User login
Medicare Rule May Needlessly Extend Hospital Stay
(Reuters Health) - A decades old Medicare rule requiring a three-day hospital stay before patients can transfer to skilled nursing facilities may needlessly prolong hospitalizations, a study suggests.
Researchers compared the average time patients were hospitalized between 2006 and 2010 in privately administered Medicare Advantage health plans that either stuck to this rule or allowed people to transfer to skilled nursing facilities sooner.
Lengths of hospital stays increased with the rule in place and declined when it was waived, the study found.
"The three-day stay rule may inappropriately lengthen the time spent in a hospital for patients who could be transferred to a skilled nursing facility earlier," senior author Dr. Amal Trivedi, a health policy researcher at Brown University in Providence, Rhode Island, said by email.
This minimum-stay rule dates back to the 1960s, when patients typically remained in the hospital for nearly two weeks, and three days was the minimum time needed to evaluate them and plan their post-hospital care, Trivedi and colleagues note in the journal Health Affairs for August.
Since then, typical stays have shortened, and skilled nursing facilities have become an increasingly common treatment setting for patients with complex medical problems who no longer require acute inpatient care.
To see how the three-day minimum stay requirement might impact hospitalization, researchers compared the typical number of hospital days for nearly 141,000 patients in 14 Medicare Advantage plans that upheld the rule and for nearly 117,000 people in 14 similar plans that waived it.
The people enrolled in plans that waived the rule were typically younger, poorer and less likely to be white.
For plans that waived the rule, 23.5% of hospitalized patients were admitted to skilled nursing facilities in the year before the rule was eliminated, compared with 25.7% in the year after it went away.
Plans that kept the rule saw a similar gain, from 22.8% to 26.3%.
But the average length of hospital stays for patients in plans that waived the three-day rule declined from 6.9 days to 6.7 days, compared with an increase from 6.1 days to 6.6 days in plans that kept the requirement in place.
Overall, the average reduction in hospital stays was 0.7 days with the rule elimination, translating into approximately $1,500 in savings for every admission that ended with a transfer to a skilled nursing facility, the researchers estimated.
One limitation of the study, however, is that it looked at hospital days over the entire year, rather then the number of days for each stay, the researchers acknowledge. It's also possible that the cost savings wouldn't be the same for people with traditional fee-for-service Medicare or other plans unlike the ones in the study.
Even so, as hospital stays become shorter and patients with complicated illnesses are treated in other settings, it makes sense to revisit whether the three days is the right cutoff to identify people who can appropriately transfer to a skilled nursing facility, said David Grabowski, a health policy researcher at Harvard Medical School in Boston.
Certain patients may also benefit from leaving the hospital sooner, because longer stays can increase their risk of infections and make it less likely that they get out of bed for physical activity that can aid recovery, Grabowski, who wasn't involved in the study, said by email.
"Some individuals with short hospital stays may be inappropriately excluded from skilled nursing facility care under the current system," he said. "Moreover, this rule has led to some unintended consequences like the growth in observational stays."
"There really aren't many benefits to staying beyond medical necessity," Grabowski added.
(Reuters Health) - A decades old Medicare rule requiring a three-day hospital stay before patients can transfer to skilled nursing facilities may needlessly prolong hospitalizations, a study suggests.
Researchers compared the average time patients were hospitalized between 2006 and 2010 in privately administered Medicare Advantage health plans that either stuck to this rule or allowed people to transfer to skilled nursing facilities sooner.
Lengths of hospital stays increased with the rule in place and declined when it was waived, the study found.
"The three-day stay rule may inappropriately lengthen the time spent in a hospital for patients who could be transferred to a skilled nursing facility earlier," senior author Dr. Amal Trivedi, a health policy researcher at Brown University in Providence, Rhode Island, said by email.
This minimum-stay rule dates back to the 1960s, when patients typically remained in the hospital for nearly two weeks, and three days was the minimum time needed to evaluate them and plan their post-hospital care, Trivedi and colleagues note in the journal Health Affairs for August.
Since then, typical stays have shortened, and skilled nursing facilities have become an increasingly common treatment setting for patients with complex medical problems who no longer require acute inpatient care.
To see how the three-day minimum stay requirement might impact hospitalization, researchers compared the typical number of hospital days for nearly 141,000 patients in 14 Medicare Advantage plans that upheld the rule and for nearly 117,000 people in 14 similar plans that waived it.
The people enrolled in plans that waived the rule were typically younger, poorer and less likely to be white.
For plans that waived the rule, 23.5% of hospitalized patients were admitted to skilled nursing facilities in the year before the rule was eliminated, compared with 25.7% in the year after it went away.
Plans that kept the rule saw a similar gain, from 22.8% to 26.3%.
But the average length of hospital stays for patients in plans that waived the three-day rule declined from 6.9 days to 6.7 days, compared with an increase from 6.1 days to 6.6 days in plans that kept the requirement in place.
Overall, the average reduction in hospital stays was 0.7 days with the rule elimination, translating into approximately $1,500 in savings for every admission that ended with a transfer to a skilled nursing facility, the researchers estimated.
One limitation of the study, however, is that it looked at hospital days over the entire year, rather then the number of days for each stay, the researchers acknowledge. It's also possible that the cost savings wouldn't be the same for people with traditional fee-for-service Medicare or other plans unlike the ones in the study.
Even so, as hospital stays become shorter and patients with complicated illnesses are treated in other settings, it makes sense to revisit whether the three days is the right cutoff to identify people who can appropriately transfer to a skilled nursing facility, said David Grabowski, a health policy researcher at Harvard Medical School in Boston.
Certain patients may also benefit from leaving the hospital sooner, because longer stays can increase their risk of infections and make it less likely that they get out of bed for physical activity that can aid recovery, Grabowski, who wasn't involved in the study, said by email.
"Some individuals with short hospital stays may be inappropriately excluded from skilled nursing facility care under the current system," he said. "Moreover, this rule has led to some unintended consequences like the growth in observational stays."
"There really aren't many benefits to staying beyond medical necessity," Grabowski added.
(Reuters Health) - A decades old Medicare rule requiring a three-day hospital stay before patients can transfer to skilled nursing facilities may needlessly prolong hospitalizations, a study suggests.
Researchers compared the average time patients were hospitalized between 2006 and 2010 in privately administered Medicare Advantage health plans that either stuck to this rule or allowed people to transfer to skilled nursing facilities sooner.
Lengths of hospital stays increased with the rule in place and declined when it was waived, the study found.
"The three-day stay rule may inappropriately lengthen the time spent in a hospital for patients who could be transferred to a skilled nursing facility earlier," senior author Dr. Amal Trivedi, a health policy researcher at Brown University in Providence, Rhode Island, said by email.
This minimum-stay rule dates back to the 1960s, when patients typically remained in the hospital for nearly two weeks, and three days was the minimum time needed to evaluate them and plan their post-hospital care, Trivedi and colleagues note in the journal Health Affairs for August.
Since then, typical stays have shortened, and skilled nursing facilities have become an increasingly common treatment setting for patients with complex medical problems who no longer require acute inpatient care.
To see how the three-day minimum stay requirement might impact hospitalization, researchers compared the typical number of hospital days for nearly 141,000 patients in 14 Medicare Advantage plans that upheld the rule and for nearly 117,000 people in 14 similar plans that waived it.
The people enrolled in plans that waived the rule were typically younger, poorer and less likely to be white.
For plans that waived the rule, 23.5% of hospitalized patients were admitted to skilled nursing facilities in the year before the rule was eliminated, compared with 25.7% in the year after it went away.
Plans that kept the rule saw a similar gain, from 22.8% to 26.3%.
But the average length of hospital stays for patients in plans that waived the three-day rule declined from 6.9 days to 6.7 days, compared with an increase from 6.1 days to 6.6 days in plans that kept the requirement in place.
Overall, the average reduction in hospital stays was 0.7 days with the rule elimination, translating into approximately $1,500 in savings for every admission that ended with a transfer to a skilled nursing facility, the researchers estimated.
One limitation of the study, however, is that it looked at hospital days over the entire year, rather then the number of days for each stay, the researchers acknowledge. It's also possible that the cost savings wouldn't be the same for people with traditional fee-for-service Medicare or other plans unlike the ones in the study.
Even so, as hospital stays become shorter and patients with complicated illnesses are treated in other settings, it makes sense to revisit whether the three days is the right cutoff to identify people who can appropriately transfer to a skilled nursing facility, said David Grabowski, a health policy researcher at Harvard Medical School in Boston.
Certain patients may also benefit from leaving the hospital sooner, because longer stays can increase their risk of infections and make it less likely that they get out of bed for physical activity that can aid recovery, Grabowski, who wasn't involved in the study, said by email.
"Some individuals with short hospital stays may be inappropriately excluded from skilled nursing facility care under the current system," he said. "Moreover, this rule has led to some unintended consequences like the growth in observational stays."
"There really aren't many benefits to staying beyond medical necessity," Grabowski added.
Toward a single, whole-body scan to detect blood clots

Image by Andre E.X. Brown
BOSTON—Researchers have devised a method that may someday allow healthcare providers to quickly scan the entire body for a blood clot.
The team developed a fibrin-specific probe, known as 64Cu-FBP8, by attaching a radionuclide to a fibrin-binding peptide.
They administered the probe to rats with thrombosis and found they could locate clots via PET imaging.
Peter Caravan, PhD, of the Athinoula A. Martinos Center for Biomedical Imaging at Massachusetts General Hospital in Boston, presented details on this work at the 250th National Meeting & Exposition of the American Chemical Society.
He and his colleagues also reported results with this method in Arteriosclerosis, Thrombosis, and Vascular Biology.
Dr Caravan noted that, at present, a physician may need to use 3 different methods to locate a blood clot: ultrasound to check the carotid arteries or legs, MRI to scan the heart, and CT to view the lungs.
“It’s a shot in the dark,” he said. “Patients could end up being scanned multiple times by multiple techniques in order to locate a clot. We sought a method that could detect blood clots anywhere in the body with a single, whole-body scan.”
He and his colleagues reported results with an early prototype of their fibrin-specific probe in 2011. With the current work, they believe they have optimized the probe, and they are now ready to proceed to clinical studies.
The researchers used different radionuclides and peptides, as well as different chemical groups for linking the radionuclide to the peptide, to identify which combination would provide the brightest PET signal in clots. They ultimately constructed and tested 15 candidate probes.
The team first analyzed how well each probe bound to fibrin in vitro. Then, they studied how well the probe detected thrombi in rats.
“The probes all had a similar affinity to fibrin in vitro, but, in rats, their performances were quite different,” Dr Caravan said.
He attributed these differences to metabolism. Some probes were broken down quickly in the body and could no longer bind to a thrombus, but others were resistant to the metabolism.
Dr Caravan said the best probe was the one that was most stable. And that proved to be 64Cu-FBP8 (copper-64—fibrin binding probe #8).
To test 64Cu-FBP8 in rats, the researchers induced thrombosis via ferric chloride application on both the carotid artery and femoral vein. They then performed 64Cu-FBP8-PET/CT imaging 1, 3, or 7 days after thrombosis induction.
The team found they could locate arterial and venous thrombi on fused PET/CT images with 97.6% accuracy. A single, whole-body PET/MRI could reveal the location of both arterial and venous thrombi as well.
Dr Caravan said the question now is how well this method will work in humans. To answer that, his group is hoping to start testing the probe in clinical trials in the fall. ![]()

Image by Andre E.X. Brown
BOSTON—Researchers have devised a method that may someday allow healthcare providers to quickly scan the entire body for a blood clot.
The team developed a fibrin-specific probe, known as 64Cu-FBP8, by attaching a radionuclide to a fibrin-binding peptide.
They administered the probe to rats with thrombosis and found they could locate clots via PET imaging.
Peter Caravan, PhD, of the Athinoula A. Martinos Center for Biomedical Imaging at Massachusetts General Hospital in Boston, presented details on this work at the 250th National Meeting & Exposition of the American Chemical Society.
He and his colleagues also reported results with this method in Arteriosclerosis, Thrombosis, and Vascular Biology.
Dr Caravan noted that, at present, a physician may need to use 3 different methods to locate a blood clot: ultrasound to check the carotid arteries or legs, MRI to scan the heart, and CT to view the lungs.
“It’s a shot in the dark,” he said. “Patients could end up being scanned multiple times by multiple techniques in order to locate a clot. We sought a method that could detect blood clots anywhere in the body with a single, whole-body scan.”
He and his colleagues reported results with an early prototype of their fibrin-specific probe in 2011. With the current work, they believe they have optimized the probe, and they are now ready to proceed to clinical studies.
The researchers used different radionuclides and peptides, as well as different chemical groups for linking the radionuclide to the peptide, to identify which combination would provide the brightest PET signal in clots. They ultimately constructed and tested 15 candidate probes.
The team first analyzed how well each probe bound to fibrin in vitro. Then, they studied how well the probe detected thrombi in rats.
“The probes all had a similar affinity to fibrin in vitro, but, in rats, their performances were quite different,” Dr Caravan said.
He attributed these differences to metabolism. Some probes were broken down quickly in the body and could no longer bind to a thrombus, but others were resistant to the metabolism.
Dr Caravan said the best probe was the one that was most stable. And that proved to be 64Cu-FBP8 (copper-64—fibrin binding probe #8).
To test 64Cu-FBP8 in rats, the researchers induced thrombosis via ferric chloride application on both the carotid artery and femoral vein. They then performed 64Cu-FBP8-PET/CT imaging 1, 3, or 7 days after thrombosis induction.
The team found they could locate arterial and venous thrombi on fused PET/CT images with 97.6% accuracy. A single, whole-body PET/MRI could reveal the location of both arterial and venous thrombi as well.
Dr Caravan said the question now is how well this method will work in humans. To answer that, his group is hoping to start testing the probe in clinical trials in the fall. ![]()

Image by Andre E.X. Brown
BOSTON—Researchers have devised a method that may someday allow healthcare providers to quickly scan the entire body for a blood clot.
The team developed a fibrin-specific probe, known as 64Cu-FBP8, by attaching a radionuclide to a fibrin-binding peptide.
They administered the probe to rats with thrombosis and found they could locate clots via PET imaging.
Peter Caravan, PhD, of the Athinoula A. Martinos Center for Biomedical Imaging at Massachusetts General Hospital in Boston, presented details on this work at the 250th National Meeting & Exposition of the American Chemical Society.
He and his colleagues also reported results with this method in Arteriosclerosis, Thrombosis, and Vascular Biology.
Dr Caravan noted that, at present, a physician may need to use 3 different methods to locate a blood clot: ultrasound to check the carotid arteries or legs, MRI to scan the heart, and CT to view the lungs.
“It’s a shot in the dark,” he said. “Patients could end up being scanned multiple times by multiple techniques in order to locate a clot. We sought a method that could detect blood clots anywhere in the body with a single, whole-body scan.”
He and his colleagues reported results with an early prototype of their fibrin-specific probe in 2011. With the current work, they believe they have optimized the probe, and they are now ready to proceed to clinical studies.
The researchers used different radionuclides and peptides, as well as different chemical groups for linking the radionuclide to the peptide, to identify which combination would provide the brightest PET signal in clots. They ultimately constructed and tested 15 candidate probes.
The team first analyzed how well each probe bound to fibrin in vitro. Then, they studied how well the probe detected thrombi in rats.
“The probes all had a similar affinity to fibrin in vitro, but, in rats, their performances were quite different,” Dr Caravan said.
He attributed these differences to metabolism. Some probes were broken down quickly in the body and could no longer bind to a thrombus, but others were resistant to the metabolism.
Dr Caravan said the best probe was the one that was most stable. And that proved to be 64Cu-FBP8 (copper-64—fibrin binding probe #8).
To test 64Cu-FBP8 in rats, the researchers induced thrombosis via ferric chloride application on both the carotid artery and femoral vein. They then performed 64Cu-FBP8-PET/CT imaging 1, 3, or 7 days after thrombosis induction.
The team found they could locate arterial and venous thrombi on fused PET/CT images with 97.6% accuracy. A single, whole-body PET/MRI could reveal the location of both arterial and venous thrombi as well.
Dr Caravan said the question now is how well this method will work in humans. To answer that, his group is hoping to start testing the probe in clinical trials in the fall. ![]()
FDA approves brentuximab vedotin as consolidation

Photo from Business Wire
The US Food and Drug Administration (FDA) has approved brentuximab vedotin (Adcetris) for use as consolidation treatment after autologous hematopoietic stem cell transplant (auto-HSCT) in patients with classical Hodgkin lymphoma (HL) at high risk of relapse or progression.
The drug is the first FDA-approved consolidation option available to these patients.
The approval was based on results of the phase 3 AETHERA trial.
Results from this trial also served to convert a prior accelerated approval of brentuximab vedotin to regular approval. The drug is now fully approved for the treatment of classical HL patients who have failed auto-HSCT and those who have failed at least 2 prior multi-agent chemotherapy regimens and are not candidates for auto-HSCT.
Brentuximab vedotin is also FDA-approved to treat patients with systemic anaplastic large-cell lymphoma who have failed at least 1 prior multi-agent chemotherapy regimen. The drug has accelerated approval for this indication based on overall response rate. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
AETHERA trial
The trial was designed to compare brentuximab vedotin to placebo, both administered for up to 16 cycles (approximately 1 year) every 3 weeks following auto-HSCT. Results from the trial were published in The Lancet in March and presented at the 2014 ASH Annual Meeting.
The study enrolled 329 HL patients at risk of relapse or progression, including 165 on the brentuximab vedotin arm and 164 on the placebo arm.
Patients were eligible for enrollment in the AETHERA trial if they had a history of primary refractory HL, relapsed within a year of receiving frontline chemotherapy, and/or had disease outside of the lymph nodes at the time of pre-auto-HSCT relapse.
Brentuximab vedotin conferred a significant increase in progression-free survival over placebo, with a hazard ratio of 0.57 (P=0.001). The median progression-free survival was 43 months for patients who received brentuximab vedotin and 24 months for patients who received placebo.
The most common adverse events (≥20%), of any grade and regardless of causality, in the brentuximab vedotin arm were neutropenia (78%), peripheral sensory neuropathy (56%), thrombocytopenia (41%), anemia (27%), upper respiratory tract infection (26%), fatigue (24%), peripheral motor neuropathy (23%), nausea (22%), cough (21%), and diarrhea (20%).
The most common adverse events (≥20%), of any grade and regardless of causality, in the placebo arm were neutropenia (34%), upper respiratory tract infection (23%), and thrombocytopenia (20%).
In all, 67% of patients on the brentuximab vedotin arm experienced peripheral neuropathy. Of those patients, 85% had resolution (59%) or partial improvement (26%) in symptoms at the time of their last evaluation, with a median time to improvement of 23 weeks (range, 0.1-138). ![]()

Photo from Business Wire
The US Food and Drug Administration (FDA) has approved brentuximab vedotin (Adcetris) for use as consolidation treatment after autologous hematopoietic stem cell transplant (auto-HSCT) in patients with classical Hodgkin lymphoma (HL) at high risk of relapse or progression.
The drug is the first FDA-approved consolidation option available to these patients.
The approval was based on results of the phase 3 AETHERA trial.
Results from this trial also served to convert a prior accelerated approval of brentuximab vedotin to regular approval. The drug is now fully approved for the treatment of classical HL patients who have failed auto-HSCT and those who have failed at least 2 prior multi-agent chemotherapy regimens and are not candidates for auto-HSCT.
Brentuximab vedotin is also FDA-approved to treat patients with systemic anaplastic large-cell lymphoma who have failed at least 1 prior multi-agent chemotherapy regimen. The drug has accelerated approval for this indication based on overall response rate. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
AETHERA trial
The trial was designed to compare brentuximab vedotin to placebo, both administered for up to 16 cycles (approximately 1 year) every 3 weeks following auto-HSCT. Results from the trial were published in The Lancet in March and presented at the 2014 ASH Annual Meeting.
The study enrolled 329 HL patients at risk of relapse or progression, including 165 on the brentuximab vedotin arm and 164 on the placebo arm.
Patients were eligible for enrollment in the AETHERA trial if they had a history of primary refractory HL, relapsed within a year of receiving frontline chemotherapy, and/or had disease outside of the lymph nodes at the time of pre-auto-HSCT relapse.
Brentuximab vedotin conferred a significant increase in progression-free survival over placebo, with a hazard ratio of 0.57 (P=0.001). The median progression-free survival was 43 months for patients who received brentuximab vedotin and 24 months for patients who received placebo.
The most common adverse events (≥20%), of any grade and regardless of causality, in the brentuximab vedotin arm were neutropenia (78%), peripheral sensory neuropathy (56%), thrombocytopenia (41%), anemia (27%), upper respiratory tract infection (26%), fatigue (24%), peripheral motor neuropathy (23%), nausea (22%), cough (21%), and diarrhea (20%).
The most common adverse events (≥20%), of any grade and regardless of causality, in the placebo arm were neutropenia (34%), upper respiratory tract infection (23%), and thrombocytopenia (20%).
In all, 67% of patients on the brentuximab vedotin arm experienced peripheral neuropathy. Of those patients, 85% had resolution (59%) or partial improvement (26%) in symptoms at the time of their last evaluation, with a median time to improvement of 23 weeks (range, 0.1-138). ![]()

Photo from Business Wire
The US Food and Drug Administration (FDA) has approved brentuximab vedotin (Adcetris) for use as consolidation treatment after autologous hematopoietic stem cell transplant (auto-HSCT) in patients with classical Hodgkin lymphoma (HL) at high risk of relapse or progression.
The drug is the first FDA-approved consolidation option available to these patients.
The approval was based on results of the phase 3 AETHERA trial.
Results from this trial also served to convert a prior accelerated approval of brentuximab vedotin to regular approval. The drug is now fully approved for the treatment of classical HL patients who have failed auto-HSCT and those who have failed at least 2 prior multi-agent chemotherapy regimens and are not candidates for auto-HSCT.
Brentuximab vedotin is also FDA-approved to treat patients with systemic anaplastic large-cell lymphoma who have failed at least 1 prior multi-agent chemotherapy regimen. The drug has accelerated approval for this indication based on overall response rate. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
AETHERA trial
The trial was designed to compare brentuximab vedotin to placebo, both administered for up to 16 cycles (approximately 1 year) every 3 weeks following auto-HSCT. Results from the trial were published in The Lancet in March and presented at the 2014 ASH Annual Meeting.
The study enrolled 329 HL patients at risk of relapse or progression, including 165 on the brentuximab vedotin arm and 164 on the placebo arm.
Patients were eligible for enrollment in the AETHERA trial if they had a history of primary refractory HL, relapsed within a year of receiving frontline chemotherapy, and/or had disease outside of the lymph nodes at the time of pre-auto-HSCT relapse.
Brentuximab vedotin conferred a significant increase in progression-free survival over placebo, with a hazard ratio of 0.57 (P=0.001). The median progression-free survival was 43 months for patients who received brentuximab vedotin and 24 months for patients who received placebo.
The most common adverse events (≥20%), of any grade and regardless of causality, in the brentuximab vedotin arm were neutropenia (78%), peripheral sensory neuropathy (56%), thrombocytopenia (41%), anemia (27%), upper respiratory tract infection (26%), fatigue (24%), peripheral motor neuropathy (23%), nausea (22%), cough (21%), and diarrhea (20%).
The most common adverse events (≥20%), of any grade and regardless of causality, in the placebo arm were neutropenia (34%), upper respiratory tract infection (23%), and thrombocytopenia (20%).
In all, 67% of patients on the brentuximab vedotin arm experienced peripheral neuropathy. Of those patients, 85% had resolution (59%) or partial improvement (26%) in symptoms at the time of their last evaluation, with a median time to improvement of 23 weeks (range, 0.1-138). ![]()
Treatments appear comparable for VTE in cancer

Results of the phase 3 CATCH trial suggest that 6 months of treatment with the low-molecular weight heparin tinzaparin produces similar results as conventional venous thromboembolism (VTE) prophylaxis in patients with active cancer and acute, symptomatic VTE.
The rates of VTE recurrence, overall death, and major bleeding were not significantly different in patients who received only tinzaparin and those who received tinzaparin followed by warfarin.
However, patients who received tinzaparin alone had a significantly lower rate of clinically relevant, nonmajor bleeding.
Agnes Y. Y. Lee, MD, of the University of British Columbia in Vancouver, Canada, and her colleagues reported these results in JAMA. The study was previously presented at ASH 2014.
The researchers enrolled 900 adult patients with active cancer and documented deep vein thrombosis or pulmonary embolism. The patients were enrolled at 164 centers in Asia, Africa, Europe, and
North, Central, and South America between August 2010 and November 2013.
The patients were randomized to receive tinzaparin (at 175 IU/kg) once daily for 6 months (n=449) or conventional therapy with tinzaparin (at 175 IU/kg) once daily for 5 to 10 days followed by dose-adjusted warfarin for the rest of the 6-month period (n=451).
The researchers saw no significant difference in the 6-month cumulative incidence of recurrent VTE between the tinzaparin and warfarin arms—7.2% (n=31) and 10.5% (n=45), respectively (hazard ratio [HR]=0.65, P=0.07).
Likewise, there was no significant difference in major bleeding (HR=0.89, P=0.77) or overall mortality (HR=1.08, P=0.54). Major bleeding occurred in 12 patients in the tinzaparin arm and 11 patients in the warfarin arm. And there were 150 deaths in the tinzaparin arm and 138 deaths in the warfarin arm.
There was a significant reduction in clinically relevant, nonmajor bleeding in the tinzaparin arm (HR=0.58, P=0.004). There were 49 such bleeds in the tinzaparin arm and 69 in the warfarin arm.
The researchers said these results suggest a full therapeutic dose of tinzaparin is safe in cancer patients for up to 6 months, and additional studies are needed to assess whether the efficacy outcomes would be different in patients at a higher risk of recurrent VTE.
This study was sponsored and funded by LEO Pharma (the company developing tinzaparin as Innohep) and had research support from the Sondra and Stephen Hardis Endowed Chair in Oncology Research and the Scott Hamilton CARES Initiative. ![]()

Results of the phase 3 CATCH trial suggest that 6 months of treatment with the low-molecular weight heparin tinzaparin produces similar results as conventional venous thromboembolism (VTE) prophylaxis in patients with active cancer and acute, symptomatic VTE.
The rates of VTE recurrence, overall death, and major bleeding were not significantly different in patients who received only tinzaparin and those who received tinzaparin followed by warfarin.
However, patients who received tinzaparin alone had a significantly lower rate of clinically relevant, nonmajor bleeding.
Agnes Y. Y. Lee, MD, of the University of British Columbia in Vancouver, Canada, and her colleagues reported these results in JAMA. The study was previously presented at ASH 2014.
The researchers enrolled 900 adult patients with active cancer and documented deep vein thrombosis or pulmonary embolism. The patients were enrolled at 164 centers in Asia, Africa, Europe, and
North, Central, and South America between August 2010 and November 2013.
The patients were randomized to receive tinzaparin (at 175 IU/kg) once daily for 6 months (n=449) or conventional therapy with tinzaparin (at 175 IU/kg) once daily for 5 to 10 days followed by dose-adjusted warfarin for the rest of the 6-month period (n=451).
The researchers saw no significant difference in the 6-month cumulative incidence of recurrent VTE between the tinzaparin and warfarin arms—7.2% (n=31) and 10.5% (n=45), respectively (hazard ratio [HR]=0.65, P=0.07).
Likewise, there was no significant difference in major bleeding (HR=0.89, P=0.77) or overall mortality (HR=1.08, P=0.54). Major bleeding occurred in 12 patients in the tinzaparin arm and 11 patients in the warfarin arm. And there were 150 deaths in the tinzaparin arm and 138 deaths in the warfarin arm.
There was a significant reduction in clinically relevant, nonmajor bleeding in the tinzaparin arm (HR=0.58, P=0.004). There were 49 such bleeds in the tinzaparin arm and 69 in the warfarin arm.
The researchers said these results suggest a full therapeutic dose of tinzaparin is safe in cancer patients for up to 6 months, and additional studies are needed to assess whether the efficacy outcomes would be different in patients at a higher risk of recurrent VTE.
This study was sponsored and funded by LEO Pharma (the company developing tinzaparin as Innohep) and had research support from the Sondra and Stephen Hardis Endowed Chair in Oncology Research and the Scott Hamilton CARES Initiative. ![]()

Results of the phase 3 CATCH trial suggest that 6 months of treatment with the low-molecular weight heparin tinzaparin produces similar results as conventional venous thromboembolism (VTE) prophylaxis in patients with active cancer and acute, symptomatic VTE.
The rates of VTE recurrence, overall death, and major bleeding were not significantly different in patients who received only tinzaparin and those who received tinzaparin followed by warfarin.
However, patients who received tinzaparin alone had a significantly lower rate of clinically relevant, nonmajor bleeding.
Agnes Y. Y. Lee, MD, of the University of British Columbia in Vancouver, Canada, and her colleagues reported these results in JAMA. The study was previously presented at ASH 2014.
The researchers enrolled 900 adult patients with active cancer and documented deep vein thrombosis or pulmonary embolism. The patients were enrolled at 164 centers in Asia, Africa, Europe, and
North, Central, and South America between August 2010 and November 2013.
The patients were randomized to receive tinzaparin (at 175 IU/kg) once daily for 6 months (n=449) or conventional therapy with tinzaparin (at 175 IU/kg) once daily for 5 to 10 days followed by dose-adjusted warfarin for the rest of the 6-month period (n=451).
The researchers saw no significant difference in the 6-month cumulative incidence of recurrent VTE between the tinzaparin and warfarin arms—7.2% (n=31) and 10.5% (n=45), respectively (hazard ratio [HR]=0.65, P=0.07).
Likewise, there was no significant difference in major bleeding (HR=0.89, P=0.77) or overall mortality (HR=1.08, P=0.54). Major bleeding occurred in 12 patients in the tinzaparin arm and 11 patients in the warfarin arm. And there were 150 deaths in the tinzaparin arm and 138 deaths in the warfarin arm.
There was a significant reduction in clinically relevant, nonmajor bleeding in the tinzaparin arm (HR=0.58, P=0.004). There were 49 such bleeds in the tinzaparin arm and 69 in the warfarin arm.
The researchers said these results suggest a full therapeutic dose of tinzaparin is safe in cancer patients for up to 6 months, and additional studies are needed to assess whether the efficacy outcomes would be different in patients at a higher risk of recurrent VTE.
This study was sponsored and funded by LEO Pharma (the company developing tinzaparin as Innohep) and had research support from the Sondra and Stephen Hardis Endowed Chair in Oncology Research and the Scott Hamilton CARES Initiative. ![]()
Return on investment slipping in biomedical research

Photo by Rhoda Baer
As more and more money has been spent on biomedical research in the US over the past 50 years, there has been diminished return on investment in terms of life expectancy gains and new drug approvals, according to a report published in PNAS.
Investigators found that the number of scientists in the US has increased about 9-fold since 1965, and the National Institutes of Health (NIH) budget has increased about 4-fold.
But the number of new drugs approved by the Food and Drug Administration has only increased about 2-fold, and life expectancy gains have remained constant, at roughly 2 months per year.
“The idea of public support for biomedical research is to make lives better, but there is increasing friction in the system,” said study author Arturo Casadevall, MD, PhD, of the Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland.
“We are spending more money now just to get the same results we always have, and this is going to keep happening if we don’t fix things.”
“There is something wrong in the process, but there are no simple answers,” said study author Anthony Bowen, an MD/PhD student at Albert Einstein College of Medicine in the Bronx, New York.
“It may be a confluence of factors that are causing us not to be getting more bang for our buck.”
Bowen and Dr Casadevall said one such factor may be that increased regulations have added to the non-scientific burdens on scientists who could otherwise spend more time at the bench.
Another potential explanation is that the “easy” cures for various conditions have been found, but to tackle cancers, Alzheimer’s disease, and autoimmune diseases, for example, is inherently more complex.
Dr Casadevall and Bowen also cited “perverse” incentives for researchers to cut corners or oversimplify their studies to gain acceptance into top-tier medical journals. The pair said this has led to an “epidemic” of retractions and findings that cannot be reproduced and are therefore worthless.
“The medical literature isn’t as good as it used to be,” Dr Casadevall said. “The culture of science appears to be changing. Less important work is being hyped, when the quality of work may not be clear until decades later when someone builds on your success to find a cure.”
In one recent study, researchers estimated that more than $28 billion, from both public and private sources, is spent each year in the US on preclinical research that can’t be reproduced, and the prevalence of these studies in the literature is 50%.
“We have more journals and more papers than ever,” Bowen said. “But the number of biomedical publications has dramatically outpaced the production of new drugs, which are key to improving people’s lives, especially in areas for which we have no good treatments.”
