User login
Senate approves bill to ban crib bumpers
The Senate on Mar. 23 approved a bill to ban the sale of padded crib bumpers, which have been deemed risky by public health experts.
The Safe Cribs Act, introduced by Sen. Rob Portman (R-Ohio) and Sen. Tammy Duckworth (D-Ill.), would prohibit making and distributing bumpers – soft pads made to protect babies from hard sides of cribs – which have been found to increase suffocation risk.
The bill will now head to the House of Representatives.
According to data from the Consumer Product Safety Commission, 107 babies died in cribs with bumpers between 1990 and 2016, and 282 nonfatal incidents with bumpers were reported, including near-misses for strangulation and suffocation.
The American Academy of Pediatrics recommends keeping babies’ cribs free of any objects, including bumpers.
Despite this, bumpers are still widely sold by retailers.
“The fact that these deadly products can still be found on shelves across the country is extremely confusing to new parents who don’t believe stores would be selling them if they were truly dangerous to babies,” Sen. Duckworth said in a statement.
A 2020 survey released by Johns Hopkins University found that many parents were unaware of the dangers posed by crib bumpers and assumed they would be removed from stores if found unsafe.
Maryland banned the sale of bumpers in 2013, followed by Ohio in 2017. Chicago became the first city to ban them in 2011.
A version of this article first appeared on WebMD.com.
The Senate on Mar. 23 approved a bill to ban the sale of padded crib bumpers, which have been deemed risky by public health experts.
The Safe Cribs Act, introduced by Sen. Rob Portman (R-Ohio) and Sen. Tammy Duckworth (D-Ill.), would prohibit making and distributing bumpers – soft pads made to protect babies from hard sides of cribs – which have been found to increase suffocation risk.
The bill will now head to the House of Representatives.
According to data from the Consumer Product Safety Commission, 107 babies died in cribs with bumpers between 1990 and 2016, and 282 nonfatal incidents with bumpers were reported, including near-misses for strangulation and suffocation.
The American Academy of Pediatrics recommends keeping babies’ cribs free of any objects, including bumpers.
Despite this, bumpers are still widely sold by retailers.
“The fact that these deadly products can still be found on shelves across the country is extremely confusing to new parents who don’t believe stores would be selling them if they were truly dangerous to babies,” Sen. Duckworth said in a statement.
A 2020 survey released by Johns Hopkins University found that many parents were unaware of the dangers posed by crib bumpers and assumed they would be removed from stores if found unsafe.
Maryland banned the sale of bumpers in 2013, followed by Ohio in 2017. Chicago became the first city to ban them in 2011.
A version of this article first appeared on WebMD.com.
The Senate on Mar. 23 approved a bill to ban the sale of padded crib bumpers, which have been deemed risky by public health experts.
The Safe Cribs Act, introduced by Sen. Rob Portman (R-Ohio) and Sen. Tammy Duckworth (D-Ill.), would prohibit making and distributing bumpers – soft pads made to protect babies from hard sides of cribs – which have been found to increase suffocation risk.
The bill will now head to the House of Representatives.
According to data from the Consumer Product Safety Commission, 107 babies died in cribs with bumpers between 1990 and 2016, and 282 nonfatal incidents with bumpers were reported, including near-misses for strangulation and suffocation.
The American Academy of Pediatrics recommends keeping babies’ cribs free of any objects, including bumpers.
Despite this, bumpers are still widely sold by retailers.
“The fact that these deadly products can still be found on shelves across the country is extremely confusing to new parents who don’t believe stores would be selling them if they were truly dangerous to babies,” Sen. Duckworth said in a statement.
A 2020 survey released by Johns Hopkins University found that many parents were unaware of the dangers posed by crib bumpers and assumed they would be removed from stores if found unsafe.
Maryland banned the sale of bumpers in 2013, followed by Ohio in 2017. Chicago became the first city to ban them in 2011.
A version of this article first appeared on WebMD.com.
Cancer of the appendix on the rise in younger patients with appendicitis
Younger patients with appendicitis appear to be increasingly likely to have cancer of the appendix, a new study suggests.
While acute appendicitis can often be managed with antibiotics instead of surgery, patients who do not have surgery need to be closely followed to avoid missed diagnoses, the authors write.
“The most important finding is that between 2004 and 2017, relative to right-sided colon cancer, the number of appendiceal cancer cases increased,” said Mustafa Raoof, MD, who was not involved in the study. He is a surgical oncologist and an assistant professor of surgical oncology at City of Hope Comprehensive Cancer Center, Duarte, Calif. “Approximately one-fourth of these were carcinoid tumors, and this category saw the greatest increase, particularly in individuals under 50 years of age.”
“There is a push to treat acute appendicitis with only antibiotics to avoid surgery,” Dr. Raoof told this news organization by email. “One underappreciated downside of this strategy is that an appendiceal cancer can be missed if the appendix is not removed.”
As reported in Journal of the American College of Surgeons, lead study author Michelle C. Salazar, MD, MHS, a general surgery resident at Yale School of Medicine in New Haven, Conn., and her colleagues conducted a retrospective analysis of the National Cancer Database (NCDB). The NCDB contains hospital registry data of around 70% of new cancer diagnoses in the United States.
The researchers extracted data on patients aged 18 years and older who were diagnosed with right-sided colon cancer between 2004 and 2017 and who underwent appendectomy. The authors also identified all patients with appendiceal cancer. They divided that group into patients with carcinoid tumors and those with other types of appendiceal cancer. They also investigated trends by age group.
Of 387,867 patients with right-sided colon cancer, 19,570 (5%) had appendiceal cancer, and 5,628 of those patients (29%) had carcinoid tumor. The odds of appendiceal cancer, compared with other right-sided colon cancers, rose over the years studied (odds ratio, 2.56; 95% confidence interval, 2.35-2.79).
This increase in odds occurred in all age groups but was steepest among patients between 40 and 49 years of age, among whom it increased from 10% in 2004 (95% CI, 9-12) to 18% in 2017 (95% CI, 16-20; P < .001).
Odds of appendiceal carcinoid, compared with other appendiceal cancers, also rose during this period (OR, 1.70; 95% CI, 1.40-2.07). The sharpest increase occurred in the likelihood of carcinoid in patients younger than 40, from 24% in 2004 (95% CI, 15-34) to 45% in 2017 (95% CI, 37-53; P < .001).
“The findings in this study are yet another reason to temper excitement about nonoperative management of acute appendicitis in adults,” Richard S. Hoehn, MD, a surgical oncologist at University Hospitals Seidman Cancer Center, Cleveland, said. “The study is important because it reveals a potential risk of deferring appendectomy in adult patients with appendiceal pathology.”
“As our pathologic examinations of appendiceal cancers improve, we are gaining better understanding of these tumors and how to best manage these patients,” Dr. Hoehn, who also was not involved in the study, added in an email. “The findings should make surgeons more suspicious of malignant causes of acute appendicitis in adults, especially those under 40. Colonoscopy and appendectomy are necessary in adult patients with appendicitis.”
Gregory Botta, MD, PhD, a medical oncologist and associate professor of medicine at the University of California San Diego Health, mentioned limitations of the study in an email. They include the NCDB’s omission of around 30% of cases nationally and the study’s omission of patients diagnosed with primary appendiceal tumor, as well as patients who underwent total colectomies and those who did not have surgery.
“Appendiceal tumors are not normally seen during colonoscopies; screening colonoscopies are not recommended to younger patients under 40, and there is less surgical management for appendicitis,” explained Dr. Botta, who also was not involved in the study. “Thus, the cause of the increasing incidence is not due to increased detection on surveillance.
“Gastrointestinal oncologists are seeing an increase in colon cancer in younger patients and a parallel increase in appendix tumors. While carcinoid tumors are usually found localized and [are] therefore curable postsurgical resection, adenocarcinoma or mucinous subtypes tend to be more diffuse, metastatic, and noncurable,” he added. “Although the increase in colon cancer is being found in our younger population, the authors hint at causes not captured by the NCDB, including environmental exposures or each patient’s diet.”
“There is no good answer as to why there is an increase in carcinoids,” Dr. Salazar said in a press release. “It could be due to environmental reasons, or it could be due to better diagnostics technology.”
The researchers and independent experts share concerns that, because surgery provides the only definitive diagnosis of appendiceal cancer, among patients managed nonsurgically, there may be a delay in cancer diagnosis.
“I would counsel patients based on age,” Dr. Salazar added. “If you’re older, you are at less risk for appendiceal cancer and greater risk for complications from surgery. Younger, healthy patients are more likely to be able to tolerate an operation and may want to rule out cancer by undergoing the operation. The characteristics of appendicitis should be considered in the decision.”
Funding information was not provided. The authors, Dr. Raoof, Dr. Hoehn, and Dr. Botta have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Younger patients with appendicitis appear to be increasingly likely to have cancer of the appendix, a new study suggests.
While acute appendicitis can often be managed with antibiotics instead of surgery, patients who do not have surgery need to be closely followed to avoid missed diagnoses, the authors write.
“The most important finding is that between 2004 and 2017, relative to right-sided colon cancer, the number of appendiceal cancer cases increased,” said Mustafa Raoof, MD, who was not involved in the study. He is a surgical oncologist and an assistant professor of surgical oncology at City of Hope Comprehensive Cancer Center, Duarte, Calif. “Approximately one-fourth of these were carcinoid tumors, and this category saw the greatest increase, particularly in individuals under 50 years of age.”
“There is a push to treat acute appendicitis with only antibiotics to avoid surgery,” Dr. Raoof told this news organization by email. “One underappreciated downside of this strategy is that an appendiceal cancer can be missed if the appendix is not removed.”
As reported in Journal of the American College of Surgeons, lead study author Michelle C. Salazar, MD, MHS, a general surgery resident at Yale School of Medicine in New Haven, Conn., and her colleagues conducted a retrospective analysis of the National Cancer Database (NCDB). The NCDB contains hospital registry data of around 70% of new cancer diagnoses in the United States.
The researchers extracted data on patients aged 18 years and older who were diagnosed with right-sided colon cancer between 2004 and 2017 and who underwent appendectomy. The authors also identified all patients with appendiceal cancer. They divided that group into patients with carcinoid tumors and those with other types of appendiceal cancer. They also investigated trends by age group.
Of 387,867 patients with right-sided colon cancer, 19,570 (5%) had appendiceal cancer, and 5,628 of those patients (29%) had carcinoid tumor. The odds of appendiceal cancer, compared with other right-sided colon cancers, rose over the years studied (odds ratio, 2.56; 95% confidence interval, 2.35-2.79).
This increase in odds occurred in all age groups but was steepest among patients between 40 and 49 years of age, among whom it increased from 10% in 2004 (95% CI, 9-12) to 18% in 2017 (95% CI, 16-20; P < .001).
Odds of appendiceal carcinoid, compared with other appendiceal cancers, also rose during this period (OR, 1.70; 95% CI, 1.40-2.07). The sharpest increase occurred in the likelihood of carcinoid in patients younger than 40, from 24% in 2004 (95% CI, 15-34) to 45% in 2017 (95% CI, 37-53; P < .001).
“The findings in this study are yet another reason to temper excitement about nonoperative management of acute appendicitis in adults,” Richard S. Hoehn, MD, a surgical oncologist at University Hospitals Seidman Cancer Center, Cleveland, said. “The study is important because it reveals a potential risk of deferring appendectomy in adult patients with appendiceal pathology.”
“As our pathologic examinations of appendiceal cancers improve, we are gaining better understanding of these tumors and how to best manage these patients,” Dr. Hoehn, who also was not involved in the study, added in an email. “The findings should make surgeons more suspicious of malignant causes of acute appendicitis in adults, especially those under 40. Colonoscopy and appendectomy are necessary in adult patients with appendicitis.”
Gregory Botta, MD, PhD, a medical oncologist and associate professor of medicine at the University of California San Diego Health, mentioned limitations of the study in an email. They include the NCDB’s omission of around 30% of cases nationally and the study’s omission of patients diagnosed with primary appendiceal tumor, as well as patients who underwent total colectomies and those who did not have surgery.
“Appendiceal tumors are not normally seen during colonoscopies; screening colonoscopies are not recommended to younger patients under 40, and there is less surgical management for appendicitis,” explained Dr. Botta, who also was not involved in the study. “Thus, the cause of the increasing incidence is not due to increased detection on surveillance.
“Gastrointestinal oncologists are seeing an increase in colon cancer in younger patients and a parallel increase in appendix tumors. While carcinoid tumors are usually found localized and [are] therefore curable postsurgical resection, adenocarcinoma or mucinous subtypes tend to be more diffuse, metastatic, and noncurable,” he added. “Although the increase in colon cancer is being found in our younger population, the authors hint at causes not captured by the NCDB, including environmental exposures or each patient’s diet.”
“There is no good answer as to why there is an increase in carcinoids,” Dr. Salazar said in a press release. “It could be due to environmental reasons, or it could be due to better diagnostics technology.”
The researchers and independent experts share concerns that, because surgery provides the only definitive diagnosis of appendiceal cancer, among patients managed nonsurgically, there may be a delay in cancer diagnosis.
“I would counsel patients based on age,” Dr. Salazar added. “If you’re older, you are at less risk for appendiceal cancer and greater risk for complications from surgery. Younger, healthy patients are more likely to be able to tolerate an operation and may want to rule out cancer by undergoing the operation. The characteristics of appendicitis should be considered in the decision.”
Funding information was not provided. The authors, Dr. Raoof, Dr. Hoehn, and Dr. Botta have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Younger patients with appendicitis appear to be increasingly likely to have cancer of the appendix, a new study suggests.
While acute appendicitis can often be managed with antibiotics instead of surgery, patients who do not have surgery need to be closely followed to avoid missed diagnoses, the authors write.
“The most important finding is that between 2004 and 2017, relative to right-sided colon cancer, the number of appendiceal cancer cases increased,” said Mustafa Raoof, MD, who was not involved in the study. He is a surgical oncologist and an assistant professor of surgical oncology at City of Hope Comprehensive Cancer Center, Duarte, Calif. “Approximately one-fourth of these were carcinoid tumors, and this category saw the greatest increase, particularly in individuals under 50 years of age.”
“There is a push to treat acute appendicitis with only antibiotics to avoid surgery,” Dr. Raoof told this news organization by email. “One underappreciated downside of this strategy is that an appendiceal cancer can be missed if the appendix is not removed.”
As reported in Journal of the American College of Surgeons, lead study author Michelle C. Salazar, MD, MHS, a general surgery resident at Yale School of Medicine in New Haven, Conn., and her colleagues conducted a retrospective analysis of the National Cancer Database (NCDB). The NCDB contains hospital registry data of around 70% of new cancer diagnoses in the United States.
The researchers extracted data on patients aged 18 years and older who were diagnosed with right-sided colon cancer between 2004 and 2017 and who underwent appendectomy. The authors also identified all patients with appendiceal cancer. They divided that group into patients with carcinoid tumors and those with other types of appendiceal cancer. They also investigated trends by age group.
Of 387,867 patients with right-sided colon cancer, 19,570 (5%) had appendiceal cancer, and 5,628 of those patients (29%) had carcinoid tumor. The odds of appendiceal cancer, compared with other right-sided colon cancers, rose over the years studied (odds ratio, 2.56; 95% confidence interval, 2.35-2.79).
This increase in odds occurred in all age groups but was steepest among patients between 40 and 49 years of age, among whom it increased from 10% in 2004 (95% CI, 9-12) to 18% in 2017 (95% CI, 16-20; P < .001).
Odds of appendiceal carcinoid, compared with other appendiceal cancers, also rose during this period (OR, 1.70; 95% CI, 1.40-2.07). The sharpest increase occurred in the likelihood of carcinoid in patients younger than 40, from 24% in 2004 (95% CI, 15-34) to 45% in 2017 (95% CI, 37-53; P < .001).
“The findings in this study are yet another reason to temper excitement about nonoperative management of acute appendicitis in adults,” Richard S. Hoehn, MD, a surgical oncologist at University Hospitals Seidman Cancer Center, Cleveland, said. “The study is important because it reveals a potential risk of deferring appendectomy in adult patients with appendiceal pathology.”
“As our pathologic examinations of appendiceal cancers improve, we are gaining better understanding of these tumors and how to best manage these patients,” Dr. Hoehn, who also was not involved in the study, added in an email. “The findings should make surgeons more suspicious of malignant causes of acute appendicitis in adults, especially those under 40. Colonoscopy and appendectomy are necessary in adult patients with appendicitis.”
Gregory Botta, MD, PhD, a medical oncologist and associate professor of medicine at the University of California San Diego Health, mentioned limitations of the study in an email. They include the NCDB’s omission of around 30% of cases nationally and the study’s omission of patients diagnosed with primary appendiceal tumor, as well as patients who underwent total colectomies and those who did not have surgery.
“Appendiceal tumors are not normally seen during colonoscopies; screening colonoscopies are not recommended to younger patients under 40, and there is less surgical management for appendicitis,” explained Dr. Botta, who also was not involved in the study. “Thus, the cause of the increasing incidence is not due to increased detection on surveillance.
“Gastrointestinal oncologists are seeing an increase in colon cancer in younger patients and a parallel increase in appendix tumors. While carcinoid tumors are usually found localized and [are] therefore curable postsurgical resection, adenocarcinoma or mucinous subtypes tend to be more diffuse, metastatic, and noncurable,” he added. “Although the increase in colon cancer is being found in our younger population, the authors hint at causes not captured by the NCDB, including environmental exposures or each patient’s diet.”
“There is no good answer as to why there is an increase in carcinoids,” Dr. Salazar said in a press release. “It could be due to environmental reasons, or it could be due to better diagnostics technology.”
The researchers and independent experts share concerns that, because surgery provides the only definitive diagnosis of appendiceal cancer, among patients managed nonsurgically, there may be a delay in cancer diagnosis.
“I would counsel patients based on age,” Dr. Salazar added. “If you’re older, you are at less risk for appendiceal cancer and greater risk for complications from surgery. Younger, healthy patients are more likely to be able to tolerate an operation and may want to rule out cancer by undergoing the operation. The characteristics of appendicitis should be considered in the decision.”
