User login
“I’m sorry, doctor, I’m afraid I can’t do that”
In “2001: A Space Odyssey,” the epic 1968 film by Stanley Kubrick and Arthur C. Clarke, humanity makes first contact with an alien intelligence, and the course of history is irreversibly altered. Hailed as a watershed moment in science fiction, “2001” was considered way ahead of its time and raised a number of philosophical questions about what would happen if we ever encountered another form of life. Interestingly, the most noteworthy character in the film isn’t human or alien, but instead a new form of life altogether: an artificial intelligence (AI) known as the Heuristically programmed ALgorithmic computer 9000. HAL (as he is known colloquially) operates the Discovery One spacecraft, ferrying several scientists bound for Jupiter on a mission of exploration. Stating that he is “foolproof and incapable of error,” HAL’s superiority complex leads him to become the film’s antagonist, as he believes that human error is the cause of the difficulties they encounter. He eventually concludes that the best way to complete the mission is to eliminate human interference. When asked by scientist Dr. David Bowman to perform a simple function essential to the survival of the crew, HAL simply states “I’m sorry, Dave, I’m afraid I can’t do that.” Bowman is forced to disconnect HAL’s higher intellectual capabilities, reverting the computer to its most basic functions to ensure human survival.
Kubrick and Clarke may have been overly ambitious in predicting the progress of human space flight, but their call for concern over the risks of artificial intelligence seems quite prescient. Recently, billionaire entrepreneur Elon Musk (CEO of Tesla Motors and SpaceX) raised his concerns about AI, warning that, left unchecked, AI could be mankind’s final invention – one that could eventually destroy us. Other giants of the tech industry, including Bill Gates and Mark Zuckerberg, disagree. They believe AI represents tremendous promise for humanity and could usher in innovations unlike any we have ever seen.
A few weeks ago, we attended a national electronic health records conference where a well-known EHR vendor unveiled the new features in the upcoming release of their software. One of the most noteworthy additions was an intelligent virtual assistant, designed to help providers care for patients. While this is not the first time AI has ventured into health care (see IBM’s “Watson”), it is the first time the idea has become mainstream and fully integrated into physician workflow. Much like the virtual assistants mentioned above, this one can use voice or mouse/keyboard interaction to find clinical information, simplify common tasks, and help with medical decision-making.
While exciting at first, the idea of artificially intelligent EHRs may sound terrifying to some who aren’t yet ready to trust any patient care to machines. Reassuringly, while the integrated virtual assistant mentioned above can make suggestions to guide physicians to the right data or offer decision support when available, it is primarily focused on interface enhancement to improve work flow. It is not yet capable of making true clinical decisions that remove the physician from care delivery, but computers that do the diagnostic work of physicians may be closer than you think.
Research done at Jefferson University in Philadelphia and published in the August 2017 edition of Radiology1 investigated the ability of deep-learning algorithms to interpret chest radiographs for the diagnosis of tuberculosis. The computers achieved an impressive reliability of 99%. While at first radiograph interpretation seems quite different than the diagnostic decision-making done in primary care, the fundamental skill required for both is similar: pattern recognition. To build those patterns, artificial intelligence requires an enormous number of data points, but that’s hardly a problem thanks to the continual collection of patient data through electronic health records. The amount of raw information available to these algorithms is growing exponentially by the day, and with time their predictive ability will be unmatched. So where will that leave us, the physicians, entrusted for generations with the responsibility of diagnosis? Possibly more satisfied than we are today.
There was a time – not long ago – when the body of available medical knowledge was incredibly limited. Diagnostic testing was primitive and often inaccurate, and the treatment provided by physicians was focused on supporting, communicating, and genuinely caring for patients and their families. In the past 50 years, medical knowledge has exploded, and diagnostic testing has become incredibly advanced. Sadly, at the same time physicians have begun to feel more like clerical workers: entering data, writing prescriptions, and filling out forms. As artificial intelligence assumes some of this busywork and takes much of the guesswork out of diagnosis, physicians may find greater job satisfaction as they provide the skills a computer never can: a human touch, a personal and reflective interpretation of a patient’s diagnosis, and a true emotional connection. Ask this of a computer, and the response will always be the same: “I’m sorry, doctor, I’m afraid I can’t do that.”
Reference
1. Lakhani, Paras & Sundaram, Baskaran, “Deep Learning at Chest Radiography: Automated Classification of Pulmonary Tuberculosis by Using Convolutional Neural Networks,” Radiology. 2017 Aug;284:574-82.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington Jefferson Health.
In “2001: A Space Odyssey,” the epic 1968 film by Stanley Kubrick and Arthur C. Clarke, humanity makes first contact with an alien intelligence, and the course of history is irreversibly altered. Hailed as a watershed moment in science fiction, “2001” was considered way ahead of its time and raised a number of philosophical questions about what would happen if we ever encountered another form of life. Interestingly, the most noteworthy character in the film isn’t human or alien, but instead a new form of life altogether: an artificial intelligence (AI) known as the Heuristically programmed ALgorithmic computer 9000. HAL (as he is known colloquially) operates the Discovery One spacecraft, ferrying several scientists bound for Jupiter on a mission of exploration. Stating that he is “foolproof and incapable of error,” HAL’s superiority complex leads him to become the film’s antagonist, as he believes that human error is the cause of the difficulties they encounter. He eventually concludes that the best way to complete the mission is to eliminate human interference. When asked by scientist Dr. David Bowman to perform a simple function essential to the survival of the crew, HAL simply states “I’m sorry, Dave, I’m afraid I can’t do that.” Bowman is forced to disconnect HAL’s higher intellectual capabilities, reverting the computer to its most basic functions to ensure human survival.
Kubrick and Clarke may have been overly ambitious in predicting the progress of human space flight, but their call for concern over the risks of artificial intelligence seems quite prescient. Recently, billionaire entrepreneur Elon Musk (CEO of Tesla Motors and SpaceX) raised his concerns about AI, warning that, left unchecked, AI could be mankind’s final invention – one that could eventually destroy us. Other giants of the tech industry, including Bill Gates and Mark Zuckerberg, disagree. They believe AI represents tremendous promise for humanity and could usher in innovations unlike any we have ever seen.
A few weeks ago, we attended a national electronic health records conference where a well-known EHR vendor unveiled the new features in the upcoming release of their software. One of the most noteworthy additions was an intelligent virtual assistant, designed to help providers care for patients. While this is not the first time AI has ventured into health care (see IBM’s “Watson”), it is the first time the idea has become mainstream and fully integrated into physician workflow. Much like the virtual assistants mentioned above, this one can use voice or mouse/keyboard interaction to find clinical information, simplify common tasks, and help with medical decision-making.
While exciting at first, the idea of artificially intelligent EHRs may sound terrifying to some who aren’t yet ready to trust any patient care to machines. Reassuringly, while the integrated virtual assistant mentioned above can make suggestions to guide physicians to the right data or offer decision support when available, it is primarily focused on interface enhancement to improve work flow. It is not yet capable of making true clinical decisions that remove the physician from care delivery, but computers that do the diagnostic work of physicians may be closer than you think.
Research done at Jefferson University in Philadelphia and published in the August 2017 edition of Radiology1 investigated the ability of deep-learning algorithms to interpret chest radiographs for the diagnosis of tuberculosis. The computers achieved an impressive reliability of 99%. While at first radiograph interpretation seems quite different than the diagnostic decision-making done in primary care, the fundamental skill required for both is similar: pattern recognition. To build those patterns, artificial intelligence requires an enormous number of data points, but that’s hardly a problem thanks to the continual collection of patient data through electronic health records. The amount of raw information available to these algorithms is growing exponentially by the day, and with time their predictive ability will be unmatched. So where will that leave us, the physicians, entrusted for generations with the responsibility of diagnosis? Possibly more satisfied than we are today.
There was a time – not long ago – when the body of available medical knowledge was incredibly limited. Diagnostic testing was primitive and often inaccurate, and the treatment provided by physicians was focused on supporting, communicating, and genuinely caring for patients and their families. In the past 50 years, medical knowledge has exploded, and diagnostic testing has become incredibly advanced. Sadly, at the same time physicians have begun to feel more like clerical workers: entering data, writing prescriptions, and filling out forms. As artificial intelligence assumes some of this busywork and takes much of the guesswork out of diagnosis, physicians may find greater job satisfaction as they provide the skills a computer never can: a human touch, a personal and reflective interpretation of a patient’s diagnosis, and a true emotional connection. Ask this of a computer, and the response will always be the same: “I’m sorry, doctor, I’m afraid I can’t do that.”
Reference
1. Lakhani, Paras & Sundaram, Baskaran, “Deep Learning at Chest Radiography: Automated Classification of Pulmonary Tuberculosis by Using Convolutional Neural Networks,” Radiology. 2017 Aug;284:574-82.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington Jefferson Health.
In “2001: A Space Odyssey,” the epic 1968 film by Stanley Kubrick and Arthur C. Clarke, humanity makes first contact with an alien intelligence, and the course of history is irreversibly altered. Hailed as a watershed moment in science fiction, “2001” was considered way ahead of its time and raised a number of philosophical questions about what would happen if we ever encountered another form of life. Interestingly, the most noteworthy character in the film isn’t human or alien, but instead a new form of life altogether: an artificial intelligence (AI) known as the Heuristically programmed ALgorithmic computer 9000. HAL (as he is known colloquially) operates the Discovery One spacecraft, ferrying several scientists bound for Jupiter on a mission of exploration. Stating that he is “foolproof and incapable of error,” HAL’s superiority complex leads him to become the film’s antagonist, as he believes that human error is the cause of the difficulties they encounter. He eventually concludes that the best way to complete the mission is to eliminate human interference. When asked by scientist Dr. David Bowman to perform a simple function essential to the survival of the crew, HAL simply states “I’m sorry, Dave, I’m afraid I can’t do that.” Bowman is forced to disconnect HAL’s higher intellectual capabilities, reverting the computer to its most basic functions to ensure human survival.
Kubrick and Clarke may have been overly ambitious in predicting the progress of human space flight, but their call for concern over the risks of artificial intelligence seems quite prescient. Recently, billionaire entrepreneur Elon Musk (CEO of Tesla Motors and SpaceX) raised his concerns about AI, warning that, left unchecked, AI could be mankind’s final invention – one that could eventually destroy us. Other giants of the tech industry, including Bill Gates and Mark Zuckerberg, disagree. They believe AI represents tremendous promise for humanity and could usher in innovations unlike any we have ever seen.
