User login
Half as many people are trying heroin, but marijuana use grows
Some good news from the front lines of the heroin crisis: Half as many people tried heroin for the first time in 2017 as in 2016. That’s according to data released Sept. 14 from the government’s annual National Survey on Drug Use and Health.
“This is what we were hoping for,” said Elinore McCance-Katz, MD, who directs the Substance Abuse and Mental Health Services Administration. “It tells us that we are getting the word out to the American people of the risks of heroin,” especially when the drug is tainted with additional powerful opioids, fentanyl or carfentanil.
The survey found that marijuana use, however, increased in 2017, especially among pregnant women and young adults. Dr. McCance-Katz said the increase was likely linked to the growing number of states that have legalized marijuana and the misperception that marijuana is harmless.
Dr. McCance-Katz attributed the drop in new heroin users to increased government funding for prevention and public messaging on the local, state and federal levels.
David Kan, MD, president of the California Society of Addiction Medicine, was surprised by the heroin finding. “This report seems to run counter to the common wisdom that everyone is migrating from prescription medications to heroin,” he said. Still, the number of drug overdose deaths continued to climb to a staggering 72,000 in 2017, with the sharpest increase among people who used fentanyl or other synthetic opioids. “All it takes is one exposure to fentanyl to die,” Dr. Kan said.
The survey also found a small increase in the number of people with substance use disorders who receive specialty treatment, particularly heroin and opioid users. Nonetheless, 92% of people with substance use disorders do not receive it.
“It’s unacceptable,” said Greg Williams, executive vice president of Facing Addiction, a nonprofit group that advocates for people struggling with substance use disorders. “We’ve had a 90% treatment gap in America for the two decades we’ve been tracking it, and we have not been able to close it.” Despite all the news coverage of the drug crisis, he said, “the response has been woefully inadequate.”
As for marijuana, it appears that public health messaging has not been as effective as marketing efforts by the burgeoning cannabis industry. “When you have an industry that does nothing but blanket our society with messages about the medicinal value of marijuana, people get the idea this is a safe substance to use. And that’s not true,” said Dr. McCance-Katz.
Cannabis does appear to have medical benefits – in June, for example, the FDA approved the first cannabinoid-derived medication for the treatment of epilepsy. But Dr. McCance-Katz said there is already ample evidence that the drug can pose serious health risks, particularly for teenagers, young adults and pregnant women.
The survey found that during 2015-2017, the percentage of pregnant women who reported marijuana use more than doubled, to 7.1%. Often, they use it to combat nausea and pain, believing it is safer than the drugs prescribed by their doctors and approved of by the Food and Drug Administration. Mounting evidence, however, suggests that marijuana can cause preterm birth and long-term neurologic problems in the babies of mothers who use it during pregnancy.
“I’m going to talk about it every chance I get,” said Dr. McCance-Katz. “Americans have the right to know that marijuana has risks.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Some good news from the front lines of the heroin crisis: Half as many people tried heroin for the first time in 2017 as in 2016. That’s according to data released Sept. 14 from the government’s annual National Survey on Drug Use and Health.
“This is what we were hoping for,” said Elinore McCance-Katz, MD, who directs the Substance Abuse and Mental Health Services Administration. “It tells us that we are getting the word out to the American people of the risks of heroin,” especially when the drug is tainted with additional powerful opioids, fentanyl or carfentanil.
The survey found that marijuana use, however, increased in 2017, especially among pregnant women and young adults. Dr. McCance-Katz said the increase was likely linked to the growing number of states that have legalized marijuana and the misperception that marijuana is harmless.
Dr. McCance-Katz attributed the drop in new heroin users to increased government funding for prevention and public messaging on the local, state and federal levels.
David Kan, MD, president of the California Society of Addiction Medicine, was surprised by the heroin finding. “This report seems to run counter to the common wisdom that everyone is migrating from prescription medications to heroin,” he said. Still, the number of drug overdose deaths continued to climb to a staggering 72,000 in 2017, with the sharpest increase among people who used fentanyl or other synthetic opioids. “All it takes is one exposure to fentanyl to die,” Dr. Kan said.
The survey also found a small increase in the number of people with substance use disorders who receive specialty treatment, particularly heroin and opioid users. Nonetheless, 92% of people with substance use disorders do not receive it.
“It’s unacceptable,” said Greg Williams, executive vice president of Facing Addiction, a nonprofit group that advocates for people struggling with substance use disorders. “We’ve had a 90% treatment gap in America for the two decades we’ve been tracking it, and we have not been able to close it.” Despite all the news coverage of the drug crisis, he said, “the response has been woefully inadequate.”
As for marijuana, it appears that public health messaging has not been as effective as marketing efforts by the burgeoning cannabis industry. “When you have an industry that does nothing but blanket our society with messages about the medicinal value of marijuana, people get the idea this is a safe substance to use. And that’s not true,” said Dr. McCance-Katz.
Cannabis does appear to have medical benefits – in June, for example, the FDA approved the first cannabinoid-derived medication for the treatment of epilepsy. But Dr. McCance-Katz said there is already ample evidence that the drug can pose serious health risks, particularly for teenagers, young adults and pregnant women.
The survey found that during 2015-2017, the percentage of pregnant women who reported marijuana use more than doubled, to 7.1%. Often, they use it to combat nausea and pain, believing it is safer than the drugs prescribed by their doctors and approved of by the Food and Drug Administration. Mounting evidence, however, suggests that marijuana can cause preterm birth and long-term neurologic problems in the babies of mothers who use it during pregnancy.
“I’m going to talk about it every chance I get,” said Dr. McCance-Katz. “Americans have the right to know that marijuana has risks.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Some good news from the front lines of the heroin crisis: Half as many people tried heroin for the first time in 2017 as in 2016. That’s according to data released Sept. 14 from the government’s annual National Survey on Drug Use and Health.
“This is what we were hoping for,” said Elinore McCance-Katz, MD, who directs the Substance Abuse and Mental Health Services Administration. “It tells us that we are getting the word out to the American people of the risks of heroin,” especially when the drug is tainted with additional powerful opioids, fentanyl or carfentanil.
The survey found that marijuana use, however, increased in 2017, especially among pregnant women and young adults. Dr. McCance-Katz said the increase was likely linked to the growing number of states that have legalized marijuana and the misperception that marijuana is harmless.
Dr. McCance-Katz attributed the drop in new heroin users to increased government funding for prevention and public messaging on the local, state and federal levels.
David Kan, MD, president of the California Society of Addiction Medicine, was surprised by the heroin finding. “This report seems to run counter to the common wisdom that everyone is migrating from prescription medications to heroin,” he said. Still, the number of drug overdose deaths continued to climb to a staggering 72,000 in 2017, with the sharpest increase among people who used fentanyl or other synthetic opioids. “All it takes is one exposure to fentanyl to die,” Dr. Kan said.
The survey also found a small increase in the number of people with substance use disorders who receive specialty treatment, particularly heroin and opioid users. Nonetheless, 92% of people with substance use disorders do not receive it.
“It’s unacceptable,” said Greg Williams, executive vice president of Facing Addiction, a nonprofit group that advocates for people struggling with substance use disorders. “We’ve had a 90% treatment gap in America for the two decades we’ve been tracking it, and we have not been able to close it.” Despite all the news coverage of the drug crisis, he said, “the response has been woefully inadequate.”
As for marijuana, it appears that public health messaging has not been as effective as marketing efforts by the burgeoning cannabis industry. “When you have an industry that does nothing but blanket our society with messages about the medicinal value of marijuana, people get the idea this is a safe substance to use. And that’s not true,” said Dr. McCance-Katz.
Cannabis does appear to have medical benefits – in June, for example, the FDA approved the first cannabinoid-derived medication for the treatment of epilepsy. But Dr. McCance-Katz said there is already ample evidence that the drug can pose serious health risks, particularly for teenagers, young adults and pregnant women.
The survey found that during 2015-2017, the percentage of pregnant women who reported marijuana use more than doubled, to 7.1%. Often, they use it to combat nausea and pain, believing it is safer than the drugs prescribed by their doctors and approved of by the Food and Drug Administration. Mounting evidence, however, suggests that marijuana can cause preterm birth and long-term neurologic problems in the babies of mothers who use it during pregnancy.
“I’m going to talk about it every chance I get,” said Dr. McCance-Katz. “Americans have the right to know that marijuana has risks.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Inpatient vs. outpatient addiction treatment: Which is best?
In the course of my general psychiatry practice, there are times when I am unable to manage a patient’s substance abuse issues, and I have referred patients to a higher level of care – often to an intensive outpatient program (IOP) that meets for 3 hours a day, or to an inpatient rehabilitation, usually for 28 days. I’m not always sure who can be managed in which setting, and I usually honor the patient’s wishes. If the patient is motivated, has a support system in place, and is concerned that his job will be in jeopardy if he takes time off work, then I refer to Kolmac Outpatient Recovery Centers, a local outpatient treatment center that gives patients the option of attending in the mornings or evenings and allows most people to continue working. If I think I may have only a single shot at getting a patient engaged in care, and the patient is willing to go to an inpatient setting, I refer to a residential treatment facility. It has occurred to me that this is not a very scientific way of making a treatment decision.
George Kolodner, MD, is the chief clinical officer of Kolmac. He has been a member of the American Society of Addiction Medicine’s (ASAM) treatment criteria committee. When I spoke with Dr. Kolodner, he noted: “Discussions between third-party payers and treatment programs about what is the appropriate level of care for a particular individual have been adversarial. ASAM has spent many years developing the ASAM Criteria, a document that attempts to mediate these disagreements by developing objective criteria for where people ought to be treated. Because it is so comprehensive and the variables are so many, it can be difficult to use. A computerized version, called ‘Continuum,’ has been developed to make the criteria more user-friendly.”
“My 45-year experience,” Dr. Kolodner continued, “is that detoxification and rehabilitation can usually be done successfully on an outpatient basis if an appropriate facility is available and the patient has both a supportive living environment and can get to the treatment. Hospitalization and residential rehabilitation is an essential level of care when those conditions do not exist or when outpatient treatment proves to be insufficient.”
One problem with comparing the success of IOPs to inpatient programs is that these settings differ widely in which services they offer to patients.
“There’s no standardization,” Dr. Kolodner said. “The services may be watered down, they may not have a medical staff or a psychiatrist, and people get sucked into inappropriate treatments. When it comes to both IOPs and inpatient facilities, there is no uniformity, and right now it’s caveat emptor.”
Marc Fishman, MD, is medical director of Maryland Treatment Centers/Mountain Manor Treatment Center, a coeditor of the ASAM Criteria, and, with Dr. Kolodner, a member of ASAM’s treatment criteria committee. He, too, talked about the absence of standardization across treatment settings.
“Bed-based and non–bed-based care exist in many flavors and subflavors. You have to remember,” Dr. Fishman said, “this is a marathon, not a sprint, and one of the most important goals of bed-based care is that it serves as a stepping stone for outpatient treatment.”
Dr. Fishman talked about a list of criteria he uses to decide whether someone can be treated as an outpatient. “First, someone has to be able to access outpatient treatment; it may not be available. Can they get back and forth? How chaotic are their lives? Is there support at home, or is it a toxic environment in which others are using? Are they likely to keep using and drop out? What is the patient’s level of motivation? If a person is very ambivalent, you may need a high-intensity motivational milieu. Are their psychiatric symptoms severe enough to require 24-hour monitoring and supervision? Most detoxification we can do on an outpatient basis, but some complex multisubstance withdrawal may need more monitoring.
“Also, we have an increasing armamentarium of medications to promote abstinence, and sometimes it makes sense to start them in higher-level treatment settings; for example long-acting injectable naltrexone (Vivitrol) needs a 10-day postdetox opioid-free washout before it can be started.”
