User login
HIV research update: March 2017
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
The prevalence of multidrug-resistant gram-negative organisms is significantly higher in HIV-positive males than in HIV-negative males, according to a study in BMC Infectious Diseases.
“[The] effects of HIV-1 on epitope evolution in M. tuberculosis may have implications for the design of [Mycobacterium] tuberculosis vaccines that are intended for use in populations with high HIV-1 infection rates,” says a report published in Molecular Biology and Evolution.
A study in AIDS Care found that depression partially mediated the relationship between basic psychological needs and quality of life in people living with HIV, suggesting that basic psychological needs and depression may be specific targets for psychosocial interventions.
HIV-infected participants who took 52 weeks of pitavastatin 4 mg daily (vs. pravastatin 40 mg daily) experienced a greater reduction in select markers of immune activation and arterial inflammation, in a 45-site study.
Plasma soluble CD163 was independently associated with incident chronic kidney disease, chronic lung disease, and liver disease in treated HIV-1 infected individuals, according to a study in the journal AIDS.
The recombinant multiepitope protein MEP1 has the potential to be developed as an effective HIV-1 vaccine candidate, a recent study found, although suitable adjuvant is necessary for this protein to generate protective immune responses.
A study in HIV Clinical Trials found that the drug combination emtricitabine/tenofovir alafenamide offers safety advantages to HIV patients over the combination emtricitabine/tenofovir disoproxil fumarate and can be an important option as a nucleoside reverse transcriptase inhibitor backbone given with a variety of third agents.
A dataset analysis found mortality and CD4 progression rates in HIV-1 infected people exhibited regional and age-specific differences, with decreased survival in African and Southeast Asian/East Asian cohorts compared with European/North American and older age groups.
Residence in supportive housing is associated with improvements in CD4 count and viral load for a sample of formerly homeless persons living with HIV/AIDS, according to an Ohio-based study of 86 participants in a supportive housing program.
People living with HIV have a higher incidence of non–AIDS-defining cancer than does the general population and HCV-coinfection is associated with a higher incidence of non–AIDS-defining cancer.
Higher body mass index, lower apolipoprotein A1 and albumin were identified as factors associated with HDL dysfunction in chronic HIV-1 infection, according to a retrospective study in JAIDS.
A study in the journal AIDS found that alcohol use trajectories characterized by persistent unhealthy drinking are associated with more advanced HIV disease severity among HIV-infected veterans in the United States.
[email protected]
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
The prevalence of multidrug-resistant gram-negative organisms is significantly higher in HIV-positive males than in HIV-negative males, according to a study in BMC Infectious Diseases.
“[The] effects of HIV-1 on epitope evolution in M. tuberculosis may have implications for the design of [Mycobacterium] tuberculosis vaccines that are intended for use in populations with high HIV-1 infection rates,” says a report published in Molecular Biology and Evolution.
A study in AIDS Care found that depression partially mediated the relationship between basic psychological needs and quality of life in people living with HIV, suggesting that basic psychological needs and depression may be specific targets for psychosocial interventions.
HIV-infected participants who took 52 weeks of pitavastatin 4 mg daily (vs. pravastatin 40 mg daily) experienced a greater reduction in select markers of immune activation and arterial inflammation, in a 45-site study.
Plasma soluble CD163 was independently associated with incident chronic kidney disease, chronic lung disease, and liver disease in treated HIV-1 infected individuals, according to a study in the journal AIDS.
The recombinant multiepitope protein MEP1 has the potential to be developed as an effective HIV-1 vaccine candidate, a recent study found, although suitable adjuvant is necessary for this protein to generate protective immune responses.
A study in HIV Clinical Trials found that the drug combination emtricitabine/tenofovir alafenamide offers safety advantages to HIV patients over the combination emtricitabine/tenofovir disoproxil fumarate and can be an important option as a nucleoside reverse transcriptase inhibitor backbone given with a variety of third agents.
A dataset analysis found mortality and CD4 progression rates in HIV-1 infected people exhibited regional and age-specific differences, with decreased survival in African and Southeast Asian/East Asian cohorts compared with European/North American and older age groups.
Residence in supportive housing is associated with improvements in CD4 count and viral load for a sample of formerly homeless persons living with HIV/AIDS, according to an Ohio-based study of 86 participants in a supportive housing program.
People living with HIV have a higher incidence of non–AIDS-defining cancer than does the general population and HCV-coinfection is associated with a higher incidence of non–AIDS-defining cancer.
Higher body mass index, lower apolipoprotein A1 and albumin were identified as factors associated with HDL dysfunction in chronic HIV-1 infection, according to a retrospective study in JAIDS.
A study in the journal AIDS found that alcohol use trajectories characterized by persistent unhealthy drinking are associated with more advanced HIV disease severity among HIV-infected veterans in the United States.
[email protected]
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
The prevalence of multidrug-resistant gram-negative organisms is significantly higher in HIV-positive males than in HIV-negative males, according to a study in BMC Infectious Diseases.
“[The] effects of HIV-1 on epitope evolution in M. tuberculosis may have implications for the design of [Mycobacterium] tuberculosis vaccines that are intended for use in populations with high HIV-1 infection rates,” says a report published in Molecular Biology and Evolution.
A study in AIDS Care found that depression partially mediated the relationship between basic psychological needs and quality of life in people living with HIV, suggesting that basic psychological needs and depression may be specific targets for psychosocial interventions.
HIV-infected participants who took 52 weeks of pitavastatin 4 mg daily (vs. pravastatin 40 mg daily) experienced a greater reduction in select markers of immune activation and arterial inflammation, in a 45-site study.
Plasma soluble CD163 was independently associated with incident chronic kidney disease, chronic lung disease, and liver disease in treated HIV-1 infected individuals, according to a study in the journal AIDS.
The recombinant multiepitope protein MEP1 has the potential to be developed as an effective HIV-1 vaccine candidate, a recent study found, although suitable adjuvant is necessary for this protein to generate protective immune responses.
A study in HIV Clinical Trials found that the drug combination emtricitabine/tenofovir alafenamide offers safety advantages to HIV patients over the combination emtricitabine/tenofovir disoproxil fumarate and can be an important option as a nucleoside reverse transcriptase inhibitor backbone given with a variety of third agents.
A dataset analysis found mortality and CD4 progression rates in HIV-1 infected people exhibited regional and age-specific differences, with decreased survival in African and Southeast Asian/East Asian cohorts compared with European/North American and older age groups.
Residence in supportive housing is associated with improvements in CD4 count and viral load for a sample of formerly homeless persons living with HIV/AIDS, according to an Ohio-based study of 86 participants in a supportive housing program.
People living with HIV have a higher incidence of non–AIDS-defining cancer than does the general population and HCV-coinfection is associated with a higher incidence of non–AIDS-defining cancer.
Higher body mass index, lower apolipoprotein A1 and albumin were identified as factors associated with HDL dysfunction in chronic HIV-1 infection, according to a retrospective study in JAIDS.
A study in the journal AIDS found that alcohol use trajectories characterized by persistent unhealthy drinking are associated with more advanced HIV disease severity among HIV-infected veterans in the United States.
[email protected]
On Twitter @richpizzi
Pegylated interferon alfa-2a induces durable responses in MPNs
Pegylated interferon alfa-2a can induce durable hematologic and molecular responses in patients with advanced essential thrombocythemia and polycythemia vera, according to a post hoc analysis of data from a prospective, open-label, phase II trial.
Of 83 patients treated with pegylated interferon alfa-2a, 66 (80%) experienced hematological response, and of 55 of the 83 who were positive for the JAK2 Val617 mutation and who were evaluable for a molecular response, 35 (64%) experienced molecular response. The median response durations were 66 months and 53 months, respectively, wrote Lucia Masarova, MD, and her colleagues at MD Anderson Cancer Center, Houston.
Of the 66 hematological responders, 26 (39%) maintained some response during a median follow-up of 83 months. Among the 40 who lost their response, 19 had dose reductions or had the drug withheld because of intolerance or toxicity, 1 developed concurrent diffuse large B-cell lymphoma, and 20 progressed despite treatment with the highest tolerable dose of pegylated interferon alfa-2a. Of note, 7 (28%) of 25 patients who were treated for at least 46 months (median of 77 months) sustained their hematologic response for a median of 6 months after discontinuation of therapy, the investigators said (Lancet Haematol. 2017 Apr;4:e165-75).
Of the 35 molecular responders, 25 (71%) maintained some response during follow-up. Of the nine evaluable patients who did not maintain response (the 10th patient was taken off the study because of concurrent non-Hodgkin lymphoma) four lost response at a median of 2 years after the drug was withheld, and five lost response while on therapy. Three maintained their complete molecular remission – for 18, 55, and 79 months – after discontinuation of therapy.
“Only one patient who achieved a complete molecular remission has relapsed after stopping therapy for 16 months (complete molecular remission duration, 66 months). The other 9 of 10 patients had durable remissions (median duration 69 months),” the investigators wrote, noting that among the 20 patients with a partial molecular remission, 5 (25%) sustained best partial remission, 7 (28%) are in minor molecular remission, 8 (32%) lost their response, and 3 of 5 (60%) with minor molecular remission sustained that remission.
The study comprised adults over age 18 years who were diagnosed with essential thrombocythemia (40 patients) or polycythemia vera (43) and were enrolled during May 2005 to October 2009. Of the 83 patients, 52 (63%) had received some form of therapy prior to enrollment, including 14 who were treated with standard interferon alfa-2a and 1 who was treated with pegylated interferon alfa-2a. The initial starting dose of pegylated interferon alfa-2a used in the study was 450 mcg delivered subcutaneously once each week, but the dose was decreased in a stepwise manner to a final starting dose of 90 mcg per week due to toxicity; starting doses include 450 mcg in 3 patients, 360 mcg in 3 patients, 270 mcg in 19 patients, 180 mcg in 26 patients, and 90 mcg in 32 patients). Treatment continued as long as clinical benefit continued, and hematological responses were assessed every 3-6 months.
Treatment-related toxicities decreased over time, but five patients had treatment-limiting grade 3 or 4 toxicities after 60 months on therapy; overall 18 patients (22%) discontinued treatment due to toxicity.
The therapeutic approach to essential thrombocythemia and polycythemia vera has mainly focused on control of blood counts and reduction of the risk of thrombosis. Those at high risk for thrombosis generally undergo cytoreductive therapy with hydroxyurea. Recombinant interferon alfa is an alternative to hydroxyurea “given its biological, anti-proliferative, immunomodulating, and anticlonal effects,” the investigators explained.
“However, the widespread use of this biological drug has been limited by high rates of discontinuation due to side effects. Pegylated forms of interferon have a better pharmacological profile than short-acting interferons: they require less frequent injection, lower immunogenicity, and possibly fewer toxic effects,” they said.
Although pegylated interferon-alfa 2a has shown promise in several trials, most had short follow-up. The nearly 7 years of follow-up in the current trial is almost twice as long as in those prior studies.
During the current study, including follow-up, eight major vascular thromboembolic events occurred. One was associated with heart catheterization, one with elective chest surgery, and one with an angiogram. The remaining five occurred with no discernible cause after a median of 38 months of therapy for an incidence of 1.22 unprovoked vascular thromboembolic events per 100 person-years, and three of those were in patients with complete hematologic response. Two of the five patients were under age 60 years and had no history of thrombosis. Another patient had a serious unprovoked cerebrovascular hemorrhage after 3 years on therapy and while in complete hematological response.
In addition, 7 of the 83 patients in the study had disease progression on therapy; 6 progressed to myelofibrosis, and 1 developed acute myeloid leukemia. The median time to transformation in these patients was 40 months.
At the time of publication, 32 patient remained in the study and 24 were receiving treatment. Nineteen were in hematologic response at last follow-up, and most (75%) were on a dose of 90 mcg or less per week.
In addition to showing that some patients achieve durable responses on pegylated interferon alfa-2a, this study provided five important observations, the investigators said: 1) Patients might continue to derive clinical benefit from pegylated interferon alfa-2a even after losing response. 2) Only complete molecular remissions are durable, and some cases can be sustained after therapy discontinuation. 3) Clinical activity of pegylated interferon alfa-2a is not correlated with JAK2 mutation status. 4) Toxic effects unrelated to dose may develop and can be treatment-limiting, even after a long exposure to the drug. 5) Disease-related vascular complications or progression to myelofibrosis can still occur in patients on therapy.
“Our findings suggest that pegylated interferon alfa-2a is a viable treatment option, especially for young patients who want to avoid prolonged cytotoxic therapy. Lower doses minimize side effects while retaining efficacy,” they wrote, suggesting – based on these and other results – a starting dose of 45 mcg weekly to limit adverse events and maximize response.
They also noted that treated patients with a history of autoimmune disease and those with mood disorder should be monitored closely for side effects.
Future studies on pegylated interferon afla-2a alone or in combination with novel immunomodulatory drugs are needed to identify patients who would benefit most from treatment, and additional objective response criteria, such as measurement of spleen size, bone marrow histology, and quality of life should be used to better assess clinical benefit, they said.
The National Cancer Institute funded the study. The authors reported having no disclosures.
The finding by Masarova et al. that interferon alfa induces durable responses that persist even after stopping treatment in a relatively large proportion of patients contradicts the main issues raised against use of interferon alfa in this setting, Jean-Jacques Kiladjian, MD, said in an editorial.
For example, despite concerns about side effects and an inability of patients to tolerate interferon alfa, the findings confirm that it can control myeloproliferative neoplasms at reduced doses, with toxicity similar to that reported with hydroxyurea and, importantly, with no new safety issues noted, he said.
Further, the findings underscore the value of achieving a molecular response, which is a subject of debate.
“In particular, patients who achieved complete molecular response derived the longest clinical benefit and none of them had disease progression,” he wrote (Lancet Haematol. 2017 Apr;4:e150-1).
While the investigators did not note a clear decrease in the expected incidence of transformation to myelofibrosis or acute leukemia among study participants, they did “underline the limitations of this study for accurate estimation of these events,” and two ongoing studies comparing interferon alfa and hydroxyurea in much larger cohorts (the Proud-PV and MPD-RC 112 studies) should provide stronger evidence regarding the leukemogenic potential of the therapies, he said.
Dr. Kiladjian is with Assistance Publique–Hopitaux de Paris and Centre d’Investigations Cliniques, Hopital Saint-Louis, Université Paris Diderot, France. He reported receiving institutional research grants from Novartis and AOP Orphan, and serving as an advisory board member for Novartis, AOP Orphan, and Shire.
The finding by Masarova et al. that interferon alfa induces durable responses that persist even after stopping treatment in a relatively large proportion of patients contradicts the main issues raised against use of interferon alfa in this setting, Jean-Jacques Kiladjian, MD, said in an editorial.
For example, despite concerns about side effects and an inability of patients to tolerate interferon alfa, the findings confirm that it can control myeloproliferative neoplasms at reduced doses, with toxicity similar to that reported with hydroxyurea and, importantly, with no new safety issues noted, he said.
Further, the findings underscore the value of achieving a molecular response, which is a subject of debate.
“In particular, patients who achieved complete molecular response derived the longest clinical benefit and none of them had disease progression,” he wrote (Lancet Haematol. 2017 Apr;4:e150-1).
While the investigators did not note a clear decrease in the expected incidence of transformation to myelofibrosis or acute leukemia among study participants, they did “underline the limitations of this study for accurate estimation of these events,” and two ongoing studies comparing interferon alfa and hydroxyurea in much larger cohorts (the Proud-PV and MPD-RC 112 studies) should provide stronger evidence regarding the leukemogenic potential of the therapies, he said.
Dr. Kiladjian is with Assistance Publique–Hopitaux de Paris and Centre d’Investigations Cliniques, Hopital Saint-Louis, Université Paris Diderot, France. He reported receiving institutional research grants from Novartis and AOP Orphan, and serving as an advisory board member for Novartis, AOP Orphan, and Shire.
