User login
U.S. maternal mortality crisis grows, yet deaths seem preventable
On June 2, 2019, 35-year-old Anne Hutchinson gave birth to her first child, Lillian. There were no problems with the pregnancy or the birth at Fairview Hospital, which is part of the Cleveland Clinic system.
But 2 days after the birth, she had shortness of breath and couldn’t lie down and breathe.
“My mom’s a nurse, and she was like, ‘You need to go to the hospital immediately,’” Ms. Hutchinson said. When she was admitted to the hospital, there were suddenly “10 doctors in the room.”
Ms. Hutchinson was diagnosed with peripartum cardiomyopathy, a weakness of the heart muscle. She had heart failure. The seriousness of heart failure is measured by the ejection fraction, or the percentage of blood the heart pumps out. Normal is 50%-70%. Ms. Hutchinson’s ejection fraction was 20%.
She was put on medication, left the hospital after 5 days, and her ejection fraction eventually rose to 35%. But she was still at risk for sudden cardiac death.
“The cardiologist said to me, ‘You probably can’t have any more children.’ My heart did not bounce back,” Ms. Hutchinson said.
By the end of 2019, her cardiologist determined that she needed an internal cardiac defibrillator, which monitors the heartbeat and delivers electric shocks to restore the heart’s normal rhythm when needed.
By 2020, when Ms. Hutchinson’s ejection fraction was near normal, she decided that she wanted another child.
“I had a daughter. She was beautiful and amazing. But I felt like I wanted to have a sibling for her,” she says. Yet when her cardiologist at Fairview Hospital heard the plan, she told her getting pregnant again “would be like Russian roulette.”
Ms. Hutchinson is one of a growing number of women whose medical condition puts them at high risk of death during and after giving birth. An estimated 30% of maternal deaths in the United States result from cardiovascular disease – a problem that has become more common with increases in diabetes and obesity.
And, in some women, hypertension can develop suddenly during pregnancy. This is called preeclampsia and is increasing in the United States, particularly in Black women. In rare cases, it can become the life-threatening condition eclampsia, with seizures and death.
Three-time Olympic medalist and world champion sprinter Tori Bowie was found dead in June of apparent complications of pregnancy. The medical examiner’s office in Orange County, Fla., said she was believed to have been in her 8th month of pregnancy and may have died of eclampsia.
Heart conditions in pregnant women are one of a long list of reasons why the United States has the highest maternal mortality rate of any developed country. But the risk is marked by significant racial differences, with death rates three times higher in Black women, compared with White women.
What troubles many experts is that it is estimated that 80% of these deaths are preventable.
“That is a ridiculous number,” said Melissa A. Simon, MD, MPH, director of the Center for Health Equity Transformation at Northwestern Medicine in Evanston, Ill.. “For a health care system in a country that is so high-resourced and high-income, for 8 out of 10 deaths for moms who are pregnant [to be preventable], that’s absolutely unacceptable.”
Pregnant women are not only at risk of death from cardiovascular complications, but other types of problems, including hemorrhage, thrombotic embolism, and infection.
But experts now are focusing attention on nonmedical reasons for maternal mortality, such as racial disparities and the fundamental issue of whether women are telling doctors about their symptoms but are not being heard.
The government has acknowledged the depth of this problem with the Centers for Disease Control and Prevention’s “Hear Her” campaign, which includes videos of women who describe how their health professionals did not take their concerns seriously.
In one such video, a woman named Sanari says 2 days after the birth of her second child, she started developing soreness.
“By day 3, it just didn’t feel right. I asked the nurses, explained my symptoms and that I was having crazy pains, and they assured me it was just gas,” she says on the video.
Sanari described how she started to have odorous discharge and ended up in an emergency room at a different hospital. Health care providers found a large abscess on her uterus.
“I’m glad I didn’t stop at no, and I’m glad someone finally heard me – someone finally listened to me,” she said.
“Hear Her” featured another woman named Lindsay, who had preeclampsia in her first pregnancy and began to get symptoms during her second pregnancy.
She describes how she voiced her concerns to her doctors, saying, “sometimes it would be, ‘Oh, you’re pregnant and your feet are supposed to swell. … It’s just fine.’ But I didn’t feel fine.”
The campaign aims to raise awareness of warning signs that require fast medical attention to prevent pregnancy-related deaths.
But Shanna Cox, associate director of the CDC’s Division of Reproductive Health, said the agency has collected many stories of women who died or nearly died because their concerns were not being addressed properly.
Ms. Cox says another part of the campaign “is really focused on health care providers and listening … to their patients, providing that respectful patient-centered care to be sure that all their concerns are addressed.”
And some experts believe the thinking has shifted even more dramatically.
“We’ve moved from beyond the days of blaming the individual, the birth person, or the woman, to say you haven’t done this, you haven’t come into health care, you are not taking care of yourself, you aren’t keeping your appointments,” says Laurie Zephyrin, MD, MPH, vice president of the Commonwealth Fund, a private foundation in New York dedicated to improving health care.
Dr. Zephyrin says the health care system falls short of providing equitable, quality care. “There’s data that shows Black people receive worse care than White people for about 40% of quality measures,” she said.
These disparities have led to the formation of organizations like National Birth Equity Collaborative, an advocacy group in New Orleans working to improve maternal care for Black patients.
Carmen Green, vice president of research and strategy, said institutional racism has been embedded into some health care providers.
“They have this hierarchy that teaches them they have to manage, they have to control, they have to direct the medical experience, and that is just not how birthing works,” she said.
She used the example of the birth experience as a car ride, where the mothers have been in the backseat with the doctor driving. “We want the birthing person in the driving seat and want [them] to be respected as a person who is deciding where that destination is going,” Ms. Green said.
She says health providers often “blame the mamas” based on assumptions, stereotypes, and biases against low-income people.
So how is American medicine responding to the medical and social causes of maternal mortality?
This news organization surveyed 10 medical centers ranked by U.S. News & World Report as the country’s top facilities for obstetrics. They were asked what programs they had and studies they had done to try to reduce maternal mortality, improve racial disparities, and target cardiovascular causes of maternal mortality.
One of the most extensive programs was founded at the Stanford School of Medicine in Stanford, Calif., in 2006. The California Maternal Quality Care Collaborative includes 200 hospitals in the state committed to ending preventable maternal mortality and racial disparities.
Nine hospitals in the collaborative have started programs to reduce hemorrhages, manage high blood pressure disorders, and reduce the rate of cesarean deliveries. All are important reasons for maternal mortality.
These programs helped bring about a 62% reduction in California’s maternal mortality rate from 2006 to 2016. And 2023 figures show that California has the lowest maternal mortality rate of any state.
Alabama has the sixth highest rate of maternal mortality in the nation. The University of Alabama at Birmingham wants to address the racial disparities in maternal mortality with a cooperative called the P3 EQUATE Network.
The network is part of a $20 million program by the American Heart Association to gain greater understanding of the disproportionate effect of maternal mortality on Black and Native American people.
The program works with pregnant and postpartum women “to discover ways to reduce racism and social problems that contribute to poor health outcomes.”
In addition to collaborative efforts, the survey found maternal mortality programs at all the top medical centers.
NewYork-Presbyterian Hospital has a Mothers Center that provides specialized care to pregnant women with complications.
The University of Chicago Medical Center established a program called “Systematic Treatment and Management of Postpartum Hypertension” that includes patient and staff education, standardized hospital discharge instructions, and a follow-up in a postpartum hypertension clinic.
A 2021 study found that the program had helped increase the number of postpartum women who correctly follow blood pressure control guidance.
A program called MOMS Navigation at Northwell Health in Long Island, N.Y., provides support to high-risk mothers. The program decreased 30-day readmission rates for all patients by 50% and for Black birthing patients by 60%. Reducing readmission is an important measure for reducing complications.
Vanderbilt University Medical Center in Nashville has what it calls the first-of-its-kind educational podcasts Healthy Mom Healthy Baby, where 30% of the content is devoted to health disparities.
And several centers, including Brigham and Women’s Hospital in Boston and NewYork-Presbyterian, make sure mothers have access to doulas – professional support people trained in the needs of the family during pregnancy and childbirth.
The survey found that 9 of the 10 centers have obstetric programs devoted to cardiac care, including the University of Chicago, Stanford Medicine, UCLA, and the Cleveland Clinic.
But the survey results raise the question: How can we have these programs and research at our best obstetrics centers devoted to reducing maternal mortality and have the highest rate of all developed countries?
“Maternal mortality largely falls on pregnant and birthing persons who do not intersect with, nor are touched, by the best obstetrical care centers in the country,” Dr. Simon said.
Unfortunately, she said, the pregnant people who face “high maternal mortality rates … face all the access-to-care barriers and do not have the privilege of birthing or accessing care at top centers.”
Anne Hutchinson believed going to a top center – the Cleveland Clinic – would give her a good chance of safely delivering a second child.
Karlee Hoffman, DO, a cardiologist in the hospital’s cardio-obstetric high-risk clinic, said Ms. Hutchinson “came to me, she was determined to have another child, and she said, ‘Please help me do this. I’m doing it regardless. So, I would really like your support in moving forward,’” Dr. Hoffman recalls.
Ms. Hutchinson said Cleveland Clinic doctors told her she had a 20%-30% chance of peripartum cardiomyopathy again if she had a second child. If that happened, the risks “ranged from mild decompensation of my heart function to death,“ she said.
Ms. Hutchinson and her husband decided to go ahead with the pregnancy. Her parents cried when they found out. But Ms. Hutchinson says she was confident in the cardio obstetric team at Cleveland Clinic.
Her fertility medicine raised the possibility of multiple births, which would be a definite threat to her life. Her heart failure medicine, Entresto, could not be used during pregnancy, so her doctors put her on older medicines.
She got pregnant in June 2022 and developed gestational diabetes, which can affect pregnancy because of raised blood sugar. Another potential risk. She was carefully monitored by the specialists and hospitalized once.
At 37 weeks, she was induced and had a forceps delivery. On Feb. 15, 2023, her second daughter, Charlotte, was born.
Ms. Hutchinson was asked to write about how she felt when she delivered Charlotte:
“I am not sure how to put into words the love, joy, and elation that I felt holding Charlotte for the first time. As I write this, I have tears of joy in my eyes thinking of that moment. I had prayed for her for so long and after being told I couldn’t or shouldn’t have any more children.”
“I felt that Charlotte and I were forever bonded in triumph from that moment on. We did it and made it out alive! And our family was now complete. I have so much joy watching the love that is growing between Charlotte and Lillian. Life is truly amazing, and I am forever grateful to have them.”
A version of this article first appeared on WebMD.com.
On June 2, 2019, 35-year-old Anne Hutchinson gave birth to her first child, Lillian. There were no problems with the pregnancy or the birth at Fairview Hospital, which is part of the Cleveland Clinic system.
But 2 days after the birth, she had shortness of breath and couldn’t lie down and breathe.
“My mom’s a nurse, and she was like, ‘You need to go to the hospital immediately,’” Ms. Hutchinson said. When she was admitted to the hospital, there were suddenly “10 doctors in the room.”
Ms. Hutchinson was diagnosed with peripartum cardiomyopathy, a weakness of the heart muscle. She had heart failure. The seriousness of heart failure is measured by the ejection fraction, or the percentage of blood the heart pumps out. Normal is 50%-70%. Ms. Hutchinson’s ejection fraction was 20%.
She was put on medication, left the hospital after 5 days, and her ejection fraction eventually rose to 35%. But she was still at risk for sudden cardiac death.
“The cardiologist said to me, ‘You probably can’t have any more children.’ My heart did not bounce back,” Ms. Hutchinson said.
By the end of 2019, her cardiologist determined that she needed an internal cardiac defibrillator, which monitors the heartbeat and delivers electric shocks to restore the heart’s normal rhythm when needed.
By 2020, when Ms. Hutchinson’s ejection fraction was near normal, she decided that she wanted another child.
“I had a daughter. She was beautiful and amazing. But I felt like I wanted to have a sibling for her,” she says. Yet when her cardiologist at Fairview Hospital heard the plan, she told her getting pregnant again “would be like Russian roulette.”
Ms. Hutchinson is one of a growing number of women whose medical condition puts them at high risk of death during and after giving birth. An estimated 30% of maternal deaths in the United States result from cardiovascular disease – a problem that has become more common with increases in diabetes and obesity.
And, in some women, hypertension can develop suddenly during pregnancy. This is called preeclampsia and is increasing in the United States, particularly in Black women. In rare cases, it can become the life-threatening condition eclampsia, with seizures and death.
Three-time Olympic medalist and world champion sprinter Tori Bowie was found dead in June of apparent complications of pregnancy. The medical examiner’s office in Orange County, Fla., said she was believed to have been in her 8th month of pregnancy and may have died of eclampsia.
Heart conditions in pregnant women are one of a long list of reasons why the United States has the highest maternal mortality rate of any developed country. But the risk is marked by significant racial differences, with death rates three times higher in Black women, compared with White women.
What troubles many experts is that it is estimated that 80% of these deaths are preventable.
“That is a ridiculous number,” said Melissa A. Simon, MD, MPH, director of the Center for Health Equity Transformation at Northwestern Medicine in Evanston, Ill.. “For a health care system in a country that is so high-resourced and high-income, for 8 out of 10 deaths for moms who are pregnant [to be preventable], that’s absolutely unacceptable.”
Pregnant women are not only at risk of death from cardiovascular complications, but other types of problems, including hemorrhage, thrombotic embolism, and infection.
But experts now are focusing attention on nonmedical reasons for maternal mortality, such as racial disparities and the fundamental issue of whether women are telling doctors about their symptoms but are not being heard.
The government has acknowledged the depth of this problem with the Centers for Disease Control and Prevention’s “Hear Her” campaign, which includes videos of women who describe how their health professionals did not take their concerns seriously.
In one such video, a woman named Sanari says 2 days after the birth of her second child, she started developing soreness.
“By day 3, it just didn’t feel right. I asked the nurses, explained my symptoms and that I was having crazy pains, and they assured me it was just gas,” she says on the video.
Sanari described how she started to have odorous discharge and ended up in an emergency room at a different hospital. Health care providers found a large abscess on her uterus.
“I’m glad I didn’t stop at no, and I’m glad someone finally heard me – someone finally listened to me,” she said.
“Hear Her” featured another woman named Lindsay, who had preeclampsia in her first pregnancy and began to get symptoms during her second pregnancy.
She describes how she voiced her concerns to her doctors, saying, “sometimes it would be, ‘Oh, you’re pregnant and your feet are supposed to swell. … It’s just fine.’ But I didn’t feel fine.”
The campaign aims to raise awareness of warning signs that require fast medical attention to prevent pregnancy-related deaths.
But Shanna Cox, associate director of the CDC’s Division of Reproductive Health, said the agency has collected many stories of women who died or nearly died because their concerns were not being addressed properly.
Ms. Cox says another part of the campaign “is really focused on health care providers and listening … to their patients, providing that respectful patient-centered care to be sure that all their concerns are addressed.”
And some experts believe the thinking has shifted even more dramatically.
“We’ve moved from beyond the days of blaming the individual, the birth person, or the woman, to say you haven’t done this, you haven’t come into health care, you are not taking care of yourself, you aren’t keeping your appointments,” says Laurie Zephyrin, MD, MPH, vice president of the Commonwealth Fund, a private foundation in New York dedicated to improving health care.
Dr. Zephyrin says the health care system falls short of providing equitable, quality care. “There’s data that shows Black people receive worse care than White people for about 40% of quality measures,” she said.
These disparities have led to the formation of organizations like National Birth Equity Collaborative, an advocacy group in New Orleans working to improve maternal care for Black patients.
Carmen Green, vice president of research and strategy, said institutional racism has been embedded into some health care providers.
“They have this hierarchy that teaches them they have to manage, they have to control, they have to direct the medical experience, and that is just not how birthing works,” she said.
She used the example of the birth experience as a car ride, where the mothers have been in the backseat with the doctor driving. “We want the birthing person in the driving seat and want [them] to be respected as a person who is deciding where that destination is going,” Ms. Green said.
She says health providers often “blame the mamas” based on assumptions, stereotypes, and biases against low-income people.
So how is American medicine responding to the medical and social causes of maternal mortality?
This news organization surveyed 10 medical centers ranked by U.S. News & World Report as the country’s top facilities for obstetrics. They were asked what programs they had and studies they had done to try to reduce maternal mortality, improve racial disparities, and target cardiovascular causes of maternal mortality.
One of the most extensive programs was founded at the Stanford School of Medicine in Stanford, Calif., in 2006. The California Maternal Quality Care Collaborative includes 200 hospitals in the state committed to ending preventable maternal mortality and racial disparities.
Nine hospitals in the collaborative have started programs to reduce hemorrhages, manage high blood pressure disorders, and reduce the rate of cesarean deliveries. All are important reasons for maternal mortality.
These programs helped bring about a 62% reduction in California’s maternal mortality rate from 2006 to 2016. And 2023 figures show that California has the lowest maternal mortality rate of any state.
Alabama has the sixth highest rate of maternal mortality in the nation. The University of Alabama at Birmingham wants to address the racial disparities in maternal mortality with a cooperative called the P3 EQUATE Network.
The network is part of a $20 million program by the American Heart Association to gain greater understanding of the disproportionate effect of maternal mortality on Black and Native American people.
The program works with pregnant and postpartum women “to discover ways to reduce racism and social problems that contribute to poor health outcomes.”
In addition to collaborative efforts, the survey found maternal mortality programs at all the top medical centers.
NewYork-Presbyterian Hospital has a Mothers Center that provides specialized care to pregnant women with complications.
The University of Chicago Medical Center established a program called “Systematic Treatment and Management of Postpartum Hypertension” that includes patient and staff education, standardized hospital discharge instructions, and a follow-up in a postpartum hypertension clinic.
A 2021 study found that the program had helped increase the number of postpartum women who correctly follow blood pressure control guidance.
A program called MOMS Navigation at Northwell Health in Long Island, N.Y., provides support to high-risk mothers. The program decreased 30-day readmission rates for all patients by 50% and for Black birthing patients by 60%. Reducing readmission is an important measure for reducing complications.
Vanderbilt University Medical Center in Nashville has what it calls the first-of-its-kind educational podcasts Healthy Mom Healthy Baby, where 30% of the content is devoted to health disparities.