Dr Casadevall said he doesn’t doubt that more cures for diseases are out there to be found, and a more efficient system of biomedical research could help push along scientific discovery.
“Scientists, regulators, and citizens need to take a hard look at the scientific enterprise and see which [problems] can be resolved,” he said. “We need a system with rigor, reproducibility, and integrity, and we need to find a way to get there as soon as we can.” ![]()

Photo by Rhoda Baer
As more and more money has been spent on biomedical research in the US over the past 50 years, there has been diminished return on investment in terms of life expectancy gains and new drug approvals, according to a report published in PNAS.
Investigators found that the number of scientists in the US has increased about 9-fold since 1965, and the National Institutes of Health (NIH) budget has increased about 4-fold.
But the number of new drugs approved by the Food and Drug Administration has only increased about 2-fold, and life expectancy gains have remained constant, at roughly 2 months per year.
“The idea of public support for biomedical research is to make lives better, but there is increasing friction in the system,” said study author Arturo Casadevall, MD, PhD, of the Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland.
“We are spending more money now just to get the same results we always have, and this is going to keep happening if we don’t fix things.”
“There is something wrong in the process, but there are no simple answers,” said study author Anthony Bowen, an MD/PhD student at Albert Einstein College of Medicine in the Bronx, New York.
“It may be a confluence of factors that are causing us not to be getting more bang for our buck.”
Bowen and Dr Casadevall said one such factor may be that increased regulations have added to the non-scientific burdens on scientists who could otherwise spend more time at the bench.
Another potential explanation is that the “easy” cures for various conditions have been found, but to tackle cancers, Alzheimer’s disease, and autoimmune diseases, for example, is inherently more complex.
Dr Casadevall and Bowen also cited “perverse” incentives for researchers to cut corners or oversimplify their studies to gain acceptance into top-tier medical journals. The pair said this has led to an “epidemic” of retractions and findings that cannot be reproduced and are therefore worthless.
“The medical literature isn’t as good as it used to be,” Dr Casadevall said. “The culture of science appears to be changing. Less important work is being hyped, when the quality of work may not be clear until decades later when someone builds on your success to find a cure.”
In one recent study, researchers estimated that more than $28 billion, from both public and private sources, is spent each year in the US on preclinical research that can’t be reproduced, and the prevalence of these studies in the literature is 50%.
“We have more journals and more papers than ever,” Bowen said. “But the number of biomedical publications has dramatically outpaced the production of new drugs, which are key to improving people’s lives, especially in areas for which we have no good treatments.”
Dr Casadevall said he doesn’t doubt that more cures for diseases are out there to be found, and a more efficient system of biomedical research could help push along scientific discovery.
“Scientists, regulators, and citizens need to take a hard look at the scientific enterprise and see which [problems] can be resolved,” he said. “We need a system with rigor, reproducibility, and integrity, and we need to find a way to get there as soon as we can.” ![]()

Photo by Rhoda Baer
As more and more money has been spent on biomedical research in the US over the past 50 years, there has been diminished return on investment in terms of life expectancy gains and new drug approvals, according to a report published in PNAS.
Investigators found that the number of scientists in the US has increased about 9-fold since 1965, and the National Institutes of Health (NIH) budget has increased about 4-fold.
But the number of new drugs approved by the Food and Drug Administration has only increased about 2-fold, and life expectancy gains have remained constant, at roughly 2 months per year.
“The idea of public support for biomedical research is to make lives better, but there is increasing friction in the system,” said study author Arturo Casadevall, MD, PhD, of the Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland.
“We are spending more money now just to get the same results we always have, and this is going to keep happening if we don’t fix things.”
“There is something wrong in the process, but there are no simple answers,” said study author Anthony Bowen, an MD/PhD student at Albert Einstein College of Medicine in the Bronx, New York.
“It may be a confluence of factors that are causing us not to be getting more bang for our buck.”
Bowen and Dr Casadevall said one such factor may be that increased regulations have added to the non-scientific burdens on scientists who could otherwise spend more time at the bench.
Another potential explanation is that the “easy” cures for various conditions have been found, but to tackle cancers, Alzheimer’s disease, and autoimmune diseases, for example, is inherently more complex.
Dr Casadevall and Bowen also cited “perverse” incentives for researchers to cut corners or oversimplify their studies to gain acceptance into top-tier medical journals. The pair said this has led to an “epidemic” of retractions and findings that cannot be reproduced and are therefore worthless.
“The medical literature isn’t as good as it used to be,” Dr Casadevall said. “The culture of science appears to be changing. Less important work is being hyped, when the quality of work may not be clear until decades later when someone builds on your success to find a cure.”
In one recent study, researchers estimated that more than $28 billion, from both public and private sources, is spent each year in the US on preclinical research that can’t be reproduced, and the prevalence of these studies in the literature is 50%.
“We have more journals and more papers than ever,” Bowen said. “But the number of biomedical publications has dramatically outpaced the production of new drugs, which are key to improving people’s lives, especially in areas for which we have no good treatments.”
Dr Casadevall said he doesn’t doubt that more cures for diseases are out there to be found, and a more efficient system of biomedical research could help push along scientific discovery.
“Scientists, regulators, and citizens need to take a hard look at the scientific enterprise and see which [problems] can be resolved,” he said. “We need a system with rigor, reproducibility, and integrity, and we need to find a way to get there as soon as we can.” ![]()
Redesigning Inpatient Care
Despite an estimated annual $2.6 trillion expenditure on healthcare, the United States performs poorly on indicators of health and harm during care.[1, 2, 3] Hospitals around the nation are working to improve the care they deliver. We describe a model developed at our institution and report the evaluation of the outcomes associated with its implementation on the general medical and surgical units. The Indiana University Institutional Review Board approved this work.
SETTING AND DEFINITIONS
Indiana University Health Methodist Hospital (MH) is an academic center in Indianapolis, Indiana, serving over 30,000 patients annually.[4] In 2012, responding to the coexisting needs to improve quality and contain costs, the MH leadership team redesigned care in the hospital. The new model centers around accountable care teams (ACTs). Each ACT is a geographically defined set of providers accepting ownership for the clinical, service, and financial outcomes of their respective inpatient unit. The units studied are described in Table 1.
| Unit | No. of Beds | Predominant Diagnosis (Maximum Domain Score)* | |
|---|---|---|---|
| |||
| Medical units with progressive‐care beds | 1 | 33 | Pulmonary (3.4, 3.5, 5) |
| 2 | 28 | Cardiology (4.8, 3.5, 4) | |
| 3 | 24 | General medical (4.8, 3.5, 4) | |
| Medical units without progressive‐care beds | 4 | 36 | Renal/diabetic (4, 3.5, 5) |
| 5 | 24 | General medical (3.75, 4, 5) | |
| Surgical units with progressive‐care beds | 6 | 51 | Cardiothoracic surgery/cardiology (4, 4, 5) |
| 7 | 29 | Trauma/general surgery (3.75, 3.5, 5) | |
| 8 | 23 | Neurosurgical/neurological (4.8, 5, 5) | |
| 9 | 24 | Neurosurgical/neurological (4.4, 4.5, 5) | |
| Surgical units without progressive‐care beds | 10 | 29 | General/urologic/gynecologic/plastic surgery (3.4, 3, 2) |
| 11 | 26 | Orthopedic surgery (4.6, 4, 5) | |
THE ACT MODEL
The model comprises 8 interventions rooted in 3 foundational domains: (1) enhancing interprofessional collaboration (IPC), (2) enabling data‐driven decisions, and (3) providing leadership. Each intervention is briefly described under its main focus (see Supporting Information, Appendix A, in the online version of this article for further details).
Enhancing IPC
Geographical Cohorting of Patients and Providers
Hospitalist providers are localized for 4 consecutive months to 1 unit. An interdisciplinary team including a case manager, clinical nurse specialist, pharmacist, nutritionist, and social worker also serve each unit. Learners (residents, pharmacy, and medical students) are embedded in the team when rotating on the hospital medicine service. The presence of unit‐based nurse managers and charge nurses predates the model and is retained.
Bedside Collaborative Rounding
Geographically cohorted providers round on their patients with the bedside nurse guided by a customizable script.
Daily Huddle
The hospitalist, learners, and the interdisciplinary team for the unit meet each weekday to discuss patients' needs for a safe transition out of the hospital. Each unit determined the timing, location, and script for the huddle while retaining the focus on discharge planning (see Supporting Information, Appendix A2, in the online version of this article for a sample script).
Hospitalist and Specialty Comanagement Agreements
Guidelines delineating responsibilities for providers of each specialty were developed. Examples include orders pertaining to the management of a dialysis catheter in a patient with end‐stage renal disease, the removal of drains in postsurgical patients, and wound care.
Unit White Board
Each unit has a white board at the nursing station. Similar to the huddle, it is focused on discharge planning.
Enabling Data‐Driven Decisions
Monthly Review of Unit‐Level Data
Data analytics at our institution developed a data dashboard. Key metrics including length of stay (LOS), patient satisfaction scores, readmission rates, and costs are tracked and attributed to the discharging unit. The data are collated monthly by the ACT program director and distributed to each unit's leadership. Monthly interdisciplinary meetings are held to review trends. Learners are encouraged but not required to attend.
Weekly Patient Satisfaction Rounding
The unit's nurse manager and physician leader conduct weekly satisfaction rounds on patients. The conversation is open‐ended and focused on eliciting positive and negative experiences.
Providing Leadership
Designated hospitalist and, where relevant, specialty leaders are committed to serve each unit for at least 1 year as a resource for both medical and operational problem solving. The leader stays closely connected with the unit's nurse manager. In addition to day‐to‐day troubleshooting, the leader is responsible for monitoring outcome trends. There is currently no stipend, training, or other incentive offered for the role.
Implementation Timelines and ACT Scores
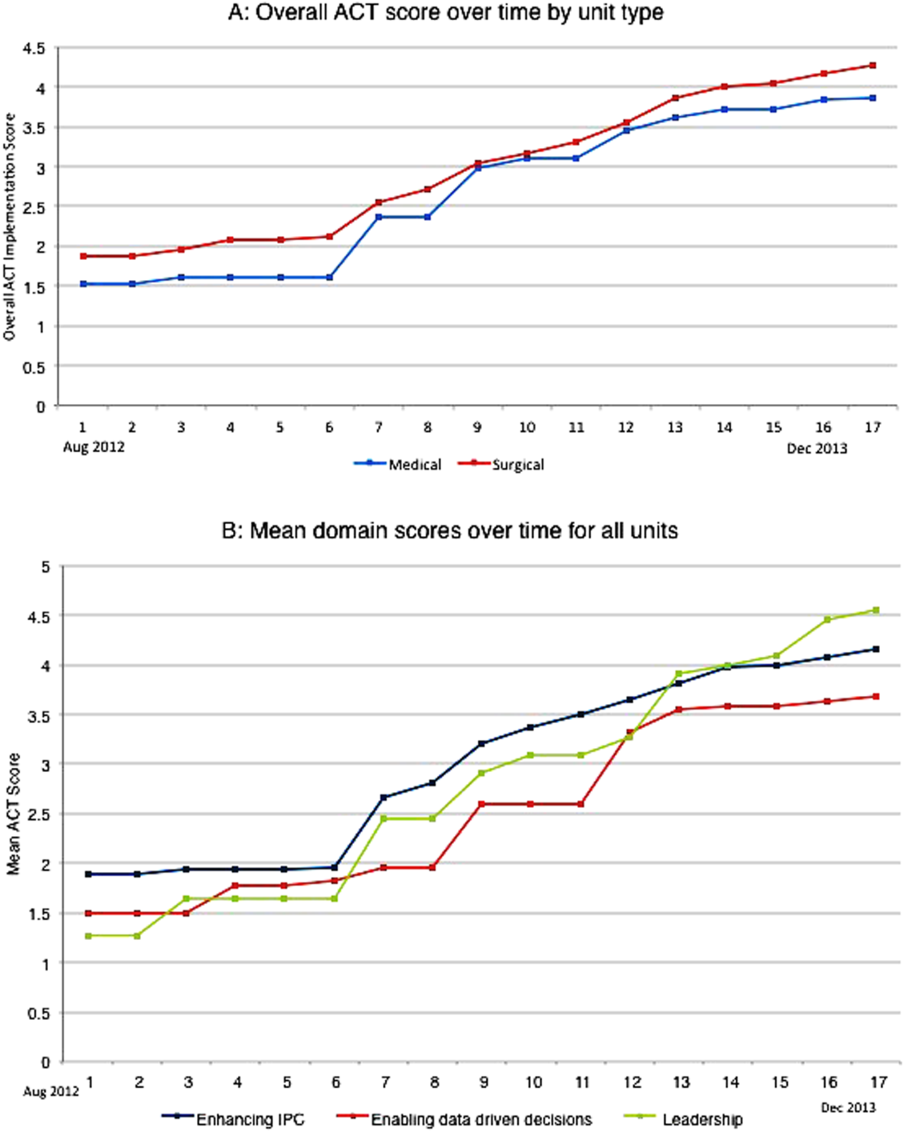
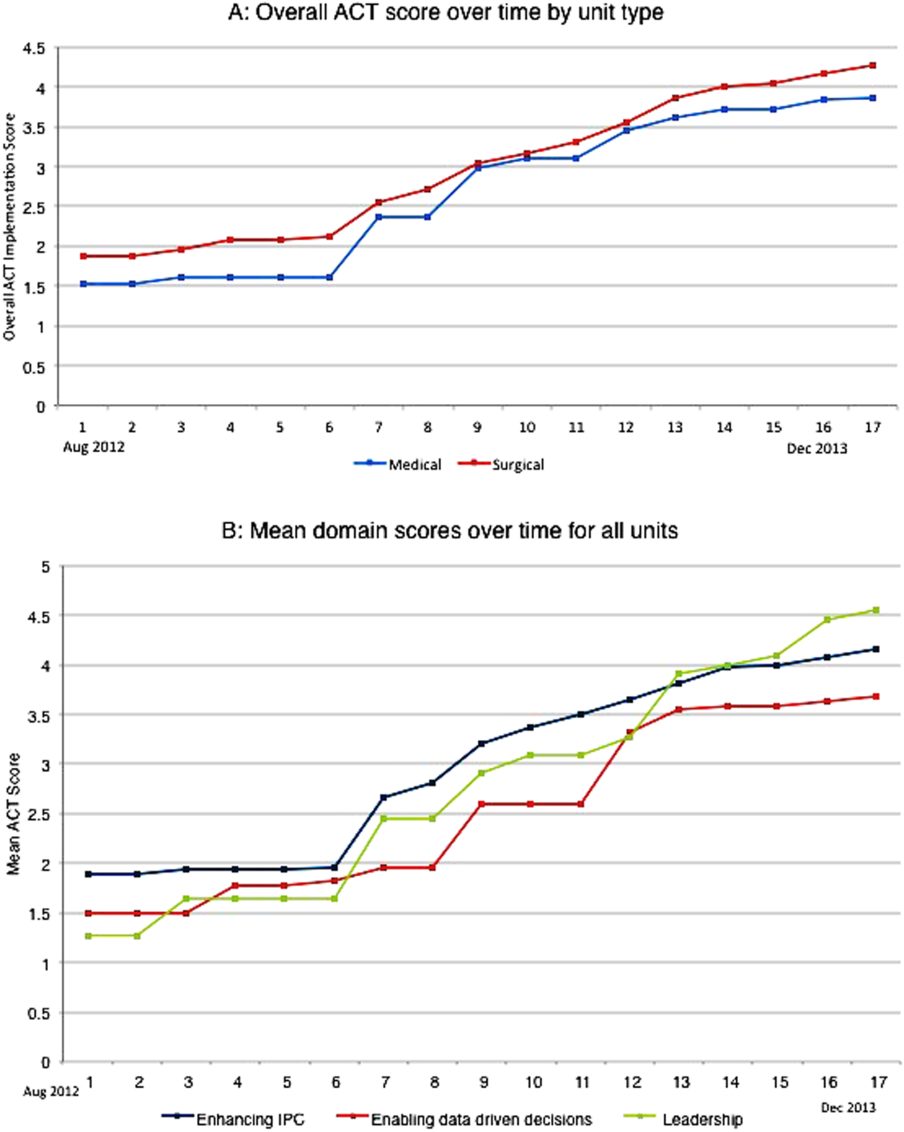
The development of the ACTs started in the spring of 2012. Physician, nursing, and pharmacy support was sought, and a pilot unit was formed in August 2012. The model was cascaded hospital wide by December 2013, with support from the ACT program director (A.N.). The program director observed and scored the uptake of each intervention by each unit monthly. A score of 1 denoted no implementation, whereas 5 denoted complete implementation. The criteria for scoring are presented in Table 2. The monthly scores for all 8 interventions in each of the 11 units were averaged as an overall ACT score, which reflects the implementation dose of the ACT model. Monthly domain scores for enhancing IPC and enabling data‐driven decisions were also calculated as the average score within each domain. This yielded 3 domain scores. Figure 1A plots by month the overall ACT score for the medical and surgical units, and Figure 1B plots the implementation score for the 3 domains between August 2012 and December 2013 for all units. The uptake of the interventions varied between units. This allowed our analysis to explore the dose relationships between the model and outcomes independent of underlying time trends that may be affected by concomitant initiatives.
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| |||||
| Geographical cohorting of patients and the ACT* | None | At least 1 discipline comprising the ACT is unit based | All disciplines comprising the ACT except the hospitalist unit based | All disciplines including the hospitalist unit based | 4 + 80% of hospitalist provider's patients on the unit |
| Bedside collaborative rounding | None | Occurring 1 day a week on at least 25% of the patients on the unit | Occurring 2 to 3 days a week on at least 50% of the patients on the unit | Occurring 3 to 4 days a week on at least 75% of the patients on the unit | Occurring MondayFriday on all patients on the unit |
| Daily huddle | None | Occurring daily, 1 out of 4 ACT disciplines represented, at least 25% of patients on the unit discussed | Occurring daily, 2 out of 4 ACT disciplines represented, at least 50% of patients on the unit discussed | Occurring daily, 3 out of 4 ACT disciplines represented, at least 75% of patients on the unit discussed | Occurring daily, all disciplines of the ACT represented, all patients on the unit discussed |
| Hospitalist and specialty comanagement agreements | None | One out of 3 specialists represented on the unit collaborating with the hospitalists on at least 25% of relevant patients | One out of 3 specialists represented on the unit collaborating with the hospitalists on at least 50% of relevant patients | Two out of 3 specialists on the unit collaborating with the hospitalists on at least 75% of relevant patients | All specialists on the unit collaborating with the hospitalists on all relevant patients on the unit |
| Unit white board | None | Present but only used by nursing | Present and used by all ACT disciplines except physician providers | Present and used by entire ACT; use inconsistent | Present and used MondayFriday by all disciplines of ACT |
| Monthly review of unit level data | None | Nurse manager reviewing data with ACT program director | Nurse manager and unit leader reviewing data with ACT program director | Meeting either not consistently occurring monthly or not consistently attended by entire ACT | Monthly meeting with entire ACT |
| Weekly patient satisfaction rounding | None | Nurse manager performing up to 1 week a month | Nurse manager performing weekly | Nurse and physician leader performing up to 3 times a month | Nurse and physician leader performing weekly |
| Leadership | None | For units with specialties, either hospitalist or specialist leader identified | Both hospitalist and specialist leader Identified | Both hospitalist and specialist leaders (where applicable) identified and partially engaged in leadership role | Both hospitalist and specialist leaders (where applicable) identified and engaged in leadership role |
Outcomes
Monthly data between August 2012 and December 2013 were analyzed.
Measures of Value
MH is a member of the University Health Consortium, which measures outcomes of participants relative to their peers. MH measures LOS index as a ratio of observed LOS to expected LOS that is adjusted for severity of illness.[5]
Variable direct costs (VDCs) are costs that a hospital can save if a service is not provided.[6] A hospital's case‐mix index (CMI) represents the average diagnosis‐related group relative weight for that hospital. We track VDCs adjusted for CMI (CMI‐adjusted VDC).[7]
Thirty‐day readmission rate is the percentage of cases that are readmitted to MH within 30 days of discharge from the index admission.[8]
Measures of Patient Satisfaction
The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey covers topics relevant to a patient's experience in the hospital.[9] Patient satisfaction scores are tracked by responses to the HCAHPS survey.
Measures of Provider Satisfaction
Hospitalist and specialty providers, leadership, and case management teams were surveyed via email through SurveyMonkey in July 2014. The survey included Likert responses that elicited opinions and comments about the ACT model.
Statistical Methods
The primary predictor of interest was the monthly overall ACT score. We also explored the domain scores as well as the individual scores for each intervention. Generalized linear mixed models were fit to investigate the association between each predictor (overall ACT score, ACT domain scores, and individual implementation scores) and each outcome (LOS index, CMI‐adjusted VDC, 30‐day readmission rate, and overall patient satisfaction). The model for testing each ACT score also included covariates of inpatient units as a random effect, as well as date and type of unit as fixed effects. We set the statistical significance level at 0.01 and reported 99% confidence intervals.
Descriptive statistics were used to report the provider satisfaction survey results.
RESULTS
The overall ACT score was associated with LOS index and CMI‐adjusted VDC (both P < 0.001). For every 1‐unit increase in the overall ACT score, LOS index decreased by 0.078 and CMI‐adjusted VDC decreased by $273.99 (Table 3).
| Length of Stay Index | CMI Adjusted VDC | |||
|---|---|---|---|---|
| Estimate (99% CI)* | P Value | Estimate (99% CI)* | P Value | |
| ||||
| Overall ACT Score | 0.078 (0.123 to 0.032) | <0.001 | 274.0 (477.31 to 70.68) | <0.001 |
| Enhancing IPC | 0.071 (0.117 to 0.026) | <0.001 | 284.7 (488.08 to 81.23) | <0.001 |
| Enabling data‐driven decisions | 0.044 (0.080 to 0.009) | 0.002 | 145.4 (304.57 to 13.81) | 0.02 |
| Providing leadership | 0.027 (0.049 to 0.005) | 0.001 | 69.9 (169.00 to 29.26) | 0.07 |
Looking at domains, enhancing IPC resulted in statistically significant decreases in both LOS index and CMI‐adjusted VDC, but providing leadership and enabling data‐driven decisions decreased only the LOS index. Most of the 8 individual interventions were associated with at least 1 of these 2 outcomes. (Even where the associations were not significant, they were all in the direction of decreasing LOS and cost). In these models, the covariate of type of units (medical vs surgical) was not associated with LOS or cost. There was no significant time trend in LOS or cost, except in models where an intervention had no association with either outcome. Inclusion of all individual effective interventions in the same statistical model to assess their relative contributions was not possible because they were highly correlated (correlations 0.450.89).
Thirty‐day readmissions and patient satisfaction were not significantly associated with the overall ACT score, but exploratory analyses showed that patient satisfaction increased with the implementation of geographical cohorting (P = 0.007).
Survey Results
The response rate was 87% (96/110). Between 85% and 96% of respondents either agreed or strongly agreed that the ACT model had improved the quality and safety of the care delivered, improved communication between providers and patients, and improved their own engagement and job satisfaction. Overall, 78% of the respondents either agreed or strongly agreed that the model improved efficiency (Table 4). Suggestions for improvements revolved around increasing the emphasis on patient centeredness and bedside nursing engagement.
| The ACT Model | Strongly Agree, n (%) | Agree, n (%) | Disagree, n (%) | Strongly Disagree, n (%) |
|---|---|---|---|---|
| ||||
| Has improved the quality and safety of patient care | 46 (47.9) | 46 (47.9) | 2 (2.1) | 2 (2.1) |
| Has improved communication with patients and families | 42 (43.7) | 47 (49.0) | 5 (5.2) | 2 (2.1) |
| Has improved your efficiency/productivity | 31 (32.6) | 43 (45.3) | 17 (17.9) | 4 (4.2) |
| Has improved your engagement and job satisfaction | 33 (34.4) | 49 (51.0) | 10 (10.4) | 4 (4.2) |
| Is a better model of delivering patient care | 45 (47.4) | 44 (46.3) | 2 (2.1) | 4 (4.2) |
DISCUSSION
The serious problems in US healthcare constitute an urgent imperative to innovate and reform.[10] Inpatient care reflects 31% of the expenditure on healthcare, and in 2010, 35.1 million patients were discharged from the hospital after spending an average of 4.8 days as an inpatient.[11] These figures represent an immense opportunity to intervene. Measuring the impact of quality improvement efforts is often complicated by concomitant changes that affect outcomes over the interval studied. Our approach allowed us to detect statistically significant changes in LOS index and CMI‐adjusted VDC associated with the ACT implementation dose that could be separated from the underlying time trends.
The ACT model we describe is rooted in improving 3 foundational domains; quantifying each intervention's compartmentalized contribution, however, proved difficult. Each intervention intertwines with the others to create changes in attitudes, knowledge, and culture that are difficult to measure yet may synergistically affect outcomes. For example, although geographical cohorting appears to have the strongest statistical association with outcomes, this may be mediated by how it enables other processes to take place more effectively. Based on this analysis, therefore, the ACT model may best be considered a bundled intervention.
The team caring for a patient during hospitalization is so complex that fewer than a quarter of patients know their physician's or nurse's name.[12] This complexity impairs communication between patients and providers and between the providers themselves. Communication failures are consistently identified as root causes in sentinel events reported to the Joint Commission.[13] IPC is the process by which different professional groups work together to positively impact health care. IPC overlaps with communication, coordination, and teamwork, and improvements in IPC may improve care.[14] Some elements of the model we describe have been tested previously.[15, 16, 17] Localization of teams may increase productivity and the frequency with which physicians and nurses communicate. Localization also decreases the number of pages received and steps walked by providers during a workday.[15, 16, 17] However, these studies reported a trend toward an increase in the LOS and neutral effects on cost and readmission rates. We found statistically significant decreases in both LOS and cost associated with the geographic cohorting of patients and providers. Notably, our model localized not only the physician providers but also the interdisciplinary team of pharmacists, clinical nurse specialists, case managers, and social workers. This proximity may facilitate IPC between all members that culminates in improved efficiency. The possibility of delays in discharges to avoid new admissions in a geographically structured team has previously been raised to explain the associated increases in LOS.[16, 17] The accountability of each unit for its metrics, the communication between nursing and physicians, and the timely availability of the unit's performance data aligns everyone toward a shared goal and provides some protection from an unintended consequence.
Structured interdisciplinary rounds decrease adverse events and improve teamwork ratings.[18, 19] The huddle in our model is a forum to collaborate between disciplines that proved to be effective in decreasing LOS and costs. Our huddle aims to discuss all the patients on the unit. This allows the team to assist each other in problem solving for the entire unit and not just the patients on the geographically cohorted team. This approach, in addition to the improved IPC fostered by the ACT model, may help explain how benefits in LOS and costs permeated across all 11 diverse units despite the presence of patients who are not directly served by the geographically cohorted team.
High‐performing clinical systems maintain an awareness of their overarching mission and unit‐based leaders can influence the frontline by reiterating the organizational mission and aligning efforts with outcomes.[20] Our leadership model is similar to those described by other institutions in the strong partnerships between physicians and nursing.[21] As outlined by Kim et al., investing in the professional development of the unit leaders may help them fulfill their roles and serve the organization better.[21]
The fragmentation and lack of ownership over the continuum of patient care causes duplication and waste. The proposal in the Accountable Care Act to create accountable care organizations is rooted in the understanding that providers and organizations will seek out new ways of improving quality when held accountable for their outcomes.[22] To foster ownership and accountability, reporting of metrics at the unit level is needed. Furthermore, an informational infrastructure is critical, as improvements cannot occur without the availability of data to both monitor performance and measure the effect of interventions.[10, 23] Even without any other interventions, providing feedback alone is an effective way of changing practices.[24] According to Berwick et al., this phenomenon reflects practitioners' intrinsic motivation to simply want to be better.[25] Our monthly review of each unit's data is an effective way to provide timely feedback to the frontline that sparks pride, ownership, and innovative thinking.
Based on our mean ACT score and CMI‐adjusted VDC reductions alone, we estimate savings of $649.36 per hospitalization (mean increase in ACT implementation of 2.37 times reduction in cost index of $273.99 per unit increase in overall ACT score). This figure does not include savings realized through reductions in LOS. This is a small decrease relative to the mean cost of hospitalization, yet when compounded over the annual MH census, it would result in substantial savings. The model relied on the restructuring of the existing workforce and the only direct additional cost was the early salary support for the ACT program director.
Limitations
We recognize several limitations. It is a single center's experience and may not be generalizable. The diffusion of knowledge and culture carried between units and the relatively rapid implementation timeline did not allow for a control unit. A single observer assigned our implementation scores, and therefore we cannot report measures of inter‐rater reliability. However, defined criteria and direct observations were used wherever possible. Although administratively available data have their limitations, where available, we used measurements that are adjusted for severity of illness and CMI. We therefore feel that this dataset is an accurate representation of currently reported national quality indicators.
FURTHER DIRECTIONS
Although there is a need to improve our healthcare system, interventions should be deliberate and evidence based wherever possible.[26] Geographic cohorting may decrease the frequency of paging interruptions for physicians and practitioners while increasing face‐to‐face interruptions.[27] The net effect on safety with this trade‐off should be investigated.
The presence of an intervention does not guarantee its success. Despite geographic cohorting and interdisciplinary meetings, communication that influences physician decision making may not improve.[28] Although instruments to measure ratings of team work and collaboration are available, focusing on clinically relevant outcomes of teamwork, such as prevention of harm, may be more empowering feedback for the frontline. Formal cost‐benefit analyses and outcomes related to physician and nursing retention will be equally important for assessing the sustainability of the model. Involving patients and their caregivers and inviting their perspectives as care is redesigned will also be critical in maintaining patient centeredness. Research addressing interventions to mediate preventable readmission risk and understanding the drivers of patient satisfaction is also needed.
The true value of the model may be in its potential to monitor and drive change within itself. Continuously aligning aims, incentives, performance measures, and feedback will help support this innovation and drive. This affects not only patient care but creates microcosms within which research and education can thrive. We hope that our experience will help guide other institutions as we all strive in our journey to improve the care we deliver.
Acknowledgements
The authors thank the Indiana University Health Physicians hospitalists at MH, Sandy Janitz and Decision Support, the Indiana University Health executive leadership team, Robert Clark, Malaz Boustani, Dennis Watson, Nadia Adams, Todd Biggerstaff, Deanne Kashiwagi, and the tireless providers at MH for their support.
Disclosure: This work was supported by a grant from the Indiana University Health Values Fund. The authors have no conflicts of interest to disclose.
- Committee on Quality of Health Care in America; Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press; 2001.
- . Is US health really the best in the world? JAMA. 2000;284(4):483–485.
- , , , , , . Temporal trends in rates of patient harm resulting from medical care. N Engl J Med. 2010;363(22):2124–2134.
- Indiana University Health. Available at: http://iuhealth.org/methodist/aboIut/. Accessed October 20, 2014.
- University Health Consortium. Available at: https://www.uhc.edu/docs/45014769_QSS_dashboard_FAQs.pdf. Accessed October 23, 2014.
- , , , et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999;281(7):644–649.
- Centers for Medicare and Medicaid Services. Case mix index. Available at: http://www.cms.gov/Medicare/Medicare‐Fee‐for‐Service‐Payment/AcuteInpatientPPS/Acute‐Inpatient‐Files‐for‐Download‐Items/CMS022630.html. Accessed May 4, 2015.
- University Health Consortium. Available at: https://www.uhc.edu. Accessed October 23, 2014.
- Centers for Medicare and Medicaid Services. Hospital Consumer Assessment of Healthcare Providers and Systems. HCAHPS survey content and administration. Centers for Medicare 280(11):1000–1005.
- Centers for Disease Control and Prevention. FastStats. Available at: http://www.cdc.gov/nchs/fastats/default.htm. Accessed October 27, 2014.
- , . Does your patient know your name? An approach to enhancing patients' awareness of their caretaker's name. J Healthc Qual. 2005;27(4):53–56.
- The Joint Commission. Sentinel event data: root causes by event type 2004‐third quarter. Available at: http://www.jointcommissionorg. Available at: http://www.jointcommission.org/assets/1/18/Root_Causes_by_Event_Type_2004-2Q2013.pdf. Accessed March 26, 2014.
- , , . Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009;(3):CD000072.
- , , , et al. Impact of localizing physicians to hospital units on nurse–physician communication and agreement on the plan of care. J Gen Intern Med. 2009;24(11):1223–1227.
- , , , et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551–556.
- , , , et al. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. J Hosp Med. 2008;3(5):361–368.
- , , , , , . Improving teamwork: impact of structured interdisciplinary rounds on a medical teaching unit. J Gen Intern Med. 2010;25(8):826–832.
