User login
Burnout takes its toll on neurology
I’m burned out.
Heck, what doctor isn’t? Politicians say we get paid too much. Lawyers say we make too many mistakes. Insurance companies say we order too many tests and too many expensive treatments. And the patients, while generally good people looking for help, can also on occasion be angry and unreasonable. The bad apples may be in the minority, but it only takes one to ruin a day full of rewarding visits.
That can’t be good.
Some of the study’s listed reasons for burnout are very familiar: complaints about maintenance of certification and about calling insurances to authorize tests and medications, crappy reimbursement for time-consuming visits, having to spend more time at work just to break even, and the constant feeling of never being caught up. I leave work, come home, have dinner with my family, do dictations, go to bed, and do it over again. No matter where I am, I’ve never left the office.
Other common complaints aren’t as much an issue for me. I don’t have, or want, an electronic health record that qualifies for meaningful use; I designed the one I have, and it works fine for me. I don’t have a nonmedical administrator telling me how many patients I’m required to see each day, and my patient population is, overall, appreciative and polite.
There are always trade-offs. When my kids have school breaks, I take that time off from the office to be with them. I enjoy it – I mean, that’s what we’re here for as parents, isn’t it? Of course, the drawback comes a few weeks later when my income drops because I wasn’t working. In solo practice, cash flow is king. I may have more freedom and control than my employed colleagues, but the downside is that I have no guaranteed salary, either. I’m the last one here who gets paid.
I see plenty of columns on how to avoid burnout, none of which seem to be written by someone who’s in a real-world practice. They all recommend taking time off for yourself, maybe seeing a counselor, finding a hobby you enjoy ... Really?
There’s no easy answer, either. We’re stuck with decreasing reimbursements, a gradual whittling away of our profession, a demand to keep putting time we don’t have into our jobs, and many other issues. It’s even worse for those who are coming out of training and are facing these same challenges with six-figure student loans over their heads and, often, the demands of young families. The idealism and energy of youth are all that seem to sustain them, and that can’t last.
I like being a doctor. I enjoy being a neurologist. I love being able to help people and have a sense of service in doing so. But the worsening financial picture for us, and the increasing demands on our often already nonexistent free time, are destroying the field. Like many other docs, I look at my savings here and there and wonder how long until I can retire. That is sad because, as we all gradually leave practice (for whatever reason), new people will need to come in and pick up the mantle. But current conditions are such that I suspect many will find something else to do unless things change.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’m burned out.
Heck, what doctor isn’t? Politicians say we get paid too much. Lawyers say we make too many mistakes. Insurance companies say we order too many tests and too many expensive treatments. And the patients, while generally good people looking for help, can also on occasion be angry and unreasonable. The bad apples may be in the minority, but it only takes one to ruin a day full of rewarding visits.
That can’t be good.
Some of the study’s listed reasons for burnout are very familiar: complaints about maintenance of certification and about calling insurances to authorize tests and medications, crappy reimbursement for time-consuming visits, having to spend more time at work just to break even, and the constant feeling of never being caught up. I leave work, come home, have dinner with my family, do dictations, go to bed, and do it over again. No matter where I am, I’ve never left the office.
Other common complaints aren’t as much an issue for me. I don’t have, or want, an electronic health record that qualifies for meaningful use; I designed the one I have, and it works fine for me. I don’t have a nonmedical administrator telling me how many patients I’m required to see each day, and my patient population is, overall, appreciative and polite.
There are always trade-offs. When my kids have school breaks, I take that time off from the office to be with them. I enjoy it – I mean, that’s what we’re here for as parents, isn’t it? Of course, the drawback comes a few weeks later when my income drops because I wasn’t working. In solo practice, cash flow is king. I may have more freedom and control than my employed colleagues, but the downside is that I have no guaranteed salary, either. I’m the last one here who gets paid.
I see plenty of columns on how to avoid burnout, none of which seem to be written by someone who’s in a real-world practice. They all recommend taking time off for yourself, maybe seeing a counselor, finding a hobby you enjoy ... Really?
There’s no easy answer, either. We’re stuck with decreasing reimbursements, a gradual whittling away of our profession, a demand to keep putting time we don’t have into our jobs, and many other issues. It’s even worse for those who are coming out of training and are facing these same challenges with six-figure student loans over their heads and, often, the demands of young families. The idealism and energy of youth are all that seem to sustain them, and that can’t last.
I like being a doctor. I enjoy being a neurologist. I love being able to help people and have a sense of service in doing so. But the worsening financial picture for us, and the increasing demands on our often already nonexistent free time, are destroying the field. Like many other docs, I look at my savings here and there and wonder how long until I can retire. That is sad because, as we all gradually leave practice (for whatever reason), new people will need to come in and pick up the mantle. But current conditions are such that I suspect many will find something else to do unless things change.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’m burned out.
Heck, what doctor isn’t? Politicians say we get paid too much. Lawyers say we make too many mistakes. Insurance companies say we order too many tests and too many expensive treatments. And the patients, while generally good people looking for help, can also on occasion be angry and unreasonable. The bad apples may be in the minority, but it only takes one to ruin a day full of rewarding visits.
That can’t be good.
Some of the study’s listed reasons for burnout are very familiar: complaints about maintenance of certification and about calling insurances to authorize tests and medications, crappy reimbursement for time-consuming visits, having to spend more time at work just to break even, and the constant feeling of never being caught up. I leave work, come home, have dinner with my family, do dictations, go to bed, and do it over again. No matter where I am, I’ve never left the office.
Other common complaints aren’t as much an issue for me. I don’t have, or want, an electronic health record that qualifies for meaningful use; I designed the one I have, and it works fine for me. I don’t have a nonmedical administrator telling me how many patients I’m required to see each day, and my patient population is, overall, appreciative and polite.
There are always trade-offs. When my kids have school breaks, I take that time off from the office to be with them. I enjoy it – I mean, that’s what we’re here for as parents, isn’t it? Of course, the drawback comes a few weeks later when my income drops because I wasn’t working. In solo practice, cash flow is king. I may have more freedom and control than my employed colleagues, but the downside is that I have no guaranteed salary, either. I’m the last one here who gets paid.
I see plenty of columns on how to avoid burnout, none of which seem to be written by someone who’s in a real-world practice. They all recommend taking time off for yourself, maybe seeing a counselor, finding a hobby you enjoy ... Really?
There’s no easy answer, either. We’re stuck with decreasing reimbursements, a gradual whittling away of our profession, a demand to keep putting time we don’t have into our jobs, and many other issues. It’s even worse for those who are coming out of training and are facing these same challenges with six-figure student loans over their heads and, often, the demands of young families. The idealism and energy of youth are all that seem to sustain them, and that can’t last.
I like being a doctor. I enjoy being a neurologist. I love being able to help people and have a sense of service in doing so. But the worsening financial picture for us, and the increasing demands on our often already nonexistent free time, are destroying the field. Like many other docs, I look at my savings here and there and wonder how long until I can retire. That is sad because, as we all gradually leave practice (for whatever reason), new people will need to come in and pick up the mantle. But current conditions are such that I suspect many will find something else to do unless things change.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Care needed using sotagliflozin as add-on to insulin in T1DM
LISBON – Further phase 3 trial data show that the investigational dual sodium-glucose cotransporter 1 and 2 (SGLT1/2) inhibitor according to results reported at the annual meeting of the European Association for the Study of Diabetes.
In the inTandem3 trial, 28.6% of 699 people with T1DM treated with sotagliflozin on top of their usual insulin therapy achieved the primary composite endpoint, which was a glycated hemoglobin (HbA1c) level of 7% or lower at Week 24, with no episodes of severe hypoglycemia or diabetic ketoacidosis (DKA). In comparison, 15.2% of the 703 individuals who received a placebo in addition to their insulin therapy achieved this endpoint (P less than .001), according to Melanie J. Davies, MD, who presented the inTandem3 study results during a symposium on the sotagliflozin clinical program. The results were published online in the New England Journal of Medicine (2017 Sep 15. doi: 10.1056/NEJMoa1708337) to coincide with their presentation at the meeting.
However, the overall rate of DKA was higher in the patients treated with sotagliflozin than in those on placebo, at 3% versus 0.6%, respectively. DKA events most often occurred in persons using insulin pumps (4.4% vs. 9.7%) than in those taking insulin via multiple daily injections (2.1% vs 0.5%). Furthermore, in a post-hoc analysis, it was found that the rate of at least one episode of DKA was significantly higher in sotagliflozin- than placebo-treated patients who failed to reach the HbA1c target of below 7% (P less than .003), reported Dr. Davies.
The study findings “build on data seen inTandem 1 and inTandem 2 but in a more pragmatic design,” said study investigator Melanie Davies, MD, professor of diabetes medicine at the University of Leicester (England).