The finding by Masarova et al. that interferon alfa induces durable responses that persist even after stopping treatment in a relatively large proportion of patients contradicts the main issues raised against use of interferon alfa in this setting, Jean-Jacques Kiladjian, MD, said in an editorial.
For example, despite concerns about side effects and an inability of patients to tolerate interferon alfa, the findings confirm that it can control myeloproliferative neoplasms at reduced doses, with toxicity similar to that reported with hydroxyurea and, importantly, with no new safety issues noted, he said.
Further, the findings underscore the value of achieving a molecular response, which is a subject of debate.
“In particular, patients who achieved complete molecular response derived the longest clinical benefit and none of them had disease progression,” he wrote (Lancet Haematol. 2017 Apr;4:e150-1).
While the investigators did not note a clear decrease in the expected incidence of transformation to myelofibrosis or acute leukemia among study participants, they did “underline the limitations of this study for accurate estimation of these events,” and two ongoing studies comparing interferon alfa and hydroxyurea in much larger cohorts (the Proud-PV and MPD-RC 112 studies) should provide stronger evidence regarding the leukemogenic potential of the therapies, he said.
Dr. Kiladjian is with Assistance Publique–Hopitaux de Paris and Centre d’Investigations Cliniques, Hopital Saint-Louis, Université Paris Diderot, France. He reported receiving institutional research grants from Novartis and AOP Orphan, and serving as an advisory board member for Novartis, AOP Orphan, and Shire.
Pegylated interferon alfa-2a can induce durable hematologic and molecular responses in patients with advanced essential thrombocythemia and polycythemia vera, according to a post hoc analysis of data from a prospective, open-label, phase II trial.
Of 83 patients treated with pegylated interferon alfa-2a, 66 (80%) experienced hematological response, and of 55 of the 83 who were positive for the JAK2 Val617 mutation and who were evaluable for a molecular response, 35 (64%) experienced molecular response. The median response durations were 66 months and 53 months, respectively, wrote Lucia Masarova, MD, and her colleagues at MD Anderson Cancer Center, Houston.
Of the 66 hematological responders, 26 (39%) maintained some response during a median follow-up of 83 months. Among the 40 who lost their response, 19 had dose reductions or had the drug withheld because of intolerance or toxicity, 1 developed concurrent diffuse large B-cell lymphoma, and 20 progressed despite treatment with the highest tolerable dose of pegylated interferon alfa-2a. Of note, 7 (28%) of 25 patients who were treated for at least 46 months (median of 77 months) sustained their hematologic response for a median of 6 months after discontinuation of therapy, the investigators said (Lancet Haematol. 2017 Apr;4:e165-75).
Of the 35 molecular responders, 25 (71%) maintained some response during follow-up. Of the nine evaluable patients who did not maintain response (the 10th patient was taken off the study because of concurrent non-Hodgkin lymphoma) four lost response at a median of 2 years after the drug was withheld, and five lost response while on therapy. Three maintained their complete molecular remission – for 18, 55, and 79 months – after discontinuation of therapy.
“Only one patient who achieved a complete molecular remission has relapsed after stopping therapy for 16 months (complete molecular remission duration, 66 months). The other 9 of 10 patients had durable remissions (median duration 69 months),” the investigators wrote, noting that among the 20 patients with a partial molecular remission, 5 (25%) sustained best partial remission, 7 (28%) are in minor molecular remission, 8 (32%) lost their response, and 3 of 5 (60%) with minor molecular remission sustained that remission.
The study comprised adults over age 18 years who were diagnosed with essential thrombocythemia (40 patients) or polycythemia vera (43) and were enrolled during May 2005 to October 2009. Of the 83 patients, 52 (63%) had received some form of therapy prior to enrollment, including 14 who were treated with standard interferon alfa-2a and 1 who was treated with pegylated interferon alfa-2a. The initial starting dose of pegylated interferon alfa-2a used in the study was 450 mcg delivered subcutaneously once each week, but the dose was decreased in a stepwise manner to a final starting dose of 90 mcg per week due to toxicity; starting doses include 450 mcg in 3 patients, 360 mcg in 3 patients, 270 mcg in 19 patients, 180 mcg in 26 patients, and 90 mcg in 32 patients). Treatment continued as long as clinical benefit continued, and hematological responses were assessed every 3-6 months.
Treatment-related toxicities decreased over time, but five patients had treatment-limiting grade 3 or 4 toxicities after 60 months on therapy; overall 18 patients (22%) discontinued treatment due to toxicity.
The therapeutic approach to essential thrombocythemia and polycythemia vera has mainly focused on control of blood counts and reduction of the risk of thrombosis. Those at high risk for thrombosis generally undergo cytoreductive therapy with hydroxyurea. Recombinant interferon alfa is an alternative to hydroxyurea “given its biological, anti-proliferative, immunomodulating, and anticlonal effects,” the investigators explained.
“However, the widespread use of this biological drug has been limited by high rates of discontinuation due to side effects. Pegylated forms of interferon have a better pharmacological profile than short-acting interferons: they require less frequent injection, lower immunogenicity, and possibly fewer toxic effects,” they said.
Although pegylated interferon-alfa 2a has shown promise in several trials, most had short follow-up. The nearly 7 years of follow-up in the current trial is almost twice as long as in those prior studies.
During the current study, including follow-up, eight major vascular thromboembolic events occurred. One was associated with heart catheterization, one with elective chest surgery, and one with an angiogram. The remaining five occurred with no discernible cause after a median of 38 months of therapy for an incidence of 1.22 unprovoked vascular thromboembolic events per 100 person-years, and three of those were in patients with complete hematologic response. Two of the five patients were under age 60 years and had no history of thrombosis. Another patient had a serious unprovoked cerebrovascular hemorrhage after 3 years on therapy and while in complete hematological response.
In addition, 7 of the 83 patients in the study had disease progression on therapy; 6 progressed to myelofibrosis, and 1 developed acute myeloid leukemia. The median time to transformation in these patients was 40 months.
At the time of publication, 32 patient remained in the study and 24 were receiving treatment. Nineteen were in hematologic response at last follow-up, and most (75%) were on a dose of 90 mcg or less per week.
In addition to showing that some patients achieve durable responses on pegylated interferon alfa-2a, this study provided five important observations, the investigators said: 1) Patients might continue to derive clinical benefit from pegylated interferon alfa-2a even after losing response. 2) Only complete molecular remissions are durable, and some cases can be sustained after therapy discontinuation. 3) Clinical activity of pegylated interferon alfa-2a is not correlated with JAK2 mutation status. 4) Toxic effects unrelated to dose may develop and can be treatment-limiting, even after a long exposure to the drug. 5) Disease-related vascular complications or progression to myelofibrosis can still occur in patients on therapy.
“Our findings suggest that pegylated interferon alfa-2a is a viable treatment option, especially for young patients who want to avoid prolonged cytotoxic therapy. Lower doses minimize side effects while retaining efficacy,” they wrote, suggesting – based on these and other results – a starting dose of 45 mcg weekly to limit adverse events and maximize response.
They also noted that treated patients with a history of autoimmune disease and those with mood disorder should be monitored closely for side effects.
Future studies on pegylated interferon afla-2a alone or in combination with novel immunomodulatory drugs are needed to identify patients who would benefit most from treatment, and additional objective response criteria, such as measurement of spleen size, bone marrow histology, and quality of life should be used to better assess clinical benefit, they said.
The National Cancer Institute funded the study. The authors reported having no disclosures.
Pegylated interferon alfa-2a can induce durable hematologic and molecular responses in patients with advanced essential thrombocythemia and polycythemia vera, according to a post hoc analysis of data from a prospective, open-label, phase II trial.
Of 83 patients treated with pegylated interferon alfa-2a, 66 (80%) experienced hematological response, and of 55 of the 83 who were positive for the JAK2 Val617 mutation and who were evaluable for a molecular response, 35 (64%) experienced molecular response. The median response durations were 66 months and 53 months, respectively, wrote Lucia Masarova, MD, and her colleagues at MD Anderson Cancer Center, Houston.
Of the 66 hematological responders, 26 (39%) maintained some response during a median follow-up of 83 months. Among the 40 who lost their response, 19 had dose reductions or had the drug withheld because of intolerance or toxicity, 1 developed concurrent diffuse large B-cell lymphoma, and 20 progressed despite treatment with the highest tolerable dose of pegylated interferon alfa-2a. Of note, 7 (28%) of 25 patients who were treated for at least 46 months (median of 77 months) sustained their hematologic response for a median of 6 months after discontinuation of therapy, the investigators said (Lancet Haematol. 2017 Apr;4:e165-75).
Of the 35 molecular responders, 25 (71%) maintained some response during follow-up. Of the nine evaluable patients who did not maintain response (the 10th patient was taken off the study because of concurrent non-Hodgkin lymphoma) four lost response at a median of 2 years after the drug was withheld, and five lost response while on therapy. Three maintained their complete molecular remission – for 18, 55, and 79 months – after discontinuation of therapy.
“Only one patient who achieved a complete molecular remission has relapsed after stopping therapy for 16 months (complete molecular remission duration, 66 months). The other 9 of 10 patients had durable remissions (median duration 69 months),” the investigators wrote, noting that among the 20 patients with a partial molecular remission, 5 (25%) sustained best partial remission, 7 (28%) are in minor molecular remission, 8 (32%) lost their response, and 3 of 5 (60%) with minor molecular remission sustained that remission.
The study comprised adults over age 18 years who were diagnosed with essential thrombocythemia (40 patients) or polycythemia vera (43) and were enrolled during May 2005 to October 2009. Of the 83 patients, 52 (63%) had received some form of therapy prior to enrollment, including 14 who were treated with standard interferon alfa-2a and 1 who was treated with pegylated interferon alfa-2a. The initial starting dose of pegylated interferon alfa-2a used in the study was 450 mcg delivered subcutaneously once each week, but the dose was decreased in a stepwise manner to a final starting dose of 90 mcg per week due to toxicity; starting doses include 450 mcg in 3 patients, 360 mcg in 3 patients, 270 mcg in 19 patients, 180 mcg in 26 patients, and 90 mcg in 32 patients). Treatment continued as long as clinical benefit continued, and hematological responses were assessed every 3-6 months.
Treatment-related toxicities decreased over time, but five patients had treatment-limiting grade 3 or 4 toxicities after 60 months on therapy; overall 18 patients (22%) discontinued treatment due to toxicity.
The therapeutic approach to essential thrombocythemia and polycythemia vera has mainly focused on control of blood counts and reduction of the risk of thrombosis. Those at high risk for thrombosis generally undergo cytoreductive therapy with hydroxyurea. Recombinant interferon alfa is an alternative to hydroxyurea “given its biological, anti-proliferative, immunomodulating, and anticlonal effects,” the investigators explained.
“However, the widespread use of this biological drug has been limited by high rates of discontinuation due to side effects. Pegylated forms of interferon have a better pharmacological profile than short-acting interferons: they require less frequent injection, lower immunogenicity, and possibly fewer toxic effects,” they said.
Although pegylated interferon-alfa 2a has shown promise in several trials, most had short follow-up. The nearly 7 years of follow-up in the current trial is almost twice as long as in those prior studies.
During the current study, including follow-up, eight major vascular thromboembolic events occurred. One was associated with heart catheterization, one with elective chest surgery, and one with an angiogram. The remaining five occurred with no discernible cause after a median of 38 months of therapy for an incidence of 1.22 unprovoked vascular thromboembolic events per 100 person-years, and three of those were in patients with complete hematologic response. Two of the five patients were under age 60 years and had no history of thrombosis. Another patient had a serious unprovoked cerebrovascular hemorrhage after 3 years on therapy and while in complete hematological response.
In addition, 7 of the 83 patients in the study had disease progression on therapy; 6 progressed to myelofibrosis, and 1 developed acute myeloid leukemia. The median time to transformation in these patients was 40 months.
At the time of publication, 32 patient remained in the study and 24 were receiving treatment. Nineteen were in hematologic response at last follow-up, and most (75%) were on a dose of 90 mcg or less per week.
In addition to showing that some patients achieve durable responses on pegylated interferon alfa-2a, this study provided five important observations, the investigators said: 1) Patients might continue to derive clinical benefit from pegylated interferon alfa-2a even after losing response. 2) Only complete molecular remissions are durable, and some cases can be sustained after therapy discontinuation. 3) Clinical activity of pegylated interferon alfa-2a is not correlated with JAK2 mutation status. 4) Toxic effects unrelated to dose may develop and can be treatment-limiting, even after a long exposure to the drug. 5) Disease-related vascular complications or progression to myelofibrosis can still occur in patients on therapy.
“Our findings suggest that pegylated interferon alfa-2a is a viable treatment option, especially for young patients who want to avoid prolonged cytotoxic therapy. Lower doses minimize side effects while retaining efficacy,” they wrote, suggesting – based on these and other results – a starting dose of 45 mcg weekly to limit adverse events and maximize response.
They also noted that treated patients with a history of autoimmune disease and those with mood disorder should be monitored closely for side effects.
Future studies on pegylated interferon afla-2a alone or in combination with novel immunomodulatory drugs are needed to identify patients who would benefit most from treatment, and additional objective response criteria, such as measurement of spleen size, bone marrow histology, and quality of life should be used to better assess clinical benefit, they said.
The National Cancer Institute funded the study. The authors reported having no disclosures.
FROM THE LANCET HAEMATOLOGY
Key clinical point:
Major finding: Eighty percent of patients experienced hematological response and 64% experienced molecular response. The median response durations were 66 months and 53 months, respectively.
Data source: A post hoc analysis of data from an open-label, phase II study of 83 patients.
Disclosures: The National Cancer Institute funded the study. The authors reported having no disclosures.
Statins in HIV-positive patients are a missed opportunity
WASHINGTON – Only one in four U.S. adults with known HIV infection is on statin therapy, even though premature coronary heart disease has become a leading cause of morbidity and mortality for HIV-positive individuals in an era of greatly extended life expectancy due to highly active antiretroviral therapy, Robert S. Rosenson, MD, reported at the annual meeting of the American College of Cardiology.
Not only are statins greatly underutilized in HIV-positive patients, but in a large national observational study, 8% of those who were on a statin were on one that was contraindicated because of concomitant use of antiretroviral therapy or other agents posing a risk for major drug interactions, added Dr. Rosenson, professor of medicine and director of cardiometabolic disorders at Icahn School of Medicine at Mount Sinai, New York.
He presented a retrospective cohort study of 23,119 HIV-positive U.S. adults with commercial health insurance in 2014. The data source was the MarketScan database.
During the study year, 5,931 HIV-positive adults (26%) were taking a statin. In a multivariate regression analysis, factors associated with increased likelihood of statin therapy were age 50 years or older, male gender, known coronary heart disease, hypertension, and diabetes.
A total of 491 patients were taking a contraindicated statin or a statin at too high a dose to be safe, given the other medications they were on.
The protease inhibitors, nonnucleoside reverse transcriptase inhibitors, and some statins are metabolized by the cytochrome P450 isoenzyme CYP3A4. As a consequence, areas under the curve for simvastatin and lovastatin skyrocket when those statins are given with some protease inhibitors, placing patients at increased risk for myopathy, including rhabdomyolysis.
As a consequence, simvastatin and lovastatin are widely considered contraindicated in HIV-positive patients.
Infectious Diseases Society of America guidelines recommend pravastatin or low-dose atorvastatin at 10 mg/day as first-line therapy for lipid-lowering and cardiovascular risk reduction in HIV-positive patients, with fluvastatin a reasonable alternative.