Funding information was not provided. The authors, Dr. Raoof, Dr. Hoehn, and Dr. Botta have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Neonatal hypoglycemia doesn’t affect childhood academics
Children at risk of neonatal hypoglycemia who were screened and treated if needed showed no difference in educational achievement from controls at age 9-10 years, based on data from 480 children.
Previous studies have shown an increased risk of poor executive and visual-motor function in children with neonatal hypoglycemia, but the effect on later childhood academic performance remains unclear, wrote Rajesh Shah, PhD, of the University of Auckland, New Zealand, and colleagues.
In a prospective cohort study published in JAMA, the researchers enrolled moderate to late preterm and term infants born at increased risk for hypoglycemia; those with episodes of hypoglycemia were treated to maintain a blood glucose concentration of at least 47 mg/dL.
The study population was enrolled between 2006 and 2010 at a regional perinatal center in New Zealand, and their educational achievement was assessed 9-10 years later. The primary outcome of low educational achievement was defined as performing below the normal curriculum level in standardized tests of reading comprehension or math. The researchers also identified 47 secondary outcomes related to executive function, visual-motor function, psychosocial adaptation, and general health.
Rates of low educational achievement were not significantly different for children with and without neonatal hypoglycemia (47% vs. 48%, adjusted risk ratio 0.95).
No significant differences appeared between the two groups for any secondary outcomes, including reading comprehension, math, behavior manifestations of executive function, fine motor function, autism traits, and overall well-being, the researchers noted.
However, children with neonatal hypoglycemia were significantly less likely to be rated as below or well below reading curriculum level by teachers compared to those without neonatal hypoglycemia (24% vs. 31%).
The researchers cited a previous study of the same patient cohort at age 4.5 years, which suggested an association between adverse neurodevelopmental outcomes and infant hypoglycemia. However, the reason this association did not persist at age 9-10 years remains unclear, the researchers wrote in their discussion. “Early disturbances in brain development may have diminishing effects over time due to neuroplasticity, that is, reorganization of neural networks, or delayed maturation with mid-childhood catch-up in neurocognitive function,” they said.
The study findings were limited by several factors including the lack of data on several measures of cognition, notably processing speed, and a lack of adjustment for intelligence quotient at age 4.5 years, the lack of data on any treatment for developmental impairment, and the inclusion of a population with well-managed hypoglycemia, the researchers said.
However, the results were strengthened by having a sample size large enough to detect associations, the prospective design, and the accurate measure of neonatal glycemic exposure, they said. Although the results suggest that at-risk children reach similar endpoints by the end of primary school, “efforts to prevent and optimize adverse pregnancy conditions remain important, and developmental surveillance after birth should be considered for at-risk infants,” they concluded.
In a related study published in JAMA, Taygen Edwards and colleagues found that prophylactic oral dextrose gel had no significant effect on neurosensory function.
The study, a prospective follow-up of a multicenter randomized trial, included 1,197 later preterm or term infants deemed at risk for neonatal hypoglycemia. The infants (49% of whom were female) were randomized to prophylactic 40% dextrose gel or a placebo, massaged into the buccal mucosa at 1 hour after birth.
The primary outcome was neurosensory impairment at 2 years of age, which was assessed by neurologic examination, parent-reported medical questionnaires, Bayley Scales of Infant and Toddler Development, Third Edition (Bayley-III), performance-based executive function, Behavior Rating Inventory of Executive Function–Preschool Version, motion coherence thresholds, growth, and body composition.
At 2 years of age, the prevalence of neurosensory impairment was 21% and 19%, respectively, in infants randomized to prophylactic oral dextrose gel and placebo, a nonsignificant difference. No differences between the two groups were noted for cognitive and language delays, or low performance-based overall executive function. However, infants randomized to dextrose gel had significantly higher risk of motor delay compared to placebo (2.5% vs. 0.7%) and significantly lower Bayley-III composite scores for cognitive, language, and motor performance.
No significant differences were noted between the groups in the areas of moderate or severe neurosensory impairment, hearing impairment, cerebral palsy, developmental delay, above-average development, socioemotional and adaptive behavior, questionnaire-based executive function, low visual processing, history of seizures, allergic and infectious diseases, growth, and body composition.
The results are consistent with previous studies on the safety of dextrose gel, the researchers wrote in their discussion. However, the absolute difference of 7% in the primary outcome may be clinically important, they noted. “Caution is warranted before using prophylactic dextrose gel,” they said.
The researchers noted the results of a dose-finding trial that suggested improved scores on language, executive function, and motor skills in unadjusted analysis with higher doses of dextrose gel, but the reason for these findings remains unknown, they said.
The study findings were limited by the potential underpowering to detect small, but significant differences, and possible lack of generalizability because the majority of the participants were children of mothers with diabetes.
The results were strengthened by the high follow-up rate and comprehensive assessments, and highlight the need for additional research with longer follow-up, the researchers said.
Findings fuel further exploration
Although hypoglycemia is common in newborns, its management and potential outcomes remain subjects for debate, Paul J. Rozance, MD, of the University of Colorado, Aurora, wrote in an editorial accompanying both studies.
“Often, the same features that increase the risk of hypoglycemia in newborns also increase the risk for poor outcomes independent of hypoglycemia,” he said.
The study by Shah and colleagues was not a randomized trial of a specific management strategy, Dr. Rozance noted. However, the high rate of low educational attainment in children not exposed to dextrose gel emphasizes the need for more effective management of infant hypoglycemia, he said. “The findings also suggest that antenatal conditions that are associated with increased risk of hypoglycemia among newborns are associated with increased risk for impaired neurodevelopment and educational achievement, independent of neonatal hypoglycemia,” he said. The study findings contrast with those of an earlier study showing low academic achievement association with early transient hypoglycemia, which could argue for earlier intervention, he noted.
The study by Edwards and colleagues addressed the potential value of dextrose gel as an early intervention to prevent neonatal hypoglycemia, said Dr. Rozance.
“The 95% CI for the primary outcome of neurosensory impairment included up to a 7% increased risk for neurosensory impairment in the prophylactic dextrose gel group. The 7% increased risk was defined by the investigators as potentially clinically important, and the study may have been underpowered to detect small differences in the primary outcome,” he wrote.
Although the reasons for adverse outcomes in children given prophylactic dextrose gel remain unclear, “incorporation of prophylactic dextrose gel into clinical practice should await further research,” he said.
Regarding such research, Dr. Rozance proposed an “ideal study,” that would “randomize newborns with hypoglycemia to treatment or no treatment, although equipoise and ethical support for such a study are lacking. Another strategy would be to randomize newborns with hypoglycemia to receive low- or high-treatment glucose concentration goals,” he noted.
The relationship between hypoglycemia and impaired neurodevelopment is yet to be determined, but the two studies provide new evidence for the clinical importance and need for management of neonatal hypoglycemia and subsequent neurodevelopmental outcomes, he concluded.
The study by Shah and colleagues was supported by the Health Research Council of New Zealand and the Maurice and Phyllis Paykel Trust. Dr. Shah disclosed a doctoral fellowship from the University of Auckland. The study by Edwards and colleagues was supported by the Health Research Council of New Zealand and the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health. Ms. Edwards had no financial conflicts to disclose. Dr. Rozance disclosed receiving a StatStrip from Nova Biomedical for use in his laboratory.
Children at risk of neonatal hypoglycemia who were screened and treated if needed showed no difference in educational achievement from controls at age 9-10 years, based on data from 480 children.
Previous studies have shown an increased risk of poor executive and visual-motor function in children with neonatal hypoglycemia, but the effect on later childhood academic performance remains unclear, wrote Rajesh Shah, PhD, of the University of Auckland, New Zealand, and colleagues.
In a prospective cohort study published in JAMA, the researchers enrolled moderate to late preterm and term infants born at increased risk for hypoglycemia; those with episodes of hypoglycemia were treated to maintain a blood glucose concentration of at least 47 mg/dL.
The study population was enrolled between 2006 and 2010 at a regional perinatal center in New Zealand, and their educational achievement was assessed 9-10 years later. The primary outcome of low educational achievement was defined as performing below the normal curriculum level in standardized tests of reading comprehension or math. The researchers also identified 47 secondary outcomes related to executive function, visual-motor function, psychosocial adaptation, and general health.
Rates of low educational achievement were not significantly different for children with and without neonatal hypoglycemia (47% vs. 48%, adjusted risk ratio 0.95).
No significant differences appeared between the two groups for any secondary outcomes, including reading comprehension, math, behavior manifestations of executive function, fine motor function, autism traits, and overall well-being, the researchers noted.
However, children with neonatal hypoglycemia were significantly less likely to be rated as below or well below reading curriculum level by teachers compared to those without neonatal hypoglycemia (24% vs. 31%).
The researchers cited a previous study of the same patient cohort at age 4.5 years, which suggested an association between adverse neurodevelopmental outcomes and infant hypoglycemia. However, the reason this association did not persist at age 9-10 years remains unclear, the researchers wrote in their discussion. “Early disturbances in brain development may have diminishing effects over time due to neuroplasticity, that is, reorganization of neural networks, or delayed maturation with mid-childhood catch-up in neurocognitive function,” they said.
The study findings were limited by several factors including the lack of data on several measures of cognition, notably processing speed, and a lack of adjustment for intelligence quotient at age 4.5 years, the lack of data on any treatment for developmental impairment, and the inclusion of a population with well-managed hypoglycemia, the researchers said.
However, the results were strengthened by having a sample size large enough to detect associations, the prospective design, and the accurate measure of neonatal glycemic exposure, they said. Although the results suggest that at-risk children reach similar endpoints by the end of primary school, “efforts to prevent and optimize adverse pregnancy conditions remain important, and developmental surveillance after birth should be considered for at-risk infants,” they concluded.
In a related study published in JAMA, Taygen Edwards and colleagues found that prophylactic oral dextrose gel had no significant effect on neurosensory function.
The study, a prospective follow-up of a multicenter randomized trial, included 1,197 later preterm or term infants deemed at risk for neonatal hypoglycemia. The infants (49% of whom were female) were randomized to prophylactic 40% dextrose gel or a placebo, massaged into the buccal mucosa at 1 hour after birth.
The primary outcome was neurosensory impairment at 2 years of age, which was assessed by neurologic examination, parent-reported medical questionnaires, Bayley Scales of Infant and Toddler Development, Third Edition (Bayley-III), performance-based executive function, Behavior Rating Inventory of Executive Function–Preschool Version, motion coherence thresholds, growth, and body composition.
At 2 years of age, the prevalence of neurosensory impairment was 21% and 19%, respectively, in infants randomized to prophylactic oral dextrose gel and placebo, a nonsignificant difference. No differences between the two groups were noted for cognitive and language delays, or low performance-based overall executive function. However, infants randomized to dextrose gel had significantly higher risk of motor delay compared to placebo (2.5% vs. 0.7%) and significantly lower Bayley-III composite scores for cognitive, language, and motor performance.
No significant differences were noted between the groups in the areas of moderate or severe neurosensory impairment, hearing impairment, cerebral palsy, developmental delay, above-average development, socioemotional and adaptive behavior, questionnaire-based executive function, low visual processing, history of seizures, allergic and infectious diseases, growth, and body composition.
The results are consistent with previous studies on the safety of dextrose gel, the researchers wrote in their discussion. However, the absolute difference of 7% in the primary outcome may be clinically important, they noted. “Caution is warranted before using prophylactic dextrose gel,” they said.
The researchers noted the results of a dose-finding trial that suggested improved scores on language, executive function, and motor skills in unadjusted analysis with higher doses of dextrose gel, but the reason for these findings remains unknown, they said.
The study findings were limited by the potential underpowering to detect small, but significant differences, and possible lack of generalizability because the majority of the participants were children of mothers with diabetes.
The results were strengthened by the high follow-up rate and comprehensive assessments, and highlight the need for additional research with longer follow-up, the researchers said.
Findings fuel further exploration
Although hypoglycemia is common in newborns, its management and potential outcomes remain subjects for debate, Paul J. Rozance, MD, of the University of Colorado, Aurora, wrote in an editorial accompanying both studies.
“Often, the same features that increase the risk of hypoglycemia in newborns also increase the risk for poor outcomes independent of hypoglycemia,” he said.
The study by Shah and colleagues was not a randomized trial of a specific management strategy, Dr. Rozance noted. However, the high rate of low educational attainment in children not exposed to dextrose gel emphasizes the need for more effective management of infant hypoglycemia, he said. “The findings also suggest that antenatal conditions that are associated with increased risk of hypoglycemia among newborns are associated with increased risk for impaired neurodevelopment and educational achievement, independent of neonatal hypoglycemia,” he said. The study findings contrast with those of an earlier study showing low academic achievement association with early transient hypoglycemia, which could argue for earlier intervention, he noted.
The study by Edwards and colleagues addressed the potential value of dextrose gel as an early intervention to prevent neonatal hypoglycemia, said Dr. Rozance.
“The 95% CI for the primary outcome of neurosensory impairment included up to a 7% increased risk for neurosensory impairment in the prophylactic dextrose gel group. The 7% increased risk was defined by the investigators as potentially clinically important, and the study may have been underpowered to detect small differences in the primary outcome,” he wrote.
Although the reasons for adverse outcomes in children given prophylactic dextrose gel remain unclear, “incorporation of prophylactic dextrose gel into clinical practice should await further research,” he said.
Regarding such research, Dr. Rozance proposed an “ideal study,” that would “randomize newborns with hypoglycemia to treatment or no treatment, although equipoise and ethical support for such a study are lacking. Another strategy would be to randomize newborns with hypoglycemia to receive low- or high-treatment glucose concentration goals,” he noted.
The relationship between hypoglycemia and impaired neurodevelopment is yet to be determined, but the two studies provide new evidence for the clinical importance and need for management of neonatal hypoglycemia and subsequent neurodevelopmental outcomes, he concluded.
The study by Shah and colleagues was supported by the Health Research Council of New Zealand and the Maurice and Phyllis Paykel Trust. Dr. Shah disclosed a doctoral fellowship from the University of Auckland. The study by Edwards and colleagues was supported by the Health Research Council of New Zealand and the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health. Ms. Edwards had no financial conflicts to disclose. Dr. Rozance disclosed receiving a StatStrip from Nova Biomedical for use in his laboratory.
Children at risk of neonatal hypoglycemia who were screened and treated if needed showed no difference in educational achievement from controls at age 9-10 years, based on data from 480 children.
Previous studies have shown an increased risk of poor executive and visual-motor function in children with neonatal hypoglycemia, but the effect on later childhood academic performance remains unclear, wrote Rajesh Shah, PhD, of the University of Auckland, New Zealand, and colleagues.
In a prospective cohort study published in JAMA, the researchers enrolled moderate to late preterm and term infants born at increased risk for hypoglycemia; those with episodes of hypoglycemia were treated to maintain a blood glucose concentration of at least 47 mg/dL.
The study population was enrolled between 2006 and 2010 at a regional perinatal center in New Zealand, and their educational achievement was assessed 9-10 years later. The primary outcome of low educational achievement was defined as performing below the normal curriculum level in standardized tests of reading comprehension or math. The researchers also identified 47 secondary outcomes related to executive function, visual-motor function, psychosocial adaptation, and general health.
Rates of low educational achievement were not significantly different for children with and without neonatal hypoglycemia (47% vs. 48%, adjusted risk ratio 0.95).
No significant differences appeared between the two groups for any secondary outcomes, including reading comprehension, math, behavior manifestations of executive function, fine motor function, autism traits, and overall well-being, the researchers noted.
However, children with neonatal hypoglycemia were significantly less likely to be rated as below or well below reading curriculum level by teachers compared to those without neonatal hypoglycemia (24% vs. 31%).
The researchers cited a previous study of the same patient cohort at age 4.5 years, which suggested an association between adverse neurodevelopmental outcomes and infant hypoglycemia. However, the reason this association did not persist at age 9-10 years remains unclear, the researchers wrote in their discussion. “Early disturbances in brain development may have diminishing effects over time due to neuroplasticity, that is, reorganization of neural networks, or delayed maturation with mid-childhood catch-up in neurocognitive function,” they said.
The study findings were limited by several factors including the lack of data on several measures of cognition, notably processing speed, and a lack of adjustment for intelligence quotient at age 4.5 years, the lack of data on any treatment for developmental impairment, and the inclusion of a population with well-managed hypoglycemia, the researchers said.
However, the results were strengthened by having a sample size large enough to detect associations, the prospective design, and the accurate measure of neonatal glycemic exposure, they said. Although the results suggest that at-risk children reach similar endpoints by the end of primary school, “efforts to prevent and optimize adverse pregnancy conditions remain important, and developmental surveillance after birth should be considered for at-risk infants,” they concluded.
In a related study published in JAMA, Taygen Edwards and colleagues found that prophylactic oral dextrose gel had no significant effect on neurosensory function.
The study, a prospective follow-up of a multicenter randomized trial, included 1,197 later preterm or term infants deemed at risk for neonatal hypoglycemia. The infants (49% of whom were female) were randomized to prophylactic 40% dextrose gel or a placebo, massaged into the buccal mucosa at 1 hour after birth.
The primary outcome was neurosensory impairment at 2 years of age, which was assessed by neurologic examination, parent-reported medical questionnaires, Bayley Scales of Infant and Toddler Development, Third Edition (Bayley-III), performance-based executive function, Behavior Rating Inventory of Executive Function–Preschool Version, motion coherence thresholds, growth, and body composition.
At 2 years of age, the prevalence of neurosensory impairment was 21% and 19%, respectively, in infants randomized to prophylactic oral dextrose gel and placebo, a nonsignificant difference. No differences between the two groups were noted for cognitive and language delays, or low performance-based overall executive function. However, infants randomized to dextrose gel had significantly higher risk of motor delay compared to placebo (2.5% vs. 0.7%) and significantly lower Bayley-III composite scores for cognitive, language, and motor performance.
No significant differences were noted between the groups in the areas of moderate or severe neurosensory impairment, hearing impairment, cerebral palsy, developmental delay, above-average development, socioemotional and adaptive behavior, questionnaire-based executive function, low visual processing, history of seizures, allergic and infectious diseases, growth, and body composition.