A few weeks ago, we attended a national electronic health records conference where a well-known EHR vendor unveiled the new features in the upcoming release of their software. One of the most noteworthy additions was an intelligent virtual assistant, designed to help providers care for patients. While this is not the first time AI has ventured into health care (see IBM’s “Watson”), it is the first time the idea has become mainstream and fully integrated into physician workflow. Much like the virtual assistants mentioned above, this one can use voice or mouse/keyboard interaction to find clinical information, simplify common tasks, and help with medical decision-making.
While exciting at first, the idea of artificially intelligent EHRs may sound terrifying to some who aren’t yet ready to trust any patient care to machines. Reassuringly, while the integrated virtual assistant mentioned above can make suggestions to guide physicians to the right data or offer decision support when available, it is primarily focused on interface enhancement to improve work flow. It is not yet capable of making true clinical decisions that remove the physician from care delivery, but computers that do the diagnostic work of physicians may be closer than you think.
Research done at Jefferson University in Philadelphia and published in the August 2017 edition of Radiology1 investigated the ability of deep-learning algorithms to interpret chest radiographs for the diagnosis of tuberculosis. The computers achieved an impressive reliability of 99%. While at first radiograph interpretation seems quite different than the diagnostic decision-making done in primary care, the fundamental skill required for both is similar: pattern recognition. To build those patterns, artificial intelligence requires an enormous number of data points, but that’s hardly a problem thanks to the continual collection of patient data through electronic health records. The amount of raw information available to these algorithms is growing exponentially by the day, and with time their predictive ability will be unmatched. So where will that leave us, the physicians, entrusted for generations with the responsibility of diagnosis? Possibly more satisfied than we are today.
There was a time – not long ago – when the body of available medical knowledge was incredibly limited. Diagnostic testing was primitive and often inaccurate, and the treatment provided by physicians was focused on supporting, communicating, and genuinely caring for patients and their families. In the past 50 years, medical knowledge has exploded, and diagnostic testing has become incredibly advanced. Sadly, at the same time physicians have begun to feel more like clerical workers: entering data, writing prescriptions, and filling out forms. As artificial intelligence assumes some of this busywork and takes much of the guesswork out of diagnosis, physicians may find greater job satisfaction as they provide the skills a computer never can: a human touch, a personal and reflective interpretation of a patient’s diagnosis, and a true emotional connection. Ask this of a computer, and the response will always be the same: “I’m sorry, doctor, I’m afraid I can’t do that.”
Reference
1. Lakhani, Paras & Sundaram, Baskaran, “Deep Learning at Chest Radiography: Automated Classification of Pulmonary Tuberculosis by Using Convolutional Neural Networks,” Radiology. 2017 Aug;284:574-82.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington Jefferson Health.
CDC: Zika-exposed newborns need intensified eye, hearing, and neurological testing
Infants with possible prenatal Zika exposure who test positive for the virus should receive an in-depth ophthalmologic exam, intensified hearing testing, and a thorough neurological evaluation with brain imaging within 1 month of birth, according to new interim guidance set forth by the Centers for Disease Control and Prevention.
The new clinical management guidelines, published in the Oct. 20 issue of the Morbidity and Mortality Weekly Report, supersede the most recent CDC guidance, issued in August 2016. The agency deemed the update necessary after a recent convocation sponsored by the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. The meeting drew dozens of practicing clinicians and federal agency representatives, who reviewed the ever-evolving body of knowledge on how to best manage the care of these infants. Since Zika emerged as a public health threat, clinicians have reported postnatal onset of some symptoms, including eye abnormalities, a developing microcephaly in infants with a normal head circumference at birth, EEG abnormalities, and diaphragmatic paralysis.
The guidance focuses on three groups: infants with clinical findings of Zika syndrome born to mothers with possible Zika exposure during pregnancy; infants without clinical findings of Zika syndrome whose mothers had lab-confirmed Zika exposure; and infants without symptoms whose mothers might have been exposed, but who did not have laboratory-confirmed infection (MMWR. 2017 Oct 20;66[41]:1089-120).
Infants with clinical findings consistent with Zika syndrome and mothers with possible prenatal Zika exposure
These infants should be tested for Zika virus with serum and urine tests. If those are negative and there is no other apparent cause of the symptoms, they should have a cerebrospinal fluid sample tested for Zika RNA and IgM Zika antibodies.
By 1 month, these infants need a head ultrasound and a detailed ophthalmologic exam. The eye exam should pick up any anomalies of the anterior and posterior eye, including microphthalmia, coloboma, intraocular calcifications, optic nerve hypoplasia and atrophy, and macular scarring with focal pigmentary retinal mottling.
A comprehensive neurological exam also is part of the recommendation. Seizures are sometimes part of Zika syndrome, but infants can also have subclinical EEG abnormalities. Advanced neuroimaging can identify both obvious and subtle brain abnormalities: cortical thinning, corpus callosum abnormalities, calcifications at the white/gray matter junction, and ventricular enlargement are possible findings.
As infants grow, clinicians should be alert for signs of increased intracranial pressure that could signal postnatal hydrocephalus. Diaphragmatic paralysis also has been seen; this manifests by respiratory distress. Dysphagia that interferes with feeding can develop as well.
The complicated clinical picture calls for a team approach, Dr. Adebanjo said. “The follow-up care of [these infants] requires a multidisciplinary team and an established medical home to facilitate the coordination of care and ensure that abnormal findings are addressed.”
Infants without clinical findings, whose mothers have lab-confirmed Zika exposure
Initially, these infants should have the same early head ultrasound, hearing, and eye exams as those who display clinical findings. All of these infants also should be tested for Zika virus in the same way as those with clinical findings.
If tests return a positive result, they should have all the investigations and follow-ups recommended for babies with clinical findings. If lab testing is negative, and clinical findings are normal, Zika infection is highly unlikely and they can receive routine care, although clinicians and parents should be on the lookout for any new symptoms that might suggest postnatal Zika syndrome.
Infants without clinical findings, whose mothers had possible, but unconfirmed, Zika exposure
This is a varied and large group, which includes women who were never tested during pregnancy, as well as those who could have had a false negative test. “Because the latter issue is not easily discerned, all mothers with possible exposure to Zika virus infection, including those who tested negative with currently available technology, should be considered in this group,” Dr. Adebanjo said.
CDC does not recommend further Zika evaluation for these infants unless additional testing confirms maternal infection. For older infants, parents and clinicians should decide together whether any further evaluations would be helpful. But, Dr. Adebanjo said, “If findings consistent with congenital Zika syndrome are identified at any time, referrals to appropriate specialties should be made, and subsequent evaluation should follow recommendations for infants with clinical findings consistent with congenital Zika.”
CDC also reiterated its special recommendations for infants who had a prenatal diagnosis of Zika infection. For now, these remain unchanged from 2016, although “as more data become available, understanding of the diagnostic role of prenatal ultrasound and amniocentesis will improve and guidance will be updated.”
No one has yet identified the optimal timing for a Zika diagnostic ultrasound. CDC recommends serial ultrasounds be done every 3-4 weeks for women with lab-confirmed prenatal Zika exposure. Women with possible exposure need only routine ultrasound screenings.
While Zika RNA has been identified in amniotic fluid, there is no consensus on the value of amniocentesis as a prenatal diagnostic tool. Investigations of serial amniocentesis suggests that viral shedding into the amniotic fluid might be transient. If the procedure is done for other reasons, Zika nucleic acid testing can be incorporated.
A shared decision-making process is key when making screening decisions that should be individually weighed, Dr. Adebanjo said. “For example, serial ultrasounds might be inconvenient, unpleasant, and expensive, and might prompt unnecessary interventions; amniocentesis carries additional known risks such as fetal loss. These potential harms of prenatal screening for congenital Zika syndrome might outweigh the clinical benefits for some patients. Therefore, these decisions should be individualized.”
Neither Dr. Adebanjo nor any of the coauthors had any financial disclosures.
Infants with possible prenatal Zika exposure who test positive for the virus should receive an in-depth ophthalmologic exam, intensified hearing testing, and a thorough neurological evaluation with brain imaging within 1 month of birth, according to new interim guidance set forth by the Centers for Disease Control and Prevention.
The new clinical management guidelines, published in the Oct. 20 issue of the Morbidity and Mortality Weekly Report, supersede the most recent CDC guidance, issued in August 2016. The agency deemed the update necessary after a recent convocation sponsored by the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. The meeting drew dozens of practicing clinicians and federal agency representatives, who reviewed the ever-evolving body of knowledge on how to best manage the care of these infants. Since Zika emerged as a public health threat, clinicians have reported postnatal onset of some symptoms, including eye abnormalities, a developing microcephaly in infants with a normal head circumference at birth, EEG abnormalities, and diaphragmatic paralysis.
The guidance focuses on three groups: infants with clinical findings of Zika syndrome born to mothers with possible Zika exposure during pregnancy; infants without clinical findings of Zika syndrome whose mothers had lab-confirmed Zika exposure; and infants without symptoms whose mothers might have been exposed, but who did not have laboratory-confirmed infection (MMWR. 2017 Oct 20;66[41]:1089-120).
Infants with clinical findings consistent with Zika syndrome and mothers with possible prenatal Zika exposure
These infants should be tested for Zika virus with serum and urine tests. If those are negative and there is no other apparent cause of the symptoms, they should have a cerebrospinal fluid sample tested for Zika RNA and IgM Zika antibodies.
By 1 month, these infants need a head ultrasound and a detailed ophthalmologic exam. The eye exam should pick up any anomalies of the anterior and posterior eye, including microphthalmia, coloboma, intraocular calcifications, optic nerve hypoplasia and atrophy, and macular scarring with focal pigmentary retinal mottling.
A comprehensive neurological exam also is part of the recommendation. Seizures are sometimes part of Zika syndrome, but infants can also have subclinical EEG abnormalities. Advanced neuroimaging can identify both obvious and subtle brain abnormalities: cortical thinning, corpus callosum abnormalities, calcifications at the white/gray matter junction, and ventricular enlargement are possible findings.
As infants grow, clinicians should be alert for signs of increased intracranial pressure that could signal postnatal hydrocephalus. Diaphragmatic paralysis also has been seen; this manifests by respiratory distress. Dysphagia that interferes with feeding can develop as well.
The complicated clinical picture calls for a team approach, Dr. Adebanjo said. “The follow-up care of [these infants] requires a multidisciplinary team and an established medical home to facilitate the coordination of care and ensure that abnormal findings are addressed.”
