User login
Encouraging early results for CB-derived NK cells in MM
CHICAGO—Cord blood (CB) is a viable source of natural killer (NK) cells for adoptive cellular therapy for multiple myeloma (MM), according to a speaker at the 2018 ASCO Annual Meeting.
Ex-vivo expanded cord blood NK cells were well tolerated without significant graft-versus-host disease (GVHD) or cytokine release syndrome (CRS) in a phase 2 study.
Nina Shah, MD, of the University of California San Francisco, reported these results as abstract 8006.*
The phase 2 study (NCT01729091) included 33 patients with symptomatic MM who were appropriate candidates for autologous stem cell transplant (ASCT).
For each patient, investigators chose cord blood units with at least a 4/6 match at HLA-A, -B and –DR.
Prior to the autologous graft, patients received lenalidomide and melphalan. Lenalidomide was given based on preclinical data suggesting synergy between that immunomodulatory agent and NK cells, Dr Shah said.
Patients were a median age of 59 (range, 25 – 72), 36% had a history of progressive disease or relapse, and 73% had adverse cytogenetics/FISH, were ISS III, or had a history of progressive disease or relapse.
Results
Dr Shah observed that in a generally high-risk population, responses to treatment with cord blood NK cells in the setting of ASCT were “encouraging,” with 79% of patients achieving very good partial response (VGPR) or better.
Twenty-one patients (64%) achieved a complete response (CR) or near CR. And 61% achieved minimal residual disease (MRD) negativity by day 100.
Patients had an estimated 3-year progression-free survival of 52%.
Three patients died, all from disease progression, and 13 patients have progressed.
The investigators observed no infusional toxicities, no GVHD, no CRS, and no neurotoxicity.
One patient experienced graft failure and was rescued with an autologous back-up graft.
"We are able to detect the donor-derived NK cells up to 13 days after infusion,” Dr Shah said, “but I think a more sensitive analysis with flow chimerism will not only allow us to detect more patients, but also better interrogate them to truly understand the in vivo phenotype and activation status of these cells."
Dr Shah indicated she and her colleagues became interested in studying cord blood for NK cell therapy because it is a known source of hematopoietic cells that is immediately available, does not require donor manipulation, and has more flexibility in genetic matching.
Previously, Dr Shah and colleagues conducted a phase 1 study, in which 12 patients received cord blood NK cells up to a dose of 1 x 108 NK cells/kg. “This was determined to be adequate and safe to move on to the phase 2,” she said.
Despite encouraging results, more research needs to be done, according to Dr Shah. “I don't think this is the end-all, be-all for NK cell therapy.”
Some future directions include combination with antibody therapy, improving NK persistence in vivo using cytokine manipulation, and possibly engineering chimeric antigen receptor (CAR)-modified NK cells, Dr Shah observed.
It’s also possible that HLA match may not be needed: “If that is the case, we will truly have an off-the-shelf source of NK cells that we can apply more readily to various patients,” she said.
The study was supported by Celgene Corporation, Stading-Younger Cancer Research Foundation, and the MD Anderson High-Risk Multiple Myeloma Moonshot Project.
*Data in the presentation differ from the abstract.
CHICAGO—Cord blood (CB) is a viable source of natural killer (NK) cells for adoptive cellular therapy for multiple myeloma (MM), according to a speaker at the 2018 ASCO Annual Meeting.
Ex-vivo expanded cord blood NK cells were well tolerated without significant graft-versus-host disease (GVHD) or cytokine release syndrome (CRS) in a phase 2 study.
Nina Shah, MD, of the University of California San Francisco, reported these results as abstract 8006.*
The phase 2 study (NCT01729091) included 33 patients with symptomatic MM who were appropriate candidates for autologous stem cell transplant (ASCT).
For each patient, investigators chose cord blood units with at least a 4/6 match at HLA-A, -B and –DR.
Prior to the autologous graft, patients received lenalidomide and melphalan. Lenalidomide was given based on preclinical data suggesting synergy between that immunomodulatory agent and NK cells, Dr Shah said.
Patients were a median age of 59 (range, 25 – 72), 36% had a history of progressive disease or relapse, and 73% had adverse cytogenetics/FISH, were ISS III, or had a history of progressive disease or relapse.
Results
Dr Shah observed that in a generally high-risk population, responses to treatment with cord blood NK cells in the setting of ASCT were “encouraging,” with 79% of patients achieving very good partial response (VGPR) or better.
Twenty-one patients (64%) achieved a complete response (CR) or near CR. And 61% achieved minimal residual disease (MRD) negativity by day 100.
Patients had an estimated 3-year progression-free survival of 52%.
Three patients died, all from disease progression, and 13 patients have progressed.
The investigators observed no infusional toxicities, no GVHD, no CRS, and no neurotoxicity.
One patient experienced graft failure and was rescued with an autologous back-up graft.
"We are able to detect the donor-derived NK cells up to 13 days after infusion,” Dr Shah said, “but I think a more sensitive analysis with flow chimerism will not only allow us to detect more patients, but also better interrogate them to truly understand the in vivo phenotype and activation status of these cells."
Dr Shah indicated she and her colleagues became interested in studying cord blood for NK cell therapy because it is a known source of hematopoietic cells that is immediately available, does not require donor manipulation, and has more flexibility in genetic matching.
Previously, Dr Shah and colleagues conducted a phase 1 study, in which 12 patients received cord blood NK cells up to a dose of 1 x 108 NK cells/kg. “This was determined to be adequate and safe to move on to the phase 2,” she said.
Despite encouraging results, more research needs to be done, according to Dr Shah. “I don't think this is the end-all, be-all for NK cell therapy.”
Some future directions include combination with antibody therapy, improving NK persistence in vivo using cytokine manipulation, and possibly engineering chimeric antigen receptor (CAR)-modified NK cells, Dr Shah observed.
It’s also possible that HLA match may not be needed: “If that is the case, we will truly have an off-the-shelf source of NK cells that we can apply more readily to various patients,” she said.
The study was supported by Celgene Corporation, Stading-Younger Cancer Research Foundation, and the MD Anderson High-Risk Multiple Myeloma Moonshot Project.
*Data in the presentation differ from the abstract.
CHICAGO—Cord blood (CB) is a viable source of natural killer (NK) cells for adoptive cellular therapy for multiple myeloma (MM), according to a speaker at the 2018 ASCO Annual Meeting.
Ex-vivo expanded cord blood NK cells were well tolerated without significant graft-versus-host disease (GVHD) or cytokine release syndrome (CRS) in a phase 2 study.
Nina Shah, MD, of the University of California San Francisco, reported these results as abstract 8006.*
The phase 2 study (NCT01729091) included 33 patients with symptomatic MM who were appropriate candidates for autologous stem cell transplant (ASCT).
For each patient, investigators chose cord blood units with at least a 4/6 match at HLA-A, -B and –DR.
Prior to the autologous graft, patients received lenalidomide and melphalan. Lenalidomide was given based on preclinical data suggesting synergy between that immunomodulatory agent and NK cells, Dr Shah said.
Patients were a median age of 59 (range, 25 – 72), 36% had a history of progressive disease or relapse, and 73% had adverse cytogenetics/FISH, were ISS III, or had a history of progressive disease or relapse.
Results
Dr Shah observed that in a generally high-risk population, responses to treatment with cord blood NK cells in the setting of ASCT were “encouraging,” with 79% of patients achieving very good partial response (VGPR) or better.
Twenty-one patients (64%) achieved a complete response (CR) or near CR. And 61% achieved minimal residual disease (MRD) negativity by day 100.
Patients had an estimated 3-year progression-free survival of 52%.
Three patients died, all from disease progression, and 13 patients have progressed.
The investigators observed no infusional toxicities, no GVHD, no CRS, and no neurotoxicity.
One patient experienced graft failure and was rescued with an autologous back-up graft.
"We are able to detect the donor-derived NK cells up to 13 days after infusion,” Dr Shah said, “but I think a more sensitive analysis with flow chimerism will not only allow us to detect more patients, but also better interrogate them to truly understand the in vivo phenotype and activation status of these cells."
Dr Shah indicated she and her colleagues became interested in studying cord blood for NK cell therapy because it is a known source of hematopoietic cells that is immediately available, does not require donor manipulation, and has more flexibility in genetic matching.
Previously, Dr Shah and colleagues conducted a phase 1 study, in which 12 patients received cord blood NK cells up to a dose of 1 x 108 NK cells/kg. “This was determined to be adequate and safe to move on to the phase 2,” she said.
Despite encouraging results, more research needs to be done, according to Dr Shah. “I don't think this is the end-all, be-all for NK cell therapy.”
Some future directions include combination with antibody therapy, improving NK persistence in vivo using cytokine manipulation, and possibly engineering chimeric antigen receptor (CAR)-modified NK cells, Dr Shah observed.
It’s also possible that HLA match may not be needed: “If that is the case, we will truly have an off-the-shelf source of NK cells that we can apply more readily to various patients,” she said.
The study was supported by Celgene Corporation, Stading-Younger Cancer Research Foundation, and the MD Anderson High-Risk Multiple Myeloma Moonshot Project.
*Data in the presentation differ from the abstract.
CAR T-cell technology making headway in MM
Chimeric antigen receptor (CAR) T-cell technology has been successfully used in the treatment of hematologic malignancies such as leukemias and lymphomas. Now, this technology has come to the forefront in multiple myeloma (MM).
Researchers at the National Cancer Institute, led by James N. Kochenderfer, MD, generated CAR T cells expressing the B-cell maturation antigen (BCMA), which is uniquely found on MM cells.
In the first in humans study, 24 patients received CAR-BCMA T cells at doses ranging between 0.3 and 3 x 106 CAR+ T cells/kg. Sixteen patients were treated at the highest dose. These patients had a median of 9.5 lines of prior therapy and 63% were refractory to their last treatment.
Thirteen patients had responses that were either partial or better and the overall response rate was 81%. Median event-free survival was 31 weeks. At the time of the report, 6 patients still have ongoing responses.
Patient cases
The report highlights a case study of a patient who had a large abdominal mass that resolved on computed tomography imaging, with λ light chains decreasing dramatically and becoming undetectable after CAR T-cell infusion. Recovery of normal plasma cells was noticeable with λ chain increases, but the ratio of κ to λ ratio remained normal 6 months after CAR T-cell infusion.
Using immunohistochemistry staining of CS138 before and 2 months after CAR-BMCA infusion, the researchers found effective depletion in bone marrow plasma cells in patients who were evaluated.
In patients who responded to treatment, decline in serum BCMA was also observed. However, in a patient who later progressed, BCMA increases were seen, leading the researchers to suggest that BCMA may be a tumor marker for MM.
The researchers noted that peak levels of CAR T cells occurred between 7 and 14 days after infusion and highest levels were seen in patients who showed antimyeloma responses.
Toxicity
CAR T-cell technology is also associated with accompanying toxicities.
At the highest dose, cytokine release syndrome (CRS) was a substantial toxicity especially in 2 patients who had a significant MM burden: in one case 80% of bone marrow cells were MM plasma cells and in the other the MM burden was 90%.
Six of the 16 patients required vasopressor support for hypotension and 1 patient required mechanical ventilation. The researchers noted that CRS of grade 3/4 was seen in patients who had a higher MM plasma cell burden.
The researchers indicated there is room for improvement. “The importance of persistence of CAR T cells in treating MM requires additional study,” they stated.
The sometimes low or absence of BCMA expression on MM cells may prompt the search for other antigens. “Treatment outcomes varied substantially between patients, and much room for improvement remains in improving the durability of antimyeloma responses and in reducing toxicity,” they concluded.
The researchers reported their findings in the Journal of Clinical Oncology.
Chimeric antigen receptor (CAR) T-cell technology has been successfully used in the treatment of hematologic malignancies such as leukemias and lymphomas. Now, this technology has come to the forefront in multiple myeloma (MM).
Researchers at the National Cancer Institute, led by James N. Kochenderfer, MD, generated CAR T cells expressing the B-cell maturation antigen (BCMA), which is uniquely found on MM cells.
In the first in humans study, 24 patients received CAR-BCMA T cells at doses ranging between 0.3 and 3 x 106 CAR+ T cells/kg. Sixteen patients were treated at the highest dose. These patients had a median of 9.5 lines of prior therapy and 63% were refractory to their last treatment.
Thirteen patients had responses that were either partial or better and the overall response rate was 81%. Median event-free survival was 31 weeks. At the time of the report, 6 patients still have ongoing responses.
Patient cases
The report highlights a case study of a patient who had a large abdominal mass that resolved on computed tomography imaging, with λ light chains decreasing dramatically and becoming undetectable after CAR T-cell infusion. Recovery of normal plasma cells was noticeable with λ chain increases, but the ratio of κ to λ ratio remained normal 6 months after CAR T-cell infusion.
Using immunohistochemistry staining of CS138 before and 2 months after CAR-BMCA infusion, the researchers found effective depletion in bone marrow plasma cells in patients who were evaluated.
In patients who responded to treatment, decline in serum BCMA was also observed. However, in a patient who later progressed, BCMA increases were seen, leading the researchers to suggest that BCMA may be a tumor marker for MM.
The researchers noted that peak levels of CAR T cells occurred between 7 and 14 days after infusion and highest levels were seen in patients who showed antimyeloma responses.
Toxicity
CAR T-cell technology is also associated with accompanying toxicities.
At the highest dose, cytokine release syndrome (CRS) was a substantial toxicity especially in 2 patients who had a significant MM burden: in one case 80% of bone marrow cells were MM plasma cells and in the other the MM burden was 90%.
Six of the 16 patients required vasopressor support for hypotension and 1 patient required mechanical ventilation. The researchers noted that CRS of grade 3/4 was seen in patients who had a higher MM plasma cell burden.
The researchers indicated there is room for improvement. “The importance of persistence of CAR T cells in treating MM requires additional study,” they stated.
The sometimes low or absence of BCMA expression on MM cells may prompt the search for other antigens. “Treatment outcomes varied substantially between patients, and much room for improvement remains in improving the durability of antimyeloma responses and in reducing toxicity,” they concluded.
The researchers reported their findings in the Journal of Clinical Oncology.
Chimeric antigen receptor (CAR) T-cell technology has been successfully used in the treatment of hematologic malignancies such as leukemias and lymphomas. Now, this technology has come to the forefront in multiple myeloma (MM).
Researchers at the National Cancer Institute, led by James N. Kochenderfer, MD, generated CAR T cells expressing the B-cell maturation antigen (BCMA), which is uniquely found on MM cells.
In the first in humans study, 24 patients received CAR-BCMA T cells at doses ranging between 0.3 and 3 x 106 CAR+ T cells/kg. Sixteen patients were treated at the highest dose. These patients had a median of 9.5 lines of prior therapy and 63% were refractory to their last treatment.
Thirteen patients had responses that were either partial or better and the overall response rate was 81%. Median event-free survival was 31 weeks. At the time of the report, 6 patients still have ongoing responses.
Patient cases
The report highlights a case study of a patient who had a large abdominal mass that resolved on computed tomography imaging, with λ light chains decreasing dramatically and becoming undetectable after CAR T-cell infusion. Recovery of normal plasma cells was noticeable with λ chain increases, but the ratio of κ to λ ratio remained normal 6 months after CAR T-cell infusion.
Using immunohistochemistry staining of CS138 before and 2 months after CAR-BMCA infusion, the researchers found effective depletion in bone marrow plasma cells in patients who were evaluated.
In patients who responded to treatment, decline in serum BCMA was also observed. However, in a patient who later progressed, BCMA increases were seen, leading the researchers to suggest that BCMA may be a tumor marker for MM.
The researchers noted that peak levels of CAR T cells occurred between 7 and 14 days after infusion and highest levels were seen in patients who showed antimyeloma responses.
Toxicity
CAR T-cell technology is also associated with accompanying toxicities.
At the highest dose, cytokine release syndrome (CRS) was a substantial toxicity especially in 2 patients who had a significant MM burden: in one case 80% of bone marrow cells were MM plasma cells and in the other the MM burden was 90%.
Six of the 16 patients required vasopressor support for hypotension and 1 patient required mechanical ventilation. The researchers noted that CRS of grade 3/4 was seen in patients who had a higher MM plasma cell burden.
The researchers indicated there is room for improvement. “The importance of persistence of CAR T cells in treating MM requires additional study,” they stated.
The sometimes low or absence of BCMA expression on MM cells may prompt the search for other antigens. “Treatment outcomes varied substantially between patients, and much room for improvement remains in improving the durability of antimyeloma responses and in reducing toxicity,” they concluded.
The researchers reported their findings in the Journal of Clinical Oncology.
FDA approves first biosimilar pegfilgrastim
The US Food and Drug Association (FDA) has approved pegfilgrastim-jmdb (Fulphila™) as the first biosimilar to Neulasta®.
The agents reduce the risk of infection or the duration of febrile neutropenia in patients treated with immunosuppressive chemotherapy for non-myeloid hematologic malignancies.
