User login
Smartphone Use During Rounds Comes Under Fire
Residents and attendings have divergent attitudes toward smartphone use during inpatient attending rounds, according to a researcher studying the topic.
Rachel Katz-Sidlow, MD, department of pediatrics, Jacobi Medical Center, Bronx, N.Y., is looking into the potential disadvantages of the phones if users are sending or receiving texts, emails, or pictures during rounds. Her preliminary research shows that a majority of faculty members believe a policy should be put in place to codify smartphone use.
“I truly think that policies to regulate smartphone use during patient management sessions are necessary, and will become commonplace in the near future until there are technology-driven solutions put into place,” says Dr. Katz-Sidlow.
Her research, currently in peer review for publication in the Journal of Hospital Medicine, comes as the ubiquity of smartphone technology has begun to be questioned by observers in the mainstream media. She says the majority of attendings and residents who responded to her initial questioning agree that smartphones “can be a serious source of distraction” during rounds.
The policy Dr. Katz-Sidlow is testing at Jacobi Medical Center defines a “smartphone” as any personal mobile communication device, including basic cellphones, Internet-enabled cellphones, and tablet computers. The beta policy restricts smartphone use during rounds to patient-care tasks, and would require all team members’ devices to be silenced or turned off at the beginning of rounds.
“Smartphones are here to stay and will become even more common in the future,” says Dr. Katz-Sidlow. “They’re such a valuable tool in medical education and patient care ... but there needs to be balance.”
Residents and attendings have divergent attitudes toward smartphone use during inpatient attending rounds, according to a researcher studying the topic.
Rachel Katz-Sidlow, MD, department of pediatrics, Jacobi Medical Center, Bronx, N.Y., is looking into the potential disadvantages of the phones if users are sending or receiving texts, emails, or pictures during rounds. Her preliminary research shows that a majority of faculty members believe a policy should be put in place to codify smartphone use.
“I truly think that policies to regulate smartphone use during patient management sessions are necessary, and will become commonplace in the near future until there are technology-driven solutions put into place,” says Dr. Katz-Sidlow.
Her research, currently in peer review for publication in the Journal of Hospital Medicine, comes as the ubiquity of smartphone technology has begun to be questioned by observers in the mainstream media. She says the majority of attendings and residents who responded to her initial questioning agree that smartphones “can be a serious source of distraction” during rounds.
The policy Dr. Katz-Sidlow is testing at Jacobi Medical Center defines a “smartphone” as any personal mobile communication device, including basic cellphones, Internet-enabled cellphones, and tablet computers. The beta policy restricts smartphone use during rounds to patient-care tasks, and would require all team members’ devices to be silenced or turned off at the beginning of rounds.
“Smartphones are here to stay and will become even more common in the future,” says Dr. Katz-Sidlow. “They’re such a valuable tool in medical education and patient care ... but there needs to be balance.”
Residents and attendings have divergent attitudes toward smartphone use during inpatient attending rounds, according to a researcher studying the topic.
Rachel Katz-Sidlow, MD, department of pediatrics, Jacobi Medical Center, Bronx, N.Y., is looking into the potential disadvantages of the phones if users are sending or receiving texts, emails, or pictures during rounds. Her preliminary research shows that a majority of faculty members believe a policy should be put in place to codify smartphone use.
“I truly think that policies to regulate smartphone use during patient management sessions are necessary, and will become commonplace in the near future until there are technology-driven solutions put into place,” says Dr. Katz-Sidlow.
Her research, currently in peer review for publication in the Journal of Hospital Medicine, comes as the ubiquity of smartphone technology has begun to be questioned by observers in the mainstream media. She says the majority of attendings and residents who responded to her initial questioning agree that smartphones “can be a serious source of distraction” during rounds.
The policy Dr. Katz-Sidlow is testing at Jacobi Medical Center defines a “smartphone” as any personal mobile communication device, including basic cellphones, Internet-enabled cellphones, and tablet computers. The beta policy restricts smartphone use during rounds to patient-care tasks, and would require all team members’ devices to be silenced or turned off at the beginning of rounds.
“Smartphones are here to stay and will become even more common in the future,” says Dr. Katz-Sidlow. “They’re such a valuable tool in medical education and patient care ... but there needs to be balance.”
Hospitalist/Palliative-Care Collaboration Aims to Reduce Readmissions
A poster presented at the Center to Advance Palliative Care national seminar in San Diego in November described a growing collaboration between the HM service and the palliative-care team at a Wisconsin medical center as part of efforts to control readmissions using tools from SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions).
On admission to 227-bed Aurora West Allis (Wis.) Medical Center, all patients assigned to a hospitalist are assessed for readmission risk factors. If a risk factor is identified, the hospital has established a set of specific interventions, including a palliative-care consultation.
“Basically, we took the BOOST tools and developed a physician action plan behind those risk factors,” says Andrew McDonagh, MD, head of the center’s hospitalist service.
Dr. McDonagh started Aurora West Allis’ HM service in 2008, and Timothy Jessick, DO, initiated the palliative-care service in 2010. “As our programs grew together, it became apparent that there were significant synergies between the two specialties, so we took the opportunity to work together in several ways,” Dr. McDonagh says.
A Palliative Care Quality Indicators Checklist, which looks for four key clinical indicators, triggers hospitalists and unit nurses to order the palliative consult. If an elderly patient has multiple admissions for the same diagnosis, the second admission triggers a geriatric consultation, and the third admission gets a palliative-care consult.
Hospitalists at the medical center are given education and modeling on how to hold family conferences with patients and their families to elicit their goals of care. Collaboration between HM and palliative care is spreading to the hospital’s ICUs, to patients transitioning out of the hospital to nursing homes, and to two other Aurora hospitals in the Milwaukee area, Dr. McDonagh explains. Since the BOOST tools have been implemented, preliminary evidence points to reduced readmissions, increased patient satisfaction, and increased palliative-care consults at the hospital.
“In the future, doing our job well as hospitalists will be more than just addressing medical needs but tailoring our care plans to the individual patient. Palliative care helps us better define appropriate care for these patients, looking beyond the trees for the forest,” he says. “I believe I’m a better clinician for being part of this relationship.”
A poster presented at the Center to Advance Palliative Care national seminar in San Diego in November described a growing collaboration between the HM service and the palliative-care team at a Wisconsin medical center as part of efforts to control readmissions using tools from SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions).
On admission to 227-bed Aurora West Allis (Wis.) Medical Center, all patients assigned to a hospitalist are assessed for readmission risk factors. If a risk factor is identified, the hospital has established a set of specific interventions, including a palliative-care consultation.
“Basically, we took the BOOST tools and developed a physician action plan behind those risk factors,” says Andrew McDonagh, MD, head of the center’s hospitalist service.
Dr. McDonagh started Aurora West Allis’ HM service in 2008, and Timothy Jessick, DO, initiated the palliative-care service in 2010. “As our programs grew together, it became apparent that there were significant synergies between the two specialties, so we took the opportunity to work together in several ways,” Dr. McDonagh says.
A Palliative Care Quality Indicators Checklist, which looks for four key clinical indicators, triggers hospitalists and unit nurses to order the palliative consult. If an elderly patient has multiple admissions for the same diagnosis, the second admission triggers a geriatric consultation, and the third admission gets a palliative-care consult.
Hospitalists at the medical center are given education and modeling on how to hold family conferences with patients and their families to elicit their goals of care. Collaboration between HM and palliative care is spreading to the hospital’s ICUs, to patients transitioning out of the hospital to nursing homes, and to two other Aurora hospitals in the Milwaukee area, Dr. McDonagh explains. Since the BOOST tools have been implemented, preliminary evidence points to reduced readmissions, increased patient satisfaction, and increased palliative-care consults at the hospital.
“In the future, doing our job well as hospitalists will be more than just addressing medical needs but tailoring our care plans to the individual patient. Palliative care helps us better define appropriate care for these patients, looking beyond the trees for the forest,” he says. “I believe I’m a better clinician for being part of this relationship.”
A poster presented at the Center to Advance Palliative Care national seminar in San Diego in November described a growing collaboration between the HM service and the palliative-care team at a Wisconsin medical center as part of efforts to control readmissions using tools from SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions).
On admission to 227-bed Aurora West Allis (Wis.) Medical Center, all patients assigned to a hospitalist are assessed for readmission risk factors. If a risk factor is identified, the hospital has established a set of specific interventions, including a palliative-care consultation.
“Basically, we took the BOOST tools and developed a physician action plan behind those risk factors,” says Andrew McDonagh, MD, head of the center’s hospitalist service.
Dr. McDonagh started Aurora West Allis’ HM service in 2008, and Timothy Jessick, DO, initiated the palliative-care service in 2010. “As our programs grew together, it became apparent that there were significant synergies between the two specialties, so we took the opportunity to work together in several ways,” Dr. McDonagh says.
A Palliative Care Quality Indicators Checklist, which looks for four key clinical indicators, triggers hospitalists and unit nurses to order the palliative consult. If an elderly patient has multiple admissions for the same diagnosis, the second admission triggers a geriatric consultation, and the third admission gets a palliative-care consult.
Hospitalists at the medical center are given education and modeling on how to hold family conferences with patients and their families to elicit their goals of care. Collaboration between HM and palliative care is spreading to the hospital’s ICUs, to patients transitioning out of the hospital to nursing homes, and to two other Aurora hospitals in the Milwaukee area, Dr. McDonagh explains. Since the BOOST tools have been implemented, preliminary evidence points to reduced readmissions, increased patient satisfaction, and increased palliative-care consults at the hospital.
“In the future, doing our job well as hospitalists will be more than just addressing medical needs but tailoring our care plans to the individual patient. Palliative care helps us better define appropriate care for these patients, looking beyond the trees for the forest,” he says. “I believe I’m a better clinician for being part of this relationship.”
FDA Approves Linagliptin/Metformin Combo For Type 2 Diabetes
The Food and Drug Administration on Jan. 30 approved a type 2 diabetes therapy that combines linagliptin and metformin in a single tablet taken twice daily.*
The approval was announced by Eli Lilly and Boehringer Ingelheim. The companies jointly developed the tablet, to be marketed as Jentadueto. Linagliptin is a dipeptidyl peptidase–4 (DPP-4) inhibitor that was approved for marketing in May 2011.
The linagliptin/metformin combination is intended to be used in conjunction with diet and exercise to improve glycemic control. Jentadueto was approved based on a 24-week, double-blind, placebo-controlled study that compared six arms: placebo, linagliptin once daily; 500 mg metformin twice daily; 2.5 mg linagliptin plus a 500-mg tablet of metformin twice daily; 1,000 mg metformin twice daily; and 2.5 mg linagliptin plus 1,000 mg metformin twice daily.
The actual combination tablet was not tested, but the FDA approved it based on bioequivalence studies, according to Lilly. The 2.5-mg linagliptin plus 1,000-mg metformin arm had the best results, reducing hemoglobin A1c by up to 1.7%. The two tablets did not cause any meaningful changes in body weight, according to a company statement.
Lilly said that Jentadueto can be used alone or in combination with a sulfonylurea. It is not indicated for type 1 diabetes or diabetic ketoacidosis. Jentadueto has a boxed warning for the risk of lactic acidosis.
*Correction, 1/31/12: An earlier version of this story noted the incorrect approval date.
The Food and Drug Administration on Jan. 30 approved a type 2 diabetes therapy that combines linagliptin and metformin in a single tablet taken twice daily.*
The approval was announced by Eli Lilly and Boehringer Ingelheim. The companies jointly developed the tablet, to be marketed as Jentadueto. Linagliptin is a dipeptidyl peptidase–4 (DPP-4) inhibitor that was approved for marketing in May 2011.
The linagliptin/metformin combination is intended to be used in conjunction with diet and exercise to improve glycemic control. Jentadueto was approved based on a 24-week, double-blind, placebo-controlled study that compared six arms: placebo, linagliptin once daily; 500 mg metformin twice daily; 2.5 mg linagliptin plus a 500-mg tablet of metformin twice daily; 1,000 mg metformin twice daily; and 2.5 mg linagliptin plus 1,000 mg metformin twice daily.
The actual combination tablet was not tested, but the FDA approved it based on bioequivalence studies, according to Lilly. The 2.5-mg linagliptin plus 1,000-mg metformin arm had the best results, reducing hemoglobin A1c by up to 1.7%. The two tablets did not cause any meaningful changes in body weight, according to a company statement.
Lilly said that Jentadueto can be used alone or in combination with a sulfonylurea. It is not indicated for type 1 diabetes or diabetic ketoacidosis. Jentadueto has a boxed warning for the risk of lactic acidosis.
*Correction, 1/31/12: An earlier version of this story noted the incorrect approval date.
The Food and Drug Administration on Jan. 30 approved a type 2 diabetes therapy that combines linagliptin and metformin in a single tablet taken twice daily.*
The approval was announced by Eli Lilly and Boehringer Ingelheim. The companies jointly developed the tablet, to be marketed as Jentadueto. Linagliptin is a dipeptidyl peptidase–4 (DPP-4) inhibitor that was approved for marketing in May 2011.
The linagliptin/metformin combination is intended to be used in conjunction with diet and exercise to improve glycemic control. Jentadueto was approved based on a 24-week, double-blind, placebo-controlled study that compared six arms: placebo, linagliptin once daily; 500 mg metformin twice daily; 2.5 mg linagliptin plus a 500-mg tablet of metformin twice daily; 1,000 mg metformin twice daily; and 2.5 mg linagliptin plus 1,000 mg metformin twice daily.
The actual combination tablet was not tested, but the FDA approved it based on bioequivalence studies, according to Lilly. The 2.5-mg linagliptin plus 1,000-mg metformin arm had the best results, reducing hemoglobin A1c by up to 1.7%. The two tablets did not cause any meaningful changes in body weight, according to a company statement.
Lilly said that Jentadueto can be used alone or in combination with a sulfonylurea. It is not indicated for type 1 diabetes or diabetic ketoacidosis. Jentadueto has a boxed warning for the risk of lactic acidosis.
*Correction, 1/31/12: An earlier version of this story noted the incorrect approval date.
Burn Size Remains Strongest Predictor of Pediatric Survival
For pediatric burn patients, the percentage of total body surface area affected remains the strongest predictor of survival, according to a report published online Jan. 31 in the Lancet.
"We have established that, in a modern pediatric burn care setting, a burn size of roughly 60% total body surface area is a crucial threshold for postburn morbidity and mortality," wrote Dr. Robert Kraft of Shriners Hospitals for Children, Galveston, Texas, and his associates.
For decades, burn size has been the main prognostic factor for both adults and children with burn injuries. But recent improvements in burn care – including novel drug treatments, new grafting techniques and materials, and improved life-support systems and monitoring methods – have dramatically improved survival, according to the investigators. Because treatment decisions, including whether to transfer a patient to a specialized burn center, are based on the probability of survival, it was important to determine whether burn size was still predictive of major complications and mortality under current treatment conditions.
To do so, Dr. Kraft and his colleagues examined outcomes in all 952 patients admitted over a 1-year period to Galveston’s Shriners Hospital with burns involving 30% or more of their total body surface area. Most of the study patients were burned on 40%-49% of their bodies.
Burn size proved to be the strongest predictor of survival, with mortality rising significantly as burn size increased. "In patient groups with burns smaller than 60% total body surface area, there were only minor increases in mortality starting at 3% and reaching up to 7%," the investigators wrote.
A large increase in mortality was noted when burn size reached 62% of the total body surface area. Such patients had a tenfold higher risk of death, compared with those who had smaller burns, the investigators reported (Lancet 2012 [doi:10.1016/S0140-6736(11)61345-7]).
Large burns also were associated with significant increases in multiorgan failure, infection during ICU stay, and the need for more surgeries to excise tissue. The rate of multiorgan failure was 6%-12% and the rate of sepsis was only 2%-6% for burns involving up to 59% of the body surface area. These rates ballooned as high as 27%-45% for multiorgan failure and 15%-26% for sepsis when burns involved 60% or more of the body surface area.
In addition, blood glucose and insulin levels rose significantly with burns involving 60% or more of the total body surface area, as did resting energy expenditure. Together with concomitant changes in liver structure and function, these findings reflect a massive hypermetabolic response to burn injury, Dr. Kraft and his associates reported.
Cytokine levels also differed by size of burn. With burns involving 60% or more of the body surface area, the levels of interleukin-6, -8, -10, and -13; macrophage inflammatory protein 1beta; tumor necrosis factor–alpha; granulocyte colony-stimulating factor; interferon-gamma; granulocyte-macrophage colony stimulating factor; and C-reactive protein rose substantially for an extended period of time.
Given these findings, "we recommend that pediatric patients with greater than 60% total body surface area burns be immediately transferred to a specialized burn center. Furthermore, at the burn center, patients should be treated with increased vigilance and improved therapies, in view of the increased risk of poor outcome associated with this burn size," the researchers wrote.
After burn size, the presence of inhalation injury in addition to external burn injury was a significant predictor of mortality. Patients who sustained inhalation injury had a threefold higher risk of death than did patients with no inhalation injuries. "We recommend that the treating physician [keep] in mind that the presence of inhalation injury significantly affects postburn outcomes," they noted.
Patient age and sex showed no association with survival, and neither did the time interval between sustaining the burn and presenting for admission.
It was noteworthy that mortality rates in this study were relatively low, even among patients who had the most extensive burns. "In our opinion, [high survival was] attributable to an improved and aggressive treatment regimen," they added.
This study was supported by Shriners Hospitals for Children, the National Institutes of Health, the National Institute on Disability and Rehabilitation Research, the Institute for Translational Sciences, the CFI Leaders Opportunity fund, and Physicians’ Services Incorporated Foundation. The investigators reported having no financial conflicts of interest.
This study shows that children with burns involving less than 62% of total body surface area can be treated successfully with standard procedures, but larger burns require the novel surgical wound management and advanced monitoring available at specialized burn centers, commented Dr. Ronald G. Tompkins.
It is also important to note that overall survival in this study was quite high. Even among children with burns involving 90% of total body surface area, half survived their injuries. And even the youngest children can be expected to survive as well as older children, now that pediatric intensive care has learned to compensate for their physiological and anatomical differences.
This means it is time to think beyond mere survival to survivors’ quality of life, he noted.
Dr. Tompkins is chief of the burn service at Massachusetts General Hospital and the Sumner M. Redstone Professor of Surgery at Harvard Medical School, both in Boston. He reported no financial conflicts of interest. These remarks were adapted from his editorial comment accompanying Dr. Kraft’s report (Lancet 2012 [doi:10.1016/S0140-6736(11)61626-7]).
This study shows that children with burns involving less than 62% of total body surface area can be treated successfully with standard procedures, but larger burns require the novel surgical wound management and advanced monitoring available at specialized burn centers, commented Dr. Ronald G. Tompkins.
It is also important to note that overall survival in this study was quite high. Even among children with burns involving 90% of total body surface area, half survived their injuries. And even the youngest children can be expected to survive as well as older children, now that pediatric intensive care has learned to compensate for their physiological and anatomical differences.
This means it is time to think beyond mere survival to survivors’ quality of life, he noted.
Dr. Tompkins is chief of the burn service at Massachusetts General Hospital and the Sumner M. Redstone Professor of Surgery at Harvard Medical School, both in Boston. He reported no financial conflicts of interest. These remarks were adapted from his editorial comment accompanying Dr. Kraft’s report (Lancet 2012 [doi:10.1016/S0140-6736(11)61626-7]).
This study shows that children with burns involving less than 62% of total body surface area can be treated successfully with standard procedures, but larger burns require the novel surgical wound management and advanced monitoring available at specialized burn centers, commented Dr. Ronald G. Tompkins.
It is also important to note that overall survival in this study was quite high. Even among children with burns involving 90% of total body surface area, half survived their injuries. And even the youngest children can be expected to survive as well as older children, now that pediatric intensive care has learned to compensate for their physiological and anatomical differences.
This means it is time to think beyond mere survival to survivors’ quality of life, he noted.
Dr. Tompkins is chief of the burn service at Massachusetts General Hospital and the Sumner M. Redstone Professor of Surgery at Harvard Medical School, both in Boston. He reported no financial conflicts of interest. These remarks were adapted from his editorial comment accompanying Dr. Kraft’s report (Lancet 2012 [doi:10.1016/S0140-6736(11)61626-7]).
For pediatric burn patients, the percentage of total body surface area affected remains the strongest predictor of survival, according to a report published online Jan. 31 in the Lancet.
"We have established that, in a modern pediatric burn care setting, a burn size of roughly 60% total body surface area is a crucial threshold for postburn morbidity and mortality," wrote Dr. Robert Kraft of Shriners Hospitals for Children, Galveston, Texas, and his associates.
For decades, burn size has been the main prognostic factor for both adults and children with burn injuries. But recent improvements in burn care – including novel drug treatments, new grafting techniques and materials, and improved life-support systems and monitoring methods – have dramatically improved survival, according to the investigators. Because treatment decisions, including whether to transfer a patient to a specialized burn center, are based on the probability of survival, it was important to determine whether burn size was still predictive of major complications and mortality under current treatment conditions.
To do so, Dr. Kraft and his colleagues examined outcomes in all 952 patients admitted over a 1-year period to Galveston’s Shriners Hospital with burns involving 30% or more of their total body surface area. Most of the study patients were burned on 40%-49% of their bodies.
Burn size proved to be the strongest predictor of survival, with mortality rising significantly as burn size increased. "In patient groups with burns smaller than 60% total body surface area, there were only minor increases in mortality starting at 3% and reaching up to 7%," the investigators wrote.
A large increase in mortality was noted when burn size reached 62% of the total body surface area. Such patients had a tenfold higher risk of death, compared with those who had smaller burns, the investigators reported (Lancet 2012 [doi:10.1016/S0140-6736(11)61345-7]).
Large burns also were associated with significant increases in multiorgan failure, infection during ICU stay, and the need for more surgeries to excise tissue. The rate of multiorgan failure was 6%-12% and the rate of sepsis was only 2%-6% for burns involving up to 59% of the body surface area. These rates ballooned as high as 27%-45% for multiorgan failure and 15%-26% for sepsis when burns involved 60% or more of the body surface area.
In addition, blood glucose and insulin levels rose significantly with burns involving 60% or more of the total body surface area, as did resting energy expenditure. Together with concomitant changes in liver structure and function, these findings reflect a massive hypermetabolic response to burn injury, Dr. Kraft and his associates reported.
Cytokine levels also differed by size of burn. With burns involving 60% or more of the body surface area, the levels of interleukin-6, -8, -10, and -13; macrophage inflammatory protein 1beta; tumor necrosis factor–alpha; granulocyte colony-stimulating factor; interferon-gamma; granulocyte-macrophage colony stimulating factor; and C-reactive protein rose substantially for an extended period of time.
Given these findings, "we recommend that pediatric patients with greater than 60% total body surface area burns be immediately transferred to a specialized burn center. Furthermore, at the burn center, patients should be treated with increased vigilance and improved therapies, in view of the increased risk of poor outcome associated with this burn size," the researchers wrote.
After burn size, the presence of inhalation injury in addition to external burn injury was a significant predictor of mortality. Patients who sustained inhalation injury had a threefold higher risk of death than did patients with no inhalation injuries. "We recommend that the treating physician [keep] in mind that the presence of inhalation injury significantly affects postburn outcomes," they noted.
Patient age and sex showed no association with survival, and neither did the time interval between sustaining the burn and presenting for admission.
It was noteworthy that mortality rates in this study were relatively low, even among patients who had the most extensive burns. "In our opinion, [high survival was] attributable to an improved and aggressive treatment regimen," they added.
This study was supported by Shriners Hospitals for Children, the National Institutes of Health, the National Institute on Disability and Rehabilitation Research, the Institute for Translational Sciences, the CFI Leaders Opportunity fund, and Physicians’ Services Incorporated Foundation. The investigators reported having no financial conflicts of interest.
For pediatric burn patients, the percentage of total body surface area affected remains the strongest predictor of survival, according to a report published online Jan. 31 in the Lancet.
"We have established that, in a modern pediatric burn care setting, a burn size of roughly 60% total body surface area is a crucial threshold for postburn morbidity and mortality," wrote Dr. Robert Kraft of Shriners Hospitals for Children, Galveston, Texas, and his associates.
For decades, burn size has been the main prognostic factor for both adults and children with burn injuries. But recent improvements in burn care – including novel drug treatments, new grafting techniques and materials, and improved life-support systems and monitoring methods – have dramatically improved survival, according to the investigators. Because treatment decisions, including whether to transfer a patient to a specialized burn center, are based on the probability of survival, it was important to determine whether burn size was still predictive of major complications and mortality under current treatment conditions.
To do so, Dr. Kraft and his colleagues examined outcomes in all 952 patients admitted over a 1-year period to Galveston’s Shriners Hospital with burns involving 30% or more of their total body surface area. Most of the study patients were burned on 40%-49% of their bodies.
Burn size proved to be the strongest predictor of survival, with mortality rising significantly as burn size increased. "In patient groups with burns smaller than 60% total body surface area, there were only minor increases in mortality starting at 3% and reaching up to 7%," the investigators wrote.
A large increase in mortality was noted when burn size reached 62% of the total body surface area. Such patients had a tenfold higher risk of death, compared with those who had smaller burns, the investigators reported (Lancet 2012 [doi:10.1016/S0140-6736(11)61345-7]).
Large burns also were associated with significant increases in multiorgan failure, infection during ICU stay, and the need for more surgeries to excise tissue. The rate of multiorgan failure was 6%-12% and the rate of sepsis was only 2%-6% for burns involving up to 59% of the body surface area. These rates ballooned as high as 27%-45% for multiorgan failure and 15%-26% for sepsis when burns involved 60% or more of the body surface area.
In addition, blood glucose and insulin levels rose significantly with burns involving 60% or more of the total body surface area, as did resting energy expenditure. Together with concomitant changes in liver structure and function, these findings reflect a massive hypermetabolic response to burn injury, Dr. Kraft and his associates reported.
Cytokine levels also differed by size of burn. With burns involving 60% or more of the body surface area, the levels of interleukin-6, -8, -10, and -13; macrophage inflammatory protein 1beta; tumor necrosis factor–alpha; granulocyte colony-stimulating factor; interferon-gamma; granulocyte-macrophage colony stimulating factor; and C-reactive protein rose substantially for an extended period of time.
Given these findings, "we recommend that pediatric patients with greater than 60% total body surface area burns be immediately transferred to a specialized burn center. Furthermore, at the burn center, patients should be treated with increased vigilance and improved therapies, in view of the increased risk of poor outcome associated with this burn size," the researchers wrote.