And several centers, including Brigham and Women’s Hospital in Boston and NewYork-Presbyterian, make sure mothers have access to doulas – professional support people trained in the needs of the family during pregnancy and childbirth.
The survey found that 9 of the 10 centers have obstetric programs devoted to cardiac care, including the University of Chicago, Stanford Medicine, UCLA, and the Cleveland Clinic.
But the survey results raise the question: How can we have these programs and research at our best obstetrics centers devoted to reducing maternal mortality and have the highest rate of all developed countries?
“Maternal mortality largely falls on pregnant and birthing persons who do not intersect with, nor are touched, by the best obstetrical care centers in the country,” Dr. Simon said.
Unfortunately, she said, the pregnant people who face “high maternal mortality rates … face all the access-to-care barriers and do not have the privilege of birthing or accessing care at top centers.”
Anne Hutchinson believed going to a top center – the Cleveland Clinic – would give her a good chance of safely delivering a second child.
Karlee Hoffman, DO, a cardiologist in the hospital’s cardio-obstetric high-risk clinic, said Ms. Hutchinson “came to me, she was determined to have another child, and she said, ‘Please help me do this. I’m doing it regardless. So, I would really like your support in moving forward,’” Dr. Hoffman recalls.
Ms. Hutchinson said Cleveland Clinic doctors told her she had a 20%-30% chance of peripartum cardiomyopathy again if she had a second child. If that happened, the risks “ranged from mild decompensation of my heart function to death,“ she said.
Ms. Hutchinson and her husband decided to go ahead with the pregnancy. Her parents cried when they found out. But Ms. Hutchinson says she was confident in the cardio obstetric team at Cleveland Clinic.
Her fertility medicine raised the possibility of multiple births, which would be a definite threat to her life. Her heart failure medicine, Entresto, could not be used during pregnancy, so her doctors put her on older medicines.
She got pregnant in June 2022 and developed gestational diabetes, which can affect pregnancy because of raised blood sugar. Another potential risk. She was carefully monitored by the specialists and hospitalized once.
At 37 weeks, she was induced and had a forceps delivery. On Feb. 15, 2023, her second daughter, Charlotte, was born.
Ms. Hutchinson was asked to write about how she felt when she delivered Charlotte:
“I am not sure how to put into words the love, joy, and elation that I felt holding Charlotte for the first time. As I write this, I have tears of joy in my eyes thinking of that moment. I had prayed for her for so long and after being told I couldn’t or shouldn’t have any more children.”
“I felt that Charlotte and I were forever bonded in triumph from that moment on. We did it and made it out alive! And our family was now complete. I have so much joy watching the love that is growing between Charlotte and Lillian. Life is truly amazing, and I am forever grateful to have them.”
A version of this article first appeared on WebMD.com.
On June 2, 2019, 35-year-old Anne Hutchinson gave birth to her first child, Lillian. There were no problems with the pregnancy or the birth at Fairview Hospital, which is part of the Cleveland Clinic system.
But 2 days after the birth, she had shortness of breath and couldn’t lie down and breathe.
“My mom’s a nurse, and she was like, ‘You need to go to the hospital immediately,’” Ms. Hutchinson said. When she was admitted to the hospital, there were suddenly “10 doctors in the room.”
Ms. Hutchinson was diagnosed with peripartum cardiomyopathy, a weakness of the heart muscle. She had heart failure. The seriousness of heart failure is measured by the ejection fraction, or the percentage of blood the heart pumps out. Normal is 50%-70%. Ms. Hutchinson’s ejection fraction was 20%.
She was put on medication, left the hospital after 5 days, and her ejection fraction eventually rose to 35%. But she was still at risk for sudden cardiac death.
“The cardiologist said to me, ‘You probably can’t have any more children.’ My heart did not bounce back,” Ms. Hutchinson said.
By the end of 2019, her cardiologist determined that she needed an internal cardiac defibrillator, which monitors the heartbeat and delivers electric shocks to restore the heart’s normal rhythm when needed.
By 2020, when Ms. Hutchinson’s ejection fraction was near normal, she decided that she wanted another child.
“I had a daughter. She was beautiful and amazing. But I felt like I wanted to have a sibling for her,” she says. Yet when her cardiologist at Fairview Hospital heard the plan, she told her getting pregnant again “would be like Russian roulette.”
Ms. Hutchinson is one of a growing number of women whose medical condition puts them at high risk of death during and after giving birth. An estimated 30% of maternal deaths in the United States result from cardiovascular disease – a problem that has become more common with increases in diabetes and obesity.
And, in some women, hypertension can develop suddenly during pregnancy. This is called preeclampsia and is increasing in the United States, particularly in Black women. In rare cases, it can become the life-threatening condition eclampsia, with seizures and death.
Three-time Olympic medalist and world champion sprinter Tori Bowie was found dead in June of apparent complications of pregnancy. The medical examiner’s office in Orange County, Fla., said she was believed to have been in her 8th month of pregnancy and may have died of eclampsia.
Heart conditions in pregnant women are one of a long list of reasons why the United States has the highest maternal mortality rate of any developed country. But the risk is marked by significant racial differences, with death rates three times higher in Black women, compared with White women.
What troubles many experts is that it is estimated that 80% of these deaths are preventable.
“That is a ridiculous number,” said Melissa A. Simon, MD, MPH, director of the Center for Health Equity Transformation at Northwestern Medicine in Evanston, Ill.. “For a health care system in a country that is so high-resourced and high-income, for 8 out of 10 deaths for moms who are pregnant [to be preventable], that’s absolutely unacceptable.”
Pregnant women are not only at risk of death from cardiovascular complications, but other types of problems, including hemorrhage, thrombotic embolism, and infection.
But experts now are focusing attention on nonmedical reasons for maternal mortality, such as racial disparities and the fundamental issue of whether women are telling doctors about their symptoms but are not being heard.
The government has acknowledged the depth of this problem with the Centers for Disease Control and Prevention’s “Hear Her” campaign, which includes videos of women who describe how their health professionals did not take their concerns seriously.
In one such video, a woman named Sanari says 2 days after the birth of her second child, she started developing soreness.
“By day 3, it just didn’t feel right. I asked the nurses, explained my symptoms and that I was having crazy pains, and they assured me it was just gas,” she says on the video.
Sanari described how she started to have odorous discharge and ended up in an emergency room at a different hospital. Health care providers found a large abscess on her uterus.
“I’m glad I didn’t stop at no, and I’m glad someone finally heard me – someone finally listened to me,” she said.
“Hear Her” featured another woman named Lindsay, who had preeclampsia in her first pregnancy and began to get symptoms during her second pregnancy.
She describes how she voiced her concerns to her doctors, saying, “sometimes it would be, ‘Oh, you’re pregnant and your feet are supposed to swell. … It’s just fine.’ But I didn’t feel fine.”
The campaign aims to raise awareness of warning signs that require fast medical attention to prevent pregnancy-related deaths.
But Shanna Cox, associate director of the CDC’s Division of Reproductive Health, said the agency has collected many stories of women who died or nearly died because their concerns were not being addressed properly.
Ms. Cox says another part of the campaign “is really focused on health care providers and listening … to their patients, providing that respectful patient-centered care to be sure that all their concerns are addressed.”
And some experts believe the thinking has shifted even more dramatically.
“We’ve moved from beyond the days of blaming the individual, the birth person, or the woman, to say you haven’t done this, you haven’t come into health care, you are not taking care of yourself, you aren’t keeping your appointments,” says Laurie Zephyrin, MD, MPH, vice president of the Commonwealth Fund, a private foundation in New York dedicated to improving health care.
Dr. Zephyrin says the health care system falls short of providing equitable, quality care. “There’s data that shows Black people receive worse care than White people for about 40% of quality measures,” she said.
These disparities have led to the formation of organizations like National Birth Equity Collaborative, an advocacy group in New Orleans working to improve maternal care for Black patients.
Carmen Green, vice president of research and strategy, said institutional racism has been embedded into some health care providers.
“They have this hierarchy that teaches them they have to manage, they have to control, they have to direct the medical experience, and that is just not how birthing works,” she said.
She used the example of the birth experience as a car ride, where the mothers have been in the backseat with the doctor driving. “We want the birthing person in the driving seat and want [them] to be respected as a person who is deciding where that destination is going,” Ms. Green said.
She says health providers often “blame the mamas” based on assumptions, stereotypes, and biases against low-income people.
So how is American medicine responding to the medical and social causes of maternal mortality?
This news organization surveyed 10 medical centers ranked by U.S. News & World Report as the country’s top facilities for obstetrics. They were asked what programs they had and studies they had done to try to reduce maternal mortality, improve racial disparities, and target cardiovascular causes of maternal mortality.
One of the most extensive programs was founded at the Stanford School of Medicine in Stanford, Calif., in 2006. The California Maternal Quality Care Collaborative includes 200 hospitals in the state committed to ending preventable maternal mortality and racial disparities.
Nine hospitals in the collaborative have started programs to reduce hemorrhages, manage high blood pressure disorders, and reduce the rate of cesarean deliveries. All are important reasons for maternal mortality.
These programs helped bring about a 62% reduction in California’s maternal mortality rate from 2006 to 2016. And 2023 figures show that California has the lowest maternal mortality rate of any state.
Alabama has the sixth highest rate of maternal mortality in the nation. The University of Alabama at Birmingham wants to address the racial disparities in maternal mortality with a cooperative called the P3 EQUATE Network.
The network is part of a $20 million program by the American Heart Association to gain greater understanding of the disproportionate effect of maternal mortality on Black and Native American people.
The program works with pregnant and postpartum women “to discover ways to reduce racism and social problems that contribute to poor health outcomes.”
In addition to collaborative efforts, the survey found maternal mortality programs at all the top medical centers.
NewYork-Presbyterian Hospital has a Mothers Center that provides specialized care to pregnant women with complications.
The University of Chicago Medical Center established a program called “Systematic Treatment and Management of Postpartum Hypertension” that includes patient and staff education, standardized hospital discharge instructions, and a follow-up in a postpartum hypertension clinic.
A 2021 study found that the program had helped increase the number of postpartum women who correctly follow blood pressure control guidance.
A program called MOMS Navigation at Northwell Health in Long Island, N.Y., provides support to high-risk mothers. The program decreased 30-day readmission rates for all patients by 50% and for Black birthing patients by 60%. Reducing readmission is an important measure for reducing complications.
Vanderbilt University Medical Center in Nashville has what it calls the first-of-its-kind educational podcasts Healthy Mom Healthy Baby, where 30% of the content is devoted to health disparities.
And several centers, including Brigham and Women’s Hospital in Boston and NewYork-Presbyterian, make sure mothers have access to doulas – professional support people trained in the needs of the family during pregnancy and childbirth.
The survey found that 9 of the 10 centers have obstetric programs devoted to cardiac care, including the University of Chicago, Stanford Medicine, UCLA, and the Cleveland Clinic.
But the survey results raise the question: How can we have these programs and research at our best obstetrics centers devoted to reducing maternal mortality and have the highest rate of all developed countries?
“Maternal mortality largely falls on pregnant and birthing persons who do not intersect with, nor are touched, by the best obstetrical care centers in the country,” Dr. Simon said.
Unfortunately, she said, the pregnant people who face “high maternal mortality rates … face all the access-to-care barriers and do not have the privilege of birthing or accessing care at top centers.”
Anne Hutchinson believed going to a top center – the Cleveland Clinic – would give her a good chance of safely delivering a second child.
Karlee Hoffman, DO, a cardiologist in the hospital’s cardio-obstetric high-risk clinic, said Ms. Hutchinson “came to me, she was determined to have another child, and she said, ‘Please help me do this. I’m doing it regardless. So, I would really like your support in moving forward,’” Dr. Hoffman recalls.
Ms. Hutchinson said Cleveland Clinic doctors told her she had a 20%-30% chance of peripartum cardiomyopathy again if she had a second child. If that happened, the risks “ranged from mild decompensation of my heart function to death,“ she said.
Ms. Hutchinson and her husband decided to go ahead with the pregnancy. Her parents cried when they found out. But Ms. Hutchinson says she was confident in the cardio obstetric team at Cleveland Clinic.
Her fertility medicine raised the possibility of multiple births, which would be a definite threat to her life. Her heart failure medicine, Entresto, could not be used during pregnancy, so her doctors put her on older medicines.
She got pregnant in June 2022 and developed gestational diabetes, which can affect pregnancy because of raised blood sugar. Another potential risk. She was carefully monitored by the specialists and hospitalized once.
At 37 weeks, she was induced and had a forceps delivery. On Feb. 15, 2023, her second daughter, Charlotte, was born.
Ms. Hutchinson was asked to write about how she felt when she delivered Charlotte:
“I am not sure how to put into words the love, joy, and elation that I felt holding Charlotte for the first time. As I write this, I have tears of joy in my eyes thinking of that moment. I had prayed for her for so long and after being told I couldn’t or shouldn’t have any more children.”
“I felt that Charlotte and I were forever bonded in triumph from that moment on. We did it and made it out alive! And our family was now complete. I have so much joy watching the love that is growing between Charlotte and Lillian. Life is truly amazing, and I am forever grateful to have them.”
A version of this article first appeared on WebMD.com.
Lawsuit alleges undisclosed stomach risks from Ozempic, Mounjaro
The two drugs, which are Food and Drug Administration approved to treat type 2 diabetes, have become well known for their weight loss properties. Ozempic is made by Danish drug maker Novo Nordisk, and Mounjaro is made by Indiana-based Eli Lilly and Co.
In the lawsuit, Jaclyn Bjorklund, 44, of Louisiana, asserts that she was “severely injured” after using Ozempic and Mounjaro and that the pharmaceutical companies failed to disclose the drugs’ risk of causing vomiting and diarrhea due to inflammation of the stomach lining, as well as the risk of gastroparesis.
The prescribing labels for Mounjaro and Ozempic state that each “delays gastric emptying” and warn of the risk of severe gastrointestinal adverse reactions. The prescribing labels for both drugs state that the most common side effects include vomiting, diarrhea, and stomach pain. The Ozempic label does not mention gastroparesis, and the Mounjaro label states that the drug has not been studied in people with the condition and is therefore not recommended for people who have it.
Ms. Bjorklund has not been diagnosed with gastroparesis, but her symptoms are “indicative of” the condition, her lawyer, Paul Pennock, told NBC News.
Ms. Bjorklund used Ozempic for more than 1 year, and in July 2023 switched to Mounjaro, the lawsuit states. The document, posted on her law firm’s website, details that using the drugs resulted in “severe vomiting, stomach pain, gastrointestinal burning, being hospitalized for stomach issues on several occasions including visits to the emergency room, [and] teeth falling out due to excessive vomiting, requiring additional medications to alleviate her excessive vomiting, and throwing up whole food hours after eating.”
Novo Nordisk spokesperson Natalia Salomao told NBC News that patient safety is “of utmost importance to Novo Nordisk,” and she also noted that gastroparesis is a known risk for people with diabetes. The Food and Drug Administration declined to comment on the case, and Eli Lilly did not immediately respond to a request for comment, NBC News reported.
A version of this article first appeared on WebMD.com.
The two drugs, which are Food and Drug Administration approved to treat type 2 diabetes, have become well known for their weight loss properties. Ozempic is made by Danish drug maker Novo Nordisk, and Mounjaro is made by Indiana-based Eli Lilly and Co.
In the lawsuit, Jaclyn Bjorklund, 44, of Louisiana, asserts that she was “severely injured” after using Ozempic and Mounjaro and that the pharmaceutical companies failed to disclose the drugs’ risk of causing vomiting and diarrhea due to inflammation of the stomach lining, as well as the risk of gastroparesis.
The prescribing labels for Mounjaro and Ozempic state that each “delays gastric emptying” and warn of the risk of severe gastrointestinal adverse reactions. The prescribing labels for both drugs state that the most common side effects include vomiting, diarrhea, and stomach pain. The Ozempic label does not mention gastroparesis, and the Mounjaro label states that the drug has not been studied in people with the condition and is therefore not recommended for people who have it.
Ms. Bjorklund has not been diagnosed with gastroparesis, but her symptoms are “indicative of” the condition, her lawyer, Paul Pennock, told NBC News.
Ms. Bjorklund used Ozempic for more than 1 year, and in July 2023 switched to Mounjaro, the lawsuit states. The document, posted on her law firm’s website, details that using the drugs resulted in “severe vomiting, stomach pain, gastrointestinal burning, being hospitalized for stomach issues on several occasions including visits to the emergency room, [and] teeth falling out due to excessive vomiting, requiring additional medications to alleviate her excessive vomiting, and throwing up whole food hours after eating.”
Novo Nordisk spokesperson Natalia Salomao told NBC News that patient safety is “of utmost importance to Novo Nordisk,” and she also noted that gastroparesis is a known risk for people with diabetes. The Food and Drug Administration declined to comment on the case, and Eli Lilly did not immediately respond to a request for comment, NBC News reported.
A version of this article first appeared on WebMD.com.
The two drugs, which are Food and Drug Administration approved to treat type 2 diabetes, have become well known for their weight loss properties. Ozempic is made by Danish drug maker Novo Nordisk, and Mounjaro is made by Indiana-based Eli Lilly and Co.
In the lawsuit, Jaclyn Bjorklund, 44, of Louisiana, asserts that she was “severely injured” after using Ozempic and Mounjaro and that the pharmaceutical companies failed to disclose the drugs’ risk of causing vomiting and diarrhea due to inflammation of the stomach lining, as well as the risk of gastroparesis.
The prescribing labels for Mounjaro and Ozempic state that each “delays gastric emptying” and warn of the risk of severe gastrointestinal adverse reactions. The prescribing labels for both drugs state that the most common side effects include vomiting, diarrhea, and stomach pain. The Ozempic label does not mention gastroparesis, and the Mounjaro label states that the drug has not been studied in people with the condition and is therefore not recommended for people who have it.
Ms. Bjorklund has not been diagnosed with gastroparesis, but her symptoms are “indicative of” the condition, her lawyer, Paul Pennock, told NBC News.
Ms. Bjorklund used Ozempic for more than 1 year, and in July 2023 switched to Mounjaro, the lawsuit states. The document, posted on her law firm’s website, details that using the drugs resulted in “severe vomiting, stomach pain, gastrointestinal burning, being hospitalized for stomach issues on several occasions including visits to the emergency room, [and] teeth falling out due to excessive vomiting, requiring additional medications to alleviate her excessive vomiting, and throwing up whole food hours after eating.”