Dr. Fishman was careful to note that imminent danger is usually not a reason to use an inpatient rehab setting. “When you’re talking about safety issues, then people usually need a hospital. Most rehabs are not equipped to deal with dangerous patients.”
In choosing from the different treatment options, the first question should be to ask which forms of treatment are available with high-quality care. Can the patient access an outpatient center, will he be able to get to treatment, and will he be able to remain sober between visits? Will he be offered a full range of treatment options in that setting? Can substance withdrawal be managed safely? If the patient fails at outpatient care, will he be willing to consider inpatient treatment as a next step? What is the risk associated with relapse in a setting that allows for access to substances between sessions? Is the patient someone who is at high risk for a fatal overdose, or at high risk for endangering others, for example, someone who has been revived from overdoses or has driven while inebriated? Would this patient benefit from more intensive psychotherapeutic care? And the question that always haunts me: If there is a bad outcome, will I regret that I did not recommend more?”
Often, I’m left with the idea that it would be nice if we were all given crystal balls at the end of training. In hindsight, if a patient does well, the treatment that was offered was enough, and perhaps even too much in terms of cost. If a patient does not do well, we may be left to ask if he would have been better off if we had recommended a higher level of care, assuming that care could be financed and accessed, and that the patient complied with the treatment recommendations.
Both experts agree that treatment is often effective, and the news here is good. But treatment only works if a patient actually follows through on it, so the best treatment is often the one the patient is willing to accept.
Dr. Miller is the coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
In the course of my general psychiatry practice, there are times when I am unable to manage a patient’s substance abuse issues, and I have referred patients to a higher level of care – often to an intensive outpatient program (IOP) that meets for 3 hours a day, or to an inpatient rehabilitation, usually for 28 days. I’m not always sure who can be managed in which setting, and I usually honor the patient’s wishes. If the patient is motivated, has a support system in place, and is concerned that his job will be in jeopardy if he takes time off work, then I refer to Kolmac Outpatient Recovery Centers, a local outpatient treatment center that gives patients the option of attending in the mornings or evenings and allows most people to continue working. If I think I may have only a single shot at getting a patient engaged in care, and the patient is willing to go to an inpatient setting, I refer to a residential treatment facility. It has occurred to me that this is not a very scientific way of making a treatment decision.
George Kolodner, MD, is the chief clinical officer of Kolmac. He has been a member of the American Society of Addiction Medicine’s (ASAM) treatment criteria committee. When I spoke with Dr. Kolodner, he noted: “Discussions between third-party payers and treatment programs about what is the appropriate level of care for a particular individual have been adversarial. ASAM has spent many years developing the ASAM Criteria, a document that attempts to mediate these disagreements by developing objective criteria for where people ought to be treated. Because it is so comprehensive and the variables are so many, it can be difficult to use. A computerized version, called ‘Continuum,’ has been developed to make the criteria more user-friendly.”
“My 45-year experience,” Dr. Kolodner continued, “is that detoxification and rehabilitation can usually be done successfully on an outpatient basis if an appropriate facility is available and the patient has both a supportive living environment and can get to the treatment. Hospitalization and residential rehabilitation is an essential level of care when those conditions do not exist or when outpatient treatment proves to be insufficient.”
One problem with comparing the success of IOPs to inpatient programs is that these settings differ widely in which services they offer to patients.
“There’s no standardization,” Dr. Kolodner said. “The services may be watered down, they may not have a medical staff or a psychiatrist, and people get sucked into inappropriate treatments. When it comes to both IOPs and inpatient facilities, there is no uniformity, and right now it’s caveat emptor.”
Marc Fishman, MD, is medical director of Maryland Treatment Centers/Mountain Manor Treatment Center, a coeditor of the ASAM Criteria, and, with Dr. Kolodner, a member of ASAM’s treatment criteria committee. He, too, talked about the absence of standardization across treatment settings.
“Bed-based and non–bed-based care exist in many flavors and subflavors. You have to remember,” Dr. Fishman said, “this is a marathon, not a sprint, and one of the most important goals of bed-based care is that it serves as a stepping stone for outpatient treatment.”
Dr. Fishman talked about a list of criteria he uses to decide whether someone can be treated as an outpatient. “First, someone has to be able to access outpatient treatment; it may not be available. Can they get back and forth? How chaotic are their lives? Is there support at home, or is it a toxic environment in which others are using? Are they likely to keep using and drop out? What is the patient’s level of motivation? If a person is very ambivalent, you may need a high-intensity motivational milieu. Are their psychiatric symptoms severe enough to require 24-hour monitoring and supervision? Most detoxification we can do on an outpatient basis, but some complex multisubstance withdrawal may need more monitoring.
“Also, we have an increasing armamentarium of medications to promote abstinence, and sometimes it makes sense to start them in higher-level treatment settings; for example long-acting injectable naltrexone (Vivitrol) needs a 10-day postdetox opioid-free washout before it can be started.”
Dr. Fishman was careful to note that imminent danger is usually not a reason to use an inpatient rehab setting. “When you’re talking about safety issues, then people usually need a hospital. Most rehabs are not equipped to deal with dangerous patients.”
In choosing from the different treatment options, the first question should be to ask which forms of treatment are available with high-quality care. Can the patient access an outpatient center, will he be able to get to treatment, and will he be able to remain sober between visits? Will he be offered a full range of treatment options in that setting? Can substance withdrawal be managed safely? If the patient fails at outpatient care, will he be willing to consider inpatient treatment as a next step? What is the risk associated with relapse in a setting that allows for access to substances between sessions? Is the patient someone who is at high risk for a fatal overdose, or at high risk for endangering others, for example, someone who has been revived from overdoses or has driven while inebriated? Would this patient benefit from more intensive psychotherapeutic care? And the question that always haunts me: If there is a bad outcome, will I regret that I did not recommend more?”
Often, I’m left with the idea that it would be nice if we were all given crystal balls at the end of training. In hindsight, if a patient does well, the treatment that was offered was enough, and perhaps even too much in terms of cost. If a patient does not do well, we may be left to ask if he would have been better off if we had recommended a higher level of care, assuming that care could be financed and accessed, and that the patient complied with the treatment recommendations.
Both experts agree that treatment is often effective, and the news here is good. But treatment only works if a patient actually follows through on it, so the best treatment is often the one the patient is willing to accept.
Dr. Miller is the coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
In the course of my general psychiatry practice, there are times when I am unable to manage a patient’s substance abuse issues, and I have referred patients to a higher level of care – often to an intensive outpatient program (IOP) that meets for 3 hours a day, or to an inpatient rehabilitation, usually for 28 days. I’m not always sure who can be managed in which setting, and I usually honor the patient’s wishes. If the patient is motivated, has a support system in place, and is concerned that his job will be in jeopardy if he takes time off work, then I refer to Kolmac Outpatient Recovery Centers, a local outpatient treatment center that gives patients the option of attending in the mornings or evenings and allows most people to continue working. If I think I may have only a single shot at getting a patient engaged in care, and the patient is willing to go to an inpatient setting, I refer to a residential treatment facility. It has occurred to me that this is not a very scientific way of making a treatment decision.
George Kolodner, MD, is the chief clinical officer of Kolmac. He has been a member of the American Society of Addiction Medicine’s (ASAM) treatment criteria committee. When I spoke with Dr. Kolodner, he noted: “Discussions between third-party payers and treatment programs about what is the appropriate level of care for a particular individual have been adversarial. ASAM has spent many years developing the ASAM Criteria, a document that attempts to mediate these disagreements by developing objective criteria for where people ought to be treated. Because it is so comprehensive and the variables are so many, it can be difficult to use. A computerized version, called ‘Continuum,’ has been developed to make the criteria more user-friendly.”
“My 45-year experience,” Dr. Kolodner continued, “is that detoxification and rehabilitation can usually be done successfully on an outpatient basis if an appropriate facility is available and the patient has both a supportive living environment and can get to the treatment. Hospitalization and residential rehabilitation is an essential level of care when those conditions do not exist or when outpatient treatment proves to be insufficient.”
One problem with comparing the success of IOPs to inpatient programs is that these settings differ widely in which services they offer to patients.
“There’s no standardization,” Dr. Kolodner said. “The services may be watered down, they may not have a medical staff or a psychiatrist, and people get sucked into inappropriate treatments. When it comes to both IOPs and inpatient facilities, there is no uniformity, and right now it’s caveat emptor.”
Marc Fishman, MD, is medical director of Maryland Treatment Centers/Mountain Manor Treatment Center, a coeditor of the ASAM Criteria, and, with Dr. Kolodner, a member of ASAM’s treatment criteria committee. He, too, talked about the absence of standardization across treatment settings.
“Bed-based and non–bed-based care exist in many flavors and subflavors. You have to remember,” Dr. Fishman said, “this is a marathon, not a sprint, and one of the most important goals of bed-based care is that it serves as a stepping stone for outpatient treatment.”
Dr. Fishman talked about a list of criteria he uses to decide whether someone can be treated as an outpatient. “First, someone has to be able to access outpatient treatment; it may not be available. Can they get back and forth? How chaotic are their lives? Is there support at home, or is it a toxic environment in which others are using? Are they likely to keep using and drop out? What is the patient’s level of motivation? If a person is very ambivalent, you may need a high-intensity motivational milieu. Are their psychiatric symptoms severe enough to require 24-hour monitoring and supervision? Most detoxification we can do on an outpatient basis, but some complex multisubstance withdrawal may need more monitoring.
“Also, we have an increasing armamentarium of medications to promote abstinence, and sometimes it makes sense to start them in higher-level treatment settings; for example long-acting injectable naltrexone (Vivitrol) needs a 10-day postdetox opioid-free washout before it can be started.”
Dr. Fishman was careful to note that imminent danger is usually not a reason to use an inpatient rehab setting. “When you’re talking about safety issues, then people usually need a hospital. Most rehabs are not equipped to deal with dangerous patients.”
In choosing from the different treatment options, the first question should be to ask which forms of treatment are available with high-quality care. Can the patient access an outpatient center, will he be able to get to treatment, and will he be able to remain sober between visits? Will he be offered a full range of treatment options in that setting? Can substance withdrawal be managed safely? If the patient fails at outpatient care, will he be willing to consider inpatient treatment as a next step? What is the risk associated with relapse in a setting that allows for access to substances between sessions? Is the patient someone who is at high risk for a fatal overdose, or at high risk for endangering others, for example, someone who has been revived from overdoses or has driven while inebriated? Would this patient benefit from more intensive psychotherapeutic care? And the question that always haunts me: If there is a bad outcome, will I regret that I did not recommend more?”
Often, I’m left with the idea that it would be nice if we were all given crystal balls at the end of training. In hindsight, if a patient does well, the treatment that was offered was enough, and perhaps even too much in terms of cost. If a patient does not do well, we may be left to ask if he would have been better off if we had recommended a higher level of care, assuming that care could be financed and accessed, and that the patient complied with the treatment recommendations.
Both experts agree that treatment is often effective, and the news here is good. But treatment only works if a patient actually follows through on it, so the best treatment is often the one the patient is willing to accept.
Dr. Miller is the coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
FDA approves device for coronary artery perforations
according to an announcement from the agency.
These small tears in the arterial wall are rare but life-threatening complications of certain procedures, such as percutaneous coronary interventions. The device uses a balloon catheter like that used with PCI and, when successful, it can spare patients more invasive procedures, such as open heart surgery.
The approval is based on survey data from 80 patients treated with this device. In 76 of the patients (95%), the device was successfully delivered to the site of the acute coronary arterial perforation, and it successfully healed the tear in 73 patients (91%). Two patients died during the procedure, and five whose perforations were sealed successfully died in the hospital after the procedure, as did one whose perforation was not sealed.
