User login
End-user agreements
Long-time readers will chuckle – but after years of affirming and reaffirming that I would never adopt electronic records in my practice, I’m in the process of doing just that. It still runs contrary to my better judgment; but the advent of ICD-10, combined with space issues and other factors that I won’t bore you with, has forced my hand.
Before implementing any electronic health record system, you first must sign an end-user license agreement (EULA) with the EHR vendor. The sales manager for the company I had chosen assured me that the EULA was a “routine” document.
“Just sign it,” he said. “It’s all basic stuff ... but you can read it, if you would like.” Of course I would like. First, it was quite clear that the agreement was designed primarily to protect the vendor. (Not surprising, since the company’s lawyer wrote it.) But then I noticed that the vendor assumed no liability at all in the event of accidental destruction of my records. And when I saw, a few paragraphs later, that the vendor would have the unrestricted right to sell my practice data to third parties, I knew I would not be “just signing” anything.
My attorney referred me to a colleague with expertise in technology contracts and HIPAA law. I asked him if EULAs were always this one-sided. “Some are much worse,” he replied. Why would any physician sign such an egregious document, I asked? “Because most of them never read it.”
Wow.
A couple of weeks later, my attorney and the vendor’s counsel signed off on a much fairer agreement. The bill was significant – but it was money well spent.
A EULA details your and your vendor’s responsibilities relating to installation of your EHR, training your staff, and ongoing software and hardware support. Sales reps will often chide you (as mine did) for “taking this much too seriously.” Any legal document that you sign – and by which you will be bound for the foreseeable future – must be taken seriously. You should never allow yourself to be pressured into signing anything that you cannot comfortably live with in perpetuity.
So if you are taking the EHR plunge, find a lawyer who understands tech contracts and medical privacy laws before you sign anything. Make certain that he or she knows your concerns, and the provisions that you can and cannot live with. Among other things, my attorney succeeded in removing clauses requiring a minimum contract term, and a hefty fee if I wanted out; a nondisclosure clause preventing any public criticism of the vendor; and that crazy provision giving them the right to sell or give practice data to anyone who asked for it.
One EHR installation in three ultimately fails, according to one management firm; so more than anything else, you need to be certain that you do not get locked into a long-term contract should your EHR turn out to be a poor performer. Be sure that the agreement allows you to terminate the contract if the product’s performance – by your criteria – proves to be inadequate.
Some seemingly obvious considerations need to be spelled out; for example, that you will have ownership of your data. You need to know exactly what happens to your data if the vendor goes out of business, or if a flood wipes out its servers, or your contract is terminated by either party, or anything else that forces you to switch vendors. The process of migrating your records to a new platform can go smoothly, or it can be a nightmare – depending on the agreement in place. It should include specific methods by which data will be migrated; and be sure to lose any clauses that force you to pay a “ransom” to regain control of your own records.
You will want to know how your data is backed up – and how the backup is backed up – and whether you can maintain a separate backup in-house if necessary. My attorney also insisted on a “guarantee of system uptime,” including the steps the vendor agrees to take in the event of a significant crash or other prolonged downtime.
The basic point, of course, is never sign a EULA without having it reviewed by an experienced technology attorney. A good one should be able to eliminate the more onerous clauses; but don’t expect perfection. My vendor refused to cave on several of my attorney’s concerns. “The agreement is still one-sided,” he told me, but it’s the best we will get at this point. Once there is more competition in the EHR field, things will be different.”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
Long-time readers will chuckle – but after years of affirming and reaffirming that I would never adopt electronic records in my practice, I’m in the process of doing just that. It still runs contrary to my better judgment; but the advent of ICD-10, combined with space issues and other factors that I won’t bore you with, has forced my hand.
Before implementing any electronic health record system, you first must sign an end-user license agreement (EULA) with the EHR vendor. The sales manager for the company I had chosen assured me that the EULA was a “routine” document.
“Just sign it,” he said. “It’s all basic stuff ... but you can read it, if you would like.” Of course I would like. First, it was quite clear that the agreement was designed primarily to protect the vendor. (Not surprising, since the company’s lawyer wrote it.) But then I noticed that the vendor assumed no liability at all in the event of accidental destruction of my records. And when I saw, a few paragraphs later, that the vendor would have the unrestricted right to sell my practice data to third parties, I knew I would not be “just signing” anything.
My attorney referred me to a colleague with expertise in technology contracts and HIPAA law. I asked him if EULAs were always this one-sided. “Some are much worse,” he replied. Why would any physician sign such an egregious document, I asked? “Because most of them never read it.”
Wow.
A couple of weeks later, my attorney and the vendor’s counsel signed off on a much fairer agreement. The bill was significant – but it was money well spent.
A EULA details your and your vendor’s responsibilities relating to installation of your EHR, training your staff, and ongoing software and hardware support. Sales reps will often chide you (as mine did) for “taking this much too seriously.” Any legal document that you sign – and by which you will be bound for the foreseeable future – must be taken seriously. You should never allow yourself to be pressured into signing anything that you cannot comfortably live with in perpetuity.
So if you are taking the EHR plunge, find a lawyer who understands tech contracts and medical privacy laws before you sign anything. Make certain that he or she knows your concerns, and the provisions that you can and cannot live with. Among other things, my attorney succeeded in removing clauses requiring a minimum contract term, and a hefty fee if I wanted out; a nondisclosure clause preventing any public criticism of the vendor; and that crazy provision giving them the right to sell or give practice data to anyone who asked for it.
One EHR installation in three ultimately fails, according to one management firm; so more than anything else, you need to be certain that you do not get locked into a long-term contract should your EHR turn out to be a poor performer. Be sure that the agreement allows you to terminate the contract if the product’s performance – by your criteria – proves to be inadequate.
Some seemingly obvious considerations need to be spelled out; for example, that you will have ownership of your data. You need to know exactly what happens to your data if the vendor goes out of business, or if a flood wipes out its servers, or your contract is terminated by either party, or anything else that forces you to switch vendors. The process of migrating your records to a new platform can go smoothly, or it can be a nightmare – depending on the agreement in place. It should include specific methods by which data will be migrated; and be sure to lose any clauses that force you to pay a “ransom” to regain control of your own records.
You will want to know how your data is backed up – and how the backup is backed up – and whether you can maintain a separate backup in-house if necessary. My attorney also insisted on a “guarantee of system uptime,” including the steps the vendor agrees to take in the event of a significant crash or other prolonged downtime.
The basic point, of course, is never sign a EULA without having it reviewed by an experienced technology attorney. A good one should be able to eliminate the more onerous clauses; but don’t expect perfection. My vendor refused to cave on several of my attorney’s concerns. “The agreement is still one-sided,” he told me, but it’s the best we will get at this point. Once there is more competition in the EHR field, things will be different.”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
Long-time readers will chuckle – but after years of affirming and reaffirming that I would never adopt electronic records in my practice, I’m in the process of doing just that. It still runs contrary to my better judgment; but the advent of ICD-10, combined with space issues and other factors that I won’t bore you with, has forced my hand.
Before implementing any electronic health record system, you first must sign an end-user license agreement (EULA) with the EHR vendor. The sales manager for the company I had chosen assured me that the EULA was a “routine” document.
“Just sign it,” he said. “It’s all basic stuff ... but you can read it, if you would like.” Of course I would like. First, it was quite clear that the agreement was designed primarily to protect the vendor. (Not surprising, since the company’s lawyer wrote it.) But then I noticed that the vendor assumed no liability at all in the event of accidental destruction of my records. And when I saw, a few paragraphs later, that the vendor would have the unrestricted right to sell my practice data to third parties, I knew I would not be “just signing” anything.
My attorney referred me to a colleague with expertise in technology contracts and HIPAA law. I asked him if EULAs were always this one-sided. “Some are much worse,” he replied. Why would any physician sign such an egregious document, I asked? “Because most of them never read it.”
Wow.
A couple of weeks later, my attorney and the vendor’s counsel signed off on a much fairer agreement. The bill was significant – but it was money well spent.
A EULA details your and your vendor’s responsibilities relating to installation of your EHR, training your staff, and ongoing software and hardware support. Sales reps will often chide you (as mine did) for “taking this much too seriously.” Any legal document that you sign – and by which you will be bound for the foreseeable future – must be taken seriously. You should never allow yourself to be pressured into signing anything that you cannot comfortably live with in perpetuity.
So if you are taking the EHR plunge, find a lawyer who understands tech contracts and medical privacy laws before you sign anything. Make certain that he or she knows your concerns, and the provisions that you can and cannot live with. Among other things, my attorney succeeded in removing clauses requiring a minimum contract term, and a hefty fee if I wanted out; a nondisclosure clause preventing any public criticism of the vendor; and that crazy provision giving them the right to sell or give practice data to anyone who asked for it.
One EHR installation in three ultimately fails, according to one management firm; so more than anything else, you need to be certain that you do not get locked into a long-term contract should your EHR turn out to be a poor performer. Be sure that the agreement allows you to terminate the contract if the product’s performance – by your criteria – proves to be inadequate.
Some seemingly obvious considerations need to be spelled out; for example, that you will have ownership of your data. You need to know exactly what happens to your data if the vendor goes out of business, or if a flood wipes out its servers, or your contract is terminated by either party, or anything else that forces you to switch vendors. The process of migrating your records to a new platform can go smoothly, or it can be a nightmare – depending on the agreement in place. It should include specific methods by which data will be migrated; and be sure to lose any clauses that force you to pay a “ransom” to regain control of your own records.
You will want to know how your data is backed up – and how the backup is backed up – and whether you can maintain a separate backup in-house if necessary. My attorney also insisted on a “guarantee of system uptime,” including the steps the vendor agrees to take in the event of a significant crash or other prolonged downtime.
The basic point, of course, is never sign a EULA without having it reviewed by an experienced technology attorney. A good one should be able to eliminate the more onerous clauses; but don’t expect perfection. My vendor refused to cave on several of my attorney’s concerns. “The agreement is still one-sided,” he told me, but it’s the best we will get at this point. Once there is more competition in the EHR field, things will be different.”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
VIDEO: Three veterans describe impact of mindfulness therapy
Mindfulness-based stress reduction therapy teaches patients to be in the present moment in nonjudgmental, accepting ways. Researchers at the Minneapolis Veterans Affairs Medical Center decided to compare a mindfulness intervention with present-centered group therapy of 116 veterans with post-traumatic stress disorder.
Those in the mindfulness group had eight weekly 2.5-hour sessions and one day-long retreat. Veterans in the present-centered group attended nine weekly 1.5-hour group sessions focusing on current problems. The results found that the veterans who used the mindfulness techniques experienced a greater decrease in the severity of their PTSD symptoms than did those in the other group.
In this video, Melissa A. Polusny, Ph.D., and Dr. Kelvin O. Lim, both of the medical center, talk with three veterans with PTSD about how mindfulness changed their quality of life and helped them find peace of mind.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Mindfulness-based stress reduction therapy teaches patients to be in the present moment in nonjudgmental, accepting ways. Researchers at the Minneapolis Veterans Affairs Medical Center decided to compare a mindfulness intervention with present-centered group therapy of 116 veterans with post-traumatic stress disorder.
Those in the mindfulness group had eight weekly 2.5-hour sessions and one day-long retreat. Veterans in the present-centered group attended nine weekly 1.5-hour group sessions focusing on current problems. The results found that the veterans who used the mindfulness techniques experienced a greater decrease in the severity of their PTSD symptoms than did those in the other group.
In this video, Melissa A. Polusny, Ph.D., and Dr. Kelvin O. Lim, both of the medical center, talk with three veterans with PTSD about how mindfulness changed their quality of life and helped them find peace of mind.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Mindfulness-based stress reduction therapy teaches patients to be in the present moment in nonjudgmental, accepting ways. Researchers at the Minneapolis Veterans Affairs Medical Center decided to compare a mindfulness intervention with present-centered group therapy of 116 veterans with post-traumatic stress disorder.
Those in the mindfulness group had eight weekly 2.5-hour sessions and one day-long retreat. Veterans in the present-centered group attended nine weekly 1.5-hour group sessions focusing on current problems. The results found that the veterans who used the mindfulness techniques experienced a greater decrease in the severity of their PTSD symptoms than did those in the other group.
In this video, Melissa A. Polusny, Ph.D., and Dr. Kelvin O. Lim, both of the medical center, talk with three veterans with PTSD about how mindfulness changed their quality of life and helped them find peace of mind.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Uveitis and Psoriasis
We are all aware of the association of psoriasis with systemic comorbidities. Psoriasis, psoriatic arthritis (PsA), and uveitis are inflammatory disorders that have notable overlap in their inflammatory pathways. In an article published online on July 29 in JAMA Dermatology, Egeberg et al investigated the potential bidirectional relationship between psoriatic disease and uveitis.
The researchers conducted a study (1997-2011) of 74,129 patients aged 18 years and older with incident psoriasis who were identified through administrative registries. There also were 13,114 patients with uveitis identified from the study cohort.
Incidence rates for uveitis per 10,000 person-years were 2.02 (95% CI [confidence interval], 1.99-2.06) for the reference population, 2.88 (95% CI, 2.33-3.56) for patients with mild psoriasis, 4.23 (2.40-7.45) for severe psoriasis, and 5.49 (95% CI, 3.36-8.96) for PsA. Incidence rate ratios per 10,000 person-years for the reference population, which included participants without uveitis, were 9.37 (95% CI, 9.30-9.45) for patients with mild psoriasis, 1.12 (95% CI, 1.10-1.15) for severe psoriasis, and 1.04 (95% CI, 1.01-1.06) for PsA. Patients with uveitis had corresponding incidence rates of 15.51 (95% CI, 12.92-18.62) for mild psoriasis, 2.66 (95% CI, 1.72-4.13) for severe psoriasis, and 4.25 (95% CI, 3.00-6.01) for PsA. Incidence rate ratios per 10,000 person-years for patients with uveitis were 1.59 (95% CI, 1.32-1.91) for mild psoriasis, 2.17 (95% CI, 1.40-3.38) for severe psoriasis, and 3.77 (95% CI, 2.66-5.34) for PsA.