Novo Nordisk spokesperson Natalia Salomao told NBC News that patient safety is “of utmost importance to Novo Nordisk,” and she also noted that gastroparesis is a known risk for people with diabetes. The Food and Drug Administration declined to comment on the case, and Eli Lilly did not immediately respond to a request for comment, NBC News reported.
A version of this article first appeared on WebMD.com.
Top U.S. neurology, neurosurgery hospitals ranked
of best hospitals for neurology and neurosurgery.
NYU Langone also claimed the top spot in last year’s ranking.
In the latest rankings, UCSF Health–UCSF Medical Center, San Francisco, holds the No. 2 spot and New York–Presbyterian Hospital–Columbia and Cornell in New York City holds the No. 3 spot for neurology care, with no change from last year.
This year, Mayo Clinic, Rochester, Minn., is ranked No. 4 in neurology and neurosurgery care, up from No. 6 last year, while Cedars-Sinai Medical Center, Los Angeles, ranks fifth this year, rising two spots from No. 7 last year.
Rounding out the top 10 hospitals for neurology and neurosurgery (in order) are UCLA Medical Center, Los Angeles; Johns Hopkins Hospital, Baltimore; Massachusetts General Hospital, Boston; Mount Sinai Hospital, New York; and Northwestern Medicine–Northwestern Memorial Hospital, Chicago.
U.S. News evaluated 1,245 hospitals and ranked the top 50 that treat patients with challenging neurological issues including stroke, conditions affecting the central nervous system, spinal disorders and injuries, seizures, and degenerative nervous system diagnoses such as multiple sclerosis.
“Consumers want useful resources to help them assess which hospital can best meet their specific care needs,” Ben Harder, chief of health analysis and managing editor at U.S. News, said in a statement.
“The 2023-2024 Best Hospitals rankings offer patients and the physicians with whom they consult a data-driven source for comparing performance in outcomes, patient satisfaction, and other metrics that matter to them,” Mr. Harder said.
Honor roll
This year, as in prior years, U.S. News recognized “honor roll” hospitals that have excelled across multiple areas of care. However, this year, for the first time, there is no ordinal ranking of hospitals making the honor roll. Instead, they are listed in alphabetical order.
In a letter to hospital leaders, U.S. News explained that the major change in format came after months of deliberation, feedback from health care organizations and professionals, and an analysis of how consumers navigate the organization’s website.
Ordinal ranking of hospitals that make the honor roll “obscures the fact that all of the honor roll hospitals have attained the highest standard of care in the nation,” the letter reads.
This year there are 22 honor roll hospitals:
- Barnes-Jewish Hospital, St. Louis
- Brigham and Women’s Hospital, Boston
- Cedars-Sinai Medical Center, Los Angeles
- Cleveland Clinic
- Hospitals of the University of Pennsylvania-Penn Medicine, Philadelphia
- Houston Methodist Hospital
- Johns Hopkins Hospital, Baltimore
- Massachusetts General Hospital, Boston
- Mayo Clinic, Rochester, Minn.
- Mount Sinai Hospital, New York City
- New York–Presbyterian Hospital–Columbia and Cornell, New York City
- North Shore University Hospital at Northwell Health, Manhasset, N.Y.
- Northwestern Memorial Hospital, Chicago
- NYU Langone Hospitals, New York City
- Rush University Medical Center, Chicago
- Stanford (Calif.) Health Care–Stanford Hospital
- UC San Diego Health–La Jolla and Hillcrest Hospitals
- UCLA Medical Center, Los Angeles
- UCSF Health–UCSF Medical Center, San Francisco
- University of Michigan Health–Ann Arbor
- UT Southwestern Medical Center, Dallas
- Vanderbilt University Medical Center, Nashville, Tenn.
U.S. News noted that to keep pace with consumers’ needs and the ever-evolving landscape of health care, “several refinements” are reflected in the latest best hospitals rankings.
These include the introduction of outpatient outcomes in key specialty rankings and surgical ratings, the expanded inclusion of other outpatient data, an increased weight on objective quality measures, and a reduced weight on expert opinion.
In addition, hospital profiles at usnews.com feature refined health equity measures, including a new measure of racial disparities in outcomes.
The full report for best hospitals, best specialty hospitals, and methodology is available online.
A version of this article first appeared on Medscape.com.
of best hospitals for neurology and neurosurgery.
NYU Langone also claimed the top spot in last year’s ranking.
In the latest rankings, UCSF Health–UCSF Medical Center, San Francisco, holds the No. 2 spot and New York–Presbyterian Hospital–Columbia and Cornell in New York City holds the No. 3 spot for neurology care, with no change from last year.
This year, Mayo Clinic, Rochester, Minn., is ranked No. 4 in neurology and neurosurgery care, up from No. 6 last year, while Cedars-Sinai Medical Center, Los Angeles, ranks fifth this year, rising two spots from No. 7 last year.
Rounding out the top 10 hospitals for neurology and neurosurgery (in order) are UCLA Medical Center, Los Angeles; Johns Hopkins Hospital, Baltimore; Massachusetts General Hospital, Boston; Mount Sinai Hospital, New York; and Northwestern Medicine–Northwestern Memorial Hospital, Chicago.
U.S. News evaluated 1,245 hospitals and ranked the top 50 that treat patients with challenging neurological issues including stroke, conditions affecting the central nervous system, spinal disorders and injuries, seizures, and degenerative nervous system diagnoses such as multiple sclerosis.
“Consumers want useful resources to help them assess which hospital can best meet their specific care needs,” Ben Harder, chief of health analysis and managing editor at U.S. News, said in a statement.
“The 2023-2024 Best Hospitals rankings offer patients and the physicians with whom they consult a data-driven source for comparing performance in outcomes, patient satisfaction, and other metrics that matter to them,” Mr. Harder said.
Honor roll
This year, as in prior years, U.S. News recognized “honor roll” hospitals that have excelled across multiple areas of care. However, this year, for the first time, there is no ordinal ranking of hospitals making the honor roll. Instead, they are listed in alphabetical order.
In a letter to hospital leaders, U.S. News explained that the major change in format came after months of deliberation, feedback from health care organizations and professionals, and an analysis of how consumers navigate the organization’s website.
Ordinal ranking of hospitals that make the honor roll “obscures the fact that all of the honor roll hospitals have attained the highest standard of care in the nation,” the letter reads.
This year there are 22 honor roll hospitals:
- Barnes-Jewish Hospital, St. Louis
- Brigham and Women’s Hospital, Boston
- Cedars-Sinai Medical Center, Los Angeles
- Cleveland Clinic
- Hospitals of the University of Pennsylvania-Penn Medicine, Philadelphia
- Houston Methodist Hospital
- Johns Hopkins Hospital, Baltimore
- Massachusetts General Hospital, Boston
- Mayo Clinic, Rochester, Minn.
- Mount Sinai Hospital, New York City
- New York–Presbyterian Hospital–Columbia and Cornell, New York City
- North Shore University Hospital at Northwell Health, Manhasset, N.Y.
- Northwestern Memorial Hospital, Chicago
- NYU Langone Hospitals, New York City
- Rush University Medical Center, Chicago
- Stanford (Calif.) Health Care–Stanford Hospital
- UC San Diego Health–La Jolla and Hillcrest Hospitals
- UCLA Medical Center, Los Angeles
- UCSF Health–UCSF Medical Center, San Francisco
- University of Michigan Health–Ann Arbor
- UT Southwestern Medical Center, Dallas
- Vanderbilt University Medical Center, Nashville, Tenn.
U.S. News noted that to keep pace with consumers’ needs and the ever-evolving landscape of health care, “several refinements” are reflected in the latest best hospitals rankings.
These include the introduction of outpatient outcomes in key specialty rankings and surgical ratings, the expanded inclusion of other outpatient data, an increased weight on objective quality measures, and a reduced weight on expert opinion.
In addition, hospital profiles at usnews.com feature refined health equity measures, including a new measure of racial disparities in outcomes.
The full report for best hospitals, best specialty hospitals, and methodology is available online.
A version of this article first appeared on Medscape.com.
of best hospitals for neurology and neurosurgery.
NYU Langone also claimed the top spot in last year’s ranking.
In the latest rankings, UCSF Health–UCSF Medical Center, San Francisco, holds the No. 2 spot and New York–Presbyterian Hospital–Columbia and Cornell in New York City holds the No. 3 spot for neurology care, with no change from last year.
This year, Mayo Clinic, Rochester, Minn., is ranked No. 4 in neurology and neurosurgery care, up from No. 6 last year, while Cedars-Sinai Medical Center, Los Angeles, ranks fifth this year, rising two spots from No. 7 last year.
Rounding out the top 10 hospitals for neurology and neurosurgery (in order) are UCLA Medical Center, Los Angeles; Johns Hopkins Hospital, Baltimore; Massachusetts General Hospital, Boston; Mount Sinai Hospital, New York; and Northwestern Medicine–Northwestern Memorial Hospital, Chicago.
U.S. News evaluated 1,245 hospitals and ranked the top 50 that treat patients with challenging neurological issues including stroke, conditions affecting the central nervous system, spinal disorders and injuries, seizures, and degenerative nervous system diagnoses such as multiple sclerosis.
“Consumers want useful resources to help them assess which hospital can best meet their specific care needs,” Ben Harder, chief of health analysis and managing editor at U.S. News, said in a statement.
“The 2023-2024 Best Hospitals rankings offer patients and the physicians with whom they consult a data-driven source for comparing performance in outcomes, patient satisfaction, and other metrics that matter to them,” Mr. Harder said.
Honor roll
This year, as in prior years, U.S. News recognized “honor roll” hospitals that have excelled across multiple areas of care. However, this year, for the first time, there is no ordinal ranking of hospitals making the honor roll. Instead, they are listed in alphabetical order.
In a letter to hospital leaders, U.S. News explained that the major change in format came after months of deliberation, feedback from health care organizations and professionals, and an analysis of how consumers navigate the organization’s website.
Ordinal ranking of hospitals that make the honor roll “obscures the fact that all of the honor roll hospitals have attained the highest standard of care in the nation,” the letter reads.
This year there are 22 honor roll hospitals:
- Barnes-Jewish Hospital, St. Louis
- Brigham and Women’s Hospital, Boston
- Cedars-Sinai Medical Center, Los Angeles
- Cleveland Clinic
- Hospitals of the University of Pennsylvania-Penn Medicine, Philadelphia
- Houston Methodist Hospital
- Johns Hopkins Hospital, Baltimore
- Massachusetts General Hospital, Boston
- Mayo Clinic, Rochester, Minn.
- Mount Sinai Hospital, New York City
- New York–Presbyterian Hospital–Columbia and Cornell, New York City
- North Shore University Hospital at Northwell Health, Manhasset, N.Y.
- Northwestern Memorial Hospital, Chicago
- NYU Langone Hospitals, New York City
- Rush University Medical Center, Chicago
- Stanford (Calif.) Health Care–Stanford Hospital
- UC San Diego Health–La Jolla and Hillcrest Hospitals
- UCLA Medical Center, Los Angeles
- UCSF Health–UCSF Medical Center, San Francisco
- University of Michigan Health–Ann Arbor
- UT Southwestern Medical Center, Dallas
- Vanderbilt University Medical Center, Nashville, Tenn.
U.S. News noted that to keep pace with consumers’ needs and the ever-evolving landscape of health care, “several refinements” are reflected in the latest best hospitals rankings.
These include the introduction of outpatient outcomes in key specialty rankings and surgical ratings, the expanded inclusion of other outpatient data, an increased weight on objective quality measures, and a reduced weight on expert opinion.
In addition, hospital profiles at usnews.com feature refined health equity measures, including a new measure of racial disparities in outcomes.
The full report for best hospitals, best specialty hospitals, and methodology is available online.
A version of this article first appeared on Medscape.com.
AI-supported breast screens may reduce radiologist workload
according to early results from a large, randomized, population-based cohort study.
The AI-supported screening also reduced radiologist workload by nearly 44%, researchers estimated.
The trial also found a 20% increase in cancer detection using AI support compared with routine double mammography reading, underscoring AI’s potential to improve screening accuracy and efficiency.
The findings, published online in Lancet Oncology, come from a planned interim safety analysis of the Swedish Mammography Screening with Artificial Intelligence (MASAI) trial.
To date, AI has shown promise in mammography screening, with retrospective evidence demonstrating similar accuracy, compared with standard double readings as well as reduced workload for radiologists. Still, randomized trials assessing the efficacy of AI-supported breast screening are needed.
The aim of the current interim randomized analysis was to assess early screening performance, which included cancer detection, recall, and false positive rates as well as cancer type detected and workload.
The MASAI trial randomized 80,033 women, with a median age of 54, to AI-supported screening (n = 40,003) or double reading without AI (n = 40,030).
The AI system provided malignancy risk scores from 1 to 10, with low-risk scores ranging from 1 to 7, intermediate risk from 8 to 9, and high risk at 10. These risk scores were used to triage screening exams to a single radiologist reading (score of 1-9) or double reading (score of 10), given that cancer prevalence “increases sharply” for those with a risk score of 10, the researchers explained. The AI system also provided computer-aided detection marks for exams with risk scores of 8-10 to radiologists.
Among nearly 40,000 women screened with AI support, 244 cancers were detected, including 184 invasive cancers (75%) and 60 in situ cancers (25%), and resulted in 861 recalls. Among 40,024 participants receiving standard screening, radiologists detected 203 cancers, including 165 invasive cancers (81%) and 38 in situ cancers (19%), and resulted in 817 recalls.
Overall, the detection rate using AI support versus standard screening was 6.1 per 1000 screened participants versus 5.1 per 1,000. The recall rates were 2.2% versus 2.0%, respectively.
The false positive rates were the same in both groups (1.5%) while the positive predictive value (PPV) of recall – how likely a recall of a participant ultimately led to a cancer diagnosis – was higher in the AI group: 28.3% versus 24.8%.
The cancer detection rate in the high-risk group – patients with a risk score of 10 – was 72.3 per 1000 participants screened, or one cancer per 14 screening exams. And, overall, 189 of 490 screening exams flagged as extra-high risk by AI (the highest 1% risk) were recalled. Of the 189 recalled participants, 136 had cancer, representing a PPV of recall of 72%.
Overall, “we found that the benefit of AI-supported screening in terms of screen-reading workload reduction was considerable,” the authors said.
Assuming a radiologist can read 50 mammograms an hour, the researchers estimated that a radiologist would take 4.6 fewer months to read more than 46,000 screening exams in the intervention group compared with more than 83,000 in the control group.
Although these early safety results are “promising,” the findings “are not enough on their own to confirm that AI is ready to be implemented in mammography screening,” lead author Kristina Lång, PhD, of Lund (Sweden) University, said in a press release.
“We still need to understand the implications on patients’ outcomes, especially whether combining radiologists’ expertise with AI can help detect interval cancers that are often missed by traditional screening, as well as the cost-effectiveness of the technology,” she said, adding that “the greatest potential of AI right now is that it could allow radiologists to be less burdened by the excessive amount of reading.”
In an accompanying editorial, Nereo Segnan, MD, and Antonio Ponti, MD, both of CPO Piemonte in Torino, Italy, said that the AI risk score for breast cancer in the trial “seems very accurate at being able to separate high-risk from low-risk women.”
However, the potential for overdiagnosis or overdetection of indolent lesions in the intervention group should “prompt caution in the interpretation of results that otherwise seem straightforward in favoring the use of AI,” the editorialists noted.
The authors agreed that increased detection of in situ cancers with AI-supported screening compared with standard screening – 25% versus 19% – “could be concerning in terms of overdiagnosis,” as the risk of overtreatment is more likely with these low-grade cancers.
In the final analysis, Dr. Lång and colleagues plan to characterize the biological features of detected lesions to provide further insight on AI-supported screening, including the risk for overdiagnosis.
In a statement to the U.K.-based Science Media Centre, Stephen Duffy, professor of cancer screening, Wolfson Institute of Population Health, Queen Mary University of London, commented that the “results illustrate the potential for artificial intelligence to reduce the burden on radiologists’ time,” which is “an issue of considerable importance in many breast screening programs.”
The MASAI study was funded by the Swedish Cancer Society, Confederation of Regional Cancer Centres, and government funding for clinical research. Dr. Lång has been an advisory board member for Siemens Healthineers and has received lecture honorarium from AstraZeneca. Dr. Segnan and Dr. Hall reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to early results from a large, randomized, population-based cohort study.
The AI-supported screening also reduced radiologist workload by nearly 44%, researchers estimated.
The trial also found a 20% increase in cancer detection using AI support compared with routine double mammography reading, underscoring AI’s potential to improve screening accuracy and efficiency.
The findings, published online in Lancet Oncology, come from a planned interim safety analysis of the Swedish Mammography Screening with Artificial Intelligence (MASAI) trial.
To date, AI has shown promise in mammography screening, with retrospective evidence demonstrating similar accuracy, compared with standard double readings as well as reduced workload for radiologists. Still, randomized trials assessing the efficacy of AI-supported breast screening are needed.
The aim of the current interim randomized analysis was to assess early screening performance, which included cancer detection, recall, and false positive rates as well as cancer type detected and workload.
The MASAI trial randomized 80,033 women, with a median age of 54, to AI-supported screening (n = 40,003) or double reading without AI (n = 40,030).
The AI system provided malignancy risk scores from 1 to 10, with low-risk scores ranging from 1 to 7, intermediate risk from 8 to 9, and high risk at 10. These risk scores were used to triage screening exams to a single radiologist reading (score of 1-9) or double reading (score of 10), given that cancer prevalence “increases sharply” for those with a risk score of 10, the researchers explained. The AI system also provided computer-aided detection marks for exams with risk scores of 8-10 to radiologists.
Among nearly 40,000 women screened with AI support, 244 cancers were detected, including 184 invasive cancers (75%) and 60 in situ cancers (25%), and resulted in 861 recalls. Among 40,024 participants receiving standard screening, radiologists detected 203 cancers, including 165 invasive cancers (81%) and 38 in situ cancers (19%), and resulted in 817 recalls.
Overall, the detection rate using AI support versus standard screening was 6.1 per 1000 screened participants versus 5.1 per 1,000. The recall rates were 2.2% versus 2.0%, respectively.
