User login
Fungal foot infections risk secondary infection in diabetic patients
VANCOUVER – Fungal foot infections in diabetic patients are often ignored and are far more than a cosmetic problem.
In patients with diabetes, tinea pedis and onychomycosis triple the likelihood of secondary bacterial infections including gram-negative intertrigo, cellulitis, and osteomyelitis. Further, they boost up to fivefold the risk of life- and limb-threatening gangrene, Dr. Manuela Papini said at the World Congress of Dermatology.
Her own work (G Ital Dermatol Venereol. 2013 Dec;148(6):603-8), as well as that of others, indicates tinea pedis and onychomycosis in diabetic patients often goes undiagnosed, ignored, or inadequately treated.
In her own experience, four out of five diabetic patients with a fungal foot infection are unaware of it, she said. Moreover, half of those with a diagnosed fungal foot infection remain untreated or insufficiently treated, added Dr. Papini, a dermatologist at the University of Perugia (Italy).
Fungal infections of the foot are three times more common among diabetic individuals than the general population. The reasons for this disparity included impaired peripheral circulation, an immunocompromised state, autonomic neuropathy, and the inability to maintain good foot hygiene because of obesity, impaired vision, or advanced age.
The causative organisms of fungal infections in diabetic patients are the same as those seen in the general population. So are the recommended first-line treatments. But treatment response is generally poor – much worse than in nondiabetics. Adherence to antifungal medication also is a real problem in diabetic patients, due in large part to the high prevalence of comorbid conditions and resultant polypharmacy.
“Most diabetic patients say their large pill burden is an issue, and they think onychomycosis is the least important of their problems,” she explained.
Photodynamic therapy and laser treatments show promise, but the supporting data aren’t yet sufficient to warrant their introduction into clinical practice, according to Dr. Papini.
As for contemporary therapy, she noted that the British Association of Dermatologists, in its current onychomycosis treatment guidelines, reserves its A-strength recommendations for two oral drugs given daily for 12 weeks: terbinafine and itraconazole, although itraconazole can alternatively be used as pulse therapy for 3-6 months. Topical therapies are advised only for superficial white onychomycosis and early distal lateral subungual onychomycosis (Br J Dermatol. 2014 Nov;171(5):937-58).
A systematic review of the published literature on treatment of diabetic fungal foot infections concluded that there is good evidence that oral terbinafine is as safe and effective as itraconazole for treating onychomycosis. The authors, however, found that there is no evidence to guide treatment of tinea pedis in the diabetic population (J Foot Ankle Res. 2011 Dec 4;4:26).
In the nondiabetic population, the first-line treatment for tinea pedis is typically a topical antifungal. A good option in diabetic patients is luliconazole (Luzu), which is active against Trichophyton rubrum – the most common causative organism – and has the advantage of simplicity: the regimen is once-daily treatment for 2 weeks, much shorter than for many other topical antifungals, Dr. Papini observed.
Until new and better treatments come along, she continued, the key to preventing relapse of fungal foot infections in diabetic patients is to choose the simplest and most effective therapy, stress to patients the importance of completing the treatment course, and provide instruction in self-inspection and disinfection of shoes and socks.
Dr. Papini reported having no financial conflicts of interest.
VANCOUVER – Fungal foot infections in diabetic patients are often ignored and are far more than a cosmetic problem.
In patients with diabetes, tinea pedis and onychomycosis triple the likelihood of secondary bacterial infections including gram-negative intertrigo, cellulitis, and osteomyelitis. Further, they boost up to fivefold the risk of life- and limb-threatening gangrene, Dr. Manuela Papini said at the World Congress of Dermatology.
Her own work (G Ital Dermatol Venereol. 2013 Dec;148(6):603-8), as well as that of others, indicates tinea pedis and onychomycosis in diabetic patients often goes undiagnosed, ignored, or inadequately treated.
In her own experience, four out of five diabetic patients with a fungal foot infection are unaware of it, she said. Moreover, half of those with a diagnosed fungal foot infection remain untreated or insufficiently treated, added Dr. Papini, a dermatologist at the University of Perugia (Italy).
Fungal infections of the foot are three times more common among diabetic individuals than the general population. The reasons for this disparity included impaired peripheral circulation, an immunocompromised state, autonomic neuropathy, and the inability to maintain good foot hygiene because of obesity, impaired vision, or advanced age.
The causative organisms of fungal infections in diabetic patients are the same as those seen in the general population. So are the recommended first-line treatments. But treatment response is generally poor – much worse than in nondiabetics. Adherence to antifungal medication also is a real problem in diabetic patients, due in large part to the high prevalence of comorbid conditions and resultant polypharmacy.
“Most diabetic patients say their large pill burden is an issue, and they think onychomycosis is the least important of their problems,” she explained.
Photodynamic therapy and laser treatments show promise, but the supporting data aren’t yet sufficient to warrant their introduction into clinical practice, according to Dr. Papini.
As for contemporary therapy, she noted that the British Association of Dermatologists, in its current onychomycosis treatment guidelines, reserves its A-strength recommendations for two oral drugs given daily for 12 weeks: terbinafine and itraconazole, although itraconazole can alternatively be used as pulse therapy for 3-6 months. Topical therapies are advised only for superficial white onychomycosis and early distal lateral subungual onychomycosis (Br J Dermatol. 2014 Nov;171(5):937-58).
A systematic review of the published literature on treatment of diabetic fungal foot infections concluded that there is good evidence that oral terbinafine is as safe and effective as itraconazole for treating onychomycosis. The authors, however, found that there is no evidence to guide treatment of tinea pedis in the diabetic population (J Foot Ankle Res. 2011 Dec 4;4:26).
In the nondiabetic population, the first-line treatment for tinea pedis is typically a topical antifungal. A good option in diabetic patients is luliconazole (Luzu), which is active against Trichophyton rubrum – the most common causative organism – and has the advantage of simplicity: the regimen is once-daily treatment for 2 weeks, much shorter than for many other topical antifungals, Dr. Papini observed.
Until new and better treatments come along, she continued, the key to preventing relapse of fungal foot infections in diabetic patients is to choose the simplest and most effective therapy, stress to patients the importance of completing the treatment course, and provide instruction in self-inspection and disinfection of shoes and socks.
Dr. Papini reported having no financial conflicts of interest.
VANCOUVER – Fungal foot infections in diabetic patients are often ignored and are far more than a cosmetic problem.
In patients with diabetes, tinea pedis and onychomycosis triple the likelihood of secondary bacterial infections including gram-negative intertrigo, cellulitis, and osteomyelitis. Further, they boost up to fivefold the risk of life- and limb-threatening gangrene, Dr. Manuela Papini said at the World Congress of Dermatology.
Her own work (G Ital Dermatol Venereol. 2013 Dec;148(6):603-8), as well as that of others, indicates tinea pedis and onychomycosis in diabetic patients often goes undiagnosed, ignored, or inadequately treated.
In her own experience, four out of five diabetic patients with a fungal foot infection are unaware of it, she said. Moreover, half of those with a diagnosed fungal foot infection remain untreated or insufficiently treated, added Dr. Papini, a dermatologist at the University of Perugia (Italy).
Fungal infections of the foot are three times more common among diabetic individuals than the general population. The reasons for this disparity included impaired peripheral circulation, an immunocompromised state, autonomic neuropathy, and the inability to maintain good foot hygiene because of obesity, impaired vision, or advanced age.
The causative organisms of fungal infections in diabetic patients are the same as those seen in the general population. So are the recommended first-line treatments. But treatment response is generally poor – much worse than in nondiabetics. Adherence to antifungal medication also is a real problem in diabetic patients, due in large part to the high prevalence of comorbid conditions and resultant polypharmacy.
“Most diabetic patients say their large pill burden is an issue, and they think onychomycosis is the least important of their problems,” she explained.
Photodynamic therapy and laser treatments show promise, but the supporting data aren’t yet sufficient to warrant their introduction into clinical practice, according to Dr. Papini.
As for contemporary therapy, she noted that the British Association of Dermatologists, in its current onychomycosis treatment guidelines, reserves its A-strength recommendations for two oral drugs given daily for 12 weeks: terbinafine and itraconazole, although itraconazole can alternatively be used as pulse therapy for 3-6 months. Topical therapies are advised only for superficial white onychomycosis and early distal lateral subungual onychomycosis (Br J Dermatol. 2014 Nov;171(5):937-58).
A systematic review of the published literature on treatment of diabetic fungal foot infections concluded that there is good evidence that oral terbinafine is as safe and effective as itraconazole for treating onychomycosis. The authors, however, found that there is no evidence to guide treatment of tinea pedis in the diabetic population (J Foot Ankle Res. 2011 Dec 4;4:26).
In the nondiabetic population, the first-line treatment for tinea pedis is typically a topical antifungal. A good option in diabetic patients is luliconazole (Luzu), which is active against Trichophyton rubrum – the most common causative organism – and has the advantage of simplicity: the regimen is once-daily treatment for 2 weeks, much shorter than for many other topical antifungals, Dr. Papini observed.
Until new and better treatments come along, she continued, the key to preventing relapse of fungal foot infections in diabetic patients is to choose the simplest and most effective therapy, stress to patients the importance of completing the treatment course, and provide instruction in self-inspection and disinfection of shoes and socks.
Dr. Papini reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM WCD 2015
One dollar and forty-two cents
No good deed goes unpunished.
We froze Myrna’s keratosis off her forehead. Gratis, of course.
This was followed by repeated calls from Myrna: the spot was red, it was painful, it wasn’t healing right.
So we mailed her an envelope filled with cream to help heal the skin. Although we used our regular postage meter, somehow Myrna got the package with $1.42 postage due.
Not going to work.
Myrna called to complain. Then she drove over and walked into the office, but we weren’t there. Then she called again and left a message. “I’m coming in this afternoon,” she said. “I expect to pick up my $1.42.”
Really.
Later that morning, Stephanie came by for a skin check. Because Stephanie is catering manager at a downtown ultra-upscale hotel, I knew she would both appreciate the tale of $1.42 and be able to top it. Everyone in her field can fill several books of client encounters no one could make up.
When I asked her to share some stories, Stephanie did not disappoint.
“Sure,” she said. “People plan lavish weddings, no expense spared. But when they send gift baskets, we have to charge $3.50 each to pay the livery people who deliver them. That they object to.
“But what’s even worse,” she went on, “is when it comes to feeding the band. We discount the meals for musicians 60%-70% below the per-plate rate for guests.
“That’s not low enough for some people, though. We explain to them that the band members do have to eat. ‘Yes,’ say some of the brides, ‘but do we have to give them a whole meal? Can’t we just give them a sandwich or something?’ This is from people who are spending six figures on food alone.”
“Sounds like Marie Antoinette,” I said. “What do you tell them?”
“We say, OK, we’ll see if we can discount the band meals even more,” Stephanie said.
Not an hour later, Ken came in. Ken manages an art-house movie theater in a close-in, affluent suburb. As I knew he would, Ken had stories, too.
“People are always angling for some kind of special privilege,” he said. ‘I’ve been a patron for years,” they say. ‘Can’t you do something for me?’
“What do they want?” I ask. “Free tickets?”
“Yes, or preferential seating,” said Ken, “but we tell them that if we do that for them, we’d have to do it for everybody.
“Or else it’s a cold, winter night and the theater is a little chilly. Some of the patrons want us to give them free popcorn.” Ken sighed.
Anybody in the service business is going to meet up with behavior like this. We probably should be grateful that most patients have enough respect for our profession to dissuade them from:
• Demanding to be seen for free or have us waive the copay since “the treatment didn’t work.”
• Refusing to hand over the copay for a follow-up, because, “It was just a quick check, didn’t take any time.”
• Insist on having us treat the wart or skin tag again at no charge, because “you missed a spot.”
And so on. At least even our demanding patients don’t ask for popcorn.
Myrna did show up that afternoon, by the way. I don’t know how much she spent on gas to come in. Our office manager Fatima took care of things. She gave Myrna her Buck-42:
Three quarters.
Two dimes.
Five nickels.
And 22 pennies.
Fatima is really good at keeping a straight face.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years.
No good deed goes unpunished.
We froze Myrna’s keratosis off her forehead. Gratis, of course.
This was followed by repeated calls from Myrna: the spot was red, it was painful, it wasn’t healing right.
So we mailed her an envelope filled with cream to help heal the skin. Although we used our regular postage meter, somehow Myrna got the package with $1.42 postage due.
Not going to work.
Myrna called to complain. Then she drove over and walked into the office, but we weren’t there. Then she called again and left a message. “I’m coming in this afternoon,” she said. “I expect to pick up my $1.42.”
Really.
Later that morning, Stephanie came by for a skin check. Because Stephanie is catering manager at a downtown ultra-upscale hotel, I knew she would both appreciate the tale of $1.42 and be able to top it. Everyone in her field can fill several books of client encounters no one could make up.
When I asked her to share some stories, Stephanie did not disappoint.
“Sure,” she said. “People plan lavish weddings, no expense spared. But when they send gift baskets, we have to charge $3.50 each to pay the livery people who deliver them. That they object to.
“But what’s even worse,” she went on, “is when it comes to feeding the band. We discount the meals for musicians 60%-70% below the per-plate rate for guests.
“That’s not low enough for some people, though. We explain to them that the band members do have to eat. ‘Yes,’ say some of the brides, ‘but do we have to give them a whole meal? Can’t we just give them a sandwich or something?’ This is from people who are spending six figures on food alone.”
“Sounds like Marie Antoinette,” I said. “What do you tell them?”
“We say, OK, we’ll see if we can discount the band meals even more,” Stephanie said.
Not an hour later, Ken came in. Ken manages an art-house movie theater in a close-in, affluent suburb. As I knew he would, Ken had stories, too.
“People are always angling for some kind of special privilege,” he said. ‘I’ve been a patron for years,” they say. ‘Can’t you do something for me?’
“What do they want?” I ask. “Free tickets?”
“Yes, or preferential seating,” said Ken, “but we tell them that if we do that for them, we’d have to do it for everybody.
“Or else it’s a cold, winter night and the theater is a little chilly. Some of the patrons want us to give them free popcorn.” Ken sighed.
Anybody in the service business is going to meet up with behavior like this. We probably should be grateful that most patients have enough respect for our profession to dissuade them from:
• Demanding to be seen for free or have us waive the copay since “the treatment didn’t work.”
• Refusing to hand over the copay for a follow-up, because, “It was just a quick check, didn’t take any time.”
• Insist on having us treat the wart or skin tag again at no charge, because “you missed a spot.”
And so on. At least even our demanding patients don’t ask for popcorn.
Myrna did show up that afternoon, by the way. I don’t know how much she spent on gas to come in. Our office manager Fatima took care of things. She gave Myrna her Buck-42:
Three quarters.
Two dimes.
Five nickels.
And 22 pennies.
Fatima is really good at keeping a straight face.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years.
No good deed goes unpunished.
We froze Myrna’s keratosis off her forehead. Gratis, of course.
This was followed by repeated calls from Myrna: the spot was red, it was painful, it wasn’t healing right.
So we mailed her an envelope filled with cream to help heal the skin. Although we used our regular postage meter, somehow Myrna got the package with $1.42 postage due.
Not going to work.
Myrna called to complain. Then she drove over and walked into the office, but we weren’t there. Then she called again and left a message. “I’m coming in this afternoon,” she said. “I expect to pick up my $1.42.”
Really.
Later that morning, Stephanie came by for a skin check. Because Stephanie is catering manager at a downtown ultra-upscale hotel, I knew she would both appreciate the tale of $1.42 and be able to top it. Everyone in her field can fill several books of client encounters no one could make up.
When I asked her to share some stories, Stephanie did not disappoint.
“Sure,” she said. “People plan lavish weddings, no expense spared. But when they send gift baskets, we have to charge $3.50 each to pay the livery people who deliver them. That they object to.
“But what’s even worse,” she went on, “is when it comes to feeding the band. We discount the meals for musicians 60%-70% below the per-plate rate for guests.
“That’s not low enough for some people, though. We explain to them that the band members do have to eat. ‘Yes,’ say some of the brides, ‘but do we have to give them a whole meal? Can’t we just give them a sandwich or something?’ This is from people who are spending six figures on food alone.”
“Sounds like Marie Antoinette,” I said. “What do you tell them?”
“We say, OK, we’ll see if we can discount the band meals even more,” Stephanie said.
Not an hour later, Ken came in. Ken manages an art-house movie theater in a close-in, affluent suburb. As I knew he would, Ken had stories, too.
“People are always angling for some kind of special privilege,” he said. ‘I’ve been a patron for years,” they say. ‘Can’t you do something for me?’
“What do they want?” I ask. “Free tickets?”
“Yes, or preferential seating,” said Ken, “but we tell them that if we do that for them, we’d have to do it for everybody.
“Or else it’s a cold, winter night and the theater is a little chilly. Some of the patrons want us to give them free popcorn.” Ken sighed.
Anybody in the service business is going to meet up with behavior like this. We probably should be grateful that most patients have enough respect for our profession to dissuade them from:
• Demanding to be seen for free or have us waive the copay since “the treatment didn’t work.”
• Refusing to hand over the copay for a follow-up, because, “It was just a quick check, didn’t take any time.”
• Insist on having us treat the wart or skin tag again at no charge, because “you missed a spot.”
And so on. At least even our demanding patients don’t ask for popcorn.
Myrna did show up that afternoon, by the way. I don’t know how much she spent on gas to come in. Our office manager Fatima took care of things. She gave Myrna her Buck-42:
Three quarters.
Two dimes.
Five nickels.
And 22 pennies.
Fatima is really good at keeping a straight face.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years.
China's Healthcare Reform Drive Stuck in First Gear
SHANGHAI (Reuters) - Li Tiantian, a Chinese doctor turned tech entrepreneur, is a leading light of the country's much-trumpeted healthcare reform drive. His medical networking platform DXY.com links two million doctors across China and has attracted funding from tech giants like Tencent.
DXY is exactly what Beijing has said it's looking to support after it pinpointed remote healthcare, Internet and technology as drivers to solve its healthcare woes in a 5-year roadmap in March.
The reality is rather different: DXY is curbing plans to work with public hospitals to help connect doctors and patients online because of a lack of support by Beijing and obstacles working with China's huge, fragmented public healthcare sector.
"We've heard a lot of good stories from the top - Internet +, driving force, policy changing - but see nothing happen at the bottom," Li told Reuters. "It's not about market, capital or even tech - these things are already developed very well ... rather it's the regulations, laws and systems of support."
Li's position reflects wider obstacles to healthcare reforms in technology, online drug sales, hospital privatization and doctors' pay, drivers that are a major lure for investors and firms betting billions of dollars on China opening up a market set to be worth around $1.3 trillion by 2020.
"(Investors) always ask: is there actually a macro tailwind, and is the government and regulatory environment - which is very important in China - supportive of this?" said Alexander Ng, associate principal at McKinsey & Co.
"If there's a lot of negative voices it might make investors back off or calculate a much higher risk premium."
China has ramped up its healthcare reform rhetoric, touting greater access for foreign investors to healthcare services, a bigger role for technology and pushing drug sales from mostly state-run hospitals towards the retail market.
This has helped draw in close to $30 billion worth of healthcare merger and acquisition investment so far this year, a fivefold leap from the same period in 2014, according to Reuters data. Healthcare M&A already leapt last year.
But, despite the government's longer-term ambitions, industry insiders say reforms are being held up because of technical issues such as crumbling and fragmented IT systems to in-fighting between regulators and push-back from the state-run firms who dominate the sector - and don't want change.
"With so many vested interests - dealers, hospitals, insurance departments and others - reform is not very fast," said Frank Zhao, chief financial officer at China Jo Jo Drugstores Inc.
Privately, some health policy advisers admit reforms are falling behind, while the public line is that reform has "hit up against the Yangtze River," a reference to the obstacle famously overcome by Mao Zedong's Communist forces in 1949.
The healthcare ministry did not respond to faxed queries seeking comment for this article.
Zhao points to the expected approval for online prescription drug sales, which he and other industry insiders say has been delayed this year due to regulatory concerns and opposition from state-run hospitals and distributors.
These hold-ups are a frustration for pharmacy chains like Jo Jo as it looks to increase its business online, but also for tech giants like Alibaba Group Holding Ltd, which wants to get into the online prescription drug space.
One big draw for investors has been China's privatization drive of healthcare services - touted as key to revamping an unpopular healthcare system, blighted by crowded hospitals, corruption and simmering tension between patients and staff.
But, despite the fast growth of private investment in hospitals, the public sector still dominates around 90% of all patient visits, according to a Deutsche Bank 2015 healthcare report. Investors cite issues with insurance schemes, access to Chinese doctors and a still tightly-controlled market.
"With things still not market-led, organizations like ours are facing huge challenges and difficulties," Hu Lan, President and Director of hospital investment firm AMCARE Corporation, said at a conference in Shanghai in June.
Healthcare spending as a slice of China's GDP also remains small at around 6% in 2013 compared to 17% in the United States, World Health Organization (WHO) data show.
Reforms to reduce hospitals' reliance on drug sales also faces a revolt from doctors who argue this will take away a key revenue stream at a time when medical staff are overworked, underpaid and often violently abused by angry patients.
"Every few days you hear about a doctor being beaten or even killed. This situation is a huge mental burden for doctors," said Wu Xiaobo a doctor at the Wangjing Hospital in Beijing in a recent viral video campaign for doctors' rights.
As for DXY's Li, his firm now plans to change tack and set up an offline clinic in the eastern city of Hangzhou this year to pilot potential healthcare reforms - outside the state sector.
"We were hoping we could leverage changing policy and do something on mobile and digital," Li said. "We found it's just too slow, so the only way to do it is out on our own."
SHANGHAI (Reuters) - Li Tiantian, a Chinese doctor turned tech entrepreneur, is a leading light of the country's much-trumpeted healthcare reform drive. His medical networking platform DXY.com links two million doctors across China and has attracted funding from tech giants like Tencent.
DXY is exactly what Beijing has said it's looking to support after it pinpointed remote healthcare, Internet and technology as drivers to solve its healthcare woes in a 5-year roadmap in March.
The reality is rather different: DXY is curbing plans to work with public hospitals to help connect doctors and patients online because of a lack of support by Beijing and obstacles working with China's huge, fragmented public healthcare sector.
"We've heard a lot of good stories from the top - Internet +, driving force, policy changing - but see nothing happen at the bottom," Li told Reuters. "It's not about market, capital or even tech - these things are already developed very well ... rather it's the regulations, laws and systems of support."
Li's position reflects wider obstacles to healthcare reforms in technology, online drug sales, hospital privatization and doctors' pay, drivers that are a major lure for investors and firms betting billions of dollars on China opening up a market set to be worth around $1.3 trillion by 2020.
"(Investors) always ask: is there actually a macro tailwind, and is the government and regulatory environment - which is very important in China - supportive of this?" said Alexander Ng, associate principal at McKinsey & Co.
"If there's a lot of negative voices it might make investors back off or calculate a much higher risk premium."
China has ramped up its healthcare reform rhetoric, touting greater access for foreign investors to healthcare services, a bigger role for technology and pushing drug sales from mostly state-run hospitals towards the retail market.
This has helped draw in close to $30 billion worth of healthcare merger and acquisition investment so far this year, a fivefold leap from the same period in 2014, according to Reuters data. Healthcare M&A already leapt last year.
But, despite the government's longer-term ambitions, industry insiders say reforms are being held up because of technical issues such as crumbling and fragmented IT systems to in-fighting between regulators and push-back from the state-run firms who dominate the sector - and don't want change.
"With so many vested interests - dealers, hospitals, insurance departments and others - reform is not very fast," said Frank Zhao, chief financial officer at China Jo Jo Drugstores Inc.
Privately, some health policy advisers admit reforms are falling behind, while the public line is that reform has "hit up against the Yangtze River," a reference to the obstacle famously overcome by Mao Zedong's Communist forces in 1949.
The healthcare ministry did not respond to faxed queries seeking comment for this article.
Zhao points to the expected approval for online prescription drug sales, which he and other industry insiders say has been delayed this year due to regulatory concerns and opposition from state-run hospitals and distributors.
These hold-ups are a frustration for pharmacy chains like Jo Jo as it looks to increase its business online, but also for tech giants like Alibaba Group Holding Ltd, which wants to get into the online prescription drug space.
One big draw for investors has been China's privatization drive of healthcare services - touted as key to revamping an unpopular healthcare system, blighted by crowded hospitals, corruption and simmering tension between patients and staff.
But, despite the fast growth of private investment in hospitals, the public sector still dominates around 90% of all patient visits, according to a Deutsche Bank 2015 healthcare report. Investors cite issues with insurance schemes, access to Chinese doctors and a still tightly-controlled market.
"With things still not market-led, organizations like ours are facing huge challenges and difficulties," Hu Lan, President and Director of hospital investment firm AMCARE Corporation, said at a conference in Shanghai in June.
Healthcare spending as a slice of China's GDP also remains small at around 6% in 2013 compared to 17% in the United States, World Health Organization (WHO) data show.
Reforms to reduce hospitals' reliance on drug sales also faces a revolt from doctors who argue this will take away a key revenue stream at a time when medical staff are overworked, underpaid and often violently abused by angry patients.
"Every few days you hear about a doctor being beaten or even killed. This situation is a huge mental burden for doctors," said Wu Xiaobo a doctor at the Wangjing Hospital in Beijing in a recent viral video campaign for doctors' rights.
As for DXY's Li, his firm now plans to change tack and set up an offline clinic in the eastern city of Hangzhou this year to pilot potential healthcare reforms - outside the state sector.
"We were hoping we could leverage changing policy and do something on mobile and digital," Li said. "We found it's just too slow, so the only way to do it is out on our own."
SHANGHAI (Reuters) - Li Tiantian, a Chinese doctor turned tech entrepreneur, is a leading light of the country's much-trumpeted healthcare reform drive. His medical networking platform DXY.com links two million doctors across China and has attracted funding from tech giants like Tencent.
DXY is exactly what Beijing has said it's looking to support after it pinpointed remote healthcare, Internet and technology as drivers to solve its healthcare woes in a 5-year roadmap in March.
The reality is rather different: DXY is curbing plans to work with public hospitals to help connect doctors and patients online because of a lack of support by Beijing and obstacles working with China's huge, fragmented public healthcare sector.
"We've heard a lot of good stories from the top - Internet +, driving force, policy changing - but see nothing happen at the bottom," Li told Reuters. "It's not about market, capital or even tech - these things are already developed very well ... rather it's the regulations, laws and systems of support."
Li's position reflects wider obstacles to healthcare reforms in technology, online drug sales, hospital privatization and doctors' pay, drivers that are a major lure for investors and firms betting billions of dollars on China opening up a market set to be worth around $1.3 trillion by 2020.
"(Investors) always ask: is there actually a macro tailwind, and is the government and regulatory environment - which is very important in China - supportive of this?" said Alexander Ng, associate principal at McKinsey & Co.
"If there's a lot of negative voices it might make investors back off or calculate a much higher risk premium."
China has ramped up its healthcare reform rhetoric, touting greater access for foreign investors to healthcare services, a bigger role for technology and pushing drug sales from mostly state-run hospitals towards the retail market.
This has helped draw in close to $30 billion worth of healthcare merger and acquisition investment so far this year, a fivefold leap from the same period in 2014, according to Reuters data. Healthcare M&A already leapt last year.
But, despite the government's longer-term ambitions, industry insiders say reforms are being held up because of technical issues such as crumbling and fragmented IT systems to in-fighting between regulators and push-back from the state-run firms who dominate the sector - and don't want change.
"With so many vested interests - dealers, hospitals, insurance departments and others - reform is not very fast," said Frank Zhao, chief financial officer at China Jo Jo Drugstores Inc.
Privately, some health policy advisers admit reforms are falling behind, while the public line is that reform has "hit up against the Yangtze River," a reference to the obstacle famously overcome by Mao Zedong's Communist forces in 1949.
The healthcare ministry did not respond to faxed queries seeking comment for this article.
Zhao points to the expected approval for online prescription drug sales, which he and other industry insiders say has been delayed this year due to regulatory concerns and opposition from state-run hospitals and distributors.
These hold-ups are a frustration for pharmacy chains like Jo Jo as it looks to increase its business online, but also for tech giants like Alibaba Group Holding Ltd, which wants to get into the online prescription drug space.
One big draw for investors has been China's privatization drive of healthcare services - touted as key to revamping an unpopular healthcare system, blighted by crowded hospitals, corruption and simmering tension between patients and staff.
But, despite the fast growth of private investment in hospitals, the public sector still dominates around 90% of all patient visits, according to a Deutsche Bank 2015 healthcare report. Investors cite issues with insurance schemes, access to Chinese doctors and a still tightly-controlled market.
"With things still not market-led, organizations like ours are facing huge challenges and difficulties," Hu Lan, President and Director of hospital investment firm AMCARE Corporation, said at a conference in Shanghai in June.
Healthcare spending as a slice of China's GDP also remains small at around 6% in 2013 compared to 17% in the United States, World Health Organization (WHO) data show.
Reforms to reduce hospitals' reliance on drug sales also faces a revolt from doctors who argue this will take away a key revenue stream at a time when medical staff are overworked, underpaid and often violently abused by angry patients.
"Every few days you hear about a doctor being beaten or even killed. This situation is a huge mental burden for doctors," said Wu Xiaobo a doctor at the Wangjing Hospital in Beijing in a recent viral video campaign for doctors' rights.
As for DXY's Li, his firm now plans to change tack and set up an offline clinic in the eastern city of Hangzhou this year to pilot potential healthcare reforms - outside the state sector.
"We were hoping we could leverage changing policy and do something on mobile and digital," Li said. "We found it's just too slow, so the only way to do it is out on our own."
Health care transition practices continue to evolve
It’s been nearly 13 years since the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Physicians released its Consensus Policy Statement on Health Care Transitions for Young Adults With Special Needs and 4 years since the AAP, AAFP, ACP Clinical Report: Supporting Health Care Transition (HCT) from Adolescence to Adulthood in the Medical Home was published, but formal adoption of suggested approaches has remained minimal.
A recent survey of 158 members of the Childhood Arthritis and Rheumatology Research Alliance in North America found that fewer than 10% of respondents were familiar with the consensus statement and the HCT clinical report, only 8% have a formal written transition policy, while 42% use an informal approach (J. Rheumatol. 2014;41:768-79). Respondents ranked fragmented adult health care and lack of time to provide sufficient services as the two major barriers to transition.
“Until recently, there hasn’t been a lot of focus on transition in fellowship training, and I don’t know how well the consensus policy statement and HCT clinical report are publicized in residency or fellowship training,” one of the study authors, Dr. Tova Ronis, said in an interview. “There’s definitely a role for more education about the policy statement and HCT clinical report.” As a result of inconsistent transition practices, some patients fall through the cracks in the transition from pediatric to adult rheumatology care. Transition can be difficult and even patients who receive transition care can have challenges, said Dr. Ronis of the pediatric rheumatology division at Children’s National Health System, Washington. She spoke of one young patient with severe systemic disease who was referred to ongoing adult care with an expert in the field. The patient “went to the adult office but didn’t like it there; she didn’t feel like she was being listened to and didn’t feel like the new doctor knew her well. She would come back to us, go back and forth, so her care became very fragmented. We communicated with the adult doctor but there wasn’t one person making the plan [of care].” In addition, other clinicians who had been providing subspecialty care and had not transitioned her to adult practice “were still at the children’s hospital, so when she experienced health problems or pain, she would come to the pediatric emergency department,” Dr. Ronis recalled. “She hadn’t identified the new institution as her medical home, so her care became very fragmented during that transition process. She actually missed some therapy because she didn’t like the new office, so wasn’t seen anywhere for a while.”
Dr. Paul T. Jensen said that most clinicians “have a gut feeling” that the current health care transition landscape has limitations, despite the availability of such tools as the Got Transition website, the Transition Readiness Assessment Questionnaire (TRAQ), as well as studies of novel approaches such as having a social worker serve as a transition coordinator(Pediatr. Rheumatol. 2015;13:17 [doi:10.1186/s12969-015-0013-0]) or having clinicians from adult practices see patients at a pediatric institution (Pediatr. Pulmonol. 2013;48:658-65). “I think that most, if not all, pediatric providers, including pediatric rheumatologists, worry about their patients as they get older, especially those who have a decreased maturity level,” said Dr. Jensen, who is a fellow in both adult and pediatric rheumatology at the Ohio State University Wexner Medical Center and Nationwide Children’s Hospital, Columbus. “But I think there’s a large lack of knowledge about what resources are available.”
Choosing transition practices that work for you
Dr. Patience White, a pediatric and adult rheumatologist who in 2011 coauthored the HCT Clinical Report, is familiar with such sentiment. She says that the topic of transition has “come to the forefront because the pediatric rheumatology field has grown. On top of that, many of our patients have grown up and moved on to other aspects of adulthood, so now pediatric providers will need to prepare to ‘let them go to adult health care.’ The perfect storm is happening.” Dr. White codirects the Got Transition Center for Health Care Transition Improvement, a federally funded program located at the National Alliance to Advance Adolescent Health. One of the center’s goals is to expand the use of the Six Core Elements of Health Care Transition that were developed to help make the 2011 Health Care Transitions Clinical Report actionable. These include practice quality improvement strategies such as establishing a transition policy, tracking progress, offering transition readiness assessments, creating a transition plan, transferring to an adult provider, and assessing the youth’s and family’s experience with the transition. The original Six Core Elements of Health Care Transition were tested in learning collaboratives across the United States and have been updated with input from the learning collaboratives and national transition experts into three separate packages of tools and evaluation approaches for transitioning youth to adult health care providers, transitioning to an adult approach to health care without changing providers, and integrating young adults into adult health care. For example, recommendations when transitioning youth to adult health care providers include developing a transition policy/statement “with input from youth and families that describes the practice’s approach to transition, including privacy and consent information,” as well as conducting regular transition readiness assessments, beginning at age 14 years, “to identify and discuss with youth and parent/caregiver their needs and goals in self-care.” Other tools available from the Got Transition website include a set of frequently asked transition questions developed by and for youth/young adults, as well as many transition resources.
While she acknowledged it may not be feasible for pediatric and adult rheumatologists to implement all Six Core Elements in their practice, Dr. White suggests providers might try implementing at least one or two and, for pediatric rheumatologists, start the discussion of the transition process when their patients reach the age of 13 years as recommended by the HCT clinical report. “Everybody says it’s hard, and I agree, changing practice processes to improve health care is hard work,” she said. “We know preparation for the youth and family needs to happen. We know transfer and communication has to occur, and that the accepting adult provider has to be informed and comfortable to make the transition process a success. It is about choosing one or two Six Core Element tools that can work for you, your practice, and your patients to help them through the transition process. If you’re an adult provider, you might choose to offer a welcome letter to my practice and a self-care assessment for the new young adult patients joining the practice so the adult health care provider can understand how proficient the young adults are with respect to their self-care skills and knowledge of the adult health care system.”
Disease-specific toolkits coming in 2016
Dr. White is also a consultant to the Pediatric to Adult Health Care Transitions Workgroup, an effort of the ACP Council of Subspecialty Societies to address gaps in care that exist with the transition of pediatric patients into adult health care. According to an ACP document describing the effort, the goal of workgroup is to identify “common tools/templates for a ‘general’ transition process, and subspecialty societies will utilize the templates to develop customized toolkits for specific diseases/conditions. The toolkits will then be collected and broadly disseminated,” with release targeted for May 2016 at the ACP national meeting. Dr. Stacy P. Ardoin, who is leading the rheumatology subspecialty group on behalf of the American College of Rheumatology, said the fact that this effort was initiated by the ACP “is great, because historically most of the interest in transition has bubbled up from the pediatric side. I think that adult providers are realizing more and more that patients who come to them with complex childhood onset conditions are challenging to manage, and that we really need to partner together to make things the best for our patients.”
Dr. Ardoin, a rheumatologist in the department of internal medicine at the Ohio State University Wexner Medical Center and in the department of pediatrics at Nationwide Children’s Hospital, characterized the final product as “not so much a definite protocol that everybody has to follow, but more just providing recommendations to the practitioner saying, ‘these are the things that we recommend and here are some tools to accomplish it.’ There’s such a lack of standardization for anything with transition despite the fact that we have consensus statements that have been put out in the past. Perhaps part of the problem is that they were too vague or not considered individually for each specialty. Hopefully, having each specialty take this on and look at their unique needs in the transition process will make people more willing to participate.”
Preparing patients to become health care self-advocates
Not all physicians are convinced that more recommendations will help clinicians navigate the intricacies of health care transition, however. “If children come to you as a physician at a young age (most of the kids with arthritis) or very ill (most of the children with systemic lupus erythematosus), good care over time represents a significant bonding experience,” said Dr. Thomas J. A. Lehman, chief of the division of pediatric rheumatology at the Hospital for Special Surgery in New York. “The children come to see you as a significant other in their life. If they then are suddenly ‘cast out’ because they reach a certain age it doesn’t go down any better than it would if a significant relative ‘cast them out.’ The doctors like to think they are transitioning the patients. The patients who have bonded feel they are being rejected. I don’t have an answer to this problem. However, none of the past HCT policy statements adequately recognize this aspect.”
For her part, Dr. White, who is also professor of medicine and pediatrics at George Washington University, Washington, said that in some published studies pediatric providers acknowledged that they are reluctant to transition patients to adult health care providers “and can overprotect their young patients as some parents do. This approach can result in the young adult being a poor self-advocate in the adult health care environment and not receiving developmentally appropriate health care. If a pediatric patient and family have not been informed of when they can no longer come to the pediatric rheumatology practice and have not discussed a transition to adult health care plan, they often assume they can stay with their pediatric rheumatologist forever.”
In addition, Dr. White continued, “some pediatric rheumatologists might say, ‘adult providers don’t know how to care for pediatric rheumatology [patients].’ Well, that may due to the adult providers not having received training in specific pediatric onset conditions. Communication between the pediatric and adult providers is key to a good transition experience for everyone. Trying to quickly build a new relationship with a new young adult patient to keep them engaged in their care and who has been used to the same pediatric provider for years is challenging, and the young adult and the adult provider need the pediatric provider’s support and availability to be a consultant to support the adult provider in the areas where they have little disease-specific experience.”
Dr. Jensen makes it a point to talk to his patients about health care transition in early adolescence, helps them set goals, and encourages them to “take more ownership in late adolescence for his or her own health: making their own appointments for follow-up visits, giving time to the patient in the room alone, and asking patients to maybe monitor medication adherence but not to lay the medications out for the patient in the morning,” he said. “When patients are given that opportunity, they may mature.”
Dr. Ronis, who is implementing a health care transition program at Children’s National Health System, thinks about health care transition as “a time where there’s risk for potentially worsening disease and negative outcomes due to perceived fragmentation of care. The more prepared we are and the more we prepare our patients to do this successfully, the better outcomes our patients will have.”
The Got Transition Center for Health Care Transition Improvement is funded by the Health Resources and Services Administration. The physicians interviewed for this story reported having no financial disclosures.
It’s been nearly 13 years since the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Physicians released its Consensus Policy Statement on Health Care Transitions for Young Adults With Special Needs and 4 years since the AAP, AAFP, ACP Clinical Report: Supporting Health Care Transition (HCT) from Adolescence to Adulthood in the Medical Home was published, but formal adoption of suggested approaches has remained minimal.
A recent survey of 158 members of the Childhood Arthritis and Rheumatology Research Alliance in North America found that fewer than 10% of respondents were familiar with the consensus statement and the HCT clinical report, only 8% have a formal written transition policy, while 42% use an informal approach (J. Rheumatol. 2014;41:768-79). Respondents ranked fragmented adult health care and lack of time to provide sufficient services as the two major barriers to transition.
“Until recently, there hasn’t been a lot of focus on transition in fellowship training, and I don’t know how well the consensus policy statement and HCT clinical report are publicized in residency or fellowship training,” one of the study authors, Dr. Tova Ronis, said in an interview. “There’s definitely a role for more education about the policy statement and HCT clinical report.” As a result of inconsistent transition practices, some patients fall through the cracks in the transition from pediatric to adult rheumatology care. Transition can be difficult and even patients who receive transition care can have challenges, said Dr. Ronis of the pediatric rheumatology division at Children’s National Health System, Washington. She spoke of one young patient with severe systemic disease who was referred to ongoing adult care with an expert in the field. The patient “went to the adult office but didn’t like it there; she didn’t feel like she was being listened to and didn’t feel like the new doctor knew her well. She would come back to us, go back and forth, so her care became very fragmented. We communicated with the adult doctor but there wasn’t one person making the plan [of care].” In addition, other clinicians who had been providing subspecialty care and had not transitioned her to adult practice “were still at the children’s hospital, so when she experienced health problems or pain, she would come to the pediatric emergency department,” Dr. Ronis recalled. “She hadn’t identified the new institution as her medical home, so her care became very fragmented during that transition process. She actually missed some therapy because she didn’t like the new office, so wasn’t seen anywhere for a while.”
Dr. Paul T. Jensen said that most clinicians “have a gut feeling” that the current health care transition landscape has limitations, despite the availability of such tools as the Got Transition website, the Transition Readiness Assessment Questionnaire (TRAQ), as well as studies of novel approaches such as having a social worker serve as a transition coordinator(Pediatr. Rheumatol. 2015;13:17 [doi:10.1186/s12969-015-0013-0]) or having clinicians from adult practices see patients at a pediatric institution (Pediatr. Pulmonol. 2013;48:658-65). “I think that most, if not all, pediatric providers, including pediatric rheumatologists, worry about their patients as they get older, especially those who have a decreased maturity level,” said Dr. Jensen, who is a fellow in both adult and pediatric rheumatology at the Ohio State University Wexner Medical Center and Nationwide Children’s Hospital, Columbus. “But I think there’s a large lack of knowledge about what resources are available.”
Choosing transition practices that work for you
Dr. Patience White, a pediatric and adult rheumatologist who in 2011 coauthored the HCT Clinical Report, is familiar with such sentiment. She says that the topic of transition has “come to the forefront because the pediatric rheumatology field has grown. On top of that, many of our patients have grown up and moved on to other aspects of adulthood, so now pediatric providers will need to prepare to ‘let them go to adult health care.’ The perfect storm is happening.” Dr. White codirects the Got Transition Center for Health Care Transition Improvement, a federally funded program located at the National Alliance to Advance Adolescent Health. One of the center’s goals is to expand the use of the Six Core Elements of Health Care Transition that were developed to help make the 2011 Health Care Transitions Clinical Report actionable. These include practice quality improvement strategies such as establishing a transition policy, tracking progress, offering transition readiness assessments, creating a transition plan, transferring to an adult provider, and assessing the youth’s and family’s experience with the transition. The original Six Core Elements of Health Care Transition were tested in learning collaboratives across the United States and have been updated with input from the learning collaboratives and national transition experts into three separate packages of tools and evaluation approaches for transitioning youth to adult health care providers, transitioning to an adult approach to health care without changing providers, and integrating young adults into adult health care. For example, recommendations when transitioning youth to adult health care providers include developing a transition policy/statement “with input from youth and families that describes the practice’s approach to transition, including privacy and consent information,” as well as conducting regular transition readiness assessments, beginning at age 14 years, “to identify and discuss with youth and parent/caregiver their needs and goals in self-care.” Other tools available from the Got Transition website include a set of frequently asked transition questions developed by and for youth/young adults, as well as many transition resources.
While she acknowledged it may not be feasible for pediatric and adult rheumatologists to implement all Six Core Elements in their practice, Dr. White suggests providers might try implementing at least one or two and, for pediatric rheumatologists, start the discussion of the transition process when their patients reach the age of 13 years as recommended by the HCT clinical report. “Everybody says it’s hard, and I agree, changing practice processes to improve health care is hard work,” she said. “We know preparation for the youth and family needs to happen. We know transfer and communication has to occur, and that the accepting adult provider has to be informed and comfortable to make the transition process a success. It is about choosing one or two Six Core Element tools that can work for you, your practice, and your patients to help them through the transition process. If you’re an adult provider, you might choose to offer a welcome letter to my practice and a self-care assessment for the new young adult patients joining the practice so the adult health care provider can understand how proficient the young adults are with respect to their self-care skills and knowledge of the adult health care system.”
Disease-specific toolkits coming in 2016
Dr. White is also a consultant to the Pediatric to Adult Health Care Transitions Workgroup, an effort of the ACP Council of Subspecialty Societies to address gaps in care that exist with the transition of pediatric patients into adult health care. According to an ACP document describing the effort, the goal of workgroup is to identify “common tools/templates for a ‘general’ transition process, and subspecialty societies will utilize the templates to develop customized toolkits for specific diseases/conditions. The toolkits will then be collected and broadly disseminated,” with release targeted for May 2016 at the ACP national meeting. Dr. Stacy P. Ardoin, who is leading the rheumatology subspecialty group on behalf of the American College of Rheumatology, said the fact that this effort was initiated by the ACP “is great, because historically most of the interest in transition has bubbled up from the pediatric side. I think that adult providers are realizing more and more that patients who come to them with complex childhood onset conditions are challenging to manage, and that we really need to partner together to make things the best for our patients.”
Dr. Ardoin, a rheumatologist in the department of internal medicine at the Ohio State University Wexner Medical Center and in the department of pediatrics at Nationwide Children’s Hospital, characterized the final product as “not so much a definite protocol that everybody has to follow, but more just providing recommendations to the practitioner saying, ‘these are the things that we recommend and here are some tools to accomplish it.’ There’s such a lack of standardization for anything with transition despite the fact that we have consensus statements that have been put out in the past. Perhaps part of the problem is that they were too vague or not considered individually for each specialty. Hopefully, having each specialty take this on and look at their unique needs in the transition process will make people more willing to participate.”
Preparing patients to become health care self-advocates
Not all physicians are convinced that more recommendations will help clinicians navigate the intricacies of health care transition, however. “If children come to you as a physician at a young age (most of the kids with arthritis) or very ill (most of the children with systemic lupus erythematosus), good care over time represents a significant bonding experience,” said Dr. Thomas J. A. Lehman, chief of the division of pediatric rheumatology at the Hospital for Special Surgery in New York. “The children come to see you as a significant other in their life. If they then are suddenly ‘cast out’ because they reach a certain age it doesn’t go down any better than it would if a significant relative ‘cast them out.’ The doctors like to think they are transitioning the patients. The patients who have bonded feel they are being rejected. I don’t have an answer to this problem. However, none of the past HCT policy statements adequately recognize this aspect.”
For her part, Dr. White, who is also professor of medicine and pediatrics at George Washington University, Washington, said that in some published studies pediatric providers acknowledged that they are reluctant to transition patients to adult health care providers “and can overprotect their young patients as some parents do. This approach can result in the young adult being a poor self-advocate in the adult health care environment and not receiving developmentally appropriate health care. If a pediatric patient and family have not been informed of when they can no longer come to the pediatric rheumatology practice and have not discussed a transition to adult health care plan, they often assume they can stay with their pediatric rheumatologist forever.”
In addition, Dr. White continued, “some pediatric rheumatologists might say, ‘adult providers don’t know how to care for pediatric rheumatology [patients].’ Well, that may due to the adult providers not having received training in specific pediatric onset conditions. Communication between the pediatric and adult providers is key to a good transition experience for everyone. Trying to quickly build a new relationship with a new young adult patient to keep them engaged in their care and who has been used to the same pediatric provider for years is challenging, and the young adult and the adult provider need the pediatric provider’s support and availability to be a consultant to support the adult provider in the areas where they have little disease-specific experience.”
Dr. Jensen makes it a point to talk to his patients about health care transition in early adolescence, helps them set goals, and encourages them to “take more ownership in late adolescence for his or her own health: making their own appointments for follow-up visits, giving time to the patient in the room alone, and asking patients to maybe monitor medication adherence but not to lay the medications out for the patient in the morning,” he said. “When patients are given that opportunity, they may mature.”
Dr. Ronis, who is implementing a health care transition program at Children’s National Health System, thinks about health care transition as “a time where there’s risk for potentially worsening disease and negative outcomes due to perceived fragmentation of care. The more prepared we are and the more we prepare our patients to do this successfully, the better outcomes our patients will have.”
The Got Transition Center for Health Care Transition Improvement is funded by the Health Resources and Services Administration. The physicians interviewed for this story reported having no financial disclosures.
It’s been nearly 13 years since the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Physicians released its Consensus Policy Statement on Health Care Transitions for Young Adults With Special Needs and 4 years since the AAP, AAFP, ACP Clinical Report: Supporting Health Care Transition (HCT) from Adolescence to Adulthood in the Medical Home was published, but formal adoption of suggested approaches has remained minimal.
A recent survey of 158 members of the Childhood Arthritis and Rheumatology Research Alliance in North America found that fewer than 10% of respondents were familiar with the consensus statement and the HCT clinical report, only 8% have a formal written transition policy, while 42% use an informal approach (J. Rheumatol. 2014;41:768-79). Respondents ranked fragmented adult health care and lack of time to provide sufficient services as the two major barriers to transition.
“Until recently, there hasn’t been a lot of focus on transition in fellowship training, and I don’t know how well the consensus policy statement and HCT clinical report are publicized in residency or fellowship training,” one of the study authors, Dr. Tova Ronis, said in an interview. “There’s definitely a role for more education about the policy statement and HCT clinical report.” As a result of inconsistent transition practices, some patients fall through the cracks in the transition from pediatric to adult rheumatology care. Transition can be difficult and even patients who receive transition care can have challenges, said Dr. Ronis of the pediatric rheumatology division at Children’s National Health System, Washington. She spoke of one young patient with severe systemic disease who was referred to ongoing adult care with an expert in the field. The patient “went to the adult office but didn’t like it there; she didn’t feel like she was being listened to and didn’t feel like the new doctor knew her well. She would come back to us, go back and forth, so her care became very fragmented. We communicated with the adult doctor but there wasn’t one person making the plan [of care].” In addition, other clinicians who had been providing subspecialty care and had not transitioned her to adult practice “were still at the children’s hospital, so when she experienced health problems or pain, she would come to the pediatric emergency department,” Dr. Ronis recalled. “She hadn’t identified the new institution as her medical home, so her care became very fragmented during that transition process. She actually missed some therapy because she didn’t like the new office, so wasn’t seen anywhere for a while.”
Dr. Paul T. Jensen said that most clinicians “have a gut feeling” that the current health care transition landscape has limitations, despite the availability of such tools as the Got Transition website, the Transition Readiness Assessment Questionnaire (TRAQ), as well as studies of novel approaches such as having a social worker serve as a transition coordinator(Pediatr. Rheumatol. 2015;13:17 [doi:10.1186/s12969-015-0013-0]) or having clinicians from adult practices see patients at a pediatric institution (Pediatr. Pulmonol. 2013;48:658-65). “I think that most, if not all, pediatric providers, including pediatric rheumatologists, worry about their patients as they get older, especially those who have a decreased maturity level,” said Dr. Jensen, who is a fellow in both adult and pediatric rheumatology at the Ohio State University Wexner Medical Center and Nationwide Children’s Hospital, Columbus. “But I think there’s a large lack of knowledge about what resources are available.”
Choosing transition practices that work for you
Dr. Patience White, a pediatric and adult rheumatologist who in 2011 coauthored the HCT Clinical Report, is familiar with such sentiment. She says that the topic of transition has “come to the forefront because the pediatric rheumatology field has grown. On top of that, many of our patients have grown up and moved on to other aspects of adulthood, so now pediatric providers will need to prepare to ‘let them go to adult health care.’ The perfect storm is happening.” Dr. White codirects the Got Transition Center for Health Care Transition Improvement, a federally funded program located at the National Alliance to Advance Adolescent Health. One of the center’s goals is to expand the use of the Six Core Elements of Health Care Transition that were developed to help make the 2011 Health Care Transitions Clinical Report actionable. These include practice quality improvement strategies such as establishing a transition policy, tracking progress, offering transition readiness assessments, creating a transition plan, transferring to an adult provider, and assessing the youth’s and family’s experience with the transition. The original Six Core Elements of Health Care Transition were tested in learning collaboratives across the United States and have been updated with input from the learning collaboratives and national transition experts into three separate packages of tools and evaluation approaches for transitioning youth to adult health care providers, transitioning to an adult approach to health care without changing providers, and integrating young adults into adult health care. For example, recommendations when transitioning youth to adult health care providers include developing a transition policy/statement “with input from youth and families that describes the practice’s approach to transition, including privacy and consent information,” as well as conducting regular transition readiness assessments, beginning at age 14 years, “to identify and discuss with youth and parent/caregiver their needs and goals in self-care.” Other tools available from the Got Transition website include a set of frequently asked transition questions developed by and for youth/young adults, as well as many transition resources.
While she acknowledged it may not be feasible for pediatric and adult rheumatologists to implement all Six Core Elements in their practice, Dr. White suggests providers might try implementing at least one or two and, for pediatric rheumatologists, start the discussion of the transition process when their patients reach the age of 13 years as recommended by the HCT clinical report. “Everybody says it’s hard, and I agree, changing practice processes to improve health care is hard work,” she said. “We know preparation for the youth and family needs to happen. We know transfer and communication has to occur, and that the accepting adult provider has to be informed and comfortable to make the transition process a success. It is about choosing one or two Six Core Element tools that can work for you, your practice, and your patients to help them through the transition process. If you’re an adult provider, you might choose to offer a welcome letter to my practice and a self-care assessment for the new young adult patients joining the practice so the adult health care provider can understand how proficient the young adults are with respect to their self-care skills and knowledge of the adult health care system.”
Disease-specific toolkits coming in 2016
Dr. White is also a consultant to the Pediatric to Adult Health Care Transitions Workgroup, an effort of the ACP Council of Subspecialty Societies to address gaps in care that exist with the transition of pediatric patients into adult health care. According to an ACP document describing the effort, the goal of workgroup is to identify “common tools/templates for a ‘general’ transition process, and subspecialty societies will utilize the templates to develop customized toolkits for specific diseases/conditions. The toolkits will then be collected and broadly disseminated,” with release targeted for May 2016 at the ACP national meeting. Dr. Stacy P. Ardoin, who is leading the rheumatology subspecialty group on behalf of the American College of Rheumatology, said the fact that this effort was initiated by the ACP “is great, because historically most of the interest in transition has bubbled up from the pediatric side. I think that adult providers are realizing more and more that patients who come to them with complex childhood onset conditions are challenging to manage, and that we really need to partner together to make things the best for our patients.”
Dr. Ardoin, a rheumatologist in the department of internal medicine at the Ohio State University Wexner Medical Center and in the department of pediatrics at Nationwide Children’s Hospital, characterized the final product as “not so much a definite protocol that everybody has to follow, but more just providing recommendations to the practitioner saying, ‘these are the things that we recommend and here are some tools to accomplish it.’ There’s such a lack of standardization for anything with transition despite the fact that we have consensus statements that have been put out in the past. Perhaps part of the problem is that they were too vague or not considered individually for each specialty. Hopefully, having each specialty take this on and look at their unique needs in the transition process will make people more willing to participate.”
Preparing patients to become health care self-advocates
Not all physicians are convinced that more recommendations will help clinicians navigate the intricacies of health care transition, however. “If children come to you as a physician at a young age (most of the kids with arthritis) or very ill (most of the children with systemic lupus erythematosus), good care over time represents a significant bonding experience,” said Dr. Thomas J. A. Lehman, chief of the division of pediatric rheumatology at the Hospital for Special Surgery in New York. “The children come to see you as a significant other in their life. If they then are suddenly ‘cast out’ because they reach a certain age it doesn’t go down any better than it would if a significant relative ‘cast them out.’ The doctors like to think they are transitioning the patients. The patients who have bonded feel they are being rejected. I don’t have an answer to this problem. However, none of the past HCT policy statements adequately recognize this aspect.”
For her part, Dr. White, who is also professor of medicine and pediatrics at George Washington University, Washington, said that in some published studies pediatric providers acknowledged that they are reluctant to transition patients to adult health care providers “and can overprotect their young patients as some parents do. This approach can result in the young adult being a poor self-advocate in the adult health care environment and not receiving developmentally appropriate health care. If a pediatric patient and family have not been informed of when they can no longer come to the pediatric rheumatology practice and have not discussed a transition to adult health care plan, they often assume they can stay with their pediatric rheumatologist forever.”
In addition, Dr. White continued, “some pediatric rheumatologists might say, ‘adult providers don’t know how to care for pediatric rheumatology [patients].’ Well, that may due to the adult providers not having received training in specific pediatric onset conditions. Communication between the pediatric and adult providers is key to a good transition experience for everyone. Trying to quickly build a new relationship with a new young adult patient to keep them engaged in their care and who has been used to the same pediatric provider for years is challenging, and the young adult and the adult provider need the pediatric provider’s support and availability to be a consultant to support the adult provider in the areas where they have little disease-specific experience.”
Dr. Jensen makes it a point to talk to his patients about health care transition in early adolescence, helps them set goals, and encourages them to “take more ownership in late adolescence for his or her own health: making their own appointments for follow-up visits, giving time to the patient in the room alone, and asking patients to maybe monitor medication adherence but not to lay the medications out for the patient in the morning,” he said. “When patients are given that opportunity, they may mature.”
Dr. Ronis, who is implementing a health care transition program at Children’s National Health System, thinks about health care transition as “a time where there’s risk for potentially worsening disease and negative outcomes due to perceived fragmentation of care. The more prepared we are and the more we prepare our patients to do this successfully, the better outcomes our patients will have.”
The Got Transition Center for Health Care Transition Improvement is funded by the Health Resources and Services Administration. The physicians interviewed for this story reported having no financial disclosures.
How CLL evades the immune system

