User login
What Is the Appropriate Use of Antibiotics In Acute Exacerbations of COPD?
Case
A 58-year-old male smoker with moderate chronic obstructive pulmonary disease (COPD) (FEV1 56% predicted) is admitted with an acute exacerbation of COPD for the second time this year. He presented to the ED with increased productive cough and shortness of breath, similar to prior exacerbations. He denies fevers, myalgias, or upper-respiratory symptoms. Physical exam is notable for bilateral inspiratory and expiratory wheezing. His sputum is purulent. He is given continuous nebulizer therapy and one dose of oral prednisone, but his dyspnea and wheezing persist. Chest X-ray does not reveal an infiltrate.
Should this patient be treated with antibiotics and, if so, what regimen is most appropriate?
Overview
Acute exacerbations of COPD (AECOPD) present a major health burden, accounting for more than 2.4% of all hospital admissions and causing significant morbidity, mortality, and costs.1 During 2006 and 2007, COPD mortality in the United States topped 39 deaths per 100,000 people, and more recently, hospital costs related to COPD were expected to exceed $13 billion annually.2 Patients with AECOPD also experience decreased quality of life and faster decline in pulmonary function, further highlighting the need for timely and appropriate treatment.1
Several guidelines have proposed treatment strategies now considered standard of care in AECOPD management.3,4,5,6 These include the use of corticosteroids, bronchodilator agents, and, in select cases, antibiotics. While there is well-established evidence for the use of steroids and bronchodilators in AECOPD, the debate continues over the appropriate use of antibiotics in the treatment of acute exacerbations. There are multiple potential factors leading to AECOPD, including viruses, bacteria, and common pollutants; as such, antibiotic treatment may not be indicated for all patients presenting with exacerbations. Further, the risks of antibiotic treatment—including adverse drug events, selection for drug-resistant bacteria, and associated costs—are not insignificant.
However, bacterial infections do play a role in approximately 50% of patients with AECOPD and, for this population, use of antibiotics may confer important benefits.7
Interestingly, a retrospective cohort study of 84,621 patients admitted for AECOPD demonstrated that 85% of patients received antibiotics at some point during hospitalization.8
Support for Antibiotics
Several randomized trials have compared clinical outcomes in patients with AECOPD who have received antibiotics versus those who received placebos. Most of these had small sample sizes and studied only ββ-lactam and tetracycline antibiotics in an outpatient setting; there are limited data involving inpatients and newer drugs. Nevertheless, antibiotic treatment has been associated with decreased risk of adverse outcomes in AECOPD.
One meta-analysis demonstrated that antibiotics reduced treatment failures by 66% and in-hospital mortality by 78% in the subset of trials involving hospitalized patients.8 Similarly, analysis of a large retrospective cohort of patients hospitalized for AECOPD found a significantly lower risk of treatment failure in antibiotic-treated versus untreated patients.9 Specifically, treated patients had lower rates of in-hospital mortality and readmission for AECOPD and a lower likelihood of requiring subsequent mechanical ventilation during the index hospitalization.
Data also suggest that antibiotic treatment during exacerbations might favorably impact subsequent exacerbations.10 A retrospective study of 18,928 Dutch patients with AECOPD compared outcomes among patients who had received antibiotics (most frequently doxycycline or a penicillin) as part of their therapy to those who did not. The authors demonstrated that the median time to the next exacerbation was significantly longer in the patients receiving antibiotics.10 Further, both mortality and overall risk of developing a subsequent exacerbation were significantly decreased in the antibiotic group, with median follow-up of approximately two years.
Indications for Antibiotics
Clinical symptoms. A landmark study by Anthonisen and colleagues set forth three clinical criteria that have formed the basis for treating AECOPD with antibiotics in subsequent studies and in clinical practice.11 Often referred to as the “cardinal symptoms” of AECOPD, these include increased dyspnea, sputum volume, and sputum purulence. In this study, 173 outpatients with COPD were randomized to a 10-day course of antibiotics or placebo at onset of an exacerbation and followed clinically. The authors found that antibiotic-treated patients were significantly more likely than the placebo group to achieve treatment success, defined as resolution of all exacerbated symptoms within 21 days (68.1% vs. 55.0%, P<0.01).
Importantly, treated patients were also significantly less likely to experience clinical deterioration after 72 hours (9.9% vs. 18.9%, P<0.05). Patients with Type I exacerbations, characterized by all three cardinal symptoms, were most likely to benefit from antibiotic therapy, followed by patients with Type II exacerbations, in whom only two of the symptoms were present. Subsequent studies have suggested that sputum purulence correlates well with the presence of acute bacterial infection and therefore may be a reliable clinical indicator of patients who are likely to benefit from antibiotic therapy.12
Laboratory data. While sputum purulence is associated with bacterial infection, sputum culture is less reliable, as pathogenic bacteria are commonly isolated from patients with both AECOPD and stable COPD. In fact, the prevalence of bacterial colonization in moderate to severe COPD might be as high as 50%.13 Therefore, a positive bacterial sputum culture, in the absence of purulence or other signs of infection, is not recommended as the sole basis for which to prescribe antibiotics.
Serum biomarkers, most notably C-reactive protein (CRP) and procalcitonin, have been studied as a newer approach to identify patients who might benefit from antibiotic therapy for AECOPD. Studies have demonstrated increased CRP levels during AECOPD, particularly in patients with purulent sputum and positive bacterial sputum cultures.12 Procalcitonin is preferentially elevated in bacterial infections.
One randomized, placebo-controlled trial in hospitalized patients with AECOPD demonstrated a significant reduction in antibiotic usage based on low procalcitonin levels, without negatively impacting clinical success rate, hospital mortality, subsequent antibiotic needs, or time to next exacerbation.14 However, due to inconsistent evidence, use of these markers to guide antibiotic administration in AECOPD has not yet been definitively established.14,15 Additionally, these laboratory results are often not available at the point of care, potentially limiting their utility in the decision to initiate antibiotics.
Severity of illness. Severity of illness is an important factor in the decision to treat AECOPD with antibiotics. Patients with advanced, underlying airway obstruction, as measured by FEV1, are more likely to have a bacterial cause of AECOPD.16 Additionally, baseline clinical characteristics including advanced age and comorbid conditions, particularly cardiovascular disease and diabetes, increase the risk of severe exacerbations.17
One meta-analysis of placebo-controlled trials found that patients with severe exacerbations were likely to benefit from antibiotic therapy, while patients with mild or moderate exacerbations had no reduction in treatment failure or mortality rates.18 Patients presenting with acute respiratory failure necessitating intensive care and/or ventilator support (noninvasive or invasive) have also been shown to benefit from antibiotics.19
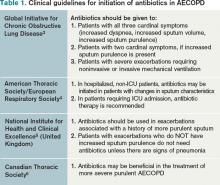
Current clinical guidelines vary slightly in their recommendations regarding when to give antibiotics in AECOPD (see Table 1). However, existing evidence favors antibiotic treatment for those patients presenting with two or three cardinal symptoms, specifically those with increased sputum purulence, and those with severe disease (i.e. pre-existing advanced airflow obstruction and/or exacerbations requiring mechanical ventilation). Conversely, studies have shown that many patients, particularly those with milder exacerbations, experience resolution of symptoms without antibiotic treatment.11,18
Antibiotic Choice in AECOPD
Risk stratification. In patients likely to benefit from antibiotic therapy, an understanding of the relationship between severity of COPD, host risk factors for poor outcomes, and microbiology is paramount to guide clinical decision-making. Historically, such bacteria as Haemophilus influenzae, Streptococcus pneumoniae, and Moraxella catarrhalis have been implicated in the pathogenesis of AECOPD.3,7 In patients with simple exacerbations, antibiotics that target these pathogens should be used (see Table 2).
However, patients with more severe underlying airway obstruction (i.e. FEV1<50%) and risk factors for poor outcomes, specifically recent hospitalization (≥2 days during the previous 90 days), frequent antibiotics (>3 courses during the previous year), and severe exacerbations are more likely to be infected with resistant strains or gram-negative organisms.3,7 Pseudomonas aeruginosa, in particular, is of increasing concern in this population. In patients with complicated exacerbations, more broad-coverage, empiric antibiotics should be initiated (see Table 2).
With this in mind, patients meeting criteria for treatment must first be stratified according to the severity of COPD and risk factors for poor outcomes before a decision regarding a specific antibiotic is reached. Figure 1 outlines a recommended approach for antibiotic administration in AECOPD. The optimal choice of antibiotics must consider cost-effectiveness, local patterns of antibiotic resistance, tissue penetration, patient adherence, and risk of such adverse drug events as diarrhea.
Comparative effectiveness. Current treatment guidelines do not favor the use of any particular antibiotic in simple AECOPD.3,4,5,6 However, as selective pressure has led to in vitro resistance to antibiotics traditionally considered first-line (e.g. doxycycline, trimethoprim/sulfamethoxazole, amoxicillin), the use of second-line antibiotics (e.g. fluoroquinolones, macrolides, cephalosporins, β-lactam/ β-lactamase inhibitors) has increased. Consequently, several studies have compared the effectiveness of different antimicrobial regimens.
One meta-analysis found that second-line antibiotics, when compared with first-line agents, provided greater clinical improvement to patients with AECOPD, without significant differences in mortality, microbiologic eradication, or incidence of adverse drug events.20 Among the subgroup of trials enrolling hospitalized patients, the clinical effectiveness of second-line agents remained significantly greater than that of first-line agents.
Another meta-analysis compared trials that studied only macrolides, quinolones, and amoxicillin-clavulanate and found no difference in terms of short-term clinical effectiveness; however, there was weak evidence to suggest that quinolones were associated with better microbiological success and fewer recurrences of AECOPD.21 Fluoroquinolones are preferred in complicated cases of AECOPD in which there is a greater risk for enterobacteriaceae and Pseudomonas species.3,7
Antibiotic Duration
The duration of antibiotic therapy in AECOPD has been studied extensively, with randomized controlled trials consistently demonstrating no additional benefit to courses extending beyond five days. One meta-analysis of 21 studies found similar clinical and microbiologic cure rates among patients randomized to antibiotic treatment for ≤5 days versus >5 days.22 A subgroup analysis of the trials evaluating different durations of the same antibiotic also demonstrated no difference in clinical effectiveness, and this finding was confirmed in a separate meta-analysis.22,23
Advantages to shorter antibiotic courses include improved compliance and decreased rates of resistance. The usual duration of antibiotic therapy is three to seven days, depending upon the response to therapy.3
Back to the Case
As the patient has no significant comorbidities or risk factors, and meets criteria for a simple Anthonisen Type I exacerbation (increased dyspnea, sputum, and sputum purulence), antibiotic therapy with trimethoprim/sulfamethoxazole is initiated on admission, in addition to the previously started steroid and bronchodilator treatments. The patient’s clinical status improves, and he is discharged on hospital Day 3 with a prescription to complete a five-day course of antibiotics.
Bottom Line
Antibiotic therapy is effective in select AECOPD patients, with maximal benefits obtained when the decision to treat is based on careful consideration of characteristic clinical symptoms and severity of illness. Choice and duration of antibiotics should follow likely bacterial causes and current guidelines.
Dr. Cunningham is an assistant professor of internal medicine and academic hospitalist in the section of hospital medicine at Vanderbilt University School of Medicine in Nashville, Tenn. Dr. LaBrin is assistant professor of internal medicine and pediatrics and an academic hospitalist at Vanderbilt. Dr. Markley is a clinical instructor and academic hospitalist at Vanderbilt.
References
- Donaldson GC, Wedzicha JA. COPD exacerbations: 1. Epidemiology. Thorax. 2006;61:164-168.
- National Heart, Lung, and Blood Institute. 2009 NHLBI Morbidity and Mortality Chartbook. National Heart, Lung, and Blood Institute website. Available at: http://www.nhlbi.nih.gov/resources/docs/cht-book.htm Accessed Oct. 10, 2011.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease. Global Initiative for Chronic Obstructive Lung Disease (GOLD) website. Available at: www.goldcopd.org/guidelines-resources.html Accessed Oct. 10, 2011.
- Celli BR, MacNee W, Agusti A, et al. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Resp J. 2004;23:932-946.
- National Clinical Guideline Centre. Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care. National Institute for Health and Clinical Excellence website. Available at: http://guidance.nice.org.uk/CG101/Guidance/pdf/English. Accessed Oct. 10, 2011.
- O’Donnell DE, Aaron S, Bourbeau J, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease—2007 update. Can Respir J. 2007;14(Suppl B):5B-32B.
- Sethi S, Murphy TF. Infection in the pathogenesis and course of chronic obstructive pulmonary disease. N Engl J Med. 2008;359:2355-2565.
- Quon BS, Qi Gan W, Sin DD. Contemporary management of acute exacerbations of COPD: a systematic review and metaanalysis. Chest. 2008;133:756-766.
- Rothberg MB, Pekow PS, Lahti M, Brody O, Skiest DJ, Lindenauer PK. Antibiotic therapy and treatment failure in patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease. JAMA. 2010;303:2035-2042.
- Roede BM, Bresser P, Bindels PJE, et al. Antibiotic treatment is associated with reduced risk of subsequent exacerbation in obstructive lung disease: a historical population based cohort study. Thorax. 2008;63:968-973.
- Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GKM, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106:196-204.
- Stockley RA, O’Brien C, Pye A, Hill SL. Relationship of sputum color to nature and outpatient management of acute exacerbations of COPD. Chest. 2000;117:1638-1645.
- Rosell A, Monso E, Soler N, et al. Microbiologic determinants of exacerbation in chronic obstructive pulmonary disease. Arch Intern Med. 2005; 165:891-897.
- Stolz D, Christ-Crain M, Bingisser R, et al. Antibiotic treatment of exacerbations of COPD: a randomized, controlled trial comparing procalcitonin-guidance with standard therapy. Chest. 2007;131:9-19.
- Daniels JMA, Schoorl M, Snijders D, et al. Procalcitonin vs C-reactive protein as predictive markers of response to antibiotic therapy in acute exacerbations of COPD. Chest. 2010;138:1108-1015.
- Miravitlles M, Espinosa C, Fernandez-Laso E, Martos JA, Maldonado JA, Gallego M. Relationship between bacterial flora in sputum and functional impairment in patients with acute exacerbations of COPD. Chest. 1999;116:40-46.
- Patil SP, Krishnan JA, Lechtzin N, Diette GB. In-hospital mortality following acute exacerbations of chronic obstructive pulmonary disease. Arch Intern Med. 2003;163:1180-1186.
- Puhan MA, Vollenweider D, Latshang T, Steurer J, Steurer-Stey C. Exacerbations of chronic obstructive lung disease: when are antibiotics indicated? A systematic review. Resp Res. 2007;8:30-40.
- Nouira S, Marghli S, Belghith M, Besbes L, Elatrous S, Abroug F. Once daily ofloxacin in chronic obstructive pulmonary disease exacerbation requiring mechanical ventilation: a randomized placebo-controlled trial. Lancet. 2001;358:2020-2025.
- Dimopoulos G, Siempos II, Korbila IP, Manta KG, Falagas ME. Comparison of first-line with second-line antibiotics for acute exacerbations of chronic bronchitis: a metaanalysis of randomized controlled trials. Chest. 2007;132:447-455.
- Siempos II, Dimopoulos G, Korbila IP, Manta KG, Falagas ME. Macrolides, quinolones and amoxicillin/clavulanate for chronic bronchitis: a meta-analysis. Eur Resp J. 2007;29:1127-1137.
- El-Moussaoui, Roede BM, Speelman P, Bresser P, Prins JM, Bossuyt PMM. Short-course antibiotic treatment in acute exacerbations of chronic bronchitis and COPD: a meta-analysis of double-blind studies. Thorax. 2008;63:415-422.
- Falagas ME, Avgeri SG, Matthaiou DK, Dimopoulos G, Siempos II. Short- versus long-duration antimicrobial treatment for exacerbations of chronic bronchitis: a meta-analysis. J Antimicrob Chemother. 2008;62:442-450.
Case
A 58-year-old male smoker with moderate chronic obstructive pulmonary disease (COPD) (FEV1 56% predicted) is admitted with an acute exacerbation of COPD for the second time this year. He presented to the ED with increased productive cough and shortness of breath, similar to prior exacerbations. He denies fevers, myalgias, or upper-respiratory symptoms. Physical exam is notable for bilateral inspiratory and expiratory wheezing. His sputum is purulent. He is given continuous nebulizer therapy and one dose of oral prednisone, but his dyspnea and wheezing persist. Chest X-ray does not reveal an infiltrate.
Should this patient be treated with antibiotics and, if so, what regimen is most appropriate?
Overview
Acute exacerbations of COPD (AECOPD) present a major health burden, accounting for more than 2.4% of all hospital admissions and causing significant morbidity, mortality, and costs.1 During 2006 and 2007, COPD mortality in the United States topped 39 deaths per 100,000 people, and more recently, hospital costs related to COPD were expected to exceed $13 billion annually.2 Patients with AECOPD also experience decreased quality of life and faster decline in pulmonary function, further highlighting the need for timely and appropriate treatment.1
Several guidelines have proposed treatment strategies now considered standard of care in AECOPD management.3,4,5,6 These include the use of corticosteroids, bronchodilator agents, and, in select cases, antibiotics. While there is well-established evidence for the use of steroids and bronchodilators in AECOPD, the debate continues over the appropriate use of antibiotics in the treatment of acute exacerbations. There are multiple potential factors leading to AECOPD, including viruses, bacteria, and common pollutants; as such, antibiotic treatment may not be indicated for all patients presenting with exacerbations. Further, the risks of antibiotic treatment—including adverse drug events, selection for drug-resistant bacteria, and associated costs—are not insignificant.
However, bacterial infections do play a role in approximately 50% of patients with AECOPD and, for this population, use of antibiotics may confer important benefits.7
Interestingly, a retrospective cohort study of 84,621 patients admitted for AECOPD demonstrated that 85% of patients received antibiotics at some point during hospitalization.8
Support for Antibiotics
Several randomized trials have compared clinical outcomes in patients with AECOPD who have received antibiotics versus those who received placebos. Most of these had small sample sizes and studied only ββ-lactam and tetracycline antibiotics in an outpatient setting; there are limited data involving inpatients and newer drugs. Nevertheless, antibiotic treatment has been associated with decreased risk of adverse outcomes in AECOPD.
