User login
Will we ever outgrow the Goldwater rule?
Since it appeared in the first edition of the American Psychiatric Association’s Principles of Medical Ethics in 1973, the “Goldwater rule” – often referred to in terms of where in the APA’s guideline it can be found, Section 7.3 – has placed a stringent prohibition on psychiatrists offering professional opinions about public figures “unless he or she has conducted an examination and has been granted proper authorization for such a statement.”1
Some psychiatrists experienced the restrictive nature of Section 7.3 more acutely perhaps than ever during the Trump presidency. This spurred numerous articles criticizing the guideline as an outdated “gag rule”2 that harms the public image of psychiatry.3 Some psychiatrists violated the rule to warn the public of the dangers of a president with “incipient dementia”4 occupying the most powerful position on earth.
Following President Trump’s exit from the White House, the alarm bells surrounding his presidency have quieted. Criticisms of the Goldwater rule, on the other hand, have persisted. Many of these criticisms now call for the rule to be refined, allowing for psychiatrists to give their professional opinions about public figures, but with certain guidelines on how to do so.5 Few have yet to make a sober case for the outright abolition of Section 7.3.6
Self-regulating and internal policing are important factors in the continued independence of the medical profession, and we should continue to hold each other to high professional standards. That being said, do psychiatrists need training wheels to prevent us from devolving into unprofessional social commentators? Other medical specialties do not see the need to implement a rule preventing their colleagues from expressing expertise in fear of embarrassment. Do we not have faith in our ability to conduct ourselves professionally? Is the Goldwater rule an admission of a juvenile lack of self-control within our field?
Not only do other medical specialties not forcibly handhold their members in public settings, but other “providers” in the realm of mental health likewise do not implement such strict self-restraints. Psychiatry staying silent on the matter of public figures leaves a void filled by other, arguably less qualified, individuals. Subsequently, the public discord risks being flooded with pseudoscientific pontification and distorted views of psychiatric illness. The cycle of speculating on the mental fitness of the president has outlived President Trump, with concerns about Joe Biden’s incoherence and waning cognition.7 Therein is an important argument to be made for the public duty of psychiatrists, with their greater expertise and clinical acumen, to weigh in on matters of societal importance in an attempt to dispel dangerous misconceptions.
Practical limitations are often raised and serve as the cornerstone for the Goldwater rule. Specifically, the limitation being that a psychiatrist cannot provide a professional opinion about an individual without a proper in-person evaluation. The psychiatric interview could be considered the most in-depth and comprehensive evaluation in all of medicine. Even so, is a trained psychiatrist presented with grandiosity, flight-of-ideas, and pressured speech unable to comment on the possibility of mania without a lengthy and comprehensive evaluation? How much disorganization of behavior and dialogue does one need to observe to recognize psychosis? For the experienced psychiatrist, many of these behavioral hallmarks are akin to an ST elevation on an EKG representing a heart attack.
When considering less extreme examples of mental affliction, such as depression and anxiety, many signs – including demeanor, motor activity, manner of speaking, and other aspects of behavior – are apparent to the perceptive psychiatrist without needing an extensive interview that dives into the depths of a person’s social history and childhood. After all, our own criteria for depression and mania do not require the presence of social stressors or childhood trauma. Even personality disorders can be reasonably postulated when a person behaves in a particular fashion. The recognition of transitional objects, items used to provide psychological comfort, including the “teddy bear sign” are common and scientifically studied methods to recognize personality disorder.8
The necessity for an in-person evaluation has become less compelling over the years. In our modern age, important social moments are memorialized in countless videos that are arguably more relevant, more accurate, and less subjective than a psychiatric interview. Furthermore, forensic psychiatrists routinely comment on individuals they have not examined for a variety of reasons, from postmortem analysis to the refusal of the client to be interviewed. Moreover, and with significant contradiction, many leaders in the field of psychiatry view integrated care, the practice of psychiatrists advising primary care doctors, often without even seeing patients, to be the future of psychiatry.9
Some reading this may scoff at the above examples. Perhaps Section 7.3 speaks to an underlying insecurity in our field regarding our ability to accurately diagnose. That insecurity is not unfounded. In terms of the DSM-5, the bar for reliability has been lowered to a kappa of 0.2-0.4, from a previous standard of 0.6, in an attempt to avoid critiques of unreliability.10 Yet herein lies a powerful recognition of the necessity of the Goldwater rule. If psychiatrists cannot reliably agree on the presence of diagnoses in the controlled setting of scientific study, how can we expect to speak with coherence and consistency on highly mediatized and provoking topics?
The defense – that the difficulty psychiatrists have at providing an accurate diagnosis stems from the immense complexity of the system being evaluated, the human mind – is a valid one. Attempts to force such complex pathology, with all its many variables, into the check-box approach implemented in the DSM inevitably leads to problems with diagnostic reliability. Still, as psychiatrists we retain a level of expertise in assessing and treating complex disorders of the mind that no other field can claim.
The duty physicians have not only to work toward the health of their individual patients, but also to act in service of the public health and well-being of communities in which our patients live, is well established. How ethical is it then for psychiatry to absolve itself from duty when it comes to public figures at the center of shaping public opinion? There are numerous recent, high-profile instances where our expertise may have helped shine light in an otherwise murky public discussion filled with disinformation. The death of George Floyd and the year of turmoil that followed is a salient example. The conservatorship of Britney Spears and the resulting societal outcry is another. Even setting the matter of diagnosis aside, we can help illuminate the societal implications of conservatorship laws,11 in addition to providing input on how to safely and responsibly approach an individual who is in crisis, under the influence of multiple illicit substances, and possibly suffering from excited delirium.
Whether psychiatry has progressed enough as a medical specialty to trust ourselves with the option of providing professional opinions on public figures is an ongoing debate. The persistence of the Goldwater rule is a strong testament to the internal lack of confidence among psychiatrists regarding our ability to provide accurate diagnoses, act with integrity in the public space, and foster a positive public image. That lack of confidence may be well deserved. However, it is possible that our field will never go through the necessary pains of maturing as long as Section 7.3 remains in place.
Dr. Compton is a psychiatry resident at University of California, San Diego. His background includes medical education, mental health advocacy, work with underserved populations, and brain cancer research. Dr. Compton has no conflicts of interest. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. American Psychiatric Association. The principles of medical ethics with annotations especially applicable to psychiatry. Section 7. American Psychiatric Association; 2013 edition.
2. Glass LL. The Goldwater rule is broken. Here’s how to fix it. STAT News. 2018 June 18.
3. Plymyer D. The Goldwater rule paradox. 2020 Aug 7.
4. Lieberman JA. Trump’s brain and the 25th Amendment. Vice. 2017 Sep 8.
5. Blotcky AD et al. The Goldwater rule is fine, if refined. Here’s how to do it. Psychiatric Times. 2022 Jan 6;39(1).
6. Blotcky AD and Norrholm SD. After Trump, end the Goldwater rule once and for all. New York Daily News. 2020 Dec 22.
7. Stephens B. Biden should not run again – And he should say he won’t. New York Times. 2021 Dec 14.
8. Schmaling KB et al. The positive teddy bear sign: Transitional objects in the medical setting. J Nerv Ment Dis. 1994 Dec;182(12):725.
9. Badre N et al. Psychopharmacologic management in integrated care: Challenges for residency education. Acad Psychiatry. 2015; 39(4):466-9.
10. Kraemer HC et al. DSM-5: How reliable is reliable enough? Am J Psychiatry. 2012 Jan;169(1):13-5.
11. Badre N and Compton C. Britney Spears – Reflections on conservatorship. Clinical Psychiatry News. 2021 Nov 16.
Since it appeared in the first edition of the American Psychiatric Association’s Principles of Medical Ethics in 1973, the “Goldwater rule” – often referred to in terms of where in the APA’s guideline it can be found, Section 7.3 – has placed a stringent prohibition on psychiatrists offering professional opinions about public figures “unless he or she has conducted an examination and has been granted proper authorization for such a statement.”1
Some psychiatrists experienced the restrictive nature of Section 7.3 more acutely perhaps than ever during the Trump presidency. This spurred numerous articles criticizing the guideline as an outdated “gag rule”2 that harms the public image of psychiatry.3 Some psychiatrists violated the rule to warn the public of the dangers of a president with “incipient dementia”4 occupying the most powerful position on earth.
Following President Trump’s exit from the White House, the alarm bells surrounding his presidency have quieted. Criticisms of the Goldwater rule, on the other hand, have persisted. Many of these criticisms now call for the rule to be refined, allowing for psychiatrists to give their professional opinions about public figures, but with certain guidelines on how to do so.5 Few have yet to make a sober case for the outright abolition of Section 7.3.6
Self-regulating and internal policing are important factors in the continued independence of the medical profession, and we should continue to hold each other to high professional standards. That being said, do psychiatrists need training wheels to prevent us from devolving into unprofessional social commentators? Other medical specialties do not see the need to implement a rule preventing their colleagues from expressing expertise in fear of embarrassment. Do we not have faith in our ability to conduct ourselves professionally? Is the Goldwater rule an admission of a juvenile lack of self-control within our field?
Not only do other medical specialties not forcibly handhold their members in public settings, but other “providers” in the realm of mental health likewise do not implement such strict self-restraints. Psychiatry staying silent on the matter of public figures leaves a void filled by other, arguably less qualified, individuals. Subsequently, the public discord risks being flooded with pseudoscientific pontification and distorted views of psychiatric illness. The cycle of speculating on the mental fitness of the president has outlived President Trump, with concerns about Joe Biden’s incoherence and waning cognition.7 Therein is an important argument to be made for the public duty of psychiatrists, with their greater expertise and clinical acumen, to weigh in on matters of societal importance in an attempt to dispel dangerous misconceptions.
Practical limitations are often raised and serve as the cornerstone for the Goldwater rule. Specifically, the limitation being that a psychiatrist cannot provide a professional opinion about an individual without a proper in-person evaluation. The psychiatric interview could be considered the most in-depth and comprehensive evaluation in all of medicine. Even so, is a trained psychiatrist presented with grandiosity, flight-of-ideas, and pressured speech unable to comment on the possibility of mania without a lengthy and comprehensive evaluation? How much disorganization of behavior and dialogue does one need to observe to recognize psychosis? For the experienced psychiatrist, many of these behavioral hallmarks are akin to an ST elevation on an EKG representing a heart attack.
When considering less extreme examples of mental affliction, such as depression and anxiety, many signs – including demeanor, motor activity, manner of speaking, and other aspects of behavior – are apparent to the perceptive psychiatrist without needing an extensive interview that dives into the depths of a person’s social history and childhood. After all, our own criteria for depression and mania do not require the presence of social stressors or childhood trauma. Even personality disorders can be reasonably postulated when a person behaves in a particular fashion. The recognition of transitional objects, items used to provide psychological comfort, including the “teddy bear sign” are common and scientifically studied methods to recognize personality disorder.8
The necessity for an in-person evaluation has become less compelling over the years. In our modern age, important social moments are memorialized in countless videos that are arguably more relevant, more accurate, and less subjective than a psychiatric interview. Furthermore, forensic psychiatrists routinely comment on individuals they have not examined for a variety of reasons, from postmortem analysis to the refusal of the client to be interviewed. Moreover, and with significant contradiction, many leaders in the field of psychiatry view integrated care, the practice of psychiatrists advising primary care doctors, often without even seeing patients, to be the future of psychiatry.9
Some reading this may scoff at the above examples. Perhaps Section 7.3 speaks to an underlying insecurity in our field regarding our ability to accurately diagnose. That insecurity is not unfounded. In terms of the DSM-5, the bar for reliability has been lowered to a kappa of 0.2-0.4, from a previous standard of 0.6, in an attempt to avoid critiques of unreliability.10 Yet herein lies a powerful recognition of the necessity of the Goldwater rule. If psychiatrists cannot reliably agree on the presence of diagnoses in the controlled setting of scientific study, how can we expect to speak with coherence and consistency on highly mediatized and provoking topics?
The defense – that the difficulty psychiatrists have at providing an accurate diagnosis stems from the immense complexity of the system being evaluated, the human mind – is a valid one. Attempts to force such complex pathology, with all its many variables, into the check-box approach implemented in the DSM inevitably leads to problems with diagnostic reliability. Still, as psychiatrists we retain a level of expertise in assessing and treating complex disorders of the mind that no other field can claim.
The duty physicians have not only to work toward the health of their individual patients, but also to act in service of the public health and well-being of communities in which our patients live, is well established. How ethical is it then for psychiatry to absolve itself from duty when it comes to public figures at the center of shaping public opinion? There are numerous recent, high-profile instances where our expertise may have helped shine light in an otherwise murky public discussion filled with disinformation. The death of George Floyd and the year of turmoil that followed is a salient example. The conservatorship of Britney Spears and the resulting societal outcry is another. Even setting the matter of diagnosis aside, we can help illuminate the societal implications of conservatorship laws,11 in addition to providing input on how to safely and responsibly approach an individual who is in crisis, under the influence of multiple illicit substances, and possibly suffering from excited delirium.
Whether psychiatry has progressed enough as a medical specialty to trust ourselves with the option of providing professional opinions on public figures is an ongoing debate. The persistence of the Goldwater rule is a strong testament to the internal lack of confidence among psychiatrists regarding our ability to provide accurate diagnoses, act with integrity in the public space, and foster a positive public image. That lack of confidence may be well deserved. However, it is possible that our field will never go through the necessary pains of maturing as long as Section 7.3 remains in place.
Dr. Compton is a psychiatry resident at University of California, San Diego. His background includes medical education, mental health advocacy, work with underserved populations, and brain cancer research. Dr. Compton has no conflicts of interest. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. American Psychiatric Association. The principles of medical ethics with annotations especially applicable to psychiatry. Section 7. American Psychiatric Association; 2013 edition.
2. Glass LL. The Goldwater rule is broken. Here’s how to fix it. STAT News. 2018 June 18.
3. Plymyer D. The Goldwater rule paradox. 2020 Aug 7.
4. Lieberman JA. Trump’s brain and the 25th Amendment. Vice. 2017 Sep 8.
5. Blotcky AD et al. The Goldwater rule is fine, if refined. Here’s how to do it. Psychiatric Times. 2022 Jan 6;39(1).
6. Blotcky AD and Norrholm SD. After Trump, end the Goldwater rule once and for all. New York Daily News. 2020 Dec 22.
7. Stephens B. Biden should not run again – And he should say he won’t. New York Times. 2021 Dec 14.
8. Schmaling KB et al. The positive teddy bear sign: Transitional objects in the medical setting. J Nerv Ment Dis. 1994 Dec;182(12):725.
9. Badre N et al. Psychopharmacologic management in integrated care: Challenges for residency education. Acad Psychiatry. 2015; 39(4):466-9.
10. Kraemer HC et al. DSM-5: How reliable is reliable enough? Am J Psychiatry. 2012 Jan;169(1):13-5.
11. Badre N and Compton C. Britney Spears – Reflections on conservatorship. Clinical Psychiatry News. 2021 Nov 16.
Since it appeared in the first edition of the American Psychiatric Association’s Principles of Medical Ethics in 1973, the “Goldwater rule” – often referred to in terms of where in the APA’s guideline it can be found, Section 7.3 – has placed a stringent prohibition on psychiatrists offering professional opinions about public figures “unless he or she has conducted an examination and has been granted proper authorization for such a statement.”1
Some psychiatrists experienced the restrictive nature of Section 7.3 more acutely perhaps than ever during the Trump presidency. This spurred numerous articles criticizing the guideline as an outdated “gag rule”2 that harms the public image of psychiatry.3 Some psychiatrists violated the rule to warn the public of the dangers of a president with “incipient dementia”4 occupying the most powerful position on earth.
Following President Trump’s exit from the White House, the alarm bells surrounding his presidency have quieted. Criticisms of the Goldwater rule, on the other hand, have persisted. Many of these criticisms now call for the rule to be refined, allowing for psychiatrists to give their professional opinions about public figures, but with certain guidelines on how to do so.5 Few have yet to make a sober case for the outright abolition of Section 7.3.6
Self-regulating and internal policing are important factors in the continued independence of the medical profession, and we should continue to hold each other to high professional standards. That being said, do psychiatrists need training wheels to prevent us from devolving into unprofessional social commentators? Other medical specialties do not see the need to implement a rule preventing their colleagues from expressing expertise in fear of embarrassment. Do we not have faith in our ability to conduct ourselves professionally? Is the Goldwater rule an admission of a juvenile lack of self-control within our field?
Not only do other medical specialties not forcibly handhold their members in public settings, but other “providers” in the realm of mental health likewise do not implement such strict self-restraints. Psychiatry staying silent on the matter of public figures leaves a void filled by other, arguably less qualified, individuals. Subsequently, the public discord risks being flooded with pseudoscientific pontification and distorted views of psychiatric illness. The cycle of speculating on the mental fitness of the president has outlived President Trump, with concerns about Joe Biden’s incoherence and waning cognition.7 Therein is an important argument to be made for the public duty of psychiatrists, with their greater expertise and clinical acumen, to weigh in on matters of societal importance in an attempt to dispel dangerous misconceptions.
Practical limitations are often raised and serve as the cornerstone for the Goldwater rule. Specifically, the limitation being that a psychiatrist cannot provide a professional opinion about an individual without a proper in-person evaluation. The psychiatric interview could be considered the most in-depth and comprehensive evaluation in all of medicine. Even so, is a trained psychiatrist presented with grandiosity, flight-of-ideas, and pressured speech unable to comment on the possibility of mania without a lengthy and comprehensive evaluation? How much disorganization of behavior and dialogue does one need to observe to recognize psychosis? For the experienced psychiatrist, many of these behavioral hallmarks are akin to an ST elevation on an EKG representing a heart attack.
When considering less extreme examples of mental affliction, such as depression and anxiety, many signs – including demeanor, motor activity, manner of speaking, and other aspects of behavior – are apparent to the perceptive psychiatrist without needing an extensive interview that dives into the depths of a person’s social history and childhood. After all, our own criteria for depression and mania do not require the presence of social stressors or childhood trauma. Even personality disorders can be reasonably postulated when a person behaves in a particular fashion. The recognition of transitional objects, items used to provide psychological comfort, including the “teddy bear sign” are common and scientifically studied methods to recognize personality disorder.8
The necessity for an in-person evaluation has become less compelling over the years. In our modern age, important social moments are memorialized in countless videos that are arguably more relevant, more accurate, and less subjective than a psychiatric interview. Furthermore, forensic psychiatrists routinely comment on individuals they have not examined for a variety of reasons, from postmortem analysis to the refusal of the client to be interviewed. Moreover, and with significant contradiction, many leaders in the field of psychiatry view integrated care, the practice of psychiatrists advising primary care doctors, often without even seeing patients, to be the future of psychiatry.9
Some reading this may scoff at the above examples. Perhaps Section 7.3 speaks to an underlying insecurity in our field regarding our ability to accurately diagnose. That insecurity is not unfounded. In terms of the DSM-5, the bar for reliability has been lowered to a kappa of 0.2-0.4, from a previous standard of 0.6, in an attempt to avoid critiques of unreliability.10 Yet herein lies a powerful recognition of the necessity of the Goldwater rule. If psychiatrists cannot reliably agree on the presence of diagnoses in the controlled setting of scientific study, how can we expect to speak with coherence and consistency on highly mediatized and provoking topics?
The defense – that the difficulty psychiatrists have at providing an accurate diagnosis stems from the immense complexity of the system being evaluated, the human mind – is a valid one. Attempts to force such complex pathology, with all its many variables, into the check-box approach implemented in the DSM inevitably leads to problems with diagnostic reliability. Still, as psychiatrists we retain a level of expertise in assessing and treating complex disorders of the mind that no other field can claim.
The duty physicians have not only to work toward the health of their individual patients, but also to act in service of the public health and well-being of communities in which our patients live, is well established. How ethical is it then for psychiatry to absolve itself from duty when it comes to public figures at the center of shaping public opinion? There are numerous recent, high-profile instances where our expertise may have helped shine light in an otherwise murky public discussion filled with disinformation. The death of George Floyd and the year of turmoil that followed is a salient example. The conservatorship of Britney Spears and the resulting societal outcry is another. Even setting the matter of diagnosis aside, we can help illuminate the societal implications of conservatorship laws,11 in addition to providing input on how to safely and responsibly approach an individual who is in crisis, under the influence of multiple illicit substances, and possibly suffering from excited delirium.
Whether psychiatry has progressed enough as a medical specialty to trust ourselves with the option of providing professional opinions on public figures is an ongoing debate. The persistence of the Goldwater rule is a strong testament to the internal lack of confidence among psychiatrists regarding our ability to provide accurate diagnoses, act with integrity in the public space, and foster a positive public image. That lack of confidence may be well deserved. However, it is possible that our field will never go through the necessary pains of maturing as long as Section 7.3 remains in place.
Dr. Compton is a psychiatry resident at University of California, San Diego. His background includes medical education, mental health advocacy, work with underserved populations, and brain cancer research. Dr. Compton has no conflicts of interest. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. American Psychiatric Association. The principles of medical ethics with annotations especially applicable to psychiatry. Section 7. American Psychiatric Association; 2013 edition.
2. Glass LL. The Goldwater rule is broken. Here’s how to fix it. STAT News. 2018 June 18.
3. Plymyer D. The Goldwater rule paradox. 2020 Aug 7.
4. Lieberman JA. Trump’s brain and the 25th Amendment. Vice. 2017 Sep 8.
5. Blotcky AD et al. The Goldwater rule is fine, if refined. Here’s how to do it. Psychiatric Times. 2022 Jan 6;39(1).
6. Blotcky AD and Norrholm SD. After Trump, end the Goldwater rule once and for all. New York Daily News. 2020 Dec 22.
7. Stephens B. Biden should not run again – And he should say he won’t. New York Times. 2021 Dec 14.
8. Schmaling KB et al. The positive teddy bear sign: Transitional objects in the medical setting. J Nerv Ment Dis. 1994 Dec;182(12):725.
9. Badre N et al. Psychopharmacologic management in integrated care: Challenges for residency education. Acad Psychiatry. 2015; 39(4):466-9.
