User login
VA Nurses Advocate for Best Care
The Nurses Organization of Veterans Affairs (NOVA) is a national nonprofit professional organization whose members are VA nurses working at VHA facilities throughout the country and caring for America’s heroes. For more than 35 years, NOVA has been the voice of VA nurses. Speaking strongly on behalf of its more than 3,000 members, NOVA leaders recently met in Washington, DC, for the annual Capitol Hill meetings and Legislative Roundtable.
With the elections over and new members taking their seats in the 115th Congress, NOVA leadership spoke candidly about ongoing VA transformation, choice, recruitment and retention, and access to care with respect to the new advanced practice registered nurse (APRN) regulation being implemented across VHA facilities. The APRN regulation allowing APRNs to practice to their full authority within the VA cleared in December. It grants 3 of the 4 APRN roles (nurse practitioners, certified nurse-midwives, and clinical nurse specialists) the ability to practice to the full extent of their education and training.
Armed with copies of the organization’s 2017 Legislative Priority Goals, NOVA leadership met with congressional members and staff of the House and Senate VA committees. Among NOVA’s priorities for the 115th Congress are the following:
- Effects of the federal hiring freeze
- VA transformation
- CHOICE/community-integrated health care
- Information technology
- Retention/recruitment and staffing
For a complete list of the 2017 Legislative Priority Goals, visit vanurse.org
Committee members were eager to hear the opinions of NOVA experts on the Choice Act and on the status of hiring initiatives at their facilities. A key staffing provision of the Veterans Access, Choice, and Accountability Act included an increase in hiring authority and a more generous loan repayment for those looking to work at the VA. In addition, Congress authorized $5 million in funding to hire more medical professionals. A VA internal audit found that the need for additional doctors, nurses, and specialty care was the highest barrier or challenge to providing access to care. NOVA testified on this issue before the 114th Congress.
Staff of House and Senate VA Committees shared other legislative priorities, including the reauthorization of the Choice Act and continued oversight of many areas within the VA, to include a sharp look at access and coordination of care and accountability.
The meeting concluded with the NOVA Legislative Roundtable discussion. Held at the Washington, DC, offices of the Disabled American Veterans service organization, the roundtable was attended by more than 25 organizations that have a stake in veterans’ health care. Leaders from various professional nursing organizations, veterans service organizations, VA Office of Nursing Services, the American Federation of Government Employees, and staff from both the House and Senate VA committees were in attendance.
A lively discussion was held regarding the future of VA health care, APRN implementation, workforce/ retention and recruitment issues, as well as telehealth and the opioid epidemic as it relates to VA patients. The release of the President’s proposed budget also was discussed. As is often the case with a new administration, a “skinny” or outline of a budget proposal is released in advance of an actual detailed budget, which included a substantial 10% increase in VA’s anticipated budget for overall discretionary items (over FY 2017) and an 8.3% increase for medical care (over FY 2017).
For more information about NOVA or to become a member, visit vanurse.org.
The Nurses Organization of Veterans Affairs (NOVA) is a national nonprofit professional organization whose members are VA nurses working at VHA facilities throughout the country and caring for America’s heroes. For more than 35 years, NOVA has been the voice of VA nurses. Speaking strongly on behalf of its more than 3,000 members, NOVA leaders recently met in Washington, DC, for the annual Capitol Hill meetings and Legislative Roundtable.
With the elections over and new members taking their seats in the 115th Congress, NOVA leadership spoke candidly about ongoing VA transformation, choice, recruitment and retention, and access to care with respect to the new advanced practice registered nurse (APRN) regulation being implemented across VHA facilities. The APRN regulation allowing APRNs to practice to their full authority within the VA cleared in December. It grants 3 of the 4 APRN roles (nurse practitioners, certified nurse-midwives, and clinical nurse specialists) the ability to practice to the full extent of their education and training.
Armed with copies of the organization’s 2017 Legislative Priority Goals, NOVA leadership met with congressional members and staff of the House and Senate VA committees. Among NOVA’s priorities for the 115th Congress are the following:
- Effects of the federal hiring freeze
- VA transformation
- CHOICE/community-integrated health care
- Information technology
- Retention/recruitment and staffing
For a complete list of the 2017 Legislative Priority Goals, visit vanurse.org
Committee members were eager to hear the opinions of NOVA experts on the Choice Act and on the status of hiring initiatives at their facilities. A key staffing provision of the Veterans Access, Choice, and Accountability Act included an increase in hiring authority and a more generous loan repayment for those looking to work at the VA. In addition, Congress authorized $5 million in funding to hire more medical professionals. A VA internal audit found that the need for additional doctors, nurses, and specialty care was the highest barrier or challenge to providing access to care. NOVA testified on this issue before the 114th Congress.
Staff of House and Senate VA Committees shared other legislative priorities, including the reauthorization of the Choice Act and continued oversight of many areas within the VA, to include a sharp look at access and coordination of care and accountability.
The meeting concluded with the NOVA Legislative Roundtable discussion. Held at the Washington, DC, offices of the Disabled American Veterans service organization, the roundtable was attended by more than 25 organizations that have a stake in veterans’ health care. Leaders from various professional nursing organizations, veterans service organizations, VA Office of Nursing Services, the American Federation of Government Employees, and staff from both the House and Senate VA committees were in attendance.
A lively discussion was held regarding the future of VA health care, APRN implementation, workforce/ retention and recruitment issues, as well as telehealth and the opioid epidemic as it relates to VA patients. The release of the President’s proposed budget also was discussed. As is often the case with a new administration, a “skinny” or outline of a budget proposal is released in advance of an actual detailed budget, which included a substantial 10% increase in VA’s anticipated budget for overall discretionary items (over FY 2017) and an 8.3% increase for medical care (over FY 2017).
For more information about NOVA or to become a member, visit vanurse.org.
The Nurses Organization of Veterans Affairs (NOVA) is a national nonprofit professional organization whose members are VA nurses working at VHA facilities throughout the country and caring for America’s heroes. For more than 35 years, NOVA has been the voice of VA nurses. Speaking strongly on behalf of its more than 3,000 members, NOVA leaders recently met in Washington, DC, for the annual Capitol Hill meetings and Legislative Roundtable.
With the elections over and new members taking their seats in the 115th Congress, NOVA leadership spoke candidly about ongoing VA transformation, choice, recruitment and retention, and access to care with respect to the new advanced practice registered nurse (APRN) regulation being implemented across VHA facilities. The APRN regulation allowing APRNs to practice to their full authority within the VA cleared in December. It grants 3 of the 4 APRN roles (nurse practitioners, certified nurse-midwives, and clinical nurse specialists) the ability to practice to the full extent of their education and training.
Armed with copies of the organization’s 2017 Legislative Priority Goals, NOVA leadership met with congressional members and staff of the House and Senate VA committees. Among NOVA’s priorities for the 115th Congress are the following:
- Effects of the federal hiring freeze
- VA transformation
- CHOICE/community-integrated health care
- Information technology
- Retention/recruitment and staffing
For a complete list of the 2017 Legislative Priority Goals, visit vanurse.org
Committee members were eager to hear the opinions of NOVA experts on the Choice Act and on the status of hiring initiatives at their facilities. A key staffing provision of the Veterans Access, Choice, and Accountability Act included an increase in hiring authority and a more generous loan repayment for those looking to work at the VA. In addition, Congress authorized $5 million in funding to hire more medical professionals. A VA internal audit found that the need for additional doctors, nurses, and specialty care was the highest barrier or challenge to providing access to care. NOVA testified on this issue before the 114th Congress.
Staff of House and Senate VA Committees shared other legislative priorities, including the reauthorization of the Choice Act and continued oversight of many areas within the VA, to include a sharp look at access and coordination of care and accountability.
The meeting concluded with the NOVA Legislative Roundtable discussion. Held at the Washington, DC, offices of the Disabled American Veterans service organization, the roundtable was attended by more than 25 organizations that have a stake in veterans’ health care. Leaders from various professional nursing organizations, veterans service organizations, VA Office of Nursing Services, the American Federation of Government Employees, and staff from both the House and Senate VA committees were in attendance.
A lively discussion was held regarding the future of VA health care, APRN implementation, workforce/ retention and recruitment issues, as well as telehealth and the opioid epidemic as it relates to VA patients. The release of the President’s proposed budget also was discussed. As is often the case with a new administration, a “skinny” or outline of a budget proposal is released in advance of an actual detailed budget, which included a substantial 10% increase in VA’s anticipated budget for overall discretionary items (over FY 2017) and an 8.3% increase for medical care (over FY 2017).
For more information about NOVA or to become a member, visit vanurse.org.
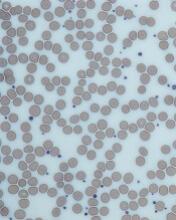
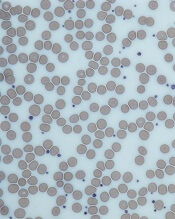
Patients with thrombocytosis should be tested for cancers, team says
Researchers have found evidence to suggest that thrombocytosis is a strong predictor of cancer, particularly lung and colorectal cancer.
The team therefore believes patients with thrombocytosis should be evaluated for an underlying malignancy, as such investigation could speed up cancer diagnosis and save lives.
“We know that early diagnosis is absolutely key in whether people survive cancer,” said Sarah Bailey, PhD, of the University of Exeter Medical School in the UK.
“Our research suggests that substantial numbers of people could have their cancer diagnosed up to 3 months earlier if thrombocytosis prompted investigation for cancer. This time could make a vital difference in achieving earlier diagnosis.”
Dr Bailey and her colleagues described their research in the British Journal of General Practice.
The team conducted a prospective cohort study using Clinical Practice Research Datalink data spanning the period from 2000 to 2013.
They compared the 1-year cancer incidence in 40,000 patients (age 40 and older) with thrombocytosis (platelet count >400 × 109/L) and 10,000 matched controls with normal platelet counts.
Patients with thrombocytosis had a higher incidence of cancer than individuals with normal platelet counts.
The cancer incidence was 6.2% (1355/21,826) in women with thrombocytosis and 2.2% (119/5370) in women with normal platelet counts.
The cancer incidence was 11.6% (1098/9435) in men with thrombocytosis and 4.1% (106/2599) in men with normal platelet counts.
If patients in the thrombocytosis group had a second raised platelet count recorded within 6 months of their index date, the risk of cancer increased to 18.1% for men and 10.1% for women.
Lung and colorectal cancer were more common among patients with thrombocytosis than among individuals with normal platelet counts.
And about one-third of patients with thrombocytosis and lung/colorectal cancer had no other symptoms that would indicate they had cancer.
In addition, the researchers found that “substantial proportions” of lung/colorectal cancer diagnoses could be expedited if thrombocytosis were routinely investigated.
The team calculated that if 5% of patients with cancer have thrombocytosis before a cancer diagnosis, one-third of them have the potential to have their diagnosis expedited by at least 3 months if their doctor investigates the possibility of cancer based on the presence of thrombocytosis. This equates to 5500 earlier diagnoses annually.
“The UK lags well behind other developed countries on early cancer diagnosis,” said study author Willie Hamilton, MD, of the University of Exeter Medical School.
“In 2014, 163,000 people died of cancer in this country. Our findings on thrombocytosis show a strong association with cancer, particularly in men—far stronger than that of a breast lump for breast cancer in women. It is now crucial that we roll out cancer investigation of thrombocytosis. It could save hundreds of lives each year.” ![]()
Researchers have found evidence to suggest that thrombocytosis is a strong predictor of cancer, particularly lung and colorectal cancer.
The team therefore believes patients with thrombocytosis should be evaluated for an underlying malignancy, as such investigation could speed up cancer diagnosis and save lives.
“We know that early diagnosis is absolutely key in whether people survive cancer,” said Sarah Bailey, PhD, of the University of Exeter Medical School in the UK.
“Our research suggests that substantial numbers of people could have their cancer diagnosed up to 3 months earlier if thrombocytosis prompted investigation for cancer. This time could make a vital difference in achieving earlier diagnosis.”
Dr Bailey and her colleagues described their research in the British Journal of General Practice.
The team conducted a prospective cohort study using Clinical Practice Research Datalink data spanning the period from 2000 to 2013.
They compared the 1-year cancer incidence in 40,000 patients (age 40 and older) with thrombocytosis (platelet count >400 × 109/L) and 10,000 matched controls with normal platelet counts.
Patients with thrombocytosis had a higher incidence of cancer than individuals with normal platelet counts.
The cancer incidence was 6.2% (1355/21,826) in women with thrombocytosis and 2.2% (119/5370) in women with normal platelet counts.
The cancer incidence was 11.6% (1098/9435) in men with thrombocytosis and 4.1% (106/2599) in men with normal platelet counts.
If patients in the thrombocytosis group had a second raised platelet count recorded within 6 months of their index date, the risk of cancer increased to 18.1% for men and 10.1% for women.
Lung and colorectal cancer were more common among patients with thrombocytosis than among individuals with normal platelet counts.
And about one-third of patients with thrombocytosis and lung/colorectal cancer had no other symptoms that would indicate they had cancer.
In addition, the researchers found that “substantial proportions” of lung/colorectal cancer diagnoses could be expedited if thrombocytosis were routinely investigated.
The team calculated that if 5% of patients with cancer have thrombocytosis before a cancer diagnosis, one-third of them have the potential to have their diagnosis expedited by at least 3 months if their doctor investigates the possibility of cancer based on the presence of thrombocytosis. This equates to 5500 earlier diagnoses annually.
“The UK lags well behind other developed countries on early cancer diagnosis,” said study author Willie Hamilton, MD, of the University of Exeter Medical School.
“In 2014, 163,000 people died of cancer in this country. Our findings on thrombocytosis show a strong association with cancer, particularly in men—far stronger than that of a breast lump for breast cancer in women. It is now crucial that we roll out cancer investigation of thrombocytosis. It could save hundreds of lives each year.” ![]()
Researchers have found evidence to suggest that thrombocytosis is a strong predictor of cancer, particularly lung and colorectal cancer.
The team therefore believes patients with thrombocytosis should be evaluated for an underlying malignancy, as such investigation could speed up cancer diagnosis and save lives.
“We know that early diagnosis is absolutely key in whether people survive cancer,” said Sarah Bailey, PhD, of the University of Exeter Medical School in the UK.
“Our research suggests that substantial numbers of people could have their cancer diagnosed up to 3 months earlier if thrombocytosis prompted investigation for cancer. This time could make a vital difference in achieving earlier diagnosis.”