Dr. Rosenson noted that in his study, 62% of the HIV-infected patients on a contraindicated statin were taking a protease inhibitor, 29% were on gemfibrozil (Lopid), and the remaining handful were on other agents posing significant risk of drug interactions, including azole antifungals, calcium channel blockers, or cobicistat (Tybost).
The statin study was jointly funded by Amgen, Mount Sinai, and the University of Alabama. Dr. Rosenson reported serving as a consultant to Amgen, Eli Lilly, Regeneron, and Sanofi.
WASHINGTON – Only one in four U.S. adults with known HIV infection is on statin therapy, even though premature coronary heart disease has become a leading cause of morbidity and mortality for HIV-positive individuals in an era of greatly extended life expectancy due to highly active antiretroviral therapy, Robert S. Rosenson, MD, reported at the annual meeting of the American College of Cardiology.
Not only are statins greatly underutilized in HIV-positive patients, but in a large national observational study, 8% of those who were on a statin were on one that was contraindicated because of concomitant use of antiretroviral therapy or other agents posing a risk for major drug interactions, added Dr. Rosenson, professor of medicine and director of cardiometabolic disorders at Icahn School of Medicine at Mount Sinai, New York.
He presented a retrospective cohort study of 23,119 HIV-positive U.S. adults with commercial health insurance in 2014. The data source was the MarketScan database.
During the study year, 5,931 HIV-positive adults (26%) were taking a statin. In a multivariate regression analysis, factors associated with increased likelihood of statin therapy were age 50 years or older, male gender, known coronary heart disease, hypertension, and diabetes.
A total of 491 patients were taking a contraindicated statin or a statin at too high a dose to be safe, given the other medications they were on.
The protease inhibitors, nonnucleoside reverse transcriptase inhibitors, and some statins are metabolized by the cytochrome P450 isoenzyme CYP3A4. As a consequence, areas under the curve for simvastatin and lovastatin skyrocket when those statins are given with some protease inhibitors, placing patients at increased risk for myopathy, including rhabdomyolysis.
As a consequence, simvastatin and lovastatin are widely considered contraindicated in HIV-positive patients.
Infectious Diseases Society of America guidelines recommend pravastatin or low-dose atorvastatin at 10 mg/day as first-line therapy for lipid-lowering and cardiovascular risk reduction in HIV-positive patients, with fluvastatin a reasonable alternative.
Dr. Rosenson noted that in his study, 62% of the HIV-infected patients on a contraindicated statin were taking a protease inhibitor, 29% were on gemfibrozil (Lopid), and the remaining handful were on other agents posing significant risk of drug interactions, including azole antifungals, calcium channel blockers, or cobicistat (Tybost).
The statin study was jointly funded by Amgen, Mount Sinai, and the University of Alabama. Dr. Rosenson reported serving as a consultant to Amgen, Eli Lilly, Regeneron, and Sanofi.
WASHINGTON – Only one in four U.S. adults with known HIV infection is on statin therapy, even though premature coronary heart disease has become a leading cause of morbidity and mortality for HIV-positive individuals in an era of greatly extended life expectancy due to highly active antiretroviral therapy, Robert S. Rosenson, MD, reported at the annual meeting of the American College of Cardiology.
Not only are statins greatly underutilized in HIV-positive patients, but in a large national observational study, 8% of those who were on a statin were on one that was contraindicated because of concomitant use of antiretroviral therapy or other agents posing a risk for major drug interactions, added Dr. Rosenson, professor of medicine and director of cardiometabolic disorders at Icahn School of Medicine at Mount Sinai, New York.
He presented a retrospective cohort study of 23,119 HIV-positive U.S. adults with commercial health insurance in 2014. The data source was the MarketScan database.
During the study year, 5,931 HIV-positive adults (26%) were taking a statin. In a multivariate regression analysis, factors associated with increased likelihood of statin therapy were age 50 years or older, male gender, known coronary heart disease, hypertension, and diabetes.
A total of 491 patients were taking a contraindicated statin or a statin at too high a dose to be safe, given the other medications they were on.
The protease inhibitors, nonnucleoside reverse transcriptase inhibitors, and some statins are metabolized by the cytochrome P450 isoenzyme CYP3A4. As a consequence, areas under the curve for simvastatin and lovastatin skyrocket when those statins are given with some protease inhibitors, placing patients at increased risk for myopathy, including rhabdomyolysis.
As a consequence, simvastatin and lovastatin are widely considered contraindicated in HIV-positive patients.
Infectious Diseases Society of America guidelines recommend pravastatin or low-dose atorvastatin at 10 mg/day as first-line therapy for lipid-lowering and cardiovascular risk reduction in HIV-positive patients, with fluvastatin a reasonable alternative.
Dr. Rosenson noted that in his study, 62% of the HIV-infected patients on a contraindicated statin were taking a protease inhibitor, 29% were on gemfibrozil (Lopid), and the remaining handful were on other agents posing significant risk of drug interactions, including azole antifungals, calcium channel blockers, or cobicistat (Tybost).
The statin study was jointly funded by Amgen, Mount Sinai, and the University of Alabama. Dr. Rosenson reported serving as a consultant to Amgen, Eli Lilly, Regeneron, and Sanofi.
AT ACC 2017
Key clinical point:
Major finding: Lipid-lowering in HIV-positive adults can be tricky: Eight percent of those who were on statin therapy were taking a statin contraindicated in HIV-infected individuals.
Data source: A retrospective study of more than 23,000 HIV-positive U.S. adults with commercial health insurance in 2014.
Disclosures: The statin study was jointly funded by Amgen and two U.S. medical schools. Dr. Rosenson reported serving as a consultant to Amgen, Eli Lilly, Regeneron, and Sanofi.
Twitter Q&A Transcript April 18, 2017
On April 18, 2017, Gary Goldenberg, MD, took over the @CutisJournal Twitter account for 1 hour to answer reader questions about updates in cosmetic dermatology. Below is a transcript of the Twitter Q&A session (#AskCutisJournal).
@carriekovarik
What can help #hyperpigmentation from prior #HIV related #prurigo in darker pts since this is a stigma of disease? #AskCutisJournal
@carriekovarik Aside from lightening agents & moisturizers, success with #microneedling. Go low & slow 2 prevent more hyperpigmentation.
RELATED ARTICLE:
Microneedling Therapy With and Without Platelet-Rich Plasma
@NailDoc12
What's new for treatment of melasma?
@NailDoc12 I recommend combo of prevention, sunscreen & lightening cream w/ microneedling w/ PRP or ktp laser such as #Cutera #ExcelV.
RELATED ARTICLE:
Dermatologists Weigh in on Skin-Lightening Agents
@NailDoc12
Is there good evidence for use of PRP for skin aging?
@NailDoc12 Pts swear by #PRP. Use after fillers/Botox & microneedling or laser. Pts say it improves skin quality, gives it a "glow" (1/2)
@NailDoc12 Growth factors in PRP improve tissue vascularity & help cells regenerate & normalize. Helps w/wound healing post procedure (2/2)
RELATED VIDEO:
Microneedling With Platelet-Rich Plasma
@anthonymrossi
@CutisJournal #AskCutisJournal What is your approach to global facial rejuvenation? Do you like to start with injectables or laser?
@anthonymrossi Total rejuvenation is just that. I rec combo tx 2 improve skin quality (laser and/or microneedling with PRP) (1/2)
@anthonymrossi Plus wrinkle relaxers for dynamic wrinkles, & fillers to address volume loss and deep wrinkles & lines (2/2)
RELATED VIDEO:
Facial Rejuvenation With Fractional Laser Resurfacing
@SkindocDLCC
@CutisJournal #AskCutisJournal Whats your favorite filler for cheek lifting?
@SkindocDLCC Filler naive pts: #RestylaneLyft or #JuvedermVoluma. Experienced pts: #Radiesse or #Bellafill
@SkindocDLCC
@CutisJournal @Goldenberg_Derm What filler do you like for a sharper jawline? #AskCutisJournal
@SkindocDLCC I prefer long-lasting fillers, such as #Radiesse or #Bellafill. This is true for both male & female pts
RELATED ARTICLE:
Efficacy and Safety of New Dermal Fillers
@SkindocDLCC
@CutisJournal @Goldenberg_Derm How do you get a smooth forehead with neurotoxin without a heavy brow? #AskCutisJournal
@SkindocDLCC Precise placement of product is important. Some pts may require more product to completely smooth out forehead (1/2)
@SkindocDLCC Those pts may need a combo tx with laser such as #CO2 or #microneedling with #PRP (2/2)
@SkindocDLCC
@CutisJournal @Goldenberg_Derm How do you combine PRP and fillers? #AskCutisJournal
@SkindocDLCC I regularly use #PRP with fillers 2 enhance the effect (1/3)
@SkindocDLCC PRP helps stimulate collagen & increase vascularity needed for collagen production (2/3)
@SkindocDLCC I use a mesotherapy needle to inject #PRP after injecting filler and/or neurotoxins (3/3)
@MilitelloDerm
@CutisJournal @Goldenberg_Derm What is your favorite filler for tear troughs?
@MilitelloDerm I prefer Restylane or Juvederm Ultra. These fillers give the best volume effect & last longer than other options in my hands
RELATED ARTICLE:
Periocular Fillers and Related Anatomy
On April 18, 2017, Gary Goldenberg, MD, took over the @CutisJournal Twitter account for 1 hour to answer reader questions about updates in cosmetic dermatology. Below is a transcript of the Twitter Q&A session (#AskCutisJournal).
@carriekovarik
What can help #hyperpigmentation from prior #HIV related #prurigo in darker pts since this is a stigma of disease? #AskCutisJournal
@carriekovarik Aside from lightening agents & moisturizers, success with #microneedling. Go low & slow 2 prevent more hyperpigmentation.
RELATED ARTICLE:
Microneedling Therapy With and Without Platelet-Rich Plasma
@NailDoc12
What's new for treatment of melasma?
@NailDoc12 I recommend combo of prevention, sunscreen & lightening cream w/ microneedling w/ PRP or ktp laser such as #Cutera #ExcelV.
RELATED ARTICLE:
Dermatologists Weigh in on Skin-Lightening Agents
@NailDoc12
Is there good evidence for use of PRP for skin aging?
@NailDoc12 Pts swear by #PRP. Use after fillers/Botox & microneedling or laser. Pts say it improves skin quality, gives it a "glow" (1/2)
@NailDoc12 Growth factors in PRP improve tissue vascularity & help cells regenerate & normalize. Helps w/wound healing post procedure (2/2)
RELATED VIDEO:
Microneedling With Platelet-Rich Plasma
@anthonymrossi
@CutisJournal #AskCutisJournal What is your approach to global facial rejuvenation? Do you like to start with injectables or laser?
@anthonymrossi Total rejuvenation is just that. I rec combo tx 2 improve skin quality (laser and/or microneedling with PRP) (1/2)
@anthonymrossi Plus wrinkle relaxers for dynamic wrinkles, & fillers to address volume loss and deep wrinkles & lines (2/2)
RELATED VIDEO:
Facial Rejuvenation With Fractional Laser Resurfacing
@SkindocDLCC
@CutisJournal #AskCutisJournal Whats your favorite filler for cheek lifting?
@SkindocDLCC Filler naive pts: #RestylaneLyft or #JuvedermVoluma. Experienced pts: #Radiesse or #Bellafill
@SkindocDLCC
@CutisJournal @Goldenberg_Derm What filler do you like for a sharper jawline? #AskCutisJournal
@SkindocDLCC I prefer long-lasting fillers, such as #Radiesse or #Bellafill. This is true for both male & female pts
RELATED ARTICLE:
Efficacy and Safety of New Dermal Fillers
@SkindocDLCC
@CutisJournal @Goldenberg_Derm How do you get a smooth forehead with neurotoxin without a heavy brow? #AskCutisJournal
@SkindocDLCC Precise placement of product is important. Some pts may require more product to completely smooth out forehead (1/2)
@SkindocDLCC Those pts may need a combo tx with laser such as #CO2 or #microneedling with #PRP (2/2)
@SkindocDLCC
@CutisJournal @Goldenberg_Derm How do you combine PRP and fillers? #AskCutisJournal
@SkindocDLCC I regularly use #PRP with fillers 2 enhance the effect (1/3)
@SkindocDLCC PRP helps stimulate collagen & increase vascularity needed for collagen production (2/3)
@SkindocDLCC I use a mesotherapy needle to inject #PRP after injecting filler and/or neurotoxins (3/3)
@MilitelloDerm
@CutisJournal @Goldenberg_Derm What is your favorite filler for tear troughs?
@MilitelloDerm I prefer Restylane or Juvederm Ultra. These fillers give the best volume effect & last longer than other options in my hands
RELATED ARTICLE:
Periocular Fillers and Related Anatomy
On April 18, 2017, Gary Goldenberg, MD, took over the @CutisJournal Twitter account for 1 hour to answer reader questions about updates in cosmetic dermatology. Below is a transcript of the Twitter Q&A session (#AskCutisJournal).
@carriekovarik
What can help #hyperpigmentation from prior #HIV related #prurigo in darker pts since this is a stigma of disease? #AskCutisJournal
@carriekovarik Aside from lightening agents & moisturizers, success with #microneedling. Go low & slow 2 prevent more hyperpigmentation.
RELATED ARTICLE:
Microneedling Therapy With and Without Platelet-Rich Plasma
@NailDoc12
What's new for treatment of melasma?
@NailDoc12 I recommend combo of prevention, sunscreen & lightening cream w/ microneedling w/ PRP or ktp laser such as #Cutera #ExcelV.
RELATED ARTICLE:
Dermatologists Weigh in on Skin-Lightening Agents
@NailDoc12
Is there good evidence for use of PRP for skin aging?
@NailDoc12 Pts swear by #PRP. Use after fillers/Botox & microneedling or laser. Pts say it improves skin quality, gives it a "glow" (1/2)
@NailDoc12 Growth factors in PRP improve tissue vascularity & help cells regenerate & normalize. Helps w/wound healing post procedure (2/2)
RELATED VIDEO:
Microneedling With Platelet-Rich Plasma
@anthonymrossi
@CutisJournal #AskCutisJournal What is your approach to global facial rejuvenation? Do you like to start with injectables or laser?
@anthonymrossi Total rejuvenation is just that. I rec combo tx 2 improve skin quality (laser and/or microneedling with PRP) (1/2)
@anthonymrossi Plus wrinkle relaxers for dynamic wrinkles, & fillers to address volume loss and deep wrinkles & lines (2/2)
RELATED VIDEO:
Facial Rejuvenation With Fractional Laser Resurfacing
@SkindocDLCC
@CutisJournal #AskCutisJournal Whats your favorite filler for cheek lifting?
@SkindocDLCC Filler naive pts: #RestylaneLyft or #JuvedermVoluma. Experienced pts: #Radiesse or #Bellafill
@SkindocDLCC
@CutisJournal @Goldenberg_Derm What filler do you like for a sharper jawline? #AskCutisJournal
@SkindocDLCC I prefer long-lasting fillers, such as #Radiesse or #Bellafill. This is true for both male & female pts
RELATED ARTICLE:
Efficacy and Safety of New Dermal Fillers
@SkindocDLCC
@CutisJournal @Goldenberg_Derm How do you get a smooth forehead with neurotoxin without a heavy brow? #AskCutisJournal
@SkindocDLCC Precise placement of product is important. Some pts may require more product to completely smooth out forehead (1/2)
@SkindocDLCC Those pts may need a combo tx with laser such as #CO2 or #microneedling with #PRP (2/2)
@SkindocDLCC
@CutisJournal @Goldenberg_Derm How do you combine PRP and fillers? #AskCutisJournal
@SkindocDLCC I regularly use #PRP with fillers 2 enhance the effect (1/3)
@SkindocDLCC PRP helps stimulate collagen & increase vascularity needed for collagen production (2/3)
@SkindocDLCC I use a mesotherapy needle to inject #PRP after injecting filler and/or neurotoxins (3/3)
@MilitelloDerm
@CutisJournal @Goldenberg_Derm What is your favorite filler for tear troughs?