The results are consistent with previous studies on the safety of dextrose gel, the researchers wrote in their discussion. However, the absolute difference of 7% in the primary outcome may be clinically important, they noted. “Caution is warranted before using prophylactic dextrose gel,” they said.
The researchers noted the results of a dose-finding trial that suggested improved scores on language, executive function, and motor skills in unadjusted analysis with higher doses of dextrose gel, but the reason for these findings remains unknown, they said.
The study findings were limited by the potential underpowering to detect small, but significant differences, and possible lack of generalizability because the majority of the participants were children of mothers with diabetes.
The results were strengthened by the high follow-up rate and comprehensive assessments, and highlight the need for additional research with longer follow-up, the researchers said.
Findings fuel further exploration
Although hypoglycemia is common in newborns, its management and potential outcomes remain subjects for debate, Paul J. Rozance, MD, of the University of Colorado, Aurora, wrote in an editorial accompanying both studies.
“Often, the same features that increase the risk of hypoglycemia in newborns also increase the risk for poor outcomes independent of hypoglycemia,” he said.
The study by Shah and colleagues was not a randomized trial of a specific management strategy, Dr. Rozance noted. However, the high rate of low educational attainment in children not exposed to dextrose gel emphasizes the need for more effective management of infant hypoglycemia, he said. “The findings also suggest that antenatal conditions that are associated with increased risk of hypoglycemia among newborns are associated with increased risk for impaired neurodevelopment and educational achievement, independent of neonatal hypoglycemia,” he said. The study findings contrast with those of an earlier study showing low academic achievement association with early transient hypoglycemia, which could argue for earlier intervention, he noted.
The study by Edwards and colleagues addressed the potential value of dextrose gel as an early intervention to prevent neonatal hypoglycemia, said Dr. Rozance.
“The 95% CI for the primary outcome of neurosensory impairment included up to a 7% increased risk for neurosensory impairment in the prophylactic dextrose gel group. The 7% increased risk was defined by the investigators as potentially clinically important, and the study may have been underpowered to detect small differences in the primary outcome,” he wrote.
Although the reasons for adverse outcomes in children given prophylactic dextrose gel remain unclear, “incorporation of prophylactic dextrose gel into clinical practice should await further research,” he said.
Regarding such research, Dr. Rozance proposed an “ideal study,” that would “randomize newborns with hypoglycemia to treatment or no treatment, although equipoise and ethical support for such a study are lacking. Another strategy would be to randomize newborns with hypoglycemia to receive low- or high-treatment glucose concentration goals,” he noted.
The relationship between hypoglycemia and impaired neurodevelopment is yet to be determined, but the two studies provide new evidence for the clinical importance and need for management of neonatal hypoglycemia and subsequent neurodevelopmental outcomes, he concluded.
The study by Shah and colleagues was supported by the Health Research Council of New Zealand and the Maurice and Phyllis Paykel Trust. Dr. Shah disclosed a doctoral fellowship from the University of Auckland. The study by Edwards and colleagues was supported by the Health Research Council of New Zealand and the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health. Ms. Edwards had no financial conflicts to disclose. Dr. Rozance disclosed receiving a StatStrip from Nova Biomedical for use in his laboratory.
FROM JAMA
Is aspirin the best way to prevent blood clots after THA/TKA?
CHICAGO – Patients discharged to facilities rather than to home after total hip arthroplasty (THA) or total knee arthroplasty (TKA) may need more potent chemoprophylaxis than aspirin to prevent blood clots, new data suggest.
Researchers led by Stefano Muscatelli, MD, an orthopedist at Michigan Medicine, Ann Arbor, first aimed to determine whether there was an increase in risk of venous thromboembolism (VTE) in patients who were discharged to facilities such as a skilled nursing facility or inpatient rehabilitation facility, compared with those discharged to home after THA or TKA.
The second aim was to determine whether VTE risk differed between home- and non–home-discharge patients when stratified by the chemoprophylaxis prescribed to prevent VTE.
Findings were presented at the annual meeting of the American Academy of Orthopaedic Surgeons by coauthor Michael McHugh, MD, also an orthopedist at Michigan Medicine in Ann Arbor.
The agents were categorized in three groups: aspirin only; more aggressive anticoagulants, including warfarin, factor Xa inhibitor, direct thrombin inhibitor, low-molecular-weight heparin, pentasaccharide, or antiplatelet agents, with or without concurrent aspirin; and other regimens.
The researchers found that rates of VTE were higher among patients discharged to facilities.
Of 6,411 patients included in the study, the overall rate of VTE was 1.05%. Among home-discharge patients (n = 5445), rates of VTE were significantly lower than among patients discharged to facilities (n = 966) (0.83% vs. 2.26%; P < .001).
However, the researchers found there was no difference in VTE rates between non-home and home discharge in patients who received more aggressive chemoprophylaxis.
Among discharged patients who received only aspirin, rates of VTE among those discharged to home were significantly lower compared to those discharged to facilities (0.76% vs. 3.83%; P < .001).
“Smoking, BMI [body mass index], procedure type, and preoperative anticoagulation were not associated with the outcome of VTE,” Dr. McHugh said.
“Although we found VTE to continue to be an uncommon complication, non-home discharge is independently associated with higher rates of VTE. Patients should be encouraged to discharge home, but those discharged to non-home facilities after total joint arthroplasty should be considered for more potent chemoprophylaxis than aspirin,” he concluded.
Stuart J. Fischer, MD, with Summit (N.J.) Orthopaedics and Sports Medicine, who was not part of the study, told this news organization that he found the results inconclusive.
He said there is the potential for confounding because “the people who are sent to a facility after total hip or total knee are inherently less mobile and less able to take care of themselves, so they are at a higher risk for VTE. They are going to be more static.”
Dr. Fischer noted that over the past few years, there has been a movement away from anticoagulation with more aggressive agents toward aspirin, for several reasons. Providers don’t have to monitor aspirin use and can instruct patients to take it once or twice a day. Initial data seem to show that it protects well against VTE.
“The question is, in certain population of patients, is it enough? And that’s where the data are unclear,” Dr. Fischer said.
“It’s certainly a useful study, and we need to find out which methods of anticoagulation are most effective in each setting,” he said.
Limitations include that it was a retrospective review and that adverse events from more aggressive chemoprophylaxis agents were not assessed. Prophylactic regimens were chosen at the discretion of the treating surgeon.
The researchers excluded bilateral cases, conversion arthroplasty, hip hemiarthroplasty, unicompartmental knee arthroplasty, and deaths.
Dr. Muscatelli and Dr. McHugh reported no relevant financial relationships. A coauthor reported being a paid consultant for DePuy and Zimmer. Dr. Fischer reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CHICAGO – Patients discharged to facilities rather than to home after total hip arthroplasty (THA) or total knee arthroplasty (TKA) may need more potent chemoprophylaxis than aspirin to prevent blood clots, new data suggest.
Researchers led by Stefano Muscatelli, MD, an orthopedist at Michigan Medicine, Ann Arbor, first aimed to determine whether there was an increase in risk of venous thromboembolism (VTE) in patients who were discharged to facilities such as a skilled nursing facility or inpatient rehabilitation facility, compared with those discharged to home after THA or TKA.
The second aim was to determine whether VTE risk differed between home- and non–home-discharge patients when stratified by the chemoprophylaxis prescribed to prevent VTE.
Findings were presented at the annual meeting of the American Academy of Orthopaedic Surgeons by coauthor Michael McHugh, MD, also an orthopedist at Michigan Medicine in Ann Arbor.
The agents were categorized in three groups: aspirin only; more aggressive anticoagulants, including warfarin, factor Xa inhibitor, direct thrombin inhibitor, low-molecular-weight heparin, pentasaccharide, or antiplatelet agents, with or without concurrent aspirin; and other regimens.
The researchers found that rates of VTE were higher among patients discharged to facilities.
Of 6,411 patients included in the study, the overall rate of VTE was 1.05%. Among home-discharge patients (n = 5445), rates of VTE were significantly lower than among patients discharged to facilities (n = 966) (0.83% vs. 2.26%; P < .001).
However, the researchers found there was no difference in VTE rates between non-home and home discharge in patients who received more aggressive chemoprophylaxis.
Among discharged patients who received only aspirin, rates of VTE among those discharged to home were significantly lower compared to those discharged to facilities (0.76% vs. 3.83%; P < .001).
“Smoking, BMI [body mass index], procedure type, and preoperative anticoagulation were not associated with the outcome of VTE,” Dr. McHugh said.
“Although we found VTE to continue to be an uncommon complication, non-home discharge is independently associated with higher rates of VTE. Patients should be encouraged to discharge home, but those discharged to non-home facilities after total joint arthroplasty should be considered for more potent chemoprophylaxis than aspirin,” he concluded.
Stuart J. Fischer, MD, with Summit (N.J.) Orthopaedics and Sports Medicine, who was not part of the study, told this news organization that he found the results inconclusive.
He said there is the potential for confounding because “the people who are sent to a facility after total hip or total knee are inherently less mobile and less able to take care of themselves, so they are at a higher risk for VTE. They are going to be more static.”
Dr. Fischer noted that over the past few years, there has been a movement away from anticoagulation with more aggressive agents toward aspirin, for several reasons. Providers don’t have to monitor aspirin use and can instruct patients to take it once or twice a day. Initial data seem to show that it protects well against VTE.
“The question is, in certain population of patients, is it enough? And that’s where the data are unclear,” Dr. Fischer said.
“It’s certainly a useful study, and we need to find out which methods of anticoagulation are most effective in each setting,” he said.
Limitations include that it was a retrospective review and that adverse events from more aggressive chemoprophylaxis agents were not assessed. Prophylactic regimens were chosen at the discretion of the treating surgeon.
The researchers excluded bilateral cases, conversion arthroplasty, hip hemiarthroplasty, unicompartmental knee arthroplasty, and deaths.
Dr. Muscatelli and Dr. McHugh reported no relevant financial relationships. A coauthor reported being a paid consultant for DePuy and Zimmer. Dr. Fischer reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CHICAGO – Patients discharged to facilities rather than to home after total hip arthroplasty (THA) or total knee arthroplasty (TKA) may need more potent chemoprophylaxis than aspirin to prevent blood clots, new data suggest.
Researchers led by Stefano Muscatelli, MD, an orthopedist at Michigan Medicine, Ann Arbor, first aimed to determine whether there was an increase in risk of venous thromboembolism (VTE) in patients who were discharged to facilities such as a skilled nursing facility or inpatient rehabilitation facility, compared with those discharged to home after THA or TKA.
The second aim was to determine whether VTE risk differed between home- and non–home-discharge patients when stratified by the chemoprophylaxis prescribed to prevent VTE.
Findings were presented at the annual meeting of the American Academy of Orthopaedic Surgeons by coauthor Michael McHugh, MD, also an orthopedist at Michigan Medicine in Ann Arbor.
The agents were categorized in three groups: aspirin only; more aggressive anticoagulants, including warfarin, factor Xa inhibitor, direct thrombin inhibitor, low-molecular-weight heparin, pentasaccharide, or antiplatelet agents, with or without concurrent aspirin; and other regimens.
The researchers found that rates of VTE were higher among patients discharged to facilities.
Of 6,411 patients included in the study, the overall rate of VTE was 1.05%. Among home-discharge patients (n = 5445), rates of VTE were significantly lower than among patients discharged to facilities (n = 966) (0.83% vs. 2.26%; P < .001).
However, the researchers found there was no difference in VTE rates between non-home and home discharge in patients who received more aggressive chemoprophylaxis.
Among discharged patients who received only aspirin, rates of VTE among those discharged to home were significantly lower compared to those discharged to facilities (0.76% vs. 3.83%; P < .001).
“Smoking, BMI [body mass index], procedure type, and preoperative anticoagulation were not associated with the outcome of VTE,” Dr. McHugh said.
“Although we found VTE to continue to be an uncommon complication, non-home discharge is independently associated with higher rates of VTE. Patients should be encouraged to discharge home, but those discharged to non-home facilities after total joint arthroplasty should be considered for more potent chemoprophylaxis than aspirin,” he concluded.
Stuart J. Fischer, MD, with Summit (N.J.) Orthopaedics and Sports Medicine, who was not part of the study, told this news organization that he found the results inconclusive.
He said there is the potential for confounding because “the people who are sent to a facility after total hip or total knee are inherently less mobile and less able to take care of themselves, so they are at a higher risk for VTE. They are going to be more static.”
Dr. Fischer noted that over the past few years, there has been a movement away from anticoagulation with more aggressive agents toward aspirin, for several reasons. Providers don’t have to monitor aspirin use and can instruct patients to take it once or twice a day. Initial data seem to show that it protects well against VTE.
“The question is, in certain population of patients, is it enough? And that’s where the data are unclear,” Dr. Fischer said.
“It’s certainly a useful study, and we need to find out which methods of anticoagulation are most effective in each setting,” he said.
Limitations include that it was a retrospective review and that adverse events from more aggressive chemoprophylaxis agents were not assessed. Prophylactic regimens were chosen at the discretion of the treating surgeon.
The researchers excluded bilateral cases, conversion arthroplasty, hip hemiarthroplasty, unicompartmental knee arthroplasty, and deaths.
Dr. Muscatelli and Dr. McHugh reported no relevant financial relationships. A coauthor reported being a paid consultant for DePuy and Zimmer. Dr. Fischer reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT AAOS 2022
Children and COVID: The long goodbye continues
COVID-19 continues to be a diminishing issue for U.S. children, as the number of new cases declined for the ninth consecutive week, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
the AAP and CHA said in their weekly COVID report. The most recently infected children brought the total number of COVID-19 cases to just over 12.8 million since the pandemic began.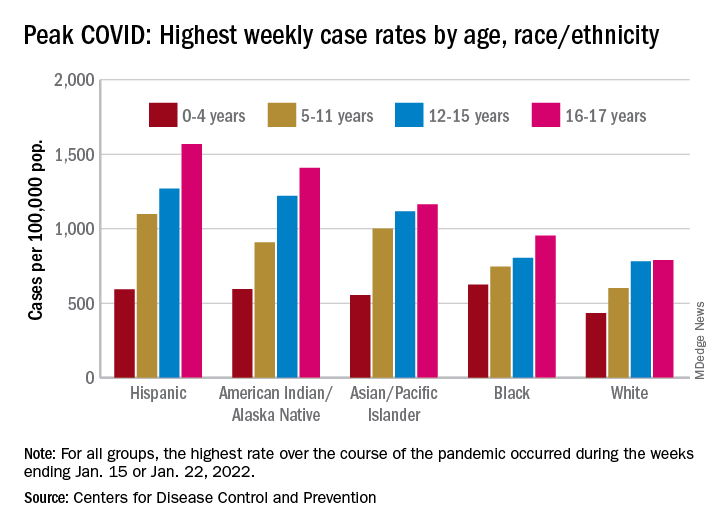
Other measures of COVID occurrence in children, such as hospital admissions and emergency department visits, also followed recent downward trends, although the sizes of the declines are beginning to decrease. Admissions dropped by 13.3% during the week ending March 26, but that followed declines of 25%, 20%, 26.5% and 24.4% for the 4 previous weeks, data from the Centers for Disease Control and Prevention show.
The slowdown in ED visits started a couple of weeks earlier, but the decline is still ongoing. As of March 25, ED visits with a confirmed COVID diagnosis represented just 0.4% of all visits for children aged 0-11 years, down from 1.1% on Feb. 25 and a peak of 14.3% on Jan. 15. For children aged 12-15, the latest figure is just 0.2%, compared with 0.5% on Feb. 25 and a peak of 14.3% on Jan. 9, the CDC reported on its COVID Data Tracker.
Although he was speaking of the nation as a whole and not specifically of children, Anthony Fauci, MD, the director of the National Institute of Allergy and Infectious Diseases, recently told the Washington Post that, “unless something changes dramatically,” another major surge isn’t on the horizon.
That sentiment, however, was not entirely shared by Moderna’s chief medical officer, Paul Burton, MD, PhD. In an interview with WebMD, he said that another COVID wave is inevitable and that it’s too soon to dismantle the vaccine infrastructure: “We’ve come so far. We’ve put so much into this to now take our foot off the gas. I think it would be a mistake for public health worldwide.”
Disparities during the Omicron surge
As the country puts Omicron in its rear view mirror, a quick look back at the CDC data shows some differences in how children were affected. At the surge’s peak in early to mid-January, Hispanic children were the most likely to get COVID-19, with incidence highest in the older groups. (See graph.)
At their peak week of Jan. 2-8, Hispanic children aged 16-17 years had a COVID rate of 1,568 cases per 100,000 population, versus 790 per 100,000 for White children, whose peak occurred a week later, from Jan. 9 to 15. Hispanic children aged 5-11 (1,098 per 100,000) and 12-15 (1,269 per 100,000) also had the highest recorded rates of the largest racial/ethnic groups, while Black children had the highest one-week rate, 625 per 100,000, among the 0- to 4-year-olds, according to the CDC.
COVID-19 continues to be a diminishing issue for U.S. children, as the number of new cases declined for the ninth consecutive week, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
the AAP and CHA said in their weekly COVID report. The most recently infected children brought the total number of COVID-19 cases to just over 12.8 million since the pandemic began.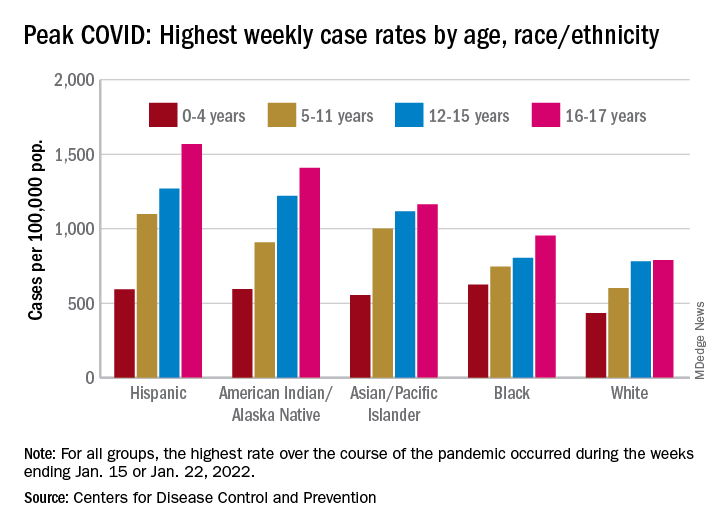
Other measures of COVID occurrence in children, such as hospital admissions and emergency department visits, also followed recent downward trends, although the sizes of the declines are beginning to decrease. Admissions dropped by 13.3% during the week ending March 26, but that followed declines of 25%, 20%, 26.5% and 24.4% for the 4 previous weeks, data from the Centers for Disease Control and Prevention show.
