User login
CSF and plasma biomarkers predict survival in sporadic Creutzfeldt-Jakob disease
, according to research published online ahead of print May 6 in JAMA Neurology. Levels of total tau in plasma and CSF are correlated, and plasma total tau is associated with survival time. These findings suggest that plasma total tau level could be a valid biomarker that guides clinical care for patients with sporadic Creutzfeldt-Jakob disease, said the investigators.
The accurate prediction of disease duration can assist clinicians and caregivers in clinical management, as well as influence the design of clinical trials. Previous studies have found that baseline protein levels in CSF and plasma are associated with disease duration in patients with sporadic Creutzfeldt-Jakob disease. To replicate these findings, Adam M. Staffaroni, PhD, of the department of neurology at the University of California, San Francisco, and colleagues conducted a longitudinal cohort study.
Evaluating fluid and nonfluid biomarkers
Dr. Staffaroni and colleagues recruited 193 participants with probable or definite sporadic Creutzfeldt-Jakob disease who had codon 129 genotyping and were referred to the UCSF Memory and Aging Center from March 2004 to January 2018. All participants underwent cognitive testing, informant measures, a neurologic examination, and CSF and blood sample collection. The researchers excluded from analysis five participants who had been placed on life-extending treatments. Participants were evaluated until death or censored at the time of statistical analysis.
Dr. Staffaroni and colleagues examined the following nonfluid biomarkers of survival: sex, age, codon 129 genotype, Barthel Index, and Medical Research Council (MRC) Prion Disease Rating Scale. In addition, they examined total tau level, phosphorylated tau level, total tau:phosphorylated tau ratio, neurofilament light (NfL) level, beta-amyloid 42 level, neuron-specific enolase level, 14-3-3 test result, and real-time quaking-induced conversion test in CSF as fluid biomarkers of survival. Finally, Dr. Staffaroni’s group analyzed total tau level, NfL level, and glial fibrillary acidic protein level in plasma as additional fluid biomarkers of survival.
The researchers fitted Cox proportional hazard models with time to event as the outcome. They log-transformed fluid biomarkers and ran models with and without nonfluid biomarkers of survival.
Plasma total tau was associated with survival
In all, 188 patients were included in the analysis. The population’s mean age was 63.8 years. Approximately 45% of participants were women. The diagnosis of sporadic Creutzfeldt-Jakob disease was pathologically confirmed for 78.2% of participants and probable for 21.8% of participants.
Dr. Staffaroni’s group observed strong correlations between plasma and CSF NfL concentrations and between plasma and CSF total tau concentrations. CSF total tau and CSF NfL concentrations were also correlated.
Among the nonfluid biomarkers, Barthel Index, MRC Scale, and codon 129 genotype were significantly associated with survival time. Lower level of function at baseline predicted a faster disease course.
Among the fluid biomarkers, greater levels of plasma total tau and NfL levels at baseline were associated with shorter survival. After the investigators controlled for Barthel Index and codon 129 genotype, the association of plasma total tau level with survival time remained significant. Plasma total tau level and Barthel Index (hazard ratio, 0.98) each independently predicted survival. Dr. Staffaroni and colleagues found that the hazard ratios for all CSF biomarkers were in the expected direction, and that those for total tau level, total tau:phosphorylated tau ratio, NfL level, and neuron-specific enolase level were statistically significant. Furthermore, positive results for 14-3-3 protein, neuron-specific enolase level, and total tau level were associated with a shorter time until death. Like the plasma biomarkers, CSF total tau level remained associated with survival after the investigators controlled for Barthel Index and codon 129 genotype. The same was true of CSF total tau:phosphorylated tau ratio, neuron-specific enolase level, and 14-3-3 result.
Plasma tau could be a diagnostic biomarker
“The hazard ratio associated with plasma total tau level was more than 40% higher than other fluid biomarkers of interest,” said the authors. “These findings further bolster the value of blood-based biomarkers, based on their minimally invasive and relatively inexpensive nature, and build on prior studies that suggested patients with sporadic Creutzfeldt-Jakob disease and controls can be discriminated with relatively high accuracy using blood-based assays.” When Dr. Staffaroni and colleagues modeled baseline functional status and plasma total tau levels together, they found that both were independent predictors of survival time. “This [finding] suggests that clinical measures and plasma total tau level could be combined to further improve prediction accuracy.”
Among the study’s limitations was its comparatively small subsample of patients for whom all plasma and CSF biomarkers were available. Disease duration and survival were longer in the study population than in the literature. “Another limitation is that the plasma biomarkers in this study, one of which showed great promise for predicting survival, were assayed using a research protocol,” said the researchers. “Widespread clinical use of these biomarkers will require well-validated commercial assays, development of which is underway.”
Before these biomarkers can be used in the clinic, these results will need to be replicated, and neurologists will need to develop consensus cutoffs for the biomarker levels. The researchers did not analyze plasma tau level as a diagnostic biomarker, but future studies should examine this potential, Dr. Staffaroni and colleagues concluded.
Grants from the National Institute on Aging and the National Institute of Allergy and Infectious Diseases supported the study.
SOURCE: Staffaroni AM et al. JAMA Neurol. 2019 May 6. doi: 10.1001/jamaneurol.2019.1071.
, according to research published online ahead of print May 6 in JAMA Neurology. Levels of total tau in plasma and CSF are correlated, and plasma total tau is associated with survival time. These findings suggest that plasma total tau level could be a valid biomarker that guides clinical care for patients with sporadic Creutzfeldt-Jakob disease, said the investigators.
The accurate prediction of disease duration can assist clinicians and caregivers in clinical management, as well as influence the design of clinical trials. Previous studies have found that baseline protein levels in CSF and plasma are associated with disease duration in patients with sporadic Creutzfeldt-Jakob disease. To replicate these findings, Adam M. Staffaroni, PhD, of the department of neurology at the University of California, San Francisco, and colleagues conducted a longitudinal cohort study.
Evaluating fluid and nonfluid biomarkers
Dr. Staffaroni and colleagues recruited 193 participants with probable or definite sporadic Creutzfeldt-Jakob disease who had codon 129 genotyping and were referred to the UCSF Memory and Aging Center from March 2004 to January 2018. All participants underwent cognitive testing, informant measures, a neurologic examination, and CSF and blood sample collection. The researchers excluded from analysis five participants who had been placed on life-extending treatments. Participants were evaluated until death or censored at the time of statistical analysis.
Dr. Staffaroni and colleagues examined the following nonfluid biomarkers of survival: sex, age, codon 129 genotype, Barthel Index, and Medical Research Council (MRC) Prion Disease Rating Scale. In addition, they examined total tau level, phosphorylated tau level, total tau:phosphorylated tau ratio, neurofilament light (NfL) level, beta-amyloid 42 level, neuron-specific enolase level, 14-3-3 test result, and real-time quaking-induced conversion test in CSF as fluid biomarkers of survival. Finally, Dr. Staffaroni’s group analyzed total tau level, NfL level, and glial fibrillary acidic protein level in plasma as additional fluid biomarkers of survival.
The researchers fitted Cox proportional hazard models with time to event as the outcome. They log-transformed fluid biomarkers and ran models with and without nonfluid biomarkers of survival.
Plasma total tau was associated with survival
In all, 188 patients were included in the analysis. The population’s mean age was 63.8 years. Approximately 45% of participants were women. The diagnosis of sporadic Creutzfeldt-Jakob disease was pathologically confirmed for 78.2% of participants and probable for 21.8% of participants.
Dr. Staffaroni’s group observed strong correlations between plasma and CSF NfL concentrations and between plasma and CSF total tau concentrations. CSF total tau and CSF NfL concentrations were also correlated.
Among the nonfluid biomarkers, Barthel Index, MRC Scale, and codon 129 genotype were significantly associated with survival time. Lower level of function at baseline predicted a faster disease course.
Among the fluid biomarkers, greater levels of plasma total tau and NfL levels at baseline were associated with shorter survival. After the investigators controlled for Barthel Index and codon 129 genotype, the association of plasma total tau level with survival time remained significant. Plasma total tau level and Barthel Index (hazard ratio, 0.98) each independently predicted survival. Dr. Staffaroni and colleagues found that the hazard ratios for all CSF biomarkers were in the expected direction, and that those for total tau level, total tau:phosphorylated tau ratio, NfL level, and neuron-specific enolase level were statistically significant. Furthermore, positive results for 14-3-3 protein, neuron-specific enolase level, and total tau level were associated with a shorter time until death. Like the plasma biomarkers, CSF total tau level remained associated with survival after the investigators controlled for Barthel Index and codon 129 genotype. The same was true of CSF total tau:phosphorylated tau ratio, neuron-specific enolase level, and 14-3-3 result.
Plasma tau could be a diagnostic biomarker
“The hazard ratio associated with plasma total tau level was more than 40% higher than other fluid biomarkers of interest,” said the authors. “These findings further bolster the value of blood-based biomarkers, based on their minimally invasive and relatively inexpensive nature, and build on prior studies that suggested patients with sporadic Creutzfeldt-Jakob disease and controls can be discriminated with relatively high accuracy using blood-based assays.” When Dr. Staffaroni and colleagues modeled baseline functional status and plasma total tau levels together, they found that both were independent predictors of survival time. “This [finding] suggests that clinical measures and plasma total tau level could be combined to further improve prediction accuracy.”
Among the study’s limitations was its comparatively small subsample of patients for whom all plasma and CSF biomarkers were available. Disease duration and survival were longer in the study population than in the literature. “Another limitation is that the plasma biomarkers in this study, one of which showed great promise for predicting survival, were assayed using a research protocol,” said the researchers. “Widespread clinical use of these biomarkers will require well-validated commercial assays, development of which is underway.”
Before these biomarkers can be used in the clinic, these results will need to be replicated, and neurologists will need to develop consensus cutoffs for the biomarker levels. The researchers did not analyze plasma tau level as a diagnostic biomarker, but future studies should examine this potential, Dr. Staffaroni and colleagues concluded.
Grants from the National Institute on Aging and the National Institute of Allergy and Infectious Diseases supported the study.
SOURCE: Staffaroni AM et al. JAMA Neurol. 2019 May 6. doi: 10.1001/jamaneurol.2019.1071.
, according to research published online ahead of print May 6 in JAMA Neurology. Levels of total tau in plasma and CSF are correlated, and plasma total tau is associated with survival time. These findings suggest that plasma total tau level could be a valid biomarker that guides clinical care for patients with sporadic Creutzfeldt-Jakob disease, said the investigators.
The accurate prediction of disease duration can assist clinicians and caregivers in clinical management, as well as influence the design of clinical trials. Previous studies have found that baseline protein levels in CSF and plasma are associated with disease duration in patients with sporadic Creutzfeldt-Jakob disease. To replicate these findings, Adam M. Staffaroni, PhD, of the department of neurology at the University of California, San Francisco, and colleagues conducted a longitudinal cohort study.
Evaluating fluid and nonfluid biomarkers
Dr. Staffaroni and colleagues recruited 193 participants with probable or definite sporadic Creutzfeldt-Jakob disease who had codon 129 genotyping and were referred to the UCSF Memory and Aging Center from March 2004 to January 2018. All participants underwent cognitive testing, informant measures, a neurologic examination, and CSF and blood sample collection. The researchers excluded from analysis five participants who had been placed on life-extending treatments. Participants were evaluated until death or censored at the time of statistical analysis.
Dr. Staffaroni and colleagues examined the following nonfluid biomarkers of survival: sex, age, codon 129 genotype, Barthel Index, and Medical Research Council (MRC) Prion Disease Rating Scale. In addition, they examined total tau level, phosphorylated tau level, total tau:phosphorylated tau ratio, neurofilament light (NfL) level, beta-amyloid 42 level, neuron-specific enolase level, 14-3-3 test result, and real-time quaking-induced conversion test in CSF as fluid biomarkers of survival. Finally, Dr. Staffaroni’s group analyzed total tau level, NfL level, and glial fibrillary acidic protein level in plasma as additional fluid biomarkers of survival.
The researchers fitted Cox proportional hazard models with time to event as the outcome. They log-transformed fluid biomarkers and ran models with and without nonfluid biomarkers of survival.
Plasma total tau was associated with survival
In all, 188 patients were included in the analysis. The population’s mean age was 63.8 years. Approximately 45% of participants were women. The diagnosis of sporadic Creutzfeldt-Jakob disease was pathologically confirmed for 78.2% of participants and probable for 21.8% of participants.
Dr. Staffaroni’s group observed strong correlations between plasma and CSF NfL concentrations and between plasma and CSF total tau concentrations. CSF total tau and CSF NfL concentrations were also correlated.
Among the nonfluid biomarkers, Barthel Index, MRC Scale, and codon 129 genotype were significantly associated with survival time. Lower level of function at baseline predicted a faster disease course.
Among the fluid biomarkers, greater levels of plasma total tau and NfL levels at baseline were associated with shorter survival. After the investigators controlled for Barthel Index and codon 129 genotype, the association of plasma total tau level with survival time remained significant. Plasma total tau level and Barthel Index (hazard ratio, 0.98) each independently predicted survival. Dr. Staffaroni and colleagues found that the hazard ratios for all CSF biomarkers were in the expected direction, and that those for total tau level, total tau:phosphorylated tau ratio, NfL level, and neuron-specific enolase level were statistically significant. Furthermore, positive results for 14-3-3 protein, neuron-specific enolase level, and total tau level were associated with a shorter time until death. Like the plasma biomarkers, CSF total tau level remained associated with survival after the investigators controlled for Barthel Index and codon 129 genotype. The same was true of CSF total tau:phosphorylated tau ratio, neuron-specific enolase level, and 14-3-3 result.
Plasma tau could be a diagnostic biomarker
“The hazard ratio associated with plasma total tau level was more than 40% higher than other fluid biomarkers of interest,” said the authors. “These findings further bolster the value of blood-based biomarkers, based on their minimally invasive and relatively inexpensive nature, and build on prior studies that suggested patients with sporadic Creutzfeldt-Jakob disease and controls can be discriminated with relatively high accuracy using blood-based assays.” When Dr. Staffaroni and colleagues modeled baseline functional status and plasma total tau levels together, they found that both were independent predictors of survival time. “This [finding] suggests that clinical measures and plasma total tau level could be combined to further improve prediction accuracy.”