The inTandem studies
Dr. Davies observed that the sotagliflozin clinical trials program in persons with T1DM involved three phase 2 and three phase 3 studies. The latter, inTandem1, inTandem2, and inTandem3, were all 24-week trials, but there were some differences in the design.
inTandem1 and inTandem2 were the pivotal studies, one conducted in 793 patients in North America and the other in 782 patients in Europe and Israel. After a 2-week screening period, participants underwent a 6-week insulin optimization program before they were randomized to one of two doses of sotagliflozin (200 mg or 400 mg) or placebo for 24 weeks, with follow-up out to 52 weeks. The primary endpoint of these studies was the reduction in HbA1c versus placebo at 24 weeks.
By comparison, inTandem3 was a global study involving 1,405 individuals with T1DM who did not undergo the 6-week insulin optimization period. Instead there was a 2-week run-in period after the initial screening, and the study ran for only 24 weeks. Only one dose (400 mg) of sotagliflozin was used and the primary endpoint was a composite to try to see what the net clinical benefit would be, Dr. Davies explained.
The results of inTandem1 and inTandem2 were reported earlier this year at the American Diabetes Association Scientific Sessions, Dr. Davies noted, and sotagliflozin had “a good efficacy and safety profile as an adjunct to insulin in type 1 diabetes.”
The quest for adjunctive treatment
“For years we’ve been looking for adjunctive therapy for people with type 1 diabetes,” said Julio Rosenstock, MD, at the EASD meeting. Dr. Rosenstock, who is the director of the Dallas Diabetes Research Center at Medical City and involved in the sotagliflozin clinical trials program, noted that the quest for an adjunctive treatment was because “glucose control in type 1 diabetes remains tough and costly, despite multiple advances in insulin therapy, delivery systems, and monitoring methods over the years.”
Several approaches to adjunctive treatment had been proposed, but so far all with limited value, Dr. Rosenstock maintained. Despite no evidence for a benefit of adding metformin, for example, registry data suggest that up to 5% of people with T1DM are using it.
The recent findings of the REMOVAL trial showed metformin did not help change the HbA1c over time and there was no change in the primary outcome, he observed but a small improvement in a tertiary endpoint. “I can’t think of a more negative cardiovascular outcomes trial,” Dr. Rosenstock asserted. “There is not enough justification to use metformin in type 1 diabetes.”
By contrast there is a strong rationale for using SGLT inhibition, partly as the glucose-lowering effects are independent of insulin’s activity. Through inhibition of SGLT1, sotagliflozin reduces glucose absorption in the proximal intestine, thus blunting or delaying rising postprandial glucose levels. By also targeting SGLT2, sotagliflozin can reduce glucose resorption by the kidneys.
Risks and clinical implications
In an editorial accompanying the published findings, David Nathan, MD, of Massachusetts General Hospital and Harvard Medical School in Boston, is not convinced that using adjunctive treatment is the future for better glycemic control in T1DM and that better automated insulin delivery systems will likely make adjunctive therapy unnecessary.
Dr. Nathan also observed “the rate of severe hypoglycemia in the whole sotagliflozin group was not significantly different from the rate in the placebo group,” and the risks and benefits of any adjunctive therapy for T1DM need to be carefully balanced.
While risks remain, one of the chairs of the session, Chantal Mathieu, MD, professor of medicine at the Katholieke Universiteit Leuven (Belgium), observed that “these are exciting times for all of us and hopefully for our patients.” She cautioned clinicians to remember, however, that “type 1 diabetes is a very different disease from type 2 diabetes, and so when we listen to [information about] all these adjunct[ive] therapies, when we read the papers, please interpret the data carefully.”
The trial was funded by Lexicon Pharmaceuticals. Sotagliflozin is being codeveloped with Sanofi. Dr. Davies disclosed acting as an advisor, consultant, or being a member of a speaker’s bureau for Sanofi-Aventis and several other companies. She was an investigator in the inTandem trials and her institution received funding from Lexicon to conduct the inTandem 2 and 3 clinical trials. Dr. Rosenstock disclosed research support and acting as an advisor to multiple pharmaceutical companies. Dr. Nathan had nothing to disclose. Dr. Mathieu chaired the session and did not present disclosures.
LISBON – Further phase 3 trial data show that the investigational dual sodium-glucose cotransporter 1 and 2 (SGLT1/2) inhibitor according to results reported at the annual meeting of the European Association for the Study of Diabetes.
In the inTandem3 trial, 28.6% of 699 people with T1DM treated with sotagliflozin on top of their usual insulin therapy achieved the primary composite endpoint, which was a glycated hemoglobin (HbA1c) level of 7% or lower at Week 24, with no episodes of severe hypoglycemia or diabetic ketoacidosis (DKA). In comparison, 15.2% of the 703 individuals who received a placebo in addition to their insulin therapy achieved this endpoint (P less than .001), according to Melanie J. Davies, MD, who presented the inTandem3 study results during a symposium on the sotagliflozin clinical program. The results were published online in the New England Journal of Medicine (2017 Sep 15. doi: 10.1056/NEJMoa1708337) to coincide with their presentation at the meeting.
However, the overall rate of DKA was higher in the patients treated with sotagliflozin than in those on placebo, at 3% versus 0.6%, respectively. DKA events most often occurred in persons using insulin pumps (4.4% vs. 9.7%) than in those taking insulin via multiple daily injections (2.1% vs 0.5%). Furthermore, in a post-hoc analysis, it was found that the rate of at least one episode of DKA was significantly higher in sotagliflozin- than placebo-treated patients who failed to reach the HbA1c target of below 7% (P less than .003), reported Dr. Davies.
The study findings “build on data seen inTandem 1 and inTandem 2 but in a more pragmatic design,” said study investigator Melanie Davies, MD, professor of diabetes medicine at the University of Leicester (England).
The inTandem studies
Dr. Davies observed that the sotagliflozin clinical trials program in persons with T1DM involved three phase 2 and three phase 3 studies. The latter, inTandem1, inTandem2, and inTandem3, were all 24-week trials, but there were some differences in the design.
inTandem1 and inTandem2 were the pivotal studies, one conducted in 793 patients in North America and the other in 782 patients in Europe and Israel. After a 2-week screening period, participants underwent a 6-week insulin optimization program before they were randomized to one of two doses of sotagliflozin (200 mg or 400 mg) or placebo for 24 weeks, with follow-up out to 52 weeks. The primary endpoint of these studies was the reduction in HbA1c versus placebo at 24 weeks.
By comparison, inTandem3 was a global study involving 1,405 individuals with T1DM who did not undergo the 6-week insulin optimization period. Instead there was a 2-week run-in period after the initial screening, and the study ran for only 24 weeks. Only one dose (400 mg) of sotagliflozin was used and the primary endpoint was a composite to try to see what the net clinical benefit would be, Dr. Davies explained.
The results of inTandem1 and inTandem2 were reported earlier this year at the American Diabetes Association Scientific Sessions, Dr. Davies noted, and sotagliflozin had “a good efficacy and safety profile as an adjunct to insulin in type 1 diabetes.”
The quest for adjunctive treatment
“For years we’ve been looking for adjunctive therapy for people with type 1 diabetes,” said Julio Rosenstock, MD, at the EASD meeting. Dr. Rosenstock, who is the director of the Dallas Diabetes Research Center at Medical City and involved in the sotagliflozin clinical trials program, noted that the quest for an adjunctive treatment was because “glucose control in type 1 diabetes remains tough and costly, despite multiple advances in insulin therapy, delivery systems, and monitoring methods over the years.”
Several approaches to adjunctive treatment had been proposed, but so far all with limited value, Dr. Rosenstock maintained. Despite no evidence for a benefit of adding metformin, for example, registry data suggest that up to 5% of people with T1DM are using it.
The recent findings of the REMOVAL trial showed metformin did not help change the HbA1c over time and there was no change in the primary outcome, he observed but a small improvement in a tertiary endpoint. “I can’t think of a more negative cardiovascular outcomes trial,” Dr. Rosenstock asserted. “There is not enough justification to use metformin in type 1 diabetes.”
By contrast there is a strong rationale for using SGLT inhibition, partly as the glucose-lowering effects are independent of insulin’s activity. Through inhibition of SGLT1, sotagliflozin reduces glucose absorption in the proximal intestine, thus blunting or delaying rising postprandial glucose levels. By also targeting SGLT2, sotagliflozin can reduce glucose resorption by the kidneys.
Risks and clinical implications
In an editorial accompanying the published findings, David Nathan, MD, of Massachusetts General Hospital and Harvard Medical School in Boston, is not convinced that using adjunctive treatment is the future for better glycemic control in T1DM and that better automated insulin delivery systems will likely make adjunctive therapy unnecessary.
Dr. Nathan also observed “the rate of severe hypoglycemia in the whole sotagliflozin group was not significantly different from the rate in the placebo group,” and the risks and benefits of any adjunctive therapy for T1DM need to be carefully balanced.
While risks remain, one of the chairs of the session, Chantal Mathieu, MD, professor of medicine at the Katholieke Universiteit Leuven (Belgium), observed that “these are exciting times for all of us and hopefully for our patients.” She cautioned clinicians to remember, however, that “type 1 diabetes is a very different disease from type 2 diabetes, and so when we listen to [information about] all these adjunct[ive] therapies, when we read the papers, please interpret the data carefully.”