One meta-analysis demonstrated that antibiotics reduced treatment failures by 66% and in-hospital mortality by 78% in the subset of trials involving hospitalized patients.8 Similarly, analysis of a large retrospective cohort of patients hospitalized for AECOPD found a significantly lower risk of treatment failure in antibiotic-treated versus untreated patients.9 Specifically, treated patients had lower rates of in-hospital mortality and readmission for AECOPD and a lower likelihood of requiring subsequent mechanical ventilation during the index hospitalization.
Data also suggest that antibiotic treatment during exacerbations might favorably impact subsequent exacerbations.10 A retrospective study of 18,928 Dutch patients with AECOPD compared outcomes among patients who had received antibiotics (most frequently doxycycline or a penicillin) as part of their therapy to those who did not. The authors demonstrated that the median time to the next exacerbation was significantly longer in the patients receiving antibiotics.10 Further, both mortality and overall risk of developing a subsequent exacerbation were significantly decreased in the antibiotic group, with median follow-up of approximately two years.
Indications for Antibiotics
Clinical symptoms. A landmark study by Anthonisen and colleagues set forth three clinical criteria that have formed the basis for treating AECOPD with antibiotics in subsequent studies and in clinical practice.11 Often referred to as the “cardinal symptoms” of AECOPD, these include increased dyspnea, sputum volume, and sputum purulence. In this study, 173 outpatients with COPD were randomized to a 10-day course of antibiotics or placebo at onset of an exacerbation and followed clinically. The authors found that antibiotic-treated patients were significantly more likely than the placebo group to achieve treatment success, defined as resolution of all exacerbated symptoms within 21 days (68.1% vs. 55.0%, P<0.01).
Importantly, treated patients were also significantly less likely to experience clinical deterioration after 72 hours (9.9% vs. 18.9%, P<0.05). Patients with Type I exacerbations, characterized by all three cardinal symptoms, were most likely to benefit from antibiotic therapy, followed by patients with Type II exacerbations, in whom only two of the symptoms were present. Subsequent studies have suggested that sputum purulence correlates well with the presence of acute bacterial infection and therefore may be a reliable clinical indicator of patients who are likely to benefit from antibiotic therapy.12
Laboratory data. While sputum purulence is associated with bacterial infection, sputum culture is less reliable, as pathogenic bacteria are commonly isolated from patients with both AECOPD and stable COPD. In fact, the prevalence of bacterial colonization in moderate to severe COPD might be as high as 50%.13 Therefore, a positive bacterial sputum culture, in the absence of purulence or other signs of infection, is not recommended as the sole basis for which to prescribe antibiotics.
Serum biomarkers, most notably C-reactive protein (CRP) and procalcitonin, have been studied as a newer approach to identify patients who might benefit from antibiotic therapy for AECOPD. Studies have demonstrated increased CRP levels during AECOPD, particularly in patients with purulent sputum and positive bacterial sputum cultures.12 Procalcitonin is preferentially elevated in bacterial infections.
One randomized, placebo-controlled trial in hospitalized patients with AECOPD demonstrated a significant reduction in antibiotic usage based on low procalcitonin levels, without negatively impacting clinical success rate, hospital mortality, subsequent antibiotic needs, or time to next exacerbation.14 However, due to inconsistent evidence, use of these markers to guide antibiotic administration in AECOPD has not yet been definitively established.14,15 Additionally, these laboratory results are often not available at the point of care, potentially limiting their utility in the decision to initiate antibiotics.
Severity of illness. Severity of illness is an important factor in the decision to treat AECOPD with antibiotics. Patients with advanced, underlying airway obstruction, as measured by FEV1, are more likely to have a bacterial cause of AECOPD.16 Additionally, baseline clinical characteristics including advanced age and comorbid conditions, particularly cardiovascular disease and diabetes, increase the risk of severe exacerbations.17
One meta-analysis of placebo-controlled trials found that patients with severe exacerbations were likely to benefit from antibiotic therapy, while patients with mild or moderate exacerbations had no reduction in treatment failure or mortality rates.18 Patients presenting with acute respiratory failure necessitating intensive care and/or ventilator support (noninvasive or invasive) have also been shown to benefit from antibiotics.19
Current clinical guidelines vary slightly in their recommendations regarding when to give antibiotics in AECOPD (see Table 1). However, existing evidence favors antibiotic treatment for those patients presenting with two or three cardinal symptoms, specifically those with increased sputum purulence, and those with severe disease (i.e. pre-existing advanced airflow obstruction and/or exacerbations requiring mechanical ventilation). Conversely, studies have shown that many patients, particularly those with milder exacerbations, experience resolution of symptoms without antibiotic treatment.11,18
Antibiotic Choice in AECOPD
Risk stratification. In patients likely to benefit from antibiotic therapy, an understanding of the relationship between severity of COPD, host risk factors for poor outcomes, and microbiology is paramount to guide clinical decision-making. Historically, such bacteria as Haemophilus influenzae, Streptococcus pneumoniae, and Moraxella catarrhalis have been implicated in the pathogenesis of AECOPD.3,7 In patients with simple exacerbations, antibiotics that target these pathogens should be used (see Table 2).
However, patients with more severe underlying airway obstruction (i.e. FEV1<50%) and risk factors for poor outcomes, specifically recent hospitalization (≥2 days during the previous 90 days), frequent antibiotics (>3 courses during the previous year), and severe exacerbations are more likely to be infected with resistant strains or gram-negative organisms.3,7 Pseudomonas aeruginosa, in particular, is of increasing concern in this population. In patients with complicated exacerbations, more broad-coverage, empiric antibiotics should be initiated (see Table 2).
With this in mind, patients meeting criteria for treatment must first be stratified according to the severity of COPD and risk factors for poor outcomes before a decision regarding a specific antibiotic is reached. Figure 1 outlines a recommended approach for antibiotic administration in AECOPD. The optimal choice of antibiotics must consider cost-effectiveness, local patterns of antibiotic resistance, tissue penetration, patient adherence, and risk of such adverse drug events as diarrhea.
Comparative effectiveness. Current treatment guidelines do not favor the use of any particular antibiotic in simple AECOPD.3,4,5,6 However, as selective pressure has led to in vitro resistance to antibiotics traditionally considered first-line (e.g. doxycycline, trimethoprim/sulfamethoxazole, amoxicillin), the use of second-line antibiotics (e.g. fluoroquinolones, macrolides, cephalosporins, β-lactam/ β-lactamase inhibitors) has increased. Consequently, several studies have compared the effectiveness of different antimicrobial regimens.
One meta-analysis found that second-line antibiotics, when compared with first-line agents, provided greater clinical improvement to patients with AECOPD, without significant differences in mortality, microbiologic eradication, or incidence of adverse drug events.20 Among the subgroup of trials enrolling hospitalized patients, the clinical effectiveness of second-line agents remained significantly greater than that of first-line agents.
Another meta-analysis compared trials that studied only macrolides, quinolones, and amoxicillin-clavulanate and found no difference in terms of short-term clinical effectiveness; however, there was weak evidence to suggest that quinolones were associated with better microbiological success and fewer recurrences of AECOPD.21 Fluoroquinolones are preferred in complicated cases of AECOPD in which there is a greater risk for enterobacteriaceae and Pseudomonas species.3,7
Antibiotic Duration
The duration of antibiotic therapy in AECOPD has been studied extensively, with randomized controlled trials consistently demonstrating no additional benefit to courses extending beyond five days. One meta-analysis of 21 studies found similar clinical and microbiologic cure rates among patients randomized to antibiotic treatment for ≤5 days versus >5 days.22 A subgroup analysis of the trials evaluating different durations of the same antibiotic also demonstrated no difference in clinical effectiveness, and this finding was confirmed in a separate meta-analysis.22,23
Advantages to shorter antibiotic courses include improved compliance and decreased rates of resistance. The usual duration of antibiotic therapy is three to seven days, depending upon the response to therapy.3
Back to the Case
As the patient has no significant comorbidities or risk factors, and meets criteria for a simple Anthonisen Type I exacerbation (increased dyspnea, sputum, and sputum purulence), antibiotic therapy with trimethoprim/sulfamethoxazole is initiated on admission, in addition to the previously started steroid and bronchodilator treatments. The patient’s clinical status improves, and he is discharged on hospital Day 3 with a prescription to complete a five-day course of antibiotics.
Bottom Line
Antibiotic therapy is effective in select AECOPD patients, with maximal benefits obtained when the decision to treat is based on careful consideration of characteristic clinical symptoms and severity of illness. Choice and duration of antibiotics should follow likely bacterial causes and current guidelines.
Dr. Cunningham is an assistant professor of internal medicine and academic hospitalist in the section of hospital medicine at Vanderbilt University School of Medicine in Nashville, Tenn. Dr. LaBrin is assistant professor of internal medicine and pediatrics and an academic hospitalist at Vanderbilt. Dr. Markley is a clinical instructor and academic hospitalist at Vanderbilt.
References
- Donaldson GC, Wedzicha JA. COPD exacerbations: 1. Epidemiology. Thorax. 2006;61:164-168.
- National Heart, Lung, and Blood Institute. 2009 NHLBI Morbidity and Mortality Chartbook. National Heart, Lung, and Blood Institute website. Available at: http://www.nhlbi.nih.gov/resources/docs/cht-book.htm Accessed Oct. 10, 2011.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease. Global Initiative for Chronic Obstructive Lung Disease (GOLD) website. Available at: www.goldcopd.org/guidelines-resources.html Accessed Oct. 10, 2011.
- Celli BR, MacNee W, Agusti A, et al. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Resp J. 2004;23:932-946.
- National Clinical Guideline Centre. Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care. National Institute for Health and Clinical Excellence website. Available at: http://guidance.nice.org.uk/CG101/Guidance/pdf/English. Accessed Oct. 10, 2011.
- O’Donnell DE, Aaron S, Bourbeau J, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease—2007 update. Can Respir J. 2007;14(Suppl B):5B-32B.
- Sethi S, Murphy TF. Infection in the pathogenesis and course of chronic obstructive pulmonary disease. N Engl J Med. 2008;359:2355-2565.
- Quon BS, Qi Gan W, Sin DD. Contemporary management of acute exacerbations of COPD: a systematic review and metaanalysis. Chest. 2008;133:756-766.
- Rothberg MB, Pekow PS, Lahti M, Brody O, Skiest DJ, Lindenauer PK. Antibiotic therapy and treatment failure in patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease. JAMA. 2010;303:2035-2042.
- Roede BM, Bresser P, Bindels PJE, et al. Antibiotic treatment is associated with reduced risk of subsequent exacerbation in obstructive lung disease: a historical population based cohort study. Thorax. 2008;63:968-973.
- Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GKM, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106:196-204.
- Stockley RA, O’Brien C, Pye A, Hill SL. Relationship of sputum color to nature and outpatient management of acute exacerbations of COPD. Chest. 2000;117:1638-1645.
- Rosell A, Monso E, Soler N, et al. Microbiologic determinants of exacerbation in chronic obstructive pulmonary disease. Arch Intern Med. 2005; 165:891-897.
- Stolz D, Christ-Crain M, Bingisser R, et al. Antibiotic treatment of exacerbations of COPD: a randomized, controlled trial comparing procalcitonin-guidance with standard therapy. Chest. 2007;131:9-19.
- Daniels JMA, Schoorl M, Snijders D, et al. Procalcitonin vs C-reactive protein as predictive markers of response to antibiotic therapy in acute exacerbations of COPD. Chest. 2010;138:1108-1015.
- Miravitlles M, Espinosa C, Fernandez-Laso E, Martos JA, Maldonado JA, Gallego M. Relationship between bacterial flora in sputum and functional impairment in patients with acute exacerbations of COPD. Chest. 1999;116:40-46.
- Patil SP, Krishnan JA, Lechtzin N, Diette GB. In-hospital mortality following acute exacerbations of chronic obstructive pulmonary disease. Arch Intern Med. 2003;163:1180-1186.
- Puhan MA, Vollenweider D, Latshang T, Steurer J, Steurer-Stey C. Exacerbations of chronic obstructive lung disease: when are antibiotics indicated? A systematic review. Resp Res. 2007;8:30-40.
- Nouira S, Marghli S, Belghith M, Besbes L, Elatrous S, Abroug F. Once daily ofloxacin in chronic obstructive pulmonary disease exacerbation requiring mechanical ventilation: a randomized placebo-controlled trial. Lancet. 2001;358:2020-2025.
- Dimopoulos G, Siempos II, Korbila IP, Manta KG, Falagas ME. Comparison of first-line with second-line antibiotics for acute exacerbations of chronic bronchitis: a metaanalysis of randomized controlled trials. Chest. 2007;132:447-455.
- Siempos II, Dimopoulos G, Korbila IP, Manta KG, Falagas ME. Macrolides, quinolones and amoxicillin/clavulanate for chronic bronchitis: a meta-analysis. Eur Resp J. 2007;29:1127-1137.
- El-Moussaoui, Roede BM, Speelman P, Bresser P, Prins JM, Bossuyt PMM. Short-course antibiotic treatment in acute exacerbations of chronic bronchitis and COPD: a meta-analysis of double-blind studies. Thorax. 2008;63:415-422.
- Falagas ME, Avgeri SG, Matthaiou DK, Dimopoulos G, Siempos II. Short- versus long-duration antimicrobial treatment for exacerbations of chronic bronchitis: a meta-analysis. J Antimicrob Chemother. 2008;62:442-450.
Case
A 58-year-old male smoker with moderate chronic obstructive pulmonary disease (COPD) (FEV1 56% predicted) is admitted with an acute exacerbation of COPD for the second time this year. He presented to the ED with increased productive cough and shortness of breath, similar to prior exacerbations. He denies fevers, myalgias, or upper-respiratory symptoms. Physical exam is notable for bilateral inspiratory and expiratory wheezing. His sputum is purulent. He is given continuous nebulizer therapy and one dose of oral prednisone, but his dyspnea and wheezing persist. Chest X-ray does not reveal an infiltrate.
Should this patient be treated with antibiotics and, if so, what regimen is most appropriate?
Overview
Acute exacerbations of COPD (AECOPD) present a major health burden, accounting for more than 2.4% of all hospital admissions and causing significant morbidity, mortality, and costs.1 During 2006 and 2007, COPD mortality in the United States topped 39 deaths per 100,000 people, and more recently, hospital costs related to COPD were expected to exceed $13 billion annually.2 Patients with AECOPD also experience decreased quality of life and faster decline in pulmonary function, further highlighting the need for timely and appropriate treatment.1
Several guidelines have proposed treatment strategies now considered standard of care in AECOPD management.3,4,5,6 These include the use of corticosteroids, bronchodilator agents, and, in select cases, antibiotics. While there is well-established evidence for the use of steroids and bronchodilators in AECOPD, the debate continues over the appropriate use of antibiotics in the treatment of acute exacerbations. There are multiple potential factors leading to AECOPD, including viruses, bacteria, and common pollutants; as such, antibiotic treatment may not be indicated for all patients presenting with exacerbations. Further, the risks of antibiotic treatment—including adverse drug events, selection for drug-resistant bacteria, and associated costs—are not insignificant.
However, bacterial infections do play a role in approximately 50% of patients with AECOPD and, for this population, use of antibiotics may confer important benefits.7
Interestingly, a retrospective cohort study of 84,621 patients admitted for AECOPD demonstrated that 85% of patients received antibiotics at some point during hospitalization.8
Support for Antibiotics
Several randomized trials have compared clinical outcomes in patients with AECOPD who have received antibiotics versus those who received placebos. Most of these had small sample sizes and studied only ββ-lactam and tetracycline antibiotics in an outpatient setting; there are limited data involving inpatients and newer drugs. Nevertheless, antibiotic treatment has been associated with decreased risk of adverse outcomes in AECOPD.
One meta-analysis demonstrated that antibiotics reduced treatment failures by 66% and in-hospital mortality by 78% in the subset of trials involving hospitalized patients.8 Similarly, analysis of a large retrospective cohort of patients hospitalized for AECOPD found a significantly lower risk of treatment failure in antibiotic-treated versus untreated patients.9 Specifically, treated patients had lower rates of in-hospital mortality and readmission for AECOPD and a lower likelihood of requiring subsequent mechanical ventilation during the index hospitalization.
Data also suggest that antibiotic treatment during exacerbations might favorably impact subsequent exacerbations.10 A retrospective study of 18,928 Dutch patients with AECOPD compared outcomes among patients who had received antibiotics (most frequently doxycycline or a penicillin) as part of their therapy to those who did not. The authors demonstrated that the median time to the next exacerbation was significantly longer in the patients receiving antibiotics.10 Further, both mortality and overall risk of developing a subsequent exacerbation were significantly decreased in the antibiotic group, with median follow-up of approximately two years.
Indications for Antibiotics
Clinical symptoms. A landmark study by Anthonisen and colleagues set forth three clinical criteria that have formed the basis for treating AECOPD with antibiotics in subsequent studies and in clinical practice.11 Often referred to as the “cardinal symptoms” of AECOPD, these include increased dyspnea, sputum volume, and sputum purulence. In this study, 173 outpatients with COPD were randomized to a 10-day course of antibiotics or placebo at onset of an exacerbation and followed clinically. The authors found that antibiotic-treated patients were significantly more likely than the placebo group to achieve treatment success, defined as resolution of all exacerbated symptoms within 21 days (68.1% vs. 55.0%, P<0.01).
Importantly, treated patients were also significantly less likely to experience clinical deterioration after 72 hours (9.9% vs. 18.9%, P<0.05). Patients with Type I exacerbations, characterized by all three cardinal symptoms, were most likely to benefit from antibiotic therapy, followed by patients with Type II exacerbations, in whom only two of the symptoms were present. Subsequent studies have suggested that sputum purulence correlates well with the presence of acute bacterial infection and therefore may be a reliable clinical indicator of patients who are likely to benefit from antibiotic therapy.12
Laboratory data. While sputum purulence is associated with bacterial infection, sputum culture is less reliable, as pathogenic bacteria are commonly isolated from patients with both AECOPD and stable COPD. In fact, the prevalence of bacterial colonization in moderate to severe COPD might be as high as 50%.13 Therefore, a positive bacterial sputum culture, in the absence of purulence or other signs of infection, is not recommended as the sole basis for which to prescribe antibiotics.
Serum biomarkers, most notably C-reactive protein (CRP) and procalcitonin, have been studied as a newer approach to identify patients who might benefit from antibiotic therapy for AECOPD. Studies have demonstrated increased CRP levels during AECOPD, particularly in patients with purulent sputum and positive bacterial sputum cultures.12 Procalcitonin is preferentially elevated in bacterial infections.