The agency noted that this is the first device approved for the indication in 17 years. More information can be found in the full FDA announcement.
according to an announcement from the agency.
These small tears in the arterial wall are rare but life-threatening complications of certain procedures, such as percutaneous coronary interventions. The device uses a balloon catheter like that used with PCI and, when successful, it can spare patients more invasive procedures, such as open heart surgery.
The approval is based on survey data from 80 patients treated with this device. In 76 of the patients (95%), the device was successfully delivered to the site of the acute coronary arterial perforation, and it successfully healed the tear in 73 patients (91%). Two patients died during the procedure, and five whose perforations were sealed successfully died in the hospital after the procedure, as did one whose perforation was not sealed.
The agency noted that this is the first device approved for the indication in 17 years. More information can be found in the full FDA announcement.
according to an announcement from the agency.
These small tears in the arterial wall are rare but life-threatening complications of certain procedures, such as percutaneous coronary interventions. The device uses a balloon catheter like that used with PCI and, when successful, it can spare patients more invasive procedures, such as open heart surgery.
The approval is based on survey data from 80 patients treated with this device. In 76 of the patients (95%), the device was successfully delivered to the site of the acute coronary arterial perforation, and it successfully healed the tear in 73 patients (91%). Two patients died during the procedure, and five whose perforations were sealed successfully died in the hospital after the procedure, as did one whose perforation was not sealed.
The agency noted that this is the first device approved for the indication in 17 years. More information can be found in the full FDA announcement.
Children with BCP-ALL show inflammatory marker differences at birth
Patients who develop B-cell precursor acute lymphoblastic leukemia (BCP-ALL) in childhood may have dysregulated immune function at birth, according to a study published in Cancer Research.
Investigators evaluated neonatal concentrations of inflammatory markers and found significant differences between children who were later diagnosed with BCP-ALL and leukemia-free control subjects.
“Our findings suggest that children who develop ALL are immunologically disparate already at birth,” said study author Signe Holst Søegaard, PhD, of Statens Serum Institut in Copenhagen. “This may link to other observations suggesting that children who develop ALL respond differently to infections in early childhood, potentially promoting subsequent genetic events required for transformation to ALL, or speculations that they are unable to eliminate preleukemic cells.”
She noted that the study could not determine if the associations shown are causal or consequential so further studies will be needed both to confirm the findings and identify the underlying mechanisms.
For this study, Dr. Søegaard and her colleagues measured concentrations of 10 inflammatory markers on neonatal dried blood spots from 178 patients with BCP-ALL and 178 matched controls. The patients were diagnosed with BCP-ALL at ages 1-9 years.
Compared with controls, children who later developed BCP-ALL had significantly different neonatal concentrations of eight inflammatory markers.
Concentrations of interleukin (IL)–8, soluble receptor sIL-6R alpha, transforming growth factor (TGF)–beta 1, monocyte chemotactic protein (MCP)–1, and C-reactive protein (CRP) were significantly lower among the BCP-ALL patients.
On the other hand, concentrations of IL-6, IL-17, and IL-18 were significantly higher among BCP-ALL patients than controls.
The investigators noted that IL-10 concentrations were too low for accurate measurement in all patients and controls. Additionally, a “large proportion” of patients and controls had IL-6 and IL-17 concentrations that were below the limit of detection.
“We also demonstrated that several previously shown ALL risk factors – namely, birth order, gestational age, and sex – were associated with the neonatal concentrations of inflammatory markers,” Dr. Søegaard said. “These findings raise the interesting possibility that the effects of some known ALL risk factors partly act through prenatal programming of immune function.”
The investigators found that increasing birth order was associated with significantly higher IL-18 and lower CRP concentrations.
Increasing gestational age was associated with significantly lower sIL-6R alpha and TGF-beta 1 concentrations and higher CRP concentrations. And boys had significantly lower sIL-6R alpha and IL-8 concentrations and higher CRP concentrations than girls.
However, none of the following factors were significantly associated with concentrations of inflammatory biomarkers: maternal age at delivery, maternal hospital contact attributable to infection during pregnancy, maternal prescription for antimicrobials during pregnancy, birth weight, and mode of delivery.
“Our findings underline the role the child’s baseline immune characteristics may play in the development of ALL,” Dr. Søegaard said. “However, we cannot yet use our research results to predict who will develop childhood ALL.”
The study was sponsored by the Dagmar Marshall Foundation, the A.P. Møller Foundation, the Danish Childhood Cancer Foundation, the Arvid Nilsson Foundation, and the Danish Cancer Research Foundation. The investigators reported having no conflicts of interest.
SOURCE: Søegaard SH et al. Cancer Res. 2018;78(18);5458-63.
Patients who develop B-cell precursor acute lymphoblastic leukemia (BCP-ALL) in childhood may have dysregulated immune function at birth, according to a study published in Cancer Research.
Investigators evaluated neonatal concentrations of inflammatory markers and found significant differences between children who were later diagnosed with BCP-ALL and leukemia-free control subjects.
“Our findings suggest that children who develop ALL are immunologically disparate already at birth,” said study author Signe Holst Søegaard, PhD, of Statens Serum Institut in Copenhagen. “This may link to other observations suggesting that children who develop ALL respond differently to infections in early childhood, potentially promoting subsequent genetic events required for transformation to ALL, or speculations that they are unable to eliminate preleukemic cells.”
She noted that the study could not determine if the associations shown are causal or consequential so further studies will be needed both to confirm the findings and identify the underlying mechanisms.
For this study, Dr. Søegaard and her colleagues measured concentrations of 10 inflammatory markers on neonatal dried blood spots from 178 patients with BCP-ALL and 178 matched controls. The patients were diagnosed with BCP-ALL at ages 1-9 years.
Compared with controls, children who later developed BCP-ALL had significantly different neonatal concentrations of eight inflammatory markers.
Concentrations of interleukin (IL)–8, soluble receptor sIL-6R alpha, transforming growth factor (TGF)–beta 1, monocyte chemotactic protein (MCP)–1, and C-reactive protein (CRP) were significantly lower among the BCP-ALL patients.
On the other hand, concentrations of IL-6, IL-17, and IL-18 were significantly higher among BCP-ALL patients than controls.
The investigators noted that IL-10 concentrations were too low for accurate measurement in all patients and controls. Additionally, a “large proportion” of patients and controls had IL-6 and IL-17 concentrations that were below the limit of detection.
“We also demonstrated that several previously shown ALL risk factors – namely, birth order, gestational age, and sex – were associated with the neonatal concentrations of inflammatory markers,” Dr. Søegaard said. “These findings raise the interesting possibility that the effects of some known ALL risk factors partly act through prenatal programming of immune function.”
The investigators found that increasing birth order was associated with significantly higher IL-18 and lower CRP concentrations.
Increasing gestational age was associated with significantly lower sIL-6R alpha and TGF-beta 1 concentrations and higher CRP concentrations. And boys had significantly lower sIL-6R alpha and IL-8 concentrations and higher CRP concentrations than girls.
However, none of the following factors were significantly associated with concentrations of inflammatory biomarkers: maternal age at delivery, maternal hospital contact attributable to infection during pregnancy, maternal prescription for antimicrobials during pregnancy, birth weight, and mode of delivery.
“Our findings underline the role the child’s baseline immune characteristics may play in the development of ALL,” Dr. Søegaard said. “However, we cannot yet use our research results to predict who will develop childhood ALL.”
The study was sponsored by the Dagmar Marshall Foundation, the A.P. Møller Foundation, the Danish Childhood Cancer Foundation, the Arvid Nilsson Foundation, and the Danish Cancer Research Foundation. The investigators reported having no conflicts of interest.
SOURCE: Søegaard SH et al. Cancer Res. 2018;78(18);5458-63.
Patients who develop B-cell precursor acute lymphoblastic leukemia (BCP-ALL) in childhood may have dysregulated immune function at birth, according to a study published in Cancer Research.
Investigators evaluated neonatal concentrations of inflammatory markers and found significant differences between children who were later diagnosed with BCP-ALL and leukemia-free control subjects.
“Our findings suggest that children who develop ALL are immunologically disparate already at birth,” said study author Signe Holst Søegaard, PhD, of Statens Serum Institut in Copenhagen. “This may link to other observations suggesting that children who develop ALL respond differently to infections in early childhood, potentially promoting subsequent genetic events required for transformation to ALL, or speculations that they are unable to eliminate preleukemic cells.”
She noted that the study could not determine if the associations shown are causal or consequential so further studies will be needed both to confirm the findings and identify the underlying mechanisms.
For this study, Dr. Søegaard and her colleagues measured concentrations of 10 inflammatory markers on neonatal dried blood spots from 178 patients with BCP-ALL and 178 matched controls. The patients were diagnosed with BCP-ALL at ages 1-9 years.
Compared with controls, children who later developed BCP-ALL had significantly different neonatal concentrations of eight inflammatory markers.
Concentrations of interleukin (IL)–8, soluble receptor sIL-6R alpha, transforming growth factor (TGF)–beta 1, monocyte chemotactic protein (MCP)–1, and C-reactive protein (CRP) were significantly lower among the BCP-ALL patients.
On the other hand, concentrations of IL-6, IL-17, and IL-18 were significantly higher among BCP-ALL patients than controls.
The investigators noted that IL-10 concentrations were too low for accurate measurement in all patients and controls. Additionally, a “large proportion” of patients and controls had IL-6 and IL-17 concentrations that were below the limit of detection.
“We also demonstrated that several previously shown ALL risk factors – namely, birth order, gestational age, and sex – were associated with the neonatal concentrations of inflammatory markers,” Dr. Søegaard said. “These findings raise the interesting possibility that the effects of some known ALL risk factors partly act through prenatal programming of immune function.”
The investigators found that increasing birth order was associated with significantly higher IL-18 and lower CRP concentrations.
Increasing gestational age was associated with significantly lower sIL-6R alpha and TGF-beta 1 concentrations and higher CRP concentrations. And boys had significantly lower sIL-6R alpha and IL-8 concentrations and higher CRP concentrations than girls.
However, none of the following factors were significantly associated with concentrations of inflammatory biomarkers: maternal age at delivery, maternal hospital contact attributable to infection during pregnancy, maternal prescription for antimicrobials during pregnancy, birth weight, and mode of delivery.
“Our findings underline the role the child’s baseline immune characteristics may play in the development of ALL,” Dr. Søegaard said. “However, we cannot yet use our research results to predict who will develop childhood ALL.”
The study was sponsored by the Dagmar Marshall Foundation, the A.P. Møller Foundation, the Danish Childhood Cancer Foundation, the Arvid Nilsson Foundation, and the Danish Cancer Research Foundation. The investigators reported having no conflicts of interest.
SOURCE: Søegaard SH et al. Cancer Res. 2018;78(18);5458-63.
FROM CANCER RESEARCH
Key clinical point:
Major finding: Neonatal concentrations of some inflammatory markers were significantly different between BCP-ALL patients and controls.
Study details: Ten markers were measured in 178 patients with BCP-ALL and 178 matched controls.
Disclosures: The study was sponsored by the Dagmar Marshall Foundation, the A.P. Møller Foundation, the Danish Childhood Cancer Foundation, the Arvid Nilsson Foundation, and the Danish Cancer Research Foundation. The investigators reported having no conflicts of interest.
Source: Søegaard SH et al. Cancer Res. 2018;78(18);5458-63.
Azithromycin for COPD exacerbations may reduce treatment failure
PARIS – In patients with a chronic obstructive pulmonary disease (provided improvement in a variety of outcomes at 90 days, including risk of death, according to a placebo-controlled trial presented as a late-breaker at the annual congress of the European Respiratory Society.