@MilitelloDerm I prefer Restylane or Juvederm Ultra. These fillers give the best volume effect & last longer than other options in my hands
RELATED ARTICLE:
Periocular Fillers and Related Anatomy
Hospitalists prepare for MACRA, seek more changes
“We heard you and will continue listening.”
Those were the words that Andrew Slavitt, then-acting administrator of the Centers for Medicare and Medicaid Services, used in a blog post on Oct. 14, 2016.1 (Slavitt no longer maintains that title since the new federal administration took office on Jan. 20, 2017.)
And, it seems they are still listening. Since issuing the final rule, CMS has continued to seek input from stakeholders. The SHM and other groups are working to clarify and pursue improvements to the bipartisan law. Reporting under MACRA begins this year and several changes that appeared in the final rule already may make living with the law less challenging for hospitalists.
For instance, 13 specialty measures were required under the final rule in order for hospitalists to begin reporting under the Quality category of the Merit-based Incentive Payment System (MIPS), one of two pathways to reimbursement available to all physicians under MACRA’s Quality Payment Program. However, of these, Dr. Greeno said that just seven are relevant to the hospitalist practice. The CMS now requires six reported measures in the Quality category, reduced from the initial nine.3
The measures include:
- Heart failure: ACE inhibitor/angiotensin receptor blocker for left ventricular systolic dysfunction
- Heart failure: Beta-blocker for LVSD
- Stroke: DC on antithrombotic therapy
- Advance Care Plan
- Prevention of catheter-related bloodstream infection: CVC (central venous catheter) Insertion Protocol
- Documentation of current medications
- Appropriate treatment of methicillin-susceptible Staphylococcus aureus bacteremia
“Of the seven available, not all will be reportable because hospitalist practices have a lot of variation, both in their practices and in their patient mix,” Dr. Greeno said. “Most hospitalists will only be able to successfully report on four measures, but we are seeking clarification on what they call a validation test and how that will function.”
In the final rule, CMS said that it will perform that “validation test” to evaluate physicians who cannot report the minimum number of measures to ensure they are not penalized for it.
In addition to Quality, the other reporting categories under the umbrella of MIPS include Advancing Care Information, Cost, and Improvement Activities. For 2017, CMS gave physicians the option to “pick your pace.”4 As long as doctors report just one quality measure, one improvement activity, or the required advancing care information measures (most hospitalists will be exempt from this category), they will avoid a penalty.1,5 Cost will not be included for 2017, the first performance year for MIPS. This year’s reporting will be used to determine payments in 2019, though all physicians will see a 0.5 percent fee increase between now and 2019.
Additionally, just for this year, physicians can choose to report for either a full or partial year (90 days). They will not be subject to the penalty and may be eligible for a positive payment adjustment. However, those who submit nothing are subject to a negative 4% adjustment penalty.
Additionally, CMS took steps to make MACRA easier on small and rural physician practices. The final rule exempts physicians who bill $30,000 or less in Medicare Part B or 100 or fewer Medicare patients, up from the previous $10,000 threshold.1
However, this is unlikely to apply to the majority of – if any – hospitalists, Dr. Dutta said. “By virtue of being a hospitalist, you are seeing all comers to your institution. We don’t really have the choice to see fewer Medicare patients, to be honest, and, [for] most hospitalists – whether employed by a hospital or contracting – one of the main reasons we are in place is to help the hospital and take the patients nobody else will take.”
The CMS has also allotted $20 million each year for five years to support training and education for practices of 15 providers or fewer, for rural providers, and for those working in geographic health professional shortage areas.1,6 According to CMS, as of December 2016, experienced organizations (regional health collaboratives, quality improvement organizations, and others) began receiving funds to help these practices choose appropriate quality measures, train in improvement techniques, select the right health information technology, and more.
Under MACRA, small practices (10 clinicians or fewer) may also join “virtual groups” in order to combine their MIPS reporting into a composite score. However, this is not yet well defined, and the option is not available in 2017. The CMS said that it will continue to seek feedback on the structure and implementation of virtual groups in future years.1
Hospitalists may find themselves presented with another option for performance measurement, Dr. Greeno said. The SHM has asked CMS to consider allowing hospitalists to align with their hospital facility instead of being measured separately.
“Hospitalists are in the unique position of working at only one acute care hospital, for the most part, and we actually floated this idea around years ago, to give hospitalists the option for all their quality metrics – not as a standalone physician group – to be judged on hospital performance metrics,” he said, adding, “It would be easier if we could do this for everybody, but not all hospitalist groups that work for hospitals may want to do that.”
Dr. Dutta said that this would be “a great and efficient option,” especially since hospitalists oversee the bulk of quality improvement activities in their hospitals.
“Hospital-level data would be a reflection of what we’re involved in, as the bulk of hospitalists not only provide clinical care but also participate in a multitude of hospital activities,” she said, like: “helping to develop and promote practices around high-value care, to serving on groups like safe transitions in care. It’s hospitalists who are usually the hospital leaders around quality improvement.”
This includes coming up with ways to work with pharmacists at patient admission and on medication reconciliation upon discharge, as well as providing input on clinical protocols, such as what should be done when someone falls or when potassium is high, Dr. Dutta said.
“Performance should be tied to the performance of the hospital. It moves in the right direction to force more collaboration and a joint fate,” Dr. Berenson added.
Alternative payment models
While MIPS is the pathway most physicians expect to find themselves on in 2017, the other option is the Alternative Payment Models (APMs) pathway, which moves away from the pay-for-performance, semi-fee-for-service structure of MIPS and, instead, follows the rules established by the models themselves, which include select qualified accountable care organizations and patient-centered medical homes.7 Participating physicians are eligible for a 5% incentive payment in 2019. Many health experts say that it’s clear CMS would like to ultimately steer most physicians from MIPS to APMs.
However, very few – if any – hospitalists will find themselves on an APM track. This is, in part, because models considered APMs require the use of Certified Electronic Health Record Technology (CEHRT) and must present “more than nominal risk” to providers.
“Right now, the only alternative payment model where hospitalists can directly take risk is BPCI [Bundled Payments for Care Improvement], but it does not qualify as an APM,” Dr. Greeno said.
It will also be difficult because CMS requires patient and payer thresholds under APMs that hospitalists simply are not poised to meet. In 2019, this means 25% of Medicare payments must come from an Advanced APM in 2017, or 20% of providers’ Medicare patients must be seen through an Advanced APM.8
Advanced APMs are those with which, at least in 2019 and 2020, providers face the risk of losing the lesser of 8% of their revenue or repaying CMS up to 3% of their total Medicare expenditures, if expenditures are higher than expected.8,9
“It is going to be very difficult for hospitalists to qualify for APMs because we’re not in the position to hit the thresholds,” said Dr. Dutta.
However, SHM has urged CMS to consider other BPCI models for qualification as APMs, and Dr. Greeno said that CMS is currently looking into developing bundles that may be appropriate for hospitalists. For instance, Dr. Dutta said, “What we do often in medicine is chronic disease management, and the time is coming to get into chronic disease bundles, such as [those for] management of heart failure or kidney disease.”
In December, SHM submitted a letter to PTAC (the Physician-Focused Payment Model Technical Advisory Committee) to show support for a model created by the American College of Surgeons, called ACS-Brandeis, which they hope will be considered as an Advanced Alternative Payment Model. In the proposal that ACS submitted, the authors noted, “The core model is focused on procedure episodes but can easily be expanded to include acute and chronic conditions.”
The SHM notes in its letter that, while the initial proposal is intended for surgical patients, the term-based nature of surgical care provides a platform for expanding the model more broadly to hospitalists and other specialties.
Some skepticism remains
Even if BPCI or other models are accepted as APMs, hospitalists may still be challenged to meet the required payment or patient thresholds, Dr. Greeno said. Additionally, Dr. Berenson is skeptical of bundled payments, particularly for hospitalists.
“Are hospitalists the right organization to be held accountable for the total cost of care for 90 days of spending, any more than oncologists under Oncology Care Models should be accountable for the total cost of cancer where some patients are getting palliative care and that’s not a driver of healthcare costs?” he asked. “I could see that as problematic for hospitalists.”
While he believes there are many positive aspects to MACRA, in general, Dr. Berenson considers it bad policy. While he does not want to see the Sustainable Growth Rate return, he believes many physicians would have seen reimbursement reductions sooner without MACRA (under the prior quality measurement programs) and that the law provides some perverse incentives.
For one thing, the Quality Payment Program is budget neutral, which means that, for every winner, there is also a loser. Before CMS expanded exemptions for smaller and rural practices, Dr. Berenson said that some larger groups – which are often better equipped to pursue APMs – were planning to stay in MIPS because they figured they were more likely to be the winners when compared with smaller physician practices. And MIPS comes with a 9% payment boost by 2022 (or 9% penalty), plus the possibility of an extra bonus for top performers, compared with the 5% incentive of APMs that same year.7
“There were literally groups saying they were going to go for the MIPS pathway because it’s a bigger upside,” Dr. Berenson said. “When CMS said it was exempting those [smaller, rural] groups, the [larger] groups turned around and said [that the smaller, rural groups] were the downside. ... That kind of game theory is bad public policy.”
Dr. Berenson also believes MACRA will be detrimental to some small and independent practices. Others may decide not to bill Medicare altogether, though that is not an option open to most hospitalists who care to stay in practice. It could, however, drive more hospitalists to consolidate or to become employees of their hospitals.10
“I don’t think there is any doubt this is going to drive consolidation,” Dr. Greeno said, citing numbers released by CMS that show an inverse relationship between practice size and the negative impact of MACRA.11 “I think it’s going to be pretty tough unless you’re big enough to commit the resources you need to do it right.”
At TeamHealth, where Dr. Greeno is senior advisor of medical affairs, he said that they have invested in information technology compliance, developed systems and trained providers to ensure the creation of favorable metrics for the organization’ and built the infrastructure to gather, report, and validate data. These are steps that may be out of reach for most smaller practices.
As Dr. Greeno said, no one expected this to be easy. “You’re trying to get doctors to change the way they practice. Anybody who has ever worked with doctors knows that’s not an easy things to do,” he said. “CMS is changing things to create enough incentive so the pain of not changing becomes greater than the pain of changing.”
While hospitalists may bear more of the pressure than other physician specialties, by virtue of their role in improving the quality of care in hospitals, they were born from reform efforts of the past, Dr. Greeno adds.
“If there had never been an attempt to change the way that physicians were paid, hospitalists wouldn’t exist,” he said. “We were created by physician groups who took capitated payments from HMOs, who had to find more efficient ways to treat patients in the hospital or go out of business.”
“Hospitalists are a delivery system reform and people look to us to lead. We can create a tremendous amount of value for whomever we work for,” Dr. Greeno said.
This is also why SHM continues to work with CMS to advocate for all its members. Dr. Greeno is in Washington at least once a month, participating in critical meetings and helping to guide decisions.
“The Public Policy Committee has to get into the weeds and get involved in advocating for measures that truly get at the work we do and push back on metrics and categories that do not relate to the care we are delivering for our patients,” said Dr. Dutta. “The group worked hard to push back on having to comply with Meaningful Use standards for hospitalists, and now we’re exempt from that category. CMS does listen. It sometimes just takes a while.”
References
1. Slavitt A. (2016 Oct 14). A letter from CMS to Medicare clinicians in the Quality Payment Program: We heard you and will continue listening. The CMS Blog (archived). Retrieved from http://wayback.archive-it.org/2744/20161109123921/https://blog.cms.gov/2016/10/14/a-letter-from-cms-to-medicare-clinicians-in-the-quality-payment-program/.
2. Department of Health & Human Services and Centers for Medicare & Medicaid Services. (2016 Oct 14). Quality Payment Program executive summary. Retrieved from https://qpp.cms.gov/docs/QPP_Executive_Summary_of_Final_Rule.pdf.
3. American Medical Association. (2016 Oct 19). Medicare Access and CHIP Reauthorization Act (MACRA) Quality Payment Program final rule AMA summary. Retrieved from https://www.ama-assn.org/sites/default/files/media-browser/public/physicians/macra/macra-qpp-summary.pdf.
4. Slavitt A. (2016 Sept 8). Plans for the Quality Payment Program in 2017: Pick your pace. The CMS Blog (archived). Retrieved from http://wayback.archive-it.org/2744/20161109123909/https://blog.cms.gov/2016/09/08/qualitypaymentprogram-pickyourpace/.
5. The Society of Hospital Medicine. Medicare physician payments are changing. Retrieved from http://www.macraforhm.org/.
6. Department of Health & Human Services and Centers for Medicare & Medicaid Services. (2016 Oct 14). Quality Payment Program fact sheet. Retrieved from https://qpp.cms.gov/docs/QPP_Small_Practice.pdf.
7. The Society of Hospital Medicine. (2017). MACRA and the Quality Payment Program. Retrieved from http://www.macraforhm.org/MACRA_FAQ_m1_final.pdf.
8. Department of Health & Human Services and Centers for Medicare & Medicaid Services. Quality Payment Program: Modernizing Medicare to provide better care and smarter spending for a healthier America. Retrieved from https://qpp.cms.gov/.
9. Wynne B. (2016 Oct 17). MACRA Final Rule: CMS strikes a balance; will docs hang on? Retrieved from http://healthaffairs.org/blog/2016/10/17/macra-final-rule-cms-strikes-a-balance-will-docs-hang-on/.
10. Quinn R. (2015 Aug). TeamHealth-IPC Deal Latest in consolidation trend. The Hospitalist. 2015(8). Retrieved from http://www.the-hospitalist.org/hospitalist/article/122210/teamhealth-ipc-deal-latest-consolidation-trend
11. Barkholz D. (2016 Jun 30). Potential MACRA byproduct: physician consolidation. Retrieved from http://www.modernhealthcare.com/article/20160630/NEWS/160639995.
“We heard you and will continue listening.”
Those were the words that Andrew Slavitt, then-acting administrator of the Centers for Medicare and Medicaid Services, used in a blog post on Oct. 14, 2016.1 (Slavitt no longer maintains that title since the new federal administration took office on Jan. 20, 2017.)
And, it seems they are still listening. Since issuing the final rule, CMS has continued to seek input from stakeholders. The SHM and other groups are working to clarify and pursue improvements to the bipartisan law. Reporting under MACRA begins this year and several changes that appeared in the final rule already may make living with the law less challenging for hospitalists.
For instance, 13 specialty measures were required under the final rule in order for hospitalists to begin reporting under the Quality category of the Merit-based Incentive Payment System (MIPS), one of two pathways to reimbursement available to all physicians under MACRA’s Quality Payment Program. However, of these, Dr. Greeno said that just seven are relevant to the hospitalist practice. The CMS now requires six reported measures in the Quality category, reduced from the initial nine.3
The measures include:
- Heart failure: ACE inhibitor/angiotensin receptor blocker for left ventricular systolic dysfunction
- Heart failure: Beta-blocker for LVSD
- Stroke: DC on antithrombotic therapy
- Advance Care Plan
- Prevention of catheter-related bloodstream infection: CVC (central venous catheter) Insertion Protocol
- Documentation of current medications
- Appropriate treatment of methicillin-susceptible Staphylococcus aureus bacteremia
“Of the seven available, not all will be reportable because hospitalist practices have a lot of variation, both in their practices and in their patient mix,” Dr. Greeno said. “Most hospitalists will only be able to successfully report on four measures, but we are seeking clarification on what they call a validation test and how that will function.”
In the final rule, CMS said that it will perform that “validation test” to evaluate physicians who cannot report the minimum number of measures to ensure they are not penalized for it.
