User login
Trichilemmoma
Trichilemmomas are benign follicular neoplasms that exhibit differentiation toward the outer root sheath of the pilosebaceous follicular epithelium.1 Trichilemmomas clinically present as individual or multiple, slowly growing, verrucous papules appearing most commonly on the face or neck. The lesions may coalesce to form small plaques. Although trichilemmomas typically are isolated, patients with multiple trichilemmomas require a cancer screening workup due to their association with Cowden disease, which results from a mutation in the phosphatase and tensin homolog tumor suppressor gene, PTEN.2 An easy way to remember the association between trichilemmomas and Cowden disease is to alter the spelling to “trichile-moo-moo,” using the “moo moo” sound of an animal cow as a clue linking the tumor to Cowden disease.
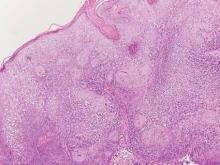
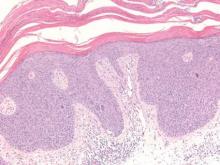
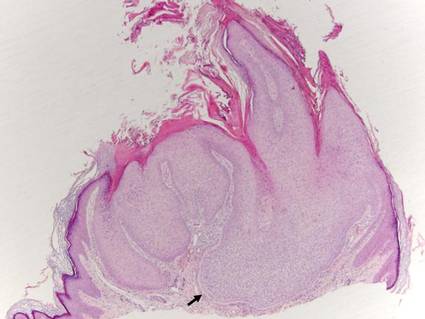
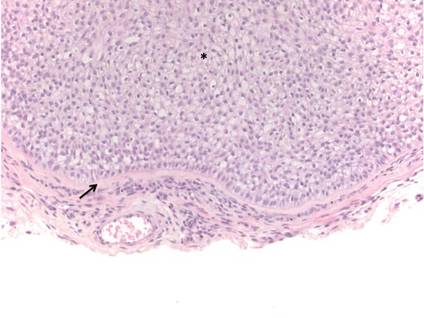
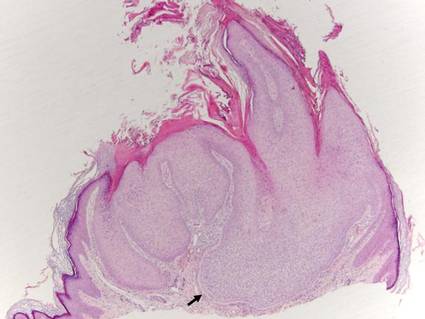
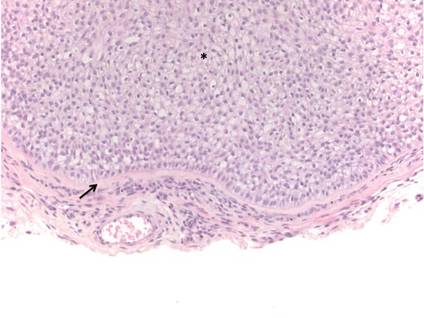
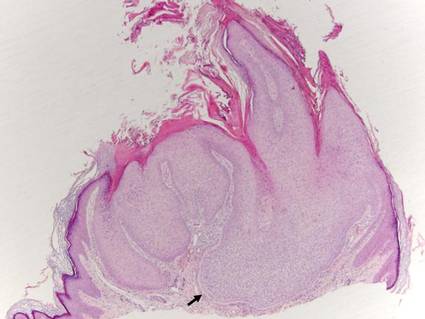
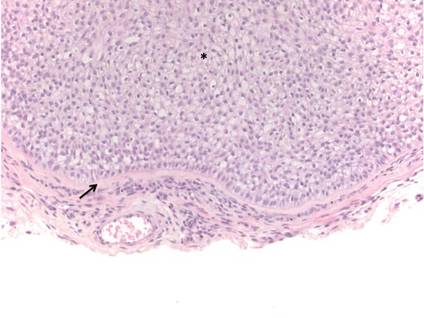
Histologically, trichilemmomas exhibit a lobular epidermal downgrowth into the dermis (Figure 1). The surface of the lesion may be hyperkeratotic and somewhat papillomatous. Cells toward the center of the lobule are pale staining, periodic acid–Schiff positive, and diastase labile due to high levels of intracellular glycogen (Figure 2). Cells toward the periphery of the lobule usually appear basophilic with a palisading arrangement of the peripheral cells. The entire lobule is enclosed within an eosinophilic basement membrane that stains positively with periodic acid–Schiff (Figure 2).1 Consistent with the tumor’s differentiation toward the outer root sheath of the hair follicle, trichilemmomas have been reported to express CD34 focally or diffusely.3
| 
|
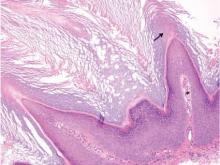
Similar to trichilemmoma, inverted follicular keratosis (IFK) commonly presents as a solitary asymptomatic papule on the face. Inverted follicular keratosis is a somewhat controversial entity, with some authorities arguing IFK is a variant of verruca vulgaris or seborrheic keratosis. Histologically, IFKs can be differentiated by the presence of squamous eddies (concentric layers of squamous cells in a whorled pattern), which are diagnostic, and central longitudinal crypts that contain keratin and are lined by squamous epithelium.4 Basaloid cells can be seen at the periphery of the tumors; however, IFKs lack an eosinophilic basement membrane surrounding the tumor (Figure 3).
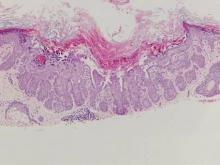
Squamous cell carcinoma in situ classically appears as an erythematous hyperkeratotic papule or plaque on sun-exposed sites that can become crusted or ulcerated. Microscopically, squamous cell carcinoma in situ displays full-thickness disorderly maturation of keratinocytes. The keratinocytes exhibit nuclear pleomorphism. Atypical mitotic figures and dyskeratotic keratinocytes also can be seen throughout the full thickness of the epidermis (Figure 4).5
Verruca vulgaris (Figure 5) histologically demonstrates hyperkeratosis with tiers of parakeratosis, digitated epidermal hyperplasia, and dilated tortuous capillaries within the dermal papillae. At the edges of the lesion there often is inward turning of elongated rete ridges,6,7 which can be thought of as the rete reaching out for a hug of sorts to spread the human papillomavirus infection. Although the surface of a trichilemmoma can bear resemblance to a verruca vulgaris, the remainder of the histologic features can be used to help differentiate these tumors. Additionally, there has been no evidence suggestive of a viral etiology for trichilemmomas.8
Warty dyskeratoma features an umbilicated papule, usually on the face, head, or neck, that is associated with a follicular unit. The papule shows a cup-shaped, keratin-filled invagination; suprabasilar clefting; and acantholytic dyskeratotic cells, which are features that are not seen in trichilemmomas (Figure 6).9
Acknowledgment—The authors would like to thank Brandon Litzner, MD, St Louis, Missouri, for proofreading the manuscript.
1. Brownstein MH, Shapiro L. Trichilemmoma: analysis of 40 new cases. Arch Dermatol. 1973;107:866-869.
2. Al-Zaid T, Ditelberg J, Prieto V, et al. Trichilemmomas show loss of PTEN in Cowden syndrome but only rarely in sporadic tumors. J Cutan Pathol. 2012;39:493-499.
3. Tardío JC. CD34-reactive tumors of the skin. an updated review of an ever-growing list of lesions. J Cutan Pathol. 2009;36:89-102.
4. Mehregan A. Inverted follicular keratosis is a distinct follicular tumor. Am J Dermatopathol. 1983;5:467-470.
5. Cockerell CJ. Histopathology of incipient intraepidermal squamous cell carcinoma (“actinic keratosis”). J Am Acad Dermatol. 2000;42(1, pt 2):11-17.
6. Jabłonska S, Majewski S, Obalek S, et al. Cutaneous warts. Clin Dermatol. 1997;15:309-319.
7. Hardin J, Gardner J, Colome M, et al. Verrucous cyst with melanocytic and sebaceous differentiation. Arch Path Lab Med. 2013;137:576-579.
8. Johnson BL, Kramer EM, Lavker RM. The keratotic tumors of Cowden’s disease: an electron microscopy study. J Cutan Pathol. 1987;14:291-298.
9. Kaddu S, Dong H, Mayer G, et al. Warty dyskeratoma—“follicular dyskeratoma”: analysis of clinicopathologic features of a distinctive follicular adnexal neoplasm. J Am Acad Dermatol. 2002;47:423-428.
Trichilemmomas are benign follicular neoplasms that exhibit differentiation toward the outer root sheath of the pilosebaceous follicular epithelium.1 Trichilemmomas clinically present as individual or multiple, slowly growing, verrucous papules appearing most commonly on the face or neck. The lesions may coalesce to form small plaques. Although trichilemmomas typically are isolated, patients with multiple trichilemmomas require a cancer screening workup due to their association with Cowden disease, which results from a mutation in the phosphatase and tensin homolog tumor suppressor gene, PTEN.2 An easy way to remember the association between trichilemmomas and Cowden disease is to alter the spelling to “trichile-moo-moo,” using the “moo moo” sound of an animal cow as a clue linking the tumor to Cowden disease.
Histologically, trichilemmomas exhibit a lobular epidermal downgrowth into the dermis (Figure 1). The surface of the lesion may be hyperkeratotic and somewhat papillomatous. Cells toward the center of the lobule are pale staining, periodic acid–Schiff positive, and diastase labile due to high levels of intracellular glycogen (Figure 2). Cells toward the periphery of the lobule usually appear basophilic with a palisading arrangement of the peripheral cells. The entire lobule is enclosed within an eosinophilic basement membrane that stains positively with periodic acid–Schiff (Figure 2).1 Consistent with the tumor’s differentiation toward the outer root sheath of the hair follicle, trichilemmomas have been reported to express CD34 focally or diffusely.3
| 
|
Similar to trichilemmoma, inverted follicular keratosis (IFK) commonly presents as a solitary asymptomatic papule on the face. Inverted follicular keratosis is a somewhat controversial entity, with some authorities arguing IFK is a variant of verruca vulgaris or seborrheic keratosis. Histologically, IFKs can be differentiated by the presence of squamous eddies (concentric layers of squamous cells in a whorled pattern), which are diagnostic, and central longitudinal crypts that contain keratin and are lined by squamous epithelium.4 Basaloid cells can be seen at the periphery of the tumors; however, IFKs lack an eosinophilic basement membrane surrounding the tumor (Figure 3).
Squamous cell carcinoma in situ classically appears as an erythematous hyperkeratotic papule or plaque on sun-exposed sites that can become crusted or ulcerated. Microscopically, squamous cell carcinoma in situ displays full-thickness disorderly maturation of keratinocytes. The keratinocytes exhibit nuclear pleomorphism. Atypical mitotic figures and dyskeratotic keratinocytes also can be seen throughout the full thickness of the epidermis (Figure 4).5
Verruca vulgaris (Figure 5) histologically demonstrates hyperkeratosis with tiers of parakeratosis, digitated epidermal hyperplasia, and dilated tortuous capillaries within the dermal papillae. At the edges of the lesion there often is inward turning of elongated rete ridges,6,7 which can be thought of as the rete reaching out for a hug of sorts to spread the human papillomavirus infection. Although the surface of a trichilemmoma can bear resemblance to a verruca vulgaris, the remainder of the histologic features can be used to help differentiate these tumors. Additionally, there has been no evidence suggestive of a viral etiology for trichilemmomas.8
Warty dyskeratoma features an umbilicated papule, usually on the face, head, or neck, that is associated with a follicular unit. The papule shows a cup-shaped, keratin-filled invagination; suprabasilar clefting; and acantholytic dyskeratotic cells, which are features that are not seen in trichilemmomas (Figure 6).9
Acknowledgment—The authors would like to thank Brandon Litzner, MD, St Louis, Missouri, for proofreading the manuscript.
Trichilemmomas are benign follicular neoplasms that exhibit differentiation toward the outer root sheath of the pilosebaceous follicular epithelium.1 Trichilemmomas clinically present as individual or multiple, slowly growing, verrucous papules appearing most commonly on the face or neck. The lesions may coalesce to form small plaques. Although trichilemmomas typically are isolated, patients with multiple trichilemmomas require a cancer screening workup due to their association with Cowden disease, which results from a mutation in the phosphatase and tensin homolog tumor suppressor gene, PTEN.2 An easy way to remember the association between trichilemmomas and Cowden disease is to alter the spelling to “trichile-moo-moo,” using the “moo moo” sound of an animal cow as a clue linking the tumor to Cowden disease.
Histologically, trichilemmomas exhibit a lobular epidermal downgrowth into the dermis (Figure 1). The surface of the lesion may be hyperkeratotic and somewhat papillomatous. Cells toward the center of the lobule are pale staining, periodic acid–Schiff positive, and diastase labile due to high levels of intracellular glycogen (Figure 2). Cells toward the periphery of the lobule usually appear basophilic with a palisading arrangement of the peripheral cells. The entire lobule is enclosed within an eosinophilic basement membrane that stains positively with periodic acid–Schiff (Figure 2).1 Consistent with the tumor’s differentiation toward the outer root sheath of the hair follicle, trichilemmomas have been reported to express CD34 focally or diffusely.3
| 
|
Similar to trichilemmoma, inverted follicular keratosis (IFK) commonly presents as a solitary asymptomatic papule on the face. Inverted follicular keratosis is a somewhat controversial entity, with some authorities arguing IFK is a variant of verruca vulgaris or seborrheic keratosis. Histologically, IFKs can be differentiated by the presence of squamous eddies (concentric layers of squamous cells in a whorled pattern), which are diagnostic, and central longitudinal crypts that contain keratin and are lined by squamous epithelium.4 Basaloid cells can be seen at the periphery of the tumors; however, IFKs lack an eosinophilic basement membrane surrounding the tumor (Figure 3).
