User login
Office visits have a chronic problem
according to the National Center for Health Statistics.
That year, chronic problems were the major reason for 40% of all office-based physician visits, making them significantly more common than the other four broad categories of visit types: new problem (26%), preventive care (19%), injury (9%), and pre- or postsurgery care (6%), the NCHS said in a recent Data Brief.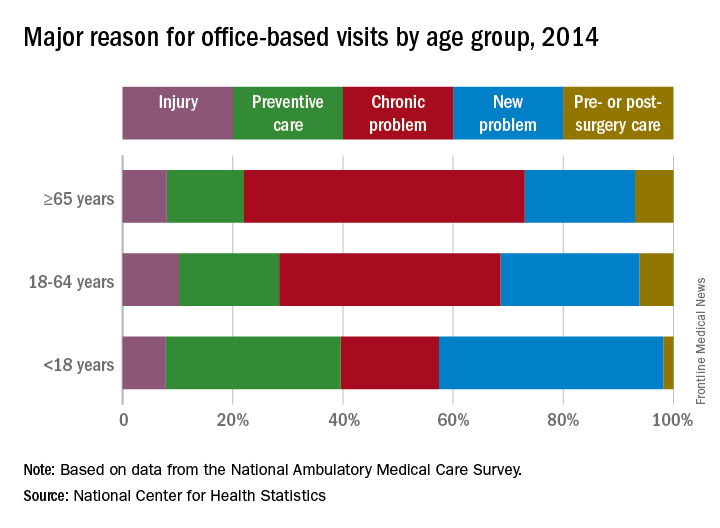
Children were significantly more likely to have a new problem (41% of visits) or get preventive care (32%) than were the other age groups and were significantly less likely to have a chronic problem (18%) or to receive pre- or postsurgery care (2%), according to data from the 2014 National Ambulatory Medical Care Survey, which included 45,710 visit records from 9,989 physicians.
SOURCE: Ashman JJ et al. NCHS Data Brief. 2017;(292):1-8e.
according to the National Center for Health Statistics.
That year, chronic problems were the major reason for 40% of all office-based physician visits, making them significantly more common than the other four broad categories of visit types: new problem (26%), preventive care (19%), injury (9%), and pre- or postsurgery care (6%), the NCHS said in a recent Data Brief.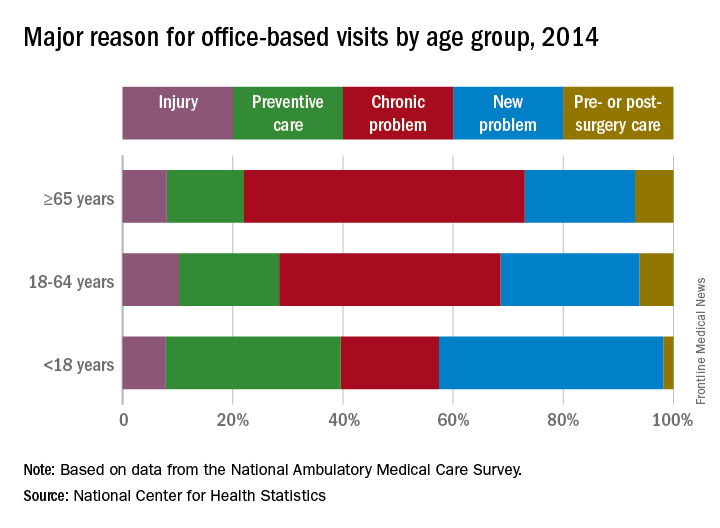
Children were significantly more likely to have a new problem (41% of visits) or get preventive care (32%) than were the other age groups and were significantly less likely to have a chronic problem (18%) or to receive pre- or postsurgery care (2%), according to data from the 2014 National Ambulatory Medical Care Survey, which included 45,710 visit records from 9,989 physicians.
SOURCE: Ashman JJ et al. NCHS Data Brief. 2017;(292):1-8e.
according to the National Center for Health Statistics.
That year, chronic problems were the major reason for 40% of all office-based physician visits, making them significantly more common than the other four broad categories of visit types: new problem (26%), preventive care (19%), injury (9%), and pre- or postsurgery care (6%), the NCHS said in a recent Data Brief.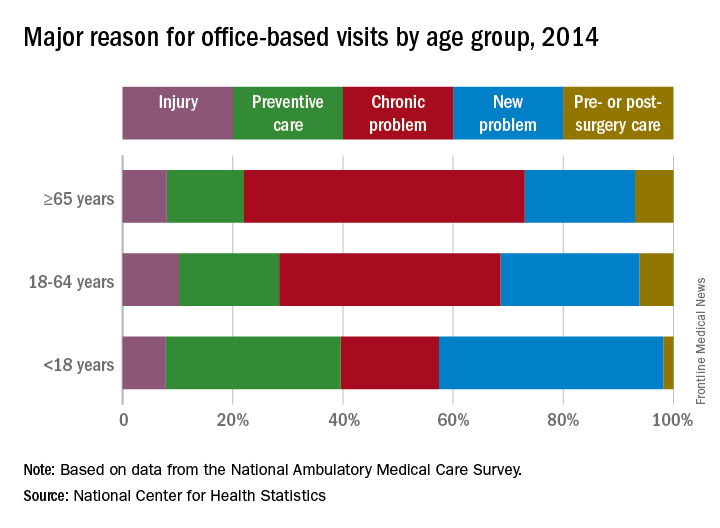
Children were significantly more likely to have a new problem (41% of visits) or get preventive care (32%) than were the other age groups and were significantly less likely to have a chronic problem (18%) or to receive pre- or postsurgery care (2%), according to data from the 2014 National Ambulatory Medical Care Survey, which included 45,710 visit records from 9,989 physicians.
SOURCE: Ashman JJ et al. NCHS Data Brief. 2017;(292):1-8e.
Waiving Medicare coinsurance for positive colorectal screening likely beneficial
Currently, Medicare covers colorectal screening at no charge to the patient, but if a polyp is removed upon discovery during the procedure, the patient would then be subject to Medicare’s coinsurance payments for both the colonoscopy and the removal.
Researchers used the Microsimulation Screening Analysis–Colon model to estimate the cost-effectiveness of waiving coinsurance for every component of colorectal cancer screening. They estimated that, currently, using the colonoscopy regimen with coinsurance, 12.8 colorectal cancer deaths occurred per 1,000 people aged 65 years and 124.1 QALYs were gained per 1,000 people aged 65 years. The total number of procedures per 1,000 Medicare beneficiaries was 1,132, of which 410 (36%) were potentially subject to coinsurance requirements.
“We estimated that the total lifetime costs for [the Centers for Medicare & Medicaid], which included colorectal cancer screening, surveillance, and treatment with coinsurance, to be $2.675 million per 1,000 65-year-olds,” Ms. Peterse and her colleagues wrote.
Researchers noted that if the coinsurance was waived but there was no follow-on increase in the screening rate, the benefits of screening would not change but the total cost of screening and treatment would increase to $2.726 million per 1,000 people aged 65 years.
However, “an assumed 5-percentage-point increase in the rates of first colonoscopy screening and surveillance decreased the number of colorectal cancer deaths by 0.9 (6.4%), accompanied by an increase of $33,000 (1.2%) in total costs, with a cost per QALY gained (or cost-effectiveness ratio) of $4,086.”
They added that estimated screening benefits were similar when fecal testing was the primary screening method.
“In general, [fecal testing] screening was associated with lower number of procedures subject to coinsurance,” the researchers added. “If [fecal testing] screening becomes more popular in the United States, following trends observed in several settings, the costs of waiving coinsurance would be even lower.” The researchers also suggest that it could lead to reducing disparities of colorectal cancer in the United States as well.
[email protected]
SOURCE: Peterse EFP et al. Health Affairs. 2017 Dec;36(12):2151-9.
Currently, Medicare covers colorectal screening at no charge to the patient, but if a polyp is removed upon discovery during the procedure, the patient would then be subject to Medicare’s coinsurance payments for both the colonoscopy and the removal.
Researchers used the Microsimulation Screening Analysis–Colon model to estimate the cost-effectiveness of waiving coinsurance for every component of colorectal cancer screening. They estimated that, currently, using the colonoscopy regimen with coinsurance, 12.8 colorectal cancer deaths occurred per 1,000 people aged 65 years and 124.1 QALYs were gained per 1,000 people aged 65 years. The total number of procedures per 1,000 Medicare beneficiaries was 1,132, of which 410 (36%) were potentially subject to coinsurance requirements.
“We estimated that the total lifetime costs for [the Centers for Medicare & Medicaid], which included colorectal cancer screening, surveillance, and treatment with coinsurance, to be $2.675 million per 1,000 65-year-olds,” Ms. Peterse and her colleagues wrote.
Researchers noted that if the coinsurance was waived but there was no follow-on increase in the screening rate, the benefits of screening would not change but the total cost of screening and treatment would increase to $2.726 million per 1,000 people aged 65 years.
However, “an assumed 5-percentage-point increase in the rates of first colonoscopy screening and surveillance decreased the number of colorectal cancer deaths by 0.9 (6.4%), accompanied by an increase of $33,000 (1.2%) in total costs, with a cost per QALY gained (or cost-effectiveness ratio) of $4,086.”
They added that estimated screening benefits were similar when fecal testing was the primary screening method.
“In general, [fecal testing] screening was associated with lower number of procedures subject to coinsurance,” the researchers added. “If [fecal testing] screening becomes more popular in the United States, following trends observed in several settings, the costs of waiving coinsurance would be even lower.” The researchers also suggest that it could lead to reducing disparities of colorectal cancer in the United States as well.
[email protected]
SOURCE: Peterse EFP et al. Health Affairs. 2017 Dec;36(12):2151-9.
Currently, Medicare covers colorectal screening at no charge to the patient, but if a polyp is removed upon discovery during the procedure, the patient would then be subject to Medicare’s coinsurance payments for both the colonoscopy and the removal.
Researchers used the Microsimulation Screening Analysis–Colon model to estimate the cost-effectiveness of waiving coinsurance for every component of colorectal cancer screening. They estimated that, currently, using the colonoscopy regimen with coinsurance, 12.8 colorectal cancer deaths occurred per 1,000 people aged 65 years and 124.1 QALYs were gained per 1,000 people aged 65 years. The total number of procedures per 1,000 Medicare beneficiaries was 1,132, of which 410 (36%) were potentially subject to coinsurance requirements.
“We estimated that the total lifetime costs for [the Centers for Medicare & Medicaid], which included colorectal cancer screening, surveillance, and treatment with coinsurance, to be $2.675 million per 1,000 65-year-olds,” Ms. Peterse and her colleagues wrote.
Researchers noted that if the coinsurance was waived but there was no follow-on increase in the screening rate, the benefits of screening would not change but the total cost of screening and treatment would increase to $2.726 million per 1,000 people aged 65 years.
However, “an assumed 5-percentage-point increase in the rates of first colonoscopy screening and surveillance decreased the number of colorectal cancer deaths by 0.9 (6.4%), accompanied by an increase of $33,000 (1.2%) in total costs, with a cost per QALY gained (or cost-effectiveness ratio) of $4,086.”
They added that estimated screening benefits were similar when fecal testing was the primary screening method.
“In general, [fecal testing] screening was associated with lower number of procedures subject to coinsurance,” the researchers added. “If [fecal testing] screening becomes more popular in the United States, following trends observed in several settings, the costs of waiving coinsurance would be even lower.” The researchers also suggest that it could lead to reducing disparities of colorectal cancer in the United States as well.
[email protected]
SOURCE: Peterse EFP et al. Health Affairs. 2017 Dec;36(12):2151-9.
FROM HEALTH AFFAIRS
Nonmalignant Cutaneous Findings Associated With Vemurafenib
To the Editor:
A 53-year-old woman was referred by her oncologist to our dermatology office with lesions on the face and body that presented 8 days after starting vemurafenib 960 mg twice daily for metastatic melanoma. The patient denied any symptoms from the lesions but was concerned they would spread to cover her entire face and body.
The patient's medical history included a diagnosis of metastatic melanoma 6 years prior to presentation. She stated that the primary cutaneous melanoma site was unknown. The patient had endured numerous surgeries to excise lymph node tumors, with some lesions up to 3 cm. The patient recently started vemurafenib, a treatment for BRAF V600E mutation-positive metastatic melanoma. The patient's personal history was notable for hepatitis A, B, and C, and her family history revealed her mother had metastatic lung cancer.
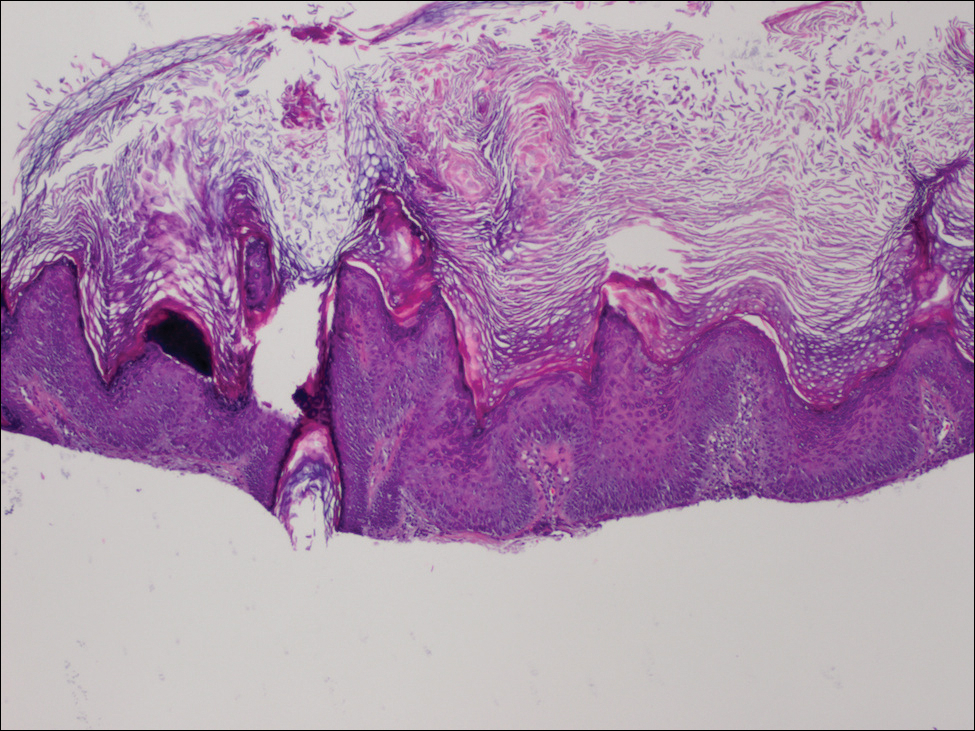
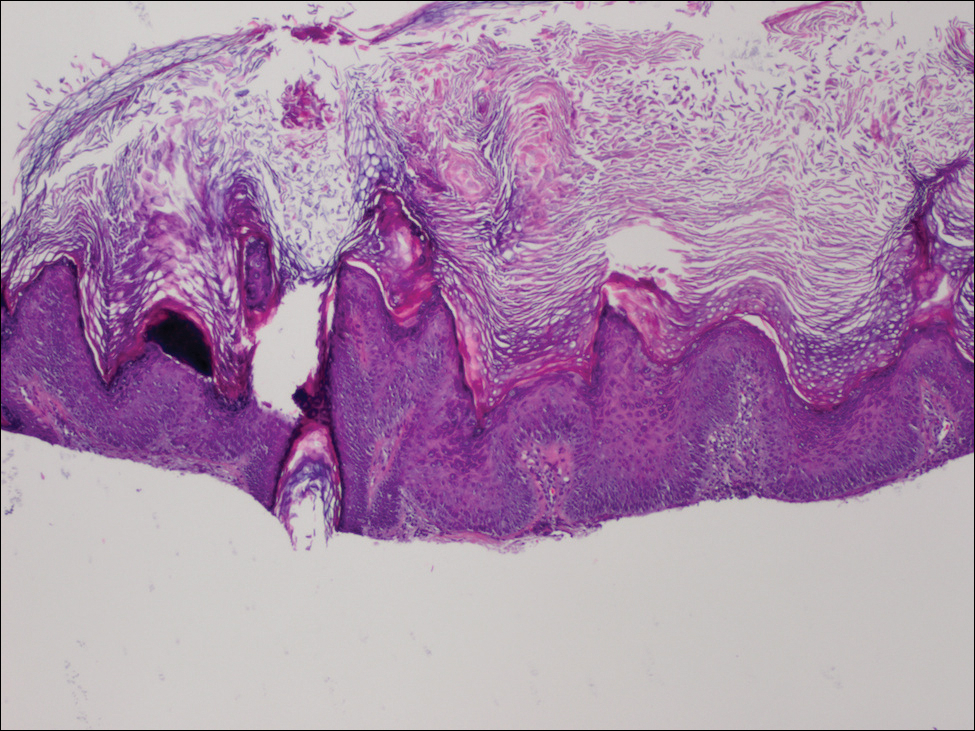
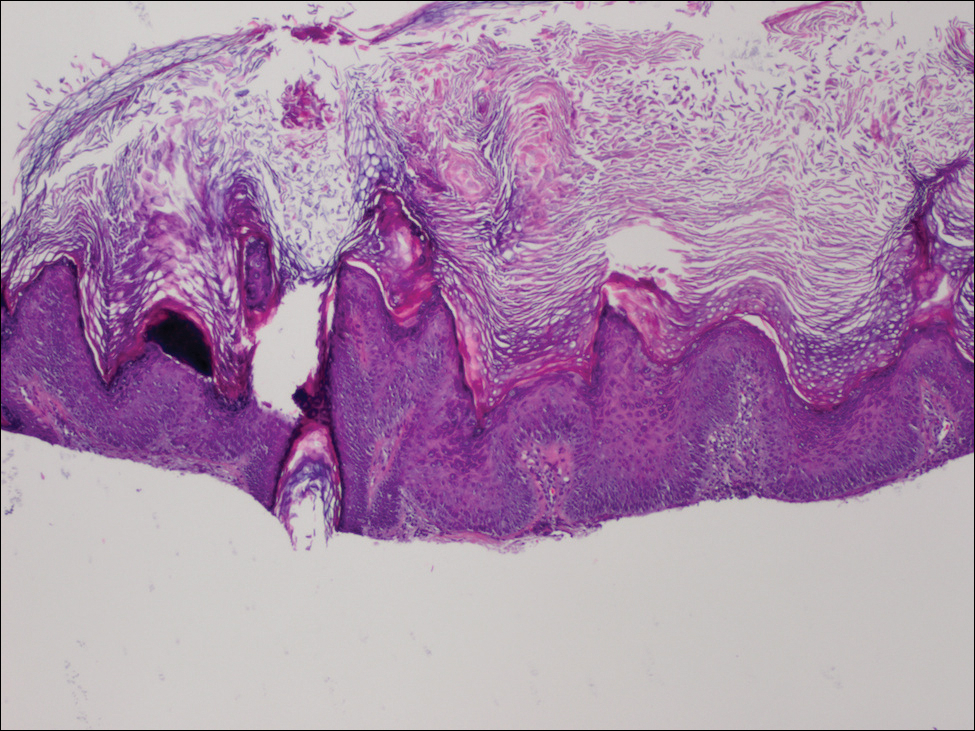
Physical examination revealed numerous 2- to 3-mm, round-oval, flesh-colored to light-brown papules on the cheeks, chest, abdomen (Figure 1), back, and both arms and legs. Some papules were inflamed and some had a stuck-on appearance. Lesions on the chest between the breasts and inframammary region were slightly inflamed. Two skin biopsies were performed. Biopsy of the lesion on the right lateral back revealed solar lentigo, early macular seborrheic keratosis, and a focus of inflamed mild solar keratosis. The dermis showed a mild superficial perivascular and interstitial inflammatory infiltrate composed mostly of lymphocytes, histiocytes, and eosinophils. There were occasional melanophages present (Figure 2). Biopsy of the lesion between the breasts revealed inflamed verrucous seborrheic keratosis (Figure 3).