After burn size, the presence of inhalation injury in addition to external burn injury was a significant predictor of mortality. Patients who sustained inhalation injury had a threefold higher risk of death than did patients with no inhalation injuries. "We recommend that the treating physician [keep] in mind that the presence of inhalation injury significantly affects postburn outcomes," they noted.
Patient age and sex showed no association with survival, and neither did the time interval between sustaining the burn and presenting for admission.
It was noteworthy that mortality rates in this study were relatively low, even among patients who had the most extensive burns. "In our opinion, [high survival was] attributable to an improved and aggressive treatment regimen," they added.
This study was supported by Shriners Hospitals for Children, the National Institutes of Health, the National Institute on Disability and Rehabilitation Research, the Institute for Translational Sciences, the CFI Leaders Opportunity fund, and Physicians’ Services Incorporated Foundation. The investigators reported having no financial conflicts of interest.
FROM LANCET
Major Finding: Larger burn size correlated with poorer prognosis, with mortality rising tenfold in patients who had 62% or more of total body surface area involved.
Data Source: A single-center, observational cohort study of 952 pediatric patients with burns covering at least 30% of their total body surface area who were treated over a 1-year period.
Disclosures: This study was supported by Shriners Hospitals for Children, the National Institutes of Health, the National Institute on Disability and Rehabilitation Research, the Institute for Translational Sciences, the CFI Leaders Opportunity fund, and Physicians’ Services Incorporated Foundation. The investigators reported having no financial conflicts of interest.
Acute Medicine in the United Kingdom
Hospital medicine has emerged in the United States (US) to address the complexity of hospital care and over the last 15 years has become the fastest growing specialty in US history.1 The field has been shaped by societal, financial, and clinical factors within American health care, several of which also exist elsewhere in the world.2, 3 Outside the US, analogs of hospital medicine have evolved; in the United Kingdom (UK), where the term and concept of a hospitalist is widely unknown, the specialty of acute medicine has evolved to meet the complex needs of the acutely unwell medical patient in the modern health care environment. The similarities are notable, as are the differences. Our objective in this brief communication is to introduce the UK model of acute medicine to counterparts in the US. We trace the development of acute medicine in the UK, describe current practice, and note features of the model potentially applicable to hospital medicine in the US. We use UK terminology but provide equivalent terms from the US, as shown in Table 1.
| UK Term | US Term |
|---|---|
| |
| General practitioner | Family practice physician |
| Consultant physician* | Attending physician (including all general internists) |
| Postgraduate trainee physicians | Interns, residents, or fellows |
| Respiratory service | Pulmonary service |
| Medicine of the elderly service | Geriatric service |
| Accident and emergency department | Emergency department |
| High‐dependency unit | Step‐down unit |
Background and Factors Contributing to the Rise of Acute Medicine in the UK
Patient care in the UK National Health Service (NHS) is separated into inpatient and outpatient care. Generally, outpatient care is provided by general practitioners (GPs). GP clinics are independent structures and interact with local NHS‐funded services via contract, in contrast to NHS hospitals that are directly controlled by their local NHS municipal‐based body. GPs have no independent admission rights to hospitals, and (with few exceptions) do not participate in direct inpatient care. Consequently, patients in GP clinics requiring hospital admission have been referred to hospital‐based providers who assume all responsibility for inpatient care. The inpatient medical physician body in the UK is comprised of consultants, each usually trained in both general internal medicine and a medical specialty very similar to US internal medicinebased subspecialists, such as endocrinology or infectious disease. Prior to the advent of acute medicine, each consultant shared responsibility for admission of medical patients with consultants from other specialties, according to a call schedule. Generalist‐focused care would be initiated by postgraduate trainee physicians at the time of admission, and continued by the accepting consultant who often conducted subspecialty inpatient and outpatient work simultaneously. Due to advances in medical care at the turn of the century, inpatient care became more specialized; as a result, a general trend developed where the contribution of some specialties to generalist‐focused care grew (respiratory and medicine of the elderly), while other specialties began to focus on specialty‐specific interventions at the expense of practice and training in the generalist approach to care (cardiology, nephrology). Consequently, interservice disparity in provision of generalist‐focused care grew, especially in larger UK teaching hospitals. These trends have manifested as recent changes in UK medical training; presently, all UK medical specialty training programs require concomitant training in general internal medicine competencies, but for some specialties, general internal medicine training is truncated (either by the training program or by allowed choice of trainees) to provide less training than what is required for recognition as a specialist in general internal medicine.
In the UK, the majority of direct clinical care is provided via supervision of postgraduate trainee physicians. Over the last 20 years, limits on resident duty‐hours have been applied, much as has happened over the previous decade in the US.4 In 1991, the NHS and the British Medical Association negotiated a compensation package for physicians in training, termed the New Deal for Junior Doctors, which called for limitation of actual work hours for postgraduate trainee physicians to 56 hours per week. Enforcement of New Deal work guidelines was implemented over the next 12 years; with the introduction of the European Working Time Directive in 2000, work hours were further limited to 48 hours a week by 2009 for consultant and trainee physicians alike. Many UK consultants had already been devoting a higher percentage of time to subspecialty‐based hospital work and, with the reduced availability of the postgraduate trainee physician resource, the quality of generalist‐focused care (for conditions out with a consultant's given specialty) became more disparate between medical specialties, with some specialties providing little generalist input during the admission process. Simultaneously, and in the context of evolving demographic and regulatory pressures (Table 2), the admission procedure required an increasingly specific set of competencies. A subset of consultants from many different specialties began to focus specifically on management of the admission process and to informally self‐identify as specialists in acute medicine.
|
| Advances in medical care leading to increased specialization |
| Increasing numbers of elderly patients with complex medical needs |
| UK‐wide targets to limit emergency department patient stays to 4 hours |
| New limits to postgraduate trainee physician work hours |
| Increased standards of supervision of trainee physicians by consultants |
| Deficiencies in availability of outpatient out‐of‐hours care |
| Locally led reconfigurations of health care resources to favor community‐based care over inpatient‐based care |
Concerns were published about the quality of initial care for the acutely unwell patient in the UK.5 The UK Royal Colleges were concerned that patients with acute medical illnesses should receive high‐quality clinical care and commissioned a number of working groups to determine how acute medicine should best be delivered. Although initial reports suggested that acute care should be delivered by physicians who maintained an organ‐specific specialty focus, subsequent reports suggested that acute medicine should be delivered by specifically trained individuals capable of managing both the acutely ill medical patient and the administration of an acute medical unit (AMU).6, 7 In response to these trends, in 2003 the Royal Colleges of Physicians Joint Committee for Higher Medical Training, now known as the Joint Royal College of Physicians Training Board (JRCPTB), introduced a training curriculum for acute medicine as a subspecialty of general medicine.8 In 2007, the Royal College of Physicians convened an Acute Medicine Task Force that published further recommendations on the purpose and design of acute medicine services.9 Application by the JRCPTB to the regulatory bodies for medical education and training in the UK led to recognition in 2009 of acute internal medicine as a separate and distinct specialty from all other specialties, including general medicine.10
Acute Medicine in Practice: the Admission Process and Prevention of Prolonged Hospital Admission
The defining characteristic of an acute medical service in the UK is the sole dedication of a team of physician, nursing, and allied health care support staff (such as therapists, pharmacists, and social workers) to the task of admission and initial care of medical inpatients during their work shifts. Admission activity usually takes place in a dedicated physical area: the AMU. The AMU is commonly located near an accident and emergency (AE) department and is often colocated with radiology services, an intensive care unit, and/or a high‐dependency unit. Patients may be admitted to the AMU from the AE department, or directly from GP clinics. Generally, an AMU is responsible for a spectrum of medical conditions identical to the conditions potentially managed by a US‐based hospitalist. Unlike general and subspecialty medical wards, where consultant bedside input may be available as infrequently as 2 to 3 times per week, twice‐daily consultant bedside input into AMU patient care is the recommended standard. AMUs provide consultant bedside input via multiple rounds during the day, or alternatively in a continuous, per‐admission rolling pattern. Existing data suggest that AMUs with daily consultant input shorten hospital length of stay and increase same‐day discharges without affecting readmissions or mortality.11 Outside the US, observational studies associate AMUs with improved hospital mortality, shortened length of stay, decreased emergency department waiting times, and improved patient satisfaction.12
Three major models of acute medicine practice have evolved in the UK, as outlined in Table 3. The model adopted by each AMU varies depending on availability of staff, AMU bed capacity, the number and variability of patients requiring admission, and even hospital philosophy regarding division of responsibility between acute medicine physicians and those of other specialties. AMUs also vary in critical care capability, with many providing noninvasive ventilation or invasive hemodynamic monitoring. Admitted medical inpatients may bypass an AMU altogether if the AMU staff are unable to provide a procedure (eg, hemodialysis), if a patient requires no further diagnostic clarification or stabilization (eg, routine chemotherapy), or if an AMU admission would delay provision of time‐sensitive care (eg, percutaneous coronary intervention for ST‐elevation myocardial infarction). In all AMUs, patients requiring inpatient care outside of the AMU will be admitted to a medical specialty ward (cardiology, general internal medicine, neurology, etc). Generalist‐focused care is then provided by postgraduate trainee physicians on the medical specialty ward, based on guidance generated by AMU physicians, per guidance form their supervising specialty consultant physician (if possible), or through the advice given by other specialty services. Whether AMU physicians continue to be responsible for the care of AMU patients transferred to a general internal medicine ward depends on arrangements based on the particular AMU model and hospital staffing factors.
| Acute Medicine Models | Acute Medicine Team Focus |
|---|---|
| |
| Triage | Inpatient care rapidly transitioned to specialty medical ward with minimal stay in AMU |
| Short stay | Short‐term inpatient care (72 hours) provided in AMU, including extensive assessment (eg, physical therapy, sequential radiologic imaging), multispecialty bedside input, medical therapy, and either coordination of postdischarge follow‐up or transition of care to specialty medical ward |
| Hybrid | Subset of patients rapidly transitioned to specialty medical ward, while others receive care in AMU for up to 72 hours; mix dependent on patient needs and available hospital/AMU resources |
Weaknesses and Strengths of Acute Medicine Model Applicable to US‐Based Hospital Medicine
The acute medicine model of care does instantiate potential risks. Utilization of an acute medicine team hardwires fragmentation of care, necessitating handovers. In the context of US hospital medicine practice, this fragmentation may compromise safety or throughput; however, no such deficit has been detected to date in the context of acute medicine practice in the UK.13 Mismatch between AMU bed or staff capacity and the number or rate of hospital admissions can generate safety risks or give away efficiency gains. Further inefficiencies can develop if hospital‐wide processes of handover, medical decision making, patient transport, and discharge are not synchronized with AMU outflow and intake. Evidence of AMU throughput failure is most often manifest by the premature transfer of patients from AMU to the main hospital ward areas, or by delay of admissions from the emergency department into the AMU (UK standards until recently mandated that 98% of AE patients complete their AE stay in 4 hours). Although some successful UK AMUs have minimized these failures, such problems are still experienced by many acute medicine services throughout the UK. Ongoing debate, both local and national, persists within the acute medicine community about how best to address these challenges.
The strengths of the acute medicine model appear to be clinically meaningful, however. The admission process is complex and occurs at a time when patients are sickest and potentially the most vulnerable. Effective management of this period offers significant opportunity to improve value for patients, hospitals, and health systems. When applied in the context of US hospitalist programs, instances of successful short stay units and active bed management do exist.1417 These documented successes represent partial application of UK‐style acute medicine activity in a US hospital setting. A multidisciplinary health care team dedicated to streamlining admissions, short stays, and follow‐up care offers many potential benefits. Standardization and accountability of admission process, especially important for quality improvement and research activity applicable to the initial portion of a hospital stay, may be more readily realized if embedded into the practice of a discrete cohort of hospital staff. In the UK, several hospital processes fall within the exclusive remit of an acute medicine service (Table 4). Optimization of several of these processes of care can reduce hospital morbidity, mortality, and length of stay.1821 As health care financing reform arrives in the US, the ability of American hospitals to manage admission‐specific processes of care with reliability will become more vital.3 In the US, programs that force hospitalists to make ad hoc, moment‐to‐moment prioritizations about when and where to perform admissions, discharges, and daily ward care may do so at the expense of system predictability, standardization, and patient‐centeredness. Where hospitalists are forced to juggle these geographically and substantively disparate care duties, data suggest significant opportunities to reduce variability and improve efficiency.22, 23
| Initiation of time‐sensitive acute care bundles (eg, stroke, sepsis, myocardial infarction) |
| Initiation of disease‐specific protocols (eg, venous thromboembolism prophylaxis, glycemic control) |
| Outpatient‐inpatient information reconciliation (medicines, code status, etc) |
| Outpatient‐to‐inpatient consultation (general practitioner phone consultation, telemedicine) |
| Stewardship of empiric antimicrobial therapy |
| Early involvement of discharge planning apparatus |
| Provision of follow‐up ambulatory care (medical assessment unit discharge with next‐day hospital follow‐up) |
| Outpatient intravenous antibiotic services |
| Frequent patient admission policies |
Integrated into US hospital medicine practices, the UK acute medicine model might capture otherwise elusive quality and efficiency gains.14 By the same token, integrating portions of the US hospital medicine model into a UK acute medicine model could be beneficial as well. For instance, when compared with the interservice handover common in UK AMUs, intraservice handover (acute care hospitalist‐to‐ward hospitalist) may promote standardization of the handover process and potentially fewer instances of failed communication. What seems certain is that greater attention should be focused on an exchange of ideas between acute medicine and hospital medicine.
Acknowledgements
The authors thank Valery Akopov for review of the manuscript.
Conflicts of Interest: Drs. Smith and Jones are employed as acute medicine physicians by NHS Lothian, and both have received reimbursement for public speaking related to acute medicine. Dr. Jones has received reimbursement for curriculum design activity for the acute medicine specialty in the UK.
- Society of Hospital Medicine. Growth of Hospital Medicine Nationwide. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Media/GrowthofHospitalMedicineNationwide/Growth_of_Hospital_M.htm. Accessed May 15, 2011.
- . The hospitalist field turns 15: new opportunities and challenges. J Hosp Med. 2011;6:E1–E4.
- . Value‐driven healthcare: implications for hospitals and hospitalists. J Hosp Med. 2009;4:507–511.
- , , . ACGME Work Group on Resident Duty Hours. Accreditation Council for Graduate Medical Education. New requirements for resident duty hours. JAMA. 2002;288:1112–1114.
- , , , et al. Confidential inquiry into quality of care before admission to intensive care. BMJ. 1998;316:1853–1858.
- Federation of Medical Royal Colleges. Acute Medicine: The Physician's Role: Proposals for the Future. A Working Party Report of the Federation of Medical Royal Colleges. London, UK: Federation of Medical Royal Colleges; 2000.
- Federation of Medical Royal Colleges. Acute Medicine: Making it Work for Patients. A Blueprint for Organization and Training. Report of a Working Party. London, UK: Federation of Medical Royal Colleges; 2004.
- Joint Royal College of Physicians Training Board. Higher medical training curriculum for subspecialty training in acute medicine for general (internal) medicine NTN holders. July 2003.
- College of Physicians, London. Acute medical care: the right person, in the right setting—first time. Report of the Acute Medicine Task Force. October 2007.
- Joint Royal College of Physicians Training Board. Specialty training curriculum for acute internal medicine. August 2009.
- , , , . What is the effect of a consultant presence in an acute medical unit? Clin Med. 2009;9:214–218.
- , , . Effectiveness of acute medical units in hospitals: a systematic review. Int J Qual Health Care. 2009;21:397–407.
- , , , , . The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5:335–338.
- , , . Implementation of a hospitalist‐run observation unit and impact on length of stay (LOS): a brief report. J Hosp Med. 2010;5:E2–E5.
- , , , , , . Active bed management by hospitalists and emergency department throughput. Ann Intern Med. 2008;149:804–811.
- , , , . Hospitalist bed management effecting throughput from the emergency department to the intensive care unit. J Crit Care. 2001;25:184–189.
- , . MSSU: a multidisciplinary approach to finding cost effective and efficient care for observation patients. Quality and Safety Fall Forum, University HealthSystem Consortium Conference; 2009.
- , , , , . Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta‐analysis of randomized controlled trials. Arch Intern Med. 2007;167:1476–1486.
- , , , et al. Results of the Medications at Transitions and Clinical Handoffs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med. 2010;25:441–447.
- , , , . Antiplatelet therapy for acute ischaemic stroke. Cochrane Database Syst Rev. 2008;16:CD000029.
- , , , et al. Early goal‐directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377.
- , , , et al. Where did the day go?—A time motion study of hospitalists. J Hosp Med. 2010;5:323–328.
- , , , , . Hospitalist time usage and cyclicality: opportunities to improve efficiency. J Hosp Med. 2010;5:329–334.
Hospital medicine has emerged in the United States (US) to address the complexity of hospital care and over the last 15 years has become the fastest growing specialty in US history.1 The field has been shaped by societal, financial, and clinical factors within American health care, several of which also exist elsewhere in the world.2, 3 Outside the US, analogs of hospital medicine have evolved; in the United Kingdom (UK), where the term and concept of a hospitalist is widely unknown, the specialty of acute medicine has evolved to meet the complex needs of the acutely unwell medical patient in the modern health care environment. The similarities are notable, as are the differences. Our objective in this brief communication is to introduce the UK model of acute medicine to counterparts in the US. We trace the development of acute medicine in the UK, describe current practice, and note features of the model potentially applicable to hospital medicine in the US. We use UK terminology but provide equivalent terms from the US, as shown in Table 1.
| UK Term | US Term |
|---|---|
| |
| General practitioner | Family practice physician |
| Consultant physician* | Attending physician (including all general internists) |
| Postgraduate trainee physicians | Interns, residents, or fellows |
| Respiratory service | Pulmonary service |
| Medicine of the elderly service | Geriatric service |
| Accident and emergency department | Emergency department |
| High‐dependency unit | Step‐down unit |
Background and Factors Contributing to the Rise of Acute Medicine in the UK
Patient care in the UK National Health Service (NHS) is separated into inpatient and outpatient care. Generally, outpatient care is provided by general practitioners (GPs). GP clinics are independent structures and interact with local NHS‐funded services via contract, in contrast to NHS hospitals that are directly controlled by their local NHS municipal‐based body. GPs have no independent admission rights to hospitals, and (with few exceptions) do not participate in direct inpatient care. Consequently, patients in GP clinics requiring hospital admission have been referred to hospital‐based providers who assume all responsibility for inpatient care. The inpatient medical physician body in the UK is comprised of consultants, each usually trained in both general internal medicine and a medical specialty very similar to US internal medicinebased subspecialists, such as endocrinology or infectious disease. Prior to the advent of acute medicine, each consultant shared responsibility for admission of medical patients with consultants from other specialties, according to a call schedule. Generalist‐focused care would be initiated by postgraduate trainee physicians at the time of admission, and continued by the accepting consultant who often conducted subspecialty inpatient and outpatient work simultaneously. Due to advances in medical care at the turn of the century, inpatient care became more specialized; as a result, a general trend developed where the contribution of some specialties to generalist‐focused care grew (respiratory and medicine of the elderly), while other specialties began to focus on specialty‐specific interventions at the expense of practice and training in the generalist approach to care (cardiology, nephrology). Consequently, interservice disparity in provision of generalist‐focused care grew, especially in larger UK teaching hospitals. These trends have manifested as recent changes in UK medical training; presently, all UK medical specialty training programs require concomitant training in general internal medicine competencies, but for some specialties, general internal medicine training is truncated (either by the training program or by allowed choice of trainees) to provide less training than what is required for recognition as a specialist in general internal medicine.
In the UK, the majority of direct clinical care is provided via supervision of postgraduate trainee physicians. Over the last 20 years, limits on resident duty‐hours have been applied, much as has happened over the previous decade in the US.4 In 1991, the NHS and the British Medical Association negotiated a compensation package for physicians in training, termed the New Deal for Junior Doctors, which called for limitation of actual work hours for postgraduate trainee physicians to 56 hours per week. Enforcement of New Deal work guidelines was implemented over the next 12 years; with the introduction of the European Working Time Directive in 2000, work hours were further limited to 48 hours a week by 2009 for consultant and trainee physicians alike. Many UK consultants had already been devoting a higher percentage of time to subspecialty‐based hospital work and, with the reduced availability of the postgraduate trainee physician resource, the quality of generalist‐focused care (for conditions out with a consultant's given specialty) became more disparate between medical specialties, with some specialties providing little generalist input during the admission process. Simultaneously, and in the context of evolving demographic and regulatory pressures (Table 2), the admission procedure required an increasingly specific set of competencies. A subset of consultants from many different specialties began to focus specifically on management of the admission process and to informally self‐identify as specialists in acute medicine.
|
| Advances in medical care leading to increased specialization |
| Increasing numbers of elderly patients with complex medical needs |
| UK‐wide targets to limit emergency department patient stays to 4 hours |
| New limits to postgraduate trainee physician work hours |
| Increased standards of supervision of trainee physicians by consultants |
| Deficiencies in availability of outpatient out‐of‐hours care |
| Locally led reconfigurations of health care resources to favor community‐based care over inpatient‐based care |
Concerns were published about the quality of initial care for the acutely unwell patient in the UK.5 The UK Royal Colleges were concerned that patients with acute medical illnesses should receive high‐quality clinical care and commissioned a number of working groups to determine how acute medicine should best be delivered. Although initial reports suggested that acute care should be delivered by physicians who maintained an organ‐specific specialty focus, subsequent reports suggested that acute medicine should be delivered by specifically trained individuals capable of managing both the acutely ill medical patient and the administration of an acute medical unit (AMU).6, 7 In response to these trends, in 2003 the Royal Colleges of Physicians Joint Committee for Higher Medical Training, now known as the Joint Royal College of Physicians Training Board (JRCPTB), introduced a training curriculum for acute medicine as a subspecialty of general medicine.8 In 2007, the Royal College of Physicians convened an Acute Medicine Task Force that published further recommendations on the purpose and design of acute medicine services.9 Application by the JRCPTB to the regulatory bodies for medical education and training in the UK led to recognition in 2009 of acute internal medicine as a separate and distinct specialty from all other specialties, including general medicine.10
Acute Medicine in Practice: the Admission Process and Prevention of Prolonged Hospital Admission
The defining characteristic of an acute medical service in the UK is the sole dedication of a team of physician, nursing, and allied health care support staff (such as therapists, pharmacists, and social workers) to the task of admission and initial care of medical inpatients during their work shifts. Admission activity usually takes place in a dedicated physical area: the AMU. The AMU is commonly located near an accident and emergency (AE) department and is often colocated with radiology services, an intensive care unit, and/or a high‐dependency unit. Patients may be admitted to the AMU from the AE department, or directly from GP clinics. Generally, an AMU is responsible for a spectrum of medical conditions identical to the conditions potentially managed by a US‐based hospitalist. Unlike general and subspecialty medical wards, where consultant bedside input may be available as infrequently as 2 to 3 times per week, twice‐daily consultant bedside input into AMU patient care is the recommended standard. AMUs provide consultant bedside input via multiple rounds during the day, or alternatively in a continuous, per‐admission rolling pattern. Existing data suggest that AMUs with daily consultant input shorten hospital length of stay and increase same‐day discharges without affecting readmissions or mortality.11 Outside the US, observational studies associate AMUs with improved hospital mortality, shortened length of stay, decreased emergency department waiting times, and improved patient satisfaction.12
Three major models of acute medicine practice have evolved in the UK, as outlined in Table 3. The model adopted by each AMU varies depending on availability of staff, AMU bed capacity, the number and variability of patients requiring admission, and even hospital philosophy regarding division of responsibility between acute medicine physicians and those of other specialties. AMUs also vary in critical care capability, with many providing noninvasive ventilation or invasive hemodynamic monitoring. Admitted medical inpatients may bypass an AMU altogether if the AMU staff are unable to provide a procedure (eg, hemodialysis), if a patient requires no further diagnostic clarification or stabilization (eg, routine chemotherapy), or if an AMU admission would delay provision of time‐sensitive care (eg, percutaneous coronary intervention for ST‐elevation myocardial infarction). In all AMUs, patients requiring inpatient care outside of the AMU will be admitted to a medical specialty ward (cardiology, general internal medicine, neurology, etc). Generalist‐focused care is then provided by postgraduate trainee physicians on the medical specialty ward, based on guidance generated by AMU physicians, per guidance form their supervising specialty consultant physician (if possible), or through the advice given by other specialty services. Whether AMU physicians continue to be responsible for the care of AMU patients transferred to a general internal medicine ward depends on arrangements based on the particular AMU model and hospital staffing factors.
| Acute Medicine Models | Acute Medicine Team Focus |
|---|---|
| |
| Triage | Inpatient care rapidly transitioned to specialty medical ward with minimal stay in AMU |
| Short stay | Short‐term inpatient care (72 hours) provided in AMU, including extensive assessment (eg, physical therapy, sequential radiologic imaging), multispecialty bedside input, medical therapy, and either coordination of postdischarge follow‐up or transition of care to specialty medical ward |
| Hybrid | Subset of patients rapidly transitioned to specialty medical ward, while others receive care in AMU for up to 72 hours; mix dependent on patient needs and available hospital/AMU resources |
Weaknesses and Strengths of Acute Medicine Model Applicable to US‐Based Hospital Medicine
The acute medicine model of care does instantiate potential risks. Utilization of an acute medicine team hardwires fragmentation of care, necessitating handovers. In the context of US hospital medicine practice, this fragmentation may compromise safety or throughput; however, no such deficit has been detected to date in the context of acute medicine practice in the UK.13 Mismatch between AMU bed or staff capacity and the number or rate of hospital admissions can generate safety risks or give away efficiency gains. Further inefficiencies can develop if hospital‐wide processes of handover, medical decision making, patient transport, and discharge are not synchronized with AMU outflow and intake. Evidence of AMU throughput failure is most often manifest by the premature transfer of patients from AMU to the main hospital ward areas, or by delay of admissions from the emergency department into the AMU (UK standards until recently mandated that 98% of AE patients complete their AE stay in 4 hours). Although some successful UK AMUs have minimized these failures, such problems are still experienced by many acute medicine services throughout the UK. Ongoing debate, both local and national, persists within the acute medicine community about how best to address these challenges.
