s also a second pneumococcal conjugate vaccine listed, PCV15, and this and PCV13 can essentially be used interchangeably.”
Minor updates to the schedule, reflected on the cover page, relate to vaccines for COVID-19, dengue fever, and pneumococcal disease, added Dr. O’Leary, a professor of pediatrics at the University of Colorado Anschutz Medical Campus and Children’s Hospital Colorado, Aurora.
The committee also changed layouts to improve the usability of the schedule. Updated annually, the guidance provides a table on recommended pediatric immunizations from birth to age 18 years, and catch-up recommendations for children aged 4 months to 18 years who start their vaccinations late or are more than 1 month behind the recommended age for vaccine administration.
“We hope this annual update will encourage clinicians to make sure all their patients are up to date on their routine vaccinations,” Dr. O’Leary said. “It’s an opportunity to develop strategies to improve vaccination rates.”
The 2023 schedule follows news from the CDC that kindergarten vaccination rates declined during the 2021-2022 school year. Only 93% of kindergarteners obtained full vaccinations, representing a drop of 1 percentage point from the year before and 2 percentage points from the 2019-2020 school year.
The dip in coverage has been attributed to disruptions caused by the COVID-19 pandemic. AAP advises health care professionals to urge families to make sure their child’s vaccines are current.
Among other additions:
In Table 1
- MMR: Second vaccine added (Priorix, GlaxoSmithKline Biologicals)
- Pneumococcal disease: second conjugate vaccine, PCV15, added (Vaxneuvance, Merck Sharp & Dohme).
- COVID-19: New row added.
- Dengue: Text changed from “Seropositive in endemic areas only” to “Seropositive in endemic dengue areas.”
- Inactivated polio vaccine: “See Notes” added to the column for children aged 18 years.
In Table 2
- PCV: Dose 3 to dose 4 interval revised to align with ACIP’s recommendation for dose 4. This dose is necessary only for children ages 12-59 months regardless of risk, or age 60-71 months with any risk who received three doses before age 12 months.
A parent-friendly vaccine schedule for children and adolescents is available on the CDC’s website.
“Vaccines are essential for the health of our whole society, including children and adolescents,” Dr. O’Leary said in a press release from AAP. “These schedules provide a road map [that] parents and pediatricians can follow to help children get the vaccines they need so their immune systems will be ready to recognize and resist diseases.”
As previously, the 2023 schedule was adjusted to ensure consistency between the formats of the childhood/adolescent and adult immunization guidance. A meeting of stakeholder organizations in October 2022 harmonized the two formats.
A version of this article first appeared on Medscape.com.
The American Academy of Pediatrics said it supports the Recommended Childhood and Adolescent Immunization Schedule: United States, 2023.
In a policy statement published online in the journal Pediatrics, the AAP said the updated recommendations do not include major changes from those released in 2022 by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
In one small shift, COVID-19 is now addressed in the main text instead of being relegated to the notes section.
“And a new vaccine – Priorix [GlaxoSmithKline] – has been added for MMR [measles, mumps, rubella], so now there are two available,” Sean T. O’Leary, MD, MPH, chair of the AAP’s Committee on Infectious Diseases, told this news organization. “There’s also a second pneumococcal conjugate vaccine listed, PCV15, and this and PCV13 can essentially be used interchangeably.”
Minor updates to the schedule, reflected on the cover page, relate to vaccines for COVID-19, dengue fever, and pneumococcal disease, added Dr. O’Leary, a professor of pediatrics at the University of Colorado Anschutz Medical Campus and Children’s Hospital Colorado, Aurora.
The committee also changed layouts to improve the usability of the schedule. Updated annually, the guidance provides a table on recommended pediatric immunizations from birth to age 18 years, and catch-up recommendations for children aged 4 months to 18 years who start their vaccinations late or are more than 1 month behind the recommended age for vaccine administration.
“We hope this annual update will encourage clinicians to make sure all their patients are up to date on their routine vaccinations,” Dr. O’Leary said. “It’s an opportunity to develop strategies to improve vaccination rates.”
The 2023 schedule follows news from the CDC that kindergarten vaccination rates declined during the 2021-2022 school year. Only 93% of kindergarteners obtained full vaccinations, representing a drop of 1 percentage point from the year before and 2 percentage points from the 2019-2020 school year.
The dip in coverage has been attributed to disruptions caused by the COVID-19 pandemic. AAP advises health care professionals to urge families to make sure their child’s vaccines are current.
Among other additions:
In Table 1
- MMR: Second vaccine added (Priorix, GlaxoSmithKline Biologicals)
- Pneumococcal disease: second conjugate vaccine, PCV15, added (Vaxneuvance, Merck Sharp & Dohme).
- COVID-19: New row added.
- Dengue: Text changed from “Seropositive in endemic areas only” to “Seropositive in endemic dengue areas.”
- Inactivated polio vaccine: “See Notes” added to the column for children aged 18 years.
In Table 2
- PCV: Dose 3 to dose 4 interval revised to align with ACIP’s recommendation for dose 4. This dose is necessary only for children ages 12-59 months regardless of risk, or age 60-71 months with any risk who received three doses before age 12 months.
A parent-friendly vaccine schedule for children and adolescents is available on the CDC’s website.
“Vaccines are essential for the health of our whole society, including children and adolescents,” Dr. O’Leary said in a press release from AAP. “These schedules provide a road map [that] parents and pediatricians can follow to help children get the vaccines they need so their immune systems will be ready to recognize and resist diseases.”
As previously, the 2023 schedule was adjusted to ensure consistency between the formats of the childhood/adolescent and adult immunization guidance. A meeting of stakeholder organizations in October 2022 harmonized the two formats.
A version of this article first appeared on Medscape.com.
FROM PEDIATRICS
Less invasive NSCLC surgery does not compromise survival
suggest results from the CALGB 140503 trial, although strict patient selection remains key.
These new results contrast with those from a previous study from 1995, which found that local recurrence was three times higher and cancer mortality was twice as high with the less invasive procedure.
Those results from nearly 30 years ago established lobectomy as the standard of surgical care in this patient population, but since then advances in imaging and staging have allowed the detection of smaller and earlier tumors, which has “rekindled interest in sublobar resection,” the authors comment.
Hence, they conducted the new trial, which involved almost 700 U.S. patients with clinical T1aN0 NSCLC and a tumor size up to 2 cm, who were randomly assigned to lobar or sublobar tumor resection, and followed for 7 years.
The rates of both disease-free and overall survival were similar between the two groups, with no significant differences observed. There were also no substantial differences in rates of distant and locoregional recurrence.
In addition, there was a suggestion of less reduction in pulmonary function following the less invasive procedure.
“These findings affirm that sublobar resection ... is an effective management approach for this subgroup of patients with NSCLC,” says lead author Nasser Altorki, MD, Weill Cornell Medicine, NewYork–Presbyterian Hospital, New York.
“It is important that these results are interpreted strictly within the constraints of the eligibility criteria mandated by the trial, he emphasizes. “Specifically, the results are applicable only to a highly selected group of patients ... in whom the absence of metastases to hilar and mediastinal lymph nodes is pathologically confirmed.”
Nevertheless, Dr. Altorki said that “these results will become increasingly relevant as the proportion of patients with early-stage lung cancer increases with expanded implementation of lung cancer screening, and as the number of older persons with early-stage disease in whom sublobar resection may be the preferred surgical option increases.”
The study was published online in the New England Journal of Medicine.
In an accompanying editorial, Valerie W. Rusch, MD, Thoracic Service, Memorial Sloan Kettering Cancer Center, New York, agrees. “As CT screening becomes more widespread, this patient population will increase in clinical practice,” she explains.
However, Dr. Rusch also urges caution around patient selection, underlining that the results do not “provide a license for suboptimal surgical care.”
She says that “safeguards” such as the meticulous and strict patient criteria used in the trial “must be preserved in routine practice.”
“Thoracic surgeons will need to expand their expertise in sublobar resections, especially complex segmentectomies, and will need to collaborate closely with pathologists in assessing margins of resection, adequacy of lymph-node staging, and tumor characteristics that may predict recurrence.”
While emphasizing that lobectomy should still be performed when appropriate, Dr. Rusch nevertheless says: “The era of ‘precision’ surgery for NSCLC has arrived.”
Consistent with Japanese results
The investigators also point out that their findings are “consistent” with those of a recent Japanese study that compared lobectomy with anatomical segmentectomy, which found that the 5-year overall survival was 91.1% for lobectomy and 94.3% for segmentectomy.
The authors suggest that the difference in overall survival rates between the two trials might be due to anatomical segmentectomy being “considered by most surgeons to be more oncologically sound than wedge resection.”
In the current trial, wedge resection was allowed, however, “because it is the most frequently practiced method of sublobar resection in North America and Europe; thus, its inclusion would make the trial more representative of a ‘real world’ setting.”
Another important difference could be that more than 90% of the patients in the Japanese trial had adenocarcinoma, 45% with an associated ground-glass component, which is associated with better survival than a completely solid adenocarcinoma.
Dr. Rusch agrees that there are likely to be various factors related to the survival differences between the two trials, including patient selection, intraoperative management, and tumor characteristics.
“However, these two landmark trials are practice-changing because they establish sublobar resection as the standard of care for a select group of patients with NSCLC,” Dr. Rusch concluded.
Study details
Dr. Altorki and colleagues conducted the multicenter, international, randomized, noninferiority, phase 3 trial in patients with clinically staged T1aN0 NSCLC from 83 academic and community-based institutions in the United States, Canada, and Australia.
Patients were required to have a peripheral lung nodule with a solid component of up to 2 cm on preoperative CT, a tumor center in the outer third of the lung, and a tumor location amenable to sublobar resection, whether wedge or segment, or lobar resection, among other criteria.
In all, 697 patients were randomly assigned to undergo either lobar resection or sublobar resection, of whom 59.1% had wedge resection and 37.9% anatomical segmental resection. The median age was 67.9 years, and 57.4% were female. The vast majority (90%) were White.
After a median follow-up of 7 years, the 5-year disease-free survival was 63.6% with sublobar resection and 64.1% following lobar resection.
The team found that sublobar resection was not inferior to lobectomy for disease-free survival, at a hazard ratio for disease recurrence or death of 1.01 (90% confidence interval, 0.83-1.24), which adjusted to 0.99 after taking into account the site where the patient was treated.
The 5-year overall survival rate was 80.3% after sublobar resection, and 78.9% following lobar resection, at a hazard ratio for death of 0.95 (95% CI, 0.72-1.26).
The results were “generally consistent” when accounting for factors such as age group, sex, tumor location, histologic type, smoking history, tumor size, and ECOG performance status, the team says.
Turning to recurrence, they showed that, among 687 patients eligible for assessment, 30.4% of those in the sublobar resection group and 29.3% of those assigned to lobar resection experienced disease recurrence, with 13.4% and 10%, respectively, having locoregional recurrence.
An exploratory analysis indicated that 5-year recurrence-free survival was similar in the two groups, at 70.2% vs. 71.2% or a hazard ratio for recurrence of 1.05 (95% CI, 0.80-1.39). The cumulative incidence of death was also similar.
It was also notable that reduction in predictive forced expiratory volume in 1 second from baseline was lower with sublobar than lobar resection, at –4.0 vs. –6.0, as was the reduction in predicted forced vital capacity, at –3.0 vs. –5.0.
“Although this difference is arguably not clinically meaningful in this patient population with normal baseline pulmonary functions,” the team writes, “it may be more clinically relevant in patients with compromised pulmonary functions, or in those with lower-lobe disease in whom lobar resection may be associated with greater impairment of pulmonary function.”
Dr. Rusch suggests that “more sensitive or functional assessments” of pulmonary function might include “diffusion capacity and 6-minute walk tests,” although she noted that even short-term differences in pulmonary function “may affect perioperative and functional outcomes, especially for tumors in the lower lobe.”
The study was supported by the National Cancer Institute of the National Institutes of Health, including via grants to the Alliance for Clinical Trials in Oncology and the Canadian Cancer Trials Group, and supported in part by Covidien and Ethicon.
Dr. Altorki reports relationships with AstraZeneca, Genentech, Johnson & Johnson, and Regeneron. Dr. Rusch reports relationships with Cancer Research UK, Genentech, and the National Cancer Institute.
A version of this article first appeared on Medscape.com.
suggest results from the CALGB 140503 trial, although strict patient selection remains key.
These new results contrast with those from a previous study from 1995, which found that local recurrence was three times higher and cancer mortality was twice as high with the less invasive procedure.
Those results from nearly 30 years ago established lobectomy as the standard of surgical care in this patient population, but since then advances in imaging and staging have allowed the detection of smaller and earlier tumors, which has “rekindled interest in sublobar resection,” the authors comment.
Hence, they conducted the new trial, which involved almost 700 U.S. patients with clinical T1aN0 NSCLC and a tumor size up to 2 cm, who were randomly assigned to lobar or sublobar tumor resection, and followed for 7 years.
The rates of both disease-free and overall survival were similar between the two groups, with no significant differences observed. There were also no substantial differences in rates of distant and locoregional recurrence.
In addition, there was a suggestion of less reduction in pulmonary function following the less invasive procedure.
“These findings affirm that sublobar resection ... is an effective management approach for this subgroup of patients with NSCLC,” says lead author Nasser Altorki, MD, Weill Cornell Medicine, NewYork–Presbyterian Hospital, New York.
“It is important that these results are interpreted strictly within the constraints of the eligibility criteria mandated by the trial, he emphasizes. “Specifically, the results are applicable only to a highly selected group of patients ... in whom the absence of metastases to hilar and mediastinal lymph nodes is pathologically confirmed.”
Nevertheless, Dr. Altorki said that “these results will become increasingly relevant as the proportion of patients with early-stage lung cancer increases with expanded implementation of lung cancer screening, and as the number of older persons with early-stage disease in whom sublobar resection may be the preferred surgical option increases.”
The study was published online in the New England Journal of Medicine.
In an accompanying editorial, Valerie W. Rusch, MD, Thoracic Service, Memorial Sloan Kettering Cancer Center, New York, agrees. “As CT screening becomes more widespread, this patient population will increase in clinical practice,” she explains.
However, Dr. Rusch also urges caution around patient selection, underlining that the results do not “provide a license for suboptimal surgical care.”
She says that “safeguards” such as the meticulous and strict patient criteria used in the trial “must be preserved in routine practice.”
“Thoracic surgeons will need to expand their expertise in sublobar resections, especially complex segmentectomies, and will need to collaborate closely with pathologists in assessing margins of resection, adequacy of lymph-node staging, and tumor characteristics that may predict recurrence.”
While emphasizing that lobectomy should still be performed when appropriate, Dr. Rusch nevertheless says: “The era of ‘precision’ surgery for NSCLC has arrived.”
Consistent with Japanese results
The investigators also point out that their findings are “consistent” with those of a recent Japanese study that compared lobectomy with anatomical segmentectomy, which found that the 5-year overall survival was 91.1% for lobectomy and 94.3% for segmentectomy.
The authors suggest that the difference in overall survival rates between the two trials might be due to anatomical segmentectomy being “considered by most surgeons to be more oncologically sound than wedge resection.”
In the current trial, wedge resection was allowed, however, “because it is the most frequently practiced method of sublobar resection in North America and Europe; thus, its inclusion would make the trial more representative of a ‘real world’ setting.”
Another important difference could be that more than 90% of the patients in the Japanese trial had adenocarcinoma, 45% with an associated ground-glass component, which is associated with better survival than a completely solid adenocarcinoma.
Dr. Rusch agrees that there are likely to be various factors related to the survival differences between the two trials, including patient selection, intraoperative management, and tumor characteristics.
“However, these two landmark trials are practice-changing because they establish sublobar resection as the standard of care for a select group of patients with NSCLC,” Dr. Rusch concluded.
Study details
Dr. Altorki and colleagues conducted the multicenter, international, randomized, noninferiority, phase 3 trial in patients with clinically staged T1aN0 NSCLC from 83 academic and community-based institutions in the United States, Canada, and Australia.
Patients were required to have a peripheral lung nodule with a solid component of up to 2 cm on preoperative CT, a tumor center in the outer third of the lung, and a tumor location amenable to sublobar resection, whether wedge or segment, or lobar resection, among other criteria.
In all, 697 patients were randomly assigned to undergo either lobar resection or sublobar resection, of whom 59.1% had wedge resection and 37.9% anatomical segmental resection. The median age was 67.9 years, and 57.4% were female. The vast majority (90%) were White.
After a median follow-up of 7 years, the 5-year disease-free survival was 63.6% with sublobar resection and 64.1% following lobar resection.
The team found that sublobar resection was not inferior to lobectomy for disease-free survival, at a hazard ratio for disease recurrence or death of 1.01 (90% confidence interval, 0.83-1.24), which adjusted to 0.99 after taking into account the site where the patient was treated.
The 5-year overall survival rate was 80.3% after sublobar resection, and 78.9% following lobar resection, at a hazard ratio for death of 0.95 (95% CI, 0.72-1.26).
The results were “generally consistent” when accounting for factors such as age group, sex, tumor location, histologic type, smoking history, tumor size, and ECOG performance status, the team says.
Turning to recurrence, they showed that, among 687 patients eligible for assessment, 30.4% of those in the sublobar resection group and 29.3% of those assigned to lobar resection experienced disease recurrence, with 13.4% and 10%, respectively, having locoregional recurrence.
An exploratory analysis indicated that 5-year recurrence-free survival was similar in the two groups, at 70.2% vs. 71.2% or a hazard ratio for recurrence of 1.05 (95% CI, 0.80-1.39). The cumulative incidence of death was also similar.
It was also notable that reduction in predictive forced expiratory volume in 1 second from baseline was lower with sublobar than lobar resection, at –4.0 vs. –6.0, as was the reduction in predicted forced vital capacity, at –3.0 vs. –5.0.
“Although this difference is arguably not clinically meaningful in this patient population with normal baseline pulmonary functions,” the team writes, “it may be more clinically relevant in patients with compromised pulmonary functions, or in those with lower-lobe disease in whom lobar resection may be associated with greater impairment of pulmonary function.”
Dr. Rusch suggests that “more sensitive or functional assessments” of pulmonary function might include “diffusion capacity and 6-minute walk tests,” although she noted that even short-term differences in pulmonary function “may affect perioperative and functional outcomes, especially for tumors in the lower lobe.”
The study was supported by the National Cancer Institute of the National Institutes of Health, including via grants to the Alliance for Clinical Trials in Oncology and the Canadian Cancer Trials Group, and supported in part by Covidien and Ethicon.
Dr. Altorki reports relationships with AstraZeneca, Genentech, Johnson & Johnson, and Regeneron. Dr. Rusch reports relationships with Cancer Research UK, Genentech, and the National Cancer Institute.
A version of this article first appeared on Medscape.com.
suggest results from the CALGB 140503 trial, although strict patient selection remains key.
These new results contrast with those from a previous study from 1995, which found that local recurrence was three times higher and cancer mortality was twice as high with the less invasive procedure.
Those results from nearly 30 years ago established lobectomy as the standard of surgical care in this patient population, but since then advances in imaging and staging have allowed the detection of smaller and earlier tumors, which has “rekindled interest in sublobar resection,” the authors comment.
Hence, they conducted the new trial, which involved almost 700 U.S. patients with clinical T1aN0 NSCLC and a tumor size up to 2 cm, who were randomly assigned to lobar or sublobar tumor resection, and followed for 7 years.
The rates of both disease-free and overall survival were similar between the two groups, with no significant differences observed. There were also no substantial differences in rates of distant and locoregional recurrence.
In addition, there was a suggestion of less reduction in pulmonary function following the less invasive procedure.
“These findings affirm that sublobar resection ... is an effective management approach for this subgroup of patients with NSCLC,” says lead author Nasser Altorki, MD, Weill Cornell Medicine, NewYork–Presbyterian Hospital, New York.
“It is important that these results are interpreted strictly within the constraints of the eligibility criteria mandated by the trial, he emphasizes. “Specifically, the results are applicable only to a highly selected group of patients ... in whom the absence of metastases to hilar and mediastinal lymph nodes is pathologically confirmed.”
Nevertheless, Dr. Altorki said that “these results will become increasingly relevant as the proportion of patients with early-stage lung cancer increases with expanded implementation of lung cancer screening, and as the number of older persons with early-stage disease in whom sublobar resection may be the preferred surgical option increases.”
The study was published online in the New England Journal of Medicine.
In an accompanying editorial, Valerie W. Rusch, MD, Thoracic Service, Memorial Sloan Kettering Cancer Center, New York, agrees. “As CT screening becomes more widespread, this patient population will increase in clinical practice,” she explains.
However, Dr. Rusch also urges caution around patient selection, underlining that the results do not “provide a license for suboptimal surgical care.”
She says that “safeguards” such as the meticulous and strict patient criteria used in the trial “must be preserved in routine practice.”
“Thoracic surgeons will need to expand their expertise in sublobar resections, especially complex segmentectomies, and will need to collaborate closely with pathologists in assessing margins of resection, adequacy of lymph-node staging, and tumor characteristics that may predict recurrence.”
While emphasizing that lobectomy should still be performed when appropriate, Dr. Rusch nevertheless says: “The era of ‘precision’ surgery for NSCLC has arrived.”
Consistent with Japanese results
The investigators also point out that their findings are “consistent” with those of a recent Japanese study that compared lobectomy with anatomical segmentectomy, which found that the 5-year overall survival was 91.1% for lobectomy and 94.3% for segmentectomy.
The authors suggest that the difference in overall survival rates between the two trials might be due to anatomical segmentectomy being “considered by most surgeons to be more oncologically sound than wedge resection.”
In the current trial, wedge resection was allowed, however, “because it is the most frequently practiced method of sublobar resection in North America and Europe; thus, its inclusion would make the trial more representative of a ‘real world’ setting.”
Another important difference could be that more than 90% of the patients in the Japanese trial had adenocarcinoma, 45% with an associated ground-glass component, which is associated with better survival than a completely solid adenocarcinoma.
Dr. Rusch agrees that there are likely to be various factors related to the survival differences between the two trials, including patient selection, intraoperative management, and tumor characteristics.
“However, these two landmark trials are practice-changing because they establish sublobar resection as the standard of care for a select group of patients with NSCLC,” Dr. Rusch concluded.
Study details
Dr. Altorki and colleagues conducted the multicenter, international, randomized, noninferiority, phase 3 trial in patients with clinically staged T1aN0 NSCLC from 83 academic and community-based institutions in the United States, Canada, and Australia.
Patients were required to have a peripheral lung nodule with a solid component of up to 2 cm on preoperative CT, a tumor center in the outer third of the lung, and a tumor location amenable to sublobar resection, whether wedge or segment, or lobar resection, among other criteria.
In all, 697 patients were randomly assigned to undergo either lobar resection or sublobar resection, of whom 59.1% had wedge resection and 37.9% anatomical segmental resection. The median age was 67.9 years, and 57.4% were female. The vast majority (90%) were White.
After a median follow-up of 7 years, the 5-year disease-free survival was 63.6% with sublobar resection and 64.1% following lobar resection.
The team found that sublobar resection was not inferior to lobectomy for disease-free survival, at a hazard ratio for disease recurrence or death of 1.01 (90% confidence interval, 0.83-1.24), which adjusted to 0.99 after taking into account the site where the patient was treated.
The 5-year overall survival rate was 80.3% after sublobar resection, and 78.9% following lobar resection, at a hazard ratio for death of 0.95 (95% CI, 0.72-1.26).
The results were “generally consistent” when accounting for factors such as age group, sex, tumor location, histologic type, smoking history, tumor size, and ECOG performance status, the team says.
Turning to recurrence, they showed that, among 687 patients eligible for assessment, 30.4% of those in the sublobar resection group and 29.3% of those assigned to lobar resection experienced disease recurrence, with 13.4% and 10%, respectively, having locoregional recurrence.
An exploratory analysis indicated that 5-year recurrence-free survival was similar in the two groups, at 70.2% vs. 71.2% or a hazard ratio for recurrence of 1.05 (95% CI, 0.80-1.39). The cumulative incidence of death was also similar.
It was also notable that reduction in predictive forced expiratory volume in 1 second from baseline was lower with sublobar than lobar resection, at –4.0 vs. –6.0, as was the reduction in predicted forced vital capacity, at –3.0 vs. –5.0.
“Although this difference is arguably not clinically meaningful in this patient population with normal baseline pulmonary functions,” the team writes, “it may be more clinically relevant in patients with compromised pulmonary functions, or in those with lower-lobe disease in whom lobar resection may be associated with greater impairment of pulmonary function.”
Dr. Rusch suggests that “more sensitive or functional assessments” of pulmonary function might include “diffusion capacity and 6-minute walk tests,” although she noted that even short-term differences in pulmonary function “may affect perioperative and functional outcomes, especially for tumors in the lower lobe.”