We treated the lesion on the right lateral back with cycles of cryotherapy and explained to the patient that the lesion between the breasts was benign. We also reiterated to the patient the importance of wearing sun-protective clothing and UVA/UVB sunblock with a sun protection factor of 30 or higher.
Our patient was diagnosed with pneumonia and subsequently had to discontinue vemurafenib. During the period of nontreatment, the keratotic lesions cleared with postinflammatory hyperpigmentation and no epidermal changes, which showed a possible inference of a direct relationship between the vemurafenib and the appearance of the nonmalignant cutaneous lesions. Although this report only represents 1 patient, other patients possibly can benefit from a modified dose of vemurafenib, which either would resolve or lessen the quantity of these lesions.
Vemurafenib is the first US Food and Drug Administration-approved treatment for nonresectable metastatic melanoma with the BRAF V600E mutation as detected by a US Food and Drug Administration-approved test.1,2 Mutated BRAF is present in approximately 60% of cutaneous melanomas.3 Vemurafenib targets the oncogenic BRAF V600E making the protein inactive, thus inhibiting cell proliferation and leading to apoptosis and shrinkage of the metastatic tumors.3-5 Vemurafenib has a response rate of more than 50% and is associated with rapid improvement in quality of life.3
Cutaneous side effects include increased incidence of squamous cell carcinoma and keratoacanthomas, appearing approximately 7 to 8 weeks after starting vemurafenib.4 The incidence of these lesions increases in patients 65 years and older and in patients with prior skin cancer and chronic sun exposure. The paradoxical activation of the mitogen-activated protein kinase pathway by mutant BRAF-selective inhibitors provides an explanation of the induction of squamous cell carcinomas.4 Prior to the initiation of vemurafenib, all patients should receive a total-body skin examination and every 2 months thereafter while on treatment. After discontinuation of the medicine, the patient should continue to receive total-body skin evaluations every 6 months indefinitely.
Patients should be aware of the potential for mild to severe photosensitivity reactions. They should be advised to limit their sun exposure time and to wear sun-protective clothing when outdoors. The use of broad-spectrum UVA/UVB sunscreen and lip protectant with a sun protection factor of 30 or higher also should be stressed.6,7 Patients should be aware that UVA rays penetrate glass; therefore, UV-protective clothing should be worn throughout the day and during all seasons.7
In clinical trials of vemurafenib, Stevens-Johnson syndrome and toxic epidermal necrolysis was reported in 2 patients.8,9 Clinical trials also reported patients developing new primary malignant melanoma lesions.10 These findings further emphasize the need for patients to undergo total-body skin examinations during and after treatment.
Other possible dermatologic reactions include a generalized rash, erythema, alopecia, and pruritus.2,3 The development of benign growths associated with patients on vemurafenib include follicular plugging seen in keratosis pilaris, palmar and plantar hyperkeratosis, seborrheic dermatitis-like rashes, verrucous keratosis, and acantholytic dyskeratosis.8,11,12
We report a case of nonmalignant growths occurring 8 days after starting vemurafenib. This case illustrates potential cutaneous adverse reactions that were benign yet still of great concern to our patient. Many of these nonmalignant cutaneous findings are associated with abnormal follicular keratinization thought to be secondary to abnormal signaling of the mitogen-activated protein kinase pathway that occurs with the use of BRAF inhibitors.8 Although in this case malignant lesions were not discovered, the need for total-body skin examinations exists during all stages of treatment. Supportive care and reassurance should be given to patients along with local treatments including topical therapies (steroids, retinoids), cryotherapy, and biopsies or excisions when necessary.13,14
- Holstein S, Hohl R. Therapeutic additions and possible deletions in oncology in 2011. Clin Pharmacol Ther. 2011;91:15-17.
- Zambon A, Niculescu-Dovaz I, Niculescu-Dovaz D, et al. Small molecule inhibitors of BRAF in clinical trials. Bioorg Med Chem Lett. 2012;22:789-792.
- Luke JJ, Hodi FS. Vemurafenib and BRAF inhibition: a new class of treatment for metastatic melanoma [published online November 14, 2011]. Clin Cancer Res. 2012;18:9-14.
- Flaherty KT, Puzanov I, Kim KB, et al. Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med. 2010; 363:809-819.
- Tsai J, Lee JT, Wang W, et al. Discovery of a selective inhibitor of oncogenic B-Raf kinase with potent antimelanoma activity. Proc Natl Acad Sci USA. 2008;105:3041-3046.
- Chapman PB, Hauschild A, Robert C, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364:2507-2516.
- Dummer R, Rinderknecht J, Goldinger SM. Ultraviolet A and photosensitivity during vemuranefib therapy. N Engl J Med. 2012;366:480-481.
- Bovd KP, Vincent B, Andrea A, et al. Nonmalignant cutaneous findings associated with vemurafenib use in patients with metastatic melanoma. J Am Acad Dermatol. 2012;67:1375-1379.
- Wang CM, Fleming KF Hsu S. A case of vemurafenib-induced keratosis pilaris-like eruption. Dermatol Online J. 2012;18:7.
- Zimmer L, Hillen U, Livingstone E, et al. Atypical melanocytic proliferations and new primary melanomas in patients with advanced melanoma undergoing selective BRAF inhibition. J Clin Oncol. 2012;30:2375-2383.
- Huang V, Hepper D, Anadkat M, et al. Cutaneous toxic effects associated with vemurafenib and inhibition of the BRAF pathway. Arch Dermatol. 2012;148:628-633.
- Gupta M, Huang V, Linette G, et al. Unusual complication of vemurafenib treatment of metastatic melanoma: exacerbation of acantholytic dyskeratosis complicated by Kaposi varicelliform eruption. Arch Dermatol. 2012;148:966-968;
- Sinha R, Edmonds K, Newton-Bishop JA, et al. Cutaneous adverse events associated with vemurafenib in patients with metastatic melanoma: practical advice on diagnosis, preventions and management of the main treatment related skin toxicities. Br J Dermatol. 2012;167:987-994.
- Boussemart L, Routier E, Mateus C, et al. Prospective study of cutaneous side effects associated with the BRAF inhibitor vemurafenib: a study of 42 patients. Ann Oncol. 2013;24:1691-1697.
To the Editor:
A 53-year-old woman was referred by her oncologist to our dermatology office with lesions on the face and body that presented 8 days after starting vemurafenib 960 mg twice daily for metastatic melanoma. The patient denied any symptoms from the lesions but was concerned they would spread to cover her entire face and body.
The patient's medical history included a diagnosis of metastatic melanoma 6 years prior to presentation. She stated that the primary cutaneous melanoma site was unknown. The patient had endured numerous surgeries to excise lymph node tumors, with some lesions up to 3 cm. The patient recently started vemurafenib, a treatment for BRAF V600E mutation-positive metastatic melanoma. The patient's personal history was notable for hepatitis A, B, and C, and her family history revealed her mother had metastatic lung cancer.
Physical examination revealed numerous 2- to 3-mm, round-oval, flesh-colored to light-brown papules on the cheeks, chest, abdomen (Figure 1), back, and both arms and legs. Some papules were inflamed and some had a stuck-on appearance. Lesions on the chest between the breasts and inframammary region were slightly inflamed. Two skin biopsies were performed. Biopsy of the lesion on the right lateral back revealed solar lentigo, early macular seborrheic keratosis, and a focus of inflamed mild solar keratosis. The dermis showed a mild superficial perivascular and interstitial inflammatory infiltrate composed mostly of lymphocytes, histiocytes, and eosinophils. There were occasional melanophages present (Figure 2). Biopsy of the lesion between the breasts revealed inflamed verrucous seborrheic keratosis (Figure 3).


We treated the lesion on the right lateral back with cycles of cryotherapy and explained to the patient that the lesion between the breasts was benign. We also reiterated to the patient the importance of wearing sun-protective clothing and UVA/UVB sunblock with a sun protection factor of 30 or higher.
Our patient was diagnosed with pneumonia and subsequently had to discontinue vemurafenib. During the period of nontreatment, the keratotic lesions cleared with postinflammatory hyperpigmentation and no epidermal changes, which showed a possible inference of a direct relationship between the vemurafenib and the appearance of the nonmalignant cutaneous lesions. Although this report only represents 1 patient, other patients possibly can benefit from a modified dose of vemurafenib, which either would resolve or lessen the quantity of these lesions.
Vemurafenib is the first US Food and Drug Administration-approved treatment for nonresectable metastatic melanoma with the BRAF V600E mutation as detected by a US Food and Drug Administration-approved test.1,2 Mutated BRAF is present in approximately 60% of cutaneous melanomas.3 Vemurafenib targets the oncogenic BRAF V600E making the protein inactive, thus inhibiting cell proliferation and leading to apoptosis and shrinkage of the metastatic tumors.3-5 Vemurafenib has a response rate of more than 50% and is associated with rapid improvement in quality of life.3
Cutaneous side effects include increased incidence of squamous cell carcinoma and keratoacanthomas, appearing approximately 7 to 8 weeks after starting vemurafenib.4 The incidence of these lesions increases in patients 65 years and older and in patients with prior skin cancer and chronic sun exposure. The paradoxical activation of the mitogen-activated protein kinase pathway by mutant BRAF-selective inhibitors provides an explanation of the induction of squamous cell carcinomas.4 Prior to the initiation of vemurafenib, all patients should receive a total-body skin examination and every 2 months thereafter while on treatment. After discontinuation of the medicine, the patient should continue to receive total-body skin evaluations every 6 months indefinitely.
Patients should be aware of the potential for mild to severe photosensitivity reactions. They should be advised to limit their sun exposure time and to wear sun-protective clothing when outdoors. The use of broad-spectrum UVA/UVB sunscreen and lip protectant with a sun protection factor of 30 or higher also should be stressed.6,7 Patients should be aware that UVA rays penetrate glass; therefore, UV-protective clothing should be worn throughout the day and during all seasons.7
In clinical trials of vemurafenib, Stevens-Johnson syndrome and toxic epidermal necrolysis was reported in 2 patients.8,9 Clinical trials also reported patients developing new primary malignant melanoma lesions.10 These findings further emphasize the need for patients to undergo total-body skin examinations during and after treatment.
Other possible dermatologic reactions include a generalized rash, erythema, alopecia, and pruritus.2,3 The development of benign growths associated with patients on vemurafenib include follicular plugging seen in keratosis pilaris, palmar and plantar hyperkeratosis, seborrheic dermatitis-like rashes, verrucous keratosis, and acantholytic dyskeratosis.8,11,12
We report a case of nonmalignant growths occurring 8 days after starting vemurafenib. This case illustrates potential cutaneous adverse reactions that were benign yet still of great concern to our patient. Many of these nonmalignant cutaneous findings are associated with abnormal follicular keratinization thought to be secondary to abnormal signaling of the mitogen-activated protein kinase pathway that occurs with the use of BRAF inhibitors.8 Although in this case malignant lesions were not discovered, the need for total-body skin examinations exists during all stages of treatment. Supportive care and reassurance should be given to patients along with local treatments including topical therapies (steroids, retinoids), cryotherapy, and biopsies or excisions when necessary.13,14
To the Editor:
A 53-year-old woman was referred by her oncologist to our dermatology office with lesions on the face and body that presented 8 days after starting vemurafenib 960 mg twice daily for metastatic melanoma. The patient denied any symptoms from the lesions but was concerned they would spread to cover her entire face and body.
The patient's medical history included a diagnosis of metastatic melanoma 6 years prior to presentation. She stated that the primary cutaneous melanoma site was unknown. The patient had endured numerous surgeries to excise lymph node tumors, with some lesions up to 3 cm. The patient recently started vemurafenib, a treatment for BRAF V600E mutation-positive metastatic melanoma. The patient's personal history was notable for hepatitis A, B, and C, and her family history revealed her mother had metastatic lung cancer.
Physical examination revealed numerous 2- to 3-mm, round-oval, flesh-colored to light-brown papules on the cheeks, chest, abdomen (Figure 1), back, and both arms and legs. Some papules were inflamed and some had a stuck-on appearance. Lesions on the chest between the breasts and inframammary region were slightly inflamed. Two skin biopsies were performed. Biopsy of the lesion on the right lateral back revealed solar lentigo, early macular seborrheic keratosis, and a focus of inflamed mild solar keratosis. The dermis showed a mild superficial perivascular and interstitial inflammatory infiltrate composed mostly of lymphocytes, histiocytes, and eosinophils. There were occasional melanophages present (Figure 2). Biopsy of the lesion between the breasts revealed inflamed verrucous seborrheic keratosis (Figure 3).


We treated the lesion on the right lateral back with cycles of cryotherapy and explained to the patient that the lesion between the breasts was benign. We also reiterated to the patient the importance of wearing sun-protective clothing and UVA/UVB sunblock with a sun protection factor of 30 or higher.
Our patient was diagnosed with pneumonia and subsequently had to discontinue vemurafenib. During the period of nontreatment, the keratotic lesions cleared with postinflammatory hyperpigmentation and no epidermal changes, which showed a possible inference of a direct relationship between the vemurafenib and the appearance of the nonmalignant cutaneous lesions. Although this report only represents 1 patient, other patients possibly can benefit from a modified dose of vemurafenib, which either would resolve or lessen the quantity of these lesions.
Vemurafenib is the first US Food and Drug Administration-approved treatment for nonresectable metastatic melanoma with the BRAF V600E mutation as detected by a US Food and Drug Administration-approved test.1,2 Mutated BRAF is present in approximately 60% of cutaneous melanomas.3 Vemurafenib targets the oncogenic BRAF V600E making the protein inactive, thus inhibiting cell proliferation and leading to apoptosis and shrinkage of the metastatic tumors.3-5 Vemurafenib has a response rate of more than 50% and is associated with rapid improvement in quality of life.3
Cutaneous side effects include increased incidence of squamous cell carcinoma and keratoacanthomas, appearing approximately 7 to 8 weeks after starting vemurafenib.4 The incidence of these lesions increases in patients 65 years and older and in patients with prior skin cancer and chronic sun exposure. The paradoxical activation of the mitogen-activated protein kinase pathway by mutant BRAF-selective inhibitors provides an explanation of the induction of squamous cell carcinomas.4 Prior to the initiation of vemurafenib, all patients should receive a total-body skin examination and every 2 months thereafter while on treatment. After discontinuation of the medicine, the patient should continue to receive total-body skin evaluations every 6 months indefinitely.