One randomized, placebo-controlled trial in hospitalized patients with AECOPD demonstrated a significant reduction in antibiotic usage based on low procalcitonin levels, without negatively impacting clinical success rate, hospital mortality, subsequent antibiotic needs, or time to next exacerbation.14 However, due to inconsistent evidence, use of these markers to guide antibiotic administration in AECOPD has not yet been definitively established.14,15 Additionally, these laboratory results are often not available at the point of care, potentially limiting their utility in the decision to initiate antibiotics.
Severity of illness. Severity of illness is an important factor in the decision to treat AECOPD with antibiotics. Patients with advanced, underlying airway obstruction, as measured by FEV1, are more likely to have a bacterial cause of AECOPD.16 Additionally, baseline clinical characteristics including advanced age and comorbid conditions, particularly cardiovascular disease and diabetes, increase the risk of severe exacerbations.17
One meta-analysis of placebo-controlled trials found that patients with severe exacerbations were likely to benefit from antibiotic therapy, while patients with mild or moderate exacerbations had no reduction in treatment failure or mortality rates.18 Patients presenting with acute respiratory failure necessitating intensive care and/or ventilator support (noninvasive or invasive) have also been shown to benefit from antibiotics.19
Current clinical guidelines vary slightly in their recommendations regarding when to give antibiotics in AECOPD (see Table 1). However, existing evidence favors antibiotic treatment for those patients presenting with two or three cardinal symptoms, specifically those with increased sputum purulence, and those with severe disease (i.e. pre-existing advanced airflow obstruction and/or exacerbations requiring mechanical ventilation). Conversely, studies have shown that many patients, particularly those with milder exacerbations, experience resolution of symptoms without antibiotic treatment.11,18
Antibiotic Choice in AECOPD
Risk stratification. In patients likely to benefit from antibiotic therapy, an understanding of the relationship between severity of COPD, host risk factors for poor outcomes, and microbiology is paramount to guide clinical decision-making. Historically, such bacteria as Haemophilus influenzae, Streptococcus pneumoniae, and Moraxella catarrhalis have been implicated in the pathogenesis of AECOPD.3,7 In patients with simple exacerbations, antibiotics that target these pathogens should be used (see Table 2).
However, patients with more severe underlying airway obstruction (i.e. FEV1<50%) and risk factors for poor outcomes, specifically recent hospitalization (≥2 days during the previous 90 days), frequent antibiotics (>3 courses during the previous year), and severe exacerbations are more likely to be infected with resistant strains or gram-negative organisms.3,7 Pseudomonas aeruginosa, in particular, is of increasing concern in this population. In patients with complicated exacerbations, more broad-coverage, empiric antibiotics should be initiated (see Table 2).
With this in mind, patients meeting criteria for treatment must first be stratified according to the severity of COPD and risk factors for poor outcomes before a decision regarding a specific antibiotic is reached. Figure 1 outlines a recommended approach for antibiotic administration in AECOPD. The optimal choice of antibiotics must consider cost-effectiveness, local patterns of antibiotic resistance, tissue penetration, patient adherence, and risk of such adverse drug events as diarrhea.
Comparative effectiveness. Current treatment guidelines do not favor the use of any particular antibiotic in simple AECOPD.3,4,5,6 However, as selective pressure has led to in vitro resistance to antibiotics traditionally considered first-line (e.g. doxycycline, trimethoprim/sulfamethoxazole, amoxicillin), the use of second-line antibiotics (e.g. fluoroquinolones, macrolides, cephalosporins, β-lactam/ β-lactamase inhibitors) has increased. Consequently, several studies have compared the effectiveness of different antimicrobial regimens.
One meta-analysis found that second-line antibiotics, when compared with first-line agents, provided greater clinical improvement to patients with AECOPD, without significant differences in mortality, microbiologic eradication, or incidence of adverse drug events.20 Among the subgroup of trials enrolling hospitalized patients, the clinical effectiveness of second-line agents remained significantly greater than that of first-line agents.
Another meta-analysis compared trials that studied only macrolides, quinolones, and amoxicillin-clavulanate and found no difference in terms of short-term clinical effectiveness; however, there was weak evidence to suggest that quinolones were associated with better microbiological success and fewer recurrences of AECOPD.21 Fluoroquinolones are preferred in complicated cases of AECOPD in which there is a greater risk for enterobacteriaceae and Pseudomonas species.3,7
Antibiotic Duration
The duration of antibiotic therapy in AECOPD has been studied extensively, with randomized controlled trials consistently demonstrating no additional benefit to courses extending beyond five days. One meta-analysis of 21 studies found similar clinical and microbiologic cure rates among patients randomized to antibiotic treatment for ≤5 days versus >5 days.22 A subgroup analysis of the trials evaluating different durations of the same antibiotic also demonstrated no difference in clinical effectiveness, and this finding was confirmed in a separate meta-analysis.22,23
Advantages to shorter antibiotic courses include improved compliance and decreased rates of resistance. The usual duration of antibiotic therapy is three to seven days, depending upon the response to therapy.3
Back to the Case
As the patient has no significant comorbidities or risk factors, and meets criteria for a simple Anthonisen Type I exacerbation (increased dyspnea, sputum, and sputum purulence), antibiotic therapy with trimethoprim/sulfamethoxazole is initiated on admission, in addition to the previously started steroid and bronchodilator treatments. The patient’s clinical status improves, and he is discharged on hospital Day 3 with a prescription to complete a five-day course of antibiotics.
Bottom Line
Antibiotic therapy is effective in select AECOPD patients, with maximal benefits obtained when the decision to treat is based on careful consideration of characteristic clinical symptoms and severity of illness. Choice and duration of antibiotics should follow likely bacterial causes and current guidelines.
Dr. Cunningham is an assistant professor of internal medicine and academic hospitalist in the section of hospital medicine at Vanderbilt University School of Medicine in Nashville, Tenn. Dr. LaBrin is assistant professor of internal medicine and pediatrics and an academic hospitalist at Vanderbilt. Dr. Markley is a clinical instructor and academic hospitalist at Vanderbilt.
References
- Donaldson GC, Wedzicha JA. COPD exacerbations: 1. Epidemiology. Thorax. 2006;61:164-168.
- National Heart, Lung, and Blood Institute. 2009 NHLBI Morbidity and Mortality Chartbook. National Heart, Lung, and Blood Institute website. Available at: http://www.nhlbi.nih.gov/resources/docs/cht-book.htm Accessed Oct. 10, 2011.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease. Global Initiative for Chronic Obstructive Lung Disease (GOLD) website. Available at: www.goldcopd.org/guidelines-resources.html Accessed Oct. 10, 2011.
- Celli BR, MacNee W, Agusti A, et al. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Resp J. 2004;23:932-946.
- National Clinical Guideline Centre. Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care. National Institute for Health and Clinical Excellence website. Available at: http://guidance.nice.org.uk/CG101/Guidance/pdf/English. Accessed Oct. 10, 2011.
- O’Donnell DE, Aaron S, Bourbeau J, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease—2007 update. Can Respir J. 2007;14(Suppl B):5B-32B.
- Sethi S, Murphy TF. Infection in the pathogenesis and course of chronic obstructive pulmonary disease. N Engl J Med. 2008;359:2355-2565.
- Quon BS, Qi Gan W, Sin DD. Contemporary management of acute exacerbations of COPD: a systematic review and metaanalysis. Chest. 2008;133:756-766.
- Rothberg MB, Pekow PS, Lahti M, Brody O, Skiest DJ, Lindenauer PK. Antibiotic therapy and treatment failure in patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease. JAMA. 2010;303:2035-2042.
- Roede BM, Bresser P, Bindels PJE, et al. Antibiotic treatment is associated with reduced risk of subsequent exacerbation in obstructive lung disease: a historical population based cohort study. Thorax. 2008;63:968-973.
- Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GKM, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106:196-204.
- Stockley RA, O’Brien C, Pye A, Hill SL. Relationship of sputum color to nature and outpatient management of acute exacerbations of COPD. Chest. 2000;117:1638-1645.
- Rosell A, Monso E, Soler N, et al. Microbiologic determinants of exacerbation in chronic obstructive pulmonary disease. Arch Intern Med. 2005; 165:891-897.
- Stolz D, Christ-Crain M, Bingisser R, et al. Antibiotic treatment of exacerbations of COPD: a randomized, controlled trial comparing procalcitonin-guidance with standard therapy. Chest. 2007;131:9-19.
- Daniels JMA, Schoorl M, Snijders D, et al. Procalcitonin vs C-reactive protein as predictive markers of response to antibiotic therapy in acute exacerbations of COPD. Chest. 2010;138:1108-1015.
- Miravitlles M, Espinosa C, Fernandez-Laso E, Martos JA, Maldonado JA, Gallego M. Relationship between bacterial flora in sputum and functional impairment in patients with acute exacerbations of COPD. Chest. 1999;116:40-46.
- Patil SP, Krishnan JA, Lechtzin N, Diette GB. In-hospital mortality following acute exacerbations of chronic obstructive pulmonary disease. Arch Intern Med. 2003;163:1180-1186.
- Puhan MA, Vollenweider D, Latshang T, Steurer J, Steurer-Stey C. Exacerbations of chronic obstructive lung disease: when are antibiotics indicated? A systematic review. Resp Res. 2007;8:30-40.
- Nouira S, Marghli S, Belghith M, Besbes L, Elatrous S, Abroug F. Once daily ofloxacin in chronic obstructive pulmonary disease exacerbation requiring mechanical ventilation: a randomized placebo-controlled trial. Lancet. 2001;358:2020-2025.
- Dimopoulos G, Siempos II, Korbila IP, Manta KG, Falagas ME. Comparison of first-line with second-line antibiotics for acute exacerbations of chronic bronchitis: a metaanalysis of randomized controlled trials. Chest. 2007;132:447-455.
- Siempos II, Dimopoulos G, Korbila IP, Manta KG, Falagas ME. Macrolides, quinolones and amoxicillin/clavulanate for chronic bronchitis: a meta-analysis. Eur Resp J. 2007;29:1127-1137.
- El-Moussaoui, Roede BM, Speelman P, Bresser P, Prins JM, Bossuyt PMM. Short-course antibiotic treatment in acute exacerbations of chronic bronchitis and COPD: a meta-analysis of double-blind studies. Thorax. 2008;63:415-422.
- Falagas ME, Avgeri SG, Matthaiou DK, Dimopoulos G, Siempos II. Short- versus long-duration antimicrobial treatment for exacerbations of chronic bronchitis: a meta-analysis. J Antimicrob Chemother. 2008;62:442-450.
Hospitalist/Nurse Collaboration Drives Multidisciplinary Rounding
Aultidisciplinary patient rounding system implemented on a non-teaching hospitalist unit at the Ohio State University Medical Center (OSUMC) has been well received by unit staff, according to an HM11 abstract presentation. Key to its success, says lead author and OSUMC hospitalist Eric Schumacher, DO, MBA, was to involve nursing staff from the start and to work closely with the unit’s nurse manager and charge nurse.
“Once we got their buy-in, we proposed what we wanted to do and asked for their suggestions,” Dr. Schumacher says.
Hospitalists partner with the nurse leaders to establish a morning bedside rounding process on the unit, using a “Physician Nurse Rounding Sheet” for each hospitalist. The sheet is prepared daily by the charge nurse and unit clerks, listing the hospitalist’s patients, assigned nurses, and phone numbers. A short debriefing is performed outside the patient’s room before each encounter, and a daily feedback sheet is given to the patient and family with a picture of the hospitalist, a list of all care-team members, and such information as goals for the day, pending tests and consultations, and anticipated discharge date.
“Part of the challenge is to create a process that is efficient for both doctors and nurses, given multiple nurses caring for multiple patients,” Dr. Schumacher says.
Charge nurses or nursing managers provide backup when the bedside nurse is not available for bedside rounding. “Right now we’re rounding with hospitalists and nurses only, but a long-term goal is to expand it to include the social worker and other ancillary professionals,” he says.
Preliminary data on the project show the feasibility of multidisciplinary rounding, with elevated Press Ganey patient satisfaction scores on the unit in the first two months after rounding began. In the third month, compliance with rounding went down, and so did satisfaction scores, but with a renewed commitment the following month, scores went back up again. Subjective reports from hospitalists also suggest fewer interruptions during the day from nursing pages, Dr. Schumacher says.
Aultidisciplinary patient rounding system implemented on a non-teaching hospitalist unit at the Ohio State University Medical Center (OSUMC) has been well received by unit staff, according to an HM11 abstract presentation. Key to its success, says lead author and OSUMC hospitalist Eric Schumacher, DO, MBA, was to involve nursing staff from the start and to work closely with the unit’s nurse manager and charge nurse.
“Once we got their buy-in, we proposed what we wanted to do and asked for their suggestions,” Dr. Schumacher says.
Hospitalists partner with the nurse leaders to establish a morning bedside rounding process on the unit, using a “Physician Nurse Rounding Sheet” for each hospitalist. The sheet is prepared daily by the charge nurse and unit clerks, listing the hospitalist’s patients, assigned nurses, and phone numbers. A short debriefing is performed outside the patient’s room before each encounter, and a daily feedback sheet is given to the patient and family with a picture of the hospitalist, a list of all care-team members, and such information as goals for the day, pending tests and consultations, and anticipated discharge date.
“Part of the challenge is to create a process that is efficient for both doctors and nurses, given multiple nurses caring for multiple patients,” Dr. Schumacher says.
Charge nurses or nursing managers provide backup when the bedside nurse is not available for bedside rounding. “Right now we’re rounding with hospitalists and nurses only, but a long-term goal is to expand it to include the social worker and other ancillary professionals,” he says.
Preliminary data on the project show the feasibility of multidisciplinary rounding, with elevated Press Ganey patient satisfaction scores on the unit in the first two months after rounding began. In the third month, compliance with rounding went down, and so did satisfaction scores, but with a renewed commitment the following month, scores went back up again. Subjective reports from hospitalists also suggest fewer interruptions during the day from nursing pages, Dr. Schumacher says.
Aultidisciplinary patient rounding system implemented on a non-teaching hospitalist unit at the Ohio State University Medical Center (OSUMC) has been well received by unit staff, according to an HM11 abstract presentation. Key to its success, says lead author and OSUMC hospitalist Eric Schumacher, DO, MBA, was to involve nursing staff from the start and to work closely with the unit’s nurse manager and charge nurse.
“Once we got their buy-in, we proposed what we wanted to do and asked for their suggestions,” Dr. Schumacher says.
Hospitalists partner with the nurse leaders to establish a morning bedside rounding process on the unit, using a “Physician Nurse Rounding Sheet” for each hospitalist. The sheet is prepared daily by the charge nurse and unit clerks, listing the hospitalist’s patients, assigned nurses, and phone numbers. A short debriefing is performed outside the patient’s room before each encounter, and a daily feedback sheet is given to the patient and family with a picture of the hospitalist, a list of all care-team members, and such information as goals for the day, pending tests and consultations, and anticipated discharge date.
“Part of the challenge is to create a process that is efficient for both doctors and nurses, given multiple nurses caring for multiple patients,” Dr. Schumacher says.
Charge nurses or nursing managers provide backup when the bedside nurse is not available for bedside rounding. “Right now we’re rounding with hospitalists and nurses only, but a long-term goal is to expand it to include the social worker and other ancillary professionals,” he says.
Preliminary data on the project show the feasibility of multidisciplinary rounding, with elevated Press Ganey patient satisfaction scores on the unit in the first two months after rounding began. In the third month, compliance with rounding went down, and so did satisfaction scores, but with a renewed commitment the following month, scores went back up again. Subjective reports from hospitalists also suggest fewer interruptions during the day from nursing pages, Dr. Schumacher says.
Adverse Events and Rural Discharges
The Center on Patient Safety at Florida State University College of Medicine in Tallahassee has been awarded a two-year, $908,000 grant from the federal Agency for Healthcare Research and Quality to study adverse events during the three weeks following hospital discharge, both for urban patients and, for the first time, those returning to rural settings.
Center director Dennis Tsilimingras, MD, MPH, says the project will enroll 600 patients, half urban and half rural, discharged by the Tallahassee Memorial Hospitalist Group, and track injuries resulting from medical errors, including medication errors, procedure-related injuries, nosocomial infections, and pressure ulcers.
Errors or injuries to patients may occur in the hospital but not be identified until after the patient goes home, he says, and such errors could contribute to rehospitalizations. “Our hypothesis is that the rate of adverse events post-discharge may be greater among rural patients because they have less access to follow-up care,” he adds.
Dr. Tsilimingras will be working closely with hospitalists, and Phase 2 of the research will use the hospital’s post-discharge transitional care clinic (see “Is a Post-Discharge Clinic in Your Hospital’s Future?,” December 2011) as an intervention strategy.
The eventual goal is to develop a screening tool to flag risk for post-discharge adverse events and develop strategies to reduce post-discharge problems, including readmissions, a quarter of which may be related to post-discharge adverse events, Dr. Tsilimingras says. He encourages hospitalists to reevaluate their patients and review their charts at the time of discharge, to see if post-discharge problems loom, and to reach out to primary care physicians by telephone, rather than just sending discharge summaries.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Armellino D, Hussain E, Schilling ME, et al. Using high-technology to enforce low-technology safety measures: the use of third-party remote video auditing and real-time feedback in healthcare [published online ahead of print Nov. 21, 2011. Clin Infect Dis. doi;10.1093/cid/cir773.
- Fuller C, Savage J, Besser S, et al. “The dirty handin the latex glove”: a study of hand hygiene compliance when gloves are worn. Infect Control Hosp Epidemiol. 2011;32(12):1194-1199.
The Center on Patient Safety at Florida State University College of Medicine in Tallahassee has been awarded a two-year, $908,000 grant from the federal Agency for Healthcare Research and Quality to study adverse events during the three weeks following hospital discharge, both for urban patients and, for the first time, those returning to rural settings.
Center director Dennis Tsilimingras, MD, MPH, says the project will enroll 600 patients, half urban and half rural, discharged by the Tallahassee Memorial Hospitalist Group, and track injuries resulting from medical errors, including medication errors, procedure-related injuries, nosocomial infections, and pressure ulcers.
Errors or injuries to patients may occur in the hospital but not be identified until after the patient goes home, he says, and such errors could contribute to rehospitalizations. “Our hypothesis is that the rate of adverse events post-discharge may be greater among rural patients because they have less access to follow-up care,” he adds.