Squamous cell carcinoma in situ classically appears as an erythematous hyperkeratotic papule or plaque on sun-exposed sites that can become crusted or ulcerated. Microscopically, squamous cell carcinoma in situ displays full-thickness disorderly maturation of keratinocytes. The keratinocytes exhibit nuclear pleomorphism. Atypical mitotic figures and dyskeratotic keratinocytes also can be seen throughout the full thickness of the epidermis (Figure 4).5
Verruca vulgaris (Figure 5) histologically demonstrates hyperkeratosis with tiers of parakeratosis, digitated epidermal hyperplasia, and dilated tortuous capillaries within the dermal papillae. At the edges of the lesion there often is inward turning of elongated rete ridges,6,7 which can be thought of as the rete reaching out for a hug of sorts to spread the human papillomavirus infection. Although the surface of a trichilemmoma can bear resemblance to a verruca vulgaris, the remainder of the histologic features can be used to help differentiate these tumors. Additionally, there has been no evidence suggestive of a viral etiology for trichilemmomas.8
Warty dyskeratoma features an umbilicated papule, usually on the face, head, or neck, that is associated with a follicular unit. The papule shows a cup-shaped, keratin-filled invagination; suprabasilar clefting; and acantholytic dyskeratotic cells, which are features that are not seen in trichilemmomas (Figure 6).9
Acknowledgment—The authors would like to thank Brandon Litzner, MD, St Louis, Missouri, for proofreading the manuscript.
1. Brownstein MH, Shapiro L. Trichilemmoma: analysis of 40 new cases. Arch Dermatol. 1973;107:866-869.
2. Al-Zaid T, Ditelberg J, Prieto V, et al. Trichilemmomas show loss of PTEN in Cowden syndrome but only rarely in sporadic tumors. J Cutan Pathol. 2012;39:493-499.
3. Tardío JC. CD34-reactive tumors of the skin. an updated review of an ever-growing list of lesions. J Cutan Pathol. 2009;36:89-102.
4. Mehregan A. Inverted follicular keratosis is a distinct follicular tumor. Am J Dermatopathol. 1983;5:467-470.
5. Cockerell CJ. Histopathology of incipient intraepidermal squamous cell carcinoma (“actinic keratosis”). J Am Acad Dermatol. 2000;42(1, pt 2):11-17.
6. Jabłonska S, Majewski S, Obalek S, et al. Cutaneous warts. Clin Dermatol. 1997;15:309-319.
7. Hardin J, Gardner J, Colome M, et al. Verrucous cyst with melanocytic and sebaceous differentiation. Arch Path Lab Med. 2013;137:576-579.
8. Johnson BL, Kramer EM, Lavker RM. The keratotic tumors of Cowden’s disease: an electron microscopy study. J Cutan Pathol. 1987;14:291-298.
9. Kaddu S, Dong H, Mayer G, et al. Warty dyskeratoma—“follicular dyskeratoma”: analysis of clinicopathologic features of a distinctive follicular adnexal neoplasm. J Am Acad Dermatol. 2002;47:423-428.
1. Brownstein MH, Shapiro L. Trichilemmoma: analysis of 40 new cases. Arch Dermatol. 1973;107:866-869.
2. Al-Zaid T, Ditelberg J, Prieto V, et al. Trichilemmomas show loss of PTEN in Cowden syndrome but only rarely in sporadic tumors. J Cutan Pathol. 2012;39:493-499.
3. Tardío JC. CD34-reactive tumors of the skin. an updated review of an ever-growing list of lesions. J Cutan Pathol. 2009;36:89-102.
4. Mehregan A. Inverted follicular keratosis is a distinct follicular tumor. Am J Dermatopathol. 1983;5:467-470.
5. Cockerell CJ. Histopathology of incipient intraepidermal squamous cell carcinoma (“actinic keratosis”). J Am Acad Dermatol. 2000;42(1, pt 2):11-17.
6. Jabłonska S, Majewski S, Obalek S, et al. Cutaneous warts. Clin Dermatol. 1997;15:309-319.
7. Hardin J, Gardner J, Colome M, et al. Verrucous cyst with melanocytic and sebaceous differentiation. Arch Path Lab Med. 2013;137:576-579.
8. Johnson BL, Kramer EM, Lavker RM. The keratotic tumors of Cowden’s disease: an electron microscopy study. J Cutan Pathol. 1987;14:291-298.
9. Kaddu S, Dong H, Mayer G, et al. Warty dyskeratoma—“follicular dyskeratoma”: analysis of clinicopathologic features of a distinctive follicular adnexal neoplasm. J Am Acad Dermatol. 2002;47:423-428.
Catching up on brain stimulation with Dr. Irving Reti
Psychiatry is a field where the treatment of our disorders remains perplexing: We’re still trying to figure out if the best way to treat psychiatric conditions is through psychotherapy, with medications, or for more resistant conditions, by stimulating activity in the brain in several different ways.
The field of brain stimulation includes electroconvulsive therapy, as well as transcranial magnetic stimulation (TMS), direct transcranial current stimulation (tDCS), and deep brain stimulation (DBS), all of which are examples of treatments that are still just coming into their own.
In search of an update on brain stimulation, I met with Dr. Irving Reti, director of the Johns Hopkins Hospital Brain Stimulation Program and editor of “Brain Stimulation: Methodologies and Interventions” (Hoboken, N.J.: Wiley-Blackwell, 2015). We met at a Starbucks in Baltimore, and I’ll tell you that a one-on-one conversation with an expert is a wonderful way to learn about state-of-the-art treatments, the only downside being that Starbucks does not offer CME credit.
Dr. Reti, who went to medical school at the University of Sydney and speaks with a charming Australian accent, trained in psychiatry at Johns Hopkins, and then did a neuroscience fellowship.
“I’d just finished residency training, and I was giving ECT to rats. We were looking at the expression of immediate-early genes. At the same time, I started doing consults in the mood disorders clinic.”
In 2006, Dr. Reti took over as director of ECT at Hopkins, and that same year, Dr. Jimmy Potash got funding to study TMS. Dr. Potash has since moved to the University of Iowa, and Dr. Reti took over TMS administration at Hopkins. Dr. Reti was flattered to be approached by Wiley to edit “Brain Stimulation,” and he talked about how he was pleased with the final edition of the book.
“I ended up getting the top people to write the chapters, people like Sarah Lisanby, Michael Nitsche, John Rothwell, and Mark George. These are the leaders in the field of brain stimulation.”
I asked Dr. Reti to walk me through what was happening in each brain stimulation area.
“In ECT,” he said, “we know a lot more now about how both the settings and the anesthesia regimen affect the outcomes. We didn’t know this when I trained in the ’90s.” Dr. Reti estimated that he’s administered ECT to close to 2,000 patients.
TMS is done less often at Hopkins; he estimated that 10-20 patients receive the treatment, and each patient comes 30-40 times, with each session lasting 40 minutes.
“It’s better than medicine but not as effective as ECT. We’re seeing an efficacy rate around 50%-60%,” and he noted that some patients have trouble tolerating the procedure as the magnetic stimulation can be uncomfortable. “The TMS coil stimulates the scalp nerves and muscles immediately under the coil, which causes discomfort.” He noted that some patients need to premedicate with over-the-counter pain medicines.
“We’re also finding that low-frequency stimulation on the right can be helpful for anxiety,” Dr. Reti said.
He talked about treating patients with psychotherapy along with TMS. The brain changes are thought to increase the brain’s plasticity and perhaps make psychotherapy more effective.
“It’s being studied in drug treatment. You can show someone with an addiction stimuli to trigger cravings, and doing this with TMS may block the response,” he said.
He talked for a while about direct transcranial brain stimulation, which I was not very familiar with. Because it is being used to improve focus-playing video games, the equipment is not being marketed as a psychiatric treatment and doesn’t fall under the domain of the Food and Drug Administration.
“Kids are using it to improve their concentration and performance with video games; all you need is a 9-volt battery and some electrodes that are attached to the scalp. The kits cost about $250, but you can burn your scalp,” he said.
Dr. Reti referred me to an article in the New Yorker on tDCS, “Electrified: Adventures in transcranial direct-current stimulation” by Elif Batuman. He noted that there are studies in progress to look at therapeutic uses for tDCS, including one at Johns Hopkins where neuropsychologist David Schretlen is looking at improving cognition in schizophrenia. Dr. Reti is interested in seeing if tDCS might be helpful in decreasing self-injurious behaviors in autistic children, as ECT has been effective in severe cases. He noted that while ECT and TMS stimulate neurons in the brain to fire, tDCS changes the stimulation threshold without directly causing the neurons to discharge.
Finally, we talked a little about deep brain stimulation. Thin electrodes directly target nodes in brain circuits that can modulate the activity of those circuits. He noted that deep brain stimulation was being used at Johns Hopkins to treat Parkinson’s disease, and other centers have looked at its use for severe obsessive-compulsive disorder and treatment-resistant depression.
“We know that the response habituates; now they are trying on-demand DBS,” Dr. Reti noted.
So, although I got no continuing medical education credits, I did get to try a new Starbucks drink while having a very stimulating discussion on the latest convulsive and nonconvulsive psychiatric brain research.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Psychiatry is a field where the treatment of our disorders remains perplexing: We’re still trying to figure out if the best way to treat psychiatric conditions is through psychotherapy, with medications, or for more resistant conditions, by stimulating activity in the brain in several different ways.
The field of brain stimulation includes electroconvulsive therapy, as well as transcranial magnetic stimulation (TMS), direct transcranial current stimulation (tDCS), and deep brain stimulation (DBS), all of which are examples of treatments that are still just coming into their own.
In search of an update on brain stimulation, I met with Dr. Irving Reti, director of the Johns Hopkins Hospital Brain Stimulation Program and editor of “Brain Stimulation: Methodologies and Interventions” (Hoboken, N.J.: Wiley-Blackwell, 2015). We met at a Starbucks in Baltimore, and I’ll tell you that a one-on-one conversation with an expert is a wonderful way to learn about state-of-the-art treatments, the only downside being that Starbucks does not offer CME credit.
Dr. Reti, who went to medical school at the University of Sydney and speaks with a charming Australian accent, trained in psychiatry at Johns Hopkins, and then did a neuroscience fellowship.
“I’d just finished residency training, and I was giving ECT to rats. We were looking at the expression of immediate-early genes. At the same time, I started doing consults in the mood disorders clinic.”
In 2006, Dr. Reti took over as director of ECT at Hopkins, and that same year, Dr. Jimmy Potash got funding to study TMS. Dr. Potash has since moved to the University of Iowa, and Dr. Reti took over TMS administration at Hopkins. Dr. Reti was flattered to be approached by Wiley to edit “Brain Stimulation,” and he talked about how he was pleased with the final edition of the book.
“I ended up getting the top people to write the chapters, people like Sarah Lisanby, Michael Nitsche, John Rothwell, and Mark George. These are the leaders in the field of brain stimulation.”
I asked Dr. Reti to walk me through what was happening in each brain stimulation area.
“In ECT,” he said, “we know a lot more now about how both the settings and the anesthesia regimen affect the outcomes. We didn’t know this when I trained in the ’90s.” Dr. Reti estimated that he’s administered ECT to close to 2,000 patients.
TMS is done less often at Hopkins; he estimated that 10-20 patients receive the treatment, and each patient comes 30-40 times, with each session lasting 40 minutes.
“It’s better than medicine but not as effective as ECT. We’re seeing an efficacy rate around 50%-60%,” and he noted that some patients have trouble tolerating the procedure as the magnetic stimulation can be uncomfortable. “The TMS coil stimulates the scalp nerves and muscles immediately under the coil, which causes discomfort.” He noted that some patients need to premedicate with over-the-counter pain medicines.
“We’re also finding that low-frequency stimulation on the right can be helpful for anxiety,” Dr. Reti said.
He talked about treating patients with psychotherapy along with TMS. The brain changes are thought to increase the brain’s plasticity and perhaps make psychotherapy more effective.
“It’s being studied in drug treatment. You can show someone with an addiction stimuli to trigger cravings, and doing this with TMS may block the response,” he said.
He talked for a while about direct transcranial brain stimulation, which I was not very familiar with. Because it is being used to improve focus-playing video games, the equipment is not being marketed as a psychiatric treatment and doesn’t fall under the domain of the Food and Drug Administration.
“Kids are using it to improve their concentration and performance with video games; all you need is a 9-volt battery and some electrodes that are attached to the scalp. The kits cost about $250, but you can burn your scalp,” he said.
Dr. Reti referred me to an article in the New Yorker on tDCS, “Electrified: Adventures in transcranial direct-current stimulation” by Elif Batuman. He noted that there are studies in progress to look at therapeutic uses for tDCS, including one at Johns Hopkins where neuropsychologist David Schretlen is looking at improving cognition in schizophrenia. Dr. Reti is interested in seeing if tDCS might be helpful in decreasing self-injurious behaviors in autistic children, as ECT has been effective in severe cases. He noted that while ECT and TMS stimulate neurons in the brain to fire, tDCS changes the stimulation threshold without directly causing the neurons to discharge.
Finally, we talked a little about deep brain stimulation. Thin electrodes directly target nodes in brain circuits that can modulate the activity of those circuits. He noted that deep brain stimulation was being used at Johns Hopkins to treat Parkinson’s disease, and other centers have looked at its use for severe obsessive-compulsive disorder and treatment-resistant depression.
“We know that the response habituates; now they are trying on-demand DBS,” Dr. Reti noted.
So, although I got no continuing medical education credits, I did get to try a new Starbucks drink while having a very stimulating discussion on the latest convulsive and nonconvulsive psychiatric brain research.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Psychiatry is a field where the treatment of our disorders remains perplexing: We’re still trying to figure out if the best way to treat psychiatric conditions is through psychotherapy, with medications, or for more resistant conditions, by stimulating activity in the brain in several different ways.
The field of brain stimulation includes electroconvulsive therapy, as well as transcranial magnetic stimulation (TMS), direct transcranial current stimulation (tDCS), and deep brain stimulation (DBS), all of which are examples of treatments that are still just coming into their own.
In search of an update on brain stimulation, I met with Dr. Irving Reti, director of the Johns Hopkins Hospital Brain Stimulation Program and editor of “Brain Stimulation: Methodologies and Interventions” (Hoboken, N.J.: Wiley-Blackwell, 2015). We met at a Starbucks in Baltimore, and I’ll tell you that a one-on-one conversation with an expert is a wonderful way to learn about state-of-the-art treatments, the only downside being that Starbucks does not offer CME credit.
Dr. Reti, who went to medical school at the University of Sydney and speaks with a charming Australian accent, trained in psychiatry at Johns Hopkins, and then did a neuroscience fellowship.