Patients should be aware of the potential for mild to severe photosensitivity reactions. They should be advised to limit their sun exposure time and to wear sun-protective clothing when outdoors. The use of broad-spectrum UVA/UVB sunscreen and lip protectant with a sun protection factor of 30 or higher also should be stressed.6,7 Patients should be aware that UVA rays penetrate glass; therefore, UV-protective clothing should be worn throughout the day and during all seasons.7
In clinical trials of vemurafenib, Stevens-Johnson syndrome and toxic epidermal necrolysis was reported in 2 patients.8,9 Clinical trials also reported patients developing new primary malignant melanoma lesions.10 These findings further emphasize the need for patients to undergo total-body skin examinations during and after treatment.
Other possible dermatologic reactions include a generalized rash, erythema, alopecia, and pruritus.2,3 The development of benign growths associated with patients on vemurafenib include follicular plugging seen in keratosis pilaris, palmar and plantar hyperkeratosis, seborrheic dermatitis-like rashes, verrucous keratosis, and acantholytic dyskeratosis.8,11,12
We report a case of nonmalignant growths occurring 8 days after starting vemurafenib. This case illustrates potential cutaneous adverse reactions that were benign yet still of great concern to our patient. Many of these nonmalignant cutaneous findings are associated with abnormal follicular keratinization thought to be secondary to abnormal signaling of the mitogen-activated protein kinase pathway that occurs with the use of BRAF inhibitors.8 Although in this case malignant lesions were not discovered, the need for total-body skin examinations exists during all stages of treatment. Supportive care and reassurance should be given to patients along with local treatments including topical therapies (steroids, retinoids), cryotherapy, and biopsies or excisions when necessary.13,14
- Holstein S, Hohl R. Therapeutic additions and possible deletions in oncology in 2011. Clin Pharmacol Ther. 2011;91:15-17.
- Zambon A, Niculescu-Dovaz I, Niculescu-Dovaz D, et al. Small molecule inhibitors of BRAF in clinical trials. Bioorg Med Chem Lett. 2012;22:789-792.
- Luke JJ, Hodi FS. Vemurafenib and BRAF inhibition: a new class of treatment for metastatic melanoma [published online November 14, 2011]. Clin Cancer Res. 2012;18:9-14.
- Flaherty KT, Puzanov I, Kim KB, et al. Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med. 2010; 363:809-819.
- Tsai J, Lee JT, Wang W, et al. Discovery of a selective inhibitor of oncogenic B-Raf kinase with potent antimelanoma activity. Proc Natl Acad Sci USA. 2008;105:3041-3046.
- Chapman PB, Hauschild A, Robert C, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364:2507-2516.
- Dummer R, Rinderknecht J, Goldinger SM. Ultraviolet A and photosensitivity during vemuranefib therapy. N Engl J Med. 2012;366:480-481.
- Bovd KP, Vincent B, Andrea A, et al. Nonmalignant cutaneous findings associated with vemurafenib use in patients with metastatic melanoma. J Am Acad Dermatol. 2012;67:1375-1379.
- Wang CM, Fleming KF Hsu S. A case of vemurafenib-induced keratosis pilaris-like eruption. Dermatol Online J. 2012;18:7.
- Zimmer L, Hillen U, Livingstone E, et al. Atypical melanocytic proliferations and new primary melanomas in patients with advanced melanoma undergoing selective BRAF inhibition. J Clin Oncol. 2012;30:2375-2383.
- Huang V, Hepper D, Anadkat M, et al. Cutaneous toxic effects associated with vemurafenib and inhibition of the BRAF pathway. Arch Dermatol. 2012;148:628-633.
- Gupta M, Huang V, Linette G, et al. Unusual complication of vemurafenib treatment of metastatic melanoma: exacerbation of acantholytic dyskeratosis complicated by Kaposi varicelliform eruption. Arch Dermatol. 2012;148:966-968;
- Sinha R, Edmonds K, Newton-Bishop JA, et al. Cutaneous adverse events associated with vemurafenib in patients with metastatic melanoma: practical advice on diagnosis, preventions and management of the main treatment related skin toxicities. Br J Dermatol. 2012;167:987-994.
- Boussemart L, Routier E, Mateus C, et al. Prospective study of cutaneous side effects associated with the BRAF inhibitor vemurafenib: a study of 42 patients. Ann Oncol. 2013;24:1691-1697.
- Holstein S, Hohl R. Therapeutic additions and possible deletions in oncology in 2011. Clin Pharmacol Ther. 2011;91:15-17.
- Zambon A, Niculescu-Dovaz I, Niculescu-Dovaz D, et al. Small molecule inhibitors of BRAF in clinical trials. Bioorg Med Chem Lett. 2012;22:789-792.
- Luke JJ, Hodi FS. Vemurafenib and BRAF inhibition: a new class of treatment for metastatic melanoma [published online November 14, 2011]. Clin Cancer Res. 2012;18:9-14.
- Flaherty KT, Puzanov I, Kim KB, et al. Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med. 2010; 363:809-819.
- Tsai J, Lee JT, Wang W, et al. Discovery of a selective inhibitor of oncogenic B-Raf kinase with potent antimelanoma activity. Proc Natl Acad Sci USA. 2008;105:3041-3046.
- Chapman PB, Hauschild A, Robert C, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364:2507-2516.
- Dummer R, Rinderknecht J, Goldinger SM. Ultraviolet A and photosensitivity during vemuranefib therapy. N Engl J Med. 2012;366:480-481.
- Bovd KP, Vincent B, Andrea A, et al. Nonmalignant cutaneous findings associated with vemurafenib use in patients with metastatic melanoma. J Am Acad Dermatol. 2012;67:1375-1379.
- Wang CM, Fleming KF Hsu S. A case of vemurafenib-induced keratosis pilaris-like eruption. Dermatol Online J. 2012;18:7.
- Zimmer L, Hillen U, Livingstone E, et al. Atypical melanocytic proliferations and new primary melanomas in patients with advanced melanoma undergoing selective BRAF inhibition. J Clin Oncol. 2012;30:2375-2383.
- Huang V, Hepper D, Anadkat M, et al. Cutaneous toxic effects associated with vemurafenib and inhibition of the BRAF pathway. Arch Dermatol. 2012;148:628-633.
- Gupta M, Huang V, Linette G, et al. Unusual complication of vemurafenib treatment of metastatic melanoma: exacerbation of acantholytic dyskeratosis complicated by Kaposi varicelliform eruption. Arch Dermatol. 2012;148:966-968;
- Sinha R, Edmonds K, Newton-Bishop JA, et al. Cutaneous adverse events associated with vemurafenib in patients with metastatic melanoma: practical advice on diagnosis, preventions and management of the main treatment related skin toxicities. Br J Dermatol. 2012;167:987-994.
- Boussemart L, Routier E, Mateus C, et al. Prospective study of cutaneous side effects associated with the BRAF inhibitor vemurafenib: a study of 42 patients. Ann Oncol. 2013;24:1691-1697.
Practice Points
- Prior to starting a BRAF inhibitor, clinicians should perform a baseline total-body skin examination and follow-up every 2 months.
- Take photographs of the patient's entire body on initial total-body skin examination.
- Encourage sun protection for exposed areas on the body in all seasons.
VcR-CVAD yields high responses, ‘excellent’ survival in MCL
Adding rituximab and bortezomib to a moderate-intensity chemotherapy regimen and following it up with maintenance rituximab produced high response rates and “excellent” survival outcomes for adults with previously untreated mantle cell lymphoma (MCL), investigators reported in long-term follow-up of a small study.
The objective response rate (ORR) among 30 patients with MCL treated with VcR-CVAD – bortezomib (Velcade), rituximab, and hyperCVAD (hyper-fractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) followed by rituximab maintenance – was 90%, including a high proportion of complete responses (CR) or unconfirmed complete responses.
After a median follow-up of 7.8 years, the rates of 6-year progression-free and overall survival (PFS and OS) were 53% and 70%, respectively, with patients older and younger than 60 years having equally good outcomes, according to Julie E. Chang, MD, of the Wisconsin Institute of Medical Research in Madison, and her colleagues.
VcR-CVAD is a moderate-intensity regimen with a favorable toxicity profile that allowed tolerability even in an older population, the investigators noted. “An important lesson illustrated by VcR-CVAD is that long-term remissions are achievable in some patients without intensive inductions or consolidation,” they wrote in Clinical Lymphoma, Myeloma & Leukemia.
The investigators previously reported that after a median follow-up of 42 months, the 3-year PFS and OS were 63% and 86%, respectively, and that these outcomes were comparable to those reported with more intensive regimens (Br J Haematol. 2011 Oct;155[2]:190-7).
As noted, the ORR was 90%, including 77% CR/unconfirmed CR, 6-year PFS was 53%, and 6-year OS was 70%.
A univariate analysis showed a significant interaction between lactate dehydrogenase levels and age for PFS, and a trend, albeit not significant, toward an interaction with LDH levels and age for OS.
In multivariate analysis, worse Eastern Cooperative Oncology Group (ECOG) performance status at baseline showed a nonsignificant trend toward worse OS. In contrast, an increase of one in the number of extranodal disease sites was associated with better OS (relative risk 0.66, 95% confidence interval 0.01-0.66).
The investigators noted that the advent of new agents with activity against MCL and the use of prognostic information, such as minimal residual disease measurements, could help clinicians develop induction and maintenance strategies with better efficacy and lower toxicity than VcR-CVAD.
The study was supported by the National Institutes of Health, Millennium Pharmaceuticals, and the University of Wisconsin Forward Lymphoma Research Fund. Dr. Chang reported research funding from Genentech. One coauthor disclosed consulting work for Genentech and Millennium and research funding from Genentech.
SOURCE: Chang J et al. Clin Lymphoma Myeloma Leuk. 2018 Jan;18(1):e61-e67. doi: 10.1016/j.clml.2017.10.006.
Adding rituximab and bortezomib to a moderate-intensity chemotherapy regimen and following it up with maintenance rituximab produced high response rates and “excellent” survival outcomes for adults with previously untreated mantle cell lymphoma (MCL), investigators reported in long-term follow-up of a small study.
The objective response rate (ORR) among 30 patients with MCL treated with VcR-CVAD – bortezomib (Velcade), rituximab, and hyperCVAD (hyper-fractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) followed by rituximab maintenance – was 90%, including a high proportion of complete responses (CR) or unconfirmed complete responses.
After a median follow-up of 7.8 years, the rates of 6-year progression-free and overall survival (PFS and OS) were 53% and 70%, respectively, with patients older and younger than 60 years having equally good outcomes, according to Julie E. Chang, MD, of the Wisconsin Institute of Medical Research in Madison, and her colleagues.
VcR-CVAD is a moderate-intensity regimen with a favorable toxicity profile that allowed tolerability even in an older population, the investigators noted. “An important lesson illustrated by VcR-CVAD is that long-term remissions are achievable in some patients without intensive inductions or consolidation,” they wrote in Clinical Lymphoma, Myeloma & Leukemia.
The investigators previously reported that after a median follow-up of 42 months, the 3-year PFS and OS were 63% and 86%, respectively, and that these outcomes were comparable to those reported with more intensive regimens (Br J Haematol. 2011 Oct;155[2]:190-7).
As noted, the ORR was 90%, including 77% CR/unconfirmed CR, 6-year PFS was 53%, and 6-year OS was 70%.
A univariate analysis showed a significant interaction between lactate dehydrogenase levels and age for PFS, and a trend, albeit not significant, toward an interaction with LDH levels and age for OS.
In multivariate analysis, worse Eastern Cooperative Oncology Group (ECOG) performance status at baseline showed a nonsignificant trend toward worse OS. In contrast, an increase of one in the number of extranodal disease sites was associated with better OS (relative risk 0.66, 95% confidence interval 0.01-0.66).
The investigators noted that the advent of new agents with activity against MCL and the use of prognostic information, such as minimal residual disease measurements, could help clinicians develop induction and maintenance strategies with better efficacy and lower toxicity than VcR-CVAD.
The study was supported by the National Institutes of Health, Millennium Pharmaceuticals, and the University of Wisconsin Forward Lymphoma Research Fund. Dr. Chang reported research funding from Genentech. One coauthor disclosed consulting work for Genentech and Millennium and research funding from Genentech.
SOURCE: Chang J et al. Clin Lymphoma Myeloma Leuk. 2018 Jan;18(1):e61-e67. doi: 10.1016/j.clml.2017.10.006.
Adding rituximab and bortezomib to a moderate-intensity chemotherapy regimen and following it up with maintenance rituximab produced high response rates and “excellent” survival outcomes for adults with previously untreated mantle cell lymphoma (MCL), investigators reported in long-term follow-up of a small study.
The objective response rate (ORR) among 30 patients with MCL treated with VcR-CVAD – bortezomib (Velcade), rituximab, and hyperCVAD (hyper-fractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) followed by rituximab maintenance – was 90%, including a high proportion of complete responses (CR) or unconfirmed complete responses.
After a median follow-up of 7.8 years, the rates of 6-year progression-free and overall survival (PFS and OS) were 53% and 70%, respectively, with patients older and younger than 60 years having equally good outcomes, according to Julie E. Chang, MD, of the Wisconsin Institute of Medical Research in Madison, and her colleagues.
VcR-CVAD is a moderate-intensity regimen with a favorable toxicity profile that allowed tolerability even in an older population, the investigators noted. “An important lesson illustrated by VcR-CVAD is that long-term remissions are achievable in some patients without intensive inductions or consolidation,” they wrote in Clinical Lymphoma, Myeloma & Leukemia.
The investigators previously reported that after a median follow-up of 42 months, the 3-year PFS and OS were 63% and 86%, respectively, and that these outcomes were comparable to those reported with more intensive regimens (Br J Haematol. 2011 Oct;155[2]:190-7).
As noted, the ORR was 90%, including 77% CR/unconfirmed CR, 6-year PFS was 53%, and 6-year OS was 70%.
A univariate analysis showed a significant interaction between lactate dehydrogenase levels and age for PFS, and a trend, albeit not significant, toward an interaction with LDH levels and age for OS.
In multivariate analysis, worse Eastern Cooperative Oncology Group (ECOG) performance status at baseline showed a nonsignificant trend toward worse OS. In contrast, an increase of one in the number of extranodal disease sites was associated with better OS (relative risk 0.66, 95% confidence interval 0.01-0.66).
The investigators noted that the advent of new agents with activity against MCL and the use of prognostic information, such as minimal residual disease measurements, could help clinicians develop induction and maintenance strategies with better efficacy and lower toxicity than VcR-CVAD.
The study was supported by the National Institutes of Health, Millennium Pharmaceuticals, and the University of Wisconsin Forward Lymphoma Research Fund. Dr. Chang reported research funding from Genentech. One coauthor disclosed consulting work for Genentech and Millennium and research funding from Genentech.
SOURCE: Chang J et al. Clin Lymphoma Myeloma Leuk. 2018 Jan;18(1):e61-e67. doi: 10.1016/j.clml.2017.10.006.
FROM CLINICAL LYMPHOMA, MYELOMA & LEUKEMIA
Key clinical point:
Major finding: The objective response rate was 90%, including 77% complete or unconfirmed complete responses.
Study details: Open-label study of 30 patients with previously untreated MCL.
Disclosures: The study was supported by the National Institutes of Health, Millennium Pharmaceuticals, and the University of Wisconsin Forward Lymphoma Research Fund. Dr. Chang reported research funding from Genentech. A coauthor reported consulting work for Genentech and Millennium and research funding from Genentech.
Source: Chang J et al. Clin Lymphoma Myeloma Leuk. 2018 Jan;18(1):e61-e67. doi: 10.1016/j.clml.2017.10.006.
High levels of neuroinflammatory markers may drive increased Alzheimer’s prevalence among blacks
Potent proinflammatory markers appear to be significantly elevated in the brains of black patients with Alzheimer’s disease, compared to the brains of white patients, while cytokines with a potentially neuroprotective role are decreased, a Food and Drug Administration researcher reported Jan. 11 at an agency grand rounds presentation
These differences may be driven by the NLRP3 gene, which, in the presence of neuronal insults like beta amyloid aggregates, can direct microglia to pump out a stew of inflammatory cytokines and chemokines, Dr. Ferguson said.
“This proposed pathway may help explain why black patients are twice as likely as white ones to develop AD, said Dr. Ferguson, acting director of FDA Division of Neurotoxicology. “Once NLRP3 is activated, it leads to chronically increased levels of inflammatory cytokines. Once they are chronically increased, it could lead to increased synaptic dysfunction, cognitive impairment, and cell death.”
Dr. Ferguson and her colleague, Vijayalakshmi Varma, PhD, FDA research biologist, obtained brain tissue samples from 12 black patients with AD and 12 white ones. She did not have baseline severity staging for the cohort, but said that the patients were a mean of 81 years old, and had confirmed AD pathology at the time of death.
The researchers examined neurodegenerative proteins and cytokine levels in the BA21 area of the brain. Located in the temporal lobe, BA21 is important in language and auditory processing. It generally exhibits atrophy and the characteristic AD lesions of beta amyloid plaques and tau tangles early in the disease.
