User login
Doc says fatal bleeding with extended DAPT is rare

Photo by Sage Ross
LONDON—Fatal bleeding is rare with extended dual antiplatelet therapy (DAPT), according to research presented at the ESC Congress 2015.
The study included patients with a coronary stent who were receiving 30 months or 12 months of DAPT to prevent stent thrombosis and major cardiovascular and cerebrovascular events.
The results showed that bleeding-related mortality accounted for a minority of deaths in both patient groups.
Laura Mauri, MD, of Harvard Medical School in Boston, Massachusetts, presented these results as abstract 3916. The study, known as the DAPT trial, was funded by a consortium of 8 device and drug manufacturers and other entities.
The trial enrolled patients who were set to receive a drug-eluting or bare-metal stent. After stent placement, they received DAPT—aspirin plus thienopyridine (clopidogrel or prasugrel)—for at least 12 months.
After 12 months of therapy, patients who were treatment-compliant and event-free (no myocardial infarction, stroke, or moderate or severe bleeding) were randomized to continued thienopyridine or placebo, each in addition to aspirin, for an additional 18 months. At month 30, patients discontinued randomized treatment but remained on aspirin for 3 months.
Results from patients with drug-eluting stents were published in NEJM in 2014.
But Dr Mauri reported on causes of death in all 11,648 randomized patients. All deaths were reviewed and adjudicated by an independent committee of cardiologists and oncologists who were blinded to the randomized treatment groups.
Any death that was possibly, probably, or definitely related to any prior clinically evident bleeding event was adjudicated as “bleeding-related,” and any death that was possibly, probably, or definitely related to a malignancy or to complications from treatments specifically administered for the malignancy was adjudicated as “cancer-related.” Fatal bleeding was defined using the Bleeding Academic Research Consortium (BARC) definition.
All-cause mortality
At 30 months (end of the randomization period), the mortality rate was 1.9% in the 30-month treatment group and 1.5% in 12-month group (P=0.07).
There was no significant difference between the groups for cardiovascular mortality—both about 1% (P=0.97)—but there was a significant difference for non-cardiovascular mortality—0.9% and 0.5%, respectively (P=0.01).
At 33 months (combined randomization and aspirin monotherapy periods), the mortality rate was 2.2% in the 30-month treatment group and 1.8% in the 12-month treatment group (P=0.05).
The rates of cardiovascular mortality were 1.2% and 1.1%, respectively (P=0.51). And the rates of non-cardiovascular mortality were 1.0% and 0.7%, respectively (P=0.02).
Bleeding-related deaths
At 33 months, there was no significant difference in bleeding-related mortality. Fatal bleeding occurred in 0.3% of patients in the 30-month group and 0.2% of those in the 12-month group (P=0.36).
There was no significant difference between the groups for bleeding-related death without cancer or trauma (P>0.99), bleeding-related death with cancer (P=0.25), bleeding-related death with trauma (P=0.58), trauma-related death (P=0.30), or trauma-related death without bleeding (P=0.50).
“This analysis of the DAPT study provides valuable insight to suggest that fatal bleeding is rare with extended dual antiplatelet therapy and may be avoided with careful patient selection,” Dr Mauri said.
Cancer-related deaths
Dr Mauri noted that there was no significant difference in the incidence of cancer between the randomized groups (P=0.12). But there was a significant difference in the incidence of cancer-related mortality at 33 months. It was 0.6% in the 30-month group and 0.3% in the 12-month group (P=0.02).
However, when the investigators excluded the cancer-related deaths that occurred in patients whose cancer was diagnosed before they enrolled in the DAPT study, the difference in cancer-related death became non-significant (0.4% and 0.3%, respectively, P=0.16).
“Given the clear benefits of dual antiplatelet therapy in reducing myocardial infarction, these medications remain essential for patients with acute coronary syndromes or coronary stents,” Dr Mauri said. “The relationship with cancer requires further investigation.” ![]()

Photo by Sage Ross
LONDON—Fatal bleeding is rare with extended dual antiplatelet therapy (DAPT), according to research presented at the ESC Congress 2015.
The study included patients with a coronary stent who were receiving 30 months or 12 months of DAPT to prevent stent thrombosis and major cardiovascular and cerebrovascular events.
The results showed that bleeding-related mortality accounted for a minority of deaths in both patient groups.
Laura Mauri, MD, of Harvard Medical School in Boston, Massachusetts, presented these results as abstract 3916. The study, known as the DAPT trial, was funded by a consortium of 8 device and drug manufacturers and other entities.
The trial enrolled patients who were set to receive a drug-eluting or bare-metal stent. After stent placement, they received DAPT—aspirin plus thienopyridine (clopidogrel or prasugrel)—for at least 12 months.
After 12 months of therapy, patients who were treatment-compliant and event-free (no myocardial infarction, stroke, or moderate or severe bleeding) were randomized to continued thienopyridine or placebo, each in addition to aspirin, for an additional 18 months. At month 30, patients discontinued randomized treatment but remained on aspirin for 3 months.
Results from patients with drug-eluting stents were published in NEJM in 2014.
But Dr Mauri reported on causes of death in all 11,648 randomized patients. All deaths were reviewed and adjudicated by an independent committee of cardiologists and oncologists who were blinded to the randomized treatment groups.
Any death that was possibly, probably, or definitely related to any prior clinically evident bleeding event was adjudicated as “bleeding-related,” and any death that was possibly, probably, or definitely related to a malignancy or to complications from treatments specifically administered for the malignancy was adjudicated as “cancer-related.” Fatal bleeding was defined using the Bleeding Academic Research Consortium (BARC) definition.
All-cause mortality
At 30 months (end of the randomization period), the mortality rate was 1.9% in the 30-month treatment group and 1.5% in 12-month group (P=0.07).
There was no significant difference between the groups for cardiovascular mortality—both about 1% (P=0.97)—but there was a significant difference for non-cardiovascular mortality—0.9% and 0.5%, respectively (P=0.01).
At 33 months (combined randomization and aspirin monotherapy periods), the mortality rate was 2.2% in the 30-month treatment group and 1.8% in the 12-month treatment group (P=0.05).
The rates of cardiovascular mortality were 1.2% and 1.1%, respectively (P=0.51). And the rates of non-cardiovascular mortality were 1.0% and 0.7%, respectively (P=0.02).
Bleeding-related deaths
At 33 months, there was no significant difference in bleeding-related mortality. Fatal bleeding occurred in 0.3% of patients in the 30-month group and 0.2% of those in the 12-month group (P=0.36).
There was no significant difference between the groups for bleeding-related death without cancer or trauma (P>0.99), bleeding-related death with cancer (P=0.25), bleeding-related death with trauma (P=0.58), trauma-related death (P=0.30), or trauma-related death without bleeding (P=0.50).
“This analysis of the DAPT study provides valuable insight to suggest that fatal bleeding is rare with extended dual antiplatelet therapy and may be avoided with careful patient selection,” Dr Mauri said.
Cancer-related deaths
Dr Mauri noted that there was no significant difference in the incidence of cancer between the randomized groups (P=0.12). But there was a significant difference in the incidence of cancer-related mortality at 33 months. It was 0.6% in the 30-month group and 0.3% in the 12-month group (P=0.02).
However, when the investigators excluded the cancer-related deaths that occurred in patients whose cancer was diagnosed before they enrolled in the DAPT study, the difference in cancer-related death became non-significant (0.4% and 0.3%, respectively, P=0.16).
“Given the clear benefits of dual antiplatelet therapy in reducing myocardial infarction, these medications remain essential for patients with acute coronary syndromes or coronary stents,” Dr Mauri said. “The relationship with cancer requires further investigation.” ![]()