In patients with COPD, “azithromycin initiated in the acute setting and continued for 3 months appears to be safe and potentially effective,” reported Wim Janssens, MD, PhD, division of respiratory medicine, University Hospital, Leuven, Belgium.
The phrase “potentially effective” was used because the primary endpoint, which was time to treatment failure, fell just short of statistical significance (P = .053), but the rate of treatment failures, which was a coprimary endpoint (P = .04), and all of the secondary endpoints, including mortality at 90 days (P = .027), need for treatment intensification (P = .02) and need for an intensive care unit (ICU) admission (P = .003), were significantly lower in the group receiving azithromycin rather than placebo.
In a previous trial, chronic azithromycin therapy on top of usual care in patients frequently hospitalized for COPD was associated with a reduction in the risk of exacerbations and an improvement in quality of life (N Engl J Med. 2011;365:689-98). However, Dr. Janssens explained that this strategy is not commonly used because it was associated with a variety of adverse events, not least of which was QTc prolongation.
The study at the meeting, called the BACE trial, was designed to test whether azithromycin could be employed in a more targeted approach to control exacerbations. In the study, 301 COPD patients hospitalized with an acute exacerbation were randomized within 48 hours of admission to azithromycin or placebo. For the first 3 days, azithromycin was administered in a 500-mg dose. Thereafter, the dose was 250 mg every second day. Treatment was stopped at 90 days.
The primary outcome was time to treatment failure, a novel composite endpoint of any of three events: the need for treatment intensification, the need for step-up hospital care (either ICU admission or hospital readmission), or death by any cause. The two treatment arms were also compared for safety, including QTc prolongation.
The treatment failure rates were 49% in the azithromycin arm and 60% in the placebo arm, producing a hazard ratio (HR) of 0.73. Although this outcome fell short of significance, Dr. Janssens suggested that benefits over the 90 days of treatment are supported by the secondary outcomes. However, he also cautioned that most relative advantages for azithromycin over placebo were found to dissipate over time.
“The maximum separation between the azithromycin and placebo arms [for the primary outcome] occurred at 120 days or 30 days after the medication was stopped,” Dr. Janssens reported. After this point, the two arms converged and eventually overlapped.
However, the acute benefits appeared to be substantial. For example, average hospital stay over the 90-day treatment period was reduced from 40 to 10 days (P = .0061), and the ICU days fell from 11 days to 3 days in the azithromycin relative to the placebo group. According to Dr. Janssens, the difference in hospital stay carries “important health economic potential that deserves further attention.”
Of the three QTc events that occurred during the course of the study, one was observed in the placebo group. There was no significant difference in this or other adverse events, according to Dr. Janssens.
It is notable that the design for the BACE trial called for 500 patients. When enrollment was slow, the design was changed on the basis of power calculations indicating that 300 patients would be sufficient to demonstrate a difference. It is unclear whether a larger study would have permitted the difference in the primary endpoint to advance from a trend.
Dr. Janssens reports no conflicts of interest relevant to this study.
PARIS – In patients with a chronic obstructive pulmonary disease (provided improvement in a variety of outcomes at 90 days, including risk of death, according to a placebo-controlled trial presented as a late-breaker at the annual congress of the European Respiratory Society.
In patients with COPD, “azithromycin initiated in the acute setting and continued for 3 months appears to be safe and potentially effective,” reported Wim Janssens, MD, PhD, division of respiratory medicine, University Hospital, Leuven, Belgium.
The phrase “potentially effective” was used because the primary endpoint, which was time to treatment failure, fell just short of statistical significance (P = .053), but the rate of treatment failures, which was a coprimary endpoint (P = .04), and all of the secondary endpoints, including mortality at 90 days (P = .027), need for treatment intensification (P = .02) and need for an intensive care unit (ICU) admission (P = .003), were significantly lower in the group receiving azithromycin rather than placebo.
In a previous trial, chronic azithromycin therapy on top of usual care in patients frequently hospitalized for COPD was associated with a reduction in the risk of exacerbations and an improvement in quality of life (N Engl J Med. 2011;365:689-98). However, Dr. Janssens explained that this strategy is not commonly used because it was associated with a variety of adverse events, not least of which was QTc prolongation.
The study at the meeting, called the BACE trial, was designed to test whether azithromycin could be employed in a more targeted approach to control exacerbations. In the study, 301 COPD patients hospitalized with an acute exacerbation were randomized within 48 hours of admission to azithromycin or placebo. For the first 3 days, azithromycin was administered in a 500-mg dose. Thereafter, the dose was 250 mg every second day. Treatment was stopped at 90 days.
The primary outcome was time to treatment failure, a novel composite endpoint of any of three events: the need for treatment intensification, the need for step-up hospital care (either ICU admission or hospital readmission), or death by any cause. The two treatment arms were also compared for safety, including QTc prolongation.
The treatment failure rates were 49% in the azithromycin arm and 60% in the placebo arm, producing a hazard ratio (HR) of 0.73. Although this outcome fell short of significance, Dr. Janssens suggested that benefits over the 90 days of treatment are supported by the secondary outcomes. However, he also cautioned that most relative advantages for azithromycin over placebo were found to dissipate over time.
“The maximum separation between the azithromycin and placebo arms [for the primary outcome] occurred at 120 days or 30 days after the medication was stopped,” Dr. Janssens reported. After this point, the two arms converged and eventually overlapped.
However, the acute benefits appeared to be substantial. For example, average hospital stay over the 90-day treatment period was reduced from 40 to 10 days (P = .0061), and the ICU days fell from 11 days to 3 days in the azithromycin relative to the placebo group. According to Dr. Janssens, the difference in hospital stay carries “important health economic potential that deserves further attention.”
Of the three QTc events that occurred during the course of the study, one was observed in the placebo group. There was no significant difference in this or other adverse events, according to Dr. Janssens.
It is notable that the design for the BACE trial called for 500 patients. When enrollment was slow, the design was changed on the basis of power calculations indicating that 300 patients would be sufficient to demonstrate a difference. It is unclear whether a larger study would have permitted the difference in the primary endpoint to advance from a trend.
Dr. Janssens reports no conflicts of interest relevant to this study.
PARIS – In patients with a chronic obstructive pulmonary disease (provided improvement in a variety of outcomes at 90 days, including risk of death, according to a placebo-controlled trial presented as a late-breaker at the annual congress of the European Respiratory Society.
In patients with COPD, “azithromycin initiated in the acute setting and continued for 3 months appears to be safe and potentially effective,” reported Wim Janssens, MD, PhD, division of respiratory medicine, University Hospital, Leuven, Belgium.
The phrase “potentially effective” was used because the primary endpoint, which was time to treatment failure, fell just short of statistical significance (P = .053), but the rate of treatment failures, which was a coprimary endpoint (P = .04), and all of the secondary endpoints, including mortality at 90 days (P = .027), need for treatment intensification (P = .02) and need for an intensive care unit (ICU) admission (P = .003), were significantly lower in the group receiving azithromycin rather than placebo.
In a previous trial, chronic azithromycin therapy on top of usual care in patients frequently hospitalized for COPD was associated with a reduction in the risk of exacerbations and an improvement in quality of life (N Engl J Med. 2011;365:689-98). However, Dr. Janssens explained that this strategy is not commonly used because it was associated with a variety of adverse events, not least of which was QTc prolongation.
The study at the meeting, called the BACE trial, was designed to test whether azithromycin could be employed in a more targeted approach to control exacerbations. In the study, 301 COPD patients hospitalized with an acute exacerbation were randomized within 48 hours of admission to azithromycin or placebo. For the first 3 days, azithromycin was administered in a 500-mg dose. Thereafter, the dose was 250 mg every second day. Treatment was stopped at 90 days.
The primary outcome was time to treatment failure, a novel composite endpoint of any of three events: the need for treatment intensification, the need for step-up hospital care (either ICU admission or hospital readmission), or death by any cause. The two treatment arms were also compared for safety, including QTc prolongation.
The treatment failure rates were 49% in the azithromycin arm and 60% in the placebo arm, producing a hazard ratio (HR) of 0.73. Although this outcome fell short of significance, Dr. Janssens suggested that benefits over the 90 days of treatment are supported by the secondary outcomes. However, he also cautioned that most relative advantages for azithromycin over placebo were found to dissipate over time.
“The maximum separation between the azithromycin and placebo arms [for the primary outcome] occurred at 120 days or 30 days after the medication was stopped,” Dr. Janssens reported. After this point, the two arms converged and eventually overlapped.
However, the acute benefits appeared to be substantial. For example, average hospital stay over the 90-day treatment period was reduced from 40 to 10 days (P = .0061), and the ICU days fell from 11 days to 3 days in the azithromycin relative to the placebo group. According to Dr. Janssens, the difference in hospital stay carries “important health economic potential that deserves further attention.”
Of the three QTc events that occurred during the course of the study, one was observed in the placebo group. There was no significant difference in this or other adverse events, according to Dr. Janssens.
It is notable that the design for the BACE trial called for 500 patients. When enrollment was slow, the design was changed on the basis of power calculations indicating that 300 patients would be sufficient to demonstrate a difference. It is unclear whether a larger study would have permitted the difference in the primary endpoint to advance from a trend.
Dr. Janssens reports no conflicts of interest relevant to this study.
REPORTING FROM THE ERS CONGRESS 2018
Key clinical point: Initiating azithromycin in patients with COPD exacerbation at the time of hospitalization improves short-term outcomes.
Major finding: Relative to placebo, azithromycin provided a borderline reduction in treatment failure (P = .053) while reducing mortality (P = .027).
Study details: Multicenter, placebo-controlled trial.
Disclosures: Dr. Janssens reports no conflicts of interest relevant to this study.
Ob.Gyn. News welcomes Dr. Badell to the Board
Dr. Badell is an assistant professor of gynecology and obstetrics in the division of maternal-fetal medicine at Emory University in Atlanta. She also is director of the Perinatal Center at Emory University Hospital Midtown.
Dr. Badell has been a primary author or coauthor of 35 articles published and accepted in refereed medical publications on topics including Zika infection during pregnancy, HIV infection during pregnancy, use of complementary and alternative medication in obstetrics and gynecology, botulism during pregnancy, maternal and fetal risk associated with assisted reproductive technology, and perinatal outcomes among women with congenital heart disease. She also has written several book chapters, and she currently is involved in research involving pediatric and maternal HIV/AIDS, as well as chronic hypertension during pregnancy.
Dr. Badell serves on a number of committees at Emory for the department of obstetrics and gynecology, including the clinical competency committee and program evaluation committee, as well as similar committees for the maternal-fetal medicine fellowship program. She also is a member of the Emory University Hospital Midtown’s quality enhancement committee.
Dr. Badell graduated with distinction from the University of Rochester (N.Y.), did a clinical research fellowship in obstetrics and gynecology at Baylor College of Medicine in Houston, and a fellowship in maternal-fetal medicine at Emory University. Dr. Badell has won too many honors and awards to mention, but a few of them are membership in Phi Beta Kappa; an outstanding clinician award in maternal-fetal medicine; an excellence in teaching, maternal-fetal medicine award; and a faculty recognition “Hidden Gem” award.
Dr. Badell is an assistant professor of gynecology and obstetrics in the division of maternal-fetal medicine at Emory University in Atlanta. She also is director of the Perinatal Center at Emory University Hospital Midtown.
Dr. Badell has been a primary author or coauthor of 35 articles published and accepted in refereed medical publications on topics including Zika infection during pregnancy, HIV infection during pregnancy, use of complementary and alternative medication in obstetrics and gynecology, botulism during pregnancy, maternal and fetal risk associated with assisted reproductive technology, and perinatal outcomes among women with congenital heart disease. She also has written several book chapters, and she currently is involved in research involving pediatric and maternal HIV/AIDS, as well as chronic hypertension during pregnancy.
