User login
Groups draft guidelines for acute leukemia

Photo courtesy of the CDC
The American Society of Hematology (ASH) and the College of American Pathologists (CAP) have opened a public comment period for a draft guideline that addresses the initial work-up of acute leukemia.
The guideline details the information required for the diagnosis of acute leukemias, as well as recommended testing and how test results and diagnosis should be correlated.
The document will be available for comment through August 31.
The guideline authors examined evidence from more than 170 articles to devise the draft guidelines. The resulting document answers the following questions:
- What clinical and laboratory information should be available during the initial diagnostic evaluation of a patient with acute leukemia?
- What specimens and sample types should be evaluated during the initial work-up of a patient with acute leukemia?
- At the time of diagnosis, what tests are required for all patients for the initial evaluation of an acute leukemia?
- What tests should be performed only on a subset of patients, including in response to results of initial tests and morphology?
- Where should testing be performed?
- How should test results and the diagnosis be correlated and reported?
“Evidence-based guidelines like these are increasingly vital to the continued improvement and continuity of patient care,” said ASH guideline co-chair James W. Vardiman, MD, of the University of Chicago in Illinois.
He and Daniel A. Arber, MD, of Stanford School of Medicine in California, (the CAP representative co-chair) are leading an interdisciplinary team of 8 physicians representing sub-specialties that include hematopathology and oncology.
“Our work on these guidelines aims at integrating the very best practices to improve outcomes for [acute leukemia] patients and their families,” Dr Arber said.
At the close of the comment period, the CAP/ASH team will review any comments and make final recommendations, which are targeted for publication in the first quarter of 2016. ![]()

Photo courtesy of the CDC
The American Society of Hematology (ASH) and the College of American Pathologists (CAP) have opened a public comment period for a draft guideline that addresses the initial work-up of acute leukemia.
The guideline details the information required for the diagnosis of acute leukemias, as well as recommended testing and how test results and diagnosis should be correlated.
The document will be available for comment through August 31.
The guideline authors examined evidence from more than 170 articles to devise the draft guidelines. The resulting document answers the following questions:
- What clinical and laboratory information should be available during the initial diagnostic evaluation of a patient with acute leukemia?
- What specimens and sample types should be evaluated during the initial work-up of a patient with acute leukemia?
- At the time of diagnosis, what tests are required for all patients for the initial evaluation of an acute leukemia?
- What tests should be performed only on a subset of patients, including in response to results of initial tests and morphology?
- Where should testing be performed?
- How should test results and the diagnosis be correlated and reported?
“Evidence-based guidelines like these are increasingly vital to the continued improvement and continuity of patient care,” said ASH guideline co-chair James W. Vardiman, MD, of the University of Chicago in Illinois.
He and Daniel A. Arber, MD, of Stanford School of Medicine in California, (the CAP representative co-chair) are leading an interdisciplinary team of 8 physicians representing sub-specialties that include hematopathology and oncology.
“Our work on these guidelines aims at integrating the very best practices to improve outcomes for [acute leukemia] patients and their families,” Dr Arber said.
At the close of the comment period, the CAP/ASH team will review any comments and make final recommendations, which are targeted for publication in the first quarter of 2016. ![]()

Photo courtesy of the CDC
The American Society of Hematology (ASH) and the College of American Pathologists (CAP) have opened a public comment period for a draft guideline that addresses the initial work-up of acute leukemia.
The guideline details the information required for the diagnosis of acute leukemias, as well as recommended testing and how test results and diagnosis should be correlated.
The document will be available for comment through August 31.
The guideline authors examined evidence from more than 170 articles to devise the draft guidelines. The resulting document answers the following questions:
- What clinical and laboratory information should be available during the initial diagnostic evaluation of a patient with acute leukemia?
- What specimens and sample types should be evaluated during the initial work-up of a patient with acute leukemia?
- At the time of diagnosis, what tests are required for all patients for the initial evaluation of an acute leukemia?
- What tests should be performed only on a subset of patients, including in response to results of initial tests and morphology?
- Where should testing be performed?
- How should test results and the diagnosis be correlated and reported?
“Evidence-based guidelines like these are increasingly vital to the continued improvement and continuity of patient care,” said ASH guideline co-chair James W. Vardiman, MD, of the University of Chicago in Illinois.
He and Daniel A. Arber, MD, of Stanford School of Medicine in California, (the CAP representative co-chair) are leading an interdisciplinary team of 8 physicians representing sub-specialties that include hematopathology and oncology.
“Our work on these guidelines aims at integrating the very best practices to improve outcomes for [acute leukemia] patients and their families,” Dr Arber said.
At the close of the comment period, the CAP/ASH team will review any comments and make final recommendations, which are targeted for publication in the first quarter of 2016. ![]()
Mutations may contribute to CTCL

mycosis fungoides
Researchers have identified 15 mutations that may drive cutaneous T-cell lymphoma (CTCL).
The team sequenced normal and cancerous samples from 73 patients with mycosis fungoides or Sézary syndrome.
This revealed recurrent alterations in the TNFR2 pathway, as well as mutations in phosphoinositide 3-kinase (PI3K)-related genes, NF-κB pathway genes, and other genes that regulate T-cell survival and proliferation.
Specifically, the researchers identified TNFRSF1B point mutations, TNFRSF1B gains, CTLA4-CD28 fusions, a TRAF3 deletion, and mutations in NFAT5, TEC, PIK3CD, PIK3R6, PIK3CG, PIK3R5, PIK3R4, VAV1, MALT1, CD28, and ITK.
Paul Khavari, MD, PhD, of Stanford University in California, and his colleagues conducted this research and described their findings in a letter to Nature Genetics.
TNFR2 mutations
The researchers noted that the most frequent recurrent point mutation they identified occurred at codon 377 of TNFRSF1B (5%; 4/73), resulting in a recurrent TNFR2 Thr377Ile mutant.
TNFR2 is a receptor that regulates T-cell signaling pathways, and the mutation locked the receptor into an always-on state, preventing the T-cell-survival pathway from shutting down.
Previous studies showed that patients with increased TNFR2 in their bloodstream had more aggressive forms of CTCL that were more likely to return quickly after treatment.
This led Dr Khavari and his colleagues to look at the other patients’ DNA to see if duplications could account for both the elevated levels in the blood and increased signaling to activate the T-cell-survival pathway. The team found that 10 of the patients had TNFRSF1B gains.
In total, TNFRSF1B was altered in 18% of patients (13/73), by point mutation or gain (both in 1 patient). The researchers said this suggests a potential role of oncogenic TNFR2 signaling in the development of CTCL.
The team uncovered evidence to support this role by growing cells in the lab with either the point mutation or the gain. Their experiment showed the T-cell-survival pathway was more active in these cells than in normal cells.
Now, the researchers are working to incorporate the mutations they identified into the DNA of mice to study the mutated genes’ effects and the actions of drugs on those genes. ![]()

mycosis fungoides
Researchers have identified 15 mutations that may drive cutaneous T-cell lymphoma (CTCL).
The team sequenced normal and cancerous samples from 73 patients with mycosis fungoides or Sézary syndrome.
This revealed recurrent alterations in the TNFR2 pathway, as well as mutations in phosphoinositide 3-kinase (PI3K)-related genes, NF-κB pathway genes, and other genes that regulate T-cell survival and proliferation.
Specifically, the researchers identified TNFRSF1B point mutations, TNFRSF1B gains, CTLA4-CD28 fusions, a TRAF3 deletion, and mutations in NFAT5, TEC, PIK3CD, PIK3R6, PIK3CG, PIK3R5, PIK3R4, VAV1, MALT1, CD28, and ITK.
Paul Khavari, MD, PhD, of Stanford University in California, and his colleagues conducted this research and described their findings in a letter to Nature Genetics.
TNFR2 mutations
The researchers noted that the most frequent recurrent point mutation they identified occurred at codon 377 of TNFRSF1B (5%; 4/73), resulting in a recurrent TNFR2 Thr377Ile mutant.
TNFR2 is a receptor that regulates T-cell signaling pathways, and the mutation locked the receptor into an always-on state, preventing the T-cell-survival pathway from shutting down.
Previous studies showed that patients with increased TNFR2 in their bloodstream had more aggressive forms of CTCL that were more likely to return quickly after treatment.
This led Dr Khavari and his colleagues to look at the other patients’ DNA to see if duplications could account for both the elevated levels in the blood and increased signaling to activate the T-cell-survival pathway. The team found that 10 of the patients had TNFRSF1B gains.
In total, TNFRSF1B was altered in 18% of patients (13/73), by point mutation or gain (both in 1 patient). The researchers said this suggests a potential role of oncogenic TNFR2 signaling in the development of CTCL.
The team uncovered evidence to support this role by growing cells in the lab with either the point mutation or the gain. Their experiment showed the T-cell-survival pathway was more active in these cells than in normal cells.
Now, the researchers are working to incorporate the mutations they identified into the DNA of mice to study the mutated genes’ effects and the actions of drugs on those genes. ![]()

mycosis fungoides
Researchers have identified 15 mutations that may drive cutaneous T-cell lymphoma (CTCL).
The team sequenced normal and cancerous samples from 73 patients with mycosis fungoides or Sézary syndrome.
This revealed recurrent alterations in the TNFR2 pathway, as well as mutations in phosphoinositide 3-kinase (PI3K)-related genes, NF-κB pathway genes, and other genes that regulate T-cell survival and proliferation.
Specifically, the researchers identified TNFRSF1B point mutations, TNFRSF1B gains, CTLA4-CD28 fusions, a TRAF3 deletion, and mutations in NFAT5, TEC, PIK3CD, PIK3R6, PIK3CG, PIK3R5, PIK3R4, VAV1, MALT1, CD28, and ITK.
Paul Khavari, MD, PhD, of Stanford University in California, and his colleagues conducted this research and described their findings in a letter to Nature Genetics.
TNFR2 mutations
The researchers noted that the most frequent recurrent point mutation they identified occurred at codon 377 of TNFRSF1B (5%; 4/73), resulting in a recurrent TNFR2 Thr377Ile mutant.
TNFR2 is a receptor that regulates T-cell signaling pathways, and the mutation locked the receptor into an always-on state, preventing the T-cell-survival pathway from shutting down.
Previous studies showed that patients with increased TNFR2 in their bloodstream had more aggressive forms of CTCL that were more likely to return quickly after treatment.
This led Dr Khavari and his colleagues to look at the other patients’ DNA to see if duplications could account for both the elevated levels in the blood and increased signaling to activate the T-cell-survival pathway. The team found that 10 of the patients had TNFRSF1B gains.
In total, TNFRSF1B was altered in 18% of patients (13/73), by point mutation or gain (both in 1 patient). The researchers said this suggests a potential role of oncogenic TNFR2 signaling in the development of CTCL.
The team uncovered evidence to support this role by growing cells in the lab with either the point mutation or the gain. Their experiment showed the T-cell-survival pathway was more active in these cells than in normal cells.
Now, the researchers are working to incorporate the mutations they identified into the DNA of mice to study the mutated genes’ effects and the actions of drugs on those genes. ![]()
Selinexor dose lowered due to sepsis in AML patients

Photo by Esther Dyson
An excess of sepsis cases has prompted dose reductions in a phase 2 trial of selinexor in older patients with relapsed/refractory acute myeloid leukemia (AML).
For this study, known as SOPRA, researchers are comparing selinexor to physician’s choice of treatment in AML patients age 60 and older.
There have only been 8 cases of sepsis in the selinexor arm thus far, but this is more than observed in the physician’s
choice arm.
So the company developing selinexor, Karyopharm Therapeutics Inc., said it has reduced the selinexor dose used in this study.
The company decided to reduce the dose from 55 mg/m2 to a fixed dose of 60 mg, which corresponds to approximately 35 mg/m2. Dosing will remain twice weekly.
The change was implemented based on ongoing safety and tolerability evaluations in the SOPRA study, as well as maturing data from AML patients in the phase 1, first-in-human trial of selinexor.
The SOPRA study uses a 2 to 1 randomization of AML patients to selinexor or physician’s choice and, therefore, approximately twice as many cases of sepsis would be expected on the selinexor arm compared with the physician’s choice arm.
As of the end of July 2015, there have been 8 reports of sepsis in 7 patients receiving selinexor at 55 mg/m2, compared with 2 reports of sepsis in 2 patients receiving physician’s choice.
Karyopharm pointed out that these numbers are small, and sepsis is often observed in patients with AML, but the incidence of sepsis appears to be higher in the patients receiving selinexor.
In addition, the company noted an apparent increase in the incidence of sepsis in patients with relapsed or refractory AML receiving high doses of selinexor twice weekly in the phase 1 trial of patients with hematologic malignancies.
Karyopharm said selinexor doses of 60 mg twice weekly do not appear to be associated with any increase in sepsis or other infection-related events in patients with hematologic malignancies or solid tumors.
In addition, most patients with AML in the phase 1 study who showed a response to selinexor, including complete responses, received the drug at doses of approximately 60 mg or lower.
As a result of the change in dose, the SOPRA study will now have an interim assessment in mid-2016.
Karyopharm is actively enrolling patients in the SOPRA study, as well as a study of selinexor in patients with relapsed/refractory diffuse large B-cell lymphoma (SADAL trial), and a study of the drug in patients with Richter’s transformation (SIRRT trial).
Preliminary top-line data from all 3 studies are anticipated in the fourth quarter of 2016.
The company has also initiated a single-arm trial of selinexor plus dexamethasone in patients with multiple myeloma (STORM trial), which will initially include 80 patients. Preliminary top-line data from this study are anticipated in mid-2016. ![]()

Photo by Esther Dyson
An excess of sepsis cases has prompted dose reductions in a phase 2 trial of selinexor in older patients with relapsed/refractory acute myeloid leukemia (AML).
For this study, known as SOPRA, researchers are comparing selinexor to physician’s choice of treatment in AML patients age 60 and older.
There have only been 8 cases of sepsis in the selinexor arm thus far, but this is more than observed in the physician’s
choice arm.
So the company developing selinexor, Karyopharm Therapeutics Inc., said it has reduced the selinexor dose used in this study.
The company decided to reduce the dose from 55 mg/m2 to a fixed dose of 60 mg, which corresponds to approximately 35 mg/m2. Dosing will remain twice weekly.
The change was implemented based on ongoing safety and tolerability evaluations in the SOPRA study, as well as maturing data from AML patients in the phase 1, first-in-human trial of selinexor.
The SOPRA study uses a 2 to 1 randomization of AML patients to selinexor or physician’s choice and, therefore, approximately twice as many cases of sepsis would be expected on the selinexor arm compared with the physician’s choice arm.
As of the end of July 2015, there have been 8 reports of sepsis in 7 patients receiving selinexor at 55 mg/m2, compared with 2 reports of sepsis in 2 patients receiving physician’s choice.
Karyopharm pointed out that these numbers are small, and sepsis is often observed in patients with AML, but the incidence of sepsis appears to be higher in the patients receiving selinexor.
In addition, the company noted an apparent increase in the incidence of sepsis in patients with relapsed or refractory AML receiving high doses of selinexor twice weekly in the phase 1 trial of patients with hematologic malignancies.
Karyopharm said selinexor doses of 60 mg twice weekly do not appear to be associated with any increase in sepsis or other infection-related events in patients with hematologic malignancies or solid tumors.
In addition, most patients with AML in the phase 1 study who showed a response to selinexor, including complete responses, received the drug at doses of approximately 60 mg or lower.
As a result of the change in dose, the SOPRA study will now have an interim assessment in mid-2016.
Karyopharm is actively enrolling patients in the SOPRA study, as well as a study of selinexor in patients with relapsed/refractory diffuse large B-cell lymphoma (SADAL trial), and a study of the drug in patients with Richter’s transformation (SIRRT trial).
Preliminary top-line data from all 3 studies are anticipated in the fourth quarter of 2016.
The company has also initiated a single-arm trial of selinexor plus dexamethasone in patients with multiple myeloma (STORM trial), which will initially include 80 patients. Preliminary top-line data from this study are anticipated in mid-2016. ![]()

Photo by Esther Dyson
An excess of sepsis cases has prompted dose reductions in a phase 2 trial of selinexor in older patients with relapsed/refractory acute myeloid leukemia (AML).
For this study, known as SOPRA, researchers are comparing selinexor to physician’s choice of treatment in AML patients age 60 and older.