Photo by Sage Ross
LONDON—Fatal bleeding is rare with extended dual antiplatelet therapy (DAPT), according to research presented at the ESC Congress 2015.
The study included patients with a coronary stent who were receiving 30 months or 12 months of DAPT to prevent stent thrombosis and major cardiovascular and cerebrovascular events.
The results showed that bleeding-related mortality accounted for a minority of deaths in both patient groups.
Laura Mauri, MD, of Harvard Medical School in Boston, Massachusetts, presented these results as abstract 3916. The study, known as the DAPT trial, was funded by a consortium of 8 device and drug manufacturers and other entities.
The trial enrolled patients who were set to receive a drug-eluting or bare-metal stent. After stent placement, they received DAPT—aspirin plus thienopyridine (clopidogrel or prasugrel)—for at least 12 months.
After 12 months of therapy, patients who were treatment-compliant and event-free (no myocardial infarction, stroke, or moderate or severe bleeding) were randomized to continued thienopyridine or placebo, each in addition to aspirin, for an additional 18 months. At month 30, patients discontinued randomized treatment but remained on aspirin for 3 months.
Results from patients with drug-eluting stents were published in NEJM in 2014.
But Dr Mauri reported on causes of death in all 11,648 randomized patients. All deaths were reviewed and adjudicated by an independent committee of cardiologists and oncologists who were blinded to the randomized treatment groups.
Any death that was possibly, probably, or definitely related to any prior clinically evident bleeding event was adjudicated as “bleeding-related,” and any death that was possibly, probably, or definitely related to a malignancy or to complications from treatments specifically administered for the malignancy was adjudicated as “cancer-related.” Fatal bleeding was defined using the Bleeding Academic Research Consortium (BARC) definition.
All-cause mortality
At 30 months (end of the randomization period), the mortality rate was 1.9% in the 30-month treatment group and 1.5% in 12-month group (P=0.07).
There was no significant difference between the groups for cardiovascular mortality—both about 1% (P=0.97)—but there was a significant difference for non-cardiovascular mortality—0.9% and 0.5%, respectively (P=0.01).
At 33 months (combined randomization and aspirin monotherapy periods), the mortality rate was 2.2% in the 30-month treatment group and 1.8% in the 12-month treatment group (P=0.05).
The rates of cardiovascular mortality were 1.2% and 1.1%, respectively (P=0.51). And the rates of non-cardiovascular mortality were 1.0% and 0.7%, respectively (P=0.02).
Bleeding-related deaths
At 33 months, there was no significant difference in bleeding-related mortality. Fatal bleeding occurred in 0.3% of patients in the 30-month group and 0.2% of those in the 12-month group (P=0.36).
There was no significant difference between the groups for bleeding-related death without cancer or trauma (P>0.99), bleeding-related death with cancer (P=0.25), bleeding-related death with trauma (P=0.58), trauma-related death (P=0.30), or trauma-related death without bleeding (P=0.50).
“This analysis of the DAPT study provides valuable insight to suggest that fatal bleeding is rare with extended dual antiplatelet therapy and may be avoided with careful patient selection,” Dr Mauri said.
Cancer-related deaths
Dr Mauri noted that there was no significant difference in the incidence of cancer between the randomized groups (P=0.12). But there was a significant difference in the incidence of cancer-related mortality at 33 months. It was 0.6% in the 30-month group and 0.3% in the 12-month group (P=0.02).
However, when the investigators excluded the cancer-related deaths that occurred in patients whose cancer was diagnosed before they enrolled in the DAPT study, the difference in cancer-related death became non-significant (0.4% and 0.3%, respectively, P=0.16).
“Given the clear benefits of dual antiplatelet therapy in reducing myocardial infarction, these medications remain essential for patients with acute coronary syndromes or coronary stents,” Dr Mauri said. “The relationship with cancer requires further investigation.” ![]()
Score ‘modestly accurate’ for predicting thromboembolism

Image by Kevin MacKEnzie
LONDON—A score used to predict the risk of thromboembolic events, ischemic stroke, and death is only modestly accurate in patients with heart failure (HF), according to researchers.
They found the accuracy of the CHA2DS2-VASc score was dependent upon the endpoint being assessed and the duration of follow-up.
The score proved least effective for predicting thromboembolism, and its negative predictive values (NPVs) were inferior at 5 years of follow-up compared to 1 year.
Gregory Y. H Lip, MD, of Aalborg University in Denmark, and his colleagues reported these findings in JAMA and at the ESC Congress 2015 (abstract 1830*).
The team noted that the CHA2DS2-VASc score (congestive heart failure, hypertension, age 75 years or older [doubled], diabetes, stroke/transient ischemic attack/thromboembolism [doubled], vascular disease [prior heart attack, peripheral artery disease, or aortic plaque], age 65-75 years, sex category [female]) is already used clinically for stroke risk stratification in patients with atrial fibrillation (AF).
But its usefulness in a population of patients with HF has been unclear. So the researchers investigated whether CHA2DS2-VASc predicts ischemic stroke, thromboembolism, and death in patients with a new diagnosis of HF, with or without AF.
Using Danish registries, the researchers compiled data from 42,987 patients (22% with concomitant AF). The patients were not receiving anticoagulation and had been diagnosed with new-onset HF from 2000 to 2012.
The end of follow-up was December 31, 2012. Levels of the CHA2DS2-VASc score (based on 10 possible points, with higher scores indicating higher risk) were stratified by the presence of AF at study entry.
Among patients without AF, the incidence of thromboembolism was 3.5%, the rate of ischemic stroke was 1%, and the death rate was 7.2%. Among patients with AF, the rates were 4.2%, 2%, and 13.2%, respectively.
Predictive accuracy
For predicting thromboembolism in patients without AF, the C statistics were 0.63 at 1 year and 0.67 at 5 years. The NPVs were 88% and 73%, respectively.
For predicting thromboembolism in patients with AF, the C statistics were 0.62 at 1 year and 0.69 at 5 years. The NPVs were 88% and 61%, respectively.
For predicting ischemic stroke in patients without AF, the C statistics were 0.67 at 1 year and 0.69 at 5 years. The NPVs were 92% and 78%, respectively.
For predicting ischemic stroke in patients with AF, the C statistics were 0.64 at 1 year and 0.71 at 5 years. The NPVs were 91% and 69%, respectively.
For predicting death in patients without AF, the C statistics were 0.64 at 1 year and 0.68 at 5 years. The NPVs were 93% and 81%, respectively.
For predicting death in patients with AF, the C statistics were 0.63 at 1 year and 0.70 at 5 years. The NPVs were 94% and 76%, respectively.
Based on these results, the researchers said the clinical usefulness of the CHA2DS2-VASc score for patients with HF remains to be determined. And preventative strategies to reduce thromboembolism and ischemic stroke among these patients require further investigation. ![]()
*Information in the abstract differs from that presented.

Image by Kevin MacKEnzie
LONDON—A score used to predict the risk of thromboembolic events, ischemic stroke, and death is only modestly accurate in patients with heart failure (HF), according to researchers.
They found the accuracy of the CHA2DS2-VASc score was dependent upon the endpoint being assessed and the duration of follow-up.
The score proved least effective for predicting thromboembolism, and its negative predictive values (NPVs) were inferior at 5 years of follow-up compared to 1 year.
Gregory Y. H Lip, MD, of Aalborg University in Denmark, and his colleagues reported these findings in JAMA and at the ESC Congress 2015 (abstract 1830*).
The team noted that the CHA2DS2-VASc score (congestive heart failure, hypertension, age 75 years or older [doubled], diabetes, stroke/transient ischemic attack/thromboembolism [doubled], vascular disease [prior heart attack, peripheral artery disease, or aortic plaque], age 65-75 years, sex category [female]) is already used clinically for stroke risk stratification in patients with atrial fibrillation (AF).
But its usefulness in a population of patients with HF has been unclear. So the researchers investigated whether CHA2DS2-VASc predicts ischemic stroke, thromboembolism, and death in patients with a new diagnosis of HF, with or without AF.
Using Danish registries, the researchers compiled data from 42,987 patients (22% with concomitant AF). The patients were not receiving anticoagulation and had been diagnosed with new-onset HF from 2000 to 2012.
The end of follow-up was December 31, 2012. Levels of the CHA2DS2-VASc score (based on 10 possible points, with higher scores indicating higher risk) were stratified by the presence of AF at study entry.
Among patients without AF, the incidence of thromboembolism was 3.5%, the rate of ischemic stroke was 1%, and the death rate was 7.2%. Among patients with AF, the rates were 4.2%, 2%, and 13.2%, respectively.
Predictive accuracy
For predicting thromboembolism in patients without AF, the C statistics were 0.63 at 1 year and 0.67 at 5 years. The NPVs were 88% and 73%, respectively.
For predicting thromboembolism in patients with AF, the C statistics were 0.62 at 1 year and 0.69 at 5 years. The NPVs were 88% and 61%, respectively.
For predicting ischemic stroke in patients without AF, the C statistics were 0.67 at 1 year and 0.69 at 5 years. The NPVs were 92% and 78%, respectively.
For predicting ischemic stroke in patients with AF, the C statistics were 0.64 at 1 year and 0.71 at 5 years. The NPVs were 91% and 69%, respectively.
For predicting death in patients without AF, the C statistics were 0.64 at 1 year and 0.68 at 5 years. The NPVs were 93% and 81%, respectively.
For predicting death in patients with AF, the C statistics were 0.63 at 1 year and 0.70 at 5 years. The NPVs were 94% and 76%, respectively.
Based on these results, the researchers said the clinical usefulness of the CHA2DS2-VASc score for patients with HF remains to be determined. And preventative strategies to reduce thromboembolism and ischemic stroke among these patients require further investigation. ![]()
*Information in the abstract differs from that presented.