- , , , ; High Performance Teams and the Hospital of the Future Project Team. Interdisciplinary teamwork in hospitals: a review and practical recommendations for improvement. J Hosp Med. 2011;7(1):48–54.
- , , , , , . Microsystems in health care: part 8. Developing people and improving work life: what front‐line staff told us. Jt Comm J Qual Saf. 2003;29(10):512–522.
- , , , , , . Unit‐based interprofessional leadership models in six US hospitals. J Hosp Med. 2014;9(8):545–550.
- , , , . Creating accountable care organizations: the extended hospital medical staff. Health Aff (Millwood). 2007;26(1):w44–w57.
- , . Using performance measurement to drive improvement: a road map for change. Med Care. 2003;41(1 suppl):I48–I60.
- , . Changing physicians' practices. N Engl J Med. 1993;329(17):1271–1273.
- , , . Connections between quality measurement and improvement. Med Care. 2003;41(1 suppl):I30–I38.
- , , . The tension between needing to improve care and knowing how to do it. N Engl J Med. 2007;357(6):608–613.
- , . A qualitative evaluation of geographical localization of hospitalists: how unintended consequences may impact quality. J Gen Intern Med. 2014;29(7):1009–1016.
- , , , , . Disengaged: a qualitative study of communication and collaboration between physicians and other professions on general internal medicine wards. BMC Health Serv Res. 2013;13:494.
Despite an estimated annual $2.6 trillion expenditure on healthcare, the United States performs poorly on indicators of health and harm during care.[1, 2, 3] Hospitals around the nation are working to improve the care they deliver. We describe a model developed at our institution and report the evaluation of the outcomes associated with its implementation on the general medical and surgical units. The Indiana University Institutional Review Board approved this work.
SETTING AND DEFINITIONS
Indiana University Health Methodist Hospital (MH) is an academic center in Indianapolis, Indiana, serving over 30,000 patients annually.[4] In 2012, responding to the coexisting needs to improve quality and contain costs, the MH leadership team redesigned care in the hospital. The new model centers around accountable care teams (ACTs). Each ACT is a geographically defined set of providers accepting ownership for the clinical, service, and financial outcomes of their respective inpatient unit. The units studied are described in Table 1.
| Unit | No. of Beds | Predominant Diagnosis (Maximum Domain Score)* | |
|---|---|---|---|
| |||
| Medical units with progressive‐care beds | 1 | 33 | Pulmonary (3.4, 3.5, 5) |
| 2 | 28 | Cardiology (4.8, 3.5, 4) | |
| 3 | 24 | General medical (4.8, 3.5, 4) | |
| Medical units without progressive‐care beds | 4 | 36 | Renal/diabetic (4, 3.5, 5) |
| 5 | 24 | General medical (3.75, 4, 5) | |
| Surgical units with progressive‐care beds | 6 | 51 | Cardiothoracic surgery/cardiology (4, 4, 5) |
| 7 | 29 | Trauma/general surgery (3.75, 3.5, 5) | |
| 8 | 23 | Neurosurgical/neurological (4.8, 5, 5) | |
| 9 | 24 | Neurosurgical/neurological (4.4, 4.5, 5) | |
| Surgical units without progressive‐care beds | 10 | 29 | General/urologic/gynecologic/plastic surgery (3.4, 3, 2) |
| 11 | 26 | Orthopedic surgery (4.6, 4, 5) | |
THE ACT MODEL
The model comprises 8 interventions rooted in 3 foundational domains: (1) enhancing interprofessional collaboration (IPC), (2) enabling data‐driven decisions, and (3) providing leadership. Each intervention is briefly described under its main focus (see Supporting Information, Appendix A, in the online version of this article for further details).
Enhancing IPC
Geographical Cohorting of Patients and Providers
Hospitalist providers are localized for 4 consecutive months to 1 unit. An interdisciplinary team including a case manager, clinical nurse specialist, pharmacist, nutritionist, and social worker also serve each unit. Learners (residents, pharmacy, and medical students) are embedded in the team when rotating on the hospital medicine service. The presence of unit‐based nurse managers and charge nurses predates the model and is retained.
Bedside Collaborative Rounding
Geographically cohorted providers round on their patients with the bedside nurse guided by a customizable script.
Daily Huddle
The hospitalist, learners, and the interdisciplinary team for the unit meet each weekday to discuss patients' needs for a safe transition out of the hospital. Each unit determined the timing, location, and script for the huddle while retaining the focus on discharge planning (see Supporting Information, Appendix A2, in the online version of this article for a sample script).
Hospitalist and Specialty Comanagement Agreements
Guidelines delineating responsibilities for providers of each specialty were developed. Examples include orders pertaining to the management of a dialysis catheter in a patient with end‐stage renal disease, the removal of drains in postsurgical patients, and wound care.
Unit White Board
Each unit has a white board at the nursing station. Similar to the huddle, it is focused on discharge planning.
Enabling Data‐Driven Decisions
Monthly Review of Unit‐Level Data
Data analytics at our institution developed a data dashboard. Key metrics including length of stay (LOS), patient satisfaction scores, readmission rates, and costs are tracked and attributed to the discharging unit. The data are collated monthly by the ACT program director and distributed to each unit's leadership. Monthly interdisciplinary meetings are held to review trends. Learners are encouraged but not required to attend.
Weekly Patient Satisfaction Rounding
The unit's nurse manager and physician leader conduct weekly satisfaction rounds on patients. The conversation is open‐ended and focused on eliciting positive and negative experiences.
Providing Leadership
Designated hospitalist and, where relevant, specialty leaders are committed to serve each unit for at least 1 year as a resource for both medical and operational problem solving. The leader stays closely connected with the unit's nurse manager. In addition to day‐to‐day troubleshooting, the leader is responsible for monitoring outcome trends. There is currently no stipend, training, or other incentive offered for the role.
Implementation Timelines and ACT Scores
The development of the ACTs started in the spring of 2012. Physician, nursing, and pharmacy support was sought, and a pilot unit was formed in August 2012. The model was cascaded hospital wide by December 2013, with support from the ACT program director (A.N.). The program director observed and scored the uptake of each intervention by each unit monthly. A score of 1 denoted no implementation, whereas 5 denoted complete implementation. The criteria for scoring are presented in Table 2. The monthly scores for all 8 interventions in each of the 11 units were averaged as an overall ACT score, which reflects the implementation dose of the ACT model. Monthly domain scores for enhancing IPC and enabling data‐driven decisions were also calculated as the average score within each domain. This yielded 3 domain scores. Figure 1A plots by month the overall ACT score for the medical and surgical units, and Figure 1B plots the implementation score for the 3 domains between August 2012 and December 2013 for all units. The uptake of the interventions varied between units. This allowed our analysis to explore the dose relationships between the model and outcomes independent of underlying time trends that may be affected by concomitant initiatives.
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| |||||
| Geographical cohorting of patients and the ACT* | None | At least 1 discipline comprising the ACT is unit based | All disciplines comprising the ACT except the hospitalist unit based | All disciplines including the hospitalist unit based | 4 + 80% of hospitalist provider's patients on the unit |
| Bedside collaborative rounding | None | Occurring 1 day a week on at least 25% of the patients on the unit | Occurring 2 to 3 days a week on at least 50% of the patients on the unit | Occurring 3 to 4 days a week on at least 75% of the patients on the unit | Occurring MondayFriday on all patients on the unit |
| Daily huddle | None | Occurring daily, 1 out of 4 ACT disciplines represented, at least 25% of patients on the unit discussed | Occurring daily, 2 out of 4 ACT disciplines represented, at least 50% of patients on the unit discussed | Occurring daily, 3 out of 4 ACT disciplines represented, at least 75% of patients on the unit discussed | Occurring daily, all disciplines of the ACT represented, all patients on the unit discussed |
| Hospitalist and specialty comanagement agreements | None | One out of 3 specialists represented on the unit collaborating with the hospitalists on at least 25% of relevant patients | One out of 3 specialists represented on the unit collaborating with the hospitalists on at least 50% of relevant patients | Two out of 3 specialists on the unit collaborating with the hospitalists on at least 75% of relevant patients | All specialists on the unit collaborating with the hospitalists on all relevant patients on the unit |
| Unit white board | None | Present but only used by nursing | Present and used by all ACT disciplines except physician providers | Present and used by entire ACT; use inconsistent | Present and used MondayFriday by all disciplines of ACT |
| Monthly review of unit level data | None | Nurse manager reviewing data with ACT program director | Nurse manager and unit leader reviewing data with ACT program director | Meeting either not consistently occurring monthly or not consistently attended by entire ACT | Monthly meeting with entire ACT |
| Weekly patient satisfaction rounding | None | Nurse manager performing up to 1 week a month | Nurse manager performing weekly | Nurse and physician leader performing up to 3 times a month | Nurse and physician leader performing weekly |
| Leadership | None | For units with specialties, either hospitalist or specialist leader identified | Both hospitalist and specialist leader Identified | Both hospitalist and specialist leaders (where applicable) identified and partially engaged in leadership role | Both hospitalist and specialist leaders (where applicable) identified and engaged in leadership role |
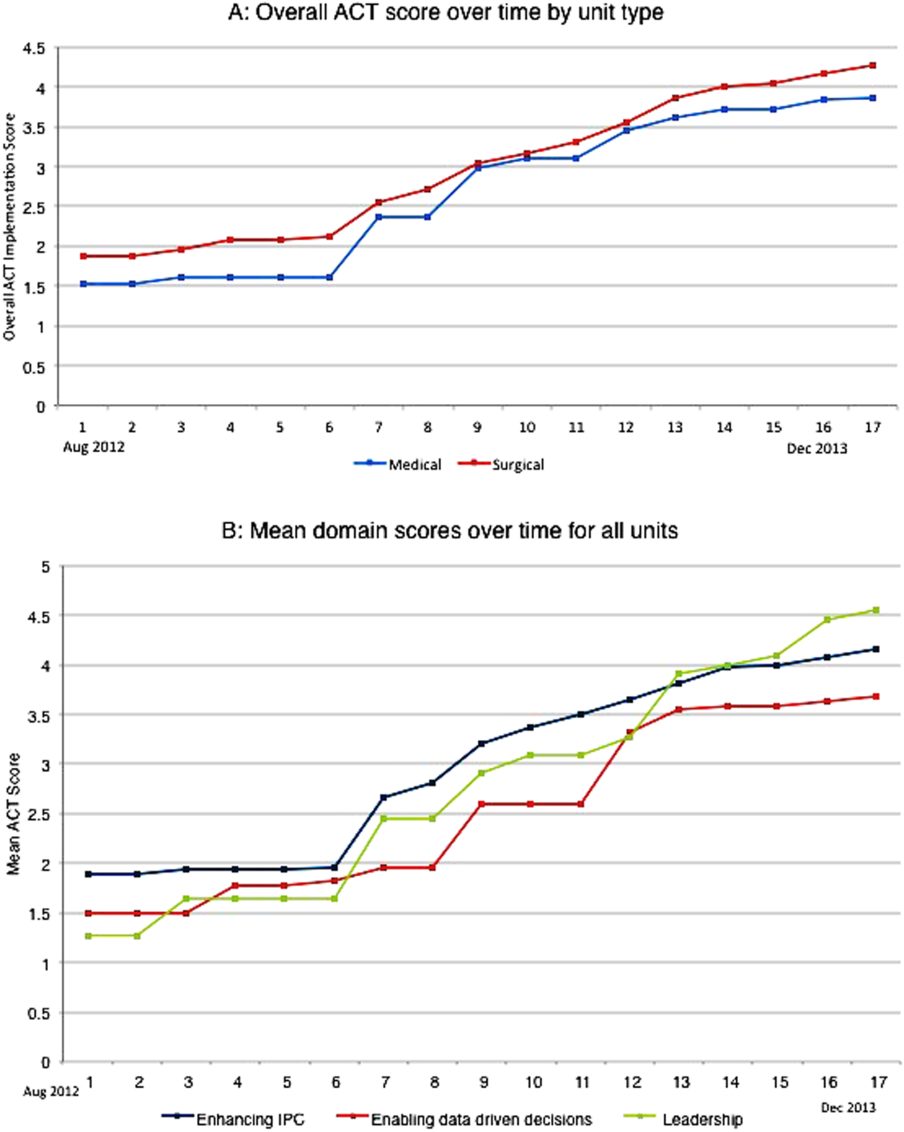
Outcomes
Monthly data between August 2012 and December 2013 were analyzed.
Measures of Value
MH is a member of the University Health Consortium, which measures outcomes of participants relative to their peers. MH measures LOS index as a ratio of observed LOS to expected LOS that is adjusted for severity of illness.[5]
Variable direct costs (VDCs) are costs that a hospital can save if a service is not provided.[6] A hospital's case‐mix index (CMI) represents the average diagnosis‐related group relative weight for that hospital. We track VDCs adjusted for CMI (CMI‐adjusted VDC).[7]
Thirty‐day readmission rate is the percentage of cases that are readmitted to MH within 30 days of discharge from the index admission.[8]
Measures of Patient Satisfaction
The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey covers topics relevant to a patient's experience in the hospital.[9] Patient satisfaction scores are tracked by responses to the HCAHPS survey.
Measures of Provider Satisfaction
Hospitalist and specialty providers, leadership, and case management teams were surveyed via email through SurveyMonkey in July 2014. The survey included Likert responses that elicited opinions and comments about the ACT model.
Statistical Methods
The primary predictor of interest was the monthly overall ACT score. We also explored the domain scores as well as the individual scores for each intervention. Generalized linear mixed models were fit to investigate the association between each predictor (overall ACT score, ACT domain scores, and individual implementation scores) and each outcome (LOS index, CMI‐adjusted VDC, 30‐day readmission rate, and overall patient satisfaction). The model for testing each ACT score also included covariates of inpatient units as a random effect, as well as date and type of unit as fixed effects. We set the statistical significance level at 0.01 and reported 99% confidence intervals.
Descriptive statistics were used to report the provider satisfaction survey results.
RESULTS
The overall ACT score was associated with LOS index and CMI‐adjusted VDC (both P < 0.001). For every 1‐unit increase in the overall ACT score, LOS index decreased by 0.078 and CMI‐adjusted VDC decreased by $273.99 (Table 3).
| Length of Stay Index | CMI Adjusted VDC | |||
|---|---|---|---|---|
| Estimate (99% CI)* | P Value | Estimate (99% CI)* | P Value | |
| ||||
| Overall ACT Score | 0.078 (0.123 to 0.032) | <0.001 | 274.0 (477.31 to 70.68) | <0.001 |
| Enhancing IPC | 0.071 (0.117 to 0.026) | <0.001 | 284.7 (488.08 to 81.23) | <0.001 |
| Enabling data‐driven decisions | 0.044 (0.080 to 0.009) | 0.002 | 145.4 (304.57 to 13.81) | 0.02 |
| Providing leadership | 0.027 (0.049 to 0.005) | 0.001 | 69.9 (169.00 to 29.26) | 0.07 |
Looking at domains, enhancing IPC resulted in statistically significant decreases in both LOS index and CMI‐adjusted VDC, but providing leadership and enabling data‐driven decisions decreased only the LOS index. Most of the 8 individual interventions were associated with at least 1 of these 2 outcomes. (Even where the associations were not significant, they were all in the direction of decreasing LOS and cost). In these models, the covariate of type of units (medical vs surgical) was not associated with LOS or cost. There was no significant time trend in LOS or cost, except in models where an intervention had no association with either outcome. Inclusion of all individual effective interventions in the same statistical model to assess their relative contributions was not possible because they were highly correlated (correlations 0.450.89).
Thirty‐day readmissions and patient satisfaction were not significantly associated with the overall ACT score, but exploratory analyses showed that patient satisfaction increased with the implementation of geographical cohorting (P = 0.007).
Survey Results
The response rate was 87% (96/110). Between 85% and 96% of respondents either agreed or strongly agreed that the ACT model had improved the quality and safety of the care delivered, improved communication between providers and patients, and improved their own engagement and job satisfaction. Overall, 78% of the respondents either agreed or strongly agreed that the model improved efficiency (Table 4). Suggestions for improvements revolved around increasing the emphasis on patient centeredness and bedside nursing engagement.
| The ACT Model | Strongly Agree, n (%) | Agree, n (%) | Disagree, n (%) | Strongly Disagree, n (%) |
|---|---|---|---|---|
| ||||
| Has improved the quality and safety of patient care | 46 (47.9) | 46 (47.9) | 2 (2.1) | 2 (2.1) |
| Has improved communication with patients and families | 42 (43.7) | 47 (49.0) | 5 (5.2) | 2 (2.1) |
| Has improved your efficiency/productivity | 31 (32.6) | 43 (45.3) | 17 (17.9) | 4 (4.2) |
| Has improved your engagement and job satisfaction | 33 (34.4) | 49 (51.0) | 10 (10.4) | 4 (4.2) |
| Is a better model of delivering patient care | 45 (47.4) | 44 (46.3) | 2 (2.1) | 4 (4.2) |
DISCUSSION
The serious problems in US healthcare constitute an urgent imperative to innovate and reform.[10] Inpatient care reflects 31% of the expenditure on healthcare, and in 2010, 35.1 million patients were discharged from the hospital after spending an average of 4.8 days as an inpatient.[11] These figures represent an immense opportunity to intervene. Measuring the impact of quality improvement efforts is often complicated by concomitant changes that affect outcomes over the interval studied. Our approach allowed us to detect statistically significant changes in LOS index and CMI‐adjusted VDC associated with the ACT implementation dose that could be separated from the underlying time trends.
The ACT model we describe is rooted in improving 3 foundational domains; quantifying each intervention's compartmentalized contribution, however, proved difficult. Each intervention intertwines with the others to create changes in attitudes, knowledge, and culture that are difficult to measure yet may synergistically affect outcomes. For example, although geographical cohorting appears to have the strongest statistical association with outcomes, this may be mediated by how it enables other processes to take place more effectively. Based on this analysis, therefore, the ACT model may best be considered a bundled intervention.
The team caring for a patient during hospitalization is so complex that fewer than a quarter of patients know their physician's or nurse's name.[12] This complexity impairs communication between patients and providers and between the providers themselves. Communication failures are consistently identified as root causes in sentinel events reported to the Joint Commission.[13] IPC is the process by which different professional groups work together to positively impact health care. IPC overlaps with communication, coordination, and teamwork, and improvements in IPC may improve care.[14] Some elements of the model we describe have been tested previously.[15, 16, 17] Localization of teams may increase productivity and the frequency with which physicians and nurses communicate. Localization also decreases the number of pages received and steps walked by providers during a workday.[15, 16, 17] However, these studies reported a trend toward an increase in the LOS and neutral effects on cost and readmission rates. We found statistically significant decreases in both LOS and cost associated with the geographic cohorting of patients and providers. Notably, our model localized not only the physician providers but also the interdisciplinary team of pharmacists, clinical nurse specialists, case managers, and social workers. This proximity may facilitate IPC between all members that culminates in improved efficiency. The possibility of delays in discharges to avoid new admissions in a geographically structured team has previously been raised to explain the associated increases in LOS.[16, 17] The accountability of each unit for its metrics, the communication between nursing and physicians, and the timely availability of the unit's performance data aligns everyone toward a shared goal and provides some protection from an unintended consequence.
Structured interdisciplinary rounds decrease adverse events and improve teamwork ratings.[18, 19] The huddle in our model is a forum to collaborate between disciplines that proved to be effective in decreasing LOS and costs. Our huddle aims to discuss all the patients on the unit. This allows the team to assist each other in problem solving for the entire unit and not just the patients on the geographically cohorted team. This approach, in addition to the improved IPC fostered by the ACT model, may help explain how benefits in LOS and costs permeated across all 11 diverse units despite the presence of patients who are not directly served by the geographically cohorted team.
High‐performing clinical systems maintain an awareness of their overarching mission and unit‐based leaders can influence the frontline by reiterating the organizational mission and aligning efforts with outcomes.[20] Our leadership model is similar to those described by other institutions in the strong partnerships between physicians and nursing.[21] As outlined by Kim et al., investing in the professional development of the unit leaders may help them fulfill their roles and serve the organization better.[21]
The fragmentation and lack of ownership over the continuum of patient care causes duplication and waste. The proposal in the Accountable Care Act to create accountable care organizations is rooted in the understanding that providers and organizations will seek out new ways of improving quality when held accountable for their outcomes.[22] To foster ownership and accountability, reporting of metrics at the unit level is needed. Furthermore, an informational infrastructure is critical, as improvements cannot occur without the availability of data to both monitor performance and measure the effect of interventions.[10, 23] Even without any other interventions, providing feedback alone is an effective way of changing practices.[24] According to Berwick et al., this phenomenon reflects practitioners' intrinsic motivation to simply want to be better.[25] Our monthly review of each unit's data is an effective way to provide timely feedback to the frontline that sparks pride, ownership, and innovative thinking.
Based on our mean ACT score and CMI‐adjusted VDC reductions alone, we estimate savings of $649.36 per hospitalization (mean increase in ACT implementation of 2.37 times reduction in cost index of $273.99 per unit increase in overall ACT score). This figure does not include savings realized through reductions in LOS. This is a small decrease relative to the mean cost of hospitalization, yet when compounded over the annual MH census, it would result in substantial savings. The model relied on the restructuring of the existing workforce and the only direct additional cost was the early salary support for the ACT program director.
Limitations
We recognize several limitations. It is a single center's experience and may not be generalizable. The diffusion of knowledge and culture carried between units and the relatively rapid implementation timeline did not allow for a control unit. A single observer assigned our implementation scores, and therefore we cannot report measures of inter‐rater reliability. However, defined criteria and direct observations were used wherever possible. Although administratively available data have their limitations, where available, we used measurements that are adjusted for severity of illness and CMI. We therefore feel that this dataset is an accurate representation of currently reported national quality indicators.
FURTHER DIRECTIONS
Although there is a need to improve our healthcare system, interventions should be deliberate and evidence based wherever possible.[26] Geographic cohorting may decrease the frequency of paging interruptions for physicians and practitioners while increasing face‐to‐face interruptions.[27] The net effect on safety with this trade‐off should be investigated.
The presence of an intervention does not guarantee its success. Despite geographic cohorting and interdisciplinary meetings, communication that influences physician decision making may not improve.[28] Although instruments to measure ratings of team work and collaboration are available, focusing on clinically relevant outcomes of teamwork, such as prevention of harm, may be more empowering feedback for the frontline. Formal cost‐benefit analyses and outcomes related to physician and nursing retention will be equally important for assessing the sustainability of the model. Involving patients and their caregivers and inviting their perspectives as care is redesigned will also be critical in maintaining patient centeredness. Research addressing interventions to mediate preventable readmission risk and understanding the drivers of patient satisfaction is also needed.
The true value of the model may be in its potential to monitor and drive change within itself. Continuously aligning aims, incentives, performance measures, and feedback will help support this innovation and drive. This affects not only patient care but creates microcosms within which research and education can thrive. We hope that our experience will help guide other institutions as we all strive in our journey to improve the care we deliver.
Acknowledgements
The authors thank the Indiana University Health Physicians hospitalists at MH, Sandy Janitz and Decision Support, the Indiana University Health executive leadership team, Robert Clark, Malaz Boustani, Dennis Watson, Nadia Adams, Todd Biggerstaff, Deanne Kashiwagi, and the tireless providers at MH for their support.
Disclosure: This work was supported by a grant from the Indiana University Health Values Fund. The authors have no conflicts of interest to disclose.
Despite an estimated annual $2.6 trillion expenditure on healthcare, the United States performs poorly on indicators of health and harm during care.[1, 2, 3] Hospitals around the nation are working to improve the care they deliver. We describe a model developed at our institution and report the evaluation of the outcomes associated with its implementation on the general medical and surgical units. The Indiana University Institutional Review Board approved this work.
SETTING AND DEFINITIONS
Indiana University Health Methodist Hospital (MH) is an academic center in Indianapolis, Indiana, serving over 30,000 patients annually.[4] In 2012, responding to the coexisting needs to improve quality and contain costs, the MH leadership team redesigned care in the hospital. The new model centers around accountable care teams (ACTs). Each ACT is a geographically defined set of providers accepting ownership for the clinical, service, and financial outcomes of their respective inpatient unit. The units studied are described in Table 1.
| Unit | No. of Beds | Predominant Diagnosis (Maximum Domain Score)* | |
|---|---|---|---|
| |||
| Medical units with progressive‐care beds | 1 | 33 | Pulmonary (3.4, 3.5, 5) |
| 2 | 28 | Cardiology (4.8, 3.5, 4) | |
| 3 | 24 | General medical (4.8, 3.5, 4) | |
| Medical units without progressive‐care beds | 4 | 36 | Renal/diabetic (4, 3.5, 5) |
| 5 | 24 | General medical (3.75, 4, 5) | |
| Surgical units with progressive‐care beds | 6 | 51 | Cardiothoracic surgery/cardiology (4, 4, 5) |
| 7 | 29 | Trauma/general surgery (3.75, 3.5, 5) | |
| 8 | 23 | Neurosurgical/neurological (4.8, 5, 5) | |
| 9 | 24 | Neurosurgical/neurological (4.4, 4.5, 5) | |
| Surgical units without progressive‐care beds | 10 | 29 | General/urologic/gynecologic/plastic surgery (3.4, 3, 2) |
| 11 | 26 | Orthopedic surgery (4.6, 4, 5) | |
THE ACT MODEL
The model comprises 8 interventions rooted in 3 foundational domains: (1) enhancing interprofessional collaboration (IPC), (2) enabling data‐driven decisions, and (3) providing leadership. Each intervention is briefly described under its main focus (see Supporting Information, Appendix A, in the online version of this article for further details).
Enhancing IPC
Geographical Cohorting of Patients and Providers
Hospitalist providers are localized for 4 consecutive months to 1 unit. An interdisciplinary team including a case manager, clinical nurse specialist, pharmacist, nutritionist, and social worker also serve each unit. Learners (residents, pharmacy, and medical students) are embedded in the team when rotating on the hospital medicine service. The presence of unit‐based nurse managers and charge nurses predates the model and is retained.
Bedside Collaborative Rounding
Geographically cohorted providers round on their patients with the bedside nurse guided by a customizable script.
Daily Huddle
The hospitalist, learners, and the interdisciplinary team for the unit meet each weekday to discuss patients' needs for a safe transition out of the hospital. Each unit determined the timing, location, and script for the huddle while retaining the focus on discharge planning (see Supporting Information, Appendix A2, in the online version of this article for a sample script).
Hospitalist and Specialty Comanagement Agreements
Guidelines delineating responsibilities for providers of each specialty were developed. Examples include orders pertaining to the management of a dialysis catheter in a patient with end‐stage renal disease, the removal of drains in postsurgical patients, and wound care.
Unit White Board
Each unit has a white board at the nursing station. Similar to the huddle, it is focused on discharge planning.
Enabling Data‐Driven Decisions
Monthly Review of Unit‐Level Data
Data analytics at our institution developed a data dashboard. Key metrics including length of stay (LOS), patient satisfaction scores, readmission rates, and costs are tracked and attributed to the discharging unit. The data are collated monthly by the ACT program director and distributed to each unit's leadership. Monthly interdisciplinary meetings are held to review trends. Learners are encouraged but not required to attend.
Weekly Patient Satisfaction Rounding
The unit's nurse manager and physician leader conduct weekly satisfaction rounds on patients. The conversation is open‐ended and focused on eliciting positive and negative experiences.
Providing Leadership
Designated hospitalist and, where relevant, specialty leaders are committed to serve each unit for at least 1 year as a resource for both medical and operational problem solving. The leader stays closely connected with the unit's nurse manager. In addition to day‐to‐day troubleshooting, the leader is responsible for monitoring outcome trends. There is currently no stipend, training, or other incentive offered for the role.
Implementation Timelines and ACT Scores
The development of the ACTs started in the spring of 2012. Physician, nursing, and pharmacy support was sought, and a pilot unit was formed in August 2012. The model was cascaded hospital wide by December 2013, with support from the ACT program director (A.N.). The program director observed and scored the uptake of each intervention by each unit monthly. A score of 1 denoted no implementation, whereas 5 denoted complete implementation. The criteria for scoring are presented in Table 2. The monthly scores for all 8 interventions in each of the 11 units were averaged as an overall ACT score, which reflects the implementation dose of the ACT model. Monthly domain scores for enhancing IPC and enabling data‐driven decisions were also calculated as the average score within each domain. This yielded 3 domain scores. Figure 1A plots by month the overall ACT score for the medical and surgical units, and Figure 1B plots the implementation score for the 3 domains between August 2012 and December 2013 for all units. The uptake of the interventions varied between units. This allowed our analysis to explore the dose relationships between the model and outcomes independent of underlying time trends that may be affected by concomitant initiatives.
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| |||||
| Geographical cohorting of patients and the ACT* | None | At least 1 discipline comprising the ACT is unit based | All disciplines comprising the ACT except the hospitalist unit based | All disciplines including the hospitalist unit based | 4 + 80% of hospitalist provider's patients on the unit |
| Bedside collaborative rounding | None | Occurring 1 day a week on at least 25% of the patients on the unit | Occurring 2 to 3 days a week on at least 50% of the patients on the unit | Occurring 3 to 4 days a week on at least 75% of the patients on the unit | Occurring MondayFriday on all patients on the unit |
| Daily huddle | None | Occurring daily, 1 out of 4 ACT disciplines represented, at least 25% of patients on the unit discussed | Occurring daily, 2 out of 4 ACT disciplines represented, at least 50% of patients on the unit discussed | Occurring daily, 3 out of 4 ACT disciplines represented, at least 75% of patients on the unit discussed | Occurring daily, all disciplines of the ACT represented, all patients on the unit discussed |
| Hospitalist and specialty comanagement agreements | None | One out of 3 specialists represented on the unit collaborating with the hospitalists on at least 25% of relevant patients | One out of 3 specialists represented on the unit collaborating with the hospitalists on at least 50% of relevant patients | Two out of 3 specialists on the unit collaborating with the hospitalists on at least 75% of relevant patients | All specialists on the unit collaborating with the hospitalists on all relevant patients on the unit |
| Unit white board | None | Present but only used by nursing | Present and used by all ACT disciplines except physician providers | Present and used by entire ACT; use inconsistent | Present and used MondayFriday by all disciplines of ACT |
| Monthly review of unit level data | None | Nurse manager reviewing data with ACT program director | Nurse manager and unit leader reviewing data with ACT program director | Meeting either not consistently occurring monthly or not consistently attended by entire ACT | Monthly meeting with entire ACT |
| Weekly patient satisfaction rounding | None | Nurse manager performing up to 1 week a month | Nurse manager performing weekly | Nurse and physician leader performing up to 3 times a month | Nurse and physician leader performing weekly |
| Leadership | None | For units with specialties, either hospitalist or specialist leader identified | Both hospitalist and specialist leader Identified | Both hospitalist and specialist leaders (where applicable) identified and partially engaged in leadership role | Both hospitalist and specialist leaders (where applicable) identified and engaged in leadership role |
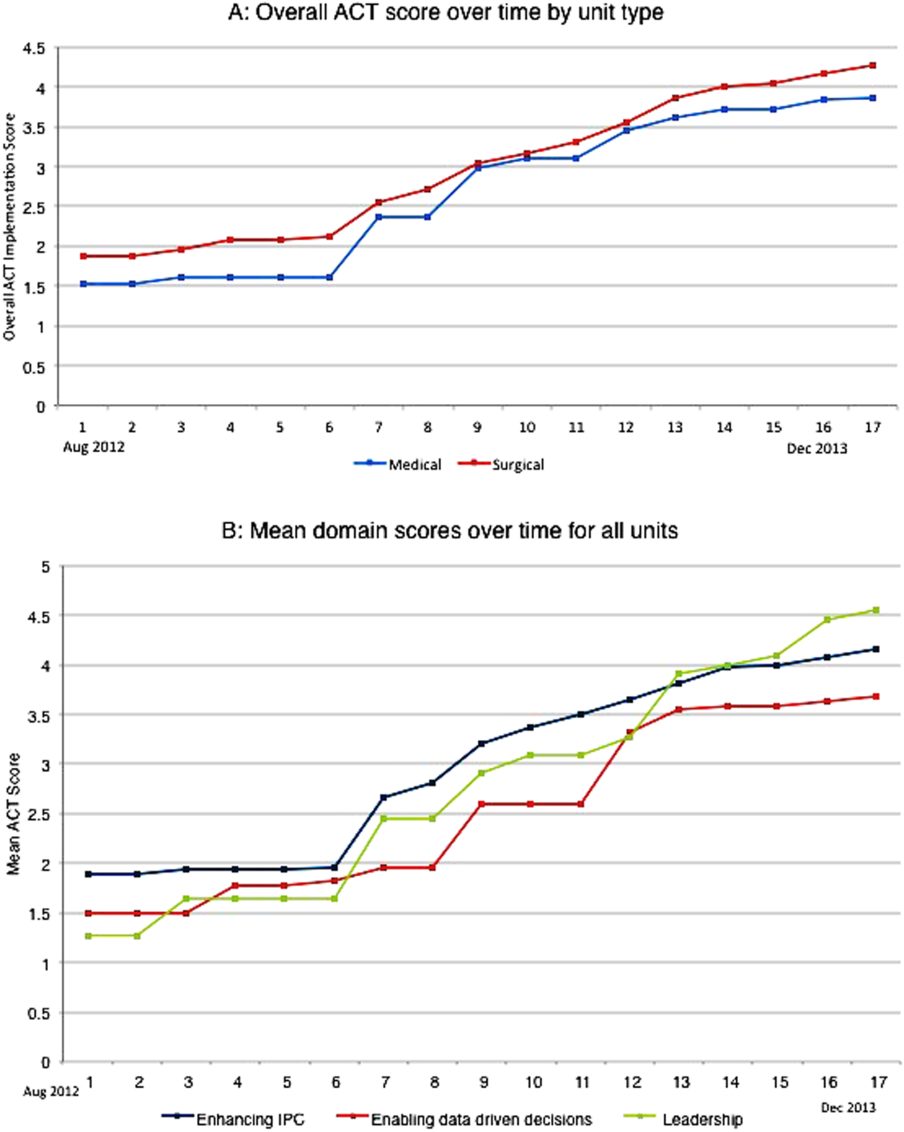
Outcomes
Monthly data between August 2012 and December 2013 were analyzed.