The trial was funded by Lexicon Pharmaceuticals. Sotagliflozin is being codeveloped with Sanofi. Dr. Davies disclosed acting as an advisor, consultant, or being a member of a speaker’s bureau for Sanofi-Aventis and several other companies. She was an investigator in the inTandem trials and her institution received funding from Lexicon to conduct the inTandem 2 and 3 clinical trials. Dr. Rosenstock disclosed research support and acting as an advisor to multiple pharmaceutical companies. Dr. Nathan had nothing to disclose. Dr. Mathieu chaired the session and did not present disclosures.
LISBON – Further phase 3 trial data show that the investigational dual sodium-glucose cotransporter 1 and 2 (SGLT1/2) inhibitor according to results reported at the annual meeting of the European Association for the Study of Diabetes.
In the inTandem3 trial, 28.6% of 699 people with T1DM treated with sotagliflozin on top of their usual insulin therapy achieved the primary composite endpoint, which was a glycated hemoglobin (HbA1c) level of 7% or lower at Week 24, with no episodes of severe hypoglycemia or diabetic ketoacidosis (DKA). In comparison, 15.2% of the 703 individuals who received a placebo in addition to their insulin therapy achieved this endpoint (P less than .001), according to Melanie J. Davies, MD, who presented the inTandem3 study results during a symposium on the sotagliflozin clinical program. The results were published online in the New England Journal of Medicine (2017 Sep 15. doi: 10.1056/NEJMoa1708337) to coincide with their presentation at the meeting.
However, the overall rate of DKA was higher in the patients treated with sotagliflozin than in those on placebo, at 3% versus 0.6%, respectively. DKA events most often occurred in persons using insulin pumps (4.4% vs. 9.7%) than in those taking insulin via multiple daily injections (2.1% vs 0.5%). Furthermore, in a post-hoc analysis, it was found that the rate of at least one episode of DKA was significantly higher in sotagliflozin- than placebo-treated patients who failed to reach the HbA1c target of below 7% (P less than .003), reported Dr. Davies.
The study findings “build on data seen inTandem 1 and inTandem 2 but in a more pragmatic design,” said study investigator Melanie Davies, MD, professor of diabetes medicine at the University of Leicester (England).
The inTandem studies
Dr. Davies observed that the sotagliflozin clinical trials program in persons with T1DM involved three phase 2 and three phase 3 studies. The latter, inTandem1, inTandem2, and inTandem3, were all 24-week trials, but there were some differences in the design.
inTandem1 and inTandem2 were the pivotal studies, one conducted in 793 patients in North America and the other in 782 patients in Europe and Israel. After a 2-week screening period, participants underwent a 6-week insulin optimization program before they were randomized to one of two doses of sotagliflozin (200 mg or 400 mg) or placebo for 24 weeks, with follow-up out to 52 weeks. The primary endpoint of these studies was the reduction in HbA1c versus placebo at 24 weeks.
By comparison, inTandem3 was a global study involving 1,405 individuals with T1DM who did not undergo the 6-week insulin optimization period. Instead there was a 2-week run-in period after the initial screening, and the study ran for only 24 weeks. Only one dose (400 mg) of sotagliflozin was used and the primary endpoint was a composite to try to see what the net clinical benefit would be, Dr. Davies explained.
The results of inTandem1 and inTandem2 were reported earlier this year at the American Diabetes Association Scientific Sessions, Dr. Davies noted, and sotagliflozin had “a good efficacy and safety profile as an adjunct to insulin in type 1 diabetes.”
The quest for adjunctive treatment
“For years we’ve been looking for adjunctive therapy for people with type 1 diabetes,” said Julio Rosenstock, MD, at the EASD meeting. Dr. Rosenstock, who is the director of the Dallas Diabetes Research Center at Medical City and involved in the sotagliflozin clinical trials program, noted that the quest for an adjunctive treatment was because “glucose control in type 1 diabetes remains tough and costly, despite multiple advances in insulin therapy, delivery systems, and monitoring methods over the years.”
Several approaches to adjunctive treatment had been proposed, but so far all with limited value, Dr. Rosenstock maintained. Despite no evidence for a benefit of adding metformin, for example, registry data suggest that up to 5% of people with T1DM are using it.
The recent findings of the REMOVAL trial showed metformin did not help change the HbA1c over time and there was no change in the primary outcome, he observed but a small improvement in a tertiary endpoint. “I can’t think of a more negative cardiovascular outcomes trial,” Dr. Rosenstock asserted. “There is not enough justification to use metformin in type 1 diabetes.”
By contrast there is a strong rationale for using SGLT inhibition, partly as the glucose-lowering effects are independent of insulin’s activity. Through inhibition of SGLT1, sotagliflozin reduces glucose absorption in the proximal intestine, thus blunting or delaying rising postprandial glucose levels. By also targeting SGLT2, sotagliflozin can reduce glucose resorption by the kidneys.
Risks and clinical implications
In an editorial accompanying the published findings, David Nathan, MD, of Massachusetts General Hospital and Harvard Medical School in Boston, is not convinced that using adjunctive treatment is the future for better glycemic control in T1DM and that better automated insulin delivery systems will likely make adjunctive therapy unnecessary.
Dr. Nathan also observed “the rate of severe hypoglycemia in the whole sotagliflozin group was not significantly different from the rate in the placebo group,” and the risks and benefits of any adjunctive therapy for T1DM need to be carefully balanced.
While risks remain, one of the chairs of the session, Chantal Mathieu, MD, professor of medicine at the Katholieke Universiteit Leuven (Belgium), observed that “these are exciting times for all of us and hopefully for our patients.” She cautioned clinicians to remember, however, that “type 1 diabetes is a very different disease from type 2 diabetes, and so when we listen to [information about] all these adjunct[ive] therapies, when we read the papers, please interpret the data carefully.”
The trial was funded by Lexicon Pharmaceuticals. Sotagliflozin is being codeveloped with Sanofi. Dr. Davies disclosed acting as an advisor, consultant, or being a member of a speaker’s bureau for Sanofi-Aventis and several other companies. She was an investigator in the inTandem trials and her institution received funding from Lexicon to conduct the inTandem 2 and 3 clinical trials. Dr. Rosenstock disclosed research support and acting as an advisor to multiple pharmaceutical companies. Dr. Nathan had nothing to disclose. Dr. Mathieu chaired the session and did not present disclosures.
AT EASD 2017
Key clinical point: A higher proportion of people with type 1 diabetes mellitus (T1DM) treated with sotagliflozin than placebo achieved the primary composite endpoint, but there is the risk of diabetic ketoacidosis (DKA) in some.
Major finding: 28.6% versus 15.2% of sotaglifozin- and placebo-treated individuals achieved an HbA1c less than 7% at week 24, with no episodes of severe hypoglycemia or DKA (P less than .001).
Data source: The phase 3, randomized, controlled, multicenter inTandem3 trial in 1,402 people with type 1 diabetes on stable insulin therapy but with poor glycemic control.
Disclosures: The trial was funded by Lexicon Pharmaceuticals. Sotagliflozin is being codeveloped with Sanofi. Two presenters have received research support to perform clinical studies. The commentators had nothing to disclose.
A Peek at Our October 2017 Issue
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
FDA panel advises approval of semaglutide to lower HbA1c in patients with type 2 diabetes
The Food and drug Administration’s Endocrinologic and Metabolic Drugs Advisory Committee (EMDAC) recommended the approval of a once-weekly semaglutide injection for adults with type 2 diabetes mellitus. The vote was 16-0 in favor of approval, with one committee member abstaining.
The committee met on Oct. 18 and discussed the safety and efficacy of new drug application (NDA) 209637 for semaglutide injection when used to help glycemic control in addition to diet and exercise. Semaglutide, manufactured and submitted for approval by Novo Nordisk, is described by the company as “an investigational analog of native human glucagonlike peptide–1,” with a half-life of approximately 1 week, making the agent appropriate for weekly dosing.
The researchers found some increase in diabetic retinopathy in the SUSTAIN trials, but a post-hoc analysis found that “To the extent that the data suggest a signal that there was progression of diabetic retinopathy in patients with significant decreases in HbA1c, these events should be expected because they are consistent with treatments that decrease HbA1c. While this decrease may result in an initial increase in retinopathy, ocular health is ultimately benefited by decreasing HbA1c.”
Novo Nordisk submitted the application for semaglutide in December 2016; the drug also is being reviewed in Europe and Japan.
The FDA is not obligated to follow the committee’s recommendation but considers it as part of the review process of new drug applications.
The Food and drug Administration’s Endocrinologic and Metabolic Drugs Advisory Committee (EMDAC) recommended the approval of a once-weekly semaglutide injection for adults with type 2 diabetes mellitus. The vote was 16-0 in favor of approval, with one committee member abstaining.
The committee met on Oct. 18 and discussed the safety and efficacy of new drug application (NDA) 209637 for semaglutide injection when used to help glycemic control in addition to diet and exercise. Semaglutide, manufactured and submitted for approval by Novo Nordisk, is described by the company as “an investigational analog of native human glucagonlike peptide–1,” with a half-life of approximately 1 week, making the agent appropriate for weekly dosing.