Image by Kevin MacKEnzie
LONDON—A score used to predict the risk of thromboembolic events, ischemic stroke, and death is only modestly accurate in patients with heart failure (HF), according to researchers.
They found the accuracy of the CHA2DS2-VASc score was dependent upon the endpoint being assessed and the duration of follow-up.
The score proved least effective for predicting thromboembolism, and its negative predictive values (NPVs) were inferior at 5 years of follow-up compared to 1 year.
Gregory Y. H Lip, MD, of Aalborg University in Denmark, and his colleagues reported these findings in JAMA and at the ESC Congress 2015 (abstract 1830*).
The team noted that the CHA2DS2-VASc score (congestive heart failure, hypertension, age 75 years or older [doubled], diabetes, stroke/transient ischemic attack/thromboembolism [doubled], vascular disease [prior heart attack, peripheral artery disease, or aortic plaque], age 65-75 years, sex category [female]) is already used clinically for stroke risk stratification in patients with atrial fibrillation (AF).
But its usefulness in a population of patients with HF has been unclear. So the researchers investigated whether CHA2DS2-VASc predicts ischemic stroke, thromboembolism, and death in patients with a new diagnosis of HF, with or without AF.
Using Danish registries, the researchers compiled data from 42,987 patients (22% with concomitant AF). The patients were not receiving anticoagulation and had been diagnosed with new-onset HF from 2000 to 2012.
The end of follow-up was December 31, 2012. Levels of the CHA2DS2-VASc score (based on 10 possible points, with higher scores indicating higher risk) were stratified by the presence of AF at study entry.
Among patients without AF, the incidence of thromboembolism was 3.5%, the rate of ischemic stroke was 1%, and the death rate was 7.2%. Among patients with AF, the rates were 4.2%, 2%, and 13.2%, respectively.
Predictive accuracy
For predicting thromboembolism in patients without AF, the C statistics were 0.63 at 1 year and 0.67 at 5 years. The NPVs were 88% and 73%, respectively.
For predicting thromboembolism in patients with AF, the C statistics were 0.62 at 1 year and 0.69 at 5 years. The NPVs were 88% and 61%, respectively.
For predicting ischemic stroke in patients without AF, the C statistics were 0.67 at 1 year and 0.69 at 5 years. The NPVs were 92% and 78%, respectively.
For predicting ischemic stroke in patients with AF, the C statistics were 0.64 at 1 year and 0.71 at 5 years. The NPVs were 91% and 69%, respectively.
For predicting death in patients without AF, the C statistics were 0.64 at 1 year and 0.68 at 5 years. The NPVs were 93% and 81%, respectively.
For predicting death in patients with AF, the C statistics were 0.63 at 1 year and 0.70 at 5 years. The NPVs were 94% and 76%, respectively.
Based on these results, the researchers said the clinical usefulness of the CHA2DS2-VASc score for patients with HF remains to be determined. And preventative strategies to reduce thromboembolism and ischemic stroke among these patients require further investigation. ![]()
*Information in the abstract differs from that presented.
Research reveals potential target for stent thrombosis

Image by Volker Brinkmann
LONDON—Immune cells may represent an important therapeutic target for preventing stent thrombosis, according to investigators from the PRESTIGE study.
The team analyzed more than 250 thrombus specimens and observed leukocyte infiltration in the context of early and late stent thrombosis.
Neutrophils were the most common leukocyte detected, and eosinophils were present in thrombi from all stent types.
The investigators reported these findings in the European Heart Journal and at the ESC Congress 2015 (abstract 1996*).
“Our results suggest that immune-cell-mediated thrombotic processes may be a realistic target for novel therapies to prevent [stent thrombosis],” said study investigator Steffen Massberg, PhD, of Ludwig-Maximilians University in Munich, Germany.
“Inhibition of triggers, such as extracellular nucleic acids activating the contact phase, may not only result in efficient anticoagulation in the setting of [stent thrombosis] but might also yield less therapy-associated bleeding. Future studies should evaluate whether inhibition of immune-cell-driven thrombotic pathways are effective and safe in clinical practice.”
The PRESTIGE study included patients with stent thrombosis who underwent thrombus aspiration at 9 centers in Europe between 2010 and 2014. In all, the investigators analyzed 253 thrombus specimens from these patients.
Seventy-nine specimens (31.2%) were from patients presenting with early stent thrombosis, and 174 (68.8%) were from patients with late stent thrombosis. Seventy-nine (31.2%) were from bare metal stents, 166 (65.6%) were from drug-eluting stents, and 8 (3.2%) were from stents of unknown type.
The thrombus specimens had heterogeneous morphology, with platelet-rich thrombus and fibrin/fibrinogen fragments being most abundant.
The investigators said leukocyte infiltrations were hallmarks of both early and late stent thrombosis, with neutrophils representing the most prominent subset. Neutrophils were found in similar amounts in early and late stent thrombosis.
“It is important to note that leukocyte counts were significantly higher compared with a control group of patients with thrombus aspiration in spontaneous myocardial infarction,” Dr Massberg said.
He and his colleagues also observed neutrophil extracellular traps (NETs) in 23% of samples.
And they found that eosinophils were present in all stent types, but there were higher numbers in patients with late stent thrombosis in sirolimus-eluting and everolimus-eluting stents.
“The presence of NETs supports their pathophysiological relevance in [stent thrombosis], while eosinophil recruitment suggests an allergic component to the process of [stent thrombosis],” Dr Massberg said. ![]()
*Information in the abstract differs from that presented.

Image by Volker Brinkmann
LONDON—Immune cells may represent an important therapeutic target for preventing stent thrombosis, according to investigators from the PRESTIGE study.
The team analyzed more than 250 thrombus specimens and observed leukocyte infiltration in the context of early and late stent thrombosis.
Neutrophils were the most common leukocyte detected, and eosinophils were present in thrombi from all stent types.
The investigators reported these findings in the European Heart Journal and at the ESC Congress 2015 (abstract 1996*).
“Our results suggest that immune-cell-mediated thrombotic processes may be a realistic target for novel therapies to prevent [stent thrombosis],” said study investigator Steffen Massberg, PhD, of Ludwig-Maximilians University in Munich, Germany.
“Inhibition of triggers, such as extracellular nucleic acids activating the contact phase, may not only result in efficient anticoagulation in the setting of [stent thrombosis] but might also yield less therapy-associated bleeding. Future studies should evaluate whether inhibition of immune-cell-driven thrombotic pathways are effective and safe in clinical practice.”
The PRESTIGE study included patients with stent thrombosis who underwent thrombus aspiration at 9 centers in Europe between 2010 and 2014. In all, the investigators analyzed 253 thrombus specimens from these patients.
Seventy-nine specimens (31.2%) were from patients presenting with early stent thrombosis, and 174 (68.8%) were from patients with late stent thrombosis. Seventy-nine (31.2%) were from bare metal stents, 166 (65.6%) were from drug-eluting stents, and 8 (3.2%) were from stents of unknown type.
The thrombus specimens had heterogeneous morphology, with platelet-rich thrombus and fibrin/fibrinogen fragments being most abundant.
The investigators said leukocyte infiltrations were hallmarks of both early and late stent thrombosis, with neutrophils representing the most prominent subset. Neutrophils were found in similar amounts in early and late stent thrombosis.
“It is important to note that leukocyte counts were significantly higher compared with a control group of patients with thrombus aspiration in spontaneous myocardial infarction,” Dr Massberg said.
He and his colleagues also observed neutrophil extracellular traps (NETs) in 23% of samples.
And they found that eosinophils were present in all stent types, but there were higher numbers in patients with late stent thrombosis in sirolimus-eluting and everolimus-eluting stents.
“The presence of NETs supports their pathophysiological relevance in [stent thrombosis], while eosinophil recruitment suggests an allergic component to the process of [stent thrombosis],” Dr Massberg said. ![]()
*Information in the abstract differs from that presented.