Measures of Value
MH is a member of the University Health Consortium, which measures outcomes of participants relative to their peers. MH measures LOS index as a ratio of observed LOS to expected LOS that is adjusted for severity of illness.[5]
Variable direct costs (VDCs) are costs that a hospital can save if a service is not provided.[6] A hospital's case‐mix index (CMI) represents the average diagnosis‐related group relative weight for that hospital. We track VDCs adjusted for CMI (CMI‐adjusted VDC).[7]
Thirty‐day readmission rate is the percentage of cases that are readmitted to MH within 30 days of discharge from the index admission.[8]
Measures of Patient Satisfaction
The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey covers topics relevant to a patient's experience in the hospital.[9] Patient satisfaction scores are tracked by responses to the HCAHPS survey.
Measures of Provider Satisfaction
Hospitalist and specialty providers, leadership, and case management teams were surveyed via email through SurveyMonkey in July 2014. The survey included Likert responses that elicited opinions and comments about the ACT model.
Statistical Methods
The primary predictor of interest was the monthly overall ACT score. We also explored the domain scores as well as the individual scores for each intervention. Generalized linear mixed models were fit to investigate the association between each predictor (overall ACT score, ACT domain scores, and individual implementation scores) and each outcome (LOS index, CMI‐adjusted VDC, 30‐day readmission rate, and overall patient satisfaction). The model for testing each ACT score also included covariates of inpatient units as a random effect, as well as date and type of unit as fixed effects. We set the statistical significance level at 0.01 and reported 99% confidence intervals.
Descriptive statistics were used to report the provider satisfaction survey results.
RESULTS
The overall ACT score was associated with LOS index and CMI‐adjusted VDC (both P < 0.001). For every 1‐unit increase in the overall ACT score, LOS index decreased by 0.078 and CMI‐adjusted VDC decreased by $273.99 (Table 3).
| Length of Stay Index | CMI Adjusted VDC | |||
|---|---|---|---|---|
| Estimate (99% CI)* | P Value | Estimate (99% CI)* | P Value | |
| ||||
| Overall ACT Score | 0.078 (0.123 to 0.032) | <0.001 | 274.0 (477.31 to 70.68) | <0.001 |
| Enhancing IPC | 0.071 (0.117 to 0.026) | <0.001 | 284.7 (488.08 to 81.23) | <0.001 |
| Enabling data‐driven decisions | 0.044 (0.080 to 0.009) | 0.002 | 145.4 (304.57 to 13.81) | 0.02 |
| Providing leadership | 0.027 (0.049 to 0.005) | 0.001 | 69.9 (169.00 to 29.26) | 0.07 |
Looking at domains, enhancing IPC resulted in statistically significant decreases in both LOS index and CMI‐adjusted VDC, but providing leadership and enabling data‐driven decisions decreased only the LOS index. Most of the 8 individual interventions were associated with at least 1 of these 2 outcomes. (Even where the associations were not significant, they were all in the direction of decreasing LOS and cost). In these models, the covariate of type of units (medical vs surgical) was not associated with LOS or cost. There was no significant time trend in LOS or cost, except in models where an intervention had no association with either outcome. Inclusion of all individual effective interventions in the same statistical model to assess their relative contributions was not possible because they were highly correlated (correlations 0.450.89).
Thirty‐day readmissions and patient satisfaction were not significantly associated with the overall ACT score, but exploratory analyses showed that patient satisfaction increased with the implementation of geographical cohorting (P = 0.007).
Survey Results
The response rate was 87% (96/110). Between 85% and 96% of respondents either agreed or strongly agreed that the ACT model had improved the quality and safety of the care delivered, improved communication between providers and patients, and improved their own engagement and job satisfaction. Overall, 78% of the respondents either agreed or strongly agreed that the model improved efficiency (Table 4). Suggestions for improvements revolved around increasing the emphasis on patient centeredness and bedside nursing engagement.
| The ACT Model | Strongly Agree, n (%) | Agree, n (%) | Disagree, n (%) | Strongly Disagree, n (%) |
|---|---|---|---|---|
| ||||
| Has improved the quality and safety of patient care | 46 (47.9) | 46 (47.9) | 2 (2.1) | 2 (2.1) |
| Has improved communication with patients and families | 42 (43.7) | 47 (49.0) | 5 (5.2) | 2 (2.1) |
| Has improved your efficiency/productivity | 31 (32.6) | 43 (45.3) | 17 (17.9) | 4 (4.2) |
| Has improved your engagement and job satisfaction | 33 (34.4) | 49 (51.0) | 10 (10.4) | 4 (4.2) |
| Is a better model of delivering patient care | 45 (47.4) | 44 (46.3) | 2 (2.1) | 4 (4.2) |
DISCUSSION
The serious problems in US healthcare constitute an urgent imperative to innovate and reform.[10] Inpatient care reflects 31% of the expenditure on healthcare, and in 2010, 35.1 million patients were discharged from the hospital after spending an average of 4.8 days as an inpatient.[11] These figures represent an immense opportunity to intervene. Measuring the impact of quality improvement efforts is often complicated by concomitant changes that affect outcomes over the interval studied. Our approach allowed us to detect statistically significant changes in LOS index and CMI‐adjusted VDC associated with the ACT implementation dose that could be separated from the underlying time trends.
The ACT model we describe is rooted in improving 3 foundational domains; quantifying each intervention's compartmentalized contribution, however, proved difficult. Each intervention intertwines with the others to create changes in attitudes, knowledge, and culture that are difficult to measure yet may synergistically affect outcomes. For example, although geographical cohorting appears to have the strongest statistical association with outcomes, this may be mediated by how it enables other processes to take place more effectively. Based on this analysis, therefore, the ACT model may best be considered a bundled intervention.
The team caring for a patient during hospitalization is so complex that fewer than a quarter of patients know their physician's or nurse's name.[12] This complexity impairs communication between patients and providers and between the providers themselves. Communication failures are consistently identified as root causes in sentinel events reported to the Joint Commission.[13] IPC is the process by which different professional groups work together to positively impact health care. IPC overlaps with communication, coordination, and teamwork, and improvements in IPC may improve care.[14] Some elements of the model we describe have been tested previously.[15, 16, 17] Localization of teams may increase productivity and the frequency with which physicians and nurses communicate. Localization also decreases the number of pages received and steps walked by providers during a workday.[15, 16, 17] However, these studies reported a trend toward an increase in the LOS and neutral effects on cost and readmission rates. We found statistically significant decreases in both LOS and cost associated with the geographic cohorting of patients and providers. Notably, our model localized not only the physician providers but also the interdisciplinary team of pharmacists, clinical nurse specialists, case managers, and social workers. This proximity may facilitate IPC between all members that culminates in improved efficiency. The possibility of delays in discharges to avoid new admissions in a geographically structured team has previously been raised to explain the associated increases in LOS.[16, 17] The accountability of each unit for its metrics, the communication between nursing and physicians, and the timely availability of the unit's performance data aligns everyone toward a shared goal and provides some protection from an unintended consequence.
Structured interdisciplinary rounds decrease adverse events and improve teamwork ratings.[18, 19] The huddle in our model is a forum to collaborate between disciplines that proved to be effective in decreasing LOS and costs. Our huddle aims to discuss all the patients on the unit. This allows the team to assist each other in problem solving for the entire unit and not just the patients on the geographically cohorted team. This approach, in addition to the improved IPC fostered by the ACT model, may help explain how benefits in LOS and costs permeated across all 11 diverse units despite the presence of patients who are not directly served by the geographically cohorted team.
High‐performing clinical systems maintain an awareness of their overarching mission and unit‐based leaders can influence the frontline by reiterating the organizational mission and aligning efforts with outcomes.[20] Our leadership model is similar to those described by other institutions in the strong partnerships between physicians and nursing.[21] As outlined by Kim et al., investing in the professional development of the unit leaders may help them fulfill their roles and serve the organization better.[21]
The fragmentation and lack of ownership over the continuum of patient care causes duplication and waste. The proposal in the Accountable Care Act to create accountable care organizations is rooted in the understanding that providers and organizations will seek out new ways of improving quality when held accountable for their outcomes.[22] To foster ownership and accountability, reporting of metrics at the unit level is needed. Furthermore, an informational infrastructure is critical, as improvements cannot occur without the availability of data to both monitor performance and measure the effect of interventions.[10, 23] Even without any other interventions, providing feedback alone is an effective way of changing practices.[24] According to Berwick et al., this phenomenon reflects practitioners' intrinsic motivation to simply want to be better.[25] Our monthly review of each unit's data is an effective way to provide timely feedback to the frontline that sparks pride, ownership, and innovative thinking.
Based on our mean ACT score and CMI‐adjusted VDC reductions alone, we estimate savings of $649.36 per hospitalization (mean increase in ACT implementation of 2.37 times reduction in cost index of $273.99 per unit increase in overall ACT score). This figure does not include savings realized through reductions in LOS. This is a small decrease relative to the mean cost of hospitalization, yet when compounded over the annual MH census, it would result in substantial savings. The model relied on the restructuring of the existing workforce and the only direct additional cost was the early salary support for the ACT program director.
Limitations
We recognize several limitations. It is a single center's experience and may not be generalizable. The diffusion of knowledge and culture carried between units and the relatively rapid implementation timeline did not allow for a control unit. A single observer assigned our implementation scores, and therefore we cannot report measures of inter‐rater reliability. However, defined criteria and direct observations were used wherever possible. Although administratively available data have their limitations, where available, we used measurements that are adjusted for severity of illness and CMI. We therefore feel that this dataset is an accurate representation of currently reported national quality indicators.
FURTHER DIRECTIONS
Although there is a need to improve our healthcare system, interventions should be deliberate and evidence based wherever possible.[26] Geographic cohorting may decrease the frequency of paging interruptions for physicians and practitioners while increasing face‐to‐face interruptions.[27] The net effect on safety with this trade‐off should be investigated.
The presence of an intervention does not guarantee its success. Despite geographic cohorting and interdisciplinary meetings, communication that influences physician decision making may not improve.[28] Although instruments to measure ratings of team work and collaboration are available, focusing on clinically relevant outcomes of teamwork, such as prevention of harm, may be more empowering feedback for the frontline. Formal cost‐benefit analyses and outcomes related to physician and nursing retention will be equally important for assessing the sustainability of the model. Involving patients and their caregivers and inviting their perspectives as care is redesigned will also be critical in maintaining patient centeredness. Research addressing interventions to mediate preventable readmission risk and understanding the drivers of patient satisfaction is also needed.
The true value of the model may be in its potential to monitor and drive change within itself. Continuously aligning aims, incentives, performance measures, and feedback will help support this innovation and drive. This affects not only patient care but creates microcosms within which research and education can thrive. We hope that our experience will help guide other institutions as we all strive in our journey to improve the care we deliver.
Acknowledgements
The authors thank the Indiana University Health Physicians hospitalists at MH, Sandy Janitz and Decision Support, the Indiana University Health executive leadership team, Robert Clark, Malaz Boustani, Dennis Watson, Nadia Adams, Todd Biggerstaff, Deanne Kashiwagi, and the tireless providers at MH for their support.
Disclosure: This work was supported by a grant from the Indiana University Health Values Fund. The authors have no conflicts of interest to disclose.
- Committee on Quality of Health Care in America; Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press; 2001.
- . Is US health really the best in the world? JAMA. 2000;284(4):483–485.
- , , , , , . Temporal trends in rates of patient harm resulting from medical care. N Engl J Med. 2010;363(22):2124–2134.
- Indiana University Health. Available at: http://iuhealth.org/methodist/aboIut/. Accessed October 20, 2014.
- University Health Consortium. Available at: https://www.uhc.edu/docs/45014769_QSS_dashboard_FAQs.pdf. Accessed October 23, 2014.
- , , , et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999;281(7):644–649.
- Centers for Medicare and Medicaid Services. Case mix index. Available at: http://www.cms.gov/Medicare/Medicare‐Fee‐for‐Service‐Payment/AcuteInpatientPPS/Acute‐Inpatient‐Files‐for‐Download‐Items/CMS022630.html. Accessed May 4, 2015.
- University Health Consortium. Available at: https://www.uhc.edu. Accessed October 23, 2014.
- Centers for Medicare and Medicaid Services. Hospital Consumer Assessment of Healthcare Providers and Systems. HCAHPS survey content and administration. Centers for Medicare 280(11):1000–1005.
- Centers for Disease Control and Prevention. FastStats. Available at: http://www.cdc.gov/nchs/fastats/default.htm. Accessed October 27, 2014.
- , . Does your patient know your name? An approach to enhancing patients' awareness of their caretaker's name. J Healthc Qual. 2005;27(4):53–56.
- The Joint Commission. Sentinel event data: root causes by event type 2004‐third quarter. Available at: http://www.jointcommissionorg. Available at: http://www.jointcommission.org/assets/1/18/Root_Causes_by_Event_Type_2004-2Q2013.pdf. Accessed March 26, 2014.
- , , . Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009;(3):CD000072.
- , , , et al. Impact of localizing physicians to hospital units on nurse–physician communication and agreement on the plan of care. J Gen Intern Med. 2009;24(11):1223–1227.
- , , , et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551–556.
- , , , et al. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. J Hosp Med. 2008;3(5):361–368.
- , , , , , . Improving teamwork: impact of structured interdisciplinary rounds on a medical teaching unit. J Gen Intern Med. 2010;25(8):826–832.
- , , , ; High Performance Teams and the Hospital of the Future Project Team. Interdisciplinary teamwork in hospitals: a review and practical recommendations for improvement. J Hosp Med. 2011;7(1):48–54.
- , , , , , . Microsystems in health care: part 8. Developing people and improving work life: what front‐line staff told us. Jt Comm J Qual Saf. 2003;29(10):512–522.
- , , , , , . Unit‐based interprofessional leadership models in six US hospitals. J Hosp Med. 2014;9(8):545–550.
- , , , . Creating accountable care organizations: the extended hospital medical staff. Health Aff (Millwood). 2007;26(1):w44–w57.
- , . Using performance measurement to drive improvement: a road map for change. Med Care. 2003;41(1 suppl):I48–I60.
- , . Changing physicians' practices. N Engl J Med. 1993;329(17):1271–1273.
- , , . Connections between quality measurement and improvement. Med Care. 2003;41(1 suppl):I30–I38.
- , , . The tension between needing to improve care and knowing how to do it. N Engl J Med. 2007;357(6):608–613.
- , . A qualitative evaluation of geographical localization of hospitalists: how unintended consequences may impact quality. J Gen Intern Med. 2014;29(7):1009–1016.
- , , , , . Disengaged: a qualitative study of communication and collaboration between physicians and other professions on general internal medicine wards. BMC Health Serv Res. 2013;13:494.
- Committee on Quality of Health Care in America; Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press; 2001.
- . Is US health really the best in the world? JAMA. 2000;284(4):483–485.
- , , , , , . Temporal trends in rates of patient harm resulting from medical care. N Engl J Med. 2010;363(22):2124–2134.
- Indiana University Health. Available at: http://iuhealth.org/methodist/aboIut/. Accessed October 20, 2014.
- University Health Consortium. Available at: https://www.uhc.edu/docs/45014769_QSS_dashboard_FAQs.pdf. Accessed October 23, 2014.
- , , , et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999;281(7):644–649.
- Centers for Medicare and Medicaid Services. Case mix index. Available at: http://www.cms.gov/Medicare/Medicare‐Fee‐for‐Service‐Payment/AcuteInpatientPPS/Acute‐Inpatient‐Files‐for‐Download‐Items/CMS022630.html. Accessed May 4, 2015.
- University Health Consortium. Available at: https://www.uhc.edu. Accessed October 23, 2014.
- Centers for Medicare and Medicaid Services. Hospital Consumer Assessment of Healthcare Providers and Systems. HCAHPS survey content and administration. Centers for Medicare 280(11):1000–1005.
- Centers for Disease Control and Prevention. FastStats. Available at: http://www.cdc.gov/nchs/fastats/default.htm. Accessed October 27, 2014.
- , . Does your patient know your name? An approach to enhancing patients' awareness of their caretaker's name. J Healthc Qual. 2005;27(4):53–56.
- The Joint Commission. Sentinel event data: root causes by event type 2004‐third quarter. Available at: http://www.jointcommissionorg. Available at: http://www.jointcommission.org/assets/1/18/Root_Causes_by_Event_Type_2004-2Q2013.pdf. Accessed March 26, 2014.
- , , . Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009;(3):CD000072.
- , , , et al. Impact of localizing physicians to hospital units on nurse–physician communication and agreement on the plan of care. J Gen Intern Med. 2009;24(11):1223–1227.
- , , , et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551–556.
- , , , et al. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. J Hosp Med. 2008;3(5):361–368.
- , , , , , . Improving teamwork: impact of structured interdisciplinary rounds on a medical teaching unit. J Gen Intern Med. 2010;25(8):826–832.
- , , , ; High Performance Teams and the Hospital of the Future Project Team. Interdisciplinary teamwork in hospitals: a review and practical recommendations for improvement. J Hosp Med. 2011;7(1):48–54.
- , , , , , . Microsystems in health care: part 8. Developing people and improving work life: what front‐line staff told us. Jt Comm J Qual Saf. 2003;29(10):512–522.
- , , , , , . Unit‐based interprofessional leadership models in six US hospitals. J Hosp Med. 2014;9(8):545–550.
- , , , . Creating accountable care organizations: the extended hospital medical staff. Health Aff (Millwood). 2007;26(1):w44–w57.
- , . Using performance measurement to drive improvement: a road map for change. Med Care. 2003;41(1 suppl):I48–I60.
- , . Changing physicians' practices. N Engl J Med. 1993;329(17):1271–1273.
- , , . Connections between quality measurement and improvement. Med Care. 2003;41(1 suppl):I30–I38.
- , , . The tension between needing to improve care and knowing how to do it. N Engl J Med. 2007;357(6):608–613.
- , . A qualitative evaluation of geographical localization of hospitalists: how unintended consequences may impact quality. J Gen Intern Med. 2014;29(7):1009–1016.
- , , , , . Disengaged: a qualitative study of communication and collaboration between physicians and other professions on general internal medicine wards. BMC Health Serv Res. 2013;13:494.
© 2015 Society of Hospital Medicine
Baseline QTc and Azithromycin Evaluation
Azithromycin, a macrolide antibiotic, received US Food and Drug Administration (FDA) approval in 1991 and is 1 of the most prescribed antibiotics used for a variety of infections, including community‐acquired pneumonia, bacterial sinusitis, urethritis, and cervicitis. In 2011, it was estimated that 40.3 million outpatients received a prescription for azithromycin.[1] In addition to treating acute bacterial infections, recent literature has pointed to using azithromycin for its unlabeled immunomodulatory and anti‐inflammatory effects, particularly in cystic fibrosis, chronic obstructive pulmonary disease (COPD), and lung transplant recipients.[2, 3, 4] Azithromycin decreases bacterial load and virulence, thus reducing airway secretion, as well as decreasing airway neutrophil accumulation through a reduction in proinflammatory cytokine expression.[4]
Cardiac toxicity can occur with macrolide antibiotics, and prolongation of the QT interval with subsequent Torsades de pointes has been documented with azithromycin.[1, 5, 6] In 2012, Ray et al. published data on a cohort of outpatients receiving azithromycin compared to amoxicillin, ciprofloxacin, or no antibiotics, and showed a small but absolute increase in cardiovascular deaths.[7, 8] Subsequent data, however, have not illustrated increased risk of death from cardiovascular causes. Mortensen et al. showed a lower risk of 90‐day mortality in older patients treated for community acquired pneumonia with azithromycin and ceftriaxone, although there was a nonstatistically significant increased risk of myocardial infarction in this group.[8, 9, 10] In March 2013, the FDA released an official statement regarding increased cardiovascular risk with azithromycin, stating that healthcare professionals should consider the risk of fatal heart rhythms with azithromycin when considering treatment options for patients who are at risk for cardiovascular events.[11]
In recent years, the potential for corrected QT (QTc) prolongation and Torsades de pointes has received increased attention due to its catastrophic nature, and it is thought that hospitalized patients are at a greater risk of drug‐induced Torsades de pointes due to the likelihood of having more risk factors.[12, 13] The American Heart Association released a statement in 2010 to raise awareness among healthcare professionals about risk, electrocardiogram (ECG) monitoring, and management of drug‐induced QT interval prolongation in hospitalized patients, although little data exist regarding quantification of risk in this patient population.[13, 14]
Prescribers currently have no standardized practice guidelines related to cardiovascular safety when prescribing QTc prolonging medications. Given the dramatic increase in azithromycin prescriptions and ongoing concern for cardiovascular risk and QTc prolongation, we investigated the prescribing practices with azithromycin within our institution. Our primary aims were 3‐fold. First, we aimed to describe the frequency azithromycin was prescribed with additional QTc prolonging medications. Second, we assessed the relationship between the number of arrhythmogenic drugs prescribed in addition to azithromycin with ordering telemetry. Finally, we assessed the relationship between baseline ECG abnormalities and telemetry monitoring in patients prescribed azithromycin. The purpose of these objectives was to better understand physician prescribing practices and to determine if patients have a potential risk of developing fatal cardiac arrhythmias
METHODS
Data
For this retrospective review, we utilized data from the University of Alabama at Birmingham Health Care system, a 1157licensed bed hospital. The institutional review board approved this study with a waiver of informed consent. Patients were eligible to be included in this study if they were 19 years of age with an inpatient hospital length of stay 3 days. Patients were considered to be receiving azithromycin and were included only when they were dispensed 1 dose of azithromycin by the pharmacy. Between October 1, 2012 and April 30, 2013, 1610 encounters were identified, of which 100 patient encounters were randomly selected for evaluation via a Microsoft Excel (Microsoft Corp., Redmond, WA) function. One patient was randomly included twice in this study, but had 2 separate admissions in which he received azithromycin.
QTc prolonging medications in our hospital formulary were identified via Micromedex and package inserts (see Supporting Information, Appendix, in the online version of this article for the full list).
Measures
The primary study measures were number of medications associated with QTc prolongation, baseline ECG findings, and telemetry monitoring. Secondary study measures include indication, dose, duration of use, formulation, length of stay, and admitting service (Table 1). Indications, dosage, and duration were defined by the FDA package insert for azithromycin (see Supporting Information, Appendix, in the online version of this article). Indication for use was defined as (1) empiric for a specific infection; (2) anti‐inflammatory for patients with COPD, lung transplant recipients, or cystic fibrosis patients; and (3) culture proven if evidence of a particular pathogen grown on culture. Indications were defined by prescriber notes. Dosage is defined as appropriate if FDA guidelines were followed for the defined indication. If patients were given azithromycin for anti‐inflammatory purposes, dosing was considered appropriate if it followed previous literature dosing of 250mg daily.
| |
| Age, y | |
| Average | 5519.5 |
| Range | 2197 |
| Gender | |
| Female | 61% |
| Male | 39% |
| Length of stay, d | |
| Average | 9.713.1 |
| Range | 3115 |
| Admitting service | |
| Hospitalist | 37% |
| Pulmonary | 23% |
| Obstetrics | 9% |
| General medicine | 8% |
| Hematology/oncology | 6% |
| Othera | 17% |
| Days of therapy | |
| Average | 4.53.9 |
| Range | 128 |
| Median | 4 |
| Indication for use | |
| Empiric | 79% |
| Anti‐inflammatory | 20% |
| Culture proven | 1% |
| Dosage | |
| Appropriate | 67% |
| Inappropriate | 14% |
| Unknown | 19% |
| Duration | |
| Appropriate | 63% |
| Inappropriate | 19% |
| Unknown | 18% |
| Formulation | |
| Intravenous only | 21% |
| Intravenous followed by tablet | 13% |
| Suspension | 2% |
| Tablet | 64% |
| Diagnosis‐related group | |
| Simple pneumonia with pleurisy | 14% |
| Septicemia with sepsis | 8% |
| Respiratory infection with inflammation | 8% |
| Chronic obstructive pulmonary disease | 8% |
| Pulmonary edema with respiratory failure | 6% |
| Vaginal delivery with complications | 6% |
| Respiratory diagnosis with ventilator support | 4% |
| Otherb | 46% |
Patients were divided into drug interaction risk levels based on the number of medications prescribed with the potential for QT prolongation (Table 2). Patients were considered low risk if they received azithromycin alone, medium risk if they received 2 to 3 QT‐prolonging medications including azithromycin, and high risk if they received 4 or more QT‐prolonging medications including azithromycin.
| Medication | % of Patients Receiving Interacting Medication With Azithromycin |
|---|---|
| |
| Ondansetron | 48 |
| Trazodone | 23 |
| Moxifloxacin | 17 |
| Promethazine, haloperidol | 10 |
| Ciprofloxacin, citalopram, fluconazole | 7 |
| Amiodarone, amitriptyline | 5 |
| Quetiapine, methadone | 4 |
| Clarithromycin, octreotide, voriconazole | 2 |
| Erythromycin, granisetron, salmeterol, sotalol, ziprasidone | 1 |
The QT interval was measured from the beginning of the QRS complex to the end of the T wave as it returns to baseline. QTc has been defined by the most universally adopted method known as Bazett's formula ( , where QT is the measured QT interval and RR is the interval in seconds).[15]
Baseline QTc was evaluated through the use of most recent ECG within the past 6 months of admission. Borderline QTc was defined as 431 to 450 ms in males and 451 to 470 ms in females. Abnormal QTc was defined as >450 ms in males and >470 ms in females.[16]
Following admission, inpatient charges for telemetry during hospitalization were included. Telemetry was documented based on telemetry charges at any point in the hospital.
Statistical Analysis
Patient data were initially collected via Excel and analyzed with SAS version 9.4 software (SAS Institute, Cary, NC). Univariate analysis including central tendency and dispersion were utilized for aim 1. P values were calculated using 2 analysis and Fisher exact test for probability if cells with numerical values were <5 for aims 2 and 3.
RESULTS
Azithromycin use within our hospital system has increased from 15 days of therapy per 1000 patient days in 2002 to 40 days of therapy per 1000 patient days in 2013 (Figure 1). At the same time, azithromycin susceptibility in Streptococcus pneumoniae isolates has decreased over the past decade from 65% to 35% in our hospital.
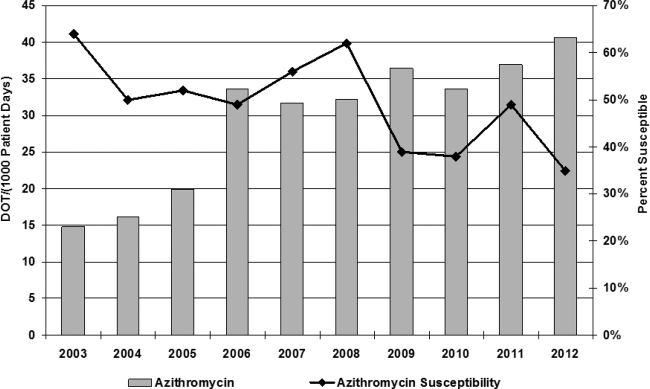
The baseline characteristics of patients included in this study are noted in Table 1. The mean age of patients was 55 years, with a range of 21 to 97 years, and 61% were female. Forty‐five percent of patients were admitted to either the general medicine teaching service or hospitalist service, and 23% were admitted to the pulmonary service, which includes intensive care unit admission. The average length of patient stay was 9.7 days (range, 3115 days; median 6 days).
Seventy‐nine percent of azithromycin use was empiric for the treatment of suspected infection. The second most common use was for anti‐inflammatory effects (20%), as documented by prescribers in the medical record for patients with cystic fibrosis, lung transplant, and chronic obstructive pulmonary disease. Azithromycin was dosed appropriately according to the documented indication in 67% of patients, with the most discrepancy in dosing noted for anti‐inflammatory use. The average duration of azithromycin therapy was 4.5 days (range, 128 days). Duration was appropriate in 63% of patients. Twenty‐one percent of patients received intravenous formulation of azithromycin, 13% received intravenous followed by oral formulation, and 64% of patient received tablet formulation alone.
Thirty‐five medications have been identified in our formulary as having a potential major drug‐drug interaction when prescribed with azithromycin (see Supporting Information, Appendix, in the online version of this article), and of these medications, 20 were prescribed with azithromycin, with an average overlap of therapy of 4.5 days (Table 2). Seventy‐six percent of patients were concomitantly prescribed a QT‐prolonging drug in addition to azithromycin. The most commonly prescribed agents were ondansetron (48%), trazodone (22%), and moxifloxacin (17%).
Telemetry monitoring was assessed for each patient based on inpatient charges during their hospitalization (Table 3). Forty‐three percent of patients were placed on telemetry. Twenty‐four (24%) of the patients were prescribed azithromycin alone, of whom 45.8% were placed on telemetry. Fifty‐seven percent of patients were prescribed azithromycin with 1 to 2 additional QT‐prolonging medications (medium‐risk arm); 38.5% of patients in this group were placed on telemetry. In the high‐risk arm, 19% of patients were prescribed at least 3 QT‐prolonging medications in addition to azithromycin, of which only 52.6% of patients were monitored with telemetry. No statistically significant association was observed between risk level and telemetry placement (P=0.07).
| Telemetry (%) | No Telemetry (%) | Total | P Valueb | |
|---|---|---|---|---|
| ||||
| Drug interaction risk levela | ||||
| Low | 11 (45.8) | 13 (54.2) | 24 | |
| Medium | 22 (38.5) | 35 (61.4) | 57 | |
| High | 10 (52.6) | 9 (47.4) | 19 | |
| Total | 43 | 57 | 100 | 0.07 |
| QTc | ||||
| Normal | 14 (50) | 14 (50) | 28 | |
| Borderline | 6 (66.7) | 3 (33.3) | 9 | |
| Abnormal | 15 (51.7) | 14 (48.3) | 29 | |
| Total | 35 | 31 | 66 | 0.22 |
Telemetry charges were further examined by analyzing baseline ECG evaluation within the past 6 months of their hospitalization (Table 3). Sixty‐six patients received baseline ECGs prior to initiation of azithromycin. Telemetry placement was not statistically correlated to abnormal QTc at baseline (P=0.22). Of those who underwent baseline ECG evaluation, 8.3% were noted to have borderline QTc, and 12.5% had abnormal QTc on admission prior to receiving azithromycin in the low‐risk level (Table 4). Within the medium‐risk level, 63.2% had baseline ECG evaluation, with 5.3% with borderline QTc and 35.7% with abnormal QTc. In the high‐risk level, 73.6% received a baseline ECG, with 21% with borderline QTc and 31.6% with abnormal QTc. No statistically significant association was observed between risk level and obtainment of baseline ECG (P=0.7). In 17 out of 66 patients, average repeat ECGs were obtained on day 3 (range, 27 days). Ten of the 17 ECGs showed increase in QTc (range, 397ms; average 27 ms), whereas the other 7 had a decrease in their QTc interval (range, 618 ms; average 13 ms; P=0.17).
| QTcb | Low, n=24 (%) | Medium, n=57 (%) | High, n=19 (%) | Total |
|---|---|---|---|---|
| ||||
| Normal | 11 (45.8%) | 13 (22.8%) | 4 (21.0%) | 28 |
| Borderline | 2 (8.3%) | 3 (5.3%) | 4 (21.0%) | 9 |
| Abnormal | 3 (12.5%) | 20 (35.7%) | 6 (31.6%) | 29 |
| Total | 16 (66.7%) | 36 (63.2%) | 14 (73.6%) | 66 |
| P valuec | 0.03 | 0.11 | ||
As risk level increased, having an abnormal QTc at baseline was statistically different between low‐ and medium‐risk levels (P=0.03), but this association was lost when comparing the low‐risk arm to the high‐risk arm (P=0.11). When the medium‐ and high‐risk categories were combined, there was a noted statistical significance of having an abnormal ECG at baseline (P=0.03).