The FDA approved Fulphila based on evidence that included extensive structural and functional characterization, animal study data, human pharmacokinetic and pharmacodynamic data, clinical immunogenicity data, and other clinical safety and effectiveness data.
The evidence demonstrated that Fulphila is biosimilar to Amgen’s Neulasta. The FDA, in its announcement, noted that Fulphila has been approved as a biosimilar and not as an interchangeable product.
A biosimilar is a biological product approved based on data showing it is highly similar to a biological product already approved by the FDA, termed the reference product.
A biosimilar has no clinically meaningful differences from the reference product in terms of safety, purity, and effectiveness.
Common side effects of Fulphila include bone pain and pain in extremities.
The FDA cautions that patients with a history of serious allergic reaction to human granulocyte colony-stimulating factors, such as pegfilgrastim or filgrastim products, should not take Fulphila.
Serious side effects from Fulphila include:
- rupture of the spleen
- acute respiratory distress syndrome
- serious allergic reactions including anaphylaxis
- glomerulonephritis
- leukocytosis
- capillary leak syndrome
- potential for tumor growth
Fatal sickle cell crises have also occurred with Fulphila use.
Fulphila is not indicated for the mobilization of peripheral blood progenitor cells for hematopoietic stem cell transplantation.
The FDA is planning to release a comprehensive new plan to advance policy efforts that promote biosimilar product development, according to FDA Commissioner Scott Gotlieb, MD.
“We want to make sure that the pathway for developing biosimilar versions of approved biologics is efficient and effective, so that patients benefit from competition to existing biologics once lawful intellectual property has lapsed on these products,” he said in the announcement.
The FDA granted approval of Fulphila to Mylan GmbH. Mylan is co-developing Fulphila with Biocon.
Last fall, the agency had issued a complete response letter saying it could not approve the proposed biosimilar pending an update to the application.
The complete response letter did not raise any questions on the biosimilarity of Fulphila (investigational drug product MYL-1401H), pharmacokinetic/pharmacodynamic data, clinical data, or immunogenicity, however.
Mylan anticipates launching Fulphila in the coming weeks.
The US Food and Drug Association (FDA) has approved pegfilgrastim-jmdb (Fulphila™) as the first biosimilar to Neulasta®.
The agents reduce the risk of infection or the duration of febrile neutropenia in patients treated with immunosuppressive chemotherapy for non-myeloid hematologic malignancies.
The FDA approved Fulphila based on evidence that included extensive structural and functional characterization, animal study data, human pharmacokinetic and pharmacodynamic data, clinical immunogenicity data, and other clinical safety and effectiveness data.
The evidence demonstrated that Fulphila is biosimilar to Amgen’s Neulasta. The FDA, in its announcement, noted that Fulphila has been approved as a biosimilar and not as an interchangeable product.
A biosimilar is a biological product approved based on data showing it is highly similar to a biological product already approved by the FDA, termed the reference product.
A biosimilar has no clinically meaningful differences from the reference product in terms of safety, purity, and effectiveness.
Common side effects of Fulphila include bone pain and pain in extremities.
The FDA cautions that patients with a history of serious allergic reaction to human granulocyte colony-stimulating factors, such as pegfilgrastim or filgrastim products, should not take Fulphila.
Serious side effects from Fulphila include:
- rupture of the spleen
- acute respiratory distress syndrome
- serious allergic reactions including anaphylaxis
- glomerulonephritis
- leukocytosis
- capillary leak syndrome
- potential for tumor growth
Fatal sickle cell crises have also occurred with Fulphila use.
Fulphila is not indicated for the mobilization of peripheral blood progenitor cells for hematopoietic stem cell transplantation.
The FDA is planning to release a comprehensive new plan to advance policy efforts that promote biosimilar product development, according to FDA Commissioner Scott Gotlieb, MD.
“We want to make sure that the pathway for developing biosimilar versions of approved biologics is efficient and effective, so that patients benefit from competition to existing biologics once lawful intellectual property has lapsed on these products,” he said in the announcement.
The FDA granted approval of Fulphila to Mylan GmbH. Mylan is co-developing Fulphila with Biocon.
Last fall, the agency had issued a complete response letter saying it could not approve the proposed biosimilar pending an update to the application.
The complete response letter did not raise any questions on the biosimilarity of Fulphila (investigational drug product MYL-1401H), pharmacokinetic/pharmacodynamic data, clinical data, or immunogenicity, however.
Mylan anticipates launching Fulphila in the coming weeks.
The US Food and Drug Association (FDA) has approved pegfilgrastim-jmdb (Fulphila™) as the first biosimilar to Neulasta®.
The agents reduce the risk of infection or the duration of febrile neutropenia in patients treated with immunosuppressive chemotherapy for non-myeloid hematologic malignancies.
The FDA approved Fulphila based on evidence that included extensive structural and functional characterization, animal study data, human pharmacokinetic and pharmacodynamic data, clinical immunogenicity data, and other clinical safety and effectiveness data.
The evidence demonstrated that Fulphila is biosimilar to Amgen’s Neulasta. The FDA, in its announcement, noted that Fulphila has been approved as a biosimilar and not as an interchangeable product.
A biosimilar is a biological product approved based on data showing it is highly similar to a biological product already approved by the FDA, termed the reference product.
A biosimilar has no clinically meaningful differences from the reference product in terms of safety, purity, and effectiveness.
Common side effects of Fulphila include bone pain and pain in extremities.
The FDA cautions that patients with a history of serious allergic reaction to human granulocyte colony-stimulating factors, such as pegfilgrastim or filgrastim products, should not take Fulphila.
Serious side effects from Fulphila include:
- rupture of the spleen
- acute respiratory distress syndrome
- serious allergic reactions including anaphylaxis
- glomerulonephritis
- leukocytosis
- capillary leak syndrome
- potential for tumor growth
Fatal sickle cell crises have also occurred with Fulphila use.
Fulphila is not indicated for the mobilization of peripheral blood progenitor cells for hematopoietic stem cell transplantation.
The FDA is planning to release a comprehensive new plan to advance policy efforts that promote biosimilar product development, according to FDA Commissioner Scott Gotlieb, MD.
“We want to make sure that the pathway for developing biosimilar versions of approved biologics is efficient and effective, so that patients benefit from competition to existing biologics once lawful intellectual property has lapsed on these products,” he said in the announcement.
The FDA granted approval of Fulphila to Mylan GmbH. Mylan is co-developing Fulphila with Biocon.
Last fall, the agency had issued a complete response letter saying it could not approve the proposed biosimilar pending an update to the application.
The complete response letter did not raise any questions on the biosimilarity of Fulphila (investigational drug product MYL-1401H), pharmacokinetic/pharmacodynamic data, clinical data, or immunogenicity, however.
Mylan anticipates launching Fulphila in the coming weeks.
Pembrolizumab monotherapy shows activity in advanced recurrent ovarian cancer
CHICAGO – Pembrolizumab monotherapy is associated with antitumor activity in patients with advanced recurrent ovarian cancer, interim results from the phase 2 KEYNOTE-100 study suggest.
Notably, objective response rates among study subjects increased in tandem with increased programmed death-ligand 1 (PD-L1) expression, which helps define the population most likely to benefit from single agent pembrolizumab (Keytruda), Ursula A. Matulonis reported during an oral abstract session at the annual meeting of the American Society of Clinical Oncology.
Further, no new safety signals were identified, said Dr. Matulonis, medical director and program leader of the Medical Gynecologic Oncology Program at of Dana-Farber Cancer Institute and professor of medicine at Harvard Medical School, both in Boston.
All patients received intravenous pembrolizumab at 200 mg every 3 weeks for 2 years or until progression, death, unacceptable toxicity, or consent withdrawal, and tumor imaging was performed every 9 weeks for a year, then every 12 weeks thereafter until progressive disease, death, or study completion.
The overall response rate (ORR) among 285 patients in Cohort A, who had one to three prior chemotherapy lines for recurrent advanced ovarian cancer and a platinum-free or treatment-free interval of 3-12 months, was 7.4%, with mean duration of response of 8.2 months. The ORR among 91 patients in Cohort B, who had four to six prior chemotherapy lines and a platinum-free or treatment-free interval of at least 3 months, was 9.9%; the mean duration of response was not reached in Cohort B.
Among all-comers, the ORR was 8.0%, including 7 complete responses and 23 partial responses. Mean duration of response was 8.2 months, and 65.5% of responses lasted at least 6 months. Further, responses were observed across all subgroups, Dr. Matulonis said, noting that responses were seen regardless of age, prior lines of treatment, progression-free/treatment-free interval duration, platinum sensitivity, and histology.
“The one factor that did predict response was a [combined positive score] of 10 or higher, where there were more responses,” she said.
The ORRs among those with PD-L1 expression as measured using the combined positive score (CPS), which is defined as the number of PD-L1–positive cells out of the total number of tumor cells x 100, was 5.0% in those with CPS less than 1, 10.2% in those with CPS of 1 or greater, and 17.1% in those with CPS of 10 or greater (vs. the 8.0% ORR in the study), she explained, noting that all complete responses occurred in those with CPS of 10 or higher.
Grade 3-4 treatment-related adverse events occurred in 19.7% of patients, and included fatigue in 2.7%, and anemia, colitis, increased amylase, increased blood alkaline phosphatase, ascites, and diarrhea in 0.8-1.3%. One treatment-related death occurred in a patient with Stevens-Johnson syndrome, and another occurred in a patient with hypoaldosteronism. Immune-mediated adverse events and infusion reactions were most commonly hyperthyroidism and hypothyroidism, and most cases were grade 1-2, she said.
KEYNOTE-100 is an ongoing study that followed KEYNOTE-028, which demonstrated the clinical activity of pembrolizumab in patients with advanced ovarian cancer. To date, KEYNOTE-100 has enrolled 376 patients with epithelial ovarian, fallopian tube, or primary peritoneal cancer and confirmed recurrence after frontline platinum-based therapy. All had a tumor sample available for biomarker analysis.
The patients had a mean age of 61 years, 64% and 35% had performance status scores of 0 and 1, respectively, and 75% had high-grade serous disease.
Median follow-up in Cohort A at the time of the current analysis was 16.7 months, and in Cohort B, the median follow-up was 17.3 months. Treatment was ongoing in 15 and 6 patients in the cohorts, respectively. Reasons for discontinuation included radiographic progression (204 and 62 patients), clinical progression (24 and 17 patients), adverse events (22 and 3 patients), and patient withdrawal (9 and 3 patients). Complete responses occurred in 1 and 0 patients in the groups, respectively.
Median progression-free survival in both cohorts was 2.1 months, and overall survival was not reached in Cohort A, while it was 17.6 months in the more heavily pretreated Cohort B.
“Recurrent ovarian cancer is the leading cause of death from gynecologic cancer. The majority of our patients relapse after first-line platinum and taxane-based chemotherapy, and the degree of platinum sensitivity will predict the tumor response rates with platinum, as well as survival time,” she said, noting that subsequent recurrences become increasingly platinum and treatment resistant.
Current treatment options in these patients include chemotherapy with or without bevacizumab; the ORRs with single-agent immune checkpoint blockade are about 10%, but in KEYNOTE-028, patients with PD-L1–positive advanced recurrent ovarian cancer had an ORR of 11.5% with pembrolizumab treatment, she said.
“With 16.9 months median follow-up, the results confirm that pembrolizumab monotherapy in recurrent ovarian cancer elicits modest antitumor efficacy,” Dr. Matulonis concluded, noting that further analysis for biomarkers predictive of pembrolizumab response are ongoing.
Invited discussant Janos Laszlo Tanyi, MD, of the University of Pennsylvania, Philadelphia, said the findings underscore the overall modest ORRs of 5.9%-15% seen with anti-PD-1 or PD-L1 monotherapy in patients with advanced recurrent ovarian cancer, but noted the importance of the finding that the subpopulation of patients with increased PD-L1 expression may experience greater benefit.
Dr. Matulonis reported consulting or advisory roles with 2X Oncology, Clovis Oncology, Fujifilm, Geneos Therapeutics, Lilly, Merck, and Myriad Genetics, and research funding from Merck and Novartis. Dr .Tanyi reported having no disclosures.
SOURCE: Matulonis UA et al. ASCO 2018, Abstract 5511.
CHICAGO – Pembrolizumab monotherapy is associated with antitumor activity in patients with advanced recurrent ovarian cancer, interim results from the phase 2 KEYNOTE-100 study suggest.
Notably, objective response rates among study subjects increased in tandem with increased programmed death-ligand 1 (PD-L1) expression, which helps define the population most likely to benefit from single agent pembrolizumab (Keytruda), Ursula A. Matulonis reported during an oral abstract session at the annual meeting of the American Society of Clinical Oncology.
Further, no new safety signals were identified, said Dr. Matulonis, medical director and program leader of the Medical Gynecologic Oncology Program at of Dana-Farber Cancer Institute and professor of medicine at Harvard Medical School, both in Boston.
All patients received intravenous pembrolizumab at 200 mg every 3 weeks for 2 years or until progression, death, unacceptable toxicity, or consent withdrawal, and tumor imaging was performed every 9 weeks for a year, then every 12 weeks thereafter until progressive disease, death, or study completion.
The overall response rate (ORR) among 285 patients in Cohort A, who had one to three prior chemotherapy lines for recurrent advanced ovarian cancer and a platinum-free or treatment-free interval of 3-12 months, was 7.4%, with mean duration of response of 8.2 months. The ORR among 91 patients in Cohort B, who had four to six prior chemotherapy lines and a platinum-free or treatment-free interval of at least 3 months, was 9.9%; the mean duration of response was not reached in Cohort B.
Among all-comers, the ORR was 8.0%, including 7 complete responses and 23 partial responses. Mean duration of response was 8.2 months, and 65.5% of responses lasted at least 6 months. Further, responses were observed across all subgroups, Dr. Matulonis said, noting that responses were seen regardless of age, prior lines of treatment, progression-free/treatment-free interval duration, platinum sensitivity, and histology.
“The one factor that did predict response was a [combined positive score] of 10 or higher, where there were more responses,” she said.
The ORRs among those with PD-L1 expression as measured using the combined positive score (CPS), which is defined as the number of PD-L1–positive cells out of the total number of tumor cells x 100, was 5.0% in those with CPS less than 1, 10.2% in those with CPS of 1 or greater, and 17.1% in those with CPS of 10 or greater (vs. the 8.0% ORR in the study), she explained, noting that all complete responses occurred in those with CPS of 10 or higher.
Grade 3-4 treatment-related adverse events occurred in 19.7% of patients, and included fatigue in 2.7%, and anemia, colitis, increased amylase, increased blood alkaline phosphatase, ascites, and diarrhea in 0.8-1.3%. One treatment-related death occurred in a patient with Stevens-Johnson syndrome, and another occurred in a patient with hypoaldosteronism. Immune-mediated adverse events and infusion reactions were most commonly hyperthyroidism and hypothyroidism, and most cases were grade 1-2, she said.
KEYNOTE-100 is an ongoing study that followed KEYNOTE-028, which demonstrated the clinical activity of pembrolizumab in patients with advanced ovarian cancer. To date, KEYNOTE-100 has enrolled 376 patients with epithelial ovarian, fallopian tube, or primary peritoneal cancer and confirmed recurrence after frontline platinum-based therapy. All had a tumor sample available for biomarker analysis.
The patients had a mean age of 61 years, 64% and 35% had performance status scores of 0 and 1, respectively, and 75% had high-grade serous disease.
Median follow-up in Cohort A at the time of the current analysis was 16.7 months, and in Cohort B, the median follow-up was 17.3 months. Treatment was ongoing in 15 and 6 patients in the cohorts, respectively. Reasons for discontinuation included radiographic progression (204 and 62 patients), clinical progression (24 and 17 patients), adverse events (22 and 3 patients), and patient withdrawal (9 and 3 patients). Complete responses occurred in 1 and 0 patients in the groups, respectively.
Median progression-free survival in both cohorts was 2.1 months, and overall survival was not reached in Cohort A, while it was 17.6 months in the more heavily pretreated Cohort B.
“Recurrent ovarian cancer is the leading cause of death from gynecologic cancer. The majority of our patients relapse after first-line platinum and taxane-based chemotherapy, and the degree of platinum sensitivity will predict the tumor response rates with platinum, as well as survival time,” she said, noting that subsequent recurrences become increasingly platinum and treatment resistant.
Current treatment options in these patients include chemotherapy with or without bevacizumab; the ORRs with single-agent immune checkpoint blockade are about 10%, but in KEYNOTE-028, patients with PD-L1–positive advanced recurrent ovarian cancer had an ORR of 11.5% with pembrolizumab treatment, she said.
“With 16.9 months median follow-up, the results confirm that pembrolizumab monotherapy in recurrent ovarian cancer elicits modest antitumor efficacy,” Dr. Matulonis concluded, noting that further analysis for biomarkers predictive of pembrolizumab response are ongoing.