Image by Volker Brinkmann
LONDON—Immune cells may represent an important therapeutic target for preventing stent thrombosis, according to investigators from the PRESTIGE study.
The team analyzed more than 250 thrombus specimens and observed leukocyte infiltration in the context of early and late stent thrombosis.
Neutrophils were the most common leukocyte detected, and eosinophils were present in thrombi from all stent types.
The investigators reported these findings in the European Heart Journal and at the ESC Congress 2015 (abstract 1996*).
“Our results suggest that immune-cell-mediated thrombotic processes may be a realistic target for novel therapies to prevent [stent thrombosis],” said study investigator Steffen Massberg, PhD, of Ludwig-Maximilians University in Munich, Germany.
“Inhibition of triggers, such as extracellular nucleic acids activating the contact phase, may not only result in efficient anticoagulation in the setting of [stent thrombosis] but might also yield less therapy-associated bleeding. Future studies should evaluate whether inhibition of immune-cell-driven thrombotic pathways are effective and safe in clinical practice.”
The PRESTIGE study included patients with stent thrombosis who underwent thrombus aspiration at 9 centers in Europe between 2010 and 2014. In all, the investigators analyzed 253 thrombus specimens from these patients.
Seventy-nine specimens (31.2%) were from patients presenting with early stent thrombosis, and 174 (68.8%) were from patients with late stent thrombosis. Seventy-nine (31.2%) were from bare metal stents, 166 (65.6%) were from drug-eluting stents, and 8 (3.2%) were from stents of unknown type.
The thrombus specimens had heterogeneous morphology, with platelet-rich thrombus and fibrin/fibrinogen fragments being most abundant.
The investigators said leukocyte infiltrations were hallmarks of both early and late stent thrombosis, with neutrophils representing the most prominent subset. Neutrophils were found in similar amounts in early and late stent thrombosis.
“It is important to note that leukocyte counts were significantly higher compared with a control group of patients with thrombus aspiration in spontaneous myocardial infarction,” Dr Massberg said.
He and his colleagues also observed neutrophil extracellular traps (NETs) in 23% of samples.
And they found that eosinophils were present in all stent types, but there were higher numbers in patients with late stent thrombosis in sirolimus-eluting and everolimus-eluting stents.
“The presence of NETs supports their pathophysiological relevance in [stent thrombosis], while eosinophil recruitment suggests an allergic component to the process of [stent thrombosis],” Dr Massberg said. ![]()
*Information in the abstract differs from that presented.
H. pylori resistance highlights need for guided therapy
Only half of Helicobacter pylori strains were pansusceptible, and almost one in three was resistant to at least one antibiotic, according to a single-center study of U.S. veterans published in Clinical Gastroenterology and Hepatology.
The analysis is the first published report of H. pylori resistance in more than a decade, said Dr. Seiji Shiota at the Michael E. DeBakey Veterans Affairs Medical Center and the Baylor College of Medicine, Houston, and his associates. “Clarithromycin, metronidazole, and levofloxacin resistances were all high among untreated patients, suggesting that they all should be avoided as components of empiric triple therapy [consisting of a] proton pump inhibitor, amoxicillin, plus a third antibiotic,” said the researchers. “The four-drug concomitant therapy and bismuth quadruple therapy, or antibiotic susceptibility–guided therapy, are likely be the best strategies locally and are recommended for previously untreated patients with H. pylori infection.”
The study assessed 656 gastric biopsies randomly selected from a cohort of 1,559 patients who underwent esophagogastroduodenoscopy at the Houston VA Medical Center between 2009 and 2013. About 90% of patients were male, and patients ranged in age from 40 to 79 years old, with an average age of 60 years. The researchers cultured tissue samples and used the E test to assess minimum inhibitory concentrations for amoxicillin, clarithromycin, metronidazole, levofloxacin, and tetracycline. (Clin Gastroenterol Hepatol. 2015 Feb 11. pii: S1542-3565(15)00122-6).
A total of 135 (20.6%) of the biopsies cultured H. pylori, of which half (65 strains) were susceptible to all five antibiotics tested, 31% were resistant to levofloxacin (95% confidence interval, 23%-39%), 20% were resistant to metronidazole (95% CI, 13%-27%), 16% were resistant to clarithromycin (95% CI, 10%-23%), 0.8% were resistant to tetracycline (95% CI, 0%-2%), and none were resistant to amoxicillin, said the researchers. The extent of levofloxacin resistance was a “new and concerning finding” that was linked in the multivariable analysis with past fluoroquinolone treatment, reflecting the rising use of fluoroquinolones in community practice, they said. “Levofloxacin has been recommended as a rescue drug to eradicate H. pylori in patients who fail first-line therapy,” they added. “Locally, it would seem to be a poor choice on the basis of the high resistance rate (31.9%), which is higher than the 10% limit suggested as a cutoff for use of fluoroquinolone-containing triple therapy for H. pylori.”
Clarithromycin resistance also rose during the study period, probably because of the rising use of macrolides in respiratory and otorhinolaryngology, the investigators noted. Patients who had been treated before for helicobacteriosis were significantly more likely to have clarithromycin-resistant H. pylori infections even after accounting for demographic factors, smoking status, gastroesophageal reflux disease, and past use of macrolides and fluoroquinolones, they said. Based on that result, patients with a history of prior helicobacteriosis should not receive clarithromycin as part of triple therapy, they emphasized.
Resistance to metronidazole also remained high, but only 1.8% of isolates were resistant to both metronidazole and clarithromycin, making combination therapy with a proton pump inhibitor, clarithromycin, metronidazole, and amoxicillin “an excellent choice as an empiric therapy,” added Dr. Shiota and his associates. Furthermore, the study might have overestimated the rate of metronidazole resistance because the E test yielded significantly higher minimum inhibitory concentration values than did agar dilution, they noted. The study cohort also was demographically dissimilar to that of the United States and might have reflected selection bias, because patients with a history of helicobacteriosis would be more likely to be referred for endoscopy, they said.
The National Institutes of Health and the Veterans Affairs Health Services Research & Development Center for Innovations in Quality, Effectiveness, and Safety supported the study. The researchers reported having no conflicts of interest.
Antimicrobial-resistant strains of H. pylori are increasing in prevalence in the United States. In the study described here, only half of H. pylori strains were susceptible to commonly used antibiotics and approximately one in three were resistant to at least one antibiotic, according to a single-center study of U.S. veterans. The study assessed 656 gastric biopsies randomly selected from a cohort of 1,559 patients who underwent esophagogastroduodenoscopy at the Houston VA Medical Center between 2009 and 2013. Patients were mostly male and had an average age of 60 years. The researchers cultured tissue samples and used the E test to assess minimum inhibitory concentrations for amoxicillin, clarithromycin, metronidazole, levofloxacin, and tetracycline.

|
Dr. Nimish Vakil |
A total of 135 (20.6%) of the biopsies cultured H. pylori, of which half (65 strains) were susceptible to all five antibiotics tested, 31% were resistant to levofloxacin (95% confidence interval, 23%-39%), 20% were resistant to metronidazole (95% CI, 13%-27%), 16% were resistant to clarithromycin (95% CI, 10%-23%), 0.8% were resistant to tetracycline (95% CI, 0%-2%), and none were resistant to amoxicillin, said the researchers.
The study mirrors findings in Europe where similar rates of resistance have been reported. European studies have also shown that levofloxacin resistance rises rapidly when it becomes widely used in the community, The study described here is not population based and consists mostly of male subjects and therefore may not be generalizable to the rest to the rest of the United States. As culture and antimicrobial sensitivity testing is not available to most gastroenterologists, the initial treatment chosen should reflect resistance data in the community. Given the rising rates of resistance, it is important that eradication be confirmed 4 weeks or more after eradication therapy ends using a stool antigen test or a breath test. Clinicians should be prepared to re-treat patients if necessary.
Dr. Nimish Vakil, AGAF, is clinical professor of medicine at the University of Wisconsin School of Medicine and Public Health in Madison. He has no conflicts of interest.
Antimicrobial-resistant strains of H. pylori are increasing in prevalence in the United States. In the study described here, only half of H. pylori strains were susceptible to commonly used antibiotics and approximately one in three were resistant to at least one antibiotic, according to a single-center study of U.S. veterans. The study assessed 656 gastric biopsies randomly selected from a cohort of 1,559 patients who underwent esophagogastroduodenoscopy at the Houston VA Medical Center between 2009 and 2013. Patients were mostly male and had an average age of 60 years. The researchers cultured tissue samples and used the E test to assess minimum inhibitory concentrations for amoxicillin, clarithromycin, metronidazole, levofloxacin, and tetracycline.

|
Dr. Nimish Vakil |
A total of 135 (20.6%) of the biopsies cultured H. pylori, of which half (65 strains) were susceptible to all five antibiotics tested, 31% were resistant to levofloxacin (95% confidence interval, 23%-39%), 20% were resistant to metronidazole (95% CI, 13%-27%), 16% were resistant to clarithromycin (95% CI, 10%-23%), 0.8% were resistant to tetracycline (95% CI, 0%-2%), and none were resistant to amoxicillin, said the researchers.
The study mirrors findings in Europe where similar rates of resistance have been reported. European studies have also shown that levofloxacin resistance rises rapidly when it becomes widely used in the community, The study described here is not population based and consists mostly of male subjects and therefore may not be generalizable to the rest to the rest of the United States. As culture and antimicrobial sensitivity testing is not available to most gastroenterologists, the initial treatment chosen should reflect resistance data in the community. Given the rising rates of resistance, it is important that eradication be confirmed 4 weeks or more after eradication therapy ends using a stool antigen test or a breath test. Clinicians should be prepared to re-treat patients if necessary.
Dr. Nimish Vakil, AGAF, is clinical professor of medicine at the University of Wisconsin School of Medicine and Public Health in Madison. He has no conflicts of interest.
Antimicrobial-resistant strains of H. pylori are increasing in prevalence in the United States. In the study described here, only half of H. pylori strains were susceptible to commonly used antibiotics and approximately one in three were resistant to at least one antibiotic, according to a single-center study of U.S. veterans. The study assessed 656 gastric biopsies randomly selected from a cohort of 1,559 patients who underwent esophagogastroduodenoscopy at the Houston VA Medical Center between 2009 and 2013. Patients were mostly male and had an average age of 60 years. The researchers cultured tissue samples and used the E test to assess minimum inhibitory concentrations for amoxicillin, clarithromycin, metronidazole, levofloxacin, and tetracycline.

