User login
Surgery for stress incontinence: Which technique for which patient?
-

-

-


Choosing appropriate surgical interventions is the focus of the second of our 2-part panel on stress urinary incontinence (SUI). The panelists discuss:
- how to weigh the factors that influence choice of technique, including Burch retropubic urethropexy and the various sling operations;
- the challenges of treating “mixed” stress and urge incontinence; and
- when to use bulking agents for intrinsic sphincteric deficiency.
The panelists also share tips on:
- how to help patients accurately describe their symptoms, and
- what issues to review with patients as they consider their options.
Part 1 covered medical therapies such as pelvic floor muscle rehabilitation, occlusive devices, and drugs. (Stress urinary incontinence: A closer look at nonsurgical therapies. OBG Management. 2003;15(9):40-51.)
Review surgical options with the patient
SAND: How do you counsel patients about surgical treatments for stress urinary incontinence?
MYERS: After the initial evaluation and diagnosis, I review the conservative options, and I also offer surgery. At this time, I discuss whether an operation is appropriate.
I work with the patient, going over her diagnosis as well as the different types of operations that are performed. Some patients are fairly well educated about their options, having looked up information on the Internet.
Next I explore whether other types of procedures need to be done concomitantly. For instance, does the patient need abdominal hysterectomy for some other reason? That would prompt me to offer an abdominal approach to the SUI. Do other types of vaginal surgery need to be done? Then I would probably opt for a vaginal approach.
I also look at the patient’s health status. Is she healthy and physically active? Or is she sedentary with comorbidities? In a woman who is a poor surgical candidate, I would consider less invasive procedures or procedures with less operative risk, such as urethral injections or the newer tape slings.
LUBER: When it comes to surgery for urinary incontinence, I like to reinforce the reconstructive nature of the repair, since patients tend to view surgical procedures as definitive. For example, when the uterus and ovaries are removed, they never bother that patient again. Incontinence procedures are different. Their effect is potentially time-limited, so it’s important to reinforce the patient’s understanding of their reconstructive and fallible nature.
At the first surgical consultation, I basically go through an informed consent. I do so again preoperatively, but I think it is a very important initial step for a patient who is considering surgery.
SAND: What if a patient isn’t sure she wants surgery?
LUBER: When a patient asks, “What should I do, Dr. Luber? Should I have an operation?” I like to use the example of standing in front of the refrigerator and asking, “Gee, am I hungry?” If you have to ask, you probably aren’t.
Potential surgical patients should feel extremely comfortable that they have exhausted all the nonsurgical options. Even if they have decided against nonsurgical therapy, they should feel very comfortable with that choice. Then I am confident we can work through any potential problems of surgery.
As for the operation itself, history has demonstrated the irresistible impulse to innovate during surgery for female stress incontinence. Literally hundreds of operations have been described, and dozens are currently in use; this reinforces the supposition that our techniques are imperfect, and the importance of basing what we do upon the available data. The 1997 American Urological Association guidelines are an excellent example. Looking forward, the National Institutes of Health are sponsoring studies comparing, for example, the goldstandard Burch to the goldstandard sling operation. In the next few years, we should have better evidence-based guidance.
Consider patient characteristics when choosing treatment
SAND: How do you select a surgical procedure for a particular patient?
MYERS: Because of all the different variables, I use various treatment arms. Since my institution does a large number of sling procedures, I am very comfortable performing those operations. I still do retropubic urethropexy. I also do the newer vaginal-tape procedures, and I use bulking agents for patients who have a demonstrated sphincter deficiency with no obvious support problems. Basically, I try to tailor my procedure to the patient.
For example, in a woman who requires a total abdominal hysterectomy for fibroids as well as an anti-incontinence procedure, I would do a Burch operation. For a woman who needed a vaginal hysterectomy, I probably would perform a sling procedure.
DAVILA: Ob/Gyns may be a bit unsure how to proceed at this point. For example, we formerly considered the Burch procedure the gold standard against which other procedures should be judged. Although I continue to view it as the standard, the Burch procedure increasingly is overlooked in favor of tension-free slings—due to increased marketing of the latter—for any form of stress incontinence. I think that has led us down a path that is not entirely beneficial for many of our patients.
In contrast to that approach, I use a basic evaluation of the patient to construct a treatment algorithm. In simple terms, 2 factors are taken into account: urethral sphincter function and bladder neck or urethral support. Using those 2 factors, I create a 2×2 table to select patients who do or don’t have urethral hypermobility and who do or don’t have sphincteric deficiency (TABLE).
For example, a patient with hypermobility and normal sphincter function has what we might consider “garden-variety” stress incontinence. Such patients do well with any form of treatment, whether it’s conservative therapy, a vaginal device, or a Burch procedure or tension-free sling.
I am more concerned when the patient has hypermobility with a significant degree of sphincteric deficiency. In recent years, the tendency has been to treat such patients with a tension-free sling. Although the literature is not absolutely clear, the success rate of tension-free slings in a patient with intrinsic sphincteric deficiency (ISD) is not as high as in a woman without ISD.1 So in these patients, I do a traditional sling.
Atrophy can cause significant urgency and nocturia symptoms.—Dr. Davila
The other 2 groups of patients have no hypermobility. I think most of us would agree that a woman with ISD and no hypermobility would best be treated with a bulking agent such as Contigen (C.R. Bard, Murray Hill, NJ) or Durasphere (Advanced Uroscience, St. Paul, Minn).
I have had good success rates with bulking agents. I do not think current data would support a tension-free sling in these patients.
Finally, there is the patient without hypermobility who has normal sphincter function. These patients do fairly well with conservative therapy, including pelvic floor exercises. They usually have mild forms of stress incontinence to begin with.
TABLE 1
Stress urinary incontinence treatment choices based on urethral support and urethral sphincteric function
| URETHRAL SUPPORT | URETHRAL SPHINCTERIC FUNCTION | |
|---|---|---|
| Bladder neck mobility (Q-tip test) | Normal urethral | Poor urethral function function |
| MUCP >20 cm H20 | LPP <20 cm H20 | |
| VLPP <60 cm H20 | VLPP >60 cm H20 | |
| Negative EBST | Positive EBST | |
| >30 degrees (hypermobility) | Kegel exercises | Traditional sling |
| Biofeedback | ||
| Vaginal device | ||
| Tension-free vaginal tape | ||
| Burch urethropexy | ||
| <30 degrees | Kegel exercises | Bulking agents |
| Biofeedback | ||
| Source: GW Davila, MD | ||
| EBST = empty bladder stress test; | ||
| MUCP = maximal urethral closure pressure; | ||
| VLPP = Valsalva leak point pressure | ||
| NOTE: Urethral plugs may function in all categories | ||
Simple method to assess sphincter function
DAVILA: This is the algorithm I tend to follow. It does entail evaluation of the urethral sphincter mechanism, but there are simpler ways to do that than with multi-channel urodynamics. For example, if the patient leaks with a Valsalva maneuver, after voiding, in a supine position, that suggests she has ISD and therefore is likely to have a low-pressure urethra or a low leak-point pressure. Multiple centers have reported on this.2,3
Role of urethral function in choice of treatment
LUBER: There seems to be 2 schools. The first dichotomizes urethral function to reasonable (“good” urethral function) versus unreasonable (“poor” urethral function or ISD) and selects the operation based on that. Thus, a Burch or supportive operation would be used for good urethral function with hypermobility, and a sling operation would be selected for poor urethral function or ISD.
More recently, some experts have preached an inclusive approach, whereby all patients undergo sling operations. That strategy evolved out of frustration over the difficulty of identifying which patients have poor urethral function. Unfortunately, we lack good long-term data on the potential downside of performing sling procedures on all patients with incontinence. Hopefully, over the next 3 years, the National Institutes of Health data will help clarify whether we need to dichotomize patients in terms of urethral function.
Meanwhile, at our center, we continue to consider urethral function the deciding factor as to whether patients will undergo a gold-standard Burch procedure or a sling. We steer toward a sling procedure when the patient clearly has poor urethral function or ISD. Of course in cases of the fixed immobile and poorly functioning urethra, we also make bulking agents available.
Additional factors in the choice of treatment
SAND: We throw 2 other things into the algorithm at our center: One is detrusor overactivity, which is very important when considering surgical treatment of stress urinary incontinence. The second is voiding function.
Activity level of the patient is an additional measure, as Dr. Myers commented on earlier. I’m not as concerned about age as I am about the patient’s physical activity and expectations for the operation over time. For example, for a woman who is relatively homebound and not physically active and has poor voiding function (underactive detrusor) and prolapse with normal intrinsic urethral function, a Kelly Kennedy procedure at the time of an anterior colporrhaphy may be more appropriate than a Burch procedure.
Detrusor overactivity is important because, in the trial that we performed, the Burch retropubic urethropexy had a 55% objective cure rate of concurrent detrusor overactivity and a 70% subjective cure rate of the symptom of urge urinary incontinence. In contrast, over the last 12 years, the sling procedure has had a resolution rate of between 20% and 28% for recurrent detrusor overactivity. Recent subjective data at 1 year for midurethral slings fall into the same range: 20% to 30% resolution of recurrent urge incontinence.
Another factor is de novo detrusor overactivity. The rate of de novo detrusor overactivity and urge incontinence in our sling patients seems consistently higher, compared with our retropubic urethropexy patients. We all know that the patient with urge incontinence is far more upset about her condition than the patient who has predictable stress incontinence, because urge incontinence can be far more destructive to quality of life. I try to encourage gynecologists to consider this factor.
Voiding function is less clear-cut. Basically, because intrinsic urethral function declines with age, it is not uncommon to see a woman in her 70s or 80s with ISD who also has absent detrusor contractions during voiding studies. The physician can assess this function by ultrasound or urodynamic testing, or by measuring the postvoid residual volume, which usually falls in the range of 100 to 200 mL, especially if no prolapse is present. Thus, even in cases in which I normally would want to do a sling for ISD, I opt against it if the patient has poor voiding function. That’s because the risk of permanent retention may rise as high as 15% to 20% in some of these patients.
Evaluation and treatment of mixed incontinence
DAVILA: I think we all agree that incontinence is easier to address than “hypercontinence” resulting from postoperative urethral obstruction, urinary retention, and irritative voiding symptoms. But what about patients with mixed incontinence? How do you evaluate them? Is there a role for surgical procedures in patients with primary urge incontinence?
I believe in offering all patients both nonsurgical and surgical options.—Dr. Sand
SAND: Many centers offer nonsurgical treatment of mixed incontinence, especially if urge incontinence predominates. But I believe in offering all patients both nonsurgical and surgical options. I end up triaging based on what patients select first, regardless of whether they have pure SUI or mixed symptoms, as long as they have been counseled appropriately about the expected outcomes of the various options.
MYERS: In my practice, I treat the urge symptoms first with anticholinergics or other medications. Then, if the stress incontinence continues, I offer a procedure.
This may be difficult in some cases, such as a patient with severe ISD. It is hard to treat detrusor overactivity when the urethral sphincter is weak, as the woman cannot hold increasing volumes of urine in the bladder.
Thus, I approach these cases by treating the stress incontinence first and then the urgency symptoms if intervention is still necessary—which is a 180-degree shift from my previous statement. In these cases, I treat the ISD first. Then, after the stress incontinence resolves, I offer medications for the urgency.
LUBER: I want to throw a little cold water on surgical treatment of overactive bladder. Clearly, this is an enormous issue. Probably 40% of women who come to my office complaining of urinary incontinence have mixed symptoms or mixed disease as determined by urodynamics. For the doctors out there caring for these patients daily, I think it is important to remember, as Dr. Sand mentioned, that in some cases, anti-incontinence operations can provoke detrusor overactivity in patients who were relatively asymptomatic previously. Dr. Myers’ suggestion that surgery may simply unmask the detrusor overactivity is also possible, of course.
Probably 40% of women who come to my office complaining of urinary incontinence have mixed symptoms.—Dr. Luber
Thus, I think it is reasonable to ask patients reporting mixed symptoms to characterize their urine loss. I usually have them pick a percentage (which isn’t always easy). I ask, “Is your urge incontinence 10%, 50% or 90% of your problem?” If urgency is 90% of the problem and stress incontinence is minimal, then naturally that patient’s care should be focused on the urge incontinence, and vice versa.
It becomes more problematic in the middle, with that 50/50 group. But I’m old-fashioned in that I like to treat the urge incontinence first and get that under control. Of course, in women with poor sphincter function, this distinction becomes more difficult because of the inevitable overlap of symptoms. But this is a small subset of the whole population.
DAVILA: Even if you operate on these patients to correct sphincter function, you must follow them closely. You shouldn’t be saying, “We’ll see you in 6 months.”
In addition, the cofactor of urogenital atrophy should be addressed. Atrophy can cause significant urinary urgency and nocturia symptoms, although most women may not report vaginal atrophy symptoms.4 Local estrogen cream at a low dosage can be used pre- and postoperatively without concern about systemic absorption.5
Which patients benefit from bulking agents?
SAND: We touched on the use of periurethral injections of bulking agents. How do you determine when bulking agents are appropriate?
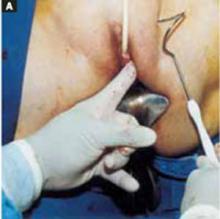
MYERS: I use periurethral injections for demonstrated sphincter deficiency. The ideal patient has a supported bladder neck and true sphincter deficiency—for example, patients whose sphincter deficiency is caused by pelvic radiation or significant surgical scarring.
In recent years, I have loosened the guidelines slightly, in that a number of my patients are elderly women with urethral hypermobility who are not healthy enough to undergo a major operation. In these patients, I use a pessary to support the bladder neck before performing an injection, and I make sure the patient understands that she will need to use the pessary even after the injection. I have better results when there is no hypermobility.
LUBER: The concept of ISD as the sole cause of urinary incontinence is less mysterious than it at first appears. In the typical patient with a fixed poorly functioning urethra, a Qtip test will be 0 degrees at rest, and will still be 0 degrees with straining. The patient will leak readily with any kind of provocative maneuver, be it coughing or slight straining. With or without urodynamics, we know that patient’s urethra is not functioning properly. Such a patient, for me, is the ideal candidate for bulking agents.
Unfortunately, bulking agents tend to have short half-lives of around 2 years. Still, you can improve the quality of life of these patients tremendously in that time by periurethrally injecting bulking agents during a very simple office or outpatient visit.
I have had less satisfaction and success using bulking agents in patients with urethral hypermobility, although I do like Dr. Myers’ idea of correcting the hypermobility with an intravaginal support device and then using collagen to improve their urethral coaptation. That’s a nice concept.
Improvements being studied
SAND: Currently, we have 2 injectables approved by the US Food and Drug Administration: collagen and carbon-coated microspheres. Are new agents coming out? Do you expect improvements in the current agents?
DAVILA: The number of bulking agents being studied right now is huge. I think the future will bring one that can be implanted without the need for cystoscopy. A couple of trials under way use a conical urethral template for needle placement, and the injection is performed without cystoscopy. Although we’re a number of years away from having enough data to support the widespread implementation of this approach, the momentum is certainly in that direction.
The half-lives of bulking agents also are increasing. Collagen was an excellent start, but we are moving toward permanence. In addition, most of the agents being studied are simpler to inject than collagen. Biotechnology is coming to the forefront with polymers that are either temperature-sensitive or able to reconfigure themselves over time. Thus, they should serve as a nidus for collagen deposition or remain in place longer, enhancing urethral sphincteric function.
It isn’t clear which agent will take a leading role in the next few years, but a number of them have great promise. This is an exciting time in the management of stress incontinence as we move from invasive procedures such as retropubic urethropexy to minimally invasive surgery—as well as from the operating room to the office.
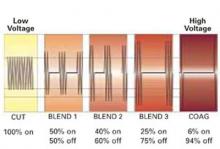
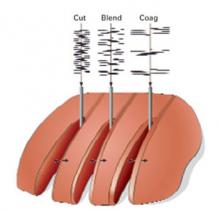
Radiofrequency technologies
SAND: What do you think about the new radiofrequency technologies being used to create support in periurethral tissues to correct hypermobility? Is there a role for this evolving technology?
LUBER: The concept of developing scar tissue adjacent to the urethra to provide better support underlies much of what we already do surgically. So there is some logic in the use of radiofrequency technologies to accomplish the same thing.
Still, there is the theoretical risk of further denervating the urethra, which is probably already denervated. Having looked at outcome studies for radiofrequency therapy, I think it’s a modality that can be embraced, but that should be done under the auspices of clinical research. Again, I’m old fashioned and am not comfortable integrating untested approaches into routine clinical care until we have adequate evidence of their effectiveness. In caring for incontinence, it is important that this effectiveness be looked at over a reasonable period of time, for example, 48 months.
It is hard to treat detrusor overactivity when the urethral sphincter is weak.—Dr. Myers
DAVILA: I have had some experience with radiofrequency therapy, and the tissue changes it stimulates are fairly impressive. I share your concern about the issue of denervation. In fact, my colleagues and I are hoping to initiate a trial in which we plan to look at pudendal latencies to the urethral sphincter in these patients. As of now, with limited experience, it appears that there is no worsening of urethral sphincter function with the therapy.
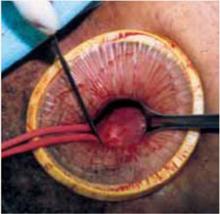
Tension-free vaginal tape
SAND: What about other new treatments on the horizon?
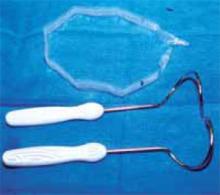
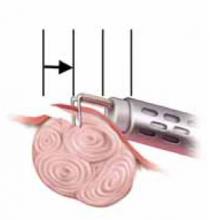
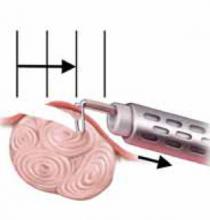
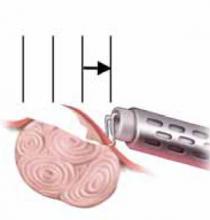
DAVILA: Like bulking agents, new minimally invasive surgical techniques are also increasing in number. The advent of the tension-free vaginal tape (TVT), a technique that moved from Sweden to the United States a couple of years ago, truly has revolutionized what we do in anti-incontinence surgery. I think we all can agree that it has changed our practice patterns quite significantly, and the modifications or theoretical improvements by different companies are likely to have a further impact.
Polypropylene mesh appears to be very well received by the body. It doesn’t get rejected or infected at a significant rate, so most physicians are comfortable with it. But I think it has become the surgeon’s preference as to which product works better.
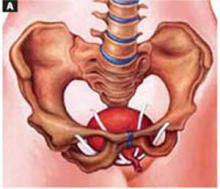
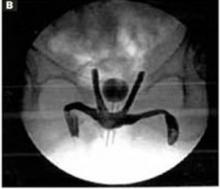
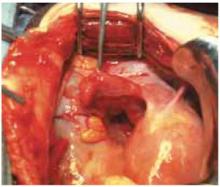
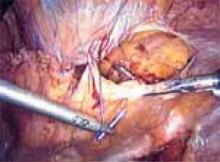
For the Ob/Gyn, the primary issue remains the small yet well-recognized risks of retropubic needle placement, beginning with bladder perforation and including vascular or bowel injury. As a result, many Ob/Gyns have probably been hesitant to perform these procedures.
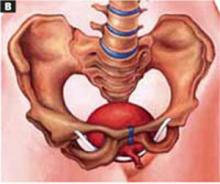
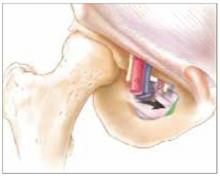
What the future holds is very exciting: the transobturator approach to surgery for stress incontinence. Instead of bringing the needle superiorly behind the pubic bone, the surgeon maneuvers it laterally beneath the pubic ramus and through the obturator membrane. This is an anti-incontinence procedure a gynecologist can embrace. It may not be necessary to perform cystoscopy afterward because the surgery is nowhere near the bladder.
The French have taken the lead in developing this technique and recently presented approximately 2 years of data.6,7 A US trial also is being initiated.
LUBER: TVT is billed as a midurethral procedure. However, when you consider where those tapes actually end up after a few months, it probably functions much like a traditional sling. Recent studies are in conflict: Some demonstrate the sling remains at the midurethra while others show that it readily migrates to the bladder neck. So the quest for a less obstructive procedure has not been fulfilled with the TVT.
In fact, in our recent TVT series that Drs. Lukacz and Nager are meticulously following, the voiding time increases and the maximum flow decreases postoperatively in roughly 30% of patients. So it definitely has some obstructive characteristics.
Quest for the Holy Grail continues
LUBER: I think we need to continue to explore these newer, less invasive procedures that offer wonderful potential. At this point, I might employ them in patients who are not able to tolerate the more invasive procedures or who flatly state that they want a less invasive operation. But I am not ready to embrace them as first-line therapy for all of my patients with stress incontinence.
Over the years, we have all seen various waves of surgical innovation, from the noincision urethropexies of the mid-1990s to the laparoscopic techniques prominent later in the decade. Now, more minimally invasive techniques are coming to the fore. At some point, we may even find the Holy Grail. But for the most part, we continue to evolve, examining new approaches until we are forced to reconcile with their limitations.
SAND: It is clear that this is a very exciting time to be treating SUI, with continuing innovation and an increased awareness of the problem by the public. While we all treat these women differently, there is a surprising consensus. We all seem to concur that the operation should be tailored to the individual, considering the relative balance of any concurrent urinary urge incontinence, urethral hypermobility, voiding dysfunction, and the woman’s health and activity level. We all use midurethral slings and periurethral bulking agents in selected women, but still also rely on Burch procedures and bladder-neck slings.
The authors report no financial relationship with any companies whose products are mentioned in this article.
1. Mutone N, Mastropietro M, Brizendine E, Hale D. Effect of tension-free vaginal tape procedure on urodynamic continence indices. Obstet Gynecol. 2001;98:638-645.
2. McLennan MT, Bent AE. Supine empty stress test as a predictor of low valsalva leak pressure. Neurourol Urodynamics. 1998;17:121-127.
3. Lobel RW, Sand PK. The empty supine stress test as a predictor of intrinsic urethral sphincter dysfunction. Obstet Gynecol. 1996;88:128-132.
4. Davila GW, Singh A, Karapanagiotou I, et al. Are women with urogenital atrophy symptomatic? Am J Obstet Gynecol. 2003;188:382-388.
5. Handa VL, Bachus KE, Johnston WW, Robboy SJ, Hammond CP. Vaginal administration of low-dose conjugated estrogens: systemic absorption and effects on the endometrium. Obstet Gynecol. 1994;84:215-218.
6. Delorme E. Transobturator sling: a minimally invasive procedure to treat female stress urinary incontinence. Prog Urol. 2001;11:1306-1313.
7. Dargent D, Bretones S, George P, Mellier G. Insertion of a suburethral sling through the obturator membrane in the treatment of female urinary incontinence. Gynecol Obstet Fertil. 2002;30:576-582.
-

-

-


Choosing appropriate surgical interventions is the focus of the second of our 2-part panel on stress urinary incontinence (SUI). The panelists discuss:
- how to weigh the factors that influence choice of technique, including Burch retropubic urethropexy and the various sling operations;
- the challenges of treating “mixed” stress and urge incontinence; and
- when to use bulking agents for intrinsic sphincteric deficiency.
The panelists also share tips on:
- how to help patients accurately describe their symptoms, and
- what issues to review with patients as they consider their options.
Part 1 covered medical therapies such as pelvic floor muscle rehabilitation, occlusive devices, and drugs. (Stress urinary incontinence: A closer look at nonsurgical therapies. OBG Management. 2003;15(9):40-51.)
Review surgical options with the patient
SAND: How do you counsel patients about surgical treatments for stress urinary incontinence?
MYERS: After the initial evaluation and diagnosis, I review the conservative options, and I also offer surgery. At this time, I discuss whether an operation is appropriate.
I work with the patient, going over her diagnosis as well as the different types of operations that are performed. Some patients are fairly well educated about their options, having looked up information on the Internet.
Next I explore whether other types of procedures need to be done concomitantly. For instance, does the patient need abdominal hysterectomy for some other reason? That would prompt me to offer an abdominal approach to the SUI. Do other types of vaginal surgery need to be done? Then I would probably opt for a vaginal approach.
I also look at the patient’s health status. Is she healthy and physically active? Or is she sedentary with comorbidities? In a woman who is a poor surgical candidate, I would consider less invasive procedures or procedures with less operative risk, such as urethral injections or the newer tape slings.
LUBER: When it comes to surgery for urinary incontinence, I like to reinforce the reconstructive nature of the repair, since patients tend to view surgical procedures as definitive. For example, when the uterus and ovaries are removed, they never bother that patient again. Incontinence procedures are different. Their effect is potentially time-limited, so it’s important to reinforce the patient’s understanding of their reconstructive and fallible nature.
At the first surgical consultation, I basically go through an informed consent. I do so again preoperatively, but I think it is a very important initial step for a patient who is considering surgery.
SAND: What if a patient isn’t sure she wants surgery?
LUBER: When a patient asks, “What should I do, Dr. Luber? Should I have an operation?” I like to use the example of standing in front of the refrigerator and asking, “Gee, am I hungry?” If you have to ask, you probably aren’t.
Potential surgical patients should feel extremely comfortable that they have exhausted all the nonsurgical options. Even if they have decided against nonsurgical therapy, they should feel very comfortable with that choice. Then I am confident we can work through any potential problems of surgery.
As for the operation itself, history has demonstrated the irresistible impulse to innovate during surgery for female stress incontinence. Literally hundreds of operations have been described, and dozens are currently in use; this reinforces the supposition that our techniques are imperfect, and the importance of basing what we do upon the available data. The 1997 American Urological Association guidelines are an excellent example. Looking forward, the National Institutes of Health are sponsoring studies comparing, for example, the goldstandard Burch to the goldstandard sling operation. In the next few years, we should have better evidence-based guidance.
Consider patient characteristics when choosing treatment
SAND: How do you select a surgical procedure for a particular patient?
MYERS: Because of all the different variables, I use various treatment arms. Since my institution does a large number of sling procedures, I am very comfortable performing those operations. I still do retropubic urethropexy. I also do the newer vaginal-tape procedures, and I use bulking agents for patients who have a demonstrated sphincter deficiency with no obvious support problems. Basically, I try to tailor my procedure to the patient.
For example, in a woman who requires a total abdominal hysterectomy for fibroids as well as an anti-incontinence procedure, I would do a Burch operation. For a woman who needed a vaginal hysterectomy, I probably would perform a sling procedure.
DAVILA: Ob/Gyns may be a bit unsure how to proceed at this point. For example, we formerly considered the Burch procedure the gold standard against which other procedures should be judged. Although I continue to view it as the standard, the Burch procedure increasingly is overlooked in favor of tension-free slings—due to increased marketing of the latter—for any form of stress incontinence. I think that has led us down a path that is not entirely beneficial for many of our patients.
In contrast to that approach, I use a basic evaluation of the patient to construct a treatment algorithm. In simple terms, 2 factors are taken into account: urethral sphincter function and bladder neck or urethral support. Using those 2 factors, I create a 2×2 table to select patients who do or don’t have urethral hypermobility and who do or don’t have sphincteric deficiency (TABLE).
For example, a patient with hypermobility and normal sphincter function has what we might consider “garden-variety” stress incontinence. Such patients do well with any form of treatment, whether it’s conservative therapy, a vaginal device, or a Burch procedure or tension-free sling.
I am more concerned when the patient has hypermobility with a significant degree of sphincteric deficiency. In recent years, the tendency has been to treat such patients with a tension-free sling. Although the literature is not absolutely clear, the success rate of tension-free slings in a patient with intrinsic sphincteric deficiency (ISD) is not as high as in a woman without ISD.1 So in these patients, I do a traditional sling.
Atrophy can cause significant urgency and nocturia symptoms.—Dr. Davila
The other 2 groups of patients have no hypermobility. I think most of us would agree that a woman with ISD and no hypermobility would best be treated with a bulking agent such as Contigen (C.R. Bard, Murray Hill, NJ) or Durasphere (Advanced Uroscience, St. Paul, Minn).
I have had good success rates with bulking agents. I do not think current data would support a tension-free sling in these patients.
Finally, there is the patient without hypermobility who has normal sphincter function. These patients do fairly well with conservative therapy, including pelvic floor exercises. They usually have mild forms of stress incontinence to begin with.
TABLE 1
Stress urinary incontinence treatment choices based on urethral support and urethral sphincteric function
| URETHRAL SUPPORT | URETHRAL SPHINCTERIC FUNCTION | |
|---|---|---|
| Bladder neck mobility (Q-tip test) | Normal urethral | Poor urethral function function |
| MUCP >20 cm H20 | LPP <20 cm H20 | |
| VLPP <60 cm H20 | VLPP >60 cm H20 | |
| Negative EBST | Positive EBST | |
| >30 degrees (hypermobility) | Kegel exercises | Traditional sling |
| Biofeedback | ||
| Vaginal device | ||
| Tension-free vaginal tape | ||
| Burch urethropexy | ||
| <30 degrees | Kegel exercises | Bulking agents |
| Biofeedback | ||
| Source: GW Davila, MD | ||
| EBST = empty bladder stress test; | ||
| MUCP = maximal urethral closure pressure; | ||
| VLPP = Valsalva leak point pressure | ||
| NOTE: Urethral plugs may function in all categories | ||
Simple method to assess sphincter function
DAVILA: This is the algorithm I tend to follow. It does entail evaluation of the urethral sphincter mechanism, but there are simpler ways to do that than with multi-channel urodynamics. For example, if the patient leaks with a Valsalva maneuver, after voiding, in a supine position, that suggests she has ISD and therefore is likely to have a low-pressure urethra or a low leak-point pressure. Multiple centers have reported on this.2,3
Role of urethral function in choice of treatment
LUBER: There seems to be 2 schools. The first dichotomizes urethral function to reasonable (“good” urethral function) versus unreasonable (“poor” urethral function or ISD) and selects the operation based on that. Thus, a Burch or supportive operation would be used for good urethral function with hypermobility, and a sling operation would be selected for poor urethral function or ISD.
More recently, some experts have preached an inclusive approach, whereby all patients undergo sling operations. That strategy evolved out of frustration over the difficulty of identifying which patients have poor urethral function. Unfortunately, we lack good long-term data on the potential downside of performing sling procedures on all patients with incontinence. Hopefully, over the next 3 years, the National Institutes of Health data will help clarify whether we need to dichotomize patients in terms of urethral function.
Meanwhile, at our center, we continue to consider urethral function the deciding factor as to whether patients will undergo a gold-standard Burch procedure or a sling. We steer toward a sling procedure when the patient clearly has poor urethral function or ISD. Of course in cases of the fixed immobile and poorly functioning urethra, we also make bulking agents available.
Additional factors in the choice of treatment
SAND: We throw 2 other things into the algorithm at our center: One is detrusor overactivity, which is very important when considering surgical treatment of stress urinary incontinence. The second is voiding function.
Activity level of the patient is an additional measure, as Dr. Myers commented on earlier. I’m not as concerned about age as I am about the patient’s physical activity and expectations for the operation over time. For example, for a woman who is relatively homebound and not physically active and has poor voiding function (underactive detrusor) and prolapse with normal intrinsic urethral function, a Kelly Kennedy procedure at the time of an anterior colporrhaphy may be more appropriate than a Burch procedure.
Detrusor overactivity is important because, in the trial that we performed, the Burch retropubic urethropexy had a 55% objective cure rate of concurrent detrusor overactivity and a 70% subjective cure rate of the symptom of urge urinary incontinence. In contrast, over the last 12 years, the sling procedure has had a resolution rate of between 20% and 28% for recurrent detrusor overactivity. Recent subjective data at 1 year for midurethral slings fall into the same range: 20% to 30% resolution of recurrent urge incontinence.
Another factor is de novo detrusor overactivity. The rate of de novo detrusor overactivity and urge incontinence in our sling patients seems consistently higher, compared with our retropubic urethropexy patients. We all know that the patient with urge incontinence is far more upset about her condition than the patient who has predictable stress incontinence, because urge incontinence can be far more destructive to quality of life. I try to encourage gynecologists to consider this factor.
Voiding function is less clear-cut. Basically, because intrinsic urethral function declines with age, it is not uncommon to see a woman in her 70s or 80s with ISD who also has absent detrusor contractions during voiding studies. The physician can assess this function by ultrasound or urodynamic testing, or by measuring the postvoid residual volume, which usually falls in the range of 100 to 200 mL, especially if no prolapse is present. Thus, even in cases in which I normally would want to do a sling for ISD, I opt against it if the patient has poor voiding function. That’s because the risk of permanent retention may rise as high as 15% to 20% in some of these patients.
Evaluation and treatment of mixed incontinence
DAVILA: I think we all agree that incontinence is easier to address than “hypercontinence” resulting from postoperative urethral obstruction, urinary retention, and irritative voiding symptoms. But what about patients with mixed incontinence? How do you evaluate them? Is there a role for surgical procedures in patients with primary urge incontinence?
I believe in offering all patients both nonsurgical and surgical options.—Dr. Sand
SAND: Many centers offer nonsurgical treatment of mixed incontinence, especially if urge incontinence predominates. But I believe in offering all patients both nonsurgical and surgical options. I end up triaging based on what patients select first, regardless of whether they have pure SUI or mixed symptoms, as long as they have been counseled appropriately about the expected outcomes of the various options.
MYERS: In my practice, I treat the urge symptoms first with anticholinergics or other medications. Then, if the stress incontinence continues, I offer a procedure.
This may be difficult in some cases, such as a patient with severe ISD. It is hard to treat detrusor overactivity when the urethral sphincter is weak, as the woman cannot hold increasing volumes of urine in the bladder.
Thus, I approach these cases by treating the stress incontinence first and then the urgency symptoms if intervention is still necessary—which is a 180-degree shift from my previous statement. In these cases, I treat the ISD first. Then, after the stress incontinence resolves, I offer medications for the urgency.
LUBER: I want to throw a little cold water on surgical treatment of overactive bladder. Clearly, this is an enormous issue. Probably 40% of women who come to my office complaining of urinary incontinence have mixed symptoms or mixed disease as determined by urodynamics. For the doctors out there caring for these patients daily, I think it is important to remember, as Dr. Sand mentioned, that in some cases, anti-incontinence operations can provoke detrusor overactivity in patients who were relatively asymptomatic previously. Dr. Myers’ suggestion that surgery may simply unmask the detrusor overactivity is also possible, of course.
Probably 40% of women who come to my office complaining of urinary incontinence have mixed symptoms.—Dr. Luber
Thus, I think it is reasonable to ask patients reporting mixed symptoms to characterize their urine loss. I usually have them pick a percentage (which isn’t always easy). I ask, “Is your urge incontinence 10%, 50% or 90% of your problem?” If urgency is 90% of the problem and stress incontinence is minimal, then naturally that patient’s care should be focused on the urge incontinence, and vice versa.
It becomes more problematic in the middle, with that 50/50 group. But I’m old-fashioned in that I like to treat the urge incontinence first and get that under control. Of course, in women with poor sphincter function, this distinction becomes more difficult because of the inevitable overlap of symptoms. But this is a small subset of the whole population.
DAVILA: Even if you operate on these patients to correct sphincter function, you must follow them closely. You shouldn’t be saying, “We’ll see you in 6 months.”
In addition, the cofactor of urogenital atrophy should be addressed. Atrophy can cause significant urinary urgency and nocturia symptoms, although most women may not report vaginal atrophy symptoms.4 Local estrogen cream at a low dosage can be used pre- and postoperatively without concern about systemic absorption.5
Which patients benefit from bulking agents?
SAND: We touched on the use of periurethral injections of bulking agents. How do you determine when bulking agents are appropriate?
MYERS: I use periurethral injections for demonstrated sphincter deficiency. The ideal patient has a supported bladder neck and true sphincter deficiency—for example, patients whose sphincter deficiency is caused by pelvic radiation or significant surgical scarring.
In recent years, I have loosened the guidelines slightly, in that a number of my patients are elderly women with urethral hypermobility who are not healthy enough to undergo a major operation. In these patients, I use a pessary to support the bladder neck before performing an injection, and I make sure the patient understands that she will need to use the pessary even after the injection. I have better results when there is no hypermobility.
LUBER: The concept of ISD as the sole cause of urinary incontinence is less mysterious than it at first appears. In the typical patient with a fixed poorly functioning urethra, a Qtip test will be 0 degrees at rest, and will still be 0 degrees with straining. The patient will leak readily with any kind of provocative maneuver, be it coughing or slight straining. With or without urodynamics, we know that patient’s urethra is not functioning properly. Such a patient, for me, is the ideal candidate for bulking agents.
Unfortunately, bulking agents tend to have short half-lives of around 2 years. Still, you can improve the quality of life of these patients tremendously in that time by periurethrally injecting bulking agents during a very simple office or outpatient visit.
I have had less satisfaction and success using bulking agents in patients with urethral hypermobility, although I do like Dr. Myers’ idea of correcting the hypermobility with an intravaginal support device and then using collagen to improve their urethral coaptation. That’s a nice concept.
Improvements being studied
SAND: Currently, we have 2 injectables approved by the US Food and Drug Administration: collagen and carbon-coated microspheres. Are new agents coming out? Do you expect improvements in the current agents?
DAVILA: The number of bulking agents being studied right now is huge. I think the future will bring one that can be implanted without the need for cystoscopy. A couple of trials under way use a conical urethral template for needle placement, and the injection is performed without cystoscopy. Although we’re a number of years away from having enough data to support the widespread implementation of this approach, the momentum is certainly in that direction.
The half-lives of bulking agents also are increasing. Collagen was an excellent start, but we are moving toward permanence. In addition, most of the agents being studied are simpler to inject than collagen. Biotechnology is coming to the forefront with polymers that are either temperature-sensitive or able to reconfigure themselves over time. Thus, they should serve as a nidus for collagen deposition or remain in place longer, enhancing urethral sphincteric function.
It isn’t clear which agent will take a leading role in the next few years, but a number of them have great promise. This is an exciting time in the management of stress incontinence as we move from invasive procedures such as retropubic urethropexy to minimally invasive surgery—as well as from the operating room to the office.
Radiofrequency technologies
SAND: What do you think about the new radiofrequency technologies being used to create support in periurethral tissues to correct hypermobility? Is there a role for this evolving technology?
LUBER: The concept of developing scar tissue adjacent to the urethra to provide better support underlies much of what we already do surgically. So there is some logic in the use of radiofrequency technologies to accomplish the same thing.
Still, there is the theoretical risk of further denervating the urethra, which is probably already denervated. Having looked at outcome studies for radiofrequency therapy, I think it’s a modality that can be embraced, but that should be done under the auspices of clinical research. Again, I’m old fashioned and am not comfortable integrating untested approaches into routine clinical care until we have adequate evidence of their effectiveness. In caring for incontinence, it is important that this effectiveness be looked at over a reasonable period of time, for example, 48 months.
It is hard to treat detrusor overactivity when the urethral sphincter is weak.—Dr. Myers
DAVILA: I have had some experience with radiofrequency therapy, and the tissue changes it stimulates are fairly impressive. I share your concern about the issue of denervation. In fact, my colleagues and I are hoping to initiate a trial in which we plan to look at pudendal latencies to the urethral sphincter in these patients. As of now, with limited experience, it appears that there is no worsening of urethral sphincter function with the therapy.
Tension-free vaginal tape
SAND: What about other new treatments on the horizon?
DAVILA: Like bulking agents, new minimally invasive surgical techniques are also increasing in number. The advent of the tension-free vaginal tape (TVT), a technique that moved from Sweden to the United States a couple of years ago, truly has revolutionized what we do in anti-incontinence surgery. I think we all can agree that it has changed our practice patterns quite significantly, and the modifications or theoretical improvements by different companies are likely to have a further impact.
Polypropylene mesh appears to be very well received by the body. It doesn’t get rejected or infected at a significant rate, so most physicians are comfortable with it. But I think it has become the surgeon’s preference as to which product works better.
For the Ob/Gyn, the primary issue remains the small yet well-recognized risks of retropubic needle placement, beginning with bladder perforation and including vascular or bowel injury. As a result, many Ob/Gyns have probably been hesitant to perform these procedures.
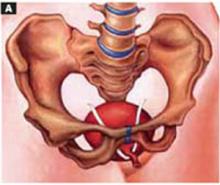
What the future holds is very exciting: the transobturator approach to surgery for stress incontinence. Instead of bringing the needle superiorly behind the pubic bone, the surgeon maneuvers it laterally beneath the pubic ramus and through the obturator membrane. This is an anti-incontinence procedure a gynecologist can embrace. It may not be necessary to perform cystoscopy afterward because the surgery is nowhere near the bladder.
The French have taken the lead in developing this technique and recently presented approximately 2 years of data.6,7 A US trial also is being initiated.
LUBER: TVT is billed as a midurethral procedure. However, when you consider where those tapes actually end up after a few months, it probably functions much like a traditional sling. Recent studies are in conflict: Some demonstrate the sling remains at the midurethra while others show that it readily migrates to the bladder neck. So the quest for a less obstructive procedure has not been fulfilled with the TVT.
In fact, in our recent TVT series that Drs. Lukacz and Nager are meticulously following, the voiding time increases and the maximum flow decreases postoperatively in roughly 30% of patients. So it definitely has some obstructive characteristics.
Quest for the Holy Grail continues
LUBER: I think we need to continue to explore these newer, less invasive procedures that offer wonderful potential. At this point, I might employ them in patients who are not able to tolerate the more invasive procedures or who flatly state that they want a less invasive operation. But I am not ready to embrace them as first-line therapy for all of my patients with stress incontinence.
Over the years, we have all seen various waves of surgical innovation, from the noincision urethropexies of the mid-1990s to the laparoscopic techniques prominent later in the decade. Now, more minimally invasive techniques are coming to the fore. At some point, we may even find the Holy Grail. But for the most part, we continue to evolve, examining new approaches until we are forced to reconcile with their limitations.
SAND: It is clear that this is a very exciting time to be treating SUI, with continuing innovation and an increased awareness of the problem by the public. While we all treat these women differently, there is a surprising consensus. We all seem to concur that the operation should be tailored to the individual, considering the relative balance of any concurrent urinary urge incontinence, urethral hypermobility, voiding dysfunction, and the woman’s health and activity level. We all use midurethral slings and periurethral bulking agents in selected women, but still also rely on Burch procedures and bladder-neck slings.
The authors report no financial relationship with any companies whose products are mentioned in this article.
-

-

-


Choosing appropriate surgical interventions is the focus of the second of our 2-part panel on stress urinary incontinence (SUI). The panelists discuss:
- how to weigh the factors that influence choice of technique, including Burch retropubic urethropexy and the various sling operations;
- the challenges of treating “mixed” stress and urge incontinence; and
- when to use bulking agents for intrinsic sphincteric deficiency.
The panelists also share tips on:
- how to help patients accurately describe their symptoms, and
- what issues to review with patients as they consider their options.
Part 1 covered medical therapies such as pelvic floor muscle rehabilitation, occlusive devices, and drugs. (Stress urinary incontinence: A closer look at nonsurgical therapies. OBG Management. 2003;15(9):40-51.)
Review surgical options with the patient
SAND: How do you counsel patients about surgical treatments for stress urinary incontinence?
MYERS: After the initial evaluation and diagnosis, I review the conservative options, and I also offer surgery. At this time, I discuss whether an operation is appropriate.
I work with the patient, going over her diagnosis as well as the different types of operations that are performed. Some patients are fairly well educated about their options, having looked up information on the Internet.
Next I explore whether other types of procedures need to be done concomitantly. For instance, does the patient need abdominal hysterectomy for some other reason? That would prompt me to offer an abdominal approach to the SUI. Do other types of vaginal surgery need to be done? Then I would probably opt for a vaginal approach.
I also look at the patient’s health status. Is she healthy and physically active? Or is she sedentary with comorbidities? In a woman who is a poor surgical candidate, I would consider less invasive procedures or procedures with less operative risk, such as urethral injections or the newer tape slings.
LUBER: When it comes to surgery for urinary incontinence, I like to reinforce the reconstructive nature of the repair, since patients tend to view surgical procedures as definitive. For example, when the uterus and ovaries are removed, they never bother that patient again. Incontinence procedures are different. Their effect is potentially time-limited, so it’s important to reinforce the patient’s understanding of their reconstructive and fallible nature.
At the first surgical consultation, I basically go through an informed consent. I do so again preoperatively, but I think it is a very important initial step for a patient who is considering surgery.
SAND: What if a patient isn’t sure she wants surgery?
LUBER: When a patient asks, “What should I do, Dr. Luber? Should I have an operation?” I like to use the example of standing in front of the refrigerator and asking, “Gee, am I hungry?” If you have to ask, you probably aren’t.
Potential surgical patients should feel extremely comfortable that they have exhausted all the nonsurgical options. Even if they have decided against nonsurgical therapy, they should feel very comfortable with that choice. Then I am confident we can work through any potential problems of surgery.
As for the operation itself, history has demonstrated the irresistible impulse to innovate during surgery for female stress incontinence. Literally hundreds of operations have been described, and dozens are currently in use; this reinforces the supposition that our techniques are imperfect, and the importance of basing what we do upon the available data. The 1997 American Urological Association guidelines are an excellent example. Looking forward, the National Institutes of Health are sponsoring studies comparing, for example, the goldstandard Burch to the goldstandard sling operation. In the next few years, we should have better evidence-based guidance.
Consider patient characteristics when choosing treatment
SAND: How do you select a surgical procedure for a particular patient?
MYERS: Because of all the different variables, I use various treatment arms. Since my institution does a large number of sling procedures, I am very comfortable performing those operations. I still do retropubic urethropexy. I also do the newer vaginal-tape procedures, and I use bulking agents for patients who have a demonstrated sphincter deficiency with no obvious support problems. Basically, I try to tailor my procedure to the patient.
For example, in a woman who requires a total abdominal hysterectomy for fibroids as well as an anti-incontinence procedure, I would do a Burch operation. For a woman who needed a vaginal hysterectomy, I probably would perform a sling procedure.
DAVILA: Ob/Gyns may be a bit unsure how to proceed at this point. For example, we formerly considered the Burch procedure the gold standard against which other procedures should be judged. Although I continue to view it as the standard, the Burch procedure increasingly is overlooked in favor of tension-free slings—due to increased marketing of the latter—for any form of stress incontinence. I think that has led us down a path that is not entirely beneficial for many of our patients.
In contrast to that approach, I use a basic evaluation of the patient to construct a treatment algorithm. In simple terms, 2 factors are taken into account: urethral sphincter function and bladder neck or urethral support. Using those 2 factors, I create a 2×2 table to select patients who do or don’t have urethral hypermobility and who do or don’t have sphincteric deficiency (TABLE).
For example, a patient with hypermobility and normal sphincter function has what we might consider “garden-variety” stress incontinence. Such patients do well with any form of treatment, whether it’s conservative therapy, a vaginal device, or a Burch procedure or tension-free sling.
I am more concerned when the patient has hypermobility with a significant degree of sphincteric deficiency. In recent years, the tendency has been to treat such patients with a tension-free sling. Although the literature is not absolutely clear, the success rate of tension-free slings in a patient with intrinsic sphincteric deficiency (ISD) is not as high as in a woman without ISD.1 So in these patients, I do a traditional sling.
Atrophy can cause significant urgency and nocturia symptoms.—Dr. Davila
The other 2 groups of patients have no hypermobility. I think most of us would agree that a woman with ISD and no hypermobility would best be treated with a bulking agent such as Contigen (C.R. Bard, Murray Hill, NJ) or Durasphere (Advanced Uroscience, St. Paul, Minn).
I have had good success rates with bulking agents. I do not think current data would support a tension-free sling in these patients.
Finally, there is the patient without hypermobility who has normal sphincter function. These patients do fairly well with conservative therapy, including pelvic floor exercises. They usually have mild forms of stress incontinence to begin with.
TABLE 1
Stress urinary incontinence treatment choices based on urethral support and urethral sphincteric function
| URETHRAL SUPPORT | URETHRAL SPHINCTERIC FUNCTION | |
|---|---|---|
| Bladder neck mobility (Q-tip test) | Normal urethral | Poor urethral function function |
| MUCP >20 cm H20 | LPP <20 cm H20 | |
| VLPP <60 cm H20 | VLPP >60 cm H20 | |
| Negative EBST | Positive EBST | |
| >30 degrees (hypermobility) | Kegel exercises | Traditional sling |
| Biofeedback | ||
| Vaginal device | ||
| Tension-free vaginal tape | ||
| Burch urethropexy | ||
| <30 degrees | Kegel exercises | Bulking agents |
| Biofeedback | ||
| Source: GW Davila, MD | ||
| EBST = empty bladder stress test; | ||
| MUCP = maximal urethral closure pressure; | ||
| VLPP = Valsalva leak point pressure | ||
| NOTE: Urethral plugs may function in all categories | ||
Simple method to assess sphincter function
DAVILA: This is the algorithm I tend to follow. It does entail evaluation of the urethral sphincter mechanism, but there are simpler ways to do that than with multi-channel urodynamics. For example, if the patient leaks with a Valsalva maneuver, after voiding, in a supine position, that suggests she has ISD and therefore is likely to have a low-pressure urethra or a low leak-point pressure. Multiple centers have reported on this.2,3
Role of urethral function in choice of treatment
LUBER: There seems to be 2 schools. The first dichotomizes urethral function to reasonable (“good” urethral function) versus unreasonable (“poor” urethral function or ISD) and selects the operation based on that. Thus, a Burch or supportive operation would be used for good urethral function with hypermobility, and a sling operation would be selected for poor urethral function or ISD.
More recently, some experts have preached an inclusive approach, whereby all patients undergo sling operations. That strategy evolved out of frustration over the difficulty of identifying which patients have poor urethral function. Unfortunately, we lack good long-term data on the potential downside of performing sling procedures on all patients with incontinence. Hopefully, over the next 3 years, the National Institutes of Health data will help clarify whether we need to dichotomize patients in terms of urethral function.
Meanwhile, at our center, we continue to consider urethral function the deciding factor as to whether patients will undergo a gold-standard Burch procedure or a sling. We steer toward a sling procedure when the patient clearly has poor urethral function or ISD. Of course in cases of the fixed immobile and poorly functioning urethra, we also make bulking agents available.
Additional factors in the choice of treatment
SAND: We throw 2 other things into the algorithm at our center: One is detrusor overactivity, which is very important when considering surgical treatment of stress urinary incontinence. The second is voiding function.
Activity level of the patient is an additional measure, as Dr. Myers commented on earlier. I’m not as concerned about age as I am about the patient’s physical activity and expectations for the operation over time. For example, for a woman who is relatively homebound and not physically active and has poor voiding function (underactive detrusor) and prolapse with normal intrinsic urethral function, a Kelly Kennedy procedure at the time of an anterior colporrhaphy may be more appropriate than a Burch procedure.
Detrusor overactivity is important because, in the trial that we performed, the Burch retropubic urethropexy had a 55% objective cure rate of concurrent detrusor overactivity and a 70% subjective cure rate of the symptom of urge urinary incontinence. In contrast, over the last 12 years, the sling procedure has had a resolution rate of between 20% and 28% for recurrent detrusor overactivity. Recent subjective data at 1 year for midurethral slings fall into the same range: 20% to 30% resolution of recurrent urge incontinence.
Another factor is de novo detrusor overactivity. The rate of de novo detrusor overactivity and urge incontinence in our sling patients seems consistently higher, compared with our retropubic urethropexy patients. We all know that the patient with urge incontinence is far more upset about her condition than the patient who has predictable stress incontinence, because urge incontinence can be far more destructive to quality of life. I try to encourage gynecologists to consider this factor.
Voiding function is less clear-cut. Basically, because intrinsic urethral function declines with age, it is not uncommon to see a woman in her 70s or 80s with ISD who also has absent detrusor contractions during voiding studies. The physician can assess this function by ultrasound or urodynamic testing, or by measuring the postvoid residual volume, which usually falls in the range of 100 to 200 mL, especially if no prolapse is present. Thus, even in cases in which I normally would want to do a sling for ISD, I opt against it if the patient has poor voiding function. That’s because the risk of permanent retention may rise as high as 15% to 20% in some of these patients.
Evaluation and treatment of mixed incontinence
DAVILA: I think we all agree that incontinence is easier to address than “hypercontinence” resulting from postoperative urethral obstruction, urinary retention, and irritative voiding symptoms. But what about patients with mixed incontinence? How do you evaluate them? Is there a role for surgical procedures in patients with primary urge incontinence?
I believe in offering all patients both nonsurgical and surgical options.—Dr. Sand
SAND: Many centers offer nonsurgical treatment of mixed incontinence, especially if urge incontinence predominates. But I believe in offering all patients both nonsurgical and surgical options. I end up triaging based on what patients select first, regardless of whether they have pure SUI or mixed symptoms, as long as they have been counseled appropriately about the expected outcomes of the various options.
MYERS: In my practice, I treat the urge symptoms first with anticholinergics or other medications. Then, if the stress incontinence continues, I offer a procedure.
This may be difficult in some cases, such as a patient with severe ISD. It is hard to treat detrusor overactivity when the urethral sphincter is weak, as the woman cannot hold increasing volumes of urine in the bladder.
Thus, I approach these cases by treating the stress incontinence first and then the urgency symptoms if intervention is still necessary—which is a 180-degree shift from my previous statement. In these cases, I treat the ISD first. Then, after the stress incontinence resolves, I offer medications for the urgency.
LUBER: I want to throw a little cold water on surgical treatment of overactive bladder. Clearly, this is an enormous issue. Probably 40% of women who come to my office complaining of urinary incontinence have mixed symptoms or mixed disease as determined by urodynamics. For the doctors out there caring for these patients daily, I think it is important to remember, as Dr. Sand mentioned, that in some cases, anti-incontinence operations can provoke detrusor overactivity in patients who were relatively asymptomatic previously. Dr. Myers’ suggestion that surgery may simply unmask the detrusor overactivity is also possible, of course.
Probably 40% of women who come to my office complaining of urinary incontinence have mixed symptoms.—Dr. Luber
Thus, I think it is reasonable to ask patients reporting mixed symptoms to characterize their urine loss. I usually have them pick a percentage (which isn’t always easy). I ask, “Is your urge incontinence 10%, 50% or 90% of your problem?” If urgency is 90% of the problem and stress incontinence is minimal, then naturally that patient’s care should be focused on the urge incontinence, and vice versa.
It becomes more problematic in the middle, with that 50/50 group. But I’m old-fashioned in that I like to treat the urge incontinence first and get that under control. Of course, in women with poor sphincter function, this distinction becomes more difficult because of the inevitable overlap of symptoms. But this is a small subset of the whole population.
DAVILA: Even if you operate on these patients to correct sphincter function, you must follow them closely. You shouldn’t be saying, “We’ll see you in 6 months.”
In addition, the cofactor of urogenital atrophy should be addressed. Atrophy can cause significant urinary urgency and nocturia symptoms, although most women may not report vaginal atrophy symptoms.4 Local estrogen cream at a low dosage can be used pre- and postoperatively without concern about systemic absorption.5
Which patients benefit from bulking agents?
SAND: We touched on the use of periurethral injections of bulking agents. How do you determine when bulking agents are appropriate?
MYERS: I use periurethral injections for demonstrated sphincter deficiency. The ideal patient has a supported bladder neck and true sphincter deficiency—for example, patients whose sphincter deficiency is caused by pelvic radiation or significant surgical scarring.
In recent years, I have loosened the guidelines slightly, in that a number of my patients are elderly women with urethral hypermobility who are not healthy enough to undergo a major operation. In these patients, I use a pessary to support the bladder neck before performing an injection, and I make sure the patient understands that she will need to use the pessary even after the injection. I have better results when there is no hypermobility.
LUBER: The concept of ISD as the sole cause of urinary incontinence is less mysterious than it at first appears. In the typical patient with a fixed poorly functioning urethra, a Qtip test will be 0 degrees at rest, and will still be 0 degrees with straining. The patient will leak readily with any kind of provocative maneuver, be it coughing or slight straining. With or without urodynamics, we know that patient’s urethra is not functioning properly. Such a patient, for me, is the ideal candidate for bulking agents.
Unfortunately, bulking agents tend to have short half-lives of around 2 years. Still, you can improve the quality of life of these patients tremendously in that time by periurethrally injecting bulking agents during a very simple office or outpatient visit.
I have had less satisfaction and success using bulking agents in patients with urethral hypermobility, although I do like Dr. Myers’ idea of correcting the hypermobility with an intravaginal support device and then using collagen to improve their urethral coaptation. That’s a nice concept.
Improvements being studied
SAND: Currently, we have 2 injectables approved by the US Food and Drug Administration: collagen and carbon-coated microspheres. Are new agents coming out? Do you expect improvements in the current agents?
DAVILA: The number of bulking agents being studied right now is huge. I think the future will bring one that can be implanted without the need for cystoscopy. A couple of trials under way use a conical urethral template for needle placement, and the injection is performed without cystoscopy. Although we’re a number of years away from having enough data to support the widespread implementation of this approach, the momentum is certainly in that direction.
The half-lives of bulking agents also are increasing. Collagen was an excellent start, but we are moving toward permanence. In addition, most of the agents being studied are simpler to inject than collagen. Biotechnology is coming to the forefront with polymers that are either temperature-sensitive or able to reconfigure themselves over time. Thus, they should serve as a nidus for collagen deposition or remain in place longer, enhancing urethral sphincteric function.
It isn’t clear which agent will take a leading role in the next few years, but a number of them have great promise. This is an exciting time in the management of stress incontinence as we move from invasive procedures such as retropubic urethropexy to minimally invasive surgery—as well as from the operating room to the office.
Radiofrequency technologies
SAND: What do you think about the new radiofrequency technologies being used to create support in periurethral tissues to correct hypermobility? Is there a role for this evolving technology?
LUBER: The concept of developing scar tissue adjacent to the urethra to provide better support underlies much of what we already do surgically. So there is some logic in the use of radiofrequency technologies to accomplish the same thing.
Still, there is the theoretical risk of further denervating the urethra, which is probably already denervated. Having looked at outcome studies for radiofrequency therapy, I think it’s a modality that can be embraced, but that should be done under the auspices of clinical research. Again, I’m old fashioned and am not comfortable integrating untested approaches into routine clinical care until we have adequate evidence of their effectiveness. In caring for incontinence, it is important that this effectiveness be looked at over a reasonable period of time, for example, 48 months.
It is hard to treat detrusor overactivity when the urethral sphincter is weak.—Dr. Myers
DAVILA: I have had some experience with radiofrequency therapy, and the tissue changes it stimulates are fairly impressive. I share your concern about the issue of denervation. In fact, my colleagues and I are hoping to initiate a trial in which we plan to look at pudendal latencies to the urethral sphincter in these patients. As of now, with limited experience, it appears that there is no worsening of urethral sphincter function with the therapy.
Tension-free vaginal tape
SAND: What about other new treatments on the horizon?
DAVILA: Like bulking agents, new minimally invasive surgical techniques are also increasing in number. The advent of the tension-free vaginal tape (TVT), a technique that moved from Sweden to the United States a couple of years ago, truly has revolutionized what we do in anti-incontinence surgery. I think we all can agree that it has changed our practice patterns quite significantly, and the modifications or theoretical improvements by different companies are likely to have a further impact.
Polypropylene mesh appears to be very well received by the body. It doesn’t get rejected or infected at a significant rate, so most physicians are comfortable with it. But I think it has become the surgeon’s preference as to which product works better.
For the Ob/Gyn, the primary issue remains the small yet well-recognized risks of retropubic needle placement, beginning with bladder perforation and including vascular or bowel injury. As a result, many Ob/Gyns have probably been hesitant to perform these procedures.
What the future holds is very exciting: the transobturator approach to surgery for stress incontinence. Instead of bringing the needle superiorly behind the pubic bone, the surgeon maneuvers it laterally beneath the pubic ramus and through the obturator membrane. This is an anti-incontinence procedure a gynecologist can embrace. It may not be necessary to perform cystoscopy afterward because the surgery is nowhere near the bladder.
The French have taken the lead in developing this technique and recently presented approximately 2 years of data.6,7 A US trial also is being initiated.
LUBER: TVT is billed as a midurethral procedure. However, when you consider where those tapes actually end up after a few months, it probably functions much like a traditional sling. Recent studies are in conflict: Some demonstrate the sling remains at the midurethra while others show that it readily migrates to the bladder neck. So the quest for a less obstructive procedure has not been fulfilled with the TVT.
In fact, in our recent TVT series that Drs. Lukacz and Nager are meticulously following, the voiding time increases and the maximum flow decreases postoperatively in roughly 30% of patients. So it definitely has some obstructive characteristics.
Quest for the Holy Grail continues
LUBER: I think we need to continue to explore these newer, less invasive procedures that offer wonderful potential. At this point, I might employ them in patients who are not able to tolerate the more invasive procedures or who flatly state that they want a less invasive operation. But I am not ready to embrace them as first-line therapy for all of my patients with stress incontinence.
Over the years, we have all seen various waves of surgical innovation, from the noincision urethropexies of the mid-1990s to the laparoscopic techniques prominent later in the decade. Now, more minimally invasive techniques are coming to the fore. At some point, we may even find the Holy Grail. But for the most part, we continue to evolve, examining new approaches until we are forced to reconcile with their limitations.
SAND: It is clear that this is a very exciting time to be treating SUI, with continuing innovation and an increased awareness of the problem by the public. While we all treat these women differently, there is a surprising consensus. We all seem to concur that the operation should be tailored to the individual, considering the relative balance of any concurrent urinary urge incontinence, urethral hypermobility, voiding dysfunction, and the woman’s health and activity level. We all use midurethral slings and periurethral bulking agents in selected women, but still also rely on Burch procedures and bladder-neck slings.
The authors report no financial relationship with any companies whose products are mentioned in this article.
1. Mutone N, Mastropietro M, Brizendine E, Hale D. Effect of tension-free vaginal tape procedure on urodynamic continence indices. Obstet Gynecol. 2001;98:638-645.
2. McLennan MT, Bent AE. Supine empty stress test as a predictor of low valsalva leak pressure. Neurourol Urodynamics. 1998;17:121-127.
3. Lobel RW, Sand PK. The empty supine stress test as a predictor of intrinsic urethral sphincter dysfunction. Obstet Gynecol. 1996;88:128-132.
4. Davila GW, Singh A, Karapanagiotou I, et al. Are women with urogenital atrophy symptomatic? Am J Obstet Gynecol. 2003;188:382-388.
5. Handa VL, Bachus KE, Johnston WW, Robboy SJ, Hammond CP. Vaginal administration of low-dose conjugated estrogens: systemic absorption and effects on the endometrium. Obstet Gynecol. 1994;84:215-218.
6. Delorme E. Transobturator sling: a minimally invasive procedure to treat female stress urinary incontinence. Prog Urol. 2001;11:1306-1313.
7. Dargent D, Bretones S, George P, Mellier G. Insertion of a suburethral sling through the obturator membrane in the treatment of female urinary incontinence. Gynecol Obstet Fertil. 2002;30:576-582.
1. Mutone N, Mastropietro M, Brizendine E, Hale D. Effect of tension-free vaginal tape procedure on urodynamic continence indices. Obstet Gynecol. 2001;98:638-645.
2. McLennan MT, Bent AE. Supine empty stress test as a predictor of low valsalva leak pressure. Neurourol Urodynamics. 1998;17:121-127.
3. Lobel RW, Sand PK. The empty supine stress test as a predictor of intrinsic urethral sphincter dysfunction. Obstet Gynecol. 1996;88:128-132.
4. Davila GW, Singh A, Karapanagiotou I, et al. Are women with urogenital atrophy symptomatic? Am J Obstet Gynecol. 2003;188:382-388.
5. Handa VL, Bachus KE, Johnston WW, Robboy SJ, Hammond CP. Vaginal administration of low-dose conjugated estrogens: systemic absorption and effects on the endometrium. Obstet Gynecol. 1994;84:215-218.
6. Delorme E. Transobturator sling: a minimally invasive procedure to treat female stress urinary incontinence. Prog Urol. 2001;11:1306-1313.
7. Dargent D, Bretones S, George P, Mellier G. Insertion of a suburethral sling through the obturator membrane in the treatment of female urinary incontinence. Gynecol Obstet Fertil. 2002;30:576-582.
Meeting the challenge of vesicovaginal fistula repair: Conservative and surgical measures
- Surgical risk factors include prior pelvic surgery, history of pelvic inflammatory disease, pelvic malignancy, endometriosis, infection, diabetes, and anatomic distortion.
- Conservative therapy should be reserved for simple fistulae that are less than 1 cm in size, diagnosed within 7 days of the index surgery, lacking associated carcinoma or radiation, and subject to at least 4 weeks of constant bladder drainage.
- In surgical repair, the Latzko partial colpocleisis or fistulectomy with flap-splitting closure is preferred.
Recent advances have improved the success of vesicovaginal fistula (VVF) repair—a challenge that can test even the most experienced gynecologic surgeon. For example, it now is apparent that some small uncomplicated fistulae respond to conservative treatment. Further, in selected cases, laparoscopic repair can eliminate the need for complicated laparotomy.
In addition, timing of fistula repair no longer requires long periods of observation, and good surgical technique for identifying and repairing bladder injuries at the time of the index surgery can often prevent the development or reduce the severity of VVF.
Vesicovaginal fistula is the most common type of urogenital fistula. Presentation and prognosis vary, depending on location and size of the defect, as well as coexisting factors such as tissue devascularization and previous radiation. However, surgical repair is associated with a high cure rate if it is performed by an experienced surgeon.
Most US cases follow gynecologic surgery
Vesicovaginal fistula was first documented in the mummified remains of Egyptian Queen Henhenit (11th Dynasty, 2050 BC), which were examined in 1923 by Derry.1 Although the exact incidence of VVF in the United States is unknown, the primary cause is gynecologic surgery, especially hysterectomy. The defect is estimated to occur in 0.01% to 0.04% of gynecologic procedures.
A study of 303 women with genitourinary fistula found that the defect was related to gynecologic surgery in 82% of cases, obstetric events in 8%, radiation therapy in 6%, and trauma or fulguration in 4%.2 Rare causes of VVF include lymphogranuloma venereum, tuberculosis, syphilis, bladder stones, and a retained foreign body in the vagina. In rare instances, spontaneous vesicouterine fistulae were reported following uncomplicated vaginal birth after cesarean section.3
Gynecologic surgery may lead to VVF due to extensive dissection between the bladder and the uterus, unrecognized bladder laceration, inappropriate stitch placement, and/or devascularization injury to the tissue planes. Concurrent ureteric involvement has been reported in as many as 10% to 15% of vesicovaginal fistula cases.
In developing countries, vesicovaginal fistulae are far more common and generally related to obstetric factors such as obstructed labor (due to unattended deliveries), small pelvic dimensions, malpresentation, poor uterine contractions, and introital stenosis.
Risk factors. Conditions that may predispose patients to VVF include prior pelvic surgery, a history of pelvic inflammatory disease, pelvic malignancy, endometriosis, infection, diabetes, and anatomic distortion. If these risk factors are present, the patient should be counseled accordingly prior to gynecologic surgery.
Correct classification crucial to surgical success
Proper classification of VVF can help the gynecologic surgeon plan operative intervention. Obstetric vesicovaginal fistulae usually are categorized according to their cause, complexity, and site of obstruction. In contrast, gynecologic fistulae are generally classified as simple or complicated (TABLE).
These levels may have important implications for the surgical approach and prognosis.4 For example, simple vesicovaginal fistulae are usually uncomplicated surgical cases with good prognosis. Complicated vesicovaginal fistulae, on the other hand, can challenge even highly practiced and skilled gynecologic surgeons and are associated with a high rate of recurrence.
Women typically present within specific intervals after the various antecedent events (pelvic surgery, childbirth, radiation therapy) with a primary complaint of constant, painless urinary incontinence. If the fistula is related to traumatic childbirth, most patients experience urine leakage within the first 24 to 48 hours. Following pelvic surgery, symptoms usually occur within the first 30 days. In contrast, radiation-induced fistulae develop over a much longer interval secondary to progressive devascularization necrosis, and may present 30 days to 30 years after the antecedent event.