Invited discussant Janos Laszlo Tanyi, MD, of the University of Pennsylvania, Philadelphia, said the findings underscore the overall modest ORRs of 5.9%-15% seen with anti-PD-1 or PD-L1 monotherapy in patients with advanced recurrent ovarian cancer, but noted the importance of the finding that the subpopulation of patients with increased PD-L1 expression may experience greater benefit.
Dr. Matulonis reported consulting or advisory roles with 2X Oncology, Clovis Oncology, Fujifilm, Geneos Therapeutics, Lilly, Merck, and Myriad Genetics, and research funding from Merck and Novartis. Dr .Tanyi reported having no disclosures.
SOURCE: Matulonis UA et al. ASCO 2018, Abstract 5511.
CHICAGO – Pembrolizumab monotherapy is associated with antitumor activity in patients with advanced recurrent ovarian cancer, interim results from the phase 2 KEYNOTE-100 study suggest.
Notably, objective response rates among study subjects increased in tandem with increased programmed death-ligand 1 (PD-L1) expression, which helps define the population most likely to benefit from single agent pembrolizumab (Keytruda), Ursula A. Matulonis reported during an oral abstract session at the annual meeting of the American Society of Clinical Oncology.
Further, no new safety signals were identified, said Dr. Matulonis, medical director and program leader of the Medical Gynecologic Oncology Program at of Dana-Farber Cancer Institute and professor of medicine at Harvard Medical School, both in Boston.
All patients received intravenous pembrolizumab at 200 mg every 3 weeks for 2 years or until progression, death, unacceptable toxicity, or consent withdrawal, and tumor imaging was performed every 9 weeks for a year, then every 12 weeks thereafter until progressive disease, death, or study completion.
The overall response rate (ORR) among 285 patients in Cohort A, who had one to three prior chemotherapy lines for recurrent advanced ovarian cancer and a platinum-free or treatment-free interval of 3-12 months, was 7.4%, with mean duration of response of 8.2 months. The ORR among 91 patients in Cohort B, who had four to six prior chemotherapy lines and a platinum-free or treatment-free interval of at least 3 months, was 9.9%; the mean duration of response was not reached in Cohort B.
Among all-comers, the ORR was 8.0%, including 7 complete responses and 23 partial responses. Mean duration of response was 8.2 months, and 65.5% of responses lasted at least 6 months. Further, responses were observed across all subgroups, Dr. Matulonis said, noting that responses were seen regardless of age, prior lines of treatment, progression-free/treatment-free interval duration, platinum sensitivity, and histology.
“The one factor that did predict response was a [combined positive score] of 10 or higher, where there were more responses,” she said.
The ORRs among those with PD-L1 expression as measured using the combined positive score (CPS), which is defined as the number of PD-L1–positive cells out of the total number of tumor cells x 100, was 5.0% in those with CPS less than 1, 10.2% in those with CPS of 1 or greater, and 17.1% in those with CPS of 10 or greater (vs. the 8.0% ORR in the study), she explained, noting that all complete responses occurred in those with CPS of 10 or higher.
Grade 3-4 treatment-related adverse events occurred in 19.7% of patients, and included fatigue in 2.7%, and anemia, colitis, increased amylase, increased blood alkaline phosphatase, ascites, and diarrhea in 0.8-1.3%. One treatment-related death occurred in a patient with Stevens-Johnson syndrome, and another occurred in a patient with hypoaldosteronism. Immune-mediated adverse events and infusion reactions were most commonly hyperthyroidism and hypothyroidism, and most cases were grade 1-2, she said.
KEYNOTE-100 is an ongoing study that followed KEYNOTE-028, which demonstrated the clinical activity of pembrolizumab in patients with advanced ovarian cancer. To date, KEYNOTE-100 has enrolled 376 patients with epithelial ovarian, fallopian tube, or primary peritoneal cancer and confirmed recurrence after frontline platinum-based therapy. All had a tumor sample available for biomarker analysis.
The patients had a mean age of 61 years, 64% and 35% had performance status scores of 0 and 1, respectively, and 75% had high-grade serous disease.
Median follow-up in Cohort A at the time of the current analysis was 16.7 months, and in Cohort B, the median follow-up was 17.3 months. Treatment was ongoing in 15 and 6 patients in the cohorts, respectively. Reasons for discontinuation included radiographic progression (204 and 62 patients), clinical progression (24 and 17 patients), adverse events (22 and 3 patients), and patient withdrawal (9 and 3 patients). Complete responses occurred in 1 and 0 patients in the groups, respectively.
Median progression-free survival in both cohorts was 2.1 months, and overall survival was not reached in Cohort A, while it was 17.6 months in the more heavily pretreated Cohort B.
“Recurrent ovarian cancer is the leading cause of death from gynecologic cancer. The majority of our patients relapse after first-line platinum and taxane-based chemotherapy, and the degree of platinum sensitivity will predict the tumor response rates with platinum, as well as survival time,” she said, noting that subsequent recurrences become increasingly platinum and treatment resistant.
Current treatment options in these patients include chemotherapy with or without bevacizumab; the ORRs with single-agent immune checkpoint blockade are about 10%, but in KEYNOTE-028, patients with PD-L1–positive advanced recurrent ovarian cancer had an ORR of 11.5% with pembrolizumab treatment, she said.
“With 16.9 months median follow-up, the results confirm that pembrolizumab monotherapy in recurrent ovarian cancer elicits modest antitumor efficacy,” Dr. Matulonis concluded, noting that further analysis for biomarkers predictive of pembrolizumab response are ongoing.
Invited discussant Janos Laszlo Tanyi, MD, of the University of Pennsylvania, Philadelphia, said the findings underscore the overall modest ORRs of 5.9%-15% seen with anti-PD-1 or PD-L1 monotherapy in patients with advanced recurrent ovarian cancer, but noted the importance of the finding that the subpopulation of patients with increased PD-L1 expression may experience greater benefit.
Dr. Matulonis reported consulting or advisory roles with 2X Oncology, Clovis Oncology, Fujifilm, Geneos Therapeutics, Lilly, Merck, and Myriad Genetics, and research funding from Merck and Novartis. Dr .Tanyi reported having no disclosures.
SOURCE: Matulonis UA et al. ASCO 2018, Abstract 5511.
REPORTING FROM ASCO 2018
Key clinical point: Pembrolizumab monotherapy shows antitumor activity in advanced recurrent OC, particularly in those with higher PD-L1 expression.
Major finding: Overall response rates: 8.0% overall, 5.0% with CPS up to 1, 10.2% with CPS of 1+, and 17.1% with CPS of 10+.
Study details: Interim findings from the 376-patient phase 2 KEYNOTE-100 study.
Disclosures: Dr. Matulonis reported consulting or advisory roles with 2X Oncology, Clovis Oncology, Fujifilm, Geneos Therapeutics, Lilly, Merck, and Myriad Genetics, and research funding from Merck and Novartis. Dr. Tanyi reported having no disclosures.
Source: Matulonis UA et al. ASCO 2018, Abstract 5511.
Bladder injection may improve sexual function
An injection to the bladder may help improve sexual function along with relieving symptoms, according to a recent statistical analysis.
In a prospective observational study, 32 women with wet idiopathic overactive bladder received a 100 U/10 mL injection of onabotulinumtoxinA (onaBoNT-A) to their detrusor muscle while sedated.
The women in the study had overactive bladder syndrome with urgency urinary incontinence that was refractory to more conservative treatments. All were aged 18 years or older, sexually active, and in a relationship with the same partner for more than 3 months.
The researchers sought to distinguish the effect of the injection treatment on sexual function for women with an idiopathic, rather than neurogenic, version of the syndrome. Sexual function was assessed through a 19-item questionnaire, the Female Sexual Function Index (FSFI), before and after the treatment. To determine the efficacy of the treatment, participants kept a 3-day voiding diary, and completed two more forms: an overactive bladder screener questionnaire and the International Consultation on Incontinence Questionnaire Short Form.
Most of the participants (88.2%) saw an improvement in their overactive bladder symptoms. They also reported statistically meaningful improvement in sexual function on the FSFI, and specifically for arousal, lubrication, orgasm, and satisfaction, though not for desire and pain (average FSFI total score before and after treatment, 20.30 vs. 24.91; P = .0008).
“Although voiding diaries and questionnaires on urinary symptoms showed an improvement after onaBoNT-A injection, we documented a significant correlation only between the reduction of episodes of [urgency urinary incontinence] and improvement of FSFI total score. This finding shows that, in our population, the most relevant urinary symptom reducing the sexual function is urgency urinary incontinence,” Matteo Balzarro, MD, of Azienda Ospedaliera Universitaria Integrata of Verona, Italy, and his coauthors wrote in the European Journal of Obstetrics & Gynecology and Reproductive Biology.
The researchers noted that the small sample size resulted from multiple exclusion criteria applied to an already small population of 157 patients. They also remarked that a control group – which was absent from their study – would be difficult to have because of “ethical considerations.”
The researchers reported having no conflicts of interest.
SOURCE: Balzarro M et al. Eur J Obstet Gynecol Reprod Biol. 2018 Jun;225:228-31.
An injection to the bladder may help improve sexual function along with relieving symptoms, according to a recent statistical analysis.
In a prospective observational study, 32 women with wet idiopathic overactive bladder received a 100 U/10 mL injection of onabotulinumtoxinA (onaBoNT-A) to their detrusor muscle while sedated.
The women in the study had overactive bladder syndrome with urgency urinary incontinence that was refractory to more conservative treatments. All were aged 18 years or older, sexually active, and in a relationship with the same partner for more than 3 months.
The researchers sought to distinguish the effect of the injection treatment on sexual function for women with an idiopathic, rather than neurogenic, version of the syndrome. Sexual function was assessed through a 19-item questionnaire, the Female Sexual Function Index (FSFI), before and after the treatment. To determine the efficacy of the treatment, participants kept a 3-day voiding diary, and completed two more forms: an overactive bladder screener questionnaire and the International Consultation on Incontinence Questionnaire Short Form.
Most of the participants (88.2%) saw an improvement in their overactive bladder symptoms. They also reported statistically meaningful improvement in sexual function on the FSFI, and specifically for arousal, lubrication, orgasm, and satisfaction, though not for desire and pain (average FSFI total score before and after treatment, 20.30 vs. 24.91; P = .0008).
“Although voiding diaries and questionnaires on urinary symptoms showed an improvement after onaBoNT-A injection, we documented a significant correlation only between the reduction of episodes of [urgency urinary incontinence] and improvement of FSFI total score. This finding shows that, in our population, the most relevant urinary symptom reducing the sexual function is urgency urinary incontinence,” Matteo Balzarro, MD, of Azienda Ospedaliera Universitaria Integrata of Verona, Italy, and his coauthors wrote in the European Journal of Obstetrics & Gynecology and Reproductive Biology.
The researchers noted that the small sample size resulted from multiple exclusion criteria applied to an already small population of 157 patients. They also remarked that a control group – which was absent from their study – would be difficult to have because of “ethical considerations.”
The researchers reported having no conflicts of interest.
SOURCE: Balzarro M et al. Eur J Obstet Gynecol Reprod Biol. 2018 Jun;225:228-31.
An injection to the bladder may help improve sexual function along with relieving symptoms, according to a recent statistical analysis.
In a prospective observational study, 32 women with wet idiopathic overactive bladder received a 100 U/10 mL injection of onabotulinumtoxinA (onaBoNT-A) to their detrusor muscle while sedated.
The women in the study had overactive bladder syndrome with urgency urinary incontinence that was refractory to more conservative treatments. All were aged 18 years or older, sexually active, and in a relationship with the same partner for more than 3 months.
The researchers sought to distinguish the effect of the injection treatment on sexual function for women with an idiopathic, rather than neurogenic, version of the syndrome. Sexual function was assessed through a 19-item questionnaire, the Female Sexual Function Index (FSFI), before and after the treatment. To determine the efficacy of the treatment, participants kept a 3-day voiding diary, and completed two more forms: an overactive bladder screener questionnaire and the International Consultation on Incontinence Questionnaire Short Form.
Most of the participants (88.2%) saw an improvement in their overactive bladder symptoms. They also reported statistically meaningful improvement in sexual function on the FSFI, and specifically for arousal, lubrication, orgasm, and satisfaction, though not for desire and pain (average FSFI total score before and after treatment, 20.30 vs. 24.91; P = .0008).
“Although voiding diaries and questionnaires on urinary symptoms showed an improvement after onaBoNT-A injection, we documented a significant correlation only between the reduction of episodes of [urgency urinary incontinence] and improvement of FSFI total score. This finding shows that, in our population, the most relevant urinary symptom reducing the sexual function is urgency urinary incontinence,” Matteo Balzarro, MD, of Azienda Ospedaliera Universitaria Integrata of Verona, Italy, and his coauthors wrote in the European Journal of Obstetrics & Gynecology and Reproductive Biology.
The researchers noted that the small sample size resulted from multiple exclusion criteria applied to an already small population of 157 patients. They also remarked that a control group – which was absent from their study – would be difficult to have because of “ethical considerations.”
The researchers reported having no conflicts of interest.
SOURCE: Balzarro M et al. Eur J Obstet Gynecol Reprod Biol. 2018 Jun;225:228-31.
FROM THE EUROPEAN JOURNAL OF OBSTETRICS & GYNECOLOGY AND REPRODUCTIVE BIOLOGY
Prostate cancer risk before age 55 higher for black men
according to a new study that drew subjects aged 40-54 years from three public and two private hospitals in the Chicago area.
Black race, rather than socioeconomic or clinical factors, appeared to be the strongest nonmodifiable predictor of prostate cancer risk in that age group, the researchers concluded, based on multivariate analyses that examined the association between prostate cancer risk and clinical setting, race, genetically determined West African ancestry, and clinical and socioeconomic risk factors.
The results suggest that screening practices should be altered, said study investigator Oluwarotimi S. Nettey, MD, of Northwestern University, Chicago. “You might want to think about screening black men who are younger than 55.”
“In the prebiopsy space, most studies have looked at race, age, PSA [level], and prostate volume, and they’ve said that the reason we see that black men have disparate prostate cancer risk on diagnosis is probably because of access to care issues, so that’s been the confounder. We tried to control for this by looking at socioeconomic status through income, marriage, and education, as well as hospital setting,” said Dr. Nettey, who presented the study at a poster session at the annual meeting of the American Urological Association.
Previous studies have examined populations and then conducted a secondary analysis on outcomes in black men. The current study has greater power and is more convincing because outcomes in black men was the primary outcome of the study, according to Robert L. Waterhouse Jr., MD, who is the public policy liaison for the R. Frank Jones Urological Society of the National Medical Association. Dr. Waterhouse, a urologist in Charlotte, N.C., attended the poster session and was not involved in the research.
“This study helps to provide some evidence that black heritage is indeed a significant risk factor in men who develop prostate cancer at an earlier age, and efforts at identifying prostate cancer at an earlier age [should consider] black race as a high-risk group,” said Dr. Waterhouse.
For patients of all ages, biopsies were positive in 63.1% of black men, compared with 41.5% of nonblack men (P less than .001). Cancers were also more advanced in black men: 47.5% were Gleason 3+4 in black men, compared with 40% in nonblack men (P less than .001), and 14.4% were Gleason 4+4 in black men, compared with 9.6% in nonblack men (P = .02).
After researchers controlled for other risk factors, black race was associated with heightened risk of prostate cancer diagnosis (OR, 5.66; P = .02), as was family history (OR, 4.98; P = .01).
There was no association between West African ancestry and prostate cancer risk either as a continuous variable or in quartiles.
Limitations of the study include the fact that race was self-reported and that this was a referred population.
The study received funding from the National Institutes of Health and the U.S. Department of Veterans Affairs. Dr. Nettey reported having no financial disclosures.
SOURCE: Nettey OS et al. AUA Annual Meeting. Abstract MP 21-17.
according to a new study that drew subjects aged 40-54 years from three public and two private hospitals in the Chicago area.
Black race, rather than socioeconomic or clinical factors, appeared to be the strongest nonmodifiable predictor of prostate cancer risk in that age group, the researchers concluded, based on multivariate analyses that examined the association between prostate cancer risk and clinical setting, race, genetically determined West African ancestry, and clinical and socioeconomic risk factors.
The results suggest that screening practices should be altered, said study investigator Oluwarotimi S. Nettey, MD, of Northwestern University, Chicago. “You might want to think about screening black men who are younger than 55.”
“In the prebiopsy space, most studies have looked at race, age, PSA [level], and prostate volume, and they’ve said that the reason we see that black men have disparate prostate cancer risk on diagnosis is probably because of access to care issues, so that’s been the confounder. We tried to control for this by looking at socioeconomic status through income, marriage, and education, as well as hospital setting,” said Dr. Nettey, who presented the study at a poster session at the annual meeting of the American Urological Association.