The slowdown in ED visits started a couple of weeks earlier, but the decline is still ongoing. As of March 25, ED visits with a confirmed COVID diagnosis represented just 0.4% of all visits for children aged 0-11 years, down from 1.1% on Feb. 25 and a peak of 14.3% on Jan. 15. For children aged 12-15, the latest figure is just 0.2%, compared with 0.5% on Feb. 25 and a peak of 14.3% on Jan. 9, the CDC reported on its COVID Data Tracker.
Although he was speaking of the nation as a whole and not specifically of children, Anthony Fauci, MD, the director of the National Institute of Allergy and Infectious Diseases, recently told the Washington Post that, “unless something changes dramatically,” another major surge isn’t on the horizon.
That sentiment, however, was not entirely shared by Moderna’s chief medical officer, Paul Burton, MD, PhD. In an interview with WebMD, he said that another COVID wave is inevitable and that it’s too soon to dismantle the vaccine infrastructure: “We’ve come so far. We’ve put so much into this to now take our foot off the gas. I think it would be a mistake for public health worldwide.”
Disparities during the Omicron surge
As the country puts Omicron in its rear view mirror, a quick look back at the CDC data shows some differences in how children were affected. At the surge’s peak in early to mid-January, Hispanic children were the most likely to get COVID-19, with incidence highest in the older groups. (See graph.)
At their peak week of Jan. 2-8, Hispanic children aged 16-17 years had a COVID rate of 1,568 cases per 100,000 population, versus 790 per 100,000 for White children, whose peak occurred a week later, from Jan. 9 to 15. Hispanic children aged 5-11 (1,098 per 100,000) and 12-15 (1,269 per 100,000) also had the highest recorded rates of the largest racial/ethnic groups, while Black children had the highest one-week rate, 625 per 100,000, among the 0- to 4-year-olds, according to the CDC.
COVID-19 continues to be a diminishing issue for U.S. children, as the number of new cases declined for the ninth consecutive week, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
the AAP and CHA said in their weekly COVID report. The most recently infected children brought the total number of COVID-19 cases to just over 12.8 million since the pandemic began.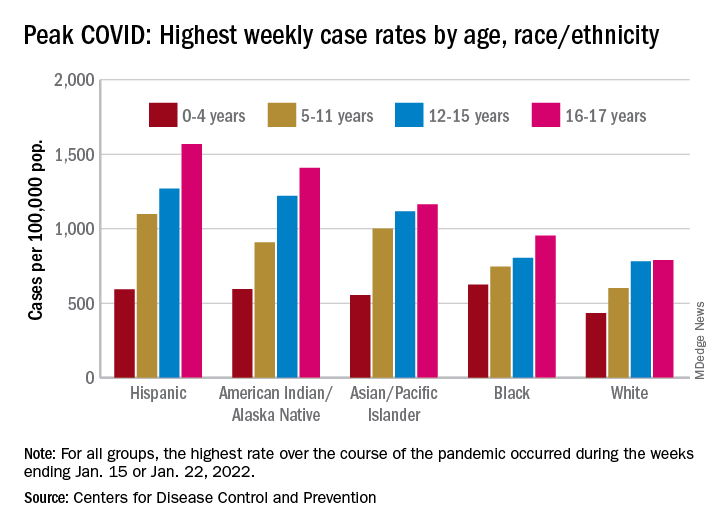
Other measures of COVID occurrence in children, such as hospital admissions and emergency department visits, also followed recent downward trends, although the sizes of the declines are beginning to decrease. Admissions dropped by 13.3% during the week ending March 26, but that followed declines of 25%, 20%, 26.5% and 24.4% for the 4 previous weeks, data from the Centers for Disease Control and Prevention show.
The slowdown in ED visits started a couple of weeks earlier, but the decline is still ongoing. As of March 25, ED visits with a confirmed COVID diagnosis represented just 0.4% of all visits for children aged 0-11 years, down from 1.1% on Feb. 25 and a peak of 14.3% on Jan. 15. For children aged 12-15, the latest figure is just 0.2%, compared with 0.5% on Feb. 25 and a peak of 14.3% on Jan. 9, the CDC reported on its COVID Data Tracker.
Although he was speaking of the nation as a whole and not specifically of children, Anthony Fauci, MD, the director of the National Institute of Allergy and Infectious Diseases, recently told the Washington Post that, “unless something changes dramatically,” another major surge isn’t on the horizon.
That sentiment, however, was not entirely shared by Moderna’s chief medical officer, Paul Burton, MD, PhD. In an interview with WebMD, he said that another COVID wave is inevitable and that it’s too soon to dismantle the vaccine infrastructure: “We’ve come so far. We’ve put so much into this to now take our foot off the gas. I think it would be a mistake for public health worldwide.”
Disparities during the Omicron surge
As the country puts Omicron in its rear view mirror, a quick look back at the CDC data shows some differences in how children were affected. At the surge’s peak in early to mid-January, Hispanic children were the most likely to get COVID-19, with incidence highest in the older groups. (See graph.)
At their peak week of Jan. 2-8, Hispanic children aged 16-17 years had a COVID rate of 1,568 cases per 100,000 population, versus 790 per 100,000 for White children, whose peak occurred a week later, from Jan. 9 to 15. Hispanic children aged 5-11 (1,098 per 100,000) and 12-15 (1,269 per 100,000) also had the highest recorded rates of the largest racial/ethnic groups, while Black children had the highest one-week rate, 625 per 100,000, among the 0- to 4-year-olds, according to the CDC.
What a sleep expert thinks of sleep trackers
The pandemic not only disrupted sleep but may have also triggered an uptick in the use of wearable tech. Sleep tracking was featured at the Cardiovascular Health Tech virtual conference 2022, sponsored by the Institute of Electrical and Electronics Engineers Engineering in Medicine & Biology Society technical committee on Cardiopulmonary Systems and Physiology-Based Engineering.
This news organization interviewed presenter Kelly Glazer Baron, PhD, MPH, DBSM, an associate professor at the University of Utah, Salt Lake City, and a clinical psychologist specializing in behavioral sleep medicine.
The interview has been edited for length and clarity.
Question: Are consumer sleep trackers mainly divided into “nearables” – things that you put at the side of the bed or under the pillow – vs. wearables?
Dr. Baron: There are so many different devices these days. There are things that you put under your mattress or pillow; there are bedside recording devices; then there are headbands, rings, wrist-worn, all kinds of things.
Q: At the conference, Philip de Chazal, PhD, (University of Sydney) described the evidence on sleep tracking smartphone apps as woeful. Would you agree with that?
A: Yes. I would agree if you’re looking at how accurate they are at recording sleep, particularly compared with what we would define as the gold standard, which is a sleep study wherein you have electrodes on the scalp and you’re measuring the electrical activity directly.
They are best at detecting when you get into the bed and when you get out. But even then, there isn’t good evidence that they do that accurately when there are two people in the bed.
Overall, they may give you a general gist of what’s happening in terms of time in and out of bed, but we’re doubtful on their recording ability to tell sleep from wake time.
Q: Are the wrist-worn devices better for sleep tracking?
A: They’re getting better. We’ve used wrist activity monitors in research for years. They use an accelerometer to measure movement, and then an algorithm determines whether an interval of time is called sleep or wake.
Recently, they’ve incorporated more sensors, such as heart rate, and they can more accurately decipher rapid eye movement (REM) sleep from non-REM. They’re still not as good as doing a full sleep study. But they’re getting closer.
Q: If asked how you slept, most of us think we can answer without needing to look at a smartphone, but maybe not. Can you explain “paradoxical insomnia”?
A: You can’t really know if you’re sleeping because if you know you’re asleep, then you can’t be asleep because it’s a state of unconsciousness. How people decide whether they had a good night’s sleep probably depends on a lot of things about how they feel when they wake up in the morning or if they remember being up in the night.
Quality of sleep is not really something that people can directly ascertain. There is a selection of people who feel awake all night but they actually are sleeping. They feel that their sleep quality is poor: They’re suffering; they have insomnia, but from the objective data, they are sleeping fine.
Q: Is this related to non-REM stage 1 sleep, when you may not be aware that you’re asleep?
A: No. I’m talking about people who come into the sleep lab for an overnight study and get hooked up. And in the morning, they’ll tell the tech I was awake all night, but the tech will see that their sleep was just fine.
There is a disconnect between how people perceive their sleep and how they actually sleep. For most people it’s impossible to be completely accurate to know how much you’re sleeping. Then there are some people who perceive it very differently.
Sleep trackers don’t have the level of detail of sleep studies that use scalp electrodes. When we get into the details of sleep measurement, we’re measuring 30-second epochs (sampling periods), where we look at broad measures of electrical activity. There is even more detail there that can be pulled out using other techniques, such as analyzing the spectrum of the EEG. For example, some studies have found a beta frequency in the EEG of people with insomnia, so even though they are sleeping, they often feel awake.
Basically, the subjective experience of sleep somewhat overlaps with the objective recording of what’s happening on a sleep study, but not completely.
Q: You said that first thing in the morning might not be the best time to assess your sleep – if you wake up groggy and are already thinking, “The day is shot.”
A: In general, people really feel worst in the morning. Their circadian drive is low, especially if they’re a little sleep deprived. You shouldn’t judge the day on the first hour after waking – most people are pretty cognitively impaired. I tell people they need some boot-up time.
You feel differently as the day goes on and even at different points of the day. There’s a lull in the early afternoon because of your circadian dip and then we get a second wind in the evening. How you feel isn’t one flat line; it’s really a rhythm throughout the day
Q: Would you say that consumer sleep trackers are okay for individuals to use to see a pattern but are maybe not accurate enough to use more globally in research?
A: I think there is a huge opportunity to understand sleep at a population level. For example, if there’s been a hurricane or an earthquake or Superbowl Sunday, companies have an opportunity to look at the impact – say, daylight saving time and how it affects sleep across different countries, or men vs. women, or different age groups.
There was a paper about sleep among hospital workers in Wuhan during the outbreak of the pandemic. That was a creative use of wearable devices to look at sleep in a large population.
Now, of course, the devices are not given out randomly; the people who buy them are probably a little bit healthier, maybe a little bit younger – that sort of thing. It is a biased sample.
Q: As you note, mobile health trackers tend to be used by the “worried well.” Can you tell us about your paper that introduced the term “orthosomnia,” or “a perfectionistic quest for the ideal sleep in order to optimize daytime function”?
A: As these devices came out, more people were coming into the clinic and shoving their data in front of us saying, “I don’t feel well, and I don’t sleep 7 hours.” They were focused on this specific number. Back when we wrote this paper, the devices were primarily movement based (now the devices are a bit more accurate). Some would say, “My sleep is light, and it’s not deep.” We’d do a sleep study that showed that they have deep sleep, but they would still believe their device even though the device really wasn’t able to classify sleep accurately.
We even found people making their sleep worse because of the device. For example, trying to get the number higher by spending more time lying in bed trying to sleep which is the opposite of what you want someone with insomnia to do. These people held the data so tight and really felt that it characterized their experience, even though we sleep medicine practitioners didn’t find it very accurate and felt that it was somewhat unhelpful to their treatment.
Q: What advice would you give the harried primary care physician presented with a patient’s hypnogram or sleep pattern?
A: As someone once pointed out to me, it’s a conversation opener about their sleep. Did they buy the device because they’re worried about their sleep? It’s unlikely that you can glean anything clinically useful from the data.
I briefly look at it to see the duration of their sleep, the regularity in their sleep pattern – the pattern of awakenings during the night might suggest that they have some insomnia. But it doesn’t take the place of clinical assessment for conditions like sleep apnea: Are they snoring? Are they unrefreshed?
I had a patient in the orthosomnia study who was given a sleep tracker by a family member. He brought the data to his doctor who ordered a sleep study that found he had sleep apnea. He would say, “The device diagnosed my sleep apnea.” But that wasn’t actually the case; it just opened the conversation and the clinician said, “Well, let’s order a sleep study.”
Q: The device told him he wasn’t getting much sleep and then the sleep study told him it was apnea.
A: Right. It’s impossible to pick up sleep apnea. Some of the latest devices have some oximetry reading but it is not a clinically validated oximetry that could diagnose sleep apnea.
When these first came out I thought I’d get more referrals. So far, I haven’t had a single person come in and ask if they have sleep apnea. If you have a patient saying, “Hey, I’m worried about my oxygen level and here’s my data,” then the clinician should consider whether they need a sleep study for sleep apnea.
Q: You did a survey that suggests that clinicians are less keen on these devices than consumers. Conor Heneghan of Fitbit/Google also mentioned a study using the Fitbit Charge and a SleepLife portal. The patients were very engaged but only one physician (out of 49) logged into the portal to look at the data.
A: Our survey of sleep professionals (which we need to publish) showed that they were wary of the data. They found it frustrating in some ways because it took time out of the clinical encounter.
Some of them said that parents are putting trackers on their children and then catastrophizing their children’s sleep.
Q: Is there such a thing as an ideal hypnogram or does it vary by individual?
A: I would say that it depends on a lot of things. If you think about a hypnogram from a sleep study, the patient is not sleeping in their home environment, and it’s only one night. There’s a range of what would be considered normal, and it’s related to your sex and your age.
One night is not going to be sufficient to characterize your percentage in this or that sleep stage. Our patients come in saying, “I’m not getting enough REM.” But there isn’t a sleep disorder called lack of REM; there’s no treatment for that. It’s probably pretty normal for them or maybe they’re taking medications that suppress their REM, such as antidepressants.
The tech world is very interested to sense REM properly and to display it. But on the treatment side of things, there’s not much that we do with that data. We’re more interested in the consolidation of their sleep, the duration of their sleep, breathing-related sleep disorders, those sorts of things.
Q: Is there any reason to be concerned about the amount of REM sleep in terms of outcomes? We know that poor sleep can lead to bad cardiovascular outcomes, but has any of that correlated to sleep stage?
A: There are studies where they’ve experimentally deprived people of certain stages of sleep, but they’re not very useful in the real world. We’re looking at sleep holistically: Do you have a good sleep pattern? Any breathing-related sleep disorders? Insomnia? We don’t treat sleep by the stage.
Q: Any concern that people who are focused on a device may be ignoring the basic tenets of good sleep hygiene?
A: If people are doing things that are obviously bad for their sleep, like working too late, not exercising enough, sleeping in on weekends to compensate for being up late during the week, or probably the biggest thing contributing to insomnia – stress. A device itself won’t fix those things but it could show you the evidence.
If somebody really has a sleep disorder, then sleep hygiene alone is probably not going to be enough. They’re going to need to engage in a more extensive program to improve their sleep, such as cognitive-behavioral therapy for insomnia.
Q: Is there anything else you want to mention?
A: I don’t want to leave with a reputation of being against sleep trackers. I think they are a great opportunity for people to get excited about and learn about their sleep and try to improve it. We have a lot to learn about what people want from their data and how we can use that data to improve people’s sleep.
As providers, we can engage with our patients – sleep is an automatic process, but improving sleep takes some effort. Buying a device is not going to automatically make you sleep better. It takes work to establish a better sleep pattern; it may require some cognitive-behavioral therapy or treating a sleep disorder. That takes some work.
Dr. Baron reported no conflicts of interest.A version of this article first appeared on Medscape.com.
The pandemic not only disrupted sleep but may have also triggered an uptick in the use of wearable tech. Sleep tracking was featured at the Cardiovascular Health Tech virtual conference 2022, sponsored by the Institute of Electrical and Electronics Engineers Engineering in Medicine & Biology Society technical committee on Cardiopulmonary Systems and Physiology-Based Engineering.
This news organization interviewed presenter Kelly Glazer Baron, PhD, MPH, DBSM, an associate professor at the University of Utah, Salt Lake City, and a clinical psychologist specializing in behavioral sleep medicine.
The interview has been edited for length and clarity.
Question: Are consumer sleep trackers mainly divided into “nearables” – things that you put at the side of the bed or under the pillow – vs. wearables?
Dr. Baron: There are so many different devices these days. There are things that you put under your mattress or pillow; there are bedside recording devices; then there are headbands, rings, wrist-worn, all kinds of things.
Q: At the conference, Philip de Chazal, PhD, (University of Sydney) described the evidence on sleep tracking smartphone apps as woeful. Would you agree with that?
A: Yes. I would agree if you’re looking at how accurate they are at recording sleep, particularly compared with what we would define as the gold standard, which is a sleep study wherein you have electrodes on the scalp and you’re measuring the electrical activity directly.
They are best at detecting when you get into the bed and when you get out. But even then, there isn’t good evidence that they do that accurately when there are two people in the bed.
Overall, they may give you a general gist of what’s happening in terms of time in and out of bed, but we’re doubtful on their recording ability to tell sleep from wake time.
Q: Are the wrist-worn devices better for sleep tracking?
A: They’re getting better. We’ve used wrist activity monitors in research for years. They use an accelerometer to measure movement, and then an algorithm determines whether an interval of time is called sleep or wake.
Recently, they’ve incorporated more sensors, such as heart rate, and they can more accurately decipher rapid eye movement (REM) sleep from non-REM. They’re still not as good as doing a full sleep study. But they’re getting closer.
Q: If asked how you slept, most of us think we can answer without needing to look at a smartphone, but maybe not. Can you explain “paradoxical insomnia”?
