User login
Product can eliminate inhibitors in hemophilia A

A plasma-derived factor VIII/von Willebrand factor product (Octanate) can eliminate inhibitors in patients with hemophilia A, according to research published in Haemophilia.
Octanate eradicated inhibitors in nearly 80% of patients studied, and patients who became inhibitor-free experienced an 86% reduction in monthly bleeding.
Adverse drug reactions occurred in about 42% of patients, and 4 of the 124 adverse events were considered serious.
Wolfhart Kreuz, MD, of HZRM (Haemophilia Centre Rhein Main) in Mörfelden-Walldorf, Germany, and his colleagues conducted this research as part of the ongoing ObsITI study. The trial enrolled 48 patients with hemophilia A and inhibitors.
Most patients–83.3% (n=40)—had 1 or more poor prognostic factors for immune tolerance induction (ITI) success. This includes age of 7 or older, having been diagnosed with inhibitors for 2 years or more, having an inhibitor titer of 10 BU or higher at the start of ITI, and prior ITI failure.
Patients received Octanate as the sole factor VIII product between December 2005 and October 2010. Patients who were “low responders” at the start of ITI (<5 BU) received 50–100 IU factor VIII kg-1 daily or every other day. And “high responders” (≥5 BU) received 100 IU factor VIII kg-1 every 12 hours.
During ITI, 4 patients received prophylaxis with bypassing agents—2 with activated prothrombin complex concentrates and 2 with recombinant factor VIIa.
The researchers assessed ITI efficacy according to 3 criteria. These were: (1) inhibitor titer <0.6 BU, (2) factor VIII recovery ≥80% of the predefined reference value of 1.5% IU-1 kg-1 body weight ≤1 hour post-injection, and (3) factor VIII half-life ≥7 hours.
The researchers defined “complete success” as meeting all 3 efficacy criteria, “partial success” as meeting 2 criteria, and “partial response” as meeting 1 criterion. If none of the criteria were met within the 36-month observation period, this was considered an ITI failure. Withdrawal from the study for administrative reasons was considered an ITI failure as well.
Treatment was deemed a complete success in 70.8% of patients (n=34) and a partial success in 6.3% (n=3). One patient (2.1%) had a partial response. Treatment failed in 20.8% of patients (n=10), all of whom had poor prognostic factors.
Overall, 79.2% of patients (38/48) became negative for inhibitors. These patients saw an 86% reduction in their monthly bleeding rate (P<0.0001), which decreased most dramatically during the initial 4 months of ITI. During that period, the mean monthly bleeding rate fell from 1.05 to 0.26.
The researchers noted that treatment outcome was significantly associated with a patient’s inhibitor titer level at the start of ITI (P=0.0068), the number of poor prognostic factors (P=0.0187), the monthly bleeding rate during ITI (P=0.0005), and peak inhibitor titer during ITI (P=0.0007).
There were 124 adverse drug reactions reported in 20 patients (41.7%). And there were 4 serious adverse drug reactions—intravenous catheter infection, febrile convulsion, gingivitis, and pyrexia. One reaction—allergic dermatitis—was considered possibly or probably related to treatment. ![]()

A plasma-derived factor VIII/von Willebrand factor product (Octanate) can eliminate inhibitors in patients with hemophilia A, according to research published in Haemophilia.
Octanate eradicated inhibitors in nearly 80% of patients studied, and patients who became inhibitor-free experienced an 86% reduction in monthly bleeding.
Adverse drug reactions occurred in about 42% of patients, and 4 of the 124 adverse events were considered serious.
Wolfhart Kreuz, MD, of HZRM (Haemophilia Centre Rhein Main) in Mörfelden-Walldorf, Germany, and his colleagues conducted this research as part of the ongoing ObsITI study. The trial enrolled 48 patients with hemophilia A and inhibitors.
Most patients–83.3% (n=40)—had 1 or more poor prognostic factors for immune tolerance induction (ITI) success. This includes age of 7 or older, having been diagnosed with inhibitors for 2 years or more, having an inhibitor titer of 10 BU or higher at the start of ITI, and prior ITI failure.
Patients received Octanate as the sole factor VIII product between December 2005 and October 2010. Patients who were “low responders” at the start of ITI (<5 BU) received 50–100 IU factor VIII kg-1 daily or every other day. And “high responders” (≥5 BU) received 100 IU factor VIII kg-1 every 12 hours.
During ITI, 4 patients received prophylaxis with bypassing agents—2 with activated prothrombin complex concentrates and 2 with recombinant factor VIIa.
The researchers assessed ITI efficacy according to 3 criteria. These were: (1) inhibitor titer <0.6 BU, (2) factor VIII recovery ≥80% of the predefined reference value of 1.5% IU-1 kg-1 body weight ≤1 hour post-injection, and (3) factor VIII half-life ≥7 hours.
The researchers defined “complete success” as meeting all 3 efficacy criteria, “partial success” as meeting 2 criteria, and “partial response” as meeting 1 criterion. If none of the criteria were met within the 36-month observation period, this was considered an ITI failure. Withdrawal from the study for administrative reasons was considered an ITI failure as well.
Treatment was deemed a complete success in 70.8% of patients (n=34) and a partial success in 6.3% (n=3). One patient (2.1%) had a partial response. Treatment failed in 20.8% of patients (n=10), all of whom had poor prognostic factors.
Overall, 79.2% of patients (38/48) became negative for inhibitors. These patients saw an 86% reduction in their monthly bleeding rate (P<0.0001), which decreased most dramatically during the initial 4 months of ITI. During that period, the mean monthly bleeding rate fell from 1.05 to 0.26.
The researchers noted that treatment outcome was significantly associated with a patient’s inhibitor titer level at the start of ITI (P=0.0068), the number of poor prognostic factors (P=0.0187), the monthly bleeding rate during ITI (P=0.0005), and peak inhibitor titer during ITI (P=0.0007).
There were 124 adverse drug reactions reported in 20 patients (41.7%). And there were 4 serious adverse drug reactions—intravenous catheter infection, febrile convulsion, gingivitis, and pyrexia. One reaction—allergic dermatitis—was considered possibly or probably related to treatment. ![]()

A plasma-derived factor VIII/von Willebrand factor product (Octanate) can eliminate inhibitors in patients with hemophilia A, according to research published in Haemophilia.
Octanate eradicated inhibitors in nearly 80% of patients studied, and patients who became inhibitor-free experienced an 86% reduction in monthly bleeding.
Adverse drug reactions occurred in about 42% of patients, and 4 of the 124 adverse events were considered serious.
Wolfhart Kreuz, MD, of HZRM (Haemophilia Centre Rhein Main) in Mörfelden-Walldorf, Germany, and his colleagues conducted this research as part of the ongoing ObsITI study. The trial enrolled 48 patients with hemophilia A and inhibitors.
Most patients–83.3% (n=40)—had 1 or more poor prognostic factors for immune tolerance induction (ITI) success. This includes age of 7 or older, having been diagnosed with inhibitors for 2 years or more, having an inhibitor titer of 10 BU or higher at the start of ITI, and prior ITI failure.
Patients received Octanate as the sole factor VIII product between December 2005 and October 2010. Patients who were “low responders” at the start of ITI (<5 BU) received 50–100 IU factor VIII kg-1 daily or every other day. And “high responders” (≥5 BU) received 100 IU factor VIII kg-1 every 12 hours.
During ITI, 4 patients received prophylaxis with bypassing agents—2 with activated prothrombin complex concentrates and 2 with recombinant factor VIIa.
The researchers assessed ITI efficacy according to 3 criteria. These were: (1) inhibitor titer <0.6 BU, (2) factor VIII recovery ≥80% of the predefined reference value of 1.5% IU-1 kg-1 body weight ≤1 hour post-injection, and (3) factor VIII half-life ≥7 hours.
The researchers defined “complete success” as meeting all 3 efficacy criteria, “partial success” as meeting 2 criteria, and “partial response” as meeting 1 criterion. If none of the criteria were met within the 36-month observation period, this was considered an ITI failure. Withdrawal from the study for administrative reasons was considered an ITI failure as well.
Treatment was deemed a complete success in 70.8% of patients (n=34) and a partial success in 6.3% (n=3). One patient (2.1%) had a partial response. Treatment failed in 20.8% of patients (n=10), all of whom had poor prognostic factors.
Overall, 79.2% of patients (38/48) became negative for inhibitors. These patients saw an 86% reduction in their monthly bleeding rate (P<0.0001), which decreased most dramatically during the initial 4 months of ITI. During that period, the mean monthly bleeding rate fell from 1.05 to 0.26.
The researchers noted that treatment outcome was significantly associated with a patient’s inhibitor titer level at the start of ITI (P=0.0068), the number of poor prognostic factors (P=0.0187), the monthly bleeding rate during ITI (P=0.0005), and peak inhibitor titer during ITI (P=0.0007).
There were 124 adverse drug reactions reported in 20 patients (41.7%). And there were 4 serious adverse drug reactions—intravenous catheter infection, febrile convulsion, gingivitis, and pyrexia. One reaction—allergic dermatitis—was considered possibly or probably related to treatment. ![]()
FDA clears automated system for testing blood

Photo courtesy of
Ortho Clinical Diagnostics
The US Food and Drug Administration (FDA) has granted 510(k) clearance to the ORTHO VISIONTM Analyzer, a system that automates in vitro testing of human blood.
The system is now commercially available in the US and Puerto Rico.
The ORTHO VISION Analyzer automates test processing functions, including liquid pipetting, reagent handling, incubation, centrifugation, reaction grading, and interpretation and data management requirements using ID-MTS Gel Cards and digital image processing.
Tests that can be performed with the system include:
- ABO/Rh/grouping
- ABO/Rh confirmation
- Antibody screen
- Antibody identification
- Selected cell panel
- Rh phenotype (C,c,E,e)
- Donor confirmation
- Crossmatch (AHG)
- Antigen typing
- Serial dilutions for titration studies
- DAT (polyspecific)
- DAT (IGG)
- Cord blood testing
The system can be used as a standalone instrument or interfaced to a laboratory information system.
The ORTHO VISION Analyzer was designed with secure monitoring technologies for safety checks and balances, and it allows transfusion medicine professionals to track steps in the immunohematology testing process.
Through Ortho Clinical Diagnostics’ proprietary Intellicheck Technology, the ORTHO VISION Analyzer verifies and documents diagnostic checks throughout the testing process, while e-Connectivity Technology provides 24/7 remote data tracking that monitors instrument performance while maximizing uptime. Laboratory personnel can log on anytime, anywhere to collaborate on interpreting results in real time.
“With the launch of the ORTHO VISION Analyzer, our goal is to help improve the safety of blood transfusions by reducing the lab’s reliance on manual methods,” said Robert Yates, chief operating officer of Ortho Clinical Diagnostics, the company developing the ORTHO VISION Analyzer.
A version of the ORTHO VISION Analyzer is already commercially available in Europe, Japan, Latin America, Canada, and Australia.
For more information on the system, visit the Ortho Clinical Diagnostics website. ![]()

Photo courtesy of
Ortho Clinical Diagnostics
The US Food and Drug Administration (FDA) has granted 510(k) clearance to the ORTHO VISIONTM Analyzer, a system that automates in vitro testing of human blood.
The system is now commercially available in the US and Puerto Rico.
The ORTHO VISION Analyzer automates test processing functions, including liquid pipetting, reagent handling, incubation, centrifugation, reaction grading, and interpretation and data management requirements using ID-MTS Gel Cards and digital image processing.
Tests that can be performed with the system include:
- ABO/Rh/grouping
- ABO/Rh confirmation
- Antibody screen
- Antibody identification
- Selected cell panel
- Rh phenotype (C,c,E,e)
- Donor confirmation
- Crossmatch (AHG)
- Antigen typing
- Serial dilutions for titration studies
- DAT (polyspecific)
- DAT (IGG)
- Cord blood testing
The system can be used as a standalone instrument or interfaced to a laboratory information system.
The ORTHO VISION Analyzer was designed with secure monitoring technologies for safety checks and balances, and it allows transfusion medicine professionals to track steps in the immunohematology testing process.
Through Ortho Clinical Diagnostics’ proprietary Intellicheck Technology, the ORTHO VISION Analyzer verifies and documents diagnostic checks throughout the testing process, while e-Connectivity Technology provides 24/7 remote data tracking that monitors instrument performance while maximizing uptime. Laboratory personnel can log on anytime, anywhere to collaborate on interpreting results in real time.
“With the launch of the ORTHO VISION Analyzer, our goal is to help improve the safety of blood transfusions by reducing the lab’s reliance on manual methods,” said Robert Yates, chief operating officer of Ortho Clinical Diagnostics, the company developing the ORTHO VISION Analyzer.
A version of the ORTHO VISION Analyzer is already commercially available in Europe, Japan, Latin America, Canada, and Australia.
For more information on the system, visit the Ortho Clinical Diagnostics website. ![]()

Photo courtesy of
Ortho Clinical Diagnostics
The US Food and Drug Administration (FDA) has granted 510(k) clearance to the ORTHO VISIONTM Analyzer, a system that automates in vitro testing of human blood.
The system is now commercially available in the US and Puerto Rico.
The ORTHO VISION Analyzer automates test processing functions, including liquid pipetting, reagent handling, incubation, centrifugation, reaction grading, and interpretation and data management requirements using ID-MTS Gel Cards and digital image processing.
Tests that can be performed with the system include:
- ABO/Rh/grouping
- ABO/Rh confirmation
- Antibody screen
- Antibody identification
- Selected cell panel
- Rh phenotype (C,c,E,e)
- Donor confirmation
- Crossmatch (AHG)
- Antigen typing
- Serial dilutions for titration studies
- DAT (polyspecific)
- DAT (IGG)
- Cord blood testing
The system can be used as a standalone instrument or interfaced to a laboratory information system.
The ORTHO VISION Analyzer was designed with secure monitoring technologies for safety checks and balances, and it allows transfusion medicine professionals to track steps in the immunohematology testing process.
Through Ortho Clinical Diagnostics’ proprietary Intellicheck Technology, the ORTHO VISION Analyzer verifies and documents diagnostic checks throughout the testing process, while e-Connectivity Technology provides 24/7 remote data tracking that monitors instrument performance while maximizing uptime. Laboratory personnel can log on anytime, anywhere to collaborate on interpreting results in real time.
“With the launch of the ORTHO VISION Analyzer, our goal is to help improve the safety of blood transfusions by reducing the lab’s reliance on manual methods,” said Robert Yates, chief operating officer of Ortho Clinical Diagnostics, the company developing the ORTHO VISION Analyzer.
A version of the ORTHO VISION Analyzer is already commercially available in Europe, Japan, Latin America, Canada, and Australia.
For more information on the system, visit the Ortho Clinical Diagnostics website. ![]()
New HMA shows early promise for MDS/AML

Image by Christoph Bock
Investigators say a novel hypomethylating agent (HMA) is safe and clinically active in patients with myelodysplastic syndromes (MDS) or acute myelogenous leukemia (AML) who have failed standard therapy.
The HMA, guadecitabine (SGI-110), reverses aberrant DNA methylation by inhibiting DNA methyltransferase enzymes.
The investigators tested guadecitabine in a phase 1 study of patients with relapsed or refractory AML or MDS.
They reported the results in The Lancet Oncology. The study was sponsored by Astex Pharmaceuticals, the company developing guadecitabine.
“In this study, we observed induced clinical responses in heavily pretreated patients, including prior treatment with current HMAs,” said study author Hagop Kantarjian, MD, of The University of Texas MD Anderson Cancer Center in Houston.
“Together with the results of a large phase 2 study to be published later, these data support further investigation, including the recently commenced global phase 3 study in treatment-naïve AML patients”.
Dr Kantarjian and his colleagues enrolled 93 patients in the phase 1 study, 74 with AML and 19 with MDS. The patients had received 1 to 9 prior treatment regimens, and most had received prior azacitidine or decitabine.
The trial had a 3+3 dose-escalation design. Patients received guadecitabine doses ranging from 3 mg/m2 to 125 mg/m2.
The patients were also randomized to receive guadecitabine either once-daily for 5 consecutive days (35 AML, 9 MDS) or once-weekly (28 AML, 6 MDS) for 3 weeks in a 28-day treatment cycle. A twice-weekly treatment schedule was added to the study after a protocol amendment (11 AML, 4 MDS).
The investigators said the 3 treatment groups were well balanced with regard to baseline characteristics. However, the initial median bone marrow blast percentage in the daily × 5 group was twice that of the once-weekly and twice-weekly groups—42%, 19%, and 20%, respectively.
Safety and efficacy
The investigators said the treatment was well-tolerated. The most common grade 3 or higher adverse events were febrile neutropenia (41%), pneumonia (29%), thrombocytopenia (25%), anemia (25%), and sepsis (17%).
The most common serious adverse events were febrile neutropenia (31%), pneumonia (28%), and sepsis (17%).
There were 2 dose-limiting toxicities in MDS patients at the 125 mg/m2 daily × 5 dose. So the maximum tolerated dose for these patients was 90 mg/m2 daily × 5. The maximum tolerated dose was not reached in patients with AML.
Six patients with AML and 6 with MDS had a clinical response to guadecitabine. The investigators said potent, dose-related DNA demethylation occurred on the daily × 5 regimen, reaching a plateau at 60 mg/m2. So the team recommended this as the phase 2 dose.
A phase 2 study of guadecitabine is ongoing. The study enrolled more than 300 patients with treatment-naïve or relapsed/refractory AML or MDS.
Investigators recently began an 800-patient, phase 3 study (ASTRAL-1), in which guadecitabine is being compared with physician’s choice of decitabine, azacitidine, or low-dose cytarabine in treatment-naïve AML patients who are not candidates for intensive induction chemotherapy. ![]()

Image by Christoph Bock
Investigators say a novel hypomethylating agent (HMA) is safe and clinically active in patients with myelodysplastic syndromes (MDS) or acute myelogenous leukemia (AML) who have failed standard therapy.
The HMA, guadecitabine (SGI-110), reverses aberrant DNA methylation by inhibiting DNA methyltransferase enzymes.
The investigators tested guadecitabine in a phase 1 study of patients with relapsed or refractory AML or MDS.
They reported the results in The Lancet Oncology. The study was sponsored by Astex Pharmaceuticals, the company developing guadecitabine.
“In this study, we observed induced clinical responses in heavily pretreated patients, including prior treatment with current HMAs,” said study author Hagop Kantarjian, MD, of The University of Texas MD Anderson Cancer Center in Houston.
“Together with the results of a large phase 2 study to be published later, these data support further investigation, including the recently commenced global phase 3 study in treatment-naïve AML patients”.
Dr Kantarjian and his colleagues enrolled 93 patients in the phase 1 study, 74 with AML and 19 with MDS. The patients had received 1 to 9 prior treatment regimens, and most had received prior azacitidine or decitabine.
The trial had a 3+3 dose-escalation design. Patients received guadecitabine doses ranging from 3 mg/m2 to 125 mg/m2.
The patients were also randomized to receive guadecitabine either once-daily for 5 consecutive days (35 AML, 9 MDS) or once-weekly (28 AML, 6 MDS) for 3 weeks in a 28-day treatment cycle. A twice-weekly treatment schedule was added to the study after a protocol amendment (11 AML, 4 MDS).
The investigators said the 3 treatment groups were well balanced with regard to baseline characteristics. However, the initial median bone marrow blast percentage in the daily × 5 group was twice that of the once-weekly and twice-weekly groups—42%, 19%, and 20%, respectively.
Safety and efficacy
The investigators said the treatment was well-tolerated. The most common grade 3 or higher adverse events were febrile neutropenia (41%), pneumonia (29%), thrombocytopenia (25%), anemia (25%), and sepsis (17%).
The most common serious adverse events were febrile neutropenia (31%), pneumonia (28%), and sepsis (17%).
There were 2 dose-limiting toxicities in MDS patients at the 125 mg/m2 daily × 5 dose. So the maximum tolerated dose for these patients was 90 mg/m2 daily × 5. The maximum tolerated dose was not reached in patients with AML.
Six patients with AML and 6 with MDS had a clinical response to guadecitabine. The investigators said potent, dose-related DNA demethylation occurred on the daily × 5 regimen, reaching a plateau at 60 mg/m2. So the team recommended this as the phase 2 dose.
A phase 2 study of guadecitabine is ongoing. The study enrolled more than 300 patients with treatment-naïve or relapsed/refractory AML or MDS.
Investigators recently began an 800-patient, phase 3 study (ASTRAL-1), in which guadecitabine is being compared with physician’s choice of decitabine, azacitidine, or low-dose cytarabine in treatment-naïve AML patients who are not candidates for intensive induction chemotherapy. ![]()

Image by Christoph Bock
Investigators say a novel hypomethylating agent (HMA) is safe and clinically active in patients with myelodysplastic syndromes (MDS) or acute myelogenous leukemia (AML) who have failed standard therapy.
The HMA, guadecitabine (SGI-110), reverses aberrant DNA methylation by inhibiting DNA methyltransferase enzymes.
The investigators tested guadecitabine in a phase 1 study of patients with relapsed or refractory AML or MDS.
They reported the results in The Lancet Oncology. The study was sponsored by Astex Pharmaceuticals, the company developing guadecitabine.
“In this study, we observed induced clinical responses in heavily pretreated patients, including prior treatment with current HMAs,” said study author Hagop Kantarjian, MD, of The University of Texas MD Anderson Cancer Center in Houston.
“Together with the results of a large phase 2 study to be published later, these data support further investigation, including the recently commenced global phase 3 study in treatment-naïve AML patients”.
Dr Kantarjian and his colleagues enrolled 93 patients in the phase 1 study, 74 with AML and 19 with MDS. The patients had received 1 to 9 prior treatment regimens, and most had received prior azacitidine or decitabine.
The trial had a 3+3 dose-escalation design. Patients received guadecitabine doses ranging from 3 mg/m2 to 125 mg/m2.
The patients were also randomized to receive guadecitabine either once-daily for 5 consecutive days (35 AML, 9 MDS) or once-weekly (28 AML, 6 MDS) for 3 weeks in a 28-day treatment cycle. A twice-weekly treatment schedule was added to the study after a protocol amendment (11 AML, 4 MDS).
The investigators said the 3 treatment groups were well balanced with regard to baseline characteristics. However, the initial median bone marrow blast percentage in the daily × 5 group was twice that of the once-weekly and twice-weekly groups—42%, 19%, and 20%, respectively.
Safety and efficacy
The investigators said the treatment was well-tolerated. The most common grade 3 or higher adverse events were febrile neutropenia (41%), pneumonia (29%), thrombocytopenia (25%), anemia (25%), and sepsis (17%).
The most common serious adverse events were febrile neutropenia (31%), pneumonia (28%), and sepsis (17%).
There were 2 dose-limiting toxicities in MDS patients at the 125 mg/m2 daily × 5 dose. So the maximum tolerated dose for these patients was 90 mg/m2 daily × 5. The maximum tolerated dose was not reached in patients with AML.