In addition to Quality, the other reporting categories under the umbrella of MIPS include Advancing Care Information, Cost, and Improvement Activities. For 2017, CMS gave physicians the option to “pick your pace.”4 As long as doctors report just one quality measure, one improvement activity, or the required advancing care information measures (most hospitalists will be exempt from this category), they will avoid a penalty.1,5 Cost will not be included for 2017, the first performance year for MIPS. This year’s reporting will be used to determine payments in 2019, though all physicians will see a 0.5 percent fee increase between now and 2019.
Additionally, just for this year, physicians can choose to report for either a full or partial year (90 days). They will not be subject to the penalty and may be eligible for a positive payment adjustment. However, those who submit nothing are subject to a negative 4% adjustment penalty.
Additionally, CMS took steps to make MACRA easier on small and rural physician practices. The final rule exempts physicians who bill $30,000 or less in Medicare Part B or 100 or fewer Medicare patients, up from the previous $10,000 threshold.1
However, this is unlikely to apply to the majority of – if any – hospitalists, Dr. Dutta said. “By virtue of being a hospitalist, you are seeing all comers to your institution. We don’t really have the choice to see fewer Medicare patients, to be honest, and, [for] most hospitalists – whether employed by a hospital or contracting – one of the main reasons we are in place is to help the hospital and take the patients nobody else will take.”
The CMS has also allotted $20 million each year for five years to support training and education for practices of 15 providers or fewer, for rural providers, and for those working in geographic health professional shortage areas.1,6 According to CMS, as of December 2016, experienced organizations (regional health collaboratives, quality improvement organizations, and others) began receiving funds to help these practices choose appropriate quality measures, train in improvement techniques, select the right health information technology, and more.
Under MACRA, small practices (10 clinicians or fewer) may also join “virtual groups” in order to combine their MIPS reporting into a composite score. However, this is not yet well defined, and the option is not available in 2017. The CMS said that it will continue to seek feedback on the structure and implementation of virtual groups in future years.1
Hospitalists may find themselves presented with another option for performance measurement, Dr. Greeno said. The SHM has asked CMS to consider allowing hospitalists to align with their hospital facility instead of being measured separately.
“Hospitalists are in the unique position of working at only one acute care hospital, for the most part, and we actually floated this idea around years ago, to give hospitalists the option for all their quality metrics – not as a standalone physician group – to be judged on hospital performance metrics,” he said, adding, “It would be easier if we could do this for everybody, but not all hospitalist groups that work for hospitals may want to do that.”
Dr. Dutta said that this would be “a great and efficient option,” especially since hospitalists oversee the bulk of quality improvement activities in their hospitals.
“Hospital-level data would be a reflection of what we’re involved in, as the bulk of hospitalists not only provide clinical care but also participate in a multitude of hospital activities,” she said, like: “helping to develop and promote practices around high-value care, to serving on groups like safe transitions in care. It’s hospitalists who are usually the hospital leaders around quality improvement.”
This includes coming up with ways to work with pharmacists at patient admission and on medication reconciliation upon discharge, as well as providing input on clinical protocols, such as what should be done when someone falls or when potassium is high, Dr. Dutta said.
“Performance should be tied to the performance of the hospital. It moves in the right direction to force more collaboration and a joint fate,” Dr. Berenson added.
Alternative payment models
While MIPS is the pathway most physicians expect to find themselves on in 2017, the other option is the Alternative Payment Models (APMs) pathway, which moves away from the pay-for-performance, semi-fee-for-service structure of MIPS and, instead, follows the rules established by the models themselves, which include select qualified accountable care organizations and patient-centered medical homes.7 Participating physicians are eligible for a 5% incentive payment in 2019. Many health experts say that it’s clear CMS would like to ultimately steer most physicians from MIPS to APMs.
However, very few – if any – hospitalists will find themselves on an APM track. This is, in part, because models considered APMs require the use of Certified Electronic Health Record Technology (CEHRT) and must present “more than nominal risk” to providers.
“Right now, the only alternative payment model where hospitalists can directly take risk is BPCI [Bundled Payments for Care Improvement], but it does not qualify as an APM,” Dr. Greeno said.
It will also be difficult because CMS requires patient and payer thresholds under APMs that hospitalists simply are not poised to meet. In 2019, this means 25% of Medicare payments must come from an Advanced APM in 2017, or 20% of providers’ Medicare patients must be seen through an Advanced APM.8
Advanced APMs are those with which, at least in 2019 and 2020, providers face the risk of losing the lesser of 8% of their revenue or repaying CMS up to 3% of their total Medicare expenditures, if expenditures are higher than expected.8,9
“It is going to be very difficult for hospitalists to qualify for APMs because we’re not in the position to hit the thresholds,” said Dr. Dutta.
However, SHM has urged CMS to consider other BPCI models for qualification as APMs, and Dr. Greeno said that CMS is currently looking into developing bundles that may be appropriate for hospitalists. For instance, Dr. Dutta said, “What we do often in medicine is chronic disease management, and the time is coming to get into chronic disease bundles, such as [those for] management of heart failure or kidney disease.”
In December, SHM submitted a letter to PTAC (the Physician-Focused Payment Model Technical Advisory Committee) to show support for a model created by the American College of Surgeons, called ACS-Brandeis, which they hope will be considered as an Advanced Alternative Payment Model. In the proposal that ACS submitted, the authors noted, “The core model is focused on procedure episodes but can easily be expanded to include acute and chronic conditions.”
The SHM notes in its letter that, while the initial proposal is intended for surgical patients, the term-based nature of surgical care provides a platform for expanding the model more broadly to hospitalists and other specialties.
Some skepticism remains
Even if BPCI or other models are accepted as APMs, hospitalists may still be challenged to meet the required payment or patient thresholds, Dr. Greeno said. Additionally, Dr. Berenson is skeptical of bundled payments, particularly for hospitalists.
“Are hospitalists the right organization to be held accountable for the total cost of care for 90 days of spending, any more than oncologists under Oncology Care Models should be accountable for the total cost of cancer where some patients are getting palliative care and that’s not a driver of healthcare costs?” he asked. “I could see that as problematic for hospitalists.”
While he believes there are many positive aspects to MACRA, in general, Dr. Berenson considers it bad policy. While he does not want to see the Sustainable Growth Rate return, he believes many physicians would have seen reimbursement reductions sooner without MACRA (under the prior quality measurement programs) and that the law provides some perverse incentives.
For one thing, the Quality Payment Program is budget neutral, which means that, for every winner, there is also a loser. Before CMS expanded exemptions for smaller and rural practices, Dr. Berenson said that some larger groups – which are often better equipped to pursue APMs – were planning to stay in MIPS because they figured they were more likely to be the winners when compared with smaller physician practices. And MIPS comes with a 9% payment boost by 2022 (or 9% penalty), plus the possibility of an extra bonus for top performers, compared with the 5% incentive of APMs that same year.7
“There were literally groups saying they were going to go for the MIPS pathway because it’s a bigger upside,” Dr. Berenson said. “When CMS said it was exempting those [smaller, rural] groups, the [larger] groups turned around and said [that the smaller, rural groups] were the downside. ... That kind of game theory is bad public policy.”
Dr. Berenson also believes MACRA will be detrimental to some small and independent practices. Others may decide not to bill Medicare altogether, though that is not an option open to most hospitalists who care to stay in practice. It could, however, drive more hospitalists to consolidate or to become employees of their hospitals.10
“I don’t think there is any doubt this is going to drive consolidation,” Dr. Greeno said, citing numbers released by CMS that show an inverse relationship between practice size and the negative impact of MACRA.11 “I think it’s going to be pretty tough unless you’re big enough to commit the resources you need to do it right.”
At TeamHealth, where Dr. Greeno is senior advisor of medical affairs, he said that they have invested in information technology compliance, developed systems and trained providers to ensure the creation of favorable metrics for the organization’ and built the infrastructure to gather, report, and validate data. These are steps that may be out of reach for most smaller practices.
As Dr. Greeno said, no one expected this to be easy. “You’re trying to get doctors to change the way they practice. Anybody who has ever worked with doctors knows that’s not an easy things to do,” he said. “CMS is changing things to create enough incentive so the pain of not changing becomes greater than the pain of changing.”
While hospitalists may bear more of the pressure than other physician specialties, by virtue of their role in improving the quality of care in hospitals, they were born from reform efforts of the past, Dr. Greeno adds.
“If there had never been an attempt to change the way that physicians were paid, hospitalists wouldn’t exist,” he said. “We were created by physician groups who took capitated payments from HMOs, who had to find more efficient ways to treat patients in the hospital or go out of business.”
“Hospitalists are a delivery system reform and people look to us to lead. We can create a tremendous amount of value for whomever we work for,” Dr. Greeno said.
This is also why SHM continues to work with CMS to advocate for all its members. Dr. Greeno is in Washington at least once a month, participating in critical meetings and helping to guide decisions.
“The Public Policy Committee has to get into the weeds and get involved in advocating for measures that truly get at the work we do and push back on metrics and categories that do not relate to the care we are delivering for our patients,” said Dr. Dutta. “The group worked hard to push back on having to comply with Meaningful Use standards for hospitalists, and now we’re exempt from that category. CMS does listen. It sometimes just takes a while.”
References
1. Slavitt A. (2016 Oct 14). A letter from CMS to Medicare clinicians in the Quality Payment Program: We heard you and will continue listening. The CMS Blog (archived). Retrieved from http://wayback.archive-it.org/2744/20161109123921/https://blog.cms.gov/2016/10/14/a-letter-from-cms-to-medicare-clinicians-in-the-quality-payment-program/.
2. Department of Health & Human Services and Centers for Medicare & Medicaid Services. (2016 Oct 14). Quality Payment Program executive summary. Retrieved from https://qpp.cms.gov/docs/QPP_Executive_Summary_of_Final_Rule.pdf.
3. American Medical Association. (2016 Oct 19). Medicare Access and CHIP Reauthorization Act (MACRA) Quality Payment Program final rule AMA summary. Retrieved from https://www.ama-assn.org/sites/default/files/media-browser/public/physicians/macra/macra-qpp-summary.pdf.
4. Slavitt A. (2016 Sept 8). Plans for the Quality Payment Program in 2017: Pick your pace. The CMS Blog (archived). Retrieved from http://wayback.archive-it.org/2744/20161109123909/https://blog.cms.gov/2016/09/08/qualitypaymentprogram-pickyourpace/.
5. The Society of Hospital Medicine. Medicare physician payments are changing. Retrieved from http://www.macraforhm.org/.
6. Department of Health & Human Services and Centers for Medicare & Medicaid Services. (2016 Oct 14). Quality Payment Program fact sheet. Retrieved from https://qpp.cms.gov/docs/QPP_Small_Practice.pdf.
7. The Society of Hospital Medicine. (2017). MACRA and the Quality Payment Program. Retrieved from http://www.macraforhm.org/MACRA_FAQ_m1_final.pdf.
8. Department of Health & Human Services and Centers for Medicare & Medicaid Services. Quality Payment Program: Modernizing Medicare to provide better care and smarter spending for a healthier America. Retrieved from https://qpp.cms.gov/.
9. Wynne B. (2016 Oct 17). MACRA Final Rule: CMS strikes a balance; will docs hang on? Retrieved from http://healthaffairs.org/blog/2016/10/17/macra-final-rule-cms-strikes-a-balance-will-docs-hang-on/.
10. Quinn R. (2015 Aug). TeamHealth-IPC Deal Latest in consolidation trend. The Hospitalist. 2015(8). Retrieved from http://www.the-hospitalist.org/hospitalist/article/122210/teamhealth-ipc-deal-latest-consolidation-trend
11. Barkholz D. (2016 Jun 30). Potential MACRA byproduct: physician consolidation. Retrieved from http://www.modernhealthcare.com/article/20160630/NEWS/160639995.
“We heard you and will continue listening.”
Those were the words that Andrew Slavitt, then-acting administrator of the Centers for Medicare and Medicaid Services, used in a blog post on Oct. 14, 2016.1 (Slavitt no longer maintains that title since the new federal administration took office on Jan. 20, 2017.)
And, it seems they are still listening. Since issuing the final rule, CMS has continued to seek input from stakeholders. The SHM and other groups are working to clarify and pursue improvements to the bipartisan law. Reporting under MACRA begins this year and several changes that appeared in the final rule already may make living with the law less challenging for hospitalists.
For instance, 13 specialty measures were required under the final rule in order for hospitalists to begin reporting under the Quality category of the Merit-based Incentive Payment System (MIPS), one of two pathways to reimbursement available to all physicians under MACRA’s Quality Payment Program. However, of these, Dr. Greeno said that just seven are relevant to the hospitalist practice. The CMS now requires six reported measures in the Quality category, reduced from the initial nine.3
The measures include:
- Heart failure: ACE inhibitor/angiotensin receptor blocker for left ventricular systolic dysfunction
- Heart failure: Beta-blocker for LVSD
- Stroke: DC on antithrombotic therapy
- Advance Care Plan
- Prevention of catheter-related bloodstream infection: CVC (central venous catheter) Insertion Protocol
- Documentation of current medications
- Appropriate treatment of methicillin-susceptible Staphylococcus aureus bacteremia
“Of the seven available, not all will be reportable because hospitalist practices have a lot of variation, both in their practices and in their patient mix,” Dr. Greeno said. “Most hospitalists will only be able to successfully report on four measures, but we are seeking clarification on what they call a validation test and how that will function.”
In the final rule, CMS said that it will perform that “validation test” to evaluate physicians who cannot report the minimum number of measures to ensure they are not penalized for it.
In addition to Quality, the other reporting categories under the umbrella of MIPS include Advancing Care Information, Cost, and Improvement Activities. For 2017, CMS gave physicians the option to “pick your pace.”4 As long as doctors report just one quality measure, one improvement activity, or the required advancing care information measures (most hospitalists will be exempt from this category), they will avoid a penalty.1,5 Cost will not be included for 2017, the first performance year for MIPS. This year’s reporting will be used to determine payments in 2019, though all physicians will see a 0.5 percent fee increase between now and 2019.
Additionally, just for this year, physicians can choose to report for either a full or partial year (90 days). They will not be subject to the penalty and may be eligible for a positive payment adjustment. However, those who submit nothing are subject to a negative 4% adjustment penalty.
Additionally, CMS took steps to make MACRA easier on small and rural physician practices. The final rule exempts physicians who bill $30,000 or less in Medicare Part B or 100 or fewer Medicare patients, up from the previous $10,000 threshold.1
However, this is unlikely to apply to the majority of – if any – hospitalists, Dr. Dutta said. “By virtue of being a hospitalist, you are seeing all comers to your institution. We don’t really have the choice to see fewer Medicare patients, to be honest, and, [for] most hospitalists – whether employed by a hospital or contracting – one of the main reasons we are in place is to help the hospital and take the patients nobody else will take.”
The CMS has also allotted $20 million each year for five years to support training and education for practices of 15 providers or fewer, for rural providers, and for those working in geographic health professional shortage areas.1,6 According to CMS, as of December 2016, experienced organizations (regional health collaboratives, quality improvement organizations, and others) began receiving funds to help these practices choose appropriate quality measures, train in improvement techniques, select the right health information technology, and more.
Under MACRA, small practices (10 clinicians or fewer) may also join “virtual groups” in order to combine their MIPS reporting into a composite score. However, this is not yet well defined, and the option is not available in 2017. The CMS said that it will continue to seek feedback on the structure and implementation of virtual groups in future years.1
Hospitalists may find themselves presented with another option for performance measurement, Dr. Greeno said. The SHM has asked CMS to consider allowing hospitalists to align with their hospital facility instead of being measured separately.