Dr. Badell serves on a number of committees at Emory for the department of obstetrics and gynecology, including the clinical competency committee and program evaluation committee, as well as similar committees for the maternal-fetal medicine fellowship program. She also is a member of the Emory University Hospital Midtown’s quality enhancement committee.
Dr. Badell graduated with distinction from the University of Rochester (N.Y.), did a clinical research fellowship in obstetrics and gynecology at Baylor College of Medicine in Houston, and a fellowship in maternal-fetal medicine at Emory University. Dr. Badell has won too many honors and awards to mention, but a few of them are membership in Phi Beta Kappa; an outstanding clinician award in maternal-fetal medicine; an excellence in teaching, maternal-fetal medicine award; and a faculty recognition “Hidden Gem” award.
Dr. Badell is an assistant professor of gynecology and obstetrics in the division of maternal-fetal medicine at Emory University in Atlanta. She also is director of the Perinatal Center at Emory University Hospital Midtown.
Dr. Badell has been a primary author or coauthor of 35 articles published and accepted in refereed medical publications on topics including Zika infection during pregnancy, HIV infection during pregnancy, use of complementary and alternative medication in obstetrics and gynecology, botulism during pregnancy, maternal and fetal risk associated with assisted reproductive technology, and perinatal outcomes among women with congenital heart disease. She also has written several book chapters, and she currently is involved in research involving pediatric and maternal HIV/AIDS, as well as chronic hypertension during pregnancy.
Dr. Badell serves on a number of committees at Emory for the department of obstetrics and gynecology, including the clinical competency committee and program evaluation committee, as well as similar committees for the maternal-fetal medicine fellowship program. She also is a member of the Emory University Hospital Midtown’s quality enhancement committee.
Dr. Badell graduated with distinction from the University of Rochester (N.Y.), did a clinical research fellowship in obstetrics and gynecology at Baylor College of Medicine in Houston, and a fellowship in maternal-fetal medicine at Emory University. Dr. Badell has won too many honors and awards to mention, but a few of them are membership in Phi Beta Kappa; an outstanding clinician award in maternal-fetal medicine; an excellence in teaching, maternal-fetal medicine award; and a faculty recognition “Hidden Gem” award.
SBRT controls oligometastatic RCC in majority of patients
Stereotactic body radiation therapy (SBRT) is a safe and effective treatment option for patients with oligometastatic renal cell carcinoma (RCC), according to investigators.
Patients with clear cell RCC who had previously received systemic therapy were more likely to achieve local control, reported Ciro Franzese, MD of Humanitas Clinical and Research Center in Milan, and his coauthors.
These findings contribute to a shifting landscape in RCC; modern techniques are opening doors once closed by disappointing historical results. Several recent SBRT studies have demonstrated local control rates of approximately 90%, compared with conventional RT rates of 20%.
“While the outcomes from conventional RT were quite poor, with SBRT, different biological mechanisms occur due to the use of higher doses per fraction,” the authors wrote in The Journal of Urology.
The present retrospective study involved 58 patients with oligometastatic RCC who were treated with SBRT between 2004 and 2006. Patients previously underwent primary tumor excision, had no greater than three distant extracranial metastases, and were not surgical candidates. Study endpoints included median overall survival (OS), progression-free survival (PFS), and in-field local control (LC). Stratified analysis was also performed in patients with clear cell RCC.
Just over 90% of patients achieved LC at 18 months. Slightly less than half (46.2%) were progression-free at 1 year, and this number dropped to one-third (35%) by 18 months. Median OS was just over 2 years (28 months). Although all patients (100%) were alive at 2 years, this rate dropped to 83% by the 5-year mark.
In patients with clear cell RCC, those treated with systemic therapy prior to SBRT were more likely to achieve LC compared with patients who did not receive systemic therapy (HR 0.15; P = .032).
Overall, SBRT was well tolerated. No grade 3 or higher adverse events occurred. The most common adverse events were pain, fatigue, nausea, and vomiting.
The authors concluded that SBRT is a safe and effective option for patients with oligometastatic RCC. They called for future research to address “the radiobiology of RCC” in order to “understand the role of SBRT and, particularly, its possible interaction with medical therapies.”
The authors reported no conflicts of interest.
SOURCE: Franzese et al. J Urol. 2018 Sep 1. doi: 10.1016/j.juro.2018.08.049.
Stereotactic body radiation therapy (SBRT) is a safe and effective treatment option for patients with oligometastatic renal cell carcinoma (RCC), according to investigators.
Patients with clear cell RCC who had previously received systemic therapy were more likely to achieve local control, reported Ciro Franzese, MD of Humanitas Clinical and Research Center in Milan, and his coauthors.
These findings contribute to a shifting landscape in RCC; modern techniques are opening doors once closed by disappointing historical results. Several recent SBRT studies have demonstrated local control rates of approximately 90%, compared with conventional RT rates of 20%.
“While the outcomes from conventional RT were quite poor, with SBRT, different biological mechanisms occur due to the use of higher doses per fraction,” the authors wrote in The Journal of Urology.
The present retrospective study involved 58 patients with oligometastatic RCC who were treated with SBRT between 2004 and 2006. Patients previously underwent primary tumor excision, had no greater than three distant extracranial metastases, and were not surgical candidates. Study endpoints included median overall survival (OS), progression-free survival (PFS), and in-field local control (LC). Stratified analysis was also performed in patients with clear cell RCC.
Just over 90% of patients achieved LC at 18 months. Slightly less than half (46.2%) were progression-free at 1 year, and this number dropped to one-third (35%) by 18 months. Median OS was just over 2 years (28 months). Although all patients (100%) were alive at 2 years, this rate dropped to 83% by the 5-year mark.
In patients with clear cell RCC, those treated with systemic therapy prior to SBRT were more likely to achieve LC compared with patients who did not receive systemic therapy (HR 0.15; P = .032).
Overall, SBRT was well tolerated. No grade 3 or higher adverse events occurred. The most common adverse events were pain, fatigue, nausea, and vomiting.
The authors concluded that SBRT is a safe and effective option for patients with oligometastatic RCC. They called for future research to address “the radiobiology of RCC” in order to “understand the role of SBRT and, particularly, its possible interaction with medical therapies.”
The authors reported no conflicts of interest.
SOURCE: Franzese et al. J Urol. 2018 Sep 1. doi: 10.1016/j.juro.2018.08.049.
Stereotactic body radiation therapy (SBRT) is a safe and effective treatment option for patients with oligometastatic renal cell carcinoma (RCC), according to investigators.
Patients with clear cell RCC who had previously received systemic therapy were more likely to achieve local control, reported Ciro Franzese, MD of Humanitas Clinical and Research Center in Milan, and his coauthors.
These findings contribute to a shifting landscape in RCC; modern techniques are opening doors once closed by disappointing historical results. Several recent SBRT studies have demonstrated local control rates of approximately 90%, compared with conventional RT rates of 20%.
“While the outcomes from conventional RT were quite poor, with SBRT, different biological mechanisms occur due to the use of higher doses per fraction,” the authors wrote in The Journal of Urology.
The present retrospective study involved 58 patients with oligometastatic RCC who were treated with SBRT between 2004 and 2006. Patients previously underwent primary tumor excision, had no greater than three distant extracranial metastases, and were not surgical candidates. Study endpoints included median overall survival (OS), progression-free survival (PFS), and in-field local control (LC). Stratified analysis was also performed in patients with clear cell RCC.
Just over 90% of patients achieved LC at 18 months. Slightly less than half (46.2%) were progression-free at 1 year, and this number dropped to one-third (35%) by 18 months. Median OS was just over 2 years (28 months). Although all patients (100%) were alive at 2 years, this rate dropped to 83% by the 5-year mark.
In patients with clear cell RCC, those treated with systemic therapy prior to SBRT were more likely to achieve LC compared with patients who did not receive systemic therapy (HR 0.15; P = .032).
Overall, SBRT was well tolerated. No grade 3 or higher adverse events occurred. The most common adverse events were pain, fatigue, nausea, and vomiting.
The authors concluded that SBRT is a safe and effective option for patients with oligometastatic RCC. They called for future research to address “the radiobiology of RCC” in order to “understand the role of SBRT and, particularly, its possible interaction with medical therapies.”
The authors reported no conflicts of interest.
SOURCE: Franzese et al. J Urol. 2018 Sep 1. doi: 10.1016/j.juro.2018.08.049.
FROM THE JOURNAL OF UROLOGY
Key clinical point: For patients with oligometastatic renal cell carcinoma (RCC), stereotactic body radiation therapy (SBRT) is a safe and effective treatment option.
Major finding: The local control rate 18 months after SBRT was 90.2%.
Study details: A retrospective study involving 58 patients with oligometastatic RCC who were treated with SBRT between 2004 and 2006.
Disclosures: None.
Source: Franzese et al. J Urol. 2018 Sep 1. doi: 10.1016/j.juro.2018.08.049.
Female Gender, High Stress Levels, and Migraine
A recent study found a 10.7% prevalence of migraines and synergism between female gender and stress on risk of migraine, suggesting health interventions targeting women under stress may be beneficial. Researchers used data from 42,282 persons aged ≥12 years who participated in a 2013–2014 community health survey. A multivariate log-binomial model was used to calculate adjusted prevalence ratios for migraines associated with individual and joint exposures of female gender and stress. They used relative excess risk due to interaction (RERI), attributable proportion (AP), and synergy index (S index) to measure additive interaction. They found:
- The prevalence of migraines was 10.7%.
- The adjusted prevalence ratios were 2.37 for female vs male, 1.63 for persons with high vs low levels of stress, and 3.38 for women with high stress vs men with low stress.
- The RERI estimate was 0.38, the AP estimate was 0.11, and the S index was 1.19.
Slatculescu AM, Chen Y. Synergism between female gender and high levels of daily stress associated with migraine headaches in Ontario, Canada. [Published online ahead of print August 28, 2018]. Neuroepidemiol. doi:10.1159/000492503.
A recent study found a 10.7% prevalence of migraines and synergism between female gender and stress on risk of migraine, suggesting health interventions targeting women under stress may be beneficial. Researchers used data from 42,282 persons aged ≥12 years who participated in a 2013–2014 community health survey. A multivariate log-binomial model was used to calculate adjusted prevalence ratios for migraines associated with individual and joint exposures of female gender and stress. They used relative excess risk due to interaction (RERI), attributable proportion (AP), and synergy index (S index) to measure additive interaction. They found:
- The prevalence of migraines was 10.7%.
- The adjusted prevalence ratios were 2.37 for female vs male, 1.63 for persons with high vs low levels of stress, and 3.38 for women with high stress vs men with low stress.
- The RERI estimate was 0.38, the AP estimate was 0.11, and the S index was 1.19.
Slatculescu AM, Chen Y. Synergism between female gender and high levels of daily stress associated with migraine headaches in Ontario, Canada. [Published online ahead of print August 28, 2018]. Neuroepidemiol. doi:10.1159/000492503.
A recent study found a 10.7% prevalence of migraines and synergism between female gender and stress on risk of migraine, suggesting health interventions targeting women under stress may be beneficial. Researchers used data from 42,282 persons aged ≥12 years who participated in a 2013–2014 community health survey. A multivariate log-binomial model was used to calculate adjusted prevalence ratios for migraines associated with individual and joint exposures of female gender and stress. They used relative excess risk due to interaction (RERI), attributable proportion (AP), and synergy index (S index) to measure additive interaction. They found:
- The prevalence of migraines was 10.7%.
- The adjusted prevalence ratios were 2.37 for female vs male, 1.63 for persons with high vs low levels of stress, and 3.38 for women with high stress vs men with low stress.