Previous studies have examined populations and then conducted a secondary analysis on outcomes in black men. The current study has greater power and is more convincing because outcomes in black men was the primary outcome of the study, according to Robert L. Waterhouse Jr., MD, who is the public policy liaison for the R. Frank Jones Urological Society of the National Medical Association. Dr. Waterhouse, a urologist in Charlotte, N.C., attended the poster session and was not involved in the research.
“This study helps to provide some evidence that black heritage is indeed a significant risk factor in men who develop prostate cancer at an earlier age, and efforts at identifying prostate cancer at an earlier age [should consider] black race as a high-risk group,” said Dr. Waterhouse.
For patients of all ages, biopsies were positive in 63.1% of black men, compared with 41.5% of nonblack men (P less than .001). Cancers were also more advanced in black men: 47.5% were Gleason 3+4 in black men, compared with 40% in nonblack men (P less than .001), and 14.4% were Gleason 4+4 in black men, compared with 9.6% in nonblack men (P = .02).
After researchers controlled for other risk factors, black race was associated with heightened risk of prostate cancer diagnosis (OR, 5.66; P = .02), as was family history (OR, 4.98; P = .01).
There was no association between West African ancestry and prostate cancer risk either as a continuous variable or in quartiles.
Limitations of the study include the fact that race was self-reported and that this was a referred population.
The study received funding from the National Institutes of Health and the U.S. Department of Veterans Affairs. Dr. Nettey reported having no financial disclosures.
SOURCE: Nettey OS et al. AUA Annual Meeting. Abstract MP 21-17.
according to a new study that drew subjects aged 40-54 years from three public and two private hospitals in the Chicago area.
Black race, rather than socioeconomic or clinical factors, appeared to be the strongest nonmodifiable predictor of prostate cancer risk in that age group, the researchers concluded, based on multivariate analyses that examined the association between prostate cancer risk and clinical setting, race, genetically determined West African ancestry, and clinical and socioeconomic risk factors.
The results suggest that screening practices should be altered, said study investigator Oluwarotimi S. Nettey, MD, of Northwestern University, Chicago. “You might want to think about screening black men who are younger than 55.”
“In the prebiopsy space, most studies have looked at race, age, PSA [level], and prostate volume, and they’ve said that the reason we see that black men have disparate prostate cancer risk on diagnosis is probably because of access to care issues, so that’s been the confounder. We tried to control for this by looking at socioeconomic status through income, marriage, and education, as well as hospital setting,” said Dr. Nettey, who presented the study at a poster session at the annual meeting of the American Urological Association.
Previous studies have examined populations and then conducted a secondary analysis on outcomes in black men. The current study has greater power and is more convincing because outcomes in black men was the primary outcome of the study, according to Robert L. Waterhouse Jr., MD, who is the public policy liaison for the R. Frank Jones Urological Society of the National Medical Association. Dr. Waterhouse, a urologist in Charlotte, N.C., attended the poster session and was not involved in the research.
“This study helps to provide some evidence that black heritage is indeed a significant risk factor in men who develop prostate cancer at an earlier age, and efforts at identifying prostate cancer at an earlier age [should consider] black race as a high-risk group,” said Dr. Waterhouse.
For patients of all ages, biopsies were positive in 63.1% of black men, compared with 41.5% of nonblack men (P less than .001). Cancers were also more advanced in black men: 47.5% were Gleason 3+4 in black men, compared with 40% in nonblack men (P less than .001), and 14.4% were Gleason 4+4 in black men, compared with 9.6% in nonblack men (P = .02).
After researchers controlled for other risk factors, black race was associated with heightened risk of prostate cancer diagnosis (OR, 5.66; P = .02), as was family history (OR, 4.98; P = .01).
There was no association between West African ancestry and prostate cancer risk either as a continuous variable or in quartiles.
Limitations of the study include the fact that race was self-reported and that this was a referred population.
The study received funding from the National Institutes of Health and the U.S. Department of Veterans Affairs. Dr. Nettey reported having no financial disclosures.
SOURCE: Nettey OS et al. AUA Annual Meeting. Abstract MP 21-17.
REPORTING FROM THE AUA ANNUAL MEETING
Key clinical point: Black race appears to be a key risk factor for prostate cancer in younger men.
Major finding: Black men younger than age 55 years undergoing prostate biopsies were 5.6 times more likely than other men to have a positive biopsy result.
Study details: Retrospective analysis of 564 men.
Disclosures: The study received funding from the National Institutes of Health and the U.S. Department of Veterans Affairs. Dr. Nettey reported having no financial disclosures.
Source: Nettey OS et al. AUA Annual Meeting. Abstract MP 21-17.
Looking for lower Medicare drug costs? Ask your pharmacist for the cash price
As part of President Donald Trump’s blueprint to bring down prescription costs, Medicare officials have warned insurers that “gag orders” keeping pharmacists from alerting seniors that they could save money by paying cash – rather than using their insurance – are “unacceptable and contrary” to the government’s effort to promote price transparency.
But the agency stopped short of requiring insurers to lift such restrictions on pharmacists.
That doesn’t mean people with Medicare drug coverage are destined to overpay for prescriptions. But first, they must ask the pharmacist about that option, said Julie Carter, federal policy associate at the Medicare Rights Center, a patient advocacy group.
“If they bring it up, then we can inform them of those prices,” said Nick Newman, PharmD, a pharmacist and the manager at Essentra Pharmacy in rural Marengo, Ohio. “It’s a moral dilemma for the pharmacist, knowing what would be best for the patient, but not being able to help them and hoping they will ask you about the comparison.”
A simple question could unlock some savings for millions of beneficiaries.
But details may be hard to find: Medicare’s website and annual handbook don’t mention it.
“If you don’t know that there are a bunch of different prices that could be available at any given pharmacy, you don’t know what you don’t know,” said Leigh Purvis, the AARP Public Policy Institute’s director of health services research.
Researchers analyzing 9.5 million Part D prescription claims reported in a letter in the Journal of the American Medical Association in March that a patient’s copayment was higher than the cash price for nearly one in four drugs purchased in 2013. For 12 of the 20 most commonly prescribed drugs, patients overpaid by more than 33%.
Although the study found that the average overpayment for a single prescription was relatively small, Dr. Newman said he had seen consumers pay as much as $30 more than the cash price.
And many beneficiaries may not know that, if they pay a lower cash price for a covered drug at a pharmacy that participates in their insurance plan and then submit the proper documentation, insurers must count it toward their out-of-pocket expenses. The total of those expenses can trigger the drug coverage gap, commonly called the doughnut hole. (This year, the gap begins after the plan and beneficiary spend $3,750 and ends once the beneficiary has spent a total of $5,000.)
Daniel Nam, executive director of federal programs at America’s Health Insurance Plans, a trade group, agreed that “patients should have access to the lowest price possible at the pharmacy.” But he said Medicare’s warning, contained in a letter in May 2018, takes aim at an increasingly rare occurrence. Gag order clauses are “not something they are incorporating into their contracts,” he said.
UnitedHealthcare, whose popular prescription drug plans dominate the market, does not include them in any of its Medicare, Medicaid, or commercial insurance contracts, said Matt Burns, a company spokesman.
Pharmacy benefit managers also said gag orders are not typical. “If it is happening, it is very much an outlier,” said Mark Merritt, president and CEO of the Pharmaceutical Care Management Association.
However, some pharmacists disagree. Kala Shankle, policy and regulatory affairs director for the National Community Pharmacists Association, which represents 22,000 independent pharmacies, said insurers have punished pharmacists who violate gag orders by dropping them from the plan’s network.
In Ohio, one of several states that have banned gag orders in insurance contracts, including some Medicare drug plans, officials responded to complaints about the problem.
“The Department has received inquiries related to entities withholding cost-saving information from consumers, which sometimes results in an insured [patient] paying more for pharmacy benefits than the actual cost of such pharmacy benefits,” the department said in April.
Illinois and Ohio state legislators are considering bills to make such restrictions illegal, and similar legislation has been introduced in the U.S. Senate.
“If we didn’t have these gag clauses, there would not be a need for the legislation and policy changes movement that’s going on in the country,” said Garth Reynolds, executive director of the Illinois Pharmacists Association.
KHN’s coverage of prescription drug development, costs and pricing is supported by the Laura and John Arnold Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
As part of President Donald Trump’s blueprint to bring down prescription costs, Medicare officials have warned insurers that “gag orders” keeping pharmacists from alerting seniors that they could save money by paying cash – rather than using their insurance – are “unacceptable and contrary” to the government’s effort to promote price transparency.
But the agency stopped short of requiring insurers to lift such restrictions on pharmacists.
That doesn’t mean people with Medicare drug coverage are destined to overpay for prescriptions. But first, they must ask the pharmacist about that option, said Julie Carter, federal policy associate at the Medicare Rights Center, a patient advocacy group.
“If they bring it up, then we can inform them of those prices,” said Nick Newman, PharmD, a pharmacist and the manager at Essentra Pharmacy in rural Marengo, Ohio. “It’s a moral dilemma for the pharmacist, knowing what would be best for the patient, but not being able to help them and hoping they will ask you about the comparison.”
A simple question could unlock some savings for millions of beneficiaries.
But details may be hard to find: Medicare’s website and annual handbook don’t mention it.
“If you don’t know that there are a bunch of different prices that could be available at any given pharmacy, you don’t know what you don’t know,” said Leigh Purvis, the AARP Public Policy Institute’s director of health services research.
Researchers analyzing 9.5 million Part D prescription claims reported in a letter in the Journal of the American Medical Association in March that a patient’s copayment was higher than the cash price for nearly one in four drugs purchased in 2013. For 12 of the 20 most commonly prescribed drugs, patients overpaid by more than 33%.
Although the study found that the average overpayment for a single prescription was relatively small, Dr. Newman said he had seen consumers pay as much as $30 more than the cash price.
And many beneficiaries may not know that, if they pay a lower cash price for a covered drug at a pharmacy that participates in their insurance plan and then submit the proper documentation, insurers must count it toward their out-of-pocket expenses. The total of those expenses can trigger the drug coverage gap, commonly called the doughnut hole. (This year, the gap begins after the plan and beneficiary spend $3,750 and ends once the beneficiary has spent a total of $5,000.)
Daniel Nam, executive director of federal programs at America’s Health Insurance Plans, a trade group, agreed that “patients should have access to the lowest price possible at the pharmacy.” But he said Medicare’s warning, contained in a letter in May 2018, takes aim at an increasingly rare occurrence. Gag order clauses are “not something they are incorporating into their contracts,” he said.
UnitedHealthcare, whose popular prescription drug plans dominate the market, does not include them in any of its Medicare, Medicaid, or commercial insurance contracts, said Matt Burns, a company spokesman.
Pharmacy benefit managers also said gag orders are not typical. “If it is happening, it is very much an outlier,” said Mark Merritt, president and CEO of the Pharmaceutical Care Management Association.
However, some pharmacists disagree. Kala Shankle, policy and regulatory affairs director for the National Community Pharmacists Association, which represents 22,000 independent pharmacies, said insurers have punished pharmacists who violate gag orders by dropping them from the plan’s network.
In Ohio, one of several states that have banned gag orders in insurance contracts, including some Medicare drug plans, officials responded to complaints about the problem.
“The Department has received inquiries related to entities withholding cost-saving information from consumers, which sometimes results in an insured [patient] paying more for pharmacy benefits than the actual cost of such pharmacy benefits,” the department said in April.
Illinois and Ohio state legislators are considering bills to make such restrictions illegal, and similar legislation has been introduced in the U.S. Senate.
“If we didn’t have these gag clauses, there would not be a need for the legislation and policy changes movement that’s going on in the country,” said Garth Reynolds, executive director of the Illinois Pharmacists Association.
KHN’s coverage of prescription drug development, costs and pricing is supported by the Laura and John Arnold Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
As part of President Donald Trump’s blueprint to bring down prescription costs, Medicare officials have warned insurers that “gag orders” keeping pharmacists from alerting seniors that they could save money by paying cash – rather than using their insurance – are “unacceptable and contrary” to the government’s effort to promote price transparency.
But the agency stopped short of requiring insurers to lift such restrictions on pharmacists.
That doesn’t mean people with Medicare drug coverage are destined to overpay for prescriptions. But first, they must ask the pharmacist about that option, said Julie Carter, federal policy associate at the Medicare Rights Center, a patient advocacy group.
“If they bring it up, then we can inform them of those prices,” said Nick Newman, PharmD, a pharmacist and the manager at Essentra Pharmacy in rural Marengo, Ohio. “It’s a moral dilemma for the pharmacist, knowing what would be best for the patient, but not being able to help them and hoping they will ask you about the comparison.”
A simple question could unlock some savings for millions of beneficiaries.
But details may be hard to find: Medicare’s website and annual handbook don’t mention it.
“If you don’t know that there are a bunch of different prices that could be available at any given pharmacy, you don’t know what you don’t know,” said Leigh Purvis, the AARP Public Policy Institute’s director of health services research.
Researchers analyzing 9.5 million Part D prescription claims reported in a letter in the Journal of the American Medical Association in March that a patient’s copayment was higher than the cash price for nearly one in four drugs purchased in 2013. For 12 of the 20 most commonly prescribed drugs, patients overpaid by more than 33%.
Although the study found that the average overpayment for a single prescription was relatively small, Dr. Newman said he had seen consumers pay as much as $30 more than the cash price.
And many beneficiaries may not know that, if they pay a lower cash price for a covered drug at a pharmacy that participates in their insurance plan and then submit the proper documentation, insurers must count it toward their out-of-pocket expenses. The total of those expenses can trigger the drug coverage gap, commonly called the doughnut hole. (This year, the gap begins after the plan and beneficiary spend $3,750 and ends once the beneficiary has spent a total of $5,000.)
Daniel Nam, executive director of federal programs at America’s Health Insurance Plans, a trade group, agreed that “patients should have access to the lowest price possible at the pharmacy.” But he said Medicare’s warning, contained in a letter in May 2018, takes aim at an increasingly rare occurrence. Gag order clauses are “not something they are incorporating into their contracts,” he said.
UnitedHealthcare, whose popular prescription drug plans dominate the market, does not include them in any of its Medicare, Medicaid, or commercial insurance contracts, said Matt Burns, a company spokesman.
Pharmacy benefit managers also said gag orders are not typical. “If it is happening, it is very much an outlier,” said Mark Merritt, president and CEO of the Pharmaceutical Care Management Association.
However, some pharmacists disagree. Kala Shankle, policy and regulatory affairs director for the National Community Pharmacists Association, which represents 22,000 independent pharmacies, said insurers have punished pharmacists who violate gag orders by dropping them from the plan’s network.
In Ohio, one of several states that have banned gag orders in insurance contracts, including some Medicare drug plans, officials responded to complaints about the problem.
“The Department has received inquiries related to entities withholding cost-saving information from consumers, which sometimes results in an insured [patient] paying more for pharmacy benefits than the actual cost of such pharmacy benefits,” the department said in April.
Illinois and Ohio state legislators are considering bills to make such restrictions illegal, and similar legislation has been introduced in the U.S. Senate.
“If we didn’t have these gag clauses, there would not be a need for the legislation and policy changes movement that’s going on in the country,” said Garth Reynolds, executive director of the Illinois Pharmacists Association.
KHN’s coverage of prescription drug development, costs and pricing is supported by the Laura and John Arnold Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Multiple therapies for NAFLD and NASH are now in phase 3 clinical trials
WASHINGTON – Several potential treatments for nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) currently in phase 3 trials show promise in treating these complex disorders.
“When we talk emerging treatments in NASH, focusing on phase 3s [trials], there are really four drugs,” said Stephen Harrison, MD, the medical director of Pinnacle Clinical Research at the annual Digestive Disease Week®. “There’s elafibranor, obeticholic acid (OCA), selonsertib, and cenicriviroc. Each of these have there own phase 3.”
The phase 3 trials for these drugs have different primary endpoints, an important factor to consider, according to Dr. Harrison.
OCA is one of the promising drugs to treat NASH. It is already approved by the Food and Drug Administration to treat primary biliary cholangitis. In FLINT (The Farnesoid X Receptor Ligand Obeticholic Acid in NASH Treatment Trial), a phase 2 study, OCA showed promise in treating NASH. In this double-blind, randomized, controlled trial, 141 patients received 25 mg of OCA daily for 72 weeks while another 142 received placebo. By the end of the study, 45% of 110 patients in the OCA group had improved their liver histology, compared with only 21% of patients receiving placebo.
Currently, the REGENERATE trial is evaluating the effects of obeticholic acid on histologic improvement and liver related outcomes in NASH patients. Patients have been randomized to receive either 10 mg of OCA, 25 mg of OCA, or placebo. As of yet, no results have been posted.