Dr Bailey and her colleagues described their research in the British Journal of General Practice.
The team conducted a prospective cohort study using Clinical Practice Research Datalink data spanning the period from 2000 to 2013.
They compared the 1-year cancer incidence in 40,000 patients (age 40 and older) with thrombocytosis (platelet count >400 × 109/L) and 10,000 matched controls with normal platelet counts.
Patients with thrombocytosis had a higher incidence of cancer than individuals with normal platelet counts.
The cancer incidence was 6.2% (1355/21,826) in women with thrombocytosis and 2.2% (119/5370) in women with normal platelet counts.
The cancer incidence was 11.6% (1098/9435) in men with thrombocytosis and 4.1% (106/2599) in men with normal platelet counts.
If patients in the thrombocytosis group had a second raised platelet count recorded within 6 months of their index date, the risk of cancer increased to 18.1% for men and 10.1% for women.
Lung and colorectal cancer were more common among patients with thrombocytosis than among individuals with normal platelet counts.
And about one-third of patients with thrombocytosis and lung/colorectal cancer had no other symptoms that would indicate they had cancer.
In addition, the researchers found that “substantial proportions” of lung/colorectal cancer diagnoses could be expedited if thrombocytosis were routinely investigated.
The team calculated that if 5% of patients with cancer have thrombocytosis before a cancer diagnosis, one-third of them have the potential to have their diagnosis expedited by at least 3 months if their doctor investigates the possibility of cancer based on the presence of thrombocytosis. This equates to 5500 earlier diagnoses annually.
“The UK lags well behind other developed countries on early cancer diagnosis,” said study author Willie Hamilton, MD, of the University of Exeter Medical School.
“In 2014, 163,000 people died of cancer in this country. Our findings on thrombocytosis show a strong association with cancer, particularly in men—far stronger than that of a breast lump for breast cancer in women. It is now crucial that we roll out cancer investigation of thrombocytosis. It could save hundreds of lives each year.” ![]()
PK-guided prophylaxis reduces dosing, still prevents bleeds
Personalized prophylaxis with a recombinant factor VIII product allowed for reduced dosing while still providing protection from bleeds in a small study of patients with severe hemophilia A.
Researchers tested pharmacokinetic (PK)-guided prophylaxis with simoctocog alfa in previously treated patients with severe hemophilia A.
The approach reduced the dose administered and increased the dosing interval compared to standard prophylaxis, without compromising protection from bleeds.
Researchers reported these results in the journal Haemophilia. The research was sponsored by Octapharma AG, the company marketing simoctocog alfa as Nuwiq.
Simoctocog alfa is a fourth-generation recombinant human factor VIII product produced in a human cell line.
In this phase 3b study, researchers tested PK-guided prophylaxis with simoctocog alfa in 66 previously treated adults with severe hemophilia A.
The patients’ mean age at baseline was 33.6. Most (62%) had received on-demand treatment in the 6 months prior to starting the study. Prophylaxis was largely irregular in the 38% of patients who received prophylaxis.
At baseline, the mean annualized bleeding rates (ABRs) were 38.9 in the entire cohort, 45.6 in the on-demand cohort, and 27.8 in the prophylaxis cohort.
Study design
The study had 3 phases. The first was the 72-hour PK phase. Patients received a single dose of simoctocog alfa (60 ± 5 IU kg–1) and had blood samples taken at various time points. This helped the researchers determine the patients’ personalized prophylaxis regimen.
The second phase of the study was the standard prophylaxis phase, which lasted 1 to 3 months. In this phase, patients received simoctocog alfa at a dose of 30 to 40 IU kg–1 every other day or 3 times a week until they began personalized prophylaxis.
The third phase was the 6-month personalized prophylaxis phase. A patient’s personalized prophylaxis regimen was based on individual PK modeling for each patient according to whether their PK profile most closely fit a 1- or 2-compartment model. In cases of uncertainty, the researchers used a non-compartment model.
A 2-compartment PK model was used for 36 patients, a 1-compartment model was used for 23 patients, and a non-compartment model was used for 7 patients.
Dosing
In total, the patients received 6612 infusions of simoctocog alfa.
During standard prophylaxis, the mean treatment duration was 2.7 months. Patients received a mean of 34.0 infusions and a total dose of 1157.6 IU kg–1.
During the personalized prophylaxis phase, the mean treatment duration was 6.2 months. Patients received a mean of 58.8 infusions and a total dose of 2574.4 IU kg–1.
The median dosing interval was 3.5 days during personalized prophylaxis, 3.5 days in the 1- and 2-compartment model groups, and 2.3 days in the non-compartment group. Fifty-seven percent of patients had twice-weekly dosing or less.
In the standard prophylaxis period, patients were dosed every other day or 3 times a week.
The median weekly dose was 100.0 IU kg–1 during standard prophylaxis and 95.0 IU kg–1 during personalized prophylaxis. It was 97.5 IU kg–1 during months 1 to 4 of personalized prophylaxis and 92.8 IU kg–1 during months 5 and 6 of personalized prophylaxis.
Bleeding and safety
Similar percentages of patients were bleed-free during the roughly 3-month standard prophylaxis period and the roughly 6-month personalized prophylaxis period—76.9% and 73.8%, respectively.
However, the mean ABR was 3.16 for the standard prophylaxis period and 1.45 for the personalized prophylaxis period. The median ABR was 0 for both periods.
In all, there were 95 breakthrough bleeds—46 during standard prophylaxis and 49 during personalized prophylaxis—in 23 of the patients. All of these bleeds were treated with at least 1 dose of simoctocog alfa.
There were no serious adverse events associated with treatment, and none of the patients developed factor VIII inhibitors.
One patient experienced malaise and dizziness after a single infusion during the standard prophylaxis period. These events were considered treatment-related, but both events resolved. ![]()
Personalized prophylaxis with a recombinant factor VIII product allowed for reduced dosing while still providing protection from bleeds in a small study of patients with severe hemophilia A.
Researchers tested pharmacokinetic (PK)-guided prophylaxis with simoctocog alfa in previously treated patients with severe hemophilia A.
The approach reduced the dose administered and increased the dosing interval compared to standard prophylaxis, without compromising protection from bleeds.
Researchers reported these results in the journal Haemophilia. The research was sponsored by Octapharma AG, the company marketing simoctocog alfa as Nuwiq.
Simoctocog alfa is a fourth-generation recombinant human factor VIII product produced in a human cell line.
In this phase 3b study, researchers tested PK-guided prophylaxis with simoctocog alfa in 66 previously treated adults with severe hemophilia A.
The patients’ mean age at baseline was 33.6. Most (62%) had received on-demand treatment in the 6 months prior to starting the study. Prophylaxis was largely irregular in the 38% of patients who received prophylaxis.
At baseline, the mean annualized bleeding rates (ABRs) were 38.9 in the entire cohort, 45.6 in the on-demand cohort, and 27.8 in the prophylaxis cohort.
Study design
The study had 3 phases. The first was the 72-hour PK phase. Patients received a single dose of simoctocog alfa (60 ± 5 IU kg–1) and had blood samples taken at various time points. This helped the researchers determine the patients’ personalized prophylaxis regimen.
The second phase of the study was the standard prophylaxis phase, which lasted 1 to 3 months. In this phase, patients received simoctocog alfa at a dose of 30 to 40 IU kg–1 every other day or 3 times a week until they began personalized prophylaxis.
The third phase was the 6-month personalized prophylaxis phase. A patient’s personalized prophylaxis regimen was based on individual PK modeling for each patient according to whether their PK profile most closely fit a 1- or 2-compartment model. In cases of uncertainty, the researchers used a non-compartment model.
A 2-compartment PK model was used for 36 patients, a 1-compartment model was used for 23 patients, and a non-compartment model was used for 7 patients.
Dosing
In total, the patients received 6612 infusions of simoctocog alfa.
During standard prophylaxis, the mean treatment duration was 2.7 months. Patients received a mean of 34.0 infusions and a total dose of 1157.6 IU kg–1.
During the personalized prophylaxis phase, the mean treatment duration was 6.2 months. Patients received a mean of 58.8 infusions and a total dose of 2574.4 IU kg–1.
The median dosing interval was 3.5 days during personalized prophylaxis, 3.5 days in the 1- and 2-compartment model groups, and 2.3 days in the non-compartment group. Fifty-seven percent of patients had twice-weekly dosing or less.
In the standard prophylaxis period, patients were dosed every other day or 3 times a week.
The median weekly dose was 100.0 IU kg–1 during standard prophylaxis and 95.0 IU kg–1 during personalized prophylaxis. It was 97.5 IU kg–1 during months 1 to 4 of personalized prophylaxis and 92.8 IU kg–1 during months 5 and 6 of personalized prophylaxis.
Bleeding and safety
Similar percentages of patients were bleed-free during the roughly 3-month standard prophylaxis period and the roughly 6-month personalized prophylaxis period—76.9% and 73.8%, respectively.
However, the mean ABR was 3.16 for the standard prophylaxis period and 1.45 for the personalized prophylaxis period. The median ABR was 0 for both periods.
In all, there were 95 breakthrough bleeds—46 during standard prophylaxis and 49 during personalized prophylaxis—in 23 of the patients. All of these bleeds were treated with at least 1 dose of simoctocog alfa.
There were no serious adverse events associated with treatment, and none of the patients developed factor VIII inhibitors.
One patient experienced malaise and dizziness after a single infusion during the standard prophylaxis period. These events were considered treatment-related, but both events resolved. ![]()
Personalized prophylaxis with a recombinant factor VIII product allowed for reduced dosing while still providing protection from bleeds in a small study of patients with severe hemophilia A.
Researchers tested pharmacokinetic (PK)-guided prophylaxis with simoctocog alfa in previously treated patients with severe hemophilia A.
The approach reduced the dose administered and increased the dosing interval compared to standard prophylaxis, without compromising protection from bleeds.
Researchers reported these results in the journal Haemophilia. The research was sponsored by Octapharma AG, the company marketing simoctocog alfa as Nuwiq.
Simoctocog alfa is a fourth-generation recombinant human factor VIII product produced in a human cell line.
In this phase 3b study, researchers tested PK-guided prophylaxis with simoctocog alfa in 66 previously treated adults with severe hemophilia A.
The patients’ mean age at baseline was 33.6. Most (62%) had received on-demand treatment in the 6 months prior to starting the study. Prophylaxis was largely irregular in the 38% of patients who received prophylaxis.
At baseline, the mean annualized bleeding rates (ABRs) were 38.9 in the entire cohort, 45.6 in the on-demand cohort, and 27.8 in the prophylaxis cohort.
Study design
The study had 3 phases. The first was the 72-hour PK phase. Patients received a single dose of simoctocog alfa (60 ± 5 IU kg–1) and had blood samples taken at various time points. This helped the researchers determine the patients’ personalized prophylaxis regimen.
The second phase of the study was the standard prophylaxis phase, which lasted 1 to 3 months. In this phase, patients received simoctocog alfa at a dose of 30 to 40 IU kg–1 every other day or 3 times a week until they began personalized prophylaxis.
The third phase was the 6-month personalized prophylaxis phase. A patient’s personalized prophylaxis regimen was based on individual PK modeling for each patient according to whether their PK profile most closely fit a 1- or 2-compartment model. In cases of uncertainty, the researchers used a non-compartment model.
A 2-compartment PK model was used for 36 patients, a 1-compartment model was used for 23 patients, and a non-compartment model was used for 7 patients.
Dosing
In total, the patients received 6612 infusions of simoctocog alfa.
During standard prophylaxis, the mean treatment duration was 2.7 months. Patients received a mean of 34.0 infusions and a total dose of 1157.6 IU kg–1.
During the personalized prophylaxis phase, the mean treatment duration was 6.2 months. Patients received a mean of 58.8 infusions and a total dose of 2574.4 IU kg–1.
The median dosing interval was 3.5 days during personalized prophylaxis, 3.5 days in the 1- and 2-compartment model groups, and 2.3 days in the non-compartment group. Fifty-seven percent of patients had twice-weekly dosing or less.
In the standard prophylaxis period, patients were dosed every other day or 3 times a week.
The median weekly dose was 100.0 IU kg–1 during standard prophylaxis and 95.0 IU kg–1 during personalized prophylaxis. It was 97.5 IU kg–1 during months 1 to 4 of personalized prophylaxis and 92.8 IU kg–1 during months 5 and 6 of personalized prophylaxis.
Bleeding and safety
Similar percentages of patients were bleed-free during the roughly 3-month standard prophylaxis period and the roughly 6-month personalized prophylaxis period—76.9% and 73.8%, respectively.
However, the mean ABR was 3.16 for the standard prophylaxis period and 1.45 for the personalized prophylaxis period. The median ABR was 0 for both periods.
In all, there were 95 breakthrough bleeds—46 during standard prophylaxis and 49 during personalized prophylaxis—in 23 of the patients. All of these bleeds were treated with at least 1 dose of simoctocog alfa.
There were no serious adverse events associated with treatment, and none of the patients developed factor VIII inhibitors.
One patient experienced malaise and dizziness after a single infusion during the standard prophylaxis period. These events were considered treatment-related, but both events resolved. ![]()
FDA approves new formulation of deferasirox
The US Food and Drug Administration (FDA) has approved a new formulation of deferasirox known as Jadenu Sprinkle granules.
The granules are approved for use in the same population as Jadenu film-coated tablets.
Both formulations of Jadenu have accelerated approval from the FDA for the treatment of chronic iron overload due to blood transfusions in patients age 2 and older.
The formulations also have accelerated FDA approval for the treatment of chronic iron overload in patients age 10 and older with non-transfusion-dependent-thalassemia and a liver iron concentration of at least 5 mg Fe per gram of dry weight and a serum ferritin greater than 300 mcg/L.
Continued FDA approval for Jadenu in these indications may be contingent upon verification and description of clinical benefit in confirmatory trials.
Jadenu Sprinkle granules are intended for patients who have difficulty swallowing whole tablets. The granules can be sprinkled over soft foods (eg, yogurt or applesauce) prior to consumption.
Like Jadenu film-coated tablets, Jadenu Sprinkle granules are available in 3 strengths—90 mg, 180 mg, and 360 mg.
Both formulations of Jadenu are products of Novartis. For more details on Jadenu, see the prescribing information. ![]()
The US Food and Drug Administration (FDA) has approved a new formulation of deferasirox known as Jadenu Sprinkle granules.