Some patients report exacerbation during physical activities, which can sometimes lead to erroneous diagnosis of uncomplicated stress incontinence. If the fistula is small, intermittent leakage with increased bladder distention or physical activity may be noted.
Other patients may complain of vaginal discharge or hematuria.
If there is concurrent ureteric involvement, the patient may experience constitutional symptoms (such as fever, chills, and flank pain) or even gastrointestinal symptoms.
Physical findings. Any pooling of fluid in the vagina that is noted should be sent for analysis if the diagnosis is unclear. Next, perform a careful speculum exam that allows visualization of the entire anterior vaginal wall to identify the fistula tract (FIGURE 1). In many cases, the fistula is grossly visible.
Determine the location of the fistula in relation to the vaginal apex and bladder trigone and assess the quality of surrounding tissue (eg, presence of inflammation, edema, or infection). Fistulas near the vaginal apex may require a more complicated abdominal approach, and those close to the trigone may be associated with increased risk of ureteral injury during repair.
If the fistula is particularly small, no tract may be apparent. In such cases, bimanual exam with careful palpation of the anterior wall may help isolate the fistula (eg, when there is a surrounding zone of induration).
Office tests. If no fistula is noted despite highly suspicious signs and symptoms and careful examination, a simple office test can be performed. Using a catheter, fill the bladder with a dyed solution such as normal saline with indigo carmine and repeat the pelvic exam with a half-speculum to visualize the anterior wall. Ask the patient to cough and bear down, and identify the fistula by visualizing urine leakage.
If this test fails to locate the fistula, insert a tampon and ask the patient to perform 10 to 15 minutes of exertional maneuvers, including stair climbing and jumping in place. Then remove the tampon. Visualization of dye beyond the most distal edge of the tampon confirms the presence of a fistula.
A variation of this technique is the double-dye test: Give the patient oral phenazopyridine (Pyridium), fill the bladder with the blue-tinted solution, and insert a tampon. The presence of blue staining suggests vesicovaginal or urethrovaginal fistula, while red staining (Pyridium) suggests ureterovaginal fistula.
Other testing. Further assessment is recommended to rule out concurrent pathology and formulate an appropriate treatment plan. Routine testing should include a urinalysis and culture to exclude coexisting urinary tract infection, an electrolyte panel to evaluate renal function, and a complete blood cell count to rule out systemic infection.
Cystoscopy should be performed to visualize the fistulous tract, assess its location in relation to the ureters and trigone, assure bilateral ureteral patency, and exclude the presence of a foreign body or suture in the bladder.
In patients with a history of urogenital malignancy, biopsy of the fistula tract and urine cytology is warranted.
Comparable success rates have been reported for early and late repair of surgery-induced fistulae.
Radiologic studies are recommended prior to surgical repair of a vesicovaginal fistula to fully assess the defect and exclude the presence of multiple fistulae. An intravenous pyelogram is helpful to exclude concurrent ureterovaginal fistulae or ureteral obstruction. A targeted fistulogram may be indicated if conservative therapy is planned, including expectant management, continuous bladder drainage, fulguration, or fibrin occlusion.
FIGURE 1 Vesicovaginal fistula
Pelvic cross section depicting high vesicovaginal fistula.TABLE
Classification of vesicovaginal fistulae17
| CLASSIFICATION | DESCRIPTION |
|---|---|
| Simple |
|
| Complicated |
|
Indications for conservative management
Because spontaneous closure is uncommon, symptomatic VVF merits treatment. Appropriate therapy depends on various factors, including fistula size and location, timing from the antecedent event, severity of symptoms, quality of surrounding tissue, and clinician experience and surgical skills.
Occasionally, a fistula heals following prolonged bladder drainage through a transurethral or suprapubic catheter—provided it is diagnosed within a few days of surgery. Zimmern5 recommends a conservative approach to small fistulae if the patient’s complaints of urinary incontinence are resolved with insertion of a Foley catheter. In this case, bladder drainage should be continued for 3 weeks, followed by reevaluation of the fistula. If the fistula has diminished in size, an additional 3 weeks of catheter drainage is associated with a high rate of spontaneous closure; if there is no change, the fistula is unlikely to resolve spontaneously.5
Varying success rates have been reported for conservative management, ranging from 2% to 80%.4,6 The chances of success are apparently greater if the fistula is:
- diagnosed within 7 days of the index surgery,
- less than 1 cm in size,
- simple, without associated carcinoma or radiation, and
- subject to at least 4 weeks of constant bladder drainage.
Persistent, large, or complex fistulae are best treated surgically.
Indications for surgical management
The basic principles of fistula closure apply. They are:
- adequate exposure,
- good hemostasis,
- wide mobilization of the bladder and vagina,
- resection of devascularized tissue,
- removal of any foreign bodies,
- tension-free closure,
- nonopposition of suture lines,
- confirmation of a water-tight seal on bladder closure, and
- bladder drainage for 10 to 14 days following the repair.
Timing of the repair has been the subject of controversy and can pose a dilemma to physician and patient alike. Traditionally, an interval of 3 months was recommended between the index surgery and fistula repair, with a delay of up to 1 year when the fistula was radiation-induced. However, little data support these recommendations.
Today most experts recommend an individualized approach, delaying the surgery until inflammation and infection of the surrounding tissue have resolved. The use of estrogen, antibiotics, or steroids to facilitate healing during this period also has been recommended.7 Comparable success rates have been reported for early and late repair of surgery-induced fistulae based on these principles.8-10
Vaginal approach. Most vesicovaginal fistulae can be surgically corrected using a vaginal approach. Traditionally, a Latzko partial colpocleisis or fistulectomy with flap-splitting closure has been advocated.
Debate continues about whether resection of the fistulous tract is necessary. Some experts believe that wide resection increases the size of the fistula and, therefore, the risk of recurrence. They also maintain that the fibrous tissue surrounding the fistula helps to reinforce the surgical repair. Proponents of fistulectomy counter that resection of the fistula and exposure of healthy tissue optimizes wound healing and improves surgical success rates. Comparable success has been reported for both techniques.11,12
We prefer an individualized approach, with minimal resection of the fistulous tract to simplify the procedure and minimize associated complications, including recurrence.
- Latzko partial colpocleisis. This technique, first reported in 1942, remains a common procedure, with success rates of 90% to 100%.13 Advantages include a short operative time, low intraoperative and postoperative morbidity, and low risk of ureteral injury.
- Fistulectomy technique. Alternatively, to perform fistulectomy with a flap-splitting closure, begin by resecting the fistulous tract to expose healthy tissue at the wound margins. Then close the defect in a multilayer fashion, beginning with the bladder mucosa, bladder serosa, pubocervical fascia, and vaginal mucosa. Be careful to avoid tension on suture lines. In addition, create a fascial flap to prevent opposition of the incision planes and reduce the risk of recurrence.
- Grafts. In cases with a high risk of recurrence, such as complex or large fistulae, a Martius fat-pad graft should be interposed between the closure layers to promote vascularization and reduce the risk of recurrence.14 Placement of a cadaveric biomaterial graft also has been reported, reducing the need for complicated flap procedures.15
Abdominal approach. Although most vesicovaginal fistulae can be surgically corrected via the vaginal approach, the abdominal route may be preferred when the fistula is high and inaccessible, large and complex, multiple in number, or when there is concurrent uterine or bowel involvement or a need for ureteral reimplantation. The abdominal approach may be facilitated by cystoscopically guided placement of a catheter through the fistulous tract to assist in subsequent identification and dissection.
To begin, make a vertical skin incision to optimize visualization and allow mobilization of an omental flap, if necessary. Expose the bladder and perform a high extraperitoneal cystotomy to visualize the fistulous tract. Place ureteral stents if the fistula is in close proximity to the ureteral orifice.
Extend the bladder incision to the fistulous tract and completely excise it following mobilization of the vagina. Then close the vagina and bladder with interrupted, delayed absorbable suture in a double layer.
Transpose an omental flap between the vaginal and bladder incisions to promote vascularization, minimize opposition of suture lines, and reduce the risk of recurrence (FIGURE 2).
Laparoscopic approach. A similar laparoscopic repair has been reported with comparable results, but requires advanced skills with endoscopic suturing and knot tying (FIGURE 3).16
FIGURE 2 Abdominal repair
Abdominal repair of vesicovaginal fistula, with closure of bladder defect and posterior cystotomy and separate closure of vaginal defect. Note the omental flap pictured in the insert.
FIGURE 3 Laparoscopic repair
Laparoscopic repair of vesicovaginal fistula.The authors report no financial relationship with any companies whose products are mentioned in this article.
1. Kremling H. Labor-induced bladder injuries: historical observations. Gynakol Geburtshilfliche Rundsch. 1996;36:197-200.
2. Lee RA, Symmonds RE, Williams TJ. Current state of genitourinary fistula. Obstet Gynecol. 1998;72:313-315.
3. Miklos JR, Sze EHM, Parobeck D, et al. Vesicouterine fistula: a rare complication of vaginal birth after cesarean. Obstet Gynecol. 1995;86:638-639.
4. Elkins TE, Thompson JR. Lower urinary tract fistulas. In: Walters M, Karram MM, eds. Urogynecology and Reconstructive Pelvic Surgery. 2nd ed. St. Louis, Mo: Mosby; 1999;355-365.
5. Zimmern PE, Hadley HR, Staskin D. Genitourinary fistulas: vaginal approach for repair of vesicovaginal fistulas. Clin Obstet Gynaecol. 1985;12:403-413.
6. Davits RJ, Miranda SI. Conservative treatment of vesicovaginal fistulas by bladder drainage alone. Br J Urol. 1991;68:155-156.
7. Margolis T, Mercer LJ. Vesicovaginal fistula. Obstet Gynecol Surv. 1995;49:840-847.
8. Blaivas JG, Heritz DM, Romanzi LJ. Early versus late repair of vesicovaginal fistulas: vaginal and abdominal approaches. J Urol. 1995;153:1110-1112.
9. Blandy JP, Badenoch DF, Fowler CG. Early repair of iatrogenic injury to the ureter or bladder after gynecological surgery. J Urol. 1991;146:761-765.
10. Cruikshank SH. Early closure of posthysterectomy vesicovaginal fistulas. South Med J. 1988;81:1525-1528.
11. Raz S, Bregg KJ, Nitti VW. Transvaginal repair of vesicovaginal fistula using a peritoneal flap. J Urol. 1993;150:56-59.
12. Iselin CE, Aslan P, Webster GD. Transvaginal repair of vesicovaginal fistulas after hysterectomy by vaginal cuff excision. J Urol. 1998;160(3 Pt 1):728-730.
13. Latzko W. Postoperative vesicovaginal fistulas: genesis and therapy. Am J Surg. 1942;58:211-218.
14. Punekar SV, Buch DN, Soni AB. Martius’ labial fat pad interposition and its modification in complex lower urinary fistulae. J Postgrad Med. 1999;10:405-406.
15. Miklos JR, Kohli N. Rectovaginal fistula repair utilizing a cadaveric dermal allograft. Int Urogynecol J Pelvic Floor Dysfunct. 1999;10:405-406.
16. Nezhat CH, Nezhat F, Nezhat C. Laparoscopic repair of a vesicovaginal fistula: a case report. Obstet Gynecol. 1994;83(5 Pt 2):899-901.
17. Walters MD, Karram MM, eds. Urogynecology and Reconstructive Pelvic Surgery. 2nd ed. St. Louis, Mo: Mosby; 1999.
- Surgical risk factors include prior pelvic surgery, history of pelvic inflammatory disease, pelvic malignancy, endometriosis, infection, diabetes, and anatomic distortion.
- Conservative therapy should be reserved for simple fistulae that are less than 1 cm in size, diagnosed within 7 days of the index surgery, lacking associated carcinoma or radiation, and subject to at least 4 weeks of constant bladder drainage.
- In surgical repair, the Latzko partial colpocleisis or fistulectomy with flap-splitting closure is preferred.
Recent advances have improved the success of vesicovaginal fistula (VVF) repair—a challenge that can test even the most experienced gynecologic surgeon. For example, it now is apparent that some small uncomplicated fistulae respond to conservative treatment. Further, in selected cases, laparoscopic repair can eliminate the need for complicated laparotomy.
In addition, timing of fistula repair no longer requires long periods of observation, and good surgical technique for identifying and repairing bladder injuries at the time of the index surgery can often prevent the development or reduce the severity of VVF.
Vesicovaginal fistula is the most common type of urogenital fistula. Presentation and prognosis vary, depending on location and size of the defect, as well as coexisting factors such as tissue devascularization and previous radiation. However, surgical repair is associated with a high cure rate if it is performed by an experienced surgeon.
Most US cases follow gynecologic surgery
Vesicovaginal fistula was first documented in the mummified remains of Egyptian Queen Henhenit (11th Dynasty, 2050 BC), which were examined in 1923 by Derry.1 Although the exact incidence of VVF in the United States is unknown, the primary cause is gynecologic surgery, especially hysterectomy. The defect is estimated to occur in 0.01% to 0.04% of gynecologic procedures.
A study of 303 women with genitourinary fistula found that the defect was related to gynecologic surgery in 82% of cases, obstetric events in 8%, radiation therapy in 6%, and trauma or fulguration in 4%.2 Rare causes of VVF include lymphogranuloma venereum, tuberculosis, syphilis, bladder stones, and a retained foreign body in the vagina. In rare instances, spontaneous vesicouterine fistulae were reported following uncomplicated vaginal birth after cesarean section.3
Gynecologic surgery may lead to VVF due to extensive dissection between the bladder and the uterus, unrecognized bladder laceration, inappropriate stitch placement, and/or devascularization injury to the tissue planes. Concurrent ureteric involvement has been reported in as many as 10% to 15% of vesicovaginal fistula cases.
In developing countries, vesicovaginal fistulae are far more common and generally related to obstetric factors such as obstructed labor (due to unattended deliveries), small pelvic dimensions, malpresentation, poor uterine contractions, and introital stenosis.
Risk factors. Conditions that may predispose patients to VVF include prior pelvic surgery, a history of pelvic inflammatory disease, pelvic malignancy, endometriosis, infection, diabetes, and anatomic distortion. If these risk factors are present, the patient should be counseled accordingly prior to gynecologic surgery.
Correct classification crucial to surgical success
Proper classification of VVF can help the gynecologic surgeon plan operative intervention. Obstetric vesicovaginal fistulae usually are categorized according to their cause, complexity, and site of obstruction. In contrast, gynecologic fistulae are generally classified as simple or complicated (TABLE).
These levels may have important implications for the surgical approach and prognosis.4 For example, simple vesicovaginal fistulae are usually uncomplicated surgical cases with good prognosis. Complicated vesicovaginal fistulae, on the other hand, can challenge even highly practiced and skilled gynecologic surgeons and are associated with a high rate of recurrence.
Women typically present within specific intervals after the various antecedent events (pelvic surgery, childbirth, radiation therapy) with a primary complaint of constant, painless urinary incontinence. If the fistula is related to traumatic childbirth, most patients experience urine leakage within the first 24 to 48 hours. Following pelvic surgery, symptoms usually occur within the first 30 days. In contrast, radiation-induced fistulae develop over a much longer interval secondary to progressive devascularization necrosis, and may present 30 days to 30 years after the antecedent event.
Some patients report exacerbation during physical activities, which can sometimes lead to erroneous diagnosis of uncomplicated stress incontinence. If the fistula is small, intermittent leakage with increased bladder distention or physical activity may be noted.
Other patients may complain of vaginal discharge or hematuria.
If there is concurrent ureteric involvement, the patient may experience constitutional symptoms (such as fever, chills, and flank pain) or even gastrointestinal symptoms.
Physical findings. Any pooling of fluid in the vagina that is noted should be sent for analysis if the diagnosis is unclear. Next, perform a careful speculum exam that allows visualization of the entire anterior vaginal wall to identify the fistula tract (FIGURE 1). In many cases, the fistula is grossly visible.
Determine the location of the fistula in relation to the vaginal apex and bladder trigone and assess the quality of surrounding tissue (eg, presence of inflammation, edema, or infection). Fistulas near the vaginal apex may require a more complicated abdominal approach, and those close to the trigone may be associated with increased risk of ureteral injury during repair.
If the fistula is particularly small, no tract may be apparent. In such cases, bimanual exam with careful palpation of the anterior wall may help isolate the fistula (eg, when there is a surrounding zone of induration).
Office tests. If no fistula is noted despite highly suspicious signs and symptoms and careful examination, a simple office test can be performed. Using a catheter, fill the bladder with a dyed solution such as normal saline with indigo carmine and repeat the pelvic exam with a half-speculum to visualize the anterior wall. Ask the patient to cough and bear down, and identify the fistula by visualizing urine leakage.
If this test fails to locate the fistula, insert a tampon and ask the patient to perform 10 to 15 minutes of exertional maneuvers, including stair climbing and jumping in place. Then remove the tampon. Visualization of dye beyond the most distal edge of the tampon confirms the presence of a fistula.
A variation of this technique is the double-dye test: Give the patient oral phenazopyridine (Pyridium), fill the bladder with the blue-tinted solution, and insert a tampon. The presence of blue staining suggests vesicovaginal or urethrovaginal fistula, while red staining (Pyridium) suggests ureterovaginal fistula.
Other testing. Further assessment is recommended to rule out concurrent pathology and formulate an appropriate treatment plan. Routine testing should include a urinalysis and culture to exclude coexisting urinary tract infection, an electrolyte panel to evaluate renal function, and a complete blood cell count to rule out systemic infection.
Cystoscopy should be performed to visualize the fistulous tract, assess its location in relation to the ureters and trigone, assure bilateral ureteral patency, and exclude the presence of a foreign body or suture in the bladder.
In patients with a history of urogenital malignancy, biopsy of the fistula tract and urine cytology is warranted.
Comparable success rates have been reported for early and late repair of surgery-induced fistulae.
Radiologic studies are recommended prior to surgical repair of a vesicovaginal fistula to fully assess the defect and exclude the presence of multiple fistulae. An intravenous pyelogram is helpful to exclude concurrent ureterovaginal fistulae or ureteral obstruction. A targeted fistulogram may be indicated if conservative therapy is planned, including expectant management, continuous bladder drainage, fulguration, or fibrin occlusion.
FIGURE 1 Vesicovaginal fistula
Pelvic cross section depicting high vesicovaginal fistula.TABLE
Classification of vesicovaginal fistulae17
| CLASSIFICATION | DESCRIPTION |
|---|---|
| Simple |
|
| Complicated |
|
Indications for conservative management
Because spontaneous closure is uncommon, symptomatic VVF merits treatment. Appropriate therapy depends on various factors, including fistula size and location, timing from the antecedent event, severity of symptoms, quality of surrounding tissue, and clinician experience and surgical skills.
Occasionally, a fistula heals following prolonged bladder drainage through a transurethral or suprapubic catheter—provided it is diagnosed within a few days of surgery. Zimmern5 recommends a conservative approach to small fistulae if the patient’s complaints of urinary incontinence are resolved with insertion of a Foley catheter. In this case, bladder drainage should be continued for 3 weeks, followed by reevaluation of the fistula. If the fistula has diminished in size, an additional 3 weeks of catheter drainage is associated with a high rate of spontaneous closure; if there is no change, the fistula is unlikely to resolve spontaneously.5
Varying success rates have been reported for conservative management, ranging from 2% to 80%.4,6 The chances of success are apparently greater if the fistula is:
- diagnosed within 7 days of the index surgery,
- less than 1 cm in size,
- simple, without associated carcinoma or radiation, and
- subject to at least 4 weeks of constant bladder drainage.
Persistent, large, or complex fistulae are best treated surgically.
Indications for surgical management
The basic principles of fistula closure apply. They are:
- adequate exposure,
- good hemostasis,
- wide mobilization of the bladder and vagina,
- resection of devascularized tissue,
- removal of any foreign bodies,
- tension-free closure,
- nonopposition of suture lines,
- confirmation of a water-tight seal on bladder closure, and
- bladder drainage for 10 to 14 days following the repair.
Timing of the repair has been the subject of controversy and can pose a dilemma to physician and patient alike. Traditionally, an interval of 3 months was recommended between the index surgery and fistula repair, with a delay of up to 1 year when the fistula was radiation-induced. However, little data support these recommendations.
Today most experts recommend an individualized approach, delaying the surgery until inflammation and infection of the surrounding tissue have resolved. The use of estrogen, antibiotics, or steroids to facilitate healing during this period also has been recommended.7 Comparable success rates have been reported for early and late repair of surgery-induced fistulae based on these principles.8-10
Vaginal approach. Most vesicovaginal fistulae can be surgically corrected using a vaginal approach. Traditionally, a Latzko partial colpocleisis or fistulectomy with flap-splitting closure has been advocated.
Debate continues about whether resection of the fistulous tract is necessary. Some experts believe that wide resection increases the size of the fistula and, therefore, the risk of recurrence. They also maintain that the fibrous tissue surrounding the fistula helps to reinforce the surgical repair. Proponents of fistulectomy counter that resection of the fistula and exposure of healthy tissue optimizes wound healing and improves surgical success rates. Comparable success has been reported for both techniques.11,12
We prefer an individualized approach, with minimal resection of the fistulous tract to simplify the procedure and minimize associated complications, including recurrence.
- Latzko partial colpocleisis. This technique, first reported in 1942, remains a common procedure, with success rates of 90% to 100%.13 Advantages include a short operative time, low intraoperative and postoperative morbidity, and low risk of ureteral injury.
- Fistulectomy technique. Alternatively, to perform fistulectomy with a flap-splitting closure, begin by resecting the fistulous tract to expose healthy tissue at the wound margins. Then close the defect in a multilayer fashion, beginning with the bladder mucosa, bladder serosa, pubocervical fascia, and vaginal mucosa. Be careful to avoid tension on suture lines. In addition, create a fascial flap to prevent opposition of the incision planes and reduce the risk of recurrence.
- Grafts. In cases with a high risk of recurrence, such as complex or large fistulae, a Martius fat-pad graft should be interposed between the closure layers to promote vascularization and reduce the risk of recurrence.14 Placement of a cadaveric biomaterial graft also has been reported, reducing the need for complicated flap procedures.15
Abdominal approach. Although most vesicovaginal fistulae can be surgically corrected via the vaginal approach, the abdominal route may be preferred when the fistula is high and inaccessible, large and complex, multiple in number, or when there is concurrent uterine or bowel involvement or a need for ureteral reimplantation. The abdominal approach may be facilitated by cystoscopically guided placement of a catheter through the fistulous tract to assist in subsequent identification and dissection.
To begin, make a vertical skin incision to optimize visualization and allow mobilization of an omental flap, if necessary. Expose the bladder and perform a high extraperitoneal cystotomy to visualize the fistulous tract. Place ureteral stents if the fistula is in close proximity to the ureteral orifice.
Extend the bladder incision to the fistulous tract and completely excise it following mobilization of the vagina. Then close the vagina and bladder with interrupted, delayed absorbable suture in a double layer.
Transpose an omental flap between the vaginal and bladder incisions to promote vascularization, minimize opposition of suture lines, and reduce the risk of recurrence (FIGURE 2).
Laparoscopic approach. A similar laparoscopic repair has been reported with comparable results, but requires advanced skills with endoscopic suturing and knot tying (FIGURE 3).16
FIGURE 2 Abdominal repair
Abdominal repair of vesicovaginal fistula, with closure of bladder defect and posterior cystotomy and separate closure of vaginal defect. Note the omental flap pictured in the insert.
FIGURE 3 Laparoscopic repair
Laparoscopic repair of vesicovaginal fistula.The authors report no financial relationship with any companies whose products are mentioned in this article.
- Surgical risk factors include prior pelvic surgery, history of pelvic inflammatory disease, pelvic malignancy, endometriosis, infection, diabetes, and anatomic distortion.
- Conservative therapy should be reserved for simple fistulae that are less than 1 cm in size, diagnosed within 7 days of the index surgery, lacking associated carcinoma or radiation, and subject to at least 4 weeks of constant bladder drainage.
- In surgical repair, the Latzko partial colpocleisis or fistulectomy with flap-splitting closure is preferred.
Recent advances have improved the success of vesicovaginal fistula (VVF) repair—a challenge that can test even the most experienced gynecologic surgeon. For example, it now is apparent that some small uncomplicated fistulae respond to conservative treatment. Further, in selected cases, laparoscopic repair can eliminate the need for complicated laparotomy.
In addition, timing of fistula repair no longer requires long periods of observation, and good surgical technique for identifying and repairing bladder injuries at the time of the index surgery can often prevent the development or reduce the severity of VVF.
Vesicovaginal fistula is the most common type of urogenital fistula. Presentation and prognosis vary, depending on location and size of the defect, as well as coexisting factors such as tissue devascularization and previous radiation. However, surgical repair is associated with a high cure rate if it is performed by an experienced surgeon.
Most US cases follow gynecologic surgery
Vesicovaginal fistula was first documented in the mummified remains of Egyptian Queen Henhenit (11th Dynasty, 2050 BC), which were examined in 1923 by Derry.1 Although the exact incidence of VVF in the United States is unknown, the primary cause is gynecologic surgery, especially hysterectomy. The defect is estimated to occur in 0.01% to 0.04% of gynecologic procedures.
A study of 303 women with genitourinary fistula found that the defect was related to gynecologic surgery in 82% of cases, obstetric events in 8%, radiation therapy in 6%, and trauma or fulguration in 4%.2 Rare causes of VVF include lymphogranuloma venereum, tuberculosis, syphilis, bladder stones, and a retained foreign body in the vagina. In rare instances, spontaneous vesicouterine fistulae were reported following uncomplicated vaginal birth after cesarean section.3
Gynecologic surgery may lead to VVF due to extensive dissection between the bladder and the uterus, unrecognized bladder laceration, inappropriate stitch placement, and/or devascularization injury to the tissue planes. Concurrent ureteric involvement has been reported in as many as 10% to 15% of vesicovaginal fistula cases.
In developing countries, vesicovaginal fistulae are far more common and generally related to obstetric factors such as obstructed labor (due to unattended deliveries), small pelvic dimensions, malpresentation, poor uterine contractions, and introital stenosis.
Risk factors. Conditions that may predispose patients to VVF include prior pelvic surgery, a history of pelvic inflammatory disease, pelvic malignancy, endometriosis, infection, diabetes, and anatomic distortion. If these risk factors are present, the patient should be counseled accordingly prior to gynecologic surgery.
Correct classification crucial to surgical success
Proper classification of VVF can help the gynecologic surgeon plan operative intervention. Obstetric vesicovaginal fistulae usually are categorized according to their cause, complexity, and site of obstruction. In contrast, gynecologic fistulae are generally classified as simple or complicated (TABLE).
These levels may have important implications for the surgical approach and prognosis.4 For example, simple vesicovaginal fistulae are usually uncomplicated surgical cases with good prognosis. Complicated vesicovaginal fistulae, on the other hand, can challenge even highly practiced and skilled gynecologic surgeons and are associated with a high rate of recurrence.
Women typically present within specific intervals after the various antecedent events (pelvic surgery, childbirth, radiation therapy) with a primary complaint of constant, painless urinary incontinence. If the fistula is related to traumatic childbirth, most patients experience urine leakage within the first 24 to 48 hours. Following pelvic surgery, symptoms usually occur within the first 30 days. In contrast, radiation-induced fistulae develop over a much longer interval secondary to progressive devascularization necrosis, and may present 30 days to 30 years after the antecedent event.
Some patients report exacerbation during physical activities, which can sometimes lead to erroneous diagnosis of uncomplicated stress incontinence. If the fistula is small, intermittent leakage with increased bladder distention or physical activity may be noted.
Other patients may complain of vaginal discharge or hematuria.
If there is concurrent ureteric involvement, the patient may experience constitutional symptoms (such as fever, chills, and flank pain) or even gastrointestinal symptoms.
Physical findings. Any pooling of fluid in the vagina that is noted should be sent for analysis if the diagnosis is unclear. Next, perform a careful speculum exam that allows visualization of the entire anterior vaginal wall to identify the fistula tract (FIGURE 1). In many cases, the fistula is grossly visible.
Determine the location of the fistula in relation to the vaginal apex and bladder trigone and assess the quality of surrounding tissue (eg, presence of inflammation, edema, or infection). Fistulas near the vaginal apex may require a more complicated abdominal approach, and those close to the trigone may be associated with increased risk of ureteral injury during repair.
If the fistula is particularly small, no tract may be apparent. In such cases, bimanual exam with careful palpation of the anterior wall may help isolate the fistula (eg, when there is a surrounding zone of induration).
Office tests. If no fistula is noted despite highly suspicious signs and symptoms and careful examination, a simple office test can be performed. Using a catheter, fill the bladder with a dyed solution such as normal saline with indigo carmine and repeat the pelvic exam with a half-speculum to visualize the anterior wall. Ask the patient to cough and bear down, and identify the fistula by visualizing urine leakage.
If this test fails to locate the fistula, insert a tampon and ask the patient to perform 10 to 15 minutes of exertional maneuvers, including stair climbing and jumping in place. Then remove the tampon. Visualization of dye beyond the most distal edge of the tampon confirms the presence of a fistula.
A variation of this technique is the double-dye test: Give the patient oral phenazopyridine (Pyridium), fill the bladder with the blue-tinted solution, and insert a tampon. The presence of blue staining suggests vesicovaginal or urethrovaginal fistula, while red staining (Pyridium) suggests ureterovaginal fistula.
Other testing. Further assessment is recommended to rule out concurrent pathology and formulate an appropriate treatment plan. Routine testing should include a urinalysis and culture to exclude coexisting urinary tract infection, an electrolyte panel to evaluate renal function, and a complete blood cell count to rule out systemic infection.
Cystoscopy should be performed to visualize the fistulous tract, assess its location in relation to the ureters and trigone, assure bilateral ureteral patency, and exclude the presence of a foreign body or suture in the bladder.
In patients with a history of urogenital malignancy, biopsy of the fistula tract and urine cytology is warranted.
Comparable success rates have been reported for early and late repair of surgery-induced fistulae.
Radiologic studies are recommended prior to surgical repair of a vesicovaginal fistula to fully assess the defect and exclude the presence of multiple fistulae. An intravenous pyelogram is helpful to exclude concurrent ureterovaginal fistulae or ureteral obstruction. A targeted fistulogram may be indicated if conservative therapy is planned, including expectant management, continuous bladder drainage, fulguration, or fibrin occlusion.
FIGURE 1 Vesicovaginal fistula
Pelvic cross section depicting high vesicovaginal fistula.TABLE
Classification of vesicovaginal fistulae17
| CLASSIFICATION | DESCRIPTION |
|---|---|
| Simple |
|
| Complicated |
|
Indications for conservative management
Because spontaneous closure is uncommon, symptomatic VVF merits treatment. Appropriate therapy depends on various factors, including fistula size and location, timing from the antecedent event, severity of symptoms, quality of surrounding tissue, and clinician experience and surgical skills.
Occasionally, a fistula heals following prolonged bladder drainage through a transurethral or suprapubic catheter—provided it is diagnosed within a few days of surgery. Zimmern5 recommends a conservative approach to small fistulae if the patient’s complaints of urinary incontinence are resolved with insertion of a Foley catheter. In this case, bladder drainage should be continued for 3 weeks, followed by reevaluation of the fistula. If the fistula has diminished in size, an additional 3 weeks of catheter drainage is associated with a high rate of spontaneous closure; if there is no change, the fistula is unlikely to resolve spontaneously.5
Varying success rates have been reported for conservative management, ranging from 2% to 80%.4,6 The chances of success are apparently greater if the fistula is:
- diagnosed within 7 days of the index surgery,
- less than 1 cm in size,
- simple, without associated carcinoma or radiation, and
- subject to at least 4 weeks of constant bladder drainage.
Persistent, large, or complex fistulae are best treated surgically.
Indications for surgical management
The basic principles of fistula closure apply. They are:
- adequate exposure,
- good hemostasis,
- wide mobilization of the bladder and vagina,
- resection of devascularized tissue,
- removal of any foreign bodies,
- tension-free closure,
- nonopposition of suture lines,
- confirmation of a water-tight seal on bladder closure, and
- bladder drainage for 10 to 14 days following the repair.
Timing of the repair has been the subject of controversy and can pose a dilemma to physician and patient alike. Traditionally, an interval of 3 months was recommended between the index surgery and fistula repair, with a delay of up to 1 year when the fistula was radiation-induced. However, little data support these recommendations.
Today most experts recommend an individualized approach, delaying the surgery until inflammation and infection of the surrounding tissue have resolved. The use of estrogen, antibiotics, or steroids to facilitate healing during this period also has been recommended.7 Comparable success rates have been reported for early and late repair of surgery-induced fistulae based on these principles.8-10
Vaginal approach. Most vesicovaginal fistulae can be surgically corrected using a vaginal approach. Traditionally, a Latzko partial colpocleisis or fistulectomy with flap-splitting closure has been advocated.
Debate continues about whether resection of the fistulous tract is necessary. Some experts believe that wide resection increases the size of the fistula and, therefore, the risk of recurrence. They also maintain that the fibrous tissue surrounding the fistula helps to reinforce the surgical repair. Proponents of fistulectomy counter that resection of the fistula and exposure of healthy tissue optimizes wound healing and improves surgical success rates. Comparable success has been reported for both techniques.11,12
We prefer an individualized approach, with minimal resection of the fistulous tract to simplify the procedure and minimize associated complications, including recurrence.
- Latzko partial colpocleisis. This technique, first reported in 1942, remains a common procedure, with success rates of 90% to 100%.13 Advantages include a short operative time, low intraoperative and postoperative morbidity, and low risk of ureteral injury.
- Fistulectomy technique. Alternatively, to perform fistulectomy with a flap-splitting closure, begin by resecting the fistulous tract to expose healthy tissue at the wound margins. Then close the defect in a multilayer fashion, beginning with the bladder mucosa, bladder serosa, pubocervical fascia, and vaginal mucosa. Be careful to avoid tension on suture lines. In addition, create a fascial flap to prevent opposition of the incision planes and reduce the risk of recurrence.
- Grafts. In cases with a high risk of recurrence, such as complex or large fistulae, a Martius fat-pad graft should be interposed between the closure layers to promote vascularization and reduce the risk of recurrence.14 Placement of a cadaveric biomaterial graft also has been reported, reducing the need for complicated flap procedures.15
Abdominal approach. Although most vesicovaginal fistulae can be surgically corrected via the vaginal approach, the abdominal route may be preferred when the fistula is high and inaccessible, large and complex, multiple in number, or when there is concurrent uterine or bowel involvement or a need for ureteral reimplantation. The abdominal approach may be facilitated by cystoscopically guided placement of a catheter through the fistulous tract to assist in subsequent identification and dissection.
To begin, make a vertical skin incision to optimize visualization and allow mobilization of an omental flap, if necessary. Expose the bladder and perform a high extraperitoneal cystotomy to visualize the fistulous tract. Place ureteral stents if the fistula is in close proximity to the ureteral orifice.
Extend the bladder incision to the fistulous tract and completely excise it following mobilization of the vagina. Then close the vagina and bladder with interrupted, delayed absorbable suture in a double layer.
Transpose an omental flap between the vaginal and bladder incisions to promote vascularization, minimize opposition of suture lines, and reduce the risk of recurrence (FIGURE 2).
Laparoscopic approach. A similar laparoscopic repair has been reported with comparable results, but requires advanced skills with endoscopic suturing and knot tying (FIGURE 3).16
FIGURE 2 Abdominal repair
Abdominal repair of vesicovaginal fistula, with closure of bladder defect and posterior cystotomy and separate closure of vaginal defect. Note the omental flap pictured in the insert.
FIGURE 3 Laparoscopic repair
Laparoscopic repair of vesicovaginal fistula.The authors report no financial relationship with any companies whose products are mentioned in this article.
1. Kremling H. Labor-induced bladder injuries: historical observations. Gynakol Geburtshilfliche Rundsch. 1996;36:197-200.
2. Lee RA, Symmonds RE, Williams TJ. Current state of genitourinary fistula. Obstet Gynecol. 1998;72:313-315.
3. Miklos JR, Sze EHM, Parobeck D, et al. Vesicouterine fistula: a rare complication of vaginal birth after cesarean. Obstet Gynecol. 1995;86:638-639.
4. Elkins TE, Thompson JR. Lower urinary tract fistulas. In: Walters M, Karram MM, eds. Urogynecology and Reconstructive Pelvic Surgery. 2nd ed. St. Louis, Mo: Mosby; 1999;355-365.
5. Zimmern PE, Hadley HR, Staskin D. Genitourinary fistulas: vaginal approach for repair of vesicovaginal fistulas. Clin Obstet Gynaecol. 1985;12:403-413.
6. Davits RJ, Miranda SI. Conservative treatment of vesicovaginal fistulas by bladder drainage alone. Br J Urol. 1991;68:155-156.
7. Margolis T, Mercer LJ. Vesicovaginal fistula. Obstet Gynecol Surv. 1995;49:840-847.
8. Blaivas JG, Heritz DM, Romanzi LJ. Early versus late repair of vesicovaginal fistulas: vaginal and abdominal approaches. J Urol. 1995;153:1110-1112.
9. Blandy JP, Badenoch DF, Fowler CG. Early repair of iatrogenic injury to the ureter or bladder after gynecological surgery. J Urol. 1991;146:761-765.
10. Cruikshank SH. Early closure of posthysterectomy vesicovaginal fistulas. South Med J. 1988;81:1525-1528.
11. Raz S, Bregg KJ, Nitti VW. Transvaginal repair of vesicovaginal fistula using a peritoneal flap. J Urol. 1993;150:56-59.
12. Iselin CE, Aslan P, Webster GD. Transvaginal repair of vesicovaginal fistulas after hysterectomy by vaginal cuff excision. J Urol. 1998;160(3 Pt 1):728-730.
13. Latzko W. Postoperative vesicovaginal fistulas: genesis and therapy. Am J Surg. 1942;58:211-218.
14. Punekar SV, Buch DN, Soni AB. Martius’ labial fat pad interposition and its modification in complex lower urinary fistulae. J Postgrad Med. 1999;10:405-406.
15. Miklos JR, Kohli N. Rectovaginal fistula repair utilizing a cadaveric dermal allograft. Int Urogynecol J Pelvic Floor Dysfunct. 1999;10:405-406.
16. Nezhat CH, Nezhat F, Nezhat C. Laparoscopic repair of a vesicovaginal fistula: a case report. Obstet Gynecol. 1994;83(5 Pt 2):899-901.
17. Walters MD, Karram MM, eds. Urogynecology and Reconstructive Pelvic Surgery. 2nd ed. St. Louis, Mo: Mosby; 1999.
1. Kremling H. Labor-induced bladder injuries: historical observations. Gynakol Geburtshilfliche Rundsch. 1996;36:197-200.
2. Lee RA, Symmonds RE, Williams TJ. Current state of genitourinary fistula. Obstet Gynecol. 1998;72:313-315.
3. Miklos JR, Sze EHM, Parobeck D, et al. Vesicouterine fistula: a rare complication of vaginal birth after cesarean. Obstet Gynecol. 1995;86:638-639.
4. Elkins TE, Thompson JR. Lower urinary tract fistulas. In: Walters M, Karram MM, eds. Urogynecology and Reconstructive Pelvic Surgery. 2nd ed. St. Louis, Mo: Mosby; 1999;355-365.
5. Zimmern PE, Hadley HR, Staskin D. Genitourinary fistulas: vaginal approach for repair of vesicovaginal fistulas. Clin Obstet Gynaecol. 1985;12:403-413.
6. Davits RJ, Miranda SI. Conservative treatment of vesicovaginal fistulas by bladder drainage alone. Br J Urol. 1991;68:155-156.
7. Margolis T, Mercer LJ. Vesicovaginal fistula. Obstet Gynecol Surv. 1995;49:840-847.
8. Blaivas JG, Heritz DM, Romanzi LJ. Early versus late repair of vesicovaginal fistulas: vaginal and abdominal approaches. J Urol. 1995;153:1110-1112.
9. Blandy JP, Badenoch DF, Fowler CG. Early repair of iatrogenic injury to the ureter or bladder after gynecological surgery. J Urol. 1991;146:761-765.
10. Cruikshank SH. Early closure of posthysterectomy vesicovaginal fistulas. South Med J. 1988;81:1525-1528.
11. Raz S, Bregg KJ, Nitti VW. Transvaginal repair of vesicovaginal fistula using a peritoneal flap. J Urol. 1993;150:56-59.
12. Iselin CE, Aslan P, Webster GD. Transvaginal repair of vesicovaginal fistulas after hysterectomy by vaginal cuff excision. J Urol. 1998;160(3 Pt 1):728-730.
13. Latzko W. Postoperative vesicovaginal fistulas: genesis and therapy. Am J Surg. 1942;58:211-218.
14. Punekar SV, Buch DN, Soni AB. Martius’ labial fat pad interposition and its modification in complex lower urinary fistulae. J Postgrad Med. 1999;10:405-406.
15. Miklos JR, Kohli N. Rectovaginal fistula repair utilizing a cadaveric dermal allograft. Int Urogynecol J Pelvic Floor Dysfunct. 1999;10:405-406.
16. Nezhat CH, Nezhat F, Nezhat C. Laparoscopic repair of a vesicovaginal fistula: a case report. Obstet Gynecol. 1994;83(5 Pt 2):899-901.
17. Walters MD, Karram MM, eds. Urogynecology and Reconstructive Pelvic Surgery. 2nd ed. St. Louis, Mo: Mosby; 1999.
New transobturator sling reduces risk of injury
- The route of the transobturator sling is strictly perineal, with a very short, blind passage through the crural region. This pathway ensures that the retropubic space is not entered and that the anatomic structures crossed by the needle passer and mesh are either muscle or fascia.
- The transobturator approach eliminates the need for routine cystoscopy in most patients.
- Short-term efficacy of the transobturator sling is similar to that of other suburethral tension-free slings.
- In our experience, the transobturator approach reduces average operating time to 17 minutes.
Potential complications associated with passing needle carriers through the retropubic space are eliminated, and cystoscopy is not routinely required with the use of a transobturator sling.
Although it is effective and easy to perform,1-6 retropubic placement of suburethral tension-free vaginal tape (TVT) for the treatment of stress urinary incontinence has been associated with a number of bowel, vascular, nerve, and bladder injuries (TABLE).7-13
Such complications appear to be related to the unique upward vaginal passage of the metallic sling trocars through the retropubic space. Newer slings eliminate the upward approach, but still require routine cystoscopy to confirm an intact bladder and urethra.
A new tension-free suburethral sling addresses these shortcomings using an innovative transobturator route.14 In the new procedure, the surgeon uses needle passers to run the sling from one obturator foramen to the other. The perineal approach reproduces the natural suspension of the urethral fascia while preserving an intact retropubic space (FIGURE 1).
TABLE
Advantages of the transobturator sling
|
FIGURE 1 Suburethral slings: Retropubic and transobturator pathways
Traditional suburethral tension-free slings require the needle passers and sling to be placed through the retropubic space.
The newer transobturator sling uses a perineal approach. The needle passer and sling are passed from one obturator foramen to the other, preserving an intact retropubic space.
What does ‘tension-free’ mean?
Tension-free slings are used to treat stress urinary incontinence caused by urethral hypermobility and intrinsic sphincter deficiency. In this approach, a synthetic transvaginal suburethral sling is placed through the retropubic space without using suspension sutures. The sling is held in place by the friction between the mesh and the tissue canals created by the metallic needle passers. Scar tissue later fixes the mesh, preventing migration.
Short-term efficacy of the Monarc transobturator sling is similar to that of the SPARC and tension-free vaginal slings.
Because the sling is not anchored to the pubic bone, ligaments, or rectus fascia, it is considered “free of tension.” The result is a midcomplex urethral support that limits urethral descent, improves the stabilization mechanism generated by pubourethral ligaments and levator ani muscles, and reinforces support of the backboard vaginal hammock.
A tension-free sling designed to reduce injury
Since its introduction in the mid 1990s, retropubic placement of suburethral tension-free tape has continued to gain in popularity.15-22 The technique has several advantages: It is simple to perform under local, regional, or general anesthesia, and has proved to be a safe treatment for stress urinary incontinence, with minimal complications in experienced hands. Still, injuries have occurred7-13 —likely due to the blind passing of metal trocars from the vagina upward through the retropubic space.9,23
Downward placement introduced. In an effort to reduce these complications, tension-free sling systems that rely on suprapubic, downward needle-carrier placement through the retropubic space were developed, such as the SPARC Female Sling System (American Medical Systems, Minnetonka, Minn), introduced in 2001.24 The manufacturer of the traditional TVT (Gynecare, a division of Ethicon, Somerville, NJ) also recently introduced suprapubic needle passers. However, because these slings still require passage through the retropubic space, their use may lead to vascular, bowel, and bladder injury. Routine cystoscopy is therefore required.
The transobturator sling. In the Netherlands in 1998, Nickel et al25 reported a successful sling procedure using a polyester ribbon passed through the obturator foramen and around the urethra for treatment of refractory urethral sphincter incompetence in female dogs. In France in 2001, Delorme14 introduced the transobturator sling procedure in humans. Dargent et al26 then performed the operation in 71 patients using a technique inspired by Delorme, and found the shortterm results similar to those of the TVT.
The Monarc transobturator sling (American Medical Systems), introduced in Europe in January 2003, has been used successfully in more than 1,000 procedures ( FIGURE 2). This new system offers significant technical improvements over the original transobturator sling devices.
The Monarc transobturator sling, introduced in Europe in January 2003, has been used successfully in more than 1,000 procedures.
Specifically, the Monarc system simplifies rotation of the needle passer during insertion and extraction around the inferior aspect of the ischiopubic ramus. The 3-mm–diameter passers are specifically designed for right-side or left-side use. They are attached to fixed handles to create a natural wrist rotation. The sling connectors, meanwhile, facilitate rapid, effortless, and secure mesh placement and fixation.
FIGURE 2 Monarc transobturator sling system
The Monarc system consists of 2 stainless steel helical-shaped needle passers and a 1-cm by 35-cm polypropylene sling mesh with a protected sheath, attached connectors, and a reabsorbable tensioning suture.
Easy to learn and perform
Anesthesia may be local, regional, or general, and prophylactic antibiotics are routinely given. FIGURES 3 through 6 offer a detailed description of how to surgically place the Monarc transobturator sling for treatment of stress urinary incontinence. What follows is a brief overview:
After making a small vertical incision along the anterior vaginal mucosa, use a finger to locate the upper-inner corner of the obturator foramen—the safe zone for needle insertion. You will incise the skin at this point and introduce the needle tip perpendicularly. Rotate the needle, with the tip following the posterior surface of the pubic ramus, until the tip exits the vaginal incision. Repeat this process on the other side.
Attach the sling and its plastic sheath, then draw both out through the skin incisions by pulling back on the needle passers. Cut the mesh, adjust the tension, and close the incisions.
A Foley catheter and vaginal packing with metronidazole gel may be used at the surgeon’s discretion.
Route minimizes anatomical hazards. The pathway described ensures that there tropubic space is not entered and that muscle or fascia are the only anatomic structures crossed by the needle passer and mesh. No major vessels or nerves come in contact with the sling (FIGURES 7 and 8).
Our fluoroscopic observations of the transobturator sling in cadavers show that insertion of the needle passer through the obturator foramen with exit through the vaginal incision under the mid-urethra is precise and simple (FIGURE 9).
Our comparative studies in cadavers revealed that, despite the different shape and placement, lengths for the SPARC and Monarc transobturator slings in the same cadaver are almost equivalent—ranging from 12 to 14 cm, depending on the patient’s height and weight (FIGURE 10).
The transobturator sling involves fewer potential anatomical hazards than retropubic placement.
These considerations strongly suggest that the transobturator sling offers a simpler approach with fewer potential anatomic hazards than retropubic tension-free slings.
FIGURE 3 Vaginal incision
Inject a diluted vasoconstrictive solution into the anterior vaginal wall, and make a small vertical incision along the anterior vaginal mucosa 0.5 cm below the urethral meatus. Separate the vaginal epithelium from the underlying periurethral fascia using sharp and digital dissection, advancing bilaterally to the inferior pubic ramus. Insert a finger into the vaginal dissection and palpate the internal edge of the ischiopubic ramus and the upper-inner corner of the obturator foramen.
FIGURE 4 Needle entry: Transobturator sling procedure
The safe zone for needle insertion is the upper-inner corner of the obturator foramen (red line). The red dot indicates the recommended insertion site (upper inner corner).
The insertion area corresponds to the point where a horizontal line at the level of the clitoris crosses a vertical line at the level of the genitofemoral fold. Make a small skin incision at this point.
FIGURE 5 Needle passage: Transobturator sling procedure
Insert your left index finger into the vaginal incision on the patient’s left side. Holding the right-side Monarc needle, introduce the needle tip perpendicularly through the skin incision.
Place the thumb of your left hand onto the outside curve of the needle and gently push until its tip penetrates the obturator membrane and muscle. Use the needle’s tip to locate the pubic ramus, and rotate the needle so that the tip follows the posterior surface of this structure.
Continue this rotation, using your left index finger to guide the needle tip to exit the vaginal incision.
Repeat steps A and B on the contralateral side.
With the needle-passer tips extending out of the vaginal incision, attach the sling and its plastic sheath using the connectors. Make sure the mesh lies flat and is not twisted before attaching the connector to the second needle.
FIGURE 7 Route of transobturator sling minimizes anatomical hazards
The needle travels around the ischiopubic ramus. Transobturator needle passage begins with penetration of the skin and subcutaneous tissue. After traversing the superficial perineal fascia, the needle crosses the adductor muscles of the thigh near their pubic bone origin and below the insertion point of the adductor longus tendon (arrow). It then penetrates the obturator membrane, obturator internus muscle, and periurethral endopelvic fascia. After passing the level of the white line—either over or under the puborectalis section of the levator—the needle exits through the vaginal incision.
FIGURE 8 The obturator foramen
The tough obturator membrane covers the foramen. The obturator canal is 2 to 3 cm long and is located at the anterolateral upper margin of the membrane. The distance between the safe zone for needle insertion and the obturator canal is approximately 3.5 to 4 cm. At the safe entry zone (green area), the anterior branch of the obturator artery is reduced to a capillary diameter and no significant arteries, veins, or nerve pedicles are present.
FIGURE 10 Routes of transobturator and retropubic slings
Graphic depiction of both the transobturator sling and the retropubic tension-free sling in place.
Fluoroscopic image of both slings in a cadaver. The transobturator sling runs horizontally while the retropubic tension-free sling forms a tighter “U.”
Clinical experience yields positive results
Early European series and our initial experience suggest that the short-term efficacy of the Monarc transobturator sling is similar to that of the SPARC and TVT slings. Average operating time is 17 minutes. The technique involves a short learning curve (approximately 4 cases).
Cystoscopy is not routinely required; we perform it only in women with significant prolapse or suspected urethral injury, and have encountered no intraoperative or post-operative complications.
No major vessels or nerves come in contact with the transobturator tension-free sling.
No patients have complained of postoperative pain in the area of the adductor muscles of the thigh, and no sling erosions have occurred. We also have found this approach useful in obese patients and women with retropubic scarring, in whom retropubic needle passage can be a challenge.
In addition to its application in the treatment of female stress urinary incontinence, the transobturator foramen route was recently used to insert the anterior wings of a large mesh in the repair of severe cystocele.27
Although long-term follow-up data are not available for the transobturator approach, short-term results are encouraging. Large comparative studies with other anti-incontinent procedures are needed.
Dr. Pelosi II reports that he is a consultant for American Medical Systems. Dr. Pelosi III reports no affiliations or financial arrangements with any companies whose products are mentioned in this article.
1. Reschers UM, Tunn R, Buczkowski M, et al. Tension-free vaginal tape for the treatment of stress urinary incontinence. Clin Obstet Gynecol. 2000;43:670-675.
2. Tamussino KF, Hanzal E, Kolle D, et al. Tension-free vaginal tape operation: results of the Austrian Registry. Obstet Gynecol. 2001;98:732-736.
3. Haab F, Sananes S, Amarenco G, et al. Results of the tension-free vaginal tape procedure for the treatment of type II stress urinary incontinence at a minimum follow up of one year. J Urol. 2001;165:159-162.
4. Rardin CR, Kohli N, Rosenblatt PL, et al. Tension-free vaginal tape: outcomes among women with primary versus recurrent stress urinary incontinence. Obstet Gynecol. 2002;100:893-897.
5. Vassallo BJ, Kleeman SD, Segal JL, et al. Tension-free vaginal tape: a quality of life assessment. Obstet Gynecol. 2002;100:518-524.
6. Karram MM, Segal JL, Vassallo BJ, et al. Complications and untoward effects of the tension-free vaginal tape procedure. Obstet Gynecol. 2003;101:929-932.
7. MAUDE: Food and Drug Administration Manufacturer and User Facility Device Experience Database. Available at http://www.fda.gov/cdrh/maude.html. Accessed June 7, 2003.
8. Peyrat L, Boutin JM, Bruyere F, et al. Intestinal perforation is a complication of TVT procedure for UI. Eur Urol. 2001;39:603-605.
9. Walters MD, Tulikangas PR, LaSala C, et al. Vascular injury during tension-free vaginal tape procedure for stress urinary incontinence. Obstet Gynecol. 2001;98:957-959.
10. Zilbert AW, Farrell SA. External iliac artery laceration during tension-free vaginal tape procedure. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12:141-143.
11. Vierhout ME. Severe hemorrhage complicating TVT: a case report. Int Urogynecol J Pelvic Floor Dysfunct. 2000;12:139-140.
12. Brink DM. Bowel injury following insertion of TVT. S Afr Med J. 2000;90:450-452.
13. Shobeiri SA, Garely AD, Chesson RR. Recognition of occult bladder injury during the tension-free vaginal tape procedure. Obstet Gynecol. 2002;99:1067-1072.
14. Delorme E. Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol. 2001;11:1306-1313.
15. Ulmstein V, Petros P. Intravaginal slingplasty (IVS): an ambulatory surgical procedure for treatment of female urinary incontinence. Scand J Urol Neprhol. 1995;29:75-82.
16. Chung MK, Chung RP. Comparison of laparoscopic Burch and tension-free vaginal tape in treating stress urinary incontinence in obese patients. JSLS. 2002;6:17-21.
17. Pelosi MA, III, Pelosi MA, II. Pubic bone suburethral stabilization sling: laparoscopic assessment of a transvaginal operation for the treatment of stress urinary incontinence. J Laparoendosc Adv Surg Tech. 1999;9:45-50.
18. Pelosi MA, II, Pelosi MA, III, Pelekanos M. The YAMA uropatch sling for treatment of female stress urinary incontinence: a pilot study. J Laparoendosc Adv Surg Tech. 2002;12:27-33.
19. Pelosi MA, II, Pelosi MA, III. Laparoscopic assessment of transvaginal suture fixation to Cooper’s ligament for suburethral slings. J Am Assoc Gynecol Laparosc. 2001;8:S53.-
20. Cundiff GW, Wright JE. A review of surgical management of genuine stress incontinence in women with a discussion of innovative procedures. J Pelvic Surg. 1998;4:271-278.
21. Sarver R, Govier FE. Pubovaginal slings: past, present, and future. Int Urogynecol J. 1997;8:358-368.
22. Kovac RS, Cruikshank SH. Pubic bone suburethral stabilization sling for recurrent urinary incontinence. Obstet Gynecol. 1997;89:624-627.
23. Muir TW, Tulikangos PK, Paraiso MF, et al. The relationship of tension-free vaginal tape insertion and the vascular anatomy. Obstet Gynecol. 2003;101:933-936.
24. Pelosi MA, II, Pelosi MA, III. Laparoscopic evaluation of a new tension-free vaginal sling (SPARC) for stress urinary incontinence. Proceedings of the 31st annual meeting of the American Association of Gynecologic Laparoscopists. November 2002; Miami, Fla.
25. Nickel RF, Wiegand U, van den Brom WE. Evaluation of a transpelvic sling procedure with and without colposuspension for treatment of female dogs with refractory urethral sphincter mechanism incompetence. Vet Surg. 1998;27:94-104.
26. Dargent D, Bretones S, George P, et al. Insertion of a suburethral sling through the obturator membrane in the treatment of female urinary incontinence. Gynecol Obstet Fertil. 2002;30:576-582.
27. Mouly P, Soulie M, Seguin P, et al. Vaginal reconstruction of a complete vaginal prolapse: the transobturator repair. J Urol. 2003;169:S182.-
- The route of the transobturator sling is strictly perineal, with a very short, blind passage through the crural region. This pathway ensures that the retropubic space is not entered and that the anatomic structures crossed by the needle passer and mesh are either muscle or fascia.
- The transobturator approach eliminates the need for routine cystoscopy in most patients.
- Short-term efficacy of the transobturator sling is similar to that of other suburethral tension-free slings.
- In our experience, the transobturator approach reduces average operating time to 17 minutes.
Potential complications associated with passing needle carriers through the retropubic space are eliminated, and cystoscopy is not routinely required with the use of a transobturator sling.
Although it is effective and easy to perform,1-6 retropubic placement of suburethral tension-free vaginal tape (TVT) for the treatment of stress urinary incontinence has been associated with a number of bowel, vascular, nerve, and bladder injuries (TABLE).7-13
Such complications appear to be related to the unique upward vaginal passage of the metallic sling trocars through the retropubic space. Newer slings eliminate the upward approach, but still require routine cystoscopy to confirm an intact bladder and urethra.
A new tension-free suburethral sling addresses these shortcomings using an innovative transobturator route.14 In the new procedure, the surgeon uses needle passers to run the sling from one obturator foramen to the other. The perineal approach reproduces the natural suspension of the urethral fascia while preserving an intact retropubic space (FIGURE 1).
TABLE
Advantages of the transobturator sling
|
FIGURE 1 Suburethral slings: Retropubic and transobturator pathways
Traditional suburethral tension-free slings require the needle passers and sling to be placed through the retropubic space.
The newer transobturator sling uses a perineal approach. The needle passer and sling are passed from one obturator foramen to the other, preserving an intact retropubic space.
What does ‘tension-free’ mean?
Tension-free slings are used to treat stress urinary incontinence caused by urethral hypermobility and intrinsic sphincter deficiency. In this approach, a synthetic transvaginal suburethral sling is placed through the retropubic space without using suspension sutures. The sling is held in place by the friction between the mesh and the tissue canals created by the metallic needle passers. Scar tissue later fixes the mesh, preventing migration.
Short-term efficacy of the Monarc transobturator sling is similar to that of the SPARC and tension-free vaginal slings.
Because the sling is not anchored to the pubic bone, ligaments, or rectus fascia, it is considered “free of tension.” The result is a midcomplex urethral support that limits urethral descent, improves the stabilization mechanism generated by pubourethral ligaments and levator ani muscles, and reinforces support of the backboard vaginal hammock.
A tension-free sling designed to reduce injury
Since its introduction in the mid 1990s, retropubic placement of suburethral tension-free tape has continued to gain in popularity.15-22 The technique has several advantages: It is simple to perform under local, regional, or general anesthesia, and has proved to be a safe treatment for stress urinary incontinence, with minimal complications in experienced hands. Still, injuries have occurred7-13 —likely due to the blind passing of metal trocars from the vagina upward through the retropubic space.9,23
Downward placement introduced. In an effort to reduce these complications, tension-free sling systems that rely on suprapubic, downward needle-carrier placement through the retropubic space were developed, such as the SPARC Female Sling System (American Medical Systems, Minnetonka, Minn), introduced in 2001.24 The manufacturer of the traditional TVT (Gynecare, a division of Ethicon, Somerville, NJ) also recently introduced suprapubic needle passers. However, because these slings still require passage through the retropubic space, their use may lead to vascular, bowel, and bladder injury. Routine cystoscopy is therefore required.
The transobturator sling. In the Netherlands in 1998, Nickel et al25 reported a successful sling procedure using a polyester ribbon passed through the obturator foramen and around the urethra for treatment of refractory urethral sphincter incompetence in female dogs. In France in 2001, Delorme14 introduced the transobturator sling procedure in humans. Dargent et al26 then performed the operation in 71 patients using a technique inspired by Delorme, and found the shortterm results similar to those of the TVT.
The Monarc transobturator sling (American Medical Systems), introduced in Europe in January 2003, has been used successfully in more than 1,000 procedures ( FIGURE 2). This new system offers significant technical improvements over the original transobturator sling devices.
The Monarc transobturator sling, introduced in Europe in January 2003, has been used successfully in more than 1,000 procedures.
Specifically, the Monarc system simplifies rotation of the needle passer during insertion and extraction around the inferior aspect of the ischiopubic ramus. The 3-mm–diameter passers are specifically designed for right-side or left-side use. They are attached to fixed handles to create a natural wrist rotation. The sling connectors, meanwhile, facilitate rapid, effortless, and secure mesh placement and fixation.
FIGURE 2 Monarc transobturator sling system
The Monarc system consists of 2 stainless steel helical-shaped needle passers and a 1-cm by 35-cm polypropylene sling mesh with a protected sheath, attached connectors, and a reabsorbable tensioning suture.
Easy to learn and perform
Anesthesia may be local, regional, or general, and prophylactic antibiotics are routinely given. FIGURES 3 through 6 offer a detailed description of how to surgically place the Monarc transobturator sling for treatment of stress urinary incontinence. What follows is a brief overview:
After making a small vertical incision along the anterior vaginal mucosa, use a finger to locate the upper-inner corner of the obturator foramen—the safe zone for needle insertion. You will incise the skin at this point and introduce the needle tip perpendicularly. Rotate the needle, with the tip following the posterior surface of the pubic ramus, until the tip exits the vaginal incision. Repeat this process on the other side.
Attach the sling and its plastic sheath, then draw both out through the skin incisions by pulling back on the needle passers. Cut the mesh, adjust the tension, and close the incisions.
A Foley catheter and vaginal packing with metronidazole gel may be used at the surgeon’s discretion.
Route minimizes anatomical hazards. The pathway described ensures that there tropubic space is not entered and that muscle or fascia are the only anatomic structures crossed by the needle passer and mesh. No major vessels or nerves come in contact with the sling (FIGURES 7 and 8).
Our fluoroscopic observations of the transobturator sling in cadavers show that insertion of the needle passer through the obturator foramen with exit through the vaginal incision under the mid-urethra is precise and simple (FIGURE 9).
Our comparative studies in cadavers revealed that, despite the different shape and placement, lengths for the SPARC and Monarc transobturator slings in the same cadaver are almost equivalent—ranging from 12 to 14 cm, depending on the patient’s height and weight (FIGURE 10).
The transobturator sling involves fewer potential anatomical hazards than retropubic placement.
These considerations strongly suggest that the transobturator sling offers a simpler approach with fewer potential anatomic hazards than retropubic tension-free slings.
FIGURE 3 Vaginal incision
Inject a diluted vasoconstrictive solution into the anterior vaginal wall, and make a small vertical incision along the anterior vaginal mucosa 0.5 cm below the urethral meatus. Separate the vaginal epithelium from the underlying periurethral fascia using sharp and digital dissection, advancing bilaterally to the inferior pubic ramus. Insert a finger into the vaginal dissection and palpate the internal edge of the ischiopubic ramus and the upper-inner corner of the obturator foramen.
FIGURE 4 Needle entry: Transobturator sling procedure
The safe zone for needle insertion is the upper-inner corner of the obturator foramen (red line). The red dot indicates the recommended insertion site (upper inner corner).
The insertion area corresponds to the point where a horizontal line at the level of the clitoris crosses a vertical line at the level of the genitofemoral fold. Make a small skin incision at this point.
FIGURE 5 Needle passage: Transobturator sling procedure
Insert your left index finger into the vaginal incision on the patient’s left side. Holding the right-side Monarc needle, introduce the needle tip perpendicularly through the skin incision.
Place the thumb of your left hand onto the outside curve of the needle and gently push until its tip penetrates the obturator membrane and muscle. Use the needle’s tip to locate the pubic ramus, and rotate the needle so that the tip follows the posterior surface of this structure.
Continue this rotation, using your left index finger to guide the needle tip to exit the vaginal incision.
Repeat steps A and B on the contralateral side.
With the needle-passer tips extending out of the vaginal incision, attach the sling and its plastic sheath using the connectors. Make sure the mesh lies flat and is not twisted before attaching the connector to the second needle.
FIGURE 7 Route of transobturator sling minimizes anatomical hazards
The needle travels around the ischiopubic ramus. Transobturator needle passage begins with penetration of the skin and subcutaneous tissue. After traversing the superficial perineal fascia, the needle crosses the adductor muscles of the thigh near their pubic bone origin and below the insertion point of the adductor longus tendon (arrow). It then penetrates the obturator membrane, obturator internus muscle, and periurethral endopelvic fascia. After passing the level of the white line—either over or under the puborectalis section of the levator—the needle exits through the vaginal incision.
FIGURE 8 The obturator foramen
The tough obturator membrane covers the foramen. The obturator canal is 2 to 3 cm long and is located at the anterolateral upper margin of the membrane. The distance between the safe zone for needle insertion and the obturator canal is approximately 3.5 to 4 cm. At the safe entry zone (green area), the anterior branch of the obturator artery is reduced to a capillary diameter and no significant arteries, veins, or nerve pedicles are present.
FIGURE 10 Routes of transobturator and retropubic slings
Graphic depiction of both the transobturator sling and the retropubic tension-free sling in place.
Fluoroscopic image of both slings in a cadaver. The transobturator sling runs horizontally while the retropubic tension-free sling forms a tighter “U.”
Clinical experience yields positive results
Early European series and our initial experience suggest that the short-term efficacy of the Monarc transobturator sling is similar to that of the SPARC and TVT slings. Average operating time is 17 minutes. The technique involves a short learning curve (approximately 4 cases).
Cystoscopy is not routinely required; we perform it only in women with significant prolapse or suspected urethral injury, and have encountered no intraoperative or post-operative complications.
No major vessels or nerves come in contact with the transobturator tension-free sling.
No patients have complained of postoperative pain in the area of the adductor muscles of the thigh, and no sling erosions have occurred. We also have found this approach useful in obese patients and women with retropubic scarring, in whom retropubic needle passage can be a challenge.
In addition to its application in the treatment of female stress urinary incontinence, the transobturator foramen route was recently used to insert the anterior wings of a large mesh in the repair of severe cystocele.27
Although long-term follow-up data are not available for the transobturator approach, short-term results are encouraging. Large comparative studies with other anti-incontinent procedures are needed.
Dr. Pelosi II reports that he is a consultant for American Medical Systems. Dr. Pelosi III reports no affiliations or financial arrangements with any companies whose products are mentioned in this article.
- The route of the transobturator sling is strictly perineal, with a very short, blind passage through the crural region. This pathway ensures that the retropubic space is not entered and that the anatomic structures crossed by the needle passer and mesh are either muscle or fascia.
- The transobturator approach eliminates the need for routine cystoscopy in most patients.
- Short-term efficacy of the transobturator sling is similar to that of other suburethral tension-free slings.
- In our experience, the transobturator approach reduces average operating time to 17 minutes.
Potential complications associated with passing needle carriers through the retropubic space are eliminated, and cystoscopy is not routinely required with the use of a transobturator sling.
Although it is effective and easy to perform,1-6 retropubic placement of suburethral tension-free vaginal tape (TVT) for the treatment of stress urinary incontinence has been associated with a number of bowel, vascular, nerve, and bladder injuries (TABLE).7-13
Such complications appear to be related to the unique upward vaginal passage of the metallic sling trocars through the retropubic space. Newer slings eliminate the upward approach, but still require routine cystoscopy to confirm an intact bladder and urethra.
A new tension-free suburethral sling addresses these shortcomings using an innovative transobturator route.14 In the new procedure, the surgeon uses needle passers to run the sling from one obturator foramen to the other. The perineal approach reproduces the natural suspension of the urethral fascia while preserving an intact retropubic space (FIGURE 1).
TABLE
Advantages of the transobturator sling
|
FIGURE 1 Suburethral slings: Retropubic and transobturator pathways
Traditional suburethral tension-free slings require the needle passers and sling to be placed through the retropubic space.
The newer transobturator sling uses a perineal approach. The needle passer and sling are passed from one obturator foramen to the other, preserving an intact retropubic space.