The study was supported by the National Cancer Institute of the National Institutes of Health, including via grants to the Alliance for Clinical Trials in Oncology and the Canadian Cancer Trials Group, and supported in part by Covidien and Ethicon.
Dr. Altorki reports relationships with AstraZeneca, Genentech, Johnson & Johnson, and Regeneron. Dr. Rusch reports relationships with Cancer Research UK, Genentech, and the National Cancer Institute.
A version of this article first appeared on Medscape.com.
FROM NEW ENGLAND JOURNAL OF MEDICINE
COVID-19 ECMO and right ventricular failure: Lessons learned and standardization of management
The SARS-CoV-2 pandemic changed the way intensivists approach extracorporeal membrane oxygenation (ECMO). Patients with COVID-19 acute respiratory distress syndrome (ARDS) placed on ECMO have a high prevalence of right ventricular (RV) failure, which is associated with reduced survival (Maharaj V et al. ASAIO Journal. 2022;68[6]:772). In 2021, our institution supported 51 patients with COVID-19 ARDS with ECMO: 51% developed RV failure, defined as a clinical syndrome (reduced cardiac output) in the presence of RV dysfunction on transthoracic echocardiogram (TTE) (Marra A et al. Chest. 2022;161[2]:535). Total numbers for RV dysfunction and RV dilation on TTE were 78% and 91% respectively, In essence then, TTE signs of RV dysfunction are sensitive but not specific for clinical RV failure.
Rates for survival to decannulation were far lower when RV failure was present (27%) vs. absent (84%). Given these numbers, we felt a reduction in RV failure would be an important target for improving outcomes for patients with COVID-19 ARDS receiving ECMO. Existing studies on RV failure in patients with ARDS receiving ECMO are plagued by scant data, small sample sizes, differences in diagnostic criteria, and heterogenous treatment approaches. Despite these limitations, we felt the need to make changes in our approach to RV management.
Because outcomes once clinical RV-failure occurs are so poor, we focused on prevention. While we’re short on data and evidence-based medicine (EBM) here, we know a lot about the physiology of COVID19, the pulmonary vasculature, and the right side of the heart. There are multiple physiologic and disease-related pathways that converge to produce RV-failure in patients with COVID-19 ARDS on ECMO (Sato R et al. Crit Care. 2021;25:172). Ongoing relative hypoxemia, hypercapnia, acidemia, and microvascular thromboses/immunothromboses can all lead to increased pulmonary vascular resistance (PVR) and an increased workload for the RV (Zochios V et al. ASAIO Journal. 2022; 68[4]:456). ARDS management typically involves high positive end-expiratory pressure (PEEP), which can produce RV-PA uncoupling (Wanner P et al. J Clin Med. 2020;9:432).
We do know that ECMO relieves the stress on the right side of the heart by improving hypoxemia, hypercapnia, and acidemia while allowing for reduction in PEEP (Zochios V et al. ASAIO Journal. 2022; 68[4]:456). In addition to ECMO, proning and pulmonary vasodilators offload RV by further reducing pulmonary pressures (Sato R et al. Crit Care. 2021;25:172). Lastly, a right ventricular assist device (RVAD) can dissipate the work required by the RV and prevent decompensation. Collectively, these therapies can be considered preventive.
Knowing the RV parameters on RV are sensitive but not specific for outcomes though, when should some of these treatments be instituted? It’s clear that once RV failure has developed it’s probably too late, but it’s hard to find data to guide us on when to act. One institution used right ventricular assist devices (RVADs) at the time of ECMO initiation with protocolized care and achieved a survival to discharge rate of 73% (Mustafa AK et al. JAMA Surgery. 2020;155[10]:990). The publication generated enthusiasm for RVAD support with ECMO, but it’s possible the protocolized care drove the high survival rate, at least in part.
At our institution, we developed our own protocol for evaluation of the RV with proactive treatment based on specific targets. We performed daily, bedside TTE and assessed the RV fractional area of change (FAC) and outflow tract velocity time integral (VTI). These parameters provide a quantitative assessment of global RV function, and FAC is directly related to ability to wean from ECMO support (Maharaj V et al. ASAIO Journal. 2022;68[6]:772). We avoided using the tricuspid annular plain systolic excursion (TAPSE) due to its poor sensitivity (Marra AM et al. Chest. 2022;161[2]:535). Patients receiving ECMO with subjective, global mild to moderate RV dysfunction on TTE with worsening clinical data, an FAC of 20%-35%, and a VTI of 10-14 cm were treated with aggressive diuresis, pulmonary vasodilators, and inotropy for 48 hours. If there was no improvement or deterioration, an RVAD was placed. For patients with signs of severe RV dysfunction (FAC < 20% or VTI < 10 cm), we proceeded directly to RVAD. We’re currently collecting data and tracking outcomes.
While data exist on various interventions in RV failure due to COVID-19 ARDS with ECMO, our understanding of this disease is still in its infancy. The optimal timing of interventions to manage and prevent RV failure is not known. We would argue that those who wait for RV failure to occur before instituting protective or supportive therapies are missing the opportunity to impact outcomes. We currently do not have the evidence to support the specific protocol we’ve outlined here and instituted at our hospital. However, we do believe there’s enough literature and experience to support the concept that close monitoring of RV function is critical for patients with COVID19 ARDS receiving ECMO. Failure to anticipate worsening function on the way to failure means reacting to it rather than staving it off. By then, it’s too late.
Dr. Thomas is Maj, USAF, assistant professor, pulmonary/critical care; Dr. O’Neil is Maj, USAF, pediatric and ECMO intensivist, PICU medical director; and Dr. Villalobos is Capt, USAF, assistant professor, pulmonary/critical care, medical ICU director, Brooke Army Medical Center, San Antonio, Tex. The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Army, the Department of the Air Force, or the Department of Defense or the U.S. government.
The SARS-CoV-2 pandemic changed the way intensivists approach extracorporeal membrane oxygenation (ECMO). Patients with COVID-19 acute respiratory distress syndrome (ARDS) placed on ECMO have a high prevalence of right ventricular (RV) failure, which is associated with reduced survival (Maharaj V et al. ASAIO Journal. 2022;68[6]:772). In 2021, our institution supported 51 patients with COVID-19 ARDS with ECMO: 51% developed RV failure, defined as a clinical syndrome (reduced cardiac output) in the presence of RV dysfunction on transthoracic echocardiogram (TTE) (Marra A et al. Chest. 2022;161[2]:535). Total numbers for RV dysfunction and RV dilation on TTE were 78% and 91% respectively, In essence then, TTE signs of RV dysfunction are sensitive but not specific for clinical RV failure.
Rates for survival to decannulation were far lower when RV failure was present (27%) vs. absent (84%). Given these numbers, we felt a reduction in RV failure would be an important target for improving outcomes for patients with COVID-19 ARDS receiving ECMO. Existing studies on RV failure in patients with ARDS receiving ECMO are plagued by scant data, small sample sizes, differences in diagnostic criteria, and heterogenous treatment approaches. Despite these limitations, we felt the need to make changes in our approach to RV management.
Because outcomes once clinical RV-failure occurs are so poor, we focused on prevention. While we’re short on data and evidence-based medicine (EBM) here, we know a lot about the physiology of COVID19, the pulmonary vasculature, and the right side of the heart. There are multiple physiologic and disease-related pathways that converge to produce RV-failure in patients with COVID-19 ARDS on ECMO (Sato R et al. Crit Care. 2021;25:172). Ongoing relative hypoxemia, hypercapnia, acidemia, and microvascular thromboses/immunothromboses can all lead to increased pulmonary vascular resistance (PVR) and an increased workload for the RV (Zochios V et al. ASAIO Journal. 2022; 68[4]:456). ARDS management typically involves high positive end-expiratory pressure (PEEP), which can produce RV-PA uncoupling (Wanner P et al. J Clin Med. 2020;9:432).
We do know that ECMO relieves the stress on the right side of the heart by improving hypoxemia, hypercapnia, and acidemia while allowing for reduction in PEEP (Zochios V et al. ASAIO Journal. 2022; 68[4]:456). In addition to ECMO, proning and pulmonary vasodilators offload RV by further reducing pulmonary pressures (Sato R et al. Crit Care. 2021;25:172). Lastly, a right ventricular assist device (RVAD) can dissipate the work required by the RV and prevent decompensation. Collectively, these therapies can be considered preventive.
Knowing the RV parameters on RV are sensitive but not specific for outcomes though, when should some of these treatments be instituted? It’s clear that once RV failure has developed it’s probably too late, but it’s hard to find data to guide us on when to act. One institution used right ventricular assist devices (RVADs) at the time of ECMO initiation with protocolized care and achieved a survival to discharge rate of 73% (Mustafa AK et al. JAMA Surgery. 2020;155[10]:990). The publication generated enthusiasm for RVAD support with ECMO, but it’s possible the protocolized care drove the high survival rate, at least in part.
At our institution, we developed our own protocol for evaluation of the RV with proactive treatment based on specific targets. We performed daily, bedside TTE and assessed the RV fractional area of change (FAC) and outflow tract velocity time integral (VTI). These parameters provide a quantitative assessment of global RV function, and FAC is directly related to ability to wean from ECMO support (Maharaj V et al. ASAIO Journal. 2022;68[6]:772). We avoided using the tricuspid annular plain systolic excursion (TAPSE) due to its poor sensitivity (Marra AM et al. Chest. 2022;161[2]:535). Patients receiving ECMO with subjective, global mild to moderate RV dysfunction on TTE with worsening clinical data, an FAC of 20%-35%, and a VTI of 10-14 cm were treated with aggressive diuresis, pulmonary vasodilators, and inotropy for 48 hours. If there was no improvement or deterioration, an RVAD was placed. For patients with signs of severe RV dysfunction (FAC < 20% or VTI < 10 cm), we proceeded directly to RVAD. We’re currently collecting data and tracking outcomes.
While data exist on various interventions in RV failure due to COVID-19 ARDS with ECMO, our understanding of this disease is still in its infancy. The optimal timing of interventions to manage and prevent RV failure is not known. We would argue that those who wait for RV failure to occur before instituting protective or supportive therapies are missing the opportunity to impact outcomes. We currently do not have the evidence to support the specific protocol we’ve outlined here and instituted at our hospital. However, we do believe there’s enough literature and experience to support the concept that close monitoring of RV function is critical for patients with COVID19 ARDS receiving ECMO. Failure to anticipate worsening function on the way to failure means reacting to it rather than staving it off. By then, it’s too late.
Dr. Thomas is Maj, USAF, assistant professor, pulmonary/critical care; Dr. O’Neil is Maj, USAF, pediatric and ECMO intensivist, PICU medical director; and Dr. Villalobos is Capt, USAF, assistant professor, pulmonary/critical care, medical ICU director, Brooke Army Medical Center, San Antonio, Tex. The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Army, the Department of the Air Force, or the Department of Defense or the U.S. government.
The SARS-CoV-2 pandemic changed the way intensivists approach extracorporeal membrane oxygenation (ECMO). Patients with COVID-19 acute respiratory distress syndrome (ARDS) placed on ECMO have a high prevalence of right ventricular (RV) failure, which is associated with reduced survival (Maharaj V et al. ASAIO Journal. 2022;68[6]:772). In 2021, our institution supported 51 patients with COVID-19 ARDS with ECMO: 51% developed RV failure, defined as a clinical syndrome (reduced cardiac output) in the presence of RV dysfunction on transthoracic echocardiogram (TTE) (Marra A et al. Chest. 2022;161[2]:535). Total numbers for RV dysfunction and RV dilation on TTE were 78% and 91% respectively, In essence then, TTE signs of RV dysfunction are sensitive but not specific for clinical RV failure.
Rates for survival to decannulation were far lower when RV failure was present (27%) vs. absent (84%). Given these numbers, we felt a reduction in RV failure would be an important target for improving outcomes for patients with COVID-19 ARDS receiving ECMO. Existing studies on RV failure in patients with ARDS receiving ECMO are plagued by scant data, small sample sizes, differences in diagnostic criteria, and heterogenous treatment approaches. Despite these limitations, we felt the need to make changes in our approach to RV management.
Because outcomes once clinical RV-failure occurs are so poor, we focused on prevention. While we’re short on data and evidence-based medicine (EBM) here, we know a lot about the physiology of COVID19, the pulmonary vasculature, and the right side of the heart. There are multiple physiologic and disease-related pathways that converge to produce RV-failure in patients with COVID-19 ARDS on ECMO (Sato R et al. Crit Care. 2021;25:172). Ongoing relative hypoxemia, hypercapnia, acidemia, and microvascular thromboses/immunothromboses can all lead to increased pulmonary vascular resistance (PVR) and an increased workload for the RV (Zochios V et al. ASAIO Journal. 2022; 68[4]:456). ARDS management typically involves high positive end-expiratory pressure (PEEP), which can produce RV-PA uncoupling (Wanner P et al. J Clin Med. 2020;9:432).
We do know that ECMO relieves the stress on the right side of the heart by improving hypoxemia, hypercapnia, and acidemia while allowing for reduction in PEEP (Zochios V et al. ASAIO Journal. 2022; 68[4]:456). In addition to ECMO, proning and pulmonary vasodilators offload RV by further reducing pulmonary pressures (Sato R et al. Crit Care. 2021;25:172). Lastly, a right ventricular assist device (RVAD) can dissipate the work required by the RV and prevent decompensation. Collectively, these therapies can be considered preventive.
Knowing the RV parameters on RV are sensitive but not specific for outcomes though, when should some of these treatments be instituted? It’s clear that once RV failure has developed it’s probably too late, but it’s hard to find data to guide us on when to act. One institution used right ventricular assist devices (RVADs) at the time of ECMO initiation with protocolized care and achieved a survival to discharge rate of 73% (Mustafa AK et al. JAMA Surgery. 2020;155[10]:990). The publication generated enthusiasm for RVAD support with ECMO, but it’s possible the protocolized care drove the high survival rate, at least in part.
At our institution, we developed our own protocol for evaluation of the RV with proactive treatment based on specific targets. We performed daily, bedside TTE and assessed the RV fractional area of change (FAC) and outflow tract velocity time integral (VTI). These parameters provide a quantitative assessment of global RV function, and FAC is directly related to ability to wean from ECMO support (Maharaj V et al. ASAIO Journal. 2022;68[6]:772). We avoided using the tricuspid annular plain systolic excursion (TAPSE) due to its poor sensitivity (Marra AM et al. Chest. 2022;161[2]:535). Patients receiving ECMO with subjective, global mild to moderate RV dysfunction on TTE with worsening clinical data, an FAC of 20%-35%, and a VTI of 10-14 cm were treated with aggressive diuresis, pulmonary vasodilators, and inotropy for 48 hours. If there was no improvement or deterioration, an RVAD was placed. For patients with signs of severe RV dysfunction (FAC < 20% or VTI < 10 cm), we proceeded directly to RVAD. We’re currently collecting data and tracking outcomes.
While data exist on various interventions in RV failure due to COVID-19 ARDS with ECMO, our understanding of this disease is still in its infancy. The optimal timing of interventions to manage and prevent RV failure is not known. We would argue that those who wait for RV failure to occur before instituting protective or supportive therapies are missing the opportunity to impact outcomes. We currently do not have the evidence to support the specific protocol we’ve outlined here and instituted at our hospital. However, we do believe there’s enough literature and experience to support the concept that close monitoring of RV function is critical for patients with COVID19 ARDS receiving ECMO. Failure to anticipate worsening function on the way to failure means reacting to it rather than staving it off. By then, it’s too late.
Dr. Thomas is Maj, USAF, assistant professor, pulmonary/critical care; Dr. O’Neil is Maj, USAF, pediatric and ECMO intensivist, PICU medical director; and Dr. Villalobos is Capt, USAF, assistant professor, pulmonary/critical care, medical ICU director, Brooke Army Medical Center, San Antonio, Tex. The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Army, the Department of the Air Force, or the Department of Defense or the U.S. government.
Management strategies for patients with COVID-19 pneumonia/ARDS
Since the first SARS-CoV-2 (COVID-19) outbreak in Wuhan, China, in December 2019, more than 6.6 million deaths have occurred. . One of the strategies for those cases refractory to traditional ARDS treatments has been the use of extracorporeal membrane oxygenation (ECMO).
Before the COVID-19 pandemic, a substantial amount of data regarding the use of ECMO in ARDS was gathered during the H1N1 influenza outbreak in 2009. Mortality ranged from 8% to 65% (Zangrillo, et al. Crit Care. 2013;17[1]:R30). From these data, we learned the importance of patient selection. Young patients with few co-morbidities and less than 7 days supported by mechanical ventilation did remarkably better than elderly patients or those who had prolonged positive-pressure ventilation prior to ECMO.
To date, the mortality rate for COVID-19 patients with ARDS requiring ECMO is 48% based on data from ELSO. Interestingly though, using May 1, 2020, as a cutoff date, mortality rates for patients with COVID-19 receiving ECMO significantly increased from 37% to 52% (Barbaro, et al. Lancet. 2021;398[10307]:1230). This escalation in mortality engendered concern that ECMO may not be useful in treating patients with COVID-19 and ARDS.
Several factors can be cited for this increase in mortality. First, many new ECMO programs launched after May 1. These new programs had a higher mortality rate (59%) compared with established programs, suggesting that program and provider experience play a significant role in patient outcomes (Barbaro, et al. Lancet. 2021;398[10307]:1230). Second, patients in the latter part of 2020 experienced much longer intervals between the onset of symptoms and time of intubation. Clinicians had a tendency to delay intubation as long as possible. Subsequently, the number of days receiving high flow nasal oxygen or noninvasive ventilation (NIV) was significantly longer (Schmidt, et al. Crit Care. 2021;25[1]:355). These data suggest that prolonged NIV on high Fio2 may be a negative prognostic indicator and should be considered when assessing a patient’s candidacy for ECMO.
Early in the pandemic, clinicians realized that average ECMO run times for patients with COVID-19 and ARDS were significantly longer, 15 vs 9 days, respectively (Jacobs, et al. Ann Thorac Surg. 2022;113[5]:1452). With such long run times, beds were slow to turn over, and a shortage of ECMO beds resulted during the height of the pandemic. In a retrospective study, Gannon looked at 90 patients, all of whom were deemed medically appropriate for ECMO. Two groups were created: (1) no capacity for ECMO vs (2) ECMO provided. Mortality rates were staggering at 89% and 43%, respectively (P =.001) (Gannon, et al. Am J Respir Crit Care Med. 2022;205[11]:1354). This study demonstrated a profound point: during a pandemic, when demand overcomes supply, there is a unique opportunity to see the effect of lifesaving therapies, such as ECMO, on outcomes. This study was particularly poignant, as the average age of the patients was 40 years old.
It is now widely accepted that prone positioning has survival benefit in ARDS. Prone positioning while receiving ECMO has generally been avoided due to concern for potential complications associated with the cannula(s). However, it has been shown that prone positioning while receiving veno-venous (VV) -ECMO reduces mortality rates, 37% proned vs 50% supine positioning (P =.02) (Giani, et al. Ann Am Thorac Soc. 2021;18[3]:495). In this study, no major complications occurred, and minor complications occurred in 6% of the proning events. Prone positioning improves ventilation-perfusion mismatch and reduces hypoxic vasoconstriction, which is thought to be right-sided heart-protective.
Right-sided heart dysfunction (RHD) is common in ARDS, whether COVID-19-related or not. The pathogenesis includes hypoxic vasoconstriction, pulmonary fibrosis, and ventilator-induced lung injury. Pulmonary microthrombi and patient-specific characteristics, such as obesity, are additional factors leading to RHD in patients with COVID-19. During the pandemic, several articles described using right-sided heart protective cannulation strategies for patients with COVID-19 requiring ECMO with favorable results (Mustafa, et al. JAMA Surg. 2020;155[10]:990; Cain, et al. J Surg Res. 2021;264:81-89). This right-sided heart protective strategy involves inserting a single access dual lumen cannula into the right internal jugular vein, which is advanced into the pulmonary artery, effectively bypassing the right ventricle. This setup is more typical of right ventricle assist device (RVAD), rather than typical VV-ECMO, which returns blood to the right atrium. Unfortunately, these studies did not include echocardiographic information to evaluate the effects of this intervention on RVD, and this is an area for future research. However, this vein to pulmonary artery strategy was found to facilitate decreased sedation, earlier liberation from mechanical ventilation, reduced need for tracheostomy, improved mobilization out of bed, and ease in prone positioning (Mustafa, et al. JAMA Surg. 2020;155[10]:990).
In conclusion, there is evidence to support the use of ECMO in patients with COVID-19 patients and ARDS failing conventional mechanical ventilation. The success of ECMO therapy is highly dependent on patient selection. Prolonged use of NIV on high Fio2 may be a negative predictor of ECMO survival and should be considered when assessing a patient for ECMO candidacy. Prone positioning with ECMO has been shown to have survival benefit and should be considered in all patients receiving ECMO.
Dr. Gaillard, Dr. Staples, and Dr. Kapoor are with the Department of Anesthesiology, Section on Critical Care, at Wake Forest School of Medicine in Winston-Salem, N.C. Dr. Gaillard is also with the Department of Emergency Medicine and Department of Internal Medicine, Section on Pulmonary, Critical Care, Allergy, and Immunology at Wake Forest School of Medicine.
Since the first SARS-CoV-2 (COVID-19) outbreak in Wuhan, China, in December 2019, more than 6.6 million deaths have occurred. . One of the strategies for those cases refractory to traditional ARDS treatments has been the use of extracorporeal membrane oxygenation (ECMO).
Before the COVID-19 pandemic, a substantial amount of data regarding the use of ECMO in ARDS was gathered during the H1N1 influenza outbreak in 2009. Mortality ranged from 8% to 65% (Zangrillo, et al. Crit Care. 2013;17[1]:R30). From these data, we learned the importance of patient selection. Young patients with few co-morbidities and less than 7 days supported by mechanical ventilation did remarkably better than elderly patients or those who had prolonged positive-pressure ventilation prior to ECMO.
To date, the mortality rate for COVID-19 patients with ARDS requiring ECMO is 48% based on data from ELSO. Interestingly though, using May 1, 2020, as a cutoff date, mortality rates for patients with COVID-19 receiving ECMO significantly increased from 37% to 52% (Barbaro, et al. Lancet. 2021;398[10307]:1230). This escalation in mortality engendered concern that ECMO may not be useful in treating patients with COVID-19 and ARDS.
Several factors can be cited for this increase in mortality. First, many new ECMO programs launched after May 1. These new programs had a higher mortality rate (59%) compared with established programs, suggesting that program and provider experience play a significant role in patient outcomes (Barbaro, et al. Lancet. 2021;398[10307]:1230). Second, patients in the latter part of 2020 experienced much longer intervals between the onset of symptoms and time of intubation. Clinicians had a tendency to delay intubation as long as possible. Subsequently, the number of days receiving high flow nasal oxygen or noninvasive ventilation (NIV) was significantly longer (Schmidt, et al. Crit Care. 2021;25[1]:355). These data suggest that prolonged NIV on high Fio2 may be a negative prognostic indicator and should be considered when assessing a patient’s candidacy for ECMO.
Early in the pandemic, clinicians realized that average ECMO run times for patients with COVID-19 and ARDS were significantly longer, 15 vs 9 days, respectively (Jacobs, et al. Ann Thorac Surg. 2022;113[5]:1452). With such long run times, beds were slow to turn over, and a shortage of ECMO beds resulted during the height of the pandemic. In a retrospective study, Gannon looked at 90 patients, all of whom were deemed medically appropriate for ECMO. Two groups were created: (1) no capacity for ECMO vs (2) ECMO provided. Mortality rates were staggering at 89% and 43%, respectively (P =.001) (Gannon, et al. Am J Respir Crit Care Med. 2022;205[11]:1354). This study demonstrated a profound point: during a pandemic, when demand overcomes supply, there is a unique opportunity to see the effect of lifesaving therapies, such as ECMO, on outcomes. This study was particularly poignant, as the average age of the patients was 40 years old.
It is now widely accepted that prone positioning has survival benefit in ARDS. Prone positioning while receiving ECMO has generally been avoided due to concern for potential complications associated with the cannula(s). However, it has been shown that prone positioning while receiving veno-venous (VV) -ECMO reduces mortality rates, 37% proned vs 50% supine positioning (P =.02) (Giani, et al. Ann Am Thorac Soc. 2021;18[3]:495). In this study, no major complications occurred, and minor complications occurred in 6% of the proning events. Prone positioning improves ventilation-perfusion mismatch and reduces hypoxic vasoconstriction, which is thought to be right-sided heart-protective.