The researchers found some increase in diabetic retinopathy in the SUSTAIN trials, but a post-hoc analysis found that “To the extent that the data suggest a signal that there was progression of diabetic retinopathy in patients with significant decreases in HbA1c, these events should be expected because they are consistent with treatments that decrease HbA1c. While this decrease may result in an initial increase in retinopathy, ocular health is ultimately benefited by decreasing HbA1c.”
Novo Nordisk submitted the application for semaglutide in December 2016; the drug also is being reviewed in Europe and Japan.
The FDA is not obligated to follow the committee’s recommendation but considers it as part of the review process of new drug applications.
The Food and drug Administration’s Endocrinologic and Metabolic Drugs Advisory Committee (EMDAC) recommended the approval of a once-weekly semaglutide injection for adults with type 2 diabetes mellitus. The vote was 16-0 in favor of approval, with one committee member abstaining.
The committee met on Oct. 18 and discussed the safety and efficacy of new drug application (NDA) 209637 for semaglutide injection when used to help glycemic control in addition to diet and exercise. Semaglutide, manufactured and submitted for approval by Novo Nordisk, is described by the company as “an investigational analog of native human glucagonlike peptide–1,” with a half-life of approximately 1 week, making the agent appropriate for weekly dosing.
The researchers found some increase in diabetic retinopathy in the SUSTAIN trials, but a post-hoc analysis found that “To the extent that the data suggest a signal that there was progression of diabetic retinopathy in patients with significant decreases in HbA1c, these events should be expected because they are consistent with treatments that decrease HbA1c. While this decrease may result in an initial increase in retinopathy, ocular health is ultimately benefited by decreasing HbA1c.”
Novo Nordisk submitted the application for semaglutide in December 2016; the drug also is being reviewed in Europe and Japan.
The FDA is not obligated to follow the committee’s recommendation but considers it as part of the review process of new drug applications.
AT AN FDA ADVISORY COMMITTEE MEETING
Home-based cognitive-behavioral therapy aids IBS
ORLANDO – A 10-week program of home-based cognitive-behavioral therapy led to significantly better improvements in irritable bowel syndrome than did a control education program in a prospective, randomized, single-center trial with 436 patients.
Study data also showed that the improvements produced by the home-based cognitive-behavioral therapy (CBT) program were durable, persisting in 63% of high responders out to 6 months after treatment, Jeffrey M. Lackner, PsyD, said at the World Congress of Gastroenterology at ACG 2017.

He suggested that the minimal contact, home-based approach actually enhanced the efficacy of the CBT training that patients received.
“Patients are given tasks to carry out. Responsibility is placed on them. It changes the dynamic between the clinician and patient,” Dr. Lackner said. Skills patients learned during the minimal contact sessions included self-monitoring, muscle relaxation, worry control, problem solving, and modification of core beliefs.
The study enrolled adults up to 70 years old with at least moderately severe IBS symptoms at least twice weekly who met the Rome III diagnostic criteria. When patients performed a self-assessment 2 weeks after the end of the 10-week intervention, 61% of those in the home-based CBT program group rated themselves as much or very much improved, compared with 55% of patients who received standard CBT and 44% of patients in the control group, who attended generic education sessions. The differences between each of the two CBT groups and the controls were statistically significant. Patient assessments performed by blinded gastroenterologists rated 56% of the home-based CBT patients as much or very much improved, compared with 51% of those who received standard CBT and 40% of the controls.
When reassessed 3 and 6 months later, the edge that home-based CBT patients showed over the control patients persisted. After 6 months off treatment, 57% of those who received home-based CBT continued to say they were much or very much improved over their baseline status, compared with 47% of the controls.
Dr. Lackner’s analysis also examined whether patients treated with CBT, either standard or home based, went into remission. He defined remission as having no or only mild symptoms during an assessment 2 weeks after the end of the intervention and then maintaining this response out to 6 months. No or only mild symptoms were reported by 35% of all CBT patients soon after treatment, compared with 23% of the controls. Six months later, 63% of the high-responding patients on CBT and 52% of the high responders with education maintained their high response.
“CBT appears to have an enduring effect that protects against subsequent relapse and recurrence in a sizable subsample of patients,” he concluded. The findings “suggest possible disease modification by CBT.”
Dr. Lackner had no relevant financial disclosures.
[email protected]
On Twitter @mitchelzoler
ORLANDO – A 10-week program of home-based cognitive-behavioral therapy led to significantly better improvements in irritable bowel syndrome than did a control education program in a prospective, randomized, single-center trial with 436 patients.
Study data also showed that the improvements produced by the home-based cognitive-behavioral therapy (CBT) program were durable, persisting in 63% of high responders out to 6 months after treatment, Jeffrey M. Lackner, PsyD, said at the World Congress of Gastroenterology at ACG 2017.

He suggested that the minimal contact, home-based approach actually enhanced the efficacy of the CBT training that patients received.
“Patients are given tasks to carry out. Responsibility is placed on them. It changes the dynamic between the clinician and patient,” Dr. Lackner said. Skills patients learned during the minimal contact sessions included self-monitoring, muscle relaxation, worry control, problem solving, and modification of core beliefs.
The study enrolled adults up to 70 years old with at least moderately severe IBS symptoms at least twice weekly who met the Rome III diagnostic criteria. When patients performed a self-assessment 2 weeks after the end of the 10-week intervention, 61% of those in the home-based CBT program group rated themselves as much or very much improved, compared with 55% of patients who received standard CBT and 44% of patients in the control group, who attended generic education sessions. The differences between each of the two CBT groups and the controls were statistically significant. Patient assessments performed by blinded gastroenterologists rated 56% of the home-based CBT patients as much or very much improved, compared with 51% of those who received standard CBT and 40% of the controls.
When reassessed 3 and 6 months later, the edge that home-based CBT patients showed over the control patients persisted. After 6 months off treatment, 57% of those who received home-based CBT continued to say they were much or very much improved over their baseline status, compared with 47% of the controls.
Dr. Lackner’s analysis also examined whether patients treated with CBT, either standard or home based, went into remission. He defined remission as having no or only mild symptoms during an assessment 2 weeks after the end of the intervention and then maintaining this response out to 6 months. No or only mild symptoms were reported by 35% of all CBT patients soon after treatment, compared with 23% of the controls. Six months later, 63% of the high-responding patients on CBT and 52% of the high responders with education maintained their high response.
“CBT appears to have an enduring effect that protects against subsequent relapse and recurrence in a sizable subsample of patients,” he concluded. The findings “suggest possible disease modification by CBT.”
Dr. Lackner had no relevant financial disclosures.
[email protected]
On Twitter @mitchelzoler
ORLANDO – A 10-week program of home-based cognitive-behavioral therapy led to significantly better improvements in irritable bowel syndrome than did a control education program in a prospective, randomized, single-center trial with 436 patients.
Study data also showed that the improvements produced by the home-based cognitive-behavioral therapy (CBT) program were durable, persisting in 63% of high responders out to 6 months after treatment, Jeffrey M. Lackner, PsyD, said at the World Congress of Gastroenterology at ACG 2017.

He suggested that the minimal contact, home-based approach actually enhanced the efficacy of the CBT training that patients received.
“Patients are given tasks to carry out. Responsibility is placed on them. It changes the dynamic between the clinician and patient,” Dr. Lackner said. Skills patients learned during the minimal contact sessions included self-monitoring, muscle relaxation, worry control, problem solving, and modification of core beliefs.
The study enrolled adults up to 70 years old with at least moderately severe IBS symptoms at least twice weekly who met the Rome III diagnostic criteria. When patients performed a self-assessment 2 weeks after the end of the 10-week intervention, 61% of those in the home-based CBT program group rated themselves as much or very much improved, compared with 55% of patients who received standard CBT and 44% of patients in the control group, who attended generic education sessions. The differences between each of the two CBT groups and the controls were statistically significant. Patient assessments performed by blinded gastroenterologists rated 56% of the home-based CBT patients as much or very much improved, compared with 51% of those who received standard CBT and 40% of the controls.
When reassessed 3 and 6 months later, the edge that home-based CBT patients showed over the control patients persisted. After 6 months off treatment, 57% of those who received home-based CBT continued to say they were much or very much improved over their baseline status, compared with 47% of the controls.
Dr. Lackner’s analysis also examined whether patients treated with CBT, either standard or home based, went into remission. He defined remission as having no or only mild symptoms during an assessment 2 weeks after the end of the intervention and then maintaining this response out to 6 months. No or only mild symptoms were reported by 35% of all CBT patients soon after treatment, compared with 23% of the controls. Six months later, 63% of the high-responding patients on CBT and 52% of the high responders with education maintained their high response.
“CBT appears to have an enduring effect that protects against subsequent relapse and recurrence in a sizable subsample of patients,” he concluded. The findings “suggest possible disease modification by CBT.”
Dr. Lackner had no relevant financial disclosures.