Among the study’s limitations was its comparatively small subsample of patients for whom all plasma and CSF biomarkers were available. Disease duration and survival were longer in the study population than in the literature. “Another limitation is that the plasma biomarkers in this study, one of which showed great promise for predicting survival, were assayed using a research protocol,” said the researchers. “Widespread clinical use of these biomarkers will require well-validated commercial assays, development of which is underway.”
Before these biomarkers can be used in the clinic, these results will need to be replicated, and neurologists will need to develop consensus cutoffs for the biomarker levels. The researchers did not analyze plasma tau level as a diagnostic biomarker, but future studies should examine this potential, Dr. Staffaroni and colleagues concluded.
Grants from the National Institute on Aging and the National Institute of Allergy and Infectious Diseases supported the study.
SOURCE: Staffaroni AM et al. JAMA Neurol. 2019 May 6. doi: 10.1001/jamaneurol.2019.1071.
FROM JAMA NEUROLOGY
Key clinical point: Invasive and minimally invasive biomarkers are associated with survival in sporadic Creutzfeldt-Jakob disease.
Major finding: The hazard ratio for plasma total tau level was more than 40% larger than any other biomarker.
Study details: A longitudinal study of 188 participants with sporadic Creutzfeldt-Jakob disease.
Disclosures: Grants from the National Institute on Aging and the National Institute of Allergy and Infectious Diseases supported the study.
Source: Staffaroni AM et al. JAMA Neurol. 2019 May 6. doi: 10.1001/jamaneurol.2019.1071.
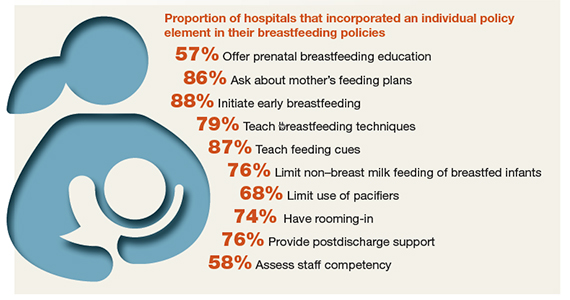
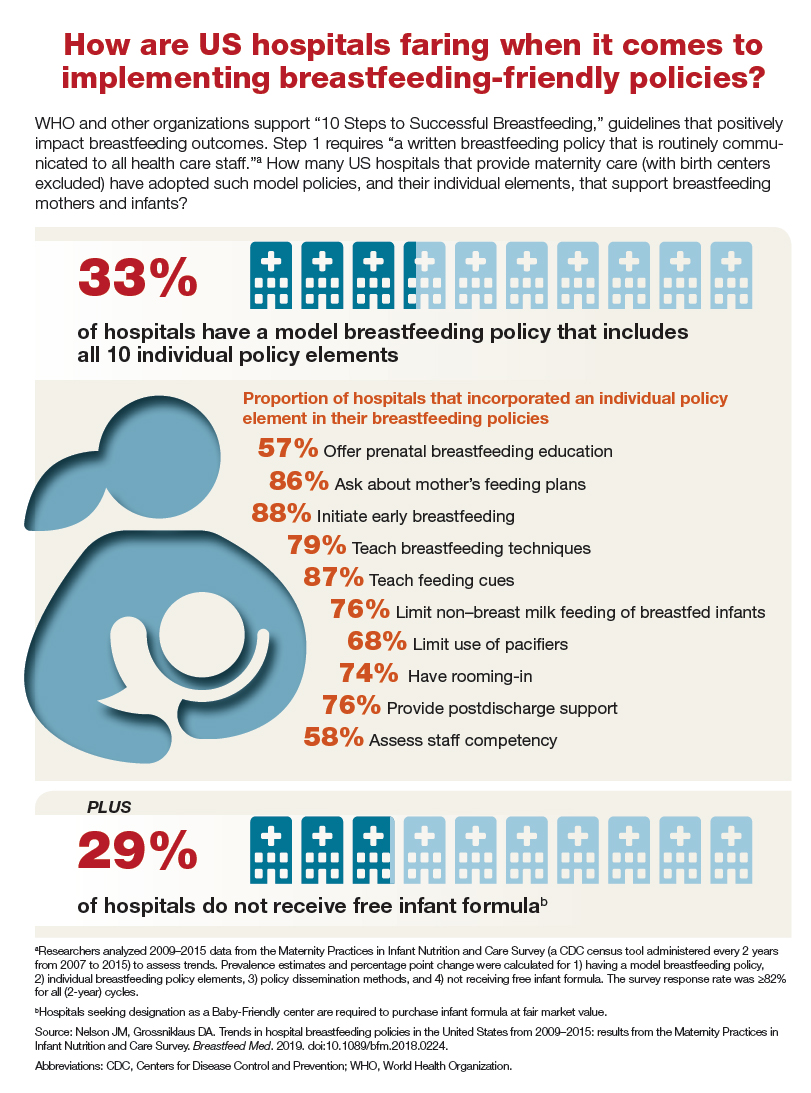
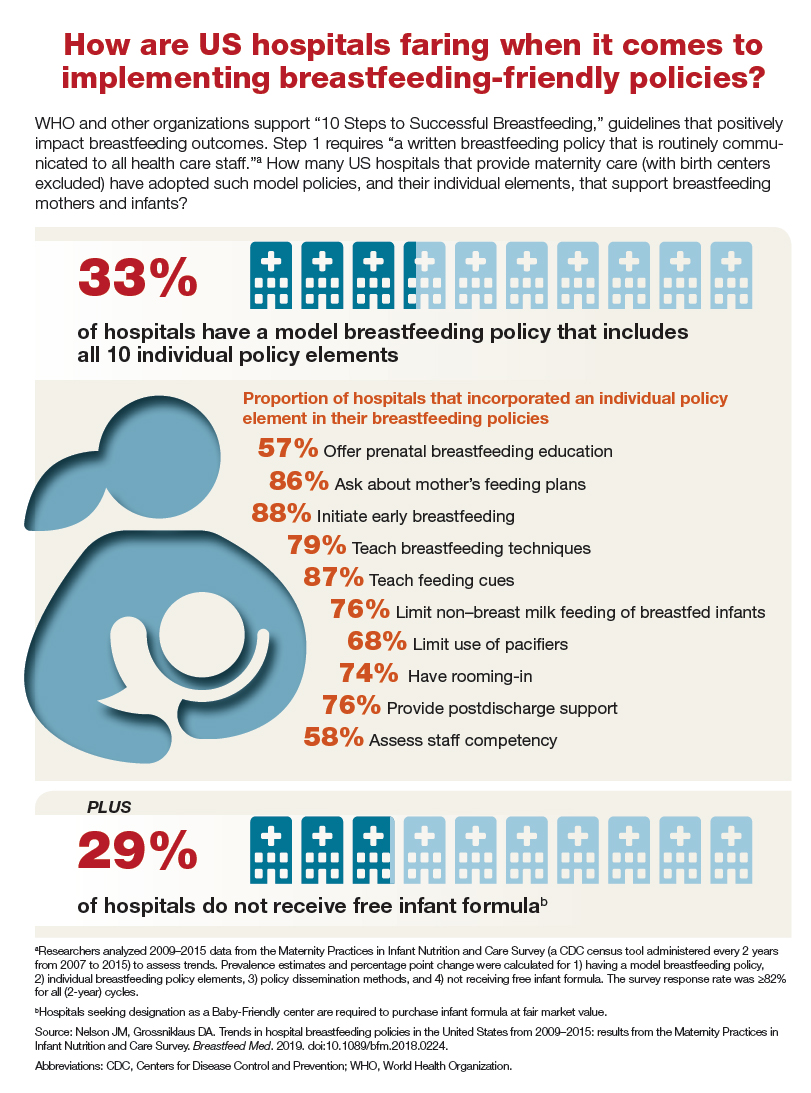
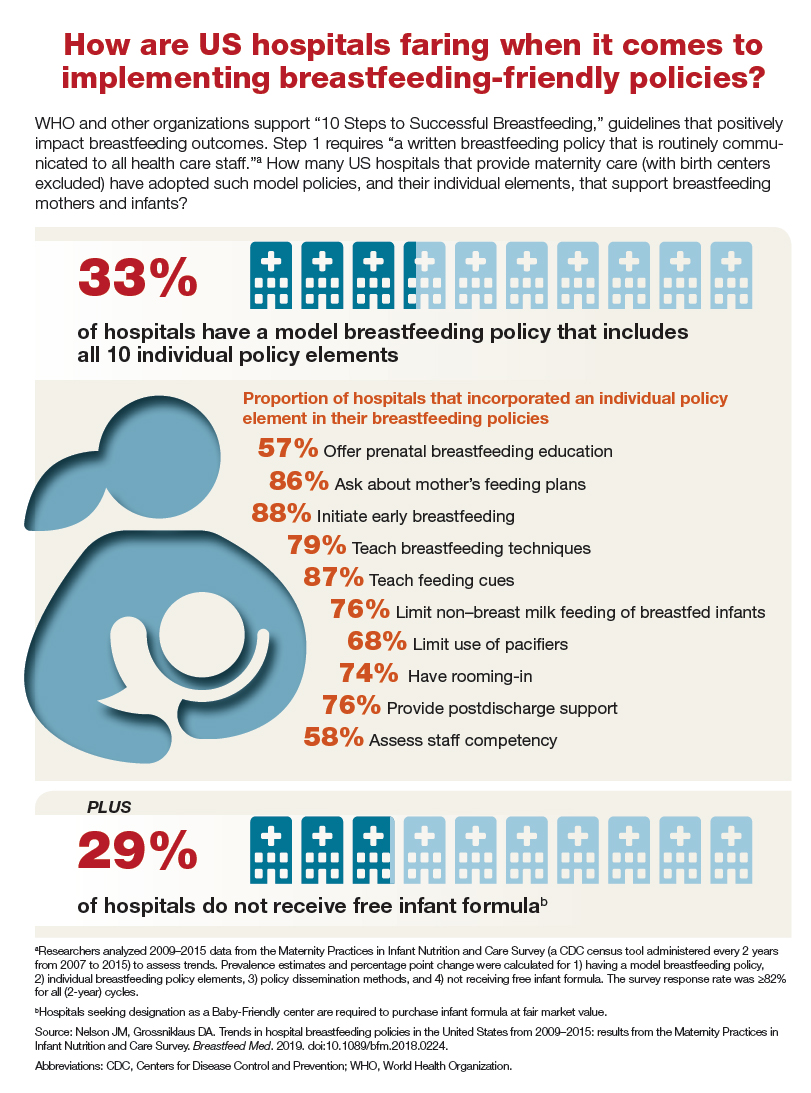
How are US hospitals faring when it comes to implementing breastfeeding-friendly policies?
Endo fellows report lack of confidence in managing some after-hour calls
LOS ANGELES – When it comes to handling after-hours phone calls from patients, endocrinology fellows generally have less confidence in their decision making than their supervising faculty have in them, as measured by faculty’s reported agreement with fellows’ management plans. In addition, their confidence varies widely depending on the reason for call, results from a small, single-center study suggest.
“The research on training in telephone medicine is sparse,” lead study author Ramya Punati, MD, said in an interview in advance of the annual scientific and clinical congress of the American Association of Clinical Endocrinologists. “Our field relies on blood sugars and patient monitoring at home. We get a large volume of such calls, so while supervising faculty are always available for questions overnight, I think it would be useful to have a formal curriculum or feedback process in place at all major medical centers for fellows to learn how to appropriately manage outpatient calls.”
In October 2018, 6 endocrinology fellows and 13 endocrinology faculty members at the Hospital of the University of Pennsylvania, Philadelphia, completed baseline surveys. Fellows were asked how often they felt confident on after-hours calls managing specific conditions, such as problems with insulin pumps, positive ketones, and hyperglycemia and hypoglycemia. Faculty were asked how often they agreed with the fellows’ management of the same conditions.
One month later, the researchers implemented a two-part intervention. Part one consisted of a 1-hour didactic session for the six fellows about how to handle common outpatient diabetes-related calls. Part two involved a process by which faculty gave feedback through the EMR on decisions that fellows make on after-hours calls. Assistance provided in real time by supervising faculty was not measured.
In April 2019, the researchers used the same surveys to reassess the fellows’ and the faculty’s confidence. In addition, “pre- and postintervention, fellows were asked two questions to reflect on the perceived utility of taking outpatient calls,” said Dr. Punati, who is an endocrinology fellow at the Hospital of the University of Pennsylvania. “One was, ‘Do you feel that taking outpatient calls allows you to impact patient care in a meaningful way?’ The other was, ‘Do you feel that taking after-hours calls is educational for you?’ ”
At baseline, all fellows reported that they rarely received feedback from outpatient faculty on decisions they make on after-hours calls. Following implementation of the intervention, most fellows reported a slight increase in the feedback received. Pre- and postintervention, most fellows said that they were able to affect care in a meaningful way by handling after-hours calls, but felt that taking such calls had more limited educational value.
She and her colleagues found that faculty confidence in after-hour decision making by endocrine fellows is generally higher than fellows’ reported confidence in the same domains. At baseline, both faculty and fellows had highest confidence in the ability of fellows to manage calls related to fluctuations in blood glucose, and both groups had lowest ratings in management of insulin pump problems and diabetic ketoacidosis. After the intervention, both fellows and faculty had increased confidence in the ability of fellows to manage all types of calls, compared with baseline.
“It’s hard to say how much of the improvement is due to the intervention versus the passage of time and experience,” Dr. Punati said. “By the nature of taking more calls and getting more experience, fellows are going to get more confident as the year goes on.”
Fellows’ responses about their confidence in handling after-hours calls and their perception of the educational value of that responsibility highlight the need for a more formalized curriculum in telephone medicine and feedback process, she said.
Dr. Punati recommends a combination of didactic instruction early in endocrinology fellowship training and ongoing feedback for decisions that fellows make during after-hours calls.