Infants without clinical findings, whose mothers have lab-confirmed Zika exposure
Initially, these infants should have the same early head ultrasound, hearing, and eye exams as those who display clinical findings. All of these infants also should be tested for Zika virus in the same way as those with clinical findings.
If tests return a positive result, they should have all the investigations and follow-ups recommended for babies with clinical findings. If lab testing is negative, and clinical findings are normal, Zika infection is highly unlikely and they can receive routine care, although clinicians and parents should be on the lookout for any new symptoms that might suggest postnatal Zika syndrome.
Infants without clinical findings, whose mothers had possible, but unconfirmed, Zika exposure
This is a varied and large group, which includes women who were never tested during pregnancy, as well as those who could have had a false negative test. “Because the latter issue is not easily discerned, all mothers with possible exposure to Zika virus infection, including those who tested negative with currently available technology, should be considered in this group,” Dr. Adebanjo said.
CDC does not recommend further Zika evaluation for these infants unless additional testing confirms maternal infection. For older infants, parents and clinicians should decide together whether any further evaluations would be helpful. But, Dr. Adebanjo said, “If findings consistent with congenital Zika syndrome are identified at any time, referrals to appropriate specialties should be made, and subsequent evaluation should follow recommendations for infants with clinical findings consistent with congenital Zika.”
CDC also reiterated its special recommendations for infants who had a prenatal diagnosis of Zika infection. For now, these remain unchanged from 2016, although “as more data become available, understanding of the diagnostic role of prenatal ultrasound and amniocentesis will improve and guidance will be updated.”
No one has yet identified the optimal timing for a Zika diagnostic ultrasound. CDC recommends serial ultrasounds be done every 3-4 weeks for women with lab-confirmed prenatal Zika exposure. Women with possible exposure need only routine ultrasound screenings.
While Zika RNA has been identified in amniotic fluid, there is no consensus on the value of amniocentesis as a prenatal diagnostic tool. Investigations of serial amniocentesis suggests that viral shedding into the amniotic fluid might be transient. If the procedure is done for other reasons, Zika nucleic acid testing can be incorporated.
A shared decision-making process is key when making screening decisions that should be individually weighed, Dr. Adebanjo said. “For example, serial ultrasounds might be inconvenient, unpleasant, and expensive, and might prompt unnecessary interventions; amniocentesis carries additional known risks such as fetal loss. These potential harms of prenatal screening for congenital Zika syndrome might outweigh the clinical benefits for some patients. Therefore, these decisions should be individualized.”
Neither Dr. Adebanjo nor any of the coauthors had any financial disclosures.
Infants with possible prenatal Zika exposure who test positive for the virus should receive an in-depth ophthalmologic exam, intensified hearing testing, and a thorough neurological evaluation with brain imaging within 1 month of birth, according to new interim guidance set forth by the Centers for Disease Control and Prevention.
The new clinical management guidelines, published in the Oct. 20 issue of the Morbidity and Mortality Weekly Report, supersede the most recent CDC guidance, issued in August 2016. The agency deemed the update necessary after a recent convocation sponsored by the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. The meeting drew dozens of practicing clinicians and federal agency representatives, who reviewed the ever-evolving body of knowledge on how to best manage the care of these infants. Since Zika emerged as a public health threat, clinicians have reported postnatal onset of some symptoms, including eye abnormalities, a developing microcephaly in infants with a normal head circumference at birth, EEG abnormalities, and diaphragmatic paralysis.
The guidance focuses on three groups: infants with clinical findings of Zika syndrome born to mothers with possible Zika exposure during pregnancy; infants without clinical findings of Zika syndrome whose mothers had lab-confirmed Zika exposure; and infants without symptoms whose mothers might have been exposed, but who did not have laboratory-confirmed infection (MMWR. 2017 Oct 20;66[41]:1089-120).
Infants with clinical findings consistent with Zika syndrome and mothers with possible prenatal Zika exposure
These infants should be tested for Zika virus with serum and urine tests. If those are negative and there is no other apparent cause of the symptoms, they should have a cerebrospinal fluid sample tested for Zika RNA and IgM Zika antibodies.
By 1 month, these infants need a head ultrasound and a detailed ophthalmologic exam. The eye exam should pick up any anomalies of the anterior and posterior eye, including microphthalmia, coloboma, intraocular calcifications, optic nerve hypoplasia and atrophy, and macular scarring with focal pigmentary retinal mottling.
A comprehensive neurological exam also is part of the recommendation. Seizures are sometimes part of Zika syndrome, but infants can also have subclinical EEG abnormalities. Advanced neuroimaging can identify both obvious and subtle brain abnormalities: cortical thinning, corpus callosum abnormalities, calcifications at the white/gray matter junction, and ventricular enlargement are possible findings.
As infants grow, clinicians should be alert for signs of increased intracranial pressure that could signal postnatal hydrocephalus. Diaphragmatic paralysis also has been seen; this manifests by respiratory distress. Dysphagia that interferes with feeding can develop as well.
The complicated clinical picture calls for a team approach, Dr. Adebanjo said. “The follow-up care of [these infants] requires a multidisciplinary team and an established medical home to facilitate the coordination of care and ensure that abnormal findings are addressed.”
Infants without clinical findings, whose mothers have lab-confirmed Zika exposure
Initially, these infants should have the same early head ultrasound, hearing, and eye exams as those who display clinical findings. All of these infants also should be tested for Zika virus in the same way as those with clinical findings.
If tests return a positive result, they should have all the investigations and follow-ups recommended for babies with clinical findings. If lab testing is negative, and clinical findings are normal, Zika infection is highly unlikely and they can receive routine care, although clinicians and parents should be on the lookout for any new symptoms that might suggest postnatal Zika syndrome.
Infants without clinical findings, whose mothers had possible, but unconfirmed, Zika exposure
This is a varied and large group, which includes women who were never tested during pregnancy, as well as those who could have had a false negative test. “Because the latter issue is not easily discerned, all mothers with possible exposure to Zika virus infection, including those who tested negative with currently available technology, should be considered in this group,” Dr. Adebanjo said.
CDC does not recommend further Zika evaluation for these infants unless additional testing confirms maternal infection. For older infants, parents and clinicians should decide together whether any further evaluations would be helpful. But, Dr. Adebanjo said, “If findings consistent with congenital Zika syndrome are identified at any time, referrals to appropriate specialties should be made, and subsequent evaluation should follow recommendations for infants with clinical findings consistent with congenital Zika.”
CDC also reiterated its special recommendations for infants who had a prenatal diagnosis of Zika infection. For now, these remain unchanged from 2016, although “as more data become available, understanding of the diagnostic role of prenatal ultrasound and amniocentesis will improve and guidance will be updated.”
No one has yet identified the optimal timing for a Zika diagnostic ultrasound. CDC recommends serial ultrasounds be done every 3-4 weeks for women with lab-confirmed prenatal Zika exposure. Women with possible exposure need only routine ultrasound screenings.
While Zika RNA has been identified in amniotic fluid, there is no consensus on the value of amniocentesis as a prenatal diagnostic tool. Investigations of serial amniocentesis suggests that viral shedding into the amniotic fluid might be transient. If the procedure is done for other reasons, Zika nucleic acid testing can be incorporated.
A shared decision-making process is key when making screening decisions that should be individually weighed, Dr. Adebanjo said. “For example, serial ultrasounds might be inconvenient, unpleasant, and expensive, and might prompt unnecessary interventions; amniocentesis carries additional known risks such as fetal loss. These potential harms of prenatal screening for congenital Zika syndrome might outweigh the clinical benefits for some patients. Therefore, these decisions should be individualized.”
Neither Dr. Adebanjo nor any of the coauthors had any financial disclosures.
FROM MMWR
VIDEO: Salvageable brain tissue can guide decision for stroke thrombectomy
SAN DIEGO – Neurologists have long suspected that some stroke patients could benefit from thrombectomy many hours after they were last seen well. But lingering doubts remained, and physicians weren’t sure which stroke patients were likely to improve.
Now, with the early stoppage of two key clinical trials, the answer is clear, Jeffrey Saver, MD, director of the stroke unit at the University of California, Los Angeles, said in a video interview at the annual meeting of the American Neurological Association.
At the European Stroke Organization Conference in May, Stryker Neurovascular announced the results of its DAWN trial, which tested the company’s mechanical thrombectomy device in patients who’d suffered a stroke within the past 6-24 hours and in whom imaging showed a clinical core mismatch. It was stopped early based on an interim analysis after it met multiple prespecified stopping criteria. At 90 days, 48.6% of patients in the treatment group were functionally independent, compared with 13.1% who received only medical management.
The DEFUSE 3 trial examined endovascular thrombectomy in patients 6-16 hours after a stroke who appeared to have salvageable brain tissue based on target mismatch profile with a less extreme core than in DAWN. It too was halted early because of a high probability of efficacy. Together, the trials suggest neurologists are entering a new era of treating based on tissue and not just time, Dr. Saver said.
SAN DIEGO – Neurologists have long suspected that some stroke patients could benefit from thrombectomy many hours after they were last seen well. But lingering doubts remained, and physicians weren’t sure which stroke patients were likely to improve.
Now, with the early stoppage of two key clinical trials, the answer is clear, Jeffrey Saver, MD, director of the stroke unit at the University of California, Los Angeles, said in a video interview at the annual meeting of the American Neurological Association.
At the European Stroke Organization Conference in May, Stryker Neurovascular announced the results of its DAWN trial, which tested the company’s mechanical thrombectomy device in patients who’d suffered a stroke within the past 6-24 hours and in whom imaging showed a clinical core mismatch. It was stopped early based on an interim analysis after it met multiple prespecified stopping criteria. At 90 days, 48.6% of patients in the treatment group were functionally independent, compared with 13.1% who received only medical management.
The DEFUSE 3 trial examined endovascular thrombectomy in patients 6-16 hours after a stroke who appeared to have salvageable brain tissue based on target mismatch profile with a less extreme core than in DAWN. It too was halted early because of a high probability of efficacy. Together, the trials suggest neurologists are entering a new era of treating based on tissue and not just time, Dr. Saver said.
SAN DIEGO – Neurologists have long suspected that some stroke patients could benefit from thrombectomy many hours after they were last seen well. But lingering doubts remained, and physicians weren’t sure which stroke patients were likely to improve.