Right-sided heart dysfunction (RHD) is common in ARDS, whether COVID-19-related or not. The pathogenesis includes hypoxic vasoconstriction, pulmonary fibrosis, and ventilator-induced lung injury. Pulmonary microthrombi and patient-specific characteristics, such as obesity, are additional factors leading to RHD in patients with COVID-19. During the pandemic, several articles described using right-sided heart protective cannulation strategies for patients with COVID-19 requiring ECMO with favorable results (Mustafa, et al. JAMA Surg. 2020;155[10]:990; Cain, et al. J Surg Res. 2021;264:81-89). This right-sided heart protective strategy involves inserting a single access dual lumen cannula into the right internal jugular vein, which is advanced into the pulmonary artery, effectively bypassing the right ventricle. This setup is more typical of right ventricle assist device (RVAD), rather than typical VV-ECMO, which returns blood to the right atrium. Unfortunately, these studies did not include echocardiographic information to evaluate the effects of this intervention on RVD, and this is an area for future research. However, this vein to pulmonary artery strategy was found to facilitate decreased sedation, earlier liberation from mechanical ventilation, reduced need for tracheostomy, improved mobilization out of bed, and ease in prone positioning (Mustafa, et al. JAMA Surg. 2020;155[10]:990).
In conclusion, there is evidence to support the use of ECMO in patients with COVID-19 patients and ARDS failing conventional mechanical ventilation. The success of ECMO therapy is highly dependent on patient selection. Prolonged use of NIV on high Fio2 may be a negative predictor of ECMO survival and should be considered when assessing a patient for ECMO candidacy. Prone positioning with ECMO has been shown to have survival benefit and should be considered in all patients receiving ECMO.
Dr. Gaillard, Dr. Staples, and Dr. Kapoor are with the Department of Anesthesiology, Section on Critical Care, at Wake Forest School of Medicine in Winston-Salem, N.C. Dr. Gaillard is also with the Department of Emergency Medicine and Department of Internal Medicine, Section on Pulmonary, Critical Care, Allergy, and Immunology at Wake Forest School of Medicine.
Since the first SARS-CoV-2 (COVID-19) outbreak in Wuhan, China, in December 2019, more than 6.6 million deaths have occurred. . One of the strategies for those cases refractory to traditional ARDS treatments has been the use of extracorporeal membrane oxygenation (ECMO).
Before the COVID-19 pandemic, a substantial amount of data regarding the use of ECMO in ARDS was gathered during the H1N1 influenza outbreak in 2009. Mortality ranged from 8% to 65% (Zangrillo, et al. Crit Care. 2013;17[1]:R30). From these data, we learned the importance of patient selection. Young patients with few co-morbidities and less than 7 days supported by mechanical ventilation did remarkably better than elderly patients or those who had prolonged positive-pressure ventilation prior to ECMO.
To date, the mortality rate for COVID-19 patients with ARDS requiring ECMO is 48% based on data from ELSO. Interestingly though, using May 1, 2020, as a cutoff date, mortality rates for patients with COVID-19 receiving ECMO significantly increased from 37% to 52% (Barbaro, et al. Lancet. 2021;398[10307]:1230). This escalation in mortality engendered concern that ECMO may not be useful in treating patients with COVID-19 and ARDS.
Several factors can be cited for this increase in mortality. First, many new ECMO programs launched after May 1. These new programs had a higher mortality rate (59%) compared with established programs, suggesting that program and provider experience play a significant role in patient outcomes (Barbaro, et al. Lancet. 2021;398[10307]:1230). Second, patients in the latter part of 2020 experienced much longer intervals between the onset of symptoms and time of intubation. Clinicians had a tendency to delay intubation as long as possible. Subsequently, the number of days receiving high flow nasal oxygen or noninvasive ventilation (NIV) was significantly longer (Schmidt, et al. Crit Care. 2021;25[1]:355). These data suggest that prolonged NIV on high Fio2 may be a negative prognostic indicator and should be considered when assessing a patient’s candidacy for ECMO.
Early in the pandemic, clinicians realized that average ECMO run times for patients with COVID-19 and ARDS were significantly longer, 15 vs 9 days, respectively (Jacobs, et al. Ann Thorac Surg. 2022;113[5]:1452). With such long run times, beds were slow to turn over, and a shortage of ECMO beds resulted during the height of the pandemic. In a retrospective study, Gannon looked at 90 patients, all of whom were deemed medically appropriate for ECMO. Two groups were created: (1) no capacity for ECMO vs (2) ECMO provided. Mortality rates were staggering at 89% and 43%, respectively (P =.001) (Gannon, et al. Am J Respir Crit Care Med. 2022;205[11]:1354). This study demonstrated a profound point: during a pandemic, when demand overcomes supply, there is a unique opportunity to see the effect of lifesaving therapies, such as ECMO, on outcomes. This study was particularly poignant, as the average age of the patients was 40 years old.
It is now widely accepted that prone positioning has survival benefit in ARDS. Prone positioning while receiving ECMO has generally been avoided due to concern for potential complications associated with the cannula(s). However, it has been shown that prone positioning while receiving veno-venous (VV) -ECMO reduces mortality rates, 37% proned vs 50% supine positioning (P =.02) (Giani, et al. Ann Am Thorac Soc. 2021;18[3]:495). In this study, no major complications occurred, and minor complications occurred in 6% of the proning events. Prone positioning improves ventilation-perfusion mismatch and reduces hypoxic vasoconstriction, which is thought to be right-sided heart-protective.
Right-sided heart dysfunction (RHD) is common in ARDS, whether COVID-19-related or not. The pathogenesis includes hypoxic vasoconstriction, pulmonary fibrosis, and ventilator-induced lung injury. Pulmonary microthrombi and patient-specific characteristics, such as obesity, are additional factors leading to RHD in patients with COVID-19. During the pandemic, several articles described using right-sided heart protective cannulation strategies for patients with COVID-19 requiring ECMO with favorable results (Mustafa, et al. JAMA Surg. 2020;155[10]:990; Cain, et al. J Surg Res. 2021;264:81-89). This right-sided heart protective strategy involves inserting a single access dual lumen cannula into the right internal jugular vein, which is advanced into the pulmonary artery, effectively bypassing the right ventricle. This setup is more typical of right ventricle assist device (RVAD), rather than typical VV-ECMO, which returns blood to the right atrium. Unfortunately, these studies did not include echocardiographic information to evaluate the effects of this intervention on RVD, and this is an area for future research. However, this vein to pulmonary artery strategy was found to facilitate decreased sedation, earlier liberation from mechanical ventilation, reduced need for tracheostomy, improved mobilization out of bed, and ease in prone positioning (Mustafa, et al. JAMA Surg. 2020;155[10]:990).
In conclusion, there is evidence to support the use of ECMO in patients with COVID-19 patients and ARDS failing conventional mechanical ventilation. The success of ECMO therapy is highly dependent on patient selection. Prolonged use of NIV on high Fio2 may be a negative predictor of ECMO survival and should be considered when assessing a patient for ECMO candidacy. Prone positioning with ECMO has been shown to have survival benefit and should be considered in all patients receiving ECMO.
Dr. Gaillard, Dr. Staples, and Dr. Kapoor are with the Department of Anesthesiology, Section on Critical Care, at Wake Forest School of Medicine in Winston-Salem, N.C. Dr. Gaillard is also with the Department of Emergency Medicine and Department of Internal Medicine, Section on Pulmonary, Critical Care, Allergy, and Immunology at Wake Forest School of Medicine.
Delays in diagnosing IPF. Noninvasive ventilation. BPA and CTEPH.
Diffuse Lung Disease & Transplant Network
Interstitial Lung Disease Section
Delay in diagnosis of IPF: How bad is the problem?
Idiopathic pulmonary fibrosis (IPF) is a devastating disease with a poor prognosis. Antifibrotic therapies for IPF are only capable of slowing disease progression without reversing established fibrosis. As such, the therapeutic efficacy of antifibrotic therapy may be reduced in patients whose diagnosis is delayed.
Unfortunately, diagnostic delay is common in IPF. Studies demonstrate that IPF diagnosis is delayed by more than a year after symptom onset in 43% of subjects, and more than 3 years in 19% of subjects (Cosgrove GP et al. BMC Pulm Med. 2018;18[9]). Approximately one-third of patients with IPF have undergone chest CT imaging more than 3 years prior to diagnosis, and around the same proportion has seen a pulmonologist within the same time span (Mooney J, et al. Ann Am Thorac Soc. 2019;16[3]:393). A median delay to IPF diagnosis of 2.2 years was noted in patients presenting to a tertiary academic medical center and was associated with an increased risk of death independent of age, sex, and forced vital capacity (adjusted hazard ratio per doubling of delay was 1.3) (Lamas DJ et al. Am J Respir Crit Care Med. 2011;184:842).
Robust improvements are clearly required for identifying patients with IPF earlier in their disease course. The Bridging Specialties Initiative from CHEST and the Three Lakes Foundation is one resource designed to improve the timely diagnosis of ILD (ILD Clinician Toolkit available at https://www.chestnet.org/Guidelines-and-Topic-Collections/Bridging-Specialties/Timely-Diagnosis-for-ILD-Patients/Clinician-Toolkit). This, and other initiatives will hopefully reduce delays in diagnosing IPF, allowing for optimal patient care.
Adrian Shifren, MBBCh, FCCP, Member-at-Large
Saniya Khan, MD, MBBS, Member-at-Large
Robert Case Jr., MD, Pulmonary & Critical Care Fellow
Critical Care Network
Mechanical Ventilation and Airways Section
Noninvasive ventilation
Noninvasive ventilation (NIV) is a ventilation modality that supports breathing by using mechanically assisted breaths without the need for intubation or a surgical airway. NIV is divided into two main types, negative-pressure ventilation (NPV) and noninvasive positive-pressure ventilation (NIPPV).
NPV
NPV periodically generates a negative (subatmospheric) pressure on the thorax wall, reflecting the natural breathing mechanism. As this negative pressure is transmitted into the thorax, normal atmospheric pressure air outside the thorax is pulled in for inhalation. Initiated by the negative pressure generator switching off, exhalation is passive due to elastic recoil of the lung and chest wall. The iron lung was a neck-to-toe horizontal cylinder used for NPV during the polio epidemic. New NPV devices are designed to fit the thorax only, using a cuirass (a torso-covering body armor molded shell).
For years, NPV use declined as NIPPV use increased. However, during the shortage of NIPPV devices during COVID and a recent recall of certain CPAP devices, NPV use has increased. NPV is an excellent alternative for those who cannot tolerate a facial mask due to facial deformity, claustrophobia, or excessive airway secretion (Corrado A et al. European Resp J. 2002;20[1]:187).
NIPPV
NIPPV is divided into several subtypes, including continuous positive airway pressure (CPAP), bilevel positive airway pressure (BPAP or BiPAP), and average volume-assured pressure support (AVAPS or VAPS). CPAP is defined as a single pressure delivered in inhalation (Pi) and exhalation (Pe). The increased mean airway pressure provides improved oxygenation (O2) but not ventilation (CO2). BPAP uses dual pressures with Pi higher than Pe. The increased mean airway pressure provides improved O2 while the difference between Pi minus Pe increases ventilation and decreases CO2.
AVAPS is a form of BPAP where Pi varies in an automated range to achieve the ordered tidal volume. In AVAPS, the generator adjusts Pi based on the average delivered tidal volume. If the average delivered tidal volume is less than the set tidal volume, Pi gradually increases while not exceeding Pi Max. Patients notice improved comfort of AVAPS with a variable Pi vs. BPAP with a fixed Pi (Frank A et al. Chest. 2018;154[4]:1060A).
Samantha Tauscher, DO, Resident-in-Training
Herbert Patrick, MD, MSEE, FCCP , Member-at-Large
Pulmonary Vascular & Cardiovascular Disease Network
Pulmonary Vascular Disease Section
A RACE to the finish: Revisiting the role of BPA in the management of CTEPH
Pulmonary thromboendarterectomy (PTE) is the treatment of choice for patients with CTEPH (Kim NH et al. Eur Respir J. 2019;53:1801915). However, this leaves about 40% of CTEPH patients who are not operative candidates due to inaccessible distal clot burden or significant comorbidities (Pepke-Zaba J et al. Circulation 2011;124:1973). For these inoperable situations, riociguat is the only FDA-approved medical therapy (Delcroix M et al. Eur Respir J. 2021;57:2002828). Balloon pulmonary angioplasty (BPA) became a treatment option for these patients in the last 2 decades. As technique refined, BPA demonstrated improved safety data along with improved hemodynamics and increased exercise capacity (Kataoka M et al. Circ Cardiovasc Interv. 2012;5:756).
A recently published crossover study, the RACE trial, compared riociguat with BPA in treating inoperable CTEPH (Jaïs X et al. Lancet Respir Med. 2022;10[10]:961). Patients were randomly assigned to either riociguat or BPA for 26 weeks. At 26 weeks, patients with pulmonary vascular resistance (PVR) more than 4 Woods Units (WU) were crossed over to receive either BPA or riociguat therapy. At 26 weeks, the BPA arm showed a greater reduction in PVR but more complications, including lung injury and hemoptysis. After a 26-week crossover period, the reduction in PVR was similar in both arms. The complication rate in the BPA arm was lower when preceded by riociguat.
In patients with inoperable CTEPH, BPA has emerged as an attractive management option in addition to the medical therapy with riociguat. However, BPA should be performed at expert centers with experience. Further studies are needed to strengthen the role and optimal timing of BPA in management of post PTE patients with residual PH.
Samantha Pettigrew, MD, Fellow-in-Training
Janine Vintich, MD, FCCP, Member-at-Large
Diffuse Lung Disease & Transplant Network
Interstitial Lung Disease Section
Delay in diagnosis of IPF: How bad is the problem?
Idiopathic pulmonary fibrosis (IPF) is a devastating disease with a poor prognosis. Antifibrotic therapies for IPF are only capable of slowing disease progression without reversing established fibrosis. As such, the therapeutic efficacy of antifibrotic therapy may be reduced in patients whose diagnosis is delayed.
Unfortunately, diagnostic delay is common in IPF. Studies demonstrate that IPF diagnosis is delayed by more than a year after symptom onset in 43% of subjects, and more than 3 years in 19% of subjects (Cosgrove GP et al. BMC Pulm Med. 2018;18[9]). Approximately one-third of patients with IPF have undergone chest CT imaging more than 3 years prior to diagnosis, and around the same proportion has seen a pulmonologist within the same time span (Mooney J, et al. Ann Am Thorac Soc. 2019;16[3]:393). A median delay to IPF diagnosis of 2.2 years was noted in patients presenting to a tertiary academic medical center and was associated with an increased risk of death independent of age, sex, and forced vital capacity (adjusted hazard ratio per doubling of delay was 1.3) (Lamas DJ et al. Am J Respir Crit Care Med. 2011;184:842).
Robust improvements are clearly required for identifying patients with IPF earlier in their disease course. The Bridging Specialties Initiative from CHEST and the Three Lakes Foundation is one resource designed to improve the timely diagnosis of ILD (ILD Clinician Toolkit available at https://www.chestnet.org/Guidelines-and-Topic-Collections/Bridging-Specialties/Timely-Diagnosis-for-ILD-Patients/Clinician-Toolkit). This, and other initiatives will hopefully reduce delays in diagnosing IPF, allowing for optimal patient care.
Adrian Shifren, MBBCh, FCCP, Member-at-Large
Saniya Khan, MD, MBBS, Member-at-Large
Robert Case Jr., MD, Pulmonary & Critical Care Fellow
Critical Care Network
Mechanical Ventilation and Airways Section
Noninvasive ventilation
Noninvasive ventilation (NIV) is a ventilation modality that supports breathing by using mechanically assisted breaths without the need for intubation or a surgical airway. NIV is divided into two main types, negative-pressure ventilation (NPV) and noninvasive positive-pressure ventilation (NIPPV).
NPV
NPV periodically generates a negative (subatmospheric) pressure on the thorax wall, reflecting the natural breathing mechanism. As this negative pressure is transmitted into the thorax, normal atmospheric pressure air outside the thorax is pulled in for inhalation. Initiated by the negative pressure generator switching off, exhalation is passive due to elastic recoil of the lung and chest wall. The iron lung was a neck-to-toe horizontal cylinder used for NPV during the polio epidemic. New NPV devices are designed to fit the thorax only, using a cuirass (a torso-covering body armor molded shell).
For years, NPV use declined as NIPPV use increased. However, during the shortage of NIPPV devices during COVID and a recent recall of certain CPAP devices, NPV use has increased. NPV is an excellent alternative for those who cannot tolerate a facial mask due to facial deformity, claustrophobia, or excessive airway secretion (Corrado A et al. European Resp J. 2002;20[1]:187).
NIPPV
NIPPV is divided into several subtypes, including continuous positive airway pressure (CPAP), bilevel positive airway pressure (BPAP or BiPAP), and average volume-assured pressure support (AVAPS or VAPS). CPAP is defined as a single pressure delivered in inhalation (Pi) and exhalation (Pe). The increased mean airway pressure provides improved oxygenation (O2) but not ventilation (CO2). BPAP uses dual pressures with Pi higher than Pe. The increased mean airway pressure provides improved O2 while the difference between Pi minus Pe increases ventilation and decreases CO2.
AVAPS is a form of BPAP where Pi varies in an automated range to achieve the ordered tidal volume. In AVAPS, the generator adjusts Pi based on the average delivered tidal volume. If the average delivered tidal volume is less than the set tidal volume, Pi gradually increases while not exceeding Pi Max. Patients notice improved comfort of AVAPS with a variable Pi vs. BPAP with a fixed Pi (Frank A et al. Chest. 2018;154[4]:1060A).
Samantha Tauscher, DO, Resident-in-Training
Herbert Patrick, MD, MSEE, FCCP , Member-at-Large
Pulmonary Vascular & Cardiovascular Disease Network
Pulmonary Vascular Disease Section
A RACE to the finish: Revisiting the role of BPA in the management of CTEPH
Pulmonary thromboendarterectomy (PTE) is the treatment of choice for patients with CTEPH (Kim NH et al. Eur Respir J. 2019;53:1801915). However, this leaves about 40% of CTEPH patients who are not operative candidates due to inaccessible distal clot burden or significant comorbidities (Pepke-Zaba J et al. Circulation 2011;124:1973). For these inoperable situations, riociguat is the only FDA-approved medical therapy (Delcroix M et al. Eur Respir J. 2021;57:2002828). Balloon pulmonary angioplasty (BPA) became a treatment option for these patients in the last 2 decades. As technique refined, BPA demonstrated improved safety data along with improved hemodynamics and increased exercise capacity (Kataoka M et al. Circ Cardiovasc Interv. 2012;5:756).
A recently published crossover study, the RACE trial, compared riociguat with BPA in treating inoperable CTEPH (Jaïs X et al. Lancet Respir Med. 2022;10[10]:961). Patients were randomly assigned to either riociguat or BPA for 26 weeks. At 26 weeks, patients with pulmonary vascular resistance (PVR) more than 4 Woods Units (WU) were crossed over to receive either BPA or riociguat therapy. At 26 weeks, the BPA arm showed a greater reduction in PVR but more complications, including lung injury and hemoptysis. After a 26-week crossover period, the reduction in PVR was similar in both arms. The complication rate in the BPA arm was lower when preceded by riociguat.
In patients with inoperable CTEPH, BPA has emerged as an attractive management option in addition to the medical therapy with riociguat. However, BPA should be performed at expert centers with experience. Further studies are needed to strengthen the role and optimal timing of BPA in management of post PTE patients with residual PH.
Samantha Pettigrew, MD, Fellow-in-Training
Janine Vintich, MD, FCCP, Member-at-Large
Diffuse Lung Disease & Transplant Network
Interstitial Lung Disease Section
Delay in diagnosis of IPF: How bad is the problem?
Idiopathic pulmonary fibrosis (IPF) is a devastating disease with a poor prognosis. Antifibrotic therapies for IPF are only capable of slowing disease progression without reversing established fibrosis. As such, the therapeutic efficacy of antifibrotic therapy may be reduced in patients whose diagnosis is delayed.
Unfortunately, diagnostic delay is common in IPF. Studies demonstrate that IPF diagnosis is delayed by more than a year after symptom onset in 43% of subjects, and more than 3 years in 19% of subjects (Cosgrove GP et al. BMC Pulm Med. 2018;18[9]). Approximately one-third of patients with IPF have undergone chest CT imaging more than 3 years prior to diagnosis, and around the same proportion has seen a pulmonologist within the same time span (Mooney J, et al. Ann Am Thorac Soc. 2019;16[3]:393). A median delay to IPF diagnosis of 2.2 years was noted in patients presenting to a tertiary academic medical center and was associated with an increased risk of death independent of age, sex, and forced vital capacity (adjusted hazard ratio per doubling of delay was 1.3) (Lamas DJ et al. Am J Respir Crit Care Med. 2011;184:842).
Robust improvements are clearly required for identifying patients with IPF earlier in their disease course. The Bridging Specialties Initiative from CHEST and the Three Lakes Foundation is one resource designed to improve the timely diagnosis of ILD (ILD Clinician Toolkit available at https://www.chestnet.org/Guidelines-and-Topic-Collections/Bridging-Specialties/Timely-Diagnosis-for-ILD-Patients/Clinician-Toolkit). This, and other initiatives will hopefully reduce delays in diagnosing IPF, allowing for optimal patient care.
Adrian Shifren, MBBCh, FCCP, Member-at-Large
Saniya Khan, MD, MBBS, Member-at-Large
Robert Case Jr., MD, Pulmonary & Critical Care Fellow
Critical Care Network
Mechanical Ventilation and Airways Section
Noninvasive ventilation
Noninvasive ventilation (NIV) is a ventilation modality that supports breathing by using mechanically assisted breaths without the need for intubation or a surgical airway. NIV is divided into two main types, negative-pressure ventilation (NPV) and noninvasive positive-pressure ventilation (NIPPV).
NPV
NPV periodically generates a negative (subatmospheric) pressure on the thorax wall, reflecting the natural breathing mechanism. As this negative pressure is transmitted into the thorax, normal atmospheric pressure air outside the thorax is pulled in for inhalation. Initiated by the negative pressure generator switching off, exhalation is passive due to elastic recoil of the lung and chest wall. The iron lung was a neck-to-toe horizontal cylinder used for NPV during the polio epidemic. New NPV devices are designed to fit the thorax only, using a cuirass (a torso-covering body armor molded shell).
For years, NPV use declined as NIPPV use increased. However, during the shortage of NIPPV devices during COVID and a recent recall of certain CPAP devices, NPV use has increased. NPV is an excellent alternative for those who cannot tolerate a facial mask due to facial deformity, claustrophobia, or excessive airway secretion (Corrado A et al. European Resp J. 2002;20[1]:187).
NIPPV
NIPPV is divided into several subtypes, including continuous positive airway pressure (CPAP), bilevel positive airway pressure (BPAP or BiPAP), and average volume-assured pressure support (AVAPS or VAPS). CPAP is defined as a single pressure delivered in inhalation (Pi) and exhalation (Pe). The increased mean airway pressure provides improved oxygenation (O2) but not ventilation (CO2). BPAP uses dual pressures with Pi higher than Pe. The increased mean airway pressure provides improved O2 while the difference between Pi minus Pe increases ventilation and decreases CO2.
AVAPS is a form of BPAP where Pi varies in an automated range to achieve the ordered tidal volume. In AVAPS, the generator adjusts Pi based on the average delivered tidal volume. If the average delivered tidal volume is less than the set tidal volume, Pi gradually increases while not exceeding Pi Max. Patients notice improved comfort of AVAPS with a variable Pi vs. BPAP with a fixed Pi (Frank A et al. Chest. 2018;154[4]:1060A).
Samantha Tauscher, DO, Resident-in-Training
Herbert Patrick, MD, MSEE, FCCP , Member-at-Large
Pulmonary Vascular & Cardiovascular Disease Network
Pulmonary Vascular Disease Section
A RACE to the finish: Revisiting the role of BPA in the management of CTEPH
Pulmonary thromboendarterectomy (PTE) is the treatment of choice for patients with CTEPH (Kim NH et al. Eur Respir J. 2019;53:1801915). However, this leaves about 40% of CTEPH patients who are not operative candidates due to inaccessible distal clot burden or significant comorbidities (Pepke-Zaba J et al. Circulation 2011;124:1973). For these inoperable situations, riociguat is the only FDA-approved medical therapy (Delcroix M et al. Eur Respir J. 2021;57:2002828). Balloon pulmonary angioplasty (BPA) became a treatment option for these patients in the last 2 decades. As technique refined, BPA demonstrated improved safety data along with improved hemodynamics and increased exercise capacity (Kataoka M et al. Circ Cardiovasc Interv. 2012;5:756).
A recently published crossover study, the RACE trial, compared riociguat with BPA in treating inoperable CTEPH (Jaïs X et al. Lancet Respir Med. 2022;10[10]:961). Patients were randomly assigned to either riociguat or BPA for 26 weeks. At 26 weeks, patients with pulmonary vascular resistance (PVR) more than 4 Woods Units (WU) were crossed over to receive either BPA or riociguat therapy. At 26 weeks, the BPA arm showed a greater reduction in PVR but more complications, including lung injury and hemoptysis. After a 26-week crossover period, the reduction in PVR was similar in both arms. The complication rate in the BPA arm was lower when preceded by riociguat.