Six patients with AML and 6 with MDS had a clinical response to guadecitabine. The investigators said potent, dose-related DNA demethylation occurred on the daily × 5 regimen, reaching a plateau at 60 mg/m2. So the team recommended this as the phase 2 dose.
A phase 2 study of guadecitabine is ongoing. The study enrolled more than 300 patients with treatment-naïve or relapsed/refractory AML or MDS.
Investigators recently began an 800-patient, phase 3 study (ASTRAL-1), in which guadecitabine is being compared with physician’s choice of decitabine, azacitidine, or low-dose cytarabine in treatment-naïve AML patients who are not candidates for intensive induction chemotherapy. ![]()
Medicare Observation Stay Liability
The problems surrounding hospital observation care and associated audits by Recovery Audit Contractors are gaining increased attention from both Congress and the Centers for Medicare & Medicaid Services (CMS).[1, 2, 3, 4, 5] On August 6, 2015, President Obama signed the NOTICE (Notice of Observation Treatment and Implication for Care Eligibility) Act (P.L. 114‐42),[4] which will require all Medicare beneficiaries receiving observation services for over 24 hours to be informed of their outpatient status. However, providers and hospitals are currently unable to answer a question that patients will certainly ask: What will an observation stay cost me compared to the same stay billed as an inpatient?
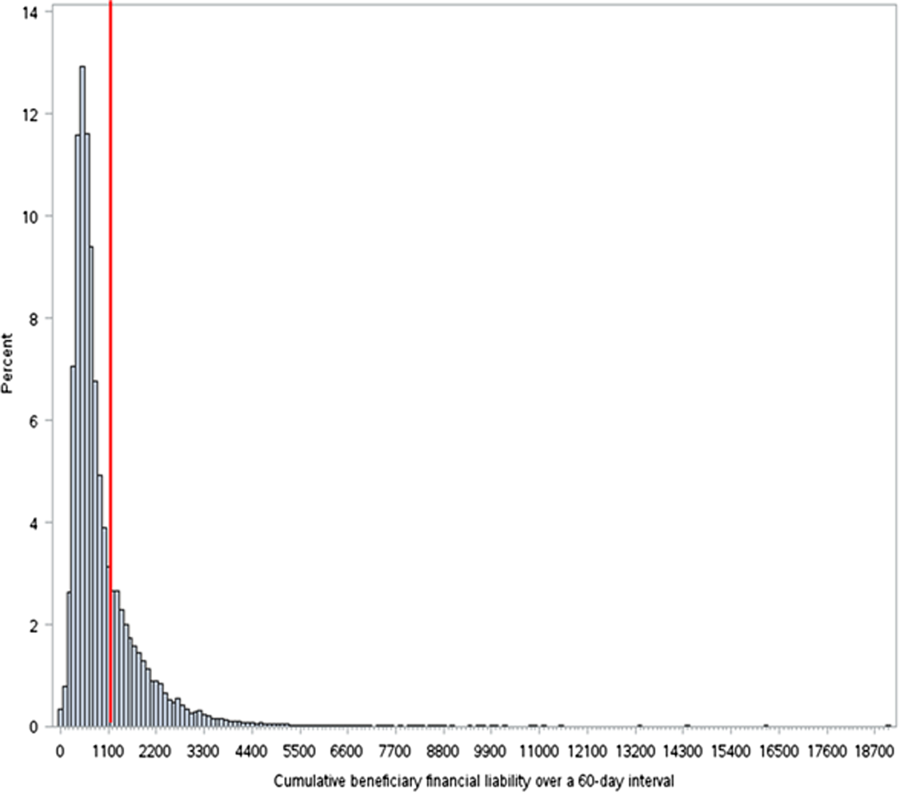
In this issue of the Journal of Hospital Medicine, Kangovi et al.[6] get a step closer to answering this question. Using 2010 to 2012 Medicare data, Kangovi and colleagues studied patient out‐of‐pocket costs per Medicare benefit period and found that the mean financial self‐pay cost per beneficiary observation stay was less ($469.42) than the 2010 inpatient deductible ($1100),[7] although about 1 in 10 observation stays exceeded the inpatient deductible. For beneficiaries with multiple observation stays per benefit period, the mean cumulative self‐pay cost ($947.40) was also less than the inpatient deductible. However, for over a quarter of beneficiaries with multiple observation stays, the cumulative patient cost exceeded the inpatient deductible. The authors also found that black beneficiaries and those with more comorbidities were more likely to have multiple observation visits per benefit period, but higher out‐of‐pocket observation liability was associated with nonblack race, lower number of chronic conditions, and not being dual eligible.
Medicare beneficiaries hospitalized as inpatients are covered by Medicare Part A, with a single deductible per benefit period, and are eligible for skilled nursing facility (SNF) coverage after 3 consecutive inpatient midnights. Medicare patients hospitalized as outpatients, including those receiving observation services, are not eligible for SNF coverage, must pay the cost of many self‐administered pharmaceuticals, and are generally responsible for 20% of each service rendered, but with the per‐service out‐of‐pocket 20% deductible capped at the equivalent to the current Part A deductible. However, there is no cumulative limit on the total out‐of‐pocket cost for outpatient observation (Part B) hospitalizations.[8]
Put in a slightly different way, while [outpatient coverage] is designed to reflect the cost of caring for each individual beneficiary, [inpatient payment structure] is designed to reflect the cost of caring for an average beneficiary.[9] Because outpatient observation payments are made per service, Medicare and beneficiary payment amounts both increase as the number of services provided increases,[9] which creates a threshold where the number and complexity of outpatient services exceeds the average inpatient stay, resulting in out‐of‐pocket observation costs exceeding the inpatient deductible. It makes sense that this threshold is more likely to be reached when the costs of multiple observation stays are added. Therefore, we should not be surprised at the findings of Kangovi et al.,[6] nor at those of the Office of Inspector General (OIG)[9] using 2012 Medicare claims data, showing higher average out‐of‐pocket patient costs for short inpatient stays compared to observation stays, but with a significant minority of out‐of‐pocket observation patient stay costs exceeding the inpatient deductible.
Dr. Kangovi and colleagues should be applauded for their efforts to address this important Medicare beneficiary issue. Yet many questions remain. First, neither the OIG study nor Kangovi et al. fully included cost of self‐administered medications in calculating patients' out‐of‐pocket patient liability. Second, Kangovi and colleagues did not account for beneficiary posthospitalization SNF costs, which would be substantially higher for any patients who did not have a qualifying 3‐day inpatient stay, including all patients hospitalized under observation. Third, both reports used data predating the 2‐midnight rule, so it is unlikely that beneficiary costs are comparable under current policy. Fewer long (>48 hours) observation stays under the 2‐midnight rule should reduce beneficiary financial burden, though this is unconfirmed. However, certain shorter, high‐acuity, procedure‐based observation stays could be more costly for patients.[9] Fourth, Kangovi et al. also did not consider patients with both an inpatient stay and an observation stay in the same benefit period; these patients would be liable for both the inpatient deductible and the outpatient fees. Fifth, to be meaningful, comparison of beneficiary out‐of‐pocket liability for inpatient versus outpatient care must occur in the context of services rendered, similar to what was proposed by the House Ways and Means Subcommittee in their Hospital Improvements for Payment draft bill.[10] Absent this, we should not conclude from this study that observation care is delivered at a discounted rate for patients when it is possible that lower out‐of‐pocket payments simply reflect, on average, fewer services rendered per observation stay when compared to an inpatient stay. Finally, the association between race, socioeconomic status, chronic conditions, and inpatient and observation stays merits further investigation. How such hospitalizations may relate to larger costs associated with lack of appropriate follow‐up care, including costs for those who have adverse consequences when they curtail or forego SNF placement, must be considered.
Even if we accept these limitations and accede that out‐of‐pocket observation cost is, on average, less than inpatient, pitfalls of observation policy remain: a cap on out‐of‐pocket financial risk for hospital care and SNF coverage are protections only afforded to those Medicare beneficiaries hospitalized as inpatients. Although the aspect of CMS' 2‐midnight rule that presumes inpatient status if a there is a physician's expectation of a medically necessary hospitalization of 2 or more midnights mitigates, but does not eliminate, the observation policy problem of uncapped out‐of‐pocket financial liability, it does not address the lack of SNF coverage following outpatient hospitalization. Further action and answers need to come from both Congress and CMS. At a recent Senate Special Committee on Aging hearing, Elizabeth Warren emphasized that CMS must accurately determine Medicare beneficiary out‐of‐pocket cost for observation care so providers can answer this question that patients undoubtedly ask.[1] CMS should be called upon to make available estimates of beneficiary costs under the 2‐midnight rule that include pharmacy charges, copayments (in the context of services rendered), and SNF costs. In addition, data should extend past beneficiary liability to detail differences in outpatient versus inpatient hospital reimbursement, systematic recovery auditing costs, and the total financial impact of maintaining 2 distinct (inpatient and outpatient) hospital reimbursement systems.[11, 12]
Congress and CMS must ultimately go beyond cost estimates and actually reform the core problems in outpatient observation policy and the Recovery Audit program charged with enforcing status determinations. Congress should pass the Improving Access to Medicare Coverage Act of 2015 (H.R. 1571 and S. 843), which would guarantee SNF coverage for Medicare beneficiaries hospitalized for 3 consecutive midnights, regardless of whether those nights are inpatient or outpatient.[13] Recovery Audit reform bills in the House (H.R. 2156)[3] and under consideration in the Senate[2] should be strongly supported. In addition, Congress and CMS should consider legislation or regulation that would cap outpatient hospitalization out‐of‐pocket liability at the inpatient Medicare beneficiary deductible. Alternatively, policymakers could finally recognize the current observation versus inpatient system for what it is: a payment structure with little clinical relevance. When the same exact medical care has 2 different hospital reimbursement rates and 2 different patient out‐of‐pocket financial liabilities, it may be time for policymakers to eliminate the false distinction altogether.
Disclosure: Nothing to report.
- Senate Special Committee on Aging hearing: challenging the status quo: solutions to the hospital observation stay crisis. May 20, 2015. Available at: http://www.aging.senate.gov/hearings/challenging‐the‐status‐quo_solutions‐to‐the‐hospital‐observation‐stay‐crisis. Accessed July 1, 2015.
- Senate Finance Committee Open Executive Session to consider an original bill entitled Audit 10(11):718–723.
- Medicare general information, eligibility, and entitlement. Chapter 3—deductibles, coninsurance amounts, and payment limitations. Available at: http://www.cms.gov/Regulations‐and‐Guidance/Guidance/Manuals/downloads/ge101c03.pdf. Accessed July 5, 2015.
- What Medicare covers: find out if you're an inpatient or an outpatient—it affects what you pay. Available at: http://www.medicare.gov/what‐medicare‐covers/part‐a/inpatient‐or‐outpatient.html. Accessed July 10, 2015.
- Department of Health and Human Services. Office of Inspector General. Hospitals' use of observation stays and short inpatient stays for Medicare beneficiaries, OEI‐02‐12‐00040. July 29, 2013. Available at: https://oig.hhs.gov/oei/reports/oei‐02‐12‐00040.pdf. Accessed July 1, 2015.
- Association of American Medical Colleges. Washington Highlights: Ways and Means Committee releases Medicare hospital bill. Available at: https://www.aamc.org/advocacy/washhigh/highlights2014/415486/112114waysandmeanscommitteereleasesmedicarehospitalbill.html. Accessed July 10, 2015.
- , , , et al. Hospitalized but not admitted: characteristics of patients with “observation status” at an academic medical center. JAMA Intern Med. 2013;173(21):1991–1998.
- , , , et al. Recovery audit contractor audits and appeals at three academic medical centers. J Hosp Med. 2015;10(4):212–219.
- Improving Access to Medicare Coverage Act of 2015 (H.R. 1571/S. 843). Available at: https://www.congress.gov/bill/114th‐congress/house‐bill/1571. Accessed July 6, 2015.
The problems surrounding hospital observation care and associated audits by Recovery Audit Contractors are gaining increased attention from both Congress and the Centers for Medicare & Medicaid Services (CMS).[1, 2, 3, 4, 5] On August 6, 2015, President Obama signed the NOTICE (Notice of Observation Treatment and Implication for Care Eligibility) Act (P.L. 114‐42),[4] which will require all Medicare beneficiaries receiving observation services for over 24 hours to be informed of their outpatient status. However, providers and hospitals are currently unable to answer a question that patients will certainly ask: What will an observation stay cost me compared to the same stay billed as an inpatient?
In this issue of the Journal of Hospital Medicine, Kangovi et al.[6] get a step closer to answering this question. Using 2010 to 2012 Medicare data, Kangovi and colleagues studied patient out‐of‐pocket costs per Medicare benefit period and found that the mean financial self‐pay cost per beneficiary observation stay was less ($469.42) than the 2010 inpatient deductible ($1100),[7] although about 1 in 10 observation stays exceeded the inpatient deductible. For beneficiaries with multiple observation stays per benefit period, the mean cumulative self‐pay cost ($947.40) was also less than the inpatient deductible. However, for over a quarter of beneficiaries with multiple observation stays, the cumulative patient cost exceeded the inpatient deductible. The authors also found that black beneficiaries and those with more comorbidities were more likely to have multiple observation visits per benefit period, but higher out‐of‐pocket observation liability was associated with nonblack race, lower number of chronic conditions, and not being dual eligible.
Medicare beneficiaries hospitalized as inpatients are covered by Medicare Part A, with a single deductible per benefit period, and are eligible for skilled nursing facility (SNF) coverage after 3 consecutive inpatient midnights. Medicare patients hospitalized as outpatients, including those receiving observation services, are not eligible for SNF coverage, must pay the cost of many self‐administered pharmaceuticals, and are generally responsible for 20% of each service rendered, but with the per‐service out‐of‐pocket 20% deductible capped at the equivalent to the current Part A deductible. However, there is no cumulative limit on the total out‐of‐pocket cost for outpatient observation (Part B) hospitalizations.[8]
Put in a slightly different way, while [outpatient coverage] is designed to reflect the cost of caring for each individual beneficiary, [inpatient payment structure] is designed to reflect the cost of caring for an average beneficiary.[9] Because outpatient observation payments are made per service, Medicare and beneficiary payment amounts both increase as the number of services provided increases,[9] which creates a threshold where the number and complexity of outpatient services exceeds the average inpatient stay, resulting in out‐of‐pocket observation costs exceeding the inpatient deductible. It makes sense that this threshold is more likely to be reached when the costs of multiple observation stays are added. Therefore, we should not be surprised at the findings of Kangovi et al.,[6] nor at those of the Office of Inspector General (OIG)[9] using 2012 Medicare claims data, showing higher average out‐of‐pocket patient costs for short inpatient stays compared to observation stays, but with a significant minority of out‐of‐pocket observation patient stay costs exceeding the inpatient deductible.
Dr. Kangovi and colleagues should be applauded for their efforts to address this important Medicare beneficiary issue. Yet many questions remain. First, neither the OIG study nor Kangovi et al. fully included cost of self‐administered medications in calculating patients' out‐of‐pocket patient liability. Second, Kangovi and colleagues did not account for beneficiary posthospitalization SNF costs, which would be substantially higher for any patients who did not have a qualifying 3‐day inpatient stay, including all patients hospitalized under observation. Third, both reports used data predating the 2‐midnight rule, so it is unlikely that beneficiary costs are comparable under current policy. Fewer long (>48 hours) observation stays under the 2‐midnight rule should reduce beneficiary financial burden, though this is unconfirmed. However, certain shorter, high‐acuity, procedure‐based observation stays could be more costly for patients.[9] Fourth, Kangovi et al. also did not consider patients with both an inpatient stay and an observation stay in the same benefit period; these patients would be liable for both the inpatient deductible and the outpatient fees. Fifth, to be meaningful, comparison of beneficiary out‐of‐pocket liability for inpatient versus outpatient care must occur in the context of services rendered, similar to what was proposed by the House Ways and Means Subcommittee in their Hospital Improvements for Payment draft bill.[10] Absent this, we should not conclude from this study that observation care is delivered at a discounted rate for patients when it is possible that lower out‐of‐pocket payments simply reflect, on average, fewer services rendered per observation stay when compared to an inpatient stay. Finally, the association between race, socioeconomic status, chronic conditions, and inpatient and observation stays merits further investigation. How such hospitalizations may relate to larger costs associated with lack of appropriate follow‐up care, including costs for those who have adverse consequences when they curtail or forego SNF placement, must be considered.
Even if we accept these limitations and accede that out‐of‐pocket observation cost is, on average, less than inpatient, pitfalls of observation policy remain: a cap on out‐of‐pocket financial risk for hospital care and SNF coverage are protections only afforded to those Medicare beneficiaries hospitalized as inpatients. Although the aspect of CMS' 2‐midnight rule that presumes inpatient status if a there is a physician's expectation of a medically necessary hospitalization of 2 or more midnights mitigates, but does not eliminate, the observation policy problem of uncapped out‐of‐pocket financial liability, it does not address the lack of SNF coverage following outpatient hospitalization. Further action and answers need to come from both Congress and CMS. At a recent Senate Special Committee on Aging hearing, Elizabeth Warren emphasized that CMS must accurately determine Medicare beneficiary out‐of‐pocket cost for observation care so providers can answer this question that patients undoubtedly ask.[1] CMS should be called upon to make available estimates of beneficiary costs under the 2‐midnight rule that include pharmacy charges, copayments (in the context of services rendered), and SNF costs. In addition, data should extend past beneficiary liability to detail differences in outpatient versus inpatient hospital reimbursement, systematic recovery auditing costs, and the total financial impact of maintaining 2 distinct (inpatient and outpatient) hospital reimbursement systems.[11, 12]
Congress and CMS must ultimately go beyond cost estimates and actually reform the core problems in outpatient observation policy and the Recovery Audit program charged with enforcing status determinations. Congress should pass the Improving Access to Medicare Coverage Act of 2015 (H.R. 1571 and S. 843), which would guarantee SNF coverage for Medicare beneficiaries hospitalized for 3 consecutive midnights, regardless of whether those nights are inpatient or outpatient.[13] Recovery Audit reform bills in the House (H.R. 2156)[3] and under consideration in the Senate[2] should be strongly supported. In addition, Congress and CMS should consider legislation or regulation that would cap outpatient hospitalization out‐of‐pocket liability at the inpatient Medicare beneficiary deductible. Alternatively, policymakers could finally recognize the current observation versus inpatient system for what it is: a payment structure with little clinical relevance. When the same exact medical care has 2 different hospital reimbursement rates and 2 different patient out‐of‐pocket financial liabilities, it may be time for policymakers to eliminate the false distinction altogether.
Disclosure: Nothing to report.
The problems surrounding hospital observation care and associated audits by Recovery Audit Contractors are gaining increased attention from both Congress and the Centers for Medicare & Medicaid Services (CMS).[1, 2, 3, 4, 5] On August 6, 2015, President Obama signed the NOTICE (Notice of Observation Treatment and Implication for Care Eligibility) Act (P.L. 114‐42),[4] which will require all Medicare beneficiaries receiving observation services for over 24 hours to be informed of their outpatient status. However, providers and hospitals are currently unable to answer a question that patients will certainly ask: What will an observation stay cost me compared to the same stay billed as an inpatient?
In this issue of the Journal of Hospital Medicine, Kangovi et al.[6] get a step closer to answering this question. Using 2010 to 2012 Medicare data, Kangovi and colleagues studied patient out‐of‐pocket costs per Medicare benefit period and found that the mean financial self‐pay cost per beneficiary observation stay was less ($469.42) than the 2010 inpatient deductible ($1100),[7] although about 1 in 10 observation stays exceeded the inpatient deductible. For beneficiaries with multiple observation stays per benefit period, the mean cumulative self‐pay cost ($947.40) was also less than the inpatient deductible. However, for over a quarter of beneficiaries with multiple observation stays, the cumulative patient cost exceeded the inpatient deductible. The authors also found that black beneficiaries and those with more comorbidities were more likely to have multiple observation visits per benefit period, but higher out‐of‐pocket observation liability was associated with nonblack race, lower number of chronic conditions, and not being dual eligible.
Medicare beneficiaries hospitalized as inpatients are covered by Medicare Part A, with a single deductible per benefit period, and are eligible for skilled nursing facility (SNF) coverage after 3 consecutive inpatient midnights. Medicare patients hospitalized as outpatients, including those receiving observation services, are not eligible for SNF coverage, must pay the cost of many self‐administered pharmaceuticals, and are generally responsible for 20% of each service rendered, but with the per‐service out‐of‐pocket 20% deductible capped at the equivalent to the current Part A deductible. However, there is no cumulative limit on the total out‐of‐pocket cost for outpatient observation (Part B) hospitalizations.[8]
Put in a slightly different way, while [outpatient coverage] is designed to reflect the cost of caring for each individual beneficiary, [inpatient payment structure] is designed to reflect the cost of caring for an average beneficiary.[9] Because outpatient observation payments are made per service, Medicare and beneficiary payment amounts both increase as the number of services provided increases,[9] which creates a threshold where the number and complexity of outpatient services exceeds the average inpatient stay, resulting in out‐of‐pocket observation costs exceeding the inpatient deductible. It makes sense that this threshold is more likely to be reached when the costs of multiple observation stays are added. Therefore, we should not be surprised at the findings of Kangovi et al.,[6] nor at those of the Office of Inspector General (OIG)[9] using 2012 Medicare claims data, showing higher average out‐of‐pocket patient costs for short inpatient stays compared to observation stays, but with a significant minority of out‐of‐pocket observation patient stay costs exceeding the inpatient deductible.
Dr. Kangovi and colleagues should be applauded for their efforts to address this important Medicare beneficiary issue. Yet many questions remain. First, neither the OIG study nor Kangovi et al. fully included cost of self‐administered medications in calculating patients' out‐of‐pocket patient liability. Second, Kangovi and colleagues did not account for beneficiary posthospitalization SNF costs, which would be substantially higher for any patients who did not have a qualifying 3‐day inpatient stay, including all patients hospitalized under observation. Third, both reports used data predating the 2‐midnight rule, so it is unlikely that beneficiary costs are comparable under current policy. Fewer long (>48 hours) observation stays under the 2‐midnight rule should reduce beneficiary financial burden, though this is unconfirmed. However, certain shorter, high‐acuity, procedure‐based observation stays could be more costly for patients.[9] Fourth, Kangovi et al. also did not consider patients with both an inpatient stay and an observation stay in the same benefit period; these patients would be liable for both the inpatient deductible and the outpatient fees. Fifth, to be meaningful, comparison of beneficiary out‐of‐pocket liability for inpatient versus outpatient care must occur in the context of services rendered, similar to what was proposed by the House Ways and Means Subcommittee in their Hospital Improvements for Payment draft bill.[10] Absent this, we should not conclude from this study that observation care is delivered at a discounted rate for patients when it is possible that lower out‐of‐pocket payments simply reflect, on average, fewer services rendered per observation stay when compared to an inpatient stay. Finally, the association between race, socioeconomic status, chronic conditions, and inpatient and observation stays merits further investigation. How such hospitalizations may relate to larger costs associated with lack of appropriate follow‐up care, including costs for those who have adverse consequences when they curtail or forego SNF placement, must be considered.