A: You can’t really know if you’re sleeping because if you know you’re asleep, then you can’t be asleep because it’s a state of unconsciousness. How people decide whether they had a good night’s sleep probably depends on a lot of things about how they feel when they wake up in the morning or if they remember being up in the night.
Quality of sleep is not really something that people can directly ascertain. There is a selection of people who feel awake all night but they actually are sleeping. They feel that their sleep quality is poor: They’re suffering; they have insomnia, but from the objective data, they are sleeping fine.
Q: Is this related to non-REM stage 1 sleep, when you may not be aware that you’re asleep?
A: No. I’m talking about people who come into the sleep lab for an overnight study and get hooked up. And in the morning, they’ll tell the tech I was awake all night, but the tech will see that their sleep was just fine.
There is a disconnect between how people perceive their sleep and how they actually sleep. For most people it’s impossible to be completely accurate to know how much you’re sleeping. Then there are some people who perceive it very differently.
Sleep trackers don’t have the level of detail of sleep studies that use scalp electrodes. When we get into the details of sleep measurement, we’re measuring 30-second epochs (sampling periods), where we look at broad measures of electrical activity. There is even more detail there that can be pulled out using other techniques, such as analyzing the spectrum of the EEG. For example, some studies have found a beta frequency in the EEG of people with insomnia, so even though they are sleeping, they often feel awake.
Basically, the subjective experience of sleep somewhat overlaps with the objective recording of what’s happening on a sleep study, but not completely.
Q: You said that first thing in the morning might not be the best time to assess your sleep – if you wake up groggy and are already thinking, “The day is shot.”
A: In general, people really feel worst in the morning. Their circadian drive is low, especially if they’re a little sleep deprived. You shouldn’t judge the day on the first hour after waking – most people are pretty cognitively impaired. I tell people they need some boot-up time.
You feel differently as the day goes on and even at different points of the day. There’s a lull in the early afternoon because of your circadian dip and then we get a second wind in the evening. How you feel isn’t one flat line; it’s really a rhythm throughout the day
Q: Would you say that consumer sleep trackers are okay for individuals to use to see a pattern but are maybe not accurate enough to use more globally in research?
A: I think there is a huge opportunity to understand sleep at a population level. For example, if there’s been a hurricane or an earthquake or Superbowl Sunday, companies have an opportunity to look at the impact – say, daylight saving time and how it affects sleep across different countries, or men vs. women, or different age groups.
There was a paper about sleep among hospital workers in Wuhan during the outbreak of the pandemic. That was a creative use of wearable devices to look at sleep in a large population.
Now, of course, the devices are not given out randomly; the people who buy them are probably a little bit healthier, maybe a little bit younger – that sort of thing. It is a biased sample.
Q: As you note, mobile health trackers tend to be used by the “worried well.” Can you tell us about your paper that introduced the term “orthosomnia,” or “a perfectionistic quest for the ideal sleep in order to optimize daytime function”?
A: As these devices came out, more people were coming into the clinic and shoving their data in front of us saying, “I don’t feel well, and I don’t sleep 7 hours.” They were focused on this specific number. Back when we wrote this paper, the devices were primarily movement based (now the devices are a bit more accurate). Some would say, “My sleep is light, and it’s not deep.” We’d do a sleep study that showed that they have deep sleep, but they would still believe their device even though the device really wasn’t able to classify sleep accurately.
We even found people making their sleep worse because of the device. For example, trying to get the number higher by spending more time lying in bed trying to sleep which is the opposite of what you want someone with insomnia to do. These people held the data so tight and really felt that it characterized their experience, even though we sleep medicine practitioners didn’t find it very accurate and felt that it was somewhat unhelpful to their treatment.
Q: What advice would you give the harried primary care physician presented with a patient’s hypnogram or sleep pattern?
A: As someone once pointed out to me, it’s a conversation opener about their sleep. Did they buy the device because they’re worried about their sleep? It’s unlikely that you can glean anything clinically useful from the data.
I briefly look at it to see the duration of their sleep, the regularity in their sleep pattern – the pattern of awakenings during the night might suggest that they have some insomnia. But it doesn’t take the place of clinical assessment for conditions like sleep apnea: Are they snoring? Are they unrefreshed?
I had a patient in the orthosomnia study who was given a sleep tracker by a family member. He brought the data to his doctor who ordered a sleep study that found he had sleep apnea. He would say, “The device diagnosed my sleep apnea.” But that wasn’t actually the case; it just opened the conversation and the clinician said, “Well, let’s order a sleep study.”
Q: The device told him he wasn’t getting much sleep and then the sleep study told him it was apnea.
A: Right. It’s impossible to pick up sleep apnea. Some of the latest devices have some oximetry reading but it is not a clinically validated oximetry that could diagnose sleep apnea.
When these first came out I thought I’d get more referrals. So far, I haven’t had a single person come in and ask if they have sleep apnea. If you have a patient saying, “Hey, I’m worried about my oxygen level and here’s my data,” then the clinician should consider whether they need a sleep study for sleep apnea.
Q: You did a survey that suggests that clinicians are less keen on these devices than consumers. Conor Heneghan of Fitbit/Google also mentioned a study using the Fitbit Charge and a SleepLife portal. The patients were very engaged but only one physician (out of 49) logged into the portal to look at the data.
A: Our survey of sleep professionals (which we need to publish) showed that they were wary of the data. They found it frustrating in some ways because it took time out of the clinical encounter.
Some of them said that parents are putting trackers on their children and then catastrophizing their children’s sleep.
Q: Is there such a thing as an ideal hypnogram or does it vary by individual?
A: I would say that it depends on a lot of things. If you think about a hypnogram from a sleep study, the patient is not sleeping in their home environment, and it’s only one night. There’s a range of what would be considered normal, and it’s related to your sex and your age.
One night is not going to be sufficient to characterize your percentage in this or that sleep stage. Our patients come in saying, “I’m not getting enough REM.” But there isn’t a sleep disorder called lack of REM; there’s no treatment for that. It’s probably pretty normal for them or maybe they’re taking medications that suppress their REM, such as antidepressants.
The tech world is very interested to sense REM properly and to display it. But on the treatment side of things, there’s not much that we do with that data. We’re more interested in the consolidation of their sleep, the duration of their sleep, breathing-related sleep disorders, those sorts of things.
Q: Is there any reason to be concerned about the amount of REM sleep in terms of outcomes? We know that poor sleep can lead to bad cardiovascular outcomes, but has any of that correlated to sleep stage?
A: There are studies where they’ve experimentally deprived people of certain stages of sleep, but they’re not very useful in the real world. We’re looking at sleep holistically: Do you have a good sleep pattern? Any breathing-related sleep disorders? Insomnia? We don’t treat sleep by the stage.
Q: Any concern that people who are focused on a device may be ignoring the basic tenets of good sleep hygiene?
A: If people are doing things that are obviously bad for their sleep, like working too late, not exercising enough, sleeping in on weekends to compensate for being up late during the week, or probably the biggest thing contributing to insomnia – stress. A device itself won’t fix those things but it could show you the evidence.
If somebody really has a sleep disorder, then sleep hygiene alone is probably not going to be enough. They’re going to need to engage in a more extensive program to improve their sleep, such as cognitive-behavioral therapy for insomnia.
Q: Is there anything else you want to mention?
A: I don’t want to leave with a reputation of being against sleep trackers. I think they are a great opportunity for people to get excited about and learn about their sleep and try to improve it. We have a lot to learn about what people want from their data and how we can use that data to improve people’s sleep.
As providers, we can engage with our patients – sleep is an automatic process, but improving sleep takes some effort. Buying a device is not going to automatically make you sleep better. It takes work to establish a better sleep pattern; it may require some cognitive-behavioral therapy or treating a sleep disorder. That takes some work.
Dr. Baron reported no conflicts of interest.A version of this article first appeared on Medscape.com.
The pandemic not only disrupted sleep but may have also triggered an uptick in the use of wearable tech. Sleep tracking was featured at the Cardiovascular Health Tech virtual conference 2022, sponsored by the Institute of Electrical and Electronics Engineers Engineering in Medicine & Biology Society technical committee on Cardiopulmonary Systems and Physiology-Based Engineering.
This news organization interviewed presenter Kelly Glazer Baron, PhD, MPH, DBSM, an associate professor at the University of Utah, Salt Lake City, and a clinical psychologist specializing in behavioral sleep medicine.
The interview has been edited for length and clarity.
Question: Are consumer sleep trackers mainly divided into “nearables” – things that you put at the side of the bed or under the pillow – vs. wearables?
Dr. Baron: There are so many different devices these days. There are things that you put under your mattress or pillow; there are bedside recording devices; then there are headbands, rings, wrist-worn, all kinds of things.
Q: At the conference, Philip de Chazal, PhD, (University of Sydney) described the evidence on sleep tracking smartphone apps as woeful. Would you agree with that?
A: Yes. I would agree if you’re looking at how accurate they are at recording sleep, particularly compared with what we would define as the gold standard, which is a sleep study wherein you have electrodes on the scalp and you’re measuring the electrical activity directly.
They are best at detecting when you get into the bed and when you get out. But even then, there isn’t good evidence that they do that accurately when there are two people in the bed.
Overall, they may give you a general gist of what’s happening in terms of time in and out of bed, but we’re doubtful on their recording ability to tell sleep from wake time.
Q: Are the wrist-worn devices better for sleep tracking?
A: They’re getting better. We’ve used wrist activity monitors in research for years. They use an accelerometer to measure movement, and then an algorithm determines whether an interval of time is called sleep or wake.
Recently, they’ve incorporated more sensors, such as heart rate, and they can more accurately decipher rapid eye movement (REM) sleep from non-REM. They’re still not as good as doing a full sleep study. But they’re getting closer.
Q: If asked how you slept, most of us think we can answer without needing to look at a smartphone, but maybe not. Can you explain “paradoxical insomnia”?
A: You can’t really know if you’re sleeping because if you know you’re asleep, then you can’t be asleep because it’s a state of unconsciousness. How people decide whether they had a good night’s sleep probably depends on a lot of things about how they feel when they wake up in the morning or if they remember being up in the night.
Quality of sleep is not really something that people can directly ascertain. There is a selection of people who feel awake all night but they actually are sleeping. They feel that their sleep quality is poor: They’re suffering; they have insomnia, but from the objective data, they are sleeping fine.
Q: Is this related to non-REM stage 1 sleep, when you may not be aware that you’re asleep?
A: No. I’m talking about people who come into the sleep lab for an overnight study and get hooked up. And in the morning, they’ll tell the tech I was awake all night, but the tech will see that their sleep was just fine.
There is a disconnect between how people perceive their sleep and how they actually sleep. For most people it’s impossible to be completely accurate to know how much you’re sleeping. Then there are some people who perceive it very differently.
Sleep trackers don’t have the level of detail of sleep studies that use scalp electrodes. When we get into the details of sleep measurement, we’re measuring 30-second epochs (sampling periods), where we look at broad measures of electrical activity. There is even more detail there that can be pulled out using other techniques, such as analyzing the spectrum of the EEG. For example, some studies have found a beta frequency in the EEG of people with insomnia, so even though they are sleeping, they often feel awake.
Basically, the subjective experience of sleep somewhat overlaps with the objective recording of what’s happening on a sleep study, but not completely.
Q: You said that first thing in the morning might not be the best time to assess your sleep – if you wake up groggy and are already thinking, “The day is shot.”
A: In general, people really feel worst in the morning. Their circadian drive is low, especially if they’re a little sleep deprived. You shouldn’t judge the day on the first hour after waking – most people are pretty cognitively impaired. I tell people they need some boot-up time.
You feel differently as the day goes on and even at different points of the day. There’s a lull in the early afternoon because of your circadian dip and then we get a second wind in the evening. How you feel isn’t one flat line; it’s really a rhythm throughout the day
Q: Would you say that consumer sleep trackers are okay for individuals to use to see a pattern but are maybe not accurate enough to use more globally in research?
A: I think there is a huge opportunity to understand sleep at a population level. For example, if there’s been a hurricane or an earthquake or Superbowl Sunday, companies have an opportunity to look at the impact – say, daylight saving time and how it affects sleep across different countries, or men vs. women, or different age groups.
There was a paper about sleep among hospital workers in Wuhan during the outbreak of the pandemic. That was a creative use of wearable devices to look at sleep in a large population.
Now, of course, the devices are not given out randomly; the people who buy them are probably a little bit healthier, maybe a little bit younger – that sort of thing. It is a biased sample.
Q: As you note, mobile health trackers tend to be used by the “worried well.” Can you tell us about your paper that introduced the term “orthosomnia,” or “a perfectionistic quest for the ideal sleep in order to optimize daytime function”?
A: As these devices came out, more people were coming into the clinic and shoving their data in front of us saying, “I don’t feel well, and I don’t sleep 7 hours.” They were focused on this specific number. Back when we wrote this paper, the devices were primarily movement based (now the devices are a bit more accurate). Some would say, “My sleep is light, and it’s not deep.” We’d do a sleep study that showed that they have deep sleep, but they would still believe their device even though the device really wasn’t able to classify sleep accurately.
We even found people making their sleep worse because of the device. For example, trying to get the number higher by spending more time lying in bed trying to sleep which is the opposite of what you want someone with insomnia to do. These people held the data so tight and really felt that it characterized their experience, even though we sleep medicine practitioners didn’t find it very accurate and felt that it was somewhat unhelpful to their treatment.
Q: What advice would you give the harried primary care physician presented with a patient’s hypnogram or sleep pattern?
A: As someone once pointed out to me, it’s a conversation opener about their sleep. Did they buy the device because they’re worried about their sleep? It’s unlikely that you can glean anything clinically useful from the data.
I briefly look at it to see the duration of their sleep, the regularity in their sleep pattern – the pattern of awakenings during the night might suggest that they have some insomnia. But it doesn’t take the place of clinical assessment for conditions like sleep apnea: Are they snoring? Are they unrefreshed?
I had a patient in the orthosomnia study who was given a sleep tracker by a family member. He brought the data to his doctor who ordered a sleep study that found he had sleep apnea. He would say, “The device diagnosed my sleep apnea.” But that wasn’t actually the case; it just opened the conversation and the clinician said, “Well, let’s order a sleep study.”
Q: The device told him he wasn’t getting much sleep and then the sleep study told him it was apnea.
A: Right. It’s impossible to pick up sleep apnea. Some of the latest devices have some oximetry reading but it is not a clinically validated oximetry that could diagnose sleep apnea.
When these first came out I thought I’d get more referrals. So far, I haven’t had a single person come in and ask if they have sleep apnea. If you have a patient saying, “Hey, I’m worried about my oxygen level and here’s my data,” then the clinician should consider whether they need a sleep study for sleep apnea.
Q: You did a survey that suggests that clinicians are less keen on these devices than consumers. Conor Heneghan of Fitbit/Google also mentioned a study using the Fitbit Charge and a SleepLife portal. The patients were very engaged but only one physician (out of 49) logged into the portal to look at the data.
A: Our survey of sleep professionals (which we need to publish) showed that they were wary of the data. They found it frustrating in some ways because it took time out of the clinical encounter.
Some of them said that parents are putting trackers on their children and then catastrophizing their children’s sleep.
Q: Is there such a thing as an ideal hypnogram or does it vary by individual?
A: I would say that it depends on a lot of things. If you think about a hypnogram from a sleep study, the patient is not sleeping in their home environment, and it’s only one night. There’s a range of what would be considered normal, and it’s related to your sex and your age.
One night is not going to be sufficient to characterize your percentage in this or that sleep stage. Our patients come in saying, “I’m not getting enough REM.” But there isn’t a sleep disorder called lack of REM; there’s no treatment for that. It’s probably pretty normal for them or maybe they’re taking medications that suppress their REM, such as antidepressants.
The tech world is very interested to sense REM properly and to display it. But on the treatment side of things, there’s not much that we do with that data. We’re more interested in the consolidation of their sleep, the duration of their sleep, breathing-related sleep disorders, those sorts of things.
Q: Is there any reason to be concerned about the amount of REM sleep in terms of outcomes? We know that poor sleep can lead to bad cardiovascular outcomes, but has any of that correlated to sleep stage?
A: There are studies where they’ve experimentally deprived people of certain stages of sleep, but they’re not very useful in the real world. We’re looking at sleep holistically: Do you have a good sleep pattern? Any breathing-related sleep disorders? Insomnia? We don’t treat sleep by the stage.
Q: Any concern that people who are focused on a device may be ignoring the basic tenets of good sleep hygiene?
A: If people are doing things that are obviously bad for their sleep, like working too late, not exercising enough, sleeping in on weekends to compensate for being up late during the week, or probably the biggest thing contributing to insomnia – stress. A device itself won’t fix those things but it could show you the evidence.
If somebody really has a sleep disorder, then sleep hygiene alone is probably not going to be enough. They’re going to need to engage in a more extensive program to improve their sleep, such as cognitive-behavioral therapy for insomnia.
Q: Is there anything else you want to mention?
A: I don’t want to leave with a reputation of being against sleep trackers. I think they are a great opportunity for people to get excited about and learn about their sleep and try to improve it. We have a lot to learn about what people want from their data and how we can use that data to improve people’s sleep.
As providers, we can engage with our patients – sleep is an automatic process, but improving sleep takes some effort. Buying a device is not going to automatically make you sleep better. It takes work to establish a better sleep pattern; it may require some cognitive-behavioral therapy or treating a sleep disorder. That takes some work.
Dr. Baron reported no conflicts of interest.A version of this article first appeared on Medscape.com.
Oscars fight highlights for many the toll alopecia may carry
The Academy Awards ceremony on March 27 is a buzzing topic of conversation.
Troy Kotsur became the first deaf man to win an Oscar – and the highly coveted best supporting actor award, at that.
But it was what happened afterward that arguably stole the show.
Viewers and audience members alike watched in awe as actor Will Smith marched on stage and struck award presenter and comedian Chris Rock in the face after he directed a joke at Smith’s wife, Jada Pinkett Smith, for her shaved head.
and can lead to feelings of depression or mental illness.
About 700,000 people in the United States have alopecia areata, according to a 2020 study. Of them, slightly more than half are women, and more than 77% are White.