|
Dr. Nimish Vakil |
A total of 135 (20.6%) of the biopsies cultured H. pylori, of which half (65 strains) were susceptible to all five antibiotics tested, 31% were resistant to levofloxacin (95% confidence interval, 23%-39%), 20% were resistant to metronidazole (95% CI, 13%-27%), 16% were resistant to clarithromycin (95% CI, 10%-23%), 0.8% were resistant to tetracycline (95% CI, 0%-2%), and none were resistant to amoxicillin, said the researchers.
The study mirrors findings in Europe where similar rates of resistance have been reported. European studies have also shown that levofloxacin resistance rises rapidly when it becomes widely used in the community, The study described here is not population based and consists mostly of male subjects and therefore may not be generalizable to the rest to the rest of the United States. As culture and antimicrobial sensitivity testing is not available to most gastroenterologists, the initial treatment chosen should reflect resistance data in the community. Given the rising rates of resistance, it is important that eradication be confirmed 4 weeks or more after eradication therapy ends using a stool antigen test or a breath test. Clinicians should be prepared to re-treat patients if necessary.
Dr. Nimish Vakil, AGAF, is clinical professor of medicine at the University of Wisconsin School of Medicine and Public Health in Madison. He has no conflicts of interest.
Only half of Helicobacter pylori strains were pansusceptible, and almost one in three was resistant to at least one antibiotic, according to a single-center study of U.S. veterans published in Clinical Gastroenterology and Hepatology.
The analysis is the first published report of H. pylori resistance in more than a decade, said Dr. Seiji Shiota at the Michael E. DeBakey Veterans Affairs Medical Center and the Baylor College of Medicine, Houston, and his associates. “Clarithromycin, metronidazole, and levofloxacin resistances were all high among untreated patients, suggesting that they all should be avoided as components of empiric triple therapy [consisting of a] proton pump inhibitor, amoxicillin, plus a third antibiotic,” said the researchers. “The four-drug concomitant therapy and bismuth quadruple therapy, or antibiotic susceptibility–guided therapy, are likely be the best strategies locally and are recommended for previously untreated patients with H. pylori infection.”
The study assessed 656 gastric biopsies randomly selected from a cohort of 1,559 patients who underwent esophagogastroduodenoscopy at the Houston VA Medical Center between 2009 and 2013. About 90% of patients were male, and patients ranged in age from 40 to 79 years old, with an average age of 60 years. The researchers cultured tissue samples and used the E test to assess minimum inhibitory concentrations for amoxicillin, clarithromycin, metronidazole, levofloxacin, and tetracycline. (Clin Gastroenterol Hepatol. 2015 Feb 11. pii: S1542-3565(15)00122-6).
A total of 135 (20.6%) of the biopsies cultured H. pylori, of which half (65 strains) were susceptible to all five antibiotics tested, 31% were resistant to levofloxacin (95% confidence interval, 23%-39%), 20% were resistant to metronidazole (95% CI, 13%-27%), 16% were resistant to clarithromycin (95% CI, 10%-23%), 0.8% were resistant to tetracycline (95% CI, 0%-2%), and none were resistant to amoxicillin, said the researchers. The extent of levofloxacin resistance was a “new and concerning finding” that was linked in the multivariable analysis with past fluoroquinolone treatment, reflecting the rising use of fluoroquinolones in community practice, they said. “Levofloxacin has been recommended as a rescue drug to eradicate H. pylori in patients who fail first-line therapy,” they added. “Locally, it would seem to be a poor choice on the basis of the high resistance rate (31.9%), which is higher than the 10% limit suggested as a cutoff for use of fluoroquinolone-containing triple therapy for H. pylori.”
Clarithromycin resistance also rose during the study period, probably because of the rising use of macrolides in respiratory and otorhinolaryngology, the investigators noted. Patients who had been treated before for helicobacteriosis were significantly more likely to have clarithromycin-resistant H. pylori infections even after accounting for demographic factors, smoking status, gastroesophageal reflux disease, and past use of macrolides and fluoroquinolones, they said. Based on that result, patients with a history of prior helicobacteriosis should not receive clarithromycin as part of triple therapy, they emphasized.
Resistance to metronidazole also remained high, but only 1.8% of isolates were resistant to both metronidazole and clarithromycin, making combination therapy with a proton pump inhibitor, clarithromycin, metronidazole, and amoxicillin “an excellent choice as an empiric therapy,” added Dr. Shiota and his associates. Furthermore, the study might have overestimated the rate of metronidazole resistance because the E test yielded significantly higher minimum inhibitory concentration values than did agar dilution, they noted. The study cohort also was demographically dissimilar to that of the United States and might have reflected selection bias, because patients with a history of helicobacteriosis would be more likely to be referred for endoscopy, they said.
The National Institutes of Health and the Veterans Affairs Health Services Research & Development Center for Innovations in Quality, Effectiveness, and Safety supported the study. The researchers reported having no conflicts of interest.
Only half of Helicobacter pylori strains were pansusceptible, and almost one in three was resistant to at least one antibiotic, according to a single-center study of U.S. veterans published in Clinical Gastroenterology and Hepatology.
The analysis is the first published report of H. pylori resistance in more than a decade, said Dr. Seiji Shiota at the Michael E. DeBakey Veterans Affairs Medical Center and the Baylor College of Medicine, Houston, and his associates. “Clarithromycin, metronidazole, and levofloxacin resistances were all high among untreated patients, suggesting that they all should be avoided as components of empiric triple therapy [consisting of a] proton pump inhibitor, amoxicillin, plus a third antibiotic,” said the researchers. “The four-drug concomitant therapy and bismuth quadruple therapy, or antibiotic susceptibility–guided therapy, are likely be the best strategies locally and are recommended for previously untreated patients with H. pylori infection.”
The study assessed 656 gastric biopsies randomly selected from a cohort of 1,559 patients who underwent esophagogastroduodenoscopy at the Houston VA Medical Center between 2009 and 2013. About 90% of patients were male, and patients ranged in age from 40 to 79 years old, with an average age of 60 years. The researchers cultured tissue samples and used the E test to assess minimum inhibitory concentrations for amoxicillin, clarithromycin, metronidazole, levofloxacin, and tetracycline. (Clin Gastroenterol Hepatol. 2015 Feb 11. pii: S1542-3565(15)00122-6).
A total of 135 (20.6%) of the biopsies cultured H. pylori, of which half (65 strains) were susceptible to all five antibiotics tested, 31% were resistant to levofloxacin (95% confidence interval, 23%-39%), 20% were resistant to metronidazole (95% CI, 13%-27%), 16% were resistant to clarithromycin (95% CI, 10%-23%), 0.8% were resistant to tetracycline (95% CI, 0%-2%), and none were resistant to amoxicillin, said the researchers. The extent of levofloxacin resistance was a “new and concerning finding” that was linked in the multivariable analysis with past fluoroquinolone treatment, reflecting the rising use of fluoroquinolones in community practice, they said. “Levofloxacin has been recommended as a rescue drug to eradicate H. pylori in patients who fail first-line therapy,” they added. “Locally, it would seem to be a poor choice on the basis of the high resistance rate (31.9%), which is higher than the 10% limit suggested as a cutoff for use of fluoroquinolone-containing triple therapy for H. pylori.”
Clarithromycin resistance also rose during the study period, probably because of the rising use of macrolides in respiratory and otorhinolaryngology, the investigators noted. Patients who had been treated before for helicobacteriosis were significantly more likely to have clarithromycin-resistant H. pylori infections even after accounting for demographic factors, smoking status, gastroesophageal reflux disease, and past use of macrolides and fluoroquinolones, they said. Based on that result, patients with a history of prior helicobacteriosis should not receive clarithromycin as part of triple therapy, they emphasized.
Resistance to metronidazole also remained high, but only 1.8% of isolates were resistant to both metronidazole and clarithromycin, making combination therapy with a proton pump inhibitor, clarithromycin, metronidazole, and amoxicillin “an excellent choice as an empiric therapy,” added Dr. Shiota and his associates. Furthermore, the study might have overestimated the rate of metronidazole resistance because the E test yielded significantly higher minimum inhibitory concentration values than did agar dilution, they noted. The study cohort also was demographically dissimilar to that of the United States and might have reflected selection bias, because patients with a history of helicobacteriosis would be more likely to be referred for endoscopy, they said.
The National Institutes of Health and the Veterans Affairs Health Services Research & Development Center for Innovations in Quality, Effectiveness, and Safety supported the study. The researchers reported having no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Because H. pylori showed high rates of resistance to clarithromycin, metronidazole, and levofloxacin, they should be excluded from triple therapy regimens for helicobacteriosis.
Major finding: Half of strains were susceptible to all five antibiotics tested, 31% were resistant to levofloxacin, 20% were resistant to metronidazole, 16% were resistant to clarithromycin, 0.8% were resistant to tetracycline, and none were resistant to amoxicillin.
Data source: Analysis of gastric biopsies from 656 U.S. veterans who underwent esophagogastroduodenoscopy in Texas between 2009 and 2013.
Disclosures: The National Institutes of Health and the VA Health Services Research & Development Center for Innovations in Quality, Effectiveness, and Safety supported the study. The researchers reported having no conflicts of interest.
Assessing progression, impact of radiofrequency ablation in Barrett’s esophagus
Patients with Barrett’s esophagus have about a 0.2% annual chance of developing esophageal adenocarcinoma in the 5 years after initial diagnosis, but the likelihood then rises so that about 9% of all patients will develop cancer by 20 years out, according to a study in the September issue of Gastroenterology.
The modeled rates of progression for the early years after diagnosis are substantially lower than are those reported by prospective studies, which involve more intensive surveillance and therefore suffer from detection bias, said Dr. Sonja Kroep of Erasmus Medical Center, Rotterdam, the Netherlands, and her associates. “Clinicians informing their patients about their cancer risk can best use this clinical progression rate, which is not influenced by surveillance-detected cancers,” they wrote.
Past analyses have yielded varying results for the rate at which Barrett’s esophagus with low-grade dysplasia progresses to high-grade dysplasia and esophageal carcinoma. For their study, Dr. Kroep and her associates calibrated a model based on the annual rate of 0.18% reported by population-level studies, and used it to simulate prospective studies and to predict results from both population-based and prospective studies for various follow-up periods (Gastroenterology 2015 Apr 29. pii: S0016-5085(15)00601-0).
For the first 5 years of follow-up, the model predicted a 0.19% annual rate of transformation to esophageal adenocarcinoma for population-based studies and a 0.36% annual rate for prospective studies, the researchers reported. At 20 years, these rates rose to 0.63% and 0.65% annually, for a cumulative incidence rate of 9.1% to 9.5%. Between the 5-year and 20-year thresholds, the gap between rates of progression for the two types of studies narrowed from 91% to 5%. Taken together, the findings suggest that for the first 5 years after a diagnosis of Barrett’s esophagus, rates of progression to esophageal adenocarcinoma reflect those from population-level studies instead of surveillance-based prospective studies, the investigators said. “Clinicians should use this information to explain to patients their short-term and long-term risks if no action is taken, and then discuss the risks and benefits of surveillance,” they added.
In a separate retrospective study, radiofrequency ablation of low-grade esophageal dysplasia was linked to substantially lower rates of progression compared with watchful waiting in the form of endoscopic surveillance, said Dr. Aaron Small of the University of Pennsylvania, Philadelphia, and his associates. Their study included 125 patients with Barrett’s esophagus and low-grade dysplasia who underwent surveillance only, and 45 patients who underwent radiofrequency ablation at three university medical centers.
Over median follow-up periods of more than 2 years, the risk of progression with radiofrequency ablation was significantly lower than with endoscopic surveillance only, even after the researchers controlled for year of diagnosis (adjusted hazard ratio, 0.06; 95% confidence interval, 0.008-0.48; P = .008). The ablation group also had fewer visible macroscopic lesions, although the difference was not significant. “We estimate that for every three patients treated with radiofrequency ablation, one additional patient with low-grade dysplasia will avoid progression to high-grade dysplasia or esophageal adenocarcinoma within 3 years,” the researchers wrote. “Although selection bias cannot be excluded, these findings provide additional evidence for the use of endoscopic ablation therapy for low-grade dysplasia” (Gastroenterology 2015 Apr 24. pii: S0016-5085(15)00569-7).
The study by Dr. Kroep and her associates was funded by grant U01 CA152926, and the investigators reported having no conflicts of interest. The study by Dr. Small and his associates was supported by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases and by institutional funds. Dr. Small reported no conflicts of interest, but seven coauthors reported ties with a number of pharmaceutical companies.
These two studies highlight two different hot topics in the management of patients with a Barrett’s esophagus. The first is the low rate of neoplastic progression in patients undergoing surveillance for nondysplastic BE. The second relates to the management of patients with low-grade dysplasia (LG