What does ‘tension-free’ mean?
Tension-free slings are used to treat stress urinary incontinence caused by urethral hypermobility and intrinsic sphincter deficiency. In this approach, a synthetic transvaginal suburethral sling is placed through the retropubic space without using suspension sutures. The sling is held in place by the friction between the mesh and the tissue canals created by the metallic needle passers. Scar tissue later fixes the mesh, preventing migration.
Short-term efficacy of the Monarc transobturator sling is similar to that of the SPARC and tension-free vaginal slings.
Because the sling is not anchored to the pubic bone, ligaments, or rectus fascia, it is considered “free of tension.” The result is a midcomplex urethral support that limits urethral descent, improves the stabilization mechanism generated by pubourethral ligaments and levator ani muscles, and reinforces support of the backboard vaginal hammock.
A tension-free sling designed to reduce injury
Since its introduction in the mid 1990s, retropubic placement of suburethral tension-free tape has continued to gain in popularity.15-22 The technique has several advantages: It is simple to perform under local, regional, or general anesthesia, and has proved to be a safe treatment for stress urinary incontinence, with minimal complications in experienced hands. Still, injuries have occurred7-13 —likely due to the blind passing of metal trocars from the vagina upward through the retropubic space.9,23
Downward placement introduced. In an effort to reduce these complications, tension-free sling systems that rely on suprapubic, downward needle-carrier placement through the retropubic space were developed, such as the SPARC Female Sling System (American Medical Systems, Minnetonka, Minn), introduced in 2001.24 The manufacturer of the traditional TVT (Gynecare, a division of Ethicon, Somerville, NJ) also recently introduced suprapubic needle passers. However, because these slings still require passage through the retropubic space, their use may lead to vascular, bowel, and bladder injury. Routine cystoscopy is therefore required.
The transobturator sling. In the Netherlands in 1998, Nickel et al25 reported a successful sling procedure using a polyester ribbon passed through the obturator foramen and around the urethra for treatment of refractory urethral sphincter incompetence in female dogs. In France in 2001, Delorme14 introduced the transobturator sling procedure in humans. Dargent et al26 then performed the operation in 71 patients using a technique inspired by Delorme, and found the shortterm results similar to those of the TVT.
The Monarc transobturator sling (American Medical Systems), introduced in Europe in January 2003, has been used successfully in more than 1,000 procedures ( FIGURE 2). This new system offers significant technical improvements over the original transobturator sling devices.
The Monarc transobturator sling, introduced in Europe in January 2003, has been used successfully in more than 1,000 procedures.
Specifically, the Monarc system simplifies rotation of the needle passer during insertion and extraction around the inferior aspect of the ischiopubic ramus. The 3-mm–diameter passers are specifically designed for right-side or left-side use. They are attached to fixed handles to create a natural wrist rotation. The sling connectors, meanwhile, facilitate rapid, effortless, and secure mesh placement and fixation.
FIGURE 2 Monarc transobturator sling system
The Monarc system consists of 2 stainless steel helical-shaped needle passers and a 1-cm by 35-cm polypropylene sling mesh with a protected sheath, attached connectors, and a reabsorbable tensioning suture.
Easy to learn and perform
Anesthesia may be local, regional, or general, and prophylactic antibiotics are routinely given. FIGURES 3 through 6 offer a detailed description of how to surgically place the Monarc transobturator sling for treatment of stress urinary incontinence. What follows is a brief overview:
After making a small vertical incision along the anterior vaginal mucosa, use a finger to locate the upper-inner corner of the obturator foramen—the safe zone for needle insertion. You will incise the skin at this point and introduce the needle tip perpendicularly. Rotate the needle, with the tip following the posterior surface of the pubic ramus, until the tip exits the vaginal incision. Repeat this process on the other side.
Attach the sling and its plastic sheath, then draw both out through the skin incisions by pulling back on the needle passers. Cut the mesh, adjust the tension, and close the incisions.
A Foley catheter and vaginal packing with metronidazole gel may be used at the surgeon’s discretion.
Route minimizes anatomical hazards. The pathway described ensures that there tropubic space is not entered and that muscle or fascia are the only anatomic structures crossed by the needle passer and mesh. No major vessels or nerves come in contact with the sling (FIGURES 7 and 8).
Our fluoroscopic observations of the transobturator sling in cadavers show that insertion of the needle passer through the obturator foramen with exit through the vaginal incision under the mid-urethra is precise and simple (FIGURE 9).
Our comparative studies in cadavers revealed that, despite the different shape and placement, lengths for the SPARC and Monarc transobturator slings in the same cadaver are almost equivalent—ranging from 12 to 14 cm, depending on the patient’s height and weight (FIGURE 10).
The transobturator sling involves fewer potential anatomical hazards than retropubic placement.
These considerations strongly suggest that the transobturator sling offers a simpler approach with fewer potential anatomic hazards than retropubic tension-free slings.
FIGURE 3 Vaginal incision
Inject a diluted vasoconstrictive solution into the anterior vaginal wall, and make a small vertical incision along the anterior vaginal mucosa 0.5 cm below the urethral meatus. Separate the vaginal epithelium from the underlying periurethral fascia using sharp and digital dissection, advancing bilaterally to the inferior pubic ramus. Insert a finger into the vaginal dissection and palpate the internal edge of the ischiopubic ramus and the upper-inner corner of the obturator foramen.
FIGURE 4 Needle entry: Transobturator sling procedure
The safe zone for needle insertion is the upper-inner corner of the obturator foramen (red line). The red dot indicates the recommended insertion site (upper inner corner).
The insertion area corresponds to the point where a horizontal line at the level of the clitoris crosses a vertical line at the level of the genitofemoral fold. Make a small skin incision at this point.
FIGURE 5 Needle passage: Transobturator sling procedure
Insert your left index finger into the vaginal incision on the patient’s left side. Holding the right-side Monarc needle, introduce the needle tip perpendicularly through the skin incision.
Place the thumb of your left hand onto the outside curve of the needle and gently push until its tip penetrates the obturator membrane and muscle. Use the needle’s tip to locate the pubic ramus, and rotate the needle so that the tip follows the posterior surface of this structure.
Continue this rotation, using your left index finger to guide the needle tip to exit the vaginal incision.
Repeat steps A and B on the contralateral side.
With the needle-passer tips extending out of the vaginal incision, attach the sling and its plastic sheath using the connectors. Make sure the mesh lies flat and is not twisted before attaching the connector to the second needle.
FIGURE 7 Route of transobturator sling minimizes anatomical hazards
The needle travels around the ischiopubic ramus. Transobturator needle passage begins with penetration of the skin and subcutaneous tissue. After traversing the superficial perineal fascia, the needle crosses the adductor muscles of the thigh near their pubic bone origin and below the insertion point of the adductor longus tendon (arrow). It then penetrates the obturator membrane, obturator internus muscle, and periurethral endopelvic fascia. After passing the level of the white line—either over or under the puborectalis section of the levator—the needle exits through the vaginal incision.
FIGURE 8 The obturator foramen
The tough obturator membrane covers the foramen. The obturator canal is 2 to 3 cm long and is located at the anterolateral upper margin of the membrane. The distance between the safe zone for needle insertion and the obturator canal is approximately 3.5 to 4 cm. At the safe entry zone (green area), the anterior branch of the obturator artery is reduced to a capillary diameter and no significant arteries, veins, or nerve pedicles are present.
FIGURE 10 Routes of transobturator and retropubic slings
Graphic depiction of both the transobturator sling and the retropubic tension-free sling in place.
Fluoroscopic image of both slings in a cadaver. The transobturator sling runs horizontally while the retropubic tension-free sling forms a tighter “U.”
Clinical experience yields positive results
Early European series and our initial experience suggest that the short-term efficacy of the Monarc transobturator sling is similar to that of the SPARC and TVT slings. Average operating time is 17 minutes. The technique involves a short learning curve (approximately 4 cases).
Cystoscopy is not routinely required; we perform it only in women with significant prolapse or suspected urethral injury, and have encountered no intraoperative or post-operative complications.
No major vessels or nerves come in contact with the transobturator tension-free sling.
No patients have complained of postoperative pain in the area of the adductor muscles of the thigh, and no sling erosions have occurred. We also have found this approach useful in obese patients and women with retropubic scarring, in whom retropubic needle passage can be a challenge.
In addition to its application in the treatment of female stress urinary incontinence, the transobturator foramen route was recently used to insert the anterior wings of a large mesh in the repair of severe cystocele.27
Although long-term follow-up data are not available for the transobturator approach, short-term results are encouraging. Large comparative studies with other anti-incontinent procedures are needed.
Dr. Pelosi II reports that he is a consultant for American Medical Systems. Dr. Pelosi III reports no affiliations or financial arrangements with any companies whose products are mentioned in this article.
1. Reschers UM, Tunn R, Buczkowski M, et al. Tension-free vaginal tape for the treatment of stress urinary incontinence. Clin Obstet Gynecol. 2000;43:670-675.
2. Tamussino KF, Hanzal E, Kolle D, et al. Tension-free vaginal tape operation: results of the Austrian Registry. Obstet Gynecol. 2001;98:732-736.
3. Haab F, Sananes S, Amarenco G, et al. Results of the tension-free vaginal tape procedure for the treatment of type II stress urinary incontinence at a minimum follow up of one year. J Urol. 2001;165:159-162.
4. Rardin CR, Kohli N, Rosenblatt PL, et al. Tension-free vaginal tape: outcomes among women with primary versus recurrent stress urinary incontinence. Obstet Gynecol. 2002;100:893-897.
5. Vassallo BJ, Kleeman SD, Segal JL, et al. Tension-free vaginal tape: a quality of life assessment. Obstet Gynecol. 2002;100:518-524.
6. Karram MM, Segal JL, Vassallo BJ, et al. Complications and untoward effects of the tension-free vaginal tape procedure. Obstet Gynecol. 2003;101:929-932.
7. MAUDE: Food and Drug Administration Manufacturer and User Facility Device Experience Database. Available at http://www.fda.gov/cdrh/maude.html. Accessed June 7, 2003.
8. Peyrat L, Boutin JM, Bruyere F, et al. Intestinal perforation is a complication of TVT procedure for UI. Eur Urol. 2001;39:603-605.
9. Walters MD, Tulikangas PR, LaSala C, et al. Vascular injury during tension-free vaginal tape procedure for stress urinary incontinence. Obstet Gynecol. 2001;98:957-959.
10. Zilbert AW, Farrell SA. External iliac artery laceration during tension-free vaginal tape procedure. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12:141-143.
11. Vierhout ME. Severe hemorrhage complicating TVT: a case report. Int Urogynecol J Pelvic Floor Dysfunct. 2000;12:139-140.
12. Brink DM. Bowel injury following insertion of TVT. S Afr Med J. 2000;90:450-452.
13. Shobeiri SA, Garely AD, Chesson RR. Recognition of occult bladder injury during the tension-free vaginal tape procedure. Obstet Gynecol. 2002;99:1067-1072.
14. Delorme E. Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol. 2001;11:1306-1313.
15. Ulmstein V, Petros P. Intravaginal slingplasty (IVS): an ambulatory surgical procedure for treatment of female urinary incontinence. Scand J Urol Neprhol. 1995;29:75-82.
16. Chung MK, Chung RP. Comparison of laparoscopic Burch and tension-free vaginal tape in treating stress urinary incontinence in obese patients. JSLS. 2002;6:17-21.
17. Pelosi MA, III, Pelosi MA, II. Pubic bone suburethral stabilization sling: laparoscopic assessment of a transvaginal operation for the treatment of stress urinary incontinence. J Laparoendosc Adv Surg Tech. 1999;9:45-50.
18. Pelosi MA, II, Pelosi MA, III, Pelekanos M. The YAMA uropatch sling for treatment of female stress urinary incontinence: a pilot study. J Laparoendosc Adv Surg Tech. 2002;12:27-33.
19. Pelosi MA, II, Pelosi MA, III. Laparoscopic assessment of transvaginal suture fixation to Cooper’s ligament for suburethral slings. J Am Assoc Gynecol Laparosc. 2001;8:S53.-
20. Cundiff GW, Wright JE. A review of surgical management of genuine stress incontinence in women with a discussion of innovative procedures. J Pelvic Surg. 1998;4:271-278.
21. Sarver R, Govier FE. Pubovaginal slings: past, present, and future. Int Urogynecol J. 1997;8:358-368.
22. Kovac RS, Cruikshank SH. Pubic bone suburethral stabilization sling for recurrent urinary incontinence. Obstet Gynecol. 1997;89:624-627.
23. Muir TW, Tulikangos PK, Paraiso MF, et al. The relationship of tension-free vaginal tape insertion and the vascular anatomy. Obstet Gynecol. 2003;101:933-936.
24. Pelosi MA, II, Pelosi MA, III. Laparoscopic evaluation of a new tension-free vaginal sling (SPARC) for stress urinary incontinence. Proceedings of the 31st annual meeting of the American Association of Gynecologic Laparoscopists. November 2002; Miami, Fla.
25. Nickel RF, Wiegand U, van den Brom WE. Evaluation of a transpelvic sling procedure with and without colposuspension for treatment of female dogs with refractory urethral sphincter mechanism incompetence. Vet Surg. 1998;27:94-104.
26. Dargent D, Bretones S, George P, et al. Insertion of a suburethral sling through the obturator membrane in the treatment of female urinary incontinence. Gynecol Obstet Fertil. 2002;30:576-582.
27. Mouly P, Soulie M, Seguin P, et al. Vaginal reconstruction of a complete vaginal prolapse: the transobturator repair. J Urol. 2003;169:S182.-
1. Reschers UM, Tunn R, Buczkowski M, et al. Tension-free vaginal tape for the treatment of stress urinary incontinence. Clin Obstet Gynecol. 2000;43:670-675.
2. Tamussino KF, Hanzal E, Kolle D, et al. Tension-free vaginal tape operation: results of the Austrian Registry. Obstet Gynecol. 2001;98:732-736.
3. Haab F, Sananes S, Amarenco G, et al. Results of the tension-free vaginal tape procedure for the treatment of type II stress urinary incontinence at a minimum follow up of one year. J Urol. 2001;165:159-162.
4. Rardin CR, Kohli N, Rosenblatt PL, et al. Tension-free vaginal tape: outcomes among women with primary versus recurrent stress urinary incontinence. Obstet Gynecol. 2002;100:893-897.
5. Vassallo BJ, Kleeman SD, Segal JL, et al. Tension-free vaginal tape: a quality of life assessment. Obstet Gynecol. 2002;100:518-524.
6. Karram MM, Segal JL, Vassallo BJ, et al. Complications and untoward effects of the tension-free vaginal tape procedure. Obstet Gynecol. 2003;101:929-932.
7. MAUDE: Food and Drug Administration Manufacturer and User Facility Device Experience Database. Available at http://www.fda.gov/cdrh/maude.html. Accessed June 7, 2003.
8. Peyrat L, Boutin JM, Bruyere F, et al. Intestinal perforation is a complication of TVT procedure for UI. Eur Urol. 2001;39:603-605.
9. Walters MD, Tulikangas PR, LaSala C, et al. Vascular injury during tension-free vaginal tape procedure for stress urinary incontinence. Obstet Gynecol. 2001;98:957-959.
10. Zilbert AW, Farrell SA. External iliac artery laceration during tension-free vaginal tape procedure. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12:141-143.
11. Vierhout ME. Severe hemorrhage complicating TVT: a case report. Int Urogynecol J Pelvic Floor Dysfunct. 2000;12:139-140.
12. Brink DM. Bowel injury following insertion of TVT. S Afr Med J. 2000;90:450-452.
13. Shobeiri SA, Garely AD, Chesson RR. Recognition of occult bladder injury during the tension-free vaginal tape procedure. Obstet Gynecol. 2002;99:1067-1072.
14. Delorme E. Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol. 2001;11:1306-1313.
15. Ulmstein V, Petros P. Intravaginal slingplasty (IVS): an ambulatory surgical procedure for treatment of female urinary incontinence. Scand J Urol Neprhol. 1995;29:75-82.
16. Chung MK, Chung RP. Comparison of laparoscopic Burch and tension-free vaginal tape in treating stress urinary incontinence in obese patients. JSLS. 2002;6:17-21.
17. Pelosi MA, III, Pelosi MA, II. Pubic bone suburethral stabilization sling: laparoscopic assessment of a transvaginal operation for the treatment of stress urinary incontinence. J Laparoendosc Adv Surg Tech. 1999;9:45-50.
18. Pelosi MA, II, Pelosi MA, III, Pelekanos M. The YAMA uropatch sling for treatment of female stress urinary incontinence: a pilot study. J Laparoendosc Adv Surg Tech. 2002;12:27-33.
19. Pelosi MA, II, Pelosi MA, III. Laparoscopic assessment of transvaginal suture fixation to Cooper’s ligament for suburethral slings. J Am Assoc Gynecol Laparosc. 2001;8:S53.-
20. Cundiff GW, Wright JE. A review of surgical management of genuine stress incontinence in women with a discussion of innovative procedures. J Pelvic Surg. 1998;4:271-278.
21. Sarver R, Govier FE. Pubovaginal slings: past, present, and future. Int Urogynecol J. 1997;8:358-368.
22. Kovac RS, Cruikshank SH. Pubic bone suburethral stabilization sling for recurrent urinary incontinence. Obstet Gynecol. 1997;89:624-627.
23. Muir TW, Tulikangos PK, Paraiso MF, et al. The relationship of tension-free vaginal tape insertion and the vascular anatomy. Obstet Gynecol. 2003;101:933-936.
24. Pelosi MA, II, Pelosi MA, III. Laparoscopic evaluation of a new tension-free vaginal sling (SPARC) for stress urinary incontinence. Proceedings of the 31st annual meeting of the American Association of Gynecologic Laparoscopists. November 2002; Miami, Fla.
25. Nickel RF, Wiegand U, van den Brom WE. Evaluation of a transpelvic sling procedure with and without colposuspension for treatment of female dogs with refractory urethral sphincter mechanism incompetence. Vet Surg. 1998;27:94-104.
26. Dargent D, Bretones S, George P, et al. Insertion of a suburethral sling through the obturator membrane in the treatment of female urinary incontinence. Gynecol Obstet Fertil. 2002;30:576-582.
27. Mouly P, Soulie M, Seguin P, et al. Vaginal reconstruction of a complete vaginal prolapse: the transobturator repair. J Urol. 2003;169:S182.-
Preventing adhesions after abdominal myomectomy: Tools and techniques
- To reduce the incidence of postoperative adhesions, follow basic principles of microsurgery: Minimize the number and extent of incisions, handle all tissue gently, strive for absolute hemostasis, and use small, nonreactive suture.
- Despite limited data from prospective, randomized studies, both fluid and barrier adjuvants have proved effective in reducing the incidence and extent of adhesions after abdominal myomectomy.
Abdominal myomectomy is the preferred treatment in women with large or numerous intramural myomas, especially in the setting of infertility, recurrent pregnancy loss, and preservation of future fertility.1,2 However, postoperative adhesions are distressingly common following this procedure, resulting in significant potential morbidity. Fortunately, a number of products can reduce their occurrence. Proper surgical techniques and a thorough knowledge of these products are invaluable in helping reduce the incidence of adhesions.
The association between adhesions and diminished fertility is well-established,3,4 particularly when peritubal involvement is present (FIGURES 1-3). Abdominopelvic adhesions also contribute to significant chronic pelvic pain, bowel obstruction, and technical difficulty in subsequent surgical or assisted-reproduction procedures.5 Unfortunately, most attempts at adhesiolysis meet with less than complete success, since adhesions recur in 55% to 100% of patients (FIGURE 4).6 Thus, preventing adhesions in the first place would seem to be key to successful outcomes in abdominal myomectomy.
This article reviews the evidence on various approaches and products. While the number of studies examining each adjuvant in the setting of abdominal myomectomy is limited, the overall evidence supports the safety and efficacy of both liquid and barrier adjuvants.
Adhesions present a significant clinical dilemma after abdominal myomectomy, occurring in 50% to 90% of patients.5,7 In 1 prospective series of women undergoing second-look laparoscopy (SLL) after myomectomy, adnexal adhesions were noted in 94% of patients with posterior uterine incisions and in 56% of patients with only anterior or fundal incisions; adhesions between the uterus and omentum or bowel occurred in 88% of all patients.5
In another study of early SLL following abdominal myomectomy, 83% of patients had adhesions between the surgical site and the bowel or omentum, and 65% had adhesions involving the adnexae.2 Removal of large, bulky fibroids (with uterine mass exceeding 13 weeks’ gestational size) resulted in higher adhesion scores than did small myomas. Again, the incidence and severity of adhesions also correlated with location of the uterine incision: Adnexal adhesions were more common after posterior uterine incisions (76%) than after anterior or fundal entries (45%).2
FIGURE 1 Peritubal adhesion
Adhesion at distal end of the fallopian tube. Peritubal involvement often leads to diminished fertility.
FIGURE 2 Adherent structures
Postoperative adhesion between fallopian tube and the uterus.
FIGURE 3 Cyst dissection
Adhesions can follow common surgeries such as paratubal cyst dissection.
FIGURE 4 Recurrent adhesions
Adhesions may recur following adhesiolysis.
Causes of pelvic adhesions
Adhesion prevention requires an understanding of risk factors and maneuvers that increase the likelihood of injury (see “Pathophysiology of adhesion formation”). A number of causes have been proposed, most of them centering on tissue and peritoneal trauma (TABLE 1).
Injury can arise from excessive or rough manipulation of tissue and peritoneal surfaces or from common effects such as cutting, abrasion, and denudation (FIGURE 5). Tissue desiccation or manual blotting may lead to peritoneal desquamation and fibrin deposition.
Exposure of surfaces to intraperitoneal blood in the setting of tissue hypoxia—virtually unavoidable during abdominal myomectomy—disrupts normal fibrinolytic activity, resulting in stimulation of angiogenesis.8
Introduction of reactive foreign bodies such as talc powder, residual suture material, and even lint from laparotomy pads can favor adhesion formation. These serve as substrates or niduses of fibrin deposition.
FIGURE 5 Conducive conditions
Raw surface area can become a potent substrate for adhesions.TABLE 1
Proposed causes of adhesion formation
| Tissue hypoxia or ischemia |
| Tissue desiccation |
| Intra-abdominal infection |
| Introduction of reactive foreign body |
| Presence of intraperitoneal blood |
| Dissection of adhesions |
Techniques that may help prevent adhesions
Based on findings from studies of second-look procedures, most physicians advocate avoiding posterior uterine incisions, as well as minimizing the number and extent of incisions, to help reduce the likelihood of adhesion formation. Further, many Ob/Gyns favor removing myomas through as few uterine incisions as possible.9 We select anterior hysterotomy sites that enable removal of multiple fibroids, avoiding posterior incisions and the uterotubal junction whenever possible.
Interestingly, reapproximation of peritoneal defects after reproductive surgery (and, probably, myomectomy) does not appear to help prevent adhesions. Tulandi and colleagues10 examined the clinical and SLL outcomes of peritoneal closure in patients undergoing Pfannenstiel incisions with or without peritoneal closure at the end of the procedure. There was no difference in postoperative complications or wound healing in the 2 groups. At the time of SLL, there was no significant difference in the incidence of adhesion formation at the anterior abdominal wall.
Principles of microsurgery have been adopted by reproductive surgeons to minimize the likelihood of adhesions after myomectomy and gynecologic surgery in general. The basic techniques reflect respect for tissue integrity:
- Gentle handling of tissue, with minimal manipulation of all peritoneal surfaces.
- Meticulous hemostasis. Examine all myomectomy sites to ensure adequate hemostasis prior to closure.
- Continuous irrigation to prevent tissue desiccation. We favor continuous saline irrigation throughout the procedure. We also use only moistened laparotomy sponges and pads, and avoid applying dry gauze to any tissue surface.
- Avoidance of foreign-body introduction. We use only talc-free gloves and remove all residual suture fragments and tissue debris before closure. We also perform copious saline suction-irrigation at the end of the procedure to remove as much residue as possible.
- Use of fine, nonreactive suture. We favor fine, resorbable sutures that incite as little tissue reactivity as possible. For closure of large myomectomy defects, we use braided multifilaments such as Vicryl (polyglactine 910) (Ethicon, Somerville, NJ) or Dexon (polyglycolic acid) (Davis and Geck, Danbury, Conn) for strength and ease of handling. These sutures are absorbed through simple hydrolysis and stimulate less tissue reactivity than do chromic or catgut sutures.
The idea is appealing, but a randomized, blinded comparison of “good” and “bad” microsurgical technique is unlikely, since no one would wish to perform “bad” technique.
With barrier adjuvants, optimal benefit is obtained when the physician can predict potential sites of adhesions.
Wide range of prevention tools has been studied
Many types of agents have been studied in an attempt to reduce postsurgical adhesions after gynecologic surgery. Although most offer little or no benefit (TABLE 2), a few have potential in myomectomy procedures.
Barriers that form mechanical separation (TABLE 3) theoretically physically separate damaged tissues during early peritoneal wound healing, when adhesions form.11 The original adhesion barriers consisted of omental and peritoneal grafts that were placed over surgical sites. However, studies demonstrated that devitalized tissue positioned on damaged peritoneum serves as a potent substrate—not inhibitor—for adhesions.12 More recent trials have examined the adhesion-prevention benefit of other types of absorbable and nonabsorbable barriers.
TABLE 2
Pharmacologic agents studied for adhesion prevention in reproductive surgery
| AGENT | THEORETICAL ACTION | EXAMPLES | MODE OF USE/APPLICATION | RISKS/PROBLEMS |
|---|---|---|---|---|
| Antibiotics | Prevent infection or inflammation | Cephalosporins Tetracyclines | Intraperitoneal irrigation with antibiotic fluid Hydrotubation fluid with antibiotic | Theoretical reaction to antibiotic |
| Anticoagulants | Clot prevention Fibrin prevention | Heparin | In conjunction with Interceed | Risk of postoperative bleeding |
| Anti-inflammatory agents | Decrease permeability and histamine release | Nonsteroidal anti-inflammatory drugs Corticosteroids | Awaiting further investigation | Theoretical reaction to agent |
| Crystalloid solutions | Hydroflotation effect, decrease surface contact between pelvic organs | Normal saline Ringer’s lactate | Intra-abdominal instillation | Possible volume overload from intravascular absorption |
| Fibrinolytic agents | Fibrinolysis Plasminogen activation | Streptokinase Trypsin Fibrinolysin | Awaiting further investigation | Theoretical risk of postoperative bleeding |
| Steroids | Decrease inflammatory response | Dexamethasone | Systemic and/or intraperitoneal | Possible suppression of hypothalamic-pituitary axis |
| Polysaccharide polymer | "Siliconizing" effect to coat raw surfaces | Dextran 70 (Hyskon) | 200 mL placed in posterior cul-de-sac or coating surgical site surfaces | Abdominal bloating, anaphylaxis, pleural effusion, liver function abnormalities, wound separation, rare diffuse intravascular coagulation |
| Other fluid and barrier agents* | Peritoneal surface separation Hydroflotation | Absorbable and nonabsorbable barriers (see Table 3) | See Table 3 | See Table 3 |
| *Adjuvants studied in the setting of abdominal myomectomy | ||||
TABLE 3
Fluid and barrier adjuvants studied for adhesion reduction after myomectomy
| AGENT | THEORETICAL ACTION | MODE OF USE/APPLICATION | PROBLEMS | EVIDENCE FOR ADHESION REDUCTION |
|---|---|---|---|---|
| ABSORBABLE (BARRIER) | ||||
| Oxidized regenerated cellulose (Interceed) | Protective layer over surgical sites to prevent surface contact | Direct placement onto surface of uterus; no suturing required | Requires hemostasis | Prospective studies and meta-analysis support benefit in reproductive surgery including abdominal myomectomy |
| Hyaluronatecarboxymethycellulose derivative film (Seprafilm) | Protective layer over surgical sites to prevent surface contact | Direct placement around entire uterine surface; no suturing required | Requires hemostasis | Multicenter prospective, randomized study supports benefit in reducing adhesions after abdominal myomectomy |
| NONABSORBABLE (BARRIER) | ||||
| Expanded polytetrafluoroethylene (GoreTex) | Prevent contact between surgical surfaces | Patch sutured onto surface of uterus | Usually must be removed Report of fistula formation when left in situ | Multicenter prospective studies support adhesion-preventive benefit after abdominal myomectomy |
| Pericardial patch (Shelhigh No-React) | Prevent contact between surgical surfaces | Patch sutured onto surface of uterus | Early clinical use in myomectomy Proven safety as pericardial patch in humans | Preliminary study (case series data only) shows potential benefit |
| FLUID | ||||
| Hyaluronic acid-coat (Sepracoat) | Diffuse coating on surgical sites and potential sites of contact | 100-mL to 250-mL aliquots injected into peritoneal cavity | Limited data on efficacy in abdominal myomectomy | Small studies (multicenter, prospective, randomized, controlled trials) demonstrated reduced postoperative adhesions after reproductive surgery via laparotomy, including myomectomy |
| Hyaluronate-carboxymethycellulose derivative gel (Intergel) | Diffuse coating on surgical sites and potential sites of contact | 300-mL aliquot into peritoneal cavity | Withdrawn from market for reports of postoperative pain, complications | Reduced adhesion formation in animal studies and in preliminary human studies |
Adhesions are fibrous or fibrovascular bands that connect tissue surfaces in abnormal locations.1,2 Their development likely results from an imbalance in inflammatory mediators or fibrin degradation during peritoneal wound healing.
Peritoneal injury initiates the release of histamine and vasoactive kinins that mediate increased capillary permeability and outpouring of serosanguineous fluid.3 This proteinaceous exudate coagulates, depositing fibrinous bands between areas of denuded tissue.
Under normal circumstances, the fibrinolytic system is activated to lyse these bands within 72 hours. Peritoneal healing occurs when mesothelial cells migrate from the underlying mesenchyme to reepithelialize the injured site.4 Disequilibrium of the fibrin deposition-fibrinolysis system results in a persistent band that will eventually undergo fibroblast and vascular invasion.
REFERENCES
1. Diamond MP, DeCherney AH. Pathogenesis of adhesion formation/reformation: application to reproductive pelvic surgery. Microsurgery. 1987;8:103-107.
2. Diamond MP, Freeman ML. Clinical implications of postsurgical adhesions. Hum Reprod. 2001;7:567-576.
3. Diamond MP, El-Mowafi DM. Pelvic adhesions. Surg Technol Int. 1998;VII:273-283.
4. Farquhar C, Vandekerckhove P, Watson A, Vail A, Wiseman D. Barrier agents for preventing adhesions after surgery for subfertility. Cochrane Database Systematic Rev. 2002;(4):1-34.
Absorbable barriers
These are largely derivatives of organic materials. Their application to myomectomy may be limited by the requirement for absolute hemostasis at the site of application.
Interceed (Gynecare, a division of Ethicon), which is derived from oxidized regenerated cellulose, is one of the first and most extensively evaluated barriers. A mesh synthetic designed to be placed over injured tissue, it is a derivative of the hemostatic agent Surgicell (Johnson & Johnson, New Brunswick, NJ), with modifications in weave and pore size.
Interceed offers ease of application: It can be cut to the size or shape necessary and requires no suturing. It forms a gelatinous protective layer within 8 hours of placement, and is degraded into monosaccharides and absorbed within 2 weeks.13
The use of Interceed has been shown to reduce adhesions following adhesiolysis and ovarian surgery. In a large, multicenter, prospective, randomized trial, it significantly decreased the incidence of adhesion reformation after adnexal adhesiolysis in infertility patients with bilateral tubal disease.14
In a retrospective series of 38 infertility patients, including 19 patients after myomectomy (13 with the barrier, 6 without), reproductive outcomes were significantly better in the Interceed group, and adhesion development was reduced.15 Pregnancy rates in the 2 years following surgery were 78% in the Interceed group, compared with 47% in controls. In addition, among 23 patients who had second-look procedures, postoperative adhesions were noted in 38% of the Interceed group, compared with 86% in controls.15
Seprafilm (hyaluronic acid-film) (Genzyme Corp, Cambridge, Mass) is a bioresorbable membrane derived from sodium hyaluronate and carboxymethylcellulose. It is absorbed from the peritoneal cavity within 1 week and is completely excreted within 1 month.
Its potential for adhesion prevention after abdominal myomectomy was examined by SLL in a multicenter, prospective, randomized, blinded study11 in which 127 women undergoing abdominal myomectomy at 19 institutions were randomized to either Seprafilm or no barrier. In the Seprafilm group, the barrier was wrapped circumferentially around the uterus, covering all uterine defects, at the time of abdominal closure. Clinical outcomes—including vital signs, adverse events (pain, fever, nausea), and abdominal wound complications—were similar in the control and Seprafilm groups.
In this study, the incidence (mean number of sites), severity, and extent (mean area) of uterine adhesions were significantly lower in the Seprafilm-treated patients. The proportion of patients undergoing anterior hysterotomies who were found to have no anterior uterine adhesions was 39% in the Seprafilm group, compared with 6% in the control group. The percentage of patients with at least 1 adnexa totally free of adhesions to the posterior uterus also was higher in the Seprafilm group—48% versus 31%.11
Nonabsorbable barriers
GoreTex Surgical Membrane (W.L. Gore and Associates, Newark, Del) is an inert expanded polytetrafluoroethylene (PTFE) derivative that must be sutured in place. It is of potential utility in myomectomy because its application does not require absolute hemostasis. However, its usefulness and application are limited by the need for later removal.
In a multicenter, randomized, controlled trial exploring its adhesion-preventive properties after myomectomy, the GoreTex membrane significantly outperformed the barrierfree group.16
In a separate multicenter, randomized clinical trial, the GoreTex membrane was more effective than Interceed in preventing adhesions after pelvic/tubal reconstructive surgery.17
Yet another multicenter, randomized trial—this one involving 27 women undergoing abdominal myomectomy—used SLL to determine the extent of adhesions and to remove the barrier. The percentage of adhesion-free surgical sites was significantly higher in the GoreTex group: 56% compared with 7% in no-barrier controls.16
The adhesion scores, determined by the extent (area of involvement), nature (filmy versus opaque), and tenacity (ease of lysis or dissection) of the adhesions, were significantly lower in the GoreTex group.16
Despite the few prospective, randomized trials, the evidence supports the efficacy of various fluid and barrier adjuvants.
Histologic examination of the removed barriers demonstrated no tissue attachment to the PTFE. Despite these positive findings, however, both fistula formation and graft infection have been reported after placement of a GoreTex barrier.18
The Shelhigh Pericardial No-React Patch (Herzog Surgical, Sacramento, Calif) is a new nonabsorbable adhesion barrier that was first described in gynecologic use by Pelosi and Pelosi in a case series of 20 patients.19 Consisting of a 12-cm-diameter patch of glutaraldehyde-treated bovine/porcine pericardium, this product has an excellent safety record as a permanent pericardial substitute in the cardiovascular literature and has been shown to resist calcification and adhesions.
In the Pelosi series, the patch was placed over the uterine fundus and secured by 4 monofilament sutures at the dome of the uterus and the parietal peritoneum.19 All patients underwent SLL at 6 weeks, and 3 patients also underwent third-look laparoscopy. None of the 20 women had adhesions between the abdominal wall and the bladder, bowel, uterus, or adnexae at SLL. However, minimal adhesions of the ovaries and tubes were found in 7 patients who had undergone posterior hysterotomy. Clinical trials are likely to follow this small pilot study.
Absorbable fluid adjuvants
With barrier adjuvants, optimal benefit is obtained when the physician can predict potential sites of adhesions. This is not a strict requirement with fluid barriers, which is their chief advantage. Among the agents described below, Sepracoat (Genzyme Corp) is available in the United States, while Intergel (Lifecore Biomedical, Chaska, Minn) was withdrawn from the market in March.
Intergel, a 0.5% ferric hyaluronade formulation, is a sterile nonpyrogenic gel of highly purified sodium hyaluronate, which is ionically cross-linked with ferric ion and adjusted to isotonicity with sodium chloride.11 (Hyaluronic acid is a major component of body tissues and fluids such as peritoneal fluid, where it performs physically supportive and mechanically protective roles.)
Johns and colleagues20 studied Intergel in a randomized, multicenter, third-party– blinded, placebo-controlled study. Of the 265 patients who completed the study, 131 were given 300 mL of Intergel and 134 were given lactated Ringer’s solution (the placebo) at the time of their surgery, through the laparoscopic port. When SLL was performed 6 to 12 weeks after surgery, the mean number and severity of adhesions—overall and at the surgical site—were significantly lower in the Intergel group. Adhesions reformed in 91% of those in the control group, compared with 63% in the Intergel group.
In myomectomy patients, the modified American Fertility Society Score, which uses 24 potential adhesion sites, was reduced by 42% in the Intergel group—a statistically significant improvement.20
One major advantage of Intergel is that it reduces adhesion formation at sites distant from the area of application, secondary to its wide intra-abdominal circulation. However, as mentioned above, sales were voluntarily suspended due to post-market reports of tissue adherence, sterile foreign-body reaction, and late-onset pain that sometimes required surgical intervention. In some patients, persistent residual material was noted at the time of subsequent surgery.
Sepracoat (hyaluronic acid-coat) is a dilute solution of 0.4% hyaluronic acid in phosphate-buffered saline. It is bioresorbable, persists at the application site less than 24 hours, and is completely cleared in less than 5 days.
In a prospective, randomized, blinded, placebo-controlled, multicenter study in 1998, Diamond and colleagues compared Sepracoat with a pure phosphate-buffered saline solution in 227 women undergoing gynecologic procedures via laparotomy.21 The aim of the study was to assess the efficacy and safety of the fluid at sites without direct surgical trauma or adhesiolysis. Both solutions were warmed to room temperature and injected into the abdominal cavity before the procedure began (250 mL after skin incision). The solution was reapplied after irrigation or every 30 minutes (100 mL), and at the end of the procedure (250 mL) before closure. The maximum volume used was 1,000 mL. After application, the fluid was left 1 minute before suctioning. Patients underwent SLL 40 days later, and adhesions were identified at the initial procedure and at SLL.
In the Sepracoat group, there was a reduction in de novo adhesions at nonsurgical sites by a factor of 2.8. The proportion of sites with de novo adhesions also decreased, and 80% of Sepracoat patients had at least 1 ovary that was adhesion-free compared with 58% of placebo-treated patients. These findings occurred in areas of indirect trauma, demonstrating that Sepracoat limited trauma at tissue injury.21
Conclusion
Adhesion prevention is of utmost importance after abdominal myomectomy, especially in patients who desire future fertility. Despite the limited number of prospective, randomized studies, the literature does support the efficacy of various fluid and barrier adjuvants.
Our practice is to use an adjuvant in all abdominal myomectomies. We have long relied on Interceed, which enjoys both ease of application and an excellent safety record. However, as reviewed above, other potentially useful products are available or in development. As ever, the reproductive surgeon should adhere to principles of microsurgery, strive for meticulous hemostasis, and demonstrate respect for tissue integrity.
Dr. DeCherney reports small holdings with Lifecore Biomedical. Drs. Chang and Marin report no affiliations or financial arrangements with any of the manufacturers of products mentioned in this article.
1. Stewart EA. Treatment of uterine leiomyomas. UpToDate (Version 10.3) 2002; 1-8. Available at: www.uptodate.com.
2. Ugur M, Tura C, Mungan T, Aydogdu T, Sahin Y, Gokmen O. Laparoscopy for adhesion prevention following myomectomy. Int J Gynecol Obstet. 1996;53:145-149.
3. Berkeley AS, DeCherney AH, Plan ML. Abdominal myomectomy and subsequent fertility. Surg Gynecol Obstet. 1983;153:319-322.
4. Tulandi T, Collin JA, Burrows E, et al. Treatment-dependent and treatment-independent pregnancy among women with periadnexal adhesions. Am J Obstet Gynecol. 1990;162:354-357.
5. Tulandi T, Murria C, Guralnick M. Adhesion formation and reproductive outcome after myomectomy and second-look laparoscopy. Obstet Gynecol. 1993;82:213-215.
6. Diamond MP, Freeman ML. Clinical implications of postsurgical adhesions. Hum Reprod. 2001;7:567-576.
7. Lau S, Tulandi T. Myomectomy and adhesion formation. In: diZerega GS, ed. Peritoneal Surgery. New York: Springer-Verlag 1999;289-290.
8. Diamond MP, El-Mowafi DM. Pelvic adhesions. Surg Technol Int. 1998;VII:273-283.
9. Guarnaccia MM, Rein MS. Traditional surgical approaches to uterine fibroids: abdominal myomectomy and hysterectomy. Clin Obstet Gynecol. 2001;44:385-400.
10. Tulandi T, Hum HS, Gelfand MM. Closure of laparotomy incisions with or without peritoneal suturing and second-look laparoscopy. Am J Obstet Gynecol. 1988;158:536-537.
11. Diamond MP. Reduction of adhesions after uterine myomectomy by Seprafilm membrane (HAL-F): a blinded, prospective, randomized, multicenter clinical study. Fertil Steril. 1996;66:904-910.
12. Johns D. Reduction of postsurgical adhesions with Intergel adhesion prevention solution: a multicenter study of safety and efficacy after conservative gynecologic surgery. Fertil Steril. 2001;76:595-604.
13. Farquhar C, vandekerckhove P, Watson A, Vail A, Wiseman D. Barrier agents for preventing adhesions after surgery for subfertility. Cochrane Database Systematic Rev. 2002(4);1-34.
14. Nordic Adhesion Prevention Study Group. The efficacy of Interceed (TC7) for prevention of reformation of postoperative adhesions on ovaries, fallopian tubes, and fimbriae in microsurgical operations for fertility: a multicenter study. Fertil Steril. 1995;63:709-714.
15. Sawada T, Nishizawa H, Nishio E, Kadowaki M. Postoperative adhesion prevention with an oxidized regenerated cellulose adhesion barrier in infertile women. J Reprod Med. 2000;45:387-389.
16. The Myomectomy Adhesions Multicenter Study Group. An expanded polytetrafluoroethylene barrier (Gore-Tex Surgical Membrane) reduces post-myomectomy adhesion formation. Fertil Steril. 1995;63:491-493.
17. Haney AF, Hesla J, Hurst BS, et al. Expanded polytetrafluoroethylene (Gore-Tex Surgical Membrane) is superior to oxidized regenerated cellulose (Interceed TC7) in preventing adhesions. Fertil Steril. 1995;63:1021-1026.
18. Monteforte CA, Queirazza R, Francescetting P, Herbst TJ. Fistula formation after implanting an ePTFE membrane. A case report. J Reprod Med. 1997;42:184-187.
19. Pelosi MA, II, Pelosi MA, III. A new nonabsorbable adhesion barrier for myomectomy. Am J Surg. 2002;184:428-432.
20. Johns D. Reduction of postsurgical adhesions with Intergel adhesion prevention solution: a multicenter study of safety and efficacy after conservative gynecologic surgery. Fertil Steril. 2001;76:596-604.
21. Diamond MP and The Sepracoat Adhesion Study Group. Reduction of de novo postsurgical adhesions by intraoperative precoating with Sepracoat (HAL-C) solution: a prospective, randomized, blinded, placebo-controlled multicenter study. Fertil Steril. 1998;69:1067-1074.
- To reduce the incidence of postoperative adhesions, follow basic principles of microsurgery: Minimize the number and extent of incisions, handle all tissue gently, strive for absolute hemostasis, and use small, nonreactive suture.
- Despite limited data from prospective, randomized studies, both fluid and barrier adjuvants have proved effective in reducing the incidence and extent of adhesions after abdominal myomectomy.
Abdominal myomectomy is the preferred treatment in women with large or numerous intramural myomas, especially in the setting of infertility, recurrent pregnancy loss, and preservation of future fertility.1,2 However, postoperative adhesions are distressingly common following this procedure, resulting in significant potential morbidity. Fortunately, a number of products can reduce their occurrence. Proper surgical techniques and a thorough knowledge of these products are invaluable in helping reduce the incidence of adhesions.
The association between adhesions and diminished fertility is well-established,3,4 particularly when peritubal involvement is present (FIGURES 1-3). Abdominopelvic adhesions also contribute to significant chronic pelvic pain, bowel obstruction, and technical difficulty in subsequent surgical or assisted-reproduction procedures.5 Unfortunately, most attempts at adhesiolysis meet with less than complete success, since adhesions recur in 55% to 100% of patients (FIGURE 4).6 Thus, preventing adhesions in the first place would seem to be key to successful outcomes in abdominal myomectomy.
This article reviews the evidence on various approaches and products. While the number of studies examining each adjuvant in the setting of abdominal myomectomy is limited, the overall evidence supports the safety and efficacy of both liquid and barrier adjuvants.
Adhesions present a significant clinical dilemma after abdominal myomectomy, occurring in 50% to 90% of patients.5,7 In 1 prospective series of women undergoing second-look laparoscopy (SLL) after myomectomy, adnexal adhesions were noted in 94% of patients with posterior uterine incisions and in 56% of patients with only anterior or fundal incisions; adhesions between the uterus and omentum or bowel occurred in 88% of all patients.5
In another study of early SLL following abdominal myomectomy, 83% of patients had adhesions between the surgical site and the bowel or omentum, and 65% had adhesions involving the adnexae.2 Removal of large, bulky fibroids (with uterine mass exceeding 13 weeks’ gestational size) resulted in higher adhesion scores than did small myomas. Again, the incidence and severity of adhesions also correlated with location of the uterine incision: Adnexal adhesions were more common after posterior uterine incisions (76%) than after anterior or fundal entries (45%).2
FIGURE 1 Peritubal adhesion
Adhesion at distal end of the fallopian tube. Peritubal involvement often leads to diminished fertility.
FIGURE 2 Adherent structures
Postoperative adhesion between fallopian tube and the uterus.
FIGURE 3 Cyst dissection
Adhesions can follow common surgeries such as paratubal cyst dissection.
FIGURE 4 Recurrent adhesions
Adhesions may recur following adhesiolysis.
Causes of pelvic adhesions
Adhesion prevention requires an understanding of risk factors and maneuvers that increase the likelihood of injury (see “Pathophysiology of adhesion formation”). A number of causes have been proposed, most of them centering on tissue and peritoneal trauma (TABLE 1).
Injury can arise from excessive or rough manipulation of tissue and peritoneal surfaces or from common effects such as cutting, abrasion, and denudation (FIGURE 5). Tissue desiccation or manual blotting may lead to peritoneal desquamation and fibrin deposition.
Exposure of surfaces to intraperitoneal blood in the setting of tissue hypoxia—virtually unavoidable during abdominal myomectomy—disrupts normal fibrinolytic activity, resulting in stimulation of angiogenesis.8
Introduction of reactive foreign bodies such as talc powder, residual suture material, and even lint from laparotomy pads can favor adhesion formation. These serve as substrates or niduses of fibrin deposition.
FIGURE 5 Conducive conditions
Raw surface area can become a potent substrate for adhesions.TABLE 1
Proposed causes of adhesion formation
| Tissue hypoxia or ischemia |
| Tissue desiccation |
| Intra-abdominal infection |
| Introduction of reactive foreign body |
| Presence of intraperitoneal blood |
| Dissection of adhesions |
Techniques that may help prevent adhesions
Based on findings from studies of second-look procedures, most physicians advocate avoiding posterior uterine incisions, as well as minimizing the number and extent of incisions, to help reduce the likelihood of adhesion formation. Further, many Ob/Gyns favor removing myomas through as few uterine incisions as possible.9 We select anterior hysterotomy sites that enable removal of multiple fibroids, avoiding posterior incisions and the uterotubal junction whenever possible.
Interestingly, reapproximation of peritoneal defects after reproductive surgery (and, probably, myomectomy) does not appear to help prevent adhesions. Tulandi and colleagues10 examined the clinical and SLL outcomes of peritoneal closure in patients undergoing Pfannenstiel incisions with or without peritoneal closure at the end of the procedure. There was no difference in postoperative complications or wound healing in the 2 groups. At the time of SLL, there was no significant difference in the incidence of adhesion formation at the anterior abdominal wall.
Principles of microsurgery have been adopted by reproductive surgeons to minimize the likelihood of adhesions after myomectomy and gynecologic surgery in general. The basic techniques reflect respect for tissue integrity:
- Gentle handling of tissue, with minimal manipulation of all peritoneal surfaces.
- Meticulous hemostasis. Examine all myomectomy sites to ensure adequate hemostasis prior to closure.
- Continuous irrigation to prevent tissue desiccation. We favor continuous saline irrigation throughout the procedure. We also use only moistened laparotomy sponges and pads, and avoid applying dry gauze to any tissue surface.
- Avoidance of foreign-body introduction. We use only talc-free gloves and remove all residual suture fragments and tissue debris before closure. We also perform copious saline suction-irrigation at the end of the procedure to remove as much residue as possible.
- Use of fine, nonreactive suture. We favor fine, resorbable sutures that incite as little tissue reactivity as possible. For closure of large myomectomy defects, we use braided multifilaments such as Vicryl (polyglactine 910) (Ethicon, Somerville, NJ) or Dexon (polyglycolic acid) (Davis and Geck, Danbury, Conn) for strength and ease of handling. These sutures are absorbed through simple hydrolysis and stimulate less tissue reactivity than do chromic or catgut sutures.
The idea is appealing, but a randomized, blinded comparison of “good” and “bad” microsurgical technique is unlikely, since no one would wish to perform “bad” technique.
With barrier adjuvants, optimal benefit is obtained when the physician can predict potential sites of adhesions.
Wide range of prevention tools has been studied
Many types of agents have been studied in an attempt to reduce postsurgical adhesions after gynecologic surgery. Although most offer little or no benefit (TABLE 2), a few have potential in myomectomy procedures.
Barriers that form mechanical separation (TABLE 3) theoretically physically separate damaged tissues during early peritoneal wound healing, when adhesions form.11 The original adhesion barriers consisted of omental and peritoneal grafts that were placed over surgical sites. However, studies demonstrated that devitalized tissue positioned on damaged peritoneum serves as a potent substrate—not inhibitor—for adhesions.12 More recent trials have examined the adhesion-prevention benefit of other types of absorbable and nonabsorbable barriers.
TABLE 2
Pharmacologic agents studied for adhesion prevention in reproductive surgery
| AGENT | THEORETICAL ACTION | EXAMPLES | MODE OF USE/APPLICATION | RISKS/PROBLEMS |
|---|---|---|---|---|
| Antibiotics | Prevent infection or inflammation | Cephalosporins Tetracyclines | Intraperitoneal irrigation with antibiotic fluid Hydrotubation fluid with antibiotic | Theoretical reaction to antibiotic |
| Anticoagulants | Clot prevention Fibrin prevention | Heparin | In conjunction with Interceed | Risk of postoperative bleeding |
| Anti-inflammatory agents | Decrease permeability and histamine release | Nonsteroidal anti-inflammatory drugs Corticosteroids | Awaiting further investigation | Theoretical reaction to agent |
| Crystalloid solutions | Hydroflotation effect, decrease surface contact between pelvic organs | Normal saline Ringer’s lactate | Intra-abdominal instillation | Possible volume overload from intravascular absorption |
| Fibrinolytic agents | Fibrinolysis Plasminogen activation | Streptokinase Trypsin Fibrinolysin | Awaiting further investigation | Theoretical risk of postoperative bleeding |
| Steroids | Decrease inflammatory response | Dexamethasone | Systemic and/or intraperitoneal | Possible suppression of hypothalamic-pituitary axis |
| Polysaccharide polymer | "Siliconizing" effect to coat raw surfaces | Dextran 70 (Hyskon) | 200 mL placed in posterior cul-de-sac or coating surgical site surfaces | Abdominal bloating, anaphylaxis, pleural effusion, liver function abnormalities, wound separation, rare diffuse intravascular coagulation |
| Other fluid and barrier agents* | Peritoneal surface separation Hydroflotation | Absorbable and nonabsorbable barriers (see Table 3) | See Table 3 | See Table 3 |
| *Adjuvants studied in the setting of abdominal myomectomy | ||||
TABLE 3
Fluid and barrier adjuvants studied for adhesion reduction after myomectomy
| AGENT | THEORETICAL ACTION | MODE OF USE/APPLICATION | PROBLEMS | EVIDENCE FOR ADHESION REDUCTION |
|---|---|---|---|---|
| ABSORBABLE (BARRIER) | ||||
| Oxidized regenerated cellulose (Interceed) | Protective layer over surgical sites to prevent surface contact | Direct placement onto surface of uterus; no suturing required | Requires hemostasis | Prospective studies and meta-analysis support benefit in reproductive surgery including abdominal myomectomy |
| Hyaluronatecarboxymethycellulose derivative film (Seprafilm) | Protective layer over surgical sites to prevent surface contact | Direct placement around entire uterine surface; no suturing required | Requires hemostasis | Multicenter prospective, randomized study supports benefit in reducing adhesions after abdominal myomectomy |
| NONABSORBABLE (BARRIER) | ||||
| Expanded polytetrafluoroethylene (GoreTex) | Prevent contact between surgical surfaces | Patch sutured onto surface of uterus | Usually must be removed Report of fistula formation when left in situ | Multicenter prospective studies support adhesion-preventive benefit after abdominal myomectomy |
| Pericardial patch (Shelhigh No-React) | Prevent contact between surgical surfaces | Patch sutured onto surface of uterus | Early clinical use in myomectomy Proven safety as pericardial patch in humans | Preliminary study (case series data only) shows potential benefit |
| FLUID | ||||
| Hyaluronic acid-coat (Sepracoat) | Diffuse coating on surgical sites and potential sites of contact | 100-mL to 250-mL aliquots injected into peritoneal cavity | Limited data on efficacy in abdominal myomectomy | Small studies (multicenter, prospective, randomized, controlled trials) demonstrated reduced postoperative adhesions after reproductive surgery via laparotomy, including myomectomy |
| Hyaluronate-carboxymethycellulose derivative gel (Intergel) | Diffuse coating on surgical sites and potential sites of contact | 300-mL aliquot into peritoneal cavity | Withdrawn from market for reports of postoperative pain, complications | Reduced adhesion formation in animal studies and in preliminary human studies |
Adhesions are fibrous or fibrovascular bands that connect tissue surfaces in abnormal locations.1,2 Their development likely results from an imbalance in inflammatory mediators or fibrin degradation during peritoneal wound healing.
Peritoneal injury initiates the release of histamine and vasoactive kinins that mediate increased capillary permeability and outpouring of serosanguineous fluid.3 This proteinaceous exudate coagulates, depositing fibrinous bands between areas of denuded tissue.
Under normal circumstances, the fibrinolytic system is activated to lyse these bands within 72 hours. Peritoneal healing occurs when mesothelial cells migrate from the underlying mesenchyme to reepithelialize the injured site.4 Disequilibrium of the fibrin deposition-fibrinolysis system results in a persistent band that will eventually undergo fibroblast and vascular invasion.
REFERENCES
1. Diamond MP, DeCherney AH. Pathogenesis of adhesion formation/reformation: application to reproductive pelvic surgery. Microsurgery. 1987;8:103-107.
2. Diamond MP, Freeman ML. Clinical implications of postsurgical adhesions. Hum Reprod. 2001;7:567-576.
3. Diamond MP, El-Mowafi DM. Pelvic adhesions. Surg Technol Int. 1998;VII:273-283.
4. Farquhar C, Vandekerckhove P, Watson A, Vail A, Wiseman D. Barrier agents for preventing adhesions after surgery for subfertility. Cochrane Database Systematic Rev. 2002;(4):1-34.
Absorbable barriers
These are largely derivatives of organic materials. Their application to myomectomy may be limited by the requirement for absolute hemostasis at the site of application.
Interceed (Gynecare, a division of Ethicon), which is derived from oxidized regenerated cellulose, is one of the first and most extensively evaluated barriers. A mesh synthetic designed to be placed over injured tissue, it is a derivative of the hemostatic agent Surgicell (Johnson & Johnson, New Brunswick, NJ), with modifications in weave and pore size.
Interceed offers ease of application: It can be cut to the size or shape necessary and requires no suturing. It forms a gelatinous protective layer within 8 hours of placement, and is degraded into monosaccharides and absorbed within 2 weeks.13
The use of Interceed has been shown to reduce adhesions following adhesiolysis and ovarian surgery. In a large, multicenter, prospective, randomized trial, it significantly decreased the incidence of adhesion reformation after adnexal adhesiolysis in infertility patients with bilateral tubal disease.14
In a retrospective series of 38 infertility patients, including 19 patients after myomectomy (13 with the barrier, 6 without), reproductive outcomes were significantly better in the Interceed group, and adhesion development was reduced.15 Pregnancy rates in the 2 years following surgery were 78% in the Interceed group, compared with 47% in controls. In addition, among 23 patients who had second-look procedures, postoperative adhesions were noted in 38% of the Interceed group, compared with 86% in controls.15
Seprafilm (hyaluronic acid-film) (Genzyme Corp, Cambridge, Mass) is a bioresorbable membrane derived from sodium hyaluronate and carboxymethylcellulose. It is absorbed from the peritoneal cavity within 1 week and is completely excreted within 1 month.
Its potential for adhesion prevention after abdominal myomectomy was examined by SLL in a multicenter, prospective, randomized, blinded study11 in which 127 women undergoing abdominal myomectomy at 19 institutions were randomized to either Seprafilm or no barrier. In the Seprafilm group, the barrier was wrapped circumferentially around the uterus, covering all uterine defects, at the time of abdominal closure. Clinical outcomes—including vital signs, adverse events (pain, fever, nausea), and abdominal wound complications—were similar in the control and Seprafilm groups.
In this study, the incidence (mean number of sites), severity, and extent (mean area) of uterine adhesions were significantly lower in the Seprafilm-treated patients. The proportion of patients undergoing anterior hysterotomies who were found to have no anterior uterine adhesions was 39% in the Seprafilm group, compared with 6% in the control group. The percentage of patients with at least 1 adnexa totally free of adhesions to the posterior uterus also was higher in the Seprafilm group—48% versus 31%.11
Nonabsorbable barriers
GoreTex Surgical Membrane (W.L. Gore and Associates, Newark, Del) is an inert expanded polytetrafluoroethylene (PTFE) derivative that must be sutured in place. It is of potential utility in myomectomy because its application does not require absolute hemostasis. However, its usefulness and application are limited by the need for later removal.
In a multicenter, randomized, controlled trial exploring its adhesion-preventive properties after myomectomy, the GoreTex membrane significantly outperformed the barrierfree group.16
In a separate multicenter, randomized clinical trial, the GoreTex membrane was more effective than Interceed in preventing adhesions after pelvic/tubal reconstructive surgery.17
Yet another multicenter, randomized trial—this one involving 27 women undergoing abdominal myomectomy—used SLL to determine the extent of adhesions and to remove the barrier. The percentage of adhesion-free surgical sites was significantly higher in the GoreTex group: 56% compared with 7% in no-barrier controls.16
The adhesion scores, determined by the extent (area of involvement), nature (filmy versus opaque), and tenacity (ease of lysis or dissection) of the adhesions, were significantly lower in the GoreTex group.16
Despite the few prospective, randomized trials, the evidence supports the efficacy of various fluid and barrier adjuvants.
Histologic examination of the removed barriers demonstrated no tissue attachment to the PTFE. Despite these positive findings, however, both fistula formation and graft infection have been reported after placement of a GoreTex barrier.18
The Shelhigh Pericardial No-React Patch (Herzog Surgical, Sacramento, Calif) is a new nonabsorbable adhesion barrier that was first described in gynecologic use by Pelosi and Pelosi in a case series of 20 patients.19 Consisting of a 12-cm-diameter patch of glutaraldehyde-treated bovine/porcine pericardium, this product has an excellent safety record as a permanent pericardial substitute in the cardiovascular literature and has been shown to resist calcification and adhesions.
In the Pelosi series, the patch was placed over the uterine fundus and secured by 4 monofilament sutures at the dome of the uterus and the parietal peritoneum.19 All patients underwent SLL at 6 weeks, and 3 patients also underwent third-look laparoscopy. None of the 20 women had adhesions between the abdominal wall and the bladder, bowel, uterus, or adnexae at SLL. However, minimal adhesions of the ovaries and tubes were found in 7 patients who had undergone posterior hysterotomy. Clinical trials are likely to follow this small pilot study.
Absorbable fluid adjuvants
With barrier adjuvants, optimal benefit is obtained when the physician can predict potential sites of adhesions. This is not a strict requirement with fluid barriers, which is their chief advantage. Among the agents described below, Sepracoat (Genzyme Corp) is available in the United States, while Intergel (Lifecore Biomedical, Chaska, Minn) was withdrawn from the market in March.
Intergel, a 0.5% ferric hyaluronade formulation, is a sterile nonpyrogenic gel of highly purified sodium hyaluronate, which is ionically cross-linked with ferric ion and adjusted to isotonicity with sodium chloride.11 (Hyaluronic acid is a major component of body tissues and fluids such as peritoneal fluid, where it performs physically supportive and mechanically protective roles.)
Johns and colleagues20 studied Intergel in a randomized, multicenter, third-party– blinded, placebo-controlled study. Of the 265 patients who completed the study, 131 were given 300 mL of Intergel and 134 were given lactated Ringer’s solution (the placebo) at the time of their surgery, through the laparoscopic port. When SLL was performed 6 to 12 weeks after surgery, the mean number and severity of adhesions—overall and at the surgical site—were significantly lower in the Intergel group. Adhesions reformed in 91% of those in the control group, compared with 63% in the Intergel group.
In myomectomy patients, the modified American Fertility Society Score, which uses 24 potential adhesion sites, was reduced by 42% in the Intergel group—a statistically significant improvement.20
One major advantage of Intergel is that it reduces adhesion formation at sites distant from the area of application, secondary to its wide intra-abdominal circulation. However, as mentioned above, sales were voluntarily suspended due to post-market reports of tissue adherence, sterile foreign-body reaction, and late-onset pain that sometimes required surgical intervention. In some patients, persistent residual material was noted at the time of subsequent surgery.
Sepracoat (hyaluronic acid-coat) is a dilute solution of 0.4% hyaluronic acid in phosphate-buffered saline. It is bioresorbable, persists at the application site less than 24 hours, and is completely cleared in less than 5 days.
In a prospective, randomized, blinded, placebo-controlled, multicenter study in 1998, Diamond and colleagues compared Sepracoat with a pure phosphate-buffered saline solution in 227 women undergoing gynecologic procedures via laparotomy.21 The aim of the study was to assess the efficacy and safety of the fluid at sites without direct surgical trauma or adhesiolysis. Both solutions were warmed to room temperature and injected into the abdominal cavity before the procedure began (250 mL after skin incision). The solution was reapplied after irrigation or every 30 minutes (100 mL), and at the end of the procedure (250 mL) before closure. The maximum volume used was 1,000 mL. After application, the fluid was left 1 minute before suctioning. Patients underwent SLL 40 days later, and adhesions were identified at the initial procedure and at SLL.
In the Sepracoat group, there was a reduction in de novo adhesions at nonsurgical sites by a factor of 2.8. The proportion of sites with de novo adhesions also decreased, and 80% of Sepracoat patients had at least 1 ovary that was adhesion-free compared with 58% of placebo-treated patients. These findings occurred in areas of indirect trauma, demonstrating that Sepracoat limited trauma at tissue injury.21
Conclusion
Adhesion prevention is of utmost importance after abdominal myomectomy, especially in patients who desire future fertility. Despite the limited number of prospective, randomized studies, the literature does support the efficacy of various fluid and barrier adjuvants.
Our practice is to use an adjuvant in all abdominal myomectomies. We have long relied on Interceed, which enjoys both ease of application and an excellent safety record. However, as reviewed above, other potentially useful products are available or in development. As ever, the reproductive surgeon should adhere to principles of microsurgery, strive for meticulous hemostasis, and demonstrate respect for tissue integrity.
Dr. DeCherney reports small holdings with Lifecore Biomedical. Drs. Chang and Marin report no affiliations or financial arrangements with any of the manufacturers of products mentioned in this article.
- To reduce the incidence of postoperative adhesions, follow basic principles of microsurgery: Minimize the number and extent of incisions, handle all tissue gently, strive for absolute hemostasis, and use small, nonreactive suture.
- Despite limited data from prospective, randomized studies, both fluid and barrier adjuvants have proved effective in reducing the incidence and extent of adhesions after abdominal myomectomy.
Abdominal myomectomy is the preferred treatment in women with large or numerous intramural myomas, especially in the setting of infertility, recurrent pregnancy loss, and preservation of future fertility.1,2 However, postoperative adhesions are distressingly common following this procedure, resulting in significant potential morbidity. Fortunately, a number of products can reduce their occurrence. Proper surgical techniques and a thorough knowledge of these products are invaluable in helping reduce the incidence of adhesions.
The association between adhesions and diminished fertility is well-established,3,4 particularly when peritubal involvement is present (FIGURES 1-3). Abdominopelvic adhesions also contribute to significant chronic pelvic pain, bowel obstruction, and technical difficulty in subsequent surgical or assisted-reproduction procedures.5 Unfortunately, most attempts at adhesiolysis meet with less than complete success, since adhesions recur in 55% to 100% of patients (FIGURE 4).6 Thus, preventing adhesions in the first place would seem to be key to successful outcomes in abdominal myomectomy.
This article reviews the evidence on various approaches and products. While the number of studies examining each adjuvant in the setting of abdominal myomectomy is limited, the overall evidence supports the safety and efficacy of both liquid and barrier adjuvants.
Adhesions present a significant clinical dilemma after abdominal myomectomy, occurring in 50% to 90% of patients.5,7 In 1 prospective series of women undergoing second-look laparoscopy (SLL) after myomectomy, adnexal adhesions were noted in 94% of patients with posterior uterine incisions and in 56% of patients with only anterior or fundal incisions; adhesions between the uterus and omentum or bowel occurred in 88% of all patients.5
In another study of early SLL following abdominal myomectomy, 83% of patients had adhesions between the surgical site and the bowel or omentum, and 65% had adhesions involving the adnexae.2 Removal of large, bulky fibroids (with uterine mass exceeding 13 weeks’ gestational size) resulted in higher adhesion scores than did small myomas. Again, the incidence and severity of adhesions also correlated with location of the uterine incision: Adnexal adhesions were more common after posterior uterine incisions (76%) than after anterior or fundal entries (45%).2
FIGURE 1 Peritubal adhesion
Adhesion at distal end of the fallopian tube. Peritubal involvement often leads to diminished fertility.
FIGURE 2 Adherent structures
Postoperative adhesion between fallopian tube and the uterus.
FIGURE 3 Cyst dissection
Adhesions can follow common surgeries such as paratubal cyst dissection.
FIGURE 4 Recurrent adhesions
Adhesions may recur following adhesiolysis.
Causes of pelvic adhesions
Adhesion prevention requires an understanding of risk factors and maneuvers that increase the likelihood of injury (see “Pathophysiology of adhesion formation”). A number of causes have been proposed, most of them centering on tissue and peritoneal trauma (TABLE 1).
Injury can arise from excessive or rough manipulation of tissue and peritoneal surfaces or from common effects such as cutting, abrasion, and denudation (FIGURE 5). Tissue desiccation or manual blotting may lead to peritoneal desquamation and fibrin deposition.
Exposure of surfaces to intraperitoneal blood in the setting of tissue hypoxia—virtually unavoidable during abdominal myomectomy—disrupts normal fibrinolytic activity, resulting in stimulation of angiogenesis.8
Introduction of reactive foreign bodies such as talc powder, residual suture material, and even lint from laparotomy pads can favor adhesion formation. These serve as substrates or niduses of fibrin deposition.
FIGURE 5 Conducive conditions
Raw surface area can become a potent substrate for adhesions.TABLE 1
Proposed causes of adhesion formation
| Tissue hypoxia or ischemia |
| Tissue desiccation |
| Intra-abdominal infection |
| Introduction of reactive foreign body |
| Presence of intraperitoneal blood |
| Dissection of adhesions |
Techniques that may help prevent adhesions
Based on findings from studies of second-look procedures, most physicians advocate avoiding posterior uterine incisions, as well as minimizing the number and extent of incisions, to help reduce the likelihood of adhesion formation. Further, many Ob/Gyns favor removing myomas through as few uterine incisions as possible.9 We select anterior hysterotomy sites that enable removal of multiple fibroids, avoiding posterior incisions and the uterotubal junction whenever possible.