“Hospitalists are in the unique position of working at only one acute care hospital, for the most part, and we actually floated this idea around years ago, to give hospitalists the option for all their quality metrics – not as a standalone physician group – to be judged on hospital performance metrics,” he said, adding, “It would be easier if we could do this for everybody, but not all hospitalist groups that work for hospitals may want to do that.”
Dr. Dutta said that this would be “a great and efficient option,” especially since hospitalists oversee the bulk of quality improvement activities in their hospitals.
“Hospital-level data would be a reflection of what we’re involved in, as the bulk of hospitalists not only provide clinical care but also participate in a multitude of hospital activities,” she said, like: “helping to develop and promote practices around high-value care, to serving on groups like safe transitions in care. It’s hospitalists who are usually the hospital leaders around quality improvement.”
This includes coming up with ways to work with pharmacists at patient admission and on medication reconciliation upon discharge, as well as providing input on clinical protocols, such as what should be done when someone falls or when potassium is high, Dr. Dutta said.
“Performance should be tied to the performance of the hospital. It moves in the right direction to force more collaboration and a joint fate,” Dr. Berenson added.
Alternative payment models
While MIPS is the pathway most physicians expect to find themselves on in 2017, the other option is the Alternative Payment Models (APMs) pathway, which moves away from the pay-for-performance, semi-fee-for-service structure of MIPS and, instead, follows the rules established by the models themselves, which include select qualified accountable care organizations and patient-centered medical homes.7 Participating physicians are eligible for a 5% incentive payment in 2019. Many health experts say that it’s clear CMS would like to ultimately steer most physicians from MIPS to APMs.
However, very few – if any – hospitalists will find themselves on an APM track. This is, in part, because models considered APMs require the use of Certified Electronic Health Record Technology (CEHRT) and must present “more than nominal risk” to providers.
“Right now, the only alternative payment model where hospitalists can directly take risk is BPCI [Bundled Payments for Care Improvement], but it does not qualify as an APM,” Dr. Greeno said.
It will also be difficult because CMS requires patient and payer thresholds under APMs that hospitalists simply are not poised to meet. In 2019, this means 25% of Medicare payments must come from an Advanced APM in 2017, or 20% of providers’ Medicare patients must be seen through an Advanced APM.8
Advanced APMs are those with which, at least in 2019 and 2020, providers face the risk of losing the lesser of 8% of their revenue or repaying CMS up to 3% of their total Medicare expenditures, if expenditures are higher than expected.8,9
“It is going to be very difficult for hospitalists to qualify for APMs because we’re not in the position to hit the thresholds,” said Dr. Dutta.
However, SHM has urged CMS to consider other BPCI models for qualification as APMs, and Dr. Greeno said that CMS is currently looking into developing bundles that may be appropriate for hospitalists. For instance, Dr. Dutta said, “What we do often in medicine is chronic disease management, and the time is coming to get into chronic disease bundles, such as [those for] management of heart failure or kidney disease.”
In December, SHM submitted a letter to PTAC (the Physician-Focused Payment Model Technical Advisory Committee) to show support for a model created by the American College of Surgeons, called ACS-Brandeis, which they hope will be considered as an Advanced Alternative Payment Model. In the proposal that ACS submitted, the authors noted, “The core model is focused on procedure episodes but can easily be expanded to include acute and chronic conditions.”
The SHM notes in its letter that, while the initial proposal is intended for surgical patients, the term-based nature of surgical care provides a platform for expanding the model more broadly to hospitalists and other specialties.
Some skepticism remains
Even if BPCI or other models are accepted as APMs, hospitalists may still be challenged to meet the required payment or patient thresholds, Dr. Greeno said. Additionally, Dr. Berenson is skeptical of bundled payments, particularly for hospitalists.
“Are hospitalists the right organization to be held accountable for the total cost of care for 90 days of spending, any more than oncologists under Oncology Care Models should be accountable for the total cost of cancer where some patients are getting palliative care and that’s not a driver of healthcare costs?” he asked. “I could see that as problematic for hospitalists.”
While he believes there are many positive aspects to MACRA, in general, Dr. Berenson considers it bad policy. While he does not want to see the Sustainable Growth Rate return, he believes many physicians would have seen reimbursement reductions sooner without MACRA (under the prior quality measurement programs) and that the law provides some perverse incentives.
For one thing, the Quality Payment Program is budget neutral, which means that, for every winner, there is also a loser. Before CMS expanded exemptions for smaller and rural practices, Dr. Berenson said that some larger groups – which are often better equipped to pursue APMs – were planning to stay in MIPS because they figured they were more likely to be the winners when compared with smaller physician practices. And MIPS comes with a 9% payment boost by 2022 (or 9% penalty), plus the possibility of an extra bonus for top performers, compared with the 5% incentive of APMs that same year.7
“There were literally groups saying they were going to go for the MIPS pathway because it’s a bigger upside,” Dr. Berenson said. “When CMS said it was exempting those [smaller, rural] groups, the [larger] groups turned around and said [that the smaller, rural groups] were the downside. ... That kind of game theory is bad public policy.”
Dr. Berenson also believes MACRA will be detrimental to some small and independent practices. Others may decide not to bill Medicare altogether, though that is not an option open to most hospitalists who care to stay in practice. It could, however, drive more hospitalists to consolidate or to become employees of their hospitals.10
“I don’t think there is any doubt this is going to drive consolidation,” Dr. Greeno said, citing numbers released by CMS that show an inverse relationship between practice size and the negative impact of MACRA.11 “I think it’s going to be pretty tough unless you’re big enough to commit the resources you need to do it right.”
At TeamHealth, where Dr. Greeno is senior advisor of medical affairs, he said that they have invested in information technology compliance, developed systems and trained providers to ensure the creation of favorable metrics for the organization’ and built the infrastructure to gather, report, and validate data. These are steps that may be out of reach for most smaller practices.
As Dr. Greeno said, no one expected this to be easy. “You’re trying to get doctors to change the way they practice. Anybody who has ever worked with doctors knows that’s not an easy things to do,” he said. “CMS is changing things to create enough incentive so the pain of not changing becomes greater than the pain of changing.”
While hospitalists may bear more of the pressure than other physician specialties, by virtue of their role in improving the quality of care in hospitals, they were born from reform efforts of the past, Dr. Greeno adds.
“If there had never been an attempt to change the way that physicians were paid, hospitalists wouldn’t exist,” he said. “We were created by physician groups who took capitated payments from HMOs, who had to find more efficient ways to treat patients in the hospital or go out of business.”
“Hospitalists are a delivery system reform and people look to us to lead. We can create a tremendous amount of value for whomever we work for,” Dr. Greeno said.
This is also why SHM continues to work with CMS to advocate for all its members. Dr. Greeno is in Washington at least once a month, participating in critical meetings and helping to guide decisions.
“The Public Policy Committee has to get into the weeds and get involved in advocating for measures that truly get at the work we do and push back on metrics and categories that do not relate to the care we are delivering for our patients,” said Dr. Dutta. “The group worked hard to push back on having to comply with Meaningful Use standards for hospitalists, and now we’re exempt from that category. CMS does listen. It sometimes just takes a while.”
References
1. Slavitt A. (2016 Oct 14). A letter from CMS to Medicare clinicians in the Quality Payment Program: We heard you and will continue listening. The CMS Blog (archived). Retrieved from http://wayback.archive-it.org/2744/20161109123921/https://blog.cms.gov/2016/10/14/a-letter-from-cms-to-medicare-clinicians-in-the-quality-payment-program/.
2. Department of Health & Human Services and Centers for Medicare & Medicaid Services. (2016 Oct 14). Quality Payment Program executive summary. Retrieved from https://qpp.cms.gov/docs/QPP_Executive_Summary_of_Final_Rule.pdf.
3. American Medical Association. (2016 Oct 19). Medicare Access and CHIP Reauthorization Act (MACRA) Quality Payment Program final rule AMA summary. Retrieved from https://www.ama-assn.org/sites/default/files/media-browser/public/physicians/macra/macra-qpp-summary.pdf.
4. Slavitt A. (2016 Sept 8). Plans for the Quality Payment Program in 2017: Pick your pace. The CMS Blog (archived). Retrieved from http://wayback.archive-it.org/2744/20161109123909/https://blog.cms.gov/2016/09/08/qualitypaymentprogram-pickyourpace/.
5. The Society of Hospital Medicine. Medicare physician payments are changing. Retrieved from http://www.macraforhm.org/.
6. Department of Health & Human Services and Centers for Medicare & Medicaid Services. (2016 Oct 14). Quality Payment Program fact sheet. Retrieved from https://qpp.cms.gov/docs/QPP_Small_Practice.pdf.
7. The Society of Hospital Medicine. (2017). MACRA and the Quality Payment Program. Retrieved from http://www.macraforhm.org/MACRA_FAQ_m1_final.pdf.
8. Department of Health & Human Services and Centers for Medicare & Medicaid Services. Quality Payment Program: Modernizing Medicare to provide better care and smarter spending for a healthier America. Retrieved from https://qpp.cms.gov/.
9. Wynne B. (2016 Oct 17). MACRA Final Rule: CMS strikes a balance; will docs hang on? Retrieved from http://healthaffairs.org/blog/2016/10/17/macra-final-rule-cms-strikes-a-balance-will-docs-hang-on/.
10. Quinn R. (2015 Aug). TeamHealth-IPC Deal Latest in consolidation trend. The Hospitalist. 2015(8). Retrieved from http://www.the-hospitalist.org/hospitalist/article/122210/teamhealth-ipc-deal-latest-consolidation-trend
11. Barkholz D. (2016 Jun 30). Potential MACRA byproduct: physician consolidation. Retrieved from http://www.modernhealthcare.com/article/20160630/NEWS/160639995.
Triple therapy found as ‘durable’ as biologic after methotrexate failure
People with active rheumatoid arthritis who have a suboptimal response to methotrexate and then switch to triple therapy with methotrexate, sulfasalazine, and hydroxychloroquine do just as well and stay on treatment just as long as do those who switch to methotrexate and etanercept, a follow-up study to the RACAT trial shows.
Although evidence shows that patients do well on combination disease-modifying antirheumatic drugs (DMARDs) following methotrexate failure, many rheumatologists still prefer to add a tumor necrosis factor inhibitor such as etanercept, wrote first author Shana M. Peper, MD, of the University of Nebraska, Omaha, and her colleagues (Arthritis Care Res. 2017 Apr 7. doi: 10.1002/acr.23255).
The observational, follow-up study involved 289 patients with active rheumatoid arthritis with a suboptimal response to methotrexate who had participated in the 48-week, multicenter, double-blind, Rheumatoid Arthritis Comparison of Active Therapies (RACAT) trial and then consented to an additional 72 weeks of open-label extended follow-up during which patients and their physicians were free to change or continue treatment. At the end of the double-blind portion, 145 were receiving triple therapy with the conventional DMARDs and 144 were receiving combination therapy with methotrexate and etanercept.
In the RACAT trial, the primary outcome was the 48-week change in 28-joint Disease Activity Score (DAS28). At 24 weeks, patients in both groups who had an inadequate response to their assigned therapy (defined by a change in DAS28 of less than 1.2) were switched to the other treatment arm in a blinded fashion.
After 1 year, 78% of patients on triple therapy remained on it, compared with 63% of patients who began the extended follow-up on the methotrexate-etanercept combination and remained on it.
More patients switched from methotrexate-etanercept to triple therapy than the other way around (P = .005), but when the researchers removed patients who switched at the start of the extended follow-up from the analysis, continuation rates were nearly identical. The results also did not change when the researchers performed analyses using only the patients who did not switch therapy at week 24 during the blinded trial and again with patients assigned to their original randomized groups.
Average DAS28 scores were similar for each group (3.8 ± 1.4 for triple therapy vs. 3.5 ± 1.3 for methotrexate-etanercept) and remained similar at follow-up. There were also no differences between swollen or tender joint counts, patient global health assessments, or erythrocyte sedimentation rates between the groups.
“Triple therapy remained at least as durable and effective as its biologic counterpart,” the authors concluded.
“Our findings suggest that the majority of patients with active disease despite methotrexate respond to triple therapy and will continue to do so with excellent tolerability,” they wrote.
The findings also supported the approach of reserving more costly biologics for patients who continue to have disease progression despite combination conventional DMARD therapy, they added.
The authors reported no relevant funding for the follow-up analysis. One author reported having consulted for Pfizer and received research support from Bristol-Myers Squibb and AstraZeneca. Another author reported having consulted for Medac, Antares, Lilly, Coherus, and GlaxoSmithKline.
People with active rheumatoid arthritis who have a suboptimal response to methotrexate and then switch to triple therapy with methotrexate, sulfasalazine, and hydroxychloroquine do just as well and stay on treatment just as long as do those who switch to methotrexate and etanercept, a follow-up study to the RACAT trial shows.
Although evidence shows that patients do well on combination disease-modifying antirheumatic drugs (DMARDs) following methotrexate failure, many rheumatologists still prefer to add a tumor necrosis factor inhibitor such as etanercept, wrote first author Shana M. Peper, MD, of the University of Nebraska, Omaha, and her colleagues (Arthritis Care Res. 2017 Apr 7. doi: 10.1002/acr.23255).
The observational, follow-up study involved 289 patients with active rheumatoid arthritis with a suboptimal response to methotrexate who had participated in the 48-week, multicenter, double-blind, Rheumatoid Arthritis Comparison of Active Therapies (RACAT) trial and then consented to an additional 72 weeks of open-label extended follow-up during which patients and their physicians were free to change or continue treatment. At the end of the double-blind portion, 145 were receiving triple therapy with the conventional DMARDs and 144 were receiving combination therapy with methotrexate and etanercept.
In the RACAT trial, the primary outcome was the 48-week change in 28-joint Disease Activity Score (DAS28). At 24 weeks, patients in both groups who had an inadequate response to their assigned therapy (defined by a change in DAS28 of less than 1.2) were switched to the other treatment arm in a blinded fashion.
After 1 year, 78% of patients on triple therapy remained on it, compared with 63% of patients who began the extended follow-up on the methotrexate-etanercept combination and remained on it.
More patients switched from methotrexate-etanercept to triple therapy than the other way around (P = .005), but when the researchers removed patients who switched at the start of the extended follow-up from the analysis, continuation rates were nearly identical. The results also did not change when the researchers performed analyses using only the patients who did not switch therapy at week 24 during the blinded trial and again with patients assigned to their original randomized groups.
Average DAS28 scores were similar for each group (3.8 ± 1.4 for triple therapy vs. 3.5 ± 1.3 for methotrexate-etanercept) and remained similar at follow-up. There were also no differences between swollen or tender joint counts, patient global health assessments, or erythrocyte sedimentation rates between the groups.
“Triple therapy remained at least as durable and effective as its biologic counterpart,” the authors concluded.
“Our findings suggest that the majority of patients with active disease despite methotrexate respond to triple therapy and will continue to do so with excellent tolerability,” they wrote.
The findings also supported the approach of reserving more costly biologics for patients who continue to have disease progression despite combination conventional DMARD therapy, they added.
The authors reported no relevant funding for the follow-up analysis. One author reported having consulted for Pfizer and received research support from Bristol-Myers Squibb and AstraZeneca. Another author reported having consulted for Medac, Antares, Lilly, Coherus, and GlaxoSmithKline.
People with active rheumatoid arthritis who have a suboptimal response to methotrexate and then switch to triple therapy with methotrexate, sulfasalazine, and hydroxychloroquine do just as well and stay on treatment just as long as do those who switch to methotrexate and etanercept, a follow-up study to the RACAT trial shows.
Although evidence shows that patients do well on combination disease-modifying antirheumatic drugs (DMARDs) following methotrexate failure, many rheumatologists still prefer to add a tumor necrosis factor inhibitor such as etanercept, wrote first author Shana M. Peper, MD, of the University of Nebraska, Omaha, and her colleagues (Arthritis Care Res. 2017 Apr 7. doi: 10.1002/acr.23255).