|
| Dr. Jacques Bergman |
Population-based BE surveillance studies have shown lower progression rates than have prospective surveillance studies. The biggest difference between these two is that not all patients in population-based studies actually undergo subsequent surveillance endoscopies and/or surveillance is carried out less rigorously than in prospective surveillance studies. Patients who have undergone a baseline endoscopy showing no neoplasia first need to develop early neoplasia (which is generally asymptomatic) that then needs to progress to a symptomatic stage before they are diagnosed. During this interval they may die from other causes or may be lost to follow-up. Patients in strict surveillance programs will be diagnosed at an earlier stage and at a higher rate. This is especially true in the first years of follow-up, when the initial screening endoscopy has its largest effect. Over time, the difference then fades away as suggested by the 9% progression rate of both types of studies at 20 years of follow-up. Both perspectives are relevant for patients. For elderly patients with significant comorbidity, the 5-year data from population-based studies reassure them not to undergo surveillance endoscopies because even when an early cancer develops it is unlikely to bear any clinical relevance, whereas for patients with a long life expectancy, the 9% cancer risk at 20 years and the dismal prognosis of a symptomatic Barrett’s cancer may be strong arguments for participating in a surveillance program.
For patients with LGD, the situation is different: The rate of progression is much higher than that reported for nondysplastic BE, and with radiofrequency ablation (RFA), an effective and safe tool is at hand to significantly reduce this rate of neoplastic progression. Small et al. reported that only three patients need to be treated with RFA to prevent one patient from progressing to high-grade dysplasia or cancer. These data are in agreement with data from a prospective randomized study on the use of RFA for patients with a confirmed diagnosis of LGD. Most societies therefore consider a confirmed histologic diagnosis of LGD a justified indication for prophylactic ablation with RFA.
However, this does not imply that all patients with LGD should be ablated. First, only patients in whom the histologic diagnosis of LGD is confirmed by an expert BE pathologist should be considered for RFA. In approximately 75% of patients, the LGD diagnosis will be downstaged to nondysplastic BE upon expert review. Second, the lessons learned from the Kroep study also apply here: For an elderly LGD patient with or without significant comorbidity, the decision to proceed to RFA is different from the decision for patients with a longer life expectancy, especially if an intermediate solution – to continue endoscopic surveillance and proceed to endoscopic management in case neoplasia is diagnosed – is also considered.
Jacques Bergman, M.D., Ph.D., is professor of gastrointestinal endoscopy, director of endoscopy, at the Academic Medical Center, Amsterdam. He received research support for clinical studies and consulted for Covidien/Medtronic GI solutions.
These two studies highlight two different hot topics in the management of patients with a Barrett’s esophagus. The first is the low rate of neoplastic progression in patients undergoing surveillance for nondysplastic BE. The second relates to the management of patients with low-grade dysplasia (LG