“I’d just finished residency training, and I was giving ECT to rats. We were looking at the expression of immediate-early genes. At the same time, I started doing consults in the mood disorders clinic.”
In 2006, Dr. Reti took over as director of ECT at Hopkins, and that same year, Dr. Jimmy Potash got funding to study TMS. Dr. Potash has since moved to the University of Iowa, and Dr. Reti took over TMS administration at Hopkins. Dr. Reti was flattered to be approached by Wiley to edit “Brain Stimulation,” and he talked about how he was pleased with the final edition of the book.
“I ended up getting the top people to write the chapters, people like Sarah Lisanby, Michael Nitsche, John Rothwell, and Mark George. These are the leaders in the field of brain stimulation.”
I asked Dr. Reti to walk me through what was happening in each brain stimulation area.
“In ECT,” he said, “we know a lot more now about how both the settings and the anesthesia regimen affect the outcomes. We didn’t know this when I trained in the ’90s.” Dr. Reti estimated that he’s administered ECT to close to 2,000 patients.
TMS is done less often at Hopkins; he estimated that 10-20 patients receive the treatment, and each patient comes 30-40 times, with each session lasting 40 minutes.
“It’s better than medicine but not as effective as ECT. We’re seeing an efficacy rate around 50%-60%,” and he noted that some patients have trouble tolerating the procedure as the magnetic stimulation can be uncomfortable. “The TMS coil stimulates the scalp nerves and muscles immediately under the coil, which causes discomfort.” He noted that some patients need to premedicate with over-the-counter pain medicines.
“We’re also finding that low-frequency stimulation on the right can be helpful for anxiety,” Dr. Reti said.
He talked about treating patients with psychotherapy along with TMS. The brain changes are thought to increase the brain’s plasticity and perhaps make psychotherapy more effective.
“It’s being studied in drug treatment. You can show someone with an addiction stimuli to trigger cravings, and doing this with TMS may block the response,” he said.
He talked for a while about direct transcranial brain stimulation, which I was not very familiar with. Because it is being used to improve focus-playing video games, the equipment is not being marketed as a psychiatric treatment and doesn’t fall under the domain of the Food and Drug Administration.
“Kids are using it to improve their concentration and performance with video games; all you need is a 9-volt battery and some electrodes that are attached to the scalp. The kits cost about $250, but you can burn your scalp,” he said.
Dr. Reti referred me to an article in the New Yorker on tDCS, “Electrified: Adventures in transcranial direct-current stimulation” by Elif Batuman. He noted that there are studies in progress to look at therapeutic uses for tDCS, including one at Johns Hopkins where neuropsychologist David Schretlen is looking at improving cognition in schizophrenia. Dr. Reti is interested in seeing if tDCS might be helpful in decreasing self-injurious behaviors in autistic children, as ECT has been effective in severe cases. He noted that while ECT and TMS stimulate neurons in the brain to fire, tDCS changes the stimulation threshold without directly causing the neurons to discharge.
Finally, we talked a little about deep brain stimulation. Thin electrodes directly target nodes in brain circuits that can modulate the activity of those circuits. He noted that deep brain stimulation was being used at Johns Hopkins to treat Parkinson’s disease, and other centers have looked at its use for severe obsessive-compulsive disorder and treatment-resistant depression.
“We know that the response habituates; now they are trying on-demand DBS,” Dr. Reti noted.
So, although I got no continuing medical education credits, I did get to try a new Starbucks drink while having a very stimulating discussion on the latest convulsive and nonconvulsive psychiatric brain research.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Top 10 treatments for vitiligo
PARK CITY, UTAH – At the annual meeting of the Pacific Dermatologic Association, Dr. Sancy A. Leachman offered a top 10 list of new agents and technologies for the treatment of vitiligo.
No. 10: Ultraviolet A1 (UVA1) phototherapy
Dr. Harvey Lui at the University of British Columbia in Vancouver is leading a phase II trial to evaluate the potential for UVA1 to induce repigmentation within vitiligo patches and to assess the side effect profile of the treatment. “I think it might work,” said Dr. Leachman, professor and chair of dermatology at Oregon Health & Science University (OHSU), Portland.
No. 9: Ginkgo biloba
The use of ginko biloba 40-60 mg 2-3 times per day, 10 minutes before a meal, was mentioned in a Cochrane Review of vitiligo treatments published on Feb. 24, 2015. “I think I’m going to give this a try in people who have failed other treatments and see if I can get some response,” Dr. Leachman said.
No. 8: Red light
Dr. Lui is leading a randomized phase II trial of low-intensity and high-intensity red light versus no treatment for vitiligo patches. Treatments will be given twice weekly for 10 weeks, with follow-up assessments at 4, 8, and 12 weeks post treatment.
No. 7: Micrografting
A novel suction blister device known as the CelluTome epidermal harvesting system uses heat and slight vacuum pressure to harvest healthy epidermal skin tissue without damaging the donor site. Dr. Leachman characterized the technology as “semiautomating the process of suction graft transplantation.”
No. 6: The ReCell device
Manufactured by Avita Medical, this investigational autologous cell harvesting device is used after CO2 abrasion and enables clinicians to create regenerative epithelial suspension with a small sample of the patient’s skin. A phase IV trial in the Netherlands is underway to assess the efficacy and safety of autologous epidermal cell suspension grafting with the ReCell device after CO2 laser abrasion, compared with CO2 laser abrasion alone and no treatment, in patients with piebaldism and stable vitiligo.
No. 5: Topical Photocil
In a pilot study sponsored by Applied Biology, researchers are enrolling patients with vitiligo to assess the safety and efficacy of Photocil. The primary outcome measure is the Vitiligo Area Severity Index (VASI). “When this cream is activated by sunlight, it degrades into narrow-band and UVB light, so you can put a topical cream on that will administer narrow-band UVB only in that spot,” said Dr. Leachman, who is also director of OHSU’s Knight Melanoma Research Program. “That’s amazing to me.”
No. 4: Afamelanotide
This is an analogue of a melanocyte-stimulating hormone. A randomized study conducted at two academic medical centers found that the combination of afamelanotide implant and narrow-band UVB phototherapy resulted in statistically superior and faster repigmentation, compared with narrow-band UVB monotherapy (JAMA Dermatol. 2015 Jan;151(1):42-50).
No. 3: Abatacept (Orencia)
This is a soluble fusion protein consisting of human cytotoxic T-lymphocyte–associated antigen 4 (CTLA4), which prevents T-cell activation. A phase I trial is underway at Brigham and Women’s Hospital in Boston to determine if weekly self-injections of the agent lead to clinical improvements of vitiligo lesions. The primary outcome measure is change in repigmentation with abatacept therapy based on the VASI score.
No. 2. Simvastatin
The notion of its use is based on STAT1 inhibition reducing interferon-gamma–dependent activation of CD8-positive T cells, according to Dr. Leachman. The concept has been successful in a mouse model, and a study in humans was recently completed by Dr. John Harris at the University of Massachusetts, Worcester. “What we have is the ability to apply an existing drug (Simvastatin) to the process and see if it works,” she said. “Wouldn’t it be cool if we could give a statin and improve vitiligo?”
No 1: Tofacitinib
This is a Janus kinase inhibitor commonly used for rheumatoid arthritis. According to Dr. Leachman, Janus kinase inhibition prevents STAT activation, “which prevents [interferon]-gamma production, which reduces activation of CD8-positive T cells via CXCL10 binding to CXCR3,” she said. A case report demonstrating its efficacy in a 53-year-old patient was recently published in JAMA Dermatology by Dr. Brett A. King and Dr. Brittany Craiglow, dermatologists at Yale School of Medicine, New Haven, Conn. “I’m hopeful that this [agent] will be made into a topical cream because these drugs do have substantial side effects,” Dr. Leachman said.
Dr. Leachman disclosed that she is a member of the medical and scientific advisory board for Myriad Genetics Laboratory. She has also participated in an advisory board meeting for Castle Biosciences and has participated in the DecisionDx registry.
PARK CITY, UTAH – At the annual meeting of the Pacific Dermatologic Association, Dr. Sancy A. Leachman offered a top 10 list of new agents and technologies for the treatment of vitiligo.
No. 10: Ultraviolet A1 (UVA1) phototherapy
Dr. Harvey Lui at the University of British Columbia in Vancouver is leading a phase II trial to evaluate the potential for UVA1 to induce repigmentation within vitiligo patches and to assess the side effect profile of the treatment. “I think it might work,” said Dr. Leachman, professor and chair of dermatology at Oregon Health & Science University (OHSU), Portland.
No. 9: Ginkgo biloba
The use of ginko biloba 40-60 mg 2-3 times per day, 10 minutes before a meal, was mentioned in a Cochrane Review of vitiligo treatments published on Feb. 24, 2015. “I think I’m going to give this a try in people who have failed other treatments and see if I can get some response,” Dr. Leachman said.
No. 8: Red light
Dr. Lui is leading a randomized phase II trial of low-intensity and high-intensity red light versus no treatment for vitiligo patches. Treatments will be given twice weekly for 10 weeks, with follow-up assessments at 4, 8, and 12 weeks post treatment.
No. 7: Micrografting
A novel suction blister device known as the CelluTome epidermal harvesting system uses heat and slight vacuum pressure to harvest healthy epidermal skin tissue without damaging the donor site. Dr. Leachman characterized the technology as “semiautomating the process of suction graft transplantation.”
No. 6: The ReCell device
Manufactured by Avita Medical, this investigational autologous cell harvesting device is used after CO2 abrasion and enables clinicians to create regenerative epithelial suspension with a small sample of the patient’s skin. A phase IV trial in the Netherlands is underway to assess the efficacy and safety of autologous epidermal cell suspension grafting with the ReCell device after CO2 laser abrasion, compared with CO2 laser abrasion alone and no treatment, in patients with piebaldism and stable vitiligo.
No. 5: Topical Photocil
In a pilot study sponsored by Applied Biology, researchers are enrolling patients with vitiligo to assess the safety and efficacy of Photocil. The primary outcome measure is the Vitiligo Area Severity Index (VASI). “When this cream is activated by sunlight, it degrades into narrow-band and UVB light, so you can put a topical cream on that will administer narrow-band UVB only in that spot,” said Dr. Leachman, who is also director of OHSU’s Knight Melanoma Research Program. “That’s amazing to me.”
No. 4: Afamelanotide
This is an analogue of a melanocyte-stimulating hormone. A randomized study conducted at two academic medical centers found that the combination of afamelanotide implant and narrow-band UVB phototherapy resulted in statistically superior and faster repigmentation, compared with narrow-band UVB monotherapy (JAMA Dermatol. 2015 Jan;151(1):42-50).
No. 3: Abatacept (Orencia)
This is a soluble fusion protein consisting of human cytotoxic T-lymphocyte–associated antigen 4 (CTLA4), which prevents T-cell activation. A phase I trial is underway at Brigham and Women’s Hospital in Boston to determine if weekly self-injections of the agent lead to clinical improvements of vitiligo lesions. The primary outcome measure is change in repigmentation with abatacept therapy based on the VASI score.
No. 2. Simvastatin
The notion of its use is based on STAT1 inhibition reducing interferon-gamma–dependent activation of CD8-positive T cells, according to Dr. Leachman. The concept has been successful in a mouse model, and a study in humans was recently completed by Dr. John Harris at the University of Massachusetts, Worcester. “What we have is the ability to apply an existing drug (Simvastatin) to the process and see if it works,” she said. “Wouldn’t it be cool if we could give a statin and improve vitiligo?”
No 1: Tofacitinib
This is a Janus kinase inhibitor commonly used for rheumatoid arthritis. According to Dr. Leachman, Janus kinase inhibition prevents STAT activation, “which prevents [interferon]-gamma production, which reduces activation of CD8-positive T cells via CXCL10 binding to CXCR3,” she said. A case report demonstrating its efficacy in a 53-year-old patient was recently published in JAMA Dermatology by Dr. Brett A. King and Dr. Brittany Craiglow, dermatologists at Yale School of Medicine, New Haven, Conn. “I’m hopeful that this [agent] will be made into a topical cream because these drugs do have substantial side effects,” Dr. Leachman said.
Dr. Leachman disclosed that she is a member of the medical and scientific advisory board for Myriad Genetics Laboratory. She has also participated in an advisory board meeting for Castle Biosciences and has participated in the DecisionDx registry.
PARK CITY, UTAH – At the annual meeting of the Pacific Dermatologic Association, Dr. Sancy A. Leachman offered a top 10 list of new agents and technologies for the treatment of vitiligo.
No. 10: Ultraviolet A1 (UVA1) phototherapy
Dr. Harvey Lui at the University of British Columbia in Vancouver is leading a phase II trial to evaluate the potential for UVA1 to induce repigmentation within vitiligo patches and to assess the side effect profile of the treatment. “I think it might work,” said Dr. Leachman, professor and chair of dermatology at Oregon Health & Science University (OHSU), Portland.
No. 9: Ginkgo biloba
The use of ginko biloba 40-60 mg 2-3 times per day, 10 minutes before a meal, was mentioned in a Cochrane Review of vitiligo treatments published on Feb. 24, 2015. “I think I’m going to give this a try in people who have failed other treatments and see if I can get some response,” Dr. Leachman said.
No. 8: Red light
Dr. Lui is leading a randomized phase II trial of low-intensity and high-intensity red light versus no treatment for vitiligo patches. Treatments will be given twice weekly for 10 weeks, with follow-up assessments at 4, 8, and 12 weeks post treatment.
No. 7: Micrografting
A novel suction blister device known as the CelluTome epidermal harvesting system uses heat and slight vacuum pressure to harvest healthy epidermal skin tissue without damaging the donor site. Dr. Leachman characterized the technology as “semiautomating the process of suction graft transplantation.”
No. 6: The ReCell device
Manufactured by Avita Medical, this investigational autologous cell harvesting device is used after CO2 abrasion and enables clinicians to create regenerative epithelial suspension with a small sample of the patient’s skin. A phase IV trial in the Netherlands is underway to assess the efficacy and safety of autologous epidermal cell suspension grafting with the ReCell device after CO2 laser abrasion, compared with CO2 laser abrasion alone and no treatment, in patients with piebaldism and stable vitiligo.
