User login
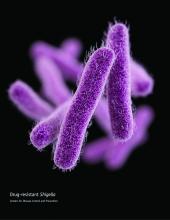
CDC: Some Shigella strains show reduced ciprofloxacin susceptibility
The Centers for Disease Control and Prevention has identified an increase in Shigella isolates with reduced susceptibility to ciprofloxacin, and has released an official health advisory outlining new recommendations for clinical diagnosis, management, and reporting, as well as for laboratories and public health officials.
The Shigella isolates of concern in the United States have minimum inhibitory concentration (MIC) values of 0.12-1 mcg/mL for ciprofloxacin, which is within the range considered susceptible. These strains, however, “often have a quinolone resistance gene that may lead to clinically significant reduced susceptibility to fluoroquinolone antibiotics,” such as ciprofloxacin, according to the CDC advisory.
It is possible that strains with MIC in the 0.12-1 mcg/mL range may have worse clinical outcome or increased risk of transmission, so the CDC made the following recommendations to clinicians:
• Order a stool culture to obtain isolates for antimicrobial susceptibility testing in suspected cases.
• Order antimicrobial susceptibility testing when ordering a stool culture for Shigella.
• Avoid routine prescribing of antibiotic therapy for Shigella infection, instead reserving antibiotics for patients with a clinical indication or when advised by public health officials in an outbreak setting.
• Tailor antibiotic choice (when antibiotics are indicated) to susceptibility results as soon as possible – with special attention given to the MIC for fluoroquinolone antibiotics.
• Obtain follow-up stool cultures in shigellosis patients who have continued or worsening symptoms despite antibiotic therapy.
• Consult local or state health departments for guidance regarding when patients may return to child care, school, or work.
• Counsel patients with active diarrhea on how they can prevent spreading the infection to others, regardless of whether antibiotic treatment is prescribed.
Additionally, the CDC noted that shigellosis is a nationally notifiable condition; all cases should be reported to the local health department. If a patient with shigellosis and a ciprofloxacin MIC of 0.12-1 mcg/mL is identified, this information should be included in the report to facilitate further testing of the isolate.
The CDC reported that it is working with state and local public health departments and clinical partners to determine if outcomes are indeed worse for patients treated with ciprofloxacin for Shigella strains harboring a quinolone resistance gene, and it will continue to monitor trends in susceptibility of Shigella isolates and to perform genetic testing on select strains to confirm the presence and type of resistance genes.
The Centers for Disease Control and Prevention has identified an increase in Shigella isolates with reduced susceptibility to ciprofloxacin, and has released an official health advisory outlining new recommendations for clinical diagnosis, management, and reporting, as well as for laboratories and public health officials.
The Shigella isolates of concern in the United States have minimum inhibitory concentration (MIC) values of 0.12-1 mcg/mL for ciprofloxacin, which is within the range considered susceptible. These strains, however, “often have a quinolone resistance gene that may lead to clinically significant reduced susceptibility to fluoroquinolone antibiotics,” such as ciprofloxacin, according to the CDC advisory.
It is possible that strains with MIC in the 0.12-1 mcg/mL range may have worse clinical outcome or increased risk of transmission, so the CDC made the following recommendations to clinicians:
• Order a stool culture to obtain isolates for antimicrobial susceptibility testing in suspected cases.
• Order antimicrobial susceptibility testing when ordering a stool culture for Shigella.
• Avoid routine prescribing of antibiotic therapy for Shigella infection, instead reserving antibiotics for patients with a clinical indication or when advised by public health officials in an outbreak setting.
• Tailor antibiotic choice (when antibiotics are indicated) to susceptibility results as soon as possible – with special attention given to the MIC for fluoroquinolone antibiotics.
• Obtain follow-up stool cultures in shigellosis patients who have continued or worsening symptoms despite antibiotic therapy.
• Consult local or state health departments for guidance regarding when patients may return to child care, school, or work.
• Counsel patients with active diarrhea on how they can prevent spreading the infection to others, regardless of whether antibiotic treatment is prescribed.
Additionally, the CDC noted that shigellosis is a nationally notifiable condition; all cases should be reported to the local health department. If a patient with shigellosis and a ciprofloxacin MIC of 0.12-1 mcg/mL is identified, this information should be included in the report to facilitate further testing of the isolate.
The CDC reported that it is working with state and local public health departments and clinical partners to determine if outcomes are indeed worse for patients treated with ciprofloxacin for Shigella strains harboring a quinolone resistance gene, and it will continue to monitor trends in susceptibility of Shigella isolates and to perform genetic testing on select strains to confirm the presence and type of resistance genes.
The Centers for Disease Control and Prevention has identified an increase in Shigella isolates with reduced susceptibility to ciprofloxacin, and has released an official health advisory outlining new recommendations for clinical diagnosis, management, and reporting, as well as for laboratories and public health officials.
The Shigella isolates of concern in the United States have minimum inhibitory concentration (MIC) values of 0.12-1 mcg/mL for ciprofloxacin, which is within the range considered susceptible. These strains, however, “often have a quinolone resistance gene that may lead to clinically significant reduced susceptibility to fluoroquinolone antibiotics,” such as ciprofloxacin, according to the CDC advisory.
It is possible that strains with MIC in the 0.12-1 mcg/mL range may have worse clinical outcome or increased risk of transmission, so the CDC made the following recommendations to clinicians:
• Order a stool culture to obtain isolates for antimicrobial susceptibility testing in suspected cases.
• Order antimicrobial susceptibility testing when ordering a stool culture for Shigella.
• Avoid routine prescribing of antibiotic therapy for Shigella infection, instead reserving antibiotics for patients with a clinical indication or when advised by public health officials in an outbreak setting.
• Tailor antibiotic choice (when antibiotics are indicated) to susceptibility results as soon as possible – with special attention given to the MIC for fluoroquinolone antibiotics.
• Obtain follow-up stool cultures in shigellosis patients who have continued or worsening symptoms despite antibiotic therapy.
• Consult local or state health departments for guidance regarding when patients may return to child care, school, or work.
• Counsel patients with active diarrhea on how they can prevent spreading the infection to others, regardless of whether antibiotic treatment is prescribed.
Additionally, the CDC noted that shigellosis is a nationally notifiable condition; all cases should be reported to the local health department. If a patient with shigellosis and a ciprofloxacin MIC of 0.12-1 mcg/mL is identified, this information should be included in the report to facilitate further testing of the isolate.
The CDC reported that it is working with state and local public health departments and clinical partners to determine if outcomes are indeed worse for patients treated with ciprofloxacin for Shigella strains harboring a quinolone resistance gene, and it will continue to monitor trends in susceptibility of Shigella isolates and to perform genetic testing on select strains to confirm the presence and type of resistance genes.
Survey insights: Unwrapping the compensation package
When approached for advice regarding the evaluation of job offers after completion of training, specific day-to-day duties (for example, shift length, teaching time, ICU coverage, and so on), and the overall gestalt of the interview experience, I find that location, lifestyle, and pay are the most consistent and common themes.
People often assume that pay is relatively straightforward, since it can be summarized in a number in the offer, whereas the other factors are harder to evaluate. However, it turns out pay is more complex. As a result, the last several State of Hospital Medicine reports have sought to evaluate compensation packages more thoroughly.
In 2016, the survey started including pay increases by years of experience, as well as CME dollars allotted per year per hospitalist. The goal was to gain deeper insight into the entire financial package, which is tied to a particular hospitalist job.
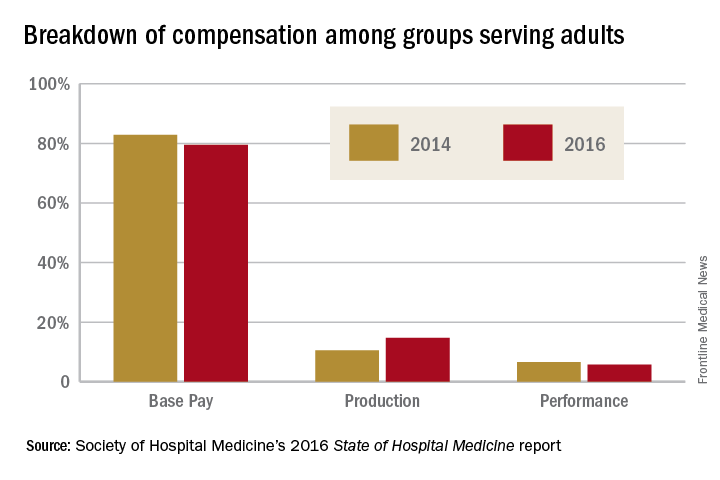
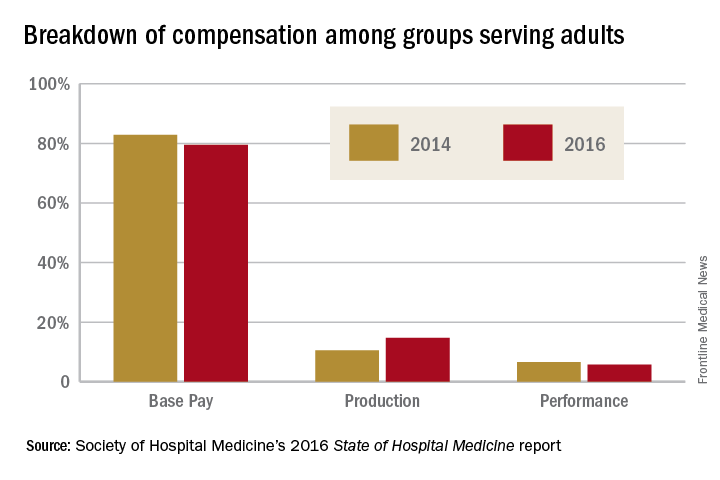
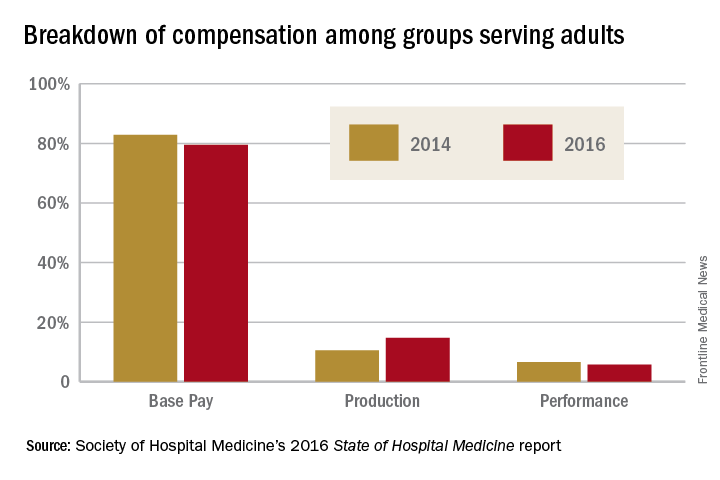
When looking at the 2014 and 2016 SHM survey results, there are several interesting findings. Base pay makes up the majority of earnings for all types of hospitalists (those seeing adults only, children only, and a mix of adults and children). In academic hospitalist groups, more of the total package of compensation comes from base pay, compared with nonacademic groups, where production and performance pay play a bigger role.
Of interest, despite the increased national attention on quality of care, productivity-based pay increased again (10.5%-14.7%), while performance-based pay (usually tied to quality and safety metrics) decreased (6.6%-5.7%) among groups serving adults. Consistent with prior trends for adults-only hospitalists, the Southern region of the country had the highest percentage of pay derived from productivity (18.8%), as well as of overall compensation in the 2016 report.
For hospitalists serving both adults and children, there was a smaller increase in pay derived from production (12.4%-13.2%), while pay derived from performance dropped more dramatically (8.9%-3.9%).
For hospitalists serving only children, the opposite occurred: Pay derived from production fell from 10.7% to 2.8%. While it is not yet clear why compensation, overall, is moving into closer alignment with productivity, rather than performance on quality and safety metrics, one hypothesis is that work relative value units used for calculating productivity are easier to tie to an individual hospitalist than are quality and safety outcomes.
Employee benefits, as previously defined, increased among hospitalists caring for adults only and those caring for adults and children, with a mean increase in both groups of $5,000. The most generous benefits were typically seen at university-based academic medical centers. Amongst adult-only hospitalists, academic groups offer benefits worth $8,000-$9,000 more per year than in nonacademic groups. Lower benefits were common among practices in the Eastern region and in groups with four or fewer full-time hospitalists. The 2016 survey data on CME dollars revealed a median of $3,000-$4,000 per year, with higher amounts provided in nonacademic groups.
Paid time off (PTO) from work is an ongoing topic of interest on venues such as HMX forum, and, in the surveys, PTO remained fairly consistent among groups caring for adults only and those caring for adults and children, with only 30%-40% of groups offering PTO. The number of PTO hours offered vary substantially, however, ranging from a mean of 126 hours up to 216.4 hours annually. Future analysis of PTO will benefit from a deeper understanding of how many hours equate to a shift (the practical definition of a “day off” for most hospitalists).
Finally, the 2016 survey asked about automatic pay increases based strictly on overall experience or length of employment with the group. Roughly one-fifth to one-third of groups provided some sort of salary increase based on experience in 2015. This practice was more common in the Southern region and in nonteaching hospitals. These data raise the complex topic of seniority among hospitalists and how to define it: years since completing training, years with a particular hospital or group, academic rank, leadership roles, other? Further, if seniority is not recognized in pay, how commonly are groups recognizing it in other ways, such as in preferences related to time on certain services, shift type, or vacation requests?
The expanded survey on hospitalist pay, in addition to the biannual comparison of prior data, will likely continue to add value in assessing and exploring the entire package of compensation. Additional topics of interest moving forward might include better understanding of parental leave, sick time, and the comparison between compensation packages for physician hospitalists and those for inpatient Nurse Practitioners and Physician Assistants. Stay tuned for the next report.
Dr. Anoff is associate professor of clinical practice, division of hospital medicine, department of medicine, University of Colorado at Denver, Aurora.
References
1. (2014). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2014.
2. (2016). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2016.
When approached for advice regarding the evaluation of job offers after completion of training, specific day-to-day duties (for example, shift length, teaching time, ICU coverage, and so on), and the overall gestalt of the interview experience, I find that location, lifestyle, and pay are the most consistent and common themes.
People often assume that pay is relatively straightforward, since it can be summarized in a number in the offer, whereas the other factors are harder to evaluate. However, it turns out pay is more complex. As a result, the last several State of Hospital Medicine reports have sought to evaluate compensation packages more thoroughly.
In 2016, the survey started including pay increases by years of experience, as well as CME dollars allotted per year per hospitalist. The goal was to gain deeper insight into the entire financial package, which is tied to a particular hospitalist job.
When looking at the 2014 and 2016 SHM survey results, there are several interesting findings. Base pay makes up the majority of earnings for all types of hospitalists (those seeing adults only, children only, and a mix of adults and children). In academic hospitalist groups, more of the total package of compensation comes from base pay, compared with nonacademic groups, where production and performance pay play a bigger role.
Of interest, despite the increased national attention on quality of care, productivity-based pay increased again (10.5%-14.7%), while performance-based pay (usually tied to quality and safety metrics) decreased (6.6%-5.7%) among groups serving adults. Consistent with prior trends for adults-only hospitalists, the Southern region of the country had the highest percentage of pay derived from productivity (18.8%), as well as of overall compensation in the 2016 report.
For hospitalists serving both adults and children, there was a smaller increase in pay derived from production (12.4%-13.2%), while pay derived from performance dropped more dramatically (8.9%-3.9%).
For hospitalists serving only children, the opposite occurred: Pay derived from production fell from 10.7% to 2.8%. While it is not yet clear why compensation, overall, is moving into closer alignment with productivity, rather than performance on quality and safety metrics, one hypothesis is that work relative value units used for calculating productivity are easier to tie to an individual hospitalist than are quality and safety outcomes.