The granules are approved for use in the same population as Jadenu film-coated tablets.
Both formulations of Jadenu have accelerated approval from the FDA for the treatment of chronic iron overload due to blood transfusions in patients age 2 and older.
The formulations also have accelerated FDA approval for the treatment of chronic iron overload in patients age 10 and older with non-transfusion-dependent-thalassemia and a liver iron concentration of at least 5 mg Fe per gram of dry weight and a serum ferritin greater than 300 mcg/L.
Continued FDA approval for Jadenu in these indications may be contingent upon verification and description of clinical benefit in confirmatory trials.
Jadenu Sprinkle granules are intended for patients who have difficulty swallowing whole tablets. The granules can be sprinkled over soft foods (eg, yogurt or applesauce) prior to consumption.
Like Jadenu film-coated tablets, Jadenu Sprinkle granules are available in 3 strengths—90 mg, 180 mg, and 360 mg.
Both formulations of Jadenu are products of Novartis. For more details on Jadenu, see the prescribing information. ![]()
The US Food and Drug Administration (FDA) has approved a new formulation of deferasirox known as Jadenu Sprinkle granules.
The granules are approved for use in the same population as Jadenu film-coated tablets.
Both formulations of Jadenu have accelerated approval from the FDA for the treatment of chronic iron overload due to blood transfusions in patients age 2 and older.
The formulations also have accelerated FDA approval for the treatment of chronic iron overload in patients age 10 and older with non-transfusion-dependent-thalassemia and a liver iron concentration of at least 5 mg Fe per gram of dry weight and a serum ferritin greater than 300 mcg/L.
Continued FDA approval for Jadenu in these indications may be contingent upon verification and description of clinical benefit in confirmatory trials.
Jadenu Sprinkle granules are intended for patients who have difficulty swallowing whole tablets. The granules can be sprinkled over soft foods (eg, yogurt or applesauce) prior to consumption.
Like Jadenu film-coated tablets, Jadenu Sprinkle granules are available in 3 strengths—90 mg, 180 mg, and 360 mg.
Both formulations of Jadenu are products of Novartis. For more details on Jadenu, see the prescribing information. ![]()
NIH releases COPD National Action Plan
WASHINGTON – The National Institutes of Health on Monday released its first COPD National Action Plan, a five-point initiative to reduce the burden of chronic obstructive pulmonary disease and increase research into prevention and treatment.
On the same day, the National Heart, Lung, and Blood Institute and other supporters of the plan described its evolution and why they thought the plan’s implementation was important.
The plan’s five goals are:
- Empower people with COPD, their families, and caregivers to recognize and reduce the burden of COPD.
- Improve the prevention, diagnosis, treatment, and management of COPD by increasing the quality of care delivered across the health care continuum.
- Collect, analyze, report, and disseminate COPD-related public health data that drive change and track progress.
- Increase and sustain research to better understand the prevention, pathogenesis, diagnosis, treatment, and management of COPD.
- Translate national policy, educational, and program recommendations into research and public health care actions.
“Chronic obstructive pulmonary disease is the third-leading cause of death in this country; it’s just behind heart disease and cancer,” Dr. Kiley noted. “What’s really disappointing and discouraging is it’s the only cause of death in this country where the numbers are not declining.”
COPD “got the attention of Congress a number of years ago,” he added. “They encouraged the National Institutes of Health to work with the community stakeholders and other federal agencies to develop a national action plan to respond to the growing burden of this disease.”
COPD’s stakeholder community, the federal government, and other partners worked together to develop a set of core goals that the National Action Plan would address, Dr. Kiley continued. “It was meant to obtain the broadest amount of input possible so that we could get it right from the start.”
Another of the plan’s advocates, MeiLan Han, MD, medical director of the women’s respiratory health program at the University of Michigan, Ann Arbor, illustrated the need to increase and sustain COPD research related to the disease.
[polldaddy:9806142]
“I see the suffering and disease toll that this takes on my patients, and I can’t convince you enough of the level of frustration that I have as a physician in not being able to provide the level of care that I want to be able to provide,” said Dr. Han, who served as a panelist at the press conference.
“We face some serious barriers to being able to provide adequate care for patients,” she added. Those barriers include lack of access to providers who are knowledgeable about COPD, as well as lack of access to affordable and conveniently located pulmonology rehabilitation and education materials. From a research standpoint, Dr. Han added, medicine still doesn’t know enough about the disease. “We certainly have good treatments, but we need better treatments,” she said.
“What’s clear is that we as society can no longer afford to brush this under the table and ignore this problem,” Dr. Han added.
The National Action Plan and information about how to get involved are available at copd.nih.gov.
WASHINGTON – The National Institutes of Health on Monday released its first COPD National Action Plan, a five-point initiative to reduce the burden of chronic obstructive pulmonary disease and increase research into prevention and treatment.
On the same day, the National Heart, Lung, and Blood Institute and other supporters of the plan described its evolution and why they thought the plan’s implementation was important.
The plan’s five goals are:
- Empower people with COPD, their families, and caregivers to recognize and reduce the burden of COPD.
- Improve the prevention, diagnosis, treatment, and management of COPD by increasing the quality of care delivered across the health care continuum.
- Collect, analyze, report, and disseminate COPD-related public health data that drive change and track progress.
- Increase and sustain research to better understand the prevention, pathogenesis, diagnosis, treatment, and management of COPD.
- Translate national policy, educational, and program recommendations into research and public health care actions.
“Chronic obstructive pulmonary disease is the third-leading cause of death in this country; it’s just behind heart disease and cancer,” Dr. Kiley noted. “What’s really disappointing and discouraging is it’s the only cause of death in this country where the numbers are not declining.”
COPD “got the attention of Congress a number of years ago,” he added. “They encouraged the National Institutes of Health to work with the community stakeholders and other federal agencies to develop a national action plan to respond to the growing burden of this disease.”
COPD’s stakeholder community, the federal government, and other partners worked together to develop a set of core goals that the National Action Plan would address, Dr. Kiley continued. “It was meant to obtain the broadest amount of input possible so that we could get it right from the start.”
Another of the plan’s advocates, MeiLan Han, MD, medical director of the women’s respiratory health program at the University of Michigan, Ann Arbor, illustrated the need to increase and sustain COPD research related to the disease.
[polldaddy:9806142]
“I see the suffering and disease toll that this takes on my patients, and I can’t convince you enough of the level of frustration that I have as a physician in not being able to provide the level of care that I want to be able to provide,” said Dr. Han, who served as a panelist at the press conference.
“We face some serious barriers to being able to provide adequate care for patients,” she added. Those barriers include lack of access to providers who are knowledgeable about COPD, as well as lack of access to affordable and conveniently located pulmonology rehabilitation and education materials. From a research standpoint, Dr. Han added, medicine still doesn’t know enough about the disease. “We certainly have good treatments, but we need better treatments,” she said.
“What’s clear is that we as society can no longer afford to brush this under the table and ignore this problem,” Dr. Han added.
The National Action Plan and information about how to get involved are available at copd.nih.gov.
WASHINGTON – The National Institutes of Health on Monday released its first COPD National Action Plan, a five-point initiative to reduce the burden of chronic obstructive pulmonary disease and increase research into prevention and treatment.
On the same day, the National Heart, Lung, and Blood Institute and other supporters of the plan described its evolution and why they thought the plan’s implementation was important.
The plan’s five goals are:
- Empower people with COPD, their families, and caregivers to recognize and reduce the burden of COPD.
- Improve the prevention, diagnosis, treatment, and management of COPD by increasing the quality of care delivered across the health care continuum.
- Collect, analyze, report, and disseminate COPD-related public health data that drive change and track progress.
- Increase and sustain research to better understand the prevention, pathogenesis, diagnosis, treatment, and management of COPD.
- Translate national policy, educational, and program recommendations into research and public health care actions.
“Chronic obstructive pulmonary disease is the third-leading cause of death in this country; it’s just behind heart disease and cancer,” Dr. Kiley noted. “What’s really disappointing and discouraging is it’s the only cause of death in this country where the numbers are not declining.”
COPD “got the attention of Congress a number of years ago,” he added. “They encouraged the National Institutes of Health to work with the community stakeholders and other federal agencies to develop a national action plan to respond to the growing burden of this disease.”
COPD’s stakeholder community, the federal government, and other partners worked together to develop a set of core goals that the National Action Plan would address, Dr. Kiley continued. “It was meant to obtain the broadest amount of input possible so that we could get it right from the start.”
Another of the plan’s advocates, MeiLan Han, MD, medical director of the women’s respiratory health program at the University of Michigan, Ann Arbor, illustrated the need to increase and sustain COPD research related to the disease.
[polldaddy:9806142]
“I see the suffering and disease toll that this takes on my patients, and I can’t convince you enough of the level of frustration that I have as a physician in not being able to provide the level of care that I want to be able to provide,” said Dr. Han, who served as a panelist at the press conference.
“We face some serious barriers to being able to provide adequate care for patients,” she added. Those barriers include lack of access to providers who are knowledgeable about COPD, as well as lack of access to affordable and conveniently located pulmonology rehabilitation and education materials. From a research standpoint, Dr. Han added, medicine still doesn’t know enough about the disease. “We certainly have good treatments, but we need better treatments,” she said.
“What’s clear is that we as society can no longer afford to brush this under the table and ignore this problem,” Dr. Han added.
The National Action Plan and information about how to get involved are available at copd.nih.gov.
AT ATS 2017
FDA okays pembrolizumab for certain solid tumors with common biomarker
In an accelerated approval process, the Food and Drug Administration has approved the use of the monoclonal antibody pembrolizumab for treatment of certain solid tumors that have a common biomarker, a first for the agency.
Pembrolizumab (Keytruda) was approved to treat patients whose tumors are metastatic or unresectable, and which have the biomarker microsatellite instability-high (MSI-H), also known as mismatch repair deficient (dMMR). This biomarker is found in many kinds of solid tumors, especially in colorectal and other gastrointestinal cancers, as well as endometrial cancer, and may make tumors more susceptible to host immune system activity. “Approximately 5% of patients with metastatic colorectal cancer have MSI-H or dMMR tumors,” according to the FDA statement announcing the approval.
Patients who are eligible for pembrolizumab under this approval are those whose solid tumors have progressed despite earlier treatment and who lack other treatment options; pembrolizumab was also approved for colorectal cancer patients whose cancers have progressed after treatment with some chemotherapy drugs.
Pembrolizumab received priority review from the FDA and was approved on the basis of five uncontrolled single-arm clinical trials. There were a total of 149 patients enrolled in the trials, and 15 different cancer types were represented. Colorectal and other gastrointestinal cancers and endometrial cancers were the most common types in the studies. Of the 149 patients, 39.6% had a complete or partial response, and of these responders, 78% had a response lasting at least 6 months.
Fatigue is a common side effect of pembrolizumab; anorexia, peripheral edema, rash, pruritis, hyperlipidemia, and electrolyte disturbances are also common. Because of the drug’s mechanism of action, it can cause immune-mediated side effects, such as pneumonitis, hepatitis, nephritis, and endocrinopathies.
Pembrolizumab is given as an intravenous infusion, usually once every 3 weeks. It targets the programmed death-1/programmed death-ligand 1 (PD-1/PDL-1) pathway to boost the immune system’s ability to target and kill cancer cells.
“This is an important first for the cancer community,” said Dr. Pazdur, who is also acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. The clinical trials were sponsored by Merck & Co., which markets Keytruda.
[email protected]
On Twitter @karioakes
In an accelerated approval process, the Food and Drug Administration has approved the use of the monoclonal antibody pembrolizumab for treatment of certain solid tumors that have a common biomarker, a first for the agency.
Pembrolizumab (Keytruda) was approved to treat patients whose tumors are metastatic or unresectable, and which have the biomarker microsatellite instability-high (MSI-H), also known as mismatch repair deficient (dMMR). This biomarker is found in many kinds of solid tumors, especially in colorectal and other gastrointestinal cancers, as well as endometrial cancer, and may make tumors more susceptible to host immune system activity. “Approximately 5% of patients with metastatic colorectal cancer have MSI-H or dMMR tumors,” according to the FDA statement announcing the approval.
Patients who are eligible for pembrolizumab under this approval are those whose solid tumors have progressed despite earlier treatment and who lack other treatment options; pembrolizumab was also approved for colorectal cancer patients whose cancers have progressed after treatment with some chemotherapy drugs.
Pembrolizumab received priority review from the FDA and was approved on the basis of five uncontrolled single-arm clinical trials. There were a total of 149 patients enrolled in the trials, and 15 different cancer types were represented. Colorectal and other gastrointestinal cancers and endometrial cancers were the most common types in the studies. Of the 149 patients, 39.6% had a complete or partial response, and of these responders, 78% had a response lasting at least 6 months.
Fatigue is a common side effect of pembrolizumab; anorexia, peripheral edema, rash, pruritis, hyperlipidemia, and electrolyte disturbances are also common. Because of the drug’s mechanism of action, it can cause immune-mediated side effects, such as pneumonitis, hepatitis, nephritis, and endocrinopathies.
Pembrolizumab is given as an intravenous infusion, usually once every 3 weeks. It targets the programmed death-1/programmed death-ligand 1 (PD-1/PDL-1) pathway to boost the immune system’s ability to target and kill cancer cells.
“This is an important first for the cancer community,” said Dr. Pazdur, who is also acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. The clinical trials were sponsored by Merck & Co., which markets Keytruda.
[email protected]
On Twitter @karioakes
In an accelerated approval process, the Food and Drug Administration has approved the use of the monoclonal antibody pembrolizumab for treatment of certain solid tumors that have a common biomarker, a first for the agency.
Pembrolizumab (Keytruda) was approved to treat patients whose tumors are metastatic or unresectable, and which have the biomarker microsatellite instability-high (MSI-H), also known as mismatch repair deficient (dMMR). This biomarker is found in many kinds of solid tumors, especially in colorectal and other gastrointestinal cancers, as well as endometrial cancer, and may make tumors more susceptible to host immune system activity. “Approximately 5% of patients with metastatic colorectal cancer have MSI-H or dMMR tumors,” according to the FDA statement announcing the approval.
Patients who are eligible for pembrolizumab under this approval are those whose solid tumors have progressed despite earlier treatment and who lack other treatment options; pembrolizumab was also approved for colorectal cancer patients whose cancers have progressed after treatment with some chemotherapy drugs.