10. Kraemer HC et al. DSM-5: How reliable is reliable enough? Am J Psychiatry. 2012 Jan;169(1):13-5.
11. Badre N and Compton C. Britney Spears – Reflections on conservatorship. Clinical Psychiatry News. 2021 Nov 16.
Chronic Vulvar Plaque in a Patient With Severe Hidradenitis Suppurativa
The Diagnosis: Acquired Lymphangioma Circumscriptum
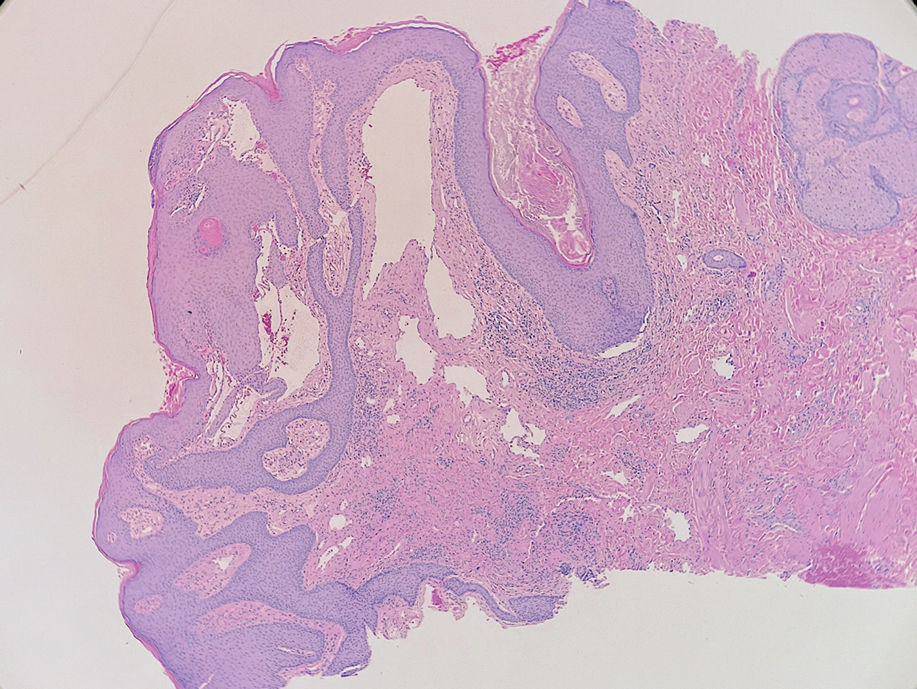
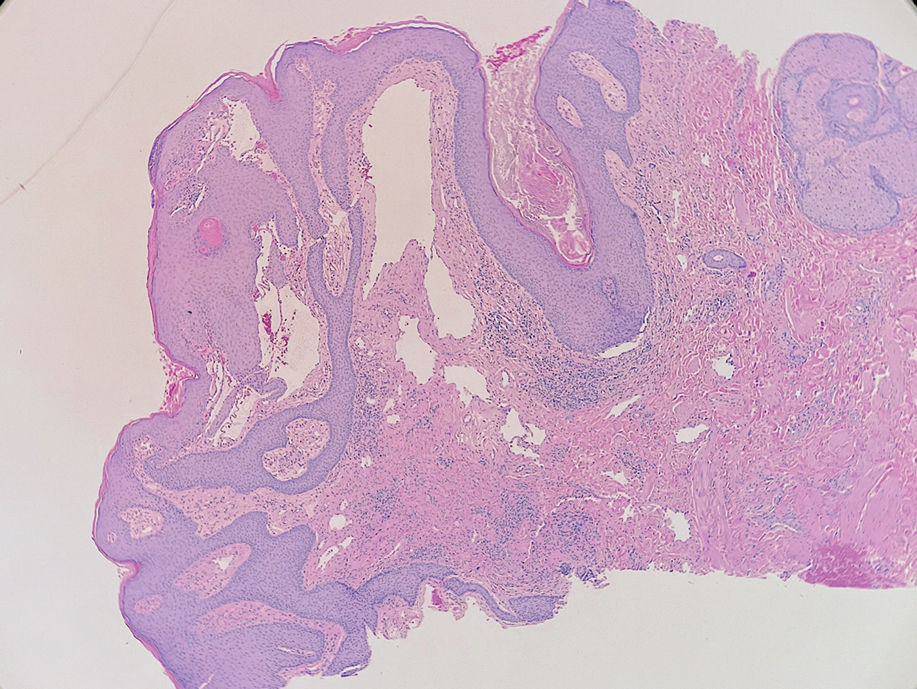
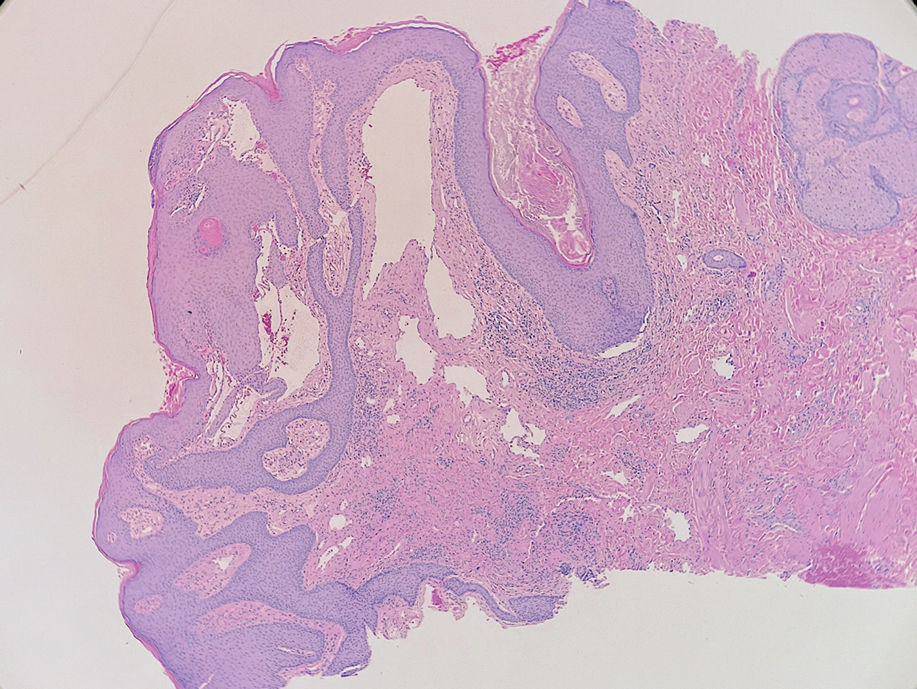
A skin biopsy of the plaque on the right labium majus showed a proliferation of well-formed, dilated lymphatic vessels lined by benign-appearing endothelial cells in the papillary dermis (Figure). These findings were consistent with a diagnosis of acquired lymphangioma circumscriptum (ALC) in the setting of severe hidradenitis suppurativa (HS).
Acquired lymphangioma circumscriptum (also known as acquired lymphangiectasia or secondary lymphangioma1) is a rare skin finding resulting from chronic lymphatic obstruction that leads to dilated lymphatic vessels within the dermis.2,3 There also is a distinct congenital form of lymphangioma circumscriptum caused by lymphatic malformations present at birth.2,4 Acquired lymphangioma circumscriptum of the vulva is a rare phenomenon.3 Identified causes include radiation or surgery for carcinoma, solid gynecologic tumors, lymphadenectomy, Crohn disease, and tuberculosis and other infections, all of which can disrupt normal lymphatics to cause ALC.2-4 Hidradenitis suppurativa is not a widely recognized cause of ALC; however, this phenomenon is reported in the literature. A long-standing history of severe HS complicated by lymphedema seems to precede the development of ALC in the reported cases, as in our patient.5-7
Acquired lymphangioma circumscriptum of the vulva can appear in women of all ages as frog spawn or cobblestone papules or vesicles, sometimes with a hyperkeratotic or verrucous appearance.2,4 Associated symptoms include serous drainage, edema, pruritus, and discomfort. The lesions may become eroded, which can predispose patients to secondary infections.1,2 Acquired lymphangioma circumscriptum of the vulva can be difficult to diagnose, as the time interval between the initial cause and the appearance of skin findings can be years, leading to the misdiagnosis of ALC as other similar-appearing genital skin conditions such as squamous cell carcinoma or condyloma.4,8 When misidentified as an infection, diagnosis can lead to substantial distress, abstinence from sexual activity, and unnecessary and painful treatments.
Skin biopsy is helpful in distinguishing ALC from other differential diagnoses such as condylomata acuminata, squamous cell carcinoma, and condyloma lata. Histopathology in ALC is notable for dilated lymphatic vessels filled with hypocellular fluid and lined with endothelial cells in the superficial dermis; the epidermis can appear hyperplastic, hyperkeratotic, or eroded.3-5,9 These lymphatic vessels stain positively for CD31 and D2-40, markers for endothelial cells and lymphatic endothelium, respectively, and negative for CD34, a marker for vascular endothelium.3,4,9 Features suggestive of condylomata acuminata such as rounded parakeratosis, hypergranulosis, and vacuolated keratinocytes9 are not present. The giant condyloma of Buschke-Löwenstein, a clinical variant of verrucous squamous cell carcinoma, also can present as a warty ulcerated papule or plaque in the genital region, but the characteristic rounded eosinophilic keratinocytes pushing down into the dermis9 are not seen in ALC. Secondary syphilis is associated with condyloma lata, which are verrucous or fleshy-appearing papules often coalescing into plaques located in the anogenital region. Pathologic features of secondary syphilis include vacuolar interface dermatitis and acanthosis with long slender rete ridges.9 Squamous cell carcinoma, which can arise from inflammation associated with long-standing HS, must be ruled out, as it is associated with a high risk of mortality in patients with HS.10
It is noteworthy to recognize the various, often confusing nomenclature used to describe cutaneous lymphatic conditions. The terms acquired lymphangioma circumscriptum, secondary lymphangioma, and lymphangiectasia are used interchangeably to describe dilated lymphatic vessels in the skin.1 The term atypical vascular lesion refers to lymphectasias of the skin of the breast due to prior radiation therapy most often used in the treatment of breast carcinoma; clinically, these present as red-brown or flesh-colored papules or telangiectatic plaques on the breast.11,12 Lymphedema also may occur alongside atypical vascular lesions, as prior radiation or surgical lymph node dissection can predispose patients to impaired lymphatic drainage.13 The lymphatic histopathologic subtype of atypical vascular lesions may appear similar to ALC; however, the vascular subtype will demonstrate collections of capillary-sized vessels and extravasated erythrocytes.11,12 Unlike ALC, the benign nature of atypical vascular lesions has been questioned, as they may be associated with a small risk for progression to angiosarcoma.11-13 It also is important to distinguish ALC from lymphangiomatosis, a generalized lymphatic anomaly that is characterized by extensive lymphatic malformations involving numerous internal organs, including the lungs and gastrointestinal tract. This condition is associated with notable morbidity and mortality.13
Although the suffix of the term lymphangioma suggests a neoplastic process, ALC is not a neoplasm and can be managed expectantly in many cases.2,3,8 However, due to cosmetic appearance, pain, discomfort, and recurrent bacterial superinfections, many patients pursue treatment. Treatment options for ALC include sclerotherapy, electrocautery, radiofrequency or carbon dioxide laser ablation, and excision, though recurrence can arise.3-5,7,8 Our patient elected to manage her asymptomatic ALC expectantly.
- Verma SB. Lymphangiectasias of the skin: victims of confusing nomenclature. Clin Exp Dermatol. 2009;34:566-569.
- Vlastos AT, Malpica A, Follen M. Lymphangioma circumscriptum of the vulva: a review of the literature. Obstet Gynecol. 2003;101:946-954.
- Chang MB, Newman CC, Davis MD, et al. Acquired lymphangiectasia (lymphangioma circumscriptum) of the vulva: clinicopathologic study of 11 patients from a single institution and 67 from the literature. Int J Dermatol. 2016;55:E482-E487.
- Stewart CJ, Chan T, Platten M. Acquired lymphangiectasia (‘lymphangioma circumscriptum’) of the vulva: a report of eight cases. Pathology. 2009;41:448-453.
- Sims SM, McLean FW, Davis JD, et al. Vulvar lymphangioma circumscriptum: a report of 3 cases, 2 associated with vulvar carcinoma and 1 with hidradenitis suppurativa. J Low Genit Tract Dis. 2010; 14:234-237.
- Moosbrugger EA, Mutasim DF. Hidradenitis suppurativa complicated by severe lymphedema and lymphangiectasias. J Am Acad Dermatol. 2011;6:1223-1224.
- Piernick DM 2nd, Mahmood SH, Daveluy S. Acquired lymphangioma circumscriptum of the genitals in an individual with chronic hidradenitis suppurativa. JAAD Case Rep. 2018;1:64-66.
- Horn LC, Kühndel K, Pawlowitsch T, et al. Acquired lymphangioma circumscriptum of the vulva mimicking genital warts. Eur J Obstet Gynecol Reprod Biol. 2005;1:118-120.
- Elston DM, Ferringer T, Ko CJ, et al. Dermatopathology. 3rd ed. Elsevier; 2019.
- Kohorst JJ, Shah KK, Hallemeier CL, et al. Squamous cell carcinoma in perineal, perianal, and gluteal hidradenitis suppurativa: experience in 12 patients. Dermatol Surg. 2019;45:519-526.
- Patton KT, Deyrup AT, Weiss SW. Atypical vascular lesions after surgery and radiation of the breast: a clinicopathologic study of 32 cases analyzing histologic heterogeneity and association with angiosarcoma. Am J Surg Pathol. 2008;32:943-950.
- Ronen S, Ivan D, Torres-Cabala CA, et al. Post-radiation vascular lesions of the breast. J Cutan Pathol. 2019;46:52-58.
- Bolognia JL, Schaffer JV, Cerroni L. Dermatology. 4th ed. Elsevier; 2018.
The Diagnosis: Acquired Lymphangioma Circumscriptum
A skin biopsy of the plaque on the right labium majus showed a proliferation of well-formed, dilated lymphatic vessels lined by benign-appearing endothelial cells in the papillary dermis (Figure). These findings were consistent with a diagnosis of acquired lymphangioma circumscriptum (ALC) in the setting of severe hidradenitis suppurativa (HS).
Acquired lymphangioma circumscriptum (also known as acquired lymphangiectasia or secondary lymphangioma1) is a rare skin finding resulting from chronic lymphatic obstruction that leads to dilated lymphatic vessels within the dermis.2,3 There also is a distinct congenital form of lymphangioma circumscriptum caused by lymphatic malformations present at birth.2,4 Acquired lymphangioma circumscriptum of the vulva is a rare phenomenon.3 Identified causes include radiation or surgery for carcinoma, solid gynecologic tumors, lymphadenectomy, Crohn disease, and tuberculosis and other infections, all of which can disrupt normal lymphatics to cause ALC.2-4 Hidradenitis suppurativa is not a widely recognized cause of ALC; however, this phenomenon is reported in the literature. A long-standing history of severe HS complicated by lymphedema seems to precede the development of ALC in the reported cases, as in our patient.5-7
Acquired lymphangioma circumscriptum of the vulva can appear in women of all ages as frog spawn or cobblestone papules or vesicles, sometimes with a hyperkeratotic or verrucous appearance.2,4 Associated symptoms include serous drainage, edema, pruritus, and discomfort. The lesions may become eroded, which can predispose patients to secondary infections.1,2 Acquired lymphangioma circumscriptum of the vulva can be difficult to diagnose, as the time interval between the initial cause and the appearance of skin findings can be years, leading to the misdiagnosis of ALC as other similar-appearing genital skin conditions such as squamous cell carcinoma or condyloma.4,8 When misidentified as an infection, diagnosis can lead to substantial distress, abstinence from sexual activity, and unnecessary and painful treatments.
Skin biopsy is helpful in distinguishing ALC from other differential diagnoses such as condylomata acuminata, squamous cell carcinoma, and condyloma lata. Histopathology in ALC is notable for dilated lymphatic vessels filled with hypocellular fluid and lined with endothelial cells in the superficial dermis; the epidermis can appear hyperplastic, hyperkeratotic, or eroded.3-5,9 These lymphatic vessels stain positively for CD31 and D2-40, markers for endothelial cells and lymphatic endothelium, respectively, and negative for CD34, a marker for vascular endothelium.3,4,9 Features suggestive of condylomata acuminata such as rounded parakeratosis, hypergranulosis, and vacuolated keratinocytes9 are not present. The giant condyloma of Buschke-Löwenstein, a clinical variant of verrucous squamous cell carcinoma, also can present as a warty ulcerated papule or plaque in the genital region, but the characteristic rounded eosinophilic keratinocytes pushing down into the dermis9 are not seen in ALC. Secondary syphilis is associated with condyloma lata, which are verrucous or fleshy-appearing papules often coalescing into plaques located in the anogenital region. Pathologic features of secondary syphilis include vacuolar interface dermatitis and acanthosis with long slender rete ridges.9 Squamous cell carcinoma, which can arise from inflammation associated with long-standing HS, must be ruled out, as it is associated with a high risk of mortality in patients with HS.10
It is noteworthy to recognize the various, often confusing nomenclature used to describe cutaneous lymphatic conditions. The terms acquired lymphangioma circumscriptum, secondary lymphangioma, and lymphangiectasia are used interchangeably to describe dilated lymphatic vessels in the skin.1 The term atypical vascular lesion refers to lymphectasias of the skin of the breast due to prior radiation therapy most often used in the treatment of breast carcinoma; clinically, these present as red-brown or flesh-colored papules or telangiectatic plaques on the breast.11,12 Lymphedema also may occur alongside atypical vascular lesions, as prior radiation or surgical lymph node dissection can predispose patients to impaired lymphatic drainage.13 The lymphatic histopathologic subtype of atypical vascular lesions may appear similar to ALC; however, the vascular subtype will demonstrate collections of capillary-sized vessels and extravasated erythrocytes.11,12 Unlike ALC, the benign nature of atypical vascular lesions has been questioned, as they may be associated with a small risk for progression to angiosarcoma.11-13 It also is important to distinguish ALC from lymphangiomatosis, a generalized lymphatic anomaly that is characterized by extensive lymphatic malformations involving numerous internal organs, including the lungs and gastrointestinal tract. This condition is associated with notable morbidity and mortality.13
Although the suffix of the term lymphangioma suggests a neoplastic process, ALC is not a neoplasm and can be managed expectantly in many cases.2,3,8 However, due to cosmetic appearance, pain, discomfort, and recurrent bacterial superinfections, many patients pursue treatment. Treatment options for ALC include sclerotherapy, electrocautery, radiofrequency or carbon dioxide laser ablation, and excision, though recurrence can arise.3-5,7,8 Our patient elected to manage her asymptomatic ALC expectantly.
The Diagnosis: Acquired Lymphangioma Circumscriptum
A skin biopsy of the plaque on the right labium majus showed a proliferation of well-formed, dilated lymphatic vessels lined by benign-appearing endothelial cells in the papillary dermis (Figure). These findings were consistent with a diagnosis of acquired lymphangioma circumscriptum (ALC) in the setting of severe hidradenitis suppurativa (HS).
Acquired lymphangioma circumscriptum (also known as acquired lymphangiectasia or secondary lymphangioma1) is a rare skin finding resulting from chronic lymphatic obstruction that leads to dilated lymphatic vessels within the dermis.2,3 There also is a distinct congenital form of lymphangioma circumscriptum caused by lymphatic malformations present at birth.2,4 Acquired lymphangioma circumscriptum of the vulva is a rare phenomenon.3 Identified causes include radiation or surgery for carcinoma, solid gynecologic tumors, lymphadenectomy, Crohn disease, and tuberculosis and other infections, all of which can disrupt normal lymphatics to cause ALC.2-4 Hidradenitis suppurativa is not a widely recognized cause of ALC; however, this phenomenon is reported in the literature. A long-standing history of severe HS complicated by lymphedema seems to precede the development of ALC in the reported cases, as in our patient.5-7
Acquired lymphangioma circumscriptum of the vulva can appear in women of all ages as frog spawn or cobblestone papules or vesicles, sometimes with a hyperkeratotic or verrucous appearance.2,4 Associated symptoms include serous drainage, edema, pruritus, and discomfort. The lesions may become eroded, which can predispose patients to secondary infections.1,2 Acquired lymphangioma circumscriptum of the vulva can be difficult to diagnose, as the time interval between the initial cause and the appearance of skin findings can be years, leading to the misdiagnosis of ALC as other similar-appearing genital skin conditions such as squamous cell carcinoma or condyloma.4,8 When misidentified as an infection, diagnosis can lead to substantial distress, abstinence from sexual activity, and unnecessary and painful treatments.
Skin biopsy is helpful in distinguishing ALC from other differential diagnoses such as condylomata acuminata, squamous cell carcinoma, and condyloma lata. Histopathology in ALC is notable for dilated lymphatic vessels filled with hypocellular fluid and lined with endothelial cells in the superficial dermis; the epidermis can appear hyperplastic, hyperkeratotic, or eroded.3-5,9 These lymphatic vessels stain positively for CD31 and D2-40, markers for endothelial cells and lymphatic endothelium, respectively, and negative for CD34, a marker for vascular endothelium.3,4,9 Features suggestive of condylomata acuminata such as rounded parakeratosis, hypergranulosis, and vacuolated keratinocytes9 are not present. The giant condyloma of Buschke-Löwenstein, a clinical variant of verrucous squamous cell carcinoma, also can present as a warty ulcerated papule or plaque in the genital region, but the characteristic rounded eosinophilic keratinocytes pushing down into the dermis9 are not seen in ALC. Secondary syphilis is associated with condyloma lata, which are verrucous or fleshy-appearing papules often coalescing into plaques located in the anogenital region. Pathologic features of secondary syphilis include vacuolar interface dermatitis and acanthosis with long slender rete ridges.9 Squamous cell carcinoma, which can arise from inflammation associated with long-standing HS, must be ruled out, as it is associated with a high risk of mortality in patients with HS.10
It is noteworthy to recognize the various, often confusing nomenclature used to describe cutaneous lymphatic conditions. The terms acquired lymphangioma circumscriptum, secondary lymphangioma, and lymphangiectasia are used interchangeably to describe dilated lymphatic vessels in the skin.1 The term atypical vascular lesion refers to lymphectasias of the skin of the breast due to prior radiation therapy most often used in the treatment of breast carcinoma; clinically, these present as red-brown or flesh-colored papules or telangiectatic plaques on the breast.11,12 Lymphedema also may occur alongside atypical vascular lesions, as prior radiation or surgical lymph node dissection can predispose patients to impaired lymphatic drainage.13 The lymphatic histopathologic subtype of atypical vascular lesions may appear similar to ALC; however, the vascular subtype will demonstrate collections of capillary-sized vessels and extravasated erythrocytes.11,12 Unlike ALC, the benign nature of atypical vascular lesions has been questioned, as they may be associated with a small risk for progression to angiosarcoma.11-13 It also is important to distinguish ALC from lymphangiomatosis, a generalized lymphatic anomaly that is characterized by extensive lymphatic malformations involving numerous internal organs, including the lungs and gastrointestinal tract. This condition is associated with notable morbidity and mortality.13
Although the suffix of the term lymphangioma suggests a neoplastic process, ALC is not a neoplasm and can be managed expectantly in many cases.2,3,8 However, due to cosmetic appearance, pain, discomfort, and recurrent bacterial superinfections, many patients pursue treatment. Treatment options for ALC include sclerotherapy, electrocautery, radiofrequency or carbon dioxide laser ablation, and excision, though recurrence can arise.3-5,7,8 Our patient elected to manage her asymptomatic ALC expectantly.
- Verma SB. Lymphangiectasias of the skin: victims of confusing nomenclature. Clin Exp Dermatol. 2009;34:566-569.
- Vlastos AT, Malpica A, Follen M. Lymphangioma circumscriptum of the vulva: a review of the literature. Obstet Gynecol. 2003;101:946-954.
- Chang MB, Newman CC, Davis MD, et al. Acquired lymphangiectasia (lymphangioma circumscriptum) of the vulva: clinicopathologic study of 11 patients from a single institution and 67 from the literature. Int J Dermatol. 2016;55:E482-E487.
- Stewart CJ, Chan T, Platten M. Acquired lymphangiectasia (‘lymphangioma circumscriptum’) of the vulva: a report of eight cases. Pathology. 2009;41:448-453.
- Sims SM, McLean FW, Davis JD, et al. Vulvar lymphangioma circumscriptum: a report of 3 cases, 2 associated with vulvar carcinoma and 1 with hidradenitis suppurativa. J Low Genit Tract Dis. 2010; 14:234-237.
- Moosbrugger EA, Mutasim DF. Hidradenitis suppurativa complicated by severe lymphedema and lymphangiectasias. J Am Acad Dermatol. 2011;6:1223-1224.
- Piernick DM 2nd, Mahmood SH, Daveluy S. Acquired lymphangioma circumscriptum of the genitals in an individual with chronic hidradenitis suppurativa. JAAD Case Rep. 2018;1:64-66.
- Horn LC, Kühndel K, Pawlowitsch T, et al. Acquired lymphangioma circumscriptum of the vulva mimicking genital warts. Eur J Obstet Gynecol Reprod Biol. 2005;1:118-120.
- Elston DM, Ferringer T, Ko CJ, et al. Dermatopathology. 3rd ed. Elsevier; 2019.
- Kohorst JJ, Shah KK, Hallemeier CL, et al. Squamous cell carcinoma in perineal, perianal, and gluteal hidradenitis suppurativa: experience in 12 patients. Dermatol Surg. 2019;45:519-526.
- Patton KT, Deyrup AT, Weiss SW. Atypical vascular lesions after surgery and radiation of the breast: a clinicopathologic study of 32 cases analyzing histologic heterogeneity and association with angiosarcoma. Am J Surg Pathol. 2008;32:943-950.
- Ronen S, Ivan D, Torres-Cabala CA, et al. Post-radiation vascular lesions of the breast. J Cutan Pathol. 2019;46:52-58.
- Bolognia JL, Schaffer JV, Cerroni L. Dermatology. 4th ed. Elsevier; 2018.
- Verma SB. Lymphangiectasias of the skin: victims of confusing nomenclature. Clin Exp Dermatol. 2009;34:566-569.
- Vlastos AT, Malpica A, Follen M. Lymphangioma circumscriptum of the vulva: a review of the literature. Obstet Gynecol. 2003;101:946-954.
- Chang MB, Newman CC, Davis MD, et al. Acquired lymphangiectasia (lymphangioma circumscriptum) of the vulva: clinicopathologic study of 11 patients from a single institution and 67 from the literature. Int J Dermatol. 2016;55:E482-E487.
- Stewart CJ, Chan T, Platten M. Acquired lymphangiectasia (‘lymphangioma circumscriptum’) of the vulva: a report of eight cases. Pathology. 2009;41:448-453.
- Sims SM, McLean FW, Davis JD, et al. Vulvar lymphangioma circumscriptum: a report of 3 cases, 2 associated with vulvar carcinoma and 1 with hidradenitis suppurativa. J Low Genit Tract Dis. 2010; 14:234-237.
- Moosbrugger EA, Mutasim DF. Hidradenitis suppurativa complicated by severe lymphedema and lymphangiectasias. J Am Acad Dermatol. 2011;6:1223-1224.
- Piernick DM 2nd, Mahmood SH, Daveluy S. Acquired lymphangioma circumscriptum of the genitals in an individual with chronic hidradenitis suppurativa. JAAD Case Rep. 2018;1:64-66.
- Horn LC, Kühndel K, Pawlowitsch T, et al. Acquired lymphangioma circumscriptum of the vulva mimicking genital warts. Eur J Obstet Gynecol Reprod Biol. 2005;1:118-120.
- Elston DM, Ferringer T, Ko CJ, et al. Dermatopathology. 3rd ed. Elsevier; 2019.