The strengths of the acute medicine model appear to be clinically meaningful, however. The admission process is complex and occurs at a time when patients are sickest and potentially the most vulnerable. Effective management of this period offers significant opportunity to improve value for patients, hospitals, and health systems. When applied in the context of US hospitalist programs, instances of successful short stay units and active bed management do exist.1417 These documented successes represent partial application of UK‐style acute medicine activity in a US hospital setting. A multidisciplinary health care team dedicated to streamlining admissions, short stays, and follow‐up care offers many potential benefits. Standardization and accountability of admission process, especially important for quality improvement and research activity applicable to the initial portion of a hospital stay, may be more readily realized if embedded into the practice of a discrete cohort of hospital staff. In the UK, several hospital processes fall within the exclusive remit of an acute medicine service (Table 4). Optimization of several of these processes of care can reduce hospital morbidity, mortality, and length of stay.1821 As health care financing reform arrives in the US, the ability of American hospitals to manage admission‐specific processes of care with reliability will become more vital.3 In the US, programs that force hospitalists to make ad hoc, moment‐to‐moment prioritizations about when and where to perform admissions, discharges, and daily ward care may do so at the expense of system predictability, standardization, and patient‐centeredness. Where hospitalists are forced to juggle these geographically and substantively disparate care duties, data suggest significant opportunities to reduce variability and improve efficiency.22, 23
| Initiation of time‐sensitive acute care bundles (eg, stroke, sepsis, myocardial infarction) |
| Initiation of disease‐specific protocols (eg, venous thromboembolism prophylaxis, glycemic control) |
| Outpatient‐inpatient information reconciliation (medicines, code status, etc) |
| Outpatient‐to‐inpatient consultation (general practitioner phone consultation, telemedicine) |
| Stewardship of empiric antimicrobial therapy |
| Early involvement of discharge planning apparatus |
| Provision of follow‐up ambulatory care (medical assessment unit discharge with next‐day hospital follow‐up) |
| Outpatient intravenous antibiotic services |
| Frequent patient admission policies |
Integrated into US hospital medicine practices, the UK acute medicine model might capture otherwise elusive quality and efficiency gains.14 By the same token, integrating portions of the US hospital medicine model into a UK acute medicine model could be beneficial as well. For instance, when compared with the interservice handover common in UK AMUs, intraservice handover (acute care hospitalist‐to‐ward hospitalist) may promote standardization of the handover process and potentially fewer instances of failed communication. What seems certain is that greater attention should be focused on an exchange of ideas between acute medicine and hospital medicine.
Acknowledgements
The authors thank Valery Akopov for review of the manuscript.
Conflicts of Interest: Drs. Smith and Jones are employed as acute medicine physicians by NHS Lothian, and both have received reimbursement for public speaking related to acute medicine. Dr. Jones has received reimbursement for curriculum design activity for the acute medicine specialty in the UK.
Hospital medicine has emerged in the United States (US) to address the complexity of hospital care and over the last 15 years has become the fastest growing specialty in US history.1 The field has been shaped by societal, financial, and clinical factors within American health care, several of which also exist elsewhere in the world.2, 3 Outside the US, analogs of hospital medicine have evolved; in the United Kingdom (UK), where the term and concept of a hospitalist is widely unknown, the specialty of acute medicine has evolved to meet the complex needs of the acutely unwell medical patient in the modern health care environment. The similarities are notable, as are the differences. Our objective in this brief communication is to introduce the UK model of acute medicine to counterparts in the US. We trace the development of acute medicine in the UK, describe current practice, and note features of the model potentially applicable to hospital medicine in the US. We use UK terminology but provide equivalent terms from the US, as shown in Table 1.
| UK Term | US Term |
|---|---|
| |
| General practitioner | Family practice physician |
| Consultant physician* | Attending physician (including all general internists) |
| Postgraduate trainee physicians | Interns, residents, or fellows |
| Respiratory service | Pulmonary service |
| Medicine of the elderly service | Geriatric service |
| Accident and emergency department | Emergency department |
| High‐dependency unit | Step‐down unit |
Background and Factors Contributing to the Rise of Acute Medicine in the UK
Patient care in the UK National Health Service (NHS) is separated into inpatient and outpatient care. Generally, outpatient care is provided by general practitioners (GPs). GP clinics are independent structures and interact with local NHS‐funded services via contract, in contrast to NHS hospitals that are directly controlled by their local NHS municipal‐based body. GPs have no independent admission rights to hospitals, and (with few exceptions) do not participate in direct inpatient care. Consequently, patients in GP clinics requiring hospital admission have been referred to hospital‐based providers who assume all responsibility for inpatient care. The inpatient medical physician body in the UK is comprised of consultants, each usually trained in both general internal medicine and a medical specialty very similar to US internal medicinebased subspecialists, such as endocrinology or infectious disease. Prior to the advent of acute medicine, each consultant shared responsibility for admission of medical patients with consultants from other specialties, according to a call schedule. Generalist‐focused care would be initiated by postgraduate trainee physicians at the time of admission, and continued by the accepting consultant who often conducted subspecialty inpatient and outpatient work simultaneously. Due to advances in medical care at the turn of the century, inpatient care became more specialized; as a result, a general trend developed where the contribution of some specialties to generalist‐focused care grew (respiratory and medicine of the elderly), while other specialties began to focus on specialty‐specific interventions at the expense of practice and training in the generalist approach to care (cardiology, nephrology). Consequently, interservice disparity in provision of generalist‐focused care grew, especially in larger UK teaching hospitals. These trends have manifested as recent changes in UK medical training; presently, all UK medical specialty training programs require concomitant training in general internal medicine competencies, but for some specialties, general internal medicine training is truncated (either by the training program or by allowed choice of trainees) to provide less training than what is required for recognition as a specialist in general internal medicine.
In the UK, the majority of direct clinical care is provided via supervision of postgraduate trainee physicians. Over the last 20 years, limits on resident duty‐hours have been applied, much as has happened over the previous decade in the US.4 In 1991, the NHS and the British Medical Association negotiated a compensation package for physicians in training, termed the New Deal for Junior Doctors, which called for limitation of actual work hours for postgraduate trainee physicians to 56 hours per week. Enforcement of New Deal work guidelines was implemented over the next 12 years; with the introduction of the European Working Time Directive in 2000, work hours were further limited to 48 hours a week by 2009 for consultant and trainee physicians alike. Many UK consultants had already been devoting a higher percentage of time to subspecialty‐based hospital work and, with the reduced availability of the postgraduate trainee physician resource, the quality of generalist‐focused care (for conditions out with a consultant's given specialty) became more disparate between medical specialties, with some specialties providing little generalist input during the admission process. Simultaneously, and in the context of evolving demographic and regulatory pressures (Table 2), the admission procedure required an increasingly specific set of competencies. A subset of consultants from many different specialties began to focus specifically on management of the admission process and to informally self‐identify as specialists in acute medicine.
|
| Advances in medical care leading to increased specialization |
| Increasing numbers of elderly patients with complex medical needs |
| UK‐wide targets to limit emergency department patient stays to 4 hours |
| New limits to postgraduate trainee physician work hours |
| Increased standards of supervision of trainee physicians by consultants |
| Deficiencies in availability of outpatient out‐of‐hours care |
| Locally led reconfigurations of health care resources to favor community‐based care over inpatient‐based care |
Concerns were published about the quality of initial care for the acutely unwell patient in the UK.5 The UK Royal Colleges were concerned that patients with acute medical illnesses should receive high‐quality clinical care and commissioned a number of working groups to determine how acute medicine should best be delivered. Although initial reports suggested that acute care should be delivered by physicians who maintained an organ‐specific specialty focus, subsequent reports suggested that acute medicine should be delivered by specifically trained individuals capable of managing both the acutely ill medical patient and the administration of an acute medical unit (AMU).6, 7 In response to these trends, in 2003 the Royal Colleges of Physicians Joint Committee for Higher Medical Training, now known as the Joint Royal College of Physicians Training Board (JRCPTB), introduced a training curriculum for acute medicine as a subspecialty of general medicine.8 In 2007, the Royal College of Physicians convened an Acute Medicine Task Force that published further recommendations on the purpose and design of acute medicine services.9 Application by the JRCPTB to the regulatory bodies for medical education and training in the UK led to recognition in 2009 of acute internal medicine as a separate and distinct specialty from all other specialties, including general medicine.10
Acute Medicine in Practice: the Admission Process and Prevention of Prolonged Hospital Admission
The defining characteristic of an acute medical service in the UK is the sole dedication of a team of physician, nursing, and allied health care support staff (such as therapists, pharmacists, and social workers) to the task of admission and initial care of medical inpatients during their work shifts. Admission activity usually takes place in a dedicated physical area: the AMU. The AMU is commonly located near an accident and emergency (AE) department and is often colocated with radiology services, an intensive care unit, and/or a high‐dependency unit. Patients may be admitted to the AMU from the AE department, or directly from GP clinics. Generally, an AMU is responsible for a spectrum of medical conditions identical to the conditions potentially managed by a US‐based hospitalist. Unlike general and subspecialty medical wards, where consultant bedside input may be available as infrequently as 2 to 3 times per week, twice‐daily consultant bedside input into AMU patient care is the recommended standard. AMUs provide consultant bedside input via multiple rounds during the day, or alternatively in a continuous, per‐admission rolling pattern. Existing data suggest that AMUs with daily consultant input shorten hospital length of stay and increase same‐day discharges without affecting readmissions or mortality.11 Outside the US, observational studies associate AMUs with improved hospital mortality, shortened length of stay, decreased emergency department waiting times, and improved patient satisfaction.12
Three major models of acute medicine practice have evolved in the UK, as outlined in Table 3. The model adopted by each AMU varies depending on availability of staff, AMU bed capacity, the number and variability of patients requiring admission, and even hospital philosophy regarding division of responsibility between acute medicine physicians and those of other specialties. AMUs also vary in critical care capability, with many providing noninvasive ventilation or invasive hemodynamic monitoring. Admitted medical inpatients may bypass an AMU altogether if the AMU staff are unable to provide a procedure (eg, hemodialysis), if a patient requires no further diagnostic clarification or stabilization (eg, routine chemotherapy), or if an AMU admission would delay provision of time‐sensitive care (eg, percutaneous coronary intervention for ST‐elevation myocardial infarction). In all AMUs, patients requiring inpatient care outside of the AMU will be admitted to a medical specialty ward (cardiology, general internal medicine, neurology, etc). Generalist‐focused care is then provided by postgraduate trainee physicians on the medical specialty ward, based on guidance generated by AMU physicians, per guidance form their supervising specialty consultant physician (if possible), or through the advice given by other specialty services. Whether AMU physicians continue to be responsible for the care of AMU patients transferred to a general internal medicine ward depends on arrangements based on the particular AMU model and hospital staffing factors.
| Acute Medicine Models | Acute Medicine Team Focus |
|---|---|
| |
| Triage | Inpatient care rapidly transitioned to specialty medical ward with minimal stay in AMU |
| Short stay | Short‐term inpatient care (72 hours) provided in AMU, including extensive assessment (eg, physical therapy, sequential radiologic imaging), multispecialty bedside input, medical therapy, and either coordination of postdischarge follow‐up or transition of care to specialty medical ward |
| Hybrid | Subset of patients rapidly transitioned to specialty medical ward, while others receive care in AMU for up to 72 hours; mix dependent on patient needs and available hospital/AMU resources |
Weaknesses and Strengths of Acute Medicine Model Applicable to US‐Based Hospital Medicine
The acute medicine model of care does instantiate potential risks. Utilization of an acute medicine team hardwires fragmentation of care, necessitating handovers. In the context of US hospital medicine practice, this fragmentation may compromise safety or throughput; however, no such deficit has been detected to date in the context of acute medicine practice in the UK.13 Mismatch between AMU bed or staff capacity and the number or rate of hospital admissions can generate safety risks or give away efficiency gains. Further inefficiencies can develop if hospital‐wide processes of handover, medical decision making, patient transport, and discharge are not synchronized with AMU outflow and intake. Evidence of AMU throughput failure is most often manifest by the premature transfer of patients from AMU to the main hospital ward areas, or by delay of admissions from the emergency department into the AMU (UK standards until recently mandated that 98% of AE patients complete their AE stay in 4 hours). Although some successful UK AMUs have minimized these failures, such problems are still experienced by many acute medicine services throughout the UK. Ongoing debate, both local and national, persists within the acute medicine community about how best to address these challenges.
The strengths of the acute medicine model appear to be clinically meaningful, however. The admission process is complex and occurs at a time when patients are sickest and potentially the most vulnerable. Effective management of this period offers significant opportunity to improve value for patients, hospitals, and health systems. When applied in the context of US hospitalist programs, instances of successful short stay units and active bed management do exist.1417 These documented successes represent partial application of UK‐style acute medicine activity in a US hospital setting. A multidisciplinary health care team dedicated to streamlining admissions, short stays, and follow‐up care offers many potential benefits. Standardization and accountability of admission process, especially important for quality improvement and research activity applicable to the initial portion of a hospital stay, may be more readily realized if embedded into the practice of a discrete cohort of hospital staff. In the UK, several hospital processes fall within the exclusive remit of an acute medicine service (Table 4). Optimization of several of these processes of care can reduce hospital morbidity, mortality, and length of stay.1821 As health care financing reform arrives in the US, the ability of American hospitals to manage admission‐specific processes of care with reliability will become more vital.3 In the US, programs that force hospitalists to make ad hoc, moment‐to‐moment prioritizations about when and where to perform admissions, discharges, and daily ward care may do so at the expense of system predictability, standardization, and patient‐centeredness. Where hospitalists are forced to juggle these geographically and substantively disparate care duties, data suggest significant opportunities to reduce variability and improve efficiency.22, 23
| Initiation of time‐sensitive acute care bundles (eg, stroke, sepsis, myocardial infarction) |
| Initiation of disease‐specific protocols (eg, venous thromboembolism prophylaxis, glycemic control) |
| Outpatient‐inpatient information reconciliation (medicines, code status, etc) |
| Outpatient‐to‐inpatient consultation (general practitioner phone consultation, telemedicine) |
| Stewardship of empiric antimicrobial therapy |
| Early involvement of discharge planning apparatus |
| Provision of follow‐up ambulatory care (medical assessment unit discharge with next‐day hospital follow‐up) |
| Outpatient intravenous antibiotic services |
| Frequent patient admission policies |
Integrated into US hospital medicine practices, the UK acute medicine model might capture otherwise elusive quality and efficiency gains.14 By the same token, integrating portions of the US hospital medicine model into a UK acute medicine model could be beneficial as well. For instance, when compared with the interservice handover common in UK AMUs, intraservice handover (acute care hospitalist‐to‐ward hospitalist) may promote standardization of the handover process and potentially fewer instances of failed communication. What seems certain is that greater attention should be focused on an exchange of ideas between acute medicine and hospital medicine.
Acknowledgements
The authors thank Valery Akopov for review of the manuscript.
Conflicts of Interest: Drs. Smith and Jones are employed as acute medicine physicians by NHS Lothian, and both have received reimbursement for public speaking related to acute medicine. Dr. Jones has received reimbursement for curriculum design activity for the acute medicine specialty in the UK.
- Society of Hospital Medicine. Growth of Hospital Medicine Nationwide. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Media/GrowthofHospitalMedicineNationwide/Growth_of_Hospital_M.htm. Accessed May 15, 2011.
- . The hospitalist field turns 15: new opportunities and challenges. J Hosp Med. 2011;6:E1–E4.
- . Value‐driven healthcare: implications for hospitals and hospitalists. J Hosp Med. 2009;4:507–511.
- , , . ACGME Work Group on Resident Duty Hours. Accreditation Council for Graduate Medical Education. New requirements for resident duty hours. JAMA. 2002;288:1112–1114.
- , , , et al. Confidential inquiry into quality of care before admission to intensive care. BMJ. 1998;316:1853–1858.
- Federation of Medical Royal Colleges. Acute Medicine: The Physician's Role: Proposals for the Future. A Working Party Report of the Federation of Medical Royal Colleges. London, UK: Federation of Medical Royal Colleges; 2000.
- Federation of Medical Royal Colleges. Acute Medicine: Making it Work for Patients. A Blueprint for Organization and Training. Report of a Working Party. London, UK: Federation of Medical Royal Colleges; 2004.
- Joint Royal College of Physicians Training Board. Higher medical training curriculum for subspecialty training in acute medicine for general (internal) medicine NTN holders. July 2003.
- College of Physicians, London. Acute medical care: the right person, in the right setting—first time. Report of the Acute Medicine Task Force. October 2007.
- Joint Royal College of Physicians Training Board. Specialty training curriculum for acute internal medicine. August 2009.
- , , , . What is the effect of a consultant presence in an acute medical unit? Clin Med. 2009;9:214–218.
- , , . Effectiveness of acute medical units in hospitals: a systematic review. Int J Qual Health Care. 2009;21:397–407.
- , , , , . The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5:335–338.
- , , . Implementation of a hospitalist‐run observation unit and impact on length of stay (LOS): a brief report. J Hosp Med. 2010;5:E2–E5.
- , , , , , . Active bed management by hospitalists and emergency department throughput. Ann Intern Med. 2008;149:804–811.
- , , , . Hospitalist bed management effecting throughput from the emergency department to the intensive care unit. J Crit Care. 2001;25:184–189.
- , . MSSU: a multidisciplinary approach to finding cost effective and efficient care for observation patients. Quality and Safety Fall Forum, University HealthSystem Consortium Conference; 2009.
- , , , , . Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta‐analysis of randomized controlled trials. Arch Intern Med. 2007;167:1476–1486.
- , , , et al. Results of the Medications at Transitions and Clinical Handoffs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med. 2010;25:441–447.
- , , , . Antiplatelet therapy for acute ischaemic stroke. Cochrane Database Syst Rev. 2008;16:CD000029.
- , , , et al. Early goal‐directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377.
- , , , et al. Where did the day go?—A time motion study of hospitalists. J Hosp Med. 2010;5:323–328.
- , , , , . Hospitalist time usage and cyclicality: opportunities to improve efficiency. J Hosp Med. 2010;5:329–334.
- Society of Hospital Medicine. Growth of Hospital Medicine Nationwide. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Media/GrowthofHospitalMedicineNationwide/Growth_of_Hospital_M.htm. Accessed May 15, 2011.
- . The hospitalist field turns 15: new opportunities and challenges. J Hosp Med. 2011;6:E1–E4.
- . Value‐driven healthcare: implications for hospitals and hospitalists. J Hosp Med. 2009;4:507–511.
- , , . ACGME Work Group on Resident Duty Hours. Accreditation Council for Graduate Medical Education. New requirements for resident duty hours. JAMA. 2002;288:1112–1114.
- , , , et al. Confidential inquiry into quality of care before admission to intensive care. BMJ. 1998;316:1853–1858.
- Federation of Medical Royal Colleges. Acute Medicine: The Physician's Role: Proposals for the Future. A Working Party Report of the Federation of Medical Royal Colleges. London, UK: Federation of Medical Royal Colleges; 2000.
- Federation of Medical Royal Colleges. Acute Medicine: Making it Work for Patients. A Blueprint for Organization and Training. Report of a Working Party. London, UK: Federation of Medical Royal Colleges; 2004.
- Joint Royal College of Physicians Training Board. Higher medical training curriculum for subspecialty training in acute medicine for general (internal) medicine NTN holders. July 2003.
- College of Physicians, London. Acute medical care: the right person, in the right setting—first time. Report of the Acute Medicine Task Force. October 2007.
- Joint Royal College of Physicians Training Board. Specialty training curriculum for acute internal medicine. August 2009.
- , , , . What is the effect of a consultant presence in an acute medical unit? Clin Med. 2009;9:214–218.
- , , . Effectiveness of acute medical units in hospitals: a systematic review. Int J Qual Health Care. 2009;21:397–407.
- , , , , . The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5:335–338.
- , , . Implementation of a hospitalist‐run observation unit and impact on length of stay (LOS): a brief report. J Hosp Med. 2010;5:E2–E5.
- , , , , , . Active bed management by hospitalists and emergency department throughput. Ann Intern Med. 2008;149:804–811.
- , , , . Hospitalist bed management effecting throughput from the emergency department to the intensive care unit. J Crit Care. 2001;25:184–189.
- , . MSSU: a multidisciplinary approach to finding cost effective and efficient care for observation patients. Quality and Safety Fall Forum, University HealthSystem Consortium Conference; 2009.
- , , , , . Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta‐analysis of randomized controlled trials. Arch Intern Med. 2007;167:1476–1486.
- , , , et al. Results of the Medications at Transitions and Clinical Handoffs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med. 2010;25:441–447.
- , , , . Antiplatelet therapy for acute ischaemic stroke. Cochrane Database Syst Rev. 2008;16:CD000029.
- , , , et al. Early goal‐directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377.
- , , , et al. Where did the day go?—A time motion study of hospitalists. J Hosp Med. 2010;5:323–328.
- , , , , . Hospitalist time usage and cyclicality: opportunities to improve efficiency. J Hosp Med. 2010;5:329–334.
Sleep and Circadian Misalignment
For hospitalists, patient care is 24 hours a day. To provide continual patient care, shift work has become a way of life for hospitalists, similar to hospital nurses, residents in training, and emergency medicine physicians. Notably, they belong to a substantial minority of the workforce as shift workers, starting after 6 PM or before 6 AM, approximately one‐fifth of the total work force in industrialized nations.1, 2 Unfortunately, shift workers suffer from misalignment of their endogenous circadian system, which regulates daily sleep and alertness patterns, and work obligations beyond daylight hours. Such a misalignment can lead to fatigue, sleep loss, and excessive sleepiness, which can adversely affect personal health and safety, as well as the quality of medical care delivered.3
The relationship between shift work, extended work hours, and medical safety is a topic currently under intense scrutiny, as reviewed in the Institute of Medicine's (IOM) controversial report on residents and sleep.4 This publication led the Accreditation Council of Graduate Medical Education (ACGME) to mandate more changes to residents' work hours,5 adding to those first implemented in 2003.6 These restrictions forbid residents from working more than 30 consecutive hours, and required at least 10 hours off between shifts and an average of 1 day off in 7. Subsequent studies suggested that the reduction in resident work hours led to greater resident well‐being, fewer attention failures. and fewer medical errors.3, 7
In 2007, amid growing public concern over sleep‐deprived residents and patient safety, Congress requested the IOM investigate additional safeguards for residents.8 In 2008, the IOM published a report calling for more protection against resident fatigue.4 They recommended integrating a protected sleep period into any 24‐hour shift. If residents cannot get protected sleep time, then the maximal shift duration should not exceed 16 hoursreduced from the previous ACGME recommendation of 30. Further provisions to allow adequate sleep include capping the number of consecutive night shifts at 4, and extending the time off after a night shift. In response, the ACGME recently updated their recommendations effective July 1, 2011,5 though not following all the IOM's recommendations (Table 1).
| 2003 ACGME Limits | 2008 IOM Recommendation | 2010 ACGME Limits | |
|---|---|---|---|
| |||
| Maximum work hours per week | 80 hr, averaged over 4 wk | No change | No change |
| Maximum shift length | 30 hr (admitting patients up to 24 hr, with 6 hr of transition activities) | 30 hr (admitting patients up to 16 hr, with 5 hr protected sleep between 10 PM to 8 AM, and remaining hours for transition activities) | PGY‐1: 16 hr; PGY‐2 and above: 28 hr (admitting patients up to 24 hr, with 4 hr of transition activities) |
| Minimum time off between shifts | 10 hr after shift | 10 hr after day shift; 12 hr after night shift; 14 hr after any extended shift of 30 hr and not return until 6 AM the next day | 10 hr after shift; 14 hr free after 24‐hr shift for intermediate level residents |
| Maximum frequency of in‐hospital night shifts | No limits | 4 night maximum, with 48 hr off after 3 or 4 consecutive shifts | 6 consecutive night maximum |
The growing nationwide emphasis on fatigue prevention within healthcare settings now clearly impacts residents and their training schedule. But why focus only on residents? Why not other physicians, such as hospitalists, who work shifts to cover 24 hours each day? Are they any less prone to making medical errors when fatigued? Given that hospitalists' represent the fastest growing specialty in the history of American medicine,9 we sought to inform decisions about their scheduling by reviewing normal regulation of sleep and wake patterns, addressing the problems associated with misalignment between sleep and work, and identifying strategies to realign circadian schedules.
NORMAL SLEEP AND CIRCADIAN RHYTHMS
An understanding of sleep physiology begins with the endogenous circadian timekeeping system. At the center of this timekeeping system is a master circadian clock, located in the suprachiasmatic nucleus (SCN) of the hypothalamus. Cells within the SCN generate a near 24‐hour rhythm, transmitted through neural connections, to rhythmically influence the entire central nervous system and other bodily systems.10
The SCN and the circadian rhythm interact with the need to sleep (sleep homeostasis) to form the 2‐process model of sleepwakefulness.11 In this model, progression of biological day (a time when wakefulness and its associated functions are promoted) coincides with a rise in homeostatic pressure to sleep (see Figure 1). Daytime alertness is maintained by increasing SCN neuronal activity to counterbalance rising sleep pressure. After peaking in the early evening, SCN activity falls to begin biological night (a time when sleep and its associated functions are promoted). To facilitate the onset of biological night, the SCN coordinates the activity of sleep‐promoting centers and the release of melatonin from the pineal gland which promotes sleep.
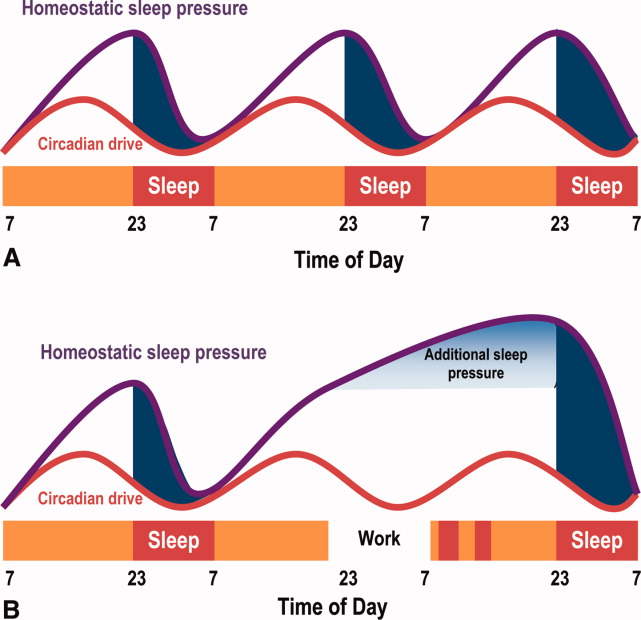
This endogenous circadian clock runs slightly longer than 24 hours and must be resynchronized daily to the 24‐hour day, a process known as entrainment. This occurs primarily through environmental exposure of retinalhypothalamic links to the lightdark cycle. The intensity, duration, and wave length of light all influence the circadian system,12 but perhaps most importantly is the timing. In general, light exposure in the evening will shift the circadian clock later (phase delay shift), whereas light exposure in the morning will shift the clock earlier (phase advance shift). Exogenous melatonin can also shift the circadian system. However, when endogenous levels of melatonin are high, ingested melatonin has little influence on sleep.13
Balancing sleep and wakefulness requires an interweaving of endogenous and exogenous factors. This balance is disturbed if we try to sleep or be wakeful during incorrect endogenous biological times, a process called circadian misalignment.