The authors concluded that there is a bidirectional association between psoriatic disease and uveitis. They noted that increased focus on ocular symptoms in patients with psoriasis and PsA and on cutaneous and joint symptoms in patients with prior or current uveitis may be appropriate.
What’s the issue?
This research adds to the potential comorbidities of psoriasis and also adds a potential comorbidity of uveitis itself. Therefore, it would be helpful to add ocular symptoms to our review of systems in those with psoriatic disease. How will this information affect your workup of psoriasis patients?
We are all aware of the association of psoriasis with systemic comorbidities. Psoriasis, psoriatic arthritis (PsA), and uveitis are inflammatory disorders that have notable overlap in their inflammatory pathways. In an article published online on July 29 in JAMA Dermatology, Egeberg et al investigated the potential bidirectional relationship between psoriatic disease and uveitis.
The researchers conducted a study (1997-2011) of 74,129 patients aged 18 years and older with incident psoriasis who were identified through administrative registries. There also were 13,114 patients with uveitis identified from the study cohort.
Incidence rates for uveitis per 10,000 person-years were 2.02 (95% CI [confidence interval], 1.99-2.06) for the reference population, 2.88 (95% CI, 2.33-3.56) for patients with mild psoriasis, 4.23 (2.40-7.45) for severe psoriasis, and 5.49 (95% CI, 3.36-8.96) for PsA. Incidence rate ratios per 10,000 person-years for the reference population, which included participants without uveitis, were 9.37 (95% CI, 9.30-9.45) for patients with mild psoriasis, 1.12 (95% CI, 1.10-1.15) for severe psoriasis, and 1.04 (95% CI, 1.01-1.06) for PsA. Patients with uveitis had corresponding incidence rates of 15.51 (95% CI, 12.92-18.62) for mild psoriasis, 2.66 (95% CI, 1.72-4.13) for severe psoriasis, and 4.25 (95% CI, 3.00-6.01) for PsA. Incidence rate ratios per 10,000 person-years for patients with uveitis were 1.59 (95% CI, 1.32-1.91) for mild psoriasis, 2.17 (95% CI, 1.40-3.38) for severe psoriasis, and 3.77 (95% CI, 2.66-5.34) for PsA.
The authors concluded that there is a bidirectional association between psoriatic disease and uveitis. They noted that increased focus on ocular symptoms in patients with psoriasis and PsA and on cutaneous and joint symptoms in patients with prior or current uveitis may be appropriate.
What’s the issue?
This research adds to the potential comorbidities of psoriasis and also adds a potential comorbidity of uveitis itself. Therefore, it would be helpful to add ocular symptoms to our review of systems in those with psoriatic disease. How will this information affect your workup of psoriasis patients?
We are all aware of the association of psoriasis with systemic comorbidities. Psoriasis, psoriatic arthritis (PsA), and uveitis are inflammatory disorders that have notable overlap in their inflammatory pathways. In an article published online on July 29 in JAMA Dermatology, Egeberg et al investigated the potential bidirectional relationship between psoriatic disease and uveitis.
The researchers conducted a study (1997-2011) of 74,129 patients aged 18 years and older with incident psoriasis who were identified through administrative registries. There also were 13,114 patients with uveitis identified from the study cohort.
Incidence rates for uveitis per 10,000 person-years were 2.02 (95% CI [confidence interval], 1.99-2.06) for the reference population, 2.88 (95% CI, 2.33-3.56) for patients with mild psoriasis, 4.23 (2.40-7.45) for severe psoriasis, and 5.49 (95% CI, 3.36-8.96) for PsA. Incidence rate ratios per 10,000 person-years for the reference population, which included participants without uveitis, were 9.37 (95% CI, 9.30-9.45) for patients with mild psoriasis, 1.12 (95% CI, 1.10-1.15) for severe psoriasis, and 1.04 (95% CI, 1.01-1.06) for PsA. Patients with uveitis had corresponding incidence rates of 15.51 (95% CI, 12.92-18.62) for mild psoriasis, 2.66 (95% CI, 1.72-4.13) for severe psoriasis, and 4.25 (95% CI, 3.00-6.01) for PsA. Incidence rate ratios per 10,000 person-years for patients with uveitis were 1.59 (95% CI, 1.32-1.91) for mild psoriasis, 2.17 (95% CI, 1.40-3.38) for severe psoriasis, and 3.77 (95% CI, 2.66-5.34) for PsA.
The authors concluded that there is a bidirectional association between psoriatic disease and uveitis. They noted that increased focus on ocular symptoms in patients with psoriasis and PsA and on cutaneous and joint symptoms in patients with prior or current uveitis may be appropriate.
What’s the issue?
This research adds to the potential comorbidities of psoriasis and also adds a potential comorbidity of uveitis itself. Therefore, it would be helpful to add ocular symptoms to our review of systems in those with psoriatic disease. How will this information affect your workup of psoriasis patients?
Better Catheter-Directed Thrombolysis Outcomes at Higher-Volume Institutions
NEW YORK - In-hospital mortality and bleeding rates after catheter-directed thrombolysis (CDT) of lower extremity proximal deep vein thrombosis are lower in institutions that perform more procedures than in those with fewer procedures, according to a new study.
"As utilization of CDT continues to increase, we propose that institutions follow a standardized CDT protocol that includes careful patient selection as well as patient monitoring," Dr. Riyaz Bashir from Temple University School of Medicine in Philadelphia, Pennsylvania, told Reuters Health by email. "In addition, establishment of centers of excellence in treating venous thromboembolic disease may provide the necessary framework within which bleeding risk to the patient can be minimized."
CDT is increasingly favored over anticoagulation for patients with lower extremity proximal deep vein thrombosis (LE-DVT), but it has been associated with increased bleeding rates and procedure-related complications, Dr. Bashir and colleagues note in Circulation, online July 21.
In light of literature implicating institutional volume as a significant factor in patient outcomes, the team used the Nationwide Inpatient Sample database to investigate the relationship between annual institutional procedure volume and adverse in-hospital patient outcomes in patients receiving CDT for acute proximal LE-DVT.
Just over half the 3,649 procedures were performed at high-volume centers (six or more procedures per year), with the remainder (43%) done at low-volume centers (less than six procedures per year).
In a propensity-matched comparison of 1,310 patients from each group, in-hospital mortality was significantly lower at high-volume centers than at low-volume centers (0.6% vs. 1.5%, p=0.04), the researchers found.
Intracranial hemorrhage rates tended to be lower at high-volume centers (0.4% vs. 1.0%, p=0.07), while inferior vena cava filter placement rates were significantly higher at high-volume centers (37.0% vs. 32.8%; p=0.03).
Institutional volume did not influence blood transfusion, GI bleeding, or pulmonary embolism rates or hospital length of stay. Median hospital charges were higher at high-volume centers ($75,870) than at low-volume centers ($65,500).
At low-volume centers, outcomes tended to be worse for CDT plus anticoagulation than for anticoagulation alone, whereas outcomes were similar for CDT plus anticoagulation and for anticoagulation alone at high-volume centers.
On multiple regression analysis, there was a significant inverse relationship between institutional volume and in-hospital mortality.
"Our observation that the major safety outcomes (death and intracranial hemorrhage) were not significantly different between patients undergoing CDT as compared to patients undergoing anticoagulation therapy alone at high volume centers suggests that these complications can be minimized," Dr. Bashir concluded. "Patients with leg DVT - especially young patients - should feel comfortable considering clot removal, particularly at a high volume center, as a viable option to prevent post-thrombotic syndrome."
NEW YORK - In-hospital mortality and bleeding rates after catheter-directed thrombolysis (CDT) of lower extremity proximal deep vein thrombosis are lower in institutions that perform more procedures than in those with fewer procedures, according to a new study.
"As utilization of CDT continues to increase, we propose that institutions follow a standardized CDT protocol that includes careful patient selection as well as patient monitoring," Dr. Riyaz Bashir from Temple University School of Medicine in Philadelphia, Pennsylvania, told Reuters Health by email. "In addition, establishment of centers of excellence in treating venous thromboembolic disease may provide the necessary framework within which bleeding risk to the patient can be minimized."
CDT is increasingly favored over anticoagulation for patients with lower extremity proximal deep vein thrombosis (LE-DVT), but it has been associated with increased bleeding rates and procedure-related complications, Dr. Bashir and colleagues note in Circulation, online July 21.
In light of literature implicating institutional volume as a significant factor in patient outcomes, the team used the Nationwide Inpatient Sample database to investigate the relationship between annual institutional procedure volume and adverse in-hospital patient outcomes in patients receiving CDT for acute proximal LE-DVT.
Just over half the 3,649 procedures were performed at high-volume centers (six or more procedures per year), with the remainder (43%) done at low-volume centers (less than six procedures per year).
In a propensity-matched comparison of 1,310 patients from each group, in-hospital mortality was significantly lower at high-volume centers than at low-volume centers (0.6% vs. 1.5%, p=0.04), the researchers found.
Intracranial hemorrhage rates tended to be lower at high-volume centers (0.4% vs. 1.0%, p=0.07), while inferior vena cava filter placement rates were significantly higher at high-volume centers (37.0% vs. 32.8%; p=0.03).
Institutional volume did not influence blood transfusion, GI bleeding, or pulmonary embolism rates or hospital length of stay. Median hospital charges were higher at high-volume centers ($75,870) than at low-volume centers ($65,500).
At low-volume centers, outcomes tended to be worse for CDT plus anticoagulation than for anticoagulation alone, whereas outcomes were similar for CDT plus anticoagulation and for anticoagulation alone at high-volume centers.
On multiple regression analysis, there was a significant inverse relationship between institutional volume and in-hospital mortality.
"Our observation that the major safety outcomes (death and intracranial hemorrhage) were not significantly different between patients undergoing CDT as compared to patients undergoing anticoagulation therapy alone at high volume centers suggests that these complications can be minimized," Dr. Bashir concluded. "Patients with leg DVT - especially young patients - should feel comfortable considering clot removal, particularly at a high volume center, as a viable option to prevent post-thrombotic syndrome."
NEW YORK - In-hospital mortality and bleeding rates after catheter-directed thrombolysis (CDT) of lower extremity proximal deep vein thrombosis are lower in institutions that perform more procedures than in those with fewer procedures, according to a new study.
"As utilization of CDT continues to increase, we propose that institutions follow a standardized CDT protocol that includes careful patient selection as well as patient monitoring," Dr. Riyaz Bashir from Temple University School of Medicine in Philadelphia, Pennsylvania, told Reuters Health by email. "In addition, establishment of centers of excellence in treating venous thromboembolic disease may provide the necessary framework within which bleeding risk to the patient can be minimized."
CDT is increasingly favored over anticoagulation for patients with lower extremity proximal deep vein thrombosis (LE-DVT), but it has been associated with increased bleeding rates and procedure-related complications, Dr. Bashir and colleagues note in Circulation, online July 21.
In light of literature implicating institutional volume as a significant factor in patient outcomes, the team used the Nationwide Inpatient Sample database to investigate the relationship between annual institutional procedure volume and adverse in-hospital patient outcomes in patients receiving CDT for acute proximal LE-DVT.
Just over half the 3,649 procedures were performed at high-volume centers (six or more procedures per year), with the remainder (43%) done at low-volume centers (less than six procedures per year).
In a propensity-matched comparison of 1,310 patients from each group, in-hospital mortality was significantly lower at high-volume centers than at low-volume centers (0.6% vs. 1.5%, p=0.04), the researchers found.
Intracranial hemorrhage rates tended to be lower at high-volume centers (0.4% vs. 1.0%, p=0.07), while inferior vena cava filter placement rates were significantly higher at high-volume centers (37.0% vs. 32.8%; p=0.03).
Institutional volume did not influence blood transfusion, GI bleeding, or pulmonary embolism rates or hospital length of stay. Median hospital charges were higher at high-volume centers ($75,870) than at low-volume centers ($65,500).
At low-volume centers, outcomes tended to be worse for CDT plus anticoagulation than for anticoagulation alone, whereas outcomes were similar for CDT plus anticoagulation and for anticoagulation alone at high-volume centers.
On multiple regression analysis, there was a significant inverse relationship between institutional volume and in-hospital mortality.
"Our observation that the major safety outcomes (death and intracranial hemorrhage) were not significantly different between patients undergoing CDT as compared to patients undergoing anticoagulation therapy alone at high volume centers suggests that these complications can be minimized," Dr. Bashir concluded. "Patients with leg DVT - especially young patients - should feel comfortable considering clot removal, particularly at a high volume center, as a viable option to prevent post-thrombotic syndrome."
ICDs in the elderly
There has been a spate of recent publications dealing with the lack of implantable cardioverter-defibrillator implantations in the elderly. The most recent indicates that only 8% of patients over age 75 years who have experienced a non–ST-segment elevation myocardial infarction (NSTEMI) or STEMI receive an ICD largely due to the restriction of implantation within 40 days of the incident infarction because of the delayed repair of ventricular function after an MI and the uncertainty of ejection fraction measurements during this period. That article indicates that despite this delay, patients who receive an ICD had an improved survival over the subsequent 2 years, compared with those who did not (JAMA. 2015;313[24]:2433-40). Some of my octogenarian friends might question whether improved survival and the prevention of sudden death is a benefit at that age.
An accompanying editorial suggests that a closer follow-up of these patients is warranted in order to improve the rate of implantation in those patients who are discharged so that they do not “fall through the cracks” and are lost to follow-up (JAMA. 2015:313[24]:2429-30).