Even if we accept these limitations and accede that out‐of‐pocket observation cost is, on average, less than inpatient, pitfalls of observation policy remain: a cap on out‐of‐pocket financial risk for hospital care and SNF coverage are protections only afforded to those Medicare beneficiaries hospitalized as inpatients. Although the aspect of CMS' 2‐midnight rule that presumes inpatient status if a there is a physician's expectation of a medically necessary hospitalization of 2 or more midnights mitigates, but does not eliminate, the observation policy problem of uncapped out‐of‐pocket financial liability, it does not address the lack of SNF coverage following outpatient hospitalization. Further action and answers need to come from both Congress and CMS. At a recent Senate Special Committee on Aging hearing, Elizabeth Warren emphasized that CMS must accurately determine Medicare beneficiary out‐of‐pocket cost for observation care so providers can answer this question that patients undoubtedly ask.[1] CMS should be called upon to make available estimates of beneficiary costs under the 2‐midnight rule that include pharmacy charges, copayments (in the context of services rendered), and SNF costs. In addition, data should extend past beneficiary liability to detail differences in outpatient versus inpatient hospital reimbursement, systematic recovery auditing costs, and the total financial impact of maintaining 2 distinct (inpatient and outpatient) hospital reimbursement systems.[11, 12]
Congress and CMS must ultimately go beyond cost estimates and actually reform the core problems in outpatient observation policy and the Recovery Audit program charged with enforcing status determinations. Congress should pass the Improving Access to Medicare Coverage Act of 2015 (H.R. 1571 and S. 843), which would guarantee SNF coverage for Medicare beneficiaries hospitalized for 3 consecutive midnights, regardless of whether those nights are inpatient or outpatient.[13] Recovery Audit reform bills in the House (H.R. 2156)[3] and under consideration in the Senate[2] should be strongly supported. In addition, Congress and CMS should consider legislation or regulation that would cap outpatient hospitalization out‐of‐pocket liability at the inpatient Medicare beneficiary deductible. Alternatively, policymakers could finally recognize the current observation versus inpatient system for what it is: a payment structure with little clinical relevance. When the same exact medical care has 2 different hospital reimbursement rates and 2 different patient out‐of‐pocket financial liabilities, it may be time for policymakers to eliminate the false distinction altogether.
Disclosure: Nothing to report.
- Senate Special Committee on Aging hearing: challenging the status quo: solutions to the hospital observation stay crisis. May 20, 2015. Available at: http://www.aging.senate.gov/hearings/challenging‐the‐status‐quo_solutions‐to‐the‐hospital‐observation‐stay‐crisis. Accessed July 1, 2015.
- Senate Finance Committee Open Executive Session to consider an original bill entitled Audit 10(11):718–723.
- Medicare general information, eligibility, and entitlement. Chapter 3—deductibles, coninsurance amounts, and payment limitations. Available at: http://www.cms.gov/Regulations‐and‐Guidance/Guidance/Manuals/downloads/ge101c03.pdf. Accessed July 5, 2015.
- What Medicare covers: find out if you're an inpatient or an outpatient—it affects what you pay. Available at: http://www.medicare.gov/what‐medicare‐covers/part‐a/inpatient‐or‐outpatient.html. Accessed July 10, 2015.
- Department of Health and Human Services. Office of Inspector General. Hospitals' use of observation stays and short inpatient stays for Medicare beneficiaries, OEI‐02‐12‐00040. July 29, 2013. Available at: https://oig.hhs.gov/oei/reports/oei‐02‐12‐00040.pdf. Accessed July 1, 2015.
- Association of American Medical Colleges. Washington Highlights: Ways and Means Committee releases Medicare hospital bill. Available at: https://www.aamc.org/advocacy/washhigh/highlights2014/415486/112114waysandmeanscommitteereleasesmedicarehospitalbill.html. Accessed July 10, 2015.
- , , , et al. Hospitalized but not admitted: characteristics of patients with “observation status” at an academic medical center. JAMA Intern Med. 2013;173(21):1991–1998.
- , , , et al. Recovery audit contractor audits and appeals at three academic medical centers. J Hosp Med. 2015;10(4):212–219.
- Improving Access to Medicare Coverage Act of 2015 (H.R. 1571/S. 843). Available at: https://www.congress.gov/bill/114th‐congress/house‐bill/1571. Accessed July 6, 2015.
- Senate Special Committee on Aging hearing: challenging the status quo: solutions to the hospital observation stay crisis. May 20, 2015. Available at: http://www.aging.senate.gov/hearings/challenging‐the‐status‐quo_solutions‐to‐the‐hospital‐observation‐stay‐crisis. Accessed July 1, 2015.
- Senate Finance Committee Open Executive Session to consider an original bill entitled Audit 10(11):718–723.
- Medicare general information, eligibility, and entitlement. Chapter 3—deductibles, coninsurance amounts, and payment limitations. Available at: http://www.cms.gov/Regulations‐and‐Guidance/Guidance/Manuals/downloads/ge101c03.pdf. Accessed July 5, 2015.
- What Medicare covers: find out if you're an inpatient or an outpatient—it affects what you pay. Available at: http://www.medicare.gov/what‐medicare‐covers/part‐a/inpatient‐or‐outpatient.html. Accessed July 10, 2015.
- Department of Health and Human Services. Office of Inspector General. Hospitals' use of observation stays and short inpatient stays for Medicare beneficiaries, OEI‐02‐12‐00040. July 29, 2013. Available at: https://oig.hhs.gov/oei/reports/oei‐02‐12‐00040.pdf. Accessed July 1, 2015.
- Association of American Medical Colleges. Washington Highlights: Ways and Means Committee releases Medicare hospital bill. Available at: https://www.aamc.org/advocacy/washhigh/highlights2014/415486/112114waysandmeanscommitteereleasesmedicarehospitalbill.html. Accessed July 10, 2015.
- , , , et al. Hospitalized but not admitted: characteristics of patients with “observation status” at an academic medical center. JAMA Intern Med. 2013;173(21):1991–1998.
- , , , et al. Recovery audit contractor audits and appeals at three academic medical centers. J Hosp Med. 2015;10(4):212–219.
- Improving Access to Medicare Coverage Act of 2015 (H.R. 1571/S. 843). Available at: https://www.congress.gov/bill/114th‐congress/house‐bill/1571. Accessed July 6, 2015.
Patient Costs for Observation Care/
When Medicare beneficiaries seek healthcare, they are increasingly likely to have that care delivered under observation status. From 2006 to 2010, the annual number of observation hours for Medicare beneficiaries rose by nearly 70%.[1] In 2012, the number of observation stays for Medicare beneficiaries reached 1.5 million.[2] One consequence of this trend is a potential change in patient financial liabilitythe amount patients are expected to pay out of pocket for care. Although observation care is usually delivered in a hospital, Medicare classifies it as an outpatient service, covered through Part B rather than inpatient Part A. In two‐thirds of US hospitals, observation care is largely an administrative classification, delivered in the same units and beds as admitted patients rather than in a protocol‐driven observation care unit.[3] Therefore, patients are often unaware of their outpatient observation status and its financial implications until they receive their hospital bill.
Observation has the potential to impact patient financial liability through 4 mechanisms.[4] First, instead of a fixed cost for an inpatient admission (eg, a fixed deductible for a hospital admission), patients pay a percentage of the cost of each service provided. Therefore, patients who have long observation stays or receive expensive services could have higher than expected liability. A recent study using all‐payer data demonstrated that patients with longer observation stays (greater than 24 hours) paid 21% more than for those with shorter stays.[5]
A second consideration is that Medicare does not cover the same hospital services for observation care as it does for inpatient care. For example, self‐administered medications are generally not covered for beneficiaries receiving observation care. However, the Office of the Inspector General (OIG)[2] recently found that the average patient cost per observation stay in 2012even including the cost of self‐administered medicationswas $528. This was significantly lower than the inpatient deductible ($1156 in 2012) that patients would have paid had they been admitted. Although on average patients paid less for observation care, the OIG report found that 6% of observation stays were more costly to patients than inpatient admissions.
Third, there are certain benefits that Medicare beneficiaries are not eligible for unless they are admitted to the hospital. For a beneficiary to receive skilled nursing facility (SNF) benefits, they must be admitted to the hospital for 3 or more days. This was the basis for Bagnall v Sebelius, a class action lawsuit against the Centers for Medicare & Medicaid Services (CMS) filed in 2009 by the Center for Medicare Advocacy.[6] The OIG estimated that in 2012, Medicare beneficiaries had 600,000 observation stays longer than 3 days that failed to qualify them for SNF services. Since then, CMS created the 2‐midnight rule,[7] stating that CMS will assign inpatient status to all medically necessary stays of 2 midnights or longer. This rule was intended, in part, to curb the use of observation stays greater than 48 hours and was a key factor in Judge Michael Shea's decision to dismiss Bagnall v Sebelius.[6]
Finally, Medicare beneficiaries who must revisit the hospital may have greater cumulative costs under observation care versus inpatient care. Medicare beneficiaries are partially protected from accumulating high costs over multiple inpatient admissions by a benefit design known as the benefit period. A benefit period begins the day a beneficiary is admitted to a hospital or SNF, and ends when he or she has not received any inpatient hospital or SNF care for 60 days in a row. Beneficiaries pay the inpatient deductible only once per benefit period, even if they have multiple readmissions during this time. So, for example, if a beneficiary was readmitted to the hospital 59 days after discharge, he or she would not have to pay the inpatient deductible again. In addition, the benefit period would be extended for an additional 60 days. In contrast, beneficiaries who receive observation care are subject to coinsurance at every subsequent visit; therefore, these beneficiaries could accrue high cumulative costs over multiple observation stays.
To our knowledge, there have been no published studies focusing on the potentially vulnerable population of Medicare beneficiaries who frequently use observation care. Our objectives were to determine the financial liability for patients who have multiple observation stays within a 60‐day period, and then compare this to the inpatient deductible they would have paid as inpatients.
METHODS
Data Sources
We used a 20% sample of the Medicare Outpatient Standard Analytic File (SAF) to identify hospital observation stays among beneficiaries over the 3‐year period 2010 to 2012. The Outpatient SAF contains all institutional outpatient claims filed on the UB‐04 form. We also used publicly available data (American Association of Medical Colleges Council of Teaching Hospitals status,[8] US Department of Agriculture rural/urban continuum codes,[9] CMS Hospital Cost Reports,[10] and census bureau region) to link hospital Medicare provider number to hospital characteristics.
Measures
Our primary measure was beneficiary financial responsibility for facilities fees. For observation care patients, this amount is the sum of the Part B coinsurance liability amount, the Part B deductible amount, and the blood deductible liability amount.[11]
Observation care claims also include information on claim date, hospital Medicare provider number, principal diagnosis (International Classification of Diseases, Ninth Revision codes), services provided, and total hours for which observation services were provided (service units). Finally, claims include unique individual identifiers, which allowed us to construct our study population and obtain beneficiary characteristics including beneficiary age, race, gender, dual eligibility for Medicare/Medicaid, and severity of illness as measured by the CMS Hierarchical Condition Category (CMS‐HCC).[12] We obtained publicly available data on hospital characteristics, including academic hospital status,[8] urban versus rural,[9] nonprofit versus for profit,[10] and census bureau region, and linked these to the hospital Medicare provider number.
Study Sample and Statistical Analysis
We first created a denominator file that included all fee‐for‐service Medicare beneficiaries who had Part A and Part B coverage for a full calendar year (or until death) during the study period 2010 to 2012. We included dually eligible individuals, provided they had fee‐for‐service Medicare rather than a Medicare Advantage Plan.
We then constructed our study sample of unique beneficiaries who had an observation stay (lasting 8 hours, which is the criteria for Medicare payment) during the study period. We identified observation stays using revenue center codes and the Healthcare Common Procedure Coding System classification, and according to coding instructions found in the Medicare Claims Processing Manual.[13] Beneficiaries were excluded if their stay was converted from observation to inpatient status, because these claims may not be reliably tracked. After creating this study sample, we calculated the mean financial liability for the first observation stay for each beneficiary.
Next, within our study sample, we divided beneficiaries receiving observation care into 2 groups: those with multiple visits (defined as 2 observation stays in any 60‐day interval over the study period) and those without multiple visits. For each beneficiary with multiple visits, we calculated the mean cumulative financial liability for all stays within the 60‐day interval. We then compared this mean cumulative financial liability to the 2010 inpatient deductible of $1100.
We compared baseline characteristics of Medicare beneficiaries not receiving observation care, those with multiple observation visits, and those without multiple visits. We did this by using 2 tests for categorical variables, 2‐tailed unpaired t tests for 2‐way comparisons of means, and analysis of variance for 3‐way comparisons of means. We compared our primary outcome, mean beneficiary financial liability with the inpatient deductible of $1100 using a 1‐sample z test. As an exploratory analysis, we compared characteristics of beneficiaries with multiple observation visits with high cumulative liability (>$1100) versus low liability using bivariate analyses. We then created a multivariable logistic regression model for high liability. All analyses were performed using SAS version 9.1 (SAS Institute, Inc., Cary, NC). This study was reviewed by the institutional review board of the University of Pennsylvania.
RESULTS
Of the 7,470,676 unique Medicare beneficiaries in the 20% denominator file, 691,760 (9.3%) had at least 1 observation visit during the 3‐year study period (Table 1). The proportion of beneficiaries using observation care rose in each year of the study; 4.1% of beneficiaries used observation care in 2010, 4.4% in 2011, and 5.0% in 2012.
| Medicare FFS Beneficiaries Not Receiving Observation Care | Observation Care (n = 691,760) | P Value | ||
|---|---|---|---|---|
| No Multiple Observation Stays in 60 Days | Multiple (2) Observation Stays in 60 Days | |||
| ||||
| No. | 6,778,916 | 650,375 | 41,385 | N/A |
| Age, y, mean (SD) | 70.5 (12.9) | 72.2 (13.1) | 70.3 (14.9) | <0.01 |
| Gender, no. (%) | <0.01 | |||
| Male | 3,720,428 (54.9) | 387,333 (59.6) | 24,462 (59.1) | |
| Female | 3,058,488 (45.1) | 263,042 (40.4) | 16,923 (40.9) | |
| Race, no. (%) | <0.01 | |||
| White | 5,673,580 (83.7) | 545,165 (83.8) | 33,586 (81.2) | |
| Black | 674,420 (10.0) | 74,367 (11.4) | 5,913 (14.3) | |
| Other | 430,916 (6.4) | 30,843 (4.7) | 1,886 (4.6) | |
| Average no. of chronic conditions, mean (SD) | 1.7 (1.7) | 2.8 (2.0) | 3.6 (2.1) | <0.01 |
| Length of stay, h, mean (SD) | N/A | 29.9 (53.7) | 32.1 (16.9) | <0.01 |
| Most common hospital diagnoses, no. (%)* | N/A | |||
| Other chest pain (786.59) | N/A | 82,550 (12.7) | 9,995 (11.5) | |
| Chest pain, unspecified (786.50) | N/A | 56,416 (8.7) | 7,578 (8.7) | |
| Syncope and collapse (780.2) | N/A | 34,183 (5.3) | 3,291 (3.8) | |
| Coronary atherosclerosis (414.01) | N/A | 16,348 (2.5) | 2,763 (3.1) | |
Of the beneficiaries receiving observation care over the entire study period, 41,385 (6.0%) had multiple visits (2 observation visits in any 60‐day interval). The number of beneficiaries with multiple visits grew by 21.9% from 2010 to 2012. There were racial differences in the use of observation care; patients with multiple visits were more likely to be black than those without multiple visits or those not receiving observation care (14.3% vs 11.4% vs 10.0, P < 0.01). Multiple observation visits were also associated with a higher number of chronic conditions (3.6 vs 2.8 vs 1.7, P < 0.01) (Table 1).
The mean financial liability for the first observation stay for each beneficiary in our study sample was $469.42 (442.43) (Table 2). This is significantly lower than the standard inpatient deductible of $1100 (p<0.01). For 9.2% of beneficiaries, the financial liability was greater than the inpatient deductible.
| Mean (SD) | 25th Percentile | 50th Percentile | 75th Percentile | 90th Percentile | 99th Percentile | |
|---|---|---|---|---|---|---|
| ||||||
| First observation stay, n = 691,760 | $469.43 (442.43) | $216.20 | $333.77 | $529.87 | $1,045.85 | $2,088.66 |
| Cumulative 60 days for beneficiaries with multiple visits, n = 41,385 | $947.40 (803.62) | $471.01 | $681.40 | $1,152.66 | $1,904.54 | $3,902.50 |
The cumulative mean financial liability for beneficiaries with 2 stays in a 60‐day interval was $947.40 (803.62) (Table 2). This is significantly lower than the standard inpatient deductible of $1100 (P < 0.01). However, for 26.6% of beneficiaries, cumulative financial liability was greater than the $1100 inpatient deductible, which is what they would have paid had these hospital visits been inpatient admissions (Figure 1).
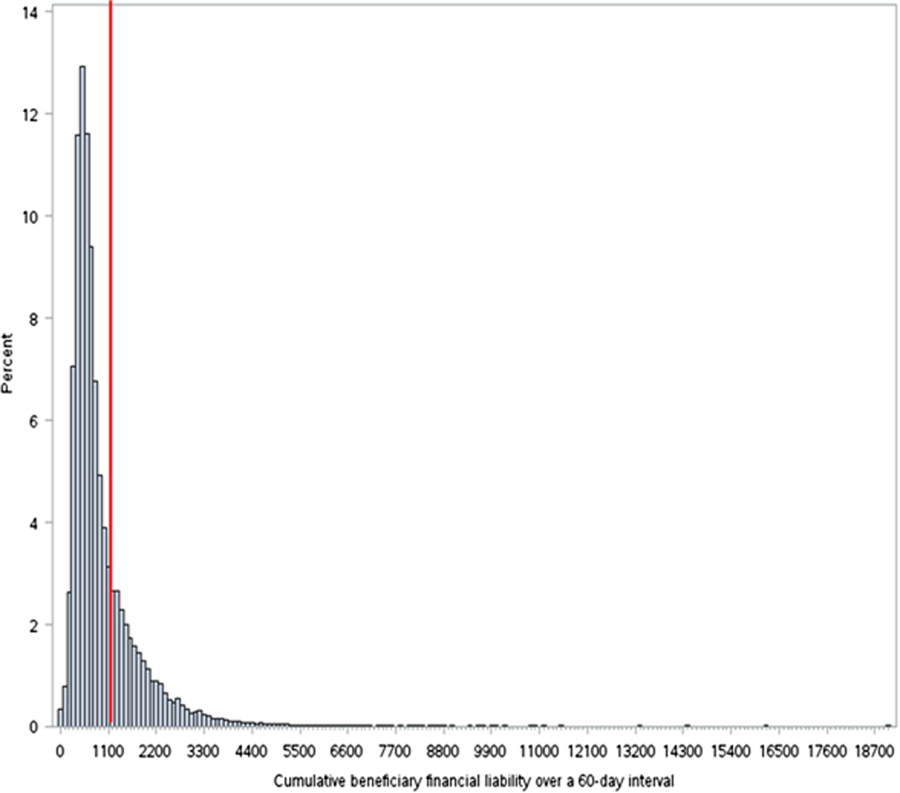
There were several factors associated with having this excess cumulative liability (Table 3). Higher frequency of observation visits within a 60‐day period was associated with high liability (odds ratio [OR]: 2.0, 95% confidence interval [CI]: 1.9‐2.1). In addition, having an index hospitalization in the Northeast region of the country was associated with lower odds of being in the high‐liability group (OR: 0.51, 95% CI: 0.47‐0.55). High liability was weakly associated with lower CMS‐HCC risk scores, nondual eligibility, nonblack race, and index hospital stay at an academic, urban, or nonprofit hospital.
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Low, n = 30,416 | High, n = 10,969 | P Value | OR (95% CI) | |
| ||||
| No. of observation visits in a 60‐day period, mean (SD) | 2.08 (0.30) | 2.18 (0.52) | <0.001 | 2.0 (1.92.1) |
| HCC risk score, mean (SD) | 2.40 (2.50) | 2.10 (2.50) | <0.001 | 0.97 (0.960.98) |
| Most common hospital diagnoses, no. (%) | Chest pain (other or unspecified); 13,381 (21.1%) | Chest pain (other or unspecified); 4,165 (17.4%) | N/A | |
| Syncope and collapse; 2,602 (4.1%) | Coronary atherosclerosis; 2,228 (9.3%) | N/A | ||
| Dehydration; 1,264 (2.0%) | Syncope and collapse; 686 (2.9%) | N/A | ||
| Altered mental status; 1,140 (1.8%) | Atrial fibrillation; 390 (1.6%) | N/A | ||
| Obstructive bronchitis with exacerbation; 1,032 (1.6%) | CHF; 350 (1.5%) | N/A | ||
| Dual eligibility, no. (%) | 10,895 (35.8%) | 3,162 (28.8%) | <0.001 | 0.76 (0.730.80) |
| Race, no. (%) | <0.001 | |||
| White | 24,283 (79.8%) | 9,303 (84.8%) | 1 | |
| Black | 4,704 (15.5%) | 1,209 (11.0%) | 0.79 (0.730.85) | |
| Other | 1,429 (4.7%) | 457 (4.2%) | 0.95 (0.851.1) | |
| Hospital census bureau region, no. (%) | <0.001 | |||
| South | 14,076 (46.3%) | 5,059 (46.1%) | 1 | |
| Midwest | 8,431 (27.7%) | 3,365 (30.7%) | 1.08 (1.021.14) | |
| West | 3,426 (11.3%) | 1,709 (15.6%) | 1.34 (1.251.44) | |
| Northeast | 4,483 (14.7%) | 832 (7.6%) | 0.51 (0.470.55) | |
| Academic hospital | 5,038 (16.9%) | 1,362 (12.9%) | <0.001 | 0.90 (0.840.96) |
| Urban hospital | 13,260 (44.4%) | 3,926 (37.1%) | <0.001 | 0.79 (0.760.83) |
| Nonprofit hospital | 20,665 (69.2%) | 7,143 (67.4%) | 0.001 | 0.89 (0.830.94) |
DISCUSSION
Our findings suggest that for 91% of Medicare beneficiaries, a single observation stay was less costly than an inpatient admission. However, when beneficiaries had to return to observation care within 60 days of a prior stay, on average, their cumulative costs went up to $947. For more than a quarter of beneficiaries with multiple observation visits, the cumulative costs of these observation visits exceeded the inpatient deductible.