There have only been 8 cases of sepsis in the selinexor arm thus far, but this is more than observed in the physician’s
choice arm.
So the company developing selinexor, Karyopharm Therapeutics Inc., said it has reduced the selinexor dose used in this study.
The company decided to reduce the dose from 55 mg/m2 to a fixed dose of 60 mg, which corresponds to approximately 35 mg/m2. Dosing will remain twice weekly.
The change was implemented based on ongoing safety and tolerability evaluations in the SOPRA study, as well as maturing data from AML patients in the phase 1, first-in-human trial of selinexor.
The SOPRA study uses a 2 to 1 randomization of AML patients to selinexor or physician’s choice and, therefore, approximately twice as many cases of sepsis would be expected on the selinexor arm compared with the physician’s choice arm.
As of the end of July 2015, there have been 8 reports of sepsis in 7 patients receiving selinexor at 55 mg/m2, compared with 2 reports of sepsis in 2 patients receiving physician’s choice.
Karyopharm pointed out that these numbers are small, and sepsis is often observed in patients with AML, but the incidence of sepsis appears to be higher in the patients receiving selinexor.
In addition, the company noted an apparent increase in the incidence of sepsis in patients with relapsed or refractory AML receiving high doses of selinexor twice weekly in the phase 1 trial of patients with hematologic malignancies.
Karyopharm said selinexor doses of 60 mg twice weekly do not appear to be associated with any increase in sepsis or other infection-related events in patients with hematologic malignancies or solid tumors.
In addition, most patients with AML in the phase 1 study who showed a response to selinexor, including complete responses, received the drug at doses of approximately 60 mg or lower.
As a result of the change in dose, the SOPRA study will now have an interim assessment in mid-2016.
Karyopharm is actively enrolling patients in the SOPRA study, as well as a study of selinexor in patients with relapsed/refractory diffuse large B-cell lymphoma (SADAL trial), and a study of the drug in patients with Richter’s transformation (SIRRT trial).
Preliminary top-line data from all 3 studies are anticipated in the fourth quarter of 2016.
The company has also initiated a single-arm trial of selinexor plus dexamethasone in patients with multiple myeloma (STORM trial), which will initially include 80 patients. Preliminary top-line data from this study are anticipated in mid-2016. ![]()
Yet another insurer demand: patient care notifications
Some insurance companies recently started sending notifications about patient care. For example, one recently sent my boss a letter about one of his patients with rheumatoid arthritis, asking why the patient is not on a disease modifier. There is an invitation to explain why by ticking any one of several boxes. Is the patient perhaps not compliant? Did the patient discontinue the medication against the doctor’s advice? Has the patient passed away? Does the patient not have rheumatoid arthritis?
Oh, to be a fly on the wall when the insurance company decided that they would start doing this! This must impose a financial burden on the insurer, one that I cannot imagine they take on out of sheer altruism. What is the end game? What do they do with this information? Will they hold this information against the patient somehow, raise their premium in the next enrollment period? Or hold it against the physician, perhaps ding their reimbursement or use the information to include or exclude physicians from their panels?
When I decided to come to the United States, one of the biggest draws was the availability of health insurance. Most of my medical school education came from American textbooks, after all, so I thought it would be fabulous to be able to practice medicine the way it should be practiced because insurance will pay for it. (I know I sound like your elderly aunt that likes to repeat herself, but if you have not read any of my columns before, I come from the Philippines where health care is mostly paid for out of pocket, so how we treated patients was severely limited by how much the patient could afford.) I was wrong. I had no idea that part of my job description would include having to ask a corporate entity’s permission to administer treatments.
My boss replied to the letter. He said: “Patient is on dialysis and cannot be on methotrexate. He was prescribed a biologic, but your insurance does not cover its cost sufficiently to make it affordable. We had obtained the biologic through foundation support, but they ran out of money. So when you send out a letter like this blaming either the patient or MD for a compliance issue, I urge you to do some soul-searching.”
Dr. Chan practices rheumatology in Pawtucket, R.I.
Some insurance companies recently started sending notifications about patient care. For example, one recently sent my boss a letter about one of his patients with rheumatoid arthritis, asking why the patient is not on a disease modifier. There is an invitation to explain why by ticking any one of several boxes. Is the patient perhaps not compliant? Did the patient discontinue the medication against the doctor’s advice? Has the patient passed away? Does the patient not have rheumatoid arthritis?
Oh, to be a fly on the wall when the insurance company decided that they would start doing this! This must impose a financial burden on the insurer, one that I cannot imagine they take on out of sheer altruism. What is the end game? What do they do with this information? Will they hold this information against the patient somehow, raise their premium in the next enrollment period? Or hold it against the physician, perhaps ding their reimbursement or use the information to include or exclude physicians from their panels?
When I decided to come to the United States, one of the biggest draws was the availability of health insurance. Most of my medical school education came from American textbooks, after all, so I thought it would be fabulous to be able to practice medicine the way it should be practiced because insurance will pay for it. (I know I sound like your elderly aunt that likes to repeat herself, but if you have not read any of my columns before, I come from the Philippines where health care is mostly paid for out of pocket, so how we treated patients was severely limited by how much the patient could afford.) I was wrong. I had no idea that part of my job description would include having to ask a corporate entity’s permission to administer treatments.
My boss replied to the letter. He said: “Patient is on dialysis and cannot be on methotrexate. He was prescribed a biologic, but your insurance does not cover its cost sufficiently to make it affordable. We had obtained the biologic through foundation support, but they ran out of money. So when you send out a letter like this blaming either the patient or MD for a compliance issue, I urge you to do some soul-searching.”
Dr. Chan practices rheumatology in Pawtucket, R.I.
Some insurance companies recently started sending notifications about patient care. For example, one recently sent my boss a letter about one of his patients with rheumatoid arthritis, asking why the patient is not on a disease modifier. There is an invitation to explain why by ticking any one of several boxes. Is the patient perhaps not compliant? Did the patient discontinue the medication against the doctor’s advice? Has the patient passed away? Does the patient not have rheumatoid arthritis?
Oh, to be a fly on the wall when the insurance company decided that they would start doing this! This must impose a financial burden on the insurer, one that I cannot imagine they take on out of sheer altruism. What is the end game? What do they do with this information? Will they hold this information against the patient somehow, raise their premium in the next enrollment period? Or hold it against the physician, perhaps ding their reimbursement or use the information to include or exclude physicians from their panels?
When I decided to come to the United States, one of the biggest draws was the availability of health insurance. Most of my medical school education came from American textbooks, after all, so I thought it would be fabulous to be able to practice medicine the way it should be practiced because insurance will pay for it. (I know I sound like your elderly aunt that likes to repeat herself, but if you have not read any of my columns before, I come from the Philippines where health care is mostly paid for out of pocket, so how we treated patients was severely limited by how much the patient could afford.) I was wrong. I had no idea that part of my job description would include having to ask a corporate entity’s permission to administer treatments.
My boss replied to the letter. He said: “Patient is on dialysis and cannot be on methotrexate. He was prescribed a biologic, but your insurance does not cover its cost sufficiently to make it affordable. We had obtained the biologic through foundation support, but they ran out of money. So when you send out a letter like this blaming either the patient or MD for a compliance issue, I urge you to do some soul-searching.”
Dr. Chan practices rheumatology in Pawtucket, R.I.
Linear Scleroderma Associated With Neurofibromatosis Type I
To the Editor:
A 12-year-old girl presented with an asymptomatic hypopigmented area on the right cheek of 2 months’ duration. Two years prior to presentation she was diagnosed with neurofibromatosis type I (NF1) based on the findings of 13 café au lait spots on the trunk, axillary and groin freckling, bilateral Lisch nodules, and mild scoliosis. She was otherwise well and had no relevant medical history or family history of neurofibromatosis.
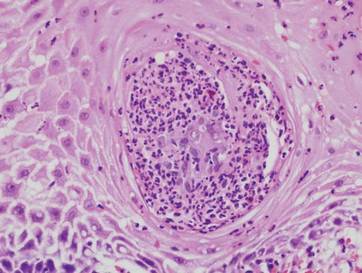
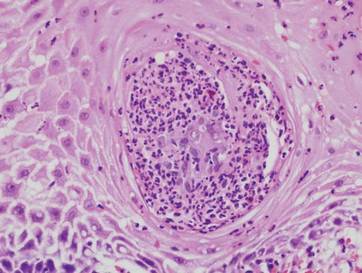
Physical examination revealed a 3×7-cm linear, shiny, sclerotic plaque extending from the right temple to the preauricular area and lower aspect of the right cheek (Figure 1) with associated facial asymmetry (Figure 2). A smaller similar plaque on the chin measured 0.5×0.5 cm. Examination of the oral cavity was unremarkable and there were no neurological signs. No other features were present to suggest a mixed connective tissue disease or lupus erythematosus, and nuclear antibodies were negative.

| 
|
An incisional biopsy from the sclerotic plaque revealed swollen eosinophilic bundles in the reticular dermis with a moderate perivascular lymphohistiocytic infiltrate extending into the subcutaneous layer. These features were compatible with the diagnosis of linear scleroderma. Due to the progressive nature of the condition and its anatomical location, she was treated with pulsed intravenous methylprednisolone 1 g daily for 3 days and commenced on oral methotrexate 20 mg weekly as well as tacrolimus ointment 0.1% daily. The plaque gradually softened and faded over a period of 8 months. The patient continued on methotrexate for another 10 months. The facial asymmetry persisted with a discernible reduction in the volume of the right cheek. New onset of ipsilateral jaw locking and pain associated with spasms of the muscles of mastication suggested the diagnosis of Parry-Romberg syndrome.
Neurofibromatosis type I is a neuroectodermal abnormality first described by Friedrich von Recklinghausen in 1882 with an incidence of 1 in 3000 births. Neurofibromatosis type I gene mutations lead to increased Ras activity, which is implicated in many NF1-related conditions such as neurofibromas and schwannomas.1 Autoimmune conditions including systemic lupus erythematosus (SLE) and mixed connective tissue rarely have been reported in NF1, but the mechanism of their association is not clear.2 Based on a review of 5 reported cases of NF1 and SLE, most patients were female, and the predominant features of NF1 were café au lait macules and neurofibromas.3-6 One case documented a family history of NF1,6 suggesting predominance of sporadic mutations in these cases. Interestingly, in 3 cases the diagnosis of SLE preceded the diagnosis of NF1, prompting the authors to suggest a viral trigger for the development of NF1 lesions.3,4 Linear scleroderma is immunologically mediated and is characterized by the onset of smooth indurated cutaneous plaques. According to a PubMed search of articles indexed for MEDLINE using the search terms morphea and neurofibromatosis as well as linear scleroderma and neurofibromatosis, there have been no reports of linear scleroderma or morphea associated with NF1. Cichowski et al7 demonstrated enhanced activation of Ras and prolonged activities of both Ras and extracellular signal-regulated kinase (ERK) signaling pathways in NF1-deficient mice. Chen et al8 showed that heparin sulfate–dependent ERK activation contributes to the development of scleroderma by promoting the expression of profibrotic proteins in scleroderma fibroblasts. It was previously noted that increased Ras/ERK signaling activities were important in connective tissue growth factor expression in normal mesenchymal cells.9
Based on these findings, we speculated that hyperactivation of Ras/ERK signaling from NF1 mutations could lead to the promotion of fibrosis seen in scleroderma. The lack of similar reports, however, suggests that the presence of both conditions in this case is coincidental. However, the growing number of reports on autoimmune and connective tissue disorders in NF1 reflects the need for further research in this area.
1. Harrisingh MC, Lloyd AC. Ras/Raf/ERK signalling and NF1. Cell Cycle. 2004;3:1255-1258.
2. Migita K, Kawabe Y, Mori M, et al. Mixed connective tissue disease associated with von Recklinghausen’s neurofibromatosis. Intern Med. 2001;40:363-364.
3. Bitnun S, Bassan H. Letter: neurofibromatosis and SLE. N Engl J Med. 1975;292:429-430.
4. Riccardi VM. Neurofibromatosis in a patient with systemic lupus erythematosus. Arthritis Rheum. 1983;26:574.
5. Corominas H, Guardiola JM, Matas L, et al. Neurofibromatosis and systemic lupus erythematosus. A matter of coincidence? Clin Rheum. 2003;22:496-497.
6. Akyüz SG, Çatlik A, Bülbül M, et al. An unusual pediatric case with neurofibromatosis and systemic lupus erythematosus. Rheum Int. 2012;32:2345-2347.
7. Cichowski K, Santiago S, Jardim M, et al. Dynamic regulation of the Ras pathway via proteolysis of the NF1 tumour suppressor. Genes Dev. 2003;17:449-454.
8. Chen Y, Leask A, Abraham DJ, et al. Heparan sulfate-dependent ERK activation contributes to the overexpression of fibrotic proteins and enhanced contraction by scleroderma fibroblasts. Arthritis Rheum. 2008;58:577-585.
9. Chen Y, Shi-wen X, van Beek J, et al. Matrix contraction by dermal fibroblasts requiring transforming growth factor-â/activin-linked kinase 5, heparin sulphate-containing proteoglycans and MEK/ERK: insights into pathological scarring in chronic fibrotic disease. Am J Pathol. 2005;167:1699-1711.
To the Editor:
A 12-year-old girl presented with an asymptomatic hypopigmented area on the right cheek of 2 months’ duration. Two years prior to presentation she was diagnosed with neurofibromatosis type I (NF1) based on the findings of 13 café au lait spots on the trunk, axillary and groin freckling, bilateral Lisch nodules, and mild scoliosis. She was otherwise well and had no relevant medical history or family history of neurofibromatosis.
Physical examination revealed a 3×7-cm linear, shiny, sclerotic plaque extending from the right temple to the preauricular area and lower aspect of the right cheek (Figure 1) with associated facial asymmetry (Figure 2). A smaller similar plaque on the chin measured 0.5×0.5 cm. Examination of the oral cavity was unremarkable and there were no neurological signs. No other features were present to suggest a mixed connective tissue disease or lupus erythematosus, and nuclear antibodies were negative.

| 
|
An incisional biopsy from the sclerotic plaque revealed swollen eosinophilic bundles in the reticular dermis with a moderate perivascular lymphohistiocytic infiltrate extending into the subcutaneous layer. These features were compatible with the diagnosis of linear scleroderma. Due to the progressive nature of the condition and its anatomical location, she was treated with pulsed intravenous methylprednisolone 1 g daily for 3 days and commenced on oral methotrexate 20 mg weekly as well as tacrolimus ointment 0.1% daily. The plaque gradually softened and faded over a period of 8 months. The patient continued on methotrexate for another 10 months. The facial asymmetry persisted with a discernible reduction in the volume of the right cheek. New onset of ipsilateral jaw locking and pain associated with spasms of the muscles of mastication suggested the diagnosis of Parry-Romberg syndrome.
Neurofibromatosis type I is a neuroectodermal abnormality first described by Friedrich von Recklinghausen in 1882 with an incidence of 1 in 3000 births. Neurofibromatosis type I gene mutations lead to increased Ras activity, which is implicated in many NF1-related conditions such as neurofibromas and schwannomas.1 Autoimmune conditions including systemic lupus erythematosus (SLE) and mixed connective tissue rarely have been reported in NF1, but the mechanism of their association is not clear.2 Based on a review of 5 reported cases of NF1 and SLE, most patients were female, and the predominant features of NF1 were café au lait macules and neurofibromas.3-6 One case documented a family history of NF1,6 suggesting predominance of sporadic mutations in these cases. Interestingly, in 3 cases the diagnosis of SLE preceded the diagnosis of NF1, prompting the authors to suggest a viral trigger for the development of NF1 lesions.3,4 Linear scleroderma is immunologically mediated and is characterized by the onset of smooth indurated cutaneous plaques. According to a PubMed search of articles indexed for MEDLINE using the search terms morphea and neurofibromatosis as well as linear scleroderma and neurofibromatosis, there have been no reports of linear scleroderma or morphea associated with NF1. Cichowski et al7 demonstrated enhanced activation of Ras and prolonged activities of both Ras and extracellular signal-regulated kinase (ERK) signaling pathways in NF1-deficient mice. Chen et al8 showed that heparin sulfate–dependent ERK activation contributes to the development of scleroderma by promoting the expression of profibrotic proteins in scleroderma fibroblasts. It was previously noted that increased Ras/ERK signaling activities were important in connective tissue growth factor expression in normal mesenchymal cells.9
Based on these findings, we speculated that hyperactivation of Ras/ERK signaling from NF1 mutations could lead to the promotion of fibrosis seen in scleroderma. The lack of similar reports, however, suggests that the presence of both conditions in this case is coincidental. However, the growing number of reports on autoimmune and connective tissue disorders in NF1 reflects the need for further research in this area.