Although there has been a tapering off of the explosive use of ICDs in the United States, almost a quarter million devices were implanted between 2010 and 2011 (Heart Rhythm. 2013 Apr;10[4]:e59-65). The U.S. number is roughly four times that of Western Europe. Primary prevention was the reason for implantation in 73.8%, and half of the implantations were in patients over 65; 29% were in the 70-79 age group, and 14% were octogenarians. A history of New York Heart Association class II-IV heart failure was present in 82% and a myocardial infarction in 49%.
There are of course other reasons why the elderly may not receive an ICD. The most frequent are the presence of concomitant diseases like stroke, cancer, and chronic renal disease. However, many elderly do not wish to have their survival tied to a device that they have no control over. Some may view sudden death as an acceptable mortality outcome considering other alternatives. Certainly, adverse lifestyle changes at advanced age may be a reason for the reluctance to choose an ICD.
The application of our new technologies like ICDs, catheter-implanted aortic valves, and mini–left ventricular assist devices have been remarkably successful and have brought lifesaving interventions to thousands of patients. Their relative ease of application has led to a casualness in regard to appropriateness in patients with concomitant diseases, and particularly in the elderly.
The definition of who is elderly has changed dramatically in clinical trials from the mid–20th century when those studies excluded patients over 65. In today’s world, the definition of the elderly has become a slippery slope, as there is no age limit and the inclusion of octogenarians is not unusual. The observation that elderly postinfarction patients with decreased ejection fraction can experience improved survival needs to be evaluated in the light of important considerations of current and expected quality of life in individual patients, as well as their own mortality expectations.
Most of the studies examining implantation rates, extensively analyze the effect of comorbidity and cost benefit of implantation. They rarely deal with how quality of life of the patient and their own mortality expectation impacts on the decision for ICD implantation. Once implanted, removal of the device is often impossible and when possible, as with an ICD, raise important and difficult ethical questions for patient, family, and doctor.
For those of us who are octogenarians and treat octogenarians, these issues are first and foremost in the decision process. The decision to use these devices for the relatively short-term benefit may become an onerous burden for the very elderly whose future quality of life can become abruptly abbreviated by the aging process. Easy exodus from life by sudden death may unfortunately be prolonged by an ICD.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
There has been a spate of recent publications dealing with the lack of implantable cardioverter-defibrillator implantations in the elderly. The most recent indicates that only 8% of patients over age 75 years who have experienced a non–ST-segment elevation myocardial infarction (NSTEMI) or STEMI receive an ICD largely due to the restriction of implantation within 40 days of the incident infarction because of the delayed repair of ventricular function after an MI and the uncertainty of ejection fraction measurements during this period. That article indicates that despite this delay, patients who receive an ICD had an improved survival over the subsequent 2 years, compared with those who did not (JAMA. 2015;313[24]:2433-40). Some of my octogenarian friends might question whether improved survival and the prevention of sudden death is a benefit at that age.
An accompanying editorial suggests that a closer follow-up of these patients is warranted in order to improve the rate of implantation in those patients who are discharged so that they do not “fall through the cracks” and are lost to follow-up (JAMA. 2015:313[24]:2429-30).
Although there has been a tapering off of the explosive use of ICDs in the United States, almost a quarter million devices were implanted between 2010 and 2011 (Heart Rhythm. 2013 Apr;10[4]:e59-65). The U.S. number is roughly four times that of Western Europe. Primary prevention was the reason for implantation in 73.8%, and half of the implantations were in patients over 65; 29% were in the 70-79 age group, and 14% were octogenarians. A history of New York Heart Association class II-IV heart failure was present in 82% and a myocardial infarction in 49%.
There are of course other reasons why the elderly may not receive an ICD. The most frequent are the presence of concomitant diseases like stroke, cancer, and chronic renal disease. However, many elderly do not wish to have their survival tied to a device that they have no control over. Some may view sudden death as an acceptable mortality outcome considering other alternatives. Certainly, adverse lifestyle changes at advanced age may be a reason for the reluctance to choose an ICD.
The application of our new technologies like ICDs, catheter-implanted aortic valves, and mini–left ventricular assist devices have been remarkably successful and have brought lifesaving interventions to thousands of patients. Their relative ease of application has led to a casualness in regard to appropriateness in patients with concomitant diseases, and particularly in the elderly.
The definition of who is elderly has changed dramatically in clinical trials from the mid–20th century when those studies excluded patients over 65. In today’s world, the definition of the elderly has become a slippery slope, as there is no age limit and the inclusion of octogenarians is not unusual. The observation that elderly postinfarction patients with decreased ejection fraction can experience improved survival needs to be evaluated in the light of important considerations of current and expected quality of life in individual patients, as well as their own mortality expectations.
Most of the studies examining implantation rates, extensively analyze the effect of comorbidity and cost benefit of implantation. They rarely deal with how quality of life of the patient and their own mortality expectation impacts on the decision for ICD implantation. Once implanted, removal of the device is often impossible and when possible, as with an ICD, raise important and difficult ethical questions for patient, family, and doctor.
For those of us who are octogenarians and treat octogenarians, these issues are first and foremost in the decision process. The decision to use these devices for the relatively short-term benefit may become an onerous burden for the very elderly whose future quality of life can become abruptly abbreviated by the aging process. Easy exodus from life by sudden death may unfortunately be prolonged by an ICD.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
There has been a spate of recent publications dealing with the lack of implantable cardioverter-defibrillator implantations in the elderly. The most recent indicates that only 8% of patients over age 75 years who have experienced a non–ST-segment elevation myocardial infarction (NSTEMI) or STEMI receive an ICD largely due to the restriction of implantation within 40 days of the incident infarction because of the delayed repair of ventricular function after an MI and the uncertainty of ejection fraction measurements during this period. That article indicates that despite this delay, patients who receive an ICD had an improved survival over the subsequent 2 years, compared with those who did not (JAMA. 2015;313[24]:2433-40). Some of my octogenarian friends might question whether improved survival and the prevention of sudden death is a benefit at that age.
An accompanying editorial suggests that a closer follow-up of these patients is warranted in order to improve the rate of implantation in those patients who are discharged so that they do not “fall through the cracks” and are lost to follow-up (JAMA. 2015:313[24]:2429-30).
Although there has been a tapering off of the explosive use of ICDs in the United States, almost a quarter million devices were implanted between 2010 and 2011 (Heart Rhythm. 2013 Apr;10[4]:e59-65). The U.S. number is roughly four times that of Western Europe. Primary prevention was the reason for implantation in 73.8%, and half of the implantations were in patients over 65; 29% were in the 70-79 age group, and 14% were octogenarians. A history of New York Heart Association class II-IV heart failure was present in 82% and a myocardial infarction in 49%.
There are of course other reasons why the elderly may not receive an ICD. The most frequent are the presence of concomitant diseases like stroke, cancer, and chronic renal disease. However, many elderly do not wish to have their survival tied to a device that they have no control over. Some may view sudden death as an acceptable mortality outcome considering other alternatives. Certainly, adverse lifestyle changes at advanced age may be a reason for the reluctance to choose an ICD.
The application of our new technologies like ICDs, catheter-implanted aortic valves, and mini–left ventricular assist devices have been remarkably successful and have brought lifesaving interventions to thousands of patients. Their relative ease of application has led to a casualness in regard to appropriateness in patients with concomitant diseases, and particularly in the elderly.
The definition of who is elderly has changed dramatically in clinical trials from the mid–20th century when those studies excluded patients over 65. In today’s world, the definition of the elderly has become a slippery slope, as there is no age limit and the inclusion of octogenarians is not unusual. The observation that elderly postinfarction patients with decreased ejection fraction can experience improved survival needs to be evaluated in the light of important considerations of current and expected quality of life in individual patients, as well as their own mortality expectations.
Most of the studies examining implantation rates, extensively analyze the effect of comorbidity and cost benefit of implantation. They rarely deal with how quality of life of the patient and their own mortality expectation impacts on the decision for ICD implantation. Once implanted, removal of the device is often impossible and when possible, as with an ICD, raise important and difficult ethical questions for patient, family, and doctor.
For those of us who are octogenarians and treat octogenarians, these issues are first and foremost in the decision process. The decision to use these devices for the relatively short-term benefit may become an onerous burden for the very elderly whose future quality of life can become abruptly abbreviated by the aging process. Easy exodus from life by sudden death may unfortunately be prolonged by an ICD.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
Method can predict prognosis in MM, group says

Photo courtesy of NIH
Assessing certain genetic abnormalities and a patient’s International Staging System (ISS) stage can reveal patients with high-risk multiple myeloma (MM), according to research published in the Journal of Clinical Oncology.
Investigators said this method can identify a majority of newly diagnosed MM patients who will relapse or die prematurely.
The team began this work by performing whole-exome sequencing on the 463 patients enrolled in the Myeloma XI trial.
This revealed 15 genes that were significantly mutated—IRF4, KRAS, NRAS, MAX, HIST1H1E, RB1, EGR1, TP53, TRAF3, FAM46C, DIS3, BRAF, LTB, CYLD, and FGFR3.
The investigators noted that mutations in the RAS (43%) and NF-κB (17%) pathways were common but proved prognostically neutral.
On the other hand, mutations in CCND1 and DNA repair pathway alterations—TP53, ATM, ATR, and ZNFHX4 mutations—were associated with poor survival.
For example, 2-year overall survival (OS) was 38.1% in patients with CCND1 mutations and 80% in those without them (P=0.005). Likewise, 2-year OS was 50% in patients with ATM mutations and 80.3% in those without them (P=0.01).
Conversely, mutations in IRF4 and EGR1 were associated with superior survival. Two-year OS was 100% in patients with IRF4 mutations and 79% in those without them (P=0.05). And 2-year OS was 100% in patients with EGR1 mutations and 78% in those without them (P=0.04).
In a multivariable analysis, an ISS stage of III, TP53 variants, CCND1 mutations, ATM and ATR mutations, amp(1q), and MYC translocations were independently associated with OS.
An ISS stage of III, age older than 70 years, t(4;14), MYC translocations, TP53 variants, ATM and ATR mutations, and ZFHX4 mutations were independently associated with progression-free survival (PFS).
In an attempt to predict PFS and OS accurately in newly diagnosed MM patients, the investigators combined the genetic risk factors they identified—mutations and copy number and structural abnormalities (CNSAs)—with clinical information captured by the ISS.
This led to 3 prognostic groups. Patients in group 1 (low-risk) had ISS I/II and no mutations/CNSAs. Patients in group 2 (moderate-risk) had ISS III with no mutations/CNSAs or ISS I/II/III with 1 mutation/CNSA. And patients in group 3 (high-risk) had 2 mutations/CNSAs regardless of their ISS.
The investigators said classifying patients in this way can identify 83% of patients who will relapse prematurely and 92% of patients who will die prematurely.
“Our study has identified genetic features which can identify those patients whose myeloma is likely to prove aggressive and to progress quickly,” said study author Gareth Morgan, MD, PhD, of The Institute of Cancer Research, London in the UK.
“We hope our study ultimately paves the way for genetic testing to pick out the minority of patients with myeloma with a poor prognosis, who might benefit from the most intensive possible treatment.” ![]()

Photo courtesy of NIH
Assessing certain genetic abnormalities and a patient’s International Staging System (ISS) stage can reveal patients with high-risk multiple myeloma (MM), according to research published in the Journal of Clinical Oncology.
Investigators said this method can identify a majority of newly diagnosed MM patients who will relapse or die prematurely.
The team began this work by performing whole-exome sequencing on the 463 patients enrolled in the Myeloma XI trial.
This revealed 15 genes that were significantly mutated—IRF4, KRAS, NRAS, MAX, HIST1H1E, RB1, EGR1, TP53, TRAF3, FAM46C, DIS3, BRAF, LTB, CYLD, and FGFR3.
The investigators noted that mutations in the RAS (43%) and NF-κB (17%) pathways were common but proved prognostically neutral.
On the other hand, mutations in CCND1 and DNA repair pathway alterations—TP53, ATM, ATR, and ZNFHX4 mutations—were associated with poor survival.
For example, 2-year overall survival (OS) was 38.1% in patients with CCND1 mutations and 80% in those without them (P=0.005). Likewise, 2-year OS was 50% in patients with ATM mutations and 80.3% in those without them (P=0.01).
Conversely, mutations in IRF4 and EGR1 were associated with superior survival. Two-year OS was 100% in patients with IRF4 mutations and 79% in those without them (P=0.05). And 2-year OS was 100% in patients with EGR1 mutations and 78% in those without them (P=0.04).
In a multivariable analysis, an ISS stage of III, TP53 variants, CCND1 mutations, ATM and ATR mutations, amp(1q), and MYC translocations were independently associated with OS.
An ISS stage of III, age older than 70 years, t(4;14), MYC translocations, TP53 variants, ATM and ATR mutations, and ZFHX4 mutations were independently associated with progression-free survival (PFS).
In an attempt to predict PFS and OS accurately in newly diagnosed MM patients, the investigators combined the genetic risk factors they identified—mutations and copy number and structural abnormalities (CNSAs)—with clinical information captured by the ISS.
This led to 3 prognostic groups. Patients in group 1 (low-risk) had ISS I/II and no mutations/CNSAs. Patients in group 2 (moderate-risk) had ISS III with no mutations/CNSAs or ISS I/II/III with 1 mutation/CNSA. And patients in group 3 (high-risk) had 2 mutations/CNSAs regardless of their ISS.
The investigators said classifying patients in this way can identify 83% of patients who will relapse prematurely and 92% of patients who will die prematurely.
“Our study has identified genetic features which can identify those patients whose myeloma is likely to prove aggressive and to progress quickly,” said study author Gareth Morgan, MD, PhD, of The Institute of Cancer Research, London in the UK.