Employee benefits, as previously defined, increased among hospitalists caring for adults only and those caring for adults and children, with a mean increase in both groups of $5,000. The most generous benefits were typically seen at university-based academic medical centers. Amongst adult-only hospitalists, academic groups offer benefits worth $8,000-$9,000 more per year than in nonacademic groups. Lower benefits were common among practices in the Eastern region and in groups with four or fewer full-time hospitalists. The 2016 survey data on CME dollars revealed a median of $3,000-$4,000 per year, with higher amounts provided in nonacademic groups.
Paid time off (PTO) from work is an ongoing topic of interest on venues such as HMX forum, and, in the surveys, PTO remained fairly consistent among groups caring for adults only and those caring for adults and children, with only 30%-40% of groups offering PTO. The number of PTO hours offered vary substantially, however, ranging from a mean of 126 hours up to 216.4 hours annually. Future analysis of PTO will benefit from a deeper understanding of how many hours equate to a shift (the practical definition of a “day off” for most hospitalists).
Finally, the 2016 survey asked about automatic pay increases based strictly on overall experience or length of employment with the group. Roughly one-fifth to one-third of groups provided some sort of salary increase based on experience in 2015. This practice was more common in the Southern region and in nonteaching hospitals. These data raise the complex topic of seniority among hospitalists and how to define it: years since completing training, years with a particular hospital or group, academic rank, leadership roles, other? Further, if seniority is not recognized in pay, how commonly are groups recognizing it in other ways, such as in preferences related to time on certain services, shift type, or vacation requests?
The expanded survey on hospitalist pay, in addition to the biannual comparison of prior data, will likely continue to add value in assessing and exploring the entire package of compensation. Additional topics of interest moving forward might include better understanding of parental leave, sick time, and the comparison between compensation packages for physician hospitalists and those for inpatient Nurse Practitioners and Physician Assistants. Stay tuned for the next report.
Dr. Anoff is associate professor of clinical practice, division of hospital medicine, department of medicine, University of Colorado at Denver, Aurora.
References
1. (2014). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2014.
2. (2016). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2016.
When approached for advice regarding the evaluation of job offers after completion of training, specific day-to-day duties (for example, shift length, teaching time, ICU coverage, and so on), and the overall gestalt of the interview experience, I find that location, lifestyle, and pay are the most consistent and common themes.
People often assume that pay is relatively straightforward, since it can be summarized in a number in the offer, whereas the other factors are harder to evaluate. However, it turns out pay is more complex. As a result, the last several State of Hospital Medicine reports have sought to evaluate compensation packages more thoroughly.
In 2016, the survey started including pay increases by years of experience, as well as CME dollars allotted per year per hospitalist. The goal was to gain deeper insight into the entire financial package, which is tied to a particular hospitalist job.
When looking at the 2014 and 2016 SHM survey results, there are several interesting findings. Base pay makes up the majority of earnings for all types of hospitalists (those seeing adults only, children only, and a mix of adults and children). In academic hospitalist groups, more of the total package of compensation comes from base pay, compared with nonacademic groups, where production and performance pay play a bigger role.
Of interest, despite the increased national attention on quality of care, productivity-based pay increased again (10.5%-14.7%), while performance-based pay (usually tied to quality and safety metrics) decreased (6.6%-5.7%) among groups serving adults. Consistent with prior trends for adults-only hospitalists, the Southern region of the country had the highest percentage of pay derived from productivity (18.8%), as well as of overall compensation in the 2016 report.
For hospitalists serving both adults and children, there was a smaller increase in pay derived from production (12.4%-13.2%), while pay derived from performance dropped more dramatically (8.9%-3.9%).
For hospitalists serving only children, the opposite occurred: Pay derived from production fell from 10.7% to 2.8%. While it is not yet clear why compensation, overall, is moving into closer alignment with productivity, rather than performance on quality and safety metrics, one hypothesis is that work relative value units used for calculating productivity are easier to tie to an individual hospitalist than are quality and safety outcomes.
Employee benefits, as previously defined, increased among hospitalists caring for adults only and those caring for adults and children, with a mean increase in both groups of $5,000. The most generous benefits were typically seen at university-based academic medical centers. Amongst adult-only hospitalists, academic groups offer benefits worth $8,000-$9,000 more per year than in nonacademic groups. Lower benefits were common among practices in the Eastern region and in groups with four or fewer full-time hospitalists. The 2016 survey data on CME dollars revealed a median of $3,000-$4,000 per year, with higher amounts provided in nonacademic groups.
Paid time off (PTO) from work is an ongoing topic of interest on venues such as HMX forum, and, in the surveys, PTO remained fairly consistent among groups caring for adults only and those caring for adults and children, with only 30%-40% of groups offering PTO. The number of PTO hours offered vary substantially, however, ranging from a mean of 126 hours up to 216.4 hours annually. Future analysis of PTO will benefit from a deeper understanding of how many hours equate to a shift (the practical definition of a “day off” for most hospitalists).
Finally, the 2016 survey asked about automatic pay increases based strictly on overall experience or length of employment with the group. Roughly one-fifth to one-third of groups provided some sort of salary increase based on experience in 2015. This practice was more common in the Southern region and in nonteaching hospitals. These data raise the complex topic of seniority among hospitalists and how to define it: years since completing training, years with a particular hospital or group, academic rank, leadership roles, other? Further, if seniority is not recognized in pay, how commonly are groups recognizing it in other ways, such as in preferences related to time on certain services, shift type, or vacation requests?
The expanded survey on hospitalist pay, in addition to the biannual comparison of prior data, will likely continue to add value in assessing and exploring the entire package of compensation. Additional topics of interest moving forward might include better understanding of parental leave, sick time, and the comparison between compensation packages for physician hospitalists and those for inpatient Nurse Practitioners and Physician Assistants. Stay tuned for the next report.
Dr. Anoff is associate professor of clinical practice, division of hospital medicine, department of medicine, University of Colorado at Denver, Aurora.
References
1. (2014). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2014.
2. (2016). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2016.
States consider abortion ‘reversal’ bills
Legislation requiring doctors to tell their patients that a medication abortion can be reversed is cropping up across the country.
Already in 2017, Colorado, Georgia, Indiana, Idaho, and North Carolina have introduced versions of the so-called abortion reversal legislation. In March, Utah became the latest state to pass a law addressing discontinuation of a medication abortion. Arkansas, South Dakota, and Arizona have similar laws on the books, but a court challenge ultimately led Arizona to amend its law, significantly toning down the language on reversal.
Utah’s law meanwhile, requires that physicians explain “the options and consequences of aborting a medication-induced abortion” and inform women that mifepristone alone is not always effective in ending a pregnancy. Women who have not yet taken the second drug and who are questioning their decision are encouraged to immediately consult their physician, according to the statute.
Calling the Utah measure an “abortion reversal law” is an inaccurate overreach, said state Sen. Curt Bramble, a Utah Republican who cosponsored the bill. A previous version included language about the potential of progesterone in reversing a medication abortion, but that section was removed after conferring with local physician groups, Sen. Bramble said.
“The purpose of this bill is to provide the most accurate information for a woman contemplating terminating a pregnancy,” Sen. Bramble said in an interview. “I want to make certain that women, if they decide to take the life of that unborn child, that they’re doing so in light of all the available information. If they take mifepristone, and they have second thoughts, that they’re aware that [the pregnancy may still be viable]. What this bill does is hopefully provide them that information before they make the decision to take the drug.”
“Generally, when a physician’s going to be providing an abortion, the physician wants to be very sure that the woman is certain about her decision and wants to address any areas of uncertainty and resolve those before moving forward,” Dr. Grossman said in an interview. “[Utah’s law] kind of implies that if you’re not sure, you can still go forward, and you may still have another chance at continuing the pregnancy. It sends a mixed message to women.”
“Last year, we thought this kind of counseling requirement wasn’t going to be a trend,” Ms. Nash said in an interview. “Yet, there’s been much more energy around these bills this year. Typically, around abortion legislation, you see similar language pop up in various states. In this case, the bills don’t mimic each other at all. I think it’s because some of the bills are trying to account for the fact there is very little scientific evidence to support this idea, so they’re trying different approaches to craft language that could withstand a legal challenge.”
“Anyone who has ever had a surgery or taken a powerful drug knows that it’s common practice to be told all the possible implications and side effects,” Ms. Hamrick said in an interview. “Women should be given all the facts about the drugs sold to them. It’s commonsense, common practice in other settings, and we should trust women with the science.”
She points to AbortionPillReversal.com, a website that assists women in locating physicians trained in the reversal process. San Diego–based family physician George Delgado, MD, who operates the website, said he has a forthcoming research study that will detail 300 successful reversals of mifepristone and that will also show that the success rate using best protocols is between 60% and 70%. The upcoming study builds on a case series he published in 2012 showing that four out of six women who took mifepristone carried their pregnancies to term after receiving 200 mg of intramuscular progesterone (Ann Pharmacother. 2012 Dec;46[12]:e36).
But the American Congress of Obstetricians and Gynecologists states that claims of medication abortion reversal are not supported by the body of scientific evidence, and the approach is not recommended in ACOG’s clinical guidance on medication abortion. In their fact sheet on the issue, they specifically rebut Dr. Delgado’s evidence, noting that it describes only “a handful of experiences” involving varying regimens of injected progesterone, and that it was not a controlled study.
Further, a 2015 study led by Dr. Grossman found that evidence is insufficient to determine whether treatment with progesterone after mifepristone results in a higher proportion of continuing pregnancies, compared with expectant management (Contraception. 2015 Sep;92[3]:206-11).
“As our paper lays out, there’s really no medical evidence that any kind of treatment given to women after taking mifepristone increases the likelihood that pregnancy will continue,” Dr. Grossman said. “It’s very concerning that these laws are being passed based on nonexistent evidence. It essentially forces doctors to tell patients about an unproven therapy and pushes them toward participating in an unmonitored research study.”
Any law that requires a physician to make false statements to patients creates a barrier between the doctor and the patient, said Sarah Prager, MD, director of the family planning division and family planning fellowship at the University of Washington, Seattle.
“These laws get in the way of a strong doctor-patient relationship and harm doctors’ ability to use their medical judgment and practice evidence-based medicine,” Dr. Prager said in an interview. “It could be difficult for patients to trust their doctors if we are legally required to give them information that has no basis in medical evidence.”
[email protected]
On Twitter @legal_med
Legislation requiring doctors to tell their patients that a medication abortion can be reversed is cropping up across the country.
Already in 2017, Colorado, Georgia, Indiana, Idaho, and North Carolina have introduced versions of the so-called abortion reversal legislation. In March, Utah became the latest state to pass a law addressing discontinuation of a medication abortion. Arkansas, South Dakota, and Arizona have similar laws on the books, but a court challenge ultimately led Arizona to amend its law, significantly toning down the language on reversal.
Utah’s law meanwhile, requires that physicians explain “the options and consequences of aborting a medication-induced abortion” and inform women that mifepristone alone is not always effective in ending a pregnancy. Women who have not yet taken the second drug and who are questioning their decision are encouraged to immediately consult their physician, according to the statute.
Calling the Utah measure an “abortion reversal law” is an inaccurate overreach, said state Sen. Curt Bramble, a Utah Republican who cosponsored the bill. A previous version included language about the potential of progesterone in reversing a medication abortion, but that section was removed after conferring with local physician groups, Sen. Bramble said.
“The purpose of this bill is to provide the most accurate information for a woman contemplating terminating a pregnancy,” Sen. Bramble said in an interview. “I want to make certain that women, if they decide to take the life of that unborn child, that they’re doing so in light of all the available information. If they take mifepristone, and they have second thoughts, that they’re aware that [the pregnancy may still be viable]. What this bill does is hopefully provide them that information before they make the decision to take the drug.”
“Generally, when a physician’s going to be providing an abortion, the physician wants to be very sure that the woman is certain about her decision and wants to address any areas of uncertainty and resolve those before moving forward,” Dr. Grossman said in an interview. “[Utah’s law] kind of implies that if you’re not sure, you can still go forward, and you may still have another chance at continuing the pregnancy. It sends a mixed message to women.”
“Last year, we thought this kind of counseling requirement wasn’t going to be a trend,” Ms. Nash said in an interview. “Yet, there’s been much more energy around these bills this year. Typically, around abortion legislation, you see similar language pop up in various states. In this case, the bills don’t mimic each other at all. I think it’s because some of the bills are trying to account for the fact there is very little scientific evidence to support this idea, so they’re trying different approaches to craft language that could withstand a legal challenge.”
“Anyone who has ever had a surgery or taken a powerful drug knows that it’s common practice to be told all the possible implications and side effects,” Ms. Hamrick said in an interview. “Women should be given all the facts about the drugs sold to them. It’s commonsense, common practice in other settings, and we should trust women with the science.”
She points to AbortionPillReversal.com, a website that assists women in locating physicians trained in the reversal process. San Diego–based family physician George Delgado, MD, who operates the website, said he has a forthcoming research study that will detail 300 successful reversals of mifepristone and that will also show that the success rate using best protocols is between 60% and 70%. The upcoming study builds on a case series he published in 2012 showing that four out of six women who took mifepristone carried their pregnancies to term after receiving 200 mg of intramuscular progesterone (Ann Pharmacother. 2012 Dec;46[12]:e36).
But the American Congress of Obstetricians and Gynecologists states that claims of medication abortion reversal are not supported by the body of scientific evidence, and the approach is not recommended in ACOG’s clinical guidance on medication abortion. In their fact sheet on the issue, they specifically rebut Dr. Delgado’s evidence, noting that it describes only “a handful of experiences” involving varying regimens of injected progesterone, and that it was not a controlled study.
Further, a 2015 study led by Dr. Grossman found that evidence is insufficient to determine whether treatment with progesterone after mifepristone results in a higher proportion of continuing pregnancies, compared with expectant management (Contraception. 2015 Sep;92[3]:206-11).
“As our paper lays out, there’s really no medical evidence that any kind of treatment given to women after taking mifepristone increases the likelihood that pregnancy will continue,” Dr. Grossman said. “It’s very concerning that these laws are being passed based on nonexistent evidence. It essentially forces doctors to tell patients about an unproven therapy and pushes them toward participating in an unmonitored research study.”
Any law that requires a physician to make false statements to patients creates a barrier between the doctor and the patient, said Sarah Prager, MD, director of the family planning division and family planning fellowship at the University of Washington, Seattle.
“These laws get in the way of a strong doctor-patient relationship and harm doctors’ ability to use their medical judgment and practice evidence-based medicine,” Dr. Prager said in an interview. “It could be difficult for patients to trust their doctors if we are legally required to give them information that has no basis in medical evidence.”
[email protected]
On Twitter @legal_med
Legislation requiring doctors to tell their patients that a medication abortion can be reversed is cropping up across the country.
Already in 2017, Colorado, Georgia, Indiana, Idaho, and North Carolina have introduced versions of the so-called abortion reversal legislation. In March, Utah became the latest state to pass a law addressing discontinuation of a medication abortion. Arkansas, South Dakota, and Arizona have similar laws on the books, but a court challenge ultimately led Arizona to amend its law, significantly toning down the language on reversal.
Utah’s law meanwhile, requires that physicians explain “the options and consequences of aborting a medication-induced abortion” and inform women that mifepristone alone is not always effective in ending a pregnancy. Women who have not yet taken the second drug and who are questioning their decision are encouraged to immediately consult their physician, according to the statute.
Calling the Utah measure an “abortion reversal law” is an inaccurate overreach, said state Sen. Curt Bramble, a Utah Republican who cosponsored the bill. A previous version included language about the potential of progesterone in reversing a medication abortion, but that section was removed after conferring with local physician groups, Sen. Bramble said.