The false positive rates were the same in both groups (1.5%) while the positive predictive value (PPV) of recall – how likely a recall of a participant ultimately led to a cancer diagnosis – was higher in the AI group: 28.3% versus 24.8%.
The cancer detection rate in the high-risk group – patients with a risk score of 10 – was 72.3 per 1000 participants screened, or one cancer per 14 screening exams. And, overall, 189 of 490 screening exams flagged as extra-high risk by AI (the highest 1% risk) were recalled. Of the 189 recalled participants, 136 had cancer, representing a PPV of recall of 72%.
Overall, “we found that the benefit of AI-supported screening in terms of screen-reading workload reduction was considerable,” the authors said.
Assuming a radiologist can read 50 mammograms an hour, the researchers estimated that a radiologist would take 4.6 fewer months to read more than 46,000 screening exams in the intervention group compared with more than 83,000 in the control group.
Although these early safety results are “promising,” the findings “are not enough on their own to confirm that AI is ready to be implemented in mammography screening,” lead author Kristina Lång, PhD, of Lund (Sweden) University, said in a press release.
“We still need to understand the implications on patients’ outcomes, especially whether combining radiologists’ expertise with AI can help detect interval cancers that are often missed by traditional screening, as well as the cost-effectiveness of the technology,” she said, adding that “the greatest potential of AI right now is that it could allow radiologists to be less burdened by the excessive amount of reading.”
In an accompanying editorial, Nereo Segnan, MD, and Antonio Ponti, MD, both of CPO Piemonte in Torino, Italy, said that the AI risk score for breast cancer in the trial “seems very accurate at being able to separate high-risk from low-risk women.”
However, the potential for overdiagnosis or overdetection of indolent lesions in the intervention group should “prompt caution in the interpretation of results that otherwise seem straightforward in favoring the use of AI,” the editorialists noted.
The authors agreed that increased detection of in situ cancers with AI-supported screening compared with standard screening – 25% versus 19% – “could be concerning in terms of overdiagnosis,” as the risk of overtreatment is more likely with these low-grade cancers.
In the final analysis, Dr. Lång and colleagues plan to characterize the biological features of detected lesions to provide further insight on AI-supported screening, including the risk for overdiagnosis.
In a statement to the U.K.-based Science Media Centre, Stephen Duffy, professor of cancer screening, Wolfson Institute of Population Health, Queen Mary University of London, commented that the “results illustrate the potential for artificial intelligence to reduce the burden on radiologists’ time,” which is “an issue of considerable importance in many breast screening programs.”
The MASAI study was funded by the Swedish Cancer Society, Confederation of Regional Cancer Centres, and government funding for clinical research. Dr. Lång has been an advisory board member for Siemens Healthineers and has received lecture honorarium from AstraZeneca. Dr. Segnan and Dr. Hall reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to early results from a large, randomized, population-based cohort study.
The AI-supported screening also reduced radiologist workload by nearly 44%, researchers estimated.
The trial also found a 20% increase in cancer detection using AI support compared with routine double mammography reading, underscoring AI’s potential to improve screening accuracy and efficiency.
The findings, published online in Lancet Oncology, come from a planned interim safety analysis of the Swedish Mammography Screening with Artificial Intelligence (MASAI) trial.
To date, AI has shown promise in mammography screening, with retrospective evidence demonstrating similar accuracy, compared with standard double readings as well as reduced workload for radiologists. Still, randomized trials assessing the efficacy of AI-supported breast screening are needed.
The aim of the current interim randomized analysis was to assess early screening performance, which included cancer detection, recall, and false positive rates as well as cancer type detected and workload.
The MASAI trial randomized 80,033 women, with a median age of 54, to AI-supported screening (n = 40,003) or double reading without AI (n = 40,030).
The AI system provided malignancy risk scores from 1 to 10, with low-risk scores ranging from 1 to 7, intermediate risk from 8 to 9, and high risk at 10. These risk scores were used to triage screening exams to a single radiologist reading (score of 1-9) or double reading (score of 10), given that cancer prevalence “increases sharply” for those with a risk score of 10, the researchers explained. The AI system also provided computer-aided detection marks for exams with risk scores of 8-10 to radiologists.
Among nearly 40,000 women screened with AI support, 244 cancers were detected, including 184 invasive cancers (75%) and 60 in situ cancers (25%), and resulted in 861 recalls. Among 40,024 participants receiving standard screening, radiologists detected 203 cancers, including 165 invasive cancers (81%) and 38 in situ cancers (19%), and resulted in 817 recalls.
Overall, the detection rate using AI support versus standard screening was 6.1 per 1000 screened participants versus 5.1 per 1,000. The recall rates were 2.2% versus 2.0%, respectively.
The false positive rates were the same in both groups (1.5%) while the positive predictive value (PPV) of recall – how likely a recall of a participant ultimately led to a cancer diagnosis – was higher in the AI group: 28.3% versus 24.8%.
The cancer detection rate in the high-risk group – patients with a risk score of 10 – was 72.3 per 1000 participants screened, or one cancer per 14 screening exams. And, overall, 189 of 490 screening exams flagged as extra-high risk by AI (the highest 1% risk) were recalled. Of the 189 recalled participants, 136 had cancer, representing a PPV of recall of 72%.
Overall, “we found that the benefit of AI-supported screening in terms of screen-reading workload reduction was considerable,” the authors said.
Assuming a radiologist can read 50 mammograms an hour, the researchers estimated that a radiologist would take 4.6 fewer months to read more than 46,000 screening exams in the intervention group compared with more than 83,000 in the control group.
Although these early safety results are “promising,” the findings “are not enough on their own to confirm that AI is ready to be implemented in mammography screening,” lead author Kristina Lång, PhD, of Lund (Sweden) University, said in a press release.
“We still need to understand the implications on patients’ outcomes, especially whether combining radiologists’ expertise with AI can help detect interval cancers that are often missed by traditional screening, as well as the cost-effectiveness of the technology,” she said, adding that “the greatest potential of AI right now is that it could allow radiologists to be less burdened by the excessive amount of reading.”
In an accompanying editorial, Nereo Segnan, MD, and Antonio Ponti, MD, both of CPO Piemonte in Torino, Italy, said that the AI risk score for breast cancer in the trial “seems very accurate at being able to separate high-risk from low-risk women.”
However, the potential for overdiagnosis or overdetection of indolent lesions in the intervention group should “prompt caution in the interpretation of results that otherwise seem straightforward in favoring the use of AI,” the editorialists noted.
The authors agreed that increased detection of in situ cancers with AI-supported screening compared with standard screening – 25% versus 19% – “could be concerning in terms of overdiagnosis,” as the risk of overtreatment is more likely with these low-grade cancers.
In the final analysis, Dr. Lång and colleagues plan to characterize the biological features of detected lesions to provide further insight on AI-supported screening, including the risk for overdiagnosis.
In a statement to the U.K.-based Science Media Centre, Stephen Duffy, professor of cancer screening, Wolfson Institute of Population Health, Queen Mary University of London, commented that the “results illustrate the potential for artificial intelligence to reduce the burden on radiologists’ time,” which is “an issue of considerable importance in many breast screening programs.”
The MASAI study was funded by the Swedish Cancer Society, Confederation of Regional Cancer Centres, and government funding for clinical research. Dr. Lång has been an advisory board member for Siemens Healthineers and has received lecture honorarium from AstraZeneca. Dr. Segnan and Dr. Hall reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM LANCET ONCOLOGY
Scrubs & Heels Summit 2023: Filling a void for women in GI
.1-3 This gender disparity arises from a multitude of factors including lack of effective mentoring, unequal leadership and career advancement opportunities, and pay inequity. In this context, The Scrubs & Heels Leadership Summit (S&H) was launched in 2022 focused on the professional and personal development of women in gastroenterology.
I had the great pleasure and honor of attending the 2023 summit which took place in February in Rancho Palos Verdes, Calif. There were nearly 200 attendees ranging from trainees to midcareer and senior gastroenterologists and other health care professionals from both academia and private practices across the nation. The weekend course was directed by S&H cofounders, Dr. Aline Charabaty and Dr. Anita Afzali, and cochaired by Dr. Amy Oxentenko and Dr. Aja McCutchen.
The 2-day summit opened with a presentation by Sally Helgesen, author of How Women Rise, describing the 12 common habits that often hold women back in career advancement, promotion, or opportunities. Dr. Aline Charabaty addressed the myth of women needing to fulfill the role of superwoman or have suprahuman abilities. Attendees were challenged to reframe this societal construct and begin to find balance and the reasonable choice to switch to part-time work and, as Dr. Aja McCutch emphasized, dial-down responsibilities to maintain wellness when life has competing priorities.
Dr. Amy Oxentenko shared her personal journey to success and instilled the importance of engaging with community and society at large. We then heard from Dr. Neena Abraham on how to gracefully embrace transitions in our professional lives, whether intentionally sought or natural progressions of a career. She encouraged attendees to control our own narrative and seek challenges that promote growth. We explored different practice models with Dr. Caroline Hwang and learned strategies of switching from academics to private practice or vice versa. We also heard from cofounder Dr. Anita Afzali on becoming a physician executive and the importance of staying connected to patient care when rising in ranks of leadership.
The second day opened with a keynote address delivered by Dr. Marla Dubinsky detailing her journey of becoming a CEO of a publicly-traded company while retaining her role as professor and chief of pediatric gastroenterology in a large academic institution. Attendees were provided with a master class on discovering ways to inspire our inner entrepreneur and highlighted the benefit of physicians, especially women, in being effective business leaders. This talk was followed by a talk by Phil Schoenfeld, MD, FACS, editor-in-chief of Evidence-Based GI for the American College of Gastroenterology. He spoke on the importance of male allyship for women in GI and shared his personal experiences and challenges with allyship.
The summit included a breakout session by Dr. Rashmi Advani designed for residents to hear tips on how to have a successful fellowship match and for fellows to embrace a steep learning curve when starting and included tips for efficiency. Additional breakout sessions included learning ergonomic strategies for positioning and scope-holding, vocal-cord exercises before giving oral presentations, and how to formulate a business plan and negotiate a contract.
We ended the summit with uplifting advice from executive coaches Sonia Narang and Dr. Dawn Sears who taught us the art of leaning into opportunities, mansizing aspirations, finding coconspirators for amplification of female GI leaders, and supporting our colleagues personally and professionally.
Three key takeaway messages:
- Recognize your self-worth and the contributions you bring to your patients and community as a whole.
- Lean into the importance of vocalizing your asks, advocating for yourself, building your brand, and showcasing your accomplishments.
- Be mindful of the balance between the time and energy you dedicate towards goals that bring you recognition and fuel your passion and your mental, physical, and emotional health.
As a trainee, I benefited tremendously from attending and expanding my professional network of mentors, sponsors and colleagues. I am encouraged by this programming and hope to see more of it in the future.
Contributors to this article included: Rashmi Advani, MD2; Anita Afzali, MD3; Aline Charabaty, MD.4
Neither Dr. Syed, nor the article contributors, had financial conflicts of interest associated with this article. The AGA was represented at the Scrubs and Heels Summit as a society partner committed to the advancement of women in GI. AGA is building on years of efforts to bolster leadership, mentorship, and sponsorship among women in GI through its annual women’s leadership conference and most recently with its 2022 regional women in GI workshops held around the country that led to the development of a comprehensive gender equity strategy designed to build an environment of gender equity in the field of GI so that all can thrive.
Institutions and social media handle
1. Santa Clara Valley Medical Center (San Jose, Calif), @noorannemd
2. Cedars Sinai (Los Angeles), @AdvaniRashmiMD
3. University of Cincinnati, @IBD_Afzali
4. Johns Hopkins Medicine (Washington), @DCharabaty
References
Advani R et al. Gender-specific attitudes of internal medicine residents toward gastroenterology. Dig Dis Sci. 2022 Nov;67(11):5044-52.
American Association of Medical Colleges. Diversity in Medicine: Facts and Figures (2019).
Elta GH. The challenges of being a female gastroenterologist. Gastroenterol Clin North Am. 2011 Jun;40(2):441-7.
Burke CA et al. Gender disparity in the practice of gastroenterology: The first 5 years of a career. Am J Gastroenterol 2005;100:259-64
David, Yakira N. et al. Gender-specific factors influencing gastroenterologists to pursue careers in advanced endoscopy: perceptions vs reality. Journal of the American College of Gastroenterology, ACG 116.3 (2021):539-50.
Rabinowitz LG et al. Gender dynamics in education and practice of gastroenterology. Gastrointest Endosc. 2021;93:1047-56.
Rabinowitz LG et al. Survey finds gender disparities impact both women mentors and mentees in gastroenterology. Journal of the American College of Gastroenterology, ACG 2021;116:1876-84.
.1-3 This gender disparity arises from a multitude of factors including lack of effective mentoring, unequal leadership and career advancement opportunities, and pay inequity. In this context, The Scrubs & Heels Leadership Summit (S&H) was launched in 2022 focused on the professional and personal development of women in gastroenterology.
I had the great pleasure and honor of attending the 2023 summit which took place in February in Rancho Palos Verdes, Calif. There were nearly 200 attendees ranging from trainees to midcareer and senior gastroenterologists and other health care professionals from both academia and private practices across the nation. The weekend course was directed by S&H cofounders, Dr. Aline Charabaty and Dr. Anita Afzali, and cochaired by Dr. Amy Oxentenko and Dr. Aja McCutchen.
The 2-day summit opened with a presentation by Sally Helgesen, author of How Women Rise, describing the 12 common habits that often hold women back in career advancement, promotion, or opportunities. Dr. Aline Charabaty addressed the myth of women needing to fulfill the role of superwoman or have suprahuman abilities. Attendees were challenged to reframe this societal construct and begin to find balance and the reasonable choice to switch to part-time work and, as Dr. Aja McCutch emphasized, dial-down responsibilities to maintain wellness when life has competing priorities.
Dr. Amy Oxentenko shared her personal journey to success and instilled the importance of engaging with community and society at large. We then heard from Dr. Neena Abraham on how to gracefully embrace transitions in our professional lives, whether intentionally sought or natural progressions of a career. She encouraged attendees to control our own narrative and seek challenges that promote growth. We explored different practice models with Dr. Caroline Hwang and learned strategies of switching from academics to private practice or vice versa. We also heard from cofounder Dr. Anita Afzali on becoming a physician executive and the importance of staying connected to patient care when rising in ranks of leadership.
The second day opened with a keynote address delivered by Dr. Marla Dubinsky detailing her journey of becoming a CEO of a publicly-traded company while retaining her role as professor and chief of pediatric gastroenterology in a large academic institution. Attendees were provided with a master class on discovering ways to inspire our inner entrepreneur and highlighted the benefit of physicians, especially women, in being effective business leaders. This talk was followed by a talk by Phil Schoenfeld, MD, FACS, editor-in-chief of Evidence-Based GI for the American College of Gastroenterology. He spoke on the importance of male allyship for women in GI and shared his personal experiences and challenges with allyship.
The summit included a breakout session by Dr. Rashmi Advani designed for residents to hear tips on how to have a successful fellowship match and for fellows to embrace a steep learning curve when starting and included tips for efficiency. Additional breakout sessions included learning ergonomic strategies for positioning and scope-holding, vocal-cord exercises before giving oral presentations, and how to formulate a business plan and negotiate a contract.
We ended the summit with uplifting advice from executive coaches Sonia Narang and Dr. Dawn Sears who taught us the art of leaning into opportunities, mansizing aspirations, finding coconspirators for amplification of female GI leaders, and supporting our colleagues personally and professionally.
Three key takeaway messages:
- Recognize your self-worth and the contributions you bring to your patients and community as a whole.
- Lean into the importance of vocalizing your asks, advocating for yourself, building your brand, and showcasing your accomplishments.
- Be mindful of the balance between the time and energy you dedicate towards goals that bring you recognition and fuel your passion and your mental, physical, and emotional health.
As a trainee, I benefited tremendously from attending and expanding my professional network of mentors, sponsors and colleagues. I am encouraged by this programming and hope to see more of it in the future.
Contributors to this article included: Rashmi Advani, MD2; Anita Afzali, MD3; Aline Charabaty, MD.4
Neither Dr. Syed, nor the article contributors, had financial conflicts of interest associated with this article. The AGA was represented at the Scrubs and Heels Summit as a society partner committed to the advancement of women in GI. AGA is building on years of efforts to bolster leadership, mentorship, and sponsorship among women in GI through its annual women’s leadership conference and most recently with its 2022 regional women in GI workshops held around the country that led to the development of a comprehensive gender equity strategy designed to build an environment of gender equity in the field of GI so that all can thrive.
Institutions and social media handle
1. Santa Clara Valley Medical Center (San Jose, Calif), @noorannemd
2. Cedars Sinai (Los Angeles), @AdvaniRashmiMD
3. University of Cincinnati, @IBD_Afzali
4. Johns Hopkins Medicine (Washington), @DCharabaty
References
Advani R et al. Gender-specific attitudes of internal medicine residents toward gastroenterology. Dig Dis Sci. 2022 Nov;67(11):5044-52.
American Association of Medical Colleges. Diversity in Medicine: Facts and Figures (2019).
Elta GH. The challenges of being a female gastroenterologist. Gastroenterol Clin North Am. 2011 Jun;40(2):441-7.
Burke CA et al. Gender disparity in the practice of gastroenterology: The first 5 years of a career. Am J Gastroenterol 2005;100:259-64
David, Yakira N. et al. Gender-specific factors influencing gastroenterologists to pursue careers in advanced endoscopy: perceptions vs reality. Journal of the American College of Gastroenterology, ACG 116.3 (2021):539-50.
Rabinowitz LG et al. Gender dynamics in education and practice of gastroenterology. Gastrointest Endosc. 2021;93:1047-56.
Rabinowitz LG et al. Survey finds gender disparities impact both women mentors and mentees in gastroenterology. Journal of the American College of Gastroenterology, ACG 2021;116:1876-84.
.1-3 This gender disparity arises from a multitude of factors including lack of effective mentoring, unequal leadership and career advancement opportunities, and pay inequity. In this context, The Scrubs & Heels Leadership Summit (S&H) was launched in 2022 focused on the professional and personal development of women in gastroenterology.