The results of this study are consistent with prior studies of observation care. We found that in 2010, 4.1% of Medicare beneficiaries used observation care, consistent with the estimated 4.0% in 2009 reported by the AARP Public Policy Institute.[14] Also, consistent with the growth rate from the AARP report, we found growth in use of observation care from 4.1% in 2010 to 5.0% in 2012. We found that the mean length of stay for observation care was 30 hours, consistent with recent studies estimating mean length of stay in 2009 as 25.9 hours.[15] We found that beneficiaries paid an average of $468.50 per observation care stay, very close to the $401 estimated by the 2013 OIG report (when self‐administered drugs were excluded).[2] The difference may be explained by the fact that OIG included observation stays of <8 hours in their sample; we excluded these stays because they did not meet criteria for Medicare payment. Like the OIG report, we also found that the vast majority (91%) of beneficiaries pay less for any given observation stay than for an inpatient stay.
However, our findings raise the concern that for a significant proportion of beneficiaries who are likely to return to the hospital, cumulative costs of multiple observation stays may be greater than the inpatient deductible. Therefore, although observation care is, on average, less expensive for beneficiaries than inpatient admission, beneficiaries lack the protection from escalating financial liability over multiple visits.
This finding is worrisome for 3 reasons. First, compared with the general beneficiary population, Medicare beneficiaries who return to the hospital frequently are also typically of lower socioeconomic status[16, 17, 18] and may be disproportionately affected by any increased financial liability. Interestingly, our analysis showed that patients with high financial liability incurred from multiple observation stays actually had a lower comorbidity burden than patients in the multiple observation stay group with lower liability, and were less likely to be black or dual eligible. This finding perhaps reflects the fact that very high‐risk patients who returned to the hospital were readmitted rather than being placed under observation status again, potentially depleting the high‐liability group of patients with these high‐risk characteristics. Second, patients have little control over their classification as observation versus inpatients. In many hospitals, observation is simply an administrative classification for care thatfrom the patients' perspectiveis identical to inpatient care.[4] It is problematic to expose patients to varying financial liability based on differences in administrative classification. Finally, we found that the number of patients with multiple observation visits within a 60‐day period rose by 22% between 2010 and 2012. This means that the problem of excess cumulative financial liability is likely to be increasingly common over the coming years. The increased incidence of multiple observation visits may be simply related to overall increases in use of observation care. Alternatively, some authors worry that this trend may be driven by hospital use of observation care for patients who are likely to be readmitted.[14, 19] A recent analysis by Gerhardt et al.[20] did not find evidence of direct substitution of observation care in the 30‐day window after an index admission. This suggests that physicians are not explicitly shifting patients to observation care in order to avert a readmission and the readmissions penalty.[21] However, it does not exclude the possibility of general shifts toward observation care for patients likely to return.
Experts have suggested capping the total out‐of‐pocket expense for observation care at the inpatient‐deductible amount.[4] This deductible cap would prevent the relatively rare case in which a single observation stay costs more than an inpatient admission. Our findings suggest that a benefit period (as in Part A) during which such a deductible would serve as a cap would also protect a small but significantly impacted population from higher than expected cumulative costs for multiple observation care visits.
This study has several limitations. First, we are only able to measure beneficiary financial responsibility and not the amount actually paid. This can differ from financial responsibility when patients do not pay their bill, when patients accrue additional charges (such as self‐administered medications) that are not reflected on outpatient claims, or when patients have additional third‐party payers who cover part or all of the financial responsibility (as with dually eligible patients). For such beneficiaries with supplemental coverage, out‐of‐pocket cost in both scenarios (inpatient or observation care) may be low or zero. However, the use of financial responsibility as an approximation of actual payment amounts is recommended by the Research Data Assistance Center and is consistent with other studies of cost in observation care.[2] Second, our data source only allowed us to assess facilities fees and not professional expenses. Our comparator of the inpatient deductible also only reflects facilities fees, making this a valid comparison. Third, we selected 60 days as the time interval for defining multiple visits. This interval is intended to approximate a Medicare benefit period, which is the time interval following a discharge from a hospital or an SNF until the time when the deductible resets. However, Medicare actually extends the benefit period another 60 days if a patient is readmitted during that 60‐day period. Thus, 60 days is actually the shortest possible benefit period. By conservatively defining the interval for recurrent observation stays in this way, we are likely underestimating the number and cost of observation stays in a true benefit period, and biasing our results toward the null.
In conclusion, our findings suggest that a significant proportion of Medicare beneficiaries who revisit observation care pay more than they would have had they been readmitted. As CMS policies on observation care continue to evolve, it may be helpful to consider measures to cap total out‐of‐pocket expenses within a benefit period to protect beneficiaries from higher than expected costs.
Disclosure
Disclosure: Nothing to report.
- June 2012 Data Book: Health Care Spending and the Medicare Program. Washington, DC: Medicare Payment Advisory Commission; 2012.
- . Hospitals' use of observation stays and short inpatient stays for Medicare beneficiaries, OEI‐02‐12‐00040. Washington, DC: Department of Health and Human Services, Office of the Inspector General; 2013.
- , , . National study of emergency department observation services. Acad Emerg Med. 2011;18(9):959–965.
- , . Observation care—high‐value care or a cost‐shifting loophole? N Engl J Med. 2013;369(4):302–305.
- , , , , . Factors associated with prolonged observation services stays and the impact of long stays on patient cost. Health Serv Res. 2014;49(3):893–909.
- Bagnall v Sebelius. No. 3:11cv1703 (MPS). September 23, 2013.
- Centers for Medicare 2 Midnight Benchmark for Inpatient Hospital Admissions. CMS‐1599‐F2013.2013. Available at: http://www.cms.gov/Outreach‐and‐Education/Outreach/OpenDoorForums/Downloads/02042014SODF.pdf. Accessed June 16, 2015
- Council of Teaching Hospitals and Health Systems (COTH). Association of American Medical Colleges website. Available at: https://www.aamc.org/members/coth/. Accessed May 5, 2006.
- United States Department of Agriculture Economic Research Service. Rural‐urban continuity codes. Available at: http://www.ers.usda.gov/data‐products/rural‐urban‐continuum‐codes.aspx. Accessed June 16, 2015.
- Centers for Medicare
When Medicare beneficiaries seek healthcare, they are increasingly likely to have that care delivered under observation status. From 2006 to 2010, the annual number of observation hours for Medicare beneficiaries rose by nearly 70%.[1] In 2012, the number of observation stays for Medicare beneficiaries reached 1.5 million.[2] One consequence of this trend is a potential change in patient financial liabilitythe amount patients are expected to pay out of pocket for care. Although observation care is usually delivered in a hospital, Medicare classifies it as an outpatient service, covered through Part B rather than inpatient Part A. In two‐thirds of US hospitals, observation care is largely an administrative classification, delivered in the same units and beds as admitted patients rather than in a protocol‐driven observation care unit.[3] Therefore, patients are often unaware of their outpatient observation status and its financial implications until they receive their hospital bill.
Observation has the potential to impact patient financial liability through 4 mechanisms.[4] First, instead of a fixed cost for an inpatient admission (eg, a fixed deductible for a hospital admission), patients pay a percentage of the cost of each service provided. Therefore, patients who have long observation stays or receive expensive services could have higher than expected liability. A recent study using all‐payer data demonstrated that patients with longer observation stays (greater than 24 hours) paid 21% more than for those with shorter stays.[5]
A second consideration is that Medicare does not cover the same hospital services for observation care as it does for inpatient care. For example, self‐administered medications are generally not covered for beneficiaries receiving observation care. However, the Office of the Inspector General (OIG)[2] recently found that the average patient cost per observation stay in 2012even including the cost of self‐administered medicationswas $528. This was significantly lower than the inpatient deductible ($1156 in 2012) that patients would have paid had they been admitted. Although on average patients paid less for observation care, the OIG report found that 6% of observation stays were more costly to patients than inpatient admissions.
Third, there are certain benefits that Medicare beneficiaries are not eligible for unless they are admitted to the hospital. For a beneficiary to receive skilled nursing facility (SNF) benefits, they must be admitted to the hospital for 3 or more days. This was the basis for Bagnall v Sebelius, a class action lawsuit against the Centers for Medicare & Medicaid Services (CMS) filed in 2009 by the Center for Medicare Advocacy.[6] The OIG estimated that in 2012, Medicare beneficiaries had 600,000 observation stays longer than 3 days that failed to qualify them for SNF services. Since then, CMS created the 2‐midnight rule,[7] stating that CMS will assign inpatient status to all medically necessary stays of 2 midnights or longer. This rule was intended, in part, to curb the use of observation stays greater than 48 hours and was a key factor in Judge Michael Shea's decision to dismiss Bagnall v Sebelius.[6]
Finally, Medicare beneficiaries who must revisit the hospital may have greater cumulative costs under observation care versus inpatient care. Medicare beneficiaries are partially protected from accumulating high costs over multiple inpatient admissions by a benefit design known as the benefit period. A benefit period begins the day a beneficiary is admitted to a hospital or SNF, and ends when he or she has not received any inpatient hospital or SNF care for 60 days in a row. Beneficiaries pay the inpatient deductible only once per benefit period, even if they have multiple readmissions during this time. So, for example, if a beneficiary was readmitted to the hospital 59 days after discharge, he or she would not have to pay the inpatient deductible again. In addition, the benefit period would be extended for an additional 60 days. In contrast, beneficiaries who receive observation care are subject to coinsurance at every subsequent visit; therefore, these beneficiaries could accrue high cumulative costs over multiple observation stays.
To our knowledge, there have been no published studies focusing on the potentially vulnerable population of Medicare beneficiaries who frequently use observation care. Our objectives were to determine the financial liability for patients who have multiple observation stays within a 60‐day period, and then compare this to the inpatient deductible they would have paid as inpatients.
METHODS
Data Sources
We used a 20% sample of the Medicare Outpatient Standard Analytic File (SAF) to identify hospital observation stays among beneficiaries over the 3‐year period 2010 to 2012. The Outpatient SAF contains all institutional outpatient claims filed on the UB‐04 form. We also used publicly available data (American Association of Medical Colleges Council of Teaching Hospitals status,[8] US Department of Agriculture rural/urban continuum codes,[9] CMS Hospital Cost Reports,[10] and census bureau region) to link hospital Medicare provider number to hospital characteristics.
Measures
Our primary measure was beneficiary financial responsibility for facilities fees. For observation care patients, this amount is the sum of the Part B coinsurance liability amount, the Part B deductible amount, and the blood deductible liability amount.[11]
Observation care claims also include information on claim date, hospital Medicare provider number, principal diagnosis (International Classification of Diseases, Ninth Revision codes), services provided, and total hours for which observation services were provided (service units). Finally, claims include unique individual identifiers, which allowed us to construct our study population and obtain beneficiary characteristics including beneficiary age, race, gender, dual eligibility for Medicare/Medicaid, and severity of illness as measured by the CMS Hierarchical Condition Category (CMS‐HCC).[12] We obtained publicly available data on hospital characteristics, including academic hospital status,[8] urban versus rural,[9] nonprofit versus for profit,[10] and census bureau region, and linked these to the hospital Medicare provider number.
Study Sample and Statistical Analysis
We first created a denominator file that included all fee‐for‐service Medicare beneficiaries who had Part A and Part B coverage for a full calendar year (or until death) during the study period 2010 to 2012. We included dually eligible individuals, provided they had fee‐for‐service Medicare rather than a Medicare Advantage Plan.
We then constructed our study sample of unique beneficiaries who had an observation stay (lasting 8 hours, which is the criteria for Medicare payment) during the study period. We identified observation stays using revenue center codes and the Healthcare Common Procedure Coding System classification, and according to coding instructions found in the Medicare Claims Processing Manual.[13] Beneficiaries were excluded if their stay was converted from observation to inpatient status, because these claims may not be reliably tracked. After creating this study sample, we calculated the mean financial liability for the first observation stay for each beneficiary.
Next, within our study sample, we divided beneficiaries receiving observation care into 2 groups: those with multiple visits (defined as 2 observation stays in any 60‐day interval over the study period) and those without multiple visits. For each beneficiary with multiple visits, we calculated the mean cumulative financial liability for all stays within the 60‐day interval. We then compared this mean cumulative financial liability to the 2010 inpatient deductible of $1100.
We compared baseline characteristics of Medicare beneficiaries not receiving observation care, those with multiple observation visits, and those without multiple visits. We did this by using 2 tests for categorical variables, 2‐tailed unpaired t tests for 2‐way comparisons of means, and analysis of variance for 3‐way comparisons of means. We compared our primary outcome, mean beneficiary financial liability with the inpatient deductible of $1100 using a 1‐sample z test. As an exploratory analysis, we compared characteristics of beneficiaries with multiple observation visits with high cumulative liability (>$1100) versus low liability using bivariate analyses. We then created a multivariable logistic regression model for high liability. All analyses were performed using SAS version 9.1 (SAS Institute, Inc., Cary, NC). This study was reviewed by the institutional review board of the University of Pennsylvania.
RESULTS
Of the 7,470,676 unique Medicare beneficiaries in the 20% denominator file, 691,760 (9.3%) had at least 1 observation visit during the 3‐year study period (Table 1). The proportion of beneficiaries using observation care rose in each year of the study; 4.1% of beneficiaries used observation care in 2010, 4.4% in 2011, and 5.0% in 2012.
| Medicare FFS Beneficiaries Not Receiving Observation Care | Observation Care (n = 691,760) | P Value | ||
|---|---|---|---|---|
| No Multiple Observation Stays in 60 Days | Multiple (2) Observation Stays in 60 Days | |||
| ||||
| No. | 6,778,916 | 650,375 | 41,385 | N/A |
| Age, y, mean (SD) | 70.5 (12.9) | 72.2 (13.1) | 70.3 (14.9) | <0.01 |
| Gender, no. (%) | <0.01 | |||
| Male | 3,720,428 (54.9) | 387,333 (59.6) | 24,462 (59.1) | |
| Female | 3,058,488 (45.1) | 263,042 (40.4) | 16,923 (40.9) | |
| Race, no. (%) | <0.01 | |||
| White | 5,673,580 (83.7) | 545,165 (83.8) | 33,586 (81.2) | |
| Black | 674,420 (10.0) | 74,367 (11.4) | 5,913 (14.3) | |
| Other | 430,916 (6.4) | 30,843 (4.7) | 1,886 (4.6) | |
| Average no. of chronic conditions, mean (SD) | 1.7 (1.7) | 2.8 (2.0) | 3.6 (2.1) | <0.01 |
| Length of stay, h, mean (SD) | N/A | 29.9 (53.7) | 32.1 (16.9) | <0.01 |
| Most common hospital diagnoses, no. (%)* | N/A | |||
| Other chest pain (786.59) | N/A | 82,550 (12.7) | 9,995 (11.5) | |
| Chest pain, unspecified (786.50) | N/A | 56,416 (8.7) | 7,578 (8.7) | |
| Syncope and collapse (780.2) | N/A | 34,183 (5.3) | 3,291 (3.8) | |
| Coronary atherosclerosis (414.01) | N/A | 16,348 (2.5) | 2,763 (3.1) | |
Of the beneficiaries receiving observation care over the entire study period, 41,385 (6.0%) had multiple visits (2 observation visits in any 60‐day interval). The number of beneficiaries with multiple visits grew by 21.9% from 2010 to 2012. There were racial differences in the use of observation care; patients with multiple visits were more likely to be black than those without multiple visits or those not receiving observation care (14.3% vs 11.4% vs 10.0, P < 0.01). Multiple observation visits were also associated with a higher number of chronic conditions (3.6 vs 2.8 vs 1.7, P < 0.01) (Table 1).
The mean financial liability for the first observation stay for each beneficiary in our study sample was $469.42 (442.43) (Table 2). This is significantly lower than the standard inpatient deductible of $1100 (p<0.01). For 9.2% of beneficiaries, the financial liability was greater than the inpatient deductible.
| Mean (SD) | 25th Percentile | 50th Percentile | 75th Percentile | 90th Percentile | 99th Percentile | |
|---|---|---|---|---|---|---|
| ||||||
| First observation stay, n = 691,760 | $469.43 (442.43) | $216.20 | $333.77 | $529.87 | $1,045.85 | $2,088.66 |
| Cumulative 60 days for beneficiaries with multiple visits, n = 41,385 | $947.40 (803.62) | $471.01 | $681.40 | $1,152.66 | $1,904.54 | $3,902.50 |
The cumulative mean financial liability for beneficiaries with 2 stays in a 60‐day interval was $947.40 (803.62) (Table 2). This is significantly lower than the standard inpatient deductible of $1100 (P < 0.01). However, for 26.6% of beneficiaries, cumulative financial liability was greater than the $1100 inpatient deductible, which is what they would have paid had these hospital visits been inpatient admissions (Figure 1).
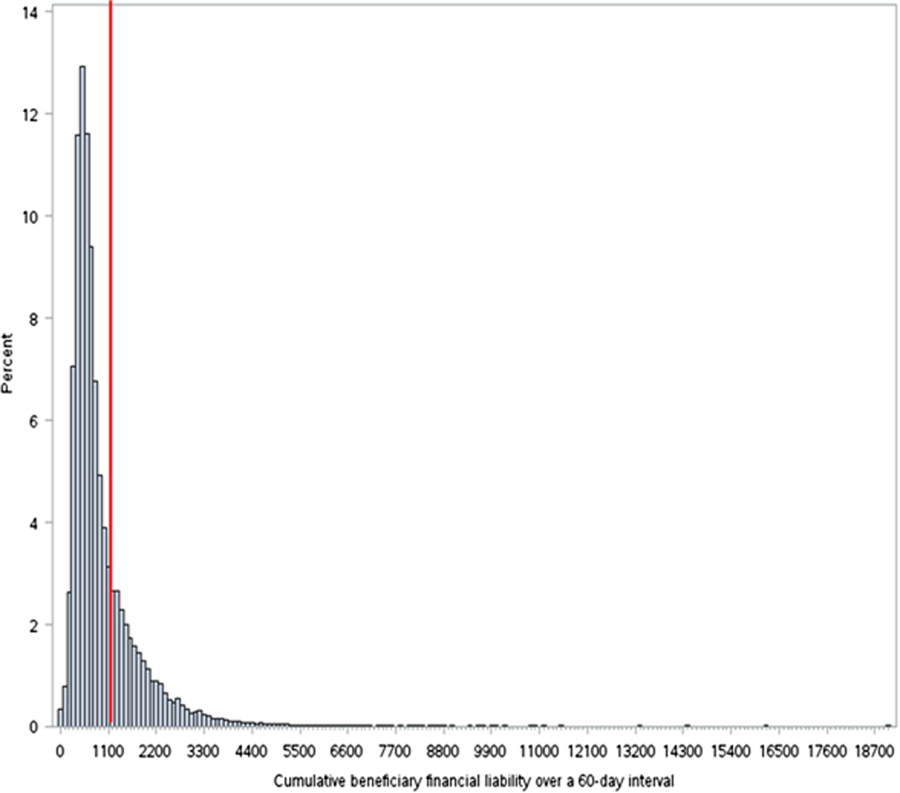
There were several factors associated with having this excess cumulative liability (Table 3). Higher frequency of observation visits within a 60‐day period was associated with high liability (odds ratio [OR]: 2.0, 95% confidence interval [CI]: 1.9‐2.1). In addition, having an index hospitalization in the Northeast region of the country was associated with lower odds of being in the high‐liability group (OR: 0.51, 95% CI: 0.47‐0.55). High liability was weakly associated with lower CMS‐HCC risk scores, nondual eligibility, nonblack race, and index hospital stay at an academic, urban, or nonprofit hospital.
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Low, n = 30,416 | High, n = 10,969 | P Value | OR (95% CI) | |
| ||||
| No. of observation visits in a 60‐day period, mean (SD) | 2.08 (0.30) | 2.18 (0.52) | <0.001 | 2.0 (1.92.1) |
| HCC risk score, mean (SD) | 2.40 (2.50) | 2.10 (2.50) | <0.001 | 0.97 (0.960.98) |
| Most common hospital diagnoses, no. (%) | Chest pain (other or unspecified); 13,381 (21.1%) | Chest pain (other or unspecified); 4,165 (17.4%) | N/A | |
| Syncope and collapse; 2,602 (4.1%) | Coronary atherosclerosis; 2,228 (9.3%) | N/A | ||
| Dehydration; 1,264 (2.0%) | Syncope and collapse; 686 (2.9%) | N/A | ||
| Altered mental status; 1,140 (1.8%) | Atrial fibrillation; 390 (1.6%) | N/A | ||
| Obstructive bronchitis with exacerbation; 1,032 (1.6%) | CHF; 350 (1.5%) | N/A | ||
| Dual eligibility, no. (%) | 10,895 (35.8%) | 3,162 (28.8%) | <0.001 | 0.76 (0.730.80) |
| Race, no. (%) | <0.001 | |||
| White | 24,283 (79.8%) | 9,303 (84.8%) | 1 | |
| Black | 4,704 (15.5%) | 1,209 (11.0%) | 0.79 (0.730.85) | |
| Other | 1,429 (4.7%) | 457 (4.2%) | 0.95 (0.851.1) | |
| Hospital census bureau region, no. (%) | <0.001 | |||
| South | 14,076 (46.3%) | 5,059 (46.1%) | 1 | |
| Midwest | 8,431 (27.7%) | 3,365 (30.7%) | 1.08 (1.021.14) | |
| West | 3,426 (11.3%) | 1,709 (15.6%) | 1.34 (1.251.44) | |
| Northeast | 4,483 (14.7%) | 832 (7.6%) | 0.51 (0.470.55) | |
| Academic hospital | 5,038 (16.9%) | 1,362 (12.9%) | <0.001 | 0.90 (0.840.96) |
| Urban hospital | 13,260 (44.4%) | 3,926 (37.1%) | <0.001 | 0.79 (0.760.83) |
| Nonprofit hospital | 20,665 (69.2%) | 7,143 (67.4%) | 0.001 | 0.89 (0.830.94) |
DISCUSSION
Our findings suggest that for 91% of Medicare beneficiaries, a single observation stay was less costly than an inpatient admission. However, when beneficiaries had to return to observation care within 60 days of a prior stay, on average, their cumulative costs went up to $947. For more than a quarter of beneficiaries with multiple observation visits, the cumulative costs of these observation visits exceeded the inpatient deductible.
The results of this study are consistent with prior studies of observation care. We found that in 2010, 4.1% of Medicare beneficiaries used observation care, consistent with the estimated 4.0% in 2009 reported by the AARP Public Policy Institute.[14] Also, consistent with the growth rate from the AARP report, we found growth in use of observation care from 4.1% in 2010 to 5.0% in 2012. We found that the mean length of stay for observation care was 30 hours, consistent with recent studies estimating mean length of stay in 2009 as 25.9 hours.[15] We found that beneficiaries paid an average of $468.50 per observation care stay, very close to the $401 estimated by the 2013 OIG report (when self‐administered drugs were excluded).[2] The difference may be explained by the fact that OIG included observation stays of <8 hours in their sample; we excluded these stays because they did not meet criteria for Medicare payment. Like the OIG report, we also found that the vast majority (91%) of beneficiaries pay less for any given observation stay than for an inpatient stay.
However, our findings raise the concern that for a significant proportion of beneficiaries who are likely to return to the hospital, cumulative costs of multiple observation stays may be greater than the inpatient deductible. Therefore, although observation care is, on average, less expensive for beneficiaries than inpatient admission, beneficiaries lack the protection from escalating financial liability over multiple visits.