Photo courtesy of
Monash University
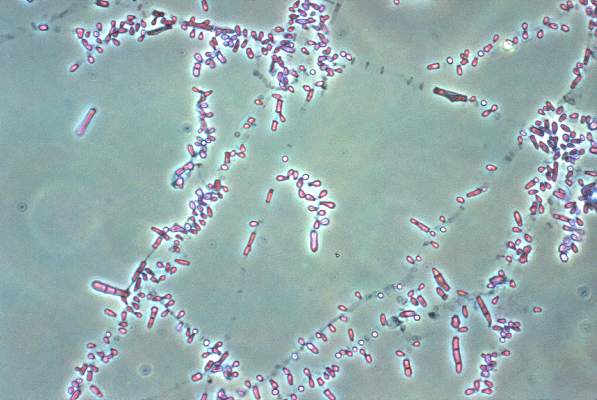
A study published in Leukemia has revealed a mechanism by which chronic lymphocytic leukemia (CLL) evades the immune system.
“It turns out that cancer cells are very good at sabotaging the immune system, using various tricks that confuse immune cells and ‘smoke screens’ preventing immune cells from recognizing the cancer,” said study author Fabienne Mackay, PhD, of Monash University in Melbourne, Victoria, Australia.
She and her colleagues believe they have determined exactly how CLL confuses the immune system and devised a way to stop it without destroying the patient’s immune system.
The team noted that B cells rely on the protein BAFF to survive. And each B cell has 3 different kinds of receptors that detect the presence of BAFF in the blood—TACI, BAFF-R, and BCMA.
The researchers discovered that, in CLL patients, the TACI receptors of cancerous B cells over-produce interleukin-10 (IL-10), which tricks the immune system into thinking nothing is wrong, allowing CLL to thrive undetected.
“We found that, when the receptor called TACI was blocked, it prevented the secretion of IL-10 without eliminating normal B cells,” Dr Mackay said. “Without IL-10, the tumor can no longer keep the immune system at bay, which means the patient’s immune system can be ‘kick-started’ again to fight infections and cancers.”
“This is very exciting because it means that B cells stay alive and well to do their job in the immune system fighting other infections. It also means the over-production of IL-10 is stopped, and the CLL cells are now exposed to immune cells specialized in fighting cancers.”
Dr Mackay said her team’s discovery may be relevant for cancers other than CLL and could change the way they are treated.
“The best weapon we have for fighting cancer is the immune system itself,” Dr Mackay noted. “It can sense the presence of an infection but also the emergence of a cancer.” ![]()