The observational, follow-up study involved 289 patients with active rheumatoid arthritis with a suboptimal response to methotrexate who had participated in the 48-week, multicenter, double-blind, Rheumatoid Arthritis Comparison of Active Therapies (RACAT) trial and then consented to an additional 72 weeks of open-label extended follow-up during which patients and their physicians were free to change or continue treatment. At the end of the double-blind portion, 145 were receiving triple therapy with the conventional DMARDs and 144 were receiving combination therapy with methotrexate and etanercept.
In the RACAT trial, the primary outcome was the 48-week change in 28-joint Disease Activity Score (DAS28). At 24 weeks, patients in both groups who had an inadequate response to their assigned therapy (defined by a change in DAS28 of less than 1.2) were switched to the other treatment arm in a blinded fashion.
After 1 year, 78% of patients on triple therapy remained on it, compared with 63% of patients who began the extended follow-up on the methotrexate-etanercept combination and remained on it.
More patients switched from methotrexate-etanercept to triple therapy than the other way around (P = .005), but when the researchers removed patients who switched at the start of the extended follow-up from the analysis, continuation rates were nearly identical. The results also did not change when the researchers performed analyses using only the patients who did not switch therapy at week 24 during the blinded trial and again with patients assigned to their original randomized groups.
Average DAS28 scores were similar for each group (3.8 ± 1.4 for triple therapy vs. 3.5 ± 1.3 for methotrexate-etanercept) and remained similar at follow-up. There were also no differences between swollen or tender joint counts, patient global health assessments, or erythrocyte sedimentation rates between the groups.
“Triple therapy remained at least as durable and effective as its biologic counterpart,” the authors concluded.
“Our findings suggest that the majority of patients with active disease despite methotrexate respond to triple therapy and will continue to do so with excellent tolerability,” they wrote.
The findings also supported the approach of reserving more costly biologics for patients who continue to have disease progression despite combination conventional DMARD therapy, they added.
The authors reported no relevant funding for the follow-up analysis. One author reported having consulted for Pfizer and received research support from Bristol-Myers Squibb and AstraZeneca. Another author reported having consulted for Medac, Antares, Lilly, Coherus, and GlaxoSmithKline.
Key clinical point:
Major finding: At 1 year, people with active RA with a suboptimal response to methotrexate were just as likely to remain on triple DMARD therapy as they were on etanercept plus methotrexate.
Data source: An observational follow-up study of 289 patients with RA who had participated in the 48-week, multicenter, double-blind, RACAT trial.
Disclosures: The authors reported no relevant funding for the follow-up analysis. One author reported having consulted for Pfizer and received research support from Bristol-Myers Squibb and AstraZeneca. Another author reported having consulted for Medac, Antares, Lilly, Coherus, and GlaxoSmithKline.
Hospitalist specialty code goes live: What ‘C6’ means for you
The long wait for the introduction of the C6 hospitalist specialty code has ended. If you are a provider, hospital, or hospitalist administrator, this new specialty designation is important.
The Centers for Medicare & Medicaid Services tracks specialty utilization and compares providers across the country using codes attached to medical specialties, such as cardiology, emergency medicine, pediatrics, etc. Until the CMS designated hospital medicine as a unique specialty, hospitalists were grouped together with office-based internal medicine physicians and general practitioners. This lack of recognition of the hospitalist specialty created two issues.
The first is one of location. Hospitalists practice in hospitals and utilize codes that are hospital based, not office based. Yet hospitalists have been benchmarked against their primary care peers’ utilization for many years. At this point in time, most if not all primary care physicians practice exclusively in the office, so comparison of CPT utilization looks unusual when benchmarked nationally. What appeared as a ‘spike’ was actually normal utilization for a hospitalist; however, this coding anomaly can lead to pre- or postpayment audits.
The second issue is being able to benchmark utilization against one’s peers. For the first time, hospitalist utilization will be considered unique, facilitating more accurate comparisons and fairer assessments of hospitalist performance.
Hospitalists can use the C6 specialty code during initial enrollment or as an update, depending on the individual situation. Note that this is a designation for the individual, not the practice, organization, or billing company. The C6 specialty code was recognized as of April 1, 2017, on submitted claims. You may now change your designation and should avoid any disruption or denial of claims.
There are two places to designate the C6 specialty codes, depending on whether the provider is new to Medicare enrollment or is an existing provider:
• Paper: Initial enrollment in the Medicare program on form CMS-855I or CMS 855O (https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/CMS-Forms-List.html).
• Electronically: Utilizing the PECOS system, provider credentialing offices can update existing specialty codes to C6 (https://pecos.cms.hhs.gov/PECOSWebMaintenance.htm).
This major milestone for hospital medicine demonstrates the continued growth and impact of the specialty. Ensure your self-election in the PECOS system reflects “C6,” your specialty as a hospitalist and your commitment to the hospital medicine movement.
For more information, visit www.hospitalmedicine.org/C6.
Dea Robinson is a member of SHM’s Practice Management Committee, Cultural Competency Workgroup and Physician Burnout Workgroup.
Reference: MLN Matters Number: MM9716 ( https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/Downloads/MM9716.pdf)
The long wait for the introduction of the C6 hospitalist specialty code has ended. If you are a provider, hospital, or hospitalist administrator, this new specialty designation is important.
The Centers for Medicare & Medicaid Services tracks specialty utilization and compares providers across the country using codes attached to medical specialties, such as cardiology, emergency medicine, pediatrics, etc. Until the CMS designated hospital medicine as a unique specialty, hospitalists were grouped together with office-based internal medicine physicians and general practitioners. This lack of recognition of the hospitalist specialty created two issues.
The first is one of location. Hospitalists practice in hospitals and utilize codes that are hospital based, not office based. Yet hospitalists have been benchmarked against their primary care peers’ utilization for many years. At this point in time, most if not all primary care physicians practice exclusively in the office, so comparison of CPT utilization looks unusual when benchmarked nationally. What appeared as a ‘spike’ was actually normal utilization for a hospitalist; however, this coding anomaly can lead to pre- or postpayment audits.
The second issue is being able to benchmark utilization against one’s peers. For the first time, hospitalist utilization will be considered unique, facilitating more accurate comparisons and fairer assessments of hospitalist performance.
Hospitalists can use the C6 specialty code during initial enrollment or as an update, depending on the individual situation. Note that this is a designation for the individual, not the practice, organization, or billing company. The C6 specialty code was recognized as of April 1, 2017, on submitted claims. You may now change your designation and should avoid any disruption or denial of claims.
There are two places to designate the C6 specialty codes, depending on whether the provider is new to Medicare enrollment or is an existing provider:
• Paper: Initial enrollment in the Medicare program on form CMS-855I or CMS 855O (https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/CMS-Forms-List.html).
• Electronically: Utilizing the PECOS system, provider credentialing offices can update existing specialty codes to C6 (https://pecos.cms.hhs.gov/PECOSWebMaintenance.htm).
This major milestone for hospital medicine demonstrates the continued growth and impact of the specialty. Ensure your self-election in the PECOS system reflects “C6,” your specialty as a hospitalist and your commitment to the hospital medicine movement.
For more information, visit www.hospitalmedicine.org/C6.
Dea Robinson is a member of SHM’s Practice Management Committee, Cultural Competency Workgroup and Physician Burnout Workgroup.
Reference: MLN Matters Number: MM9716 ( https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/Downloads/MM9716.pdf)
The long wait for the introduction of the C6 hospitalist specialty code has ended. If you are a provider, hospital, or hospitalist administrator, this new specialty designation is important.
The Centers for Medicare & Medicaid Services tracks specialty utilization and compares providers across the country using codes attached to medical specialties, such as cardiology, emergency medicine, pediatrics, etc. Until the CMS designated hospital medicine as a unique specialty, hospitalists were grouped together with office-based internal medicine physicians and general practitioners. This lack of recognition of the hospitalist specialty created two issues.
The first is one of location. Hospitalists practice in hospitals and utilize codes that are hospital based, not office based. Yet hospitalists have been benchmarked against their primary care peers’ utilization for many years. At this point in time, most if not all primary care physicians practice exclusively in the office, so comparison of CPT utilization looks unusual when benchmarked nationally. What appeared as a ‘spike’ was actually normal utilization for a hospitalist; however, this coding anomaly can lead to pre- or postpayment audits.
The second issue is being able to benchmark utilization against one’s peers. For the first time, hospitalist utilization will be considered unique, facilitating more accurate comparisons and fairer assessments of hospitalist performance.
Hospitalists can use the C6 specialty code during initial enrollment or as an update, depending on the individual situation. Note that this is a designation for the individual, not the practice, organization, or billing company. The C6 specialty code was recognized as of April 1, 2017, on submitted claims. You may now change your designation and should avoid any disruption or denial of claims.
There are two places to designate the C6 specialty codes, depending on whether the provider is new to Medicare enrollment or is an existing provider:
• Paper: Initial enrollment in the Medicare program on form CMS-855I or CMS 855O (https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/CMS-Forms-List.html).
• Electronically: Utilizing the PECOS system, provider credentialing offices can update existing specialty codes to C6 (https://pecos.cms.hhs.gov/PECOSWebMaintenance.htm).
This major milestone for hospital medicine demonstrates the continued growth and impact of the specialty. Ensure your self-election in the PECOS system reflects “C6,” your specialty as a hospitalist and your commitment to the hospital medicine movement.
For more information, visit www.hospitalmedicine.org/C6.
Dea Robinson is a member of SHM’s Practice Management Committee, Cultural Competency Workgroup and Physician Burnout Workgroup.
Reference: MLN Matters Number: MM9716 ( https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/Downloads/MM9716.pdf)
If you ask me ...
In a feature article in Pediatric News entitled “What do doctors want from health reform,” Alicia Gallegos reports on the results of a recent online Frontline Medical News poll of 390 physicians who were asked what one thing about the ACA they would change. The answers were scattered, but “Stabilize premiums and out of pocket expenses for patients” garnered 50% of the votes.
I suspect that this result was an anguished cry for some leadership in Washington. It could come from the left or the right or, even better, from a coalition. But please, we just need some clear leadership, some direction, and a plan that would allow all of us – physicians, patients, hospitals, and insurance companies – to get on with our various missions.
The cost of medication is another major driver of health care cost. Any new plan or adjustments to the ACA should more forcefully rein in or outright eliminate the pharmacy benefit managers who needlessly add cost to medication. Although most of us grumble when faced with cookbook recipes for care that constrain our prescribing choices, we must accept that, in most cases, these evidence-based guidelines are necessary evils. At the same time, we should vigorously support and cooperate with the efforts to discipline the flagrant overprescribers in our midst.
It is not surprising that the ACA has had difficulty attracting young healthy people to buy health insurance that is costly even at a discount. Offering a lower price, no frills, catastrophic care option might be more appealing to young people who still see themselves as invincible. While, as pediatricians, we can see the benefit of immunizations and preventive care in the first year of life, it may be time for a more critical look at the cost benefit ratio for other preventive initiatives in older age groups that may sound good but are making health insurance more expensive.
Finally, an improved ACA should make reduction of the administrative burden of prior authorizations a high priority. Michael L. Munger, MD, president-elect of the American Academy of Family Physicians, suggests that a standard process for both private and publicly funded patients would allow physicians to focus their time and talents on more efficient patient care. The failure of the ACA to mandate even basic standardization for electronic health records has left us with a nonsystem made up of mini-systems that are neither user friendly nor capable of effectively communicating with one another.
It appears that this country doesn’t yet have the stomach for a single payer model. While I usually believe that compromise will yield a good result, the ACA is an example of when a leadership vacuum can result in a collection of bad compromises.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
[polldaddy:9708248]
In a feature article in Pediatric News entitled “What do doctors want from health reform,” Alicia Gallegos reports on the results of a recent online Frontline Medical News poll of 390 physicians who were asked what one thing about the ACA they would change. The answers were scattered, but “Stabilize premiums and out of pocket expenses for patients” garnered 50% of the votes.
I suspect that this result was an anguished cry for some leadership in Washington. It could come from the left or the right or, even better, from a coalition. But please, we just need some clear leadership, some direction, and a plan that would allow all of us – physicians, patients, hospitals, and insurance companies – to get on with our various missions.
The cost of medication is another major driver of health care cost. Any new plan or adjustments to the ACA should more forcefully rein in or outright eliminate the pharmacy benefit managers who needlessly add cost to medication. Although most of us grumble when faced with cookbook recipes for care that constrain our prescribing choices, we must accept that, in most cases, these evidence-based guidelines are necessary evils. At the same time, we should vigorously support and cooperate with the efforts to discipline the flagrant overprescribers in our midst.
It is not surprising that the ACA has had difficulty attracting young healthy people to buy health insurance that is costly even at a discount. Offering a lower price, no frills, catastrophic care option might be more appealing to young people who still see themselves as invincible. While, as pediatricians, we can see the benefit of immunizations and preventive care in the first year of life, it may be time for a more critical look at the cost benefit ratio for other preventive initiatives in older age groups that may sound good but are making health insurance more expensive.
Finally, an improved ACA should make reduction of the administrative burden of prior authorizations a high priority. Michael L. Munger, MD, president-elect of the American Academy of Family Physicians, suggests that a standard process for both private and publicly funded patients would allow physicians to focus their time and talents on more efficient patient care. The failure of the ACA to mandate even basic standardization for electronic health records has left us with a nonsystem made up of mini-systems that are neither user friendly nor capable of effectively communicating with one another.
It appears that this country doesn’t yet have the stomach for a single payer model. While I usually believe that compromise will yield a good result, the ACA is an example of when a leadership vacuum can result in a collection of bad compromises.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
[polldaddy:9708248]
In a feature article in Pediatric News entitled “What do doctors want from health reform,” Alicia Gallegos reports on the results of a recent online Frontline Medical News poll of 390 physicians who were asked what one thing about the ACA they would change. The answers were scattered, but “Stabilize premiums and out of pocket expenses for patients” garnered 50% of the votes.
I suspect that this result was an anguished cry for some leadership in Washington. It could come from the left or the right or, even better, from a coalition. But please, we just need some clear leadership, some direction, and a plan that would allow all of us – physicians, patients, hospitals, and insurance companies – to get on with our various missions.
The cost of medication is another major driver of health care cost. Any new plan or adjustments to the ACA should more forcefully rein in or outright eliminate the pharmacy benefit managers who needlessly add cost to medication. Although most of us grumble when faced with cookbook recipes for care that constrain our prescribing choices, we must accept that, in most cases, these evidence-based guidelines are necessary evils. At the same time, we should vigorously support and cooperate with the efforts to discipline the flagrant overprescribers in our midst.
It is not surprising that the ACA has had difficulty attracting young healthy people to buy health insurance that is costly even at a discount. Offering a lower price, no frills, catastrophic care option might be more appealing to young people who still see themselves as invincible. While, as pediatricians, we can see the benefit of immunizations and preventive care in the first year of life, it may be time for a more critical look at the cost benefit ratio for other preventive initiatives in older age groups that may sound good but are making health insurance more expensive.
Finally, an improved ACA should make reduction of the administrative burden of prior authorizations a high priority. Michael L. Munger, MD, president-elect of the American Academy of Family Physicians, suggests that a standard process for both private and publicly funded patients would allow physicians to focus their time and talents on more efficient patient care. The failure of the ACA to mandate even basic standardization for electronic health records has left us with a nonsystem made up of mini-systems that are neither user friendly nor capable of effectively communicating with one another.