To the Editor:
A 12-year-old girl presented with an asymptomatic hypopigmented area on the right cheek of 2 months’ duration. Two years prior to presentation she was diagnosed with neurofibromatosis type I (NF1) based on the findings of 13 café au lait spots on the trunk, axillary and groin freckling, bilateral Lisch nodules, and mild scoliosis. She was otherwise well and had no relevant medical history or family history of neurofibromatosis.
Physical examination revealed a 3×7-cm linear, shiny, sclerotic plaque extending from the right temple to the preauricular area and lower aspect of the right cheek (Figure 1) with associated facial asymmetry (Figure 2). A smaller similar plaque on the chin measured 0.5×0.5 cm. Examination of the oral cavity was unremarkable and there were no neurological signs. No other features were present to suggest a mixed connective tissue disease or lupus erythematosus, and nuclear antibodies were negative.

| 
|
An incisional biopsy from the sclerotic plaque revealed swollen eosinophilic bundles in the reticular dermis with a moderate perivascular lymphohistiocytic infiltrate extending into the subcutaneous layer. These features were compatible with the diagnosis of linear scleroderma. Due to the progressive nature of the condition and its anatomical location, she was treated with pulsed intravenous methylprednisolone 1 g daily for 3 days and commenced on oral methotrexate 20 mg weekly as well as tacrolimus ointment 0.1% daily. The plaque gradually softened and faded over a period of 8 months. The patient continued on methotrexate for another 10 months. The facial asymmetry persisted with a discernible reduction in the volume of the right cheek. New onset of ipsilateral jaw locking and pain associated with spasms of the muscles of mastication suggested the diagnosis of Parry-Romberg syndrome.
Neurofibromatosis type I is a neuroectodermal abnormality first described by Friedrich von Recklinghausen in 1882 with an incidence of 1 in 3000 births. Neurofibromatosis type I gene mutations lead to increased Ras activity, which is implicated in many NF1-related conditions such as neurofibromas and schwannomas.1 Autoimmune conditions including systemic lupus erythematosus (SLE) and mixed connective tissue rarely have been reported in NF1, but the mechanism of their association is not clear.2 Based on a review of 5 reported cases of NF1 and SLE, most patients were female, and the predominant features of NF1 were café au lait macules and neurofibromas.3-6 One case documented a family history of NF1,6 suggesting predominance of sporadic mutations in these cases. Interestingly, in 3 cases the diagnosis of SLE preceded the diagnosis of NF1, prompting the authors to suggest a viral trigger for the development of NF1 lesions.3,4 Linear scleroderma is immunologically mediated and is characterized by the onset of smooth indurated cutaneous plaques. According to a PubMed search of articles indexed for MEDLINE using the search terms morphea and neurofibromatosis as well as linear scleroderma and neurofibromatosis, there have been no reports of linear scleroderma or morphea associated with NF1. Cichowski et al7 demonstrated enhanced activation of Ras and prolonged activities of both Ras and extracellular signal-regulated kinase (ERK) signaling pathways in NF1-deficient mice. Chen et al8 showed that heparin sulfate–dependent ERK activation contributes to the development of scleroderma by promoting the expression of profibrotic proteins in scleroderma fibroblasts. It was previously noted that increased Ras/ERK signaling activities were important in connective tissue growth factor expression in normal mesenchymal cells.9
Based on these findings, we speculated that hyperactivation of Ras/ERK signaling from NF1 mutations could lead to the promotion of fibrosis seen in scleroderma. The lack of similar reports, however, suggests that the presence of both conditions in this case is coincidental. However, the growing number of reports on autoimmune and connective tissue disorders in NF1 reflects the need for further research in this area.
1. Harrisingh MC, Lloyd AC. Ras/Raf/ERK signalling and NF1. Cell Cycle. 2004;3:1255-1258.
2. Migita K, Kawabe Y, Mori M, et al. Mixed connective tissue disease associated with von Recklinghausen’s neurofibromatosis. Intern Med. 2001;40:363-364.
3. Bitnun S, Bassan H. Letter: neurofibromatosis and SLE. N Engl J Med. 1975;292:429-430.
4. Riccardi VM. Neurofibromatosis in a patient with systemic lupus erythematosus. Arthritis Rheum. 1983;26:574.
5. Corominas H, Guardiola JM, Matas L, et al. Neurofibromatosis and systemic lupus erythematosus. A matter of coincidence? Clin Rheum. 2003;22:496-497.
6. Akyüz SG, Çatlik A, Bülbül M, et al. An unusual pediatric case with neurofibromatosis and systemic lupus erythematosus. Rheum Int. 2012;32:2345-2347.
7. Cichowski K, Santiago S, Jardim M, et al. Dynamic regulation of the Ras pathway via proteolysis of the NF1 tumour suppressor. Genes Dev. 2003;17:449-454.
8. Chen Y, Leask A, Abraham DJ, et al. Heparan sulfate-dependent ERK activation contributes to the overexpression of fibrotic proteins and enhanced contraction by scleroderma fibroblasts. Arthritis Rheum. 2008;58:577-585.
9. Chen Y, Shi-wen X, van Beek J, et al. Matrix contraction by dermal fibroblasts requiring transforming growth factor-â/activin-linked kinase 5, heparin sulphate-containing proteoglycans and MEK/ERK: insights into pathological scarring in chronic fibrotic disease. Am J Pathol. 2005;167:1699-1711.
1. Harrisingh MC, Lloyd AC. Ras/Raf/ERK signalling and NF1. Cell Cycle. 2004;3:1255-1258.
2. Migita K, Kawabe Y, Mori M, et al. Mixed connective tissue disease associated with von Recklinghausen’s neurofibromatosis. Intern Med. 2001;40:363-364.
3. Bitnun S, Bassan H. Letter: neurofibromatosis and SLE. N Engl J Med. 1975;292:429-430.
4. Riccardi VM. Neurofibromatosis in a patient with systemic lupus erythematosus. Arthritis Rheum. 1983;26:574.
5. Corominas H, Guardiola JM, Matas L, et al. Neurofibromatosis and systemic lupus erythematosus. A matter of coincidence? Clin Rheum. 2003;22:496-497.
6. Akyüz SG, Çatlik A, Bülbül M, et al. An unusual pediatric case with neurofibromatosis and systemic lupus erythematosus. Rheum Int. 2012;32:2345-2347.
7. Cichowski K, Santiago S, Jardim M, et al. Dynamic regulation of the Ras pathway via proteolysis of the NF1 tumour suppressor. Genes Dev. 2003;17:449-454.
8. Chen Y, Leask A, Abraham DJ, et al. Heparan sulfate-dependent ERK activation contributes to the overexpression of fibrotic proteins and enhanced contraction by scleroderma fibroblasts. Arthritis Rheum. 2008;58:577-585.
9. Chen Y, Shi-wen X, van Beek J, et al. Matrix contraction by dermal fibroblasts requiring transforming growth factor-â/activin-linked kinase 5, heparin sulphate-containing proteoglycans and MEK/ERK: insights into pathological scarring in chronic fibrotic disease. Am J Pathol. 2005;167:1699-1711.
Stopping intergenerational cycles of trauma
Understanding the root of stress and trauma experienced by patients as individuals is a key charge of psychiatry. But patients also can experience psychological distress because of the traumatic experiences of previous generations. The mental health community must be prepared to treat patients who fall into the latter category.
My colleagues and I recently analyzed representative samples of First Nations adults and youth living on a reserve in Canada. We found that the number of previous generations in which families were forced to attend Indian residential schools was cumulatively linked with higher levels of psychological distress and suicidal ideation among those who did not attend themselves (Transcultural Psychiatry. 2014, 51:320-338).
The forced removal of Indigenous children from their homes for the purposes of assimilation occurred over generations in many countries around the world. In Canada, these government-mandated church-run residential schools ran from the mid-1800s until 1996, and resulted in generations of indigenous children being exposed to chronic neglect, abuse, trauma, racism, and cultural shaming (“Honouring the Truth: Reconciling for the Future,” Truth and Reconciliation Commission of Canada, 2015).
Some of our more recent analyses revealed that having a family history of residential school attendance has been linked to a greater likelihood of early-onset mental health symptoms, which in turn, has been tied to an increased risk of suicidality and other unique outcomes that have implications for treatment and prevention. Furthermore, other negative outcomes experienced by indigenous peoples, such as low family income and limited educational opportunities, also appear to be involved in the intergenerational transmission of residential school trauma.
Against this backdrop in Canada, we have a prevailing sense of blaming the victim that is counterproductive to healing. According to a 2014 report by the Royal Canadian Mounted Police (RCMP), 1,017 indigenous women and girls were murdered between 1980 and 2012 across Canada. About one-third of the women died as a result of physical beating, and more than 90% of the victims had a “previous relationship” with the person who killed them, according to the RCMP report. Yet, despite evidence to the contrary, the prime minister of Canada shared his view last year that those staggering numbers should be viewed as a criminal issue and not a “sociological phenomenon” (CBC News, Aug. 21, 2014).
Members of other groups whose previous generations also were exposed indirectly to unspeakable trauma include Americans of African descent, Native Americans, and adult offspring of Holocaust survivors. Rachel Yehuda, Ph.D., has studied the latter group extensively.
In one study, Dr. Yehuda and her associates found significantly reduced cortisol excretion in Holocaust offspring, compared with controls (Psychoneuroendocrinology. 2014 Oct;48:1-10). In another study of the adult offspring of Holocaust survivors, Dr. Yehuda, professor of psychiatry at the Icahn School of Medicine at Mount Sinai in New York, found that “offspring with paternal [posttraumatic stress disorder] showed higher GR-1F promoter methylation, whereas offspring with both maternal and paternal PTSD showed lower methylation.” Furthermore, lower methylation was tied to greater suppression of cortisol (Am J Psychiatry. 2014 Aug;171(8)872-880).
An appreciation for the power of epigenetics, or “soul wounds,” can help us stop blaming indigenous and other traumatized populations, and start tending to their mental health needs. Furthermore, getting individuals to understand these concepts can be yet another step on the path toward healing.
A study of 19 staff members and clients in a Native American healing lodge who began a discourse on the legacy of historical trauma found that counselors understood that their clients carried pain “leading to adult dysfunction, including substance abuse” (J Consult Clin Psychol. 2009 Aug;77(4):751-762). Second, the counselors believed that the pain needed to be confessed. Third, the counselors thought that expressing the pain would help the clients become more introspective. Finally, the process included reclaiming “indigenous heritage, identity, and spirituality that program staff thought would neutralize the pathogenic effects of colonization.”
We do not know the extent to which epigenetics are involved in specific diseases. Epigenetic mechanisms have not yet been tested as pathways involved in the intergenerational transmission of trauma in indigenous peoples. But Dr. Yehuda’s work with the children of Holocaust survivors shows that these mechanisms do indeed exist.
In light of what we do understand and the DSM-5’s emphasis on cultural competency, mental health professionals have a role to play in reversing the negative intergenerational cycles experienced by people across the globe. Only when we start paying attention to the plight of indigenous peoples across the globe will true healing begin.
Dr. Bombay is assistant professor of psychiatry at Dalhousie University, Halifax, N.S.
Understanding the root of stress and trauma experienced by patients as individuals is a key charge of psychiatry. But patients also can experience psychological distress because of the traumatic experiences of previous generations. The mental health community must be prepared to treat patients who fall into the latter category.
My colleagues and I recently analyzed representative samples of First Nations adults and youth living on a reserve in Canada. We found that the number of previous generations in which families were forced to attend Indian residential schools was cumulatively linked with higher levels of psychological distress and suicidal ideation among those who did not attend themselves (Transcultural Psychiatry. 2014, 51:320-338).
The forced removal of Indigenous children from their homes for the purposes of assimilation occurred over generations in many countries around the world. In Canada, these government-mandated church-run residential schools ran from the mid-1800s until 1996, and resulted in generations of indigenous children being exposed to chronic neglect, abuse, trauma, racism, and cultural shaming (“Honouring the Truth: Reconciling for the Future,” Truth and Reconciliation Commission of Canada, 2015).
Some of our more recent analyses revealed that having a family history of residential school attendance has been linked to a greater likelihood of early-onset mental health symptoms, which in turn, has been tied to an increased risk of suicidality and other unique outcomes that have implications for treatment and prevention. Furthermore, other negative outcomes experienced by indigenous peoples, such as low family income and limited educational opportunities, also appear to be involved in the intergenerational transmission of residential school trauma.
Against this backdrop in Canada, we have a prevailing sense of blaming the victim that is counterproductive to healing. According to a 2014 report by the Royal Canadian Mounted Police (RCMP), 1,017 indigenous women and girls were murdered between 1980 and 2012 across Canada. About one-third of the women died as a result of physical beating, and more than 90% of the victims had a “previous relationship” with the person who killed them, according to the RCMP report. Yet, despite evidence to the contrary, the prime minister of Canada shared his view last year that those staggering numbers should be viewed as a criminal issue and not a “sociological phenomenon” (CBC News, Aug. 21, 2014).
Members of other groups whose previous generations also were exposed indirectly to unspeakable trauma include Americans of African descent, Native Americans, and adult offspring of Holocaust survivors. Rachel Yehuda, Ph.D., has studied the latter group extensively.
In one study, Dr. Yehuda and her associates found significantly reduced cortisol excretion in Holocaust offspring, compared with controls (Psychoneuroendocrinology. 2014 Oct;48:1-10). In another study of the adult offspring of Holocaust survivors, Dr. Yehuda, professor of psychiatry at the Icahn School of Medicine at Mount Sinai in New York, found that “offspring with paternal [posttraumatic stress disorder] showed higher GR-1F promoter methylation, whereas offspring with both maternal and paternal PTSD showed lower methylation.” Furthermore, lower methylation was tied to greater suppression of cortisol (Am J Psychiatry. 2014 Aug;171(8)872-880).
An appreciation for the power of epigenetics, or “soul wounds,” can help us stop blaming indigenous and other traumatized populations, and start tending to their mental health needs. Furthermore, getting individuals to understand these concepts can be yet another step on the path toward healing.
A study of 19 staff members and clients in a Native American healing lodge who began a discourse on the legacy of historical trauma found that counselors understood that their clients carried pain “leading to adult dysfunction, including substance abuse” (J Consult Clin Psychol. 2009 Aug;77(4):751-762). Second, the counselors believed that the pain needed to be confessed. Third, the counselors thought that expressing the pain would help the clients become more introspective. Finally, the process included reclaiming “indigenous heritage, identity, and spirituality that program staff thought would neutralize the pathogenic effects of colonization.”
We do not know the extent to which epigenetics are involved in specific diseases. Epigenetic mechanisms have not yet been tested as pathways involved in the intergenerational transmission of trauma in indigenous peoples. But Dr. Yehuda’s work with the children of Holocaust survivors shows that these mechanisms do indeed exist.
In light of what we do understand and the DSM-5’s emphasis on cultural competency, mental health professionals have a role to play in reversing the negative intergenerational cycles experienced by people across the globe. Only when we start paying attention to the plight of indigenous peoples across the globe will true healing begin.
Dr. Bombay is assistant professor of psychiatry at Dalhousie University, Halifax, N.S.
Understanding the root of stress and trauma experienced by patients as individuals is a key charge of psychiatry. But patients also can experience psychological distress because of the traumatic experiences of previous generations. The mental health community must be prepared to treat patients who fall into the latter category.
My colleagues and I recently analyzed representative samples of First Nations adults and youth living on a reserve in Canada. We found that the number of previous generations in which families were forced to attend Indian residential schools was cumulatively linked with higher levels of psychological distress and suicidal ideation among those who did not attend themselves (Transcultural Psychiatry. 2014, 51:320-338).
The forced removal of Indigenous children from their homes for the purposes of assimilation occurred over generations in many countries around the world. In Canada, these government-mandated church-run residential schools ran from the mid-1800s until 1996, and resulted in generations of indigenous children being exposed to chronic neglect, abuse, trauma, racism, and cultural shaming (“Honouring the Truth: Reconciling for the Future,” Truth and Reconciliation Commission of Canada, 2015).