This finding is worrisome for 3 reasons. First, compared with the general beneficiary population, Medicare beneficiaries who return to the hospital frequently are also typically of lower socioeconomic status[16, 17, 18] and may be disproportionately affected by any increased financial liability. Interestingly, our analysis showed that patients with high financial liability incurred from multiple observation stays actually had a lower comorbidity burden than patients in the multiple observation stay group with lower liability, and were less likely to be black or dual eligible. This finding perhaps reflects the fact that very high‐risk patients who returned to the hospital were readmitted rather than being placed under observation status again, potentially depleting the high‐liability group of patients with these high‐risk characteristics. Second, patients have little control over their classification as observation versus inpatients. In many hospitals, observation is simply an administrative classification for care thatfrom the patients' perspectiveis identical to inpatient care.[4] It is problematic to expose patients to varying financial liability based on differences in administrative classification. Finally, we found that the number of patients with multiple observation visits within a 60‐day period rose by 22% between 2010 and 2012. This means that the problem of excess cumulative financial liability is likely to be increasingly common over the coming years. The increased incidence of multiple observation visits may be simply related to overall increases in use of observation care. Alternatively, some authors worry that this trend may be driven by hospital use of observation care for patients who are likely to be readmitted.[14, 19] A recent analysis by Gerhardt et al.[20] did not find evidence of direct substitution of observation care in the 30‐day window after an index admission. This suggests that physicians are not explicitly shifting patients to observation care in order to avert a readmission and the readmissions penalty.[21] However, it does not exclude the possibility of general shifts toward observation care for patients likely to return.
Experts have suggested capping the total out‐of‐pocket expense for observation care at the inpatient‐deductible amount.[4] This deductible cap would prevent the relatively rare case in which a single observation stay costs more than an inpatient admission. Our findings suggest that a benefit period (as in Part A) during which such a deductible would serve as a cap would also protect a small but significantly impacted population from higher than expected cumulative costs for multiple observation care visits.
This study has several limitations. First, we are only able to measure beneficiary financial responsibility and not the amount actually paid. This can differ from financial responsibility when patients do not pay their bill, when patients accrue additional charges (such as self‐administered medications) that are not reflected on outpatient claims, or when patients have additional third‐party payers who cover part or all of the financial responsibility (as with dually eligible patients). For such beneficiaries with supplemental coverage, out‐of‐pocket cost in both scenarios (inpatient or observation care) may be low or zero. However, the use of financial responsibility as an approximation of actual payment amounts is recommended by the Research Data Assistance Center and is consistent with other studies of cost in observation care.[2] Second, our data source only allowed us to assess facilities fees and not professional expenses. Our comparator of the inpatient deductible also only reflects facilities fees, making this a valid comparison. Third, we selected 60 days as the time interval for defining multiple visits. This interval is intended to approximate a Medicare benefit period, which is the time interval following a discharge from a hospital or an SNF until the time when the deductible resets. However, Medicare actually extends the benefit period another 60 days if a patient is readmitted during that 60‐day period. Thus, 60 days is actually the shortest possible benefit period. By conservatively defining the interval for recurrent observation stays in this way, we are likely underestimating the number and cost of observation stays in a true benefit period, and biasing our results toward the null.
In conclusion, our findings suggest that a significant proportion of Medicare beneficiaries who revisit observation care pay more than they would have had they been readmitted. As CMS policies on observation care continue to evolve, it may be helpful to consider measures to cap total out‐of‐pocket expenses within a benefit period to protect beneficiaries from higher than expected costs.
Disclosure
Disclosure: Nothing to report.
When Medicare beneficiaries seek healthcare, they are increasingly likely to have that care delivered under observation status. From 2006 to 2010, the annual number of observation hours for Medicare beneficiaries rose by nearly 70%.[1] In 2012, the number of observation stays for Medicare beneficiaries reached 1.5 million.[2] One consequence of this trend is a potential change in patient financial liabilitythe amount patients are expected to pay out of pocket for care. Although observation care is usually delivered in a hospital, Medicare classifies it as an outpatient service, covered through Part B rather than inpatient Part A. In two‐thirds of US hospitals, observation care is largely an administrative classification, delivered in the same units and beds as admitted patients rather than in a protocol‐driven observation care unit.[3] Therefore, patients are often unaware of their outpatient observation status and its financial implications until they receive their hospital bill.
Observation has the potential to impact patient financial liability through 4 mechanisms.[4] First, instead of a fixed cost for an inpatient admission (eg, a fixed deductible for a hospital admission), patients pay a percentage of the cost of each service provided. Therefore, patients who have long observation stays or receive expensive services could have higher than expected liability. A recent study using all‐payer data demonstrated that patients with longer observation stays (greater than 24 hours) paid 21% more than for those with shorter stays.[5]
A second consideration is that Medicare does not cover the same hospital services for observation care as it does for inpatient care. For example, self‐administered medications are generally not covered for beneficiaries receiving observation care. However, the Office of the Inspector General (OIG)[2] recently found that the average patient cost per observation stay in 2012even including the cost of self‐administered medicationswas $528. This was significantly lower than the inpatient deductible ($1156 in 2012) that patients would have paid had they been admitted. Although on average patients paid less for observation care, the OIG report found that 6% of observation stays were more costly to patients than inpatient admissions.
Third, there are certain benefits that Medicare beneficiaries are not eligible for unless they are admitted to the hospital. For a beneficiary to receive skilled nursing facility (SNF) benefits, they must be admitted to the hospital for 3 or more days. This was the basis for Bagnall v Sebelius, a class action lawsuit against the Centers for Medicare & Medicaid Services (CMS) filed in 2009 by the Center for Medicare Advocacy.[6] The OIG estimated that in 2012, Medicare beneficiaries had 600,000 observation stays longer than 3 days that failed to qualify them for SNF services. Since then, CMS created the 2‐midnight rule,[7] stating that CMS will assign inpatient status to all medically necessary stays of 2 midnights or longer. This rule was intended, in part, to curb the use of observation stays greater than 48 hours and was a key factor in Judge Michael Shea's decision to dismiss Bagnall v Sebelius.[6]
Finally, Medicare beneficiaries who must revisit the hospital may have greater cumulative costs under observation care versus inpatient care. Medicare beneficiaries are partially protected from accumulating high costs over multiple inpatient admissions by a benefit design known as the benefit period. A benefit period begins the day a beneficiary is admitted to a hospital or SNF, and ends when he or she has not received any inpatient hospital or SNF care for 60 days in a row. Beneficiaries pay the inpatient deductible only once per benefit period, even if they have multiple readmissions during this time. So, for example, if a beneficiary was readmitted to the hospital 59 days after discharge, he or she would not have to pay the inpatient deductible again. In addition, the benefit period would be extended for an additional 60 days. In contrast, beneficiaries who receive observation care are subject to coinsurance at every subsequent visit; therefore, these beneficiaries could accrue high cumulative costs over multiple observation stays.
To our knowledge, there have been no published studies focusing on the potentially vulnerable population of Medicare beneficiaries who frequently use observation care. Our objectives were to determine the financial liability for patients who have multiple observation stays within a 60‐day period, and then compare this to the inpatient deductible they would have paid as inpatients.
METHODS
Data Sources
We used a 20% sample of the Medicare Outpatient Standard Analytic File (SAF) to identify hospital observation stays among beneficiaries over the 3‐year period 2010 to 2012. The Outpatient SAF contains all institutional outpatient claims filed on the UB‐04 form. We also used publicly available data (American Association of Medical Colleges Council of Teaching Hospitals status,[8] US Department of Agriculture rural/urban continuum codes,[9] CMS Hospital Cost Reports,[10] and census bureau region) to link hospital Medicare provider number to hospital characteristics.
Measures
Our primary measure was beneficiary financial responsibility for facilities fees. For observation care patients, this amount is the sum of the Part B coinsurance liability amount, the Part B deductible amount, and the blood deductible liability amount.[11]
Observation care claims also include information on claim date, hospital Medicare provider number, principal diagnosis (International Classification of Diseases, Ninth Revision codes), services provided, and total hours for which observation services were provided (service units). Finally, claims include unique individual identifiers, which allowed us to construct our study population and obtain beneficiary characteristics including beneficiary age, race, gender, dual eligibility for Medicare/Medicaid, and severity of illness as measured by the CMS Hierarchical Condition Category (CMS‐HCC).[12] We obtained publicly available data on hospital characteristics, including academic hospital status,[8] urban versus rural,[9] nonprofit versus for profit,[10] and census bureau region, and linked these to the hospital Medicare provider number.
Study Sample and Statistical Analysis
We first created a denominator file that included all fee‐for‐service Medicare beneficiaries who had Part A and Part B coverage for a full calendar year (or until death) during the study period 2010 to 2012. We included dually eligible individuals, provided they had fee‐for‐service Medicare rather than a Medicare Advantage Plan.
We then constructed our study sample of unique beneficiaries who had an observation stay (lasting 8 hours, which is the criteria for Medicare payment) during the study period. We identified observation stays using revenue center codes and the Healthcare Common Procedure Coding System classification, and according to coding instructions found in the Medicare Claims Processing Manual.[13] Beneficiaries were excluded if their stay was converted from observation to inpatient status, because these claims may not be reliably tracked. After creating this study sample, we calculated the mean financial liability for the first observation stay for each beneficiary.
Next, within our study sample, we divided beneficiaries receiving observation care into 2 groups: those with multiple visits (defined as 2 observation stays in any 60‐day interval over the study period) and those without multiple visits. For each beneficiary with multiple visits, we calculated the mean cumulative financial liability for all stays within the 60‐day interval. We then compared this mean cumulative financial liability to the 2010 inpatient deductible of $1100.
We compared baseline characteristics of Medicare beneficiaries not receiving observation care, those with multiple observation visits, and those without multiple visits. We did this by using 2 tests for categorical variables, 2‐tailed unpaired t tests for 2‐way comparisons of means, and analysis of variance for 3‐way comparisons of means. We compared our primary outcome, mean beneficiary financial liability with the inpatient deductible of $1100 using a 1‐sample z test. As an exploratory analysis, we compared characteristics of beneficiaries with multiple observation visits with high cumulative liability (>$1100) versus low liability using bivariate analyses. We then created a multivariable logistic regression model for high liability. All analyses were performed using SAS version 9.1 (SAS Institute, Inc., Cary, NC). This study was reviewed by the institutional review board of the University of Pennsylvania.
RESULTS
Of the 7,470,676 unique Medicare beneficiaries in the 20% denominator file, 691,760 (9.3%) had at least 1 observation visit during the 3‐year study period (Table 1). The proportion of beneficiaries using observation care rose in each year of the study; 4.1% of beneficiaries used observation care in 2010, 4.4% in 2011, and 5.0% in 2012.
| Medicare FFS Beneficiaries Not Receiving Observation Care | Observation Care (n = 691,760) | P Value | ||
|---|---|---|---|---|
| No Multiple Observation Stays in 60 Days | Multiple (2) Observation Stays in 60 Days | |||
| ||||
| No. | 6,778,916 | 650,375 | 41,385 | N/A |
| Age, y, mean (SD) | 70.5 (12.9) | 72.2 (13.1) | 70.3 (14.9) | <0.01 |
| Gender, no. (%) | <0.01 | |||
| Male | 3,720,428 (54.9) | 387,333 (59.6) | 24,462 (59.1) | |
| Female | 3,058,488 (45.1) | 263,042 (40.4) | 16,923 (40.9) | |
| Race, no. (%) | <0.01 | |||
| White | 5,673,580 (83.7) | 545,165 (83.8) | 33,586 (81.2) | |
| Black | 674,420 (10.0) | 74,367 (11.4) | 5,913 (14.3) | |
| Other | 430,916 (6.4) | 30,843 (4.7) | 1,886 (4.6) | |
| Average no. of chronic conditions, mean (SD) | 1.7 (1.7) | 2.8 (2.0) | 3.6 (2.1) | <0.01 |
| Length of stay, h, mean (SD) | N/A | 29.9 (53.7) | 32.1 (16.9) | <0.01 |
| Most common hospital diagnoses, no. (%)* | N/A | |||
| Other chest pain (786.59) | N/A | 82,550 (12.7) | 9,995 (11.5) | |
| Chest pain, unspecified (786.50) | N/A | 56,416 (8.7) | 7,578 (8.7) | |
| Syncope and collapse (780.2) | N/A | 34,183 (5.3) | 3,291 (3.8) | |
| Coronary atherosclerosis (414.01) | N/A | 16,348 (2.5) | 2,763 (3.1) | |
Of the beneficiaries receiving observation care over the entire study period, 41,385 (6.0%) had multiple visits (2 observation visits in any 60‐day interval). The number of beneficiaries with multiple visits grew by 21.9% from 2010 to 2012. There were racial differences in the use of observation care; patients with multiple visits were more likely to be black than those without multiple visits or those not receiving observation care (14.3% vs 11.4% vs 10.0, P < 0.01). Multiple observation visits were also associated with a higher number of chronic conditions (3.6 vs 2.8 vs 1.7, P < 0.01) (Table 1).
The mean financial liability for the first observation stay for each beneficiary in our study sample was $469.42 (442.43) (Table 2). This is significantly lower than the standard inpatient deductible of $1100 (p<0.01). For 9.2% of beneficiaries, the financial liability was greater than the inpatient deductible.
| Mean (SD) | 25th Percentile | 50th Percentile | 75th Percentile | 90th Percentile | 99th Percentile | |
|---|---|---|---|---|---|---|
| ||||||
| First observation stay, n = 691,760 | $469.43 (442.43) | $216.20 | $333.77 | $529.87 | $1,045.85 | $2,088.66 |
| Cumulative 60 days for beneficiaries with multiple visits, n = 41,385 | $947.40 (803.62) | $471.01 | $681.40 | $1,152.66 | $1,904.54 | $3,902.50 |
The cumulative mean financial liability for beneficiaries with 2 stays in a 60‐day interval was $947.40 (803.62) (Table 2). This is significantly lower than the standard inpatient deductible of $1100 (P < 0.01). However, for 26.6% of beneficiaries, cumulative financial liability was greater than the $1100 inpatient deductible, which is what they would have paid had these hospital visits been inpatient admissions (Figure 1).
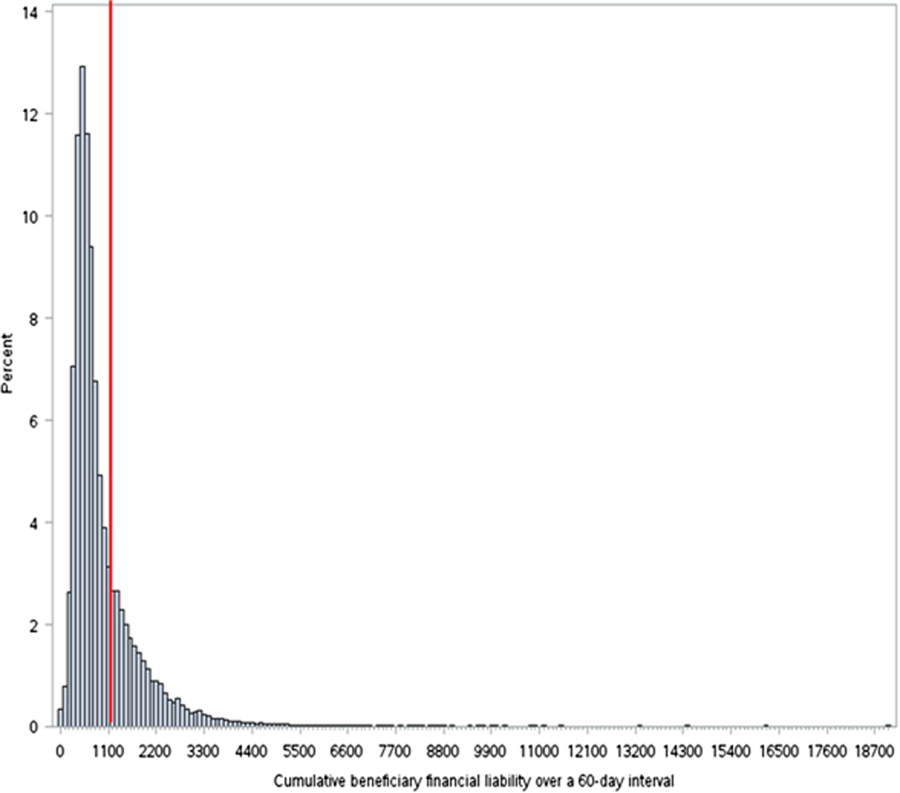
There were several factors associated with having this excess cumulative liability (Table 3). Higher frequency of observation visits within a 60‐day period was associated with high liability (odds ratio [OR]: 2.0, 95% confidence interval [CI]: 1.9‐2.1). In addition, having an index hospitalization in the Northeast region of the country was associated with lower odds of being in the high‐liability group (OR: 0.51, 95% CI: 0.47‐0.55). High liability was weakly associated with lower CMS‐HCC risk scores, nondual eligibility, nonblack race, and index hospital stay at an academic, urban, or nonprofit hospital.
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Low, n = 30,416 | High, n = 10,969 | P Value | OR (95% CI) | |
| ||||
| No. of observation visits in a 60‐day period, mean (SD) | 2.08 (0.30) | 2.18 (0.52) | <0.001 | 2.0 (1.92.1) |
| HCC risk score, mean (SD) | 2.40 (2.50) | 2.10 (2.50) | <0.001 | 0.97 (0.960.98) |
| Most common hospital diagnoses, no. (%) | Chest pain (other or unspecified); 13,381 (21.1%) | Chest pain (other or unspecified); 4,165 (17.4%) | N/A | |
| Syncope and collapse; 2,602 (4.1%) | Coronary atherosclerosis; 2,228 (9.3%) | N/A | ||
| Dehydration; 1,264 (2.0%) | Syncope and collapse; 686 (2.9%) | N/A | ||
| Altered mental status; 1,140 (1.8%) | Atrial fibrillation; 390 (1.6%) | N/A | ||
| Obstructive bronchitis with exacerbation; 1,032 (1.6%) | CHF; 350 (1.5%) | N/A | ||
| Dual eligibility, no. (%) | 10,895 (35.8%) | 3,162 (28.8%) | <0.001 | 0.76 (0.730.80) |
| Race, no. (%) | <0.001 | |||
| White | 24,283 (79.8%) | 9,303 (84.8%) | 1 | |
| Black | 4,704 (15.5%) | 1,209 (11.0%) | 0.79 (0.730.85) | |
| Other | 1,429 (4.7%) | 457 (4.2%) | 0.95 (0.851.1) | |
| Hospital census bureau region, no. (%) | <0.001 | |||
| South | 14,076 (46.3%) | 5,059 (46.1%) | 1 | |
| Midwest | 8,431 (27.7%) | 3,365 (30.7%) | 1.08 (1.021.14) | |
| West | 3,426 (11.3%) | 1,709 (15.6%) | 1.34 (1.251.44) | |
| Northeast | 4,483 (14.7%) | 832 (7.6%) | 0.51 (0.470.55) | |
| Academic hospital | 5,038 (16.9%) | 1,362 (12.9%) | <0.001 | 0.90 (0.840.96) |
| Urban hospital | 13,260 (44.4%) | 3,926 (37.1%) | <0.001 | 0.79 (0.760.83) |
| Nonprofit hospital | 20,665 (69.2%) | 7,143 (67.4%) | 0.001 | 0.89 (0.830.94) |
DISCUSSION
Our findings suggest that for 91% of Medicare beneficiaries, a single observation stay was less costly than an inpatient admission. However, when beneficiaries had to return to observation care within 60 days of a prior stay, on average, their cumulative costs went up to $947. For more than a quarter of beneficiaries with multiple observation visits, the cumulative costs of these observation visits exceeded the inpatient deductible.
The results of this study are consistent with prior studies of observation care. We found that in 2010, 4.1% of Medicare beneficiaries used observation care, consistent with the estimated 4.0% in 2009 reported by the AARP Public Policy Institute.[14] Also, consistent with the growth rate from the AARP report, we found growth in use of observation care from 4.1% in 2010 to 5.0% in 2012. We found that the mean length of stay for observation care was 30 hours, consistent with recent studies estimating mean length of stay in 2009 as 25.9 hours.[15] We found that beneficiaries paid an average of $468.50 per observation care stay, very close to the $401 estimated by the 2013 OIG report (when self‐administered drugs were excluded).[2] The difference may be explained by the fact that OIG included observation stays of <8 hours in their sample; we excluded these stays because they did not meet criteria for Medicare payment. Like the OIG report, we also found that the vast majority (91%) of beneficiaries pay less for any given observation stay than for an inpatient stay.
However, our findings raise the concern that for a significant proportion of beneficiaries who are likely to return to the hospital, cumulative costs of multiple observation stays may be greater than the inpatient deductible. Therefore, although observation care is, on average, less expensive for beneficiaries than inpatient admission, beneficiaries lack the protection from escalating financial liability over multiple visits.
This finding is worrisome for 3 reasons. First, compared with the general beneficiary population, Medicare beneficiaries who return to the hospital frequently are also typically of lower socioeconomic status[16, 17, 18] and may be disproportionately affected by any increased financial liability. Interestingly, our analysis showed that patients with high financial liability incurred from multiple observation stays actually had a lower comorbidity burden than patients in the multiple observation stay group with lower liability, and were less likely to be black or dual eligible. This finding perhaps reflects the fact that very high‐risk patients who returned to the hospital were readmitted rather than being placed under observation status again, potentially depleting the high‐liability group of patients with these high‐risk characteristics. Second, patients have little control over their classification as observation versus inpatients. In many hospitals, observation is simply an administrative classification for care thatfrom the patients' perspectiveis identical to inpatient care.[4] It is problematic to expose patients to varying financial liability based on differences in administrative classification. Finally, we found that the number of patients with multiple observation visits within a 60‐day period rose by 22% between 2010 and 2012. This means that the problem of excess cumulative financial liability is likely to be increasingly common over the coming years. The increased incidence of multiple observation visits may be simply related to overall increases in use of observation care. Alternatively, some authors worry that this trend may be driven by hospital use of observation care for patients who are likely to be readmitted.[14, 19] A recent analysis by Gerhardt et al.[20] did not find evidence of direct substitution of observation care in the 30‐day window after an index admission. This suggests that physicians are not explicitly shifting patients to observation care in order to avert a readmission and the readmissions penalty.[21] However, it does not exclude the possibility of general shifts toward observation care for patients likely to return.
Experts have suggested capping the total out‐of‐pocket expense for observation care at the inpatient‐deductible amount.[4] This deductible cap would prevent the relatively rare case in which a single observation stay costs more than an inpatient admission. Our findings suggest that a benefit period (as in Part A) during which such a deductible would serve as a cap would also protect a small but significantly impacted population from higher than expected cumulative costs for multiple observation care visits.