Photo courtesy of
Monash University
A study published in Leukemia has revealed a mechanism by which chronic lymphocytic leukemia (CLL) evades the immune system.
“It turns out that cancer cells are very good at sabotaging the immune system, using various tricks that confuse immune cells and ‘smoke screens’ preventing immune cells from recognizing the cancer,” said study author Fabienne Mackay, PhD, of Monash University in Melbourne, Victoria, Australia.
She and her colleagues believe they have determined exactly how CLL confuses the immune system and devised a way to stop it without destroying the patient’s immune system.
The team noted that B cells rely on the protein BAFF to survive. And each B cell has 3 different kinds of receptors that detect the presence of BAFF in the blood—TACI, BAFF-R, and BCMA.
The researchers discovered that, in CLL patients, the TACI receptors of cancerous B cells over-produce interleukin-10 (IL-10), which tricks the immune system into thinking nothing is wrong, allowing CLL to thrive undetected.
“We found that, when the receptor called TACI was blocked, it prevented the secretion of IL-10 without eliminating normal B cells,” Dr Mackay said. “Without IL-10, the tumor can no longer keep the immune system at bay, which means the patient’s immune system can be ‘kick-started’ again to fight infections and cancers.”
“This is very exciting because it means that B cells stay alive and well to do their job in the immune system fighting other infections. It also means the over-production of IL-10 is stopped, and the CLL cells are now exposed to immune cells specialized in fighting cancers.”
Dr Mackay said her team’s discovery may be relevant for cancers other than CLL and could change the way they are treated.
“The best weapon we have for fighting cancer is the immune system itself,” Dr Mackay noted. “It can sense the presence of an infection but also the emergence of a cancer.” ![]()