“That process of feedback is the only way fellows will improve their knowledge and their confidence in handling these calls,” she said. In fact, as a result of the study, the university’s endocrinology fellowship program has already implemented changes in the academic curriculum to enhance the fellows’ educational experience and provide them with tools they need to confidently manage these calls.
Dr. Punati reported having no financial disclosures.
LOS ANGELES – When it comes to handling after-hours phone calls from patients, endocrinology fellows generally have less confidence in their decision making than their supervising faculty have in them, as measured by faculty’s reported agreement with fellows’ management plans. In addition, their confidence varies widely depending on the reason for call, results from a small, single-center study suggest.
“The research on training in telephone medicine is sparse,” lead study author Ramya Punati, MD, said in an interview in advance of the annual scientific and clinical congress of the American Association of Clinical Endocrinologists. “Our field relies on blood sugars and patient monitoring at home. We get a large volume of such calls, so while supervising faculty are always available for questions overnight, I think it would be useful to have a formal curriculum or feedback process in place at all major medical centers for fellows to learn how to appropriately manage outpatient calls.”
In October 2018, 6 endocrinology fellows and 13 endocrinology faculty members at the Hospital of the University of Pennsylvania, Philadelphia, completed baseline surveys. Fellows were asked how often they felt confident on after-hours calls managing specific conditions, such as problems with insulin pumps, positive ketones, and hyperglycemia and hypoglycemia. Faculty were asked how often they agreed with the fellows’ management of the same conditions.
One month later, the researchers implemented a two-part intervention. Part one consisted of a 1-hour didactic session for the six fellows about how to handle common outpatient diabetes-related calls. Part two involved a process by which faculty gave feedback through the EMR on decisions that fellows make on after-hours calls. Assistance provided in real time by supervising faculty was not measured.
In April 2019, the researchers used the same surveys to reassess the fellows’ and the faculty’s confidence. In addition, “pre- and postintervention, fellows were asked two questions to reflect on the perceived utility of taking outpatient calls,” said Dr. Punati, who is an endocrinology fellow at the Hospital of the University of Pennsylvania. “One was, ‘Do you feel that taking outpatient calls allows you to impact patient care in a meaningful way?’ The other was, ‘Do you feel that taking after-hours calls is educational for you?’ ”
At baseline, all fellows reported that they rarely received feedback from outpatient faculty on decisions they make on after-hours calls. Following implementation of the intervention, most fellows reported a slight increase in the feedback received. Pre- and postintervention, most fellows said that they were able to affect care in a meaningful way by handling after-hours calls, but felt that taking such calls had more limited educational value.
She and her colleagues found that faculty confidence in after-hour decision making by endocrine fellows is generally higher than fellows’ reported confidence in the same domains. At baseline, both faculty and fellows had highest confidence in the ability of fellows to manage calls related to fluctuations in blood glucose, and both groups had lowest ratings in management of insulin pump problems and diabetic ketoacidosis. After the intervention, both fellows and faculty had increased confidence in the ability of fellows to manage all types of calls, compared with baseline.
“It’s hard to say how much of the improvement is due to the intervention versus the passage of time and experience,” Dr. Punati said. “By the nature of taking more calls and getting more experience, fellows are going to get more confident as the year goes on.”
Fellows’ responses about their confidence in handling after-hours calls and their perception of the educational value of that responsibility highlight the need for a more formalized curriculum in telephone medicine and feedback process, she said.
Dr. Punati recommends a combination of didactic instruction early in endocrinology fellowship training and ongoing feedback for decisions that fellows make during after-hours calls.
“That process of feedback is the only way fellows will improve their knowledge and their confidence in handling these calls,” she said. In fact, as a result of the study, the university’s endocrinology fellowship program has already implemented changes in the academic curriculum to enhance the fellows’ educational experience and provide them with tools they need to confidently manage these calls.
Dr. Punati reported having no financial disclosures.
LOS ANGELES – When it comes to handling after-hours phone calls from patients, endocrinology fellows generally have less confidence in their decision making than their supervising faculty have in them, as measured by faculty’s reported agreement with fellows’ management plans. In addition, their confidence varies widely depending on the reason for call, results from a small, single-center study suggest.
“The research on training in telephone medicine is sparse,” lead study author Ramya Punati, MD, said in an interview in advance of the annual scientific and clinical congress of the American Association of Clinical Endocrinologists. “Our field relies on blood sugars and patient monitoring at home. We get a large volume of such calls, so while supervising faculty are always available for questions overnight, I think it would be useful to have a formal curriculum or feedback process in place at all major medical centers for fellows to learn how to appropriately manage outpatient calls.”
In October 2018, 6 endocrinology fellows and 13 endocrinology faculty members at the Hospital of the University of Pennsylvania, Philadelphia, completed baseline surveys. Fellows were asked how often they felt confident on after-hours calls managing specific conditions, such as problems with insulin pumps, positive ketones, and hyperglycemia and hypoglycemia. Faculty were asked how often they agreed with the fellows’ management of the same conditions.
One month later, the researchers implemented a two-part intervention. Part one consisted of a 1-hour didactic session for the six fellows about how to handle common outpatient diabetes-related calls. Part two involved a process by which faculty gave feedback through the EMR on decisions that fellows make on after-hours calls. Assistance provided in real time by supervising faculty was not measured.
In April 2019, the researchers used the same surveys to reassess the fellows’ and the faculty’s confidence. In addition, “pre- and postintervention, fellows were asked two questions to reflect on the perceived utility of taking outpatient calls,” said Dr. Punati, who is an endocrinology fellow at the Hospital of the University of Pennsylvania. “One was, ‘Do you feel that taking outpatient calls allows you to impact patient care in a meaningful way?’ The other was, ‘Do you feel that taking after-hours calls is educational for you?’ ”
At baseline, all fellows reported that they rarely received feedback from outpatient faculty on decisions they make on after-hours calls. Following implementation of the intervention, most fellows reported a slight increase in the feedback received. Pre- and postintervention, most fellows said that they were able to affect care in a meaningful way by handling after-hours calls, but felt that taking such calls had more limited educational value.
She and her colleagues found that faculty confidence in after-hour decision making by endocrine fellows is generally higher than fellows’ reported confidence in the same domains. At baseline, both faculty and fellows had highest confidence in the ability of fellows to manage calls related to fluctuations in blood glucose, and both groups had lowest ratings in management of insulin pump problems and diabetic ketoacidosis. After the intervention, both fellows and faculty had increased confidence in the ability of fellows to manage all types of calls, compared with baseline.
“It’s hard to say how much of the improvement is due to the intervention versus the passage of time and experience,” Dr. Punati said. “By the nature of taking more calls and getting more experience, fellows are going to get more confident as the year goes on.”
Fellows’ responses about their confidence in handling after-hours calls and their perception of the educational value of that responsibility highlight the need for a more formalized curriculum in telephone medicine and feedback process, she said.
Dr. Punati recommends a combination of didactic instruction early in endocrinology fellowship training and ongoing feedback for decisions that fellows make during after-hours calls.
“That process of feedback is the only way fellows will improve their knowledge and their confidence in handling these calls,” she said. In fact, as a result of the study, the university’s endocrinology fellowship program has already implemented changes in the academic curriculum to enhance the fellows’ educational experience and provide them with tools they need to confidently manage these calls.
Dr. Punati reported having no financial disclosures.
REPORTING FROM AACE 2019
Key clinical point:
Major finding: Before and after intervention, most fellows said that they were able to affect care in a meaningful way by handling after-hours calls, but felt that taking such calls had more limited educational value.
Study details: A survey of 6 endocrinology fellows and 13 endocrinology faculty members at the Hospital of the University of Pennsylvania, Philadelphia.
Disclosures: Dr. Punati reported having no financial disclosures.
New adventures of an old device: Clinic delivers cortisol via the insulin pump
LOS ANGELES – The venerable insulin pump is being repurposed: A Detroit-area endocrinology
“We’ve seen amazing results,” said endocrinologist Opada Alzohaili, MD, MBA, of Wayne State University, Detroit, coauthor of a study released at the annual scientific and clinical congress of the American Association of Clinical Endocrinologists.
Dr. Alzohaili said he and his colleagues developed the approach to manage patients who are “so sick that they go to the hospital 10-12 times a year.” Oral medication just did not control their disorder.
“Most of the time, we end up way overdosing them [on oral medication] just to prevent them from going to the hospital in adrenal crisis,” he said in an interview.
Dr. Alzohaili said his clinic has tested delivering hydrocortisone via insulin pump in about 20 patients. The report presented at the conference focused on six patients who had failed oral hydrocortisone treatment for adrenal insufficiency. Testing showed that all had malabsorption of the drug.
The patients underwent training in how to use and adjust the pump, which allows dosing adjustments in increments of 1 mg. They learned how to adjust their doses based on their situation, Dr. Alzohaili said.
According to the report, the average number of adrenal crises in the patients over a 6-month period fell from a mean of 2.3 before baseline to 0.5 after treatment began. The maximum dose of hydrocortisone dose fell by 38%, while the average mean weight of patients rose from 182 pounds to 199 pounds.
In addition, the mean dose of hydrocortisone decreased with the use of the pump delivery system, from 85.8 mg with oral treatment to 32.4 mg on pump therapy, and the mean level of cortisol increased from 11.8 mcg/dL with oral treatment to 12.3 mcg/dL on pump therapy.
The researchers said that the pump provides better delivery of the medication compared with the oral route, and that the patients experienced fewer interactions with other medications.
Some patients developed skin reactions to the pump, but those adverse events were resolved by changing the pump’s location on the body and by using hypoallergenic needles, Dr. Alzohaili said.
There were fewer cases of clogging with the pumps than is normally seen when they’re used with insulin, he added.
As for expense, Dr. Alzohaili said the pumps cost thousands of dollars and supplies can cost between $100 and $150 a month. In the first couple of cases, patients paid for the treatment themselves, he said, but in later cases, insurers were willing to pay for the treatment once they learned about the results.
Other researchers have successfully used insulin pumps to deliver hydrocortisone to small numbers of patients with adrenal insufficiency, including British and U.S. teams that reported positive results in 2015 and 2018, respectively.
The next step, Dr. Alzohaili said, is to attract the interest of insulin pump manufacturers by using the treatment in more patients. “I’ve spoken to CEOs, but none of them is interested in using cortisol in their pumps,” he said. “If you don’t have the company supporting the research, it becomes difficult for it to become standard of care. So I’m trying to build awareness [of its use] and the number of patients [who use the pump].”
Dr. Alzohaili reported no financial conflicts of interest or disclosures.
LOS ANGELES – The venerable insulin pump is being repurposed: A Detroit-area endocrinology
“We’ve seen amazing results,” said endocrinologist Opada Alzohaili, MD, MBA, of Wayne State University, Detroit, coauthor of a study released at the annual scientific and clinical congress of the American Association of Clinical Endocrinologists.
Dr. Alzohaili said he and his colleagues developed the approach to manage patients who are “so sick that they go to the hospital 10-12 times a year.” Oral medication just did not control their disorder.
“Most of the time, we end up way overdosing them [on oral medication] just to prevent them from going to the hospital in adrenal crisis,” he said in an interview.
Dr. Alzohaili said his clinic has tested delivering hydrocortisone via insulin pump in about 20 patients. The report presented at the conference focused on six patients who had failed oral hydrocortisone treatment for adrenal insufficiency. Testing showed that all had malabsorption of the drug.
The patients underwent training in how to use and adjust the pump, which allows dosing adjustments in increments of 1 mg. They learned how to adjust their doses based on their situation, Dr. Alzohaili said.
According to the report, the average number of adrenal crises in the patients over a 6-month period fell from a mean of 2.3 before baseline to 0.5 after treatment began. The maximum dose of hydrocortisone dose fell by 38%, while the average mean weight of patients rose from 182 pounds to 199 pounds.
In addition, the mean dose of hydrocortisone decreased with the use of the pump delivery system, from 85.8 mg with oral treatment to 32.4 mg on pump therapy, and the mean level of cortisol increased from 11.8 mcg/dL with oral treatment to 12.3 mcg/dL on pump therapy.
The researchers said that the pump provides better delivery of the medication compared with the oral route, and that the patients experienced fewer interactions with other medications.
Some patients developed skin reactions to the pump, but those adverse events were resolved by changing the pump’s location on the body and by using hypoallergenic needles, Dr. Alzohaili said.
There were fewer cases of clogging with the pumps than is normally seen when they’re used with insulin, he added.
As for expense, Dr. Alzohaili said the pumps cost thousands of dollars and supplies can cost between $100 and $150 a month. In the first couple of cases, patients paid for the treatment themselves, he said, but in later cases, insurers were willing to pay for the treatment once they learned about the results.
Other researchers have successfully used insulin pumps to deliver hydrocortisone to small numbers of patients with adrenal insufficiency, including British and U.S. teams that reported positive results in 2015 and 2018, respectively.
The next step, Dr. Alzohaili said, is to attract the interest of insulin pump manufacturers by using the treatment in more patients. “I’ve spoken to CEOs, but none of them is interested in using cortisol in their pumps,” he said. “If you don’t have the company supporting the research, it becomes difficult for it to become standard of care. So I’m trying to build awareness [of its use] and the number of patients [who use the pump].”
Dr. Alzohaili reported no financial conflicts of interest or disclosures.
LOS ANGELES – The venerable insulin pump is being repurposed: A Detroit-area endocrinology
“We’ve seen amazing results,” said endocrinologist Opada Alzohaili, MD, MBA, of Wayne State University, Detroit, coauthor of a study released at the annual scientific and clinical congress of the American Association of Clinical Endocrinologists.
Dr. Alzohaili said he and his colleagues developed the approach to manage patients who are “so sick that they go to the hospital 10-12 times a year.” Oral medication just did not control their disorder.
“Most of the time, we end up way overdosing them [on oral medication] just to prevent them from going to the hospital in adrenal crisis,” he said in an interview.
Dr. Alzohaili said his clinic has tested delivering hydrocortisone via insulin pump in about 20 patients. The report presented at the conference focused on six patients who had failed oral hydrocortisone treatment for adrenal insufficiency. Testing showed that all had malabsorption of the drug.