Interestingly, reapproximation of peritoneal defects after reproductive surgery (and, probably, myomectomy) does not appear to help prevent adhesions. Tulandi and colleagues10 examined the clinical and SLL outcomes of peritoneal closure in patients undergoing Pfannenstiel incisions with or without peritoneal closure at the end of the procedure. There was no difference in postoperative complications or wound healing in the 2 groups. At the time of SLL, there was no significant difference in the incidence of adhesion formation at the anterior abdominal wall.
Principles of microsurgery have been adopted by reproductive surgeons to minimize the likelihood of adhesions after myomectomy and gynecologic surgery in general. The basic techniques reflect respect for tissue integrity:
- Gentle handling of tissue, with minimal manipulation of all peritoneal surfaces.
- Meticulous hemostasis. Examine all myomectomy sites to ensure adequate hemostasis prior to closure.
- Continuous irrigation to prevent tissue desiccation. We favor continuous saline irrigation throughout the procedure. We also use only moistened laparotomy sponges and pads, and avoid applying dry gauze to any tissue surface.
- Avoidance of foreign-body introduction. We use only talc-free gloves and remove all residual suture fragments and tissue debris before closure. We also perform copious saline suction-irrigation at the end of the procedure to remove as much residue as possible.
- Use of fine, nonreactive suture. We favor fine, resorbable sutures that incite as little tissue reactivity as possible. For closure of large myomectomy defects, we use braided multifilaments such as Vicryl (polyglactine 910) (Ethicon, Somerville, NJ) or Dexon (polyglycolic acid) (Davis and Geck, Danbury, Conn) for strength and ease of handling. These sutures are absorbed through simple hydrolysis and stimulate less tissue reactivity than do chromic or catgut sutures.
The idea is appealing, but a randomized, blinded comparison of “good” and “bad” microsurgical technique is unlikely, since no one would wish to perform “bad” technique.
With barrier adjuvants, optimal benefit is obtained when the physician can predict potential sites of adhesions.
Wide range of prevention tools has been studied
Many types of agents have been studied in an attempt to reduce postsurgical adhesions after gynecologic surgery. Although most offer little or no benefit (TABLE 2), a few have potential in myomectomy procedures.
Barriers that form mechanical separation (TABLE 3) theoretically physically separate damaged tissues during early peritoneal wound healing, when adhesions form.11 The original adhesion barriers consisted of omental and peritoneal grafts that were placed over surgical sites. However, studies demonstrated that devitalized tissue positioned on damaged peritoneum serves as a potent substrate—not inhibitor—for adhesions.12 More recent trials have examined the adhesion-prevention benefit of other types of absorbable and nonabsorbable barriers.
TABLE 2
Pharmacologic agents studied for adhesion prevention in reproductive surgery
| AGENT | THEORETICAL ACTION | EXAMPLES | MODE OF USE/APPLICATION | RISKS/PROBLEMS |
|---|---|---|---|---|
| Antibiotics | Prevent infection or inflammation | Cephalosporins Tetracyclines | Intraperitoneal irrigation with antibiotic fluid Hydrotubation fluid with antibiotic | Theoretical reaction to antibiotic |
| Anticoagulants | Clot prevention Fibrin prevention | Heparin | In conjunction with Interceed | Risk of postoperative bleeding |
| Anti-inflammatory agents | Decrease permeability and histamine release | Nonsteroidal anti-inflammatory drugs Corticosteroids | Awaiting further investigation | Theoretical reaction to agent |
| Crystalloid solutions | Hydroflotation effect, decrease surface contact between pelvic organs | Normal saline Ringer’s lactate | Intra-abdominal instillation | Possible volume overload from intravascular absorption |
| Fibrinolytic agents | Fibrinolysis Plasminogen activation | Streptokinase Trypsin Fibrinolysin | Awaiting further investigation | Theoretical risk of postoperative bleeding |
| Steroids | Decrease inflammatory response | Dexamethasone | Systemic and/or intraperitoneal | Possible suppression of hypothalamic-pituitary axis |
| Polysaccharide polymer | "Siliconizing" effect to coat raw surfaces | Dextran 70 (Hyskon) | 200 mL placed in posterior cul-de-sac or coating surgical site surfaces | Abdominal bloating, anaphylaxis, pleural effusion, liver function abnormalities, wound separation, rare diffuse intravascular coagulation |
| Other fluid and barrier agents* | Peritoneal surface separation Hydroflotation | Absorbable and nonabsorbable barriers (see Table 3) | See Table 3 | See Table 3 |
| *Adjuvants studied in the setting of abdominal myomectomy | ||||
TABLE 3
Fluid and barrier adjuvants studied for adhesion reduction after myomectomy
| AGENT | THEORETICAL ACTION | MODE OF USE/APPLICATION | PROBLEMS | EVIDENCE FOR ADHESION REDUCTION |
|---|---|---|---|---|
| ABSORBABLE (BARRIER) | ||||
| Oxidized regenerated cellulose (Interceed) | Protective layer over surgical sites to prevent surface contact | Direct placement onto surface of uterus; no suturing required | Requires hemostasis | Prospective studies and meta-analysis support benefit in reproductive surgery including abdominal myomectomy |
| Hyaluronatecarboxymethycellulose derivative film (Seprafilm) | Protective layer over surgical sites to prevent surface contact | Direct placement around entire uterine surface; no suturing required | Requires hemostasis | Multicenter prospective, randomized study supports benefit in reducing adhesions after abdominal myomectomy |
| NONABSORBABLE (BARRIER) | ||||
| Expanded polytetrafluoroethylene (GoreTex) | Prevent contact between surgical surfaces | Patch sutured onto surface of uterus | Usually must be removed Report of fistula formation when left in situ | Multicenter prospective studies support adhesion-preventive benefit after abdominal myomectomy |
| Pericardial patch (Shelhigh No-React) | Prevent contact between surgical surfaces | Patch sutured onto surface of uterus | Early clinical use in myomectomy Proven safety as pericardial patch in humans | Preliminary study (case series data only) shows potential benefit |
| FLUID | ||||
| Hyaluronic acid-coat (Sepracoat) | Diffuse coating on surgical sites and potential sites of contact | 100-mL to 250-mL aliquots injected into peritoneal cavity | Limited data on efficacy in abdominal myomectomy | Small studies (multicenter, prospective, randomized, controlled trials) demonstrated reduced postoperative adhesions after reproductive surgery via laparotomy, including myomectomy |
| Hyaluronate-carboxymethycellulose derivative gel (Intergel) | Diffuse coating on surgical sites and potential sites of contact | 300-mL aliquot into peritoneal cavity | Withdrawn from market for reports of postoperative pain, complications | Reduced adhesion formation in animal studies and in preliminary human studies |
Adhesions are fibrous or fibrovascular bands that connect tissue surfaces in abnormal locations.1,2 Their development likely results from an imbalance in inflammatory mediators or fibrin degradation during peritoneal wound healing.
Peritoneal injury initiates the release of histamine and vasoactive kinins that mediate increased capillary permeability and outpouring of serosanguineous fluid.3 This proteinaceous exudate coagulates, depositing fibrinous bands between areas of denuded tissue.
Under normal circumstances, the fibrinolytic system is activated to lyse these bands within 72 hours. Peritoneal healing occurs when mesothelial cells migrate from the underlying mesenchyme to reepithelialize the injured site.4 Disequilibrium of the fibrin deposition-fibrinolysis system results in a persistent band that will eventually undergo fibroblast and vascular invasion.
REFERENCES
1. Diamond MP, DeCherney AH. Pathogenesis of adhesion formation/reformation: application to reproductive pelvic surgery. Microsurgery. 1987;8:103-107.
2. Diamond MP, Freeman ML. Clinical implications of postsurgical adhesions. Hum Reprod. 2001;7:567-576.
3. Diamond MP, El-Mowafi DM. Pelvic adhesions. Surg Technol Int. 1998;VII:273-283.
4. Farquhar C, Vandekerckhove P, Watson A, Vail A, Wiseman D. Barrier agents for preventing adhesions after surgery for subfertility. Cochrane Database Systematic Rev. 2002;(4):1-34.
Absorbable barriers
These are largely derivatives of organic materials. Their application to myomectomy may be limited by the requirement for absolute hemostasis at the site of application.
Interceed (Gynecare, a division of Ethicon), which is derived from oxidized regenerated cellulose, is one of the first and most extensively evaluated barriers. A mesh synthetic designed to be placed over injured tissue, it is a derivative of the hemostatic agent Surgicell (Johnson & Johnson, New Brunswick, NJ), with modifications in weave and pore size.
Interceed offers ease of application: It can be cut to the size or shape necessary and requires no suturing. It forms a gelatinous protective layer within 8 hours of placement, and is degraded into monosaccharides and absorbed within 2 weeks.13
The use of Interceed has been shown to reduce adhesions following adhesiolysis and ovarian surgery. In a large, multicenter, prospective, randomized trial, it significantly decreased the incidence of adhesion reformation after adnexal adhesiolysis in infertility patients with bilateral tubal disease.14
In a retrospective series of 38 infertility patients, including 19 patients after myomectomy (13 with the barrier, 6 without), reproductive outcomes were significantly better in the Interceed group, and adhesion development was reduced.15 Pregnancy rates in the 2 years following surgery were 78% in the Interceed group, compared with 47% in controls. In addition, among 23 patients who had second-look procedures, postoperative adhesions were noted in 38% of the Interceed group, compared with 86% in controls.15
Seprafilm (hyaluronic acid-film) (Genzyme Corp, Cambridge, Mass) is a bioresorbable membrane derived from sodium hyaluronate and carboxymethylcellulose. It is absorbed from the peritoneal cavity within 1 week and is completely excreted within 1 month.
Its potential for adhesion prevention after abdominal myomectomy was examined by SLL in a multicenter, prospective, randomized, blinded study11 in which 127 women undergoing abdominal myomectomy at 19 institutions were randomized to either Seprafilm or no barrier. In the Seprafilm group, the barrier was wrapped circumferentially around the uterus, covering all uterine defects, at the time of abdominal closure. Clinical outcomes—including vital signs, adverse events (pain, fever, nausea), and abdominal wound complications—were similar in the control and Seprafilm groups.
In this study, the incidence (mean number of sites), severity, and extent (mean area) of uterine adhesions were significantly lower in the Seprafilm-treated patients. The proportion of patients undergoing anterior hysterotomies who were found to have no anterior uterine adhesions was 39% in the Seprafilm group, compared with 6% in the control group. The percentage of patients with at least 1 adnexa totally free of adhesions to the posterior uterus also was higher in the Seprafilm group—48% versus 31%.11
Nonabsorbable barriers
GoreTex Surgical Membrane (W.L. Gore and Associates, Newark, Del) is an inert expanded polytetrafluoroethylene (PTFE) derivative that must be sutured in place. It is of potential utility in myomectomy because its application does not require absolute hemostasis. However, its usefulness and application are limited by the need for later removal.
In a multicenter, randomized, controlled trial exploring its adhesion-preventive properties after myomectomy, the GoreTex membrane significantly outperformed the barrierfree group.16
In a separate multicenter, randomized clinical trial, the GoreTex membrane was more effective than Interceed in preventing adhesions after pelvic/tubal reconstructive surgery.17
Yet another multicenter, randomized trial—this one involving 27 women undergoing abdominal myomectomy—used SLL to determine the extent of adhesions and to remove the barrier. The percentage of adhesion-free surgical sites was significantly higher in the GoreTex group: 56% compared with 7% in no-barrier controls.16
The adhesion scores, determined by the extent (area of involvement), nature (filmy versus opaque), and tenacity (ease of lysis or dissection) of the adhesions, were significantly lower in the GoreTex group.16
Despite the few prospective, randomized trials, the evidence supports the efficacy of various fluid and barrier adjuvants.
Histologic examination of the removed barriers demonstrated no tissue attachment to the PTFE. Despite these positive findings, however, both fistula formation and graft infection have been reported after placement of a GoreTex barrier.18
The Shelhigh Pericardial No-React Patch (Herzog Surgical, Sacramento, Calif) is a new nonabsorbable adhesion barrier that was first described in gynecologic use by Pelosi and Pelosi in a case series of 20 patients.19 Consisting of a 12-cm-diameter patch of glutaraldehyde-treated bovine/porcine pericardium, this product has an excellent safety record as a permanent pericardial substitute in the cardiovascular literature and has been shown to resist calcification and adhesions.
In the Pelosi series, the patch was placed over the uterine fundus and secured by 4 monofilament sutures at the dome of the uterus and the parietal peritoneum.19 All patients underwent SLL at 6 weeks, and 3 patients also underwent third-look laparoscopy. None of the 20 women had adhesions between the abdominal wall and the bladder, bowel, uterus, or adnexae at SLL. However, minimal adhesions of the ovaries and tubes were found in 7 patients who had undergone posterior hysterotomy. Clinical trials are likely to follow this small pilot study.
Absorbable fluid adjuvants
With barrier adjuvants, optimal benefit is obtained when the physician can predict potential sites of adhesions. This is not a strict requirement with fluid barriers, which is their chief advantage. Among the agents described below, Sepracoat (Genzyme Corp) is available in the United States, while Intergel (Lifecore Biomedical, Chaska, Minn) was withdrawn from the market in March.
Intergel, a 0.5% ferric hyaluronade formulation, is a sterile nonpyrogenic gel of highly purified sodium hyaluronate, which is ionically cross-linked with ferric ion and adjusted to isotonicity with sodium chloride.11 (Hyaluronic acid is a major component of body tissues and fluids such as peritoneal fluid, where it performs physically supportive and mechanically protective roles.)
Johns and colleagues20 studied Intergel in a randomized, multicenter, third-party– blinded, placebo-controlled study. Of the 265 patients who completed the study, 131 were given 300 mL of Intergel and 134 were given lactated Ringer’s solution (the placebo) at the time of their surgery, through the laparoscopic port. When SLL was performed 6 to 12 weeks after surgery, the mean number and severity of adhesions—overall and at the surgical site—were significantly lower in the Intergel group. Adhesions reformed in 91% of those in the control group, compared with 63% in the Intergel group.
In myomectomy patients, the modified American Fertility Society Score, which uses 24 potential adhesion sites, was reduced by 42% in the Intergel group—a statistically significant improvement.20
One major advantage of Intergel is that it reduces adhesion formation at sites distant from the area of application, secondary to its wide intra-abdominal circulation. However, as mentioned above, sales were voluntarily suspended due to post-market reports of tissue adherence, sterile foreign-body reaction, and late-onset pain that sometimes required surgical intervention. In some patients, persistent residual material was noted at the time of subsequent surgery.
Sepracoat (hyaluronic acid-coat) is a dilute solution of 0.4% hyaluronic acid in phosphate-buffered saline. It is bioresorbable, persists at the application site less than 24 hours, and is completely cleared in less than 5 days.
In a prospective, randomized, blinded, placebo-controlled, multicenter study in 1998, Diamond and colleagues compared Sepracoat with a pure phosphate-buffered saline solution in 227 women undergoing gynecologic procedures via laparotomy.21 The aim of the study was to assess the efficacy and safety of the fluid at sites without direct surgical trauma or adhesiolysis. Both solutions were warmed to room temperature and injected into the abdominal cavity before the procedure began (250 mL after skin incision). The solution was reapplied after irrigation or every 30 minutes (100 mL), and at the end of the procedure (250 mL) before closure. The maximum volume used was 1,000 mL. After application, the fluid was left 1 minute before suctioning. Patients underwent SLL 40 days later, and adhesions were identified at the initial procedure and at SLL.
In the Sepracoat group, there was a reduction in de novo adhesions at nonsurgical sites by a factor of 2.8. The proportion of sites with de novo adhesions also decreased, and 80% of Sepracoat patients had at least 1 ovary that was adhesion-free compared with 58% of placebo-treated patients. These findings occurred in areas of indirect trauma, demonstrating that Sepracoat limited trauma at tissue injury.21
Conclusion
Adhesion prevention is of utmost importance after abdominal myomectomy, especially in patients who desire future fertility. Despite the limited number of prospective, randomized studies, the literature does support the efficacy of various fluid and barrier adjuvants.
Our practice is to use an adjuvant in all abdominal myomectomies. We have long relied on Interceed, which enjoys both ease of application and an excellent safety record. However, as reviewed above, other potentially useful products are available or in development. As ever, the reproductive surgeon should adhere to principles of microsurgery, strive for meticulous hemostasis, and demonstrate respect for tissue integrity.
Dr. DeCherney reports small holdings with Lifecore Biomedical. Drs. Chang and Marin report no affiliations or financial arrangements with any of the manufacturers of products mentioned in this article.
1. Stewart EA. Treatment of uterine leiomyomas. UpToDate (Version 10.3) 2002; 1-8. Available at: www.uptodate.com.
2. Ugur M, Tura C, Mungan T, Aydogdu T, Sahin Y, Gokmen O. Laparoscopy for adhesion prevention following myomectomy. Int J Gynecol Obstet. 1996;53:145-149.
3. Berkeley AS, DeCherney AH, Plan ML. Abdominal myomectomy and subsequent fertility. Surg Gynecol Obstet. 1983;153:319-322.
4. Tulandi T, Collin JA, Burrows E, et al. Treatment-dependent and treatment-independent pregnancy among women with periadnexal adhesions. Am J Obstet Gynecol. 1990;162:354-357.
5. Tulandi T, Murria C, Guralnick M. Adhesion formation and reproductive outcome after myomectomy and second-look laparoscopy. Obstet Gynecol. 1993;82:213-215.
6. Diamond MP, Freeman ML. Clinical implications of postsurgical adhesions. Hum Reprod. 2001;7:567-576.
7. Lau S, Tulandi T. Myomectomy and adhesion formation. In: diZerega GS, ed. Peritoneal Surgery. New York: Springer-Verlag 1999;289-290.
8. Diamond MP, El-Mowafi DM. Pelvic adhesions. Surg Technol Int. 1998;VII:273-283.
9. Guarnaccia MM, Rein MS. Traditional surgical approaches to uterine fibroids: abdominal myomectomy and hysterectomy. Clin Obstet Gynecol. 2001;44:385-400.
10. Tulandi T, Hum HS, Gelfand MM. Closure of laparotomy incisions with or without peritoneal suturing and second-look laparoscopy. Am J Obstet Gynecol. 1988;158:536-537.
11. Diamond MP. Reduction of adhesions after uterine myomectomy by Seprafilm membrane (HAL-F): a blinded, prospective, randomized, multicenter clinical study. Fertil Steril. 1996;66:904-910.
12. Johns D. Reduction of postsurgical adhesions with Intergel adhesion prevention solution: a multicenter study of safety and efficacy after conservative gynecologic surgery. Fertil Steril. 2001;76:595-604.
13. Farquhar C, vandekerckhove P, Watson A, Vail A, Wiseman D. Barrier agents for preventing adhesions after surgery for subfertility. Cochrane Database Systematic Rev. 2002(4);1-34.
14. Nordic Adhesion Prevention Study Group. The efficacy of Interceed (TC7) for prevention of reformation of postoperative adhesions on ovaries, fallopian tubes, and fimbriae in microsurgical operations for fertility: a multicenter study. Fertil Steril. 1995;63:709-714.
15. Sawada T, Nishizawa H, Nishio E, Kadowaki M. Postoperative adhesion prevention with an oxidized regenerated cellulose adhesion barrier in infertile women. J Reprod Med. 2000;45:387-389.
16. The Myomectomy Adhesions Multicenter Study Group. An expanded polytetrafluoroethylene barrier (Gore-Tex Surgical Membrane) reduces post-myomectomy adhesion formation. Fertil Steril. 1995;63:491-493.
17. Haney AF, Hesla J, Hurst BS, et al. Expanded polytetrafluoroethylene (Gore-Tex Surgical Membrane) is superior to oxidized regenerated cellulose (Interceed TC7) in preventing adhesions. Fertil Steril. 1995;63:1021-1026.
18. Monteforte CA, Queirazza R, Francescetting P, Herbst TJ. Fistula formation after implanting an ePTFE membrane. A case report. J Reprod Med. 1997;42:184-187.
19. Pelosi MA, II, Pelosi MA, III. A new nonabsorbable adhesion barrier for myomectomy. Am J Surg. 2002;184:428-432.
20. Johns D. Reduction of postsurgical adhesions with Intergel adhesion prevention solution: a multicenter study of safety and efficacy after conservative gynecologic surgery. Fertil Steril. 2001;76:596-604.
21. Diamond MP and The Sepracoat Adhesion Study Group. Reduction of de novo postsurgical adhesions by intraoperative precoating with Sepracoat (HAL-C) solution: a prospective, randomized, blinded, placebo-controlled multicenter study. Fertil Steril. 1998;69:1067-1074.
1. Stewart EA. Treatment of uterine leiomyomas. UpToDate (Version 10.3) 2002; 1-8. Available at: www.uptodate.com.
2. Ugur M, Tura C, Mungan T, Aydogdu T, Sahin Y, Gokmen O. Laparoscopy for adhesion prevention following myomectomy. Int J Gynecol Obstet. 1996;53:145-149.
3. Berkeley AS, DeCherney AH, Plan ML. Abdominal myomectomy and subsequent fertility. Surg Gynecol Obstet. 1983;153:319-322.
4. Tulandi T, Collin JA, Burrows E, et al. Treatment-dependent and treatment-independent pregnancy among women with periadnexal adhesions. Am J Obstet Gynecol. 1990;162:354-357.
5. Tulandi T, Murria C, Guralnick M. Adhesion formation and reproductive outcome after myomectomy and second-look laparoscopy. Obstet Gynecol. 1993;82:213-215.
6. Diamond MP, Freeman ML. Clinical implications of postsurgical adhesions. Hum Reprod. 2001;7:567-576.
7. Lau S, Tulandi T. Myomectomy and adhesion formation. In: diZerega GS, ed. Peritoneal Surgery. New York: Springer-Verlag 1999;289-290.
8. Diamond MP, El-Mowafi DM. Pelvic adhesions. Surg Technol Int. 1998;VII:273-283.
9. Guarnaccia MM, Rein MS. Traditional surgical approaches to uterine fibroids: abdominal myomectomy and hysterectomy. Clin Obstet Gynecol. 2001;44:385-400.
10. Tulandi T, Hum HS, Gelfand MM. Closure of laparotomy incisions with or without peritoneal suturing and second-look laparoscopy. Am J Obstet Gynecol. 1988;158:536-537.
11. Diamond MP. Reduction of adhesions after uterine myomectomy by Seprafilm membrane (HAL-F): a blinded, prospective, randomized, multicenter clinical study. Fertil Steril. 1996;66:904-910.
12. Johns D. Reduction of postsurgical adhesions with Intergel adhesion prevention solution: a multicenter study of safety and efficacy after conservative gynecologic surgery. Fertil Steril. 2001;76:595-604.
13. Farquhar C, vandekerckhove P, Watson A, Vail A, Wiseman D. Barrier agents for preventing adhesions after surgery for subfertility. Cochrane Database Systematic Rev. 2002(4);1-34.
14. Nordic Adhesion Prevention Study Group. The efficacy of Interceed (TC7) for prevention of reformation of postoperative adhesions on ovaries, fallopian tubes, and fimbriae in microsurgical operations for fertility: a multicenter study. Fertil Steril. 1995;63:709-714.
15. Sawada T, Nishizawa H, Nishio E, Kadowaki M. Postoperative adhesion prevention with an oxidized regenerated cellulose adhesion barrier in infertile women. J Reprod Med. 2000;45:387-389.
16. The Myomectomy Adhesions Multicenter Study Group. An expanded polytetrafluoroethylene barrier (Gore-Tex Surgical Membrane) reduces post-myomectomy adhesion formation. Fertil Steril. 1995;63:491-493.
17. Haney AF, Hesla J, Hurst BS, et al. Expanded polytetrafluoroethylene (Gore-Tex Surgical Membrane) is superior to oxidized regenerated cellulose (Interceed TC7) in preventing adhesions. Fertil Steril. 1995;63:1021-1026.
18. Monteforte CA, Queirazza R, Francescetting P, Herbst TJ. Fistula formation after implanting an ePTFE membrane. A case report. J Reprod Med. 1997;42:184-187.
19. Pelosi MA, II, Pelosi MA, III. A new nonabsorbable adhesion barrier for myomectomy. Am J Surg. 2002;184:428-432.
20. Johns D. Reduction of postsurgical adhesions with Intergel adhesion prevention solution: a multicenter study of safety and efficacy after conservative gynecologic surgery. Fertil Steril. 2001;76:596-604.
21. Diamond MP and The Sepracoat Adhesion Study Group. Reduction of de novo postsurgical adhesions by intraoperative precoating with Sepracoat (HAL-C) solution: a prospective, randomized, blinded, placebo-controlled multicenter study. Fertil Steril. 1998;69:1067-1074.
Energy-based techniques to ensure hemostasis and limit damage during laparoscopy
- Inspect all vascular sites with and without insufflation before assuming hemostasis is complete.
- In monopolar electrosurgery, electrode contact using low-voltage current leads to deeper, more effective penetration than higher-voltage current.
- To minimize unwanted thermal damage during bipolar electrosurgery, stop current flow at the end of the visible vapor phase, apply current in a pulsatile fashion, and secure pedicles by alternating between partial desiccation and incremental cutting.
- Since ultrasonic energy does not generate the high temperatures created by electrosurgery, it is less dependable for deep-tissue coagulation.
Compared with laparotomy, laparoscopic surgery achieves better hemostasis with less blood loss. Not only does this approach avoid an abdominal incision and the trauma associated with traction, manual manipulation, mechanical dissection, and larger tissue pedicles, but its illumination and magnification afford superior anatomical clarity, allowing the surgeon to seal a vessel before it is incised.
Still, keen surgical judgment remains critical—despite the availability of innovative electrosurgical, ultrasonic, and mechanical laparoscopic devices. Incomplete hemostasis or incision of an active vascular core can occur even with ideal application.
This article outlines the key ingredients of hemostasis during laparoscopy, focusing on the following modalities:
- monopolar electrosurgery
- bipolar electrosurgery
- ultrasonic energy
An orderly protocol minimizes risk
The art of surgical hemostasis is preventing vascular trauma while leaving the least-possible collateral tissue damage. When bleeding is encountered, the surgeon’s ability to attain hemostasis using a particular modality depends largely on how well he or she understands its technical aspects. Of course, thorough knowledge of anatomy also is crucial to prevent inadvertent damage to vital structures.
Surgical hemostasis should not be driven by reflex alone. Instead, surgeons should always follow this orderly sequence of steps to minimize risk:
Identify source of bleeding. Before taking any action, make every effort to accurately determine the source of bleeding and its proximity to vital anatomy. Even in the face of active hemorrhage, you can usually identify the bleeders by combining mechanical tamponade (using the jaws of a grasper or the side of a simple metallic probe) with active hydrolavage (using an irrigator-aspirator to break up and remove blood and clots).
Protect vital structures. If the bowel, bladder, or ureter is in close proximity to the bleeder, mobilize that structure sufficiently before applying energy. You can usually protect these entities by using a combination of countertraction and incremental tissue dissection. Whenever the peritoneum is involved, a relaxing incision parallel to the structure of concern also may be useful.
This protocol mandates withholding thermal energy until an orderly sequence of anatomical triage is carried out. Whenever a vital structure cannot be adequately mobilized, make every effort to control hemorrhage by using mechanical tamponade alone for up to 5 minutes. If access to the bleeding site or vessel caliber render pressure-alone unrealistic, employ either a carefully applied thermal energy or a suture ligature. If the surgeon is uncomfortable using either of these, conversion to laparotomy may be warranted.
Inspect vascular sites. Finally, because pneumoperitoneal pressure alone can tamponade venous bleeders—as well as small arterial ones—inspect all vascular sites with and without insufflation before assuming hemostasis is complete.
Monopolar electrosurgery
With conventional electrosurgery, tissue is coagulated when an electric field is applied across it using high-frequency alternating current. Whether cutting or coagulation occurs depends on the rate and extent of thermodynamic effects (FIGURE 1).
Mechanism of coagulation. When tissue comes into contact with the surface of an activated monopolar electrode, a relatively low-current circuit is completed.
- As the tissue is slowly heated to and maintained at temperatures above 50°C, irreversible cellular damage occurs. This is caused by deconfiguration of regulatory proteins and denaturation of cellular proteins.
- If the tissue is heated to 100°C, cellular water completely evaporates (desiccation), localized hemostasis occurs due to contraction of blood vessels and the surrounding tissues (coagulation), and collagens convert to glucose, which creates an adhesive effect between the tissue and electrode.
- Temperatures above 200°C cause carbonization and charring.
Select the best output voltage. Since the output voltage of “coag” current is very high (FIGURE 2), contact coagulation is generally limited to superficial layers. That is because of the accelerated buildup of tissue resistance from rapid desiccation and carbonization. Conversely, electrode contact using the lower-voltage “cut” current heats tissue more gradually, leading to deeper and more reliable penetration. Thus, both contact and coaptive coagulation with monopolar electrosurgery are more effectively performed using “cut” current.
Since superficial-appearing endometriotic implants may extend deeply into the retroperitoneal tissues, I thermally ablate these lesions using a broad-surface electrode in contact with “cut” current. In contrast, I treat superficial implants on the ovarian cortex with “coag” current to minimize unwanted thermal injury to adjacent follicular tissue.
Interrupt the blood flow. Coaptive vessel sealing using any type of monopolar current may be ineffective if the blood flow remains uninterrupted. Unless a vessel is sufficiently squeezed before electricity is applied, current density is dramatically reduced by conduction in blood, and luminal temperatures undergo little change, as any heat is dissipated by convection. Deceived by the appearance of well-coagulated tissue, a surgeon may discover an alarmingly viable core at the time of incision. Regardless of the selected output current (that is, “cut,” “blend,” or “coag”), coaptive desiccation with monopolar electrosurgery is usually insufficient to reliably secure the uterine or ovarian vessels during hysterectomy and oophorectomy.
Achieve the appropriate cutting arc. Electrosurgical cutting (vaporization/ablation) is possible whenever voltage is sufficient to create an electrical spark between an electrode and underlying tissue; tissue cutting is more apt to occur if the arcing remains unabated. When it does, cellular water is superheated to temperatures greater than 600°C, causing explosive vaporization secondary to the production of highly disruptive pressure (since steam occupies 6 times the volume of liquid water).
Although all of the typical output currents (“cut,” “blend,” and “coag”) provide sufficient voltage to ionize the air gap and arc to tissue, the higher voltages of “blend” and “coag” create progressively wider zones of thermal damage at the margins of the incision (FIGURE 3) These effects are amplified by using broad-surface electrodes.
Wide versus narrow hemostasis. Using “blend” or “coag” current to cut in order to provide wider hemostasis can be helpful during myomectomy, as well as when operating down the broad ligament and along the vaginal fornices during hysterectomy, across vascular adhesions, and to clarify the space of Retzius in preparation for colposuspension and paravaginal repair. Higher-voltage currents also facilitate incision of tissues that have greater impedance, such as fatty or desiccated pedicles and adhesions.
On the other hand, it is more prudent to utilize the lower-voltage “cut” current via the edge of an electrode for electrosurgical incision whenever lateral thermal spread may pose extra liability to adjacent tissues, such as the ovarian cortex during cystectomy and the ureter or rectum during excision of endometriosis from the lateral pelvic sidewall or cul-de-sac.
Deceived by the appearance of well-coagulated tissue, surgeons may discover an alarmingly viable core at the time of incision.
- Fulguration is the use of high-voltage sparking produced by “coag” current to coagulate a broad surface with open bleeders. As opposed to the continuous arcing produced by “cut” current, the highly interrupted output of “coag” current causes the arcs to strike the tissue surface in a widely dispersed and random fashion. This leads to more rapid thermal change, creating a zone of superficial coagulation.
I typically employ fulguration to control small bleeders and vessels cut on end along the undersurface of the ovarian cortex during cystectomy, atop the myometrial bed during myomectomy, and alongside Cooper’s ligament during colposuspension.
Protect vital structures with short bursts of “coag” current. If bleeding near the bowel, bladder, or ureter cannot be controlled with pressure alone, carefully directed short bursts of noncontact “coag” current with a broad-surface electrode may help you attain effective hemostasis with the least-possible amount of electrosurgical penetration.
Despite the high-voltage output involved, fulguration is useless in a wet, conductive surgical field due to the random diffusion of current.
FIGURE 2 Range of output voltages
Relative changes in voltage and average current related to “cut,” “blend,” and “coag” currents.
FIGURE 3Zones of thermal damage related to voltage
Using a conventional electrosurgical generator for tissue cutting, the margin of thermal necrosis expands with increasing voltage.
Bipolar electrosurgery
Mechanism of action. Bipolar electrosurgery consolidates an active electrode and return electrode into an instrument with 2 small poles. These poles can be the tines of a forceps, blades of a scissors, or an electrode matched to a more proximal conductive collar separated by an insulator. The output typically used is the low-voltage “cut” current.
Advantages of bipolar energy. Localization of current between the poles offers distinct advantages. Thermal damage is generally limited to a discrete volume of tissue. A bipolar forceps can be used to coapt and thermally weld blood vessels. The concentrated current and small distance between the poles also make it possible to desiccate tissue that is immersed in fluid. This modality is less useful, however, when open blood vessels are retracted or tissue pedicles are very thick.
Because it tends to promote the flow of energy well beyond desiccation, an ammeter should not be used to determine the treatment endpoint for coagulation of blood vessels in the vicinity of vital tissue.
Know when to terminate current to prevent vital-tissue damage. Although the flow of current and primary thermal effects are restricted to the tissue between the poles, this does not eliminate the risk of thermal injury to tissue that is distant from the site of directed hemostasis. As current is applied between the poles, the intervening tissue gradually desiccates until it becomes thoroughly dehydrated. Desiccation is complete when the tissue whitens and visible steam emission stops. If the application of current continues, the heat spreads well beyond the electrical limits of the instrument.
This secondary thermal bloom is caused by the bubbling of steam into the tissue parenchyma as heat is rapidly generated (due to dry tissue’s high resistance to the flow of electrical current). This explains why structures such as the ureter or bowel may suffer irreversible thermal damage despite being at some distance from an operative or bleeding site.
Use of an in-line ammeter does not prevent this problem. Rather, it tends to promote the flow of energy well beyond desiccation. Consequently, an ammeter should not be used to determine the treatment endpoint for coagulation of blood vessels in the vicinity of vital tissue.
Whenever bipolar electrosurgery is used for hemostasis, unwanted thermal damage can be minimized by:
- terminating the flow of current at the end of the visible vapor phase,
- applying current in a pulsatile fashion to permit tissue cooling,
- avoiding the use of an in-line ammeter to determine the coagulation endpoint, and
- securing pedicles by a stepwise process that alternates between partial desiccation and incremental cutting (TABLE 1).
Since the rate of temperature generation is a direct function of the volume of tissue being desiccated, thermal spread can also be reduced by using the sides or tips of a slightly open forceps to press or lift, rather than coapt for hemostasis (FIGURE 4).
Free adherent tissue gently. As with contact monopolar coagulation, tissue between the electrodes of a bipolar instrument may become adherent during desiccation. Repeated attempts to shake the tissue free may lead to traumatic avulsion of a key vascular pedicle. A stuck vascular pedicle can usually be unglued by energizing the opened device while immersing it in a conductive irrigant, such as saline. Once the solution is boiled by the high current density between the electrodes, the mechanical action of bubbling is usually sufficient to atraumatically free the pedicle.
FIGURE 4 Minimizing bipolar thermal damage
Using contact rather than coaptation is one way to limit thermal injury during bipolar electrosurgery.TABLE 1
Minimizing bipolar thermal damage
|
Ultrasonic energy
Mechanism of action. Ultrasonic shears produce mechanical energy to cut and coagulate tissue. Housed in the hand piece of this laparoscopic device is a piezoelectric crystal that vibrates a titanium blade 55,500 times per second over a variable excursion of 50 microns to 100 microns. As energy is transmitted to tissue, hydrogen bonds of tissue proteins are ruptured, leading to a denatured protein coagulum without significant charring. The tissue cutting that occurs is secondary to mechanical vibration and cavitational fragmentation of tissue parenchyma.
Since ultrasonic energy does not generate the high temperatures created by electrosurgery, it is less dependable for deep-tissue coagulation. Rather, thermal change is gradual, requiring a modicum of patience.
Available instrument configurations include 5-mm curved or hook blades. In addition, 5-mm or 10-mm ligating and cutting shears coaptively desiccate and cut the tissue by securing it between a grooved plastic pad and the vibrating blade.
Tissue effects depend on interplay of factors. By using various combinations of blade shapes, blade excursions, and tissue tensions, surgeons can accomplish a variety of specific effects. Cutting velocity is directly proportional to blade excursion, tissue traction, and blade surface area (energy density), and is inversely related to tissue density and elasticity. Thus, the fastest cutting with the least amount of coagulation occurs when tissue is placed on tension and firmly squeezed, lifted, or rotated with the sharpest side of a blade set at maximum excursion.
Coagulation is the obverse of cutting: It is inversely related to tissue tension, blade sharpness, blade excursion, and cutting speed. Therefore, coagulation is best achieved by relaxing tension, minimizing blade excursion, and using a blunt edge or flattened blade surface.
A stuck vascular pedicle can usually be unglued by energizing the opened bipolar device while immersing it in a conductive irrigant.
Avoid excessive traction and torsion. Be mindful of the potential for premature incision of an incompletely coagulated tissue pedicle when excessive traction or torsion is applied. When used to coaptively desiccate and incise a vascular pedicle, ultrasonic energy should be applied patiently, taking great care to minimize tissue tension while using the broadest blade surface set to the lowest excursion (TABLE 2). Hemostatic incision is best ensured by first coagulating several overlapping areas along an untracted pedicle, limiting each application to the point of tissue blanching and initial vapor emission. Only then should the pedicle be incised by gradually lifting, squeezing, or rotating the distal device. In this fashion, ultrasonic energy can be successfully used to secure both the ovarian and uterine vessels.
TABLE 2
Factors likely to cause premature incision with ultrasonic energy
|
Summary
The use of electrical and ultrasonic energy during operative laparoscopy poses several challenges, including the reduction of unwanted thermal injury and the elimination of incomplete hemostasis.
Since the depth of penetration during monopolar electrosurgery is proportional to both output voltage and surface area, unwanted thermal change can be reduced by using the smallest electrode surface with “cut” current for tissue cutting, and “coag” current with a broad-surface electrode for contact or noncontact (fulguration) coagulation.
Bipolar electrosurgery is the preferred modality for coaptive desiccation of a vascular pedicle with electricity. Despite the isolation of current to the intervening tissue, surgeons must take steps to reduce the lateral percolation of heat into adjacent tissues.
Ultrasonic energy provides reliable coaptive hemostasis and incision with little tissue damage. However, the surgeon must be mindful of the forces that promulgate premature incision. Knowledge of the biophysical behavior of electrical and ultrasonic energy is a prelude to safety and efficacy during laparoscopic dissection.
Dr. Brill reports no affiliations or financial arrangements with any of the manufacturers of products mentioned in this article.
1. Brill AI. Energy systems for operative laparoscopy. J Am Assoc Gynecol Laparosc. 1998;5:335-345.
2. Friedman J. The technical aspects of electrosurgery. Oral Surg. 1973;36:177-187.
3. Honig WM. The mechanism of cutting in electrosurgery. IEEE Trans Biomed Eng BME. 1975;22:55-58.
4. Sigel B, Dunn MR. The mechanism of blood vessel closure by high frequency electrocoagulation. Surg Gynecol Obstet. 1965;121:823-831.
5. Phipps JH. Thermometry studies with bipolar diathermy during hysterectomy. Gynecol Laparosc. 1994;1:146-149.
6. Ryder RM, Hulka JF. Bladder and bowel injury after electrodesiccation with Kleppinger bipolar forceps: A clinicopathologic study. J Reprod Med. 1993;3:595-598.
7. McCarus SD. Physiologic mechanism of the ultrasonically activated scalpel. J Am Assoc Gynecol Laparosc. 1996;3:601-608.
- Inspect all vascular sites with and without insufflation before assuming hemostasis is complete.
- In monopolar electrosurgery, electrode contact using low-voltage current leads to deeper, more effective penetration than higher-voltage current.
- To minimize unwanted thermal damage during bipolar electrosurgery, stop current flow at the end of the visible vapor phase, apply current in a pulsatile fashion, and secure pedicles by alternating between partial desiccation and incremental cutting.
- Since ultrasonic energy does not generate the high temperatures created by electrosurgery, it is less dependable for deep-tissue coagulation.
Compared with laparotomy, laparoscopic surgery achieves better hemostasis with less blood loss. Not only does this approach avoid an abdominal incision and the trauma associated with traction, manual manipulation, mechanical dissection, and larger tissue pedicles, but its illumination and magnification afford superior anatomical clarity, allowing the surgeon to seal a vessel before it is incised.
Still, keen surgical judgment remains critical—despite the availability of innovative electrosurgical, ultrasonic, and mechanical laparoscopic devices. Incomplete hemostasis or incision of an active vascular core can occur even with ideal application.
This article outlines the key ingredients of hemostasis during laparoscopy, focusing on the following modalities:
- monopolar electrosurgery
- bipolar electrosurgery
- ultrasonic energy
An orderly protocol minimizes risk
The art of surgical hemostasis is preventing vascular trauma while leaving the least-possible collateral tissue damage. When bleeding is encountered, the surgeon’s ability to attain hemostasis using a particular modality depends largely on how well he or she understands its technical aspects. Of course, thorough knowledge of anatomy also is crucial to prevent inadvertent damage to vital structures.
Surgical hemostasis should not be driven by reflex alone. Instead, surgeons should always follow this orderly sequence of steps to minimize risk:
Identify source of bleeding. Before taking any action, make every effort to accurately determine the source of bleeding and its proximity to vital anatomy. Even in the face of active hemorrhage, you can usually identify the bleeders by combining mechanical tamponade (using the jaws of a grasper or the side of a simple metallic probe) with active hydrolavage (using an irrigator-aspirator to break up and remove blood and clots).
Protect vital structures. If the bowel, bladder, or ureter is in close proximity to the bleeder, mobilize that structure sufficiently before applying energy. You can usually protect these entities by using a combination of countertraction and incremental tissue dissection. Whenever the peritoneum is involved, a relaxing incision parallel to the structure of concern also may be useful.
This protocol mandates withholding thermal energy until an orderly sequence of anatomical triage is carried out. Whenever a vital structure cannot be adequately mobilized, make every effort to control hemorrhage by using mechanical tamponade alone for up to 5 minutes. If access to the bleeding site or vessel caliber render pressure-alone unrealistic, employ either a carefully applied thermal energy or a suture ligature. If the surgeon is uncomfortable using either of these, conversion to laparotomy may be warranted.
Inspect vascular sites. Finally, because pneumoperitoneal pressure alone can tamponade venous bleeders—as well as small arterial ones—inspect all vascular sites with and without insufflation before assuming hemostasis is complete.
Monopolar electrosurgery
With conventional electrosurgery, tissue is coagulated when an electric field is applied across it using high-frequency alternating current. Whether cutting or coagulation occurs depends on the rate and extent of thermodynamic effects (FIGURE 1).
Mechanism of coagulation. When tissue comes into contact with the surface of an activated monopolar electrode, a relatively low-current circuit is completed.
- As the tissue is slowly heated to and maintained at temperatures above 50°C, irreversible cellular damage occurs. This is caused by deconfiguration of regulatory proteins and denaturation of cellular proteins.
- If the tissue is heated to 100°C, cellular water completely evaporates (desiccation), localized hemostasis occurs due to contraction of blood vessels and the surrounding tissues (coagulation), and collagens convert to glucose, which creates an adhesive effect between the tissue and electrode.
- Temperatures above 200°C cause carbonization and charring.
Select the best output voltage. Since the output voltage of “coag” current is very high (FIGURE 2), contact coagulation is generally limited to superficial layers. That is because of the accelerated buildup of tissue resistance from rapid desiccation and carbonization. Conversely, electrode contact using the lower-voltage “cut” current heats tissue more gradually, leading to deeper and more reliable penetration. Thus, both contact and coaptive coagulation with monopolar electrosurgery are more effectively performed using “cut” current.
Since superficial-appearing endometriotic implants may extend deeply into the retroperitoneal tissues, I thermally ablate these lesions using a broad-surface electrode in contact with “cut” current. In contrast, I treat superficial implants on the ovarian cortex with “coag” current to minimize unwanted thermal injury to adjacent follicular tissue.
Interrupt the blood flow. Coaptive vessel sealing using any type of monopolar current may be ineffective if the blood flow remains uninterrupted. Unless a vessel is sufficiently squeezed before electricity is applied, current density is dramatically reduced by conduction in blood, and luminal temperatures undergo little change, as any heat is dissipated by convection. Deceived by the appearance of well-coagulated tissue, a surgeon may discover an alarmingly viable core at the time of incision. Regardless of the selected output current (that is, “cut,” “blend,” or “coag”), coaptive desiccation with monopolar electrosurgery is usually insufficient to reliably secure the uterine or ovarian vessels during hysterectomy and oophorectomy.
Achieve the appropriate cutting arc. Electrosurgical cutting (vaporization/ablation) is possible whenever voltage is sufficient to create an electrical spark between an electrode and underlying tissue; tissue cutting is more apt to occur if the arcing remains unabated. When it does, cellular water is superheated to temperatures greater than 600°C, causing explosive vaporization secondary to the production of highly disruptive pressure (since steam occupies 6 times the volume of liquid water).
Although all of the typical output currents (“cut,” “blend,” and “coag”) provide sufficient voltage to ionize the air gap and arc to tissue, the higher voltages of “blend” and “coag” create progressively wider zones of thermal damage at the margins of the incision (FIGURE 3) These effects are amplified by using broad-surface electrodes.
Wide versus narrow hemostasis. Using “blend” or “coag” current to cut in order to provide wider hemostasis can be helpful during myomectomy, as well as when operating down the broad ligament and along the vaginal fornices during hysterectomy, across vascular adhesions, and to clarify the space of Retzius in preparation for colposuspension and paravaginal repair. Higher-voltage currents also facilitate incision of tissues that have greater impedance, such as fatty or desiccated pedicles and adhesions.
On the other hand, it is more prudent to utilize the lower-voltage “cut” current via the edge of an electrode for electrosurgical incision whenever lateral thermal spread may pose extra liability to adjacent tissues, such as the ovarian cortex during cystectomy and the ureter or rectum during excision of endometriosis from the lateral pelvic sidewall or cul-de-sac.
Deceived by the appearance of well-coagulated tissue, surgeons may discover an alarmingly viable core at the time of incision.
- Fulguration is the use of high-voltage sparking produced by “coag” current to coagulate a broad surface with open bleeders. As opposed to the continuous arcing produced by “cut” current, the highly interrupted output of “coag” current causes the arcs to strike the tissue surface in a widely dispersed and random fashion. This leads to more rapid thermal change, creating a zone of superficial coagulation.
I typically employ fulguration to control small bleeders and vessels cut on end along the undersurface of the ovarian cortex during cystectomy, atop the myometrial bed during myomectomy, and alongside Cooper’s ligament during colposuspension.
Protect vital structures with short bursts of “coag” current. If bleeding near the bowel, bladder, or ureter cannot be controlled with pressure alone, carefully directed short bursts of noncontact “coag” current with a broad-surface electrode may help you attain effective hemostasis with the least-possible amount of electrosurgical penetration.
Despite the high-voltage output involved, fulguration is useless in a wet, conductive surgical field due to the random diffusion of current.
FIGURE 2 Range of output voltages
Relative changes in voltage and average current related to “cut,” “blend,” and “coag” currents.
FIGURE 3Zones of thermal damage related to voltage
Using a conventional electrosurgical generator for tissue cutting, the margin of thermal necrosis expands with increasing voltage.
Bipolar electrosurgery
Mechanism of action. Bipolar electrosurgery consolidates an active electrode and return electrode into an instrument with 2 small poles. These poles can be the tines of a forceps, blades of a scissors, or an electrode matched to a more proximal conductive collar separated by an insulator. The output typically used is the low-voltage “cut” current.
Advantages of bipolar energy. Localization of current between the poles offers distinct advantages. Thermal damage is generally limited to a discrete volume of tissue. A bipolar forceps can be used to coapt and thermally weld blood vessels. The concentrated current and small distance between the poles also make it possible to desiccate tissue that is immersed in fluid. This modality is less useful, however, when open blood vessels are retracted or tissue pedicles are very thick.
Because it tends to promote the flow of energy well beyond desiccation, an ammeter should not be used to determine the treatment endpoint for coagulation of blood vessels in the vicinity of vital tissue.
Know when to terminate current to prevent vital-tissue damage. Although the flow of current and primary thermal effects are restricted to the tissue between the poles, this does not eliminate the risk of thermal injury to tissue that is distant from the site of directed hemostasis. As current is applied between the poles, the intervening tissue gradually desiccates until it becomes thoroughly dehydrated. Desiccation is complete when the tissue whitens and visible steam emission stops. If the application of current continues, the heat spreads well beyond the electrical limits of the instrument.
This secondary thermal bloom is caused by the bubbling of steam into the tissue parenchyma as heat is rapidly generated (due to dry tissue’s high resistance to the flow of electrical current). This explains why structures such as the ureter or bowel may suffer irreversible thermal damage despite being at some distance from an operative or bleeding site.
Use of an in-line ammeter does not prevent this problem. Rather, it tends to promote the flow of energy well beyond desiccation. Consequently, an ammeter should not be used to determine the treatment endpoint for coagulation of blood vessels in the vicinity of vital tissue.
Whenever bipolar electrosurgery is used for hemostasis, unwanted thermal damage can be minimized by:
- terminating the flow of current at the end of the visible vapor phase,
- applying current in a pulsatile fashion to permit tissue cooling,
- avoiding the use of an in-line ammeter to determine the coagulation endpoint, and
- securing pedicles by a stepwise process that alternates between partial desiccation and incremental cutting (TABLE 1).
Since the rate of temperature generation is a direct function of the volume of tissue being desiccated, thermal spread can also be reduced by using the sides or tips of a slightly open forceps to press or lift, rather than coapt for hemostasis (FIGURE 4).
Free adherent tissue gently. As with contact monopolar coagulation, tissue between the electrodes of a bipolar instrument may become adherent during desiccation. Repeated attempts to shake the tissue free may lead to traumatic avulsion of a key vascular pedicle. A stuck vascular pedicle can usually be unglued by energizing the opened device while immersing it in a conductive irrigant, such as saline. Once the solution is boiled by the high current density between the electrodes, the mechanical action of bubbling is usually sufficient to atraumatically free the pedicle.
FIGURE 4 Minimizing bipolar thermal damage
Using contact rather than coaptation is one way to limit thermal injury during bipolar electrosurgery.TABLE 1
Minimizing bipolar thermal damage
|
Ultrasonic energy
Mechanism of action. Ultrasonic shears produce mechanical energy to cut and coagulate tissue. Housed in the hand piece of this laparoscopic device is a piezoelectric crystal that vibrates a titanium blade 55,500 times per second over a variable excursion of 50 microns to 100 microns. As energy is transmitted to tissue, hydrogen bonds of tissue proteins are ruptured, leading to a denatured protein coagulum without significant charring. The tissue cutting that occurs is secondary to mechanical vibration and cavitational fragmentation of tissue parenchyma.
Since ultrasonic energy does not generate the high temperatures created by electrosurgery, it is less dependable for deep-tissue coagulation. Rather, thermal change is gradual, requiring a modicum of patience.
Available instrument configurations include 5-mm curved or hook blades. In addition, 5-mm or 10-mm ligating and cutting shears coaptively desiccate and cut the tissue by securing it between a grooved plastic pad and the vibrating blade.
Tissue effects depend on interplay of factors. By using various combinations of blade shapes, blade excursions, and tissue tensions, surgeons can accomplish a variety of specific effects. Cutting velocity is directly proportional to blade excursion, tissue traction, and blade surface area (energy density), and is inversely related to tissue density and elasticity. Thus, the fastest cutting with the least amount of coagulation occurs when tissue is placed on tension and firmly squeezed, lifted, or rotated with the sharpest side of a blade set at maximum excursion.
Coagulation is the obverse of cutting: It is inversely related to tissue tension, blade sharpness, blade excursion, and cutting speed. Therefore, coagulation is best achieved by relaxing tension, minimizing blade excursion, and using a blunt edge or flattened blade surface.
A stuck vascular pedicle can usually be unglued by energizing the opened bipolar device while immersing it in a conductive irrigant.
Avoid excessive traction and torsion. Be mindful of the potential for premature incision of an incompletely coagulated tissue pedicle when excessive traction or torsion is applied. When used to coaptively desiccate and incise a vascular pedicle, ultrasonic energy should be applied patiently, taking great care to minimize tissue tension while using the broadest blade surface set to the lowest excursion (TABLE 2). Hemostatic incision is best ensured by first coagulating several overlapping areas along an untracted pedicle, limiting each application to the point of tissue blanching and initial vapor emission. Only then should the pedicle be incised by gradually lifting, squeezing, or rotating the distal device. In this fashion, ultrasonic energy can be successfully used to secure both the ovarian and uterine vessels.
TABLE 2
Factors likely to cause premature incision with ultrasonic energy
|
Summary
The use of electrical and ultrasonic energy during operative laparoscopy poses several challenges, including the reduction of unwanted thermal injury and the elimination of incomplete hemostasis.
Since the depth of penetration during monopolar electrosurgery is proportional to both output voltage and surface area, unwanted thermal change can be reduced by using the smallest electrode surface with “cut” current for tissue cutting, and “coag” current with a broad-surface electrode for contact or noncontact (fulguration) coagulation.
Bipolar electrosurgery is the preferred modality for coaptive desiccation of a vascular pedicle with electricity. Despite the isolation of current to the intervening tissue, surgeons must take steps to reduce the lateral percolation of heat into adjacent tissues.
Ultrasonic energy provides reliable coaptive hemostasis and incision with little tissue damage. However, the surgeon must be mindful of the forces that promulgate premature incision. Knowledge of the biophysical behavior of electrical and ultrasonic energy is a prelude to safety and efficacy during laparoscopic dissection.
Dr. Brill reports no affiliations or financial arrangements with any of the manufacturers of products mentioned in this article.
- Inspect all vascular sites with and without insufflation before assuming hemostasis is complete.
- In monopolar electrosurgery, electrode contact using low-voltage current leads to deeper, more effective penetration than higher-voltage current.
- To minimize unwanted thermal damage during bipolar electrosurgery, stop current flow at the end of the visible vapor phase, apply current in a pulsatile fashion, and secure pedicles by alternating between partial desiccation and incremental cutting.
- Since ultrasonic energy does not generate the high temperatures created by electrosurgery, it is less dependable for deep-tissue coagulation.
Compared with laparotomy, laparoscopic surgery achieves better hemostasis with less blood loss. Not only does this approach avoid an abdominal incision and the trauma associated with traction, manual manipulation, mechanical dissection, and larger tissue pedicles, but its illumination and magnification afford superior anatomical clarity, allowing the surgeon to seal a vessel before it is incised.
Still, keen surgical judgment remains critical—despite the availability of innovative electrosurgical, ultrasonic, and mechanical laparoscopic devices. Incomplete hemostasis or incision of an active vascular core can occur even with ideal application.
This article outlines the key ingredients of hemostasis during laparoscopy, focusing on the following modalities:
- monopolar electrosurgery
- bipolar electrosurgery
- ultrasonic energy
An orderly protocol minimizes risk
The art of surgical hemostasis is preventing vascular trauma while leaving the least-possible collateral tissue damage. When bleeding is encountered, the surgeon’s ability to attain hemostasis using a particular modality depends largely on how well he or she understands its technical aspects. Of course, thorough knowledge of anatomy also is crucial to prevent inadvertent damage to vital structures.
Surgical hemostasis should not be driven by reflex alone. Instead, surgeons should always follow this orderly sequence of steps to minimize risk:
Identify source of bleeding. Before taking any action, make every effort to accurately determine the source of bleeding and its proximity to vital anatomy. Even in the face of active hemorrhage, you can usually identify the bleeders by combining mechanical tamponade (using the jaws of a grasper or the side of a simple metallic probe) with active hydrolavage (using an irrigator-aspirator to break up and remove blood and clots).
Protect vital structures. If the bowel, bladder, or ureter is in close proximity to the bleeder, mobilize that structure sufficiently before applying energy. You can usually protect these entities by using a combination of countertraction and incremental tissue dissection. Whenever the peritoneum is involved, a relaxing incision parallel to the structure of concern also may be useful.
This protocol mandates withholding thermal energy until an orderly sequence of anatomical triage is carried out. Whenever a vital structure cannot be adequately mobilized, make every effort to control hemorrhage by using mechanical tamponade alone for up to 5 minutes. If access to the bleeding site or vessel caliber render pressure-alone unrealistic, employ either a carefully applied thermal energy or a suture ligature. If the surgeon is uncomfortable using either of these, conversion to laparotomy may be warranted.
Inspect vascular sites. Finally, because pneumoperitoneal pressure alone can tamponade venous bleeders—as well as small arterial ones—inspect all vascular sites with and without insufflation before assuming hemostasis is complete.
Monopolar electrosurgery
With conventional electrosurgery, tissue is coagulated when an electric field is applied across it using high-frequency alternating current. Whether cutting or coagulation occurs depends on the rate and extent of thermodynamic effects (FIGURE 1).
Mechanism of coagulation. When tissue comes into contact with the surface of an activated monopolar electrode, a relatively low-current circuit is completed.
- As the tissue is slowly heated to and maintained at temperatures above 50°C, irreversible cellular damage occurs. This is caused by deconfiguration of regulatory proteins and denaturation of cellular proteins.
- If the tissue is heated to 100°C, cellular water completely evaporates (desiccation), localized hemostasis occurs due to contraction of blood vessels and the surrounding tissues (coagulation), and collagens convert to glucose, which creates an adhesive effect between the tissue and electrode.
- Temperatures above 200°C cause carbonization and charring.
Select the best output voltage. Since the output voltage of “coag” current is very high (FIGURE 2), contact coagulation is generally limited to superficial layers. That is because of the accelerated buildup of tissue resistance from rapid desiccation and carbonization. Conversely, electrode contact using the lower-voltage “cut” current heats tissue more gradually, leading to deeper and more reliable penetration. Thus, both contact and coaptive coagulation with monopolar electrosurgery are more effectively performed using “cut” current.
Since superficial-appearing endometriotic implants may extend deeply into the retroperitoneal tissues, I thermally ablate these lesions using a broad-surface electrode in contact with “cut” current. In contrast, I treat superficial implants on the ovarian cortex with “coag” current to minimize unwanted thermal injury to adjacent follicular tissue.
Interrupt the blood flow. Coaptive vessel sealing using any type of monopolar current may be ineffective if the blood flow remains uninterrupted. Unless a vessel is sufficiently squeezed before electricity is applied, current density is dramatically reduced by conduction in blood, and luminal temperatures undergo little change, as any heat is dissipated by convection. Deceived by the appearance of well-coagulated tissue, a surgeon may discover an alarmingly viable core at the time of incision. Regardless of the selected output current (that is, “cut,” “blend,” or “coag”), coaptive desiccation with monopolar electrosurgery is usually insufficient to reliably secure the uterine or ovarian vessels during hysterectomy and oophorectomy.
Achieve the appropriate cutting arc. Electrosurgical cutting (vaporization/ablation) is possible whenever voltage is sufficient to create an electrical spark between an electrode and underlying tissue; tissue cutting is more apt to occur if the arcing remains unabated. When it does, cellular water is superheated to temperatures greater than 600°C, causing explosive vaporization secondary to the production of highly disruptive pressure (since steam occupies 6 times the volume of liquid water).
Although all of the typical output currents (“cut,” “blend,” and “coag”) provide sufficient voltage to ionize the air gap and arc to tissue, the higher voltages of “blend” and “coag” create progressively wider zones of thermal damage at the margins of the incision (FIGURE 3) These effects are amplified by using broad-surface electrodes.
Wide versus narrow hemostasis. Using “blend” or “coag” current to cut in order to provide wider hemostasis can be helpful during myomectomy, as well as when operating down the broad ligament and along the vaginal fornices during hysterectomy, across vascular adhesions, and to clarify the space of Retzius in preparation for colposuspension and paravaginal repair. Higher-voltage currents also facilitate incision of tissues that have greater impedance, such as fatty or desiccated pedicles and adhesions.
On the other hand, it is more prudent to utilize the lower-voltage “cut” current via the edge of an electrode for electrosurgical incision whenever lateral thermal spread may pose extra liability to adjacent tissues, such as the ovarian cortex during cystectomy and the ureter or rectum during excision of endometriosis from the lateral pelvic sidewall or cul-de-sac.
Deceived by the appearance of well-coagulated tissue, surgeons may discover an alarmingly viable core at the time of incision.
- Fulguration is the use of high-voltage sparking produced by “coag” current to coagulate a broad surface with open bleeders. As opposed to the continuous arcing produced by “cut” current, the highly interrupted output of “coag” current causes the arcs to strike the tissue surface in a widely dispersed and random fashion. This leads to more rapid thermal change, creating a zone of superficial coagulation.
I typically employ fulguration to control small bleeders and vessels cut on end along the undersurface of the ovarian cortex during cystectomy, atop the myometrial bed during myomectomy, and alongside Cooper’s ligament during colposuspension.
Protect vital structures with short bursts of “coag” current. If bleeding near the bowel, bladder, or ureter cannot be controlled with pressure alone, carefully directed short bursts of noncontact “coag” current with a broad-surface electrode may help you attain effective hemostasis with the least-possible amount of electrosurgical penetration.
Despite the high-voltage output involved, fulguration is useless in a wet, conductive surgical field due to the random diffusion of current.
FIGURE 2 Range of output voltages
Relative changes in voltage and average current related to “cut,” “blend,” and “coag” currents.
FIGURE 3Zones of thermal damage related to voltage
Using a conventional electrosurgical generator for tissue cutting, the margin of thermal necrosis expands with increasing voltage.
Bipolar electrosurgery
Mechanism of action. Bipolar electrosurgery consolidates an active electrode and return electrode into an instrument with 2 small poles. These poles can be the tines of a forceps, blades of a scissors, or an electrode matched to a more proximal conductive collar separated by an insulator. The output typically used is the low-voltage “cut” current.
Advantages of bipolar energy. Localization of current between the poles offers distinct advantages. Thermal damage is generally limited to a discrete volume of tissue. A bipolar forceps can be used to coapt and thermally weld blood vessels. The concentrated current and small distance between the poles also make it possible to desiccate tissue that is immersed in fluid. This modality is less useful, however, when open blood vessels are retracted or tissue pedicles are very thick.
Because it tends to promote the flow of energy well beyond desiccation, an ammeter should not be used to determine the treatment endpoint for coagulation of blood vessels in the vicinity of vital tissue.
Know when to terminate current to prevent vital-tissue damage. Although the flow of current and primary thermal effects are restricted to the tissue between the poles, this does not eliminate the risk of thermal injury to tissue that is distant from the site of directed hemostasis. As current is applied between the poles, the intervening tissue gradually desiccates until it becomes thoroughly dehydrated. Desiccation is complete when the tissue whitens and visible steam emission stops. If the application of current continues, the heat spreads well beyond the electrical limits of the instrument.
This secondary thermal bloom is caused by the bubbling of steam into the tissue parenchyma as heat is rapidly generated (due to dry tissue’s high resistance to the flow of electrical current). This explains why structures such as the ureter or bowel may suffer irreversible thermal damage despite being at some distance from an operative or bleeding site.
Use of an in-line ammeter does not prevent this problem. Rather, it tends to promote the flow of energy well beyond desiccation. Consequently, an ammeter should not be used to determine the treatment endpoint for coagulation of blood vessels in the vicinity of vital tissue.
Whenever bipolar electrosurgery is used for hemostasis, unwanted thermal damage can be minimized by:
- terminating the flow of current at the end of the visible vapor phase,
- applying current in a pulsatile fashion to permit tissue cooling,
- avoiding the use of an in-line ammeter to determine the coagulation endpoint, and
- securing pedicles by a stepwise process that alternates between partial desiccation and incremental cutting (TABLE 1).
Since the rate of temperature generation is a direct function of the volume of tissue being desiccated, thermal spread can also be reduced by using the sides or tips of a slightly open forceps to press or lift, rather than coapt for hemostasis (FIGURE 4).
Free adherent tissue gently. As with contact monopolar coagulation, tissue between the electrodes of a bipolar instrument may become adherent during desiccation. Repeated attempts to shake the tissue free may lead to traumatic avulsion of a key vascular pedicle. A stuck vascular pedicle can usually be unglued by energizing the opened device while immersing it in a conductive irrigant, such as saline. Once the solution is boiled by the high current density between the electrodes, the mechanical action of bubbling is usually sufficient to atraumatically free the pedicle.
FIGURE 4 Minimizing bipolar thermal damage
Using contact rather than coaptation is one way to limit thermal injury during bipolar electrosurgery.TABLE 1
Minimizing bipolar thermal damage
|
Ultrasonic energy
Mechanism of action. Ultrasonic shears produce mechanical energy to cut and coagulate tissue. Housed in the hand piece of this laparoscopic device is a piezoelectric crystal that vibrates a titanium blade 55,500 times per second over a variable excursion of 50 microns to 100 microns. As energy is transmitted to tissue, hydrogen bonds of tissue proteins are ruptured, leading to a denatured protein coagulum without significant charring. The tissue cutting that occurs is secondary to mechanical vibration and cavitational fragmentation of tissue parenchyma.
Since ultrasonic energy does not generate the high temperatures created by electrosurgery, it is less dependable for deep-tissue coagulation. Rather, thermal change is gradual, requiring a modicum of patience.
Available instrument configurations include 5-mm curved or hook blades. In addition, 5-mm or 10-mm ligating and cutting shears coaptively desiccate and cut the tissue by securing it between a grooved plastic pad and the vibrating blade.
Tissue effects depend on interplay of factors. By using various combinations of blade shapes, blade excursions, and tissue tensions, surgeons can accomplish a variety of specific effects. Cutting velocity is directly proportional to blade excursion, tissue traction, and blade surface area (energy density), and is inversely related to tissue density and elasticity. Thus, the fastest cutting with the least amount of coagulation occurs when tissue is placed on tension and firmly squeezed, lifted, or rotated with the sharpest side of a blade set at maximum excursion.
Coagulation is the obverse of cutting: It is inversely related to tissue tension, blade sharpness, blade excursion, and cutting speed. Therefore, coagulation is best achieved by relaxing tension, minimizing blade excursion, and using a blunt edge or flattened blade surface.
A stuck vascular pedicle can usually be unglued by energizing the opened bipolar device while immersing it in a conductive irrigant.
Avoid excessive traction and torsion. Be mindful of the potential for premature incision of an incompletely coagulated tissue pedicle when excessive traction or torsion is applied. When used to coaptively desiccate and incise a vascular pedicle, ultrasonic energy should be applied patiently, taking great care to minimize tissue tension while using the broadest blade surface set to the lowest excursion (TABLE 2). Hemostatic incision is best ensured by first coagulating several overlapping areas along an untracted pedicle, limiting each application to the point of tissue blanching and initial vapor emission. Only then should the pedicle be incised by gradually lifting, squeezing, or rotating the distal device. In this fashion, ultrasonic energy can be successfully used to secure both the ovarian and uterine vessels.
TABLE 2
Factors likely to cause premature incision with ultrasonic energy
|
Summary
The use of electrical and ultrasonic energy during operative laparoscopy poses several challenges, including the reduction of unwanted thermal injury and the elimination of incomplete hemostasis.
Since the depth of penetration during monopolar electrosurgery is proportional to both output voltage and surface area, unwanted thermal change can be reduced by using the smallest electrode surface with “cut” current for tissue cutting, and “coag” current with a broad-surface electrode for contact or noncontact (fulguration) coagulation.
Bipolar electrosurgery is the preferred modality for coaptive desiccation of a vascular pedicle with electricity. Despite the isolation of current to the intervening tissue, surgeons must take steps to reduce the lateral percolation of heat into adjacent tissues.