Photo courtesy of
Monash University
A study published in Leukemia has revealed a mechanism by which chronic lymphocytic leukemia (CLL) evades the immune system.
“It turns out that cancer cells are very good at sabotaging the immune system, using various tricks that confuse immune cells and ‘smoke screens’ preventing immune cells from recognizing the cancer,” said study author Fabienne Mackay, PhD, of Monash University in Melbourne, Victoria, Australia.
She and her colleagues believe they have determined exactly how CLL confuses the immune system and devised a way to stop it without destroying the patient’s immune system.
The team noted that B cells rely on the protein BAFF to survive. And each B cell has 3 different kinds of receptors that detect the presence of BAFF in the blood—TACI, BAFF-R, and BCMA.
The researchers discovered that, in CLL patients, the TACI receptors of cancerous B cells over-produce interleukin-10 (IL-10), which tricks the immune system into thinking nothing is wrong, allowing CLL to thrive undetected.
“We found that, when the receptor called TACI was blocked, it prevented the secretion of IL-10 without eliminating normal B cells,” Dr Mackay said. “Without IL-10, the tumor can no longer keep the immune system at bay, which means the patient’s immune system can be ‘kick-started’ again to fight infections and cancers.”
“This is very exciting because it means that B cells stay alive and well to do their job in the immune system fighting other infections. It also means the over-production of IL-10 is stopped, and the CLL cells are now exposed to immune cells specialized in fighting cancers.”
Dr Mackay said her team’s discovery may be relevant for cancers other than CLL and could change the way they are treated.
“The best weapon we have for fighting cancer is the immune system itself,” Dr Mackay noted. “It can sense the presence of an infection but also the emergence of a cancer.” ![]()
FDA extends storage of platelets in plasma