In a previously published report of this neuropathological cohort, the team examined a number of markers of neurodegeneration including S100B, the soluble form of the receptor for advanced glycation end-products (sRAGE); glial cell-derived neurotrophic factor (GDNF); and amyloid beta (AB) 40 and AB42 (J Alzheimers Dis. 2017:59; 57-66).
RAGE helps mediate the transport of AB through the cell membrane and the blood brain barrier. S100B is a protein that has been implicated in the formation of tau tangles; other studies suggest that it interacts with RAGE to promote tau phosphorylation.
Compared to levels in the brains of white patients, brains of black patients contained 17% more S100B and 121% more AB42. The AB42/40 ratio was increased by almost 500% over that seen in the white sample.
The new, unpublished data used this same neuropathological cohort, but examined 40 known neuroinflammatory markers. Compared to the white sample, the black sample showed:
IL-1B, thought to increase amyloid precursor protein and promote tau phosphorylation, increased by 109% MIG, an attractant for activated T-cells, increased by 37%
TRAIL, a ligand that induces apoptosis. increased by 50%
“S 100 B is an astrocytic calcium binding protein,” Dr. Ferguson said. “We know that there are increased brain and cerebrospinal levels of S100 be in mild-moderate Alzheimer’s. S100 B can trigger neuroinflammatory signaling pathways. S100 B is also a potential biomarker of blood-brain barrier permeability. We see increased serum levels in such things as unmedicated schizophrenia and depression as well as brain injury.”
However, Dr. Ferguson said, “There were a couple of cytokines significantly that were decreased in African-American sample, including IL-8. Decreased IL-8 brain levels have been described in those with Alzheimer’s and recent studies have indicated that IL-8 may have a protective role in Alzheimer’s pathogenesis.”
IL-3, which activates mature neutrophils and macrophages, was also significantly decreased.
The researchers also saw some gender differences. Women had about 20% less CCL25 and CCL26 than men, and 32% less CxCL1 (fracktalkine). CCL26 (Eotaxin-3) was decreased significantly (19%) in women. Fractalkine is essential for microglial cell migration. CCL25 and CCL26 are also mobilizers of immune cells.
Dr. Ferguson postulated that at least some of this neuroinflammatory profile could be related to the formation of inflammasomes – multi-protein oligomeric structures formed in microglia in the brain by the influence of the NLRP3 gene.
“There is a lot of evidence that inflammasomes are involved in AD pathogenesis,” she said. Messenger RNA for the NLRP3 inflammasome is up-regulated in blood from AD patients. Alzheimer’s transgenic mice without the gene show decreased hippocampal and cortical AB40 and 42, increased microglial phagocytosis, and better memory. There is also some evidence that the NLRP3 inflammasome releases minute protein particles called apoptosis-associated (ASC) specks. Some researchers think these particles help seed amyloid throughout the brain. Based on these findings, Dr. Ferguson postulated a potential pathway for the increased prevalence and severity of AD among blacks.
Proinflammatory cytokines are released in response to rising AB levels. These promote the formation of the NLRP3 inflammasome within activated microglia. The inflammasome releases more chemokines and cytokines, leading to a chronic proinflammatory state that may actually promote amyloid seeding. This leads to synaptic dysfunction, cognitive dysfunction, and neuronal death
Dr. Ferguson said work on the samples will continue.
“We also have CSF and hippocampal tissue and intend to look at similar endpoints in those,” she said. “If as a result of this, we can find gene variants associated with ethnicity and Alzheimer’s, we may be able to establish genetic profiles to identify those at high risk. If we can do that, we may be able to intervene early before the person starts showing cognitive deficits and slow the progression of the disease – even develop precision medications for disease intervention.”
This article was updated 1/11/18.
Potent proinflammatory markers appear to be significantly elevated in the brains of black patients with Alzheimer’s disease, compared to the brains of white patients, while cytokines with a potentially neuroprotective role are decreased, a Food and Drug Administration researcher reported Jan. 11 at an agency grand rounds presentation
These differences may be driven by the NLRP3 gene, which, in the presence of neuronal insults like beta amyloid aggregates, can direct microglia to pump out a stew of inflammatory cytokines and chemokines, Dr. Ferguson said.
“This proposed pathway may help explain why black patients are twice as likely as white ones to develop AD, said Dr. Ferguson, acting director of FDA Division of Neurotoxicology. “Once NLRP3 is activated, it leads to chronically increased levels of inflammatory cytokines. Once they are chronically increased, it could lead to increased synaptic dysfunction, cognitive impairment, and cell death.”
Dr. Ferguson and her colleague, Vijayalakshmi Varma, PhD, FDA research biologist, obtained brain tissue samples from 12 black patients with AD and 12 white ones. She did not have baseline severity staging for the cohort, but said that the patients were a mean of 81 years old, and had confirmed AD pathology at the time of death.
The researchers examined neurodegenerative proteins and cytokine levels in the BA21 area of the brain. Located in the temporal lobe, BA21 is important in language and auditory processing. It generally exhibits atrophy and the characteristic AD lesions of beta amyloid plaques and tau tangles early in the disease.
In a previously published report of this neuropathological cohort, the team examined a number of markers of neurodegeneration including S100B, the soluble form of the receptor for advanced glycation end-products (sRAGE); glial cell-derived neurotrophic factor (GDNF); and amyloid beta (AB) 40 and AB42 (J Alzheimers Dis. 2017:59; 57-66).
RAGE helps mediate the transport of AB through the cell membrane and the blood brain barrier. S100B is a protein that has been implicated in the formation of tau tangles; other studies suggest that it interacts with RAGE to promote tau phosphorylation.
Compared to levels in the brains of white patients, brains of black patients contained 17% more S100B and 121% more AB42. The AB42/40 ratio was increased by almost 500% over that seen in the white sample.
The new, unpublished data used this same neuropathological cohort, but examined 40 known neuroinflammatory markers. Compared to the white sample, the black sample showed:
IL-1B, thought to increase amyloid precursor protein and promote tau phosphorylation, increased by 109% MIG, an attractant for activated T-cells, increased by 37%
TRAIL, a ligand that induces apoptosis. increased by 50%
“S 100 B is an astrocytic calcium binding protein,” Dr. Ferguson said. “We know that there are increased brain and cerebrospinal levels of S100 be in mild-moderate Alzheimer’s. S100 B can trigger neuroinflammatory signaling pathways. S100 B is also a potential biomarker of blood-brain barrier permeability. We see increased serum levels in such things as unmedicated schizophrenia and depression as well as brain injury.”
However, Dr. Ferguson said, “There were a couple of cytokines significantly that were decreased in African-American sample, including IL-8. Decreased IL-8 brain levels have been described in those with Alzheimer’s and recent studies have indicated that IL-8 may have a protective role in Alzheimer’s pathogenesis.”
IL-3, which activates mature neutrophils and macrophages, was also significantly decreased.
The researchers also saw some gender differences. Women had about 20% less CCL25 and CCL26 than men, and 32% less CxCL1 (fracktalkine). CCL26 (Eotaxin-3) was decreased significantly (19%) in women. Fractalkine is essential for microglial cell migration. CCL25 and CCL26 are also mobilizers of immune cells.
Dr. Ferguson postulated that at least some of this neuroinflammatory profile could be related to the formation of inflammasomes – multi-protein oligomeric structures formed in microglia in the brain by the influence of the NLRP3 gene.
“There is a lot of evidence that inflammasomes are involved in AD pathogenesis,” she said. Messenger RNA for the NLRP3 inflammasome is up-regulated in blood from AD patients. Alzheimer’s transgenic mice without the gene show decreased hippocampal and cortical AB40 and 42, increased microglial phagocytosis, and better memory. There is also some evidence that the NLRP3 inflammasome releases minute protein particles called apoptosis-associated (ASC) specks. Some researchers think these particles help seed amyloid throughout the brain. Based on these findings, Dr. Ferguson postulated a potential pathway for the increased prevalence and severity of AD among blacks.
Proinflammatory cytokines are released in response to rising AB levels. These promote the formation of the NLRP3 inflammasome within activated microglia. The inflammasome releases more chemokines and cytokines, leading to a chronic proinflammatory state that may actually promote amyloid seeding. This leads to synaptic dysfunction, cognitive dysfunction, and neuronal death
Dr. Ferguson said work on the samples will continue.
“We also have CSF and hippocampal tissue and intend to look at similar endpoints in those,” she said. “If as a result of this, we can find gene variants associated with ethnicity and Alzheimer’s, we may be able to establish genetic profiles to identify those at high risk. If we can do that, we may be able to intervene early before the person starts showing cognitive deficits and slow the progression of the disease – even develop precision medications for disease intervention.”
This article was updated 1/11/18.
Potent proinflammatory markers appear to be significantly elevated in the brains of black patients with Alzheimer’s disease, compared to the brains of white patients, while cytokines with a potentially neuroprotective role are decreased, a Food and Drug Administration researcher reported Jan. 11 at an agency grand rounds presentation
These differences may be driven by the NLRP3 gene, which, in the presence of neuronal insults like beta amyloid aggregates, can direct microglia to pump out a stew of inflammatory cytokines and chemokines, Dr. Ferguson said.
“This proposed pathway may help explain why black patients are twice as likely as white ones to develop AD, said Dr. Ferguson, acting director of FDA Division of Neurotoxicology. “Once NLRP3 is activated, it leads to chronically increased levels of inflammatory cytokines. Once they are chronically increased, it could lead to increased synaptic dysfunction, cognitive impairment, and cell death.”
Dr. Ferguson and her colleague, Vijayalakshmi Varma, PhD, FDA research biologist, obtained brain tissue samples from 12 black patients with AD and 12 white ones. She did not have baseline severity staging for the cohort, but said that the patients were a mean of 81 years old, and had confirmed AD pathology at the time of death.
The researchers examined neurodegenerative proteins and cytokine levels in the BA21 area of the brain. Located in the temporal lobe, BA21 is important in language and auditory processing. It generally exhibits atrophy and the characteristic AD lesions of beta amyloid plaques and tau tangles early in the disease.
In a previously published report of this neuropathological cohort, the team examined a number of markers of neurodegeneration including S100B, the soluble form of the receptor for advanced glycation end-products (sRAGE); glial cell-derived neurotrophic factor (GDNF); and amyloid beta (AB) 40 and AB42 (J Alzheimers Dis. 2017:59; 57-66).
RAGE helps mediate the transport of AB through the cell membrane and the blood brain barrier. S100B is a protein that has been implicated in the formation of tau tangles; other studies suggest that it interacts with RAGE to promote tau phosphorylation.
Compared to levels in the brains of white patients, brains of black patients contained 17% more S100B and 121% more AB42. The AB42/40 ratio was increased by almost 500% over that seen in the white sample.
The new, unpublished data used this same neuropathological cohort, but examined 40 known neuroinflammatory markers. Compared to the white sample, the black sample showed:
IL-1B, thought to increase amyloid precursor protein and promote tau phosphorylation, increased by 109% MIG, an attractant for activated T-cells, increased by 37%
TRAIL, a ligand that induces apoptosis. increased by 50%
“S 100 B is an astrocytic calcium binding protein,” Dr. Ferguson said. “We know that there are increased brain and cerebrospinal levels of S100 be in mild-moderate Alzheimer’s. S100 B can trigger neuroinflammatory signaling pathways. S100 B is also a potential biomarker of blood-brain barrier permeability. We see increased serum levels in such things as unmedicated schizophrenia and depression as well as brain injury.”
However, Dr. Ferguson said, “There were a couple of cytokines significantly that were decreased in African-American sample, including IL-8. Decreased IL-8 brain levels have been described in those with Alzheimer’s and recent studies have indicated that IL-8 may have a protective role in Alzheimer’s pathogenesis.”
IL-3, which activates mature neutrophils and macrophages, was also significantly decreased.
The researchers also saw some gender differences. Women had about 20% less CCL25 and CCL26 than men, and 32% less CxCL1 (fracktalkine). CCL26 (Eotaxin-3) was decreased significantly (19%) in women. Fractalkine is essential for microglial cell migration. CCL25 and CCL26 are also mobilizers of immune cells.
Dr. Ferguson postulated that at least some of this neuroinflammatory profile could be related to the formation of inflammasomes – multi-protein oligomeric structures formed in microglia in the brain by the influence of the NLRP3 gene.
“There is a lot of evidence that inflammasomes are involved in AD pathogenesis,” she said. Messenger RNA for the NLRP3 inflammasome is up-regulated in blood from AD patients. Alzheimer’s transgenic mice without the gene show decreased hippocampal and cortical AB40 and 42, increased microglial phagocytosis, and better memory. There is also some evidence that the NLRP3 inflammasome releases minute protein particles called apoptosis-associated (ASC) specks. Some researchers think these particles help seed amyloid throughout the brain. Based on these findings, Dr. Ferguson postulated a potential pathway for the increased prevalence and severity of AD among blacks.
Proinflammatory cytokines are released in response to rising AB levels. These promote the formation of the NLRP3 inflammasome within activated microglia. The inflammasome releases more chemokines and cytokines, leading to a chronic proinflammatory state that may actually promote amyloid seeding. This leads to synaptic dysfunction, cognitive dysfunction, and neuronal death
Dr. Ferguson said work on the samples will continue.
“We also have CSF and hippocampal tissue and intend to look at similar endpoints in those,” she said. “If as a result of this, we can find gene variants associated with ethnicity and Alzheimer’s, we may be able to establish genetic profiles to identify those at high risk. If we can do that, we may be able to intervene early before the person starts showing cognitive deficits and slow the progression of the disease – even develop precision medications for disease intervention.”
This article was updated 1/11/18.
REPORTING FROM FDA GRAND ROUNDS
S-1 regimen noninferior to other frontline mCRC options
to other commonly used regimens, according to results of a randomized, open-label, phase 3 trial.
Median progression-free survival for patients receiving the S-1–containing regimen was 14.0 months, compared with 10.8 months for patients receiving either mFOLFOX6 or CapeOX plus bevacizumab (P less than .0001 for noninferiority; P less than .0815 for superiority), Yuji Yamada, MD, of National Cancer Center Hospital, Tokyo, and coauthors reported.
Based on these results, “we consider S-1 and irinotecan plus bevacizumab to be an effective first-line therapy for mCRC and believe that it can be included as one of the recommended standard regimens,” Dr. Yamada and colleagues said (Ann Oncol. 2017 Dec 17. doi: 10.1093/annonc/mdx816).
S-1, a combination preparation that includes the 5-fluorouracil prodrug tegafur plus the modulators gimeracil and oteracil potassium, has been approved in Japan and is approved by the European Medicines Agency for gastric cancer, authors wrote.
Their phase 3 trial, known as TRICOLORE, included 487 patients randomly assigned to receive S-1 and irinotecan plus bevacizumab or a control group that received an oxaliplatin-based regimen (either mFOLFOX6 or CapeOX).
Oxaliplatin-based regimens are associated with milder alopecia and gastrointestinal toxicity, compared with irinotecan-based regimens but can result in prolonged peripheral neuropathy that can negatively impact quality of life and may lead to treatment discontinuation, Dr. Yamada and associates said.
Adverse events of grade 3 or higher occurred in 58.6% of the S-1/irinotecan/bevacizumab group and 64.9% of the control group. The most common grade 3 or greater adverse events were neutropenia and diarrhea in the S-1 group, and neutropenia and peripheral sensory neuropathy in the controls.
The median 14-month progression-free survival for S-1/irinotecan/bevacizumab establishes its noninferiority to the standard regimens, according to the authors: “Although superiority could not be proven, the median progression-free survival was 3.2 months longer in the experimental group than in the control group, and the quality of life results were favorable,” they wrote.
Quality of life was not statistically different between arms as measured by the Functional Assessment of Cancer Therapy-Colorectal Trial Outcome Index, according to the report. However, scores on the FACT/Gynecologic Oncology Group-Neurotoxicity subscale showed a “significantly more favorable trend over time in the experimental group,” authors noted.
The study was supported in part by Taiho Pharmaceutical. Dr. Yamada reported receiving honoraria from Taiho, Chugai, and Yakult.
SOURCE: Yamada Y et al. Ann Oncol. 2017 Dec 17. doi: 10.1093/annonc/mdx816.
to other commonly used regimens, according to results of a randomized, open-label, phase 3 trial.
Median progression-free survival for patients receiving the S-1–containing regimen was 14.0 months, compared with 10.8 months for patients receiving either mFOLFOX6 or CapeOX plus bevacizumab (P less than .0001 for noninferiority; P less than .0815 for superiority), Yuji Yamada, MD, of National Cancer Center Hospital, Tokyo, and coauthors reported.
Based on these results, “we consider S-1 and irinotecan plus bevacizumab to be an effective first-line therapy for mCRC and believe that it can be included as one of the recommended standard regimens,” Dr. Yamada and colleagues said (Ann Oncol. 2017 Dec 17. doi: 10.1093/annonc/mdx816).
S-1, a combination preparation that includes the 5-fluorouracil prodrug tegafur plus the modulators gimeracil and oteracil potassium, has been approved in Japan and is approved by the European Medicines Agency for gastric cancer, authors wrote.
Their phase 3 trial, known as TRICOLORE, included 487 patients randomly assigned to receive S-1 and irinotecan plus bevacizumab or a control group that received an oxaliplatin-based regimen (either mFOLFOX6 or CapeOX).