- Kohorst JJ, Shah KK, Hallemeier CL, et al. Squamous cell carcinoma in perineal, perianal, and gluteal hidradenitis suppurativa: experience in 12 patients. Dermatol Surg. 2019;45:519-526.
- Patton KT, Deyrup AT, Weiss SW. Atypical vascular lesions after surgery and radiation of the breast: a clinicopathologic study of 32 cases analyzing histologic heterogeneity and association with angiosarcoma. Am J Surg Pathol. 2008;32:943-950.
- Ronen S, Ivan D, Torres-Cabala CA, et al. Post-radiation vascular lesions of the breast. J Cutan Pathol. 2019;46:52-58.
- Bolognia JL, Schaffer JV, Cerroni L. Dermatology. 4th ed. Elsevier; 2018.
A 38-year-old woman with long-standing severe hidradenitis suppurativa presented to our dermatology clinic with an asymptomatic, slowly enlarging growth on the right labium majus of 2 years’ duration. She also had severe persistent drainage from nodules and sinus tracts involving the abdominal pannus, inguinal folds, vulva, perineum, buttocks, and upper thighs. After treatment failure with oral antibiotics and adalimumab, her regimen included infliximab-dyyb, chronic systemic steroids, spironolactone, topical clindamycin, and benzoyl peroxide, with plans for eventual surgical intervention. Physical examination revealed the patient had numerous pink papules coalescing into a plaque on the right labium majus. She also had innumerable papulonodules, sinus tracts, and indurated scars in the inguinal folds, genitalia, and perineal region from severe hidradenitis suppurativa.

Patient blinded in one eye from surgery wins $1.2 million
Carola Rozon visited New York ophthalmologic surgeon Edwin Schottenstein, MD, in 2013 to undergo a second eye surgery, according to court documents. As with the previous surgery, Dr. Schottenstein performed phacoemulsification, a technique by which the tip of an ultrasonic machine is inserted into the lens through a small incision in the anterior chamber. The machine’s vibrations break up the hard, inner portion of the nucleus that is affected by the cataract, and the lens is then extracted with irrigation and suction, leaving the capsular bag filled with fluid.
Dr. Schottenstein made a 2.75-mm incision in the anterior chamber and successfully removed most of the nucleus of the cataract lens, according to the appellate decision. However, complications arose during the surgery when the capsular bag tore, and a piece of the lens dropped through the tear into the back of the patient’s eye.
Following the complications, Dr. Schottenstein injected a folded 6-mm intraocular lens (IOL) into the patient’s eye, but it was off center and moved toward the back, according to court documents. He removed it with holding forceps, pulling the unfolded 6-mm IOL through the 2.75-mm incision.
Because it was New Years Eve, Dr. Schottenstein did not immediately seek assistance from a vitreoretinal surgeon. Two days later, on Jan. 2, 2014, the patient was referred to a vitreoretinal surgeon for removal of the dropped lens. The vitreoretinal surgeon reported signs of trauma to the patient’s eye, including corneal edema and blood from a vitreous hemorrhage. Neither the ophthalmologist nor the vitreoretinal surgeon reported any injury to the patient’s iris.
Because of the vitreous hemorrhage, the vitreoretinal surgeon could not visualize the back of the eye. He used a B-scan ultrasound to create an image of the back of the eye to determine whether there were any retinal tears. According to court records, the vitreoretinal surgeon reported that the B-scan did not detect any retinal tears, and the vitreoretinal surgeon scheduled the patient for a follow-up the following week.
On Jan. 9, 2014, there was still blood in the patient’s eye from the hemorrhage. The vitreoretinal surgeon did not perform another B scan and stated that, with a fundoscope, he could see the back of the eye and the piece of fallen lens, according to court documents. No retinal tears were seen. Surgery was scheduled for 6 days later.
During the surgery, the vitreoretinal surgeon noted a choroidal effusion, swelling of the blood vessels that feed the retina. After draining it, he saw a giant retinal tear and retinal detachment at the top of the patient’s eye. Over the course of a year, the vitreoretinal surgeon performed five more surgeries to repair the giant retinal tear, but they were unsuccessful. Ultimately, the patient lost sight in her right eye.
The patient sued Dr. Schottenstein for malpractice in 2016, alleging that, as a result of his negligence, she suffered the retinal tear and is now blind in her right eye. A trial took place in November 2019.
What did the experts say?
At trial, the plaintiff’s expert, an ophthalmologic surgeon, testified that removing the 6-mm IOL through the 2.75-mm incision and the associated manipulations of the patient’s eye caused the retinal tear and the ensuing retinal detachment, according to court documents. The small tear was not immediately seen by the physician because he was not looking at that part of the eye. The tear grew to become the giant tear eventually seen by the vitreoretinal surgeon, the expert testified.
The vitreoretinal surgeon would not have seen the small retinal tear when he first examined the patient because B-scan ultrasounds are not generally used to diagnose retinal tears, he testified.
A vitreoretinal expert for Dr. Schottenstein testified that retinal tears that are tractional in origin tend to have a retinal flap that can be seen as a small indentation on a B-scan ultrasound. However, a tear with no flap would not be visualized by the scan. An ophthalmologic surgeon who testified for Dr. Schottenstein said it’s possible the retinal tear would not have been visible to Dr. Schottenstein or the vitreoretinal surgeon if vitreous fluid that was pulled into the anterior chamber was not a strand but just a blob too small to distort the pupil.
The jury found for the plaintiff, awarding the patient $1.2 million. Dr. Schottenstein requested the trial court to overturn the jury’s verdict and award judgment in his favor or grant a new trial, which was denied.
On March 1, 2022, the Supreme Court Appellate Division of the First Judicial Department affirmed the decision.
“To be against the weight of the evidence, a verdict must be palpably wrong,” the judges wrote in their opinion. “In this case, we cannot say the verdict is palpably wrong. The jury found that plaintiff’s injuries were proximately caused by defendant. They deemed the testimony of plaintiff’s expert, when considered with the documentary evidence and all the other evidence in the case, more credible than the testimony of the vitreoretinal surgeon, and defendant’s expert witnesses. The differing testimony and conclusions on causation given by defendant’s witnesses do not require a different outcome.”
Attorneys for the parties in this case did not return messages seeking comment.
A version of this article first appeared on Medscape.com.
Carola Rozon visited New York ophthalmologic surgeon Edwin Schottenstein, MD, in 2013 to undergo a second eye surgery, according to court documents. As with the previous surgery, Dr. Schottenstein performed phacoemulsification, a technique by which the tip of an ultrasonic machine is inserted into the lens through a small incision in the anterior chamber. The machine’s vibrations break up the hard, inner portion of the nucleus that is affected by the cataract, and the lens is then extracted with irrigation and suction, leaving the capsular bag filled with fluid.
Dr. Schottenstein made a 2.75-mm incision in the anterior chamber and successfully removed most of the nucleus of the cataract lens, according to the appellate decision. However, complications arose during the surgery when the capsular bag tore, and a piece of the lens dropped through the tear into the back of the patient’s eye.
Following the complications, Dr. Schottenstein injected a folded 6-mm intraocular lens (IOL) into the patient’s eye, but it was off center and moved toward the back, according to court documents. He removed it with holding forceps, pulling the unfolded 6-mm IOL through the 2.75-mm incision.
Because it was New Years Eve, Dr. Schottenstein did not immediately seek assistance from a vitreoretinal surgeon. Two days later, on Jan. 2, 2014, the patient was referred to a vitreoretinal surgeon for removal of the dropped lens. The vitreoretinal surgeon reported signs of trauma to the patient’s eye, including corneal edema and blood from a vitreous hemorrhage. Neither the ophthalmologist nor the vitreoretinal surgeon reported any injury to the patient’s iris.
Because of the vitreous hemorrhage, the vitreoretinal surgeon could not visualize the back of the eye. He used a B-scan ultrasound to create an image of the back of the eye to determine whether there were any retinal tears. According to court records, the vitreoretinal surgeon reported that the B-scan did not detect any retinal tears, and the vitreoretinal surgeon scheduled the patient for a follow-up the following week.
On Jan. 9, 2014, there was still blood in the patient’s eye from the hemorrhage. The vitreoretinal surgeon did not perform another B scan and stated that, with a fundoscope, he could see the back of the eye and the piece of fallen lens, according to court documents. No retinal tears were seen. Surgery was scheduled for 6 days later.
During the surgery, the vitreoretinal surgeon noted a choroidal effusion, swelling of the blood vessels that feed the retina. After draining it, he saw a giant retinal tear and retinal detachment at the top of the patient’s eye. Over the course of a year, the vitreoretinal surgeon performed five more surgeries to repair the giant retinal tear, but they were unsuccessful. Ultimately, the patient lost sight in her right eye.
The patient sued Dr. Schottenstein for malpractice in 2016, alleging that, as a result of his negligence, she suffered the retinal tear and is now blind in her right eye. A trial took place in November 2019.
What did the experts say?
At trial, the plaintiff’s expert, an ophthalmologic surgeon, testified that removing the 6-mm IOL through the 2.75-mm incision and the associated manipulations of the patient’s eye caused the retinal tear and the ensuing retinal detachment, according to court documents. The small tear was not immediately seen by the physician because he was not looking at that part of the eye. The tear grew to become the giant tear eventually seen by the vitreoretinal surgeon, the expert testified.
The vitreoretinal surgeon would not have seen the small retinal tear when he first examined the patient because B-scan ultrasounds are not generally used to diagnose retinal tears, he testified.
A vitreoretinal expert for Dr. Schottenstein testified that retinal tears that are tractional in origin tend to have a retinal flap that can be seen as a small indentation on a B-scan ultrasound. However, a tear with no flap would not be visualized by the scan. An ophthalmologic surgeon who testified for Dr. Schottenstein said it’s possible the retinal tear would not have been visible to Dr. Schottenstein or the vitreoretinal surgeon if vitreous fluid that was pulled into the anterior chamber was not a strand but just a blob too small to distort the pupil.
The jury found for the plaintiff, awarding the patient $1.2 million. Dr. Schottenstein requested the trial court to overturn the jury’s verdict and award judgment in his favor or grant a new trial, which was denied.
On March 1, 2022, the Supreme Court Appellate Division of the First Judicial Department affirmed the decision.
“To be against the weight of the evidence, a verdict must be palpably wrong,” the judges wrote in their opinion. “In this case, we cannot say the verdict is palpably wrong. The jury found that plaintiff’s injuries were proximately caused by defendant. They deemed the testimony of plaintiff’s expert, when considered with the documentary evidence and all the other evidence in the case, more credible than the testimony of the vitreoretinal surgeon, and defendant’s expert witnesses. The differing testimony and conclusions on causation given by defendant’s witnesses do not require a different outcome.”
Attorneys for the parties in this case did not return messages seeking comment.
A version of this article first appeared on Medscape.com.
Carola Rozon visited New York ophthalmologic surgeon Edwin Schottenstein, MD, in 2013 to undergo a second eye surgery, according to court documents. As with the previous surgery, Dr. Schottenstein performed phacoemulsification, a technique by which the tip of an ultrasonic machine is inserted into the lens through a small incision in the anterior chamber. The machine’s vibrations break up the hard, inner portion of the nucleus that is affected by the cataract, and the lens is then extracted with irrigation and suction, leaving the capsular bag filled with fluid.
Dr. Schottenstein made a 2.75-mm incision in the anterior chamber and successfully removed most of the nucleus of the cataract lens, according to the appellate decision. However, complications arose during the surgery when the capsular bag tore, and a piece of the lens dropped through the tear into the back of the patient’s eye.
Following the complications, Dr. Schottenstein injected a folded 6-mm intraocular lens (IOL) into the patient’s eye, but it was off center and moved toward the back, according to court documents. He removed it with holding forceps, pulling the unfolded 6-mm IOL through the 2.75-mm incision.
Because it was New Years Eve, Dr. Schottenstein did not immediately seek assistance from a vitreoretinal surgeon. Two days later, on Jan. 2, 2014, the patient was referred to a vitreoretinal surgeon for removal of the dropped lens. The vitreoretinal surgeon reported signs of trauma to the patient’s eye, including corneal edema and blood from a vitreous hemorrhage. Neither the ophthalmologist nor the vitreoretinal surgeon reported any injury to the patient’s iris.
Because of the vitreous hemorrhage, the vitreoretinal surgeon could not visualize the back of the eye. He used a B-scan ultrasound to create an image of the back of the eye to determine whether there were any retinal tears. According to court records, the vitreoretinal surgeon reported that the B-scan did not detect any retinal tears, and the vitreoretinal surgeon scheduled the patient for a follow-up the following week.
On Jan. 9, 2014, there was still blood in the patient’s eye from the hemorrhage. The vitreoretinal surgeon did not perform another B scan and stated that, with a fundoscope, he could see the back of the eye and the piece of fallen lens, according to court documents. No retinal tears were seen. Surgery was scheduled for 6 days later.
During the surgery, the vitreoretinal surgeon noted a choroidal effusion, swelling of the blood vessels that feed the retina. After draining it, he saw a giant retinal tear and retinal detachment at the top of the patient’s eye. Over the course of a year, the vitreoretinal surgeon performed five more surgeries to repair the giant retinal tear, but they were unsuccessful. Ultimately, the patient lost sight in her right eye.
The patient sued Dr. Schottenstein for malpractice in 2016, alleging that, as a result of his negligence, she suffered the retinal tear and is now blind in her right eye. A trial took place in November 2019.
What did the experts say?
At trial, the plaintiff’s expert, an ophthalmologic surgeon, testified that removing the 6-mm IOL through the 2.75-mm incision and the associated manipulations of the patient’s eye caused the retinal tear and the ensuing retinal detachment, according to court documents. The small tear was not immediately seen by the physician because he was not looking at that part of the eye. The tear grew to become the giant tear eventually seen by the vitreoretinal surgeon, the expert testified.
The vitreoretinal surgeon would not have seen the small retinal tear when he first examined the patient because B-scan ultrasounds are not generally used to diagnose retinal tears, he testified.
A vitreoretinal expert for Dr. Schottenstein testified that retinal tears that are tractional in origin tend to have a retinal flap that can be seen as a small indentation on a B-scan ultrasound. However, a tear with no flap would not be visualized by the scan. An ophthalmologic surgeon who testified for Dr. Schottenstein said it’s possible the retinal tear would not have been visible to Dr. Schottenstein or the vitreoretinal surgeon if vitreous fluid that was pulled into the anterior chamber was not a strand but just a blob too small to distort the pupil.
The jury found for the plaintiff, awarding the patient $1.2 million. Dr. Schottenstein requested the trial court to overturn the jury’s verdict and award judgment in his favor or grant a new trial, which was denied.
On March 1, 2022, the Supreme Court Appellate Division of the First Judicial Department affirmed the decision.
“To be against the weight of the evidence, a verdict must be palpably wrong,” the judges wrote in their opinion. “In this case, we cannot say the verdict is palpably wrong. The jury found that plaintiff’s injuries were proximately caused by defendant. They deemed the testimony of plaintiff’s expert, when considered with the documentary evidence and all the other evidence in the case, more credible than the testimony of the vitreoretinal surgeon, and defendant’s expert witnesses. The differing testimony and conclusions on causation given by defendant’s witnesses do not require a different outcome.”
Attorneys for the parties in this case did not return messages seeking comment.
A version of this article first appeared on Medscape.com.
Hybrid ACC 2022 resurrects the live scientific session
Regardless of the pandemic’s sometimes mercurial behavior, the cardiology community appears set to reclaim valued traditions perhaps taken for granted in the pre-COVID era.
They include the bustling scientific congress and its myriad educational and networking prospects, along with pleiotropic effects like unplanned reunions with colleagues and catching up face-to-face with old friends.
That seems evident in the growing number of registrants for live attendance at at the annual scientific sessions of the American College of Cardiology, set for this Saturday through Monday in Washington as well as virtually, for a global reach that was unattainable in the pre-COVID era.
Registrations had hit the 11,000 mark and were picking up speed in recent weeks, ACC 2022 cochair Pamela B. Morris, MD, Medical University of South Carolina, Charleston, said at a mid-March presentation to the media.
They had reached about 12,880 and were still climbing a week before the conference, the ACC confirmed to this news organization. By then the professional registration had surpassed 9,900, of whom more than two-thirds reported plans to attend in person.
Dr. Morris said there had been 117 international submissions for what turned out to be 39 coveted spots on the meeting’s Late-Breaking Clinical Trial (LBCT) and Featured Clinical Research agenda spread across eight separate sessions.
On-site participants at the Walter E. Washington Convention Center should head for the Main Tent in Hall D for all LBCT presentations; venues for the Featured Clinical Research sessions are as noted below. Their real-time virtual equivalents will reside on the online platform’s Hot Topics channel. All noted session times are Eastern Daylight Time.
Saturday, April 2, 9:30 a.m.–10:30 a.m. Joint American College of Cardiology/Journal of the American College of Cardiology LBCT (I)
Leading off the conference’s first LBCT session, the randomized VALOR-HCM trial explored whether 16 weeks of mavacamten (MyoKardia) could help patients with severe obstructive hypertrophic cardiomyopathy (HCM) avoid septal reduction therapy, either surgical or by alcohol ablation.
The 22-center VALOR-HCM trial with an estimated enrollment of 100 follows EXPLORER-HCM, which in 2020 suggested the novel myosin-inhibiting agent could improve symptoms, exercise capacity, cardiac remodeling, and quality of life in such patients.
Simply advising people with heart failure (HF) to consume less salt is one thing, but it’s another to show them clinical trial evidence that it might help keep them out of the hospital. The SODIUM-HF (Study of Dietary Intervention Under 100 mmol in Heart Failure) study, conducted at 27 sites in six countries, sought to provide that evidence.
The trial randomly assigned 1,000 patients with NYHA class 2-3 HF to consume no more than 1,500 mg/day in sodium or to receive standard advice to limit sodium intake, and followed them for a year for the endpoint of death from any cause, cardiovascular (CV) hospitalization, or CV emergency department visit.
SODIUM-HF “may provide a rigorous evidence base for sodium restriction in patients with heart failure and may truly change our practice and how we recommend dietary modification,” ACC 2022 vice chair Douglas E. Drachman, MD, Massachusetts General Hospital, Boston, said at the media presentation.
In the same session, the CHAP (Chronic Hypertension and Pregnancy) study explored whether blood pressure (BP) control in pregnant women with new or untreated chronic hypertension could help avert preeclampsia, poor fetal outcomes, and other adverse events.
CHAP assigned about 2,400 women to receive either stepwise antihypertensive therapy to a BP goal of 140/90 mm Hg or lower or no such meds unless their BP reached or exceeded 160/105 mm Hg. Stepwise therapy featured either labetalol or extended-release nifedipine to start, the other agent added as necessary.
The LBCT block also includes the POISE-3 (Perioperative Ischemic Evaluation-3) comparison of the hemostatic agent tranexamic acid vs. placebo in nearly 10,000 patients undergoing noncardiac surgery. A separate randomization of the same cohort, to be reported at a Monday LBCT session, compared pre- and perioperative BP-control strategies.
Saturday, April 2, 12:00 p.m.–1:15 p.m. Featured Clinical Research I. Room 143A
This session features a subgroup analysis by age from the REVERSE-IT trial, which had previously showcased the monoclonal antibody bentracimab (PhaseBio Pharmaceuticals) for its ability to reverse the antiplatelet effects of ticagrelor.
REVERSE-IT is accompanied on the schedule by several secondary-endpoint presentations from trials whose primary outcomes have already been presented at meetings or in the journals.
They include the SCORED trial of sotagliflozin in patients with diabetes and chronic kidney disease (CKD); COMPLETE, which explored complete revascularization of multivessel coronary disease at primary stenting; and the FAME-3 comparison of coronary bypass surgery (CABG) vs. percutaneous coronary intervention (PCI) guided by fractional flow reserve (FFR) readings.
The session is to conclude with EDIT-CMD, which was a small, randomized assessment of diltiazem for improving microvascular dysfunction in patients with chronic angina despite nonobstructive coronary disease.
Sunday, April 3, 8:00 a.m.–9:15 a.m. Joint American College of Cardiology/Journal of the American Medical Association LBCT (II)
The SuperWIN (Supermarket Web Intervention) study tested an innovative strategy for community-based promotion of healthy lifestyle choices: point-of-purchase dietary education for grocery shoppers with an online instructional component, and follow-up to determine whether it influenced future food choices.
“Dietary interventions are notoriously difficult for us to implement, let alone to study scientifically,” Dr. Drachman observed. “So we think that there may be opportunity for dietary interventions to be best implemented at grocery stores where people are doing their shopping for food.”
SuperWIN compared supermarket shoppers with at least one CV risk factor who participated in the education intervention to a nonintervention control group for any changes in their DASH scores. The scores reflected consistency with the venerable DASH diet based on participants’ food purchases over 3 months.
In the same session, the MITIGATE trial explored whether daily administration of icosapent ethyl (Vascepa) might cut the risk of upper respiratory infection (especially from SARS-CoV-2 or seasonal influenza virus) in persons 50 or older with a history of clinical coronary, neurovascular, or peripheral vascular disease or revascularization. The trial has an estimated enrollment of 39,600.
Accompanying SuperWIN and MITIGATE are studies of several dyslipidemia drugs, including the discontinued antisense agent vupanorsen (Pfizer), as tested in TRANSLATE-TIMI 70; the PCSK9 inhibitor alirocumab (Praluent), explored for its effects on coronary plaque volume and composition in the PACMAN-AMI trial; and the APOLLO trial, a phase 1 evaluation of SLN360 (Silence Therapeutics), a short interfering ribonucleic acid (siRNA) that suppresses the molecular machinery in the liver that produces lipoprotein(a), or Lp(a).
The 32-patient APOLLO trial’s recently released top-line results suggested that SLN360 at varying dosages reduced Lp(a) levels by about one-half to more than 90%. Although elevated Lp(a) is known to track with CV risk, it remains to be shown whether dropping Lp(a) levels pharmacologically is protective.
Sunday, April 3, 9:45 a.m.–11:00 a.m. Joint American College of Cardiology/New England Journal of Medicine LBCT (III)
The meeting’s all-HF late-breaker session includes the METEORIC-HF trial, which compared the myotropic agent omecamtiv mecarbil (Cytokinetics) against placebo for effects on exercise performance over 20 weeks. The trial entered 276 patients with HF with reduced ejection fraction (HFrEF) and reduced peak VO2.
The GALACTIC-HF trial had previously suggested that the drug improved the risk of HF-related events or CV death in more than 8000 patients with HFrEF, those with the lowest ejection fractions benefiting the most.
This block of trials also features DIAMOND, the latest trial with a gemologic name to look at the potassium sequestrant patiromer (Veltassa) for any protection against hyperkalemia, a familiar side effect of renin-angiotensin-aldosterone inhibitors. DIAMOND tested patiromer in 878 patients with HFrEF who were on beta-blockers and other HF-appropriate medications and had a history of drug-associated hyperkalemia.
Previously, the AMBER trial of patients with CKD or refractory hypertension on spironolactone had suggested the drug might be protective enough against hyperkalemia to allow higher and more consistent dosing of BP-lowering agents.
Also in the session: the randomized IVVE (Influenza Vaccine to Prevent Adverse Vascular Events) trial, with an estimated 5,000 patients with HF in Africa, Asia, and the Middle East; PROMPT-HF, with a projected 1,310 HF patients and billed as a cluster-randomized pragmatic trial of a strategy for improving guideline-directed outpatient medical therapy; and MAVA-LTE, the long-term extension study of an estimated 310 patients who were in the MAVERICK-HCM and EXPLORER-HCM mavacamten trials.
Sunday, April 3, 12:15–1:30 p.m. Featured Clinical Research II. Main Tent, Hall D
The arrhythmia-centric session includes PARTITA, with its estimated 590 patients with primary- or secondary-prevention implantable cardioverter-defibrillators (ICDs). The trial followed them initially for burden of untreated nonsustained ventricular tachycardia (VT) or events treated with anti-tachycardia pacing. Then it randomly assigned those who experienced a first appropriate ICD shock to either immediate VT ablation or standard care. The latter included ablation on next occurrence of arrhythmic storm.
Investigational oral factor XIa inhibitors, viewed by many as potentially safer as anticoagulants than contemporary oral inhibitors of factor Xa, are now on the scene and include milvexian (Bristol-Myers Squibb/Janssen) and, lately, asundexian (BAY 2433334; Bayer). The latter agent was compared to the factor Xa inhibitor apixaban (Eliquis) in 753 patients with AF in the phase 2 PACIFIC-AF trial, which looked at the newer drug’s safety and optimal dosing.
Also on the bill: a long-term follow-up of the mAFA-2 (Mobile AF Application 2) extension study, which explored the value of a smartphone-based atrial fibrillation (AF) screening app for improving risk of AF-related events; a presentation billed as “Residual Leaks Post Left Atrial Appendage Occlusion”; and one that declares “low rates of guideline-directed care” to be “associated with higher mortality” in patients with pacemakers or ICDs.