“We hope our study ultimately paves the way for genetic testing to pick out the minority of patients with myeloma with a poor prognosis, who might benefit from the most intensive possible treatment.” ![]()

Photo courtesy of NIH
Assessing certain genetic abnormalities and a patient’s International Staging System (ISS) stage can reveal patients with high-risk multiple myeloma (MM), according to research published in the Journal of Clinical Oncology.
Investigators said this method can identify a majority of newly diagnosed MM patients who will relapse or die prematurely.
The team began this work by performing whole-exome sequencing on the 463 patients enrolled in the Myeloma XI trial.
This revealed 15 genes that were significantly mutated—IRF4, KRAS, NRAS, MAX, HIST1H1E, RB1, EGR1, TP53, TRAF3, FAM46C, DIS3, BRAF, LTB, CYLD, and FGFR3.
The investigators noted that mutations in the RAS (43%) and NF-κB (17%) pathways were common but proved prognostically neutral.
On the other hand, mutations in CCND1 and DNA repair pathway alterations—TP53, ATM, ATR, and ZNFHX4 mutations—were associated with poor survival.
For example, 2-year overall survival (OS) was 38.1% in patients with CCND1 mutations and 80% in those without them (P=0.005). Likewise, 2-year OS was 50% in patients with ATM mutations and 80.3% in those without them (P=0.01).
Conversely, mutations in IRF4 and EGR1 were associated with superior survival. Two-year OS was 100% in patients with IRF4 mutations and 79% in those without them (P=0.05). And 2-year OS was 100% in patients with EGR1 mutations and 78% in those without them (P=0.04).
In a multivariable analysis, an ISS stage of III, TP53 variants, CCND1 mutations, ATM and ATR mutations, amp(1q), and MYC translocations were independently associated with OS.
An ISS stage of III, age older than 70 years, t(4;14), MYC translocations, TP53 variants, ATM and ATR mutations, and ZFHX4 mutations were independently associated with progression-free survival (PFS).
In an attempt to predict PFS and OS accurately in newly diagnosed MM patients, the investigators combined the genetic risk factors they identified—mutations and copy number and structural abnormalities (CNSAs)—with clinical information captured by the ISS.
This led to 3 prognostic groups. Patients in group 1 (low-risk) had ISS I/II and no mutations/CNSAs. Patients in group 2 (moderate-risk) had ISS III with no mutations/CNSAs or ISS I/II/III with 1 mutation/CNSA. And patients in group 3 (high-risk) had 2 mutations/CNSAs regardless of their ISS.
The investigators said classifying patients in this way can identify 83% of patients who will relapse prematurely and 92% of patients who will die prematurely.
“Our study has identified genetic features which can identify those patients whose myeloma is likely to prove aggressive and to progress quickly,” said study author Gareth Morgan, MD, PhD, of The Institute of Cancer Research, London in the UK.
“We hope our study ultimately paves the way for genetic testing to pick out the minority of patients with myeloma with a poor prognosis, who might benefit from the most intensive possible treatment.” ![]()
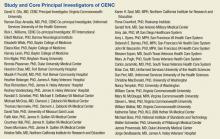
The VA/DoD Chronic Effects of Neurotrauma Consortium: An Overview at Year 1
The Chronic Effects of Neuro-trauma Consortium (CENC) is a federally funded research project devised to address the long-term effects of mild traumatic brain injury (mTBI) in military service members (SMs) and veterans. Announced by President Barack Obama on August 20, 2013, the CENC is one of 2 major initiatives developed in response to injuries incurred by U.S. service personnel during Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) as part of the National Research Action Plan. The CENC is jointly funded by the DoD and the VA, with a budget of $62.175 million over 5 years.
The consortium funds basic science, clinical, and translational research efforts with a closely integrated supportive infrastructure, including administrative services, regulatory guidance, study design, biostatistical consultation, data management, common data element application, and interdisciplinary communication. In addition, the consortium facilitates and integrates the activities of a diverse group of skilled specialty research teams, allowing them to fully focus their efforts on understanding and clarifying the relationship between combat-related mTBI and chronic neurotrauma effects, including neurodegeneration.
Background
Nearly 20% of the more than 2.6 million U.S. SMs deployed since 2003 to OEF and OIF have sustained at least 1 TBI, predominantly mTBI. Almost 8% of all OEF/OIF veterans demonstrate persistent post-TBI symptoms more than 6 months postinjury. Acute mTBI effects are typically transient, with headache, cognitive, behavioral, balance, and sleep symptoms most often seen, but symptoms may persist and even lead to lifelong disability. In these individuals, additional chronic effects, such as neuroendocrinologic abnormalities, seizures and seizurelike disorders, fatigue, vision and hearing abnormalities, and numerous other somatic symptoms are more common over time. The long-term effects from single or repeated mTBIs on the persistence of these symptoms, on combat and trauma-related comorbidities, and on long-term brain functioning are unknown.
Increasing evidence supports the link between both concussions and combat-related trauma with chronic traumatic encephalopathy (CTE), which results in progressive cognitive and behavioral decline in subpopulations 5 to 50 years out from repeated or cumulative mTBI exposures. The possibility of a link between mTBI, persistent symptoms, and early dementia has widespread implications for SMs and veterans; however, these chronic and late-life effects of mTBI are poorly understood.
Traumatic brain injuries of mixed severity have been linked to a higher incidence of Alzheimer disease (AD) and other dementias and an earlier onset of AD, although negative findings have also been reported. Chronic traumatic encephalopathy has been reported to occur in retired boxers at higher rates and at younger ages compared with dementia in the general population. More recently, brain autopsies of athletes from a variety of sports with confirmed CTE have demonstrated elevated tau proteins, tau-immunoreactive neurofibrillary tangles, and neuropil threads, suggesting that pathologic processes similar to those occurring in AD may be involved. Longitudinal research bridging SMs, veterans, and athletes with neurotrauma has been fragmented and incompletely focused on the strategic needs (eg, troop readiness) and vision of the DoD and VA.
Critical gaps exist in the literature with few prospective, well-controlled, longitudinal studies on late-life outcomes and neurodegeneration after mTBI, as well as in related basic science research. These research gaps are particularly prominent in the potentially unique injuries and difficulties seen in combat-exposed populations. The existing research, although suggestive, is not rigorous or robust enough to allow for a clear understanding of the relationships, risks, and potential effective interventions for mTBI, chronic symptoms, and neurodegeneration.
The CENC was developed to create a road map of existing knowledge gaps, to recruit the top relevant subject matter experts in the country, to develop and establish a cohesive set of rigorously designed studies to address these knowledge voids, and to leverage core consortium resources both efficiently and effectively.
Related: The Right Care at the Right Time and in the Right Place: The Role of Technology in the VHA
Given these gaps in scientific research and knowledge, the DoD and VA jointly issued a request for proposals to fund a project to address these concerns. After a competitive application process, an integrated proposal, led by researchers at Virginia Commonwealth University (VCU) was announced as the recipient of the Presidential award.
Consortium Structure
The CENC, serving as the comprehensive research network for DoD and VA, focuses on (1) identifying and characterizing the anatomic, molecular, and physiologic mechanisms of chronic injury from mTBI and potential neurodegeneration; (2) investigating the relationship of comorbidities (psychological, neurologic, sensory, motor, pain, cognitive, and neuroendocrine) of trauma and combat exposure to TBI with neurodegeneration; and (3) assessing the efficacy of existing and novel treatment and rehabilitation strategies for chronic effects and neurodegeneration following TBI.
The consortium is a collaboration among more than 30 universities, nonprofit research organizations, VAMCs, and military medical centers made up of a leadership core, 5 research infrastructure cores, 8 active studies, a data safety monitoring committee, a consumer advisory board, a scientific advisory board, and an independent granting mechanism to foster additional research in chronic effects after mTBI.
Leadership Core
The principal investigator for CENC is David X. Cifu, MD, chairman and professor of the VCU Department of Physical Medicine and Rehabilitation in Richmond, Virginia. The consortium co-principal investigators are Ramon Diaz-Arrastia, MD, PhD, professor of neurology, Uniformed Services University of the Health Sciences (USUHS) and director of the clinical research at the Center for Neuroscience and Regenerative Medicine in Bethesda, Maryland, and Rick L. Williams, PhD, co-principal investigator for CENC and senior statistician at RTI International in Raleigh, North Carolina.
Research Cores
The CENC operates 5 research infrastructure cores. The Biorepository Core, led by Dr. Diaz-Arrastia at USUHS, manages the storage and processing of biologic (blood and saliva) samples collected through all CENC protocols. The Biostatistics Core, led by Dr. Williams; Nancy Temkin, PhD; and Heather Belanger, PhD at RTI, provides study design guidance and biostatistical analysis to facilitate knowledge translation and dissemination.
The Data and Study Management Core is led by Dr. Williams at RTI. It centrally and securely maintains all collected data; oversees the clinical monitoring of research sites; provides a consortium research manager for each study who interacts with the study leadership, study site leaders, and staff; expedites and guides clinical protocols through regulatory approval processes; coordinates patient accrual and study activities across sites; develops and monitors data acquisition compliance; and facilitates exportation of all data collection to the Federal Interagency Traumatic Brain Injury Research informatics system.
The Neuroimaging Core is led by Elisabeth Wilde, PhD, at Baylor College of Medicine and the Michael E. DeBakey VAMC in Houston, Texas. This core facilitates sequence development and pulse programming; provides training and supervision of technologists and support personnel; ensures acquisition, transfer, and storage of imaging data; oversees quality assurance; performs conventional and advanced imaging analysis; and interprets neuroimaging data.
The Neuropathology Core is led by Dr. Dan Perl and colocated at USUHS and Edith Norse Rogers Memorial Veterans Hospital/VA Boston Healthcare System. Dr. Perl manages the collection of brain specimens from the participants, using an existing national network of dieners and neuropathologists, catalogs and stores tissues, and administers requests for use of these tissues.
Active Research Studies
The Longitudinal Cohort Study addresses a critical research gap by identifying and characterizing the late effects of mTBI and assessing the influence and interaction of the many potential risk factors for early dementia. The study uses a wide array of self-report, laboratory, biophysical, neuropsychologic, and imaging assessment tools to evaluate a cohort (n = 880) of U.S. OEF/OIF combatants who have had at least 1 mTBI and a control group of participants (n = 220) who have experienced combat but have not had a mTBI, and then re-assesses them annually (in person or via telephone), with the goal of following the cohort for as long as resources are available.
Collaborating sites for this study include Hunter Holmes McGuire VAMC in Richmond, Virginia; James A. Haley Veterans’ Hospital in Tampa, Florida; Michael E. DeBakey VAMC in Houston, Texas; Audie L. Murphy Memorial Veterans Hospital in San Antonio, Texas; VA Boston Healthcare System; Minneapolis VA Health Care System in Minnesota; and Fort Belvoir in Virginia. Dr. Cifu and Dr. William Walker lead this study.
Epidemiology of mTBI and Neurosensory Outcomes
This project integrates and analyzes several VA, DoD, and Centers for Medicare and Medicaid Services health care system data sets to study the chronic effects of mTBI on neurodegenerative disease and other comorbidities. The primary aims of the project include evaluating the association between mTBI and short-term clinical outcomes, including factors associated with resilience and effects of treatment; investigating long-term clinical outcomes, including neurosensory disorders and mortality; and identifying factors associated with low- and high-distress trajectories of comorbid burden after mTBI. Dr. Kristine Yaffe, Dr. Mary Jo Pugh, and Dr. Michael McCrea, are the leads of this study.
Tau Modification and Aggregation in TBI
This study aims to develop an animal model of repetitive-mTBI, which will allow the tracking of progressive intraneuronal tau alterations that can be correlated with behavioral dysfunction, neuronal protein, and gene expression signatures that can be used to assess the effects of interventions. The observations made in the animal model will be compared with findings generated from tissue obtained at autopsy from deceased SMs and veterans who sustained repetitive-mTBI. Dr. Fiona Crawford and Dr. Elliott Mufson lead this study.
Otolith Dysfunction
This study is examining the effect of inner ear dysfunction on balance, gait, and quality of life (QOL). Recent evidence suggests that otolith organ dysfunction can occur in patients with mTBI or blast exposure. If the dizziness and imbalance symptoms that occur following head injury or blast exposure are related to injury to the otolith organs rather than to the horizontal semicircular canal, then new treatment approaches may be necessary to focus on otolith organ pathway recovery. Performance on balance tasks while standing and walking and questionnaires on the impact on QOL will be compared in 4 groups of individuals (n = 120) with and without head injury/blast exposure (otolith organ dysfunction, horizontal canal dysfunction, both otolith and horizontal canal dysfunction, and healthy individuals). Dr. Faith Akin leads this study.
ADAPT
The ADAPT study (Assessment and Long-term Outcome and Disability in Active Duty Military Prospectively Examined following Concussive TBI) is investigating the association of early clinical and imaging measures with late (5 year) clinical outcome after blast-related mTBI from combat. The study (n = 100) will use 5-year follow-up advanced magnetic resonance imaging (MRI) and clinical outcome measures of combat mTBI, as a continuation of previous longitudinal research efforts (n = 575). Two groups of subjects will be studied: subjects who sustained a mTBI from blast during deployment and subjects without history of blast exposure and no diagnosis of deployment mTBI. Dr. Christine MacDonald leads this study.
Diffusion Tensor Imaging Phantom Study
This study involves the development and testing of a novel phantom that would be used to enhance accuracy, consistency, and reliability in both isotropic and anisotropic measurements derived from diffusion imaging, as well as other MRI-based measurements, using universal fluid disk chambers in a single phantom. Currently, the acquisition of diffusion data in large studies and clinical trials lacks standardization, and important differences exist in how data are acquired on scanners of different manufacturers, using different hardware or software, or when different acquisition parameters are used. As a result, development of large pools of data and the creation of normative data are hampered by inhomogeneity in the data set, which is difficult to analyze. The study team will perform detailed testing of the phantom materials and phantoms themselves, as well as examine diffusion imaging on 1 to 2 human volunteers at each of the 4 sites. Intra- and interscanner differences will be measured, and based on these findings, a more standardized imaging protocol that will provide optimal uniformity of diffusion imaging will be designed. Dr. Elisabeth Wilde leads this study.