Pembrolizumab received priority review from the FDA and was approved on the basis of five uncontrolled single-arm clinical trials. There were a total of 149 patients enrolled in the trials, and 15 different cancer types were represented. Colorectal and other gastrointestinal cancers and endometrial cancers were the most common types in the studies. Of the 149 patients, 39.6% had a complete or partial response, and of these responders, 78% had a response lasting at least 6 months.
Fatigue is a common side effect of pembrolizumab; anorexia, peripheral edema, rash, pruritis, hyperlipidemia, and electrolyte disturbances are also common. Because of the drug’s mechanism of action, it can cause immune-mediated side effects, such as pneumonitis, hepatitis, nephritis, and endocrinopathies.
Pembrolizumab is given as an intravenous infusion, usually once every 3 weeks. It targets the programmed death-1/programmed death-ligand 1 (PD-1/PDL-1) pathway to boost the immune system’s ability to target and kill cancer cells.
“This is an important first for the cancer community,” said Dr. Pazdur, who is also acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. The clinical trials were sponsored by Merck & Co., which markets Keytruda.
[email protected]
On Twitter @karioakes
ECG finding predicts AFib in ibrutinib-treated CLL
NEW YORK – A left atrial abnormality on a pretreatment electrocardiogram (ECG) is a moderately specific and sensitive finding that independently predicts risk for developing atrial fibrillation in chronic lymphocytic leukemia patients starting on ibrutinib, findings from a retrospective cohort study indicate.
ECGs are inexpensive and available in most physician’s offices. Routinely checking for a left atrial abnormality before starting ibrutinib would identify a patient subgroup that would benefit from increased monitoring and allow for proactive intervention strategies to reduce complications should atrial fibrillation develop, Anthony Mato, MD, said at the annual meeting of the International Workshop on Chronic Lymphocytic Leukemia.
Prior studies, including the RESONATE and RESONATE 2 trials, have clearly demonstrated a link between ibrutinib exposure and the development of AFib. Long-term follow-up data suggest an estimated incidence of 9% to 11%.
Dr. Mato and his colleagues used a case-control design within a two-center retrospective cohort study to test the hypothesis that pre-ibrutinib left atrial abnormality, as determined by the ECG, can identify patients at increased risk for AFib during ibrutinib-based therapy.
Of 153 consecutive CLL patients who were treated with ibrutinib 420 mg/day, 11% developed new AFib at a median of 7 months after starting treatment. Discontinuation of ibrutinib because of AFib was low, with less than 2% of the entire cohort discontinuing treatment.
Based on findings in 20 case patients and 24 controls with an available pretreatment ECG, the presence of a left atrial abnormality before ibrutinib therapy was associated with a nine times increased risk of subsequently developing AFib.
“We looked at baseline hypertension, coronary disease, diabetes, age, and sex, and, although hypertension, coronary disease, and age appeared to have some effect, they weren’t as significant as left atrial abnormality” for predicting risk of AFib, Dr. Mato noted.
On multivariate analysis, controlling for hypertension, coronary disease, and age, a left atrial abnormality continued to be a significant predictor of AFib (odds ratio, 6.6).
“We then wanted to make this more practical for clinicians who may potentially perform an ECG to estimate risk,” he said, noting that ECG test characteristics associated with left atrial abnormality were defined: Sensitivity was estimated to be 79%, specificity was 71%, positive and negative likelihood ratios were 2.7 and 0.3, respectively. Positive predictive value was 68%, and negative predictive value was 81%.
The area under the ROC curve for this single predictor was 75%, he said.
The median age of the cohort at CLL diagnosis was 61 years, and the median age at ibrutinib start was 70. Patients had undergone a median of 2 prior lines of therapy, and 87% were treated in the relapsed/refractory setting.
The median follow-up was 17 months, and the median time from CLL diagnosis to the start of ibrutinib was 73 months.
Cardiovascular characteristics prior to treatment included smoking or former smoking in 49%, hypertension in 42%, hyperlipidemia in 39%, diabetes in 17%, coronary artery disease in 12%, and valvular heart disease in 5%.
Controls were matched to cases on baseline characteristics, and only those with no pretreatment history of AFib, a pretreatment ECG, and therapeutic ibrutinib dosing (420 mg/day for at least 4 months) were included.
To minimize bias, all ECGs were reviewed by a cardio-oncologist blinded to clinical outcomes.
The findings need prospective validation, as they are limited by the retrospective study design, lack of balance with respect to cardiovascular characteristics among cases and controls, a small number of atrial fibrillation cases, and variable timing of pre-ibrutinib ECG, he said.
Patients should be educated about the signs and symptoms of AFib. “The development of AFib during ibrutinib treatment should not prevent its continuation. These patients should be managed medically,” he added.
Dr. Mato reported having no disclosures.
NEW YORK – A left atrial abnormality on a pretreatment electrocardiogram (ECG) is a moderately specific and sensitive finding that independently predicts risk for developing atrial fibrillation in chronic lymphocytic leukemia patients starting on ibrutinib, findings from a retrospective cohort study indicate.
ECGs are inexpensive and available in most physician’s offices. Routinely checking for a left atrial abnormality before starting ibrutinib would identify a patient subgroup that would benefit from increased monitoring and allow for proactive intervention strategies to reduce complications should atrial fibrillation develop, Anthony Mato, MD, said at the annual meeting of the International Workshop on Chronic Lymphocytic Leukemia.
Prior studies, including the RESONATE and RESONATE 2 trials, have clearly demonstrated a link between ibrutinib exposure and the development of AFib. Long-term follow-up data suggest an estimated incidence of 9% to 11%.
Dr. Mato and his colleagues used a case-control design within a two-center retrospective cohort study to test the hypothesis that pre-ibrutinib left atrial abnormality, as determined by the ECG, can identify patients at increased risk for AFib during ibrutinib-based therapy.
Of 153 consecutive CLL patients who were treated with ibrutinib 420 mg/day, 11% developed new AFib at a median of 7 months after starting treatment. Discontinuation of ibrutinib because of AFib was low, with less than 2% of the entire cohort discontinuing treatment.
Based on findings in 20 case patients and 24 controls with an available pretreatment ECG, the presence of a left atrial abnormality before ibrutinib therapy was associated with a nine times increased risk of subsequently developing AFib.
“We looked at baseline hypertension, coronary disease, diabetes, age, and sex, and, although hypertension, coronary disease, and age appeared to have some effect, they weren’t as significant as left atrial abnormality” for predicting risk of AFib, Dr. Mato noted.
On multivariate analysis, controlling for hypertension, coronary disease, and age, a left atrial abnormality continued to be a significant predictor of AFib (odds ratio, 6.6).
“We then wanted to make this more practical for clinicians who may potentially perform an ECG to estimate risk,” he said, noting that ECG test characteristics associated with left atrial abnormality were defined: Sensitivity was estimated to be 79%, specificity was 71%, positive and negative likelihood ratios were 2.7 and 0.3, respectively. Positive predictive value was 68%, and negative predictive value was 81%.
The area under the ROC curve for this single predictor was 75%, he said.
The median age of the cohort at CLL diagnosis was 61 years, and the median age at ibrutinib start was 70. Patients had undergone a median of 2 prior lines of therapy, and 87% were treated in the relapsed/refractory setting.
The median follow-up was 17 months, and the median time from CLL diagnosis to the start of ibrutinib was 73 months.
Cardiovascular characteristics prior to treatment included smoking or former smoking in 49%, hypertension in 42%, hyperlipidemia in 39%, diabetes in 17%, coronary artery disease in 12%, and valvular heart disease in 5%.
Controls were matched to cases on baseline characteristics, and only those with no pretreatment history of AFib, a pretreatment ECG, and therapeutic ibrutinib dosing (420 mg/day for at least 4 months) were included.
To minimize bias, all ECGs were reviewed by a cardio-oncologist blinded to clinical outcomes.
The findings need prospective validation, as they are limited by the retrospective study design, lack of balance with respect to cardiovascular characteristics among cases and controls, a small number of atrial fibrillation cases, and variable timing of pre-ibrutinib ECG, he said.
Patients should be educated about the signs and symptoms of AFib. “The development of AFib during ibrutinib treatment should not prevent its continuation. These patients should be managed medically,” he added.
Dr. Mato reported having no disclosures.
NEW YORK – A left atrial abnormality on a pretreatment electrocardiogram (ECG) is a moderately specific and sensitive finding that independently predicts risk for developing atrial fibrillation in chronic lymphocytic leukemia patients starting on ibrutinib, findings from a retrospective cohort study indicate.
ECGs are inexpensive and available in most physician’s offices. Routinely checking for a left atrial abnormality before starting ibrutinib would identify a patient subgroup that would benefit from increased monitoring and allow for proactive intervention strategies to reduce complications should atrial fibrillation develop, Anthony Mato, MD, said at the annual meeting of the International Workshop on Chronic Lymphocytic Leukemia.
Prior studies, including the RESONATE and RESONATE 2 trials, have clearly demonstrated a link between ibrutinib exposure and the development of AFib. Long-term follow-up data suggest an estimated incidence of 9% to 11%.
Dr. Mato and his colleagues used a case-control design within a two-center retrospective cohort study to test the hypothesis that pre-ibrutinib left atrial abnormality, as determined by the ECG, can identify patients at increased risk for AFib during ibrutinib-based therapy.
Of 153 consecutive CLL patients who were treated with ibrutinib 420 mg/day, 11% developed new AFib at a median of 7 months after starting treatment. Discontinuation of ibrutinib because of AFib was low, with less than 2% of the entire cohort discontinuing treatment.
Based on findings in 20 case patients and 24 controls with an available pretreatment ECG, the presence of a left atrial abnormality before ibrutinib therapy was associated with a nine times increased risk of subsequently developing AFib.
“We looked at baseline hypertension, coronary disease, diabetes, age, and sex, and, although hypertension, coronary disease, and age appeared to have some effect, they weren’t as significant as left atrial abnormality” for predicting risk of AFib, Dr. Mato noted.
On multivariate analysis, controlling for hypertension, coronary disease, and age, a left atrial abnormality continued to be a significant predictor of AFib (odds ratio, 6.6).
“We then wanted to make this more practical for clinicians who may potentially perform an ECG to estimate risk,” he said, noting that ECG test characteristics associated with left atrial abnormality were defined: Sensitivity was estimated to be 79%, specificity was 71%, positive and negative likelihood ratios were 2.7 and 0.3, respectively. Positive predictive value was 68%, and negative predictive value was 81%.
The area under the ROC curve for this single predictor was 75%, he said.
The median age of the cohort at CLL diagnosis was 61 years, and the median age at ibrutinib start was 70. Patients had undergone a median of 2 prior lines of therapy, and 87% were treated in the relapsed/refractory setting.
The median follow-up was 17 months, and the median time from CLL diagnosis to the start of ibrutinib was 73 months.
Cardiovascular characteristics prior to treatment included smoking or former smoking in 49%, hypertension in 42%, hyperlipidemia in 39%, diabetes in 17%, coronary artery disease in 12%, and valvular heart disease in 5%.
Controls were matched to cases on baseline characteristics, and only those with no pretreatment history of AFib, a pretreatment ECG, and therapeutic ibrutinib dosing (420 mg/day for at least 4 months) were included.
To minimize bias, all ECGs were reviewed by a cardio-oncologist blinded to clinical outcomes.
The findings need prospective validation, as they are limited by the retrospective study design, lack of balance with respect to cardiovascular characteristics among cases and controls, a small number of atrial fibrillation cases, and variable timing of pre-ibrutinib ECG, he said.
Patients should be educated about the signs and symptoms of AFib. “The development of AFib during ibrutinib treatment should not prevent its continuation. These patients should be managed medically,” he added.
Dr. Mato reported having no disclosures.
AT THE IWCLL MEETING
Key clinical point:
Major finding: Left atrial abnormality as measured using ECG was a significant predictor of AFIB (adjusted odds ratio, 6.6).
Data source: A case-control study of 44 patients within a retrospective cohort.
Disclosures: Dr. Mato reported having no disclosures.
Benefits, safety of dupilumab-steroid combination in adults with AD sustained
Dupilumab significantly improved symptoms when used in conjunction with topical steroids over one year in a phase III randomized trial of adults with moderate to severe atopic dermatitis (AD) conducted at 161 centers in 14 countries.
The study is “the first large, randomized, double-blinded placebo-controlled study of long-term systemic treatment in patients with moderate-to-severe atopic dermatitis,” wrote Andrew Blauvelt, MD, president of the Oregon Medical Research Center, Portland, and his coauthors. “These results validate the fundamental role for interleukin 4 and interleukin 13 in the pathogenesis of atopic dermatitis,” they added. The findings were published online (Lancet. 2017 May 4. doi: 10.1016/S0140-6736[17]31191-1).
Dupilumab (Dupixent), a monoclonal antibody that inhibits signaling of both interleukin-4 and interleukin-13, was approved by the Food and Drug Administration in March for treating moderate-to-severe AD in adults.
In the study, known as LIBERTY AD CHRONOS, 740 patients were enrolled and 1-year data were available for 270 adults who received 300 mg of dupilumab once a week plus topical corticosteroids, 89 patients who received 300 mg of dupilumab every two weeks plus topical corticosteroids, and 264 patients who received a placebo plus topical corticosteroids. The two efficacy endpoints were the percent of patients with Investigator’s Global Assessment (IGA) of 0/1 and a 2-point or higher improvement from baseline and a 75% improvement from baseline on the Eczema Area and Severity Index.
At week 16, significantly more patients who received dupilumab plus topical corticosteroids achieved IGA 0/1 (39% of weekly dupilumab plus topical corticosteroids and 39% of those who received dupilumab every 2 weeks plus topical corticosteroids), compared with 12% of placebo/corticosteroid patients. The percentages of patients in each group who met the EASI-75 endpoint were 64%, 69%, and 23%, respectively (P less than .0001).
“The improvement was sustained over the 52-week treatment period,” and the combination therapy was also associated with improvements in “several other measures of clinical signs and symptoms of atopic dermatitis including pruritus, as well as symptoms of anxiety and depression and health-related quality of life, over the 52-week treatment period,” they wrote.
Adverse events were similar among the groups, with 83%, 88%, and 84% of patients in the weekly dupilumab, biweekly dupilumab, and placebo groups, respectively, reporting at least one adverse event. Nonherpetic skin infections were less common among dupilumab patients than among placebo patients, but conjunctivitis was more common among those on dupilumab (14%-19% vs. 8%). “Dupilumab might be the first targeted immune biologic that is neither immunosuppressive nor associated with increased risk of infection but, rather, restorative of barrier and immune function,” the researchers noted.