Dr. Tsilimingras will be working closely with hospitalists, and Phase 2 of the research will use the hospital’s post-discharge transitional care clinic (see “Is a Post-Discharge Clinic in Your Hospital’s Future?,” December 2011) as an intervention strategy.
The eventual goal is to develop a screening tool to flag risk for post-discharge adverse events and develop strategies to reduce post-discharge problems, including readmissions, a quarter of which may be related to post-discharge adverse events, Dr. Tsilimingras says. He encourages hospitalists to reevaluate their patients and review their charts at the time of discharge, to see if post-discharge problems loom, and to reach out to primary care physicians by telephone, rather than just sending discharge summaries.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Armellino D, Hussain E, Schilling ME, et al. Using high-technology to enforce low-technology safety measures: the use of third-party remote video auditing and real-time feedback in healthcare [published online ahead of print Nov. 21, 2011. Clin Infect Dis. doi;10.1093/cid/cir773.
- Fuller C, Savage J, Besser S, et al. “The dirty handin the latex glove”: a study of hand hygiene compliance when gloves are worn. Infect Control Hosp Epidemiol. 2011;32(12):1194-1199.
The Center on Patient Safety at Florida State University College of Medicine in Tallahassee has been awarded a two-year, $908,000 grant from the federal Agency for Healthcare Research and Quality to study adverse events during the three weeks following hospital discharge, both for urban patients and, for the first time, those returning to rural settings.
Center director Dennis Tsilimingras, MD, MPH, says the project will enroll 600 patients, half urban and half rural, discharged by the Tallahassee Memorial Hospitalist Group, and track injuries resulting from medical errors, including medication errors, procedure-related injuries, nosocomial infections, and pressure ulcers.
Errors or injuries to patients may occur in the hospital but not be identified until after the patient goes home, he says, and such errors could contribute to rehospitalizations. “Our hypothesis is that the rate of adverse events post-discharge may be greater among rural patients because they have less access to follow-up care,” he adds.
Dr. Tsilimingras will be working closely with hospitalists, and Phase 2 of the research will use the hospital’s post-discharge transitional care clinic (see “Is a Post-Discharge Clinic in Your Hospital’s Future?,” December 2011) as an intervention strategy.
The eventual goal is to develop a screening tool to flag risk for post-discharge adverse events and develop strategies to reduce post-discharge problems, including readmissions, a quarter of which may be related to post-discharge adverse events, Dr. Tsilimingras says. He encourages hospitalists to reevaluate their patients and review their charts at the time of discharge, to see if post-discharge problems loom, and to reach out to primary care physicians by telephone, rather than just sending discharge summaries.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Armellino D, Hussain E, Schilling ME, et al. Using high-technology to enforce low-technology safety measures: the use of third-party remote video auditing and real-time feedback in healthcare [published online ahead of print Nov. 21, 2011. Clin Infect Dis. doi;10.1093/cid/cir773.
- Fuller C, Savage J, Besser S, et al. “The dirty handin the latex glove”: a study of hand hygiene compliance when gloves are worn. Infect Control Hosp Epidemiol. 2011;32(12):1194-1199.
Hand Hygiene Makes Headlines
Recent efforts to raise awareness about proper hand hygiene in health facilities in order to prevent disease transmission, range from the ScrubUp! campaign in Ohio to the World Health Organization’s global Clean Care is Safer Care campaign (www.who.int/gpsc/en/), which advocates for improving hand hygiene practices of health care workers around the world.
Twenty hospitals in Central Ohio staged ScrubUp! rallies on Dec. 5, 2011, during National Handwashing Awareness Week, not only to raise awareness of the hospitals’ commitment to hand hygiene, but also to encourage hospital visitors to wash their hands. The Ohio Hospital Association estimates that 50,000 people were exposed to these messages via a full-page ad in the Columbus Dispatch, overhead announcements and distribution tables in each hospital, handing out hand sanitizers to visitors, and engaging staff with humor, food, and prizes.
A recent study conducted at North Shore University Hospital in Manhasset, N.Y., found that hand hygiene compliance rates improve when remote video auditing platforms provide professionals with continuous feedback.1 During 16 weeks of real-time feedback on compliance with strict hand hygiene (i.e. within 10 seconds of entering/leaving patients’ rooms) via LED screens mounted on the walls of a MICU, compliance jumped to more than 80%.
A British study of 7,000 contacts in ICUs and geriatric units found that wearing latex gloves may discourage guideline-recommended hand washing, even though such failures to wash may contribute to spreading disease.2 Compliance was 47.7% without gloves, and 41% with gloves.
One of the study’s authors calls for further study of the behavioral reasons why healthcare workers are less likely to wash their hands when gloved, but urges that hand hygiene associated with gloving be part of educational campaigns.
Recent efforts to raise awareness about proper hand hygiene in health facilities in order to prevent disease transmission, range from the ScrubUp! campaign in Ohio to the World Health Organization’s global Clean Care is Safer Care campaign (www.who.int/gpsc/en/), which advocates for improving hand hygiene practices of health care workers around the world.
Twenty hospitals in Central Ohio staged ScrubUp! rallies on Dec. 5, 2011, during National Handwashing Awareness Week, not only to raise awareness of the hospitals’ commitment to hand hygiene, but also to encourage hospital visitors to wash their hands. The Ohio Hospital Association estimates that 50,000 people were exposed to these messages via a full-page ad in the Columbus Dispatch, overhead announcements and distribution tables in each hospital, handing out hand sanitizers to visitors, and engaging staff with humor, food, and prizes.
A recent study conducted at North Shore University Hospital in Manhasset, N.Y., found that hand hygiene compliance rates improve when remote video auditing platforms provide professionals with continuous feedback.1 During 16 weeks of real-time feedback on compliance with strict hand hygiene (i.e. within 10 seconds of entering/leaving patients’ rooms) via LED screens mounted on the walls of a MICU, compliance jumped to more than 80%.
A British study of 7,000 contacts in ICUs and geriatric units found that wearing latex gloves may discourage guideline-recommended hand washing, even though such failures to wash may contribute to spreading disease.2 Compliance was 47.7% without gloves, and 41% with gloves.
One of the study’s authors calls for further study of the behavioral reasons why healthcare workers are less likely to wash their hands when gloved, but urges that hand hygiene associated with gloving be part of educational campaigns.
Recent efforts to raise awareness about proper hand hygiene in health facilities in order to prevent disease transmission, range from the ScrubUp! campaign in Ohio to the World Health Organization’s global Clean Care is Safer Care campaign (www.who.int/gpsc/en/), which advocates for improving hand hygiene practices of health care workers around the world.
Twenty hospitals in Central Ohio staged ScrubUp! rallies on Dec. 5, 2011, during National Handwashing Awareness Week, not only to raise awareness of the hospitals’ commitment to hand hygiene, but also to encourage hospital visitors to wash their hands. The Ohio Hospital Association estimates that 50,000 people were exposed to these messages via a full-page ad in the Columbus Dispatch, overhead announcements and distribution tables in each hospital, handing out hand sanitizers to visitors, and engaging staff with humor, food, and prizes.
A recent study conducted at North Shore University Hospital in Manhasset, N.Y., found that hand hygiene compliance rates improve when remote video auditing platforms provide professionals with continuous feedback.1 During 16 weeks of real-time feedback on compliance with strict hand hygiene (i.e. within 10 seconds of entering/leaving patients’ rooms) via LED screens mounted on the walls of a MICU, compliance jumped to more than 80%.
A British study of 7,000 contacts in ICUs and geriatric units found that wearing latex gloves may discourage guideline-recommended hand washing, even though such failures to wash may contribute to spreading disease.2 Compliance was 47.7% without gloves, and 41% with gloves.
One of the study’s authors calls for further study of the behavioral reasons why healthcare workers are less likely to wash their hands when gloved, but urges that hand hygiene associated with gloving be part of educational campaigns.
By the Numbers: 57
Percentage of responding physicians who say they are using electronic health records (EHR), according to a survey of 10,000 office-based physicians by the National Center for Health Statistics, up from 51% usage in 2010. More than half say they intend to apply for meaningful use incentives offered by the government for implementing EHR, and 43% of those respondents report having computerized systems meeting Stage 1 Core Set criteria to qualify.
Percentage of responding physicians who say they are using electronic health records (EHR), according to a survey of 10,000 office-based physicians by the National Center for Health Statistics, up from 51% usage in 2010. More than half say they intend to apply for meaningful use incentives offered by the government for implementing EHR, and 43% of those respondents report having computerized systems meeting Stage 1 Core Set criteria to qualify.
Percentage of responding physicians who say they are using electronic health records (EHR), according to a survey of 10,000 office-based physicians by the National Center for Health Statistics, up from 51% usage in 2010. More than half say they intend to apply for meaningful use incentives offered by the government for implementing EHR, and 43% of those respondents report having computerized systems meeting Stage 1 Core Set criteria to qualify.
Resume Red Flags
Fifteen seconds: That’s approximately how long an employer looks at a CV. Recruiters and employers know what they want; they skim even the best resumes. They are on the lookout for applicants who meet their requirements; sometimes they’ll take a chance on a long shot whose pitch catches their eye.
So what happens when a resume stands out for the wrong reasons? Work histories aren’t always perfect, and recruiters and prospective employers will notice any blemishes.
“The thing about red flags is they’re just an indicator that the applicant is an outlier,” says Kim Bell, MD, FACP, SFHM, regional medical director of the Pacific West Region for EmCare, a Dallas-based company that provides outsourced physician services to more than 500 hospitals in 40 states. “It doesn’t necessarily rule them out.”
Preempt Suspicion
For hospitalists, resume imperfections that attract attention include:
- Gaps in employment;
- Frequent changes in employment;
- Changes in residency;
- Medical board sanctions or probation;
- Failures on the board exam; and
- Forced resignations or firings.
—Cheryl O’Malley, MD, FACP, program director, Department of Internal Medicine and Pediatrics, Banner Good Samaritan Medical Center, Phoenix
When recruiters or employers notice a red flag, they look for other problems to see if patterns emerge and to discern if the applicant exhibited bad judgment, has character flaws, or shows an inability to learn from a mistake, says Jeff Kaplan, PhD, MBA, MCC, a licensed psychologist and Philadelphia-based executive coach whose clients include healthcare industry executives. If such signs exist, the applicant is generally eliminated from consideration. Therefore, it’s critical that applicants explain clearly and succinctly the reason for any resume shortcoming.
“A good way is to actually write a cover letter to explain some uniqueness in their CV that they want [recruiters] to understand,” says Alpesh Amin, MD, MBA, FACP, SFHM, professor and chairman of the Department of Medicine and executive director of the hospitalist program at the University of California at Irvine.
By explaining the situation, Dr. Bell says, the hospitalist doesn’t give the employer a chance to guess a reason for the red flag—and potentially guess wrong.
“There’s a big difference between there’s been some sort of serious censure and they’ve been driven out, versus they thought another setting might be more interesting or they just wanted to make a geographic move,” says Thomas E. Thorsheim, PhD, a licensed psychologist and physician leadership coach based in Greenville, S.C. “It’s important to preempt any concerns about how reliable or stable they’re going to be.”
Applicants with resume red flags should show that they’ve taken responsibility for what happened and grown from the experience, say Dr. Thorsheim and Cheryl O’Malley, MD, FACP, program director in the department of internal medicine and pediatrics at Banner Good Samaritan Medical Center in Phoenix.
“Everyone wants to know that you have learned from your mistakes. Try to have a demonstrated remediation of the concern and go above and beyond the minimum requirements,” Dr. O’Malley says. “For example, if the red flag is academic concerns or not passing your board exams, then bring in documentation of your schedule for reading daily and all of the CME and MKSAP you complete. If it is interpersonal issues, then give examples of recent successes that show how you have improved.”
Brand Recognition
Physicians with a resume blemish should concentrate on highlighting their strengths and “branding” themselves as a workplace contributor, says Bernadette Norz, MBA, ACC, a certified physician development coach. While this advice applies to all applicants, it is particularly critical for those with resume problems, as it will demonstrate they have skills that set them apart from others.
“What people are really looking for is what did you do and what was the result,” Norz says. “Things that one accomplished as a volunteer or on a committee count, too, because that’s where people gain a lot of leadership skills.”
Resumes should not be recitations of job descriptions, she advises. They should be lists of achievements described with action verbs that give the applicant a clear identity and brand. “When you read a resume, you should walk away from it knowing who this person is,” says Dr. Kaplan. “If you don’t see that on their resume, then you’ve got to question it.”
The best applicants network. The more you can develop a relationship and rapport with peers and potential employers, the more likely you will be given a greater chance to sell your strengths and explain weaknesses, says career strategist Ellen Dunagan, president of Traverse Management Solutions in Arlington, Va. “You really want to step it up and be much more active with your own pitch,” she says.
Attitude Matters
But before a hospitalist or any applicant with a resume shortcoming begins to look for a job, they must resolve the issue internally, Dr. Kaplan notes. Taking responsibility will allow you to speak clearly and comfortably about what happened, without negativity or blame.
“If you don’t, you will fumble,” he says. “The prospective employer will start seeing those red flags and they will ask you about it, and you thought you had your pitch ready. Then they ask you two more questions, and before you know it, they’re not going to feel a sense of transparency with you.”
More and more, what employers are looking for is positivity, Dunagan says. It’s a trait applicants won’t have if they still harbor negative feelings toward a previous employer. “It’s just very important to be not only a team player, but to have a really good attitude,” she says. “So present yourself in the best possible light.”
Lisa Ryan is a freelance writer based in New Jersey.
Fifteen seconds: That’s approximately how long an employer looks at a CV. Recruiters and employers know what they want; they skim even the best resumes. They are on the lookout for applicants who meet their requirements; sometimes they’ll take a chance on a long shot whose pitch catches their eye.
So what happens when a resume stands out for the wrong reasons? Work histories aren’t always perfect, and recruiters and prospective employers will notice any blemishes.
“The thing about red flags is they’re just an indicator that the applicant is an outlier,” says Kim Bell, MD, FACP, SFHM, regional medical director of the Pacific West Region for EmCare, a Dallas-based company that provides outsourced physician services to more than 500 hospitals in 40 states. “It doesn’t necessarily rule them out.”
Preempt Suspicion
For hospitalists, resume imperfections that attract attention include:
- Gaps in employment;
- Frequent changes in employment;
- Changes in residency;
- Medical board sanctions or probation;
- Failures on the board exam; and
- Forced resignations or firings.
—Cheryl O’Malley, MD, FACP, program director, Department of Internal Medicine and Pediatrics, Banner Good Samaritan Medical Center, Phoenix
When recruiters or employers notice a red flag, they look for other problems to see if patterns emerge and to discern if the applicant exhibited bad judgment, has character flaws, or shows an inability to learn from a mistake, says Jeff Kaplan, PhD, MBA, MCC, a licensed psychologist and Philadelphia-based executive coach whose clients include healthcare industry executives. If such signs exist, the applicant is generally eliminated from consideration. Therefore, it’s critical that applicants explain clearly and succinctly the reason for any resume shortcoming.
“A good way is to actually write a cover letter to explain some uniqueness in their CV that they want [recruiters] to understand,” says Alpesh Amin, MD, MBA, FACP, SFHM, professor and chairman of the Department of Medicine and executive director of the hospitalist program at the University of California at Irvine.
By explaining the situation, Dr. Bell says, the hospitalist doesn’t give the employer a chance to guess a reason for the red flag—and potentially guess wrong.
“There’s a big difference between there’s been some sort of serious censure and they’ve been driven out, versus they thought another setting might be more interesting or they just wanted to make a geographic move,” says Thomas E. Thorsheim, PhD, a licensed psychologist and physician leadership coach based in Greenville, S.C. “It’s important to preempt any concerns about how reliable or stable they’re going to be.”
Applicants with resume red flags should show that they’ve taken responsibility for what happened and grown from the experience, say Dr. Thorsheim and Cheryl O’Malley, MD, FACP, program director in the department of internal medicine and pediatrics at Banner Good Samaritan Medical Center in Phoenix.
“Everyone wants to know that you have learned from your mistakes. Try to have a demonstrated remediation of the concern and go above and beyond the minimum requirements,” Dr. O’Malley says. “For example, if the red flag is academic concerns or not passing your board exams, then bring in documentation of your schedule for reading daily and all of the CME and MKSAP you complete. If it is interpersonal issues, then give examples of recent successes that show how you have improved.”
Brand Recognition
Physicians with a resume blemish should concentrate on highlighting their strengths and “branding” themselves as a workplace contributor, says Bernadette Norz, MBA, ACC, a certified physician development coach. While this advice applies to all applicants, it is particularly critical for those with resume problems, as it will demonstrate they have skills that set them apart from others.
“What people are really looking for is what did you do and what was the result,” Norz says. “Things that one accomplished as a volunteer or on a committee count, too, because that’s where people gain a lot of leadership skills.”
Resumes should not be recitations of job descriptions, she advises. They should be lists of achievements described with action verbs that give the applicant a clear identity and brand. “When you read a resume, you should walk away from it knowing who this person is,” says Dr. Kaplan. “If you don’t see that on their resume, then you’ve got to question it.”
The best applicants network. The more you can develop a relationship and rapport with peers and potential employers, the more likely you will be given a greater chance to sell your strengths and explain weaknesses, says career strategist Ellen Dunagan, president of Traverse Management Solutions in Arlington, Va. “You really want to step it up and be much more active with your own pitch,” she says.
Attitude Matters
But before a hospitalist or any applicant with a resume shortcoming begins to look for a job, they must resolve the issue internally, Dr. Kaplan notes. Taking responsibility will allow you to speak clearly and comfortably about what happened, without negativity or blame.
“If you don’t, you will fumble,” he says. “The prospective employer will start seeing those red flags and they will ask you about it, and you thought you had your pitch ready. Then they ask you two more questions, and before you know it, they’re not going to feel a sense of transparency with you.”
More and more, what employers are looking for is positivity, Dunagan says. It’s a trait applicants won’t have if they still harbor negative feelings toward a previous employer. “It’s just very important to be not only a team player, but to have a really good attitude,” she says. “So present yourself in the best possible light.”
Lisa Ryan is a freelance writer based in New Jersey.
Fifteen seconds: That’s approximately how long an employer looks at a CV. Recruiters and employers know what they want; they skim even the best resumes. They are on the lookout for applicants who meet their requirements; sometimes they’ll take a chance on a long shot whose pitch catches their eye.
So what happens when a resume stands out for the wrong reasons? Work histories aren’t always perfect, and recruiters and prospective employers will notice any blemishes.