Novel White Matter Imaging to Improve mTBI Diagnosis
This study will use myelin-sensitive novel imaging techniques (McDespot [multi-component driven equilibrium single pulse observation of T1/T2]) to improve correspondence with diagnostic groups after trauma exposure and correlation with cognitive deficits in mTBI. The study will recruit individuals (n = 82) from 4 groups, comorbid mTBI and posttraumatic stress disorder (PTSD), only mTBI, only PTSD, and controls who will be prospectively comprehensively assessed clinically (clinical interview, physical exam, neuropsychological assessment) and with advanced imaging (including McDespot, diffusion tensor imaging, and other forms of imaging). Dr. Amy Jak leads this study.
Peer Review Program
The CENC has an integrated grant program to identify scientifically valid and strategically important research projects. To date, 2 rounds of proposal requests and project support have been completed. Scientific review is conducted under the CENC Peer Review Program. Scientifically meritorious studies are identified by independent peer review and then undergo a Programmatic Review by CENC leadership before being recommended for funding to the Government Steering Committee (GSC). Studies that are recommended must address road map gaps, develop innovative approaches, or provide an avenue for new researchers and novel research approaches to contribute to the consortium mission to advance the science of brain injury treatment and prevention. The CENC grant program is administered by Dr. Steven L. West.
Consumer Advisory Board
The Consumer Advisory Board (CAB) advises and makes nonbinding recommendations to CENC. The responsibilities of the committee members include (1) providing information that helps CENC leadership better appreciate and understand the issues and needs of TBI survivors and their support networks so appropriate research can be designed and implemented; (2) evaluating existing research and making recommendations for additions and/or modifications to project procedures; (3) providing input for the road map for future research based on members’ personal experiences and knowledge; and (4) providing linkages to targeted communities for direct feedback and to assist in forming collaborative partnerships.
The CAB is composed of survivors of TBI, family members of survivors of TBI, providers of TBI services, service organizations with specific ties to SMs and veterans, and clinical and corporate representatives of transportation services for the disabled, the independent living movement, and assistive technology. Persons who are heavily engaged in political activity or who actively endorse a specific device or product are not eligible for membership on the CAB. Membership is composed of persons nominated by CENC leadership and approved by the GSC. The CAB is co-chaired by Charles Gatlin, MS, and General (Ret.) Peter Chiarelli.
Scientific Advisory Board
The members of the Scientific Advisory Board (SAB) advise and make nonbinding recommendations to CENC. Responsibilities of the committee members include (1) providing information that may help the consortium leadership better understand the issues related to TBI; (2) evaluating existing research; (3) recommending additions and/or modifications to project procedures; and (4) assisting CENC by helping leverage relationships with other researchers. The SAB is composed of members of the research community on TBI who are not part of CENC. Persons who may be considered to have positions of authority, such as active or retired flag officers or chief executive officers, may be eligible for general SAB membership but are not be eligible for chair positions. Membership is composed of persons nominated by CENC leadership and approved by the GSC. Col. Jamie Grimes, MD, and Henry Lew, MD, PhD, co-chair the SAB.
Federal Oversight
The GSC oversees CENC. Members of the GSC are DoD and VA appointed and represent both government agencies and nongovernment subject matter experts. The GSC approves all studies to be conducted, recommends new studies, and identifies existing and new requirements. The GSC is the overall main governing and management committee for the project and the committee through which the DoD and VA interact and collaborate with the CENC. The GSC determines all major scientific decisions, and clinical studies proposed by the CENC committee proceed to the implementation stage only with the approval of the GSC.
Acknowledgements
This research is supported by grants 1-I01-RX-001135-01-A2 (PI: F. Aiken), 1-I01-RX-001774-01 (PI: F. Crawford), 1-I01-RX-001880-01 (PI: E. Wilde), 1-I01-CX-001135-01 (PI: S. Cifu), and 1-I01-CX-001246-01 (PI: K. Yaffe) from the U.S. Department of Veterans Affairs and by grant W81XWH-13-2-0095 (PI: D. Cifu) from the U.S. Department of Defense, Congressionally Directed Medical Research Programs. The ideas and opinions expressed in this paper do not necessarily represent the views of the Department of Veterans Affairs, the Department of Defense, or the U.S. Government.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
The Chronic Effects of Neuro-trauma Consortium (CENC) is a federally funded research project devised to address the long-term effects of mild traumatic brain injury (mTBI) in military service members (SMs) and veterans. Announced by President Barack Obama on August 20, 2013, the CENC is one of 2 major initiatives developed in response to injuries incurred by U.S. service personnel during Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) as part of the National Research Action Plan. The CENC is jointly funded by the DoD and the VA, with a budget of $62.175 million over 5 years.
The consortium funds basic science, clinical, and translational research efforts with a closely integrated supportive infrastructure, including administrative services, regulatory guidance, study design, biostatistical consultation, data management, common data element application, and interdisciplinary communication. In addition, the consortium facilitates and integrates the activities of a diverse group of skilled specialty research teams, allowing them to fully focus their efforts on understanding and clarifying the relationship between combat-related mTBI and chronic neurotrauma effects, including neurodegeneration.
Background
Nearly 20% of the more than 2.6 million U.S. SMs deployed since 2003 to OEF and OIF have sustained at least 1 TBI, predominantly mTBI. Almost 8% of all OEF/OIF veterans demonstrate persistent post-TBI symptoms more than 6 months postinjury. Acute mTBI effects are typically transient, with headache, cognitive, behavioral, balance, and sleep symptoms most often seen, but symptoms may persist and even lead to lifelong disability. In these individuals, additional chronic effects, such as neuroendocrinologic abnormalities, seizures and seizurelike disorders, fatigue, vision and hearing abnormalities, and numerous other somatic symptoms are more common over time. The long-term effects from single or repeated mTBIs on the persistence of these symptoms, on combat and trauma-related comorbidities, and on long-term brain functioning are unknown.
Increasing evidence supports the link between both concussions and combat-related trauma with chronic traumatic encephalopathy (CTE), which results in progressive cognitive and behavioral decline in subpopulations 5 to 50 years out from repeated or cumulative mTBI exposures. The possibility of a link between mTBI, persistent symptoms, and early dementia has widespread implications for SMs and veterans; however, these chronic and late-life effects of mTBI are poorly understood.
Traumatic brain injuries of mixed severity have been linked to a higher incidence of Alzheimer disease (AD) and other dementias and an earlier onset of AD, although negative findings have also been reported. Chronic traumatic encephalopathy has been reported to occur in retired boxers at higher rates and at younger ages compared with dementia in the general population. More recently, brain autopsies of athletes from a variety of sports with confirmed CTE have demonstrated elevated tau proteins, tau-immunoreactive neurofibrillary tangles, and neuropil threads, suggesting that pathologic processes similar to those occurring in AD may be involved. Longitudinal research bridging SMs, veterans, and athletes with neurotrauma has been fragmented and incompletely focused on the strategic needs (eg, troop readiness) and vision of the DoD and VA.
Critical gaps exist in the literature with few prospective, well-controlled, longitudinal studies on late-life outcomes and neurodegeneration after mTBI, as well as in related basic science research. These research gaps are particularly prominent in the potentially unique injuries and difficulties seen in combat-exposed populations. The existing research, although suggestive, is not rigorous or robust enough to allow for a clear understanding of the relationships, risks, and potential effective interventions for mTBI, chronic symptoms, and neurodegeneration.
The CENC was developed to create a road map of existing knowledge gaps, to recruit the top relevant subject matter experts in the country, to develop and establish a cohesive set of rigorously designed studies to address these knowledge voids, and to leverage core consortium resources both efficiently and effectively.
Related: The Right Care at the Right Time and in the Right Place: The Role of Technology in the VHA
Given these gaps in scientific research and knowledge, the DoD and VA jointly issued a request for proposals to fund a project to address these concerns. After a competitive application process, an integrated proposal, led by researchers at Virginia Commonwealth University (VCU) was announced as the recipient of the Presidential award.
Consortium Structure
The CENC, serving as the comprehensive research network for DoD and VA, focuses on (1) identifying and characterizing the anatomic, molecular, and physiologic mechanisms of chronic injury from mTBI and potential neurodegeneration; (2) investigating the relationship of comorbidities (psychological, neurologic, sensory, motor, pain, cognitive, and neuroendocrine) of trauma and combat exposure to TBI with neurodegeneration; and (3) assessing the efficacy of existing and novel treatment and rehabilitation strategies for chronic effects and neurodegeneration following TBI.
The consortium is a collaboration among more than 30 universities, nonprofit research organizations, VAMCs, and military medical centers made up of a leadership core, 5 research infrastructure cores, 8 active studies, a data safety monitoring committee, a consumer advisory board, a scientific advisory board, and an independent granting mechanism to foster additional research in chronic effects after mTBI.
Leadership Core
The principal investigator for CENC is David X. Cifu, MD, chairman and professor of the VCU Department of Physical Medicine and Rehabilitation in Richmond, Virginia. The consortium co-principal investigators are Ramon Diaz-Arrastia, MD, PhD, professor of neurology, Uniformed Services University of the Health Sciences (USUHS) and director of the clinical research at the Center for Neuroscience and Regenerative Medicine in Bethesda, Maryland, and Rick L. Williams, PhD, co-principal investigator for CENC and senior statistician at RTI International in Raleigh, North Carolina.
Research Cores
The CENC operates 5 research infrastructure cores. The Biorepository Core, led by Dr. Diaz-Arrastia at USUHS, manages the storage and processing of biologic (blood and saliva) samples collected through all CENC protocols. The Biostatistics Core, led by Dr. Williams; Nancy Temkin, PhD; and Heather Belanger, PhD at RTI, provides study design guidance and biostatistical analysis to facilitate knowledge translation and dissemination.
The Data and Study Management Core is led by Dr. Williams at RTI. It centrally and securely maintains all collected data; oversees the clinical monitoring of research sites; provides a consortium research manager for each study who interacts with the study leadership, study site leaders, and staff; expedites and guides clinical protocols through regulatory approval processes; coordinates patient accrual and study activities across sites; develops and monitors data acquisition compliance; and facilitates exportation of all data collection to the Federal Interagency Traumatic Brain Injury Research informatics system.
The Neuroimaging Core is led by Elisabeth Wilde, PhD, at Baylor College of Medicine and the Michael E. DeBakey VAMC in Houston, Texas. This core facilitates sequence development and pulse programming; provides training and supervision of technologists and support personnel; ensures acquisition, transfer, and storage of imaging data; oversees quality assurance; performs conventional and advanced imaging analysis; and interprets neuroimaging data.
The Neuropathology Core is led by Dr. Dan Perl and colocated at USUHS and Edith Norse Rogers Memorial Veterans Hospital/VA Boston Healthcare System. Dr. Perl manages the collection of brain specimens from the participants, using an existing national network of dieners and neuropathologists, catalogs and stores tissues, and administers requests for use of these tissues.
Active Research Studies
The Longitudinal Cohort Study addresses a critical research gap by identifying and characterizing the late effects of mTBI and assessing the influence and interaction of the many potential risk factors for early dementia. The study uses a wide array of self-report, laboratory, biophysical, neuropsychologic, and imaging assessment tools to evaluate a cohort (n = 880) of U.S. OEF/OIF combatants who have had at least 1 mTBI and a control group of participants (n = 220) who have experienced combat but have not had a mTBI, and then re-assesses them annually (in person or via telephone), with the goal of following the cohort for as long as resources are available.
Collaborating sites for this study include Hunter Holmes McGuire VAMC in Richmond, Virginia; James A. Haley Veterans’ Hospital in Tampa, Florida; Michael E. DeBakey VAMC in Houston, Texas; Audie L. Murphy Memorial Veterans Hospital in San Antonio, Texas; VA Boston Healthcare System; Minneapolis VA Health Care System in Minnesota; and Fort Belvoir in Virginia. Dr. Cifu and Dr. William Walker lead this study.
Epidemiology of mTBI and Neurosensory Outcomes
This project integrates and analyzes several VA, DoD, and Centers for Medicare and Medicaid Services health care system data sets to study the chronic effects of mTBI on neurodegenerative disease and other comorbidities. The primary aims of the project include evaluating the association between mTBI and short-term clinical outcomes, including factors associated with resilience and effects of treatment; investigating long-term clinical outcomes, including neurosensory disorders and mortality; and identifying factors associated with low- and high-distress trajectories of comorbid burden after mTBI. Dr. Kristine Yaffe, Dr. Mary Jo Pugh, and Dr. Michael McCrea, are the leads of this study.
Tau Modification and Aggregation in TBI
This study aims to develop an animal model of repetitive-mTBI, which will allow the tracking of progressive intraneuronal tau alterations that can be correlated with behavioral dysfunction, neuronal protein, and gene expression signatures that can be used to assess the effects of interventions. The observations made in the animal model will be compared with findings generated from tissue obtained at autopsy from deceased SMs and veterans who sustained repetitive-mTBI. Dr. Fiona Crawford and Dr. Elliott Mufson lead this study.
Otolith Dysfunction
This study is examining the effect of inner ear dysfunction on balance, gait, and quality of life (QOL). Recent evidence suggests that otolith organ dysfunction can occur in patients with mTBI or blast exposure. If the dizziness and imbalance symptoms that occur following head injury or blast exposure are related to injury to the otolith organs rather than to the horizontal semicircular canal, then new treatment approaches may be necessary to focus on otolith organ pathway recovery. Performance on balance tasks while standing and walking and questionnaires on the impact on QOL will be compared in 4 groups of individuals (n = 120) with and without head injury/blast exposure (otolith organ dysfunction, horizontal canal dysfunction, both otolith and horizontal canal dysfunction, and healthy individuals). Dr. Faith Akin leads this study.