The results were limited by several factors including the challenges of determining how much topical medication was actually used by patients across multiple study sites, they wrote. However, the data suggest that “the emerging benefit-to-risk profile in this 52-week study supports the role of dupilumab as a primary targeted biologic therapy for up to 1 year in patients with moderate-to-severe atopic dermatitis who are not controlled with topical medications alone,” they said.
The study was funded by Sanofi and Regeneron Pharmaceuticals. Dr. Blauvelt and coauthors disclosed relationships with companies including Sanofi and Regeneron. Several authors were employees of the two companies.
Dupilumab significantly improved symptoms when used in conjunction with topical steroids over one year in a phase III randomized trial of adults with moderate to severe atopic dermatitis (AD) conducted at 161 centers in 14 countries.
The study is “the first large, randomized, double-blinded placebo-controlled study of long-term systemic treatment in patients with moderate-to-severe atopic dermatitis,” wrote Andrew Blauvelt, MD, president of the Oregon Medical Research Center, Portland, and his coauthors. “These results validate the fundamental role for interleukin 4 and interleukin 13 in the pathogenesis of atopic dermatitis,” they added. The findings were published online (Lancet. 2017 May 4. doi: 10.1016/S0140-6736[17]31191-1).
Dupilumab (Dupixent), a monoclonal antibody that inhibits signaling of both interleukin-4 and interleukin-13, was approved by the Food and Drug Administration in March for treating moderate-to-severe AD in adults.
In the study, known as LIBERTY AD CHRONOS, 740 patients were enrolled and 1-year data were available for 270 adults who received 300 mg of dupilumab once a week plus topical corticosteroids, 89 patients who received 300 mg of dupilumab every two weeks plus topical corticosteroids, and 264 patients who received a placebo plus topical corticosteroids. The two efficacy endpoints were the percent of patients with Investigator’s Global Assessment (IGA) of 0/1 and a 2-point or higher improvement from baseline and a 75% improvement from baseline on the Eczema Area and Severity Index.
At week 16, significantly more patients who received dupilumab plus topical corticosteroids achieved IGA 0/1 (39% of weekly dupilumab plus topical corticosteroids and 39% of those who received dupilumab every 2 weeks plus topical corticosteroids), compared with 12% of placebo/corticosteroid patients. The percentages of patients in each group who met the EASI-75 endpoint were 64%, 69%, and 23%, respectively (P less than .0001).
“The improvement was sustained over the 52-week treatment period,” and the combination therapy was also associated with improvements in “several other measures of clinical signs and symptoms of atopic dermatitis including pruritus, as well as symptoms of anxiety and depression and health-related quality of life, over the 52-week treatment period,” they wrote.
Adverse events were similar among the groups, with 83%, 88%, and 84% of patients in the weekly dupilumab, biweekly dupilumab, and placebo groups, respectively, reporting at least one adverse event. Nonherpetic skin infections were less common among dupilumab patients than among placebo patients, but conjunctivitis was more common among those on dupilumab (14%-19% vs. 8%). “Dupilumab might be the first targeted immune biologic that is neither immunosuppressive nor associated with increased risk of infection but, rather, restorative of barrier and immune function,” the researchers noted.
The results were limited by several factors including the challenges of determining how much topical medication was actually used by patients across multiple study sites, they wrote. However, the data suggest that “the emerging benefit-to-risk profile in this 52-week study supports the role of dupilumab as a primary targeted biologic therapy for up to 1 year in patients with moderate-to-severe atopic dermatitis who are not controlled with topical medications alone,” they said.
The study was funded by Sanofi and Regeneron Pharmaceuticals. Dr. Blauvelt and coauthors disclosed relationships with companies including Sanofi and Regeneron. Several authors were employees of the two companies.
Dupilumab significantly improved symptoms when used in conjunction with topical steroids over one year in a phase III randomized trial of adults with moderate to severe atopic dermatitis (AD) conducted at 161 centers in 14 countries.
The study is “the first large, randomized, double-blinded placebo-controlled study of long-term systemic treatment in patients with moderate-to-severe atopic dermatitis,” wrote Andrew Blauvelt, MD, president of the Oregon Medical Research Center, Portland, and his coauthors. “These results validate the fundamental role for interleukin 4 and interleukin 13 in the pathogenesis of atopic dermatitis,” they added. The findings were published online (Lancet. 2017 May 4. doi: 10.1016/S0140-6736[17]31191-1).
Dupilumab (Dupixent), a monoclonal antibody that inhibits signaling of both interleukin-4 and interleukin-13, was approved by the Food and Drug Administration in March for treating moderate-to-severe AD in adults.
In the study, known as LIBERTY AD CHRONOS, 740 patients were enrolled and 1-year data were available for 270 adults who received 300 mg of dupilumab once a week plus topical corticosteroids, 89 patients who received 300 mg of dupilumab every two weeks plus topical corticosteroids, and 264 patients who received a placebo plus topical corticosteroids. The two efficacy endpoints were the percent of patients with Investigator’s Global Assessment (IGA) of 0/1 and a 2-point or higher improvement from baseline and a 75% improvement from baseline on the Eczema Area and Severity Index.
At week 16, significantly more patients who received dupilumab plus topical corticosteroids achieved IGA 0/1 (39% of weekly dupilumab plus topical corticosteroids and 39% of those who received dupilumab every 2 weeks plus topical corticosteroids), compared with 12% of placebo/corticosteroid patients. The percentages of patients in each group who met the EASI-75 endpoint were 64%, 69%, and 23%, respectively (P less than .0001).
“The improvement was sustained over the 52-week treatment period,” and the combination therapy was also associated with improvements in “several other measures of clinical signs and symptoms of atopic dermatitis including pruritus, as well as symptoms of anxiety and depression and health-related quality of life, over the 52-week treatment period,” they wrote.
Adverse events were similar among the groups, with 83%, 88%, and 84% of patients in the weekly dupilumab, biweekly dupilumab, and placebo groups, respectively, reporting at least one adverse event. Nonherpetic skin infections were less common among dupilumab patients than among placebo patients, but conjunctivitis was more common among those on dupilumab (14%-19% vs. 8%). “Dupilumab might be the first targeted immune biologic that is neither immunosuppressive nor associated with increased risk of infection but, rather, restorative of barrier and immune function,” the researchers noted.
The results were limited by several factors including the challenges of determining how much topical medication was actually used by patients across multiple study sites, they wrote. However, the data suggest that “the emerging benefit-to-risk profile in this 52-week study supports the role of dupilumab as a primary targeted biologic therapy for up to 1 year in patients with moderate-to-severe atopic dermatitis who are not controlled with topical medications alone,” they said.
The study was funded by Sanofi and Regeneron Pharmaceuticals. Dr. Blauvelt and coauthors disclosed relationships with companies including Sanofi and Regeneron. Several authors were employees of the two companies.
FROM THE LANCET
Key clinical point: One year data on the efficacy and safety of dupilumab, combined with topical steroids, in adults with atopic dermatitis reflected the positive 16-week results, with encouraging safety data.
Major finding: After 16 weeks, 39% of atopic dermatitis patients who received dupilumab in addition to topical steroids met endpoints for improved symptoms, vs. 12% of patients who received topical steroids plus placebo. These benefits were sustained through one year.
Data source: An international phase III randomized trial of adults with moderate to severe atopic dermatitis.
Disclosures: The study was funded by Sanofi and Regeneron Pharmaceuticals. The lead author and coauthors disclosed relationships with companies including Sanofi and Regeneron. Several authors were employees of the two companies.
Infliximab biosimilar noninferior to originator in IBD – NOR-SWITCH
CHICAGO – The biosimilar infliximab CT-P13 is not inferior to the originator infliximab in terms of efficacy, safety, and immunogenicity in the treatment of inflammatory bowel disease (IBD), a phase IV randomized trial showed.
Patient outcomes were not compromised with the use of the biosimilar, and the cost of treatment was much lower, said lead author Kristin K. Jørgensen, MD, PhD, at Digestive Disease Week®.
“Biologics represent a substantial source of IBD expenditure,” said Dr. Jørgensen of Akershus University Hospital, Lørenskog, Norway. “The medication is expensive, patients are treated on a long-term basis, and the incidence of IBD is increasing.”
Biosimilars are biotherapeutic products that are similar in terms of quality, safety, and efficacy to the already licensed reference biologic product. “Use of biosimilars can potentially dramatically decrease costs and may lead to better patient care,” said Dr. Jørgensen. “The patient gets increased access to biologic therapy, and it is easier to intensify dosing if indicated.”
Tumor necrosis factor–inhibitors are commonly used to treat Crohn’s disease, ulcerative colitis, spondyloarthritis, rheumatoid arthritis, psoriatic arthritis, and chronic plaque psoriasis, and, while they have altered the treatment paradigm, they are expensive products.
The goal of the NOR-SWITCH was to evaluate switching from originator infliximab to CT-P13, in terms of efficacy, safety, and immunogenicity.
Dr. Jørgensen and her colleagues conducted a randomized phase IV trial that enrolled 482 patients who were randomly assigned to either infliximab originator (n = 241) or CT-P13 (n = 241). The primary endpoint was disease worsening during follow-up.
Of the group, 155 patients (32%) had Crohn’s disease, 93 (19%) had ulcerative colitis, 91 (19%) had spondyloarthritis, 77 (16%) had rheumatoid arthritis, 30 (6%) had psoriatic arthritis, and 35 (7%) had chronic plaque psoriasis.
Disease worsening occurred at a similar rate in both groups. In the infliximab originator group, 53 patients (26%) experienced a worsening of their symptoms, compared with 61 patients (30%) in the CT-P13 group. The 95% confidence interval of the adjusted risk difference (−4.4%) was −12.7% to 3.9%, which fell within the prespecified noninferiority margin of 15%.
Therefore, the findings demonstrated that CT-P13 is not inferior to infliximab originator, and the adjusted relative risk of disease worsening for CT-P13 patients was 1.17 (95% CI, 0.82-1.52), compared with the infliximab originator group.
An almost equal number of patients achieved disease remission, 123 patients (61%) in the infliximab originator group and 126 patients (61%) in the CT-P13 group, and the adjusted rate difference was 0.6% (95% CI, –7.5%-8.8%; per-protocol set).
An explorative subgroup analysis that looked at patients with Crohn’s disease and ulcerative colitis showed similar findings between patients treated with either agent.
“Our results support switching from the originator to a biosimilar for nonmedical reasons,” concluded Dr. Jørgensen.
However, she urged caution in generalizing these findings to other biologic agents.
The study was funded by the Norwegian Ministry of Health and Care Services. Dr. Jorgensen reported receiving personal fees from Tillotts, Intercept, and Celltrion. Several coauthors also reported relationships with industry.
Digestive Disease Week® is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
CHICAGO – The biosimilar infliximab CT-P13 is not inferior to the originator infliximab in terms of efficacy, safety, and immunogenicity in the treatment of inflammatory bowel disease (IBD), a phase IV randomized trial showed.
Patient outcomes were not compromised with the use of the biosimilar, and the cost of treatment was much lower, said lead author Kristin K. Jørgensen, MD, PhD, at Digestive Disease Week®.
“Biologics represent a substantial source of IBD expenditure,” said Dr. Jørgensen of Akershus University Hospital, Lørenskog, Norway. “The medication is expensive, patients are treated on a long-term basis, and the incidence of IBD is increasing.”
Biosimilars are biotherapeutic products that are similar in terms of quality, safety, and efficacy to the already licensed reference biologic product. “Use of biosimilars can potentially dramatically decrease costs and may lead to better patient care,” said Dr. Jørgensen. “The patient gets increased access to biologic therapy, and it is easier to intensify dosing if indicated.”
Tumor necrosis factor–inhibitors are commonly used to treat Crohn’s disease, ulcerative colitis, spondyloarthritis, rheumatoid arthritis, psoriatic arthritis, and chronic plaque psoriasis, and, while they have altered the treatment paradigm, they are expensive products.
The goal of the NOR-SWITCH was to evaluate switching from originator infliximab to CT-P13, in terms of efficacy, safety, and immunogenicity.
Dr. Jørgensen and her colleagues conducted a randomized phase IV trial that enrolled 482 patients who were randomly assigned to either infliximab originator (n = 241) or CT-P13 (n = 241). The primary endpoint was disease worsening during follow-up.
Of the group, 155 patients (32%) had Crohn’s disease, 93 (19%) had ulcerative colitis, 91 (19%) had spondyloarthritis, 77 (16%) had rheumatoid arthritis, 30 (6%) had psoriatic arthritis, and 35 (7%) had chronic plaque psoriasis.
Disease worsening occurred at a similar rate in both groups. In the infliximab originator group, 53 patients (26%) experienced a worsening of their symptoms, compared with 61 patients (30%) in the CT-P13 group. The 95% confidence interval of the adjusted risk difference (−4.4%) was −12.7% to 3.9%, which fell within the prespecified noninferiority margin of 15%.
Therefore, the findings demonstrated that CT-P13 is not inferior to infliximab originator, and the adjusted relative risk of disease worsening for CT-P13 patients was 1.17 (95% CI, 0.82-1.52), compared with the infliximab originator group.
An almost equal number of patients achieved disease remission, 123 patients (61%) in the infliximab originator group and 126 patients (61%) in the CT-P13 group, and the adjusted rate difference was 0.6% (95% CI, –7.5%-8.8%; per-protocol set).
An explorative subgroup analysis that looked at patients with Crohn’s disease and ulcerative colitis showed similar findings between patients treated with either agent.
“Our results support switching from the originator to a biosimilar for nonmedical reasons,” concluded Dr. Jørgensen.
However, she urged caution in generalizing these findings to other biologic agents.
The study was funded by the Norwegian Ministry of Health and Care Services. Dr. Jorgensen reported receiving personal fees from Tillotts, Intercept, and Celltrion. Several coauthors also reported relationships with industry.
Digestive Disease Week® is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
CHICAGO – The biosimilar infliximab CT-P13 is not inferior to the originator infliximab in terms of efficacy, safety, and immunogenicity in the treatment of inflammatory bowel disease (IBD), a phase IV randomized trial showed.
Patient outcomes were not compromised with the use of the biosimilar, and the cost of treatment was much lower, said lead author Kristin K. Jørgensen, MD, PhD, at Digestive Disease Week®.