This study has several limitations. First, we are only able to measure beneficiary financial responsibility and not the amount actually paid. This can differ from financial responsibility when patients do not pay their bill, when patients accrue additional charges (such as self‐administered medications) that are not reflected on outpatient claims, or when patients have additional third‐party payers who cover part or all of the financial responsibility (as with dually eligible patients). For such beneficiaries with supplemental coverage, out‐of‐pocket cost in both scenarios (inpatient or observation care) may be low or zero. However, the use of financial responsibility as an approximation of actual payment amounts is recommended by the Research Data Assistance Center and is consistent with other studies of cost in observation care.[2] Second, our data source only allowed us to assess facilities fees and not professional expenses. Our comparator of the inpatient deductible also only reflects facilities fees, making this a valid comparison. Third, we selected 60 days as the time interval for defining multiple visits. This interval is intended to approximate a Medicare benefit period, which is the time interval following a discharge from a hospital or an SNF until the time when the deductible resets. However, Medicare actually extends the benefit period another 60 days if a patient is readmitted during that 60‐day period. Thus, 60 days is actually the shortest possible benefit period. By conservatively defining the interval for recurrent observation stays in this way, we are likely underestimating the number and cost of observation stays in a true benefit period, and biasing our results toward the null.
In conclusion, our findings suggest that a significant proportion of Medicare beneficiaries who revisit observation care pay more than they would have had they been readmitted. As CMS policies on observation care continue to evolve, it may be helpful to consider measures to cap total out‐of‐pocket expenses within a benefit period to protect beneficiaries from higher than expected costs.
Disclosure
Disclosure: Nothing to report.
- June 2012 Data Book: Health Care Spending and the Medicare Program. Washington, DC: Medicare Payment Advisory Commission; 2012.
- . Hospitals' use of observation stays and short inpatient stays for Medicare beneficiaries, OEI‐02‐12‐00040. Washington, DC: Department of Health and Human Services, Office of the Inspector General; 2013.
- , , . National study of emergency department observation services. Acad Emerg Med. 2011;18(9):959–965.
- , . Observation care—high‐value care or a cost‐shifting loophole? N Engl J Med. 2013;369(4):302–305.
- , , , , . Factors associated with prolonged observation services stays and the impact of long stays on patient cost. Health Serv Res. 2014;49(3):893–909.
- Bagnall v Sebelius. No. 3:11cv1703 (MPS). September 23, 2013.
- Centers for Medicare 2 Midnight Benchmark for Inpatient Hospital Admissions. CMS‐1599‐F2013.2013. Available at: http://www.cms.gov/Outreach‐and‐Education/Outreach/OpenDoorForums/Downloads/02042014SODF.pdf. Accessed June 16, 2015
- Council of Teaching Hospitals and Health Systems (COTH). Association of American Medical Colleges website. Available at: https://www.aamc.org/members/coth/. Accessed May 5, 2006.
- United States Department of Agriculture Economic Research Service. Rural‐urban continuity codes. Available at: http://www.ers.usda.gov/data‐products/rural‐urban‐continuum‐codes.aspx. Accessed June 16, 2015.
- Centers for Medicare
- June 2012 Data Book: Health Care Spending and the Medicare Program. Washington, DC: Medicare Payment Advisory Commission; 2012.
- . Hospitals' use of observation stays and short inpatient stays for Medicare beneficiaries, OEI‐02‐12‐00040. Washington, DC: Department of Health and Human Services, Office of the Inspector General; 2013.
- , , . National study of emergency department observation services. Acad Emerg Med. 2011;18(9):959–965.
- , . Observation care—high‐value care or a cost‐shifting loophole? N Engl J Med. 2013;369(4):302–305.
- , , , , . Factors associated with prolonged observation services stays and the impact of long stays on patient cost. Health Serv Res. 2014;49(3):893–909.
- Bagnall v Sebelius. No. 3:11cv1703 (MPS). September 23, 2013.
- Centers for Medicare 2 Midnight Benchmark for Inpatient Hospital Admissions. CMS‐1599‐F2013.2013. Available at: http://www.cms.gov/Outreach‐and‐Education/Outreach/OpenDoorForums/Downloads/02042014SODF.pdf. Accessed June 16, 2015
- Council of Teaching Hospitals and Health Systems (COTH). Association of American Medical Colleges website. Available at: https://www.aamc.org/members/coth/. Accessed May 5, 2006.
- United States Department of Agriculture Economic Research Service. Rural‐urban continuity codes. Available at: http://www.ers.usda.gov/data‐products/rural‐urban‐continuum‐codes.aspx. Accessed June 16, 2015.
- Centers for Medicare
© 2015 Society of Hospital Medicine
Grandparents and the new baby
A couple having a baby brings together two family traditions that themselves blended the previous generations’ experiences and perspectives. Each of the new parents has been raised by two parents with their own histories, values, successes, and crises all available and potentially playing a part in the new baby’s future. A baby’s arrival can call forth memories of past successes, failures, hopes, and dreams – some fulfilled and some not.
As the pediatrician, you serve as an authority and a resource for the new parents. You will hear questions that have roots that may go back one, two, or more generations. Some may involve discipline, approaches to food, religious issues, or more subtle concerns relating to control and autonomy. And you may find that they will bring you the challenge of managing the beliefs, values, and expectations of the new grandparents. You may even find these new grandparents in your office! You have a unique opportunity to help new parents set a course with their own parents or in-laws that can promote family cohesion and honor family traditions or values, while empowering parents to trust themselves and truly be in charge of raising their own children.
Imagine this scenario: A young couple has just had their first baby, a son. The paternal grandfather, who played soccer in high school and college, presents his first grandchild with his own college soccer ball, proclaiming with great emotion that soccer will certainly be a part of his grandson’s future.
While this simple act may seem touching, it might also be perceived by the new parents as intrusive or controlling. How does the new father (who was maybe more bookish than athletic) feel the burden of this expectation? Perhaps the mother may wish her son to be more of a scholar than an athlete, or may want no expectation set, but may feel uncomfortable speaking honestly with her father-in-law. And this scenario is just about the gift of a soccer ball!
Grandparents (like parents) come with expectations, with beliefs about what practices worked and what failed over a wide range of areas from child rearing to managing finances to career to marriage. The arrival of a new grandchild will likely prompt them to share these beliefs, and do so in the way they usually communicate with their own children, be it blunt, emotional, indirect, or mute. These views might be forcefully presented, if a grandparent feels guilty or unfulfilled because a meaningful hope for their own child did not materialize: The new grandchild is their “last chance.” While their love and interest, their experience and wisdom can be invaluable, they might also arouse insecurity in a new parent or be disruptive. If they share opinions in a way that is stressful, devaluing, or confusing for new parents, that can translate into anxious, uncertain interactions with their new baby or a climate at home that is full of conflict instead of calm.
Parents are already blending their two styles and values, challenging enough before also trying to blend the elements of four grandparents.
The first weeks after the arrival of the new baby is a crucial time in the baby’s development, as well as in the development of the new parents, as all are rapidly acquiring new skills, adjusting to a new schedule, and learning how to understand and respond to each other. During these hard early days, grandparents often will be present, staying in the home or nearby to offer support to their children. Very commonly, they will share their opinions about such basics as nutrition and sleep. These are areas that are fundamentally important for a baby’s healthy development, but can be mysterious and challenging for new parents. They may seek out guidance from friends, books, websites, and pediatricians, as well as the new grandparents.
While their accumulated wisdom may be as helpful as their helping with laundry or meal preparation (think, “sleep when the baby sleeps”), it also might not. Perhaps the opinions are misguided (think, “sleeping on the tummy was always fine in my day”). And grandparents who are inadvertently undermining (“I don’t understand the difficulty, nursing was so easy for me”), or highly anxious might add to the new parents’ stress and uncertainty rather than alleviate it.
Grandparents also may come with strong cultural beliefs about child rearing. In families that are only one or two generations removed from immigration to this country, there may be powerfully held ideas about newborns, ones that might be inextricably linked for the grandparents with their drive to preserve their own cultural background. These may include ideas about when a child can eat solid food or what he or she should start eating. They may include beliefs that a child should never be put down or should be left to cry for long periods, lest they be “spoiled.” They might include ideas about when a baby can swim or how best to bathe them, what sorts of toys are appropriate or when their hair can be cut. While many of these beliefs have cultural value and no medical implications (like the timing of the first haircut), some may fly in the face of current scientific evidence (such as eating solids before they are able). And even when they are “safe,” new parents may experience these beliefs as fraught directives: ones that they may not believe in, but which will make them guilty of some cultural betrayal if they do not follow them.
Along a similar vein, grandparents may enter the home of their new grandchild with passionately held religious beliefs. While few of these may have direct medical implications for the new baby (such as circumcision), they can still have profound implications for life in the family’s home. When parents and grandparents all share the same religious beliefs, there is less possibility of conflict. But when new parents come from different religious traditions or no longer share their parents’ faith, there is high potential for emotionally charged differences. And if the new parents have not anticipated these conversations (say, whether or not to circumcise a baby boy when one parent is Jewish and the other is Protestant), trying to sort out these matters while also learning to change diapers or nurse a colicky baby can make a challenging situation into an overwhelming one.
Lastly, about 1% of all households have same-sex partners or marriages and about one in four are raising children. While same-sex parenthood has rapidly gained cultural acceptance over the past decade, it is possible that some grandparents will not have fully accepted the reality of their own child’s sexual orientation and committed relationship. If the parents speak to you about such a fraught situation, listen supportively. When it sounds like there is ambivalence in the grandparents, the new parents can try to nurture the love that is there and be patient when their own parents still struggle. They should nurture the connections with those in their families that offer unconditional support and who can model love and acceptance for the new grandparents. In situations in which there is deeper alienation and little or no contact, offer that they might want to find a way to share photos and stories through one who remains close to their parents and periodically offer opportunities to rebuild relationships. A new grandchild can be a loving moment to take a fresh look at unresolved anger and loss, and as clinicians we have seen families resolve differences as they look to a new baby’s future.
Pediatricians are in a unique position of both neutrality and authority with their new patient’s parents and grandparents. When parents come to a newborn check or well-baby check, it can be invaluable to determine “who else is helping you?” After finding out about nursing or feeding the baby and about sleep, inquire about where they are getting any guidance or support. Friends or siblings with children? Books or websites? Grandparents? What has been helpful and what has not? When you hear about grandparents and see an eye-roll or hear a deep sigh, be curious about what has been helpful and what has been challenging. It is vitally helpful to first-time parents to be validated in their feeling that their own parents are a valuable resource, but not without their challenges.
While it may be important to offer a “medical” opinion about certain matters (back-sleeping, cosleeping, and introducing solids, for example), on most matters, the pediatrician’s role will be to help parents set a framework that will help them to cultivate what is precious and helpful from grandparents while minimizing conflict or unnecessary stress. For new parents, this may be as simple as reminding them that while this is an vital time for the baby’s development, it is also a big transition for them into parenthood and a significant transition for their parents or in-laws into grandparenthood. Help the new parents to understand that there is sometimes no one “right” way to handle certain decisions or challenges, and they will have to try a variety of strategies before finding the one that fits them as parents to this particular child. Remind them that parenting is a learning curve and it is common to feel stressed in new territory with high stakes. But they will find the right rhythm with being attuned to their new baby and eventually managing routines and limits. They are allowed to embrace the support that they find helpful and limit that which they experience as deeply undermining, dismissive, or judgmental.
When you notice that parents sound very angry at or alienated from grandparents, particularly when it is causing some marital conflict, it can be powerful for you to suggest that they should sort out their wishes and beliefs as parents first and then find a clear and loving way to communicate these to the grandparents. Remind them that they are becoming the experts on their children and that they will best be able to set appropriate routines and expectations. But remind them also that grandparents are potentially a treasure to their grandchildren, beyond the help with laundry and meal preparation at the very start of a child’s life.
There can never be enough loving, interested adults in a child’s orbit or a big enough cheering section. And grandparents can be uniquely passionate, patient, curious, and supportive to their growing grandchildren. They bring perspective on a family’s history, wonderful as a growing child builds a story about who they are and where they come from. And their interest and love will help a growing child build a sense of what characteristics make them a treasure to others. Few people can do this as well as grandparents, and letting them begin this involvement at the start of their grandchild’s life only supports this role.
While the arrival of a new baby will be a joyful event for a family, it will also be emotionally complex. Providing your patient’s parents with support and even some language that may help them cultivate the grandparents’ interest and love, while building healthy boundaries around their own parenting, may help set the stage for the healthiest development of your very young patient.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor of psychiatry and of pediatrics at Harvard Medical School, Boston. E-mail them at [email protected].
A couple having a baby brings together two family traditions that themselves blended the previous generations’ experiences and perspectives. Each of the new parents has been raised by two parents with their own histories, values, successes, and crises all available and potentially playing a part in the new baby’s future. A baby’s arrival can call forth memories of past successes, failures, hopes, and dreams – some fulfilled and some not.
As the pediatrician, you serve as an authority and a resource for the new parents. You will hear questions that have roots that may go back one, two, or more generations. Some may involve discipline, approaches to food, religious issues, or more subtle concerns relating to control and autonomy. And you may find that they will bring you the challenge of managing the beliefs, values, and expectations of the new grandparents. You may even find these new grandparents in your office! You have a unique opportunity to help new parents set a course with their own parents or in-laws that can promote family cohesion and honor family traditions or values, while empowering parents to trust themselves and truly be in charge of raising their own children.
Imagine this scenario: A young couple has just had their first baby, a son. The paternal grandfather, who played soccer in high school and college, presents his first grandchild with his own college soccer ball, proclaiming with great emotion that soccer will certainly be a part of his grandson’s future.
While this simple act may seem touching, it might also be perceived by the new parents as intrusive or controlling. How does the new father (who was maybe more bookish than athletic) feel the burden of this expectation? Perhaps the mother may wish her son to be more of a scholar than an athlete, or may want no expectation set, but may feel uncomfortable speaking honestly with her father-in-law. And this scenario is just about the gift of a soccer ball!
Grandparents (like parents) come with expectations, with beliefs about what practices worked and what failed over a wide range of areas from child rearing to managing finances to career to marriage. The arrival of a new grandchild will likely prompt them to share these beliefs, and do so in the way they usually communicate with their own children, be it blunt, emotional, indirect, or mute. These views might be forcefully presented, if a grandparent feels guilty or unfulfilled because a meaningful hope for their own child did not materialize: The new grandchild is their “last chance.” While their love and interest, their experience and wisdom can be invaluable, they might also arouse insecurity in a new parent or be disruptive. If they share opinions in a way that is stressful, devaluing, or confusing for new parents, that can translate into anxious, uncertain interactions with their new baby or a climate at home that is full of conflict instead of calm.
Parents are already blending their two styles and values, challenging enough before also trying to blend the elements of four grandparents.
The first weeks after the arrival of the new baby is a crucial time in the baby’s development, as well as in the development of the new parents, as all are rapidly acquiring new skills, adjusting to a new schedule, and learning how to understand and respond to each other. During these hard early days, grandparents often will be present, staying in the home or nearby to offer support to their children. Very commonly, they will share their opinions about such basics as nutrition and sleep. These are areas that are fundamentally important for a baby’s healthy development, but can be mysterious and challenging for new parents. They may seek out guidance from friends, books, websites, and pediatricians, as well as the new grandparents.
While their accumulated wisdom may be as helpful as their helping with laundry or meal preparation (think, “sleep when the baby sleeps”), it also might not. Perhaps the opinions are misguided (think, “sleeping on the tummy was always fine in my day”). And grandparents who are inadvertently undermining (“I don’t understand the difficulty, nursing was so easy for me”), or highly anxious might add to the new parents’ stress and uncertainty rather than alleviate it.
Grandparents also may come with strong cultural beliefs about child rearing. In families that are only one or two generations removed from immigration to this country, there may be powerfully held ideas about newborns, ones that might be inextricably linked for the grandparents with their drive to preserve their own cultural background. These may include ideas about when a child can eat solid food or what he or she should start eating. They may include beliefs that a child should never be put down or should be left to cry for long periods, lest they be “spoiled.” They might include ideas about when a baby can swim or how best to bathe them, what sorts of toys are appropriate or when their hair can be cut. While many of these beliefs have cultural value and no medical implications (like the timing of the first haircut), some may fly in the face of current scientific evidence (such as eating solids before they are able). And even when they are “safe,” new parents may experience these beliefs as fraught directives: ones that they may not believe in, but which will make them guilty of some cultural betrayal if they do not follow them.
Along a similar vein, grandparents may enter the home of their new grandchild with passionately held religious beliefs. While few of these may have direct medical implications for the new baby (such as circumcision), they can still have profound implications for life in the family’s home. When parents and grandparents all share the same religious beliefs, there is less possibility of conflict. But when new parents come from different religious traditions or no longer share their parents’ faith, there is high potential for emotionally charged differences. And if the new parents have not anticipated these conversations (say, whether or not to circumcise a baby boy when one parent is Jewish and the other is Protestant), trying to sort out these matters while also learning to change diapers or nurse a colicky baby can make a challenging situation into an overwhelming one.
Lastly, about 1% of all households have same-sex partners or marriages and about one in four are raising children. While same-sex parenthood has rapidly gained cultural acceptance over the past decade, it is possible that some grandparents will not have fully accepted the reality of their own child’s sexual orientation and committed relationship. If the parents speak to you about such a fraught situation, listen supportively. When it sounds like there is ambivalence in the grandparents, the new parents can try to nurture the love that is there and be patient when their own parents still struggle. They should nurture the connections with those in their families that offer unconditional support and who can model love and acceptance for the new grandparents. In situations in which there is deeper alienation and little or no contact, offer that they might want to find a way to share photos and stories through one who remains close to their parents and periodically offer opportunities to rebuild relationships. A new grandchild can be a loving moment to take a fresh look at unresolved anger and loss, and as clinicians we have seen families resolve differences as they look to a new baby’s future.
Pediatricians are in a unique position of both neutrality and authority with their new patient’s parents and grandparents. When parents come to a newborn check or well-baby check, it can be invaluable to determine “who else is helping you?” After finding out about nursing or feeding the baby and about sleep, inquire about where they are getting any guidance or support. Friends or siblings with children? Books or websites? Grandparents? What has been helpful and what has not? When you hear about grandparents and see an eye-roll or hear a deep sigh, be curious about what has been helpful and what has been challenging. It is vitally helpful to first-time parents to be validated in their feeling that their own parents are a valuable resource, but not without their challenges.
While it may be important to offer a “medical” opinion about certain matters (back-sleeping, cosleeping, and introducing solids, for example), on most matters, the pediatrician’s role will be to help parents set a framework that will help them to cultivate what is precious and helpful from grandparents while minimizing conflict or unnecessary stress. For new parents, this may be as simple as reminding them that while this is an vital time for the baby’s development, it is also a big transition for them into parenthood and a significant transition for their parents or in-laws into grandparenthood. Help the new parents to understand that there is sometimes no one “right” way to handle certain decisions or challenges, and they will have to try a variety of strategies before finding the one that fits them as parents to this particular child. Remind them that parenting is a learning curve and it is common to feel stressed in new territory with high stakes. But they will find the right rhythm with being attuned to their new baby and eventually managing routines and limits. They are allowed to embrace the support that they find helpful and limit that which they experience as deeply undermining, dismissive, or judgmental.
When you notice that parents sound very angry at or alienated from grandparents, particularly when it is causing some marital conflict, it can be powerful for you to suggest that they should sort out their wishes and beliefs as parents first and then find a clear and loving way to communicate these to the grandparents. Remind them that they are becoming the experts on their children and that they will best be able to set appropriate routines and expectations. But remind them also that grandparents are potentially a treasure to their grandchildren, beyond the help with laundry and meal preparation at the very start of a child’s life.
There can never be enough loving, interested adults in a child’s orbit or a big enough cheering section. And grandparents can be uniquely passionate, patient, curious, and supportive to their growing grandchildren. They bring perspective on a family’s history, wonderful as a growing child builds a story about who they are and where they come from. And their interest and love will help a growing child build a sense of what characteristics make them a treasure to others. Few people can do this as well as grandparents, and letting them begin this involvement at the start of their grandchild’s life only supports this role.
While the arrival of a new baby will be a joyful event for a family, it will also be emotionally complex. Providing your patient’s parents with support and even some language that may help them cultivate the grandparents’ interest and love, while building healthy boundaries around their own parenting, may help set the stage for the healthiest development of your very young patient.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor of psychiatry and of pediatrics at Harvard Medical School, Boston. E-mail them at [email protected].
A couple having a baby brings together two family traditions that themselves blended the previous generations’ experiences and perspectives. Each of the new parents has been raised by two parents with their own histories, values, successes, and crises all available and potentially playing a part in the new baby’s future. A baby’s arrival can call forth memories of past successes, failures, hopes, and dreams – some fulfilled and some not.
As the pediatrician, you serve as an authority and a resource for the new parents. You will hear questions that have roots that may go back one, two, or more generations. Some may involve discipline, approaches to food, religious issues, or more subtle concerns relating to control and autonomy. And you may find that they will bring you the challenge of managing the beliefs, values, and expectations of the new grandparents. You may even find these new grandparents in your office! You have a unique opportunity to help new parents set a course with their own parents or in-laws that can promote family cohesion and honor family traditions or values, while empowering parents to trust themselves and truly be in charge of raising their own children.
Imagine this scenario: A young couple has just had their first baby, a son. The paternal grandfather, who played soccer in high school and college, presents his first grandchild with his own college soccer ball, proclaiming with great emotion that soccer will certainly be a part of his grandson’s future.
While this simple act may seem touching, it might also be perceived by the new parents as intrusive or controlling. How does the new father (who was maybe more bookish than athletic) feel the burden of this expectation? Perhaps the mother may wish her son to be more of a scholar than an athlete, or may want no expectation set, but may feel uncomfortable speaking honestly with her father-in-law. And this scenario is just about the gift of a soccer ball!
Grandparents (like parents) come with expectations, with beliefs about what practices worked and what failed over a wide range of areas from child rearing to managing finances to career to marriage. The arrival of a new grandchild will likely prompt them to share these beliefs, and do so in the way they usually communicate with their own children, be it blunt, emotional, indirect, or mute. These views might be forcefully presented, if a grandparent feels guilty or unfulfilled because a meaningful hope for their own child did not materialize: The new grandchild is their “last chance.” While their love and interest, their experience and wisdom can be invaluable, they might also arouse insecurity in a new parent or be disruptive. If they share opinions in a way that is stressful, devaluing, or confusing for new parents, that can translate into anxious, uncertain interactions with their new baby or a climate at home that is full of conflict instead of calm.
Parents are already blending their two styles and values, challenging enough before also trying to blend the elements of four grandparents.
The first weeks after the arrival of the new baby is a crucial time in the baby’s development, as well as in the development of the new parents, as all are rapidly acquiring new skills, adjusting to a new schedule, and learning how to understand and respond to each other. During these hard early days, grandparents often will be present, staying in the home or nearby to offer support to their children. Very commonly, they will share their opinions about such basics as nutrition and sleep. These are areas that are fundamentally important for a baby’s healthy development, but can be mysterious and challenging for new parents. They may seek out guidance from friends, books, websites, and pediatricians, as well as the new grandparents.