[email protected]
On Twitter @mitchelzoler
AT THE WORLD CONGRESS OF GASTROENTEROLOGY
Key clinical point:
Major finding: After completion of a 10-week treatment, 61% of CBT patients and 44% of controls showed either much or very much improvement.
Data source: A prospective, randomized, single-center study with 436 patients.
Disclosures: Dr. Lackner had no relevant financial disclosures.
Mental health risks higher in sexual minorities with acne
Among young adults with acne, nonheterosexuals are much more likely to report mental health problems, according to data from a national cross-sectional study.
Since previous studies have shown that both acne and sexual minority status are associated with increased risk of depression and suicidal ideation, the investigators used data from the National Longitudinal Study on Adolescent to Adult Health, which included 4,094 heterosexual (167 with acne) and 564 sexual minority (35 with acne) adults aged 18-28 years, to examine the relationship between the two.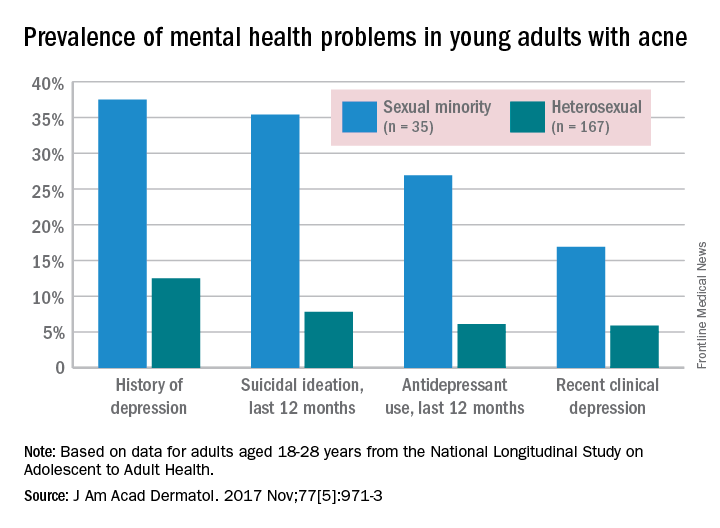
Past-year antidepressant use (AOR, 8.21) and current clinical depression (AOR, 4.1) also were both more common among sexual minorities, who were defined as “those indicating same-sex attraction or sexual orientation other than ‘100% heterosexual,’ ” they said.
“Validated screening tools to assess sexual orientation and depression among patients with acne may identify at-risk individuals and expedite referral for psychological care,” Mr. Gao and his associates wrote.
The investigators did not declare any conflicts of interest. The work of one of Mr. Gao’s associates was supported through a grant from the California Pacific Medical Center Foundation.
Among young adults with acne, nonheterosexuals are much more likely to report mental health problems, according to data from a national cross-sectional study.
Since previous studies have shown that both acne and sexual minority status are associated with increased risk of depression and suicidal ideation, the investigators used data from the National Longitudinal Study on Adolescent to Adult Health, which included 4,094 heterosexual (167 with acne) and 564 sexual minority (35 with acne) adults aged 18-28 years, to examine the relationship between the two.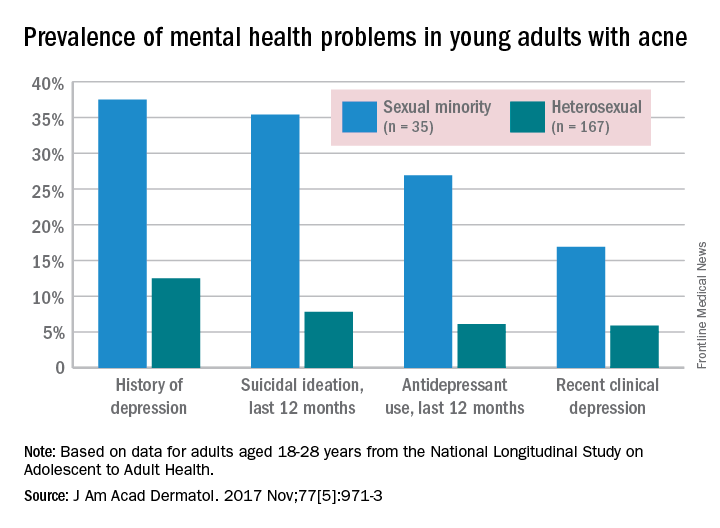
Past-year antidepressant use (AOR, 8.21) and current clinical depression (AOR, 4.1) also were both more common among sexual minorities, who were defined as “those indicating same-sex attraction or sexual orientation other than ‘100% heterosexual,’ ” they said.
“Validated screening tools to assess sexual orientation and depression among patients with acne may identify at-risk individuals and expedite referral for psychological care,” Mr. Gao and his associates wrote.
The investigators did not declare any conflicts of interest. The work of one of Mr. Gao’s associates was supported through a grant from the California Pacific Medical Center Foundation.
Among young adults with acne, nonheterosexuals are much more likely to report mental health problems, according to data from a national cross-sectional study.
Since previous studies have shown that both acne and sexual minority status are associated with increased risk of depression and suicidal ideation, the investigators used data from the National Longitudinal Study on Adolescent to Adult Health, which included 4,094 heterosexual (167 with acne) and 564 sexual minority (35 with acne) adults aged 18-28 years, to examine the relationship between the two.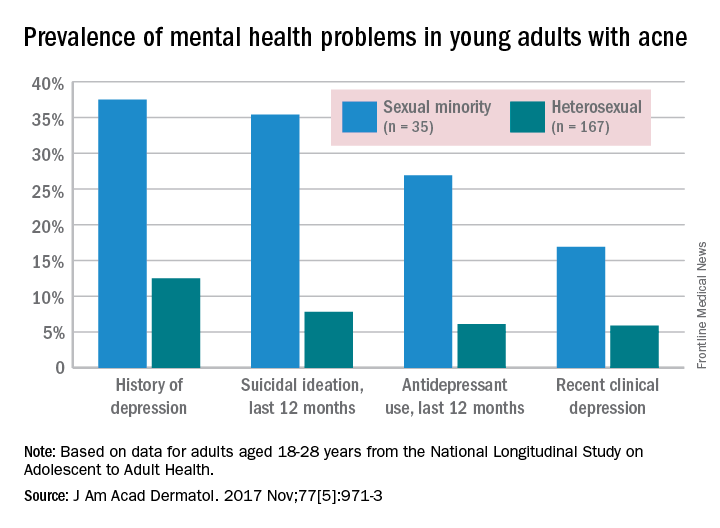
Past-year antidepressant use (AOR, 8.21) and current clinical depression (AOR, 4.1) also were both more common among sexual minorities, who were defined as “those indicating same-sex attraction or sexual orientation other than ‘100% heterosexual,’ ” they said.
“Validated screening tools to assess sexual orientation and depression among patients with acne may identify at-risk individuals and expedite referral for psychological care,” Mr. Gao and his associates wrote.
The investigators did not declare any conflicts of interest. The work of one of Mr. Gao’s associates was supported through a grant from the California Pacific Medical Center Foundation.
FROM JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Docs should engage employers directly if they want better payment models
WASHINGTON – If doctors want to improve their reimbursement and at the same time be a catalyst for reducing costs to the overall health care delivery system, they need to be stronger advocates for themselves.
This was the message of Harold D. Miller, president and CEO of the Center for Healthcare Quality and Payment Reform, in his presentation to the American Gastroenterological Association Partners in Value meeting on Oct. 6.

He called specifically on doctors to exercise initiative and accept the accountability that comes with leading the charge for payment reform.
“I think there is a much better way, which is bottom up, which is to say ask the physicians and the hospitals to say what are the ways you can improve care and reduce costs,” he continued. “Then get payers to provide adequate support for that but have physicians take accountability for actually achieving those results they think are possible. And then you have patients who get good care and you keep physicians and hospitals financially sustainable, which nobody in Washington is talking about how to actually do.”
Getting to that point is going to require physicians to be much more proactive in who they communicate with to get the information that is necessary to build payment models from the bottom up.
“I think there are lots of potential solutions, but I think it needs to be talked about,” Mr. Miller said. “If I were to leave you with one message, the problem is that employers, Congress, etc., are not hearing from physicians that you want to do something different.”
He noted that part of the issue is the adversarial relationship doctors have with the payer community, noting that most “health plans demonize you all.”
Mr. Miller added: “They go in to employers and they tell employers that the only thing standing between the employers and certain health insurance bankruptcy is the health plan because all the doctors want to do is spend more money.”
To change that, it is going to require doctors to be much more proactive in reaching out past the payer middleman to start engaging directly with employers.
“Employers do not see doctors as their partners,” Mr. Miller noted. “The people who pay have to start seeing you as wanting to solve the same problem they are trying to solve.”
And working with employers could help physicians insofar as getting access to data that would be crucial in developing the kinds of payment models that would benefit all of the financial aspects of health care delivery while at the same time improving care.
Mr. Miller recounted how various state and local governments in Maine were trying to extract clinical information that might not be ascertained from claims data from Anthem, the largest or second largest health insurance company in America. Initially, Anthem balked, prompting the state and local entities to issue requests for information and seek to replace Anthem as the main provider for its health insurance coverage.