“Biologics represent a substantial source of IBD expenditure,” said Dr. Jørgensen of Akershus University Hospital, Lørenskog, Norway. “The medication is expensive, patients are treated on a long-term basis, and the incidence of IBD is increasing.”
Biosimilars are biotherapeutic products that are similar in terms of quality, safety, and efficacy to the already licensed reference biologic product. “Use of biosimilars can potentially dramatically decrease costs and may lead to better patient care,” said Dr. Jørgensen. “The patient gets increased access to biologic therapy, and it is easier to intensify dosing if indicated.”
Tumor necrosis factor–inhibitors are commonly used to treat Crohn’s disease, ulcerative colitis, spondyloarthritis, rheumatoid arthritis, psoriatic arthritis, and chronic plaque psoriasis, and, while they have altered the treatment paradigm, they are expensive products.
The goal of the NOR-SWITCH was to evaluate switching from originator infliximab to CT-P13, in terms of efficacy, safety, and immunogenicity.
Dr. Jørgensen and her colleagues conducted a randomized phase IV trial that enrolled 482 patients who were randomly assigned to either infliximab originator (n = 241) or CT-P13 (n = 241). The primary endpoint was disease worsening during follow-up.
Of the group, 155 patients (32%) had Crohn’s disease, 93 (19%) had ulcerative colitis, 91 (19%) had spondyloarthritis, 77 (16%) had rheumatoid arthritis, 30 (6%) had psoriatic arthritis, and 35 (7%) had chronic plaque psoriasis.
Disease worsening occurred at a similar rate in both groups. In the infliximab originator group, 53 patients (26%) experienced a worsening of their symptoms, compared with 61 patients (30%) in the CT-P13 group. The 95% confidence interval of the adjusted risk difference (−4.4%) was −12.7% to 3.9%, which fell within the prespecified noninferiority margin of 15%.
Therefore, the findings demonstrated that CT-P13 is not inferior to infliximab originator, and the adjusted relative risk of disease worsening for CT-P13 patients was 1.17 (95% CI, 0.82-1.52), compared with the infliximab originator group.
An almost equal number of patients achieved disease remission, 123 patients (61%) in the infliximab originator group and 126 patients (61%) in the CT-P13 group, and the adjusted rate difference was 0.6% (95% CI, –7.5%-8.8%; per-protocol set).
An explorative subgroup analysis that looked at patients with Crohn’s disease and ulcerative colitis showed similar findings between patients treated with either agent.
“Our results support switching from the originator to a biosimilar for nonmedical reasons,” concluded Dr. Jørgensen.
However, she urged caution in generalizing these findings to other biologic agents.
The study was funded by the Norwegian Ministry of Health and Care Services. Dr. Jorgensen reported receiving personal fees from Tillotts, Intercept, and Celltrion. Several coauthors also reported relationships with industry.
Digestive Disease Week® is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
AT DDW
Key clinical point: An infliximab biosimilar was not inferior to the originator in terms of efficacy, safety, and immunogenicity in the treatment of inflammatory bowel disease (IBD).
Major finding: In the infliximab originator group, 53 patients (26%) experienced disease worsening, vs. 61 patients (30%) in the CT-P13 group, which fell within the prespecified noninferiority margin of 15%.
Data source: A phase IV randomized trial that included 482 patients with inflammatory bowel disease.
Disclosures: The study was funded by the Norwegian Ministry of Health and Care Services. Dr. Jorgensen reported receiving personal fees from Tillotts, Intercept, and Celltrion. Several coauthors also reported relationships with industry.
Experts bust common sports medicine myths
SAN DIEGO – Is it okay for pregnant women to attend CrossFit classes? Are patients who run for fun at increased risk for osteoarthritis? Does stretching before exercise provide any benefits to athletes?
Experts discussed these topics during a session titled “Mythbusters in sports medicine” at the annual meeting of the American Medical Society for Sports Medicine.
Does exercise negatively impact pregnancy?
The idea that strenuous exercise during pregnancy can harm a baby’s health is a myth, according to Elizabeth A. Joy, MD.
“Women having healthy, uncomplicated pregnancies should be encouraged to be physically active throughout pregnancy, with a goal of achieving 150 minutes per week of moderate-intensity activity,” she said. “Fit pregnant women who were habitually performing high-intensity exercise before pregnancy can continue to do so during pregnancy, assuming an otherwise healthy, uncomplicated pregnancy.”
Results from more than 600 studies in the medical literature indicate that exercise during pregnancy is safe for moms and babies, noted Dr. Joy, medical director for community health and food and nutrition at Intermountain Healthcare in Salt Lake City, Utah.
In fact, the 2008 Physical Activity Guidelines for Americans state that pregnant women who habitually engage in vigorous-intensity aerobic activity or who are highly active “can continue physical activity during pregnancy and the postpartum period, provided that they remain healthy and discuss with their health care provider how and when activity should be adjusted over time.”
Such advice wasn’t always supported by the medical profession. In fact, 1985 guidelines from the American College of Obstetricians and Gynecologists recommended that women limit exercise to no more than 15 minutes at a time during pregnancy and keep their maternal heart rate less than 140 beats per minute. ACOG also discouraged previously sedentary women from beginning an exercise program during pregnancy.
“Sadly, women are still getting this advice,” said Dr. Joy, who is also president of the American College of Sports Medicine. According to the 2005-2010 National Ambulatory Medical Care Survey, only 18% of pregnant women reported receiving counseling to be physically active during their pregnancies (Matern Child Health J. 2014 Sep;18[7]:1610-18). “That is just unacceptable,” she said.
In a prospective study of the association between vigorous physical activity during pregnancy and length of gestation and birth weight, researchers evaluated 1,647 births among primiparous women (Matern Child Health J. 2012 Jul;16[5]:1031-44).
They conducted telephone interviews with the women between 7-20 weeks gestation and assigned metabolic equivalent of task values to self-reported levels of physical activity. Of the 1,647 births, 7% were preterm.
Slightly more than one-third of the women (35%) performed first-trimester vigorous physical activity. The average total vigorous activity reported was 76 minutes per week, 38% of which was vigorous recreational activity.
Women who performed first-trimester vigorous recreational physical activity tended to have lower odds of preterm birth. They also tended to have lighter-weight babies, but this did not reach statistical significance (P = .08). The authors concluded that first-trimester vigorous physical activity “does not appear to be detrimental to the timing of birth or birth weight.”
In a separate analysis, researchers evaluated acute fetal responses to individually prescribed exercise according to existing physical activity guidelines in active and inactive pregnant women (Obstet Gynecol. 2012 Mar;119[3]:603-10).
Of the 45 study participants, 15 were classified as nonexercisers, 15 were regularly active, and 15 were highly active. The women underwent treadmill assessment between 28 weeks and 33 weeks, while fetal assessment included umbilical artery Doppler, fetal heart tracing and rate, and biophysical profile at rest and immediately post exercise.
The researchers observed no differences between the groups in mode of delivery, birth weight, and Apgar scores. During vigorous-intensity exercise, all umbilical artery indices showed decreases post exercise.
“Although statistically significant, this decrease is likely not clinically significant,” the researchers wrote. “We did not identify any adverse acute fetal responses to current exercise recommendations.” They went on to conclude that the potential health benefits of exercise “are too great for [physicians] to miss the opportunity to effectively counsel pregnant women about this important heath-enhancing behavior.”
In a more recent randomized study, Swedish researchers evaluated the efficacy of moderate-to-vigorous resistance exercise in 92 pregnant women (Acta Obstet Gynecol Scand. 2015 Jan; 94[1]:35-42).
The intervention group received supervised resistance exercise twice per week at moderate-to-vigorous intensity between 14-25 weeks of their pregnancy, while the control group received a generalized home exercise program. Outcome measures included health-related quality of life, physical strength, pain, weight, blood pressure, functional status, activity level, and perinatal data.
The researchers found no significant differences between the two groups and concluded that “supervised regular, moderate-to-vigorous resistance exercise performed twice per week does not adversely impact childbirth outcome, pain, or blood pressure.”
Despite all that’s known about exercise during pregnancy, a few practice and research gaps remain.
For one, Dr. Joy said, the relationship between performing physically demanding work during pregnancy in combination with moderate-to-vigorous exercise remains largely unknown.
“Even within health care, you have residents, nurses, and others working in hospitals,” she said. “That’s demanding work, but we don’t know whether or not moderate-to-vigorous exercise in combination with that kind of work is safe. Also, although women tend to thermoregulate better during pregnancy, we still don’t fully understand the impact of elevated core body temperature, which may occur with regularly performed vigorous-intensity exercise over the course of pregnancy.”
Does running cause knee OA?
During another talk at the meeting, William O. Roberts, MD, characterized the notion that running causes knee osteoarthritis as largely a myth for recreational runners. However, elite runners and athletes who participate in other sports may face an increased risk of developing the condition.
Well-established risk factors for knee OA include post–joint injury proteases and cytokines and injury load stress on articular cartilage. “Other risk factors include overweight and obesity, a family history of OA, exercise, heavy work that involved squatting and kneeling, and being female,” said Dr. Roberts, professor of family medicine and community health at the University of Minnesota, Minneapolis.
He discussed three articles on the topic drawn from medical literature. One was a retrospective cross-sectional analysis of 2,637 Osteoarthritis Initiative participants, 45-79 years of age, who had knee-specific pain or knee x-ray data 4 years into the 10-year–long study (Arthritis Care Res. 2017 Feb;69[2]:183-91).
More than half of the participants (56%) were female, their mean body mass index was 28.5 kg/m2, only 20% reported more than 2,000 bouts of running during their lifetime, and about 5% had run competitively.
Adjusted odds ratios of pain, radiographic OA, and symptomatic OA for those prior runners and current runners, compared with those who never ran, were 0.82 and 0.76 (P for trend = .02), 0.98 and 0.91 (P for trend = .05), and 0.88 and 0.71 (P for trend = .03), respectively.
The authors concluded that running does not appear to be detrimental to the knees, and the strength of recommendation taxonomy was rated as 2B.
In a separate analysis, researchers performed a systematic review and meta-analysis of 11 cohort (6 retrospective) and 4 case-control studies related to running and knee arthritis (Am J Sports Med. 2016 May;45[6]:1447-57). The mean ages of subjects at outcome assessment ranged from 27 years to 69 years, and the sample size ranged from 15 to 1,279 participants. The four case control studies assessed exposure by mailed questionnaire or by personal interview.
The meta-analysis suggests that runners have a 50% reduced odds of requiring a total knee replacement because of OA.
“It contradicts some previous studies, and there were confounders,” Dr. Roberts said of the analysis. “The one that I noticed is that people would delay surgery to keep running. That’s what I find in my practice.”
The researchers were unable to link running to knee OA development. Moderate- to low-quality evidence suggests a positive association with OA diagnosis but a negative association with requirement for a total knee replacement.
Based on published evidence, they concluded there is no clear advice to give regarding the potential effect of running on musculoskeletal health and rated the strength of evidence as 1A.
A third study Dr. Roberts discussed investigated the association between specific sports participation and knee OA (J Athl Train. 2015 Jan. 9. doi: 10.4085/1062-6050-50.2.08). After locating nearly 18,000 articles on the topic, the researchers limited their meta-analysis to 17 published studies.
They found that the overall risk of knee OA prevalence in sports participants was 7.7%, compared with 7.3% among nonexposed controls (odds ratio, 0.9). However, risks for knee OA were elevated among those who participated in the following sports: soccer (OR, 3.5), elite long-distance running (OR, 3.3), competitive weightlifting (OR, 6.9), and wrestling (OR, 3.8). The researchers concluded that athletes who participate in those sports “should be targeted for risk-reduction strategies.”
“So, does running cause knee OA? It depends,” said Dr. Roberts, who is also medical director of Twin Cities in Motion. “There is a potential risk to high-volume, high-intensity, and long-distance runners, but there does not appear to be a risk in fitness or recreational runners. Of course, you can’t erase your genetics.”
He called for more research on the topic, including prospective longitudinal outcomes studies, those that study the role of genetics/epigenetics in runners and nonrunners who develop knee OA and those focused on the knee joint “chemical environment,” referring to recent work that suggests that running appears to decrease knee intra-articular proinflammatory cytokine concentration (Eur J Appl Physiol. 2016 Dec;116[11-12]:2305-14).
“It’s okay to run for fitness, because the health benefits far outweigh the risk of knee OA,” Dr. Roberts said. “If you run hard and long, it could be a problem. We probably should be screening for neuromuscular control to reduce anterior cruciate ligament disruption.”
Does it help to stretch before exercise?
Stretching before engaging in exercise is a common practice often recommended by coaches and clinicians – but it appears to have no role in preventing injuries during exercise itself.
Several decades ago, investigators subscribed to muscle spasm theory, which held that unaccustomed exercise caused muscle spasms.
“The thought was that muscle spasms impeded blood flow to the muscle, causing ischemic pain and further spasm,” Valerie E. Cothran, MD, said during a presentation at the meeting. “Stretching the muscle was thought to restore blood flow to the muscle and interrupt the pain-spasm-pain cycle. This theory has been discredited for 40 years, but the practice of stretching before exercise persists.”
According to Dr. Cothran, of the department of family and community medicine at the University of Maryland, Baltimore, a limited number of randomized, controlled trials exist on the topic – and many are fraught with limitations, such as the evaluation of multiple stretching methods and variable types of sports activities and the inclusion of multiple cointerventions.
One systematic review evaluated 361 randomized, controlled trials and cohort studies of interventions that included stretching and that appeared in the medical literature from 1966 to 2002 (Med Sci Sports Exerc. 2004 Mar;36[3]:371-8). Studies with no controls were excluded from the analysis, as were those in which stretching could not be assessed independently or those that did not include people engaged in sports or fitness activities.
The researchers determined that stretching was not significantly associated with a reduction in total injuries (OR, 0.93). “There is not sufficient evidence to endorse or discontinue routine stretching before or after exercise to prevent injury among competitive or recreational athletes,” they concluded.
The following year, Lawrence Hart, MBBch, of McMaster University, Hamilton, Ont., assessed the same set of data but eliminated some of the confounding factors of the previous analysis, including studies that had limited statistical power (Clin J Sport Med. 2005 Mar;15[2]:113). The final meta-analysis included six studies.