No. 5: Topical Photocil
In a pilot study sponsored by Applied Biology, researchers are enrolling patients with vitiligo to assess the safety and efficacy of Photocil. The primary outcome measure is the Vitiligo Area Severity Index (VASI). “When this cream is activated by sunlight, it degrades into narrow-band and UVB light, so you can put a topical cream on that will administer narrow-band UVB only in that spot,” said Dr. Leachman, who is also director of OHSU’s Knight Melanoma Research Program. “That’s amazing to me.”
No. 4: Afamelanotide
This is an analogue of a melanocyte-stimulating hormone. A randomized study conducted at two academic medical centers found that the combination of afamelanotide implant and narrow-band UVB phototherapy resulted in statistically superior and faster repigmentation, compared with narrow-band UVB monotherapy (JAMA Dermatol. 2015 Jan;151(1):42-50).
No. 3: Abatacept (Orencia)
This is a soluble fusion protein consisting of human cytotoxic T-lymphocyte–associated antigen 4 (CTLA4), which prevents T-cell activation. A phase I trial is underway at Brigham and Women’s Hospital in Boston to determine if weekly self-injections of the agent lead to clinical improvements of vitiligo lesions. The primary outcome measure is change in repigmentation with abatacept therapy based on the VASI score.
No. 2. Simvastatin
The notion of its use is based on STAT1 inhibition reducing interferon-gamma–dependent activation of CD8-positive T cells, according to Dr. Leachman. The concept has been successful in a mouse model, and a study in humans was recently completed by Dr. John Harris at the University of Massachusetts, Worcester. “What we have is the ability to apply an existing drug (Simvastatin) to the process and see if it works,” she said. “Wouldn’t it be cool if we could give a statin and improve vitiligo?”
No 1: Tofacitinib
This is a Janus kinase inhibitor commonly used for rheumatoid arthritis. According to Dr. Leachman, Janus kinase inhibition prevents STAT activation, “which prevents [interferon]-gamma production, which reduces activation of CD8-positive T cells via CXCL10 binding to CXCR3,” she said. A case report demonstrating its efficacy in a 53-year-old patient was recently published in JAMA Dermatology by Dr. Brett A. King and Dr. Brittany Craiglow, dermatologists at Yale School of Medicine, New Haven, Conn. “I’m hopeful that this [agent] will be made into a topical cream because these drugs do have substantial side effects,” Dr. Leachman said.
Dr. Leachman disclosed that she is a member of the medical and scientific advisory board for Myriad Genetics Laboratory. She has also participated in an advisory board meeting for Castle Biosciences and has participated in the DecisionDx registry.
EXPERT ANALYSIS AT PDA 2015
LISTEN NOW: Tales from the Research, Innovations, and Clinical Vignette (RIV) Poster Competition
Hospitalists who presented RIV posters at HM15 talk about their projects. Dr. Brian Poustinchian worked on a bedside rounding study at Midwestern University in Illinois, and Dr. Jennifer Pascoe worked on a poster about patients leaving the hospital against medical advice, focusing on a case of her own at the University of Rochester.
Hospitalists who presented RIV posters at HM15 talk about their projects. Dr. Brian Poustinchian worked on a bedside rounding study at Midwestern University in Illinois, and Dr. Jennifer Pascoe worked on a poster about patients leaving the hospital against medical advice, focusing on a case of her own at the University of Rochester.
Hospitalists who presented RIV posters at HM15 talk about their projects. Dr. Brian Poustinchian worked on a bedside rounding study at Midwestern University in Illinois, and Dr. Jennifer Pascoe worked on a poster about patients leaving the hospital against medical advice, focusing on a case of her own at the University of Rochester.
Similar Early Outcomes in nvAF Regardless of Anticoagulant Type
NEW YORK - In the early months of anticoagulant treatment, patients with nonvalvular atrial fibrillation (nvAF) have similar rates of bleeding and arterial clots with dabigatran, rivaroxaban and vitamin K antagonists (VKA) like warfarin, researchers from France report.
Large randomized trials have shown the newer non-VKA oral anticoagulants (NOAC) to have superior safety and efficacy relative to warfarin, but subsequent observational studies have yielded conflicting results.
Dr. Géric Maura from National Health Insurance (CNAMTS) in Paris and colleagues used the French National Health Insurance information system to assess the bleeding and arterial thrombotic risks of dabigatran and rivaroxaban, each compared with VKA, during the first few months of therapy in 32,807 newly treated patients with nvAF.
There was no significant difference in bleeding between VKA- and dabigatran- or rivaroxaban-treated patients on propensity-matched analysis, regardless of whether patients were treated with low or high doses of each NOAC, the researchers report in Circulation, online July 21.
The composite outcome comprising hospitalization for bleeding and death occurred with similar frequency in the different treatment groups.
Among the secondary endpoints, there were no significant differences between treatments in arterial thromboembolic events or in the composite outcome comprising stroke, systemic embolism and death.
"Although our overall results are reassuring in relation to initiation of NOAC in nvAF patients in France with no marked excess thromboembolic or bleeding risk, they also suggest that particular caution is required when initiating NOAC," the researchers conclude. "But on the basis of this study comparing NOAC to VKA, NOAC cannot be considered to be safer than VKA during the early phase of treatment. On the contrary, the clinical implications of our results are that physicians must be just as cautious when initiating NOAC as when initiating VKA, particularly in view of the absence of an antidote and objective monitoring of the extent of anticoagulation."
"Similar analyses should be extended to other NOAC such as apixaban and observational studies should now focus on NOAC head-to-head comparison in a non-inferiority design," they suggest.
The study had no commercial funding and the authors reported no conflicts of interest.
Dr. Maura did not respond to a request for comment.
NEW YORK - In the early months of anticoagulant treatment, patients with nonvalvular atrial fibrillation (nvAF) have similar rates of bleeding and arterial clots with dabigatran, rivaroxaban and vitamin K antagonists (VKA) like warfarin, researchers from France report.
Large randomized trials have shown the newer non-VKA oral anticoagulants (NOAC) to have superior safety and efficacy relative to warfarin, but subsequent observational studies have yielded conflicting results.
Dr. Géric Maura from National Health Insurance (CNAMTS) in Paris and colleagues used the French National Health Insurance information system to assess the bleeding and arterial thrombotic risks of dabigatran and rivaroxaban, each compared with VKA, during the first few months of therapy in 32,807 newly treated patients with nvAF.
There was no significant difference in bleeding between VKA- and dabigatran- or rivaroxaban-treated patients on propensity-matched analysis, regardless of whether patients were treated with low or high doses of each NOAC, the researchers report in Circulation, online July 21.
The composite outcome comprising hospitalization for bleeding and death occurred with similar frequency in the different treatment groups.
Among the secondary endpoints, there were no significant differences between treatments in arterial thromboembolic events or in the composite outcome comprising stroke, systemic embolism and death.
"Although our overall results are reassuring in relation to initiation of NOAC in nvAF patients in France with no marked excess thromboembolic or bleeding risk, they also suggest that particular caution is required when initiating NOAC," the researchers conclude. "But on the basis of this study comparing NOAC to VKA, NOAC cannot be considered to be safer than VKA during the early phase of treatment. On the contrary, the clinical implications of our results are that physicians must be just as cautious when initiating NOAC as when initiating VKA, particularly in view of the absence of an antidote and objective monitoring of the extent of anticoagulation."
"Similar analyses should be extended to other NOAC such as apixaban and observational studies should now focus on NOAC head-to-head comparison in a non-inferiority design," they suggest.
The study had no commercial funding and the authors reported no conflicts of interest.
Dr. Maura did not respond to a request for comment.
NEW YORK - In the early months of anticoagulant treatment, patients with nonvalvular atrial fibrillation (nvAF) have similar rates of bleeding and arterial clots with dabigatran, rivaroxaban and vitamin K antagonists (VKA) like warfarin, researchers from France report.
Large randomized trials have shown the newer non-VKA oral anticoagulants (NOAC) to have superior safety and efficacy relative to warfarin, but subsequent observational studies have yielded conflicting results.
Dr. Géric Maura from National Health Insurance (CNAMTS) in Paris and colleagues used the French National Health Insurance information system to assess the bleeding and arterial thrombotic risks of dabigatran and rivaroxaban, each compared with VKA, during the first few months of therapy in 32,807 newly treated patients with nvAF.
There was no significant difference in bleeding between VKA- and dabigatran- or rivaroxaban-treated patients on propensity-matched analysis, regardless of whether patients were treated with low or high doses of each NOAC, the researchers report in Circulation, online July 21.
The composite outcome comprising hospitalization for bleeding and death occurred with similar frequency in the different treatment groups.
Among the secondary endpoints, there were no significant differences between treatments in arterial thromboembolic events or in the composite outcome comprising stroke, systemic embolism and death.
"Although our overall results are reassuring in relation to initiation of NOAC in nvAF patients in France with no marked excess thromboembolic or bleeding risk, they also suggest that particular caution is required when initiating NOAC," the researchers conclude. "But on the basis of this study comparing NOAC to VKA, NOAC cannot be considered to be safer than VKA during the early phase of treatment. On the contrary, the clinical implications of our results are that physicians must be just as cautious when initiating NOAC as when initiating VKA, particularly in view of the absence of an antidote and objective monitoring of the extent of anticoagulation."
"Similar analyses should be extended to other NOAC such as apixaban and observational studies should now focus on NOAC head-to-head comparison in a non-inferiority design," they suggest.
The study had no commercial funding and the authors reported no conflicts of interest.
Dr. Maura did not respond to a request for comment.
New prognostic model for follicular lymphoma

Photo courtesy of NIH
A newly developed prognostic model can identify follicular lymphoma (FL) patients at the highest risk for treatment failure, according to researchers.
To create this model, called m7-FLIPI, the team combined the Follicular Lymphoma International Prognostic Index (FLIPI), Eastern Cooperative Oncology Group (ECOG) performance status, and the mutation status of 7 genes—EZH2, ARID1A, MEF2B, EP300, FOXO1, CREBBP, and CARD11.
The researchers said this is the first prognostic model for FL that accounts for both clinical factors and genetic mutations.
They described the creation and testing of the model in The Lancet Oncology.
“We set out to determine, at the time of diagnosis, which patients’ disease will have sustained responses after treatment and whether new genetic data could help inform which patients are at risk for developing progressive lymphoma so clinicians would be able to offer these high-risk patients more effective therapies,” said Randy Gascoyne, MD, of the British Columbia Cancer Agency in Vancouver, Canada.
He and his colleagues created the m7-FLIPI by conducting a retrospective analysis of genetic mutations and clinical risk factors in 2 cohorts of patients with symptomatic, advanced stage, or bulky FL grade 1, 2, or 3A.
The patients had a biopsy specimen collected 12 months or less before they began first-line treatment with an immunochemotherapy regimen containing rituximab.
Training cohort
The training cohort consisted of 151 FL patients who received R-CHOP. The median follow-up for these patients was 7.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found 28% of patients (43/151) were defined as high-risk, with a 5-year failure-free survival (FFS) rate of 38.29%.
And 72% of patients (108/151) were defined as low-risk, with a 5-year FFS of 77.21%. The hazard ratio was 4.14 (P<0.0001).
The positive predictive value for 5-year FFS was 64%, and the negative predictive value was 78%. The m7-FLIPI outperformed a prognostic model of only gene mutations and the FLIPI-2.
Validation cohort
The validation cohort consisted of 107 patients who received R-CVP. The median follow-up for these patients was 6.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found that 22% of patients (24/107) were defined as high-risk, with a 5-year FFS of 25%.
And 78% of patients (83/107) were defined as low-risk, with a 5-year FFS of 68.24%. The hazard ratio was 3.58 (P<0.0001).
The positive predictive value for 5-year FFS was 72%, and the negative predictive value was 68%. The m7-FLIPI outperformed the FLIPI alone and the FLIPI combined with ECOG performance status.
Overall survival
Although the m7-FLIPI was designed specifically for FFS, the researchers also tested its prognostic utility for overall survival (OS).
In the training cohort, high-risk disease according to the m7-FLIPI was associated with a 5-year OS of 65.25%, compared to 89.98% for low-risk disease (P=0.00031).
In the validation cohort, 5-year OS was 41.67% for patients with high-risk disease and 84.01% for patients with low-risk disease (P<0.0001). In both cohorts, the m7-FLIPI outperformed the FLIPI alone.
Based on these results, the researchers believe the m7-FLIPI could be utilized in a clinical setting to test all new FL patients at diagnosis and identify patients who harbor the most aggressive disease.
“The m7-FLIPI could be extremely significant for the medical community,” Dr Gascoyne said, “changing the story for high-risk patients who are currently destined to not respond well to standard treatment.” ![]()

Photo courtesy of NIH
A newly developed prognostic model can identify follicular lymphoma (FL) patients at the highest risk for treatment failure, according to researchers.
To create this model, called m7-FLIPI, the team combined the Follicular Lymphoma International Prognostic Index (FLIPI), Eastern Cooperative Oncology Group (ECOG) performance status, and the mutation status of 7 genes—EZH2, ARID1A, MEF2B, EP300, FOXO1, CREBBP, and CARD11.
The researchers said this is the first prognostic model for FL that accounts for both clinical factors and genetic mutations.
They described the creation and testing of the model in The Lancet Oncology.
“We set out to determine, at the time of diagnosis, which patients’ disease will have sustained responses after treatment and whether new genetic data could help inform which patients are at risk for developing progressive lymphoma so clinicians would be able to offer these high-risk patients more effective therapies,” said Randy Gascoyne, MD, of the British Columbia Cancer Agency in Vancouver, Canada.
He and his colleagues created the m7-FLIPI by conducting a retrospective analysis of genetic mutations and clinical risk factors in 2 cohorts of patients with symptomatic, advanced stage, or bulky FL grade 1, 2, or 3A.
The patients had a biopsy specimen collected 12 months or less before they began first-line treatment with an immunochemotherapy regimen containing rituximab.
Training cohort
The training cohort consisted of 151 FL patients who received R-CHOP. The median follow-up for these patients was 7.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found 28% of patients (43/151) were defined as high-risk, with a 5-year failure-free survival (FFS) rate of 38.29%.