“The thing about red flags is they’re just an indicator that the applicant is an outlier,” says Kim Bell, MD, FACP, SFHM, regional medical director of the Pacific West Region for EmCare, a Dallas-based company that provides outsourced physician services to more than 500 hospitals in 40 states. “It doesn’t necessarily rule them out.”
Preempt Suspicion
For hospitalists, resume imperfections that attract attention include:
- Gaps in employment;
- Frequent changes in employment;
- Changes in residency;
- Medical board sanctions or probation;
- Failures on the board exam; and
- Forced resignations or firings.
—Cheryl O’Malley, MD, FACP, program director, Department of Internal Medicine and Pediatrics, Banner Good Samaritan Medical Center, Phoenix
When recruiters or employers notice a red flag, they look for other problems to see if patterns emerge and to discern if the applicant exhibited bad judgment, has character flaws, or shows an inability to learn from a mistake, says Jeff Kaplan, PhD, MBA, MCC, a licensed psychologist and Philadelphia-based executive coach whose clients include healthcare industry executives. If such signs exist, the applicant is generally eliminated from consideration. Therefore, it’s critical that applicants explain clearly and succinctly the reason for any resume shortcoming.
“A good way is to actually write a cover letter to explain some uniqueness in their CV that they want [recruiters] to understand,” says Alpesh Amin, MD, MBA, FACP, SFHM, professor and chairman of the Department of Medicine and executive director of the hospitalist program at the University of California at Irvine.
By explaining the situation, Dr. Bell says, the hospitalist doesn’t give the employer a chance to guess a reason for the red flag—and potentially guess wrong.
“There’s a big difference between there’s been some sort of serious censure and they’ve been driven out, versus they thought another setting might be more interesting or they just wanted to make a geographic move,” says Thomas E. Thorsheim, PhD, a licensed psychologist and physician leadership coach based in Greenville, S.C. “It’s important to preempt any concerns about how reliable or stable they’re going to be.”
Applicants with resume red flags should show that they’ve taken responsibility for what happened and grown from the experience, say Dr. Thorsheim and Cheryl O’Malley, MD, FACP, program director in the department of internal medicine and pediatrics at Banner Good Samaritan Medical Center in Phoenix.
“Everyone wants to know that you have learned from your mistakes. Try to have a demonstrated remediation of the concern and go above and beyond the minimum requirements,” Dr. O’Malley says. “For example, if the red flag is academic concerns or not passing your board exams, then bring in documentation of your schedule for reading daily and all of the CME and MKSAP you complete. If it is interpersonal issues, then give examples of recent successes that show how you have improved.”
Brand Recognition
Physicians with a resume blemish should concentrate on highlighting their strengths and “branding” themselves as a workplace contributor, says Bernadette Norz, MBA, ACC, a certified physician development coach. While this advice applies to all applicants, it is particularly critical for those with resume problems, as it will demonstrate they have skills that set them apart from others.
“What people are really looking for is what did you do and what was the result,” Norz says. “Things that one accomplished as a volunteer or on a committee count, too, because that’s where people gain a lot of leadership skills.”
Resumes should not be recitations of job descriptions, she advises. They should be lists of achievements described with action verbs that give the applicant a clear identity and brand. “When you read a resume, you should walk away from it knowing who this person is,” says Dr. Kaplan. “If you don’t see that on their resume, then you’ve got to question it.”
The best applicants network. The more you can develop a relationship and rapport with peers and potential employers, the more likely you will be given a greater chance to sell your strengths and explain weaknesses, says career strategist Ellen Dunagan, president of Traverse Management Solutions in Arlington, Va. “You really want to step it up and be much more active with your own pitch,” she says.
Attitude Matters
But before a hospitalist or any applicant with a resume shortcoming begins to look for a job, they must resolve the issue internally, Dr. Kaplan notes. Taking responsibility will allow you to speak clearly and comfortably about what happened, without negativity or blame.
“If you don’t, you will fumble,” he says. “The prospective employer will start seeing those red flags and they will ask you about it, and you thought you had your pitch ready. Then they ask you two more questions, and before you know it, they’re not going to feel a sense of transparency with you.”
More and more, what employers are looking for is positivity, Dunagan says. It’s a trait applicants won’t have if they still harbor negative feelings toward a previous employer. “It’s just very important to be not only a team player, but to have a really good attitude,” she says. “So present yourself in the best possible light.”
Lisa Ryan is a freelance writer based in New Jersey.
Medical Decision-Making Factors Include Quantity of Information, Complexity
Physicians should formulate a complete and accurate description of a patient’s condition with an equivalent plan of care for each encounter. While acuity and severity can be inferred by healthcare professionals without excessive detail or repetitive documentation of previously entered information, adequate documentation for every service date assists in conveying patient complexity during medical record review.
Regardless of how complex a patient’s condition might be, physicians tend to undervalue their services. This is due, in part, to the routine nature of patient care for seasoned physicians; it is also due in part to a general lack of understanding with respect to the documentation guidelines.
Consider the following scenario: A 68-year-old male with diabetes and a history of chronic obstructive bronchitis was hospitalized after a five-day history of progressive cough with increasing purulent sputum, shortness of breath, and fever. He was treated for an exacerbation of chronic bronchitis within the past six weeks. Upon admission, the patient had an increased temperature (102°F), increased heart rate (96 beats per minute), and increased respiratory rate (28 shallow breaths per minute). His breath sounds included in the right lower lobe rhonchi, and his pulse oximetry was 89% on room air. Chest X-ray confirmed right lower lobe infiltrates along with chronic changes.
Although some physicians would consider this “low complexity” due to the frequency in which they encounter this type of case, others will more appropriately identify this as moderately complex.
MDM Categories
Medical decision-making (MDM) remains consistent in both the 1995 and 1997 guidelines.1,2 Complexity is categorized as straightforward, low, moderate, or high, based on the content of physician documentation. Each visit level is associated with a particular level of complexity. Only the care plan for a given date of service is considered when assigning MDM complexity. For each encounter, the physician receives credit for the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality (see Table 1).
Number of diagnoses or treatment options. Physicians should document problems addressed and managed daily despite any changes to the treatment plan. Credit is provided for each problem with an associated plan, even if the plan states “continue treatment.” Credit also depends upon the quantity of problems addressed, as well as the problem type. An established problem in which the care plan has been established by the physician or group practice member during the current hospitalization is less complex than a new problem for which a diagnosis, prognosis, or plan has not been determined. Severity of the problem affects the weight of complexity. A worsening problem is more complex than an improving problem. Physician documentation should:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- When documentation indicates a continuation of current management options (e.g. “continue meds”), be sure that the management options to be continued are noted somewhere in the progress note for that encounter (e.g. medication list).
The plan of care outlines problems that the physician personally manages and those that impact management options, even if another physician directly oversees the problem. For example, the hospitalist might primarily manage diabetes, while the pulmonologist manages pneumonia. Since the pneumonia may impact the hospitalist’s plan for diabetic management, the hospitalist can receive credit for the pneumonia diagnosis if there is a non-overlapping, hospitalist-related care plan or comment about the pneumonia.
Amount and/or complexity of data ordered/reviewed. “Data” is classified as pathology/laboratory testing, radiology, and medicine-based diagnostics. Pertinent orders or results could be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”);
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary;
- Indicate when images, tracings, or specimens are “personally reviewed”; and
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Risks of complication and/or morbidity or mortality. Risk involves the patient’s presenting problem, diagnostic procedures ordered, and management options selected. It is measured as minimal, low, moderate, or high when compared with corresponding items assigned to each risk level (see Table 2). The highest individual item detected on the table determines the overall patient risk for that encounter.
Chronic conditions and invasive procedures pose more risk than acute, uncomplicated illnesses or non-invasive procedures. Stable or improving problems are not as menacing as progressing problems; minor exacerbations are less hazardous than severe exacerbations; and medication risk varies with the type and potential for adverse effects. A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change. Physicians should:
- Status all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), when applicable;
- Document all diagnostic or therapeutic procedures considered;
- Identify surgical risk factors involving comorbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding medication (e.g. “Continue Coumadin, monitor PT/INR”).
Determining complexity of medical decision-making. The final complexity of MDM depends upon the second-highest MDM category. The physician does not have to meet the requirements for all three MDM categories. For example, if a physician satisfies the requirements for a “multiple” number of diagnoses/treatment options, “limited” data, and “high” risk, the physician achieves moderate complexity decision-making (see Table 3). Remember that decision-making is just one of three components in evaluation and management services, along with history and exam.
Beware of payor variation, as it could have a significant impact on visit-level selection.3 Become acquainted with rules applicable to the geographical area. Review insurer websites for guidelines, policies, and “frequently asked questions” that can help improve documentation skills and support billing practices.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Nov. 14, 2011.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Nov. 14, 2011.
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
Physicians should formulate a complete and accurate description of a patient’s condition with an equivalent plan of care for each encounter. While acuity and severity can be inferred by healthcare professionals without excessive detail or repetitive documentation of previously entered information, adequate documentation for every service date assists in conveying patient complexity during medical record review.
Regardless of how complex a patient’s condition might be, physicians tend to undervalue their services. This is due, in part, to the routine nature of patient care for seasoned physicians; it is also due in part to a general lack of understanding with respect to the documentation guidelines.
Consider the following scenario: A 68-year-old male with diabetes and a history of chronic obstructive bronchitis was hospitalized after a five-day history of progressive cough with increasing purulent sputum, shortness of breath, and fever. He was treated for an exacerbation of chronic bronchitis within the past six weeks. Upon admission, the patient had an increased temperature (102°F), increased heart rate (96 beats per minute), and increased respiratory rate (28 shallow breaths per minute). His breath sounds included in the right lower lobe rhonchi, and his pulse oximetry was 89% on room air. Chest X-ray confirmed right lower lobe infiltrates along with chronic changes.
Although some physicians would consider this “low complexity” due to the frequency in which they encounter this type of case, others will more appropriately identify this as moderately complex.
MDM Categories
Medical decision-making (MDM) remains consistent in both the 1995 and 1997 guidelines.1,2 Complexity is categorized as straightforward, low, moderate, or high, based on the content of physician documentation. Each visit level is associated with a particular level of complexity. Only the care plan for a given date of service is considered when assigning MDM complexity. For each encounter, the physician receives credit for the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality (see Table 1).
Number of diagnoses or treatment options. Physicians should document problems addressed and managed daily despite any changes to the treatment plan. Credit is provided for each problem with an associated plan, even if the plan states “continue treatment.” Credit also depends upon the quantity of problems addressed, as well as the problem type. An established problem in which the care plan has been established by the physician or group practice member during the current hospitalization is less complex than a new problem for which a diagnosis, prognosis, or plan has not been determined. Severity of the problem affects the weight of complexity. A worsening problem is more complex than an improving problem. Physician documentation should:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- When documentation indicates a continuation of current management options (e.g. “continue meds”), be sure that the management options to be continued are noted somewhere in the progress note for that encounter (e.g. medication list).
The plan of care outlines problems that the physician personally manages and those that impact management options, even if another physician directly oversees the problem. For example, the hospitalist might primarily manage diabetes, while the pulmonologist manages pneumonia. Since the pneumonia may impact the hospitalist’s plan for diabetic management, the hospitalist can receive credit for the pneumonia diagnosis if there is a non-overlapping, hospitalist-related care plan or comment about the pneumonia.
Amount and/or complexity of data ordered/reviewed. “Data” is classified as pathology/laboratory testing, radiology, and medicine-based diagnostics. Pertinent orders or results could be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”);
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary;
- Indicate when images, tracings, or specimens are “personally reviewed”; and
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Risks of complication and/or morbidity or mortality. Risk involves the patient’s presenting problem, diagnostic procedures ordered, and management options selected. It is measured as minimal, low, moderate, or high when compared with corresponding items assigned to each risk level (see Table 2). The highest individual item detected on the table determines the overall patient risk for that encounter.
Chronic conditions and invasive procedures pose more risk than acute, uncomplicated illnesses or non-invasive procedures. Stable or improving problems are not as menacing as progressing problems; minor exacerbations are less hazardous than severe exacerbations; and medication risk varies with the type and potential for adverse effects. A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change. Physicians should:
- Status all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), when applicable;
- Document all diagnostic or therapeutic procedures considered;
- Identify surgical risk factors involving comorbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding medication (e.g. “Continue Coumadin, monitor PT/INR”).
Determining complexity of medical decision-making. The final complexity of MDM depends upon the second-highest MDM category. The physician does not have to meet the requirements for all three MDM categories. For example, if a physician satisfies the requirements for a “multiple” number of diagnoses/treatment options, “limited” data, and “high” risk, the physician achieves moderate complexity decision-making (see Table 3). Remember that decision-making is just one of three components in evaluation and management services, along with history and exam.
Beware of payor variation, as it could have a significant impact on visit-level selection.3 Become acquainted with rules applicable to the geographical area. Review insurer websites for guidelines, policies, and “frequently asked questions” that can help improve documentation skills and support billing practices.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Nov. 14, 2011.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Nov. 14, 2011.
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
Physicians should formulate a complete and accurate description of a patient’s condition with an equivalent plan of care for each encounter. While acuity and severity can be inferred by healthcare professionals without excessive detail or repetitive documentation of previously entered information, adequate documentation for every service date assists in conveying patient complexity during medical record review.
Regardless of how complex a patient’s condition might be, physicians tend to undervalue their services. This is due, in part, to the routine nature of patient care for seasoned physicians; it is also due in part to a general lack of understanding with respect to the documentation guidelines.
Consider the following scenario: A 68-year-old male with diabetes and a history of chronic obstructive bronchitis was hospitalized after a five-day history of progressive cough with increasing purulent sputum, shortness of breath, and fever. He was treated for an exacerbation of chronic bronchitis within the past six weeks. Upon admission, the patient had an increased temperature (102°F), increased heart rate (96 beats per minute), and increased respiratory rate (28 shallow breaths per minute). His breath sounds included in the right lower lobe rhonchi, and his pulse oximetry was 89% on room air. Chest X-ray confirmed right lower lobe infiltrates along with chronic changes.
Although some physicians would consider this “low complexity” due to the frequency in which they encounter this type of case, others will more appropriately identify this as moderately complex.
MDM Categories
Medical decision-making (MDM) remains consistent in both the 1995 and 1997 guidelines.1,2 Complexity is categorized as straightforward, low, moderate, or high, based on the content of physician documentation. Each visit level is associated with a particular level of complexity. Only the care plan for a given date of service is considered when assigning MDM complexity. For each encounter, the physician receives credit for the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality (see Table 1).
Number of diagnoses or treatment options. Physicians should document problems addressed and managed daily despite any changes to the treatment plan. Credit is provided for each problem with an associated plan, even if the plan states “continue treatment.” Credit also depends upon the quantity of problems addressed, as well as the problem type. An established problem in which the care plan has been established by the physician or group practice member during the current hospitalization is less complex than a new problem for which a diagnosis, prognosis, or plan has not been determined. Severity of the problem affects the weight of complexity. A worsening problem is more complex than an improving problem. Physician documentation should:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- When documentation indicates a continuation of current management options (e.g. “continue meds”), be sure that the management options to be continued are noted somewhere in the progress note for that encounter (e.g. medication list).
The plan of care outlines problems that the physician personally manages and those that impact management options, even if another physician directly oversees the problem. For example, the hospitalist might primarily manage diabetes, while the pulmonologist manages pneumonia. Since the pneumonia may impact the hospitalist’s plan for diabetic management, the hospitalist can receive credit for the pneumonia diagnosis if there is a non-overlapping, hospitalist-related care plan or comment about the pneumonia.
Amount and/or complexity of data ordered/reviewed. “Data” is classified as pathology/laboratory testing, radiology, and medicine-based diagnostics. Pertinent orders or results could be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”);
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary;
- Indicate when images, tracings, or specimens are “personally reviewed”; and
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Risks of complication and/or morbidity or mortality. Risk involves the patient’s presenting problem, diagnostic procedures ordered, and management options selected. It is measured as minimal, low, moderate, or high when compared with corresponding items assigned to each risk level (see Table 2). The highest individual item detected on the table determines the overall patient risk for that encounter.
Chronic conditions and invasive procedures pose more risk than acute, uncomplicated illnesses or non-invasive procedures. Stable or improving problems are not as menacing as progressing problems; minor exacerbations are less hazardous than severe exacerbations; and medication risk varies with the type and potential for adverse effects. A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change. Physicians should:
- Status all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), when applicable;
- Document all diagnostic or therapeutic procedures considered;
- Identify surgical risk factors involving comorbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding medication (e.g. “Continue Coumadin, monitor PT/INR”).
Determining complexity of medical decision-making. The final complexity of MDM depends upon the second-highest MDM category. The physician does not have to meet the requirements for all three MDM categories. For example, if a physician satisfies the requirements for a “multiple” number of diagnoses/treatment options, “limited” data, and “high” risk, the physician achieves moderate complexity decision-making (see Table 3). Remember that decision-making is just one of three components in evaluation and management services, along with history and exam.
Beware of payor variation, as it could have a significant impact on visit-level selection.3 Become acquainted with rules applicable to the geographical area. Review insurer websites for guidelines, policies, and “frequently asked questions” that can help improve documentation skills and support billing practices.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Nov. 14, 2011.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Nov. 14, 2011.
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
IPAB is Medicare's New Hammer for Spending Accountability
Now that the latest annual “doc fix” is in, physicians have been granted another reprieve from potentially crippling cuts to their Medicare reimbursement under the flawed sustainable growth rate (SGR) payment formula.
Beginning this year, there’s a new player in town that will have the authority to achieve what Congress has consistently failed to do—cut Medicare provider spending to keep it below a cap—and it can do so with unprecedented autonomy.
Say hello to the Independent Payment Advisory Board (IPAB), a creature of the Affordable Care Act (ACA) that will propose ways to reduce “overpayment” to Medicare providers if target-spending levels are exceeded.
What distinguishes the IPAB from the Medicare Payment Advisory Commission (MedPAC) is that its proposals will automatically become law, unless Congress enacts its own proposals that reduce Medicare provider spending by at least as much as IPAB’s, or the Senate musters a three-fifths majority vote to override IPAB’s proposals entirely. Further, the IPAB’s changes to Medicare cannot be overruled by the executive branch or a court of law.
MedPAC never wielded such authority; in fact, many of its cost-control recommendations were ignored.