In patients with inoperable CTEPH, BPA has emerged as an attractive management option in addition to the medical therapy with riociguat. However, BPA should be performed at expert centers with experience. Further studies are needed to strengthen the role and optimal timing of BPA in management of post PTE patients with residual PH.
Samantha Pettigrew, MD, Fellow-in-Training
Janine Vintich, MD, FCCP, Member-at-Large
Continuing our list of CHEST 2022 Winners
CHEST FOUNDATION GRANT AWARDS
CHEST Foundation Research Grant in Women’s Lung Health Disparities
Laura Sanapo, MD, The Miriam Hospital, Providence, R.I.
This grant is jointly supported by the CHEST Foundation and the Respiratory Health Association.
CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease
Benjamin Wu, MD, New York University
This grant is supported by AstraZeneca.
CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease
Richard Zou, MD, University of Pittsburgh Medical Center
This grant is supported by the CHEST Foundation.
CHEST Foundation and AASM Foundation Research Grant in Sleep Medicine
Gonzalo Labarca, MD, Universidad San Sebastian, Concepción, Chile
This grant is jointly supported by the CHEST Foundation and AASM Foundation.
CHEST Foundation and American Academy of Dental Sleep Medicine Research Grant in Sleep Apnea
Sherri Katz, MD, FCCP, Children’s Hospital of Eastern Ontario, Ottawa
This grant is supported by the CHEST Foundation and American Academy of Dental Sleep Medicine.
CHEST Foundation Research Grant in Sleep Medicine
Nancy Stewart, DO, University of Kansas Medical Center, Kansas City
This grant is supported by Jazz Pharmaceuticals.
CHEST Foundation Research Grant in Severe Asthma
Gareth Walters, MD, University Hospitals Birmingham (England)
This grant is supported by AstraZeneca.
CHEST Foundation Research Grant in Severe Asthma
Andréanne Côté, MD, Institut Universitaire de Cardiologie et de Pneumologie de Québec, Quebec
This grant is supported by AstraZeneca.
CHEST Foundation and APCCMPD Research Grant in Medical Education
Christopher Leba, MD, MPH, University of California, San Francisco
This grant is jointly supported by the CHEST Foundation and APCCMPD.
CHEST Foundation Research Grant in COVID-19
Clea Barnett, MD, New York University
This grant is supported by the CHEST Foundation.
CHEST Foundation Research Grant in Critical Care
Katherine Walker, MD, Brigham and Women’s Hospital, Harvard Medical School, Boston
This grant is supported by the CHEST Foundation.
CHEST Foundation Research Grant in Venous Thromboembolism
Daniel Lachant, DO, University of Rochester (N.Y.) Medical Center/Strong Memorial Hospital
This grant is supported by the CHEST Foundation.
CHEST Foundation Research Grant in Pulmonary Hypertension
Christina Thornton, MD, PhD, University of Calgary (Alta.)
This grant is supported by the CHEST Foundation.
CHEST Foundation Research Grant in Pulmonary Fibrosis
Christina Eckhardt, MD, Columbia University, New York
This grant is supported by an independent grant from Boehringer Ingelheim Pharmaceuticals and Genentech.
CHEST Foundation Research Grant in Pulmonary Fibrosis
John Kim, MD, University of Virginia, Charlottesville
This grant is supported by an independent grant from Boehringer Ingelheim Pharmaceuticals and Genentech.
John R. Addrizzo, MD, FCCP Research Grant in Sarcoidosis
Kerry Hena, MD, New York University
This grant is in honor of John R. Addrizzo, MD, FCCP and is jointly supported by the Addrizzo family and the CHEST Foundation.
CHEST Foundation Research Grant in Pediatric Lung Health
Adam Shapiro, MD, McGill University Health Centre, Montreal
This grant is supported by the CHEST Foundation.
CHEST Foundation Young Investigator Grant
Sameer Avasarala, MD, Case Western Reserve University, Cleveland
This grant is supported by the CHEST Foundation.
CHEST/ALA/ATS Respiratory Health Equity Research Award
Matthew Triplette, MD, Fred Hutchinson Cancer Research Center, Seattle
The Respiratory Health Equity Research Award is jointly supported by the American Lung Association, the American Thoracic Society, and the CHEST Foundation.
CHEST/ALA/ATS Respiratory Health Equity Research Award
Ayobami Akenroye, MD, MPH, Brigham and Women’s Hospital, Boston
The Respiratory Health Equity Research Award is jointly supported by the American Lung Association, the American Thoracic Society, and the CHEST Foundation.
CHEST Foundation Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP
Lorriane Odhiambo, PhD, Augusta (Ga.) University
This grant is supported by the CHEST Foundation.
CHEST Foundation Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP
Katie Stevens, Team Telomere, New York
This grant is supported by the CHEST Foundation.
CHEST Foundation Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP
Matthew Sharpe, MD, The University of Kansas Medical Center, Kansas City
This grant is supported by the CHEST Foundation.
SCIENTIFIC ABSTRACT AWARDS
Alfred Soffer Research Awards
Presented abstracts will be judged by session moderators, and award recipients will be selected for their outstanding original scientific research. Finalists will be evaluated on the basis of their written abstract and the quality of their oral presentation. This award is named in honor of Alfred Soffer, MD, Master FCCP, who was Editor in Chief of the journal CHEST® from 1968 to 1993, and Executive Director of CHEST from 1969 to 1992.
Young Investigator Awards
Investigators who are enrolled in a training or fellowship program or who have completed a fellowship program within 5 years prior to CHEST 2022 are eligible for Young Investigator Awards.
Presenters will be evaluated on the basis of their written abstract and presentation. Recipients will be selected by judges from the Scientific Presentations and Awards Committee for their outstanding original scientific research.
Top Rapid Fire Abstract Award
Awards are granted to two presenters from all the rapid fire sessions at the CHEST Annual Meeting for outstanding original scientific research and presentation
Top Case Report Award
Awards are granted to one presenter in each oral case report session at the CHEST Annual Meeting for outstanding original scientific research and presentation
Top Rapid Fire Case Report Award
Awards are granted to one presenter in each rapid fire oral case report session at the CHEST Annual Meeting for outstanding original scientific research and presentation
ALFRED SOFFER RESEARCH AWARD WINNERS
Palak Rath, MD
A Sense Of Urgency: Boarding Of Critical Care Medicine Patients In The ED
Syed Nazeer Mahmood, MD
Quantifying The Risk For Overtreatment And Undertreatment Of Severe Community Onset Pneumonia
YOUNG INVESTIGATOR AWARD WINNERS
Anusha Devarajan, MD, MBBS
Pneumomediastinum And Pneumothorax In COVID-19 Pneumonia: A Matched Case-Control Study
Marjan Islam, MD
Thoracic Ultrasound In COVID-19: Use Of Lung And Diaphragm Ultrasound In Evaluating Dyspnea In Survivors Of Critical Illness From COVID-19 Pneumonia In A Post-ICU Clinic
Aaron St Laurent, MD
Duchenne Muscular Dystrophy Respiratory Profiles From Real-World Registry Data: A Retrospective Longitudinal Study
ABSTRACT RAPID FIRE WINNERS
Andrew J.O. Davis, MD
Early Gas Exchange Parameters Not Associated With Survival In COVID-19-Associated ARDS Patients Requiring Prolonged Venovenous Extracorporeal Membrane Oxygenation
Benjamin Emmanuel
Clinical Outcomes In Patients With Severe Asthma Who Had Or Had Not Initiated Biologic Therapy: Results From The CLEAR Study
CASE REPORT SESSION WINNERS
Sathya Alekhya Bukkuri
Smarca4-Deficient Undifferentiated Tumor: A Rare Thoracic Malignancy
Zachary A. Banbury, MD
Fungal Aortitis In A Patient For Whom Blood Transfusion Is Not An Option: A Rare But Potentially Fatal Complication Of Aortic Valve Replacement
Harinivaas Shanmugavel Geetha, MD
Respiratory Distress After Potentially Fatal Aspirin Overdose: When To Intubate?
Lisa Hayes
Systemic Epstein-Barr Virus-Related T-Cell Lymphoproliferative Disorder: A Rare Cause Of Dyspnea And Pulmonary Infiltrates In An Immunocompetent Adult
Mohammed Alsaggaf, MBBS
Calcium Oxalate Deposition In Pulmonary Aspergillosis
Cheyenne Snavely
Traffic Jam In The Vasculature: A Case Of Pulmonary Leukostasis
Clarissa Smith, MD
Talcoma In Lung Cancer Screening: A Rare Benign Cause Of PET Scan Avidity
Nitin Gupta, MD
The Clue Is In The Blood Gas: A Rare Manifestation Of Lactic Acidosis
Moses Hayrabedian, MD
A Century-Old Infection Mimicking Malignancy: A Case Of Diffuse Histoplasmosis
Gabriel R. Schroeder, MD
A Case Of Wind-Instrument Associated Hypersensitivity Pneumonitis
Fizza Sajid, DO
Leaping From Lush Tropical Environments To The L-Train: A Case Of Severe Leptospirosis In New York City
Krista R. Dollar, MD
Looking Past The Ground Glass: It Was Only Skin Deep
Konstantin Golubykh, MD
Point-Of-Care Ultrasound In The Timely Diagnosis Of Colonic Necrosis
Arsal Tharwani
Abdominal Compression In End-Stage Fibrotic Interstitial Lung Disease (ILD) Improves Respiratory Compliance
Ryan Kozloski
When Asthma Isn’t: Multispecialty Approach To Fibrosing Mediastinitis
Zach S. Jarrett, DO
Vanishing Cancer: A Case Of Smoking-Related Organizing Pneumonia
Stephen Simeone
Intravascular Papillary Endothelial Hyperplasia Presenting As Thrombus In Transit With Acute Pulmonary Embolism
David Gruen, MD
Tackling Posterior Reversible Encephalopathy Syndrome (PRES): A Rare Case Of Subtherapeutic Tacrolimus Causing PRES In Steroid-Resistant Nephropathy
Nicholas Kunce, MD
An Unusual Case Of Subacute Bacterial Endocarditis Presenting With Catastrophic Subarachnoid Hemorrhage
Phillip J. Gary, MD
Sarcoid-Like Reaction After Treatment With Pembrolizumab
Shreya Podder, MD
Endobronchial Valves For Treatment Of Persistent Air Leak After Secondary Spontaneous Pneumothorax In Patients With Cystic Fibrosis
Alina Aw Wasim, MD, MBBS
Chest-Wall Castleman Disease Mimicking Thymoma Drop Metastasis
Ndausung Udongwo
The ‘Rat Bite Sign” On Cardiac MRI: Left Dominant Arrhythmogenic Cardiomyopathy As An Atypical Etiology Of Sudden Cardiac Arrest
Grant Senyei, MD
Management Of Ventriculopleural Shunt-Associated Pleural Effusion
Garima Singh, MD
COVID-19-Associated Thrombotic Thrombocytopenia Purpura (TTP)
CASE REPORT RAPID FIRE WINNERS
Sandeep Patri
Hyperammonemia Postlung Transplantation: An Uncommon But Life-Threatening Complication
Trung Nguyen
Dyspnea During Pregnancy Revealing Multiple Pulmonary Arteriovenous Malformations And A New Diagnosis Of Hereditary Hemorrhagic Telangiectasia
Pedro J. Baez, MD
Adenoid Cystic Adenocarcinoma: A Rare Esophageal Malignancy Misdiagnosed As COPD
Brette Guckian, DO
Management Of Pulmonary Cement Emboli After Kyphoplasty
Brinn Demars, DO
Tumor Emboli In The Pulmonary Artery Secondary To Chondrosarcoma: A Rare Presentation Mimicking Pulmonary Thromboembolism
Aakriti Arora
A Case Of Pulmonary Hypertension As A Possible Extracranial Manifestation Of Moyamoya Disease
Racine Elaine Reinoso
Clot In Transit: The Role Of Point-Of-Care Ultrasound In Early Diagnosis And Improved Outcomes
Qiraat Azeem, MD
A Case Of Autosomal-Dominant Hyper-IgE Syndrome Masquerading As Cystic Fibrosis
Jason R. Ballengee, DO
Third-Trimester Pregnancy Complicated By Non-Small Cell Lung Cancer Initially Presenting With Central Airway Obstruction And Stenosis
Sam Shafer
Caught In The Fray: Neurosarcoidosis Presenting As Chronic Respiratory Failure
Takkin Lo, MD, MPH
China White In Asthmatic Recreational Drug Users: Does It Contribute To Pneumatocele Development?
Sanjeev Shrestha, MD
Successful Treatment Of Microscopic Polyangiitis Using Novel Steroid-Sparing Agent Avacopan
Kristina Menchaca, MD
Cardiac Tamponade Without The Beck Triad: A Complication Of Severe Hypothyroidism
Olivia Millay, BS
Spontaneous Coronary Artery Dissection Of Left Anterior Descending Artery Complicated By Ventricular Septal Rupture
Akruti P. Prabhakar, DO
Delayed Lead Perforation Of The Right Atrium In The Presence Of Persistent Left Superior Vena Cava: A Rare Coincidence
Kevin Hsu, MD
A Modified Valsalva Maneuver For Ventilated And Sedated Patients With Unstable Supraventricular Tachycardia
Nang San Hti Lar Seng
Cardiovascular Manifestations Of Paraaortic Paragangliomas
Rocio Castillo-Larios
Membranous Dehiscence After Tracheal Resection And Reconstruction Healed Spontaneously With Conservative Treatment
Fizza Sajid, DO
A Young Broken Heart, Reversed
Janeen Grant-Sittol, MD
Inhaled Tranexamic Acid Use For Massive Hemoptysis In Vasculitis-Induced Bronchoalveolar Hemorrhage
Raman G. Kutty, Md, PhD
Progressive Lung Infiltrates In Patient With Acquired Immunodeficiency: A Rare Case Of GLILD
Tanwe Shende
Mycobacterium Shimoidei: A Rare Nontuberculous Infection In A U.S. Patient
Sarah M. Upson, MD
Not Your Typical Lactic Acidosis
Prachi Saluja, MD
Late-Onset Immune Thrombotic Thrombocytopenic Purpura (TTP) After Asymptomatic COVID-19 Infection
Steven S. Wu, MD
Type 1 Multiple Endocrine Neoplasia-Associated Tracheobronchial Tumors Managed By Rigid Bronchoscopy-Directed Multimodal Tumor Destruction
Konstantin Golubykh, MD
The Reversal That Helped: Role Of Bedside Echocardiography In Takotsubo Cardiomyopathy
Eric Salomon, MD
Obstructive Tracheobronchial Pulmonary Aspergillosis Managed With Local Bronchoscopic Intervention Alone
Daniel Hoesterey, MD
A Rare Case Of Critical Illness Due To Eczema Herpeticum With Disseminated Herpes Simplex Virus Infection
Awab U. Khan, DO
Severe Colchicine Toxicity In A Suicide Attempt Causing Multiorgan Failure: A Survival Story
Jacob Cebulko
Disseminated Strongyloidiasis In A Patient With Acute Lymphocytic Leukemia
Hasan Baher, MD
Hiding In Plain Sight: Disseminated Pulmonary TB
Navneet Ramesh
Multimodal Management Of Gastric Variceal Bleeding In Hemorrhagic Shock
Jason L. Peng, MD
Improving Compliance With Continuous Anterior Chest Compression In ARDS Caused By COVID-19: A Case Series
Sushan Gupta, MD
Complete Resolution Of Vasoreactive Pulmonary Artery Hypertension In Chronic Hypersensitive Pneumonitis
Mamta S. Chhabria, MD
A Fistulous Issue: Gastropleural Fistula As A Complication Of Gastrectomy
Anita Singh, DO, MBA
Identifying A Novel Surfactant Protein Mutation In A Family With Pulmonary Fibrosis
Rana Prathap Padappayil, MBBS
Delayed Cerebral Venous Sinus Thrombosis (CSVT) After An Invasive Meningioma Resection: An Uncommon Presentation Of A Common Complication
Rubabin Tooba, MD
The Morphing Cavity: An Image Series Of A Patient’s Pulmonary Infarction Over Time
Sally Ziatabar, DO
A Rare Case Of Disseminated Blastomycosis
Sumukh Arun Kumar
Incidental Pulmonary Cavitary Lesions As An Uncommon Presentation Of Lemierre Syndrome
Sophia Emetu
Pet Peeve: Dyspnea From Undiagnosed Pasteurella Multocida Empyema
Chidambaram Ramasamy, MD
A Case Of Diffuse Alveolar-Septal Pulmonary Amyloidosis And Cardiomyopathy
Rachel Swier
Acid-Fast Bacteria In Bronchiectasis: If The Glass Slipper Does Not Fit, Non-TB Mycobacteria, Consider Tsukamurella
Catherine Durant, MD
Idiopathic Multicentric Castleman Disease With Tafro Syndrome And Sjögren Syndrome
Ali Al-Hilli, MD, MSc
Sarcoidosis-Like Reaction During Treatment For Metastatic Breast Cancer With CDK 4/6 Inhibitors: Just An Epiphenomenon Or A Causal Relationship?
Scott Slusarenko, DO
Rapidly Progressive Perimyocarditis In SARS-CoV-2 Infection
Agatha M. Formoso, MD
Two Infants Presenting With Polymicrobial Pneumonia And Hypoxemic Respiratory Failure Associated With Heterozygous Variants In Carmil2 And Itk
Juan Adams-Chahin
The Silence Of “Lam”: A Case Of Tuberous Sclerosis Complex Associated With Lymphangioleiomyomatosis (Lam)
Kathleen Capaccione, MD
Lung Cancer Is Not Always The Answer: Exploring The Differential Diagnosis Of Thoracic Masses
Joann Wongvravit, DO
West Nile-Induced Myasthenia Gravis Crisis: An Unexpected Case Of Respiratory Failure
Ethan Karle, Do
A Rare Cause Of Community-Acquired Bacterial Pneumonia In A Patient With Poorly Controlled Diabetes
Taylor C. Becker, MD
Calcified Cavitary Conundrum: Delayed Diagnosis Of Histoplasmosis
Anneka Hutton, MD
Disseminated Listeriosis: A Deadly Triplicate
Omar Kandah, DO
COVID-19 Cardiac Tamponade With Cardiogenic Shock In A Previously Vaccinated Young Adult: A Case Report
Cihan Caglayan, MD
Partial Anomalous Pulmonary Venous Connection Diagnosed After Central Venous Catheter Placement
Michelle Jones, DO
Delayed Hemophagocytic Lymphohistiocytosis (HLH) Diagnosis In A Patient With Pulmonary Sarcoidosis And Newly Diagnosed T-Cell Lymphoma: A Case Report
Mariah Evarts, MD
A Normotensive Woman With Profound Lactic Acidosis And Stress-Induced Cardiomyopathy
Rachel V. Tan, MD
A Four-Boding Future: Polyviral Infection With SARS-CoV-2, Parainfluenza Virus Type 3, Influenza A, And Adenovirus
Thanh Hoang
Recurrent Syncope From Intermittent Torsades In Loperamide Abuse
Alissa Ali, MD
Ground Glass Opacities In A Patient Receiving Treatment With All-Trans Retinoic Acid And Arsenic Trioxide
Sean M. Masi, DO, MBA
Ferritin-Guided Therapeutic Plasma Exchange (TPE) Administration In COVID-19-Induced Cytokine Storm Syndrome: A Case Series
Anjali Sachdeva
Successful Biopsy Of Aortopulmonary Window Lymph Node With Robotic-Assisted Bronchoscopy
Rehan Saeed, MD
Multiple Sclerosis After COVID-19: A Sign Of Things To Come?
Harshitha Mergey Devender
Invasive Pulmonary Aspergillosis Associated With Nonspecific Interstitial Pneumonia Causing Recurrent Respiratory Failure
Be sure to check out the other award winners on page 20 in the January issue of CHEST Physician: https://tinyurl.com/2bcdcbj3 .
CHEST FOUNDATION GRANT AWARDS
CHEST Foundation Research Grant in Women’s Lung Health Disparities
Laura Sanapo, MD, The Miriam Hospital, Providence, R.I.
This grant is jointly supported by the CHEST Foundation and the Respiratory Health Association.
CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease
Benjamin Wu, MD, New York University
This grant is supported by AstraZeneca.
CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease
Richard Zou, MD, University of Pittsburgh Medical Center
This grant is supported by the CHEST Foundation.
CHEST Foundation and AASM Foundation Research Grant in Sleep Medicine
Gonzalo Labarca, MD, Universidad San Sebastian, Concepción, Chile
This grant is jointly supported by the CHEST Foundation and AASM Foundation.
CHEST Foundation and American Academy of Dental Sleep Medicine Research Grant in Sleep Apnea
Sherri Katz, MD, FCCP, Children’s Hospital of Eastern Ontario, Ottawa
This grant is supported by the CHEST Foundation and American Academy of Dental Sleep Medicine.
CHEST Foundation Research Grant in Sleep Medicine
Nancy Stewart, DO, University of Kansas Medical Center, Kansas City
This grant is supported by Jazz Pharmaceuticals.
CHEST Foundation Research Grant in Severe Asthma
Gareth Walters, MD, University Hospitals Birmingham (England)
This grant is supported by AstraZeneca.
CHEST Foundation Research Grant in Severe Asthma
Andréanne Côté, MD, Institut Universitaire de Cardiologie et de Pneumologie de Québec, Quebec
This grant is supported by AstraZeneca.
CHEST Foundation and APCCMPD Research Grant in Medical Education
Christopher Leba, MD, MPH, University of California, San Francisco
This grant is jointly supported by the CHEST Foundation and APCCMPD.
CHEST Foundation Research Grant in COVID-19
Clea Barnett, MD, New York University
This grant is supported by the CHEST Foundation.
CHEST Foundation Research Grant in Critical Care
Katherine Walker, MD, Brigham and Women’s Hospital, Harvard Medical School, Boston
This grant is supported by the CHEST Foundation.
CHEST Foundation Research Grant in Venous Thromboembolism
Daniel Lachant, DO, University of Rochester (N.Y.) Medical Center/Strong Memorial Hospital
This grant is supported by the CHEST Foundation.
CHEST Foundation Research Grant in Pulmonary Hypertension
Christina Thornton, MD, PhD, University of Calgary (Alta.)
This grant is supported by the CHEST Foundation.
CHEST Foundation Research Grant in Pulmonary Fibrosis
Christina Eckhardt, MD, Columbia University, New York
This grant is supported by an independent grant from Boehringer Ingelheim Pharmaceuticals and Genentech.
CHEST Foundation Research Grant in Pulmonary Fibrosis
John Kim, MD, University of Virginia, Charlottesville
This grant is supported by an independent grant from Boehringer Ingelheim Pharmaceuticals and Genentech.
John R. Addrizzo, MD, FCCP Research Grant in Sarcoidosis
Kerry Hena, MD, New York University
This grant is in honor of John R. Addrizzo, MD, FCCP and is jointly supported by the Addrizzo family and the CHEST Foundation.
CHEST Foundation Research Grant in Pediatric Lung Health
Adam Shapiro, MD, McGill University Health Centre, Montreal
This grant is supported by the CHEST Foundation.
CHEST Foundation Young Investigator Grant
Sameer Avasarala, MD, Case Western Reserve University, Cleveland
This grant is supported by the CHEST Foundation.
CHEST/ALA/ATS Respiratory Health Equity Research Award
Matthew Triplette, MD, Fred Hutchinson Cancer Research Center, Seattle
The Respiratory Health Equity Research Award is jointly supported by the American Lung Association, the American Thoracic Society, and the CHEST Foundation.
CHEST/ALA/ATS Respiratory Health Equity Research Award
Ayobami Akenroye, MD, MPH, Brigham and Women’s Hospital, Boston
The Respiratory Health Equity Research Award is jointly supported by the American Lung Association, the American Thoracic Society, and the CHEST Foundation.
CHEST Foundation Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP
Lorriane Odhiambo, PhD, Augusta (Ga.) University
This grant is supported by the CHEST Foundation.
CHEST Foundation Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP
Katie Stevens, Team Telomere, New York
This grant is supported by the CHEST Foundation.
CHEST Foundation Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP
Matthew Sharpe, MD, The University of Kansas Medical Center, Kansas City
This grant is supported by the CHEST Foundation.
SCIENTIFIC ABSTRACT AWARDS
Alfred Soffer Research Awards
Presented abstracts will be judged by session moderators, and award recipients will be selected for their outstanding original scientific research. Finalists will be evaluated on the basis of their written abstract and the quality of their oral presentation. This award is named in honor of Alfred Soffer, MD, Master FCCP, who was Editor in Chief of the journal CHEST® from 1968 to 1993, and Executive Director of CHEST from 1969 to 1992.