Shortly after the awards show, the Los Angeles Police Department released a statement saying it was aware of the incident and Mr. Rock had not pressed charges against Mr. Smith.
The incident set social media ablaze, and strong sentiments were heard from those who have been personally affected by alopecia.
Illness is never funny
Mr. Rock’s comment can be triggering to the millions who have been affected by hair loss, said Carolyn Goh, MD, a dermatologist at UCLA Health.
“As someone with alopecia myself, I consider it a microaggression,” Dr. Goh said. “I’ve experienced many similar comments. These build up over time and wear us down.”
One U.K.-based Instagram user, Kitty Dry, said the expression on Ms. Pinkett Smith’s face represented the hurt felt by so many with this condition.
“I want to preface this post by saying that in no way do I condone any sort of violence, but thank you Will Smith,” said Ms. Dry, 23, who was diagnosed with alopecia universalis after losing all her hair in 12 weeks.
“That slap was for anyone with alopecia who has ever been at the butt of an unwanted joke, comment or stare,” Ms. Dry said.
Others posted comments raising awareness of the tragic passing of Rio Allred, a 12-year-old girl with alopecia who recently died by suicide.
Rio Allred is said to have endured serious bullying at school, with classmates pulling off her wig and smacking her head, according to the Canadian Alopecia Areata Foundation.
It’s common for those who have hair loss conditions to feel helpless, and sometimes confused, said Amy McMichael, MD, a professor and chair of the dermatology department at Wake Forest University, Winston-Salem, N.C. That’s why it’s critical for those people to see a board-certified dermatologist, so they know they are not alone.
“As dermatologists, we can not only diagnose the type of alopecia, but we can also render treatment,” Dr. McMichael said.
Alopecia awareness
Dermatologists can also help connect patients to organizations that address the physical and emotional struggles of those who have hair loss, such as the National Alopecia Areata Foundation and the Scarring Alopecia Foundation, Dr. McMichael said.
She hopes the event shows people the “many faces of hair loss” and shows that these conditions can happen to people of all ages, ethnicities, and genders.
The National Alopecia Areata Foundation calls what happened at the Oscars a “teachable” moment.
“We encourage both our community and the broader public to learn more about alopecia areata so we can end the stigma around this disease,” the organization said in a statement.
Dr. Goh said that anyone with hair loss should feel free to explore potential medical causes and, if needed, seek out mental health treatment, too.
A version of this article first appeared on WebMD.com.
The Academy Awards ceremony on March 27 is a buzzing topic of conversation.
Troy Kotsur became the first deaf man to win an Oscar – and the highly coveted best supporting actor award, at that.
But it was what happened afterward that arguably stole the show.
Viewers and audience members alike watched in awe as actor Will Smith marched on stage and struck award presenter and comedian Chris Rock in the face after he directed a joke at Smith’s wife, Jada Pinkett Smith, for her shaved head.
and can lead to feelings of depression or mental illness.
About 700,000 people in the United States have alopecia areata, according to a 2020 study. Of them, slightly more than half are women, and more than 77% are White.
Shortly after the awards show, the Los Angeles Police Department released a statement saying it was aware of the incident and Mr. Rock had not pressed charges against Mr. Smith.
The incident set social media ablaze, and strong sentiments were heard from those who have been personally affected by alopecia.
Illness is never funny
Mr. Rock’s comment can be triggering to the millions who have been affected by hair loss, said Carolyn Goh, MD, a dermatologist at UCLA Health.
“As someone with alopecia myself, I consider it a microaggression,” Dr. Goh said. “I’ve experienced many similar comments. These build up over time and wear us down.”
One U.K.-based Instagram user, Kitty Dry, said the expression on Ms. Pinkett Smith’s face represented the hurt felt by so many with this condition.
“I want to preface this post by saying that in no way do I condone any sort of violence, but thank you Will Smith,” said Ms. Dry, 23, who was diagnosed with alopecia universalis after losing all her hair in 12 weeks.
“That slap was for anyone with alopecia who has ever been at the butt of an unwanted joke, comment or stare,” Ms. Dry said.
Others posted comments raising awareness of the tragic passing of Rio Allred, a 12-year-old girl with alopecia who recently died by suicide.
Rio Allred is said to have endured serious bullying at school, with classmates pulling off her wig and smacking her head, according to the Canadian Alopecia Areata Foundation.
It’s common for those who have hair loss conditions to feel helpless, and sometimes confused, said Amy McMichael, MD, a professor and chair of the dermatology department at Wake Forest University, Winston-Salem, N.C. That’s why it’s critical for those people to see a board-certified dermatologist, so they know they are not alone.
“As dermatologists, we can not only diagnose the type of alopecia, but we can also render treatment,” Dr. McMichael said.
Alopecia awareness
Dermatologists can also help connect patients to organizations that address the physical and emotional struggles of those who have hair loss, such as the National Alopecia Areata Foundation and the Scarring Alopecia Foundation, Dr. McMichael said.
She hopes the event shows people the “many faces of hair loss” and shows that these conditions can happen to people of all ages, ethnicities, and genders.
The National Alopecia Areata Foundation calls what happened at the Oscars a “teachable” moment.
“We encourage both our community and the broader public to learn more about alopecia areata so we can end the stigma around this disease,” the organization said in a statement.
Dr. Goh said that anyone with hair loss should feel free to explore potential medical causes and, if needed, seek out mental health treatment, too.
A version of this article first appeared on WebMD.com.
The Academy Awards ceremony on March 27 is a buzzing topic of conversation.
Troy Kotsur became the first deaf man to win an Oscar – and the highly coveted best supporting actor award, at that.
But it was what happened afterward that arguably stole the show.
Viewers and audience members alike watched in awe as actor Will Smith marched on stage and struck award presenter and comedian Chris Rock in the face after he directed a joke at Smith’s wife, Jada Pinkett Smith, for her shaved head.
and can lead to feelings of depression or mental illness.
About 700,000 people in the United States have alopecia areata, according to a 2020 study. Of them, slightly more than half are women, and more than 77% are White.
Shortly after the awards show, the Los Angeles Police Department released a statement saying it was aware of the incident and Mr. Rock had not pressed charges against Mr. Smith.
The incident set social media ablaze, and strong sentiments were heard from those who have been personally affected by alopecia.
Illness is never funny
Mr. Rock’s comment can be triggering to the millions who have been affected by hair loss, said Carolyn Goh, MD, a dermatologist at UCLA Health.
“As someone with alopecia myself, I consider it a microaggression,” Dr. Goh said. “I’ve experienced many similar comments. These build up over time and wear us down.”
One U.K.-based Instagram user, Kitty Dry, said the expression on Ms. Pinkett Smith’s face represented the hurt felt by so many with this condition.
“I want to preface this post by saying that in no way do I condone any sort of violence, but thank you Will Smith,” said Ms. Dry, 23, who was diagnosed with alopecia universalis after losing all her hair in 12 weeks.
“That slap was for anyone with alopecia who has ever been at the butt of an unwanted joke, comment or stare,” Ms. Dry said.
Others posted comments raising awareness of the tragic passing of Rio Allred, a 12-year-old girl with alopecia who recently died by suicide.
Rio Allred is said to have endured serious bullying at school, with classmates pulling off her wig and smacking her head, according to the Canadian Alopecia Areata Foundation.
It’s common for those who have hair loss conditions to feel helpless, and sometimes confused, said Amy McMichael, MD, a professor and chair of the dermatology department at Wake Forest University, Winston-Salem, N.C. That’s why it’s critical for those people to see a board-certified dermatologist, so they know they are not alone.
“As dermatologists, we can not only diagnose the type of alopecia, but we can also render treatment,” Dr. McMichael said.
Alopecia awareness
Dermatologists can also help connect patients to organizations that address the physical and emotional struggles of those who have hair loss, such as the National Alopecia Areata Foundation and the Scarring Alopecia Foundation, Dr. McMichael said.
She hopes the event shows people the “many faces of hair loss” and shows that these conditions can happen to people of all ages, ethnicities, and genders.
The National Alopecia Areata Foundation calls what happened at the Oscars a “teachable” moment.
“We encourage both our community and the broader public to learn more about alopecia areata so we can end the stigma around this disease,” the organization said in a statement.
Dr. Goh said that anyone with hair loss should feel free to explore potential medical causes and, if needed, seek out mental health treatment, too.
A version of this article first appeared on WebMD.com.
Surgery in CJD patients a potential risk factor for transmission
About one in six patients with Creutzfeldt-Jakob disease (CJD) undergo surgery, raising the risk of iatrogenic transmission of this rare but universally fatal prion disease.
In a retrospective analysis, researchers found that 26 of 121 (21%) patients with probable or definite CJD at four U.S. academic medical centers underwent a total of 55 procedures.
These included high-risk procedures for two patients with neuropathologically proven CJD. One underwent ophthalmic artery aneurysm clipping for unruptured aneurysm, and the other underwent diagnostic brain biopsy.
“The findings were definitely surprising to me and my team – particularly the high frequency with which patients with an irreversible and particularly transmissible neurologic disease underwent invasive medical procedures either just before or shortly after the emergence of symptoms later attributed to CJD,” study investigator Gregory Day, MD, with the Mayo Clinic, Jacksonville, Fla., said in an interview.
The study was published online March 9, 2022, in JAMA Network Open.
Poor infection control
The investigators noted that the majority of CJD cases are sporadic or are inherited, but research shows that prion transmission can occur via contaminated tissues or reusable medical equipment.
While the risk of iatrogenic transmission is highest following procedures involving the central nervous system, where prion burden is highest, experimental models suggest CJD transmission can occur after contact with other tissues, including nasal mucosa, lung, lymph nodes, and spleen, the researchers noted.
“If these models are accurate, surgical procedures involving these tissues may pose a risk to patients,” the investigators wrote.
To determine the potential scope of this problem, the researchers examined the frequency of invasive procedures performed in patients with CJD at four tertiary care centers.
“In several cases, these procedures were done with clear indications [such as] fixation or joint replacement following a fracture. In several others, however, the procedures were unlikely to help the patient. For instance, a hip replacement for walking difficulties that were actually due to changes in the brain due to CJD,” Dr. Day said.
“Even more surprising was the low frequency with which appropriate surgical precautions/infection control procedures were used in patients with established diagnoses of CJD,” he noted.
Only one procedure was performed with sterilization techniques adequate to prevent CJD.
Dr. Day said the findings aren’t necessarily cause for immediate alarm, but they do highlight an area for potential improvement, including better screening of patients who have new and unexplained symptoms before proceeding with surgery, especially surgery of the central nervous system, where prion burden is high.
Another potential solution is to develop and support program surveillance and to work with public health organizations such the Centers for Disease Control and Prevention and the National Prion Disease Pathology Surveillance Center to elicit a surgical history in patients diagnosed with prion disease.
“Active nationwide surveillance is needed to determine the true scope of this potential problem and to develop strategies to mitigate the potential risk of iatrogenic prion transmission to future patients,” Dr. Day said.
True prevalence unknown
The authors of an invited commentary noted that, while most CJD infections occur sporadically, iatrogenic transmission is possible. Approximately 500 such cases have been reported worldwide to date.
“Yet, reported transmission from surgical procedures remains rare, with fewer than 10 confirmed CJD cases described in the literature, although the true prevalence is difficult to quantify as confirmed diagnosis requires autopsy,” wrote Beatrice Sun, MD, and Joseph Forrester, MD, with the department of surgery, Stanford (Calif.) University.
They noted that, over a 15-year period, 19 suspected iatrogenic CJD exposures were reported to the CDC – two from ophthalmology procedures, and 17 from neurosurgical procedures.
In all 19 cases, the diagnosis of CJD was unknown before the intervention, and all surgical instruments underwent normal decontamination protocols, which are inadequate to eradicate prion disease.
For patients with suspected or confirmed CJD, the World Health Organization has published infection control guidelines to prevent transmission of spongiform encephalopathies.
The guidelines recommend proper communication with all staff involved in the surgical procedure and the sterilization of supplies to be aware of potential exposure; minimizing the number of staff in the operating room; using single-use equipment whenever possible and disposing of it by incineration; using protective coverings for all nondisposable equipment; and scheduling such procedures at the end of the day to allow adequate time for decontamination.
Funding for the study was provided by the National Institutes of Health. Dr. Day owns stock in ANI Pharmaceuticals; serves as a consultant for Parabon Nanolabs, as a topic editor (dementia) for DynaMed, and as the clinical director of the Anti-NMDA Receptor Encephalitis Foundation (uncompensated). Dr. Forrester reported receiving unrestricted research funding from Varian and has received grant funding from the Surgical Infections Society.
A version of this article first appeared on Medscape.com.
About one in six patients with Creutzfeldt-Jakob disease (CJD) undergo surgery, raising the risk of iatrogenic transmission of this rare but universally fatal prion disease.
In a retrospective analysis, researchers found that 26 of 121 (21%) patients with probable or definite CJD at four U.S. academic medical centers underwent a total of 55 procedures.
These included high-risk procedures for two patients with neuropathologically proven CJD. One underwent ophthalmic artery aneurysm clipping for unruptured aneurysm, and the other underwent diagnostic brain biopsy.
“The findings were definitely surprising to me and my team – particularly the high frequency with which patients with an irreversible and particularly transmissible neurologic disease underwent invasive medical procedures either just before or shortly after the emergence of symptoms later attributed to CJD,” study investigator Gregory Day, MD, with the Mayo Clinic, Jacksonville, Fla., said in an interview.
The study was published online March 9, 2022, in JAMA Network Open.
Poor infection control
The investigators noted that the majority of CJD cases are sporadic or are inherited, but research shows that prion transmission can occur via contaminated tissues or reusable medical equipment.
While the risk of iatrogenic transmission is highest following procedures involving the central nervous system, where prion burden is highest, experimental models suggest CJD transmission can occur after contact with other tissues, including nasal mucosa, lung, lymph nodes, and spleen, the researchers noted.
“If these models are accurate, surgical procedures involving these tissues may pose a risk to patients,” the investigators wrote.
To determine the potential scope of this problem, the researchers examined the frequency of invasive procedures performed in patients with CJD at four tertiary care centers.
“In several cases, these procedures were done with clear indications [such as] fixation or joint replacement following a fracture. In several others, however, the procedures were unlikely to help the patient. For instance, a hip replacement for walking difficulties that were actually due to changes in the brain due to CJD,” Dr. Day said.
“Even more surprising was the low frequency with which appropriate surgical precautions/infection control procedures were used in patients with established diagnoses of CJD,” he noted.
Only one procedure was performed with sterilization techniques adequate to prevent CJD.
Dr. Day said the findings aren’t necessarily cause for immediate alarm, but they do highlight an area for potential improvement, including better screening of patients who have new and unexplained symptoms before proceeding with surgery, especially surgery of the central nervous system, where prion burden is high.
Another potential solution is to develop and support program surveillance and to work with public health organizations such the Centers for Disease Control and Prevention and the National Prion Disease Pathology Surveillance Center to elicit a surgical history in patients diagnosed with prion disease.
“Active nationwide surveillance is needed to determine the true scope of this potential problem and to develop strategies to mitigate the potential risk of iatrogenic prion transmission to future patients,” Dr. Day said.
True prevalence unknown
The authors of an invited commentary noted that, while most CJD infections occur sporadically, iatrogenic transmission is possible. Approximately 500 such cases have been reported worldwide to date.
“Yet, reported transmission from surgical procedures remains rare, with fewer than 10 confirmed CJD cases described in the literature, although the true prevalence is difficult to quantify as confirmed diagnosis requires autopsy,” wrote Beatrice Sun, MD, and Joseph Forrester, MD, with the department of surgery, Stanford (Calif.) University.
They noted that, over a 15-year period, 19 suspected iatrogenic CJD exposures were reported to the CDC – two from ophthalmology procedures, and 17 from neurosurgical procedures.
In all 19 cases, the diagnosis of CJD was unknown before the intervention, and all surgical instruments underwent normal decontamination protocols, which are inadequate to eradicate prion disease.
For patients with suspected or confirmed CJD, the World Health Organization has published infection control guidelines to prevent transmission of spongiform encephalopathies.
The guidelines recommend proper communication with all staff involved in the surgical procedure and the sterilization of supplies to be aware of potential exposure; minimizing the number of staff in the operating room; using single-use equipment whenever possible and disposing of it by incineration; using protective coverings for all nondisposable equipment; and scheduling such procedures at the end of the day to allow adequate time for decontamination.
Funding for the study was provided by the National Institutes of Health. Dr. Day owns stock in ANI Pharmaceuticals; serves as a consultant for Parabon Nanolabs, as a topic editor (dementia) for DynaMed, and as the clinical director of the Anti-NMDA Receptor Encephalitis Foundation (uncompensated). Dr. Forrester reported receiving unrestricted research funding from Varian and has received grant funding from the Surgical Infections Society.
A version of this article first appeared on Medscape.com.
About one in six patients with Creutzfeldt-Jakob disease (CJD) undergo surgery, raising the risk of iatrogenic transmission of this rare but universally fatal prion disease.
In a retrospective analysis, researchers found that 26 of 121 (21%) patients with probable or definite CJD at four U.S. academic medical centers underwent a total of 55 procedures.
These included high-risk procedures for two patients with neuropathologically proven CJD. One underwent ophthalmic artery aneurysm clipping for unruptured aneurysm, and the other underwent diagnostic brain biopsy.
“The findings were definitely surprising to me and my team – particularly the high frequency with which patients with an irreversible and particularly transmissible neurologic disease underwent invasive medical procedures either just before or shortly after the emergence of symptoms later attributed to CJD,” study investigator Gregory Day, MD, with the Mayo Clinic, Jacksonville, Fla., said in an interview.
The study was published online March 9, 2022, in JAMA Network Open.
Poor infection control
The investigators noted that the majority of CJD cases are sporadic or are inherited, but research shows that prion transmission can occur via contaminated tissues or reusable medical equipment.
While the risk of iatrogenic transmission is highest following procedures involving the central nervous system, where prion burden is highest, experimental models suggest CJD transmission can occur after contact with other tissues, including nasal mucosa, lung, lymph nodes, and spleen, the researchers noted.