—Judith Feder, PhD, professor of public policy, Georgetown University, Washington, D.C., former dean, Georgetown Public Policy Institute, fellow, the Urban Institute
The IPAB comes to life this year, with a $15 million appropriation from the ACA, and begins ramping up its operations (see “The IPAB Timetable,” p. 26). The board will be comprised of a 15-member, multi-stakeholder group—expected to include physicians, nurses, medical experts, economists, consumer advocates, and others—appointed by the President and subject to Senate confirmation.
Incendiary Reactions
Dubbed by its most vociferous and largely Republican critics as “dangerously powerful,” “the real death panel,” and “bureaucrats deciding whether you get care,” the IPAB even has some Democrats decrying its power grab. Rep. Pete Stark (D-Calif.) called the IPAB “an unprecedented abrogation of Congressional authority to an unelected, unaccountable body of so-called experts.”1
Even Allyson Schwartz (D-Pa.), who helped draft the ACA, has come out against the IPAB, joining a handful of Democrats and more than 200 Republicans in signing on to a bill (H.R. 452) to repeal the ACA’s IPAB provision. The Senate has a similar bill (S. 668).
Although the IPAB legally is barred from formally making recommendations to ration care, increase beneficiary premiums or cost sharing, and from restricting benefits or eligibility criteria, critics worry that its authority to control prices could hurt patients by driving Medicare payments so low that physicians cease to offer certain services to them.
Enforcement Power
IPAB will have unprecedented power to enforce Medicare’s provider spending benchmarks. Beginning in 2014, if Medicare’s projected spending growth rate per beneficiary rises above an inflation threshold of Gross Domestic Product per capita plus 1%, the IPAB would be triggered and would propose ways to trim provider payments. President Obama has since proposed a lower threshold of GDP per capita plus 0.5%, meaning that the IPAB would be triggered earlier and likely would have deeper cuts to make.
It is unclear how the spending growth benchmark will be affected by the $123 billion in Medicare payment cuts to hospitals and other providers over nine years, which were triggered when the so-called “super committee” failed to reach a budget-cutting consensus last fall.
U.S. Department of Health and Human Services (HHS) Secretary Kathleen Sebelius describes the IPAB as a “backstop to ensure that rising costs don’t accelerate out of control, threatening Medicare’s stability,” and she maintains that the board is a necessary fallback mechanism to enforce Medicare spending within budget while healthcare providers continue to prove the effectiveness of various value-based delivery and reimbursement reform projects the ACA is funding.2
Impact on Physicians
“The IPAB is a structural intervention to put pressure on Congress, the Executive, and CMS [Centers for Medicare & Medicaid Services] to guarantee the ACA’s investment in cost-containment, and it gives physicians the incentive to act on its principles,” says Judith Feder, PhD, professor of public policy at Georgetown University, former dean of the Georgetown Public Policy Institute, and a fellow at the Urban Institute.
Dr. Feder was a co-signer of a letter sent by 100 health policy experts and economists—including Congressional Budget Office founding director Alice Rivlin, now with the Brookings Institute—to congressional leaders last May urging them to abandon attempts to repeal the IPAB provision. Dr. Feder maintains that the IPAB will marshal “the expertise of professionals who can weigh evidence on how payment incentives affect care delivery and suggest sensible improvements, while forcing debate on difficult choices that Congress has thus far failed to address.”
Because of the changes the ACA has already made to provider reimbursement and Medicare Advantage plan funding, Feder says that Medicare’s average annual growth rate for the next decade is projected to be a full percentage point below per capita growth in GDP. On top of that, she says, “the ACA’s other payment reform experiments have the potential to improve quality and cut spending growth even further by reducing payment for overpriced or undesirable care–like unnecessary hospital readmissions–and rewarding efficiently provided, coordinated care.” By Feder’s analysis, the IPAB would not likely be triggered for a decade, but stands ready as a backup, if needed. Indeed, she favors extending IPAB’s authority beyond Medicare, to allow a system-wide spending target that creates an all-payer incentive to assure that providers really change their behavior to boost quality and efficiency.
Impact on Hospitalists
If the IPAB does come into play, Feder believes that hospitalists have less to worry about than other physician specialists, because the Board’s cost-reduction proposals would likely focus on services where overpayment is the most acute – like imaging and high-cost specialty procedures. “If hospitalists are promoting efficient, coordinated care, their position can only be enhanced by IPAB’s recommendations, to the extent that they can demonstrate value for the healthcare dollar spent,” she says.
Necessary quality and cost reforms that patients deserve, and physicians want to deliver, have been stymied for too long by a crippled Congress, and by powerful special interest agendas, says SHM Public Policy Committee member Bradley Flansbaum DO, MPH, FACP, SFHM, director of the HM program at Lenox Hill Hospital in New York City, and clinical assistant professor of medicine at NYU School of Medicine. Reform requires some real enforcement authority to put value-based quality above the fray, he adds.
“CMS just does not have the teeth to do that right now; they are in the cross-hairs, and an IPAB-like body is needed to insulate Congress from the politically-risky choices, bring evidence and expertise to the decisions, bust through the politics, and get the job done,” Dr. Flansbaum says.
Dr. Flansbaum illustrates the problem by pointing to recent clinical studies that show percutaneous vertebroplasty, which injects bone cement into the spine to treat fractures, to be no better than a placebo in relieving pain. Medicare and private health insurers have been covering vertebroplasty for many years, despite the absence of rigorous study of its effectiveness. The same likely holds true for scores of other expensive treatments and surgical procedures. “Who, exactly, is going to put the kibosh on this?” Dr. Flansbaum asks. “The free market, which includes surgeons, hospitals, and device companies, each with their agendas, or regulators?”
Dr. Flansbaum believes that, in order to effectively bring down costs, the IPAB should not be restricted to supply-side proposals (i.e. provider reimbursement), but also should be allowed to propose demand-side changes to Medicare’s benefit plans, such as tiered network pricing with higher premiums to cover the latest and most expensive technologies.
SHM supports the need for an independent entity to check the growth in Medicare spending, but it does not support the IPAB as it is currently established under the ACA because certain groups (including hospitals) are protected from its scrutiny during its first several years—a limitation that SHM says puts the board’s legitimacy into question and seriously weakens its potential cost-saving effectiveness. SHM supports replacing the IPAB with an independent board that (1) subjects all Medicare providers and suppliers to the same scrutiny without special interest carve-outs, (2) balances cost-saving with QI considerations, (3) protects delivery of quality services, and (4) ensures board membership that represents all potentially affected groups, including physicians. (Read the entire statement in the “Where We Stand” section of SHM’s Advocacy microsite at www.hospitalmedicine.org/advocacy.)
By removing the IPAB’s present handcuffs—opening its scope to all providers, as well as to demand-side changes in Medicare’s benefit structure—an IPAB-like entity with the proper staff and expertise can rationally think-out the choices that Congress will never make, according to Dr. Flansbaum.
“For the sake of our economy and our future generations, healthcare costs have to come down, even if that means some short-term pain,” he says. “Hospitals may take a hit. Some physician income might take a hit. Otherwise, there won’t be any hospitals or salaries to be hit.”
Christopher Guadagnino is a freelance writer in Philadelphia.
Reference
- Statement of Congressman Pete Stark Supporting Health Care Reform, March 21, 2010. Available at: http://www.stark.house.gov/index.php?option=com_content&view=article&id=1534:statement-of-congressman-pete-stark-supporting-health-care-reform&catid=67:floor-statements-2010-. Accessed Jan. 5, 2012.
- Kathleen Sebelius, “IPAB Will Protect Medicare.” Politico, June 23, 2011. Available at: http://dyn.politico.com/printstory.cfm?uuid=FDE594BA-87EE-4DA5-9841-33804926EF36. Accessed Jan. 5, 2012.
Now that the latest annual “doc fix” is in, physicians have been granted another reprieve from potentially crippling cuts to their Medicare reimbursement under the flawed sustainable growth rate (SGR) payment formula.
Beginning this year, there’s a new player in town that will have the authority to achieve what Congress has consistently failed to do—cut Medicare provider spending to keep it below a cap—and it can do so with unprecedented autonomy.
Say hello to the Independent Payment Advisory Board (IPAB), a creature of the Affordable Care Act (ACA) that will propose ways to reduce “overpayment” to Medicare providers if target-spending levels are exceeded.
What distinguishes the IPAB from the Medicare Payment Advisory Commission (MedPAC) is that its proposals will automatically become law, unless Congress enacts its own proposals that reduce Medicare provider spending by at least as much as IPAB’s, or the Senate musters a three-fifths majority vote to override IPAB’s proposals entirely. Further, the IPAB’s changes to Medicare cannot be overruled by the executive branch or a court of law.
MedPAC never wielded such authority; in fact, many of its cost-control recommendations were ignored.

—Judith Feder, PhD, professor of public policy, Georgetown University, Washington, D.C., former dean, Georgetown Public Policy Institute, fellow, the Urban Institute
The IPAB comes to life this year, with a $15 million appropriation from the ACA, and begins ramping up its operations (see “The IPAB Timetable,” p. 26). The board will be comprised of a 15-member, multi-stakeholder group—expected to include physicians, nurses, medical experts, economists, consumer advocates, and others—appointed by the President and subject to Senate confirmation.
Incendiary Reactions
Dubbed by its most vociferous and largely Republican critics as “dangerously powerful,” “the real death panel,” and “bureaucrats deciding whether you get care,” the IPAB even has some Democrats decrying its power grab. Rep. Pete Stark (D-Calif.) called the IPAB “an unprecedented abrogation of Congressional authority to an unelected, unaccountable body of so-called experts.”1
Even Allyson Schwartz (D-Pa.), who helped draft the ACA, has come out against the IPAB, joining a handful of Democrats and more than 200 Republicans in signing on to a bill (H.R. 452) to repeal the ACA’s IPAB provision. The Senate has a similar bill (S. 668).
Although the IPAB legally is barred from formally making recommendations to ration care, increase beneficiary premiums or cost sharing, and from restricting benefits or eligibility criteria, critics worry that its authority to control prices could hurt patients by driving Medicare payments so low that physicians cease to offer certain services to them.
Enforcement Power
IPAB will have unprecedented power to enforce Medicare’s provider spending benchmarks. Beginning in 2014, if Medicare’s projected spending growth rate per beneficiary rises above an inflation threshold of Gross Domestic Product per capita plus 1%, the IPAB would be triggered and would propose ways to trim provider payments. President Obama has since proposed a lower threshold of GDP per capita plus 0.5%, meaning that the IPAB would be triggered earlier and likely would have deeper cuts to make.
It is unclear how the spending growth benchmark will be affected by the $123 billion in Medicare payment cuts to hospitals and other providers over nine years, which were triggered when the so-called “super committee” failed to reach a budget-cutting consensus last fall.
U.S. Department of Health and Human Services (HHS) Secretary Kathleen Sebelius describes the IPAB as a “backstop to ensure that rising costs don’t accelerate out of control, threatening Medicare’s stability,” and she maintains that the board is a necessary fallback mechanism to enforce Medicare spending within budget while healthcare providers continue to prove the effectiveness of various value-based delivery and reimbursement reform projects the ACA is funding.2
Impact on Physicians
“The IPAB is a structural intervention to put pressure on Congress, the Executive, and CMS [Centers for Medicare & Medicaid Services] to guarantee the ACA’s investment in cost-containment, and it gives physicians the incentive to act on its principles,” says Judith Feder, PhD, professor of public policy at Georgetown University, former dean of the Georgetown Public Policy Institute, and a fellow at the Urban Institute.
Dr. Feder was a co-signer of a letter sent by 100 health policy experts and economists—including Congressional Budget Office founding director Alice Rivlin, now with the Brookings Institute—to congressional leaders last May urging them to abandon attempts to repeal the IPAB provision. Dr. Feder maintains that the IPAB will marshal “the expertise of professionals who can weigh evidence on how payment incentives affect care delivery and suggest sensible improvements, while forcing debate on difficult choices that Congress has thus far failed to address.”
Because of the changes the ACA has already made to provider reimbursement and Medicare Advantage plan funding, Feder says that Medicare’s average annual growth rate for the next decade is projected to be a full percentage point below per capita growth in GDP. On top of that, she says, “the ACA’s other payment reform experiments have the potential to improve quality and cut spending growth even further by reducing payment for overpriced or undesirable care–like unnecessary hospital readmissions–and rewarding efficiently provided, coordinated care.” By Feder’s analysis, the IPAB would not likely be triggered for a decade, but stands ready as a backup, if needed. Indeed, she favors extending IPAB’s authority beyond Medicare, to allow a system-wide spending target that creates an all-payer incentive to assure that providers really change their behavior to boost quality and efficiency.
Impact on Hospitalists
If the IPAB does come into play, Feder believes that hospitalists have less to worry about than other physician specialists, because the Board’s cost-reduction proposals would likely focus on services where overpayment is the most acute – like imaging and high-cost specialty procedures. “If hospitalists are promoting efficient, coordinated care, their position can only be enhanced by IPAB’s recommendations, to the extent that they can demonstrate value for the healthcare dollar spent,” she says.
Necessary quality and cost reforms that patients deserve, and physicians want to deliver, have been stymied for too long by a crippled Congress, and by powerful special interest agendas, says SHM Public Policy Committee member Bradley Flansbaum DO, MPH, FACP, SFHM, director of the HM program at Lenox Hill Hospital in New York City, and clinical assistant professor of medicine at NYU School of Medicine. Reform requires some real enforcement authority to put value-based quality above the fray, he adds.
“CMS just does not have the teeth to do that right now; they are in the cross-hairs, and an IPAB-like body is needed to insulate Congress from the politically-risky choices, bring evidence and expertise to the decisions, bust through the politics, and get the job done,” Dr. Flansbaum says.
Dr. Flansbaum illustrates the problem by pointing to recent clinical studies that show percutaneous vertebroplasty, which injects bone cement into the spine to treat fractures, to be no better than a placebo in relieving pain. Medicare and private health insurers have been covering vertebroplasty for many years, despite the absence of rigorous study of its effectiveness. The same likely holds true for scores of other expensive treatments and surgical procedures. “Who, exactly, is going to put the kibosh on this?” Dr. Flansbaum asks. “The free market, which includes surgeons, hospitals, and device companies, each with their agendas, or regulators?”
Dr. Flansbaum believes that, in order to effectively bring down costs, the IPAB should not be restricted to supply-side proposals (i.e. provider reimbursement), but also should be allowed to propose demand-side changes to Medicare’s benefit plans, such as tiered network pricing with higher premiums to cover the latest and most expensive technologies.
SHM supports the need for an independent entity to check the growth in Medicare spending, but it does not support the IPAB as it is currently established under the ACA because certain groups (including hospitals) are protected from its scrutiny during its first several years—a limitation that SHM says puts the board’s legitimacy into question and seriously weakens its potential cost-saving effectiveness. SHM supports replacing the IPAB with an independent board that (1) subjects all Medicare providers and suppliers to the same scrutiny without special interest carve-outs, (2) balances cost-saving with QI considerations, (3) protects delivery of quality services, and (4) ensures board membership that represents all potentially affected groups, including physicians. (Read the entire statement in the “Where We Stand” section of SHM’s Advocacy microsite at www.hospitalmedicine.org/advocacy.)
By removing the IPAB’s present handcuffs—opening its scope to all providers, as well as to demand-side changes in Medicare’s benefit structure—an IPAB-like entity with the proper staff and expertise can rationally think-out the choices that Congress will never make, according to Dr. Flansbaum.
“For the sake of our economy and our future generations, healthcare costs have to come down, even if that means some short-term pain,” he says. “Hospitals may take a hit. Some physician income might take a hit. Otherwise, there won’t be any hospitals or salaries to be hit.”
Christopher Guadagnino is a freelance writer in Philadelphia.
Reference
- Statement of Congressman Pete Stark Supporting Health Care Reform, March 21, 2010. Available at: http://www.stark.house.gov/index.php?option=com_content&view=article&id=1534:statement-of-congressman-pete-stark-supporting-health-care-reform&catid=67:floor-statements-2010-. Accessed Jan. 5, 2012.
- Kathleen Sebelius, “IPAB Will Protect Medicare.” Politico, June 23, 2011. Available at: http://dyn.politico.com/printstory.cfm?uuid=FDE594BA-87EE-4DA5-9841-33804926EF36. Accessed Jan. 5, 2012.
Now that the latest annual “doc fix” is in, physicians have been granted another reprieve from potentially crippling cuts to their Medicare reimbursement under the flawed sustainable growth rate (SGR) payment formula.
Beginning this year, there’s a new player in town that will have the authority to achieve what Congress has consistently failed to do—cut Medicare provider spending to keep it below a cap—and it can do so with unprecedented autonomy.
Say hello to the Independent Payment Advisory Board (IPAB), a creature of the Affordable Care Act (ACA) that will propose ways to reduce “overpayment” to Medicare providers if target-spending levels are exceeded.
What distinguishes the IPAB from the Medicare Payment Advisory Commission (MedPAC) is that its proposals will automatically become law, unless Congress enacts its own proposals that reduce Medicare provider spending by at least as much as IPAB’s, or the Senate musters a three-fifths majority vote to override IPAB’s proposals entirely. Further, the IPAB’s changes to Medicare cannot be overruled by the executive branch or a court of law.
MedPAC never wielded such authority; in fact, many of its cost-control recommendations were ignored.

—Judith Feder, PhD, professor of public policy, Georgetown University, Washington, D.C., former dean, Georgetown Public Policy Institute, fellow, the Urban Institute
The IPAB comes to life this year, with a $15 million appropriation from the ACA, and begins ramping up its operations (see “The IPAB Timetable,” p. 26). The board will be comprised of a 15-member, multi-stakeholder group—expected to include physicians, nurses, medical experts, economists, consumer advocates, and others—appointed by the President and subject to Senate confirmation.
Incendiary Reactions
Dubbed by its most vociferous and largely Republican critics as “dangerously powerful,” “the real death panel,” and “bureaucrats deciding whether you get care,” the IPAB even has some Democrats decrying its power grab. Rep. Pete Stark (D-Calif.) called the IPAB “an unprecedented abrogation of Congressional authority to an unelected, unaccountable body of so-called experts.”1
Even Allyson Schwartz (D-Pa.), who helped draft the ACA, has come out against the IPAB, joining a handful of Democrats and more than 200 Republicans in signing on to a bill (H.R. 452) to repeal the ACA’s IPAB provision. The Senate has a similar bill (S. 668).