And 72% of patients (108/151) were defined as low-risk, with a 5-year FFS of 77.21%. The hazard ratio was 4.14 (P<0.0001).
The positive predictive value for 5-year FFS was 64%, and the negative predictive value was 78%. The m7-FLIPI outperformed a prognostic model of only gene mutations and the FLIPI-2.
Validation cohort
The validation cohort consisted of 107 patients who received R-CVP. The median follow-up for these patients was 6.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found that 22% of patients (24/107) were defined as high-risk, with a 5-year FFS of 25%.
And 78% of patients (83/107) were defined as low-risk, with a 5-year FFS of 68.24%. The hazard ratio was 3.58 (P<0.0001).
The positive predictive value for 5-year FFS was 72%, and the negative predictive value was 68%. The m7-FLIPI outperformed the FLIPI alone and the FLIPI combined with ECOG performance status.
Overall survival
Although the m7-FLIPI was designed specifically for FFS, the researchers also tested its prognostic utility for overall survival (OS).
In the training cohort, high-risk disease according to the m7-FLIPI was associated with a 5-year OS of 65.25%, compared to 89.98% for low-risk disease (P=0.00031).
In the validation cohort, 5-year OS was 41.67% for patients with high-risk disease and 84.01% for patients with low-risk disease (P<0.0001). In both cohorts, the m7-FLIPI outperformed the FLIPI alone.
Based on these results, the researchers believe the m7-FLIPI could be utilized in a clinical setting to test all new FL patients at diagnosis and identify patients who harbor the most aggressive disease.
“The m7-FLIPI could be extremely significant for the medical community,” Dr Gascoyne said, “changing the story for high-risk patients who are currently destined to not respond well to standard treatment.” ![]()

Photo courtesy of NIH
A newly developed prognostic model can identify follicular lymphoma (FL) patients at the highest risk for treatment failure, according to researchers.
To create this model, called m7-FLIPI, the team combined the Follicular Lymphoma International Prognostic Index (FLIPI), Eastern Cooperative Oncology Group (ECOG) performance status, and the mutation status of 7 genes—EZH2, ARID1A, MEF2B, EP300, FOXO1, CREBBP, and CARD11.
The researchers said this is the first prognostic model for FL that accounts for both clinical factors and genetic mutations.
They described the creation and testing of the model in The Lancet Oncology.
“We set out to determine, at the time of diagnosis, which patients’ disease will have sustained responses after treatment and whether new genetic data could help inform which patients are at risk for developing progressive lymphoma so clinicians would be able to offer these high-risk patients more effective therapies,” said Randy Gascoyne, MD, of the British Columbia Cancer Agency in Vancouver, Canada.
He and his colleagues created the m7-FLIPI by conducting a retrospective analysis of genetic mutations and clinical risk factors in 2 cohorts of patients with symptomatic, advanced stage, or bulky FL grade 1, 2, or 3A.
The patients had a biopsy specimen collected 12 months or less before they began first-line treatment with an immunochemotherapy regimen containing rituximab.
Training cohort
The training cohort consisted of 151 FL patients who received R-CHOP. The median follow-up for these patients was 7.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found 28% of patients (43/151) were defined as high-risk, with a 5-year failure-free survival (FFS) rate of 38.29%.
And 72% of patients (108/151) were defined as low-risk, with a 5-year FFS of 77.21%. The hazard ratio was 4.14 (P<0.0001).
The positive predictive value for 5-year FFS was 64%, and the negative predictive value was 78%. The m7-FLIPI outperformed a prognostic model of only gene mutations and the FLIPI-2.
Validation cohort
The validation cohort consisted of 107 patients who received R-CVP. The median follow-up for these patients was 6.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found that 22% of patients (24/107) were defined as high-risk, with a 5-year FFS of 25%.
And 78% of patients (83/107) were defined as low-risk, with a 5-year FFS of 68.24%. The hazard ratio was 3.58 (P<0.0001).
The positive predictive value for 5-year FFS was 72%, and the negative predictive value was 68%. The m7-FLIPI outperformed the FLIPI alone and the FLIPI combined with ECOG performance status.
Overall survival
Although the m7-FLIPI was designed specifically for FFS, the researchers also tested its prognostic utility for overall survival (OS).
In the training cohort, high-risk disease according to the m7-FLIPI was associated with a 5-year OS of 65.25%, compared to 89.98% for low-risk disease (P=0.00031).
In the validation cohort, 5-year OS was 41.67% for patients with high-risk disease and 84.01% for patients with low-risk disease (P<0.0001). In both cohorts, the m7-FLIPI outperformed the FLIPI alone.
Based on these results, the researchers believe the m7-FLIPI could be utilized in a clinical setting to test all new FL patients at diagnosis and identify patients who harbor the most aggressive disease.
“The m7-FLIPI could be extremely significant for the medical community,” Dr Gascoyne said, “changing the story for high-risk patients who are currently destined to not respond well to standard treatment.” ![]()
Rivaroxaban monitoring kit launched in Europe

Instrumentation Laboratory, a company that develops in vitro diagnostic instruments, has announced the commercialization of the HemosIL Rivaroxaban Testing Solution in Europe.
This testing kit consists of the HemosIL Liquid Anti-Xa Assay, Rivaroxaban Calibrators, and Rivaroxaban Controls, which can be used with ACL TOP Hemostasis Testing Systems to monitor patients taking the oral anticoagulant rivaroxaban (Xarelto).
The assay, calibrators, and controls are now CE IVD Marked under the European IVD Directive 98/79/EC.
This allows Instrumentation Laboratory to distribute the HemosIL Rivaroxaban Testing Solution in the European Union and other international territories.
Although monitoring is generally not required for patients on rivaroxaban, there are cases in which measuring rivaroxaban may be necessary.
This includes patients who present with bleeding, require reversal of anticoagulation, experience deteriorating renal function, or must undergo surgery or an invasive procedure and have taken rivaroxaban within 24 hours or longer if creatinine clearance is < 50 mL min-1.
Liquid Anti-Xa Assay
The HemosIL Liquid Anti-Xa kit is a one-stage chromogenic assay based on a synthetic chromogenic substrate and factor Xa inactivation. Rivaroxaban levels in patient plasma are measured automatically on an ACL TOP Hemostasis Testing System when this assay is calibrated with the HemosIL Rivaroxaban Calibrators.
The Anti-Xa Assay kit consists of:
- Factor Xa reagent: 5 x 2.5 mL vial of a liquid preparation containing purified bovine factor Xa (approximately 5.5 nkat/mL), Tris-Buffer, EDTA, dextran sulfate, sodium chloride, and bovine serum albumin.
- Chromogenic substrate: 5 x 3 mL vial of liquid chromogenic substrate S-2732 (approximately 1.2 mg/mL) and bulking agent.
Rivaroxaban Calibrators
The HemosIL Rivaroxaban Calibrators are intended for the calibration of the Liquid Anti-Xa Assay when testing for rivaroxaban on an ACL TOP Hemostasis Testing System.
Two levels of lyophilized calibrators prepared from human citrated plasma by means of a dedicated process at 2 different concentrations of rivaroxaban are used by the instrument to automatically prepare a calibration curve.
The Rivaroxaban Calibrator kit consists of:
- Rivaroxaban Calibrator 1: 5 x 1 mL vials of a lyophilized human plasma containing buffers and stabilizers.
- Rivaroxaban Calibrator 2: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, buffers, and stabilizers.
Rivaroxaban Controls
HemosIL Rivaroxaban Controls are intended for the quality control of the Liquid Anti-Xa Assay when testing for rivaroxaban on an ACL TOP Hemostasis Testing System.
Two levels of lyophilized controls are prepared from human citrated plasma by means of a dedicated process at 2 different concentrations of rivaroxaban. Use of both controls is recommended for a complete quality control program.
The Rivaroxaban Controls kit consists of:
- Rivaroxaban Low Control: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, stabilizers, and buffer solution.
- Rivaroxaban High Control: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, stabilizers, and buffer solution.


Instrumentation Laboratory, a company that develops in vitro diagnostic instruments, has announced the commercialization of the HemosIL Rivaroxaban Testing Solution in Europe.
This testing kit consists of the HemosIL Liquid Anti-Xa Assay, Rivaroxaban Calibrators, and Rivaroxaban Controls, which can be used with ACL TOP Hemostasis Testing Systems to monitor patients taking the oral anticoagulant rivaroxaban (Xarelto).
The assay, calibrators, and controls are now CE IVD Marked under the European IVD Directive 98/79/EC.
This allows Instrumentation Laboratory to distribute the HemosIL Rivaroxaban Testing Solution in the European Union and other international territories.
Although monitoring is generally not required for patients on rivaroxaban, there are cases in which measuring rivaroxaban may be necessary.
This includes patients who present with bleeding, require reversal of anticoagulation, experience deteriorating renal function, or must undergo surgery or an invasive procedure and have taken rivaroxaban within 24 hours or longer if creatinine clearance is < 50 mL min-1.
Liquid Anti-Xa Assay
The HemosIL Liquid Anti-Xa kit is a one-stage chromogenic assay based on a synthetic chromogenic substrate and factor Xa inactivation. Rivaroxaban levels in patient plasma are measured automatically on an ACL TOP Hemostasis Testing System when this assay is calibrated with the HemosIL Rivaroxaban Calibrators.
The Anti-Xa Assay kit consists of:
- Factor Xa reagent: 5 x 2.5 mL vial of a liquid preparation containing purified bovine factor Xa (approximately 5.5 nkat/mL), Tris-Buffer, EDTA, dextran sulfate, sodium chloride, and bovine serum albumin.
- Chromogenic substrate: 5 x 3 mL vial of liquid chromogenic substrate S-2732 (approximately 1.2 mg/mL) and bulking agent.
Rivaroxaban Calibrators
The HemosIL Rivaroxaban Calibrators are intended for the calibration of the Liquid Anti-Xa Assay when testing for rivaroxaban on an ACL TOP Hemostasis Testing System.
Two levels of lyophilized calibrators prepared from human citrated plasma by means of a dedicated process at 2 different concentrations of rivaroxaban are used by the instrument to automatically prepare a calibration curve.
The Rivaroxaban Calibrator kit consists of:
- Rivaroxaban Calibrator 1: 5 x 1 mL vials of a lyophilized human plasma containing buffers and stabilizers.
- Rivaroxaban Calibrator 2: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, buffers, and stabilizers.
Rivaroxaban Controls
HemosIL Rivaroxaban Controls are intended for the quality control of the Liquid Anti-Xa Assay when testing for rivaroxaban on an ACL TOP Hemostasis Testing System.
Two levels of lyophilized controls are prepared from human citrated plasma by means of a dedicated process at 2 different concentrations of rivaroxaban. Use of both controls is recommended for a complete quality control program.
The Rivaroxaban Controls kit consists of:
- Rivaroxaban Low Control: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, stabilizers, and buffer solution.
- Rivaroxaban High Control: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, stabilizers, and buffer solution.


Instrumentation Laboratory, a company that develops in vitro diagnostic instruments, has announced the commercialization of the HemosIL Rivaroxaban Testing Solution in Europe.
This testing kit consists of the HemosIL Liquid Anti-Xa Assay, Rivaroxaban Calibrators, and Rivaroxaban Controls, which can be used with ACL TOP Hemostasis Testing Systems to monitor patients taking the oral anticoagulant rivaroxaban (Xarelto).
The assay, calibrators, and controls are now CE IVD Marked under the European IVD Directive 98/79/EC.
This allows Instrumentation Laboratory to distribute the HemosIL Rivaroxaban Testing Solution in the European Union and other international territories.
Although monitoring is generally not required for patients on rivaroxaban, there are cases in which measuring rivaroxaban may be necessary.
This includes patients who present with bleeding, require reversal of anticoagulation, experience deteriorating renal function, or must undergo surgery or an invasive procedure and have taken rivaroxaban within 24 hours or longer if creatinine clearance is < 50 mL min-1.
Liquid Anti-Xa Assay
The HemosIL Liquid Anti-Xa kit is a one-stage chromogenic assay based on a synthetic chromogenic substrate and factor Xa inactivation. Rivaroxaban levels in patient plasma are measured automatically on an ACL TOP Hemostasis Testing System when this assay is calibrated with the HemosIL Rivaroxaban Calibrators.
The Anti-Xa Assay kit consists of:
- Factor Xa reagent: 5 x 2.5 mL vial of a liquid preparation containing purified bovine factor Xa (approximately 5.5 nkat/mL), Tris-Buffer, EDTA, dextran sulfate, sodium chloride, and bovine serum albumin.
- Chromogenic substrate: 5 x 3 mL vial of liquid chromogenic substrate S-2732 (approximately 1.2 mg/mL) and bulking agent.
Rivaroxaban Calibrators
The HemosIL Rivaroxaban Calibrators are intended for the calibration of the Liquid Anti-Xa Assay when testing for rivaroxaban on an ACL TOP Hemostasis Testing System.
Two levels of lyophilized calibrators prepared from human citrated plasma by means of a dedicated process at 2 different concentrations of rivaroxaban are used by the instrument to automatically prepare a calibration curve.
The Rivaroxaban Calibrator kit consists of:
- Rivaroxaban Calibrator 1: 5 x 1 mL vials of a lyophilized human plasma containing buffers and stabilizers.
- Rivaroxaban Calibrator 2: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, buffers, and stabilizers.
Rivaroxaban Controls
HemosIL Rivaroxaban Controls are intended for the quality control of the Liquid Anti-Xa Assay when testing for rivaroxaban on an ACL TOP Hemostasis Testing System.
Two levels of lyophilized controls are prepared from human citrated plasma by means of a dedicated process at 2 different concentrations of rivaroxaban. Use of both controls is recommended for a complete quality control program.
The Rivaroxaban Controls kit consists of:
- Rivaroxaban Low Control: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, stabilizers, and buffer solution.
- Rivaroxaban High Control: 5 x 1 mL vials of a lyophilized human plasma containing rivaroxaban, stabilizers, and buffer solution.

Platform simplifies data analysis, team says

Photo by Rhoda Baer
Researchers say they have developed a user-friendly platform for analyzing transcriptomic and epigenomic sequencing data.
This platform, BioWardrobe, was designed to help biomedical researchers analyze data that might answer questions about diseases and basic biology.