Much as he did for trials involving OCA, Dr. Harrison also detailed the results of a phase 2b elafibranor study that led to a registration trial that is currently underway. In Golden 505 (Phase IIb Study to Evaluate the Efficacy and Safety of GFT505 Versus Placebo in Patients With Non-Alcoholic Steatohepatitis), patients were randomized to receive either GFT505 80 mg, GFT505 120 mg, or placebo. The aim of the study was to identify the percentage of responders with disappearance of steatohepatitis without worsening of fibrosis. Unfortunately, there was no difference between placebo and the treatment groups for this outcome, although a post hoc analysis did reveal that NASH resolved in a higher proportion of the 120-mg elafibranor group, compared with the placebo group (19% vs. 12%, respectively). This also translated into a reduction of 0.65 in liver fibrosis stages in responders, compared with a 0.10 increase in nonresponders (P less than .001).
Now, elafibranor is being further examined in RESOLVE-IT (Phase 3 Study to Evaluate the Efficacy and Safety of Elafibranor Versus Placebo in Patients With Nonalcoholic Steatohepatitis), but no results have been posted at press time.
Cenicriviroc has followed a similar path, with a phase 2b leading to a phase 3 study.
CENTAUR (Efficacy and Safety Study of Cenicriviroc for the Treatment of NASH in Adult Subjects With Liver Fibrosis) looked at histologic improvement in NAFLD over the course of 2 years. Patients were randomized into either the cenicriviroc 150-mg group (group A) or two placebo groups (groups B and C) for the first year of the study. In the second year of the study patients in placebo group B started to receive 150 mg cenicriviroc and group C remained as the placebo until the end of year 2. NAFLD activity scores were similar between placebo and cenicriviroc. But, fibrosis outcomes were met at a much higher rate in the cenicriviroc group, compared with those seen with placebo (20% vs. 10%, respectively; P = 0.02).
Based on these findings, AURORA (Phase 3 Study for the Efficacy and Safety of Cenicriviroc for the Treatment of Liver Fibrosis in Adults With NASH) is now evaluating the safety and efficacy of cenicriviroc in the treatment of liver fibrosis in adults with NASH.
Finally, there is selonsertib, an ASK1 inhibitor. A phase 2 trial showed that it had the potential to induce stage reduction in fibrosis at an 18-mg dose.
Now there are two phase 3 studies, STELLAR 3 and STELLAR 4, evaluating the effects of selonsertib in adults with NASH and NASH with compensated cirrhosis.
Dr. Harrison recognizes that, because of the complexity of NASH and other fatty liver diseases, trials testing therapies for these conditions face unique challenges in the approval process.
“In fatty liver disease it’s been recognized that, to do those types of studies, it’s going to take a long time to get FDA approval,” he said. “So there’s a way to get conditional approval; it’s called the Subpart H pathway, and the FDA has accepted a couple reasonable, likely surrogates. One is resolution of NASH without worsening of fibrosis, and you need to know what that definition is: resolution of NASH.” He explained this means eliminating inflammation and ballooning rather than worrying about fat on the liver biopsy.With these four drugs in the development pipeline, Dr. Harrison sees them becoming available sometime next year.
“Looking at the data, the earliest that we are looking at therapy getting into the clinic is mid-2019,” Dr. Harrison said.
Dr. Harrison has received research grants from Genfit, Intercept, and Gilead among others. He consults for Medpace, Innovate Biopharmaceuticals, and other companies. He is also on the speakers bureau for Alexion Pharmaceuticals and AbbVie.
SOURCE: Harrison S. DDW 2018, Presentation 2230.
WASHINGTON – Several potential treatments for nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) currently in phase 3 trials show promise in treating these complex disorders.
“When we talk emerging treatments in NASH, focusing on phase 3s [trials], there are really four drugs,” said Stephen Harrison, MD, the medical director of Pinnacle Clinical Research at the annual Digestive Disease Week®. “There’s elafibranor, obeticholic acid (OCA), selonsertib, and cenicriviroc. Each of these have there own phase 3.”
The phase 3 trials for these drugs have different primary endpoints, an important factor to consider, according to Dr. Harrison.
OCA is one of the promising drugs to treat NASH. It is already approved by the Food and Drug Administration to treat primary biliary cholangitis. In FLINT (The Farnesoid X Receptor Ligand Obeticholic Acid in NASH Treatment Trial), a phase 2 study, OCA showed promise in treating NASH. In this double-blind, randomized, controlled trial, 141 patients received 25 mg of OCA daily for 72 weeks while another 142 received placebo. By the end of the study, 45% of 110 patients in the OCA group had improved their liver histology, compared with only 21% of patients receiving placebo.
Currently, the REGENERATE trial is evaluating the effects of obeticholic acid on histologic improvement and liver related outcomes in NASH patients. Patients have been randomized to receive either 10 mg of OCA, 25 mg of OCA, or placebo. As of yet, no results have been posted.
Much as he did for trials involving OCA, Dr. Harrison also detailed the results of a phase 2b elafibranor study that led to a registration trial that is currently underway. In Golden 505 (Phase IIb Study to Evaluate the Efficacy and Safety of GFT505 Versus Placebo in Patients With Non-Alcoholic Steatohepatitis), patients were randomized to receive either GFT505 80 mg, GFT505 120 mg, or placebo. The aim of the study was to identify the percentage of responders with disappearance of steatohepatitis without worsening of fibrosis. Unfortunately, there was no difference between placebo and the treatment groups for this outcome, although a post hoc analysis did reveal that NASH resolved in a higher proportion of the 120-mg elafibranor group, compared with the placebo group (19% vs. 12%, respectively). This also translated into a reduction of 0.65 in liver fibrosis stages in responders, compared with a 0.10 increase in nonresponders (P less than .001).
Now, elafibranor is being further examined in RESOLVE-IT (Phase 3 Study to Evaluate the Efficacy and Safety of Elafibranor Versus Placebo in Patients With Nonalcoholic Steatohepatitis), but no results have been posted at press time.
Cenicriviroc has followed a similar path, with a phase 2b leading to a phase 3 study.
CENTAUR (Efficacy and Safety Study of Cenicriviroc for the Treatment of NASH in Adult Subjects With Liver Fibrosis) looked at histologic improvement in NAFLD over the course of 2 years. Patients were randomized into either the cenicriviroc 150-mg group (group A) or two placebo groups (groups B and C) for the first year of the study. In the second year of the study patients in placebo group B started to receive 150 mg cenicriviroc and group C remained as the placebo until the end of year 2. NAFLD activity scores were similar between placebo and cenicriviroc. But, fibrosis outcomes were met at a much higher rate in the cenicriviroc group, compared with those seen with placebo (20% vs. 10%, respectively; P = 0.02).
Based on these findings, AURORA (Phase 3 Study for the Efficacy and Safety of Cenicriviroc for the Treatment of Liver Fibrosis in Adults With NASH) is now evaluating the safety and efficacy of cenicriviroc in the treatment of liver fibrosis in adults with NASH.
Finally, there is selonsertib, an ASK1 inhibitor. A phase 2 trial showed that it had the potential to induce stage reduction in fibrosis at an 18-mg dose.
Now there are two phase 3 studies, STELLAR 3 and STELLAR 4, evaluating the effects of selonsertib in adults with NASH and NASH with compensated cirrhosis.
Dr. Harrison recognizes that, because of the complexity of NASH and other fatty liver diseases, trials testing therapies for these conditions face unique challenges in the approval process.
“In fatty liver disease it’s been recognized that, to do those types of studies, it’s going to take a long time to get FDA approval,” he said. “So there’s a way to get conditional approval; it’s called the Subpart H pathway, and the FDA has accepted a couple reasonable, likely surrogates. One is resolution of NASH without worsening of fibrosis, and you need to know what that definition is: resolution of NASH.” He explained this means eliminating inflammation and ballooning rather than worrying about fat on the liver biopsy.With these four drugs in the development pipeline, Dr. Harrison sees them becoming available sometime next year.
“Looking at the data, the earliest that we are looking at therapy getting into the clinic is mid-2019,” Dr. Harrison said.
Dr. Harrison has received research grants from Genfit, Intercept, and Gilead among others. He consults for Medpace, Innovate Biopharmaceuticals, and other companies. He is also on the speakers bureau for Alexion Pharmaceuticals and AbbVie.
SOURCE: Harrison S. DDW 2018, Presentation 2230.
WASHINGTON – Several potential treatments for nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) currently in phase 3 trials show promise in treating these complex disorders.
“When we talk emerging treatments in NASH, focusing on phase 3s [trials], there are really four drugs,” said Stephen Harrison, MD, the medical director of Pinnacle Clinical Research at the annual Digestive Disease Week®. “There’s elafibranor, obeticholic acid (OCA), selonsertib, and cenicriviroc. Each of these have there own phase 3.”
The phase 3 trials for these drugs have different primary endpoints, an important factor to consider, according to Dr. Harrison.
OCA is one of the promising drugs to treat NASH. It is already approved by the Food and Drug Administration to treat primary biliary cholangitis. In FLINT (The Farnesoid X Receptor Ligand Obeticholic Acid in NASH Treatment Trial), a phase 2 study, OCA showed promise in treating NASH. In this double-blind, randomized, controlled trial, 141 patients received 25 mg of OCA daily for 72 weeks while another 142 received placebo. By the end of the study, 45% of 110 patients in the OCA group had improved their liver histology, compared with only 21% of patients receiving placebo.
Currently, the REGENERATE trial is evaluating the effects of obeticholic acid on histologic improvement and liver related outcomes in NASH patients. Patients have been randomized to receive either 10 mg of OCA, 25 mg of OCA, or placebo. As of yet, no results have been posted.
Much as he did for trials involving OCA, Dr. Harrison also detailed the results of a phase 2b elafibranor study that led to a registration trial that is currently underway. In Golden 505 (Phase IIb Study to Evaluate the Efficacy and Safety of GFT505 Versus Placebo in Patients With Non-Alcoholic Steatohepatitis), patients were randomized to receive either GFT505 80 mg, GFT505 120 mg, or placebo. The aim of the study was to identify the percentage of responders with disappearance of steatohepatitis without worsening of fibrosis. Unfortunately, there was no difference between placebo and the treatment groups for this outcome, although a post hoc analysis did reveal that NASH resolved in a higher proportion of the 120-mg elafibranor group, compared with the placebo group (19% vs. 12%, respectively). This also translated into a reduction of 0.65 in liver fibrosis stages in responders, compared with a 0.10 increase in nonresponders (P less than .001).
Now, elafibranor is being further examined in RESOLVE-IT (Phase 3 Study to Evaluate the Efficacy and Safety of Elafibranor Versus Placebo in Patients With Nonalcoholic Steatohepatitis), but no results have been posted at press time.
Cenicriviroc has followed a similar path, with a phase 2b leading to a phase 3 study.
CENTAUR (Efficacy and Safety Study of Cenicriviroc for the Treatment of NASH in Adult Subjects With Liver Fibrosis) looked at histologic improvement in NAFLD over the course of 2 years. Patients were randomized into either the cenicriviroc 150-mg group (group A) or two placebo groups (groups B and C) for the first year of the study. In the second year of the study patients in placebo group B started to receive 150 mg cenicriviroc and group C remained as the placebo until the end of year 2. NAFLD activity scores were similar between placebo and cenicriviroc. But, fibrosis outcomes were met at a much higher rate in the cenicriviroc group, compared with those seen with placebo (20% vs. 10%, respectively; P = 0.02).
Based on these findings, AURORA (Phase 3 Study for the Efficacy and Safety of Cenicriviroc for the Treatment of Liver Fibrosis in Adults With NASH) is now evaluating the safety and efficacy of cenicriviroc in the treatment of liver fibrosis in adults with NASH.
Finally, there is selonsertib, an ASK1 inhibitor. A phase 2 trial showed that it had the potential to induce stage reduction in fibrosis at an 18-mg dose.
Now there are two phase 3 studies, STELLAR 3 and STELLAR 4, evaluating the effects of selonsertib in adults with NASH and NASH with compensated cirrhosis.
Dr. Harrison recognizes that, because of the complexity of NASH and other fatty liver diseases, trials testing therapies for these conditions face unique challenges in the approval process.
“In fatty liver disease it’s been recognized that, to do those types of studies, it’s going to take a long time to get FDA approval,” he said. “So there’s a way to get conditional approval; it’s called the Subpart H pathway, and the FDA has accepted a couple reasonable, likely surrogates. One is resolution of NASH without worsening of fibrosis, and you need to know what that definition is: resolution of NASH.” He explained this means eliminating inflammation and ballooning rather than worrying about fat on the liver biopsy.With these four drugs in the development pipeline, Dr. Harrison sees them becoming available sometime next year.
“Looking at the data, the earliest that we are looking at therapy getting into the clinic is mid-2019,” Dr. Harrison said.
Dr. Harrison has received research grants from Genfit, Intercept, and Gilead among others. He consults for Medpace, Innovate Biopharmaceuticals, and other companies. He is also on the speakers bureau for Alexion Pharmaceuticals and AbbVie.
SOURCE: Harrison S. DDW 2018, Presentation 2230.
REPORTING FROM DDW 2018
Myocarditis shows causal role in frequent PVCs
BOSTON – About half of patients who present with a new onset of frequent premature ventricular contractions without obvious underlying heart disease had an underlying myocardial inflammation that was often responsive to immunosuppressive treatment, according to a single-center series of 107 patients.
“Early diagnosis and appropriate treatment with immunosuppressive therapy can significantly affect the clinical course,” although large-scale, multicenter, randomized trials must confirm this as an effective management approach, Dhanunjaya Lakkireddy, MD, said at the annual scientific sessions of the Heart Rhythm Society. He stressed that the anecdotal efficacy seen in this series with immunosuppressive therapy and selected use of ablation treatment for the premature ventricular contractions (PVCs) applies only to patients with new-onset PVCs that occur at a rate of at least 5,000 during 24 hours who also have myocardial inflammation identified by a PET scan showing increased fluorodeoxyglucose (FDG) uptake.
The apparent impact of immunosuppressive treatment was “profound,” Dr. Lakkireddy said. The treatment usually involved prednisone and, in many patients, a second immunosuppressant agent such as azathioprine, cyclophosphamide, or methotrexate. The results suggest “a unique opportunity to intervene early with immunosuppression to change the natural course of the disease. PVCs may be the earliest sign of a disease process” featuring myocardial inflammation.
The data came from the Myocarditis and Ventricular Arrhythmia (MAVERIC) registry that Dr. Lakkireddy and his associates started because “we began seeing patients referred for ablations without underlying heart disease who had suddenly presented with a lot of PVCs,” he recalled, an observation that led them to systematically study these patients in an “arduous” process that involved several tests. One hundred seven patients met the registry’s inclusion criteria for new onset of frequent PVCs without apparent underlying heart disease, and roughly half of these patients showed clear evidence of myocardial inflammation by FDG and PET imaging. “If the PET is negative, I don’t worry about myocarditis, “ Dr. Lakkireddy said.
The 55 patients with apparent myocarditis on PET imaging, out of the 107 patients examined generally, had lower left ventricular (LV) ejection fractions averaging 46%, compared with 51% among the patients without myocarditis The patients with myocarditis further subdivided into 27 with preserved LV function, with an average ejection fraction of 60%, and 28 with a reduced LV function, with an average ejection fraction of 40%. The researchers saw an optimal response to immunosuppressive therapy in 18 of the 23 patients (78%) with preserved ejection fractions who received this treatment and in 13 of the 24 patients (54%) with diminished LV ejection fractions who got immunosuppressive therapy.
Twenty-eight of the 55 patients with myocarditis on PET imaging underwent a right-sided biopsy during their work-up, and 13 of these 28 biopsies (46%) showed a lymphocytic infiltrate of a type often seen in patients with postviral myocarditis. Seven of the 28 biopsied patients (25%) had completely normal-appearing cardiac tissue.
Dr. Lakkireddy has been a consultant to or has received research support from Biosense Webster, Boehinger Ingelheim, Bristol-Myers Squibb, Estech, Janssen, Pfizer, SentreHeart, and St. Jude.
SOURCE: Lakkireddy D et al. Heart Rhythm 2018, Abstract B-LBCT02-02.
I was quite taken by this study, which produced results that raise shock and alarm. I believe that the clinical condition that this study highlights is a real biological phenomenon that affects patients who were not on my radar screen.
From now on, I will certainly be more alert for and concerned about patients whom I see with an abrupt onset of frequent premature ventricular contractions, especially those who also have a reduced left ventricular ejection fraction. However the potential need to use serial PET examinations to identify and then follow these patients also raises concern about the cumulative radiation exposure patients could receive from serial PET studies.
David J. Callans, MD , is professor of medicine and associate director of electrophysiology at the University of Pennsylvania in Philadelphia. He has been a consultant to Abbott, Biosense Webster, Biotronik, Boston Scientific, Medtronic, and St. Jude. He made these comments as designated discussant for the report.
I was quite taken by this study, which produced results that raise shock and alarm. I believe that the clinical condition that this study highlights is a real biological phenomenon that affects patients who were not on my radar screen.
From now on, I will certainly be more alert for and concerned about patients whom I see with an abrupt onset of frequent premature ventricular contractions, especially those who also have a reduced left ventricular ejection fraction. However the potential need to use serial PET examinations to identify and then follow these patients also raises concern about the cumulative radiation exposure patients could receive from serial PET studies.