Dr. Hart found that neither stretching of specific leg-muscle groups or multiple muscle groups led to a reduction in total injuries, such as shin splints, tibial stress reaction, or sprains/strains (OR, 0.93). In addition, reduction in injuries was not significantly greater for stretching of specific muscles or multiple muscle groups (OR, 0.80, and OR, 0.96, respectively). “Limited evidence showed stretching had no effects on injuries,” he concluded.
A more recent systematic review analyzed the efficacy of static stretching as part of a warm-up for the prevention of exercise-related injury (Res Sports Med. 2008;16[3]:213-31). The researchers reviewed 364 studies published after 1990 but before 2008, and they included seven in the final analysis: four randomized, controlled trials and three controlled trials.
All four randomized, controlled trials concluded that static stretching was ineffective in reducing the incidence of exercise-related injury, and only one of the three controlled trials concluded that static stretching reduced the incidence of exercise-related injury. In addition, three of the seven studies reported significant reductions in musculotendinous and ligament injuries following a static stretching protocol.
“There is moderate to strong evidence that routine application of static stretching does not reduce overall injury rates,” the researchers concluded. “There is preliminary evidence, however, that static stretching may reduce musculotendinous injuries.”
The final study Dr. Cothran discussed was a systematic review of two randomized, controlled trials and two prospective cohort studies on the effect of stretching in sports injury prevention that appeared in the literature between 1998 and 2008 (J Comm Health Sci. 2008;3[1]:51-8).
One cohort study found that stretching reduced the incidence of exercise-related injuries, while two randomized, controlled trials and one cohort study found that stretching did not produce a practical reduction on the occurrence of injuries. The researchers concluded that stretching exercises “do not give a practical, useful reduction in the risk of injuries.”
Some studies have demonstrated that explosive athletic performance such as sprinting may be compromised by acute stretching, noted Dr. Cothran, who is also program director of the primary care sports medicine fellowship at the University of Maryland, Baltimore. Current practice and research gaps include few recent randomized, controlled trials; few studies isolating stretching alone; and few that compare the different forms of stretching, such as dynamic and static stretching, she added.
“There is moderate to strong evidence that routine stretching before exercise will not reduce injury rates,” she concluded. “There is evidence that stretching before exercise may negatively affect performance. Flexibility training can be beneficial but should take place at alternative times and not before exercise.”
Dr. Joy disclosed that she receives funding from Savvysherpa and Dexcom for a project on the prevention of gestational diabetes. Dr. Roberts and Dr. Cothran reported having no financial disclosures.
SAN DIEGO – Is it okay for pregnant women to attend CrossFit classes? Are patients who run for fun at increased risk for osteoarthritis? Does stretching before exercise provide any benefits to athletes?
Experts discussed these topics during a session titled “Mythbusters in sports medicine” at the annual meeting of the American Medical Society for Sports Medicine.
Does exercise negatively impact pregnancy?
The idea that strenuous exercise during pregnancy can harm a baby’s health is a myth, according to Elizabeth A. Joy, MD.
“Women having healthy, uncomplicated pregnancies should be encouraged to be physically active throughout pregnancy, with a goal of achieving 150 minutes per week of moderate-intensity activity,” she said. “Fit pregnant women who were habitually performing high-intensity exercise before pregnancy can continue to do so during pregnancy, assuming an otherwise healthy, uncomplicated pregnancy.”
Results from more than 600 studies in the medical literature indicate that exercise during pregnancy is safe for moms and babies, noted Dr. Joy, medical director for community health and food and nutrition at Intermountain Healthcare in Salt Lake City, Utah.
In fact, the 2008 Physical Activity Guidelines for Americans state that pregnant women who habitually engage in vigorous-intensity aerobic activity or who are highly active “can continue physical activity during pregnancy and the postpartum period, provided that they remain healthy and discuss with their health care provider how and when activity should be adjusted over time.”
Such advice wasn’t always supported by the medical profession. In fact, 1985 guidelines from the American College of Obstetricians and Gynecologists recommended that women limit exercise to no more than 15 minutes at a time during pregnancy and keep their maternal heart rate less than 140 beats per minute. ACOG also discouraged previously sedentary women from beginning an exercise program during pregnancy.
“Sadly, women are still getting this advice,” said Dr. Joy, who is also president of the American College of Sports Medicine. According to the 2005-2010 National Ambulatory Medical Care Survey, only 18% of pregnant women reported receiving counseling to be physically active during their pregnancies (Matern Child Health J. 2014 Sep;18[7]:1610-18). “That is just unacceptable,” she said.
In a prospective study of the association between vigorous physical activity during pregnancy and length of gestation and birth weight, researchers evaluated 1,647 births among primiparous women (Matern Child Health J. 2012 Jul;16[5]:1031-44).
They conducted telephone interviews with the women between 7-20 weeks gestation and assigned metabolic equivalent of task values to self-reported levels of physical activity. Of the 1,647 births, 7% were preterm.
Slightly more than one-third of the women (35%) performed first-trimester vigorous physical activity. The average total vigorous activity reported was 76 minutes per week, 38% of which was vigorous recreational activity.
Women who performed first-trimester vigorous recreational physical activity tended to have lower odds of preterm birth. They also tended to have lighter-weight babies, but this did not reach statistical significance (P = .08). The authors concluded that first-trimester vigorous physical activity “does not appear to be detrimental to the timing of birth or birth weight.”
In a separate analysis, researchers evaluated acute fetal responses to individually prescribed exercise according to existing physical activity guidelines in active and inactive pregnant women (Obstet Gynecol. 2012 Mar;119[3]:603-10).
Of the 45 study participants, 15 were classified as nonexercisers, 15 were regularly active, and 15 were highly active. The women underwent treadmill assessment between 28 weeks and 33 weeks, while fetal assessment included umbilical artery Doppler, fetal heart tracing and rate, and biophysical profile at rest and immediately post exercise.
The researchers observed no differences between the groups in mode of delivery, birth weight, and Apgar scores. During vigorous-intensity exercise, all umbilical artery indices showed decreases post exercise.
“Although statistically significant, this decrease is likely not clinically significant,” the researchers wrote. “We did not identify any adverse acute fetal responses to current exercise recommendations.” They went on to conclude that the potential health benefits of exercise “are too great for [physicians] to miss the opportunity to effectively counsel pregnant women about this important heath-enhancing behavior.”
In a more recent randomized study, Swedish researchers evaluated the efficacy of moderate-to-vigorous resistance exercise in 92 pregnant women (Acta Obstet Gynecol Scand. 2015 Jan; 94[1]:35-42).
The intervention group received supervised resistance exercise twice per week at moderate-to-vigorous intensity between 14-25 weeks of their pregnancy, while the control group received a generalized home exercise program. Outcome measures included health-related quality of life, physical strength, pain, weight, blood pressure, functional status, activity level, and perinatal data.
The researchers found no significant differences between the two groups and concluded that “supervised regular, moderate-to-vigorous resistance exercise performed twice per week does not adversely impact childbirth outcome, pain, or blood pressure.”
Despite all that’s known about exercise during pregnancy, a few practice and research gaps remain.
For one, Dr. Joy said, the relationship between performing physically demanding work during pregnancy in combination with moderate-to-vigorous exercise remains largely unknown.
“Even within health care, you have residents, nurses, and others working in hospitals,” she said. “That’s demanding work, but we don’t know whether or not moderate-to-vigorous exercise in combination with that kind of work is safe. Also, although women tend to thermoregulate better during pregnancy, we still don’t fully understand the impact of elevated core body temperature, which may occur with regularly performed vigorous-intensity exercise over the course of pregnancy.”
Does running cause knee OA?
During another talk at the meeting, William O. Roberts, MD, characterized the notion that running causes knee osteoarthritis as largely a myth for recreational runners. However, elite runners and athletes who participate in other sports may face an increased risk of developing the condition.
Well-established risk factors for knee OA include post–joint injury proteases and cytokines and injury load stress on articular cartilage. “Other risk factors include overweight and obesity, a family history of OA, exercise, heavy work that involved squatting and kneeling, and being female,” said Dr. Roberts, professor of family medicine and community health at the University of Minnesota, Minneapolis.
He discussed three articles on the topic drawn from medical literature. One was a retrospective cross-sectional analysis of 2,637 Osteoarthritis Initiative participants, 45-79 years of age, who had knee-specific pain or knee x-ray data 4 years into the 10-year–long study (Arthritis Care Res. 2017 Feb;69[2]:183-91).
More than half of the participants (56%) were female, their mean body mass index was 28.5 kg/m2, only 20% reported more than 2,000 bouts of running during their lifetime, and about 5% had run competitively.
Adjusted odds ratios of pain, radiographic OA, and symptomatic OA for those prior runners and current runners, compared with those who never ran, were 0.82 and 0.76 (P for trend = .02), 0.98 and 0.91 (P for trend = .05), and 0.88 and 0.71 (P for trend = .03), respectively.
The authors concluded that running does not appear to be detrimental to the knees, and the strength of recommendation taxonomy was rated as 2B.
In a separate analysis, researchers performed a systematic review and meta-analysis of 11 cohort (6 retrospective) and 4 case-control studies related to running and knee arthritis (Am J Sports Med. 2016 May;45[6]:1447-57). The mean ages of subjects at outcome assessment ranged from 27 years to 69 years, and the sample size ranged from 15 to 1,279 participants. The four case control studies assessed exposure by mailed questionnaire or by personal interview.
The meta-analysis suggests that runners have a 50% reduced odds of requiring a total knee replacement because of OA.
“It contradicts some previous studies, and there were confounders,” Dr. Roberts said of the analysis. “The one that I noticed is that people would delay surgery to keep running. That’s what I find in my practice.”
The researchers were unable to link running to knee OA development. Moderate- to low-quality evidence suggests a positive association with OA diagnosis but a negative association with requirement for a total knee replacement.
Based on published evidence, they concluded there is no clear advice to give regarding the potential effect of running on musculoskeletal health and rated the strength of evidence as 1A.
A third study Dr. Roberts discussed investigated the association between specific sports participation and knee OA (J Athl Train. 2015 Jan. 9. doi: 10.4085/1062-6050-50.2.08). After locating nearly 18,000 articles on the topic, the researchers limited their meta-analysis to 17 published studies.
They found that the overall risk of knee OA prevalence in sports participants was 7.7%, compared with 7.3% among nonexposed controls (odds ratio, 0.9). However, risks for knee OA were elevated among those who participated in the following sports: soccer (OR, 3.5), elite long-distance running (OR, 3.3), competitive weightlifting (OR, 6.9), and wrestling (OR, 3.8). The researchers concluded that athletes who participate in those sports “should be targeted for risk-reduction strategies.”
“So, does running cause knee OA? It depends,” said Dr. Roberts, who is also medical director of Twin Cities in Motion. “There is a potential risk to high-volume, high-intensity, and long-distance runners, but there does not appear to be a risk in fitness or recreational runners. Of course, you can’t erase your genetics.”
He called for more research on the topic, including prospective longitudinal outcomes studies, those that study the role of genetics/epigenetics in runners and nonrunners who develop knee OA and those focused on the knee joint “chemical environment,” referring to recent work that suggests that running appears to decrease knee intra-articular proinflammatory cytokine concentration (Eur J Appl Physiol. 2016 Dec;116[11-12]:2305-14).
“It’s okay to run for fitness, because the health benefits far outweigh the risk of knee OA,” Dr. Roberts said. “If you run hard and long, it could be a problem. We probably should be screening for neuromuscular control to reduce anterior cruciate ligament disruption.”
Does it help to stretch before exercise?
Stretching before engaging in exercise is a common practice often recommended by coaches and clinicians – but it appears to have no role in preventing injuries during exercise itself.
Several decades ago, investigators subscribed to muscle spasm theory, which held that unaccustomed exercise caused muscle spasms.
“The thought was that muscle spasms impeded blood flow to the muscle, causing ischemic pain and further spasm,” Valerie E. Cothran, MD, said during a presentation at the meeting. “Stretching the muscle was thought to restore blood flow to the muscle and interrupt the pain-spasm-pain cycle. This theory has been discredited for 40 years, but the practice of stretching before exercise persists.”
According to Dr. Cothran, of the department of family and community medicine at the University of Maryland, Baltimore, a limited number of randomized, controlled trials exist on the topic – and many are fraught with limitations, such as the evaluation of multiple stretching methods and variable types of sports activities and the inclusion of multiple cointerventions.
One systematic review evaluated 361 randomized, controlled trials and cohort studies of interventions that included stretching and that appeared in the medical literature from 1966 to 2002 (Med Sci Sports Exerc. 2004 Mar;36[3]:371-8). Studies with no controls were excluded from the analysis, as were those in which stretching could not be assessed independently or those that did not include people engaged in sports or fitness activities.
The researchers determined that stretching was not significantly associated with a reduction in total injuries (OR, 0.93). “There is not sufficient evidence to endorse or discontinue routine stretching before or after exercise to prevent injury among competitive or recreational athletes,” they concluded.
The following year, Lawrence Hart, MBBch, of McMaster University, Hamilton, Ont., assessed the same set of data but eliminated some of the confounding factors of the previous analysis, including studies that had limited statistical power (Clin J Sport Med. 2005 Mar;15[2]:113). The final meta-analysis included six studies.
Dr. Hart found that neither stretching of specific leg-muscle groups or multiple muscle groups led to a reduction in total injuries, such as shin splints, tibial stress reaction, or sprains/strains (OR, 0.93). In addition, reduction in injuries was not significantly greater for stretching of specific muscles or multiple muscle groups (OR, 0.80, and OR, 0.96, respectively). “Limited evidence showed stretching had no effects on injuries,” he concluded.
A more recent systematic review analyzed the efficacy of static stretching as part of a warm-up for the prevention of exercise-related injury (Res Sports Med. 2008;16[3]:213-31). The researchers reviewed 364 studies published after 1990 but before 2008, and they included seven in the final analysis: four randomized, controlled trials and three controlled trials.
All four randomized, controlled trials concluded that static stretching was ineffective in reducing the incidence of exercise-related injury, and only one of the three controlled trials concluded that static stretching reduced the incidence of exercise-related injury. In addition, three of the seven studies reported significant reductions in musculotendinous and ligament injuries following a static stretching protocol.
“There is moderate to strong evidence that routine application of static stretching does not reduce overall injury rates,” the researchers concluded. “There is preliminary evidence, however, that static stretching may reduce musculotendinous injuries.”