Of the 9 patients prescribed azithromycin chronically, 3 patients were in the low‐risk category, 4 in the medium‐risk category, and 2 in the high‐risk category. Only 2 had baseline ECGs obtained, 1 of which was noted to have abnormal QTc and was in the high‐risk category. Only 1 patient was placed on telemetry, but was considered low risk based on medications prescribed.
DISCUSSION
In this study, 76% of patients were prescribed azithromycin with 1 or more medications known to affect QT prolongation; 19% received 3 or more QT‐prolonging medications in addition to azithromycin. Of patients who received a baseline ECG, 43% were documented to have borderline or prolonged QTc on admission. Telemetry monitoring was ordered 43% of the time, but there was no significant association between telemetry placement and risk level (P=0.07), suggesting that telemetry was ordered based on symptoms more than risk. Despite more drug‐druginteracting medications prescribed, there was no association to either telemetry orders or baseline ECG evaluation. Furthermore, if an abnormal QTc was documented on admission, there was no relationship to ordering telemetry as an inpatient (P=0.215), suggesting that healthcare providers are not considering risk of QTc medication accumulation. Given increased warnings issued by the FDA for azithromycin, further prospective studies are indicated to fully assess risk of QTc prolongation and arrhythmias in the setting of multiple drug interactions. This study elucidates the potential for drug‐drug interactions and need for increased vigilance and education of providers in the healthcare setting for QTc prolongation and subsequent arrhythmias.
Forty‐eight percent of patients receiving other QTc prolonging medications were prescribed ondansetron, followed by 23% of patients prescribed trazodone. Both of these medications are included on the admission order set in our institution and can be easily ordered for patients. Despite ordering multiple medications that have potential for QTc prolongation, there are no current alerts set up in our electronic medical record. When patients are separated into drug interaction risk levels, there is a trend of having an abnormal QTc on admission, but this is driven by the large number of patients in the medium‐risk category, and the rate does not increase (and is not significant) when comparing high risk to low risk. However, patients who receive any QTc‐prolonging medication are more likely to have an abnormal QTc when compared to azithromycin prescription alone (P=0.03). The small sample size limits the power and generalizability of this study, and further larger studies are indicated to assess if risk of QTc prolongation is additive.
In the 9 patients prescribed azithromycin chronically, dosing was not consistent, and a vast majority of patients were not placed on telemetry nor had baseline ECGs on admission. This further correlates with the idea that risk of arrhythmia is not fully considered in this patient population, as patients prescribed more than 1 QTc‐prolonging medication were not included in prior studies that examined azithromycin for its anti‐inflammatory effects.[2]
Azithromycin was added to our hospital formulary in 1998, and prescription of this agent remained relatively low until 2006, when azithromycin use increased dramatically from 15 days of therapy (DOT) per 1000 patient days to 40 DOT per 1000 patient days. Although numerous factors may have led to this increase, literature was published in 2006 and 2011 citing benefit from the anti‐inflammatory effects of azithromycin.[2, 17] At the same time, azithromycin susceptibility among Streptococcus pneumoniae in patients within our hospital has decreased over the past decade; studies have found a correlation between increasing use of macrolides and the development of resistance in Streptococcus species.[18, 19, 20] In this study, 79% of patients were prescribed azithromycin empirically for treatment of bacterial infections, whereas 20% were given azithromycin for its anti‐inflammatory effects; both dose and frequency varied among patients, raising the concern for development of resistance. Published studies have shown improvement in quality of life and decreased frequency of exacerbation and infection when azithromycin is used as an anti‐inflammatory agent; however, no QTc monitoring was noted.[2] Drug‐induced QTc prolongation>10 ms above baseline suggests the potential for clinical significance, whereas a QTc prolongation >20 milliseconds above baseline has a substantially increased likelihood of being proarrhythmic.[1] Unfortunately, drug‐induced QT prolongation is unpredictable, and additional risk factors play a role in facilitating Torsades de pointes, including female sex, advanced age, electrolyte disturbances, intravenous formulation, and concurrent use of more than 1 drug that can prolong the QT interval.[15] Azithromycin has recently been added to the growing list of medications that can prolong the QT interval, with 12 cases of Torsades de pointes reported in the literature. In March 2013, the FDA released a warning regarding prescribing azithromycin, but there is a lack of guidance for clinicians in identifying risk of cardiovascular events in susceptible patients.
There are some limitations to this study. Given data were acquired retrospectively and telemetry sheets were unable to be reviewed. Some patients were noted to have arrhythmias, but these data were obtained through physician notes and not examined directly from telemetry sheets. Seventeen patients had repeat ECGs, but most were performed serially for chest pain and not QTc monitoring. Four patients died in this study, but cause of death could not be determined through electronic medical records provided for all 4 patients; families pursued withdrawal of care.
Despite the published FDA warning, there are no national guidelines for clinicians in prescribing QTc‐prolonging medications. The American Heart Association published recommendations in 2010 for prescribing these drugs in the inpatient setting, but because hospitals differ in cardiac monitoring, there is no one‐size‐fits‐all strategy in reducing risk of cardiac events.[14] If the benefit of azithromycin outweighs the risk, QTc prolongation should not limit therapy; however, institutional awareness is necessary, whether it be through automatic stop dates on azithromycin, electronic alerts regarding drug‐drug interaction, enhanced prescriber education, or a combination of all of the above.
Disclosure: Nothing to report.
- , , . Azithromycin and the risk of cardiovascular complications. J Pharm Pract. 2014;27(5):496–500.
- , , , et al., Azithromycin for prevention of exacerbations of COPD. N Engl J Med. 2011;365(8):689–698.
- , , , . Macrolide antibiotics for cystic fibrosis. Cochrane Database Syst Rev. 2012;11:CD002203.
- , , . Long‐term macrolide treatment for chronic respiratory disease. Eur Respir J. 2013;42(1):239–251.
- , . Antimicrobial‐associated QT interval prolongation: pointes of interest. Clin Infect Dis. 2006;43(12):1603–1611.
- . Azithromycin‐induced proarrhythmia and cardiovascular death. Ann Pharmacother. 2013;47(11):1547–1551.
- , , , , . Azithromycin and the risk of cardiovascular death. N Engl J Med. 2012;366(20):1881–1890.
- , , , et al. Azithromycin and levofloxacin use and increased risk of cardiac arrhythmia and death. Ann Fam Med. 2014;12(2):121–127.
- , , , et al. Association of azithromycin with mortality and cardiovascular events among older patients hospitalized with pneumonia. JAMA. 2014;311(21):2199–2208.
- , , . Use of azithromycin and death from cardiovascular causes. N Engl J Med. 2013;368(18):1704–1712.
- U.S. Food and Drug Administration Drug Information. FDA drug safety communication: azithromycin (zithromax or zmax) and the risk of potentially fatal heart rhythms. Available at: http://www.fda.gov/Drugs/DrugSafety/ucm341822.htm. Accessed December 1, 2014.
- , , , , . QT interval prolongation and the risk of torsades de pointes: essentials for clinicians. Curr Med Res Opin. 2013;29(12):1719–1726.
- , , , et al., Development and validation of a risk score to predict QT interval prolongation in hospitalized patients. Circ Cardiovasc Qual Outcomes. 2013;6(4):479–487.
- , , , et al.; American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology; Council on Cardiovascular Nursing; American College of Cardiology Foundation. Prevention of torsade de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. J Am Coll Cardiol. 2010;55(9):934–947.
- , , . Drug‐induced QT interval prolongation: mechanisms and clinical management. Ther Adv Drug Saf. 2012;3(5):241–253.
- , , . QT interval: how to measure it and what is “normal”. J Cardiovasc Electrophysiol. 2006;17(3):333–336.
- , , , , . Anti‐inflammatory effects of azithromycin in cystic fibrosis airway epithelial cells. Biochem Biophys Res Commun. 2006;350(4):977–982.
- , , , , , ; Finnish Study Group for Antimicrobial Resistance (FiRe‐Network). Macrolide‐resistant Streptococcus pneumoniae and use of antimicrobial agents. Clin Infect Dis. 2001;33(4):483–488.
- , , , , , . Community prescribing and resistant Streptococcus pneumoniae. Emerg Infect Dis. 2005;11(6):829–837.
- , , , , ; Finnish Study Group for Antimicrobial Resistance (FiRe Network). Macrolide and azithromycin use are linked to increased macrolide resistance in Streptococcus pneumoniae. Antimicrob Agents Chemother. 2006;50(11):3646–3650.
Azithromycin, a macrolide antibiotic, received US Food and Drug Administration (FDA) approval in 1991 and is 1 of the most prescribed antibiotics used for a variety of infections, including community‐acquired pneumonia, bacterial sinusitis, urethritis, and cervicitis. In 2011, it was estimated that 40.3 million outpatients received a prescription for azithromycin.[1] In addition to treating acute bacterial infections, recent literature has pointed to using azithromycin for its unlabeled immunomodulatory and anti‐inflammatory effects, particularly in cystic fibrosis, chronic obstructive pulmonary disease (COPD), and lung transplant recipients.[2, 3, 4] Azithromycin decreases bacterial load and virulence, thus reducing airway secretion, as well as decreasing airway neutrophil accumulation through a reduction in proinflammatory cytokine expression.[4]
Cardiac toxicity can occur with macrolide antibiotics, and prolongation of the QT interval with subsequent Torsades de pointes has been documented with azithromycin.[1, 5, 6] In 2012, Ray et al. published data on a cohort of outpatients receiving azithromycin compared to amoxicillin, ciprofloxacin, or no antibiotics, and showed a small but absolute increase in cardiovascular deaths.[7, 8] Subsequent data, however, have not illustrated increased risk of death from cardiovascular causes. Mortensen et al. showed a lower risk of 90‐day mortality in older patients treated for community acquired pneumonia with azithromycin and ceftriaxone, although there was a nonstatistically significant increased risk of myocardial infarction in this group.[8, 9, 10] In March 2013, the FDA released an official statement regarding increased cardiovascular risk with azithromycin, stating that healthcare professionals should consider the risk of fatal heart rhythms with azithromycin when considering treatment options for patients who are at risk for cardiovascular events.[11]
In recent years, the potential for corrected QT (QTc) prolongation and Torsades de pointes has received increased attention due to its catastrophic nature, and it is thought that hospitalized patients are at a greater risk of drug‐induced Torsades de pointes due to the likelihood of having more risk factors.[12, 13] The American Heart Association released a statement in 2010 to raise awareness among healthcare professionals about risk, electrocardiogram (ECG) monitoring, and management of drug‐induced QT interval prolongation in hospitalized patients, although little data exist regarding quantification of risk in this patient population.[13, 14]
Prescribers currently have no standardized practice guidelines related to cardiovascular safety when prescribing QTc prolonging medications. Given the dramatic increase in azithromycin prescriptions and ongoing concern for cardiovascular risk and QTc prolongation, we investigated the prescribing practices with azithromycin within our institution. Our primary aims were 3‐fold. First, we aimed to describe the frequency azithromycin was prescribed with additional QTc prolonging medications. Second, we assessed the relationship between the number of arrhythmogenic drugs prescribed in addition to azithromycin with ordering telemetry. Finally, we assessed the relationship between baseline ECG abnormalities and telemetry monitoring in patients prescribed azithromycin. The purpose of these objectives was to better understand physician prescribing practices and to determine if patients have a potential risk of developing fatal cardiac arrhythmias
METHODS
Data
For this retrospective review, we utilized data from the University of Alabama at Birmingham Health Care system, a 1157licensed bed hospital. The institutional review board approved this study with a waiver of informed consent. Patients were eligible to be included in this study if they were 19 years of age with an inpatient hospital length of stay 3 days. Patients were considered to be receiving azithromycin and were included only when they were dispensed 1 dose of azithromycin by the pharmacy. Between October 1, 2012 and April 30, 2013, 1610 encounters were identified, of which 100 patient encounters were randomly selected for evaluation via a Microsoft Excel (Microsoft Corp., Redmond, WA) function. One patient was randomly included twice in this study, but had 2 separate admissions in which he received azithromycin.
QTc prolonging medications in our hospital formulary were identified via Micromedex and package inserts (see Supporting Information, Appendix, in the online version of this article for the full list).
Measures
The primary study measures were number of medications associated with QTc prolongation, baseline ECG findings, and telemetry monitoring. Secondary study measures include indication, dose, duration of use, formulation, length of stay, and admitting service (Table 1). Indications, dosage, and duration were defined by the FDA package insert for azithromycin (see Supporting Information, Appendix, in the online version of this article). Indication for use was defined as (1) empiric for a specific infection; (2) anti‐inflammatory for patients with COPD, lung transplant recipients, or cystic fibrosis patients; and (3) culture proven if evidence of a particular pathogen grown on culture. Indications were defined by prescriber notes. Dosage is defined as appropriate if FDA guidelines were followed for the defined indication. If patients were given azithromycin for anti‐inflammatory purposes, dosing was considered appropriate if it followed previous literature dosing of 250mg daily.
| |
| Age, y | |
| Average | 5519.5 |
| Range | 2197 |
| Gender | |
| Female | 61% |
| Male | 39% |
| Length of stay, d | |
| Average | 9.713.1 |
| Range | 3115 |
| Admitting service | |
| Hospitalist | 37% |
| Pulmonary | 23% |
| Obstetrics | 9% |
| General medicine | 8% |
| Hematology/oncology | 6% |
| Othera | 17% |
| Days of therapy | |
| Average | 4.53.9 |
| Range | 128 |
| Median | 4 |
| Indication for use | |
| Empiric | 79% |
| Anti‐inflammatory | 20% |
| Culture proven | 1% |
| Dosage | |
| Appropriate | 67% |
| Inappropriate | 14% |
| Unknown | 19% |
| Duration | |
| Appropriate | 63% |
| Inappropriate | 19% |
| Unknown | 18% |
| Formulation | |
| Intravenous only | 21% |
| Intravenous followed by tablet | 13% |
| Suspension | 2% |
| Tablet | 64% |
| Diagnosis‐related group | |
| Simple pneumonia with pleurisy | 14% |
| Septicemia with sepsis | 8% |
| Respiratory infection with inflammation | 8% |
| Chronic obstructive pulmonary disease | 8% |
| Pulmonary edema with respiratory failure | 6% |
| Vaginal delivery with complications | 6% |
| Respiratory diagnosis with ventilator support | 4% |
| Otherb | 46% |
Patients were divided into drug interaction risk levels based on the number of medications prescribed with the potential for QT prolongation (Table 2). Patients were considered low risk if they received azithromycin alone, medium risk if they received 2 to 3 QT‐prolonging medications including azithromycin, and high risk if they received 4 or more QT‐prolonging medications including azithromycin.
| Medication | % of Patients Receiving Interacting Medication With Azithromycin |
|---|---|
| |
| Ondansetron | 48 |
| Trazodone | 23 |
| Moxifloxacin | 17 |
| Promethazine, haloperidol | 10 |
| Ciprofloxacin, citalopram, fluconazole | 7 |
| Amiodarone, amitriptyline | 5 |
| Quetiapine, methadone | 4 |
| Clarithromycin, octreotide, voriconazole | 2 |
| Erythromycin, granisetron, salmeterol, sotalol, ziprasidone | 1 |
The QT interval was measured from the beginning of the QRS complex to the end of the T wave as it returns to baseline. QTc has been defined by the most universally adopted method known as Bazett's formula ( , where QT is the measured QT interval and RR is the interval in seconds).[15]
Baseline QTc was evaluated through the use of most recent ECG within the past 6 months of admission. Borderline QTc was defined as 431 to 450 ms in males and 451 to 470 ms in females. Abnormal QTc was defined as >450 ms in males and >470 ms in females.[16]
Following admission, inpatient charges for telemetry during hospitalization were included. Telemetry was documented based on telemetry charges at any point in the hospital.
Statistical Analysis
Patient data were initially collected via Excel and analyzed with SAS version 9.4 software (SAS Institute, Cary, NC). Univariate analysis including central tendency and dispersion were utilized for aim 1. P values were calculated using 2 analysis and Fisher exact test for probability if cells with numerical values were <5 for aims 2 and 3.
RESULTS
Azithromycin use within our hospital system has increased from 15 days of therapy per 1000 patient days in 2002 to 40 days of therapy per 1000 patient days in 2013 (Figure 1). At the same time, azithromycin susceptibility in Streptococcus pneumoniae isolates has decreased over the past decade from 65% to 35% in our hospital.
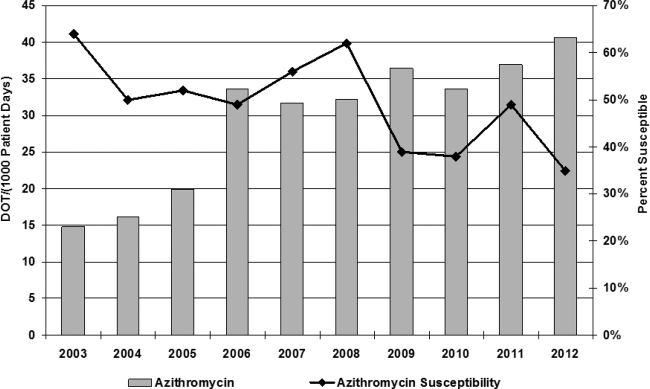
The baseline characteristics of patients included in this study are noted in Table 1. The mean age of patients was 55 years, with a range of 21 to 97 years, and 61% were female. Forty‐five percent of patients were admitted to either the general medicine teaching service or hospitalist service, and 23% were admitted to the pulmonary service, which includes intensive care unit admission. The average length of patient stay was 9.7 days (range, 3115 days; median 6 days).
Seventy‐nine percent of azithromycin use was empiric for the treatment of suspected infection. The second most common use was for anti‐inflammatory effects (20%), as documented by prescribers in the medical record for patients with cystic fibrosis, lung transplant, and chronic obstructive pulmonary disease. Azithromycin was dosed appropriately according to the documented indication in 67% of patients, with the most discrepancy in dosing noted for anti‐inflammatory use. The average duration of azithromycin therapy was 4.5 days (range, 128 days). Duration was appropriate in 63% of patients. Twenty‐one percent of patients received intravenous formulation of azithromycin, 13% received intravenous followed by oral formulation, and 64% of patient received tablet formulation alone.
Thirty‐five medications have been identified in our formulary as having a potential major drug‐drug interaction when prescribed with azithromycin (see Supporting Information, Appendix, in the online version of this article), and of these medications, 20 were prescribed with azithromycin, with an average overlap of therapy of 4.5 days (Table 2). Seventy‐six percent of patients were concomitantly prescribed a QT‐prolonging drug in addition to azithromycin. The most commonly prescribed agents were ondansetron (48%), trazodone (22%), and moxifloxacin (17%).
Telemetry monitoring was assessed for each patient based on inpatient charges during their hospitalization (Table 3). Forty‐three percent of patients were placed on telemetry. Twenty‐four (24%) of the patients were prescribed azithromycin alone, of whom 45.8% were placed on telemetry. Fifty‐seven percent of patients were prescribed azithromycin with 1 to 2 additional QT‐prolonging medications (medium‐risk arm); 38.5% of patients in this group were placed on telemetry. In the high‐risk arm, 19% of patients were prescribed at least 3 QT‐prolonging medications in addition to azithromycin, of which only 52.6% of patients were monitored with telemetry. No statistically significant association was observed between risk level and telemetry placement (P=0.07).
| Telemetry (%) | No Telemetry (%) | Total | P Valueb | |
|---|---|---|---|---|
| ||||
| Drug interaction risk levela | ||||
| Low | 11 (45.8) | 13 (54.2) | 24 | |
| Medium | 22 (38.5) | 35 (61.4) | 57 | |
| High | 10 (52.6) | 9 (47.4) | 19 | |
| Total | 43 | 57 | 100 | 0.07 |
| QTc | ||||
| Normal | 14 (50) | 14 (50) | 28 | |
| Borderline | 6 (66.7) | 3 (33.3) | 9 | |
| Abnormal | 15 (51.7) | 14 (48.3) | 29 | |
| Total | 35 | 31 | 66 | 0.22 |
Telemetry charges were further examined by analyzing baseline ECG evaluation within the past 6 months of their hospitalization (Table 3). Sixty‐six patients received baseline ECGs prior to initiation of azithromycin. Telemetry placement was not statistically correlated to abnormal QTc at baseline (P=0.22). Of those who underwent baseline ECG evaluation, 8.3% were noted to have borderline QTc, and 12.5% had abnormal QTc on admission prior to receiving azithromycin in the low‐risk level (Table 4). Within the medium‐risk level, 63.2% had baseline ECG evaluation, with 5.3% with borderline QTc and 35.7% with abnormal QTc. In the high‐risk level, 73.6% received a baseline ECG, with 21% with borderline QTc and 31.6% with abnormal QTc. No statistically significant association was observed between risk level and obtainment of baseline ECG (P=0.7). In 17 out of 66 patients, average repeat ECGs were obtained on day 3 (range, 27 days). Ten of the 17 ECGs showed increase in QTc (range, 397ms; average 27 ms), whereas the other 7 had a decrease in their QTc interval (range, 618 ms; average 13 ms; P=0.17).
| QTcb | Low, n=24 (%) | Medium, n=57 (%) | High, n=19 (%) | Total |
|---|---|---|---|---|
| ||||
| Normal | 11 (45.8%) | 13 (22.8%) | 4 (21.0%) | 28 |
| Borderline | 2 (8.3%) | 3 (5.3%) | 4 (21.0%) | 9 |
| Abnormal | 3 (12.5%) | 20 (35.7%) | 6 (31.6%) | 29 |
| Total | 16 (66.7%) | 36 (63.2%) | 14 (73.6%) | 66 |
| P valuec | 0.03 | 0.11 | ||
As risk level increased, having an abnormal QTc at baseline was statistically different between low‐ and medium‐risk levels (P=0.03), but this association was lost when comparing the low‐risk arm to the high‐risk arm (P=0.11). When the medium‐ and high‐risk categories were combined, there was a noted statistical significance of having an abnormal ECG at baseline (P=0.03).
Of the 9 patients prescribed azithromycin chronically, 3 patients were in the low‐risk category, 4 in the medium‐risk category, and 2 in the high‐risk category. Only 2 had baseline ECGs obtained, 1 of which was noted to have abnormal QTc and was in the high‐risk category. Only 1 patient was placed on telemetry, but was considered low risk based on medications prescribed.
DISCUSSION
In this study, 76% of patients were prescribed azithromycin with 1 or more medications known to affect QT prolongation; 19% received 3 or more QT‐prolonging medications in addition to azithromycin. Of patients who received a baseline ECG, 43% were documented to have borderline or prolonged QTc on admission. Telemetry monitoring was ordered 43% of the time, but there was no significant association between telemetry placement and risk level (P=0.07), suggesting that telemetry was ordered based on symptoms more than risk. Despite more drug‐druginteracting medications prescribed, there was no association to either telemetry orders or baseline ECG evaluation. Furthermore, if an abnormal QTc was documented on admission, there was no relationship to ordering telemetry as an inpatient (P=0.215), suggesting that healthcare providers are not considering risk of QTc medication accumulation. Given increased warnings issued by the FDA for azithromycin, further prospective studies are indicated to fully assess risk of QTc prolongation and arrhythmias in the setting of multiple drug interactions. This study elucidates the potential for drug‐drug interactions and need for increased vigilance and education of providers in the healthcare setting for QTc prolongation and subsequent arrhythmias.
Forty‐eight percent of patients receiving other QTc prolonging medications were prescribed ondansetron, followed by 23% of patients prescribed trazodone. Both of these medications are included on the admission order set in our institution and can be easily ordered for patients. Despite ordering multiple medications that have potential for QTc prolongation, there are no current alerts set up in our electronic medical record. When patients are separated into drug interaction risk levels, there is a trend of having an abnormal QTc on admission, but this is driven by the large number of patients in the medium‐risk category, and the rate does not increase (and is not significant) when comparing high risk to low risk. However, patients who receive any QTc‐prolonging medication are more likely to have an abnormal QTc when compared to azithromycin prescription alone (P=0.03). The small sample size limits the power and generalizability of this study, and further larger studies are indicated to assess if risk of QTc prolongation is additive.
In the 9 patients prescribed azithromycin chronically, dosing was not consistent, and a vast majority of patients were not placed on telemetry nor had baseline ECGs on admission. This further correlates with the idea that risk of arrhythmia is not fully considered in this patient population, as patients prescribed more than 1 QTc‐prolonging medication were not included in prior studies that examined azithromycin for its anti‐inflammatory effects.[2]
Azithromycin was added to our hospital formulary in 1998, and prescription of this agent remained relatively low until 2006, when azithromycin use increased dramatically from 15 days of therapy (DOT) per 1000 patient days to 40 DOT per 1000 patient days. Although numerous factors may have led to this increase, literature was published in 2006 and 2011 citing benefit from the anti‐inflammatory effects of azithromycin.[2, 17] At the same time, azithromycin susceptibility among Streptococcus pneumoniae in patients within our hospital has decreased over the past decade; studies have found a correlation between increasing use of macrolides and the development of resistance in Streptococcus species.[18, 19, 20] In this study, 79% of patients were prescribed azithromycin empirically for treatment of bacterial infections, whereas 20% were given azithromycin for its anti‐inflammatory effects; both dose and frequency varied among patients, raising the concern for development of resistance. Published studies have shown improvement in quality of life and decreased frequency of exacerbation and infection when azithromycin is used as an anti‐inflammatory agent; however, no QTc monitoring was noted.[2] Drug‐induced QTc prolongation>10 ms above baseline suggests the potential for clinical significance, whereas a QTc prolongation >20 milliseconds above baseline has a substantially increased likelihood of being proarrhythmic.[1] Unfortunately, drug‐induced QT prolongation is unpredictable, and additional risk factors play a role in facilitating Torsades de pointes, including female sex, advanced age, electrolyte disturbances, intravenous formulation, and concurrent use of more than 1 drug that can prolong the QT interval.[15] Azithromycin has recently been added to the growing list of medications that can prolong the QT interval, with 12 cases of Torsades de pointes reported in the literature. In March 2013, the FDA released a warning regarding prescribing azithromycin, but there is a lack of guidance for clinicians in identifying risk of cardiovascular events in susceptible patients.
There are some limitations to this study. Given data were acquired retrospectively and telemetry sheets were unable to be reviewed. Some patients were noted to have arrhythmias, but these data were obtained through physician notes and not examined directly from telemetry sheets. Seventeen patients had repeat ECGs, but most were performed serially for chest pain and not QTc monitoring. Four patients died in this study, but cause of death could not be determined through electronic medical records provided for all 4 patients; families pursued withdrawal of care.
Despite the published FDA warning, there are no national guidelines for clinicians in prescribing QTc‐prolonging medications. The American Heart Association published recommendations in 2010 for prescribing these drugs in the inpatient setting, but because hospitals differ in cardiac monitoring, there is no one‐size‐fits‐all strategy in reducing risk of cardiac events.[14] If the benefit of azithromycin outweighs the risk, QTc prolongation should not limit therapy; however, institutional awareness is necessary, whether it be through automatic stop dates on azithromycin, electronic alerts regarding drug‐drug interaction, enhanced prescriber education, or a combination of all of the above.
Disclosure: Nothing to report.
Azithromycin, a macrolide antibiotic, received US Food and Drug Administration (FDA) approval in 1991 and is 1 of the most prescribed antibiotics used for a variety of infections, including community‐acquired pneumonia, bacterial sinusitis, urethritis, and cervicitis. In 2011, it was estimated that 40.3 million outpatients received a prescription for azithromycin.[1] In addition to treating acute bacterial infections, recent literature has pointed to using azithromycin for its unlabeled immunomodulatory and anti‐inflammatory effects, particularly in cystic fibrosis, chronic obstructive pulmonary disease (COPD), and lung transplant recipients.[2, 3, 4] Azithromycin decreases bacterial load and virulence, thus reducing airway secretion, as well as decreasing airway neutrophil accumulation through a reduction in proinflammatory cytokine expression.[4]
Cardiac toxicity can occur with macrolide antibiotics, and prolongation of the QT interval with subsequent Torsades de pointes has been documented with azithromycin.[1, 5, 6] In 2012, Ray et al. published data on a cohort of outpatients receiving azithromycin compared to amoxicillin, ciprofloxacin, or no antibiotics, and showed a small but absolute increase in cardiovascular deaths.[7, 8] Subsequent data, however, have not illustrated increased risk of death from cardiovascular causes. Mortensen et al. showed a lower risk of 90‐day mortality in older patients treated for community acquired pneumonia with azithromycin and ceftriaxone, although there was a nonstatistically significant increased risk of myocardial infarction in this group.[8, 9, 10] In March 2013, the FDA released an official statement regarding increased cardiovascular risk with azithromycin, stating that healthcare professionals should consider the risk of fatal heart rhythms with azithromycin when considering treatment options for patients who are at risk for cardiovascular events.[11]
In recent years, the potential for corrected QT (QTc) prolongation and Torsades de pointes has received increased attention due to its catastrophic nature, and it is thought that hospitalized patients are at a greater risk of drug‐induced Torsades de pointes due to the likelihood of having more risk factors.[12, 13] The American Heart Association released a statement in 2010 to raise awareness among healthcare professionals about risk, electrocardiogram (ECG) monitoring, and management of drug‐induced QT interval prolongation in hospitalized patients, although little data exist regarding quantification of risk in this patient population.[13, 14]
Prescribers currently have no standardized practice guidelines related to cardiovascular safety when prescribing QTc prolonging medications. Given the dramatic increase in azithromycin prescriptions and ongoing concern for cardiovascular risk and QTc prolongation, we investigated the prescribing practices with azithromycin within our institution. Our primary aims were 3‐fold. First, we aimed to describe the frequency azithromycin was prescribed with additional QTc prolonging medications. Second, we assessed the relationship between the number of arrhythmogenic drugs prescribed in addition to azithromycin with ordering telemetry. Finally, we assessed the relationship between baseline ECG abnormalities and telemetry monitoring in patients prescribed azithromycin. The purpose of these objectives was to better understand physician prescribing practices and to determine if patients have a potential risk of developing fatal cardiac arrhythmias
METHODS
Data
For this retrospective review, we utilized data from the University of Alabama at Birmingham Health Care system, a 1157licensed bed hospital. The institutional review board approved this study with a waiver of informed consent. Patients were eligible to be included in this study if they were 19 years of age with an inpatient hospital length of stay 3 days. Patients were considered to be receiving azithromycin and were included only when they were dispensed 1 dose of azithromycin by the pharmacy. Between October 1, 2012 and April 30, 2013, 1610 encounters were identified, of which 100 patient encounters were randomly selected for evaluation via a Microsoft Excel (Microsoft Corp., Redmond, WA) function. One patient was randomly included twice in this study, but had 2 separate admissions in which he received azithromycin.
QTc prolonging medications in our hospital formulary were identified via Micromedex and package inserts (see Supporting Information, Appendix, in the online version of this article for the full list).