“Although biologists can perform experiments and obtain the data, they often lack the programming expertise required to perform computational data analysis,” said Artem Barski, PhD, of the University of Cincinnati in Ohio.
“BioWardrobe aims to empower researchers by bridging this gap between data and knowledge.”
Dr Barski and Andrey Kartashov, also of the University of Cincinnati, described BioWardrobe in Genome Biology.
The pair said the recent proliferation of sequencing-based methods for analysis of gene expression, chromatin structure, and protein-DNA interactions has widened our horizons, but the volume of data obtained from sequencing requires computational data analysis.
Unfortunately, the bioinformatics and programming expertise required for this analysis may be absent in biomedical laboratories. And this can result in data inaccessibility or delays in applying modern sequencing-based technologies to pressing questions in basic and health-related research.
Dr Barski and Kartashov believe BioWardrobe can solve those problems by providing a “biologist-friendly” web interface.
BioWardrobe users can download data from institutional facilities or public databases, map reads, and visualize results on a genome browser. The platform also allows for differential gene expression and binding analysis, and it can create average tag-density profiles and heatmaps.
Dr Barski and Kartashov plan to continue improving BioWardrobe and continue using the platform in their own research on epigenetic regulation in the immune system, as well as in collaborative projects with other investigators. ![]()

Photo by Rhoda Baer
Researchers say they have developed a user-friendly platform for analyzing transcriptomic and epigenomic sequencing data.
This platform, BioWardrobe, was designed to help biomedical researchers analyze data that might answer questions about diseases and basic biology.
“Although biologists can perform experiments and obtain the data, they often lack the programming expertise required to perform computational data analysis,” said Artem Barski, PhD, of the University of Cincinnati in Ohio.
“BioWardrobe aims to empower researchers by bridging this gap between data and knowledge.”
Dr Barski and Andrey Kartashov, also of the University of Cincinnati, described BioWardrobe in Genome Biology.
The pair said the recent proliferation of sequencing-based methods for analysis of gene expression, chromatin structure, and protein-DNA interactions has widened our horizons, but the volume of data obtained from sequencing requires computational data analysis.
Unfortunately, the bioinformatics and programming expertise required for this analysis may be absent in biomedical laboratories. And this can result in data inaccessibility or delays in applying modern sequencing-based technologies to pressing questions in basic and health-related research.
Dr Barski and Kartashov believe BioWardrobe can solve those problems by providing a “biologist-friendly” web interface.
BioWardrobe users can download data from institutional facilities or public databases, map reads, and visualize results on a genome browser. The platform also allows for differential gene expression and binding analysis, and it can create average tag-density profiles and heatmaps.
Dr Barski and Kartashov plan to continue improving BioWardrobe and continue using the platform in their own research on epigenetic regulation in the immune system, as well as in collaborative projects with other investigators. ![]()

Photo by Rhoda Baer
Researchers say they have developed a user-friendly platform for analyzing transcriptomic and epigenomic sequencing data.
This platform, BioWardrobe, was designed to help biomedical researchers analyze data that might answer questions about diseases and basic biology.
“Although biologists can perform experiments and obtain the data, they often lack the programming expertise required to perform computational data analysis,” said Artem Barski, PhD, of the University of Cincinnati in Ohio.
“BioWardrobe aims to empower researchers by bridging this gap between data and knowledge.”
Dr Barski and Andrey Kartashov, also of the University of Cincinnati, described BioWardrobe in Genome Biology.
The pair said the recent proliferation of sequencing-based methods for analysis of gene expression, chromatin structure, and protein-DNA interactions has widened our horizons, but the volume of data obtained from sequencing requires computational data analysis.
Unfortunately, the bioinformatics and programming expertise required for this analysis may be absent in biomedical laboratories. And this can result in data inaccessibility or delays in applying modern sequencing-based technologies to pressing questions in basic and health-related research.
Dr Barski and Kartashov believe BioWardrobe can solve those problems by providing a “biologist-friendly” web interface.
BioWardrobe users can download data from institutional facilities or public databases, map reads, and visualize results on a genome browser. The platform also allows for differential gene expression and binding analysis, and it can create average tag-density profiles and heatmaps.
Dr Barski and Kartashov plan to continue improving BioWardrobe and continue using the platform in their own research on epigenetic regulation in the immune system, as well as in collaborative projects with other investigators. ![]()
Family-centered care in the NICU
Hospitals are slow to change, especially when changes – such as the inclusion of families in patient care – are not big money makers. Even so, in a competitive marketplace, hospitals are beginning to realize that patient and family satisfaction develops loyal customers.
When patients and families have a good experience, they are likely to return to the hospital and recommend the hospital to others. From a business perspective, it makes sense to develop family-oriented care in hospital specialty units such as the neonatal intensive care unit.
Involving families in the NICU also reduces the neonate’s length of stay (Nurs Adm Q. 2009 Jan-Mar;33[1]32-7).
COPE is a manualized intervention program comprising DVDs and a workbook.
The DVDs provide parents with educational information about the appearance and behavioral characteristics of their premature infants and about how they can participate in their infants’ care, meet their needs, enhance the quality of interaction with their infants, and facilitate their development.
The workbook skills-building activities assist parents in implementing the educational information (for example, learning how to read their infants’ awake states and stress cues, keeping track of important developmental milestones, determining what behaviors are helpful when their infants are stressed).
Parents listen to the COPE educational information on DVDs as they read it in their workbooks. The first intervention in COPE is delivered to the parents 2-4 days after the infant is admitted to the NICU. The second COPE intervention is delivered 2-4 days after the first intervention, and the third intervention is delivered to parents 1-4 days prior to the infant’s discharge from the NICU. Parents receive the fourth COPE intervention 1 week after the infant is discharged from the hospital. Each of the four DVDs has corresponding skills-building activities that parents complete after they listen to the educational information on the DVDs.
The problem
In NICUs, families are not the primary focus of care. To nursing staff, parents are an unknown factor. Parents may silence alarms or open cribs to touch the baby, not realizing that by doing so, they are dysregulating the neonate’s delicate environment. They see nurses moving things around, and so feel they should be able to do it, too. Parents come in many varieties. Some parents sit quietly and appear overwhelmed. Some parents behave erratically. Some parents may smell of alcohol or marijuana, putting everyone in the NICU on alert. Assessing and intervening with parents is helpful to nurses, reduces tension between nurse and parent, and ensures that the daily caring for the neonate is smooth and optimal. Nurses are eager to help with parents.
Nursing perspective
From the nurses’ perspective, the parents are not the patient! Nurses have not been trained to assess and manage distressed parents. Nurses can provide basic education about the baby’s medical condition but do not have time to explain the details that overanxious parents might demand. The nurses recognize that some parents are under severe stress and do not want to leave the bedside, even to care for their own needs. The nurses recognize that some parents have their own health conditions but are unsure how to approach this issue. Nurses welcome education about how to intervene and how to refer parents to appropriate resources.
Parental perspective
Parents are distressed and uncertain about the fate of their newborns. There is an immediate need to gain as much information as possible about the baby’s medical condition and to understand what the nurses are “doing to our baby.” There may be concern that the nurse seems more bonded to the baby than the parents. There may be a lack of understanding of when the babies can be handled and what and when they can be fed. There is significant emotional distress about “not being able to take the baby home.” Parents may want to assign blame or may feel overwhelmed with guilt. For families with poor coping skills, fear and anger may predominate and can be directed at the nurses – an immediate and ever available target. Generally, parents want to be included as much as possible in the care of their children.
Postpartum disorders in the NICU
It is expected that having a baby in the NICU is stressful. However, a meta-analysis of 38 studies of stress in parents of preterm infants, compared with term infants, found that parents of preterm children experience only slightly more stress than do parents of term children. There is decreasing parental stress from the 1980s onward, probably because of the increased quality of care for preterm infants. These studies included 3,025 parents of preterm and low-birth-weight infants (PLoS One 2013;8[2]:e54992).
Over the long term, the psychological functioning of NICU parents is no different from that of control parents. A prospective randomized controlled study defined psychological distress as meeting one or more of the following criteria: any psychiatric diagnosis on the Mini-International Neuropsychiatric Interview at 2 years; Edinburgh Postnatal Depression Scale score more than 12.5 at 2 years; Hospital Anxiety and Depression Scale score more than 11.0 at 2 years, receiving treatment with antidepressants/psychotherapy/counseling over the previous 15 months (Psychosomatics 2014;55[6]:613-20).
In the short term, NICU parents are at risk for postpartum depression (PPD) with the resultant difficulty in establishing good attachment with their babies. The prevalence of PPD in mothers of term newborns is 10%-15%, compared with 28%-70% among NICU mothers (Int J Womens Health. 2014;2014[6]:975-87).
Fathers are known as the forgotten parents and experience a high prevalence of depressive symptoms. Fathers of term newborns experience depression at rates of 2%-10%, but rates of up to 60% have been reported in NICU fathers (Adv Neonatal Care. 2010 Aug;10[4]:200-3).
Prevention of psychiatric illness in family members
The NICU environment is often dimly lighted, and improving lighting prevents depression in NICU mothers. A 3-week bright-light therapy intervention improved the sleep and health outcomes of NICU mothers, who experienced less morning fatigue and depressive symptoms, and improved quality of life, compared with the control group (Biol Res Nurs. 2013 Oct;15[4] 398-406). An architect on our team is designing “quiet spaces” for parents and creating more ambient light and daylighting in our NICU.
For parents who do not want to leave the NICU, mobile computer terminals can bring education to the bedside. For parents who can leave the bedside, family educational interventions are well received (Adv Neonatal Care. 2013 Apr;13[2]:115-26).
In current practice, in our labor and delivery suite and in many NICUs, mothers are screened for postpartum depression via the Edinburgh Postnatal Depression Scale (EPDS) (Br J Psychiatry 1987 Jun;150[6]:782-6). If mothers score over 13, they are referred for further assessment. Treatment often consists of referral for individual intervention for the mother (usually sertraline and disclosures/instructions about breastfeeding, as well as supportive psychotherapy).
What does family-centered care look like?
A family perspective supports the screening of both parents, using the EPDS. This can occur on admission of the baby to the NICU and at 2-week intervals thereafter and again at discharge (J Perinatol 2013 Oct;33[10]748-53). Ideally, family functioning also can be assessed, and if needed, intervention can be offered to the whole family system.
Family screening occurs in other pediatric medical settings. High-risk families can be identified with the Psychosocial Assessment Tool (PAT) (Acta Oncol. 2015 May;54[5]:574-80).
The PAT is a brief parent self-report composed of items that assess risk associated with the child, family, and broader systems. It is currently used at 50 sites in 28 states in the United States. The PAT has been translated into Spanish, Columbian Spanish, Dutch, Brazilian Portuguese, Hebrew, Greek, Polish, Italian, Japanese, Chinese, and Korean, and is used internationally. English adaptations for Canada, the United Kingdom, Australia, New Zealand, and Singapore also are available. It has been modified for use in NICUs.
The screening enables health care providers to refer families to the appropriate service: support groups (low risk), psychoeducation (medium risk), or intensive outpatient services (high risk). This stratification allows for the appropriate use of services.
Likewise, family interventions can be thought about in tiers, similar to the risk stratification of the PAT. Tier 1 is a universal educational intervention for all parents, tier 2 parents have higher needs, and tier 3 parents need immediate intervention. The following descriptions show how this might work in practice.
Family intervention: Tier 1
•All families can be given educational material about the mental health needs of parents with a newborn in the NICU. Ideally, this material can be provided through handouts, references for further reading, and through websites accessed in the NICU. For parents who are willing to leave the NICU, they can attend support groups.
•All parents can be screened at initial contact in the NICU and then on discharge from the NICU. If the neonate stays an extended time, the parents can be screened at 2-week intervals. A high score on the EPDS screen indicates an immediate need to refer a parent. A family assessment tool, such as the PAT, can identify high-risk families for immediate referral.
•NICU nursing staff can actively address coparenting struggles. Our NICU nurses provide formal letters between nurses and parents to establish the parameters of the care of the baby, and provide direction for coparenting.
Family intervention: Tier 2
Parents identified on the PAT as having higher needs can be enrolled in psychoeducational groups, led by staff members who have behavioral health training and experience.
Family intervention: Tier 3
These parents are identified on the PAT as high risk and need significant health care services. The NICU social worker can actively work on consultation with addiction medicine, mental health, or social services.
In summary, a family approach in the NICU improves nurse-parent interactions. A focus on coparenting sets the stage for cooperation, trust, and better family outcomes. Some basic training in systems concepts and family dynamics can provide NICU staff with basic clinical skills to provide psychoeducation. Adequate screening can triage high-risk parents appropriately. For NICUs that want to implement a psychoeducational program, Melnyk’s COPE program is an evidenced-based program that is well worth implementation.
Dr. Heru is with the department of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She thanks other members of the NICU team at the University of Colorado Hospital: Christy Math, Katherine Perica, and John J. White.
Hospitals are slow to change, especially when changes – such as the inclusion of families in patient care – are not big money makers. Even so, in a competitive marketplace, hospitals are beginning to realize that patient and family satisfaction develops loyal customers.
When patients and families have a good experience, they are likely to return to the hospital and recommend the hospital to others. From a business perspective, it makes sense to develop family-oriented care in hospital specialty units such as the neonatal intensive care unit.
Involving families in the NICU also reduces the neonate’s length of stay (Nurs Adm Q. 2009 Jan-Mar;33[1]32-7).
COPE is a manualized intervention program comprising DVDs and a workbook.
The DVDs provide parents with educational information about the appearance and behavioral characteristics of their premature infants and about how they can participate in their infants’ care, meet their needs, enhance the quality of interaction with their infants, and facilitate their development.
The workbook skills-building activities assist parents in implementing the educational information (for example, learning how to read their infants’ awake states and stress cues, keeping track of important developmental milestones, determining what behaviors are helpful when their infants are stressed).
Parents listen to the COPE educational information on DVDs as they read it in their workbooks. The first intervention in COPE is delivered to the parents 2-4 days after the infant is admitted to the NICU. The second COPE intervention is delivered 2-4 days after the first intervention, and the third intervention is delivered to parents 1-4 days prior to the infant’s discharge from the NICU. Parents receive the fourth COPE intervention 1 week after the infant is discharged from the hospital. Each of the four DVDs has corresponding skills-building activities that parents complete after they listen to the educational information on the DVDs.