I had the great pleasure and honor of attending the 2023 summit which took place in February in Rancho Palos Verdes, Calif. There were nearly 200 attendees ranging from trainees to midcareer and senior gastroenterologists and other health care professionals from both academia and private practices across the nation. The weekend course was directed by S&H cofounders, Dr. Aline Charabaty and Dr. Anita Afzali, and cochaired by Dr. Amy Oxentenko and Dr. Aja McCutchen.
The 2-day summit opened with a presentation by Sally Helgesen, author of How Women Rise, describing the 12 common habits that often hold women back in career advancement, promotion, or opportunities. Dr. Aline Charabaty addressed the myth of women needing to fulfill the role of superwoman or have suprahuman abilities. Attendees were challenged to reframe this societal construct and begin to find balance and the reasonable choice to switch to part-time work and, as Dr. Aja McCutch emphasized, dial-down responsibilities to maintain wellness when life has competing priorities.
Dr. Amy Oxentenko shared her personal journey to success and instilled the importance of engaging with community and society at large. We then heard from Dr. Neena Abraham on how to gracefully embrace transitions in our professional lives, whether intentionally sought or natural progressions of a career. She encouraged attendees to control our own narrative and seek challenges that promote growth. We explored different practice models with Dr. Caroline Hwang and learned strategies of switching from academics to private practice or vice versa. We also heard from cofounder Dr. Anita Afzali on becoming a physician executive and the importance of staying connected to patient care when rising in ranks of leadership.
The second day opened with a keynote address delivered by Dr. Marla Dubinsky detailing her journey of becoming a CEO of a publicly-traded company while retaining her role as professor and chief of pediatric gastroenterology in a large academic institution. Attendees were provided with a master class on discovering ways to inspire our inner entrepreneur and highlighted the benefit of physicians, especially women, in being effective business leaders. This talk was followed by a talk by Phil Schoenfeld, MD, FACS, editor-in-chief of Evidence-Based GI for the American College of Gastroenterology. He spoke on the importance of male allyship for women in GI and shared his personal experiences and challenges with allyship.
The summit included a breakout session by Dr. Rashmi Advani designed for residents to hear tips on how to have a successful fellowship match and for fellows to embrace a steep learning curve when starting and included tips for efficiency. Additional breakout sessions included learning ergonomic strategies for positioning and scope-holding, vocal-cord exercises before giving oral presentations, and how to formulate a business plan and negotiate a contract.
We ended the summit with uplifting advice from executive coaches Sonia Narang and Dr. Dawn Sears who taught us the art of leaning into opportunities, mansizing aspirations, finding coconspirators for amplification of female GI leaders, and supporting our colleagues personally and professionally.
Three key takeaway messages:
- Recognize your self-worth and the contributions you bring to your patients and community as a whole.
- Lean into the importance of vocalizing your asks, advocating for yourself, building your brand, and showcasing your accomplishments.
- Be mindful of the balance between the time and energy you dedicate towards goals that bring you recognition and fuel your passion and your mental, physical, and emotional health.
As a trainee, I benefited tremendously from attending and expanding my professional network of mentors, sponsors and colleagues. I am encouraged by this programming and hope to see more of it in the future.
Contributors to this article included: Rashmi Advani, MD2; Anita Afzali, MD3; Aline Charabaty, MD.4
Neither Dr. Syed, nor the article contributors, had financial conflicts of interest associated with this article. The AGA was represented at the Scrubs and Heels Summit as a society partner committed to the advancement of women in GI. AGA is building on years of efforts to bolster leadership, mentorship, and sponsorship among women in GI through its annual women’s leadership conference and most recently with its 2022 regional women in GI workshops held around the country that led to the development of a comprehensive gender equity strategy designed to build an environment of gender equity in the field of GI so that all can thrive.
Institutions and social media handle
1. Santa Clara Valley Medical Center (San Jose, Calif), @noorannemd
2. Cedars Sinai (Los Angeles), @AdvaniRashmiMD
3. University of Cincinnati, @IBD_Afzali
4. Johns Hopkins Medicine (Washington), @DCharabaty
References
Advani R et al. Gender-specific attitudes of internal medicine residents toward gastroenterology. Dig Dis Sci. 2022 Nov;67(11):5044-52.
American Association of Medical Colleges. Diversity in Medicine: Facts and Figures (2019).
Elta GH. The challenges of being a female gastroenterologist. Gastroenterol Clin North Am. 2011 Jun;40(2):441-7.
Burke CA et al. Gender disparity in the practice of gastroenterology: The first 5 years of a career. Am J Gastroenterol 2005;100:259-64
David, Yakira N. et al. Gender-specific factors influencing gastroenterologists to pursue careers in advanced endoscopy: perceptions vs reality. Journal of the American College of Gastroenterology, ACG 116.3 (2021):539-50.
Rabinowitz LG et al. Gender dynamics in education and practice of gastroenterology. Gastrointest Endosc. 2021;93:1047-56.
Rabinowitz LG et al. Survey finds gender disparities impact both women mentors and mentees in gastroenterology. Journal of the American College of Gastroenterology, ACG 2021;116:1876-84.
Bipolar disorder tied to a sixfold increased risk of early death
In addition, patients with BD are three times more likely to die prematurely of all causes, compared with the general population, with alcohol-related diseases contributing to more premature deaths than cardiovascular disease (CVD), diabetes, and cancer.
The study results emphasize the need for personalized approaches to risk prediction and prevention of premature cause-specific mortality over the life-course of individuals with BD, lead investigator Tapio Paljärvi, PhD, an epidemiologist at Niuvanniemi Hospital in Kuopio, Finland, told this news organization.
The findings were published online in BMJ Mental Health.
Alcohol a major contributor to early death
A number of studies have established that those with BD have twice the risk of dying prematurely, compared with those without the disorder.
To learn more about the factors contributing to early death in this patient population, the investigators analyzed data from nationwide Finnish medical and insurance registries. They identified and tracked the health of 47,000 patients, aged 15-64 years, with BD between 2004 and 2018.
The average age at the beginning of the monitoring period was 38 years, and 57% of the cohort were women.
To determine the excess deaths directly attributable to BD, the researchers compared the ratio of deaths observed over the monitoring period in those with BD to the number expected to die in the general population, also known as the standard mortality ratio.
Of the group with BD, 3,300 died during the monitoring period. The average age at death was 50, and almost two-thirds (65%, or 2,137) of those who died were men.
Investigators grouped excess deaths in BD patients into two categories – somatic and external.
Of those with BD who died from somatic or disease-related causes, alcohol caused the highest rate of death (29%). The second-leading cause was heart disease and stroke (27%), followed by cancer (22%), respiratory diseases (4%), and diabetes (2%).
Among the 595 patients with BD who died because of alcohol consumption, liver disease was the leading cause of death (48%). The second cause was accidental alcohol poisoning (28%), followed by alcohol dependence (10%).
The leading cause of death from external causes in BD patients was suicide (58%, or 740), nearly half of which (48%) were from an overdose with prescribed psychotropic medications.
Overall, 64%, or 2,104, of the deaths in BD patients from any cause were considered excess deaths, that is, the number of deaths above those expected for those without BD of comparable age and sex.
Most of the excess deaths from somatic illness were either from alcohol-related causes (40%) – a rate three times higher than that of the general population – CVD (26%), or cancer (10%).
High suicide rate
When the team examined excess deaths from external causes, they found that 61% (651) were attributable to suicide, a rate eight times higher than that of the general population.
“In terms of absolute numbers, somatic causes of death represented the majority of all deaths in BD, as also reported in previous research,” Dr. Paljärvi said.
“However, this finding reflects the fact that in many high-income countries most of the deaths are due to somatic causes; with CVD, cancers, and diseases of the nervous system as the leading causes of death in the older age groups,” he added.
Dr. Paljärvi advised that clinicians treating patients with BD balance therapeutic response with potentially serious long-term medication side effects, to prevent premature deaths.
A stronger emphasis on identifying and treating comorbid substance abuse is also warranted, he noted.
Dr. Paljärvi noted that the underlying causes of the excess somatic mortality in people with BD are not fully understood, but may result from the “complex interaction between various established risk factors, including tobacco use, alcohol abuse, physical inactivity, unhealthy diet, obesity, hypertension, etc.”
Regarding the generalizability of the findings, he said many previous studies have been based only on inpatient data and noted that the current study included individuals from various sources including inpatient and outpatient registries as well as social insurance registries.
“While the reported excess all-cause mortality rates are strikingly similar across populations globally, there is a paucity of more detailed cause-specific analyses of excess mortality in BD,” said Dr. Paljärvi, adding that these findings should be replicated in other countries, including the United States.
Chronic inflammation
Commenting on the findings, Benjamin Goldstein, MD, PhD, professor of psychiatry and pharmacology at the University of Toronto, noted that there are clear disparities in access to, and quality of care among, patients with BD and other serious mental illnesses.
“Taking heart disease as an example, disparities exist at virtually every point of contact, ranging from the point of preventive care to the time it takes to be assessed in the ER, to the likelihood of receiving cardiac catheterization, to the quality of postdischarge care,” said Dr. Goldstein.
He also noted that CVD occurs in patients with BD, on average, 10-15 years earlier than the general population. However, he added, “there is important evidence that when people with BD receive the same standard of care as those without BD their cardiovascular outcomes are similar.”
Dr. Goldstein also noted that inflammation, which is a driver of cardiovascular risk, is elevated among patients with BD, particularly during mania and depression.
“Given that the average person with BD has some degree of mood symptoms about 40% of the time, chronically elevated inflammation likely contributes in part to the excess risk of heart disease in bipolar disorder,” he said.
Dr. Goldstein’s team’s research focuses on microvessels. “We have found that microvessel function in both the heart and the brain, determined by MRI, is reduced among teens with BD,” he said.
His team has also found that endothelial function in fingertip microvessels, an indicator of future heart disease risk, varies according to mood states.
“Collectively, these findings suggest the microvascular problems may explain, in part, the extra risk of heart disease beyond traditional risk factors in BD,” he added.
The study was funded by a Wellcome Trust Senior Clinical Research Fellowship and by the Oxford Health Biomedical Research Centre. Dr. Paljärvi and Dr. Goldstein report no relevant financial relationships.
A version of this article appeared on Medscape.com.
In addition, patients with BD are three times more likely to die prematurely of all causes, compared with the general population, with alcohol-related diseases contributing to more premature deaths than cardiovascular disease (CVD), diabetes, and cancer.
The study results emphasize the need for personalized approaches to risk prediction and prevention of premature cause-specific mortality over the life-course of individuals with BD, lead investigator Tapio Paljärvi, PhD, an epidemiologist at Niuvanniemi Hospital in Kuopio, Finland, told this news organization.
The findings were published online in BMJ Mental Health.
Alcohol a major contributor to early death
A number of studies have established that those with BD have twice the risk of dying prematurely, compared with those without the disorder.
To learn more about the factors contributing to early death in this patient population, the investigators analyzed data from nationwide Finnish medical and insurance registries. They identified and tracked the health of 47,000 patients, aged 15-64 years, with BD between 2004 and 2018.
The average age at the beginning of the monitoring period was 38 years, and 57% of the cohort were women.
To determine the excess deaths directly attributable to BD, the researchers compared the ratio of deaths observed over the monitoring period in those with BD to the number expected to die in the general population, also known as the standard mortality ratio.
Of the group with BD, 3,300 died during the monitoring period. The average age at death was 50, and almost two-thirds (65%, or 2,137) of those who died were men.
Investigators grouped excess deaths in BD patients into two categories – somatic and external.
Of those with BD who died from somatic or disease-related causes, alcohol caused the highest rate of death (29%). The second-leading cause was heart disease and stroke (27%), followed by cancer (22%), respiratory diseases (4%), and diabetes (2%).
Among the 595 patients with BD who died because of alcohol consumption, liver disease was the leading cause of death (48%). The second cause was accidental alcohol poisoning (28%), followed by alcohol dependence (10%).
The leading cause of death from external causes in BD patients was suicide (58%, or 740), nearly half of which (48%) were from an overdose with prescribed psychotropic medications.
Overall, 64%, or 2,104, of the deaths in BD patients from any cause were considered excess deaths, that is, the number of deaths above those expected for those without BD of comparable age and sex.
Most of the excess deaths from somatic illness were either from alcohol-related causes (40%) – a rate three times higher than that of the general population – CVD (26%), or cancer (10%).
High suicide rate
When the team examined excess deaths from external causes, they found that 61% (651) were attributable to suicide, a rate eight times higher than that of the general population.
“In terms of absolute numbers, somatic causes of death represented the majority of all deaths in BD, as also reported in previous research,” Dr. Paljärvi said.
“However, this finding reflects the fact that in many high-income countries most of the deaths are due to somatic causes; with CVD, cancers, and diseases of the nervous system as the leading causes of death in the older age groups,” he added.
Dr. Paljärvi advised that clinicians treating patients with BD balance therapeutic response with potentially serious long-term medication side effects, to prevent premature deaths.
A stronger emphasis on identifying and treating comorbid substance abuse is also warranted, he noted.
Dr. Paljärvi noted that the underlying causes of the excess somatic mortality in people with BD are not fully understood, but may result from the “complex interaction between various established risk factors, including tobacco use, alcohol abuse, physical inactivity, unhealthy diet, obesity, hypertension, etc.”
Regarding the generalizability of the findings, he said many previous studies have been based only on inpatient data and noted that the current study included individuals from various sources including inpatient and outpatient registries as well as social insurance registries.
“While the reported excess all-cause mortality rates are strikingly similar across populations globally, there is a paucity of more detailed cause-specific analyses of excess mortality in BD,” said Dr. Paljärvi, adding that these findings should be replicated in other countries, including the United States.
Chronic inflammation
Commenting on the findings, Benjamin Goldstein, MD, PhD, professor of psychiatry and pharmacology at the University of Toronto, noted that there are clear disparities in access to, and quality of care among, patients with BD and other serious mental illnesses.
“Taking heart disease as an example, disparities exist at virtually every point of contact, ranging from the point of preventive care to the time it takes to be assessed in the ER, to the likelihood of receiving cardiac catheterization, to the quality of postdischarge care,” said Dr. Goldstein.
He also noted that CVD occurs in patients with BD, on average, 10-15 years earlier than the general population. However, he added, “there is important evidence that when people with BD receive the same standard of care as those without BD their cardiovascular outcomes are similar.”
Dr. Goldstein also noted that inflammation, which is a driver of cardiovascular risk, is elevated among patients with BD, particularly during mania and depression.
“Given that the average person with BD has some degree of mood symptoms about 40% of the time, chronically elevated inflammation likely contributes in part to the excess risk of heart disease in bipolar disorder,” he said.
Dr. Goldstein’s team’s research focuses on microvessels. “We have found that microvessel function in both the heart and the brain, determined by MRI, is reduced among teens with BD,” he said.
His team has also found that endothelial function in fingertip microvessels, an indicator of future heart disease risk, varies according to mood states.
“Collectively, these findings suggest the microvascular problems may explain, in part, the extra risk of heart disease beyond traditional risk factors in BD,” he added.
The study was funded by a Wellcome Trust Senior Clinical Research Fellowship and by the Oxford Health Biomedical Research Centre. Dr. Paljärvi and Dr. Goldstein report no relevant financial relationships.
A version of this article appeared on Medscape.com.
In addition, patients with BD are three times more likely to die prematurely of all causes, compared with the general population, with alcohol-related diseases contributing to more premature deaths than cardiovascular disease (CVD), diabetes, and cancer.
The study results emphasize the need for personalized approaches to risk prediction and prevention of premature cause-specific mortality over the life-course of individuals with BD, lead investigator Tapio Paljärvi, PhD, an epidemiologist at Niuvanniemi Hospital in Kuopio, Finland, told this news organization.
The findings were published online in BMJ Mental Health.
Alcohol a major contributor to early death
A number of studies have established that those with BD have twice the risk of dying prematurely, compared with those without the disorder.
To learn more about the factors contributing to early death in this patient population, the investigators analyzed data from nationwide Finnish medical and insurance registries. They identified and tracked the health of 47,000 patients, aged 15-64 years, with BD between 2004 and 2018.
The average age at the beginning of the monitoring period was 38 years, and 57% of the cohort were women.
To determine the excess deaths directly attributable to BD, the researchers compared the ratio of deaths observed over the monitoring period in those with BD to the number expected to die in the general population, also known as the standard mortality ratio.
Of the group with BD, 3,300 died during the monitoring period. The average age at death was 50, and almost two-thirds (65%, or 2,137) of those who died were men.
Investigators grouped excess deaths in BD patients into two categories – somatic and external.
Of those with BD who died from somatic or disease-related causes, alcohol caused the highest rate of death (29%). The second-leading cause was heart disease and stroke (27%), followed by cancer (22%), respiratory diseases (4%), and diabetes (2%).
Among the 595 patients with BD who died because of alcohol consumption, liver disease was the leading cause of death (48%). The second cause was accidental alcohol poisoning (28%), followed by alcohol dependence (10%).
The leading cause of death from external causes in BD patients was suicide (58%, or 740), nearly half of which (48%) were from an overdose with prescribed psychotropic medications.
Overall, 64%, or 2,104, of the deaths in BD patients from any cause were considered excess deaths, that is, the number of deaths above those expected for those without BD of comparable age and sex.
Most of the excess deaths from somatic illness were either from alcohol-related causes (40%) – a rate three times higher than that of the general population – CVD (26%), or cancer (10%).
High suicide rate
When the team examined excess deaths from external causes, they found that 61% (651) were attributable to suicide, a rate eight times higher than that of the general population.
“In terms of absolute numbers, somatic causes of death represented the majority of all deaths in BD, as also reported in previous research,” Dr. Paljärvi said.
“However, this finding reflects the fact that in many high-income countries most of the deaths are due to somatic causes; with CVD, cancers, and diseases of the nervous system as the leading causes of death in the older age groups,” he added.
Dr. Paljärvi advised that clinicians treating patients with BD balance therapeutic response with potentially serious long-term medication side effects, to prevent premature deaths.
A stronger emphasis on identifying and treating comorbid substance abuse is also warranted, he noted.
Dr. Paljärvi noted that the underlying causes of the excess somatic mortality in people with BD are not fully understood, but may result from the “complex interaction between various established risk factors, including tobacco use, alcohol abuse, physical inactivity, unhealthy diet, obesity, hypertension, etc.”
Regarding the generalizability of the findings, he said many previous studies have been based only on inpatient data and noted that the current study included individuals from various sources including inpatient and outpatient registries as well as social insurance registries.
