User login
PARP inhibitor plus trabectedin shows promise for sarcoma
A combination of trabectedin and the PARP inhibitor olaparib may be a safe and effective therapy for patients with sarcoma, the recent TOMAS trial found.
High PARP1 expression was associated with treatment response, reported Giovanni Grignani, MD, of the Medical Oncology_Sarcoma Unit at Istituto di Ricovero e Cura a Carattere Scientifico in Candiolo, Italy, and his colleagues.
PARP inhibitors prevent repair of DNA damage, suggesting potential synergisms with DNA-damaging anticancer agents. Preclinical models support this strategy; however, clinical trials have found that toxicities restrict doses below antitumor activity levels.
“In view of these findings, trabectedin could be an ideal drug to use in combination with PARP1/2 inhibitors for two reasons: its favourable haemopoietic toxicity profile and its unique mechanisms of action,” the authors wrote in The Lancet Oncology. Trabectedin bends the minor groove of DNA toward the major groove, which activates PARP1 in an attempt to repair the damage. Preclinical trials showed that a PARP inhibitor such as olaparib would block this PARP1 activation, ultimately resulting in a more robust response than with either drug alone.
The phase 1b, open-label TOMAS trial involved 50 patients with sarcoma who had experienced disease progression after standard therapy. The study was divided into two cohorts: dose-escalation and dose-expansion. Patients received a median of four cycles of therapy with a median follow-up of 10 months (some patients are still undergoing treatment). The primary endpoint was maximum tolerated dose. The investigators also evaluated pharmacokinetics, pharmacodynamics, and various response measures.
Although adverse events occurred, these were manageable, and the authors concluded that the combination is safe for further investigation. The most common grade 3 or higher adverse events were lymphopenia (64%), neutropenia (62%), thrombocytopenia (28%), anemia (26%), hypophosphatemia (40%), and alanine aminotransferase elevation (18%). The maximum tolerated dose (recommended phase 2 dose) was olaparib 150 mg twice daily and trabectedin 1.1 mg/m2 every 3 weeks.
“These doses allowed us to minimize the need for dose reductions and continue treatment for as long as tumour control was maintained,” the authors wrote. Previous treatments impacted tolerability. The researchers noted that “patients who had received more than two lines of therapy had a higher risk of developing dose-limiting toxicities than those patients who had been treated with only one line of therapy.”
Overall, 14% of patients responded to therapy. Six-month progression-free survival was more common in patients with soft tissue sarcoma (38%) than other tumor types. More patients with high PARP1 expression achieved 6-month PFS compared with patients who had low PARP1 expression (59% vs. 8%; P = .01).
“The combination of olaparib and trabectedin exploits the potential of two different first-in-class drugs and shows tolerability and activity in homologous repair-proficient tumors,” the authors concluded.
They are planning two phase 2 studies in the future; one “comparing trabectedin alone versus the combination of trabectedin and olaparib, stratifying patients according to PARP1 expression,” and an “after-platinum-failure study of patients with ovarian cancer regardless of patients’ BRCA1/2 and BRCAness status.”
The TOMAS trial was funded by the Italian Association for Cancer Research, the Foundation for Research on Musculoskeletal and Rare Tumors, the Italian Ministry of Health, and PharmaMar. The authors reported compensation from Lilly, Novartis, Bayer, Eisai, Amgen, and others.
SOURCE: Grignani et al. Lancet Oncol. 2018 Sep 11. doi: 10.1016/S1470-2045(18)30438-8.
The phase 1b TOMAS trial by Grignani et al. showed that PARP inhibitor combination therapy may be a safe and effective option for patients with sarcoma, and a phase 2 study is warranted, according to Benjamin A. Nacev, MD, and William D. Tap, MD.
PARP inhibitors mitigate DNA damage repair, suggesting potential for synergistic combinations with DNA-damaging anticancer agents. Unfortunately, previous combinations have revealed toxicity issues.
“The first clinical example of this approach was the combination of the alkylating drug temozolomide and the PARP inhibitor rucaparib, which was hampered by dose-limiting myelosuppression,” Dr. Nacev and Dr. Tap wrote in an editorial in The Lancet Oncology.
In the TOMAS trial, Grignani et al. assessed a combination of trabectedin and the PARP inhibitor olaparib. Preclinical data showed synergistic activity in sarcoma cell lines, and the authors predicted tolerable myelosuppression with trabectedin.
Their predictions yielded promising results: Approximately one-third of patients with soft-tissue sarcoma were progression free at 6 months. Although myelosuppression did occur, the adverse event profile was tolerable.
As drug synergisms are biologically complex, “a key success of the TOMAS trial is the effective use of exploratory pharmacodynamic endpoints including PARP1 expression, PARylation, and mutational status of the DNA damage repair pathway.”
“For example, efficacy in the TOMAS trial correlated with PARP1 expression, with greater 6-month progression-free survival in the high PARP1 expression group than the low expression group.”
“The TOMAS investigators should be commended for doing the important bench-to-bedside approach of rationally designing and testing a drug combination to leverage available active drugs. We agree with the authors’ call for further investigation of trabectedin and olaparib in a randomised phase 2 trial in soft tissue sarcoma.”
William D. Tap, MD is chief of the Sarcoma Medical Oncology Service and Benjamin A. Nacev, MD is a third-year medical oncology/hematology fellow at Memorial Sloan Kettering Cancer Center in New York. Dr. Tap reported personal fees from Eli Lilly, Novartis, Eisai, and others. These comments are adapted from their accompanying editorial .
The phase 1b TOMAS trial by Grignani et al. showed that PARP inhibitor combination therapy may be a safe and effective option for patients with sarcoma, and a phase 2 study is warranted, according to Benjamin A. Nacev, MD, and William D. Tap, MD.
PARP inhibitors mitigate DNA damage repair, suggesting potential for synergistic combinations with DNA-damaging anticancer agents. Unfortunately, previous combinations have revealed toxicity issues.
“The first clinical example of this approach was the combination of the alkylating drug temozolomide and the PARP inhibitor rucaparib, which was hampered by dose-limiting myelosuppression,” Dr. Nacev and Dr. Tap wrote in an editorial in The Lancet Oncology.
In the TOMAS trial, Grignani et al. assessed a combination of trabectedin and the PARP inhibitor olaparib. Preclinical data showed synergistic activity in sarcoma cell lines, and the authors predicted tolerable myelosuppression with trabectedin.
Their predictions yielded promising results: Approximately one-third of patients with soft-tissue sarcoma were progression free at 6 months. Although myelosuppression did occur, the adverse event profile was tolerable.
As drug synergisms are biologically complex, “a key success of the TOMAS trial is the effective use of exploratory pharmacodynamic endpoints including PARP1 expression, PARylation, and mutational status of the DNA damage repair pathway.”
“For example, efficacy in the TOMAS trial correlated with PARP1 expression, with greater 6-month progression-free survival in the high PARP1 expression group than the low expression group.”
“The TOMAS investigators should be commended for doing the important bench-to-bedside approach of rationally designing and testing a drug combination to leverage available active drugs. We agree with the authors’ call for further investigation of trabectedin and olaparib in a randomised phase 2 trial in soft tissue sarcoma.”
William D. Tap, MD is chief of the Sarcoma Medical Oncology Service and Benjamin A. Nacev, MD is a third-year medical oncology/hematology fellow at Memorial Sloan Kettering Cancer Center in New York. Dr. Tap reported personal fees from Eli Lilly, Novartis, Eisai, and others. These comments are adapted from their accompanying editorial .
The phase 1b TOMAS trial by Grignani et al. showed that PARP inhibitor combination therapy may be a safe and effective option for patients with sarcoma, and a phase 2 study is warranted, according to Benjamin A. Nacev, MD, and William D. Tap, MD.
PARP inhibitors mitigate DNA damage repair, suggesting potential for synergistic combinations with DNA-damaging anticancer agents. Unfortunately, previous combinations have revealed toxicity issues.
“The first clinical example of this approach was the combination of the alkylating drug temozolomide and the PARP inhibitor rucaparib, which was hampered by dose-limiting myelosuppression,” Dr. Nacev and Dr. Tap wrote in an editorial in The Lancet Oncology.
In the TOMAS trial, Grignani et al. assessed a combination of trabectedin and the PARP inhibitor olaparib. Preclinical data showed synergistic activity in sarcoma cell lines, and the authors predicted tolerable myelosuppression with trabectedin.
Their predictions yielded promising results: Approximately one-third of patients with soft-tissue sarcoma were progression free at 6 months. Although myelosuppression did occur, the adverse event profile was tolerable.
As drug synergisms are biologically complex, “a key success of the TOMAS trial is the effective use of exploratory pharmacodynamic endpoints including PARP1 expression, PARylation, and mutational status of the DNA damage repair pathway.”
“For example, efficacy in the TOMAS trial correlated with PARP1 expression, with greater 6-month progression-free survival in the high PARP1 expression group than the low expression group.”
“The TOMAS investigators should be commended for doing the important bench-to-bedside approach of rationally designing and testing a drug combination to leverage available active drugs. We agree with the authors’ call for further investigation of trabectedin and olaparib in a randomised phase 2 trial in soft tissue sarcoma.”
William D. Tap, MD is chief of the Sarcoma Medical Oncology Service and Benjamin A. Nacev, MD is a third-year medical oncology/hematology fellow at Memorial Sloan Kettering Cancer Center in New York. Dr. Tap reported personal fees from Eli Lilly, Novartis, Eisai, and others. These comments are adapted from their accompanying editorial .
A combination of trabectedin and the PARP inhibitor olaparib may be a safe and effective therapy for patients with sarcoma, the recent TOMAS trial found.
High PARP1 expression was associated with treatment response, reported Giovanni Grignani, MD, of the Medical Oncology_Sarcoma Unit at Istituto di Ricovero e Cura a Carattere Scientifico in Candiolo, Italy, and his colleagues.
PARP inhibitors prevent repair of DNA damage, suggesting potential synergisms with DNA-damaging anticancer agents. Preclinical models support this strategy; however, clinical trials have found that toxicities restrict doses below antitumor activity levels.
“In view of these findings, trabectedin could be an ideal drug to use in combination with PARP1/2 inhibitors for two reasons: its favourable haemopoietic toxicity profile and its unique mechanisms of action,” the authors wrote in The Lancet Oncology. Trabectedin bends the minor groove of DNA toward the major groove, which activates PARP1 in an attempt to repair the damage. Preclinical trials showed that a PARP inhibitor such as olaparib would block this PARP1 activation, ultimately resulting in a more robust response than with either drug alone.
The phase 1b, open-label TOMAS trial involved 50 patients with sarcoma who had experienced disease progression after standard therapy. The study was divided into two cohorts: dose-escalation and dose-expansion. Patients received a median of four cycles of therapy with a median follow-up of 10 months (some patients are still undergoing treatment). The primary endpoint was maximum tolerated dose. The investigators also evaluated pharmacokinetics, pharmacodynamics, and various response measures.
Although adverse events occurred, these were manageable, and the authors concluded that the combination is safe for further investigation. The most common grade 3 or higher adverse events were lymphopenia (64%), neutropenia (62%), thrombocytopenia (28%), anemia (26%), hypophosphatemia (40%), and alanine aminotransferase elevation (18%). The maximum tolerated dose (recommended phase 2 dose) was olaparib 150 mg twice daily and trabectedin 1.1 mg/m2 every 3 weeks.
“These doses allowed us to minimize the need for dose reductions and continue treatment for as long as tumour control was maintained,” the authors wrote. Previous treatments impacted tolerability. The researchers noted that “patients who had received more than two lines of therapy had a higher risk of developing dose-limiting toxicities than those patients who had been treated with only one line of therapy.”
Overall, 14% of patients responded to therapy. Six-month progression-free survival was more common in patients with soft tissue sarcoma (38%) than other tumor types. More patients with high PARP1 expression achieved 6-month PFS compared with patients who had low PARP1 expression (59% vs. 8%; P = .01).
“The combination of olaparib and trabectedin exploits the potential of two different first-in-class drugs and shows tolerability and activity in homologous repair-proficient tumors,” the authors concluded.
They are planning two phase 2 studies in the future; one “comparing trabectedin alone versus the combination of trabectedin and olaparib, stratifying patients according to PARP1 expression,” and an “after-platinum-failure study of patients with ovarian cancer regardless of patients’ BRCA1/2 and BRCAness status.”
The TOMAS trial was funded by the Italian Association for Cancer Research, the Foundation for Research on Musculoskeletal and Rare Tumors, the Italian Ministry of Health, and PharmaMar. The authors reported compensation from Lilly, Novartis, Bayer, Eisai, Amgen, and others.
SOURCE: Grignani et al. Lancet Oncol. 2018 Sep 11. doi: 10.1016/S1470-2045(18)30438-8.
A combination of trabectedin and the PARP inhibitor olaparib may be a safe and effective therapy for patients with sarcoma, the recent TOMAS trial found.
High PARP1 expression was associated with treatment response, reported Giovanni Grignani, MD, of the Medical Oncology_Sarcoma Unit at Istituto di Ricovero e Cura a Carattere Scientifico in Candiolo, Italy, and his colleagues.
PARP inhibitors prevent repair of DNA damage, suggesting potential synergisms with DNA-damaging anticancer agents. Preclinical models support this strategy; however, clinical trials have found that toxicities restrict doses below antitumor activity levels.
“In view of these findings, trabectedin could be an ideal drug to use in combination with PARP1/2 inhibitors for two reasons: its favourable haemopoietic toxicity profile and its unique mechanisms of action,” the authors wrote in The Lancet Oncology. Trabectedin bends the minor groove of DNA toward the major groove, which activates PARP1 in an attempt to repair the damage. Preclinical trials showed that a PARP inhibitor such as olaparib would block this PARP1 activation, ultimately resulting in a more robust response than with either drug alone.
The phase 1b, open-label TOMAS trial involved 50 patients with sarcoma who had experienced disease progression after standard therapy. The study was divided into two cohorts: dose-escalation and dose-expansion. Patients received a median of four cycles of therapy with a median follow-up of 10 months (some patients are still undergoing treatment). The primary endpoint was maximum tolerated dose. The investigators also evaluated pharmacokinetics, pharmacodynamics, and various response measures.
Although adverse events occurred, these were manageable, and the authors concluded that the combination is safe for further investigation. The most common grade 3 or higher adverse events were lymphopenia (64%), neutropenia (62%), thrombocytopenia (28%), anemia (26%), hypophosphatemia (40%), and alanine aminotransferase elevation (18%). The maximum tolerated dose (recommended phase 2 dose) was olaparib 150 mg twice daily and trabectedin 1.1 mg/m2 every 3 weeks.
“These doses allowed us to minimize the need for dose reductions and continue treatment for as long as tumour control was maintained,” the authors wrote. Previous treatments impacted tolerability. The researchers noted that “patients who had received more than two lines of therapy had a higher risk of developing dose-limiting toxicities than those patients who had been treated with only one line of therapy.”
Overall, 14% of patients responded to therapy. Six-month progression-free survival was more common in patients with soft tissue sarcoma (38%) than other tumor types. More patients with high PARP1 expression achieved 6-month PFS compared with patients who had low PARP1 expression (59% vs. 8%; P = .01).
“The combination of olaparib and trabectedin exploits the potential of two different first-in-class drugs and shows tolerability and activity in homologous repair-proficient tumors,” the authors concluded.
They are planning two phase 2 studies in the future; one “comparing trabectedin alone versus the combination of trabectedin and olaparib, stratifying patients according to PARP1 expression,” and an “after-platinum-failure study of patients with ovarian cancer regardless of patients’ BRCA1/2 and BRCAness status.”
The TOMAS trial was funded by the Italian Association for Cancer Research, the Foundation for Research on Musculoskeletal and Rare Tumors, the Italian Ministry of Health, and PharmaMar. The authors reported compensation from Lilly, Novartis, Bayer, Eisai, Amgen, and others.
SOURCE: Grignani et al. Lancet Oncol. 2018 Sep 11. doi: 10.1016/S1470-2045(18)30438-8.
FROM THE LANCET ONCOLOGY
Key clinical point: A combination of trabectedin and the PARP inhibitor olaparib may be a safe and effective therapy for patients with sarcoma.
Major finding: Of those with high PARP1 expression, 59% were progression free 6 months after treatment.
Study details: TOMAS was an open-label phase 1b trial involving 50 patients with sarcoma who had disease progression after standard therapy.
Disclosures: The study was funded by the Italian Association for Cancer Research, the Foundation for Research on Musculoskeletal and Rare Tumors, the Italian Ministry of Health, and PharmaMar. The authors reported compensation from Lilly, Novartis, Bayer, Eisai, Amgen, and others.