Monday, April 4, 8:30 a.m.–9:45 a.m. LBCT IV
This session is to open with the PROTECT trial, which sought to determine whether perioperative “aggressive warming” may be cardioprotective in patients with CV risk factors undergoing noncardiac surgery. Its estimated 5,100 patients were randomly assigned to a procedure that achieves normothermia, that is 37° C (98.6° F), vs. standard care in which patients’ core temperature may decline to no further than 35.5° C (95.9° F).
Next on the list are a second POISE-3 comparison of BP-control strategies comparing hypotension avoidance vs. hypertension avoidance in patients undergoing noncardiac surgery; the pivotal CLASP 2 TR trial of patients with symptomatic tricuspid regurgitation on optimal medical therapy with vs. without treatment with the Edwards PASCAL Transcatheter Repair System; and one said to provide “insights from the Corevalve US Pivotal and SURTAVI trials” on 5-year incidence, timing, and predictors of hemodynamic valve deterioration transcatheter and surgical aortic bioprostheses.”
Rounding out the block of presentations: the ADAPT-TAVR comparison of the factor Xa inhibitor edoxaban (Lixiana) to dual-antiplatelet therapy for prevention of leaflet thrombosis after successful transcatheter aortic valve replacement (TAVR). The 235-patient trial was conducted at five centers in South Korea, Hong Kong, and Taiwan.
Monday, April 4, 11:00–12:15 p.m. LBCT V
This session includes the FLAVOUR randomized comparison of PCI guided by either FFR or intravascular ultrasound (IVUS) in 1,700 patients with 40%-70% stenoses. The patients from centers in China and South Korea were followed for death from any cause, MI, or any repeat revascularization at 24 months.
Also scheduled: the 2-year report on 4,000 patients with ST-segment elevation MI (STEMI) in the ACC-sponsored quality improvement program GHATI (Global Heart Attack Treatment Initiative); the GIPS-4 myocardial protection study of an estimated 380 patients with STEMI assigned to receive pre- and post-PCI infusions of sodium thiosulfate or placebo, with infarct size at 4 months as the primary endpoint; and a randomized test of an arrhythmia-monitoring implant for influence on clinical outcomes in 802 patients with a history of MI but no pacemaker or ICD indication, called BIO-GUARD-MI,
Last in the session: the Chocolate Touch Study of peripheral-artery angioplasty using a drug-coated balloon (DCB) with a confectionery name that treats lesions not with theobromine, but the antiproliferative mainstay paclitaxel.
The randomized comparison of the Chocolate Touch DCB (TriReme Medical) and the more established Lutonix DCB (Bard) assigned a projected 585 patients with symptomatic peripheral vascular disease to treatment of superficial femoral or popliteal artery lesions with one of the two paclitaxel-coated balloon catheters.
Monday, April 4, 12:45–2 p.m. Featured Clinical Research III. Room 143A
The final session features five subgroup analyses or other updates from trials that have already reported their primary outcomes. Among them is the SPYRAL HTN-ON MED trial, which helped to revitalize hopes for renal denervation therapy as a catheter-based treatment for drug-resistant hypertension by showing significant effects on both systolic and diastolic blood pressure. The new data follow the trial’s more than 400 patients out to 3 years.
There is also a symptom and quality-of-life analysis from the 530-patient EMPULSE trial of 530 patients with stabilized acute HF assigned in-hospital to start on empagliflozin (Jardiance) or placebo. The trial made a splash last year when it reported a significant improvement in risk for death or HF rehospitalization for its patients put on the SGLT2 inhibitor.
A secondary analysis from CANTOS is also featured; the trial had randomly assigned more than 10,000 patients with recent acute MI and elevated C-reactive protein (CRP) levels to receive or not receive the anti-inflammatory canakinumab (Ilaris). Those assigned to active therapy showed benefits for a range of outcomes, including CV mortality and stroke, but no decreases in cholesterol levels. Billing for the new CANTOS analysis promises insights on the “differential impact of residual inflammatory risk and residual cholesterol risk among atherosclerosis patients with and without chronic kidney disease.”
The session also features “trends and final results” from the NACMI (North American COVID-19 Myocardial Infarction) registry, which had shown excellent primary-PCI results without compromise of door-to-balloon times in patients with confirmed SARS-CoV-2 infection; and a FIDELITY analysis of cardiorenal endpoints by history of CV disease in the study’s more than 13,000 patients with diabetes and CKD assigned to placebo or finerenone (Kerendia), a mineralocorticoid receptor antagonist.
A version of this article first appeared on Medscape.com.
Regardless of the pandemic’s sometimes mercurial behavior, the cardiology community appears set to reclaim valued traditions perhaps taken for granted in the pre-COVID era.
They include the bustling scientific congress and its myriad educational and networking prospects, along with pleiotropic effects like unplanned reunions with colleagues and catching up face-to-face with old friends.
That seems evident in the growing number of registrants for live attendance at at the annual scientific sessions of the American College of Cardiology, set for this Saturday through Monday in Washington as well as virtually, for a global reach that was unattainable in the pre-COVID era.
Registrations had hit the 11,000 mark and were picking up speed in recent weeks, ACC 2022 cochair Pamela B. Morris, MD, Medical University of South Carolina, Charleston, said at a mid-March presentation to the media.
They had reached about 12,880 and were still climbing a week before the conference, the ACC confirmed to this news organization. By then the professional registration had surpassed 9,900, of whom more than two-thirds reported plans to attend in person.
Dr. Morris said there had been 117 international submissions for what turned out to be 39 coveted spots on the meeting’s Late-Breaking Clinical Trial (LBCT) and Featured Clinical Research agenda spread across eight separate sessions.
On-site participants at the Walter E. Washington Convention Center should head for the Main Tent in Hall D for all LBCT presentations; venues for the Featured Clinical Research sessions are as noted below. Their real-time virtual equivalents will reside on the online platform’s Hot Topics channel. All noted session times are Eastern Daylight Time.
Saturday, April 2, 9:30 a.m.–10:30 a.m. Joint American College of Cardiology/Journal of the American College of Cardiology LBCT (I)
Leading off the conference’s first LBCT session, the randomized VALOR-HCM trial explored whether 16 weeks of mavacamten (MyoKardia) could help patients with severe obstructive hypertrophic cardiomyopathy (HCM) avoid septal reduction therapy, either surgical or by alcohol ablation.
The 22-center VALOR-HCM trial with an estimated enrollment of 100 follows EXPLORER-HCM, which in 2020 suggested the novel myosin-inhibiting agent could improve symptoms, exercise capacity, cardiac remodeling, and quality of life in such patients.
Simply advising people with heart failure (HF) to consume less salt is one thing, but it’s another to show them clinical trial evidence that it might help keep them out of the hospital. The SODIUM-HF (Study of Dietary Intervention Under 100 mmol in Heart Failure) study, conducted at 27 sites in six countries, sought to provide that evidence.
The trial randomly assigned 1,000 patients with NYHA class 2-3 HF to consume no more than 1,500 mg/day in sodium or to receive standard advice to limit sodium intake, and followed them for a year for the endpoint of death from any cause, cardiovascular (CV) hospitalization, or CV emergency department visit.
SODIUM-HF “may provide a rigorous evidence base for sodium restriction in patients with heart failure and may truly change our practice and how we recommend dietary modification,” ACC 2022 vice chair Douglas E. Drachman, MD, Massachusetts General Hospital, Boston, said at the media presentation.
In the same session, the CHAP (Chronic Hypertension and Pregnancy) study explored whether blood pressure (BP) control in pregnant women with new or untreated chronic hypertension could help avert preeclampsia, poor fetal outcomes, and other adverse events.
CHAP assigned about 2,400 women to receive either stepwise antihypertensive therapy to a BP goal of 140/90 mm Hg or lower or no such meds unless their BP reached or exceeded 160/105 mm Hg. Stepwise therapy featured either labetalol or extended-release nifedipine to start, the other agent added as necessary.
The LBCT block also includes the POISE-3 (Perioperative Ischemic Evaluation-3) comparison of the hemostatic agent tranexamic acid vs. placebo in nearly 10,000 patients undergoing noncardiac surgery. A separate randomization of the same cohort, to be reported at a Monday LBCT session, compared pre- and perioperative BP-control strategies.
Saturday, April 2, 12:00 p.m.–1:15 p.m. Featured Clinical Research I. Room 143A
This session features a subgroup analysis by age from the REVERSE-IT trial, which had previously showcased the monoclonal antibody bentracimab (PhaseBio Pharmaceuticals) for its ability to reverse the antiplatelet effects of ticagrelor.
REVERSE-IT is accompanied on the schedule by several secondary-endpoint presentations from trials whose primary outcomes have already been presented at meetings or in the journals.
They include the SCORED trial of sotagliflozin in patients with diabetes and chronic kidney disease (CKD); COMPLETE, which explored complete revascularization of multivessel coronary disease at primary stenting; and the FAME-3 comparison of coronary bypass surgery (CABG) vs. percutaneous coronary intervention (PCI) guided by fractional flow reserve (FFR) readings.
The session is to conclude with EDIT-CMD, which was a small, randomized assessment of diltiazem for improving microvascular dysfunction in patients with chronic angina despite nonobstructive coronary disease.
Sunday, April 3, 8:00 a.m.–9:15 a.m. Joint American College of Cardiology/Journal of the American Medical Association LBCT (II)
The SuperWIN (Supermarket Web Intervention) study tested an innovative strategy for community-based promotion of healthy lifestyle choices: point-of-purchase dietary education for grocery shoppers with an online instructional component, and follow-up to determine whether it influenced future food choices.
“Dietary interventions are notoriously difficult for us to implement, let alone to study scientifically,” Dr. Drachman observed. “So we think that there may be opportunity for dietary interventions to be best implemented at grocery stores where people are doing their shopping for food.”
SuperWIN compared supermarket shoppers with at least one CV risk factor who participated in the education intervention to a nonintervention control group for any changes in their DASH scores. The scores reflected consistency with the venerable DASH diet based on participants’ food purchases over 3 months.
In the same session, the MITIGATE trial explored whether daily administration of icosapent ethyl (Vascepa) might cut the risk of upper respiratory infection (especially from SARS-CoV-2 or seasonal influenza virus) in persons 50 or older with a history of clinical coronary, neurovascular, or peripheral vascular disease or revascularization. The trial has an estimated enrollment of 39,600.
Accompanying SuperWIN and MITIGATE are studies of several dyslipidemia drugs, including the discontinued antisense agent vupanorsen (Pfizer), as tested in TRANSLATE-TIMI 70; the PCSK9 inhibitor alirocumab (Praluent), explored for its effects on coronary plaque volume and composition in the PACMAN-AMI trial; and the APOLLO trial, a phase 1 evaluation of SLN360 (Silence Therapeutics), a short interfering ribonucleic acid (siRNA) that suppresses the molecular machinery in the liver that produces lipoprotein(a), or Lp(a).
The 32-patient APOLLO trial’s recently released top-line results suggested that SLN360 at varying dosages reduced Lp(a) levels by about one-half to more than 90%. Although elevated Lp(a) is known to track with CV risk, it remains to be shown whether dropping Lp(a) levels pharmacologically is protective.
Sunday, April 3, 9:45 a.m.–11:00 a.m. Joint American College of Cardiology/New England Journal of Medicine LBCT (III)
The meeting’s all-HF late-breaker session includes the METEORIC-HF trial, which compared the myotropic agent omecamtiv mecarbil (Cytokinetics) against placebo for effects on exercise performance over 20 weeks. The trial entered 276 patients with HF with reduced ejection fraction (HFrEF) and reduced peak VO2.
The GALACTIC-HF trial had previously suggested that the drug improved the risk of HF-related events or CV death in more than 8000 patients with HFrEF, those with the lowest ejection fractions benefiting the most.
This block of trials also features DIAMOND, the latest trial with a gemologic name to look at the potassium sequestrant patiromer (Veltassa) for any protection against hyperkalemia, a familiar side effect of renin-angiotensin-aldosterone inhibitors. DIAMOND tested patiromer in 878 patients with HFrEF who were on beta-blockers and other HF-appropriate medications and had a history of drug-associated hyperkalemia.
Previously, the AMBER trial of patients with CKD or refractory hypertension on spironolactone had suggested the drug might be protective enough against hyperkalemia to allow higher and more consistent dosing of BP-lowering agents.
Also in the session: the randomized IVVE (Influenza Vaccine to Prevent Adverse Vascular Events) trial, with an estimated 5,000 patients with HF in Africa, Asia, and the Middle East; PROMPT-HF, with a projected 1,310 HF patients and billed as a cluster-randomized pragmatic trial of a strategy for improving guideline-directed outpatient medical therapy; and MAVA-LTE, the long-term extension study of an estimated 310 patients who were in the MAVERICK-HCM and EXPLORER-HCM mavacamten trials.
Sunday, April 3, 12:15–1:30 p.m. Featured Clinical Research II. Main Tent, Hall D
The arrhythmia-centric session includes PARTITA, with its estimated 590 patients with primary- or secondary-prevention implantable cardioverter-defibrillators (ICDs). The trial followed them initially for burden of untreated nonsustained ventricular tachycardia (VT) or events treated with anti-tachycardia pacing. Then it randomly assigned those who experienced a first appropriate ICD shock to either immediate VT ablation or standard care. The latter included ablation on next occurrence of arrhythmic storm.
Investigational oral factor XIa inhibitors, viewed by many as potentially safer as anticoagulants than contemporary oral inhibitors of factor Xa, are now on the scene and include milvexian (Bristol-Myers Squibb/Janssen) and, lately, asundexian (BAY 2433334; Bayer). The latter agent was compared to the factor Xa inhibitor apixaban (Eliquis) in 753 patients with AF in the phase 2 PACIFIC-AF trial, which looked at the newer drug’s safety and optimal dosing.
Also on the bill: a long-term follow-up of the mAFA-2 (Mobile AF Application 2) extension study, which explored the value of a smartphone-based atrial fibrillation (AF) screening app for improving risk of AF-related events; a presentation billed as “Residual Leaks Post Left Atrial Appendage Occlusion”; and one that declares “low rates of guideline-directed care” to be “associated with higher mortality” in patients with pacemakers or ICDs.
Monday, April 4, 8:30 a.m.–9:45 a.m. LBCT IV
This session is to open with the PROTECT trial, which sought to determine whether perioperative “aggressive warming” may be cardioprotective in patients with CV risk factors undergoing noncardiac surgery. Its estimated 5,100 patients were randomly assigned to a procedure that achieves normothermia, that is 37° C (98.6° F), vs. standard care in which patients’ core temperature may decline to no further than 35.5° C (95.9° F).
Next on the list are a second POISE-3 comparison of BP-control strategies comparing hypotension avoidance vs. hypertension avoidance in patients undergoing noncardiac surgery; the pivotal CLASP 2 TR trial of patients with symptomatic tricuspid regurgitation on optimal medical therapy with vs. without treatment with the Edwards PASCAL Transcatheter Repair System; and one said to provide “insights from the Corevalve US Pivotal and SURTAVI trials” on 5-year incidence, timing, and predictors of hemodynamic valve deterioration transcatheter and surgical aortic bioprostheses.”
Rounding out the block of presentations: the ADAPT-TAVR comparison of the factor Xa inhibitor edoxaban (Lixiana) to dual-antiplatelet therapy for prevention of leaflet thrombosis after successful transcatheter aortic valve replacement (TAVR). The 235-patient trial was conducted at five centers in South Korea, Hong Kong, and Taiwan.
Monday, April 4, 11:00–12:15 p.m. LBCT V
This session includes the FLAVOUR randomized comparison of PCI guided by either FFR or intravascular ultrasound (IVUS) in 1,700 patients with 40%-70% stenoses. The patients from centers in China and South Korea were followed for death from any cause, MI, or any repeat revascularization at 24 months.
Also scheduled: the 2-year report on 4,000 patients with ST-segment elevation MI (STEMI) in the ACC-sponsored quality improvement program GHATI (Global Heart Attack Treatment Initiative); the GIPS-4 myocardial protection study of an estimated 380 patients with STEMI assigned to receive pre- and post-PCI infusions of sodium thiosulfate or placebo, with infarct size at 4 months as the primary endpoint; and a randomized test of an arrhythmia-monitoring implant for influence on clinical outcomes in 802 patients with a history of MI but no pacemaker or ICD indication, called BIO-GUARD-MI,
Last in the session: the Chocolate Touch Study of peripheral-artery angioplasty using a drug-coated balloon (DCB) with a confectionery name that treats lesions not with theobromine, but the antiproliferative mainstay paclitaxel.
The randomized comparison of the Chocolate Touch DCB (TriReme Medical) and the more established Lutonix DCB (Bard) assigned a projected 585 patients with symptomatic peripheral vascular disease to treatment of superficial femoral or popliteal artery lesions with one of the two paclitaxel-coated balloon catheters.
Monday, April 4, 12:45–2 p.m. Featured Clinical Research III. Room 143A
The final session features five subgroup analyses or other updates from trials that have already reported their primary outcomes. Among them is the SPYRAL HTN-ON MED trial, which helped to revitalize hopes for renal denervation therapy as a catheter-based treatment for drug-resistant hypertension by showing significant effects on both systolic and diastolic blood pressure. The new data follow the trial’s more than 400 patients out to 3 years.
There is also a symptom and quality-of-life analysis from the 530-patient EMPULSE trial of 530 patients with stabilized acute HF assigned in-hospital to start on empagliflozin (Jardiance) or placebo. The trial made a splash last year when it reported a significant improvement in risk for death or HF rehospitalization for its patients put on the SGLT2 inhibitor.
A secondary analysis from CANTOS is also featured; the trial had randomly assigned more than 10,000 patients with recent acute MI and elevated C-reactive protein (CRP) levels to receive or not receive the anti-inflammatory canakinumab (Ilaris). Those assigned to active therapy showed benefits for a range of outcomes, including CV mortality and stroke, but no decreases in cholesterol levels. Billing for the new CANTOS analysis promises insights on the “differential impact of residual inflammatory risk and residual cholesterol risk among atherosclerosis patients with and without chronic kidney disease.”
The session also features “trends and final results” from the NACMI (North American COVID-19 Myocardial Infarction) registry, which had shown excellent primary-PCI results without compromise of door-to-balloon times in patients with confirmed SARS-CoV-2 infection; and a FIDELITY analysis of cardiorenal endpoints by history of CV disease in the study’s more than 13,000 patients with diabetes and CKD assigned to placebo or finerenone (Kerendia), a mineralocorticoid receptor antagonist.
A version of this article first appeared on Medscape.com.
Regardless of the pandemic’s sometimes mercurial behavior, the cardiology community appears set to reclaim valued traditions perhaps taken for granted in the pre-COVID era.
They include the bustling scientific congress and its myriad educational and networking prospects, along with pleiotropic effects like unplanned reunions with colleagues and catching up face-to-face with old friends.
That seems evident in the growing number of registrants for live attendance at at the annual scientific sessions of the American College of Cardiology, set for this Saturday through Monday in Washington as well as virtually, for a global reach that was unattainable in the pre-COVID era.
Registrations had hit the 11,000 mark and were picking up speed in recent weeks, ACC 2022 cochair Pamela B. Morris, MD, Medical University of South Carolina, Charleston, said at a mid-March presentation to the media.
They had reached about 12,880 and were still climbing a week before the conference, the ACC confirmed to this news organization. By then the professional registration had surpassed 9,900, of whom more than two-thirds reported plans to attend in person.
Dr. Morris said there had been 117 international submissions for what turned out to be 39 coveted spots on the meeting’s Late-Breaking Clinical Trial (LBCT) and Featured Clinical Research agenda spread across eight separate sessions.
On-site participants at the Walter E. Washington Convention Center should head for the Main Tent in Hall D for all LBCT presentations; venues for the Featured Clinical Research sessions are as noted below. Their real-time virtual equivalents will reside on the online platform’s Hot Topics channel. All noted session times are Eastern Daylight Time.
Saturday, April 2, 9:30 a.m.–10:30 a.m. Joint American College of Cardiology/Journal of the American College of Cardiology LBCT (I)
Leading off the conference’s first LBCT session, the randomized VALOR-HCM trial explored whether 16 weeks of mavacamten (MyoKardia) could help patients with severe obstructive hypertrophic cardiomyopathy (HCM) avoid septal reduction therapy, either surgical or by alcohol ablation.
The 22-center VALOR-HCM trial with an estimated enrollment of 100 follows EXPLORER-HCM, which in 2020 suggested the novel myosin-inhibiting agent could improve symptoms, exercise capacity, cardiac remodeling, and quality of life in such patients.
Simply advising people with heart failure (HF) to consume less salt is one thing, but it’s another to show them clinical trial evidence that it might help keep them out of the hospital. The SODIUM-HF (Study of Dietary Intervention Under 100 mmol in Heart Failure) study, conducted at 27 sites in six countries, sought to provide that evidence.
The trial randomly assigned 1,000 patients with NYHA class 2-3 HF to consume no more than 1,500 mg/day in sodium or to receive standard advice to limit sodium intake, and followed them for a year for the endpoint of death from any cause, cardiovascular (CV) hospitalization, or CV emergency department visit.
SODIUM-HF “may provide a rigorous evidence base for sodium restriction in patients with heart failure and may truly change our practice and how we recommend dietary modification,” ACC 2022 vice chair Douglas E. Drachman, MD, Massachusetts General Hospital, Boston, said at the media presentation.
In the same session, the CHAP (Chronic Hypertension and Pregnancy) study explored whether blood pressure (BP) control in pregnant women with new or untreated chronic hypertension could help avert preeclampsia, poor fetal outcomes, and other adverse events.
CHAP assigned about 2,400 women to receive either stepwise antihypertensive therapy to a BP goal of 140/90 mm Hg or lower or no such meds unless their BP reached or exceeded 160/105 mm Hg. Stepwise therapy featured either labetalol or extended-release nifedipine to start, the other agent added as necessary.
The LBCT block also includes the POISE-3 (Perioperative Ischemic Evaluation-3) comparison of the hemostatic agent tranexamic acid vs. placebo in nearly 10,000 patients undergoing noncardiac surgery. A separate randomization of the same cohort, to be reported at a Monday LBCT session, compared pre- and perioperative BP-control strategies.
Saturday, April 2, 12:00 p.m.–1:15 p.m. Featured Clinical Research I. Room 143A
This session features a subgroup analysis by age from the REVERSE-IT trial, which had previously showcased the monoclonal antibody bentracimab (PhaseBio Pharmaceuticals) for its ability to reverse the antiplatelet effects of ticagrelor.
REVERSE-IT is accompanied on the schedule by several secondary-endpoint presentations from trials whose primary outcomes have already been presented at meetings or in the journals.
They include the SCORED trial of sotagliflozin in patients with diabetes and chronic kidney disease (CKD); COMPLETE, which explored complete revascularization of multivessel coronary disease at primary stenting; and the FAME-3 comparison of coronary bypass surgery (CABG) vs. percutaneous coronary intervention (PCI) guided by fractional flow reserve (FFR) readings.
The session is to conclude with EDIT-CMD, which was a small, randomized assessment of diltiazem for improving microvascular dysfunction in patients with chronic angina despite nonobstructive coronary disease.
Sunday, April 3, 8:00 a.m.–9:15 a.m. Joint American College of Cardiology/Journal of the American Medical Association LBCT (II)
The SuperWIN (Supermarket Web Intervention) study tested an innovative strategy for community-based promotion of healthy lifestyle choices: point-of-purchase dietary education for grocery shoppers with an online instructional component, and follow-up to determine whether it influenced future food choices.
“Dietary interventions are notoriously difficult for us to implement, let alone to study scientifically,” Dr. Drachman observed. “So we think that there may be opportunity for dietary interventions to be best implemented at grocery stores where people are doing their shopping for food.”
SuperWIN compared supermarket shoppers with at least one CV risk factor who participated in the education intervention to a nonintervention control group for any changes in their DASH scores. The scores reflected consistency with the venerable DASH diet based on participants’ food purchases over 3 months.
In the same session, the MITIGATE trial explored whether daily administration of icosapent ethyl (Vascepa) might cut the risk of upper respiratory infection (especially from SARS-CoV-2 or seasonal influenza virus) in persons 50 or older with a history of clinical coronary, neurovascular, or peripheral vascular disease or revascularization. The trial has an estimated enrollment of 39,600.
Accompanying SuperWIN and MITIGATE are studies of several dyslipidemia drugs, including the discontinued antisense agent vupanorsen (Pfizer), as tested in TRANSLATE-TIMI 70; the PCSK9 inhibitor alirocumab (Praluent), explored for its effects on coronary plaque volume and composition in the PACMAN-AMI trial; and the APOLLO trial, a phase 1 evaluation of SLN360 (Silence Therapeutics), a short interfering ribonucleic acid (siRNA) that suppresses the molecular machinery in the liver that produces lipoprotein(a), or Lp(a).
The 32-patient APOLLO trial’s recently released top-line results suggested that SLN360 at varying dosages reduced Lp(a) levels by about one-half to more than 90%. Although elevated Lp(a) is known to track with CV risk, it remains to be shown whether dropping Lp(a) levels pharmacologically is protective.