Although the IPAB legally is barred from formally making recommendations to ration care, increase beneficiary premiums or cost sharing, and from restricting benefits or eligibility criteria, critics worry that its authority to control prices could hurt patients by driving Medicare payments so low that physicians cease to offer certain services to them.
Enforcement Power
IPAB will have unprecedented power to enforce Medicare’s provider spending benchmarks. Beginning in 2014, if Medicare’s projected spending growth rate per beneficiary rises above an inflation threshold of Gross Domestic Product per capita plus 1%, the IPAB would be triggered and would propose ways to trim provider payments. President Obama has since proposed a lower threshold of GDP per capita plus 0.5%, meaning that the IPAB would be triggered earlier and likely would have deeper cuts to make.
It is unclear how the spending growth benchmark will be affected by the $123 billion in Medicare payment cuts to hospitals and other providers over nine years, which were triggered when the so-called “super committee” failed to reach a budget-cutting consensus last fall.
U.S. Department of Health and Human Services (HHS) Secretary Kathleen Sebelius describes the IPAB as a “backstop to ensure that rising costs don’t accelerate out of control, threatening Medicare’s stability,” and she maintains that the board is a necessary fallback mechanism to enforce Medicare spending within budget while healthcare providers continue to prove the effectiveness of various value-based delivery and reimbursement reform projects the ACA is funding.2
Impact on Physicians
“The IPAB is a structural intervention to put pressure on Congress, the Executive, and CMS [Centers for Medicare & Medicaid Services] to guarantee the ACA’s investment in cost-containment, and it gives physicians the incentive to act on its principles,” says Judith Feder, PhD, professor of public policy at Georgetown University, former dean of the Georgetown Public Policy Institute, and a fellow at the Urban Institute.
Dr. Feder was a co-signer of a letter sent by 100 health policy experts and economists—including Congressional Budget Office founding director Alice Rivlin, now with the Brookings Institute—to congressional leaders last May urging them to abandon attempts to repeal the IPAB provision. Dr. Feder maintains that the IPAB will marshal “the expertise of professionals who can weigh evidence on how payment incentives affect care delivery and suggest sensible improvements, while forcing debate on difficult choices that Congress has thus far failed to address.”
Because of the changes the ACA has already made to provider reimbursement and Medicare Advantage plan funding, Feder says that Medicare’s average annual growth rate for the next decade is projected to be a full percentage point below per capita growth in GDP. On top of that, she says, “the ACA’s other payment reform experiments have the potential to improve quality and cut spending growth even further by reducing payment for overpriced or undesirable care–like unnecessary hospital readmissions–and rewarding efficiently provided, coordinated care.” By Feder’s analysis, the IPAB would not likely be triggered for a decade, but stands ready as a backup, if needed. Indeed, she favors extending IPAB’s authority beyond Medicare, to allow a system-wide spending target that creates an all-payer incentive to assure that providers really change their behavior to boost quality and efficiency.
Impact on Hospitalists
If the IPAB does come into play, Feder believes that hospitalists have less to worry about than other physician specialists, because the Board’s cost-reduction proposals would likely focus on services where overpayment is the most acute – like imaging and high-cost specialty procedures. “If hospitalists are promoting efficient, coordinated care, their position can only be enhanced by IPAB’s recommendations, to the extent that they can demonstrate value for the healthcare dollar spent,” she says.
Necessary quality and cost reforms that patients deserve, and physicians want to deliver, have been stymied for too long by a crippled Congress, and by powerful special interest agendas, says SHM Public Policy Committee member Bradley Flansbaum DO, MPH, FACP, SFHM, director of the HM program at Lenox Hill Hospital in New York City, and clinical assistant professor of medicine at NYU School of Medicine. Reform requires some real enforcement authority to put value-based quality above the fray, he adds.
“CMS just does not have the teeth to do that right now; they are in the cross-hairs, and an IPAB-like body is needed to insulate Congress from the politically-risky choices, bring evidence and expertise to the decisions, bust through the politics, and get the job done,” Dr. Flansbaum says.
Dr. Flansbaum illustrates the problem by pointing to recent clinical studies that show percutaneous vertebroplasty, which injects bone cement into the spine to treat fractures, to be no better than a placebo in relieving pain. Medicare and private health insurers have been covering vertebroplasty for many years, despite the absence of rigorous study of its effectiveness. The same likely holds true for scores of other expensive treatments and surgical procedures. “Who, exactly, is going to put the kibosh on this?” Dr. Flansbaum asks. “The free market, which includes surgeons, hospitals, and device companies, each with their agendas, or regulators?”
Dr. Flansbaum believes that, in order to effectively bring down costs, the IPAB should not be restricted to supply-side proposals (i.e. provider reimbursement), but also should be allowed to propose demand-side changes to Medicare’s benefit plans, such as tiered network pricing with higher premiums to cover the latest and most expensive technologies.
SHM supports the need for an independent entity to check the growth in Medicare spending, but it does not support the IPAB as it is currently established under the ACA because certain groups (including hospitals) are protected from its scrutiny during its first several years—a limitation that SHM says puts the board’s legitimacy into question and seriously weakens its potential cost-saving effectiveness. SHM supports replacing the IPAB with an independent board that (1) subjects all Medicare providers and suppliers to the same scrutiny without special interest carve-outs, (2) balances cost-saving with QI considerations, (3) protects delivery of quality services, and (4) ensures board membership that represents all potentially affected groups, including physicians. (Read the entire statement in the “Where We Stand” section of SHM’s Advocacy microsite at www.hospitalmedicine.org/advocacy.)
By removing the IPAB’s present handcuffs—opening its scope to all providers, as well as to demand-side changes in Medicare’s benefit structure—an IPAB-like entity with the proper staff and expertise can rationally think-out the choices that Congress will never make, according to Dr. Flansbaum.
“For the sake of our economy and our future generations, healthcare costs have to come down, even if that means some short-term pain,” he says. “Hospitals may take a hit. Some physician income might take a hit. Otherwise, there won’t be any hospitals or salaries to be hit.”
Christopher Guadagnino is a freelance writer in Philadelphia.
Reference
- Statement of Congressman Pete Stark Supporting Health Care Reform, March 21, 2010. Available at: http://www.stark.house.gov/index.php?option=com_content&view=article&id=1534:statement-of-congressman-pete-stark-supporting-health-care-reform&catid=67:floor-statements-2010-. Accessed Jan. 5, 2012.
- Kathleen Sebelius, “IPAB Will Protect Medicare.” Politico, June 23, 2011. Available at: http://dyn.politico.com/printstory.cfm?uuid=FDE594BA-87EE-4DA5-9841-33804926EF36. Accessed Jan. 5, 2012.
Patients, Many of Whom are in Crisis, are Tracy Cardin’s Reason for Being
Tracy Cardin, ACNP-BC, entered college as a criminal justice major, believing her talent for crafting sound arguments and her passion for defending her point of view would translate into a successful law career.
Less than a year later, Cardin visited her gravely ill aunt and discovered her true calling. “I noticed a lot of small things: Her fingernails were a little long, her hair was sort of unkempt, and the environment wasn’t as clean as I would have liked,” Cardin says. “I didn’t feel the people who were caring for her were putting in the time or effort to make her as comfortable as possible. I didn’t see a lot of tender loving care, and I honestly felt I could do a better job.”
Cardin changed her major, pursued a nursing career, and now has 22 years of experience providing inpatient care.
“It’s a privilege to take care of patients, and hospitalists have a wonderful opportunity to impact the quality of care they receive,” says Cardin, one of seven nonphysician providers (NPPs) in the Section of Hospital Medicine at the University of Chicago Medical Center. She also is Team Hospitalist’s only NPP member. “They are the reason I do what I do—and the reason I love what I do.”
Are there similarities between being a nurse practitioner (NP) and a litigator?
You definitely have to advocate for your patients. Both fields allow you to see the stories of the human condition. In my job, it’s all about the patients’ stories—how they came to be here and fitting your care for the patient within their narrative. And like the legal setting, people often find themselves in the healthcare world at a time of crisis. I like being there to help people in those times.
Why did you choose to practice in a hospital setting?
I like the objective data you get in a hospital. You have lab work, imaging, and vital signs. It helps create a better picture of what’s going on. I like that it’s very acute. Patients have a problem, hopefully you fix the problem or at least stabilize the person, and then they can go home. I also like that it’s fast-paced and varied. The hospital truly is one of the places I’m most comfortable.
What is your biggest professional reward?
When a patient knows it’s time to go home and die—when it’s their time and they are ready to go—and they need someone to help them get through that process. When patients and their families move from trying to solve unsolvable problems to an acceptance of their mortality, it’s a beautiful journey, and I really like helping them navigate that journey.
How would you describe the relationship between the physicians and NPPs in your program?
Like all relationships, it has gone through an evolution. It started with the “getting to know you” stage, during which the physicians weren’t sure what the NPPs do and the NPPs were very anxious to show our capabilities. There was this pushing and pulling. Over time, thanks to excellent leadership, we have a model that utilizes NPPs to the maximum of their capabilities. We have a very collaborative, collegial group, and it’s a special place to work. I have the utmost respect for the physicians, and I feel they have the utmost respect for our abilities.
Do most HM programs that bring on NPPs go through growing pains?
In the beginning, often there’s a little drama or controversy. Someone oversteps their bounds, someone is too rigid and doesn’t allow a mid-level provider to do something, or someone gets their feelings hurt.
How can you survive that process without the partnership breaking down?
It’s like when you’re driving a car and it starts to pull off the road. If you overcorrect and turn the wheel too hard, you’re going to end up crashing. Instead, you just turn the wheel a little bit. It’s very important that you don’t panic and try to overcorrect. Sometimes only a small adjustment needs to be made. If everyone is committed to one another, it will work out.
What advice would you give to NPPs who are thinking about joining an HM program?
First, be ready to work hard. It’s very rewarding, but it’s a rapid pace and it’s stressful. Second, align yourself with someone who is sympathetic to and supportive of the role of a mid-level provider within a hospitalist group. Third, never give up, because hospital medicine is a great career.
What advice would you give to physicians whose programs are considering hiring NPPs?
Check out the SHM website (www.hospitalmedicine.org), because it is a tremendous resource. Also, treat the NPPs the same way they would treat another physician. Give them the same assistance, invite them to the same meetings, and give them the same education or training. Realize that even though physicians, NPs, and physician assistants have different educations, everyone brings their own skill set to the table that adds to this stew of excellence.
How do you see the role of NPPs evolving as they become more prevalent in HM?
Given residency work-hour reforms and the fact there are not physicians to do all of the work, NPPs are going to be utilized much more. NPPs bring a ton of experience to the care of inpatients, so a hospital medicine group should utilize them in all kinds of roles, whether it’s orienting new physicians or educating nursing staff about the care of their specialized patients. NPPs also can take on leadership roles as part of quality improvement projects. We are going to be needed in patient care, but we shouldn’t just be relegated to patient care. The experience is there to help in many other areas.
You have spoken about the integration of NPs in hospitalist programs at two HM meetings and will do so again at HM12. What does that mean to you?
It’s my passion. I’m fascinated by the entire process. I always say, “Why am I up here speaking about this? Because I’ve made every mistake; learn from me.” My program director [Chad Whelan, MD, FHM], who was so calm and so rational and helped me integrate so well, has impacted me so greatly. I get to pass that on to other people, and it’s a tremendous opportunity.
Mark Leiser is a freelance writer in New Jersey.
Tracy Cardin, ACNP-BC, entered college as a criminal justice major, believing her talent for crafting sound arguments and her passion for defending her point of view would translate into a successful law career.
Less than a year later, Cardin visited her gravely ill aunt and discovered her true calling. “I noticed a lot of small things: Her fingernails were a little long, her hair was sort of unkempt, and the environment wasn’t as clean as I would have liked,” Cardin says. “I didn’t feel the people who were caring for her were putting in the time or effort to make her as comfortable as possible. I didn’t see a lot of tender loving care, and I honestly felt I could do a better job.”
Cardin changed her major, pursued a nursing career, and now has 22 years of experience providing inpatient care.
“It’s a privilege to take care of patients, and hospitalists have a wonderful opportunity to impact the quality of care they receive,” says Cardin, one of seven nonphysician providers (NPPs) in the Section of Hospital Medicine at the University of Chicago Medical Center. She also is Team Hospitalist’s only NPP member. “They are the reason I do what I do—and the reason I love what I do.”
Are there similarities between being a nurse practitioner (NP) and a litigator?
You definitely have to advocate for your patients. Both fields allow you to see the stories of the human condition. In my job, it’s all about the patients’ stories—how they came to be here and fitting your care for the patient within their narrative. And like the legal setting, people often find themselves in the healthcare world at a time of crisis. I like being there to help people in those times.
Why did you choose to practice in a hospital setting?
I like the objective data you get in a hospital. You have lab work, imaging, and vital signs. It helps create a better picture of what’s going on. I like that it’s very acute. Patients have a problem, hopefully you fix the problem or at least stabilize the person, and then they can go home. I also like that it’s fast-paced and varied. The hospital truly is one of the places I’m most comfortable.
What is your biggest professional reward?
When a patient knows it’s time to go home and die—when it’s their time and they are ready to go—and they need someone to help them get through that process. When patients and their families move from trying to solve unsolvable problems to an acceptance of their mortality, it’s a beautiful journey, and I really like helping them navigate that journey.
How would you describe the relationship between the physicians and NPPs in your program?
Like all relationships, it has gone through an evolution. It started with the “getting to know you” stage, during which the physicians weren’t sure what the NPPs do and the NPPs were very anxious to show our capabilities. There was this pushing and pulling. Over time, thanks to excellent leadership, we have a model that utilizes NPPs to the maximum of their capabilities. We have a very collaborative, collegial group, and it’s a special place to work. I have the utmost respect for the physicians, and I feel they have the utmost respect for our abilities.
Do most HM programs that bring on NPPs go through growing pains?
In the beginning, often there’s a little drama or controversy. Someone oversteps their bounds, someone is too rigid and doesn’t allow a mid-level provider to do something, or someone gets their feelings hurt.
How can you survive that process without the partnership breaking down?
It’s like when you’re driving a car and it starts to pull off the road. If you overcorrect and turn the wheel too hard, you’re going to end up crashing. Instead, you just turn the wheel a little bit. It’s very important that you don’t panic and try to overcorrect. Sometimes only a small adjustment needs to be made. If everyone is committed to one another, it will work out.
What advice would you give to NPPs who are thinking about joining an HM program?
First, be ready to work hard. It’s very rewarding, but it’s a rapid pace and it’s stressful. Second, align yourself with someone who is sympathetic to and supportive of the role of a mid-level provider within a hospitalist group. Third, never give up, because hospital medicine is a great career.
What advice would you give to physicians whose programs are considering hiring NPPs?
Check out the SHM website (www.hospitalmedicine.org), because it is a tremendous resource. Also, treat the NPPs the same way they would treat another physician. Give them the same assistance, invite them to the same meetings, and give them the same education or training. Realize that even though physicians, NPs, and physician assistants have different educations, everyone brings their own skill set to the table that adds to this stew of excellence.
How do you see the role of NPPs evolving as they become more prevalent in HM?
Given residency work-hour reforms and the fact there are not physicians to do all of the work, NPPs are going to be utilized much more. NPPs bring a ton of experience to the care of inpatients, so a hospital medicine group should utilize them in all kinds of roles, whether it’s orienting new physicians or educating nursing staff about the care of their specialized patients. NPPs also can take on leadership roles as part of quality improvement projects. We are going to be needed in patient care, but we shouldn’t just be relegated to patient care. The experience is there to help in many other areas.
You have spoken about the integration of NPs in hospitalist programs at two HM meetings and will do so again at HM12. What does that mean to you?
It’s my passion. I’m fascinated by the entire process. I always say, “Why am I up here speaking about this? Because I’ve made every mistake; learn from me.” My program director [Chad Whelan, MD, FHM], who was so calm and so rational and helped me integrate so well, has impacted me so greatly. I get to pass that on to other people, and it’s a tremendous opportunity.
Mark Leiser is a freelance writer in New Jersey.
Tracy Cardin, ACNP-BC, entered college as a criminal justice major, believing her talent for crafting sound arguments and her passion for defending her point of view would translate into a successful law career.
Less than a year later, Cardin visited her gravely ill aunt and discovered her true calling. “I noticed a lot of small things: Her fingernails were a little long, her hair was sort of unkempt, and the environment wasn’t as clean as I would have liked,” Cardin says. “I didn’t feel the people who were caring for her were putting in the time or effort to make her as comfortable as possible. I didn’t see a lot of tender loving care, and I honestly felt I could do a better job.”
Cardin changed her major, pursued a nursing career, and now has 22 years of experience providing inpatient care.
“It’s a privilege to take care of patients, and hospitalists have a wonderful opportunity to impact the quality of care they receive,” says Cardin, one of seven nonphysician providers (NPPs) in the Section of Hospital Medicine at the University of Chicago Medical Center. She also is Team Hospitalist’s only NPP member. “They are the reason I do what I do—and the reason I love what I do.”
Are there similarities between being a nurse practitioner (NP) and a litigator?
You definitely have to advocate for your patients. Both fields allow you to see the stories of the human condition. In my job, it’s all about the patients’ stories—how they came to be here and fitting your care for the patient within their narrative. And like the legal setting, people often find themselves in the healthcare world at a time of crisis. I like being there to help people in those times.
Why did you choose to practice in a hospital setting?
I like the objective data you get in a hospital. You have lab work, imaging, and vital signs. It helps create a better picture of what’s going on. I like that it’s very acute. Patients have a problem, hopefully you fix the problem or at least stabilize the person, and then they can go home. I also like that it’s fast-paced and varied. The hospital truly is one of the places I’m most comfortable.
What is your biggest professional reward?
When a patient knows it’s time to go home and die—when it’s their time and they are ready to go—and they need someone to help them get through that process. When patients and their families move from trying to solve unsolvable problems to an acceptance of their mortality, it’s a beautiful journey, and I really like helping them navigate that journey.
How would you describe the relationship between the physicians and NPPs in your program?
Like all relationships, it has gone through an evolution. It started with the “getting to know you” stage, during which the physicians weren’t sure what the NPPs do and the NPPs were very anxious to show our capabilities. There was this pushing and pulling. Over time, thanks to excellent leadership, we have a model that utilizes NPPs to the maximum of their capabilities. We have a very collaborative, collegial group, and it’s a special place to work. I have the utmost respect for the physicians, and I feel they have the utmost respect for our abilities.
Do most HM programs that bring on NPPs go through growing pains?