Young Investigator Awards
Investigators who are enrolled in a training or fellowship program or who have completed a fellowship program within 5 years prior to CHEST 2022 are eligible for Young Investigator Awards.
Presenters will be evaluated on the basis of their written abstract and presentation. Recipients will be selected by judges from the Scientific Presentations and Awards Committee for their outstanding original scientific research.
Top Rapid Fire Abstract Award
Awards are granted to two presenters from all the rapid fire sessions at the CHEST Annual Meeting for outstanding original scientific research and presentation
Top Case Report Award
Awards are granted to one presenter in each oral case report session at the CHEST Annual Meeting for outstanding original scientific research and presentation
Top Rapid Fire Case Report Award
Awards are granted to one presenter in each rapid fire oral case report session at the CHEST Annual Meeting for outstanding original scientific research and presentation
ALFRED SOFFER RESEARCH AWARD WINNERS
Palak Rath, MD
A Sense Of Urgency: Boarding Of Critical Care Medicine Patients In The ED
Syed Nazeer Mahmood, MD
Quantifying The Risk For Overtreatment And Undertreatment Of Severe Community Onset Pneumonia
YOUNG INVESTIGATOR AWARD WINNERS
Anusha Devarajan, MD, MBBS
Pneumomediastinum And Pneumothorax In COVID-19 Pneumonia: A Matched Case-Control Study
Marjan Islam, MD
Thoracic Ultrasound In COVID-19: Use Of Lung And Diaphragm Ultrasound In Evaluating Dyspnea In Survivors Of Critical Illness From COVID-19 Pneumonia In A Post-ICU Clinic
Aaron St Laurent, MD
Duchenne Muscular Dystrophy Respiratory Profiles From Real-World Registry Data: A Retrospective Longitudinal Study
ABSTRACT RAPID FIRE WINNERS
Andrew J.O. Davis, MD
Early Gas Exchange Parameters Not Associated With Survival In COVID-19-Associated ARDS Patients Requiring Prolonged Venovenous Extracorporeal Membrane Oxygenation
Benjamin Emmanuel
Clinical Outcomes In Patients With Severe Asthma Who Had Or Had Not Initiated Biologic Therapy: Results From The CLEAR Study
CASE REPORT SESSION WINNERS
Sathya Alekhya Bukkuri
Smarca4-Deficient Undifferentiated Tumor: A Rare Thoracic Malignancy
Zachary A. Banbury, MD
Fungal Aortitis In A Patient For Whom Blood Transfusion Is Not An Option: A Rare But Potentially Fatal Complication Of Aortic Valve Replacement
Harinivaas Shanmugavel Geetha, MD
Respiratory Distress After Potentially Fatal Aspirin Overdose: When To Intubate?
Lisa Hayes
Systemic Epstein-Barr Virus-Related T-Cell Lymphoproliferative Disorder: A Rare Cause Of Dyspnea And Pulmonary Infiltrates In An Immunocompetent Adult
Mohammed Alsaggaf, MBBS
Calcium Oxalate Deposition In Pulmonary Aspergillosis
Cheyenne Snavely
Traffic Jam In The Vasculature: A Case Of Pulmonary Leukostasis
Clarissa Smith, MD
Talcoma In Lung Cancer Screening: A Rare Benign Cause Of PET Scan Avidity
Nitin Gupta, MD
The Clue Is In The Blood Gas: A Rare Manifestation Of Lactic Acidosis
Moses Hayrabedian, MD
A Century-Old Infection Mimicking Malignancy: A Case Of Diffuse Histoplasmosis
Gabriel R. Schroeder, MD
A Case Of Wind-Instrument Associated Hypersensitivity Pneumonitis
Fizza Sajid, DO
Leaping From Lush Tropical Environments To The L-Train: A Case Of Severe Leptospirosis In New York City
Krista R. Dollar, MD
Looking Past The Ground Glass: It Was Only Skin Deep
Konstantin Golubykh, MD
Point-Of-Care Ultrasound In The Timely Diagnosis Of Colonic Necrosis
Arsal Tharwani
Abdominal Compression In End-Stage Fibrotic Interstitial Lung Disease (ILD) Improves Respiratory Compliance
Ryan Kozloski
When Asthma Isn’t: Multispecialty Approach To Fibrosing Mediastinitis
Zach S. Jarrett, DO
Vanishing Cancer: A Case Of Smoking-Related Organizing Pneumonia
Stephen Simeone
Intravascular Papillary Endothelial Hyperplasia Presenting As Thrombus In Transit With Acute Pulmonary Embolism
David Gruen, MD
Tackling Posterior Reversible Encephalopathy Syndrome (PRES): A Rare Case Of Subtherapeutic Tacrolimus Causing PRES In Steroid-Resistant Nephropathy
Nicholas Kunce, MD
An Unusual Case Of Subacute Bacterial Endocarditis Presenting With Catastrophic Subarachnoid Hemorrhage
Phillip J. Gary, MD
Sarcoid-Like Reaction After Treatment With Pembrolizumab
Shreya Podder, MD
Endobronchial Valves For Treatment Of Persistent Air Leak After Secondary Spontaneous Pneumothorax In Patients With Cystic Fibrosis
Alina Aw Wasim, MD, MBBS
Chest-Wall Castleman Disease Mimicking Thymoma Drop Metastasis
Ndausung Udongwo
The ‘Rat Bite Sign” On Cardiac MRI: Left Dominant Arrhythmogenic Cardiomyopathy As An Atypical Etiology Of Sudden Cardiac Arrest
Grant Senyei, MD
Management Of Ventriculopleural Shunt-Associated Pleural Effusion
Garima Singh, MD
COVID-19-Associated Thrombotic Thrombocytopenia Purpura (TTP)
CASE REPORT RAPID FIRE WINNERS
Sandeep Patri
Hyperammonemia Postlung Transplantation: An Uncommon But Life-Threatening Complication
Trung Nguyen
Dyspnea During Pregnancy Revealing Multiple Pulmonary Arteriovenous Malformations And A New Diagnosis Of Hereditary Hemorrhagic Telangiectasia
Pedro J. Baez, MD
Adenoid Cystic Adenocarcinoma: A Rare Esophageal Malignancy Misdiagnosed As COPD
Brette Guckian, DO
Management Of Pulmonary Cement Emboli After Kyphoplasty
Brinn Demars, DO
Tumor Emboli In The Pulmonary Artery Secondary To Chondrosarcoma: A Rare Presentation Mimicking Pulmonary Thromboembolism
Aakriti Arora
A Case Of Pulmonary Hypertension As A Possible Extracranial Manifestation Of Moyamoya Disease
Racine Elaine Reinoso
Clot In Transit: The Role Of Point-Of-Care Ultrasound In Early Diagnosis And Improved Outcomes
Qiraat Azeem, MD
A Case Of Autosomal-Dominant Hyper-IgE Syndrome Masquerading As Cystic Fibrosis
Jason R. Ballengee, DO
Third-Trimester Pregnancy Complicated By Non-Small Cell Lung Cancer Initially Presenting With Central Airway Obstruction And Stenosis
Sam Shafer
Caught In The Fray: Neurosarcoidosis Presenting As Chronic Respiratory Failure
Takkin Lo, MD, MPH
China White In Asthmatic Recreational Drug Users: Does It Contribute To Pneumatocele Development?
Sanjeev Shrestha, MD
Successful Treatment Of Microscopic Polyangiitis Using Novel Steroid-Sparing Agent Avacopan
Kristina Menchaca, MD
Cardiac Tamponade Without The Beck Triad: A Complication Of Severe Hypothyroidism
Olivia Millay, BS
Spontaneous Coronary Artery Dissection Of Left Anterior Descending Artery Complicated By Ventricular Septal Rupture
Akruti P. Prabhakar, DO
Delayed Lead Perforation Of The Right Atrium In The Presence Of Persistent Left Superior Vena Cava: A Rare Coincidence
Kevin Hsu, MD
A Modified Valsalva Maneuver For Ventilated And Sedated Patients With Unstable Supraventricular Tachycardia
Nang San Hti Lar Seng
Cardiovascular Manifestations Of Paraaortic Paragangliomas
Rocio Castillo-Larios
Membranous Dehiscence After Tracheal Resection And Reconstruction Healed Spontaneously With Conservative Treatment
Fizza Sajid, DO
A Young Broken Heart, Reversed
Janeen Grant-Sittol, MD
Inhaled Tranexamic Acid Use For Massive Hemoptysis In Vasculitis-Induced Bronchoalveolar Hemorrhage
Raman G. Kutty, Md, PhD
Progressive Lung Infiltrates In Patient With Acquired Immunodeficiency: A Rare Case Of GLILD
Tanwe Shende
Mycobacterium Shimoidei: A Rare Nontuberculous Infection In A U.S. Patient
Sarah M. Upson, MD
Not Your Typical Lactic Acidosis
Prachi Saluja, MD
Late-Onset Immune Thrombotic Thrombocytopenic Purpura (TTP) After Asymptomatic COVID-19 Infection
Steven S. Wu, MD
Type 1 Multiple Endocrine Neoplasia-Associated Tracheobronchial Tumors Managed By Rigid Bronchoscopy-Directed Multimodal Tumor Destruction
Konstantin Golubykh, MD
The Reversal That Helped: Role Of Bedside Echocardiography In Takotsubo Cardiomyopathy
Eric Salomon, MD
Obstructive Tracheobronchial Pulmonary Aspergillosis Managed With Local Bronchoscopic Intervention Alone
Daniel Hoesterey, MD
A Rare Case Of Critical Illness Due To Eczema Herpeticum With Disseminated Herpes Simplex Virus Infection
Awab U. Khan, DO
Severe Colchicine Toxicity In A Suicide Attempt Causing Multiorgan Failure: A Survival Story
Jacob Cebulko
Disseminated Strongyloidiasis In A Patient With Acute Lymphocytic Leukemia
Hasan Baher, MD
Hiding In Plain Sight: Disseminated Pulmonary TB
Navneet Ramesh
Multimodal Management Of Gastric Variceal Bleeding In Hemorrhagic Shock
Jason L. Peng, MD
Improving Compliance With Continuous Anterior Chest Compression In ARDS Caused By COVID-19: A Case Series
Sushan Gupta, MD
Complete Resolution Of Vasoreactive Pulmonary Artery Hypertension In Chronic Hypersensitive Pneumonitis
Mamta S. Chhabria, MD
A Fistulous Issue: Gastropleural Fistula As A Complication Of Gastrectomy
Anita Singh, DO, MBA
Identifying A Novel Surfactant Protein Mutation In A Family With Pulmonary Fibrosis
Rana Prathap Padappayil, MBBS
Delayed Cerebral Venous Sinus Thrombosis (CSVT) After An Invasive Meningioma Resection: An Uncommon Presentation Of A Common Complication
Rubabin Tooba, MD
The Morphing Cavity: An Image Series Of A Patient’s Pulmonary Infarction Over Time
Sally Ziatabar, DO
A Rare Case Of Disseminated Blastomycosis
Sumukh Arun Kumar
Incidental Pulmonary Cavitary Lesions As An Uncommon Presentation Of Lemierre Syndrome
Sophia Emetu
Pet Peeve: Dyspnea From Undiagnosed Pasteurella Multocida Empyema
Chidambaram Ramasamy, MD
A Case Of Diffuse Alveolar-Septal Pulmonary Amyloidosis And Cardiomyopathy
Rachel Swier
Acid-Fast Bacteria In Bronchiectasis: If The Glass Slipper Does Not Fit, Non-TB Mycobacteria, Consider Tsukamurella
Catherine Durant, MD
Idiopathic Multicentric Castleman Disease With Tafro Syndrome And Sjögren Syndrome
Ali Al-Hilli, MD, MSc
Sarcoidosis-Like Reaction During Treatment For Metastatic Breast Cancer With CDK 4/6 Inhibitors: Just An Epiphenomenon Or A Causal Relationship?
Scott Slusarenko, DO
Rapidly Progressive Perimyocarditis In SARS-CoV-2 Infection
Agatha M. Formoso, MD
Two Infants Presenting With Polymicrobial Pneumonia And Hypoxemic Respiratory Failure Associated With Heterozygous Variants In Carmil2 And Itk
Juan Adams-Chahin
The Silence Of “Lam”: A Case Of Tuberous Sclerosis Complex Associated With Lymphangioleiomyomatosis (Lam)
Kathleen Capaccione, MD
Lung Cancer Is Not Always The Answer: Exploring The Differential Diagnosis Of Thoracic Masses
Joann Wongvravit, DO
West Nile-Induced Myasthenia Gravis Crisis: An Unexpected Case Of Respiratory Failure
Ethan Karle, Do
A Rare Cause Of Community-Acquired Bacterial Pneumonia In A Patient With Poorly Controlled Diabetes
Taylor C. Becker, MD
Calcified Cavitary Conundrum: Delayed Diagnosis Of Histoplasmosis
Anneka Hutton, MD
Disseminated Listeriosis: A Deadly Triplicate
Omar Kandah, DO
COVID-19 Cardiac Tamponade With Cardiogenic Shock In A Previously Vaccinated Young Adult: A Case Report
Cihan Caglayan, MD
Partial Anomalous Pulmonary Venous Connection Diagnosed After Central Venous Catheter Placement
Michelle Jones, DO
Delayed Hemophagocytic Lymphohistiocytosis (HLH) Diagnosis In A Patient With Pulmonary Sarcoidosis And Newly Diagnosed T-Cell Lymphoma: A Case Report
Mariah Evarts, MD
A Normotensive Woman With Profound Lactic Acidosis And Stress-Induced Cardiomyopathy
Rachel V. Tan, MD
A Four-Boding Future: Polyviral Infection With SARS-CoV-2, Parainfluenza Virus Type 3, Influenza A, And Adenovirus
Thanh Hoang
Recurrent Syncope From Intermittent Torsades In Loperamide Abuse
Alissa Ali, MD
Ground Glass Opacities In A Patient Receiving Treatment With All-Trans Retinoic Acid And Arsenic Trioxide
Sean M. Masi, DO, MBA
Ferritin-Guided Therapeutic Plasma Exchange (TPE) Administration In COVID-19-Induced Cytokine Storm Syndrome: A Case Series
Anjali Sachdeva
Successful Biopsy Of Aortopulmonary Window Lymph Node With Robotic-Assisted Bronchoscopy
Rehan Saeed, MD
Multiple Sclerosis After COVID-19: A Sign Of Things To Come?
Harshitha Mergey Devender
Invasive Pulmonary Aspergillosis Associated With Nonspecific Interstitial Pneumonia Causing Recurrent Respiratory Failure
Be sure to check out the other award winners on page 20 in the January issue of CHEST Physician: https://tinyurl.com/2bcdcbj3 .
CHEST FOUNDATION GRANT AWARDS
CHEST Foundation Research Grant in Women’s Lung Health Disparities
Laura Sanapo, MD, The Miriam Hospital, Providence, R.I.
This grant is jointly supported by the CHEST Foundation and the Respiratory Health Association.
CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease
Benjamin Wu, MD, New York University
This grant is supported by AstraZeneca.
CHEST Foundation Research Grant in Chronic Obstructive Pulmonary Disease
Richard Zou, MD, University of Pittsburgh Medical Center
This grant is supported by the CHEST Foundation.
CHEST Foundation and AASM Foundation Research Grant in Sleep Medicine
Gonzalo Labarca, MD, Universidad San Sebastian, Concepción, Chile
This grant is jointly supported by the CHEST Foundation and AASM Foundation.
CHEST Foundation and American Academy of Dental Sleep Medicine Research Grant in Sleep Apnea
Sherri Katz, MD, FCCP, Children’s Hospital of Eastern Ontario, Ottawa
This grant is supported by the CHEST Foundation and American Academy of Dental Sleep Medicine.
CHEST Foundation Research Grant in Sleep Medicine
Nancy Stewart, DO, University of Kansas Medical Center, Kansas City
This grant is supported by Jazz Pharmaceuticals.
CHEST Foundation Research Grant in Severe Asthma
Gareth Walters, MD, University Hospitals Birmingham (England)
This grant is supported by AstraZeneca.
CHEST Foundation Research Grant in Severe Asthma
Andréanne Côté, MD, Institut Universitaire de Cardiologie et de Pneumologie de Québec, Quebec
This grant is supported by AstraZeneca.
CHEST Foundation and APCCMPD Research Grant in Medical Education
Christopher Leba, MD, MPH, University of California, San Francisco
This grant is jointly supported by the CHEST Foundation and APCCMPD.
CHEST Foundation Research Grant in COVID-19
Clea Barnett, MD, New York University
This grant is supported by the CHEST Foundation.
CHEST Foundation Research Grant in Critical Care
Katherine Walker, MD, Brigham and Women’s Hospital, Harvard Medical School, Boston
This grant is supported by the CHEST Foundation.
CHEST Foundation Research Grant in Venous Thromboembolism
Daniel Lachant, DO, University of Rochester (N.Y.) Medical Center/Strong Memorial Hospital
This grant is supported by the CHEST Foundation.
CHEST Foundation Research Grant in Pulmonary Hypertension
Christina Thornton, MD, PhD, University of Calgary (Alta.)
This grant is supported by the CHEST Foundation.
CHEST Foundation Research Grant in Pulmonary Fibrosis
Christina Eckhardt, MD, Columbia University, New York
This grant is supported by an independent grant from Boehringer Ingelheim Pharmaceuticals and Genentech.
CHEST Foundation Research Grant in Pulmonary Fibrosis
John Kim, MD, University of Virginia, Charlottesville
This grant is supported by an independent grant from Boehringer Ingelheim Pharmaceuticals and Genentech.
John R. Addrizzo, MD, FCCP Research Grant in Sarcoidosis
Kerry Hena, MD, New York University
This grant is in honor of John R. Addrizzo, MD, FCCP and is jointly supported by the Addrizzo family and the CHEST Foundation.
CHEST Foundation Research Grant in Pediatric Lung Health
Adam Shapiro, MD, McGill University Health Centre, Montreal
This grant is supported by the CHEST Foundation.
CHEST Foundation Young Investigator Grant
Sameer Avasarala, MD, Case Western Reserve University, Cleveland
This grant is supported by the CHEST Foundation.
CHEST/ALA/ATS Respiratory Health Equity Research Award
Matthew Triplette, MD, Fred Hutchinson Cancer Research Center, Seattle
The Respiratory Health Equity Research Award is jointly supported by the American Lung Association, the American Thoracic Society, and the CHEST Foundation.
CHEST/ALA/ATS Respiratory Health Equity Research Award
Ayobami Akenroye, MD, MPH, Brigham and Women’s Hospital, Boston
The Respiratory Health Equity Research Award is jointly supported by the American Lung Association, the American Thoracic Society, and the CHEST Foundation.
CHEST Foundation Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP
Lorriane Odhiambo, PhD, Augusta (Ga.) University
This grant is supported by the CHEST Foundation.
CHEST Foundation Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP
Katie Stevens, Team Telomere, New York
This grant is supported by the CHEST Foundation.
CHEST Foundation Community Service Grant Honoring D. Robert McCaffree, MD, Master FCCP
Matthew Sharpe, MD, The University of Kansas Medical Center, Kansas City
This grant is supported by the CHEST Foundation.
SCIENTIFIC ABSTRACT AWARDS
Alfred Soffer Research Awards
Presented abstracts will be judged by session moderators, and award recipients will be selected for their outstanding original scientific research. Finalists will be evaluated on the basis of their written abstract and the quality of their oral presentation. This award is named in honor of Alfred Soffer, MD, Master FCCP, who was Editor in Chief of the journal CHEST® from 1968 to 1993, and Executive Director of CHEST from 1969 to 1992.
Young Investigator Awards
Investigators who are enrolled in a training or fellowship program or who have completed a fellowship program within 5 years prior to CHEST 2022 are eligible for Young Investigator Awards.
Presenters will be evaluated on the basis of their written abstract and presentation. Recipients will be selected by judges from the Scientific Presentations and Awards Committee for their outstanding original scientific research.
Top Rapid Fire Abstract Award
Awards are granted to two presenters from all the rapid fire sessions at the CHEST Annual Meeting for outstanding original scientific research and presentation
Top Case Report Award
Awards are granted to one presenter in each oral case report session at the CHEST Annual Meeting for outstanding original scientific research and presentation
Top Rapid Fire Case Report Award
Awards are granted to one presenter in each rapid fire oral case report session at the CHEST Annual Meeting for outstanding original scientific research and presentation
ALFRED SOFFER RESEARCH AWARD WINNERS
Palak Rath, MD
A Sense Of Urgency: Boarding Of Critical Care Medicine Patients In The ED
Syed Nazeer Mahmood, MD
Quantifying The Risk For Overtreatment And Undertreatment Of Severe Community Onset Pneumonia
YOUNG INVESTIGATOR AWARD WINNERS
Anusha Devarajan, MD, MBBS
Pneumomediastinum And Pneumothorax In COVID-19 Pneumonia: A Matched Case-Control Study
Marjan Islam, MD
Thoracic Ultrasound In COVID-19: Use Of Lung And Diaphragm Ultrasound In Evaluating Dyspnea In Survivors Of Critical Illness From COVID-19 Pneumonia In A Post-ICU Clinic
Aaron St Laurent, MD
Duchenne Muscular Dystrophy Respiratory Profiles From Real-World Registry Data: A Retrospective Longitudinal Study
ABSTRACT RAPID FIRE WINNERS
Andrew J.O. Davis, MD
Early Gas Exchange Parameters Not Associated With Survival In COVID-19-Associated ARDS Patients Requiring Prolonged Venovenous Extracorporeal Membrane Oxygenation
Benjamin Emmanuel
Clinical Outcomes In Patients With Severe Asthma Who Had Or Had Not Initiated Biologic Therapy: Results From The CLEAR Study
CASE REPORT SESSION WINNERS
Sathya Alekhya Bukkuri
Smarca4-Deficient Undifferentiated Tumor: A Rare Thoracic Malignancy
Zachary A. Banbury, MD
Fungal Aortitis In A Patient For Whom Blood Transfusion Is Not An Option: A Rare But Potentially Fatal Complication Of Aortic Valve Replacement
Harinivaas Shanmugavel Geetha, MD
Respiratory Distress After Potentially Fatal Aspirin Overdose: When To Intubate?
Lisa Hayes
Systemic Epstein-Barr Virus-Related T-Cell Lymphoproliferative Disorder: A Rare Cause Of Dyspnea And Pulmonary Infiltrates In An Immunocompetent Adult
Mohammed Alsaggaf, MBBS
Calcium Oxalate Deposition In Pulmonary Aspergillosis
Cheyenne Snavely
Traffic Jam In The Vasculature: A Case Of Pulmonary Leukostasis
Clarissa Smith, MD
Talcoma In Lung Cancer Screening: A Rare Benign Cause Of PET Scan Avidity
Nitin Gupta, MD
The Clue Is In The Blood Gas: A Rare Manifestation Of Lactic Acidosis
Moses Hayrabedian, MD
A Century-Old Infection Mimicking Malignancy: A Case Of Diffuse Histoplasmosis
Gabriel R. Schroeder, MD
A Case Of Wind-Instrument Associated Hypersensitivity Pneumonitis
Fizza Sajid, DO
Leaping From Lush Tropical Environments To The L-Train: A Case Of Severe Leptospirosis In New York City
Krista R. Dollar, MD
Looking Past The Ground Glass: It Was Only Skin Deep
Konstantin Golubykh, MD
Point-Of-Care Ultrasound In The Timely Diagnosis Of Colonic Necrosis
Arsal Tharwani
Abdominal Compression In End-Stage Fibrotic Interstitial Lung Disease (ILD) Improves Respiratory Compliance
Ryan Kozloski
When Asthma Isn’t: Multispecialty Approach To Fibrosing Mediastinitis
Zach S. Jarrett, DO
Vanishing Cancer: A Case Of Smoking-Related Organizing Pneumonia
Stephen Simeone
Intravascular Papillary Endothelial Hyperplasia Presenting As Thrombus In Transit With Acute Pulmonary Embolism
David Gruen, MD
Tackling Posterior Reversible Encephalopathy Syndrome (PRES): A Rare Case Of Subtherapeutic Tacrolimus Causing PRES In Steroid-Resistant Nephropathy
Nicholas Kunce, MD
An Unusual Case Of Subacute Bacterial Endocarditis Presenting With Catastrophic Subarachnoid Hemorrhage
Phillip J. Gary, MD
Sarcoid-Like Reaction After Treatment With Pembrolizumab
Shreya Podder, MD
Endobronchial Valves For Treatment Of Persistent Air Leak After Secondary Spontaneous Pneumothorax In Patients With Cystic Fibrosis
Alina Aw Wasim, MD, MBBS
Chest-Wall Castleman Disease Mimicking Thymoma Drop Metastasis
Ndausung Udongwo
The ‘Rat Bite Sign” On Cardiac MRI: Left Dominant Arrhythmogenic Cardiomyopathy As An Atypical Etiology Of Sudden Cardiac Arrest
Grant Senyei, MD
Management Of Ventriculopleural Shunt-Associated Pleural Effusion
Garima Singh, MD
COVID-19-Associated Thrombotic Thrombocytopenia Purpura (TTP)
CASE REPORT RAPID FIRE WINNERS
Sandeep Patri
Hyperammonemia Postlung Transplantation: An Uncommon But Life-Threatening Complication
Trung Nguyen
Dyspnea During Pregnancy Revealing Multiple Pulmonary Arteriovenous Malformations And A New Diagnosis Of Hereditary Hemorrhagic Telangiectasia
Pedro J. Baez, MD
Adenoid Cystic Adenocarcinoma: A Rare Esophageal Malignancy Misdiagnosed As COPD
Brette Guckian, DO
Management Of Pulmonary Cement Emboli After Kyphoplasty
Brinn Demars, DO
Tumor Emboli In The Pulmonary Artery Secondary To Chondrosarcoma: A Rare Presentation Mimicking Pulmonary Thromboembolism
Aakriti Arora
A Case Of Pulmonary Hypertension As A Possible Extracranial Manifestation Of Moyamoya Disease
Racine Elaine Reinoso
Clot In Transit: The Role Of Point-Of-Care Ultrasound In Early Diagnosis And Improved Outcomes
Qiraat Azeem, MD
A Case Of Autosomal-Dominant Hyper-IgE Syndrome Masquerading As Cystic Fibrosis
Jason R. Ballengee, DO
Third-Trimester Pregnancy Complicated By Non-Small Cell Lung Cancer Initially Presenting With Central Airway Obstruction And Stenosis
Sam Shafer
Caught In The Fray: Neurosarcoidosis Presenting As Chronic Respiratory Failure
Takkin Lo, MD, MPH
China White In Asthmatic Recreational Drug Users: Does It Contribute To Pneumatocele Development?