Photo by Charles Haymond
The US Food and Drug Administration (FDA) has cleared a labeling change for the Terumo BCT Trima Accel Automated Blood Collection System.
The change means platelets in plasma that are collected via this system can now be stored for 7 days instead of 5, but the blood products must be tested for bacterial contamination.
The label change also allows for use of a wireless feature designed to enhance the mobility and flexibility of the system.
The Trima Accel system includes the Trima Accel device, a tubing set, and Trima Accel software. The system uses a centrifuge to separate whole blood into platelets, plasma, and red blood cells. It then collects the components based on customer-configured priorities and the donor’s physiology and blood count.
Platelet storage
The FDA is now allowing platelets in 100% plasma that are collected via the Trima Accel system to be stored for up to 7 days post-collection. But platelets in isoplate solution can only be stored for up to 5 days.
For platelet storage up to 7 days, the FDA requires that every product be tested with a bacterial detection device cleared by the FDA and labeled as a “safety measure.”
Wireless feature
The newly cleared wireless feature connects the Trima Accel system to software applications such as the Cadence Data Collection System or the Vista Information System through the blood center’s or hospital’s existing wireless network.
This enables access to electronic donor information and reporting capabilities, with the goals of streamlining collections, simplifying data management, and allowing operators to focus on donor care, even when a wired connection is unavailable.
The wireless feature enables blood centers to either purchase a compatible wireless appliance from Terumo BCT or choose an appliance of their own for attachment to the Trima Accel system using a mounting bracket on the back of the system. ![]()