While their accumulated wisdom may be as helpful as their helping with laundry or meal preparation (think, “sleep when the baby sleeps”), it also might not. Perhaps the opinions are misguided (think, “sleeping on the tummy was always fine in my day”). And grandparents who are inadvertently undermining (“I don’t understand the difficulty, nursing was so easy for me”), or highly anxious might add to the new parents’ stress and uncertainty rather than alleviate it.
Grandparents also may come with strong cultural beliefs about child rearing. In families that are only one or two generations removed from immigration to this country, there may be powerfully held ideas about newborns, ones that might be inextricably linked for the grandparents with their drive to preserve their own cultural background. These may include ideas about when a child can eat solid food or what he or she should start eating. They may include beliefs that a child should never be put down or should be left to cry for long periods, lest they be “spoiled.” They might include ideas about when a baby can swim or how best to bathe them, what sorts of toys are appropriate or when their hair can be cut. While many of these beliefs have cultural value and no medical implications (like the timing of the first haircut), some may fly in the face of current scientific evidence (such as eating solids before they are able). And even when they are “safe,” new parents may experience these beliefs as fraught directives: ones that they may not believe in, but which will make them guilty of some cultural betrayal if they do not follow them.
Along a similar vein, grandparents may enter the home of their new grandchild with passionately held religious beliefs. While few of these may have direct medical implications for the new baby (such as circumcision), they can still have profound implications for life in the family’s home. When parents and grandparents all share the same religious beliefs, there is less possibility of conflict. But when new parents come from different religious traditions or no longer share their parents’ faith, there is high potential for emotionally charged differences. And if the new parents have not anticipated these conversations (say, whether or not to circumcise a baby boy when one parent is Jewish and the other is Protestant), trying to sort out these matters while also learning to change diapers or nurse a colicky baby can make a challenging situation into an overwhelming one.
Lastly, about 1% of all households have same-sex partners or marriages and about one in four are raising children. While same-sex parenthood has rapidly gained cultural acceptance over the past decade, it is possible that some grandparents will not have fully accepted the reality of their own child’s sexual orientation and committed relationship. If the parents speak to you about such a fraught situation, listen supportively. When it sounds like there is ambivalence in the grandparents, the new parents can try to nurture the love that is there and be patient when their own parents still struggle. They should nurture the connections with those in their families that offer unconditional support and who can model love and acceptance for the new grandparents. In situations in which there is deeper alienation and little or no contact, offer that they might want to find a way to share photos and stories through one who remains close to their parents and periodically offer opportunities to rebuild relationships. A new grandchild can be a loving moment to take a fresh look at unresolved anger and loss, and as clinicians we have seen families resolve differences as they look to a new baby’s future.
Pediatricians are in a unique position of both neutrality and authority with their new patient’s parents and grandparents. When parents come to a newborn check or well-baby check, it can be invaluable to determine “who else is helping you?” After finding out about nursing or feeding the baby and about sleep, inquire about where they are getting any guidance or support. Friends or siblings with children? Books or websites? Grandparents? What has been helpful and what has not? When you hear about grandparents and see an eye-roll or hear a deep sigh, be curious about what has been helpful and what has been challenging. It is vitally helpful to first-time parents to be validated in their feeling that their own parents are a valuable resource, but not without their challenges.
While it may be important to offer a “medical” opinion about certain matters (back-sleeping, cosleeping, and introducing solids, for example), on most matters, the pediatrician’s role will be to help parents set a framework that will help them to cultivate what is precious and helpful from grandparents while minimizing conflict or unnecessary stress. For new parents, this may be as simple as reminding them that while this is an vital time for the baby’s development, it is also a big transition for them into parenthood and a significant transition for their parents or in-laws into grandparenthood. Help the new parents to understand that there is sometimes no one “right” way to handle certain decisions or challenges, and they will have to try a variety of strategies before finding the one that fits them as parents to this particular child. Remind them that parenting is a learning curve and it is common to feel stressed in new territory with high stakes. But they will find the right rhythm with being attuned to their new baby and eventually managing routines and limits. They are allowed to embrace the support that they find helpful and limit that which they experience as deeply undermining, dismissive, or judgmental.
When you notice that parents sound very angry at or alienated from grandparents, particularly when it is causing some marital conflict, it can be powerful for you to suggest that they should sort out their wishes and beliefs as parents first and then find a clear and loving way to communicate these to the grandparents. Remind them that they are becoming the experts on their children and that they will best be able to set appropriate routines and expectations. But remind them also that grandparents are potentially a treasure to their grandchildren, beyond the help with laundry and meal preparation at the very start of a child’s life.
There can never be enough loving, interested adults in a child’s orbit or a big enough cheering section. And grandparents can be uniquely passionate, patient, curious, and supportive to their growing grandchildren. They bring perspective on a family’s history, wonderful as a growing child builds a story about who they are and where they come from. And their interest and love will help a growing child build a sense of what characteristics make them a treasure to others. Few people can do this as well as grandparents, and letting them begin this involvement at the start of their grandchild’s life only supports this role.
While the arrival of a new baby will be a joyful event for a family, it will also be emotionally complex. Providing your patient’s parents with support and even some language that may help them cultivate the grandparents’ interest and love, while building healthy boundaries around their own parenting, may help set the stage for the healthiest development of your very young patient.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor of psychiatry and of pediatrics at Harvard Medical School, Boston. E-mail them at [email protected].
Recognizing and treating vulvar cancer
Vulvar cancer is a rare gynecologic cancer comprising only 5% of gynecologic malignancies. Given the low incidence of disease, many primary providers and even obstetricians and gynecologists many never encounter a case. Increased awareness of vulvar cancer and vulvar dysplasia among patients and physicians may decrease diagnostic delays and expedite patient therapy.
Diagnosis
There is a well documented delay in diagnosis of vulvar cancer that is attributed to both the patient and the physician. Patients may feel uncomfortable or embarrassed telling their physicians about vulvar symptoms and providers may not recognize the risk for malignancy and provide alternative therapies prior to biopsy (J Reprod Med. 1999;44[9]:766-8.).
Risk factors for vulvar cancer include human papillomavirus (HPV) infection, a history of smoking, immunosuppression, and a history of an abnormal pap smear. Vulvar dystrophy, lichen sclerosis, and squamous intraepithelial lesions have also been suggested as precursor lesions of invasive cancers. The key to early diagnosis and treatment is immediate in-office biopsy.
When evaluating a patient with a vulvar lesion, the initial evaluation should include a thorough exam with a measurement of the lesion and evaluation of inguinal lymph nodes. Also, a detailed description of a lesion’s relationship to the midline (how many centimeters away) and other vital structures (clitoris, urethra, anus) is important.
An in-office biopsy can be done on initial presentation and should include the lesion in question and underlying stroma in an effort to delineate depth of invasion. While shave biopsies may be appropriate for some skin lesions, if there is any concern for malignancy, a punch biopsy is preferred.
Pathology
Squamous cell carcinoma is the most common histologic subtype (greater than 90%) followed by malignant melanoma. Malignant melanoma poses a diagnostic challenge as 25% may present with nonpigmented lesions. These lesions may arise from a junctional nevus and are more common in postmenopausal white women.
The measurement of tumor thickness is essential in evaluation of melanoma. A diagnosis of vulvar melanoma should be referred to a gynecologic oncologist for further evaluation and treatment. Frequently these patients require a multidisciplinary approach with other medical and surgical subspecialties consulting.
Adenocarcinoma of the vulva frequently arises within the Bartholin glands. Bartholin gland disease is typically a disease of young women. Any abscess or lesion in the bartholin gland in women older than 50 years should raise awareness of the possibility of malignancy. Providers should have a low threshold for biopsy of any Bartholin lesion in older women and for any Bartholin gland lesion or cyst that returns or persists after initial drainage.
Staging pearls
Vulvar cancer spreads by direct extension, lymphatic embolization and hematogenous spread. Lymphatic spread can occur early in the disease and portends a much worse prognosis. In 2009, the International Federation of Gynecology and Obstetrics (FIGO) revised the staging system. The most significant change was in stage III disease, which now includes any patient with lymph node involvement. This change emphasizes lymph node status as the single most important prognostic factor. The 5-year overall survival of patients with locally advanced tumors but negative regional lymph nodes (62%) has been found to be significantly better than those with positive nodal status (39%, P value less than.0001) (Gynecol Oncol. 2008;110[1]:83-6.).
In patients with stage IA disease, which includes lesions less than 2 cm in size with stromal invasion of less than 1 mm, the risk of lymph node metastasis is low. These patients do not require inguinal lymph node dissection. If lesions are greater than 2 cm and/or have greater than 1 mm depth of invasion, a lymph node dissection is indicated. Lymph node dissection is performed on the ipsilateral side of the lesion as long as the lesion is more than 2 cm from a midline structure. If the lesion is in the midline or within 2 cm of the midline, a bilateral inguinal lymph node dissection is recommended.
There has been a recent uptake of the sentinel inguinal lymph node biopsy technique after two large prospective studies (the GROINSS V trial and GOG 173) validated this methodology (Lancet Oncol. 2010 Jul;11[7]:646-52 and Gynecol Oncol. 2013 Feb;128[2]:155-9).
Treatment
Surgical management of stage I and II disease involves a wide radical excision of the tumor with a 1-cm circumferential margin. Tumors with a depth of invasion of less than 1 mm do not require lymphadenectomy (Gynecol Oncol. 1992 Mar;44[3]:240-4). Stage I/II disease with deeper than 1-mm invasion requires a 2-cm margin and either sentinel node evaluation or lymphadenectomy. Survival for women with adequate resection of primary squamous carcinoma with negative lymph node involvement is greater than 90%.
Patients with metastasis to the groin frequently receive bilateral groin and pelvic radiation; however, recommendations are individualized based on size and number of metastasis. Patients should expect to receive recommendations for therapy after pathologic review and multidisciplinary consultation; therapy should be individualized for each clinical situation.
This disease is one of the elderly, but it is important to remember that treatment recommendations should not be made according to age alone. A British study found that when women over the age of 80 received standard treatment, their recurrence rate was 25% compared with a 53% recurrence rate in those whose treatment was modified (Int J Gynecol Cancer. 2009;19[4]:752-5.). In patients with advanced disease, preoperative radiation, with or without chemotherapy, is frequently regarded as the treatment of choice and may eliminate the need for radical surgery.
While vulvar cancer is a rare gynecologic malignancy, it can be devastating for patients and families, especially at late stages. Early diagnosis and treatment is imperative for improved patient outcomes. An increased awareness among patients and physicians alike may allow for earlier diagnosis and treatment.
Dr. Sullivan is a fellow in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Gehrig is professor and director of gynecologic oncology at the university. Dr. Sullivan and Dr. Gehrig reported having no relevant financial disclosures.
Vulvar cancer is a rare gynecologic cancer comprising only 5% of gynecologic malignancies. Given the low incidence of disease, many primary providers and even obstetricians and gynecologists many never encounter a case. Increased awareness of vulvar cancer and vulvar dysplasia among patients and physicians may decrease diagnostic delays and expedite patient therapy.
Diagnosis
There is a well documented delay in diagnosis of vulvar cancer that is attributed to both the patient and the physician. Patients may feel uncomfortable or embarrassed telling their physicians about vulvar symptoms and providers may not recognize the risk for malignancy and provide alternative therapies prior to biopsy (J Reprod Med. 1999;44[9]:766-8.).
Risk factors for vulvar cancer include human papillomavirus (HPV) infection, a history of smoking, immunosuppression, and a history of an abnormal pap smear. Vulvar dystrophy, lichen sclerosis, and squamous intraepithelial lesions have also been suggested as precursor lesions of invasive cancers. The key to early diagnosis and treatment is immediate in-office biopsy.
When evaluating a patient with a vulvar lesion, the initial evaluation should include a thorough exam with a measurement of the lesion and evaluation of inguinal lymph nodes. Also, a detailed description of a lesion’s relationship to the midline (how many centimeters away) and other vital structures (clitoris, urethra, anus) is important.
An in-office biopsy can be done on initial presentation and should include the lesion in question and underlying stroma in an effort to delineate depth of invasion. While shave biopsies may be appropriate for some skin lesions, if there is any concern for malignancy, a punch biopsy is preferred.
Pathology
Squamous cell carcinoma is the most common histologic subtype (greater than 90%) followed by malignant melanoma. Malignant melanoma poses a diagnostic challenge as 25% may present with nonpigmented lesions. These lesions may arise from a junctional nevus and are more common in postmenopausal white women.
The measurement of tumor thickness is essential in evaluation of melanoma. A diagnosis of vulvar melanoma should be referred to a gynecologic oncologist for further evaluation and treatment. Frequently these patients require a multidisciplinary approach with other medical and surgical subspecialties consulting.
Adenocarcinoma of the vulva frequently arises within the Bartholin glands. Bartholin gland disease is typically a disease of young women. Any abscess or lesion in the bartholin gland in women older than 50 years should raise awareness of the possibility of malignancy. Providers should have a low threshold for biopsy of any Bartholin lesion in older women and for any Bartholin gland lesion or cyst that returns or persists after initial drainage.
Staging pearls
Vulvar cancer spreads by direct extension, lymphatic embolization and hematogenous spread. Lymphatic spread can occur early in the disease and portends a much worse prognosis. In 2009, the International Federation of Gynecology and Obstetrics (FIGO) revised the staging system. The most significant change was in stage III disease, which now includes any patient with lymph node involvement. This change emphasizes lymph node status as the single most important prognostic factor. The 5-year overall survival of patients with locally advanced tumors but negative regional lymph nodes (62%) has been found to be significantly better than those with positive nodal status (39%, P value less than.0001) (Gynecol Oncol. 2008;110[1]:83-6.).
In patients with stage IA disease, which includes lesions less than 2 cm in size with stromal invasion of less than 1 mm, the risk of lymph node metastasis is low. These patients do not require inguinal lymph node dissection. If lesions are greater than 2 cm and/or have greater than 1 mm depth of invasion, a lymph node dissection is indicated. Lymph node dissection is performed on the ipsilateral side of the lesion as long as the lesion is more than 2 cm from a midline structure. If the lesion is in the midline or within 2 cm of the midline, a bilateral inguinal lymph node dissection is recommended.
There has been a recent uptake of the sentinel inguinal lymph node biopsy technique after two large prospective studies (the GROINSS V trial and GOG 173) validated this methodology (Lancet Oncol. 2010 Jul;11[7]:646-52 and Gynecol Oncol. 2013 Feb;128[2]:155-9).
Treatment
Surgical management of stage I and II disease involves a wide radical excision of the tumor with a 1-cm circumferential margin. Tumors with a depth of invasion of less than 1 mm do not require lymphadenectomy (Gynecol Oncol. 1992 Mar;44[3]:240-4). Stage I/II disease with deeper than 1-mm invasion requires a 2-cm margin and either sentinel node evaluation or lymphadenectomy. Survival for women with adequate resection of primary squamous carcinoma with negative lymph node involvement is greater than 90%.
Patients with metastasis to the groin frequently receive bilateral groin and pelvic radiation; however, recommendations are individualized based on size and number of metastasis. Patients should expect to receive recommendations for therapy after pathologic review and multidisciplinary consultation; therapy should be individualized for each clinical situation.
This disease is one of the elderly, but it is important to remember that treatment recommendations should not be made according to age alone. A British study found that when women over the age of 80 received standard treatment, their recurrence rate was 25% compared with a 53% recurrence rate in those whose treatment was modified (Int J Gynecol Cancer. 2009;19[4]:752-5.). In patients with advanced disease, preoperative radiation, with or without chemotherapy, is frequently regarded as the treatment of choice and may eliminate the need for radical surgery.
While vulvar cancer is a rare gynecologic malignancy, it can be devastating for patients and families, especially at late stages. Early diagnosis and treatment is imperative for improved patient outcomes. An increased awareness among patients and physicians alike may allow for earlier diagnosis and treatment.
Dr. Sullivan is a fellow in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Gehrig is professor and director of gynecologic oncology at the university. Dr. Sullivan and Dr. Gehrig reported having no relevant financial disclosures.
Vulvar cancer is a rare gynecologic cancer comprising only 5% of gynecologic malignancies. Given the low incidence of disease, many primary providers and even obstetricians and gynecologists many never encounter a case. Increased awareness of vulvar cancer and vulvar dysplasia among patients and physicians may decrease diagnostic delays and expedite patient therapy.
Diagnosis
There is a well documented delay in diagnosis of vulvar cancer that is attributed to both the patient and the physician. Patients may feel uncomfortable or embarrassed telling their physicians about vulvar symptoms and providers may not recognize the risk for malignancy and provide alternative therapies prior to biopsy (J Reprod Med. 1999;44[9]:766-8.).
Risk factors for vulvar cancer include human papillomavirus (HPV) infection, a history of smoking, immunosuppression, and a history of an abnormal pap smear. Vulvar dystrophy, lichen sclerosis, and squamous intraepithelial lesions have also been suggested as precursor lesions of invasive cancers. The key to early diagnosis and treatment is immediate in-office biopsy.
When evaluating a patient with a vulvar lesion, the initial evaluation should include a thorough exam with a measurement of the lesion and evaluation of inguinal lymph nodes. Also, a detailed description of a lesion’s relationship to the midline (how many centimeters away) and other vital structures (clitoris, urethra, anus) is important.
An in-office biopsy can be done on initial presentation and should include the lesion in question and underlying stroma in an effort to delineate depth of invasion. While shave biopsies may be appropriate for some skin lesions, if there is any concern for malignancy, a punch biopsy is preferred.
Pathology
Squamous cell carcinoma is the most common histologic subtype (greater than 90%) followed by malignant melanoma. Malignant melanoma poses a diagnostic challenge as 25% may present with nonpigmented lesions. These lesions may arise from a junctional nevus and are more common in postmenopausal white women.
The measurement of tumor thickness is essential in evaluation of melanoma. A diagnosis of vulvar melanoma should be referred to a gynecologic oncologist for further evaluation and treatment. Frequently these patients require a multidisciplinary approach with other medical and surgical subspecialties consulting.
Adenocarcinoma of the vulva frequently arises within the Bartholin glands. Bartholin gland disease is typically a disease of young women. Any abscess or lesion in the bartholin gland in women older than 50 years should raise awareness of the possibility of malignancy. Providers should have a low threshold for biopsy of any Bartholin lesion in older women and for any Bartholin gland lesion or cyst that returns or persists after initial drainage.
Staging pearls
Vulvar cancer spreads by direct extension, lymphatic embolization and hematogenous spread. Lymphatic spread can occur early in the disease and portends a much worse prognosis. In 2009, the International Federation of Gynecology and Obstetrics (FIGO) revised the staging system. The most significant change was in stage III disease, which now includes any patient with lymph node involvement. This change emphasizes lymph node status as the single most important prognostic factor. The 5-year overall survival of patients with locally advanced tumors but negative regional lymph nodes (62%) has been found to be significantly better than those with positive nodal status (39%, P value less than.0001) (Gynecol Oncol. 2008;110[1]:83-6.).
In patients with stage IA disease, which includes lesions less than 2 cm in size with stromal invasion of less than 1 mm, the risk of lymph node metastasis is low. These patients do not require inguinal lymph node dissection. If lesions are greater than 2 cm and/or have greater than 1 mm depth of invasion, a lymph node dissection is indicated. Lymph node dissection is performed on the ipsilateral side of the lesion as long as the lesion is more than 2 cm from a midline structure. If the lesion is in the midline or within 2 cm of the midline, a bilateral inguinal lymph node dissection is recommended.
There has been a recent uptake of the sentinel inguinal lymph node biopsy technique after two large prospective studies (the GROINSS V trial and GOG 173) validated this methodology (Lancet Oncol. 2010 Jul;11[7]:646-52 and Gynecol Oncol. 2013 Feb;128[2]:155-9).
Treatment
Surgical management of stage I and II disease involves a wide radical excision of the tumor with a 1-cm circumferential margin. Tumors with a depth of invasion of less than 1 mm do not require lymphadenectomy (Gynecol Oncol. 1992 Mar;44[3]:240-4). Stage I/II disease with deeper than 1-mm invasion requires a 2-cm margin and either sentinel node evaluation or lymphadenectomy. Survival for women with adequate resection of primary squamous carcinoma with negative lymph node involvement is greater than 90%.
Patients with metastasis to the groin frequently receive bilateral groin and pelvic radiation; however, recommendations are individualized based on size and number of metastasis. Patients should expect to receive recommendations for therapy after pathologic review and multidisciplinary consultation; therapy should be individualized for each clinical situation.
This disease is one of the elderly, but it is important to remember that treatment recommendations should not be made according to age alone. A British study found that when women over the age of 80 received standard treatment, their recurrence rate was 25% compared with a 53% recurrence rate in those whose treatment was modified (Int J Gynecol Cancer. 2009;19[4]:752-5.). In patients with advanced disease, preoperative radiation, with or without chemotherapy, is frequently regarded as the treatment of choice and may eliminate the need for radical surgery.
While vulvar cancer is a rare gynecologic malignancy, it can be devastating for patients and families, especially at late stages. Early diagnosis and treatment is imperative for improved patient outcomes. An increased awareness among patients and physicians alike may allow for earlier diagnosis and treatment.
Dr. Sullivan is a fellow in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Gehrig is professor and director of gynecologic oncology at the university. Dr. Sullivan and Dr. Gehrig reported having no relevant financial disclosures.
VA Hospital Deficiencies Contributed to Marine’s Death
On August 30, 2014, a 35-year-old marine died during inpatient treatment for mental health at the Tomah VAMC in Wisconsin. A year later, the VA Office of Inspector General (OIG) Office of Healthcare Inspections determined a number of deficiencies in hospital operations as a result of the investigation of this patient’s death.
Among these deficiencies were a lack of documenting patient consent for treatment and insufficient response to the patient’s cardiopulmonary emergency.
“We are deeply saddened by the tragic, avoidable death of this veteran and are committed to learning from this event and making improvements in the care we provide to our veterans,” the Tomah VAMC said in a statement.
Related: Negligence Settlement Reached After Army Hospital Death
Neither of the 2 psychiatrists treating the patient, Jason Simcakoski, obtained informed consent, verbal or written, for the buprenorphine/naloxone, according to both the patient’s electronic health record and the treating psychiatrists’ accounts. The prescription was administered to the patient with an off-label indication beginning the day prior to his death.
In addition, when the patient was found unresponsive in his room, “unit staff did not immediately assess the patient and determine the need for cardiopulmonary resuscitation,” nor did they use the in-room emergency call system or determine cardiac activity with the automatic external defibrillator, as noted in the OIG report.
Mr. Simcakoski served with the U.S. Marine Corp from 1998 until his honorable discharge in 2002. Mr. Simcakoski established VA medical care in 2003, according to the OIG report. Two years later, he sought help for his addiction to oxycodone, a medication he said he obtained from a friend; no VA provider ever prescribed Mr. Simcakoski oxycodone or other Schedule II opioid analgesic. The patient was treated for addiction at a non-VA clinic through 2007 and again in 2010.