“Anthem completely changed its attitude,” he said. “All of a sudden, Anthem was back in. ... Anthem felt that impact all the way in Indianapolis. Sam Nussbaum, MD [former chief medical officer at Anthem], said to me, ‘We were punished in Maine.’ ”
He noted that some big employers are seeking out direct contracts with health systems because they are not getting support from the health plans.
“But they need to hear from you and what it is you need and what you are going to do with it,” he said. “It is not just give us data, see ya. It is here’s what we are trying to do. Here is the information we need and why we need it. If you say to an employer ‘I want to know how many patients are being hospitalized so that I can help you reduce hospitalizations,’ do you think they are going to say nah, we are too busy for that?”
WASHINGTON – If doctors want to improve their reimbursement and at the same time be a catalyst for reducing costs to the overall health care delivery system, they need to be stronger advocates for themselves.
This was the message of Harold D. Miller, president and CEO of the Center for Healthcare Quality and Payment Reform, in his presentation to the American Gastroenterological Association Partners in Value meeting on Oct. 6.

He called specifically on doctors to exercise initiative and accept the accountability that comes with leading the charge for payment reform.
“I think there is a much better way, which is bottom up, which is to say ask the physicians and the hospitals to say what are the ways you can improve care and reduce costs,” he continued. “Then get payers to provide adequate support for that but have physicians take accountability for actually achieving those results they think are possible. And then you have patients who get good care and you keep physicians and hospitals financially sustainable, which nobody in Washington is talking about how to actually do.”
Getting to that point is going to require physicians to be much more proactive in who they communicate with to get the information that is necessary to build payment models from the bottom up.
“I think there are lots of potential solutions, but I think it needs to be talked about,” Mr. Miller said. “If I were to leave you with one message, the problem is that employers, Congress, etc., are not hearing from physicians that you want to do something different.”
He noted that part of the issue is the adversarial relationship doctors have with the payer community, noting that most “health plans demonize you all.”
Mr. Miller added: “They go in to employers and they tell employers that the only thing standing between the employers and certain health insurance bankruptcy is the health plan because all the doctors want to do is spend more money.”
To change that, it is going to require doctors to be much more proactive in reaching out past the payer middleman to start engaging directly with employers.
“Employers do not see doctors as their partners,” Mr. Miller noted. “The people who pay have to start seeing you as wanting to solve the same problem they are trying to solve.”
And working with employers could help physicians insofar as getting access to data that would be crucial in developing the kinds of payment models that would benefit all of the financial aspects of health care delivery while at the same time improving care.
Mr. Miller recounted how various state and local governments in Maine were trying to extract clinical information that might not be ascertained from claims data from Anthem, the largest or second largest health insurance company in America. Initially, Anthem balked, prompting the state and local entities to issue requests for information and seek to replace Anthem as the main provider for its health insurance coverage.
“Anthem completely changed its attitude,” he said. “All of a sudden, Anthem was back in. ... Anthem felt that impact all the way in Indianapolis. Sam Nussbaum, MD [former chief medical officer at Anthem], said to me, ‘We were punished in Maine.’ ”
He noted that some big employers are seeking out direct contracts with health systems because they are not getting support from the health plans.
“But they need to hear from you and what it is you need and what you are going to do with it,” he said. “It is not just give us data, see ya. It is here’s what we are trying to do. Here is the information we need and why we need it. If you say to an employer ‘I want to know how many patients are being hospitalized so that I can help you reduce hospitalizations,’ do you think they are going to say nah, we are too busy for that?”
WASHINGTON – If doctors want to improve their reimbursement and at the same time be a catalyst for reducing costs to the overall health care delivery system, they need to be stronger advocates for themselves.
This was the message of Harold D. Miller, president and CEO of the Center for Healthcare Quality and Payment Reform, in his presentation to the American Gastroenterological Association Partners in Value meeting on Oct. 6.

He called specifically on doctors to exercise initiative and accept the accountability that comes with leading the charge for payment reform.
“I think there is a much better way, which is bottom up, which is to say ask the physicians and the hospitals to say what are the ways you can improve care and reduce costs,” he continued. “Then get payers to provide adequate support for that but have physicians take accountability for actually achieving those results they think are possible. And then you have patients who get good care and you keep physicians and hospitals financially sustainable, which nobody in Washington is talking about how to actually do.”
Getting to that point is going to require physicians to be much more proactive in who they communicate with to get the information that is necessary to build payment models from the bottom up.
“I think there are lots of potential solutions, but I think it needs to be talked about,” Mr. Miller said. “If I were to leave you with one message, the problem is that employers, Congress, etc., are not hearing from physicians that you want to do something different.”
He noted that part of the issue is the adversarial relationship doctors have with the payer community, noting that most “health plans demonize you all.”
Mr. Miller added: “They go in to employers and they tell employers that the only thing standing between the employers and certain health insurance bankruptcy is the health plan because all the doctors want to do is spend more money.”
To change that, it is going to require doctors to be much more proactive in reaching out past the payer middleman to start engaging directly with employers.
“Employers do not see doctors as their partners,” Mr. Miller noted. “The people who pay have to start seeing you as wanting to solve the same problem they are trying to solve.”
And working with employers could help physicians insofar as getting access to data that would be crucial in developing the kinds of payment models that would benefit all of the financial aspects of health care delivery while at the same time improving care.
Mr. Miller recounted how various state and local governments in Maine were trying to extract clinical information that might not be ascertained from claims data from Anthem, the largest or second largest health insurance company in America. Initially, Anthem balked, prompting the state and local entities to issue requests for information and seek to replace Anthem as the main provider for its health insurance coverage.
“Anthem completely changed its attitude,” he said. “All of a sudden, Anthem was back in. ... Anthem felt that impact all the way in Indianapolis. Sam Nussbaum, MD [former chief medical officer at Anthem], said to me, ‘We were punished in Maine.’ ”
He noted that some big employers are seeking out direct contracts with health systems because they are not getting support from the health plans.
“But they need to hear from you and what it is you need and what you are going to do with it,” he said. “It is not just give us data, see ya. It is here’s what we are trying to do. Here is the information we need and why we need it. If you say to an employer ‘I want to know how many patients are being hospitalized so that I can help you reduce hospitalizations,’ do you think they are going to say nah, we are too busy for that?”
Role grows for heart failure patient-reported outcomes
DALLAS – The Food and Drug Administration is keenly seeking patient-reported outcomes as endpoints in cardiovascular drug or device trials, particularly for heart failure patients, but the bar remains high for getting such an outcome into labeling, said agency officials who regulate cardiovascular disease therapies.
The FDA issued guidance nearly 8 years ago on how to integrate patient-reported outcome (PRO) measures into medical product development, but so far no heart failure drug nor device has met the agency’s standards for documented success in improving a PRO, despite the clear need for these patients to receive patient-centered care, clinicians said.

“We don’t yet have a patient-reported outcome in a label for heart failure,” Paul A. Heidenreich, MD, said during a session on PROs at the annual scientific meeting of the Heart Failure Society of America. He voiced hope that a PRO might end up on the label of a heart failure drug or device sometime in 2018. “Almost half of FDA submissions now include a PRO” as part of the data package, added Dr. Heidenreich, a cardiologist and professor of medicine at Stanford (Calif.) University.
For years, PROs for heart failure weren’t often used in trials, and they remain largely absent from routine practice – an absence Dr. Heidenreich lamented. “Just focusing on mortality in heart failure is really not patient centered,” he said.
Heart failure physicians “are very good at disease-centered care” that focuses on survival and reducing hospitalizations, but “survival is often not as important to patients,” noted Mary Norine Walsh, MD, medical director of the heart failure and cardiac transplantation program at St. Vincent Medical Group in Indianapolis. She suggested “tailoring treatment to improve patient symptoms, physical function, and quality of life” without necessarily reducing hospital readmissions or increasing survival rates. “Self-reported measures have more meaning for patients,” she said, and called for using PROs to better target interventions to the patients who can most benefit from them.
Two FDA representatives who spoke during the session agreed on the importance of PROs and attested to the agency’s interest in greater reliance on them.
“PROs are a critical complement to the other measures made in device trials,” said Bram Zuckerman, MD, director of the FDA’s division of cardiovascular devices. “We need PRO information because it reflects important aspects of patients’ health-related quality of life.”
The most commonly used PRO measures in device trials today are the Kansas City Cardiomyopathy Questionnaire (J Am Coll Cardiol. 2000 Apr;35[5]:1245-55) and the Minnesota Living With Heart Failure questionnaire, he noted.
“Neither is perfect, but there is a track record in heart failure device development that these two PROs can be helpful.” The FDA’s cardiovascular device division “wants to use PRO information,” Dr. Zuckerman said.
“All-cause mortality is the most unbiased endpoint, but there is interest in PROs,” agreed Ebony Dashiell-Aje, PhD, from the FDA’s office of new drugs in the Center for Drug Evaluation and Research. She highlighted the encouragement that the FDA gave to drug and device developers to include PROs in trials, both in its 2009 guidance document as well as in a “roadmap” from the agency on how to measure PROs in clinical trials. “Unfortunately, in heart failure we struggle to find tools that can adequately measure the patient’s perspective and be sensitive enough to detect a treatment benefit,” she said.