David J. Callans, MD , is professor of medicine and associate director of electrophysiology at the University of Pennsylvania in Philadelphia. He has been a consultant to Abbott, Biosense Webster, Biotronik, Boston Scientific, Medtronic, and St. Jude. He made these comments as designated discussant for the report.
I was quite taken by this study, which produced results that raise shock and alarm. I believe that the clinical condition that this study highlights is a real biological phenomenon that affects patients who were not on my radar screen.
From now on, I will certainly be more alert for and concerned about patients whom I see with an abrupt onset of frequent premature ventricular contractions, especially those who also have a reduced left ventricular ejection fraction. However the potential need to use serial PET examinations to identify and then follow these patients also raises concern about the cumulative radiation exposure patients could receive from serial PET studies.
David J. Callans, MD , is professor of medicine and associate director of electrophysiology at the University of Pennsylvania in Philadelphia. He has been a consultant to Abbott, Biosense Webster, Biotronik, Boston Scientific, Medtronic, and St. Jude. He made these comments as designated discussant for the report.
BOSTON – About half of patients who present with a new onset of frequent premature ventricular contractions without obvious underlying heart disease had an underlying myocardial inflammation that was often responsive to immunosuppressive treatment, according to a single-center series of 107 patients.
“Early diagnosis and appropriate treatment with immunosuppressive therapy can significantly affect the clinical course,” although large-scale, multicenter, randomized trials must confirm this as an effective management approach, Dhanunjaya Lakkireddy, MD, said at the annual scientific sessions of the Heart Rhythm Society. He stressed that the anecdotal efficacy seen in this series with immunosuppressive therapy and selected use of ablation treatment for the premature ventricular contractions (PVCs) applies only to patients with new-onset PVCs that occur at a rate of at least 5,000 during 24 hours who also have myocardial inflammation identified by a PET scan showing increased fluorodeoxyglucose (FDG) uptake.
The apparent impact of immunosuppressive treatment was “profound,” Dr. Lakkireddy said. The treatment usually involved prednisone and, in many patients, a second immunosuppressant agent such as azathioprine, cyclophosphamide, or methotrexate. The results suggest “a unique opportunity to intervene early with immunosuppression to change the natural course of the disease. PVCs may be the earliest sign of a disease process” featuring myocardial inflammation.
The data came from the Myocarditis and Ventricular Arrhythmia (MAVERIC) registry that Dr. Lakkireddy and his associates started because “we began seeing patients referred for ablations without underlying heart disease who had suddenly presented with a lot of PVCs,” he recalled, an observation that led them to systematically study these patients in an “arduous” process that involved several tests. One hundred seven patients met the registry’s inclusion criteria for new onset of frequent PVCs without apparent underlying heart disease, and roughly half of these patients showed clear evidence of myocardial inflammation by FDG and PET imaging. “If the PET is negative, I don’t worry about myocarditis, “ Dr. Lakkireddy said.
The 55 patients with apparent myocarditis on PET imaging, out of the 107 patients examined generally, had lower left ventricular (LV) ejection fractions averaging 46%, compared with 51% among the patients without myocarditis The patients with myocarditis further subdivided into 27 with preserved LV function, with an average ejection fraction of 60%, and 28 with a reduced LV function, with an average ejection fraction of 40%. The researchers saw an optimal response to immunosuppressive therapy in 18 of the 23 patients (78%) with preserved ejection fractions who received this treatment and in 13 of the 24 patients (54%) with diminished LV ejection fractions who got immunosuppressive therapy.
Twenty-eight of the 55 patients with myocarditis on PET imaging underwent a right-sided biopsy during their work-up, and 13 of these 28 biopsies (46%) showed a lymphocytic infiltrate of a type often seen in patients with postviral myocarditis. Seven of the 28 biopsied patients (25%) had completely normal-appearing cardiac tissue.
Dr. Lakkireddy has been a consultant to or has received research support from Biosense Webster, Boehinger Ingelheim, Bristol-Myers Squibb, Estech, Janssen, Pfizer, SentreHeart, and St. Jude.
SOURCE: Lakkireddy D et al. Heart Rhythm 2018, Abstract B-LBCT02-02.
BOSTON – About half of patients who present with a new onset of frequent premature ventricular contractions without obvious underlying heart disease had an underlying myocardial inflammation that was often responsive to immunosuppressive treatment, according to a single-center series of 107 patients.
“Early diagnosis and appropriate treatment with immunosuppressive therapy can significantly affect the clinical course,” although large-scale, multicenter, randomized trials must confirm this as an effective management approach, Dhanunjaya Lakkireddy, MD, said at the annual scientific sessions of the Heart Rhythm Society. He stressed that the anecdotal efficacy seen in this series with immunosuppressive therapy and selected use of ablation treatment for the premature ventricular contractions (PVCs) applies only to patients with new-onset PVCs that occur at a rate of at least 5,000 during 24 hours who also have myocardial inflammation identified by a PET scan showing increased fluorodeoxyglucose (FDG) uptake.
The apparent impact of immunosuppressive treatment was “profound,” Dr. Lakkireddy said. The treatment usually involved prednisone and, in many patients, a second immunosuppressant agent such as azathioprine, cyclophosphamide, or methotrexate. The results suggest “a unique opportunity to intervene early with immunosuppression to change the natural course of the disease. PVCs may be the earliest sign of a disease process” featuring myocardial inflammation.
The data came from the Myocarditis and Ventricular Arrhythmia (MAVERIC) registry that Dr. Lakkireddy and his associates started because “we began seeing patients referred for ablations without underlying heart disease who had suddenly presented with a lot of PVCs,” he recalled, an observation that led them to systematically study these patients in an “arduous” process that involved several tests. One hundred seven patients met the registry’s inclusion criteria for new onset of frequent PVCs without apparent underlying heart disease, and roughly half of these patients showed clear evidence of myocardial inflammation by FDG and PET imaging. “If the PET is negative, I don’t worry about myocarditis, “ Dr. Lakkireddy said.
The 55 patients with apparent myocarditis on PET imaging, out of the 107 patients examined generally, had lower left ventricular (LV) ejection fractions averaging 46%, compared with 51% among the patients without myocarditis The patients with myocarditis further subdivided into 27 with preserved LV function, with an average ejection fraction of 60%, and 28 with a reduced LV function, with an average ejection fraction of 40%. The researchers saw an optimal response to immunosuppressive therapy in 18 of the 23 patients (78%) with preserved ejection fractions who received this treatment and in 13 of the 24 patients (54%) with diminished LV ejection fractions who got immunosuppressive therapy.
Twenty-eight of the 55 patients with myocarditis on PET imaging underwent a right-sided biopsy during their work-up, and 13 of these 28 biopsies (46%) showed a lymphocytic infiltrate of a type often seen in patients with postviral myocarditis. Seven of the 28 biopsied patients (25%) had completely normal-appearing cardiac tissue.
Dr. Lakkireddy has been a consultant to or has received research support from Biosense Webster, Boehinger Ingelheim, Bristol-Myers Squibb, Estech, Janssen, Pfizer, SentreHeart, and St. Jude.
SOURCE: Lakkireddy D et al. Heart Rhythm 2018, Abstract B-LBCT02-02.
REPORTING FROM HEART RHYTHM 2018
Key clinical point:
Major finding: Immunosuppressive therapy resolved myocarditis in two-thirds of 51% of patients with new-onset, frequents PVCs.
Study details: Single-center series with 107 patients.
Disclosures: Dr. Lakkireddy has been a consultant to or has received research support from Biosense Webster, Boehinger Ingelheim, Bristol-Myers Squibb, Estech, Janssen, Pfizer, SentreHeart, and St. Jude.
Source: Lakkireddy D et al. Heart Rhythm 2018, Abstract B-LBCT02-02.
New models of gastroenterology practice
The variety of employment models available to gastroenterologists reflects the dynamic changes we are experiencing in medicine today. Delivery of gastrointestinal (GI) care in the United States continues to evolve in light of health care reform and the Affordable Care Act.1 Within the past decade, as health systems and payers continue to consolidate, regulatory pressures have increased steadily and new policies such as electronic documentation and mandatory quality metrics reporting have added new challenges to the emerging generation of gastroenterologists.2 Although the lay press tends to focus on health care costs, coverage, physician reimbursement, provider burnout, health system consolidation, and value-based payment models, relatively less has been published about emerging employment and practice models.
Here,
Background
When the senior author graduated from fellowship in 1983 (J.I.A.), gastroenterology practice model choices were limited to essentially 4: independent community-based, single-specialty, physician-owned practice (solo or small group); independent multispecialty physician-owned practice; hospital or health system–owned multispecialty practice; and academic practice (including the Veterans Administration Medical Centers).
In the private sector, young community gastroenterologists typically would join a physician-owned practice and spend time (2–5 y) as an employed physician in a partnership track. During this time, his/her salary was subsidized while he/she built a practice base. Then, they would buy into the Professional Association with cash or equity equivalents and become a partner. As a partner, he/she then had the opportunity to share in ancillary revenue streams such as facility fees derived from a practice-owned ambulatory endoscopy center (AEC). By contrast, young academic faculty would be hired as an instructor and, if successful, climb the traditional ladder track to assistant, associate, and professor of medicine in an academic medical center (AMC).
In the 1980s, a typical community GI practice comprised 1 to 8 physicians, with most having been formed by 1 or 2 male gastroenterologists in the early 1970s when flexible endoscopy moved into clinical practice. The three practices that eventually would become Minnesota Gastroenterology (where J.I.A. practiced) opened in 1972. In 1996, the three practices merged into a single group of 38 physicians with ownership in three AECs. Advanced practice nurses and physician assistants were not yet part of the equation. Colonoscopy represented 48% of procedure volume, accounts receivable (time between submitting an insurance claim and being paid) averaged 88 days, and physicians averaged 9000 work relative value units (wRVUs) per partner annually. By comparison, median wRVUs for a full-time community GI in 1996 was 10,422 according to the Medical Group Management Association.3 Annual gross revenue (before expenses) per physician was approximately $400,000, and overhead reached 38% and 47% of revenue (there were 2 divisions). Partner incomes were at the 12% level of the Medical Group Management Association for gastroenterologists (personal management notes of J.I.A.). Minnesota Gastroenterology was the largest single-specialty GI practice in 1996 and its consolidation foreshadowed a trend that has accelerated over the ensuing generation.
When one of the authors (N.K.) graduated from the University of California Los Angeles in 2017, the GI employment landscape had evolved considerably. At least five new models of GI practice had emerged: individual incorporation with a Professional Services Agreement (PSA), a clinician track within an AMC, large single-specialty group practice (partnership or employee), private equity-backed multistate practice, and locum tenens (Figure 1).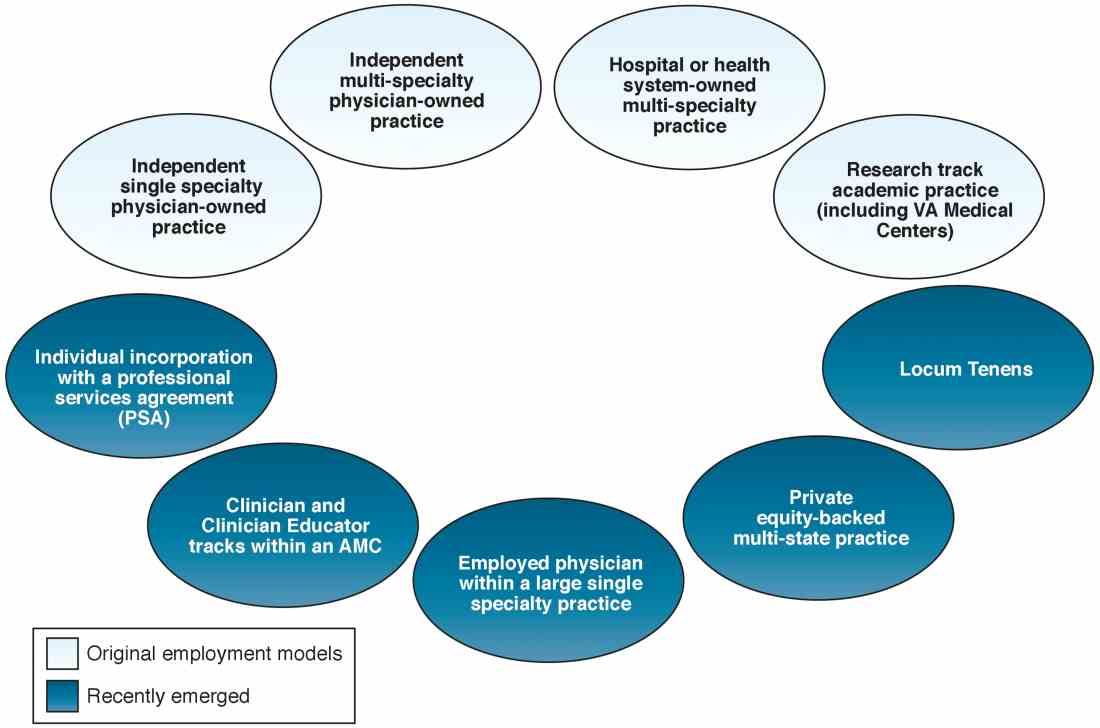
Employment models (light blue) available in the 1980s and those that have emerged as common models in the last decade (dark blue).
An individual corporation with a professional services agreement
For gastroenterologists at any career stage, the prospect of employment within a corporate entity, be it an academic university, hospital system, or private practice group, can be daunting. To that end, one central question facing nearly all gastroenterologists is: how much independence and flexibility, both clinically and financially, do I really want, and what can I do to realize my ideal job description?
An interesting alternative to direct health system employment occurs when a physician forms a solo corporation and then contracts with a hospital or health system under a PSA. Here, the physician provides professional services on a contractual basis, but retains control of finances and has more autonomy compared with employment. Essentially, the physician is a corporation of one, with hospital alignment rather than employment. For full disclosure, this is the employment model of one of the authors (N.K.).
A PSA arrangement is common for larger independent GI practices. Many practices have PSA arrangements with hospitals ranging from call coverage to full professional services. For an individual working within a PSA, income is not the traditional W-2 Internal Revenue Service arrangement in which taxes are removed automatically. Income derived from a PSA usually falls under an Internal Revenue Service Form 1099. The physician actually is employed through their practice corporation and relates to the hospital as an independent contractor.
There are four common variants of the PSA model.4 A Global Payment PSA is when a hospital contracts with the physician practice for specific services and pays a global rate linked to wRVUs. The rate is negotiated to encompass physician compensation, benefits, and practice overhead. The practice retains control of its own office functions and staff.
In a traditional PSA, the hospital contracts with physicians and pays them based on RVU production, but the hospital owns the administrative part of the practice (staff, billing, collections, equipment, and supplies).
A practice management arrangement occurs when the hospital employs the physician who provides professional services and a separate third party manages the practice via a separate management contract. Finally, a Carve-Out PSA can use any of the earlier-described PSA arrangements and certain services are carved out under line-item provisions. For example, a hospital could contract with a private GI group for endoscopic services or night call and write a PSA expressly for these purposes.
Some notable benefits of the PSA are that physicians can maintain financial and employment independence from the hospital and have more control over benefits packages, retirement savings options, and health insurance. Physicians also can provide services outside of the hospital (e.g., telemedicine or locums tenens — see later) without institutional restrictions or conflicts. Finally, physicians benefit from tax advantages of self-employment (with associated business-related tax deductions) through their corporation. The potential downsides of a PSA contract are the subtle expansion of services demanded (known as scope creep) or the possibility of contract termination (or nonrenewal) by the hospital. In addition, medical training does not equip physicians with the knowledge to navigate personal and corporate finances, benefits packages, and tax structures, so the learning curve can be quite steep. Nevertheless, PSAs can be an innovative employment model for gastroenterologists who wish to preserve autonomy and financial flexibility. In this model, legal advice by an attorney skilled in employment law is mandatory.
Academic clinicians track
Until recently, clinically oriented academic faculty were channeled into the traditional ladder faculty model in which advancement was contingent on publications, national recognition, grant support, and teaching. As competition for market share has intensified among regional health systems, many AMCs have developed purely clinical tracks in which research, publication, and teaching are not expected; salaries are linked to clinical productivity; and income may approximate the professional (but not ancillary) income of a community gastroenterologist.
Various models of this arrangement exist as well. For example, clinicians can be employed within a group that has a board and management structure distinct from the faculty group practice, as in the case of the Northeast Medical Group at Yale New Haven Health System5 and the University of Maryland Community Medical Group. In addition, clinicians can form an operating group separate from the faculty practice but as a controlled subsidiary (such as the University of Pittsburgh Community Medicine), separate operating group for primary care but specialists are employed within their respective departments (Emory Specialty Associates) or as a distinct clinical department within a faculty practice (University of California Los Angeles Medical Group Staff Physicians).