“The purpose of this bill is to provide the most accurate information for a woman contemplating terminating a pregnancy,” Sen. Bramble said in an interview. “I want to make certain that women, if they decide to take the life of that unborn child, that they’re doing so in light of all the available information. If they take mifepristone, and they have second thoughts, that they’re aware that [the pregnancy may still be viable]. What this bill does is hopefully provide them that information before they make the decision to take the drug.”
“Generally, when a physician’s going to be providing an abortion, the physician wants to be very sure that the woman is certain about her decision and wants to address any areas of uncertainty and resolve those before moving forward,” Dr. Grossman said in an interview. “[Utah’s law] kind of implies that if you’re not sure, you can still go forward, and you may still have another chance at continuing the pregnancy. It sends a mixed message to women.”
“Last year, we thought this kind of counseling requirement wasn’t going to be a trend,” Ms. Nash said in an interview. “Yet, there’s been much more energy around these bills this year. Typically, around abortion legislation, you see similar language pop up in various states. In this case, the bills don’t mimic each other at all. I think it’s because some of the bills are trying to account for the fact there is very little scientific evidence to support this idea, so they’re trying different approaches to craft language that could withstand a legal challenge.”
“Anyone who has ever had a surgery or taken a powerful drug knows that it’s common practice to be told all the possible implications and side effects,” Ms. Hamrick said in an interview. “Women should be given all the facts about the drugs sold to them. It’s commonsense, common practice in other settings, and we should trust women with the science.”
She points to AbortionPillReversal.com, a website that assists women in locating physicians trained in the reversal process. San Diego–based family physician George Delgado, MD, who operates the website, said he has a forthcoming research study that will detail 300 successful reversals of mifepristone and that will also show that the success rate using best protocols is between 60% and 70%. The upcoming study builds on a case series he published in 2012 showing that four out of six women who took mifepristone carried their pregnancies to term after receiving 200 mg of intramuscular progesterone (Ann Pharmacother. 2012 Dec;46[12]:e36).
But the American Congress of Obstetricians and Gynecologists states that claims of medication abortion reversal are not supported by the body of scientific evidence, and the approach is not recommended in ACOG’s clinical guidance on medication abortion. In their fact sheet on the issue, they specifically rebut Dr. Delgado’s evidence, noting that it describes only “a handful of experiences” involving varying regimens of injected progesterone, and that it was not a controlled study.
Further, a 2015 study led by Dr. Grossman found that evidence is insufficient to determine whether treatment with progesterone after mifepristone results in a higher proportion of continuing pregnancies, compared with expectant management (Contraception. 2015 Sep;92[3]:206-11).
“As our paper lays out, there’s really no medical evidence that any kind of treatment given to women after taking mifepristone increases the likelihood that pregnancy will continue,” Dr. Grossman said. “It’s very concerning that these laws are being passed based on nonexistent evidence. It essentially forces doctors to tell patients about an unproven therapy and pushes them toward participating in an unmonitored research study.”
Any law that requires a physician to make false statements to patients creates a barrier between the doctor and the patient, said Sarah Prager, MD, director of the family planning division and family planning fellowship at the University of Washington, Seattle.
“These laws get in the way of a strong doctor-patient relationship and harm doctors’ ability to use their medical judgment and practice evidence-based medicine,” Dr. Prager said in an interview. “It could be difficult for patients to trust their doctors if we are legally required to give them information that has no basis in medical evidence.”
[email protected]
On Twitter @legal_med
Suspected Clozapine-Induced Cardiomyopathy and Heart Failure With Reduced Ejection Fraction
Clozapine is an atypical antipsychotic that is usually reserved for use in patients with treatment-resistant schizophrenia or schizoaffective disorder with suicidalit
Clozapine-induced cardiomyopathy is a diagnosis of exclusion that requires the absence of other etiologies of cardiac dysfunction (ie, coronary artery disease, hypertension, valvular disease, congenital heart disease, etc). Diagnosing a clozapine-related cardiomyopathy may be a long and laborious task. Patients with cardiomyopathy may present with many nonspecific signs and symptoms, such as fatigue, dyspnea, edema, and/or nausea and vomiting, which are present in other diseases; therefore, multiple encounters and lab tests may be needed until a cardiac source is implicated. The exact mechanism is unknown; however, Chow and colleagues believe that clozapine is a direct toxin of the myocardium.5-7
Case Presentation
A 30-year-old woman with a history of asthma, hypothyroidism (euthyroid with supplementation), posttraumatic stress disorder, and schizoaffective disorder was started on clozapine due to major depression and increased suicidal ideation despite previous treatment with several other antipsychotic agents. Clozapine was gradually titrated to a dose of 150 mg twice a day during an inpatient psychiatric admission. Prior to starting clozapine, this patient had been admitted to the psychiatry unit 11 times within the prior 2 years. After initiating and titrating clozapine over 4 months, her psychiatric symptoms markedly improved.
More than 4 years after the initiation of clozapine and after various treatments for multiple symptoms (Sidebar), the patient was diagnosed with heart failure (HF) with a reduced ejection fraction (EF) of 10% to 15%. She was referred to the cardiology HF clinic. Her dose of clozapine 150 mg at bedtime was discontinued after a discussion with psychiatry. She had a negative workup for other HF etiologies and was started on HF medications that included carvedilol, losartan, and spironolactone. After discontinuation of clozapine, her psychiatric symptoms worsened, and she was admitted to the psychiatry unit twice within a year. Two months after clozapine was discontinued, a repeat echocardiogram (ECHO) was obtained and was essentially unchanged. A chest X-ray (CXR) obtained 4 months after clozapine discontinuation demonstrated a normalized cardio-mediastinal silhouette. A third ECHO was ordered during her second psychiatric admission, which was 11 months after clozapine discontinuation; this revealed an improved left ventricular EF (LVEF) of 30% to 35% and resolution of left ventricular (LV) dilation.
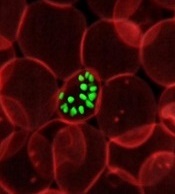
This patient’s clinical course led to an extensive chart review that investigated whether there may have been earlier signs and symptoms of HF or cardiomyopathy. It was discovered that the initial HF signs and symptoms were likely present for about 1 year before the diagnosis was made and after having been on clozapine for about 40 months (Patient’s ECHO before and after clozapine discontinuation, click here for additional ECHO perspectives ).
Discussion
In retrospect, this patient likely had HF for many months prior to the official diagnosis; however, given this patient’s young age, prior history of asthma, respiratory disorders, underlying severe psychiatric disease, and confounding symptoms, it is easy to understand why the diagnosis was initially overlooked and delayed.
This patient did not have significant lower extremity edema, but she reported nausea, vomiting, and weight loss. Typical patients with HF exhibit edema and weight gain unless they experience cardiac cachexia. It is not clear whether this patient had a coexisting gastrointestinal (GI) disorder or whether the GI symptoms were secondary to cardiac cachexia. Additionally, weight gain and metabolic syndrome have been documented with clozapine therapy.
It is interesting that a repeat ECHO within 2 months of clozapine discontinuation did not show an improvement, whereas a CXR at 4 months showed a normal cardiac silhouette, and an ECHO at 11 months showed an improvement in EF and normalization of LV size while on appropriate HF medications. It would have been interesting if an ECHO had been completed at 4 months to correspond with the time when the CXR normalized.
There does not seem to be a high level of awareness regarding this potentially fatal diagnosis of cardiomyopathy related to the use of clozapine. A recent review of clozapine-induced cardiomyopathy by Alawami and colleagues revealed characteristics, including median age of diagnosis of 33.5 years, a mean daily dose of 360 mg (range 125-700 mg/d), average time of therapy until the development of symptoms 14.4 months (range between 3 weeks and 4 years), and the presence of ventricular dilation in 39%.8 The most common symptoms on clinical presentation were shortness of breath (60%), palpitations (36%), cough (16%), fatigue (16%), and chest pain (8%).8
It is interesting that edema was not present in the patients studied in their review; this difference from the usual presentation of severe HF may lower clinical suspicion and makes diagnosing this type of cardiomyopathy more difficult. Alawami also noted that patients with an LVEF < 25% at the time of diagnosis tended to have a poorer prognosis with the highest risk of mortality and limited recovery. Fortunately, in this case, the patient’s LVEF improved significantly, and it will be interesting to continue to monitor the patient for further improvement.
As a result of this case, the authors have performed a chart review on all patients prescribed clozapine at VA Loma Linda Healthcare System. Additionally, this case supports the implementation of better cardiomyopathy monitoring of all clozapine patients. It may be recommended to obtain a baseline CXR in all patients starting clozapine, conduct monthly cardiomyopathy symptom screening that coincides with ANC monitoring, and perform an ECHO immediately on any clinical suspicion of cardiomyopathy.
Conclusion
Better awareness and regular screening for signs and symptoms of HF may help prevent a delay in diagnosing a rare but serious and potentially fatal condition associated with clozapine. Chest X-rays demonstrating cardiomegaly can be helpful when the early diagnosis of HF is suspected and may be the first diagnostic imaging test to normalize after clozapine discontinuation.
Since clozapine is a REMS medication and all patients are scheduled for regular ANC follow-up, it would seem prudent that patients also should be screened for signs and symptoms of HF, including the new onset or worsening of baseline shortness of breath, palpitations, cough, fatigue, chest pain, edema, gastroparesis, and perhaps extreme weight loss. Once a physician suspects HF, an ECHO should be obtained immediately.
In addition to the clozapine boxed warning for cardiomyopathy, it would be helpful if the clozapine patient counseling information section had a specific warning that advises patients to contact their clinician if they develop the signs and symptoms of HF.
1. Clozaril [package insert]. Rosemont, PA: HLS Therapeutics (USA), Inc; 2015.
2. Youssef DL, Narayanan P, Gill N. Incidence and risk factors for clozapine-induced myocarditis and cardiomyopathy at a regional mental health service in Australia. Austalas Psychiatry. 2016;24(2):176-180.
3. La Grenade L, Graham D, Trontell A. Myocarditis and cardiomyopathy associated with clozapine use in the United States. N Eng J Med. 2001;345(3):224-225.
4. Kilian JG, Kerr K, Lawrence C, Celermajer DS. Myocarditis and cardiomyopathy associated with clozapine. Lancet. 1999;354(9193):1841-1845.
5. Chow V, Yeoh T, Ng AC, et al. Asymptomatic left ventricular dysfunction with long-term clozapine treatment for schizophrenia: a multicenter cross-sectional cohort study. Open Heart 2014;1(1):e000030.
6. Scelsa SN, Simpson DM, McQuistion HL, Fineman A, Ault K, Reichler B. Clozapine-induced myotoxicity in patients with chronic psychotic disorders. Neurology. 1996;47(6):1518-1523.
7. Reznik I, Volchek L, Mester R, et al. Myotoxicity and neurotoxicity during clozapine treatment. Clin Neuropharmacol. 2000;23(5):276-280.
8. Alawami A, Wasywich C, Cicovic A, Kenedi C. A systematic review of clozapine induced cardiomyopathy. Int J Cardiol. 2014;176(2):315-320.
Clozapine is an atypical antipsychotic that is usually reserved for use in patients with treatment-resistant schizophrenia or schizoaffective disorder with suicidalit
Clozapine-induced cardiomyopathy is a diagnosis of exclusion that requires the absence of other etiologies of cardiac dysfunction (ie, coronary artery disease, hypertension, valvular disease, congenital heart disease, etc). Diagnosing a clozapine-related cardiomyopathy may be a long and laborious task. Patients with cardiomyopathy may present with many nonspecific signs and symptoms, such as fatigue, dyspnea, edema, and/or nausea and vomiting, which are present in other diseases; therefore, multiple encounters and lab tests may be needed until a cardiac source is implicated. The exact mechanism is unknown; however, Chow and colleagues believe that clozapine is a direct toxin of the myocardium.5-7
Case Presentation
A 30-year-old woman with a history of asthma, hypothyroidism (euthyroid with supplementation), posttraumatic stress disorder, and schizoaffective disorder was started on clozapine due to major depression and increased suicidal ideation despite previous treatment with several other antipsychotic agents. Clozapine was gradually titrated to a dose of 150 mg twice a day during an inpatient psychiatric admission. Prior to starting clozapine, this patient had been admitted to the psychiatry unit 11 times within the prior 2 years. After initiating and titrating clozapine over 4 months, her psychiatric symptoms markedly improved.
More than 4 years after the initiation of clozapine and after various treatments for multiple symptoms (Sidebar), the patient was diagnosed with heart failure (HF) with a reduced ejection fraction (EF) of 10% to 15%. She was referred to the cardiology HF clinic. Her dose of clozapine 150 mg at bedtime was discontinued after a discussion with psychiatry. She had a negative workup for other HF etiologies and was started on HF medications that included carvedilol, losartan, and spironolactone. After discontinuation of clozapine, her psychiatric symptoms worsened, and she was admitted to the psychiatry unit twice within a year. Two months after clozapine was discontinued, a repeat echocardiogram (ECHO) was obtained and was essentially unchanged. A chest X-ray (CXR) obtained 4 months after clozapine discontinuation demonstrated a normalized cardio-mediastinal silhouette. A third ECHO was ordered during her second psychiatric admission, which was 11 months after clozapine discontinuation; this revealed an improved left ventricular EF (LVEF) of 30% to 35% and resolution of left ventricular (LV) dilation.
This patient’s clinical course led to an extensive chart review that investigated whether there may have been earlier signs and symptoms of HF or cardiomyopathy. It was discovered that the initial HF signs and symptoms were likely present for about 1 year before the diagnosis was made and after having been on clozapine for about 40 months (Patient’s ECHO before and after clozapine discontinuation, click here for additional ECHO perspectives ).
Discussion
In retrospect, this patient likely had HF for many months prior to the official diagnosis; however, given this patient’s young age, prior history of asthma, respiratory disorders, underlying severe psychiatric disease, and confounding symptoms, it is easy to understand why the diagnosis was initially overlooked and delayed.
This patient did not have significant lower extremity edema, but she reported nausea, vomiting, and weight loss. Typical patients with HF exhibit edema and weight gain unless they experience cardiac cachexia. It is not clear whether this patient had a coexisting gastrointestinal (GI) disorder or whether the GI symptoms were secondary to cardiac cachexia. Additionally, weight gain and metabolic syndrome have been documented with clozapine therapy.
It is interesting that a repeat ECHO within 2 months of clozapine discontinuation did not show an improvement, whereas a CXR at 4 months showed a normal cardiac silhouette, and an ECHO at 11 months showed an improvement in EF and normalization of LV size while on appropriate HF medications. It would have been interesting if an ECHO had been completed at 4 months to correspond with the time when the CXR normalized.
There does not seem to be a high level of awareness regarding this potentially fatal diagnosis of cardiomyopathy related to the use of clozapine. A recent review of clozapine-induced cardiomyopathy by Alawami and colleagues revealed characteristics, including median age of diagnosis of 33.5 years, a mean daily dose of 360 mg (range 125-700 mg/d), average time of therapy until the development of symptoms 14.4 months (range between 3 weeks and 4 years), and the presence of ventricular dilation in 39%.8 The most common symptoms on clinical presentation were shortness of breath (60%), palpitations (36%), cough (16%), fatigue (16%), and chest pain (8%).8
It is interesting that edema was not present in the patients studied in their review; this difference from the usual presentation of severe HF may lower clinical suspicion and makes diagnosing this type of cardiomyopathy more difficult. Alawami also noted that patients with an LVEF < 25% at the time of diagnosis tended to have a poorer prognosis with the highest risk of mortality and limited recovery. Fortunately, in this case, the patient’s LVEF improved significantly, and it will be interesting to continue to monitor the patient for further improvement.
As a result of this case, the authors have performed a chart review on all patients prescribed clozapine at VA Loma Linda Healthcare System. Additionally, this case supports the implementation of better cardiomyopathy monitoring of all clozapine patients. It may be recommended to obtain a baseline CXR in all patients starting clozapine, conduct monthly cardiomyopathy symptom screening that coincides with ANC monitoring, and perform an ECHO immediately on any clinical suspicion of cardiomyopathy.