Source: Grignani et al. Lancet Oncol. 2018 Sep 11. doi: 10.1016/S1470-2045(18)30438-8.
Researchers propose new acute leukemia subtypes
An extensive analysis of mixed phenotype acute leukemia (MPAL) has led to new insights that may have implications for disease classification and treatment.
Researchers believe they have identified new subtypes of MPAL that should be included in the World Health Organization classification for acute leukemia.
Each of these subtypes share genomic characteristics with other acute leukemias, which suggests they might respond to treatments that are already in use.
This research also has shed light on how MPAL evolves and appears to provide an explanation for why MPAL displays characteristics of both acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL).
“ALL and AML have very different treatments, but MPAL has features of both, so the question of how best to treat patients with MPAL has been challenging the leukemia community worldwide, and long-term survival of patients has been poor,” said study author Charles G. Mullighan, MD, of St. Jude Children’s Research Hospital in Memphis, Tenn.
In the current study, published in Nature, Dr. Mullighan and his colleagues used whole-genome, whole-exome, and RNA sequencing to analyze 115 samples from pediatric patients with MPAL.
The analysis revealed mutations that define the two most common subtypes of MPAL – B/myeloid and T/myeloid – and suggested these subtypes share similarities with other leukemia subtypes.
The researchers found that 48% of B/myeloid MPAL cases carried rearrangements in ZNF384, a characteristic that is also found in cases of B-cell ALL. In fact, the team said the gene expression profiles of ZNF384r B-ALL and ZNF384r MPAL were indistinguishable.
“That is biologically and clinically important,” Dr. Mullighan said. “The findings suggest the ZNF384 rearrangement defines a distinct leukemia subtype, and the alteration should be used to guide treatment.”
The researchers noted that patients with ZNF384r exhibited higher FLT3 expression than that of patients with other types of B/myeloid or T/myeloid MPAL, so patients with ZNF384r MPAL might respond well to treatment with a FLT3 inhibitor.
This study also showed that cases of B/myeloid MPAL without ZNF384r shared genomic features with other B-ALL subtypes, such as Ph-like B-ALL.
In addition, the analysis showed that T/myeloid MPAL and early T-cell precursor ALL have similar gene expression profiles.
The team identified several genes that were mutated at similar frequencies in T/myeloid MPAL and early T-cell precursor ALL, including WT1, ETV6, EZH2, and FLT3.
WT1 was the most frequently mutated transcription factor gene in T/myeloid MPAL.
Based on these findings, the researchers said the WHO classification of acute leukemia should be updated to include: ZNF384r acute leukemia (either B-ALL or MPAL), WT1-mutant T/myeloid MPAL, and Ph-like B/myeloid MPAL.
This research was supported by the National Cancer Institute, the National Institutes of Health, Cookies for Kids’ Cancer, and other organizations. The researchers reported having no competing interests.
SOURCE: Alexander TB et al. Nature. 2018 Sep 12. doi: 10.1038/s41586-018-0436-0.
An extensive analysis of mixed phenotype acute leukemia (MPAL) has led to new insights that may have implications for disease classification and treatment.
Researchers believe they have identified new subtypes of MPAL that should be included in the World Health Organization classification for acute leukemia.
Each of these subtypes share genomic characteristics with other acute leukemias, which suggests they might respond to treatments that are already in use.
This research also has shed light on how MPAL evolves and appears to provide an explanation for why MPAL displays characteristics of both acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL).
“ALL and AML have very different treatments, but MPAL has features of both, so the question of how best to treat patients with MPAL has been challenging the leukemia community worldwide, and long-term survival of patients has been poor,” said study author Charles G. Mullighan, MD, of St. Jude Children’s Research Hospital in Memphis, Tenn.
In the current study, published in Nature, Dr. Mullighan and his colleagues used whole-genome, whole-exome, and RNA sequencing to analyze 115 samples from pediatric patients with MPAL.
The analysis revealed mutations that define the two most common subtypes of MPAL – B/myeloid and T/myeloid – and suggested these subtypes share similarities with other leukemia subtypes.
The researchers found that 48% of B/myeloid MPAL cases carried rearrangements in ZNF384, a characteristic that is also found in cases of B-cell ALL. In fact, the team said the gene expression profiles of ZNF384r B-ALL and ZNF384r MPAL were indistinguishable.
“That is biologically and clinically important,” Dr. Mullighan said. “The findings suggest the ZNF384 rearrangement defines a distinct leukemia subtype, and the alteration should be used to guide treatment.”
The researchers noted that patients with ZNF384r exhibited higher FLT3 expression than that of patients with other types of B/myeloid or T/myeloid MPAL, so patients with ZNF384r MPAL might respond well to treatment with a FLT3 inhibitor.
This study also showed that cases of B/myeloid MPAL without ZNF384r shared genomic features with other B-ALL subtypes, such as Ph-like B-ALL.
In addition, the analysis showed that T/myeloid MPAL and early T-cell precursor ALL have similar gene expression profiles.
The team identified several genes that were mutated at similar frequencies in T/myeloid MPAL and early T-cell precursor ALL, including WT1, ETV6, EZH2, and FLT3.
WT1 was the most frequently mutated transcription factor gene in T/myeloid MPAL.
Based on these findings, the researchers said the WHO classification of acute leukemia should be updated to include: ZNF384r acute leukemia (either B-ALL or MPAL), WT1-mutant T/myeloid MPAL, and Ph-like B/myeloid MPAL.
This research was supported by the National Cancer Institute, the National Institutes of Health, Cookies for Kids’ Cancer, and other organizations. The researchers reported having no competing interests.
SOURCE: Alexander TB et al. Nature. 2018 Sep 12. doi: 10.1038/s41586-018-0436-0.
An extensive analysis of mixed phenotype acute leukemia (MPAL) has led to new insights that may have implications for disease classification and treatment.
Researchers believe they have identified new subtypes of MPAL that should be included in the World Health Organization classification for acute leukemia.
Each of these subtypes share genomic characteristics with other acute leukemias, which suggests they might respond to treatments that are already in use.
This research also has shed light on how MPAL evolves and appears to provide an explanation for why MPAL displays characteristics of both acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL).
“ALL and AML have very different treatments, but MPAL has features of both, so the question of how best to treat patients with MPAL has been challenging the leukemia community worldwide, and long-term survival of patients has been poor,” said study author Charles G. Mullighan, MD, of St. Jude Children’s Research Hospital in Memphis, Tenn.
In the current study, published in Nature, Dr. Mullighan and his colleagues used whole-genome, whole-exome, and RNA sequencing to analyze 115 samples from pediatric patients with MPAL.
The analysis revealed mutations that define the two most common subtypes of MPAL – B/myeloid and T/myeloid – and suggested these subtypes share similarities with other leukemia subtypes.
The researchers found that 48% of B/myeloid MPAL cases carried rearrangements in ZNF384, a characteristic that is also found in cases of B-cell ALL. In fact, the team said the gene expression profiles of ZNF384r B-ALL and ZNF384r MPAL were indistinguishable.
“That is biologically and clinically important,” Dr. Mullighan said. “The findings suggest the ZNF384 rearrangement defines a distinct leukemia subtype, and the alteration should be used to guide treatment.”
The researchers noted that patients with ZNF384r exhibited higher FLT3 expression than that of patients with other types of B/myeloid or T/myeloid MPAL, so patients with ZNF384r MPAL might respond well to treatment with a FLT3 inhibitor.
This study also showed that cases of B/myeloid MPAL without ZNF384r shared genomic features with other B-ALL subtypes, such as Ph-like B-ALL.
In addition, the analysis showed that T/myeloid MPAL and early T-cell precursor ALL have similar gene expression profiles.
The team identified several genes that were mutated at similar frequencies in T/myeloid MPAL and early T-cell precursor ALL, including WT1, ETV6, EZH2, and FLT3.
WT1 was the most frequently mutated transcription factor gene in T/myeloid MPAL.
Based on these findings, the researchers said the WHO classification of acute leukemia should be updated to include: ZNF384r acute leukemia (either B-ALL or MPAL), WT1-mutant T/myeloid MPAL, and Ph-like B/myeloid MPAL.
This research was supported by the National Cancer Institute, the National Institutes of Health, Cookies for Kids’ Cancer, and other organizations. The researchers reported having no competing interests.
SOURCE: Alexander TB et al. Nature. 2018 Sep 12. doi: 10.1038/s41586-018-0436-0.
FROM NATURE
Key clinical point:
Major finding: In total, 48% of B/myeloid MPAL cases carried rearrangements in ZNF384, a characteristic that is also found in cases of B-cell ALL.
Study details: Whole-genome, -exome, and RNA sequencing of 115 samples from pediatric patients with MPAL.
Disclosures: This research was supported by the National Cancer Institute and other organizations. The researchers reported having no competing interests.
Source: Alexander TB et al. Nature. 2018 Sep 12. doi: 10.1038/s41586-018-0436-0.
Vaginal intraepithelial neoplasia: What to do when dysplasia persists after hysterectomy
Vaginal intraepithelial neoplasia (VAIN) is a condition that frequently poses therapeutic dilemmas for gynecologists. VAIN represents dysplastic changes to the epithelium of the vaginal mucosa, and like cervical neoplasia, the extent of disease is characterized as levels I, II, or III dependent upon the depth of involvement in the epithelial layer by dysplastic cells. While VAIN itself typically is asymptomatic and not a harmful condition, it carries a 12% risk of progression to invasive vaginal carcinoma, so accurate identification, thorough treatment, and ongoing surveillance are essential.1
VAIN is associated with high-risk human papillomavirus (HPV) infection, tobacco use, and prior cervical dysplasia. Of women with VAIN, 65% have undergone a prior hysterectomy for cervical dysplasia, which emphasizes the nondefinitive nature of such an intervention.2 These women should be very closely followed for at least 20 years with vaginal cytologic and/or HPV surveillance. High-risk HPV infection is present in 85% of women with VAIN, and the presence of high-risk HPV is a predictor for recurrent VAIN. Recurrent and persistent VAIN also is more common in postmenopausal women and those with multifocal disease.
The most common location for VAIN is at the upper third of the vagina (including the vaginal cuff). It commonly arises within the vaginal fornices, which may be difficult to fully visualize because of their puckered appearance, redundant vaginal tissues, and extensive vaginal rogation.
A diagnosis of VAIN is typically obtained from vaginal cytology which reveals atypical or dysplastic cells. Such a result should prompt the physician to perform vaginal colposcopy and directed biopsies. Comprehensive visualization of the vaginal cuff can be limited in cases where the vaginal fornices are tethered, deeply puckered, or when there is significant mucosal rogation.
The application of 4% acetic acid or Lugol’s iodine are techniques that can enhance the detection of dysplastic vaginal mucosa. Lugol’s iodine selectively stains normal, glycogenated cells, and spares dysplastic glycogen-free cells. The sharp contrast between the brown iodine-stained tissues and the white dysplastic tissues aids in detection of dysplastic areas.
If colposcopic biopsy reveals low grade dysplasia (VAIN I) it does not require intervention, and has a very low rate of conversion to invasive vaginal carcinoma. However moderate- and high-grade vaginal dysplastic lesions should be treated because of the potential for malignant transformation.
Options for treatment of VAIN include topical, ablative, and excisional procedures. Observation also is an option but should be reserved for patients who are closely monitored with repeated colposcopic examinations, and probably should best be reserved for patients with VAIN I or II lesions.
Excisional procedures
The most common excisional procedure employed for VAIN is upper vaginectomy. In this procedure, the surgeon grasps and tents up the vaginal mucosa, incises the mucosa without penetrating the subepithelial tissue layers such as bladder and rectum. The vaginal mucosa then is carefully separated from the underlying endopelvic fascial plane. The specimen should be oriented, ideally on a cork board, with pins or sutures to ascribe margins and borders. Excision is best utilized for women with unifocal disease, or those who fail or do not tolerate ablative or topical interventions.
The most significant risks of excision include the potential for damage to underlying pelvic visceral structures, which is particularly concerning in postmenopausal women with thin vaginal epithelium. Vaginectomy is commonly associated with vaginal shortening or narrowing, which can be deleterious for quality of life. Retrospective series have described a 30% incidence of recurrence after vaginectomy, likely secondary to incomplete excision of all affected tissue.3
Ablation
Ablation of dysplastic foci with a carbon dioxide (CO2) laser is a common method for treatment of VAIN. CO2 laser should ablate tissue to a 1.5 mm minimum depth.3 The benefit of using CO2 laser is its ability to treat multifocal disease in situ without an extensive excisional procedure.
It is technically more straightforward than upper vaginectomy with less blood loss and shorter surgical times, and it can be easily accomplished in an outpatient surgical or office setting. However, one of its greatest limitations is the difficulty in visualizing all lesions and therefore adequately treating all sites. The vaginal rogations also make adequate laser ablation challenging because laser only is able to effectively ablate tissue that is oriented perpendicular to the laser beam.
In addition, there is no pathologic confirmation of adequacy of excision or margin status. These features may contribute to the modestly higher rates of recurrence of dysplasia following laser ablation, compared with vaginectomy.3 It also has been associated with more vaginal scarring than vaginectomy, which can have a negative effect on sexual health.
Topical agents
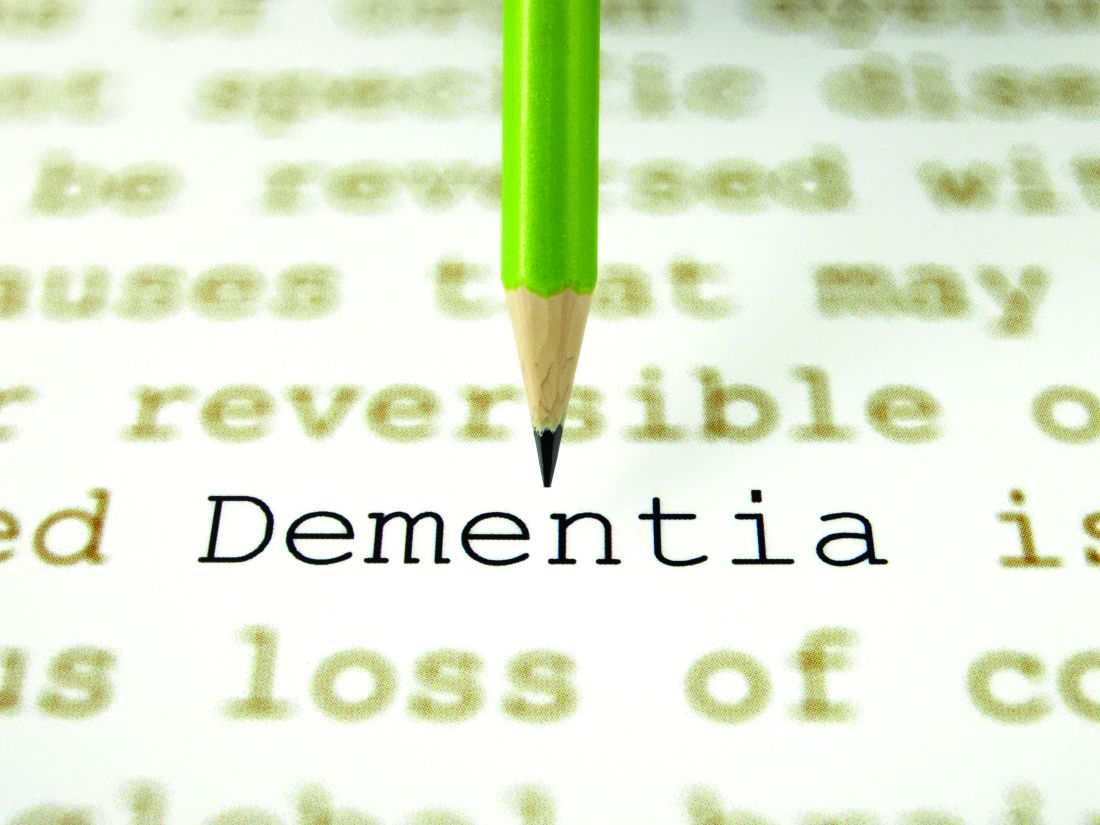
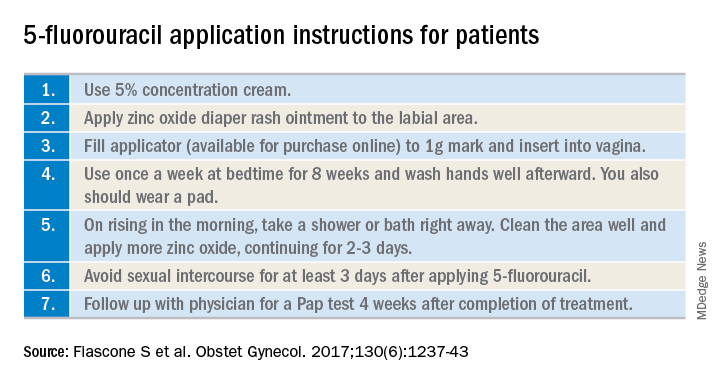
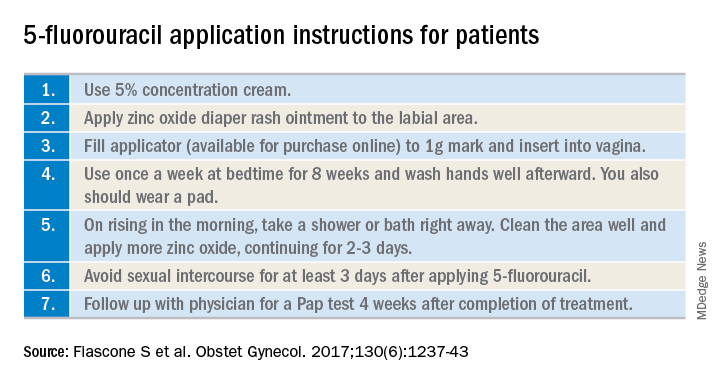
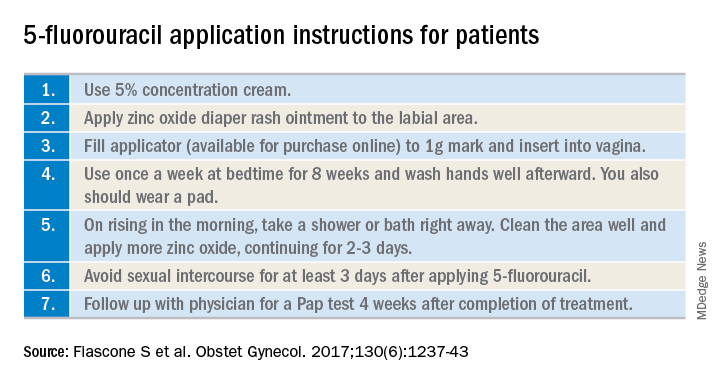
The most commonly utilized topical therapy for VAIN is the antimetabolite chemotherapeutic agent 5-fluorouracil (5FU). A typical schedule for 5FU treatment is to apply vaginally, at night, once a week for 8 weeks.4 Because it can cause extensive irritation to the vulvar and urethral epithelium, patients are recommended to apply barrier creams or ointments before and following the use of 5FU for several days, wash hands thoroughly after application, and to rinse and shower in the morning after rising. Severe irritation occurs in up to 16% of patients, but in general it is very well tolerated.