DELETERIOUS EFFECTS OF CIRCADIAN MISALIGNMENT
Hospitalists and other shift workers required to work during the biological night risk circadian misalignment and, consequently, poor sleep, shift work disorder, errors on the job, and possibly long‐term health consequences.
Chronic Sleep Loss
When working at night or in the early morning, nearly 75% of shift workers encounter some amount of at‐work fatigue and sleepiness.14 After the shift is over, objective assessments among rotating shift workers15, 16 and interns7 demonstrated that day sleep is 1 to 4 hours shorter than night sleep. Chronic or recurring night shifts can therefore lead to chronic sleep loss. While it seems reasonable that permanent night shift workers have greater circadian adjustment to suit their work schedule, little evidence supports this argument.17 Permanent night shift workers may sleep a little longer during the day than rotating shift workers. Yet, the sleep quality does not match night sleep, presumably from conflict between external factors, such as light and activity, and the scheduled sleep period.
Shift Work Disorder
If severe and chronic, sleepiness and impaired performance during work hours and poor sleep during the day can be enough to warrant a diagnosis of shift work disorder (SWD), one of the several circadian rhythm sleep disorders (CRSD). The prevalence of SWD among rotating and night workers is estimated to be 10%25%.18 Patients with SWD can experience similar levels of nighttime sleepiness as patients with narcolepsy and sleep apnea.19 These patients experience reduced satisfaction with the work schedule, and suffer higher rates of depression, ulcers, and sleepiness‐related accidents, compared to other shift workers.18 What distinguishes those shift workers who suffer from normal fatigue and those with SWD is not easily identified. The International Classification of Sleep Disorders‐2 (ICSD‐2) lists the diagnostic criteria for SWD20:
-
Symptoms of insomnia associated with a work schedule that overlaps the usual time for sleep.
-
Symptoms are directly associated with shift work schedule over the course of at least 1 month.
-
Sleep log monitoring for at least 7 days demonstrates circadian and sleep‐time misalignment.
-
Sleep disturbance is not better explained by another sleep disorder or by a medical, neurological, or mental disorder; medication use; or substance‐use disorder.
Symptoms must be present for at least 1 month, and comorbid mood or sleep/wake disorders (commonly found in this disorder) need to be treated. SWD is more common among night shift workers, although those workers starting shifts between 4 AM and 7 AM (early morning shift) are also subject to SWD.21 Type of work schedule, along with physical or mental disorders, domestic responsibilities, and commute times are examples of factors that may increase vulnerability for SWD.18 In addition, genetic factors may explain the considerable inter‐individual differences in susceptibility to SWD. For example, a polymorphism in the circadian gene, PER 3, present in 10%15% of the population, is believed to decrease tolerability to acute sleep loss,22 while genetic variation in the adenosine A2A receptor may be associated with resistance to the effects of sleep loss.23 If a hospitalist suspects a diagnosis SWD, they should seek evaluation by a physician specializing in sleep medicine.
Errors
Disruption of the circadian rhythm influences neurocognitive and psychomotor function, and can lead to human error. Human errors that result in serious accidents or injuries typically result from interaction of circadian rhythm misalignment with multiple other factors, including task duration and complexity, motivation and proficiency, and level of sleep deprivation.24 Though difficult to isolate from the environmental and work experience factors, consistent evidence identifies circadian misalignment as a cause of errors and serious accidents. Most evidence comes from night shift workers trying to remain awake when the circadian signal for alertness is low, or attempting sleep when the circadian alerting signal is high. Compared to day workers, night shift workers are 1.63 times more likely to suffer a fatal accident.25 A study of critical care nurses revealed a prominent circadian pattern of inadvertent sleep episodes during work with the highest peak between 2 AM and 6 AM.26 In addition, nurses working the night shift have been shown to commit more medication administration errors than day workers.27
Medical errors among resident physicians during extended shift durations is well documented.28 On the other hand, not much research has examined error rates among attending physicians. In 1 small study, attending surgeons made more cognitive errors using a simulated laparoscopic exercise as the amount of on‐call overnight sleep decreased.29 A large, single‐center review reported an increased rate of complications among post‐nighttime surgical procedures performed by attendings who slept 6 hours or less the preceding night.30 Notably, proposed legislation would require physicians who have been awake 22 of the preceding 24 hours to inform patients of the potential safety impact of their sleep deprivation prior to providing clinical care.31
Chronic Health Morbidity
Several studies reveal the effect of shift work on chronic health conditions among healthcare workers, such as obesity, cardiovascular disease, and certain cancers (eg, breast, colorectal). These results are summarized in Table 2, with the largest evaluation of healthcare shift workers coming from the Nurses' Health Study.3234
| Disease | Study Design | Population | Comparison | Health Risk | Adjusted Risk Factors |
|---|---|---|---|---|---|
| |||||
| Acute myocardial infarction | Prospective cohort32 | 79,109 US nurses | Working 3 night shifts/mo for 6 yr | RR 1.51 | CAD risk factors, aspirin use, hormone replacement therapy |
| 95% CI (1.12‐2.03) | |||||
| Obesity (BMI 30) | Cross‐sectional72 | 27,485 Swedish workers | Shift‐workers vs day workers | OR 1.41 | Age, socioeconomic status |
| 95% CI (1.25‐1.59) | |||||
| Breast cancer | Prospective cohort33 | 116,087 US nurses | Working 3 night shifts/mo for 20 yr | RR 1.79 | Breast cancer risk factors |
| 95% CI (1.06‐3.01) | |||||
| Colon cancer | Prospective cohort34 | 78,586 US nurses | Working 3 night shifts/mo for 15 yr | RR 1.35 | Family history of colon cancer, dietary intake, activity |
| 95% CI (1.03‐1.77) | |||||
Some believe that adverse health outcomes in shift workers derive from circadian stressan alteration of psychosocial and physiological homeostasis (eg, increased cortisol and catecholamine output) resulting from circadian misalignment.35 Based on data suggesting an increased risk for certain cancers among shift workers, the International Agency for Research of Cancer, a unit of the World Health Organization, announced that shift work resulting in circadian misalignment is probably carcinogenic.36 Researchers propose several biologic mechanisms to explain the increased cancer riskmost revolve around the alteration of the melatonin circadian cycle, found in night shift workers,37 and subsequent disruption of its believed cancer‐protective biologic pathways.
Overall, however, the heterogeneous nature of shift work limits conclusions regarding the long‐term health of shift workers. That is, as the shift work intensity and composition varies, and as the number and timing of these shifts change, so too can the adverse health consequences.
HOSPITALISTS AND NIGHT SHIFTS
Hospital medicine is the fastest growing specialty in the history of medicine, with an estimated 30,000 practicing hospitalists in 2010.38 Survey results from 2009 indicate that hospitalists staff 58% of hospitals; 89% of hospitals with more than 200 beds (J. Miller, Society of Hospital Medicine, personal communication). One reason for the growth in the number of hospitalists at academic medical centers has been the imposed work‐hour restrictions for residents.39
Across the county, hospitalist programs use a variety of shift work systems to ensure 24‐hour patient care. Among those programs that provide continuous on‐site coverage, many staff 3 shiftsday, late afternoon/evening (swing), and night shifts. Some permanently partition the scheduling, with dedicated night hospitalists or nocturnists.40
Hospitalists do not have mandated work‐hour restrictions and, in general, are older than resident physicians. Whether or not hospitalists who trained before the era of work‐hour regulations are better prepared for practicing in a real‐world, after‐hours scenario than hospitalists with previous work‐hour restrictions is a matter of debate. That said, hospitalists who are fatigued, just like residents, may be at increased risk for committing medical errors, particularly when the fatigue is unrecognized. Yet, limiting hospitalists' work hours would have obvious financial implications, likely similar those from resident work‐hour reductions.41 As part of the ACGME 2011 recommendations, faculty and residents now must be trained to recognize signs of fatigue and sleep deprivation, and adopt management strategies such as naps or backup call schedules. Fatigue that results in excessive sleepiness while at work may manifest as weariness, difficulty concentrating, headache, irritability or depressed mood, and feeling unrefreshed after sleeping.42
STRATEGIES TO IMPROVE CIRCADIAN ADAPTATION
Hospitalists can help limit fatigue and improve performance and safety through circadian adaptation: a multimodal approach to realign work and circadian schedules. Depending on whether the shift starts at night or in the early morning (4 AM to 7 AM), circadian adaptation aims may differ. For night shift workers, the overall aim is to delay the timing of circadian rhythms such that the highest propensity of wakefulness occurs during the night work period, while the highest propensity for sleep occurs during the day.17, 43 For early morning shift workers, circadian rhythms for wakefulness and sleep propensity should be shifted earlier. Circadian adaptation involves not only sleeping well before work, but also preventing dips in wakefulness during work. Adaptation strategies are listed in Table 3.
| Night Shift60 | Early Day Shift (Starting at 4 AM‐7 AM) | |
|---|---|---|
| Prior to shift | Avoid sleep debt | Avoid sleep debt |
| Proper sleep hygiene | Proper sleep hygiene | |
| Planned napping | Bright light exposure | |
| Caffeine use | ||
| During the shift | Bright light exposure | Caffeine use |
| Planned napping | ||
| After the shift | Avoid bright light | Avoid late evening bright light (when applicable) |
| Melatonin prior to sleep | ||
| Careful use of other hypnotics | Initiate sleep early |
Improved Sleep Before Work
As an essential first step, hospitalists must get a full night's rest before starting a night shift, as sleep debt will worsen fatigue while at work. Tips for proper sleep hygiene are listed in Table 4. Some shift workers stay up late the night before a scheduled night shift, in order to sleep during the day and awaken shortly before their scheduled night shift, to combat fatigue at work. Such an approach to shift work is typically met with 3 barriers. First, environmental factors often prevent 6 hours of uninterrupted day sleep. Second, 6 hours of continual day sleep is typically difficult because rising circadian activity often limits the sleep period to just a few hours. Third, an adequate amount of sleep prior to a night shift will itself not be enough to prevent sleepiness from occurring after midnightreducing the fall in circadian activity is also essential to maintaining alertness and performance.
| Physical | Adhere to regular wake and sleep schedule |
| activities73 | Engage in regular exercise early in the day |
| Avoid caffeine, nicotine, and alcohol use 6 hr prior to sleeping | |
| Avoid stimulating or stressful activities 30 min prior to sleeping | |
| Proper sleep | Well ventilated, temperature‐controlled bedroom |
| environment | Use heavy curtains to provide as much darkness as possible |
| Comfortable mattress and pillow | |
| Remove television and pets from the bedroom | |
| Housemates should help provide quiet sleep environment |
Napping
Napping prior to a night shift, or during the work shift, can improve alertness and performance and decrease accident rates.44, 45 During shift work, naps of 20 to 50 minutes in duration have demonstrated improvements in reaction time, and restoration of performance to that seen at the start of the shift. Napping early in the night shift can improve objective measures of alertness.44 To avoid increased drowsiness that sometimes occurs when waking from a nap, naps should not be longer than 50 minutes, and can be as short as 10 to 15 minutes.44, 46 Although effective, napping may be impractical for many workers due to time or space constraints. To facilitate brief naps, hospitalist practices should ensure they have a dark, quiet call room for use by overnight hospitalists.
Bright Light Exposure
Studies demonstrate that light exposure during the night shift improves circadian alignment, mood, and performance during the night shift.47, 48 Light exposure ranged from 6 hours to 5 light treatments of 15 minutes each, with brightness ranging from 2,500 to 10,000 lux (approximating outdoor daylight; typical office lighting provides 200‐500 lux).47, 49 Results demonstrate that bright light exposure during the night shift acutely improves alertness and performance, though not to daytime levels.50 The greatest circadian adjustments occur in groups using both bright light during the night shift and light avoidance the following morning.51 Dark sunglasses and a dark home environment can decrease bright light exposure during the day. Though little evidence exists to support widespread application of bright light devices in hospitalists' call‐rooms, a hospitalist practice should consider installing one to promote circadian adaptation if physicians working overnight have multiple consecutive shifts. Likewise, these physicians should be vigilant and wear dark sunglasses during the day after their night shifteven a few minutes of light exposure at the wrong time of the day may disrupt the intended circadian adaptation.
Wake‐Promoting Agents
Numerous studies demonstrate that 150 mg to 400 mg of caffeine (a 16 oz grande cup of coffee from Starbucks contains between 200 to 500 mg of caffeine52; a Diet Coke contains 46 mg/12 oz53) reduces sleepiness, increases alertness, and improves performance during the night shift.54, 55 Thus, judicious use of caffeine may be recommended in hospital practices during extended work hours. Other wake‐promoting agents, such as modafinil and armodafinil, are US Food and Drug Administration (FDA)‐approved in the treatment of excessive sleepiness associated with SWD. Typically taken 3060 minutes before the start of the night shift, these medications have been shown in trials, enrolling mostly permanent night shift workers, to reduce excessive nighttime sleepiness and improve performance.19, 56 Armodafinil used to treat SWD‐associated excessive sleepiness, has been safely tolerated for durations of 1 year or more.57 However, these agents are not approved for use in patients without a diagnosed sleep disorder.
Melatonin
Exogenous melatonin has been used to reset circadian rhythms in patients with CRSDs.58 Melatonin administered in the late afternoon to early evening directs the largest phase advance. In contrast, melatonin given in the morning produces the largest phase delays.59 When taken after a night shift, melatonin (at a dose 1.8 to 3.0 mg) can improve day sleep quality and duration.60 Despite this result, melatonin's effectiveness in improving circadian adaptation has been mixed.61 For example, improvements in nighttime alertness during the night shift were not seen, despite the use of melatonin to facilitate daytime sleep beforehand.62 Hospitalists may consider a trial of melatonin to improve circadian alignment and facilitate daytime sleep, but its chronic use and long‐term safety has not been adequately studied.
Hypnotics After Work
Hypnotics such as temazepam 20 mg,63 triazolam,64 and zolpidem65 taken after night shift work have been shown to improve day sleep quality under simulated conditions, but do not improve shift work performance. These medications should be reserved for judicious short‐term use in patients with insomnia associated with SWD.
NIGHT SHIFT SCHEDULING TO REDUCE CIRCADIAN MISALIGNMENT
When providing 24‐hour, on‐site medical care, questions may arise about how to incorporate circadian adaptation into the daily schedule.
How Should Shifts Be Rotated?
When scheduling shifts with different start times, evidence suggests that sleep disturbance is reduced with a clockwise progression in shifts (eg, day shift to evening shift to night shift). This reduction in sleep disturbance is thought due to increased time between shifts and the circadian timekeeping tendency to extend beyond 24 hours.66
When Should the Night Shift Start?
Those hospitalist programs using an evening swing shift from afternoon to late evening may have the option of using a 12‐hour night shift starting around 7 PM, or a shorter night shift beginning later at night. Though there are no data among hospitalists to suggest which night shift start time and duration would lead to the least amount of fatigue and errors, healthcare providers working a 12‐hour night shift may have increased morale due to fewer shifts, but may suffer a reduction in the quality of care provided compared with working an 8‐hour night shift.67 In either case, shift workers given flexibility in scheduling have been shown to have positive effects on sleep.68
Should Night Shifts Be Bunched?
The decision to bunch night shifts together depends on how many night shifts are required, and how quickly circadian adaptation can occur. Under simulated conditions, circadian adaptation can yield significant changes in sleep/wake cycles in as little as 4 days.48 In real‐world settings, more time may be required to achieve significant shifts in the circadian cycle. Therefore, hospitalists who have 7 or fewer night shifts during the academic year may want to space the shifts out to prevent sleep debt on consecutive shifts, since significant circadian adaptation would be difficult to achieve in less than a week. In this situation, after a night shift, the hospitalist should have at least one 9‐hour sleep period at night to relieve their sleep debt before staffing another night shift.69 Consecutive night shifts require at least 2 nighttime sleep periods of 9 hours to recover from sleep debt.70 The IOM recommends setting a limit of 4 consecutive night float shifts for resident physicians, however, a recent systematic review of resident night float models did not find data supporting use of a 4‐night‐maximum model.28
If more than 7 night shifts are required, then scheduling the shifts close together with use of circadian adaptation techniques may result in increased nighttime alertness, less fatigue, and fewer errors while at work than widely spacing out the shifts. For example, 1 recent study simulated 8 night shifts over a 10‐day period, and compared circadian schedules and work performance between those subjects who used circadian adaptation strategies and those that did not.71 Circadian adaptation techniques included: four 15‐minute bright light pulses during each night shift, dark sunglasses when outside, dark bedrooms and delayed sleeping until 3 AM on the nights off in between the night shift blocks. The group who shifted their circadian schedule improved night shift alertness and performance as measured by neurophysiological testing, while permitting sufficient daytime sleep after work, as well as late‐night sleep on days off. The group without circadian interventions did not shift their circadian schedule as significantly as the intervention group, and performed worse on the performance testing.
CONCLUSIONS
The nationwide use of hospitalists to provide 24‐hour patient care continues to expand, thus subjecting more hospitalists to work hours asynchronous with the lightdark cycle. Resultant circadian misalignment can result in fatigue while at work, shift work disorder, and, potentially, an increased rate of medical errors. Recognition of these dangers among resident physicians has prompted the ACGME to intensify their regulations on work hours, shift schedules, and time off between shifts. However, no such recommendations exist for hospitalists or emergency physicians and nurses.
Given the potential risk to both physicians and patients, we recommend more research examining the effects of circadian misalignment within the hospitalist community. Sample research questions are offered in Table 5. More information is urgently needed to provide evidence‐based practice guidelines to ensure the safety of this growing workforce and the patients they treat.
| Are hospitalists more immune to fatigue than resident physicians? |
| Are hospitalists better able to recognize fatigue while at work than resident physicians? |
| Does 1 shift work schedule promote better circadian alignment than other shift schedules? |
| Do consistent nighttime hours of nocturnists make them more prone to commit medical errors than hospitalists rotating their shifts? |
- .Job, family, and gender: determinants of nonstandard work schedules among employed Americans in 1991.Demography.1995;32:577–598.
- ,.Shift work among dual‐earner couples with children.Science.1983;219:876–879.
- ,,, et al.Effect of reducing interns' work hours on serious medical errors in intensive care units.N Engl J Med.2004;351:1838–1848.
- Institute of Medicine. Resident Duty Hours: Enhancing Sleep, Supervision and Safety. Released December 15,2008. Available at: http://www.iom.edu/Reports/2008/Resident‐Duty‐Hours‐Enhancing‐Sleep‐Supervision‐and‐Safety.aspx. Accessed on October 20, 2010.
- ACGME. ACGME Approved Standards. Effective July2011. Available at: http://acgme‐2010standards.org/. Accessed on January 6, 2011
- ACGME. Common Program Requirements: Resident Duty Hours in the Learning and Work Environment. Effective July 1, 2007. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_ComProgrRequirmentsDutyHours0707.pdf. Accessed October 20,2010.
- ,,, et al.Effect of reducing interns' weekly work hours on sleep and attentional failures.N Engl J Med.2004;351:1829–1837.
- Letter written to William Munier, Agency for Healthcare Research and Quality.Washington, DC:US House of Representatives, Committee on Energy and Commerce, March 29,2007. Available at: http://energycommerce.house.gov/Press_110/110‐ltr.032907.HHS.Munier.pdf. Accessed on October 24, 2010.
- ,.The evolution and future of hospital medicine.Mt Sinai J Med.2008;75:418–423.
- .Brain structures and receptors involved in alertness.Sleep Med.2005;6(suppl 1):S3–S7.
- .A two process model of sleep regulation.Hum Neurobiol.1982;1:195–204.
- ,.Entrainment of the human circadian system by light.J Biol Rhythms.2005;20:326–338.
- ,.Sleep‐promoting and hypothermic effects of daytime melatonin administration in humans.Sleep.1997;20:124–131.
- .Sleepiness as a consequence of shift work.Sleep.1988;11:17–34.
- ,,,,.The sleep of long‐haul truck drivers.N Engl J Med.1997;337:755–761.
- ,,,.Sleep on the night shift: 24‐hour EEG monitoring of spontaneous sleep/wake behavior.Psychophysiology.1989;26:352–358.
- .Do permanent night workers show circadian adjustment? A review based on the endogenous melatonin rhythm.Chronobiol Int.2008;25:215–224.
- ,,,,.Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers.Sleep.2004;27:1453–1462.
- ,,, et al.Modafinil for excessive sleepiness associated with shift‐work sleep disorder.N Engl J Med.2005;353:476–486.
- American Academy of Sleep Medicine.The International Classification of Sleep Disorders (ICSD).2nd ed.Chicago, IL:American Academy of Sleep Medicine;2005.
- ,.Circadian rhythm sleep disorders.Chest.2006;130:1915–1923.
- ,,,,,.Early morning executive functioning during sleep deprivation is compromised by a PERIOD3 polymorphism.Sleep.2008;31:1159–1167.
- ,,,,,.Genetic variation in the adenosine A2A receptor gene modulates performance on the psychomotor vigilance task.Sleep Biol Rhythms.2007;5:A47.
- ,.Circadian rhythms in cognitive performance: methodological constraints, protocols, theoretical underpinnings.Physiol Behav.2007;90:196–208.
- ,,,.A prospective study of fatal occupational accidents—relationship to sleeping difficulties and occupational factors.J Sleep Res.2002;11:69–71.
- ,,,.Effects of critical care nurses' work hours on vigilance and patients' safety.Am J Crit Care.2006;15:30–37.
- ,,,,.Daytime sleepiness, sleep habits and occupational accidents among hospital nurses.J Adv Nurs.2005;52:445–453.
- ,,.Systematic review: association of shift length, protected sleep time, and night float with patient care, residents' health, and education.Ann Intern Med.2010;153:829–842.
- ,,,,.Jack Barney Award: the effect of fatigue on cognitive and psychomotor skills of trauma residents and attending surgeons.Am J Surg.2008;196:813–819; discussion 9–20.
- ,,, et al.Risks of complications by attending physicians after performing nighttime procedures.JAMA.2009;302:1565–1572.
- ,,.Sleep deprivation, elective surgical procedures, and informed consent.N Engl J Med.2010;363:2577–2579.
- ,,,,.A prospective study of anger and coronary heart disease. The Normative Aging Study.Circulation.1996;94:2090–2095.
- ,,,.Night work and risk of breast cancer.Epidemiology.2006;17:108–111.
- ,,, et al.Night‐shift work and risk of colorectal cancer in the nurses' health study.J Natl Cancer Inst.2003;95:825–828.
- ,,.Shift work and cardiovascular disease—pathways from circadian stress to morbidity.Scand J Work Environ Health.2010;36:96–108.
- IARC. IARC monographs on the evalutaion of carcinogenic risks to humans. Vol 98. Painting, firefighting, and shiftwork. 2007. Available at: monographs.iarc.fr/ENG/Monographs/vol98/mono98.pdf. Accessed January 16,2011.
- ,,,.Influence of melatonin on invasive and metastatic properties of MCF‐7 human breast cancer cells.Cancer Res.1998;58:4383–4390.
- Society of Hospital Medicine. Society of Hospital Medicine releases results of the 2007–2008 survey on the state of the hospital medicine movement. 2008. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Press_Releases3:247–255.
- ,,.Hospitalists: A Guide to Building and Sustaining a Successful Program.Chicago, IL:Health Administration Press;2008.
- ,,,,.The increased financial burden of further proposed orthopaedic resident work‐hour reductions.J Bone Joint Surg Am.2011;93:e31.
- ,,,,,.Fatigue and shift work.J Sleep Res.2006;15:1–5.
- ,,, et al.Rapid shift in peak melatonin secretion associated with improved performance in short shift work schedule.Sleep.1997;20:1145–1150.
- ,,.The impact of a nap opportunity during the night shift on the performance and alertness of 12‐h shift workers.J Sleep Res.2002;11:219–227.
- ,,, et al.Improving alertness and performance in emergency department physicians and nurses: the use of planned naps.Ann Emerg Med.2006;48:596–604, e1‐e3.
- ,,,,.Promoting alertness with a short nap during a night shift.J Sleep Res.1998;7:240–247.
- ,.Circadian adaptation to night‐shift work by judicious light and darkness exposure.J Biol Rhythms.2002;17:556–567.
- ,,,,,.Exposure to bright light and darkness to treat physiologic maladaptation to night work.N Engl J Med.1990;322:1253–1259.
- ,.Night shift performance is improved by a compromise circadian phase position: study 3. Circadian phase after 7 night shifts with an intervening weekend off.Sleep.2008;31:1639–1645.
- ,,,.Dose‐response relationship for light intensity and ocular and electroencephalographic correlates of human alertness.Behav Brain Res.2000;115:75–83.
- ,,,,.Dark goggles and bright light improve circadian rhythm adaptation to night‐shift work.Sleep.1994;17:535–543.
- ,,.Caffeine content of specialty coffees.J Anal Toxicol.2003;27:520–522.
- ,.Caffeine content of prepackaged national‐brand and private‐label carbonated beverages.J Food Sci.2007;72:C337–C342.
- ,,, et al.The effects of coffee and napping on nighttime highway driving: a randomized trial.Ann Intern Med.2006;144:785–791.
- ,,,,.Laboratory and field studies of naps and caffeine as practical countermeasures for sleep‐wake problems associated with night work.Sleep.2006;29:39–50.
- ,,,,.Armodafinil for treatment of excessive sleepiness associated with shift work disorder: a randomized controlled study.Mayo Clin Proc.2009;84:958–972.
- ,,,,.The long‐term tolerability and efficacy of armodafinil in patients with excessive sleepiness associated with treated obstructive sleep apnea, shift work disorder, or narcolepsy: an open‐label extension study.J Clin Sleep Med.2010;6:458–466.
- ,,.Circadian rhythm sleep disorders.Med Clin North Am.2004;88:631–651, viii.
- ,,.A three pulse phase response curve to three milligrams of melatonin in humans.J Physiol.2008;586:639–647.
- ,,, et al.Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report.Sleep.2007;30:1445–1459.