Conclusion
Better awareness and regular screening for signs and symptoms of HF may help prevent a delay in diagnosing a rare but serious and potentially fatal condition associated with clozapine. Chest X-rays demonstrating cardiomegaly can be helpful when the early diagnosis of HF is suspected and may be the first diagnostic imaging test to normalize after clozapine discontinuation.
Since clozapine is a REMS medication and all patients are scheduled for regular ANC follow-up, it would seem prudent that patients also should be screened for signs and symptoms of HF, including the new onset or worsening of baseline shortness of breath, palpitations, cough, fatigue, chest pain, edema, gastroparesis, and perhaps extreme weight loss. Once a physician suspects HF, an ECHO should be obtained immediately.
In addition to the clozapine boxed warning for cardiomyopathy, it would be helpful if the clozapine patient counseling information section had a specific warning that advises patients to contact their clinician if they develop the signs and symptoms of HF.
Clozapine is an atypical antipsychotic that is usually reserved for use in patients with treatment-resistant schizophrenia or schizoaffective disorder with suicidalit
Clozapine-induced cardiomyopathy is a diagnosis of exclusion that requires the absence of other etiologies of cardiac dysfunction (ie, coronary artery disease, hypertension, valvular disease, congenital heart disease, etc). Diagnosing a clozapine-related cardiomyopathy may be a long and laborious task. Patients with cardiomyopathy may present with many nonspecific signs and symptoms, such as fatigue, dyspnea, edema, and/or nausea and vomiting, which are present in other diseases; therefore, multiple encounters and lab tests may be needed until a cardiac source is implicated. The exact mechanism is unknown; however, Chow and colleagues believe that clozapine is a direct toxin of the myocardium.5-7
Case Presentation
A 30-year-old woman with a history of asthma, hypothyroidism (euthyroid with supplementation), posttraumatic stress disorder, and schizoaffective disorder was started on clozapine due to major depression and increased suicidal ideation despite previous treatment with several other antipsychotic agents. Clozapine was gradually titrated to a dose of 150 mg twice a day during an inpatient psychiatric admission. Prior to starting clozapine, this patient had been admitted to the psychiatry unit 11 times within the prior 2 years. After initiating and titrating clozapine over 4 months, her psychiatric symptoms markedly improved.
More than 4 years after the initiation of clozapine and after various treatments for multiple symptoms (Sidebar), the patient was diagnosed with heart failure (HF) with a reduced ejection fraction (EF) of 10% to 15%. She was referred to the cardiology HF clinic. Her dose of clozapine 150 mg at bedtime was discontinued after a discussion with psychiatry. She had a negative workup for other HF etiologies and was started on HF medications that included carvedilol, losartan, and spironolactone. After discontinuation of clozapine, her psychiatric symptoms worsened, and she was admitted to the psychiatry unit twice within a year. Two months after clozapine was discontinued, a repeat echocardiogram (ECHO) was obtained and was essentially unchanged. A chest X-ray (CXR) obtained 4 months after clozapine discontinuation demonstrated a normalized cardio-mediastinal silhouette. A third ECHO was ordered during her second psychiatric admission, which was 11 months after clozapine discontinuation; this revealed an improved left ventricular EF (LVEF) of 30% to 35% and resolution of left ventricular (LV) dilation.
This patient’s clinical course led to an extensive chart review that investigated whether there may have been earlier signs and symptoms of HF or cardiomyopathy. It was discovered that the initial HF signs and symptoms were likely present for about 1 year before the diagnosis was made and after having been on clozapine for about 40 months (Patient’s ECHO before and after clozapine discontinuation, click here for additional ECHO perspectives ).
Discussion
In retrospect, this patient likely had HF for many months prior to the official diagnosis; however, given this patient’s young age, prior history of asthma, respiratory disorders, underlying severe psychiatric disease, and confounding symptoms, it is easy to understand why the diagnosis was initially overlooked and delayed.
This patient did not have significant lower extremity edema, but she reported nausea, vomiting, and weight loss. Typical patients with HF exhibit edema and weight gain unless they experience cardiac cachexia. It is not clear whether this patient had a coexisting gastrointestinal (GI) disorder or whether the GI symptoms were secondary to cardiac cachexia. Additionally, weight gain and metabolic syndrome have been documented with clozapine therapy.
It is interesting that a repeat ECHO within 2 months of clozapine discontinuation did not show an improvement, whereas a CXR at 4 months showed a normal cardiac silhouette, and an ECHO at 11 months showed an improvement in EF and normalization of LV size while on appropriate HF medications. It would have been interesting if an ECHO had been completed at 4 months to correspond with the time when the CXR normalized.
There does not seem to be a high level of awareness regarding this potentially fatal diagnosis of cardiomyopathy related to the use of clozapine. A recent review of clozapine-induced cardiomyopathy by Alawami and colleagues revealed characteristics, including median age of diagnosis of 33.5 years, a mean daily dose of 360 mg (range 125-700 mg/d), average time of therapy until the development of symptoms 14.4 months (range between 3 weeks and 4 years), and the presence of ventricular dilation in 39%.8 The most common symptoms on clinical presentation were shortness of breath (60%), palpitations (36%), cough (16%), fatigue (16%), and chest pain (8%).8
It is interesting that edema was not present in the patients studied in their review; this difference from the usual presentation of severe HF may lower clinical suspicion and makes diagnosing this type of cardiomyopathy more difficult. Alawami also noted that patients with an LVEF < 25% at the time of diagnosis tended to have a poorer prognosis with the highest risk of mortality and limited recovery. Fortunately, in this case, the patient’s LVEF improved significantly, and it will be interesting to continue to monitor the patient for further improvement.
As a result of this case, the authors have performed a chart review on all patients prescribed clozapine at VA Loma Linda Healthcare System. Additionally, this case supports the implementation of better cardiomyopathy monitoring of all clozapine patients. It may be recommended to obtain a baseline CXR in all patients starting clozapine, conduct monthly cardiomyopathy symptom screening that coincides with ANC monitoring, and perform an ECHO immediately on any clinical suspicion of cardiomyopathy.
Conclusion
Better awareness and regular screening for signs and symptoms of HF may help prevent a delay in diagnosing a rare but serious and potentially fatal condition associated with clozapine. Chest X-rays demonstrating cardiomegaly can be helpful when the early diagnosis of HF is suspected and may be the first diagnostic imaging test to normalize after clozapine discontinuation.
Since clozapine is a REMS medication and all patients are scheduled for regular ANC follow-up, it would seem prudent that patients also should be screened for signs and symptoms of HF, including the new onset or worsening of baseline shortness of breath, palpitations, cough, fatigue, chest pain, edema, gastroparesis, and perhaps extreme weight loss. Once a physician suspects HF, an ECHO should be obtained immediately.
In addition to the clozapine boxed warning for cardiomyopathy, it would be helpful if the clozapine patient counseling information section had a specific warning that advises patients to contact their clinician if they develop the signs and symptoms of HF.
1. Clozaril [package insert]. Rosemont, PA: HLS Therapeutics (USA), Inc; 2015.
2. Youssef DL, Narayanan P, Gill N. Incidence and risk factors for clozapine-induced myocarditis and cardiomyopathy at a regional mental health service in Australia. Austalas Psychiatry. 2016;24(2):176-180.
3. La Grenade L, Graham D, Trontell A. Myocarditis and cardiomyopathy associated with clozapine use in the United States. N Eng J Med. 2001;345(3):224-225.
4. Kilian JG, Kerr K, Lawrence C, Celermajer DS. Myocarditis and cardiomyopathy associated with clozapine. Lancet. 1999;354(9193):1841-1845.
5. Chow V, Yeoh T, Ng AC, et al. Asymptomatic left ventricular dysfunction with long-term clozapine treatment for schizophrenia: a multicenter cross-sectional cohort study. Open Heart 2014;1(1):e000030.
6. Scelsa SN, Simpson DM, McQuistion HL, Fineman A, Ault K, Reichler B. Clozapine-induced myotoxicity in patients with chronic psychotic disorders. Neurology. 1996;47(6):1518-1523.
7. Reznik I, Volchek L, Mester R, et al. Myotoxicity and neurotoxicity during clozapine treatment. Clin Neuropharmacol. 2000;23(5):276-280.
8. Alawami A, Wasywich C, Cicovic A, Kenedi C. A systematic review of clozapine induced cardiomyopathy. Int J Cardiol. 2014;176(2):315-320.
1. Clozaril [package insert]. Rosemont, PA: HLS Therapeutics (USA), Inc; 2015.
2. Youssef DL, Narayanan P, Gill N. Incidence and risk factors for clozapine-induced myocarditis and cardiomyopathy at a regional mental health service in Australia. Austalas Psychiatry. 2016;24(2):176-180.
3. La Grenade L, Graham D, Trontell A. Myocarditis and cardiomyopathy associated with clozapine use in the United States. N Eng J Med. 2001;345(3):224-225.
4. Kilian JG, Kerr K, Lawrence C, Celermajer DS. Myocarditis and cardiomyopathy associated with clozapine. Lancet. 1999;354(9193):1841-1845.
5. Chow V, Yeoh T, Ng AC, et al. Asymptomatic left ventricular dysfunction with long-term clozapine treatment for schizophrenia: a multicenter cross-sectional cohort study. Open Heart 2014;1(1):e000030.
6. Scelsa SN, Simpson DM, McQuistion HL, Fineman A, Ault K, Reichler B. Clozapine-induced myotoxicity in patients with chronic psychotic disorders. Neurology. 1996;47(6):1518-1523.
7. Reznik I, Volchek L, Mester R, et al. Myotoxicity and neurotoxicity during clozapine treatment. Clin Neuropharmacol. 2000;23(5):276-280.
8. Alawami A, Wasywich C, Cicovic A, Kenedi C. A systematic review of clozapine induced cardiomyopathy. Int J Cardiol. 2014;176(2):315-320.
Second cancers take greater toll on younger patients
Second cancers take a greater toll on patients under the age of 40, according to research published in JAMA Oncology.
Researchers studied 14 types of cancer occurring in more than 1 million patients.
For nearly all of the cancers studied, 5-year survival rates were much higher if the cancer occurred as a first malignancy rather than a second cancer.
These survival differences were more pronounced in pediatric patients and adolescents and young adults (AYAs) than they were in patients age 40 and older.
Researchers hope these findings will help guide clinicians in providing age-specific recommendations on cancer prevention, screening, treatment, and survivorship, especially among the AYA population.
“Although the increased incidence of second cancers is well known among cancer survivors, less is known about outcomes of these cancers or the influence of age,” said Theresa Keegan, PhD, of the UC Davis Comprehensive Cancer Center in Sacramento, California.
With this in mind, Dr Keegan and her colleagues analyzed data on patients diagnosed with either a single cancer or a first and second malignancy during 1992 through 2008. The researchers used Surveillance, Epidemiology and End Results program data collected from 13 cancer registries.
The team collected data on the 14 most common cancer types that affect AYAs: acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), Hodgkin lymphoma (HL), non-Hodgkin lymphoma (NHL), soft tissue sarcoma, and bone sarcoma, as well as female breast, thyroid, testicular, colorectal, central nervous system, cervical, and ovarian cancers.
There were a total of 15,954 pediatric patients (younger than 15 years at diagnosis), 125,750 AYAs (ages 15 to 39), and 878,370 older adult patients (age 40 and older).
Survival rates
For pediatric patients, the 5-year relative survival was 80% for a first cancer and 47% for a second primary malignancy.
For AYAs, the 5-year relative survival was 81% for a first cancer and 60% for a second primary malignancy.
For older adults, the 5-year relative survival was 70% for a first cancer and 61% for a second primary malignancy.
When the researchers looked at 5-year survival by age and individual cancer types, they found striking differences depending on whether it was a first or second malignancy in all but 2 of the 14 cancer types, testicular cancer and melanoma.
“For almost every type of cancer, the AYA population did worse with a secondary cancer,” said study author Melanie Goldfarb, MD, of John Wayne Cancer Institute at Providence Saint John’s Health Center in Santa Monica, California.
“What struck us was that the second cancer caused such an increased risk of death.”
Lymphomas
For pediatric patients with HL, the 5-year relative survival was 95% when patients had HL as a first cancer. There were no data on HL as a second primary malignancy.
For AYAs, the 5-year relative survival was 93% when patients had HL as a first cancer and 72% when they had HL as a second primary malignancy.
For older adults, the 5-year relative survival was 69% when patients had HL as a first cancer and 54% when they had HL as a second primary malignancy.
For pediatric patients with NHL, the 5-year relative survival was 84% when patients had NHL as a first cancer and 63% when they had NHL as a second primary malignancy.
For AYAs, the 5-year relative survival was 64% when patients had NHL as a first cancer and 22% when they had NHL as a second primary malignancy.
For older adults, the 5-year relative survival was 57% when patients had NHL as a first cancer and 54% when they had NHL as a second primary malignancy.
Leukemias
For pediatric patients with ALL, the 5-year relative survival was 87% when patients had ALL as a first cancer and 63% when they had ALL as a second primary malignancy.
For AYAs, the 5-year relative survival was 48% when patients had ALL as a first cancer and 26% when they had ALL as a second primary malignancy.
For older adults, the 5-year relative survival was 17% when patients had ALL as a first cancer and 11% when they had ALL as a second primary malignancy.
For pediatric patients with AML, the 5-year relative survival was 57% when patients had AML as a first cancer and 29% when they had AML as a second primary malignancy.
For AYAs, the 5-year relative survival was 46% when patients had AML as a first cancer and 23% when they had AML as a second primary malignancy.
For older adults, the 5-year relative survival was 12% when patients had AML as a first cancer and 10% when they had AML as a second primary malignancy.
Why younger patients tend to fare worse after a second cancer than older patients is not fully understood or specifically addressed in the current study, the researchers noted.
Now, the team plans to examine how the time between getting a first and second cancer affects survival and whether the type of treatment for the first cancer influences the outcome of a second cancer. ![]()
Second cancers take a greater toll on patients under the age of 40, according to research published in JAMA Oncology.
Researchers studied 14 types of cancer occurring in more than 1 million patients.
For nearly all of the cancers studied, 5-year survival rates were much higher if the cancer occurred as a first malignancy rather than a second cancer.
These survival differences were more pronounced in pediatric patients and adolescents and young adults (AYAs) than they were in patients age 40 and older.
Researchers hope these findings will help guide clinicians in providing age-specific recommendations on cancer prevention, screening, treatment, and survivorship, especially among the AYA population.
“Although the increased incidence of second cancers is well known among cancer survivors, less is known about outcomes of these cancers or the influence of age,” said Theresa Keegan, PhD, of the UC Davis Comprehensive Cancer Center in Sacramento, California.
With this in mind, Dr Keegan and her colleagues analyzed data on patients diagnosed with either a single cancer or a first and second malignancy during 1992 through 2008. The researchers used Surveillance, Epidemiology and End Results program data collected from 13 cancer registries.
The team collected data on the 14 most common cancer types that affect AYAs: acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), Hodgkin lymphoma (HL), non-Hodgkin lymphoma (NHL), soft tissue sarcoma, and bone sarcoma, as well as female breast, thyroid, testicular, colorectal, central nervous system, cervical, and ovarian cancers.
There were a total of 15,954 pediatric patients (younger than 15 years at diagnosis), 125,750 AYAs (ages 15 to 39), and 878,370 older adult patients (age 40 and older).
Survival rates
For pediatric patients, the 5-year relative survival was 80% for a first cancer and 47% for a second primary malignancy.
For AYAs, the 5-year relative survival was 81% for a first cancer and 60% for a second primary malignancy.
For older adults, the 5-year relative survival was 70% for a first cancer and 61% for a second primary malignancy.
When the researchers looked at 5-year survival by age and individual cancer types, they found striking differences depending on whether it was a first or second malignancy in all but 2 of the 14 cancer types, testicular cancer and melanoma.