The patients underwent training in how to use and adjust the pump, which allows dosing adjustments in increments of 1 mg. They learned how to adjust their doses based on their situation, Dr. Alzohaili said.
According to the report, the average number of adrenal crises in the patients over a 6-month period fell from a mean of 2.3 before baseline to 0.5 after treatment began. The maximum dose of hydrocortisone dose fell by 38%, while the average mean weight of patients rose from 182 pounds to 199 pounds.
In addition, the mean dose of hydrocortisone decreased with the use of the pump delivery system, from 85.8 mg with oral treatment to 32.4 mg on pump therapy, and the mean level of cortisol increased from 11.8 mcg/dL with oral treatment to 12.3 mcg/dL on pump therapy.
The researchers said that the pump provides better delivery of the medication compared with the oral route, and that the patients experienced fewer interactions with other medications.
Some patients developed skin reactions to the pump, but those adverse events were resolved by changing the pump’s location on the body and by using hypoallergenic needles, Dr. Alzohaili said.
There were fewer cases of clogging with the pumps than is normally seen when they’re used with insulin, he added.
As for expense, Dr. Alzohaili said the pumps cost thousands of dollars and supplies can cost between $100 and $150 a month. In the first couple of cases, patients paid for the treatment themselves, he said, but in later cases, insurers were willing to pay for the treatment once they learned about the results.
Other researchers have successfully used insulin pumps to deliver hydrocortisone to small numbers of patients with adrenal insufficiency, including British and U.S. teams that reported positive results in 2015 and 2018, respectively.
The next step, Dr. Alzohaili said, is to attract the interest of insulin pump manufacturers by using the treatment in more patients. “I’ve spoken to CEOs, but none of them is interested in using cortisol in their pumps,” he said. “If you don’t have the company supporting the research, it becomes difficult for it to become standard of care. So I’m trying to build awareness [of its use] and the number of patients [who use the pump].”
Dr. Alzohaili reported no financial conflicts of interest or disclosures.
REPORTING FROM AACE 2019
FDA approves T-DM1 as adjuvant treatment
The Food and Drug Administration has approved the antibody-drug conjugate trastuzumab emtansine (T-DM1) for adjuvant treatment of patients with HER2-positive early breast cancer who have residual invasive disease after neoadjuvant treatment with a taxane and trastuzumab (Herceptin).
Approval of adjuvant T-DM1, marketed as Kadcyla, was based on a reduced risk of breast cancer recurrence or death in the phase 3 KATHERINE trial. In KATHERINE, over 1,400 patients with HER2-positive early breast cancer who had residual invasive disease after neoadjuvant taxane and trastuzumab-based treatment were randomized to adjuvant therapy with T-DM1 or trastuzumab. The 3-year invasive disease-free survival rate was 88.3% for those taking T-DM1, compared with 77.0% for patients assigned to adjuvant trastuzumab (hazard ratio, 0.50; 95% confidence interval, 0.39-0.64; P less than .0001). Results of KATHERINE were presented at the 2018 San Antonio Breast Cancer Symposium and simultaneously published in the New England Journal of Medicine.
The most common grade 3 or greater adverse events for those in the T-DM1 arm included decreased platelet count in 5.7% and hypertension in 2.0%. The most common side effects with T-DM1 were fatigue, nausea, increased blood levels of liver enzymes, musculoskeletal pain, bleeding, decreased platelet count, headache, numbness in the hands or feet, and joint pain.
T-DM1 was previously approved to treat metastatic HER2-positive breast cancer after prior treatment with trastuzumab and a taxane.
“This approval is a significant treatment advance for HER2-positive early breast cancer. By working closely with the FDA and participating in the Real-Time Oncology Review pilot program, we are able to make Kadcyla available for people with residual invasive disease after neoadjuvant therapy much sooner than anticipated,” said Sandra Horning, MD, chief medical officer and head of global product development at Genentech (Roche), the developer of T-DM1, in a press release announcing the current approval.
The Food and Drug Administration has approved the antibody-drug conjugate trastuzumab emtansine (T-DM1) for adjuvant treatment of patients with HER2-positive early breast cancer who have residual invasive disease after neoadjuvant treatment with a taxane and trastuzumab (Herceptin).
Approval of adjuvant T-DM1, marketed as Kadcyla, was based on a reduced risk of breast cancer recurrence or death in the phase 3 KATHERINE trial. In KATHERINE, over 1,400 patients with HER2-positive early breast cancer who had residual invasive disease after neoadjuvant taxane and trastuzumab-based treatment were randomized to adjuvant therapy with T-DM1 or trastuzumab. The 3-year invasive disease-free survival rate was 88.3% for those taking T-DM1, compared with 77.0% for patients assigned to adjuvant trastuzumab (hazard ratio, 0.50; 95% confidence interval, 0.39-0.64; P less than .0001). Results of KATHERINE were presented at the 2018 San Antonio Breast Cancer Symposium and simultaneously published in the New England Journal of Medicine.
The most common grade 3 or greater adverse events for those in the T-DM1 arm included decreased platelet count in 5.7% and hypertension in 2.0%. The most common side effects with T-DM1 were fatigue, nausea, increased blood levels of liver enzymes, musculoskeletal pain, bleeding, decreased platelet count, headache, numbness in the hands or feet, and joint pain.
T-DM1 was previously approved to treat metastatic HER2-positive breast cancer after prior treatment with trastuzumab and a taxane.
“This approval is a significant treatment advance for HER2-positive early breast cancer. By working closely with the FDA and participating in the Real-Time Oncology Review pilot program, we are able to make Kadcyla available for people with residual invasive disease after neoadjuvant therapy much sooner than anticipated,” said Sandra Horning, MD, chief medical officer and head of global product development at Genentech (Roche), the developer of T-DM1, in a press release announcing the current approval.
The Food and Drug Administration has approved the antibody-drug conjugate trastuzumab emtansine (T-DM1) for adjuvant treatment of patients with HER2-positive early breast cancer who have residual invasive disease after neoadjuvant treatment with a taxane and trastuzumab (Herceptin).
Approval of adjuvant T-DM1, marketed as Kadcyla, was based on a reduced risk of breast cancer recurrence or death in the phase 3 KATHERINE trial. In KATHERINE, over 1,400 patients with HER2-positive early breast cancer who had residual invasive disease after neoadjuvant taxane and trastuzumab-based treatment were randomized to adjuvant therapy with T-DM1 or trastuzumab. The 3-year invasive disease-free survival rate was 88.3% for those taking T-DM1, compared with 77.0% for patients assigned to adjuvant trastuzumab (hazard ratio, 0.50; 95% confidence interval, 0.39-0.64; P less than .0001). Results of KATHERINE were presented at the 2018 San Antonio Breast Cancer Symposium and simultaneously published in the New England Journal of Medicine.
The most common grade 3 or greater adverse events for those in the T-DM1 arm included decreased platelet count in 5.7% and hypertension in 2.0%. The most common side effects with T-DM1 were fatigue, nausea, increased blood levels of liver enzymes, musculoskeletal pain, bleeding, decreased platelet count, headache, numbness in the hands or feet, and joint pain.
T-DM1 was previously approved to treat metastatic HER2-positive breast cancer after prior treatment with trastuzumab and a taxane.
“This approval is a significant treatment advance for HER2-positive early breast cancer. By working closely with the FDA and participating in the Real-Time Oncology Review pilot program, we are able to make Kadcyla available for people with residual invasive disease after neoadjuvant therapy much sooner than anticipated,” said Sandra Horning, MD, chief medical officer and head of global product development at Genentech (Roche), the developer of T-DM1, in a press release announcing the current approval.
Restroom, locker room restrictions foster abuse of transgender teens
Transgender youth with restricted restroom and locker room use at school were significantly more likely to experience sexual assault at school than those without such restrictions, based on surveys from more than 3,000 teens in the United States who identified as transgender or nonbinary.
“Little is known about risk factors for sexual assault in gender minority adolescents, but school policies and practices play an important role in other forms of victimization,” including restricting transgender students from using restrooms or locker rooms that match their gender identities, wrote Gabriel R. Murchison, MPH, of Harvard University, Boston, Mass., and colleagues in Pediatrics (2019 May 6. doi: https://doi.org/10.1542/peds.2018-2902).
To examine the relationship between school restroom/locker room policies and sexual assault on transgender teens, the researchers reviewed data from the Lesbian, Gay, Bisexual, Transgender, and Queer or Questioning (LGBTQ) Teen Study, an anonymous web-based survey of U.S. adolescents aged 13 to 17 years who could read and write in English. Participants were assigned to one of four gender groups: trans male, trans female, nonbinary who were assigned male at birth (AMAB), or nonbinary who were assigned female at birth (AFAB) based on the survey questions asking their sex assigned at birth and current gender identity. The final study population of 3,673 individuals included 1,359 boys and 1,947 nonbinary youth AFAB and 158 transgender girls and 209 nonbinary youth AMAB. The results were published in Pediatrics.
with risk ratios of 1.26 for transgender boys and 2.49 for transgender girls, and 1.42 for nonbinary AFAB youth. Restroom/locker room restrictions were not significantly associated with sexual abuse in nonbinary AMAB youth.
The 12-month prevalence of sexual assault was highest among nonbinary youth AFAB (27%), followed by 26.5% among transgender boys, 18.5% among transgender girls, and 17.6% among nonbinary youth AMAB.
Sexual assault was determined based on participants’ response to the question, “During the past 12 months, how many times did anyone force you to do sexual things that you did not want to do? (Count such things as kissing, touching, or being physically forced to have sexual intercourse.)” The researchers adjusted for multiple factors associated with adolescent sexual assault including alcohol use, family connectedness, and educational attainment of caregivers; as well as variables including exposure to antitransgender stigma and perception of teacher support at school.
The researchers also identified four mediating variables: sexual harassment, feeling safe in restrooms and locker rooms, feeling safe in other locations at school, and classmates’ knowledge of gender status.
“Significant indirect effects were present for all 4 mediating variables,” which included feel safe in restrooms and locker rooms, feel safe elsewhere in school, classmates know gender minority status, and sexual harassment. The fourth mediating variable mentioned fully explains “the association between restroom and locker room restrictions and sexual assault victimization,” the researchers wrote.
The findings were limited by several factors including the lack of racial diversity and the reliance on cross-sectional, nonprobability data, the researchers said.
However, the results are strengthened by the large sample size and suggest that avoiding restrictive policies at school can make a difference in reducing abuse of transgender teens, they wrote.
“From a prevention perspective, pediatricians are key advocates for transgender and nonbinary patients, and their role may include educating school officials and submitting letters confirming the patient’s need to express their gender identity,” that emphasize the importance of “safe, identity-congruent restrooms and locker rooms,” the researchers concluded.
The study was supported in part by the Office of Vice President for Research at the University of Connecticut, and the Human Rights Campaign Foundation provided in-kind support for the LGBTQ Teen Study. Mr. Murchison disclosed participation in survey development and data collection for the LGBTQ Teen Study as an employee of the Human Rights Campaign Foundation.
SOURCE: Murchison G et al. Pediatrics . 2019 May 6. doi: https://doi.org/10.1542/peds.2018-2902 .
The study findings “make a compelling case for what we as gender specialist providers witness every day in our work: failure to support transgender and gender-expansive youth in being able to fully live in their affirmed gender puts them at physical as well as psychological risk,” wrote Diane Ehrensaft, PhD, and Stephen M. Rosenthal, MD, in an accompanying editorial.
What can reduce the risk of these youth experiencing abuse and assault, according to the editorialists, is putting policies in place that support them. Dr. Ehrensaft and Dr. Rosenthal cited the state of California’s 2013 decision to allow all students in public schools, from kindergarten through 12th grade “the right to use the bathroom and locker room consistent with their affirmed gender identity” as an example of something pediatricians should be advocating for in other states.
Restrictions on bathroom use to their assigned birth identity may cause transgender youth to be at increased risk for verbal and physical harassment and abuse, they said. It may also lead some to avoid restroom use and increase their risk for urinary tract infections, impacted stool, and school avoidance, the editorialists noted. They added that “[such] policies are often fear based, with nontransgender students thought to be the ones at risk for sexual assault by transgender intruders, by anyone whose genitalia does not match the one associated with the sign on the door, or by predators posing as transgender students.” The editorialists noted that these attitudes can come from school personnel or parents and that pediatricians should be aware of “the high prevalence of sexual assault” on transgender and gender nonbinary youth” (Pediatrics. 2019 May 6. doi: 10.1542/peds.2019-0554).
Dr. Ehrensaft and Dr. Rosenthal are affiliated with the Benioff Children’s Hospital at the University of California, San Francisco. They had no financial conflicts to disclose.
The study findings “make a compelling case for what we as gender specialist providers witness every day in our work: failure to support transgender and gender-expansive youth in being able to fully live in their affirmed gender puts them at physical as well as psychological risk,” wrote Diane Ehrensaft, PhD, and Stephen M. Rosenthal, MD, in an accompanying editorial.
What can reduce the risk of these youth experiencing abuse and assault, according to the editorialists, is putting policies in place that support them. Dr. Ehrensaft and Dr. Rosenthal cited the state of California’s 2013 decision to allow all students in public schools, from kindergarten through 12th grade “the right to use the bathroom and locker room consistent with their affirmed gender identity” as an example of something pediatricians should be advocating for in other states.
Restrictions on bathroom use to their assigned birth identity may cause transgender youth to be at increased risk for verbal and physical harassment and abuse, they said. It may also lead some to avoid restroom use and increase their risk for urinary tract infections, impacted stool, and school avoidance, the editorialists noted. They added that “[such] policies are often fear based, with nontransgender students thought to be the ones at risk for sexual assault by transgender intruders, by anyone whose genitalia does not match the one associated with the sign on the door, or by predators posing as transgender students.” The editorialists noted that these attitudes can come from school personnel or parents and that pediatricians should be aware of “the high prevalence of sexual assault” on transgender and gender nonbinary youth” (Pediatrics. 2019 May 6. doi: 10.1542/peds.2019-0554).