Photo by Charles Haymond
The US Food and Drug Administration (FDA) has cleared a labeling change for the Terumo BCT Trima Accel Automated Blood Collection System.
The change means platelets in plasma that are collected via this system can now be stored for 7 days instead of 5, but the blood products must be tested for bacterial contamination.
The label change also allows for use of a wireless feature designed to enhance the mobility and flexibility of the system.
The Trima Accel system includes the Trima Accel device, a tubing set, and Trima Accel software. The system uses a centrifuge to separate whole blood into platelets, plasma, and red blood cells. It then collects the components based on customer-configured priorities and the donor’s physiology and blood count.
Platelet storage
The FDA is now allowing platelets in 100% plasma that are collected via the Trima Accel system to be stored for up to 7 days post-collection. But platelets in isoplate solution can only be stored for up to 5 days.
For platelet storage up to 7 days, the FDA requires that every product be tested with a bacterial detection device cleared by the FDA and labeled as a “safety measure.”
Wireless feature
The newly cleared wireless feature connects the Trima Accel system to software applications such as the Cadence Data Collection System or the Vista Information System through the blood center’s or hospital’s existing wireless network.
This enables access to electronic donor information and reporting capabilities, with the goals of streamlining collections, simplifying data management, and allowing operators to focus on donor care, even when a wired connection is unavailable.
The wireless feature enables blood centers to either purchase a compatible wireless appliance from Terumo BCT or choose an appliance of their own for attachment to the Trima Accel system using a mounting bracket on the back of the system. ![]()

Photo by Charles Haymond
The US Food and Drug Administration (FDA) has cleared a labeling change for the Terumo BCT Trima Accel Automated Blood Collection System.
The change means platelets in plasma that are collected via this system can now be stored for 7 days instead of 5, but the blood products must be tested for bacterial contamination.
The label change also allows for use of a wireless feature designed to enhance the mobility and flexibility of the system.
The Trima Accel system includes the Trima Accel device, a tubing set, and Trima Accel software. The system uses a centrifuge to separate whole blood into platelets, plasma, and red blood cells. It then collects the components based on customer-configured priorities and the donor’s physiology and blood count.
Platelet storage
The FDA is now allowing platelets in 100% plasma that are collected via the Trima Accel system to be stored for up to 7 days post-collection. But platelets in isoplate solution can only be stored for up to 5 days.
For platelet storage up to 7 days, the FDA requires that every product be tested with a bacterial detection device cleared by the FDA and labeled as a “safety measure.”
Wireless feature
The newly cleared wireless feature connects the Trima Accel system to software applications such as the Cadence Data Collection System or the Vista Information System through the blood center’s or hospital’s existing wireless network.
This enables access to electronic donor information and reporting capabilities, with the goals of streamlining collections, simplifying data management, and allowing operators to focus on donor care, even when a wired connection is unavailable.
The wireless feature enables blood centers to either purchase a compatible wireless appliance from Terumo BCT or choose an appliance of their own for attachment to the Trima Accel system using a mounting bracket on the back of the system. ![]()
NICE recommends edoxaban for NVAF

Photo courtesy of the CDC
The UK’s National Institute for Health and Care Excellence (NICE) has issued a draft guidance recommending the oral anticoagulant edoxaban tosylate (Lixiana) as an option for preventing stroke and systemic embolism in adults with non-valvular atrial fibrillation (NVAF).
The patients must have 1 or more risk factors for stroke, including congestive heart failure, hypertension, diabetes, prior stroke or transient ischemic attack, and age of 75 years or older.
Such patients are generally treated with warfarin or the newer oral anticoagulants dabigatran, rivaroxaban, and apixaban.
NICE said it wants to add edoxaban to that list because the drug is a clinically and cost-effective treatment option for these patients.
NICE’s draft guidance says the decision about whether to start treatment with edoxaban should be made after an informed discussion between the clinician and the patient about the risks and benefits of edoxaban compared with warfarin, apixaban, dabigatran, and rivaroxaban.
For patients considering switching from warfarin, edoxaban’s potential benefits should be weighed against its potential risks, taking into account the patient’s level of international normalized ratio control.
Clinical effectiveness
NICE’s conclusion that edoxaban is clinically effective was based primarily on results of the ENGAGE AF-TIMI 48 trial. In this trial, researchers compared edoxaban and warfarin as prophylaxis for stroke or systemic embolism in patients with NVAF.
Results suggested edoxaban was at least non-inferior to warfarin with regard to efficacy, and edoxaban was associated with a significantly lower rate of major and fatal bleeding.
A committee advising NICE also reviewed a meta-analysis prepared by Daiichi Sankyo Co., Ltd., the company developing edoxaban.
The goal of the meta-analysis was to compare edoxaban with rivaroxaban, apixaban, and dabigatran. The analysis included 4 trials: ENGAGE AF-TIMI 48, ARISTOTLE (apixaban), RE-LY (dabigatran), and ROCKET-AF (rivaroxaban). All 4 trials had a warfarin comparator arm.
The results of the meta-analysis indicated that, for the composite endpoint of stroke and systemic embolism, efficacy was similar for high-dose edoxaban and the other newer oral anticoagulants.
However, edoxaban significantly reduced major bleeding risk by 24% compared to rivaroxaban, 28% compared to dabigatran at 150 mg, and 17% compared to dabigatran at 110 mg. Major bleeding rates were similar for high-dose edoxaban and apixaban.
The committee advising NICE said these results should be interpreted with caution, but edoxaban is unlikely to be different from rivaroxaban, apixaban, and dabigatran in clinical practice.
Cost-effectiveness
Edoxaban costs £58.80 for a 28-tablet pack (60 mg or 30 mg), and the daily cost of treatment is £2.10 (excluding value-added tax). However, costs may vary in different settings because of negotiated procurement discounts.
The committee advising NICE analyzed cost information and concluded that edoxaban is cost-effective compared with warfarin, but there is insufficient evidence to distinguish between the clinical and cost-effectiveness of edoxaban and the newer oral anticoagulants.
Nevertheless, the committee recommended edoxaban as a cost-effective treatment for patients with NVAF who have 1 or more risk factors for stroke.
NICE’s draft guidance is now with consultees, who have the opportunity to appeal against it. Once NICE issues its final guidance on a technology, it replaces local recommendations. ![]()

Photo courtesy of the CDC
The UK’s National Institute for Health and Care Excellence (NICE) has issued a draft guidance recommending the oral anticoagulant edoxaban tosylate (Lixiana) as an option for preventing stroke and systemic embolism in adults with non-valvular atrial fibrillation (NVAF).
The patients must have 1 or more risk factors for stroke, including congestive heart failure, hypertension, diabetes, prior stroke or transient ischemic attack, and age of 75 years or older.
Such patients are generally treated with warfarin or the newer oral anticoagulants dabigatran, rivaroxaban, and apixaban.
NICE said it wants to add edoxaban to that list because the drug is a clinically and cost-effective treatment option for these patients.
NICE’s draft guidance says the decision about whether to start treatment with edoxaban should be made after an informed discussion between the clinician and the patient about the risks and benefits of edoxaban compared with warfarin, apixaban, dabigatran, and rivaroxaban.
For patients considering switching from warfarin, edoxaban’s potential benefits should be weighed against its potential risks, taking into account the patient’s level of international normalized ratio control.
Clinical effectiveness
NICE’s conclusion that edoxaban is clinically effective was based primarily on results of the ENGAGE AF-TIMI 48 trial. In this trial, researchers compared edoxaban and warfarin as prophylaxis for stroke or systemic embolism in patients with NVAF.
Results suggested edoxaban was at least non-inferior to warfarin with regard to efficacy, and edoxaban was associated with a significantly lower rate of major and fatal bleeding.
A committee advising NICE also reviewed a meta-analysis prepared by Daiichi Sankyo Co., Ltd., the company developing edoxaban.
The goal of the meta-analysis was to compare edoxaban with rivaroxaban, apixaban, and dabigatran. The analysis included 4 trials: ENGAGE AF-TIMI 48, ARISTOTLE (apixaban), RE-LY (dabigatran), and ROCKET-AF (rivaroxaban). All 4 trials had a warfarin comparator arm.
The results of the meta-analysis indicated that, for the composite endpoint of stroke and systemic embolism, efficacy was similar for high-dose edoxaban and the other newer oral anticoagulants.
However, edoxaban significantly reduced major bleeding risk by 24% compared to rivaroxaban, 28% compared to dabigatran at 150 mg, and 17% compared to dabigatran at 110 mg. Major bleeding rates were similar for high-dose edoxaban and apixaban.
The committee advising NICE said these results should be interpreted with caution, but edoxaban is unlikely to be different from rivaroxaban, apixaban, and dabigatran in clinical practice.
Cost-effectiveness
Edoxaban costs £58.80 for a 28-tablet pack (60 mg or 30 mg), and the daily cost of treatment is £2.10 (excluding value-added tax). However, costs may vary in different settings because of negotiated procurement discounts.
The committee advising NICE analyzed cost information and concluded that edoxaban is cost-effective compared with warfarin, but there is insufficient evidence to distinguish between the clinical and cost-effectiveness of edoxaban and the newer oral anticoagulants.
Nevertheless, the committee recommended edoxaban as a cost-effective treatment for patients with NVAF who have 1 or more risk factors for stroke.
NICE’s draft guidance is now with consultees, who have the opportunity to appeal against it. Once NICE issues its final guidance on a technology, it replaces local recommendations. ![]()