Sunday, April 3, 9:45 a.m.–11:00 a.m. Joint American College of Cardiology/New England Journal of Medicine LBCT (III)
The meeting’s all-HF late-breaker session includes the METEORIC-HF trial, which compared the myotropic agent omecamtiv mecarbil (Cytokinetics) against placebo for effects on exercise performance over 20 weeks. The trial entered 276 patients with HF with reduced ejection fraction (HFrEF) and reduced peak VO2.
The GALACTIC-HF trial had previously suggested that the drug improved the risk of HF-related events or CV death in more than 8000 patients with HFrEF, those with the lowest ejection fractions benefiting the most.
This block of trials also features DIAMOND, the latest trial with a gemologic name to look at the potassium sequestrant patiromer (Veltassa) for any protection against hyperkalemia, a familiar side effect of renin-angiotensin-aldosterone inhibitors. DIAMOND tested patiromer in 878 patients with HFrEF who were on beta-blockers and other HF-appropriate medications and had a history of drug-associated hyperkalemia.
Previously, the AMBER trial of patients with CKD or refractory hypertension on spironolactone had suggested the drug might be protective enough against hyperkalemia to allow higher and more consistent dosing of BP-lowering agents.
Also in the session: the randomized IVVE (Influenza Vaccine to Prevent Adverse Vascular Events) trial, with an estimated 5,000 patients with HF in Africa, Asia, and the Middle East; PROMPT-HF, with a projected 1,310 HF patients and billed as a cluster-randomized pragmatic trial of a strategy for improving guideline-directed outpatient medical therapy; and MAVA-LTE, the long-term extension study of an estimated 310 patients who were in the MAVERICK-HCM and EXPLORER-HCM mavacamten trials.
Sunday, April 3, 12:15–1:30 p.m. Featured Clinical Research II. Main Tent, Hall D
The arrhythmia-centric session includes PARTITA, with its estimated 590 patients with primary- or secondary-prevention implantable cardioverter-defibrillators (ICDs). The trial followed them initially for burden of untreated nonsustained ventricular tachycardia (VT) or events treated with anti-tachycardia pacing. Then it randomly assigned those who experienced a first appropriate ICD shock to either immediate VT ablation or standard care. The latter included ablation on next occurrence of arrhythmic storm.
Investigational oral factor XIa inhibitors, viewed by many as potentially safer as anticoagulants than contemporary oral inhibitors of factor Xa, are now on the scene and include milvexian (Bristol-Myers Squibb/Janssen) and, lately, asundexian (BAY 2433334; Bayer). The latter agent was compared to the factor Xa inhibitor apixaban (Eliquis) in 753 patients with AF in the phase 2 PACIFIC-AF trial, which looked at the newer drug’s safety and optimal dosing.
Also on the bill: a long-term follow-up of the mAFA-2 (Mobile AF Application 2) extension study, which explored the value of a smartphone-based atrial fibrillation (AF) screening app for improving risk of AF-related events; a presentation billed as “Residual Leaks Post Left Atrial Appendage Occlusion”; and one that declares “low rates of guideline-directed care” to be “associated with higher mortality” in patients with pacemakers or ICDs.
Monday, April 4, 8:30 a.m.–9:45 a.m. LBCT IV
This session is to open with the PROTECT trial, which sought to determine whether perioperative “aggressive warming” may be cardioprotective in patients with CV risk factors undergoing noncardiac surgery. Its estimated 5,100 patients were randomly assigned to a procedure that achieves normothermia, that is 37° C (98.6° F), vs. standard care in which patients’ core temperature may decline to no further than 35.5° C (95.9° F).
Next on the list are a second POISE-3 comparison of BP-control strategies comparing hypotension avoidance vs. hypertension avoidance in patients undergoing noncardiac surgery; the pivotal CLASP 2 TR trial of patients with symptomatic tricuspid regurgitation on optimal medical therapy with vs. without treatment with the Edwards PASCAL Transcatheter Repair System; and one said to provide “insights from the Corevalve US Pivotal and SURTAVI trials” on 5-year incidence, timing, and predictors of hemodynamic valve deterioration transcatheter and surgical aortic bioprostheses.”
Rounding out the block of presentations: the ADAPT-TAVR comparison of the factor Xa inhibitor edoxaban (Lixiana) to dual-antiplatelet therapy for prevention of leaflet thrombosis after successful transcatheter aortic valve replacement (TAVR). The 235-patient trial was conducted at five centers in South Korea, Hong Kong, and Taiwan.
Monday, April 4, 11:00–12:15 p.m. LBCT V
This session includes the FLAVOUR randomized comparison of PCI guided by either FFR or intravascular ultrasound (IVUS) in 1,700 patients with 40%-70% stenoses. The patients from centers in China and South Korea were followed for death from any cause, MI, or any repeat revascularization at 24 months.
Also scheduled: the 2-year report on 4,000 patients with ST-segment elevation MI (STEMI) in the ACC-sponsored quality improvement program GHATI (Global Heart Attack Treatment Initiative); the GIPS-4 myocardial protection study of an estimated 380 patients with STEMI assigned to receive pre- and post-PCI infusions of sodium thiosulfate or placebo, with infarct size at 4 months as the primary endpoint; and a randomized test of an arrhythmia-monitoring implant for influence on clinical outcomes in 802 patients with a history of MI but no pacemaker or ICD indication, called BIO-GUARD-MI,
Last in the session: the Chocolate Touch Study of peripheral-artery angioplasty using a drug-coated balloon (DCB) with a confectionery name that treats lesions not with theobromine, but the antiproliferative mainstay paclitaxel.
The randomized comparison of the Chocolate Touch DCB (TriReme Medical) and the more established Lutonix DCB (Bard) assigned a projected 585 patients with symptomatic peripheral vascular disease to treatment of superficial femoral or popliteal artery lesions with one of the two paclitaxel-coated balloon catheters.
Monday, April 4, 12:45–2 p.m. Featured Clinical Research III. Room 143A
The final session features five subgroup analyses or other updates from trials that have already reported their primary outcomes. Among them is the SPYRAL HTN-ON MED trial, which helped to revitalize hopes for renal denervation therapy as a catheter-based treatment for drug-resistant hypertension by showing significant effects on both systolic and diastolic blood pressure. The new data follow the trial’s more than 400 patients out to 3 years.
There is also a symptom and quality-of-life analysis from the 530-patient EMPULSE trial of 530 patients with stabilized acute HF assigned in-hospital to start on empagliflozin (Jardiance) or placebo. The trial made a splash last year when it reported a significant improvement in risk for death or HF rehospitalization for its patients put on the SGLT2 inhibitor.
A secondary analysis from CANTOS is also featured; the trial had randomly assigned more than 10,000 patients with recent acute MI and elevated C-reactive protein (CRP) levels to receive or not receive the anti-inflammatory canakinumab (Ilaris). Those assigned to active therapy showed benefits for a range of outcomes, including CV mortality and stroke, but no decreases in cholesterol levels. Billing for the new CANTOS analysis promises insights on the “differential impact of residual inflammatory risk and residual cholesterol risk among atherosclerosis patients with and without chronic kidney disease.”
The session also features “trends and final results” from the NACMI (North American COVID-19 Myocardial Infarction) registry, which had shown excellent primary-PCI results without compromise of door-to-balloon times in patients with confirmed SARS-CoV-2 infection; and a FIDELITY analysis of cardiorenal endpoints by history of CV disease in the study’s more than 13,000 patients with diabetes and CKD assigned to placebo or finerenone (Kerendia), a mineralocorticoid receptor antagonist.
A version of this article first appeared on Medscape.com.
Gastric band failures drive many to safer weight loss surgeries
Jessica Furby struggled with weight most of her life, constantly dieting and exercising to shed pounds. But nothing seemed to help. By her 22nd birthday, she tipped the scales at more than 300 pounds.
So, in 2011, while a college student in Pittsburgh, she decided to have gastric band surgery. Doctors placed a synthetic belt around her stomach to limit what she could eat. It seemed like a good option at the time and, after her surgery, she lost about 60 pounds.
But the benefits didn’t last. In the months that followed, she had pain and other complications. Worst of all, she eventually regained all the weight she’d lost – and then some. By 2016, she weighed 350 pounds and was becoming prediabetic.
That’s when she decided to have the band removed and, on her doctor’s recommendation, had gastric sleeve surgery.
Studies have found the sleeve surgeries carry fewer complications and a much higher success rate than gastric band procedures, which Ms. Furby’s experience has confirmed.
Today, at age 32, she’s down to 288 pounds and says she is on her way to hitting her ultimate goal of 200 pounds.
“The surgery has been a godsend,” she said. “I have not had any complications with it at all. The sleeve was life-changing for me.”
Ms. Furby’s experience has become more common as the risks, complications, and failures of gastric band surgeries have been rising over the past decade.
, because of problems like Ms. Furby’s.
According to the latest figures from the American Society for Metabolic and Bariatric Surgery, gastric band procedures account for fewer than 1% of the 256,000 bariatric operations done in the United States each year, while gastric sleeves add up to nearly 60%. That makes sleeve surgeries the most commonly performed bariatric operation today.
By comparison, 35% of bariatric surgeries were gastric band procedures in 2011, while sleeve operations accounted for under 18%.
Ms. Furby’s surgeon, Anita P. Courcoulas, MD, said the trend is being driven by many of the things Ms.Furby experienced firsthand.
Dr. Courcoulas, chief of minimally invasive bariatric and general surgery at the University of Pittsburgh, said there are two main reasons for the decline in gastric band procedures.
“It has been shown to be less effective for weight loss [than] other bariatric surgical procedures, and band intolerance often results in band removal,” she noted.
Gastric sleeve, followed by gastric bypass, are the two most commonly performed operations in the United States and worldwide, she said.
Dr. Courcoulas said the shift from gastric bypass to gastric sleeve procedures “is likely driven by the decline in the band usage, patient preferences for a less invasive operation, such as the sleeve compared to bypass, and surgeon preferences about which operation(s) to offer a given patient.”
Ali Aminian, MD, director of the Bariatric and Metabolic Institute at the Cleveland Clinic, agrees that gastric band complications and failures, in addition to ineffective weight loss, are behind the trend, driving patients and doctors to choose safer and more effective procedures.
He said the Cleveland Clinic no longer does band operations, and he has done a lot of conversions.
“Around 50%-60% of [gastric band] patients require reoperation to take care of the complications,” he says. “So, when you have a surgery where more than half of the time the patients require reoperation, we cannot claim that’s a safe operation.”
Evolution in bariatric surgery
Bariatric surgeries for weight loss date back to the 1950s and 1960s, when surgeons at the University of Minnesota first did experimental bypass operations. Adjustable gastric banding appeared in the late 1970s and early 1980s.
But these procedures didn’t gain widespread mainstream use until gastric band procedures gained full Food and Drug Administration approval in 2001. Clinical trials have found people who have bariatric surgery have a significantly lower risk of heart disease and other obesity-related health problems.
In the decade that followed the FDA’s approval of gastric band surgery, it became a popular weight loss procedure, accounting for more than a third of all bariatric surgeries by 2011.
“Fifteen to 20 years ago, [gastric] band was the most commonly performed procedure for bariatric surgery worldwide and in the United States,” Dr. Aminian said. “It was very easy to do, it was quick – it takes 20 minutes to do the procedure – recovery was short, and initially patients had great outcomes. They would lose weight and were healthy.”
But over the past decade, surgeons found that patients often regained the weight they’d lost, and complication and failure rates rose.
“Because the [gastric] band is a foreign body that we place inside the body, many patients had complications related to that foreign body,” Dr. Aminian said.
The band can sometimes move or be displaced, causing blockage of the stomach, experts noted. Other common complications include nausea, vomiting, acid reflux, and esophageal issues (such as a hard time swallowing). Some patients feel pain, constant food cravings, or that they can’t eat or drink anything. And painful infections and other problems can develop with the tubing or the port placed under the skin that is connected to the band, which doctors use to make adjustments after surgery.
“Scar tissue can also form around the [gastric] band that can cause a blockage in the stomach,” Dr. Aminian said. “Then if the band is too tight, it can erode into the stomach tissue or even go inside the stomach and cause perforation or bleeding.”
By contrast, gastric sleeve and bypass procedures have been found to be safer, result in longer-lasting weight loss, carry fewer complications, and require fewer patient reoperations. Dr. Aminian estimates that 2%-3% of patients need second operations.
Another key factor: Metabolic ‘reset’
Sleeve and bypass procedures offer another critical advantage over band operations: They help reset the body’s metabolism better, changing appetite- and weight-related hormones in the body.
Those hormones can affect food cravings, help people feel full after eating, or boost weight gain in ways that can trump willpower, experts say.
“The [gastric] band doesn’t change the hormones in the body, it’s just a restrictive band around the esophagus or the upper part of the stomach, so it limits the patient’s ability to eat too much,” Dr. Aminian said. “That’s why it doesn’t have the metabolic effects.”
But other procedures, like the gastric sleeve, change the hormones in the body. Removing the source of those hormones means the patient won’t have the same appetite, Dr. Aminian said.
“And that’s why it’s very effective. The problem with the [gastric] band is the patient always has the feeling and desire to eat – they’re always hungry. That’s why in the long run, they fail,” he said.
“They change the setpoints,” Dr. Aminian said. “When the hormones in your body change, the [metabolic] setpoint in the brain also changes.”
He likens the metabolic setpoint to a thermostat in your home that regulates temperature inside.
“When a patient goes on a diet or goes on the [gastric] band, the thermostat doesn’t change,” he says. “They may lose some weight, but they’re going to regain it because the thermostat is the same. But when the hormones in your body change, then the thermostat will change and you’re not going to regain the weight that you have lost.”
Sachin Kukreja, MD, a surgeon and CEO at DFW Bariatrics and General Surgery in Dallas, said he believes these metabolic changes are the biggest things behind successful surgeries.
“People synonymize bariatric surgery with weight loss surgery, but really the metrics we should be using are more related to metabolic measures,” said Dr. Kukreja, who hasn’t done a band surgery since 2013. “And so, the metabolic parameters that change with bariatric surgery are much more significant in the setting with sleeve and gastric sleeve, and much less significant with [gastric] band.”
David Arterburn, MD, agrees that resetting metabolism is important but said the issue is “controversial and challenging” among bariatric surgeons.
“The metabolic setpoint is the idea that we have a biologically controlled set body weight that we will always return to. Clearly, this is not the case for everyone, as some people lose and maintain long-term weight loss,” said Dr. Arterburn, a general internist and bariatric surgery researcher at Kaiser Permanente Washington Health Research Institute in Seattle.
Postop lifestyle changes critical to success
Bariatric surgeons and patients alike also say that no surgical procedure is a magic-bullet solution for weight loss. Patients who have any type of bariatric surgery must embrace postop lifestyle changes – adopting healthier diets, getting more exercise, cutting out unhealthy habits – to lose weight and maintain weight loss.
Jan Lasecki, 54, a health care specialist in Akron, Ohio, who had band-to-sleeve conversion surgery in 2020, said the postop follow-up was at least as important as the surgery itself in helping her shed pounds.
She said at first, she chose gastric band surgery several years ago because it was “less invasive” than gastric sleeve or bypass. But while she lost about 50 pounds, she regained it after about 6 years and had other complications.
So, 2 years ago, Ms. Lasecki had two surgeries 6 months apart – one to remove her band, and a second to create a gastric sleeve. And the results, she said, have been very successful, in part because of the changes she made after surgery, with the help of her doctor’s staff.
“I have now lost about 90 pounds and have kept if off since surgery,” she says. “I would tell anyone considering any bariatric surgery, it was definitely worth it [and] having the sleeve resulted in greater weight loss.”
The follow-up was key to the success, she said.
The staff “have the tools and support to help you when you tend to fall back on old behaviors and start to regain weight,” Ms. Lasecki said. “They can help you before it gets out of control. I had no issues following either procedure from a surgery perspective.”
Sally and Robert Cordova – who had gastric bypass and sleeve surgeries, respectively, 3 years ago – agreed that the postop lifestyle changes are critical to success.
“When we agreed to have this surgery, we agreed that this will be a lifestyle change for the rest of our lives,” said Sally, 48, an accounting specialist who’s lost 150 pounds – half her body weight – since her surgery. “You can’t just get to your ideal weight and then stop.”
Robert, 47, a federal border control agent whose workmates nicknamed him “Big Rob” when he tipped the scales at 336 pounds, said it’s a mistake to think of the surgery as a “magic-bullet” solution to obesity. There’s more to it than that, he said.
“One of the things I like about the process I’ve taken is, in my opinion, they set you up for success,” he said. “Because it’s not just having the surgery and you’re done; it’s all the classes educating you about all the lifestyle changes you have to do, and starting them before the surgery. The only people that I know personally who haven’t been successful with the surgery are those who haven’t made the lifestyle changes.”
Today, at 230 pounds, Robert says he’s never felt better.
“I feel great,” he says. “I have become more active, obviously doing everything is a lot easier. It got to the point where it was a task to just tying up my shoes!”
Should band patients convert to sleeve or bypass?
Bariatric surgeons interviewed for this article were reluctant to say that all people who had gastric band procedures should convert to gastric sleeve or bypass. But they made it clear that sleeve and bypass procedures are safer and more effective than gastric band surgery, which is why it is rarely done today.
“If a patient experiences poor weight loss or complications from a band, they can consider conversion/revision to a sleeve or bypass,” said Dr. Courcoulas, echoing the views of other doctors.
“The choice of revision procedure should be based on patient factors, including diabetes and total weight. Converting a band to a sleeve is a technically easier operation, and some studies show that there are fewer complications, compared to conversion to a bypass. These considerations need to be balanced with data that show that both weight loss and metabolic improvements such as diabetes are greater after bypass, compared to sleeve.”
Doctors and experts also say it’s important for patients who are considering a gastric band conversion to gastric sleeve or bypass to understand the differences among these three primary procedures, all endorsed by the American Society for Metabolic and Bariatric Surgery.
Here’s a primer, including the pros and cons of each procedure:
Gastric band
In gastric band surgery, an adjustable gastric band made of silicone is placed around the top part of the stomach, creating a small pouch above it, to limit the amount of food a person can eat. The size of the opening between the pouch and the stomach can be adjusted with fluid injections through a port placed underneath the skin.
Food goes through the stomach but is limited by the smaller opening of the band.
Advantages:
- Lowest rate of complications right after surgery.
- No division of the stomach or intestines.
- Patients go home on the day of surgery, and recovery is quick.
- The band can be removed, if necessary.
Disadvantages:
- The band may need to be adjusted from time to time, and patients must make monthly office visits during the first year.
- There’s less weight loss than with other surgical procedures.
- It comes with the risk of band movement (slippage) or damage to the stomach over time (erosion).
- The surgery means that a foreign implant has to remain in the body.
- It has a high rate of reoperation.
- The surgery can bring swallowing problems, enlargement of the esophagus, and other complications.
Gastric sleeve
For laparoscopic sleeve gastrectomy – often called gastric sleeve – surgeons remove about 80% of the stomach, so the remaining stomach is the size and shape of a banana.
The new, smaller stomach holds less food and liquid, reducing how much food (and how many calories) the patient can get. By removing the portion of the stomach that produces hunger and appetite hormones, the surgery also helps reset the body’s metabolism – decreasing hunger, increasing feelings of fullness, and allowing the body to reach and maintain a healthy weight as well as control blood sugar.
Advantages:
- It’s technically simple and has a short surgery time.
- It can be done in certain patients with high-risk medical conditions.
- It may be the first step for patients with severe obesity or as a bridge to gastric bypass.
- The surgery brings effective weight loss and improvement of obesity-related conditions (typically 50%-60%, by Mayo Clinic estimates), with a low complication rate (2%-3%).
Disadvantages:
- Nonreversible procedure.
- May worsen or cause new reflux and heartburn.
- Less impact on metabolism, compared to bypass procedures.
Gastric bypass
Gastric bypass, also known as the Roux-en-Y gastric bypass (French for “in the form of a Y”) is another effective procedure used to treat obesity and obesity-related diseases (done laparoscopically since the 1990s).
For the operation, surgeons divide the stomach into a smaller top portion (pouch) about the size of an egg, then the larger part of the stomach is bypassed and no longer stores or digests food.
The small intestine is divided and connected to the new egg-sized stomach pouch to allow food to pass.
Gastric bypass works by limiting the amount of food and calories a patient can consume. It also decreases hunger and increases fullness, allowing the patient to reach and maintain a healthy weight. The impact on hormones and metabolic health often results in improvement of diabetes and helps patients with reflux.
Advantages:
- Reliable and long-lasting weight loss.
- Effective for remission of obesity-associated conditions.
- Effective weight loss (60%-70%, by Mayo Clinic estimates).
Disadvantages:
- Technically more complex when compared to gastric sleeve or band.
- More vitamin and mineral deficiencies than with gastric sleeve or band.
- Risk for small bowel complications and obstruction, as well as ulcers, especially with NSAID or tobacco use.
- May cause “dumping syndrome,” a feeling of sickness after eating or drinking, especially sweets.
A version of this article first appeared on WebMD.com.
Editor’s Note: This story has been updated to properly identify a product referenced in the story.
Jessica Furby struggled with weight most of her life, constantly dieting and exercising to shed pounds. But nothing seemed to help. By her 22nd birthday, she tipped the scales at more than 300 pounds.
So, in 2011, while a college student in Pittsburgh, she decided to have gastric band surgery. Doctors placed a synthetic belt around her stomach to limit what she could eat. It seemed like a good option at the time and, after her surgery, she lost about 60 pounds.
But the benefits didn’t last. In the months that followed, she had pain and other complications. Worst of all, she eventually regained all the weight she’d lost – and then some. By 2016, she weighed 350 pounds and was becoming prediabetic.
That’s when she decided to have the band removed and, on her doctor’s recommendation, had gastric sleeve surgery.
Studies have found the sleeve surgeries carry fewer complications and a much higher success rate than gastric band procedures, which Ms. Furby’s experience has confirmed.
Today, at age 32, she’s down to 288 pounds and says she is on her way to hitting her ultimate goal of 200 pounds.
“The surgery has been a godsend,” she said. “I have not had any complications with it at all. The sleeve was life-changing for me.”
Ms. Furby’s experience has become more common as the risks, complications, and failures of gastric band surgeries have been rising over the past decade.
, because of problems like Ms. Furby’s.
According to the latest figures from the American Society for Metabolic and Bariatric Surgery, gastric band procedures account for fewer than 1% of the 256,000 bariatric operations done in the United States each year, while gastric sleeves add up to nearly 60%. That makes sleeve surgeries the most commonly performed bariatric operation today.
By comparison, 35% of bariatric surgeries were gastric band procedures in 2011, while sleeve operations accounted for under 18%.
Ms. Furby’s surgeon, Anita P. Courcoulas, MD, said the trend is being driven by many of the things Ms.Furby experienced firsthand.
Dr. Courcoulas, chief of minimally invasive bariatric and general surgery at the University of Pittsburgh, said there are two main reasons for the decline in gastric band procedures.
“It has been shown to be less effective for weight loss [than] other bariatric surgical procedures, and band intolerance often results in band removal,” she noted.
Gastric sleeve, followed by gastric bypass, are the two most commonly performed operations in the United States and worldwide, she said.
Dr. Courcoulas said the shift from gastric bypass to gastric sleeve procedures “is likely driven by the decline in the band usage, patient preferences for a less invasive operation, such as the sleeve compared to bypass, and surgeon preferences about which operation(s) to offer a given patient.”
Ali Aminian, MD, director of the Bariatric and Metabolic Institute at the Cleveland Clinic, agrees that gastric band complications and failures, in addition to ineffective weight loss, are behind the trend, driving patients and doctors to choose safer and more effective procedures.
He said the Cleveland Clinic no longer does band operations, and he has done a lot of conversions.
“Around 50%-60% of [gastric band] patients require reoperation to take care of the complications,” he says. “So, when you have a surgery where more than half of the time the patients require reoperation, we cannot claim that’s a safe operation.”
Evolution in bariatric surgery
Bariatric surgeries for weight loss date back to the 1950s and 1960s, when surgeons at the University of Minnesota first did experimental bypass operations. Adjustable gastric banding appeared in the late 1970s and early 1980s.
But these procedures didn’t gain widespread mainstream use until gastric band procedures gained full Food and Drug Administration approval in 2001. Clinical trials have found people who have bariatric surgery have a significantly lower risk of heart disease and other obesity-related health problems.
In the decade that followed the FDA’s approval of gastric band surgery, it became a popular weight loss procedure, accounting for more than a third of all bariatric surgeries by 2011.
“Fifteen to 20 years ago, [gastric] band was the most commonly performed procedure for bariatric surgery worldwide and in the United States,” Dr. Aminian said. “It was very easy to do, it was quick – it takes 20 minutes to do the procedure – recovery was short, and initially patients had great outcomes. They would lose weight and were healthy.”