Measures
The primary study measures were number of medications associated with QTc prolongation, baseline ECG findings, and telemetry monitoring. Secondary study measures include indication, dose, duration of use, formulation, length of stay, and admitting service (Table 1). Indications, dosage, and duration were defined by the FDA package insert for azithromycin (see Supporting Information, Appendix, in the online version of this article). Indication for use was defined as (1) empiric for a specific infection; (2) anti‐inflammatory for patients with COPD, lung transplant recipients, or cystic fibrosis patients; and (3) culture proven if evidence of a particular pathogen grown on culture. Indications were defined by prescriber notes. Dosage is defined as appropriate if FDA guidelines were followed for the defined indication. If patients were given azithromycin for anti‐inflammatory purposes, dosing was considered appropriate if it followed previous literature dosing of 250mg daily.
| |
| Age, y | |
| Average | 5519.5 |
| Range | 2197 |
| Gender | |
| Female | 61% |
| Male | 39% |
| Length of stay, d | |
| Average | 9.713.1 |
| Range | 3115 |
| Admitting service | |
| Hospitalist | 37% |
| Pulmonary | 23% |
| Obstetrics | 9% |
| General medicine | 8% |
| Hematology/oncology | 6% |
| Othera | 17% |
| Days of therapy | |
| Average | 4.53.9 |
| Range | 128 |
| Median | 4 |
| Indication for use | |
| Empiric | 79% |
| Anti‐inflammatory | 20% |
| Culture proven | 1% |
| Dosage | |
| Appropriate | 67% |
| Inappropriate | 14% |
| Unknown | 19% |
| Duration | |
| Appropriate | 63% |
| Inappropriate | 19% |
| Unknown | 18% |
| Formulation | |
| Intravenous only | 21% |
| Intravenous followed by tablet | 13% |
| Suspension | 2% |
| Tablet | 64% |
| Diagnosis‐related group | |
| Simple pneumonia with pleurisy | 14% |
| Septicemia with sepsis | 8% |
| Respiratory infection with inflammation | 8% |
| Chronic obstructive pulmonary disease | 8% |
| Pulmonary edema with respiratory failure | 6% |
| Vaginal delivery with complications | 6% |
| Respiratory diagnosis with ventilator support | 4% |
| Otherb | 46% |
Patients were divided into drug interaction risk levels based on the number of medications prescribed with the potential for QT prolongation (Table 2). Patients were considered low risk if they received azithromycin alone, medium risk if they received 2 to 3 QT‐prolonging medications including azithromycin, and high risk if they received 4 or more QT‐prolonging medications including azithromycin.
| Medication | % of Patients Receiving Interacting Medication With Azithromycin |
|---|---|
| |
| Ondansetron | 48 |
| Trazodone | 23 |
| Moxifloxacin | 17 |
| Promethazine, haloperidol | 10 |
| Ciprofloxacin, citalopram, fluconazole | 7 |
| Amiodarone, amitriptyline | 5 |
| Quetiapine, methadone | 4 |
| Clarithromycin, octreotide, voriconazole | 2 |
| Erythromycin, granisetron, salmeterol, sotalol, ziprasidone | 1 |
The QT interval was measured from the beginning of the QRS complex to the end of the T wave as it returns to baseline. QTc has been defined by the most universally adopted method known as Bazett's formula ( , where QT is the measured QT interval and RR is the interval in seconds).[15]
Baseline QTc was evaluated through the use of most recent ECG within the past 6 months of admission. Borderline QTc was defined as 431 to 450 ms in males and 451 to 470 ms in females. Abnormal QTc was defined as >450 ms in males and >470 ms in females.[16]
Following admission, inpatient charges for telemetry during hospitalization were included. Telemetry was documented based on telemetry charges at any point in the hospital.
Statistical Analysis
Patient data were initially collected via Excel and analyzed with SAS version 9.4 software (SAS Institute, Cary, NC). Univariate analysis including central tendency and dispersion were utilized for aim 1. P values were calculated using 2 analysis and Fisher exact test for probability if cells with numerical values were <5 for aims 2 and 3.
RESULTS
Azithromycin use within our hospital system has increased from 15 days of therapy per 1000 patient days in 2002 to 40 days of therapy per 1000 patient days in 2013 (Figure 1). At the same time, azithromycin susceptibility in Streptococcus pneumoniae isolates has decreased over the past decade from 65% to 35% in our hospital.
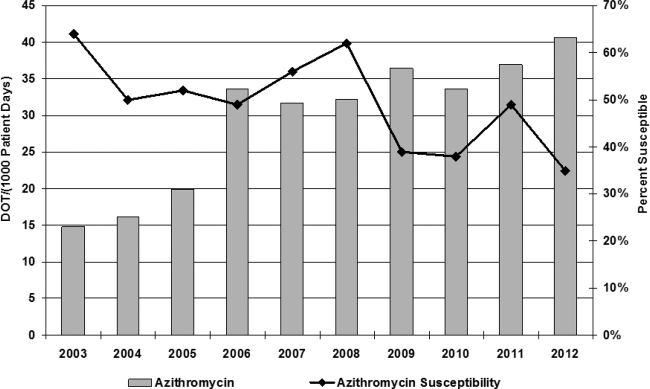
The baseline characteristics of patients included in this study are noted in Table 1. The mean age of patients was 55 years, with a range of 21 to 97 years, and 61% were female. Forty‐five percent of patients were admitted to either the general medicine teaching service or hospitalist service, and 23% were admitted to the pulmonary service, which includes intensive care unit admission. The average length of patient stay was 9.7 days (range, 3115 days; median 6 days).
Seventy‐nine percent of azithromycin use was empiric for the treatment of suspected infection. The second most common use was for anti‐inflammatory effects (20%), as documented by prescribers in the medical record for patients with cystic fibrosis, lung transplant, and chronic obstructive pulmonary disease. Azithromycin was dosed appropriately according to the documented indication in 67% of patients, with the most discrepancy in dosing noted for anti‐inflammatory use. The average duration of azithromycin therapy was 4.5 days (range, 128 days). Duration was appropriate in 63% of patients. Twenty‐one percent of patients received intravenous formulation of azithromycin, 13% received intravenous followed by oral formulation, and 64% of patient received tablet formulation alone.
Thirty‐five medications have been identified in our formulary as having a potential major drug‐drug interaction when prescribed with azithromycin (see Supporting Information, Appendix, in the online version of this article), and of these medications, 20 were prescribed with azithromycin, with an average overlap of therapy of 4.5 days (Table 2). Seventy‐six percent of patients were concomitantly prescribed a QT‐prolonging drug in addition to azithromycin. The most commonly prescribed agents were ondansetron (48%), trazodone (22%), and moxifloxacin (17%).
Telemetry monitoring was assessed for each patient based on inpatient charges during their hospitalization (Table 3). Forty‐three percent of patients were placed on telemetry. Twenty‐four (24%) of the patients were prescribed azithromycin alone, of whom 45.8% were placed on telemetry. Fifty‐seven percent of patients were prescribed azithromycin with 1 to 2 additional QT‐prolonging medications (medium‐risk arm); 38.5% of patients in this group were placed on telemetry. In the high‐risk arm, 19% of patients were prescribed at least 3 QT‐prolonging medications in addition to azithromycin, of which only 52.6% of patients were monitored with telemetry. No statistically significant association was observed between risk level and telemetry placement (P=0.07).
| Telemetry (%) | No Telemetry (%) | Total | P Valueb | |
|---|---|---|---|---|
| ||||
| Drug interaction risk levela | ||||
| Low | 11 (45.8) | 13 (54.2) | 24 | |
| Medium | 22 (38.5) | 35 (61.4) | 57 | |
| High | 10 (52.6) | 9 (47.4) | 19 | |
| Total | 43 | 57 | 100 | 0.07 |
| QTc | ||||
| Normal | 14 (50) | 14 (50) | 28 | |
| Borderline | 6 (66.7) | 3 (33.3) | 9 | |
| Abnormal | 15 (51.7) | 14 (48.3) | 29 | |
| Total | 35 | 31 | 66 | 0.22 |
Telemetry charges were further examined by analyzing baseline ECG evaluation within the past 6 months of their hospitalization (Table 3). Sixty‐six patients received baseline ECGs prior to initiation of azithromycin. Telemetry placement was not statistically correlated to abnormal QTc at baseline (P=0.22). Of those who underwent baseline ECG evaluation, 8.3% were noted to have borderline QTc, and 12.5% had abnormal QTc on admission prior to receiving azithromycin in the low‐risk level (Table 4). Within the medium‐risk level, 63.2% had baseline ECG evaluation, with 5.3% with borderline QTc and 35.7% with abnormal QTc. In the high‐risk level, 73.6% received a baseline ECG, with 21% with borderline QTc and 31.6% with abnormal QTc. No statistically significant association was observed between risk level and obtainment of baseline ECG (P=0.7). In 17 out of 66 patients, average repeat ECGs were obtained on day 3 (range, 27 days). Ten of the 17 ECGs showed increase in QTc (range, 397ms; average 27 ms), whereas the other 7 had a decrease in their QTc interval (range, 618 ms; average 13 ms; P=0.17).
| QTcb | Low, n=24 (%) | Medium, n=57 (%) | High, n=19 (%) | Total |
|---|---|---|---|---|
| ||||
| Normal | 11 (45.8%) | 13 (22.8%) | 4 (21.0%) | 28 |
| Borderline | 2 (8.3%) | 3 (5.3%) | 4 (21.0%) | 9 |
| Abnormal | 3 (12.5%) | 20 (35.7%) | 6 (31.6%) | 29 |
| Total | 16 (66.7%) | 36 (63.2%) | 14 (73.6%) | 66 |
| P valuec | 0.03 | 0.11 | ||
As risk level increased, having an abnormal QTc at baseline was statistically different between low‐ and medium‐risk levels (P=0.03), but this association was lost when comparing the low‐risk arm to the high‐risk arm (P=0.11). When the medium‐ and high‐risk categories were combined, there was a noted statistical significance of having an abnormal ECG at baseline (P=0.03).
Of the 9 patients prescribed azithromycin chronically, 3 patients were in the low‐risk category, 4 in the medium‐risk category, and 2 in the high‐risk category. Only 2 had baseline ECGs obtained, 1 of which was noted to have abnormal QTc and was in the high‐risk category. Only 1 patient was placed on telemetry, but was considered low risk based on medications prescribed.
DISCUSSION
In this study, 76% of patients were prescribed azithromycin with 1 or more medications known to affect QT prolongation; 19% received 3 or more QT‐prolonging medications in addition to azithromycin. Of patients who received a baseline ECG, 43% were documented to have borderline or prolonged QTc on admission. Telemetry monitoring was ordered 43% of the time, but there was no significant association between telemetry placement and risk level (P=0.07), suggesting that telemetry was ordered based on symptoms more than risk. Despite more drug‐druginteracting medications prescribed, there was no association to either telemetry orders or baseline ECG evaluation. Furthermore, if an abnormal QTc was documented on admission, there was no relationship to ordering telemetry as an inpatient (P=0.215), suggesting that healthcare providers are not considering risk of QTc medication accumulation. Given increased warnings issued by the FDA for azithromycin, further prospective studies are indicated to fully assess risk of QTc prolongation and arrhythmias in the setting of multiple drug interactions. This study elucidates the potential for drug‐drug interactions and need for increased vigilance and education of providers in the healthcare setting for QTc prolongation and subsequent arrhythmias.
Forty‐eight percent of patients receiving other QTc prolonging medications were prescribed ondansetron, followed by 23% of patients prescribed trazodone. Both of these medications are included on the admission order set in our institution and can be easily ordered for patients. Despite ordering multiple medications that have potential for QTc prolongation, there are no current alerts set up in our electronic medical record. When patients are separated into drug interaction risk levels, there is a trend of having an abnormal QTc on admission, but this is driven by the large number of patients in the medium‐risk category, and the rate does not increase (and is not significant) when comparing high risk to low risk. However, patients who receive any QTc‐prolonging medication are more likely to have an abnormal QTc when compared to azithromycin prescription alone (P=0.03). The small sample size limits the power and generalizability of this study, and further larger studies are indicated to assess if risk of QTc prolongation is additive.
In the 9 patients prescribed azithromycin chronically, dosing was not consistent, and a vast majority of patients were not placed on telemetry nor had baseline ECGs on admission. This further correlates with the idea that risk of arrhythmia is not fully considered in this patient population, as patients prescribed more than 1 QTc‐prolonging medication were not included in prior studies that examined azithromycin for its anti‐inflammatory effects.[2]
Azithromycin was added to our hospital formulary in 1998, and prescription of this agent remained relatively low until 2006, when azithromycin use increased dramatically from 15 days of therapy (DOT) per 1000 patient days to 40 DOT per 1000 patient days. Although numerous factors may have led to this increase, literature was published in 2006 and 2011 citing benefit from the anti‐inflammatory effects of azithromycin.[2, 17] At the same time, azithromycin susceptibility among Streptococcus pneumoniae in patients within our hospital has decreased over the past decade; studies have found a correlation between increasing use of macrolides and the development of resistance in Streptococcus species.[18, 19, 20] In this study, 79% of patients were prescribed azithromycin empirically for treatment of bacterial infections, whereas 20% were given azithromycin for its anti‐inflammatory effects; both dose and frequency varied among patients, raising the concern for development of resistance. Published studies have shown improvement in quality of life and decreased frequency of exacerbation and infection when azithromycin is used as an anti‐inflammatory agent; however, no QTc monitoring was noted.[2] Drug‐induced QTc prolongation>10 ms above baseline suggests the potential for clinical significance, whereas a QTc prolongation >20 milliseconds above baseline has a substantially increased likelihood of being proarrhythmic.[1] Unfortunately, drug‐induced QT prolongation is unpredictable, and additional risk factors play a role in facilitating Torsades de pointes, including female sex, advanced age, electrolyte disturbances, intravenous formulation, and concurrent use of more than 1 drug that can prolong the QT interval.[15] Azithromycin has recently been added to the growing list of medications that can prolong the QT interval, with 12 cases of Torsades de pointes reported in the literature. In March 2013, the FDA released a warning regarding prescribing azithromycin, but there is a lack of guidance for clinicians in identifying risk of cardiovascular events in susceptible patients.
There are some limitations to this study. Given data were acquired retrospectively and telemetry sheets were unable to be reviewed. Some patients were noted to have arrhythmias, but these data were obtained through physician notes and not examined directly from telemetry sheets. Seventeen patients had repeat ECGs, but most were performed serially for chest pain and not QTc monitoring. Four patients died in this study, but cause of death could not be determined through electronic medical records provided for all 4 patients; families pursued withdrawal of care.
Despite the published FDA warning, there are no national guidelines for clinicians in prescribing QTc‐prolonging medications. The American Heart Association published recommendations in 2010 for prescribing these drugs in the inpatient setting, but because hospitals differ in cardiac monitoring, there is no one‐size‐fits‐all strategy in reducing risk of cardiac events.[14] If the benefit of azithromycin outweighs the risk, QTc prolongation should not limit therapy; however, institutional awareness is necessary, whether it be through automatic stop dates on azithromycin, electronic alerts regarding drug‐drug interaction, enhanced prescriber education, or a combination of all of the above.
Disclosure: Nothing to report.
- , , . Azithromycin and the risk of cardiovascular complications. J Pharm Pract. 2014;27(5):496–500.
- , , , et al., Azithromycin for prevention of exacerbations of COPD. N Engl J Med. 2011;365(8):689–698.
- , , , . Macrolide antibiotics for cystic fibrosis. Cochrane Database Syst Rev. 2012;11:CD002203.
- , , . Long‐term macrolide treatment for chronic respiratory disease. Eur Respir J. 2013;42(1):239–251.
- , . Antimicrobial‐associated QT interval prolongation: pointes of interest. Clin Infect Dis. 2006;43(12):1603–1611.
- . Azithromycin‐induced proarrhythmia and cardiovascular death. Ann Pharmacother. 2013;47(11):1547–1551.
- , , , , . Azithromycin and the risk of cardiovascular death. N Engl J Med. 2012;366(20):1881–1890.
- , , , et al. Azithromycin and levofloxacin use and increased risk of cardiac arrhythmia and death. Ann Fam Med. 2014;12(2):121–127.
- , , , et al. Association of azithromycin with mortality and cardiovascular events among older patients hospitalized with pneumonia. JAMA. 2014;311(21):2199–2208.
- , , . Use of azithromycin and death from cardiovascular causes. N Engl J Med. 2013;368(18):1704–1712.
- U.S. Food and Drug Administration Drug Information. FDA drug safety communication: azithromycin (zithromax or zmax) and the risk of potentially fatal heart rhythms. Available at: http://www.fda.gov/Drugs/DrugSafety/ucm341822.htm. Accessed December 1, 2014.
- , , , , . QT interval prolongation and the risk of torsades de pointes: essentials for clinicians. Curr Med Res Opin. 2013;29(12):1719–1726.
- , , , et al., Development and validation of a risk score to predict QT interval prolongation in hospitalized patients. Circ Cardiovasc Qual Outcomes. 2013;6(4):479–487.
- , , , et al.; American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology; Council on Cardiovascular Nursing; American College of Cardiology Foundation. Prevention of torsade de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. J Am Coll Cardiol. 2010;55(9):934–947.
- , , . Drug‐induced QT interval prolongation: mechanisms and clinical management. Ther Adv Drug Saf. 2012;3(5):241–253.
- , , . QT interval: how to measure it and what is “normal”. J Cardiovasc Electrophysiol. 2006;17(3):333–336.
- , , , , . Anti‐inflammatory effects of azithromycin in cystic fibrosis airway epithelial cells. Biochem Biophys Res Commun. 2006;350(4):977–982.
- , , , , , ; Finnish Study Group for Antimicrobial Resistance (FiRe‐Network). Macrolide‐resistant Streptococcus pneumoniae and use of antimicrobial agents. Clin Infect Dis. 2001;33(4):483–488.
- , , , , , . Community prescribing and resistant Streptococcus pneumoniae. Emerg Infect Dis. 2005;11(6):829–837.
- , , , , ; Finnish Study Group for Antimicrobial Resistance (FiRe Network). Macrolide and azithromycin use are linked to increased macrolide resistance in Streptococcus pneumoniae. Antimicrob Agents Chemother. 2006;50(11):3646–3650.
- , , . Azithromycin and the risk of cardiovascular complications. J Pharm Pract. 2014;27(5):496–500.
- , , , et al., Azithromycin for prevention of exacerbations of COPD. N Engl J Med. 2011;365(8):689–698.
- , , , . Macrolide antibiotics for cystic fibrosis. Cochrane Database Syst Rev. 2012;11:CD002203.
- , , . Long‐term macrolide treatment for chronic respiratory disease. Eur Respir J. 2013;42(1):239–251.
- , . Antimicrobial‐associated QT interval prolongation: pointes of interest. Clin Infect Dis. 2006;43(12):1603–1611.
- . Azithromycin‐induced proarrhythmia and cardiovascular death. Ann Pharmacother. 2013;47(11):1547–1551.
- , , , , . Azithromycin and the risk of cardiovascular death. N Engl J Med. 2012;366(20):1881–1890.
- , , , et al. Azithromycin and levofloxacin use and increased risk of cardiac arrhythmia and death. Ann Fam Med. 2014;12(2):121–127.
- , , , et al. Association of azithromycin with mortality and cardiovascular events among older patients hospitalized with pneumonia. JAMA. 2014;311(21):2199–2208.
- , , . Use of azithromycin and death from cardiovascular causes. N Engl J Med. 2013;368(18):1704–1712.
- U.S. Food and Drug Administration Drug Information. FDA drug safety communication: azithromycin (zithromax or zmax) and the risk of potentially fatal heart rhythms. Available at: http://www.fda.gov/Drugs/DrugSafety/ucm341822.htm. Accessed December 1, 2014.
- , , , , . QT interval prolongation and the risk of torsades de pointes: essentials for clinicians. Curr Med Res Opin. 2013;29(12):1719–1726.
- , , , et al., Development and validation of a risk score to predict QT interval prolongation in hospitalized patients. Circ Cardiovasc Qual Outcomes. 2013;6(4):479–487.
- , , , et al.; American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology; Council on Cardiovascular Nursing; American College of Cardiology Foundation. Prevention of torsade de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. J Am Coll Cardiol. 2010;55(9):934–947.
- , , . Drug‐induced QT interval prolongation: mechanisms and clinical management. Ther Adv Drug Saf. 2012;3(5):241–253.
- , , . QT interval: how to measure it and what is “normal”. J Cardiovasc Electrophysiol. 2006;17(3):333–336.
- , , , , . Anti‐inflammatory effects of azithromycin in cystic fibrosis airway epithelial cells. Biochem Biophys Res Commun. 2006;350(4):977–982.
- , , , , , ; Finnish Study Group for Antimicrobial Resistance (FiRe‐Network). Macrolide‐resistant Streptococcus pneumoniae and use of antimicrobial agents. Clin Infect Dis. 2001;33(4):483–488.
- , , , , , . Community prescribing and resistant Streptococcus pneumoniae. Emerg Infect Dis. 2005;11(6):829–837.
- , , , , ; Finnish Study Group for Antimicrobial Resistance (FiRe Network). Macrolide and azithromycin use are linked to increased macrolide resistance in Streptococcus pneumoniae. Antimicrob Agents Chemother. 2006;50(11):3646–3650.
© 2015 Society of Hospital Medicine
The Puzzle of Posthospital Recovery
Admission to a hospital for acute care is often a puzzling and traumatic experience for patients.[1, 2] Even after overcoming important hurdles such as receiving the right diagnosis, being treated with appropriate therapies, and experiencing initial improvement, the ultimate goal of complete recovery after discharge remains elusive for many. Dozens of interventions have been tested to reduce failed recoveries and readmissions with mixed results. Most of these have relied on system‐level changes such as improved medication reconciliation and postdischarge phone calls.[3, 4] Physicians have largely been ignored in such efforts. Most systems leave it up to individual physicians to decide how much time and effort to invest in postdischarge care, and patient outcomes are often highly dependent on a physician's skill, interest, and experience.
We are both hospitalists who attend regularly on general internal medicine services in the United States and Canada. In that capacity, we have experienced many successes and failures in helping patients recover after discharge. This Perspective frames the problem of engaging both hospitalists and office‐based physicians in transitions of care within the current context of readmission reduction efforts, and proposes a more structured approach for integrating those physicians into postdischarge care to promote recovery. Although we also consider broader policy efforts to reduce fragmentation and misaligned incentives such as electronic health records (EHRs), accountable care organizations (ACOs), and the patient‐centered medical home (PCMH), our focus is on how these may (or may not) help front‐line physicians to solve the puzzle of posthospital recovery in the current state of affairs.
THE PROBLEMLACK OF TIME, VARIABLE ENGAGEMENT, SILOED COMMUNICATION
Perhaps the most important barrier to engaging physicians in the posthospital recovery phase is their limited time and energy. Today's rapid throughput and the complexity of acute care leave little bandwidth for issues that are not right in front of hospitalists. Once discharged, patients are often out of sight, out of mind.[5] Office‐based physicians face similar time constraints.[6] In both settings, physicians find themselves operating in silos with significant communication barriers that are time consuming and difficult to overcome.
There are many current policy efforts to break down these silos, a prominent example being recent incentives to speed the widespread use of EHRs. Although EHR implementation progress has been steady, nearly half of US hospitals still do not have a basic EHR, and more advanced functions required for sharing care summaries and allowing patients to access their EHR are not in place at most hospitals that have implemented basic EHRs already.[7] Furthermore, the state of implementation in office‐based settings lags even farther behind hospitals.[8] Finally, our personal experience working in systems with fully integrated EHR systems has suggested to us that sometimes more shared information simply becomes part of the problem, as it is far too easy to include too many complex details of hospitalization in discharge summaries.
Moreover, as front‐line hospitalists, we generally want to help with transitional issues that occur after patients have left our hospital, and we are very mindful of the tradition of the physician who takes responsibility for all aspects of their patients' care in all settings. Yet this tradition may be more representative of the 20th century ideal of continuity than the new continuity that we see emerging in the 21st century.[9] Thus, the question at hand now is how individual physicians should prioritize and execute these tasks without overreaching.
EFFECTS OF THE PROBLEM IN PRACTICEVARIATIONS IN PHYSICIAN ENGAGEMENT
Patient needs after discharge are not uniform, and risk prediction is still imprecise despite many studies.[10] Some patients need no help; others need only targeted help with specific gaps; still others need full‐time navigators to meaningfully reduce their risk of ending up back in the emergency department.[11] The goal is to piece together the resources required to create a complete picture of patient support; much like the way ones solves a jigsaw puzzle (Figure 1A). Despite best efforts, the gaps in careor missing pieces[12]may only become apparent after discharge. Recent research suggests physicians do not see the same gaps as patients do and agree on causes for readmission less than 50% of the time.[13, 14] Often, these gaps come to light when an outside pharmacist, home health nurse, or case manager reaches out to the hospital or primary care physician to address a new problem (Figure 1B). As frequent recipients of those calls for help, we are conflicted in our reaction. On the one hand, we want to know when our carefully crafted plans fall apart. On the other hand, neither of us looks forward to voice mail messages informing us that the specialist to whom we referred the patient for follow‐up never called with an appointment. Micromanaging this kind of care can be very frustrating, both when we are the first person called or resource of last resort.
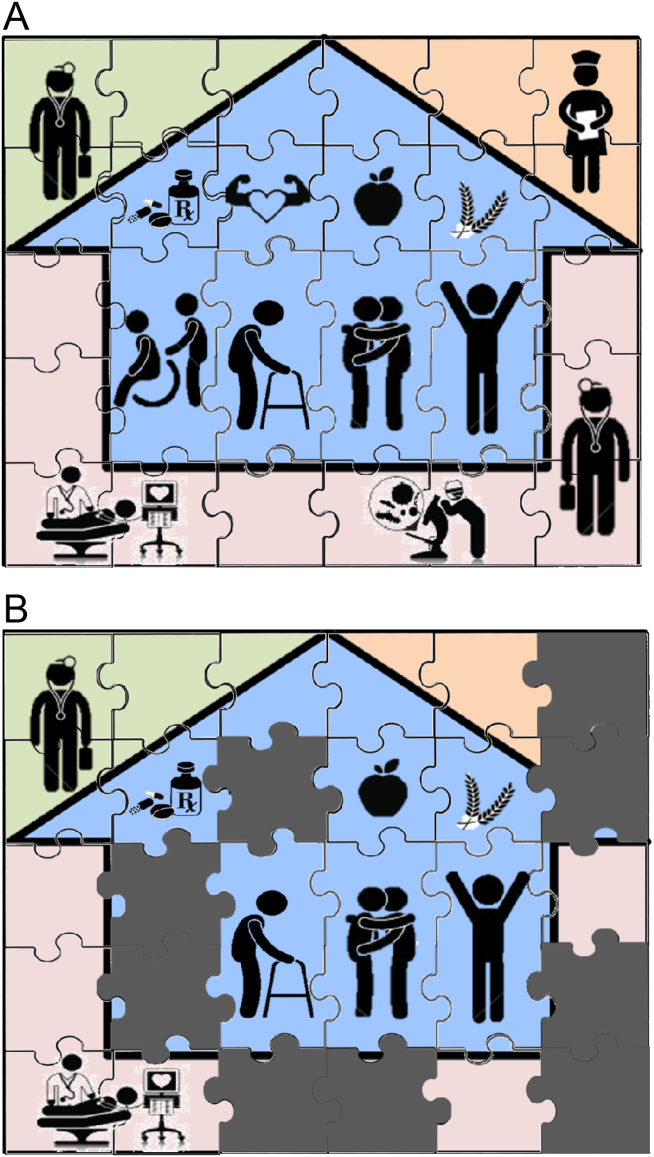
Even when physicians do not feel burdened by postdischarge care, they may be ineffective due to a lack of experience or resources. These efforts can leave them feeling demoralized, which in turn may further discourage them from future engagement, solidifying a pattern of missing (or perhaps lost) pieces (Figure 1B). Too often, a well‐intentioned but underpowered effort becomes a solution crushed by the weight of the problem. Successful physician models for care coordination must balance competing ideals of the 1 doctor, 1 patient strategy that preserve continuity,[15] with the need to focus individual physicians' time on those postdischarge tasks in which their engagement is clearly needed.
Certain payment models, such as ACOs, may help catalyze specific solutions to these problems by creating incentives for better coordination at the organizational level (eg, hospitals, skilled nursing facilities, and clinics), but these incentives may not necessarily translate into changes in physician practice, particularly as physicians payments are not yet part of bundled hospital care payments.[16] Likewise, innovative practice models such as the PCMH have promise to reshape the way healthcare is delivered, particularly by fortifying the role of primary care providers; but again, we note the lack of specific guidance for providers, particularly hospitalists. The Agency for Healthcare Research and Quality defines care coordination as 1 of the 5 pillars of the PCMH, but notes considerable uncertainty about how to operationalize coordination around transitions from hospital care: A clearer understanding of, and research on, the optimal role of the PCMH in terms of leadership and care coordination in inpatient care is needed. Specifically, a better understanding of the possible approaches and the tradeoffs involved with eachin terms of access, quality, cost, and patient experiencewould be useful.[17] Early studies of these outcomes from both ACOs and PCMHs suggest improvements in some areas of patient and provider experience but not in others.[18, 19, 20, 21] Thus, we believe that although EHRs, ACOs, and PCMHs provide laudable and fundamentally necessary organizational changes to spur innovation and quality in transitions, more discussion about the specific roles for physicians is still needed. Though certainly not a definitive or exhaustive list, we provide a few specific suggestions for more effective physician engagement below.
ENABLING STRUCTURESAPPROACHES FOR MORE EFFECTIVE POSTDISCHARGE ENGAGEMENT
One approach for structuring physician participation is to create new roles for physicians as transitionalists,[22] extensivists,[23] or comprehensive‐care physicians[24] to help patients migrate from the volatile postacute period into a more stable state of recovery. Much as hospital‐based rapid response teams add a layer of additional expertise and availability without replacing the role of the attending physician, in this model, transitionalist or extensivist teams could respond to postacute issues in concert with inpatient and outpatient physicians of record.
Another approach could be to integrate the patients' hospitalists or primary care physicians into interprofessional teams modeled after hospital transfer centers, robust interdisciplinary teams that manage intense care‐coordination issues for complex inpatients. A similar approach could be used to elevate care transitions from hospital to homea postdischarge recovery center. In the same way that transfer centers develop ongoing relationships with referring hospitals and communities, postdischarge recovery centers will also need to develop working relationships with community resources like senior centers, transportation services, and the patients' physicians that provide ongoing care to be effective. A recent study of a similar concept (a virtual ward) [25] provides both a framework for this type of interprofessional collaboration and also caution in underestimating the dose or intensity of such interventions needed for those interventions to succeed. In that study, the interprofessional team was not fully integrated into the ecosystem in which patients lived, and providers frequently had difficulty communicating with the patients' ongoing caregivers, including both physicians and personal support workers.
Certainly, there are many other approaches that could be imagined, and there are pros and cons for those suggested here. Although some of these roles may seem like new types of physicians, which could worsen fragmentation, what we are suggesting is more akin to hybridization of current hospitalist and primary care provider roles. A first step could be just giving a name to the additional effort asked of these providers, and paying for time spent when they are not acting in either the inpatient attending or outpatient attending role but in the coordinating role. Fortunately, Medicare's new initiative to pay for chronic‐care management will allow physicians, clinics, and hospitals more flexibility to bill for such services that are not based on face‐to‐face encounters in the hospital or clinic.[26]
Moreover, although solving the puzzle of posthospital recovery cannot be fixed with hospitalist‐centric solutions alone, we believe more discourse is needed to define contributions from these physicians. Current policies, such as the PCMH, focus on the clinic and primary‐care providers, whereas the Medicare Readmission Reduction Program focuses on the hospital but not the hospitalist. Thus, there is a specific gap in engaging hospitalists in ongoing efforts to solve this puzzle and answer important questions about the specific role(s) of the hospitalist[27] as well as the primary care provider[28] in preventing readmissions and facilitating recovery. Certainly, integration of any new roles is needed to avoid fragmentation by default, and our suggestion of roles such as transitionalists or transfer center physicians are intended as examples to facilitate broader discussion about individual physician roles. As is often the case in healthcare, a 1 size fits all solution is unlikely, and a variety of complimentary roles may be needed to accommodate the diversity of patients and providers as well as the delivery systems where they interact.
CONCLUSION
Although the emphasis on interdisciplinary care and systems approaches in promoting recovery is welcome, individual physicians are usually overlooked in these discussions. Most physicians want to help but cannot simply do more in the absence of more creative and structured approaches. As a recent commentary on care transitions suggested, It's the how, not just the what.[29] We agree but would add, It's also about who. Thus, the time has come to engage physicians within care‐delivery models specifically designed to solve this puzzle. Although interprofessional teams are clearly needed, patients look to individuals who know them, not teams, when they run into trouble, and their first move is often to call the doctor. Because physicians play such an important role in the acute phase of illness, their struggles and efforts in the postacute phase need to be recognized and streamlined if we are to improve our patients' chances of full recovery.
Disclosure: Nothing to report.
- . Post‐hospital syndrome‐an acquired transient condition of generalized risk. N Engl J Med. 2013;368:2169–2170.
- , . Reducing the trauma of hospitalization. JAMA. 2014;311(21):2169–2170.
- , , , et al. Hospital‐initiated transitional care interventions as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158:433–440.
- , , , et al. Interventions to reduce 30‐day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–528.
- , , , , . “Out of sight, out of mind”: housestaff perceptions of quality‐limiting factors in discharge care at teaching hospitals. J Hosp Med. 2012;7(5):376–381.
- . Instant replay—a quarterback's view of care coordination. N Engl J Med. 2014;371:489–491.
- , , , et al. More than half of US hospitals have at least a basic EHR, but stage 2 criteria remain challenging for most. Health Aff (Millwood). 2014;33(9):1664–1671.