Dr. Ehrensaft and Dr. Rosenthal are affiliated with the Benioff Children’s Hospital at the University of California, San Francisco. They had no financial conflicts to disclose.
The study findings “make a compelling case for what we as gender specialist providers witness every day in our work: failure to support transgender and gender-expansive youth in being able to fully live in their affirmed gender puts them at physical as well as psychological risk,” wrote Diane Ehrensaft, PhD, and Stephen M. Rosenthal, MD, in an accompanying editorial.
What can reduce the risk of these youth experiencing abuse and assault, according to the editorialists, is putting policies in place that support them. Dr. Ehrensaft and Dr. Rosenthal cited the state of California’s 2013 decision to allow all students in public schools, from kindergarten through 12th grade “the right to use the bathroom and locker room consistent with their affirmed gender identity” as an example of something pediatricians should be advocating for in other states.
Restrictions on bathroom use to their assigned birth identity may cause transgender youth to be at increased risk for verbal and physical harassment and abuse, they said. It may also lead some to avoid restroom use and increase their risk for urinary tract infections, impacted stool, and school avoidance, the editorialists noted. They added that “[such] policies are often fear based, with nontransgender students thought to be the ones at risk for sexual assault by transgender intruders, by anyone whose genitalia does not match the one associated with the sign on the door, or by predators posing as transgender students.” The editorialists noted that these attitudes can come from school personnel or parents and that pediatricians should be aware of “the high prevalence of sexual assault” on transgender and gender nonbinary youth” (Pediatrics. 2019 May 6. doi: 10.1542/peds.2019-0554).
Dr. Ehrensaft and Dr. Rosenthal are affiliated with the Benioff Children’s Hospital at the University of California, San Francisco. They had no financial conflicts to disclose.
Transgender youth with restricted restroom and locker room use at school were significantly more likely to experience sexual assault at school than those without such restrictions, based on surveys from more than 3,000 teens in the United States who identified as transgender or nonbinary.
“Little is known about risk factors for sexual assault in gender minority adolescents, but school policies and practices play an important role in other forms of victimization,” including restricting transgender students from using restrooms or locker rooms that match their gender identities, wrote Gabriel R. Murchison, MPH, of Harvard University, Boston, Mass., and colleagues in Pediatrics (2019 May 6. doi: https://doi.org/10.1542/peds.2018-2902).
To examine the relationship between school restroom/locker room policies and sexual assault on transgender teens, the researchers reviewed data from the Lesbian, Gay, Bisexual, Transgender, and Queer or Questioning (LGBTQ) Teen Study, an anonymous web-based survey of U.S. adolescents aged 13 to 17 years who could read and write in English. Participants were assigned to one of four gender groups: trans male, trans female, nonbinary who were assigned male at birth (AMAB), or nonbinary who were assigned female at birth (AFAB) based on the survey questions asking their sex assigned at birth and current gender identity. The final study population of 3,673 individuals included 1,359 boys and 1,947 nonbinary youth AFAB and 158 transgender girls and 209 nonbinary youth AMAB. The results were published in Pediatrics.
with risk ratios of 1.26 for transgender boys and 2.49 for transgender girls, and 1.42 for nonbinary AFAB youth. Restroom/locker room restrictions were not significantly associated with sexual abuse in nonbinary AMAB youth.
The 12-month prevalence of sexual assault was highest among nonbinary youth AFAB (27%), followed by 26.5% among transgender boys, 18.5% among transgender girls, and 17.6% among nonbinary youth AMAB.
Sexual assault was determined based on participants’ response to the question, “During the past 12 months, how many times did anyone force you to do sexual things that you did not want to do? (Count such things as kissing, touching, or being physically forced to have sexual intercourse.)” The researchers adjusted for multiple factors associated with adolescent sexual assault including alcohol use, family connectedness, and educational attainment of caregivers; as well as variables including exposure to antitransgender stigma and perception of teacher support at school.
The researchers also identified four mediating variables: sexual harassment, feeling safe in restrooms and locker rooms, feeling safe in other locations at school, and classmates’ knowledge of gender status.
“Significant indirect effects were present for all 4 mediating variables,” which included feel safe in restrooms and locker rooms, feel safe elsewhere in school, classmates know gender minority status, and sexual harassment. The fourth mediating variable mentioned fully explains “the association between restroom and locker room restrictions and sexual assault victimization,” the researchers wrote.
The findings were limited by several factors including the lack of racial diversity and the reliance on cross-sectional, nonprobability data, the researchers said.
However, the results are strengthened by the large sample size and suggest that avoiding restrictive policies at school can make a difference in reducing abuse of transgender teens, they wrote.
“From a prevention perspective, pediatricians are key advocates for transgender and nonbinary patients, and their role may include educating school officials and submitting letters confirming the patient’s need to express their gender identity,” that emphasize the importance of “safe, identity-congruent restrooms and locker rooms,” the researchers concluded.
The study was supported in part by the Office of Vice President for Research at the University of Connecticut, and the Human Rights Campaign Foundation provided in-kind support for the LGBTQ Teen Study. Mr. Murchison disclosed participation in survey development and data collection for the LGBTQ Teen Study as an employee of the Human Rights Campaign Foundation.
SOURCE: Murchison G et al. Pediatrics . 2019 May 6. doi: https://doi.org/10.1542/peds.2018-2902 .
Transgender youth with restricted restroom and locker room use at school were significantly more likely to experience sexual assault at school than those without such restrictions, based on surveys from more than 3,000 teens in the United States who identified as transgender or nonbinary.
“Little is known about risk factors for sexual assault in gender minority adolescents, but school policies and practices play an important role in other forms of victimization,” including restricting transgender students from using restrooms or locker rooms that match their gender identities, wrote Gabriel R. Murchison, MPH, of Harvard University, Boston, Mass., and colleagues in Pediatrics (2019 May 6. doi: https://doi.org/10.1542/peds.2018-2902).
To examine the relationship between school restroom/locker room policies and sexual assault on transgender teens, the researchers reviewed data from the Lesbian, Gay, Bisexual, Transgender, and Queer or Questioning (LGBTQ) Teen Study, an anonymous web-based survey of U.S. adolescents aged 13 to 17 years who could read and write in English. Participants were assigned to one of four gender groups: trans male, trans female, nonbinary who were assigned male at birth (AMAB), or nonbinary who were assigned female at birth (AFAB) based on the survey questions asking their sex assigned at birth and current gender identity. The final study population of 3,673 individuals included 1,359 boys and 1,947 nonbinary youth AFAB and 158 transgender girls and 209 nonbinary youth AMAB. The results were published in Pediatrics.
with risk ratios of 1.26 for transgender boys and 2.49 for transgender girls, and 1.42 for nonbinary AFAB youth. Restroom/locker room restrictions were not significantly associated with sexual abuse in nonbinary AMAB youth.
The 12-month prevalence of sexual assault was highest among nonbinary youth AFAB (27%), followed by 26.5% among transgender boys, 18.5% among transgender girls, and 17.6% among nonbinary youth AMAB.
Sexual assault was determined based on participants’ response to the question, “During the past 12 months, how many times did anyone force you to do sexual things that you did not want to do? (Count such things as kissing, touching, or being physically forced to have sexual intercourse.)” The researchers adjusted for multiple factors associated with adolescent sexual assault including alcohol use, family connectedness, and educational attainment of caregivers; as well as variables including exposure to antitransgender stigma and perception of teacher support at school.
The researchers also identified four mediating variables: sexual harassment, feeling safe in restrooms and locker rooms, feeling safe in other locations at school, and classmates’ knowledge of gender status.
“Significant indirect effects were present for all 4 mediating variables,” which included feel safe in restrooms and locker rooms, feel safe elsewhere in school, classmates know gender minority status, and sexual harassment. The fourth mediating variable mentioned fully explains “the association between restroom and locker room restrictions and sexual assault victimization,” the researchers wrote.
The findings were limited by several factors including the lack of racial diversity and the reliance on cross-sectional, nonprobability data, the researchers said.
However, the results are strengthened by the large sample size and suggest that avoiding restrictive policies at school can make a difference in reducing abuse of transgender teens, they wrote.
“From a prevention perspective, pediatricians are key advocates for transgender and nonbinary patients, and their role may include educating school officials and submitting letters confirming the patient’s need to express their gender identity,” that emphasize the importance of “safe, identity-congruent restrooms and locker rooms,” the researchers concluded.
The study was supported in part by the Office of Vice President for Research at the University of Connecticut, and the Human Rights Campaign Foundation provided in-kind support for the LGBTQ Teen Study. Mr. Murchison disclosed participation in survey development and data collection for the LGBTQ Teen Study as an employee of the Human Rights Campaign Foundation.
SOURCE: Murchison G et al. Pediatrics . 2019 May 6. doi: https://doi.org/10.1542/peds.2018-2902 .
FROM PEDIATRICS
Key clinical point: Restrictive restroom and locker room environments in schools promote abuse of transgender teens.
Major finding: Sexual assault was significantly more likely against transgender teens with restroom and locker room restrictions vs those without restrictions, with risk ratios of 1.26 for transgender boys and 2.49 for transgender girls.
Study details: The data came from web-based surveys of 3,673 teens aged 13 to 17 years who identified as transgender or nonbinary.
Disclosures: The study was supported in part by the Office of Vice President for Research at the University of Connecticut, and the Human Rights Campaign Foundation provided in-kind support for the LGBTQ Teen Study. Mr. Murchison disclosed participation in survey development and data collection for the LGBTQ Teen Study as an employee of the Human Rights Campaign Foundation.
Source: Murchison G et al. Pediatrics. 2019 May 6. doi: https://doi.org/10.1542/peds.2018-2902
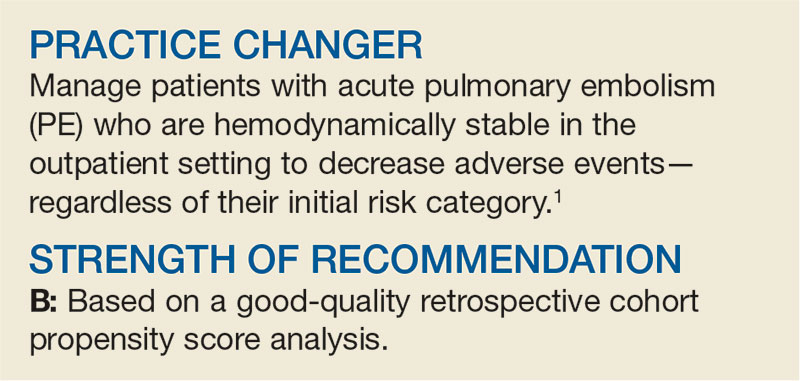
What’s the Best Treatment Setting for Stable Pulmonary Embolism?
A 63-year-old woman with a history of hypertension presents to the emergency department (ED) with acute-onset shortness of breath and pleuritic chest pain after traveling across the country for a work conference. She has no history of cancer, liver disease, or renal disease. Her blood pressure is 140/80 mm Hg, and her heart rate, 90 beats/min. You diagnose an acute PE in this patient and start anticoagulation. Should you admit her to the hospital to decrease morbidity and mortality?
According to the CDC, venous thromboembolism (VTE) affects about 900,000 people each year, and about 60,000 to 100,000 of these patients die annually.2 Pulmonary embolism is the third leading cause of death from cardiovascular disease, following heart attack and stroke.3 Prompt diagnosis and treatment with systemic anticoagulation improves patient outcomes and decreases the risk for long-term complications.
The 2016 American College of Chest Physicians (CHEST) guideline on antithrombotic therapy for VTE recommends home treatment or early discharge over standard discharge (after the first 5 days of treatment) for patients who meet the following clinical criteria: “clinically stable with good cardiopulmonary reserve; no contraindications such as recent bleeding, severe renal or liver disease, or severe thrombocytopenia (ie, < 70,000/mm3); expected to be compliant with treatment; and feels well enough to be treated at home.”3
The guideline states that various clinical decision tools, such as the Pulmonary Embolism Severity Index (PESI), can aid in identifying low-risk patients to be considered for treatment at home. The PESI uses age, gender, vital signs, mental status, and a history of cancer, lung, and cardiac disease to stratify patients by risk.4
A systematic review of 1 randomized controlled trial (RCT) and 7 observational studies found that in low-risk patients, outpatient treatment was as safe as inpatient treatment.5 This more recent study determines the net clinical benefit of hospitalized versus outpatient management in a wider range of patients with acute PE, regardless of initial risk.1
STUDY SUMMARY
Hospitalization confers no benefit to stable PE patients
This retrospective, propensity-matched cohort study compared rates of adverse events in 1127 patients with acute PE managed in the hospital versus outpatient setting.1 Patients were classified as outpatients if they were discharged from the ED or discharged from the hospital within 48 hours of admission. Patients were included if a symptomatic acute PE was diagnosed via CT or high-probability ventilation-perfusion scan and excluded if they were younger than 19, were diagnosed with a PE during hospitalization, had chronic PE, or were hemodynamically unstable, among other factors. The investigators calculated PESI scores for all patients.
Propensity scores matched patients on 28 characteristics and known risk factors for adverse events to ensure the groups were similar. The primary outcome was rate of adverse events, including recurrent VTE, major bleeding, or death at 14 days. The secondary outcome included rates of the above during the 3-month follow-up period.
Continue to: Of the 1127 eligible patients...