Now, with the early stoppage of two key clinical trials, the answer is clear, Jeffrey Saver, MD, director of the stroke unit at the University of California, Los Angeles, said in a video interview at the annual meeting of the American Neurological Association.
At the European Stroke Organization Conference in May, Stryker Neurovascular announced the results of its DAWN trial, which tested the company’s mechanical thrombectomy device in patients who’d suffered a stroke within the past 6-24 hours and in whom imaging showed a clinical core mismatch. It was stopped early based on an interim analysis after it met multiple prespecified stopping criteria. At 90 days, 48.6% of patients in the treatment group were functionally independent, compared with 13.1% who received only medical management.
The DEFUSE 3 trial examined endovascular thrombectomy in patients 6-16 hours after a stroke who appeared to have salvageable brain tissue based on target mismatch profile with a less extreme core than in DAWN. It too was halted early because of a high probability of efficacy. Together, the trials suggest neurologists are entering a new era of treating based on tissue and not just time, Dr. Saver said.
AT ANA 2017
Burnout takes its toll on neurology
I’m burned out.
Heck, what doctor isn’t? Politicians say we get paid too much. Lawyers say we make too many mistakes. Insurance companies say we order too many tests and too many expensive treatments. And the patients, while generally good people looking for help, can also on occasion be angry and unreasonable. The bad apples may be in the minority, but it only takes one to ruin a day full of rewarding visits.
That can’t be good.
Some of the study’s listed reasons for burnout are very familiar: complaints about maintenance of certification and about calling insurances to authorize tests and medications, crappy reimbursement for time-consuming visits, having to spend more time at work just to break even, and the constant feeling of never being caught up. I leave work, come home, have dinner with my family, do dictations, go to bed, and do it over again. No matter where I am, I’ve never left the office.
Other common complaints aren’t as much an issue for me. I don’t have, or want, an electronic health record that qualifies for meaningful use; I designed the one I have, and it works fine for me. I don’t have a nonmedical administrator telling me how many patients I’m required to see each day, and my patient population is, overall, appreciative and polite.
There are always trade-offs. When my kids have school breaks, I take that time off from the office to be with them. I enjoy it – I mean, that’s what we’re here for as parents, isn’t it? Of course, the drawback comes a few weeks later when my income drops because I wasn’t working. In solo practice, cash flow is king. I may have more freedom and control than my employed colleagues, but the downside is that I have no guaranteed salary, either. I’m the last one here who gets paid.
I see plenty of columns on how to avoid burnout, none of which seem to be written by someone who’s in a real-world practice. They all recommend taking time off for yourself, maybe seeing a counselor, finding a hobby you enjoy ... Really?
There’s no easy answer, either. We’re stuck with decreasing reimbursements, a gradual whittling away of our profession, a demand to keep putting time we don’t have into our jobs, and many other issues. It’s even worse for those who are coming out of training and are facing these same challenges with six-figure student loans over their heads and, often, the demands of young families. The idealism and energy of youth are all that seem to sustain them, and that can’t last.
I like being a doctor. I enjoy being a neurologist. I love being able to help people and have a sense of service in doing so. But the worsening financial picture for us, and the increasing demands on our often already nonexistent free time, are destroying the field. Like many other docs, I look at my savings here and there and wonder how long until I can retire. That is sad because, as we all gradually leave practice (for whatever reason), new people will need to come in and pick up the mantle. But current conditions are such that I suspect many will find something else to do unless things change.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’m burned out.
Heck, what doctor isn’t? Politicians say we get paid too much. Lawyers say we make too many mistakes. Insurance companies say we order too many tests and too many expensive treatments. And the patients, while generally good people looking for help, can also on occasion be angry and unreasonable. The bad apples may be in the minority, but it only takes one to ruin a day full of rewarding visits.
That can’t be good.
Some of the study’s listed reasons for burnout are very familiar: complaints about maintenance of certification and about calling insurances to authorize tests and medications, crappy reimbursement for time-consuming visits, having to spend more time at work just to break even, and the constant feeling of never being caught up. I leave work, come home, have dinner with my family, do dictations, go to bed, and do it over again. No matter where I am, I’ve never left the office.
Other common complaints aren’t as much an issue for me. I don’t have, or want, an electronic health record that qualifies for meaningful use; I designed the one I have, and it works fine for me. I don’t have a nonmedical administrator telling me how many patients I’m required to see each day, and my patient population is, overall, appreciative and polite.
There are always trade-offs. When my kids have school breaks, I take that time off from the office to be with them. I enjoy it – I mean, that’s what we’re here for as parents, isn’t it? Of course, the drawback comes a few weeks later when my income drops because I wasn’t working. In solo practice, cash flow is king. I may have more freedom and control than my employed colleagues, but the downside is that I have no guaranteed salary, either. I’m the last one here who gets paid.
I see plenty of columns on how to avoid burnout, none of which seem to be written by someone who’s in a real-world practice. They all recommend taking time off for yourself, maybe seeing a counselor, finding a hobby you enjoy ... Really?
There’s no easy answer, either. We’re stuck with decreasing reimbursements, a gradual whittling away of our profession, a demand to keep putting time we don’t have into our jobs, and many other issues. It’s even worse for those who are coming out of training and are facing these same challenges with six-figure student loans over their heads and, often, the demands of young families. The idealism and energy of youth are all that seem to sustain them, and that can’t last.
I like being a doctor. I enjoy being a neurologist. I love being able to help people and have a sense of service in doing so. But the worsening financial picture for us, and the increasing demands on our often already nonexistent free time, are destroying the field. Like many other docs, I look at my savings here and there and wonder how long until I can retire. That is sad because, as we all gradually leave practice (for whatever reason), new people will need to come in and pick up the mantle. But current conditions are such that I suspect many will find something else to do unless things change.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’m burned out.
Heck, what doctor isn’t? Politicians say we get paid too much. Lawyers say we make too many mistakes. Insurance companies say we order too many tests and too many expensive treatments. And the patients, while generally good people looking for help, can also on occasion be angry and unreasonable. The bad apples may be in the minority, but it only takes one to ruin a day full of rewarding visits.
That can’t be good.
Some of the study’s listed reasons for burnout are very familiar: complaints about maintenance of certification and about calling insurances to authorize tests and medications, crappy reimbursement for time-consuming visits, having to spend more time at work just to break even, and the constant feeling of never being caught up. I leave work, come home, have dinner with my family, do dictations, go to bed, and do it over again. No matter where I am, I’ve never left the office.
Other common complaints aren’t as much an issue for me. I don’t have, or want, an electronic health record that qualifies for meaningful use; I designed the one I have, and it works fine for me. I don’t have a nonmedical administrator telling me how many patients I’m required to see each day, and my patient population is, overall, appreciative and polite.
There are always trade-offs. When my kids have school breaks, I take that time off from the office to be with them. I enjoy it – I mean, that’s what we’re here for as parents, isn’t it? Of course, the drawback comes a few weeks later when my income drops because I wasn’t working. In solo practice, cash flow is king. I may have more freedom and control than my employed colleagues, but the downside is that I have no guaranteed salary, either. I’m the last one here who gets paid.
I see plenty of columns on how to avoid burnout, none of which seem to be written by someone who’s in a real-world practice. They all recommend taking time off for yourself, maybe seeing a counselor, finding a hobby you enjoy ... Really?
There’s no easy answer, either. We’re stuck with decreasing reimbursements, a gradual whittling away of our profession, a demand to keep putting time we don’t have into our jobs, and many other issues. It’s even worse for those who are coming out of training and are facing these same challenges with six-figure student loans over their heads and, often, the demands of young families. The idealism and energy of youth are all that seem to sustain them, and that can’t last.
I like being a doctor. I enjoy being a neurologist. I love being able to help people and have a sense of service in doing so. But the worsening financial picture for us, and the increasing demands on our often already nonexistent free time, are destroying the field. Like many other docs, I look at my savings here and there and wonder how long until I can retire. That is sad because, as we all gradually leave practice (for whatever reason), new people will need to come in and pick up the mantle. But current conditions are such that I suspect many will find something else to do unless things change.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Care needed using sotagliflozin as add-on to insulin in T1DM
LISBON – Further phase 3 trial data show that the investigational dual sodium-glucose cotransporter 1 and 2 (SGLT1/2) inhibitor according to results reported at the annual meeting of the European Association for the Study of Diabetes.
In the inTandem3 trial, 28.6% of 699 people with T1DM treated with sotagliflozin on top of their usual insulin therapy achieved the primary composite endpoint, which was a glycated hemoglobin (HbA1c) level of 7% or lower at Week 24, with no episodes of severe hypoglycemia or diabetic ketoacidosis (DKA). In comparison, 15.2% of the 703 individuals who received a placebo in addition to their insulin therapy achieved this endpoint (P less than .001), according to Melanie J. Davies, MD, who presented the inTandem3 study results during a symposium on the sotagliflozin clinical program. The results were published online in the New England Journal of Medicine (2017 Sep 15. doi: 10.1056/NEJMoa1708337) to coincide with their presentation at the meeting.
However, the overall rate of DKA was higher in the patients treated with sotagliflozin than in those on placebo, at 3% versus 0.6%, respectively. DKA events most often occurred in persons using insulin pumps (4.4% vs. 9.7%) than in those taking insulin via multiple daily injections (2.1% vs 0.5%). Furthermore, in a post-hoc analysis, it was found that the rate of at least one episode of DKA was significantly higher in sotagliflozin- than placebo-treated patients who failed to reach the HbA1c target of below 7% (P less than .003), reported Dr. Davies.
The study findings “build on data seen inTandem 1 and inTandem 2 but in a more pragmatic design,” said study investigator Melanie Davies, MD, professor of diabetes medicine at the University of Leicester (England).
The inTandem studies
Dr. Davies observed that the sotagliflozin clinical trials program in persons with T1DM involved three phase 2 and three phase 3 studies. The latter, inTandem1, inTandem2, and inTandem3, were all 24-week trials, but there were some differences in the design.
inTandem1 and inTandem2 were the pivotal studies, one conducted in 793 patients in North America and the other in 782 patients in Europe and Israel. After a 2-week screening period, participants underwent a 6-week insulin optimization program before they were randomized to one of two doses of sotagliflozin (200 mg or 400 mg) or placebo for 24 weeks, with follow-up out to 52 weeks. The primary endpoint of these studies was the reduction in HbA1c versus placebo at 24 weeks.