Ultrasonic energy provides reliable coaptive hemostasis and incision with little tissue damage. However, the surgeon must be mindful of the forces that promulgate premature incision. Knowledge of the biophysical behavior of electrical and ultrasonic energy is a prelude to safety and efficacy during laparoscopic dissection.
Dr. Brill reports no affiliations or financial arrangements with any of the manufacturers of products mentioned in this article.
1. Brill AI. Energy systems for operative laparoscopy. J Am Assoc Gynecol Laparosc. 1998;5:335-345.
2. Friedman J. The technical aspects of electrosurgery. Oral Surg. 1973;36:177-187.
3. Honig WM. The mechanism of cutting in electrosurgery. IEEE Trans Biomed Eng BME. 1975;22:55-58.
4. Sigel B, Dunn MR. The mechanism of blood vessel closure by high frequency electrocoagulation. Surg Gynecol Obstet. 1965;121:823-831.
5. Phipps JH. Thermometry studies with bipolar diathermy during hysterectomy. Gynecol Laparosc. 1994;1:146-149.
6. Ryder RM, Hulka JF. Bladder and bowel injury after electrodesiccation with Kleppinger bipolar forceps: A clinicopathologic study. J Reprod Med. 1993;3:595-598.
7. McCarus SD. Physiologic mechanism of the ultrasonically activated scalpel. J Am Assoc Gynecol Laparosc. 1996;3:601-608.
1. Brill AI. Energy systems for operative laparoscopy. J Am Assoc Gynecol Laparosc. 1998;5:335-345.
2. Friedman J. The technical aspects of electrosurgery. Oral Surg. 1973;36:177-187.
3. Honig WM. The mechanism of cutting in electrosurgery. IEEE Trans Biomed Eng BME. 1975;22:55-58.
4. Sigel B, Dunn MR. The mechanism of blood vessel closure by high frequency electrocoagulation. Surg Gynecol Obstet. 1965;121:823-831.
5. Phipps JH. Thermometry studies with bipolar diathermy during hysterectomy. Gynecol Laparosc. 1994;1:146-149.
6. Ryder RM, Hulka JF. Bladder and bowel injury after electrodesiccation with Kleppinger bipolar forceps: A clinicopathologic study. J Reprod Med. 1993;3:595-598.
7. McCarus SD. Physiologic mechanism of the ultrasonically activated scalpel. J Am Assoc Gynecol Laparosc. 1996;3:601-608.
Pelosi minilaparotomy hysterectomy: Effective alternative to laparoscopy and laparotomy
Although laparoscopic hysterectomy offers a minimally invasive alternative to laparotomy when vaginal hysterectomy is contraindicated, it has its drawbacks. Among them: the cost of expensive equipment, the long learning curve, and prolonged operating time.
We describe another alternative to open surgery that is comparable to laparoscopic hysterectomy in postoperative pain, cosmetic results, and time to return to normal activities. Our procedure—a redesigned minilaparotomy hysterectomy—relies on traditional open techniques and inexpensive novel instrumentation, making it significantly faster than laparoscopy and easy to perform and teach.
For patients who cannot undergo vaginal hysterectomy, this new modality offers an expeditious, minimal-access option. Gynecologists reluctant to relinquish the routine use of standard laparotomy may find this approach an appealing, less-invasive alternative.
Position, incision, and retraction are crucial to success
Our minilaparotomy hysterectomy is a systemized approach with elements derived from both open and laparoscopic surgery. Three preparatory components are involved:
- position
- incision
- retraction
All are critical to a successful hysterectomy, ensuring that the procedure never becomes a haphazard struggle through an improvised, scaled-down, conventional Pfannenstiel or vertical incision. Our approach also avoids cumbersome traditional laparotomy exposure maneuvers and positioning.
Position: Modified lithotomy. After regional or general anesthesia is given, position the patient in a modified lithotomy with both arms tucked as for laparoscopic surgery. Place the legs in boot-type stirrups, with no hip flexion and sufficient thigh abduction to expose the vagina.
Next, perform a thorough pelvic examination and place an indwelling, transurethral catheter. A sturdy, hinged uterine manipulator is of paramount importance for the hysterectomy, as it facilitates exposure of the adnexa as well as elevation/rotation of the uterus and the uterine attachments. We recommend the Pelosi Uterine Manipulator (Apple Medical Corporation, Marlboro, Mass) or its equivalent (FIGURE 1).
Standard minilaparotomy
The use of standard minilaparotomy—which is nothing more than a conventional laparotomy of limited length (3 cm to 6 cm), performed either transversely or vertically—has been confined to the surgical treatment of benign pelvic pathology of limited extent.
To generate sufficient exposure to work effectively, surgeons using the standard minilaparotomy have relied on the length of the abdominal incision and, secondarily, bowel packing and metal handheld or self-retaining fixed retraction systems. When exposure is difficult to achieve or maintain, however, routine surgical maneuvers become frustrating and time-consuming—unless the clinician uses extensive traction force, extends the incision length, or performs muscle-splitting. These alternatives often result in an uncomfortable, slow recovery typical of most laparotomies, thereby negating the primary goal of minimally invasive surgery.
Use of traditional minilaparotomy for hysterectomy has been reported only rarely. Hoffman et al1 found the procedure safe and effective in nonobese women in whom a vaginal approach was precluded. Benedetti Panicci et al2,3 also have used minilaparotomy successfully in benign gynecologic disease and hysterectomy.
The Kustner incision
Originally reported in 1896,4 this incision is avoided by most surgeons in favor of complete transverse or complete vertical incisions—largely due to difficulties with exposure, troublesome seroma formation, and wound complications secondary to increased fluid accumulation in the large dead space that results from wide dissection of the subcutaneous flap.
In the early 1990s, we realized the potential benefits of a scaled-down Kustner’s incision (2 cm to 5 cm) when assistance was needed via minilaparotomy during such laparoscopic-assisted procedures as uterine morcellation, tubal reanastomosis, and extensive uterine suture and reconstruction following complex laparoscopic myomectomy.5 As a substitute for laparoscopy and laparotomy, we then tried a minilaparotomy Kustner’s incision (3 cm to 5 cm) as the sole means of surgical access, assessment, and treatment for benign pelvic conditions.
Benefits of this incision. When a sturdy uterine manipulator was used to facilitate exposure of the adnexa and uterine elevation/rotation, we found this technique more effective than similar procedures using a scaled-down Pfannenstiel or Maylard incision. In addition, because the incision was small and the extent of subcutaneous dissection required to expose the rectus fascia in a vertical fashion was limited, there was no need for incision drainage. Nor was the procedure associated with seroma formation, as the full-sized Kustner’s incision had been.3 However, the minilaparotomy Kustner’s incision still suffered from limited surgical exposure.
Adding the retractor
It became clear that a soft, self-retaining abdominal retractor that is capable of creating a rapid, effective, nontraumatic, and predictable circular area of abdominal retraction would be helpful, particularly one that could be placed through the minilaparotomy Kustner’s incision.6 Once this retractor system was developed, using technology borrowed from hand-assisted laparoscopy,7-10 the minilaparotomy hysterectomy became a much simpler, more useful surgical option.
REFERENCES
1. Hoffman MS, Lynch CM. Minilaparotomy hysterectomy. Am J Obstet Gynecol. 1998;179:316-320.
2. Benedetti Panicci P, Maneschi F, Cutillo G, et al. Surgery by minilaparotomy in benign gynecologic disease. Obstet Gynecol. 1996;87:456-459.
3. Benedetti Panicci P, Zullo MA, Casalino B, et al. Subcutaneous drainage versus no drainage after minilaparotomy in gynecologic benign conditions. Am J Obstet Gynecol. 2003;188:71-75.
4. Kustner O. Der suprasymphysare kruzschnitt, eine methode der coeliotomie bei wening umfanglichen affektionen der weiblichen beckenorgane. Monatsschr Geburtshilfe Gynakol. 1896;4:197-206.
5. Pelosi MA, II, Pelosi MA, III. The suprapubic cruciate incision for laparoscopic assisted microceliotomy. J Soc Laparoendosc Surg. 1997;1:269-272.
6. Pelosi MA, II, Pelosi MA, III. Self-retaining abdominal retractor for minilaparotomy. Obstet Gynecol. 2000;96:775-778.
7. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopy for complex hysterectomy. J Am Assoc Gynecol Laparosc. 1999;6:183-188.
8. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopic cholecystectomy at cesarean section. J Am Assoc Gynecol Laparosc. 1999;6:491-495.
9. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopy (handoscopy) for megamyomectomy: A case study. J Reprod Med. 2000;45:519-525.
10. Pelosi MA, II, Pelosi MA, III, Eim J. Hand-assisted laparoscopy for pelvic malignancy. J Laparoendosc Adv Surg Tech. 2000;10:143-150.
Incision: Modified Kustner’s. Open the abdomen with a cruciate incision. Using a conventional scalpel and the Bovie device, make a 2.5-cm to 5-cm transverse incision through the skin and subcutaneous fat until you reach the anterior rectus fascia (FIGURE 2A). Clear the fat from the midline superiorly and inferiorly to expose approximately 5 cm to 6 cm of fascia in the vertical axis. Then incise the anterior rectus fascia in a vertical direction through the full length of the cleared area (FIGURE 2B).
Retract the rectus muscles from the midline, exposing the transversalis fascia and the underlying peritoneum. Enter the peritoneum digitally or with scissors above the level of the bladder dome, incising vertically until the entrance extends the full length of the fascial incision (FIGURE 2C).
This modified Kustner’s incision is essentially a vertical midline incision in its deeper layers.1 The rapid surgical dissection of the fascia and rectus muscles and the intraperitoneal entry are relatively bloodless. This approach yields a surgical exposure superior to that of a small Pfannenstiel or Maylard incision.
Note that, in some patients, a vertical incision can be selected if there is a prior vertical incision or if the perioperative workup suggests a malignancy that may require a later extension of the original minilaparotomy incision.
Retraction: Soft, sleeve-type, self-retaining abdominal retractor. This device consists of a flexible plastic inner ring and a firmer outer ring connected by a soft plastic sleeve (FIGURE 3A). Two models are available: the Mobius (Apple Medical Corporation) and the Protractor (Weck Closure Systems, Research Triangle Park, NC).
Squeeze the inner ring into the peritoneal cavity through the minilaparotomy incision, allowing it to spring open against the parietal peritoneum. Conduct a digital assessment to ensure that no viscera are trapped by elevating the outer ring. Next, roll the outer ring onto the sleeve, collecting excess length, until it sits firmly against the skin (FIGURES 3B and 3C). The result, when there is adequate tension within the sleeve, is a circular area of retraction offering excellent exposure of the pelvis. Note that during surgery you may need to adjust the outer ring if the sleeve loosens.
The soft, self-retaining abdominal retractor offers several advantages over traditional abdominal retraction:
- Atraumatic retraction. This device distributes retraction force evenly around the entire incision. Because standard retractors concentrate retraction force at only a few points, they often lead to tissue trauma, nerve damage, bruising, and postoperative pain.
- Incision protection. The retractor’s flexible material lines the incision, protecting the wound’s edges from contamination and potential implantation of malignant cells.
- Improved access. Because the continuous retraction force is delivered more effectively to the incision, exposure is maximized. As a result, the need for intensive surgical assistance is dramatically reduced.
- Adjustable height. The retractor’s design lets it adapt to wounds of varying depth—a feature that makes it ideal for obese patients. The device compresses the patient’s skin and peritoneum between the external and internal rings, keeping the full thickness of the abdominal incision constant throughout the surgery.
- Cost-effectiveness. The device, which costs under $100, is simple and fast to set up. In our experience, placement takes approximately 2 minutes; this compares favorably with table-mounted or self-retaining rigid retraction systems, which may require significant capital expenditures (cost may run in the thousands), repair costs, and complicated set-ups.
FIGURE 1 Hinged uterine manipulator
A sturdy hinged uterine manipulator facilitates exposure of the adnexa as well as elevation/rotation of the uterus.
FIGURE 2 Cruciate incision
A. Make a transverse incision suprapubically through the skin and the subcutaneous fat to reach the anterior rectus fascia.
FIGURE 2 Cruciate incision
B. Clear the fat from the midline to expose the rectus fascia in the vertical axis, then incise the fascia in a vertical direction through the full length of the previously cleared area. The rectus muscles are retracted, thereby exposing the peritoneum.
FIGURE 2 Cruciate incision
C. Incise the peritoneum vertically until it extends the full length of the fascial incision.
FIGURE 3 Soft, sleeve-type, self-retaining abdominal retractor
A. At left, the Protractor (Weck Closure Systems); at right, the Mobius (Apple Medical Corporation).
FIGURE 3 Soft, sleeve-type, self-retaining abdominal retractor
B. After inserting the inner ring into the peritoneal cavity, twist the outer ring downward until it inverts and rests snuggly against the skin.
FIGURE 3 Soft, sleeve-type, self-retaining abdominal retractor
C. An atraumatic, circular, self-retaining area of retraction is created.
Standard technique: Exteriorize the uterus; divide uterine attachments, vessels
Assess the anatomy. Using your index finger and the uterine manipulator to rotate and flex the uterus, carefully assess the uterus, adnexa, and pelvis, noting the location of the ureters. Determine the extent of any unexpected pelvic pathology or adhesions, using traditional small retractors or gentle packing to gain additional exposure. Perform any adhesiolysis that is necessary.
Exteriorize the uterus. Next, bring the uterus and the adnexa above the abdominal wall in order to perform as much of the hysterectomy extracorporeally as possible. Pass the uterus or adnexa through the incision with the upward assistance of the uterine manipulator, then divide the upper uterine attachments (FIGURE 4A).
Increase exposure. You can achieve additional uterine elevation and targeted exposure in several ways. For example, a strong traction suture can be placed in the uterine fundus, left long, and secured with a clamp. To achieve uterine elevation, place long clamps lateral to the corpus. Another effective approach is to place a heavy tenaculum on the uterine fundus.
When lateral exposure is limited, divide the proximal adnexal pedicles and round ligaments to begin the operation, and remove the adnexa separately following the completion of the hysterectomy.
Divide the uterine vessels through the small incision using clamping, division, and ligation. Unless you intend to preserve the cervix, mobilize the bladder to the level of the anterior vaginal fornix. Inward pressure on the uterine manipulator provides additional elevation of the lower uterine vasculature and the cardinal and uterosacral ligaments as these structures are ligated and divided. Amputate the uterine specimen from the vaginal cuff using the uterine manipulator to guide the vaginal circumcision (FIGURE 4B). Close the vaginal cuff using standard closure.
If the cervix is to be preserved, amputate the uterus supracervically following division of the uterine vessels. Then suture the cervical stump in the traditional fashion. Upward elevation of the cervix using the uterine manipulator expedites this step.
Complete the procedure. Once the surgery is completed, remove the retractor, hooking the bottom ring by inserting a finger into it and pulling it up and out of the incision (FIGURE 4C). Closing a cruciate incision is faster and requires less exposure than closing a mini-Pfannenstiel incision. Eliminate the possibility of postoperative wound hematoma or seroma formation by applying a vertical pressure dressing over the incision (FIGURE 4D). Remove the dressing 24 hours later.
FIGURE 4 Hysterectomy for the normal to moderately enlarged uterus
A. Exteriorize the uterus as much as possible with both upward assistance of the manipulator and uterine fundal elevation (using clamps lateral to the uterus, a heavy tenaculum, or a traction suture). Then conduct a standard hysterectomy.
FIGURE 4 Hysterectomy for the normal to moderately enlarged uterus
B. Separate the uterus from the vagina using the manipulator to guide the vaginal circumcision. (If the cervix is to be preserved, a supracervical amputation is performed instead.)
FIGURE 4 Hysterectomy for the normal to moderately enlarged uterus
C. After completing the surgery, remove the retractor from the incision.
FIGURE 4 Hysterectomy for the normal to moderately enlarged uterus
D. Apply a vertical pressure dressing over the incision.
Variations for abnormal uteri
The large fibroid uterus: Begin with the dominant myoma. A large fibroid uterus can be easily removed with our minilaparotomy technique using 3 basic steps:
- Reduce size by selective myomectomy.
- Deliver the debulked uterus through the abdominal incision.
- Perform extracorporeal hysterectomy.
First, you must conduct a thorough assessment of the number, size, and location of the myomas. Begin the myomectomy on the largest tumor of those closest to the minilaparotomy incision. (Minimize bleeding by injecting diluted vasopressin subserosally prior to the procedure.)
Incise the uterine serosa, myometrium, and pseudocapsule of the myoma via scalpel or Bovie electrocautery until the whorly appearance of the myoma is apparent. Next, grasp the myoma with claw-toothed forceps to stabilize it and place it under traction. Then, using a combination of sharp and digital dissection, develop a plane of dissection between the fibroid and the myometrium (FIGURE 5A).
After securing the dominant myoma, deliver it through the abdominal incision. If the myoma is too large to be removed intact from the abdominal cavity, morcellate it using a scalpel or scissors (FIGURE 5B). Then continue systematic removal of the remaining myomas using the same approach. It is not necessary to remove all myomas—the goal of this process is merely to permit delivery of the uterine body for subsequent hysterectomy.
Once the uterus is debulked, deliver it through the abdominal incision. Hysterectomy then is easily completed (FIGURE 5C).
The ‘solid’ uterus: In situ supracervical hysterectomy and uterine morcellation.
Very large uteri are sometimes homogeneous and solid in nature, possessing few or no individual myomas. This so-called cannonball fibroid uterus is the most challenging type of uterus to remove. The selective-myomectomy approach cannot be used because of the potential for massive bleeding and the technical anatomical difficulties that arise when operating through such a small abdominal incision.
Instead, manage this type of uterus by performing a deliberate in situ supracervical hysterectomy through the minilaparotomy incision. At the end of this procedure, morcellate the amputated fibroid uterus.
Begin the surgery by dividing the upper uterine attachments. Regardless of uterine size, the origins of the round and adnexal ligaments will always be lateral to and within easy reach of a transverse minilaparotomy incision. (Access to these areas is the only factor that determines the feasibility of this procedure; uterine size is completely irrelevant.) We have found that these elongated ligaments are quite lax. Thus, in most cases it is relatively simple to navigate your index finger laterally and, using digital traction, elevate these structures into the minilaparotomy incision (FIGURE 6A). You can then clamp, cut, and suture the ligaments in the standard fashion in whatever sequence is most efficient.
Thanks to the retractor, minimal assistance is necessary during the surgery. You can create additional exposure by deflecting the uterus toward the opposite side of the pelvis using external abdominal pressure and the uterine manipulator.
Once both round ligaments and adnexal pedicles are divided, dissect the bladder flap to expose the uterine arteries (inward pressure on the uterine manipulator provides helpful countertraction). Then clamp, divide, and ligate the uterine arteries (FIGURE 6B).
The uterus is now ready for supracervical amputation. Upward traction on the isthmus by means of a rubber tourniquet facilitates uterine division (FIGURE 6C). After the uterus is amputated, push it toward the upper abdomen to increase exposure for suturing of the cervical stump (if the cervix is preserved) or for cervical excision and vaginal cuff closure (when total hysterectomy is chosen).
Next, remove the uterine specimen by morcellation through the minilaparotomy incision. Using the Doyen ladder-shaped uterine morcellation technique (originally described in the early 1920s) grasp an area of the uterus and, alternating right and left, make deep but incomplete incisions on the uterus, creating a ladder shape.2 Because of its elasticity, the retractor can stretch quite significantly without tearing the edges of the abdominal incision (FIGURE 6D). This allows the easy exteriorization of uteri with diameters considerably larger than that of the retractor, mimicking the stretching of the perineum during the crowning of the fetal head.
When the surgery is complete, remove the retractor, close the minilaparotomy incision, and apply a vertical pressure dressing over the incision. Neither vaginal packing nor bladder catheterization is required.
FIGURE 5 Hysterectomy for the fibroid uterus
A. Develop a plane of dissection between the myoma and myometrium.
FIGURE 5 Hysterectomy for the fibroid uterus
B. Deliver the myoma through the incision; if it is too large to remove intact, morcellate it with a scalpel or scissors.
FIGURE 5 Hysterectomy for the fibroid uterus
C. After reducing the uterine size by selective myomectomy, deliver the debulked uterus through the abdominal incision. Then proceed with an extracorporeal total or subtotal hysterectomy.
A short learning curve
Since it uses conventional open techniques and traditional instrumentation, this method can be learned and mastered quickly.
We tend to think of this procedure as a transabdominal “vaginal” hysterectomy, since the average diameter of the minilaparotomy opening is approximately the same as the vaginal canal. Further, as in vaginal hysterectomy, only 1 portion of the uterus, adnexa, or ligaments must be exteriorized at a given time. Thus, this approach requires less general exposure but offers effective targeted exposure.
The technique also removes the need for frequent use of traumatic metal retractors, extensive bowel packing, and extended incision exposure. The benefits: diminished postoperative discomfort and bowel dysfunction.
High success rates. We have performed more than 100 minilaparotomy procedures using this technique in patients in whom vaginal hysterectomy was contraindicated. Uterine weight ranged from 80 g to 2,500 g. Mean operating time was 50 minutes. All patients were discharged within 36 hours. Mean return to work time was 12 days, and there have been no intraoperative or postoperative complications. All surgeries were successfully completed without laparoscopy or conversion to traditional laparotomy.
FIGURE 6 Hysterectomy for the large, solid, fibroid uterus
A. Draw the upper uterine attachments to the surgical field with finger traction.
FIGURE 6 Hysterectomy for the large, solid, fibroid uterus
B. Divide the round ligaments and proximal adnexal pedicles, then carry out division of the uterine vessels bilaterally.
FIGURE 6 Hysterectomy for the large, solid, fibroid uterus
C. After dividing both round ligaments, adnexal pedicles, and uterine vessels, place the uterine isthmus in traction with a rubber tourniquet and perform an in situ supracervical amputation.
FIGURE 6 Hysterectomy for the large, solid, fibroid uterus
D. After trachelectomy, the large uterine specimen is removed by morcellation. Notice that the retractor is able to stretch significantly, allowing the exteriorization of uteri with diameters considerably larger than that of the retractor.
Devices that simplify the procedure
Occasionally, hysterectomy using traditional clamp, division, and suture ligation can be tedious, frustrating, and time-consuming, especially when exposure is limited or difficult. Several devices developed for laparoscopic surgery can ease suture ligation and the division of blood vessels, ligaments, and tissue bundles during minilaparotomy hysterectomy. They include the Hem-o-lok ligating clip (Weck Closure Systems); the LigaSure Atlas, a vessel sealer-divider (Valleylab, Tyco Healthcare, Boulder, Colo); the ETS 45-Flex endoscopic linear cutter (Ethicon Endo-Surgery, Cincinnati, Ohio); and the PK bipolar cutting forceps (Gyrus Medical, Maple Grove, Minn).
Additional concerns
Is the incision too large? Fears that incisions over 5 cm might nullify minimally invasive surgery’s benefits have proven unfounded.
Laparoscopic procedures that use a 7-cm to 8-cm incision to introduce the hand into the abdomen, as well as those performed in conjunction with minilaparotomy, have consistently failed to identify a link between these combinations and morbidity or lengthy recovery. A “large” minilaparotomy incision is still superior to a standard abdominal hysterectomy in terms of convalescence, and it is significantly faster and more cost-effective than a prolonged laparoscopic or laparoscopic-assisted vaginal hysterectomy.3-10
Do any conditions contraindicate minilaparotomy? In patients with documented or strongly suspected severe pelvic conditions (for example, advanced endometriosis, pelvic inflammatory disease, bowel disease, or malignancy), preliminary laparoscopic evaluation to determine the pathologic condition’s severity and extent is strongly recommended.
If during this assessment you detect pathology that is not appropriate for laparoscopic surgery or minilaparotomy, perform a traditional laparotomy. If, however, this evaluation demonstrates that pelvic pathology is amenable to laparoscopic surgery, a laparoscopic hysterectomy or laparoscopic-assisted minilaparotomy hysterectomy is indicated.
Dr. Pelosi II reports that he is a consultant for Apple Medical Corporation. Dr. Pelosi III reports no affiliations or financial arrangements with any of the manufacturers of products mentioned in this article or their competitors.
1. Kustner O. Der suprasymphysare kruzschnitt, eine methode der coeliotomie bei wening umfanglichen affektionen der weiblichen beckenorgane. Monatsschr Geburtshilfe Gynakol. 1896;4:197-206.
2. Doyen E. Surgical Therapeutics and Operative Technique. Vol. III. Spencer-Browne H, translator. London, England: Bailliere, Tindal and Cox; 1920.
3. Benedetti Panicci P, Maneschi F, Cutillo G, et al. Surgery by minilaparotomy in benign gynecologic disease. Obstet Gynecol. 1996;87:456-459.
4. Benedetti Panicci P, Zullo MA, Casalino B, et al. Subcutaneous drainage versus no drainage after minilaparotomy in gynecologic benign conditions. Am J Obstet Gynecol. 2003;188:71-75.
5. Pelosi MA, II, Pelosi MA, III. The suprapubic cruciate incision for laparoscopic assisted microceliotomy. J Soc Laparoendosc Surg. 1997;1:269-272.
6. Pelosi MA, II, Pelosi MA, III. Self-retaining abdominal retractor for minilaparotomy. Obstet Gynecol. 2000;96:775-778.
7. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopy for complex hysterectomy. J Am Assoc Gynecol Laparosc. 1999;6:183-188.
8. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopic cholecystectomy at cesarean section. J Am Assoc Gynecol Laparosc. 1999;6:491-495.
9. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopy (handoscopy) for megamyomectomy: A case study. J Reprod Med. 2000;45:519-525.
10. Pelosi MA, II, Pelosi MA, III, Eim J. Hand-assisted laparoscopy for pelvic malignancy. J Laparoendosc Adv Surg Tech. 2000;10:143-150.
Although laparoscopic hysterectomy offers a minimally invasive alternative to laparotomy when vaginal hysterectomy is contraindicated, it has its drawbacks. Among them: the cost of expensive equipment, the long learning curve, and prolonged operating time.
We describe another alternative to open surgery that is comparable to laparoscopic hysterectomy in postoperative pain, cosmetic results, and time to return to normal activities. Our procedure—a redesigned minilaparotomy hysterectomy—relies on traditional open techniques and inexpensive novel instrumentation, making it significantly faster than laparoscopy and easy to perform and teach.
For patients who cannot undergo vaginal hysterectomy, this new modality offers an expeditious, minimal-access option. Gynecologists reluctant to relinquish the routine use of standard laparotomy may find this approach an appealing, less-invasive alternative.
Position, incision, and retraction are crucial to success
Our minilaparotomy hysterectomy is a systemized approach with elements derived from both open and laparoscopic surgery. Three preparatory components are involved:
- position
- incision
- retraction
All are critical to a successful hysterectomy, ensuring that the procedure never becomes a haphazard struggle through an improvised, scaled-down, conventional Pfannenstiel or vertical incision. Our approach also avoids cumbersome traditional laparotomy exposure maneuvers and positioning.
Position: Modified lithotomy. After regional or general anesthesia is given, position the patient in a modified lithotomy with both arms tucked as for laparoscopic surgery. Place the legs in boot-type stirrups, with no hip flexion and sufficient thigh abduction to expose the vagina.
Next, perform a thorough pelvic examination and place an indwelling, transurethral catheter. A sturdy, hinged uterine manipulator is of paramount importance for the hysterectomy, as it facilitates exposure of the adnexa as well as elevation/rotation of the uterus and the uterine attachments. We recommend the Pelosi Uterine Manipulator (Apple Medical Corporation, Marlboro, Mass) or its equivalent (FIGURE 1).
Standard minilaparotomy
The use of standard minilaparotomy—which is nothing more than a conventional laparotomy of limited length (3 cm to 6 cm), performed either transversely or vertically—has been confined to the surgical treatment of benign pelvic pathology of limited extent.
To generate sufficient exposure to work effectively, surgeons using the standard minilaparotomy have relied on the length of the abdominal incision and, secondarily, bowel packing and metal handheld or self-retaining fixed retraction systems. When exposure is difficult to achieve or maintain, however, routine surgical maneuvers become frustrating and time-consuming—unless the clinician uses extensive traction force, extends the incision length, or performs muscle-splitting. These alternatives often result in an uncomfortable, slow recovery typical of most laparotomies, thereby negating the primary goal of minimally invasive surgery.
Use of traditional minilaparotomy for hysterectomy has been reported only rarely. Hoffman et al1 found the procedure safe and effective in nonobese women in whom a vaginal approach was precluded. Benedetti Panicci et al2,3 also have used minilaparotomy successfully in benign gynecologic disease and hysterectomy.
The Kustner incision
Originally reported in 1896,4 this incision is avoided by most surgeons in favor of complete transverse or complete vertical incisions—largely due to difficulties with exposure, troublesome seroma formation, and wound complications secondary to increased fluid accumulation in the large dead space that results from wide dissection of the subcutaneous flap.
In the early 1990s, we realized the potential benefits of a scaled-down Kustner’s incision (2 cm to 5 cm) when assistance was needed via minilaparotomy during such laparoscopic-assisted procedures as uterine morcellation, tubal reanastomosis, and extensive uterine suture and reconstruction following complex laparoscopic myomectomy.5 As a substitute for laparoscopy and laparotomy, we then tried a minilaparotomy Kustner’s incision (3 cm to 5 cm) as the sole means of surgical access, assessment, and treatment for benign pelvic conditions.
Benefits of this incision. When a sturdy uterine manipulator was used to facilitate exposure of the adnexa and uterine elevation/rotation, we found this technique more effective than similar procedures using a scaled-down Pfannenstiel or Maylard incision. In addition, because the incision was small and the extent of subcutaneous dissection required to expose the rectus fascia in a vertical fashion was limited, there was no need for incision drainage. Nor was the procedure associated with seroma formation, as the full-sized Kustner’s incision had been.3 However, the minilaparotomy Kustner’s incision still suffered from limited surgical exposure.
Adding the retractor
It became clear that a soft, self-retaining abdominal retractor that is capable of creating a rapid, effective, nontraumatic, and predictable circular area of abdominal retraction would be helpful, particularly one that could be placed through the minilaparotomy Kustner’s incision.6 Once this retractor system was developed, using technology borrowed from hand-assisted laparoscopy,7-10 the minilaparotomy hysterectomy became a much simpler, more useful surgical option.
REFERENCES
1. Hoffman MS, Lynch CM. Minilaparotomy hysterectomy. Am J Obstet Gynecol. 1998;179:316-320.
2. Benedetti Panicci P, Maneschi F, Cutillo G, et al. Surgery by minilaparotomy in benign gynecologic disease. Obstet Gynecol. 1996;87:456-459.
3. Benedetti Panicci P, Zullo MA, Casalino B, et al. Subcutaneous drainage versus no drainage after minilaparotomy in gynecologic benign conditions. Am J Obstet Gynecol. 2003;188:71-75.
4. Kustner O. Der suprasymphysare kruzschnitt, eine methode der coeliotomie bei wening umfanglichen affektionen der weiblichen beckenorgane. Monatsschr Geburtshilfe Gynakol. 1896;4:197-206.
5. Pelosi MA, II, Pelosi MA, III. The suprapubic cruciate incision for laparoscopic assisted microceliotomy. J Soc Laparoendosc Surg. 1997;1:269-272.
6. Pelosi MA, II, Pelosi MA, III. Self-retaining abdominal retractor for minilaparotomy. Obstet Gynecol. 2000;96:775-778.
7. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopy for complex hysterectomy. J Am Assoc Gynecol Laparosc. 1999;6:183-188.
8. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopic cholecystectomy at cesarean section. J Am Assoc Gynecol Laparosc. 1999;6:491-495.
9. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopy (handoscopy) for megamyomectomy: A case study. J Reprod Med. 2000;45:519-525.
10. Pelosi MA, II, Pelosi MA, III, Eim J. Hand-assisted laparoscopy for pelvic malignancy. J Laparoendosc Adv Surg Tech. 2000;10:143-150.
Incision: Modified Kustner’s. Open the abdomen with a cruciate incision. Using a conventional scalpel and the Bovie device, make a 2.5-cm to 5-cm transverse incision through the skin and subcutaneous fat until you reach the anterior rectus fascia (FIGURE 2A). Clear the fat from the midline superiorly and inferiorly to expose approximately 5 cm to 6 cm of fascia in the vertical axis. Then incise the anterior rectus fascia in a vertical direction through the full length of the cleared area (FIGURE 2B).
Retract the rectus muscles from the midline, exposing the transversalis fascia and the underlying peritoneum. Enter the peritoneum digitally or with scissors above the level of the bladder dome, incising vertically until the entrance extends the full length of the fascial incision (FIGURE 2C).
This modified Kustner’s incision is essentially a vertical midline incision in its deeper layers.1 The rapid surgical dissection of the fascia and rectus muscles and the intraperitoneal entry are relatively bloodless. This approach yields a surgical exposure superior to that of a small Pfannenstiel or Maylard incision.
Note that, in some patients, a vertical incision can be selected if there is a prior vertical incision or if the perioperative workup suggests a malignancy that may require a later extension of the original minilaparotomy incision.
Retraction: Soft, sleeve-type, self-retaining abdominal retractor. This device consists of a flexible plastic inner ring and a firmer outer ring connected by a soft plastic sleeve (FIGURE 3A). Two models are available: the Mobius (Apple Medical Corporation) and the Protractor (Weck Closure Systems, Research Triangle Park, NC).
Squeeze the inner ring into the peritoneal cavity through the minilaparotomy incision, allowing it to spring open against the parietal peritoneum. Conduct a digital assessment to ensure that no viscera are trapped by elevating the outer ring. Next, roll the outer ring onto the sleeve, collecting excess length, until it sits firmly against the skin (FIGURES 3B and 3C). The result, when there is adequate tension within the sleeve, is a circular area of retraction offering excellent exposure of the pelvis. Note that during surgery you may need to adjust the outer ring if the sleeve loosens.
The soft, self-retaining abdominal retractor offers several advantages over traditional abdominal retraction:
- Atraumatic retraction. This device distributes retraction force evenly around the entire incision. Because standard retractors concentrate retraction force at only a few points, they often lead to tissue trauma, nerve damage, bruising, and postoperative pain.
- Incision protection. The retractor’s flexible material lines the incision, protecting the wound’s edges from contamination and potential implantation of malignant cells.
- Improved access. Because the continuous retraction force is delivered more effectively to the incision, exposure is maximized. As a result, the need for intensive surgical assistance is dramatically reduced.
- Adjustable height. The retractor’s design lets it adapt to wounds of varying depth—a feature that makes it ideal for obese patients. The device compresses the patient’s skin and peritoneum between the external and internal rings, keeping the full thickness of the abdominal incision constant throughout the surgery.
- Cost-effectiveness. The device, which costs under $100, is simple and fast to set up. In our experience, placement takes approximately 2 minutes; this compares favorably with table-mounted or self-retaining rigid retraction systems, which may require significant capital expenditures (cost may run in the thousands), repair costs, and complicated set-ups.
FIGURE 1 Hinged uterine manipulator
A sturdy hinged uterine manipulator facilitates exposure of the adnexa as well as elevation/rotation of the uterus.
FIGURE 2 Cruciate incision
A. Make a transverse incision suprapubically through the skin and the subcutaneous fat to reach the anterior rectus fascia.
FIGURE 2 Cruciate incision
B. Clear the fat from the midline to expose the rectus fascia in the vertical axis, then incise the fascia in a vertical direction through the full length of the previously cleared area. The rectus muscles are retracted, thereby exposing the peritoneum.
FIGURE 2 Cruciate incision
C. Incise the peritoneum vertically until it extends the full length of the fascial incision.
FIGURE 3 Soft, sleeve-type, self-retaining abdominal retractor
A. At left, the Protractor (Weck Closure Systems); at right, the Mobius (Apple Medical Corporation).
FIGURE 3 Soft, sleeve-type, self-retaining abdominal retractor
B. After inserting the inner ring into the peritoneal cavity, twist the outer ring downward until it inverts and rests snuggly against the skin.
FIGURE 3 Soft, sleeve-type, self-retaining abdominal retractor
C. An atraumatic, circular, self-retaining area of retraction is created.
Standard technique: Exteriorize the uterus; divide uterine attachments, vessels
Assess the anatomy. Using your index finger and the uterine manipulator to rotate and flex the uterus, carefully assess the uterus, adnexa, and pelvis, noting the location of the ureters. Determine the extent of any unexpected pelvic pathology or adhesions, using traditional small retractors or gentle packing to gain additional exposure. Perform any adhesiolysis that is necessary.
Exteriorize the uterus. Next, bring the uterus and the adnexa above the abdominal wall in order to perform as much of the hysterectomy extracorporeally as possible. Pass the uterus or adnexa through the incision with the upward assistance of the uterine manipulator, then divide the upper uterine attachments (FIGURE 4A).
Increase exposure. You can achieve additional uterine elevation and targeted exposure in several ways. For example, a strong traction suture can be placed in the uterine fundus, left long, and secured with a clamp. To achieve uterine elevation, place long clamps lateral to the corpus. Another effective approach is to place a heavy tenaculum on the uterine fundus.
When lateral exposure is limited, divide the proximal adnexal pedicles and round ligaments to begin the operation, and remove the adnexa separately following the completion of the hysterectomy.
Divide the uterine vessels through the small incision using clamping, division, and ligation. Unless you intend to preserve the cervix, mobilize the bladder to the level of the anterior vaginal fornix. Inward pressure on the uterine manipulator provides additional elevation of the lower uterine vasculature and the cardinal and uterosacral ligaments as these structures are ligated and divided. Amputate the uterine specimen from the vaginal cuff using the uterine manipulator to guide the vaginal circumcision (FIGURE 4B). Close the vaginal cuff using standard closure.
If the cervix is to be preserved, amputate the uterus supracervically following division of the uterine vessels. Then suture the cervical stump in the traditional fashion. Upward elevation of the cervix using the uterine manipulator expedites this step.
Complete the procedure. Once the surgery is completed, remove the retractor, hooking the bottom ring by inserting a finger into it and pulling it up and out of the incision (FIGURE 4C). Closing a cruciate incision is faster and requires less exposure than closing a mini-Pfannenstiel incision. Eliminate the possibility of postoperative wound hematoma or seroma formation by applying a vertical pressure dressing over the incision (FIGURE 4D). Remove the dressing 24 hours later.
FIGURE 4 Hysterectomy for the normal to moderately enlarged uterus
A. Exteriorize the uterus as much as possible with both upward assistance of the manipulator and uterine fundal elevation (using clamps lateral to the uterus, a heavy tenaculum, or a traction suture). Then conduct a standard hysterectomy.
FIGURE 4 Hysterectomy for the normal to moderately enlarged uterus
B. Separate the uterus from the vagina using the manipulator to guide the vaginal circumcision. (If the cervix is to be preserved, a supracervical amputation is performed instead.)
FIGURE 4 Hysterectomy for the normal to moderately enlarged uterus
C. After completing the surgery, remove the retractor from the incision.
FIGURE 4 Hysterectomy for the normal to moderately enlarged uterus
D. Apply a vertical pressure dressing over the incision.
Variations for abnormal uteri
The large fibroid uterus: Begin with the dominant myoma. A large fibroid uterus can be easily removed with our minilaparotomy technique using 3 basic steps:
- Reduce size by selective myomectomy.
- Deliver the debulked uterus through the abdominal incision.
- Perform extracorporeal hysterectomy.
First, you must conduct a thorough assessment of the number, size, and location of the myomas. Begin the myomectomy on the largest tumor of those closest to the minilaparotomy incision. (Minimize bleeding by injecting diluted vasopressin subserosally prior to the procedure.)
Incise the uterine serosa, myometrium, and pseudocapsule of the myoma via scalpel or Bovie electrocautery until the whorly appearance of the myoma is apparent. Next, grasp the myoma with claw-toothed forceps to stabilize it and place it under traction. Then, using a combination of sharp and digital dissection, develop a plane of dissection between the fibroid and the myometrium (FIGURE 5A).
After securing the dominant myoma, deliver it through the abdominal incision. If the myoma is too large to be removed intact from the abdominal cavity, morcellate it using a scalpel or scissors (FIGURE 5B). Then continue systematic removal of the remaining myomas using the same approach. It is not necessary to remove all myomas—the goal of this process is merely to permit delivery of the uterine body for subsequent hysterectomy.
Once the uterus is debulked, deliver it through the abdominal incision. Hysterectomy then is easily completed (FIGURE 5C).
The ‘solid’ uterus: In situ supracervical hysterectomy and uterine morcellation.
Very large uteri are sometimes homogeneous and solid in nature, possessing few or no individual myomas. This so-called cannonball fibroid uterus is the most challenging type of uterus to remove. The selective-myomectomy approach cannot be used because of the potential for massive bleeding and the technical anatomical difficulties that arise when operating through such a small abdominal incision.
Instead, manage this type of uterus by performing a deliberate in situ supracervical hysterectomy through the minilaparotomy incision. At the end of this procedure, morcellate the amputated fibroid uterus.
Begin the surgery by dividing the upper uterine attachments. Regardless of uterine size, the origins of the round and adnexal ligaments will always be lateral to and within easy reach of a transverse minilaparotomy incision. (Access to these areas is the only factor that determines the feasibility of this procedure; uterine size is completely irrelevant.) We have found that these elongated ligaments are quite lax. Thus, in most cases it is relatively simple to navigate your index finger laterally and, using digital traction, elevate these structures into the minilaparotomy incision (FIGURE 6A). You can then clamp, cut, and suture the ligaments in the standard fashion in whatever sequence is most efficient.
Thanks to the retractor, minimal assistance is necessary during the surgery. You can create additional exposure by deflecting the uterus toward the opposite side of the pelvis using external abdominal pressure and the uterine manipulator.
Once both round ligaments and adnexal pedicles are divided, dissect the bladder flap to expose the uterine arteries (inward pressure on the uterine manipulator provides helpful countertraction). Then clamp, divide, and ligate the uterine arteries (FIGURE 6B).
The uterus is now ready for supracervical amputation. Upward traction on the isthmus by means of a rubber tourniquet facilitates uterine division (FIGURE 6C). After the uterus is amputated, push it toward the upper abdomen to increase exposure for suturing of the cervical stump (if the cervix is preserved) or for cervical excision and vaginal cuff closure (when total hysterectomy is chosen).
Next, remove the uterine specimen by morcellation through the minilaparotomy incision. Using the Doyen ladder-shaped uterine morcellation technique (originally described in the early 1920s) grasp an area of the uterus and, alternating right and left, make deep but incomplete incisions on the uterus, creating a ladder shape.2 Because of its elasticity, the retractor can stretch quite significantly without tearing the edges of the abdominal incision (FIGURE 6D). This allows the easy exteriorization of uteri with diameters considerably larger than that of the retractor, mimicking the stretching of the perineum during the crowning of the fetal head.
When the surgery is complete, remove the retractor, close the minilaparotomy incision, and apply a vertical pressure dressing over the incision. Neither vaginal packing nor bladder catheterization is required.
FIGURE 5 Hysterectomy for the fibroid uterus
A. Develop a plane of dissection between the myoma and myometrium.
FIGURE 5 Hysterectomy for the fibroid uterus
B. Deliver the myoma through the incision; if it is too large to remove intact, morcellate it with a scalpel or scissors.
FIGURE 5 Hysterectomy for the fibroid uterus
C. After reducing the uterine size by selective myomectomy, deliver the debulked uterus through the abdominal incision. Then proceed with an extracorporeal total or subtotal hysterectomy.
A short learning curve
Since it uses conventional open techniques and traditional instrumentation, this method can be learned and mastered quickly.
We tend to think of this procedure as a transabdominal “vaginal” hysterectomy, since the average diameter of the minilaparotomy opening is approximately the same as the vaginal canal. Further, as in vaginal hysterectomy, only 1 portion of the uterus, adnexa, or ligaments must be exteriorized at a given time. Thus, this approach requires less general exposure but offers effective targeted exposure.
The technique also removes the need for frequent use of traumatic metal retractors, extensive bowel packing, and extended incision exposure. The benefits: diminished postoperative discomfort and bowel dysfunction.
High success rates. We have performed more than 100 minilaparotomy procedures using this technique in patients in whom vaginal hysterectomy was contraindicated. Uterine weight ranged from 80 g to 2,500 g. Mean operating time was 50 minutes. All patients were discharged within 36 hours. Mean return to work time was 12 days, and there have been no intraoperative or postoperative complications. All surgeries were successfully completed without laparoscopy or conversion to traditional laparotomy.
FIGURE 6 Hysterectomy for the large, solid, fibroid uterus
A. Draw the upper uterine attachments to the surgical field with finger traction.
FIGURE 6 Hysterectomy for the large, solid, fibroid uterus
B. Divide the round ligaments and proximal adnexal pedicles, then carry out division of the uterine vessels bilaterally.
FIGURE 6 Hysterectomy for the large, solid, fibroid uterus
C. After dividing both round ligaments, adnexal pedicles, and uterine vessels, place the uterine isthmus in traction with a rubber tourniquet and perform an in situ supracervical amputation.
FIGURE 6 Hysterectomy for the large, solid, fibroid uterus
D. After trachelectomy, the large uterine specimen is removed by morcellation. Notice that the retractor is able to stretch significantly, allowing the exteriorization of uteri with diameters considerably larger than that of the retractor.
Devices that simplify the procedure
Occasionally, hysterectomy using traditional clamp, division, and suture ligation can be tedious, frustrating, and time-consuming, especially when exposure is limited or difficult. Several devices developed for laparoscopic surgery can ease suture ligation and the division of blood vessels, ligaments, and tissue bundles during minilaparotomy hysterectomy. They include the Hem-o-lok ligating clip (Weck Closure Systems); the LigaSure Atlas, a vessel sealer-divider (Valleylab, Tyco Healthcare, Boulder, Colo); the ETS 45-Flex endoscopic linear cutter (Ethicon Endo-Surgery, Cincinnati, Ohio); and the PK bipolar cutting forceps (Gyrus Medical, Maple Grove, Minn).
Additional concerns
Is the incision too large? Fears that incisions over 5 cm might nullify minimally invasive surgery’s benefits have proven unfounded.
Laparoscopic procedures that use a 7-cm to 8-cm incision to introduce the hand into the abdomen, as well as those performed in conjunction with minilaparotomy, have consistently failed to identify a link between these combinations and morbidity or lengthy recovery. A “large” minilaparotomy incision is still superior to a standard abdominal hysterectomy in terms of convalescence, and it is significantly faster and more cost-effective than a prolonged laparoscopic or laparoscopic-assisted vaginal hysterectomy.3-10
Do any conditions contraindicate minilaparotomy? In patients with documented or strongly suspected severe pelvic conditions (for example, advanced endometriosis, pelvic inflammatory disease, bowel disease, or malignancy), preliminary laparoscopic evaluation to determine the pathologic condition’s severity and extent is strongly recommended.
If during this assessment you detect pathology that is not appropriate for laparoscopic surgery or minilaparotomy, perform a traditional laparotomy. If, however, this evaluation demonstrates that pelvic pathology is amenable to laparoscopic surgery, a laparoscopic hysterectomy or laparoscopic-assisted minilaparotomy hysterectomy is indicated.
Dr. Pelosi II reports that he is a consultant for Apple Medical Corporation. Dr. Pelosi III reports no affiliations or financial arrangements with any of the manufacturers of products mentioned in this article or their competitors.
Although laparoscopic hysterectomy offers a minimally invasive alternative to laparotomy when vaginal hysterectomy is contraindicated, it has its drawbacks. Among them: the cost of expensive equipment, the long learning curve, and prolonged operating time.
We describe another alternative to open surgery that is comparable to laparoscopic hysterectomy in postoperative pain, cosmetic results, and time to return to normal activities. Our procedure—a redesigned minilaparotomy hysterectomy—relies on traditional open techniques and inexpensive novel instrumentation, making it significantly faster than laparoscopy and easy to perform and teach.
For patients who cannot undergo vaginal hysterectomy, this new modality offers an expeditious, minimal-access option. Gynecologists reluctant to relinquish the routine use of standard laparotomy may find this approach an appealing, less-invasive alternative.
Position, incision, and retraction are crucial to success
Our minilaparotomy hysterectomy is a systemized approach with elements derived from both open and laparoscopic surgery. Three preparatory components are involved:
- position
- incision
- retraction
All are critical to a successful hysterectomy, ensuring that the procedure never becomes a haphazard struggle through an improvised, scaled-down, conventional Pfannenstiel or vertical incision. Our approach also avoids cumbersome traditional laparotomy exposure maneuvers and positioning.
Position: Modified lithotomy. After regional or general anesthesia is given, position the patient in a modified lithotomy with both arms tucked as for laparoscopic surgery. Place the legs in boot-type stirrups, with no hip flexion and sufficient thigh abduction to expose the vagina.
Next, perform a thorough pelvic examination and place an indwelling, transurethral catheter. A sturdy, hinged uterine manipulator is of paramount importance for the hysterectomy, as it facilitates exposure of the adnexa as well as elevation/rotation of the uterus and the uterine attachments. We recommend the Pelosi Uterine Manipulator (Apple Medical Corporation, Marlboro, Mass) or its equivalent (FIGURE 1).
Standard minilaparotomy
The use of standard minilaparotomy—which is nothing more than a conventional laparotomy of limited length (3 cm to 6 cm), performed either transversely or vertically—has been confined to the surgical treatment of benign pelvic pathology of limited extent.
To generate sufficient exposure to work effectively, surgeons using the standard minilaparotomy have relied on the length of the abdominal incision and, secondarily, bowel packing and metal handheld or self-retaining fixed retraction systems. When exposure is difficult to achieve or maintain, however, routine surgical maneuvers become frustrating and time-consuming—unless the clinician uses extensive traction force, extends the incision length, or performs muscle-splitting. These alternatives often result in an uncomfortable, slow recovery typical of most laparotomies, thereby negating the primary goal of minimally invasive surgery.
Use of traditional minilaparotomy for hysterectomy has been reported only rarely. Hoffman et al1 found the procedure safe and effective in nonobese women in whom a vaginal approach was precluded. Benedetti Panicci et al2,3 also have used minilaparotomy successfully in benign gynecologic disease and hysterectomy.
The Kustner incision
Originally reported in 1896,4 this incision is avoided by most surgeons in favor of complete transverse or complete vertical incisions—largely due to difficulties with exposure, troublesome seroma formation, and wound complications secondary to increased fluid accumulation in the large dead space that results from wide dissection of the subcutaneous flap.
In the early 1990s, we realized the potential benefits of a scaled-down Kustner’s incision (2 cm to 5 cm) when assistance was needed via minilaparotomy during such laparoscopic-assisted procedures as uterine morcellation, tubal reanastomosis, and extensive uterine suture and reconstruction following complex laparoscopic myomectomy.5 As a substitute for laparoscopy and laparotomy, we then tried a minilaparotomy Kustner’s incision (3 cm to 5 cm) as the sole means of surgical access, assessment, and treatment for benign pelvic conditions.
Benefits of this incision. When a sturdy uterine manipulator was used to facilitate exposure of the adnexa and uterine elevation/rotation, we found this technique more effective than similar procedures using a scaled-down Pfannenstiel or Maylard incision. In addition, because the incision was small and the extent of subcutaneous dissection required to expose the rectus fascia in a vertical fashion was limited, there was no need for incision drainage. Nor was the procedure associated with seroma formation, as the full-sized Kustner’s incision had been.3 However, the minilaparotomy Kustner’s incision still suffered from limited surgical exposure.
Adding the retractor
It became clear that a soft, self-retaining abdominal retractor that is capable of creating a rapid, effective, nontraumatic, and predictable circular area of abdominal retraction would be helpful, particularly one that could be placed through the minilaparotomy Kustner’s incision.6 Once this retractor system was developed, using technology borrowed from hand-assisted laparoscopy,7-10 the minilaparotomy hysterectomy became a much simpler, more useful surgical option.
REFERENCES
1. Hoffman MS, Lynch CM. Minilaparotomy hysterectomy. Am J Obstet Gynecol. 1998;179:316-320.
2. Benedetti Panicci P, Maneschi F, Cutillo G, et al. Surgery by minilaparotomy in benign gynecologic disease. Obstet Gynecol. 1996;87:456-459.
3. Benedetti Panicci P, Zullo MA, Casalino B, et al. Subcutaneous drainage versus no drainage after minilaparotomy in gynecologic benign conditions. Am J Obstet Gynecol. 2003;188:71-75.
4. Kustner O. Der suprasymphysare kruzschnitt, eine methode der coeliotomie bei wening umfanglichen affektionen der weiblichen beckenorgane. Monatsschr Geburtshilfe Gynakol. 1896;4:197-206.
5. Pelosi MA, II, Pelosi MA, III. The suprapubic cruciate incision for laparoscopic assisted microceliotomy. J Soc Laparoendosc Surg. 1997;1:269-272.
6. Pelosi MA, II, Pelosi MA, III. Self-retaining abdominal retractor for minilaparotomy. Obstet Gynecol. 2000;96:775-778.
7. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopy for complex hysterectomy. J Am Assoc Gynecol Laparosc. 1999;6:183-188.
8. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopic cholecystectomy at cesarean section. J Am Assoc Gynecol Laparosc. 1999;6:491-495.
9. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopy (handoscopy) for megamyomectomy: A case study. J Reprod Med. 2000;45:519-525.
10. Pelosi MA, II, Pelosi MA, III, Eim J. Hand-assisted laparoscopy for pelvic malignancy. J Laparoendosc Adv Surg Tech. 2000;10:143-150.
Incision: Modified Kustner’s. Open the abdomen with a cruciate incision. Using a conventional scalpel and the Bovie device, make a 2.5-cm to 5-cm transverse incision through the skin and subcutaneous fat until you reach the anterior rectus fascia (FIGURE 2A). Clear the fat from the midline superiorly and inferiorly to expose approximately 5 cm to 6 cm of fascia in the vertical axis. Then incise the anterior rectus fascia in a vertical direction through the full length of the cleared area (FIGURE 2B).
Retract the rectus muscles from the midline, exposing the transversalis fascia and the underlying peritoneum. Enter the peritoneum digitally or with scissors above the level of the bladder dome, incising vertically until the entrance extends the full length of the fascial incision (FIGURE 2C).
This modified Kustner’s incision is essentially a vertical midline incision in its deeper layers.1 The rapid surgical dissection of the fascia and rectus muscles and the intraperitoneal entry are relatively bloodless. This approach yields a surgical exposure superior to that of a small Pfannenstiel or Maylard incision.
Note that, in some patients, a vertical incision can be selected if there is a prior vertical incision or if the perioperative workup suggests a malignancy that may require a later extension of the original minilaparotomy incision.
Retraction: Soft, sleeve-type, self-retaining abdominal retractor. This device consists of a flexible plastic inner ring and a firmer outer ring connected by a soft plastic sleeve (FIGURE 3A). Two models are available: the Mobius (Apple Medical Corporation) and the Protractor (Weck Closure Systems, Research Triangle Park, NC).
Squeeze the inner ring into the peritoneal cavity through the minilaparotomy incision, allowing it to spring open against the parietal peritoneum. Conduct a digital assessment to ensure that no viscera are trapped by elevating the outer ring. Next, roll the outer ring onto the sleeve, collecting excess length, until it sits firmly against the skin (FIGURES 3B and 3C). The result, when there is adequate tension within the sleeve, is a circular area of retraction offering excellent exposure of the pelvis. Note that during surgery you may need to adjust the outer ring if the sleeve loosens.
The soft, self-retaining abdominal retractor offers several advantages over traditional abdominal retraction:
- Atraumatic retraction. This device distributes retraction force evenly around the entire incision. Because standard retractors concentrate retraction force at only a few points, they often lead to tissue trauma, nerve damage, bruising, and postoperative pain.
- Incision protection. The retractor’s flexible material lines the incision, protecting the wound’s edges from contamination and potential implantation of malignant cells.
- Improved access. Because the continuous retraction force is delivered more effectively to the incision, exposure is maximized. As a result, the need for intensive surgical assistance is dramatically reduced.
- Adjustable height. The retractor’s design lets it adapt to wounds of varying depth—a feature that makes it ideal for obese patients. The device compresses the patient’s skin and peritoneum between the external and internal rings, keeping the full thickness of the abdominal incision constant throughout the surgery.
- Cost-effectiveness. The device, which costs under $100, is simple and fast to set up. In our experience, placement takes approximately 2 minutes; this compares favorably with table-mounted or self-retaining rigid retraction systems, which may require significant capital expenditures (cost may run in the thousands), repair costs, and complicated set-ups.
FIGURE 1 Hinged uterine manipulator
A sturdy hinged uterine manipulator facilitates exposure of the adnexa as well as elevation/rotation of the uterus.
FIGURE 2 Cruciate incision
A. Make a transverse incision suprapubically through the skin and the subcutaneous fat to reach the anterior rectus fascia.
FIGURE 2 Cruciate incision
B. Clear the fat from the midline to expose the rectus fascia in the vertical axis, then incise the fascia in a vertical direction through the full length of the previously cleared area. The rectus muscles are retracted, thereby exposing the peritoneum.
FIGURE 2 Cruciate incision
C. Incise the peritoneum vertically until it extends the full length of the fascial incision.
FIGURE 3 Soft, sleeve-type, self-retaining abdominal retractor
A. At left, the Protractor (Weck Closure Systems); at right, the Mobius (Apple Medical Corporation).
FIGURE 3 Soft, sleeve-type, self-retaining abdominal retractor
B. After inserting the inner ring into the peritoneal cavity, twist the outer ring downward until it inverts and rests snuggly against the skin.
FIGURE 3 Soft, sleeve-type, self-retaining abdominal retractor
C. An atraumatic, circular, self-retaining area of retraction is created.
Standard technique: Exteriorize the uterus; divide uterine attachments, vessels
Assess the anatomy. Using your index finger and the uterine manipulator to rotate and flex the uterus, carefully assess the uterus, adnexa, and pelvis, noting the location of the ureters. Determine the extent of any unexpected pelvic pathology or adhesions, using traditional small retractors or gentle packing to gain additional exposure. Perform any adhesiolysis that is necessary.
Exteriorize the uterus. Next, bring the uterus and the adnexa above the abdominal wall in order to perform as much of the hysterectomy extracorporeally as possible. Pass the uterus or adnexa through the incision with the upward assistance of the uterine manipulator, then divide the upper uterine attachments (FIGURE 4A).
Increase exposure. You can achieve additional uterine elevation and targeted exposure in several ways. For example, a strong traction suture can be placed in the uterine fundus, left long, and secured with a clamp. To achieve uterine elevation, place long clamps lateral to the corpus. Another effective approach is to place a heavy tenaculum on the uterine fundus.
When lateral exposure is limited, divide the proximal adnexal pedicles and round ligaments to begin the operation, and remove the adnexa separately following the completion of the hysterectomy.
Divide the uterine vessels through the small incision using clamping, division, and ligation. Unless you intend to preserve the cervix, mobilize the bladder to the level of the anterior vaginal fornix. Inward pressure on the uterine manipulator provides additional elevation of the lower uterine vasculature and the cardinal and uterosacral ligaments as these structures are ligated and divided. Amputate the uterine specimen from the vaginal cuff using the uterine manipulator to guide the vaginal circumcision (FIGURE 4B). Close the vaginal cuff using standard closure.
If the cervix is to be preserved, amputate the uterus supracervically following division of the uterine vessels. Then suture the cervical stump in the traditional fashion. Upward elevation of the cervix using the uterine manipulator expedites this step.
Complete the procedure. Once the surgery is completed, remove the retractor, hooking the bottom ring by inserting a finger into it and pulling it up and out of the incision (FIGURE 4C). Closing a cruciate incision is faster and requires less exposure than closing a mini-Pfannenstiel incision. Eliminate the possibility of postoperative wound hematoma or seroma formation by applying a vertical pressure dressing over the incision (FIGURE 4D). Remove the dressing 24 hours later.
FIGURE 4 Hysterectomy for the normal to moderately enlarged uterus
A. Exteriorize the uterus as much as possible with both upward assistance of the manipulator and uterine fundal elevation (using clamps lateral to the uterus, a heavy tenaculum, or a traction suture). Then conduct a standard hysterectomy.
FIGURE 4 Hysterectomy for the normal to moderately enlarged uterus
B. Separate the uterus from the vagina using the manipulator to guide the vaginal circumcision. (If the cervix is to be preserved, a supracervical amputation is performed instead.)
FIGURE 4 Hysterectomy for the normal to moderately enlarged uterus
C. After completing the surgery, remove the retractor from the incision.
FIGURE 4 Hysterectomy for the normal to moderately enlarged uterus
D. Apply a vertical pressure dressing over the incision.
Variations for abnormal uteri
The large fibroid uterus: Begin with the dominant myoma. A large fibroid uterus can be easily removed with our minilaparotomy technique using 3 basic steps:
- Reduce size by selective myomectomy.
- Deliver the debulked uterus through the abdominal incision.
- Perform extracorporeal hysterectomy.
First, you must conduct a thorough assessment of the number, size, and location of the myomas. Begin the myomectomy on the largest tumor of those closest to the minilaparotomy incision. (Minimize bleeding by injecting diluted vasopressin subserosally prior to the procedure.)
Incise the uterine serosa, myometrium, and pseudocapsule of the myoma via scalpel or Bovie electrocautery until the whorly appearance of the myoma is apparent. Next, grasp the myoma with claw-toothed forceps to stabilize it and place it under traction. Then, using a combination of sharp and digital dissection, develop a plane of dissection between the fibroid and the myometrium (FIGURE 5A).
After securing the dominant myoma, deliver it through the abdominal incision. If the myoma is too large to be removed intact from the abdominal cavity, morcellate it using a scalpel or scissors (FIGURE 5B). Then continue systematic removal of the remaining myomas using the same approach. It is not necessary to remove all myomas—the goal of this process is merely to permit delivery of the uterine body for subsequent hysterectomy.
Once the uterus is debulked, deliver it through the abdominal incision. Hysterectomy then is easily completed (FIGURE 5C).
The ‘solid’ uterus: In situ supracervical hysterectomy and uterine morcellation.
Very large uteri are sometimes homogeneous and solid in nature, possessing few or no individual myomas. This so-called cannonball fibroid uterus is the most challenging type of uterus to remove. The selective-myomectomy approach cannot be used because of the potential for massive bleeding and the technical anatomical difficulties that arise when operating through such a small abdominal incision.
Instead, manage this type of uterus by performing a deliberate in situ supracervical hysterectomy through the minilaparotomy incision. At the end of this procedure, morcellate the amputated fibroid uterus.
Begin the surgery by dividing the upper uterine attachments. Regardless of uterine size, the origins of the round and adnexal ligaments will always be lateral to and within easy reach of a transverse minilaparotomy incision. (Access to these areas is the only factor that determines the feasibility of this procedure; uterine size is completely irrelevant.) We have found that these elongated ligaments are quite lax. Thus, in most cases it is relatively simple to navigate your index finger laterally and, using digital traction, elevate these structures into the minilaparotomy incision (FIGURE 6A). You can then clamp, cut, and suture the ligaments in the standard fashion in whatever sequence is most efficient.
Thanks to the retractor, minimal assistance is necessary during the surgery. You can create additional exposure by deflecting the uterus toward the opposite side of the pelvis using external abdominal pressure and the uterine manipulator.
Once both round ligaments and adnexal pedicles are divided, dissect the bladder flap to expose the uterine arteries (inward pressure on the uterine manipulator provides helpful countertraction). Then clamp, divide, and ligate the uterine arteries (FIGURE 6B).
The uterus is now ready for supracervical amputation. Upward traction on the isthmus by means of a rubber tourniquet facilitates uterine division (FIGURE 6C). After the uterus is amputated, push it toward the upper abdomen to increase exposure for suturing of the cervical stump (if the cervix is preserved) or for cervical excision and vaginal cuff closure (when total hysterectomy is chosen).
Next, remove the uterine specimen by morcellation through the minilaparotomy incision. Using the Doyen ladder-shaped uterine morcellation technique (originally described in the early 1920s) grasp an area of the uterus and, alternating right and left, make deep but incomplete incisions on the uterus, creating a ladder shape.2 Because of its elasticity, the retractor can stretch quite significantly without tearing the edges of the abdominal incision (FIGURE 6D). This allows the easy exteriorization of uteri with diameters considerably larger than that of the retractor, mimicking the stretching of the perineum during the crowning of the fetal head.
When the surgery is complete, remove the retractor, close the minilaparotomy incision, and apply a vertical pressure dressing over the incision. Neither vaginal packing nor bladder catheterization is required.
FIGURE 5 Hysterectomy for the fibroid uterus
A. Develop a plane of dissection between the myoma and myometrium.
FIGURE 5 Hysterectomy for the fibroid uterus
B. Deliver the myoma through the incision; if it is too large to remove intact, morcellate it with a scalpel or scissors.
FIGURE 5 Hysterectomy for the fibroid uterus
C. After reducing the uterine size by selective myomectomy, deliver the debulked uterus through the abdominal incision. Then proceed with an extracorporeal total or subtotal hysterectomy.
A short learning curve
Since it uses conventional open techniques and traditional instrumentation, this method can be learned and mastered quickly.
We tend to think of this procedure as a transabdominal “vaginal” hysterectomy, since the average diameter of the minilaparotomy opening is approximately the same as the vaginal canal. Further, as in vaginal hysterectomy, only 1 portion of the uterus, adnexa, or ligaments must be exteriorized at a given time. Thus, this approach requires less general exposure but offers effective targeted exposure.
The technique also removes the need for frequent use of traumatic metal retractors, extensive bowel packing, and extended incision exposure. The benefits: diminished postoperative discomfort and bowel dysfunction.
High success rates. We have performed more than 100 minilaparotomy procedures using this technique in patients in whom vaginal hysterectomy was contraindicated. Uterine weight ranged from 80 g to 2,500 g. Mean operating time was 50 minutes. All patients were discharged within 36 hours. Mean return to work time was 12 days, and there have been no intraoperative or postoperative complications. All surgeries were successfully completed without laparoscopy or conversion to traditional laparotomy.
FIGURE 6 Hysterectomy for the large, solid, fibroid uterus
A. Draw the upper uterine attachments to the surgical field with finger traction.
FIGURE 6 Hysterectomy for the large, solid, fibroid uterus
B. Divide the round ligaments and proximal adnexal pedicles, then carry out division of the uterine vessels bilaterally.
FIGURE 6 Hysterectomy for the large, solid, fibroid uterus
C. After dividing both round ligaments, adnexal pedicles, and uterine vessels, place the uterine isthmus in traction with a rubber tourniquet and perform an in situ supracervical amputation.
FIGURE 6 Hysterectomy for the large, solid, fibroid uterus
D. After trachelectomy, the large uterine specimen is removed by morcellation. Notice that the retractor is able to stretch significantly, allowing the exteriorization of uteri with diameters considerably larger than that of the retractor.
Devices that simplify the procedure
Occasionally, hysterectomy using traditional clamp, division, and suture ligation can be tedious, frustrating, and time-consuming, especially when exposure is limited or difficult. Several devices developed for laparoscopic surgery can ease suture ligation and the division of blood vessels, ligaments, and tissue bundles during minilaparotomy hysterectomy. They include the Hem-o-lok ligating clip (Weck Closure Systems); the LigaSure Atlas, a vessel sealer-divider (Valleylab, Tyco Healthcare, Boulder, Colo); the ETS 45-Flex endoscopic linear cutter (Ethicon Endo-Surgery, Cincinnati, Ohio); and the PK bipolar cutting forceps (Gyrus Medical, Maple Grove, Minn).
Additional concerns
Is the incision too large? Fears that incisions over 5 cm might nullify minimally invasive surgery’s benefits have proven unfounded.
Laparoscopic procedures that use a 7-cm to 8-cm incision to introduce the hand into the abdomen, as well as those performed in conjunction with minilaparotomy, have consistently failed to identify a link between these combinations and morbidity or lengthy recovery. A “large” minilaparotomy incision is still superior to a standard abdominal hysterectomy in terms of convalescence, and it is significantly faster and more cost-effective than a prolonged laparoscopic or laparoscopic-assisted vaginal hysterectomy.3-10
Do any conditions contraindicate minilaparotomy? In patients with documented or strongly suspected severe pelvic conditions (for example, advanced endometriosis, pelvic inflammatory disease, bowel disease, or malignancy), preliminary laparoscopic evaluation to determine the pathologic condition’s severity and extent is strongly recommended.