Its virtue is that it is able to conform and travel to all parts of the vaginal mucosa, including those that are poorly visualized within the fornices or vaginal folds. 5FU does not require a hospitalization or surgical procedure, can be applied by the patient at home, and preserves vaginal length and function. In recent reports, 5FU is associated with the lowest rates of recurrence (10%-30%), compared with excision or ablation, and therefore is a very attractive option for primary therapy.3 However, it requires patients to have a degree of comfort with vaginal application of drug and adherence with perineal care strategies to minimize the likelihood of toxicity.
The immune response modifier, imiquimod, that is commonly used in the treatment of vulvar dysplasia also has been described in the treatment of VAIN. It appears to have high rates of clearance (greater than 75%) and be most effective in the treatment of VAIN I.5 It requires application under colposcopic guidance three times a week for 8 weeks, which is a laborious undertaking for both patient and physician. Like 5FU, imiquimod is associated with vulvar and perineal irritation.
Vaginal estrogens are an alternative topical therapy for moderate- and high-grade VAIN and particularly useful for postmenopausal patients. They have been associated with a high rate (up to 90%) of resolution on follow-up vaginal cytology testing and are not associated with toxicities of the above stated therapies.6 Vaginal estrogen can be used alone or in addition to other therapeutic strategies. For example, it can be added to the nontreatment days of 5FU or postoperatively prescribed following laser or excisional procedures.
Radiation
Intracavitary brachytherapy is a technique in which a radiation source is placed within a cylinder or ovoids and placed within the vagina.7 Typically 45 Gy is delivered to a depth 0.5mm below the vaginal mucosal surface (“point z”). Recurrence occurs is approximately 10%-15% of patients, and toxicities can be severe, including vaginal stenosis and ulceration. This aggressive therapy typically is best reserved for cases that are refractory to other therapies. Following radiation, subsequent treatments are more difficult because of radiation-induced changes to the vaginal mucosa that can affect healing.
Vaginal dysplasia is a relatively common sequelae of high-risk HPV, particularly among women who have had a prior hysterectomy for cervical dysplasia. Because of anatomic changes following hysterectomy, adequate visualization and comprehensive vaginal treatment is difficult. Therefore, surgeons should avoid utilization of hysterectomy as a routine strategy to “cure” dysplasia as it may fail to achieve this cure and make subsequent evaluations and treatments of persistent dysplasia more difficult. Women who have had a hysterectomy for dysplasia should be closely followed for several decades, and they should be counseled that they have a persistent risk for vaginal disease. When VAIN develops, clinicians should consider topical therapies as primary treatment options because they may minimize toxicity and have high rates of enduring response.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant conflicts of interest.
References
1. Gynecol Oncol. 2016 Jun;141(3):507-10.
2. Arch Gynecol Obstet. 2016 Feb;293(2):415-9.
3. Anticancer Res. 2013 Jan;33(1):29-38.
4. Obstet Gynecol. 2017 Dec;130(6):1237-43.
5. Eur J Obstet Gynecol Reprod Biol. 2017 Nov;218:129-36.
6. J Low Genit Tract Dis. 2014 Apr;18(2):115-21.
7. Gynecol Oncol. 2007 Jul;106(1):105-11.
Vaginal intraepithelial neoplasia (VAIN) is a condition that frequently poses therapeutic dilemmas for gynecologists. VAIN represents dysplastic changes to the epithelium of the vaginal mucosa, and like cervical neoplasia, the extent of disease is characterized as levels I, II, or III dependent upon the depth of involvement in the epithelial layer by dysplastic cells. While VAIN itself typically is asymptomatic and not a harmful condition, it carries a 12% risk of progression to invasive vaginal carcinoma, so accurate identification, thorough treatment, and ongoing surveillance are essential.1
VAIN is associated with high-risk human papillomavirus (HPV) infection, tobacco use, and prior cervical dysplasia. Of women with VAIN, 65% have undergone a prior hysterectomy for cervical dysplasia, which emphasizes the nondefinitive nature of such an intervention.2 These women should be very closely followed for at least 20 years with vaginal cytologic and/or HPV surveillance. High-risk HPV infection is present in 85% of women with VAIN, and the presence of high-risk HPV is a predictor for recurrent VAIN. Recurrent and persistent VAIN also is more common in postmenopausal women and those with multifocal disease.
The most common location for VAIN is at the upper third of the vagina (including the vaginal cuff). It commonly arises within the vaginal fornices, which may be difficult to fully visualize because of their puckered appearance, redundant vaginal tissues, and extensive vaginal rogation.
A diagnosis of VAIN is typically obtained from vaginal cytology which reveals atypical or dysplastic cells. Such a result should prompt the physician to perform vaginal colposcopy and directed biopsies. Comprehensive visualization of the vaginal cuff can be limited in cases where the vaginal fornices are tethered, deeply puckered, or when there is significant mucosal rogation.
The application of 4% acetic acid or Lugol’s iodine are techniques that can enhance the detection of dysplastic vaginal mucosa. Lugol’s iodine selectively stains normal, glycogenated cells, and spares dysplastic glycogen-free cells. The sharp contrast between the brown iodine-stained tissues and the white dysplastic tissues aids in detection of dysplastic areas.
If colposcopic biopsy reveals low grade dysplasia (VAIN I) it does not require intervention, and has a very low rate of conversion to invasive vaginal carcinoma. However moderate- and high-grade vaginal dysplastic lesions should be treated because of the potential for malignant transformation.
Options for treatment of VAIN include topical, ablative, and excisional procedures. Observation also is an option but should be reserved for patients who are closely monitored with repeated colposcopic examinations, and probably should best be reserved for patients with VAIN I or II lesions.
Excisional procedures
The most common excisional procedure employed for VAIN is upper vaginectomy. In this procedure, the surgeon grasps and tents up the vaginal mucosa, incises the mucosa without penetrating the subepithelial tissue layers such as bladder and rectum. The vaginal mucosa then is carefully separated from the underlying endopelvic fascial plane. The specimen should be oriented, ideally on a cork board, with pins or sutures to ascribe margins and borders. Excision is best utilized for women with unifocal disease, or those who fail or do not tolerate ablative or topical interventions.
The most significant risks of excision include the potential for damage to underlying pelvic visceral structures, which is particularly concerning in postmenopausal women with thin vaginal epithelium. Vaginectomy is commonly associated with vaginal shortening or narrowing, which can be deleterious for quality of life. Retrospective series have described a 30% incidence of recurrence after vaginectomy, likely secondary to incomplete excision of all affected tissue.3
Ablation
Ablation of dysplastic foci with a carbon dioxide (CO2) laser is a common method for treatment of VAIN. CO2 laser should ablate tissue to a 1.5 mm minimum depth.3 The benefit of using CO2 laser is its ability to treat multifocal disease in situ without an extensive excisional procedure.
It is technically more straightforward than upper vaginectomy with less blood loss and shorter surgical times, and it can be easily accomplished in an outpatient surgical or office setting. However, one of its greatest limitations is the difficulty in visualizing all lesions and therefore adequately treating all sites. The vaginal rogations also make adequate laser ablation challenging because laser only is able to effectively ablate tissue that is oriented perpendicular to the laser beam.
In addition, there is no pathologic confirmation of adequacy of excision or margin status. These features may contribute to the modestly higher rates of recurrence of dysplasia following laser ablation, compared with vaginectomy.3 It also has been associated with more vaginal scarring than vaginectomy, which can have a negative effect on sexual health.
Topical agents
The most commonly utilized topical therapy for VAIN is the antimetabolite chemotherapeutic agent 5-fluorouracil (5FU). A typical schedule for 5FU treatment is to apply vaginally, at night, once a week for 8 weeks.4 Because it can cause extensive irritation to the vulvar and urethral epithelium, patients are recommended to apply barrier creams or ointments before and following the use of 5FU for several days, wash hands thoroughly after application, and to rinse and shower in the morning after rising. Severe irritation occurs in up to 16% of patients, but in general it is very well tolerated.
Its virtue is that it is able to conform and travel to all parts of the vaginal mucosa, including those that are poorly visualized within the fornices or vaginal folds. 5FU does not require a hospitalization or surgical procedure, can be applied by the patient at home, and preserves vaginal length and function. In recent reports, 5FU is associated with the lowest rates of recurrence (10%-30%), compared with excision or ablation, and therefore is a very attractive option for primary therapy.3 However, it requires patients to have a degree of comfort with vaginal application of drug and adherence with perineal care strategies to minimize the likelihood of toxicity.
The immune response modifier, imiquimod, that is commonly used in the treatment of vulvar dysplasia also has been described in the treatment of VAIN. It appears to have high rates of clearance (greater than 75%) and be most effective in the treatment of VAIN I.5 It requires application under colposcopic guidance three times a week for 8 weeks, which is a laborious undertaking for both patient and physician. Like 5FU, imiquimod is associated with vulvar and perineal irritation.
Vaginal estrogens are an alternative topical therapy for moderate- and high-grade VAIN and particularly useful for postmenopausal patients. They have been associated with a high rate (up to 90%) of resolution on follow-up vaginal cytology testing and are not associated with toxicities of the above stated therapies.6 Vaginal estrogen can be used alone or in addition to other therapeutic strategies. For example, it can be added to the nontreatment days of 5FU or postoperatively prescribed following laser or excisional procedures.
Radiation
Intracavitary brachytherapy is a technique in which a radiation source is placed within a cylinder or ovoids and placed within the vagina.7 Typically 45 Gy is delivered to a depth 0.5mm below the vaginal mucosal surface (“point z”). Recurrence occurs is approximately 10%-15% of patients, and toxicities can be severe, including vaginal stenosis and ulceration. This aggressive therapy typically is best reserved for cases that are refractory to other therapies. Following radiation, subsequent treatments are more difficult because of radiation-induced changes to the vaginal mucosa that can affect healing.
Vaginal dysplasia is a relatively common sequelae of high-risk HPV, particularly among women who have had a prior hysterectomy for cervical dysplasia. Because of anatomic changes following hysterectomy, adequate visualization and comprehensive vaginal treatment is difficult. Therefore, surgeons should avoid utilization of hysterectomy as a routine strategy to “cure” dysplasia as it may fail to achieve this cure and make subsequent evaluations and treatments of persistent dysplasia more difficult. Women who have had a hysterectomy for dysplasia should be closely followed for several decades, and they should be counseled that they have a persistent risk for vaginal disease. When VAIN develops, clinicians should consider topical therapies as primary treatment options because they may minimize toxicity and have high rates of enduring response.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant conflicts of interest.
References
1. Gynecol Oncol. 2016 Jun;141(3):507-10.
2. Arch Gynecol Obstet. 2016 Feb;293(2):415-9.
3. Anticancer Res. 2013 Jan;33(1):29-38.
4. Obstet Gynecol. 2017 Dec;130(6):1237-43.
5. Eur J Obstet Gynecol Reprod Biol. 2017 Nov;218:129-36.
6. J Low Genit Tract Dis. 2014 Apr;18(2):115-21.
7. Gynecol Oncol. 2007 Jul;106(1):105-11.
Vaginal intraepithelial neoplasia (VAIN) is a condition that frequently poses therapeutic dilemmas for gynecologists. VAIN represents dysplastic changes to the epithelium of the vaginal mucosa, and like cervical neoplasia, the extent of disease is characterized as levels I, II, or III dependent upon the depth of involvement in the epithelial layer by dysplastic cells. While VAIN itself typically is asymptomatic and not a harmful condition, it carries a 12% risk of progression to invasive vaginal carcinoma, so accurate identification, thorough treatment, and ongoing surveillance are essential.1
VAIN is associated with high-risk human papillomavirus (HPV) infection, tobacco use, and prior cervical dysplasia. Of women with VAIN, 65% have undergone a prior hysterectomy for cervical dysplasia, which emphasizes the nondefinitive nature of such an intervention.2 These women should be very closely followed for at least 20 years with vaginal cytologic and/or HPV surveillance. High-risk HPV infection is present in 85% of women with VAIN, and the presence of high-risk HPV is a predictor for recurrent VAIN. Recurrent and persistent VAIN also is more common in postmenopausal women and those with multifocal disease.
The most common location for VAIN is at the upper third of the vagina (including the vaginal cuff). It commonly arises within the vaginal fornices, which may be difficult to fully visualize because of their puckered appearance, redundant vaginal tissues, and extensive vaginal rogation.
A diagnosis of VAIN is typically obtained from vaginal cytology which reveals atypical or dysplastic cells. Such a result should prompt the physician to perform vaginal colposcopy and directed biopsies. Comprehensive visualization of the vaginal cuff can be limited in cases where the vaginal fornices are tethered, deeply puckered, or when there is significant mucosal rogation.
The application of 4% acetic acid or Lugol’s iodine are techniques that can enhance the detection of dysplastic vaginal mucosa. Lugol’s iodine selectively stains normal, glycogenated cells, and spares dysplastic glycogen-free cells. The sharp contrast between the brown iodine-stained tissues and the white dysplastic tissues aids in detection of dysplastic areas.
If colposcopic biopsy reveals low grade dysplasia (VAIN I) it does not require intervention, and has a very low rate of conversion to invasive vaginal carcinoma. However moderate- and high-grade vaginal dysplastic lesions should be treated because of the potential for malignant transformation.
Options for treatment of VAIN include topical, ablative, and excisional procedures. Observation also is an option but should be reserved for patients who are closely monitored with repeated colposcopic examinations, and probably should best be reserved for patients with VAIN I or II lesions.
Excisional procedures
The most common excisional procedure employed for VAIN is upper vaginectomy. In this procedure, the surgeon grasps and tents up the vaginal mucosa, incises the mucosa without penetrating the subepithelial tissue layers such as bladder and rectum. The vaginal mucosa then is carefully separated from the underlying endopelvic fascial plane. The specimen should be oriented, ideally on a cork board, with pins or sutures to ascribe margins and borders. Excision is best utilized for women with unifocal disease, or those who fail or do not tolerate ablative or topical interventions.