It appears that this country doesn’t yet have the stomach for a single payer model. While I usually believe that compromise will yield a good result, the ACA is an example of when a leadership vacuum can result in a collection of bad compromises.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
[polldaddy:9708248]
Genital HPV prevalence tops 42% in adults
The overall prevalence of genital human papillomavirus (HPV) among adults aged 18-59 years was 42.5% in 2013-2014, with more than half of that representing infection with high-risk types, according to the National Center for Health Statistics.
Prevalence of the 14 HPV types (out of 37 total) considered to be high risk was almost 23% in 2013-2014. Men were significantly more likely than women to have any genital HPV (45% vs. 40%) and high-risk genital HPV (25% vs. 20%), the NCHS reported.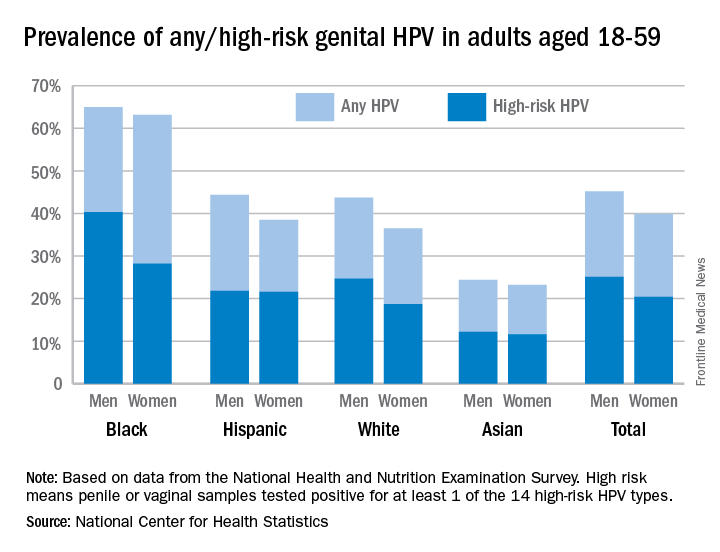
Oral rinse samples were collected as well for adults aged 18-69 years, and the overall prevalence was 7.3% for any oral HPV and 4% for high-risk HPV in 2011-2014. Prevalence among men was significantly higher than among women for all oral HPV (11.5% vs. 3.3%) and for high-risk HPV (6.8% vs. 1.2%), the NCHS said.
The overall prevalence of genital human papillomavirus (HPV) among adults aged 18-59 years was 42.5% in 2013-2014, with more than half of that representing infection with high-risk types, according to the National Center for Health Statistics.
Prevalence of the 14 HPV types (out of 37 total) considered to be high risk was almost 23% in 2013-2014. Men were significantly more likely than women to have any genital HPV (45% vs. 40%) and high-risk genital HPV (25% vs. 20%), the NCHS reported.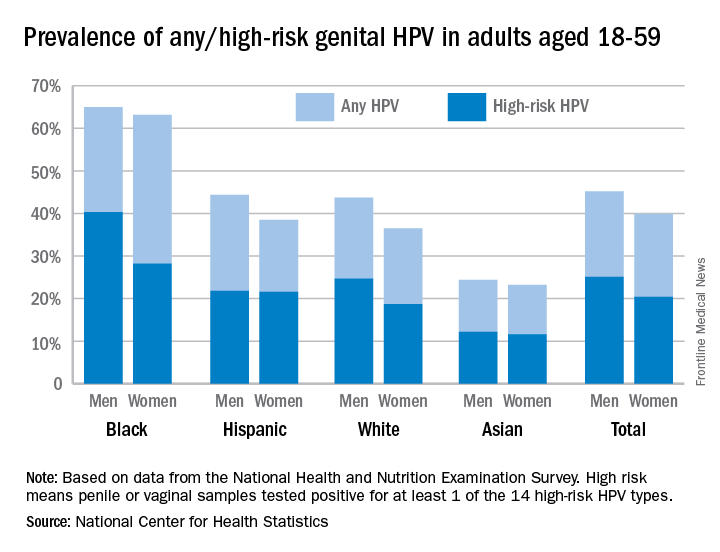
Oral rinse samples were collected as well for adults aged 18-69 years, and the overall prevalence was 7.3% for any oral HPV and 4% for high-risk HPV in 2011-2014. Prevalence among men was significantly higher than among women for all oral HPV (11.5% vs. 3.3%) and for high-risk HPV (6.8% vs. 1.2%), the NCHS said.
The overall prevalence of genital human papillomavirus (HPV) among adults aged 18-59 years was 42.5% in 2013-2014, with more than half of that representing infection with high-risk types, according to the National Center for Health Statistics.
Prevalence of the 14 HPV types (out of 37 total) considered to be high risk was almost 23% in 2013-2014. Men were significantly more likely than women to have any genital HPV (45% vs. 40%) and high-risk genital HPV (25% vs. 20%), the NCHS reported.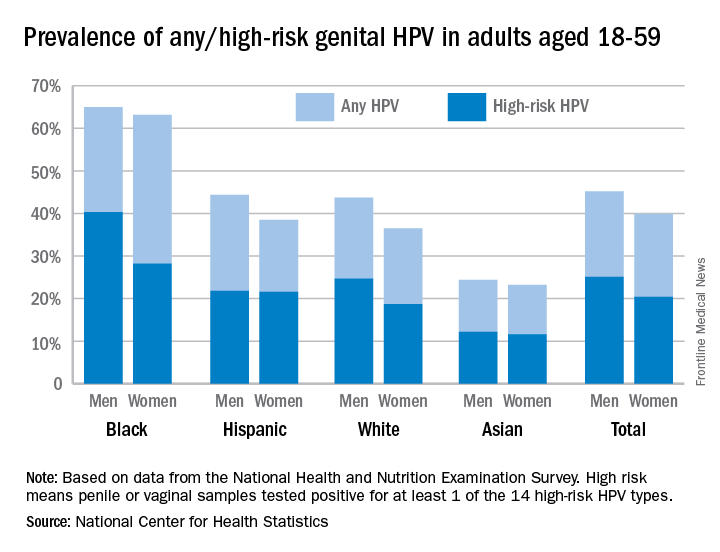
Oral rinse samples were collected as well for adults aged 18-69 years, and the overall prevalence was 7.3% for any oral HPV and 4% for high-risk HPV in 2011-2014. Prevalence among men was significantly higher than among women for all oral HPV (11.5% vs. 3.3%) and for high-risk HPV (6.8% vs. 1.2%), the NCHS said.
Hepatitis Outlook: March 2017
If you work on the front lines of medical care, treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering the major hepatitis viruses.
Preliver transplant treatment with a highly effective, all-oral direct-acting antiviral agent regimen provides the best health outcomes and is the most cost-effective strategy for the treatment of patients with hepatitis C virus with hepatocellular carcinoma or decompensated cirrhosis who are waitlisted for liver transplant, a study in Hepatology revealed.
A recent study in the Journal of Viral Hepatitis found that patients with chronic HCV and compensated or decompensated cirrhosis who achieve sustained viral response can have clinically meaningful reductions in hepatic venous pressure gradient at long-term follow-up.
The hepatic expressions of cannabinoid receptor 1 and cannabinoid receptor 2 play important roles during the progression of fibrosis induced by chronic hepatitis B virus, according to a study in the International Journal of Infectious Diseases.
A study in the Journal of Viral Hepatitis found that the Pooled Cohort atherosclerotic cardiovascular disease risk equation overestimated the risk of cardiovascular disease among lower-risk patients and underestimated risk among higher-risk patients in both HCV-infected and uninfected groups.
A multinational study in Hepatology found that hemoglobin levels and international normalized ratio values were similar in patients with inherited bleeding disorders and HCV infection who received elbasvir/grazoprevir and placebo.
The number of HBV patients in the United States requiring liver transplantation remained stable, according to a recent study in the Journal of Viral Hepatitis, but the proportion of HBV patients with hepatocellular carcinoma continues to rise.
A research letter in the Morbidity and Mortality Weekly Report reported the transmission of HCV from the inappropriate reuse of saline flush syringes for multiple patients in an acute care hospital in Texas.
A large German study in the Journal of Viral Hepatitis found that ombitasvir/paritaprevir/ritonavir plus/minus dasabuvir plus/minus ribavirin for treatment of HCV genotype 1 and genotype 4 infection was effective and generally well tolerated in clinical practice.
A study, conducted in South Korea, in Hepatology found that monotherapy with tenofovir disoproxil fumarate was efficacious and safe for up to 144 weeks in heavily pretreated patients with multidrug-resistant HBV infection.
Overt and occult HBV infection of children was more serious in underdeveloped northwest regions of China, a study in the Journal of Viral Hepatitis found, suggesting that HBV neonatal immunization and catch-up programs should be strengthened and supplemented.
A study in Hepatology found that long-term entecavir monotherapy is highly effective in preventing HBV reactivation after liver transplantation for chronic HBV, with a durable HBV surface antigen seroclearance rate of 92%, undetectable HBV DNA rate of 100% at 8 years, and excellent long-term survival of 85% at 9 years.
An Italian study in the Journal of Viral Hepatitis found that treatment with direct-acting antivirals was effective and well tolerated in people who inject drugs, although cirrhotic subjects with Model For End-Stage Liver Disease scores greater than 10 and albumin levels below 3 g/dL showed a higher risk of developing serious adverse events and treatment failure.
Direct-acting antiviral–based treatments for severe posttransplant HCV recurrence, comprising fibrosing cholestatic hepatitis, significantly improves liver function even without viral clearance and permits excellent long-term survival, according to a study in the Journal of Viral Hepatitis.
[email protected]
On Twitter @richpizzi
If you work on the front lines of medical care, treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering the major hepatitis viruses.
Preliver transplant treatment with a highly effective, all-oral direct-acting antiviral agent regimen provides the best health outcomes and is the most cost-effective strategy for the treatment of patients with hepatitis C virus with hepatocellular carcinoma or decompensated cirrhosis who are waitlisted for liver transplant, a study in Hepatology revealed.
A recent study in the Journal of Viral Hepatitis found that patients with chronic HCV and compensated or decompensated cirrhosis who achieve sustained viral response can have clinically meaningful reductions in hepatic venous pressure gradient at long-term follow-up.
The hepatic expressions of cannabinoid receptor 1 and cannabinoid receptor 2 play important roles during the progression of fibrosis induced by chronic hepatitis B virus, according to a study in the International Journal of Infectious Diseases.
A study in the Journal of Viral Hepatitis found that the Pooled Cohort atherosclerotic cardiovascular disease risk equation overestimated the risk of cardiovascular disease among lower-risk patients and underestimated risk among higher-risk patients in both HCV-infected and uninfected groups.
A multinational study in Hepatology found that hemoglobin levels and international normalized ratio values were similar in patients with inherited bleeding disorders and HCV infection who received elbasvir/grazoprevir and placebo.
The number of HBV patients in the United States requiring liver transplantation remained stable, according to a recent study in the Journal of Viral Hepatitis, but the proportion of HBV patients with hepatocellular carcinoma continues to rise.
A research letter in the Morbidity and Mortality Weekly Report reported the transmission of HCV from the inappropriate reuse of saline flush syringes for multiple patients in an acute care hospital in Texas.
A large German study in the Journal of Viral Hepatitis found that ombitasvir/paritaprevir/ritonavir plus/minus dasabuvir plus/minus ribavirin for treatment of HCV genotype 1 and genotype 4 infection was effective and generally well tolerated in clinical practice.
A study, conducted in South Korea, in Hepatology found that monotherapy with tenofovir disoproxil fumarate was efficacious and safe for up to 144 weeks in heavily pretreated patients with multidrug-resistant HBV infection.
Overt and occult HBV infection of children was more serious in underdeveloped northwest regions of China, a study in the Journal of Viral Hepatitis found, suggesting that HBV neonatal immunization and catch-up programs should be strengthened and supplemented.
A study in Hepatology found that long-term entecavir monotherapy is highly effective in preventing HBV reactivation after liver transplantation for chronic HBV, with a durable HBV surface antigen seroclearance rate of 92%, undetectable HBV DNA rate of 100% at 8 years, and excellent long-term survival of 85% at 9 years.
An Italian study in the Journal of Viral Hepatitis found that treatment with direct-acting antivirals was effective and well tolerated in people who inject drugs, although cirrhotic subjects with Model For End-Stage Liver Disease scores greater than 10 and albumin levels below 3 g/dL showed a higher risk of developing serious adverse events and treatment failure.
Direct-acting antiviral–based treatments for severe posttransplant HCV recurrence, comprising fibrosing cholestatic hepatitis, significantly improves liver function even without viral clearance and permits excellent long-term survival, according to a study in the Journal of Viral Hepatitis.
[email protected]
On Twitter @richpizzi
If you work on the front lines of medical care, treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering the major hepatitis viruses.
Preliver transplant treatment with a highly effective, all-oral direct-acting antiviral agent regimen provides the best health outcomes and is the most cost-effective strategy for the treatment of patients with hepatitis C virus with hepatocellular carcinoma or decompensated cirrhosis who are waitlisted for liver transplant, a study in Hepatology revealed.
A recent study in the Journal of Viral Hepatitis found that patients with chronic HCV and compensated or decompensated cirrhosis who achieve sustained viral response can have clinically meaningful reductions in hepatic venous pressure gradient at long-term follow-up.
The hepatic expressions of cannabinoid receptor 1 and cannabinoid receptor 2 play important roles during the progression of fibrosis induced by chronic hepatitis B virus, according to a study in the International Journal of Infectious Diseases.
A study in the Journal of Viral Hepatitis found that the Pooled Cohort atherosclerotic cardiovascular disease risk equation overestimated the risk of cardiovascular disease among lower-risk patients and underestimated risk among higher-risk patients in both HCV-infected and uninfected groups.
A multinational study in Hepatology found that hemoglobin levels and international normalized ratio values were similar in patients with inherited bleeding disorders and HCV infection who received elbasvir/grazoprevir and placebo.
The number of HBV patients in the United States requiring liver transplantation remained stable, according to a recent study in the Journal of Viral Hepatitis, but the proportion of HBV patients with hepatocellular carcinoma continues to rise.
A research letter in the Morbidity and Mortality Weekly Report reported the transmission of HCV from the inappropriate reuse of saline flush syringes for multiple patients in an acute care hospital in Texas.
A large German study in the Journal of Viral Hepatitis found that ombitasvir/paritaprevir/ritonavir plus/minus dasabuvir plus/minus ribavirin for treatment of HCV genotype 1 and genotype 4 infection was effective and generally well tolerated in clinical practice.
A study, conducted in South Korea, in Hepatology found that monotherapy with tenofovir disoproxil fumarate was efficacious and safe for up to 144 weeks in heavily pretreated patients with multidrug-resistant HBV infection.
Overt and occult HBV infection of children was more serious in underdeveloped northwest regions of China, a study in the Journal of Viral Hepatitis found, suggesting that HBV neonatal immunization and catch-up programs should be strengthened and supplemented.
A study in Hepatology found that long-term entecavir monotherapy is highly effective in preventing HBV reactivation after liver transplantation for chronic HBV, with a durable HBV surface antigen seroclearance rate of 92%, undetectable HBV DNA rate of 100% at 8 years, and excellent long-term survival of 85% at 9 years.
An Italian study in the Journal of Viral Hepatitis found that treatment with direct-acting antivirals was effective and well tolerated in people who inject drugs, although cirrhotic subjects with Model For End-Stage Liver Disease scores greater than 10 and albumin levels below 3 g/dL showed a higher risk of developing serious adverse events and treatment failure.
Direct-acting antiviral–based treatments for severe posttransplant HCV recurrence, comprising fibrosing cholestatic hepatitis, significantly improves liver function even without viral clearance and permits excellent long-term survival, according to a study in the Journal of Viral Hepatitis.
[email protected]
On Twitter @richpizzi