If during this assessment you detect pathology that is not appropriate for laparoscopic surgery or minilaparotomy, perform a traditional laparotomy. If, however, this evaluation demonstrates that pelvic pathology is amenable to laparoscopic surgery, a laparoscopic hysterectomy or laparoscopic-assisted minilaparotomy hysterectomy is indicated.
Dr. Pelosi II reports that he is a consultant for Apple Medical Corporation. Dr. Pelosi III reports no affiliations or financial arrangements with any of the manufacturers of products mentioned in this article or their competitors.
1. Kustner O. Der suprasymphysare kruzschnitt, eine methode der coeliotomie bei wening umfanglichen affektionen der weiblichen beckenorgane. Monatsschr Geburtshilfe Gynakol. 1896;4:197-206.
2. Doyen E. Surgical Therapeutics and Operative Technique. Vol. III. Spencer-Browne H, translator. London, England: Bailliere, Tindal and Cox; 1920.
3. Benedetti Panicci P, Maneschi F, Cutillo G, et al. Surgery by minilaparotomy in benign gynecologic disease. Obstet Gynecol. 1996;87:456-459.
4. Benedetti Panicci P, Zullo MA, Casalino B, et al. Subcutaneous drainage versus no drainage after minilaparotomy in gynecologic benign conditions. Am J Obstet Gynecol. 2003;188:71-75.
5. Pelosi MA, II, Pelosi MA, III. The suprapubic cruciate incision for laparoscopic assisted microceliotomy. J Soc Laparoendosc Surg. 1997;1:269-272.
6. Pelosi MA, II, Pelosi MA, III. Self-retaining abdominal retractor for minilaparotomy. Obstet Gynecol. 2000;96:775-778.
7. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopy for complex hysterectomy. J Am Assoc Gynecol Laparosc. 1999;6:183-188.
8. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopic cholecystectomy at cesarean section. J Am Assoc Gynecol Laparosc. 1999;6:491-495.
9. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopy (handoscopy) for megamyomectomy: A case study. J Reprod Med. 2000;45:519-525.
10. Pelosi MA, II, Pelosi MA, III, Eim J. Hand-assisted laparoscopy for pelvic malignancy. J Laparoendosc Adv Surg Tech. 2000;10:143-150.
1. Kustner O. Der suprasymphysare kruzschnitt, eine methode der coeliotomie bei wening umfanglichen affektionen der weiblichen beckenorgane. Monatsschr Geburtshilfe Gynakol. 1896;4:197-206.
2. Doyen E. Surgical Therapeutics and Operative Technique. Vol. III. Spencer-Browne H, translator. London, England: Bailliere, Tindal and Cox; 1920.
3. Benedetti Panicci P, Maneschi F, Cutillo G, et al. Surgery by minilaparotomy in benign gynecologic disease. Obstet Gynecol. 1996;87:456-459.
4. Benedetti Panicci P, Zullo MA, Casalino B, et al. Subcutaneous drainage versus no drainage after minilaparotomy in gynecologic benign conditions. Am J Obstet Gynecol. 2003;188:71-75.
5. Pelosi MA, II, Pelosi MA, III. The suprapubic cruciate incision for laparoscopic assisted microceliotomy. J Soc Laparoendosc Surg. 1997;1:269-272.
6. Pelosi MA, II, Pelosi MA, III. Self-retaining abdominal retractor for minilaparotomy. Obstet Gynecol. 2000;96:775-778.
7. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopy for complex hysterectomy. J Am Assoc Gynecol Laparosc. 1999;6:183-188.
8. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopic cholecystectomy at cesarean section. J Am Assoc Gynecol Laparosc. 1999;6:491-495.
9. Pelosi MA, II, Pelosi MA, III. Hand-assisted laparoscopy (handoscopy) for megamyomectomy: A case study. J Reprod Med. 2000;45:519-525.
10. Pelosi MA, II, Pelosi MA, III, Eim J. Hand-assisted laparoscopy for pelvic malignancy. J Laparoendosc Adv Surg Tech. 2000;10:143-150.
Uterine artery embolization for symptomatic fibroids: Pros and cons
- Uterine artery embolization (UAE) may be especially useful in women who are poor surgical candidates or have extensive adhesive disease, or who refuse blood products or are perimenopausal.
- The average reported symptom improvement is 87%; the mean reduction in fibroid volume is 46%.
- Most patients are discharged within 24 hours of the procedure and experience an average recovery period of 8 days.
- Women undergoing UAE for fibroids are more likely than those undergoing myomectomy to need further invasive treatment within 3 to 5 years.
- Although several series and case reports have noted successful pregnancies following UAE, desire for fertility is considered a relative contraindication by some authorities.
With the increasing demand for nonsurgical alternatives to hysterectomy or myomectomy for fibroids, uterine artery embolization (UAE) has grown in use and popularity—and most patients report a high level of satisfaction after the procedure.
UAE has been shown to be safe and effective in selected patients with symptomatic fibroids unresponsive to medical treatment. If they are not contemplating pregnancy and do not have additional pelvic pathology, these women may elect UAE as an appropriate alternative to hysterectomy or myomectomy. This article reviews the indications, contraindications, technique, complications, and outcomes of UAE.
Limits of primary surgeries increase demand for UAE
Most of the 590,000 hysterectomies performed each year in the United States are for symptomatic fibroids, the most common tumors of the female reproductive tract.1 Although hysterectomy is the definitive treatment, increasing numbers of patients express a desire for alternatives, primarily to preserve the uterus. While myomectomy spares the uterus, as many as 25% of women who undergo this procedure require another surgery for recurrent symptoms.2 These limitations of the primary surgeries for fibroids have increased the demand for UAE.
Embolization of the uterine arteries has been utilized for more than 20 years to treat pelvic hemorrhage following delivery or abortion, ectopic or cervical pregnancy, gestational trophoblastic disease, or malignancy.3,4 It was first reported as an effective intervention for fibroids in 1995, when Ravina et al5 noted that several women with symptomatic leiomyomata who underwent UAE as a pre-hysterectomy treatment had such significant clinical improvement that hysterectoMy was no longer required.
In a study involving 200 patients undergoing UAE for leiomyomata, Spies et al6 noted improvement in heavy bleeding in 90% (95% confidence interval [CI], 86%, 95%) and a reduction in bulk-related symptoms in 91% (95% CI, 86%, 95%) at 1 year.
Because data are limited on the safety of pregnancy following uterine artery embolization, some authorities consider the desire for future fertility a relative contraindication.
On a global level, more than 30,000 UAE procedures have been performed for symptomatic uterine fibroids.
The economic considerations surrounding uterine artery embolization (UAE) have led to a turf war of sorts between gynecologists and interventional radiologists. In Philadelphia, Pa, the average reimbursement to an interventional radiologist for a UAE is approximately $1,650; for a gynecologist performing a hysterectomy or myomectomy, it is approximately $1,000.
Some Ob/Gyns are reluctant to recommend UAE for their patients for a variety of reasons. Because of this reluctance, UAE is increasingly marketed directly to the consumer over the Internet and in print media. Large proportions of women undergoing UAE are self-referrals or are referred by their gynecologist after specifically requesting the procedure.
UAE may represent a societal savings in terms of direct and indirect costs. For example, a Canadian cost analysis found that UAE was associated with significantly lower hospital costs ($1007.44 Canadian) than abdominal myomectomy ($1,781.73 Canadian).1
Reference
1. Al-Fozan H, Dufort J, Kaplow M, Valenti D, Tulandi T. Cost analysis of myomectomy, hysterectomy, and uterine artery embolization. Am J Obstet Gynecol. 2002;187:1401-1404.
Technique
UAE is a radiologic procedure performed with either local or regional anesthesia. Most commonly, an approach through the right femoral artery is used, after a preliminary arteriogram (FIGURE 1) has been made to visualize the pelvic vasculature.
Fluoroscopic guidance enables a catheter to be passed into the right femoral artery and through the right external iliac artery to the aorta, then down the left common iliac artery to the left internal iliac, down the anterior division, and finally to the left uterine artery. When the catheter is properly positioned, polyvinyl alcohol particles or acrylic copolymer beads (300 microns to 700 microns) are infused until slow flow or stasis occurs in the uterine artery and the fibroid vasculature is occluded (FIGURE 2). The catheter is then pulled back and manipulated into the right uterine artery, which is similarly embolized. Procedure time ranges from 15 to 120 minutes, depending on the patient’s anatomy and the skill of the operator.1,6,7
FIGURE 1 Pre—uterine-artery-embolization arteriograms
Preprocedure right and left arteriograms for vasculature of a 12-week size fibroid uterus.
Preprocedure right and left arteriograms for vasculature of a 24-week size fibroid uterus.
FIGURE 2 Embolization catheter infusing microparticles within uterine artery
A catheter is passed into the right femoral artery, through the right external iliac artery to the aorta, then down the left common iliac artery to the left internal iliac, down the anterior division to the left uterine artery. Embolization material—polyvinyl alcohol particles or acrylic copolymer beads—is then delivered via catheter in the uterine artery until slow flow or stasis occurs in the artery.
Indications
Like hysterectomy and myomectomy, the indications for UAE are symptomatic fibroids that are unresponsive to medical management (with hormonal agents or analgesics). Common symptoms of fibroids include abdominal or pelvic pain, abnormal menstrual bleeding, anemia, urinary frequency, dyspareunia, and infertility.
UAE may be an especially useful option for women who are poor surgical candidates or have extensive adhesive disease, as well as for those who refuse blood products or are perimenopausal.6,8,9
Contraindications
Pelvic infection, severe contrast allergy, arteriovenous shunting, the presence of an undiagnosed pelvic mass, coagulopathy, renal insufficiency, a history of pelvic radiation, and genital tract malignancy all are contraindications.
Because data are limited on the safety of pregnancy following UAE, some authorities consider the desire for future fertility a relative contraindication.4,7,10
Preoperative evaluation
The preoperative workup should include a thorough history and physical examination by both an interventional radiologist and a gynecologist, a pregnancy test, pelvic imaging via ultrasound or magnetic resonance imaging, and endometrial biopsy to exclude endometrial hyperplasia or cancer. (Patients without abnormal bleeding may not require an endometrial biopsy.)
Outcomes
The average reported symptom improvement is 87%, and the mean reduction in fibroid volume is 46%.1 Most patients see improvement within 3 months of the procedure, with control over the symptoms lasting at least 2 years. At 1 year, 90% of patients report improvement in heavy menstrual bleeding.4
Most patients are discharged within 24 hours of the procedure, compared with 48 to 72 hours for abdominal hysterectomy or myomectomy. They also experience an average recovery period of 8 days, compared with 4 to 6 weeks for abdominal hysterectomy or myomectomy.6
However, a recent study found that women undergoing embolization for fibroids were more likely than those undergoing myomectomy to need further invasive treatment (i.e., repeat embolization or surgery) within 3 to 5 years (29% versus 3%).11
Complications
Most patients report some degree of “post-embolization syndrome,” which is characterized by low-grade fever, pain, malaise, nausea, and leukocytosis, generally within the first 4 days.4 This may be caused by the systemic effects of transient fibroid and uterine ischemia. Although the condition is usually self-limiting and observable on an outpatient basis, these patients are often admitted for antibiotic therapy.
“Post-embolization syndrome” is characterized by low-grade fever, pain, malaise, nausea, and leukocytosis, generally within the first 4 days.
In the most recent series published,12 major complications occurred in 0.5% of embolizations performed for symptomatic fibroids. They include pulmonary embolism, arterial thrombosis, groin hematomas, local infection, guide-wire perforation of arteries, allergic reaction to contrast medium, endometritis, ischemia of pelvic organs, sepsis, and death. Among more than 30,000 procedures performed to date worldwide, there have been 4 related fatalities. In 2 cases, pulmonary embolism occurred within a few days of the procedure; the 2 other deaths occurred within 2 weeks and were related to septicemia and disseminated intravascular coagulation.
There have been reports of total uterine necrosis, transient and permanent ovarian failure, and external sexual dysfunction. These complications may occur up to 2 years after the procedure.1,4,7,10,13-16 Nontarget vascular embolizations of the gluteus muscle, ovaries, labia minora, and bladder wall also have been noted.17,18
When viewed in the context of the large number of procedures performed—and considering the complications associated with myomectomy and hysterectomy—these rare complications show that, overall, UAE is a very safe procedure.
Pregnancy after embolization
Because we lack controlled studies and abundant data, the role of UAE in women contemplating childbearing is unclear. More studies are needed before UAE can be confidently recommended for these women. Premature ovarian failure is an uncommon but recognized complication of UAE.13
Several series and case reports have noted successful pregnancies following UAE.19,20 Our recent report21 on 50 pregnancies following UAE for leiomyomata noted higher rates of cesarean delivery, preterm delivery, malpresentation, spontaneous abortion, and postpartum hemorrhage than in the general population (TABLE). It is unclear whether the increased rate of premature delivery and malpresentation is due to residual fibroids, changes in myometrial vascularity or elasticity, or other unknown labor-associated processes.
Pregnancy outcomes following myomectomy have been reported in several case series, with rates of premature delivery and other complications similar to those for the general population.22,23 Confounding factors (for example, residual fibroids) and the absence of randomized controlled trials, however, make well-founded comparisons of pregnancy outcomes following UAE and myomectomy difficult.
Theoretical concerns about risk of growth restriction and preeclampsia following UAE have been raised. In our study, we did not observe an increase of small-for-gestational-age infants following embolization.21 Uterine rupture during pregnancy after UAE also has been reported.24
TABLE
Rates of pregnancy complications after UAE and in the general population
| PREGNANCY | COMPLICATIONS OF PREGNANCY % (NUMBER AFFECTED/NUMBER OF SUBJECTS STUDIED) | |||||
|---|---|---|---|---|---|---|
| SPONTANEOUS ABORTION | POSTPARTUM HEMORRHAGE | PREMATURE DELIVERY | CESAREAN DELIVERY | SMALL FOR GESTATIONAL AGE | MAL.* | |
| After UAE for leiomyomata | 32 (11/34) | 9(2/23) | 22 (5/23) | 65 (15/23) | 9 (2/22) | 22 (5/23) |
| In the general population | 10-15 | 4-6 | 5-10 | 22 | 10 | 5 |
| UAE=uterine artery embolization | ||||||
| *MAL=malpresentation | ||||||
| Reprinted from the American Journal of Obstetrics and Gynecology, 100, Goldberg J, Pereira L, Berghella V, Pregnancy after uterine artery embolization, 869-872, 2002, with permission from Elsevier. | ||||||
Internet Resources
- Society of Cardiovascular and Interventional Radiologists (www.SIRweb.org)
- Fibroid Uterine Artery Embolization Registry (www.fibroidregistry.org)
- American College of Obstetricians and Gynecologists (www.acog.org)
The authors report no financial relationships with any companies whose products are mentioned in this article.
1. Floridon C, Lund N, Thomsen SG. Alternative treatment for symptomatic fibroids. Curr Opin Obstet Gynecol. 2001;13:491-495.
2. Stenchever MA, Droegemueller W, Herbst AL, Mishell DR. Comprehensive Gynecology. 4th ed. St. Louis, Mo: Mosby; 2001.
3. Goodwin SC, Walker WJ. Uterine artery embolization for the treatment of uterine fibroids. Curr Opin Obstet Gynecol. 1998;10:315-320.
4. Schwartz ML, Klein A, McLucas B. Using uterine artery embolization to treat fibroids. Contemporary OB/GYN. 2001;8:14-37.
5. Ravina J, Herbreteau D, Ciraru-Vigneron N, et al. Arterial embolization to treat uterine myomata. Lancet. 1995;346:671-672.
6. Spies JB, Ascher SA, Roth AR, Kim J, Levy EB, Gomez-Jorge J. Uterine artery embolization for leiomyomata. Obstet Gynecol. 2001;98:29-34.
7. Demello AB. Uterine artery embolization. AORN J. 2001;73:788-814.
8. Bradley EA, Reidy JF, Forman RG, Jarosz J, Braude PR. Transcatheter uterine artery embolization to treat large uterine fibroids. Br J Obstet Gynaecol. 1998;15:235-240.
9. Goodwin SC, Vedantham S, McLucas B, Forno A, Perrella R. Preliminary experience with uterine artery embolization for uterine fibroids. J Vasc Interv Radiol. 1997;8:517-520.
10. Godfrey CD, Zbella EA. Uterine necrosis after uterine artery embolization for leiomyoma. Obstet Gynecol. 2001;98:950-952.
11. Broder MS, Goodwin S, Chen G, et al. Comparison of long-term outcomes of myomectomy and uterine artery embolization. Obstet Gynecol. 2002;100:864-868.
12. Spies JB, Spector A, Roth A, Baker C, Mauro L, Murphy-Skyrynarz K. Complications after uterine artery embolization for leiomyomas. Obstet Gynecol. 2002;100:873-880.
13. Amato P, Roberts AC. Transient ovarian failure: a complication of uterine artery embolization. Fertil Steril. 2001;75:438-439.
14. Lai AC, Goodwin SC, Bonilla SM, et al. Sexual dysfunction after uterine artery embolization. J Vasc Interv Radiol. 2000;11:755-758.
15. Stringer N. Diagnosis and management of long-term complications of uterine artery embolization. Female Patient. 2002;27(11):13-24.
16. Vashisht A, Studd J, Carey A, Burn P. Fatal septicaemia after fibroid embolisation. Lancet. 1999;354:307-308.
17. Sultana CJ, Goldberg J, Aizenman L, Chon JK. Vesicouterine fistula after uterine artery embolization: a case report. Am J Obstet Gynecol. 2002;187:1726-1727.
18. Yeagley T, Goldberg J, Klein T, Bonn J. Labial necrosis after uterine artery embolization for leiomyomas. Obstet Gynecol. 2002;100:881.-
19. Vashisht A, Smith JR, Thorpe-Beeston G, McCall J. Pregnancy subsequent to uterine artery embolization. Fertil Steril. 2001;75:1246-1247.
20. Ravina JH, Vigneron NC, Aymard A, Le Dref O, Merland JJ. Pregnancy after embolization of uterine myoma: Report of 12 cases. Fertil Steril. 2000;73:1241-1243.
21. Goldberg J, Pereira L, Berghella V. Pregnancy after uterine artery embolization. Obstet Gynecol. 2002;100:869-872.
22. Seracchioli R, Rossi S, Govoni F, et al. Fertility and obstetric outcome after laparoscopic myomectomy of large myomata: A randomized comparison with abdominal myomectomy. Hum Reprod. 2000;15:2663-2668.
23. Dessolle L, Soriano D, Poncelet C, Benifla JL, Madelenat P, Darai E. Determinants of pregnancy rate and obstetric outcome after laparoscopic myomectomy for infertility. Fertil Steril. 2001;76:370-374.
24. Walker W, Green A, Sutton C. Bilateral uterine artery embolization for myomata: Results, complications, and failures. Min Invas Ther Allied Technol. 1999;8:449-454.
- Uterine artery embolization (UAE) may be especially useful in women who are poor surgical candidates or have extensive adhesive disease, or who refuse blood products or are perimenopausal.
- The average reported symptom improvement is 87%; the mean reduction in fibroid volume is 46%.
- Most patients are discharged within 24 hours of the procedure and experience an average recovery period of 8 days.
- Women undergoing UAE for fibroids are more likely than those undergoing myomectomy to need further invasive treatment within 3 to 5 years.
- Although several series and case reports have noted successful pregnancies following UAE, desire for fertility is considered a relative contraindication by some authorities.
With the increasing demand for nonsurgical alternatives to hysterectomy or myomectomy for fibroids, uterine artery embolization (UAE) has grown in use and popularity—and most patients report a high level of satisfaction after the procedure.
UAE has been shown to be safe and effective in selected patients with symptomatic fibroids unresponsive to medical treatment. If they are not contemplating pregnancy and do not have additional pelvic pathology, these women may elect UAE as an appropriate alternative to hysterectomy or myomectomy. This article reviews the indications, contraindications, technique, complications, and outcomes of UAE.
Limits of primary surgeries increase demand for UAE
Most of the 590,000 hysterectomies performed each year in the United States are for symptomatic fibroids, the most common tumors of the female reproductive tract.1 Although hysterectomy is the definitive treatment, increasing numbers of patients express a desire for alternatives, primarily to preserve the uterus. While myomectomy spares the uterus, as many as 25% of women who undergo this procedure require another surgery for recurrent symptoms.2 These limitations of the primary surgeries for fibroids have increased the demand for UAE.
Embolization of the uterine arteries has been utilized for more than 20 years to treat pelvic hemorrhage following delivery or abortion, ectopic or cervical pregnancy, gestational trophoblastic disease, or malignancy.3,4 It was first reported as an effective intervention for fibroids in 1995, when Ravina et al5 noted that several women with symptomatic leiomyomata who underwent UAE as a pre-hysterectomy treatment had such significant clinical improvement that hysterectoMy was no longer required.
In a study involving 200 patients undergoing UAE for leiomyomata, Spies et al6 noted improvement in heavy bleeding in 90% (95% confidence interval [CI], 86%, 95%) and a reduction in bulk-related symptoms in 91% (95% CI, 86%, 95%) at 1 year.
Because data are limited on the safety of pregnancy following uterine artery embolization, some authorities consider the desire for future fertility a relative contraindication.
On a global level, more than 30,000 UAE procedures have been performed for symptomatic uterine fibroids.
The economic considerations surrounding uterine artery embolization (UAE) have led to a turf war of sorts between gynecologists and interventional radiologists. In Philadelphia, Pa, the average reimbursement to an interventional radiologist for a UAE is approximately $1,650; for a gynecologist performing a hysterectomy or myomectomy, it is approximately $1,000.
Some Ob/Gyns are reluctant to recommend UAE for their patients for a variety of reasons. Because of this reluctance, UAE is increasingly marketed directly to the consumer over the Internet and in print media. Large proportions of women undergoing UAE are self-referrals or are referred by their gynecologist after specifically requesting the procedure.
UAE may represent a societal savings in terms of direct and indirect costs. For example, a Canadian cost analysis found that UAE was associated with significantly lower hospital costs ($1007.44 Canadian) than abdominal myomectomy ($1,781.73 Canadian).1
Reference
1. Al-Fozan H, Dufort J, Kaplow M, Valenti D, Tulandi T. Cost analysis of myomectomy, hysterectomy, and uterine artery embolization. Am J Obstet Gynecol. 2002;187:1401-1404.
Technique
UAE is a radiologic procedure performed with either local or regional anesthesia. Most commonly, an approach through the right femoral artery is used, after a preliminary arteriogram (FIGURE 1) has been made to visualize the pelvic vasculature.
Fluoroscopic guidance enables a catheter to be passed into the right femoral artery and through the right external iliac artery to the aorta, then down the left common iliac artery to the left internal iliac, down the anterior division, and finally to the left uterine artery. When the catheter is properly positioned, polyvinyl alcohol particles or acrylic copolymer beads (300 microns to 700 microns) are infused until slow flow or stasis occurs in the uterine artery and the fibroid vasculature is occluded (FIGURE 2). The catheter is then pulled back and manipulated into the right uterine artery, which is similarly embolized. Procedure time ranges from 15 to 120 minutes, depending on the patient’s anatomy and the skill of the operator.1,6,7
FIGURE 1 Pre—uterine-artery-embolization arteriograms
Preprocedure right and left arteriograms for vasculature of a 12-week size fibroid uterus.
Preprocedure right and left arteriograms for vasculature of a 24-week size fibroid uterus.
FIGURE 2 Embolization catheter infusing microparticles within uterine artery
A catheter is passed into the right femoral artery, through the right external iliac artery to the aorta, then down the left common iliac artery to the left internal iliac, down the anterior division to the left uterine artery. Embolization material—polyvinyl alcohol particles or acrylic copolymer beads—is then delivered via catheter in the uterine artery until slow flow or stasis occurs in the artery.
Indications
Like hysterectomy and myomectomy, the indications for UAE are symptomatic fibroids that are unresponsive to medical management (with hormonal agents or analgesics). Common symptoms of fibroids include abdominal or pelvic pain, abnormal menstrual bleeding, anemia, urinary frequency, dyspareunia, and infertility.
UAE may be an especially useful option for women who are poor surgical candidates or have extensive adhesive disease, as well as for those who refuse blood products or are perimenopausal.6,8,9
Contraindications
Pelvic infection, severe contrast allergy, arteriovenous shunting, the presence of an undiagnosed pelvic mass, coagulopathy, renal insufficiency, a history of pelvic radiation, and genital tract malignancy all are contraindications.
Because data are limited on the safety of pregnancy following UAE, some authorities consider the desire for future fertility a relative contraindication.4,7,10
Preoperative evaluation
The preoperative workup should include a thorough history and physical examination by both an interventional radiologist and a gynecologist, a pregnancy test, pelvic imaging via ultrasound or magnetic resonance imaging, and endometrial biopsy to exclude endometrial hyperplasia or cancer. (Patients without abnormal bleeding may not require an endometrial biopsy.)
Outcomes
The average reported symptom improvement is 87%, and the mean reduction in fibroid volume is 46%.1 Most patients see improvement within 3 months of the procedure, with control over the symptoms lasting at least 2 years. At 1 year, 90% of patients report improvement in heavy menstrual bleeding.4
Most patients are discharged within 24 hours of the procedure, compared with 48 to 72 hours for abdominal hysterectomy or myomectomy. They also experience an average recovery period of 8 days, compared with 4 to 6 weeks for abdominal hysterectomy or myomectomy.6
However, a recent study found that women undergoing embolization for fibroids were more likely than those undergoing myomectomy to need further invasive treatment (i.e., repeat embolization or surgery) within 3 to 5 years (29% versus 3%).11
Complications
Most patients report some degree of “post-embolization syndrome,” which is characterized by low-grade fever, pain, malaise, nausea, and leukocytosis, generally within the first 4 days.4 This may be caused by the systemic effects of transient fibroid and uterine ischemia. Although the condition is usually self-limiting and observable on an outpatient basis, these patients are often admitted for antibiotic therapy.
“Post-embolization syndrome” is characterized by low-grade fever, pain, malaise, nausea, and leukocytosis, generally within the first 4 days.
In the most recent series published,12 major complications occurred in 0.5% of embolizations performed for symptomatic fibroids. They include pulmonary embolism, arterial thrombosis, groin hematomas, local infection, guide-wire perforation of arteries, allergic reaction to contrast medium, endometritis, ischemia of pelvic organs, sepsis, and death. Among more than 30,000 procedures performed to date worldwide, there have been 4 related fatalities. In 2 cases, pulmonary embolism occurred within a few days of the procedure; the 2 other deaths occurred within 2 weeks and were related to septicemia and disseminated intravascular coagulation.
There have been reports of total uterine necrosis, transient and permanent ovarian failure, and external sexual dysfunction. These complications may occur up to 2 years after the procedure.1,4,7,10,13-16 Nontarget vascular embolizations of the gluteus muscle, ovaries, labia minora, and bladder wall also have been noted.17,18
When viewed in the context of the large number of procedures performed—and considering the complications associated with myomectomy and hysterectomy—these rare complications show that, overall, UAE is a very safe procedure.
Pregnancy after embolization
Because we lack controlled studies and abundant data, the role of UAE in women contemplating childbearing is unclear. More studies are needed before UAE can be confidently recommended for these women. Premature ovarian failure is an uncommon but recognized complication of UAE.13
Several series and case reports have noted successful pregnancies following UAE.19,20 Our recent report21 on 50 pregnancies following UAE for leiomyomata noted higher rates of cesarean delivery, preterm delivery, malpresentation, spontaneous abortion, and postpartum hemorrhage than in the general population (TABLE). It is unclear whether the increased rate of premature delivery and malpresentation is due to residual fibroids, changes in myometrial vascularity or elasticity, or other unknown labor-associated processes.
Pregnancy outcomes following myomectomy have been reported in several case series, with rates of premature delivery and other complications similar to those for the general population.22,23 Confounding factors (for example, residual fibroids) and the absence of randomized controlled trials, however, make well-founded comparisons of pregnancy outcomes following UAE and myomectomy difficult.
Theoretical concerns about risk of growth restriction and preeclampsia following UAE have been raised. In our study, we did not observe an increase of small-for-gestational-age infants following embolization.21 Uterine rupture during pregnancy after UAE also has been reported.24
TABLE
Rates of pregnancy complications after UAE and in the general population
| PREGNANCY | COMPLICATIONS OF PREGNANCY % (NUMBER AFFECTED/NUMBER OF SUBJECTS STUDIED) | |||||
|---|---|---|---|---|---|---|
| SPONTANEOUS ABORTION | POSTPARTUM HEMORRHAGE | PREMATURE DELIVERY | CESAREAN DELIVERY | SMALL FOR GESTATIONAL AGE | MAL.* | |
| After UAE for leiomyomata | 32 (11/34) | 9(2/23) | 22 (5/23) | 65 (15/23) | 9 (2/22) | 22 (5/23) |
| In the general population | 10-15 | 4-6 | 5-10 | 22 | 10 | 5 |
| UAE=uterine artery embolization | ||||||
| *MAL=malpresentation | ||||||
| Reprinted from the American Journal of Obstetrics and Gynecology, 100, Goldberg J, Pereira L, Berghella V, Pregnancy after uterine artery embolization, 869-872, 2002, with permission from Elsevier. | ||||||
Internet Resources
- Society of Cardiovascular and Interventional Radiologists (www.SIRweb.org)
- Fibroid Uterine Artery Embolization Registry (www.fibroidregistry.org)
- American College of Obstetricians and Gynecologists (www.acog.org)
The authors report no financial relationships with any companies whose products are mentioned in this article.
- Uterine artery embolization (UAE) may be especially useful in women who are poor surgical candidates or have extensive adhesive disease, or who refuse blood products or are perimenopausal.
- The average reported symptom improvement is 87%; the mean reduction in fibroid volume is 46%.
- Most patients are discharged within 24 hours of the procedure and experience an average recovery period of 8 days.
- Women undergoing UAE for fibroids are more likely than those undergoing myomectomy to need further invasive treatment within 3 to 5 years.
- Although several series and case reports have noted successful pregnancies following UAE, desire for fertility is considered a relative contraindication by some authorities.
With the increasing demand for nonsurgical alternatives to hysterectomy or myomectomy for fibroids, uterine artery embolization (UAE) has grown in use and popularity—and most patients report a high level of satisfaction after the procedure.
UAE has been shown to be safe and effective in selected patients with symptomatic fibroids unresponsive to medical treatment. If they are not contemplating pregnancy and do not have additional pelvic pathology, these women may elect UAE as an appropriate alternative to hysterectomy or myomectomy. This article reviews the indications, contraindications, technique, complications, and outcomes of UAE.
Limits of primary surgeries increase demand for UAE
Most of the 590,000 hysterectomies performed each year in the United States are for symptomatic fibroids, the most common tumors of the female reproductive tract.1 Although hysterectomy is the definitive treatment, increasing numbers of patients express a desire for alternatives, primarily to preserve the uterus. While myomectomy spares the uterus, as many as 25% of women who undergo this procedure require another surgery for recurrent symptoms.2 These limitations of the primary surgeries for fibroids have increased the demand for UAE.
Embolization of the uterine arteries has been utilized for more than 20 years to treat pelvic hemorrhage following delivery or abortion, ectopic or cervical pregnancy, gestational trophoblastic disease, or malignancy.3,4 It was first reported as an effective intervention for fibroids in 1995, when Ravina et al5 noted that several women with symptomatic leiomyomata who underwent UAE as a pre-hysterectomy treatment had such significant clinical improvement that hysterectoMy was no longer required.
In a study involving 200 patients undergoing UAE for leiomyomata, Spies et al6 noted improvement in heavy bleeding in 90% (95% confidence interval [CI], 86%, 95%) and a reduction in bulk-related symptoms in 91% (95% CI, 86%, 95%) at 1 year.
Because data are limited on the safety of pregnancy following uterine artery embolization, some authorities consider the desire for future fertility a relative contraindication.
On a global level, more than 30,000 UAE procedures have been performed for symptomatic uterine fibroids.
The economic considerations surrounding uterine artery embolization (UAE) have led to a turf war of sorts between gynecologists and interventional radiologists. In Philadelphia, Pa, the average reimbursement to an interventional radiologist for a UAE is approximately $1,650; for a gynecologist performing a hysterectomy or myomectomy, it is approximately $1,000.
Some Ob/Gyns are reluctant to recommend UAE for their patients for a variety of reasons. Because of this reluctance, UAE is increasingly marketed directly to the consumer over the Internet and in print media. Large proportions of women undergoing UAE are self-referrals or are referred by their gynecologist after specifically requesting the procedure.
UAE may represent a societal savings in terms of direct and indirect costs. For example, a Canadian cost analysis found that UAE was associated with significantly lower hospital costs ($1007.44 Canadian) than abdominal myomectomy ($1,781.73 Canadian).1
Reference
1. Al-Fozan H, Dufort J, Kaplow M, Valenti D, Tulandi T. Cost analysis of myomectomy, hysterectomy, and uterine artery embolization. Am J Obstet Gynecol. 2002;187:1401-1404.
Technique
UAE is a radiologic procedure performed with either local or regional anesthesia. Most commonly, an approach through the right femoral artery is used, after a preliminary arteriogram (FIGURE 1) has been made to visualize the pelvic vasculature.
Fluoroscopic guidance enables a catheter to be passed into the right femoral artery and through the right external iliac artery to the aorta, then down the left common iliac artery to the left internal iliac, down the anterior division, and finally to the left uterine artery. When the catheter is properly positioned, polyvinyl alcohol particles or acrylic copolymer beads (300 microns to 700 microns) are infused until slow flow or stasis occurs in the uterine artery and the fibroid vasculature is occluded (FIGURE 2). The catheter is then pulled back and manipulated into the right uterine artery, which is similarly embolized. Procedure time ranges from 15 to 120 minutes, depending on the patient’s anatomy and the skill of the operator.1,6,7
FIGURE 1 Pre—uterine-artery-embolization arteriograms
Preprocedure right and left arteriograms for vasculature of a 12-week size fibroid uterus.
Preprocedure right and left arteriograms for vasculature of a 24-week size fibroid uterus.
FIGURE 2 Embolization catheter infusing microparticles within uterine artery
A catheter is passed into the right femoral artery, through the right external iliac artery to the aorta, then down the left common iliac artery to the left internal iliac, down the anterior division to the left uterine artery. Embolization material—polyvinyl alcohol particles or acrylic copolymer beads—is then delivered via catheter in the uterine artery until slow flow or stasis occurs in the artery.
Indications
Like hysterectomy and myomectomy, the indications for UAE are symptomatic fibroids that are unresponsive to medical management (with hormonal agents or analgesics). Common symptoms of fibroids include abdominal or pelvic pain, abnormal menstrual bleeding, anemia, urinary frequency, dyspareunia, and infertility.
UAE may be an especially useful option for women who are poor surgical candidates or have extensive adhesive disease, as well as for those who refuse blood products or are perimenopausal.6,8,9
Contraindications
Pelvic infection, severe contrast allergy, arteriovenous shunting, the presence of an undiagnosed pelvic mass, coagulopathy, renal insufficiency, a history of pelvic radiation, and genital tract malignancy all are contraindications.
Because data are limited on the safety of pregnancy following UAE, some authorities consider the desire for future fertility a relative contraindication.4,7,10
Preoperative evaluation
The preoperative workup should include a thorough history and physical examination by both an interventional radiologist and a gynecologist, a pregnancy test, pelvic imaging via ultrasound or magnetic resonance imaging, and endometrial biopsy to exclude endometrial hyperplasia or cancer. (Patients without abnormal bleeding may not require an endometrial biopsy.)
Outcomes
The average reported symptom improvement is 87%, and the mean reduction in fibroid volume is 46%.1 Most patients see improvement within 3 months of the procedure, with control over the symptoms lasting at least 2 years. At 1 year, 90% of patients report improvement in heavy menstrual bleeding.4
Most patients are discharged within 24 hours of the procedure, compared with 48 to 72 hours for abdominal hysterectomy or myomectomy. They also experience an average recovery period of 8 days, compared with 4 to 6 weeks for abdominal hysterectomy or myomectomy.6
However, a recent study found that women undergoing embolization for fibroids were more likely than those undergoing myomectomy to need further invasive treatment (i.e., repeat embolization or surgery) within 3 to 5 years (29% versus 3%).11
Complications
Most patients report some degree of “post-embolization syndrome,” which is characterized by low-grade fever, pain, malaise, nausea, and leukocytosis, generally within the first 4 days.4 This may be caused by the systemic effects of transient fibroid and uterine ischemia. Although the condition is usually self-limiting and observable on an outpatient basis, these patients are often admitted for antibiotic therapy.
“Post-embolization syndrome” is characterized by low-grade fever, pain, malaise, nausea, and leukocytosis, generally within the first 4 days.
In the most recent series published,12 major complications occurred in 0.5% of embolizations performed for symptomatic fibroids. They include pulmonary embolism, arterial thrombosis, groin hematomas, local infection, guide-wire perforation of arteries, allergic reaction to contrast medium, endometritis, ischemia of pelvic organs, sepsis, and death. Among more than 30,000 procedures performed to date worldwide, there have been 4 related fatalities. In 2 cases, pulmonary embolism occurred within a few days of the procedure; the 2 other deaths occurred within 2 weeks and were related to septicemia and disseminated intravascular coagulation.
There have been reports of total uterine necrosis, transient and permanent ovarian failure, and external sexual dysfunction. These complications may occur up to 2 years after the procedure.1,4,7,10,13-16 Nontarget vascular embolizations of the gluteus muscle, ovaries, labia minora, and bladder wall also have been noted.17,18
When viewed in the context of the large number of procedures performed—and considering the complications associated with myomectomy and hysterectomy—these rare complications show that, overall, UAE is a very safe procedure.
Pregnancy after embolization
Because we lack controlled studies and abundant data, the role of UAE in women contemplating childbearing is unclear. More studies are needed before UAE can be confidently recommended for these women. Premature ovarian failure is an uncommon but recognized complication of UAE.13
Several series and case reports have noted successful pregnancies following UAE.19,20 Our recent report21 on 50 pregnancies following UAE for leiomyomata noted higher rates of cesarean delivery, preterm delivery, malpresentation, spontaneous abortion, and postpartum hemorrhage than in the general population (TABLE). It is unclear whether the increased rate of premature delivery and malpresentation is due to residual fibroids, changes in myometrial vascularity or elasticity, or other unknown labor-associated processes.
Pregnancy outcomes following myomectomy have been reported in several case series, with rates of premature delivery and other complications similar to those for the general population.22,23 Confounding factors (for example, residual fibroids) and the absence of randomized controlled trials, however, make well-founded comparisons of pregnancy outcomes following UAE and myomectomy difficult.
Theoretical concerns about risk of growth restriction and preeclampsia following UAE have been raised. In our study, we did not observe an increase of small-for-gestational-age infants following embolization.21 Uterine rupture during pregnancy after UAE also has been reported.24
TABLE
Rates of pregnancy complications after UAE and in the general population
| PREGNANCY | COMPLICATIONS OF PREGNANCY % (NUMBER AFFECTED/NUMBER OF SUBJECTS STUDIED) | |||||
|---|---|---|---|---|---|---|
| SPONTANEOUS ABORTION | POSTPARTUM HEMORRHAGE | PREMATURE DELIVERY | CESAREAN DELIVERY | SMALL FOR GESTATIONAL AGE | MAL.* | |
| After UAE for leiomyomata | 32 (11/34) | 9(2/23) | 22 (5/23) | 65 (15/23) | 9 (2/22) | 22 (5/23) |
| In the general population | 10-15 | 4-6 | 5-10 | 22 | 10 | 5 |
| UAE=uterine artery embolization | ||||||
| *MAL=malpresentation | ||||||
| Reprinted from the American Journal of Obstetrics and Gynecology, 100, Goldberg J, Pereira L, Berghella V, Pregnancy after uterine artery embolization, 869-872, 2002, with permission from Elsevier. | ||||||
Internet Resources
- Society of Cardiovascular and Interventional Radiologists (www.SIRweb.org)
- Fibroid Uterine Artery Embolization Registry (www.fibroidregistry.org)
- American College of Obstetricians and Gynecologists (www.acog.org)
The authors report no financial relationships with any companies whose products are mentioned in this article.
1. Floridon C, Lund N, Thomsen SG. Alternative treatment for symptomatic fibroids. Curr Opin Obstet Gynecol. 2001;13:491-495.
2. Stenchever MA, Droegemueller W, Herbst AL, Mishell DR. Comprehensive Gynecology. 4th ed. St. Louis, Mo: Mosby; 2001.
3. Goodwin SC, Walker WJ. Uterine artery embolization for the treatment of uterine fibroids. Curr Opin Obstet Gynecol. 1998;10:315-320.
4. Schwartz ML, Klein A, McLucas B. Using uterine artery embolization to treat fibroids. Contemporary OB/GYN. 2001;8:14-37.
5. Ravina J, Herbreteau D, Ciraru-Vigneron N, et al. Arterial embolization to treat uterine myomata. Lancet. 1995;346:671-672.
6. Spies JB, Ascher SA, Roth AR, Kim J, Levy EB, Gomez-Jorge J. Uterine artery embolization for leiomyomata. Obstet Gynecol. 2001;98:29-34.
7. Demello AB. Uterine artery embolization. AORN J. 2001;73:788-814.
8. Bradley EA, Reidy JF, Forman RG, Jarosz J, Braude PR. Transcatheter uterine artery embolization to treat large uterine fibroids. Br J Obstet Gynaecol. 1998;15:235-240.
9. Goodwin SC, Vedantham S, McLucas B, Forno A, Perrella R. Preliminary experience with uterine artery embolization for uterine fibroids. J Vasc Interv Radiol. 1997;8:517-520.
10. Godfrey CD, Zbella EA. Uterine necrosis after uterine artery embolization for leiomyoma. Obstet Gynecol. 2001;98:950-952.
11. Broder MS, Goodwin S, Chen G, et al. Comparison of long-term outcomes of myomectomy and uterine artery embolization. Obstet Gynecol. 2002;100:864-868.
12. Spies JB, Spector A, Roth A, Baker C, Mauro L, Murphy-Skyrynarz K. Complications after uterine artery embolization for leiomyomas. Obstet Gynecol. 2002;100:873-880.
13. Amato P, Roberts AC. Transient ovarian failure: a complication of uterine artery embolization. Fertil Steril. 2001;75:438-439.
14. Lai AC, Goodwin SC, Bonilla SM, et al. Sexual dysfunction after uterine artery embolization. J Vasc Interv Radiol. 2000;11:755-758.
15. Stringer N. Diagnosis and management of long-term complications of uterine artery embolization. Female Patient. 2002;27(11):13-24.
16. Vashisht A, Studd J, Carey A, Burn P. Fatal septicaemia after fibroid embolisation. Lancet. 1999;354:307-308.
17. Sultana CJ, Goldberg J, Aizenman L, Chon JK. Vesicouterine fistula after uterine artery embolization: a case report. Am J Obstet Gynecol. 2002;187:1726-1727.
18. Yeagley T, Goldberg J, Klein T, Bonn J. Labial necrosis after uterine artery embolization for leiomyomas. Obstet Gynecol. 2002;100:881.-
19. Vashisht A, Smith JR, Thorpe-Beeston G, McCall J. Pregnancy subsequent to uterine artery embolization. Fertil Steril. 2001;75:1246-1247.
20. Ravina JH, Vigneron NC, Aymard A, Le Dref O, Merland JJ. Pregnancy after embolization of uterine myoma: Report of 12 cases. Fertil Steril. 2000;73:1241-1243.
21. Goldberg J, Pereira L, Berghella V. Pregnancy after uterine artery embolization. Obstet Gynecol. 2002;100:869-872.
22. Seracchioli R, Rossi S, Govoni F, et al. Fertility and obstetric outcome after laparoscopic myomectomy of large myomata: A randomized comparison with abdominal myomectomy. Hum Reprod. 2000;15:2663-2668.
23. Dessolle L, Soriano D, Poncelet C, Benifla JL, Madelenat P, Darai E. Determinants of pregnancy rate and obstetric outcome after laparoscopic myomectomy for infertility. Fertil Steril. 2001;76:370-374.
24. Walker W, Green A, Sutton C. Bilateral uterine artery embolization for myomata: Results, complications, and failures. Min Invas Ther Allied Technol. 1999;8:449-454.
1. Floridon C, Lund N, Thomsen SG. Alternative treatment for symptomatic fibroids. Curr Opin Obstet Gynecol. 2001;13:491-495.
2. Stenchever MA, Droegemueller W, Herbst AL, Mishell DR. Comprehensive Gynecology. 4th ed. St. Louis, Mo: Mosby; 2001.
3. Goodwin SC, Walker WJ. Uterine artery embolization for the treatment of uterine fibroids. Curr Opin Obstet Gynecol. 1998;10:315-320.
4. Schwartz ML, Klein A, McLucas B. Using uterine artery embolization to treat fibroids. Contemporary OB/GYN. 2001;8:14-37.
5. Ravina J, Herbreteau D, Ciraru-Vigneron N, et al. Arterial embolization to treat uterine myomata. Lancet. 1995;346:671-672.
6. Spies JB, Ascher SA, Roth AR, Kim J, Levy EB, Gomez-Jorge J. Uterine artery embolization for leiomyomata. Obstet Gynecol. 2001;98:29-34.
7. Demello AB. Uterine artery embolization. AORN J. 2001;73:788-814.
8. Bradley EA, Reidy JF, Forman RG, Jarosz J, Braude PR. Transcatheter uterine artery embolization to treat large uterine fibroids. Br J Obstet Gynaecol. 1998;15:235-240.
9. Goodwin SC, Vedantham S, McLucas B, Forno A, Perrella R. Preliminary experience with uterine artery embolization for uterine fibroids. J Vasc Interv Radiol. 1997;8:517-520.
10. Godfrey CD, Zbella EA. Uterine necrosis after uterine artery embolization for leiomyoma. Obstet Gynecol. 2001;98:950-952.
11. Broder MS, Goodwin S, Chen G, et al. Comparison of long-term outcomes of myomectomy and uterine artery embolization. Obstet Gynecol. 2002;100:864-868.
12. Spies JB, Spector A, Roth A, Baker C, Mauro L, Murphy-Skyrynarz K. Complications after uterine artery embolization for leiomyomas. Obstet Gynecol. 2002;100:873-880.
13. Amato P, Roberts AC. Transient ovarian failure: a complication of uterine artery embolization. Fertil Steril. 2001;75:438-439.
14. Lai AC, Goodwin SC, Bonilla SM, et al. Sexual dysfunction after uterine artery embolization. J Vasc Interv Radiol. 2000;11:755-758.
15. Stringer N. Diagnosis and management of long-term complications of uterine artery embolization. Female Patient. 2002;27(11):13-24.
16. Vashisht A, Studd J, Carey A, Burn P. Fatal septicaemia after fibroid embolisation. Lancet. 1999;354:307-308.
17. Sultana CJ, Goldberg J, Aizenman L, Chon JK. Vesicouterine fistula after uterine artery embolization: a case report. Am J Obstet Gynecol. 2002;187:1726-1727.
18. Yeagley T, Goldberg J, Klein T, Bonn J. Labial necrosis after uterine artery embolization for leiomyomas. Obstet Gynecol. 2002;100:881.-
19. Vashisht A, Smith JR, Thorpe-Beeston G, McCall J. Pregnancy subsequent to uterine artery embolization. Fertil Steril. 2001;75:1246-1247.
20. Ravina JH, Vigneron NC, Aymard A, Le Dref O, Merland JJ. Pregnancy after embolization of uterine myoma: Report of 12 cases. Fertil Steril. 2000;73:1241-1243.
21. Goldberg J, Pereira L, Berghella V. Pregnancy after uterine artery embolization. Obstet Gynecol. 2002;100:869-872.
22. Seracchioli R, Rossi S, Govoni F, et al. Fertility and obstetric outcome after laparoscopic myomectomy of large myomata: A randomized comparison with abdominal myomectomy. Hum Reprod. 2000;15:2663-2668.
23. Dessolle L, Soriano D, Poncelet C, Benifla JL, Madelenat P, Darai E. Determinants of pregnancy rate and obstetric outcome after laparoscopic myomectomy for infertility. Fertil Steril. 2001;76:370-374.
24. Walker W, Green A, Sutton C. Bilateral uterine artery embolization for myomata: Results, complications, and failures. Min Invas Ther Allied Technol. 1999;8:449-454.
Hysteroscopic myomectomy: Fertility-preserving yet underutilized
- The goal of hysteroscopic myomectomy is complete removal of the fibroid without trauma to normal uterine tissue.
- Patients with Type 0 and Type I fibroids often require only 1 surgery; patients with Type II fibroids should be advised that 2 surgeries may be needed to remove the entire fibroid.
- Adjuvant preoperative hormonal therapy facilitates surgical scheduling, helps prevent further blood loss in patients already suffering from anemia, and reduces distention media intravasation.
- The monopolar loop electrode is the fibroid removal system that is used most often.
Hysteroscopic myomectomy should be offered to all patients with symptomatic submucous fibroids who desire to avoid hysterectomy. Although it is a highly effective, minimally invasive technique, it is underutilized.
Unfortunately, fewer than one third of US gynecologists perform this procedure. In a 1997 survey of members of the American Association of Gynecologic Laparoscopists—an organization committed to minimally invasive surgery—only half of the respondents reported that they perform this surgery.1
The reasons for learning to perform hysteroscopic myomectomy are compelling:
- A large cohort of patients could benefit, since most heavy vaginal bleeding from fibroids is due to the submucous location, and hysteroscopic resection is a much more benign approach than hysterectomy. Symptomatic fibroids account for 27% of all hysterectomies performed in the US (the largest single diagnostic category) and more than 100,000 are performed for fibroids that cause abnormal uterine bleeding.2
- Removing these lesions hysteroscopically greatly improves prognosis in women with recurrent pregnancy loss and infertility due to submucous fibroids.3 Up to 15% of patients presenting with infertility have otherwise asymptomatic uterine defects, including submucous fibroids. For example, a meta-analysis of patients undergoing in vitro fertilization determined that, compared with controls, the relative risk of pregnancy for women with submucous fibroids was 0.32 (95% confidence interval [CI], 0.13–0.70). When the submucous fibroids were resected, the relative risk of pregnancy rose to 1.72 (CI, 1.13–2.58).3
Preoperative evaluation of fibroids
Severity of menorrhagia (the most common symptom) is considered directly related to the volume of the myoma within the endometrial cavity. It is not uncommon to see large tortuous vessels covering the surface of the fibroids; although the exact mechanism of fibroid-related menorrhagia is undetermined, the fragility of these vessels is probably responsible, at least in part.
Additionally, fibroids involving the uterine mucosa or submucosa may interfere with the muscular contraction necessary for hemostasis.
Surgical options and pretreatment depend on fibroid type. Submucous fibroids are classified according to the percentage of the fibroid within the endometrial cavity:4
- Type 0: pedunculated; 100% within the cavity
- Type I: more than 50% within the cavity
- Type II: more than 50% within the myometrium
The type dictates surgical options, determines endometrial pretreatment, and shapes patient expectations. Type 0 and Type I submucosal fibroids are more successfully removed in a single surgery, whereas Type II submucous fibroids usually require 2 procedures for complete removal.5
My preference is office hysteroscopy to evaluate the endometrial cavity combined with vaginal ultrasound to assess intramural disease. The view with the office hysteroscope is the same view you will have during surgery.
Patients with Type II myomas should be informed of the potential need for 2 procedures, as this fact often influences their treatment decisions. In addition, whenever a patient with a Type II myoma is pretreated with a gonadotropin-releasing hormone (GnRH) agonist, the physician should reassess the fibroid preoperatively to ensure that it has not become completely intramural.
Office assessment: Hysteroscopy plus ultrasound. Preoperative assessment can be achieved with a hysterosalpingogram, vaginal ultrasound, hysterosonogram, or office hysteroscopy.
Method. My preference is office hysteroscopy to evaluate the endometrial cavity combined with vaginal ultrasound to assess intramural disease. The view with the office hysteroscope is the same view you will have during surgery. There will be no surprises. With a small flexible hysteroscope using saline for distention, the procedure is done with no tenaculum, no paracervical block, and can be completed with 60 to 100 cc of fluid in less than 1 minute.
Patients are often intrigued to view the myoma responsible for their heavy vaginal bleeding.
Several advantages of preoperative hormonal therapy
Preoperative hormonal therapy has several advantages:
- Since it is best to resect submucous myomas when the endometrium is thin, hormonal therapy facilitates surgical scheduling.
- Since preoperative therapy creates a state of amenorrhea, it enables patients suffering from menorrhagia and anemia to build up their blood counts, reducing the need for transfusion.
- Most importantly, preoperative therapy can reduce blood flow to the uterus, thereby reducing the rate of fluid intravasation.
Adjuvants used for these functions include oral contraceptives, progestogens, danazol, and GnRH agonists. However, a recent Cochrane review suggests that only GnRH agonists reduce fluid absorption during operative hysteroscopy.6
Method. Numerous protocols have been published, but my preference is to administer 1 intramuscular injection of depot leuprolide acetate (7.5 mg) 6 weeks prior to surgery.
A review of ‘systems’
Submucous myomas have been hysteroscopically removed using the neodymium/yttrium aluminum-garnet (Nd:YAG) laser, a monopolar resectoscope loop, a monopolar radiofrequency (RF) vaporizing electrode, a bipolar RF vaporizing electrode, and a bipolar RF loop.
Laser. The Nd:YAG laser is an expensive device that was popular in the late 1980s and early 1990s. It can be used as a cutting tool for pedunculated Type 0 myomas, or it can be used for myolysis by burning numerous holes in the myoma, causing devascularization and shrinkage.7,8
The sole advantage of the Nd:YAG laser is that it can be used in an isotonic-fluid-filled cavity. Now that accurate fluid-monitoring devices are available, the Nd:YAG laser is rarely used for this indication.
Vaporizing electrodes. Both the bipolar system and monopolar vaporizing electrodes utilize very high RF power (200 W to 300 W) to vaporize fibroids. The advantage is that the fibroids are eradicated very quickly, without any bothersome fibroid chips to remove. The bipolar system can be used with isotonic fluid, whereas the monopolar vaporizing electrodes require non-electrolyte-containing distention media.
The main disadvantages of vaporizing electrodes are:
- They do not produce a tissue sample for pathology. While uterine sarcomas are very rare, they are not homogeneous. Therefore, a simple sample prior to vaporization does not rule out the disease.
- Since vaporizing electrodes are used at high power, numerous gas bubbles are produced and enter the vascular system. Fortunately, these bubbles dissipate rapidly in the blood. As long as the rate of formation does not exceed the rate of dissipation, there are no significant clinical sequelae. The surgeon can avoid complications by monitoring the patient’s endtidal CO2 and maintaining communication with the anesthesiologist. If a sudden drop in endtidal CO2 is observed, the surgeon should stop the case until it resolves.9
Monopolar loop electrode. The instrument most commonly used to remove submucosal myomas is the monopolar loop electrode with a continuous-flow resectoscope. This is quite similar to the instrument used to resect the prostate; it has been slightly modified for gynecologic use to provide enhanced fluid inflow and outflow. A key instrument now considered standard is an accurate fluid-monitoring device that can be attached to the resectoscope.
Distention media for monopolar resection. Prior to the introduction of continuous high-flow resectoscopes and fluid-management systems, monopolar resectoscopy could only be performed using a solution of 32% dextran 70 and water because of that formulation’s viscosity and facilitation of visualization in the presence of blood. However, due to complications related to absorption, allergies, and the solution’s sticky residue, it is not used with today’s high-flow technology.
The instrument most commonly used to remove submucosal myomas is the monopolar loop electrode with a continuous-flow resectoscope.
When using nonviscous fluids with monopolar RF energy, a distention medium without electrolytes must be selected. Isotonic physiologic media such as normal saline or lactated Ringer’s solution would cause the energy at the electrode to disperse, eliminating the cutting effect. Contrary to popular belief, there would be no burning of the uterine cavity and no subsequent danger to the patient.
The 3 most commonly used fluids for uterine distention are 1.5% glycine, 3% sorbitol, and 5% mannitol. All 3 lack electrolytes. The glycine and sorbitol solutions are hypotonic, while 5% mannitol is isotonic. Although there is some debate over whether an isotonic non-electrolyte-containing medium is safer than a hypotonic one, the guidelines for fluid monitoring are the same for all 3.
The goal of a hysteroscopic myomectomy is to alleviate symptoms without causing a weak myometrium or intracavitary synechia. This is accomplished by removing the fibroid without traumatizing normal uterine tissue.
As a general rule, the serum sodium level will decrease approximately 10 meq for every liter absorbed in the blood stream. That is why, to predict hyponatremia, the gynecologist must rely on exact measurements of fluid deficits rather than operating time or total volume used.
Fluid management. Significant hyponatremia can result in pulmonary edema, transient blindness, cerebral edema, brainstem herniation, and death. Catastrophic as these complications are, they are almost 100% avoidable with accurate deficit measurements and adherence to sound fluid-management protocols.
At our institution, fluids are monitored using a weighted system, and the fluid deficit is displayed on the surgical screen in real time. When the deficit reaches 1 L, electrolytes are drawn, the patient is given 10 mg of intravenous (IV) furosemide, and attempts are made to finish the surgery as soon as possible. When the deficit reaches 1.5 L, the surgery is discontinued no matter how much or how little remains to complete it.
It is important that the protocol at each institution be agreed upon by the chief of service and anesthesia as well as the director of nursing so that there are no conflicts at the time of surgery.
Uterine distention methods
Numerous methods have been used to distend the uterus: gravity, gas pressure, and electronic pumps and pressure bags. The optimal intrauterine pressure is the minimum pressure that allows for flow, distention, and visualization. Most of the time this ranges from 40 mm Hg to 60 mm Hg. The higher the intrauterine pressure, the more rapid the fluid intravasation, particularly when intrauterine pressure exceeds the mean arterial pressure.
Rapid fluid loss can occur even with low intrauterine pressures. That is because a large venous sinus will have a pressure of 8 mm Hg to 10 mm Hg, while the minimum uterine distention pressure is much greater. Strict adherence to fluid-deficit protocols will minimize the risk of complications from fluid overload.
Surgical technique
The goal of a hysteroscopic myomectomy is to alleviate symptoms without causing a weak myometrium or intracavitary synechia. Ideally, this is accomplished by completely removing the fibroid without traumatizing normal uterine tissue. Removal of the entire myoma reduces the likelihood of recurrence and regrowth.
Surgical technique for removal of Types 0, I, and II fibroids is illustrated and explained on (FIGURES1-4).
Within a given range (40 W to 100 W), it makes little difference which cutting-current setting on the RF generator you use; the principles are the same. The loop must be in contact with the tissue to be resected. Energy is applied and, once the circuit is completed (through tissue, the dispersive electrode, the generator and back to the loop), the loop is able to cut with minimal tactile feedback.
The lower the wattage, the more contact necessary between the loop and the tissue and the longer it takes to complete the circuit. Conversely, the higher the power, the faster the circuit is completed and cutting occurs.
Though it does not matter what setting is used, the operator must choose a setting based on his or her comfort level. Lower power gives the operator more control. Higher power should be used only by the most experienced hysteroscopist, since it involves very little tactile feedback and a higher risk of uterine perforation. At our teaching institution, we use 60 W of pure cutting current.
The technique for removing a submucous fibroid depends on its type and location within the endometrial cavity.
Type 0. Because these fibroids are pedunculated, the operator has the option of cutting the stalk (FIGURE 1) or shaving the myoma to remove it in pieces through the cervix. If the stalk is cut, it often is difficult to remove the fibroid through the cervix due to its large size. Nor can the fibroid be cut with monopolar energy because of the difficulty of completing the circuit. Type 0 myomas can be grabbed blindly with a Corson forceps or under direct visualization with an Isaacson optical tenaculum (Karl Storz Endoscopy, Culver City, Calif.). It also is acceptable to leave the fibroid in the cavity and let it degenerate and be expelled spontaneously. The risk of infection is very small.
My preference is to shave the fibroid down to the endometrium while it is attached to the stalk. I find it easier to remove when it is anchored rather than trying to pull out a single large specimen.
Type I. In a Type I myoma, more than 50% of the fibroid is within the uterine cavity, with a smaller portion embedded in the myometrium. To remove these fibroids, shave each to the level of the endometrium. To do so, place the loop behind the fibroid to be resected (FIGURE 5). Next, activate the RF energy using a foot pedal and, once the circuit is complete, draw the loop back into the resectoscope. Be careful to maintain visualization of the fibroid, loop, and cavity (FIGURE 6). This becomes difficult as the fibroid approaches the resectoscope and obstructs the hysteroscopic lens. To avoid this, bring the loop—which begins its cut fully extended—only halfway back to the resectoscope (FIGURE 7). Then retract the resectoscope itself, with the loop halfway extended, until the cut through the fibroid is complete (FIGURE 8). The loop then is retracted back into the resectoscope. The angle of the resectoscope must be adjusted to maintain loop contact with the fibroid tissue.
When more than 70% or 80% of the fibroid has been resected, the remainder will slough spontaneously over the next 2 to 4 months.
Once the fibroid is resected to the level of the endometrium, remove the fibroid chips (FIGURE 2). Often, when the hysteroscope is removed and uterine distention is reestablished, more of the fibroid will protrude into the cavity, facilitating safe resection. At some point, the fibroid will no longer protrude into the cavity; it will have been removed or only a small percentage will remain intramural.
Often, when more than 70% or 80% of the fibroid has been resected, the remainder will slough spontaneously over the next 2 to 4 months. The technique for removing the intramural fibroid is described on page 78 (FIGURE 3).
Type II. The first step in resecting a Type II myoma is shaving the intracavitary portion to the level of the endometrium, as in the resection of a Type I fibroid. Often, once a small Type II myoma is “unroofed,” the remainder will spontaneously fall into the cavity and can easily be removed.
Larger Type II myomas require a different approach. In these, the goal is to identify the pseudo-capsular plane that allows for blunt dissection. Once you have identified it, use the loop electrode to bluntly dissect (without RF activation) the fibroid from the myometrium. Place the electrode in the capsular plane and retract as much of the myoma into the cavity as possible (FIGURE 4). Another way to do this is to use a twisting motion—similar to those performed in open myomectomies—with the optical tenaculum. Once the fibroid is in the cavity, shave it to the level of the endometrium. Repeat this technique until you have removed as much of the fibroid as possible. Use minimal distention pressure when you perform this technique so that the fibroid will not be pressed back into the myometrium.
Underutilization of hysteroscopic myomectomy may be due to inadequate training in the technique or a misconception that it is difficult to learn. Fortunately, hysteroscope manufacturers are beginning to offer physicians and operating room personnel didactic and hands-on laboratory courses.
FIGURE 1 Surgical technique for removing Type 0, I, II fibroids
Type 0. The loop is placed behind the fibroid. Once activated, the loop is drawn toward the operator to resect the pedicle.
FIGURE 2 Surgical technique for removing Type 0, I, II fibroids
Type I. The myoma is resected to the level of the myometrium.
FIGURE 3 Surgical technique for removing Type 0, I, II fibroids
Resection of intramural portion of Type I and II. The resectoscopic loop is placed in the pseudocapsular lane between the fibroid and the myometrium to bluntly dissect the fibroid into the cavity for further resection.
FIGURE 4 Surgical technique for removing Type 0, I, II fibroids
Type II. The roof of the myoma is shaved off to the level of the myometrium. The insert demonstrates the intramural portion of the myoma that will protrude into the cavity with a reduction in uterine distension pressure.
FIGURE 5 Resect technique—4 steps in resecting a submucous myoma
The loop is placed behind the fibroid with maximal contact with the tissue before RF activation.
FIGURE 6 Resect technique—4 steps in resecting a submucous myoma
The loop is withdrawn toward the operator (see arrow) while cutting the myoma but not so far as to obstruct the hysteroscopic view.
FIGURE 7 Resect technique—4 steps in resecting a submucous myoma
The loop is held in place while the hysteroscope is withdrawn (arrows indicate how to remain in direct contact with myoma) continuing to cut the myoma with visualization.
FIGURE 8 Resect technique—4 steps in resecting a submucous myoma
Once through the myoma, the loop is withdrawn into the hysteroscope.
Management of complications
The primary complications of hysteroscopic myomectomy are bleeding, infection, uterine perforation, and fluid overload.
Bleeding. If postoperative hemorrhage occurs, use a 30-cc Foley balloon to tamponade the vessels, or pack the uterus with gauze soaked in a vasopressin solution. Both can be removed any time from 4 hours to 24 hours following placement. If bleeding persists, uterine artery embolization should be considered prior to hysterectomy.
Most attempts at controlling bleeding with a rollerball are futile because the intrauterine distention pressure necessary to see the venous bleeders hides the actual bleeding. Arterial bleeders can be seen and controlled with the rollerball, but they are much less common.
Infection. Because infection is uncommon with hysteroscopic surgery, routine prophylaxis is unnecessary.
Antibiotics should be used if the patient had cervical laminaria placed preoperatively.
Uterine perforation. The management of uterine perforation depends on the site of perforation and whether energy was used during the perforation. For example, if the perforation was at the fundus and occurred with a blunt, non-energized instrument, observation without laparoscopy is sufficient. If the perforation was lateral or occurred with RF energy, laparoscopy is suggested to rule out a broad ligament hematoma or injury to intraperitoneal vessels and viscera. If the perforation is anterior, a cystoscopy is recommended; internal colon inspection is necessary if the perforation is posterior.
Fluid overload. Complications and prevention can be avoided and treated as previously discussed.
New training opportunities may include virtual reality
Underutilization of hysteroscopic myomectomy may be due to inadequate training in the technique during residency or the misconception that it is difficult to learn. (Training has been further hampered by the lack of a suitable animal model.)
Fortunately, hysteroscope manufacturers are beginning to offer physicians and operating room personnel didactic and hands-on laboratory courses. In the near future, we hope, these companies will hire gynecologic hysteroscopists to support physicians and nurses in the field, as has been done in many other specialties.
The creation of new tools such as virtual-reality simulators will undoubtedly enhance the teaching of operative hysteroscopy.
Dr. Isaacson teaches hysteroscopy courses sponsored by Karl Storz Endoscopy.
1. Hulka JF, Levy BS, Luciano AA, Parker WH, Phillips JM. 1997 AAGL membership survey: practice profiles. J Amer Assoc Gynecol Laparosc. 1998;5:93-96.
2. Carlson KJ, Nichols DH, Schiff I. Indications for hysterectomy. N Eng J Med. 1993;328:856-860.
3. Pritts E. Fibroids and infertility: a systematic review of the evidence. Obstet Gynecol Survey. 2001;56:483-491.
4. deBlok S, Dijkman AB, Hemrika DJ. Transcervical resection of fibroids (TCRM): results related to hysteroscopic classification. Gynaecol Endosc. 1995;4:243-246.
5. Istre O. Transcervical resection of endometrium and fibroids: the outcome of 412 operations performed over 5 years. Acta Obstet Gynecol Scand. 1996;75:567-574.
6. Sowter MC, Lethaby A, Singla AA. Preoperative endometrial thinning agents before hysteroscopic surgery for heavy menstrual bleeding. Cochrane Database Syst Rev. 2002;(3):CD001124.-
7. Baggish MS, Sze EM, Morgan G. Hysteroscopic treatment of symptomatic submucous myomas with the Nd:YAG laser. J Gynecol Surg. 1989;5:27-36.
8. Donnez J, Gillerot S, Bourgonjon D, et al. Neodymium:YAG laser hysteroscopy in large submucous fibroids. Fertil Steril. 1990;54:999-1003.
9. Bloomstone J, Chen C, Isselbacher E, Isaacson K. A pilot study examining the frequency and quantity of gas embolization during operative hysteroscopy using a monopolar resectoscope. J Am Assoc Gynecol Laparosc. 2002;9:9-14.
- The goal of hysteroscopic myomectomy is complete removal of the fibroid without trauma to normal uterine tissue.