“For almost every type of cancer, the AYA population did worse with a secondary cancer,” said study author Melanie Goldfarb, MD, of John Wayne Cancer Institute at Providence Saint John’s Health Center in Santa Monica, California.
“What struck us was that the second cancer caused such an increased risk of death.”
Lymphomas
For pediatric patients with HL, the 5-year relative survival was 95% when patients had HL as a first cancer. There were no data on HL as a second primary malignancy.
For AYAs, the 5-year relative survival was 93% when patients had HL as a first cancer and 72% when they had HL as a second primary malignancy.
For older adults, the 5-year relative survival was 69% when patients had HL as a first cancer and 54% when they had HL as a second primary malignancy.
For pediatric patients with NHL, the 5-year relative survival was 84% when patients had NHL as a first cancer and 63% when they had NHL as a second primary malignancy.
For AYAs, the 5-year relative survival was 64% when patients had NHL as a first cancer and 22% when they had NHL as a second primary malignancy.
For older adults, the 5-year relative survival was 57% when patients had NHL as a first cancer and 54% when they had NHL as a second primary malignancy.
Leukemias
For pediatric patients with ALL, the 5-year relative survival was 87% when patients had ALL as a first cancer and 63% when they had ALL as a second primary malignancy.
For AYAs, the 5-year relative survival was 48% when patients had ALL as a first cancer and 26% when they had ALL as a second primary malignancy.
For older adults, the 5-year relative survival was 17% when patients had ALL as a first cancer and 11% when they had ALL as a second primary malignancy.
For pediatric patients with AML, the 5-year relative survival was 57% when patients had AML as a first cancer and 29% when they had AML as a second primary malignancy.
For AYAs, the 5-year relative survival was 46% when patients had AML as a first cancer and 23% when they had AML as a second primary malignancy.
For older adults, the 5-year relative survival was 12% when patients had AML as a first cancer and 10% when they had AML as a second primary malignancy.
Why younger patients tend to fare worse after a second cancer than older patients is not fully understood or specifically addressed in the current study, the researchers noted.
Now, the team plans to examine how the time between getting a first and second cancer affects survival and whether the type of treatment for the first cancer influences the outcome of a second cancer. ![]()
Second cancers take a greater toll on patients under the age of 40, according to research published in JAMA Oncology.
Researchers studied 14 types of cancer occurring in more than 1 million patients.
For nearly all of the cancers studied, 5-year survival rates were much higher if the cancer occurred as a first malignancy rather than a second cancer.
These survival differences were more pronounced in pediatric patients and adolescents and young adults (AYAs) than they were in patients age 40 and older.
Researchers hope these findings will help guide clinicians in providing age-specific recommendations on cancer prevention, screening, treatment, and survivorship, especially among the AYA population.
“Although the increased incidence of second cancers is well known among cancer survivors, less is known about outcomes of these cancers or the influence of age,” said Theresa Keegan, PhD, of the UC Davis Comprehensive Cancer Center in Sacramento, California.
With this in mind, Dr Keegan and her colleagues analyzed data on patients diagnosed with either a single cancer or a first and second malignancy during 1992 through 2008. The researchers used Surveillance, Epidemiology and End Results program data collected from 13 cancer registries.
The team collected data on the 14 most common cancer types that affect AYAs: acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), Hodgkin lymphoma (HL), non-Hodgkin lymphoma (NHL), soft tissue sarcoma, and bone sarcoma, as well as female breast, thyroid, testicular, colorectal, central nervous system, cervical, and ovarian cancers.
There were a total of 15,954 pediatric patients (younger than 15 years at diagnosis), 125,750 AYAs (ages 15 to 39), and 878,370 older adult patients (age 40 and older).
Survival rates
For pediatric patients, the 5-year relative survival was 80% for a first cancer and 47% for a second primary malignancy.
For AYAs, the 5-year relative survival was 81% for a first cancer and 60% for a second primary malignancy.
For older adults, the 5-year relative survival was 70% for a first cancer and 61% for a second primary malignancy.
When the researchers looked at 5-year survival by age and individual cancer types, they found striking differences depending on whether it was a first or second malignancy in all but 2 of the 14 cancer types, testicular cancer and melanoma.
“For almost every type of cancer, the AYA population did worse with a secondary cancer,” said study author Melanie Goldfarb, MD, of John Wayne Cancer Institute at Providence Saint John’s Health Center in Santa Monica, California.
“What struck us was that the second cancer caused such an increased risk of death.”
Lymphomas
For pediatric patients with HL, the 5-year relative survival was 95% when patients had HL as a first cancer. There were no data on HL as a second primary malignancy.
For AYAs, the 5-year relative survival was 93% when patients had HL as a first cancer and 72% when they had HL as a second primary malignancy.
For older adults, the 5-year relative survival was 69% when patients had HL as a first cancer and 54% when they had HL as a second primary malignancy.
For pediatric patients with NHL, the 5-year relative survival was 84% when patients had NHL as a first cancer and 63% when they had NHL as a second primary malignancy.
For AYAs, the 5-year relative survival was 64% when patients had NHL as a first cancer and 22% when they had NHL as a second primary malignancy.
For older adults, the 5-year relative survival was 57% when patients had NHL as a first cancer and 54% when they had NHL as a second primary malignancy.
Leukemias
For pediatric patients with ALL, the 5-year relative survival was 87% when patients had ALL as a first cancer and 63% when they had ALL as a second primary malignancy.
For AYAs, the 5-year relative survival was 48% when patients had ALL as a first cancer and 26% when they had ALL as a second primary malignancy.
For older adults, the 5-year relative survival was 17% when patients had ALL as a first cancer and 11% when they had ALL as a second primary malignancy.
For pediatric patients with AML, the 5-year relative survival was 57% when patients had AML as a first cancer and 29% when they had AML as a second primary malignancy.
For AYAs, the 5-year relative survival was 46% when patients had AML as a first cancer and 23% when they had AML as a second primary malignancy.
For older adults, the 5-year relative survival was 12% when patients had AML as a first cancer and 10% when they had AML as a second primary malignancy.
Why younger patients tend to fare worse after a second cancer than older patients is not fully understood or specifically addressed in the current study, the researchers noted.
Now, the team plans to examine how the time between getting a first and second cancer affects survival and whether the type of treatment for the first cancer influences the outcome of a second cancer. ![]()
Cord blood product bests standard UCB transplant
The expanded umbilical cord blood (UCB) product NiCord can provide benefits over standard UCB transplant, according to research published in Biology of Blood and Marrow Transplantation.
NiCord is a stand-alone graft derived from a single UCB unit that has been expanded in culture and enriched with stem and progenitor cells.
The study showed that patients transplanted with NiCord had shorter time to engraftment, a lower risk of infection, and shorter hospital stays than patients who received standard UCB transplants.
On the other hand, there was no significant difference between the transplant groups when it came to grade 2-4 acute graft-versus-host disease (GVHD), relapse, or survival within 100 days of transplant.
“Our results indicate that rapid hematopoietic recovery from Gamida Cell’s NiCord transplantation approach is associated with clinical benefit,” said study author Mitchell Horwitz, MD, of Duke University School of Medicine in Durham, North Carolina.
Dr Horwitz receives research support from Gamida Cell Ltd., makers of NiCord.
Patient characteristics
The researchers compared 18 consecutive NiCord-transplanted patients and 86 consecutive patients who received standard UCB transplants. All of the patients received total body irradiation-based myeloablative conditioning.
In both arms, most patients received a double transplant. In the NiCord arm, 61.1% of patients (n=11) received NiCord along with a second unmanipulated UCB unit. In the standard UCB arm, 95.3% of patients (n=82) received a double UCB transplant.
Patients in the NiCord arm were older than patients in the standard UCB arm, with median ages of 45.5 (range, 42-57) and 37.5 (range, 28-51), respectively.
Most patients in both arms had acute leukemia or myelodysplastic syndromes (about 89%), although roughly 11% had lymphoid malignancies.
There were no significant differences between the arms when it came to patient sex, pre-transplant weight, cytomegalovirus serostatus, and Karnofsky Performance Status.
Results
The median time to neutrophil engraftment was 12.5 days (range, 10-18) in the NiCord arm and 27 days (range, 23-28) in the standard UCB arm (P<0.001).
All of the patients studied had at least 1 infection of any severity. However, patients in the NiCord arm had a significantly lower risk of infection than patients in the standard UCB arm.
In an analysis adjusted for age, disease stage, and grade 2-4 acute GVHD, the risk ratios (RRs) for NiCord versus standard UCB transplant were as follows:
- Total infection—RR=0.72, P=0.03
- Grade 2-3 infection—RR=0.38, P=0.001
- Bacterial infection—RR=0.42, P=0.008
- Grade 2-3 bacterial infection—RR=0.23, P=0.006.
Patients in the NiCord arm spent a mean of 72.4 days out of the hospital in the first 100 days after transplant, compared to 48.6 days for the standard UCB arm (P=0.001).
After the researchers adjusted for age and Karnofsky Performance Status, patients in the NiCord arm had a mean of 20.2 more days out of the hospital than their peers who received standard UCB (P=0.005).
The incidence of grade 2-4 acute GHVD was 55.6% in the NiCord arm and 41.9% in the standard UCB arm (P=0.31). The rate of second transplant was 5.6% and 11.6%, respectively (P=0.68).
The rate of relapse was 0% in the NiCord arm and 7% in the standard UCB arm (P=0.59). And the rate of death was 5.6% and 16.3%, respectively (P=0.46). ![]()
The expanded umbilical cord blood (UCB) product NiCord can provide benefits over standard UCB transplant, according to research published in Biology of Blood and Marrow Transplantation.
NiCord is a stand-alone graft derived from a single UCB unit that has been expanded in culture and enriched with stem and progenitor cells.
The study showed that patients transplanted with NiCord had shorter time to engraftment, a lower risk of infection, and shorter hospital stays than patients who received standard UCB transplants.
On the other hand, there was no significant difference between the transplant groups when it came to grade 2-4 acute graft-versus-host disease (GVHD), relapse, or survival within 100 days of transplant.
“Our results indicate that rapid hematopoietic recovery from Gamida Cell’s NiCord transplantation approach is associated with clinical benefit,” said study author Mitchell Horwitz, MD, of Duke University School of Medicine in Durham, North Carolina.
Dr Horwitz receives research support from Gamida Cell Ltd., makers of NiCord.
Patient characteristics
The researchers compared 18 consecutive NiCord-transplanted patients and 86 consecutive patients who received standard UCB transplants. All of the patients received total body irradiation-based myeloablative conditioning.
In both arms, most patients received a double transplant. In the NiCord arm, 61.1% of patients (n=11) received NiCord along with a second unmanipulated UCB unit. In the standard UCB arm, 95.3% of patients (n=82) received a double UCB transplant.
Patients in the NiCord arm were older than patients in the standard UCB arm, with median ages of 45.5 (range, 42-57) and 37.5 (range, 28-51), respectively.
Most patients in both arms had acute leukemia or myelodysplastic syndromes (about 89%), although roughly 11% had lymphoid malignancies.
There were no significant differences between the arms when it came to patient sex, pre-transplant weight, cytomegalovirus serostatus, and Karnofsky Performance Status.
Results
The median time to neutrophil engraftment was 12.5 days (range, 10-18) in the NiCord arm and 27 days (range, 23-28) in the standard UCB arm (P<0.001).
All of the patients studied had at least 1 infection of any severity. However, patients in the NiCord arm had a significantly lower risk of infection than patients in the standard UCB arm.
In an analysis adjusted for age, disease stage, and grade 2-4 acute GVHD, the risk ratios (RRs) for NiCord versus standard UCB transplant were as follows:
- Total infection—RR=0.72, P=0.03
- Grade 2-3 infection—RR=0.38, P=0.001
- Bacterial infection—RR=0.42, P=0.008
- Grade 2-3 bacterial infection—RR=0.23, P=0.006.
Patients in the NiCord arm spent a mean of 72.4 days out of the hospital in the first 100 days after transplant, compared to 48.6 days for the standard UCB arm (P=0.001).
After the researchers adjusted for age and Karnofsky Performance Status, patients in the NiCord arm had a mean of 20.2 more days out of the hospital than their peers who received standard UCB (P=0.005).
The incidence of grade 2-4 acute GHVD was 55.6% in the NiCord arm and 41.9% in the standard UCB arm (P=0.31). The rate of second transplant was 5.6% and 11.6%, respectively (P=0.68).
The rate of relapse was 0% in the NiCord arm and 7% in the standard UCB arm (P=0.59). And the rate of death was 5.6% and 16.3%, respectively (P=0.46). ![]()
The expanded umbilical cord blood (UCB) product NiCord can provide benefits over standard UCB transplant, according to research published in Biology of Blood and Marrow Transplantation.
NiCord is a stand-alone graft derived from a single UCB unit that has been expanded in culture and enriched with stem and progenitor cells.
The study showed that patients transplanted with NiCord had shorter time to engraftment, a lower risk of infection, and shorter hospital stays than patients who received standard UCB transplants.
On the other hand, there was no significant difference between the transplant groups when it came to grade 2-4 acute graft-versus-host disease (GVHD), relapse, or survival within 100 days of transplant.
“Our results indicate that rapid hematopoietic recovery from Gamida Cell’s NiCord transplantation approach is associated with clinical benefit,” said study author Mitchell Horwitz, MD, of Duke University School of Medicine in Durham, North Carolina.
Dr Horwitz receives research support from Gamida Cell Ltd., makers of NiCord.
Patient characteristics
The researchers compared 18 consecutive NiCord-transplanted patients and 86 consecutive patients who received standard UCB transplants. All of the patients received total body irradiation-based myeloablative conditioning.
In both arms, most patients received a double transplant. In the NiCord arm, 61.1% of patients (n=11) received NiCord along with a second unmanipulated UCB unit. In the standard UCB arm, 95.3% of patients (n=82) received a double UCB transplant.
Patients in the NiCord arm were older than patients in the standard UCB arm, with median ages of 45.5 (range, 42-57) and 37.5 (range, 28-51), respectively.
Most patients in both arms had acute leukemia or myelodysplastic syndromes (about 89%), although roughly 11% had lymphoid malignancies.
There were no significant differences between the arms when it came to patient sex, pre-transplant weight, cytomegalovirus serostatus, and Karnofsky Performance Status.
Results
The median time to neutrophil engraftment was 12.5 days (range, 10-18) in the NiCord arm and 27 days (range, 23-28) in the standard UCB arm (P<0.001).
All of the patients studied had at least 1 infection of any severity. However, patients in the NiCord arm had a significantly lower risk of infection than patients in the standard UCB arm.
In an analysis adjusted for age, disease stage, and grade 2-4 acute GVHD, the risk ratios (RRs) for NiCord versus standard UCB transplant were as follows:
- Total infection—RR=0.72, P=0.03
- Grade 2-3 infection—RR=0.38, P=0.001
- Bacterial infection—RR=0.42, P=0.008
- Grade 2-3 bacterial infection—RR=0.23, P=0.006.
Patients in the NiCord arm spent a mean of 72.4 days out of the hospital in the first 100 days after transplant, compared to 48.6 days for the standard UCB arm (P=0.001).
After the researchers adjusted for age and Karnofsky Performance Status, patients in the NiCord arm had a mean of 20.2 more days out of the hospital than their peers who received standard UCB (P=0.005).
The incidence of grade 2-4 acute GHVD was 55.6% in the NiCord arm and 41.9% in the standard UCB arm (P=0.31). The rate of second transplant was 5.6% and 11.6%, respectively (P=0.68).
The rate of relapse was 0% in the NiCord arm and 7% in the standard UCB arm (P=0.59). And the rate of death was 5.6% and 16.3%, respectively (P=0.46). ![]()
TGA approves therapy for hemophilia A
The Australian Therapeutic Goods Administration (TGA) has approved use of lonoctocog alfa (AFSTYLA®), a recombinant single-chain coagulation factor VIII (FVIII) therapy, in patients with hemophilia A.