- ,,, et al.Efficacy and safety of exogenous melatonin for secondary sleep disorders and sleep disorders accompanying sleep restriction: meta‐analysis.BMJ.2006;332:385–393.
- ,,.Effects of melatonin administration on daytime sleep after simulated night shift work.J Sleep Res.2001;10:181–192.
- ,,,.Performance, ability to stay awake, and tendency to fall asleep during the night after a diurnal sleep with temazepam or placebo.Sleep.1997;20:535–541.
- ,,,,,.Sleepiness/alertness on a simulated night shift following sleep at home with triazolam.Sleep.1991;14:140–146.
- ,,,.Zolpidem‐related effects on performance and mood during simulated night‐shift work.Exp Clin Psychopharmacol.2003;11:259–268.
- ,,,,.Intrinsic near‐24‐h pacemaker period determines limits of circadian entrainment to a weak synchronizer in humans.Proc Natl Acad Sci USA.2001;98:14027–14032.
- ,,,.Work shift duration: a review comparing eight hour and 12 hour shift systems.Occup Environ Med.1998;55:217–229.
- ,,.Influence of flexibility and variability of working hours on health and well‐being.Chronobiol Int.2006;23:1125–1137.
- ,,.Impact of night‐float rotation on sleep, mood, and alertness: the resident's perception.Chronobiol Int.2002;19:893–902.
- ,,,,,.The characteristics of recovery sleep when recovery opportunity is restricted.Sleep.2007;30:353–360.
- ,,.Practical interventions to promote circadian adaptation to permanent night shift work: study 4.J Biol Rhythms.2009;24:161–172.
- ,,.Is there an association between shift work and having a metabolic syndrome? Results from a population based study of 27,485 people.Occup Environ Med.2001;58:747–752.
- ,.Use of sleep hygiene in the treatment of insomnia.Sleep Med Rev.2003;7:215–225.
For hospitalists, patient care is 24 hours a day. To provide continual patient care, shift work has become a way of life for hospitalists, similar to hospital nurses, residents in training, and emergency medicine physicians. Notably, they belong to a substantial minority of the workforce as shift workers, starting after 6 PM or before 6 AM, approximately one‐fifth of the total work force in industrialized nations.1, 2 Unfortunately, shift workers suffer from misalignment of their endogenous circadian system, which regulates daily sleep and alertness patterns, and work obligations beyond daylight hours. Such a misalignment can lead to fatigue, sleep loss, and excessive sleepiness, which can adversely affect personal health and safety, as well as the quality of medical care delivered.3
The relationship between shift work, extended work hours, and medical safety is a topic currently under intense scrutiny, as reviewed in the Institute of Medicine's (IOM) controversial report on residents and sleep.4 This publication led the Accreditation Council of Graduate Medical Education (ACGME) to mandate more changes to residents' work hours,5 adding to those first implemented in 2003.6 These restrictions forbid residents from working more than 30 consecutive hours, and required at least 10 hours off between shifts and an average of 1 day off in 7. Subsequent studies suggested that the reduction in resident work hours led to greater resident well‐being, fewer attention failures. and fewer medical errors.3, 7
In 2007, amid growing public concern over sleep‐deprived residents and patient safety, Congress requested the IOM investigate additional safeguards for residents.8 In 2008, the IOM published a report calling for more protection against resident fatigue.4 They recommended integrating a protected sleep period into any 24‐hour shift. If residents cannot get protected sleep time, then the maximal shift duration should not exceed 16 hoursreduced from the previous ACGME recommendation of 30. Further provisions to allow adequate sleep include capping the number of consecutive night shifts at 4, and extending the time off after a night shift. In response, the ACGME recently updated their recommendations effective July 1, 2011,5 though not following all the IOM's recommendations (Table 1).
| 2003 ACGME Limits | 2008 IOM Recommendation | 2010 ACGME Limits | |
|---|---|---|---|
| |||
| Maximum work hours per week | 80 hr, averaged over 4 wk | No change | No change |
| Maximum shift length | 30 hr (admitting patients up to 24 hr, with 6 hr of transition activities) | 30 hr (admitting patients up to 16 hr, with 5 hr protected sleep between 10 PM to 8 AM, and remaining hours for transition activities) | PGY‐1: 16 hr; PGY‐2 and above: 28 hr (admitting patients up to 24 hr, with 4 hr of transition activities) |
| Minimum time off between shifts | 10 hr after shift | 10 hr after day shift; 12 hr after night shift; 14 hr after any extended shift of 30 hr and not return until 6 AM the next day | 10 hr after shift; 14 hr free after 24‐hr shift for intermediate level residents |
| Maximum frequency of in‐hospital night shifts | No limits | 4 night maximum, with 48 hr off after 3 or 4 consecutive shifts | 6 consecutive night maximum |
The growing nationwide emphasis on fatigue prevention within healthcare settings now clearly impacts residents and their training schedule. But why focus only on residents? Why not other physicians, such as hospitalists, who work shifts to cover 24 hours each day? Are they any less prone to making medical errors when fatigued? Given that hospitalists' represent the fastest growing specialty in the history of American medicine,9 we sought to inform decisions about their scheduling by reviewing normal regulation of sleep and wake patterns, addressing the problems associated with misalignment between sleep and work, and identifying strategies to realign circadian schedules.
NORMAL SLEEP AND CIRCADIAN RHYTHMS
An understanding of sleep physiology begins with the endogenous circadian timekeeping system. At the center of this timekeeping system is a master circadian clock, located in the suprachiasmatic nucleus (SCN) of the hypothalamus. Cells within the SCN generate a near 24‐hour rhythm, transmitted through neural connections, to rhythmically influence the entire central nervous system and other bodily systems.10
The SCN and the circadian rhythm interact with the need to sleep (sleep homeostasis) to form the 2‐process model of sleepwakefulness.11 In this model, progression of biological day (a time when wakefulness and its associated functions are promoted) coincides with a rise in homeostatic pressure to sleep (see Figure 1). Daytime alertness is maintained by increasing SCN neuronal activity to counterbalance rising sleep pressure. After peaking in the early evening, SCN activity falls to begin biological night (a time when sleep and its associated functions are promoted). To facilitate the onset of biological night, the SCN coordinates the activity of sleep‐promoting centers and the release of melatonin from the pineal gland which promotes sleep.
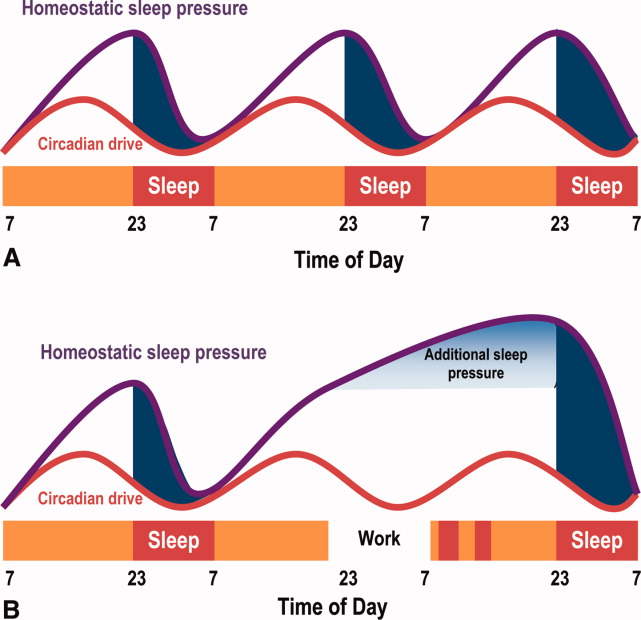
This endogenous circadian clock runs slightly longer than 24 hours and must be resynchronized daily to the 24‐hour day, a process known as entrainment. This occurs primarily through environmental exposure of retinalhypothalamic links to the lightdark cycle. The intensity, duration, and wave length of light all influence the circadian system,12 but perhaps most importantly is the timing. In general, light exposure in the evening will shift the circadian clock later (phase delay shift), whereas light exposure in the morning will shift the clock earlier (phase advance shift). Exogenous melatonin can also shift the circadian system. However, when endogenous levels of melatonin are high, ingested melatonin has little influence on sleep.13
Balancing sleep and wakefulness requires an interweaving of endogenous and exogenous factors. This balance is disturbed if we try to sleep or be wakeful during incorrect endogenous biological times, a process called circadian misalignment.
DELETERIOUS EFFECTS OF CIRCADIAN MISALIGNMENT
Hospitalists and other shift workers required to work during the biological night risk circadian misalignment and, consequently, poor sleep, shift work disorder, errors on the job, and possibly long‐term health consequences.
Chronic Sleep Loss
When working at night or in the early morning, nearly 75% of shift workers encounter some amount of at‐work fatigue and sleepiness.14 After the shift is over, objective assessments among rotating shift workers15, 16 and interns7 demonstrated that day sleep is 1 to 4 hours shorter than night sleep. Chronic or recurring night shifts can therefore lead to chronic sleep loss. While it seems reasonable that permanent night shift workers have greater circadian adjustment to suit their work schedule, little evidence supports this argument.17 Permanent night shift workers may sleep a little longer during the day than rotating shift workers. Yet, the sleep quality does not match night sleep, presumably from conflict between external factors, such as light and activity, and the scheduled sleep period.
Shift Work Disorder
If severe and chronic, sleepiness and impaired performance during work hours and poor sleep during the day can be enough to warrant a diagnosis of shift work disorder (SWD), one of the several circadian rhythm sleep disorders (CRSD). The prevalence of SWD among rotating and night workers is estimated to be 10%25%.18 Patients with SWD can experience similar levels of nighttime sleepiness as patients with narcolepsy and sleep apnea.19 These patients experience reduced satisfaction with the work schedule, and suffer higher rates of depression, ulcers, and sleepiness‐related accidents, compared to other shift workers.18 What distinguishes those shift workers who suffer from normal fatigue and those with SWD is not easily identified. The International Classification of Sleep Disorders‐2 (ICSD‐2) lists the diagnostic criteria for SWD20:
-
Symptoms of insomnia associated with a work schedule that overlaps the usual time for sleep.
-
Symptoms are directly associated with shift work schedule over the course of at least 1 month.
-
Sleep log monitoring for at least 7 days demonstrates circadian and sleep‐time misalignment.
-
Sleep disturbance is not better explained by another sleep disorder or by a medical, neurological, or mental disorder; medication use; or substance‐use disorder.
Symptoms must be present for at least 1 month, and comorbid mood or sleep/wake disorders (commonly found in this disorder) need to be treated. SWD is more common among night shift workers, although those workers starting shifts between 4 AM and 7 AM (early morning shift) are also subject to SWD.21 Type of work schedule, along with physical or mental disorders, domestic responsibilities, and commute times are examples of factors that may increase vulnerability for SWD.18 In addition, genetic factors may explain the considerable inter‐individual differences in susceptibility to SWD. For example, a polymorphism in the circadian gene, PER 3, present in 10%15% of the population, is believed to decrease tolerability to acute sleep loss,22 while genetic variation in the adenosine A2A receptor may be associated with resistance to the effects of sleep loss.23 If a hospitalist suspects a diagnosis SWD, they should seek evaluation by a physician specializing in sleep medicine.
Errors
Disruption of the circadian rhythm influences neurocognitive and psychomotor function, and can lead to human error. Human errors that result in serious accidents or injuries typically result from interaction of circadian rhythm misalignment with multiple other factors, including task duration and complexity, motivation and proficiency, and level of sleep deprivation.24 Though difficult to isolate from the environmental and work experience factors, consistent evidence identifies circadian misalignment as a cause of errors and serious accidents. Most evidence comes from night shift workers trying to remain awake when the circadian signal for alertness is low, or attempting sleep when the circadian alerting signal is high. Compared to day workers, night shift workers are 1.63 times more likely to suffer a fatal accident.25 A study of critical care nurses revealed a prominent circadian pattern of inadvertent sleep episodes during work with the highest peak between 2 AM and 6 AM.26 In addition, nurses working the night shift have been shown to commit more medication administration errors than day workers.27
Medical errors among resident physicians during extended shift durations is well documented.28 On the other hand, not much research has examined error rates among attending physicians. In 1 small study, attending surgeons made more cognitive errors using a simulated laparoscopic exercise as the amount of on‐call overnight sleep decreased.29 A large, single‐center review reported an increased rate of complications among post‐nighttime surgical procedures performed by attendings who slept 6 hours or less the preceding night.30 Notably, proposed legislation would require physicians who have been awake 22 of the preceding 24 hours to inform patients of the potential safety impact of their sleep deprivation prior to providing clinical care.31
Chronic Health Morbidity
Several studies reveal the effect of shift work on chronic health conditions among healthcare workers, such as obesity, cardiovascular disease, and certain cancers (eg, breast, colorectal). These results are summarized in Table 2, with the largest evaluation of healthcare shift workers coming from the Nurses' Health Study.3234
| Disease | Study Design | Population | Comparison | Health Risk | Adjusted Risk Factors |
|---|---|---|---|---|---|
| |||||
| Acute myocardial infarction | Prospective cohort32 | 79,109 US nurses | Working 3 night shifts/mo for 6 yr | RR 1.51 | CAD risk factors, aspirin use, hormone replacement therapy |
| 95% CI (1.12‐2.03) | |||||
| Obesity (BMI 30) | Cross‐sectional72 | 27,485 Swedish workers | Shift‐workers vs day workers | OR 1.41 | Age, socioeconomic status |
| 95% CI (1.25‐1.59) | |||||
| Breast cancer | Prospective cohort33 | 116,087 US nurses | Working 3 night shifts/mo for 20 yr | RR 1.79 | Breast cancer risk factors |
| 95% CI (1.06‐3.01) | |||||
| Colon cancer | Prospective cohort34 | 78,586 US nurses | Working 3 night shifts/mo for 15 yr | RR 1.35 | Family history of colon cancer, dietary intake, activity |
| 95% CI (1.03‐1.77) | |||||
Some believe that adverse health outcomes in shift workers derive from circadian stressan alteration of psychosocial and physiological homeostasis (eg, increased cortisol and catecholamine output) resulting from circadian misalignment.35 Based on data suggesting an increased risk for certain cancers among shift workers, the International Agency for Research of Cancer, a unit of the World Health Organization, announced that shift work resulting in circadian misalignment is probably carcinogenic.36 Researchers propose several biologic mechanisms to explain the increased cancer riskmost revolve around the alteration of the melatonin circadian cycle, found in night shift workers,37 and subsequent disruption of its believed cancer‐protective biologic pathways.
Overall, however, the heterogeneous nature of shift work limits conclusions regarding the long‐term health of shift workers. That is, as the shift work intensity and composition varies, and as the number and timing of these shifts change, so too can the adverse health consequences.
HOSPITALISTS AND NIGHT SHIFTS
Hospital medicine is the fastest growing specialty in the history of medicine, with an estimated 30,000 practicing hospitalists in 2010.38 Survey results from 2009 indicate that hospitalists staff 58% of hospitals; 89% of hospitals with more than 200 beds (J. Miller, Society of Hospital Medicine, personal communication). One reason for the growth in the number of hospitalists at academic medical centers has been the imposed work‐hour restrictions for residents.39
Across the county, hospitalist programs use a variety of shift work systems to ensure 24‐hour patient care. Among those programs that provide continuous on‐site coverage, many staff 3 shiftsday, late afternoon/evening (swing), and night shifts. Some permanently partition the scheduling, with dedicated night hospitalists or nocturnists.40
Hospitalists do not have mandated work‐hour restrictions and, in general, are older than resident physicians. Whether or not hospitalists who trained before the era of work‐hour regulations are better prepared for practicing in a real‐world, after‐hours scenario than hospitalists with previous work‐hour restrictions is a matter of debate. That said, hospitalists who are fatigued, just like residents, may be at increased risk for committing medical errors, particularly when the fatigue is unrecognized. Yet, limiting hospitalists' work hours would have obvious financial implications, likely similar those from resident work‐hour reductions.41 As part of the ACGME 2011 recommendations, faculty and residents now must be trained to recognize signs of fatigue and sleep deprivation, and adopt management strategies such as naps or backup call schedules. Fatigue that results in excessive sleepiness while at work may manifest as weariness, difficulty concentrating, headache, irritability or depressed mood, and feeling unrefreshed after sleeping.42
STRATEGIES TO IMPROVE CIRCADIAN ADAPTATION
Hospitalists can help limit fatigue and improve performance and safety through circadian adaptation: a multimodal approach to realign work and circadian schedules. Depending on whether the shift starts at night or in the early morning (4 AM to 7 AM), circadian adaptation aims may differ. For night shift workers, the overall aim is to delay the timing of circadian rhythms such that the highest propensity of wakefulness occurs during the night work period, while the highest propensity for sleep occurs during the day.17, 43 For early morning shift workers, circadian rhythms for wakefulness and sleep propensity should be shifted earlier. Circadian adaptation involves not only sleeping well before work, but also preventing dips in wakefulness during work. Adaptation strategies are listed in Table 3.
| Night Shift60 | Early Day Shift (Starting at 4 AM‐7 AM) | |
|---|---|---|
| Prior to shift | Avoid sleep debt | Avoid sleep debt |
| Proper sleep hygiene | Proper sleep hygiene | |
| Planned napping | Bright light exposure | |
| Caffeine use | ||
| During the shift | Bright light exposure | Caffeine use |
| Planned napping | ||
| After the shift | Avoid bright light | Avoid late evening bright light (when applicable) |
| Melatonin prior to sleep | ||
| Careful use of other hypnotics | Initiate sleep early |
Improved Sleep Before Work
As an essential first step, hospitalists must get a full night's rest before starting a night shift, as sleep debt will worsen fatigue while at work. Tips for proper sleep hygiene are listed in Table 4. Some shift workers stay up late the night before a scheduled night shift, in order to sleep during the day and awaken shortly before their scheduled night shift, to combat fatigue at work. Such an approach to shift work is typically met with 3 barriers. First, environmental factors often prevent 6 hours of uninterrupted day sleep. Second, 6 hours of continual day sleep is typically difficult because rising circadian activity often limits the sleep period to just a few hours. Third, an adequate amount of sleep prior to a night shift will itself not be enough to prevent sleepiness from occurring after midnightreducing the fall in circadian activity is also essential to maintaining alertness and performance.
| Physical | Adhere to regular wake and sleep schedule |
| activities73 | Engage in regular exercise early in the day |
| Avoid caffeine, nicotine, and alcohol use 6 hr prior to sleeping | |
| Avoid stimulating or stressful activities 30 min prior to sleeping | |
| Proper sleep | Well ventilated, temperature‐controlled bedroom |
| environment | Use heavy curtains to provide as much darkness as possible |
| Comfortable mattress and pillow | |
| Remove television and pets from the bedroom | |
| Housemates should help provide quiet sleep environment |
Napping
Napping prior to a night shift, or during the work shift, can improve alertness and performance and decrease accident rates.44, 45 During shift work, naps of 20 to 50 minutes in duration have demonstrated improvements in reaction time, and restoration of performance to that seen at the start of the shift. Napping early in the night shift can improve objective measures of alertness.44 To avoid increased drowsiness that sometimes occurs when waking from a nap, naps should not be longer than 50 minutes, and can be as short as 10 to 15 minutes.44, 46 Although effective, napping may be impractical for many workers due to time or space constraints. To facilitate brief naps, hospitalist practices should ensure they have a dark, quiet call room for use by overnight hospitalists.
Bright Light Exposure
Studies demonstrate that light exposure during the night shift improves circadian alignment, mood, and performance during the night shift.47, 48 Light exposure ranged from 6 hours to 5 light treatments of 15 minutes each, with brightness ranging from 2,500 to 10,000 lux (approximating outdoor daylight; typical office lighting provides 200‐500 lux).47, 49 Results demonstrate that bright light exposure during the night shift acutely improves alertness and performance, though not to daytime levels.50 The greatest circadian adjustments occur in groups using both bright light during the night shift and light avoidance the following morning.51 Dark sunglasses and a dark home environment can decrease bright light exposure during the day. Though little evidence exists to support widespread application of bright light devices in hospitalists' call‐rooms, a hospitalist practice should consider installing one to promote circadian adaptation if physicians working overnight have multiple consecutive shifts. Likewise, these physicians should be vigilant and wear dark sunglasses during the day after their night shifteven a few minutes of light exposure at the wrong time of the day may disrupt the intended circadian adaptation.
Wake‐Promoting Agents
Numerous studies demonstrate that 150 mg to 400 mg of caffeine (a 16 oz grande cup of coffee from Starbucks contains between 200 to 500 mg of caffeine52; a Diet Coke contains 46 mg/12 oz53) reduces sleepiness, increases alertness, and improves performance during the night shift.54, 55 Thus, judicious use of caffeine may be recommended in hospital practices during extended work hours. Other wake‐promoting agents, such as modafinil and armodafinil, are US Food and Drug Administration (FDA)‐approved in the treatment of excessive sleepiness associated with SWD. Typically taken 3060 minutes before the start of the night shift, these medications have been shown in trials, enrolling mostly permanent night shift workers, to reduce excessive nighttime sleepiness and improve performance.19, 56 Armodafinil used to treat SWD‐associated excessive sleepiness, has been safely tolerated for durations of 1 year or more.57 However, these agents are not approved for use in patients without a diagnosed sleep disorder.
Melatonin
Exogenous melatonin has been used to reset circadian rhythms in patients with CRSDs.58 Melatonin administered in the late afternoon to early evening directs the largest phase advance. In contrast, melatonin given in the morning produces the largest phase delays.59 When taken after a night shift, melatonin (at a dose 1.8 to 3.0 mg) can improve day sleep quality and duration.60 Despite this result, melatonin's effectiveness in improving circadian adaptation has been mixed.61 For example, improvements in nighttime alertness during the night shift were not seen, despite the use of melatonin to facilitate daytime sleep beforehand.62 Hospitalists may consider a trial of melatonin to improve circadian alignment and facilitate daytime sleep, but its chronic use and long‐term safety has not been adequately studied.
Hypnotics After Work
Hypnotics such as temazepam 20 mg,63 triazolam,64 and zolpidem65 taken after night shift work have been shown to improve day sleep quality under simulated conditions, but do not improve shift work performance. These medications should be reserved for judicious short‐term use in patients with insomnia associated with SWD.
NIGHT SHIFT SCHEDULING TO REDUCE CIRCADIAN MISALIGNMENT
When providing 24‐hour, on‐site medical care, questions may arise about how to incorporate circadian adaptation into the daily schedule.
How Should Shifts Be Rotated?
When scheduling shifts with different start times, evidence suggests that sleep disturbance is reduced with a clockwise progression in shifts (eg, day shift to evening shift to night shift). This reduction in sleep disturbance is thought due to increased time between shifts and the circadian timekeeping tendency to extend beyond 24 hours.66
When Should the Night Shift Start?
Those hospitalist programs using an evening swing shift from afternoon to late evening may have the option of using a 12‐hour night shift starting around 7 PM, or a shorter night shift beginning later at night. Though there are no data among hospitalists to suggest which night shift start time and duration would lead to the least amount of fatigue and errors, healthcare providers working a 12‐hour night shift may have increased morale due to fewer shifts, but may suffer a reduction in the quality of care provided compared with working an 8‐hour night shift.67 In either case, shift workers given flexibility in scheduling have been shown to have positive effects on sleep.68
Should Night Shifts Be Bunched?
The decision to bunch night shifts together depends on how many night shifts are required, and how quickly circadian adaptation can occur. Under simulated conditions, circadian adaptation can yield significant changes in sleep/wake cycles in as little as 4 days.48 In real‐world settings, more time may be required to achieve significant shifts in the circadian cycle. Therefore, hospitalists who have 7 or fewer night shifts during the academic year may want to space the shifts out to prevent sleep debt on consecutive shifts, since significant circadian adaptation would be difficult to achieve in less than a week. In this situation, after a night shift, the hospitalist should have at least one 9‐hour sleep period at night to relieve their sleep debt before staffing another night shift.69 Consecutive night shifts require at least 2 nighttime sleep periods of 9 hours to recover from sleep debt.70 The IOM recommends setting a limit of 4 consecutive night float shifts for resident physicians, however, a recent systematic review of resident night float models did not find data supporting use of a 4‐night‐maximum model.28
If more than 7 night shifts are required, then scheduling the shifts close together with use of circadian adaptation techniques may result in increased nighttime alertness, less fatigue, and fewer errors while at work than widely spacing out the shifts. For example, 1 recent study simulated 8 night shifts over a 10‐day period, and compared circadian schedules and work performance between those subjects who used circadian adaptation strategies and those that did not.71 Circadian adaptation techniques included: four 15‐minute bright light pulses during each night shift, dark sunglasses when outside, dark bedrooms and delayed sleeping until 3 AM on the nights off in between the night shift blocks. The group who shifted their circadian schedule improved night shift alertness and performance as measured by neurophysiological testing, while permitting sufficient daytime sleep after work, as well as late‐night sleep on days off. The group without circadian interventions did not shift their circadian schedule as significantly as the intervention group, and performed worse on the performance testing.
CONCLUSIONS
The nationwide use of hospitalists to provide 24‐hour patient care continues to expand, thus subjecting more hospitalists to work hours asynchronous with the lightdark cycle. Resultant circadian misalignment can result in fatigue while at work, shift work disorder, and, potentially, an increased rate of medical errors. Recognition of these dangers among resident physicians has prompted the ACGME to intensify their regulations on work hours, shift schedules, and time off between shifts. However, no such recommendations exist for hospitalists or emergency physicians and nurses.