- Patients with Type 0 and Type I fibroids often require only 1 surgery; patients with Type II fibroids should be advised that 2 surgeries may be needed to remove the entire fibroid.
- Adjuvant preoperative hormonal therapy facilitates surgical scheduling, helps prevent further blood loss in patients already suffering from anemia, and reduces distention media intravasation.
- The monopolar loop electrode is the fibroid removal system that is used most often.
Hysteroscopic myomectomy should be offered to all patients with symptomatic submucous fibroids who desire to avoid hysterectomy. Although it is a highly effective, minimally invasive technique, it is underutilized.
Unfortunately, fewer than one third of US gynecologists perform this procedure. In a 1997 survey of members of the American Association of Gynecologic Laparoscopists—an organization committed to minimally invasive surgery—only half of the respondents reported that they perform this surgery.1
The reasons for learning to perform hysteroscopic myomectomy are compelling:
- A large cohort of patients could benefit, since most heavy vaginal bleeding from fibroids is due to the submucous location, and hysteroscopic resection is a much more benign approach than hysterectomy. Symptomatic fibroids account for 27% of all hysterectomies performed in the US (the largest single diagnostic category) and more than 100,000 are performed for fibroids that cause abnormal uterine bleeding.2
- Removing these lesions hysteroscopically greatly improves prognosis in women with recurrent pregnancy loss and infertility due to submucous fibroids.3 Up to 15% of patients presenting with infertility have otherwise asymptomatic uterine defects, including submucous fibroids. For example, a meta-analysis of patients undergoing in vitro fertilization determined that, compared with controls, the relative risk of pregnancy for women with submucous fibroids was 0.32 (95% confidence interval [CI], 0.13–0.70). When the submucous fibroids were resected, the relative risk of pregnancy rose to 1.72 (CI, 1.13–2.58).3
Preoperative evaluation of fibroids
Severity of menorrhagia (the most common symptom) is considered directly related to the volume of the myoma within the endometrial cavity. It is not uncommon to see large tortuous vessels covering the surface of the fibroids; although the exact mechanism of fibroid-related menorrhagia is undetermined, the fragility of these vessels is probably responsible, at least in part.
Additionally, fibroids involving the uterine mucosa or submucosa may interfere with the muscular contraction necessary for hemostasis.
Surgical options and pretreatment depend on fibroid type. Submucous fibroids are classified according to the percentage of the fibroid within the endometrial cavity:4
- Type 0: pedunculated; 100% within the cavity
- Type I: more than 50% within the cavity
- Type II: more than 50% within the myometrium
The type dictates surgical options, determines endometrial pretreatment, and shapes patient expectations. Type 0 and Type I submucosal fibroids are more successfully removed in a single surgery, whereas Type II submucous fibroids usually require 2 procedures for complete removal.5
My preference is office hysteroscopy to evaluate the endometrial cavity combined with vaginal ultrasound to assess intramural disease. The view with the office hysteroscope is the same view you will have during surgery.
Patients with Type II myomas should be informed of the potential need for 2 procedures, as this fact often influences their treatment decisions. In addition, whenever a patient with a Type II myoma is pretreated with a gonadotropin-releasing hormone (GnRH) agonist, the physician should reassess the fibroid preoperatively to ensure that it has not become completely intramural.
Office assessment: Hysteroscopy plus ultrasound. Preoperative assessment can be achieved with a hysterosalpingogram, vaginal ultrasound, hysterosonogram, or office hysteroscopy.
Method. My preference is office hysteroscopy to evaluate the endometrial cavity combined with vaginal ultrasound to assess intramural disease. The view with the office hysteroscope is the same view you will have during surgery. There will be no surprises. With a small flexible hysteroscope using saline for distention, the procedure is done with no tenaculum, no paracervical block, and can be completed with 60 to 100 cc of fluid in less than 1 minute.
Patients are often intrigued to view the myoma responsible for their heavy vaginal bleeding.
Several advantages of preoperative hormonal therapy
Preoperative hormonal therapy has several advantages:
- Since it is best to resect submucous myomas when the endometrium is thin, hormonal therapy facilitates surgical scheduling.
- Since preoperative therapy creates a state of amenorrhea, it enables patients suffering from menorrhagia and anemia to build up their blood counts, reducing the need for transfusion.
- Most importantly, preoperative therapy can reduce blood flow to the uterus, thereby reducing the rate of fluid intravasation.
Adjuvants used for these functions include oral contraceptives, progestogens, danazol, and GnRH agonists. However, a recent Cochrane review suggests that only GnRH agonists reduce fluid absorption during operative hysteroscopy.6
Method. Numerous protocols have been published, but my preference is to administer 1 intramuscular injection of depot leuprolide acetate (7.5 mg) 6 weeks prior to surgery.
A review of ‘systems’
Submucous myomas have been hysteroscopically removed using the neodymium/yttrium aluminum-garnet (Nd:YAG) laser, a monopolar resectoscope loop, a monopolar radiofrequency (RF) vaporizing electrode, a bipolar RF vaporizing electrode, and a bipolar RF loop.
Laser. The Nd:YAG laser is an expensive device that was popular in the late 1980s and early 1990s. It can be used as a cutting tool for pedunculated Type 0 myomas, or it can be used for myolysis by burning numerous holes in the myoma, causing devascularization and shrinkage.7,8
The sole advantage of the Nd:YAG laser is that it can be used in an isotonic-fluid-filled cavity. Now that accurate fluid-monitoring devices are available, the Nd:YAG laser is rarely used for this indication.
Vaporizing electrodes. Both the bipolar system and monopolar vaporizing electrodes utilize very high RF power (200 W to 300 W) to vaporize fibroids. The advantage is that the fibroids are eradicated very quickly, without any bothersome fibroid chips to remove. The bipolar system can be used with isotonic fluid, whereas the monopolar vaporizing electrodes require non-electrolyte-containing distention media.
The main disadvantages of vaporizing electrodes are:
- They do not produce a tissue sample for pathology. While uterine sarcomas are very rare, they are not homogeneous. Therefore, a simple sample prior to vaporization does not rule out the disease.
- Since vaporizing electrodes are used at high power, numerous gas bubbles are produced and enter the vascular system. Fortunately, these bubbles dissipate rapidly in the blood. As long as the rate of formation does not exceed the rate of dissipation, there are no significant clinical sequelae. The surgeon can avoid complications by monitoring the patient’s endtidal CO2 and maintaining communication with the anesthesiologist. If a sudden drop in endtidal CO2 is observed, the surgeon should stop the case until it resolves.9
Monopolar loop electrode. The instrument most commonly used to remove submucosal myomas is the monopolar loop electrode with a continuous-flow resectoscope. This is quite similar to the instrument used to resect the prostate; it has been slightly modified for gynecologic use to provide enhanced fluid inflow and outflow. A key instrument now considered standard is an accurate fluid-monitoring device that can be attached to the resectoscope.
Distention media for monopolar resection. Prior to the introduction of continuous high-flow resectoscopes and fluid-management systems, monopolar resectoscopy could only be performed using a solution of 32% dextran 70 and water because of that formulation’s viscosity and facilitation of visualization in the presence of blood. However, due to complications related to absorption, allergies, and the solution’s sticky residue, it is not used with today’s high-flow technology.
The instrument most commonly used to remove submucosal myomas is the monopolar loop electrode with a continuous-flow resectoscope.
When using nonviscous fluids with monopolar RF energy, a distention medium without electrolytes must be selected. Isotonic physiologic media such as normal saline or lactated Ringer’s solution would cause the energy at the electrode to disperse, eliminating the cutting effect. Contrary to popular belief, there would be no burning of the uterine cavity and no subsequent danger to the patient.
The 3 most commonly used fluids for uterine distention are 1.5% glycine, 3% sorbitol, and 5% mannitol. All 3 lack electrolytes. The glycine and sorbitol solutions are hypotonic, while 5% mannitol is isotonic. Although there is some debate over whether an isotonic non-electrolyte-containing medium is safer than a hypotonic one, the guidelines for fluid monitoring are the same for all 3.
The goal of a hysteroscopic myomectomy is to alleviate symptoms without causing a weak myometrium or intracavitary synechia. This is accomplished by removing the fibroid without traumatizing normal uterine tissue.
As a general rule, the serum sodium level will decrease approximately 10 meq for every liter absorbed in the blood stream. That is why, to predict hyponatremia, the gynecologist must rely on exact measurements of fluid deficits rather than operating time or total volume used.
Fluid management. Significant hyponatremia can result in pulmonary edema, transient blindness, cerebral edema, brainstem herniation, and death. Catastrophic as these complications are, they are almost 100% avoidable with accurate deficit measurements and adherence to sound fluid-management protocols.
At our institution, fluids are monitored using a weighted system, and the fluid deficit is displayed on the surgical screen in real time. When the deficit reaches 1 L, electrolytes are drawn, the patient is given 10 mg of intravenous (IV) furosemide, and attempts are made to finish the surgery as soon as possible. When the deficit reaches 1.5 L, the surgery is discontinued no matter how much or how little remains to complete it.
It is important that the protocol at each institution be agreed upon by the chief of service and anesthesia as well as the director of nursing so that there are no conflicts at the time of surgery.
Uterine distention methods
Numerous methods have been used to distend the uterus: gravity, gas pressure, and electronic pumps and pressure bags. The optimal intrauterine pressure is the minimum pressure that allows for flow, distention, and visualization. Most of the time this ranges from 40 mm Hg to 60 mm Hg. The higher the intrauterine pressure, the more rapid the fluid intravasation, particularly when intrauterine pressure exceeds the mean arterial pressure.
Rapid fluid loss can occur even with low intrauterine pressures. That is because a large venous sinus will have a pressure of 8 mm Hg to 10 mm Hg, while the minimum uterine distention pressure is much greater. Strict adherence to fluid-deficit protocols will minimize the risk of complications from fluid overload.
Surgical technique
The goal of a hysteroscopic myomectomy is to alleviate symptoms without causing a weak myometrium or intracavitary synechia. Ideally, this is accomplished by completely removing the fibroid without traumatizing normal uterine tissue. Removal of the entire myoma reduces the likelihood of recurrence and regrowth.
Surgical technique for removal of Types 0, I, and II fibroids is illustrated and explained on (FIGURES1-4).
Within a given range (40 W to 100 W), it makes little difference which cutting-current setting on the RF generator you use; the principles are the same. The loop must be in contact with the tissue to be resected. Energy is applied and, once the circuit is completed (through tissue, the dispersive electrode, the generator and back to the loop), the loop is able to cut with minimal tactile feedback.
The lower the wattage, the more contact necessary between the loop and the tissue and the longer it takes to complete the circuit. Conversely, the higher the power, the faster the circuit is completed and cutting occurs.
Though it does not matter what setting is used, the operator must choose a setting based on his or her comfort level. Lower power gives the operator more control. Higher power should be used only by the most experienced hysteroscopist, since it involves very little tactile feedback and a higher risk of uterine perforation. At our teaching institution, we use 60 W of pure cutting current.
The technique for removing a submucous fibroid depends on its type and location within the endometrial cavity.
Type 0. Because these fibroids are pedunculated, the operator has the option of cutting the stalk (FIGURE 1) or shaving the myoma to remove it in pieces through the cervix. If the stalk is cut, it often is difficult to remove the fibroid through the cervix due to its large size. Nor can the fibroid be cut with monopolar energy because of the difficulty of completing the circuit. Type 0 myomas can be grabbed blindly with a Corson forceps or under direct visualization with an Isaacson optical tenaculum (Karl Storz Endoscopy, Culver City, Calif.). It also is acceptable to leave the fibroid in the cavity and let it degenerate and be expelled spontaneously. The risk of infection is very small.
My preference is to shave the fibroid down to the endometrium while it is attached to the stalk. I find it easier to remove when it is anchored rather than trying to pull out a single large specimen.
Type I. In a Type I myoma, more than 50% of the fibroid is within the uterine cavity, with a smaller portion embedded in the myometrium. To remove these fibroids, shave each to the level of the endometrium. To do so, place the loop behind the fibroid to be resected (FIGURE 5). Next, activate the RF energy using a foot pedal and, once the circuit is complete, draw the loop back into the resectoscope. Be careful to maintain visualization of the fibroid, loop, and cavity (FIGURE 6). This becomes difficult as the fibroid approaches the resectoscope and obstructs the hysteroscopic lens. To avoid this, bring the loop—which begins its cut fully extended—only halfway back to the resectoscope (FIGURE 7). Then retract the resectoscope itself, with the loop halfway extended, until the cut through the fibroid is complete (FIGURE 8). The loop then is retracted back into the resectoscope. The angle of the resectoscope must be adjusted to maintain loop contact with the fibroid tissue.
When more than 70% or 80% of the fibroid has been resected, the remainder will slough spontaneously over the next 2 to 4 months.
Once the fibroid is resected to the level of the endometrium, remove the fibroid chips (FIGURE 2). Often, when the hysteroscope is removed and uterine distention is reestablished, more of the fibroid will protrude into the cavity, facilitating safe resection. At some point, the fibroid will no longer protrude into the cavity; it will have been removed or only a small percentage will remain intramural.
Often, when more than 70% or 80% of the fibroid has been resected, the remainder will slough spontaneously over the next 2 to 4 months. The technique for removing the intramural fibroid is described on page 78 (FIGURE 3).
Type II. The first step in resecting a Type II myoma is shaving the intracavitary portion to the level of the endometrium, as in the resection of a Type I fibroid. Often, once a small Type II myoma is “unroofed,” the remainder will spontaneously fall into the cavity and can easily be removed.
Larger Type II myomas require a different approach. In these, the goal is to identify the pseudo-capsular plane that allows for blunt dissection. Once you have identified it, use the loop electrode to bluntly dissect (without RF activation) the fibroid from the myometrium. Place the electrode in the capsular plane and retract as much of the myoma into the cavity as possible (FIGURE 4). Another way to do this is to use a twisting motion—similar to those performed in open myomectomies—with the optical tenaculum. Once the fibroid is in the cavity, shave it to the level of the endometrium. Repeat this technique until you have removed as much of the fibroid as possible. Use minimal distention pressure when you perform this technique so that the fibroid will not be pressed back into the myometrium.
Underutilization of hysteroscopic myomectomy may be due to inadequate training in the technique or a misconception that it is difficult to learn. Fortunately, hysteroscope manufacturers are beginning to offer physicians and operating room personnel didactic and hands-on laboratory courses.
FIGURE 1 Surgical technique for removing Type 0, I, II fibroids
Type 0. The loop is placed behind the fibroid. Once activated, the loop is drawn toward the operator to resect the pedicle.
FIGURE 2 Surgical technique for removing Type 0, I, II fibroids
Type I. The myoma is resected to the level of the myometrium.
FIGURE 3 Surgical technique for removing Type 0, I, II fibroids
Resection of intramural portion of Type I and II. The resectoscopic loop is placed in the pseudocapsular lane between the fibroid and the myometrium to bluntly dissect the fibroid into the cavity for further resection.
FIGURE 4 Surgical technique for removing Type 0, I, II fibroids
Type II. The roof of the myoma is shaved off to the level of the myometrium. The insert demonstrates the intramural portion of the myoma that will protrude into the cavity with a reduction in uterine distension pressure.
FIGURE 5 Resect technique—4 steps in resecting a submucous myoma
The loop is placed behind the fibroid with maximal contact with the tissue before RF activation.
FIGURE 6 Resect technique—4 steps in resecting a submucous myoma
The loop is withdrawn toward the operator (see arrow) while cutting the myoma but not so far as to obstruct the hysteroscopic view.
FIGURE 7 Resect technique—4 steps in resecting a submucous myoma
The loop is held in place while the hysteroscope is withdrawn (arrows indicate how to remain in direct contact with myoma) continuing to cut the myoma with visualization.
FIGURE 8 Resect technique—4 steps in resecting a submucous myoma
Once through the myoma, the loop is withdrawn into the hysteroscope.
Management of complications
The primary complications of hysteroscopic myomectomy are bleeding, infection, uterine perforation, and fluid overload.
Bleeding. If postoperative hemorrhage occurs, use a 30-cc Foley balloon to tamponade the vessels, or pack the uterus with gauze soaked in a vasopressin solution. Both can be removed any time from 4 hours to 24 hours following placement. If bleeding persists, uterine artery embolization should be considered prior to hysterectomy.
Most attempts at controlling bleeding with a rollerball are futile because the intrauterine distention pressure necessary to see the venous bleeders hides the actual bleeding. Arterial bleeders can be seen and controlled with the rollerball, but they are much less common.
Infection. Because infection is uncommon with hysteroscopic surgery, routine prophylaxis is unnecessary.
Antibiotics should be used if the patient had cervical laminaria placed preoperatively.
Uterine perforation. The management of uterine perforation depends on the site of perforation and whether energy was used during the perforation. For example, if the perforation was at the fundus and occurred with a blunt, non-energized instrument, observation without laparoscopy is sufficient. If the perforation was lateral or occurred with RF energy, laparoscopy is suggested to rule out a broad ligament hematoma or injury to intraperitoneal vessels and viscera. If the perforation is anterior, a cystoscopy is recommended; internal colon inspection is necessary if the perforation is posterior.
Fluid overload. Complications and prevention can be avoided and treated as previously discussed.
New training opportunities may include virtual reality
Underutilization of hysteroscopic myomectomy may be due to inadequate training in the technique during residency or the misconception that it is difficult to learn. (Training has been further hampered by the lack of a suitable animal model.)
Fortunately, hysteroscope manufacturers are beginning to offer physicians and operating room personnel didactic and hands-on laboratory courses. In the near future, we hope, these companies will hire gynecologic hysteroscopists to support physicians and nurses in the field, as has been done in many other specialties.
The creation of new tools such as virtual-reality simulators will undoubtedly enhance the teaching of operative hysteroscopy.
Dr. Isaacson teaches hysteroscopy courses sponsored by Karl Storz Endoscopy.
- The goal of hysteroscopic myomectomy is complete removal of the fibroid without trauma to normal uterine tissue.
- Patients with Type 0 and Type I fibroids often require only 1 surgery; patients with Type II fibroids should be advised that 2 surgeries may be needed to remove the entire fibroid.
- Adjuvant preoperative hormonal therapy facilitates surgical scheduling, helps prevent further blood loss in patients already suffering from anemia, and reduces distention media intravasation.
- The monopolar loop electrode is the fibroid removal system that is used most often.
Hysteroscopic myomectomy should be offered to all patients with symptomatic submucous fibroids who desire to avoid hysterectomy. Although it is a highly effective, minimally invasive technique, it is underutilized.
Unfortunately, fewer than one third of US gynecologists perform this procedure. In a 1997 survey of members of the American Association of Gynecologic Laparoscopists—an organization committed to minimally invasive surgery—only half of the respondents reported that they perform this surgery.1
The reasons for learning to perform hysteroscopic myomectomy are compelling:
- A large cohort of patients could benefit, since most heavy vaginal bleeding from fibroids is due to the submucous location, and hysteroscopic resection is a much more benign approach than hysterectomy. Symptomatic fibroids account for 27% of all hysterectomies performed in the US (the largest single diagnostic category) and more than 100,000 are performed for fibroids that cause abnormal uterine bleeding.2
- Removing these lesions hysteroscopically greatly improves prognosis in women with recurrent pregnancy loss and infertility due to submucous fibroids.3 Up to 15% of patients presenting with infertility have otherwise asymptomatic uterine defects, including submucous fibroids. For example, a meta-analysis of patients undergoing in vitro fertilization determined that, compared with controls, the relative risk of pregnancy for women with submucous fibroids was 0.32 (95% confidence interval [CI], 0.13–0.70). When the submucous fibroids were resected, the relative risk of pregnancy rose to 1.72 (CI, 1.13–2.58).3
Preoperative evaluation of fibroids
Severity of menorrhagia (the most common symptom) is considered directly related to the volume of the myoma within the endometrial cavity. It is not uncommon to see large tortuous vessels covering the surface of the fibroids; although the exact mechanism of fibroid-related menorrhagia is undetermined, the fragility of these vessels is probably responsible, at least in part.
Additionally, fibroids involving the uterine mucosa or submucosa may interfere with the muscular contraction necessary for hemostasis.
Surgical options and pretreatment depend on fibroid type. Submucous fibroids are classified according to the percentage of the fibroid within the endometrial cavity:4
- Type 0: pedunculated; 100% within the cavity
- Type I: more than 50% within the cavity
- Type II: more than 50% within the myometrium
The type dictates surgical options, determines endometrial pretreatment, and shapes patient expectations. Type 0 and Type I submucosal fibroids are more successfully removed in a single surgery, whereas Type II submucous fibroids usually require 2 procedures for complete removal.5
My preference is office hysteroscopy to evaluate the endometrial cavity combined with vaginal ultrasound to assess intramural disease. The view with the office hysteroscope is the same view you will have during surgery.
Patients with Type II myomas should be informed of the potential need for 2 procedures, as this fact often influences their treatment decisions. In addition, whenever a patient with a Type II myoma is pretreated with a gonadotropin-releasing hormone (GnRH) agonist, the physician should reassess the fibroid preoperatively to ensure that it has not become completely intramural.
Office assessment: Hysteroscopy plus ultrasound. Preoperative assessment can be achieved with a hysterosalpingogram, vaginal ultrasound, hysterosonogram, or office hysteroscopy.
Method. My preference is office hysteroscopy to evaluate the endometrial cavity combined with vaginal ultrasound to assess intramural disease. The view with the office hysteroscope is the same view you will have during surgery. There will be no surprises. With a small flexible hysteroscope using saline for distention, the procedure is done with no tenaculum, no paracervical block, and can be completed with 60 to 100 cc of fluid in less than 1 minute.
Patients are often intrigued to view the myoma responsible for their heavy vaginal bleeding.
Several advantages of preoperative hormonal therapy
Preoperative hormonal therapy has several advantages:
- Since it is best to resect submucous myomas when the endometrium is thin, hormonal therapy facilitates surgical scheduling.
- Since preoperative therapy creates a state of amenorrhea, it enables patients suffering from menorrhagia and anemia to build up their blood counts, reducing the need for transfusion.
- Most importantly, preoperative therapy can reduce blood flow to the uterus, thereby reducing the rate of fluid intravasation.
Adjuvants used for these functions include oral contraceptives, progestogens, danazol, and GnRH agonists. However, a recent Cochrane review suggests that only GnRH agonists reduce fluid absorption during operative hysteroscopy.6
Method. Numerous protocols have been published, but my preference is to administer 1 intramuscular injection of depot leuprolide acetate (7.5 mg) 6 weeks prior to surgery.
A review of ‘systems’
Submucous myomas have been hysteroscopically removed using the neodymium/yttrium aluminum-garnet (Nd:YAG) laser, a monopolar resectoscope loop, a monopolar radiofrequency (RF) vaporizing electrode, a bipolar RF vaporizing electrode, and a bipolar RF loop.
Laser. The Nd:YAG laser is an expensive device that was popular in the late 1980s and early 1990s. It can be used as a cutting tool for pedunculated Type 0 myomas, or it can be used for myolysis by burning numerous holes in the myoma, causing devascularization and shrinkage.7,8
The sole advantage of the Nd:YAG laser is that it can be used in an isotonic-fluid-filled cavity. Now that accurate fluid-monitoring devices are available, the Nd:YAG laser is rarely used for this indication.
Vaporizing electrodes. Both the bipolar system and monopolar vaporizing electrodes utilize very high RF power (200 W to 300 W) to vaporize fibroids. The advantage is that the fibroids are eradicated very quickly, without any bothersome fibroid chips to remove. The bipolar system can be used with isotonic fluid, whereas the monopolar vaporizing electrodes require non-electrolyte-containing distention media.
The main disadvantages of vaporizing electrodes are:
- They do not produce a tissue sample for pathology. While uterine sarcomas are very rare, they are not homogeneous. Therefore, a simple sample prior to vaporization does not rule out the disease.
- Since vaporizing electrodes are used at high power, numerous gas bubbles are produced and enter the vascular system. Fortunately, these bubbles dissipate rapidly in the blood. As long as the rate of formation does not exceed the rate of dissipation, there are no significant clinical sequelae. The surgeon can avoid complications by monitoring the patient’s endtidal CO2 and maintaining communication with the anesthesiologist. If a sudden drop in endtidal CO2 is observed, the surgeon should stop the case until it resolves.9
Monopolar loop electrode. The instrument most commonly used to remove submucosal myomas is the monopolar loop electrode with a continuous-flow resectoscope. This is quite similar to the instrument used to resect the prostate; it has been slightly modified for gynecologic use to provide enhanced fluid inflow and outflow. A key instrument now considered standard is an accurate fluid-monitoring device that can be attached to the resectoscope.
Distention media for monopolar resection. Prior to the introduction of continuous high-flow resectoscopes and fluid-management systems, monopolar resectoscopy could only be performed using a solution of 32% dextran 70 and water because of that formulation’s viscosity and facilitation of visualization in the presence of blood. However, due to complications related to absorption, allergies, and the solution’s sticky residue, it is not used with today’s high-flow technology.
The instrument most commonly used to remove submucosal myomas is the monopolar loop electrode with a continuous-flow resectoscope.
When using nonviscous fluids with monopolar RF energy, a distention medium without electrolytes must be selected. Isotonic physiologic media such as normal saline or lactated Ringer’s solution would cause the energy at the electrode to disperse, eliminating the cutting effect. Contrary to popular belief, there would be no burning of the uterine cavity and no subsequent danger to the patient.
The 3 most commonly used fluids for uterine distention are 1.5% glycine, 3% sorbitol, and 5% mannitol. All 3 lack electrolytes. The glycine and sorbitol solutions are hypotonic, while 5% mannitol is isotonic. Although there is some debate over whether an isotonic non-electrolyte-containing medium is safer than a hypotonic one, the guidelines for fluid monitoring are the same for all 3.
The goal of a hysteroscopic myomectomy is to alleviate symptoms without causing a weak myometrium or intracavitary synechia. This is accomplished by removing the fibroid without traumatizing normal uterine tissue.
As a general rule, the serum sodium level will decrease approximately 10 meq for every liter absorbed in the blood stream. That is why, to predict hyponatremia, the gynecologist must rely on exact measurements of fluid deficits rather than operating time or total volume used.
Fluid management. Significant hyponatremia can result in pulmonary edema, transient blindness, cerebral edema, brainstem herniation, and death. Catastrophic as these complications are, they are almost 100% avoidable with accurate deficit measurements and adherence to sound fluid-management protocols.
At our institution, fluids are monitored using a weighted system, and the fluid deficit is displayed on the surgical screen in real time. When the deficit reaches 1 L, electrolytes are drawn, the patient is given 10 mg of intravenous (IV) furosemide, and attempts are made to finish the surgery as soon as possible. When the deficit reaches 1.5 L, the surgery is discontinued no matter how much or how little remains to complete it.
It is important that the protocol at each institution be agreed upon by the chief of service and anesthesia as well as the director of nursing so that there are no conflicts at the time of surgery.
Uterine distention methods
Numerous methods have been used to distend the uterus: gravity, gas pressure, and electronic pumps and pressure bags. The optimal intrauterine pressure is the minimum pressure that allows for flow, distention, and visualization. Most of the time this ranges from 40 mm Hg to 60 mm Hg. The higher the intrauterine pressure, the more rapid the fluid intravasation, particularly when intrauterine pressure exceeds the mean arterial pressure.
Rapid fluid loss can occur even with low intrauterine pressures. That is because a large venous sinus will have a pressure of 8 mm Hg to 10 mm Hg, while the minimum uterine distention pressure is much greater. Strict adherence to fluid-deficit protocols will minimize the risk of complications from fluid overload.
Surgical technique
The goal of a hysteroscopic myomectomy is to alleviate symptoms without causing a weak myometrium or intracavitary synechia. Ideally, this is accomplished by completely removing the fibroid without traumatizing normal uterine tissue. Removal of the entire myoma reduces the likelihood of recurrence and regrowth.
Surgical technique for removal of Types 0, I, and II fibroids is illustrated and explained on (FIGURES1-4).
Within a given range (40 W to 100 W), it makes little difference which cutting-current setting on the RF generator you use; the principles are the same. The loop must be in contact with the tissue to be resected. Energy is applied and, once the circuit is completed (through tissue, the dispersive electrode, the generator and back to the loop), the loop is able to cut with minimal tactile feedback.
The lower the wattage, the more contact necessary between the loop and the tissue and the longer it takes to complete the circuit. Conversely, the higher the power, the faster the circuit is completed and cutting occurs.
Though it does not matter what setting is used, the operator must choose a setting based on his or her comfort level. Lower power gives the operator more control. Higher power should be used only by the most experienced hysteroscopist, since it involves very little tactile feedback and a higher risk of uterine perforation. At our teaching institution, we use 60 W of pure cutting current.
The technique for removing a submucous fibroid depends on its type and location within the endometrial cavity.
Type 0. Because these fibroids are pedunculated, the operator has the option of cutting the stalk (FIGURE 1) or shaving the myoma to remove it in pieces through the cervix. If the stalk is cut, it often is difficult to remove the fibroid through the cervix due to its large size. Nor can the fibroid be cut with monopolar energy because of the difficulty of completing the circuit. Type 0 myomas can be grabbed blindly with a Corson forceps or under direct visualization with an Isaacson optical tenaculum (Karl Storz Endoscopy, Culver City, Calif.). It also is acceptable to leave the fibroid in the cavity and let it degenerate and be expelled spontaneously. The risk of infection is very small.
My preference is to shave the fibroid down to the endometrium while it is attached to the stalk. I find it easier to remove when it is anchored rather than trying to pull out a single large specimen.
Type I. In a Type I myoma, more than 50% of the fibroid is within the uterine cavity, with a smaller portion embedded in the myometrium. To remove these fibroids, shave each to the level of the endometrium. To do so, place the loop behind the fibroid to be resected (FIGURE 5). Next, activate the RF energy using a foot pedal and, once the circuit is complete, draw the loop back into the resectoscope. Be careful to maintain visualization of the fibroid, loop, and cavity (FIGURE 6). This becomes difficult as the fibroid approaches the resectoscope and obstructs the hysteroscopic lens. To avoid this, bring the loop—which begins its cut fully extended—only halfway back to the resectoscope (FIGURE 7). Then retract the resectoscope itself, with the loop halfway extended, until the cut through the fibroid is complete (FIGURE 8). The loop then is retracted back into the resectoscope. The angle of the resectoscope must be adjusted to maintain loop contact with the fibroid tissue.
When more than 70% or 80% of the fibroid has been resected, the remainder will slough spontaneously over the next 2 to 4 months.
Once the fibroid is resected to the level of the endometrium, remove the fibroid chips (FIGURE 2). Often, when the hysteroscope is removed and uterine distention is reestablished, more of the fibroid will protrude into the cavity, facilitating safe resection. At some point, the fibroid will no longer protrude into the cavity; it will have been removed or only a small percentage will remain intramural.
Often, when more than 70% or 80% of the fibroid has been resected, the remainder will slough spontaneously over the next 2 to 4 months. The technique for removing the intramural fibroid is described on page 78 (FIGURE 3).
Type II. The first step in resecting a Type II myoma is shaving the intracavitary portion to the level of the endometrium, as in the resection of a Type I fibroid. Often, once a small Type II myoma is “unroofed,” the remainder will spontaneously fall into the cavity and can easily be removed.
Larger Type II myomas require a different approach. In these, the goal is to identify the pseudo-capsular plane that allows for blunt dissection. Once you have identified it, use the loop electrode to bluntly dissect (without RF activation) the fibroid from the myometrium. Place the electrode in the capsular plane and retract as much of the myoma into the cavity as possible (FIGURE 4). Another way to do this is to use a twisting motion—similar to those performed in open myomectomies—with the optical tenaculum. Once the fibroid is in the cavity, shave it to the level of the endometrium. Repeat this technique until you have removed as much of the fibroid as possible. Use minimal distention pressure when you perform this technique so that the fibroid will not be pressed back into the myometrium.
Underutilization of hysteroscopic myomectomy may be due to inadequate training in the technique or a misconception that it is difficult to learn. Fortunately, hysteroscope manufacturers are beginning to offer physicians and operating room personnel didactic and hands-on laboratory courses.
FIGURE 1 Surgical technique for removing Type 0, I, II fibroids
Type 0. The loop is placed behind the fibroid. Once activated, the loop is drawn toward the operator to resect the pedicle.
FIGURE 2 Surgical technique for removing Type 0, I, II fibroids
Type I. The myoma is resected to the level of the myometrium.
FIGURE 3 Surgical technique for removing Type 0, I, II fibroids
Resection of intramural portion of Type I and II. The resectoscopic loop is placed in the pseudocapsular lane between the fibroid and the myometrium to bluntly dissect the fibroid into the cavity for further resection.
FIGURE 4 Surgical technique for removing Type 0, I, II fibroids
Type II. The roof of the myoma is shaved off to the level of the myometrium. The insert demonstrates the intramural portion of the myoma that will protrude into the cavity with a reduction in uterine distension pressure.
FIGURE 5 Resect technique—4 steps in resecting a submucous myoma
The loop is placed behind the fibroid with maximal contact with the tissue before RF activation.
FIGURE 6 Resect technique—4 steps in resecting a submucous myoma
The loop is withdrawn toward the operator (see arrow) while cutting the myoma but not so far as to obstruct the hysteroscopic view.
FIGURE 7 Resect technique—4 steps in resecting a submucous myoma
The loop is held in place while the hysteroscope is withdrawn (arrows indicate how to remain in direct contact with myoma) continuing to cut the myoma with visualization.
FIGURE 8 Resect technique—4 steps in resecting a submucous myoma
Once through the myoma, the loop is withdrawn into the hysteroscope.
Management of complications
The primary complications of hysteroscopic myomectomy are bleeding, infection, uterine perforation, and fluid overload.
Bleeding. If postoperative hemorrhage occurs, use a 30-cc Foley balloon to tamponade the vessels, or pack the uterus with gauze soaked in a vasopressin solution. Both can be removed any time from 4 hours to 24 hours following placement. If bleeding persists, uterine artery embolization should be considered prior to hysterectomy.
Most attempts at controlling bleeding with a rollerball are futile because the intrauterine distention pressure necessary to see the venous bleeders hides the actual bleeding. Arterial bleeders can be seen and controlled with the rollerball, but they are much less common.
Infection. Because infection is uncommon with hysteroscopic surgery, routine prophylaxis is unnecessary.
Antibiotics should be used if the patient had cervical laminaria placed preoperatively.
Uterine perforation. The management of uterine perforation depends on the site of perforation and whether energy was used during the perforation. For example, if the perforation was at the fundus and occurred with a blunt, non-energized instrument, observation without laparoscopy is sufficient. If the perforation was lateral or occurred with RF energy, laparoscopy is suggested to rule out a broad ligament hematoma or injury to intraperitoneal vessels and viscera. If the perforation is anterior, a cystoscopy is recommended; internal colon inspection is necessary if the perforation is posterior.
Fluid overload. Complications and prevention can be avoided and treated as previously discussed.
New training opportunities may include virtual reality
Underutilization of hysteroscopic myomectomy may be due to inadequate training in the technique during residency or the misconception that it is difficult to learn. (Training has been further hampered by the lack of a suitable animal model.)
Fortunately, hysteroscope manufacturers are beginning to offer physicians and operating room personnel didactic and hands-on laboratory courses. In the near future, we hope, these companies will hire gynecologic hysteroscopists to support physicians and nurses in the field, as has been done in many other specialties.
The creation of new tools such as virtual-reality simulators will undoubtedly enhance the teaching of operative hysteroscopy.
Dr. Isaacson teaches hysteroscopy courses sponsored by Karl Storz Endoscopy.
1. Hulka JF, Levy BS, Luciano AA, Parker WH, Phillips JM. 1997 AAGL membership survey: practice profiles. J Amer Assoc Gynecol Laparosc. 1998;5:93-96.
2. Carlson KJ, Nichols DH, Schiff I. Indications for hysterectomy. N Eng J Med. 1993;328:856-860.
3. Pritts E. Fibroids and infertility: a systematic review of the evidence. Obstet Gynecol Survey. 2001;56:483-491.
4. deBlok S, Dijkman AB, Hemrika DJ. Transcervical resection of fibroids (TCRM): results related to hysteroscopic classification. Gynaecol Endosc. 1995;4:243-246.
5. Istre O. Transcervical resection of endometrium and fibroids: the outcome of 412 operations performed over 5 years. Acta Obstet Gynecol Scand. 1996;75:567-574.
6. Sowter MC, Lethaby A, Singla AA. Preoperative endometrial thinning agents before hysteroscopic surgery for heavy menstrual bleeding. Cochrane Database Syst Rev. 2002;(3):CD001124.-
7. Baggish MS, Sze EM, Morgan G. Hysteroscopic treatment of symptomatic submucous myomas with the Nd:YAG laser. J Gynecol Surg. 1989;5:27-36.
8. Donnez J, Gillerot S, Bourgonjon D, et al. Neodymium:YAG laser hysteroscopy in large submucous fibroids. Fertil Steril. 1990;54:999-1003.
9. Bloomstone J, Chen C, Isselbacher E, Isaacson K. A pilot study examining the frequency and quantity of gas embolization during operative hysteroscopy using a monopolar resectoscope. J Am Assoc Gynecol Laparosc. 2002;9:9-14.
1. Hulka JF, Levy BS, Luciano AA, Parker WH, Phillips JM. 1997 AAGL membership survey: practice profiles. J Amer Assoc Gynecol Laparosc. 1998;5:93-96.
2. Carlson KJ, Nichols DH, Schiff I. Indications for hysterectomy. N Eng J Med. 1993;328:856-860.
3. Pritts E. Fibroids and infertility: a systematic review of the evidence. Obstet Gynecol Survey. 2001;56:483-491.
4. deBlok S, Dijkman AB, Hemrika DJ. Transcervical resection of fibroids (TCRM): results related to hysteroscopic classification. Gynaecol Endosc. 1995;4:243-246.
5. Istre O. Transcervical resection of endometrium and fibroids: the outcome of 412 operations performed over 5 years. Acta Obstet Gynecol Scand. 1996;75:567-574.
6. Sowter MC, Lethaby A, Singla AA. Preoperative endometrial thinning agents before hysteroscopic surgery for heavy menstrual bleeding. Cochrane Database Syst Rev. 2002;(3):CD001124.-
7. Baggish MS, Sze EM, Morgan G. Hysteroscopic treatment of symptomatic submucous myomas with the Nd:YAG laser. J Gynecol Surg. 1989;5:27-36.
8. Donnez J, Gillerot S, Bourgonjon D, et al. Neodymium:YAG laser hysteroscopy in large submucous fibroids. Fertil Steril. 1990;54:999-1003.
9. Bloomstone J, Chen C, Isselbacher E, Isaacson K. A pilot study examining the frequency and quantity of gas embolization during operative hysteroscopy using a monopolar resectoscope. J Am Assoc Gynecol Laparosc. 2002;9:9-14.
Laparoscopic Burch colposuspension for stress urinary incontinence: When, how, and why?
- Laparoscopic Burch colposuspension provides high long-term success rates, reduced morbidity, and accelerated convalescence.
- A growing number of studies have shown the laparoscopic Burch to have results similar to traditional laparotomy when conventional surgical techniques and suture materials are used.
- When we limit the discussion to 2 comparable techniques—a laparoscopic versus open 2-suture procedure—there is moderately strong evidence that the laparoscopic approach maintains efficacy while modestly reducing morbidity.
- The selection of suture material and the total number and placement of sutures are crucial to the long-term cure rate.
Despite the growing body of medical knowledge on stress urinary incontinence (SUI), controversies over its management remain.
SUI is the most common type of inconti-nence and occurs almost exclusively in females. A recent survey by the National Association for Continence revealed that SUI affects approximately 16.5 million women in the United States.1 Nearly two thirds of these women are under 50 years of age.
Still, there is no surgical procedure of choice for women with this condition. In fact, a recent systematic review of the literature by Black and Downs could not determine the “best procedure” based on scientific clinical evidence.2
Among the large number of surgical options for SUI treatment is bladder-neck suspension via a laparoscopic Burch colposus-pension. When it is properly executed, this procedure offers high long-term success rates, reduced morbidity, and accelerated convalescence. In this article, we describe how to perform the laparoscopic Burch procedure (reviewing both conventional suturing techniques and the Tanagho modification)3 and discuss when to consider a laparoscopic approach. In addition, we explain why the procedure should be part of your surgical options for female SUI.
Retropubic versus transvaginal suspensions
With so many surgeries to choose from, determining which procedure would be best for a woman with genuine stress urinary incontinence is a challenge. In 1997, the American Urological Association published a report designed to offer some guidance.
An 8-member panel reviewed data from 282 articles, all of which followed patients for a minimum of 12 months for short-term cure/dry results, and 48 months for long-term results. The Report on the Surgical Management of Female Stress Urinary Incontinence—based on expert opinion and evidence from the literature (as determined by probability estimates)—stated that retropubic suspensions and slings are the most efficacious procedures for long-term success.
Still, the panel noted that these interventions are associated with slightly higher complication rates—including an increased incidence of voiding dysfunction—and longer convalescence than other SUI procedures. For patients willing to accept these complication rates for the sake of improved long-term success, the panel concluded, retropubic suspension and slings are appropriate. However, for patients valuing a decreased hospital stay, reduced morbidity, and an earlier return to normal activity, transvaginal suspensions—the only minimally invasive option widely offered at that time—were the better option.4
The Burch procedure
In the classic Burch colposuspension, a physician places 2 bilateral nonabsorbable sutures through the pubocervical fascia—1 at the level of the midurethra, the other at the urethrovesical junction (UVJ)—and fixes them to Cooper’s ligament. But since 1991, when Vancaille and Schuessler introduced a laparoscopic approach to a retropubic colposuspension (MMK technique),5 a growing number of studies have shown the laparoscopic Burch to have results similar to traditional laparotomy when conventional surgical techniques and suture materials are used.6-24
A number of reports have also described modifications or alternatives to the classic laparoscopic Burch.25-28 These variations—which use stapling devices, mesh placement, bone anchors, and even fibrin glue—avoid laparoscopic suturing, thereby reducing the surgical complexity and shortening the learning curve. They also may lower the cost per procedure by decreasing time in the operating room.29-32 Still, an experienced laparoscopist who has mastered endoscopic suturing can perform a laparoscopic Burch using “standard” suturing in a time frame comparable to that of one of the modifications.33
Retropubic suspensions and slings are associated with slightly higher complication rates than other SUI procedures.
As far as outcomes go, it is the selection of suture material, the total number of sutures used, and their proper placement that are crucial to an optimal long-term cure rate—regardless of the surgical access to the space of Retzius.34-36 In fact, if a surgeon laparoscopically employs the identical operative technique, “suture for suture,” that he or she would use via laparotomy, there is no biological reason why the continence cure rates would be any different.
When? Burch procedure versus the TVT sling
Several studies have demonstrated that for patients with intrinsic sphincter deficiency (ISD) the Burch colposuspension cure/dry rate is less than that of a standard sling procedure.37 We therefore obtain urodynamic studies on all patients presenting with SUI who we feel are at risk for ISD ( TABLE). For patients with ISD and urethral hypermobility, we recommend the minimally invasive pubovaginal sling tension-free vaginal tape (TVT) procedure. In the absence of urethral hypermobility, we first utilize periurethral bulking agents to correct the ISD. If this is not successful, we proceed with urethrolysis and a traditional sling procedure.
For women who have concomitant pelvic-support defects such as uterine prolapse, vaginal vault inversion, or lateral cystoceles, we routinely perform laparoscopic reconstructive surgery, including the laparoscopic Burch for correction of the SUI.
Still, the difficult question remains: Which minimally invasive procedure—a laparoscopic Burch or a TVT—is preferable for the patient with genuine SUI without ISD or any additional pelvic-support defects aside from urethral hypermobility? Only a few studies comparing the clinical outcomes of the TVT and laparoscopic Burch procedures have reported preliminary findings. One retrospective study of 74 women followed for at least 1 year demonstrated an overall objective cure rate of 88% for the laparoscopic Burch versus 92% for the TVT procedure.38 There were no significant differences in time to resumption of normal voiding or in irritative symptoms such as frequency, urgency, and urge incontinence. The TVT group, however, was noted to have a shorter operative time and hospital stay.
Another study reported a higher cure or improvement rate (94%) among patients undergoing the laparoscopic Burch than the TVT (82%). Postoperative voiding difficulty was also significantly less in the laparoscopic group (0% versus 18%).39
Although these early studies suggest that laparoscopic Burch and TVT are comparable, we anxiously await the results of welldesigned, prospective, randomized clinical trials currently under way. One recent report (level I evidence) has demonstrated that the open Burch and the TVT procedure have equivalent results.40
TABLE
Patients at risk for intrinsic sphincter deficiency
|
How? The laparoscopic Burch technique
Preparing the patient. As always, obtain informed consent prior to the procedure. Beyond the usual surgical risks of blood loss, infection, surgical injury, failure rate, and thromboembolic complications, patients also face potential postoperative voiding dysfunction, as mentioned earlier, as well as de novo detrusor instability. Also inform your patients of the possible conversion to laparotomy.
Administer a single intravenous dose of an appropriate broad-spectrum antibiotic no more than 1 hour prior to surgery. For patients undergoing additional laparoscopic reconstructive surgery, we recommend a modified bowel preparation to improve visualization by decompressing the sigmoid colon.
Administer general anesthesia and place the patient in a dorsal lithotomy position with both arms tucked. Support the patient’s lower extremities with Allen Universal Stirrups (Allen Medical Systems, Mayfield, Ohio) and avoid excessive flexion of the knees or hips. Insert a 16F 3-way Foley catheter into the bladder—this allows intermittent bladder filling during the procedure—and inflate the bulb to 10 cc to facilitate identification of the UVJ throughout surgery.
Entering the space of Retzius. We routinely perform operative laparoscopy after Veress needle insertion and insufflation through an umbilical incision. (Use open laparoscopy for patients with prior abdominal surgery and paraumbilical scarring.)
Under direct visualization, place 2 additional accessory 10-mm trocars in the lower quadrants, just lateral to the inferior epigastric arteries. Brief insufflation to greater than 20 mm Hg intra-abdominal pressure facilitates safe entry for these secondary trocars. Although you may opt for smaller trocars, the 10-mm size allows unhindered passage of suture, thus providing more options for maximizing favorable ergonomics with future suture placement.
Although a preperitoneal, or extraperitoneal, approach has been described, we favor a transperitoneal entrance into the space of Retzius. The extraperitoneal approach allows the use of regional anesthesia, avoids intraabdominal adhesions, and eliminates the associated risks of peritoneal entry.31 The disadvantages, however, are significant, including failure to enter the retropubic space secondary to abdominal wall scarring, the inability to perform concomitant vault suspension, and the cost of commercially available dissecting balloons. With experience, a transperitoneal approach will not prolong operative time.
With experience, a transperitoneal approach into the space of Retzius will not prolong operative time.
Approaching the bladder. Distend the bladder in a retrograde fashion with 300 mL to 400 mL of normal saline. This allows identification of the superior margin of the bladder dome and provides mass traction posteriorly. Use the urachus to identify the midline; then, grasp the anterior abdominal wall peritoneum and apply downward traction ( FIGURE 1). Next, create a transverse incision 3 cm to 4 cm above the bladder reflection, using monopolar endoscopic scissors on a 70-watt pure-cut setting ( FIGURE 2). The incision should be within the obliterated umbilical ligaments, but can be extended slightly beyond for patients undergoing a combined laparoscopic Burch-paravaginal repair.41 Using a combination of blunt and electrocautery dissection, you then can easily dissect the loose areolar tissue of the prevesicle space down to the level of the pubic symphysis and ramus ( FIGURE 3).
FIGURE 1
Pictured is the distended bladder, forceps (right) at the bladder margin, endoshears (left) at level of incision, and urachus.
FIGURE 2
Create a transverse incision using monopolar scissors. Note the loose areolar tissue of prevesicle space.
FIGURE 3
Locate the pubic symphysis and ramus using the pelvic brim as a landmark.As the paravesical space is further developed, the pubocervical fascia will become exposed at the level of the UVJ. You must carefully protect the urethra, avoiding aggressive midline dissection as well as the obturator neurovascular bundle laterally. Medial traction on the bladder, perpendicular to the slope of the pubic ramus, encourages identification of the proper surgical plane. Use electrocautery to maintain meticulous hemostasis at all times. Identify Cooper’s ligament, and bluntly dissect away any obstructing fat or areolar tissue (FIGURE 4). To encourage scarification, gently remove excessive overlying periurethral and perivesical fat from pubocervical fascia at the level of the bladder neck, while avoiding any dissection within 1 cm lateral to the urethra ( FIGURE 5).
Placing the sutures. Using an extra-long (36-in), doubled-armed, nonabsorbable suture on an SH needle, place the sutures in the consistent sequence outlined below (note that sturdy needle drivers will facilitate secure needle placement):
First, introduce a needle from the contralateral port and pass it through the pubocervical fascia at the level of the midurethra, using your index finger for transvaginal guidance. If you think the tissue bite will not purchase nearly the entire thickness of the anterior vaginal wall, place a second helical throw (FIGURE 6). Next, bring the suture up through Cooper’s ligament and “store” it by hooking the anterior wall peritoneum (FIGURE 7). Bring up the second arm (needle) of the suture through Cooper’s ligament, but at a different depth than the first pass so ligament fibers are truly encircled by the suture (FIGURE 8). Retrieve both needles, bringing them out through the same port, but do not yet tie the suture.
Introduce the second suture through the ipsilateral port and place it in the same fashion at the level of the UVJ. Again, use helical throws as necessary. Once both sutures have been placed, tie them extracorporeally in sequence using a closed-loop knot pusher. (Waiting until both sutures are placed before tying allows exposure for easy placement of the second suture [FIGURE 9].) The appropriate tension should create a small, localized “knuckle” of pubocervical fascia that approximates laterally to the obturator internus fascia ( FIGURE 10).
Repeat this procedure in the same sequence on the opposite side of the pelvis ( FIGURE 11), then close the retropubic space using a running continuous 2-0 suture reapproximating the peritoneum (FIGURE 12). Close the laparoscopic ports at the fascia level using a Veress needle threaded with a 0-Vicryl. Both ends of the suture are passed on either side of the fascial incision. Using a contralateral grasping forceps, the suture end is freed from the Veress needle, then retrieved using an ipsilateral forceps. This port closure technique is easy to perform as well as cost-effective.
Postoperative care. Place a suprapubic catheter with a 2-way stop clock; this makes postoperative voiding trials easier for both patients and nursing staff.
Most patients will be discharged the day after surgery. If the patient still has an elevated postvoid residual, she’ll likely find going home with the suprapubic catheter more acceptable than intermittent self-catheterization or an indwelling Foley running to a leg bag. For postoperative discomfort, acetaminophen and nonsteroidal anti-inflammatory preparations are generally sufficient. Patients can resume normal living activities within days, but should be cautioned to delay strenuous work or exercise for at least 8 weeks.
FIGURE 4
Apply medial traction to the bladder as the paravesical space is developed down to the level of pubocervical fascia. Note Cooper’s ligament, seen anteriorly.
FIGURE 5
Gently remove the overlying periurethral and perivesical fat to expose white pubocervical fascia.
FIGURE 6
Apply counter traction on the suture from the first pass to facilitate better tissue purchase on the second pass of the helical suture.
FIGURE 7
Place the needle through Cooper’s ligament.
FIGURE 8
Pass the second needle at a deeper depth through Cooper’s ligament to encircle fibers within the suture. This will minimize the risk of “pull out.”
FIGURE 9
Place both sutures before extracorporeal tying.
FIGURE 10
Suture tension should create only a small knuckle of pubocervical fascia, approximating obturator fascia laterally.
FIGURE 11
Both sides completed.
FIGURE 12
Close the retropubic space.
Why? A look at the evidence
The learning curve for laparoscopic Burch is steep and somewhat long—approximately 20 cases. The real question, therefore, is whether the benefits justify the time needed to master this procedure. In other words, is there clinical evidence that, once the plateau of this curve has been reached, we can reduce patient morbidity while maintaining efficacy compared to the traditional open technique? If not, there’s little reason for surgeons to learn the technique. If there is, however, more physicians should include the laparoscopic Burch in their surgical arsenal.
The real question is whether the benefits of the laparoscopic Burch justify the time needed to master the procedure.
When we limit the discussion to 2 comparable techniques, a laparoscopic versus open 2-suture procedure, there is moderately strong evidence that the laparoscopic approach maintains efficacy while modestly reducing morbidity.42 The strength of this evidence is established in 6 studies, including 3 randomized trials (level I evidence).8,18,23,24,43,44
Currently, data are insufficient regarding a laparoscopic approach to make concomitant site-specific defect repairs.45-51 However, if the procedures are performed in the same fashion, “suture for suture,” as their abdominal counterparts, we should expect to see, as we have with the laparoscopic Burch, similar efficacy rates between the laparoscopic and open approaches.
So, in closing, we encourage our colleagues to reignite their interest in learning laparoscopic reconstructive surgery and recommit to reaching that learning curve plateau. Why? We owe it to our patients.
Dr. Lucente is a consultant for GyneCare. Dr. Murphy reports no financial relationship with any companies whose products are mentioned in this article.
1. National Association for Incontinence Quarterly Report. Summer 2002, Vol 20 No 3.
2. Black NA, Down SH. The effectiveness of surgery for stress incontinence in women: A systematic review. Br J Urol. 1996;78:497.-
3. Tanagho E. Colpocystourethropexy: The way we do it. J Urol. 1976;116:751-753.
4. Leach GE, Dinochowski RR, Appell RA, et al. Female stress urinary incontinence clinical guidelines panel: Report on the surgical management of female stress urinary incontinence. Baltimore, Md: American Urological Association, Inc.; 1997.
5. Vancaille TG, Schuessler W. Laparoscopic bladder neck suspension. J Laparoendosc Surg. 1991;1:169-173.
6. Albala DM, Schuessler WW, Vancaillie TG. Laparoscopic bladder suspension for the treatment of stress incontinence. Semin Urol. 1992;10:222-225.
7. Burton G. A randomized comparison of laparoscopic and open colposuspension [abstract]. Neurourol Urodyn. 1993;16:353-354.
8. Polascik TJ, Moore RG, Roseberg MT, Kavoussi LR. Comparison of laparoscopic and open retropubic colposuspension for treatment of stress urinary incontinence. Urology. 1995;45:647-652.
9. Liu CY. Laparoscopic treatment of genuine urinary stress incontinence. Clin Obstet Gynecol. 1994;8:789-798.
10. Gunn GC, Cooper RP, Gordon NS, Gragnon L. Use of a new device for endoscopic suturing in the laparoscopic Burch procedure. J Am Assoc Gynecol Laparosc. 1994;2:65-70.
11. Nezhat CH, Nezhat F, Nezhat CR, et al. Laparoscopic retropubic cystocolposuspension. J Am Assoc Gynecol Laparosc. 1994;1:339-349.
12. Lyons TL, Winer WK. Clinical outcomes with laparoscopic approaches and open Burch procedures for urinary stress incontinence. J Am Assoc Gynecol Laparosc. 1995;2:193-197.
13. McDougal EM, Klutke CG, Cornell T. Comparison of transvaginal versus laparoscopic bladder neck suspension for stress urinary incontinence. Adult Urol. 1995;45:641-645.
14. Ross JW. Laparoscopic Burch repair compared to laparotomy Burch for cure of urinary stress incontinence. Int Urogynecol. 1995;6:323-328.
15. Langebrekke A, Dahlstrom B, Eraker R, Urnes A. The laparoscopic Burch procedure: a preliminary report. Acta Obstet Gynecol Scand. 1995;74:153-155.
16. Radomski SB, Herschorn S. Laparoscopic Burch bladder neck suspension: early results. J Urol. 1996;155:515-518.
17. Ross JW. Two techniques of laparoscopic Burch repair for stress incontinence: a prospective randomized study. J Am Assoc Gynecol Laparoscopists. 1996;3:351-357.
18. Lam AM, Jenkins GJ, Hyslop RS. Laparoscopic results. Med J Aust. 1995;162:18-22.
19. Su TH, Wang KG, Hsu CY, Wei H, Hong BK. Prospective comparison of laparoscopic and traditional colposuspensions in the treatment of genuine stress inconti-nence. Acta Obstet Gynecol. 1997;76:576-582.
20. Papasakelariou C, Papasakelariou B. Laparoscopic bladder neck suspension. J Am Assoc Gynecol Laparosc. 1997;4:185-188.
21. Lobel RW, Davis GD. Long-term results of laparoscopic Burch colposuspension. J Am Assoc Gynecol Laparosc. 1997;4:341-345.
22. Ross JW. Multichannel urodynamic evaluation of laparoscopic Burch colposuspension for genuine stress incontinence. Obstet Gynecol. 1998;91:55-59.
23. Miannay E, Cosson M, Querleu D, et al. [Comparison of laparoscopic and laparotomy colposuspension in the treatment of urinary stress incontinence. Comparative study of 72 matched cases][French]. Contracept Fertil Sex. 1998;26:376-385.
24. Saidi MH, Gallagher MS, Skop IP, et al. Extrperitoneal laparoscopic colposuspension: short-term cure rate, complications and duration of hospital stay in comparison with Burch colposuspension. Obstet Gynecol. 1998;92:619-625.
25. Henley C. The Henley staple-suture technique for laparoscopic Burch colposuspension. J Am Assoc Gynecol Laparosc. 1995;2:441-444.
26. Das S, Palmer JK. Laparoscopic colposuspension. J Urol. 1995;154:1119-1121.
27. Ou CS, Presthus J, Beadle E. Laparoscopic bladder neck suspension using hernia mesh and surgical staples. J Laparoendosc Surg. 1993;3:563-566.
28. Kiilholma P, Haarala M, Polvi II, Makinen J, Chancellor MB. Sutureless colposuspension with fibrin sealant. Tech Urol. 1995;1:81-83.
29. Lose G. Laparoscopic Burch colposuspension. Acta Obstet Gynecol Scand Suppl. 1998;168:29-33.
30. Miannay E, Cosson M, Lanvin D, et al. Comparison of open retropubic and laparoscopic colposuspension for treatment of stress urinary incontinence. Eur J Obstet Gynecol Reprod Biol. 1998;79:159-166.
31. Saidi MH, Sadler RK, Saidi JA. Extraperitoneal laparoscopic colposuspension for genuine urinary stress incontinence. J Am Assoc Gynecol Laparosc. 1998;9:249-252.
32. Ou CS, Rowbotham R. Five-year follow-up of a laparoscopic bladder neck suspension using synthetic mesh and surgical staples. J Laparoendosc Adv Surg Techn A. 1999;9:249-252.
33. Zullo F, Morelli M, Russo T, et al. Two techniques of laparoscopic retropubic urethropexy. J Am Assoc Gynecol Laparosc. 2001;12:323-327.
34. Langer R, Lipshitz Y, Halperin R, et al. Long-term (10-15 years) follow-up after Burch colposuspension for urinary stress incontinence. Int Urogynecol J. 2001;12:323-327.
35. Herbertsson G, Iosif CS. Surgical results and urodynamic studies 10 years after retropubic colpurethropexy. Acta Obstet Gynecol Scand. 1993;72:298-301.
36. Parasio M, Falcone T, Walters M. Laparoscopic surgery for genuine stress incontinence. Int Urogynecol J. 1999;10:237-247.
37. Horbach NS. Suburethral sling procedures. Urogynecology and Urodynamics: Theory and Practice. 4th ed. Baltimore, Md: Williams and Wilkins 1996;569-579.
38. Vassallo B, Murphy M, Lucente V, Karram M. TVT versus Laparoscopic Burch: a retrospective review at 1-4 years. 27th Scientific Meeting of the Society of Gynecologic Surgeons. March 5-7, 2001.
39. Fotte A. Which is the best minimally invasive procedure? TVT versus laparoscopic colposuspension. Presented at the 31st annual meeting of the International Continence Society; September 18-21, 2001; Seoul, Korea.
40. Ward KL, Hilton P. Prospective multicentre randomized trial of tension-free vaginal tape and colposuspension as primary treatment for stress incontinence. BMJ. 2002;326:67.-
41. Miklos J, Kohli N. Laparoscopic paravaginal repair plus Burch colposuspension: review and descriptive technique. Urology. 2000;56:64-68.
42. Walter A. Laparoscopic repairs for stress urinary incontinence and pelvic organ prolapse: “show me the evidence.” Presented at the annual meeting of the American Urogynecologic Society; 2002; San Diego, Calif.
43. Summitt RL, Lucente V, Karram MM, Shull BL, Bent AE. Randomized comparison of laparoscopic and transabdominal Burch urethropexy for the treatment of genuine stress incontinence. Obstet Gynecol. 2000;95:(suppl):2.-
44. Fatthy H, El Hao M, Samaha I, Abdallah K. Modified Burch colposuspension: laparoscopy versus laparotomy. J Am Assoc Gynecol Laparosc. 2001;8:99-106.
45. Ross JW. Techniques of laparoscopic repair for total vault eversion after hysterectomy. J Am Assoc Gynecol Laparosc. 1997;4:173-183.
46. Ross JW. Laparoscopic approach for severe pelvic vault prolapse. J Am Assoc Gynecol Laparosc. 1996;3(suppl):43.-
47. Lyons TL, Winer WK. Laparoscopic rectocele repair using polyglactin mesh. J Am Assoc Gynecol Laparosc. 1997;4:381-384.
48. Ostrzenski A. Laparoscopic colposuspension for total vaginal prolapse. Int J Gynaecol Obstet. 1996;55:147-152.
49. Carter JE, Winter M, Mendehlsohn S, Saye W, Richardson AC. Vaginal vault suspension and enterocele repair by Richardson-Saye laparoscopic technique: description of training technique and results. JSLS. 2001;5:29-36.
50. Cosson M, Rajabally R, Bogaert E, Querleu D, Crepin G. Laparoscopic sacrocolpopexy, hysterectomy and Burch colposuspension: feasibility and short-term complications of 77 procedures. JSLS. 2002;6:115-119.
51. Miklos JR, Moore RD, Kohli N. Laparoscopic surgery for pelvic support defects. Curr Opin Obstet Gynecol. 2002;14:387-395.
- Laparoscopic Burch colposuspension provides high long-term success rates, reduced morbidity, and accelerated convalescence.
- A growing number of studies have shown the laparoscopic Burch to have results similar to traditional laparotomy when conventional surgical techniques and suture materials are used.
- When we limit the discussion to 2 comparable techniques—a laparoscopic versus open 2-suture procedure—there is moderately strong evidence that the laparoscopic approach maintains efficacy while modestly reducing morbidity.
- The selection of suture material and the total number and placement of sutures are crucial to the long-term cure rate.
Despite the growing body of medical knowledge on stress urinary incontinence (SUI), controversies over its management remain.
SUI is the most common type of inconti-nence and occurs almost exclusively in females. A recent survey by the National Association for Continence revealed that SUI affects approximately 16.5 million women in the United States.1 Nearly two thirds of these women are under 50 years of age.
Still, there is no surgical procedure of choice for women with this condition. In fact, a recent systematic review of the literature by Black and Downs could not determine the “best procedure” based on scientific clinical evidence.2
Among the large number of surgical options for SUI treatment is bladder-neck suspension via a laparoscopic Burch colposus-pension. When it is properly executed, this procedure offers high long-term success rates, reduced morbidity, and accelerated convalescence. In this article, we describe how to perform the laparoscopic Burch procedure (reviewing both conventional suturing techniques and the Tanagho modification)3 and discuss when to consider a laparoscopic approach. In addition, we explain why the procedure should be part of your surgical options for female SUI.
Retropubic versus transvaginal suspensions
With so many surgeries to choose from, determining which procedure would be best for a woman with genuine stress urinary incontinence is a challenge. In 1997, the American Urological Association published a report designed to offer some guidance.
An 8-member panel reviewed data from 282 articles, all of which followed patients for a minimum of 12 months for short-term cure/dry results, and 48 months for long-term results. The Report on the Surgical Management of Female Stress Urinary Incontinence—based on expert opinion and evidence from the literature (as determined by probability estimates)—stated that retropubic suspensions and slings are the most efficacious procedures for long-term success.
Still, the panel noted that these interventions are associated with slightly higher complication rates—including an increased incidence of voiding dysfunction—and longer convalescence than other SUI procedures. For patients willing to accept these complication rates for the sake of improved long-term success, the panel concluded, retropubic suspension and slings are appropriate. However, for patients valuing a decreased hospital stay, reduced morbidity, and an earlier return to normal activity, transvaginal suspensions—the only minimally invasive option widely offered at that time—were the better option.4
The Burch procedure
In the classic Burch colposuspension, a physician places 2 bilateral nonabsorbable sutures through the pubocervical fascia—1 at the level of the midurethra, the other at the urethrovesical junction (UVJ)—and fixes them to Cooper’s ligament. But since 1991, when Vancaille and Schuessler introduced a laparoscopic approach to a retropubic colposuspension (MMK technique),5 a growing number of studies have shown the laparoscopic Burch to have results similar to traditional laparotomy when conventional surgical techniques and suture materials are used.6-24
A number of reports have also described modifications or alternatives to the classic laparoscopic Burch.25-28 These variations—which use stapling devices, mesh placement, bone anchors, and even fibrin glue—avoid laparoscopic suturing, thereby reducing the surgical complexity and shortening the learning curve. They also may lower the cost per procedure by decreasing time in the operating room.29-32 Still, an experienced laparoscopist who has mastered endoscopic suturing can perform a laparoscopic Burch using “standard” suturing in a time frame comparable to that of one of the modifications.33
Retropubic suspensions and slings are associated with slightly higher complication rates than other SUI procedures.
As far as outcomes go, it is the selection of suture material, the total number of sutures used, and their proper placement that are crucial to an optimal long-term cure rate—regardless of the surgical access to the space of Retzius.34-36 In fact, if a surgeon laparoscopically employs the identical operative technique, “suture for suture,” that he or she would use via laparotomy, there is no biological reason why the continence cure rates would be any different.
When? Burch procedure versus the TVT sling
Several studies have demonstrated that for patients with intrinsic sphincter deficiency (ISD) the Burch colposuspension cure/dry rate is less than that of a standard sling procedure.37 We therefore obtain urodynamic studies on all patients presenting with SUI who we feel are at risk for ISD ( TABLE). For patients with ISD and urethral hypermobility, we recommend the minimally invasive pubovaginal sling tension-free vaginal tape (TVT) procedure. In the absence of urethral hypermobility, we first utilize periurethral bulking agents to correct the ISD. If this is not successful, we proceed with urethrolysis and a traditional sling procedure.
For women who have concomitant pelvic-support defects such as uterine prolapse, vaginal vault inversion, or lateral cystoceles, we routinely perform laparoscopic reconstructive surgery, including the laparoscopic Burch for correction of the SUI.
Still, the difficult question remains: Which minimally invasive procedure—a laparoscopic Burch or a TVT—is preferable for the patient with genuine SUI without ISD or any additional pelvic-support defects aside from urethral hypermobility? Only a few studies comparing the clinical outcomes of the TVT and laparoscopic Burch procedures have reported preliminary findings. One retrospective study of 74 women followed for at least 1 year demonstrated an overall objective cure rate of 88% for the laparoscopic Burch versus 92% for the TVT procedure.38 There were no significant differences in time to resumption of normal voiding or in irritative symptoms such as frequency, urgency, and urge incontinence. The TVT group, however, was noted to have a shorter operative time and hospital stay.
Another study reported a higher cure or improvement rate (94%) among patients undergoing the laparoscopic Burch than the TVT (82%). Postoperative voiding difficulty was also significantly less in the laparoscopic group (0% versus 18%).39
Although these early studies suggest that laparoscopic Burch and TVT are comparable, we anxiously await the results of welldesigned, prospective, randomized clinical trials currently under way. One recent report (level I evidence) has demonstrated that the open Burch and the TVT procedure have equivalent results.40
TABLE
Patients at risk for intrinsic sphincter deficiency
|
How? The laparoscopic Burch technique
Preparing the patient. As always, obtain informed consent prior to the procedure. Beyond the usual surgical risks of blood loss, infection, surgical injury, failure rate, and thromboembolic complications, patients also face potential postoperative voiding dysfunction, as mentioned earlier, as well as de novo detrusor instability. Also inform your patients of the possible conversion to laparotomy.