Photo courtesy of the CDC
The UK’s National Institute for Health and Care Excellence (NICE) has issued a draft guidance recommending the oral anticoagulant edoxaban tosylate (Lixiana) as an option for preventing stroke and systemic embolism in adults with non-valvular atrial fibrillation (NVAF).
The patients must have 1 or more risk factors for stroke, including congestive heart failure, hypertension, diabetes, prior stroke or transient ischemic attack, and age of 75 years or older.
Such patients are generally treated with warfarin or the newer oral anticoagulants dabigatran, rivaroxaban, and apixaban.
NICE said it wants to add edoxaban to that list because the drug is a clinically and cost-effective treatment option for these patients.
NICE’s draft guidance says the decision about whether to start treatment with edoxaban should be made after an informed discussion between the clinician and the patient about the risks and benefits of edoxaban compared with warfarin, apixaban, dabigatran, and rivaroxaban.
For patients considering switching from warfarin, edoxaban’s potential benefits should be weighed against its potential risks, taking into account the patient’s level of international normalized ratio control.
Clinical effectiveness
NICE’s conclusion that edoxaban is clinically effective was based primarily on results of the ENGAGE AF-TIMI 48 trial. In this trial, researchers compared edoxaban and warfarin as prophylaxis for stroke or systemic embolism in patients with NVAF.
Results suggested edoxaban was at least non-inferior to warfarin with regard to efficacy, and edoxaban was associated with a significantly lower rate of major and fatal bleeding.
A committee advising NICE also reviewed a meta-analysis prepared by Daiichi Sankyo Co., Ltd., the company developing edoxaban.
The goal of the meta-analysis was to compare edoxaban with rivaroxaban, apixaban, and dabigatran. The analysis included 4 trials: ENGAGE AF-TIMI 48, ARISTOTLE (apixaban), RE-LY (dabigatran), and ROCKET-AF (rivaroxaban). All 4 trials had a warfarin comparator arm.
The results of the meta-analysis indicated that, for the composite endpoint of stroke and systemic embolism, efficacy was similar for high-dose edoxaban and the other newer oral anticoagulants.
However, edoxaban significantly reduced major bleeding risk by 24% compared to rivaroxaban, 28% compared to dabigatran at 150 mg, and 17% compared to dabigatran at 110 mg. Major bleeding rates were similar for high-dose edoxaban and apixaban.
The committee advising NICE said these results should be interpreted with caution, but edoxaban is unlikely to be different from rivaroxaban, apixaban, and dabigatran in clinical practice.
Cost-effectiveness
Edoxaban costs £58.80 for a 28-tablet pack (60 mg or 30 mg), and the daily cost of treatment is £2.10 (excluding value-added tax). However, costs may vary in different settings because of negotiated procurement discounts.
The committee advising NICE analyzed cost information and concluded that edoxaban is cost-effective compared with warfarin, but there is insufficient evidence to distinguish between the clinical and cost-effectiveness of edoxaban and the newer oral anticoagulants.
Nevertheless, the committee recommended edoxaban as a cost-effective treatment for patients with NVAF who have 1 or more risk factors for stroke.
NICE’s draft guidance is now with consultees, who have the opportunity to appeal against it. Once NICE issues its final guidance on a technology, it replaces local recommendations. ![]()
Method can predict genes likely to cause diseases

Photo by Darren Baker
A new computational method improves the detection of genes linked to complex diseases and biological traits, according to researchers.
The method, PrediXcan, estimates gene expression levels across the whole genome and integrates this data with genome-wide association study (GWAS) data.
Researchers say PrediXcan has the potential to identify gene targets for therapeutic applications faster and with greater accuracy than traditional methods.
“PrediXcan tells us which genes are more likely to affect a disease or trait by learning the relationship between genotype, gene expression levels from large-scale transcriptome studies, and disease associations from GWAS studies,” said Hae Kyung Im, PhD, of the University of Chicago in Illinois.
“This is the first method that accounts for the mechanisms of gene regulation and can be applied to any heritable disease or phenotype.”
Dr Im and her colleagues described the method in Nature Genetics.
They said PrediXcan uses computational algorithms to learn how genome sequence influences gene expression, based on large-scale transcriptome datasets. This can then be used to create computational estimates of gene expression levels from any whole-genome sequence or chip dataset.
Genomes that have been sequenced as part of a GWAS can be run through PrediXcan to generate a gene expression level profile, which is then analyzed to determine the association between gene expression levels and the disease states or the trait of interest being studied.
The researchers said this method can reveal potentially causal genes and determine directionality—whether high or low levels of expression might cause the disease or trait.
As calculations are based on DNA sequence data and not physical measurements, PrediXcan can tease apart the genetically determined component of gene expression from the effects of the trait itself (avoiding reverse causality) and other factors such as environment.
The researchers said that, with PrediXcan, validation studies need to test a few thousand genes, instead of millions of potential single mutations. In addition, the method can be used to re-analyze existing genomic datasets, with a focus on mechanism, in a high-throughput manner.
“This integrates what we know about consequences of genetic variation in the transcriptome in order to discover genes, instead of just looking at mutations,” Dr Im said. “In a way, we’re modeling one mechanism through which genes affect disease or traits, which is the regulation of gene expression level.”
Dr Im noted that, because PrediXcan creates estimates based on genome sequence data, it is most accurate for strongly heritable traits. However, almost every complex trait or disease has a genetic component. The method can be used to predict the influence of that component, reducing the complexity of follow-up studies.
Dr Im is now working to improve the prediction of PrediXcan and applying it to mental health disorders. In addition, she is working to expand it beyond gene expression levels, to predict the links between diseases or traits and protein levels, epigenetics, and other measurements that can be estimated based on genomic data.
“GWAS studies have been incredibly successful at finding genetic links to disease, but they have been unable to account for mechanism,” Dr Im said. “We now have a computational method that allows us to understand the consequences of GWAS studies.” ![]()

Photo by Darren Baker
A new computational method improves the detection of genes linked to complex diseases and biological traits, according to researchers.
The method, PrediXcan, estimates gene expression levels across the whole genome and integrates this data with genome-wide association study (GWAS) data.
Researchers say PrediXcan has the potential to identify gene targets for therapeutic applications faster and with greater accuracy than traditional methods.
“PrediXcan tells us which genes are more likely to affect a disease or trait by learning the relationship between genotype, gene expression levels from large-scale transcriptome studies, and disease associations from GWAS studies,” said Hae Kyung Im, PhD, of the University of Chicago in Illinois.
“This is the first method that accounts for the mechanisms of gene regulation and can be applied to any heritable disease or phenotype.”
Dr Im and her colleagues described the method in Nature Genetics.
They said PrediXcan uses computational algorithms to learn how genome sequence influences gene expression, based on large-scale transcriptome datasets. This can then be used to create computational estimates of gene expression levels from any whole-genome sequence or chip dataset.
Genomes that have been sequenced as part of a GWAS can be run through PrediXcan to generate a gene expression level profile, which is then analyzed to determine the association between gene expression levels and the disease states or the trait of interest being studied.
The researchers said this method can reveal potentially causal genes and determine directionality—whether high or low levels of expression might cause the disease or trait.
As calculations are based on DNA sequence data and not physical measurements, PrediXcan can tease apart the genetically determined component of gene expression from the effects of the trait itself (avoiding reverse causality) and other factors such as environment.
The researchers said that, with PrediXcan, validation studies need to test a few thousand genes, instead of millions of potential single mutations. In addition, the method can be used to re-analyze existing genomic datasets, with a focus on mechanism, in a high-throughput manner.
“This integrates what we know about consequences of genetic variation in the transcriptome in order to discover genes, instead of just looking at mutations,” Dr Im said. “In a way, we’re modeling one mechanism through which genes affect disease or traits, which is the regulation of gene expression level.”
Dr Im noted that, because PrediXcan creates estimates based on genome sequence data, it is most accurate for strongly heritable traits. However, almost every complex trait or disease has a genetic component. The method can be used to predict the influence of that component, reducing the complexity of follow-up studies.
Dr Im is now working to improve the prediction of PrediXcan and applying it to mental health disorders. In addition, she is working to expand it beyond gene expression levels, to predict the links between diseases or traits and protein levels, epigenetics, and other measurements that can be estimated based on genomic data.
“GWAS studies have been incredibly successful at finding genetic links to disease, but they have been unable to account for mechanism,” Dr Im said. “We now have a computational method that allows us to understand the consequences of GWAS studies.” ![]()

Photo by Darren Baker
A new computational method improves the detection of genes linked to complex diseases and biological traits, according to researchers.
The method, PrediXcan, estimates gene expression levels across the whole genome and integrates this data with genome-wide association study (GWAS) data.
Researchers say PrediXcan has the potential to identify gene targets for therapeutic applications faster and with greater accuracy than traditional methods.
“PrediXcan tells us which genes are more likely to affect a disease or trait by learning the relationship between genotype, gene expression levels from large-scale transcriptome studies, and disease associations from GWAS studies,” said Hae Kyung Im, PhD, of the University of Chicago in Illinois.
“This is the first method that accounts for the mechanisms of gene regulation and can be applied to any heritable disease or phenotype.”
Dr Im and her colleagues described the method in Nature Genetics.
They said PrediXcan uses computational algorithms to learn how genome sequence influences gene expression, based on large-scale transcriptome datasets. This can then be used to create computational estimates of gene expression levels from any whole-genome sequence or chip dataset.
Genomes that have been sequenced as part of a GWAS can be run through PrediXcan to generate a gene expression level profile, which is then analyzed to determine the association between gene expression levels and the disease states or the trait of interest being studied.
The researchers said this method can reveal potentially causal genes and determine directionality—whether high or low levels of expression might cause the disease or trait.
As calculations are based on DNA sequence data and not physical measurements, PrediXcan can tease apart the genetically determined component of gene expression from the effects of the trait itself (avoiding reverse causality) and other factors such as environment.
The researchers said that, with PrediXcan, validation studies need to test a few thousand genes, instead of millions of potential single mutations. In addition, the method can be used to re-analyze existing genomic datasets, with a focus on mechanism, in a high-throughput manner.
“This integrates what we know about consequences of genetic variation in the transcriptome in order to discover genes, instead of just looking at mutations,” Dr Im said. “In a way, we’re modeling one mechanism through which genes affect disease or traits, which is the regulation of gene expression level.”
Dr Im noted that, because PrediXcan creates estimates based on genome sequence data, it is most accurate for strongly heritable traits. However, almost every complex trait or disease has a genetic component. The method can be used to predict the influence of that component, reducing the complexity of follow-up studies.
Dr Im is now working to improve the prediction of PrediXcan and applying it to mental health disorders. In addition, she is working to expand it beyond gene expression levels, to predict the links between diseases or traits and protein levels, epigenetics, and other measurements that can be estimated based on genomic data.
“GWAS studies have been incredibly successful at finding genetic links to disease, but they have been unable to account for mechanism,” Dr Im said. “We now have a computational method that allows us to understand the consequences of GWAS studies.” ![]()
The Skin Cancer Vitamin?

Martin et al recently presented a study at the 2015 American Society of Clinical Oncology Annual Meeting (J Clin Oncol. 2015;33[suppl]:9000) that reported on a phase 3 double-blind randomized trial to assess the use of oral nicotinamide to reduce actinic skin cancers, namely basal cell carcinoma (BCC) and squamous cell carcinoma (SCC).
This study was conducted in 2 tertiary treatment centers in Sydney, Australia, from 2012 to 2014, and it included 386 immunocompetent participants with 2 or more histologically confirmed nonmelanoma skin cancers (NMSCs) in the last 5 years. Two groups were randomized (1:1 ratio) to either receive oral nicotinamide 500 mg twice daily or matched placebo for 12 months. The primary end point measured was the number of new NMSCs to 12 months. Other secondary end points included number of SCCs, BCCs, and actinic keratoses to 12 months. Dermatologists performed skin checks every 3 months on the participants.
The results of the study showed that the average NMSC rate was significantly lower for the oral nicotinamide group (1.77) compared to the placebo group (2.42). The estimated relative rate reduction (RRR) was 0.23 (95% confidence interval [CI], 0.04-0.38; P=.02) adjusting for center and NMSC history, and 0.27 (95% CI, 0.05-0.44; P=.02) with no adjustment. The effects for BCC were comparable to SCC: BCC (RRR, 0.20; 95% CI, -0.06 to 0.39; P=.1) and SCC (RRR, 0.30; 95% CI, 0-0.51; P=.05). Additionally, actinic keratosis counts were reduced by 11% at 3 months (P=.01), 14% at 6 months (P<.001), 20% at 9 months (P<.0001), and 13% at 12 months (P<.005) for the oral nicotinamide group compared to the placebo group. There was no difference in the adverse event rates between the 2 groups.
What’s the issue?
This study reported the results of a double-blind randomized study of nicotinamide (vitamin B3) to reduce actinic cancer, called the ONTRAC (Oral Nicotinamide to Reduce Actinic Cancer) study, with favorable results for the use of oral nicotinamide, an inexpensive vitamin. There was a 20% reduction in BCC and a 30% reduction in SCC in the nicotinamide group compared to the group taking a placebo with no active ingredients. This study was conducted in a heavily sun-damaged group and it is postulated that nicotinamide helps cells repair DNA damage.
The thought of using a vitamin to reduce skin cancer rates is exciting; however, this study is singular, and while it did show promising results, the number of participants is not very large. There also was no evidence that nicotinamide prevents melanoma formation. Also, there was no protective effect seen once the vitamin B3 treatment was stopped. One must be cognizant that nicotinamide is not interchangeable with other forms of vitamin B3 such as niacin.
Although this study is promising, more research is needed to determine nicotinamide’s preventative effects. Of course, strict sun protection and skin checks are the first line in the prevention of skin cancer. Will you be prescribing oral nicotinamide to your patients to prevent NMSC?