In the beginning, often there’s a little drama or controversy. Someone oversteps their bounds, someone is too rigid and doesn’t allow a mid-level provider to do something, or someone gets their feelings hurt.
How can you survive that process without the partnership breaking down?
It’s like when you’re driving a car and it starts to pull off the road. If you overcorrect and turn the wheel too hard, you’re going to end up crashing. Instead, you just turn the wheel a little bit. It’s very important that you don’t panic and try to overcorrect. Sometimes only a small adjustment needs to be made. If everyone is committed to one another, it will work out.
What advice would you give to NPPs who are thinking about joining an HM program?
First, be ready to work hard. It’s very rewarding, but it’s a rapid pace and it’s stressful. Second, align yourself with someone who is sympathetic to and supportive of the role of a mid-level provider within a hospitalist group. Third, never give up, because hospital medicine is a great career.
What advice would you give to physicians whose programs are considering hiring NPPs?
Check out the SHM website (www.hospitalmedicine.org), because it is a tremendous resource. Also, treat the NPPs the same way they would treat another physician. Give them the same assistance, invite them to the same meetings, and give them the same education or training. Realize that even though physicians, NPs, and physician assistants have different educations, everyone brings their own skill set to the table that adds to this stew of excellence.
How do you see the role of NPPs evolving as they become more prevalent in HM?
Given residency work-hour reforms and the fact there are not physicians to do all of the work, NPPs are going to be utilized much more. NPPs bring a ton of experience to the care of inpatients, so a hospital medicine group should utilize them in all kinds of roles, whether it’s orienting new physicians or educating nursing staff about the care of their specialized patients. NPPs also can take on leadership roles as part of quality improvement projects. We are going to be needed in patient care, but we shouldn’t just be relegated to patient care. The experience is there to help in many other areas.
You have spoken about the integration of NPs in hospitalist programs at two HM meetings and will do so again at HM12. What does that mean to you?
It’s my passion. I’m fascinated by the entire process. I always say, “Why am I up here speaking about this? Because I’ve made every mistake; learn from me.” My program director [Chad Whelan, MD, FHM], who was so calm and so rational and helped me integrate so well, has impacted me so greatly. I get to pass that on to other people, and it’s a tremendous opportunity.
Mark Leiser is a freelance writer in New Jersey.
Pioneer Participants Work to Define Hospitalist Role in ACOs
In December, the U.S. Department of Health and Human Services (HHS) announced the selection of 32 organizations from 18 states as participants in the Pioneer Accountable Care Organization (ACO) initiative.
HHS developed this initiative with the hopes that they could save $1.1 billion over the next five years. Five of the 32 participating organizations are Massachusetts-based, including Beth Israel Deaconess Physician Organization (BIDPO) and Atrius Health. My hospitalist colleagues and I at Beth Israel Deaconess Medical Center (BIDMC) are BIDPO members; we also care for hospitalized patients for Atrius Health in Boston. So we will be caring for hospitalized patients involved in two of the 32 Pioneer ACOs.
Many of us are excited, but also understandably a bit anxious. Some of us are outright concerned. I suspect we are not alone. Many of you are in a similar position—being providers in a Pioneer ACO. My colleagues and are having conversations to increase our understanding of ACOs and the role of hospitalists in an ACO.
Nuts and Bolts
An ACO is a system to deliver and pay for healthcare by linking provider reimbursement to quality and cost of care for a defined population of patients. Think of it as a group of providers (primary-care physicians, ED doctors, hospitalists, medical and surgical specialists, etc.) who are bound by shared financial risks and rewards to work together to provide coordinated, high-quality, low-cost care for patients.
In the Pioneer ACO, groups of providers agree to manage the quality, costs, and overall care of the Medicare beneficiaries enrolled in the traditional fee-for-service program assigned to their ACO. The ACO model is designed to address some of the concerns of the traditional fee-for-service payment model, in which each provider offers services and submits their own bills separately. Under the fee-for-service model, the incentive is for each provider to provide as much care as possible, because payment is dependent on provision of more care rather than the provision of higher-quality care.
For example, there is little disincentive for PCPs to send patients to the ED if a patient needs evaluation, for any reason, when it is inconvenient for the PCP. Why keep outpatient clinic open during evenings and weekends when you could simply send the patient to the ED if they needed any sort of care? As an ED doctor, why not set a low threshold to admit patients to the hospital and mitigate any risk of a lawsuit by discharging the patient from the ED? As a hospitalist, why not discharge the patient to a skilled nursing care facility, where they will have more nursing supervision than at home, especially if the hospital, who is contributing to the hospitalist program bottom line, is monitoring your patients’ average length of stay?
Everyone is playing with everyone else’s money. Under the current system, there is little financial incentive for providers to work together in the provision of high-quality care. The ACO model is an attempt to create a model that will provide more integrated care by linking provider reimbursement to quality and cost of care.
Dr. Elliott Fisher at Dartmouth Medical School at Dartmouth College and others have identified several key principles for all ACOs:
- A strong primary-care base capable of being accountable for the quality and costs of care across the full continuum of care for a patient population;
- Provider reimbursement tied to quality improvements that also reduce overall costs; and
- Reliable performance measurement, to support quality improvement.
“ACO” may be a new term to many, but it is not new. Kaiser Permanente and HealthCare Partners Medical Group are examples of longstanding, successful ACOs.
You might be reading this and have arrived at the conclusion that Joe Li is convinced ACOs are the panacea for that ill known as the American healthcare system. That could not be further from the truth. I don’t think that the folks at Medicare are convinced, either. That is why there was a competitive process to select the 32 ACOs for this initiative. They chose provider groups that have experience working together. If ACOs are going to work, Medicare thinks these are the types of organizations that will be successful.
Interestingly, when one looks on the list of Pioneer participants, there are some notable absences. I don’t see Mayo Clinic or Cleveland Clinic. Hmmm. If these ACO “poster children” are not participating, should we? Perhaps they applied and HHS declined to accept their application, but I doubt it. These are the groups who already are ACOs. One can only assume that these organizations didn’t like the rules, or the financial rewards were not sufficiently attractive for them to participate.
Change Is Brewing
Regardless, the big question for hospitalists working in Pioneer groups is, How do we “succeed” in an ACO model? I believe that some of the same principles that allow hospitalists to succeed under the current model also apply under the ACO model. High-performing hospitalists and HM programs have:
Systems to monitor performance and provide feedback to providers with a plan for continuous quality improvement;
Established expectations for hospitalist communication with other providers, including PCPs, ED providers, subspecialists, nurses, and post-discharge care center facilities, among others; and
Multidisciplinary care teams providing evidence-based care with a focus on minimizing variations in care.
If ACOs are successful at providing high-quality care at lower costs, one could imagine changes to our healthcare system that will directly impact hospitalists. If ACOs are able to provide timely and comprehensive outpatient care, fewer patients will need care at acute-care hospitals. Efforts will be made to hospitalize patients at less-expensive community hospitals, instead of tertiary academic medical centers. The resultant smaller population of hospitalized patients will be sicker.
It’s not difficult to extrapolate on this new paradigm, as I can imagine hospitalists seeing fewer, sicker patients daily. These patients, as we all know, often require multiple visits per day. It is difficult to provide high-quality care to sick patients without doctors available in the hospital 24 hours a day, seven days a week. All hospitalists will need the skills to attend to critically ill, hospitalized patients. Hospitalists—and perhaps hospitals, if they are part of the ACO—will focus less on patient length of stay and more on keeping patients out of the hospitals. The cost of an entire readmission dwarfs the cost of one additional day in the hospital.
If you are a hospitalist providing care in a Pioneer ACO, I would love to hear how your practice is changing. Send me an email at [email protected], or message me via Twitter (@JosephLi) or LinkedIn: Joseph Li.
Dr. Li is president of SHM.
In December, the U.S. Department of Health and Human Services (HHS) announced the selection of 32 organizations from 18 states as participants in the Pioneer Accountable Care Organization (ACO) initiative.
HHS developed this initiative with the hopes that they could save $1.1 billion over the next five years. Five of the 32 participating organizations are Massachusetts-based, including Beth Israel Deaconess Physician Organization (BIDPO) and Atrius Health. My hospitalist colleagues and I at Beth Israel Deaconess Medical Center (BIDMC) are BIDPO members; we also care for hospitalized patients for Atrius Health in Boston. So we will be caring for hospitalized patients involved in two of the 32 Pioneer ACOs.
Many of us are excited, but also understandably a bit anxious. Some of us are outright concerned. I suspect we are not alone. Many of you are in a similar position—being providers in a Pioneer ACO. My colleagues and are having conversations to increase our understanding of ACOs and the role of hospitalists in an ACO.
Nuts and Bolts
An ACO is a system to deliver and pay for healthcare by linking provider reimbursement to quality and cost of care for a defined population of patients. Think of it as a group of providers (primary-care physicians, ED doctors, hospitalists, medical and surgical specialists, etc.) who are bound by shared financial risks and rewards to work together to provide coordinated, high-quality, low-cost care for patients.
In the Pioneer ACO, groups of providers agree to manage the quality, costs, and overall care of the Medicare beneficiaries enrolled in the traditional fee-for-service program assigned to their ACO. The ACO model is designed to address some of the concerns of the traditional fee-for-service payment model, in which each provider offers services and submits their own bills separately. Under the fee-for-service model, the incentive is for each provider to provide as much care as possible, because payment is dependent on provision of more care rather than the provision of higher-quality care.
For example, there is little disincentive for PCPs to send patients to the ED if a patient needs evaluation, for any reason, when it is inconvenient for the PCP. Why keep outpatient clinic open during evenings and weekends when you could simply send the patient to the ED if they needed any sort of care? As an ED doctor, why not set a low threshold to admit patients to the hospital and mitigate any risk of a lawsuit by discharging the patient from the ED? As a hospitalist, why not discharge the patient to a skilled nursing care facility, where they will have more nursing supervision than at home, especially if the hospital, who is contributing to the hospitalist program bottom line, is monitoring your patients’ average length of stay?
Everyone is playing with everyone else’s money. Under the current system, there is little financial incentive for providers to work together in the provision of high-quality care. The ACO model is an attempt to create a model that will provide more integrated care by linking provider reimbursement to quality and cost of care.
Dr. Elliott Fisher at Dartmouth Medical School at Dartmouth College and others have identified several key principles for all ACOs:
- A strong primary-care base capable of being accountable for the quality and costs of care across the full continuum of care for a patient population;
- Provider reimbursement tied to quality improvements that also reduce overall costs; and
- Reliable performance measurement, to support quality improvement.
“ACO” may be a new term to many, but it is not new. Kaiser Permanente and HealthCare Partners Medical Group are examples of longstanding, successful ACOs.
You might be reading this and have arrived at the conclusion that Joe Li is convinced ACOs are the panacea for that ill known as the American healthcare system. That could not be further from the truth. I don’t think that the folks at Medicare are convinced, either. That is why there was a competitive process to select the 32 ACOs for this initiative. They chose provider groups that have experience working together. If ACOs are going to work, Medicare thinks these are the types of organizations that will be successful.
Interestingly, when one looks on the list of Pioneer participants, there are some notable absences. I don’t see Mayo Clinic or Cleveland Clinic. Hmmm. If these ACO “poster children” are not participating, should we? Perhaps they applied and HHS declined to accept their application, but I doubt it. These are the groups who already are ACOs. One can only assume that these organizations didn’t like the rules, or the financial rewards were not sufficiently attractive for them to participate.
Change Is Brewing
Regardless, the big question for hospitalists working in Pioneer groups is, How do we “succeed” in an ACO model? I believe that some of the same principles that allow hospitalists to succeed under the current model also apply under the ACO model. High-performing hospitalists and HM programs have:
Systems to monitor performance and provide feedback to providers with a plan for continuous quality improvement;
Established expectations for hospitalist communication with other providers, including PCPs, ED providers, subspecialists, nurses, and post-discharge care center facilities, among others; and
Multidisciplinary care teams providing evidence-based care with a focus on minimizing variations in care.
If ACOs are successful at providing high-quality care at lower costs, one could imagine changes to our healthcare system that will directly impact hospitalists. If ACOs are able to provide timely and comprehensive outpatient care, fewer patients will need care at acute-care hospitals. Efforts will be made to hospitalize patients at less-expensive community hospitals, instead of tertiary academic medical centers. The resultant smaller population of hospitalized patients will be sicker.
It’s not difficult to extrapolate on this new paradigm, as I can imagine hospitalists seeing fewer, sicker patients daily. These patients, as we all know, often require multiple visits per day. It is difficult to provide high-quality care to sick patients without doctors available in the hospital 24 hours a day, seven days a week. All hospitalists will need the skills to attend to critically ill, hospitalized patients. Hospitalists—and perhaps hospitals, if they are part of the ACO—will focus less on patient length of stay and more on keeping patients out of the hospitals. The cost of an entire readmission dwarfs the cost of one additional day in the hospital.
If you are a hospitalist providing care in a Pioneer ACO, I would love to hear how your practice is changing. Send me an email at [email protected], or message me via Twitter (@JosephLi) or LinkedIn: Joseph Li.
Dr. Li is president of SHM.
In December, the U.S. Department of Health and Human Services (HHS) announced the selection of 32 organizations from 18 states as participants in the Pioneer Accountable Care Organization (ACO) initiative.
HHS developed this initiative with the hopes that they could save $1.1 billion over the next five years. Five of the 32 participating organizations are Massachusetts-based, including Beth Israel Deaconess Physician Organization (BIDPO) and Atrius Health. My hospitalist colleagues and I at Beth Israel Deaconess Medical Center (BIDMC) are BIDPO members; we also care for hospitalized patients for Atrius Health in Boston. So we will be caring for hospitalized patients involved in two of the 32 Pioneer ACOs.
Many of us are excited, but also understandably a bit anxious. Some of us are outright concerned. I suspect we are not alone. Many of you are in a similar position—being providers in a Pioneer ACO. My colleagues and are having conversations to increase our understanding of ACOs and the role of hospitalists in an ACO.
Nuts and Bolts
An ACO is a system to deliver and pay for healthcare by linking provider reimbursement to quality and cost of care for a defined population of patients. Think of it as a group of providers (primary-care physicians, ED doctors, hospitalists, medical and surgical specialists, etc.) who are bound by shared financial risks and rewards to work together to provide coordinated, high-quality, low-cost care for patients.
In the Pioneer ACO, groups of providers agree to manage the quality, costs, and overall care of the Medicare beneficiaries enrolled in the traditional fee-for-service program assigned to their ACO. The ACO model is designed to address some of the concerns of the traditional fee-for-service payment model, in which each provider offers services and submits their own bills separately. Under the fee-for-service model, the incentive is for each provider to provide as much care as possible, because payment is dependent on provision of more care rather than the provision of higher-quality care.
For example, there is little disincentive for PCPs to send patients to the ED if a patient needs evaluation, for any reason, when it is inconvenient for the PCP. Why keep outpatient clinic open during evenings and weekends when you could simply send the patient to the ED if they needed any sort of care? As an ED doctor, why not set a low threshold to admit patients to the hospital and mitigate any risk of a lawsuit by discharging the patient from the ED? As a hospitalist, why not discharge the patient to a skilled nursing care facility, where they will have more nursing supervision than at home, especially if the hospital, who is contributing to the hospitalist program bottom line, is monitoring your patients’ average length of stay?
Everyone is playing with everyone else’s money. Under the current system, there is little financial incentive for providers to work together in the provision of high-quality care. The ACO model is an attempt to create a model that will provide more integrated care by linking provider reimbursement to quality and cost of care.
Dr. Elliott Fisher at Dartmouth Medical School at Dartmouth College and others have identified several key principles for all ACOs:
- A strong primary-care base capable of being accountable for the quality and costs of care across the full continuum of care for a patient population;
- Provider reimbursement tied to quality improvements that also reduce overall costs; and
- Reliable performance measurement, to support quality improvement.
“ACO” may be a new term to many, but it is not new. Kaiser Permanente and HealthCare Partners Medical Group are examples of longstanding, successful ACOs.
You might be reading this and have arrived at the conclusion that Joe Li is convinced ACOs are the panacea for that ill known as the American healthcare system. That could not be further from the truth. I don’t think that the folks at Medicare are convinced, either. That is why there was a competitive process to select the 32 ACOs for this initiative. They chose provider groups that have experience working together. If ACOs are going to work, Medicare thinks these are the types of organizations that will be successful.
Interestingly, when one looks on the list of Pioneer participants, there are some notable absences. I don’t see Mayo Clinic or Cleveland Clinic. Hmmm. If these ACO “poster children” are not participating, should we? Perhaps they applied and HHS declined to accept their application, but I doubt it. These are the groups who already are ACOs. One can only assume that these organizations didn’t like the rules, or the financial rewards were not sufficiently attractive for them to participate.
Change Is Brewing
Regardless, the big question for hospitalists working in Pioneer groups is, How do we “succeed” in an ACO model? I believe that some of the same principles that allow hospitalists to succeed under the current model also apply under the ACO model. High-performing hospitalists and HM programs have:
Systems to monitor performance and provide feedback to providers with a plan for continuous quality improvement;
Established expectations for hospitalist communication with other providers, including PCPs, ED providers, subspecialists, nurses, and post-discharge care center facilities, among others; and
Multidisciplinary care teams providing evidence-based care with a focus on minimizing variations in care.
If ACOs are successful at providing high-quality care at lower costs, one could imagine changes to our healthcare system that will directly impact hospitalists. If ACOs are able to provide timely and comprehensive outpatient care, fewer patients will need care at acute-care hospitals. Efforts will be made to hospitalize patients at less-expensive community hospitals, instead of tertiary academic medical centers. The resultant smaller population of hospitalized patients will be sicker.
It’s not difficult to extrapolate on this new paradigm, as I can imagine hospitalists seeing fewer, sicker patients daily. These patients, as we all know, often require multiple visits per day. It is difficult to provide high-quality care to sick patients without doctors available in the hospital 24 hours a day, seven days a week. All hospitalists will need the skills to attend to critically ill, hospitalized patients. Hospitalists—and perhaps hospitals, if they are part of the ACO—will focus less on patient length of stay and more on keeping patients out of the hospitals. The cost of an entire readmission dwarfs the cost of one additional day in the hospital.
If you are a hospitalist providing care in a Pioneer ACO, I would love to hear how your practice is changing. Send me an email at [email protected], or message me via Twitter (@JosephLi) or LinkedIn: Joseph Li.
Dr. Li is president of SHM.