Norman Stockbridge, MD, director of the division of cardiovascular and renal products in the agency’s Office of Drug Evaluation, cited even bigger barriers to FDA approval of PROs as labeled effects from drugs or devices.
Getting a PRO endpoint supported by clinical-trial results that qualify it for an FDA label faces two big challenges. One challenge, he said, is “how much of an effect we need to see in a complex scoring algorithm to know that patients actually received some benefit in a disease that often varies from day to day and from week to week.” The second challenge is that, “in a disease with a high background rate of bad outcomes, you need some evidence that the benefit [from the treatment] is worth any risk,” which is something that can be hard to prove in heart failure when many patients don’t live more than 2 years with the disease, Dr. Stockbridge said in an interview.
“You need to be able to make the argument that the [PRO] benefit is likely perceptible to patients, but that is only half the problem. The other half is whether the developer can rule out that survival is not less than it would have been with no treatment. If patients take this, will they feel better but have a greater risk of being hurt?”
So far, no drug or device developer has succeeded in proving this to the FDA, despite the agency’s 2009 guidance on how it could be done.
That guidance “is one of the two worst and most destructive guidance documents we ever published,” Dr. Stockbridge declared.
Dr. Walsh, Dr. Heidenreich, Dr. Zuckerman, Dr. Dashiell-Aje, and Dr. Stockbridge had no relevant disclosures.
[email protected]
On Twitter @mitchelzoler
DALLAS – The Food and Drug Administration is keenly seeking patient-reported outcomes as endpoints in cardiovascular drug or device trials, particularly for heart failure patients, but the bar remains high for getting such an outcome into labeling, said agency officials who regulate cardiovascular disease therapies.
The FDA issued guidance nearly 8 years ago on how to integrate patient-reported outcome (PRO) measures into medical product development, but so far no heart failure drug nor device has met the agency’s standards for documented success in improving a PRO, despite the clear need for these patients to receive patient-centered care, clinicians said.

“We don’t yet have a patient-reported outcome in a label for heart failure,” Paul A. Heidenreich, MD, said during a session on PROs at the annual scientific meeting of the Heart Failure Society of America. He voiced hope that a PRO might end up on the label of a heart failure drug or device sometime in 2018. “Almost half of FDA submissions now include a PRO” as part of the data package, added Dr. Heidenreich, a cardiologist and professor of medicine at Stanford (Calif.) University.
For years, PROs for heart failure weren’t often used in trials, and they remain largely absent from routine practice – an absence Dr. Heidenreich lamented. “Just focusing on mortality in heart failure is really not patient centered,” he said.
Heart failure physicians “are very good at disease-centered care” that focuses on survival and reducing hospitalizations, but “survival is often not as important to patients,” noted Mary Norine Walsh, MD, medical director of the heart failure and cardiac transplantation program at St. Vincent Medical Group in Indianapolis. She suggested “tailoring treatment to improve patient symptoms, physical function, and quality of life” without necessarily reducing hospital readmissions or increasing survival rates. “Self-reported measures have more meaning for patients,” she said, and called for using PROs to better target interventions to the patients who can most benefit from them.
Two FDA representatives who spoke during the session agreed on the importance of PROs and attested to the agency’s interest in greater reliance on them.
“PROs are a critical complement to the other measures made in device trials,” said Bram Zuckerman, MD, director of the FDA’s division of cardiovascular devices. “We need PRO information because it reflects important aspects of patients’ health-related quality of life.”
The most commonly used PRO measures in device trials today are the Kansas City Cardiomyopathy Questionnaire (J Am Coll Cardiol. 2000 Apr;35[5]:1245-55) and the Minnesota Living With Heart Failure questionnaire, he noted.
“Neither is perfect, but there is a track record in heart failure device development that these two PROs can be helpful.” The FDA’s cardiovascular device division “wants to use PRO information,” Dr. Zuckerman said.
“All-cause mortality is the most unbiased endpoint, but there is interest in PROs,” agreed Ebony Dashiell-Aje, PhD, from the FDA’s office of new drugs in the Center for Drug Evaluation and Research. She highlighted the encouragement that the FDA gave to drug and device developers to include PROs in trials, both in its 2009 guidance document as well as in a “roadmap” from the agency on how to measure PROs in clinical trials. “Unfortunately, in heart failure we struggle to find tools that can adequately measure the patient’s perspective and be sensitive enough to detect a treatment benefit,” she said.
Norman Stockbridge, MD, director of the division of cardiovascular and renal products in the agency’s Office of Drug Evaluation, cited even bigger barriers to FDA approval of PROs as labeled effects from drugs or devices.
Getting a PRO endpoint supported by clinical-trial results that qualify it for an FDA label faces two big challenges. One challenge, he said, is “how much of an effect we need to see in a complex scoring algorithm to know that patients actually received some benefit in a disease that often varies from day to day and from week to week.” The second challenge is that, “in a disease with a high background rate of bad outcomes, you need some evidence that the benefit [from the treatment] is worth any risk,” which is something that can be hard to prove in heart failure when many patients don’t live more than 2 years with the disease, Dr. Stockbridge said in an interview.
“You need to be able to make the argument that the [PRO] benefit is likely perceptible to patients, but that is only half the problem. The other half is whether the developer can rule out that survival is not less than it would have been with no treatment. If patients take this, will they feel better but have a greater risk of being hurt?”
So far, no drug or device developer has succeeded in proving this to the FDA, despite the agency’s 2009 guidance on how it could be done.
That guidance “is one of the two worst and most destructive guidance documents we ever published,” Dr. Stockbridge declared.
Dr. Walsh, Dr. Heidenreich, Dr. Zuckerman, Dr. Dashiell-Aje, and Dr. Stockbridge had no relevant disclosures.
[email protected]
On Twitter @mitchelzoler
DALLAS – The Food and Drug Administration is keenly seeking patient-reported outcomes as endpoints in cardiovascular drug or device trials, particularly for heart failure patients, but the bar remains high for getting such an outcome into labeling, said agency officials who regulate cardiovascular disease therapies.
The FDA issued guidance nearly 8 years ago on how to integrate patient-reported outcome (PRO) measures into medical product development, but so far no heart failure drug nor device has met the agency’s standards for documented success in improving a PRO, despite the clear need for these patients to receive patient-centered care, clinicians said.

“We don’t yet have a patient-reported outcome in a label for heart failure,” Paul A. Heidenreich, MD, said during a session on PROs at the annual scientific meeting of the Heart Failure Society of America. He voiced hope that a PRO might end up on the label of a heart failure drug or device sometime in 2018. “Almost half of FDA submissions now include a PRO” as part of the data package, added Dr. Heidenreich, a cardiologist and professor of medicine at Stanford (Calif.) University.
For years, PROs for heart failure weren’t often used in trials, and they remain largely absent from routine practice – an absence Dr. Heidenreich lamented. “Just focusing on mortality in heart failure is really not patient centered,” he said.
Heart failure physicians “are very good at disease-centered care” that focuses on survival and reducing hospitalizations, but “survival is often not as important to patients,” noted Mary Norine Walsh, MD, medical director of the heart failure and cardiac transplantation program at St. Vincent Medical Group in Indianapolis. She suggested “tailoring treatment to improve patient symptoms, physical function, and quality of life” without necessarily reducing hospital readmissions or increasing survival rates. “Self-reported measures have more meaning for patients,” she said, and called for using PROs to better target interventions to the patients who can most benefit from them.
Two FDA representatives who spoke during the session agreed on the importance of PROs and attested to the agency’s interest in greater reliance on them.
“PROs are a critical complement to the other measures made in device trials,” said Bram Zuckerman, MD, director of the FDA’s division of cardiovascular devices. “We need PRO information because it reflects important aspects of patients’ health-related quality of life.”
The most commonly used PRO measures in device trials today are the Kansas City Cardiomyopathy Questionnaire (J Am Coll Cardiol. 2000 Apr;35[5]:1245-55) and the Minnesota Living With Heart Failure questionnaire, he noted.
“Neither is perfect, but there is a track record in heart failure device development that these two PROs can be helpful.” The FDA’s cardiovascular device division “wants to use PRO information,” Dr. Zuckerman said.
“All-cause mortality is the most unbiased endpoint, but there is interest in PROs,” agreed Ebony Dashiell-Aje, PhD, from the FDA’s office of new drugs in the Center for Drug Evaluation and Research. She highlighted the encouragement that the FDA gave to drug and device developers to include PROs in trials, both in its 2009 guidance document as well as in a “roadmap” from the agency on how to measure PROs in clinical trials. “Unfortunately, in heart failure we struggle to find tools that can adequately measure the patient’s perspective and be sensitive enough to detect a treatment benefit,” she said.
Norman Stockbridge, MD, director of the division of cardiovascular and renal products in the agency’s Office of Drug Evaluation, cited even bigger barriers to FDA approval of PROs as labeled effects from drugs or devices.