Of the 1127 eligible patients, 1081 were included in the matched cohort, with 576 (53%) treated as hospitalized patients and 505 (47%) treated as outpatients. The mean age of the matched cohorts wa
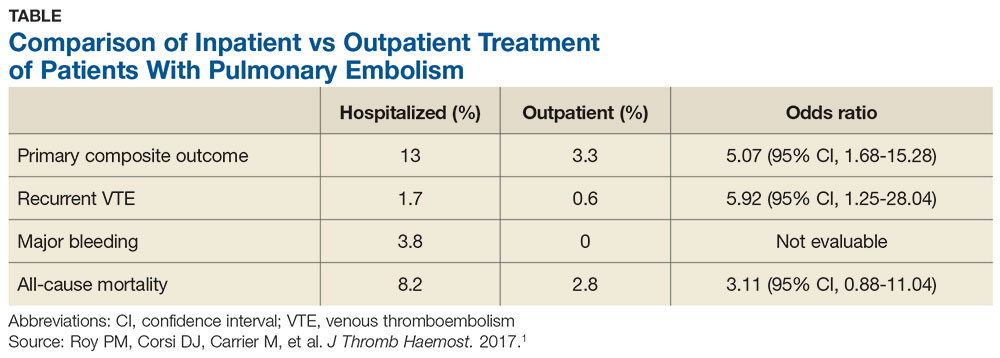
The 14-day rate of adverse events was higher in hospitalized patients than in outpatients (13% vs 3.3%; odds ratio [OR], 5.07), with each of the adverse events that made up the primary outcome occurring more frequently in the hospitalized group (see Table). The rate of adverse events at 3 months was also greater for hospitalized patients compared with outpatients (21.7% vs 6.9%; OR, 4.9). The results remained similar for high-risk patients (Class III-V) based on their PESI score.
WHAT’S NEW
Higher rate of adverse events in inpatients
This trial supports the CHEST guideline recommendations to manage hemodynamically stable patients with acute PE as outpatients.3 It adds to the conversation by demonstrating higher rates of adverse events with hospitalization, even in high-risk subgroups (PESI Class III-V).
CAVEATS
Good study, but it wasn’t an RCT
While this is a well-designed cohort study, it is not an RCT. This study defined outpatient management as patients discharged from the ED or hospitalized for < 48 hours. However, only 59 of the 544 patients in the outpatient group were early hospital discharges; the rest were never admitted. Finally, a specialized thrombosis clinic followed up with the patients within 24 hours of discharge, and patients had telephone access to specialized health care professionals; such organization of care contributed to the safe outpatient management of these PE patients.
CHALLENGES TO IMPLEMENTATION
Insurance coverage may present an issue
Medication coverage of direct oral anticoagulants and low-molecular-weight heparin may present a barrier to patients treated in the outpatient setting who have no insurance or are insured by certain carriers.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2018. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2018;67[12]:777-779).
1. Roy PM, Corsi DJ, Carrier M, et al. Net clinical benefit of hospitalization versus outpatient management of patients with acute pulmonary embolism. J Thromb Haemost. 2017;15:685-694.
2. CDC. Venous thromboembolism data & statistics. www.cdc.gov/ncbddd/dvt/data.html. Accessed April 26, 2019.
3. Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. CHEST. 2016;149:315-352.
4. Aujesky D, Obrosky DS, Stone RA, et al. Derivation and validation of a prognostic model for pulmonary embolism. Am J Respir Crit Care Med. 2005;172:1041-1046.
5. Vinson DR, Zehtabchi S, Yealy DM. Can selected patients with newly diagnosed pulmonary embolism be safely treated without hospitalization? A systematic review. Ann Emerg Med. 2012;60:651-662.
A 63-year-old woman with a history of hypertension presents to the emergency department (ED) with acute-onset shortness of breath and pleuritic chest pain after traveling across the country for a work conference. She has no history of cancer, liver disease, or renal disease. Her blood pressure is 140/80 mm Hg, and her heart rate, 90 beats/min. You diagnose an acute PE in this patient and start anticoagulation. Should you admit her to the hospital to decrease morbidity and mortality?
According to the CDC, venous thromboembolism (VTE) affects about 900,000 people each year, and about 60,000 to 100,000 of these patients die annually.2 Pulmonary embolism is the third leading cause of death from cardiovascular disease, following heart attack and stroke.3 Prompt diagnosis and treatment with systemic anticoagulation improves patient outcomes and decreases the risk for long-term complications.
The 2016 American College of Chest Physicians (CHEST) guideline on antithrombotic therapy for VTE recommends home treatment or early discharge over standard discharge (after the first 5 days of treatment) for patients who meet the following clinical criteria: “clinically stable with good cardiopulmonary reserve; no contraindications such as recent bleeding, severe renal or liver disease, or severe thrombocytopenia (ie, < 70,000/mm3); expected to be compliant with treatment; and feels well enough to be treated at home.”3
The guideline states that various clinical decision tools, such as the Pulmonary Embolism Severity Index (PESI), can aid in identifying low-risk patients to be considered for treatment at home. The PESI uses age, gender, vital signs, mental status, and a history of cancer, lung, and cardiac disease to stratify patients by risk.4
A systematic review of 1 randomized controlled trial (RCT) and 7 observational studies found that in low-risk patients, outpatient treatment was as safe as inpatient treatment.5 This more recent study determines the net clinical benefit of hospitalized versus outpatient management in a wider range of patients with acute PE, regardless of initial risk.1
STUDY SUMMARY
Hospitalization confers no benefit to stable PE patients
This retrospective, propensity-matched cohort study compared rates of adverse events in 1127 patients with acute PE managed in the hospital versus outpatient setting.1 Patients were classified as outpatients if they were discharged from the ED or discharged from the hospital within 48 hours of admission. Patients were included if a symptomatic acute PE was diagnosed via CT or high-probability ventilation-perfusion scan and excluded if they were younger than 19, were diagnosed with a PE during hospitalization, had chronic PE, or were hemodynamically unstable, among other factors. The investigators calculated PESI scores for all patients.
Propensity scores matched patients on 28 characteristics and known risk factors for adverse events to ensure the groups were similar. The primary outcome was rate of adverse events, including recurrent VTE, major bleeding, or death at 14 days. The secondary outcome included rates of the above during the 3-month follow-up period.
Continue to: Of the 1127 eligible patients...
Of the 1127 eligible patients, 1081 were included in the matched cohort, with 576 (53%) treated as hospitalized patients and 505 (47%) treated as outpatients. The mean age of the matched cohorts wa
The 14-day rate of adverse events was higher in hospitalized patients than in outpatients (13% vs 3.3%; odds ratio [OR], 5.07), with each of the adverse events that made up the primary outcome occurring more frequently in the hospitalized group (see Table). The rate of adverse events at 3 months was also greater for hospitalized patients compared with outpatients (21.7% vs 6.9%; OR, 4.9). The results remained similar for high-risk patients (Class III-V) based on their PESI score.
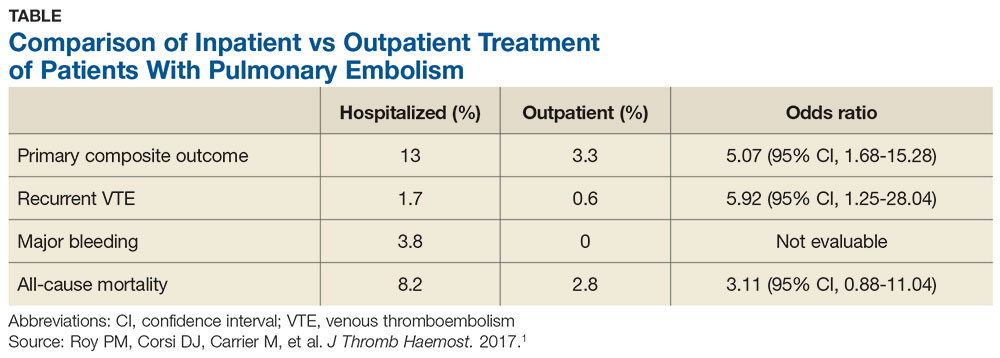
WHAT’S NEW
Higher rate of adverse events in inpatients
This trial supports the CHEST guideline recommendations to manage hemodynamically stable patients with acute PE as outpatients.3 It adds to the conversation by demonstrating higher rates of adverse events with hospitalization, even in high-risk subgroups (PESI Class III-V).
CAVEATS
Good study, but it wasn’t an RCT
While this is a well-designed cohort study, it is not an RCT. This study defined outpatient management as patients discharged from the ED or hospitalized for < 48 hours. However, only 59 of the 544 patients in the outpatient group were early hospital discharges; the rest were never admitted. Finally, a specialized thrombosis clinic followed up with the patients within 24 hours of discharge, and patients had telephone access to specialized health care professionals; such organization of care contributed to the safe outpatient management of these PE patients.
CHALLENGES TO IMPLEMENTATION
Insurance coverage may present an issue
Medication coverage of direct oral anticoagulants and low-molecular-weight heparin may present a barrier to patients treated in the outpatient setting who have no insurance or are insured by certain carriers.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2018. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2018;67[12]:777-779).
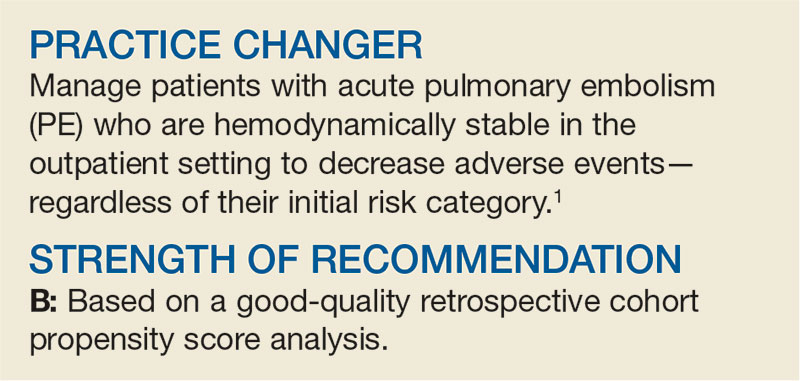
A 63-year-old woman with a history of hypertension presents to the emergency department (ED) with acute-onset shortness of breath and pleuritic chest pain after traveling across the country for a work conference. She has no history of cancer, liver disease, or renal disease. Her blood pressure is 140/80 mm Hg, and her heart rate, 90 beats/min. You diagnose an acute PE in this patient and start anticoagulation. Should you admit her to the hospital to decrease morbidity and mortality?
According to the CDC, venous thromboembolism (VTE) affects about 900,000 people each year, and about 60,000 to 100,000 of these patients die annually.2 Pulmonary embolism is the third leading cause of death from cardiovascular disease, following heart attack and stroke.3 Prompt diagnosis and treatment with systemic anticoagulation improves patient outcomes and decreases the risk for long-term complications.
The 2016 American College of Chest Physicians (CHEST) guideline on antithrombotic therapy for VTE recommends home treatment or early discharge over standard discharge (after the first 5 days of treatment) for patients who meet the following clinical criteria: “clinically stable with good cardiopulmonary reserve; no contraindications such as recent bleeding, severe renal or liver disease, or severe thrombocytopenia (ie, < 70,000/mm3); expected to be compliant with treatment; and feels well enough to be treated at home.”3
The guideline states that various clinical decision tools, such as the Pulmonary Embolism Severity Index (PESI), can aid in identifying low-risk patients to be considered for treatment at home. The PESI uses age, gender, vital signs, mental status, and a history of cancer, lung, and cardiac disease to stratify patients by risk.4
A systematic review of 1 randomized controlled trial (RCT) and 7 observational studies found that in low-risk patients, outpatient treatment was as safe as inpatient treatment.5 This more recent study determines the net clinical benefit of hospitalized versus outpatient management in a wider range of patients with acute PE, regardless of initial risk.1
STUDY SUMMARY
Hospitalization confers no benefit to stable PE patients
This retrospective, propensity-matched cohort study compared rates of adverse events in 1127 patients with acute PE managed in the hospital versus outpatient setting.1 Patients were classified as outpatients if they were discharged from the ED or discharged from the hospital within 48 hours of admission. Patients were included if a symptomatic acute PE was diagnosed via CT or high-probability ventilation-perfusion scan and excluded if they were younger than 19, were diagnosed with a PE during hospitalization, had chronic PE, or were hemodynamically unstable, among other factors. The investigators calculated PESI scores for all patients.
Propensity scores matched patients on 28 characteristics and known risk factors for adverse events to ensure the groups were similar. The primary outcome was rate of adverse events, including recurrent VTE, major bleeding, or death at 14 days. The secondary outcome included rates of the above during the 3-month follow-up period.
Continue to: Of the 1127 eligible patients...
Of the 1127 eligible patients, 1081 were included in the matched cohort, with 576 (53%) treated as hospitalized patients and 505 (47%) treated as outpatients. The mean age of the matched cohorts wa
The 14-day rate of adverse events was higher in hospitalized patients than in outpatients (13% vs 3.3%; odds ratio [OR], 5.07), with each of the adverse events that made up the primary outcome occurring more frequently in the hospitalized group (see Table). The rate of adverse events at 3 months was also greater for hospitalized patients compared with outpatients (21.7% vs 6.9%; OR, 4.9). The results remained similar for high-risk patients (Class III-V) based on their PESI score.
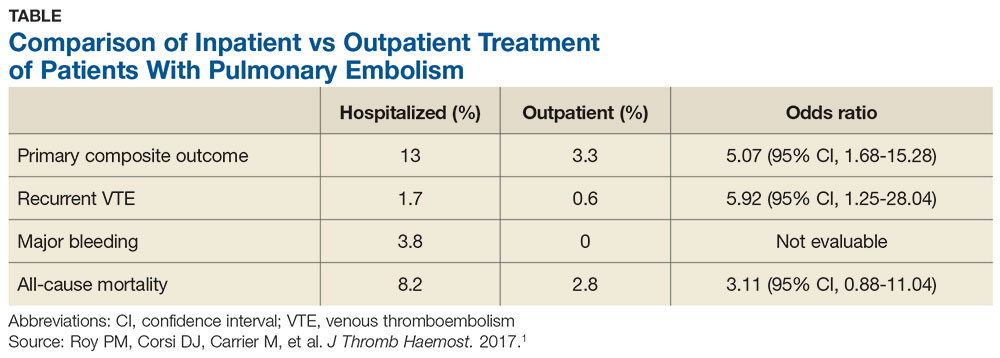
WHAT’S NEW
Higher rate of adverse events in inpatients
This trial supports the CHEST guideline recommendations to manage hemodynamically stable patients with acute PE as outpatients.3 It adds to the conversation by demonstrating higher rates of adverse events with hospitalization, even in high-risk subgroups (PESI Class III-V).