|
| Dr. Jacques Bergman |
Population-based BE surveillance studies have shown lower progression rates than have prospective surveillance studies. The biggest difference between these two is that not all patients in population-based studies actually undergo subsequent surveillance endoscopies and/or surveillance is carried out less rigorously than in prospective surveillance studies. Patients who have undergone a baseline endoscopy showing no neoplasia first need to develop early neoplasia (which is generally asymptomatic) that then needs to progress to a symptomatic stage before they are diagnosed. During this interval they may die from other causes or may be lost to follow-up. Patients in strict surveillance programs will be diagnosed at an earlier stage and at a higher rate. This is especially true in the first years of follow-up, when the initial screening endoscopy has its largest effect. Over time, the difference then fades away as suggested by the 9% progression rate of both types of studies at 20 years of follow-up. Both perspectives are relevant for patients. For elderly patients with significant comorbidity, the 5-year data from population-based studies reassure them not to undergo surveillance endoscopies because even when an early cancer develops it is unlikely to bear any clinical relevance, whereas for patients with a long life expectancy, the 9% cancer risk at 20 years and the dismal prognosis of a symptomatic Barrett’s cancer may be strong arguments for participating in a surveillance program.
For patients with LGD, the situation is different: The rate of progression is much higher than that reported for nondysplastic BE, and with radiofrequency ablation (RFA), an effective and safe tool is at hand to significantly reduce this rate of neoplastic progression. Small et al. reported that only three patients need to be treated with RFA to prevent one patient from progressing to high-grade dysplasia or cancer. These data are in agreement with data from a prospective randomized study on the use of RFA for patients with a confirmed diagnosis of LGD. Most societies therefore consider a confirmed histologic diagnosis of LGD a justified indication for prophylactic ablation with RFA.
However, this does not imply that all patients with LGD should be ablated. First, only patients in whom the histologic diagnosis of LGD is confirmed by an expert BE pathologist should be considered for RFA. In approximately 75% of patients, the LGD diagnosis will be downstaged to nondysplastic BE upon expert review. Second, the lessons learned from the Kroep study also apply here: For an elderly LGD patient with or without significant comorbidity, the decision to proceed to RFA is different from the decision for patients with a longer life expectancy, especially if an intermediate solution – to continue endoscopic surveillance and proceed to endoscopic management in case neoplasia is diagnosed – is also considered.
Jacques Bergman, M.D., Ph.D., is professor of gastrointestinal endoscopy, director of endoscopy, at the Academic Medical Center, Amsterdam. He received research support for clinical studies and consulted for Covidien/Medtronic GI solutions.
These two studies highlight two different hot topics in the management of patients with a Barrett’s esophagus. The first is the low rate of neoplastic progression in patients undergoing surveillance for nondysplastic BE. The second relates to the management of patients with low-grade dysplasia (LG

|
| Dr. Jacques Bergman |
Population-based BE surveillance studies have shown lower progression rates than have prospective surveillance studies. The biggest difference between these two is that not all patients in population-based studies actually undergo subsequent surveillance endoscopies and/or surveillance is carried out less rigorously than in prospective surveillance studies. Patients who have undergone a baseline endoscopy showing no neoplasia first need to develop early neoplasia (which is generally asymptomatic) that then needs to progress to a symptomatic stage before they are diagnosed. During this interval they may die from other causes or may be lost to follow-up. Patients in strict surveillance programs will be diagnosed at an earlier stage and at a higher rate. This is especially true in the first years of follow-up, when the initial screening endoscopy has its largest effect. Over time, the difference then fades away as suggested by the 9% progression rate of both types of studies at 20 years of follow-up. Both perspectives are relevant for patients. For elderly patients with significant comorbidity, the 5-year data from population-based studies reassure them not to undergo surveillance endoscopies because even when an early cancer develops it is unlikely to bear any clinical relevance, whereas for patients with a long life expectancy, the 9% cancer risk at 20 years and the dismal prognosis of a symptomatic Barrett’s cancer may be strong arguments for participating in a surveillance program.
For patients with LGD, the situation is different: The rate of progression is much higher than that reported for nondysplastic BE, and with radiofrequency ablation (RFA), an effective and safe tool is at hand to significantly reduce this rate of neoplastic progression. Small et al. reported that only three patients need to be treated with RFA to prevent one patient from progressing to high-grade dysplasia or cancer. These data are in agreement with data from a prospective randomized study on the use of RFA for patients with a confirmed diagnosis of LGD. Most societies therefore consider a confirmed histologic diagnosis of LGD a justified indication for prophylactic ablation with RFA.
However, this does not imply that all patients with LGD should be ablated. First, only patients in whom the histologic diagnosis of LGD is confirmed by an expert BE pathologist should be considered for RFA. In approximately 75% of patients, the LGD diagnosis will be downstaged to nondysplastic BE upon expert review. Second, the lessons learned from the Kroep study also apply here: For an elderly LGD patient with or without significant comorbidity, the decision to proceed to RFA is different from the decision for patients with a longer life expectancy, especially if an intermediate solution – to continue endoscopic surveillance and proceed to endoscopic management in case neoplasia is diagnosed – is also considered.
Jacques Bergman, M.D., Ph.D., is professor of gastrointestinal endoscopy, director of endoscopy, at the Academic Medical Center, Amsterdam. He received research support for clinical studies and consulted for Covidien/Medtronic GI solutions.
Patients with Barrett’s esophagus have about a 0.2% annual chance of developing esophageal adenocarcinoma in the 5 years after initial diagnosis, but the likelihood then rises so that about 9% of all patients will develop cancer by 20 years out, according to a study in the September issue of Gastroenterology.
The modeled rates of progression for the early years after diagnosis are substantially lower than are those reported by prospective studies, which involve more intensive surveillance and therefore suffer from detection bias, said Dr. Sonja Kroep of Erasmus Medical Center, Rotterdam, the Netherlands, and her associates. “Clinicians informing their patients about their cancer risk can best use this clinical progression rate, which is not influenced by surveillance-detected cancers,” they wrote.
Past analyses have yielded varying results for the rate at which Barrett’s esophagus with low-grade dysplasia progresses to high-grade dysplasia and esophageal carcinoma. For their study, Dr. Kroep and her associates calibrated a model based on the annual rate of 0.18% reported by population-level studies, and used it to simulate prospective studies and to predict results from both population-based and prospective studies for various follow-up periods (Gastroenterology 2015 Apr 29. pii: S0016-5085(15)00601-0).
For the first 5 years of follow-up, the model predicted a 0.19% annual rate of transformation to esophageal adenocarcinoma for population-based studies and a 0.36% annual rate for prospective studies, the researchers reported. At 20 years, these rates rose to 0.63% and 0.65% annually, for a cumulative incidence rate of 9.1% to 9.5%. Between the 5-year and 20-year thresholds, the gap between rates of progression for the two types of studies narrowed from 91% to 5%. Taken together, the findings suggest that for the first 5 years after a diagnosis of Barrett’s esophagus, rates of progression to esophageal adenocarcinoma reflect those from population-level studies instead of surveillance-based prospective studies, the investigators said. “Clinicians should use this information to explain to patients their short-term and long-term risks if no action is taken, and then discuss the risks and benefits of surveillance,” they added.
In a separate retrospective study, radiofrequency ablation of low-grade esophageal dysplasia was linked to substantially lower rates of progression compared with watchful waiting in the form of endoscopic surveillance, said Dr. Aaron Small of the University of Pennsylvania, Philadelphia, and his associates. Their study included 125 patients with Barrett’s esophagus and low-grade dysplasia who underwent surveillance only, and 45 patients who underwent radiofrequency ablation at three university medical centers.
Over median follow-up periods of more than 2 years, the risk of progression with radiofrequency ablation was significantly lower than with endoscopic surveillance only, even after the researchers controlled for year of diagnosis (adjusted hazard ratio, 0.06; 95% confidence interval, 0.008-0.48; P = .008). The ablation group also had fewer visible macroscopic lesions, although the difference was not significant. “We estimate that for every three patients treated with radiofrequency ablation, one additional patient with low-grade dysplasia will avoid progression to high-grade dysplasia or esophageal adenocarcinoma within 3 years,” the researchers wrote. “Although selection bias cannot be excluded, these findings provide additional evidence for the use of endoscopic ablation therapy for low-grade dysplasia” (Gastroenterology 2015 Apr 24. pii: S0016-5085(15)00569-7).
The study by Dr. Kroep and her associates was funded by grant U01 CA152926, and the investigators reported having no conflicts of interest. The study by Dr. Small and his associates was supported by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases and by institutional funds. Dr. Small reported no conflicts of interest, but seven coauthors reported ties with a number of pharmaceutical companies.
Patients with Barrett’s esophagus have about a 0.2% annual chance of developing esophageal adenocarcinoma in the 5 years after initial diagnosis, but the likelihood then rises so that about 9% of all patients will develop cancer by 20 years out, according to a study in the September issue of Gastroenterology.
The modeled rates of progression for the early years after diagnosis are substantially lower than are those reported by prospective studies, which involve more intensive surveillance and therefore suffer from detection bias, said Dr. Sonja Kroep of Erasmus Medical Center, Rotterdam, the Netherlands, and her associates. “Clinicians informing their patients about their cancer risk can best use this clinical progression rate, which is not influenced by surveillance-detected cancers,” they wrote.
Past analyses have yielded varying results for the rate at which Barrett’s esophagus with low-grade dysplasia progresses to high-grade dysplasia and esophageal carcinoma. For their study, Dr. Kroep and her associates calibrated a model based on the annual rate of 0.18% reported by population-level studies, and used it to simulate prospective studies and to predict results from both population-based and prospective studies for various follow-up periods (Gastroenterology 2015 Apr 29. pii: S0016-5085(15)00601-0).
For the first 5 years of follow-up, the model predicted a 0.19% annual rate of transformation to esophageal adenocarcinoma for population-based studies and a 0.36% annual rate for prospective studies, the researchers reported. At 20 years, these rates rose to 0.63% and 0.65% annually, for a cumulative incidence rate of 9.1% to 9.5%. Between the 5-year and 20-year thresholds, the gap between rates of progression for the two types of studies narrowed from 91% to 5%. Taken together, the findings suggest that for the first 5 years after a diagnosis of Barrett’s esophagus, rates of progression to esophageal adenocarcinoma reflect those from population-level studies instead of surveillance-based prospective studies, the investigators said. “Clinicians should use this information to explain to patients their short-term and long-term risks if no action is taken, and then discuss the risks and benefits of surveillance,” they added.
In a separate retrospective study, radiofrequency ablation of low-grade esophageal dysplasia was linked to substantially lower rates of progression compared with watchful waiting in the form of endoscopic surveillance, said Dr. Aaron Small of the University of Pennsylvania, Philadelphia, and his associates. Their study included 125 patients with Barrett’s esophagus and low-grade dysplasia who underwent surveillance only, and 45 patients who underwent radiofrequency ablation at three university medical centers.
Over median follow-up periods of more than 2 years, the risk of progression with radiofrequency ablation was significantly lower than with endoscopic surveillance only, even after the researchers controlled for year of diagnosis (adjusted hazard ratio, 0.06; 95% confidence interval, 0.008-0.48; P = .008). The ablation group also had fewer visible macroscopic lesions, although the difference was not significant. “We estimate that for every three patients treated with radiofrequency ablation, one additional patient with low-grade dysplasia will avoid progression to high-grade dysplasia or esophageal adenocarcinoma within 3 years,” the researchers wrote. “Although selection bias cannot be excluded, these findings provide additional evidence for the use of endoscopic ablation therapy for low-grade dysplasia” (Gastroenterology 2015 Apr 24. pii: S0016-5085(15)00569-7).
The study by Dr. Kroep and her associates was funded by grant U01 CA152926, and the investigators reported having no conflicts of interest. The study by Dr. Small and his associates was supported by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases and by institutional funds. Dr. Small reported no conflicts of interest, but seven coauthors reported ties with a number of pharmaceutical companies.
FROM GASTROENTEROLOGY
Key clinical point: Barrett’s esophagus with low-grade dysplasia had a lower rate of progression to cancer than that suggested by prospective surveillance studies, but radiofrequency ablation might further cut the risk.
Major finding: About 0.2% of cases progress during the 5 years after diagnosis, and RFA might significantly decrease risk of progression (adjusted hazard ratio, 0.06).
Data source: A model of rates of progression based on population-level studies, and a multicenter retrospective study of 170 patients with Barrett’s esophagus and low-grade dysplasia.
Disclosures: The study by Dr. Small and associates was supported by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases and by institutional funds. Dr. Small reported no conflicts of interest; seven coauthors reported ties with a number of pharmaceutical companies. The study by Dr. Kroep and her associates was funded by grant U01 CA152926, and the investigators reported having no conflicts of interest.
Circulating tumor DNA marked progressive liver cancer
A personalized PCR test for circulating tumor DNA identified cases of progressive hepatocellular carcinoma, investigators reported in the September issue of Cellular and Molecular Gastroenterology and Hepatology.
Patients with liver cancer who underwent resection or transplantation and were positive for ctDNA had significantly higher rates of recurrence (P <.0102) and metastasis (P <.0386), reported Dr. Atsushi Ono of Hiroshima (Japan) University and the RIKEN Center for Integrative Medical Sciences and associates. The study also found that transcatheter arterial chemoembolization [TACE] increased levels of ctDNA, compared with total cell-free DNA, making the marker easier to detect.
“Analyzing cell-free DNA after TACE in unresectable and recurrent cases as a liquid biopsy to establish cancer genome profiles might … guide selection of an individualized therapeutic regimen without requiring percutaneous biopsy,” they added.
Assays for ctDNA have shown promise for diagnosing other cancers and targeting their treatments, but HCC diagnosis relies primarily on imaging, and HCC ctDNA has not been well characterized, noted the investigators. They performed massively parallel whole-genome sequencing of DNA extracted from resected HCCs from 46 patients. They serially measured plasma ctDNA levels before and after surgery using personalized quantitative PCR assays that targeted somatic rearrangements. They also used chemiluminescent immunoassays to test for two conventional tumor markers, alpha-fetoprotein and des-gamma-carboxy prothrombin (Cell Mol Gastroenterol Hepatol. 2015 Jul 2 [doi: 10.1016/j.jcmgh.2015.06.009]).
In all, 25 somatic mutations were present in both primary tumor tissue and in cell-free DNA samples, and 83% of mutations in the primary tumor were detectable in cell-free DNA. Among seven patients who tested positive for ctDNA before surgery, six developed recurrent disease and four developed extrahepatic metastases, Dr. Ono and associates said.
Levels of ctDNA increased as disease progressed and dropped in response to treatment, and one case remained positive for ctDNA even after alpha-fetoprotein and des-gamma-carboxy prothrombin became negative or dropped below threshold after resection. “This suggests that, in some patients, ctDNA might be a better and more sensitive biomarker for HCC than the conventional tumor markers,” they said.
The assay analyzed plasma instead of serum because serum was likely to have more normal cell-free nucleic acids, which would make it harder to detect mutant alleles, the investigators noted. Testing for ctDNA could help address the problem of tumor heterogeneity because ctDNA contains the entire tumor genome, including variants from independent tumors, but the assay will need further validation, especially because its lower limits varied by primer sets, which reduced its sensitivity and meant that some cases went undetected, they added.
The study was funded by the government of Japan, the RIKEN President’s Fund, the Princess Takamatsu Cancer Research Fund, and the Takeda Science Foundation. The investigators declared no competing interests.
As the oncology field advances toward implementation of personalized medicine programs, molecular and genomic analysis of circulating tumor DNA (ctDNA) represents a promising approach for diagnosis, prognosis, therapy selection, and minimal residual disease monitoring of a wide array of malignancies.