The most significant risks of excision include the potential for damage to underlying pelvic visceral structures, which is particularly concerning in postmenopausal women with thin vaginal epithelium. Vaginectomy is commonly associated with vaginal shortening or narrowing, which can be deleterious for quality of life. Retrospective series have described a 30% incidence of recurrence after vaginectomy, likely secondary to incomplete excision of all affected tissue.3
Ablation
Ablation of dysplastic foci with a carbon dioxide (CO2) laser is a common method for treatment of VAIN. CO2 laser should ablate tissue to a 1.5 mm minimum depth.3 The benefit of using CO2 laser is its ability to treat multifocal disease in situ without an extensive excisional procedure.
It is technically more straightforward than upper vaginectomy with less blood loss and shorter surgical times, and it can be easily accomplished in an outpatient surgical or office setting. However, one of its greatest limitations is the difficulty in visualizing all lesions and therefore adequately treating all sites. The vaginal rogations also make adequate laser ablation challenging because laser only is able to effectively ablate tissue that is oriented perpendicular to the laser beam.
In addition, there is no pathologic confirmation of adequacy of excision or margin status. These features may contribute to the modestly higher rates of recurrence of dysplasia following laser ablation, compared with vaginectomy.3 It also has been associated with more vaginal scarring than vaginectomy, which can have a negative effect on sexual health.
Topical agents
The most commonly utilized topical therapy for VAIN is the antimetabolite chemotherapeutic agent 5-fluorouracil (5FU). A typical schedule for 5FU treatment is to apply vaginally, at night, once a week for 8 weeks.4 Because it can cause extensive irritation to the vulvar and urethral epithelium, patients are recommended to apply barrier creams or ointments before and following the use of 5FU for several days, wash hands thoroughly after application, and to rinse and shower in the morning after rising. Severe irritation occurs in up to 16% of patients, but in general it is very well tolerated.
Its virtue is that it is able to conform and travel to all parts of the vaginal mucosa, including those that are poorly visualized within the fornices or vaginal folds. 5FU does not require a hospitalization or surgical procedure, can be applied by the patient at home, and preserves vaginal length and function. In recent reports, 5FU is associated with the lowest rates of recurrence (10%-30%), compared with excision or ablation, and therefore is a very attractive option for primary therapy.3 However, it requires patients to have a degree of comfort with vaginal application of drug and adherence with perineal care strategies to minimize the likelihood of toxicity.
The immune response modifier, imiquimod, that is commonly used in the treatment of vulvar dysplasia also has been described in the treatment of VAIN. It appears to have high rates of clearance (greater than 75%) and be most effective in the treatment of VAIN I.5 It requires application under colposcopic guidance three times a week for 8 weeks, which is a laborious undertaking for both patient and physician. Like 5FU, imiquimod is associated with vulvar and perineal irritation.
Vaginal estrogens are an alternative topical therapy for moderate- and high-grade VAIN and particularly useful for postmenopausal patients. They have been associated with a high rate (up to 90%) of resolution on follow-up vaginal cytology testing and are not associated with toxicities of the above stated therapies.6 Vaginal estrogen can be used alone or in addition to other therapeutic strategies. For example, it can be added to the nontreatment days of 5FU or postoperatively prescribed following laser or excisional procedures.
Radiation
Intracavitary brachytherapy is a technique in which a radiation source is placed within a cylinder or ovoids and placed within the vagina.7 Typically 45 Gy is delivered to a depth 0.5mm below the vaginal mucosal surface (“point z”). Recurrence occurs is approximately 10%-15% of patients, and toxicities can be severe, including vaginal stenosis and ulceration. This aggressive therapy typically is best reserved for cases that are refractory to other therapies. Following radiation, subsequent treatments are more difficult because of radiation-induced changes to the vaginal mucosa that can affect healing.
Vaginal dysplasia is a relatively common sequelae of high-risk HPV, particularly among women who have had a prior hysterectomy for cervical dysplasia. Because of anatomic changes following hysterectomy, adequate visualization and comprehensive vaginal treatment is difficult. Therefore, surgeons should avoid utilization of hysterectomy as a routine strategy to “cure” dysplasia as it may fail to achieve this cure and make subsequent evaluations and treatments of persistent dysplasia more difficult. Women who have had a hysterectomy for dysplasia should be closely followed for several decades, and they should be counseled that they have a persistent risk for vaginal disease. When VAIN develops, clinicians should consider topical therapies as primary treatment options because they may minimize toxicity and have high rates of enduring response.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant conflicts of interest.
References
1. Gynecol Oncol. 2016 Jun;141(3):507-10.
2. Arch Gynecol Obstet. 2016 Feb;293(2):415-9.
3. Anticancer Res. 2013 Jan;33(1):29-38.
4. Obstet Gynecol. 2017 Dec;130(6):1237-43.
5. Eur J Obstet Gynecol Reprod Biol. 2017 Nov;218:129-36.
6. J Low Genit Tract Dis. 2014 Apr;18(2):115-21.
7. Gynecol Oncol. 2007 Jul;106(1):105-11.
ASCO addresses financial barriers to cancer clinical trials
The American Society of Clinical Oncology (ASCO) has released a policy statement addressing financial barriers that may prevent cancer patients from participating in clinical trials.
The four main recommendations in ASCO’s policy statement are:
- Payers should create clear, consistent, streamlined, and transparent policies regarding clinical trial coverage.
- Patients should receive easy-to-understand information about potential out-of-pocket costs.
- “Ethically appropriate” financial compensation for out-of-pocket costs should be allowed.
- Researchers should be incentivized to investigate and “better characterize” costs incurred by cancer patients in clinical trials as well as identify ways to “mitigate the risk of trial-associated financial hardship.”
ASCO’s full policy statement, “Addressing Financial Barriers to Patient Participation in Clinical Trials,” is available on the Journal of Clinical Oncology website.
SOURCE: Winkfield KM et al. J Clin Oncol. 2018 Sep 13:JCO1801132. doi: 10.1200/JCO.18.01132.
The American Society of Clinical Oncology (ASCO) has released a policy statement addressing financial barriers that may prevent cancer patients from participating in clinical trials.
The four main recommendations in ASCO’s policy statement are:
- Payers should create clear, consistent, streamlined, and transparent policies regarding clinical trial coverage.
- Patients should receive easy-to-understand information about potential out-of-pocket costs.
- “Ethically appropriate” financial compensation for out-of-pocket costs should be allowed.
- Researchers should be incentivized to investigate and “better characterize” costs incurred by cancer patients in clinical trials as well as identify ways to “mitigate the risk of trial-associated financial hardship.”
ASCO’s full policy statement, “Addressing Financial Barriers to Patient Participation in Clinical Trials,” is available on the Journal of Clinical Oncology website.
SOURCE: Winkfield KM et al. J Clin Oncol. 2018 Sep 13:JCO1801132. doi: 10.1200/JCO.18.01132.
The American Society of Clinical Oncology (ASCO) has released a policy statement addressing financial barriers that may prevent cancer patients from participating in clinical trials.
The four main recommendations in ASCO’s policy statement are:
- Payers should create clear, consistent, streamlined, and transparent policies regarding clinical trial coverage.
- Patients should receive easy-to-understand information about potential out-of-pocket costs.
- “Ethically appropriate” financial compensation for out-of-pocket costs should be allowed.
- Researchers should be incentivized to investigate and “better characterize” costs incurred by cancer patients in clinical trials as well as identify ways to “mitigate the risk of trial-associated financial hardship.”
ASCO’s full policy statement, “Addressing Financial Barriers to Patient Participation in Clinical Trials,” is available on the Journal of Clinical Oncology website.
SOURCE: Winkfield KM et al. J Clin Oncol. 2018 Sep 13:JCO1801132. doi: 10.1200/JCO.18.01132.
FROM JOURNAL OF CLINICAL ONCOLOGY
One-step gestational diabetes screening doesn’t improve outcomes
according to data from a before-and-after cohort study of women in the state of Washington.
The one-step test, a 75-g 2-hour oral glucose tolerance test (OGTT), was recommended for all pregnant women in 2010, although the traditional two-step test – a 50-g screening glucose challenge test followed by a 100-g 3-hour OGTT – remains widely used, wrote Gaia Pocobelli, PhD, of Kaiser Permanente Washington Health Research Institute, Seattle, and her colleagues. “No randomized trial has been published comparing outcomes of the two approaches.”
In a study published in Obstetrics & Gynecology, the researchers compared data from 23,257 women who received prenatal care in Washington State between January 2009 and December 2014, including 8,363 women who received care before the guideline change, 4,103 who received care during a transition period, and 10,791 after the guideline change. Approximately 60% of the women received care from clinicians internal to Kaiser Permanente; 40% received care from external providers. Most (87%) of the internal clinicians switched to the one-step approach, the researchers said. Only 5% of external providers did so.
Overall, adopting the one-step approach was associated with a 41% increase in the diagnosis of GDM without improved maternal or neonatal outcomes, the researchers noted.
The incidence of GDM increased from 7% before the guideline change to 11% afterward for women seen by internal providers. For women seen by external providers, gestational diabetes incidence increased from 10% to 11%.
For women seen by internal providers, the use of insulin increased from 1% before the guideline change to 4% afterward; for women seen by external providers, use of insulin increased from 1.3% to 1.4% (change between the groups P less than .001).
In addition, women seen by internal providers were more likely to undergo induction of labor after the guideline change (25% to 29%), while labor induction decreased for women seen by external providers (31% to 29%) for a relative risk of 1.2.
Neonatal hypoglycemia increased from 1% to 2% among women seen by internal providers, but decreased slightly from 2.4% to 2.1% for women seen by external providers, for a relative risk of 1.77.
There were no significant differences between the women seen by internal and external providers in risk of primary cesarean section, large for gestational age, small for gestational age, or neonatal ICU admission.
The main limitation of the study was the potential confounding variables including maternal diet and exercise, and possible underreporting of risk factors such as smoking, the researchers noted. However, the results were strengthened by the large study population, and the results “do not suggest a benefit of adopting the one-step over the two-step approach.
“Kaiser Permanente Washington has revised [its] guidelines to return to a two-step process. We recommend that any health care system considering switching to the one-step approach incorporate a rigorous evaluation of changes in maternal and neonatal outcomes,” Dr. Pocobelli and her associates added.
Dr. Pocobelli disclosed funding from Jazz Pharmaceuticals for work unrelated to this study. The study was supported in part by a grant from the Group Health Foundation Momentum Fund.
Diabetes is a significant global public health concern, but is especially problematic for women of reproductive age because diabetes in pregnancy can cause significant health complications for the mother and baby. Gestational diabetes mellitus (GDM) affects up to 10% of pregnancies in the United States annually, and is associated with perinatal loss, operative delivery, macrosomia, hypoglycemia, respiratory distress syndrome, and metabolic derangements for the offspring. For the mother, GDM is associated with hypertensive disorders, infections, hydramnios, and increased risk for developing type 2 diabetes later in life. As the incidence of GDM continues to rise, studies examining how to reduce, manage or prevent this condition become increasingly important.
The authors’ conclusions, that adopting the one-step approach increased the number of women with diagnosed GDM but did not significantly improve maternal or neonatal outcomes, are not surprising. Since the initial publication of the Hyperglycemia and Adverse Pregnancy Outcome Study, upon which the International Association of the Diabetes in Pregnancy Study Groups based its recommendations to go to a one-step approach, much debate has ensued about the best method to diagnose GDM. Indeed, the National Institutes of Health convened a consensus panel to review the literature and determine whether the one-step approach should be universally adopted (the panel concluded that more information was needed, and that the current two-step approach should continue to be used).
As the authors concede, studies have shown conflicting results, and no large-scale randomized controlled trial has been conducted to date. However, the literature does not bear out the idea that the one-step approach is truly better. The current study, although including a significant number of women and a reasonable control group, only serves as yet another study to reinforce what has previously been published.
I would agree with the researchers’ conclusions that the one-step approach is not necessarily beneficial. Although the one-step approach may identify a subset of patients who might not otherwise be diagnosed with GDM, it still remains unclear whether the outcomes for these patients will be improved. Furthermore, additional testing, need for insulin or other oral antidiabetic medications, etc., would result in additional stress to the patient and the health care system. Based on the authors’ findings, and results of other studies, it remains to be determined if the effort (diagnosing additional patients with GDM) is justified medically, economically, or otherwise.
As ob.gyns., we must continually ask ourselves: “By not doing something, are we causing harm to our patients?” If we change the diagnostic criteria for GDM, thereby increasing the number of women with the condition who would then require additional care, medications, and, potentially, more complex decisions around timing and mode of delivery, we need to be certain that we are not doing harm. This, and other studies examining the use of the one- versus two-step approach have yet to demonstrate, unequivocally, that changing the criteria reduces harm, and, perhaps, might – unintentionally – cause more.
As the study authors and the NIH consensus panel concluded, more rigorous evaluation is needed; that is, a large, multicenter randomized controlled trial that examines not only the benefits during pregnancy but also the long-term benefits to women and their children.
E. Albert Reece, MD, PhD, MBA, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He provided commentary on the study by Pocobelli et al. Dr. Reece said he had no relevant financial disclosures.
Diabetes is a significant global public health concern, but is especially problematic for women of reproductive age because diabetes in pregnancy can cause significant health complications for the mother and baby. Gestational diabetes mellitus (GDM) affects up to 10% of pregnancies in the United States annually, and is associated with perinatal loss, operative delivery, macrosomia, hypoglycemia, respiratory distress syndrome, and metabolic derangements for the offspring. For the mother, GDM is associated with hypertensive disorders, infections, hydramnios, and increased risk for developing type 2 diabetes later in life. As the incidence of GDM continues to rise, studies examining how to reduce, manage or prevent this condition become increasingly important.
The authors’ conclusions, that adopting the one-step approach increased the number of women with diagnosed GDM but did not significantly improve maternal or neonatal outcomes, are not surprising. Since the initial publication of the Hyperglycemia and Adverse Pregnancy Outcome Study, upon which the International Association of the Diabetes in Pregnancy Study Groups based its recommendations to go to a one-step approach, much debate has ensued about the best method to diagnose GDM. Indeed, the National Institutes of Health convened a consensus panel to review the literature and determine whether the one-step approach should be universally adopted (the panel concluded that more information was needed, and that the current two-step approach should continue to be used).
As the authors concede, studies have shown conflicting results, and no large-scale randomized controlled trial has been conducted to date. However, the literature does not bear out the idea that the one-step approach is truly better. The current study, although including a significant number of women and a reasonable control group, only serves as yet another study to reinforce what has previously been published.
I would agree with the researchers’ conclusions that the one-step approach is not necessarily beneficial. Although the one-step approach may identify a subset of patients who might not otherwise be diagnosed with GDM, it still remains unclear whether the outcomes for these patients will be improved. Furthermore, additional testing, need for insulin or other oral antidiabetic medications, etc., would result in additional stress to the patient and the health care system. Based on the authors’ findings, and results of other studies, it remains to be determined if the effort (diagnosing additional patients with GDM) is justified medically, economically, or otherwise.
As ob.gyns., we must continually ask ourselves: “By not doing something, are we causing harm to our patients?” If we change the diagnostic criteria for GDM, thereby increasing the number of women with the condition who would then require additional care, medications, and, potentially, more complex decisions around timing and mode of delivery, we need to be certain that we are not doing harm. This, and other studies examining the use of the one- versus two-step approach have yet to demonstrate, unequivocally, that changing the criteria reduces harm, and, perhaps, might – unintentionally – cause more.
As the study authors and the NIH consensus panel concluded, more rigorous evaluation is needed; that is, a large, multicenter randomized controlled trial that examines not only the benefits during pregnancy but also the long-term benefits to women and their children.
E. Albert Reece, MD, PhD, MBA, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He provided commentary on the study by Pocobelli et al. Dr. Reece said he had no relevant financial disclosures.
Diabetes is a significant global public health concern, but is especially problematic for women of reproductive age because diabetes in pregnancy can cause significant health complications for the mother and baby. Gestational diabetes mellitus (GDM) affects up to 10% of pregnancies in the United States annually, and is associated with perinatal loss, operative delivery, macrosomia, hypoglycemia, respiratory distress syndrome, and metabolic derangements for the offspring. For the mother, GDM is associated with hypertensive disorders, infections, hydramnios, and increased risk for developing type 2 diabetes later in life. As the incidence of GDM continues to rise, studies examining how to reduce, manage or prevent this condition become increasingly important.
The authors’ conclusions, that adopting the one-step approach increased the number of women with diagnosed GDM but did not significantly improve maternal or neonatal outcomes, are not surprising. Since the initial publication of the Hyperglycemia and Adverse Pregnancy Outcome Study, upon which the International Association of the Diabetes in Pregnancy Study Groups based its recommendations to go to a one-step approach, much debate has ensued about the best method to diagnose GDM. Indeed, the National Institutes of Health convened a consensus panel to review the literature and determine whether the one-step approach should be universally adopted (the panel concluded that more information was needed, and that the current two-step approach should continue to be used).