The product is indicated for use as routine prophylaxis to prevent or reduce the frequency of bleeding episodes, for control and prevention of bleeding episodes, and for perioperative management.
Lonoctocog alfa is designed to provide long-lasting protection from bleeds with 2- to 3-times weekly dosing, according to CSL Behring, the company developing the product.
The company says lonoctocog alfa uses a covalent bond that forms one structural entity—a single polypeptide chain—to improve the stability of FVIII and provide FVIII activity with the option of twice-weekly dosing.
The TGA’s approval of lonoctocog alfa is based on results from the AFFINITY clinical development program, which includes a trial of children (n=84) and a trial of adolescents and adults (n=175).
Among patients who received lonoctocog alfa prophylactically in these trials, the median annualized bleeding rate was 1.14 in the adults/adolescents and 3.69 in children younger than 12.
In all, there were 1195 bleeding events—848 in the adults/adolescents and 347 in the children.
Ninety-four percent of bleeds in adults/adolescents and 96% of bleeds in pediatric patients were effectively controlled with no more than 2 infusions of lonoctocog alfa weekly.
Eighty-one percent of bleeds in adults/adolescents and 86% of bleeds in pediatric patients were controlled by a single infusion.
Researchers assessed safety in 258 patients from both studies. Adverse reactions occurred in 14 patients and included hypersensitivity (n=4), dizziness (n=2), paresthesia (n=1), rash (n=1), erythema (n=1), pruritus (n=1), pyrexia (n=1), injection-site pain (n=1), chills (n=1), and feeling hot (n=1).
One patient withdrew from treatment due to hypersensitivity.
None of the patients developed neutralizing antibodies to FVIII or antibodies to host cell proteins. There were no reports of anaphylaxis or thrombosis.
Results from the trial of adolescents/adults were published in Blood in August 2016. Results from the trial of children were published in the Journal of Thrombosis and Haemostasis in March 2017. ![]()
The Australian Therapeutic Goods Administration (TGA) has approved use of lonoctocog alfa (AFSTYLA®), a recombinant single-chain coagulation factor VIII (FVIII) therapy, in patients with hemophilia A.
The product is indicated for use as routine prophylaxis to prevent or reduce the frequency of bleeding episodes, for control and prevention of bleeding episodes, and for perioperative management.
Lonoctocog alfa is designed to provide long-lasting protection from bleeds with 2- to 3-times weekly dosing, according to CSL Behring, the company developing the product.
The company says lonoctocog alfa uses a covalent bond that forms one structural entity—a single polypeptide chain—to improve the stability of FVIII and provide FVIII activity with the option of twice-weekly dosing.
The TGA’s approval of lonoctocog alfa is based on results from the AFFINITY clinical development program, which includes a trial of children (n=84) and a trial of adolescents and adults (n=175).
Among patients who received lonoctocog alfa prophylactically in these trials, the median annualized bleeding rate was 1.14 in the adults/adolescents and 3.69 in children younger than 12.
In all, there were 1195 bleeding events—848 in the adults/adolescents and 347 in the children.
Ninety-four percent of bleeds in adults/adolescents and 96% of bleeds in pediatric patients were effectively controlled with no more than 2 infusions of lonoctocog alfa weekly.
Eighty-one percent of bleeds in adults/adolescents and 86% of bleeds in pediatric patients were controlled by a single infusion.
Researchers assessed safety in 258 patients from both studies. Adverse reactions occurred in 14 patients and included hypersensitivity (n=4), dizziness (n=2), paresthesia (n=1), rash (n=1), erythema (n=1), pruritus (n=1), pyrexia (n=1), injection-site pain (n=1), chills (n=1), and feeling hot (n=1).
One patient withdrew from treatment due to hypersensitivity.
None of the patients developed neutralizing antibodies to FVIII or antibodies to host cell proteins. There were no reports of anaphylaxis or thrombosis.
Results from the trial of adolescents/adults were published in Blood in August 2016. Results from the trial of children were published in the Journal of Thrombosis and Haemostasis in March 2017. ![]()
The Australian Therapeutic Goods Administration (TGA) has approved use of lonoctocog alfa (AFSTYLA®), a recombinant single-chain coagulation factor VIII (FVIII) therapy, in patients with hemophilia A.
The product is indicated for use as routine prophylaxis to prevent or reduce the frequency of bleeding episodes, for control and prevention of bleeding episodes, and for perioperative management.
Lonoctocog alfa is designed to provide long-lasting protection from bleeds with 2- to 3-times weekly dosing, according to CSL Behring, the company developing the product.
The company says lonoctocog alfa uses a covalent bond that forms one structural entity—a single polypeptide chain—to improve the stability of FVIII and provide FVIII activity with the option of twice-weekly dosing.
The TGA’s approval of lonoctocog alfa is based on results from the AFFINITY clinical development program, which includes a trial of children (n=84) and a trial of adolescents and adults (n=175).
Among patients who received lonoctocog alfa prophylactically in these trials, the median annualized bleeding rate was 1.14 in the adults/adolescents and 3.69 in children younger than 12.
In all, there were 1195 bleeding events—848 in the adults/adolescents and 347 in the children.
Ninety-four percent of bleeds in adults/adolescents and 96% of bleeds in pediatric patients were effectively controlled with no more than 2 infusions of lonoctocog alfa weekly.
Eighty-one percent of bleeds in adults/adolescents and 86% of bleeds in pediatric patients were controlled by a single infusion.
Researchers assessed safety in 258 patients from both studies. Adverse reactions occurred in 14 patients and included hypersensitivity (n=4), dizziness (n=2), paresthesia (n=1), rash (n=1), erythema (n=1), pruritus (n=1), pyrexia (n=1), injection-site pain (n=1), chills (n=1), and feeling hot (n=1).
One patient withdrew from treatment due to hypersensitivity.
None of the patients developed neutralizing antibodies to FVIII or antibodies to host cell proteins. There were no reports of anaphylaxis or thrombosis.
Results from the trial of adolescents/adults were published in Blood in August 2016. Results from the trial of children were published in the Journal of Thrombosis and Haemostasis in March 2017. ![]()
How malaria parasites weaken RBCs’ defenses
Malaria parasites change the properties of red blood cells (RBCs) in a way that helps the parasites achieve cell entry, according to research published in PNAS.
Researchers found that Plasmodium parasites, upon binding to the surface of RBCs, cause the cell membranes to become more pliable, making it easier for the parasites to push inside the cells.
This suggests that differences in RBC stiffness, due to age or increased cholesterol content, could influence the parasites’ ability to invade.
“We have discovered that red cell entry is not just down to the ability of the parasite itself but that parasite-initiated changes to the red blood cells appear to contribute to the process of invasion,” said study author Marion Koch, a PhD student at Imperial College London in the UK.
“This could also mean that naturally more flexible cells would be easier for parasites to invade, which raises some interesting questions. Are parasites choosy about which cells to invade, picking the most deformable? Is susceptibility to malaria modified by fat or cholesterol content, or the age of circulating red blood cells?”
In the PNAS paper, the researchers noted that erythrocyte-binding antigen 175 (EBA175), a protein that’s required for entry in most parasite strains, binds to glycophorin A (GPA) on the RBC surface. However, the function of this binding interaction was unknown.
The team took a closer look at the interaction using real-time deformability cytometry and flicker spectroscopy.
They filmed 1000 RBCs per second passing through a narrow channel. Using this approach, the researchers were able to determine cell deformability by measuring how elongated the cells became during transit through the channel.
The team then measured where this deformation came from. They measured how much the RBCs deviate from their normally circular shape as their membranes naturally fluctuate or flicker.
The researchers found that EBA175 binding to GPA leads to an increase in the cytoskeletal tension of the RBC and a reduction in the bending modulus of the cell’s membrane. (The bending modulus is a measure of how much energy it takes to bend the cell membrane.)
The team then showed that the reduction in the bending modulus was “directly correlated with parasite invasion efficiency.”
The researchers said these results suggest the parasite primes the RBC surface through its binding antigens, altering the cell and reducing a barrier to invasion.
“This suggests we should be investigating not just parasite biology, but also how the body’s own red blood cells respond,” said study author Jake Baum, PhD, of Imperial College London.
“There are therapies developed for diseases like HIV that strengthen the body’s responses in addition to tackling the ‘invader.’ It’s not impossible to imagine something similar for malaria; for example, looking at a host-directed drug target and not just the parasite.” ![]()
Malaria parasites change the properties of red blood cells (RBCs) in a way that helps the parasites achieve cell entry, according to research published in PNAS.
Researchers found that Plasmodium parasites, upon binding to the surface of RBCs, cause the cell membranes to become more pliable, making it easier for the parasites to push inside the cells.
This suggests that differences in RBC stiffness, due to age or increased cholesterol content, could influence the parasites’ ability to invade.
“We have discovered that red cell entry is not just down to the ability of the parasite itself but that parasite-initiated changes to the red blood cells appear to contribute to the process of invasion,” said study author Marion Koch, a PhD student at Imperial College London in the UK.
“This could also mean that naturally more flexible cells would be easier for parasites to invade, which raises some interesting questions. Are parasites choosy about which cells to invade, picking the most deformable? Is susceptibility to malaria modified by fat or cholesterol content, or the age of circulating red blood cells?”
In the PNAS paper, the researchers noted that erythrocyte-binding antigen 175 (EBA175), a protein that’s required for entry in most parasite strains, binds to glycophorin A (GPA) on the RBC surface. However, the function of this binding interaction was unknown.
The team took a closer look at the interaction using real-time deformability cytometry and flicker spectroscopy.
They filmed 1000 RBCs per second passing through a narrow channel. Using this approach, the researchers were able to determine cell deformability by measuring how elongated the cells became during transit through the channel.
The team then measured where this deformation came from. They measured how much the RBCs deviate from their normally circular shape as their membranes naturally fluctuate or flicker.
The researchers found that EBA175 binding to GPA leads to an increase in the cytoskeletal tension of the RBC and a reduction in the bending modulus of the cell’s membrane. (The bending modulus is a measure of how much energy it takes to bend the cell membrane.)
The team then showed that the reduction in the bending modulus was “directly correlated with parasite invasion efficiency.”
The researchers said these results suggest the parasite primes the RBC surface through its binding antigens, altering the cell and reducing a barrier to invasion.
“This suggests we should be investigating not just parasite biology, but also how the body’s own red blood cells respond,” said study author Jake Baum, PhD, of Imperial College London.
“There are therapies developed for diseases like HIV that strengthen the body’s responses in addition to tackling the ‘invader.’ It’s not impossible to imagine something similar for malaria; for example, looking at a host-directed drug target and not just the parasite.” ![]()
Malaria parasites change the properties of red blood cells (RBCs) in a way that helps the parasites achieve cell entry, according to research published in PNAS.
Researchers found that Plasmodium parasites, upon binding to the surface of RBCs, cause the cell membranes to become more pliable, making it easier for the parasites to push inside the cells.
This suggests that differences in RBC stiffness, due to age or increased cholesterol content, could influence the parasites’ ability to invade.
“We have discovered that red cell entry is not just down to the ability of the parasite itself but that parasite-initiated changes to the red blood cells appear to contribute to the process of invasion,” said study author Marion Koch, a PhD student at Imperial College London in the UK.
“This could also mean that naturally more flexible cells would be easier for parasites to invade, which raises some interesting questions. Are parasites choosy about which cells to invade, picking the most deformable? Is susceptibility to malaria modified by fat or cholesterol content, or the age of circulating red blood cells?”
In the PNAS paper, the researchers noted that erythrocyte-binding antigen 175 (EBA175), a protein that’s required for entry in most parasite strains, binds to glycophorin A (GPA) on the RBC surface. However, the function of this binding interaction was unknown.
The team took a closer look at the interaction using real-time deformability cytometry and flicker spectroscopy.
They filmed 1000 RBCs per second passing through a narrow channel. Using this approach, the researchers were able to determine cell deformability by measuring how elongated the cells became during transit through the channel.
The team then measured where this deformation came from. They measured how much the RBCs deviate from their normally circular shape as their membranes naturally fluctuate or flicker.
The researchers found that EBA175 binding to GPA leads to an increase in the cytoskeletal tension of the RBC and a reduction in the bending modulus of the cell’s membrane. (The bending modulus is a measure of how much energy it takes to bend the cell membrane.)
The team then showed that the reduction in the bending modulus was “directly correlated with parasite invasion efficiency.”
The researchers said these results suggest the parasite primes the RBC surface through its binding antigens, altering the cell and reducing a barrier to invasion.
“This suggests we should be investigating not just parasite biology, but also how the body’s own red blood cells respond,” said study author Jake Baum, PhD, of Imperial College London.
“There are therapies developed for diseases like HIV that strengthen the body’s responses in addition to tackling the ‘invader.’ It’s not impossible to imagine something similar for malaria; for example, looking at a host-directed drug target and not just the parasite.” ![]()
MEDtalk presentations
Is HCAHPS Hurting Our Patients?
Speakers: Suparna Dutta, MD, MS, MPH, and John Biebelhausen, MD, MBA
Explore the unintended consequences of assessing patient satisfaction and labeling pain as “the fifth vital sign” in the midst of a national opioid epidemic. The Hospital Consumer Assessment of Healthcare Providers and Systems, which was developed by the Centers for Medicare & Medicaid Services to assess the inpatient experience and impacts hospital reimbursement, includes directed questions about pain management.
Join us as we review the background of HCAHPS, its potential unintended impacts over the years, as well as current and future efforts of SHM toward improving health policy in this domain.
Hello, My Name Is POCUS (Point-of-Care Ultrasound)
Speaker: Nilam Soni, MD, MS, FHM
Point-of-care ultrasound is being used by more hospitalists to perform bedside diagnostics and to guide invasive procedures. However, most practicing hospitalists completed their training before point-of-care ultrasound education was common in medical school and residency curricula. This interactive session will:
- Explain what point-of-care ultrasonography is and how hospitalists are currently using it.
- Highlight some of the unique point-of-care ultrasound activities at HM17.
- Describe the launch of a new point-of-care ultrasound certification program offered by SHM & ACCP.
The Best-Kept Secrets from the State of Hospital Medicine Report
Speaker: Johnbuck Creamer, MD, SFHM
The State of Hospital Medicine Report is powered by SHM’s biannual survey that recently captured data from nearly 600 HM groups, augmented by additional hospitalist data licensed from MGMA. We’ll explore trends and difference among groups, including:
- Compensation per wRVU and use of nocturnists are increasing.
- Turnover rates are decreasing.
- Compensation for quality performance varies greatly among academic, nonacademic, and pediatric practice groups.
- NP/PA utilization rates are very different between East and West U.S. regions.
- Family Practice presence is increasing in adult-only practice groups.
- Academic groups are falling further behind in CPT coding levels.
We Need to Talk: Opioid-Related Respiratory Failure & Death
Speaker: Thomas Frederickson, MD, SFHM
Discussion topics:
- The opioid epidemic – not just an outpatient issue.
- How opioids can cause respiratory arrest and death, and why current screening and monitoring strategies can fail.
- What works – examples of successful strategies that have been implemented and have saved lives.
PediBOOST®: Kids Need Better Care Transitions, Too!
Speaker: James O’Callaghan, MD, SFHM
PediBOOST is a pediatric-specific adaption of the SHM Project BOOST® (Better Outcomes by Optimizing Safe Transitions) quality initiative. The goal is to improve poor discharge processes (demonstrated by low patient satisfaction and worse clinical outcomes, not just higher hospital readmission rates).
It considers unique problems for hospitalized children, including:
- Medication issues – palatability and adherence concerns, need for compounding.
- Equipment issues – portability use for home and school.
- Education issues – engagement of patient, as developmentally appropriate, along with training of all providers who might care for the patient (parents, teachers).