Some of our more recent analyses revealed that having a family history of residential school attendance has been linked to a greater likelihood of early-onset mental health symptoms, which in turn, has been tied to an increased risk of suicidality and other unique outcomes that have implications for treatment and prevention. Furthermore, other negative outcomes experienced by indigenous peoples, such as low family income and limited educational opportunities, also appear to be involved in the intergenerational transmission of residential school trauma.
Against this backdrop in Canada, we have a prevailing sense of blaming the victim that is counterproductive to healing. According to a 2014 report by the Royal Canadian Mounted Police (RCMP), 1,017 indigenous women and girls were murdered between 1980 and 2012 across Canada. About one-third of the women died as a result of physical beating, and more than 90% of the victims had a “previous relationship” with the person who killed them, according to the RCMP report. Yet, despite evidence to the contrary, the prime minister of Canada shared his view last year that those staggering numbers should be viewed as a criminal issue and not a “sociological phenomenon” (CBC News, Aug. 21, 2014).
Members of other groups whose previous generations also were exposed indirectly to unspeakable trauma include Americans of African descent, Native Americans, and adult offspring of Holocaust survivors. Rachel Yehuda, Ph.D., has studied the latter group extensively.
In one study, Dr. Yehuda and her associates found significantly reduced cortisol excretion in Holocaust offspring, compared with controls (Psychoneuroendocrinology. 2014 Oct;48:1-10). In another study of the adult offspring of Holocaust survivors, Dr. Yehuda, professor of psychiatry at the Icahn School of Medicine at Mount Sinai in New York, found that “offspring with paternal [posttraumatic stress disorder] showed higher GR-1F promoter methylation, whereas offspring with both maternal and paternal PTSD showed lower methylation.” Furthermore, lower methylation was tied to greater suppression of cortisol (Am J Psychiatry. 2014 Aug;171(8)872-880).
An appreciation for the power of epigenetics, or “soul wounds,” can help us stop blaming indigenous and other traumatized populations, and start tending to their mental health needs. Furthermore, getting individuals to understand these concepts can be yet another step on the path toward healing.
A study of 19 staff members and clients in a Native American healing lodge who began a discourse on the legacy of historical trauma found that counselors understood that their clients carried pain “leading to adult dysfunction, including substance abuse” (J Consult Clin Psychol. 2009 Aug;77(4):751-762). Second, the counselors believed that the pain needed to be confessed. Third, the counselors thought that expressing the pain would help the clients become more introspective. Finally, the process included reclaiming “indigenous heritage, identity, and spirituality that program staff thought would neutralize the pathogenic effects of colonization.”
We do not know the extent to which epigenetics are involved in specific diseases. Epigenetic mechanisms have not yet been tested as pathways involved in the intergenerational transmission of trauma in indigenous peoples. But Dr. Yehuda’s work with the children of Holocaust survivors shows that these mechanisms do indeed exist.
In light of what we do understand and the DSM-5’s emphasis on cultural competency, mental health professionals have a role to play in reversing the negative intergenerational cycles experienced by people across the globe. Only when we start paying attention to the plight of indigenous peoples across the globe will true healing begin.
Dr. Bombay is assistant professor of psychiatry at Dalhousie University, Halifax, N.S.
Perianal North American Blastomycosis
Cutaneous North American blastomycosis is a deep fungal infection caused by Blastomyces dermatitidis, a thermally dimorphic fungus that is endemic to the Great Lakes region as well as the Mississippi and Ohio River valleys where it thrives in moist acidic soil enriched with organic material.1,2 In humans, the annual incidence rate is estimated to be 0.6 cases per million,3 though it may be as high as 42 cases per 100,000 in endemic areas.4 Infection typically results from the inhalation of conidia and manifests as either acute or chronic pneumonia.5 Most patients with acute disease present with nonspecific flulike symptoms and a nonproductive cough.
Dissemination occurs in approximately 25% of cases,6 most commonly affecting the skin. Other potential sites of dissemination include bone, the genitourinary tract, and the central nervous system. Cutaneous lesions, which may be either verrucous or ulcerative plaques, often occur on or around orifices contiguous to the respiratory tract.7 Verrucous lesions tend to have an irregular shape with well-defined borders and surface crusting. Ulcerative lesions have heaped-up borders and often have an exudative base.8 The differential diagnosis of cutaneous North American blastomycosis lesions includes squamous cell carcinoma, giant keratoacanthoma, verrucae, basal cell carcinoma, scrofuloderma, lupus vulgaris, nocardiosis, syphilis, bromoderma, iododerma, granuloma inguinale, tuberculosis verrucosa cutis, mycetoma, and actinomycosis.7,8
Although periorificial cutaneous manifestations of disseminated blastomycosis are common, perianal lesions are rare. The differential diagnosis of perianal verrucous plaques includes condyloma acuminatum, squamous cell carcinoma, adenocarcinoma, Buschke-Löwenstein tumor, actinomycosis, and localized fungal infections such as blastomycosis.9
Case Report
A 57-year-old man presented with a palpable perianal mass that produced small amounts of blood in his underwear and on toilet paper. The patient reported no history of hemorrhoids, anoreceptive intercourse, or sexually transmitted disease. Four months prior to presentation, he had a prolonged upper respiratory tract illness with a subjective fever and productive cough of 2 months’ duration. The patient described himself as an avid outdoorsman who worked at a summer resort and spent a great deal of time in the forests of central Wisconsin last autumn. Physical examination revealed a well-demarcated, firm, moist plaque with a verrucous surface that measured 3.5×2.7 cm and extended from the anal verge to the perianal skin (Figure 1).
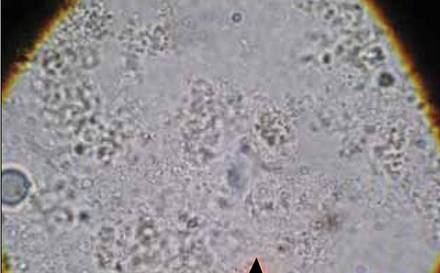
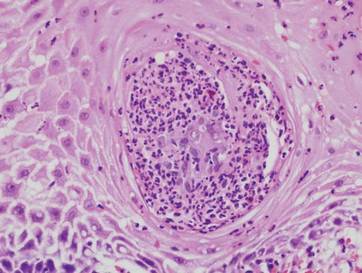
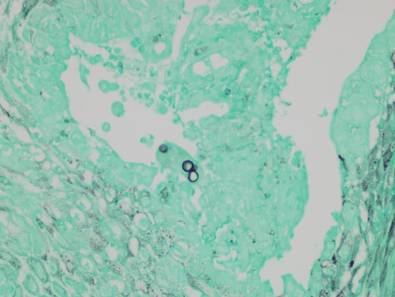
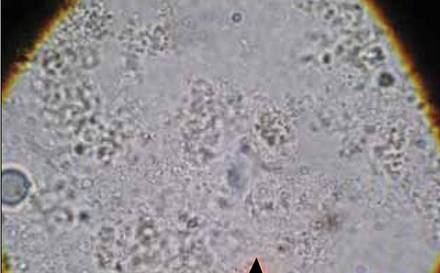
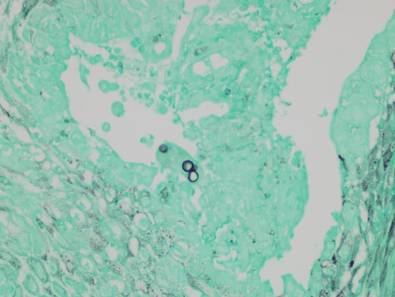
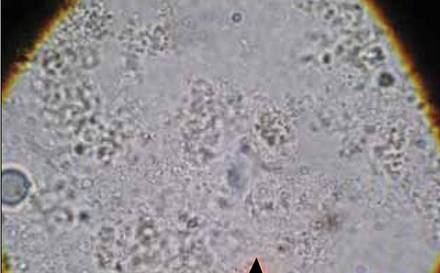
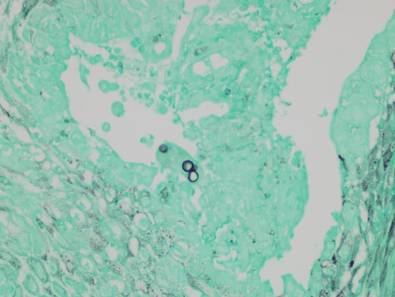
Potassium hydroxide preparation of a biopsy specimen (Figure 2), a punch biopsy of the lesion (Figure 3), and Gomori methenamine-silver staining (Figure 4) revealed scattered yeast spores, some demonstrating broad-based budding, with pseudoepitheliomatous hyperplasia, dermal neutrophils, and intraepithelial microabscesses. The patient’s urine was positive for Blastomyces antigen (1.04 ng/mL). Chest radiography demonstrated a localized infiltrate in the right hilum with possible mass effect. Computed tomography showed a consolidative opacity measuring 4.0×3.4 cm in the upper lobe of the right lung (Figure 5).
| 
|
The patient was diagnosed with cutaneous North American blastomycosis and prescribed a 6-month course of oral itraconazole 200 mg twice daily. At his 3-month follow-up visit, the perianal plaque hadalmost completely resolved (Figure 6). However, because the patient had increasing lower extremity edema, subjective hearing loss, and abnormal liver function tests, itraconazole treatment was discontinued and replaced with oral fluconazole 400 mg daily for the next 3 months. The right hilar mass had visibly improved on follow-up chest radiography 2 months after the patient started antifungal therapy with itraconazole and had resolved within another 3 months of treatment.
| 
|
Comment
Cutaneous blastomycosis results most often from the hematogenous spread of B dermatitidis from the lungs and rarely from direct inoculation.5,10 Skin lesions tend to occur on exposed areas, such as the face, scalp, hands, wrists, feet, and ankles.7,11-13 Dissemination to the perianal skin is rare, though it has been reported in 2 other patients; both patients, similar to our patient, had evidence of pulmonary involvement at some point in their clinical course.9,14
Diagnosis is based on identification of B dermatitidis by microscopy or culture. Potassium hydroxide preparation of biopsy specimens typically shows broad-based budding yeast.13 Characteristic findings of histopathologic studies include pseudo-epitheliomatous hyperplasia, intraepidermal abscesses, and a dermal infiltrate of polymorphonuclear leukocytes.15 On fungal culture, B dermatitidis is slow growing and may require a 2- to 4-week incubation period. Serologic tests are available, but sensitivity is low, at 9%, 28%, and 77% for complement fixation, immunodiffusion, and enzyme immunoassay, respectively.16
Conclusion
North American blastomycosis should be considered in patients who have verrucous or ulcerative perianal lesions and have lived in or traveled to endemic regions, especially if they have recent or ongoing pulmonary symptoms. Potassium hydroxide preparation and fungal staining of biopsy specimens can aid in diagnosis.
Acknowledgment
The authors thank the Marshfield Clinic Research Foundation’s Office of Scientific Writing and Publication (Marshfield, Wisconsin) for editorial assistance in the preparation of this manuscript.
1. Klein BS, Vergeront JM, Davis JP. Epidemiologic aspects of blastomycosis, the enigmatic systemic mycosis. Semin Respir Infect. 1986;1:29-39.
2. Klein BS, Vergeront JM, Weeks RJ, et al. Isolation of Blastomyces dermatitidis in soil associated with a large outbreak of blastomycosis in Wisconsin. N Engl J Med. 1986;314:529-534.
3. Reingold AL, Lu XD, Plikaytis BD, et al. Systemic mycoses in the United States, 1980-1982. J Med Vet Mycol. 1986;24:433-436.
4. Centers for Disease Control and Prevention (CDC). Blastomycosis—Wisconsin, 1986-1995. MMWR Morb Mortal Wkly Rep. 1996;45:601-603.
5. Smith JA, Kauffman CA. Blastomycosis. Proc Am Thorac Soc. 2010;7:173-180.
6. Goldman M, Johnson PC, Sarosi GA. Fungal pneumonias. the endemic mycoses. Clin Chest Med. 1999;20:507-519.
7. Mercurio MG, Elewski BE. Cutaneous blastomycosis. Cutis. 1992;50:422-424.
8. Saccente M, Woods GL. Clinical and laboratory update on blastomycosis. Clin Microbiol Rev. 2010;23:367-381.
9. Ricciardi R, Alavi K, Filice GA, et al. Blastomyces dermatitidis of the perianal skin: report of a case. Dis Colon Rectum. 2007;50:118-121.
10. Gray NA, Baddour LM. Cutaneous inoculation blastomycosis [published online ahead of print April 17, 2002]. Clin Infect Dis. 2002;34:e44-e49.
11. Kisso B, Mahmoud F, Thakkar JR. Blastomycosis presenting as recurrent tender cutaneous nodules. S D Med. 2006;59:255-259.
12. Mandell GL, Bennett JE, Dolin R. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 7th ed. Philadelphia, PA: Churchill Livingstone/Elsevier; 2010.
13. Mason AR, Cortes GY, Cook J, et al. Cutaneous blastomycosis: a diagnostic challenge. Int J Dermatol. 2008;47:824-830.
14. Linn JE. Pseudo-epitheliomatous lesions of the perirectal tissue: report of a case of squamous epithelioma due to blastomycosis. South Med J. 1958;51:1101-1104.
15. Woofter MJ, Cripps DJ, Warner TF. Verrucous plaques on the face. North American blastomycosis. Arch Dermatol. 2000;136:547, 550.
16. Klein BS, Vergeront JM, Kaufman L, et al. Serological tests for blastomycosis: assessments during a large point-source outbreak in Wisconsin. J Infect Dis. 1987;155:262-268.
Cutaneous North American blastomycosis is a deep fungal infection caused by Blastomyces dermatitidis, a thermally dimorphic fungus that is endemic to the Great Lakes region as well as the Mississippi and Ohio River valleys where it thrives in moist acidic soil enriched with organic material.1,2 In humans, the annual incidence rate is estimated to be 0.6 cases per million,3 though it may be as high as 42 cases per 100,000 in endemic areas.4 Infection typically results from the inhalation of conidia and manifests as either acute or chronic pneumonia.5 Most patients with acute disease present with nonspecific flulike symptoms and a nonproductive cough.
Dissemination occurs in approximately 25% of cases,6 most commonly affecting the skin. Other potential sites of dissemination include bone, the genitourinary tract, and the central nervous system. Cutaneous lesions, which may be either verrucous or ulcerative plaques, often occur on or around orifices contiguous to the respiratory tract.7 Verrucous lesions tend to have an irregular shape with well-defined borders and surface crusting. Ulcerative lesions have heaped-up borders and often have an exudative base.8 The differential diagnosis of cutaneous North American blastomycosis lesions includes squamous cell carcinoma, giant keratoacanthoma, verrucae, basal cell carcinoma, scrofuloderma, lupus vulgaris, nocardiosis, syphilis, bromoderma, iododerma, granuloma inguinale, tuberculosis verrucosa cutis, mycetoma, and actinomycosis.7,8
Although periorificial cutaneous manifestations of disseminated blastomycosis are common, perianal lesions are rare. The differential diagnosis of perianal verrucous plaques includes condyloma acuminatum, squamous cell carcinoma, adenocarcinoma, Buschke-Löwenstein tumor, actinomycosis, and localized fungal infections such as blastomycosis.9
Case Report
A 57-year-old man presented with a palpable perianal mass that produced small amounts of blood in his underwear and on toilet paper. The patient reported no history of hemorrhoids, anoreceptive intercourse, or sexually transmitted disease. Four months prior to presentation, he had a prolonged upper respiratory tract illness with a subjective fever and productive cough of 2 months’ duration. The patient described himself as an avid outdoorsman who worked at a summer resort and spent a great deal of time in the forests of central Wisconsin last autumn. Physical examination revealed a well-demarcated, firm, moist plaque with a verrucous surface that measured 3.5×2.7 cm and extended from the anal verge to the perianal skin (Figure 1).