CAVEATS
Good study, but it wasn’t an RCT
While this is a well-designed cohort study, it is not an RCT. This study defined outpatient management as patients discharged from the ED or hospitalized for < 48 hours. However, only 59 of the 544 patients in the outpatient group were early hospital discharges; the rest were never admitted. Finally, a specialized thrombosis clinic followed up with the patients within 24 hours of discharge, and patients had telephone access to specialized health care professionals; such organization of care contributed to the safe outpatient management of these PE patients.
CHALLENGES TO IMPLEMENTATION
Insurance coverage may present an issue
Medication coverage of direct oral anticoagulants and low-molecular-weight heparin may present a barrier to patients treated in the outpatient setting who have no insurance or are insured by certain carriers.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2018. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2018;67[12]:777-779).
1. Roy PM, Corsi DJ, Carrier M, et al. Net clinical benefit of hospitalization versus outpatient management of patients with acute pulmonary embolism. J Thromb Haemost. 2017;15:685-694.
2. CDC. Venous thromboembolism data & statistics. www.cdc.gov/ncbddd/dvt/data.html. Accessed April 26, 2019.
3. Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. CHEST. 2016;149:315-352.
4. Aujesky D, Obrosky DS, Stone RA, et al. Derivation and validation of a prognostic model for pulmonary embolism. Am J Respir Crit Care Med. 2005;172:1041-1046.
5. Vinson DR, Zehtabchi S, Yealy DM. Can selected patients with newly diagnosed pulmonary embolism be safely treated without hospitalization? A systematic review. Ann Emerg Med. 2012;60:651-662.
1. Roy PM, Corsi DJ, Carrier M, et al. Net clinical benefit of hospitalization versus outpatient management of patients with acute pulmonary embolism. J Thromb Haemost. 2017;15:685-694.
2. CDC. Venous thromboembolism data & statistics. www.cdc.gov/ncbddd/dvt/data.html. Accessed April 26, 2019.
3. Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. CHEST. 2016;149:315-352.
4. Aujesky D, Obrosky DS, Stone RA, et al. Derivation and validation of a prognostic model for pulmonary embolism. Am J Respir Crit Care Med. 2005;172:1041-1046.
5. Vinson DR, Zehtabchi S, Yealy DM. Can selected patients with newly diagnosed pulmonary embolism be safely treated without hospitalization? A systematic review. Ann Emerg Med. 2012;60:651-662.
Online counseling clarifies treatment options for menopausal women
NASHVILLE, TENN. – a post-intervention survey showed.
Of 36 women who completed the counseling, 72% were able to express a clear preference for a particular treatment. Additionally, 90% to 100% of those who completed the final survey said the various components of the counseling–such as an educational brochure or a telephone call from a research nurse–made them feel more prepared to speak with their provider about treatment options, Sandra Dayaratna, MD, reported during a poster session at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
Among 18 women with vasomotor symptoms, 6 (33%) preferred non-hormone treatment, 7 (39%) preferred hormone treatment, and 5 (28%) were unsure; among 18 with genitourinary symptoms of menopause, 6 (33%) preferred non-prescription treatment, 7 (39%) preferred topical hormone therapy, and 5 (28%) were unsure, Dr. Dayaratna, division director and clinical associate professor at Thomas Jefferson University Hospital and Sidney Kimmel Medical College, Philadelphia, found.
Of women who were not being treated for vasomotor symptoms, 5 (56%) expressed a clear treatment preference after counseling, whereas 8 (80%) of those not receiving treatment for genitourinary symptoms expressed a clear preference. Among 7 women receiving systemic hormone therapy for vasomotor symptoms, 86% preferred this treatment after counseling, and 3 women (50%) receiving topical hormone therapy preferred topical treatment after counseling.
The study included women aged 36-50 years from diverse educational and racial backgrounds who were referred to the counseling program after reporting menopausal symptoms, completing a baseline survey, and providing consent. The counseling, which was adapted from a tool developed at Thomas Jefferson University Hospital for the assessment of patients with colon and cancer or lung cancer, involved an educational brochure that was mailed to participants. It also offered access to an online tool that provided information about systemic hormone therapy, non-hormone prescription therapy, topical hormone treatment, and non-prescription treatment for vasomotor and genitourinary symptoms of menopause.
A research nurse contacted participants by phone and used the online program to review the brochure, clarify treatment preference, and produce a summary of the results.
In an interview, Dr. Dayaratna noted that the concept of “shared decision making” is often misunderstood to mean that patients are provided with information about options and then they make a choice.
Actually, this study demonstrates that shared decision making really involves a “values clarification” component, she explained. In this study, counseling that incorporates this type of shared decision making helped women feel more prepared to speak with their providers about treatment and thus may add value to care of menopausal women, she concluded.
“This is relevant because we know that over 50% of patients within 90 minutes of leaving their doctor’s office have forgotten what they were told, and over 50% do not comply with their treatment prescriptions,” she said. “So if patients can do this process ahead of time, when they come to speak to their physician about their symptoms and selection of medication, it’s a more effective and efficient conversation.”
Further research should evaluate impact on the subsequent office visit, she added.
This study was funded by an educational grant from Pfizer, Inc. and by the National Cancer Institute. Dr. Dayaratna reported having no disclosures.
SOURCE: Dayaratna S et al., ACOG 2019: Abstract 21M.
NASHVILLE, TENN. – a post-intervention survey showed.
Of 36 women who completed the counseling, 72% were able to express a clear preference for a particular treatment. Additionally, 90% to 100% of those who completed the final survey said the various components of the counseling–such as an educational brochure or a telephone call from a research nurse–made them feel more prepared to speak with their provider about treatment options, Sandra Dayaratna, MD, reported during a poster session at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
Among 18 women with vasomotor symptoms, 6 (33%) preferred non-hormone treatment, 7 (39%) preferred hormone treatment, and 5 (28%) were unsure; among 18 with genitourinary symptoms of menopause, 6 (33%) preferred non-prescription treatment, 7 (39%) preferred topical hormone therapy, and 5 (28%) were unsure, Dr. Dayaratna, division director and clinical associate professor at Thomas Jefferson University Hospital and Sidney Kimmel Medical College, Philadelphia, found.
Of women who were not being treated for vasomotor symptoms, 5 (56%) expressed a clear treatment preference after counseling, whereas 8 (80%) of those not receiving treatment for genitourinary symptoms expressed a clear preference. Among 7 women receiving systemic hormone therapy for vasomotor symptoms, 86% preferred this treatment after counseling, and 3 women (50%) receiving topical hormone therapy preferred topical treatment after counseling.
The study included women aged 36-50 years from diverse educational and racial backgrounds who were referred to the counseling program after reporting menopausal symptoms, completing a baseline survey, and providing consent. The counseling, which was adapted from a tool developed at Thomas Jefferson University Hospital for the assessment of patients with colon and cancer or lung cancer, involved an educational brochure that was mailed to participants. It also offered access to an online tool that provided information about systemic hormone therapy, non-hormone prescription therapy, topical hormone treatment, and non-prescription treatment for vasomotor and genitourinary symptoms of menopause.
A research nurse contacted participants by phone and used the online program to review the brochure, clarify treatment preference, and produce a summary of the results.
In an interview, Dr. Dayaratna noted that the concept of “shared decision making” is often misunderstood to mean that patients are provided with information about options and then they make a choice.
Actually, this study demonstrates that shared decision making really involves a “values clarification” component, she explained. In this study, counseling that incorporates this type of shared decision making helped women feel more prepared to speak with their providers about treatment and thus may add value to care of menopausal women, she concluded.
“This is relevant because we know that over 50% of patients within 90 minutes of leaving their doctor’s office have forgotten what they were told, and over 50% do not comply with their treatment prescriptions,” she said. “So if patients can do this process ahead of time, when they come to speak to their physician about their symptoms and selection of medication, it’s a more effective and efficient conversation.”
Further research should evaluate impact on the subsequent office visit, she added.
This study was funded by an educational grant from Pfizer, Inc. and by the National Cancer Institute. Dr. Dayaratna reported having no disclosures.
SOURCE: Dayaratna S et al., ACOG 2019: Abstract 21M.
NASHVILLE, TENN. – a post-intervention survey showed.
Of 36 women who completed the counseling, 72% were able to express a clear preference for a particular treatment. Additionally, 90% to 100% of those who completed the final survey said the various components of the counseling–such as an educational brochure or a telephone call from a research nurse–made them feel more prepared to speak with their provider about treatment options, Sandra Dayaratna, MD, reported during a poster session at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
Among 18 women with vasomotor symptoms, 6 (33%) preferred non-hormone treatment, 7 (39%) preferred hormone treatment, and 5 (28%) were unsure; among 18 with genitourinary symptoms of menopause, 6 (33%) preferred non-prescription treatment, 7 (39%) preferred topical hormone therapy, and 5 (28%) were unsure, Dr. Dayaratna, division director and clinical associate professor at Thomas Jefferson University Hospital and Sidney Kimmel Medical College, Philadelphia, found.
Of women who were not being treated for vasomotor symptoms, 5 (56%) expressed a clear treatment preference after counseling, whereas 8 (80%) of those not receiving treatment for genitourinary symptoms expressed a clear preference. Among 7 women receiving systemic hormone therapy for vasomotor symptoms, 86% preferred this treatment after counseling, and 3 women (50%) receiving topical hormone therapy preferred topical treatment after counseling.
The study included women aged 36-50 years from diverse educational and racial backgrounds who were referred to the counseling program after reporting menopausal symptoms, completing a baseline survey, and providing consent. The counseling, which was adapted from a tool developed at Thomas Jefferson University Hospital for the assessment of patients with colon and cancer or lung cancer, involved an educational brochure that was mailed to participants. It also offered access to an online tool that provided information about systemic hormone therapy, non-hormone prescription therapy, topical hormone treatment, and non-prescription treatment for vasomotor and genitourinary symptoms of menopause.
A research nurse contacted participants by phone and used the online program to review the brochure, clarify treatment preference, and produce a summary of the results.
In an interview, Dr. Dayaratna noted that the concept of “shared decision making” is often misunderstood to mean that patients are provided with information about options and then they make a choice.
Actually, this study demonstrates that shared decision making really involves a “values clarification” component, she explained. In this study, counseling that incorporates this type of shared decision making helped women feel more prepared to speak with their providers about treatment and thus may add value to care of menopausal women, she concluded.
“This is relevant because we know that over 50% of patients within 90 minutes of leaving their doctor’s office have forgotten what they were told, and over 50% do not comply with their treatment prescriptions,” she said. “So if patients can do this process ahead of time, when they come to speak to their physician about their symptoms and selection of medication, it’s a more effective and efficient conversation.”
Further research should evaluate impact on the subsequent office visit, she added.
This study was funded by an educational grant from Pfizer, Inc. and by the National Cancer Institute. Dr. Dayaratna reported having no disclosures.
SOURCE: Dayaratna S et al., ACOG 2019: Abstract 21M.
REPORTING FROM ACOG 2019
A gentler approach to gastroschisis improves outcomes
BALTIMORE – a condition in which infants are born with their intestines and sometimes other organs protruding through a hole beside the umbilicus.
Neonatologists, maternal-fetal health experts, and pediatric surgeons standardized a literature-based approach that was gentler and less invasive than usual management, emphasizing sutureless closure, sometimes at bedside on the first day of life, and early feeding. Often, it turned out, that’s all that children require.
It’s made a big difference. “We reduced the number of trips to the operating room and exposure to general anesthesia. We reduced the number of babies intubated and days on the ventilator. We reduced opioid days and antibiotic days” without increasing bacteremia, and “there are probably long-term benefits beyond the NICU,” said Kara Calkins, MD, at the Pediatric Academic Societies annual meeting.
I think this is definitely ahead of the curve for NICUs. My hope is that the vast majority of universities adopt a similar approach,” said Dr. Calkins, who is an assistant professor of neonatology at the University of California, Los Angeles.
“When I was a fellow,” she explained, “we took all of these babies and intubated them right away and put them on a drip to paralyze and sedate them. We put their bowels into a silo,” essentially a plastic bag suspended by a string, in the hopes that gravity would pull the bowels back into the abdomen. More often than not, however, “the surgeon would come by every day and slowly push them” back in over a week or so. “The fear was if you did it too quickly, you’d invoke an abdominal compartment syndrome, or respiratory decompensation. You had a baby intubated for a week, sedated and paralyzed.”
Infants were kept on total parenteral nutrition for weeks, sometimes through a Broviac central catheter.
It was overkill, Dr. Calkins said, when only the intestines are out and the abdominal wall defect isn’t too large or too small, which is the case for many infants.
For those children, sutureless closure over 1-3 days is the new goal. The bowel is worked back into the abdomen and the umbilical cord is pulled to the side to approximate the edges of the wound, and tacked down; the defect then heals itself. Antibiotics are discontinued 48 hours after closure. Gastric and rectal decompression helps with reduction.
Also, “we give drops of breast milk in their cheek right away, every couple of hours starting on the first day of life. Once the output from the gastric tube is clear, we start feeds. We still give total parenteral nutrition, but through a [peripherally inserted central catheter] in the arm,” Dr. Calkins said. “Use of breast milk for this population is important” to help establish a healthy microbiome, among other reasons.
Another improvement that had been made, according to Dr. Calkins, is that if only the intestines are out, women carry their baby to term and deliver vaginally. The old practice was to deliver babies preterm by Cesarean section, she explained.
To see how it’s worked out, Dr. Calkins and her colleagues reviewed 70 gastroschisis cases managed under the new guidelines. They were uncomplicated cases, with no intestinal atresia, stricture, or ischemia.
Paralysis was avoided for silo placement in 53 infants (76%) and 32 (46%) avoided intubation. Antibiotics were discontinued in 56 (80%) within 48 hours of abdominal wall closure, and routine narcotics were discontinued in 53 infants (76%). Feeds were initiated in almost all children within 48 hours of non-bilious gastric tube output.
Compared with 168 infants treated before the changes were made, silo placement dropped from 71% to 58% of infants, and total ventilator days from a median of 5 to 2.
There was no difference in length of stay, perhaps because the “intestinal dysmotility intrinsic to gastroschisis remains a rate limiting factor for discharge,” the team concluded.