How Hospitalists Really Feel about EMRs
Speaker: Rupesh Prasad, MD, MPH, SFHM
Electronic medical record use has tremendously increased in the last few years.
- What are the potential benefits of use – have they been realized?
- What do the hospitalists think:
- How have EMRs impacted patient safety?
- How have EMRs impacted patient face to face time?
- What are hospitalists’ frustrations about EMRs?
Improve Your Interactions with the 5 Rs of Cultural Humility
Speaker: O’Neil Pyke, MD, SFHM
As the proverbial stranger at the bedside, HM providers are tasked with a very challenging proposition: meet a new patient in their most vulnerable state and quickly establish effective lines of communication and trust and provide patient-centric care, ultimately yielding a satisfied patient (and family) irrespective of the clinical outcome. With increased focus on patient experience and satisfaction, it is imperative that hospitals and health systems equip all hospitalists with the tools needed to deliver culturally competent care to all patients served.
The goal of the 5 Rs is to equip HM providers with tangible resources and easy to understand reminders that focus on encouraging awareness and, ultimately, deliver culturally “humble” care to all patients (and family members).
- Respect: Hospitalists will treat every person with the utmost respect and strive to preserve patient dignity.
- Regard: Hospitalists will hold every person in their highest regard and not allow unconscious biases to manifest, exercising utmost sensitivity to anticipated differences in beliefs, value systems, and preferences.
- Relevance: Hospitalists will expect cultural humility to be relevant and apply this practice to every encounter.
- Reflection: Hospitalists will approach every encounter with humility and understanding that there is always something to learn from everyone.
- Resiliency: In order to provide better care for hospitalized patients, hospitalists will embody the practice of cultural humility to enhance personal resiliency and compassion for all.
It’s Critical: Hospitalists in the ICU
Speaker: Joseph Sweigart, MD
We hope to:
- Describe formation of purpose of the critical care task force within the Education Committee.
- Discuss the creation and execution of the SHM critical care survey.
- Present selected results including:
- Introduce strategies to address the practice gaps identified including:
Palliative Care in Hospital Medicine: Figuring Out What Matters Most
Speaker: Rab Razzak, MBBS, MD
We aim to:
- Discuss the overall definition of palliative care. It is for all seriously ill patients and focuses on human-centered care and quality of life, best provided early in an illness.
- Idea of primary palliative care and role of hospitalists. Most palliative care is provided by frontline clinicians, and hospitalists are optimally positioned to support seriously ill patients and their families. It is crucial for HM to involve palliative care specialists when needed.
- Effective communication about serious illness – words that work and how to operationalize human-centered care while honestly discussing serious illness.
Is HCAHPS Hurting Our Patients?
Speakers: Suparna Dutta, MD, MS, MPH, and John Biebelhausen, MD, MBA
Explore the unintended consequences of assessing patient satisfaction and labeling pain as “the fifth vital sign” in the midst of a national opioid epidemic. The Hospital Consumer Assessment of Healthcare Providers and Systems, which was developed by the Centers for Medicare & Medicaid Services to assess the inpatient experience and impacts hospital reimbursement, includes directed questions about pain management.
Join us as we review the background of HCAHPS, its potential unintended impacts over the years, as well as current and future efforts of SHM toward improving health policy in this domain.
Hello, My Name Is POCUS (Point-of-Care Ultrasound)
Speaker: Nilam Soni, MD, MS, FHM
Point-of-care ultrasound is being used by more hospitalists to perform bedside diagnostics and to guide invasive procedures. However, most practicing hospitalists completed their training before point-of-care ultrasound education was common in medical school and residency curricula. This interactive session will:
- Explain what point-of-care ultrasonography is and how hospitalists are currently using it.
- Highlight some of the unique point-of-care ultrasound activities at HM17.
- Describe the launch of a new point-of-care ultrasound certification program offered by SHM & ACCP.
The Best-Kept Secrets from the State of Hospital Medicine Report
Speaker: Johnbuck Creamer, MD, SFHM
The State of Hospital Medicine Report is powered by SHM’s biannual survey that recently captured data from nearly 600 HM groups, augmented by additional hospitalist data licensed from MGMA. We’ll explore trends and difference among groups, including:
- Compensation per wRVU and use of nocturnists are increasing.
- Turnover rates are decreasing.
- Compensation for quality performance varies greatly among academic, nonacademic, and pediatric practice groups.
- NP/PA utilization rates are very different between East and West U.S. regions.
- Family Practice presence is increasing in adult-only practice groups.
- Academic groups are falling further behind in CPT coding levels.
We Need to Talk: Opioid-Related Respiratory Failure & Death
Speaker: Thomas Frederickson, MD, SFHM
Discussion topics:
- The opioid epidemic – not just an outpatient issue.
- How opioids can cause respiratory arrest and death, and why current screening and monitoring strategies can fail.
- What works – examples of successful strategies that have been implemented and have saved lives.
PediBOOST®: Kids Need Better Care Transitions, Too!
Speaker: James O’Callaghan, MD, SFHM
PediBOOST is a pediatric-specific adaption of the SHM Project BOOST® (Better Outcomes by Optimizing Safe Transitions) quality initiative. The goal is to improve poor discharge processes (demonstrated by low patient satisfaction and worse clinical outcomes, not just higher hospital readmission rates).
It considers unique problems for hospitalized children, including:
- Medication issues – palatability and adherence concerns, need for compounding.
- Equipment issues – portability use for home and school.
- Education issues – engagement of patient, as developmentally appropriate, along with training of all providers who might care for the patient (parents, teachers).
How Hospitalists Really Feel about EMRs
Speaker: Rupesh Prasad, MD, MPH, SFHM
Electronic medical record use has tremendously increased in the last few years.
- What are the potential benefits of use – have they been realized?
- What do the hospitalists think:
- How have EMRs impacted patient safety?
- How have EMRs impacted patient face to face time?
- What are hospitalists’ frustrations about EMRs?
Improve Your Interactions with the 5 Rs of Cultural Humility
Speaker: O’Neil Pyke, MD, SFHM
As the proverbial stranger at the bedside, HM providers are tasked with a very challenging proposition: meet a new patient in their most vulnerable state and quickly establish effective lines of communication and trust and provide patient-centric care, ultimately yielding a satisfied patient (and family) irrespective of the clinical outcome. With increased focus on patient experience and satisfaction, it is imperative that hospitals and health systems equip all hospitalists with the tools needed to deliver culturally competent care to all patients served.
The goal of the 5 Rs is to equip HM providers with tangible resources and easy to understand reminders that focus on encouraging awareness and, ultimately, deliver culturally “humble” care to all patients (and family members).
- Respect: Hospitalists will treat every person with the utmost respect and strive to preserve patient dignity.
- Regard: Hospitalists will hold every person in their highest regard and not allow unconscious biases to manifest, exercising utmost sensitivity to anticipated differences in beliefs, value systems, and preferences.
- Relevance: Hospitalists will expect cultural humility to be relevant and apply this practice to every encounter.
- Reflection: Hospitalists will approach every encounter with humility and understanding that there is always something to learn from everyone.
- Resiliency: In order to provide better care for hospitalized patients, hospitalists will embody the practice of cultural humility to enhance personal resiliency and compassion for all.
It’s Critical: Hospitalists in the ICU
Speaker: Joseph Sweigart, MD
We hope to:
- Describe formation of purpose of the critical care task force within the Education Committee.
- Discuss the creation and execution of the SHM critical care survey.
- Present selected results including:
- Introduce strategies to address the practice gaps identified including:
Palliative Care in Hospital Medicine: Figuring Out What Matters Most
Speaker: Rab Razzak, MBBS, MD
We aim to:
- Discuss the overall definition of palliative care. It is for all seriously ill patients and focuses on human-centered care and quality of life, best provided early in an illness.
- Idea of primary palliative care and role of hospitalists. Most palliative care is provided by frontline clinicians, and hospitalists are optimally positioned to support seriously ill patients and their families. It is crucial for HM to involve palliative care specialists when needed.
- Effective communication about serious illness – words that work and how to operationalize human-centered care while honestly discussing serious illness.
Is HCAHPS Hurting Our Patients?
Speakers: Suparna Dutta, MD, MS, MPH, and John Biebelhausen, MD, MBA
Explore the unintended consequences of assessing patient satisfaction and labeling pain as “the fifth vital sign” in the midst of a national opioid epidemic. The Hospital Consumer Assessment of Healthcare Providers and Systems, which was developed by the Centers for Medicare & Medicaid Services to assess the inpatient experience and impacts hospital reimbursement, includes directed questions about pain management.
Join us as we review the background of HCAHPS, its potential unintended impacts over the years, as well as current and future efforts of SHM toward improving health policy in this domain.
Hello, My Name Is POCUS (Point-of-Care Ultrasound)
Speaker: Nilam Soni, MD, MS, FHM
Point-of-care ultrasound is being used by more hospitalists to perform bedside diagnostics and to guide invasive procedures. However, most practicing hospitalists completed their training before point-of-care ultrasound education was common in medical school and residency curricula. This interactive session will:
- Explain what point-of-care ultrasonography is and how hospitalists are currently using it.
- Highlight some of the unique point-of-care ultrasound activities at HM17.
- Describe the launch of a new point-of-care ultrasound certification program offered by SHM & ACCP.
The Best-Kept Secrets from the State of Hospital Medicine Report
Speaker: Johnbuck Creamer, MD, SFHM
The State of Hospital Medicine Report is powered by SHM’s biannual survey that recently captured data from nearly 600 HM groups, augmented by additional hospitalist data licensed from MGMA. We’ll explore trends and difference among groups, including:
- Compensation per wRVU and use of nocturnists are increasing.
- Turnover rates are decreasing.
- Compensation for quality performance varies greatly among academic, nonacademic, and pediatric practice groups.
- NP/PA utilization rates are very different between East and West U.S. regions.
- Family Practice presence is increasing in adult-only practice groups.
- Academic groups are falling further behind in CPT coding levels.
We Need to Talk: Opioid-Related Respiratory Failure & Death
Speaker: Thomas Frederickson, MD, SFHM
Discussion topics:
- The opioid epidemic – not just an outpatient issue.
- How opioids can cause respiratory arrest and death, and why current screening and monitoring strategies can fail.
- What works – examples of successful strategies that have been implemented and have saved lives.
PediBOOST®: Kids Need Better Care Transitions, Too!
Speaker: James O’Callaghan, MD, SFHM
PediBOOST is a pediatric-specific adaption of the SHM Project BOOST® (Better Outcomes by Optimizing Safe Transitions) quality initiative. The goal is to improve poor discharge processes (demonstrated by low patient satisfaction and worse clinical outcomes, not just higher hospital readmission rates).
It considers unique problems for hospitalized children, including:
- Medication issues – palatability and adherence concerns, need for compounding.
- Equipment issues – portability use for home and school.
- Education issues – engagement of patient, as developmentally appropriate, along with training of all providers who might care for the patient (parents, teachers).
How Hospitalists Really Feel about EMRs
Speaker: Rupesh Prasad, MD, MPH, SFHM
Electronic medical record use has tremendously increased in the last few years.
- What are the potential benefits of use – have they been realized?
- What do the hospitalists think:
- How have EMRs impacted patient safety?
- How have EMRs impacted patient face to face time?
- What are hospitalists’ frustrations about EMRs?
Improve Your Interactions with the 5 Rs of Cultural Humility
Speaker: O’Neil Pyke, MD, SFHM
As the proverbial stranger at the bedside, HM providers are tasked with a very challenging proposition: meet a new patient in their most vulnerable state and quickly establish effective lines of communication and trust and provide patient-centric care, ultimately yielding a satisfied patient (and family) irrespective of the clinical outcome. With increased focus on patient experience and satisfaction, it is imperative that hospitals and health systems equip all hospitalists with the tools needed to deliver culturally competent care to all patients served.
The goal of the 5 Rs is to equip HM providers with tangible resources and easy to understand reminders that focus on encouraging awareness and, ultimately, deliver culturally “humble” care to all patients (and family members).
- Respect: Hospitalists will treat every person with the utmost respect and strive to preserve patient dignity.
- Regard: Hospitalists will hold every person in their highest regard and not allow unconscious biases to manifest, exercising utmost sensitivity to anticipated differences in beliefs, value systems, and preferences.
- Relevance: Hospitalists will expect cultural humility to be relevant and apply this practice to every encounter.
- Reflection: Hospitalists will approach every encounter with humility and understanding that there is always something to learn from everyone.
- Resiliency: In order to provide better care for hospitalized patients, hospitalists will embody the practice of cultural humility to enhance personal resiliency and compassion for all.
It’s Critical: Hospitalists in the ICU
Speaker: Joseph Sweigart, MD
We hope to:
- Describe formation of purpose of the critical care task force within the Education Committee.
- Discuss the creation and execution of the SHM critical care survey.
- Present selected results including:
- Introduce strategies to address the practice gaps identified including:
Palliative Care in Hospital Medicine: Figuring Out What Matters Most
Speaker: Rab Razzak, MBBS, MD
We aim to:
- Discuss the overall definition of palliative care. It is for all seriously ill patients and focuses on human-centered care and quality of life, best provided early in an illness.
- Idea of primary palliative care and role of hospitalists. Most palliative care is provided by frontline clinicians, and hospitalists are optimally positioned to support seriously ill patients and their families. It is crucial for HM to involve palliative care specialists when needed.
- Effective communication about serious illness – words that work and how to operationalize human-centered care while honestly discussing serious illness.
AATS publishes guidelines for infective endocarditis
Infective endocarditis (IE) is a devastating complication of heart valve disease that, left untreated, can be fatal. Management requires a multidisciplinary approach, and many of the respective medical societies that represent the participating specialties have developed guidelines. Now, the American Association for Thoracic Surgery has published “Consensus Guidelines for the Surgical Treatment of Infective Endocarditis” to guide thoracic and cardiovascular surgeons in making decisions of when to operate in cases of IE (J Thorac Cardiovasc Surg. 2017 Jan 24. doi: 10.1016/j.jtcvs.2016.09.093).
The rationale for developing the guidelines is a growing prevalence of IE, including in patients with normal valves and no previous diagnosis of heart disease. “These new AATS consensus guidelines primarily address questions related to active and suspected active IE affective valves and intracardiac structures,” Dr. Pettersson and his coauthors said. The AATS guidelines for infective endocarditis address complications including risk of embolism and the timing of surgery in patients with neurological complications, while acknowledging the the need for additional research into these topics.* “It is understood that surgery is beneficial only if the patient’s complications and other comorbidities do not preclude survival and meaningful recovery,” the guideline authors said.
The guidelines confirm the team approach for managing patients with IE. The team should include cardiology, infectious disease, cardiac surgery, and other specialties needed to handle IE-related complications (class of recommendation [COR] I, level of evidence [LOE] B). Before surgery, the surgeon should know the patient is on effective antimicrobial therapy (COR I, LOE B). Transesophageal echocardiography (TEE) is indicated to yield the clearest understanding of the pathology (COR I, LOE B).
Dr. Pettersson and the guideline writing team also clarified indications for surgery in patients with IE. They include when valve dysfunction causes heart failure (COR I, LOE B); when, after a full course of antibiotics, the patient has signs of heart block, annular or aortic abscess or destructive penetrating lesions (COR I, LOE B); and in the setting of recurrent emboli and persistent vegetations despite appropriate antibiotic therapy (COR IIA, LOE B).
The guideline writers acknowledged potential disagreement between the AATS guidelines and those of the American College of Cardiology/American Heart Association with regard to early surgery in IE. Debate surrounds whether to operate early or wait for symptoms of heart failure to manifest in patients with native valve endocarditis (NVE). The AATS guideline authors cite work by Duk-Hyun Kang, MD, PhD, and coauthors in South Korea (N Engl J Med. 2012;366;2466-73) and others advocating for early surgery. “For this reason, once a surgical indication is evident, surgery should not be delayed,” Dr. Pettersson and his coauthors said.