Potassium hydroxide preparation of a biopsy specimen (Figure 2), a punch biopsy of the lesion (Figure 3), and Gomori methenamine-silver staining (Figure 4) revealed scattered yeast spores, some demonstrating broad-based budding, with pseudoepitheliomatous hyperplasia, dermal neutrophils, and intraepithelial microabscesses. The patient’s urine was positive for Blastomyces antigen (1.04 ng/mL). Chest radiography demonstrated a localized infiltrate in the right hilum with possible mass effect. Computed tomography showed a consolidative opacity measuring 4.0×3.4 cm in the upper lobe of the right lung (Figure 5).
| 
|
The patient was diagnosed with cutaneous North American blastomycosis and prescribed a 6-month course of oral itraconazole 200 mg twice daily. At his 3-month follow-up visit, the perianal plaque hadalmost completely resolved (Figure 6). However, because the patient had increasing lower extremity edema, subjective hearing loss, and abnormal liver function tests, itraconazole treatment was discontinued and replaced with oral fluconazole 400 mg daily for the next 3 months. The right hilar mass had visibly improved on follow-up chest radiography 2 months after the patient started antifungal therapy with itraconazole and had resolved within another 3 months of treatment.
| 
|
Comment
Cutaneous blastomycosis results most often from the hematogenous spread of B dermatitidis from the lungs and rarely from direct inoculation.5,10 Skin lesions tend to occur on exposed areas, such as the face, scalp, hands, wrists, feet, and ankles.7,11-13 Dissemination to the perianal skin is rare, though it has been reported in 2 other patients; both patients, similar to our patient, had evidence of pulmonary involvement at some point in their clinical course.9,14
Diagnosis is based on identification of B dermatitidis by microscopy or culture. Potassium hydroxide preparation of biopsy specimens typically shows broad-based budding yeast.13 Characteristic findings of histopathologic studies include pseudo-epitheliomatous hyperplasia, intraepidermal abscesses, and a dermal infiltrate of polymorphonuclear leukocytes.15 On fungal culture, B dermatitidis is slow growing and may require a 2- to 4-week incubation period. Serologic tests are available, but sensitivity is low, at 9%, 28%, and 77% for complement fixation, immunodiffusion, and enzyme immunoassay, respectively.16
Conclusion
North American blastomycosis should be considered in patients who have verrucous or ulcerative perianal lesions and have lived in or traveled to endemic regions, especially if they have recent or ongoing pulmonary symptoms. Potassium hydroxide preparation and fungal staining of biopsy specimens can aid in diagnosis.
Acknowledgment
The authors thank the Marshfield Clinic Research Foundation’s Office of Scientific Writing and Publication (Marshfield, Wisconsin) for editorial assistance in the preparation of this manuscript.
Cutaneous North American blastomycosis is a deep fungal infection caused by Blastomyces dermatitidis, a thermally dimorphic fungus that is endemic to the Great Lakes region as well as the Mississippi and Ohio River valleys where it thrives in moist acidic soil enriched with organic material.1,2 In humans, the annual incidence rate is estimated to be 0.6 cases per million,3 though it may be as high as 42 cases per 100,000 in endemic areas.4 Infection typically results from the inhalation of conidia and manifests as either acute or chronic pneumonia.5 Most patients with acute disease present with nonspecific flulike symptoms and a nonproductive cough.
Dissemination occurs in approximately 25% of cases,6 most commonly affecting the skin. Other potential sites of dissemination include bone, the genitourinary tract, and the central nervous system. Cutaneous lesions, which may be either verrucous or ulcerative plaques, often occur on or around orifices contiguous to the respiratory tract.7 Verrucous lesions tend to have an irregular shape with well-defined borders and surface crusting. Ulcerative lesions have heaped-up borders and often have an exudative base.8 The differential diagnosis of cutaneous North American blastomycosis lesions includes squamous cell carcinoma, giant keratoacanthoma, verrucae, basal cell carcinoma, scrofuloderma, lupus vulgaris, nocardiosis, syphilis, bromoderma, iododerma, granuloma inguinale, tuberculosis verrucosa cutis, mycetoma, and actinomycosis.7,8
Although periorificial cutaneous manifestations of disseminated blastomycosis are common, perianal lesions are rare. The differential diagnosis of perianal verrucous plaques includes condyloma acuminatum, squamous cell carcinoma, adenocarcinoma, Buschke-Löwenstein tumor, actinomycosis, and localized fungal infections such as blastomycosis.9
Case Report
A 57-year-old man presented with a palpable perianal mass that produced small amounts of blood in his underwear and on toilet paper. The patient reported no history of hemorrhoids, anoreceptive intercourse, or sexually transmitted disease. Four months prior to presentation, he had a prolonged upper respiratory tract illness with a subjective fever and productive cough of 2 months’ duration. The patient described himself as an avid outdoorsman who worked at a summer resort and spent a great deal of time in the forests of central Wisconsin last autumn. Physical examination revealed a well-demarcated, firm, moist plaque with a verrucous surface that measured 3.5×2.7 cm and extended from the anal verge to the perianal skin (Figure 1).
Potassium hydroxide preparation of a biopsy specimen (Figure 2), a punch biopsy of the lesion (Figure 3), and Gomori methenamine-silver staining (Figure 4) revealed scattered yeast spores, some demonstrating broad-based budding, with pseudoepitheliomatous hyperplasia, dermal neutrophils, and intraepithelial microabscesses. The patient’s urine was positive for Blastomyces antigen (1.04 ng/mL). Chest radiography demonstrated a localized infiltrate in the right hilum with possible mass effect. Computed tomography showed a consolidative opacity measuring 4.0×3.4 cm in the upper lobe of the right lung (Figure 5).
| 
|
The patient was diagnosed with cutaneous North American blastomycosis and prescribed a 6-month course of oral itraconazole 200 mg twice daily. At his 3-month follow-up visit, the perianal plaque hadalmost completely resolved (Figure 6). However, because the patient had increasing lower extremity edema, subjective hearing loss, and abnormal liver function tests, itraconazole treatment was discontinued and replaced with oral fluconazole 400 mg daily for the next 3 months. The right hilar mass had visibly improved on follow-up chest radiography 2 months after the patient started antifungal therapy with itraconazole and had resolved within another 3 months of treatment.
| 
|
Comment
Cutaneous blastomycosis results most often from the hematogenous spread of B dermatitidis from the lungs and rarely from direct inoculation.5,10 Skin lesions tend to occur on exposed areas, such as the face, scalp, hands, wrists, feet, and ankles.7,11-13 Dissemination to the perianal skin is rare, though it has been reported in 2 other patients; both patients, similar to our patient, had evidence of pulmonary involvement at some point in their clinical course.9,14
Diagnosis is based on identification of B dermatitidis by microscopy or culture. Potassium hydroxide preparation of biopsy specimens typically shows broad-based budding yeast.13 Characteristic findings of histopathologic studies include pseudo-epitheliomatous hyperplasia, intraepidermal abscesses, and a dermal infiltrate of polymorphonuclear leukocytes.15 On fungal culture, B dermatitidis is slow growing and may require a 2- to 4-week incubation period. Serologic tests are available, but sensitivity is low, at 9%, 28%, and 77% for complement fixation, immunodiffusion, and enzyme immunoassay, respectively.16
Conclusion
North American blastomycosis should be considered in patients who have verrucous or ulcerative perianal lesions and have lived in or traveled to endemic regions, especially if they have recent or ongoing pulmonary symptoms. Potassium hydroxide preparation and fungal staining of biopsy specimens can aid in diagnosis.
Acknowledgment
The authors thank the Marshfield Clinic Research Foundation’s Office of Scientific Writing and Publication (Marshfield, Wisconsin) for editorial assistance in the preparation of this manuscript.
1. Klein BS, Vergeront JM, Davis JP. Epidemiologic aspects of blastomycosis, the enigmatic systemic mycosis. Semin Respir Infect. 1986;1:29-39.
2. Klein BS, Vergeront JM, Weeks RJ, et al. Isolation of Blastomyces dermatitidis in soil associated with a large outbreak of blastomycosis in Wisconsin. N Engl J Med. 1986;314:529-534.
3. Reingold AL, Lu XD, Plikaytis BD, et al. Systemic mycoses in the United States, 1980-1982. J Med Vet Mycol. 1986;24:433-436.
4. Centers for Disease Control and Prevention (CDC). Blastomycosis—Wisconsin, 1986-1995. MMWR Morb Mortal Wkly Rep. 1996;45:601-603.
5. Smith JA, Kauffman CA. Blastomycosis. Proc Am Thorac Soc. 2010;7:173-180.
6. Goldman M, Johnson PC, Sarosi GA. Fungal pneumonias. the endemic mycoses. Clin Chest Med. 1999;20:507-519.
7. Mercurio MG, Elewski BE. Cutaneous blastomycosis. Cutis. 1992;50:422-424.
8. Saccente M, Woods GL. Clinical and laboratory update on blastomycosis. Clin Microbiol Rev. 2010;23:367-381.
9. Ricciardi R, Alavi K, Filice GA, et al. Blastomyces dermatitidis of the perianal skin: report of a case. Dis Colon Rectum. 2007;50:118-121.
10. Gray NA, Baddour LM. Cutaneous inoculation blastomycosis [published online ahead of print April 17, 2002]. Clin Infect Dis. 2002;34:e44-e49.
11. Kisso B, Mahmoud F, Thakkar JR. Blastomycosis presenting as recurrent tender cutaneous nodules. S D Med. 2006;59:255-259.
12. Mandell GL, Bennett JE, Dolin R. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 7th ed. Philadelphia, PA: Churchill Livingstone/Elsevier; 2010.
13. Mason AR, Cortes GY, Cook J, et al. Cutaneous blastomycosis: a diagnostic challenge. Int J Dermatol. 2008;47:824-830.
14. Linn JE. Pseudo-epitheliomatous lesions of the perirectal tissue: report of a case of squamous epithelioma due to blastomycosis. South Med J. 1958;51:1101-1104.
15. Woofter MJ, Cripps DJ, Warner TF. Verrucous plaques on the face. North American blastomycosis. Arch Dermatol. 2000;136:547, 550.
16. Klein BS, Vergeront JM, Kaufman L, et al. Serological tests for blastomycosis: assessments during a large point-source outbreak in Wisconsin. J Infect Dis. 1987;155:262-268.
1. Klein BS, Vergeront JM, Davis JP. Epidemiologic aspects of blastomycosis, the enigmatic systemic mycosis. Semin Respir Infect. 1986;1:29-39.
2. Klein BS, Vergeront JM, Weeks RJ, et al. Isolation of Blastomyces dermatitidis in soil associated with a large outbreak of blastomycosis in Wisconsin. N Engl J Med. 1986;314:529-534.
3. Reingold AL, Lu XD, Plikaytis BD, et al. Systemic mycoses in the United States, 1980-1982. J Med Vet Mycol. 1986;24:433-436.
4. Centers for Disease Control and Prevention (CDC). Blastomycosis—Wisconsin, 1986-1995. MMWR Morb Mortal Wkly Rep. 1996;45:601-603.
5. Smith JA, Kauffman CA. Blastomycosis. Proc Am Thorac Soc. 2010;7:173-180.
6. Goldman M, Johnson PC, Sarosi GA. Fungal pneumonias. the endemic mycoses. Clin Chest Med. 1999;20:507-519.
7. Mercurio MG, Elewski BE. Cutaneous blastomycosis. Cutis. 1992;50:422-424.
8. Saccente M, Woods GL. Clinical and laboratory update on blastomycosis. Clin Microbiol Rev. 2010;23:367-381.
9. Ricciardi R, Alavi K, Filice GA, et al. Blastomyces dermatitidis of the perianal skin: report of a case. Dis Colon Rectum. 2007;50:118-121.
10. Gray NA, Baddour LM. Cutaneous inoculation blastomycosis [published online ahead of print April 17, 2002]. Clin Infect Dis. 2002;34:e44-e49.
11. Kisso B, Mahmoud F, Thakkar JR. Blastomycosis presenting as recurrent tender cutaneous nodules. S D Med. 2006;59:255-259.
12. Mandell GL, Bennett JE, Dolin R. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 7th ed. Philadelphia, PA: Churchill Livingstone/Elsevier; 2010.
13. Mason AR, Cortes GY, Cook J, et al. Cutaneous blastomycosis: a diagnostic challenge. Int J Dermatol. 2008;47:824-830.
14. Linn JE. Pseudo-epitheliomatous lesions of the perirectal tissue: report of a case of squamous epithelioma due to blastomycosis. South Med J. 1958;51:1101-1104.
15. Woofter MJ, Cripps DJ, Warner TF. Verrucous plaques on the face. North American blastomycosis. Arch Dermatol. 2000;136:547, 550.
16. Klein BS, Vergeront JM, Kaufman L, et al. Serological tests for blastomycosis: assessments during a large point-source outbreak in Wisconsin. J Infect Dis. 1987;155:262-268.
Practice Points
- Cutaneous North American blastomycosis usually occurs in a periorificial distribution.
- The perianal region should be included in the periorificial regions considered in North American blastomycosis infections.
From the Washington Office
Last month’s edition of this column ended by calling Fellows’ attention to a new Web-based tool developed by the ACS Division of Advocacy and Health Policy to assist them in avoiding significant penalties in Medicare physician payment. This new online tool was highlighted in an e-mail sent to Fellows on June 24, 2015.
Based on follow-up inquiries since received, I would like to delve deeper into the specifics of how to successfully participate in the Physician Quality Reporting System (PQRS) and hopefully assist Fellows in avoiding penalties of up to 9% in their Medicare physician payment in the year 2017 secondary to failure to successfully participate in the current law Medicare quality programs in the current calendar year of 2015.
Despite the much publicized, and laudable, permanent repeal of the Sustainable Growth Rate (SGR), current law quality programs are still in effect. Medicare oversees several programs that offer physicians incentives for successful participation and/or penalties for failure to nonparticipation. These programs include the PQRS, the Value-Based Payment Modifier (VM) and the Electronic Health Record (EHR) Incentive Program, also known as the “EHR Meaningful Use program.”
Calendar year 2014 was the last year that physicians could earn incentives for some of these programs. Failure to participate in the Medicare quality programs leads to the potential for penalties that are applied 2 years after the performance period. Penalties in 2015 already are being assessed based on how successfully physicians participated in 2013. Thus, performance in 2015 will impact payment in 2017. Specifically, failure to participate in the programs in 2015 could result in a total penalty of 9% applied in 2017.
The College has developed resources to assist Fellows in being successful reporters. For most Fellows, the options found in the Surgeon Specific Registry (SSR) will be applicable. The SSR, formerly known as the ACS Case Log system, allows surgeons to track their cases and outcomes in a convenient and confidential manner. The SSR can also be utilized to comply with the regulatory requirements of submitting PQRS data as they have been approved to provide PQRS registry-based reporting for 2015. Use of the SSR is offered free of charge to ACS surgeon members and is available to nonmember surgeons for an annual fee.
The SSR offers a total of three options for surgeons to utilize to participate in PQRS reporting. Those options are: 1) General Surgery Measures Group; 2) Individual Measure reporting, which includes options for surgical specialties; and 3) Trauma Measures Option through the SSR’s Qualified Clinical Data Registry (QCDR). The deadline for submitting calendar year 2015 patient information in the SSR is January 31, 2016. The SSR will submit the PQRS data to Centers for Medicare & Medicaid Services (CMS).
For those surgeons for whom it could be applicable, the General Surgery Measures Group option is perhaps the least onerous in its requirements. Surgeons need report on a minimum of 20 patients, at least 11 of whom must be Medicare Part B patients. Should this option be selected, ALL seven of the included measures along with all nine risk factor variables must be reported for each of the 20 patients.
Surgeons may also choose to report individual measures data through the SSR. Those choosing this option are required to report on nine measures in three National Quality Strategy (NQS) categories, called “Domains.” One of the measures selected must further be designated as a “cross-cutting measure,” for example the documentation of current medications in the medical record, medication reconciliation, advanced care plan, or tobacco-use screening and cessation, as mentioned above. However, individual measures data must be entered for at least 50% of the provider’s Medicare Part B patients in order to be successful using this option. In order to assist one in determining whether this option is suitable for reporting, I would refer Fellows to the ACS website, www.facs.org/quality-programs/ssr/pqrs/options for a more expansive list of the individual measures, their “domains,” and whether or not they are designated as “cross-cutting.”
The SSR also provides the opportunity to leverage measures applicable to trauma surgery for successful PQRS reporting via the 2015 PQRS Trauma QCDR., which allow providers to submit non-PQRS measures, for example, measures not contained in the approved measure set or a measure that may be in the set but has substantive differences in the manner in which it is reported by the QCDR. The SSR Trauma QCDR includes 10 non-PQRS measures and one PQRS measure in this reporting option. Those choosing this option must report on 9 of the 11 designated measures, including 2 outcomes measures across three of the NQS domains. Reports must be completed on 50% of the surgeon’s Medicare Part B patients that meet the measurement requirements. One can also view the complete list of measures included in the Trauma Measures Option at the ACS website referenced above.