“While the reported excess all-cause mortality rates are strikingly similar across populations globally, there is a paucity of more detailed cause-specific analyses of excess mortality in BD,” said Dr. Paljärvi, adding that these findings should be replicated in other countries, including the United States.
Chronic inflammation
Commenting on the findings, Benjamin Goldstein, MD, PhD, professor of psychiatry and pharmacology at the University of Toronto, noted that there are clear disparities in access to, and quality of care among, patients with BD and other serious mental illnesses.
“Taking heart disease as an example, disparities exist at virtually every point of contact, ranging from the point of preventive care to the time it takes to be assessed in the ER, to the likelihood of receiving cardiac catheterization, to the quality of postdischarge care,” said Dr. Goldstein.
He also noted that CVD occurs in patients with BD, on average, 10-15 years earlier than the general population. However, he added, “there is important evidence that when people with BD receive the same standard of care as those without BD their cardiovascular outcomes are similar.”
Dr. Goldstein also noted that inflammation, which is a driver of cardiovascular risk, is elevated among patients with BD, particularly during mania and depression.
“Given that the average person with BD has some degree of mood symptoms about 40% of the time, chronically elevated inflammation likely contributes in part to the excess risk of heart disease in bipolar disorder,” he said.
Dr. Goldstein’s team’s research focuses on microvessels. “We have found that microvessel function in both the heart and the brain, determined by MRI, is reduced among teens with BD,” he said.
His team has also found that endothelial function in fingertip microvessels, an indicator of future heart disease risk, varies according to mood states.
“Collectively, these findings suggest the microvascular problems may explain, in part, the extra risk of heart disease beyond traditional risk factors in BD,” he added.
The study was funded by a Wellcome Trust Senior Clinical Research Fellowship and by the Oxford Health Biomedical Research Centre. Dr. Paljärvi and Dr. Goldstein report no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM BMJ MENTAL HEALTH
Higher occurrence of kidney stones with more added sugar
Consuming a higher percentage of calories from added sugars is linked with a higher prevalence of kidney stones, new research suggests.
Though added sugars have been linked with multiple poor health outcomes, their link with kidney stones has been unclear.
Added sugars are sugars or caloric sweeteners added to foods or drinks during processing or preparation to add flavor or shelf life. They do not include natural sugars such as lactose in milk and fructose in fruits.
Researchers, led by Shan Yin, a urologist at Affiliated Hospital of North Sichuan Medical College, in Nanchong, China, compared the added-sugar intake by quartiles in the U.S. National Health and Nutrition Examination Survey 2007-2018.
A total of 28,303 adults were included in this study, with an average age of 48. Women who consumed less than 600 or more than 3,500 kcal or men who consumed less than 800 or more than 4,200 kcal were excluded.
Researchers adjusted for factors including age, race, education, income, physical activity, and marital, employment, and smoking status.
Compared with the first quartile of percentage added-sugar calorie intake, the population in the fourth quartile, with the highest added sugar intake, had a higher prevalence of kidney stones (odds ratio, 1.39; 95% confidence interval, 1.17-1.65).
Compared with the group with fewer than 5% of calories from added sugar, the group that consumed at least 25% of calories from added sugar had nearly twice the prevalence of kidney stones (OR, 1.88; 95% CI, 1.52-2.32).
Findings were published online in Frontiers in Nutrition.
“By identifying this association, policymakers and health professionals can emphasize the need for public health initiatives to reduce added sugar consumption and promote healthy dietary habits,” the authors write.
Added sugar in the U.S. diet
Sugar-sweetened beverages such as soft drinks and energy and sports drinks account for 34.4% of added sugars in the American diet. Previous studies have shown the relationship between consuming sugar-sweetened beverages and a higher risk of obesity, diabetes, and cardiovascular disease, diseases that often co-occur with kidney stones.
Researchers note that even though most added sugars in the United States come from sugar-sweetened beverages, it’s unclear whether the association between added sugars and kidney stones is caused by the beverages or other sources. For instance, fructose intake has been found to be independently associated with kidney stones.
How much is too much?
The recommended upper limit on added sugar is controversial and varies widely by health organization. The American Heart Association says daily average intake from added sugars should be no more than 150 kcal for adult males (about 9 teaspoons) and no more than 100 kcal for women (about 6 teaspoons). The Institute of Medicine allows up to 25% of calories to be consumed from added sugars. The 2020 Dietary Guidelines for Americans and World Health Organization set 10% of calories as the recommended upper limit.
Further investigating what causes kidney stones is critical as kidney stones are common worldwide, affecting about 1 in 10 people in the United States alone, and occurrence is increasing. Kidney stones have a high recurrence rate – about half of people who get them have a second episode within 10 years, the authors note.
The researchers acknowledge that because participants self-reported food intake, there is the potential for recall bias. Additionally, because of the cross-sectional design, the researchers were not able to determine whether sugar intake or kidney stone occurrence came first.
This work was supported by the Doctoral Fund Project of North Sichuan Medical College. The authors declare no relevant financial relationships.
Consuming a higher percentage of calories from added sugars is linked with a higher prevalence of kidney stones, new research suggests.
Though added sugars have been linked with multiple poor health outcomes, their link with kidney stones has been unclear.
Added sugars are sugars or caloric sweeteners added to foods or drinks during processing or preparation to add flavor or shelf life. They do not include natural sugars such as lactose in milk and fructose in fruits.
Researchers, led by Shan Yin, a urologist at Affiliated Hospital of North Sichuan Medical College, in Nanchong, China, compared the added-sugar intake by quartiles in the U.S. National Health and Nutrition Examination Survey 2007-2018.
A total of 28,303 adults were included in this study, with an average age of 48. Women who consumed less than 600 or more than 3,500 kcal or men who consumed less than 800 or more than 4,200 kcal were excluded.
Researchers adjusted for factors including age, race, education, income, physical activity, and marital, employment, and smoking status.
Compared with the first quartile of percentage added-sugar calorie intake, the population in the fourth quartile, with the highest added sugar intake, had a higher prevalence of kidney stones (odds ratio, 1.39; 95% confidence interval, 1.17-1.65).
Compared with the group with fewer than 5% of calories from added sugar, the group that consumed at least 25% of calories from added sugar had nearly twice the prevalence of kidney stones (OR, 1.88; 95% CI, 1.52-2.32).
Findings were published online in Frontiers in Nutrition.
“By identifying this association, policymakers and health professionals can emphasize the need for public health initiatives to reduce added sugar consumption and promote healthy dietary habits,” the authors write.
Added sugar in the U.S. diet
Sugar-sweetened beverages such as soft drinks and energy and sports drinks account for 34.4% of added sugars in the American diet. Previous studies have shown the relationship between consuming sugar-sweetened beverages and a higher risk of obesity, diabetes, and cardiovascular disease, diseases that often co-occur with kidney stones.
Researchers note that even though most added sugars in the United States come from sugar-sweetened beverages, it’s unclear whether the association between added sugars and kidney stones is caused by the beverages or other sources. For instance, fructose intake has been found to be independently associated with kidney stones.
How much is too much?
The recommended upper limit on added sugar is controversial and varies widely by health organization. The American Heart Association says daily average intake from added sugars should be no more than 150 kcal for adult males (about 9 teaspoons) and no more than 100 kcal for women (about 6 teaspoons). The Institute of Medicine allows up to 25% of calories to be consumed from added sugars. The 2020 Dietary Guidelines for Americans and World Health Organization set 10% of calories as the recommended upper limit.
Further investigating what causes kidney stones is critical as kidney stones are common worldwide, affecting about 1 in 10 people in the United States alone, and occurrence is increasing. Kidney stones have a high recurrence rate – about half of people who get them have a second episode within 10 years, the authors note.
The researchers acknowledge that because participants self-reported food intake, there is the potential for recall bias. Additionally, because of the cross-sectional design, the researchers were not able to determine whether sugar intake or kidney stone occurrence came first.
This work was supported by the Doctoral Fund Project of North Sichuan Medical College. The authors declare no relevant financial relationships.
Consuming a higher percentage of calories from added sugars is linked with a higher prevalence of kidney stones, new research suggests.
Though added sugars have been linked with multiple poor health outcomes, their link with kidney stones has been unclear.
Added sugars are sugars or caloric sweeteners added to foods or drinks during processing or preparation to add flavor or shelf life. They do not include natural sugars such as lactose in milk and fructose in fruits.
Researchers, led by Shan Yin, a urologist at Affiliated Hospital of North Sichuan Medical College, in Nanchong, China, compared the added-sugar intake by quartiles in the U.S. National Health and Nutrition Examination Survey 2007-2018.
A total of 28,303 adults were included in this study, with an average age of 48. Women who consumed less than 600 or more than 3,500 kcal or men who consumed less than 800 or more than 4,200 kcal were excluded.
Researchers adjusted for factors including age, race, education, income, physical activity, and marital, employment, and smoking status.
Compared with the first quartile of percentage added-sugar calorie intake, the population in the fourth quartile, with the highest added sugar intake, had a higher prevalence of kidney stones (odds ratio, 1.39; 95% confidence interval, 1.17-1.65).
Compared with the group with fewer than 5% of calories from added sugar, the group that consumed at least 25% of calories from added sugar had nearly twice the prevalence of kidney stones (OR, 1.88; 95% CI, 1.52-2.32).
Findings were published online in Frontiers in Nutrition.
“By identifying this association, policymakers and health professionals can emphasize the need for public health initiatives to reduce added sugar consumption and promote healthy dietary habits,” the authors write.
Added sugar in the U.S. diet
Sugar-sweetened beverages such as soft drinks and energy and sports drinks account for 34.4% of added sugars in the American diet. Previous studies have shown the relationship between consuming sugar-sweetened beverages and a higher risk of obesity, diabetes, and cardiovascular disease, diseases that often co-occur with kidney stones.
Researchers note that even though most added sugars in the United States come from sugar-sweetened beverages, it’s unclear whether the association between added sugars and kidney stones is caused by the beverages or other sources. For instance, fructose intake has been found to be independently associated with kidney stones.
How much is too much?
The recommended upper limit on added sugar is controversial and varies widely by health organization. The American Heart Association says daily average intake from added sugars should be no more than 150 kcal for adult males (about 9 teaspoons) and no more than 100 kcal for women (about 6 teaspoons). The Institute of Medicine allows up to 25% of calories to be consumed from added sugars. The 2020 Dietary Guidelines for Americans and World Health Organization set 10% of calories as the recommended upper limit.
Further investigating what causes kidney stones is critical as kidney stones are common worldwide, affecting about 1 in 10 people in the United States alone, and occurrence is increasing. Kidney stones have a high recurrence rate – about half of people who get them have a second episode within 10 years, the authors note.
The researchers acknowledge that because participants self-reported food intake, there is the potential for recall bias. Additionally, because of the cross-sectional design, the researchers were not able to determine whether sugar intake or kidney stone occurrence came first.
This work was supported by the Doctoral Fund Project of North Sichuan Medical College. The authors declare no relevant financial relationships.
FROM FRONTIERS IN NUTRITION
High parathyroid hormone level a marker for NAFLD and possibly NASH
TOPLINE:
METHODOLOGY:
- The researchers conducted a systematic review and meta-analysis of 12 case-control studies of patients with NAFLD/NASH and a comparison group without NAFLD/NASH.
- All studies had data on mean PTH levels in cases and controls.
- Pooled weighted mean difference (WMD) was calculated by combining WMDs of each study using a random-effects model.
TAKEAWAY:
- A meta-analysis of 10 studies with 1,051 patients with NAFLD and 1,510 controls revealed a significant association between high PTH level and NAFLD, with a pooled WMD of 5.479.
- A meta-analysis of four studies with 99 patients with NASH and 143 controls revealed a trend toward an association of high PTH level and NASH, with a pooled WMD of 11.995; statistical significance was not achieved owing to inadequate power.
- Both meta-analyses had high statistical heterogeneity (I2 of 82.4% for NAFLD and 81.0% for NASH).
IN PRACTICE:
“These findings may have clinical implications as they may suggest that high PTH level could be another biochemical marker of presence of NAFLD and possibly NASH,” the researchers wrote.
SOURCE:
This study was led by Aunchalee Jaroenlapnopparat, MD, Mount Auburn Hospital/Beth Israel Lahey Health, Cambridge, Mass. It was published online in Diabetes & Metabolic Syndrome: Research & Reviews. The study had no funding.
LIMITATIONS:
This systematic review and meta-analysis included observational studies, which might not show a causal relationship owing to potential confounding effects. Both meta-analyses demonstrated high statistical heterogeneity, probably because of differences in study design, population, and quality among the included studies. The number of studies and participants in the NASH-related analysis were limited, which may have compromised the statistical power of the analysis.
DISCLOSURES:
The authors have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The researchers conducted a systematic review and meta-analysis of 12 case-control studies of patients with NAFLD/NASH and a comparison group without NAFLD/NASH.
- All studies had data on mean PTH levels in cases and controls.
- Pooled weighted mean difference (WMD) was calculated by combining WMDs of each study using a random-effects model.
TAKEAWAY:
- A meta-analysis of 10 studies with 1,051 patients with NAFLD and 1,510 controls revealed a significant association between high PTH level and NAFLD, with a pooled WMD of 5.479.
- A meta-analysis of four studies with 99 patients with NASH and 143 controls revealed a trend toward an association of high PTH level and NASH, with a pooled WMD of 11.995; statistical significance was not achieved owing to inadequate power.
- Both meta-analyses had high statistical heterogeneity (I2 of 82.4% for NAFLD and 81.0% for NASH).
IN PRACTICE:
“These findings may have clinical implications as they may suggest that high PTH level could be another biochemical marker of presence of NAFLD and possibly NASH,” the researchers wrote.
SOURCE:
This study was led by Aunchalee Jaroenlapnopparat, MD, Mount Auburn Hospital/Beth Israel Lahey Health, Cambridge, Mass. It was published online in Diabetes & Metabolic Syndrome: Research & Reviews. The study had no funding.
LIMITATIONS:
This systematic review and meta-analysis included observational studies, which might not show a causal relationship owing to potential confounding effects. Both meta-analyses demonstrated high statistical heterogeneity, probably because of differences in study design, population, and quality among the included studies. The number of studies and participants in the NASH-related analysis were limited, which may have compromised the statistical power of the analysis.
DISCLOSURES:
The authors have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The researchers conducted a systematic review and meta-analysis of 12 case-control studies of patients with NAFLD/NASH and a comparison group without NAFLD/NASH.
- All studies had data on mean PTH levels in cases and controls.
- Pooled weighted mean difference (WMD) was calculated by combining WMDs of each study using a random-effects model.
TAKEAWAY:
- A meta-analysis of 10 studies with 1,051 patients with NAFLD and 1,510 controls revealed a significant association between high PTH level and NAFLD, with a pooled WMD of 5.479.
- A meta-analysis of four studies with 99 patients with NASH and 143 controls revealed a trend toward an association of high PTH level and NASH, with a pooled WMD of 11.995; statistical significance was not achieved owing to inadequate power.
- Both meta-analyses had high statistical heterogeneity (I2 of 82.4% for NAFLD and 81.0% for NASH).
IN PRACTICE:
“These findings may have clinical implications as they may suggest that high PTH level could be another biochemical marker of presence of NAFLD and possibly NASH,” the researchers wrote.
SOURCE:
This study was led by Aunchalee Jaroenlapnopparat, MD, Mount Auburn Hospital/Beth Israel Lahey Health, Cambridge, Mass. It was published online in Diabetes & Metabolic Syndrome: Research & Reviews. The study had no funding.
LIMITATIONS:
This systematic review and meta-analysis included observational studies, which might not show a causal relationship owing to potential confounding effects. Both meta-analyses demonstrated high statistical heterogeneity, probably because of differences in study design, population, and quality among the included studies. The number of studies and participants in the NASH-related analysis were limited, which may have compromised the statistical power of the analysis.
DISCLOSURES:
The authors have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM DIABETES & METABOLIC SYNDROME: RESEARCH & REVIEWS
Medical students are skipping class lectures: Does it matter?
New technologies, including online lectures and guided-lesson websites, along with alternative teaching methods, such as the flipped classroom model, in which med students complete before-class assignments and participate in group projects, are helping to train future physicians for their medical careers.
So though students may not be attending in-person lectures like they did in the past, proponents of online learning say the education students receive and the subsequent care they deliver remains the same.
The Association of American Medical Colleges’ most recent annual survey of 2nd-year medical students found that 25% “almost never” attended their in-person lectures in 2022. The figure has steadily improved since 2020 but mirrors what AAMC recorded in 2017.
“The pandemic may have exacerbated the trend, but it’s a long-standing issue,” said Katherine McOwen, senior director of educational and student affairs at AAMC. She said in an interview that she’s witnessed the pattern for 24 years in her work with medical schools.
“I know it sounds alarming that students aren’t attending lectures. But that doesn’t mean they’re not learning,” said Ahmed Ahmed, MD, MPP, MSc, a recent graduate of Harvard Medical School and now a resident at Brigham and Women’s Hospital, Boston.
Today’s generation of medical students grew up in the age of technology. They are comfortable in front of the screen, so it makes sense for them to learn certain aspects of medical sciences and public health in the same way, Dr. Ahmed told this news organization.
Dr. Ahmed said that at Harvard he participated in one or two case-based classes per week that followed a flipped classroom model, which allows students to study topics on their own before discussing in a lecture format as a group. “We had to come up with a diagnostic plan and walk through the case slide by slide,” he said. “It got us to think like a clinician.”
The flipped classroom allows students to study at their own pace using their preferred learning style, leading to more collaboration in the classroom and between students, according to a 2022 article on the “new standard in medical education” published in Trends in Anaesthesia & Critical Care.
Students use online education tools to complete pre-class assignments such as watching short videos, listening to podcasts, or reading journal articles. In-class time can then be used to cement and create connections through discussions, interactive exercises, group learning, and case studies, the article stated.
Benefits of the flipped classroom include student satisfaction, learner motivation, and faculty interest in learning new teaching methods, according to the article: “Students are performing at least as well as those who attended traditional lectures, while some studies in select health care settings show increased retention in flipped classroom settings.”
Another study on the flipped classroom, published in 2018 in BMC Medical Education found that the teaching method was superior to traditional classrooms for health professions education. Researchers focused specifically on flipped classrooms that provided prerecorded videos to students.