Sanjeev Shrestha, MD
Successful Treatment Of Microscopic Polyangiitis Using Novel Steroid-Sparing Agent Avacopan
Kristina Menchaca, MD
Cardiac Tamponade Without The Beck Triad: A Complication Of Severe Hypothyroidism
Olivia Millay, BS
Spontaneous Coronary Artery Dissection Of Left Anterior Descending Artery Complicated By Ventricular Septal Rupture
Akruti P. Prabhakar, DO
Delayed Lead Perforation Of The Right Atrium In The Presence Of Persistent Left Superior Vena Cava: A Rare Coincidence
Kevin Hsu, MD
A Modified Valsalva Maneuver For Ventilated And Sedated Patients With Unstable Supraventricular Tachycardia
Nang San Hti Lar Seng
Cardiovascular Manifestations Of Paraaortic Paragangliomas
Rocio Castillo-Larios
Membranous Dehiscence After Tracheal Resection And Reconstruction Healed Spontaneously With Conservative Treatment
Fizza Sajid, DO
A Young Broken Heart, Reversed
Janeen Grant-Sittol, MD
Inhaled Tranexamic Acid Use For Massive Hemoptysis In Vasculitis-Induced Bronchoalveolar Hemorrhage
Raman G. Kutty, Md, PhD
Progressive Lung Infiltrates In Patient With Acquired Immunodeficiency: A Rare Case Of GLILD
Tanwe Shende
Mycobacterium Shimoidei: A Rare Nontuberculous Infection In A U.S. Patient
Sarah M. Upson, MD
Not Your Typical Lactic Acidosis
Prachi Saluja, MD
Late-Onset Immune Thrombotic Thrombocytopenic Purpura (TTP) After Asymptomatic COVID-19 Infection
Steven S. Wu, MD
Type 1 Multiple Endocrine Neoplasia-Associated Tracheobronchial Tumors Managed By Rigid Bronchoscopy-Directed Multimodal Tumor Destruction
Konstantin Golubykh, MD
The Reversal That Helped: Role Of Bedside Echocardiography In Takotsubo Cardiomyopathy
Eric Salomon, MD
Obstructive Tracheobronchial Pulmonary Aspergillosis Managed With Local Bronchoscopic Intervention Alone
Daniel Hoesterey, MD
A Rare Case Of Critical Illness Due To Eczema Herpeticum With Disseminated Herpes Simplex Virus Infection
Awab U. Khan, DO
Severe Colchicine Toxicity In A Suicide Attempt Causing Multiorgan Failure: A Survival Story
Jacob Cebulko
Disseminated Strongyloidiasis In A Patient With Acute Lymphocytic Leukemia
Hasan Baher, MD
Hiding In Plain Sight: Disseminated Pulmonary TB
Navneet Ramesh
Multimodal Management Of Gastric Variceal Bleeding In Hemorrhagic Shock
Jason L. Peng, MD
Improving Compliance With Continuous Anterior Chest Compression In ARDS Caused By COVID-19: A Case Series
Sushan Gupta, MD
Complete Resolution Of Vasoreactive Pulmonary Artery Hypertension In Chronic Hypersensitive Pneumonitis
Mamta S. Chhabria, MD
A Fistulous Issue: Gastropleural Fistula As A Complication Of Gastrectomy
Anita Singh, DO, MBA
Identifying A Novel Surfactant Protein Mutation In A Family With Pulmonary Fibrosis
Rana Prathap Padappayil, MBBS
Delayed Cerebral Venous Sinus Thrombosis (CSVT) After An Invasive Meningioma Resection: An Uncommon Presentation Of A Common Complication
Rubabin Tooba, MD
The Morphing Cavity: An Image Series Of A Patient’s Pulmonary Infarction Over Time
Sally Ziatabar, DO
A Rare Case Of Disseminated Blastomycosis
Sumukh Arun Kumar
Incidental Pulmonary Cavitary Lesions As An Uncommon Presentation Of Lemierre Syndrome
Sophia Emetu
Pet Peeve: Dyspnea From Undiagnosed Pasteurella Multocida Empyema
Chidambaram Ramasamy, MD
A Case Of Diffuse Alveolar-Septal Pulmonary Amyloidosis And Cardiomyopathy
Rachel Swier
Acid-Fast Bacteria In Bronchiectasis: If The Glass Slipper Does Not Fit, Non-TB Mycobacteria, Consider Tsukamurella
Catherine Durant, MD
Idiopathic Multicentric Castleman Disease With Tafro Syndrome And Sjögren Syndrome
Ali Al-Hilli, MD, MSc
Sarcoidosis-Like Reaction During Treatment For Metastatic Breast Cancer With CDK 4/6 Inhibitors: Just An Epiphenomenon Or A Causal Relationship?
Scott Slusarenko, DO
Rapidly Progressive Perimyocarditis In SARS-CoV-2 Infection
Agatha M. Formoso, MD
Two Infants Presenting With Polymicrobial Pneumonia And Hypoxemic Respiratory Failure Associated With Heterozygous Variants In Carmil2 And Itk
Juan Adams-Chahin
The Silence Of “Lam”: A Case Of Tuberous Sclerosis Complex Associated With Lymphangioleiomyomatosis (Lam)
Kathleen Capaccione, MD
Lung Cancer Is Not Always The Answer: Exploring The Differential Diagnosis Of Thoracic Masses
Joann Wongvravit, DO
West Nile-Induced Myasthenia Gravis Crisis: An Unexpected Case Of Respiratory Failure
Ethan Karle, Do
A Rare Cause Of Community-Acquired Bacterial Pneumonia In A Patient With Poorly Controlled Diabetes
Taylor C. Becker, MD
Calcified Cavitary Conundrum: Delayed Diagnosis Of Histoplasmosis
Anneka Hutton, MD
Disseminated Listeriosis: A Deadly Triplicate
Omar Kandah, DO
COVID-19 Cardiac Tamponade With Cardiogenic Shock In A Previously Vaccinated Young Adult: A Case Report
Cihan Caglayan, MD
Partial Anomalous Pulmonary Venous Connection Diagnosed After Central Venous Catheter Placement
Michelle Jones, DO
Delayed Hemophagocytic Lymphohistiocytosis (HLH) Diagnosis In A Patient With Pulmonary Sarcoidosis And Newly Diagnosed T-Cell Lymphoma: A Case Report
Mariah Evarts, MD
A Normotensive Woman With Profound Lactic Acidosis And Stress-Induced Cardiomyopathy
Rachel V. Tan, MD
A Four-Boding Future: Polyviral Infection With SARS-CoV-2, Parainfluenza Virus Type 3, Influenza A, And Adenovirus
Thanh Hoang
Recurrent Syncope From Intermittent Torsades In Loperamide Abuse
Alissa Ali, MD
Ground Glass Opacities In A Patient Receiving Treatment With All-Trans Retinoic Acid And Arsenic Trioxide
Sean M. Masi, DO, MBA
Ferritin-Guided Therapeutic Plasma Exchange (TPE) Administration In COVID-19-Induced Cytokine Storm Syndrome: A Case Series
Anjali Sachdeva
Successful Biopsy Of Aortopulmonary Window Lymph Node With Robotic-Assisted Bronchoscopy
Rehan Saeed, MD
Multiple Sclerosis After COVID-19: A Sign Of Things To Come?
Harshitha Mergey Devender
Invasive Pulmonary Aspergillosis Associated With Nonspecific Interstitial Pneumonia Causing Recurrent Respiratory Failure
Be sure to check out the other award winners on page 20 in the January issue of CHEST Physician: https://tinyurl.com/2bcdcbj3 .
More evidence suggests oxytocin can be discontinued early in labor
A new randomized, open-label French trial offers more evidence that the discontinuation of oxytocin treatment after the earliest stages of labor may be safe. Stopping oxytocin didn’t appear to affect neonatal outcomes, compared with continual use of the medication. However, the first stage of labor lasted slightly longer – not surprisingly – in those in the intervention group, and many of those who stopped oxytocin treatment resumed it later.
“Our trial did not show any impact of oxytocin discontinuation in the active [labor] stage on neonatal morbidity cesarean delivery, postpartum hemorrhage, birth experience, and postpartum depression,” said Aude Girault, MD, PhD, of Paris Cité University, in a presentation in San Francisco at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The goal of the STOPOXY study is to build upon previous research that found oxytocin discontinuation didn’t boost the risk of cesarean delivery rates, uterine hyperstimulation, and abnormal fetal heart rate, Dr. Girault said. “These studies were underpowered to show any effects on neonatal morbidity,” so she and colleagues decided to dig deeper into the issue by launching the new trial.
From 2020 to 2022, researchers assigned 2,367 women who received oxytocin before 4 centimeters dilation to either continue with the drug (n = 1,192) or discontinue it before reaching 6 centimeters dilation (n = 1,175). Overall, the women were pregnant for the first time (around 55%) with a median age around 32 years and body mass index around 24.1 kg/m2. All had live, singleton, full-term babies.
More than a third – 37% – of those who discontinued oxytocin resumed treatment with the medication, while 5% of those in the control group stopped taking it.
The neonatal morbidity rate – defined via a composite variable based on umbilical arterial pH, umbilical arterial lactates, Apgar score, and/or neonatal ICU admission – was 10.0% in the intervention group and 10.1% in the control group (P = .94), the researchers reported. Cesarean delivery rates were similar (18.8% vs. 16.5%, respectively; P = .22). Apart from the duration of the active first stage, which was significantly higher in the intervention group (100 min [ interquartile range, 50-208 min] vs. 90 min [IQR, 45-150 min]; P = .001), there were no significant differences between the groups.
Dr. Girault said this increase in labor duration was “moderate and clinically debatable.”
In an interview, oncologist-gynecologist George Saade, MD, of the University of Texas Medical Branch, Galveston, noted that “oxytocin is frequently used for either induction or augmentation of labor ... with the goal of improving maternal and neonatal outcomes.”
Oxytocin itself is not expensive, Dr. Saade said. “However, when it is given, the patient requires more monitoring, which may increase cost.”
There’s debate over the proper use of oxytocin, which is available in a synthetic version as Pitocin, and researchers have been trying to understand whether it can safely be discontinued early in labor.
Potential side effects of oxytocin include heart disorders such as arrhythmia, asphyxia, neonatal seizure, and jaundice, low Apgar score, and fetal death. A boxed warning says: “Because the available data are inadequate to evaluate the benefits-to-risks considerations, oxytocin is not indicated for elective induction of labor.”
However, “overall oxytocin is commonly used and very safe as long as careful protocols are followed,” David N. Hackney, MD, MS, of University Hospitals Cleveland, said in an interview. “The medication itself does not have many negative side effects. With very high doses there can be a concern for water intoxication, though this is clinically very uncommon. Some prior studies have raised concerns about the use of oxytocin and subsequent long-term neurodevelopmental outcomes, though these associations are likely confounders and the mainstream opinion is that these are not truly biologically causative associations.”
A 2021 study in The BMJ randomly assigned 1,200 women to continue or discontinue oxytocin. There was a slight increase in cesarean sections in the discontinuation group but significantly lower risks of uterine hyperstimulation and abnormal fetal heart rate.
Dr. Hackney, who didn’t take part in the new study, said the trial is “well conducted and well executed.” However, it needs peer review before any of its findings should change practice.
He added that differences in delivery protocols between the United States and France should be considered. As he noted, Dr. Girault mentioned in a Q&A after her presentation that delayed second-stage labor is more common in France than in the United States.
The study was funded by the French National Ministry of Health. Disclosures for the authors were not provided. Dr. Saade and Dr. Hackney have no disclosures.
A new randomized, open-label French trial offers more evidence that the discontinuation of oxytocin treatment after the earliest stages of labor may be safe. Stopping oxytocin didn’t appear to affect neonatal outcomes, compared with continual use of the medication. However, the first stage of labor lasted slightly longer – not surprisingly – in those in the intervention group, and many of those who stopped oxytocin treatment resumed it later.
“Our trial did not show any impact of oxytocin discontinuation in the active [labor] stage on neonatal morbidity cesarean delivery, postpartum hemorrhage, birth experience, and postpartum depression,” said Aude Girault, MD, PhD, of Paris Cité University, in a presentation in San Francisco at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The goal of the STOPOXY study is to build upon previous research that found oxytocin discontinuation didn’t boost the risk of cesarean delivery rates, uterine hyperstimulation, and abnormal fetal heart rate, Dr. Girault said. “These studies were underpowered to show any effects on neonatal morbidity,” so she and colleagues decided to dig deeper into the issue by launching the new trial.
From 2020 to 2022, researchers assigned 2,367 women who received oxytocin before 4 centimeters dilation to either continue with the drug (n = 1,192) or discontinue it before reaching 6 centimeters dilation (n = 1,175). Overall, the women were pregnant for the first time (around 55%) with a median age around 32 years and body mass index around 24.1 kg/m2. All had live, singleton, full-term babies.
More than a third – 37% – of those who discontinued oxytocin resumed treatment with the medication, while 5% of those in the control group stopped taking it.
The neonatal morbidity rate – defined via a composite variable based on umbilical arterial pH, umbilical arterial lactates, Apgar score, and/or neonatal ICU admission – was 10.0% in the intervention group and 10.1% in the control group (P = .94), the researchers reported. Cesarean delivery rates were similar (18.8% vs. 16.5%, respectively; P = .22). Apart from the duration of the active first stage, which was significantly higher in the intervention group (100 min [ interquartile range, 50-208 min] vs. 90 min [IQR, 45-150 min]; P = .001), there were no significant differences between the groups.
Dr. Girault said this increase in labor duration was “moderate and clinically debatable.”
In an interview, oncologist-gynecologist George Saade, MD, of the University of Texas Medical Branch, Galveston, noted that “oxytocin is frequently used for either induction or augmentation of labor ... with the goal of improving maternal and neonatal outcomes.”
Oxytocin itself is not expensive, Dr. Saade said. “However, when it is given, the patient requires more monitoring, which may increase cost.”
There’s debate over the proper use of oxytocin, which is available in a synthetic version as Pitocin, and researchers have been trying to understand whether it can safely be discontinued early in labor.
Potential side effects of oxytocin include heart disorders such as arrhythmia, asphyxia, neonatal seizure, and jaundice, low Apgar score, and fetal death. A boxed warning says: “Because the available data are inadequate to evaluate the benefits-to-risks considerations, oxytocin is not indicated for elective induction of labor.”
However, “overall oxytocin is commonly used and very safe as long as careful protocols are followed,” David N. Hackney, MD, MS, of University Hospitals Cleveland, said in an interview. “The medication itself does not have many negative side effects. With very high doses there can be a concern for water intoxication, though this is clinically very uncommon. Some prior studies have raised concerns about the use of oxytocin and subsequent long-term neurodevelopmental outcomes, though these associations are likely confounders and the mainstream opinion is that these are not truly biologically causative associations.”
A 2021 study in The BMJ randomly assigned 1,200 women to continue or discontinue oxytocin. There was a slight increase in cesarean sections in the discontinuation group but significantly lower risks of uterine hyperstimulation and abnormal fetal heart rate.
Dr. Hackney, who didn’t take part in the new study, said the trial is “well conducted and well executed.” However, it needs peer review before any of its findings should change practice.
He added that differences in delivery protocols between the United States and France should be considered. As he noted, Dr. Girault mentioned in a Q&A after her presentation that delayed second-stage labor is more common in France than in the United States.
The study was funded by the French National Ministry of Health. Disclosures for the authors were not provided. Dr. Saade and Dr. Hackney have no disclosures.
A new randomized, open-label French trial offers more evidence that the discontinuation of oxytocin treatment after the earliest stages of labor may be safe. Stopping oxytocin didn’t appear to affect neonatal outcomes, compared with continual use of the medication. However, the first stage of labor lasted slightly longer – not surprisingly – in those in the intervention group, and many of those who stopped oxytocin treatment resumed it later.
“Our trial did not show any impact of oxytocin discontinuation in the active [labor] stage on neonatal morbidity cesarean delivery, postpartum hemorrhage, birth experience, and postpartum depression,” said Aude Girault, MD, PhD, of Paris Cité University, in a presentation in San Francisco at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The goal of the STOPOXY study is to build upon previous research that found oxytocin discontinuation didn’t boost the risk of cesarean delivery rates, uterine hyperstimulation, and abnormal fetal heart rate, Dr. Girault said. “These studies were underpowered to show any effects on neonatal morbidity,” so she and colleagues decided to dig deeper into the issue by launching the new trial.
From 2020 to 2022, researchers assigned 2,367 women who received oxytocin before 4 centimeters dilation to either continue with the drug (n = 1,192) or discontinue it before reaching 6 centimeters dilation (n = 1,175). Overall, the women were pregnant for the first time (around 55%) with a median age around 32 years and body mass index around 24.1 kg/m2. All had live, singleton, full-term babies.
More than a third – 37% – of those who discontinued oxytocin resumed treatment with the medication, while 5% of those in the control group stopped taking it.
The neonatal morbidity rate – defined via a composite variable based on umbilical arterial pH, umbilical arterial lactates, Apgar score, and/or neonatal ICU admission – was 10.0% in the intervention group and 10.1% in the control group (P = .94), the researchers reported. Cesarean delivery rates were similar (18.8% vs. 16.5%, respectively; P = .22). Apart from the duration of the active first stage, which was significantly higher in the intervention group (100 min [ interquartile range, 50-208 min] vs. 90 min [IQR, 45-150 min]; P = .001), there were no significant differences between the groups.
Dr. Girault said this increase in labor duration was “moderate and clinically debatable.”
In an interview, oncologist-gynecologist George Saade, MD, of the University of Texas Medical Branch, Galveston, noted that “oxytocin is frequently used for either induction or augmentation of labor ... with the goal of improving maternal and neonatal outcomes.”
Oxytocin itself is not expensive, Dr. Saade said. “However, when it is given, the patient requires more monitoring, which may increase cost.”
There’s debate over the proper use of oxytocin, which is available in a synthetic version as Pitocin, and researchers have been trying to understand whether it can safely be discontinued early in labor.
Potential side effects of oxytocin include heart disorders such as arrhythmia, asphyxia, neonatal seizure, and jaundice, low Apgar score, and fetal death. A boxed warning says: “Because the available data are inadequate to evaluate the benefits-to-risks considerations, oxytocin is not indicated for elective induction of labor.”
However, “overall oxytocin is commonly used and very safe as long as careful protocols are followed,” David N. Hackney, MD, MS, of University Hospitals Cleveland, said in an interview. “The medication itself does not have many negative side effects. With very high doses there can be a concern for water intoxication, though this is clinically very uncommon. Some prior studies have raised concerns about the use of oxytocin and subsequent long-term neurodevelopmental outcomes, though these associations are likely confounders and the mainstream opinion is that these are not truly biologically causative associations.”
A 2021 study in The BMJ randomly assigned 1,200 women to continue or discontinue oxytocin. There was a slight increase in cesarean sections in the discontinuation group but significantly lower risks of uterine hyperstimulation and abnormal fetal heart rate.
Dr. Hackney, who didn’t take part in the new study, said the trial is “well conducted and well executed.” However, it needs peer review before any of its findings should change practice.
He added that differences in delivery protocols between the United States and France should be considered. As he noted, Dr. Girault mentioned in a Q&A after her presentation that delayed second-stage labor is more common in France than in the United States.
The study was funded by the French National Ministry of Health. Disclosures for the authors were not provided. Dr. Saade and Dr. Hackney have no disclosures.
FROM THE PREGNANCY MEETING
Finding catatonia requires knowing what to look for
Catatonia is a psychomotor syndrome identified by its clinical phenotype. Unlike common psychiatric syndromes such as major depression that are characterized by self-report of symptoms, catatonia is identified chiefly by empirically evaluated signs on clinical evaluation. Its signs are recognized through observation, physical examination, or elicitation by clinical maneuvers or the presentation of stimuli. However, catatonia is often overlooked even though its clinical signs are often visibly apparent, including to the casual observer.
Why is catatonia underdiagnosed? A key modifiable factor appears to be a prevalent misunderstanding over what catatonia looks like.1 We have sought to address this in a few ways.
First identified was the need for comprehensive educational resources on how to assess for and recognize catatonia. Using the Bush-Francis Catatonia Rating Scale – the most widely used scale for catatonia in both research and clinical settings and the most cited publication in the catatonia literature – our team developed the BFCRS Training Manual and Coding Guide.2,3 This manual expands on the definitions of each BFCRS item based on how it was originally operationalized by the scale’s authors. Subsequently, we created a comprehensive set of educational resources including videos illustrating how to assess for catatonia, a video for each of the 23 items on the BFCRS, and self-assessment tools. All resources are freely available online at https://bfcrs.urmc.edu.4
Through this project it became apparent that there are many discrepancies across the field regarding the phenotype of catatonia. Specifically, a recent review inspired by this project set about to characterize the scope of distinctions across diagnostic systems and rating scales.5 For instance, each diagnostic system and rating scale includes a unique set of signs, approaches diagnostic thresholds differently, and often operationalizes clinical features in ways that lead either to criterion overlap (for example, combativeness would be scored both as combativeness and agitation on ICD-11) or contradictions with other systems or scales (for example, varied definitions of waxy flexibility). In the face of so many inconsistencies, what is a clinician to do? What follows is a discussion of how to apply the insights from this recent review in clinical and research settings.
Starting with DSM-5-TR and ICD-11 – the current editions of the two leading diagnostic systems – one might ask: How do they compare?6,7 Overall, these two systems are broadly aligned in terms of the catatonic syndrome. Both systems identify individual clinical signs (as opposed to symptom complexes). Both require three features as a diagnostic threshold. Most of the same clinical signs are included in both systems, and the definitions of individual items are largely equivalent. Additionally, both systems allow for diagnosis of catatonia in association with psychiatric and medical conditions and include a category for unspecified catatonia.
Despite these core agreements, though, there are several important distinctions. First, whereas all 12 signs included in DSM-5-TR count toward an ICD-11 catatonia diagnosis, the opposite cannot be said. ICD-11 includes several features that are not in DSM-5-TR: rigidity, verbigeration, withdrawal, staring, ambitendency, impulsivity, and combativeness. Next, autonomic abnormality, which signifies the most severe type of catatonia called malignant catatonia, is included as a potential comorbidity in ICD-11 but not mentioned in DSM-5-TR. Third, ICD-11 includes a separate diagnosis for substance-induced catatonia, whereas this condition would be diagnosed as unspecified catatonia in DSM-5-TR.