“If these models are accurate, surgical procedures involving these tissues may pose a risk to patients,” the investigators wrote.
To determine the potential scope of this problem, the researchers examined the frequency of invasive procedures performed in patients with CJD at four tertiary care centers.
“In several cases, these procedures were done with clear indications [such as] fixation or joint replacement following a fracture. In several others, however, the procedures were unlikely to help the patient. For instance, a hip replacement for walking difficulties that were actually due to changes in the brain due to CJD,” Dr. Day said.
“Even more surprising was the low frequency with which appropriate surgical precautions/infection control procedures were used in patients with established diagnoses of CJD,” he noted.
Only one procedure was performed with sterilization techniques adequate to prevent CJD.
Dr. Day said the findings aren’t necessarily cause for immediate alarm, but they do highlight an area for potential improvement, including better screening of patients who have new and unexplained symptoms before proceeding with surgery, especially surgery of the central nervous system, where prion burden is high.
Another potential solution is to develop and support program surveillance and to work with public health organizations such the Centers for Disease Control and Prevention and the National Prion Disease Pathology Surveillance Center to elicit a surgical history in patients diagnosed with prion disease.
“Active nationwide surveillance is needed to determine the true scope of this potential problem and to develop strategies to mitigate the potential risk of iatrogenic prion transmission to future patients,” Dr. Day said.
True prevalence unknown
The authors of an invited commentary noted that, while most CJD infections occur sporadically, iatrogenic transmission is possible. Approximately 500 such cases have been reported worldwide to date.
“Yet, reported transmission from surgical procedures remains rare, with fewer than 10 confirmed CJD cases described in the literature, although the true prevalence is difficult to quantify as confirmed diagnosis requires autopsy,” wrote Beatrice Sun, MD, and Joseph Forrester, MD, with the department of surgery, Stanford (Calif.) University.
They noted that, over a 15-year period, 19 suspected iatrogenic CJD exposures were reported to the CDC – two from ophthalmology procedures, and 17 from neurosurgical procedures.
In all 19 cases, the diagnosis of CJD was unknown before the intervention, and all surgical instruments underwent normal decontamination protocols, which are inadequate to eradicate prion disease.
For patients with suspected or confirmed CJD, the World Health Organization has published infection control guidelines to prevent transmission of spongiform encephalopathies.
The guidelines recommend proper communication with all staff involved in the surgical procedure and the sterilization of supplies to be aware of potential exposure; minimizing the number of staff in the operating room; using single-use equipment whenever possible and disposing of it by incineration; using protective coverings for all nondisposable equipment; and scheduling such procedures at the end of the day to allow adequate time for decontamination.
Funding for the study was provided by the National Institutes of Health. Dr. Day owns stock in ANI Pharmaceuticals; serves as a consultant for Parabon Nanolabs, as a topic editor (dementia) for DynaMed, and as the clinical director of the Anti-NMDA Receptor Encephalitis Foundation (uncompensated). Dr. Forrester reported receiving unrestricted research funding from Varian and has received grant funding from the Surgical Infections Society.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
As FDA OKs another COVID booster, some experts question need
, even though many top infectious disease experts questioned the need before the agency’s decision.
The FDA granted emergency use authorization for both Pfizer and Moderna to offer the second booster – and fourth shot overall – for adults over 50 as well as those over 18 with compromised immune systems.
The Centers for Control and Prevention must still sign off before those doses start reaching American arms. That approval could come at any time.
“The general consensus, certainly the CDC’s consensus, is that the current vaccines are still really quite effective against Omicron and this new BA.2 variant in keeping people out of the hospital, and preventing the development of severe disease,” William Schaffner, MD, an infectious disease specialist at Vanderbilt University in Nashville said prior to the FDA’s announcement March 29.
Of the 217.4 million Americans who are “fully vaccinated,” i.e., received two doses of either Pfizer or Moderna’s vaccines or one dose of the Johnson & Johnson vaccine, only 45% have also received a booster shot, according to the CDC.
“Given that, there’s no need at the moment for the general population to get a fourth inoculation,” Dr. Schaffner says. “Our current focus ought to be on making sure that as many people as possible get that [first] booster who are eligible.”
Monica Gandhi, MD, an infectious disease specialist at the University of California, San Francisco, agreed that another booster for everyone was unnecessary. The only people who would need a fourth shot (or third, if they had the Johnson & Johnson vaccine initially) are those over age 65 or 70 years, Dr. Gandhi says.
“Older people need those antibodies up high because they’re more susceptible to severe breakthroughs,” she said, also before the latest development.
To boost or not to boost
Daniel Kuritzkes, MD, chief of infectious diseases at Brigham & Women’s Hospital in Boston, said the timing of a booster and who should be eligible depends on what the nation is trying to achieve with its vaccination strategy.
“Is the goal to prevent any symptomatic infection with COVID-19, is the goal to prevent the spread of COVID-19, or is the goal to prevent severe disease that requires hospitalization?” asked Dr. Kuritzkes.
The current vaccine — with a booster — has prevented severe disease, he said.
An Israeli study showed, for instance, that a third Pfizer dose was 93% effective against hospitalization, 92% effective against severe illness, and 81% effective against death.
A just-published study in the New England Journal of Medicine found that a booster of the Pfizer vaccine was 95% effective against COVID-19 infection and that it did not raise any new safety issues.
A small Israeli study, also published in NEJM, of a fourth Pfizer dose given to health care workers found that it prevented symptomatic infection and illness, but that it was much less effective than previous doses — maybe 65% effective against symptomatic illness, the authors write.
Giving Americans another booster now — which has been shown to lose some effectiveness after about 4 months — means it might not offer protection this fall and winter, when there could be a seasonal surge of the virus, Dr. Kuritzkes says.
And, even if people receive boosters every few months, they are still likely to get a mild respiratory virus infection, he said.
“I’m pretty convinced that we cannot boost ourselves out of this pandemic,” said Dr. Kuritzkes. “We need to first of all ensure there’s global immunization so that all the people who have not been vaccinated at all get vaccinated. That’s far more important than boosting people a fourth time.”
Booster confusion
The April 6 FDA meeting of the agency’s Vaccines and Related Biological Products Advisory Committee comes as the two major COVID vaccine makers — Pfizer and Moderna — have applied for emergency use authorization for an additional booster.
Pfizer had asked for authorization for a fourth shot in patients over age 65 years, while Moderna wanted a booster to be available to all Americans over 18. The FDA instead granted authorization to both companies for those over 50 and anyone 18 or older who is immunocompromised.
What this means for the committee’s April 6 meeting is not clear. The original agenda says the committee will consider the evidence on safety and effectiveness of the additional vaccine doses and discuss how to set up a process — similar to that used for the influenza vaccine — to be able to determine the makeup of COVID vaccines as new variants emerge. That could lay the groundwork for an annual COVID shot, if needed.
The FDA advisers will not make recommendations nor vote on whether — and which — Americans should get a COVID booster. That is the job of the CDC’s Advisory Committee on Immunization Practices (ACIP).
The last time a booster was considered, CDC Director Rochelle Walensky, MD, overrode the committee and recommended that all Americans — not just older individuals — get an additional COVID shot, which became the first booster.
That past action worries Dr. Gandhi, who calls it confusing, and says it may have contributed to the fact that less than half of Americans have since chosen to get a booster.
Dr. Schaffner says he expects the FDA to authorize emergency use for fourth doses of the Pfizer and Moderna vaccines, but he doesn’t think the CDC committee will recommend routine use. As was seen before, however, the CDC director does not have to follow the committee’s advice.
The members of ACIP “might be more conservative or narrower in scope in terms of recommending who needs to be boosted and when boosting is appropriate,” Dr. Kuritzkes says.
Dr. Gandhi says she’s concerned the FDA’s deliberations could be swayed by Moderna and Pfizer’s influence and that “pharmaceutical companies are going to have more of a say than they should in the scientific process.”
There are similar worries for Dr. Schaffner. He says he’s “a bit grumpy” that the vaccine makers have been using press releases to argue for boosters.
“Press releases are no way to make vaccine recommendations,” Dr. Schaffner said, adding that he “would advise [vaccine makers] to sit down and be quiet and let the FDA and CDC advisory committee do their thing.”
Moderna Chief Medical Officer Paul Burton, MD, however, told WebMD last week that the signs point to why a fourth shot may be needed.
“We see waning of effectiveness, antibody levels come down, and certainly effectiveness against Omicron comes down in 3 to 6 months,” Burton said. “The natural history, from what we’re seeing around the world, is that BA.2 is definitely here, it’s highly transmissible, and I think we are going to get an additional wave of BA.2 here in the United States.”
Another wave is coming, he said, and “I think there will be waning of effectiveness. We need to be prepared for that, so that’s why we need the fourth dose.”
Supply issues?
Meanwhile, the United Kingdom has begun offering boosters to anyone over 75, and Sweden’s health authority has recommended a fourth shot to people over age 80.
That puts pressure on the United States — at least on its politicians and policymakers — to, in a sense, keep up, said the infectious disease specialists.
Indeed, the White House has been keeping fourth shots in the news, warning that it is running out of money to ensure that all Americans would have access to one, if recommended.
On March 23, outgoing White House COVID-19 Response Coordinator Jeff Zients said the federal government had enough vaccine for the immunocompromised to get a fourth dose “and, if authorized in the coming weeks, enough supply for fourth doses for our most vulnerable, including seniors.”
But he warned that without congressional approval of a COVID-19 funding package, “We can’t procure the necessary vaccine supply to support fourth shots for all Americans.”
Mr. Zients also noted that other countries, including Japan, Vietnam, and the Philippines had already secured future booster doses and added, “We should be securing additional supply right now.”
Dr. Schaffner says that while it would be nice to “have a booster on the shelf,” the United States needs to put more effort into creating a globally-coordinated process for ensuring that vaccines match circulating strains and that they are manufactured on a timely basis.
He says he and others “have been reminding the public that the COVID pandemic may indeed be diminishing and moving into the endemic, but that doesn’t mean COVID is over or finished or disappeared.”
Dr. Schaffner says that it may be that “perhaps we’d need a periodic reminder to our immune system to remain protected. In other words, we might have to get boosted perhaps annually like we do with influenza.”
A version of this article first appeared on WebMD.com.
, even though many top infectious disease experts questioned the need before the agency’s decision.
The FDA granted emergency use authorization for both Pfizer and Moderna to offer the second booster – and fourth shot overall – for adults over 50 as well as those over 18 with compromised immune systems.
The Centers for Control and Prevention must still sign off before those doses start reaching American arms. That approval could come at any time.
“The general consensus, certainly the CDC’s consensus, is that the current vaccines are still really quite effective against Omicron and this new BA.2 variant in keeping people out of the hospital, and preventing the development of severe disease,” William Schaffner, MD, an infectious disease specialist at Vanderbilt University in Nashville said prior to the FDA’s announcement March 29.
Of the 217.4 million Americans who are “fully vaccinated,” i.e., received two doses of either Pfizer or Moderna’s vaccines or one dose of the Johnson & Johnson vaccine, only 45% have also received a booster shot, according to the CDC.
“Given that, there’s no need at the moment for the general population to get a fourth inoculation,” Dr. Schaffner says. “Our current focus ought to be on making sure that as many people as possible get that [first] booster who are eligible.”
Monica Gandhi, MD, an infectious disease specialist at the University of California, San Francisco, agreed that another booster for everyone was unnecessary. The only people who would need a fourth shot (or third, if they had the Johnson & Johnson vaccine initially) are those over age 65 or 70 years, Dr. Gandhi says.
“Older people need those antibodies up high because they’re more susceptible to severe breakthroughs,” she said, also before the latest development.
To boost or not to boost
Daniel Kuritzkes, MD, chief of infectious diseases at Brigham & Women’s Hospital in Boston, said the timing of a booster and who should be eligible depends on what the nation is trying to achieve with its vaccination strategy.
“Is the goal to prevent any symptomatic infection with COVID-19, is the goal to prevent the spread of COVID-19, or is the goal to prevent severe disease that requires hospitalization?” asked Dr. Kuritzkes.
The current vaccine — with a booster — has prevented severe disease, he said.
An Israeli study showed, for instance, that a third Pfizer dose was 93% effective against hospitalization, 92% effective against severe illness, and 81% effective against death.
A just-published study in the New England Journal of Medicine found that a booster of the Pfizer vaccine was 95% effective against COVID-19 infection and that it did not raise any new safety issues.
A small Israeli study, also published in NEJM, of a fourth Pfizer dose given to health care workers found that it prevented symptomatic infection and illness, but that it was much less effective than previous doses — maybe 65% effective against symptomatic illness, the authors write.
Giving Americans another booster now — which has been shown to lose some effectiveness after about 4 months — means it might not offer protection this fall and winter, when there could be a seasonal surge of the virus, Dr. Kuritzkes says.
And, even if people receive boosters every few months, they are still likely to get a mild respiratory virus infection, he said.
“I’m pretty convinced that we cannot boost ourselves out of this pandemic,” said Dr. Kuritzkes. “We need to first of all ensure there’s global immunization so that all the people who have not been vaccinated at all get vaccinated. That’s far more important than boosting people a fourth time.”
Booster confusion
The April 6 FDA meeting of the agency’s Vaccines and Related Biological Products Advisory Committee comes as the two major COVID vaccine makers — Pfizer and Moderna — have applied for emergency use authorization for an additional booster.
Pfizer had asked for authorization for a fourth shot in patients over age 65 years, while Moderna wanted a booster to be available to all Americans over 18. The FDA instead granted authorization to both companies for those over 50 and anyone 18 or older who is immunocompromised.
What this means for the committee’s April 6 meeting is not clear. The original agenda says the committee will consider the evidence on safety and effectiveness of the additional vaccine doses and discuss how to set up a process — similar to that used for the influenza vaccine — to be able to determine the makeup of COVID vaccines as new variants emerge. That could lay the groundwork for an annual COVID shot, if needed.
The FDA advisers will not make recommendations nor vote on whether — and which — Americans should get a COVID booster. That is the job of the CDC’s Advisory Committee on Immunization Practices (ACIP).
The last time a booster was considered, CDC Director Rochelle Walensky, MD, overrode the committee and recommended that all Americans — not just older individuals — get an additional COVID shot, which became the first booster.
That past action worries Dr. Gandhi, who calls it confusing, and says it may have contributed to the fact that less than half of Americans have since chosen to get a booster.
Dr. Schaffner says he expects the FDA to authorize emergency use for fourth doses of the Pfizer and Moderna vaccines, but he doesn’t think the CDC committee will recommend routine use. As was seen before, however, the CDC director does not have to follow the committee’s advice.
The members of ACIP “might be more conservative or narrower in scope in terms of recommending who needs to be boosted and when boosting is appropriate,” Dr. Kuritzkes says.
Dr. Gandhi says she’s concerned the FDA’s deliberations could be swayed by Moderna and Pfizer’s influence and that “pharmaceutical companies are going to have more of a say than they should in the scientific process.”
There are similar worries for Dr. Schaffner. He says he’s “a bit grumpy” that the vaccine makers have been using press releases to argue for boosters.
“Press releases are no way to make vaccine recommendations,” Dr. Schaffner said, adding that he “would advise [vaccine makers] to sit down and be quiet and let the FDA and CDC advisory committee do their thing.”
Moderna Chief Medical Officer Paul Burton, MD, however, told WebMD last week that the signs point to why a fourth shot may be needed.
“We see waning of effectiveness, antibody levels come down, and certainly effectiveness against Omicron comes down in 3 to 6 months,” Burton said. “The natural history, from what we’re seeing around the world, is that BA.2 is definitely here, it’s highly transmissible, and I think we are going to get an additional wave of BA.2 here in the United States.”
Another wave is coming, he said, and “I think there will be waning of effectiveness. We need to be prepared for that, so that’s why we need the fourth dose.”
Supply issues?
Meanwhile, the United Kingdom has begun offering boosters to anyone over 75, and Sweden’s health authority has recommended a fourth shot to people over age 80.
That puts pressure on the United States — at least on its politicians and policymakers — to, in a sense, keep up, said the infectious disease specialists.
Indeed, the White House has been keeping fourth shots in the news, warning that it is running out of money to ensure that all Americans would have access to one, if recommended.
On March 23, outgoing White House COVID-19 Response Coordinator Jeff Zients said the federal government had enough vaccine for the immunocompromised to get a fourth dose “and, if authorized in the coming weeks, enough supply for fourth doses for our most vulnerable, including seniors.”
But he warned that without congressional approval of a COVID-19 funding package, “We can’t procure the necessary vaccine supply to support fourth shots for all Americans.”
Mr. Zients also noted that other countries, including Japan, Vietnam, and the Philippines had already secured future booster doses and added, “We should be securing additional supply right now.”
Dr. Schaffner says that while it would be nice to “have a booster on the shelf,” the United States needs to put more effort into creating a globally-coordinated process for ensuring that vaccines match circulating strains and that they are manufactured on a timely basis.
He says he and others “have been reminding the public that the COVID pandemic may indeed be diminishing and moving into the endemic, but that doesn’t mean COVID is over or finished or disappeared.”
Dr. Schaffner says that it may be that “perhaps we’d need a periodic reminder to our immune system to remain protected. In other words, we might have to get boosted perhaps annually like we do with influenza.”
A version of this article first appeared on WebMD.com.
, even though many top infectious disease experts questioned the need before the agency’s decision.
The FDA granted emergency use authorization for both Pfizer and Moderna to offer the second booster – and fourth shot overall – for adults over 50 as well as those over 18 with compromised immune systems.
The Centers for Control and Prevention must still sign off before those doses start reaching American arms. That approval could come at any time.
“The general consensus, certainly the CDC’s consensus, is that the current vaccines are still really quite effective against Omicron and this new BA.2 variant in keeping people out of the hospital, and preventing the development of severe disease,” William Schaffner, MD, an infectious disease specialist at Vanderbilt University in Nashville said prior to the FDA’s announcement March 29.
Of the 217.4 million Americans who are “fully vaccinated,” i.e., received two doses of either Pfizer or Moderna’s vaccines or one dose of the Johnson & Johnson vaccine, only 45% have also received a booster shot, according to the CDC.