Molly Cooke, MD, director of education for global health sciences at the University of California, San Francisco, School of Medicine, said that the school no longer requires attendance at lectures. “Personally, my position is that medical students are very busy people and make, by and large, rational decisions about how to spend their time. As learning and retention from 50-minute lectures has been shown for decades to be poor, I think it’s perfectly reasonable to watch lectures on their own time.”
Dr. Ahmed agrees. “By our standards, the old model is archaic. It’s passive, and instead we should be encouraging lifelong, self-directed learning.”
To that end, Dr. Ahmed and his fellow students also relied heavily during medical school on secondary educational sources such as Boards and Beyond and Sketchy. “There’s an entire community of medical school students across the country using them,” Dr. Ahmed explained. “You can learn what you need in a tenth of the time of lectures.”
Today lectures only provide a portion of the information delivered to students, Dr. McGowen said. “They also learn in small groups, in problem-solving sessions, and in clinical experiences, all of which make up the meat of their education.”
The purpose of medical school is to prepare students for residency, she added. “Medical school education is very different from other types of education. Students are examined in a variety of ways before they move on to residency and ultimately, practice.”
For example, every student must pass the three-part United States Medical Licensing Examination. Students complete the first two parts in medical school and the third part during residency. “The tests represent a combination of everything students have learned, from lectures, clinical time, and in self-directed learning,” Dr. McGowen said.
Post pandemic, the tools and styles of learning in medical education have changed, and they are likely to continue to evolve along with students and technology, according to the 2022 article on the flipped classroom. “The future of medical education will continue to move in ways that embrace digital technology, as this is what digital native learners are increasingly expecting for their health care education,” states the article.
A version of this article first appeared on Medscape.com.
New technologies, including online lectures and guided-lesson websites, along with alternative teaching methods, such as the flipped classroom model, in which med students complete before-class assignments and participate in group projects, are helping to train future physicians for their medical careers.
So though students may not be attending in-person lectures like they did in the past, proponents of online learning say the education students receive and the subsequent care they deliver remains the same.
The Association of American Medical Colleges’ most recent annual survey of 2nd-year medical students found that 25% “almost never” attended their in-person lectures in 2022. The figure has steadily improved since 2020 but mirrors what AAMC recorded in 2017.
“The pandemic may have exacerbated the trend, but it’s a long-standing issue,” said Katherine McOwen, senior director of educational and student affairs at AAMC. She said in an interview that she’s witnessed the pattern for 24 years in her work with medical schools.
“I know it sounds alarming that students aren’t attending lectures. But that doesn’t mean they’re not learning,” said Ahmed Ahmed, MD, MPP, MSc, a recent graduate of Harvard Medical School and now a resident at Brigham and Women’s Hospital, Boston.
Today’s generation of medical students grew up in the age of technology. They are comfortable in front of the screen, so it makes sense for them to learn certain aspects of medical sciences and public health in the same way, Dr. Ahmed told this news organization.
Dr. Ahmed said that at Harvard he participated in one or two case-based classes per week that followed a flipped classroom model, which allows students to study topics on their own before discussing in a lecture format as a group. “We had to come up with a diagnostic plan and walk through the case slide by slide,” he said. “It got us to think like a clinician.”
The flipped classroom allows students to study at their own pace using their preferred learning style, leading to more collaboration in the classroom and between students, according to a 2022 article on the “new standard in medical education” published in Trends in Anaesthesia & Critical Care.
Students use online education tools to complete pre-class assignments such as watching short videos, listening to podcasts, or reading journal articles. In-class time can then be used to cement and create connections through discussions, interactive exercises, group learning, and case studies, the article stated.
Benefits of the flipped classroom include student satisfaction, learner motivation, and faculty interest in learning new teaching methods, according to the article: “Students are performing at least as well as those who attended traditional lectures, while some studies in select health care settings show increased retention in flipped classroom settings.”
Another study on the flipped classroom, published in 2018 in BMC Medical Education found that the teaching method was superior to traditional classrooms for health professions education. Researchers focused specifically on flipped classrooms that provided prerecorded videos to students.
Molly Cooke, MD, director of education for global health sciences at the University of California, San Francisco, School of Medicine, said that the school no longer requires attendance at lectures. “Personally, my position is that medical students are very busy people and make, by and large, rational decisions about how to spend their time. As learning and retention from 50-minute lectures has been shown for decades to be poor, I think it’s perfectly reasonable to watch lectures on their own time.”
Dr. Ahmed agrees. “By our standards, the old model is archaic. It’s passive, and instead we should be encouraging lifelong, self-directed learning.”
To that end, Dr. Ahmed and his fellow students also relied heavily during medical school on secondary educational sources such as Boards and Beyond and Sketchy. “There’s an entire community of medical school students across the country using them,” Dr. Ahmed explained. “You can learn what you need in a tenth of the time of lectures.”
Today lectures only provide a portion of the information delivered to students, Dr. McGowen said. “They also learn in small groups, in problem-solving sessions, and in clinical experiences, all of which make up the meat of their education.”
The purpose of medical school is to prepare students for residency, she added. “Medical school education is very different from other types of education. Students are examined in a variety of ways before they move on to residency and ultimately, practice.”
For example, every student must pass the three-part United States Medical Licensing Examination. Students complete the first two parts in medical school and the third part during residency. “The tests represent a combination of everything students have learned, from lectures, clinical time, and in self-directed learning,” Dr. McGowen said.
Post pandemic, the tools and styles of learning in medical education have changed, and they are likely to continue to evolve along with students and technology, according to the 2022 article on the flipped classroom. “The future of medical education will continue to move in ways that embrace digital technology, as this is what digital native learners are increasingly expecting for their health care education,” states the article.
A version of this article first appeared on Medscape.com.
New technologies, including online lectures and guided-lesson websites, along with alternative teaching methods, such as the flipped classroom model, in which med students complete before-class assignments and participate in group projects, are helping to train future physicians for their medical careers.
So though students may not be attending in-person lectures like they did in the past, proponents of online learning say the education students receive and the subsequent care they deliver remains the same.
The Association of American Medical Colleges’ most recent annual survey of 2nd-year medical students found that 25% “almost never” attended their in-person lectures in 2022. The figure has steadily improved since 2020 but mirrors what AAMC recorded in 2017.
“The pandemic may have exacerbated the trend, but it’s a long-standing issue,” said Katherine McOwen, senior director of educational and student affairs at AAMC. She said in an interview that she’s witnessed the pattern for 24 years in her work with medical schools.
“I know it sounds alarming that students aren’t attending lectures. But that doesn’t mean they’re not learning,” said Ahmed Ahmed, MD, MPP, MSc, a recent graduate of Harvard Medical School and now a resident at Brigham and Women’s Hospital, Boston.
Today’s generation of medical students grew up in the age of technology. They are comfortable in front of the screen, so it makes sense for them to learn certain aspects of medical sciences and public health in the same way, Dr. Ahmed told this news organization.
Dr. Ahmed said that at Harvard he participated in one or two case-based classes per week that followed a flipped classroom model, which allows students to study topics on their own before discussing in a lecture format as a group. “We had to come up with a diagnostic plan and walk through the case slide by slide,” he said. “It got us to think like a clinician.”
The flipped classroom allows students to study at their own pace using their preferred learning style, leading to more collaboration in the classroom and between students, according to a 2022 article on the “new standard in medical education” published in Trends in Anaesthesia & Critical Care.
Students use online education tools to complete pre-class assignments such as watching short videos, listening to podcasts, or reading journal articles. In-class time can then be used to cement and create connections through discussions, interactive exercises, group learning, and case studies, the article stated.
Benefits of the flipped classroom include student satisfaction, learner motivation, and faculty interest in learning new teaching methods, according to the article: “Students are performing at least as well as those who attended traditional lectures, while some studies in select health care settings show increased retention in flipped classroom settings.”
Another study on the flipped classroom, published in 2018 in BMC Medical Education found that the teaching method was superior to traditional classrooms for health professions education. Researchers focused specifically on flipped classrooms that provided prerecorded videos to students.
Molly Cooke, MD, director of education for global health sciences at the University of California, San Francisco, School of Medicine, said that the school no longer requires attendance at lectures. “Personally, my position is that medical students are very busy people and make, by and large, rational decisions about how to spend their time. As learning and retention from 50-minute lectures has been shown for decades to be poor, I think it’s perfectly reasonable to watch lectures on their own time.”
Dr. Ahmed agrees. “By our standards, the old model is archaic. It’s passive, and instead we should be encouraging lifelong, self-directed learning.”
To that end, Dr. Ahmed and his fellow students also relied heavily during medical school on secondary educational sources such as Boards and Beyond and Sketchy. “There’s an entire community of medical school students across the country using them,” Dr. Ahmed explained. “You can learn what you need in a tenth of the time of lectures.”
Today lectures only provide a portion of the information delivered to students, Dr. McGowen said. “They also learn in small groups, in problem-solving sessions, and in clinical experiences, all of which make up the meat of their education.”
The purpose of medical school is to prepare students for residency, she added. “Medical school education is very different from other types of education. Students are examined in a variety of ways before they move on to residency and ultimately, practice.”
For example, every student must pass the three-part United States Medical Licensing Examination. Students complete the first two parts in medical school and the third part during residency. “The tests represent a combination of everything students have learned, from lectures, clinical time, and in self-directed learning,” Dr. McGowen said.
Post pandemic, the tools and styles of learning in medical education have changed, and they are likely to continue to evolve along with students and technology, according to the 2022 article on the flipped classroom. “The future of medical education will continue to move in ways that embrace digital technology, as this is what digital native learners are increasingly expecting for their health care education,” states the article.
A version of this article first appeared on Medscape.com.
Evaluation of Micrographic Surgery and Dermatologic Oncology Fellowship Program Websites
To the Editor:
Micrographic surgery and dermatologic oncology (MSDO) is a highly competitive subspecialty fellowship in dermatology. Prospective applicants often depend on the Internet to obtain pertinent information about fellowship programs to navigate the application process. An up-to-date and comprehensive fellowship website has the potential to be advantageous for both applicants and programs—applicants can more readily identify programs that align with their goals and values, and programs can effectively attract compatible applicants. These advantages are increasingly relevant with the virtual application process that has become essential considering the COVID-19 pandemic. At the height of the COVID-19 pandemic in 2020, we sought to evaluate the comprehensiveness of the content of Accreditation Council for Graduate Medical Education (ACGME) MSDO fellowship program websites to identify possible areas for improvement.
We obtained a list of all ACGME MSDO fellowships from the ACGME website (https://www.acgme.org/) and verified it against the list of MSDO programs in FREIDA, the American Medical Association residency and fellowship database (https://freida.ama-assn.org/). All programs without a website were excluded from further analysis. All data collection from currently accessible fellowship websites and evaluation occurred in April 2020.
The remaining MSDO fellowship program websites were evaluated using 25 criteria distributed among 5 domains: education/research, clinical training, program information, application process, and incentives. These criteria were determined based on earlier studies that similarly evaluated the website content of fellowship programs with inclusion of information that was considered valuable in the appraisal of fellowship programs.1,2 Criteria were further refined by direct consideration of relevance and importance to MSDO fellowship applicants (eg, inclusion of case volume, exclusion of call schedule).
Each criterion was independently assessed by 2 investigators (J.Y.C. and S.J.E.S.). A third investigator (J.R.P.) then independently evaluated those 2 assessments for agreement. Where disagreement was discovered, the third evaluator (J.R.P.) provided a final appraisal. Cohen’s kappa (κ) was conducted to evaluate for concordance between the 2 primary website evaluators. We found there to be substantial agreement between the reviewers within the education/research (κ [SD]=0.772 [0.077]), clinical training (κ [SD]=0.740 [0.051]), application process (κ [SD]=0.726 [0.103]), and incentives domains (κ [SD]=0.730 [0.110]). There was moderate agreement (κ [SD]=0.603 [0.128]) between the reviewers within the program information domain.
We identified 77 active MSDO fellowship programs. Sixty of those 77 programs (77.9%) had a dedicated fellowship website that was readily accessible. Most programs that had a dedicated fellowship website had a core or affiliated residency program (49/60 [81.7%]).
Websites that we evaluated fulfilled a mean (SD) of 9.37 (4.17) of the 25 identified criteria. Only 13 of 60 (21.7%) websites fulfilled more than 50% of evaluated criteria.
There was no statistical difference in the number of criteria fulfilled based on whether the fellowship program had a core or affiliated residency program.
Upon reviewing website accessibility directly from FREIDA, only 5 of 60 programs (8.3%) provided applicants with a link directly to their fellowship page (Table). Most programs (41 [68.3%]) provided a link to the dermatology department website, not to the specific fellowship program page, thus requiring a multistep process to find the fellowship-specific page. The remaining programs had an inaccessible (4 [6.7%]) or absent (10 [16.7%]) link on FREIDA, though a fellowship website could be identified by an Internet search of the program name.
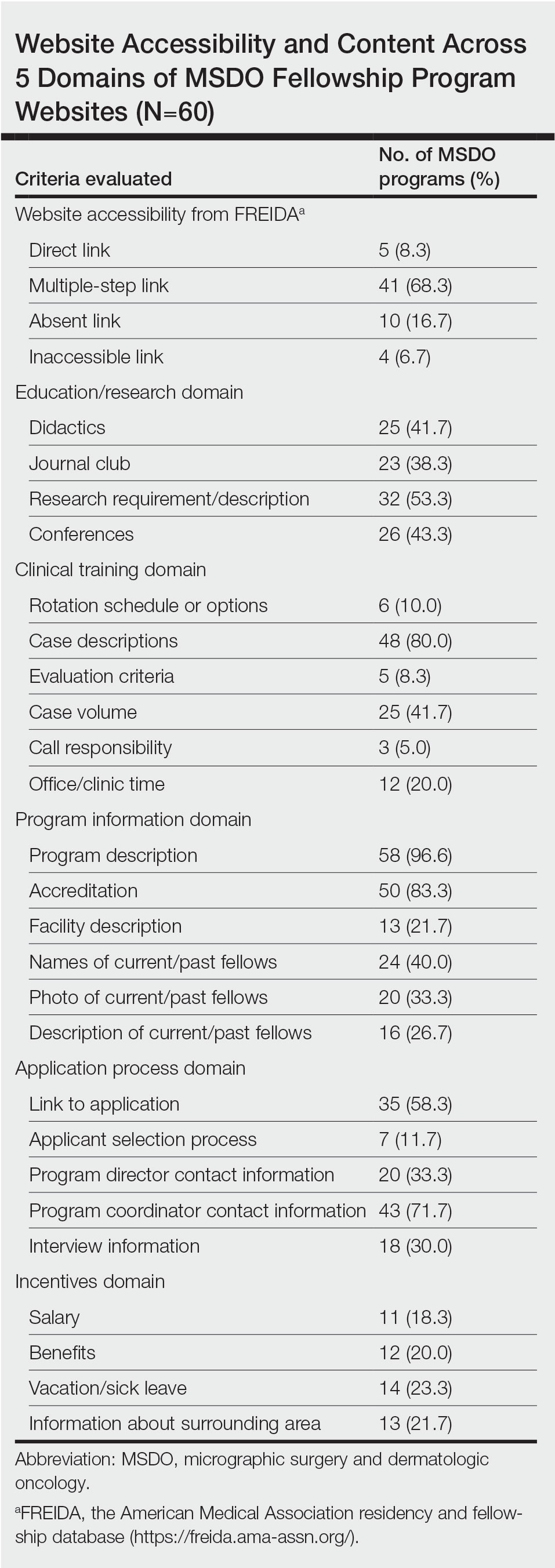
The domain most fulfilled was program information with an average of 51.1% of programs satisfying the criteria, whereas the incentives domain was least fulfilled with an average of only 20.8% of programs satisfying the criteria. Across the various criteria, websites more often included a description of the program (58 [96.6%]), mentioned accreditation (53 [88.3%]), and provided case descriptions (48 [80.0%]). They less often reported information regarding a fellow’s call responsibility (3 [5%]); evaluation criteria (5 [8.3%]); and rotation schedule or options (6 [10.0%]).
The highest number of criteria fulfilled by a single program was 19 (76%). The lowest number of criteria met was 2 (8%). These findings suggest a large variation in comprehensiveness across fellowship websites.
Our research suggests that many current MSDO fellowship programs have room to maximize the information provided to applicants through their websites, which is particularly relevant following the COVID-19 pandemic, as the value of providing comprehensive and transparent information through an online platform is greater than ever. Given the ongoing desire to limit travel, virtual methods for navigating the application process have been readily used, including online videoconferencing for interviews and virtual program visits. This scenario has placed applicants in a challenging situation—their ability to directly evaluate their compatibility with a given program has been limited.3
Earlier studies that analyzed rheumatology fellowship recruitment during the COVID-19 pandemic found that programs may have more difficulty highlighting the strengths of their institution (eg, clinical facilities, professional opportunities, educational environment).4 An updated and comprehensive fellowship website was recommended4 as a key part in facing these new challenges. On the other hand, given the large number of applicants each year for fellowship positions in any given program, we acknowledge the potential benefit programs may obtain from limiting electronic information that is readily accessible to all applicants, as doing so may encourage applicants to communicate directly with a program and allow programs to identify candidates who are more interested.
In light of the movement to a more virtual-friendly and technology-driven fellowship application process, we identified 25 content areas that fellowships may want to include on their websites so that potential applicants can be well informed about the program before submitting an application and scheduling an interview. Efforts to improve accessibility and maximize the content of these websites may help programs attract compatible candidates, improve transparency, and guide applicants throughout the application process.