There are also elements missing from both systems. The most notable of these is that neither system specifies the period over which findings must be present for diagnosis. By clinical convention, the practical definition of 24 hours is appropriate in most instances. The clinical features identified during direct evaluation are usually sufficient for diagnosis, but additional signs observed or documented over the prior 24 hours should be incorporated as part of the clinical evaluation. Another distinction is how to handle clinical features before and after lorazepam challenge. As noted in the BFCRS Training Manual, it would be appropriate to compare “state assessments” (that is, restricted to features identified only during direct, in-person assessment) from before and after lorazepam administration to document improvement.4
Whereas DSM-5-TR and ICD-11 are broadly in agreement, comparing these systems with catatonia rating scales reveals many sources of potential confusion, but also concrete guidance on operationalizing individual items.5 How exactly should each of catatonia’s clinical signs be defined? Descriptions differ, and thresholds of duration and frequency vary considerably across scales. As a result, clinicians who use different scales and then convert these results to diagnostic criteria are liable to come to different clinical conclusions. For instance, both echophenomena and negativism must be elicited more than five times to be scored per Northoff,8 but even a single convincing instance of either would be scored on the BFCRS as “occasional.”2
Such discrepancies are important because, whereas the psychometric properties of several catatonia scales have been documented, there are no analogous studies on the DSM-5-TR and ICD-11 criteria. Therefore, it is essential for clinicians and researchers to document how diagnostic criteria have been operationalized. The most practical and evidence-based way to do this is to use a clinically validated scale and convert these to diagnostic criteria, yet in doing so a few modifications will be necessary.
Of the available clinical scales, the BFCRS is best positioned for clinical use. The BFCRS has been validated clinically and has good reliability, detailed item definitions and audiovisual examples available. In addition, it is the only scale with a published semistructured evaluation (see initial paper and Training Manual), which takes about 5 minutes.2,4 In terms of utility, all 12 signs included by DSM-5-TR are among the first 14 items on the BFCRS, which constitutes a standalone tool known as the Bush-Francis Catatonia Screening Instrument (BFCSI, see Table).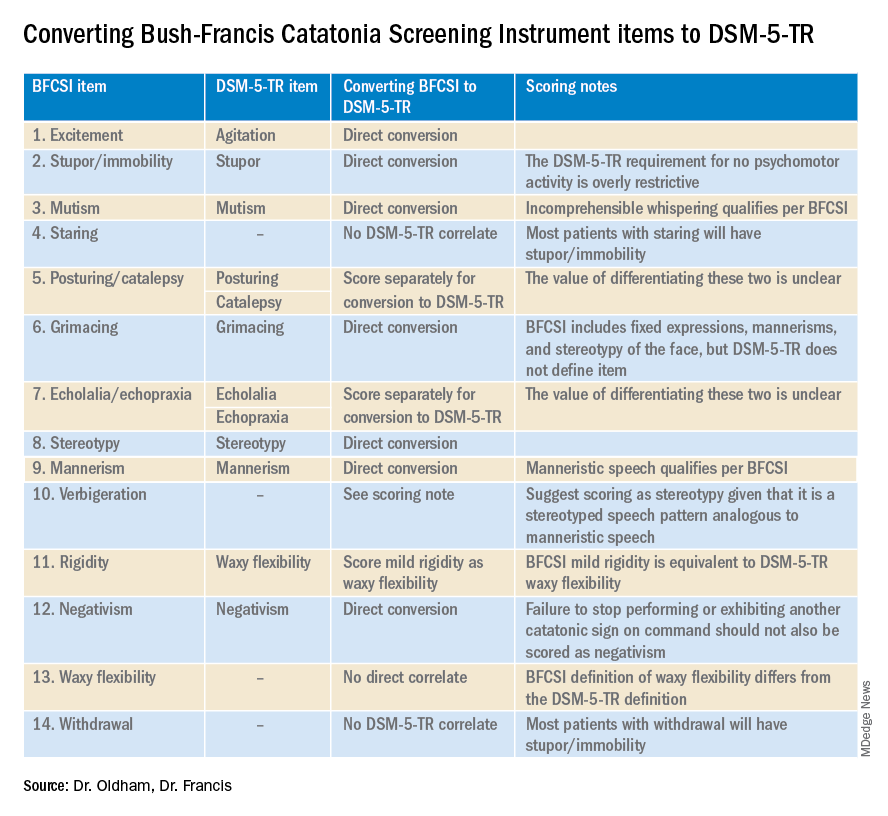
Many fundamental questions remain about catatonia,but the importance of a shared understanding of its clinical features is clear.9 Catatonia should be on the differential whenever a patient exhibits a markedly altered level of activity or grossly abnormal behavior, especially when inappropriate to context. We encourage readers to familiarize themselves with the phenotype of catatonia through online educational resources4 because the optimal care of patients with catatonia requires – at a minimum – that we know what we’re looking for.
Dr. Oldham is assistant professor of psychiatry at the University of Rochester (N.Y.) Medical Center. Dr. Francis is professor of psychiatry at Penn State University, Hershey. The authors declare no relevant conflicts of interest. Funding for the educational project hosted at https://bfcrs.urmc.edu was provided by the department of psychiatry at the University of Rochester Medical Center. Dr. Oldham is currently supported by a K23 career development award from the National Institute on Aging (AG072383). The educational resources referenced in this piece could not have been created were it not for the intellectual and thespian collaboration of Joshua R. Wortzel, MD, who is currently a fellow in child and adolescent psychiatry at Brown University, Providence, R.I. The authors are also indebted to Hochang B. Lee, MD, for his gracious support of this project.
References
1. Wortzel JR et al. J Clin Psychiatry. 2021 Aug 17;82(5):21m14025. doi: 10.4088/JCP.21m14025.
2. Bush G et al. Acta Psychiatr Scand. 1996 Feb;93(2):129-36. doi: 10.1111/j.1600-0447.1996.tb09814.x.
3. Weleff J et al. J Acad Consult Liaison Psychiatry. 2023 Jan-Feb;64(1):13-27. doi:10.1016/j.jaclp.2022.07.002.
4. Oldham MA et al. Bush-Francis Catatonia Rating Scale Assessment Resources. University of Rochester Medical Center, Department of Psychiatry. https://bfcrs.urmc.edu.
5. Oldham MA. Schizophr Res. 2022 Aug 19;S0920-9964(22)00294-8. doi: 10.1016/j.schres.2022.08.002.
6. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5-TR. Washington, D.C.: American Psychiatric Association Publishing, 2022.
7. World Health Organization. ICD-11 for Mortality and Morbidity Stastistics. 2022. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/486722075.
8. Northoff G et al. Mov Disord. May 1999;14(3):404-16. doi: 10.1002/1531-8257(199905)14:3<404::AID-MDS1004>3.0.CO;2-5.
9. Walther S et al. The Lancet Psychiatry. 2019 Jul;6(7):610-9. doi: 10.1016/S2215-0366(18)30474-7.
Catatonia is a psychomotor syndrome identified by its clinical phenotype. Unlike common psychiatric syndromes such as major depression that are characterized by self-report of symptoms, catatonia is identified chiefly by empirically evaluated signs on clinical evaluation. Its signs are recognized through observation, physical examination, or elicitation by clinical maneuvers or the presentation of stimuli. However, catatonia is often overlooked even though its clinical signs are often visibly apparent, including to the casual observer.
Why is catatonia underdiagnosed? A key modifiable factor appears to be a prevalent misunderstanding over what catatonia looks like.1 We have sought to address this in a few ways.
First identified was the need for comprehensive educational resources on how to assess for and recognize catatonia. Using the Bush-Francis Catatonia Rating Scale – the most widely used scale for catatonia in both research and clinical settings and the most cited publication in the catatonia literature – our team developed the BFCRS Training Manual and Coding Guide.2,3 This manual expands on the definitions of each BFCRS item based on how it was originally operationalized by the scale’s authors. Subsequently, we created a comprehensive set of educational resources including videos illustrating how to assess for catatonia, a video for each of the 23 items on the BFCRS, and self-assessment tools. All resources are freely available online at https://bfcrs.urmc.edu.4
Through this project it became apparent that there are many discrepancies across the field regarding the phenotype of catatonia. Specifically, a recent review inspired by this project set about to characterize the scope of distinctions across diagnostic systems and rating scales.5 For instance, each diagnostic system and rating scale includes a unique set of signs, approaches diagnostic thresholds differently, and often operationalizes clinical features in ways that lead either to criterion overlap (for example, combativeness would be scored both as combativeness and agitation on ICD-11) or contradictions with other systems or scales (for example, varied definitions of waxy flexibility). In the face of so many inconsistencies, what is a clinician to do? What follows is a discussion of how to apply the insights from this recent review in clinical and research settings.
Starting with DSM-5-TR and ICD-11 – the current editions of the two leading diagnostic systems – one might ask: How do they compare?6,7 Overall, these two systems are broadly aligned in terms of the catatonic syndrome. Both systems identify individual clinical signs (as opposed to symptom complexes). Both require three features as a diagnostic threshold. Most of the same clinical signs are included in both systems, and the definitions of individual items are largely equivalent. Additionally, both systems allow for diagnosis of catatonia in association with psychiatric and medical conditions and include a category for unspecified catatonia.
Despite these core agreements, though, there are several important distinctions. First, whereas all 12 signs included in DSM-5-TR count toward an ICD-11 catatonia diagnosis, the opposite cannot be said. ICD-11 includes several features that are not in DSM-5-TR: rigidity, verbigeration, withdrawal, staring, ambitendency, impulsivity, and combativeness. Next, autonomic abnormality, which signifies the most severe type of catatonia called malignant catatonia, is included as a potential comorbidity in ICD-11 but not mentioned in DSM-5-TR. Third, ICD-11 includes a separate diagnosis for substance-induced catatonia, whereas this condition would be diagnosed as unspecified catatonia in DSM-5-TR.
There are also elements missing from both systems. The most notable of these is that neither system specifies the period over which findings must be present for diagnosis. By clinical convention, the practical definition of 24 hours is appropriate in most instances. The clinical features identified during direct evaluation are usually sufficient for diagnosis, but additional signs observed or documented over the prior 24 hours should be incorporated as part of the clinical evaluation. Another distinction is how to handle clinical features before and after lorazepam challenge. As noted in the BFCRS Training Manual, it would be appropriate to compare “state assessments” (that is, restricted to features identified only during direct, in-person assessment) from before and after lorazepam administration to document improvement.4
Whereas DSM-5-TR and ICD-11 are broadly in agreement, comparing these systems with catatonia rating scales reveals many sources of potential confusion, but also concrete guidance on operationalizing individual items.5 How exactly should each of catatonia’s clinical signs be defined? Descriptions differ, and thresholds of duration and frequency vary considerably across scales. As a result, clinicians who use different scales and then convert these results to diagnostic criteria are liable to come to different clinical conclusions. For instance, both echophenomena and negativism must be elicited more than five times to be scored per Northoff,8 but even a single convincing instance of either would be scored on the BFCRS as “occasional.”2
Such discrepancies are important because, whereas the psychometric properties of several catatonia scales have been documented, there are no analogous studies on the DSM-5-TR and ICD-11 criteria. Therefore, it is essential for clinicians and researchers to document how diagnostic criteria have been operationalized. The most practical and evidence-based way to do this is to use a clinically validated scale and convert these to diagnostic criteria, yet in doing so a few modifications will be necessary.
Of the available clinical scales, the BFCRS is best positioned for clinical use. The BFCRS has been validated clinically and has good reliability, detailed item definitions and audiovisual examples available. In addition, it is the only scale with a published semistructured evaluation (see initial paper and Training Manual), which takes about 5 minutes.2,4 In terms of utility, all 12 signs included by DSM-5-TR are among the first 14 items on the BFCRS, which constitutes a standalone tool known as the Bush-Francis Catatonia Screening Instrument (BFCSI, see Table).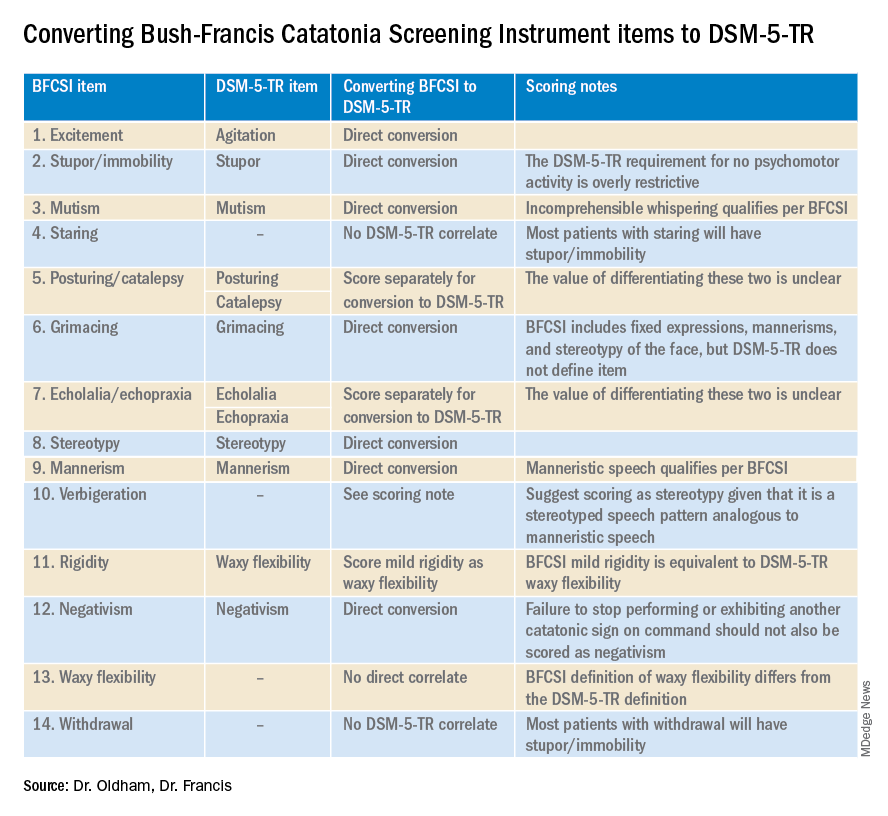
Many fundamental questions remain about catatonia,but the importance of a shared understanding of its clinical features is clear.9 Catatonia should be on the differential whenever a patient exhibits a markedly altered level of activity or grossly abnormal behavior, especially when inappropriate to context. We encourage readers to familiarize themselves with the phenotype of catatonia through online educational resources4 because the optimal care of patients with catatonia requires – at a minimum – that we know what we’re looking for.
Dr. Oldham is assistant professor of psychiatry at the University of Rochester (N.Y.) Medical Center. Dr. Francis is professor of psychiatry at Penn State University, Hershey. The authors declare no relevant conflicts of interest. Funding for the educational project hosted at https://bfcrs.urmc.edu was provided by the department of psychiatry at the University of Rochester Medical Center. Dr. Oldham is currently supported by a K23 career development award from the National Institute on Aging (AG072383). The educational resources referenced in this piece could not have been created were it not for the intellectual and thespian collaboration of Joshua R. Wortzel, MD, who is currently a fellow in child and adolescent psychiatry at Brown University, Providence, R.I. The authors are also indebted to Hochang B. Lee, MD, for his gracious support of this project.
References
1. Wortzel JR et al. J Clin Psychiatry. 2021 Aug 17;82(5):21m14025. doi: 10.4088/JCP.21m14025.
2. Bush G et al. Acta Psychiatr Scand. 1996 Feb;93(2):129-36. doi: 10.1111/j.1600-0447.1996.tb09814.x.
3. Weleff J et al. J Acad Consult Liaison Psychiatry. 2023 Jan-Feb;64(1):13-27. doi:10.1016/j.jaclp.2022.07.002.
4. Oldham MA et al. Bush-Francis Catatonia Rating Scale Assessment Resources. University of Rochester Medical Center, Department of Psychiatry. https://bfcrs.urmc.edu.
5. Oldham MA. Schizophr Res. 2022 Aug 19;S0920-9964(22)00294-8. doi: 10.1016/j.schres.2022.08.002.
6. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5-TR. Washington, D.C.: American Psychiatric Association Publishing, 2022.
7. World Health Organization. ICD-11 for Mortality and Morbidity Stastistics. 2022. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/486722075.
8. Northoff G et al. Mov Disord. May 1999;14(3):404-16. doi: 10.1002/1531-8257(199905)14:3<404::AID-MDS1004>3.0.CO;2-5.
9. Walther S et al. The Lancet Psychiatry. 2019 Jul;6(7):610-9. doi: 10.1016/S2215-0366(18)30474-7.
Catatonia is a psychomotor syndrome identified by its clinical phenotype. Unlike common psychiatric syndromes such as major depression that are characterized by self-report of symptoms, catatonia is identified chiefly by empirically evaluated signs on clinical evaluation. Its signs are recognized through observation, physical examination, or elicitation by clinical maneuvers or the presentation of stimuli. However, catatonia is often overlooked even though its clinical signs are often visibly apparent, including to the casual observer.
Why is catatonia underdiagnosed? A key modifiable factor appears to be a prevalent misunderstanding over what catatonia looks like.1 We have sought to address this in a few ways.
First identified was the need for comprehensive educational resources on how to assess for and recognize catatonia. Using the Bush-Francis Catatonia Rating Scale – the most widely used scale for catatonia in both research and clinical settings and the most cited publication in the catatonia literature – our team developed the BFCRS Training Manual and Coding Guide.2,3 This manual expands on the definitions of each BFCRS item based on how it was originally operationalized by the scale’s authors. Subsequently, we created a comprehensive set of educational resources including videos illustrating how to assess for catatonia, a video for each of the 23 items on the BFCRS, and self-assessment tools. All resources are freely available online at https://bfcrs.urmc.edu.4
Through this project it became apparent that there are many discrepancies across the field regarding the phenotype of catatonia. Specifically, a recent review inspired by this project set about to characterize the scope of distinctions across diagnostic systems and rating scales.5 For instance, each diagnostic system and rating scale includes a unique set of signs, approaches diagnostic thresholds differently, and often operationalizes clinical features in ways that lead either to criterion overlap (for example, combativeness would be scored both as combativeness and agitation on ICD-11) or contradictions with other systems or scales (for example, varied definitions of waxy flexibility). In the face of so many inconsistencies, what is a clinician to do? What follows is a discussion of how to apply the insights from this recent review in clinical and research settings.
Starting with DSM-5-TR and ICD-11 – the current editions of the two leading diagnostic systems – one might ask: How do they compare?6,7 Overall, these two systems are broadly aligned in terms of the catatonic syndrome. Both systems identify individual clinical signs (as opposed to symptom complexes). Both require three features as a diagnostic threshold. Most of the same clinical signs are included in both systems, and the definitions of individual items are largely equivalent. Additionally, both systems allow for diagnosis of catatonia in association with psychiatric and medical conditions and include a category for unspecified catatonia.
Despite these core agreements, though, there are several important distinctions. First, whereas all 12 signs included in DSM-5-TR count toward an ICD-11 catatonia diagnosis, the opposite cannot be said. ICD-11 includes several features that are not in DSM-5-TR: rigidity, verbigeration, withdrawal, staring, ambitendency, impulsivity, and combativeness. Next, autonomic abnormality, which signifies the most severe type of catatonia called malignant catatonia, is included as a potential comorbidity in ICD-11 but not mentioned in DSM-5-TR. Third, ICD-11 includes a separate diagnosis for substance-induced catatonia, whereas this condition would be diagnosed as unspecified catatonia in DSM-5-TR.
There are also elements missing from both systems. The most notable of these is that neither system specifies the period over which findings must be present for diagnosis. By clinical convention, the practical definition of 24 hours is appropriate in most instances. The clinical features identified during direct evaluation are usually sufficient for diagnosis, but additional signs observed or documented over the prior 24 hours should be incorporated as part of the clinical evaluation. Another distinction is how to handle clinical features before and after lorazepam challenge. As noted in the BFCRS Training Manual, it would be appropriate to compare “state assessments” (that is, restricted to features identified only during direct, in-person assessment) from before and after lorazepam administration to document improvement.4
Whereas DSM-5-TR and ICD-11 are broadly in agreement, comparing these systems with catatonia rating scales reveals many sources of potential confusion, but also concrete guidance on operationalizing individual items.5 How exactly should each of catatonia’s clinical signs be defined? Descriptions differ, and thresholds of duration and frequency vary considerably across scales. As a result, clinicians who use different scales and then convert these results to diagnostic criteria are liable to come to different clinical conclusions. For instance, both echophenomena and negativism must be elicited more than five times to be scored per Northoff,8 but even a single convincing instance of either would be scored on the BFCRS as “occasional.”2
Such discrepancies are important because, whereas the psychometric properties of several catatonia scales have been documented, there are no analogous studies on the DSM-5-TR and ICD-11 criteria. Therefore, it is essential for clinicians and researchers to document how diagnostic criteria have been operationalized. The most practical and evidence-based way to do this is to use a clinically validated scale and convert these to diagnostic criteria, yet in doing so a few modifications will be necessary.
Of the available clinical scales, the BFCRS is best positioned for clinical use. The BFCRS has been validated clinically and has good reliability, detailed item definitions and audiovisual examples available. In addition, it is the only scale with a published semistructured evaluation (see initial paper and Training Manual), which takes about 5 minutes.2,4 In terms of utility, all 12 signs included by DSM-5-TR are among the first 14 items on the BFCRS, which constitutes a standalone tool known as the Bush-Francis Catatonia Screening Instrument (BFCSI, see Table).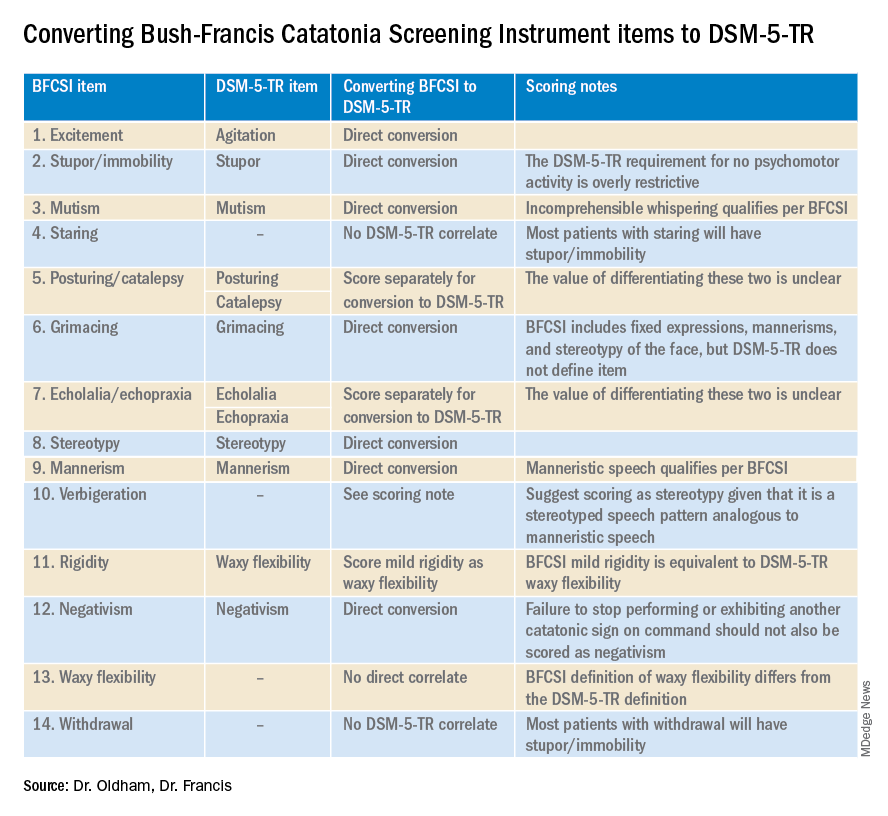
Many fundamental questions remain about catatonia,but the importance of a shared understanding of its clinical features is clear.9 Catatonia should be on the differential whenever a patient exhibits a markedly altered level of activity or grossly abnormal behavior, especially when inappropriate to context. We encourage readers to familiarize themselves with the phenotype of catatonia through online educational resources4 because the optimal care of patients with catatonia requires – at a minimum – that we know what we’re looking for.
Dr. Oldham is assistant professor of psychiatry at the University of Rochester (N.Y.) Medical Center. Dr. Francis is professor of psychiatry at Penn State University, Hershey. The authors declare no relevant conflicts of interest. Funding for the educational project hosted at https://bfcrs.urmc.edu was provided by the department of psychiatry at the University of Rochester Medical Center. Dr. Oldham is currently supported by a K23 career development award from the National Institute on Aging (AG072383). The educational resources referenced in this piece could not have been created were it not for the intellectual and thespian collaboration of Joshua R. Wortzel, MD, who is currently a fellow in child and adolescent psychiatry at Brown University, Providence, R.I. The authors are also indebted to Hochang B. Lee, MD, for his gracious support of this project.
References
1. Wortzel JR et al. J Clin Psychiatry. 2021 Aug 17;82(5):21m14025. doi: 10.4088/JCP.21m14025.
2. Bush G et al. Acta Psychiatr Scand. 1996 Feb;93(2):129-36. doi: 10.1111/j.1600-0447.1996.tb09814.x.
3. Weleff J et al. J Acad Consult Liaison Psychiatry. 2023 Jan-Feb;64(1):13-27. doi:10.1016/j.jaclp.2022.07.002.
4. Oldham MA et al. Bush-Francis Catatonia Rating Scale Assessment Resources. University of Rochester Medical Center, Department of Psychiatry. https://bfcrs.urmc.edu.