ADAPT
The ADAPT study (Assessment and Long-term Outcome and Disability in Active Duty Military Prospectively Examined following Concussive TBI) is investigating the association of early clinical and imaging measures with late (5 year) clinical outcome after blast-related mTBI from combat. The study (n = 100) will use 5-year follow-up advanced magnetic resonance imaging (MRI) and clinical outcome measures of combat mTBI, as a continuation of previous longitudinal research efforts (n = 575). Two groups of subjects will be studied: subjects who sustained a mTBI from blast during deployment and subjects without history of blast exposure and no diagnosis of deployment mTBI. Dr. Christine MacDonald leads this study.
Diffusion Tensor Imaging Phantom Study
This study involves the development and testing of a novel phantom that would be used to enhance accuracy, consistency, and reliability in both isotropic and anisotropic measurements derived from diffusion imaging, as well as other MRI-based measurements, using universal fluid disk chambers in a single phantom. Currently, the acquisition of diffusion data in large studies and clinical trials lacks standardization, and important differences exist in how data are acquired on scanners of different manufacturers, using different hardware or software, or when different acquisition parameters are used. As a result, development of large pools of data and the creation of normative data are hampered by inhomogeneity in the data set, which is difficult to analyze. The study team will perform detailed testing of the phantom materials and phantoms themselves, as well as examine diffusion imaging on 1 to 2 human volunteers at each of the 4 sites. Intra- and interscanner differences will be measured, and based on these findings, a more standardized imaging protocol that will provide optimal uniformity of diffusion imaging will be designed. Dr. Elisabeth Wilde leads this study.
Novel White Matter Imaging to Improve mTBI Diagnosis
This study will use myelin-sensitive novel imaging techniques (McDespot [multi-component driven equilibrium single pulse observation of T1/T2]) to improve correspondence with diagnostic groups after trauma exposure and correlation with cognitive deficits in mTBI. The study will recruit individuals (n = 82) from 4 groups, comorbid mTBI and posttraumatic stress disorder (PTSD), only mTBI, only PTSD, and controls who will be prospectively comprehensively assessed clinically (clinical interview, physical exam, neuropsychological assessment) and with advanced imaging (including McDespot, diffusion tensor imaging, and other forms of imaging). Dr. Amy Jak leads this study.
Peer Review Program
The CENC has an integrated grant program to identify scientifically valid and strategically important research projects. To date, 2 rounds of proposal requests and project support have been completed. Scientific review is conducted under the CENC Peer Review Program. Scientifically meritorious studies are identified by independent peer review and then undergo a Programmatic Review by CENC leadership before being recommended for funding to the Government Steering Committee (GSC). Studies that are recommended must address road map gaps, develop innovative approaches, or provide an avenue for new researchers and novel research approaches to contribute to the consortium mission to advance the science of brain injury treatment and prevention. The CENC grant program is administered by Dr. Steven L. West.
Consumer Advisory Board
The Consumer Advisory Board (CAB) advises and makes nonbinding recommendations to CENC. The responsibilities of the committee members include (1) providing information that helps CENC leadership better appreciate and understand the issues and needs of TBI survivors and their support networks so appropriate research can be designed and implemented; (2) evaluating existing research and making recommendations for additions and/or modifications to project procedures; (3) providing input for the road map for future research based on members’ personal experiences and knowledge; and (4) providing linkages to targeted communities for direct feedback and to assist in forming collaborative partnerships.
The CAB is composed of survivors of TBI, family members of survivors of TBI, providers of TBI services, service organizations with specific ties to SMs and veterans, and clinical and corporate representatives of transportation services for the disabled, the independent living movement, and assistive technology. Persons who are heavily engaged in political activity or who actively endorse a specific device or product are not eligible for membership on the CAB. Membership is composed of persons nominated by CENC leadership and approved by the GSC. The CAB is co-chaired by Charles Gatlin, MS, and General (Ret.) Peter Chiarelli.
Scientific Advisory Board
The members of the Scientific Advisory Board (SAB) advise and make nonbinding recommendations to CENC. Responsibilities of the committee members include (1) providing information that may help the consortium leadership better understand the issues related to TBI; (2) evaluating existing research; (3) recommending additions and/or modifications to project procedures; and (4) assisting CENC by helping leverage relationships with other researchers. The SAB is composed of members of the research community on TBI who are not part of CENC. Persons who may be considered to have positions of authority, such as active or retired flag officers or chief executive officers, may be eligible for general SAB membership but are not be eligible for chair positions. Membership is composed of persons nominated by CENC leadership and approved by the GSC. Col. Jamie Grimes, MD, and Henry Lew, MD, PhD, co-chair the SAB.
Federal Oversight
The GSC oversees CENC. Members of the GSC are DoD and VA appointed and represent both government agencies and nongovernment subject matter experts. The GSC approves all studies to be conducted, recommends new studies, and identifies existing and new requirements. The GSC is the overall main governing and management committee for the project and the committee through which the DoD and VA interact and collaborate with the CENC. The GSC determines all major scientific decisions, and clinical studies proposed by the CENC committee proceed to the implementation stage only with the approval of the GSC.
Acknowledgements
This research is supported by grants 1-I01-RX-001135-01-A2 (PI: F. Aiken), 1-I01-RX-001774-01 (PI: F. Crawford), 1-I01-RX-001880-01 (PI: E. Wilde), 1-I01-CX-001135-01 (PI: S. Cifu), and 1-I01-CX-001246-01 (PI: K. Yaffe) from the U.S. Department of Veterans Affairs and by grant W81XWH-13-2-0095 (PI: D. Cifu) from the U.S. Department of Defense, Congressionally Directed Medical Research Programs. The ideas and opinions expressed in this paper do not necessarily represent the views of the Department of Veterans Affairs, the Department of Defense, or the U.S. Government.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
The Chronic Effects of Neuro-trauma Consortium (CENC) is a federally funded research project devised to address the long-term effects of mild traumatic brain injury (mTBI) in military service members (SMs) and veterans. Announced by President Barack Obama on August 20, 2013, the CENC is one of 2 major initiatives developed in response to injuries incurred by U.S. service personnel during Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) as part of the National Research Action Plan. The CENC is jointly funded by the DoD and the VA, with a budget of $62.175 million over 5 years.
The consortium funds basic science, clinical, and translational research efforts with a closely integrated supportive infrastructure, including administrative services, regulatory guidance, study design, biostatistical consultation, data management, common data element application, and interdisciplinary communication. In addition, the consortium facilitates and integrates the activities of a diverse group of skilled specialty research teams, allowing them to fully focus their efforts on understanding and clarifying the relationship between combat-related mTBI and chronic neurotrauma effects, including neurodegeneration.
Background
Nearly 20% of the more than 2.6 million U.S. SMs deployed since 2003 to OEF and OIF have sustained at least 1 TBI, predominantly mTBI. Almost 8% of all OEF/OIF veterans demonstrate persistent post-TBI symptoms more than 6 months postinjury. Acute mTBI effects are typically transient, with headache, cognitive, behavioral, balance, and sleep symptoms most often seen, but symptoms may persist and even lead to lifelong disability. In these individuals, additional chronic effects, such as neuroendocrinologic abnormalities, seizures and seizurelike disorders, fatigue, vision and hearing abnormalities, and numerous other somatic symptoms are more common over time. The long-term effects from single or repeated mTBIs on the persistence of these symptoms, on combat and trauma-related comorbidities, and on long-term brain functioning are unknown.
Increasing evidence supports the link between both concussions and combat-related trauma with chronic traumatic encephalopathy (CTE), which results in progressive cognitive and behavioral decline in subpopulations 5 to 50 years out from repeated or cumulative mTBI exposures. The possibility of a link between mTBI, persistent symptoms, and early dementia has widespread implications for SMs and veterans; however, these chronic and late-life effects of mTBI are poorly understood.
Traumatic brain injuries of mixed severity have been linked to a higher incidence of Alzheimer disease (AD) and other dementias and an earlier onset of AD, although negative findings have also been reported. Chronic traumatic encephalopathy has been reported to occur in retired boxers at higher rates and at younger ages compared with dementia in the general population. More recently, brain autopsies of athletes from a variety of sports with confirmed CTE have demonstrated elevated tau proteins, tau-immunoreactive neurofibrillary tangles, and neuropil threads, suggesting that pathologic processes similar to those occurring in AD may be involved. Longitudinal research bridging SMs, veterans, and athletes with neurotrauma has been fragmented and incompletely focused on the strategic needs (eg, troop readiness) and vision of the DoD and VA.
Critical gaps exist in the literature with few prospective, well-controlled, longitudinal studies on late-life outcomes and neurodegeneration after mTBI, as well as in related basic science research. These research gaps are particularly prominent in the potentially unique injuries and difficulties seen in combat-exposed populations. The existing research, although suggestive, is not rigorous or robust enough to allow for a clear understanding of the relationships, risks, and potential effective interventions for mTBI, chronic symptoms, and neurodegeneration.
The CENC was developed to create a road map of existing knowledge gaps, to recruit the top relevant subject matter experts in the country, to develop and establish a cohesive set of rigorously designed studies to address these knowledge voids, and to leverage core consortium resources both efficiently and effectively.
Related: The Right Care at the Right Time and in the Right Place: The Role of Technology in the VHA
Given these gaps in scientific research and knowledge, the DoD and VA jointly issued a request for proposals to fund a project to address these concerns. After a competitive application process, an integrated proposal, led by researchers at Virginia Commonwealth University (VCU) was announced as the recipient of the Presidential award.
Consortium Structure
The CENC, serving as the comprehensive research network for DoD and VA, focuses on (1) identifying and characterizing the anatomic, molecular, and physiologic mechanisms of chronic injury from mTBI and potential neurodegeneration; (2) investigating the relationship of comorbidities (psychological, neurologic, sensory, motor, pain, cognitive, and neuroendocrine) of trauma and combat exposure to TBI with neurodegeneration; and (3) assessing the efficacy of existing and novel treatment and rehabilitation strategies for chronic effects and neurodegeneration following TBI.
The consortium is a collaboration among more than 30 universities, nonprofit research organizations, VAMCs, and military medical centers made up of a leadership core, 5 research infrastructure cores, 8 active studies, a data safety monitoring committee, a consumer advisory board, a scientific advisory board, and an independent granting mechanism to foster additional research in chronic effects after mTBI.
Leadership Core
The principal investigator for CENC is David X. Cifu, MD, chairman and professor of the VCU Department of Physical Medicine and Rehabilitation in Richmond, Virginia. The consortium co-principal investigators are Ramon Diaz-Arrastia, MD, PhD, professor of neurology, Uniformed Services University of the Health Sciences (USUHS) and director of the clinical research at the Center for Neuroscience and Regenerative Medicine in Bethesda, Maryland, and Rick L. Williams, PhD, co-principal investigator for CENC and senior statistician at RTI International in Raleigh, North Carolina.
Research Cores
The CENC operates 5 research infrastructure cores. The Biorepository Core, led by Dr. Diaz-Arrastia at USUHS, manages the storage and processing of biologic (blood and saliva) samples collected through all CENC protocols. The Biostatistics Core, led by Dr. Williams; Nancy Temkin, PhD; and Heather Belanger, PhD at RTI, provides study design guidance and biostatistical analysis to facilitate knowledge translation and dissemination.
The Data and Study Management Core is led by Dr. Williams at RTI. It centrally and securely maintains all collected data; oversees the clinical monitoring of research sites; provides a consortium research manager for each study who interacts with the study leadership, study site leaders, and staff; expedites and guides clinical protocols through regulatory approval processes; coordinates patient accrual and study activities across sites; develops and monitors data acquisition compliance; and facilitates exportation of all data collection to the Federal Interagency Traumatic Brain Injury Research informatics system.
The Neuroimaging Core is led by Elisabeth Wilde, PhD, at Baylor College of Medicine and the Michael E. DeBakey VAMC in Houston, Texas. This core facilitates sequence development and pulse programming; provides training and supervision of technologists and support personnel; ensures acquisition, transfer, and storage of imaging data; oversees quality assurance; performs conventional and advanced imaging analysis; and interprets neuroimaging data.
The Neuropathology Core is led by Dr. Dan Perl and colocated at USUHS and Edith Norse Rogers Memorial Veterans Hospital/VA Boston Healthcare System. Dr. Perl manages the collection of brain specimens from the participants, using an existing national network of dieners and neuropathologists, catalogs and stores tissues, and administers requests for use of these tissues.
Active Research Studies
The Longitudinal Cohort Study addresses a critical research gap by identifying and characterizing the late effects of mTBI and assessing the influence and interaction of the many potential risk factors for early dementia. The study uses a wide array of self-report, laboratory, biophysical, neuropsychologic, and imaging assessment tools to evaluate a cohort (n = 880) of U.S. OEF/OIF combatants who have had at least 1 mTBI and a control group of participants (n = 220) who have experienced combat but have not had a mTBI, and then re-assesses them annually (in person or via telephone), with the goal of following the cohort for as long as resources are available.
Collaborating sites for this study include Hunter Holmes McGuire VAMC in Richmond, Virginia; James A. Haley Veterans’ Hospital in Tampa, Florida; Michael E. DeBakey VAMC in Houston, Texas; Audie L. Murphy Memorial Veterans Hospital in San Antonio, Texas; VA Boston Healthcare System; Minneapolis VA Health Care System in Minnesota; and Fort Belvoir in Virginia. Dr. Cifu and Dr. William Walker lead this study.