But over the past decade, surgeons found that patients often regained the weight they’d lost, and complication and failure rates rose.
“Because the [gastric] band is a foreign body that we place inside the body, many patients had complications related to that foreign body,” Dr. Aminian said.
The band can sometimes move or be displaced, causing blockage of the stomach, experts noted. Other common complications include nausea, vomiting, acid reflux, and esophageal issues (such as a hard time swallowing). Some patients feel pain, constant food cravings, or that they can’t eat or drink anything. And painful infections and other problems can develop with the tubing or the port placed under the skin that is connected to the band, which doctors use to make adjustments after surgery.
“Scar tissue can also form around the [gastric] band that can cause a blockage in the stomach,” Dr. Aminian said. “Then if the band is too tight, it can erode into the stomach tissue or even go inside the stomach and cause perforation or bleeding.”
By contrast, gastric sleeve and bypass procedures have been found to be safer, result in longer-lasting weight loss, carry fewer complications, and require fewer patient reoperations. Dr. Aminian estimates that 2%-3% of patients need second operations.
Another key factor: Metabolic ‘reset’
Sleeve and bypass procedures offer another critical advantage over band operations: They help reset the body’s metabolism better, changing appetite- and weight-related hormones in the body.
Those hormones can affect food cravings, help people feel full after eating, or boost weight gain in ways that can trump willpower, experts say.
“The [gastric] band doesn’t change the hormones in the body, it’s just a restrictive band around the esophagus or the upper part of the stomach, so it limits the patient’s ability to eat too much,” Dr. Aminian said. “That’s why it doesn’t have the metabolic effects.”
But other procedures, like the gastric sleeve, change the hormones in the body. Removing the source of those hormones means the patient won’t have the same appetite, Dr. Aminian said.
“And that’s why it’s very effective. The problem with the [gastric] band is the patient always has the feeling and desire to eat – they’re always hungry. That’s why in the long run, they fail,” he said.
“They change the setpoints,” Dr. Aminian said. “When the hormones in your body change, the [metabolic] setpoint in the brain also changes.”
He likens the metabolic setpoint to a thermostat in your home that regulates temperature inside.
“When a patient goes on a diet or goes on the [gastric] band, the thermostat doesn’t change,” he says. “They may lose some weight, but they’re going to regain it because the thermostat is the same. But when the hormones in your body change, then the thermostat will change and you’re not going to regain the weight that you have lost.”
Sachin Kukreja, MD, a surgeon and CEO at DFW Bariatrics and General Surgery in Dallas, said he believes these metabolic changes are the biggest things behind successful surgeries.
“People synonymize bariatric surgery with weight loss surgery, but really the metrics we should be using are more related to metabolic measures,” said Dr. Kukreja, who hasn’t done a band surgery since 2013. “And so, the metabolic parameters that change with bariatric surgery are much more significant in the setting with sleeve and gastric sleeve, and much less significant with [gastric] band.”
David Arterburn, MD, agrees that resetting metabolism is important but said the issue is “controversial and challenging” among bariatric surgeons.
“The metabolic setpoint is the idea that we have a biologically controlled set body weight that we will always return to. Clearly, this is not the case for everyone, as some people lose and maintain long-term weight loss,” said Dr. Arterburn, a general internist and bariatric surgery researcher at Kaiser Permanente Washington Health Research Institute in Seattle.
Postop lifestyle changes critical to success
Bariatric surgeons and patients alike also say that no surgical procedure is a magic-bullet solution for weight loss. Patients who have any type of bariatric surgery must embrace postop lifestyle changes – adopting healthier diets, getting more exercise, cutting out unhealthy habits – to lose weight and maintain weight loss.
Jan Lasecki, 54, a health care specialist in Akron, Ohio, who had band-to-sleeve conversion surgery in 2020, said the postop follow-up was at least as important as the surgery itself in helping her shed pounds.
She said at first, she chose gastric band surgery several years ago because it was “less invasive” than gastric sleeve or bypass. But while she lost about 50 pounds, she regained it after about 6 years and had other complications.
So, 2 years ago, Ms. Lasecki had two surgeries 6 months apart – one to remove her band, and a second to create a gastric sleeve. And the results, she said, have been very successful, in part because of the changes she made after surgery, with the help of her doctor’s staff.
“I have now lost about 90 pounds and have kept if off since surgery,” she says. “I would tell anyone considering any bariatric surgery, it was definitely worth it [and] having the sleeve resulted in greater weight loss.”
The follow-up was key to the success, she said.
The staff “have the tools and support to help you when you tend to fall back on old behaviors and start to regain weight,” Ms. Lasecki said. “They can help you before it gets out of control. I had no issues following either procedure from a surgery perspective.”
Sally and Robert Cordova – who had gastric bypass and sleeve surgeries, respectively, 3 years ago – agreed that the postop lifestyle changes are critical to success.
“When we agreed to have this surgery, we agreed that this will be a lifestyle change for the rest of our lives,” said Sally, 48, an accounting specialist who’s lost 150 pounds – half her body weight – since her surgery. “You can’t just get to your ideal weight and then stop.”
Robert, 47, a federal border control agent whose workmates nicknamed him “Big Rob” when he tipped the scales at 336 pounds, said it’s a mistake to think of the surgery as a “magic-bullet” solution to obesity. There’s more to it than that, he said.
“One of the things I like about the process I’ve taken is, in my opinion, they set you up for success,” he said. “Because it’s not just having the surgery and you’re done; it’s all the classes educating you about all the lifestyle changes you have to do, and starting them before the surgery. The only people that I know personally who haven’t been successful with the surgery are those who haven’t made the lifestyle changes.”
Today, at 230 pounds, Robert says he’s never felt better.
“I feel great,” he says. “I have become more active, obviously doing everything is a lot easier. It got to the point where it was a task to just tying up my shoes!”
Should band patients convert to sleeve or bypass?
Bariatric surgeons interviewed for this article were reluctant to say that all people who had gastric band procedures should convert to gastric sleeve or bypass. But they made it clear that sleeve and bypass procedures are safer and more effective than gastric band surgery, which is why it is rarely done today.
“If a patient experiences poor weight loss or complications from a band, they can consider conversion/revision to a sleeve or bypass,” said Dr. Courcoulas, echoing the views of other doctors.
“The choice of revision procedure should be based on patient factors, including diabetes and total weight. Converting a band to a sleeve is a technically easier operation, and some studies show that there are fewer complications, compared to conversion to a bypass. These considerations need to be balanced with data that show that both weight loss and metabolic improvements such as diabetes are greater after bypass, compared to sleeve.”
Doctors and experts also say it’s important for patients who are considering a gastric band conversion to gastric sleeve or bypass to understand the differences among these three primary procedures, all endorsed by the American Society for Metabolic and Bariatric Surgery.
Here’s a primer, including the pros and cons of each procedure:
Gastric band
In gastric band surgery, an adjustable gastric band made of silicone is placed around the top part of the stomach, creating a small pouch above it, to limit the amount of food a person can eat. The size of the opening between the pouch and the stomach can be adjusted with fluid injections through a port placed underneath the skin.
Food goes through the stomach but is limited by the smaller opening of the band.
Advantages:
- Lowest rate of complications right after surgery.
- No division of the stomach or intestines.
- Patients go home on the day of surgery, and recovery is quick.
- The band can be removed, if necessary.
Disadvantages:
- The band may need to be adjusted from time to time, and patients must make monthly office visits during the first year.
- There’s less weight loss than with other surgical procedures.
- It comes with the risk of band movement (slippage) or damage to the stomach over time (erosion).
- The surgery means that a foreign implant has to remain in the body.
- It has a high rate of reoperation.
- The surgery can bring swallowing problems, enlargement of the esophagus, and other complications.
Gastric sleeve
For laparoscopic sleeve gastrectomy – often called gastric sleeve – surgeons remove about 80% of the stomach, so the remaining stomach is the size and shape of a banana.
The new, smaller stomach holds less food and liquid, reducing how much food (and how many calories) the patient can get. By removing the portion of the stomach that produces hunger and appetite hormones, the surgery also helps reset the body’s metabolism – decreasing hunger, increasing feelings of fullness, and allowing the body to reach and maintain a healthy weight as well as control blood sugar.
Advantages:
- It’s technically simple and has a short surgery time.
- It can be done in certain patients with high-risk medical conditions.
- It may be the first step for patients with severe obesity or as a bridge to gastric bypass.
- The surgery brings effective weight loss and improvement of obesity-related conditions (typically 50%-60%, by Mayo Clinic estimates), with a low complication rate (2%-3%).
Disadvantages:
- Nonreversible procedure.
- May worsen or cause new reflux and heartburn.
- Less impact on metabolism, compared to bypass procedures.
Gastric bypass
Gastric bypass, also known as the Roux-en-Y gastric bypass (French for “in the form of a Y”) is another effective procedure used to treat obesity and obesity-related diseases (done laparoscopically since the 1990s).
For the operation, surgeons divide the stomach into a smaller top portion (pouch) about the size of an egg, then the larger part of the stomach is bypassed and no longer stores or digests food.
The small intestine is divided and connected to the new egg-sized stomach pouch to allow food to pass.
Gastric bypass works by limiting the amount of food and calories a patient can consume. It also decreases hunger and increases fullness, allowing the patient to reach and maintain a healthy weight. The impact on hormones and metabolic health often results in improvement of diabetes and helps patients with reflux.
Advantages:
- Reliable and long-lasting weight loss.
- Effective for remission of obesity-associated conditions.
- Effective weight loss (60%-70%, by Mayo Clinic estimates).
Disadvantages:
- Technically more complex when compared to gastric sleeve or band.
- More vitamin and mineral deficiencies than with gastric sleeve or band.
- Risk for small bowel complications and obstruction, as well as ulcers, especially with NSAID or tobacco use.
- May cause “dumping syndrome,” a feeling of sickness after eating or drinking, especially sweets.
A version of this article first appeared on WebMD.com.
Editor’s Note: This story has been updated to properly identify a product referenced in the story.
Jessica Furby struggled with weight most of her life, constantly dieting and exercising to shed pounds. But nothing seemed to help. By her 22nd birthday, she tipped the scales at more than 300 pounds.
So, in 2011, while a college student in Pittsburgh, she decided to have gastric band surgery. Doctors placed a synthetic belt around her stomach to limit what she could eat. It seemed like a good option at the time and, after her surgery, she lost about 60 pounds.
But the benefits didn’t last. In the months that followed, she had pain and other complications. Worst of all, she eventually regained all the weight she’d lost – and then some. By 2016, she weighed 350 pounds and was becoming prediabetic.
That’s when she decided to have the band removed and, on her doctor’s recommendation, had gastric sleeve surgery.
Studies have found the sleeve surgeries carry fewer complications and a much higher success rate than gastric band procedures, which Ms. Furby’s experience has confirmed.
Today, at age 32, she’s down to 288 pounds and says she is on her way to hitting her ultimate goal of 200 pounds.
“The surgery has been a godsend,” she said. “I have not had any complications with it at all. The sleeve was life-changing for me.”
Ms. Furby’s experience has become more common as the risks, complications, and failures of gastric band surgeries have been rising over the past decade.
, because of problems like Ms. Furby’s.
According to the latest figures from the American Society for Metabolic and Bariatric Surgery, gastric band procedures account for fewer than 1% of the 256,000 bariatric operations done in the United States each year, while gastric sleeves add up to nearly 60%. That makes sleeve surgeries the most commonly performed bariatric operation today.
By comparison, 35% of bariatric surgeries were gastric band procedures in 2011, while sleeve operations accounted for under 18%.
Ms. Furby’s surgeon, Anita P. Courcoulas, MD, said the trend is being driven by many of the things Ms.Furby experienced firsthand.
Dr. Courcoulas, chief of minimally invasive bariatric and general surgery at the University of Pittsburgh, said there are two main reasons for the decline in gastric band procedures.
“It has been shown to be less effective for weight loss [than] other bariatric surgical procedures, and band intolerance often results in band removal,” she noted.
Gastric sleeve, followed by gastric bypass, are the two most commonly performed operations in the United States and worldwide, she said.
Dr. Courcoulas said the shift from gastric bypass to gastric sleeve procedures “is likely driven by the decline in the band usage, patient preferences for a less invasive operation, such as the sleeve compared to bypass, and surgeon preferences about which operation(s) to offer a given patient.”
Ali Aminian, MD, director of the Bariatric and Metabolic Institute at the Cleveland Clinic, agrees that gastric band complications and failures, in addition to ineffective weight loss, are behind the trend, driving patients and doctors to choose safer and more effective procedures.
He said the Cleveland Clinic no longer does band operations, and he has done a lot of conversions.
“Around 50%-60% of [gastric band] patients require reoperation to take care of the complications,” he says. “So, when you have a surgery where more than half of the time the patients require reoperation, we cannot claim that’s a safe operation.”
Evolution in bariatric surgery
Bariatric surgeries for weight loss date back to the 1950s and 1960s, when surgeons at the University of Minnesota first did experimental bypass operations. Adjustable gastric banding appeared in the late 1970s and early 1980s.
But these procedures didn’t gain widespread mainstream use until gastric band procedures gained full Food and Drug Administration approval in 2001. Clinical trials have found people who have bariatric surgery have a significantly lower risk of heart disease and other obesity-related health problems.
In the decade that followed the FDA’s approval of gastric band surgery, it became a popular weight loss procedure, accounting for more than a third of all bariatric surgeries by 2011.
“Fifteen to 20 years ago, [gastric] band was the most commonly performed procedure for bariatric surgery worldwide and in the United States,” Dr. Aminian said. “It was very easy to do, it was quick – it takes 20 minutes to do the procedure – recovery was short, and initially patients had great outcomes. They would lose weight and were healthy.”
But over the past decade, surgeons found that patients often regained the weight they’d lost, and complication and failure rates rose.
“Because the [gastric] band is a foreign body that we place inside the body, many patients had complications related to that foreign body,” Dr. Aminian said.
The band can sometimes move or be displaced, causing blockage of the stomach, experts noted. Other common complications include nausea, vomiting, acid reflux, and esophageal issues (such as a hard time swallowing). Some patients feel pain, constant food cravings, or that they can’t eat or drink anything. And painful infections and other problems can develop with the tubing or the port placed under the skin that is connected to the band, which doctors use to make adjustments after surgery.
“Scar tissue can also form around the [gastric] band that can cause a blockage in the stomach,” Dr. Aminian said. “Then if the band is too tight, it can erode into the stomach tissue or even go inside the stomach and cause perforation or bleeding.”
By contrast, gastric sleeve and bypass procedures have been found to be safer, result in longer-lasting weight loss, carry fewer complications, and require fewer patient reoperations. Dr. Aminian estimates that 2%-3% of patients need second operations.
Another key factor: Metabolic ‘reset’
Sleeve and bypass procedures offer another critical advantage over band operations: They help reset the body’s metabolism better, changing appetite- and weight-related hormones in the body.
Those hormones can affect food cravings, help people feel full after eating, or boost weight gain in ways that can trump willpower, experts say.
“The [gastric] band doesn’t change the hormones in the body, it’s just a restrictive band around the esophagus or the upper part of the stomach, so it limits the patient’s ability to eat too much,” Dr. Aminian said. “That’s why it doesn’t have the metabolic effects.”
But other procedures, like the gastric sleeve, change the hormones in the body. Removing the source of those hormones means the patient won’t have the same appetite, Dr. Aminian said.
“And that’s why it’s very effective. The problem with the [gastric] band is the patient always has the feeling and desire to eat – they’re always hungry. That’s why in the long run, they fail,” he said.
“They change the setpoints,” Dr. Aminian said. “When the hormones in your body change, the [metabolic] setpoint in the brain also changes.”
He likens the metabolic setpoint to a thermostat in your home that regulates temperature inside.
“When a patient goes on a diet or goes on the [gastric] band, the thermostat doesn’t change,” he says. “They may lose some weight, but they’re going to regain it because the thermostat is the same. But when the hormones in your body change, then the thermostat will change and you’re not going to regain the weight that you have lost.”
Sachin Kukreja, MD, a surgeon and CEO at DFW Bariatrics and General Surgery in Dallas, said he believes these metabolic changes are the biggest things behind successful surgeries.
“People synonymize bariatric surgery with weight loss surgery, but really the metrics we should be using are more related to metabolic measures,” said Dr. Kukreja, who hasn’t done a band surgery since 2013. “And so, the metabolic parameters that change with bariatric surgery are much more significant in the setting with sleeve and gastric sleeve, and much less significant with [gastric] band.”
David Arterburn, MD, agrees that resetting metabolism is important but said the issue is “controversial and challenging” among bariatric surgeons.
“The metabolic setpoint is the idea that we have a biologically controlled set body weight that we will always return to. Clearly, this is not the case for everyone, as some people lose and maintain long-term weight loss,” said Dr. Arterburn, a general internist and bariatric surgery researcher at Kaiser Permanente Washington Health Research Institute in Seattle.
Postop lifestyle changes critical to success
Bariatric surgeons and patients alike also say that no surgical procedure is a magic-bullet solution for weight loss. Patients who have any type of bariatric surgery must embrace postop lifestyle changes – adopting healthier diets, getting more exercise, cutting out unhealthy habits – to lose weight and maintain weight loss.
Jan Lasecki, 54, a health care specialist in Akron, Ohio, who had band-to-sleeve conversion surgery in 2020, said the postop follow-up was at least as important as the surgery itself in helping her shed pounds.
She said at first, she chose gastric band surgery several years ago because it was “less invasive” than gastric sleeve or bypass. But while she lost about 50 pounds, she regained it after about 6 years and had other complications.
So, 2 years ago, Ms. Lasecki had two surgeries 6 months apart – one to remove her band, and a second to create a gastric sleeve. And the results, she said, have been very successful, in part because of the changes she made after surgery, with the help of her doctor’s staff.
“I have now lost about 90 pounds and have kept if off since surgery,” she says. “I would tell anyone considering any bariatric surgery, it was definitely worth it [and] having the sleeve resulted in greater weight loss.”
The follow-up was key to the success, she said.
The staff “have the tools and support to help you when you tend to fall back on old behaviors and start to regain weight,” Ms. Lasecki said. “They can help you before it gets out of control. I had no issues following either procedure from a surgery perspective.”
Sally and Robert Cordova – who had gastric bypass and sleeve surgeries, respectively, 3 years ago – agreed that the postop lifestyle changes are critical to success.
“When we agreed to have this surgery, we agreed that this will be a lifestyle change for the rest of our lives,” said Sally, 48, an accounting specialist who’s lost 150 pounds – half her body weight – since her surgery. “You can’t just get to your ideal weight and then stop.”
Robert, 47, a federal border control agent whose workmates nicknamed him “Big Rob” when he tipped the scales at 336 pounds, said it’s a mistake to think of the surgery as a “magic-bullet” solution to obesity. There’s more to it than that, he said.
“One of the things I like about the process I’ve taken is, in my opinion, they set you up for success,” he said. “Because it’s not just having the surgery and you’re done; it’s all the classes educating you about all the lifestyle changes you have to do, and starting them before the surgery. The only people that I know personally who haven’t been successful with the surgery are those who haven’t made the lifestyle changes.”
Today, at 230 pounds, Robert says he’s never felt better.
“I feel great,” he says. “I have become more active, obviously doing everything is a lot easier. It got to the point where it was a task to just tying up my shoes!”
Should band patients convert to sleeve or bypass?
Bariatric surgeons interviewed for this article were reluctant to say that all people who had gastric band procedures should convert to gastric sleeve or bypass. But they made it clear that sleeve and bypass procedures are safer and more effective than gastric band surgery, which is why it is rarely done today.
“If a patient experiences poor weight loss or complications from a band, they can consider conversion/revision to a sleeve or bypass,” said Dr. Courcoulas, echoing the views of other doctors.
“The choice of revision procedure should be based on patient factors, including diabetes and total weight. Converting a band to a sleeve is a technically easier operation, and some studies show that there are fewer complications, compared to conversion to a bypass. These considerations need to be balanced with data that show that both weight loss and metabolic improvements such as diabetes are greater after bypass, compared to sleeve.”
Doctors and experts also say it’s important for patients who are considering a gastric band conversion to gastric sleeve or bypass to understand the differences among these three primary procedures, all endorsed by the American Society for Metabolic and Bariatric Surgery.
Here’s a primer, including the pros and cons of each procedure:
Gastric band
In gastric band surgery, an adjustable gastric band made of silicone is placed around the top part of the stomach, creating a small pouch above it, to limit the amount of food a person can eat. The size of the opening between the pouch and the stomach can be adjusted with fluid injections through a port placed underneath the skin.
Food goes through the stomach but is limited by the smaller opening of the band.
Advantages:
- Lowest rate of complications right after surgery.
- No division of the stomach or intestines.
- Patients go home on the day of surgery, and recovery is quick.
- The band can be removed, if necessary.
Disadvantages:
- The band may need to be adjusted from time to time, and patients must make monthly office visits during the first year.
- There’s less weight loss than with other surgical procedures.
- It comes with the risk of band movement (slippage) or damage to the stomach over time (erosion).
- The surgery means that a foreign implant has to remain in the body.
- It has a high rate of reoperation.
- The surgery can bring swallowing problems, enlargement of the esophagus, and other complications.
Gastric sleeve
For laparoscopic sleeve gastrectomy – often called gastric sleeve – surgeons remove about 80% of the stomach, so the remaining stomach is the size and shape of a banana.
The new, smaller stomach holds less food and liquid, reducing how much food (and how many calories) the patient can get. By removing the portion of the stomach that produces hunger and appetite hormones, the surgery also helps reset the body’s metabolism – decreasing hunger, increasing feelings of fullness, and allowing the body to reach and maintain a healthy weight as well as control blood sugar.
Advantages:
- It’s technically simple and has a short surgery time.
- It can be done in certain patients with high-risk medical conditions.
- It may be the first step for patients with severe obesity or as a bridge to gastric bypass.
- The surgery brings effective weight loss and improvement of obesity-related conditions (typically 50%-60%, by Mayo Clinic estimates), with a low complication rate (2%-3%).
Disadvantages:
- Nonreversible procedure.
- May worsen or cause new reflux and heartburn.
- Less impact on metabolism, compared to bypass procedures.
Gastric bypass
Gastric bypass, also known as the Roux-en-Y gastric bypass (French for “in the form of a Y”) is another effective procedure used to treat obesity and obesity-related diseases (done laparoscopically since the 1990s).
For the operation, surgeons divide the stomach into a smaller top portion (pouch) about the size of an egg, then the larger part of the stomach is bypassed and no longer stores or digests food.
The small intestine is divided and connected to the new egg-sized stomach pouch to allow food to pass.
Gastric bypass works by limiting the amount of food and calories a patient can consume. It also decreases hunger and increases fullness, allowing the patient to reach and maintain a healthy weight. The impact on hormones and metabolic health often results in improvement of diabetes and helps patients with reflux.
Advantages:
- Reliable and long-lasting weight loss.
- Effective for remission of obesity-associated conditions.
- Effective weight loss (60%-70%, by Mayo Clinic estimates).
Disadvantages:
- Technically more complex when compared to gastric sleeve or band.
- More vitamin and mineral deficiencies than with gastric sleeve or band.
- Risk for small bowel complications and obstruction, as well as ulcers, especially with NSAID or tobacco use.
- May cause “dumping syndrome,” a feeling of sickness after eating or drinking, especially sweets.
A version of this article first appeared on WebMD.com.
Editor’s Note: This story has been updated to properly identify a product referenced in the story.
High-intensity exercise helps patients with anxiety quit smoking
DENVER –
Results from a randomized study of 150 participants reporting symptoms of anxiety showed that among daily smokers who received a personalized, high-intensity aerobic intervention, rates of smoking abstinence were nearly twice as great as for those who received a lower-intensity exercise intervention.
“We are encouraged in the sense that we feel we have a targeted [smoking cessation] intervention to tailor to people with high anxiety sensitivity,” lead author Jasper A. Smits, PhD, professor at the Institute for Mental Health Research and the department of psychology, the University of Texas at Austin, told attendees during a presentation of the findings at the Anxiety and Depression Association of America (ADAA) 2022. The findings were recently published in Addiction.
Effective as CBT
Previous research shows that relatively short periods of exercise, lasting as little as 2 weeks, were associated with reductions in anxiety equivalent to 12 weeks of cognitive-behavioral therapy (CBT).
In light of these earlier findings, Dr. Smits and colleagues investigated the effect of an exercise intervention for smoking cessation based on the knowledge that individuals with anxiety disorders are more likely to smoke and less likely to succeed in quitting.
The initial study, which was published in 2016, included 136 smokers with high “anxiety sensitivity,” a heightened sensitivity to normal sensations associated with anxiety, potentially leading to panic attacks or other disorders.
Results showed that participation in the researchers’ Smoking Treatment Enhancement Program (STEP) was associated with significant improvements in prolonged smoking abstinence among those with high anxiety sensitivity but not those with low anxiety.