- The RERI estimate was 0.38, the AP estimate was 0.11, and the S index was 1.19.
Slatculescu AM, Chen Y. Synergism between female gender and high levels of daily stress associated with migraine headaches in Ontario, Canada. [Published online ahead of print August 28, 2018]. Neuroepidemiol. doi:10.1159/000492503.
Decrease Found in ED Return Rates for Migraine
For patients with migraine in the emergency department (ED), the use of IV fluids, dopamine receptor antagonists (DRA), nonsteroidal anti-Inflammatory drugs, and corticosteroids increased whereas the use of narcotics and discharge prescriptions for narcotics decreased, according to a recent study. Researchers also found that the return rates for migraines decreased and they speculate that the increased use of non-narcotic medications contributed to this decrease. In this study, they examined a multi-hospital retrospective cohort consisting of consecutive ED patients from January 1, 1999, to September 31, 2014. They examined charts at the beginning and end of the time period and found:
- Of the 2,824,710 total visits, 8046 (0.28%) were for migraine.
- 290 charts (147 in 1999–2000 and 143 in 2014) were reviewed to determine migraine treatments.
- Of the 8046 migraine patients, 624 (8%) returned within 72 hours.
- The return rate decreased from 1999–2000 to 2014 from 12% to 4% (difference = 8%).
Ruzek M, Richman P, Eskin B, Allegra JR. ED treatment of migraine patients has changed. [Published online ahead of print August 20, 2018]. Am J Emerg Med. doi:10.1016/j.ajem.2018.08.051.
For patients with migraine in the emergency department (ED), the use of IV fluids, dopamine receptor antagonists (DRA), nonsteroidal anti-Inflammatory drugs, and corticosteroids increased whereas the use of narcotics and discharge prescriptions for narcotics decreased, according to a recent study. Researchers also found that the return rates for migraines decreased and they speculate that the increased use of non-narcotic medications contributed to this decrease. In this study, they examined a multi-hospital retrospective cohort consisting of consecutive ED patients from January 1, 1999, to September 31, 2014. They examined charts at the beginning and end of the time period and found:
- Of the 2,824,710 total visits, 8046 (0.28%) were for migraine.
- 290 charts (147 in 1999–2000 and 143 in 2014) were reviewed to determine migraine treatments.
- Of the 8046 migraine patients, 624 (8%) returned within 72 hours.
- The return rate decreased from 1999–2000 to 2014 from 12% to 4% (difference = 8%).
Ruzek M, Richman P, Eskin B, Allegra JR. ED treatment of migraine patients has changed. [Published online ahead of print August 20, 2018]. Am J Emerg Med. doi:10.1016/j.ajem.2018.08.051.
For patients with migraine in the emergency department (ED), the use of IV fluids, dopamine receptor antagonists (DRA), nonsteroidal anti-Inflammatory drugs, and corticosteroids increased whereas the use of narcotics and discharge prescriptions for narcotics decreased, according to a recent study. Researchers also found that the return rates for migraines decreased and they speculate that the increased use of non-narcotic medications contributed to this decrease. In this study, they examined a multi-hospital retrospective cohort consisting of consecutive ED patients from January 1, 1999, to September 31, 2014. They examined charts at the beginning and end of the time period and found:
- Of the 2,824,710 total visits, 8046 (0.28%) were for migraine.
- 290 charts (147 in 1999–2000 and 143 in 2014) were reviewed to determine migraine treatments.
- Of the 8046 migraine patients, 624 (8%) returned within 72 hours.
- The return rate decreased from 1999–2000 to 2014 from 12% to 4% (difference = 8%).
Ruzek M, Richman P, Eskin B, Allegra JR. ED treatment of migraine patients has changed. [Published online ahead of print August 20, 2018]. Am J Emerg Med. doi:10.1016/j.ajem.2018.08.051.
Sunscreens: Survey of the Cutis Editorial Board
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on sunscreens. Here’s what we found.
What sun protection factor (SPF) do you recommend for the majority of your patients?

Fifty percent of dermatologists we surveyed recommend SPF 30. SPF 50 was recommended by 26%, SPF 50+ by 21%, and SPF 15 by only 2%.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Half of our Editorial Board recommends sunscreen with SPF 30, with many recommending SPF 50 or higher. This trend toward sunscreens with higher SPF is consistent with a survey-based study with 97% of dermatologists stating they were comfortable recommending sunscreens with an SPF of 50 or higher and 83.3% stating that they believe that high SPF sunscreens provide an additional margin of safety (Farberg et al). These trends are supported by a randomized, double-blind, split-face clinical trial in which participants applied either SPF 50+ or SPF 100+ sunscreen after exposure to natural sunlight. The results showed that SPF 100+ sunscreen was remarkably more effective in protecting against sunburn than SPF 50+ sunscreen in actual use conditions (Williams et al).
Next page: Spray sunscreens
Which patient populations do you feel may benefit from spray sunscreens?
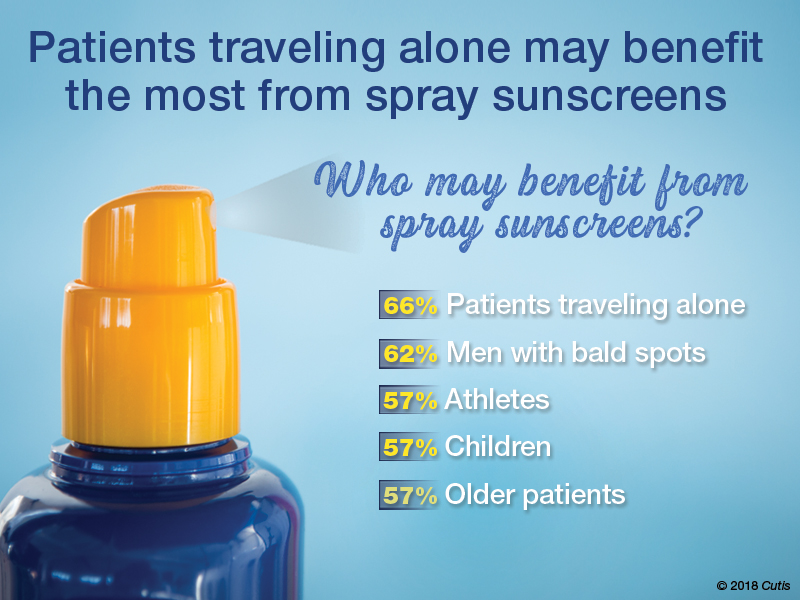
Two-thirds of dermatologists indicated that spray sunscreens may benefit patients traveling alone. Men with bald spots also may benefit (62%), as well as athletes, children, and older patients (57% each).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
As dermatologists, we tell our patients that the best sunscreens are ones that are used consistently. Spray sunscreens are likely as effective as lotions (Ou-Yang et al). There has been a clear trend in consumer purchasing of spray sunscreens from 2011 to 2016 (Teplitz et al). Spray sunscreens may benefit those traveling alone, particularly for hard-to-reach areas.
Next page: Supplemental vitamin D
In patients who apply sunscreen regularly, do you recommend supplemental vitamin D3?

More than half (53%) of dermatologists recommend supplemental vitamin D3.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Because use of photoprotection results in decreased vitamin D levels in most individuals, it is good practice to recommend vitamin D supplementation in patients who are applying sunscreen regularly (Bogaczewicz et al).
Next page: Sunscreen compliance
What is the most often heard reason(s) for not using sunscreen in your patients?
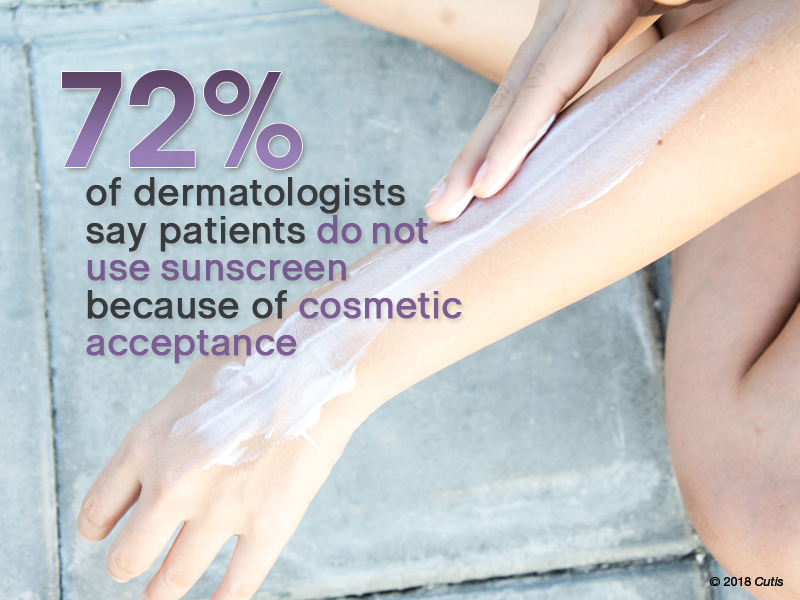
Nearly three-quarters (72%) of dermatologists reported that patients do not use sunscreen because of cosmetic acceptance. Almost one-third (31%) said their patients prefer “natural” products. Price was a factor for 26%. Fewer dermatologists indicated risk of environmental damage (14%), allergy (12%), cancer induction (5%), and hormonal alteration (5%) were reasons patients are not compliant.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Cosmetic acceptance is paramount for patient compliance for sunscreen application. These results from our Editorial Board echo a study on sunscreen product performance and other determinants of consumer preferences, which cited “cosmetic elegance” as an important factor in choosing sunscreens (Xu et al). Dermatologists must stress to patients to find a sunscreen that they find acceptable in terms of vehicle and price to increase compliance.
Next page: Sunscreens in pregnant women
What sunscreens do you recommend to pregnant women and children?

Most dermatologists (86%) recommend physical blockers “chemical-free” only sunscreens to pregnant women and children.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
While absorption of sunscreen by human embryos is likely negligible, because there is limited data on sunscreen effects in embryos and children, it is reasonable to recommend physical blockers for pregnant women and children.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
As a dermatologist married to a pediatrician, I try to get my kids to embrace sun-protection strategies. For the little ones it’s hard, but as they have gotten older and been exposed to more derm journals sitting around with pretty graphic pictures, they seem to get on board, even when away at summer camp on their own. If only our patients knew what our kids do.—Joel L. Cohen, MD (Denver, Colorado)
The most important factor in getting patient compliance with sunscreen usage is “cosmetic acceptance.” If they or their children or their spouse don’t like the feel, they won’t use it.—Vincent A. DeLeo, MD (Los Angeles, California)
Not using photoprotection with sunscreen is like crossing a busy road without looking both ways first.—James Q. Del Rosso, DO (Las Vegas, Nevada)
I do not recommend spray sunscreens. At least half of the spray seems to go in the air rather than on the skin. And people often do not rub the spray into their skin well enough. Lotions are better!—Lawrence J. Green, MD (Washington, DC)
The most important factor in sunscreen is not SPF; educate patients on the important role vehicle and sweating play in the length of sun protection.—Orit Markowitz, MD (New York, New York)
Reapplying sunscreen in the appropriate amount is key to blocking the danger rays of the sun.—Vineet Mishra, MD (San Antonio, Texas)
A good sunscreen is the one you put on properly. Regardless of the formulation, make sure you apply the sunscreen evenly to all exposed skin and reapply according to directions on the container. Remember, a regular white T-shirt has minimal SPF 4-5. Either wear sun-protective clothing or wear sunscreen underneath!—Larisa Ravitskiy, MD (Gahanna, Ohio)
Sun protection and sunscreen application go hand-in-hand. We can still enjoy the outdoors without getting excessive UV exposure.—Anthony M. Rossi, MD (New York, New York)
Sunscreens are only part of sun protection. Make sure to reapply them regularly, try to avoid direct sun between about 10 AM and 2 PM if possible, and wear a hat with a wide brim (not a baseball cap, which, after all, is designed for catching baseballs, not sun protection).—Robert I. Rudolph, MD (Wyomissing, Pennsylvania)
Sunscreens keep you younger looking longer!—Richard K. Scher, MD (New York, New York)
The dentist says only floss the teeth you want to keep. I tell patients to only sun block the skin they want to keep.—Daniel M. Siegel, MD, MS (Brooklyn, New York)
The best sunscreen is the one that is used! If it's too greasy or drying, smells bad or stings, it won't be used. Stick to the one YOU like, but at least SPF 30 or better.—Stephen P. Stone, MD, (Springfield, Illinois)
Sunscreen can be a meaningful part of your sun-protection regimen used in conjunction with sun-protective clothing, sun safe behaviors, and a diet rich in natural antioxidants.—Michelle Tarbox, MD (Lubbock, Texas)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from August 2, 2018, to September 2, 2018. A total of 42 usable responses were received.