Given the potential risk to both physicians and patients, we recommend more research examining the effects of circadian misalignment within the hospitalist community. Sample research questions are offered in Table 5. More information is urgently needed to provide evidence‐based practice guidelines to ensure the safety of this growing workforce and the patients they treat.
| Are hospitalists more immune to fatigue than resident physicians? |
| Are hospitalists better able to recognize fatigue while at work than resident physicians? |
| Does 1 shift work schedule promote better circadian alignment than other shift schedules? |
| Do consistent nighttime hours of nocturnists make them more prone to commit medical errors than hospitalists rotating their shifts? |
For hospitalists, patient care is 24 hours a day. To provide continual patient care, shift work has become a way of life for hospitalists, similar to hospital nurses, residents in training, and emergency medicine physicians. Notably, they belong to a substantial minority of the workforce as shift workers, starting after 6 PM or before 6 AM, approximately one‐fifth of the total work force in industrialized nations.1, 2 Unfortunately, shift workers suffer from misalignment of their endogenous circadian system, which regulates daily sleep and alertness patterns, and work obligations beyond daylight hours. Such a misalignment can lead to fatigue, sleep loss, and excessive sleepiness, which can adversely affect personal health and safety, as well as the quality of medical care delivered.3
The relationship between shift work, extended work hours, and medical safety is a topic currently under intense scrutiny, as reviewed in the Institute of Medicine's (IOM) controversial report on residents and sleep.4 This publication led the Accreditation Council of Graduate Medical Education (ACGME) to mandate more changes to residents' work hours,5 adding to those first implemented in 2003.6 These restrictions forbid residents from working more than 30 consecutive hours, and required at least 10 hours off between shifts and an average of 1 day off in 7. Subsequent studies suggested that the reduction in resident work hours led to greater resident well‐being, fewer attention failures. and fewer medical errors.3, 7
In 2007, amid growing public concern over sleep‐deprived residents and patient safety, Congress requested the IOM investigate additional safeguards for residents.8 In 2008, the IOM published a report calling for more protection against resident fatigue.4 They recommended integrating a protected sleep period into any 24‐hour shift. If residents cannot get protected sleep time, then the maximal shift duration should not exceed 16 hoursreduced from the previous ACGME recommendation of 30. Further provisions to allow adequate sleep include capping the number of consecutive night shifts at 4, and extending the time off after a night shift. In response, the ACGME recently updated their recommendations effective July 1, 2011,5 though not following all the IOM's recommendations (Table 1).
| 2003 ACGME Limits | 2008 IOM Recommendation | 2010 ACGME Limits | |
|---|---|---|---|
| |||
| Maximum work hours per week | 80 hr, averaged over 4 wk | No change | No change |
| Maximum shift length | 30 hr (admitting patients up to 24 hr, with 6 hr of transition activities) | 30 hr (admitting patients up to 16 hr, with 5 hr protected sleep between 10 PM to 8 AM, and remaining hours for transition activities) | PGY‐1: 16 hr; PGY‐2 and above: 28 hr (admitting patients up to 24 hr, with 4 hr of transition activities) |
| Minimum time off between shifts | 10 hr after shift | 10 hr after day shift; 12 hr after night shift; 14 hr after any extended shift of 30 hr and not return until 6 AM the next day | 10 hr after shift; 14 hr free after 24‐hr shift for intermediate level residents |
| Maximum frequency of in‐hospital night shifts | No limits | 4 night maximum, with 48 hr off after 3 or 4 consecutive shifts | 6 consecutive night maximum |
The growing nationwide emphasis on fatigue prevention within healthcare settings now clearly impacts residents and their training schedule. But why focus only on residents? Why not other physicians, such as hospitalists, who work shifts to cover 24 hours each day? Are they any less prone to making medical errors when fatigued? Given that hospitalists' represent the fastest growing specialty in the history of American medicine,9 we sought to inform decisions about their scheduling by reviewing normal regulation of sleep and wake patterns, addressing the problems associated with misalignment between sleep and work, and identifying strategies to realign circadian schedules.
NORMAL SLEEP AND CIRCADIAN RHYTHMS
An understanding of sleep physiology begins with the endogenous circadian timekeeping system. At the center of this timekeeping system is a master circadian clock, located in the suprachiasmatic nucleus (SCN) of the hypothalamus. Cells within the SCN generate a near 24‐hour rhythm, transmitted through neural connections, to rhythmically influence the entire central nervous system and other bodily systems.10
The SCN and the circadian rhythm interact with the need to sleep (sleep homeostasis) to form the 2‐process model of sleepwakefulness.11 In this model, progression of biological day (a time when wakefulness and its associated functions are promoted) coincides with a rise in homeostatic pressure to sleep (see Figure 1). Daytime alertness is maintained by increasing SCN neuronal activity to counterbalance rising sleep pressure. After peaking in the early evening, SCN activity falls to begin biological night (a time when sleep and its associated functions are promoted). To facilitate the onset of biological night, the SCN coordinates the activity of sleep‐promoting centers and the release of melatonin from the pineal gland which promotes sleep.
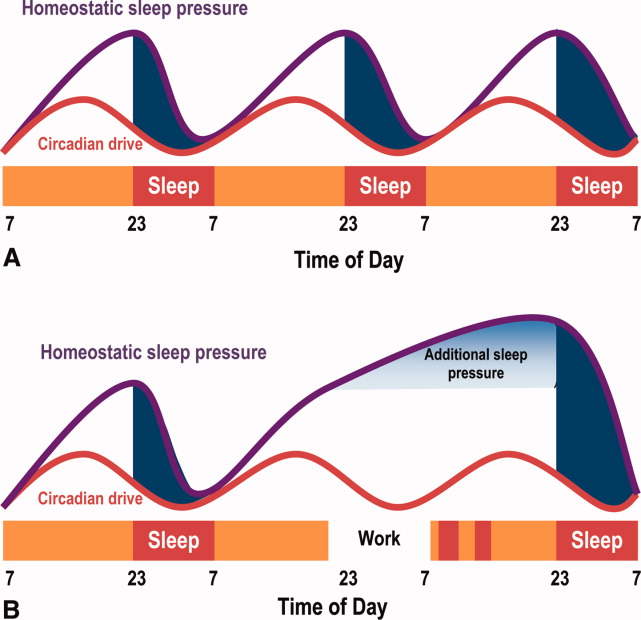
This endogenous circadian clock runs slightly longer than 24 hours and must be resynchronized daily to the 24‐hour day, a process known as entrainment. This occurs primarily through environmental exposure of retinalhypothalamic links to the lightdark cycle. The intensity, duration, and wave length of light all influence the circadian system,12 but perhaps most importantly is the timing. In general, light exposure in the evening will shift the circadian clock later (phase delay shift), whereas light exposure in the morning will shift the clock earlier (phase advance shift). Exogenous melatonin can also shift the circadian system. However, when endogenous levels of melatonin are high, ingested melatonin has little influence on sleep.13
Balancing sleep and wakefulness requires an interweaving of endogenous and exogenous factors. This balance is disturbed if we try to sleep or be wakeful during incorrect endogenous biological times, a process called circadian misalignment.
DELETERIOUS EFFECTS OF CIRCADIAN MISALIGNMENT
Hospitalists and other shift workers required to work during the biological night risk circadian misalignment and, consequently, poor sleep, shift work disorder, errors on the job, and possibly long‐term health consequences.
Chronic Sleep Loss
When working at night or in the early morning, nearly 75% of shift workers encounter some amount of at‐work fatigue and sleepiness.14 After the shift is over, objective assessments among rotating shift workers15, 16 and interns7 demonstrated that day sleep is 1 to 4 hours shorter than night sleep. Chronic or recurring night shifts can therefore lead to chronic sleep loss. While it seems reasonable that permanent night shift workers have greater circadian adjustment to suit their work schedule, little evidence supports this argument.17 Permanent night shift workers may sleep a little longer during the day than rotating shift workers. Yet, the sleep quality does not match night sleep, presumably from conflict between external factors, such as light and activity, and the scheduled sleep period.
Shift Work Disorder
If severe and chronic, sleepiness and impaired performance during work hours and poor sleep during the day can be enough to warrant a diagnosis of shift work disorder (SWD), one of the several circadian rhythm sleep disorders (CRSD). The prevalence of SWD among rotating and night workers is estimated to be 10%25%.18 Patients with SWD can experience similar levels of nighttime sleepiness as patients with narcolepsy and sleep apnea.19 These patients experience reduced satisfaction with the work schedule, and suffer higher rates of depression, ulcers, and sleepiness‐related accidents, compared to other shift workers.18 What distinguishes those shift workers who suffer from normal fatigue and those with SWD is not easily identified. The International Classification of Sleep Disorders‐2 (ICSD‐2) lists the diagnostic criteria for SWD20:
-
Symptoms of insomnia associated with a work schedule that overlaps the usual time for sleep.
-
Symptoms are directly associated with shift work schedule over the course of at least 1 month.
-
Sleep log monitoring for at least 7 days demonstrates circadian and sleep‐time misalignment.
-
Sleep disturbance is not better explained by another sleep disorder or by a medical, neurological, or mental disorder; medication use; or substance‐use disorder.
Symptoms must be present for at least 1 month, and comorbid mood or sleep/wake disorders (commonly found in this disorder) need to be treated. SWD is more common among night shift workers, although those workers starting shifts between 4 AM and 7 AM (early morning shift) are also subject to SWD.21 Type of work schedule, along with physical or mental disorders, domestic responsibilities, and commute times are examples of factors that may increase vulnerability for SWD.18 In addition, genetic factors may explain the considerable inter‐individual differences in susceptibility to SWD. For example, a polymorphism in the circadian gene, PER 3, present in 10%15% of the population, is believed to decrease tolerability to acute sleep loss,22 while genetic variation in the adenosine A2A receptor may be associated with resistance to the effects of sleep loss.23 If a hospitalist suspects a diagnosis SWD, they should seek evaluation by a physician specializing in sleep medicine.
Errors
Disruption of the circadian rhythm influences neurocognitive and psychomotor function, and can lead to human error. Human errors that result in serious accidents or injuries typically result from interaction of circadian rhythm misalignment with multiple other factors, including task duration and complexity, motivation and proficiency, and level of sleep deprivation.24 Though difficult to isolate from the environmental and work experience factors, consistent evidence identifies circadian misalignment as a cause of errors and serious accidents. Most evidence comes from night shift workers trying to remain awake when the circadian signal for alertness is low, or attempting sleep when the circadian alerting signal is high. Compared to day workers, night shift workers are 1.63 times more likely to suffer a fatal accident.25 A study of critical care nurses revealed a prominent circadian pattern of inadvertent sleep episodes during work with the highest peak between 2 AM and 6 AM.26 In addition, nurses working the night shift have been shown to commit more medication administration errors than day workers.27
Medical errors among resident physicians during extended shift durations is well documented.28 On the other hand, not much research has examined error rates among attending physicians. In 1 small study, attending surgeons made more cognitive errors using a simulated laparoscopic exercise as the amount of on‐call overnight sleep decreased.29 A large, single‐center review reported an increased rate of complications among post‐nighttime surgical procedures performed by attendings who slept 6 hours or less the preceding night.30 Notably, proposed legislation would require physicians who have been awake 22 of the preceding 24 hours to inform patients of the potential safety impact of their sleep deprivation prior to providing clinical care.31
Chronic Health Morbidity
Several studies reveal the effect of shift work on chronic health conditions among healthcare workers, such as obesity, cardiovascular disease, and certain cancers (eg, breast, colorectal). These results are summarized in Table 2, with the largest evaluation of healthcare shift workers coming from the Nurses' Health Study.3234
| Disease | Study Design | Population | Comparison | Health Risk | Adjusted Risk Factors |
|---|---|---|---|---|---|
| |||||
| Acute myocardial infarction | Prospective cohort32 | 79,109 US nurses | Working 3 night shifts/mo for 6 yr | RR 1.51 | CAD risk factors, aspirin use, hormone replacement therapy |
| 95% CI (1.12‐2.03) | |||||
| Obesity (BMI 30) | Cross‐sectional72 | 27,485 Swedish workers | Shift‐workers vs day workers | OR 1.41 | Age, socioeconomic status |
| 95% CI (1.25‐1.59) | |||||
| Breast cancer | Prospective cohort33 | 116,087 US nurses | Working 3 night shifts/mo for 20 yr | RR 1.79 | Breast cancer risk factors |
| 95% CI (1.06‐3.01) | |||||
| Colon cancer | Prospective cohort34 | 78,586 US nurses | Working 3 night shifts/mo for 15 yr | RR 1.35 | Family history of colon cancer, dietary intake, activity |
| 95% CI (1.03‐1.77) | |||||
Some believe that adverse health outcomes in shift workers derive from circadian stressan alteration of psychosocial and physiological homeostasis (eg, increased cortisol and catecholamine output) resulting from circadian misalignment.35 Based on data suggesting an increased risk for certain cancers among shift workers, the International Agency for Research of Cancer, a unit of the World Health Organization, announced that shift work resulting in circadian misalignment is probably carcinogenic.36 Researchers propose several biologic mechanisms to explain the increased cancer riskmost revolve around the alteration of the melatonin circadian cycle, found in night shift workers,37 and subsequent disruption of its believed cancer‐protective biologic pathways.
Overall, however, the heterogeneous nature of shift work limits conclusions regarding the long‐term health of shift workers. That is, as the shift work intensity and composition varies, and as the number and timing of these shifts change, so too can the adverse health consequences.
HOSPITALISTS AND NIGHT SHIFTS
Hospital medicine is the fastest growing specialty in the history of medicine, with an estimated 30,000 practicing hospitalists in 2010.38 Survey results from 2009 indicate that hospitalists staff 58% of hospitals; 89% of hospitals with more than 200 beds (J. Miller, Society of Hospital Medicine, personal communication). One reason for the growth in the number of hospitalists at academic medical centers has been the imposed work‐hour restrictions for residents.39
Across the county, hospitalist programs use a variety of shift work systems to ensure 24‐hour patient care. Among those programs that provide continuous on‐site coverage, many staff 3 shiftsday, late afternoon/evening (swing), and night shifts. Some permanently partition the scheduling, with dedicated night hospitalists or nocturnists.40
Hospitalists do not have mandated work‐hour restrictions and, in general, are older than resident physicians. Whether or not hospitalists who trained before the era of work‐hour regulations are better prepared for practicing in a real‐world, after‐hours scenario than hospitalists with previous work‐hour restrictions is a matter of debate. That said, hospitalists who are fatigued, just like residents, may be at increased risk for committing medical errors, particularly when the fatigue is unrecognized. Yet, limiting hospitalists' work hours would have obvious financial implications, likely similar those from resident work‐hour reductions.41 As part of the ACGME 2011 recommendations, faculty and residents now must be trained to recognize signs of fatigue and sleep deprivation, and adopt management strategies such as naps or backup call schedules. Fatigue that results in excessive sleepiness while at work may manifest as weariness, difficulty concentrating, headache, irritability or depressed mood, and feeling unrefreshed after sleeping.42
STRATEGIES TO IMPROVE CIRCADIAN ADAPTATION
Hospitalists can help limit fatigue and improve performance and safety through circadian adaptation: a multimodal approach to realign work and circadian schedules. Depending on whether the shift starts at night or in the early morning (4 AM to 7 AM), circadian adaptation aims may differ. For night shift workers, the overall aim is to delay the timing of circadian rhythms such that the highest propensity of wakefulness occurs during the night work period, while the highest propensity for sleep occurs during the day.17, 43 For early morning shift workers, circadian rhythms for wakefulness and sleep propensity should be shifted earlier. Circadian adaptation involves not only sleeping well before work, but also preventing dips in wakefulness during work. Adaptation strategies are listed in Table 3.
| Night Shift60 | Early Day Shift (Starting at 4 AM‐7 AM) | |
|---|---|---|
| Prior to shift | Avoid sleep debt | Avoid sleep debt |
| Proper sleep hygiene | Proper sleep hygiene | |
| Planned napping | Bright light exposure | |
| Caffeine use | ||
| During the shift | Bright light exposure | Caffeine use |
| Planned napping | ||
| After the shift | Avoid bright light | Avoid late evening bright light (when applicable) |
| Melatonin prior to sleep | ||
| Careful use of other hypnotics | Initiate sleep early |
Improved Sleep Before Work
As an essential first step, hospitalists must get a full night's rest before starting a night shift, as sleep debt will worsen fatigue while at work. Tips for proper sleep hygiene are listed in Table 4. Some shift workers stay up late the night before a scheduled night shift, in order to sleep during the day and awaken shortly before their scheduled night shift, to combat fatigue at work. Such an approach to shift work is typically met with 3 barriers. First, environmental factors often prevent 6 hours of uninterrupted day sleep. Second, 6 hours of continual day sleep is typically difficult because rising circadian activity often limits the sleep period to just a few hours. Third, an adequate amount of sleep prior to a night shift will itself not be enough to prevent sleepiness from occurring after midnightreducing the fall in circadian activity is also essential to maintaining alertness and performance.
| Physical | Adhere to regular wake and sleep schedule |
| activities73 | Engage in regular exercise early in the day |
| Avoid caffeine, nicotine, and alcohol use 6 hr prior to sleeping | |
| Avoid stimulating or stressful activities 30 min prior to sleeping | |
| Proper sleep | Well ventilated, temperature‐controlled bedroom |
| environment | Use heavy curtains to provide as much darkness as possible |
| Comfortable mattress and pillow | |
| Remove television and pets from the bedroom | |
| Housemates should help provide quiet sleep environment |
Napping
Napping prior to a night shift, or during the work shift, can improve alertness and performance and decrease accident rates.44, 45 During shift work, naps of 20 to 50 minutes in duration have demonstrated improvements in reaction time, and restoration of performance to that seen at the start of the shift. Napping early in the night shift can improve objective measures of alertness.44 To avoid increased drowsiness that sometimes occurs when waking from a nap, naps should not be longer than 50 minutes, and can be as short as 10 to 15 minutes.44, 46 Although effective, napping may be impractical for many workers due to time or space constraints. To facilitate brief naps, hospitalist practices should ensure they have a dark, quiet call room for use by overnight hospitalists.
Bright Light Exposure
Studies demonstrate that light exposure during the night shift improves circadian alignment, mood, and performance during the night shift.47, 48 Light exposure ranged from 6 hours to 5 light treatments of 15 minutes each, with brightness ranging from 2,500 to 10,000 lux (approximating outdoor daylight; typical office lighting provides 200‐500 lux).47, 49 Results demonstrate that bright light exposure during the night shift acutely improves alertness and performance, though not to daytime levels.50 The greatest circadian adjustments occur in groups using both bright light during the night shift and light avoidance the following morning.51 Dark sunglasses and a dark home environment can decrease bright light exposure during the day. Though little evidence exists to support widespread application of bright light devices in hospitalists' call‐rooms, a hospitalist practice should consider installing one to promote circadian adaptation if physicians working overnight have multiple consecutive shifts. Likewise, these physicians should be vigilant and wear dark sunglasses during the day after their night shifteven a few minutes of light exposure at the wrong time of the day may disrupt the intended circadian adaptation.
Wake‐Promoting Agents
Numerous studies demonstrate that 150 mg to 400 mg of caffeine (a 16 oz grande cup of coffee from Starbucks contains between 200 to 500 mg of caffeine52; a Diet Coke contains 46 mg/12 oz53) reduces sleepiness, increases alertness, and improves performance during the night shift.54, 55 Thus, judicious use of caffeine may be recommended in hospital practices during extended work hours. Other wake‐promoting agents, such as modafinil and armodafinil, are US Food and Drug Administration (FDA)‐approved in the treatment of excessive sleepiness associated with SWD. Typically taken 3060 minutes before the start of the night shift, these medications have been shown in trials, enrolling mostly permanent night shift workers, to reduce excessive nighttime sleepiness and improve performance.19, 56 Armodafinil used to treat SWD‐associated excessive sleepiness, has been safely tolerated for durations of 1 year or more.57 However, these agents are not approved for use in patients without a diagnosed sleep disorder.
Melatonin
Exogenous melatonin has been used to reset circadian rhythms in patients with CRSDs.58 Melatonin administered in the late afternoon to early evening directs the largest phase advance. In contrast, melatonin given in the morning produces the largest phase delays.59 When taken after a night shift, melatonin (at a dose 1.8 to 3.0 mg) can improve day sleep quality and duration.60 Despite this result, melatonin's effectiveness in improving circadian adaptation has been mixed.61 For example, improvements in nighttime alertness during the night shift were not seen, despite the use of melatonin to facilitate daytime sleep beforehand.62 Hospitalists may consider a trial of melatonin to improve circadian alignment and facilitate daytime sleep, but its chronic use and long‐term safety has not been adequately studied.
Hypnotics After Work
Hypnotics such as temazepam 20 mg,63 triazolam,64 and zolpidem65 taken after night shift work have been shown to improve day sleep quality under simulated conditions, but do not improve shift work performance. These medications should be reserved for judicious short‐term use in patients with insomnia associated with SWD.
NIGHT SHIFT SCHEDULING TO REDUCE CIRCADIAN MISALIGNMENT
When providing 24‐hour, on‐site medical care, questions may arise about how to incorporate circadian adaptation into the daily schedule.
How Should Shifts Be Rotated?
When scheduling shifts with different start times, evidence suggests that sleep disturbance is reduced with a clockwise progression in shifts (eg, day shift to evening shift to night shift). This reduction in sleep disturbance is thought due to increased time between shifts and the circadian timekeeping tendency to extend beyond 24 hours.66
When Should the Night Shift Start?
Those hospitalist programs using an evening swing shift from afternoon to late evening may have the option of using a 12‐hour night shift starting around 7 PM, or a shorter night shift beginning later at night. Though there are no data among hospitalists to suggest which night shift start time and duration would lead to the least amount of fatigue and errors, healthcare providers working a 12‐hour night shift may have increased morale due to fewer shifts, but may suffer a reduction in the quality of care provided compared with working an 8‐hour night shift.67 In either case, shift workers given flexibility in scheduling have been shown to have positive effects on sleep.68
Should Night Shifts Be Bunched?
The decision to bunch night shifts together depends on how many night shifts are required, and how quickly circadian adaptation can occur. Under simulated conditions, circadian adaptation can yield significant changes in sleep/wake cycles in as little as 4 days.48 In real‐world settings, more time may be required to achieve significant shifts in the circadian cycle. Therefore, hospitalists who have 7 or fewer night shifts during the academic year may want to space the shifts out to prevent sleep debt on consecutive shifts, since significant circadian adaptation would be difficult to achieve in less than a week. In this situation, after a night shift, the hospitalist should have at least one 9‐hour sleep period at night to relieve their sleep debt before staffing another night shift.69 Consecutive night shifts require at least 2 nighttime sleep periods of 9 hours to recover from sleep debt.70 The IOM recommends setting a limit of 4 consecutive night float shifts for resident physicians, however, a recent systematic review of resident night float models did not find data supporting use of a 4‐night‐maximum model.28
If more than 7 night shifts are required, then scheduling the shifts close together with use of circadian adaptation techniques may result in increased nighttime alertness, less fatigue, and fewer errors while at work than widely spacing out the shifts. For example, 1 recent study simulated 8 night shifts over a 10‐day period, and compared circadian schedules and work performance between those subjects who used circadian adaptation strategies and those that did not.71 Circadian adaptation techniques included: four 15‐minute bright light pulses during each night shift, dark sunglasses when outside, dark bedrooms and delayed sleeping until 3 AM on the nights off in between the night shift blocks. The group who shifted their circadian schedule improved night shift alertness and performance as measured by neurophysiological testing, while permitting sufficient daytime sleep after work, as well as late‐night sleep on days off. The group without circadian interventions did not shift their circadian schedule as significantly as the intervention group, and performed worse on the performance testing.
CONCLUSIONS
The nationwide use of hospitalists to provide 24‐hour patient care continues to expand, thus subjecting more hospitalists to work hours asynchronous with the lightdark cycle. Resultant circadian misalignment can result in fatigue while at work, shift work disorder, and, potentially, an increased rate of medical errors. Recognition of these dangers among resident physicians has prompted the ACGME to intensify their regulations on work hours, shift schedules, and time off between shifts. However, no such recommendations exist for hospitalists or emergency physicians and nurses.
Given the potential risk to both physicians and patients, we recommend more research examining the effects of circadian misalignment within the hospitalist community. Sample research questions are offered in Table 5. More information is urgently needed to provide evidence‐based practice guidelines to ensure the safety of this growing workforce and the patients they treat.
| Are hospitalists more immune to fatigue than resident physicians? |
| Are hospitalists better able to recognize fatigue while at work than resident physicians? |
| Does 1 shift work schedule promote better circadian alignment than other shift schedules? |
| Do consistent nighttime hours of nocturnists make them more prone to commit medical errors than hospitalists rotating their shifts? |
- .Job, family, and gender: determinants of nonstandard work schedules among employed Americans in 1991.Demography.1995;32:577–598.
- ,.Shift work among dual‐earner couples with children.Science.1983;219:876–879.
- ,,, et al.Effect of reducing interns' work hours on serious medical errors in intensive care units.N Engl J Med.2004;351:1838–1848.
- Institute of Medicine. Resident Duty Hours: Enhancing Sleep, Supervision and Safety. Released December 15,2008. Available at: http://www.iom.edu/Reports/2008/Resident‐Duty‐Hours‐Enhancing‐Sleep‐Supervision‐and‐Safety.aspx. Accessed on October 20, 2010.
- ACGME. ACGME Approved Standards. Effective July2011. Available at: http://acgme‐2010standards.org/. Accessed on January 6, 2011
- ACGME. Common Program Requirements: Resident Duty Hours in the Learning and Work Environment. Effective July 1, 2007. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_ComProgrRequirmentsDutyHours0707.pdf. Accessed October 20,2010.
- ,,, et al.Effect of reducing interns' weekly work hours on sleep and attentional failures.N Engl J Med.2004;351:1829–1837.
- Letter written to William Munier, Agency for Healthcare Research and Quality.Washington, DC:US House of Representatives, Committee on Energy and Commerce, March 29,2007. Available at: http://energycommerce.house.gov/Press_110/110‐ltr.032907.HHS.Munier.pdf. Accessed on October 24, 2010.
- ,.The evolution and future of hospital medicine.Mt Sinai J Med.2008;75:418–423.
- .Brain structures and receptors involved in alertness.Sleep Med.2005;6(suppl 1):S3–S7.
- .A two process model of sleep regulation.Hum Neurobiol.1982;1:195–204.
- ,.Entrainment of the human circadian system by light.J Biol Rhythms.2005;20:326–338.
- ,.Sleep‐promoting and hypothermic effects of daytime melatonin administration in humans.Sleep.1997;20:124–131.
- .Sleepiness as a consequence of shift work.Sleep.1988;11:17–34.
- ,,,,.The sleep of long‐haul truck drivers.N Engl J Med.1997;337:755–761.
- ,,,.Sleep on the night shift: 24‐hour EEG monitoring of spontaneous sleep/wake behavior.Psychophysiology.1989;26:352–358.
- .Do permanent night workers show circadian adjustment? A review based on the endogenous melatonin rhythm.Chronobiol Int.2008;25:215–224.
- ,,,,.Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers.Sleep.2004;27:1453–1462.
- ,,, et al.Modafinil for excessive sleepiness associated with shift‐work sleep disorder.N Engl J Med.2005;353:476–486.
- American Academy of Sleep Medicine.The International Classification of Sleep Disorders (ICSD).2nd ed.Chicago, IL:American Academy of Sleep Medicine;2005.
- ,.Circadian rhythm sleep disorders.Chest.2006;130:1915–1923.
- ,,,,,.Early morning executive functioning during sleep deprivation is compromised by a PERIOD3 polymorphism.Sleep.2008;31:1159–1167.