Building on these results, the new study evaluated the exercise program at a community level at four YMCA centers. This time all participants had high anxiety sensitivity, defined as a score of 23 or higher on the Anxiety Sensitivity Index–3.
The study included 150 adult participants who had high anxiety, were daily smokers, were motivated to quit smoking, and who reported that they did not currently participate in regular moderate exercise.
All participants (67.3% women; mean age, 38.6 years) took part in STEP, which included a 15-week exercise intervention with a personal trainer. Of the participants, 77 individuals were randomly assigned to receive high-intensity aerobic training that targeted 60%-85% of their heart rate reserve (HRR), while the other 73 were assigned to a lower-intensity control group in which training was only targeted to 20%-40% of their HRR.
All participants also received standard behavioral support with phone- or text-based CBT and nicotine replacement therapy (NRT).
The centers’ fitness instructors served as case managers who oversaw the smoking cessation exercise regimens of high-intensity versus low-intensity exercise. A broad array of aerobic exercise options were permitted, with the instructors working with participants to personalize their regimens.
“It’s important to take into consideration patients’ preferences [and] to work with the fitness instructors to find the right activity,” Dr. Smits said. He noted that options may include intense yoga or swimming. “So I think we just need to be creative in thinking about exercise as being more than just running,” he noted.
Abstinence rate doubled
The study’s primary endpoint was abstinence, defined as biologically verified 7-day point prevalence abstinence.
Results at 6-month follow-up showed that the primary endpoint was achieved by 27.6% of the higher-intensity intervention group, compared with just 14.8% of the lower-intensity group (odds ratio, 2.2; P = .005).
“It was encouraging to see we roughly doubled the abstinence rate at the 6-month follow-up,” Dr. Smits said. “Those receiving the high-intensity exercise intervention had greater abstinence rates spanning the entire study period versus the standard treatment.”
Of note, declines in anxiety sensitivity, as measured on the Reiss-Epstein-Gursky Anxiety Sensitivity Index, were observed in both groups. However, there was no significant difference in changes between the two groups.
Dr. Smits noted the investigators initially speculated that exercise would improve cessation success in individuals with anxiety sensitivity by providing exposure to the types of sensations that may trigger their anxiety, such as sweating and an accelerated heart rate, providing an opportunity for “extinction training” by desensitizing them to these experiences.
In addition, high-intensity exercise may also mitigate other anxiety symptoms, including panic disorder, pain, depression, overeating, and posttraumatic stress disorder, Dr. Smits said.
Real-world evidence
Commenting on the findings, Sahib S. Khalsa, MD, PhD, director of clinical operations at the Laureate Institute for Brain Research and associate professor at the University of Tulsa, Oklahoma, noted that the real-world nature of the study suggests its results are widely applicable.
It is also important to note that both the current and previous studies conducted by the investigators included NRT, “and thus the effects are more likely to be reflective of a grouping of therapies, something that is more reflective of current practice,” said Dr. Khalsa, who was not involved in the research.
He noted that initiating as well as maintaining exercise motivation over longer periods is challenging.
“The study likely addressed this challenge by using fitness instructors, which may be an important criterion for successful deployment of the intervention. We also don’t know whether maintaining an active exercise regimen is critical to maintaining smoking cessation,” Dr. Khalsa added.
Dr. Smits is a consultant for Big Health. Dr. Khalsa has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
DENVER –
Results from a randomized study of 150 participants reporting symptoms of anxiety showed that among daily smokers who received a personalized, high-intensity aerobic intervention, rates of smoking abstinence were nearly twice as great as for those who received a lower-intensity exercise intervention.
“We are encouraged in the sense that we feel we have a targeted [smoking cessation] intervention to tailor to people with high anxiety sensitivity,” lead author Jasper A. Smits, PhD, professor at the Institute for Mental Health Research and the department of psychology, the University of Texas at Austin, told attendees during a presentation of the findings at the Anxiety and Depression Association of America (ADAA) 2022. The findings were recently published in Addiction.
Effective as CBT
Previous research shows that relatively short periods of exercise, lasting as little as 2 weeks, were associated with reductions in anxiety equivalent to 12 weeks of cognitive-behavioral therapy (CBT).
In light of these earlier findings, Dr. Smits and colleagues investigated the effect of an exercise intervention for smoking cessation based on the knowledge that individuals with anxiety disorders are more likely to smoke and less likely to succeed in quitting.
The initial study, which was published in 2016, included 136 smokers with high “anxiety sensitivity,” a heightened sensitivity to normal sensations associated with anxiety, potentially leading to panic attacks or other disorders.
Results showed that participation in the researchers’ Smoking Treatment Enhancement Program (STEP) was associated with significant improvements in prolonged smoking abstinence among those with high anxiety sensitivity but not those with low anxiety.
Building on these results, the new study evaluated the exercise program at a community level at four YMCA centers. This time all participants had high anxiety sensitivity, defined as a score of 23 or higher on the Anxiety Sensitivity Index–3.
The study included 150 adult participants who had high anxiety, were daily smokers, were motivated to quit smoking, and who reported that they did not currently participate in regular moderate exercise.
All participants (67.3% women; mean age, 38.6 years) took part in STEP, which included a 15-week exercise intervention with a personal trainer. Of the participants, 77 individuals were randomly assigned to receive high-intensity aerobic training that targeted 60%-85% of their heart rate reserve (HRR), while the other 73 were assigned to a lower-intensity control group in which training was only targeted to 20%-40% of their HRR.
All participants also received standard behavioral support with phone- or text-based CBT and nicotine replacement therapy (NRT).
The centers’ fitness instructors served as case managers who oversaw the smoking cessation exercise regimens of high-intensity versus low-intensity exercise. A broad array of aerobic exercise options were permitted, with the instructors working with participants to personalize their regimens.
“It’s important to take into consideration patients’ preferences [and] to work with the fitness instructors to find the right activity,” Dr. Smits said. He noted that options may include intense yoga or swimming. “So I think we just need to be creative in thinking about exercise as being more than just running,” he noted.
Abstinence rate doubled
The study’s primary endpoint was abstinence, defined as biologically verified 7-day point prevalence abstinence.
Results at 6-month follow-up showed that the primary endpoint was achieved by 27.6% of the higher-intensity intervention group, compared with just 14.8% of the lower-intensity group (odds ratio, 2.2; P = .005).
“It was encouraging to see we roughly doubled the abstinence rate at the 6-month follow-up,” Dr. Smits said. “Those receiving the high-intensity exercise intervention had greater abstinence rates spanning the entire study period versus the standard treatment.”
Of note, declines in anxiety sensitivity, as measured on the Reiss-Epstein-Gursky Anxiety Sensitivity Index, were observed in both groups. However, there was no significant difference in changes between the two groups.
Dr. Smits noted the investigators initially speculated that exercise would improve cessation success in individuals with anxiety sensitivity by providing exposure to the types of sensations that may trigger their anxiety, such as sweating and an accelerated heart rate, providing an opportunity for “extinction training” by desensitizing them to these experiences.
In addition, high-intensity exercise may also mitigate other anxiety symptoms, including panic disorder, pain, depression, overeating, and posttraumatic stress disorder, Dr. Smits said.
Real-world evidence
Commenting on the findings, Sahib S. Khalsa, MD, PhD, director of clinical operations at the Laureate Institute for Brain Research and associate professor at the University of Tulsa, Oklahoma, noted that the real-world nature of the study suggests its results are widely applicable.
It is also important to note that both the current and previous studies conducted by the investigators included NRT, “and thus the effects are more likely to be reflective of a grouping of therapies, something that is more reflective of current practice,” said Dr. Khalsa, who was not involved in the research.
He noted that initiating as well as maintaining exercise motivation over longer periods is challenging.
“The study likely addressed this challenge by using fitness instructors, which may be an important criterion for successful deployment of the intervention. We also don’t know whether maintaining an active exercise regimen is critical to maintaining smoking cessation,” Dr. Khalsa added.
Dr. Smits is a consultant for Big Health. Dr. Khalsa has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
DENVER –
Results from a randomized study of 150 participants reporting symptoms of anxiety showed that among daily smokers who received a personalized, high-intensity aerobic intervention, rates of smoking abstinence were nearly twice as great as for those who received a lower-intensity exercise intervention.
“We are encouraged in the sense that we feel we have a targeted [smoking cessation] intervention to tailor to people with high anxiety sensitivity,” lead author Jasper A. Smits, PhD, professor at the Institute for Mental Health Research and the department of psychology, the University of Texas at Austin, told attendees during a presentation of the findings at the Anxiety and Depression Association of America (ADAA) 2022. The findings were recently published in Addiction.
Effective as CBT
Previous research shows that relatively short periods of exercise, lasting as little as 2 weeks, were associated with reductions in anxiety equivalent to 12 weeks of cognitive-behavioral therapy (CBT).
In light of these earlier findings, Dr. Smits and colleagues investigated the effect of an exercise intervention for smoking cessation based on the knowledge that individuals with anxiety disorders are more likely to smoke and less likely to succeed in quitting.
The initial study, which was published in 2016, included 136 smokers with high “anxiety sensitivity,” a heightened sensitivity to normal sensations associated with anxiety, potentially leading to panic attacks or other disorders.
Results showed that participation in the researchers’ Smoking Treatment Enhancement Program (STEP) was associated with significant improvements in prolonged smoking abstinence among those with high anxiety sensitivity but not those with low anxiety.
Building on these results, the new study evaluated the exercise program at a community level at four YMCA centers. This time all participants had high anxiety sensitivity, defined as a score of 23 or higher on the Anxiety Sensitivity Index–3.
The study included 150 adult participants who had high anxiety, were daily smokers, were motivated to quit smoking, and who reported that they did not currently participate in regular moderate exercise.
All participants (67.3% women; mean age, 38.6 years) took part in STEP, which included a 15-week exercise intervention with a personal trainer. Of the participants, 77 individuals were randomly assigned to receive high-intensity aerobic training that targeted 60%-85% of their heart rate reserve (HRR), while the other 73 were assigned to a lower-intensity control group in which training was only targeted to 20%-40% of their HRR.
All participants also received standard behavioral support with phone- or text-based CBT and nicotine replacement therapy (NRT).
The centers’ fitness instructors served as case managers who oversaw the smoking cessation exercise regimens of high-intensity versus low-intensity exercise. A broad array of aerobic exercise options were permitted, with the instructors working with participants to personalize their regimens.
“It’s important to take into consideration patients’ preferences [and] to work with the fitness instructors to find the right activity,” Dr. Smits said. He noted that options may include intense yoga or swimming. “So I think we just need to be creative in thinking about exercise as being more than just running,” he noted.
Abstinence rate doubled
The study’s primary endpoint was abstinence, defined as biologically verified 7-day point prevalence abstinence.
Results at 6-month follow-up showed that the primary endpoint was achieved by 27.6% of the higher-intensity intervention group, compared with just 14.8% of the lower-intensity group (odds ratio, 2.2; P = .005).
“It was encouraging to see we roughly doubled the abstinence rate at the 6-month follow-up,” Dr. Smits said. “Those receiving the high-intensity exercise intervention had greater abstinence rates spanning the entire study period versus the standard treatment.”
Of note, declines in anxiety sensitivity, as measured on the Reiss-Epstein-Gursky Anxiety Sensitivity Index, were observed in both groups. However, there was no significant difference in changes between the two groups.
Dr. Smits noted the investigators initially speculated that exercise would improve cessation success in individuals with anxiety sensitivity by providing exposure to the types of sensations that may trigger their anxiety, such as sweating and an accelerated heart rate, providing an opportunity for “extinction training” by desensitizing them to these experiences.
In addition, high-intensity exercise may also mitigate other anxiety symptoms, including panic disorder, pain, depression, overeating, and posttraumatic stress disorder, Dr. Smits said.
Real-world evidence
Commenting on the findings, Sahib S. Khalsa, MD, PhD, director of clinical operations at the Laureate Institute for Brain Research and associate professor at the University of Tulsa, Oklahoma, noted that the real-world nature of the study suggests its results are widely applicable.
It is also important to note that both the current and previous studies conducted by the investigators included NRT, “and thus the effects are more likely to be reflective of a grouping of therapies, something that is more reflective of current practice,” said Dr. Khalsa, who was not involved in the research.
He noted that initiating as well as maintaining exercise motivation over longer periods is challenging.
“The study likely addressed this challenge by using fitness instructors, which may be an important criterion for successful deployment of the intervention. We also don’t know whether maintaining an active exercise regimen is critical to maintaining smoking cessation,” Dr. Khalsa added.
Dr. Smits is a consultant for Big Health. Dr. Khalsa has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ADAA 2022
Cancer Data Trends 2022
Federal Practitioner, in collaboration with the Association of VA Hematology/Oncology (AVAHO), present the 2022 edition of Cancer Data Trends (click to view the digital edition). This special issue provides updates on some of the top cancers and related concerns affecting veterans through original infographics and visual storytelling.
In this issue:
- Exposure-Related Cancers
- Cancer in Women
- Genitourinary Cancers
- Gastrointestinal Cancers
- Telehealth in Oncology
- Precision Oncology
- Palliative and Hospice Care
- Alcohol and Cancer
- Lung Cancer
- Oropharyngeal Cancer
- Hematologic Cancers
Federal Practitioner and AVAHO would like to thank the following experts for their contributions to this issue:
Anita Aggarwal, DO, PhD; Sara Ahmed, PhD; Katherine Faricy-Anderson, MD; Apar Kishor Ganti, MD, MS; Solomon A Graf, MD; Kate Hendricks Thomas, PhD; Michael Kelley, MD; Mark Klein, MD, Gina McWhirter, MSN, MBA, RN; Bruce Montgomery, MD; Vida Almario Passero, MD, MBA; Thomas D Rodgers, MD; Vlad C Sandulache, MD, PhD; David H Wang, MD, PhD.
Federal Practitioner, in collaboration with the Association of VA Hematology/Oncology (AVAHO), present the 2022 edition of Cancer Data Trends (click to view the digital edition). This special issue provides updates on some of the top cancers and related concerns affecting veterans through original infographics and visual storytelling.
In this issue:
- Exposure-Related Cancers
- Cancer in Women
- Genitourinary Cancers
- Gastrointestinal Cancers
- Telehealth in Oncology
- Precision Oncology
- Palliative and Hospice Care
- Alcohol and Cancer
- Lung Cancer
- Oropharyngeal Cancer
- Hematologic Cancers
Federal Practitioner and AVAHO would like to thank the following experts for their contributions to this issue:
Anita Aggarwal, DO, PhD; Sara Ahmed, PhD; Katherine Faricy-Anderson, MD; Apar Kishor Ganti, MD, MS; Solomon A Graf, MD; Kate Hendricks Thomas, PhD; Michael Kelley, MD; Mark Klein, MD, Gina McWhirter, MSN, MBA, RN; Bruce Montgomery, MD; Vida Almario Passero, MD, MBA; Thomas D Rodgers, MD; Vlad C Sandulache, MD, PhD; David H Wang, MD, PhD.
Federal Practitioner, in collaboration with the Association of VA Hematology/Oncology (AVAHO), present the 2022 edition of Cancer Data Trends (click to view the digital edition). This special issue provides updates on some of the top cancers and related concerns affecting veterans through original infographics and visual storytelling.
In this issue:
- Exposure-Related Cancers
- Cancer in Women
- Genitourinary Cancers
- Gastrointestinal Cancers
- Telehealth in Oncology
- Precision Oncology
- Palliative and Hospice Care
- Alcohol and Cancer
- Lung Cancer
- Oropharyngeal Cancer
- Hematologic Cancers
Federal Practitioner and AVAHO would like to thank the following experts for their contributions to this issue:
Anita Aggarwal, DO, PhD; Sara Ahmed, PhD; Katherine Faricy-Anderson, MD; Apar Kishor Ganti, MD, MS; Solomon A Graf, MD; Kate Hendricks Thomas, PhD; Michael Kelley, MD; Mark Klein, MD, Gina McWhirter, MSN, MBA, RN; Bruce Montgomery, MD; Vida Almario Passero, MD, MBA; Thomas D Rodgers, MD; Vlad C Sandulache, MD, PhD; David H Wang, MD, PhD.
Cellulitis care costly from misdiagnosis, needless hospitalizations
BOSTON – The cost of care for the more than 14 million cases of cellulitis that occur each year in the United States is in the billions of dollars, but there are multiple opportunities, many involving dermatologists, to dramatically reduce these costs, according to an outline of strategies presented at the American Academy of Dermatology 2022 annual meeting in Boston.
“Cellulitis is misdiagnosed about one-third of the time, and that cost is very high,” reported Jennifer L. Adams, MD, assistant professor of dermatology, University of Nebraska, Omaha. She sees opportunities for dermatological consults to help weed through the many cellulitis mimickers, such as venous insufficiency or psoriasiform drug reactions, to prevent unnecessary admissions and ineffective therapy.
“There is a huge need for diagnostic accuracy as a means to deliver more cost-effective care,” Dr. Adams said.
Solving misdiagnosis is only part of the story. Costs of care are also ramped up by unnecessary hospitalizations. According to Dr. Adams, published criteria to triage emergency room patients with cellulitis to outpatient care are not always followed. In one review, 14% of admitted patients had met the criteria for outpatient treatment.
Cellulitis is a common skin infection that causes redness, swelling, and pain in the infected area, most often on the legs and feet.
Unnecessary hospitalizations for misdiagnosed cellulitis, which is associated with an average 4-day hospital stay, “range from $200 million to $500 million in avoidable direct healthcare costs,” Dr. Adams said.
Even for justifiable hospitalizations, there are still opportunities for cost savings. In one study, blood cultures were ordered in 73% of patients even though only 2% produced a finding relevant to care. According to Dr. Adams, most cellulitis cases are caused by the “usual suspects” – group A beta-hemolytic streptococcus, Streptococcus pneumoniae, and Staphylococcus aureus. The exceptions stand out by clinical criteria, such as known neutropenia, history of an animal bite, signs of Systemic Inflammatory Response Syndrome (SIRS), or a purulent appearance.
“Blood cultures are not cost-effective in uncomplicated cellulitis,” Dr. Adams said. She said there are numerous published algorithms to guide clinicians on decision-making in the management of soft tissue infections, including cellulitis, including a much-cited algorithm first published more than 15 years ago and updated in 2014.
Similarly, labs and imaging are commonly ordered with no strong likelihood that they will change management, she said. These types of decisions are also covered in published algorithms.
Strategies to prevent rehospitalization are another area where there is a large opportunity to reduce health care resources consumed by cellulitis. The rehospitalization rate at 30 days is approximately 10%, but many patients have recurrent episodes over years, according to Dr. Adams. The risk factors and the preventative measures have been well described.
“Scrupulous clinical care can reduce recurrence, and it is cost-effective,” said Dr. Adams, referring to control of edema, control of underlying conditions associated with increased risk, such as diabetes, and managing dry skin and erosions with topical agents or even moisturizers. Compression socks are a simple but effective tool, she added.
For patients with repeat episodes of cellulitis over years, Dr. Adams referred to a double-blind trial that associated a twice-daily dose of 250 mg penicillin with a 45% reduction in the risk of cellulitis recurrence over 1 year. At approximately $10 a month for this treatment, she said it is very cost-effective, although she acknowledged that recurrence rates of cellulitis climb back up when the penicillin is stopped.
“I think of this as a bridge while you work on addressing the venous insufficiency or other risk factors for cellulitis,” Dr. Adams said.
For reducing the costs of cellulitis, there is evidence that dermatologists can play a role. Dr. Adams cited a study that evaluated the impact of a dermatologist consultation for suspected cellulitis in the emergency room or within 24 hours of admission. Of 34 patients already prescribed antibiotics for presumed cellulitis, discontinuation was recommended in 82%. Of 39 admissions, pseudocellulitis was identified in 51%.
Extrapolating these data to national rates of cellulitis, there was an estimated savings of up to $200 million annually without any apparent increased risk of adverse outcomes, according to Dr. Adams.
When contacted about his experience, the senior investigator of that study, Arash Mostaghimi, MD, director of the Inpatient Dermatology Consult Service, Brigham and Women’s Hospital, Boston, largely agreed with the premise of Adam’s analysis. In particular, he said, avoiding misdiagnosis of cellulitis offers a major opportunity to lower costs while possibly improving care.
True of national practice and at the local level, “misdiagnosis of noninfectious inflammatory reactions such as cellulitis has substantial cost impacts,” Dr. Mostaghimi said in an interview. Based on evidence, the savings are derived directly from “unnecessary antibiotic exposure as well as inappropriate hospitalization.”
Following publication of his study, he became involved in addressing this issue at his institution.
“At Brigham and Women’s, we collaborated with colleagues in infectious disease and in the emergency department to create cellulitis protocols that identify patients at risk for misdiagnosis and facilitate early dermatology consultation for diagnostic confirmation,” he said.
Although there are algorithms to achieve this goal, he indicated that the expertise of dermatologists can quickly and efficiently differentiate inflammatory skin reactions and expedite appropriate care.
Dr. Adams and Dr. Mostaghimi have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON – The cost of care for the more than 14 million cases of cellulitis that occur each year in the United States is in the billions of dollars, but there are multiple opportunities, many involving dermatologists, to dramatically reduce these costs, according to an outline of strategies presented at the American Academy of Dermatology 2022 annual meeting in Boston.
“Cellulitis is misdiagnosed about one-third of the time, and that cost is very high,” reported Jennifer L. Adams, MD, assistant professor of dermatology, University of Nebraska, Omaha. She sees opportunities for dermatological consults to help weed through the many cellulitis mimickers, such as venous insufficiency or psoriasiform drug reactions, to prevent unnecessary admissions and ineffective therapy.
“There is a huge need for diagnostic accuracy as a means to deliver more cost-effective care,” Dr. Adams said.
Solving misdiagnosis is only part of the story. Costs of care are also ramped up by unnecessary hospitalizations. According to Dr. Adams, published criteria to triage emergency room patients with cellulitis to outpatient care are not always followed. In one review, 14% of admitted patients had met the criteria for outpatient treatment.
Cellulitis is a common skin infection that causes redness, swelling, and pain in the infected area, most often on the legs and feet.
Unnecessary hospitalizations for misdiagnosed cellulitis, which is associated with an average 4-day hospital stay, “range from $200 million to $500 million in avoidable direct healthcare costs,” Dr. Adams said.
Even for justifiable hospitalizations, there are still opportunities for cost savings. In one study, blood cultures were ordered in 73% of patients even though only 2% produced a finding relevant to care. According to Dr. Adams, most cellulitis cases are caused by the “usual suspects” – group A beta-hemolytic streptococcus, Streptococcus pneumoniae, and Staphylococcus aureus. The exceptions stand out by clinical criteria, such as known neutropenia, history of an animal bite, signs of Systemic Inflammatory Response Syndrome (SIRS), or a purulent appearance.
“Blood cultures are not cost-effective in uncomplicated cellulitis,” Dr. Adams said. She said there are numerous published algorithms to guide clinicians on decision-making in the management of soft tissue infections, including cellulitis, including a much-cited algorithm first published more than 15 years ago and updated in 2014.
Similarly, labs and imaging are commonly ordered with no strong likelihood that they will change management, she said. These types of decisions are also covered in published algorithms.
Strategies to prevent rehospitalization are another area where there is a large opportunity to reduce health care resources consumed by cellulitis. The rehospitalization rate at 30 days is approximately 10%, but many patients have recurrent episodes over years, according to Dr. Adams. The risk factors and the preventative measures have been well described.
“Scrupulous clinical care can reduce recurrence, and it is cost-effective,” said Dr. Adams, referring to control of edema, control of underlying conditions associated with increased risk, such as diabetes, and managing dry skin and erosions with topical agents or even moisturizers. Compression socks are a simple but effective tool, she added.
For patients with repeat episodes of cellulitis over years, Dr. Adams referred to a double-blind trial that associated a twice-daily dose of 250 mg penicillin with a 45% reduction in the risk of cellulitis recurrence over 1 year. At approximately $10 a month for this treatment, she said it is very cost-effective, although she acknowledged that recurrence rates of cellulitis climb back up when the penicillin is stopped.
“I think of this as a bridge while you work on addressing the venous insufficiency or other risk factors for cellulitis,” Dr. Adams said.
For reducing the costs of cellulitis, there is evidence that dermatologists can play a role. Dr. Adams cited a study that evaluated the impact of a dermatologist consultation for suspected cellulitis in the emergency room or within 24 hours of admission. Of 34 patients already prescribed antibiotics for presumed cellulitis, discontinuation was recommended in 82%. Of 39 admissions, pseudocellulitis was identified in 51%.
Extrapolating these data to national rates of cellulitis, there was an estimated savings of up to $200 million annually without any apparent increased risk of adverse outcomes, according to Dr. Adams.
When contacted about his experience, the senior investigator of that study, Arash Mostaghimi, MD, director of the Inpatient Dermatology Consult Service, Brigham and Women’s Hospital, Boston, largely agreed with the premise of Adam’s analysis. In particular, he said, avoiding misdiagnosis of cellulitis offers a major opportunity to lower costs while possibly improving care.