Lastly, for bariatric surgeons, the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) has also been approved as a QCDR for PQRS for 2015 reporting. MBSAQIP participants have the opportunity to voluntarily elect that their QCDR quality measures be submitted for PQRS participation. Metabolic and bariatric surgeons will receive reports of their QCDR measure results such that they can track their results. MBSAQIP will submit approved QCDR measures on behalf of participants who elect to have such done on their behalf. Specifics on the approved MBSAQIP QCDR quality measures are available at www.facs.org/quality-programs/mbsaqip/resources/data-registry.
As always, ACS staff in both Washington and Chicago are available to answer questions and assist members in participating in the 2015 PQRS program:
• General PQRS questions: ACS Division of Advocacy and Health Policy, 202-337-6701 or [email protected].
• Specific SSR questions: ACS Division of Research and Optimal Patient Care, 312-202-5000 or [email protected].
• Information on MBSAQIP: ACS Division of Research and Optimal Patient Care, 312-202-5000 or [email protected].
I highly encourage all Fellows to invest the time necessary to successfully participate in PQRS and thereby avoid penalties in their 2017 Medicare payment.
Until next month …
Dr. Bailey is a pediatric surgeon and Medical Director, Advocacy for the Division of Advocacy and Health Policy in the ACS offices in Washington.
Last month’s edition of this column ended by calling Fellows’ attention to a new Web-based tool developed by the ACS Division of Advocacy and Health Policy to assist them in avoiding significant penalties in Medicare physician payment. This new online tool was highlighted in an e-mail sent to Fellows on June 24, 2015.
Based on follow-up inquiries since received, I would like to delve deeper into the specifics of how to successfully participate in the Physician Quality Reporting System (PQRS) and hopefully assist Fellows in avoiding penalties of up to 9% in their Medicare physician payment in the year 2017 secondary to failure to successfully participate in the current law Medicare quality programs in the current calendar year of 2015.
Despite the much publicized, and laudable, permanent repeal of the Sustainable Growth Rate (SGR), current law quality programs are still in effect. Medicare oversees several programs that offer physicians incentives for successful participation and/or penalties for failure to nonparticipation. These programs include the PQRS, the Value-Based Payment Modifier (VM) and the Electronic Health Record (EHR) Incentive Program, also known as the “EHR Meaningful Use program.”
Calendar year 2014 was the last year that physicians could earn incentives for some of these programs. Failure to participate in the Medicare quality programs leads to the potential for penalties that are applied 2 years after the performance period. Penalties in 2015 already are being assessed based on how successfully physicians participated in 2013. Thus, performance in 2015 will impact payment in 2017. Specifically, failure to participate in the programs in 2015 could result in a total penalty of 9% applied in 2017.
The College has developed resources to assist Fellows in being successful reporters. For most Fellows, the options found in the Surgeon Specific Registry (SSR) will be applicable. The SSR, formerly known as the ACS Case Log system, allows surgeons to track their cases and outcomes in a convenient and confidential manner. The SSR can also be utilized to comply with the regulatory requirements of submitting PQRS data as they have been approved to provide PQRS registry-based reporting for 2015. Use of the SSR is offered free of charge to ACS surgeon members and is available to nonmember surgeons for an annual fee.
The SSR offers a total of three options for surgeons to utilize to participate in PQRS reporting. Those options are: 1) General Surgery Measures Group; 2) Individual Measure reporting, which includes options for surgical specialties; and 3) Trauma Measures Option through the SSR’s Qualified Clinical Data Registry (QCDR). The deadline for submitting calendar year 2015 patient information in the SSR is January 31, 2016. The SSR will submit the PQRS data to Centers for Medicare & Medicaid Services (CMS).
For those surgeons for whom it could be applicable, the General Surgery Measures Group option is perhaps the least onerous in its requirements. Surgeons need report on a minimum of 20 patients, at least 11 of whom must be Medicare Part B patients. Should this option be selected, ALL seven of the included measures along with all nine risk factor variables must be reported for each of the 20 patients.
Surgeons may also choose to report individual measures data through the SSR. Those choosing this option are required to report on nine measures in three National Quality Strategy (NQS) categories, called “Domains.” One of the measures selected must further be designated as a “cross-cutting measure,” for example the documentation of current medications in the medical record, medication reconciliation, advanced care plan, or tobacco-use screening and cessation, as mentioned above. However, individual measures data must be entered for at least 50% of the provider’s Medicare Part B patients in order to be successful using this option. In order to assist one in determining whether this option is suitable for reporting, I would refer Fellows to the ACS website, www.facs.org/quality-programs/ssr/pqrs/options for a more expansive list of the individual measures, their “domains,” and whether or not they are designated as “cross-cutting.”
The SSR also provides the opportunity to leverage measures applicable to trauma surgery for successful PQRS reporting via the 2015 PQRS Trauma QCDR., which allow providers to submit non-PQRS measures, for example, measures not contained in the approved measure set or a measure that may be in the set but has substantive differences in the manner in which it is reported by the QCDR. The SSR Trauma QCDR includes 10 non-PQRS measures and one PQRS measure in this reporting option. Those choosing this option must report on 9 of the 11 designated measures, including 2 outcomes measures across three of the NQS domains. Reports must be completed on 50% of the surgeon’s Medicare Part B patients that meet the measurement requirements. One can also view the complete list of measures included in the Trauma Measures Option at the ACS website referenced above.
Lastly, for bariatric surgeons, the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) has also been approved as a QCDR for PQRS for 2015 reporting. MBSAQIP participants have the opportunity to voluntarily elect that their QCDR quality measures be submitted for PQRS participation. Metabolic and bariatric surgeons will receive reports of their QCDR measure results such that they can track their results. MBSAQIP will submit approved QCDR measures on behalf of participants who elect to have such done on their behalf. Specifics on the approved MBSAQIP QCDR quality measures are available at www.facs.org/quality-programs/mbsaqip/resources/data-registry.
As always, ACS staff in both Washington and Chicago are available to answer questions and assist members in participating in the 2015 PQRS program:
• General PQRS questions: ACS Division of Advocacy and Health Policy, 202-337-6701 or [email protected].
• Specific SSR questions: ACS Division of Research and Optimal Patient Care, 312-202-5000 or [email protected].
• Information on MBSAQIP: ACS Division of Research and Optimal Patient Care, 312-202-5000 or [email protected].
I highly encourage all Fellows to invest the time necessary to successfully participate in PQRS and thereby avoid penalties in their 2017 Medicare payment.
Until next month …
Dr. Bailey is a pediatric surgeon and Medical Director, Advocacy for the Division of Advocacy and Health Policy in the ACS offices in Washington.
Last month’s edition of this column ended by calling Fellows’ attention to a new Web-based tool developed by the ACS Division of Advocacy and Health Policy to assist them in avoiding significant penalties in Medicare physician payment. This new online tool was highlighted in an e-mail sent to Fellows on June 24, 2015.
Based on follow-up inquiries since received, I would like to delve deeper into the specifics of how to successfully participate in the Physician Quality Reporting System (PQRS) and hopefully assist Fellows in avoiding penalties of up to 9% in their Medicare physician payment in the year 2017 secondary to failure to successfully participate in the current law Medicare quality programs in the current calendar year of 2015.
Despite the much publicized, and laudable, permanent repeal of the Sustainable Growth Rate (SGR), current law quality programs are still in effect. Medicare oversees several programs that offer physicians incentives for successful participation and/or penalties for failure to nonparticipation. These programs include the PQRS, the Value-Based Payment Modifier (VM) and the Electronic Health Record (EHR) Incentive Program, also known as the “EHR Meaningful Use program.”
Calendar year 2014 was the last year that physicians could earn incentives for some of these programs. Failure to participate in the Medicare quality programs leads to the potential for penalties that are applied 2 years after the performance period. Penalties in 2015 already are being assessed based on how successfully physicians participated in 2013. Thus, performance in 2015 will impact payment in 2017. Specifically, failure to participate in the programs in 2015 could result in a total penalty of 9% applied in 2017.
The College has developed resources to assist Fellows in being successful reporters. For most Fellows, the options found in the Surgeon Specific Registry (SSR) will be applicable. The SSR, formerly known as the ACS Case Log system, allows surgeons to track their cases and outcomes in a convenient and confidential manner. The SSR can also be utilized to comply with the regulatory requirements of submitting PQRS data as they have been approved to provide PQRS registry-based reporting for 2015. Use of the SSR is offered free of charge to ACS surgeon members and is available to nonmember surgeons for an annual fee.
The SSR offers a total of three options for surgeons to utilize to participate in PQRS reporting. Those options are: 1) General Surgery Measures Group; 2) Individual Measure reporting, which includes options for surgical specialties; and 3) Trauma Measures Option through the SSR’s Qualified Clinical Data Registry (QCDR). The deadline for submitting calendar year 2015 patient information in the SSR is January 31, 2016. The SSR will submit the PQRS data to Centers for Medicare & Medicaid Services (CMS).
For those surgeons for whom it could be applicable, the General Surgery Measures Group option is perhaps the least onerous in its requirements. Surgeons need report on a minimum of 20 patients, at least 11 of whom must be Medicare Part B patients. Should this option be selected, ALL seven of the included measures along with all nine risk factor variables must be reported for each of the 20 patients.
Surgeons may also choose to report individual measures data through the SSR. Those choosing this option are required to report on nine measures in three National Quality Strategy (NQS) categories, called “Domains.” One of the measures selected must further be designated as a “cross-cutting measure,” for example the documentation of current medications in the medical record, medication reconciliation, advanced care plan, or tobacco-use screening and cessation, as mentioned above. However, individual measures data must be entered for at least 50% of the provider’s Medicare Part B patients in order to be successful using this option. In order to assist one in determining whether this option is suitable for reporting, I would refer Fellows to the ACS website, www.facs.org/quality-programs/ssr/pqrs/options for a more expansive list of the individual measures, their “domains,” and whether or not they are designated as “cross-cutting.”
The SSR also provides the opportunity to leverage measures applicable to trauma surgery for successful PQRS reporting via the 2015 PQRS Trauma QCDR., which allow providers to submit non-PQRS measures, for example, measures not contained in the approved measure set or a measure that may be in the set but has substantive differences in the manner in which it is reported by the QCDR. The SSR Trauma QCDR includes 10 non-PQRS measures and one PQRS measure in this reporting option. Those choosing this option must report on 9 of the 11 designated measures, including 2 outcomes measures across three of the NQS domains. Reports must be completed on 50% of the surgeon’s Medicare Part B patients that meet the measurement requirements. One can also view the complete list of measures included in the Trauma Measures Option at the ACS website referenced above.
Lastly, for bariatric surgeons, the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) has also been approved as a QCDR for PQRS for 2015 reporting. MBSAQIP participants have the opportunity to voluntarily elect that their QCDR quality measures be submitted for PQRS participation. Metabolic and bariatric surgeons will receive reports of their QCDR measure results such that they can track their results. MBSAQIP will submit approved QCDR measures on behalf of participants who elect to have such done on their behalf. Specifics on the approved MBSAQIP QCDR quality measures are available at www.facs.org/quality-programs/mbsaqip/resources/data-registry.
As always, ACS staff in both Washington and Chicago are available to answer questions and assist members in participating in the 2015 PQRS program:
• General PQRS questions: ACS Division of Advocacy and Health Policy, 202-337-6701 or [email protected].
• Specific SSR questions: ACS Division of Research and Optimal Patient Care, 312-202-5000 or [email protected].
• Information on MBSAQIP: ACS Division of Research and Optimal Patient Care, 312-202-5000 or [email protected].
I highly encourage all Fellows to invest the time necessary to successfully participate in PQRS and thereby avoid penalties in their 2017 Medicare payment.
Until next month …
Dr. Bailey is a pediatric surgeon and Medical Director, Advocacy for the Division of Advocacy and Health Policy in the ACS offices in Washington.
The Rural Surgeon: The burden of transfer
I have been on both ends of the phone call. I began my career at a several-hundred bed community hospital in a town without a university medical center. We took all the local knife-and-gun club incidents, and whatever other surgical emergencies might arise, while receiving phone calls from nearly every point of the magnetic compass. It’s easy to recall the sagging feeling when you realize more serious work is coming in on the helicopter from Podunk, USA, and you’re not off call for another few hours. These memories linger as now I’m the one making the phone calls. When I state that I am the one, I mean the one and only; this is solo general surgery practice and I’m the only general surgeon in my county.
When I do speak with colleagues kind enough to accept our patients, I feel relieved. But the burden of transfer doesn’t travel away with the patient in the ambulance or on the airplane. There always seem to be questions or looks of concern lately, and I don’t just mean from other medical professionals. Maybe it is an Internet thing, but everyone is a critic these days. We are being watched by more than partners and employers, more than payers and agencies, more than our government bean counters. Families, allied health professionals, and even nonclinical staff all have opinions about which patients stay and which leaves our 14-bed, critical access hospital. Gods may have once walked these halls, but nowadays it’s just me!
Of course, any interested party can also criticize my decisions to keep any particular patient; why would anybody restrict their furrowed glare only to transfers? When we keep patients at the edge of our practice, or perform a procedure that is only done rarely locally, we incite more than just the volume debate on the ACS Communities. Goodness – my wife has heard about cases I have done via town chitter-chatter before I even get home!
How does one deal with being whipsawed? This phenomenon is defined in the business world as being subjected to two difficult situations or opposing pressures at the same time. If you transfer, you are criticized. The only thing that changes are the critics if you keep and care for that very same patient! For many rural colleagues, being whipsawed is on the short list of job dissatisfaction drivers; somewhere behind the heavyweight champ of being asked to be in two different places at the same time.
Transferring a patient rarely leads to the lasting criticism that keeping an ill patient locally can. Obviously keeping a patient extends the time period where others can knowingly shake their heads in disbelief. That extra time allows us to educate staff and others as to why a patient with more than simple hernia or appendicitis is being admitted to our little hospital. We can detail why this is a really good thing for everyone – including the patient!
So many of our locals are elderly, and when we keep one for serious surgical illness, so much goes into that decision besides just the patient’s age and comorbid conditions. Immediate family, friends, or existing social support all must be examined and understood. A significant number of geriatric couples are only “independent” together; send one off for surgery a hundred or more miles away and the remaining spouse suffers measurably. Sometimes there is no local family, as nuclear members live in neighboring states or even overseas. I’m always surprised when my patients have trouble even arranging rides to and from our facilities for the routine procedures we do regularly. I think to myself, what will they do when the inevitable happens?
Our geography plays a serious role for those patients who don’t drive any appreciable distances. The mountains to our east are difficult to negotiate and west, well, you’ll get wet rather quickly. Going north and south on Highway 101 can be tricky during summer and dangerous any time in bad weather. I talk to some patients about sending them to Portland and I get looks in response like I’m proposing surgical care in some exotic foreign capital. Urban anxiety, traffic, and unfamiliarity with our largest metropolis make the 300-mile journey untenable for many of our patients; and the TV show isn’t helping our cause! Even cases that define themselves from the get-go as major university referrals return afterward and ask us to assume their postoperative care. Our patients often can’t make the trip to follow-up with the experts who provided their life-saving care.
Stretching our surgical muscles is obviously important for all ACS members. In bigger facilities you can see and sometimes scrub into fascinating cases in other subspecialties, or at least participate in discussions about such in the surgery lounge. I won’t attach a photo of the desk space that serves as my lounge, dictation station, bathroom, and locker. Let’s just say it’s probably not quite the same as many Fellows are used to.
For the rural solo practitioner, a bigger case, done perhaps with a medical student or just scrub technicians, may not be done as slickly as it would be by a surgical team approaching the same at the university. If the case can be done safely though, it pays dividends. After all, it could be tonight when a major car wreck happens, or a hemodynamically unstable abdominal sepsis case presents, and we are forced to do a serious case – perhaps surgery at the edge of my comfort zone or something we don’t do with frequency. Keeping some bigger cases makes those scenarios just a bit less scary.