- ,,,,,.Genetic variation in the adenosine A2A receptor gene modulates performance on the psychomotor vigilance task.Sleep Biol Rhythms.2007;5:A47.
- ,.Circadian rhythms in cognitive performance: methodological constraints, protocols, theoretical underpinnings.Physiol Behav.2007;90:196–208.
- ,,,.A prospective study of fatal occupational accidents—relationship to sleeping difficulties and occupational factors.J Sleep Res.2002;11:69–71.
- ,,,.Effects of critical care nurses' work hours on vigilance and patients' safety.Am J Crit Care.2006;15:30–37.
- ,,,,.Daytime sleepiness, sleep habits and occupational accidents among hospital nurses.J Adv Nurs.2005;52:445–453.
- ,,.Systematic review: association of shift length, protected sleep time, and night float with patient care, residents' health, and education.Ann Intern Med.2010;153:829–842.
- ,,,,.Jack Barney Award: the effect of fatigue on cognitive and psychomotor skills of trauma residents and attending surgeons.Am J Surg.2008;196:813–819; discussion 9–20.
- ,,, et al.Risks of complications by attending physicians after performing nighttime procedures.JAMA.2009;302:1565–1572.
- ,,.Sleep deprivation, elective surgical procedures, and informed consent.N Engl J Med.2010;363:2577–2579.
- ,,,,.A prospective study of anger and coronary heart disease. The Normative Aging Study.Circulation.1996;94:2090–2095.
- ,,,.Night work and risk of breast cancer.Epidemiology.2006;17:108–111.
- ,,, et al.Night‐shift work and risk of colorectal cancer in the nurses' health study.J Natl Cancer Inst.2003;95:825–828.
- ,,.Shift work and cardiovascular disease—pathways from circadian stress to morbidity.Scand J Work Environ Health.2010;36:96–108.
- IARC. IARC monographs on the evalutaion of carcinogenic risks to humans. Vol 98. Painting, firefighting, and shiftwork. 2007. Available at: monographs.iarc.fr/ENG/Monographs/vol98/mono98.pdf. Accessed January 16,2011.
- ,,,.Influence of melatonin on invasive and metastatic properties of MCF‐7 human breast cancer cells.Cancer Res.1998;58:4383–4390.
- Society of Hospital Medicine. Society of Hospital Medicine releases results of the 2007–2008 survey on the state of the hospital medicine movement. 2008. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Press_Releases3:247–255.
- ,,.Hospitalists: A Guide to Building and Sustaining a Successful Program.Chicago, IL:Health Administration Press;2008.
- ,,,,.The increased financial burden of further proposed orthopaedic resident work‐hour reductions.J Bone Joint Surg Am.2011;93:e31.
- ,,,,,.Fatigue and shift work.J Sleep Res.2006;15:1–5.
- ,,, et al.Rapid shift in peak melatonin secretion associated with improved performance in short shift work schedule.Sleep.1997;20:1145–1150.
- ,,.The impact of a nap opportunity during the night shift on the performance and alertness of 12‐h shift workers.J Sleep Res.2002;11:219–227.
- ,,, et al.Improving alertness and performance in emergency department physicians and nurses: the use of planned naps.Ann Emerg Med.2006;48:596–604, e1‐e3.
- ,,,,.Promoting alertness with a short nap during a night shift.J Sleep Res.1998;7:240–247.
- ,.Circadian adaptation to night‐shift work by judicious light and darkness exposure.J Biol Rhythms.2002;17:556–567.
- ,,,,,.Exposure to bright light and darkness to treat physiologic maladaptation to night work.N Engl J Med.1990;322:1253–1259.
- ,.Night shift performance is improved by a compromise circadian phase position: study 3. Circadian phase after 7 night shifts with an intervening weekend off.Sleep.2008;31:1639–1645.
- ,,,.Dose‐response relationship for light intensity and ocular and electroencephalographic correlates of human alertness.Behav Brain Res.2000;115:75–83.
- ,,,,.Dark goggles and bright light improve circadian rhythm adaptation to night‐shift work.Sleep.1994;17:535–543.
- ,,.Caffeine content of specialty coffees.J Anal Toxicol.2003;27:520–522.
- ,.Caffeine content of prepackaged national‐brand and private‐label carbonated beverages.J Food Sci.2007;72:C337–C342.
- ,,, et al.The effects of coffee and napping on nighttime highway driving: a randomized trial.Ann Intern Med.2006;144:785–791.
- ,,,,.Laboratory and field studies of naps and caffeine as practical countermeasures for sleep‐wake problems associated with night work.Sleep.2006;29:39–50.
- ,,,,.Armodafinil for treatment of excessive sleepiness associated with shift work disorder: a randomized controlled study.Mayo Clin Proc.2009;84:958–972.
- ,,,,.The long‐term tolerability and efficacy of armodafinil in patients with excessive sleepiness associated with treated obstructive sleep apnea, shift work disorder, or narcolepsy: an open‐label extension study.J Clin Sleep Med.2010;6:458–466.
- ,,.Circadian rhythm sleep disorders.Med Clin North Am.2004;88:631–651, viii.
- ,,.A three pulse phase response curve to three milligrams of melatonin in humans.J Physiol.2008;586:639–647.
- ,,, et al.Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report.Sleep.2007;30:1445–1459.
- ,,, et al.Efficacy and safety of exogenous melatonin for secondary sleep disorders and sleep disorders accompanying sleep restriction: meta‐analysis.BMJ.2006;332:385–393.
- ,,.Effects of melatonin administration on daytime sleep after simulated night shift work.J Sleep Res.2001;10:181–192.
- ,,,.Performance, ability to stay awake, and tendency to fall asleep during the night after a diurnal sleep with temazepam or placebo.Sleep.1997;20:535–541.
- ,,,,,.Sleepiness/alertness on a simulated night shift following sleep at home with triazolam.Sleep.1991;14:140–146.
- ,,,.Zolpidem‐related effects on performance and mood during simulated night‐shift work.Exp Clin Psychopharmacol.2003;11:259–268.
- ,,,,.Intrinsic near‐24‐h pacemaker period determines limits of circadian entrainment to a weak synchronizer in humans.Proc Natl Acad Sci USA.2001;98:14027–14032.
- ,,,.Work shift duration: a review comparing eight hour and 12 hour shift systems.Occup Environ Med.1998;55:217–229.
- ,,.Influence of flexibility and variability of working hours on health and well‐being.Chronobiol Int.2006;23:1125–1137.
- ,,.Impact of night‐float rotation on sleep, mood, and alertness: the resident's perception.Chronobiol Int.2002;19:893–902.
- ,,,,,.The characteristics of recovery sleep when recovery opportunity is restricted.Sleep.2007;30:353–360.
- ,,.Practical interventions to promote circadian adaptation to permanent night shift work: study 4.J Biol Rhythms.2009;24:161–172.
- ,,.Is there an association between shift work and having a metabolic syndrome? Results from a population based study of 27,485 people.Occup Environ Med.2001;58:747–752.
- ,.Use of sleep hygiene in the treatment of insomnia.Sleep Med Rev.2003;7:215–225.
- .Job, family, and gender: determinants of nonstandard work schedules among employed Americans in 1991.Demography.1995;32:577–598.
- ,.Shift work among dual‐earner couples with children.Science.1983;219:876–879.
- ,,, et al.Effect of reducing interns' work hours on serious medical errors in intensive care units.N Engl J Med.2004;351:1838–1848.
- Institute of Medicine. Resident Duty Hours: Enhancing Sleep, Supervision and Safety. Released December 15,2008. Available at: http://www.iom.edu/Reports/2008/Resident‐Duty‐Hours‐Enhancing‐Sleep‐Supervision‐and‐Safety.aspx. Accessed on October 20, 2010.
- ACGME. ACGME Approved Standards. Effective July2011. Available at: http://acgme‐2010standards.org/. Accessed on January 6, 2011
- ACGME. Common Program Requirements: Resident Duty Hours in the Learning and Work Environment. Effective July 1, 2007. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_ComProgrRequirmentsDutyHours0707.pdf. Accessed October 20,2010.
- ,,, et al.Effect of reducing interns' weekly work hours on sleep and attentional failures.N Engl J Med.2004;351:1829–1837.
- Letter written to William Munier, Agency for Healthcare Research and Quality.Washington, DC:US House of Representatives, Committee on Energy and Commerce, March 29,2007. Available at: http://energycommerce.house.gov/Press_110/110‐ltr.032907.HHS.Munier.pdf. Accessed on October 24, 2010.
- ,.The evolution and future of hospital medicine.Mt Sinai J Med.2008;75:418–423.
- .Brain structures and receptors involved in alertness.Sleep Med.2005;6(suppl 1):S3–S7.
- .A two process model of sleep regulation.Hum Neurobiol.1982;1:195–204.
- ,.Entrainment of the human circadian system by light.J Biol Rhythms.2005;20:326–338.
- ,.Sleep‐promoting and hypothermic effects of daytime melatonin administration in humans.Sleep.1997;20:124–131.
- .Sleepiness as a consequence of shift work.Sleep.1988;11:17–34.
- ,,,,.The sleep of long‐haul truck drivers.N Engl J Med.1997;337:755–761.
- ,,,.Sleep on the night shift: 24‐hour EEG monitoring of spontaneous sleep/wake behavior.Psychophysiology.1989;26:352–358.
- .Do permanent night workers show circadian adjustment? A review based on the endogenous melatonin rhythm.Chronobiol Int.2008;25:215–224.
- ,,,,.Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers.Sleep.2004;27:1453–1462.
- ,,, et al.Modafinil for excessive sleepiness associated with shift‐work sleep disorder.N Engl J Med.2005;353:476–486.
- American Academy of Sleep Medicine.The International Classification of Sleep Disorders (ICSD).2nd ed.Chicago, IL:American Academy of Sleep Medicine;2005.
- ,.Circadian rhythm sleep disorders.Chest.2006;130:1915–1923.
- ,,,,,.Early morning executive functioning during sleep deprivation is compromised by a PERIOD3 polymorphism.Sleep.2008;31:1159–1167.
- ,,,,,.Genetic variation in the adenosine A2A receptor gene modulates performance on the psychomotor vigilance task.Sleep Biol Rhythms.2007;5:A47.
- ,.Circadian rhythms in cognitive performance: methodological constraints, protocols, theoretical underpinnings.Physiol Behav.2007;90:196–208.
- ,,,.A prospective study of fatal occupational accidents—relationship to sleeping difficulties and occupational factors.J Sleep Res.2002;11:69–71.
- ,,,.Effects of critical care nurses' work hours on vigilance and patients' safety.Am J Crit Care.2006;15:30–37.
- ,,,,.Daytime sleepiness, sleep habits and occupational accidents among hospital nurses.J Adv Nurs.2005;52:445–453.
- ,,.Systematic review: association of shift length, protected sleep time, and night float with patient care, residents' health, and education.Ann Intern Med.2010;153:829–842.
- ,,,,.Jack Barney Award: the effect of fatigue on cognitive and psychomotor skills of trauma residents and attending surgeons.Am J Surg.2008;196:813–819; discussion 9–20.
- ,,, et al.Risks of complications by attending physicians after performing nighttime procedures.JAMA.2009;302:1565–1572.
- ,,.Sleep deprivation, elective surgical procedures, and informed consent.N Engl J Med.2010;363:2577–2579.
- ,,,,.A prospective study of anger and coronary heart disease. The Normative Aging Study.Circulation.1996;94:2090–2095.
- ,,,.Night work and risk of breast cancer.Epidemiology.2006;17:108–111.
- ,,, et al.Night‐shift work and risk of colorectal cancer in the nurses' health study.J Natl Cancer Inst.2003;95:825–828.
- ,,.Shift work and cardiovascular disease—pathways from circadian stress to morbidity.Scand J Work Environ Health.2010;36:96–108.
- IARC. IARC monographs on the evalutaion of carcinogenic risks to humans. Vol 98. Painting, firefighting, and shiftwork. 2007. Available at: monographs.iarc.fr/ENG/Monographs/vol98/mono98.pdf. Accessed January 16,2011.
- ,,,.Influence of melatonin on invasive and metastatic properties of MCF‐7 human breast cancer cells.Cancer Res.1998;58:4383–4390.
- Society of Hospital Medicine. Society of Hospital Medicine releases results of the 2007–2008 survey on the state of the hospital medicine movement. 2008. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Press_Releases3:247–255.
- ,,.Hospitalists: A Guide to Building and Sustaining a Successful Program.Chicago, IL:Health Administration Press;2008.
- ,,,,.The increased financial burden of further proposed orthopaedic resident work‐hour reductions.J Bone Joint Surg Am.2011;93:e31.
- ,,,,,.Fatigue and shift work.J Sleep Res.2006;15:1–5.
- ,,, et al.Rapid shift in peak melatonin secretion associated with improved performance in short shift work schedule.Sleep.1997;20:1145–1150.
- ,,.The impact of a nap opportunity during the night shift on the performance and alertness of 12‐h shift workers.J Sleep Res.2002;11:219–227.
- ,,, et al.Improving alertness and performance in emergency department physicians and nurses: the use of planned naps.Ann Emerg Med.2006;48:596–604, e1‐e3.
- ,,,,.Promoting alertness with a short nap during a night shift.J Sleep Res.1998;7:240–247.
- ,.Circadian adaptation to night‐shift work by judicious light and darkness exposure.J Biol Rhythms.2002;17:556–567.
- ,,,,,.Exposure to bright light and darkness to treat physiologic maladaptation to night work.N Engl J Med.1990;322:1253–1259.
- ,.Night shift performance is improved by a compromise circadian phase position: study 3. Circadian phase after 7 night shifts with an intervening weekend off.Sleep.2008;31:1639–1645.
- ,,,.Dose‐response relationship for light intensity and ocular and electroencephalographic correlates of human alertness.Behav Brain Res.2000;115:75–83.
- ,,,,.Dark goggles and bright light improve circadian rhythm adaptation to night‐shift work.Sleep.1994;17:535–543.
- ,,.Caffeine content of specialty coffees.J Anal Toxicol.2003;27:520–522.
- ,.Caffeine content of prepackaged national‐brand and private‐label carbonated beverages.J Food Sci.2007;72:C337–C342.
- ,,, et al.The effects of coffee and napping on nighttime highway driving: a randomized trial.Ann Intern Med.2006;144:785–791.
- ,,,,.Laboratory and field studies of naps and caffeine as practical countermeasures for sleep‐wake problems associated with night work.Sleep.2006;29:39–50.
- ,,,,.Armodafinil for treatment of excessive sleepiness associated with shift work disorder: a randomized controlled study.Mayo Clin Proc.2009;84:958–972.
- ,,,,.The long‐term tolerability and efficacy of armodafinil in patients with excessive sleepiness associated with treated obstructive sleep apnea, shift work disorder, or narcolepsy: an open‐label extension study.J Clin Sleep Med.2010;6:458–466.
- ,,.Circadian rhythm sleep disorders.Med Clin North Am.2004;88:631–651, viii.
- ,,.A three pulse phase response curve to three milligrams of melatonin in humans.J Physiol.2008;586:639–647.
- ,,, et al.Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report.Sleep.2007;30:1445–1459.
- ,,, et al.Efficacy and safety of exogenous melatonin for secondary sleep disorders and sleep disorders accompanying sleep restriction: meta‐analysis.BMJ.2006;332:385–393.
- ,,.Effects of melatonin administration on daytime sleep after simulated night shift work.J Sleep Res.2001;10:181–192.
- ,,,.Performance, ability to stay awake, and tendency to fall asleep during the night after a diurnal sleep with temazepam or placebo.Sleep.1997;20:535–541.
- ,,,,,.Sleepiness/alertness on a simulated night shift following sleep at home with triazolam.Sleep.1991;14:140–146.
- ,,,.Zolpidem‐related effects on performance and mood during simulated night‐shift work.Exp Clin Psychopharmacol.2003;11:259–268.
- ,,,,.Intrinsic near‐24‐h pacemaker period determines limits of circadian entrainment to a weak synchronizer in humans.Proc Natl Acad Sci USA.2001;98:14027–14032.
- ,,,.Work shift duration: a review comparing eight hour and 12 hour shift systems.Occup Environ Med.1998;55:217–229.
- ,,.Influence of flexibility and variability of working hours on health and well‐being.Chronobiol Int.2006;23:1125–1137.
- ,,.Impact of night‐float rotation on sleep, mood, and alertness: the resident's perception.Chronobiol Int.2002;19:893–902.
- ,,,,,.The characteristics of recovery sleep when recovery opportunity is restricted.Sleep.2007;30:353–360.
- ,,.Practical interventions to promote circadian adaptation to permanent night shift work: study 4.J Biol Rhythms.2009;24:161–172.
- ,,.Is there an association between shift work and having a metabolic syndrome? Results from a population based study of 27,485 people.Occup Environ Med.2001;58:747–752.
- ,.Use of sleep hygiene in the treatment of insomnia.Sleep Med Rev.2003;7:215–225.
FDA Approves Long-Acting Form of Diabetes Drug Exenatide
The first once weekly diabetes drug has been approved by the Food and Drug Administration. An extended-release formulation of the type 2 diabetes medication exenatide, a glucagon-like peptide-1 (GLP-1) receptor, was approved on Jan. 27, the manufacturer announced.
The formulation, called Bydureon, is administered once a week in a subcutaneous injection, and is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes. The regular formulation of exenatide (Byetta), approved in 2005, is administered twice a day.
Approval was based on the results of the DURATION-5 study, which compared treatment with the two formulations in 252 patients with type 2 diabetes and inadequate glycemic control (mean baseline hemoglobin A1c was 8.4%) with diet and exercise alone or with oral therapy, including metformin, a sulfonylurea, a thiazolidinedione, or a combination of two of these treatments.
The mean reduction in HbA1c was 1.6 percentage points among those treated with 2 mg of extended-release exenatide once weekly, compared with a mean reduction of 0.9 percentage points among those treated with the regular form of exenatide (starting at 5 mcg twice daily increasing to 10 mcg twice daily after 4 weeks), a statistically significant difference, according to the prescribing information and the press release.
Extended-release exenatide has been approved with a Risk Evaluation and Mitigation Strategy (REMS), to ensure that the benefits of the drug outweigh the risks of acute pancreatitis and the "potential" risk of medullary thyroid cancer with treatment. There have been postmarketing reports of pancreatitis associated with exenatide, including nonfatal hemorrhagic or necrotizing pancreatitis.
In rats, extended-release exenatide causes thyroid C-cell tumors at clinically relevant exposures, but at this point, the relevance to humans is not known, according to a boxed warning in the prescribing information. It is contraindicated in people with a personal or family history of medullary thyroid cancer or those with Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
The first once weekly diabetes drug has been approved by the Food and Drug Administration. An extended-release formulation of the type 2 diabetes medication exenatide, a glucagon-like peptide-1 (GLP-1) receptor, was approved on Jan. 27, the manufacturer announced.
The formulation, called Bydureon, is administered once a week in a subcutaneous injection, and is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes. The regular formulation of exenatide (Byetta), approved in 2005, is administered twice a day.
Approval was based on the results of the DURATION-5 study, which compared treatment with the two formulations in 252 patients with type 2 diabetes and inadequate glycemic control (mean baseline hemoglobin A1c was 8.4%) with diet and exercise alone or with oral therapy, including metformin, a sulfonylurea, a thiazolidinedione, or a combination of two of these treatments.
The mean reduction in HbA1c was 1.6 percentage points among those treated with 2 mg of extended-release exenatide once weekly, compared with a mean reduction of 0.9 percentage points among those treated with the regular form of exenatide (starting at 5 mcg twice daily increasing to 10 mcg twice daily after 4 weeks), a statistically significant difference, according to the prescribing information and the press release.
Extended-release exenatide has been approved with a Risk Evaluation and Mitigation Strategy (REMS), to ensure that the benefits of the drug outweigh the risks of acute pancreatitis and the "potential" risk of medullary thyroid cancer with treatment. There have been postmarketing reports of pancreatitis associated with exenatide, including nonfatal hemorrhagic or necrotizing pancreatitis.
In rats, extended-release exenatide causes thyroid C-cell tumors at clinically relevant exposures, but at this point, the relevance to humans is not known, according to a boxed warning in the prescribing information. It is contraindicated in people with a personal or family history of medullary thyroid cancer or those with Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
The first once weekly diabetes drug has been approved by the Food and Drug Administration. An extended-release formulation of the type 2 diabetes medication exenatide, a glucagon-like peptide-1 (GLP-1) receptor, was approved on Jan. 27, the manufacturer announced.
The formulation, called Bydureon, is administered once a week in a subcutaneous injection, and is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes. The regular formulation of exenatide (Byetta), approved in 2005, is administered twice a day.
Approval was based on the results of the DURATION-5 study, which compared treatment with the two formulations in 252 patients with type 2 diabetes and inadequate glycemic control (mean baseline hemoglobin A1c was 8.4%) with diet and exercise alone or with oral therapy, including metformin, a sulfonylurea, a thiazolidinedione, or a combination of two of these treatments.
The mean reduction in HbA1c was 1.6 percentage points among those treated with 2 mg of extended-release exenatide once weekly, compared with a mean reduction of 0.9 percentage points among those treated with the regular form of exenatide (starting at 5 mcg twice daily increasing to 10 mcg twice daily after 4 weeks), a statistically significant difference, according to the prescribing information and the press release.
Extended-release exenatide has been approved with a Risk Evaluation and Mitigation Strategy (REMS), to ensure that the benefits of the drug outweigh the risks of acute pancreatitis and the "potential" risk of medullary thyroid cancer with treatment. There have been postmarketing reports of pancreatitis associated with exenatide, including nonfatal hemorrhagic or necrotizing pancreatitis.
In rats, extended-release exenatide causes thyroid C-cell tumors at clinically relevant exposures, but at this point, the relevance to humans is not known, according to a boxed warning in the prescribing information. It is contraindicated in people with a personal or family history of medullary thyroid cancer or those with Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
Study: Booster Seat Use During Carpooling Inconsistent
Only 55% of parents with children aged 4-8 years always have their child use a car booster seat when driving with other children in the car, according to a study published Jan. 30 in Pediatrics.
The researchers surveyed 681 parents with 4- to 8-year-old children to ask about their safety seat practices, especially when carpooling. They found that most parents – 76% – reported using a booster seat when riding in the family car.
However, among the 64% of parents who carpool, 45% said they do not always have their child use their booster seat when driving with friends who don’t have boosters. "These findings suggest that social norms and self-efficacy for booster seat use may be influential in carpooling situations," wrote Dr. Michelle L. Macy of the University of Michigan, Ann Arbor, and her associates (Pediatrics 2012;129:290-98).
Still, 54% of parents who frequently carpool said they would always ask another driver to use a booster seat for their child; that percentage rose to 64% in parents who occasionally carpool. In addition, parents who occasionally carpool were significantly more likely than were parents who carpool frequently to report their child always uses a booster seat, they found.
Physician should ask not just about use of size-appropriate child safety seats during office visits, but also whether parents consistently use them for their children and if there are any barriers to their use, such as perceived difficulty making arrangements to have booster seats available for other people’s children or problems transferring child safety seats between vehicles, Dr. Macy and her colleagues said.
Dr. Macy and her associates said they had no relevant financial disclosures. This research was conducted as part of the C.S. Mott Children’s Hospital National Poll on Children’s Health, sponsored by the department of pediatrics and communicable diseases at the University of Michigan and the University of Michigan Health System. The study was funded by a grant from the Michigan Center for Advancing Safe Transportation Throughout the Lifespan.
Only 55% of parents with children aged 4-8 years always have their child use a car booster seat when driving with other children in the car, according to a study published Jan. 30 in Pediatrics.
The researchers surveyed 681 parents with 4- to 8-year-old children to ask about their safety seat practices, especially when carpooling. They found that most parents – 76% – reported using a booster seat when riding in the family car.
However, among the 64% of parents who carpool, 45% said they do not always have their child use their booster seat when driving with friends who don’t have boosters. "These findings suggest that social norms and self-efficacy for booster seat use may be influential in carpooling situations," wrote Dr. Michelle L. Macy of the University of Michigan, Ann Arbor, and her associates (Pediatrics 2012;129:290-98).
Still, 54% of parents who frequently carpool said they would always ask another driver to use a booster seat for their child; that percentage rose to 64% in parents who occasionally carpool. In addition, parents who occasionally carpool were significantly more likely than were parents who carpool frequently to report their child always uses a booster seat, they found.
Physician should ask not just about use of size-appropriate child safety seats during office visits, but also whether parents consistently use them for their children and if there are any barriers to their use, such as perceived difficulty making arrangements to have booster seats available for other people’s children or problems transferring child safety seats between vehicles, Dr. Macy and her colleagues said.
Dr. Macy and her associates said they had no relevant financial disclosures. This research was conducted as part of the C.S. Mott Children’s Hospital National Poll on Children’s Health, sponsored by the department of pediatrics and communicable diseases at the University of Michigan and the University of Michigan Health System. The study was funded by a grant from the Michigan Center for Advancing Safe Transportation Throughout the Lifespan.
Only 55% of parents with children aged 4-8 years always have their child use a car booster seat when driving with other children in the car, according to a study published Jan. 30 in Pediatrics.
The researchers surveyed 681 parents with 4- to 8-year-old children to ask about their safety seat practices, especially when carpooling. They found that most parents – 76% – reported using a booster seat when riding in the family car.
However, among the 64% of parents who carpool, 45% said they do not always have their child use their booster seat when driving with friends who don’t have boosters. "These findings suggest that social norms and self-efficacy for booster seat use may be influential in carpooling situations," wrote Dr. Michelle L. Macy of the University of Michigan, Ann Arbor, and her associates (Pediatrics 2012;129:290-98).
Still, 54% of parents who frequently carpool said they would always ask another driver to use a booster seat for their child; that percentage rose to 64% in parents who occasionally carpool. In addition, parents who occasionally carpool were significantly more likely than were parents who carpool frequently to report their child always uses a booster seat, they found.
Physician should ask not just about use of size-appropriate child safety seats during office visits, but also whether parents consistently use them for their children and if there are any barriers to their use, such as perceived difficulty making arrangements to have booster seats available for other people’s children or problems transferring child safety seats between vehicles, Dr. Macy and her colleagues said.
Dr. Macy and her associates said they had no relevant financial disclosures. This research was conducted as part of the C.S. Mott Children’s Hospital National Poll on Children’s Health, sponsored by the department of pediatrics and communicable diseases at the University of Michigan and the University of Michigan Health System. The study was funded by a grant from the Michigan Center for Advancing Safe Transportation Throughout the Lifespan.