As the authors concede, studies have shown conflicting results, and no large-scale randomized controlled trial has been conducted to date. However, the literature does not bear out the idea that the one-step approach is truly better. The current study, although including a significant number of women and a reasonable control group, only serves as yet another study to reinforce what has previously been published.
I would agree with the researchers’ conclusions that the one-step approach is not necessarily beneficial. Although the one-step approach may identify a subset of patients who might not otherwise be diagnosed with GDM, it still remains unclear whether the outcomes for these patients will be improved. Furthermore, additional testing, need for insulin or other oral antidiabetic medications, etc., would result in additional stress to the patient and the health care system. Based on the authors’ findings, and results of other studies, it remains to be determined if the effort (diagnosing additional patients with GDM) is justified medically, economically, or otherwise.
As ob.gyns., we must continually ask ourselves: “By not doing something, are we causing harm to our patients?” If we change the diagnostic criteria for GDM, thereby increasing the number of women with the condition who would then require additional care, medications, and, potentially, more complex decisions around timing and mode of delivery, we need to be certain that we are not doing harm. This, and other studies examining the use of the one- versus two-step approach have yet to demonstrate, unequivocally, that changing the criteria reduces harm, and, perhaps, might – unintentionally – cause more.
As the study authors and the NIH consensus panel concluded, more rigorous evaluation is needed; that is, a large, multicenter randomized controlled trial that examines not only the benefits during pregnancy but also the long-term benefits to women and their children.
E. Albert Reece, MD, PhD, MBA, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He provided commentary on the study by Pocobelli et al. Dr. Reece said he had no relevant financial disclosures.
according to data from a before-and-after cohort study of women in the state of Washington.
The one-step test, a 75-g 2-hour oral glucose tolerance test (OGTT), was recommended for all pregnant women in 2010, although the traditional two-step test – a 50-g screening glucose challenge test followed by a 100-g 3-hour OGTT – remains widely used, wrote Gaia Pocobelli, PhD, of Kaiser Permanente Washington Health Research Institute, Seattle, and her colleagues. “No randomized trial has been published comparing outcomes of the two approaches.”
In a study published in Obstetrics & Gynecology, the researchers compared data from 23,257 women who received prenatal care in Washington State between January 2009 and December 2014, including 8,363 women who received care before the guideline change, 4,103 who received care during a transition period, and 10,791 after the guideline change. Approximately 60% of the women received care from clinicians internal to Kaiser Permanente; 40% received care from external providers. Most (87%) of the internal clinicians switched to the one-step approach, the researchers said. Only 5% of external providers did so.
Overall, adopting the one-step approach was associated with a 41% increase in the diagnosis of GDM without improved maternal or neonatal outcomes, the researchers noted.
The incidence of GDM increased from 7% before the guideline change to 11% afterward for women seen by internal providers. For women seen by external providers, gestational diabetes incidence increased from 10% to 11%.
For women seen by internal providers, the use of insulin increased from 1% before the guideline change to 4% afterward; for women seen by external providers, use of insulin increased from 1.3% to 1.4% (change between the groups P less than .001).
In addition, women seen by internal providers were more likely to undergo induction of labor after the guideline change (25% to 29%), while labor induction decreased for women seen by external providers (31% to 29%) for a relative risk of 1.2.
Neonatal hypoglycemia increased from 1% to 2% among women seen by internal providers, but decreased slightly from 2.4% to 2.1% for women seen by external providers, for a relative risk of 1.77.
There were no significant differences between the women seen by internal and external providers in risk of primary cesarean section, large for gestational age, small for gestational age, or neonatal ICU admission.
The main limitation of the study was the potential confounding variables including maternal diet and exercise, and possible underreporting of risk factors such as smoking, the researchers noted. However, the results were strengthened by the large study population, and the results “do not suggest a benefit of adopting the one-step over the two-step approach.
“Kaiser Permanente Washington has revised [its] guidelines to return to a two-step process. We recommend that any health care system considering switching to the one-step approach incorporate a rigorous evaluation of changes in maternal and neonatal outcomes,” Dr. Pocobelli and her associates added.
Dr. Pocobelli disclosed funding from Jazz Pharmaceuticals for work unrelated to this study. The study was supported in part by a grant from the Group Health Foundation Momentum Fund.
according to data from a before-and-after cohort study of women in the state of Washington.
The one-step test, a 75-g 2-hour oral glucose tolerance test (OGTT), was recommended for all pregnant women in 2010, although the traditional two-step test – a 50-g screening glucose challenge test followed by a 100-g 3-hour OGTT – remains widely used, wrote Gaia Pocobelli, PhD, of Kaiser Permanente Washington Health Research Institute, Seattle, and her colleagues. “No randomized trial has been published comparing outcomes of the two approaches.”
In a study published in Obstetrics & Gynecology, the researchers compared data from 23,257 women who received prenatal care in Washington State between January 2009 and December 2014, including 8,363 women who received care before the guideline change, 4,103 who received care during a transition period, and 10,791 after the guideline change. Approximately 60% of the women received care from clinicians internal to Kaiser Permanente; 40% received care from external providers. Most (87%) of the internal clinicians switched to the one-step approach, the researchers said. Only 5% of external providers did so.
Overall, adopting the one-step approach was associated with a 41% increase in the diagnosis of GDM without improved maternal or neonatal outcomes, the researchers noted.
The incidence of GDM increased from 7% before the guideline change to 11% afterward for women seen by internal providers. For women seen by external providers, gestational diabetes incidence increased from 10% to 11%.
For women seen by internal providers, the use of insulin increased from 1% before the guideline change to 4% afterward; for women seen by external providers, use of insulin increased from 1.3% to 1.4% (change between the groups P less than .001).
In addition, women seen by internal providers were more likely to undergo induction of labor after the guideline change (25% to 29%), while labor induction decreased for women seen by external providers (31% to 29%) for a relative risk of 1.2.
Neonatal hypoglycemia increased from 1% to 2% among women seen by internal providers, but decreased slightly from 2.4% to 2.1% for women seen by external providers, for a relative risk of 1.77.
There were no significant differences between the women seen by internal and external providers in risk of primary cesarean section, large for gestational age, small for gestational age, or neonatal ICU admission.
The main limitation of the study was the potential confounding variables including maternal diet and exercise, and possible underreporting of risk factors such as smoking, the researchers noted. However, the results were strengthened by the large study population, and the results “do not suggest a benefit of adopting the one-step over the two-step approach.
“Kaiser Permanente Washington has revised [its] guidelines to return to a two-step process. We recommend that any health care system considering switching to the one-step approach incorporate a rigorous evaluation of changes in maternal and neonatal outcomes,” Dr. Pocobelli and her associates added.
Dr. Pocobelli disclosed funding from Jazz Pharmaceuticals for work unrelated to this study. The study was supported in part by a grant from the Group Health Foundation Momentum Fund.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: Increased diagnoses of gestational diabetes did not significantly improve maternal or fetal outcomes.
Major finding: Adoption of a one-step screening process for gestational diabetes increased diagnoses by 41%.
Study details: The data come from a before-and-after cohort study with a population of 23,257 women.
Disclosures: Dr. Pocobelli disclosed funding from Jazz Pharmaceuticals for work unrelated to this study. The study was supported in part by a grant from the Group Health Foundation Momentum Fund.
Source: Pocobelli G et al. Obstet Gynecol. 2018;132:859-67.
Tau PET tracer distinguishes Alzheimer’s from other disorders
PET imaging with an investigational tau tracer, 18F-flortaucipir, distinguished Alzheimer’s disease from other neurodegenerative disorders with a high degree of accuracy in a multicenter study.
PET with 18F-flortaucipir also outperformed structural MRI markers for Alzheimer’s disease (AD), and when compared against amyloid-beta (Abeta) biomarkers, showed higher specificity for an AD dementia diagnosis, researchers wrote in a report published online Sept. 18 in JAMA.
“The accuracy and potential utility of this test in patient care require further research in clinically more representative populations,” they wrote.
The study included 719 participants recruited from memory disorder clinics in Sweden, Korea, and California. That cohort included 179 patients with AD dementia, 254 who had non-AD neurodegenerative diseases, 126 with mild cognitive impairment (MCI), and 160 controls who were cognitively normal. All participants underwent 18F-flortaucipir PET between June 2014 and November 2017.
They found that 18F-flortaucipir showed “high accuracy” for distinguishing AD dementia from non-AD neurodegenerative disorders across all five regions of interest (ROI) evaluated in the study.
For example, 18F-flortaucipir PET had 90.3% accuracy, 89.9% sensitivity, and 90.6% specificity in the temporal meta-ROI, they reported.
By contrast, the accuracy of 18F-flortaucipir was lower for distinguishing MCI caused by AD versus non-AD neurodegenerative conditions. In the temporal meta-ROI, that translated into an 83.4% accuracy, 61.5% sensitivity, and 90.6% specificity, according to the report.
The 18F-flortaucipir tracer outperformed state-of-the-art MRI measures for distinguishing AD dementia from non-AD neurodegenerative disorders, including hippocampal volumes, AD-signature thickness, and whole-brain cortical thickness, Dr. Ossenkoppele and his colleagues found in a secondary analysis.
Likewise, certain analyses showed that specificity for AD dementia versus non-AD neurodegenerative disorders was higher with 18F-flortaucipir than with Abeta status.
While both MRI measures and Abeta status are increasingly used to evaluate cognitive impairment adjunctively in a clinical setting, the utility of 18F-flortaucipir PET as a diagnostic biomarker still must be determined, the investigators wrote in a discussion of their results.
“An intended clinical use of 18F-flortaucipir PET might be to improve the diagnostic work-up as an add-on test to Abeta biomarkers in patients with early-onset dementia and possibly as a triage or even replacement test in patients with late-onset dementia in whom incidental Abeta pathology is common,” they wrote.
The study was sponsored by different sources at each of the clinic sites. Many authors disclosed relationships with companies that are marketing and/or developing PET imaging tracers, including Avid Radiopharmaceuticals/Eli Lilly, GE Healthcare, and Piramal, as well as other pharmaceutical companies.
SOURCE: Ossenkoppele R et al. JAMA. 2018;320(11):1151-62.
PET imaging with an investigational tau tracer, 18F-flortaucipir, distinguished Alzheimer’s disease from other neurodegenerative disorders with a high degree of accuracy in a multicenter study.
PET with 18F-flortaucipir also outperformed structural MRI markers for Alzheimer’s disease (AD), and when compared against amyloid-beta (Abeta) biomarkers, showed higher specificity for an AD dementia diagnosis, researchers wrote in a report published online Sept. 18 in JAMA.
“The accuracy and potential utility of this test in patient care require further research in clinically more representative populations,” they wrote.
The study included 719 participants recruited from memory disorder clinics in Sweden, Korea, and California. That cohort included 179 patients with AD dementia, 254 who had non-AD neurodegenerative diseases, 126 with mild cognitive impairment (MCI), and 160 controls who were cognitively normal. All participants underwent 18F-flortaucipir PET between June 2014 and November 2017.
They found that 18F-flortaucipir showed “high accuracy” for distinguishing AD dementia from non-AD neurodegenerative disorders across all five regions of interest (ROI) evaluated in the study.
For example, 18F-flortaucipir PET had 90.3% accuracy, 89.9% sensitivity, and 90.6% specificity in the temporal meta-ROI, they reported.
By contrast, the accuracy of 18F-flortaucipir was lower for distinguishing MCI caused by AD versus non-AD neurodegenerative conditions. In the temporal meta-ROI, that translated into an 83.4% accuracy, 61.5% sensitivity, and 90.6% specificity, according to the report.
The 18F-flortaucipir tracer outperformed state-of-the-art MRI measures for distinguishing AD dementia from non-AD neurodegenerative disorders, including hippocampal volumes, AD-signature thickness, and whole-brain cortical thickness, Dr. Ossenkoppele and his colleagues found in a secondary analysis.
Likewise, certain analyses showed that specificity for AD dementia versus non-AD neurodegenerative disorders was higher with 18F-flortaucipir than with Abeta status.
While both MRI measures and Abeta status are increasingly used to evaluate cognitive impairment adjunctively in a clinical setting, the utility of 18F-flortaucipir PET as a diagnostic biomarker still must be determined, the investigators wrote in a discussion of their results.
“An intended clinical use of 18F-flortaucipir PET might be to improve the diagnostic work-up as an add-on test to Abeta biomarkers in patients with early-onset dementia and possibly as a triage or even replacement test in patients with late-onset dementia in whom incidental Abeta pathology is common,” they wrote.
The study was sponsored by different sources at each of the clinic sites. Many authors disclosed relationships with companies that are marketing and/or developing PET imaging tracers, including Avid Radiopharmaceuticals/Eli Lilly, GE Healthcare, and Piramal, as well as other pharmaceutical companies.
SOURCE: Ossenkoppele R et al. JAMA. 2018;320(11):1151-62.
PET imaging with an investigational tau tracer, 18F-flortaucipir, distinguished Alzheimer’s disease from other neurodegenerative disorders with a high degree of accuracy in a multicenter study.
PET with 18F-flortaucipir also outperformed structural MRI markers for Alzheimer’s disease (AD), and when compared against amyloid-beta (Abeta) biomarkers, showed higher specificity for an AD dementia diagnosis, researchers wrote in a report published online Sept. 18 in JAMA.
“The accuracy and potential utility of this test in patient care require further research in clinically more representative populations,” they wrote.
The study included 719 participants recruited from memory disorder clinics in Sweden, Korea, and California. That cohort included 179 patients with AD dementia, 254 who had non-AD neurodegenerative diseases, 126 with mild cognitive impairment (MCI), and 160 controls who were cognitively normal. All participants underwent 18F-flortaucipir PET between June 2014 and November 2017.
They found that 18F-flortaucipir showed “high accuracy” for distinguishing AD dementia from non-AD neurodegenerative disorders across all five regions of interest (ROI) evaluated in the study.
For example, 18F-flortaucipir PET had 90.3% accuracy, 89.9% sensitivity, and 90.6% specificity in the temporal meta-ROI, they reported.
By contrast, the accuracy of 18F-flortaucipir was lower for distinguishing MCI caused by AD versus non-AD neurodegenerative conditions. In the temporal meta-ROI, that translated into an 83.4% accuracy, 61.5% sensitivity, and 90.6% specificity, according to the report.
The 18F-flortaucipir tracer outperformed state-of-the-art MRI measures for distinguishing AD dementia from non-AD neurodegenerative disorders, including hippocampal volumes, AD-signature thickness, and whole-brain cortical thickness, Dr. Ossenkoppele and his colleagues found in a secondary analysis.
Likewise, certain analyses showed that specificity for AD dementia versus non-AD neurodegenerative disorders was higher with 18F-flortaucipir than with Abeta status.
While both MRI measures and Abeta status are increasingly used to evaluate cognitive impairment adjunctively in a clinical setting, the utility of 18F-flortaucipir PET as a diagnostic biomarker still must be determined, the investigators wrote in a discussion of their results.
“An intended clinical use of 18F-flortaucipir PET might be to improve the diagnostic work-up as an add-on test to Abeta biomarkers in patients with early-onset dementia and possibly as a triage or even replacement test in patients with late-onset dementia in whom incidental Abeta pathology is common,” they wrote.
The study was sponsored by different sources at each of the clinic sites. Many authors disclosed relationships with companies that are marketing and/or developing PET imaging tracers, including Avid Radiopharmaceuticals/Eli Lilly, GE Healthcare, and Piramal, as well as other pharmaceutical companies.
SOURCE: Ossenkoppele R et al. JAMA. 2018;320(11):1151-62.
FROM JAMA
Key clinical point:
Major finding: PET with 18F-flortaucipir PET had 90.3% accuracy, 89.9% sensitivity, and 90.6% specificity in the temporal metaregion of interest.
Study details: A multicenter, cross-sectional study including 719 participants recruited from memory disorder clinics in Sweden, Korea, and California.
Disclosures: The study was sponsored by different sources at each of the clinic sites. Many authors disclosed relationships with companies marketing and/or developing PET imaging tracers, including Avid Radiopharmaceuticals/Eli Lilly, GE Healthcare, and Piramal, as well as other pharmaceutical companies.
Source: Ossenkoppele R et al. JAMA. 2018;320(11):1151-62.