Related: VISN 22 Evidence-Based Psychotherapy Telemental Health Center and Regional Pilot
The patient’s psychiatric diagnoses included posttraumatic stress disorder, bipolar I disorder, generalized anxiety disorder, attention deficit/hyperactivity disorder, panic disorder, opioid dependence, and alcohol and benzodiazepine abuse.
As a result of OIG recommendations, one of the psychiatrists involved in this case was terminated and the second awaits administrative proceedings. Under the direction of the Tomah VAMC acting chief of staff, all appropriate providers will be required to take relevant VHA training on informed consent, and all patients currently on buprenorphine will be reviewed to ensure consent has been obtained, both of which have an October 2015 target date of completion.
“I feel some comfort knowing they have admitted they failed Jason,” Heather Fluty Simcakoski, the victim’s widow, told Gannett Wisconsin Media. “It doesn't bring him back, but I know it's a step closer to getting justice for him.”
On August 30, 2014, a 35-year-old marine died during inpatient treatment for mental health at the Tomah VAMC in Wisconsin. A year later, the VA Office of Inspector General (OIG) Office of Healthcare Inspections determined a number of deficiencies in hospital operations as a result of the investigation of this patient’s death.
Among these deficiencies were a lack of documenting patient consent for treatment and insufficient response to the patient’s cardiopulmonary emergency.
“We are deeply saddened by the tragic, avoidable death of this veteran and are committed to learning from this event and making improvements in the care we provide to our veterans,” the Tomah VAMC said in a statement.
Related: Negligence Settlement Reached After Army Hospital Death
Neither of the 2 psychiatrists treating the patient, Jason Simcakoski, obtained informed consent, verbal or written, for the buprenorphine/naloxone, according to both the patient’s electronic health record and the treating psychiatrists’ accounts. The prescription was administered to the patient with an off-label indication beginning the day prior to his death.
In addition, when the patient was found unresponsive in his room, “unit staff did not immediately assess the patient and determine the need for cardiopulmonary resuscitation,” nor did they use the in-room emergency call system or determine cardiac activity with the automatic external defibrillator, as noted in the OIG report.
Mr. Simcakoski served with the U.S. Marine Corp from 1998 until his honorable discharge in 2002. Mr. Simcakoski established VA medical care in 2003, according to the OIG report. Two years later, he sought help for his addiction to oxycodone, a medication he said he obtained from a friend; no VA provider ever prescribed Mr. Simcakoski oxycodone or other Schedule II opioid analgesic. The patient was treated for addiction at a non-VA clinic through 2007 and again in 2010.
Related: VISN 22 Evidence-Based Psychotherapy Telemental Health Center and Regional Pilot
The patient’s psychiatric diagnoses included posttraumatic stress disorder, bipolar I disorder, generalized anxiety disorder, attention deficit/hyperactivity disorder, panic disorder, opioid dependence, and alcohol and benzodiazepine abuse.
As a result of OIG recommendations, one of the psychiatrists involved in this case was terminated and the second awaits administrative proceedings. Under the direction of the Tomah VAMC acting chief of staff, all appropriate providers will be required to take relevant VHA training on informed consent, and all patients currently on buprenorphine will be reviewed to ensure consent has been obtained, both of which have an October 2015 target date of completion.
“I feel some comfort knowing they have admitted they failed Jason,” Heather Fluty Simcakoski, the victim’s widow, told Gannett Wisconsin Media. “It doesn't bring him back, but I know it's a step closer to getting justice for him.”
On August 30, 2014, a 35-year-old marine died during inpatient treatment for mental health at the Tomah VAMC in Wisconsin. A year later, the VA Office of Inspector General (OIG) Office of Healthcare Inspections determined a number of deficiencies in hospital operations as a result of the investigation of this patient’s death.
Among these deficiencies were a lack of documenting patient consent for treatment and insufficient response to the patient’s cardiopulmonary emergency.
“We are deeply saddened by the tragic, avoidable death of this veteran and are committed to learning from this event and making improvements in the care we provide to our veterans,” the Tomah VAMC said in a statement.
Related: Negligence Settlement Reached After Army Hospital Death
Neither of the 2 psychiatrists treating the patient, Jason Simcakoski, obtained informed consent, verbal or written, for the buprenorphine/naloxone, according to both the patient’s electronic health record and the treating psychiatrists’ accounts. The prescription was administered to the patient with an off-label indication beginning the day prior to his death.
In addition, when the patient was found unresponsive in his room, “unit staff did not immediately assess the patient and determine the need for cardiopulmonary resuscitation,” nor did they use the in-room emergency call system or determine cardiac activity with the automatic external defibrillator, as noted in the OIG report.
Mr. Simcakoski served with the U.S. Marine Corp from 1998 until his honorable discharge in 2002. Mr. Simcakoski established VA medical care in 2003, according to the OIG report. Two years later, he sought help for his addiction to oxycodone, a medication he said he obtained from a friend; no VA provider ever prescribed Mr. Simcakoski oxycodone or other Schedule II opioid analgesic. The patient was treated for addiction at a non-VA clinic through 2007 and again in 2010.
Related: VISN 22 Evidence-Based Psychotherapy Telemental Health Center and Regional Pilot
The patient’s psychiatric diagnoses included posttraumatic stress disorder, bipolar I disorder, generalized anxiety disorder, attention deficit/hyperactivity disorder, panic disorder, opioid dependence, and alcohol and benzodiazepine abuse.
As a result of OIG recommendations, one of the psychiatrists involved in this case was terminated and the second awaits administrative proceedings. Under the direction of the Tomah VAMC acting chief of staff, all appropriate providers will be required to take relevant VHA training on informed consent, and all patients currently on buprenorphine will be reviewed to ensure consent has been obtained, both of which have an October 2015 target date of completion.
“I feel some comfort knowing they have admitted they failed Jason,” Heather Fluty Simcakoski, the victim’s widow, told Gannett Wisconsin Media. “It doesn't bring him back, but I know it's a step closer to getting justice for him.”
Warfarin as effective as LMWH to prevent recurrent VTEs in cancer patients
In cancer patients with acute, symptomatic venous thromboembolisms, daily tinzaparin does not significantly reduce recurrent venous thromboembolisms, overall mortality, or major bleeding compared with warfarin, but does reduce clinically-relevant nonmajor bleeding, according to a 900-patient randomized trial published in JAMA.
Tinzaparin (Innohep) is a low-molecular-weight heparin (LMWH) marketed outside the United States. LMWHs are generally recommended over warfarin to treat acute venous thromboembolism (VTE) in cancer patients, but the recommendation is based mostly on a single trial over a decade old; that might explain why, worldwide, vitamin K antagonists are still heavily used in patients with cancer-associated thrombosis, said the authors, led by Dr. Agnes Lee, of the University of British Columbia (Vancouver).
To revisit the issue in the modern treatment era, Dr. Lee and her colleagues randomized 449 adults with active cancer and documented deep vein thrombosis or pulmonary embolism to tinzaparin (175 IU/kg) once daily for 6 months, and 451 others to 6 months of conventional therapy with tinzaparin (175 IU/kg) once daily for 5-10 days followed by warfarin dose adjusted to maintain therapeutic range (JAMA. 2015;314[7]:677-86).
The subjects were recruited from 164 centers in Asia, Africa, Europe, Canada, and Central and South America; all had a life expectancy greater than 6 months. The mean age in the study was 59 years, and 60% of the subjects were women. Gynecologic and colorectal cancers were the most common in the study.
Recurrent VTE occurred in 31 patients in the tinzaparin group and 45 in the warfarin group, giving a 6-month cumulative incidence of 7.2% for tinzaparin versus 10.5% for warfarin (hazard ratio [HR] 0.65; 95% CI 0.41-1.03; P = .07).
There was major bleeding in 12 (2.7%) tinzaparin patients and 11 (2.4%) warfarin patients, an insignificant difference (HR 0.89; 95% CI 0.40-1.99; P = .77); 150 tinzaparin patients (33.4%) and 138 warfarin patients (30.6%) died in the trial, also an insignificant difference (HR, 1.08; 95% CI 0.85-1.36; P = .54).
There were 49 (10.9%) clinically relevant but nonmajor bleeds in the tinzaparin group versus 69 (15.3%) among warfarin patients, a difference that was significant (HR 0.58; 95% CI 0.40-0.84; P = .004). Clinically relevant nonmajor bleeding meant nonfatal bleeding outside of a critical area or organ that still required intervention but did not cause a fall in hemoglobin greater than 2 g/dL.
There were fewer than anticipated thrombotic events in the warfarin group. “We had expected a recurrence rate of 12.6% with warfarin; the observed rate was only 10.5%. This potentially affected the power of the trial to detect a benefit associated with tinzaparin.” Also, “a significant reduction in recurrent [VTEs] might be observed with tinzaparin” among patients at higher risk for them than were in the study, the investigators said.
Even so, the trial did demonstrate “that tinzaparin, even when given at a full therapeutic dose for up to 6 months, is safe in a broad oncology population,” they said.
LEO Pharma, makers of tinzaparin, funded the study. The company was involved throughout the trial, including data analysis and approval of the manuscript. Dr. Lee reported honoraria, consulting fees, and research funding from the company. Other authors reported payments from LEO for those or other reasons.
In cancer patients with acute, symptomatic venous thromboembolisms, daily tinzaparin does not significantly reduce recurrent venous thromboembolisms, overall mortality, or major bleeding compared with warfarin, but does reduce clinically-relevant nonmajor bleeding, according to a 900-patient randomized trial published in JAMA.
Tinzaparin (Innohep) is a low-molecular-weight heparin (LMWH) marketed outside the United States. LMWHs are generally recommended over warfarin to treat acute venous thromboembolism (VTE) in cancer patients, but the recommendation is based mostly on a single trial over a decade old; that might explain why, worldwide, vitamin K antagonists are still heavily used in patients with cancer-associated thrombosis, said the authors, led by Dr. Agnes Lee, of the University of British Columbia (Vancouver).
To revisit the issue in the modern treatment era, Dr. Lee and her colleagues randomized 449 adults with active cancer and documented deep vein thrombosis or pulmonary embolism to tinzaparin (175 IU/kg) once daily for 6 months, and 451 others to 6 months of conventional therapy with tinzaparin (175 IU/kg) once daily for 5-10 days followed by warfarin dose adjusted to maintain therapeutic range (JAMA. 2015;314[7]:677-86).
The subjects were recruited from 164 centers in Asia, Africa, Europe, Canada, and Central and South America; all had a life expectancy greater than 6 months. The mean age in the study was 59 years, and 60% of the subjects were women. Gynecologic and colorectal cancers were the most common in the study.
Recurrent VTE occurred in 31 patients in the tinzaparin group and 45 in the warfarin group, giving a 6-month cumulative incidence of 7.2% for tinzaparin versus 10.5% for warfarin (hazard ratio [HR] 0.65; 95% CI 0.41-1.03; P = .07).
There was major bleeding in 12 (2.7%) tinzaparin patients and 11 (2.4%) warfarin patients, an insignificant difference (HR 0.89; 95% CI 0.40-1.99; P = .77); 150 tinzaparin patients (33.4%) and 138 warfarin patients (30.6%) died in the trial, also an insignificant difference (HR, 1.08; 95% CI 0.85-1.36; P = .54).
There were 49 (10.9%) clinically relevant but nonmajor bleeds in the tinzaparin group versus 69 (15.3%) among warfarin patients, a difference that was significant (HR 0.58; 95% CI 0.40-0.84; P = .004). Clinically relevant nonmajor bleeding meant nonfatal bleeding outside of a critical area or organ that still required intervention but did not cause a fall in hemoglobin greater than 2 g/dL.
There were fewer than anticipated thrombotic events in the warfarin group. “We had expected a recurrence rate of 12.6% with warfarin; the observed rate was only 10.5%. This potentially affected the power of the trial to detect a benefit associated with tinzaparin.” Also, “a significant reduction in recurrent [VTEs] might be observed with tinzaparin” among patients at higher risk for them than were in the study, the investigators said.
Even so, the trial did demonstrate “that tinzaparin, even when given at a full therapeutic dose for up to 6 months, is safe in a broad oncology population,” they said.
LEO Pharma, makers of tinzaparin, funded the study. The company was involved throughout the trial, including data analysis and approval of the manuscript. Dr. Lee reported honoraria, consulting fees, and research funding from the company. Other authors reported payments from LEO for those or other reasons.
In cancer patients with acute, symptomatic venous thromboembolisms, daily tinzaparin does not significantly reduce recurrent venous thromboembolisms, overall mortality, or major bleeding compared with warfarin, but does reduce clinically-relevant nonmajor bleeding, according to a 900-patient randomized trial published in JAMA.
Tinzaparin (Innohep) is a low-molecular-weight heparin (LMWH) marketed outside the United States. LMWHs are generally recommended over warfarin to treat acute venous thromboembolism (VTE) in cancer patients, but the recommendation is based mostly on a single trial over a decade old; that might explain why, worldwide, vitamin K antagonists are still heavily used in patients with cancer-associated thrombosis, said the authors, led by Dr. Agnes Lee, of the University of British Columbia (Vancouver).
To revisit the issue in the modern treatment era, Dr. Lee and her colleagues randomized 449 adults with active cancer and documented deep vein thrombosis or pulmonary embolism to tinzaparin (175 IU/kg) once daily for 6 months, and 451 others to 6 months of conventional therapy with tinzaparin (175 IU/kg) once daily for 5-10 days followed by warfarin dose adjusted to maintain therapeutic range (JAMA. 2015;314[7]:677-86).
The subjects were recruited from 164 centers in Asia, Africa, Europe, Canada, and Central and South America; all had a life expectancy greater than 6 months. The mean age in the study was 59 years, and 60% of the subjects were women. Gynecologic and colorectal cancers were the most common in the study.
Recurrent VTE occurred in 31 patients in the tinzaparin group and 45 in the warfarin group, giving a 6-month cumulative incidence of 7.2% for tinzaparin versus 10.5% for warfarin (hazard ratio [HR] 0.65; 95% CI 0.41-1.03; P = .07).
There was major bleeding in 12 (2.7%) tinzaparin patients and 11 (2.4%) warfarin patients, an insignificant difference (HR 0.89; 95% CI 0.40-1.99; P = .77); 150 tinzaparin patients (33.4%) and 138 warfarin patients (30.6%) died in the trial, also an insignificant difference (HR, 1.08; 95% CI 0.85-1.36; P = .54).
There were 49 (10.9%) clinically relevant but nonmajor bleeds in the tinzaparin group versus 69 (15.3%) among warfarin patients, a difference that was significant (HR 0.58; 95% CI 0.40-0.84; P = .004). Clinically relevant nonmajor bleeding meant nonfatal bleeding outside of a critical area or organ that still required intervention but did not cause a fall in hemoglobin greater than 2 g/dL.
There were fewer than anticipated thrombotic events in the warfarin group. “We had expected a recurrence rate of 12.6% with warfarin; the observed rate was only 10.5%. This potentially affected the power of the trial to detect a benefit associated with tinzaparin.” Also, “a significant reduction in recurrent [VTEs] might be observed with tinzaparin” among patients at higher risk for them than were in the study, the investigators said.
Even so, the trial did demonstrate “that tinzaparin, even when given at a full therapeutic dose for up to 6 months, is safe in a broad oncology population,” they said.
LEO Pharma, makers of tinzaparin, funded the study. The company was involved throughout the trial, including data analysis and approval of the manuscript. Dr. Lee reported honoraria, consulting fees, and research funding from the company. Other authors reported payments from LEO for those or other reasons.
FROM JAMA
Key clinical point: In cancer patients, tinzaparin (Innohep) does not significantly reduce recurrent venous thromboembolisms, overall mortality, or major bleeding when compared to warfarin.
Major finding: Recurrent VTE occurred in 31 patients in the tinzaparin group and 45 in the warfarin group, giving a 6-month cumulative incidence of 7.2% for tinzaparin versus 10.5% for warfarin (HR 0.65; 95% CI 0.41-1.03; P = .07).
Data source: Randomized trial with 900 subjects.
Disclosures: LEO Pharma, maker of tinzaparin, funded the study. The company was involved throughout the trial, including data analysis and approval of the manuscript. The investigators reported honoraria, consulting fees, and other payments from the company.
Prescribing drugs outside your specialty
I prescribe medications. You do, too. It’s part of what we do.
What I don’t do is prescribe meds for other docs, or expect them to prescribe mine.
Seems reasonable, right? Yet, I’ve seen several recent posts on physician gripe boards talking about doctors dodging out on this in a few ways. Some examples follow:
• Specialists who diagnose a patient with epilepsy, and send a note back to the internists suggesting they start Tegretol.
• Internists who want the patient to take a drug for neuropathy, and give them a note to take to the specialist asking them to start Lyrica.
• Specialists who want the internist to manage another field entirely, such as a dermatologist telling the internist what to prescribe for a patient’s diabetes.
Personally, I wouldn’t expect any internist to continue a medication that I started prescribing. If they referred the patient to me, I assume they want me to handle it. If they’d prefer the patient return to them for continuing care of the condition, that’s fine, but I generally figure it’s now my issue.
On the flip side, it always bugs me when someone who’s not in my field tells a patient what they think I should prescribe. Sometimes I agree with the choice, but to me it undermines my relationship with the patient. If you want me to handle the case, then don’t give the patient expectations of what should be used. Otherwise, if I decide to try something else, Mr. Smith feels like he’s been short-changed and may call the internist to complain.
I wouldn’t dream of handing a patient a card that says, “Needs to be started on (Actos/Coreg/amiodarone/whatever),” so am always surprised when they bring a note saying, “Please start Dilantin, I think he has seizures.”
This isn’t, I admit, a common occurrence. In my little world, I can count on one hand the number of times it happens per year, almost always from a physician whom I haven’t previously worked with. My referral sources (hopefully) trust me to handle neurology, and I feel the same way about them to handle other issues.
But it must be happening to others, or it wouldn’t be showing up on Sermo and other sites. I have to wonder about the background mindset. Is it just laziness on the part of other doctors? A reluctance to prescribe, knowing that then you’ll be the one stuck with the prior authorization and refill requests? A paternalistic approach to medicine, where you feel you’re right, and therefore another doc should unquestioningly follow your instructions (if you know what’s best, why refer at all?).
More disturbingly, are a few docs seeing patients as someone else’s problem? I really hope not. I’d like to think that the affront, when present, is simply from a lack of practice experience and/or social skills, and will fade with time. Things that irritate other physicians only end up hurting the patient, which isn’t what we’re here for.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I prescribe medications. You do, too. It’s part of what we do.
What I don’t do is prescribe meds for other docs, or expect them to prescribe mine.
Seems reasonable, right? Yet, I’ve seen several recent posts on physician gripe boards talking about doctors dodging out on this in a few ways. Some examples follow:
• Specialists who diagnose a patient with epilepsy, and send a note back to the internists suggesting they start Tegretol.
• Internists who want the patient to take a drug for neuropathy, and give them a note to take to the specialist asking them to start Lyrica.
• Specialists who want the internist to manage another field entirely, such as a dermatologist telling the internist what to prescribe for a patient’s diabetes.
Personally, I wouldn’t expect any internist to continue a medication that I started prescribing. If they referred the patient to me, I assume they want me to handle it. If they’d prefer the patient return to them for continuing care of the condition, that’s fine, but I generally figure it’s now my issue.
On the flip side, it always bugs me when someone who’s not in my field tells a patient what they think I should prescribe. Sometimes I agree with the choice, but to me it undermines my relationship with the patient. If you want me to handle the case, then don’t give the patient expectations of what should be used. Otherwise, if I decide to try something else, Mr. Smith feels like he’s been short-changed and may call the internist to complain.
I wouldn’t dream of handing a patient a card that says, “Needs to be started on (Actos/Coreg/amiodarone/whatever),” so am always surprised when they bring a note saying, “Please start Dilantin, I think he has seizures.”
This isn’t, I admit, a common occurrence. In my little world, I can count on one hand the number of times it happens per year, almost always from a physician whom I haven’t previously worked with. My referral sources (hopefully) trust me to handle neurology, and I feel the same way about them to handle other issues.
But it must be happening to others, or it wouldn’t be showing up on Sermo and other sites. I have to wonder about the background mindset. Is it just laziness on the part of other doctors? A reluctance to prescribe, knowing that then you’ll be the one stuck with the prior authorization and refill requests? A paternalistic approach to medicine, where you feel you’re right, and therefore another doc should unquestioningly follow your instructions (if you know what’s best, why refer at all?).
More disturbingly, are a few docs seeing patients as someone else’s problem? I really hope not. I’d like to think that the affront, when present, is simply from a lack of practice experience and/or social skills, and will fade with time. Things that irritate other physicians only end up hurting the patient, which isn’t what we’re here for.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I prescribe medications. You do, too. It’s part of what we do.
What I don’t do is prescribe meds for other docs, or expect them to prescribe mine.
Seems reasonable, right? Yet, I’ve seen several recent posts on physician gripe boards talking about doctors dodging out on this in a few ways. Some examples follow:
• Specialists who diagnose a patient with epilepsy, and send a note back to the internists suggesting they start Tegretol.
• Internists who want the patient to take a drug for neuropathy, and give them a note to take to the specialist asking them to start Lyrica.
• Specialists who want the internist to manage another field entirely, such as a dermatologist telling the internist what to prescribe for a patient’s diabetes.
Personally, I wouldn’t expect any internist to continue a medication that I started prescribing. If they referred the patient to me, I assume they want me to handle it. If they’d prefer the patient return to them for continuing care of the condition, that’s fine, but I generally figure it’s now my issue.
On the flip side, it always bugs me when someone who’s not in my field tells a patient what they think I should prescribe. Sometimes I agree with the choice, but to me it undermines my relationship with the patient. If you want me to handle the case, then don’t give the patient expectations of what should be used. Otherwise, if I decide to try something else, Mr. Smith feels like he’s been short-changed and may call the internist to complain.
I wouldn’t dream of handing a patient a card that says, “Needs to be started on (Actos/Coreg/amiodarone/whatever),” so am always surprised when they bring a note saying, “Please start Dilantin, I think he has seizures.”
This isn’t, I admit, a common occurrence. In my little world, I can count on one hand the number of times it happens per year, almost always from a physician whom I haven’t previously worked with. My referral sources (hopefully) trust me to handle neurology, and I feel the same way about them to handle other issues.
But it must be happening to others, or it wouldn’t be showing up on Sermo and other sites. I have to wonder about the background mindset. Is it just laziness on the part of other doctors? A reluctance to prescribe, knowing that then you’ll be the one stuck with the prior authorization and refill requests? A paternalistic approach to medicine, where you feel you’re right, and therefore another doc should unquestioningly follow your instructions (if you know what’s best, why refer at all?).
More disturbingly, are a few docs seeing patients as someone else’s problem? I really hope not. I’d like to think that the affront, when present, is simply from a lack of practice experience and/or social skills, and will fade with time. Things that irritate other physicians only end up hurting the patient, which isn’t what we’re here for.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.