There was no industry funding, and Dr. Calkins didn’t have any disclosures.
SOURCE: Rottkamp CA et al., PAS 2019. Abstract 51.
BALTIMORE – a condition in which infants are born with their intestines and sometimes other organs protruding through a hole beside the umbilicus.
Neonatologists, maternal-fetal health experts, and pediatric surgeons standardized a literature-based approach that was gentler and less invasive than usual management, emphasizing sutureless closure, sometimes at bedside on the first day of life, and early feeding. Often, it turned out, that’s all that children require.
It’s made a big difference. “We reduced the number of trips to the operating room and exposure to general anesthesia. We reduced the number of babies intubated and days on the ventilator. We reduced opioid days and antibiotic days” without increasing bacteremia, and “there are probably long-term benefits beyond the NICU,” said Kara Calkins, MD, at the Pediatric Academic Societies annual meeting.
I think this is definitely ahead of the curve for NICUs. My hope is that the vast majority of universities adopt a similar approach,” said Dr. Calkins, who is an assistant professor of neonatology at the University of California, Los Angeles.
“When I was a fellow,” she explained, “we took all of these babies and intubated them right away and put them on a drip to paralyze and sedate them. We put their bowels into a silo,” essentially a plastic bag suspended by a string, in the hopes that gravity would pull the bowels back into the abdomen. More often than not, however, “the surgeon would come by every day and slowly push them” back in over a week or so. “The fear was if you did it too quickly, you’d invoke an abdominal compartment syndrome, or respiratory decompensation. You had a baby intubated for a week, sedated and paralyzed.”
Infants were kept on total parenteral nutrition for weeks, sometimes through a Broviac central catheter.
It was overkill, Dr. Calkins said, when only the intestines are out and the abdominal wall defect isn’t too large or too small, which is the case for many infants.
For those children, sutureless closure over 1-3 days is the new goal. The bowel is worked back into the abdomen and the umbilical cord is pulled to the side to approximate the edges of the wound, and tacked down; the defect then heals itself. Antibiotics are discontinued 48 hours after closure. Gastric and rectal decompression helps with reduction.
Also, “we give drops of breast milk in their cheek right away, every couple of hours starting on the first day of life. Once the output from the gastric tube is clear, we start feeds. We still give total parenteral nutrition, but through a [peripherally inserted central catheter] in the arm,” Dr. Calkins said. “Use of breast milk for this population is important” to help establish a healthy microbiome, among other reasons.
Another improvement that had been made, according to Dr. Calkins, is that if only the intestines are out, women carry their baby to term and deliver vaginally. The old practice was to deliver babies preterm by Cesarean section, she explained.
To see how it’s worked out, Dr. Calkins and her colleagues reviewed 70 gastroschisis cases managed under the new guidelines. They were uncomplicated cases, with no intestinal atresia, stricture, or ischemia.
Paralysis was avoided for silo placement in 53 infants (76%) and 32 (46%) avoided intubation. Antibiotics were discontinued in 56 (80%) within 48 hours of abdominal wall closure, and routine narcotics were discontinued in 53 infants (76%). Feeds were initiated in almost all children within 48 hours of non-bilious gastric tube output.
Compared with 168 infants treated before the changes were made, silo placement dropped from 71% to 58% of infants, and total ventilator days from a median of 5 to 2.
There was no difference in length of stay, perhaps because the “intestinal dysmotility intrinsic to gastroschisis remains a rate limiting factor for discharge,” the team concluded.
There was no industry funding, and Dr. Calkins didn’t have any disclosures.
SOURCE: Rottkamp CA et al., PAS 2019. Abstract 51.
BALTIMORE – a condition in which infants are born with their intestines and sometimes other organs protruding through a hole beside the umbilicus.
Neonatologists, maternal-fetal health experts, and pediatric surgeons standardized a literature-based approach that was gentler and less invasive than usual management, emphasizing sutureless closure, sometimes at bedside on the first day of life, and early feeding. Often, it turned out, that’s all that children require.
It’s made a big difference. “We reduced the number of trips to the operating room and exposure to general anesthesia. We reduced the number of babies intubated and days on the ventilator. We reduced opioid days and antibiotic days” without increasing bacteremia, and “there are probably long-term benefits beyond the NICU,” said Kara Calkins, MD, at the Pediatric Academic Societies annual meeting.
I think this is definitely ahead of the curve for NICUs. My hope is that the vast majority of universities adopt a similar approach,” said Dr. Calkins, who is an assistant professor of neonatology at the University of California, Los Angeles.
“When I was a fellow,” she explained, “we took all of these babies and intubated them right away and put them on a drip to paralyze and sedate them. We put their bowels into a silo,” essentially a plastic bag suspended by a string, in the hopes that gravity would pull the bowels back into the abdomen. More often than not, however, “the surgeon would come by every day and slowly push them” back in over a week or so. “The fear was if you did it too quickly, you’d invoke an abdominal compartment syndrome, or respiratory decompensation. You had a baby intubated for a week, sedated and paralyzed.”
Infants were kept on total parenteral nutrition for weeks, sometimes through a Broviac central catheter.
It was overkill, Dr. Calkins said, when only the intestines are out and the abdominal wall defect isn’t too large or too small, which is the case for many infants.
For those children, sutureless closure over 1-3 days is the new goal. The bowel is worked back into the abdomen and the umbilical cord is pulled to the side to approximate the edges of the wound, and tacked down; the defect then heals itself. Antibiotics are discontinued 48 hours after closure. Gastric and rectal decompression helps with reduction.
Also, “we give drops of breast milk in their cheek right away, every couple of hours starting on the first day of life. Once the output from the gastric tube is clear, we start feeds. We still give total parenteral nutrition, but through a [peripherally inserted central catheter] in the arm,” Dr. Calkins said. “Use of breast milk for this population is important” to help establish a healthy microbiome, among other reasons.
Another improvement that had been made, according to Dr. Calkins, is that if only the intestines are out, women carry their baby to term and deliver vaginally. The old practice was to deliver babies preterm by Cesarean section, she explained.
To see how it’s worked out, Dr. Calkins and her colleagues reviewed 70 gastroschisis cases managed under the new guidelines. They were uncomplicated cases, with no intestinal atresia, stricture, or ischemia.
Paralysis was avoided for silo placement in 53 infants (76%) and 32 (46%) avoided intubation. Antibiotics were discontinued in 56 (80%) within 48 hours of abdominal wall closure, and routine narcotics were discontinued in 53 infants (76%). Feeds were initiated in almost all children within 48 hours of non-bilious gastric tube output.
Compared with 168 infants treated before the changes were made, silo placement dropped from 71% to 58% of infants, and total ventilator days from a median of 5 to 2.
There was no difference in length of stay, perhaps because the “intestinal dysmotility intrinsic to gastroschisis remains a rate limiting factor for discharge,” the team concluded.
There was no industry funding, and Dr. Calkins didn’t have any disclosures.
SOURCE: Rottkamp CA et al., PAS 2019. Abstract 51.
REPORTING FROM PAS 2019
Brain volumes after TBI correlate with clinical features
PHILADELPHIA – ” according to a study presented at the annual meeting of the American Academy of Neurology.
Traumatic brain injury (TBI) damages brain tissue and causes subsequent volume loss, which may result in clinical symptoms. It is a prevalent worldwide health problem caused by a mechanical insult to the head, resulting in transient or permanent alteration to brain tissue and/or function. Standard neuroimaging with computerized cranial tomography (CT) and structural magnetic resonance imaging (MRI) is often unrevealing during the evaluation of patients with TBI, particularly those classified as mild TBI. I
In this study, James Rock, MD, of Penn Presbyterian Medical Center and the University of Pennsylvania, and his colleagues sought to examine the value of quantitative analysis of regional brain volumes in the evaluation of TBI. The investigators reviewed the medical records and MRI imaging from 44 patients with TBI evaluated at a Level I trauma center. They also read clinical notes to assess reported symptoms and physical findings.
Regional volumes from TBI subjects were derived using the software package Freesurfer image analysis suite, which utilizes a T1-weighted structural scan to calculate volumetric information. A machine learning algorithm, random forests, was employed across volume measurements from 25 regions of interest to determine the most important regions for classifying subjects based on clinical outcome and symptomology.
Basal ganglia volume showed the highest variable importance with regards to classifying subjects who exhibited symptoms of cognitive dysfunction (Mean Decrease in Gini = 1.067, Mean Decrease in Accuracy = 5.966e-03) in quantitative analysis. Left lateral ventricle volume was important in classifying subjects with motor and vestibular alterations (Mean Decrease in Gini = 2.037, Mean Decrease in Accuracy = 2.92e-02). Left choroid plexus volume was the most important region for classifying subjects with sensation and somatic dysfunction (Mean Decrease in Gini = 0.271, Mean Decrease in Accuracy = 4.82e-03).
The researchers noted that their study is ongoing, in an abstract. “It will be extended to a larger cohort to determine whether volume changes in specific [regions of interest] can act as useful clinical biomarkers for chronic symptoms,” they said.
Dr. Diaz-Arrastia received personal compensation from Neural Analytics, Inc, BrainBox Solutions, Inc, and Bioscience Pharma Partners. Dr. Diaz-Arrastia holds stock and/or stock options in Neural Analytics, Inc. and has received research support from BrainBox Solutions. The other authors reported not having anything to disclose..
SOURCE: Rock J et al. AAN 2019. Abstract S2.006 .
PHILADELPHIA – ” according to a study presented at the annual meeting of the American Academy of Neurology.
Traumatic brain injury (TBI) damages brain tissue and causes subsequent volume loss, which may result in clinical symptoms. It is a prevalent worldwide health problem caused by a mechanical insult to the head, resulting in transient or permanent alteration to brain tissue and/or function. Standard neuroimaging with computerized cranial tomography (CT) and structural magnetic resonance imaging (MRI) is often unrevealing during the evaluation of patients with TBI, particularly those classified as mild TBI. I
In this study, James Rock, MD, of Penn Presbyterian Medical Center and the University of Pennsylvania, and his colleagues sought to examine the value of quantitative analysis of regional brain volumes in the evaluation of TBI. The investigators reviewed the medical records and MRI imaging from 44 patients with TBI evaluated at a Level I trauma center. They also read clinical notes to assess reported symptoms and physical findings.
Regional volumes from TBI subjects were derived using the software package Freesurfer image analysis suite, which utilizes a T1-weighted structural scan to calculate volumetric information. A machine learning algorithm, random forests, was employed across volume measurements from 25 regions of interest to determine the most important regions for classifying subjects based on clinical outcome and symptomology.
Basal ganglia volume showed the highest variable importance with regards to classifying subjects who exhibited symptoms of cognitive dysfunction (Mean Decrease in Gini = 1.067, Mean Decrease in Accuracy = 5.966e-03) in quantitative analysis. Left lateral ventricle volume was important in classifying subjects with motor and vestibular alterations (Mean Decrease in Gini = 2.037, Mean Decrease in Accuracy = 2.92e-02). Left choroid plexus volume was the most important region for classifying subjects with sensation and somatic dysfunction (Mean Decrease in Gini = 0.271, Mean Decrease in Accuracy = 4.82e-03).
The researchers noted that their study is ongoing, in an abstract. “It will be extended to a larger cohort to determine whether volume changes in specific [regions of interest] can act as useful clinical biomarkers for chronic symptoms,” they said.
Dr. Diaz-Arrastia received personal compensation from Neural Analytics, Inc, BrainBox Solutions, Inc, and Bioscience Pharma Partners. Dr. Diaz-Arrastia holds stock and/or stock options in Neural Analytics, Inc. and has received research support from BrainBox Solutions. The other authors reported not having anything to disclose..
SOURCE: Rock J et al. AAN 2019. Abstract S2.006 .
PHILADELPHIA – ” according to a study presented at the annual meeting of the American Academy of Neurology.
Traumatic brain injury (TBI) damages brain tissue and causes subsequent volume loss, which may result in clinical symptoms. It is a prevalent worldwide health problem caused by a mechanical insult to the head, resulting in transient or permanent alteration to brain tissue and/or function. Standard neuroimaging with computerized cranial tomography (CT) and structural magnetic resonance imaging (MRI) is often unrevealing during the evaluation of patients with TBI, particularly those classified as mild TBI. I
In this study, James Rock, MD, of Penn Presbyterian Medical Center and the University of Pennsylvania, and his colleagues sought to examine the value of quantitative analysis of regional brain volumes in the evaluation of TBI. The investigators reviewed the medical records and MRI imaging from 44 patients with TBI evaluated at a Level I trauma center. They also read clinical notes to assess reported symptoms and physical findings.
Regional volumes from TBI subjects were derived using the software package Freesurfer image analysis suite, which utilizes a T1-weighted structural scan to calculate volumetric information. A machine learning algorithm, random forests, was employed across volume measurements from 25 regions of interest to determine the most important regions for classifying subjects based on clinical outcome and symptomology.
Basal ganglia volume showed the highest variable importance with regards to classifying subjects who exhibited symptoms of cognitive dysfunction (Mean Decrease in Gini = 1.067, Mean Decrease in Accuracy = 5.966e-03) in quantitative analysis. Left lateral ventricle volume was important in classifying subjects with motor and vestibular alterations (Mean Decrease in Gini = 2.037, Mean Decrease in Accuracy = 2.92e-02). Left choroid plexus volume was the most important region for classifying subjects with sensation and somatic dysfunction (Mean Decrease in Gini = 0.271, Mean Decrease in Accuracy = 4.82e-03).
The researchers noted that their study is ongoing, in an abstract. “It will be extended to a larger cohort to determine whether volume changes in specific [regions of interest] can act as useful clinical biomarkers for chronic symptoms,” they said.
Dr. Diaz-Arrastia received personal compensation from Neural Analytics, Inc, BrainBox Solutions, Inc, and Bioscience Pharma Partners. Dr. Diaz-Arrastia holds stock and/or stock options in Neural Analytics, Inc. and has received research support from BrainBox Solutions. The other authors reported not having anything to disclose..
SOURCE: Rock J et al. AAN 2019. Abstract S2.006 .
REPORTING FROM AAN 2019