Amantadine-Induced Livedo Reticularis in a Child Treated Off Label for Neurobehavioral Disorders
Livedo reticularis (LR) is a common dermatologic finding consisting of diffuse, reticulated, violaceous patches. It often is a benign physical finding known as cutis marmorata; however, LR can be associated with other medical conditions as well as with the use of some medications.1,2 Amantadine is a common cause of LR in Parkinson disease patients.3,4 We present a rare case of amantadine-induced LR in a pediatric patient and highlight the off-label use of this medication in children.
Case Report
An 8-year-old boy presented with a diffuse rash on the trunk, arms, and legs of 9 months’ duration. The patient denied any associated symptoms as well as alleviating or exacerbating factors. He also denied any changes with temperature. He had no recent international travel and no prior drug allergies. His medical history was remarkable for attention deficit hyperactivity disorder (ADHD), bipolar disorder, and autism spectrum disorder. His previously prescribed medications included atomoxetine, quetiapine, and valproic acid. The only new medication that had been started within the last year was amantadine. Physical examination revealed a diffuse, reticulated, erythematous to violaceous, blanching rash that was most notable on the legs (Figure 1A) but also was present on the trunk (Figure 1B) and arms (Figure 1C). The clinical examination was consistent with LR, which was presumed to be secondary to amantadine use. Given the multiple psychiatric diagnoses and medication history in this young patient, a consultation with child psychiatry was facilitated. His medications and diagnosis were reviewed, and amantadine was discontinued. At a follow-up visit 5 months later, the patient’s LR had improved (Figure 2).
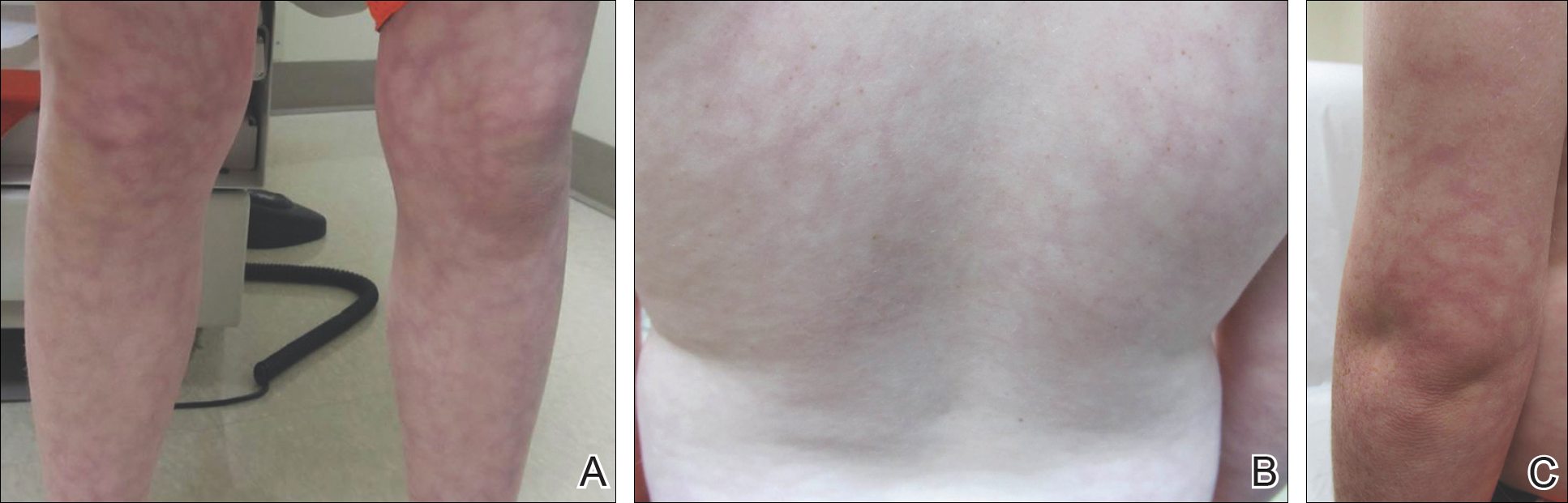

Comment
Amantadine has a well-documented association with LR in patients with Parkinson disease,3,4 which has been reported in up to 40% of those taking amantadine.2 More recently, amantadine has been used off label to treat neurobehavioral disorders in children due to beneficial effects including improvement in attention and concentration, distractibility, and fatigue.5 Our patient was being treated off label with amantadine for ADHD and bipolar disorder. Amantadine acts as a noncompetitive antagonist of the N-methyl-D-aspartate receptor, enhancing dopamine release to reduce symptoms of ADHD.5,6 Additionally, amantadine can cause a depletion of catecholamines in the peripheral nerve terminals, which may lead to dilatation of dermal vessels.4,6 This sequence of events has been proposed as a possible mechanism contributing to amantadine-induced LR, though the pathophysiology is not fully understood.1,3,4
Our case of LR likely was induced by amantadine given the temporal relationship between initiation of the medication, onset of the rash, and the considerable improvement of the rash upon discontinuation of amantadine. Barrera and Browning6 reported another case of amantadine-induced LR in a pediatric patient. Because amantadine is increasingly being used off label to treat childhood neurobehavioral disorders, amantadine-induced LR may become more prevalent in patients who do not have Parkinson disease; therefore, physicians who treat pediatric patients must be aware of this side effect.5
- Quaresma MV, Gomes-Dias AC, Serruya A, et al. Amantadine-induced livedo reticularis: a case report. An Bras Dermatol. 2015;90:745-747.
- Gibbs MB, English JC, Zirwas MJ. Livedo reticularis: an update. J Am Acad Dermatol. 2005;52:1009-1019.
- Silva SB, Miot HA. Case for diagnosis. amantadine-induced livedo reticularis. An Bras Dermatol. 2012;87:319-321.
- Vollum DI, Parkes JD, Doyle D. Livedo reticularis during amantadine treatment. Br Med J. 1971;2:627-628.
- Hosenbocus S, Chahal R. Amantadine: a review of use in child and adolescent psychiatry. J Can Acad Child Adolesc Psychiatry. 2013;22:55-60.
- Barrera F, Browning JC. Likely amantadine-induced livedo reticularis in a child. Pediatr Dermatol. 2012;29:329-330.
Livedo reticularis (LR) is a common dermatologic finding consisting of diffuse, reticulated, violaceous patches. It often is a benign physical finding known as cutis marmorata; however, LR can be associated with other medical conditions as well as with the use of some medications.1,2 Amantadine is a common cause of LR in Parkinson disease patients.3,4 We present a rare case of amantadine-induced LR in a pediatric patient and highlight the off-label use of this medication in children.
Case Report
An 8-year-old boy presented with a diffuse rash on the trunk, arms, and legs of 9 months’ duration. The patient denied any associated symptoms as well as alleviating or exacerbating factors. He also denied any changes with temperature. He had no recent international travel and no prior drug allergies. His medical history was remarkable for attention deficit hyperactivity disorder (ADHD), bipolar disorder, and autism spectrum disorder. His previously prescribed medications included atomoxetine, quetiapine, and valproic acid. The only new medication that had been started within the last year was amantadine. Physical examination revealed a diffuse, reticulated, erythematous to violaceous, blanching rash that was most notable on the legs (Figure 1A) but also was present on the trunk (Figure 1B) and arms (Figure 1C). The clinical examination was consistent with LR, which was presumed to be secondary to amantadine use. Given the multiple psychiatric diagnoses and medication history in this young patient, a consultation with child psychiatry was facilitated. His medications and diagnosis were reviewed, and amantadine was discontinued. At a follow-up visit 5 months later, the patient’s LR had improved (Figure 2).
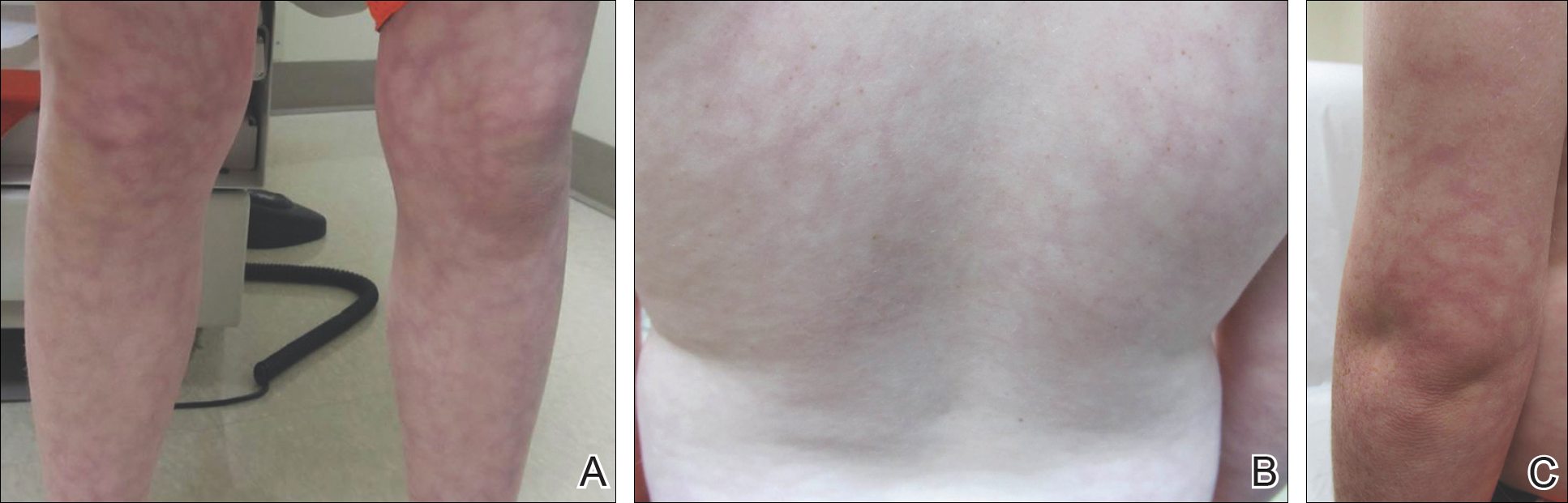

Comment
Amantadine has a well-documented association with LR in patients with Parkinson disease,3,4 which has been reported in up to 40% of those taking amantadine.2 More recently, amantadine has been used off label to treat neurobehavioral disorders in children due to beneficial effects including improvement in attention and concentration, distractibility, and fatigue.5 Our patient was being treated off label with amantadine for ADHD and bipolar disorder. Amantadine acts as a noncompetitive antagonist of the N-methyl-D-aspartate receptor, enhancing dopamine release to reduce symptoms of ADHD.5,6 Additionally, amantadine can cause a depletion of catecholamines in the peripheral nerve terminals, which may lead to dilatation of dermal vessels.4,6 This sequence of events has been proposed as a possible mechanism contributing to amantadine-induced LR, though the pathophysiology is not fully understood.1,3,4
Our case of LR likely was induced by amantadine given the temporal relationship between initiation of the medication, onset of the rash, and the considerable improvement of the rash upon discontinuation of amantadine. Barrera and Browning6 reported another case of amantadine-induced LR in a pediatric patient. Because amantadine is increasingly being used off label to treat childhood neurobehavioral disorders, amantadine-induced LR may become more prevalent in patients who do not have Parkinson disease; therefore, physicians who treat pediatric patients must be aware of this side effect.5
Livedo reticularis (LR) is a common dermatologic finding consisting of diffuse, reticulated, violaceous patches. It often is a benign physical finding known as cutis marmorata; however, LR can be associated with other medical conditions as well as with the use of some medications.1,2 Amantadine is a common cause of LR in Parkinson disease patients.3,4 We present a rare case of amantadine-induced LR in a pediatric patient and highlight the off-label use of this medication in children.
Case Report
An 8-year-old boy presented with a diffuse rash on the trunk, arms, and legs of 9 months’ duration. The patient denied any associated symptoms as well as alleviating or exacerbating factors. He also denied any changes with temperature. He had no recent international travel and no prior drug allergies. His medical history was remarkable for attention deficit hyperactivity disorder (ADHD), bipolar disorder, and autism spectrum disorder. His previously prescribed medications included atomoxetine, quetiapine, and valproic acid. The only new medication that had been started within the last year was amantadine. Physical examination revealed a diffuse, reticulated, erythematous to violaceous, blanching rash that was most notable on the legs (Figure 1A) but also was present on the trunk (Figure 1B) and arms (Figure 1C). The clinical examination was consistent with LR, which was presumed to be secondary to amantadine use. Given the multiple psychiatric diagnoses and medication history in this young patient, a consultation with child psychiatry was facilitated. His medications and diagnosis were reviewed, and amantadine was discontinued. At a follow-up visit 5 months later, the patient’s LR had improved (Figure 2).
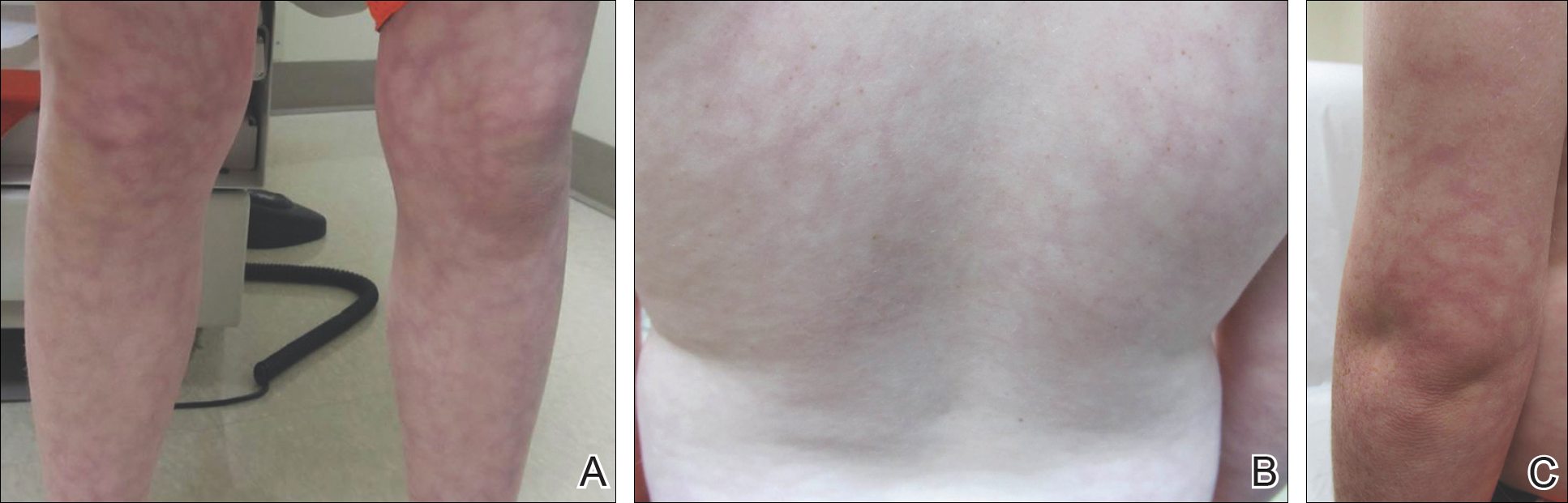

Comment
Amantadine has a well-documented association with LR in patients with Parkinson disease,3,4 which has been reported in up to 40% of those taking amantadine.2 More recently, amantadine has been used off label to treat neurobehavioral disorders in children due to beneficial effects including improvement in attention and concentration, distractibility, and fatigue.5 Our patient was being treated off label with amantadine for ADHD and bipolar disorder. Amantadine acts as a noncompetitive antagonist of the N-methyl-D-aspartate receptor, enhancing dopamine release to reduce symptoms of ADHD.5,6 Additionally, amantadine can cause a depletion of catecholamines in the peripheral nerve terminals, which may lead to dilatation of dermal vessels.4,6 This sequence of events has been proposed as a possible mechanism contributing to amantadine-induced LR, though the pathophysiology is not fully understood.1,3,4
Our case of LR likely was induced by amantadine given the temporal relationship between initiation of the medication, onset of the rash, and the considerable improvement of the rash upon discontinuation of amantadine. Barrera and Browning6 reported another case of amantadine-induced LR in a pediatric patient. Because amantadine is increasingly being used off label to treat childhood neurobehavioral disorders, amantadine-induced LR may become more prevalent in patients who do not have Parkinson disease; therefore, physicians who treat pediatric patients must be aware of this side effect.5
- Quaresma MV, Gomes-Dias AC, Serruya A, et al. Amantadine-induced livedo reticularis: a case report. An Bras Dermatol. 2015;90:745-747.
- Gibbs MB, English JC, Zirwas MJ. Livedo reticularis: an update. J Am Acad Dermatol. 2005;52:1009-1019.
- Silva SB, Miot HA. Case for diagnosis. amantadine-induced livedo reticularis. An Bras Dermatol. 2012;87:319-321.