Oxaliplatin-based regimens are associated with milder alopecia and gastrointestinal toxicity, compared with irinotecan-based regimens but can result in prolonged peripheral neuropathy that can negatively impact quality of life and may lead to treatment discontinuation, Dr. Yamada and associates said.
Adverse events of grade 3 or higher occurred in 58.6% of the S-1/irinotecan/bevacizumab group and 64.9% of the control group. The most common grade 3 or greater adverse events were neutropenia and diarrhea in the S-1 group, and neutropenia and peripheral sensory neuropathy in the controls.
The median 14-month progression-free survival for S-1/irinotecan/bevacizumab establishes its noninferiority to the standard regimens, according to the authors: “Although superiority could not be proven, the median progression-free survival was 3.2 months longer in the experimental group than in the control group, and the quality of life results were favorable,” they wrote.
Quality of life was not statistically different between arms as measured by the Functional Assessment of Cancer Therapy-Colorectal Trial Outcome Index, according to the report. However, scores on the FACT/Gynecologic Oncology Group-Neurotoxicity subscale showed a “significantly more favorable trend over time in the experimental group,” authors noted.
The study was supported in part by Taiho Pharmaceutical. Dr. Yamada reported receiving honoraria from Taiho, Chugai, and Yakult.
SOURCE: Yamada Y et al. Ann Oncol. 2017 Dec 17. doi: 10.1093/annonc/mdx816.
to other commonly used regimens, according to results of a randomized, open-label, phase 3 trial.
Median progression-free survival for patients receiving the S-1–containing regimen was 14.0 months, compared with 10.8 months for patients receiving either mFOLFOX6 or CapeOX plus bevacizumab (P less than .0001 for noninferiority; P less than .0815 for superiority), Yuji Yamada, MD, of National Cancer Center Hospital, Tokyo, and coauthors reported.
Based on these results, “we consider S-1 and irinotecan plus bevacizumab to be an effective first-line therapy for mCRC and believe that it can be included as one of the recommended standard regimens,” Dr. Yamada and colleagues said (Ann Oncol. 2017 Dec 17. doi: 10.1093/annonc/mdx816).
S-1, a combination preparation that includes the 5-fluorouracil prodrug tegafur plus the modulators gimeracil and oteracil potassium, has been approved in Japan and is approved by the European Medicines Agency for gastric cancer, authors wrote.
Their phase 3 trial, known as TRICOLORE, included 487 patients randomly assigned to receive S-1 and irinotecan plus bevacizumab or a control group that received an oxaliplatin-based regimen (either mFOLFOX6 or CapeOX).
Oxaliplatin-based regimens are associated with milder alopecia and gastrointestinal toxicity, compared with irinotecan-based regimens but can result in prolonged peripheral neuropathy that can negatively impact quality of life and may lead to treatment discontinuation, Dr. Yamada and associates said.
Adverse events of grade 3 or higher occurred in 58.6% of the S-1/irinotecan/bevacizumab group and 64.9% of the control group. The most common grade 3 or greater adverse events were neutropenia and diarrhea in the S-1 group, and neutropenia and peripheral sensory neuropathy in the controls.
The median 14-month progression-free survival for S-1/irinotecan/bevacizumab establishes its noninferiority to the standard regimens, according to the authors: “Although superiority could not be proven, the median progression-free survival was 3.2 months longer in the experimental group than in the control group, and the quality of life results were favorable,” they wrote.
Quality of life was not statistically different between arms as measured by the Functional Assessment of Cancer Therapy-Colorectal Trial Outcome Index, according to the report. However, scores on the FACT/Gynecologic Oncology Group-Neurotoxicity subscale showed a “significantly more favorable trend over time in the experimental group,” authors noted.
The study was supported in part by Taiho Pharmaceutical. Dr. Yamada reported receiving honoraria from Taiho, Chugai, and Yakult.
SOURCE: Yamada Y et al. Ann Oncol. 2017 Dec 17. doi: 10.1093/annonc/mdx816.
FROM Annals of Oncology
Key clinical point: The oral fluoropyrimidine S-1 combined with irinotecan and bevacizumab was noninferior to other commonly used first-line regimens in patients with metastatic colorectal cancer (mCRC).
Major finding: Median progression-free-survival was 14.0 months for that regimen, compared with 10.8 months for patients receiving either mFOLFOX6 or CapeOX plus bevacizumab (P less than .0001 for noninferiority; P less than .0815 for superiority).
Data source: TRICOLORE, a randomized, open-label, phase 3, noninferiority trial including 487 mCRC patients enrolled at 53 institutions in Japan.
Disclosures: The study was supported by Tokyo Cooperative Oncology Group with funding from Taiho Pharmaceutica. Study authors reported disclosures related to Taiho, Chugai, Yakult, Ono, Eli Lilly, Eisai, Bayer, and others.
Source: Yamada Y et al. Ann Oncol. 2017 Dec 17. doi: 10.1093/annonc/mdx816.
Successive antiepileptic drug treatments offer diminished chances for seizure freedom
despite the wide availability of a variety of new antiepileptic drugs, according to Zhibin Chen, PhD, and his associates
The study included a total of 1,795 patients who were treated at the epilepsy unit of the Western Infirmary in Glasgow, Scotland, from July 1, 1982, to Oct. 31, 2012, and followed until Oct. 31, 2014, or until their deaths. They had a median follow-up of 11 years. Of this group, 1,144 patients were seizure free for a year or longer, including 816 who achieved seizure freedom after the first antiepileptic drug and 212 after receiving their second antiepileptic drug.
The odds ratio for each successive antiepileptic drug regimen’s failing if the first regimen failed was 1.73. The first antiepileptic drug regimen offered about a 50% probability of seizure freedom for 1 year or longer, but the probability of success was only 12% with the second regimen and 4% with the third. Attempts after the third regimen all had a probability of seizure freedom of around or below 1%. Patients who had a greater number of seizures prior to treatment, reported recreational drug use, or had first-degree relatives with a history of seizure were significantly less likely to achieve seizure freedom in a multivariate regression analysis.
“A paradigm shift in treatment and research strategies is needed to improve the long-term outcomes of newly diagnosed epilepsy. Patients with drug-resistant epilepsy should be considered early for nonpharmacological therapies, such as resective surgery and brain stimulation techniques,” the study investigators wrote.
SOURCE: Chen Z et al. JAMA Neurol. 2017 Dec 26. doi: 10.1001/jamaneurol.2017.3949
despite the wide availability of a variety of new antiepileptic drugs, according to Zhibin Chen, PhD, and his associates
The study included a total of 1,795 patients who were treated at the epilepsy unit of the Western Infirmary in Glasgow, Scotland, from July 1, 1982, to Oct. 31, 2012, and followed until Oct. 31, 2014, or until their deaths. They had a median follow-up of 11 years. Of this group, 1,144 patients were seizure free for a year or longer, including 816 who achieved seizure freedom after the first antiepileptic drug and 212 after receiving their second antiepileptic drug.
The odds ratio for each successive antiepileptic drug regimen’s failing if the first regimen failed was 1.73. The first antiepileptic drug regimen offered about a 50% probability of seizure freedom for 1 year or longer, but the probability of success was only 12% with the second regimen and 4% with the third. Attempts after the third regimen all had a probability of seizure freedom of around or below 1%. Patients who had a greater number of seizures prior to treatment, reported recreational drug use, or had first-degree relatives with a history of seizure were significantly less likely to achieve seizure freedom in a multivariate regression analysis.
“A paradigm shift in treatment and research strategies is needed to improve the long-term outcomes of newly diagnosed epilepsy. Patients with drug-resistant epilepsy should be considered early for nonpharmacological therapies, such as resective surgery and brain stimulation techniques,” the study investigators wrote.
SOURCE: Chen Z et al. JAMA Neurol. 2017 Dec 26. doi: 10.1001/jamaneurol.2017.3949
despite the wide availability of a variety of new antiepileptic drugs, according to Zhibin Chen, PhD, and his associates
The study included a total of 1,795 patients who were treated at the epilepsy unit of the Western Infirmary in Glasgow, Scotland, from July 1, 1982, to Oct. 31, 2012, and followed until Oct. 31, 2014, or until their deaths. They had a median follow-up of 11 years. Of this group, 1,144 patients were seizure free for a year or longer, including 816 who achieved seizure freedom after the first antiepileptic drug and 212 after receiving their second antiepileptic drug.
The odds ratio for each successive antiepileptic drug regimen’s failing if the first regimen failed was 1.73. The first antiepileptic drug regimen offered about a 50% probability of seizure freedom for 1 year or longer, but the probability of success was only 12% with the second regimen and 4% with the third. Attempts after the third regimen all had a probability of seizure freedom of around or below 1%. Patients who had a greater number of seizures prior to treatment, reported recreational drug use, or had first-degree relatives with a history of seizure were significantly less likely to achieve seizure freedom in a multivariate regression analysis.
“A paradigm shift in treatment and research strategies is needed to improve the long-term outcomes of newly diagnosed epilepsy. Patients with drug-resistant epilepsy should be considered early for nonpharmacological therapies, such as resective surgery and brain stimulation techniques,” the study investigators wrote.
SOURCE: Chen Z et al. JAMA Neurol. 2017 Dec 26. doi: 10.1001/jamaneurol.2017.3949
FROM JAMA NEUROLOGY
Sales of antiradiation drug skyrocket following Trump tweets
A Twitter battle over the size of each “nuclear button” possessed by President Donald Trump and North Korea’s Kim Jong-un has spiked sales of a drug that protects against radiation poisoning.
Troy Jones, who runs the website www.nukepills.com, said demand for potassium iodide soared last week, after President Trump tweeted that he had a “much bigger & more powerful” button than Kim – a statement that raised new fears about an escalating threat of nuclear war.
“North Korean Leader Kim Jong Un just stated that the ‘Nuclear Button is on his desk at all times.’ Will someone from his depleted and food starved regime please inform him that I too have a Nuclear Button, but it is a much bigger & more powerful one than his, and my Button works!”
– Donald J. Trump (@realDonaldTrump) Jan. 3, 2018
“On Jan. 2, I basically got in a month’s supply of potassium iodide and I sold out in 48 hours,” said Mr. Jones, who is a top U.S. distributor of the drug. His Mooresville, N.C., firm sells all three types of the product approved by the Food and Drug Administration. No prescription is required.
, he said.
Mr. Jones also sells to government agencies, hospitals and universities, which aren’t included in that count.
Alan Morris, president of the Williamsburg, Va.–based pharmaceutical firm Anbex, which also distributes KI, said he’s seen a bump in demand, too.
“We are a wonderful barometer of the level of anxiety in the country,” he said.
A spokeswoman for a third firm, Recipharm, which sells low-dose KI tablets, declined to comment on recent sales.
Mr. Jones said this is not the first time in recent months that jitters over growing nuclear tensions have boosted sales of KI, which comes in tablet and liquid form and should be taken within hours of exposure to radiation.
It’s the same substance often added to table salt to provide trace amounts of iodine that ensure proper thyroid function. Mr. Jones sells his tablets for about 65 cents each, though they’re cheaper in bulk. Mr. Morris said he sells the pills to the federal government for about 1 cent apiece.
Yet, neither the FDA nor the Centers for Disease Control and Prevention recommends that families stockpile potassium iodide as an antidote against nuclear emergency.
“KI cannot protect the body from radioactive elements other than radioactive iodine – if radioactive iodine is not present, taking KI is not protective and could cause harm,” the CDC’s website states.
The drug, which has a shelf life of up to 7 years, protects against absorption of radioactive iodine into the thyroid. But that means that it protects only the thyroid, not other organs or body systems, said Anupam Kotwal, MBBS, an endocrinologist speaking for the Endocrine Society.
“This is kind of mostly to protect children, people ages less than 18 and pregnant women,” Dr. Kotwal said.
States with nuclear reactors and populations within a 10-mile radius of the reactors stockpile potassium iodide to distribute in case of an emergency, according to the Nuclear Regulatory Commission. An accident involving one of those reactors is far more likely than any nuclear threat from Kim Jong-un, Anbex’s Mr. Morris said.
Still, the escalating war of words between the United States and North Korea has unsettled many people, Mr. Jones said. Although some of his buyers may hold what could be regarded as fringe views, many others do not.
“It’s moms and dads,” he said. “They’re worried and they find that these products exist.”
Such concern was underscored last week, when the CDC announced a briefing on the “Public Health Response to a Nuclear Detonation.” One of the planned sessions is titled “Preparing for the Unthinkable.”
Hundreds of people shared the announcement on social media, with varying degrees of alarm that it could have been inspired by the presidential tweet.
A CDC spokeswoman, however, said the briefing had been “in the works” since last spring. The agency held a similar session on nuclear disaster preparedness in 2010.
“CDC has been active in this area for several years, including back in 2011, when the Fukushima nuclear power plant was damaged during a major earthquake,” the agency’s Kathy Harben said in an email.
Indeed, Jones saw big spikes in potassium iodide sales after the Fukushima Daichii disaster, after North Korea started launching missiles – and after President Trump was elected.
“I now follow his Twitter feed just to gauge the day’s sales and determine how much to stock and how many radiation emergency kits to prep for the coming week,” Mr. Jones said, adding later: “I don’t think he intended to have this kind of effect.”
KHN’s coverage of these topics is supported by Laura and John Arnold Foundation and Gordon and Betty Moore Foundation. Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
A Twitter battle over the size of each “nuclear button” possessed by President Donald Trump and North Korea’s Kim Jong-un has spiked sales of a drug that protects against radiation poisoning.
Troy Jones, who runs the website www.nukepills.com, said demand for potassium iodide soared last week, after President Trump tweeted that he had a “much bigger & more powerful” button than Kim – a statement that raised new fears about an escalating threat of nuclear war.
“North Korean Leader Kim Jong Un just stated that the ‘Nuclear Button is on his desk at all times.’ Will someone from his depleted and food starved regime please inform him that I too have a Nuclear Button, but it is a much bigger & more powerful one than his, and my Button works!”
– Donald J. Trump (@realDonaldTrump) Jan. 3, 2018
“On Jan. 2, I basically got in a month’s supply of potassium iodide and I sold out in 48 hours,” said Mr. Jones, who is a top U.S. distributor of the drug. His Mooresville, N.C., firm sells all three types of the product approved by the Food and Drug Administration. No prescription is required.
, he said.
Mr. Jones also sells to government agencies, hospitals and universities, which aren’t included in that count.
Alan Morris, president of the Williamsburg, Va.–based pharmaceutical firm Anbex, which also distributes KI, said he’s seen a bump in demand, too.
“We are a wonderful barometer of the level of anxiety in the country,” he said.
A spokeswoman for a third firm, Recipharm, which sells low-dose KI tablets, declined to comment on recent sales.
Mr. Jones said this is not the first time in recent months that jitters over growing nuclear tensions have boosted sales of KI, which comes in tablet and liquid form and should be taken within hours of exposure to radiation.
It’s the same substance often added to table salt to provide trace amounts of iodine that ensure proper thyroid function. Mr. Jones sells his tablets for about 65 cents each, though they’re cheaper in bulk. Mr. Morris said he sells the pills to the federal government for about 1 cent apiece.
Yet, neither the FDA nor the Centers for Disease Control and Prevention recommends that families stockpile potassium iodide as an antidote against nuclear emergency.
“KI cannot protect the body from radioactive elements other than radioactive iodine – if radioactive iodine is not present, taking KI is not protective and could cause harm,” the CDC’s website states.
The drug, which has a shelf life of up to 7 years, protects against absorption of radioactive iodine into the thyroid. But that means that it protects only the thyroid, not other organs or body systems, said Anupam Kotwal, MBBS, an endocrinologist speaking for the Endocrine Society.
“This is kind of mostly to protect children, people ages less than 18 and pregnant women,” Dr. Kotwal said.
States with nuclear reactors and populations within a 10-mile radius of the reactors stockpile potassium iodide to distribute in case of an emergency, according to the Nuclear Regulatory Commission. An accident involving one of those reactors is far more likely than any nuclear threat from Kim Jong-un, Anbex’s Mr. Morris said.
Still, the escalating war of words between the United States and North Korea has unsettled many people, Mr. Jones said. Although some of his buyers may hold what could be regarded as fringe views, many others do not.
“It’s moms and dads,” he said. “They’re worried and they find that these products exist.”
Such concern was underscored last week, when the CDC announced a briefing on the “Public Health Response to a Nuclear Detonation.” One of the planned sessions is titled “Preparing for the Unthinkable.”
Hundreds of people shared the announcement on social media, with varying degrees of alarm that it could have been inspired by the presidential tweet.
A CDC spokeswoman, however, said the briefing had been “in the works” since last spring. The agency held a similar session on nuclear disaster preparedness in 2010.
“CDC has been active in this area for several years, including back in 2011, when the Fukushima nuclear power plant was damaged during a major earthquake,” the agency’s Kathy Harben said in an email.
Indeed, Jones saw big spikes in potassium iodide sales after the Fukushima Daichii disaster, after North Korea started launching missiles – and after President Trump was elected.
“I now follow his Twitter feed just to gauge the day’s sales and determine how much to stock and how many radiation emergency kits to prep for the coming week,” Mr. Jones said, adding later: “I don’t think he intended to have this kind of effect.”