Epidemiology of mTBI and Neurosensory Outcomes
This project integrates and analyzes several VA, DoD, and Centers for Medicare and Medicaid Services health care system data sets to study the chronic effects of mTBI on neurodegenerative disease and other comorbidities. The primary aims of the project include evaluating the association between mTBI and short-term clinical outcomes, including factors associated with resilience and effects of treatment; investigating long-term clinical outcomes, including neurosensory disorders and mortality; and identifying factors associated with low- and high-distress trajectories of comorbid burden after mTBI. Dr. Kristine Yaffe, Dr. Mary Jo Pugh, and Dr. Michael McCrea, are the leads of this study.
Tau Modification and Aggregation in TBI
This study aims to develop an animal model of repetitive-mTBI, which will allow the tracking of progressive intraneuronal tau alterations that can be correlated with behavioral dysfunction, neuronal protein, and gene expression signatures that can be used to assess the effects of interventions. The observations made in the animal model will be compared with findings generated from tissue obtained at autopsy from deceased SMs and veterans who sustained repetitive-mTBI. Dr. Fiona Crawford and Dr. Elliott Mufson lead this study.
Otolith Dysfunction
This study is examining the effect of inner ear dysfunction on balance, gait, and quality of life (QOL). Recent evidence suggests that otolith organ dysfunction can occur in patients with mTBI or blast exposure. If the dizziness and imbalance symptoms that occur following head injury or blast exposure are related to injury to the otolith organs rather than to the horizontal semicircular canal, then new treatment approaches may be necessary to focus on otolith organ pathway recovery. Performance on balance tasks while standing and walking and questionnaires on the impact on QOL will be compared in 4 groups of individuals (n = 120) with and without head injury/blast exposure (otolith organ dysfunction, horizontal canal dysfunction, both otolith and horizontal canal dysfunction, and healthy individuals). Dr. Faith Akin leads this study.
ADAPT
The ADAPT study (Assessment and Long-term Outcome and Disability in Active Duty Military Prospectively Examined following Concussive TBI) is investigating the association of early clinical and imaging measures with late (5 year) clinical outcome after blast-related mTBI from combat. The study (n = 100) will use 5-year follow-up advanced magnetic resonance imaging (MRI) and clinical outcome measures of combat mTBI, as a continuation of previous longitudinal research efforts (n = 575). Two groups of subjects will be studied: subjects who sustained a mTBI from blast during deployment and subjects without history of blast exposure and no diagnosis of deployment mTBI. Dr. Christine MacDonald leads this study.
Diffusion Tensor Imaging Phantom Study
This study involves the development and testing of a novel phantom that would be used to enhance accuracy, consistency, and reliability in both isotropic and anisotropic measurements derived from diffusion imaging, as well as other MRI-based measurements, using universal fluid disk chambers in a single phantom. Currently, the acquisition of diffusion data in large studies and clinical trials lacks standardization, and important differences exist in how data are acquired on scanners of different manufacturers, using different hardware or software, or when different acquisition parameters are used. As a result, development of large pools of data and the creation of normative data are hampered by inhomogeneity in the data set, which is difficult to analyze. The study team will perform detailed testing of the phantom materials and phantoms themselves, as well as examine diffusion imaging on 1 to 2 human volunteers at each of the 4 sites. Intra- and interscanner differences will be measured, and based on these findings, a more standardized imaging protocol that will provide optimal uniformity of diffusion imaging will be designed. Dr. Elisabeth Wilde leads this study.
Novel White Matter Imaging to Improve mTBI Diagnosis
This study will use myelin-sensitive novel imaging techniques (McDespot [multi-component driven equilibrium single pulse observation of T1/T2]) to improve correspondence with diagnostic groups after trauma exposure and correlation with cognitive deficits in mTBI. The study will recruit individuals (n = 82) from 4 groups, comorbid mTBI and posttraumatic stress disorder (PTSD), only mTBI, only PTSD, and controls who will be prospectively comprehensively assessed clinically (clinical interview, physical exam, neuropsychological assessment) and with advanced imaging (including McDespot, diffusion tensor imaging, and other forms of imaging). Dr. Amy Jak leads this study.
Peer Review Program
The CENC has an integrated grant program to identify scientifically valid and strategically important research projects. To date, 2 rounds of proposal requests and project support have been completed. Scientific review is conducted under the CENC Peer Review Program. Scientifically meritorious studies are identified by independent peer review and then undergo a Programmatic Review by CENC leadership before being recommended for funding to the Government Steering Committee (GSC). Studies that are recommended must address road map gaps, develop innovative approaches, or provide an avenue for new researchers and novel research approaches to contribute to the consortium mission to advance the science of brain injury treatment and prevention. The CENC grant program is administered by Dr. Steven L. West.
Consumer Advisory Board
The Consumer Advisory Board (CAB) advises and makes nonbinding recommendations to CENC. The responsibilities of the committee members include (1) providing information that helps CENC leadership better appreciate and understand the issues and needs of TBI survivors and their support networks so appropriate research can be designed and implemented; (2) evaluating existing research and making recommendations for additions and/or modifications to project procedures; (3) providing input for the road map for future research based on members’ personal experiences and knowledge; and (4) providing linkages to targeted communities for direct feedback and to assist in forming collaborative partnerships.
The CAB is composed of survivors of TBI, family members of survivors of TBI, providers of TBI services, service organizations with specific ties to SMs and veterans, and clinical and corporate representatives of transportation services for the disabled, the independent living movement, and assistive technology. Persons who are heavily engaged in political activity or who actively endorse a specific device or product are not eligible for membership on the CAB. Membership is composed of persons nominated by CENC leadership and approved by the GSC. The CAB is co-chaired by Charles Gatlin, MS, and General (Ret.) Peter Chiarelli.
Scientific Advisory Board
The members of the Scientific Advisory Board (SAB) advise and make nonbinding recommendations to CENC. Responsibilities of the committee members include (1) providing information that may help the consortium leadership better understand the issues related to TBI; (2) evaluating existing research; (3) recommending additions and/or modifications to project procedures; and (4) assisting CENC by helping leverage relationships with other researchers. The SAB is composed of members of the research community on TBI who are not part of CENC. Persons who may be considered to have positions of authority, such as active or retired flag officers or chief executive officers, may be eligible for general SAB membership but are not be eligible for chair positions. Membership is composed of persons nominated by CENC leadership and approved by the GSC. Col. Jamie Grimes, MD, and Henry Lew, MD, PhD, co-chair the SAB.
Federal Oversight
The GSC oversees CENC. Members of the GSC are DoD and VA appointed and represent both government agencies and nongovernment subject matter experts. The GSC approves all studies to be conducted, recommends new studies, and identifies existing and new requirements. The GSC is the overall main governing and management committee for the project and the committee through which the DoD and VA interact and collaborate with the CENC. The GSC determines all major scientific decisions, and clinical studies proposed by the CENC committee proceed to the implementation stage only with the approval of the GSC.
Acknowledgements
This research is supported by grants 1-I01-RX-001135-01-A2 (PI: F. Aiken), 1-I01-RX-001774-01 (PI: F. Crawford), 1-I01-RX-001880-01 (PI: E. Wilde), 1-I01-CX-001135-01 (PI: S. Cifu), and 1-I01-CX-001246-01 (PI: K. Yaffe) from the U.S. Department of Veterans Affairs and by grant W81XWH-13-2-0095 (PI: D. Cifu) from the U.S. Department of Defense, Congressionally Directed Medical Research Programs. The ideas and opinions expressed in this paper do not necessarily represent the views of the Department of Veterans Affairs, the Department of Defense, or the U.S. Government.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Study shows rivaroxaban can cross placenta

Photo by Nina Matthews
New research suggests the anticoagulant rivaroxaban can cross the placenta in pregnant women, raising concerns that the drug might
cause side effects in unborn children.
The ex vivo study, published in the American Journal of Obstetrics & Gynecology, showed that rivaroxaban can rapidly cross the human placenta in both directions.
The researchers did not draw any conclusions about the potential link between rivaroxaban and birth defects, but they said additional research is needed to explore this possibility.
Gideon Koren, MD, of the Hospital for Sick Children in Toronto, Ontario, Canada, and his colleagues conducted this study using an ex vivo placenta perfusion model.
They added rivaroxaban (250 ng/mL) to the maternal circulation, the fetal circulation, or both and observed the effects over 3 hours. They measured rivaroxaban concentrations via liquid chromatography-tandem mass spectrometry.
The researchers said they saw “rapid transfer” of rivaroxaban across the placenta, both in the maternal-to-fetal and fetal-to-maternal directions.
Three hours after they added rivaroxaban to the maternal reservoir, the median fetal concentration of the drug was 69.5 ng/mL, and the median fetal-to-maternal ratio was 0.69.
Three hours after they added rivaroxaban to the fetal reservoir, the maternal concentration of rivaroxaban was 58.2 ng/mL, and the maternal-to-fetal ratio was 0.69.
When the researchers added equal concentrations of rivaroxaban to both reservoirs, the fetal-to-maternal ratio remained relatively constant over the 3-hour period. And the rate of rivaroxaban disappearance was similar in both reservoirs—1.51 ng/mL/min in the maternal reservoir and 1.86 ng/mL/min in the fetal reservoir.
The researchers said this is the first direct evidence of rivaroxaban transfer across the placenta from both directions.
However, they also noted that, because rivaroxaban is highly bound to plasma proteins, the amount of unbound drug that may reach the fetus is likely much lower than observed in these experiments.
Nevertheless, additional studies should be conducted before rivaroxaban can be safely administered to pregnant women. ![]()

Photo by Nina Matthews
New research suggests the anticoagulant rivaroxaban can cross the placenta in pregnant women, raising concerns that the drug might
cause side effects in unborn children.
The ex vivo study, published in the American Journal of Obstetrics & Gynecology, showed that rivaroxaban can rapidly cross the human placenta in both directions.
The researchers did not draw any conclusions about the potential link between rivaroxaban and birth defects, but they said additional research is needed to explore this possibility.
Gideon Koren, MD, of the Hospital for Sick Children in Toronto, Ontario, Canada, and his colleagues conducted this study using an ex vivo placenta perfusion model.
They added rivaroxaban (250 ng/mL) to the maternal circulation, the fetal circulation, or both and observed the effects over 3 hours. They measured rivaroxaban concentrations via liquid chromatography-tandem mass spectrometry.
The researchers said they saw “rapid transfer” of rivaroxaban across the placenta, both in the maternal-to-fetal and fetal-to-maternal directions.
Three hours after they added rivaroxaban to the maternal reservoir, the median fetal concentration of the drug was 69.5 ng/mL, and the median fetal-to-maternal ratio was 0.69.
Three hours after they added rivaroxaban to the fetal reservoir, the maternal concentration of rivaroxaban was 58.2 ng/mL, and the maternal-to-fetal ratio was 0.69.
When the researchers added equal concentrations of rivaroxaban to both reservoirs, the fetal-to-maternal ratio remained relatively constant over the 3-hour period. And the rate of rivaroxaban disappearance was similar in both reservoirs—1.51 ng/mL/min in the maternal reservoir and 1.86 ng/mL/min in the fetal reservoir.
The researchers said this is the first direct evidence of rivaroxaban transfer across the placenta from both directions.
However, they also noted that, because rivaroxaban is highly bound to plasma proteins, the amount of unbound drug that may reach the fetus is likely much lower than observed in these experiments.
Nevertheless, additional studies should be conducted before rivaroxaban can be safely administered to pregnant women. ![]()

Photo by Nina Matthews
New research suggests the anticoagulant rivaroxaban can cross the placenta in pregnant women, raising concerns that the drug might
cause side effects in unborn children.
The ex vivo study, published in the American Journal of Obstetrics & Gynecology, showed that rivaroxaban can rapidly cross the human placenta in both directions.
The researchers did not draw any conclusions about the potential link between rivaroxaban and birth defects, but they said additional research is needed to explore this possibility.
Gideon Koren, MD, of the Hospital for Sick Children in Toronto, Ontario, Canada, and his colleagues conducted this study using an ex vivo placenta perfusion model.
They added rivaroxaban (250 ng/mL) to the maternal circulation, the fetal circulation, or both and observed the effects over 3 hours. They measured rivaroxaban concentrations via liquid chromatography-tandem mass spectrometry.
The researchers said they saw “rapid transfer” of rivaroxaban across the placenta, both in the maternal-to-fetal and fetal-to-maternal directions.
Three hours after they added rivaroxaban to the maternal reservoir, the median fetal concentration of the drug was 69.5 ng/mL, and the median fetal-to-maternal ratio was 0.69.
Three hours after they added rivaroxaban to the fetal reservoir, the maternal concentration of rivaroxaban was 58.2 ng/mL, and the maternal-to-fetal ratio was 0.69.
When the researchers added equal concentrations of rivaroxaban to both reservoirs, the fetal-to-maternal ratio remained relatively constant over the 3-hour period. And the rate of rivaroxaban disappearance was similar in both reservoirs—1.51 ng/mL/min in the maternal reservoir and 1.86 ng/mL/min in the fetal reservoir.
The researchers said this is the first direct evidence of rivaroxaban transfer across the placenta from both directions.
However, they also noted that, because rivaroxaban is highly bound to plasma proteins, the amount of unbound drug that may reach the fetus is likely much lower than observed in these experiments.
Nevertheless, additional studies should be conducted before rivaroxaban can be safely administered to pregnant women. ![]()
PICCs linked to lower- and upper-extremity DVT

A study of more than 70,000 patients suggests the use of peripherally inserted central catheters (PICCs) is not only associated with upper-extremity deep vein thrombosis (DVT).
It’s linked to lower-extremity DVT as well. However, PICC use was not associated with pulmonary embolism (PE).
Vineet Chopra, MD, of the University of Michigan in Ann Arbor, and his colleagues reported these findings in The American Journal of Medicine.