Bogaczewicz J, Karczmarewicz E, Pludowski P, et al. Requirement for vitamin D supplementation in patients using photoprotection: variations in vitamin D levels and bone formation markers. Int J Dermatol. 2016;55:e176-e183.
Farberg AS, Glazer AM, Rigel AC, et al. Dermatologists’ perceptions, recommendations, and use of sunscreen. JAMA Dermatol. 2017;153:99-101.
Ou-Yang H, Stanfield J, Cole C, et al. High-SPF sunscreens (SPF ≥ 70) may provide ultraviolet protection above minimal recommended levels by adequately compensating for lower sunscreen user application amounts. J Am Acad Dermatol. 2012;67:1220-1227.
Teplitz RW, Glazer AM, Svoboda RM, et al. Trends in US sunscreen formulations: impact of increasing spray usage. J Am Acad Dermatol. 2018;78:187-189.
Williams JD, Maitra P, Atillasoy E, et al. SPF 100+ sunscreen is more protective against sunburn than SPF 50+ in actual use: Results of a randomized, double-blind, split-face, natural sunlight exposure clinical trial. J Am Acad Dermatol. 2018;78:902.e2-910.e2.
Xu S, Kwa M, Agarwal A, et al. Sunscreen product performance and other determinants of consumer preferences. JAMA Dermatol. 2016;152:920-927.
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on sunscreens. Here’s what we found.
What sun protection factor (SPF) do you recommend for the majority of your patients?

Fifty percent of dermatologists we surveyed recommend SPF 30. SPF 50 was recommended by 26%, SPF 50+ by 21%, and SPF 15 by only 2%.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Half of our Editorial Board recommends sunscreen with SPF 30, with many recommending SPF 50 or higher. This trend toward sunscreens with higher SPF is consistent with a survey-based study with 97% of dermatologists stating they were comfortable recommending sunscreens with an SPF of 50 or higher and 83.3% stating that they believe that high SPF sunscreens provide an additional margin of safety (Farberg et al). These trends are supported by a randomized, double-blind, split-face clinical trial in which participants applied either SPF 50+ or SPF 100+ sunscreen after exposure to natural sunlight. The results showed that SPF 100+ sunscreen was remarkably more effective in protecting against sunburn than SPF 50+ sunscreen in actual use conditions (Williams et al).
Next page: Spray sunscreens
Which patient populations do you feel may benefit from spray sunscreens?
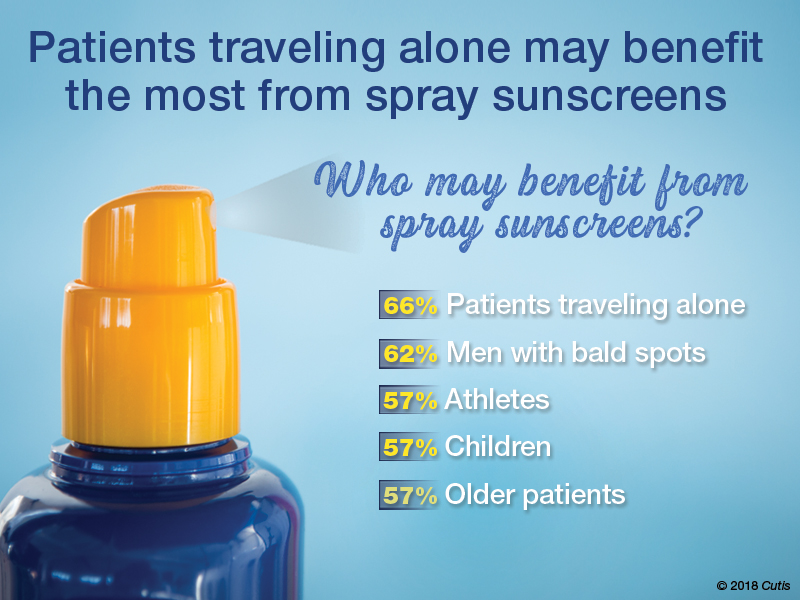
Two-thirds of dermatologists indicated that spray sunscreens may benefit patients traveling alone. Men with bald spots also may benefit (62%), as well as athletes, children, and older patients (57% each).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
As dermatologists, we tell our patients that the best sunscreens are ones that are used consistently. Spray sunscreens are likely as effective as lotions (Ou-Yang et al). There has been a clear trend in consumer purchasing of spray sunscreens from 2011 to 2016 (Teplitz et al). Spray sunscreens may benefit those traveling alone, particularly for hard-to-reach areas.
Next page: Supplemental vitamin D
In patients who apply sunscreen regularly, do you recommend supplemental vitamin D3?

More than half (53%) of dermatologists recommend supplemental vitamin D3.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Because use of photoprotection results in decreased vitamin D levels in most individuals, it is good practice to recommend vitamin D supplementation in patients who are applying sunscreen regularly (Bogaczewicz et al).
Next page: Sunscreen compliance
What is the most often heard reason(s) for not using sunscreen in your patients?
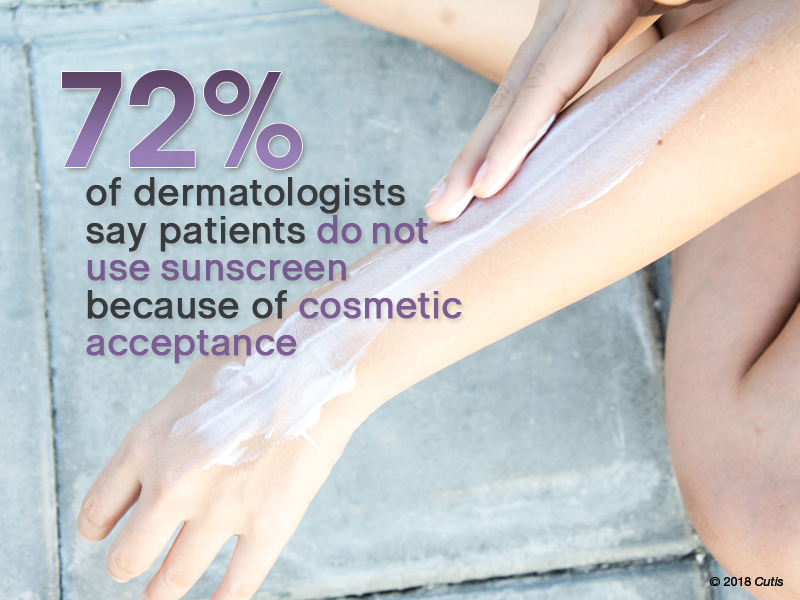
Nearly three-quarters (72%) of dermatologists reported that patients do not use sunscreen because of cosmetic acceptance. Almost one-third (31%) said their patients prefer “natural” products. Price was a factor for 26%. Fewer dermatologists indicated risk of environmental damage (14%), allergy (12%), cancer induction (5%), and hormonal alteration (5%) were reasons patients are not compliant.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Cosmetic acceptance is paramount for patient compliance for sunscreen application. These results from our Editorial Board echo a study on sunscreen product performance and other determinants of consumer preferences, which cited “cosmetic elegance” as an important factor in choosing sunscreens (Xu et al). Dermatologists must stress to patients to find a sunscreen that they find acceptable in terms of vehicle and price to increase compliance.
Next page: Sunscreens in pregnant women
What sunscreens do you recommend to pregnant women and children?

Most dermatologists (86%) recommend physical blockers “chemical-free” only sunscreens to pregnant women and children.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
While absorption of sunscreen by human embryos is likely negligible, because there is limited data on sunscreen effects in embryos and children, it is reasonable to recommend physical blockers for pregnant women and children.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
As a dermatologist married to a pediatrician, I try to get my kids to embrace sun-protection strategies. For the little ones it’s hard, but as they have gotten older and been exposed to more derm journals sitting around with pretty graphic pictures, they seem to get on board, even when away at summer camp on their own. If only our patients knew what our kids do.—Joel L. Cohen, MD (Denver, Colorado)
The most important factor in getting patient compliance with sunscreen usage is “cosmetic acceptance.” If they or their children or their spouse don’t like the feel, they won’t use it.—Vincent A. DeLeo, MD (Los Angeles, California)
Not using photoprotection with sunscreen is like crossing a busy road without looking both ways first.—James Q. Del Rosso, DO (Las Vegas, Nevada)
I do not recommend spray sunscreens. At least half of the spray seems to go in the air rather than on the skin. And people often do not rub the spray into their skin well enough. Lotions are better!—Lawrence J. Green, MD (Washington, DC)
The most important factor in sunscreen is not SPF; educate patients on the important role vehicle and sweating play in the length of sun protection.—Orit Markowitz, MD (New York, New York)
Reapplying sunscreen in the appropriate amount is key to blocking the danger rays of the sun.—Vineet Mishra, MD (San Antonio, Texas)
A good sunscreen is the one you put on properly. Regardless of the formulation, make sure you apply the sunscreen evenly to all exposed skin and reapply according to directions on the container. Remember, a regular white T-shirt has minimal SPF 4-5. Either wear sun-protective clothing or wear sunscreen underneath!—Larisa Ravitskiy, MD (Gahanna, Ohio)
Sun protection and sunscreen application go hand-in-hand. We can still enjoy the outdoors without getting excessive UV exposure.—Anthony M. Rossi, MD (New York, New York)
Sunscreens are only part of sun protection. Make sure to reapply them regularly, try to avoid direct sun between about 10 AM and 2 PM if possible, and wear a hat with a wide brim (not a baseball cap, which, after all, is designed for catching baseballs, not sun protection).—Robert I. Rudolph, MD (Wyomissing, Pennsylvania)
Sunscreens keep you younger looking longer!—Richard K. Scher, MD (New York, New York)
The dentist says only floss the teeth you want to keep. I tell patients to only sun block the skin they want to keep.—Daniel M. Siegel, MD, MS (Brooklyn, New York)
The best sunscreen is the one that is used! If it's too greasy or drying, smells bad or stings, it won't be used. Stick to the one YOU like, but at least SPF 30 or better.—Stephen P. Stone, MD, (Springfield, Illinois)
Sunscreen can be a meaningful part of your sun-protection regimen used in conjunction with sun-protective clothing, sun safe behaviors, and a diet rich in natural antioxidants.—Michelle Tarbox, MD (Lubbock, Texas)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from August 2, 2018, to September 2, 2018. A total of 42 usable responses were received.
To improve patient care and outcomes, leading dermatologists from the Cutis Editorial Board answered 5 questions on sunscreens. Here’s what we found.
What sun protection factor (SPF) do you recommend for the majority of your patients?