By comparison, inTandem3 was a global study involving 1,405 individuals with T1DM who did not undergo the 6-week insulin optimization period. Instead there was a 2-week run-in period after the initial screening, and the study ran for only 24 weeks. Only one dose (400 mg) of sotagliflozin was used and the primary endpoint was a composite to try to see what the net clinical benefit would be, Dr. Davies explained.
The results of inTandem1 and inTandem2 were reported earlier this year at the American Diabetes Association Scientific Sessions, Dr. Davies noted, and sotagliflozin had “a good efficacy and safety profile as an adjunct to insulin in type 1 diabetes.”
The quest for adjunctive treatment
“For years we’ve been looking for adjunctive therapy for people with type 1 diabetes,” said Julio Rosenstock, MD, at the EASD meeting. Dr. Rosenstock, who is the director of the Dallas Diabetes Research Center at Medical City and involved in the sotagliflozin clinical trials program, noted that the quest for an adjunctive treatment was because “glucose control in type 1 diabetes remains tough and costly, despite multiple advances in insulin therapy, delivery systems, and monitoring methods over the years.”
Several approaches to adjunctive treatment had been proposed, but so far all with limited value, Dr. Rosenstock maintained. Despite no evidence for a benefit of adding metformin, for example, registry data suggest that up to 5% of people with T1DM are using it.
The recent findings of the REMOVAL trial showed metformin did not help change the HbA1c over time and there was no change in the primary outcome, he observed but a small improvement in a tertiary endpoint. “I can’t think of a more negative cardiovascular outcomes trial,” Dr. Rosenstock asserted. “There is not enough justification to use metformin in type 1 diabetes.”
By contrast there is a strong rationale for using SGLT inhibition, partly as the glucose-lowering effects are independent of insulin’s activity. Through inhibition of SGLT1, sotagliflozin reduces glucose absorption in the proximal intestine, thus blunting or delaying rising postprandial glucose levels. By also targeting SGLT2, sotagliflozin can reduce glucose resorption by the kidneys.
Risks and clinical implications
In an editorial accompanying the published findings, David Nathan, MD, of Massachusetts General Hospital and Harvard Medical School in Boston, is not convinced that using adjunctive treatment is the future for better glycemic control in T1DM and that better automated insulin delivery systems will likely make adjunctive therapy unnecessary.
Dr. Nathan also observed “the rate of severe hypoglycemia in the whole sotagliflozin group was not significantly different from the rate in the placebo group,” and the risks and benefits of any adjunctive therapy for T1DM need to be carefully balanced.
While risks remain, one of the chairs of the session, Chantal Mathieu, MD, professor of medicine at the Katholieke Universiteit Leuven (Belgium), observed that “these are exciting times for all of us and hopefully for our patients.” She cautioned clinicians to remember, however, that “type 1 diabetes is a very different disease from type 2 diabetes, and so when we listen to [information about] all these adjunct[ive] therapies, when we read the papers, please interpret the data carefully.”
The trial was funded by Lexicon Pharmaceuticals. Sotagliflozin is being codeveloped with Sanofi. Dr. Davies disclosed acting as an advisor, consultant, or being a member of a speaker’s bureau for Sanofi-Aventis and several other companies. She was an investigator in the inTandem trials and her institution received funding from Lexicon to conduct the inTandem 2 and 3 clinical trials. Dr. Rosenstock disclosed research support and acting as an advisor to multiple pharmaceutical companies. Dr. Nathan had nothing to disclose. Dr. Mathieu chaired the session and did not present disclosures.
LISBON – Further phase 3 trial data show that the investigational dual sodium-glucose cotransporter 1 and 2 (SGLT1/2) inhibitor according to results reported at the annual meeting of the European Association for the Study of Diabetes.
In the inTandem3 trial, 28.6% of 699 people with T1DM treated with sotagliflozin on top of their usual insulin therapy achieved the primary composite endpoint, which was a glycated hemoglobin (HbA1c) level of 7% or lower at Week 24, with no episodes of severe hypoglycemia or diabetic ketoacidosis (DKA). In comparison, 15.2% of the 703 individuals who received a placebo in addition to their insulin therapy achieved this endpoint (P less than .001), according to Melanie J. Davies, MD, who presented the inTandem3 study results during a symposium on the sotagliflozin clinical program. The results were published online in the New England Journal of Medicine (2017 Sep 15. doi: 10.1056/NEJMoa1708337) to coincide with their presentation at the meeting.
However, the overall rate of DKA was higher in the patients treated with sotagliflozin than in those on placebo, at 3% versus 0.6%, respectively. DKA events most often occurred in persons using insulin pumps (4.4% vs. 9.7%) than in those taking insulin via multiple daily injections (2.1% vs 0.5%). Furthermore, in a post-hoc analysis, it was found that the rate of at least one episode of DKA was significantly higher in sotagliflozin- than placebo-treated patients who failed to reach the HbA1c target of below 7% (P less than .003), reported Dr. Davies.
The study findings “build on data seen inTandem 1 and inTandem 2 but in a more pragmatic design,” said study investigator Melanie Davies, MD, professor of diabetes medicine at the University of Leicester (England).
The inTandem studies
Dr. Davies observed that the sotagliflozin clinical trials program in persons with T1DM involved three phase 2 and three phase 3 studies. The latter, inTandem1, inTandem2, and inTandem3, were all 24-week trials, but there were some differences in the design.
inTandem1 and inTandem2 were the pivotal studies, one conducted in 793 patients in North America and the other in 782 patients in Europe and Israel. After a 2-week screening period, participants underwent a 6-week insulin optimization program before they were randomized to one of two doses of sotagliflozin (200 mg or 400 mg) or placebo for 24 weeks, with follow-up out to 52 weeks. The primary endpoint of these studies was the reduction in HbA1c versus placebo at 24 weeks.
By comparison, inTandem3 was a global study involving 1,405 individuals with T1DM who did not undergo the 6-week insulin optimization period. Instead there was a 2-week run-in period after the initial screening, and the study ran for only 24 weeks. Only one dose (400 mg) of sotagliflozin was used and the primary endpoint was a composite to try to see what the net clinical benefit would be, Dr. Davies explained.
The results of inTandem1 and inTandem2 were reported earlier this year at the American Diabetes Association Scientific Sessions, Dr. Davies noted, and sotagliflozin had “a good efficacy and safety profile as an adjunct to insulin in type 1 diabetes.”
The quest for adjunctive treatment
“For years we’ve been looking for adjunctive therapy for people with type 1 diabetes,” said Julio Rosenstock, MD, at the EASD meeting. Dr. Rosenstock, who is the director of the Dallas Diabetes Research Center at Medical City and involved in the sotagliflozin clinical trials program, noted that the quest for an adjunctive treatment was because “glucose control in type 1 diabetes remains tough and costly, despite multiple advances in insulin therapy, delivery systems, and monitoring methods over the years.”
Several approaches to adjunctive treatment had been proposed, but so far all with limited value, Dr. Rosenstock maintained. Despite no evidence for a benefit of adding metformin, for example, registry data suggest that up to 5% of people with T1DM are using it.
The recent findings of the REMOVAL trial showed metformin did not help change the HbA1c over time and there was no change in the primary outcome, he observed but a small improvement in a tertiary endpoint. “I can’t think of a more negative cardiovascular outcomes trial,” Dr. Rosenstock asserted. “There is not enough justification to use metformin in type 1 diabetes.”
By contrast there is a strong rationale for using SGLT inhibition, partly as the glucose-lowering effects are independent of insulin’s activity. Through inhibition of SGLT1, sotagliflozin reduces glucose absorption in the proximal intestine, thus blunting or delaying rising postprandial glucose levels. By also targeting SGLT2, sotagliflozin can reduce glucose resorption by the kidneys.
Risks and clinical implications
In an editorial accompanying the published findings, David Nathan, MD, of Massachusetts General Hospital and Harvard Medical School in Boston, is not convinced that using adjunctive treatment is the future for better glycemic control in T1DM and that better automated insulin delivery systems will likely make adjunctive therapy unnecessary.
Dr. Nathan also observed “the rate of severe hypoglycemia in the whole sotagliflozin group was not significantly different from the rate in the placebo group,” and the risks and benefits of any adjunctive therapy for T1DM need to be carefully balanced.
While risks remain, one of the chairs of the session, Chantal Mathieu, MD, professor of medicine at the Katholieke Universiteit Leuven (Belgium), observed that “these are exciting times for all of us and hopefully for our patients.” She cautioned clinicians to remember, however, that “type 1 diabetes is a very different disease from type 2 diabetes, and so when we listen to [information about] all these adjunct[ive] therapies, when we read the papers, please interpret the data carefully.”
The trial was funded by Lexicon Pharmaceuticals. Sotagliflozin is being codeveloped with Sanofi. Dr. Davies disclosed acting as an advisor, consultant, or being a member of a speaker’s bureau for Sanofi-Aventis and several other companies. She was an investigator in the inTandem trials and her institution received funding from Lexicon to conduct the inTandem 2 and 3 clinical trials. Dr. Rosenstock disclosed research support and acting as an advisor to multiple pharmaceutical companies. Dr. Nathan had nothing to disclose. Dr. Mathieu chaired the session and did not present disclosures.
LISBON – Further phase 3 trial data show that the investigational dual sodium-glucose cotransporter 1 and 2 (SGLT1/2) inhibitor according to results reported at the annual meeting of the European Association for the Study of Diabetes.
In the inTandem3 trial, 28.6% of 699 people with T1DM treated with sotagliflozin on top of their usual insulin therapy achieved the primary composite endpoint, which was a glycated hemoglobin (HbA1c) level of 7% or lower at Week 24, with no episodes of severe hypoglycemia or diabetic ketoacidosis (DKA). In comparison, 15.2% of the 703 individuals who received a placebo in addition to their insulin therapy achieved this endpoint (P less than .001), according to Melanie J. Davies, MD, who presented the inTandem3 study results during a symposium on the sotagliflozin clinical program. The results were published online in the New England Journal of Medicine (2017 Sep 15. doi: 10.1056/NEJMoa1708337) to coincide with their presentation at the meeting.
However, the overall rate of DKA was higher in the patients treated with sotagliflozin than in those on placebo, at 3% versus 0.6%, respectively. DKA events most often occurred in persons using insulin pumps (4.4% vs. 9.7%) than in those taking insulin via multiple daily injections (2.1% vs 0.5%). Furthermore, in a post-hoc analysis, it was found that the rate of at least one episode of DKA was significantly higher in sotagliflozin- than placebo-treated patients who failed to reach the HbA1c target of below 7% (P less than .003), reported Dr. Davies.