Irrespective of the employment model, these clinicians essentially work similar to community gastroenterologists but within the umbrella of an AMC. For young faculty whose interest is not in research or teaching, this can be an attractive option that maintains a tie to a university health system. For a seasoned clinician in community practice, this is an option to return to an academic environment. Usually, productivity expectations within the clinician track approximate those of a community practice gastroenterologist, but again total compensation may not be as great because ancillary income streams usually are not available. We expect this AMC employment track to become more prevalent as universities expand their footprints and acquire practices, hospitals, and ambulatory facilities distant from the main campus.
Large single-specialty practice
Consolidation of independent practices has been evident for 20 years and has accelerated as physicians in smaller practices have aged and burdens of practice have increased. Now, most urban centers have large mega-sized practices or super groups that have grown through practice mergers, acquisitions, and successful recruitment. Large practices can be modeled as a single integrated corporation (with ancillary components such as an AEC or infusion center) or as individual business units that are grouped under a single corporate entity.6
Within these large and mega-sized practices, differing employment options have emerged in addition to the traditional partnership track. These include payment on a per-diem basis, annual salary, or a mix of both. As opposed to partnership, the employment track avoids responsibility for governance and corporate liability, although not individual liability, and usually does not involve after-hours call. An employed physician usually does not benefit from ancillary income that derives from AEC facility fees, infusion centers, and pathology and anesthesia services.
Private equity ownership of gastroenterology practices
In June 2016, private equity entered the GI space with the investment of the Audax Group in a community GI practice based in Miami, Florida. The term private equity refers to capital that is not reported in public forums and comprises funds that investors directly invest into private companies or use to buy out public companies and turn them private.
According to their website, when the Audax Group invests in a medical practice, they provide capital for substantial infrastructure support, business experience, and acumen, but retain medical practice leaders as their clinical decision makers. They also bring proven expertise and economies of scale to resource-intensive aspects of a medical practice including information technology, regulation compliance, human resources, revenue cycle management, payroll, benefits, rents, and lease as examples. These components can be difficult to manage efficiently within independent medical practices, so many maturing practices are selling their practices to regional health systems. This multistate equity-backed medical practice is an alternative to health system acquisition, and may help physicians feel more in control of their practices and potentially share in the equity investment.
It is important to understand the employment structure and associations of any practice you are contemplating joining. The model devised by this group is meant to retain physician authority and responsibility while providing capital to support innovation and the development of needed infrastructure. Growth of market share and revenues can accrue back to physician owners. This is distinct from practices that are part of a health system in which there may be more of a corporate feeling and centralized governance.
Locum tenens
Locum tenens is a Latin phrase that means “to hold the place of.” According to the website of a large locum tenens company, this practice model originated in the 1970s when the federal government provided a grant to the University of Utah to provide physician services for underserved areas in the Western United States. The program proved so successful that hospital administrators who had difficulty recruiting staff physicians began asking for staffing assistance.
Today, a substantial number of physicians at all stages of their careers are working as locum tenens. They work as independent contractors so that income taxes are not withheld and benefits are the responsibility of the individual. As with the PSA arrangement, a physician would meet with both an accountant and labor lawyer to establish him or herself as a corporate entity for tax advantages and limited liability from litigation.
Early stage physicians who might be following a significant other or spouse to specific locations sometimes consider a locum tenens as a bridge to permanent positions. Late-stage physicians who no longer want to be tied to a small group or solo practice have become locum tenens physicians who enjoy multiple temporary employment positions nationwide. This pathway no longer is unusual and can be a satisfying means to expand employment horizons. As with all employment situations, due diligence is mandatory before signing with any locum tenens company.
Conclusions
The employment spectrum for gastroenterologists and other medical professionals has expanded greatly between the time the senior author and the junior author entered the workforce. Change is now the one constant in medicine, and medicine today largely is fast-paced, corporatized, and highly regulated. Finding an employment model that is comfortable for current physicians, whose life situations are quite diverse, can be challenging. but a variety of opportunities now exist.
Think carefully about what you truly desire as a medical professional and how you might shape your employment to realize your goals. Options are available for those with an open mind and persistence.
References
1. Sheen E, Dorn SD, Brill JV, et al. Health care reform and the road ahead for gastroenterology. Clin Gastroenterol Hepatol. 2012;10:1062-5.
2. Kosinski LR. Meaningful use and electronic medical records for the gastroenterology practice. Clin Gastroenterol Hepatol. 2010;8:494-7.
3. Medical Group Management Association (MGMA). Accessed January 20, 2017.
4. The Coker Group. PSAs as an Alternative to Employment: A Contemporary Option for Alignment and Integration. In: The Coker Group Thought Leadership – White Papers. March 2016.
5. Houston R, McGinnis T. Accountable care organizations: looking back and moving forward. Centers for Health Care Strategies Inc. Brief. January 2016. Accessed January 20, 2017.
6. Pallardy C. 7 gastroenterologists leading GI mega-practices. Becker’s GI and endoscopy 2015. Accessed January 20, 2017.
Dr. Allen is in the division of gastroenterology and hepatology, department of medicine, University of Michigan School of Medicine, Ann Arbor; he is also the Editor in Chief of GI & Hepatology News. Dr. Kaushal is in the division of gastroenterology, Adventist Health Systems, Sonora, Calif. The authors disclose no conflicts.
The variety of employment models available to gastroenterologists reflects the dynamic changes we are experiencing in medicine today. Delivery of gastrointestinal (GI) care in the United States continues to evolve in light of health care reform and the Affordable Care Act.1 Within the past decade, as health systems and payers continue to consolidate, regulatory pressures have increased steadily and new policies such as electronic documentation and mandatory quality metrics reporting have added new challenges to the emerging generation of gastroenterologists.2 Although the lay press tends to focus on health care costs, coverage, physician reimbursement, provider burnout, health system consolidation, and value-based payment models, relatively less has been published about emerging employment and practice models.
Here,
Background
When the senior author graduated from fellowship in 1983 (J.I.A.), gastroenterology practice model choices were limited to essentially 4: independent community-based, single-specialty, physician-owned practice (solo or small group); independent multispecialty physician-owned practice; hospital or health system–owned multispecialty practice; and academic practice (including the Veterans Administration Medical Centers).
In the private sector, young community gastroenterologists typically would join a physician-owned practice and spend time (2–5 y) as an employed physician in a partnership track. During this time, his/her salary was subsidized while he/she built a practice base. Then, they would buy into the Professional Association with cash or equity equivalents and become a partner. As a partner, he/she then had the opportunity to share in ancillary revenue streams such as facility fees derived from a practice-owned ambulatory endoscopy center (AEC). By contrast, young academic faculty would be hired as an instructor and, if successful, climb the traditional ladder track to assistant, associate, and professor of medicine in an academic medical center (AMC).
In the 1980s, a typical community GI practice comprised 1 to 8 physicians, with most having been formed by 1 or 2 male gastroenterologists in the early 1970s when flexible endoscopy moved into clinical practice. The three practices that eventually would become Minnesota Gastroenterology (where J.I.A. practiced) opened in 1972. In 1996, the three practices merged into a single group of 38 physicians with ownership in three AECs. Advanced practice nurses and physician assistants were not yet part of the equation. Colonoscopy represented 48% of procedure volume, accounts receivable (time between submitting an insurance claim and being paid) averaged 88 days, and physicians averaged 9000 work relative value units (wRVUs) per partner annually. By comparison, median wRVUs for a full-time community GI in 1996 was 10,422 according to the Medical Group Management Association.3 Annual gross revenue (before expenses) per physician was approximately $400,000, and overhead reached 38% and 47% of revenue (there were 2 divisions). Partner incomes were at the 12% level of the Medical Group Management Association for gastroenterologists (personal management notes of J.I.A.). Minnesota Gastroenterology was the largest single-specialty GI practice in 1996 and its consolidation foreshadowed a trend that has accelerated over the ensuing generation.
When one of the authors (N.K.) graduated from the University of California Los Angeles in 2017, the GI employment landscape had evolved considerably. At least five new models of GI practice had emerged: individual incorporation with a Professional Services Agreement (PSA), a clinician track within an AMC, large single-specialty group practice (partnership or employee), private equity-backed multistate practice, and locum tenens (Figure 1).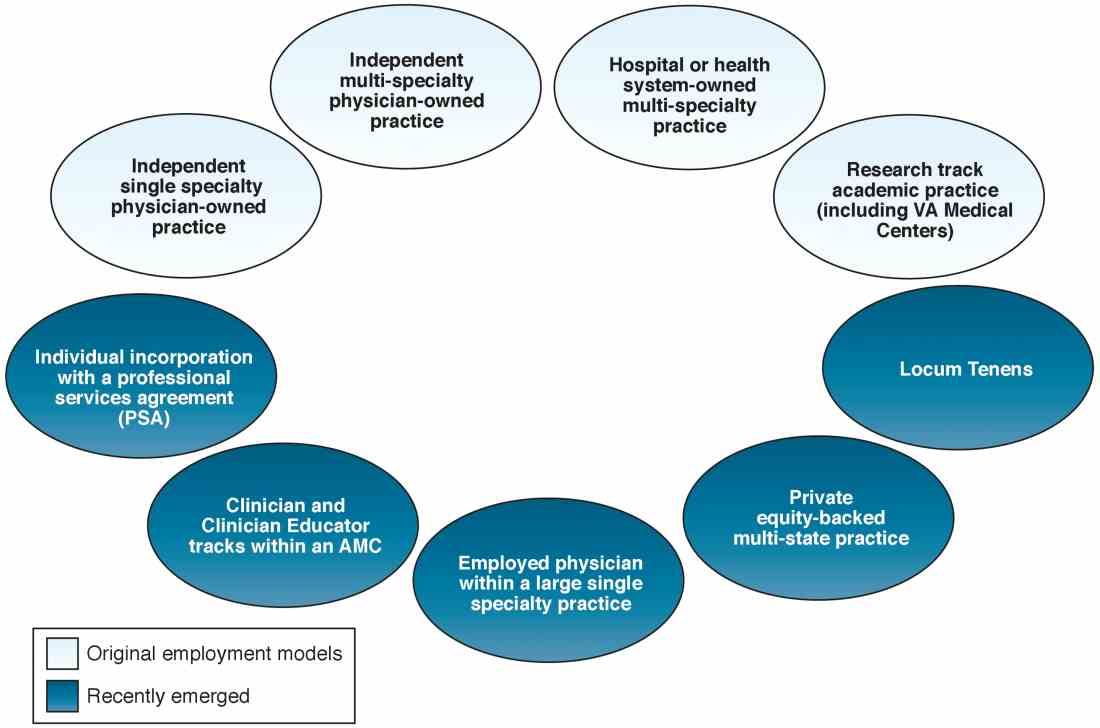
Employment models (light blue) available in the 1980s and those that have emerged as common models in the last decade (dark blue).
An individual corporation with a professional services agreement
For gastroenterologists at any career stage, the prospect of employment within a corporate entity, be it an academic university, hospital system, or private practice group, can be daunting. To that end, one central question facing nearly all gastroenterologists is: how much independence and flexibility, both clinically and financially, do I really want, and what can I do to realize my ideal job description?
An interesting alternative to direct health system employment occurs when a physician forms a solo corporation and then contracts with a hospital or health system under a PSA. Here, the physician provides professional services on a contractual basis, but retains control of finances and has more autonomy compared with employment. Essentially, the physician is a corporation of one, with hospital alignment rather than employment. For full disclosure, this is the employment model of one of the authors (N.K.).
A PSA arrangement is common for larger independent GI practices. Many practices have PSA arrangements with hospitals ranging from call coverage to full professional services. For an individual working within a PSA, income is not the traditional W-2 Internal Revenue Service arrangement in which taxes are removed automatically. Income derived from a PSA usually falls under an Internal Revenue Service Form 1099. The physician actually is employed through their practice corporation and relates to the hospital as an independent contractor.
There are four common variants of the PSA model.4 A Global Payment PSA is when a hospital contracts with the physician practice for specific services and pays a global rate linked to wRVUs. The rate is negotiated to encompass physician compensation, benefits, and practice overhead. The practice retains control of its own office functions and staff.
In a traditional PSA, the hospital contracts with physicians and pays them based on RVU production, but the hospital owns the administrative part of the practice (staff, billing, collections, equipment, and supplies).
A practice management arrangement occurs when the hospital employs the physician who provides professional services and a separate third party manages the practice via a separate management contract. Finally, a Carve-Out PSA can use any of the earlier-described PSA arrangements and certain services are carved out under line-item provisions. For example, a hospital could contract with a private GI group for endoscopic services or night call and write a PSA expressly for these purposes.
Some notable benefits of the PSA are that physicians can maintain financial and employment independence from the hospital and have more control over benefits packages, retirement savings options, and health insurance. Physicians also can provide services outside of the hospital (e.g., telemedicine or locums tenens — see later) without institutional restrictions or conflicts. Finally, physicians benefit from tax advantages of self-employment (with associated business-related tax deductions) through their corporation. The potential downsides of a PSA contract are the subtle expansion of services demanded (known as scope creep) or the possibility of contract termination (or nonrenewal) by the hospital. In addition, medical training does not equip physicians with the knowledge to navigate personal and corporate finances, benefits packages, and tax structures, so the learning curve can be quite steep. Nevertheless, PSAs can be an innovative employment model for gastroenterologists who wish to preserve autonomy and financial flexibility. In this model, legal advice by an attorney skilled in employment law is mandatory.
Academic clinicians track
Until recently, clinically oriented academic faculty were channeled into the traditional ladder faculty model in which advancement was contingent on publications, national recognition, grant support, and teaching. As competition for market share has intensified among regional health systems, many AMCs have developed purely clinical tracks in which research, publication, and teaching are not expected; salaries are linked to clinical productivity; and income may approximate the professional (but not ancillary) income of a community gastroenterologist.
Various models of this arrangement exist as well. For example, clinicians can be employed within a group that has a board and management structure distinct from the faculty group practice, as in the case of the Northeast Medical Group at Yale New Haven Health System5 and the University of Maryland Community Medical Group. In addition, clinicians can form an operating group separate from the faculty practice but as a controlled subsidiary (such as the University of Pittsburgh Community Medicine), separate operating group for primary care but specialists are employed within their respective departments (Emory Specialty Associates) or as a distinct clinical department within a faculty practice (University of California Los Angeles Medical Group Staff Physicians).
Irrespective of the employment model, these clinicians essentially work similar to community gastroenterologists but within the umbrella of an AMC. For young faculty whose interest is not in research or teaching, this can be an attractive option that maintains a tie to a university health system. For a seasoned clinician in community practice, this is an option to return to an academic environment. Usually, productivity expectations within the clinician track approximate those of a community practice gastroenterologist, but again total compensation may not be as great because ancillary income streams usually are not available. We expect this AMC employment track to become more prevalent as universities expand their footprints and acquire practices, hospitals, and ambulatory facilities distant from the main campus.
Large single-specialty practice
Consolidation of independent practices has been evident for 20 years and has accelerated as physicians in smaller practices have aged and burdens of practice have increased. Now, most urban centers have large mega-sized practices or super groups that have grown through practice mergers, acquisitions, and successful recruitment. Large practices can be modeled as a single integrated corporation (with ancillary components such as an AEC or infusion center) or as individual business units that are grouped under a single corporate entity.6
Within these large and mega-sized practices, differing employment options have emerged in addition to the traditional partnership track. These include payment on a per-diem basis, annual salary, or a mix of both. As opposed to partnership, the employment track avoids responsibility for governance and corporate liability, although not individual liability, and usually does not involve after-hours call. An employed physician usually does not benefit from ancillary income that derives from AEC facility fees, infusion centers, and pathology and anesthesia services.
Private equity ownership of gastroenterology practices
In June 2016, private equity entered the GI space with the investment of the Audax Group in a community GI practice based in Miami, Florida. The term private equity refers to capital that is not reported in public forums and comprises funds that investors directly invest into private companies or use to buy out public companies and turn them private.
According to their website, when the Audax Group invests in a medical practice, they provide capital for substantial infrastructure support, business experience, and acumen, but retain medical practice leaders as their clinical decision makers. They also bring proven expertise and economies of scale to resource-intensive aspects of a medical practice including information technology, regulation compliance, human resources, revenue cycle management, payroll, benefits, rents, and lease as examples. These components can be difficult to manage efficiently within independent medical practices, so many maturing practices are selling their practices to regional health systems. This multistate equity-backed medical practice is an alternative to health system acquisition, and may help physicians feel more in control of their practices and potentially share in the equity investment.
It is important to understand the employment structure and associations of any practice you are contemplating joining. The model devised by this group is meant to retain physician authority and responsibility while providing capital to support innovation and the development of needed infrastructure. Growth of market share and revenues can accrue back to physician owners. This is distinct from practices that are part of a health system in which there may be more of a corporate feeling and centralized governance.