- Vollum DI, Parkes JD, Doyle D. Livedo reticularis during amantadine treatment. Br Med J. 1971;2:627-628.
- Hosenbocus S, Chahal R. Amantadine: a review of use in child and adolescent psychiatry. J Can Acad Child Adolesc Psychiatry. 2013;22:55-60.
- Barrera F, Browning JC. Likely amantadine-induced livedo reticularis in a child. Pediatr Dermatol. 2012;29:329-330.
- Quaresma MV, Gomes-Dias AC, Serruya A, et al. Amantadine-induced livedo reticularis: a case report. An Bras Dermatol. 2015;90:745-747.
- Gibbs MB, English JC, Zirwas MJ. Livedo reticularis: an update. J Am Acad Dermatol. 2005;52:1009-1019.
- Silva SB, Miot HA. Case for diagnosis. amantadine-induced livedo reticularis. An Bras Dermatol. 2012;87:319-321.
- Vollum DI, Parkes JD, Doyle D. Livedo reticularis during amantadine treatment. Br Med J. 1971;2:627-628.
- Hosenbocus S, Chahal R. Amantadine: a review of use in child and adolescent psychiatry. J Can Acad Child Adolesc Psychiatry. 2013;22:55-60.
- Barrera F, Browning JC. Likely amantadine-induced livedo reticularis in a child. Pediatr Dermatol. 2012;29:329-330.
Practice Points
- Amantadine is a generally well-tolerated medication that is more commonly used for off-label treatment of several pediatric neurobehavioral conditions such as attention deficit hyperactivity disorder, autism spectrum disorders, obsessive compulsive disorder, depression, and others.
- Livedo reticularis has known associations with several medications and diseases; however, the most common presentation is cutis marmorata, a benign condition that typically affects newborns.
Inframammary Macerated Erosion
The Diagnosis: Hailey-Hailey Disease (Benign Familial Chronic Pemphigus)
Our patient had a long-standing history of Hailey-Hailey disease, as confirmed by multiple prior skin biopsies at outside institutions as well as our affiliated site. He began treatment with oral doxycycline 50 mg twice daily for 2 weeks, triamcinolone cream 0.1% twice daily to the affected region, and aluminum acetate solution soaks and chlorhexidine wash daily along with petroleum jelly, which resulted in good control of the disease. The differential diagnosis of eroded plaques, particularly in the axillary, crural, and inframammary folds, is broad and includes candidiasis, inverse psoriasis, contact dermatitis, dermatophyte infection, pemphigus vegetans or foliaceus, and granular parakeratosis.
Hailey-Hailey disease is a genetic disorder with a prevalence of 1 in 50,000 individuals. Most patients develop symptoms during the second or third decades of life.1 Hailey-Hailey disease exhibits an autosomal-dominant pattern of inheritance secondary to mutation in the human ATP2C1 gene, which codes for the ATPase secretory pathway of the Ca2+ transporting pump type 1 (SPCA1) localized in the Golgi apparatus.2 Altered SPCA1 protein reduces concentration of Ca2+ within the Golgi lumen, which in turn impairs the processing of junctional proteins needed for normal cell-to-cell adhesion.1
Clinically, Hailey-Hailey disease is characterized by vesicular or erosive plaques that have a predilection for intertriginous areas of the body.1 The primary lesions often are flaccid vesicles that easily rupture, leaving behind crusted erosions that spread peripherally. The lesions also can appear as macerated plaques resembling torn tissue paper, as in our case. Friction, heat, and sweat exacerbate the disease. Complications occur from secondary bacterial, fungal, and viral colonization. Malodor and vegetations can indicate bacterial or fungal infections and can lead to persistence of skin lesions. Herpes simplex virus infections can exacerbate preexisting lesions.3 Hailey-Hailey disease of the anogenital region also can be complicated by infection with oncogenic strains of human papillomavirus and lead to cutaneous squamous cell carcinoma.4
Hailey-Hailey disease histologically appears as suprabasal and intraepidermal keratinocyte acantholysis,5 which typically is widespread in the epidermis, with large areas of dyscohesion with a dilapidated brick wall-like appearance.1 In more chronic lesions, epidermal hyperplasia, parakeratosis, and focal crusts may be observed. A moderate perivascular lymphocytic infiltrate can be observed in the superficial dermis. Direct immunofluorescence typically is negative.
Topical corticosteroids and antimicrobials are first-line therapies that often only provide temporary suppression. When the disease is refractory to topical therapies, intralesional corticosteroids may be attempted. There is no strong evidence to support the use of systemic therapy, aside from antimicrobial agents (eg, doxycycline) for the use of superinfections. In severe cases, immunomodulating therapies such as prednisone, cyclosporine, methotrexate, dapsone, alefacept, and oral retinoids may be effective.6-8 Surgical therapy also can be considered for recalcitrant disease, including wide excision and grafting, though these techniques can be associated with morbidity.9
Superficial ablative techniques including dermabrasion, laser therapy with CO2 and erbium-doped YAG, photodynamic therapy, and electron beam radiation have been shown to be effective modalities in severe cases.5,9-11 It has been hypothesized that keratinocytes expressing the molecular defect are ablated, while the surrounding normal adnexal epithelium can regenerate normal epithelium. It also is thought that dermal fibrosis leads to better support of the diseased epidermis and decreases the risk for ulceration and fissuring.9
- Hohl D. Darier disease and Hailey-Hailey disease. In: Bolognia JL, Jorizzo JL, Schaffer JV, eds. Dermatology. 3rd ed. China: Elsevier Saunders; 2012:887-896.
- Micaroni M, Giacchetti G, Plebani R, et al. ATP2C1 gene mutations in Hailey-Hailey disease and possible roles of SPCA1 isoforms in membrane trafficking. Cell Death Dis. 2016;7:E2259.
- Peppiatt T, Keefe M,White JE. Hailey-Hailey disease--exacerbation by herpes simplex virus and patch tests. Clin Exp Dermatol. 1992;17:201-202.
- Chen MY, Chiu HC, Su LH, et al. Presence of human papillomavirus type 6 DNA in the perineal verrucoid lesions of Hailey-Hailey disease. J Eur Acad Dermatol Venereol. 2006;20:1356-1357.
- Graham PM, Melkonian A, Fivenson D. Familial benign chronic pemphigus (Hailey-Hailey disease) treated with electron beam radiation. JAAD Case Rep. 2016;2:159-161.
- Berth-Jones J, Smith SG, Graham-Brown RA, et al. Benign familial chronic pemphigus (Hailey-Hailey disease) responds to cyclosporin. Clin Exp Dermatol. 1995;20:70-72.
- Sire DJ, Johnson BL. Benign familial chronic pemphigus treated with dapsone. Arch Dermatol. 1971;103:262-265.
- Hunt MJ, Salisbury EL, Painter DM. Vesiculobullous Hailey-Hailey disease: successful treatment with oral retinoids. Australas J Dermatol. 1996;37:196-198.
- Ortiz AE, Zachary CB. Laser therapy for Hailey-Hailey disease: review of the literature and a case report. Dermatol Reports. 2011;3:E28.
- Don PC, Carney PS, Lynch WS, et al. Carbon dioxide laserabrasion: a new approach to management of familial benign chronic pemphigus (Hailey-Hailey disease). J Dermatol Surg Oncol. 1987;13:1187-1194.
- Beier C, Kaufmann R. Efficacy of erbium:YAG laser ablation in Darier disease and Hailey-Hailey disease. Arch Dermatol. 1999;135:423-427.
The Diagnosis: Hailey-Hailey Disease (Benign Familial Chronic Pemphigus)
Our patient had a long-standing history of Hailey-Hailey disease, as confirmed by multiple prior skin biopsies at outside institutions as well as our affiliated site. He began treatment with oral doxycycline 50 mg twice daily for 2 weeks, triamcinolone cream 0.1% twice daily to the affected region, and aluminum acetate solution soaks and chlorhexidine wash daily along with petroleum jelly, which resulted in good control of the disease. The differential diagnosis of eroded plaques, particularly in the axillary, crural, and inframammary folds, is broad and includes candidiasis, inverse psoriasis, contact dermatitis, dermatophyte infection, pemphigus vegetans or foliaceus, and granular parakeratosis.
Hailey-Hailey disease is a genetic disorder with a prevalence of 1 in 50,000 individuals. Most patients develop symptoms during the second or third decades of life.1 Hailey-Hailey disease exhibits an autosomal-dominant pattern of inheritance secondary to mutation in the human ATP2C1 gene, which codes for the ATPase secretory pathway of the Ca2+ transporting pump type 1 (SPCA1) localized in the Golgi apparatus.2 Altered SPCA1 protein reduces concentration of Ca2+ within the Golgi lumen, which in turn impairs the processing of junctional proteins needed for normal cell-to-cell adhesion.1
Clinically, Hailey-Hailey disease is characterized by vesicular or erosive plaques that have a predilection for intertriginous areas of the body.1 The primary lesions often are flaccid vesicles that easily rupture, leaving behind crusted erosions that spread peripherally. The lesions also can appear as macerated plaques resembling torn tissue paper, as in our case. Friction, heat, and sweat exacerbate the disease. Complications occur from secondary bacterial, fungal, and viral colonization. Malodor and vegetations can indicate bacterial or fungal infections and can lead to persistence of skin lesions. Herpes simplex virus infections can exacerbate preexisting lesions.3 Hailey-Hailey disease of the anogenital region also can be complicated by infection with oncogenic strains of human papillomavirus and lead to cutaneous squamous cell carcinoma.4
Hailey-Hailey disease histologically appears as suprabasal and intraepidermal keratinocyte acantholysis,5 which typically is widespread in the epidermis, with large areas of dyscohesion with a dilapidated brick wall-like appearance.1 In more chronic lesions, epidermal hyperplasia, parakeratosis, and focal crusts may be observed. A moderate perivascular lymphocytic infiltrate can be observed in the superficial dermis. Direct immunofluorescence typically is negative.
Topical corticosteroids and antimicrobials are first-line therapies that often only provide temporary suppression. When the disease is refractory to topical therapies, intralesional corticosteroids may be attempted. There is no strong evidence to support the use of systemic therapy, aside from antimicrobial agents (eg, doxycycline) for the use of superinfections. In severe cases, immunomodulating therapies such as prednisone, cyclosporine, methotrexate, dapsone, alefacept, and oral retinoids may be effective.6-8 Surgical therapy also can be considered for recalcitrant disease, including wide excision and grafting, though these techniques can be associated with morbidity.9
Superficial ablative techniques including dermabrasion, laser therapy with CO2 and erbium-doped YAG, photodynamic therapy, and electron beam radiation have been shown to be effective modalities in severe cases.5,9-11 It has been hypothesized that keratinocytes expressing the molecular defect are ablated, while the surrounding normal adnexal epithelium can regenerate normal epithelium. It also is thought that dermal fibrosis leads to better support of the diseased epidermis and decreases the risk for ulceration and fissuring.9
The Diagnosis: Hailey-Hailey Disease (Benign Familial Chronic Pemphigus)
Our patient had a long-standing history of Hailey-Hailey disease, as confirmed by multiple prior skin biopsies at outside institutions as well as our affiliated site. He began treatment with oral doxycycline 50 mg twice daily for 2 weeks, triamcinolone cream 0.1% twice daily to the affected region, and aluminum acetate solution soaks and chlorhexidine wash daily along with petroleum jelly, which resulted in good control of the disease. The differential diagnosis of eroded plaques, particularly in the axillary, crural, and inframammary folds, is broad and includes candidiasis, inverse psoriasis, contact dermatitis, dermatophyte infection, pemphigus vegetans or foliaceus, and granular parakeratosis.
Hailey-Hailey disease is a genetic disorder with a prevalence of 1 in 50,000 individuals. Most patients develop symptoms during the second or third decades of life.1 Hailey-Hailey disease exhibits an autosomal-dominant pattern of inheritance secondary to mutation in the human ATP2C1 gene, which codes for the ATPase secretory pathway of the Ca2+ transporting pump type 1 (SPCA1) localized in the Golgi apparatus.2 Altered SPCA1 protein reduces concentration of Ca2+ within the Golgi lumen, which in turn impairs the processing of junctional proteins needed for normal cell-to-cell adhesion.1
Clinically, Hailey-Hailey disease is characterized by vesicular or erosive plaques that have a predilection for intertriginous areas of the body.1 The primary lesions often are flaccid vesicles that easily rupture, leaving behind crusted erosions that spread peripherally. The lesions also can appear as macerated plaques resembling torn tissue paper, as in our case. Friction, heat, and sweat exacerbate the disease. Complications occur from secondary bacterial, fungal, and viral colonization. Malodor and vegetations can indicate bacterial or fungal infections and can lead to persistence of skin lesions. Herpes simplex virus infections can exacerbate preexisting lesions.3 Hailey-Hailey disease of the anogenital region also can be complicated by infection with oncogenic strains of human papillomavirus and lead to cutaneous squamous cell carcinoma.4
Hailey-Hailey disease histologically appears as suprabasal and intraepidermal keratinocyte acantholysis,5 which typically is widespread in the epidermis, with large areas of dyscohesion with a dilapidated brick wall-like appearance.1 In more chronic lesions, epidermal hyperplasia, parakeratosis, and focal crusts may be observed. A moderate perivascular lymphocytic infiltrate can be observed in the superficial dermis. Direct immunofluorescence typically is negative.
Topical corticosteroids and antimicrobials are first-line therapies that often only provide temporary suppression. When the disease is refractory to topical therapies, intralesional corticosteroids may be attempted. There is no strong evidence to support the use of systemic therapy, aside from antimicrobial agents (eg, doxycycline) for the use of superinfections. In severe cases, immunomodulating therapies such as prednisone, cyclosporine, methotrexate, dapsone, alefacept, and oral retinoids may be effective.6-8 Surgical therapy also can be considered for recalcitrant disease, including wide excision and grafting, though these techniques can be associated with morbidity.9
Superficial ablative techniques including dermabrasion, laser therapy with CO2 and erbium-doped YAG, photodynamic therapy, and electron beam radiation have been shown to be effective modalities in severe cases.5,9-11 It has been hypothesized that keratinocytes expressing the molecular defect are ablated, while the surrounding normal adnexal epithelium can regenerate normal epithelium. It also is thought that dermal fibrosis leads to better support of the diseased epidermis and decreases the risk for ulceration and fissuring.9
- Hohl D. Darier disease and Hailey-Hailey disease. In: Bolognia JL, Jorizzo JL, Schaffer JV, eds. Dermatology. 3rd ed. China: Elsevier Saunders; 2012:887-896.
- Micaroni M, Giacchetti G, Plebani R, et al. ATP2C1 gene mutations in Hailey-Hailey disease and possible roles of SPCA1 isoforms in membrane trafficking. Cell Death Dis. 2016;7:E2259.
- Peppiatt T, Keefe M,White JE. Hailey-Hailey disease--exacerbation by herpes simplex virus and patch tests. Clin Exp Dermatol. 1992;17:201-202.
- Chen MY, Chiu HC, Su LH, et al. Presence of human papillomavirus type 6 DNA in the perineal verrucoid lesions of Hailey-Hailey disease. J Eur Acad Dermatol Venereol. 2006;20:1356-1357.
- Graham PM, Melkonian A, Fivenson D. Familial benign chronic pemphigus (Hailey-Hailey disease) treated with electron beam radiation. JAAD Case Rep. 2016;2:159-161.
- Berth-Jones J, Smith SG, Graham-Brown RA, et al. Benign familial chronic pemphigus (Hailey-Hailey disease) responds to cyclosporin. Clin Exp Dermatol. 1995;20:70-72.
- Sire DJ, Johnson BL. Benign familial chronic pemphigus treated with dapsone. Arch Dermatol. 1971;103:262-265.
- Hunt MJ, Salisbury EL, Painter DM. Vesiculobullous Hailey-Hailey disease: successful treatment with oral retinoids. Australas J Dermatol. 1996;37:196-198.
- Ortiz AE, Zachary CB. Laser therapy for Hailey-Hailey disease: review of the literature and a case report. Dermatol Reports. 2011;3:E28.
- Don PC, Carney PS, Lynch WS, et al. Carbon dioxide laserabrasion: a new approach to management of familial benign chronic pemphigus (Hailey-Hailey disease). J Dermatol Surg Oncol. 1987;13:1187-1194.
- Beier C, Kaufmann R. Efficacy of erbium:YAG laser ablation in Darier disease and Hailey-Hailey disease. Arch Dermatol. 1999;135:423-427.
- Hohl D. Darier disease and Hailey-Hailey disease. In: Bolognia JL, Jorizzo JL, Schaffer JV, eds. Dermatology. 3rd ed. China: Elsevier Saunders; 2012:887-896.