The problem
In NICUs, families are not the primary focus of care. To nursing staff, parents are an unknown factor. Parents may silence alarms or open cribs to touch the baby, not realizing that by doing so, they are dysregulating the neonate’s delicate environment. They see nurses moving things around, and so feel they should be able to do it, too. Parents come in many varieties. Some parents sit quietly and appear overwhelmed. Some parents behave erratically. Some parents may smell of alcohol or marijuana, putting everyone in the NICU on alert. Assessing and intervening with parents is helpful to nurses, reduces tension between nurse and parent, and ensures that the daily caring for the neonate is smooth and optimal. Nurses are eager to help with parents.
Nursing perspective
From the nurses’ perspective, the parents are not the patient! Nurses have not been trained to assess and manage distressed parents. Nurses can provide basic education about the baby’s medical condition but do not have time to explain the details that overanxious parents might demand. The nurses recognize that some parents are under severe stress and do not want to leave the bedside, even to care for their own needs. The nurses recognize that some parents have their own health conditions but are unsure how to approach this issue. Nurses welcome education about how to intervene and how to refer parents to appropriate resources.
Parental perspective
Parents are distressed and uncertain about the fate of their newborns. There is an immediate need to gain as much information as possible about the baby’s medical condition and to understand what the nurses are “doing to our baby.” There may be concern that the nurse seems more bonded to the baby than the parents. There may be a lack of understanding of when the babies can be handled and what and when they can be fed. There is significant emotional distress about “not being able to take the baby home.” Parents may want to assign blame or may feel overwhelmed with guilt. For families with poor coping skills, fear and anger may predominate and can be directed at the nurses – an immediate and ever available target. Generally, parents want to be included as much as possible in the care of their children.
Postpartum disorders in the NICU
It is expected that having a baby in the NICU is stressful. However, a meta-analysis of 38 studies of stress in parents of preterm infants, compared with term infants, found that parents of preterm children experience only slightly more stress than do parents of term children. There is decreasing parental stress from the 1980s onward, probably because of the increased quality of care for preterm infants. These studies included 3,025 parents of preterm and low-birth-weight infants (PLoS One 2013;8[2]:e54992).
Over the long term, the psychological functioning of NICU parents is no different from that of control parents. A prospective randomized controlled study defined psychological distress as meeting one or more of the following criteria: any psychiatric diagnosis on the Mini-International Neuropsychiatric Interview at 2 years; Edinburgh Postnatal Depression Scale score more than 12.5 at 2 years; Hospital Anxiety and Depression Scale score more than 11.0 at 2 years, receiving treatment with antidepressants/psychotherapy/counseling over the previous 15 months (Psychosomatics 2014;55[6]:613-20).
In the short term, NICU parents are at risk for postpartum depression (PPD) with the resultant difficulty in establishing good attachment with their babies. The prevalence of PPD in mothers of term newborns is 10%-15%, compared with 28%-70% among NICU mothers (Int J Womens Health. 2014;2014[6]:975-87).
Fathers are known as the forgotten parents and experience a high prevalence of depressive symptoms. Fathers of term newborns experience depression at rates of 2%-10%, but rates of up to 60% have been reported in NICU fathers (Adv Neonatal Care. 2010 Aug;10[4]:200-3).
Prevention of psychiatric illness in family members
The NICU environment is often dimly lighted, and improving lighting prevents depression in NICU mothers. A 3-week bright-light therapy intervention improved the sleep and health outcomes of NICU mothers, who experienced less morning fatigue and depressive symptoms, and improved quality of life, compared with the control group (Biol Res Nurs. 2013 Oct;15[4] 398-406). An architect on our team is designing “quiet spaces” for parents and creating more ambient light and daylighting in our NICU.
For parents who do not want to leave the NICU, mobile computer terminals can bring education to the bedside. For parents who can leave the bedside, family educational interventions are well received (Adv Neonatal Care. 2013 Apr;13[2]:115-26).
In current practice, in our labor and delivery suite and in many NICUs, mothers are screened for postpartum depression via the Edinburgh Postnatal Depression Scale (EPDS) (Br J Psychiatry 1987 Jun;150[6]:782-6). If mothers score over 13, they are referred for further assessment. Treatment often consists of referral for individual intervention for the mother (usually sertraline and disclosures/instructions about breastfeeding, as well as supportive psychotherapy).
What does family-centered care look like?
A family perspective supports the screening of both parents, using the EPDS. This can occur on admission of the baby to the NICU and at 2-week intervals thereafter and again at discharge (J Perinatol 2013 Oct;33[10]748-53). Ideally, family functioning also can be assessed, and if needed, intervention can be offered to the whole family system.
Family screening occurs in other pediatric medical settings. High-risk families can be identified with the Psychosocial Assessment Tool (PAT) (Acta Oncol. 2015 May;54[5]:574-80).
The PAT is a brief parent self-report composed of items that assess risk associated with the child, family, and broader systems. It is currently used at 50 sites in 28 states in the United States. The PAT has been translated into Spanish, Columbian Spanish, Dutch, Brazilian Portuguese, Hebrew, Greek, Polish, Italian, Japanese, Chinese, and Korean, and is used internationally. English adaptations for Canada, the United Kingdom, Australia, New Zealand, and Singapore also are available. It has been modified for use in NICUs.
The screening enables health care providers to refer families to the appropriate service: support groups (low risk), psychoeducation (medium risk), or intensive outpatient services (high risk). This stratification allows for the appropriate use of services.
Likewise, family interventions can be thought about in tiers, similar to the risk stratification of the PAT. Tier 1 is a universal educational intervention for all parents, tier 2 parents have higher needs, and tier 3 parents need immediate intervention. The following descriptions show how this might work in practice.
Family intervention: Tier 1
•All families can be given educational material about the mental health needs of parents with a newborn in the NICU. Ideally, this material can be provided through handouts, references for further reading, and through websites accessed in the NICU. For parents who are willing to leave the NICU, they can attend support groups.
•All parents can be screened at initial contact in the NICU and then on discharge from the NICU. If the neonate stays an extended time, the parents can be screened at 2-week intervals. A high score on the EPDS screen indicates an immediate need to refer a parent. A family assessment tool, such as the PAT, can identify high-risk families for immediate referral.
•NICU nursing staff can actively address coparenting struggles. Our NICU nurses provide formal letters between nurses and parents to establish the parameters of the care of the baby, and provide direction for coparenting.
Family intervention: Tier 2
Parents identified on the PAT as having higher needs can be enrolled in psychoeducational groups, led by staff members who have behavioral health training and experience.
Family intervention: Tier 3
These parents are identified on the PAT as high risk and need significant health care services. The NICU social worker can actively work on consultation with addiction medicine, mental health, or social services.
In summary, a family approach in the NICU improves nurse-parent interactions. A focus on coparenting sets the stage for cooperation, trust, and better family outcomes. Some basic training in systems concepts and family dynamics can provide NICU staff with basic clinical skills to provide psychoeducation. Adequate screening can triage high-risk parents appropriately. For NICUs that want to implement a psychoeducational program, Melnyk’s COPE program is an evidenced-based program that is well worth implementation.
Dr. Heru is with the department of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She thanks other members of the NICU team at the University of Colorado Hospital: Christy Math, Katherine Perica, and John J. White.
Hospitals are slow to change, especially when changes – such as the inclusion of families in patient care – are not big money makers. Even so, in a competitive marketplace, hospitals are beginning to realize that patient and family satisfaction develops loyal customers.
When patients and families have a good experience, they are likely to return to the hospital and recommend the hospital to others. From a business perspective, it makes sense to develop family-oriented care in hospital specialty units such as the neonatal intensive care unit.
Involving families in the NICU also reduces the neonate’s length of stay (Nurs Adm Q. 2009 Jan-Mar;33[1]32-7).
COPE is a manualized intervention program comprising DVDs and a workbook.
The DVDs provide parents with educational information about the appearance and behavioral characteristics of their premature infants and about how they can participate in their infants’ care, meet their needs, enhance the quality of interaction with their infants, and facilitate their development.
The workbook skills-building activities assist parents in implementing the educational information (for example, learning how to read their infants’ awake states and stress cues, keeping track of important developmental milestones, determining what behaviors are helpful when their infants are stressed).
Parents listen to the COPE educational information on DVDs as they read it in their workbooks. The first intervention in COPE is delivered to the parents 2-4 days after the infant is admitted to the NICU. The second COPE intervention is delivered 2-4 days after the first intervention, and the third intervention is delivered to parents 1-4 days prior to the infant’s discharge from the NICU. Parents receive the fourth COPE intervention 1 week after the infant is discharged from the hospital. Each of the four DVDs has corresponding skills-building activities that parents complete after they listen to the educational information on the DVDs.
The problem
In NICUs, families are not the primary focus of care. To nursing staff, parents are an unknown factor. Parents may silence alarms or open cribs to touch the baby, not realizing that by doing so, they are dysregulating the neonate’s delicate environment. They see nurses moving things around, and so feel they should be able to do it, too. Parents come in many varieties. Some parents sit quietly and appear overwhelmed. Some parents behave erratically. Some parents may smell of alcohol or marijuana, putting everyone in the NICU on alert. Assessing and intervening with parents is helpful to nurses, reduces tension between nurse and parent, and ensures that the daily caring for the neonate is smooth and optimal. Nurses are eager to help with parents.
Nursing perspective
From the nurses’ perspective, the parents are not the patient! Nurses have not been trained to assess and manage distressed parents. Nurses can provide basic education about the baby’s medical condition but do not have time to explain the details that overanxious parents might demand. The nurses recognize that some parents are under severe stress and do not want to leave the bedside, even to care for their own needs. The nurses recognize that some parents have their own health conditions but are unsure how to approach this issue. Nurses welcome education about how to intervene and how to refer parents to appropriate resources.
Parental perspective
Parents are distressed and uncertain about the fate of their newborns. There is an immediate need to gain as much information as possible about the baby’s medical condition and to understand what the nurses are “doing to our baby.” There may be concern that the nurse seems more bonded to the baby than the parents. There may be a lack of understanding of when the babies can be handled and what and when they can be fed. There is significant emotional distress about “not being able to take the baby home.” Parents may want to assign blame or may feel overwhelmed with guilt. For families with poor coping skills, fear and anger may predominate and can be directed at the nurses – an immediate and ever available target. Generally, parents want to be included as much as possible in the care of their children.
Postpartum disorders in the NICU
It is expected that having a baby in the NICU is stressful. However, a meta-analysis of 38 studies of stress in parents of preterm infants, compared with term infants, found that parents of preterm children experience only slightly more stress than do parents of term children. There is decreasing parental stress from the 1980s onward, probably because of the increased quality of care for preterm infants. These studies included 3,025 parents of preterm and low-birth-weight infants (PLoS One 2013;8[2]:e54992).
Over the long term, the psychological functioning of NICU parents is no different from that of control parents. A prospective randomized controlled study defined psychological distress as meeting one or more of the following criteria: any psychiatric diagnosis on the Mini-International Neuropsychiatric Interview at 2 years; Edinburgh Postnatal Depression Scale score more than 12.5 at 2 years; Hospital Anxiety and Depression Scale score more than 11.0 at 2 years, receiving treatment with antidepressants/psychotherapy/counseling over the previous 15 months (Psychosomatics 2014;55[6]:613-20).
In the short term, NICU parents are at risk for postpartum depression (PPD) with the resultant difficulty in establishing good attachment with their babies. The prevalence of PPD in mothers of term newborns is 10%-15%, compared with 28%-70% among NICU mothers (Int J Womens Health. 2014;2014[6]:975-87).
Fathers are known as the forgotten parents and experience a high prevalence of depressive symptoms. Fathers of term newborns experience depression at rates of 2%-10%, but rates of up to 60% have been reported in NICU fathers (Adv Neonatal Care. 2010 Aug;10[4]:200-3).
Prevention of psychiatric illness in family members
The NICU environment is often dimly lighted, and improving lighting prevents depression in NICU mothers. A 3-week bright-light therapy intervention improved the sleep and health outcomes of NICU mothers, who experienced less morning fatigue and depressive symptoms, and improved quality of life, compared with the control group (Biol Res Nurs. 2013 Oct;15[4] 398-406). An architect on our team is designing “quiet spaces” for parents and creating more ambient light and daylighting in our NICU.
For parents who do not want to leave the NICU, mobile computer terminals can bring education to the bedside. For parents who can leave the bedside, family educational interventions are well received (Adv Neonatal Care. 2013 Apr;13[2]:115-26).
In current practice, in our labor and delivery suite and in many NICUs, mothers are screened for postpartum depression via the Edinburgh Postnatal Depression Scale (EPDS) (Br J Psychiatry 1987 Jun;150[6]:782-6). If mothers score over 13, they are referred for further assessment. Treatment often consists of referral for individual intervention for the mother (usually sertraline and disclosures/instructions about breastfeeding, as well as supportive psychotherapy).
What does family-centered care look like?
A family perspective supports the screening of both parents, using the EPDS. This can occur on admission of the baby to the NICU and at 2-week intervals thereafter and again at discharge (J Perinatol 2013 Oct;33[10]748-53). Ideally, family functioning also can be assessed, and if needed, intervention can be offered to the whole family system.
Family screening occurs in other pediatric medical settings. High-risk families can be identified with the Psychosocial Assessment Tool (PAT) (Acta Oncol. 2015 May;54[5]:574-80).
The PAT is a brief parent self-report composed of items that assess risk associated with the child, family, and broader systems. It is currently used at 50 sites in 28 states in the United States. The PAT has been translated into Spanish, Columbian Spanish, Dutch, Brazilian Portuguese, Hebrew, Greek, Polish, Italian, Japanese, Chinese, and Korean, and is used internationally. English adaptations for Canada, the United Kingdom, Australia, New Zealand, and Singapore also are available. It has been modified for use in NICUs.
The screening enables health care providers to refer families to the appropriate service: support groups (low risk), psychoeducation (medium risk), or intensive outpatient services (high risk). This stratification allows for the appropriate use of services.