“Our study confirmed that PICCs are strongly associated with DVT in upper limbs,” Dr Chopra said. “However, what is novel and noteworthy in this study is that the presence of a PICC was also associated with an increased risk of lower-extremity DVT. Prior studies had not assessed whether PICCs are independently associated with an increase in the risk of subsequent lower-extremity DVT.”
Dr Chopra and his colleagues analyzed data from 76,242 patients hospitalized at 48 Michigan hospitals.
The team reviewed PICC placement, existing medical conditions, risk factors for venous thromboembolism (VTE), and thrombotic events occurring within 90 days of hospital admission.
A total of 3790 patients received a PICC during hospitalization. And there were 876 VTEs, including 208 upper-extremity DVTs, 372 lower-extremity DVTs, and 296 PEs.
After adjusting for risk factors other than PICC use, the researchers found that PICCs were independently associated with all-cause VTE, upper-extremity DVT, and lower-extremity DVT, but not PE. The hazard ratios were 3.16, 10.49, 1.48, and 1.34, respectively.
The team also found that VTE prophylaxis did not reduce the risk of DVT.
“Taken together, these findings suggest that the thrombotic burden associated with peripherally inserted central catheters may not be restricted to the extremity where the device resides or easily attenuated after insertion,” Dr Chopra said.
He and his colleagues therefore concluded that clinicians should weigh the risks and benefits of PICC use and consider using alternative devices in patients at high risk of DVT. And clinicians should not focus only on the extremity where a PICC resides but the composite risk of VTE among patients who receive a PICC. ![]()

A study of more than 70,000 patients suggests the use of peripherally inserted central catheters (PICCs) is not only associated with upper-extremity deep vein thrombosis (DVT).
It’s linked to lower-extremity DVT as well. However, PICC use was not associated with pulmonary embolism (PE).
Vineet Chopra, MD, of the University of Michigan in Ann Arbor, and his colleagues reported these findings in The American Journal of Medicine.
“Our study confirmed that PICCs are strongly associated with DVT in upper limbs,” Dr Chopra said. “However, what is novel and noteworthy in this study is that the presence of a PICC was also associated with an increased risk of lower-extremity DVT. Prior studies had not assessed whether PICCs are independently associated with an increase in the risk of subsequent lower-extremity DVT.”
Dr Chopra and his colleagues analyzed data from 76,242 patients hospitalized at 48 Michigan hospitals.
The team reviewed PICC placement, existing medical conditions, risk factors for venous thromboembolism (VTE), and thrombotic events occurring within 90 days of hospital admission.
A total of 3790 patients received a PICC during hospitalization. And there were 876 VTEs, including 208 upper-extremity DVTs, 372 lower-extremity DVTs, and 296 PEs.
After adjusting for risk factors other than PICC use, the researchers found that PICCs were independently associated with all-cause VTE, upper-extremity DVT, and lower-extremity DVT, but not PE. The hazard ratios were 3.16, 10.49, 1.48, and 1.34, respectively.
The team also found that VTE prophylaxis did not reduce the risk of DVT.
“Taken together, these findings suggest that the thrombotic burden associated with peripherally inserted central catheters may not be restricted to the extremity where the device resides or easily attenuated after insertion,” Dr Chopra said.
He and his colleagues therefore concluded that clinicians should weigh the risks and benefits of PICC use and consider using alternative devices in patients at high risk of DVT. And clinicians should not focus only on the extremity where a PICC resides but the composite risk of VTE among patients who receive a PICC. ![]()

A study of more than 70,000 patients suggests the use of peripherally inserted central catheters (PICCs) is not only associated with upper-extremity deep vein thrombosis (DVT).
It’s linked to lower-extremity DVT as well. However, PICC use was not associated with pulmonary embolism (PE).
Vineet Chopra, MD, of the University of Michigan in Ann Arbor, and his colleagues reported these findings in The American Journal of Medicine.
“Our study confirmed that PICCs are strongly associated with DVT in upper limbs,” Dr Chopra said. “However, what is novel and noteworthy in this study is that the presence of a PICC was also associated with an increased risk of lower-extremity DVT. Prior studies had not assessed whether PICCs are independently associated with an increase in the risk of subsequent lower-extremity DVT.”
Dr Chopra and his colleagues analyzed data from 76,242 patients hospitalized at 48 Michigan hospitals.
The team reviewed PICC placement, existing medical conditions, risk factors for venous thromboembolism (VTE), and thrombotic events occurring within 90 days of hospital admission.
A total of 3790 patients received a PICC during hospitalization. And there were 876 VTEs, including 208 upper-extremity DVTs, 372 lower-extremity DVTs, and 296 PEs.
After adjusting for risk factors other than PICC use, the researchers found that PICCs were independently associated with all-cause VTE, upper-extremity DVT, and lower-extremity DVT, but not PE. The hazard ratios were 3.16, 10.49, 1.48, and 1.34, respectively.
The team also found that VTE prophylaxis did not reduce the risk of DVT.
“Taken together, these findings suggest that the thrombotic burden associated with peripherally inserted central catheters may not be restricted to the extremity where the device resides or easily attenuated after insertion,” Dr Chopra said.
He and his colleagues therefore concluded that clinicians should weigh the risks and benefits of PICC use and consider using alternative devices in patients at high risk of DVT. And clinicians should not focus only on the extremity where a PICC resides but the composite risk of VTE among patients who receive a PICC. ![]()
FDA approves new formulation of pain patch for cancer patients

receiving treatment
Photo by Rhoda Baer
The US Food and Drug Administration (FDA) has approved a new formulation of fentanyl buccal soluble film CII (Onsolis), a patch used to manage breakthrough pain in adult cancer patients who are opioid-tolerant.
This decision allows BioDelivery Sciences International, Inc. (BDSI), the company developing Onsolis, to bring the product back to the US marketplace.
However, the company said this will not happen before 2016.
Onsolis is an opioid agonist indicated for the management of breakthrough pain in cancer patients 18 years of age and older who are already receiving and are tolerant to opioid therapy for their underlying persistent cancer pain.
Onsolis utilizes BioErodible MucoAdhesive drug delivery technology, which consists of a small, bioerodible polymer film that is applied to the inner lining of the cheek. Onsolis is the only differentiated fentanyl-containing product for this indication that provides buccal administration.
Onsolis off the US market
Onsolis was originally approved by the FDA in July 2009, but BDSI stopped manufacturing the product in March 2012, after the FDA uncovered 2 issues with Onsolis.
The FDA found that, during Onsolis’s 24-month shelf-life, microscopic crystals formed on the product, and the color faded slightly. BDSI said these changes did not affect the product’s underlying integrity or safety, but the FDA thought the fading color in particular might cause patients to question the product’s efficacy.
So the FDA required that Onsolis be modified before additional product could be manufactured and distributed. Supplies of Onsolis that were already on the market remained on the market.
An analysis by BDSI showed that the changes in Onsolis were related to an excipient used in the manufacturing process that could be removed to resolve the problem.
The excipient was specific to the manufacture of Onsolis in the US. Therefore, it did not impact the launch of Breakyl, which is the brand name for Onsolis in the European Union.
Return to market
After BDSI reformulated Onsolis to prevent the aforementioned changes in the product’s appearance, the FDA approved the product’s return to market.
“We are pleased to have obtained FDA approval of our [supplemental new drug application] and to now be in a position to move toward returning Onsolis to the US marketplace,” said Mark A. Sirgo, PharmD, President and Chief Executive Officer of BDSI.
“Although we have options for Onsolis, including commercializing it on our own, our current plan is to determine the value we can secure in a partnership with a company that has access to the target physician audience. We have been engaged with a number of potential partners, and, with this approval, we can now proceed forward with those discussions in earnest. We will provide more definitive timing in the near future about the reintroduction, but this would not be prior to 2016.”
Once Onsolis does return to the market, it will only be available via the Transmucosal Immediate Release Fentanyl (TIRF) Risk Evaluation and Mitigation Strategy (REMS) program. This is an FDA-required program designed to mitigate the risk of misuse, abuse, addiction, overdose, and serious complications due to medication errors with the use of TIRF medicines.
Outpatients, healthcare professionals who prescribe to outpatients, pharmacies, and distributors must enroll in the program to receive Onsolis. Further information is available at www.TIRFREMSAccess.com. ![]()

receiving treatment
Photo by Rhoda Baer
The US Food and Drug Administration (FDA) has approved a new formulation of fentanyl buccal soluble film CII (Onsolis), a patch used to manage breakthrough pain in adult cancer patients who are opioid-tolerant.
This decision allows BioDelivery Sciences International, Inc. (BDSI), the company developing Onsolis, to bring the product back to the US marketplace.
However, the company said this will not happen before 2016.
Onsolis is an opioid agonist indicated for the management of breakthrough pain in cancer patients 18 years of age and older who are already receiving and are tolerant to opioid therapy for their underlying persistent cancer pain.
Onsolis utilizes BioErodible MucoAdhesive drug delivery technology, which consists of a small, bioerodible polymer film that is applied to the inner lining of the cheek. Onsolis is the only differentiated fentanyl-containing product for this indication that provides buccal administration.
Onsolis off the US market
Onsolis was originally approved by the FDA in July 2009, but BDSI stopped manufacturing the product in March 2012, after the FDA uncovered 2 issues with Onsolis.
The FDA found that, during Onsolis’s 24-month shelf-life, microscopic crystals formed on the product, and the color faded slightly. BDSI said these changes did not affect the product’s underlying integrity or safety, but the FDA thought the fading color in particular might cause patients to question the product’s efficacy.
So the FDA required that Onsolis be modified before additional product could be manufactured and distributed. Supplies of Onsolis that were already on the market remained on the market.
An analysis by BDSI showed that the changes in Onsolis were related to an excipient used in the manufacturing process that could be removed to resolve the problem.
The excipient was specific to the manufacture of Onsolis in the US. Therefore, it did not impact the launch of Breakyl, which is the brand name for Onsolis in the European Union.
Return to market
After BDSI reformulated Onsolis to prevent the aforementioned changes in the product’s appearance, the FDA approved the product’s return to market.
“We are pleased to have obtained FDA approval of our [supplemental new drug application] and to now be in a position to move toward returning Onsolis to the US marketplace,” said Mark A. Sirgo, PharmD, President and Chief Executive Officer of BDSI.
“Although we have options for Onsolis, including commercializing it on our own, our current plan is to determine the value we can secure in a partnership with a company that has access to the target physician audience. We have been engaged with a number of potential partners, and, with this approval, we can now proceed forward with those discussions in earnest. We will provide more definitive timing in the near future about the reintroduction, but this would not be prior to 2016.”
Once Onsolis does return to the market, it will only be available via the Transmucosal Immediate Release Fentanyl (TIRF) Risk Evaluation and Mitigation Strategy (REMS) program. This is an FDA-required program designed to mitigate the risk of misuse, abuse, addiction, overdose, and serious complications due to medication errors with the use of TIRF medicines.
Outpatients, healthcare professionals who prescribe to outpatients, pharmacies, and distributors must enroll in the program to receive Onsolis. Further information is available at www.TIRFREMSAccess.com. ![]()

receiving treatment
Photo by Rhoda Baer
The US Food and Drug Administration (FDA) has approved a new formulation of fentanyl buccal soluble film CII (Onsolis), a patch used to manage breakthrough pain in adult cancer patients who are opioid-tolerant.
This decision allows BioDelivery Sciences International, Inc. (BDSI), the company developing Onsolis, to bring the product back to the US marketplace.
However, the company said this will not happen before 2016.
Onsolis is an opioid agonist indicated for the management of breakthrough pain in cancer patients 18 years of age and older who are already receiving and are tolerant to opioid therapy for their underlying persistent cancer pain.
Onsolis utilizes BioErodible MucoAdhesive drug delivery technology, which consists of a small, bioerodible polymer film that is applied to the inner lining of the cheek. Onsolis is the only differentiated fentanyl-containing product for this indication that provides buccal administration.
Onsolis off the US market
Onsolis was originally approved by the FDA in July 2009, but BDSI stopped manufacturing the product in March 2012, after the FDA uncovered 2 issues with Onsolis.
The FDA found that, during Onsolis’s 24-month shelf-life, microscopic crystals formed on the product, and the color faded slightly. BDSI said these changes did not affect the product’s underlying integrity or safety, but the FDA thought the fading color in particular might cause patients to question the product’s efficacy.
So the FDA required that Onsolis be modified before additional product could be manufactured and distributed. Supplies of Onsolis that were already on the market remained on the market.
An analysis by BDSI showed that the changes in Onsolis were related to an excipient used in the manufacturing process that could be removed to resolve the problem.
The excipient was specific to the manufacture of Onsolis in the US. Therefore, it did not impact the launch of Breakyl, which is the brand name for Onsolis in the European Union.
Return to market
After BDSI reformulated Onsolis to prevent the aforementioned changes in the product’s appearance, the FDA approved the product’s return to market.
“We are pleased to have obtained FDA approval of our [supplemental new drug application] and to now be in a position to move toward returning Onsolis to the US marketplace,” said Mark A. Sirgo, PharmD, President and Chief Executive Officer of BDSI.
“Although we have options for Onsolis, including commercializing it on our own, our current plan is to determine the value we can secure in a partnership with a company that has access to the target physician audience. We have been engaged with a number of potential partners, and, with this approval, we can now proceed forward with those discussions in earnest. We will provide more definitive timing in the near future about the reintroduction, but this would not be prior to 2016.”
Once Onsolis does return to the market, it will only be available via the Transmucosal Immediate Release Fentanyl (TIRF) Risk Evaluation and Mitigation Strategy (REMS) program. This is an FDA-required program designed to mitigate the risk of misuse, abuse, addiction, overdose, and serious complications due to medication errors with the use of TIRF medicines.
Outpatients, healthcare professionals who prescribe to outpatients, pharmacies, and distributors must enroll in the program to receive Onsolis. Further information is available at www.TIRFREMSAccess.com. ![]()