- Micaroni M, Giacchetti G, Plebani R, et al. ATP2C1 gene mutations in Hailey-Hailey disease and possible roles of SPCA1 isoforms in membrane trafficking. Cell Death Dis. 2016;7:E2259.
- Peppiatt T, Keefe M,White JE. Hailey-Hailey disease--exacerbation by herpes simplex virus and patch tests. Clin Exp Dermatol. 1992;17:201-202.
- Chen MY, Chiu HC, Su LH, et al. Presence of human papillomavirus type 6 DNA in the perineal verrucoid lesions of Hailey-Hailey disease. J Eur Acad Dermatol Venereol. 2006;20:1356-1357.
- Graham PM, Melkonian A, Fivenson D. Familial benign chronic pemphigus (Hailey-Hailey disease) treated with electron beam radiation. JAAD Case Rep. 2016;2:159-161.
- Berth-Jones J, Smith SG, Graham-Brown RA, et al. Benign familial chronic pemphigus (Hailey-Hailey disease) responds to cyclosporin. Clin Exp Dermatol. 1995;20:70-72.
- Sire DJ, Johnson BL. Benign familial chronic pemphigus treated with dapsone. Arch Dermatol. 1971;103:262-265.
- Hunt MJ, Salisbury EL, Painter DM. Vesiculobullous Hailey-Hailey disease: successful treatment with oral retinoids. Australas J Dermatol. 1996;37:196-198.
- Ortiz AE, Zachary CB. Laser therapy for Hailey-Hailey disease: review of the literature and a case report. Dermatol Reports. 2011;3:E28.
- Don PC, Carney PS, Lynch WS, et al. Carbon dioxide laserabrasion: a new approach to management of familial benign chronic pemphigus (Hailey-Hailey disease). J Dermatol Surg Oncol. 1987;13:1187-1194.
- Beier C, Kaufmann R. Efficacy of erbium:YAG laser ablation in Darier disease and Hailey-Hailey disease. Arch Dermatol. 1999;135:423-427.

An 81-year-old man presented with a painful erosion in the left inframammary region of 2 weeks' duration. He described the lesion as pruritic and burning. He reported having prior similar episodes in the bilateral groin, axilla, and lower abdomen that often were malodorous. Use of triamcinolone cream 0.1% up to 4 times daily resulted in little relief of the erosion. Of note, the patient reported therapies for prior sites had included oral doxycycline 50 mg twice daily, clobetasol cream, and clindamycin solution, which provided limited relief but eventual resolution. Application of cold aluminum acetate solution compresses for 5 minutes daily irritated the skin even further and led to bleeding at the affected sites. The patient's father had a history of similar skin lesions.
Best practices defined for proton therapy in mediastinal lymphomas
Proton therapy can help mitigate toxicity in adults with mediastinal lymphomas, but only when this modality offers a clear advantage over intensity-modulated radiotherapy, according to new guidelines from the International Lymphoma Radiation Oncology Group.
Proton therapy reduces radiation dose to organs at risk in certain clinical presentations, such as when the mediastinal target is on both sides of the heart. The advantages are not always clear in other situations, such as when the target spans the right side of the heart, or when the target is above the heart with no axillary involvement, according to guideline authors Bouthaina Dabaja, MD, professor and section chief of hematology in the department of radiation oncology at the University of Texas MD Anderson Cancer Center, Houston, and her colleagues.
“The limited availability of proton therapy calls for case selection based on a clear understanding of which cases will derive most benefit from proton therapy as compared to advanced photon techniques,” Dr. Dabaja and her coauthors said in the guidelines, which were published in the journal Blood (doi: 10.1182/blood-2018-03-837633).
Along with intensity-modulated radiotherapy and 3-dimensional conformal radiotherapy, proton therapy presents “another opportunity” for more conformal dose distribution and better sparing of organs at risk, according to the consensus recommendations. Proton therapy can greatly benefit certain patients with mediastinal disease. These include young female patients to reduce breast dose and risk of a secondary breast cancer, patients at high risk of radiation-related toxicity due to previous treatment, and patients with disease spanning below the origin of the left main stem coronary artery that is anterior to, posterior to, or on the left side of the heart.
“The relation of disease to organs at risk determines the situations in which proton therapy is most beneficial,” the experts said in the guidelines. However, the consideration of proton therapy needs to factor the complexities of proton therapy planning, the need to manage uncertainties, and the “evolving nature of the technology,” which includes the development of pencil beam scanning.
While passive scattering proton therapy (PSPT) is the least complex delivery technique, it is challenging because beams can conform only to one side of the target; by contrast, the experts said, active mode pencil beam scanning proton therapy (PBSPT) potentially provides better conformity and sparing of organs at risk.
“Because treatment involves delivery of individual controlled spots, inhomogenous doses can be created deliberately,” the guideline authors said in their report.
However, motion management is “of prime importance” with PBSPT, which is more sensitive to density changes in the beam path as compared to PSPT, they added. Toward that end, physicians should pay close attention to evaluating intrafractional movement, which is frequently tied to the breathing cycle.
The guidelines list a total of 11 authors representing The University of Texas MD Anderson Cancer Center; University of Florida, Jacksonville; University of Pennsylvania, Philadelphia; University of Louisiana, Baton Rouge; Proton Therapy Center Czech, Prague; Motol University Hospital, Czech Republic; St. Thomas and Guy Hospital, London; Institut Curie, Paris; and Rigshospitalet, Copenhagen.
Dr. Dabaja and her guideline coauthors reported no funding or conflicts of interest.
Proton therapy can help mitigate toxicity in adults with mediastinal lymphomas, but only when this modality offers a clear advantage over intensity-modulated radiotherapy, according to new guidelines from the International Lymphoma Radiation Oncology Group.
Proton therapy reduces radiation dose to organs at risk in certain clinical presentations, such as when the mediastinal target is on both sides of the heart. The advantages are not always clear in other situations, such as when the target spans the right side of the heart, or when the target is above the heart with no axillary involvement, according to guideline authors Bouthaina Dabaja, MD, professor and section chief of hematology in the department of radiation oncology at the University of Texas MD Anderson Cancer Center, Houston, and her colleagues.
“The limited availability of proton therapy calls for case selection based on a clear understanding of which cases will derive most benefit from proton therapy as compared to advanced photon techniques,” Dr. Dabaja and her coauthors said in the guidelines, which were published in the journal Blood (doi: 10.1182/blood-2018-03-837633).
Along with intensity-modulated radiotherapy and 3-dimensional conformal radiotherapy, proton therapy presents “another opportunity” for more conformal dose distribution and better sparing of organs at risk, according to the consensus recommendations. Proton therapy can greatly benefit certain patients with mediastinal disease. These include young female patients to reduce breast dose and risk of a secondary breast cancer, patients at high risk of radiation-related toxicity due to previous treatment, and patients with disease spanning below the origin of the left main stem coronary artery that is anterior to, posterior to, or on the left side of the heart.
“The relation of disease to organs at risk determines the situations in which proton therapy is most beneficial,” the experts said in the guidelines. However, the consideration of proton therapy needs to factor the complexities of proton therapy planning, the need to manage uncertainties, and the “evolving nature of the technology,” which includes the development of pencil beam scanning.
While passive scattering proton therapy (PSPT) is the least complex delivery technique, it is challenging because beams can conform only to one side of the target; by contrast, the experts said, active mode pencil beam scanning proton therapy (PBSPT) potentially provides better conformity and sparing of organs at risk.
“Because treatment involves delivery of individual controlled spots, inhomogenous doses can be created deliberately,” the guideline authors said in their report.
However, motion management is “of prime importance” with PBSPT, which is more sensitive to density changes in the beam path as compared to PSPT, they added. Toward that end, physicians should pay close attention to evaluating intrafractional movement, which is frequently tied to the breathing cycle.
The guidelines list a total of 11 authors representing The University of Texas MD Anderson Cancer Center; University of Florida, Jacksonville; University of Pennsylvania, Philadelphia; University of Louisiana, Baton Rouge; Proton Therapy Center Czech, Prague; Motol University Hospital, Czech Republic; St. Thomas and Guy Hospital, London; Institut Curie, Paris; and Rigshospitalet, Copenhagen.
Dr. Dabaja and her guideline coauthors reported no funding or conflicts of interest.
Proton therapy can help mitigate toxicity in adults with mediastinal lymphomas, but only when this modality offers a clear advantage over intensity-modulated radiotherapy, according to new guidelines from the International Lymphoma Radiation Oncology Group.
Proton therapy reduces radiation dose to organs at risk in certain clinical presentations, such as when the mediastinal target is on both sides of the heart. The advantages are not always clear in other situations, such as when the target spans the right side of the heart, or when the target is above the heart with no axillary involvement, according to guideline authors Bouthaina Dabaja, MD, professor and section chief of hematology in the department of radiation oncology at the University of Texas MD Anderson Cancer Center, Houston, and her colleagues.
“The limited availability of proton therapy calls for case selection based on a clear understanding of which cases will derive most benefit from proton therapy as compared to advanced photon techniques,” Dr. Dabaja and her coauthors said in the guidelines, which were published in the journal Blood (doi: 10.1182/blood-2018-03-837633).
Along with intensity-modulated radiotherapy and 3-dimensional conformal radiotherapy, proton therapy presents “another opportunity” for more conformal dose distribution and better sparing of organs at risk, according to the consensus recommendations. Proton therapy can greatly benefit certain patients with mediastinal disease. These include young female patients to reduce breast dose and risk of a secondary breast cancer, patients at high risk of radiation-related toxicity due to previous treatment, and patients with disease spanning below the origin of the left main stem coronary artery that is anterior to, posterior to, or on the left side of the heart.
“The relation of disease to organs at risk determines the situations in which proton therapy is most beneficial,” the experts said in the guidelines. However, the consideration of proton therapy needs to factor the complexities of proton therapy planning, the need to manage uncertainties, and the “evolving nature of the technology,” which includes the development of pencil beam scanning.
While passive scattering proton therapy (PSPT) is the least complex delivery technique, it is challenging because beams can conform only to one side of the target; by contrast, the experts said, active mode pencil beam scanning proton therapy (PBSPT) potentially provides better conformity and sparing of organs at risk.
“Because treatment involves delivery of individual controlled spots, inhomogenous doses can be created deliberately,” the guideline authors said in their report.
However, motion management is “of prime importance” with PBSPT, which is more sensitive to density changes in the beam path as compared to PSPT, they added. Toward that end, physicians should pay close attention to evaluating intrafractional movement, which is frequently tied to the breathing cycle.
The guidelines list a total of 11 authors representing The University of Texas MD Anderson Cancer Center; University of Florida, Jacksonville; University of Pennsylvania, Philadelphia; University of Louisiana, Baton Rouge; Proton Therapy Center Czech, Prague; Motol University Hospital, Czech Republic; St. Thomas and Guy Hospital, London; Institut Curie, Paris; and Rigshospitalet, Copenhagen.
Dr. Dabaja and her guideline coauthors reported no funding or conflicts of interest.
FROM BLOOD
U.S. perspective: Euro hypertension guidelines look a lot like ours
MUNICH – The “overwhelming impression” that Paul K. Whelton, MD, has of the newly revised hypertension diagnosis and management guidelines of the European Society of Cardiology is their similarity to hypertension guidelines released by the American College of Cardiology and American Heart Association in November 2017.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“We both recommend the same treatment target, of less than 130/80 mm Hg,” noted Dr. Whelton, professor at Tulane University in New Orleans, although the European guidelines (Euro J Cardiology. 2018 Sep 1; 39[33]:3021-104) put more qualifications on this target and specify treating to no lower than 130 mm Hg systolic pressure in patients who are at least 65 years old as well as in patients with chronic kidney disease at any age. In a video interview, Dr. Whelton also cited areas of disagreement, such as how patients with an untreated blood pressure of 130-139 mm Hg are classified (high normal in the European guidelines, stage 1 hypertension in the U.S. guidelines), and whether initial drug monotherapy is a reasonable treatment strategy (U.S. says yes, Europe says no).
Dr. Whelton noted that recent modeling studies have documented the potential public health benefits from following the diagnosis and management approaches set forth in the 2017 U.S. guidelines (J Am Coll Cardiol. 2018 May;71[19]:e127-e248). For example, an analysis based on data collected by the U.S. National Health and Nutrition Examination Survey during 2013-2016 showed that following the 2017 guidelines for diagnosing and treating hypertension would have resulted in prevention of more than twice the number of cardiovascular disease events nationally as compared with application of the prior, 2014 U.S. hypertension guideline (JAMA. 2014 Feb 5;311[5]:507-20): 610,000 events prevented, compared with 270,000 events prevented. The same study showed that the 2017 guidelines would have nearly doubled the number of all-cause deaths prevented, with 334,000 deaths prevented, compared with 177,000 prevented by applying the 2014 guidelines (JAMA Cardiology. 2018 July;3[7]:572-81).
Dr. Whelton had no commercial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MUNICH – The “overwhelming impression” that Paul K. Whelton, MD, has of the newly revised hypertension diagnosis and management guidelines of the European Society of Cardiology is their similarity to hypertension guidelines released by the American College of Cardiology and American Heart Association in November 2017.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“We both recommend the same treatment target, of less than 130/80 mm Hg,” noted Dr. Whelton, professor at Tulane University in New Orleans, although the European guidelines (Euro J Cardiology. 2018 Sep 1; 39[33]:3021-104) put more qualifications on this target and specify treating to no lower than 130 mm Hg systolic pressure in patients who are at least 65 years old as well as in patients with chronic kidney disease at any age. In a video interview, Dr. Whelton also cited areas of disagreement, such as how patients with an untreated blood pressure of 130-139 mm Hg are classified (high normal in the European guidelines, stage 1 hypertension in the U.S. guidelines), and whether initial drug monotherapy is a reasonable treatment strategy (U.S. says yes, Europe says no).
Dr. Whelton noted that recent modeling studies have documented the potential public health benefits from following the diagnosis and management approaches set forth in the 2017 U.S. guidelines (J Am Coll Cardiol. 2018 May;71[19]:e127-e248). For example, an analysis based on data collected by the U.S. National Health and Nutrition Examination Survey during 2013-2016 showed that following the 2017 guidelines for diagnosing and treating hypertension would have resulted in prevention of more than twice the number of cardiovascular disease events nationally as compared with application of the prior, 2014 U.S. hypertension guideline (JAMA. 2014 Feb 5;311[5]:507-20): 610,000 events prevented, compared with 270,000 events prevented. The same study showed that the 2017 guidelines would have nearly doubled the number of all-cause deaths prevented, with 334,000 deaths prevented, compared with 177,000 prevented by applying the 2014 guidelines (JAMA Cardiology. 2018 July;3[7]:572-81).
Dr. Whelton had no commercial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MUNICH – The “overwhelming impression” that Paul K. Whelton, MD, has of the newly revised hypertension diagnosis and management guidelines of the European Society of Cardiology is their similarity to hypertension guidelines released by the American College of Cardiology and American Heart Association in November 2017.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“We both recommend the same treatment target, of less than 130/80 mm Hg,” noted Dr. Whelton, professor at Tulane University in New Orleans, although the European guidelines (Euro J Cardiology. 2018 Sep 1; 39[33]:3021-104) put more qualifications on this target and specify treating to no lower than 130 mm Hg systolic pressure in patients who are at least 65 years old as well as in patients with chronic kidney disease at any age. In a video interview, Dr. Whelton also cited areas of disagreement, such as how patients with an untreated blood pressure of 130-139 mm Hg are classified (high normal in the European guidelines, stage 1 hypertension in the U.S. guidelines), and whether initial drug monotherapy is a reasonable treatment strategy (U.S. says yes, Europe says no).
Dr. Whelton noted that recent modeling studies have documented the potential public health benefits from following the diagnosis and management approaches set forth in the 2017 U.S. guidelines (J Am Coll Cardiol. 2018 May;71[19]:e127-e248). For example, an analysis based on data collected by the U.S. National Health and Nutrition Examination Survey during 2013-2016 showed that following the 2017 guidelines for diagnosing and treating hypertension would have resulted in prevention of more than twice the number of cardiovascular disease events nationally as compared with application of the prior, 2014 U.S. hypertension guideline (JAMA. 2014 Feb 5;311[5]:507-20): 610,000 events prevented, compared with 270,000 events prevented. The same study showed that the 2017 guidelines would have nearly doubled the number of all-cause deaths prevented, with 334,000 deaths prevented, compared with 177,000 prevented by applying the 2014 guidelines (JAMA Cardiology. 2018 July;3[7]:572-81).
Dr. Whelton had no commercial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
REPORTING FROM THE ESC CONGRESS 2018