- , , , , , . Despite substantial progress In EHR adoption, health information exchange and patient engagement remain low in office settings. Health Aff (Millwood). 2014;33(9):1672–1679.
- , . Understanding the value of continuity in the 21st century [published online May 18, 2015]. JAMA Intern Med. doi: 10.1001/jamainternmed.2015.1345.
- , , , et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–1698.
- , , , , , . Perceptions of readmitted patients on the transition from hospital to home. J Hosp Med. 2012;7(9):709–712.
- , , , et al. “Missing pieces”—functional, social, and environmental barriers to recovery for vulnerable older adults transitioning from hospital to home. J Am Geriatr Soc. 2014;62:1556–1561.
- , , , et al. Readmissions in the era of patient engagement. JAMA Intern Med. 2014;174(11):1870–1872.
- , , , et al. Challenges faced by patients with low socioeconomic status during the post‐hospital transition. J Gen Intern Med. 2014;29(2):283–289.
- , . Teaching physicians to care amid chaos. JAMA. 2013;309(10):987–988.
- , . Including physicians in bundled hospital care payments: time to revisit an old idea? JAMA. 2015;313(19):1907–1908.
- Agency for Healthcare Research and Quality. Coordinating care for adults with complex care needs in the patient‐centered medical home: challenges and solutions. Available at: http://www.pcmh.ahrq.gov/sites/default/files/attachments/Coordinating%20Care%20for%20Adults%20with%20Complex%20Care%20Needs.pdf. Accessed June 8, 2015.
- , , , . Performance differences in year 1 of pioneer accountable care organizations. N Engl J Med. 2015;372(20):1927–1936.
- , , , . Changes in patients' experiences in Medicare Accountable Care Organizations. N Engl J Med. 2014;371(18):1715–1724.
- , , , , . Association between participation in a multipayer medical home intervention and changes in quality, utilization, and costs of care. JAMA. 2014;311(8):815–825.
- , , , et al. Patient‐centered medical home intervention at an internal medicine resident safety‐net clinic. JAMA Intern Med. 2013;173(18):1694–1701.
- . Walking the walk in transitional care: the “hospitalist” role expands far beyond hospital walls. Today's Hospitalist. Available at: http://www.todayshospitalist.com/index.php?b=articles_read33(5):770–777.
- , , , et al. Effect of a post‐discharge virtual ward on readmission or death for high‐risk patients: a randomized clinical trial. JAMA. 2014;312:1305–1312.
- , , . Medicare and care coordination: expanding the clinician's toolbox. JAMA. 2015;313(8):797–798.
- . Hospitalists' responsibility, role in readmission prevention. The Hospitalist. Available at: http://www.the‐hospitalist.org/article/hospitalists‐responsibility‐role‐in‐readmission‐prevention. Published April 3, 2015. Accessed July 7, 2015.
- , . Bridging the hospitalist‐primary care divide through collaborative care. N Engl J Med. 2015;372(4):308–309.
- , . Care transitions: it's the how, not just the what. J Gen Intern Med. 2015;30(5):539–540.
Admission to a hospital for acute care is often a puzzling and traumatic experience for patients.[1, 2] Even after overcoming important hurdles such as receiving the right diagnosis, being treated with appropriate therapies, and experiencing initial improvement, the ultimate goal of complete recovery after discharge remains elusive for many. Dozens of interventions have been tested to reduce failed recoveries and readmissions with mixed results. Most of these have relied on system‐level changes such as improved medication reconciliation and postdischarge phone calls.[3, 4] Physicians have largely been ignored in such efforts. Most systems leave it up to individual physicians to decide how much time and effort to invest in postdischarge care, and patient outcomes are often highly dependent on a physician's skill, interest, and experience.
We are both hospitalists who attend regularly on general internal medicine services in the United States and Canada. In that capacity, we have experienced many successes and failures in helping patients recover after discharge. This Perspective frames the problem of engaging both hospitalists and office‐based physicians in transitions of care within the current context of readmission reduction efforts, and proposes a more structured approach for integrating those physicians into postdischarge care to promote recovery. Although we also consider broader policy efforts to reduce fragmentation and misaligned incentives such as electronic health records (EHRs), accountable care organizations (ACOs), and the patient‐centered medical home (PCMH), our focus is on how these may (or may not) help front‐line physicians to solve the puzzle of posthospital recovery in the current state of affairs.
THE PROBLEMLACK OF TIME, VARIABLE ENGAGEMENT, SILOED COMMUNICATION
Perhaps the most important barrier to engaging physicians in the posthospital recovery phase is their limited time and energy. Today's rapid throughput and the complexity of acute care leave little bandwidth for issues that are not right in front of hospitalists. Once discharged, patients are often out of sight, out of mind.[5] Office‐based physicians face similar time constraints.[6] In both settings, physicians find themselves operating in silos with significant communication barriers that are time consuming and difficult to overcome.
There are many current policy efforts to break down these silos, a prominent example being recent incentives to speed the widespread use of EHRs. Although EHR implementation progress has been steady, nearly half of US hospitals still do not have a basic EHR, and more advanced functions required for sharing care summaries and allowing patients to access their EHR are not in place at most hospitals that have implemented basic EHRs already.[7] Furthermore, the state of implementation in office‐based settings lags even farther behind hospitals.[8] Finally, our personal experience working in systems with fully integrated EHR systems has suggested to us that sometimes more shared information simply becomes part of the problem, as it is far too easy to include too many complex details of hospitalization in discharge summaries.
Moreover, as front‐line hospitalists, we generally want to help with transitional issues that occur after patients have left our hospital, and we are very mindful of the tradition of the physician who takes responsibility for all aspects of their patients' care in all settings. Yet this tradition may be more representative of the 20th century ideal of continuity than the new continuity that we see emerging in the 21st century.[9] Thus, the question at hand now is how individual physicians should prioritize and execute these tasks without overreaching.
EFFECTS OF THE PROBLEM IN PRACTICEVARIATIONS IN PHYSICIAN ENGAGEMENT
Patient needs after discharge are not uniform, and risk prediction is still imprecise despite many studies.[10] Some patients need no help; others need only targeted help with specific gaps; still others need full‐time navigators to meaningfully reduce their risk of ending up back in the emergency department.[11] The goal is to piece together the resources required to create a complete picture of patient support; much like the way ones solves a jigsaw puzzle (Figure 1A). Despite best efforts, the gaps in careor missing pieces[12]may only become apparent after discharge. Recent research suggests physicians do not see the same gaps as patients do and agree on causes for readmission less than 50% of the time.[13, 14] Often, these gaps come to light when an outside pharmacist, home health nurse, or case manager reaches out to the hospital or primary care physician to address a new problem (Figure 1B). As frequent recipients of those calls for help, we are conflicted in our reaction. On the one hand, we want to know when our carefully crafted plans fall apart. On the other hand, neither of us looks forward to voice mail messages informing us that the specialist to whom we referred the patient for follow‐up never called with an appointment. Micromanaging this kind of care can be very frustrating, both when we are the first person called or resource of last resort.
Even when physicians do not feel burdened by postdischarge care, they may be ineffective due to a lack of experience or resources. These efforts can leave them feeling demoralized, which in turn may further discourage them from future engagement, solidifying a pattern of missing (or perhaps lost) pieces (Figure 1B). Too often, a well‐intentioned but underpowered effort becomes a solution crushed by the weight of the problem. Successful physician models for care coordination must balance competing ideals of the 1 doctor, 1 patient strategy that preserve continuity,[15] with the need to focus individual physicians' time on those postdischarge tasks in which their engagement is clearly needed.
Certain payment models, such as ACOs, may help catalyze specific solutions to these problems by creating incentives for better coordination at the organizational level (eg, hospitals, skilled nursing facilities, and clinics), but these incentives may not necessarily translate into changes in physician practice, particularly as physicians payments are not yet part of bundled hospital care payments.[16] Likewise, innovative practice models such as the PCMH have promise to reshape the way healthcare is delivered, particularly by fortifying the role of primary care providers; but again, we note the lack of specific guidance for providers, particularly hospitalists. The Agency for Healthcare Research and Quality defines care coordination as 1 of the 5 pillars of the PCMH, but notes considerable uncertainty about how to operationalize coordination around transitions from hospital care: A clearer understanding of, and research on, the optimal role of the PCMH in terms of leadership and care coordination in inpatient care is needed. Specifically, a better understanding of the possible approaches and the tradeoffs involved with eachin terms of access, quality, cost, and patient experiencewould be useful.[17] Early studies of these outcomes from both ACOs and PCMHs suggest improvements in some areas of patient and provider experience but not in others.[18, 19, 20, 21] Thus, we believe that although EHRs, ACOs, and PCMHs provide laudable and fundamentally necessary organizational changes to spur innovation and quality in transitions, more discussion about the specific roles for physicians is still needed. Though certainly not a definitive or exhaustive list, we provide a few specific suggestions for more effective physician engagement below.
ENABLING STRUCTURESAPPROACHES FOR MORE EFFECTIVE POSTDISCHARGE ENGAGEMENT
One approach for structuring physician participation is to create new roles for physicians as transitionalists,[22] extensivists,[23] or comprehensive‐care physicians[24] to help patients migrate from the volatile postacute period into a more stable state of recovery. Much as hospital‐based rapid response teams add a layer of additional expertise and availability without replacing the role of the attending physician, in this model, transitionalist or extensivist teams could respond to postacute issues in concert with inpatient and outpatient physicians of record.
Another approach could be to integrate the patients' hospitalists or primary care physicians into interprofessional teams modeled after hospital transfer centers, robust interdisciplinary teams that manage intense care‐coordination issues for complex inpatients. A similar approach could be used to elevate care transitions from hospital to homea postdischarge recovery center. In the same way that transfer centers develop ongoing relationships with referring hospitals and communities, postdischarge recovery centers will also need to develop working relationships with community resources like senior centers, transportation services, and the patients' physicians that provide ongoing care to be effective. A recent study of a similar concept (a virtual ward) [25] provides both a framework for this type of interprofessional collaboration and also caution in underestimating the dose or intensity of such interventions needed for those interventions to succeed. In that study, the interprofessional team was not fully integrated into the ecosystem in which patients lived, and providers frequently had difficulty communicating with the patients' ongoing caregivers, including both physicians and personal support workers.
Certainly, there are many other approaches that could be imagined, and there are pros and cons for those suggested here. Although some of these roles may seem like new types of physicians, which could worsen fragmentation, what we are suggesting is more akin to hybridization of current hospitalist and primary care provider roles. A first step could be just giving a name to the additional effort asked of these providers, and paying for time spent when they are not acting in either the inpatient attending or outpatient attending role but in the coordinating role. Fortunately, Medicare's new initiative to pay for chronic‐care management will allow physicians, clinics, and hospitals more flexibility to bill for such services that are not based on face‐to‐face encounters in the hospital or clinic.[26]
Moreover, although solving the puzzle of posthospital recovery cannot be fixed with hospitalist‐centric solutions alone, we believe more discourse is needed to define contributions from these physicians. Current policies, such as the PCMH, focus on the clinic and primary‐care providers, whereas the Medicare Readmission Reduction Program focuses on the hospital but not the hospitalist. Thus, there is a specific gap in engaging hospitalists in ongoing efforts to solve this puzzle and answer important questions about the specific role(s) of the hospitalist[27] as well as the primary care provider[28] in preventing readmissions and facilitating recovery. Certainly, integration of any new roles is needed to avoid fragmentation by default, and our suggestion of roles such as transitionalists or transfer center physicians are intended as examples to facilitate broader discussion about individual physician roles. As is often the case in healthcare, a 1 size fits all solution is unlikely, and a variety of complimentary roles may be needed to accommodate the diversity of patients and providers as well as the delivery systems where they interact.
CONCLUSION
Although the emphasis on interdisciplinary care and systems approaches in promoting recovery is welcome, individual physicians are usually overlooked in these discussions. Most physicians want to help but cannot simply do more in the absence of more creative and structured approaches. As a recent commentary on care transitions suggested, It's the how, not just the what.[29] We agree but would add, It's also about who. Thus, the time has come to engage physicians within care‐delivery models specifically designed to solve this puzzle. Although interprofessional teams are clearly needed, patients look to individuals who know them, not teams, when they run into trouble, and their first move is often to call the doctor. Because physicians play such an important role in the acute phase of illness, their struggles and efforts in the postacute phase need to be recognized and streamlined if we are to improve our patients' chances of full recovery.
Disclosure: Nothing to report.
Admission to a hospital for acute care is often a puzzling and traumatic experience for patients.[1, 2] Even after overcoming important hurdles such as receiving the right diagnosis, being treated with appropriate therapies, and experiencing initial improvement, the ultimate goal of complete recovery after discharge remains elusive for many. Dozens of interventions have been tested to reduce failed recoveries and readmissions with mixed results. Most of these have relied on system‐level changes such as improved medication reconciliation and postdischarge phone calls.[3, 4] Physicians have largely been ignored in such efforts. Most systems leave it up to individual physicians to decide how much time and effort to invest in postdischarge care, and patient outcomes are often highly dependent on a physician's skill, interest, and experience.
We are both hospitalists who attend regularly on general internal medicine services in the United States and Canada. In that capacity, we have experienced many successes and failures in helping patients recover after discharge. This Perspective frames the problem of engaging both hospitalists and office‐based physicians in transitions of care within the current context of readmission reduction efforts, and proposes a more structured approach for integrating those physicians into postdischarge care to promote recovery. Although we also consider broader policy efforts to reduce fragmentation and misaligned incentives such as electronic health records (EHRs), accountable care organizations (ACOs), and the patient‐centered medical home (PCMH), our focus is on how these may (or may not) help front‐line physicians to solve the puzzle of posthospital recovery in the current state of affairs.
THE PROBLEMLACK OF TIME, VARIABLE ENGAGEMENT, SILOED COMMUNICATION
Perhaps the most important barrier to engaging physicians in the posthospital recovery phase is their limited time and energy. Today's rapid throughput and the complexity of acute care leave little bandwidth for issues that are not right in front of hospitalists. Once discharged, patients are often out of sight, out of mind.[5] Office‐based physicians face similar time constraints.[6] In both settings, physicians find themselves operating in silos with significant communication barriers that are time consuming and difficult to overcome.
There are many current policy efforts to break down these silos, a prominent example being recent incentives to speed the widespread use of EHRs. Although EHR implementation progress has been steady, nearly half of US hospitals still do not have a basic EHR, and more advanced functions required for sharing care summaries and allowing patients to access their EHR are not in place at most hospitals that have implemented basic EHRs already.[7] Furthermore, the state of implementation in office‐based settings lags even farther behind hospitals.[8] Finally, our personal experience working in systems with fully integrated EHR systems has suggested to us that sometimes more shared information simply becomes part of the problem, as it is far too easy to include too many complex details of hospitalization in discharge summaries.
Moreover, as front‐line hospitalists, we generally want to help with transitional issues that occur after patients have left our hospital, and we are very mindful of the tradition of the physician who takes responsibility for all aspects of their patients' care in all settings. Yet this tradition may be more representative of the 20th century ideal of continuity than the new continuity that we see emerging in the 21st century.[9] Thus, the question at hand now is how individual physicians should prioritize and execute these tasks without overreaching.
EFFECTS OF THE PROBLEM IN PRACTICEVARIATIONS IN PHYSICIAN ENGAGEMENT
Patient needs after discharge are not uniform, and risk prediction is still imprecise despite many studies.[10] Some patients need no help; others need only targeted help with specific gaps; still others need full‐time navigators to meaningfully reduce their risk of ending up back in the emergency department.[11] The goal is to piece together the resources required to create a complete picture of patient support; much like the way ones solves a jigsaw puzzle (Figure 1A). Despite best efforts, the gaps in careor missing pieces[12]may only become apparent after discharge. Recent research suggests physicians do not see the same gaps as patients do and agree on causes for readmission less than 50% of the time.[13, 14] Often, these gaps come to light when an outside pharmacist, home health nurse, or case manager reaches out to the hospital or primary care physician to address a new problem (Figure 1B). As frequent recipients of those calls for help, we are conflicted in our reaction. On the one hand, we want to know when our carefully crafted plans fall apart. On the other hand, neither of us looks forward to voice mail messages informing us that the specialist to whom we referred the patient for follow‐up never called with an appointment. Micromanaging this kind of care can be very frustrating, both when we are the first person called or resource of last resort.
Even when physicians do not feel burdened by postdischarge care, they may be ineffective due to a lack of experience or resources. These efforts can leave them feeling demoralized, which in turn may further discourage them from future engagement, solidifying a pattern of missing (or perhaps lost) pieces (Figure 1B). Too often, a well‐intentioned but underpowered effort becomes a solution crushed by the weight of the problem. Successful physician models for care coordination must balance competing ideals of the 1 doctor, 1 patient strategy that preserve continuity,[15] with the need to focus individual physicians' time on those postdischarge tasks in which their engagement is clearly needed.
Certain payment models, such as ACOs, may help catalyze specific solutions to these problems by creating incentives for better coordination at the organizational level (eg, hospitals, skilled nursing facilities, and clinics), but these incentives may not necessarily translate into changes in physician practice, particularly as physicians payments are not yet part of bundled hospital care payments.[16] Likewise, innovative practice models such as the PCMH have promise to reshape the way healthcare is delivered, particularly by fortifying the role of primary care providers; but again, we note the lack of specific guidance for providers, particularly hospitalists. The Agency for Healthcare Research and Quality defines care coordination as 1 of the 5 pillars of the PCMH, but notes considerable uncertainty about how to operationalize coordination around transitions from hospital care: A clearer understanding of, and research on, the optimal role of the PCMH in terms of leadership and care coordination in inpatient care is needed. Specifically, a better understanding of the possible approaches and the tradeoffs involved with eachin terms of access, quality, cost, and patient experiencewould be useful.[17] Early studies of these outcomes from both ACOs and PCMHs suggest improvements in some areas of patient and provider experience but not in others.[18, 19, 20, 21] Thus, we believe that although EHRs, ACOs, and PCMHs provide laudable and fundamentally necessary organizational changes to spur innovation and quality in transitions, more discussion about the specific roles for physicians is still needed. Though certainly not a definitive or exhaustive list, we provide a few specific suggestions for more effective physician engagement below.
ENABLING STRUCTURESAPPROACHES FOR MORE EFFECTIVE POSTDISCHARGE ENGAGEMENT
One approach for structuring physician participation is to create new roles for physicians as transitionalists,[22] extensivists,[23] or comprehensive‐care physicians[24] to help patients migrate from the volatile postacute period into a more stable state of recovery. Much as hospital‐based rapid response teams add a layer of additional expertise and availability without replacing the role of the attending physician, in this model, transitionalist or extensivist teams could respond to postacute issues in concert with inpatient and outpatient physicians of record.
Another approach could be to integrate the patients' hospitalists or primary care physicians into interprofessional teams modeled after hospital transfer centers, robust interdisciplinary teams that manage intense care‐coordination issues for complex inpatients. A similar approach could be used to elevate care transitions from hospital to homea postdischarge recovery center. In the same way that transfer centers develop ongoing relationships with referring hospitals and communities, postdischarge recovery centers will also need to develop working relationships with community resources like senior centers, transportation services, and the patients' physicians that provide ongoing care to be effective. A recent study of a similar concept (a virtual ward) [25] provides both a framework for this type of interprofessional collaboration and also caution in underestimating the dose or intensity of such interventions needed for those interventions to succeed. In that study, the interprofessional team was not fully integrated into the ecosystem in which patients lived, and providers frequently had difficulty communicating with the patients' ongoing caregivers, including both physicians and personal support workers.
Certainly, there are many other approaches that could be imagined, and there are pros and cons for those suggested here. Although some of these roles may seem like new types of physicians, which could worsen fragmentation, what we are suggesting is more akin to hybridization of current hospitalist and primary care provider roles. A first step could be just giving a name to the additional effort asked of these providers, and paying for time spent when they are not acting in either the inpatient attending or outpatient attending role but in the coordinating role. Fortunately, Medicare's new initiative to pay for chronic‐care management will allow physicians, clinics, and hospitals more flexibility to bill for such services that are not based on face‐to‐face encounters in the hospital or clinic.[26]
Moreover, although solving the puzzle of posthospital recovery cannot be fixed with hospitalist‐centric solutions alone, we believe more discourse is needed to define contributions from these physicians. Current policies, such as the PCMH, focus on the clinic and primary‐care providers, whereas the Medicare Readmission Reduction Program focuses on the hospital but not the hospitalist. Thus, there is a specific gap in engaging hospitalists in ongoing efforts to solve this puzzle and answer important questions about the specific role(s) of the hospitalist[27] as well as the primary care provider[28] in preventing readmissions and facilitating recovery. Certainly, integration of any new roles is needed to avoid fragmentation by default, and our suggestion of roles such as transitionalists or transfer center physicians are intended as examples to facilitate broader discussion about individual physician roles. As is often the case in healthcare, a 1 size fits all solution is unlikely, and a variety of complimentary roles may be needed to accommodate the diversity of patients and providers as well as the delivery systems where they interact.
CONCLUSION
Although the emphasis on interdisciplinary care and systems approaches in promoting recovery is welcome, individual physicians are usually overlooked in these discussions. Most physicians want to help but cannot simply do more in the absence of more creative and structured approaches. As a recent commentary on care transitions suggested, It's the how, not just the what.[29] We agree but would add, It's also about who. Thus, the time has come to engage physicians within care‐delivery models specifically designed to solve this puzzle. Although interprofessional teams are clearly needed, patients look to individuals who know them, not teams, when they run into trouble, and their first move is often to call the doctor. Because physicians play such an important role in the acute phase of illness, their struggles and efforts in the postacute phase need to be recognized and streamlined if we are to improve our patients' chances of full recovery.
Disclosure: Nothing to report.
- . Post‐hospital syndrome‐an acquired transient condition of generalized risk. N Engl J Med. 2013;368:2169–2170.
- , . Reducing the trauma of hospitalization. JAMA. 2014;311(21):2169–2170.
- , , , et al. Hospital‐initiated transitional care interventions as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158:433–440.
- , , , et al. Interventions to reduce 30‐day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–528.
- , , , , . “Out of sight, out of mind”: housestaff perceptions of quality‐limiting factors in discharge care at teaching hospitals. J Hosp Med. 2012;7(5):376–381.
- . Instant replay—a quarterback's view of care coordination. N Engl J Med. 2014;371:489–491.
- , , , et al. More than half of US hospitals have at least a basic EHR, but stage 2 criteria remain challenging for most. Health Aff (Millwood). 2014;33(9):1664–1671.
- , , , , , . Despite substantial progress In EHR adoption, health information exchange and patient engagement remain low in office settings. Health Aff (Millwood). 2014;33(9):1672–1679.
- , . Understanding the value of continuity in the 21st century [published online May 18, 2015]. JAMA Intern Med. doi: 10.1001/jamainternmed.2015.1345.
- , , , et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–1698.
- , , , , , . Perceptions of readmitted patients on the transition from hospital to home. J Hosp Med. 2012;7(9):709–712.
- , , , et al. “Missing pieces”—functional, social, and environmental barriers to recovery for vulnerable older adults transitioning from hospital to home. J Am Geriatr Soc. 2014;62:1556–1561.
- , , , et al. Readmissions in the era of patient engagement. JAMA Intern Med. 2014;174(11):1870–1872.
- , , , et al. Challenges faced by patients with low socioeconomic status during the post‐hospital transition. J Gen Intern Med. 2014;29(2):283–289.
- , . Teaching physicians to care amid chaos. JAMA. 2013;309(10):987–988.
- , . Including physicians in bundled hospital care payments: time to revisit an old idea? JAMA. 2015;313(19):1907–1908.
- Agency for Healthcare Research and Quality. Coordinating care for adults with complex care needs in the patient‐centered medical home: challenges and solutions. Available at: http://www.pcmh.ahrq.gov/sites/default/files/attachments/Coordinating%20Care%20for%20Adults%20with%20Complex%20Care%20Needs.pdf. Accessed June 8, 2015.
- , , , . Performance differences in year 1 of pioneer accountable care organizations. N Engl J Med. 2015;372(20):1927–1936.
- , , , . Changes in patients' experiences in Medicare Accountable Care Organizations. N Engl J Med. 2014;371(18):1715–1724.
- , , , , . Association between participation in a multipayer medical home intervention and changes in quality, utilization, and costs of care. JAMA. 2014;311(8):815–825.
- , , , et al. Patient‐centered medical home intervention at an internal medicine resident safety‐net clinic. JAMA Intern Med. 2013;173(18):1694–1701.
- . Walking the walk in transitional care: the “hospitalist” role expands far beyond hospital walls. Today's Hospitalist. Available at: http://www.todayshospitalist.com/index.php?b=articles_read33(5):770–777.
- , , , et al. Effect of a post‐discharge virtual ward on readmission or death for high‐risk patients: a randomized clinical trial. JAMA. 2014;312:1305–1312.
- , , . Medicare and care coordination: expanding the clinician's toolbox. JAMA. 2015;313(8):797–798.
- . Hospitalists' responsibility, role in readmission prevention. The Hospitalist. Available at: http://www.the‐hospitalist.org/article/hospitalists‐responsibility‐role‐in‐readmission‐prevention. Published April 3, 2015. Accessed July 7, 2015.
- , . Bridging the hospitalist‐primary care divide through collaborative care. N Engl J Med. 2015;372(4):308–309.
- , . Care transitions: it's the how, not just the what. J Gen Intern Med. 2015;30(5):539–540.
- . Post‐hospital syndrome‐an acquired transient condition of generalized risk. N Engl J Med. 2013;368:2169–2170.
- , . Reducing the trauma of hospitalization. JAMA. 2014;311(21):2169–2170.
- , , , et al. Hospital‐initiated transitional care interventions as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158:433–440.
- , , , et al. Interventions to reduce 30‐day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–528.
- , , , , . “Out of sight, out of mind”: housestaff perceptions of quality‐limiting factors in discharge care at teaching hospitals. J Hosp Med. 2012;7(5):376–381.
- . Instant replay—a quarterback's view of care coordination. N Engl J Med. 2014;371:489–491.
- , , , et al. More than half of US hospitals have at least a basic EHR, but stage 2 criteria remain challenging for most. Health Aff (Millwood). 2014;33(9):1664–1671.
- , , , , , . Despite substantial progress In EHR adoption, health information exchange and patient engagement remain low in office settings. Health Aff (Millwood). 2014;33(9):1672–1679.
- , . Understanding the value of continuity in the 21st century [published online May 18, 2015]. JAMA Intern Med. doi: 10.1001/jamainternmed.2015.1345.
- , , , et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–1698.
- , , , , , . Perceptions of readmitted patients on the transition from hospital to home. J Hosp Med. 2012;7(9):709–712.
- , , , et al. “Missing pieces”—functional, social, and environmental barriers to recovery for vulnerable older adults transitioning from hospital to home. J Am Geriatr Soc. 2014;62:1556–1561.
- , , , et al. Readmissions in the era of patient engagement. JAMA Intern Med. 2014;174(11):1870–1872.
- , , , et al. Challenges faced by patients with low socioeconomic status during the post‐hospital transition. J Gen Intern Med. 2014;29(2):283–289.
- , . Teaching physicians to care amid chaos. JAMA. 2013;309(10):987–988.
- , . Including physicians in bundled hospital care payments: time to revisit an old idea? JAMA. 2015;313(19):1907–1908.
- Agency for Healthcare Research and Quality. Coordinating care for adults with complex care needs in the patient‐centered medical home: challenges and solutions. Available at: http://www.pcmh.ahrq.gov/sites/default/files/attachments/Coordinating%20Care%20for%20Adults%20with%20Complex%20Care%20Needs.pdf. Accessed June 8, 2015.
- , , , . Performance differences in year 1 of pioneer accountable care organizations. N Engl J Med. 2015;372(20):1927–1936.
- , , , . Changes in patients' experiences in Medicare Accountable Care Organizations. N Engl J Med. 2014;371(18):1715–1724.
- , , , , . Association between participation in a multipayer medical home intervention and changes in quality, utilization, and costs of care. JAMA. 2014;311(8):815–825.
- , , , et al. Patient‐centered medical home intervention at an internal medicine resident safety‐net clinic. JAMA Intern Med. 2013;173(18):1694–1701.
- . Walking the walk in transitional care: the “hospitalist” role expands far beyond hospital walls. Today's Hospitalist. Available at: http://www.todayshospitalist.com/index.php?b=articles_read33(5):770–777.
- , , , et al. Effect of a post‐discharge virtual ward on readmission or death for high‐risk patients: a randomized clinical trial. JAMA. 2014;312:1305–1312.
- , , . Medicare and care coordination: expanding the clinician's toolbox. JAMA. 2015;313(8):797–798.
- . Hospitalists' responsibility, role in readmission prevention. The Hospitalist. Available at: http://www.the‐hospitalist.org/article/hospitalists‐responsibility‐role‐in‐readmission‐prevention. Published April 3, 2015. Accessed July 7, 2015.
- , . Bridging the hospitalist‐primary care divide through collaborative care. N Engl J Med. 2015;372(4):308–309.
- , . Care transitions: it's the how, not just the what. J Gen Intern Med. 2015;30(5):539–540.
Indoor Tanning Is More Harmful Than Americans Believe
The Surgeon General has called on partners in prevention from various sectors to address skin cancer as a major public health problem. One of the main goals outlined in The Surgeon General’s Call to Action to Prevent Skin Cancer is to reduce harm from indoor tanning, which has been linked to increased risk for skin cancer, including melanoma, basal cell carcinoma, and squamous cell carcinoma.
Based on reports from the American Cancer Society, Centers for Disease Control and Prevention, Federal Trade Commission, Mayo Clinic, and US Food and Drug Administration, the following common myths about indoor tanning should be communicated to dermatology patients.
Myth: Indoor tanning will not increase your risk for skin cancer.
Fact: As many as 90% of melanomas are caused by UV exposure. Indoor tanning exposure to UVA and UVB radiation damages the skin and may lead to cancer. Melanoma is linked to severe sunburns, especially at a young age.
Myth: Indoor tanning is safer than tanning outdoors because it is a controlled dose of UV radiation.
Fact: Both indoor tanning and tanning outside are dangerous. Tanning beds may be more dangerous than the sun because they can be used at the same high intensity every day of the year, regardless of time of day, season, or cloud cover. Furthermore, the Surgeon General and US Food and Drug Administration report that an estimated 3000 Americans each year go to emergency departments with injuries caused by indoor tanning, including burns, eye injuries, immune suppression, and allergic reactions. Indoor tanning also causes premature skin aging.
Myth: A “base tan” protects your skin from sunburn.
Fact: Although many patients believe that a few sessions of indoor tanning will prevent them from burning in the sun, a tan does little to protect the skin from future UV exposure. In fact, the Centers for Disease Control and Prevention notes that people who tan indoors are more likely to report getting sunburned. The best way to protect the skin from sunburn is by using sun protection and avoiding indoor tanning.
Myth: Indoor tanning is a safe way to increase vitamin D levels.
Fact: It is important to get enough vitamin D; however, the safest way is through what you eat. Although UVB radiation helps the body produce vitamin D, patients do not need a tan to get that benefit. Ten to 15 minutes of unprotected natural sun exposure on the face and hands 2 to 3 times a week during the summer allows for a healthy dose of vitamin D. Dietary sources, such as low-fat milk, salmon, tuna, and fortified orange juice, are the safest way to get enough vitamin D.
Myth: Indoor tanning is approved by the government.
Fact: According to the Federal Trade Commission, no US government agency recommends the use of indoor tanning equipment. Tanning bed use by minors has been banned in many states, and efforts are ongoing to protect consumers younger than 18 years on local, state, and federal levels. In July 2009, the International Agency for Research on Cancer, part of the World Health Organization, moved tanning devices that emit UV radiation into the highest cancer risk category—carcinogenic to humans—concluding that they are more dangerous than previously thought.
Studies have consistently shown that indoor tanning increases a person’s risk of getting skin cancer and indoor tanning at a young age appears to be more strongly related to lifetime skin cancer risk. Patients should be reminded that every time they tan, they increase their risk of melanoma as well as premature skin aging and other skin cancers. Dermatologists should counsel patients on using sun protection and avoiding indoor tanning.
The Surgeon General has called on partners in prevention from various sectors to address skin cancer as a major public health problem. One of the main goals outlined in The Surgeon General’s Call to Action to Prevent Skin Cancer is to reduce harm from indoor tanning, which has been linked to increased risk for skin cancer, including melanoma, basal cell carcinoma, and squamous cell carcinoma.
Based on reports from the American Cancer Society, Centers for Disease Control and Prevention, Federal Trade Commission, Mayo Clinic, and US Food and Drug Administration, the following common myths about indoor tanning should be communicated to dermatology patients.
Myth: Indoor tanning will not increase your risk for skin cancer.