Locum tenens
Locum tenens is a Latin phrase that means “to hold the place of.” According to the website of a large locum tenens company, this practice model originated in the 1970s when the federal government provided a grant to the University of Utah to provide physician services for underserved areas in the Western United States. The program proved so successful that hospital administrators who had difficulty recruiting staff physicians began asking for staffing assistance.
Today, a substantial number of physicians at all stages of their careers are working as locum tenens. They work as independent contractors so that income taxes are not withheld and benefits are the responsibility of the individual. As with the PSA arrangement, a physician would meet with both an accountant and labor lawyer to establish him or herself as a corporate entity for tax advantages and limited liability from litigation.
Early stage physicians who might be following a significant other or spouse to specific locations sometimes consider a locum tenens as a bridge to permanent positions. Late-stage physicians who no longer want to be tied to a small group or solo practice have become locum tenens physicians who enjoy multiple temporary employment positions nationwide. This pathway no longer is unusual and can be a satisfying means to expand employment horizons. As with all employment situations, due diligence is mandatory before signing with any locum tenens company.
Conclusions
The employment spectrum for gastroenterologists and other medical professionals has expanded greatly between the time the senior author and the junior author entered the workforce. Change is now the one constant in medicine, and medicine today largely is fast-paced, corporatized, and highly regulated. Finding an employment model that is comfortable for current physicians, whose life situations are quite diverse, can be challenging. but a variety of opportunities now exist.
Think carefully about what you truly desire as a medical professional and how you might shape your employment to realize your goals. Options are available for those with an open mind and persistence.
References
1. Sheen E, Dorn SD, Brill JV, et al. Health care reform and the road ahead for gastroenterology. Clin Gastroenterol Hepatol. 2012;10:1062-5.
2. Kosinski LR. Meaningful use and electronic medical records for the gastroenterology practice. Clin Gastroenterol Hepatol. 2010;8:494-7.
3. Medical Group Management Association (MGMA). Accessed January 20, 2017.
4. The Coker Group. PSAs as an Alternative to Employment: A Contemporary Option for Alignment and Integration. In: The Coker Group Thought Leadership – White Papers. March 2016.
5. Houston R, McGinnis T. Accountable care organizations: looking back and moving forward. Centers for Health Care Strategies Inc. Brief. January 2016. Accessed January 20, 2017.
6. Pallardy C. 7 gastroenterologists leading GI mega-practices. Becker’s GI and endoscopy 2015. Accessed January 20, 2017.
Dr. Allen is in the division of gastroenterology and hepatology, department of medicine, University of Michigan School of Medicine, Ann Arbor; he is also the Editor in Chief of GI & Hepatology News. Dr. Kaushal is in the division of gastroenterology, Adventist Health Systems, Sonora, Calif. The authors disclose no conflicts.
The variety of employment models available to gastroenterologists reflects the dynamic changes we are experiencing in medicine today. Delivery of gastrointestinal (GI) care in the United States continues to evolve in light of health care reform and the Affordable Care Act.1 Within the past decade, as health systems and payers continue to consolidate, regulatory pressures have increased steadily and new policies such as electronic documentation and mandatory quality metrics reporting have added new challenges to the emerging generation of gastroenterologists.2 Although the lay press tends to focus on health care costs, coverage, physician reimbursement, provider burnout, health system consolidation, and value-based payment models, relatively less has been published about emerging employment and practice models.
Here,
Background
When the senior author graduated from fellowship in 1983 (J.I.A.), gastroenterology practice model choices were limited to essentially 4: independent community-based, single-specialty, physician-owned practice (solo or small group); independent multispecialty physician-owned practice; hospital or health system–owned multispecialty practice; and academic practice (including the Veterans Administration Medical Centers).
In the private sector, young community gastroenterologists typically would join a physician-owned practice and spend time (2–5 y) as an employed physician in a partnership track. During this time, his/her salary was subsidized while he/she built a practice base. Then, they would buy into the Professional Association with cash or equity equivalents and become a partner. As a partner, he/she then had the opportunity to share in ancillary revenue streams such as facility fees derived from a practice-owned ambulatory endoscopy center (AEC). By contrast, young academic faculty would be hired as an instructor and, if successful, climb the traditional ladder track to assistant, associate, and professor of medicine in an academic medical center (AMC).
In the 1980s, a typical community GI practice comprised 1 to 8 physicians, with most having been formed by 1 or 2 male gastroenterologists in the early 1970s when flexible endoscopy moved into clinical practice. The three practices that eventually would become Minnesota Gastroenterology (where J.I.A. practiced) opened in 1972. In 1996, the three practices merged into a single group of 38 physicians with ownership in three AECs. Advanced practice nurses and physician assistants were not yet part of the equation. Colonoscopy represented 48% of procedure volume, accounts receivable (time between submitting an insurance claim and being paid) averaged 88 days, and physicians averaged 9000 work relative value units (wRVUs) per partner annually. By comparison, median wRVUs for a full-time community GI in 1996 was 10,422 according to the Medical Group Management Association.3 Annual gross revenue (before expenses) per physician was approximately $400,000, and overhead reached 38% and 47% of revenue (there were 2 divisions). Partner incomes were at the 12% level of the Medical Group Management Association for gastroenterologists (personal management notes of J.I.A.). Minnesota Gastroenterology was the largest single-specialty GI practice in 1996 and its consolidation foreshadowed a trend that has accelerated over the ensuing generation.
When one of the authors (N.K.) graduated from the University of California Los Angeles in 2017, the GI employment landscape had evolved considerably. At least five new models of GI practice had emerged: individual incorporation with a Professional Services Agreement (PSA), a clinician track within an AMC, large single-specialty group practice (partnership or employee), private equity-backed multistate practice, and locum tenens (Figure 1).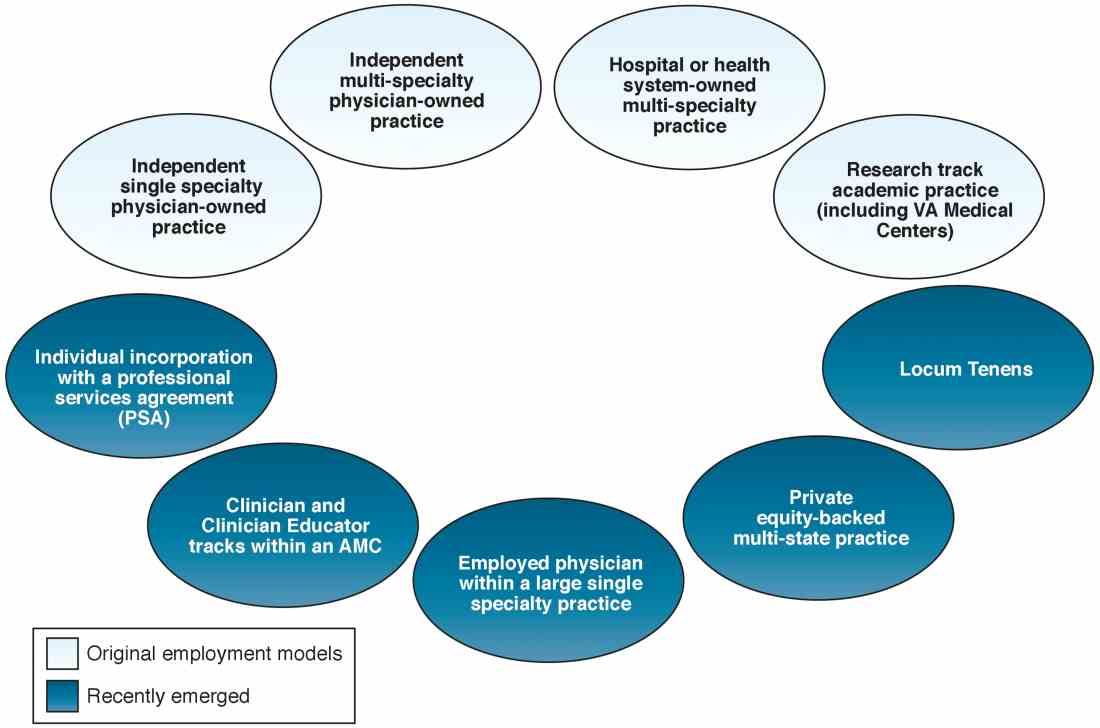
Employment models (light blue) available in the 1980s and those that have emerged as common models in the last decade (dark blue).
An individual corporation with a professional services agreement
For gastroenterologists at any career stage, the prospect of employment within a corporate entity, be it an academic university, hospital system, or private practice group, can be daunting. To that end, one central question facing nearly all gastroenterologists is: how much independence and flexibility, both clinically and financially, do I really want, and what can I do to realize my ideal job description?
An interesting alternative to direct health system employment occurs when a physician forms a solo corporation and then contracts with a hospital or health system under a PSA. Here, the physician provides professional services on a contractual basis, but retains control of finances and has more autonomy compared with employment. Essentially, the physician is a corporation of one, with hospital alignment rather than employment. For full disclosure, this is the employment model of one of the authors (N.K.).
A PSA arrangement is common for larger independent GI practices. Many practices have PSA arrangements with hospitals ranging from call coverage to full professional services. For an individual working within a PSA, income is not the traditional W-2 Internal Revenue Service arrangement in which taxes are removed automatically. Income derived from a PSA usually falls under an Internal Revenue Service Form 1099. The physician actually is employed through their practice corporation and relates to the hospital as an independent contractor.
There are four common variants of the PSA model.4 A Global Payment PSA is when a hospital contracts with the physician practice for specific services and pays a global rate linked to wRVUs. The rate is negotiated to encompass physician compensation, benefits, and practice overhead. The practice retains control of its own office functions and staff.
In a traditional PSA, the hospital contracts with physicians and pays them based on RVU production, but the hospital owns the administrative part of the practice (staff, billing, collections, equipment, and supplies).
A practice management arrangement occurs when the hospital employs the physician who provides professional services and a separate third party manages the practice via a separate management contract. Finally, a Carve-Out PSA can use any of the earlier-described PSA arrangements and certain services are carved out under line-item provisions. For example, a hospital could contract with a private GI group for endoscopic services or night call and write a PSA expressly for these purposes.
Some notable benefits of the PSA are that physicians can maintain financial and employment independence from the hospital and have more control over benefits packages, retirement savings options, and health insurance. Physicians also can provide services outside of the hospital (e.g., telemedicine or locums tenens — see later) without institutional restrictions or conflicts. Finally, physicians benefit from tax advantages of self-employment (with associated business-related tax deductions) through their corporation. The potential downsides of a PSA contract are the subtle expansion of services demanded (known as scope creep) or the possibility of contract termination (or nonrenewal) by the hospital. In addition, medical training does not equip physicians with the knowledge to navigate personal and corporate finances, benefits packages, and tax structures, so the learning curve can be quite steep. Nevertheless, PSAs can be an innovative employment model for gastroenterologists who wish to preserve autonomy and financial flexibility. In this model, legal advice by an attorney skilled in employment law is mandatory.
Academic clinicians track
Until recently, clinically oriented academic faculty were channeled into the traditional ladder faculty model in which advancement was contingent on publications, national recognition, grant support, and teaching. As competition for market share has intensified among regional health systems, many AMCs have developed purely clinical tracks in which research, publication, and teaching are not expected; salaries are linked to clinical productivity; and income may approximate the professional (but not ancillary) income of a community gastroenterologist.
Various models of this arrangement exist as well. For example, clinicians can be employed within a group that has a board and management structure distinct from the faculty group practice, as in the case of the Northeast Medical Group at Yale New Haven Health System5 and the University of Maryland Community Medical Group. In addition, clinicians can form an operating group separate from the faculty practice but as a controlled subsidiary (such as the University of Pittsburgh Community Medicine), separate operating group for primary care but specialists are employed within their respective departments (Emory Specialty Associates) or as a distinct clinical department within a faculty practice (University of California Los Angeles Medical Group Staff Physicians).
Irrespective of the employment model, these clinicians essentially work similar to community gastroenterologists but within the umbrella of an AMC. For young faculty whose interest is not in research or teaching, this can be an attractive option that maintains a tie to a university health system. For a seasoned clinician in community practice, this is an option to return to an academic environment. Usually, productivity expectations within the clinician track approximate those of a community practice gastroenterologist, but again total compensation may not be as great because ancillary income streams usually are not available. We expect this AMC employment track to become more prevalent as universities expand their footprints and acquire practices, hospitals, and ambulatory facilities distant from the main campus.
Large single-specialty practice
Consolidation of independent practices has been evident for 20 years and has accelerated as physicians in smaller practices have aged and burdens of practice have increased. Now, most urban centers have large mega-sized practices or super groups that have grown through practice mergers, acquisitions, and successful recruitment. Large practices can be modeled as a single integrated corporation (with ancillary components such as an AEC or infusion center) or as individual business units that are grouped under a single corporate entity.6
Within these large and mega-sized practices, differing employment options have emerged in addition to the traditional partnership track. These include payment on a per-diem basis, annual salary, or a mix of both. As opposed to partnership, the employment track avoids responsibility for governance and corporate liability, although not individual liability, and usually does not involve after-hours call. An employed physician usually does not benefit from ancillary income that derives from AEC facility fees, infusion centers, and pathology and anesthesia services.
Private equity ownership of gastroenterology practices
In June 2016, private equity entered the GI space with the investment of the Audax Group in a community GI practice based in Miami, Florida. The term private equity refers to capital that is not reported in public forums and comprises funds that investors directly invest into private companies or use to buy out public companies and turn them private.
According to their website, when the Audax Group invests in a medical practice, they provide capital for substantial infrastructure support, business experience, and acumen, but retain medical practice leaders as their clinical decision makers. They also bring proven expertise and economies of scale to resource-intensive aspects of a medical practice including information technology, regulation compliance, human resources, revenue cycle management, payroll, benefits, rents, and lease as examples. These components can be difficult to manage efficiently within independent medical practices, so many maturing practices are selling their practices to regional health systems. This multistate equity-backed medical practice is an alternative to health system acquisition, and may help physicians feel more in control of their practices and potentially share in the equity investment.
It is important to understand the employment structure and associations of any practice you are contemplating joining. The model devised by this group is meant to retain physician authority and responsibility while providing capital to support innovation and the development of needed infrastructure. Growth of market share and revenues can accrue back to physician owners. This is distinct from practices that are part of a health system in which there may be more of a corporate feeling and centralized governance.
Locum tenens
Locum tenens is a Latin phrase that means “to hold the place of.” According to the website of a large locum tenens company, this practice model originated in the 1970s when the federal government provided a grant to the University of Utah to provide physician services for underserved areas in the Western United States. The program proved so successful that hospital administrators who had difficulty recruiting staff physicians began asking for staffing assistance.
Today, a substantial number of physicians at all stages of their careers are working as locum tenens. They work as independent contractors so that income taxes are not withheld and benefits are the responsibility of the individual. As with the PSA arrangement, a physician would meet with both an accountant and labor lawyer to establish him or herself as a corporate entity for tax advantages and limited liability from litigation.
Early stage physicians who might be following a significant other or spouse to specific locations sometimes consider a locum tenens as a bridge to permanent positions. Late-stage physicians who no longer want to be tied to a small group or solo practice have become locum tenens physicians who enjoy multiple temporary employment positions nationwide. This pathway no longer is unusual and can be a satisfying means to expand employment horizons. As with all employment situations, due diligence is mandatory before signing with any locum tenens company.
Conclusions
The employment spectrum for gastroenterologists and other medical professionals has expanded greatly between the time the senior author and the junior author entered the workforce. Change is now the one constant in medicine, and medicine today largely is fast-paced, corporatized, and highly regulated. Finding an employment model that is comfortable for current physicians, whose life situations are quite diverse, can be challenging. but a variety of opportunities now exist.
Think carefully about what you truly desire as a medical professional and how you might shape your employment to realize your goals. Options are available for those with an open mind and persistence.
References
1. Sheen E, Dorn SD, Brill JV, et al. Health care reform and the road ahead for gastroenterology. Clin Gastroenterol Hepatol. 2012;10:1062-5.
2. Kosinski LR. Meaningful use and electronic medical records for the gastroenterology practice. Clin Gastroenterol Hepatol. 2010;8:494-7.
3. Medical Group Management Association (MGMA). Accessed January 20, 2017.
4. The Coker Group. PSAs as an Alternative to Employment: A Contemporary Option for Alignment and Integration. In: The Coker Group Thought Leadership – White Papers. March 2016.
5. Houston R, McGinnis T. Accountable care organizations: looking back and moving forward. Centers for Health Care Strategies Inc. Brief. January 2016. Accessed January 20, 2017.
6. Pallardy C. 7 gastroenterologists leading GI mega-practices. Becker’s GI and endoscopy 2015. Accessed January 20, 2017.
Dr. Allen is in the division of gastroenterology and hepatology, department of medicine, University of Michigan School of Medicine, Ann Arbor; he is also the Editor in Chief of GI & Hepatology News. Dr. Kaushal is in the division of gastroenterology, Adventist Health Systems, Sonora, Calif. The authors disclose no conflicts.