Fifty percent of dermatologists we surveyed recommend SPF 30. SPF 50 was recommended by 26%, SPF 50+ by 21%, and SPF 15 by only 2%.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Half of our Editorial Board recommends sunscreen with SPF 30, with many recommending SPF 50 or higher. This trend toward sunscreens with higher SPF is consistent with a survey-based study with 97% of dermatologists stating they were comfortable recommending sunscreens with an SPF of 50 or higher and 83.3% stating that they believe that high SPF sunscreens provide an additional margin of safety (Farberg et al). These trends are supported by a randomized, double-blind, split-face clinical trial in which participants applied either SPF 50+ or SPF 100+ sunscreen after exposure to natural sunlight. The results showed that SPF 100+ sunscreen was remarkably more effective in protecting against sunburn than SPF 50+ sunscreen in actual use conditions (Williams et al).
Next page: Spray sunscreens
Which patient populations do you feel may benefit from spray sunscreens?
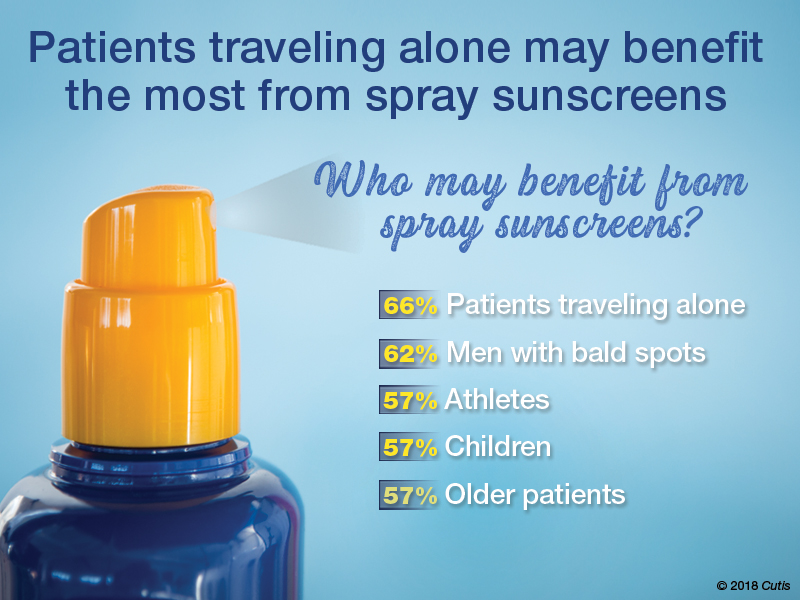
Two-thirds of dermatologists indicated that spray sunscreens may benefit patients traveling alone. Men with bald spots also may benefit (62%), as well as athletes, children, and older patients (57% each).
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
As dermatologists, we tell our patients that the best sunscreens are ones that are used consistently. Spray sunscreens are likely as effective as lotions (Ou-Yang et al). There has been a clear trend in consumer purchasing of spray sunscreens from 2011 to 2016 (Teplitz et al). Spray sunscreens may benefit those traveling alone, particularly for hard-to-reach areas.
Next page: Supplemental vitamin D
In patients who apply sunscreen regularly, do you recommend supplemental vitamin D3?

More than half (53%) of dermatologists recommend supplemental vitamin D3.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Because use of photoprotection results in decreased vitamin D levels in most individuals, it is good practice to recommend vitamin D supplementation in patients who are applying sunscreen regularly (Bogaczewicz et al).
Next page: Sunscreen compliance
What is the most often heard reason(s) for not using sunscreen in your patients?
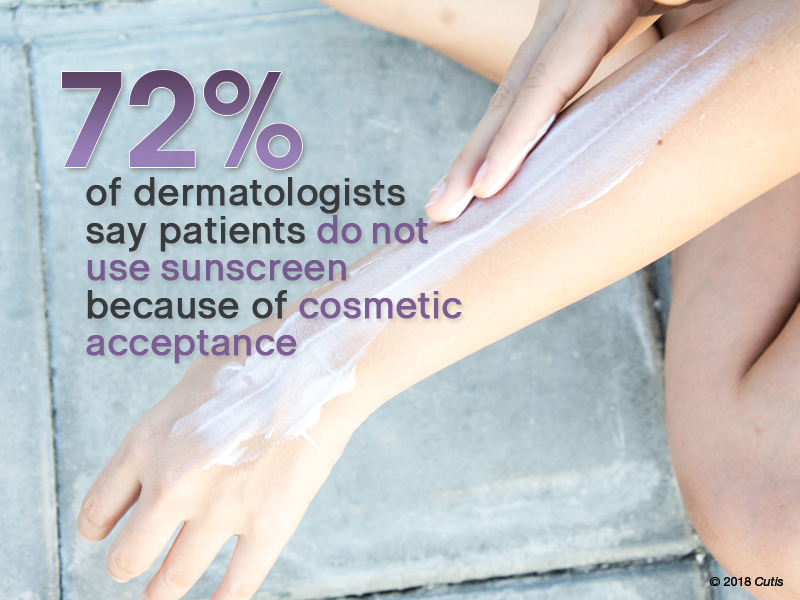
Nearly three-quarters (72%) of dermatologists reported that patients do not use sunscreen because of cosmetic acceptance. Almost one-third (31%) said their patients prefer “natural” products. Price was a factor for 26%. Fewer dermatologists indicated risk of environmental damage (14%), allergy (12%), cancer induction (5%), and hormonal alteration (5%) were reasons patients are not compliant.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
Cosmetic acceptance is paramount for patient compliance for sunscreen application. These results from our Editorial Board echo a study on sunscreen product performance and other determinants of consumer preferences, which cited “cosmetic elegance” as an important factor in choosing sunscreens (Xu et al). Dermatologists must stress to patients to find a sunscreen that they find acceptable in terms of vehicle and price to increase compliance.
Next page: Sunscreens in pregnant women
What sunscreens do you recommend to pregnant women and children?

Most dermatologists (86%) recommend physical blockers “chemical-free” only sunscreens to pregnant women and children.
Expert Commentary
Provided by Shari R. Lipner, MD, PhD (New York, New York)
While absorption of sunscreen by human embryos is likely negligible, because there is limited data on sunscreen effects in embryos and children, it is reasonable to recommend physical blockers for pregnant women and children.
Next page: More tips from derms
More Tips From Dermatologists
The dermatologists we polled had the following advice for their peers:
As a dermatologist married to a pediatrician, I try to get my kids to embrace sun-protection strategies. For the little ones it’s hard, but as they have gotten older and been exposed to more derm journals sitting around with pretty graphic pictures, they seem to get on board, even when away at summer camp on their own. If only our patients knew what our kids do.—Joel L. Cohen, MD (Denver, Colorado)
The most important factor in getting patient compliance with sunscreen usage is “cosmetic acceptance.” If they or their children or their spouse don’t like the feel, they won’t use it.—Vincent A. DeLeo, MD (Los Angeles, California)
Not using photoprotection with sunscreen is like crossing a busy road without looking both ways first.—James Q. Del Rosso, DO (Las Vegas, Nevada)
I do not recommend spray sunscreens. At least half of the spray seems to go in the air rather than on the skin. And people often do not rub the spray into their skin well enough. Lotions are better!—Lawrence J. Green, MD (Washington, DC)
The most important factor in sunscreen is not SPF; educate patients on the important role vehicle and sweating play in the length of sun protection.—Orit Markowitz, MD (New York, New York)
Reapplying sunscreen in the appropriate amount is key to blocking the danger rays of the sun.—Vineet Mishra, MD (San Antonio, Texas)
A good sunscreen is the one you put on properly. Regardless of the formulation, make sure you apply the sunscreen evenly to all exposed skin and reapply according to directions on the container. Remember, a regular white T-shirt has minimal SPF 4-5. Either wear sun-protective clothing or wear sunscreen underneath!—Larisa Ravitskiy, MD (Gahanna, Ohio)
Sun protection and sunscreen application go hand-in-hand. We can still enjoy the outdoors without getting excessive UV exposure.—Anthony M. Rossi, MD (New York, New York)
Sunscreens are only part of sun protection. Make sure to reapply them regularly, try to avoid direct sun between about 10 AM and 2 PM if possible, and wear a hat with a wide brim (not a baseball cap, which, after all, is designed for catching baseballs, not sun protection).—Robert I. Rudolph, MD (Wyomissing, Pennsylvania)
Sunscreens keep you younger looking longer!—Richard K. Scher, MD (New York, New York)
The dentist says only floss the teeth you want to keep. I tell patients to only sun block the skin they want to keep.—Daniel M. Siegel, MD, MS (Brooklyn, New York)
The best sunscreen is the one that is used! If it's too greasy or drying, smells bad or stings, it won't be used. Stick to the one YOU like, but at least SPF 30 or better.—Stephen P. Stone, MD, (Springfield, Illinois)
Sunscreen can be a meaningful part of your sun-protection regimen used in conjunction with sun-protective clothing, sun safe behaviors, and a diet rich in natural antioxidants.—Michelle Tarbox, MD (Lubbock, Texas)
About This Survey
The survey was fielded electronically to Cutis Editorial Board Members within the United States from August 2, 2018, to September 2, 2018. A total of 42 usable responses were received.
Bogaczewicz J, Karczmarewicz E, Pludowski P, et al. Requirement for vitamin D supplementation in patients using photoprotection: variations in vitamin D levels and bone formation markers. Int J Dermatol. 2016;55:e176-e183.
Farberg AS, Glazer AM, Rigel AC, et al. Dermatologists’ perceptions, recommendations, and use of sunscreen. JAMA Dermatol. 2017;153:99-101.
Ou-Yang H, Stanfield J, Cole C, et al. High-SPF sunscreens (SPF ≥ 70) may provide ultraviolet protection above minimal recommended levels by adequately compensating for lower sunscreen user application amounts. J Am Acad Dermatol. 2012;67:1220-1227.
Teplitz RW, Glazer AM, Svoboda RM, et al. Trends in US sunscreen formulations: impact of increasing spray usage. J Am Acad Dermatol. 2018;78:187-189.
Williams JD, Maitra P, Atillasoy E, et al. SPF 100+ sunscreen is more protective against sunburn than SPF 50+ in actual use: Results of a randomized, double-blind, split-face, natural sunlight exposure clinical trial. J Am Acad Dermatol. 2018;78:902.e2-910.e2.
Xu S, Kwa M, Agarwal A, et al. Sunscreen product performance and other determinants of consumer preferences. JAMA Dermatol. 2016;152:920-927.
Bogaczewicz J, Karczmarewicz E, Pludowski P, et al. Requirement for vitamin D supplementation in patients using photoprotection: variations in vitamin D levels and bone formation markers. Int J Dermatol. 2016;55:e176-e183.
Farberg AS, Glazer AM, Rigel AC, et al. Dermatologists’ perceptions, recommendations, and use of sunscreen. JAMA Dermatol. 2017;153:99-101.
Ou-Yang H, Stanfield J, Cole C, et al. High-SPF sunscreens (SPF ≥ 70) may provide ultraviolet protection above minimal recommended levels by adequately compensating for lower sunscreen user application amounts. J Am Acad Dermatol. 2012;67:1220-1227.
Teplitz RW, Glazer AM, Svoboda RM, et al. Trends in US sunscreen formulations: impact of increasing spray usage. J Am Acad Dermatol. 2018;78:187-189.
Williams JD, Maitra P, Atillasoy E, et al. SPF 100+ sunscreen is more protective against sunburn than SPF 50+ in actual use: Results of a randomized, double-blind, split-face, natural sunlight exposure clinical trial. J Am Acad Dermatol. 2018;78:902.e2-910.e2.
Xu S, Kwa M, Agarwal A, et al. Sunscreen product performance and other determinants of consumer preferences. JAMA Dermatol. 2016;152:920-927.