5. Oldham MA. Schizophr Res. 2022 Aug 19;S0920-9964(22)00294-8. doi: 10.1016/j.schres.2022.08.002.
6. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5-TR. Washington, D.C.: American Psychiatric Association Publishing, 2022.
7. World Health Organization. ICD-11 for Mortality and Morbidity Stastistics. 2022. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/486722075.
8. Northoff G et al. Mov Disord. May 1999;14(3):404-16. doi: 10.1002/1531-8257(199905)14:3<404::AID-MDS1004>3.0.CO;2-5.
9. Walther S et al. The Lancet Psychiatry. 2019 Jul;6(7):610-9. doi: 10.1016/S2215-0366(18)30474-7.
Anti-CD20 Monoclonal Antibodies for Treating Multiple Sclerosis
Multiple sclerosis (MS) is one of the most common causes of neurological disability in young adults, occurring more frequently in women than men. The development of anti-cluster of differentiation 20 (CD20) monoclonal antibodies (mAbs) in recent years has significantly changed the way we treat MS. Compared to older standards of care, such as chemotherapy and immunosuppressive drugs, anti-CD20 mAbs have been shown to be more effective in treating MS with fewer side effects.
Data have shown that B cells play a crucial role in the pathogenesis of MS via antigen-driven autoantibody responses and the cross-regulation of T-helper cells. CD20 is a protein that is expressed on the surface of B cells. Since B cells express the surface molecule CD20 at all points of differentiation, they provide a specific target for mAbs and are used to treat certain types of cancer and autoimmune disorders, including MS.
In people living with MS, the immune system mistakenly attacks the myelin sheath, a protective layer that surrounds nerve fibers in the central nervous system. This attack can cause inflammation and damage to the myelin sheath, leading to the development of various symptoms such as muscle weakness, vision problems, and issues with coordination and balance.
Anti-CD20 antibodies work by targeting and destroying B cells, which play a role in the immune system's attack on the myelin sheath. By targeting and destroying these cells, anti-CD20 antibodies may help to reduce the inflammation and damage to the myelin sheath and improve symptoms of MS.
There are several anti-CD20 mAbs used for the treatment of MS, including ocrelizumab, ofatumumab, ublituximab, and rituximab. Each drug has a unique mechanism of action and safety profile and distinct monitoring requirements. These therapies have been shown to deplete circulating B cells significantly for a certain amount of time, and they may be used in combination with other medications to treat MS.
Ocrelizumab, a humanized anti-CD20 mAb administered by intravenous (IV) infusion, was approved in March 2017 by the US Food and Drug Administration (FDA) and is the first proven treatment to reduce disability progression in both primary progressive MS and relapsing MS. Interestingly, ocrelizumab binds to a CD20 epitope that overlaps partially with the epitope to which rituximab binds.
Ofatumumab is the first fully human anti-CD20 mAb and was approved by the FDA in August 2020 for treating relapsing forms of MS. The approval was on the basis of data from the phase 3 ASCLEPIOS I and II trials, which compared ofatumumab with teriflunomide, an oral agent that reduces the activity of proliferating T lymphocytes and B lymphocytes, mitigating the overall inflammatory response in MS. Subcutaneous ofatumumab demonstrated better efficacy than oral teriflunomide in reducing the annualized relapse rate in patients with MS.
Ublituximab was recently approved by the FDA for treatment of relapsing forms of MS, including relapsing-remitting MS and active secondary progressive MS. Ublituximab works much like other anti-CD20 antibodies; however, it has been glycoengineered so that certain altered sugar molecules attached to the antibody increase its effectiveness.
Rituximab is a chimeric monoclonal B-cell–depleting anti-CD20 antibody that has also showed promise as an escalation and as a first-line therapy for MS. The FDA has not approved it for this specific use yet, so its use is considered “off label.” A 2017 study showed that ofatumumab was more effective at depleting B cells than high doses of IV rituximab.
It is important to note that anti-CD20 antibodies are not a cure for MS, and although they show promise for some patients, these agents do not work for everyone. The progress, severity, and specific symptoms of MS in any individual cannot yet be predicted; however, advances in research and treatment are leading to better understanding and moving us closer to curing this unpredictable, debilitating disease.
Multiple sclerosis (MS) is one of the most common causes of neurological disability in young adults, occurring more frequently in women than men. The development of anti-cluster of differentiation 20 (CD20) monoclonal antibodies (mAbs) in recent years has significantly changed the way we treat MS. Compared to older standards of care, such as chemotherapy and immunosuppressive drugs, anti-CD20 mAbs have been shown to be more effective in treating MS with fewer side effects.
Data have shown that B cells play a crucial role in the pathogenesis of MS via antigen-driven autoantibody responses and the cross-regulation of T-helper cells. CD20 is a protein that is expressed on the surface of B cells. Since B cells express the surface molecule CD20 at all points of differentiation, they provide a specific target for mAbs and are used to treat certain types of cancer and autoimmune disorders, including MS.
In people living with MS, the immune system mistakenly attacks the myelin sheath, a protective layer that surrounds nerve fibers in the central nervous system. This attack can cause inflammation and damage to the myelin sheath, leading to the development of various symptoms such as muscle weakness, vision problems, and issues with coordination and balance.
Anti-CD20 antibodies work by targeting and destroying B cells, which play a role in the immune system's attack on the myelin sheath. By targeting and destroying these cells, anti-CD20 antibodies may help to reduce the inflammation and damage to the myelin sheath and improve symptoms of MS.
There are several anti-CD20 mAbs used for the treatment of MS, including ocrelizumab, ofatumumab, ublituximab, and rituximab. Each drug has a unique mechanism of action and safety profile and distinct monitoring requirements. These therapies have been shown to deplete circulating B cells significantly for a certain amount of time, and they may be used in combination with other medications to treat MS.
Ocrelizumab, a humanized anti-CD20 mAb administered by intravenous (IV) infusion, was approved in March 2017 by the US Food and Drug Administration (FDA) and is the first proven treatment to reduce disability progression in both primary progressive MS and relapsing MS. Interestingly, ocrelizumab binds to a CD20 epitope that overlaps partially with the epitope to which rituximab binds.
Ofatumumab is the first fully human anti-CD20 mAb and was approved by the FDA in August 2020 for treating relapsing forms of MS. The approval was on the basis of data from the phase 3 ASCLEPIOS I and II trials, which compared ofatumumab with teriflunomide, an oral agent that reduces the activity of proliferating T lymphocytes and B lymphocytes, mitigating the overall inflammatory response in MS. Subcutaneous ofatumumab demonstrated better efficacy than oral teriflunomide in reducing the annualized relapse rate in patients with MS.
Ublituximab was recently approved by the FDA for treatment of relapsing forms of MS, including relapsing-remitting MS and active secondary progressive MS. Ublituximab works much like other anti-CD20 antibodies; however, it has been glycoengineered so that certain altered sugar molecules attached to the antibody increase its effectiveness.
Rituximab is a chimeric monoclonal B-cell–depleting anti-CD20 antibody that has also showed promise as an escalation and as a first-line therapy for MS. The FDA has not approved it for this specific use yet, so its use is considered “off label.” A 2017 study showed that ofatumumab was more effective at depleting B cells than high doses of IV rituximab.
It is important to note that anti-CD20 antibodies are not a cure for MS, and although they show promise for some patients, these agents do not work for everyone. The progress, severity, and specific symptoms of MS in any individual cannot yet be predicted; however, advances in research and treatment are leading to better understanding and moving us closer to curing this unpredictable, debilitating disease.
Multiple sclerosis (MS) is one of the most common causes of neurological disability in young adults, occurring more frequently in women than men. The development of anti-cluster of differentiation 20 (CD20) monoclonal antibodies (mAbs) in recent years has significantly changed the way we treat MS. Compared to older standards of care, such as chemotherapy and immunosuppressive drugs, anti-CD20 mAbs have been shown to be more effective in treating MS with fewer side effects.
Data have shown that B cells play a crucial role in the pathogenesis of MS via antigen-driven autoantibody responses and the cross-regulation of T-helper cells. CD20 is a protein that is expressed on the surface of B cells. Since B cells express the surface molecule CD20 at all points of differentiation, they provide a specific target for mAbs and are used to treat certain types of cancer and autoimmune disorders, including MS.
In people living with MS, the immune system mistakenly attacks the myelin sheath, a protective layer that surrounds nerve fibers in the central nervous system. This attack can cause inflammation and damage to the myelin sheath, leading to the development of various symptoms such as muscle weakness, vision problems, and issues with coordination and balance.
Anti-CD20 antibodies work by targeting and destroying B cells, which play a role in the immune system's attack on the myelin sheath. By targeting and destroying these cells, anti-CD20 antibodies may help to reduce the inflammation and damage to the myelin sheath and improve symptoms of MS.
There are several anti-CD20 mAbs used for the treatment of MS, including ocrelizumab, ofatumumab, ublituximab, and rituximab. Each drug has a unique mechanism of action and safety profile and distinct monitoring requirements. These therapies have been shown to deplete circulating B cells significantly for a certain amount of time, and they may be used in combination with other medications to treat MS.
Ocrelizumab, a humanized anti-CD20 mAb administered by intravenous (IV) infusion, was approved in March 2017 by the US Food and Drug Administration (FDA) and is the first proven treatment to reduce disability progression in both primary progressive MS and relapsing MS. Interestingly, ocrelizumab binds to a CD20 epitope that overlaps partially with the epitope to which rituximab binds.
Ofatumumab is the first fully human anti-CD20 mAb and was approved by the FDA in August 2020 for treating relapsing forms of MS. The approval was on the basis of data from the phase 3 ASCLEPIOS I and II trials, which compared ofatumumab with teriflunomide, an oral agent that reduces the activity of proliferating T lymphocytes and B lymphocytes, mitigating the overall inflammatory response in MS. Subcutaneous ofatumumab demonstrated better efficacy than oral teriflunomide in reducing the annualized relapse rate in patients with MS.
Ublituximab was recently approved by the FDA for treatment of relapsing forms of MS, including relapsing-remitting MS and active secondary progressive MS. Ublituximab works much like other anti-CD20 antibodies; however, it has been glycoengineered so that certain altered sugar molecules attached to the antibody increase its effectiveness.
Rituximab is a chimeric monoclonal B-cell–depleting anti-CD20 antibody that has also showed promise as an escalation and as a first-line therapy for MS. The FDA has not approved it for this specific use yet, so its use is considered “off label.” A 2017 study showed that ofatumumab was more effective at depleting B cells than high doses of IV rituximab.
It is important to note that anti-CD20 antibodies are not a cure for MS, and although they show promise for some patients, these agents do not work for everyone. The progress, severity, and specific symptoms of MS in any individual cannot yet be predicted; however, advances in research and treatment are leading to better understanding and moving us closer to curing this unpredictable, debilitating disease.
Commentary: Pregnancy, neck pain, and diet in migraine, February 2023
Migraine is a condition that particularly affects the population of reproductive-aged women. A significant amount of the literature discusses the effect of estrogen as a migraine trigger and specifically migraine with aura as a vascular risk factor. One topic that is not discussed in the literature is whether migraine could be a risk for miscarriage, also known as spontaneous abortion. The National Institutes of Health (NIH)-funded study by Crowe and colleagues looks at this risk, especially as it relates to the frequency of migraine, the use of acute migraine medications, and caffeine intake.
This was a broad study, including nearly 2000 patients with migraine, and was a continuation of a prior ongoing NIH-funded epidemiologic study. The initial study enrolled nearly 8000 participants, all of whom were women aged 21-45 years, were in a pregnancy planning stage, and were followed for up to 12 months or until a reported pregnancy. Questionnaires were given preconception, as well as early in pregnancy (defined as 8-9 weeks' gestation), and late in pregnancy (defined as 32 weeks' gestation).
During this study 19% of pregnancies ended in spontaneous abortion. A history of migraine preconception was not associated with spontaneous abortion risk on the basis of hazard ratios. There was a slight risk in those taking some migraine medication daily, either prophylactic or analgesic. Frequency of migraine itself was not noted as a risk for spontaneous abortion.
It is necessary that this important study be followed by further investigations looking at specific medication classes and their potential risk for spontaneous abortion. Migraine itself does not appear to be a risk for miscarriage; however, there remains the possibility that some preventive or acute medications may elevate this risk. At the current moment, there is not enough information to draw a conclusion. All clinicians who treat people with migraine, particularly women who are in their reproductive years, should continue to have conversations regarding pregnancy planning and the adjustment of both preventive and acute medications prior to conception.
Neck pain is a common comorbidity of both chronic and acute migraine, and botulinum toxin is a US Food and Drug Administration–approved treatment both for chronic migraine and certain painful neck conditions, including cervical dystonia. Migraine itself can be a disabling condition; when migraine is combined with other painful comorbidities the likelihood of disability becomes increased significantly. The standard PREEMPT protocol for botulinum toxin injection in chronic migraine of 155 units includes a number of injections in the trapezius and cervical paraspinal muscles. Many clinicians will give additional injections into these muscles and other areas around the neck, specifically targeting areas of neck and shoulder spasm and tenderness. Onan and colleagues investigated the quality of life and disability scores of patients who received these additional injections.
This was an open study, in which participants were given an additional 30 units of botulinum toxin into the general neck areas in a follow-the-pain protocol. The authors, used as a primary outcome, the reduction in the Migraine Disability Assessment (MIDAS) and Neck Disability Index (NDI) scores at 4 weeks and 3 months. The secondary outcome was the Headache Impact Test (HIT-6) score. An objective assessment of neck mobility or a quantification of trigger points were not calculated.
All scores, both the primary and secondary outcomes, were significantly decreased, and quality of life was also noted to be significantly improved with these additional injections. Most clinicians receive a 200-unit vial of botulinum toxin for each of their chronic migraine protocol injections. There is a growing body of evidence to argue that the additional units of botulinum toxin significantly improve outcomes, both regarding headache and neck pain. This study argues for delivering these additional injections of botulinum toxin, especially when neck pain is more prominent.
Much has been written about diet triggers and migraine recently. There has been some evidence for specific diet changes, ie, the addition of foods or nutrients that can be helpful or preventive for migraine. There is some evidence for the addition of omega-3 fatty acids. Huang and He investigated the effect of a high fiber diet on migraine frequency and severity.
This was a cross-sectional study involving data collected from the NIH/Centers for Disease Control and Prevention–sponsored National Health and Nutrition Examination Survey trial from 1999 to 2004. In the studied population, severe headache and migraine was present in approximately 20%, and dietary fiber intake was delineated on the basis of whether it was more than or less than 100 g/d. This study assessed dietary intake of fiber, via a 24-hour dietary recall that was conducted by trained interviewers during two interviews conducted over the course of 2 years.
A total of 12,000 participants were included in the study. There was a significant decrease in migraine severity between those with a higher and lower dietary fiber intake. The incidence of severe headache or migraine, as defined by frequency and severity, decreased in participants who had a dietary fiber intake > 100 g/d. The authors found that for every 10 g/d increase in dietary fiber intake, the prevalence of severe headache or migraine decreased by approximately 11%.
Although much has been written about the association between diet and migraine, most of the literature focuses on the avoidance of specific dietary triggers. A different consideration now exists, one that will likely increase compliance with dietary recommendations. Specifically, people treating patients with migraine can make recommendations regarding dietary changes that focus on adding specific healthy foods or other changes that can actually be associated with improving migraine frequency long-term. Recommending healthy fats, such as omega-3 fatty acids, and high fiber should be done for nearly all patients with migraine.
Migraine is a condition that particularly affects the population of reproductive-aged women. A significant amount of the literature discusses the effect of estrogen as a migraine trigger and specifically migraine with aura as a vascular risk factor. One topic that is not discussed in the literature is whether migraine could be a risk for miscarriage, also known as spontaneous abortion. The National Institutes of Health (NIH)-funded study by Crowe and colleagues looks at this risk, especially as it relates to the frequency of migraine, the use of acute migraine medications, and caffeine intake.
This was a broad study, including nearly 2000 patients with migraine, and was a continuation of a prior ongoing NIH-funded epidemiologic study. The initial study enrolled nearly 8000 participants, all of whom were women aged 21-45 years, were in a pregnancy planning stage, and were followed for up to 12 months or until a reported pregnancy. Questionnaires were given preconception, as well as early in pregnancy (defined as 8-9 weeks' gestation), and late in pregnancy (defined as 32 weeks' gestation).
During this study 19% of pregnancies ended in spontaneous abortion. A history of migraine preconception was not associated with spontaneous abortion risk on the basis of hazard ratios. There was a slight risk in those taking some migraine medication daily, either prophylactic or analgesic. Frequency of migraine itself was not noted as a risk for spontaneous abortion.
It is necessary that this important study be followed by further investigations looking at specific medication classes and their potential risk for spontaneous abortion. Migraine itself does not appear to be a risk for miscarriage; however, there remains the possibility that some preventive or acute medications may elevate this risk. At the current moment, there is not enough information to draw a conclusion. All clinicians who treat people with migraine, particularly women who are in their reproductive years, should continue to have conversations regarding pregnancy planning and the adjustment of both preventive and acute medications prior to conception.
Neck pain is a common comorbidity of both chronic and acute migraine, and botulinum toxin is a US Food and Drug Administration–approved treatment both for chronic migraine and certain painful neck conditions, including cervical dystonia. Migraine itself can be a disabling condition; when migraine is combined with other painful comorbidities the likelihood of disability becomes increased significantly. The standard PREEMPT protocol for botulinum toxin injection in chronic migraine of 155 units includes a number of injections in the trapezius and cervical paraspinal muscles. Many clinicians will give additional injections into these muscles and other areas around the neck, specifically targeting areas of neck and shoulder spasm and tenderness. Onan and colleagues investigated the quality of life and disability scores of patients who received these additional injections.
This was an open study, in which participants were given an additional 30 units of botulinum toxin into the general neck areas in a follow-the-pain protocol. The authors, used as a primary outcome, the reduction in the Migraine Disability Assessment (MIDAS) and Neck Disability Index (NDI) scores at 4 weeks and 3 months. The secondary outcome was the Headache Impact Test (HIT-6) score. An objective assessment of neck mobility or a quantification of trigger points were not calculated.
All scores, both the primary and secondary outcomes, were significantly decreased, and quality of life was also noted to be significantly improved with these additional injections. Most clinicians receive a 200-unit vial of botulinum toxin for each of their chronic migraine protocol injections. There is a growing body of evidence to argue that the additional units of botulinum toxin significantly improve outcomes, both regarding headache and neck pain. This study argues for delivering these additional injections of botulinum toxin, especially when neck pain is more prominent.
Much has been written about diet triggers and migraine recently. There has been some evidence for specific diet changes, ie, the addition of foods or nutrients that can be helpful or preventive for migraine. There is some evidence for the addition of omega-3 fatty acids. Huang and He investigated the effect of a high fiber diet on migraine frequency and severity.
This was a cross-sectional study involving data collected from the NIH/Centers for Disease Control and Prevention–sponsored National Health and Nutrition Examination Survey trial from 1999 to 2004. In the studied population, severe headache and migraine was present in approximately 20%, and dietary fiber intake was delineated on the basis of whether it was more than or less than 100 g/d. This study assessed dietary intake of fiber, via a 24-hour dietary recall that was conducted by trained interviewers during two interviews conducted over the course of 2 years.
A total of 12,000 participants were included in the study. There was a significant decrease in migraine severity between those with a higher and lower dietary fiber intake. The incidence of severe headache or migraine, as defined by frequency and severity, decreased in participants who had a dietary fiber intake > 100 g/d. The authors found that for every 10 g/d increase in dietary fiber intake, the prevalence of severe headache or migraine decreased by approximately 11%.
Although much has been written about the association between diet and migraine, most of the literature focuses on the avoidance of specific dietary triggers. A different consideration now exists, one that will likely increase compliance with dietary recommendations. Specifically, people treating patients with migraine can make recommendations regarding dietary changes that focus on adding specific healthy foods or other changes that can actually be associated with improving migraine frequency long-term. Recommending healthy fats, such as omega-3 fatty acids, and high fiber should be done for nearly all patients with migraine.
Migraine is a condition that particularly affects the population of reproductive-aged women. A significant amount of the literature discusses the effect of estrogen as a migraine trigger and specifically migraine with aura as a vascular risk factor. One topic that is not discussed in the literature is whether migraine could be a risk for miscarriage, also known as spontaneous abortion. The National Institutes of Health (NIH)-funded study by Crowe and colleagues looks at this risk, especially as it relates to the frequency of migraine, the use of acute migraine medications, and caffeine intake.
This was a broad study, including nearly 2000 patients with migraine, and was a continuation of a prior ongoing NIH-funded epidemiologic study. The initial study enrolled nearly 8000 participants, all of whom were women aged 21-45 years, were in a pregnancy planning stage, and were followed for up to 12 months or until a reported pregnancy. Questionnaires were given preconception, as well as early in pregnancy (defined as 8-9 weeks' gestation), and late in pregnancy (defined as 32 weeks' gestation).
During this study 19% of pregnancies ended in spontaneous abortion. A history of migraine preconception was not associated with spontaneous abortion risk on the basis of hazard ratios. There was a slight risk in those taking some migraine medication daily, either prophylactic or analgesic. Frequency of migraine itself was not noted as a risk for spontaneous abortion.
It is necessary that this important study be followed by further investigations looking at specific medication classes and their potential risk for spontaneous abortion. Migraine itself does not appear to be a risk for miscarriage; however, there remains the possibility that some preventive or acute medications may elevate this risk. At the current moment, there is not enough information to draw a conclusion. All clinicians who treat people with migraine, particularly women who are in their reproductive years, should continue to have conversations regarding pregnancy planning and the adjustment of both preventive and acute medications prior to conception.
Neck pain is a common comorbidity of both chronic and acute migraine, and botulinum toxin is a US Food and Drug Administration–approved treatment both for chronic migraine and certain painful neck conditions, including cervical dystonia. Migraine itself can be a disabling condition; when migraine is combined with other painful comorbidities the likelihood of disability becomes increased significantly. The standard PREEMPT protocol for botulinum toxin injection in chronic migraine of 155 units includes a number of injections in the trapezius and cervical paraspinal muscles. Many clinicians will give additional injections into these muscles and other areas around the neck, specifically targeting areas of neck and shoulder spasm and tenderness. Onan and colleagues investigated the quality of life and disability scores of patients who received these additional injections.
This was an open study, in which participants were given an additional 30 units of botulinum toxin into the general neck areas in a follow-the-pain protocol. The authors, used as a primary outcome, the reduction in the Migraine Disability Assessment (MIDAS) and Neck Disability Index (NDI) scores at 4 weeks and 3 months. The secondary outcome was the Headache Impact Test (HIT-6) score. An objective assessment of neck mobility or a quantification of trigger points were not calculated.
All scores, both the primary and secondary outcomes, were significantly decreased, and quality of life was also noted to be significantly improved with these additional injections. Most clinicians receive a 200-unit vial of botulinum toxin for each of their chronic migraine protocol injections. There is a growing body of evidence to argue that the additional units of botulinum toxin significantly improve outcomes, both regarding headache and neck pain. This study argues for delivering these additional injections of botulinum toxin, especially when neck pain is more prominent.
Much has been written about diet triggers and migraine recently. There has been some evidence for specific diet changes, ie, the addition of foods or nutrients that can be helpful or preventive for migraine. There is some evidence for the addition of omega-3 fatty acids. Huang and He investigated the effect of a high fiber diet on migraine frequency and severity.
This was a cross-sectional study involving data collected from the NIH/Centers for Disease Control and Prevention–sponsored National Health and Nutrition Examination Survey trial from 1999 to 2004. In the studied population, severe headache and migraine was present in approximately 20%, and dietary fiber intake was delineated on the basis of whether it was more than or less than 100 g/d. This study assessed dietary intake of fiber, via a 24-hour dietary recall that was conducted by trained interviewers during two interviews conducted over the course of 2 years.
A total of 12,000 participants were included in the study. There was a significant decrease in migraine severity between those with a higher and lower dietary fiber intake. The incidence of severe headache or migraine, as defined by frequency and severity, decreased in participants who had a dietary fiber intake > 100 g/d. The authors found that for every 10 g/d increase in dietary fiber intake, the prevalence of severe headache or migraine decreased by approximately 11%.
Although much has been written about the association between diet and migraine, most of the literature focuses on the avoidance of specific dietary triggers. A different consideration now exists, one that will likely increase compliance with dietary recommendations. Specifically, people treating patients with migraine can make recommendations regarding dietary changes that focus on adding specific healthy foods or other changes that can actually be associated with improving migraine frequency long-term. Recommending healthy fats, such as omega-3 fatty acids, and high fiber should be done for nearly all patients with migraine.