The final study Dr. Cothran discussed was a systematic review of two randomized, controlled trials and two prospective cohort studies on the effect of stretching in sports injury prevention that appeared in the literature between 1998 and 2008 (J Comm Health Sci. 2008;3[1]:51-8).
One cohort study found that stretching reduced the incidence of exercise-related injuries, while two randomized, controlled trials and one cohort study found that stretching did not produce a practical reduction on the occurrence of injuries. The researchers concluded that stretching exercises “do not give a practical, useful reduction in the risk of injuries.”
Some studies have demonstrated that explosive athletic performance such as sprinting may be compromised by acute stretching, noted Dr. Cothran, who is also program director of the primary care sports medicine fellowship at the University of Maryland, Baltimore. Current practice and research gaps include few recent randomized, controlled trials; few studies isolating stretching alone; and few that compare the different forms of stretching, such as dynamic and static stretching, she added.
“There is moderate to strong evidence that routine stretching before exercise will not reduce injury rates,” she concluded. “There is evidence that stretching before exercise may negatively affect performance. Flexibility training can be beneficial but should take place at alternative times and not before exercise.”
Dr. Joy disclosed that she receives funding from Savvysherpa and Dexcom for a project on the prevention of gestational diabetes. Dr. Roberts and Dr. Cothran reported having no financial disclosures.
SAN DIEGO – Is it okay for pregnant women to attend CrossFit classes? Are patients who run for fun at increased risk for osteoarthritis? Does stretching before exercise provide any benefits to athletes?
Experts discussed these topics during a session titled “Mythbusters in sports medicine” at the annual meeting of the American Medical Society for Sports Medicine.
Does exercise negatively impact pregnancy?
The idea that strenuous exercise during pregnancy can harm a baby’s health is a myth, according to Elizabeth A. Joy, MD.
“Women having healthy, uncomplicated pregnancies should be encouraged to be physically active throughout pregnancy, with a goal of achieving 150 minutes per week of moderate-intensity activity,” she said. “Fit pregnant women who were habitually performing high-intensity exercise before pregnancy can continue to do so during pregnancy, assuming an otherwise healthy, uncomplicated pregnancy.”
Results from more than 600 studies in the medical literature indicate that exercise during pregnancy is safe for moms and babies, noted Dr. Joy, medical director for community health and food and nutrition at Intermountain Healthcare in Salt Lake City, Utah.
In fact, the 2008 Physical Activity Guidelines for Americans state that pregnant women who habitually engage in vigorous-intensity aerobic activity or who are highly active “can continue physical activity during pregnancy and the postpartum period, provided that they remain healthy and discuss with their health care provider how and when activity should be adjusted over time.”
Such advice wasn’t always supported by the medical profession. In fact, 1985 guidelines from the American College of Obstetricians and Gynecologists recommended that women limit exercise to no more than 15 minutes at a time during pregnancy and keep their maternal heart rate less than 140 beats per minute. ACOG also discouraged previously sedentary women from beginning an exercise program during pregnancy.
“Sadly, women are still getting this advice,” said Dr. Joy, who is also president of the American College of Sports Medicine. According to the 2005-2010 National Ambulatory Medical Care Survey, only 18% of pregnant women reported receiving counseling to be physically active during their pregnancies (Matern Child Health J. 2014 Sep;18[7]:1610-18). “That is just unacceptable,” she said.
In a prospective study of the association between vigorous physical activity during pregnancy and length of gestation and birth weight, researchers evaluated 1,647 births among primiparous women (Matern Child Health J. 2012 Jul;16[5]:1031-44).
They conducted telephone interviews with the women between 7-20 weeks gestation and assigned metabolic equivalent of task values to self-reported levels of physical activity. Of the 1,647 births, 7% were preterm.
Slightly more than one-third of the women (35%) performed first-trimester vigorous physical activity. The average total vigorous activity reported was 76 minutes per week, 38% of which was vigorous recreational activity.
Women who performed first-trimester vigorous recreational physical activity tended to have lower odds of preterm birth. They also tended to have lighter-weight babies, but this did not reach statistical significance (P = .08). The authors concluded that first-trimester vigorous physical activity “does not appear to be detrimental to the timing of birth or birth weight.”
In a separate analysis, researchers evaluated acute fetal responses to individually prescribed exercise according to existing physical activity guidelines in active and inactive pregnant women (Obstet Gynecol. 2012 Mar;119[3]:603-10).
Of the 45 study participants, 15 were classified as nonexercisers, 15 were regularly active, and 15 were highly active. The women underwent treadmill assessment between 28 weeks and 33 weeks, while fetal assessment included umbilical artery Doppler, fetal heart tracing and rate, and biophysical profile at rest and immediately post exercise.
The researchers observed no differences between the groups in mode of delivery, birth weight, and Apgar scores. During vigorous-intensity exercise, all umbilical artery indices showed decreases post exercise.
“Although statistically significant, this decrease is likely not clinically significant,” the researchers wrote. “We did not identify any adverse acute fetal responses to current exercise recommendations.” They went on to conclude that the potential health benefits of exercise “are too great for [physicians] to miss the opportunity to effectively counsel pregnant women about this important heath-enhancing behavior.”
In a more recent randomized study, Swedish researchers evaluated the efficacy of moderate-to-vigorous resistance exercise in 92 pregnant women (Acta Obstet Gynecol Scand. 2015 Jan; 94[1]:35-42).
The intervention group received supervised resistance exercise twice per week at moderate-to-vigorous intensity between 14-25 weeks of their pregnancy, while the control group received a generalized home exercise program. Outcome measures included health-related quality of life, physical strength, pain, weight, blood pressure, functional status, activity level, and perinatal data.
The researchers found no significant differences between the two groups and concluded that “supervised regular, moderate-to-vigorous resistance exercise performed twice per week does not adversely impact childbirth outcome, pain, or blood pressure.”
Despite all that’s known about exercise during pregnancy, a few practice and research gaps remain.
For one, Dr. Joy said, the relationship between performing physically demanding work during pregnancy in combination with moderate-to-vigorous exercise remains largely unknown.
“Even within health care, you have residents, nurses, and others working in hospitals,” she said. “That’s demanding work, but we don’t know whether or not moderate-to-vigorous exercise in combination with that kind of work is safe. Also, although women tend to thermoregulate better during pregnancy, we still don’t fully understand the impact of elevated core body temperature, which may occur with regularly performed vigorous-intensity exercise over the course of pregnancy.”
Does running cause knee OA?
During another talk at the meeting, William O. Roberts, MD, characterized the notion that running causes knee osteoarthritis as largely a myth for recreational runners. However, elite runners and athletes who participate in other sports may face an increased risk of developing the condition.
Well-established risk factors for knee OA include post–joint injury proteases and cytokines and injury load stress on articular cartilage. “Other risk factors include overweight and obesity, a family history of OA, exercise, heavy work that involved squatting and kneeling, and being female,” said Dr. Roberts, professor of family medicine and community health at the University of Minnesota, Minneapolis.
He discussed three articles on the topic drawn from medical literature. One was a retrospective cross-sectional analysis of 2,637 Osteoarthritis Initiative participants, 45-79 years of age, who had knee-specific pain or knee x-ray data 4 years into the 10-year–long study (Arthritis Care Res. 2017 Feb;69[2]:183-91).
More than half of the participants (56%) were female, their mean body mass index was 28.5 kg/m2, only 20% reported more than 2,000 bouts of running during their lifetime, and about 5% had run competitively.
Adjusted odds ratios of pain, radiographic OA, and symptomatic OA for those prior runners and current runners, compared with those who never ran, were 0.82 and 0.76 (P for trend = .02), 0.98 and 0.91 (P for trend = .05), and 0.88 and 0.71 (P for trend = .03), respectively.
The authors concluded that running does not appear to be detrimental to the knees, and the strength of recommendation taxonomy was rated as 2B.
In a separate analysis, researchers performed a systematic review and meta-analysis of 11 cohort (6 retrospective) and 4 case-control studies related to running and knee arthritis (Am J Sports Med. 2016 May;45[6]:1447-57). The mean ages of subjects at outcome assessment ranged from 27 years to 69 years, and the sample size ranged from 15 to 1,279 participants. The four case control studies assessed exposure by mailed questionnaire or by personal interview.
The meta-analysis suggests that runners have a 50% reduced odds of requiring a total knee replacement because of OA.
“It contradicts some previous studies, and there were confounders,” Dr. Roberts said of the analysis. “The one that I noticed is that people would delay surgery to keep running. That’s what I find in my practice.”
The researchers were unable to link running to knee OA development. Moderate- to low-quality evidence suggests a positive association with OA diagnosis but a negative association with requirement for a total knee replacement.
Based on published evidence, they concluded there is no clear advice to give regarding the potential effect of running on musculoskeletal health and rated the strength of evidence as 1A.
A third study Dr. Roberts discussed investigated the association between specific sports participation and knee OA (J Athl Train. 2015 Jan. 9. doi: 10.4085/1062-6050-50.2.08). After locating nearly 18,000 articles on the topic, the researchers limited their meta-analysis to 17 published studies.
They found that the overall risk of knee OA prevalence in sports participants was 7.7%, compared with 7.3% among nonexposed controls (odds ratio, 0.9). However, risks for knee OA were elevated among those who participated in the following sports: soccer (OR, 3.5), elite long-distance running (OR, 3.3), competitive weightlifting (OR, 6.9), and wrestling (OR, 3.8). The researchers concluded that athletes who participate in those sports “should be targeted for risk-reduction strategies.”
“So, does running cause knee OA? It depends,” said Dr. Roberts, who is also medical director of Twin Cities in Motion. “There is a potential risk to high-volume, high-intensity, and long-distance runners, but there does not appear to be a risk in fitness or recreational runners. Of course, you can’t erase your genetics.”
He called for more research on the topic, including prospective longitudinal outcomes studies, those that study the role of genetics/epigenetics in runners and nonrunners who develop knee OA and those focused on the knee joint “chemical environment,” referring to recent work that suggests that running appears to decrease knee intra-articular proinflammatory cytokine concentration (Eur J Appl Physiol. 2016 Dec;116[11-12]:2305-14).
“It’s okay to run for fitness, because the health benefits far outweigh the risk of knee OA,” Dr. Roberts said. “If you run hard and long, it could be a problem. We probably should be screening for neuromuscular control to reduce anterior cruciate ligament disruption.”
Does it help to stretch before exercise?
Stretching before engaging in exercise is a common practice often recommended by coaches and clinicians – but it appears to have no role in preventing injuries during exercise itself.
Several decades ago, investigators subscribed to muscle spasm theory, which held that unaccustomed exercise caused muscle spasms.
“The thought was that muscle spasms impeded blood flow to the muscle, causing ischemic pain and further spasm,” Valerie E. Cothran, MD, said during a presentation at the meeting. “Stretching the muscle was thought to restore blood flow to the muscle and interrupt the pain-spasm-pain cycle. This theory has been discredited for 40 years, but the practice of stretching before exercise persists.”
According to Dr. Cothran, of the department of family and community medicine at the University of Maryland, Baltimore, a limited number of randomized, controlled trials exist on the topic – and many are fraught with limitations, such as the evaluation of multiple stretching methods and variable types of sports activities and the inclusion of multiple cointerventions.
One systematic review evaluated 361 randomized, controlled trials and cohort studies of interventions that included stretching and that appeared in the medical literature from 1966 to 2002 (Med Sci Sports Exerc. 2004 Mar;36[3]:371-8). Studies with no controls were excluded from the analysis, as were those in which stretching could not be assessed independently or those that did not include people engaged in sports or fitness activities.
The researchers determined that stretching was not significantly associated with a reduction in total injuries (OR, 0.93). “There is not sufficient evidence to endorse or discontinue routine stretching before or after exercise to prevent injury among competitive or recreational athletes,” they concluded.
The following year, Lawrence Hart, MBBch, of McMaster University, Hamilton, Ont., assessed the same set of data but eliminated some of the confounding factors of the previous analysis, including studies that had limited statistical power (Clin J Sport Med. 2005 Mar;15[2]:113). The final meta-analysis included six studies.
Dr. Hart found that neither stretching of specific leg-muscle groups or multiple muscle groups led to a reduction in total injuries, such as shin splints, tibial stress reaction, or sprains/strains (OR, 0.93). In addition, reduction in injuries was not significantly greater for stretching of specific muscles or multiple muscle groups (OR, 0.80, and OR, 0.96, respectively). “Limited evidence showed stretching had no effects on injuries,” he concluded.
A more recent systematic review analyzed the efficacy of static stretching as part of a warm-up for the prevention of exercise-related injury (Res Sports Med. 2008;16[3]:213-31). The researchers reviewed 364 studies published after 1990 but before 2008, and they included seven in the final analysis: four randomized, controlled trials and three controlled trials.
All four randomized, controlled trials concluded that static stretching was ineffective in reducing the incidence of exercise-related injury, and only one of the three controlled trials concluded that static stretching reduced the incidence of exercise-related injury. In addition, three of the seven studies reported significant reductions in musculotendinous and ligament injuries following a static stretching protocol.
“There is moderate to strong evidence that routine application of static stretching does not reduce overall injury rates,” the researchers concluded. “There is preliminary evidence, however, that static stretching may reduce musculotendinous injuries.”
The final study Dr. Cothran discussed was a systematic review of two randomized, controlled trials and two prospective cohort studies on the effect of stretching in sports injury prevention that appeared in the literature between 1998 and 2008 (J Comm Health Sci. 2008;3[1]:51-8).
One cohort study found that stretching reduced the incidence of exercise-related injuries, while two randomized, controlled trials and one cohort study found that stretching did not produce a practical reduction on the occurrence of injuries. The researchers concluded that stretching exercises “do not give a practical, useful reduction in the risk of injuries.”
Some studies have demonstrated that explosive athletic performance such as sprinting may be compromised by acute stretching, noted Dr. Cothran, who is also program director of the primary care sports medicine fellowship at the University of Maryland, Baltimore. Current practice and research gaps include few recent randomized, controlled trials; few studies isolating stretching alone; and few that compare the different forms of stretching, such as dynamic and static stretching, she added.
“There is moderate to strong evidence that routine stretching before exercise will not reduce injury rates,” she concluded. “There is evidence that stretching before exercise may negatively affect performance. Flexibility training can be beneficial but should take place at alternative times and not before exercise.”
Dr. Joy disclosed that she receives funding from Savvysherpa and Dexcom for a project on the prevention of gestational diabetes. Dr. Roberts and Dr. Cothran reported having no financial disclosures.