The study findings “build on data seen inTandem 1 and inTandem 2 but in a more pragmatic design,” said study investigator Melanie Davies, MD, professor of diabetes medicine at the University of Leicester (England).
The inTandem studies
Dr. Davies observed that the sotagliflozin clinical trials program in persons with T1DM involved three phase 2 and three phase 3 studies. The latter, inTandem1, inTandem2, and inTandem3, were all 24-week trials, but there were some differences in the design.
inTandem1 and inTandem2 were the pivotal studies, one conducted in 793 patients in North America and the other in 782 patients in Europe and Israel. After a 2-week screening period, participants underwent a 6-week insulin optimization program before they were randomized to one of two doses of sotagliflozin (200 mg or 400 mg) or placebo for 24 weeks, with follow-up out to 52 weeks. The primary endpoint of these studies was the reduction in HbA1c versus placebo at 24 weeks.
By comparison, inTandem3 was a global study involving 1,405 individuals with T1DM who did not undergo the 6-week insulin optimization period. Instead there was a 2-week run-in period after the initial screening, and the study ran for only 24 weeks. Only one dose (400 mg) of sotagliflozin was used and the primary endpoint was a composite to try to see what the net clinical benefit would be, Dr. Davies explained.
The results of inTandem1 and inTandem2 were reported earlier this year at the American Diabetes Association Scientific Sessions, Dr. Davies noted, and sotagliflozin had “a good efficacy and safety profile as an adjunct to insulin in type 1 diabetes.”
The quest for adjunctive treatment
“For years we’ve been looking for adjunctive therapy for people with type 1 diabetes,” said Julio Rosenstock, MD, at the EASD meeting. Dr. Rosenstock, who is the director of the Dallas Diabetes Research Center at Medical City and involved in the sotagliflozin clinical trials program, noted that the quest for an adjunctive treatment was because “glucose control in type 1 diabetes remains tough and costly, despite multiple advances in insulin therapy, delivery systems, and monitoring methods over the years.”
Several approaches to adjunctive treatment had been proposed, but so far all with limited value, Dr. Rosenstock maintained. Despite no evidence for a benefit of adding metformin, for example, registry data suggest that up to 5% of people with T1DM are using it.
The recent findings of the REMOVAL trial showed metformin did not help change the HbA1c over time and there was no change in the primary outcome, he observed but a small improvement in a tertiary endpoint. “I can’t think of a more negative cardiovascular outcomes trial,” Dr. Rosenstock asserted. “There is not enough justification to use metformin in type 1 diabetes.”
By contrast there is a strong rationale for using SGLT inhibition, partly as the glucose-lowering effects are independent of insulin’s activity. Through inhibition of SGLT1, sotagliflozin reduces glucose absorption in the proximal intestine, thus blunting or delaying rising postprandial glucose levels. By also targeting SGLT2, sotagliflozin can reduce glucose resorption by the kidneys.
Risks and clinical implications
In an editorial accompanying the published findings, David Nathan, MD, of Massachusetts General Hospital and Harvard Medical School in Boston, is not convinced that using adjunctive treatment is the future for better glycemic control in T1DM and that better automated insulin delivery systems will likely make adjunctive therapy unnecessary.
Dr. Nathan also observed “the rate of severe hypoglycemia in the whole sotagliflozin group was not significantly different from the rate in the placebo group,” and the risks and benefits of any adjunctive therapy for T1DM need to be carefully balanced.
While risks remain, one of the chairs of the session, Chantal Mathieu, MD, professor of medicine at the Katholieke Universiteit Leuven (Belgium), observed that “these are exciting times for all of us and hopefully for our patients.” She cautioned clinicians to remember, however, that “type 1 diabetes is a very different disease from type 2 diabetes, and so when we listen to [information about] all these adjunct[ive] therapies, when we read the papers, please interpret the data carefully.”
The trial was funded by Lexicon Pharmaceuticals. Sotagliflozin is being codeveloped with Sanofi. Dr. Davies disclosed acting as an advisor, consultant, or being a member of a speaker’s bureau for Sanofi-Aventis and several other companies. She was an investigator in the inTandem trials and her institution received funding from Lexicon to conduct the inTandem 2 and 3 clinical trials. Dr. Rosenstock disclosed research support and acting as an advisor to multiple pharmaceutical companies. Dr. Nathan had nothing to disclose. Dr. Mathieu chaired the session and did not present disclosures.
AT EASD 2017
Key clinical point: A higher proportion of people with type 1 diabetes mellitus (T1DM) treated with sotagliflozin than placebo achieved the primary composite endpoint, but there is the risk of diabetic ketoacidosis (DKA) in some.
Major finding: 28.6% versus 15.2% of sotaglifozin- and placebo-treated individuals achieved an HbA1c less than 7% at week 24, with no episodes of severe hypoglycemia or DKA (P less than .001).
Data source: The phase 3, randomized, controlled, multicenter inTandem3 trial in 1,402 people with type 1 diabetes on stable insulin therapy but with poor glycemic control.
Disclosures: The trial was funded by Lexicon Pharmaceuticals. Sotagliflozin is being codeveloped with Sanofi. Two presenters have received research support to perform clinical studies. The commentators had nothing to disclose.
A Peek at Our October 2017 Issue
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
FDA panel advises approval of semaglutide to lower HbA1c in patients with type 2 diabetes
The Food and drug Administration’s Endocrinologic and Metabolic Drugs Advisory Committee (EMDAC) recommended the approval of a once-weekly semaglutide injection for adults with type 2 diabetes mellitus. The vote was 16-0 in favor of approval, with one committee member abstaining.
The committee met on Oct. 18 and discussed the safety and efficacy of new drug application (NDA) 209637 for semaglutide injection when used to help glycemic control in addition to diet and exercise. Semaglutide, manufactured and submitted for approval by Novo Nordisk, is described by the company as “an investigational analog of native human glucagonlike peptide–1,” with a half-life of approximately 1 week, making the agent appropriate for weekly dosing.
The researchers found some increase in diabetic retinopathy in the SUSTAIN trials, but a post-hoc analysis found that “To the extent that the data suggest a signal that there was progression of diabetic retinopathy in patients with significant decreases in HbA1c, these events should be expected because they are consistent with treatments that decrease HbA1c. While this decrease may result in an initial increase in retinopathy, ocular health is ultimately benefited by decreasing HbA1c.”
Novo Nordisk submitted the application for semaglutide in December 2016; the drug also is being reviewed in Europe and Japan.
The FDA is not obligated to follow the committee’s recommendation but considers it as part of the review process of new drug applications.
The Food and drug Administration’s Endocrinologic and Metabolic Drugs Advisory Committee (EMDAC) recommended the approval of a once-weekly semaglutide injection for adults with type 2 diabetes mellitus. The vote was 16-0 in favor of approval, with one committee member abstaining.
The committee met on Oct. 18 and discussed the safety and efficacy of new drug application (NDA) 209637 for semaglutide injection when used to help glycemic control in addition to diet and exercise. Semaglutide, manufactured and submitted for approval by Novo Nordisk, is described by the company as “an investigational analog of native human glucagonlike peptide–1,” with a half-life of approximately 1 week, making the agent appropriate for weekly dosing.
The researchers found some increase in diabetic retinopathy in the SUSTAIN trials, but a post-hoc analysis found that “To the extent that the data suggest a signal that there was progression of diabetic retinopathy in patients with significant decreases in HbA1c, these events should be expected because they are consistent with treatments that decrease HbA1c. While this decrease may result in an initial increase in retinopathy, ocular health is ultimately benefited by decreasing HbA1c.”
Novo Nordisk submitted the application for semaglutide in December 2016; the drug also is being reviewed in Europe and Japan.
The FDA is not obligated to follow the committee’s recommendation but considers it as part of the review process of new drug applications.
The Food and drug Administration’s Endocrinologic and Metabolic Drugs Advisory Committee (EMDAC) recommended the approval of a once-weekly semaglutide injection for adults with type 2 diabetes mellitus. The vote was 16-0 in favor of approval, with one committee member abstaining.
The committee met on Oct. 18 and discussed the safety and efficacy of new drug application (NDA) 209637 for semaglutide injection when used to help glycemic control in addition to diet and exercise. Semaglutide, manufactured and submitted for approval by Novo Nordisk, is described by the company as “an investigational analog of native human glucagonlike peptide–1,” with a half-life of approximately 1 week, making the agent appropriate for weekly dosing.
The researchers found some increase in diabetic retinopathy in the SUSTAIN trials, but a post-hoc analysis found that “To the extent that the data suggest a signal that there was progression of diabetic retinopathy in patients with significant decreases in HbA1c, these events should be expected because they are consistent with treatments that decrease HbA1c. While this decrease may result in an initial increase in retinopathy, ocular health is ultimately benefited by decreasing HbA1c.”
Novo Nordisk submitted the application for semaglutide in December 2016; the drug also is being reviewed in Europe and Japan.
The FDA is not obligated to follow the committee’s recommendation but considers it as part of the review process of new drug applications.
AT AN FDA ADVISORY COMMITTEE MEETING
Home-based cognitive-behavioral therapy aids IBS
ORLANDO – A 10-week program of home-based cognitive-behavioral therapy led to significantly better improvements in irritable bowel syndrome than did a control education program in a prospective, randomized, single-center trial with 436 patients.
Study data also showed that the improvements produced by the home-based cognitive-behavioral therapy (CBT) program were durable, persisting in 63% of high responders out to 6 months after treatment, Jeffrey M. Lackner, PsyD, said at the World Congress of Gastroenterology at ACG 2017.

He suggested that the minimal contact, home-based approach actually enhanced the efficacy of the CBT training that patients received.
“Patients are given tasks to carry out. Responsibility is placed on them. It changes the dynamic between the clinician and patient,” Dr. Lackner said. Skills patients learned during the minimal contact sessions included self-monitoring, muscle relaxation, worry control, problem solving, and modification of core beliefs.
The study enrolled adults up to 70 years old with at least moderately severe IBS symptoms at least twice weekly who met the Rome III diagnostic criteria. When patients performed a self-assessment 2 weeks after the end of the 10-week intervention, 61% of those in the home-based CBT program group rated themselves as much or very much improved, compared with 55% of patients who received standard CBT and 44% of patients in the control group, who attended generic education sessions. The differences between each of the two CBT groups and the controls were statistically significant. Patient assessments performed by blinded gastroenterologists rated 56% of the home-based CBT patients as much or very much improved, compared with 51% of those who received standard CBT and 40% of the controls.