KHN’s coverage of these topics is supported by Laura and John Arnold Foundation and Gordon and Betty Moore Foundation. Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
A Twitter battle over the size of each “nuclear button” possessed by President Donald Trump and North Korea’s Kim Jong-un has spiked sales of a drug that protects against radiation poisoning.
Troy Jones, who runs the website www.nukepills.com, said demand for potassium iodide soared last week, after President Trump tweeted that he had a “much bigger & more powerful” button than Kim – a statement that raised new fears about an escalating threat of nuclear war.
“North Korean Leader Kim Jong Un just stated that the ‘Nuclear Button is on his desk at all times.’ Will someone from his depleted and food starved regime please inform him that I too have a Nuclear Button, but it is a much bigger & more powerful one than his, and my Button works!”
– Donald J. Trump (@realDonaldTrump) Jan. 3, 2018
“On Jan. 2, I basically got in a month’s supply of potassium iodide and I sold out in 48 hours,” said Mr. Jones, who is a top U.S. distributor of the drug. His Mooresville, N.C., firm sells all three types of the product approved by the Food and Drug Administration. No prescription is required.
, he said.
Mr. Jones also sells to government agencies, hospitals and universities, which aren’t included in that count.
Alan Morris, president of the Williamsburg, Va.–based pharmaceutical firm Anbex, which also distributes KI, said he’s seen a bump in demand, too.
“We are a wonderful barometer of the level of anxiety in the country,” he said.
A spokeswoman for a third firm, Recipharm, which sells low-dose KI tablets, declined to comment on recent sales.
Mr. Jones said this is not the first time in recent months that jitters over growing nuclear tensions have boosted sales of KI, which comes in tablet and liquid form and should be taken within hours of exposure to radiation.
It’s the same substance often added to table salt to provide trace amounts of iodine that ensure proper thyroid function. Mr. Jones sells his tablets for about 65 cents each, though they’re cheaper in bulk. Mr. Morris said he sells the pills to the federal government for about 1 cent apiece.
Yet, neither the FDA nor the Centers for Disease Control and Prevention recommends that families stockpile potassium iodide as an antidote against nuclear emergency.
“KI cannot protect the body from radioactive elements other than radioactive iodine – if radioactive iodine is not present, taking KI is not protective and could cause harm,” the CDC’s website states.
The drug, which has a shelf life of up to 7 years, protects against absorption of radioactive iodine into the thyroid. But that means that it protects only the thyroid, not other organs or body systems, said Anupam Kotwal, MBBS, an endocrinologist speaking for the Endocrine Society.
“This is kind of mostly to protect children, people ages less than 18 and pregnant women,” Dr. Kotwal said.
States with nuclear reactors and populations within a 10-mile radius of the reactors stockpile potassium iodide to distribute in case of an emergency, according to the Nuclear Regulatory Commission. An accident involving one of those reactors is far more likely than any nuclear threat from Kim Jong-un, Anbex’s Mr. Morris said.
Still, the escalating war of words between the United States and North Korea has unsettled many people, Mr. Jones said. Although some of his buyers may hold what could be regarded as fringe views, many others do not.
“It’s moms and dads,” he said. “They’re worried and they find that these products exist.”
Such concern was underscored last week, when the CDC announced a briefing on the “Public Health Response to a Nuclear Detonation.” One of the planned sessions is titled “Preparing for the Unthinkable.”
Hundreds of people shared the announcement on social media, with varying degrees of alarm that it could have been inspired by the presidential tweet.
A CDC spokeswoman, however, said the briefing had been “in the works” since last spring. The agency held a similar session on nuclear disaster preparedness in 2010.
“CDC has been active in this area for several years, including back in 2011, when the Fukushima nuclear power plant was damaged during a major earthquake,” the agency’s Kathy Harben said in an email.
Indeed, Jones saw big spikes in potassium iodide sales after the Fukushima Daichii disaster, after North Korea started launching missiles – and after President Trump was elected.
“I now follow his Twitter feed just to gauge the day’s sales and determine how much to stock and how many radiation emergency kits to prep for the coming week,” Mr. Jones said, adding later: “I don’t think he intended to have this kind of effect.”
KHN’s coverage of these topics is supported by Laura and John Arnold Foundation and Gordon and Betty Moore Foundation. Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Graft-versus-host Disease Presenting Along Blaschko Lines: Cutaneous Mosaicism
To the Editor:
Graft-versus-host disease (GVHD) is a common and serious complication seen most often with bone marrow transplantation and peripheral blood stem cell transplantation. With these therapies, functional lymphoid cells are transferred from an immunocompetent donor into a nongenetically identical recipient, or "host." Because of the allogeneic nature of these transplants, the transplanted lymphoid cells have a high potential to recognize and treat the host's cells as foreign, and the resultant clinical and pathologic picture is that of GVHD. The primary organ systems affected in this immune response are the skin, gastrointestinal tract, and hepatobiliary system.1,2 Cutaneous manifestations are by far the most common.3
Although notable gains have been made in elucidating the causes, risk factors, and mechanisms that result in the clinical picture of GVHD, gaps in our knowledge and understanding still exist. Our patient represents a unique case of unilateral GVHD occurring along Blaschko lines, which has important implications for both recognizing and understanding the pathogenesis of GVHD.
A 35-year-old woman was diagnosed with stage IV follicular lymphoma and received various chemotherapy regimens over the next 4 years. Unfortunately, her disease progressed despite treatment. At 39 years of age, she underwent a nonmyeloablative allogeneic peripheral blood stem cell transplantation from a single HLA-mismatched sibling. She was placed on prednisone and cyclosporine for immunosuppression. High-dose acyclovir prophylaxis also was initiated given her history of zoster affecting the right C3 dermatome. Successful engraftment was achieved, with molecular studies showing 100% of cells following transplantation were of donor origin. Restaging at 1 and 2 years following transplantation found her to be in complete remission.
At 2 years following transplantation, she began a slow taper of immunosuppressive medications. She was successfully weaned off prednisone and continued to gradually reduce the cyclosporine dose. Toward the end of the cyclosporine taper 3 months later, she developed a pruritic eruption on the left proximal arm.
She was seen in a bone marrow transplant clinic 4 weeks after the rash developed. On examination, she had multiple, violaceous, lichenoid papules coalescing into linear bandlike plaques. One plaque extended along the left upper arm and 2 others encircled the left hemithorax, respecting the midline. She was treated empirically for zoster with valacyclovir 1 g 3 times daily based on the presumed dermatomal distribution of the eruption. Despite treatment, the rash progressed, and she developed fever. Eight days later, she was admitted with concern for disseminated zoster (Figure). Viral tissue cultures and polymerase chain reaction analysis of the lesions were negative for varicella-zoster virus and herpes simplex viruses 1 and 2. Biopsies of skin lesions on the arm and trunk were both consistent with GVHD.
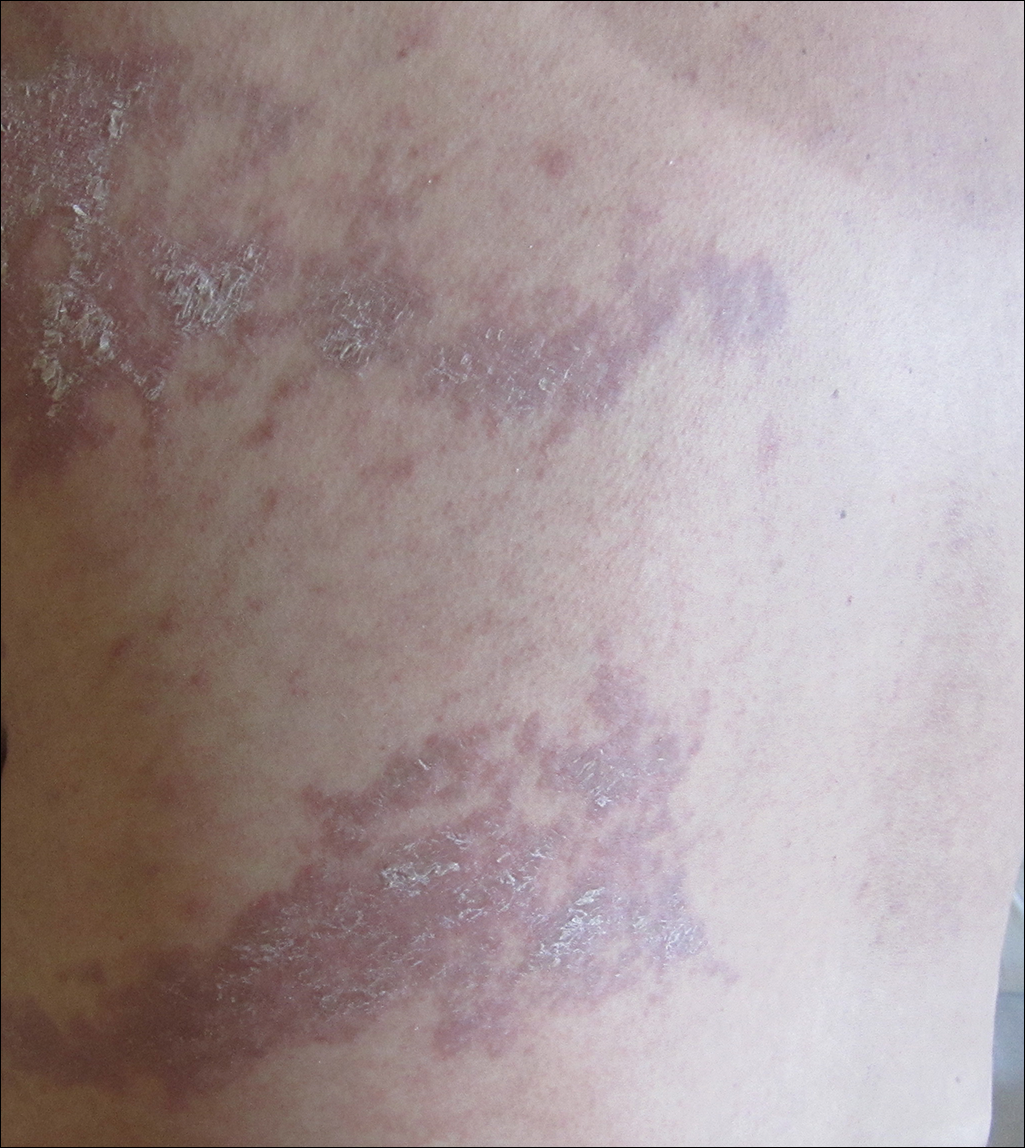
Given the clinical history, characteristic lesion morphology, and distinct linear distribution along with histopathological confirmation, a diagnosis of GVHD along Blaschko lines was made. Recognizing the cause to be immunogenic rather than infectious, immunosuppressive medications were started. In addition to increasing the prednisone and cyclosporine back to therapeutic levels, she received weekly methylprednisolone. With treatment, she showed gradual but marked improvement.
Six cases of linear GVHD have occurred as an isotopic response along dermatomes previously affected by varicella-zoster virus.4-8 These cases give credence to the idea that a cutaneous viral infection may alter the skin through unknown mechanisms, predisposing it to become affected by GVHD. Notably, this phenomenon occurred despite absence of a persistent viral genome when assessed using polymerase chain reaction analysis.4
An additional 3 cases of GVHD occurring in a dermatomal distribution without any prior infections in those areas have been reported.9,10 Of note, 2 of 3 patients did have episodes of zoster occur at other sites following transplantation and did not develop GVHD symptoms in any of those locations.9 Interestingly, controversy exists as to whether the distribution of these lesions was dermatomal or followed Blaschko lines.11
Two cases of linear GVHD have been reported in which lesions were identified as occurring along Blaschko lines.12,13 The lines of Blaschko, first described in 1901, correspond to cellular migration patterns during embryological development.14 Postzygotic mutations causing epidermal cell mosaicism may result in skin disorders occurring in segmental areas defined by the Blaschko lines.15-17 Accordingly, the Blaschko-linear pattern in GVHD suggests cellular mosaicism as the etiology in this case. Although the host's immune system develops immunotolerance to both cellular lineages during maturation, transplanted lymphoid cells from a nongenetically identical sibling may identify just one of the cell lines as nonself, producing a selective pattern of GVHD18 confined to the distribution of the genetically disparate cell line, which occurs along the lines of Blaschko in the skin. Candidate genes for mutations that would produce a mosaic following transplant GVHD include any of the 25 to 30 known minor histocompatibility antigens (or any of the several hundred yet to be found).19 Although well established for monogenic dominant disorders, in 2007 it was recognized that a postzygotic mutation can cause many complex polygenetic disorders, including GVHD, to manifest in a limited segmental pattern. This understanding, along with retrospective case review, has brought into question previously reported "dermatomal" or "zosteriform" presentations of GVHD, asserting that the linear patterns were misidentified and thus inappropriately attributed to a postviral response.20 Recognition of the Blaschko-linear distribution holds significance in both identifying lesion etiology and understanding disease pathogenesis and treatment.
Our patient illustrates a case of a Blaschko-linear GVHD. The distinctive pattern of her physical findings strongly favored epidermal cell mosaicism as the etiology of her disease. More than just a phenotypically unique case, it provided further insight into the complex etiology underlying GVHD and iterated the basic concepts of Blaschko lines and genetic alterations in development.
- Thomas ED, Storb R, Clift RA, et al. Bone-marrow transplantation. N Engl J Med. 1975;292:895-902.
- Lee SJ, Vogelsang G, Flowers ME. Chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2003;9:215-233.
- Johnson ML, Farmer ER. Graft versus host reactions in dermatology. J Am Acad Dermatol. 1998;38:369-384.
- Baselga E, Drolet BA, Segura AD, et al. Dermatomal lichenoid chronic graft-vs-host disease following varicella-zoster infection despite absence of viral genome. J Cutan Pathol. 1996;23:576-581.
- Lacour JP, Sirvent N, Monpoux F, et al. Dermatomal chronic cutaneous graft versus host disease at the site of prior herpes zoster. Br J Dermatol. 1999;141:587-589.
- Cordoba S, Fraga J, Bartolome B, et al. Giant cell lichenoid dermatitis within herpes zoster scars in a bone marrow recipient. J Cutan Pathol. 2000;27:255-257.
- Sanli H, Anadolu R, Arat M, et al. Dermatomal lichenoid graft-versus-host disease within herpes zoster scars. Int J Dermatol. 2003;42:562-564.
- Martires KJ, Baird K, Citrin DE, et al. Localization of sclerotic-type chronic graft-versus-host disease to sites of skin injury: potential insight into the mechanism of isomorphic and isotopic responses. Arch Dermatol. 2011;147:1081-1086.
- Freemer CS, Farmer ER, Corio RL, et al. Lichenoid chronic graft-vs-host disease occurring in a dermatomal distribution. Arch Dermatol. 1994;130:70-72.
- Cohen PR, Hymes SR. Linear and dermatomal cutaneous graft-versus-host disease. South Med J. 1994;87:758-761.
- Reisfeld PL. Linear lichenoid graft-vs-host disease. Arch Dermatol. 1994;130:1207-1208.
- Beers B, Kalish RS, Kaye VN, et al. Unilateral linear lichenoid eruption after bone marrow transplantation: an unmasking of tolerance to an abnormal keratinocyte clone? J Am Acad Dermatol. 1993;28(5, pt 2):888-892.
- Wilson BB, Lockman DW. Linear lichenoid graft-vs-host disease. Arch Dermatol. 1994;130:1206-1207.
- Goldberg I, Sprecher E. Patterned disorders in dermatology. Clin Dermatol. 2011;29:498-503.
- Colman SD, Rasmussen SA, Ho VT, et al. Somatic mosaicism in a patient with neurofibromatosis type 1. Am J Hum Genet. 1996;58:484-490.
- Munro CS, Wilkie AO. Epidermal mosaicism producing localised acne: somatic mutation in FGFR2. Lancet. 1998;352:704-705.
- Sakuntabhai A, Dhitavat J, Burge S, et al. Mosaicism for ATP2A2 mutations causes segmental Darier's disease. J Invest Dermatol. 2000;115:1144-1147.
- Dickinson AM, Wang XN, Sviland L, et al. In situ dissection of the graft-versus-host activities of cytotoxic T cells specific for minor histocompatibility antigens. Nat Med. 2002;8:410-414.
- Hansen JA, Chien JW, Warren EH, et al. Defining genetic risk for graft- versus-host disease and mortality following allogeneic hematopoietic stem cell transplantation. Curr Opin Hematol. 2010;17:483-492.
- Happle R. Superimposed segmental manifestation of polygenic skin disorders. J Am Acad Dermatol. 2007;57:690-699.
To the Editor:
Graft-versus-host disease (GVHD) is a common and serious complication seen most often with bone marrow transplantation and peripheral blood stem cell transplantation. With these therapies, functional lymphoid cells are transferred from an immunocompetent donor into a nongenetically identical recipient, or "host." Because of the allogeneic nature of these transplants, the transplanted lymphoid cells have a high potential to recognize and treat the host's cells as foreign, and the resultant clinical and pathologic picture is that of GVHD. The primary organ systems affected in this immune response are the skin, gastrointestinal tract, and hepatobiliary system.1,2 Cutaneous manifestations are by far the most common.3
Although notable gains have been made in elucidating the causes, risk factors, and mechanisms that result in the clinical picture of GVHD, gaps in our knowledge and understanding still exist. Our patient represents a unique case of unilateral GVHD occurring along Blaschko lines, which has important implications for both recognizing and understanding the pathogenesis of GVHD.