Several conditions can influence the timing of surgery. Patients with cerebral mycotic aneurysm should be managed closely with neurology or neurosurgery (COR I, LOE C). Patients with a recent intracranial hemorrhage should wait at least 3 weeks for surgery (COR IIA, LOE B), but those with nonhemorrhagic strokes could go in for urgent surgery (COR IIA, LOE B). Brain imaging is indicated for IE patients with neurological symptoms (COR I, LOE B), but anticoagulation management requires a nuanced approach that takes all risks and benefits into consideration (COR I, LOE C).
Key steps during surgery involve mandatory intraoperative TEE (COR I, LOE B), median sternotomy with few exceptions (COR I, LOE B), and radical debridement and removal of all infected and necrotic tissue (COR I, LOE B). The writers also provided four guidelines for reconstruction and valve replacement:
- Repair when possible for patients with NVE (COR I, LOE B).
- When replacement is indicated, the surgeon should base valve choice on normal criteria – age, life expectancy, comorbidities, and expected compliance with anticoagulation (COR I, LOE B).
- Avoid use of mechanical valves in patients with intracranial bleeding or who have had a major stroke (COR IIA, LOE C).
- In patients with invasive disease and deconstruction, reconstruction should depend on the involved valve, severity of destruction, and available options for cardiac reconstruction (COR I, LOE B).
The AATS guidelines also challenge conventional thinking on the practice of soaking a gel-impregnated graft with antimicrobials targeting a specific organism. “We found no evidence to support this practice,” Dr. Pettersson and his coauthors said (COR IIB, LOE B). They came to the same conclusion with regard to the use of local antimicrobials or antiseptics during irrigation after debridement and local injection of antimicrobials around the infected area (COR I, LOE C).
The guidelines provide direction on a host of other surgical issues in IE: use of aortic valve grafts; when to remove or replace noninfected grafts; when to remove pacemakers; the role of drainage; postoperative management; follow-up; and additional screening. They also shed insight into what the guideline authors call “residual controversies,” including surgery for injection drug users (use “all available resources and options for drug rehabilitation”) and dialysis patients (“it is reasonable to offer surgery when the additional burden of comorbidities is not overwhelming”). They also acknowledge seven different scenarios that lack clear evidence for intervention but require the surgeon to determine the need for surgery, ranging from timing of surgery for IE in patients with neurologic complications to how to treat patients with functional valve issues after being cured of IE.
The guideline writers acknowledged that institutional funds supported the work. Dr. Pettersson had no financial relationships to disclose.
*Correction 5/172017: It was incorrectly stated that these complications were not addressed in the guidelines due to lack of evidence
Whether they’re intended to or not, guidelines like the AATS Consensus Guidelines for the Surgical Treatment of Infected Endocarditis “can evolve into hard and fast principles, sometimes leading to incorrect decision making and even creating medicolegal problems for treating physicians,” Gus J. Vlahakes, MD, of Harvard Medical School and Massachusetts General Hospital, Boston, said in his invited commentary (J Thorac Cardiovasc Surg. 2016 Nov 3. doi: 10.1016/j.jtcvs.2016.10.041).
Guidelines cannot “integrate all the necessary considerations,” Dr. Vlahakes said, so surgeons should view them as “a set of general principles to guide decision making.” In IE, that means having an experienced cardiac surgeon who can apply the guidelines on a case-by-case basis and a multidisciplinary team that includes an infectious disease specialist, he said. The surgeon must participate in preoperative management.
Dr. Vlahakes had no relevant financial disclosures.
Whether they’re intended to or not, guidelines like the AATS Consensus Guidelines for the Surgical Treatment of Infected Endocarditis “can evolve into hard and fast principles, sometimes leading to incorrect decision making and even creating medicolegal problems for treating physicians,” Gus J. Vlahakes, MD, of Harvard Medical School and Massachusetts General Hospital, Boston, said in his invited commentary (J Thorac Cardiovasc Surg. 2016 Nov 3. doi: 10.1016/j.jtcvs.2016.10.041).
Guidelines cannot “integrate all the necessary considerations,” Dr. Vlahakes said, so surgeons should view them as “a set of general principles to guide decision making.” In IE, that means having an experienced cardiac surgeon who can apply the guidelines on a case-by-case basis and a multidisciplinary team that includes an infectious disease specialist, he said. The surgeon must participate in preoperative management.
Dr. Vlahakes had no relevant financial disclosures.
Whether they’re intended to or not, guidelines like the AATS Consensus Guidelines for the Surgical Treatment of Infected Endocarditis “can evolve into hard and fast principles, sometimes leading to incorrect decision making and even creating medicolegal problems for treating physicians,” Gus J. Vlahakes, MD, of Harvard Medical School and Massachusetts General Hospital, Boston, said in his invited commentary (J Thorac Cardiovasc Surg. 2016 Nov 3. doi: 10.1016/j.jtcvs.2016.10.041).
Guidelines cannot “integrate all the necessary considerations,” Dr. Vlahakes said, so surgeons should view them as “a set of general principles to guide decision making.” In IE, that means having an experienced cardiac surgeon who can apply the guidelines on a case-by-case basis and a multidisciplinary team that includes an infectious disease specialist, he said. The surgeon must participate in preoperative management.
Dr. Vlahakes had no relevant financial disclosures.
Infective endocarditis (IE) is a devastating complication of heart valve disease that, left untreated, can be fatal. Management requires a multidisciplinary approach, and many of the respective medical societies that represent the participating specialties have developed guidelines. Now, the American Association for Thoracic Surgery has published “Consensus Guidelines for the Surgical Treatment of Infective Endocarditis” to guide thoracic and cardiovascular surgeons in making decisions of when to operate in cases of IE (J Thorac Cardiovasc Surg. 2017 Jan 24. doi: 10.1016/j.jtcvs.2016.09.093).
The rationale for developing the guidelines is a growing prevalence of IE, including in patients with normal valves and no previous diagnosis of heart disease. “These new AATS consensus guidelines primarily address questions related to active and suspected active IE affective valves and intracardiac structures,” Dr. Pettersson and his coauthors said. The AATS guidelines for infective endocarditis address complications including risk of embolism and the timing of surgery in patients with neurological complications, while acknowledging the the need for additional research into these topics.* “It is understood that surgery is beneficial only if the patient’s complications and other comorbidities do not preclude survival and meaningful recovery,” the guideline authors said.
The guidelines confirm the team approach for managing patients with IE. The team should include cardiology, infectious disease, cardiac surgery, and other specialties needed to handle IE-related complications (class of recommendation [COR] I, level of evidence [LOE] B). Before surgery, the surgeon should know the patient is on effective antimicrobial therapy (COR I, LOE B). Transesophageal echocardiography (TEE) is indicated to yield the clearest understanding of the pathology (COR I, LOE B).
Dr. Pettersson and the guideline writing team also clarified indications for surgery in patients with IE. They include when valve dysfunction causes heart failure (COR I, LOE B); when, after a full course of antibiotics, the patient has signs of heart block, annular or aortic abscess or destructive penetrating lesions (COR I, LOE B); and in the setting of recurrent emboli and persistent vegetations despite appropriate antibiotic therapy (COR IIA, LOE B).
The guideline writers acknowledged potential disagreement between the AATS guidelines and those of the American College of Cardiology/American Heart Association with regard to early surgery in IE. Debate surrounds whether to operate early or wait for symptoms of heart failure to manifest in patients with native valve endocarditis (NVE). The AATS guideline authors cite work by Duk-Hyun Kang, MD, PhD, and coauthors in South Korea (N Engl J Med. 2012;366;2466-73) and others advocating for early surgery. “For this reason, once a surgical indication is evident, surgery should not be delayed,” Dr. Pettersson and his coauthors said.
Several conditions can influence the timing of surgery. Patients with cerebral mycotic aneurysm should be managed closely with neurology or neurosurgery (COR I, LOE C). Patients with a recent intracranial hemorrhage should wait at least 3 weeks for surgery (COR IIA, LOE B), but those with nonhemorrhagic strokes could go in for urgent surgery (COR IIA, LOE B). Brain imaging is indicated for IE patients with neurological symptoms (COR I, LOE B), but anticoagulation management requires a nuanced approach that takes all risks and benefits into consideration (COR I, LOE C).
Key steps during surgery involve mandatory intraoperative TEE (COR I, LOE B), median sternotomy with few exceptions (COR I, LOE B), and radical debridement and removal of all infected and necrotic tissue (COR I, LOE B). The writers also provided four guidelines for reconstruction and valve replacement:
- Repair when possible for patients with NVE (COR I, LOE B).
- When replacement is indicated, the surgeon should base valve choice on normal criteria – age, life expectancy, comorbidities, and expected compliance with anticoagulation (COR I, LOE B).
- Avoid use of mechanical valves in patients with intracranial bleeding or who have had a major stroke (COR IIA, LOE C).
- In patients with invasive disease and deconstruction, reconstruction should depend on the involved valve, severity of destruction, and available options for cardiac reconstruction (COR I, LOE B).
The AATS guidelines also challenge conventional thinking on the practice of soaking a gel-impregnated graft with antimicrobials targeting a specific organism. “We found no evidence to support this practice,” Dr. Pettersson and his coauthors said (COR IIB, LOE B). They came to the same conclusion with regard to the use of local antimicrobials or antiseptics during irrigation after debridement and local injection of antimicrobials around the infected area (COR I, LOE C).
The guidelines provide direction on a host of other surgical issues in IE: use of aortic valve grafts; when to remove or replace noninfected grafts; when to remove pacemakers; the role of drainage; postoperative management; follow-up; and additional screening. They also shed insight into what the guideline authors call “residual controversies,” including surgery for injection drug users (use “all available resources and options for drug rehabilitation”) and dialysis patients (“it is reasonable to offer surgery when the additional burden of comorbidities is not overwhelming”). They also acknowledge seven different scenarios that lack clear evidence for intervention but require the surgeon to determine the need for surgery, ranging from timing of surgery for IE in patients with neurologic complications to how to treat patients with functional valve issues after being cured of IE.
The guideline writers acknowledged that institutional funds supported the work. Dr. Pettersson had no financial relationships to disclose.
*Correction 5/172017: It was incorrectly stated that these complications were not addressed in the guidelines due to lack of evidence
Infective endocarditis (IE) is a devastating complication of heart valve disease that, left untreated, can be fatal. Management requires a multidisciplinary approach, and many of the respective medical societies that represent the participating specialties have developed guidelines. Now, the American Association for Thoracic Surgery has published “Consensus Guidelines for the Surgical Treatment of Infective Endocarditis” to guide thoracic and cardiovascular surgeons in making decisions of when to operate in cases of IE (J Thorac Cardiovasc Surg. 2017 Jan 24. doi: 10.1016/j.jtcvs.2016.09.093).
The rationale for developing the guidelines is a growing prevalence of IE, including in patients with normal valves and no previous diagnosis of heart disease. “These new AATS consensus guidelines primarily address questions related to active and suspected active IE affective valves and intracardiac structures,” Dr. Pettersson and his coauthors said. The AATS guidelines for infective endocarditis address complications including risk of embolism and the timing of surgery in patients with neurological complications, while acknowledging the the need for additional research into these topics.* “It is understood that surgery is beneficial only if the patient’s complications and other comorbidities do not preclude survival and meaningful recovery,” the guideline authors said.
The guidelines confirm the team approach for managing patients with IE. The team should include cardiology, infectious disease, cardiac surgery, and other specialties needed to handle IE-related complications (class of recommendation [COR] I, level of evidence [LOE] B). Before surgery, the surgeon should know the patient is on effective antimicrobial therapy (COR I, LOE B). Transesophageal echocardiography (TEE) is indicated to yield the clearest understanding of the pathology (COR I, LOE B).
Dr. Pettersson and the guideline writing team also clarified indications for surgery in patients with IE. They include when valve dysfunction causes heart failure (COR I, LOE B); when, after a full course of antibiotics, the patient has signs of heart block, annular or aortic abscess or destructive penetrating lesions (COR I, LOE B); and in the setting of recurrent emboli and persistent vegetations despite appropriate antibiotic therapy (COR IIA, LOE B).
The guideline writers acknowledged potential disagreement between the AATS guidelines and those of the American College of Cardiology/American Heart Association with regard to early surgery in IE. Debate surrounds whether to operate early or wait for symptoms of heart failure to manifest in patients with native valve endocarditis (NVE). The AATS guideline authors cite work by Duk-Hyun Kang, MD, PhD, and coauthors in South Korea (N Engl J Med. 2012;366;2466-73) and others advocating for early surgery. “For this reason, once a surgical indication is evident, surgery should not be delayed,” Dr. Pettersson and his coauthors said.
Several conditions can influence the timing of surgery. Patients with cerebral mycotic aneurysm should be managed closely with neurology or neurosurgery (COR I, LOE C). Patients with a recent intracranial hemorrhage should wait at least 3 weeks for surgery (COR IIA, LOE B), but those with nonhemorrhagic strokes could go in for urgent surgery (COR IIA, LOE B). Brain imaging is indicated for IE patients with neurological symptoms (COR I, LOE B), but anticoagulation management requires a nuanced approach that takes all risks and benefits into consideration (COR I, LOE C).
Key steps during surgery involve mandatory intraoperative TEE (COR I, LOE B), median sternotomy with few exceptions (COR I, LOE B), and radical debridement and removal of all infected and necrotic tissue (COR I, LOE B). The writers also provided four guidelines for reconstruction and valve replacement:
- Repair when possible for patients with NVE (COR I, LOE B).
- When replacement is indicated, the surgeon should base valve choice on normal criteria – age, life expectancy, comorbidities, and expected compliance with anticoagulation (COR I, LOE B).
- Avoid use of mechanical valves in patients with intracranial bleeding or who have had a major stroke (COR IIA, LOE C).
- In patients with invasive disease and deconstruction, reconstruction should depend on the involved valve, severity of destruction, and available options for cardiac reconstruction (COR I, LOE B).
The AATS guidelines also challenge conventional thinking on the practice of soaking a gel-impregnated graft with antimicrobials targeting a specific organism. “We found no evidence to support this practice,” Dr. Pettersson and his coauthors said (COR IIB, LOE B). They came to the same conclusion with regard to the use of local antimicrobials or antiseptics during irrigation after debridement and local injection of antimicrobials around the infected area (COR I, LOE C).
The guidelines provide direction on a host of other surgical issues in IE: use of aortic valve grafts; when to remove or replace noninfected grafts; when to remove pacemakers; the role of drainage; postoperative management; follow-up; and additional screening. They also shed insight into what the guideline authors call “residual controversies,” including surgery for injection drug users (use “all available resources and options for drug rehabilitation”) and dialysis patients (“it is reasonable to offer surgery when the additional burden of comorbidities is not overwhelming”). They also acknowledge seven different scenarios that lack clear evidence for intervention but require the surgeon to determine the need for surgery, ranging from timing of surgery for IE in patients with neurologic complications to how to treat patients with functional valve issues after being cured of IE.
The guideline writers acknowledged that institutional funds supported the work. Dr. Pettersson had no financial relationships to disclose.
*Correction 5/172017: It was incorrectly stated that these complications were not addressed in the guidelines due to lack of evidence
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: The American Association for Thoracic Surgery charged a committee of eight members to author “Consensus Guidelines: Surgical Treatment of Infective Endocarditis.”
Major finding: Patients with infective endocarditis need early input from the responsible cardiac surgeon, who must also lead the care team in evaluation, decision- making, and ultimately carrying out surgery as needed.
Data source: The writing committee followed Institute of Medicine standards for clinical practice guidelines, invited comment from a group of 12 multidisciplinary specialists and reviewed 288 articles in drafting the guidelines.
Disclosures: Institutional funds supported the work. Dr. Pettersson and his coauthors had no financial relationships to disclose.