When reassessed 3 and 6 months later, the edge that home-based CBT patients showed over the control patients persisted. After 6 months off treatment, 57% of those who received home-based CBT continued to say they were much or very much improved over their baseline status, compared with 47% of the controls.
Dr. Lackner’s analysis also examined whether patients treated with CBT, either standard or home based, went into remission. He defined remission as having no or only mild symptoms during an assessment 2 weeks after the end of the intervention and then maintaining this response out to 6 months. No or only mild symptoms were reported by 35% of all CBT patients soon after treatment, compared with 23% of the controls. Six months later, 63% of the high-responding patients on CBT and 52% of the high responders with education maintained their high response.
“CBT appears to have an enduring effect that protects against subsequent relapse and recurrence in a sizable subsample of patients,” he concluded. The findings “suggest possible disease modification by CBT.”
Dr. Lackner had no relevant financial disclosures.
[email protected]
On Twitter @mitchelzoler
ORLANDO – A 10-week program of home-based cognitive-behavioral therapy led to significantly better improvements in irritable bowel syndrome than did a control education program in a prospective, randomized, single-center trial with 436 patients.
Study data also showed that the improvements produced by the home-based cognitive-behavioral therapy (CBT) program were durable, persisting in 63% of high responders out to 6 months after treatment, Jeffrey M. Lackner, PsyD, said at the World Congress of Gastroenterology at ACG 2017.

He suggested that the minimal contact, home-based approach actually enhanced the efficacy of the CBT training that patients received.
“Patients are given tasks to carry out. Responsibility is placed on them. It changes the dynamic between the clinician and patient,” Dr. Lackner said. Skills patients learned during the minimal contact sessions included self-monitoring, muscle relaxation, worry control, problem solving, and modification of core beliefs.
The study enrolled adults up to 70 years old with at least moderately severe IBS symptoms at least twice weekly who met the Rome III diagnostic criteria. When patients performed a self-assessment 2 weeks after the end of the 10-week intervention, 61% of those in the home-based CBT program group rated themselves as much or very much improved, compared with 55% of patients who received standard CBT and 44% of patients in the control group, who attended generic education sessions. The differences between each of the two CBT groups and the controls were statistically significant. Patient assessments performed by blinded gastroenterologists rated 56% of the home-based CBT patients as much or very much improved, compared with 51% of those who received standard CBT and 40% of the controls.
When reassessed 3 and 6 months later, the edge that home-based CBT patients showed over the control patients persisted. After 6 months off treatment, 57% of those who received home-based CBT continued to say they were much or very much improved over their baseline status, compared with 47% of the controls.
Dr. Lackner’s analysis also examined whether patients treated with CBT, either standard or home based, went into remission. He defined remission as having no or only mild symptoms during an assessment 2 weeks after the end of the intervention and then maintaining this response out to 6 months. No or only mild symptoms were reported by 35% of all CBT patients soon after treatment, compared with 23% of the controls. Six months later, 63% of the high-responding patients on CBT and 52% of the high responders with education maintained their high response.
“CBT appears to have an enduring effect that protects against subsequent relapse and recurrence in a sizable subsample of patients,” he concluded. The findings “suggest possible disease modification by CBT.”
Dr. Lackner had no relevant financial disclosures.
[email protected]
On Twitter @mitchelzoler
ORLANDO – A 10-week program of home-based cognitive-behavioral therapy led to significantly better improvements in irritable bowel syndrome than did a control education program in a prospective, randomized, single-center trial with 436 patients.
Study data also showed that the improvements produced by the home-based cognitive-behavioral therapy (CBT) program were durable, persisting in 63% of high responders out to 6 months after treatment, Jeffrey M. Lackner, PsyD, said at the World Congress of Gastroenterology at ACG 2017.

He suggested that the minimal contact, home-based approach actually enhanced the efficacy of the CBT training that patients received.
“Patients are given tasks to carry out. Responsibility is placed on them. It changes the dynamic between the clinician and patient,” Dr. Lackner said. Skills patients learned during the minimal contact sessions included self-monitoring, muscle relaxation, worry control, problem solving, and modification of core beliefs.
The study enrolled adults up to 70 years old with at least moderately severe IBS symptoms at least twice weekly who met the Rome III diagnostic criteria. When patients performed a self-assessment 2 weeks after the end of the 10-week intervention, 61% of those in the home-based CBT program group rated themselves as much or very much improved, compared with 55% of patients who received standard CBT and 44% of patients in the control group, who attended generic education sessions. The differences between each of the two CBT groups and the controls were statistically significant. Patient assessments performed by blinded gastroenterologists rated 56% of the home-based CBT patients as much or very much improved, compared with 51% of those who received standard CBT and 40% of the controls.
When reassessed 3 and 6 months later, the edge that home-based CBT patients showed over the control patients persisted. After 6 months off treatment, 57% of those who received home-based CBT continued to say they were much or very much improved over their baseline status, compared with 47% of the controls.
Dr. Lackner’s analysis also examined whether patients treated with CBT, either standard or home based, went into remission. He defined remission as having no or only mild symptoms during an assessment 2 weeks after the end of the intervention and then maintaining this response out to 6 months. No or only mild symptoms were reported by 35% of all CBT patients soon after treatment, compared with 23% of the controls. Six months later, 63% of the high-responding patients on CBT and 52% of the high responders with education maintained their high response.
“CBT appears to have an enduring effect that protects against subsequent relapse and recurrence in a sizable subsample of patients,” he concluded. The findings “suggest possible disease modification by CBT.”
Dr. Lackner had no relevant financial disclosures.
[email protected]
On Twitter @mitchelzoler
AT THE WORLD CONGRESS OF GASTROENTEROLOGY
Key clinical point:
Major finding: After completion of a 10-week treatment, 61% of CBT patients and 44% of controls showed either much or very much improvement.
Data source: A prospective, randomized, single-center study with 436 patients.
Disclosures: Dr. Lackner had no relevant financial disclosures.
Mental health risks higher in sexual minorities with acne
Among young adults with acne, nonheterosexuals are much more likely to report mental health problems, according to data from a national cross-sectional study.
Since previous studies have shown that both acne and sexual minority status are associated with increased risk of depression and suicidal ideation, the investigators used data from the National Longitudinal Study on Adolescent to Adult Health, which included 4,094 heterosexual (167 with acne) and 564 sexual minority (35 with acne) adults aged 18-28 years, to examine the relationship between the two.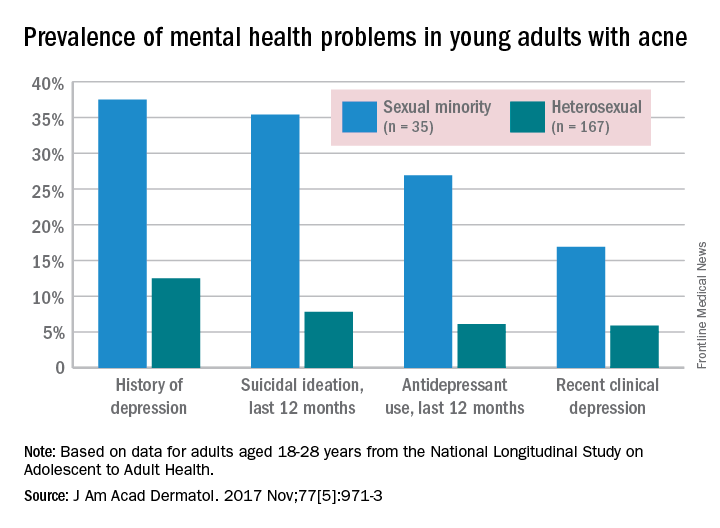
Past-year antidepressant use (AOR, 8.21) and current clinical depression (AOR, 4.1) also were both more common among sexual minorities, who were defined as “those indicating same-sex attraction or sexual orientation other than ‘100% heterosexual,’ ” they said.
“Validated screening tools to assess sexual orientation and depression among patients with acne may identify at-risk individuals and expedite referral for psychological care,” Mr. Gao and his associates wrote.
The investigators did not declare any conflicts of interest. The work of one of Mr. Gao’s associates was supported through a grant from the California Pacific Medical Center Foundation.
Among young adults with acne, nonheterosexuals are much more likely to report mental health problems, according to data from a national cross-sectional study.
Since previous studies have shown that both acne and sexual minority status are associated with increased risk of depression and suicidal ideation, the investigators used data from the National Longitudinal Study on Adolescent to Adult Health, which included 4,094 heterosexual (167 with acne) and 564 sexual minority (35 with acne) adults aged 18-28 years, to examine the relationship between the two.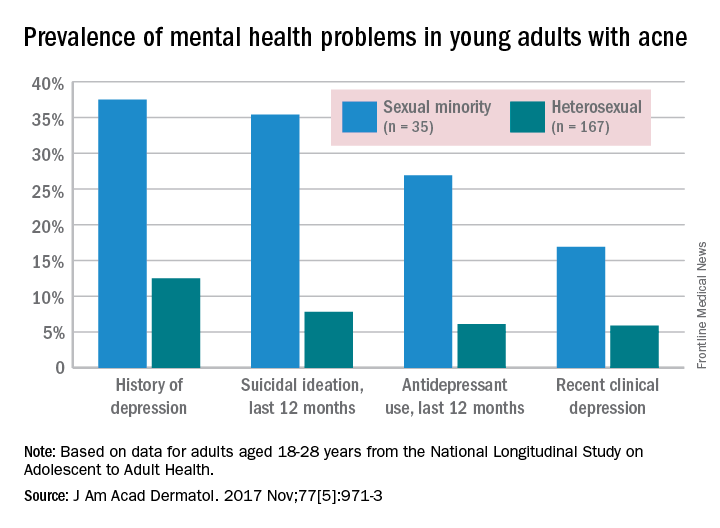
Past-year antidepressant use (AOR, 8.21) and current clinical depression (AOR, 4.1) also were both more common among sexual minorities, who were defined as “those indicating same-sex attraction or sexual orientation other than ‘100% heterosexual,’ ” they said.
“Validated screening tools to assess sexual orientation and depression among patients with acne may identify at-risk individuals and expedite referral for psychological care,” Mr. Gao and his associates wrote.
The investigators did not declare any conflicts of interest. The work of one of Mr. Gao’s associates was supported through a grant from the California Pacific Medical Center Foundation.
Among young adults with acne, nonheterosexuals are much more likely to report mental health problems, according to data from a national cross-sectional study.