I have been recruited as an advocate for our College, trying to influence those in our nation’s capital to reexamine the 96-hour rule as it applies to critical access hospitals. A phone call to my senior senator’s staff leads to a conference call and follow-up I remain involved with – a first in my professional career. One issue that resonated with D.C. staffers was recruiting my successor. How do we entice the young surgeon to a rural practice if all we do are lumps and bumps, appendectomies, and inguinal hernias? Regionalization of surgical care may be coming but that can’t excite our younger and future colleagues. In each of the last 2 years my third-year medical students parked here for their first rotation and got hustled into the OR to assist with emergency surgery. The enthusiasm was palpable and energizing, but one was a case that raised some eyebrows: pneumatosis intestinalis requiring two small bowel resections with anastomoses and an open abdomen in an elderly male. This fellow did great; I see him doing his grocery shopping these days. My perspective is that case enabled this year’s day 1 emergency, making the surgery safer here in rural America.
When we call to transfer a patient, please understand real thought and a piece of who we are as surgeons accompanies that patient. Transfer is very rarely a reflex action. Also, realize that not every case we keep is a weak fastball over the middle of the plate; sometimes we do real work here at the limit of our comfort zone, but we do so for myriad good reasons.
Dr. Levine is a general surgeon practicing in coastal southwestern Oregon. Despite growing up in Brooklyn and on Long Island in New York, he has been a practicing rural surgeon since 1999. Folks barely even notice the accent anymore!
I have been on both ends of the phone call. I began my career at a several-hundred bed community hospital in a town without a university medical center. We took all the local knife-and-gun club incidents, and whatever other surgical emergencies might arise, while receiving phone calls from nearly every point of the magnetic compass. It’s easy to recall the sagging feeling when you realize more serious work is coming in on the helicopter from Podunk, USA, and you’re not off call for another few hours. These memories linger as now I’m the one making the phone calls. When I state that I am the one, I mean the one and only; this is solo general surgery practice and I’m the only general surgeon in my county.
When I do speak with colleagues kind enough to accept our patients, I feel relieved. But the burden of transfer doesn’t travel away with the patient in the ambulance or on the airplane. There always seem to be questions or looks of concern lately, and I don’t just mean from other medical professionals. Maybe it is an Internet thing, but everyone is a critic these days. We are being watched by more than partners and employers, more than payers and agencies, more than our government bean counters. Families, allied health professionals, and even nonclinical staff all have opinions about which patients stay and which leaves our 14-bed, critical access hospital. Gods may have once walked these halls, but nowadays it’s just me!
Of course, any interested party can also criticize my decisions to keep any particular patient; why would anybody restrict their furrowed glare only to transfers? When we keep patients at the edge of our practice, or perform a procedure that is only done rarely locally, we incite more than just the volume debate on the ACS Communities. Goodness – my wife has heard about cases I have done via town chitter-chatter before I even get home!
How does one deal with being whipsawed? This phenomenon is defined in the business world as being subjected to two difficult situations or opposing pressures at the same time. If you transfer, you are criticized. The only thing that changes are the critics if you keep and care for that very same patient! For many rural colleagues, being whipsawed is on the short list of job dissatisfaction drivers; somewhere behind the heavyweight champ of being asked to be in two different places at the same time.
Transferring a patient rarely leads to the lasting criticism that keeping an ill patient locally can. Obviously keeping a patient extends the time period where others can knowingly shake their heads in disbelief. That extra time allows us to educate staff and others as to why a patient with more than simple hernia or appendicitis is being admitted to our little hospital. We can detail why this is a really good thing for everyone – including the patient!
So many of our locals are elderly, and when we keep one for serious surgical illness, so much goes into that decision besides just the patient’s age and comorbid conditions. Immediate family, friends, or existing social support all must be examined and understood. A significant number of geriatric couples are only “independent” together; send one off for surgery a hundred or more miles away and the remaining spouse suffers measurably. Sometimes there is no local family, as nuclear members live in neighboring states or even overseas. I’m always surprised when my patients have trouble even arranging rides to and from our facilities for the routine procedures we do regularly. I think to myself, what will they do when the inevitable happens?
Our geography plays a serious role for those patients who don’t drive any appreciable distances. The mountains to our east are difficult to negotiate and west, well, you’ll get wet rather quickly. Going north and south on Highway 101 can be tricky during summer and dangerous any time in bad weather. I talk to some patients about sending them to Portland and I get looks in response like I’m proposing surgical care in some exotic foreign capital. Urban anxiety, traffic, and unfamiliarity with our largest metropolis make the 300-mile journey untenable for many of our patients; and the TV show isn’t helping our cause! Even cases that define themselves from the get-go as major university referrals return afterward and ask us to assume their postoperative care. Our patients often can’t make the trip to follow-up with the experts who provided their life-saving care.
Stretching our surgical muscles is obviously important for all ACS members. In bigger facilities you can see and sometimes scrub into fascinating cases in other subspecialties, or at least participate in discussions about such in the surgery lounge. I won’t attach a photo of the desk space that serves as my lounge, dictation station, bathroom, and locker. Let’s just say it’s probably not quite the same as many Fellows are used to.
For the rural solo practitioner, a bigger case, done perhaps with a medical student or just scrub technicians, may not be done as slickly as it would be by a surgical team approaching the same at the university. If the case can be done safely though, it pays dividends. After all, it could be tonight when a major car wreck happens, or a hemodynamically unstable abdominal sepsis case presents, and we are forced to do a serious case – perhaps surgery at the edge of my comfort zone or something we don’t do with frequency. Keeping some bigger cases makes those scenarios just a bit less scary.
I have been recruited as an advocate for our College, trying to influence those in our nation’s capital to reexamine the 96-hour rule as it applies to critical access hospitals. A phone call to my senior senator’s staff leads to a conference call and follow-up I remain involved with – a first in my professional career. One issue that resonated with D.C. staffers was recruiting my successor. How do we entice the young surgeon to a rural practice if all we do are lumps and bumps, appendectomies, and inguinal hernias? Regionalization of surgical care may be coming but that can’t excite our younger and future colleagues. In each of the last 2 years my third-year medical students parked here for their first rotation and got hustled into the OR to assist with emergency surgery. The enthusiasm was palpable and energizing, but one was a case that raised some eyebrows: pneumatosis intestinalis requiring two small bowel resections with anastomoses and an open abdomen in an elderly male. This fellow did great; I see him doing his grocery shopping these days. My perspective is that case enabled this year’s day 1 emergency, making the surgery safer here in rural America.
When we call to transfer a patient, please understand real thought and a piece of who we are as surgeons accompanies that patient. Transfer is very rarely a reflex action. Also, realize that not every case we keep is a weak fastball over the middle of the plate; sometimes we do real work here at the limit of our comfort zone, but we do so for myriad good reasons.
Dr. Levine is a general surgeon practicing in coastal southwestern Oregon. Despite growing up in Brooklyn and on Long Island in New York, he has been a practicing rural surgeon since 1999. Folks barely even notice the accent anymore!
I have been on both ends of the phone call. I began my career at a several-hundred bed community hospital in a town without a university medical center. We took all the local knife-and-gun club incidents, and whatever other surgical emergencies might arise, while receiving phone calls from nearly every point of the magnetic compass. It’s easy to recall the sagging feeling when you realize more serious work is coming in on the helicopter from Podunk, USA, and you’re not off call for another few hours. These memories linger as now I’m the one making the phone calls. When I state that I am the one, I mean the one and only; this is solo general surgery practice and I’m the only general surgeon in my county.
When I do speak with colleagues kind enough to accept our patients, I feel relieved. But the burden of transfer doesn’t travel away with the patient in the ambulance or on the airplane. There always seem to be questions or looks of concern lately, and I don’t just mean from other medical professionals. Maybe it is an Internet thing, but everyone is a critic these days. We are being watched by more than partners and employers, more than payers and agencies, more than our government bean counters. Families, allied health professionals, and even nonclinical staff all have opinions about which patients stay and which leaves our 14-bed, critical access hospital. Gods may have once walked these halls, but nowadays it’s just me!
Of course, any interested party can also criticize my decisions to keep any particular patient; why would anybody restrict their furrowed glare only to transfers? When we keep patients at the edge of our practice, or perform a procedure that is only done rarely locally, we incite more than just the volume debate on the ACS Communities. Goodness – my wife has heard about cases I have done via town chitter-chatter before I even get home!
How does one deal with being whipsawed? This phenomenon is defined in the business world as being subjected to two difficult situations or opposing pressures at the same time. If you transfer, you are criticized. The only thing that changes are the critics if you keep and care for that very same patient! For many rural colleagues, being whipsawed is on the short list of job dissatisfaction drivers; somewhere behind the heavyweight champ of being asked to be in two different places at the same time.
Transferring a patient rarely leads to the lasting criticism that keeping an ill patient locally can. Obviously keeping a patient extends the time period where others can knowingly shake their heads in disbelief. That extra time allows us to educate staff and others as to why a patient with more than simple hernia or appendicitis is being admitted to our little hospital. We can detail why this is a really good thing for everyone – including the patient!
So many of our locals are elderly, and when we keep one for serious surgical illness, so much goes into that decision besides just the patient’s age and comorbid conditions. Immediate family, friends, or existing social support all must be examined and understood. A significant number of geriatric couples are only “independent” together; send one off for surgery a hundred or more miles away and the remaining spouse suffers measurably. Sometimes there is no local family, as nuclear members live in neighboring states or even overseas. I’m always surprised when my patients have trouble even arranging rides to and from our facilities for the routine procedures we do regularly. I think to myself, what will they do when the inevitable happens?
Our geography plays a serious role for those patients who don’t drive any appreciable distances. The mountains to our east are difficult to negotiate and west, well, you’ll get wet rather quickly. Going north and south on Highway 101 can be tricky during summer and dangerous any time in bad weather. I talk to some patients about sending them to Portland and I get looks in response like I’m proposing surgical care in some exotic foreign capital. Urban anxiety, traffic, and unfamiliarity with our largest metropolis make the 300-mile journey untenable for many of our patients; and the TV show isn’t helping our cause! Even cases that define themselves from the get-go as major university referrals return afterward and ask us to assume their postoperative care. Our patients often can’t make the trip to follow-up with the experts who provided their life-saving care.
Stretching our surgical muscles is obviously important for all ACS members. In bigger facilities you can see and sometimes scrub into fascinating cases in other subspecialties, or at least participate in discussions about such in the surgery lounge. I won’t attach a photo of the desk space that serves as my lounge, dictation station, bathroom, and locker. Let’s just say it’s probably not quite the same as many Fellows are used to.
For the rural solo practitioner, a bigger case, done perhaps with a medical student or just scrub technicians, may not be done as slickly as it would be by a surgical team approaching the same at the university. If the case can be done safely though, it pays dividends. After all, it could be tonight when a major car wreck happens, or a hemodynamically unstable abdominal sepsis case presents, and we are forced to do a serious case – perhaps surgery at the edge of my comfort zone or something we don’t do with frequency. Keeping some bigger cases makes those scenarios just a bit less scary.
I have been recruited as an advocate for our College, trying to influence those in our nation’s capital to reexamine the 96-hour rule as it applies to critical access hospitals. A phone call to my senior senator’s staff leads to a conference call and follow-up I remain involved with – a first in my professional career. One issue that resonated with D.C. staffers was recruiting my successor. How do we entice the young surgeon to a rural practice if all we do are lumps and bumps, appendectomies, and inguinal hernias? Regionalization of surgical care may be coming but that can’t excite our younger and future colleagues. In each of the last 2 years my third-year medical students parked here for their first rotation and got hustled into the OR to assist with emergency surgery. The enthusiasm was palpable and energizing, but one was a case that raised some eyebrows: pneumatosis intestinalis requiring two small bowel resections with anastomoses and an open abdomen in an elderly male. This fellow did great; I see him doing his grocery shopping these days. My perspective is that case enabled this year’s day 1 emergency, making the surgery safer here in rural America.
When we call to transfer a patient, please understand real thought and a piece of who we are as surgeons accompanies that patient. Transfer is very rarely a reflex action. Also, realize that not every case we keep is a weak fastball over the middle of the plate; sometimes we do real work here at the limit of our comfort zone, but we do so for myriad good reasons.
Dr. Levine is a general surgeon practicing in coastal southwestern Oregon. Despite growing up in Brooklyn and on Long Island in New York, he has been a practicing rural surgeon since 1999. Folks barely even notice the accent anymore!
Verrucous Carcinoma on the Lower Extremities
To the Editor:
A 38-year-old black man presented with a slowly enlarging growth on the left thigh of 7 years’ duration. The lesion would occasionally scrape off but always recurred. He reported that the tumor developed in the area of a prior nevus. He reported no direct trauma to the area, chronic inflammation, or similar lesions elsewhere. His medical history included gastroesophageal reflux disease and inactive sarcoidosis. Physical examination revealed a 3×3×1-cm exophytic, hyperkeratotic, erythematous nodule with surrounding stellate and branching hyperpigmentation on the anterior aspect of the thigh (Figure 1). Pathologic examination demonstrated hyperkeratosis with an endophytic proliferation of mildly atypical keratinocytes with broad blunted rete ridges (Figure 2). Complete excision of the lesion was performed.
A 33-year-old black man presented with a rapidly growing lesion on the right fifth toe of 3 months’ duration. The patient originally believed the initial small papule was a corn, and after attempts to shave it down with a razor blade, the lesion grew rapidly into a large painful tumor. He reported no prior trauma to the area or history of a similar lesion. Physical examination revealed a 2×2×0.5-cm hyperkeratotic, papillated, hard nodule with a heaped-up border and no ulceration or drainage (Figure 3). A shave biopsy of the lesion was obtained. Microscopic examination revealed hyperkeratosis, parakeratosis, and papillomatosis with deep extension of mildly atypical keratinocytes into the dermis. Small toe amputation was performed by an orthopedic surgeon.
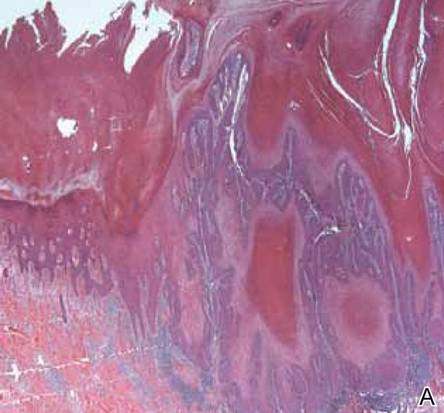
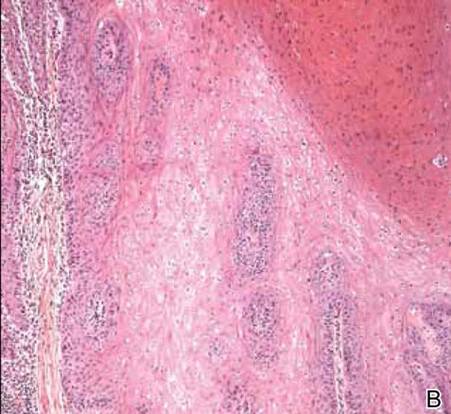
|
Verrucous carcinoma, first described by Ackerman1 in 1948, is an uncommon, low-grade, well-differentiated variant of squamous cell carcinoma. It presents as a slow-growing, bulky, exophytic tumor with a broad base. The tumor can ulcerate or present with surface sinus tracts that drain foul-smelling material. Typically, the tumor occurs in the fifth to sixth decades of life, with men outnumbering women by a ratio of 5.3 to 1.2 The prevalence of verrucous carcinoma in black individuals is unknown. A review of nonmelanoma skin cancers in skin of color identifies squamous cell carcinoma as the most common cutaneous carcinoma but does not report on the rare verrucous variant.3
Verrucous carcinoma is found in a variety of mucosal and skin surfaces. Verrucous carcinoma of the oral cavity, found most commonly on the buccal mucosa, is known as florid oral papillomatosis or Ackerman carcinoma. Cutaneous verrucous carcinoma is referred to as carcinoma cuniculatum or epithelioma cuniculatum and is predominantly located on the plantar surface of the foot. It is less commonly reported on the palm, scalp, face, extremities, and back. Verrucous carcinoma found in the anogenital area is referred to as the Buschke-Löwenstein tumor.4
Histologically, the lesion shows minimal cytologic atypia. Topped by an undulating keratinized mass, the deep margin of the tumor advances as a broad bulbous projection, compressing the underlying connective tissue in a bulldozing manner. Typically there also are keratin-filled sinuses and intraepidermal microabscesses.1
Human papillomavirus types 6, 11, 16, and 18 may be involved in the induction of the tumor. Human papillomavirus types 6 and 11 are frequently associated with the Buschke-Löwenstein tumor,2,4 while carcinoma cuniculatum is most commonly associated with human papillomavirus 16.5-7 In several cases of verrucous carcinoma, the tumor was reported to arise from preexisting lesions with chronic inflammation, such as a chronic ulcer, inflamed cyst, or burn scar.2 Ackerman carcinoma has been associated with the use of snuff, chewing tobacco, and betel nuts.