Likewise, family interventions can be thought about in tiers, similar to the risk stratification of the PAT. Tier 1 is a universal educational intervention for all parents, tier 2 parents have higher needs, and tier 3 parents need immediate intervention. The following descriptions show how this might work in practice.
Family intervention: Tier 1
•All families can be given educational material about the mental health needs of parents with a newborn in the NICU. Ideally, this material can be provided through handouts, references for further reading, and through websites accessed in the NICU. For parents who are willing to leave the NICU, they can attend support groups.
•All parents can be screened at initial contact in the NICU and then on discharge from the NICU. If the neonate stays an extended time, the parents can be screened at 2-week intervals. A high score on the EPDS screen indicates an immediate need to refer a parent. A family assessment tool, such as the PAT, can identify high-risk families for immediate referral.
•NICU nursing staff can actively address coparenting struggles. Our NICU nurses provide formal letters between nurses and parents to establish the parameters of the care of the baby, and provide direction for coparenting.
Family intervention: Tier 2
Parents identified on the PAT as having higher needs can be enrolled in psychoeducational groups, led by staff members who have behavioral health training and experience.
Family intervention: Tier 3
These parents are identified on the PAT as high risk and need significant health care services. The NICU social worker can actively work on consultation with addiction medicine, mental health, or social services.
In summary, a family approach in the NICU improves nurse-parent interactions. A focus on coparenting sets the stage for cooperation, trust, and better family outcomes. Some basic training in systems concepts and family dynamics can provide NICU staff with basic clinical skills to provide psychoeducation. Adequate screening can triage high-risk parents appropriately. For NICUs that want to implement a psychoeducational program, Melnyk’s COPE program is an evidenced-based program that is well worth implementation.
Dr. Heru is with the department of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She thanks other members of the NICU team at the University of Colorado Hospital: Christy Math, Katherine Perica, and John J. White.
OpenNotes: Transparency in health care
Transparency, until recently, was rarely associated with health care. Not anymore. For better and sometimes worse, there is a revolutionary movement toward transparency in all facets of health care: transparency of costs, outcomes, quality, service, and reputation. Full transparency has now come to medical records in the form of OpenNotes. This is a patient-centered initiative that allows patients full access to their charts, including all their doctors’ notes.
Patients have always had the right to see their records. Ordinarily though, they would be required to go to the medical records office, fill out paperwork, and request copies of their charts. They’d have to supply a reason and usually pay a fee. OpenNotes changes that. Open patient charts are free and easy to access, usually digitally. OpenNotes programs are still rare, and before we go any further, it’s important to examine what we’ve learned about them.
In 2010, Beth Israel Deaconess Medical Center in Boston, Geisinger Health System in Pennsylvania, and Harborview Medical Center in Seattle invited 105 primary care physicians to open their notes to nearly 14,000 patients. The results were overwhelmingly (and to me, surprisingly) positive: More than 85% of patients accessed their notes at least once. Nearly 100% of patients wanted the program to continue. Patients reported a better understanding of their medical issues, better medication adherence, increased adoption of healthy habits, and less anxiety about their health. I would have expected more confusion and anxiety among the patients.
What about the physicians? According to the initiative, whereas 1 in 3 patients thought they should have unfettered access to their physicians’ notes, only 1 in 10 physicians did. That’s understandable. The physicians in the pilot shared many of the same concerns you and I have, namely that OpenNotes would lead to an increased workload to explain esoteric notes to patients and to allay anxieties.
Yet, this extra workload didn’t occur. Only 3% of physicians reported spending more time answering patients’ questions. One-fifth did report that they changed the language they used when writing notes, primarily to avoid offending patients. Every physician in the initiative said he or she would continue using OpenNotes. Surprised? So was I.
Even the usually conservative SERMO physician audience responded in an unexpected manner. According to a poll conducted this June, SERMO asked 2,300 physicians if patients should have access to their medical records (including MD notes). Forty-nine percent said “only on a case-by-case basis,” 34% said “yes, always,” and 17% said “no, never.”
So, are OpenNotes a success? Let’s take a closer look at some of the challenges: First, we physicians use language that will confuse patients at best and lead them to incorrect conclusions at worst. “Acne necrotica?” Sounds like a case of medieval pimples, but actually it’s pretty harmless. Or consider, “Differential diagnosis includes neuroendocrine tumor.” It doesn’t mean you have it, but some patients will believe they do. Will we have to dumb down our charts then to appease them? Won’t this degrade note quality, one of the primary objectives we are trying to avoid? It’s unclear.
The purpose of a patient note is to inform other providers and to remind ourselves of the critical information needed to care for a patient. It must be pithy and honest. It often reflects our inchoate thoughts as much as our diagnoses. It must also include the sundry requirements we know and love that are needed only to bill for the visit. These are not characteristics that make for a good patient read.
Indeed, the benefits of transparency are not limitless. In some instances, more transparency is worse. Imagine if all your emails and texts were transparent to everyone. Or if everything you’ve ever said about your mother-in-law were viewable by her. That would clearly be a case of bad transparency. Not sharing everything doesn’t mean we are dishonest or duplicitous. It means we are civil. It doesn’t mean we don’t care; it means we do care. We care about our friends and family. We care about our patients and the best way to make them well.
Unless we make it clear to patients that the notes they are viewing are not written for them, I’m worried simply opening charts could damage the doctor-patient relationship as much as it fosters it. Interestingly, there are companies trying to build a technical solution for this conundrum. Others are advocating for standardization of pathology and lab reports that are patient friendly. I’ll research these topics and let you know what I find out in a future column.
Perhaps I shouldn’t have been surprised by the positive results from the OpenNotes initiative. After all, for the last several years, I have given patients their actual pathology report for every biopsy I’ve done (which numbers in the many thousands). I have had fewer than five follow-up questions from patients that I can remember. Pretty much all were legitimate, as I recall, including a wrong site error in a report.
Today, more than 5 million patients have access to their providers’ notes on OpenNotes. That number will grow. Our biggest risk is to not be involved. “Just say no” didn’t work for Nancy Reagan; it won’t do our cause any good either.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter.
Transparency, until recently, was rarely associated with health care. Not anymore. For better and sometimes worse, there is a revolutionary movement toward transparency in all facets of health care: transparency of costs, outcomes, quality, service, and reputation. Full transparency has now come to medical records in the form of OpenNotes. This is a patient-centered initiative that allows patients full access to their charts, including all their doctors’ notes.
Patients have always had the right to see their records. Ordinarily though, they would be required to go to the medical records office, fill out paperwork, and request copies of their charts. They’d have to supply a reason and usually pay a fee. OpenNotes changes that. Open patient charts are free and easy to access, usually digitally. OpenNotes programs are still rare, and before we go any further, it’s important to examine what we’ve learned about them.
In 2010, Beth Israel Deaconess Medical Center in Boston, Geisinger Health System in Pennsylvania, and Harborview Medical Center in Seattle invited 105 primary care physicians to open their notes to nearly 14,000 patients. The results were overwhelmingly (and to me, surprisingly) positive: More than 85% of patients accessed their notes at least once. Nearly 100% of patients wanted the program to continue. Patients reported a better understanding of their medical issues, better medication adherence, increased adoption of healthy habits, and less anxiety about their health. I would have expected more confusion and anxiety among the patients.
What about the physicians? According to the initiative, whereas 1 in 3 patients thought they should have unfettered access to their physicians’ notes, only 1 in 10 physicians did. That’s understandable. The physicians in the pilot shared many of the same concerns you and I have, namely that OpenNotes would lead to an increased workload to explain esoteric notes to patients and to allay anxieties.
Yet, this extra workload didn’t occur. Only 3% of physicians reported spending more time answering patients’ questions. One-fifth did report that they changed the language they used when writing notes, primarily to avoid offending patients. Every physician in the initiative said he or she would continue using OpenNotes. Surprised? So was I.
Even the usually conservative SERMO physician audience responded in an unexpected manner. According to a poll conducted this June, SERMO asked 2,300 physicians if patients should have access to their medical records (including MD notes). Forty-nine percent said “only on a case-by-case basis,” 34% said “yes, always,” and 17% said “no, never.”
So, are OpenNotes a success? Let’s take a closer look at some of the challenges: First, we physicians use language that will confuse patients at best and lead them to incorrect conclusions at worst. “Acne necrotica?” Sounds like a case of medieval pimples, but actually it’s pretty harmless. Or consider, “Differential diagnosis includes neuroendocrine tumor.” It doesn’t mean you have it, but some patients will believe they do. Will we have to dumb down our charts then to appease them? Won’t this degrade note quality, one of the primary objectives we are trying to avoid? It’s unclear.
The purpose of a patient note is to inform other providers and to remind ourselves of the critical information needed to care for a patient. It must be pithy and honest. It often reflects our inchoate thoughts as much as our diagnoses. It must also include the sundry requirements we know and love that are needed only to bill for the visit. These are not characteristics that make for a good patient read.
Indeed, the benefits of transparency are not limitless. In some instances, more transparency is worse. Imagine if all your emails and texts were transparent to everyone. Or if everything you’ve ever said about your mother-in-law were viewable by her. That would clearly be a case of bad transparency. Not sharing everything doesn’t mean we are dishonest or duplicitous. It means we are civil. It doesn’t mean we don’t care; it means we do care. We care about our friends and family. We care about our patients and the best way to make them well.
Unless we make it clear to patients that the notes they are viewing are not written for them, I’m worried simply opening charts could damage the doctor-patient relationship as much as it fosters it. Interestingly, there are companies trying to build a technical solution for this conundrum. Others are advocating for standardization of pathology and lab reports that are patient friendly. I’ll research these topics and let you know what I find out in a future column.
Perhaps I shouldn’t have been surprised by the positive results from the OpenNotes initiative. After all, for the last several years, I have given patients their actual pathology report for every biopsy I’ve done (which numbers in the many thousands). I have had fewer than five follow-up questions from patients that I can remember. Pretty much all were legitimate, as I recall, including a wrong site error in a report.
Today, more than 5 million patients have access to their providers’ notes on OpenNotes. That number will grow. Our biggest risk is to not be involved. “Just say no” didn’t work for Nancy Reagan; it won’t do our cause any good either.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter.
Transparency, until recently, was rarely associated with health care. Not anymore. For better and sometimes worse, there is a revolutionary movement toward transparency in all facets of health care: transparency of costs, outcomes, quality, service, and reputation. Full transparency has now come to medical records in the form of OpenNotes. This is a patient-centered initiative that allows patients full access to their charts, including all their doctors’ notes.
Patients have always had the right to see their records. Ordinarily though, they would be required to go to the medical records office, fill out paperwork, and request copies of their charts. They’d have to supply a reason and usually pay a fee. OpenNotes changes that. Open patient charts are free and easy to access, usually digitally. OpenNotes programs are still rare, and before we go any further, it’s important to examine what we’ve learned about them.
In 2010, Beth Israel Deaconess Medical Center in Boston, Geisinger Health System in Pennsylvania, and Harborview Medical Center in Seattle invited 105 primary care physicians to open their notes to nearly 14,000 patients. The results were overwhelmingly (and to me, surprisingly) positive: More than 85% of patients accessed their notes at least once. Nearly 100% of patients wanted the program to continue. Patients reported a better understanding of their medical issues, better medication adherence, increased adoption of healthy habits, and less anxiety about their health. I would have expected more confusion and anxiety among the patients.
What about the physicians? According to the initiative, whereas 1 in 3 patients thought they should have unfettered access to their physicians’ notes, only 1 in 10 physicians did. That’s understandable. The physicians in the pilot shared many of the same concerns you and I have, namely that OpenNotes would lead to an increased workload to explain esoteric notes to patients and to allay anxieties.
Yet, this extra workload didn’t occur. Only 3% of physicians reported spending more time answering patients’ questions. One-fifth did report that they changed the language they used when writing notes, primarily to avoid offending patients. Every physician in the initiative said he or she would continue using OpenNotes. Surprised? So was I.
Even the usually conservative SERMO physician audience responded in an unexpected manner. According to a poll conducted this June, SERMO asked 2,300 physicians if patients should have access to their medical records (including MD notes). Forty-nine percent said “only on a case-by-case basis,” 34% said “yes, always,” and 17% said “no, never.”
So, are OpenNotes a success? Let’s take a closer look at some of the challenges: First, we physicians use language that will confuse patients at best and lead them to incorrect conclusions at worst. “Acne necrotica?” Sounds like a case of medieval pimples, but actually it’s pretty harmless. Or consider, “Differential diagnosis includes neuroendocrine tumor.” It doesn’t mean you have it, but some patients will believe they do. Will we have to dumb down our charts then to appease them? Won’t this degrade note quality, one of the primary objectives we are trying to avoid? It’s unclear.
The purpose of a patient note is to inform other providers and to remind ourselves of the critical information needed to care for a patient. It must be pithy and honest. It often reflects our inchoate thoughts as much as our diagnoses. It must also include the sundry requirements we know and love that are needed only to bill for the visit. These are not characteristics that make for a good patient read.
Indeed, the benefits of transparency are not limitless. In some instances, more transparency is worse. Imagine if all your emails and texts were transparent to everyone. Or if everything you’ve ever said about your mother-in-law were viewable by her. That would clearly be a case of bad transparency. Not sharing everything doesn’t mean we are dishonest or duplicitous. It means we are civil. It doesn’t mean we don’t care; it means we do care. We care about our friends and family. We care about our patients and the best way to make them well.
Unless we make it clear to patients that the notes they are viewing are not written for them, I’m worried simply opening charts could damage the doctor-patient relationship as much as it fosters it. Interestingly, there are companies trying to build a technical solution for this conundrum. Others are advocating for standardization of pathology and lab reports that are patient friendly. I’ll research these topics and let you know what I find out in a future column.
Perhaps I shouldn’t have been surprised by the positive results from the OpenNotes initiative. After all, for the last several years, I have given patients their actual pathology report for every biopsy I’ve done (which numbers in the many thousands). I have had fewer than five follow-up questions from patients that I can remember. Pretty much all were legitimate, as I recall, including a wrong site error in a report.
Today, more than 5 million patients have access to their providers’ notes on OpenNotes. That number will grow. Our biggest risk is to not be involved. “Just say no” didn’t work for Nancy Reagan; it won’t do our cause any good either.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @dermdoc on Twitter.