- Lu F, Vijayasarathi A, Murray N, et al. Evaluation of pediatric radiology fellowship website content in USA and Canada. Curr Prob Diagn Radiol. 2021;50:151-155. doi:10.1067/j.cpradiol.2020.01.007
- Cantrell CK, Bergstresser SL, Schuh AC, et al. Accessibility and content of abdominal transplant fellowship program websites in the United States. J Surg Res. 2018;232:271-274. doi:10.1016/j.jss.2018.06.052
- Nesemeier BR, Lebo NL, Schmalbach CE, et al. Impact of the COVID-19 global pandemic on the otolaryngology fellowship application process. Otolaryngol Head Neck Surg. 2020;163:712-713. doi:10.1177/0194599820934370
- Kilian A, Dua AB, Bolster MB, et al. Rheumatology fellowship recruitment in 2020: benefits, challenges, and adaptations. Arthritis Care Res (Hoboken). 2021;73:459-461. doi:10.1002/acr.24445
To the Editor:
Micrographic surgery and dermatologic oncology (MSDO) is a highly competitive subspecialty fellowship in dermatology. Prospective applicants often depend on the Internet to obtain pertinent information about fellowship programs to navigate the application process. An up-to-date and comprehensive fellowship website has the potential to be advantageous for both applicants and programs—applicants can more readily identify programs that align with their goals and values, and programs can effectively attract compatible applicants. These advantages are increasingly relevant with the virtual application process that has become essential considering the COVID-19 pandemic. At the height of the COVID-19 pandemic in 2020, we sought to evaluate the comprehensiveness of the content of Accreditation Council for Graduate Medical Education (ACGME) MSDO fellowship program websites to identify possible areas for improvement.
We obtained a list of all ACGME MSDO fellowships from the ACGME website (https://www.acgme.org/) and verified it against the list of MSDO programs in FREIDA, the American Medical Association residency and fellowship database (https://freida.ama-assn.org/). All programs without a website were excluded from further analysis. All data collection from currently accessible fellowship websites and evaluation occurred in April 2020.
The remaining MSDO fellowship program websites were evaluated using 25 criteria distributed among 5 domains: education/research, clinical training, program information, application process, and incentives. These criteria were determined based on earlier studies that similarly evaluated the website content of fellowship programs with inclusion of information that was considered valuable in the appraisal of fellowship programs.1,2 Criteria were further refined by direct consideration of relevance and importance to MSDO fellowship applicants (eg, inclusion of case volume, exclusion of call schedule).
Each criterion was independently assessed by 2 investigators (J.Y.C. and S.J.E.S.). A third investigator (J.R.P.) then independently evaluated those 2 assessments for agreement. Where disagreement was discovered, the third evaluator (J.R.P.) provided a final appraisal. Cohen’s kappa (κ) was conducted to evaluate for concordance between the 2 primary website evaluators. We found there to be substantial agreement between the reviewers within the education/research (κ [SD]=0.772 [0.077]), clinical training (κ [SD]=0.740 [0.051]), application process (κ [SD]=0.726 [0.103]), and incentives domains (κ [SD]=0.730 [0.110]). There was moderate agreement (κ [SD]=0.603 [0.128]) between the reviewers within the program information domain.
We identified 77 active MSDO fellowship programs. Sixty of those 77 programs (77.9%) had a dedicated fellowship website that was readily accessible. Most programs that had a dedicated fellowship website had a core or affiliated residency program (49/60 [81.7%]).
Websites that we evaluated fulfilled a mean (SD) of 9.37 (4.17) of the 25 identified criteria. Only 13 of 60 (21.7%) websites fulfilled more than 50% of evaluated criteria.
There was no statistical difference in the number of criteria fulfilled based on whether the fellowship program had a core or affiliated residency program.
Upon reviewing website accessibility directly from FREIDA, only 5 of 60 programs (8.3%) provided applicants with a link directly to their fellowship page (Table). Most programs (41 [68.3%]) provided a link to the dermatology department website, not to the specific fellowship program page, thus requiring a multistep process to find the fellowship-specific page. The remaining programs had an inaccessible (4 [6.7%]) or absent (10 [16.7%]) link on FREIDA, though a fellowship website could be identified by an Internet search of the program name.
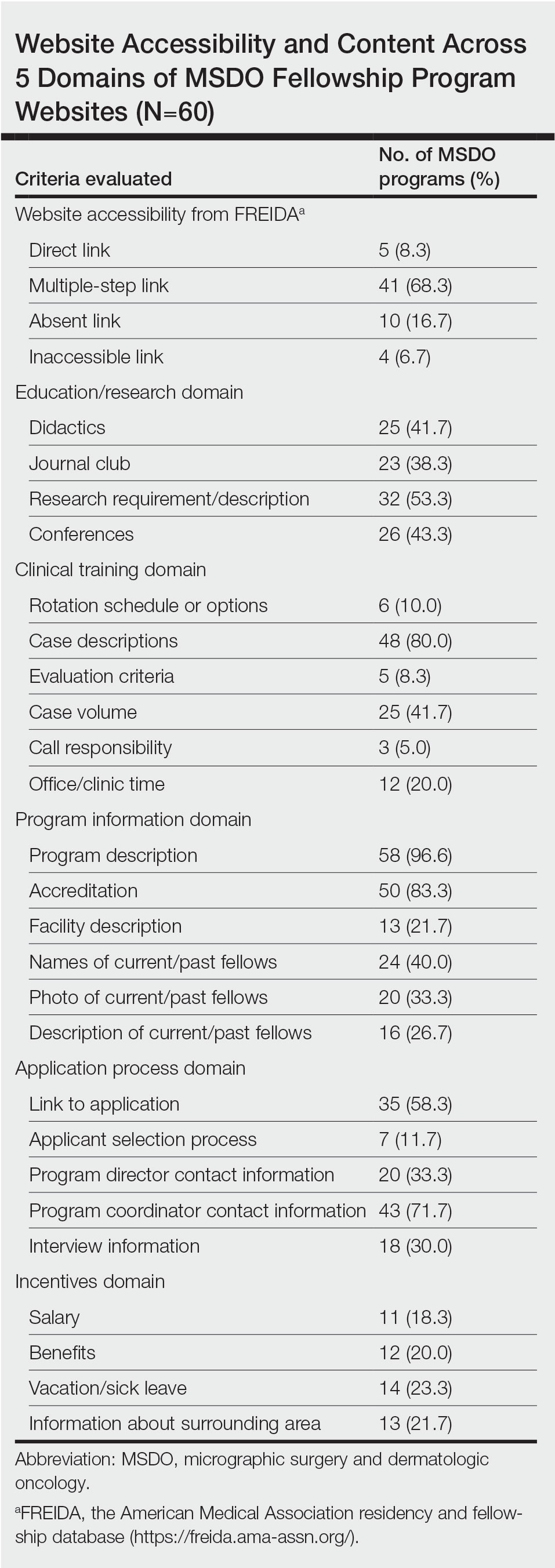
The domain most fulfilled was program information with an average of 51.1% of programs satisfying the criteria, whereas the incentives domain was least fulfilled with an average of only 20.8% of programs satisfying the criteria. Across the various criteria, websites more often included a description of the program (58 [96.6%]), mentioned accreditation (53 [88.3%]), and provided case descriptions (48 [80.0%]). They less often reported information regarding a fellow’s call responsibility (3 [5%]); evaluation criteria (5 [8.3%]); and rotation schedule or options (6 [10.0%]).
The highest number of criteria fulfilled by a single program was 19 (76%). The lowest number of criteria met was 2 (8%). These findings suggest a large variation in comprehensiveness across fellowship websites.
Our research suggests that many current MSDO fellowship programs have room to maximize the information provided to applicants through their websites, which is particularly relevant following the COVID-19 pandemic, as the value of providing comprehensive and transparent information through an online platform is greater than ever. Given the ongoing desire to limit travel, virtual methods for navigating the application process have been readily used, including online videoconferencing for interviews and virtual program visits. This scenario has placed applicants in a challenging situation—their ability to directly evaluate their compatibility with a given program has been limited.3
Earlier studies that analyzed rheumatology fellowship recruitment during the COVID-19 pandemic found that programs may have more difficulty highlighting the strengths of their institution (eg, clinical facilities, professional opportunities, educational environment).4 An updated and comprehensive fellowship website was recommended4 as a key part in facing these new challenges. On the other hand, given the large number of applicants each year for fellowship positions in any given program, we acknowledge the potential benefit programs may obtain from limiting electronic information that is readily accessible to all applicants, as doing so may encourage applicants to communicate directly with a program and allow programs to identify candidates who are more interested.
In light of the movement to a more virtual-friendly and technology-driven fellowship application process, we identified 25 content areas that fellowships may want to include on their websites so that potential applicants can be well informed about the program before submitting an application and scheduling an interview. Efforts to improve accessibility and maximize the content of these websites may help programs attract compatible candidates, improve transparency, and guide applicants throughout the application process.
To the Editor:
Micrographic surgery and dermatologic oncology (MSDO) is a highly competitive subspecialty fellowship in dermatology. Prospective applicants often depend on the Internet to obtain pertinent information about fellowship programs to navigate the application process. An up-to-date and comprehensive fellowship website has the potential to be advantageous for both applicants and programs—applicants can more readily identify programs that align with their goals and values, and programs can effectively attract compatible applicants. These advantages are increasingly relevant with the virtual application process that has become essential considering the COVID-19 pandemic. At the height of the COVID-19 pandemic in 2020, we sought to evaluate the comprehensiveness of the content of Accreditation Council for Graduate Medical Education (ACGME) MSDO fellowship program websites to identify possible areas for improvement.
We obtained a list of all ACGME MSDO fellowships from the ACGME website (https://www.acgme.org/) and verified it against the list of MSDO programs in FREIDA, the American Medical Association residency and fellowship database (https://freida.ama-assn.org/). All programs without a website were excluded from further analysis. All data collection from currently accessible fellowship websites and evaluation occurred in April 2020.
The remaining MSDO fellowship program websites were evaluated using 25 criteria distributed among 5 domains: education/research, clinical training, program information, application process, and incentives. These criteria were determined based on earlier studies that similarly evaluated the website content of fellowship programs with inclusion of information that was considered valuable in the appraisal of fellowship programs.1,2 Criteria were further refined by direct consideration of relevance and importance to MSDO fellowship applicants (eg, inclusion of case volume, exclusion of call schedule).
Each criterion was independently assessed by 2 investigators (J.Y.C. and S.J.E.S.). A third investigator (J.R.P.) then independently evaluated those 2 assessments for agreement. Where disagreement was discovered, the third evaluator (J.R.P.) provided a final appraisal. Cohen’s kappa (κ) was conducted to evaluate for concordance between the 2 primary website evaluators. We found there to be substantial agreement between the reviewers within the education/research (κ [SD]=0.772 [0.077]), clinical training (κ [SD]=0.740 [0.051]), application process (κ [SD]=0.726 [0.103]), and incentives domains (κ [SD]=0.730 [0.110]). There was moderate agreement (κ [SD]=0.603 [0.128]) between the reviewers within the program information domain.
We identified 77 active MSDO fellowship programs. Sixty of those 77 programs (77.9%) had a dedicated fellowship website that was readily accessible. Most programs that had a dedicated fellowship website had a core or affiliated residency program (49/60 [81.7%]).
Websites that we evaluated fulfilled a mean (SD) of 9.37 (4.17) of the 25 identified criteria. Only 13 of 60 (21.7%) websites fulfilled more than 50% of evaluated criteria.
There was no statistical difference in the number of criteria fulfilled based on whether the fellowship program had a core or affiliated residency program.
Upon reviewing website accessibility directly from FREIDA, only 5 of 60 programs (8.3%) provided applicants with a link directly to their fellowship page (Table). Most programs (41 [68.3%]) provided a link to the dermatology department website, not to the specific fellowship program page, thus requiring a multistep process to find the fellowship-specific page. The remaining programs had an inaccessible (4 [6.7%]) or absent (10 [16.7%]) link on FREIDA, though a fellowship website could be identified by an Internet search of the program name.
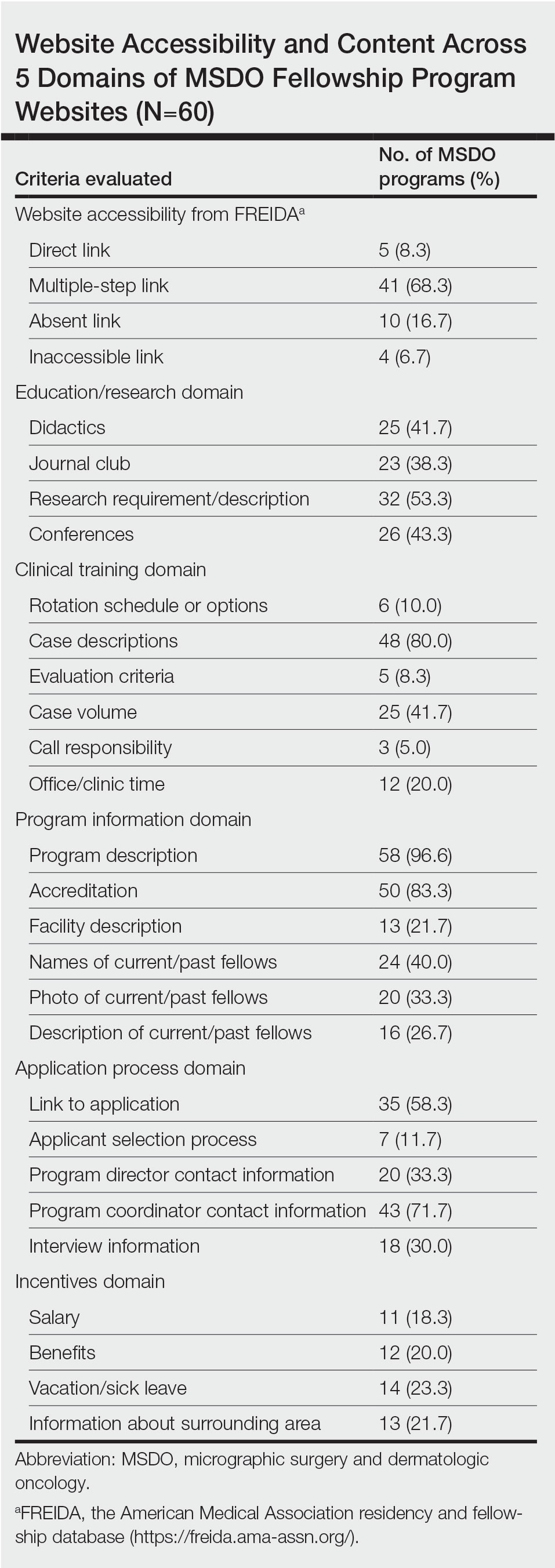
The domain most fulfilled was program information with an average of 51.1% of programs satisfying the criteria, whereas the incentives domain was least fulfilled with an average of only 20.8% of programs satisfying the criteria. Across the various criteria, websites more often included a description of the program (58 [96.6%]), mentioned accreditation (53 [88.3%]), and provided case descriptions (48 [80.0%]). They less often reported information regarding a fellow’s call responsibility (3 [5%]); evaluation criteria (5 [8.3%]); and rotation schedule or options (6 [10.0%]).
The highest number of criteria fulfilled by a single program was 19 (76%). The lowest number of criteria met was 2 (8%). These findings suggest a large variation in comprehensiveness across fellowship websites.
Our research suggests that many current MSDO fellowship programs have room to maximize the information provided to applicants through their websites, which is particularly relevant following the COVID-19 pandemic, as the value of providing comprehensive and transparent information through an online platform is greater than ever. Given the ongoing desire to limit travel, virtual methods for navigating the application process have been readily used, including online videoconferencing for interviews and virtual program visits. This scenario has placed applicants in a challenging situation—their ability to directly evaluate their compatibility with a given program has been limited.3
Earlier studies that analyzed rheumatology fellowship recruitment during the COVID-19 pandemic found that programs may have more difficulty highlighting the strengths of their institution (eg, clinical facilities, professional opportunities, educational environment).4 An updated and comprehensive fellowship website was recommended4 as a key part in facing these new challenges. On the other hand, given the large number of applicants each year for fellowship positions in any given program, we acknowledge the potential benefit programs may obtain from limiting electronic information that is readily accessible to all applicants, as doing so may encourage applicants to communicate directly with a program and allow programs to identify candidates who are more interested.
In light of the movement to a more virtual-friendly and technology-driven fellowship application process, we identified 25 content areas that fellowships may want to include on their websites so that potential applicants can be well informed about the program before submitting an application and scheduling an interview. Efforts to improve accessibility and maximize the content of these websites may help programs attract compatible candidates, improve transparency, and guide applicants throughout the application process.
- Lu F, Vijayasarathi A, Murray N, et al. Evaluation of pediatric radiology fellowship website content in USA and Canada. Curr Prob Diagn Radiol. 2021;50:151-155. doi:10.1067/j.cpradiol.2020.01.007
- Cantrell CK, Bergstresser SL, Schuh AC, et al. Accessibility and content of abdominal transplant fellowship program websites in the United States. J Surg Res. 2018;232:271-274. doi:10.1016/j.jss.2018.06.052
- Nesemeier BR, Lebo NL, Schmalbach CE, et al. Impact of the COVID-19 global pandemic on the otolaryngology fellowship application process. Otolaryngol Head Neck Surg. 2020;163:712-713. doi:10.1177/0194599820934370
- Kilian A, Dua AB, Bolster MB, et al. Rheumatology fellowship recruitment in 2020: benefits, challenges, and adaptations. Arthritis Care Res (Hoboken). 2021;73:459-461. doi:10.1002/acr.24445
- Lu F, Vijayasarathi A, Murray N, et al. Evaluation of pediatric radiology fellowship website content in USA and Canada. Curr Prob Diagn Radiol. 2021;50:151-155. doi:10.1067/j.cpradiol.2020.01.007
- Cantrell CK, Bergstresser SL, Schuh AC, et al. Accessibility and content of abdominal transplant fellowship program websites in the United States. J Surg Res. 2018;232:271-274. doi:10.1016/j.jss.2018.06.052
- Nesemeier BR, Lebo NL, Schmalbach CE, et al. Impact of the COVID-19 global pandemic on the otolaryngology fellowship application process. Otolaryngol Head Neck Surg. 2020;163:712-713. doi:10.1177/0194599820934370
- Kilian A, Dua AB, Bolster MB, et al. Rheumatology fellowship recruitment in 2020: benefits, challenges, and adaptations. Arthritis Care Res (Hoboken). 2021;73:459-461. doi:10.1002/acr.24445
Practice Points
- With the COVID-19 pandemic and the movement to a virtual fellowship application process, fellowship program websites that are comprehensive and accessible may help programs attract compatible candidates, improve transparency, and guide applicants through the application process.
- There is variation in the content of current micrographic surgery and dermatologic oncology fellowship program websites and areas upon which programs may seek to augment their website content to better reflect program strengths while attracting competitive candidates best suited for their program.