A 35-year-old woman was diagnosed with stage IV follicular lymphoma and received various chemotherapy regimens over the next 4 years. Unfortunately, her disease progressed despite treatment. At 39 years of age, she underwent a nonmyeloablative allogeneic peripheral blood stem cell transplantation from a single HLA-mismatched sibling. She was placed on prednisone and cyclosporine for immunosuppression. High-dose acyclovir prophylaxis also was initiated given her history of zoster affecting the right C3 dermatome. Successful engraftment was achieved, with molecular studies showing 100% of cells following transplantation were of donor origin. Restaging at 1 and 2 years following transplantation found her to be in complete remission.
At 2 years following transplantation, she began a slow taper of immunosuppressive medications. She was successfully weaned off prednisone and continued to gradually reduce the cyclosporine dose. Toward the end of the cyclosporine taper 3 months later, she developed a pruritic eruption on the left proximal arm.
She was seen in a bone marrow transplant clinic 4 weeks after the rash developed. On examination, she had multiple, violaceous, lichenoid papules coalescing into linear bandlike plaques. One plaque extended along the left upper arm and 2 others encircled the left hemithorax, respecting the midline. She was treated empirically for zoster with valacyclovir 1 g 3 times daily based on the presumed dermatomal distribution of the eruption. Despite treatment, the rash progressed, and she developed fever. Eight days later, she was admitted with concern for disseminated zoster (Figure). Viral tissue cultures and polymerase chain reaction analysis of the lesions were negative for varicella-zoster virus and herpes simplex viruses 1 and 2. Biopsies of skin lesions on the arm and trunk were both consistent with GVHD.
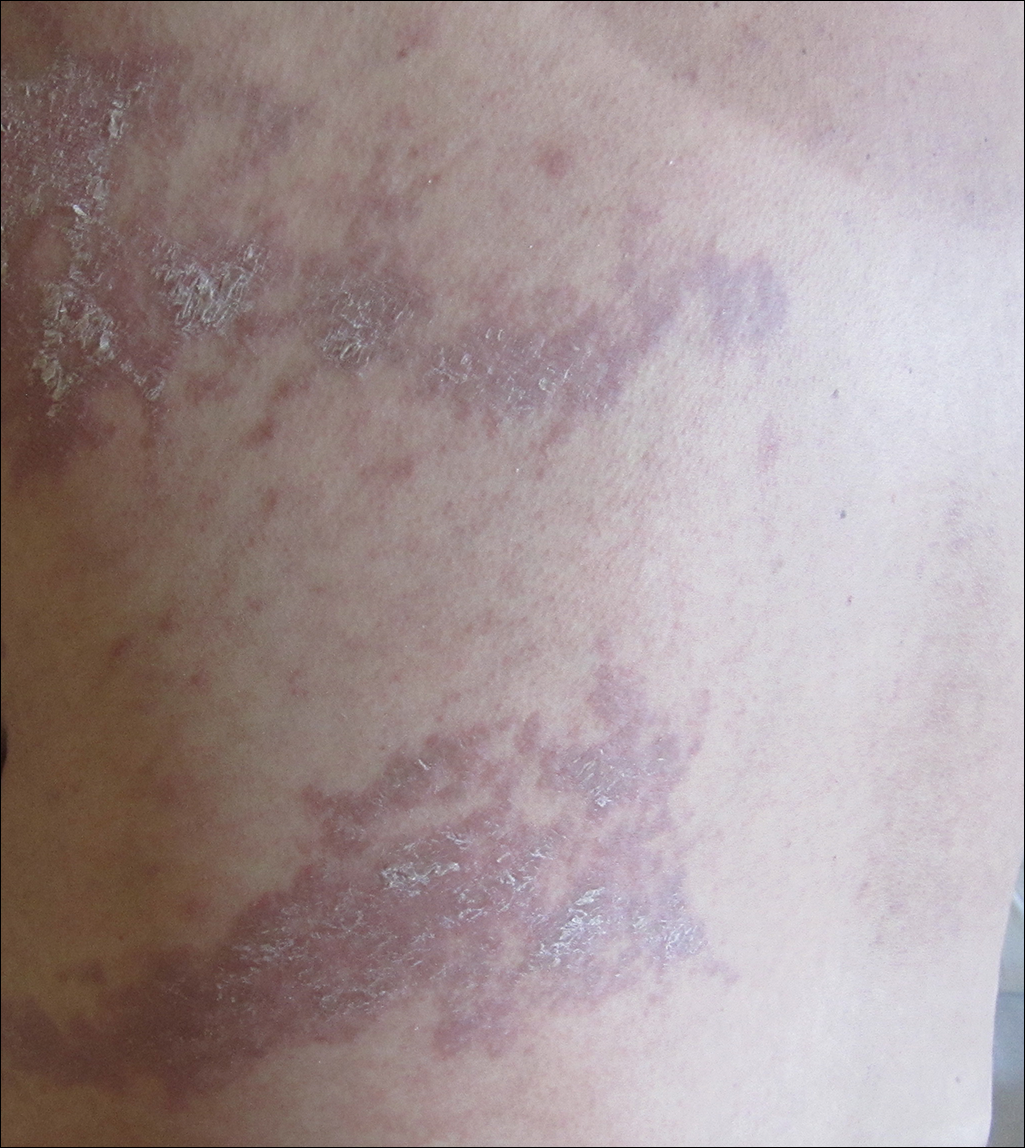
Given the clinical history, characteristic lesion morphology, and distinct linear distribution along with histopathological confirmation, a diagnosis of GVHD along Blaschko lines was made. Recognizing the cause to be immunogenic rather than infectious, immunosuppressive medications were started. In addition to increasing the prednisone and cyclosporine back to therapeutic levels, she received weekly methylprednisolone. With treatment, she showed gradual but marked improvement.
Six cases of linear GVHD have occurred as an isotopic response along dermatomes previously affected by varicella-zoster virus.4-8 These cases give credence to the idea that a cutaneous viral infection may alter the skin through unknown mechanisms, predisposing it to become affected by GVHD. Notably, this phenomenon occurred despite absence of a persistent viral genome when assessed using polymerase chain reaction analysis.4
An additional 3 cases of GVHD occurring in a dermatomal distribution without any prior infections in those areas have been reported.9,10 Of note, 2 of 3 patients did have episodes of zoster occur at other sites following transplantation and did not develop GVHD symptoms in any of those locations.9 Interestingly, controversy exists as to whether the distribution of these lesions was dermatomal or followed Blaschko lines.11
Two cases of linear GVHD have been reported in which lesions were identified as occurring along Blaschko lines.12,13 The lines of Blaschko, first described in 1901, correspond to cellular migration patterns during embryological development.14 Postzygotic mutations causing epidermal cell mosaicism may result in skin disorders occurring in segmental areas defined by the Blaschko lines.15-17 Accordingly, the Blaschko-linear pattern in GVHD suggests cellular mosaicism as the etiology in this case. Although the host's immune system develops immunotolerance to both cellular lineages during maturation, transplanted lymphoid cells from a nongenetically identical sibling may identify just one of the cell lines as nonself, producing a selective pattern of GVHD18 confined to the distribution of the genetically disparate cell line, which occurs along the lines of Blaschko in the skin. Candidate genes for mutations that would produce a mosaic following transplant GVHD include any of the 25 to 30 known minor histocompatibility antigens (or any of the several hundred yet to be found).19 Although well established for monogenic dominant disorders, in 2007 it was recognized that a postzygotic mutation can cause many complex polygenetic disorders, including GVHD, to manifest in a limited segmental pattern. This understanding, along with retrospective case review, has brought into question previously reported "dermatomal" or "zosteriform" presentations of GVHD, asserting that the linear patterns were misidentified and thus inappropriately attributed to a postviral response.20 Recognition of the Blaschko-linear distribution holds significance in both identifying lesion etiology and understanding disease pathogenesis and treatment.
Our patient illustrates a case of a Blaschko-linear GVHD. The distinctive pattern of her physical findings strongly favored epidermal cell mosaicism as the etiology of her disease. More than just a phenotypically unique case, it provided further insight into the complex etiology underlying GVHD and iterated the basic concepts of Blaschko lines and genetic alterations in development.
To the Editor:
Graft-versus-host disease (GVHD) is a common and serious complication seen most often with bone marrow transplantation and peripheral blood stem cell transplantation. With these therapies, functional lymphoid cells are transferred from an immunocompetent donor into a nongenetically identical recipient, or "host." Because of the allogeneic nature of these transplants, the transplanted lymphoid cells have a high potential to recognize and treat the host's cells as foreign, and the resultant clinical and pathologic picture is that of GVHD. The primary organ systems affected in this immune response are the skin, gastrointestinal tract, and hepatobiliary system.1,2 Cutaneous manifestations are by far the most common.3
Although notable gains have been made in elucidating the causes, risk factors, and mechanisms that result in the clinical picture of GVHD, gaps in our knowledge and understanding still exist. Our patient represents a unique case of unilateral GVHD occurring along Blaschko lines, which has important implications for both recognizing and understanding the pathogenesis of GVHD.
A 35-year-old woman was diagnosed with stage IV follicular lymphoma and received various chemotherapy regimens over the next 4 years. Unfortunately, her disease progressed despite treatment. At 39 years of age, she underwent a nonmyeloablative allogeneic peripheral blood stem cell transplantation from a single HLA-mismatched sibling. She was placed on prednisone and cyclosporine for immunosuppression. High-dose acyclovir prophylaxis also was initiated given her history of zoster affecting the right C3 dermatome. Successful engraftment was achieved, with molecular studies showing 100% of cells following transplantation were of donor origin. Restaging at 1 and 2 years following transplantation found her to be in complete remission.
At 2 years following transplantation, she began a slow taper of immunosuppressive medications. She was successfully weaned off prednisone and continued to gradually reduce the cyclosporine dose. Toward the end of the cyclosporine taper 3 months later, she developed a pruritic eruption on the left proximal arm.
She was seen in a bone marrow transplant clinic 4 weeks after the rash developed. On examination, she had multiple, violaceous, lichenoid papules coalescing into linear bandlike plaques. One plaque extended along the left upper arm and 2 others encircled the left hemithorax, respecting the midline. She was treated empirically for zoster with valacyclovir 1 g 3 times daily based on the presumed dermatomal distribution of the eruption. Despite treatment, the rash progressed, and she developed fever. Eight days later, she was admitted with concern for disseminated zoster (Figure). Viral tissue cultures and polymerase chain reaction analysis of the lesions were negative for varicella-zoster virus and herpes simplex viruses 1 and 2. Biopsies of skin lesions on the arm and trunk were both consistent with GVHD.
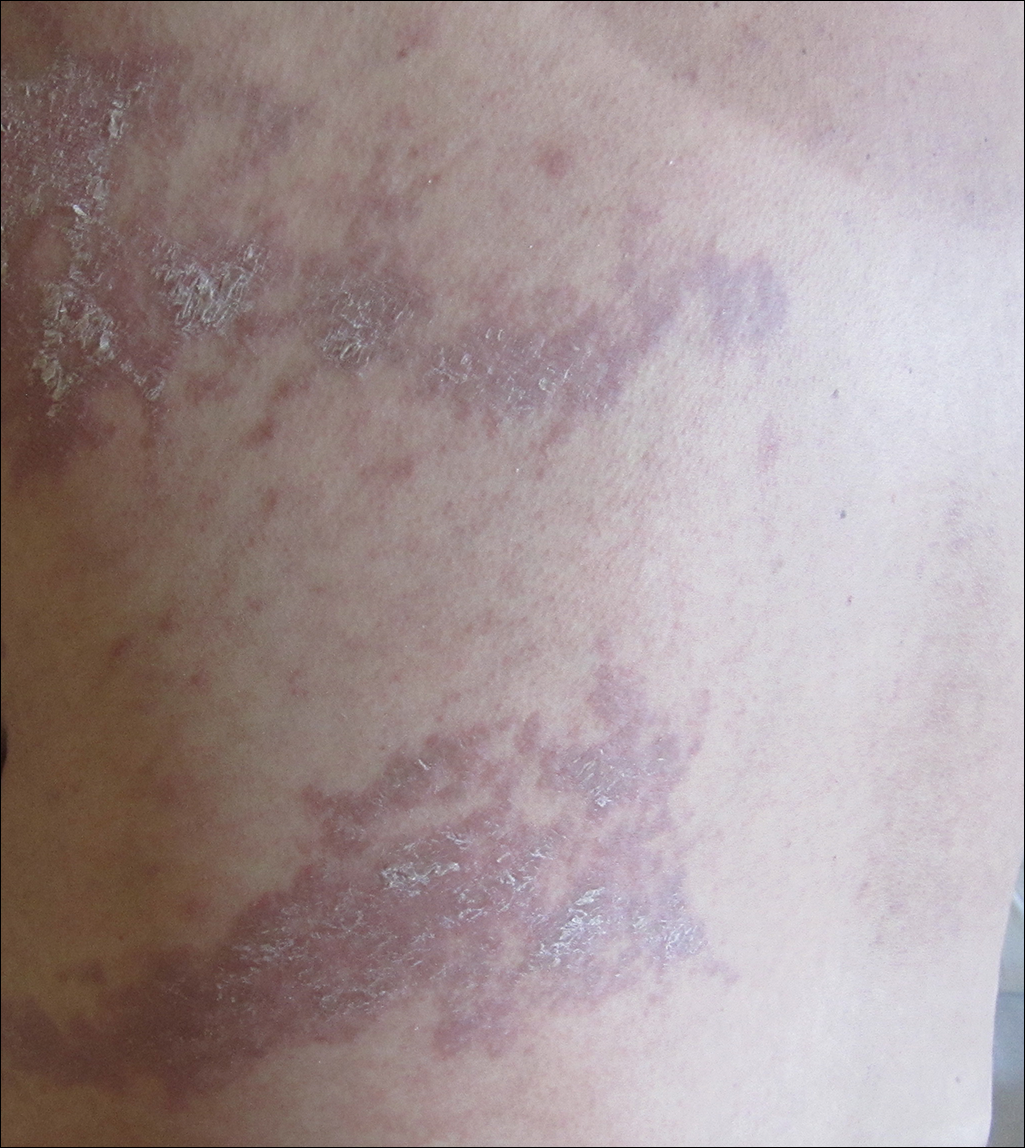
Given the clinical history, characteristic lesion morphology, and distinct linear distribution along with histopathological confirmation, a diagnosis of GVHD along Blaschko lines was made. Recognizing the cause to be immunogenic rather than infectious, immunosuppressive medications were started. In addition to increasing the prednisone and cyclosporine back to therapeutic levels, she received weekly methylprednisolone. With treatment, she showed gradual but marked improvement.
Six cases of linear GVHD have occurred as an isotopic response along dermatomes previously affected by varicella-zoster virus.4-8 These cases give credence to the idea that a cutaneous viral infection may alter the skin through unknown mechanisms, predisposing it to become affected by GVHD. Notably, this phenomenon occurred despite absence of a persistent viral genome when assessed using polymerase chain reaction analysis.4
An additional 3 cases of GVHD occurring in a dermatomal distribution without any prior infections in those areas have been reported.9,10 Of note, 2 of 3 patients did have episodes of zoster occur at other sites following transplantation and did not develop GVHD symptoms in any of those locations.9 Interestingly, controversy exists as to whether the distribution of these lesions was dermatomal or followed Blaschko lines.11
Two cases of linear GVHD have been reported in which lesions were identified as occurring along Blaschko lines.12,13 The lines of Blaschko, first described in 1901, correspond to cellular migration patterns during embryological development.14 Postzygotic mutations causing epidermal cell mosaicism may result in skin disorders occurring in segmental areas defined by the Blaschko lines.15-17 Accordingly, the Blaschko-linear pattern in GVHD suggests cellular mosaicism as the etiology in this case. Although the host's immune system develops immunotolerance to both cellular lineages during maturation, transplanted lymphoid cells from a nongenetically identical sibling may identify just one of the cell lines as nonself, producing a selective pattern of GVHD18 confined to the distribution of the genetically disparate cell line, which occurs along the lines of Blaschko in the skin. Candidate genes for mutations that would produce a mosaic following transplant GVHD include any of the 25 to 30 known minor histocompatibility antigens (or any of the several hundred yet to be found).19 Although well established for monogenic dominant disorders, in 2007 it was recognized that a postzygotic mutation can cause many complex polygenetic disorders, including GVHD, to manifest in a limited segmental pattern. This understanding, along with retrospective case review, has brought into question previously reported "dermatomal" or "zosteriform" presentations of GVHD, asserting that the linear patterns were misidentified and thus inappropriately attributed to a postviral response.20 Recognition of the Blaschko-linear distribution holds significance in both identifying lesion etiology and understanding disease pathogenesis and treatment.
Our patient illustrates a case of a Blaschko-linear GVHD. The distinctive pattern of her physical findings strongly favored epidermal cell mosaicism as the etiology of her disease. More than just a phenotypically unique case, it provided further insight into the complex etiology underlying GVHD and iterated the basic concepts of Blaschko lines and genetic alterations in development.