Martin et al recently presented a study at the 2015 American Society of Clinical Oncology Annual Meeting (J Clin Oncol. 2015;33[suppl]:9000) that reported on a phase 3 double-blind randomized trial to assess the use of oral nicotinamide to reduce actinic skin cancers, namely basal cell carcinoma (BCC) and squamous cell carcinoma (SCC).
This study was conducted in 2 tertiary treatment centers in Sydney, Australia, from 2012 to 2014, and it included 386 immunocompetent participants with 2 or more histologically confirmed nonmelanoma skin cancers (NMSCs) in the last 5 years. Two groups were randomized (1:1 ratio) to either receive oral nicotinamide 500 mg twice daily or matched placebo for 12 months. The primary end point measured was the number of new NMSCs to 12 months. Other secondary end points included number of SCCs, BCCs, and actinic keratoses to 12 months. Dermatologists performed skin checks every 3 months on the participants.
The results of the study showed that the average NMSC rate was significantly lower for the oral nicotinamide group (1.77) compared to the placebo group (2.42). The estimated relative rate reduction (RRR) was 0.23 (95% confidence interval [CI], 0.04-0.38; P=.02) adjusting for center and NMSC history, and 0.27 (95% CI, 0.05-0.44; P=.02) with no adjustment. The effects for BCC were comparable to SCC: BCC (RRR, 0.20; 95% CI, -0.06 to 0.39; P=.1) and SCC (RRR, 0.30; 95% CI, 0-0.51; P=.05). Additionally, actinic keratosis counts were reduced by 11% at 3 months (P=.01), 14% at 6 months (P<.001), 20% at 9 months (P<.0001), and 13% at 12 months (P<.005) for the oral nicotinamide group compared to the placebo group. There was no difference in the adverse event rates between the 2 groups.
What’s the issue?
This study reported the results of a double-blind randomized study of nicotinamide (vitamin B3) to reduce actinic cancer, called the ONTRAC (Oral Nicotinamide to Reduce Actinic Cancer) study, with favorable results for the use of oral nicotinamide, an inexpensive vitamin. There was a 20% reduction in BCC and a 30% reduction in SCC in the nicotinamide group compared to the group taking a placebo with no active ingredients. This study was conducted in a heavily sun-damaged group and it is postulated that nicotinamide helps cells repair DNA damage.
The thought of using a vitamin to reduce skin cancer rates is exciting; however, this study is singular, and while it did show promising results, the number of participants is not very large. There also was no evidence that nicotinamide prevents melanoma formation. Also, there was no protective effect seen once the vitamin B3 treatment was stopped. One must be cognizant that nicotinamide is not interchangeable with other forms of vitamin B3 such as niacin.
Although this study is promising, more research is needed to determine nicotinamide’s preventative effects. Of course, strict sun protection and skin checks are the first line in the prevention of skin cancer. Will you be prescribing oral nicotinamide to your patients to prevent NMSC?

Martin et al recently presented a study at the 2015 American Society of Clinical Oncology Annual Meeting (J Clin Oncol. 2015;33[suppl]:9000) that reported on a phase 3 double-blind randomized trial to assess the use of oral nicotinamide to reduce actinic skin cancers, namely basal cell carcinoma (BCC) and squamous cell carcinoma (SCC).
This study was conducted in 2 tertiary treatment centers in Sydney, Australia, from 2012 to 2014, and it included 386 immunocompetent participants with 2 or more histologically confirmed nonmelanoma skin cancers (NMSCs) in the last 5 years. Two groups were randomized (1:1 ratio) to either receive oral nicotinamide 500 mg twice daily or matched placebo for 12 months. The primary end point measured was the number of new NMSCs to 12 months. Other secondary end points included number of SCCs, BCCs, and actinic keratoses to 12 months. Dermatologists performed skin checks every 3 months on the participants.
The results of the study showed that the average NMSC rate was significantly lower for the oral nicotinamide group (1.77) compared to the placebo group (2.42). The estimated relative rate reduction (RRR) was 0.23 (95% confidence interval [CI], 0.04-0.38; P=.02) adjusting for center and NMSC history, and 0.27 (95% CI, 0.05-0.44; P=.02) with no adjustment. The effects for BCC were comparable to SCC: BCC (RRR, 0.20; 95% CI, -0.06 to 0.39; P=.1) and SCC (RRR, 0.30; 95% CI, 0-0.51; P=.05). Additionally, actinic keratosis counts were reduced by 11% at 3 months (P=.01), 14% at 6 months (P<.001), 20% at 9 months (P<.0001), and 13% at 12 months (P<.005) for the oral nicotinamide group compared to the placebo group. There was no difference in the adverse event rates between the 2 groups.
What’s the issue?
This study reported the results of a double-blind randomized study of nicotinamide (vitamin B3) to reduce actinic cancer, called the ONTRAC (Oral Nicotinamide to Reduce Actinic Cancer) study, with favorable results for the use of oral nicotinamide, an inexpensive vitamin. There was a 20% reduction in BCC and a 30% reduction in SCC in the nicotinamide group compared to the group taking a placebo with no active ingredients. This study was conducted in a heavily sun-damaged group and it is postulated that nicotinamide helps cells repair DNA damage.
The thought of using a vitamin to reduce skin cancer rates is exciting; however, this study is singular, and while it did show promising results, the number of participants is not very large. There also was no evidence that nicotinamide prevents melanoma formation. Also, there was no protective effect seen once the vitamin B3 treatment was stopped. One must be cognizant that nicotinamide is not interchangeable with other forms of vitamin B3 such as niacin.
Although this study is promising, more research is needed to determine nicotinamide’s preventative effects. Of course, strict sun protection and skin checks are the first line in the prevention of skin cancer. Will you be prescribing oral nicotinamide to your patients to prevent NMSC?
Poor Inpatient Memory Can Undermine Teachable Moments
Memory loss is prevalent among adult hospitalized patients and can complicate hospitalists' job of teaching them about their conditions and home care, recent research suggests. But just what is behind patients’ memory impairment is not clear.
In a recent study published in the Journal of Hospital Medicine, researchers assessed the memory and in-hospital sleep habits of older adult patients to determine whether the two are linked.
"Since the hospital is considered a 'teachable moment,' and hospitalized patients have to learn about their care but also face sleep loss due to a disruptive environment and their own illness, we thought it would be interesting to see if there was an association," says study co-author Vineet M. Arora, MD, MAPP, a hospitalist and associate professor of medicine at the University of Chicago.
Nearly half of hospitalized patients in the study showed poor memory, based on their recall of word lists and medical vignettes. The results led Dr. Arora to conclude that hospitalists need to rethink the idea of hospitalization as a teachable moment and try reinforcing techniques when teaching patients.
"When trying to teach something that hospitalized patients need to remember, consider adopting strategies that use reminders or tools that people can take home, such as written instructions or video," Dr. Arora says. She also suggests hospitalists consider involving a patient's caregiver during the teaching, to have someone who can serve as a backup for the patient later.
The study also found that patients averaged 5.4 hours of in-hospital sleep per night and below-normal sleep efficiency, with 44% of patients' sleep-quality scores measured in the insomniac range. But they saw no statistically significant association between sleep loss and memory impairment in this study, Dr. Arora says.
"Our study was observational; it may be that everyone was too sleep deprived," she adds. "We may not have enough variation in sleep to detect difference in memory."
In future studies, having some well-rested subjects might make it possible to detect the association between sleep loss and memory impairment, Dr. Arora notes.
"If we did an intervention and tried to improve sleep in half our patients," she says, "then it would be worth seeing if memory was improved because we would have two groups: one that had better sleep and one that had worse sleep." TH
Visit our website for more information on inpatients and memory loss.
Memory loss is prevalent among adult hospitalized patients and can complicate hospitalists' job of teaching them about their conditions and home care, recent research suggests. But just what is behind patients’ memory impairment is not clear.
In a recent study published in the Journal of Hospital Medicine, researchers assessed the memory and in-hospital sleep habits of older adult patients to determine whether the two are linked.
"Since the hospital is considered a 'teachable moment,' and hospitalized patients have to learn about their care but also face sleep loss due to a disruptive environment and their own illness, we thought it would be interesting to see if there was an association," says study co-author Vineet M. Arora, MD, MAPP, a hospitalist and associate professor of medicine at the University of Chicago.
Nearly half of hospitalized patients in the study showed poor memory, based on their recall of word lists and medical vignettes. The results led Dr. Arora to conclude that hospitalists need to rethink the idea of hospitalization as a teachable moment and try reinforcing techniques when teaching patients.
"When trying to teach something that hospitalized patients need to remember, consider adopting strategies that use reminders or tools that people can take home, such as written instructions or video," Dr. Arora says. She also suggests hospitalists consider involving a patient's caregiver during the teaching, to have someone who can serve as a backup for the patient later.
The study also found that patients averaged 5.4 hours of in-hospital sleep per night and below-normal sleep efficiency, with 44% of patients' sleep-quality scores measured in the insomniac range. But they saw no statistically significant association between sleep loss and memory impairment in this study, Dr. Arora says.
"Our study was observational; it may be that everyone was too sleep deprived," she adds. "We may not have enough variation in sleep to detect difference in memory."
In future studies, having some well-rested subjects might make it possible to detect the association between sleep loss and memory impairment, Dr. Arora notes.
"If we did an intervention and tried to improve sleep in half our patients," she says, "then it would be worth seeing if memory was improved because we would have two groups: one that had better sleep and one that had worse sleep." TH
Visit our website for more information on inpatients and memory loss.
Memory loss is prevalent among adult hospitalized patients and can complicate hospitalists' job of teaching them about their conditions and home care, recent research suggests. But just what is behind patients’ memory impairment is not clear.
In a recent study published in the Journal of Hospital Medicine, researchers assessed the memory and in-hospital sleep habits of older adult patients to determine whether the two are linked.
"Since the hospital is considered a 'teachable moment,' and hospitalized patients have to learn about their care but also face sleep loss due to a disruptive environment and their own illness, we thought it would be interesting to see if there was an association," says study co-author Vineet M. Arora, MD, MAPP, a hospitalist and associate professor of medicine at the University of Chicago.
Nearly half of hospitalized patients in the study showed poor memory, based on their recall of word lists and medical vignettes. The results led Dr. Arora to conclude that hospitalists need to rethink the idea of hospitalization as a teachable moment and try reinforcing techniques when teaching patients.
"When trying to teach something that hospitalized patients need to remember, consider adopting strategies that use reminders or tools that people can take home, such as written instructions or video," Dr. Arora says. She also suggests hospitalists consider involving a patient's caregiver during the teaching, to have someone who can serve as a backup for the patient later.
The study also found that patients averaged 5.4 hours of in-hospital sleep per night and below-normal sleep efficiency, with 44% of patients' sleep-quality scores measured in the insomniac range. But they saw no statistically significant association between sleep loss and memory impairment in this study, Dr. Arora says.
"Our study was observational; it may be that everyone was too sleep deprived," she adds. "We may not have enough variation in sleep to detect difference in memory."
In future studies, having some well-rested subjects might make it possible to detect the association between sleep loss and memory impairment, Dr. Arora notes.
"If we did an intervention and tried to improve sleep in half our patients," she says, "then it would be worth seeing if memory was improved because we would have two groups: one that had better sleep and one that had worse sleep." TH