FROM PEDIATRICS
Major Finding: Only 55% of parents with children aged 4-8 years always have their child use a booster seat when carpooling.
Data Source: Cross-sectional Web-based survey of 681 U.S. parents.
Disclosures: Dr. Macy and her associates said they had no relevant financial disclosures. This research was conducted as part of the C.S. Mott Children’s Hospital National Poll on Children Health, sponsored by the department of pediatrics and communicable diseases at the University of Michigan and the University of Michigan Health System. The study was funded by a grant from the Michigan Center for Advancing Safe Transportation Throughout the Lifespan.
Vytorin Falls Short of New Indication for CKD Patients
The Food and Drug Administration approved a revised label for Vytorin that now includes data from a study showing a benefit of treatment in patients with moderate to severe kidney disease, but the agency did not approve a new indication that reflects these findings for Vytorin or for ezetemibe, one of the components of the combination product, according to Merck.
In a Jan. 25 press release, Merck, the manufacturer of ezetimibe (Zetia) and Vytorin – a combination of ezetimibe and simvastatin – said that the FDA had approved the new labeling that now includes data from the Study of Heart and Renal Protection (SHARP). Themultinational, randomized, double-blind placebo controlled study of almost 9,500 patients with moderate to severe chronic kidney disease who did not have a history of myocardial infarction or coronary revascularization found that the lipid-lowering treatment reduced the risk of major vascular events, compared with placebo.
However, the FDA did not approve a new indication to reflect these results, because SHARP compared the combination of the two drugs with placebo and "was not designed to assess the independent contributions of each drug to the observed effect," the Merck release said, adding: "For this reason, the FDA did not approve a new indication for Vytorin or for Zetia," and the SHARP results have not been added to the ezetimibe label.
This was despite the unanimous recommendation of the FDA’s Endocrinologic and Metabolic Drugs Advisory Committee in November to approve Vytorin for reducing major cardiovascular events in patients with CKD who are not on dialysis. The panel also voted 10-6 that the data did not support approval of the combination for the same indication in patients with end-stage renal disease who are on dialysis.
Merck had filed for approval of the claim that 10 mg of ezetimibe plus 20 mg of simvastatin (in the fixed-dose combination pill or taken separately) reduces the risk of major cardiovascular events in patients with chronic kidney disease on the basis of the SHARP results.
About two-thirds of the patients enrolled in SHARP were not on dialysis at baseline, and in these patients, there was a 23% reduction in the primary end point – the risk of a major vascular event (nonfatal MI or cardiac death, stroke, or a revascularization procedure that excluded dialysis access–related procedures) – compared with those on placebo over a mean of 5 years (Lancet 2011;377:2181-92).
Among the patients who were on dialysis at baseline, the risk reduction was less (about 6% over placebo).
The two drugs remain approved for lipid-lowering indications only: Ezetimibe, a selective inhibitor of the absorption of intestinal cholesterol and related phytosterol, was approved in 2002; Vytorin, a combination of ezetimibe and the HMG-CoA reductase inhibitor simvastatin was approved in 2004; simvastatin was approved in 1991.
In an interview, Dr. William Hiatt, one of the members of the FDA panel that reviewed the SHARP data, said that "by allowing Merck to add the information from the SHARP trial to the product label, physicians will be able to use that information to help guide their decisions to use this medication for their CKD patients." Dr. Hiatt is professor of medicine, division of cardiology, University of Colorado, Denver. Members of FDA advisory panels are cleared of potential conflicts related to the topic of the meeting.
The agency usually follows FDA panel recommendations, which are not binding. At press time, no statement was available from the FDA to explain the decision.
SHARP was funded by Merck and Schering-Plough, but was independently conducted by the Oxford (England) University Clinical Trials Service Unit.
The Food and Drug Administration approved a revised label for Vytorin that now includes data from a study showing a benefit of treatment in patients with moderate to severe kidney disease, but the agency did not approve a new indication that reflects these findings for Vytorin or for ezetemibe, one of the components of the combination product, according to Merck.
In a Jan. 25 press release, Merck, the manufacturer of ezetimibe (Zetia) and Vytorin – a combination of ezetimibe and simvastatin – said that the FDA had approved the new labeling that now includes data from the Study of Heart and Renal Protection (SHARP). Themultinational, randomized, double-blind placebo controlled study of almost 9,500 patients with moderate to severe chronic kidney disease who did not have a history of myocardial infarction or coronary revascularization found that the lipid-lowering treatment reduced the risk of major vascular events, compared with placebo.
However, the FDA did not approve a new indication to reflect these results, because SHARP compared the combination of the two drugs with placebo and "was not designed to assess the independent contributions of each drug to the observed effect," the Merck release said, adding: "For this reason, the FDA did not approve a new indication for Vytorin or for Zetia," and the SHARP results have not been added to the ezetimibe label.
This was despite the unanimous recommendation of the FDA’s Endocrinologic and Metabolic Drugs Advisory Committee in November to approve Vytorin for reducing major cardiovascular events in patients with CKD who are not on dialysis. The panel also voted 10-6 that the data did not support approval of the combination for the same indication in patients with end-stage renal disease who are on dialysis.
Merck had filed for approval of the claim that 10 mg of ezetimibe plus 20 mg of simvastatin (in the fixed-dose combination pill or taken separately) reduces the risk of major cardiovascular events in patients with chronic kidney disease on the basis of the SHARP results.
About two-thirds of the patients enrolled in SHARP were not on dialysis at baseline, and in these patients, there was a 23% reduction in the primary end point – the risk of a major vascular event (nonfatal MI or cardiac death, stroke, or a revascularization procedure that excluded dialysis access–related procedures) – compared with those on placebo over a mean of 5 years (Lancet 2011;377:2181-92).
Among the patients who were on dialysis at baseline, the risk reduction was less (about 6% over placebo).
The two drugs remain approved for lipid-lowering indications only: Ezetimibe, a selective inhibitor of the absorption of intestinal cholesterol and related phytosterol, was approved in 2002; Vytorin, a combination of ezetimibe and the HMG-CoA reductase inhibitor simvastatin was approved in 2004; simvastatin was approved in 1991.
In an interview, Dr. William Hiatt, one of the members of the FDA panel that reviewed the SHARP data, said that "by allowing Merck to add the information from the SHARP trial to the product label, physicians will be able to use that information to help guide their decisions to use this medication for their CKD patients." Dr. Hiatt is professor of medicine, division of cardiology, University of Colorado, Denver. Members of FDA advisory panels are cleared of potential conflicts related to the topic of the meeting.
The agency usually follows FDA panel recommendations, which are not binding. At press time, no statement was available from the FDA to explain the decision.
SHARP was funded by Merck and Schering-Plough, but was independently conducted by the Oxford (England) University Clinical Trials Service Unit.
The Food and Drug Administration approved a revised label for Vytorin that now includes data from a study showing a benefit of treatment in patients with moderate to severe kidney disease, but the agency did not approve a new indication that reflects these findings for Vytorin or for ezetemibe, one of the components of the combination product, according to Merck.
In a Jan. 25 press release, Merck, the manufacturer of ezetimibe (Zetia) and Vytorin – a combination of ezetimibe and simvastatin – said that the FDA had approved the new labeling that now includes data from the Study of Heart and Renal Protection (SHARP). Themultinational, randomized, double-blind placebo controlled study of almost 9,500 patients with moderate to severe chronic kidney disease who did not have a history of myocardial infarction or coronary revascularization found that the lipid-lowering treatment reduced the risk of major vascular events, compared with placebo.
However, the FDA did not approve a new indication to reflect these results, because SHARP compared the combination of the two drugs with placebo and "was not designed to assess the independent contributions of each drug to the observed effect," the Merck release said, adding: "For this reason, the FDA did not approve a new indication for Vytorin or for Zetia," and the SHARP results have not been added to the ezetimibe label.
This was despite the unanimous recommendation of the FDA’s Endocrinologic and Metabolic Drugs Advisory Committee in November to approve Vytorin for reducing major cardiovascular events in patients with CKD who are not on dialysis. The panel also voted 10-6 that the data did not support approval of the combination for the same indication in patients with end-stage renal disease who are on dialysis.
Merck had filed for approval of the claim that 10 mg of ezetimibe plus 20 mg of simvastatin (in the fixed-dose combination pill or taken separately) reduces the risk of major cardiovascular events in patients with chronic kidney disease on the basis of the SHARP results.
About two-thirds of the patients enrolled in SHARP were not on dialysis at baseline, and in these patients, there was a 23% reduction in the primary end point – the risk of a major vascular event (nonfatal MI or cardiac death, stroke, or a revascularization procedure that excluded dialysis access–related procedures) – compared with those on placebo over a mean of 5 years (Lancet 2011;377:2181-92).
Among the patients who were on dialysis at baseline, the risk reduction was less (about 6% over placebo).
The two drugs remain approved for lipid-lowering indications only: Ezetimibe, a selective inhibitor of the absorption of intestinal cholesterol and related phytosterol, was approved in 2002; Vytorin, a combination of ezetimibe and the HMG-CoA reductase inhibitor simvastatin was approved in 2004; simvastatin was approved in 1991.
In an interview, Dr. William Hiatt, one of the members of the FDA panel that reviewed the SHARP data, said that "by allowing Merck to add the information from the SHARP trial to the product label, physicians will be able to use that information to help guide their decisions to use this medication for their CKD patients." Dr. Hiatt is professor of medicine, division of cardiology, University of Colorado, Denver. Members of FDA advisory panels are cleared of potential conflicts related to the topic of the meeting.
The agency usually follows FDA panel recommendations, which are not binding. At press time, no statement was available from the FDA to explain the decision.
SHARP was funded by Merck and Schering-Plough, but was independently conducted by the Oxford (England) University Clinical Trials Service Unit.
Physician Involvement in Hospital Quality and Safety Programs
Should or must? That was the sticking point. After months of hard work, it had come down to this.
In a sense, these words are synonyms. In reality, they are words, and they are worlds apart.
This discourse occurred within a task force I am working with to clinically transform our medical center—that is, making an institutional commitment to quality improvement (QI), patient safety, and clinical efficiency. The effort, in part, is driven by value-based purchasing, public reporting, payment reform, and the like. But mostly it’s being driven by the fundamental premise of doing right by our patients.
We all agreed that we have to change, that it will be hard and even what types of change are needed. The struggle came down to “should” or “must.”
I’ve used several columns imploring hospitalists to lead the quality evolution. I’ve spent less time explaining how to do this. It’s one thing to say, “Hospitalists are perfectly positioned to fundamentally change the quality, safety, and efficiency of hospital care.” It’s another to fundamentally change the quality, safety, and efficiency of hospital care. So, with the disclaimer that my HM group’s efforts to improve quality have only begun to scratch the surface of success, here are some of the lessons I’ve learned.
Start Urgently
Change is very hard for hominids. We favor the devil we know. Therefore, change requires establishing a sense of urgency for the change. Conceptually, QI is enticing—until it gets hard. Then the inevitable changes in workflow start to feel like a lot of work, often without obvious or immediate benefit.
As such, people have to believe there is a problem before they can muster the energy it takes to change. I’d submit to you that the problem with patient safety and quality in healthcare is that most of us don’t think there is a problem.
It takes someone to show us there is a problem before we can change. If you cannot create this sense of urgency for change, you should stop. Don’t continue to try to lead change. You will fail. Guaranteed.
Thus, the most important step in transformation toward quality is convincing people of the need to change. This is hard to do and requires our second step.
Leading The Ship
Leadership. By which I’m not talking about the person in charge, the autocrat, the boss. Leadership is getting people to go somewhere they otherwise wouldn’t have gone. A boss can do this, but most often this is done by the people in the trenches, by front-line people who see a problem and aspire for change, by people like you.
Quality needs leadership; we are its leaders.
20/20 Vision
A vision is the end game; it’s the finish line, that thing we are all striving for. It’s a big, inspirational, audacious goal that we can all rally behind. It’s things like “zero harm” or “no avoidable errors.”
The vision should not be confused with the plan. Plans are great. But plans that don’t tie back to a vision are destined to fail. Why? Because change is hard, and as soon as a plan (e.g. call PCPs on each discharge, reconcile 24 medications in a demented patient) gets hard, people stop doing it.
Show them, however, how the plan (often something they don’t want to do) ties back to the vision (something they want to do), and people are more likely to follow. I’ll put in the extra effort for medication reconciliation (plan) if I believe there is a problem (sense of urgency) and that this plan helps achieve the vision (no avoidable errors).
Have Patience
Administrators rightly want solutions yesterday. But clinical transformation of this type takes time. We will not unfurl the “Mission Accomplished” banner in three months. This will take years, probably a decade. For two reasons:
- This requires culture change, which takes time.
- We need bench strength.
A focus on quality cannot be accomplished with five or even 50 people working on this. Rather, it requires 500 to 5,000 people—indeed, the entire organization. It takes time to change the culture, engage the people, and make the mistakes that success requires.
Make It Easier To Do The Right Thing
We have to remove the barriers that limit success. This means not asking high-paid physicians to do chart abstraction, analyze data, and coordinate meetings—support staff should perform these tasks.
We also need institution- and provider-level data. Without valid and timely provider-level data, it is exceptionally difficult to create the needed sense of urgency for change. Show me I’m not meeting my expectations, and I’ll do what it takes to change. Leave me to believe that I’m the best doctor in the world—as we all are, of course—and I have no impetus to improve.
Success requires the infrastructure that makes it harder to do the wrong thing and easier to do the right thing.
Show Me The Money
Quality cannot be an unfunded mandate. Infrastructure needs to be built, support staff hired, and physician time protected to devote to this work.
That being said, I’d submit that if after five years an institution doesn’t see a return on investment (in cost avoidance and increased revenue) of at least 5:1 for every dollar spent, then either you’ve built it wrong or we are all misreading the tea leaves in terms of value-based purchasing. I wouldn’t bet on the latter.
Partner With Your Partners
Medicine is a team sport. True success hinges on a multiprofessional approach. Our success will be directly proportional to the degree to which we engage our clinical-care partners.
This is a less autonomous way of thinking than most of us were taught. We studied alone, took tests alone, saw patients alone. To engage nurses, therapists, pharmacists, and hospital administrators in a dynamic team is outside most of our comfort zones.
Culturing Change
We cannot mend our broken system until we begin to do things differently. Success demands that we work in teams, partner with our hospital administrators, and agree to be measured. We must better communicate with other providers, reduce variability, forgo some autonomy, and shift from physician- to patient-centric care models. This will be hard. This will be uncomfortable. This will require tough decisions.
Failure or Success
Which brings me back to our task force’s definitional divide. The issue was how strongly we push physician involvement in our quality and safety program. Do we encourage all doctors to participate (doctors “should”), or do we require all doctors to participate (doctors “must”)? The task force was divided.
On the one hand, it’s hard to mandate involvement. This would be a huge physician commitment. It would take a lot of training, time, effort, and money. There would be innumerable challenges, perhaps physician turnover.
Was this a battle worth fighting? The difference between “should” and “must” is quite small. They say nearly the same thing. Except they don’t. “Should” says it’s optional; “must” is a mandate. “Should” says it’d be nice if you’d do this; “must” states it’s an institutional priority.
This distinction is not small. It is the difference between indifference and commitment, between our present and our future, between failure and success.
Dr. Glasheen is physician editor of The Hospitalist.
For more tips on getting quality programs started at your hospital, visit www.hospitalmedicine.org/thecenter.
Should or must? That was the sticking point. After months of hard work, it had come down to this.
In a sense, these words are synonyms. In reality, they are words, and they are worlds apart.
This discourse occurred within a task force I am working with to clinically transform our medical center—that is, making an institutional commitment to quality improvement (QI), patient safety, and clinical efficiency. The effort, in part, is driven by value-based purchasing, public reporting, payment reform, and the like. But mostly it’s being driven by the fundamental premise of doing right by our patients.
We all agreed that we have to change, that it will be hard and even what types of change are needed. The struggle came down to “should” or “must.”
I’ve used several columns imploring hospitalists to lead the quality evolution. I’ve spent less time explaining how to do this. It’s one thing to say, “Hospitalists are perfectly positioned to fundamentally change the quality, safety, and efficiency of hospital care.” It’s another to fundamentally change the quality, safety, and efficiency of hospital care. So, with the disclaimer that my HM group’s efforts to improve quality have only begun to scratch the surface of success, here are some of the lessons I’ve learned.
Start Urgently
Change is very hard for hominids. We favor the devil we know. Therefore, change requires establishing a sense of urgency for the change. Conceptually, QI is enticing—until it gets hard. Then the inevitable changes in workflow start to feel like a lot of work, often without obvious or immediate benefit.
As such, people have to believe there is a problem before they can muster the energy it takes to change. I’d submit to you that the problem with patient safety and quality in healthcare is that most of us don’t think there is a problem.
It takes someone to show us there is a problem before we can change. If you cannot create this sense of urgency for change, you should stop. Don’t continue to try to lead change. You will fail. Guaranteed.
Thus, the most important step in transformation toward quality is convincing people of the need to change. This is hard to do and requires our second step.
Leading The Ship
Leadership. By which I’m not talking about the person in charge, the autocrat, the boss. Leadership is getting people to go somewhere they otherwise wouldn’t have gone. A boss can do this, but most often this is done by the people in the trenches, by front-line people who see a problem and aspire for change, by people like you.
Quality needs leadership; we are its leaders.
20/20 Vision
A vision is the end game; it’s the finish line, that thing we are all striving for. It’s a big, inspirational, audacious goal that we can all rally behind. It’s things like “zero harm” or “no avoidable errors.”
The vision should not be confused with the plan. Plans are great. But plans that don’t tie back to a vision are destined to fail. Why? Because change is hard, and as soon as a plan (e.g. call PCPs on each discharge, reconcile 24 medications in a demented patient) gets hard, people stop doing it.
Show them, however, how the plan (often something they don’t want to do) ties back to the vision (something they want to do), and people are more likely to follow. I’ll put in the extra effort for medication reconciliation (plan) if I believe there is a problem (sense of urgency) and that this plan helps achieve the vision (no avoidable errors).
Have Patience
Administrators rightly want solutions yesterday. But clinical transformation of this type takes time. We will not unfurl the “Mission Accomplished” banner in three months. This will take years, probably a decade. For two reasons:
- This requires culture change, which takes time.
- We need bench strength.
A focus on quality cannot be accomplished with five or even 50 people working on this. Rather, it requires 500 to 5,000 people—indeed, the entire organization. It takes time to change the culture, engage the people, and make the mistakes that success requires.
Make It Easier To Do The Right Thing
We have to remove the barriers that limit success. This means not asking high-paid physicians to do chart abstraction, analyze data, and coordinate meetings—support staff should perform these tasks.
We also need institution- and provider-level data. Without valid and timely provider-level data, it is exceptionally difficult to create the needed sense of urgency for change. Show me I’m not meeting my expectations, and I’ll do what it takes to change. Leave me to believe that I’m the best doctor in the world—as we all are, of course—and I have no impetus to improve.
Success requires the infrastructure that makes it harder to do the wrong thing and easier to do the right thing.
Show Me The Money
Quality cannot be an unfunded mandate. Infrastructure needs to be built, support staff hired, and physician time protected to devote to this work.
That being said, I’d submit that if after five years an institution doesn’t see a return on investment (in cost avoidance and increased revenue) of at least 5:1 for every dollar spent, then either you’ve built it wrong or we are all misreading the tea leaves in terms of value-based purchasing. I wouldn’t bet on the latter.
Partner With Your Partners
Medicine is a team sport. True success hinges on a multiprofessional approach. Our success will be directly proportional to the degree to which we engage our clinical-care partners.
This is a less autonomous way of thinking than most of us were taught. We studied alone, took tests alone, saw patients alone. To engage nurses, therapists, pharmacists, and hospital administrators in a dynamic team is outside most of our comfort zones.
Culturing Change
We cannot mend our broken system until we begin to do things differently. Success demands that we work in teams, partner with our hospital administrators, and agree to be measured. We must better communicate with other providers, reduce variability, forgo some autonomy, and shift from physician- to patient-centric care models. This will be hard. This will be uncomfortable. This will require tough decisions.
Failure or Success
Which brings me back to our task force’s definitional divide. The issue was how strongly we push physician involvement in our quality and safety program. Do we encourage all doctors to participate (doctors “should”), or do we require all doctors to participate (doctors “must”)? The task force was divided.
On the one hand, it’s hard to mandate involvement. This would be a huge physician commitment. It would take a lot of training, time, effort, and money. There would be innumerable challenges, perhaps physician turnover.
Was this a battle worth fighting? The difference between “should” and “must” is quite small. They say nearly the same thing. Except they don’t. “Should” says it’s optional; “must” is a mandate. “Should” says it’d be nice if you’d do this; “must” states it’s an institutional priority.
This distinction is not small. It is the difference between indifference and commitment, between our present and our future, between failure and success.
Dr. Glasheen is physician editor of The Hospitalist.
For more tips on getting quality programs started at your hospital, visit www.hospitalmedicine.org/thecenter.
Should or must? That was the sticking point. After months of hard work, it had come down to this.
In a sense, these words are synonyms. In reality, they are words, and they are worlds apart.
This discourse occurred within a task force I am working with to clinically transform our medical center—that is, making an institutional commitment to quality improvement (QI), patient safety, and clinical efficiency. The effort, in part, is driven by value-based purchasing, public reporting, payment reform, and the like. But mostly it’s being driven by the fundamental premise of doing right by our patients.
We all agreed that we have to change, that it will be hard and even what types of change are needed. The struggle came down to “should” or “must.”
I’ve used several columns imploring hospitalists to lead the quality evolution. I’ve spent less time explaining how to do this. It’s one thing to say, “Hospitalists are perfectly positioned to fundamentally change the quality, safety, and efficiency of hospital care.” It’s another to fundamentally change the quality, safety, and efficiency of hospital care. So, with the disclaimer that my HM group’s efforts to improve quality have only begun to scratch the surface of success, here are some of the lessons I’ve learned.
Start Urgently
Change is very hard for hominids. We favor the devil we know. Therefore, change requires establishing a sense of urgency for the change. Conceptually, QI is enticing—until it gets hard. Then the inevitable changes in workflow start to feel like a lot of work, often without obvious or immediate benefit.
As such, people have to believe there is a problem before they can muster the energy it takes to change. I’d submit to you that the problem with patient safety and quality in healthcare is that most of us don’t think there is a problem.
It takes someone to show us there is a problem before we can change. If you cannot create this sense of urgency for change, you should stop. Don’t continue to try to lead change. You will fail. Guaranteed.
Thus, the most important step in transformation toward quality is convincing people of the need to change. This is hard to do and requires our second step.
Leading The Ship
Leadership. By which I’m not talking about the person in charge, the autocrat, the boss. Leadership is getting people to go somewhere they otherwise wouldn’t have gone. A boss can do this, but most often this is done by the people in the trenches, by front-line people who see a problem and aspire for change, by people like you.
Quality needs leadership; we are its leaders.
20/20 Vision
A vision is the end game; it’s the finish line, that thing we are all striving for. It’s a big, inspirational, audacious goal that we can all rally behind. It’s things like “zero harm” or “no avoidable errors.”
The vision should not be confused with the plan. Plans are great. But plans that don’t tie back to a vision are destined to fail. Why? Because change is hard, and as soon as a plan (e.g. call PCPs on each discharge, reconcile 24 medications in a demented patient) gets hard, people stop doing it.
Show them, however, how the plan (often something they don’t want to do) ties back to the vision (something they want to do), and people are more likely to follow. I’ll put in the extra effort for medication reconciliation (plan) if I believe there is a problem (sense of urgency) and that this plan helps achieve the vision (no avoidable errors).
Have Patience
Administrators rightly want solutions yesterday. But clinical transformation of this type takes time. We will not unfurl the “Mission Accomplished” banner in three months. This will take years, probably a decade. For two reasons:
- This requires culture change, which takes time.
- We need bench strength.
A focus on quality cannot be accomplished with five or even 50 people working on this. Rather, it requires 500 to 5,000 people—indeed, the entire organization. It takes time to change the culture, engage the people, and make the mistakes that success requires.
Make It Easier To Do The Right Thing
We have to remove the barriers that limit success. This means not asking high-paid physicians to do chart abstraction, analyze data, and coordinate meetings—support staff should perform these tasks.
We also need institution- and provider-level data. Without valid and timely provider-level data, it is exceptionally difficult to create the needed sense of urgency for change. Show me I’m not meeting my expectations, and I’ll do what it takes to change. Leave me to believe that I’m the best doctor in the world—as we all are, of course—and I have no impetus to improve.
Success requires the infrastructure that makes it harder to do the wrong thing and easier to do the right thing.
Show Me The Money
Quality cannot be an unfunded mandate. Infrastructure needs to be built, support staff hired, and physician time protected to devote to this work.
That being said, I’d submit that if after five years an institution doesn’t see a return on investment (in cost avoidance and increased revenue) of at least 5:1 for every dollar spent, then either you’ve built it wrong or we are all misreading the tea leaves in terms of value-based purchasing. I wouldn’t bet on the latter.
Partner With Your Partners
Medicine is a team sport. True success hinges on a multiprofessional approach. Our success will be directly proportional to the degree to which we engage our clinical-care partners.
This is a less autonomous way of thinking than most of us were taught. We studied alone, took tests alone, saw patients alone. To engage nurses, therapists, pharmacists, and hospital administrators in a dynamic team is outside most of our comfort zones.
Culturing Change
We cannot mend our broken system until we begin to do things differently. Success demands that we work in teams, partner with our hospital administrators, and agree to be measured. We must better communicate with other providers, reduce variability, forgo some autonomy, and shift from physician- to patient-centric care models. This will be hard. This will be uncomfortable. This will require tough decisions.
Failure or Success
Which brings me back to our task force’s definitional divide. The issue was how strongly we push physician involvement in our quality and safety program. Do we encourage all doctors to participate (doctors “should”), or do we require all doctors to participate (doctors “must”)? The task force was divided.
On the one hand, it’s hard to mandate involvement. This would be a huge physician commitment. It would take a lot of training, time, effort, and money. There would be innumerable challenges, perhaps physician turnover.
Was this a battle worth fighting? The difference between “should” and “must” is quite small. They say nearly the same thing. Except they don’t. “Should” says it’s optional; “must” is a mandate. “Should” says it’d be nice if you’d do this; “must” states it’s an institutional priority.
This distinction is not small. It is the difference between indifference and commitment, between our present and our future, between failure and success.
Dr. Glasheen is physician editor of The Hospitalist.
For more tips on getting quality programs started at your hospital, visit www.hospitalmedicine.org/thecenter.