- Thomas ED, Storb R, Clift RA, et al. Bone-marrow transplantation. N Engl J Med. 1975;292:895-902.
- Lee SJ, Vogelsang G, Flowers ME. Chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2003;9:215-233.
- Johnson ML, Farmer ER. Graft versus host reactions in dermatology. J Am Acad Dermatol. 1998;38:369-384.
- Baselga E, Drolet BA, Segura AD, et al. Dermatomal lichenoid chronic graft-vs-host disease following varicella-zoster infection despite absence of viral genome. J Cutan Pathol. 1996;23:576-581.
- Lacour JP, Sirvent N, Monpoux F, et al. Dermatomal chronic cutaneous graft versus host disease at the site of prior herpes zoster. Br J Dermatol. 1999;141:587-589.
- Cordoba S, Fraga J, Bartolome B, et al. Giant cell lichenoid dermatitis within herpes zoster scars in a bone marrow recipient. J Cutan Pathol. 2000;27:255-257.
- Sanli H, Anadolu R, Arat M, et al. Dermatomal lichenoid graft-versus-host disease within herpes zoster scars. Int J Dermatol. 2003;42:562-564.
- Martires KJ, Baird K, Citrin DE, et al. Localization of sclerotic-type chronic graft-versus-host disease to sites of skin injury: potential insight into the mechanism of isomorphic and isotopic responses. Arch Dermatol. 2011;147:1081-1086.
- Freemer CS, Farmer ER, Corio RL, et al. Lichenoid chronic graft-vs-host disease occurring in a dermatomal distribution. Arch Dermatol. 1994;130:70-72.
- Cohen PR, Hymes SR. Linear and dermatomal cutaneous graft-versus-host disease. South Med J. 1994;87:758-761.
- Reisfeld PL. Linear lichenoid graft-vs-host disease. Arch Dermatol. 1994;130:1207-1208.
- Beers B, Kalish RS, Kaye VN, et al. Unilateral linear lichenoid eruption after bone marrow transplantation: an unmasking of tolerance to an abnormal keratinocyte clone? J Am Acad Dermatol. 1993;28(5, pt 2):888-892.
- Wilson BB, Lockman DW. Linear lichenoid graft-vs-host disease. Arch Dermatol. 1994;130:1206-1207.
- Goldberg I, Sprecher E. Patterned disorders in dermatology. Clin Dermatol. 2011;29:498-503.
- Colman SD, Rasmussen SA, Ho VT, et al. Somatic mosaicism in a patient with neurofibromatosis type 1. Am J Hum Genet. 1996;58:484-490.
- Munro CS, Wilkie AO. Epidermal mosaicism producing localised acne: somatic mutation in FGFR2. Lancet. 1998;352:704-705.
- Sakuntabhai A, Dhitavat J, Burge S, et al. Mosaicism for ATP2A2 mutations causes segmental Darier's disease. J Invest Dermatol. 2000;115:1144-1147.
- Dickinson AM, Wang XN, Sviland L, et al. In situ dissection of the graft-versus-host activities of cytotoxic T cells specific for minor histocompatibility antigens. Nat Med. 2002;8:410-414.
- Hansen JA, Chien JW, Warren EH, et al. Defining genetic risk for graft- versus-host disease and mortality following allogeneic hematopoietic stem cell transplantation. Curr Opin Hematol. 2010;17:483-492.
- Happle R. Superimposed segmental manifestation of polygenic skin disorders. J Am Acad Dermatol. 2007;57:690-699.
- Thomas ED, Storb R, Clift RA, et al. Bone-marrow transplantation. N Engl J Med. 1975;292:895-902.
- Lee SJ, Vogelsang G, Flowers ME. Chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2003;9:215-233.
- Johnson ML, Farmer ER. Graft versus host reactions in dermatology. J Am Acad Dermatol. 1998;38:369-384.
- Baselga E, Drolet BA, Segura AD, et al. Dermatomal lichenoid chronic graft-vs-host disease following varicella-zoster infection despite absence of viral genome. J Cutan Pathol. 1996;23:576-581.
- Lacour JP, Sirvent N, Monpoux F, et al. Dermatomal chronic cutaneous graft versus host disease at the site of prior herpes zoster. Br J Dermatol. 1999;141:587-589.
- Cordoba S, Fraga J, Bartolome B, et al. Giant cell lichenoid dermatitis within herpes zoster scars in a bone marrow recipient. J Cutan Pathol. 2000;27:255-257.
- Sanli H, Anadolu R, Arat M, et al. Dermatomal lichenoid graft-versus-host disease within herpes zoster scars. Int J Dermatol. 2003;42:562-564.
- Martires KJ, Baird K, Citrin DE, et al. Localization of sclerotic-type chronic graft-versus-host disease to sites of skin injury: potential insight into the mechanism of isomorphic and isotopic responses. Arch Dermatol. 2011;147:1081-1086.
- Freemer CS, Farmer ER, Corio RL, et al. Lichenoid chronic graft-vs-host disease occurring in a dermatomal distribution. Arch Dermatol. 1994;130:70-72.
- Cohen PR, Hymes SR. Linear and dermatomal cutaneous graft-versus-host disease. South Med J. 1994;87:758-761.
- Reisfeld PL. Linear lichenoid graft-vs-host disease. Arch Dermatol. 1994;130:1207-1208.
- Beers B, Kalish RS, Kaye VN, et al. Unilateral linear lichenoid eruption after bone marrow transplantation: an unmasking of tolerance to an abnormal keratinocyte clone? J Am Acad Dermatol. 1993;28(5, pt 2):888-892.
- Wilson BB, Lockman DW. Linear lichenoid graft-vs-host disease. Arch Dermatol. 1994;130:1206-1207.
- Goldberg I, Sprecher E. Patterned disorders in dermatology. Clin Dermatol. 2011;29:498-503.
- Colman SD, Rasmussen SA, Ho VT, et al. Somatic mosaicism in a patient with neurofibromatosis type 1. Am J Hum Genet. 1996;58:484-490.
- Munro CS, Wilkie AO. Epidermal mosaicism producing localised acne: somatic mutation in FGFR2. Lancet. 1998;352:704-705.
- Sakuntabhai A, Dhitavat J, Burge S, et al. Mosaicism for ATP2A2 mutations causes segmental Darier's disease. J Invest Dermatol. 2000;115:1144-1147.
- Dickinson AM, Wang XN, Sviland L, et al. In situ dissection of the graft-versus-host activities of cytotoxic T cells specific for minor histocompatibility antigens. Nat Med. 2002;8:410-414.
- Hansen JA, Chien JW, Warren EH, et al. Defining genetic risk for graft- versus-host disease and mortality following allogeneic hematopoietic stem cell transplantation. Curr Opin Hematol. 2010;17:483-492.
- Happle R. Superimposed segmental manifestation of polygenic skin disorders. J Am Acad Dermatol. 2007;57:690-699.
Practice Points
- Recognizing the characteristic manners in which different linear dermatoses present can aid in correctly identifying disorders that most commonly present in either a dermatomal or Blaschko-linear-type distribution.
- A blaschkoid-type distribution is the result of cutaneous mosaicism that occurs during embryological development and therefore subsequently produces a unique phenotypical presentation for various genetically influenced skin disorders, including graft-versus-host disease.
Hormone therapy may reduce depressive symptoms in early menopause
Hormone therapy may reduce the likelihood of depressive symptoms during early menopause, according to data from a placebo-controlled study published online Jan. 10 in JAMA Psychiatry.
Researchers randomized 172 medically healthy women who were perimenopausal or early postmenopausal to either patches of 0.1 mg of 17 beta-estradiol or placebo patches for 12 months, as well as oral micronized progesterone or placebo every 2-3 months.
Women in the placebo arm were more than twice as likely to score at least 16 on the Center for Epidemiologic Studies–Depression Scale (CES-D) at least once during the study, compared with women in the hormone therapy arm (32.3% vs. 17.3%; odds ratio, 2.5; 95% confidence interval, 1.1-5.7; P = .03). They also scored at least 16 on the scale during more visits than did women in the intervention arm (P = .002).
Women who received placebo had a significantly higher mean CES-D score over the course of the 12-month study, compared with those in the intervention arm. At 6 months, mean unadjusted CES-D scores were 5.6 in the placebo group and 4.2 in the intervention group. At 12 months, the scores were 5.7 and 4 respectively.
“Importantly, these results were significant despite statistically adjusting for change in vasomotor symptom bother, suggesting that TE+IMP [transdermal estradiol + intermittent micronized progesterone] has direct prophylactic mood benefits that are independent from its beneficial effects on menopausal symptoms, as previously observed in women with major depressive disorder treated with TE+IMP,” wrote Jennifer L. Gordon, PhD, of the psychology department at the University of Regina, Saskatchewan, and her associates.
The effect of hormone therapy on depression scores changed significantly depending on the women’s stage of menopause. Women in the early menopause transition experienced significant mood benefits, but women in the late menopause transition and those who were postmenopausal did not.
Treatment effects also were influenced by stress, as women who reported experiencing more stressful life events in the 6 months before enrolling in the study showed greater mood benefits than did those with fewer stressful life events.
However, baseline estradiol levels, baseline vasomotor symptoms, history of depression, and history of abuse did not significantly change the effects of treatment.
, compared with the placebo group, and one woman in the treatment group experienced acute deep vein thrombosis that led her to stop treatment and receive medical care. Two cases of major depressive disorder were noted in the placebo group.
Dr. Gordon and her associates cited several limitations. For example, they said, the active and placebo patches used in the study were not identical. “However, our findings remain significant when adjusting for participants’ beliefs about their treatment condition,” they wrote.
The study was supported by the National Institutes of Health, and one author was supported by a fellowship of the Fonds de la Recherche du Québec–Santé. No conflicts of interest were declared.
SOURCE: Gordon JL et al. JAMA Psychiatry. 2018 Jan 10. doi: 1010/jamapsychiatry.2018.3998.
Hormone therapy may reduce the likelihood of depressive symptoms during early menopause, according to data from a placebo-controlled study published online Jan. 10 in JAMA Psychiatry.
Researchers randomized 172 medically healthy women who were perimenopausal or early postmenopausal to either patches of 0.1 mg of 17 beta-estradiol or placebo patches for 12 months, as well as oral micronized progesterone or placebo every 2-3 months.
Women in the placebo arm were more than twice as likely to score at least 16 on the Center for Epidemiologic Studies–Depression Scale (CES-D) at least once during the study, compared with women in the hormone therapy arm (32.3% vs. 17.3%; odds ratio, 2.5; 95% confidence interval, 1.1-5.7; P = .03). They also scored at least 16 on the scale during more visits than did women in the intervention arm (P = .002).
Women who received placebo had a significantly higher mean CES-D score over the course of the 12-month study, compared with those in the intervention arm. At 6 months, mean unadjusted CES-D scores were 5.6 in the placebo group and 4.2 in the intervention group. At 12 months, the scores were 5.7 and 4 respectively.
“Importantly, these results were significant despite statistically adjusting for change in vasomotor symptom bother, suggesting that TE+IMP [transdermal estradiol + intermittent micronized progesterone] has direct prophylactic mood benefits that are independent from its beneficial effects on menopausal symptoms, as previously observed in women with major depressive disorder treated with TE+IMP,” wrote Jennifer L. Gordon, PhD, of the psychology department at the University of Regina, Saskatchewan, and her associates.
The effect of hormone therapy on depression scores changed significantly depending on the women’s stage of menopause. Women in the early menopause transition experienced significant mood benefits, but women in the late menopause transition and those who were postmenopausal did not.
Treatment effects also were influenced by stress, as women who reported experiencing more stressful life events in the 6 months before enrolling in the study showed greater mood benefits than did those with fewer stressful life events.
However, baseline estradiol levels, baseline vasomotor symptoms, history of depression, and history of abuse did not significantly change the effects of treatment.
, compared with the placebo group, and one woman in the treatment group experienced acute deep vein thrombosis that led her to stop treatment and receive medical care. Two cases of major depressive disorder were noted in the placebo group.
Dr. Gordon and her associates cited several limitations. For example, they said, the active and placebo patches used in the study were not identical. “However, our findings remain significant when adjusting for participants’ beliefs about their treatment condition,” they wrote.
The study was supported by the National Institutes of Health, and one author was supported by a fellowship of the Fonds de la Recherche du Québec–Santé. No conflicts of interest were declared.
SOURCE: Gordon JL et al. JAMA Psychiatry. 2018 Jan 10. doi: 1010/jamapsychiatry.2018.3998.
Hormone therapy may reduce the likelihood of depressive symptoms during early menopause, according to data from a placebo-controlled study published online Jan. 10 in JAMA Psychiatry.
Researchers randomized 172 medically healthy women who were perimenopausal or early postmenopausal to either patches of 0.1 mg of 17 beta-estradiol or placebo patches for 12 months, as well as oral micronized progesterone or placebo every 2-3 months.
Women in the placebo arm were more than twice as likely to score at least 16 on the Center for Epidemiologic Studies–Depression Scale (CES-D) at least once during the study, compared with women in the hormone therapy arm (32.3% vs. 17.3%; odds ratio, 2.5; 95% confidence interval, 1.1-5.7; P = .03). They also scored at least 16 on the scale during more visits than did women in the intervention arm (P = .002).
Women who received placebo had a significantly higher mean CES-D score over the course of the 12-month study, compared with those in the intervention arm. At 6 months, mean unadjusted CES-D scores were 5.6 in the placebo group and 4.2 in the intervention group. At 12 months, the scores were 5.7 and 4 respectively.
“Importantly, these results were significant despite statistically adjusting for change in vasomotor symptom bother, suggesting that TE+IMP [transdermal estradiol + intermittent micronized progesterone] has direct prophylactic mood benefits that are independent from its beneficial effects on menopausal symptoms, as previously observed in women with major depressive disorder treated with TE+IMP,” wrote Jennifer L. Gordon, PhD, of the psychology department at the University of Regina, Saskatchewan, and her associates.
The effect of hormone therapy on depression scores changed significantly depending on the women’s stage of menopause. Women in the early menopause transition experienced significant mood benefits, but women in the late menopause transition and those who were postmenopausal did not.
Treatment effects also were influenced by stress, as women who reported experiencing more stressful life events in the 6 months before enrolling in the study showed greater mood benefits than did those with fewer stressful life events.
However, baseline estradiol levels, baseline vasomotor symptoms, history of depression, and history of abuse did not significantly change the effects of treatment.
, compared with the placebo group, and one woman in the treatment group experienced acute deep vein thrombosis that led her to stop treatment and receive medical care. Two cases of major depressive disorder were noted in the placebo group.
Dr. Gordon and her associates cited several limitations. For example, they said, the active and placebo patches used in the study were not identical. “However, our findings remain significant when adjusting for participants’ beliefs about their treatment condition,” they wrote.
The study was supported by the National Institutes of Health, and one author was supported by a fellowship of the Fonds de la Recherche du Québec–Santé. No conflicts of interest were declared.
SOURCE: Gordon JL et al. JAMA Psychiatry. 2018 Jan 10. doi: 1010/jamapsychiatry.2018.3998.
FROM JAMA PSYCHIATRY
Key clinical point: Transdermal hormone therapy may reduce the likelihood of depressive symptoms in early menopause.
Major finding: Women who did not receive hormone therapy had more than a twofold higher likelihood of high depression scores, compared with women who were treated with transdermal estradiol.
Data source: Placebo-controlled, double-blind, randomized trial of 172 perimenopausal women.
Disclosures: The study was supported by the National Institutes of Health, and one author was supported by a fellowship of the Fonds de la Recherche du Québec–Santé. No conflicts of interest were declared.
Source: Gordon JL et al. JAMA Psychiatry. 2018 Jan 10. doi: 1010/jamapsychiatry.2018.3998.
views
The authors of this study are to be commended for conducting this randomized controlled trial to investigate the efficacy of a biologically rational strategy to prevent depressive symptoms in menopausal women, Hadine Joffe, MD, and Martha Hickey, MD, wrote in an accompanying editorial (JAMA Psychiatry. 2018 Jan 10. doi: 10.1001/jamapsychiatry.2017.3945).
The mechanisms of depression in menopause are not well understood, but increased changes in estradiol concentrations, nocturnal hot flashes, and sleep disturbance have been linked to the emergence of depressive symptoms. However, this study did not report accurate measures of hot flashes and sleep disturbance, which is important because of the central role of those symptoms in menopause associated mood disturbance.
Using hormone therapy in an effort to prevent depressive symptoms throughout perimenopause must be balanced with the adverse effects associated with extended exposure to hormone therapy, such as breast cancer. The results of this trial illustrate a potential role of hormone therapy in mood regulation, but they do not support changes in clinical guidance.
Dr. Joffe is affiliated with the Connors Center for Women’s Health and Gender Biology at Brigham and Women’s Hospital, the department of psychiatry at the hospital, and Harvard Medical School, all in Boston. Dr. Hickey is affiliated with the department of obstetrics and gynaecology at The University of Melbourne. Dr. Joffe was supported by the National Institute on Aging, and she declared research funding and consultancies from private industry, including Merck and SAGE. Dr. Hickey was supported by the Australian National Health and Medical Research Council and had no conflicts of interest to declare.