Fact: As many as 90% of melanomas are caused by UV exposure. Indoor tanning exposure to UVA and UVB radiation damages the skin and may lead to cancer. Melanoma is linked to severe sunburns, especially at a young age.
Myth: Indoor tanning is safer than tanning outdoors because it is a controlled dose of UV radiation.
Fact: Both indoor tanning and tanning outside are dangerous. Tanning beds may be more dangerous than the sun because they can be used at the same high intensity every day of the year, regardless of time of day, season, or cloud cover. Furthermore, the Surgeon General and US Food and Drug Administration report that an estimated 3000 Americans each year go to emergency departments with injuries caused by indoor tanning, including burns, eye injuries, immune suppression, and allergic reactions. Indoor tanning also causes premature skin aging.
Myth: A “base tan” protects your skin from sunburn.
Fact: Although many patients believe that a few sessions of indoor tanning will prevent them from burning in the sun, a tan does little to protect the skin from future UV exposure. In fact, the Centers for Disease Control and Prevention notes that people who tan indoors are more likely to report getting sunburned. The best way to protect the skin from sunburn is by using sun protection and avoiding indoor tanning.
Myth: Indoor tanning is a safe way to increase vitamin D levels.
Fact: It is important to get enough vitamin D; however, the safest way is through what you eat. Although UVB radiation helps the body produce vitamin D, patients do not need a tan to get that benefit. Ten to 15 minutes of unprotected natural sun exposure on the face and hands 2 to 3 times a week during the summer allows for a healthy dose of vitamin D. Dietary sources, such as low-fat milk, salmon, tuna, and fortified orange juice, are the safest way to get enough vitamin D.
Myth: Indoor tanning is approved by the government.
Fact: According to the Federal Trade Commission, no US government agency recommends the use of indoor tanning equipment. Tanning bed use by minors has been banned in many states, and efforts are ongoing to protect consumers younger than 18 years on local, state, and federal levels. In July 2009, the International Agency for Research on Cancer, part of the World Health Organization, moved tanning devices that emit UV radiation into the highest cancer risk category—carcinogenic to humans—concluding that they are more dangerous than previously thought.
Studies have consistently shown that indoor tanning increases a person’s risk of getting skin cancer and indoor tanning at a young age appears to be more strongly related to lifetime skin cancer risk. Patients should be reminded that every time they tan, they increase their risk of melanoma as well as premature skin aging and other skin cancers. Dermatologists should counsel patients on using sun protection and avoiding indoor tanning.
The Surgeon General has called on partners in prevention from various sectors to address skin cancer as a major public health problem. One of the main goals outlined in The Surgeon General’s Call to Action to Prevent Skin Cancer is to reduce harm from indoor tanning, which has been linked to increased risk for skin cancer, including melanoma, basal cell carcinoma, and squamous cell carcinoma.
Based on reports from the American Cancer Society, Centers for Disease Control and Prevention, Federal Trade Commission, Mayo Clinic, and US Food and Drug Administration, the following common myths about indoor tanning should be communicated to dermatology patients.
Myth: Indoor tanning will not increase your risk for skin cancer.
Fact: As many as 90% of melanomas are caused by UV exposure. Indoor tanning exposure to UVA and UVB radiation damages the skin and may lead to cancer. Melanoma is linked to severe sunburns, especially at a young age.
Myth: Indoor tanning is safer than tanning outdoors because it is a controlled dose of UV radiation.
Fact: Both indoor tanning and tanning outside are dangerous. Tanning beds may be more dangerous than the sun because they can be used at the same high intensity every day of the year, regardless of time of day, season, or cloud cover. Furthermore, the Surgeon General and US Food and Drug Administration report that an estimated 3000 Americans each year go to emergency departments with injuries caused by indoor tanning, including burns, eye injuries, immune suppression, and allergic reactions. Indoor tanning also causes premature skin aging.
Myth: A “base tan” protects your skin from sunburn.
Fact: Although many patients believe that a few sessions of indoor tanning will prevent them from burning in the sun, a tan does little to protect the skin from future UV exposure. In fact, the Centers for Disease Control and Prevention notes that people who tan indoors are more likely to report getting sunburned. The best way to protect the skin from sunburn is by using sun protection and avoiding indoor tanning.
Myth: Indoor tanning is a safe way to increase vitamin D levels.
Fact: It is important to get enough vitamin D; however, the safest way is through what you eat. Although UVB radiation helps the body produce vitamin D, patients do not need a tan to get that benefit. Ten to 15 minutes of unprotected natural sun exposure on the face and hands 2 to 3 times a week during the summer allows for a healthy dose of vitamin D. Dietary sources, such as low-fat milk, salmon, tuna, and fortified orange juice, are the safest way to get enough vitamin D.
Myth: Indoor tanning is approved by the government.
Fact: According to the Federal Trade Commission, no US government agency recommends the use of indoor tanning equipment. Tanning bed use by minors has been banned in many states, and efforts are ongoing to protect consumers younger than 18 years on local, state, and federal levels. In July 2009, the International Agency for Research on Cancer, part of the World Health Organization, moved tanning devices that emit UV radiation into the highest cancer risk category—carcinogenic to humans—concluding that they are more dangerous than previously thought.
Studies have consistently shown that indoor tanning increases a person’s risk of getting skin cancer and indoor tanning at a young age appears to be more strongly related to lifetime skin cancer risk. Patients should be reminded that every time they tan, they increase their risk of melanoma as well as premature skin aging and other skin cancers. Dermatologists should counsel patients on using sun protection and avoiding indoor tanning.
Postpartum psychosis and ill-advised discharge
Muslim Bangladeshi female presents
The patient is a 31-year-old married Muslim Bangladeshi female homemaker admitted to an inpatient unit in a private hospital in a large urban area in the northeastern United States because of postpartum psychosis. She recently had immigrated to the United States and spoke no English. She lived with her husband, his parents, and his siblings in a city neighborhood predominantly comprised of South Asian immigrants. Her sole source of financial support was her husband, who worked as a cab driver. Both patient and her husband were uninsured. They identified strongly with their religion and culture of origin.
Key questions
Communication was a challenge and was accomplished using an interpreter, who was not always available. The patient did not seem to respond to treatment, and there was a question about the possibility that she was “cheeking” her medications. Her husband requested her discharge against medical advice, despite her still showing signs of psychosis. He appeared ambivalent about outpatient follow-up.
What is the duty of care in this situation, given the complexities inherent in a cross-cultural situation, the presence of communication barriers, the question of patient and infant safety, the husband’s role (given the understanding that his actions were probably culturally sanctioned and consistent with his role), issues regarding financing their current and follow-up care, and their ambivalence toward follow-up care?
Family perspective
Working with a qualified medical interpreter is imperative, and hospitals and health care providers who accept federal funds are obliged to provide language assistance services under Title VI of the Civil Rights Act of 1964.
First, it is important to accurately assess the woman’s psychosis, including risk of self-harm, risk of harming the infant or others, and capacity to care adequately and safely for the infant.
Second, the team should assess the patient’s and husband’s beliefs about the illness, hospitalization, and treatment. For some Muslim patients, the daily practice of Islam may necessitate the separation of sexes, meaning that female nurses and physicians might be optimal. Accessing professional spiritual or pastoral care in meeting the patient’s and family’s religious needs should be considered. Additional cultural practices that might help increase the acceptability of inpatient psychiatric care for the family include practices regarding diet, dress, hygiene, and prayer. The husband also might want to stay and sleep in the patient’s room during her hospitalization.
It also might be challenging for some North American therapists to understand and focus on the entire family as a functioning unit, rather than seeing the issues as only between husband and wife. Learning about how “normal family functioning” is defined, especially in terms of roles, hierarchy, and intimacy, is critical to supporting this mother and baby. Cultivating “cultural humility” in working with patients and families from diverse backgrounds is extremely important.
During the hospitalization as the patient improves, a plan for care needs to be developed with the patient and her family. This plan should include adequate support of the mother and her baby. The husband should bring his parents and siblings to an initial meeting early during the hospitalization, being mindful of addressing any HIPAA-related issues. This will allow for a uniform understanding of the patient’s illness and treatment. At this meeting, all family members should express their concerns, worries, beliefs, and perceived barriers to optimal care. If the family members feel listened to, they are more likely to feel understood and adhere to recommendations.
At the initial meeting and subsequent ones, the following questions might be helpful to ask to gather information in negotiating a mutually acceptable treatment plan:
1. What is the family’s understanding of her illness? What do they think may have caused it? How do they understand postpartum psychosis? Do they think there is a role for medication? Are any other alternative healing modalities being considered or used?
2. Who is caring for the baby now? Is the baby healthy? Does the family understand how the mother’s illness affects the baby? Can the family provide adequate care for the baby?
3. How are decisions made in the family? Are there any other issues in the family, such as ill health in a parent?
4. Was this an arranged marriage? How long have they known the patient? Do they care for her? What is the family’s attitude toward her?
5. Besides the mother-in-law, are there other adult females (for example, her husband’s sisters and his brothers’ wives) living in the household? How old is the mother-in-law? Who runs the household? Who does all the work? If possible, it will be important to interview anyone else in the household. How long have the couple and the family been in the United States? Did they all come at the same time?
6. Does the family have a supportive community? What are their beliefs about mental illness? Whom do they trust in their community? A religious leader? A local doctor? Who treats the women in the community?
7. If there is time, other issues can be explored. For example, what were the circumstances of their immigration? What has the transition from Bangladesh to life in the United States been like for the family?
8. Who will care for her at home? Who will ensure she takes her medications? Who will take her to follow-up visits?
There are many unknowns in this case that require further exploration. Time taken to arrange for a medically qualified interpreter and an extended family meeting will help the physician and psychiatric team understand the current situation and set up an appropriate plan of care.
Cultural perspective
The case material raises many questions. In the first place, there is no need to assume that the husband was behaving in a “culturally sanctioned and consistent way.” In a large population like that of Bangladeshi Muslims, significant heterogeneity exists, and there are more ways than one to respond. Although access to care is increasing for some population segments, Bangladesh still has limited mental health services and resources.
What were the reasons for the patient to be admitted to a psychiatric unit? How many days after the delivery? Were there any hostile actions or reactions to the baby? What is the patient’s pregnancy history? What meaning was ascribed to the symptoms and behavior that the patient manifested prior to hospitalization? Was this the first episode of psychiatric illness for the patient? Has she shown any dangerous behaviors before?
The reason why the husband is taking the wife home against medical advice is unclear. What reason did the husband give for this decision? Could stigma toward mental illness or hospitalization play a role? Was an interpreter used to help understand his reasoning? Was the husband dissatisfied about something? This is important, because it is likely that the husband brought the wife for hospitalization in the first place. Were the inpatient physician and nurses male or female, and could gender-related issues have been a barrier to accepting care? Might there have been a Muslim chaplain in the hospital or in the community or someone else who could have served as a cultural broker earlier in the hospitalization to have prevented this impasse?
The Cultural Formulation Interview (CFI) in the DSM-5 and the CFI-Informant Version for family members provide a framework to explore these questions and the questions recommended in the Family Perspective throughout the course of treatment.
Additional relevant questions include the following: What are cultural norms for their expectations for support of a new mother during the postpartum period? What are the norms for who, besides the mother, provides infant care? Are normative postpartum practices possible, or have they been disrupted in the hospital setting and/or in their home? If the mother and baby are both on the unit, is the request motivated by a desire to bring the baby home? If the baby is not on the unit, is this driving the family’s concern?
How isolated will the woman feel when she is home with the baby and her husband is out working as a taxi driver? Are there community-based organizations that the clinicians could collaborate with to provide resources and support for this woman (for example, women’s groups, immigrant groups, religious groups)? This would require learning more about what appeals to her, which groups she might identify with, and what is available in her neighborhood/community that aligns with what appeals to her.
It also would be important to determine if the patient was having any side effects from her psychotropic medications. Many South Asians have a low tolerance for side effects. Did the patient or family have any religious or cultural concerns about how the medications were manufactured or their composition (for example, worries about alcohol content)? Could any of these factors be related to the patient’s possible “cheeking” of her medications?
The major ethical/legal question to address is the patient’s attitude toward and relationship with the baby, and whether she was and is currently a danger to herself or others. Was the baby with the patient in the hospital? Did she feed the baby? What were the signs of psychosis that the patient exhibited, and what were the bases of her diagnosis? Was there an opportunity to discuss these issues with the husband? If so, what was his response?
Unless the patient is found to be dangerous to herself or others, including the baby, there is no option but to discharge. If a Bengali-speaking psychiatrist/therapist could be located within a reasonable driving distance, every effort should be made to connect the two. Husband and wife certainly should be instructed at the first sign of trouble to seek medical/psychiatric assistance, with or without insurance. Is there a possibility of home visits with an interpreter given the potential risks of patient and infant safety? Close follow-up and coordination of care with the patient’s and baby’s primary care physician is needed. Seeking support from the patient’s religious community also is worth considering.
Contributors
Alison M. Heru, M.D. – University of Colorado Denver, Aurora
Ellen Berman, M.D. – University of Pennsylvania, Philadelphia
Annelle B. Primm, M.D., M.P.H. – Johns Hopkins University, Baltimore (adjunct faculty)
Anne E. Becker, M.D., Ph.D. – Harvard Medical School, Boston
Robert C. Like, M.D., M.S. – Rutgers University, Robert Wood Johnson Medical School, New Brunswick
Resources
Farooq S., Fear C. Working Through Interpreters. (Adv Psychiatr Treat. 2003 Mar;9[2]:104-9. doi: 10.1192/apt.01.12 http://apt.rcpsych.org/content/9/2/104.full.)
Chandra P.S. Postpartum Psychiatric Care in India: The need for Integration and Innovation. (World Psychiatry. 2004;3[2]:99-100.)
Ahmad F., Shik A., Vanza R., Cheung A.M., George U, Stewart D.E. Voices of South Asian Women: Immigration and Mental Health. (Women Health 2004; 40[4]:113-130.)
Mantle F. Developing a Culture-Specific Tool to Assess Postnatal Depression in the Indian Community. (Br J Community Nurs. 2003;8[4]:176-180.)
To read about the goals of Curbside Consult, the guiding principles for assessment, and the guidelines for case submission, see “Considering patients’ family, culture,” Clinical Psychiatry News, January 2015, p. 12. The contributors have revised selected patient details to shield the identities of the patients/cases and to comply with HIPAA requirements. This column is meant to be educational and does not constitute medical advice. The opinions expressed are those of the contributors and do not represent those of the organizations they are employed by or affiliated with or the Group for the Advancement of Psychiatry (GAP).
This column is in memory of Dr. Prakash N. Desai, who contributed to this piece before his death earlier this year.
Muslim Bangladeshi female presents
The patient is a 31-year-old married Muslim Bangladeshi female homemaker admitted to an inpatient unit in a private hospital in a large urban area in the northeastern United States because of postpartum psychosis. She recently had immigrated to the United States and spoke no English. She lived with her husband, his parents, and his siblings in a city neighborhood predominantly comprised of South Asian immigrants. Her sole source of financial support was her husband, who worked as a cab driver. Both patient and her husband were uninsured. They identified strongly with their religion and culture of origin.
Key questions
Communication was a challenge and was accomplished using an interpreter, who was not always available. The patient did not seem to respond to treatment, and there was a question about the possibility that she was “cheeking” her medications. Her husband requested her discharge against medical advice, despite her still showing signs of psychosis. He appeared ambivalent about outpatient follow-up.
What is the duty of care in this situation, given the complexities inherent in a cross-cultural situation, the presence of communication barriers, the question of patient and infant safety, the husband’s role (given the understanding that his actions were probably culturally sanctioned and consistent with his role), issues regarding financing their current and follow-up care, and their ambivalence toward follow-up care?
Family perspective
Working with a qualified medical interpreter is imperative, and hospitals and health care providers who accept federal funds are obliged to provide language assistance services under Title VI of the Civil Rights Act of 1964.
First, it is important to accurately assess the woman’s psychosis, including risk of self-harm, risk of harming the infant or others, and capacity to care adequately and safely for the infant.
Second, the team should assess the patient’s and husband’s beliefs about the illness, hospitalization, and treatment. For some Muslim patients, the daily practice of Islam may necessitate the separation of sexes, meaning that female nurses and physicians might be optimal. Accessing professional spiritual or pastoral care in meeting the patient’s and family’s religious needs should be considered. Additional cultural practices that might help increase the acceptability of inpatient psychiatric care for the family include practices regarding diet, dress, hygiene, and prayer. The husband also might want to stay and sleep in the patient’s room during her hospitalization.
It also might be challenging for some North American therapists to understand and focus on the entire family as a functioning unit, rather than seeing the issues as only between husband and wife. Learning about how “normal family functioning” is defined, especially in terms of roles, hierarchy, and intimacy, is critical to supporting this mother and baby. Cultivating “cultural humility” in working with patients and families from diverse backgrounds is extremely important.
During the hospitalization as the patient improves, a plan for care needs to be developed with the patient and her family. This plan should include adequate support of the mother and her baby. The husband should bring his parents and siblings to an initial meeting early during the hospitalization, being mindful of addressing any HIPAA-related issues. This will allow for a uniform understanding of the patient’s illness and treatment. At this meeting, all family members should express their concerns, worries, beliefs, and perceived barriers to optimal care. If the family members feel listened to, they are more likely to feel understood and adhere to recommendations.
At the initial meeting and subsequent ones, the following questions might be helpful to ask to gather information in negotiating a mutually acceptable treatment plan:
1. What is the family’s understanding of her illness? What do they think may have caused it? How do they understand postpartum psychosis? Do they think there is a role for medication? Are any other alternative healing modalities being considered or used?
2. Who is caring for the baby now? Is the baby healthy? Does the family understand how the mother’s illness affects the baby? Can the family provide adequate care for the baby?
3. How are decisions made in the family? Are there any other issues in the family, such as ill health in a parent?
4. Was this an arranged marriage? How long have they known the patient? Do they care for her? What is the family’s attitude toward her?
5. Besides the mother-in-law, are there other adult females (for example, her husband’s sisters and his brothers’ wives) living in the household? How old is the mother-in-law? Who runs the household? Who does all the work? If possible, it will be important to interview anyone else in the household. How long have the couple and the family been in the United States? Did they all come at the same time?
6. Does the family have a supportive community? What are their beliefs about mental illness? Whom do they trust in their community? A religious leader? A local doctor? Who treats the women in the community?
7. If there is time, other issues can be explored. For example, what were the circumstances of their immigration? What has the transition from Bangladesh to life in the United States been like for the family?
8. Who will care for her at home? Who will ensure she takes her medications? Who will take her to follow-up visits?
There are many unknowns in this case that require further exploration. Time taken to arrange for a medically qualified interpreter and an extended family meeting will help the physician and psychiatric team understand the current situation and set up an appropriate plan of care.
Cultural perspective
The case material raises many questions. In the first place, there is no need to assume that the husband was behaving in a “culturally sanctioned and consistent way.” In a large population like that of Bangladeshi Muslims, significant heterogeneity exists, and there are more ways than one to respond. Although access to care is increasing for some population segments, Bangladesh still has limited mental health services and resources.
What were the reasons for the patient to be admitted to a psychiatric unit? How many days after the delivery? Were there any hostile actions or reactions to the baby? What is the patient’s pregnancy history? What meaning was ascribed to the symptoms and behavior that the patient manifested prior to hospitalization? Was this the first episode of psychiatric illness for the patient? Has she shown any dangerous behaviors before?
The reason why the husband is taking the wife home against medical advice is unclear. What reason did the husband give for this decision? Could stigma toward mental illness or hospitalization play a role? Was an interpreter used to help understand his reasoning? Was the husband dissatisfied about something? This is important, because it is likely that the husband brought the wife for hospitalization in the first place. Were the inpatient physician and nurses male or female, and could gender-related issues have been a barrier to accepting care? Might there have been a Muslim chaplain in the hospital or in the community or someone else who could have served as a cultural broker earlier in the hospitalization to have prevented this impasse?
The Cultural Formulation Interview (CFI) in the DSM-5 and the CFI-Informant Version for family members provide a framework to explore these questions and the questions recommended in the Family Perspective throughout the course of treatment.
Additional relevant questions include the following: What are cultural norms for their expectations for support of a new mother during the postpartum period? What are the norms for who, besides the mother, provides infant care? Are normative postpartum practices possible, or have they been disrupted in the hospital setting and/or in their home? If the mother and baby are both on the unit, is the request motivated by a desire to bring the baby home? If the baby is not on the unit, is this driving the family’s concern?
How isolated will the woman feel when she is home with the baby and her husband is out working as a taxi driver? Are there community-based organizations that the clinicians could collaborate with to provide resources and support for this woman (for example, women’s groups, immigrant groups, religious groups)? This would require learning more about what appeals to her, which groups she might identify with, and what is available in her neighborhood/community that aligns with what appeals to her.
It also would be important to determine if the patient was having any side effects from her psychotropic medications. Many South Asians have a low tolerance for side effects. Did the patient or family have any religious or cultural concerns about how the medications were manufactured or their composition (for example, worries about alcohol content)? Could any of these factors be related to the patient’s possible “cheeking” of her medications?
The major ethical/legal question to address is the patient’s attitude toward and relationship with the baby, and whether she was and is currently a danger to herself or others. Was the baby with the patient in the hospital? Did she feed the baby? What were the signs of psychosis that the patient exhibited, and what were the bases of her diagnosis? Was there an opportunity to discuss these issues with the husband? If so, what was his response?
Unless the patient is found to be dangerous to herself or others, including the baby, there is no option but to discharge. If a Bengali-speaking psychiatrist/therapist could be located within a reasonable driving distance, every effort should be made to connect the two. Husband and wife certainly should be instructed at the first sign of trouble to seek medical/psychiatric assistance, with or without insurance. Is there a possibility of home visits with an interpreter given the potential risks of patient and infant safety? Close follow-up and coordination of care with the patient’s and baby’s primary care physician is needed. Seeking support from the patient’s religious community also is worth considering.
Contributors
Alison M. Heru, M.D. – University of Colorado Denver, Aurora
Ellen Berman, M.D. – University of Pennsylvania, Philadelphia
Annelle B. Primm, M.D., M.P.H. – Johns Hopkins University, Baltimore (adjunct faculty)
Anne E. Becker, M.D., Ph.D. – Harvard Medical School, Boston
Robert C. Like, M.D., M.S. – Rutgers University, Robert Wood Johnson Medical School, New Brunswick
Resources
Farooq S., Fear C. Working Through Interpreters. (Adv Psychiatr Treat. 2003 Mar;9[2]:104-9. doi: 10.1192/apt.01.12 http://apt.rcpsych.org/content/9/2/104.full.)
Chandra P.S. Postpartum Psychiatric Care in India: The need for Integration and Innovation. (World Psychiatry. 2004;3[2]:99-100.)
Ahmad F., Shik A., Vanza R., Cheung A.M., George U, Stewart D.E. Voices of South Asian Women: Immigration and Mental Health. (Women Health 2004; 40[4]:113-130.)
Mantle F. Developing a Culture-Specific Tool to Assess Postnatal Depression in the Indian Community. (Br J Community Nurs. 2003;8[4]:176-180.)
To read about the goals of Curbside Consult, the guiding principles for assessment, and the guidelines for case submission, see “Considering patients’ family, culture,” Clinical Psychiatry News, January 2015, p. 12. The contributors have revised selected patient details to shield the identities of the patients/cases and to comply with HIPAA requirements. This column is meant to be educational and does not constitute medical advice. The opinions expressed are those of the contributors and do not represent those of the organizations they are employed by or affiliated with or the Group for the Advancement of Psychiatry (GAP).
This column is in memory of Dr. Prakash N. Desai, who contributed to this piece before his death earlier this year.
Muslim Bangladeshi female presents
The patient is a 31-year-old married Muslim Bangladeshi female homemaker admitted to an inpatient unit in a private hospital in a large urban area in the northeastern United States because of postpartum psychosis. She recently had immigrated to the United States and spoke no English. She lived with her husband, his parents, and his siblings in a city neighborhood predominantly comprised of South Asian immigrants. Her sole source of financial support was her husband, who worked as a cab driver. Both patient and her husband were uninsured. They identified strongly with their religion and culture of origin.
Key questions
Communication was a challenge and was accomplished using an interpreter, who was not always available. The patient did not seem to respond to treatment, and there was a question about the possibility that she was “cheeking” her medications. Her husband requested her discharge against medical advice, despite her still showing signs of psychosis. He appeared ambivalent about outpatient follow-up.
What is the duty of care in this situation, given the complexities inherent in a cross-cultural situation, the presence of communication barriers, the question of patient and infant safety, the husband’s role (given the understanding that his actions were probably culturally sanctioned and consistent with his role), issues regarding financing their current and follow-up care, and their ambivalence toward follow-up care?
Family perspective
Working with a qualified medical interpreter is imperative, and hospitals and health care providers who accept federal funds are obliged to provide language assistance services under Title VI of the Civil Rights Act of 1964.
First, it is important to accurately assess the woman’s psychosis, including risk of self-harm, risk of harming the infant or others, and capacity to care adequately and safely for the infant.
Second, the team should assess the patient’s and husband’s beliefs about the illness, hospitalization, and treatment. For some Muslim patients, the daily practice of Islam may necessitate the separation of sexes, meaning that female nurses and physicians might be optimal. Accessing professional spiritual or pastoral care in meeting the patient’s and family’s religious needs should be considered. Additional cultural practices that might help increase the acceptability of inpatient psychiatric care for the family include practices regarding diet, dress, hygiene, and prayer. The husband also might want to stay and sleep in the patient’s room during her hospitalization.
It also might be challenging for some North American therapists to understand and focus on the entire family as a functioning unit, rather than seeing the issues as only between husband and wife. Learning about how “normal family functioning” is defined, especially in terms of roles, hierarchy, and intimacy, is critical to supporting this mother and baby. Cultivating “cultural humility” in working with patients and families from diverse backgrounds is extremely important.
During the hospitalization as the patient improves, a plan for care needs to be developed with the patient and her family. This plan should include adequate support of the mother and her baby. The husband should bring his parents and siblings to an initial meeting early during the hospitalization, being mindful of addressing any HIPAA-related issues. This will allow for a uniform understanding of the patient’s illness and treatment. At this meeting, all family members should express their concerns, worries, beliefs, and perceived barriers to optimal care. If the family members feel listened to, they are more likely to feel understood and adhere to recommendations.
At the initial meeting and subsequent ones, the following questions might be helpful to ask to gather information in negotiating a mutually acceptable treatment plan:
1. What is the family’s understanding of her illness? What do they think may have caused it? How do they understand postpartum psychosis? Do they think there is a role for medication? Are any other alternative healing modalities being considered or used?
2. Who is caring for the baby now? Is the baby healthy? Does the family understand how the mother’s illness affects the baby? Can the family provide adequate care for the baby?
3. How are decisions made in the family? Are there any other issues in the family, such as ill health in a parent?
4. Was this an arranged marriage? How long have they known the patient? Do they care for her? What is the family’s attitude toward her?
5. Besides the mother-in-law, are there other adult females (for example, her husband’s sisters and his brothers’ wives) living in the household? How old is the mother-in-law? Who runs the household? Who does all the work? If possible, it will be important to interview anyone else in the household. How long have the couple and the family been in the United States? Did they all come at the same time?
6. Does the family have a supportive community? What are their beliefs about mental illness? Whom do they trust in their community? A religious leader? A local doctor? Who treats the women in the community?
7. If there is time, other issues can be explored. For example, what were the circumstances of their immigration? What has the transition from Bangladesh to life in the United States been like for the family?
8. Who will care for her at home? Who will ensure she takes her medications? Who will take her to follow-up visits?
There are many unknowns in this case that require further exploration. Time taken to arrange for a medically qualified interpreter and an extended family meeting will help the physician and psychiatric team understand the current situation and set up an appropriate plan of care.
Cultural perspective
The case material raises many questions. In the first place, there is no need to assume that the husband was behaving in a “culturally sanctioned and consistent way.” In a large population like that of Bangladeshi Muslims, significant heterogeneity exists, and there are more ways than one to respond. Although access to care is increasing for some population segments, Bangladesh still has limited mental health services and resources.
What were the reasons for the patient to be admitted to a psychiatric unit? How many days after the delivery? Were there any hostile actions or reactions to the baby? What is the patient’s pregnancy history? What meaning was ascribed to the symptoms and behavior that the patient manifested prior to hospitalization? Was this the first episode of psychiatric illness for the patient? Has she shown any dangerous behaviors before?
The reason why the husband is taking the wife home against medical advice is unclear. What reason did the husband give for this decision? Could stigma toward mental illness or hospitalization play a role? Was an interpreter used to help understand his reasoning? Was the husband dissatisfied about something? This is important, because it is likely that the husband brought the wife for hospitalization in the first place. Were the inpatient physician and nurses male or female, and could gender-related issues have been a barrier to accepting care? Might there have been a Muslim chaplain in the hospital or in the community or someone else who could have served as a cultural broker earlier in the hospitalization to have prevented this impasse?
The Cultural Formulation Interview (CFI) in the DSM-5 and the CFI-Informant Version for family members provide a framework to explore these questions and the questions recommended in the Family Perspective throughout the course of treatment.
Additional relevant questions include the following: What are cultural norms for their expectations for support of a new mother during the postpartum period? What are the norms for who, besides the mother, provides infant care? Are normative postpartum practices possible, or have they been disrupted in the hospital setting and/or in their home? If the mother and baby are both on the unit, is the request motivated by a desire to bring the baby home? If the baby is not on the unit, is this driving the family’s concern?
How isolated will the woman feel when she is home with the baby and her husband is out working as a taxi driver? Are there community-based organizations that the clinicians could collaborate with to provide resources and support for this woman (for example, women’s groups, immigrant groups, religious groups)? This would require learning more about what appeals to her, which groups she might identify with, and what is available in her neighborhood/community that aligns with what appeals to her.
It also would be important to determine if the patient was having any side effects from her psychotropic medications. Many South Asians have a low tolerance for side effects. Did the patient or family have any religious or cultural concerns about how the medications were manufactured or their composition (for example, worries about alcohol content)? Could any of these factors be related to the patient’s possible “cheeking” of her medications?
The major ethical/legal question to address is the patient’s attitude toward and relationship with the baby, and whether she was and is currently a danger to herself or others. Was the baby with the patient in the hospital? Did she feed the baby? What were the signs of psychosis that the patient exhibited, and what were the bases of her diagnosis? Was there an opportunity to discuss these issues with the husband? If so, what was his response?
Unless the patient is found to be dangerous to herself or others, including the baby, there is no option but to discharge. If a Bengali-speaking psychiatrist/therapist could be located within a reasonable driving distance, every effort should be made to connect the two. Husband and wife certainly should be instructed at the first sign of trouble to seek medical/psychiatric assistance, with or without insurance. Is there a possibility of home visits with an interpreter given the potential risks of patient and infant safety? Close follow-up and coordination of care with the patient’s and baby’s primary care physician is needed. Seeking support from the patient’s religious community also is worth considering.
Contributors
Alison M. Heru, M.D. – University of Colorado Denver, Aurora
Ellen Berman, M.D. – University of Pennsylvania, Philadelphia
Annelle B. Primm, M.D., M.P.H. – Johns Hopkins University, Baltimore (adjunct faculty)
Anne E. Becker, M.D., Ph.D. – Harvard Medical School, Boston
Robert C. Like, M.D., M.S. – Rutgers University, Robert Wood Johnson Medical School, New Brunswick
Resources
Farooq S., Fear C. Working Through Interpreters. (Adv Psychiatr Treat. 2003 Mar;9[2]:104-9. doi: 10.1192/apt.01.12 http://apt.rcpsych.org/content/9/2/104.full.)
Chandra P.S. Postpartum Psychiatric Care in India: The need for Integration and Innovation. (World Psychiatry. 2004;3[2]:99-100.)
Ahmad F., Shik A., Vanza R., Cheung A.M., George U, Stewart D.E. Voices of South Asian Women: Immigration and Mental Health. (Women Health 2004; 40[4]:113-130.)
Mantle F. Developing a Culture-Specific Tool to Assess Postnatal Depression in the Indian Community. (Br J Community Nurs. 2003;8[4]:176-180.)
To read about the goals of Curbside Consult, the guiding principles for assessment, and the guidelines for case submission, see “Considering patients’ family, culture,” Clinical Psychiatry News, January 2015, p. 12. The contributors have revised selected patient details to shield the identities of the patients/cases and to comply with HIPAA requirements. This column is meant to be educational and does not constitute medical advice. The opinions expressed are those of the contributors and do not represent those of the organizations they are employed by or affiliated with or the Group for the Advancement of Psychiatry (GAP).
This column is in memory of Dr. Prakash N. Desai, who contributed to this piece before his death earlier this year.