Getting a PRO endpoint supported by clinical-trial results that qualify it for an FDA label faces two big challenges. One challenge, he said, is “how much of an effect we need to see in a complex scoring algorithm to know that patients actually received some benefit in a disease that often varies from day to day and from week to week.” The second challenge is that, “in a disease with a high background rate of bad outcomes, you need some evidence that the benefit [from the treatment] is worth any risk,” which is something that can be hard to prove in heart failure when many patients don’t live more than 2 years with the disease, Dr. Stockbridge said in an interview.
“You need to be able to make the argument that the [PRO] benefit is likely perceptible to patients, but that is only half the problem. The other half is whether the developer can rule out that survival is not less than it would have been with no treatment. If patients take this, will they feel better but have a greater risk of being hurt?”
So far, no drug or device developer has succeeded in proving this to the FDA, despite the agency’s 2009 guidance on how it could be done.
That guidance “is one of the two worst and most destructive guidance documents we ever published,” Dr. Stockbridge declared.
Dr. Walsh, Dr. Heidenreich, Dr. Zuckerman, Dr. Dashiell-Aje, and Dr. Stockbridge had no relevant disclosures.
[email protected]
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM THE HFSA ANNUAL SCIENTIFIC MEETING
VIDEO: Measuring, treating brain hypoxia looks promising for TBI
SAN DIEGO – It’s been possible for over 15 years for neurointensivists to measure the partial pressure of oxygen in the brain of patients following traumatic brain injury.
But the technology has not been widely adopted because there have been no high-quality data showing that it’s useful. As a result, in most hospitals, TBI treatment is guided mostly by intracranial pressure.
The evidence gap is being filled. In a recent phase 2 trial, there was a trend towards benefit when treatment was guided by both intracranial pressure and the brain oxygenation (Crit Care Med. 2017 Nov;45[11]:1907-14). The study was powered for nonfutility, not clinically meaningful change, but the National Institute of Neurological Disorders and Stroke has recently funded a 45-site, phase 3 trial that will definitively answer whether treatment protocols informed by both pressure and oxygen improve neurologic outcomes, said principal investigator Ramon Diaz-Arrastia, MD, PhD, a professor of neurology at the University of Pennsylvania, Philadelphia.
In an interview at the annual meeting of the American Neurological Association, he explained the work, and exactly how paying attention to brain oxygen levels changed treatment in the phase 2 study. It didn’t take anything unusual to maintain oxygen partial pressure above 20 mm Hg.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – It’s been possible for over 15 years for neurointensivists to measure the partial pressure of oxygen in the brain of patients following traumatic brain injury.
But the technology has not been widely adopted because there have been no high-quality data showing that it’s useful. As a result, in most hospitals, TBI treatment is guided mostly by intracranial pressure.
The evidence gap is being filled. In a recent phase 2 trial, there was a trend towards benefit when treatment was guided by both intracranial pressure and the brain oxygenation (Crit Care Med. 2017 Nov;45[11]:1907-14). The study was powered for nonfutility, not clinically meaningful change, but the National Institute of Neurological Disorders and Stroke has recently funded a 45-site, phase 3 trial that will definitively answer whether treatment protocols informed by both pressure and oxygen improve neurologic outcomes, said principal investigator Ramon Diaz-Arrastia, MD, PhD, a professor of neurology at the University of Pennsylvania, Philadelphia.
In an interview at the annual meeting of the American Neurological Association, he explained the work, and exactly how paying attention to brain oxygen levels changed treatment in the phase 2 study. It didn’t take anything unusual to maintain oxygen partial pressure above 20 mm Hg.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – It’s been possible for over 15 years for neurointensivists to measure the partial pressure of oxygen in the brain of patients following traumatic brain injury.
But the technology has not been widely adopted because there have been no high-quality data showing that it’s useful. As a result, in most hospitals, TBI treatment is guided mostly by intracranial pressure.
The evidence gap is being filled. In a recent phase 2 trial, there was a trend towards benefit when treatment was guided by both intracranial pressure and the brain oxygenation (Crit Care Med. 2017 Nov;45[11]:1907-14). The study was powered for nonfutility, not clinically meaningful change, but the National Institute of Neurological Disorders and Stroke has recently funded a 45-site, phase 3 trial that will definitively answer whether treatment protocols informed by both pressure and oxygen improve neurologic outcomes, said principal investigator Ramon Diaz-Arrastia, MD, PhD, a professor of neurology at the University of Pennsylvania, Philadelphia.
In an interview at the annual meeting of the American Neurological Association, he explained the work, and exactly how paying attention to brain oxygen levels changed treatment in the phase 2 study. It didn’t take anything unusual to maintain oxygen partial pressure above 20 mm Hg.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ANA 2017
VIDEO: Alzheimer’s blood test expected soon
SAN DIEGO – A blood test that could be on the market in as little as 2 years has an accuracy of 89% for detecting amyloid plaques in the brain, according to a report at the annual meeting of the American Neurological Association.
It measures the ratio of amyloid-beta 42 to amyloid-beta 40; the numbers refer to how many amino acids are in the proteins. In healthy individuals, the ratio is “remarkably consistent, but when beta-42 starts to stick to plaques in the brain, it doesn’t get out into the blood, and the ratio drops; that’s what we are detecting.” It’s highly accurate in both “Alzheimer’s patients and people who are completely normal who have amyloid plaques in their brains,” said Randall Bateman, MD, a professor of neurology at Washington University, St. Louis.
The test is being developed by C2N Diagnostics; Dr. Bateman is a cofounder and scientific adviser. The company is working with the Food and Drug Administration and the Centers for Medicare and Medicaid Services to commercialize the test.
If it makes it to market – which seems likely – it could be a game changer, not only for Alzheimer’s research, but also for screening, preclinical detection, and early treatment. At present, CNS amyloidosis is detected largely by positron emission tomography and radioactive tracers.
In an interview at the meeting, Dr. Bateman explained the test, the research behind it, and what it could mean for neurologists and patients. In short, “when effective drugs are found, the blood beta-amyloid test [could] be used to screen millions of people in the general public to identify who is at risk for Alzheimer’s disease” so they can “start treatments even before memory loss and brain damage begin,” he said.

SAN DIEGO – A blood test that could be on the market in as little as 2 years has an accuracy of 89% for detecting amyloid plaques in the brain, according to a report at the annual meeting of the American Neurological Association.
It measures the ratio of amyloid-beta 42 to amyloid-beta 40; the numbers refer to how many amino acids are in the proteins. In healthy individuals, the ratio is “remarkably consistent, but when beta-42 starts to stick to plaques in the brain, it doesn’t get out into the blood, and the ratio drops; that’s what we are detecting.” It’s highly accurate in both “Alzheimer’s patients and people who are completely normal who have amyloid plaques in their brains,” said Randall Bateman, MD, a professor of neurology at Washington University, St. Louis.
The test is being developed by C2N Diagnostics; Dr. Bateman is a cofounder and scientific adviser. The company is working with the Food and Drug Administration and the Centers for Medicare and Medicaid Services to commercialize the test.
If it makes it to market – which seems likely – it could be a game changer, not only for Alzheimer’s research, but also for screening, preclinical detection, and early treatment. At present, CNS amyloidosis is detected largely by positron emission tomography and radioactive tracers.
In an interview at the meeting, Dr. Bateman explained the test, the research behind it, and what it could mean for neurologists and patients. In short, “when effective drugs are found, the blood beta-amyloid test [could] be used to screen millions of people in the general public to identify who is at risk for Alzheimer’s disease” so they can “start treatments even before memory loss and brain damage begin,” he said.

SAN DIEGO – A blood test that could be on the market in as little as 2 years has an accuracy of 89% for detecting amyloid plaques in the brain, according to a report at the annual meeting of the American Neurological Association.
It measures the ratio of amyloid-beta 42 to amyloid-beta 40; the numbers refer to how many amino acids are in the proteins. In healthy individuals, the ratio is “remarkably consistent, but when beta-42 starts to stick to plaques in the brain, it doesn’t get out into the blood, and the ratio drops; that’s what we are detecting.” It’s highly accurate in both “Alzheimer’s patients and people who are completely normal who have amyloid plaques in their brains,” said Randall Bateman, MD, a professor of neurology at Washington University, St. Louis.
The test is being developed by C2N Diagnostics; Dr. Bateman is a cofounder and scientific adviser. The company is working with the Food and Drug Administration and the Centers for Medicare and Medicaid Services to commercialize the test.
If it makes it to market – which seems likely – it could be a game changer, not only for Alzheimer’s research, but also for screening, preclinical detection, and early treatment. At present, CNS amyloidosis is detected largely by positron emission tomography and radioactive tracers.
In an interview at the meeting, Dr. Bateman explained the test, the research behind it, and what it could mean for neurologists and patients. In short, “when effective drugs are found, the blood beta-amyloid test [could] be used to screen millions of people in the general public to identify who is at risk for Alzheimer’s disease” so they can “start treatments even before memory loss and brain damage begin,” he said.

AT ANA 2017