True of national practice and at the local level, “misdiagnosis of noninfectious inflammatory reactions such as cellulitis has substantial cost impacts,” Dr. Mostaghimi said in an interview. Based on evidence, the savings are derived directly from “unnecessary antibiotic exposure as well as inappropriate hospitalization.”
Following publication of his study, he became involved in addressing this issue at his institution.
“At Brigham and Women’s, we collaborated with colleagues in infectious disease and in the emergency department to create cellulitis protocols that identify patients at risk for misdiagnosis and facilitate early dermatology consultation for diagnostic confirmation,” he said.
Although there are algorithms to achieve this goal, he indicated that the expertise of dermatologists can quickly and efficiently differentiate inflammatory skin reactions and expedite appropriate care.
Dr. Adams and Dr. Mostaghimi have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON – The cost of care for the more than 14 million cases of cellulitis that occur each year in the United States is in the billions of dollars, but there are multiple opportunities, many involving dermatologists, to dramatically reduce these costs, according to an outline of strategies presented at the American Academy of Dermatology 2022 annual meeting in Boston.
“Cellulitis is misdiagnosed about one-third of the time, and that cost is very high,” reported Jennifer L. Adams, MD, assistant professor of dermatology, University of Nebraska, Omaha. She sees opportunities for dermatological consults to help weed through the many cellulitis mimickers, such as venous insufficiency or psoriasiform drug reactions, to prevent unnecessary admissions and ineffective therapy.
“There is a huge need for diagnostic accuracy as a means to deliver more cost-effective care,” Dr. Adams said.
Solving misdiagnosis is only part of the story. Costs of care are also ramped up by unnecessary hospitalizations. According to Dr. Adams, published criteria to triage emergency room patients with cellulitis to outpatient care are not always followed. In one review, 14% of admitted patients had met the criteria for outpatient treatment.
Cellulitis is a common skin infection that causes redness, swelling, and pain in the infected area, most often on the legs and feet.
Unnecessary hospitalizations for misdiagnosed cellulitis, which is associated with an average 4-day hospital stay, “range from $200 million to $500 million in avoidable direct healthcare costs,” Dr. Adams said.
Even for justifiable hospitalizations, there are still opportunities for cost savings. In one study, blood cultures were ordered in 73% of patients even though only 2% produced a finding relevant to care. According to Dr. Adams, most cellulitis cases are caused by the “usual suspects” – group A beta-hemolytic streptococcus, Streptococcus pneumoniae, and Staphylococcus aureus. The exceptions stand out by clinical criteria, such as known neutropenia, history of an animal bite, signs of Systemic Inflammatory Response Syndrome (SIRS), or a purulent appearance.
“Blood cultures are not cost-effective in uncomplicated cellulitis,” Dr. Adams said. She said there are numerous published algorithms to guide clinicians on decision-making in the management of soft tissue infections, including cellulitis, including a much-cited algorithm first published more than 15 years ago and updated in 2014.
Similarly, labs and imaging are commonly ordered with no strong likelihood that they will change management, she said. These types of decisions are also covered in published algorithms.
Strategies to prevent rehospitalization are another area where there is a large opportunity to reduce health care resources consumed by cellulitis. The rehospitalization rate at 30 days is approximately 10%, but many patients have recurrent episodes over years, according to Dr. Adams. The risk factors and the preventative measures have been well described.
“Scrupulous clinical care can reduce recurrence, and it is cost-effective,” said Dr. Adams, referring to control of edema, control of underlying conditions associated with increased risk, such as diabetes, and managing dry skin and erosions with topical agents or even moisturizers. Compression socks are a simple but effective tool, she added.
For patients with repeat episodes of cellulitis over years, Dr. Adams referred to a double-blind trial that associated a twice-daily dose of 250 mg penicillin with a 45% reduction in the risk of cellulitis recurrence over 1 year. At approximately $10 a month for this treatment, she said it is very cost-effective, although she acknowledged that recurrence rates of cellulitis climb back up when the penicillin is stopped.
“I think of this as a bridge while you work on addressing the venous insufficiency or other risk factors for cellulitis,” Dr. Adams said.
For reducing the costs of cellulitis, there is evidence that dermatologists can play a role. Dr. Adams cited a study that evaluated the impact of a dermatologist consultation for suspected cellulitis in the emergency room or within 24 hours of admission. Of 34 patients already prescribed antibiotics for presumed cellulitis, discontinuation was recommended in 82%. Of 39 admissions, pseudocellulitis was identified in 51%.
Extrapolating these data to national rates of cellulitis, there was an estimated savings of up to $200 million annually without any apparent increased risk of adverse outcomes, according to Dr. Adams.
When contacted about his experience, the senior investigator of that study, Arash Mostaghimi, MD, director of the Inpatient Dermatology Consult Service, Brigham and Women’s Hospital, Boston, largely agreed with the premise of Adam’s analysis. In particular, he said, avoiding misdiagnosis of cellulitis offers a major opportunity to lower costs while possibly improving care.
True of national practice and at the local level, “misdiagnosis of noninfectious inflammatory reactions such as cellulitis has substantial cost impacts,” Dr. Mostaghimi said in an interview. Based on evidence, the savings are derived directly from “unnecessary antibiotic exposure as well as inappropriate hospitalization.”
Following publication of his study, he became involved in addressing this issue at his institution.
“At Brigham and Women’s, we collaborated with colleagues in infectious disease and in the emergency department to create cellulitis protocols that identify patients at risk for misdiagnosis and facilitate early dermatology consultation for diagnostic confirmation,” he said.
Although there are algorithms to achieve this goal, he indicated that the expertise of dermatologists can quickly and efficiently differentiate inflammatory skin reactions and expedite appropriate care.
Dr. Adams and Dr. Mostaghimi have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT AAD 2022
Global registry tracks COVID-19 outcomes in atopic dermatitis patients
BOSTON – , results from a global registry demonstrated.
Moreover, combination systemic treatment, especially those that included systemic corticosteroids, was associated with the highest risk of COVID-19–related hospitalization.
“Patients with inflammatory skin diseases such as AD may be at higher risk of COVID-19,” Annelie H. Musters, MD, said during a late-breaking abstract session at the annual meeting of the American Academy of Dermatology. “Another factor to consider is that AD patients are often treated with systemic immunomodulatory therapy, including systemic corticosteroids and nonsteroidal immunosuppressants such as methotrexate, cyclosporin, biologics, and Janus kinase inhibitors. Different mechanisms of action and levels of immunosuppression may impart variable risks of serious infections.”
On the other hand, some degree of immunomodulation may have beneficial effects on the course of COVID-19 in AD patients, said Dr. Musters, of the department of dermatology at Academic Medical Center, University of Amsterdam. Targeting of specific immune pathways could reduce the development of a hyperinflammatory state in severe COVID-19. Dual blockade of interleukin (IL)-4 and IL-13 with dupilumab may have a protective effect in the context of COVID-19 infection, because expression of Th2 cytokines, including IL-4 and IL-13, may be increased during COVID-19.
“At the start of the pandemic, many of us were faced with important questions, like do systemic immunomodulatory treatments influence outcomes of COVID-19 in patients with AD?” she said. “Do patients on dupilumab or other novel systemics fare better than those on conventional systemic treatment?”
To answer these questions, she and her colleagues launched a web-based registry in April 2020 to investigate COVID-19 outcomes in patients with AD treated with or without systemic immunomodulatory treatments. For the registry, known as Surveillance Epidemiology of Coronavirus Under Research Exclusion for Atopic Dermatitis (SECURE-AD), clinicians in 27 countries used a web-based form to enter anonymized data after patients had fully recovered from COVID-19. Eligibility criteria included having proven or highly suspected COVID-19, and there were no restrictions on age nor the type of AD treatment they were receiving.
Dr. Musters reported results from 442 patients who were recruited between April 2, 2020, and Oct. 31, 2021. Their mean age was 35.6 years, their median body mass index was 23.7 kg/m2, and there was an even sex distribution. Most patients were White and were recruited from Italy. Of the 442 patients, 216 (48.8%) received dupilumab monotherapy, 131 (29.6%) received topical treatments, and 14 (3.16%) received combination systemic treatments, including systemic corticosteroids. About 12% presented to the emergency department and 6% were hospitalized. Of those hospitalized, 2% required intensive care and/or ventilation, and no deaths have occurred in the registry to date.
By treatment group, hospitalization rates were highest among those on combination treatments (35.7%), followed by systemic corticosteroids (14.3%), topical treatments only (9.9%), other conventional systemics (3.6%), methotrexate (3.3%), and dupilumab (2.3%).
To further explore the differences between hospitalization rates in treatment groups, the researchers performed a multivariable logistic regression analysis, adjusted for age, sex, ethnicity, and comorbidity score. Compared with those who received dupilumab, the adjusted odds ratios (ORs) for hospitalization were highest among those who received topical treatments (OR, 4.95), followed by those who received systemic corticosteroids (OR, 2.81), and those who received other conventional systemic treatments (OR, 2.36).
Dr. Musters and colleagues also found that compared with patients on nonsteroidal immunosuppressive therapy, patients on combination systemic therapy had a significantly higher odds of hospitalization, specifically an OR of 45.75 for those on combination treatment including corticosteroids, an OR of 37.57 for those on combination treatment not including steroids, and an OR of 1.87 for those on systemic corticosteroids as monotherapy.
“Overall, the risk of COVID-19 complications appears to be low in patients with AD, even when treated with systemic immunomodulatory agents,” Dr. Musters concluded. “Dupilumab monotherapy was associated with lower odds of hospitalizations compared with other therapies. Moreover, combination systemic treatment, especially combinations including systemic corticosteroids, was associated with the highest risk of severe COVID-19.”
She added that other population-based study designs are more suitable to answer other important questions, such as whether the overall risk of COVID-19 in patients with AD is higher or lower compared to healthy controls.
Amy S. Paller, MD, professor and chair of the department of dermatology at Northwestern University, Chicago, who was asked to comment on the study, characterized the results as reassuring. In this patient population, “we expected that dupilumab would not cause any problems,” she said. “We wouldn’t necessarily expect it to [confer] a benefit, but I think it’s because the patients who need a systemic medication are going on something that’s very targeted (dupilumab) rather than something that has a broader immunosuppressing function. It was interesting but not surprising that those on systemic steroids had more of a problem. Get them on something that’s very targeted if you can and don’t suppress the immune systems that might be handling COVID-19.”
Dr. Musters reported having no disclosures. Dr. Paller disclosed that she is consultant to and/or an investigator for many pharmaceutical companies.
BOSTON – , results from a global registry demonstrated.
Moreover, combination systemic treatment, especially those that included systemic corticosteroids, was associated with the highest risk of COVID-19–related hospitalization.
“Patients with inflammatory skin diseases such as AD may be at higher risk of COVID-19,” Annelie H. Musters, MD, said during a late-breaking abstract session at the annual meeting of the American Academy of Dermatology. “Another factor to consider is that AD patients are often treated with systemic immunomodulatory therapy, including systemic corticosteroids and nonsteroidal immunosuppressants such as methotrexate, cyclosporin, biologics, and Janus kinase inhibitors. Different mechanisms of action and levels of immunosuppression may impart variable risks of serious infections.”
On the other hand, some degree of immunomodulation may have beneficial effects on the course of COVID-19 in AD patients, said Dr. Musters, of the department of dermatology at Academic Medical Center, University of Amsterdam. Targeting of specific immune pathways could reduce the development of a hyperinflammatory state in severe COVID-19. Dual blockade of interleukin (IL)-4 and IL-13 with dupilumab may have a protective effect in the context of COVID-19 infection, because expression of Th2 cytokines, including IL-4 and IL-13, may be increased during COVID-19.
“At the start of the pandemic, many of us were faced with important questions, like do systemic immunomodulatory treatments influence outcomes of COVID-19 in patients with AD?” she said. “Do patients on dupilumab or other novel systemics fare better than those on conventional systemic treatment?”
To answer these questions, she and her colleagues launched a web-based registry in April 2020 to investigate COVID-19 outcomes in patients with AD treated with or without systemic immunomodulatory treatments. For the registry, known as Surveillance Epidemiology of Coronavirus Under Research Exclusion for Atopic Dermatitis (SECURE-AD), clinicians in 27 countries used a web-based form to enter anonymized data after patients had fully recovered from COVID-19. Eligibility criteria included having proven or highly suspected COVID-19, and there were no restrictions on age nor the type of AD treatment they were receiving.
Dr. Musters reported results from 442 patients who were recruited between April 2, 2020, and Oct. 31, 2021. Their mean age was 35.6 years, their median body mass index was 23.7 kg/m2, and there was an even sex distribution. Most patients were White and were recruited from Italy. Of the 442 patients, 216 (48.8%) received dupilumab monotherapy, 131 (29.6%) received topical treatments, and 14 (3.16%) received combination systemic treatments, including systemic corticosteroids. About 12% presented to the emergency department and 6% were hospitalized. Of those hospitalized, 2% required intensive care and/or ventilation, and no deaths have occurred in the registry to date.
By treatment group, hospitalization rates were highest among those on combination treatments (35.7%), followed by systemic corticosteroids (14.3%), topical treatments only (9.9%), other conventional systemics (3.6%), methotrexate (3.3%), and dupilumab (2.3%).
To further explore the differences between hospitalization rates in treatment groups, the researchers performed a multivariable logistic regression analysis, adjusted for age, sex, ethnicity, and comorbidity score. Compared with those who received dupilumab, the adjusted odds ratios (ORs) for hospitalization were highest among those who received topical treatments (OR, 4.95), followed by those who received systemic corticosteroids (OR, 2.81), and those who received other conventional systemic treatments (OR, 2.36).
Dr. Musters and colleagues also found that compared with patients on nonsteroidal immunosuppressive therapy, patients on combination systemic therapy had a significantly higher odds of hospitalization, specifically an OR of 45.75 for those on combination treatment including corticosteroids, an OR of 37.57 for those on combination treatment not including steroids, and an OR of 1.87 for those on systemic corticosteroids as monotherapy.
“Overall, the risk of COVID-19 complications appears to be low in patients with AD, even when treated with systemic immunomodulatory agents,” Dr. Musters concluded. “Dupilumab monotherapy was associated with lower odds of hospitalizations compared with other therapies. Moreover, combination systemic treatment, especially combinations including systemic corticosteroids, was associated with the highest risk of severe COVID-19.”
She added that other population-based study designs are more suitable to answer other important questions, such as whether the overall risk of COVID-19 in patients with AD is higher or lower compared to healthy controls.
Amy S. Paller, MD, professor and chair of the department of dermatology at Northwestern University, Chicago, who was asked to comment on the study, characterized the results as reassuring. In this patient population, “we expected that dupilumab would not cause any problems,” she said. “We wouldn’t necessarily expect it to [confer] a benefit, but I think it’s because the patients who need a systemic medication are going on something that’s very targeted (dupilumab) rather than something that has a broader immunosuppressing function. It was interesting but not surprising that those on systemic steroids had more of a problem. Get them on something that’s very targeted if you can and don’t suppress the immune systems that might be handling COVID-19.”
Dr. Musters reported having no disclosures. Dr. Paller disclosed that she is consultant to and/or an investigator for many pharmaceutical companies.
BOSTON – , results from a global registry demonstrated.
Moreover, combination systemic treatment, especially those that included systemic corticosteroids, was associated with the highest risk of COVID-19–related hospitalization.
“Patients with inflammatory skin diseases such as AD may be at higher risk of COVID-19,” Annelie H. Musters, MD, said during a late-breaking abstract session at the annual meeting of the American Academy of Dermatology. “Another factor to consider is that AD patients are often treated with systemic immunomodulatory therapy, including systemic corticosteroids and nonsteroidal immunosuppressants such as methotrexate, cyclosporin, biologics, and Janus kinase inhibitors. Different mechanisms of action and levels of immunosuppression may impart variable risks of serious infections.”
On the other hand, some degree of immunomodulation may have beneficial effects on the course of COVID-19 in AD patients, said Dr. Musters, of the department of dermatology at Academic Medical Center, University of Amsterdam. Targeting of specific immune pathways could reduce the development of a hyperinflammatory state in severe COVID-19. Dual blockade of interleukin (IL)-4 and IL-13 with dupilumab may have a protective effect in the context of COVID-19 infection, because expression of Th2 cytokines, including IL-4 and IL-13, may be increased during COVID-19.
“At the start of the pandemic, many of us were faced with important questions, like do systemic immunomodulatory treatments influence outcomes of COVID-19 in patients with AD?” she said. “Do patients on dupilumab or other novel systemics fare better than those on conventional systemic treatment?”
To answer these questions, she and her colleagues launched a web-based registry in April 2020 to investigate COVID-19 outcomes in patients with AD treated with or without systemic immunomodulatory treatments. For the registry, known as Surveillance Epidemiology of Coronavirus Under Research Exclusion for Atopic Dermatitis (SECURE-AD), clinicians in 27 countries used a web-based form to enter anonymized data after patients had fully recovered from COVID-19. Eligibility criteria included having proven or highly suspected COVID-19, and there were no restrictions on age nor the type of AD treatment they were receiving.
Dr. Musters reported results from 442 patients who were recruited between April 2, 2020, and Oct. 31, 2021. Their mean age was 35.6 years, their median body mass index was 23.7 kg/m2, and there was an even sex distribution. Most patients were White and were recruited from Italy. Of the 442 patients, 216 (48.8%) received dupilumab monotherapy, 131 (29.6%) received topical treatments, and 14 (3.16%) received combination systemic treatments, including systemic corticosteroids. About 12% presented to the emergency department and 6% were hospitalized. Of those hospitalized, 2% required intensive care and/or ventilation, and no deaths have occurred in the registry to date.
By treatment group, hospitalization rates were highest among those on combination treatments (35.7%), followed by systemic corticosteroids (14.3%), topical treatments only (9.9%), other conventional systemics (3.6%), methotrexate (3.3%), and dupilumab (2.3%).
To further explore the differences between hospitalization rates in treatment groups, the researchers performed a multivariable logistic regression analysis, adjusted for age, sex, ethnicity, and comorbidity score. Compared with those who received dupilumab, the adjusted odds ratios (ORs) for hospitalization were highest among those who received topical treatments (OR, 4.95), followed by those who received systemic corticosteroids (OR, 2.81), and those who received other conventional systemic treatments (OR, 2.36).
Dr. Musters and colleagues also found that compared with patients on nonsteroidal immunosuppressive therapy, patients on combination systemic therapy had a significantly higher odds of hospitalization, specifically an OR of 45.75 for those on combination treatment including corticosteroids, an OR of 37.57 for those on combination treatment not including steroids, and an OR of 1.87 for those on systemic corticosteroids as monotherapy.
“Overall, the risk of COVID-19 complications appears to be low in patients with AD, even when treated with systemic immunomodulatory agents,” Dr. Musters concluded. “Dupilumab monotherapy was associated with lower odds of hospitalizations compared with other therapies. Moreover, combination systemic treatment, especially combinations including systemic corticosteroids, was associated with the highest risk of severe COVID-19.”
She added that other population-based study designs are more suitable to answer other important questions, such as whether the overall risk of COVID-19 in patients with AD is higher or lower compared to healthy controls.
Amy S. Paller, MD, professor and chair of the department of dermatology at Northwestern University, Chicago, who was asked to comment on the study, characterized the results as reassuring. In this patient population, “we expected that dupilumab would not cause any problems,” she said. “We wouldn’t necessarily expect it to [confer] a benefit, but I think it’s because the patients who need a systemic medication are going on something that’s very targeted (dupilumab) rather than something that has a broader immunosuppressing function. It was interesting but not surprising that those on systemic steroids had more of a problem. Get them on something that’s very targeted if you can and don’t suppress the immune systems that might be handling COVID-19.”
Dr. Musters reported having no disclosures. Dr. Paller disclosed that she is consultant to and/or an investigator for many pharmaceutical companies.
AT AAD 22
FDA okays semaglutide higher dose, 2 mg/week, for type 2 diabetes
The U.S. Food and Drug Administration has approved a higher 2-mg dose of the GLP-1 agonist semaglutide (Ozempic, Novo Nordisk) for adults with type 2 diabetes, giving a higher-dose alternative to the previous maximum 1-mg dose of semaglutide, administered by subcutaneous injection once weekly.
Semaglutide is currently available as 0.5-mg and 1-mg doses.
Results from the pivotal SUSTAIN FORTE study of the 2-mg dose (which, like lower-dose semaglutide for type 2 diabetes, comes in a single-use pen injector) showed that when compared head-to-head with a 1-mg/week dose in a 40-week study with 961 randomized patients, the 2-mg regimen led to a significant average incremental reduction in A1c levels of 0.23 percentage points. The 2-mg dose also produced a significant incremental increase in weight loss, with patients losing 0.93 kg more on the higher dose.
The 2-mg dose gives patients with type 2 diabetes and clinicians an “additional option” when a bigger “shift” in blood glucose is needed, said Juan Pablo Frias, MD, National Research Institute, Los Angeles, California, who was lead investigator for SUSTAIN FORTE, in a written statement.
As well as reducing glucose levels, semaglutide has been shown to reduce the risk of major cardiovascular events in adults with type 2 diabetes and known cardiovascular disease.
Semaglutide was approved as a 2.4-mg injectable dose, as Wegovy, in 2021 for weight loss in patients with overweight or obesity.
SUSTAIN FORTE and other trials of semaglutide were sponsored by Novo Nordisk. SURPASS-2 and other trials of tirzepatide were sponsored by Lilly. Dr. Frias was lead investigator for both SUSTAIN FORTE and SURPASS-2, as well as an investigator for other trials sponsored by Lilly, Novo Nordisk, and other companies.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved a higher 2-mg dose of the GLP-1 agonist semaglutide (Ozempic, Novo Nordisk) for adults with type 2 diabetes, giving a higher-dose alternative to the previous maximum 1-mg dose of semaglutide, administered by subcutaneous injection once weekly.
Semaglutide is currently available as 0.5-mg and 1-mg doses.
Results from the pivotal SUSTAIN FORTE study of the 2-mg dose (which, like lower-dose semaglutide for type 2 diabetes, comes in a single-use pen injector) showed that when compared head-to-head with a 1-mg/week dose in a 40-week study with 961 randomized patients, the 2-mg regimen led to a significant average incremental reduction in A1c levels of 0.23 percentage points. The 2-mg dose also produced a significant incremental increase in weight loss, with patients losing 0.93 kg more on the higher dose.
The 2-mg dose gives patients with type 2 diabetes and clinicians an “additional option” when a bigger “shift” in blood glucose is needed, said Juan Pablo Frias, MD, National Research Institute, Los Angeles, California, who was lead investigator for SUSTAIN FORTE, in a written statement.
As well as reducing glucose levels, semaglutide has been shown to reduce the risk of major cardiovascular events in adults with type 2 diabetes and known cardiovascular disease.
Semaglutide was approved as a 2.4-mg injectable dose, as Wegovy, in 2021 for weight loss in patients with overweight or obesity.
SUSTAIN FORTE and other trials of semaglutide were sponsored by Novo Nordisk. SURPASS-2 and other trials of tirzepatide were sponsored by Lilly. Dr. Frias was lead investigator for both SUSTAIN FORTE and SURPASS-2, as well as an investigator for other trials sponsored by Lilly, Novo Nordisk, and other companies.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved a higher 2-mg dose of the GLP-1 agonist semaglutide (Ozempic, Novo Nordisk) for adults with type 2 diabetes, giving a higher-dose alternative to the previous maximum 1-mg dose of semaglutide, administered by subcutaneous injection once weekly.
Semaglutide is currently available as 0.5-mg and 1-mg doses.
Results from the pivotal SUSTAIN FORTE study of the 2-mg dose (which, like lower-dose semaglutide for type 2 diabetes, comes in a single-use pen injector) showed that when compared head-to-head with a 1-mg/week dose in a 40-week study with 961 randomized patients, the 2-mg regimen led to a significant average incremental reduction in A1c levels of 0.23 percentage points. The 2-mg dose also produced a significant incremental increase in weight loss, with patients losing 0.93 kg more on the higher dose.
The 2-mg dose gives patients with type 2 diabetes and clinicians an “additional option” when a bigger “shift” in blood glucose is needed, said Juan Pablo Frias, MD, National Research Institute, Los Angeles, California, who was lead investigator for SUSTAIN FORTE, in a written statement.
As well as reducing glucose levels, semaglutide has been shown to reduce the risk of major cardiovascular events in adults with type 2 diabetes and known cardiovascular disease.
Semaglutide was approved as a 2.4-mg injectable dose, as Wegovy, in 2021 for weight loss in patients with overweight or obesity.
SUSTAIN FORTE and other trials of semaglutide were sponsored by Novo Nordisk. SURPASS-2 and other trials of tirzepatide were sponsored by Lilly. Dr. Frias was lead investigator for both SUSTAIN FORTE and SURPASS-2, as well as an investigator for other trials sponsored by Lilly, Novo Nordisk, and other companies.
A version of this article first appeared on Medscape.com.