“Given that, there’s no need at the moment for the general population to get a fourth inoculation,” Dr. Schaffner says. “Our current focus ought to be on making sure that as many people as possible get that [first] booster who are eligible.”
Monica Gandhi, MD, an infectious disease specialist at the University of California, San Francisco, agreed that another booster for everyone was unnecessary. The only people who would need a fourth shot (or third, if they had the Johnson & Johnson vaccine initially) are those over age 65 or 70 years, Dr. Gandhi says.
“Older people need those antibodies up high because they’re more susceptible to severe breakthroughs,” she said, also before the latest development.
To boost or not to boost
Daniel Kuritzkes, MD, chief of infectious diseases at Brigham & Women’s Hospital in Boston, said the timing of a booster and who should be eligible depends on what the nation is trying to achieve with its vaccination strategy.
“Is the goal to prevent any symptomatic infection with COVID-19, is the goal to prevent the spread of COVID-19, or is the goal to prevent severe disease that requires hospitalization?” asked Dr. Kuritzkes.
The current vaccine — with a booster — has prevented severe disease, he said.
An Israeli study showed, for instance, that a third Pfizer dose was 93% effective against hospitalization, 92% effective against severe illness, and 81% effective against death.
A just-published study in the New England Journal of Medicine found that a booster of the Pfizer vaccine was 95% effective against COVID-19 infection and that it did not raise any new safety issues.
A small Israeli study, also published in NEJM, of a fourth Pfizer dose given to health care workers found that it prevented symptomatic infection and illness, but that it was much less effective than previous doses — maybe 65% effective against symptomatic illness, the authors write.
Giving Americans another booster now — which has been shown to lose some effectiveness after about 4 months — means it might not offer protection this fall and winter, when there could be a seasonal surge of the virus, Dr. Kuritzkes says.
And, even if people receive boosters every few months, they are still likely to get a mild respiratory virus infection, he said.
“I’m pretty convinced that we cannot boost ourselves out of this pandemic,” said Dr. Kuritzkes. “We need to first of all ensure there’s global immunization so that all the people who have not been vaccinated at all get vaccinated. That’s far more important than boosting people a fourth time.”
Booster confusion
The April 6 FDA meeting of the agency’s Vaccines and Related Biological Products Advisory Committee comes as the two major COVID vaccine makers — Pfizer and Moderna — have applied for emergency use authorization for an additional booster.
Pfizer had asked for authorization for a fourth shot in patients over age 65 years, while Moderna wanted a booster to be available to all Americans over 18. The FDA instead granted authorization to both companies for those over 50 and anyone 18 or older who is immunocompromised.
What this means for the committee’s April 6 meeting is not clear. The original agenda says the committee will consider the evidence on safety and effectiveness of the additional vaccine doses and discuss how to set up a process — similar to that used for the influenza vaccine — to be able to determine the makeup of COVID vaccines as new variants emerge. That could lay the groundwork for an annual COVID shot, if needed.
The FDA advisers will not make recommendations nor vote on whether — and which — Americans should get a COVID booster. That is the job of the CDC’s Advisory Committee on Immunization Practices (ACIP).
The last time a booster was considered, CDC Director Rochelle Walensky, MD, overrode the committee and recommended that all Americans — not just older individuals — get an additional COVID shot, which became the first booster.
That past action worries Dr. Gandhi, who calls it confusing, and says it may have contributed to the fact that less than half of Americans have since chosen to get a booster.
Dr. Schaffner says he expects the FDA to authorize emergency use for fourth doses of the Pfizer and Moderna vaccines, but he doesn’t think the CDC committee will recommend routine use. As was seen before, however, the CDC director does not have to follow the committee’s advice.
The members of ACIP “might be more conservative or narrower in scope in terms of recommending who needs to be boosted and when boosting is appropriate,” Dr. Kuritzkes says.
Dr. Gandhi says she’s concerned the FDA’s deliberations could be swayed by Moderna and Pfizer’s influence and that “pharmaceutical companies are going to have more of a say than they should in the scientific process.”
There are similar worries for Dr. Schaffner. He says he’s “a bit grumpy” that the vaccine makers have been using press releases to argue for boosters.
“Press releases are no way to make vaccine recommendations,” Dr. Schaffner said, adding that he “would advise [vaccine makers] to sit down and be quiet and let the FDA and CDC advisory committee do their thing.”
Moderna Chief Medical Officer Paul Burton, MD, however, told WebMD last week that the signs point to why a fourth shot may be needed.
“We see waning of effectiveness, antibody levels come down, and certainly effectiveness against Omicron comes down in 3 to 6 months,” Burton said. “The natural history, from what we’re seeing around the world, is that BA.2 is definitely here, it’s highly transmissible, and I think we are going to get an additional wave of BA.2 here in the United States.”
Another wave is coming, he said, and “I think there will be waning of effectiveness. We need to be prepared for that, so that’s why we need the fourth dose.”
Supply issues?
Meanwhile, the United Kingdom has begun offering boosters to anyone over 75, and Sweden’s health authority has recommended a fourth shot to people over age 80.
That puts pressure on the United States — at least on its politicians and policymakers — to, in a sense, keep up, said the infectious disease specialists.
Indeed, the White House has been keeping fourth shots in the news, warning that it is running out of money to ensure that all Americans would have access to one, if recommended.
On March 23, outgoing White House COVID-19 Response Coordinator Jeff Zients said the federal government had enough vaccine for the immunocompromised to get a fourth dose “and, if authorized in the coming weeks, enough supply for fourth doses for our most vulnerable, including seniors.”
But he warned that without congressional approval of a COVID-19 funding package, “We can’t procure the necessary vaccine supply to support fourth shots for all Americans.”
Mr. Zients also noted that other countries, including Japan, Vietnam, and the Philippines had already secured future booster doses and added, “We should be securing additional supply right now.”
Dr. Schaffner says that while it would be nice to “have a booster on the shelf,” the United States needs to put more effort into creating a globally-coordinated process for ensuring that vaccines match circulating strains and that they are manufactured on a timely basis.
He says he and others “have been reminding the public that the COVID pandemic may indeed be diminishing and moving into the endemic, but that doesn’t mean COVID is over or finished or disappeared.”
Dr. Schaffner says that it may be that “perhaps we’d need a periodic reminder to our immune system to remain protected. In other words, we might have to get boosted perhaps annually like we do with influenza.”
A version of this article first appeared on WebMD.com.
‘Staggeringly high’ rates of psychiatric symptoms after COVID-19
DENVER – Neurocognitive and psychiatric symptoms of mental illness, including posttraumatic stress disorder, are alarmingly high among patients who have previously had COVID-19 – even among those who were not hospitalized with the virus, new research shows.
The findings are from an online survey of more than 800 respondents.
“Regardless of how long ago they had been infected with COVID-19, all respondents had persistent symptoms,” co-investigator Beth Patterson, MSc, adjunct clinical professor at McMaster University, MacAnxiety Research Centre, Hamilton, Ont., told this news organization.
“The take-home message for clinicians is to be aware that if you have patients who had COVID-19, it’s quite likely that they may also experience a psychiatric issue and that they may have reduced resilience and lower quality-of-life [issues],” Ms. Patterson said.
The survey results were presented here at the Anxiety and Depression Association of America (ADAA) Conference 2022.
100% report symptoms
The study included 827 respondents (81% women) to an online survey who had contracted COVID.
Using validated symptom severity scores, respondents were assessed for mental health and neurocognitive issues, as well as some physical and quality-of-life factors.
Remarkably, all participants (100%) reported having current, persistent symptoms of COVID. In addition, 88% (n = 729) reported persistent neurocognitive symptoms, even though only 15.5% reported they had been hospitalized for COVID.
Of those hospitalized, 28.9% were treated in the intensive care unit; 42.2% stayed in hospital for less than 1 week; and 13.3% remained hospitalized for at least 3 weeks.
Data were not available on how long it had been since the patients were diagnosed or hospitalized, but most participants (68%) said they had not returned to normal functioning since contracting COVID.
The most common persistent symptoms were fatigue (75.9%), brain fog (67.9%), difficulty concentrating (61%), and weakness (51.2%).
More than half of respondents reported neurocognitive symptoms, including poor memory (57.4%) and word-finding problems in processing information (46.9%). Only 11% reported no persistent neurocognitive symptoms.
A total of 41.7% of respondents reported anxiety using the Generalized Anxiety Disorder-7 (GAD-7) scale, and rates of depression were 61.4% as assessed with the Patient Health Questionnaire (PHQ-9).
Rates of probable posttraumatic stress disorder were 40.5% as assessed via the PTSD checklist (PCL-5).
Although it wasn’t possible to use diagnostic screens, the assessment scores suggest strikingly high rates of mental health disorders among the respondents, Ms. Patterson said.
“When we look at the mean scores on the validated scales, we see percentages of probable diagnoses that are staggeringly higher than you would find in the population,” she added.
Of note, about 44% of respondents reported having had mental health treatment in the past, and 33.7% were receiving current mental health treatment.
Although the study had no control group, the findings are consistent with larger studies that have had comparator groups, including research recently published in the BMJ.
Poor understanding of COVID’s fallout
In an editorial accompanying the BMJ study, Scott Weich, MD, Mental Health Research Unit, School of Health and Related Research, University of Sheffield, United Kingdom, emphasized the need to better understand the lingering mental health aspects of COVID-19 infection.
“Our attachment to syndromal phenotypes means that we have learned remarkably little about the causes of mental ill health – in this case psychopathology associated with a viral pandemic,” Dr. Weich writes.
Dr. Weich called for improved efforts to understanding long COVID, as well as the establishment of more effective responses to the mental health fallout from the pandemic.
Commenting on the current study, Dr. Weich elaborated on the challenges in disentangling the causes of mental health effects in illness.
“In terms of other viruses, etc., there is a long history of debate and pitched battles between those that attribute mental health effects to predominantly biological processes, [involving] immunological and other responses, and those who understand these responses are mediated by psychological and social processes,” he noted.
“The story of myalgic encephalomyelitis/chronic fatigue syndrome speaks volumes about these different positions, and how difficult it can be to find a middle ground,” he said.
“This has been going on for centuries and may never be fully resolved, at least until we have clearer and more definitive evidence of pathophysiology, though this seems incredibly elusive,” Dr. Weich said.
The authors and Dr. Weich have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
DENVER – Neurocognitive and psychiatric symptoms of mental illness, including posttraumatic stress disorder, are alarmingly high among patients who have previously had COVID-19 – even among those who were not hospitalized with the virus, new research shows.
The findings are from an online survey of more than 800 respondents.
“Regardless of how long ago they had been infected with COVID-19, all respondents had persistent symptoms,” co-investigator Beth Patterson, MSc, adjunct clinical professor at McMaster University, MacAnxiety Research Centre, Hamilton, Ont., told this news organization.
“The take-home message for clinicians is to be aware that if you have patients who had COVID-19, it’s quite likely that they may also experience a psychiatric issue and that they may have reduced resilience and lower quality-of-life [issues],” Ms. Patterson said.
The survey results were presented here at the Anxiety and Depression Association of America (ADAA) Conference 2022.
100% report symptoms
The study included 827 respondents (81% women) to an online survey who had contracted COVID.
Using validated symptom severity scores, respondents were assessed for mental health and neurocognitive issues, as well as some physical and quality-of-life factors.
Remarkably, all participants (100%) reported having current, persistent symptoms of COVID. In addition, 88% (n = 729) reported persistent neurocognitive symptoms, even though only 15.5% reported they had been hospitalized for COVID.
Of those hospitalized, 28.9% were treated in the intensive care unit; 42.2% stayed in hospital for less than 1 week; and 13.3% remained hospitalized for at least 3 weeks.
Data were not available on how long it had been since the patients were diagnosed or hospitalized, but most participants (68%) said they had not returned to normal functioning since contracting COVID.
The most common persistent symptoms were fatigue (75.9%), brain fog (67.9%), difficulty concentrating (61%), and weakness (51.2%).
More than half of respondents reported neurocognitive symptoms, including poor memory (57.4%) and word-finding problems in processing information (46.9%). Only 11% reported no persistent neurocognitive symptoms.
A total of 41.7% of respondents reported anxiety using the Generalized Anxiety Disorder-7 (GAD-7) scale, and rates of depression were 61.4% as assessed with the Patient Health Questionnaire (PHQ-9).
Rates of probable posttraumatic stress disorder were 40.5% as assessed via the PTSD checklist (PCL-5).
Although it wasn’t possible to use diagnostic screens, the assessment scores suggest strikingly high rates of mental health disorders among the respondents, Ms. Patterson said.
“When we look at the mean scores on the validated scales, we see percentages of probable diagnoses that are staggeringly higher than you would find in the population,” she added.
Of note, about 44% of respondents reported having had mental health treatment in the past, and 33.7% were receiving current mental health treatment.
Although the study had no control group, the findings are consistent with larger studies that have had comparator groups, including research recently published in the BMJ.
Poor understanding of COVID’s fallout
In an editorial accompanying the BMJ study, Scott Weich, MD, Mental Health Research Unit, School of Health and Related Research, University of Sheffield, United Kingdom, emphasized the need to better understand the lingering mental health aspects of COVID-19 infection.
“Our attachment to syndromal phenotypes means that we have learned remarkably little about the causes of mental ill health – in this case psychopathology associated with a viral pandemic,” Dr. Weich writes.
Dr. Weich called for improved efforts to understanding long COVID, as well as the establishment of more effective responses to the mental health fallout from the pandemic.
Commenting on the current study, Dr. Weich elaborated on the challenges in disentangling the causes of mental health effects in illness.
“In terms of other viruses, etc., there is a long history of debate and pitched battles between those that attribute mental health effects to predominantly biological processes, [involving] immunological and other responses, and those who understand these responses are mediated by psychological and social processes,” he noted.
“The story of myalgic encephalomyelitis/chronic fatigue syndrome speaks volumes about these different positions, and how difficult it can be to find a middle ground,” he said.
“This has been going on for centuries and may never be fully resolved, at least until we have clearer and more definitive evidence of pathophysiology, though this seems incredibly elusive,” Dr. Weich said.
The authors and Dr. Weich have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
DENVER – Neurocognitive and psychiatric symptoms of mental illness, including posttraumatic stress disorder, are alarmingly high among patients who have previously had COVID-19 – even among those who were not hospitalized with the virus, new research shows.
The findings are from an online survey of more than 800 respondents.
“Regardless of how long ago they had been infected with COVID-19, all respondents had persistent symptoms,” co-investigator Beth Patterson, MSc, adjunct clinical professor at McMaster University, MacAnxiety Research Centre, Hamilton, Ont., told this news organization.
“The take-home message for clinicians is to be aware that if you have patients who had COVID-19, it’s quite likely that they may also experience a psychiatric issue and that they may have reduced resilience and lower quality-of-life [issues],” Ms. Patterson said.
The survey results were presented here at the Anxiety and Depression Association of America (ADAA) Conference 2022.
100% report symptoms
The study included 827 respondents (81% women) to an online survey who had contracted COVID.
Using validated symptom severity scores, respondents were assessed for mental health and neurocognitive issues, as well as some physical and quality-of-life factors.
Remarkably, all participants (100%) reported having current, persistent symptoms of COVID. In addition, 88% (n = 729) reported persistent neurocognitive symptoms, even though only 15.5% reported they had been hospitalized for COVID.
Of those hospitalized, 28.9% were treated in the intensive care unit; 42.2% stayed in hospital for less than 1 week; and 13.3% remained hospitalized for at least 3 weeks.
Data were not available on how long it had been since the patients were diagnosed or hospitalized, but most participants (68%) said they had not returned to normal functioning since contracting COVID.
The most common persistent symptoms were fatigue (75.9%), brain fog (67.9%), difficulty concentrating (61%), and weakness (51.2%).
More than half of respondents reported neurocognitive symptoms, including poor memory (57.4%) and word-finding problems in processing information (46.9%). Only 11% reported no persistent neurocognitive symptoms.
A total of 41.7% of respondents reported anxiety using the Generalized Anxiety Disorder-7 (GAD-7) scale, and rates of depression were 61.4% as assessed with the Patient Health Questionnaire (PHQ-9).
Rates of probable posttraumatic stress disorder were 40.5% as assessed via the PTSD checklist (PCL-5).
Although it wasn’t possible to use diagnostic screens, the assessment scores suggest strikingly high rates of mental health disorders among the respondents, Ms. Patterson said.
“When we look at the mean scores on the validated scales, we see percentages of probable diagnoses that are staggeringly higher than you would find in the population,” she added.
Of note, about 44% of respondents reported having had mental health treatment in the past, and 33.7% were receiving current mental health treatment.
Although the study had no control group, the findings are consistent with larger studies that have had comparator groups, including research recently published in the BMJ.
Poor understanding of COVID’s fallout
In an editorial accompanying the BMJ study, Scott Weich, MD, Mental Health Research Unit, School of Health and Related Research, University of Sheffield, United Kingdom, emphasized the need to better understand the lingering mental health aspects of COVID-19 infection.
“Our attachment to syndromal phenotypes means that we have learned remarkably little about the causes of mental ill health – in this case psychopathology associated with a viral pandemic,” Dr. Weich writes.
Dr. Weich called for improved efforts to understanding long COVID, as well as the establishment of more effective responses to the mental health fallout from the pandemic.
Commenting on the current study, Dr. Weich elaborated on the challenges in disentangling the causes of mental health effects in illness.
“In terms of other viruses, etc., there is a long history of debate and pitched battles between those that attribute mental health effects to predominantly biological processes, [involving] immunological and other responses, and those who understand these responses are mediated by psychological and social processes,” he noted.
“The story of myalgic encephalomyelitis/chronic fatigue syndrome speaks volumes about these different positions, and how difficult it can be to find a middle ground,” he said.
“This has been going on for centuries and may never be fully resolved, at least until we have clearer and more definitive evidence of pathophysiology, though this seems incredibly elusive,” Dr. Weich said.
The authors and Dr. Weich have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ADAA 2022