Administer a single intravenous dose of an appropriate broad-spectrum antibiotic no more than 1 hour prior to surgery. For patients undergoing additional laparoscopic reconstructive surgery, we recommend a modified bowel preparation to improve visualization by decompressing the sigmoid colon.
Administer general anesthesia and place the patient in a dorsal lithotomy position with both arms tucked. Support the patient’s lower extremities with Allen Universal Stirrups (Allen Medical Systems, Mayfield, Ohio) and avoid excessive flexion of the knees or hips. Insert a 16F 3-way Foley catheter into the bladder—this allows intermittent bladder filling during the procedure—and inflate the bulb to 10 cc to facilitate identification of the UVJ throughout surgery.
Entering the space of Retzius. We routinely perform operative laparoscopy after Veress needle insertion and insufflation through an umbilical incision. (Use open laparoscopy for patients with prior abdominal surgery and paraumbilical scarring.)
Under direct visualization, place 2 additional accessory 10-mm trocars in the lower quadrants, just lateral to the inferior epigastric arteries. Brief insufflation to greater than 20 mm Hg intra-abdominal pressure facilitates safe entry for these secondary trocars. Although you may opt for smaller trocars, the 10-mm size allows unhindered passage of suture, thus providing more options for maximizing favorable ergonomics with future suture placement.
Although a preperitoneal, or extraperitoneal, approach has been described, we favor a transperitoneal entrance into the space of Retzius. The extraperitoneal approach allows the use of regional anesthesia, avoids intraabdominal adhesions, and eliminates the associated risks of peritoneal entry.31 The disadvantages, however, are significant, including failure to enter the retropubic space secondary to abdominal wall scarring, the inability to perform concomitant vault suspension, and the cost of commercially available dissecting balloons. With experience, a transperitoneal approach will not prolong operative time.
With experience, a transperitoneal approach into the space of Retzius will not prolong operative time.
Approaching the bladder. Distend the bladder in a retrograde fashion with 300 mL to 400 mL of normal saline. This allows identification of the superior margin of the bladder dome and provides mass traction posteriorly. Use the urachus to identify the midline; then, grasp the anterior abdominal wall peritoneum and apply downward traction ( FIGURE 1). Next, create a transverse incision 3 cm to 4 cm above the bladder reflection, using monopolar endoscopic scissors on a 70-watt pure-cut setting ( FIGURE 2). The incision should be within the obliterated umbilical ligaments, but can be extended slightly beyond for patients undergoing a combined laparoscopic Burch-paravaginal repair.41 Using a combination of blunt and electrocautery dissection, you then can easily dissect the loose areolar tissue of the prevesicle space down to the level of the pubic symphysis and ramus ( FIGURE 3).
FIGURE 1
Pictured is the distended bladder, forceps (right) at the bladder margin, endoshears (left) at level of incision, and urachus.
FIGURE 2
Create a transverse incision using monopolar scissors. Note the loose areolar tissue of prevesicle space.
FIGURE 3
Locate the pubic symphysis and ramus using the pelvic brim as a landmark.As the paravesical space is further developed, the pubocervical fascia will become exposed at the level of the UVJ. You must carefully protect the urethra, avoiding aggressive midline dissection as well as the obturator neurovascular bundle laterally. Medial traction on the bladder, perpendicular to the slope of the pubic ramus, encourages identification of the proper surgical plane. Use electrocautery to maintain meticulous hemostasis at all times. Identify Cooper’s ligament, and bluntly dissect away any obstructing fat or areolar tissue (FIGURE 4). To encourage scarification, gently remove excessive overlying periurethral and perivesical fat from pubocervical fascia at the level of the bladder neck, while avoiding any dissection within 1 cm lateral to the urethra ( FIGURE 5).
Placing the sutures. Using an extra-long (36-in), doubled-armed, nonabsorbable suture on an SH needle, place the sutures in the consistent sequence outlined below (note that sturdy needle drivers will facilitate secure needle placement):
First, introduce a needle from the contralateral port and pass it through the pubocervical fascia at the level of the midurethra, using your index finger for transvaginal guidance. If you think the tissue bite will not purchase nearly the entire thickness of the anterior vaginal wall, place a second helical throw (FIGURE 6). Next, bring the suture up through Cooper’s ligament and “store” it by hooking the anterior wall peritoneum (FIGURE 7). Bring up the second arm (needle) of the suture through Cooper’s ligament, but at a different depth than the first pass so ligament fibers are truly encircled by the suture (FIGURE 8). Retrieve both needles, bringing them out through the same port, but do not yet tie the suture.
Introduce the second suture through the ipsilateral port and place it in the same fashion at the level of the UVJ. Again, use helical throws as necessary. Once both sutures have been placed, tie them extracorporeally in sequence using a closed-loop knot pusher. (Waiting until both sutures are placed before tying allows exposure for easy placement of the second suture [FIGURE 9].) The appropriate tension should create a small, localized “knuckle” of pubocervical fascia that approximates laterally to the obturator internus fascia ( FIGURE 10).
Repeat this procedure in the same sequence on the opposite side of the pelvis ( FIGURE 11), then close the retropubic space using a running continuous 2-0 suture reapproximating the peritoneum (FIGURE 12). Close the laparoscopic ports at the fascia level using a Veress needle threaded with a 0-Vicryl. Both ends of the suture are passed on either side of the fascial incision. Using a contralateral grasping forceps, the suture end is freed from the Veress needle, then retrieved using an ipsilateral forceps. This port closure technique is easy to perform as well as cost-effective.
Postoperative care. Place a suprapubic catheter with a 2-way stop clock; this makes postoperative voiding trials easier for both patients and nursing staff.
Most patients will be discharged the day after surgery. If the patient still has an elevated postvoid residual, she’ll likely find going home with the suprapubic catheter more acceptable than intermittent self-catheterization or an indwelling Foley running to a leg bag. For postoperative discomfort, acetaminophen and nonsteroidal anti-inflammatory preparations are generally sufficient. Patients can resume normal living activities within days, but should be cautioned to delay strenuous work or exercise for at least 8 weeks.
FIGURE 4
Apply medial traction to the bladder as the paravesical space is developed down to the level of pubocervical fascia. Note Cooper’s ligament, seen anteriorly.
FIGURE 5
Gently remove the overlying periurethral and perivesical fat to expose white pubocervical fascia.
FIGURE 6
Apply counter traction on the suture from the first pass to facilitate better tissue purchase on the second pass of the helical suture.
FIGURE 7
Place the needle through Cooper’s ligament.
FIGURE 8
Pass the second needle at a deeper depth through Cooper’s ligament to encircle fibers within the suture. This will minimize the risk of “pull out.”
FIGURE 9
Place both sutures before extracorporeal tying.
FIGURE 10
Suture tension should create only a small knuckle of pubocervical fascia, approximating obturator fascia laterally.
FIGURE 11
Both sides completed.
FIGURE 12
Close the retropubic space.
Why? A look at the evidence
The learning curve for laparoscopic Burch is steep and somewhat long—approximately 20 cases. The real question, therefore, is whether the benefits justify the time needed to master this procedure. In other words, is there clinical evidence that, once the plateau of this curve has been reached, we can reduce patient morbidity while maintaining efficacy compared to the traditional open technique? If not, there’s little reason for surgeons to learn the technique. If there is, however, more physicians should include the laparoscopic Burch in their surgical arsenal.
The real question is whether the benefits of the laparoscopic Burch justify the time needed to master the procedure.
When we limit the discussion to 2 comparable techniques, a laparoscopic versus open 2-suture procedure, there is moderately strong evidence that the laparoscopic approach maintains efficacy while modestly reducing morbidity.42 The strength of this evidence is established in 6 studies, including 3 randomized trials (level I evidence).8,18,23,24,43,44
Currently, data are insufficient regarding a laparoscopic approach to make concomitant site-specific defect repairs.45-51 However, if the procedures are performed in the same fashion, “suture for suture,” as their abdominal counterparts, we should expect to see, as we have with the laparoscopic Burch, similar efficacy rates between the laparoscopic and open approaches.
So, in closing, we encourage our colleagues to reignite their interest in learning laparoscopic reconstructive surgery and recommit to reaching that learning curve plateau. Why? We owe it to our patients.
Dr. Lucente is a consultant for GyneCare. Dr. Murphy reports no financial relationship with any companies whose products are mentioned in this article.
- Laparoscopic Burch colposuspension provides high long-term success rates, reduced morbidity, and accelerated convalescence.
- A growing number of studies have shown the laparoscopic Burch to have results similar to traditional laparotomy when conventional surgical techniques and suture materials are used.
- When we limit the discussion to 2 comparable techniques—a laparoscopic versus open 2-suture procedure—there is moderately strong evidence that the laparoscopic approach maintains efficacy while modestly reducing morbidity.
- The selection of suture material and the total number and placement of sutures are crucial to the long-term cure rate.
Despite the growing body of medical knowledge on stress urinary incontinence (SUI), controversies over its management remain.
SUI is the most common type of inconti-nence and occurs almost exclusively in females. A recent survey by the National Association for Continence revealed that SUI affects approximately 16.5 million women in the United States.1 Nearly two thirds of these women are under 50 years of age.
Still, there is no surgical procedure of choice for women with this condition. In fact, a recent systematic review of the literature by Black and Downs could not determine the “best procedure” based on scientific clinical evidence.2
Among the large number of surgical options for SUI treatment is bladder-neck suspension via a laparoscopic Burch colposus-pension. When it is properly executed, this procedure offers high long-term success rates, reduced morbidity, and accelerated convalescence. In this article, we describe how to perform the laparoscopic Burch procedure (reviewing both conventional suturing techniques and the Tanagho modification)3 and discuss when to consider a laparoscopic approach. In addition, we explain why the procedure should be part of your surgical options for female SUI.
Retropubic versus transvaginal suspensions
With so many surgeries to choose from, determining which procedure would be best for a woman with genuine stress urinary incontinence is a challenge. In 1997, the American Urological Association published a report designed to offer some guidance.
An 8-member panel reviewed data from 282 articles, all of which followed patients for a minimum of 12 months for short-term cure/dry results, and 48 months for long-term results. The Report on the Surgical Management of Female Stress Urinary Incontinence—based on expert opinion and evidence from the literature (as determined by probability estimates)—stated that retropubic suspensions and slings are the most efficacious procedures for long-term success.
Still, the panel noted that these interventions are associated with slightly higher complication rates—including an increased incidence of voiding dysfunction—and longer convalescence than other SUI procedures. For patients willing to accept these complication rates for the sake of improved long-term success, the panel concluded, retropubic suspension and slings are appropriate. However, for patients valuing a decreased hospital stay, reduced morbidity, and an earlier return to normal activity, transvaginal suspensions—the only minimally invasive option widely offered at that time—were the better option.4
The Burch procedure
In the classic Burch colposuspension, a physician places 2 bilateral nonabsorbable sutures through the pubocervical fascia—1 at the level of the midurethra, the other at the urethrovesical junction (UVJ)—and fixes them to Cooper’s ligament. But since 1991, when Vancaille and Schuessler introduced a laparoscopic approach to a retropubic colposuspension (MMK technique),5 a growing number of studies have shown the laparoscopic Burch to have results similar to traditional laparotomy when conventional surgical techniques and suture materials are used.6-24
A number of reports have also described modifications or alternatives to the classic laparoscopic Burch.25-28 These variations—which use stapling devices, mesh placement, bone anchors, and even fibrin glue—avoid laparoscopic suturing, thereby reducing the surgical complexity and shortening the learning curve. They also may lower the cost per procedure by decreasing time in the operating room.29-32 Still, an experienced laparoscopist who has mastered endoscopic suturing can perform a laparoscopic Burch using “standard” suturing in a time frame comparable to that of one of the modifications.33
Retropubic suspensions and slings are associated with slightly higher complication rates than other SUI procedures.
As far as outcomes go, it is the selection of suture material, the total number of sutures used, and their proper placement that are crucial to an optimal long-term cure rate—regardless of the surgical access to the space of Retzius.34-36 In fact, if a surgeon laparoscopically employs the identical operative technique, “suture for suture,” that he or she would use via laparotomy, there is no biological reason why the continence cure rates would be any different.
When? Burch procedure versus the TVT sling
Several studies have demonstrated that for patients with intrinsic sphincter deficiency (ISD) the Burch colposuspension cure/dry rate is less than that of a standard sling procedure.37 We therefore obtain urodynamic studies on all patients presenting with SUI who we feel are at risk for ISD ( TABLE). For patients with ISD and urethral hypermobility, we recommend the minimally invasive pubovaginal sling tension-free vaginal tape (TVT) procedure. In the absence of urethral hypermobility, we first utilize periurethral bulking agents to correct the ISD. If this is not successful, we proceed with urethrolysis and a traditional sling procedure.
For women who have concomitant pelvic-support defects such as uterine prolapse, vaginal vault inversion, or lateral cystoceles, we routinely perform laparoscopic reconstructive surgery, including the laparoscopic Burch for correction of the SUI.
Still, the difficult question remains: Which minimally invasive procedure—a laparoscopic Burch or a TVT—is preferable for the patient with genuine SUI without ISD or any additional pelvic-support defects aside from urethral hypermobility? Only a few studies comparing the clinical outcomes of the TVT and laparoscopic Burch procedures have reported preliminary findings. One retrospective study of 74 women followed for at least 1 year demonstrated an overall objective cure rate of 88% for the laparoscopic Burch versus 92% for the TVT procedure.38 There were no significant differences in time to resumption of normal voiding or in irritative symptoms such as frequency, urgency, and urge incontinence. The TVT group, however, was noted to have a shorter operative time and hospital stay.
Another study reported a higher cure or improvement rate (94%) among patients undergoing the laparoscopic Burch than the TVT (82%). Postoperative voiding difficulty was also significantly less in the laparoscopic group (0% versus 18%).39
Although these early studies suggest that laparoscopic Burch and TVT are comparable, we anxiously await the results of welldesigned, prospective, randomized clinical trials currently under way. One recent report (level I evidence) has demonstrated that the open Burch and the TVT procedure have equivalent results.40
TABLE
Patients at risk for intrinsic sphincter deficiency
|
How? The laparoscopic Burch technique
Preparing the patient. As always, obtain informed consent prior to the procedure. Beyond the usual surgical risks of blood loss, infection, surgical injury, failure rate, and thromboembolic complications, patients also face potential postoperative voiding dysfunction, as mentioned earlier, as well as de novo detrusor instability. Also inform your patients of the possible conversion to laparotomy.
Administer a single intravenous dose of an appropriate broad-spectrum antibiotic no more than 1 hour prior to surgery. For patients undergoing additional laparoscopic reconstructive surgery, we recommend a modified bowel preparation to improve visualization by decompressing the sigmoid colon.
Administer general anesthesia and place the patient in a dorsal lithotomy position with both arms tucked. Support the patient’s lower extremities with Allen Universal Stirrups (Allen Medical Systems, Mayfield, Ohio) and avoid excessive flexion of the knees or hips. Insert a 16F 3-way Foley catheter into the bladder—this allows intermittent bladder filling during the procedure—and inflate the bulb to 10 cc to facilitate identification of the UVJ throughout surgery.
Entering the space of Retzius. We routinely perform operative laparoscopy after Veress needle insertion and insufflation through an umbilical incision. (Use open laparoscopy for patients with prior abdominal surgery and paraumbilical scarring.)
Under direct visualization, place 2 additional accessory 10-mm trocars in the lower quadrants, just lateral to the inferior epigastric arteries. Brief insufflation to greater than 20 mm Hg intra-abdominal pressure facilitates safe entry for these secondary trocars. Although you may opt for smaller trocars, the 10-mm size allows unhindered passage of suture, thus providing more options for maximizing favorable ergonomics with future suture placement.
Although a preperitoneal, or extraperitoneal, approach has been described, we favor a transperitoneal entrance into the space of Retzius. The extraperitoneal approach allows the use of regional anesthesia, avoids intraabdominal adhesions, and eliminates the associated risks of peritoneal entry.31 The disadvantages, however, are significant, including failure to enter the retropubic space secondary to abdominal wall scarring, the inability to perform concomitant vault suspension, and the cost of commercially available dissecting balloons. With experience, a transperitoneal approach will not prolong operative time.
With experience, a transperitoneal approach into the space of Retzius will not prolong operative time.
Approaching the bladder. Distend the bladder in a retrograde fashion with 300 mL to 400 mL of normal saline. This allows identification of the superior margin of the bladder dome and provides mass traction posteriorly. Use the urachus to identify the midline; then, grasp the anterior abdominal wall peritoneum and apply downward traction ( FIGURE 1). Next, create a transverse incision 3 cm to 4 cm above the bladder reflection, using monopolar endoscopic scissors on a 70-watt pure-cut setting ( FIGURE 2). The incision should be within the obliterated umbilical ligaments, but can be extended slightly beyond for patients undergoing a combined laparoscopic Burch-paravaginal repair.41 Using a combination of blunt and electrocautery dissection, you then can easily dissect the loose areolar tissue of the prevesicle space down to the level of the pubic symphysis and ramus ( FIGURE 3).
FIGURE 1
Pictured is the distended bladder, forceps (right) at the bladder margin, endoshears (left) at level of incision, and urachus.
FIGURE 2
Create a transverse incision using monopolar scissors. Note the loose areolar tissue of prevesicle space.
FIGURE 3
Locate the pubic symphysis and ramus using the pelvic brim as a landmark.As the paravesical space is further developed, the pubocervical fascia will become exposed at the level of the UVJ. You must carefully protect the urethra, avoiding aggressive midline dissection as well as the obturator neurovascular bundle laterally. Medial traction on the bladder, perpendicular to the slope of the pubic ramus, encourages identification of the proper surgical plane. Use electrocautery to maintain meticulous hemostasis at all times. Identify Cooper’s ligament, and bluntly dissect away any obstructing fat or areolar tissue (FIGURE 4). To encourage scarification, gently remove excessive overlying periurethral and perivesical fat from pubocervical fascia at the level of the bladder neck, while avoiding any dissection within 1 cm lateral to the urethra ( FIGURE 5).
Placing the sutures. Using an extra-long (36-in), doubled-armed, nonabsorbable suture on an SH needle, place the sutures in the consistent sequence outlined below (note that sturdy needle drivers will facilitate secure needle placement):
First, introduce a needle from the contralateral port and pass it through the pubocervical fascia at the level of the midurethra, using your index finger for transvaginal guidance. If you think the tissue bite will not purchase nearly the entire thickness of the anterior vaginal wall, place a second helical throw (FIGURE 6). Next, bring the suture up through Cooper’s ligament and “store” it by hooking the anterior wall peritoneum (FIGURE 7). Bring up the second arm (needle) of the suture through Cooper’s ligament, but at a different depth than the first pass so ligament fibers are truly encircled by the suture (FIGURE 8). Retrieve both needles, bringing them out through the same port, but do not yet tie the suture.
Introduce the second suture through the ipsilateral port and place it in the same fashion at the level of the UVJ. Again, use helical throws as necessary. Once both sutures have been placed, tie them extracorporeally in sequence using a closed-loop knot pusher. (Waiting until both sutures are placed before tying allows exposure for easy placement of the second suture [FIGURE 9].) The appropriate tension should create a small, localized “knuckle” of pubocervical fascia that approximates laterally to the obturator internus fascia ( FIGURE 10).
Repeat this procedure in the same sequence on the opposite side of the pelvis ( FIGURE 11), then close the retropubic space using a running continuous 2-0 suture reapproximating the peritoneum (FIGURE 12). Close the laparoscopic ports at the fascia level using a Veress needle threaded with a 0-Vicryl. Both ends of the suture are passed on either side of the fascial incision. Using a contralateral grasping forceps, the suture end is freed from the Veress needle, then retrieved using an ipsilateral forceps. This port closure technique is easy to perform as well as cost-effective.
Postoperative care. Place a suprapubic catheter with a 2-way stop clock; this makes postoperative voiding trials easier for both patients and nursing staff.
Most patients will be discharged the day after surgery. If the patient still has an elevated postvoid residual, she’ll likely find going home with the suprapubic catheter more acceptable than intermittent self-catheterization or an indwelling Foley running to a leg bag. For postoperative discomfort, acetaminophen and nonsteroidal anti-inflammatory preparations are generally sufficient. Patients can resume normal living activities within days, but should be cautioned to delay strenuous work or exercise for at least 8 weeks.
FIGURE 4
Apply medial traction to the bladder as the paravesical space is developed down to the level of pubocervical fascia. Note Cooper’s ligament, seen anteriorly.
FIGURE 5
Gently remove the overlying periurethral and perivesical fat to expose white pubocervical fascia.
FIGURE 6
Apply counter traction on the suture from the first pass to facilitate better tissue purchase on the second pass of the helical suture.
FIGURE 7
Place the needle through Cooper’s ligament.
FIGURE 8
Pass the second needle at a deeper depth through Cooper’s ligament to encircle fibers within the suture. This will minimize the risk of “pull out.”
FIGURE 9
Place both sutures before extracorporeal tying.
FIGURE 10
Suture tension should create only a small knuckle of pubocervical fascia, approximating obturator fascia laterally.
FIGURE 11
Both sides completed.
FIGURE 12
Close the retropubic space.
Why? A look at the evidence
The learning curve for laparoscopic Burch is steep and somewhat long—approximately 20 cases. The real question, therefore, is whether the benefits justify the time needed to master this procedure. In other words, is there clinical evidence that, once the plateau of this curve has been reached, we can reduce patient morbidity while maintaining efficacy compared to the traditional open technique? If not, there’s little reason for surgeons to learn the technique. If there is, however, more physicians should include the laparoscopic Burch in their surgical arsenal.
The real question is whether the benefits of the laparoscopic Burch justify the time needed to master the procedure.
When we limit the discussion to 2 comparable techniques, a laparoscopic versus open 2-suture procedure, there is moderately strong evidence that the laparoscopic approach maintains efficacy while modestly reducing morbidity.42 The strength of this evidence is established in 6 studies, including 3 randomized trials (level I evidence).8,18,23,24,43,44
Currently, data are insufficient regarding a laparoscopic approach to make concomitant site-specific defect repairs.45-51 However, if the procedures are performed in the same fashion, “suture for suture,” as their abdominal counterparts, we should expect to see, as we have with the laparoscopic Burch, similar efficacy rates between the laparoscopic and open approaches.
So, in closing, we encourage our colleagues to reignite their interest in learning laparoscopic reconstructive surgery and recommit to reaching that learning curve plateau. Why? We owe it to our patients.
Dr. Lucente is a consultant for GyneCare. Dr. Murphy reports no financial relationship with any companies whose products are mentioned in this article.
1. National Association for Incontinence Quarterly Report. Summer 2002, Vol 20 No 3.
2. Black NA, Down SH. The effectiveness of surgery for stress incontinence in women: A systematic review. Br J Urol. 1996;78:497.-
3. Tanagho E. Colpocystourethropexy: The way we do it. J Urol. 1976;116:751-753.
4. Leach GE, Dinochowski RR, Appell RA, et al. Female stress urinary incontinence clinical guidelines panel: Report on the surgical management of female stress urinary incontinence. Baltimore, Md: American Urological Association, Inc.; 1997.
5. Vancaille TG, Schuessler W. Laparoscopic bladder neck suspension. J Laparoendosc Surg. 1991;1:169-173.
6. Albala DM, Schuessler WW, Vancaillie TG. Laparoscopic bladder suspension for the treatment of stress incontinence. Semin Urol. 1992;10:222-225.
7. Burton G. A randomized comparison of laparoscopic and open colposuspension [abstract]. Neurourol Urodyn. 1993;16:353-354.
8. Polascik TJ, Moore RG, Roseberg MT, Kavoussi LR. Comparison of laparoscopic and open retropubic colposuspension for treatment of stress urinary incontinence. Urology. 1995;45:647-652.
9. Liu CY. Laparoscopic treatment of genuine urinary stress incontinence. Clin Obstet Gynecol. 1994;8:789-798.
10. Gunn GC, Cooper RP, Gordon NS, Gragnon L. Use of a new device for endoscopic suturing in the laparoscopic Burch procedure. J Am Assoc Gynecol Laparosc. 1994;2:65-70.
11. Nezhat CH, Nezhat F, Nezhat CR, et al. Laparoscopic retropubic cystocolposuspension. J Am Assoc Gynecol Laparosc. 1994;1:339-349.
12. Lyons TL, Winer WK. Clinical outcomes with laparoscopic approaches and open Burch procedures for urinary stress incontinence. J Am Assoc Gynecol Laparosc. 1995;2:193-197.
13. McDougal EM, Klutke CG, Cornell T. Comparison of transvaginal versus laparoscopic bladder neck suspension for stress urinary incontinence. Adult Urol. 1995;45:641-645.
14. Ross JW. Laparoscopic Burch repair compared to laparotomy Burch for cure of urinary stress incontinence. Int Urogynecol. 1995;6:323-328.
15. Langebrekke A, Dahlstrom B, Eraker R, Urnes A. The laparoscopic Burch procedure: a preliminary report. Acta Obstet Gynecol Scand. 1995;74:153-155.
16. Radomski SB, Herschorn S. Laparoscopic Burch bladder neck suspension: early results. J Urol. 1996;155:515-518.
17. Ross JW. Two techniques of laparoscopic Burch repair for stress incontinence: a prospective randomized study. J Am Assoc Gynecol Laparoscopists. 1996;3:351-357.
18. Lam AM, Jenkins GJ, Hyslop RS. Laparoscopic results. Med J Aust. 1995;162:18-22.
19. Su TH, Wang KG, Hsu CY, Wei H, Hong BK. Prospective comparison of laparoscopic and traditional colposuspensions in the treatment of genuine stress inconti-nence. Acta Obstet Gynecol. 1997;76:576-582.
20. Papasakelariou C, Papasakelariou B. Laparoscopic bladder neck suspension. J Am Assoc Gynecol Laparosc. 1997;4:185-188.
21. Lobel RW, Davis GD. Long-term results of laparoscopic Burch colposuspension. J Am Assoc Gynecol Laparosc. 1997;4:341-345.
22. Ross JW. Multichannel urodynamic evaluation of laparoscopic Burch colposuspension for genuine stress incontinence. Obstet Gynecol. 1998;91:55-59.
23. Miannay E, Cosson M, Querleu D, et al. [Comparison of laparoscopic and laparotomy colposuspension in the treatment of urinary stress incontinence. Comparative study of 72 matched cases][French]. Contracept Fertil Sex. 1998;26:376-385.
24. Saidi MH, Gallagher MS, Skop IP, et al. Extrperitoneal laparoscopic colposuspension: short-term cure rate, complications and duration of hospital stay in comparison with Burch colposuspension. Obstet Gynecol. 1998;92:619-625.
25. Henley C. The Henley staple-suture technique for laparoscopic Burch colposuspension. J Am Assoc Gynecol Laparosc. 1995;2:441-444.
26. Das S, Palmer JK. Laparoscopic colposuspension. J Urol. 1995;154:1119-1121.
27. Ou CS, Presthus J, Beadle E. Laparoscopic bladder neck suspension using hernia mesh and surgical staples. J Laparoendosc Surg. 1993;3:563-566.
28. Kiilholma P, Haarala M, Polvi II, Makinen J, Chancellor MB. Sutureless colposuspension with fibrin sealant. Tech Urol. 1995;1:81-83.
29. Lose G. Laparoscopic Burch colposuspension. Acta Obstet Gynecol Scand Suppl. 1998;168:29-33.
30. Miannay E, Cosson M, Lanvin D, et al. Comparison of open retropubic and laparoscopic colposuspension for treatment of stress urinary incontinence. Eur J Obstet Gynecol Reprod Biol. 1998;79:159-166.
31. Saidi MH, Sadler RK, Saidi JA. Extraperitoneal laparoscopic colposuspension for genuine urinary stress incontinence. J Am Assoc Gynecol Laparosc. 1998;9:249-252.
32. Ou CS, Rowbotham R. Five-year follow-up of a laparoscopic bladder neck suspension using synthetic mesh and surgical staples. J Laparoendosc Adv Surg Techn A. 1999;9:249-252.
33. Zullo F, Morelli M, Russo T, et al. Two techniques of laparoscopic retropubic urethropexy. J Am Assoc Gynecol Laparosc. 2001;12:323-327.
34. Langer R, Lipshitz Y, Halperin R, et al. Long-term (10-15 years) follow-up after Burch colposuspension for urinary stress incontinence. Int Urogynecol J. 2001;12:323-327.
35. Herbertsson G, Iosif CS. Surgical results and urodynamic studies 10 years after retropubic colpurethropexy. Acta Obstet Gynecol Scand. 1993;72:298-301.
36. Parasio M, Falcone T, Walters M. Laparoscopic surgery for genuine stress incontinence. Int Urogynecol J. 1999;10:237-247.
37. Horbach NS. Suburethral sling procedures. Urogynecology and Urodynamics: Theory and Practice. 4th ed. Baltimore, Md: Williams and Wilkins 1996;569-579.
38. Vassallo B, Murphy M, Lucente V, Karram M. TVT versus Laparoscopic Burch: a retrospective review at 1-4 years. 27th Scientific Meeting of the Society of Gynecologic Surgeons. March 5-7, 2001.
39. Fotte A. Which is the best minimally invasive procedure? TVT versus laparoscopic colposuspension. Presented at the 31st annual meeting of the International Continence Society; September 18-21, 2001; Seoul, Korea.
40. Ward KL, Hilton P. Prospective multicentre randomized trial of tension-free vaginal tape and colposuspension as primary treatment for stress incontinence. BMJ. 2002;326:67.-
41. Miklos J, Kohli N. Laparoscopic paravaginal repair plus Burch colposuspension: review and descriptive technique. Urology. 2000;56:64-68.
42. Walter A. Laparoscopic repairs for stress urinary incontinence and pelvic organ prolapse: “show me the evidence.” Presented at the annual meeting of the American Urogynecologic Society; 2002; San Diego, Calif.
43. Summitt RL, Lucente V, Karram MM, Shull BL, Bent AE. Randomized comparison of laparoscopic and transabdominal Burch urethropexy for the treatment of genuine stress incontinence. Obstet Gynecol. 2000;95:(suppl):2.-
44. Fatthy H, El Hao M, Samaha I, Abdallah K. Modified Burch colposuspension: laparoscopy versus laparotomy. J Am Assoc Gynecol Laparosc. 2001;8:99-106.
45. Ross JW. Techniques of laparoscopic repair for total vault eversion after hysterectomy. J Am Assoc Gynecol Laparosc. 1997;4:173-183.
46. Ross JW. Laparoscopic approach for severe pelvic vault prolapse. J Am Assoc Gynecol Laparosc. 1996;3(suppl):43.-
47. Lyons TL, Winer WK. Laparoscopic rectocele repair using polyglactin mesh. J Am Assoc Gynecol Laparosc. 1997;4:381-384.
48. Ostrzenski A. Laparoscopic colposuspension for total vaginal prolapse. Int J Gynaecol Obstet. 1996;55:147-152.
49. Carter JE, Winter M, Mendehlsohn S, Saye W, Richardson AC. Vaginal vault suspension and enterocele repair by Richardson-Saye laparoscopic technique: description of training technique and results. JSLS. 2001;5:29-36.
50. Cosson M, Rajabally R, Bogaert E, Querleu D, Crepin G. Laparoscopic sacrocolpopexy, hysterectomy and Burch colposuspension: feasibility and short-term complications of 77 procedures. JSLS. 2002;6:115-119.
51. Miklos JR, Moore RD, Kohli N. Laparoscopic surgery for pelvic support defects. Curr Opin Obstet Gynecol. 2002;14:387-395.
1. National Association for Incontinence Quarterly Report. Summer 2002, Vol 20 No 3.
2. Black NA, Down SH. The effectiveness of surgery for stress incontinence in women: A systematic review. Br J Urol. 1996;78:497.-
3. Tanagho E. Colpocystourethropexy: The way we do it. J Urol. 1976;116:751-753.
4. Leach GE, Dinochowski RR, Appell RA, et al. Female stress urinary incontinence clinical guidelines panel: Report on the surgical management of female stress urinary incontinence. Baltimore, Md: American Urological Association, Inc.; 1997.
5. Vancaille TG, Schuessler W. Laparoscopic bladder neck suspension. J Laparoendosc Surg. 1991;1:169-173.
6. Albala DM, Schuessler WW, Vancaillie TG. Laparoscopic bladder suspension for the treatment of stress incontinence. Semin Urol. 1992;10:222-225.
7. Burton G. A randomized comparison of laparoscopic and open colposuspension [abstract]. Neurourol Urodyn. 1993;16:353-354.
8. Polascik TJ, Moore RG, Roseberg MT, Kavoussi LR. Comparison of laparoscopic and open retropubic colposuspension for treatment of stress urinary incontinence. Urology. 1995;45:647-652.
9. Liu CY. Laparoscopic treatment of genuine urinary stress incontinence. Clin Obstet Gynecol. 1994;8:789-798.
10. Gunn GC, Cooper RP, Gordon NS, Gragnon L. Use of a new device for endoscopic suturing in the laparoscopic Burch procedure. J Am Assoc Gynecol Laparosc. 1994;2:65-70.
11. Nezhat CH, Nezhat F, Nezhat CR, et al. Laparoscopic retropubic cystocolposuspension. J Am Assoc Gynecol Laparosc. 1994;1:339-349.
12. Lyons TL, Winer WK. Clinical outcomes with laparoscopic approaches and open Burch procedures for urinary stress incontinence. J Am Assoc Gynecol Laparosc. 1995;2:193-197.
13. McDougal EM, Klutke CG, Cornell T. Comparison of transvaginal versus laparoscopic bladder neck suspension for stress urinary incontinence. Adult Urol. 1995;45:641-645.
14. Ross JW. Laparoscopic Burch repair compared to laparotomy Burch for cure of urinary stress incontinence. Int Urogynecol. 1995;6:323-328.
15. Langebrekke A, Dahlstrom B, Eraker R, Urnes A. The laparoscopic Burch procedure: a preliminary report. Acta Obstet Gynecol Scand. 1995;74:153-155.
16. Radomski SB, Herschorn S. Laparoscopic Burch bladder neck suspension: early results. J Urol. 1996;155:515-518.
17. Ross JW. Two techniques of laparoscopic Burch repair for stress incontinence: a prospective randomized study. J Am Assoc Gynecol Laparoscopists. 1996;3:351-357.
18. Lam AM, Jenkins GJ, Hyslop RS. Laparoscopic results. Med J Aust. 1995;162:18-22.
19. Su TH, Wang KG, Hsu CY, Wei H, Hong BK. Prospective comparison of laparoscopic and traditional colposuspensions in the treatment of genuine stress inconti-nence. Acta Obstet Gynecol. 1997;76:576-582.
20. Papasakelariou C, Papasakelariou B. Laparoscopic bladder neck suspension. J Am Assoc Gynecol Laparosc. 1997;4:185-188.
21. Lobel RW, Davis GD. Long-term results of laparoscopic Burch colposuspension. J Am Assoc Gynecol Laparosc. 1997;4:341-345.
22. Ross JW. Multichannel urodynamic evaluation of laparoscopic Burch colposuspension for genuine stress incontinence. Obstet Gynecol. 1998;91:55-59.
23. Miannay E, Cosson M, Querleu D, et al. [Comparison of laparoscopic and laparotomy colposuspension in the treatment of urinary stress incontinence. Comparative study of 72 matched cases][French]. Contracept Fertil Sex. 1998;26:376-385.
24. Saidi MH, Gallagher MS, Skop IP, et al. Extrperitoneal laparoscopic colposuspension: short-term cure rate, complications and duration of hospital stay in comparison with Burch colposuspension. Obstet Gynecol. 1998;92:619-625.
25. Henley C. The Henley staple-suture technique for laparoscopic Burch colposuspension. J Am Assoc Gynecol Laparosc. 1995;2:441-444.
26. Das S, Palmer JK. Laparoscopic colposuspension. J Urol. 1995;154:1119-1121.
27. Ou CS, Presthus J, Beadle E. Laparoscopic bladder neck suspension using hernia mesh and surgical staples. J Laparoendosc Surg. 1993;3:563-566.
28. Kiilholma P, Haarala M, Polvi II, Makinen J, Chancellor MB. Sutureless colposuspension with fibrin sealant. Tech Urol. 1995;1:81-83.
29. Lose G. Laparoscopic Burch colposuspension. Acta Obstet Gynecol Scand Suppl. 1998;168:29-33.
30. Miannay E, Cosson M, Lanvin D, et al. Comparison of open retropubic and laparoscopic colposuspension for treatment of stress urinary incontinence. Eur J Obstet Gynecol Reprod Biol. 1998;79:159-166.
31. Saidi MH, Sadler RK, Saidi JA. Extraperitoneal laparoscopic colposuspension for genuine urinary stress incontinence. J Am Assoc Gynecol Laparosc. 1998;9:249-252.
32. Ou CS, Rowbotham R. Five-year follow-up of a laparoscopic bladder neck suspension using synthetic mesh and surgical staples. J Laparoendosc Adv Surg Techn A. 1999;9:249-252.
33. Zullo F, Morelli M, Russo T, et al. Two techniques of laparoscopic retropubic urethropexy. J Am Assoc Gynecol Laparosc. 2001;12:323-327.
34. Langer R, Lipshitz Y, Halperin R, et al. Long-term (10-15 years) follow-up after Burch colposuspension for urinary stress incontinence. Int Urogynecol J. 2001;12:323-327.
35. Herbertsson G, Iosif CS. Surgical results and urodynamic studies 10 years after retropubic colpurethropexy. Acta Obstet Gynecol Scand. 1993;72:298-301.
36. Parasio M, Falcone T, Walters M. Laparoscopic surgery for genuine stress incontinence. Int Urogynecol J. 1999;10:237-247.
37. Horbach NS. Suburethral sling procedures. Urogynecology and Urodynamics: Theory and Practice. 4th ed. Baltimore, Md: Williams and Wilkins 1996;569-579.
38. Vassallo B, Murphy M, Lucente V, Karram M. TVT versus Laparoscopic Burch: a retrospective review at 1-4 years. 27th Scientific Meeting of the Society of Gynecologic Surgeons. March 5-7, 2001.
39. Fotte A. Which is the best minimally invasive procedure? TVT versus laparoscopic colposuspension. Presented at the 31st annual meeting of the International Continence Society; September 18-21, 2001; Seoul, Korea.
40. Ward KL, Hilton P. Prospective multicentre randomized trial of tension-free vaginal tape and colposuspension as primary treatment for stress incontinence. BMJ. 2002;326:67.-
41. Miklos J, Kohli N. Laparoscopic paravaginal repair plus Burch colposuspension: review and descriptive technique. Urology. 2000;56:64-68.
42. Walter A. Laparoscopic repairs for stress urinary incontinence and pelvic organ prolapse: “show me the evidence.” Presented at the annual meeting of the American Urogynecologic Society; 2002; San Diego, Calif.
43. Summitt RL, Lucente V, Karram MM, Shull BL, Bent AE. Randomized comparison of laparoscopic and transabdominal Burch urethropexy for the treatment of genuine stress incontinence. Obstet Gynecol. 2000;95:(suppl):2.-
44. Fatthy H, El Hao M, Samaha I, Abdallah K. Modified Burch colposuspension: laparoscopy versus laparotomy. J Am Assoc Gynecol Laparosc. 2001;8:99-106.
45. Ross JW. Techniques of laparoscopic repair for total vault eversion after hysterectomy. J Am Assoc Gynecol Laparosc. 1997;4:173-183.
46. Ross JW. Laparoscopic approach for severe pelvic vault prolapse. J Am Assoc Gynecol Laparosc. 1996;3(suppl):43.-
47. Lyons TL, Winer WK. Laparoscopic rectocele repair using polyglactin mesh. J Am Assoc Gynecol Laparosc. 1997;4:381-384.
48. Ostrzenski A. Laparoscopic colposuspension for total vaginal prolapse. Int J Gynaecol Obstet. 1996;55:147-152.
49. Carter JE, Winter M, Mendehlsohn S, Saye W, Richardson AC. Vaginal vault suspension and enterocele repair by Richardson-Saye laparoscopic technique: description of training technique and results. JSLS. 2001;5:29-36.
50. Cosson M, Rajabally R, Bogaert E, Querleu D, Crepin G. Laparoscopic sacrocolpopexy, hysterectomy and Burch colposuspension: feasibility and short-term complications of 77 procedures. JSLS. 2002;6:115-119.
51. Miklos JR, Moore RD, Kohli N. Laparoscopic surgery for pelvic support defects. Curr Opin Obstet Gynecol. 2002;14:387-395.
Safe delivery of the fetal head during cesarean section
- Position yourself so your upper trunk, arm, and hand move as a unit to elevate the head.
- Elevate the head to the level of the uterine incision, rather than bringing the incision down to the head.
- Rotate the occiput anteriorly to present the shortest fetal head diameters to the incision.
- Reduce the lower lip of the uterine incision beneath the fetal head, as you would reduce a posterior cervical lip at a vaginal delivery.
Although it’s a skill vital for cesarean birth, manual delivery of the fetal head from a low pelvic station is given only cursory coverage in standard obstetrics texts and reviews.1-4 To learn successful methods, therefore, physicians are forced to rely on observation, anecdotal experience, and—least desirably—trial and error.
Possibly the most frequently employed maneuver in this scenario is to have an assistant elevate the head with his or her hand.1,3,4 However, this technique may not provide sufficient elevation. Furthermore, subsequent manipulation by the clinician may extend the uterine incision and risk injury to the uterine vessels and bladder. It is an untested assumption that such extensions increase the risk of uterine rupture during subsequent trials of labor.
With the goals of minimizing delay, head compression, and strain on the uterine incision, I developed the elevate, rotate, and reduce (ERR) technique for expeditious delivery of the head from a deep pelvic station.
Approaching the head
Begin the procedure by identifying the fetal position; if it is occiput posterior, you may wish to have a disposable vacuum extractor available. Then stand so that your dominant hand is closest to the patient’s pelvis.
When making the abdominal incision, consider fetal size and maternal body habitus. Be sure all layers of the incision are long enough to permit manipulation and delivery—don’t let surgical pride force you to struggle with an inadequate Pfannenstiel incision. Be prepared to identify and extend any layer of the incision that gives considerable resistance at the time of delivery.
Before proceeding to the uterine incision, make sure there is adequate rectus separation. Check the clearance by separating the right and left bodies of the rectus muscle with manual traction. If more room is needed, create a “partial Maylard incision” by cutting bilateral transverse incisions with Mayo scissors across the medial third of each body. This gives the fetus more room while avoiding damage to the inferior epigastric vessels.
The uterine incision should be as wide as the mean fetal head diameter—usually the same 10 cm that we expect of the fully dilated cervix at term. In patients with an undeveloped lower uterine segment, varices, adhesions, or leiomyomata, there may be insufficient width for a low-transverse incision. In these cases you may need to convert to a U, J, or vertical incision.
Take advantage of a well-developed lower uterine segment and avoid tight U- or V-shaped transverse incisions. Identify the uterine vessels with adequate retraction, and incise laterally right up to them. An alternate technique would be to extend the initial incision by pulling apart the ends with your index fingers, laterally and cephalad (towards the mother’s axillae). Blunt dissection may cause less bleeding from the uterine vessels.5
The ERR technique
“Don’t break the wrist” is a classic admonition, familiar to generations of obstetricians. It warns against a practice that begins by reaching for the head with extended wrist, not elevating the head enough, and delivering the head from whatever position it presents in. The head is delivered with firm wrist flexion (breaking, cocking, or levering the wrist) and anterior traction. This puts caudal leverage upon the lower edge of the uterine incision, which may cause an extension down to the bladder or into the cervix. The ERR technique corrects these errors and minimizes strain on the incision.
Elevate. The first goal of ERR is to elevate the fetal vertex to the lower edge of the uterine incision. Bringing the incision down to the presenting part may strain it. Start by holding the fingers of your dominant hand together, with the thumb tucked against the lateral base Safe delivery of the fetal head during cesarean section of the index finger and the fingers extended straight.
Next, insert your fingertips into the uterine incision and advance them around the fetal head—but not while standing erect with your wrist extended. Such a posture would cause 2 problems: First, you would have insufficient leverage and strength to advance your fingers deep into the pelvis. Second, the angle of your wrist would be obstructed by the uterine incision, the lower edge of the abdominal incision, and the pubis.
Instead, try 1 of the following 2 approaches: The first option is to extend your arm in a straight line from shoulder to fingertip, keeping it almost parallel to the patient’s longitudinal axis. This is accomplished by flexing forward at the waist while facing cross-table, and abducting your arm out from your shoulder. Another option is to turn and face the head of the table, flex at the waist, and extend your arm behind you while pronating your hand. Both of these positions keep your wrist angle neutral and allow you to use the strength and leverage of your entire upper trunk to move your hand.
In order to elevate the head, your fingers need to achieve at least a quarter-circle grip around the vertex (FIGURE 1). If the head is so deep or tightly applied that you cannot achieve this in 1 continuous movement, proceed in stages. First, have an assistant apply transvaginal digital pressure to elevate the head from below. Then, advance your fingers as far as you can around the fetal head while flexing and extending the fingers in a worm-like wiggling movement. Flex and lock your fingers against the fetal cranium, and lean your entire upper trunk and arm away from the maternal pelvis. This generally elevates the head by roughly a centimeter, enough to advance your fingers a little further. Repeat these motions until your fingers have achieved the desired quarter-circle, at which point your assistant may withdraw from below.
Now lock your arm from shoulder to fingertip, and lean out of the patient’s pelvis 1 more time. You may note the sensation and sound of breaking suction as the fetal head escapes the pelvic grip. Maintain this steady traction for several seconds. When the vertex has reached the level of the lower margin of the uterine incision, you can rotate the fetus.
Rotate. Before you begin rotation, confirm the fetal position (the fetal ears are useful as a landmark). If the head is not already in occiput anterior, grasp it and rotate the occiput into the incision (FIGURE 2). As in vaginal delivery, this presents the shortest fetal-head diameters to the birth orifice. If the head has been markedly molded by labor, rotation will bring the narrow end of a dilating cone into the uterine incision. This helps direct the head anteriorly, rather than back into the pelvis, when fundal pressure is applied.
Reduce. Using your hand like a pair of forceps may cause uterine extensions or lacerations if the uterine incision is not large enough to accommodate both your hand and the fetal head. Instead, use 4 fingers in shoehorn fashion to guide the head out of the incision. First, however, there is usually another obstacle to overcome: Fundal pressure may merely force the head back toward the pelvis. Your fingers cannot present a shallow enough angle to direct the head anteriorly, unless your hand is in so deep that your palm fills the uterine incision.
You may substitute instruments for the guiding fingers, using the Murless head extractor, the Torpin vectis blade, or 1 blade of a short-shank Simpson forceps. However, a lack of availability may limit your choices. Although you may use a disposable vacuum extractor system, consider saving that expense with this alternative: Using your fingertips, reduce the lower lip of the uterine incision beneath the fetal head, as you would reduce a posterior cervical lip at a vaginal delivery. (FIGURE 3). The reduced lip tends to extend the head anteriorly and direct it away from the pelvis. Withdraw your hand so only your fingertips remain to guide the head, while the back of your fingers retract the lower abdominal wall. With fundal pressure the head should move anteriorly out of the abdomen.
A head in the occiput-posterior position may resist attempts to rotate to occiput anterior. Should this occur, try following the incision reduction with direct manual flexion of the head out of the abdomen. If reduction flexion puts excess strain on the incision, abandon the attempt. Instead, use a disposable vacuum extractor cup—placed on the fetal brow as close to the vertex as possible—to flex the head out of the incision. Should this fail as well, extend the low-transverse uterine incision cranially into a generous U-incision, and repeat the vacuum procedure.
FIGURE 1 THE ERR SEQUENCE
Elevate. Lock the fingers into a quarter-circle around the vertex. Apply traction out of the pelvis with the hand and the entire extended arm.
FIGURE 2 THE ERR SEQUENCE
Rotate. Grasp the fetal head between the thumb and fingers and rotate it so the occiput faces the incision.
FIGURE 3 THE ERR SEQUENCE
Reduce. Push the lower edge of the uterine incision down until it is posterior to the fetal head.
Conclusion
This technique for delivering the fetal head offers minimal risk of uterine laceration and lends itself to instruction and recollection.
I have not evaluated ERR by clinical trial, both due to absence of a gold-standard technique for the control group and because ERR has yielded satisfactory outcomes in the 20 years over which I have developed, applied, and taught it. Still, the technique raises opportunities for clinical investigation. For example, residency training programs concerned over their incidence of uterine extensions and lacerations may wish to adopt this method and subsequently produce a historical-controlled, retrospective cohort study as a quality-improvement project.
Dr. Chao reports no financial relationship with any companies whose products are mentioned in this article.
1. Cunningham FG, MacDonald PC, Gant NF, et al. Williams Obstetrics. 20th ed. Stamford, Conn: Appleton & Lange; 1997;518.-
2. Scott JR. Cesarean delivery. In: Scott JR, Disaia PJ, Hammond CB, Spellacy WN, eds. Danforth’s Obstetrics and Gynecology. 8th ed. Philadelphia: Lippincott Williams and Wilkins; 1999;462.-
3. Depp R. Cesarean delivery. In: Gabbe SG, Niebyl JR, Simpson JL. Obstetrics: Normal and Problem Pregnancies. 4th ed. New York: Churchill Livingstone, 2002;554.-
4. Field CS. Surgical techniques for cesarean section. Obstet Gynecol Clin NA. 1988;15:664-665.
5. Magann EF, Chauhan SP, Bufkin L, Field K, Roberts WE, Martin JN, Jr. Intraoperative hemorrhage by blunt versus sharp expansion of the uterine incision at caesarean delivery: a randomized clinical trial. BJOG. 2002;109:448-452.
- Position yourself so your upper trunk, arm, and hand move as a unit to elevate the head.
- Elevate the head to the level of the uterine incision, rather than bringing the incision down to the head.
- Rotate the occiput anteriorly to present the shortest fetal head diameters to the incision.
- Reduce the lower lip of the uterine incision beneath the fetal head, as you would reduce a posterior cervical lip at a vaginal delivery.
Although it’s a skill vital for cesarean birth, manual delivery of the fetal head from a low pelvic station is given only cursory coverage in standard obstetrics texts and reviews.1-4 To learn successful methods, therefore, physicians are forced to rely on observation, anecdotal experience, and—least desirably—trial and error.
Possibly the most frequently employed maneuver in this scenario is to have an assistant elevate the head with his or her hand.1,3,4 However, this technique may not provide sufficient elevation. Furthermore, subsequent manipulation by the clinician may extend the uterine incision and risk injury to the uterine vessels and bladder. It is an untested assumption that such extensions increase the risk of uterine rupture during subsequent trials of labor.
With the goals of minimizing delay, head compression, and strain on the uterine incision, I developed the elevate, rotate, and reduce (ERR) technique for expeditious delivery of the head from a deep pelvic station.
Approaching the head
Begin the procedure by identifying the fetal position; if it is occiput posterior, you may wish to have a disposable vacuum extractor available. Then stand so that your dominant hand is closest to the patient’s pelvis.
When making the abdominal incision, consider fetal size and maternal body habitus. Be sure all layers of the incision are long enough to permit manipulation and delivery—don’t let surgical pride force you to struggle with an inadequate Pfannenstiel incision. Be prepared to identify and extend any layer of the incision that gives considerable resistance at the time of delivery.
Before proceeding to the uterine incision, make sure there is adequate rectus separation. Check the clearance by separating the right and left bodies of the rectus muscle with manual traction. If more room is needed, create a “partial Maylard incision” by cutting bilateral transverse incisions with Mayo scissors across the medial third of each body. This gives the fetus more room while avoiding damage to the inferior epigastric vessels.
The uterine incision should be as wide as the mean fetal head diameter—usually the same 10 cm that we expect of the fully dilated cervix at term. In patients with an undeveloped lower uterine segment, varices, adhesions, or leiomyomata, there may be insufficient width for a low-transverse incision. In these cases you may need to convert to a U, J, or vertical incision.
Take advantage of a well-developed lower uterine segment and avoid tight U- or V-shaped transverse incisions. Identify the uterine vessels with adequate retraction, and incise laterally right up to them. An alternate technique would be to extend the initial incision by pulling apart the ends with your index fingers, laterally and cephalad (towards the mother’s axillae). Blunt dissection may cause less bleeding from the uterine vessels.5
The ERR technique
“Don’t break the wrist” is a classic admonition, familiar to generations of obstetricians. It warns against a practice that begins by reaching for the head with extended wrist, not elevating the head enough, and delivering the head from whatever position it presents in. The head is delivered with firm wrist flexion (breaking, cocking, or levering the wrist) and anterior traction. This puts caudal leverage upon the lower edge of the uterine incision, which may cause an extension down to the bladder or into the cervix. The ERR technique corrects these errors and minimizes strain on the incision.
Elevate. The first goal of ERR is to elevate the fetal vertex to the lower edge of the uterine incision. Bringing the incision down to the presenting part may strain it. Start by holding the fingers of your dominant hand together, with the thumb tucked against the lateral base Safe delivery of the fetal head during cesarean section of the index finger and the fingers extended straight.
Next, insert your fingertips into the uterine incision and advance them around the fetal head—but not while standing erect with your wrist extended. Such a posture would cause 2 problems: First, you would have insufficient leverage and strength to advance your fingers deep into the pelvis. Second, the angle of your wrist would be obstructed by the uterine incision, the lower edge of the abdominal incision, and the pubis.
Instead, try 1 of the following 2 approaches: The first option is to extend your arm in a straight line from shoulder to fingertip, keeping it almost parallel to the patient’s longitudinal axis. This is accomplished by flexing forward at the waist while facing cross-table, and abducting your arm out from your shoulder. Another option is to turn and face the head of the table, flex at the waist, and extend your arm behind you while pronating your hand. Both of these positions keep your wrist angle neutral and allow you to use the strength and leverage of your entire upper trunk to move your hand.
In order to elevate the head, your fingers need to achieve at least a quarter-circle grip around the vertex (FIGURE 1). If the head is so deep or tightly applied that you cannot achieve this in 1 continuous movement, proceed in stages. First, have an assistant apply transvaginal digital pressure to elevate the head from below. Then, advance your fingers as far as you can around the fetal head while flexing and extending the fingers in a worm-like wiggling movement. Flex and lock your fingers against the fetal cranium, and lean your entire upper trunk and arm away from the maternal pelvis. This generally elevates the head by roughly a centimeter, enough to advance your fingers a little further. Repeat these motions until your fingers have achieved the desired quarter-circle, at which point your assistant may withdraw from below.
Now lock your arm from shoulder to fingertip, and lean out of the patient’s pelvis 1 more time. You may note the sensation and sound of breaking suction as the fetal head escapes the pelvic grip. Maintain this steady traction for several seconds. When the vertex has reached the level of the lower margin of the uterine incision, you can rotate the fetus.
Rotate. Before you begin rotation, confirm the fetal position (the fetal ears are useful as a landmark). If the head is not already in occiput anterior, grasp it and rotate the occiput into the incision (FIGURE 2). As in vaginal delivery, this presents the shortest fetal-head diameters to the birth orifice. If the head has been markedly molded by labor, rotation will bring the narrow end of a dilating cone into the uterine incision. This helps direct the head anteriorly, rather than back into the pelvis, when fundal pressure is applied.
Reduce. Using your hand like a pair of forceps may cause uterine extensions or lacerations if the uterine incision is not large enough to accommodate both your hand and the fetal head. Instead, use 4 fingers in shoehorn fashion to guide the head out of the incision. First, however, there is usually another obstacle to overcome: Fundal pressure may merely force the head back toward the pelvis. Your fingers cannot present a shallow enough angle to direct the head anteriorly, unless your hand is in so deep that your palm fills the uterine incision.
You may substitute instruments for the guiding fingers, using the Murless head extractor, the Torpin vectis blade, or 1 blade of a short-shank Simpson forceps. However, a lack of availability may limit your choices. Although you may use a disposable vacuum extractor system, consider saving that expense with this alternative: Using your fingertips, reduce the lower lip of the uterine incision beneath the fetal head, as you would reduce a posterior cervical lip at a vaginal delivery. (FIGURE 3). The reduced lip tends to extend the head anteriorly and direct it away from the pelvis. Withdraw your hand so only your fingertips remain to guide the head, while the back of your fingers retract the lower abdominal wall. With fundal pressure the head should move anteriorly out of the abdomen.
A head in the occiput-posterior position may resist attempts to rotate to occiput anterior. Should this occur, try following the incision reduction with direct manual flexion of the head out of the abdomen. If reduction flexion puts excess strain on the incision, abandon the attempt. Instead, use a disposable vacuum extractor cup—placed on the fetal brow as close to the vertex as possible—to flex the head out of the incision. Should this fail as well, extend the low-transverse uterine incision cranially into a generous U-incision, and repeat the vacuum procedure.
FIGURE 1 THE ERR SEQUENCE
Elevate. Lock the fingers into a quarter-circle around the vertex. Apply traction out of the pelvis with the hand and the entire extended arm.
FIGURE 2 THE ERR SEQUENCE
Rotate. Grasp the fetal head between the thumb and fingers and rotate it so the occiput faces the incision.
FIGURE 3 THE ERR SEQUENCE
Reduce. Push the lower edge of the uterine incision down until it is posterior to the fetal head.
Conclusion
This technique for delivering the fetal head offers minimal risk of uterine laceration and lends itself to instruction and recollection.
I have not evaluated ERR by clinical trial, both due to absence of a gold-standard technique for the control group and because ERR has yielded satisfactory outcomes in the 20 years over which I have developed, applied, and taught it. Still, the technique raises opportunities for clinical investigation. For example, residency training programs concerned over their incidence of uterine extensions and lacerations may wish to adopt this method and subsequently produce a historical-controlled, retrospective cohort study as a quality-improvement project.
Dr. Chao reports no financial relationship with any companies whose products are mentioned in this article.
- Position yourself so your upper trunk, arm, and hand move as a unit to elevate the head.
- Elevate the head to the level of the uterine incision, rather than bringing the incision down to the head.
- Rotate the occiput anteriorly to present the shortest fetal head diameters to the incision.
- Reduce the lower lip of the uterine incision beneath the fetal head, as you would reduce a posterior cervical lip at a vaginal delivery.
Although it’s a skill vital for cesarean birth, manual delivery of the fetal head from a low pelvic station is given only cursory coverage in standard obstetrics texts and reviews.1-4 To learn successful methods, therefore, physicians are forced to rely on observation, anecdotal experience, and—least desirably—trial and error.
Possibly the most frequently employed maneuver in this scenario is to have an assistant elevate the head with his or her hand.1,3,4 However, this technique may not provide sufficient elevation. Furthermore, subsequent manipulation by the clinician may extend the uterine incision and risk injury to the uterine vessels and bladder. It is an untested assumption that such extensions increase the risk of uterine rupture during subsequent trials of labor.
With the goals of minimizing delay, head compression, and strain on the uterine incision, I developed the elevate, rotate, and reduce (ERR) technique for expeditious delivery of the head from a deep pelvic station.
Approaching the head
Begin the procedure by identifying the fetal position; if it is occiput posterior, you may wish to have a disposable vacuum extractor available. Then stand so that your dominant hand is closest to the patient’s pelvis.
When making the abdominal incision, consider fetal size and maternal body habitus. Be sure all layers of the incision are long enough to permit manipulation and delivery—don’t let surgical pride force you to struggle with an inadequate Pfannenstiel incision. Be prepared to identify and extend any layer of the incision that gives considerable resistance at the time of delivery.
Before proceeding to the uterine incision, make sure there is adequate rectus separation. Check the clearance by separating the right and left bodies of the rectus muscle with manual traction. If more room is needed, create a “partial Maylard incision” by cutting bilateral transverse incisions with Mayo scissors across the medial third of each body. This gives the fetus more room while avoiding damage to the inferior epigastric vessels.
The uterine incision should be as wide as the mean fetal head diameter—usually the same 10 cm that we expect of the fully dilated cervix at term. In patients with an undeveloped lower uterine segment, varices, adhesions, or leiomyomata, there may be insufficient width for a low-transverse incision. In these cases you may need to convert to a U, J, or vertical incision.
Take advantage of a well-developed lower uterine segment and avoid tight U- or V-shaped transverse incisions. Identify the uterine vessels with adequate retraction, and incise laterally right up to them. An alternate technique would be to extend the initial incision by pulling apart the ends with your index fingers, laterally and cephalad (towards the mother’s axillae). Blunt dissection may cause less bleeding from the uterine vessels.5
The ERR technique
“Don’t break the wrist” is a classic admonition, familiar to generations of obstetricians. It warns against a practice that begins by reaching for the head with extended wrist, not elevating the head enough, and delivering the head from whatever position it presents in. The head is delivered with firm wrist flexion (breaking, cocking, or levering the wrist) and anterior traction. This puts caudal leverage upon the lower edge of the uterine incision, which may cause an extension down to the bladder or into the cervix. The ERR technique corrects these errors and minimizes strain on the incision.
Elevate. The first goal of ERR is to elevate the fetal vertex to the lower edge of the uterine incision. Bringing the incision down to the presenting part may strain it. Start by holding the fingers of your dominant hand together, with the thumb tucked against the lateral base Safe delivery of the fetal head during cesarean section of the index finger and the fingers extended straight.
Next, insert your fingertips into the uterine incision and advance them around the fetal head—but not while standing erect with your wrist extended. Such a posture would cause 2 problems: First, you would have insufficient leverage and strength to advance your fingers deep into the pelvis. Second, the angle of your wrist would be obstructed by the uterine incision, the lower edge of the abdominal incision, and the pubis.
Instead, try 1 of the following 2 approaches: The first option is to extend your arm in a straight line from shoulder to fingertip, keeping it almost parallel to the patient’s longitudinal axis. This is accomplished by flexing forward at the waist while facing cross-table, and abducting your arm out from your shoulder. Another option is to turn and face the head of the table, flex at the waist, and extend your arm behind you while pronating your hand. Both of these positions keep your wrist angle neutral and allow you to use the strength and leverage of your entire upper trunk to move your hand.
In order to elevate the head, your fingers need to achieve at least a quarter-circle grip around the vertex (FIGURE 1). If the head is so deep or tightly applied that you cannot achieve this in 1 continuous movement, proceed in stages. First, have an assistant apply transvaginal digital pressure to elevate the head from below. Then, advance your fingers as far as you can around the fetal head while flexing and extending the fingers in a worm-like wiggling movement. Flex and lock your fingers against the fetal cranium, and lean your entire upper trunk and arm away from the maternal pelvis. This generally elevates the head by roughly a centimeter, enough to advance your fingers a little further. Repeat these motions until your fingers have achieved the desired quarter-circle, at which point your assistant may withdraw from below.
Now lock your arm from shoulder to fingertip, and lean out of the patient’s pelvis 1 more time. You may note the sensation and sound of breaking suction as the fetal head escapes the pelvic grip. Maintain this steady traction for several seconds. When the vertex has reached the level of the lower margin of the uterine incision, you can rotate the fetus.
Rotate. Before you begin rotation, confirm the fetal position (the fetal ears are useful as a landmark). If the head is not already in occiput anterior, grasp it and rotate the occiput into the incision (FIGURE 2). As in vaginal delivery, this presents the shortest fetal-head diameters to the birth orifice. If the head has been markedly molded by labor, rotation will bring the narrow end of a dilating cone into the uterine incision. This helps direct the head anteriorly, rather than back into the pelvis, when fundal pressure is applied.
Reduce. Using your hand like a pair of forceps may cause uterine extensions or lacerations if the uterine incision is not large enough to accommodate both your hand and the fetal head. Instead, use 4 fingers in shoehorn fashion to guide the head out of the incision. First, however, there is usually another obstacle to overcome: Fundal pressure may merely force the head back toward the pelvis. Your fingers cannot present a shallow enough angle to direct the head anteriorly, unless your hand is in so deep that your palm fills the uterine incision.
You may substitute instruments for the guiding fingers, using the Murless head extractor, the Torpin vectis blade, or 1 blade of a short-shank Simpson forceps. However, a lack of availability may limit your choices. Although you may use a disposable vacuum extractor system, consider saving that expense with this alternative: Using your fingertips, reduce the lower lip of the uterine incision beneath the fetal head, as you would reduce a posterior cervical lip at a vaginal delivery. (FIGURE 3). The reduced lip tends to extend the head anteriorly and direct it away from the pelvis. Withdraw your hand so only your fingertips remain to guide the head, while the back of your fingers retract the lower abdominal wall. With fundal pressure the head should move anteriorly out of the abdomen.
A head in the occiput-posterior position may resist attempts to rotate to occiput anterior. Should this occur, try following the incision reduction with direct manual flexion of the head out of the abdomen. If reduction flexion puts excess strain on the incision, abandon the attempt. Instead, use a disposable vacuum extractor cup—placed on the fetal brow as close to the vertex as possible—to flex the head out of the incision. Should this fail as well, extend the low-transverse uterine incision cranially into a generous U-incision, and repeat the vacuum procedure.
FIGURE 1 THE ERR SEQUENCE
Elevate. Lock the fingers into a quarter-circle around the vertex. Apply traction out of the pelvis with the hand and the entire extended arm.
FIGURE 2 THE ERR SEQUENCE
Rotate. Grasp the fetal head between the thumb and fingers and rotate it so the occiput faces the incision.
FIGURE 3 THE ERR SEQUENCE
Reduce. Push the lower edge of the uterine incision down until it is posterior to the fetal head.
Conclusion
This technique for delivering the fetal head offers minimal risk of uterine laceration and lends itself to instruction and recollection.
I have not evaluated ERR by clinical trial, both due to absence of a gold-standard technique for the control group and because ERR has yielded satisfactory outcomes in the 20 years over which I have developed, applied, and taught it. Still, the technique raises opportunities for clinical investigation. For example, residency training programs concerned over their incidence of uterine extensions and lacerations may wish to adopt this method and subsequently produce a historical-controlled, retrospective cohort study as a quality-improvement project.
Dr. Chao reports no financial relationship with any companies whose products are mentioned in this article.
1. Cunningham FG, MacDonald PC, Gant NF, et al. Williams Obstetrics. 20th ed. Stamford, Conn: Appleton & Lange; 1997;518.-
2. Scott JR. Cesarean delivery. In: Scott JR, Disaia PJ, Hammond CB, Spellacy WN, eds. Danforth’s Obstetrics and Gynecology. 8th ed. Philadelphia: Lippincott Williams and Wilkins; 1999;462.-
3. Depp R. Cesarean delivery. In: Gabbe SG, Niebyl JR, Simpson JL. Obstetrics: Normal and Problem Pregnancies. 4th ed. New York: Churchill Livingstone, 2002;554.-
4. Field CS. Surgical techniques for cesarean section. Obstet Gynecol Clin NA. 1988;15:664-665.
5. Magann EF, Chauhan SP, Bufkin L, Field K, Roberts WE, Martin JN, Jr. Intraoperative hemorrhage by blunt versus sharp expansion of the uterine incision at caesarean delivery: a randomized clinical trial. BJOG. 2002;109:448-452.
1. Cunningham FG, MacDonald PC, Gant NF, et al. Williams Obstetrics. 20th ed. Stamford, Conn: Appleton & Lange; 1997;518.-
2. Scott JR. Cesarean delivery. In: Scott JR, Disaia PJ, Hammond CB, Spellacy WN, eds. Danforth’s Obstetrics and Gynecology. 8th ed. Philadelphia: Lippincott Williams and Wilkins; 1999;462.-
3. Depp R. Cesarean delivery. In: Gabbe SG, Niebyl JR, Simpson JL. Obstetrics: Normal and Problem Pregnancies. 4th ed. New York: Churchill Livingstone, 2002;554.-
4. Field CS. Surgical techniques for cesarean section. Obstet Gynecol Clin NA. 1988;15:664-665.
5. Magann EF, Chauhan SP, Bufkin L, Field K, Roberts WE, Martin JN, Jr. Intraoperative hemorrhage by blunt versus sharp expansion of the uterine incision at caesarean delivery: a randomized clinical trial. BJOG. 2002;109:448-452.