Since previous studies have shown that both acne and sexual minority status are associated with increased risk of depression and suicidal ideation, the investigators used data from the National Longitudinal Study on Adolescent to Adult Health, which included 4,094 heterosexual (167 with acne) and 564 sexual minority (35 with acne) adults aged 18-28 years, to examine the relationship between the two.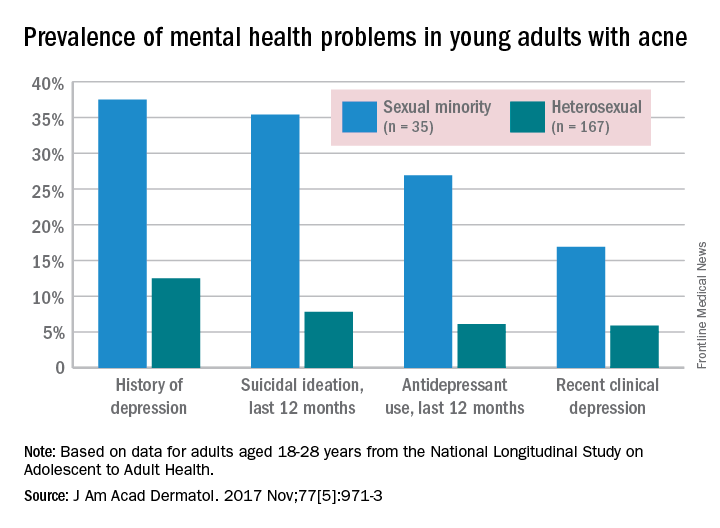
Past-year antidepressant use (AOR, 8.21) and current clinical depression (AOR, 4.1) also were both more common among sexual minorities, who were defined as “those indicating same-sex attraction or sexual orientation other than ‘100% heterosexual,’ ” they said.
“Validated screening tools to assess sexual orientation and depression among patients with acne may identify at-risk individuals and expedite referral for psychological care,” Mr. Gao and his associates wrote.
The investigators did not declare any conflicts of interest. The work of one of Mr. Gao’s associates was supported through a grant from the California Pacific Medical Center Foundation.
FROM JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Docs should engage employers directly if they want better payment models
WASHINGTON – If doctors want to improve their reimbursement and at the same time be a catalyst for reducing costs to the overall health care delivery system, they need to be stronger advocates for themselves.
This was the message of Harold D. Miller, president and CEO of the Center for Healthcare Quality and Payment Reform, in his presentation to the American Gastroenterological Association Partners in Value meeting on Oct. 6.
He called specifically on doctors to exercise initiative and accept the accountability that comes with leading the charge for payment reform.
“I think there is a much better way, which is bottom up, which is to say ask the physicians and the hospitals to say what are the ways you can improve care and reduce costs,” he continued. “Then get payers to provide adequate support for that but have physicians take accountability for actually achieving those results they think are possible. And then you have patients who get good care and you keep physicians and hospitals financially sustainable, which nobody in Washington is talking about how to actually do.”
Getting to that point is going to require physicians to be much more proactive in who they communicate with to get the information that is necessary to build payment models from the bottom up.
“I think there are lots of potential solutions, but I think it needs to be talked about,” Mr. Miller said. “If I were to leave you with one message, the problem is that employers, Congress, etc., are not hearing from physicians that you want to do something different.”
He noted that part of the issue is the adversarial relationship doctors have with the payer community, noting that most “health plans demonize you all.”
Mr. Miller added: “They go in to employers and they tell employers that the only thing standing between the employers and certain health insurance bankruptcy is the health plan because all the doctors want to do is spend more money.”
To change that, it is going to require doctors to be much more proactive in reaching out past the payer middleman to start engaging directly with employers.
“Employers do not see doctors as their partners,” Mr. Miller noted. “The people who pay have to start seeing you as wanting to solve the same problem they are trying to solve.”
And working with employers could help physicians insofar as getting access to data that would be crucial in developing the kinds of payment models that would benefit all of the financial aspects of health care delivery while at the same time improving care.
Mr. Miller recounted how various state and local governments in Maine were trying to extract clinical information that might not be ascertained from claims data from Anthem, the largest or second largest health insurance company in America. Initially, Anthem balked, prompting the state and local entities to issue requests for information and seek to replace Anthem as the main provider for its health insurance coverage.
“Anthem completely changed its attitude,” he said. “All of a sudden, Anthem was back in. ... Anthem felt that impact all the way in Indianapolis. Sam Nussbaum, MD [former chief medical officer at Anthem], said to me, ‘We were punished in Maine.’ ”
He noted that some big employers are seeking out direct contracts with health systems because they are not getting support from the health plans.
“But they need to hear from you and what it is you need and what you are going to do with it,” he said. “It is not just give us data, see ya. It is here’s what we are trying to do. Here is the information we need and why we need it. If you say to an employer ‘I want to know how many patients are being hospitalized so that I can help you reduce hospitalizations,’ do you think they are going to say nah, we are too busy for that?”
WASHINGTON – If doctors want to improve their reimbursement and at the same time be a catalyst for reducing costs to the overall health care delivery system, they need to be stronger advocates for themselves.
This was the message of Harold D. Miller, president and CEO of the Center for Healthcare Quality and Payment Reform, in his presentation to the American Gastroenterological Association Partners in Value meeting on Oct. 6.
He called specifically on doctors to exercise initiative and accept the accountability that comes with leading the charge for payment reform.
“I think there is a much better way, which is bottom up, which is to say ask the physicians and the hospitals to say what are the ways you can improve care and reduce costs,” he continued. “Then get payers to provide adequate support for that but have physicians take accountability for actually achieving those results they think are possible. And then you have patients who get good care and you keep physicians and hospitals financially sustainable, which nobody in Washington is talking about how to actually do.”
Getting to that point is going to require physicians to be much more proactive in who they communicate with to get the information that is necessary to build payment models from the bottom up.
“I think there are lots of potential solutions, but I think it needs to be talked about,” Mr. Miller said. “If I were to leave you with one message, the problem is that employers, Congress, etc., are not hearing from physicians that you want to do something different.”
He noted that part of the issue is the adversarial relationship doctors have with the payer community, noting that most “health plans demonize you all.”
Mr. Miller added: “They go in to employers and they tell employers that the only thing standing between the employers and certain health insurance bankruptcy is the health plan because all the doctors want to do is spend more money.”
To change that, it is going to require doctors to be much more proactive in reaching out past the payer middleman to start engaging directly with employers.
“Employers do not see doctors as their partners,” Mr. Miller noted. “The people who pay have to start seeing you as wanting to solve the same problem they are trying to solve.”
And working with employers could help physicians insofar as getting access to data that would be crucial in developing the kinds of payment models that would benefit all of the financial aspects of health care delivery while at the same time improving care.
Mr. Miller recounted how various state and local governments in Maine were trying to extract clinical information that might not be ascertained from claims data from Anthem, the largest or second largest health insurance company in America. Initially, Anthem balked, prompting the state and local entities to issue requests for information and seek to replace Anthem as the main provider for its health insurance coverage.
“Anthem completely changed its attitude,” he said. “All of a sudden, Anthem was back in. ... Anthem felt that impact all the way in Indianapolis. Sam Nussbaum, MD [former chief medical officer at Anthem], said to me, ‘We were punished in Maine.’ ”
He noted that some big employers are seeking out direct contracts with health systems because they are not getting support from the health plans.
“But they need to hear from you and what it is you need and what you are going to do with it,” he said. “It is not just give us data, see ya. It is here’s what we are trying to do. Here is the information we need and why we need it. If you say to an employer ‘I want to know how many patients are being hospitalized so that I can help you reduce hospitalizations,’ do you think they are going to say nah, we are too busy for that?”
WASHINGTON – If doctors want to improve their reimbursement and at the same time be a catalyst for reducing costs to the overall health care delivery system, they need to be stronger advocates for themselves.
This was the message of Harold D. Miller, president and CEO of the Center for Healthcare Quality and Payment Reform, in his presentation to the American Gastroenterological Association Partners in Value meeting on Oct. 6.
He called specifically on doctors to exercise initiative and accept the accountability that comes with leading the charge for payment reform.
“I think there is a much better way, which is bottom up, which is to say ask the physicians and the hospitals to say what are the ways you can improve care and reduce costs,” he continued. “Then get payers to provide adequate support for that but have physicians take accountability for actually achieving those results they think are possible. And then you have patients who get good care and you keep physicians and hospitals financially sustainable, which nobody in Washington is talking about how to actually do.”
Getting to that point is going to require physicians to be much more proactive in who they communicate with to get the information that is necessary to build payment models from the bottom up.
“I think there are lots of potential solutions, but I think it needs to be talked about,” Mr. Miller said. “If I were to leave you with one message, the problem is that employers, Congress, etc., are not hearing from physicians that you want to do something different.”
He noted that part of the issue is the adversarial relationship doctors have with the payer community, noting that most “health plans demonize you all.”
Mr. Miller added: “They go in to employers and they tell employers that the only thing standing between the employers and certain health insurance bankruptcy is the health plan because all the doctors want to do is spend more money.”
To change that, it is going to require doctors to be much more proactive in reaching out past the payer middleman to start engaging directly with employers.
“Employers do not see doctors as their partners,” Mr. Miller noted. “The people who pay have to start seeing you as wanting to solve the same problem they are trying to solve.”
And working with employers could help physicians insofar as getting access to data that would be crucial in developing the kinds of payment models that would benefit all of the financial aspects of health care delivery while at the same time improving care.
Mr. Miller recounted how various state and local governments in Maine were trying to extract clinical information that might not be ascertained from claims data from Anthem, the largest or second largest health insurance company in America. Initially, Anthem balked, prompting the state and local entities to issue requests for information and seek to replace Anthem as the main provider for its health insurance coverage.
“Anthem completely changed its attitude,” he said. “All of a sudden, Anthem was back in. ... Anthem felt that impact all the way in Indianapolis. Sam Nussbaum, MD [former chief medical officer at Anthem], said to me, ‘We were punished in Maine.’ ”
He noted that some big employers are seeking out direct contracts with health systems because they are not getting support from the health plans.
“But they need to hear from you and what it is you need and what you are going to do with it,” he said. “It is not just give us data, see ya. It is here’s what we are trying to do. Here is the information we need and why we need it. If you say to an employer ‘I want to know how many patients are being hospitalized so that I can help you reduce hospitalizations,’ do you think they are going to say nah, we are too busy for that?”