Morbidity and mortality from verrucous carcinoma arises from local invasion and infiltration into adjacent bone. The tumor rarely metastasizes, with regional lymph nodes being the only reported site of metastasis.8 The treatment of cutaneous verrucous carcinoma is complete surgical excision. Mohs micrographic surgery is preferred because it minimizes recurrence risk.4 Radiation therapy is contraindicated because it has been reported to cause the tumor to become more aggressive.9,10 Although local recurrence may occur, the prognosis is usually favorable.
1. Ackerman LV. Verrucous carcinoma of the oral cavity. Surgery. 1948;23:670-678.
2. Kao GF, Graham JH, Helwig EB. Carcinoma cuniculatum (verrucous carcinoma of the skin). a clinicopathologic study of 46 cases with ultrastructural observations. Cancer. 1982;49:2395-2403.
3. Jackson BA. Nonmelanoma skin cancer in persons of color. Semin Cutan Med Surg. 2009;28:93-95.
4. Schwartz RA. Verrucous carcinoma of the skin and mucosa. J Am Acad Dermatol. 1995;32:1-21; quiz 22-24.
5. Assaf C, Steinhoff M, Petrov I, et al. Verrucous carcinoma of the axilla: case report and review. J Cutan Pathol. 2004;31:199-204.
6. Schell BJ, Rosen T, Rády P, et al. Verrucous carcinoma of the foot associated with human papillomavirus type 16. J Am Acad Dermatol. 2001;45:49-55.
7. Miyamoto T, Sasaoka R, Hagari Y, et al. Association of cutaneous verrucous carcinoma with human papillomavirus type 16. Br J Dermatol. 1999;140:168-169.
8. Walvekar RR, Chaukar DA, Deshpande MS, et al. Verrucous carcinoma of the oral cavity: a clinical and pathological study of 101 cases [published online ahead of print July 11, 2008]. Oral Oncol. 2009;45:47-51.
9. Perez CA, Krans FT, Evans JC, et al. Anaplastic transformation in verrucous carcinoma of the oral cavity after radiation therapy. Radiology. 1966;86:108-115.
10. Proffett SD, Spooner TR, Kosek JC. Origin of undifferentiated neoplasm from verrucous epidermal carcinoma of oral cavity following irradiation. Cancer. 1970;26:389-393.
To the Editor:
A 38-year-old black man presented with a slowly enlarging growth on the left thigh of 7 years’ duration. The lesion would occasionally scrape off but always recurred. He reported that the tumor developed in the area of a prior nevus. He reported no direct trauma to the area, chronic inflammation, or similar lesions elsewhere. His medical history included gastroesophageal reflux disease and inactive sarcoidosis. Physical examination revealed a 3×3×1-cm exophytic, hyperkeratotic, erythematous nodule with surrounding stellate and branching hyperpigmentation on the anterior aspect of the thigh (Figure 1). Pathologic examination demonstrated hyperkeratosis with an endophytic proliferation of mildly atypical keratinocytes with broad blunted rete ridges (Figure 2). Complete excision of the lesion was performed.
A 33-year-old black man presented with a rapidly growing lesion on the right fifth toe of 3 months’ duration. The patient originally believed the initial small papule was a corn, and after attempts to shave it down with a razor blade, the lesion grew rapidly into a large painful tumor. He reported no prior trauma to the area or history of a similar lesion. Physical examination revealed a 2×2×0.5-cm hyperkeratotic, papillated, hard nodule with a heaped-up border and no ulceration or drainage (Figure 3). A shave biopsy of the lesion was obtained. Microscopic examination revealed hyperkeratosis, parakeratosis, and papillomatosis with deep extension of mildly atypical keratinocytes into the dermis. Small toe amputation was performed by an orthopedic surgeon.
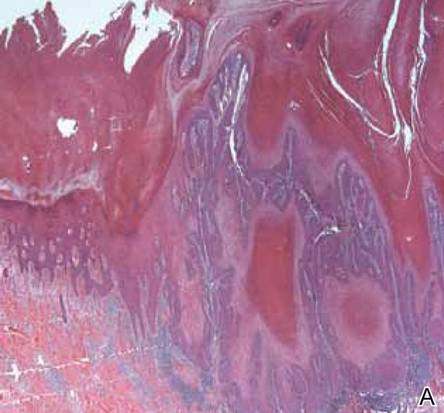
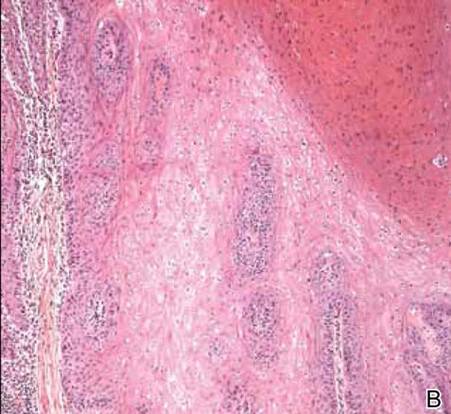
|
Verrucous carcinoma, first described by Ackerman1 in 1948, is an uncommon, low-grade, well-differentiated variant of squamous cell carcinoma. It presents as a slow-growing, bulky, exophytic tumor with a broad base. The tumor can ulcerate or present with surface sinus tracts that drain foul-smelling material. Typically, the tumor occurs in the fifth to sixth decades of life, with men outnumbering women by a ratio of 5.3 to 1.2 The prevalence of verrucous carcinoma in black individuals is unknown. A review of nonmelanoma skin cancers in skin of color identifies squamous cell carcinoma as the most common cutaneous carcinoma but does not report on the rare verrucous variant.3
Verrucous carcinoma is found in a variety of mucosal and skin surfaces. Verrucous carcinoma of the oral cavity, found most commonly on the buccal mucosa, is known as florid oral papillomatosis or Ackerman carcinoma. Cutaneous verrucous carcinoma is referred to as carcinoma cuniculatum or epithelioma cuniculatum and is predominantly located on the plantar surface of the foot. It is less commonly reported on the palm, scalp, face, extremities, and back. Verrucous carcinoma found in the anogenital area is referred to as the Buschke-Löwenstein tumor.4
Histologically, the lesion shows minimal cytologic atypia. Topped by an undulating keratinized mass, the deep margin of the tumor advances as a broad bulbous projection, compressing the underlying connective tissue in a bulldozing manner. Typically there also are keratin-filled sinuses and intraepidermal microabscesses.1
Human papillomavirus types 6, 11, 16, and 18 may be involved in the induction of the tumor. Human papillomavirus types 6 and 11 are frequently associated with the Buschke-Löwenstein tumor,2,4 while carcinoma cuniculatum is most commonly associated with human papillomavirus 16.5-7 In several cases of verrucous carcinoma, the tumor was reported to arise from preexisting lesions with chronic inflammation, such as a chronic ulcer, inflamed cyst, or burn scar.2 Ackerman carcinoma has been associated with the use of snuff, chewing tobacco, and betel nuts.
Morbidity and mortality from verrucous carcinoma arises from local invasion and infiltration into adjacent bone. The tumor rarely metastasizes, with regional lymph nodes being the only reported site of metastasis.8 The treatment of cutaneous verrucous carcinoma is complete surgical excision. Mohs micrographic surgery is preferred because it minimizes recurrence risk.4 Radiation therapy is contraindicated because it has been reported to cause the tumor to become more aggressive.9,10 Although local recurrence may occur, the prognosis is usually favorable.
To the Editor:
A 38-year-old black man presented with a slowly enlarging growth on the left thigh of 7 years’ duration. The lesion would occasionally scrape off but always recurred. He reported that the tumor developed in the area of a prior nevus. He reported no direct trauma to the area, chronic inflammation, or similar lesions elsewhere. His medical history included gastroesophageal reflux disease and inactive sarcoidosis. Physical examination revealed a 3×3×1-cm exophytic, hyperkeratotic, erythematous nodule with surrounding stellate and branching hyperpigmentation on the anterior aspect of the thigh (Figure 1). Pathologic examination demonstrated hyperkeratosis with an endophytic proliferation of mildly atypical keratinocytes with broad blunted rete ridges (Figure 2). Complete excision of the lesion was performed.
A 33-year-old black man presented with a rapidly growing lesion on the right fifth toe of 3 months’ duration. The patient originally believed the initial small papule was a corn, and after attempts to shave it down with a razor blade, the lesion grew rapidly into a large painful tumor. He reported no prior trauma to the area or history of a similar lesion. Physical examination revealed a 2×2×0.5-cm hyperkeratotic, papillated, hard nodule with a heaped-up border and no ulceration or drainage (Figure 3). A shave biopsy of the lesion was obtained. Microscopic examination revealed hyperkeratosis, parakeratosis, and papillomatosis with deep extension of mildly atypical keratinocytes into the dermis. Small toe amputation was performed by an orthopedic surgeon.
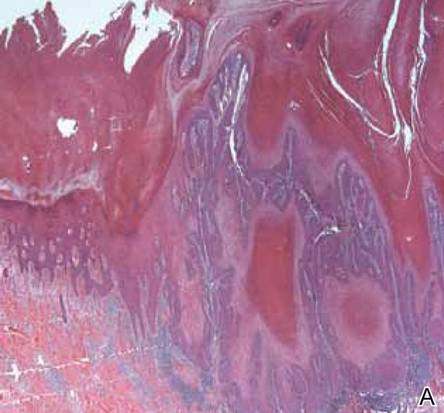
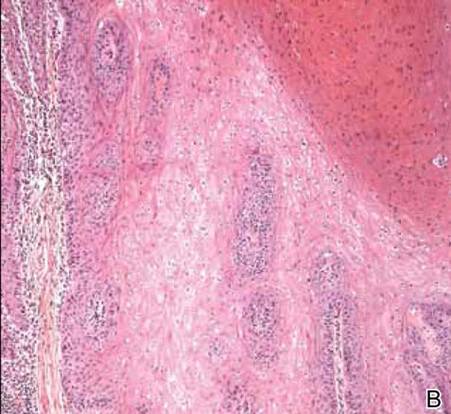
|
Verrucous carcinoma, first described by Ackerman1 in 1948, is an uncommon, low-grade, well-differentiated variant of squamous cell carcinoma. It presents as a slow-growing, bulky, exophytic tumor with a broad base. The tumor can ulcerate or present with surface sinus tracts that drain foul-smelling material. Typically, the tumor occurs in the fifth to sixth decades of life, with men outnumbering women by a ratio of 5.3 to 1.2 The prevalence of verrucous carcinoma in black individuals is unknown. A review of nonmelanoma skin cancers in skin of color identifies squamous cell carcinoma as the most common cutaneous carcinoma but does not report on the rare verrucous variant.3
Verrucous carcinoma is found in a variety of mucosal and skin surfaces. Verrucous carcinoma of the oral cavity, found most commonly on the buccal mucosa, is known as florid oral papillomatosis or Ackerman carcinoma. Cutaneous verrucous carcinoma is referred to as carcinoma cuniculatum or epithelioma cuniculatum and is predominantly located on the plantar surface of the foot. It is less commonly reported on the palm, scalp, face, extremities, and back. Verrucous carcinoma found in the anogenital area is referred to as the Buschke-Löwenstein tumor.4
Histologically, the lesion shows minimal cytologic atypia. Topped by an undulating keratinized mass, the deep margin of the tumor advances as a broad bulbous projection, compressing the underlying connective tissue in a bulldozing manner. Typically there also are keratin-filled sinuses and intraepidermal microabscesses.1
Human papillomavirus types 6, 11, 16, and 18 may be involved in the induction of the tumor. Human papillomavirus types 6 and 11 are frequently associated with the Buschke-Löwenstein tumor,2,4 while carcinoma cuniculatum is most commonly associated with human papillomavirus 16.5-7 In several cases of verrucous carcinoma, the tumor was reported to arise from preexisting lesions with chronic inflammation, such as a chronic ulcer, inflamed cyst, or burn scar.2 Ackerman carcinoma has been associated with the use of snuff, chewing tobacco, and betel nuts.
Morbidity and mortality from verrucous carcinoma arises from local invasion and infiltration into adjacent bone. The tumor rarely metastasizes, with regional lymph nodes being the only reported site of metastasis.8 The treatment of cutaneous verrucous carcinoma is complete surgical excision. Mohs micrographic surgery is preferred because it minimizes recurrence risk.4 Radiation therapy is contraindicated because it has been reported to cause the tumor to become more aggressive.9,10 Although local recurrence may occur, the prognosis is usually favorable.
1. Ackerman LV. Verrucous carcinoma of the oral cavity. Surgery. 1948;23:670-678.
2. Kao GF, Graham JH, Helwig EB. Carcinoma cuniculatum (verrucous carcinoma of the skin). a clinicopathologic study of 46 cases with ultrastructural observations. Cancer. 1982;49:2395-2403.
3. Jackson BA. Nonmelanoma skin cancer in persons of color. Semin Cutan Med Surg. 2009;28:93-95.
4. Schwartz RA. Verrucous carcinoma of the skin and mucosa. J Am Acad Dermatol. 1995;32:1-21; quiz 22-24.
5. Assaf C, Steinhoff M, Petrov I, et al. Verrucous carcinoma of the axilla: case report and review. J Cutan Pathol. 2004;31:199-204.
6. Schell BJ, Rosen T, Rády P, et al. Verrucous carcinoma of the foot associated with human papillomavirus type 16. J Am Acad Dermatol. 2001;45:49-55.
7. Miyamoto T, Sasaoka R, Hagari Y, et al. Association of cutaneous verrucous carcinoma with human papillomavirus type 16. Br J Dermatol. 1999;140:168-169.
8. Walvekar RR, Chaukar DA, Deshpande MS, et al. Verrucous carcinoma of the oral cavity: a clinical and pathological study of 101 cases [published online ahead of print July 11, 2008]. Oral Oncol. 2009;45:47-51.
9. Perez CA, Krans FT, Evans JC, et al. Anaplastic transformation in verrucous carcinoma of the oral cavity after radiation therapy. Radiology. 1966;86:108-115.
10. Proffett SD, Spooner TR, Kosek JC. Origin of undifferentiated neoplasm from verrucous epidermal carcinoma of oral cavity following irradiation. Cancer. 1970;26:389-393.
1. Ackerman LV. Verrucous carcinoma of the oral cavity. Surgery. 1948;23:670-678.
2. Kao GF, Graham JH, Helwig EB. Carcinoma cuniculatum (verrucous carcinoma of the skin). a clinicopathologic study of 46 cases with ultrastructural observations. Cancer. 1982;49:2395-2403.
3. Jackson BA. Nonmelanoma skin cancer in persons of color. Semin Cutan Med Surg. 2009;28:93-95.
4. Schwartz RA. Verrucous carcinoma of the skin and mucosa. J Am Acad Dermatol. 1995;32:1-21; quiz 22-24.
5. Assaf C, Steinhoff M, Petrov I, et al. Verrucous carcinoma of the axilla: case report and review. J Cutan Pathol. 2004;31:199-204.
6. Schell BJ, Rosen T, Rády P, et al. Verrucous carcinoma of the foot associated with human papillomavirus type 16. J Am Acad Dermatol. 2001;45:49-55.
7. Miyamoto T, Sasaoka R, Hagari Y, et al. Association of cutaneous verrucous carcinoma with human papillomavirus type 16. Br J Dermatol. 1999;140:168-169.
8. Walvekar RR, Chaukar DA, Deshpande MS, et al. Verrucous carcinoma of the oral cavity: a clinical and pathological study of 101 cases [published online ahead of print July 11, 2008]. Oral Oncol. 2009;45:47-51.
9. Perez CA, Krans FT, Evans JC, et al. Anaplastic transformation in verrucous carcinoma of the oral cavity after radiation therapy. Radiology. 1966;86:108-115.
10. Proffett SD, Spooner TR, Kosek JC. Origin of undifferentiated neoplasm from verrucous epidermal carcinoma of oral cavity following irradiation. Cancer. 1970;26:389-393.