|
| Dr. Larissa Furtado |
With the purpose of assessing the utility of extracellular tumor DNA as a potential biomarker for hepatocellular carcinoma (HCC), Dr. Ono and colleagues analyzed serum ctDNA from 46 HCC patients using quantitative PCR assays for somatic rearrangements uncovered by whole-genome sequencing of their primary tumors.
For the seven patients with detectable ctDNA in preoperative serum, the incidence of recurrence and extrahepatic metastasis within 2 years following hepatectomy were significantly worse than in the ctDNA-negative group, although no significant difference in the cumulative survival rate was observed between these patients. The ctDNA positivity also was found to be an independent predictor of microscopic vascular invasion of the portal vein, and it correlated with larger tumor size and higher alpha-fetoprotein and des-gamma-carboxy prothrombin levels.
In addition, the investigators demonstrated that transcatheter arterial chemoembolization (TACE) enriched ctDNA levels in cell-free DNA in blood, and that serum ctDNA levels were increased with disease progression and reflected response to treatments.

|
| Dr. Jeremy Segal |
The diagnosis of HCC is currently based on imaging and/or biopsies. Even though there are no well-established biomarkers for early detection and monitoring of HCC at present, the data presented here indicate the potential utility of personalized ctDNA testing for individualized management of hepatocellular carcinoma patients.
Dr. Larissa V. Furtado and Dr. Jeremy P. Segal are both assistant professors and assistant directors of the division of genomic and molecular pathology in the department of pathology at the University of Chicago Medical Center. Neither has conflicts of interest.
As the oncology field advances toward implementation of personalized medicine programs, molecular and genomic analysis of circulating tumor DNA (ctDNA) represents a promising approach for diagnosis, prognosis, therapy selection, and minimal residual disease monitoring of a wide array of malignancies.

|
| Dr. Larissa Furtado |
With the purpose of assessing the utility of extracellular tumor DNA as a potential biomarker for hepatocellular carcinoma (HCC), Dr. Ono and colleagues analyzed serum ctDNA from 46 HCC patients using quantitative PCR assays for somatic rearrangements uncovered by whole-genome sequencing of their primary tumors.
For the seven patients with detectable ctDNA in preoperative serum, the incidence of recurrence and extrahepatic metastasis within 2 years following hepatectomy were significantly worse than in the ctDNA-negative group, although no significant difference in the cumulative survival rate was observed between these patients. The ctDNA positivity also was found to be an independent predictor of microscopic vascular invasion of the portal vein, and it correlated with larger tumor size and higher alpha-fetoprotein and des-gamma-carboxy prothrombin levels.
In addition, the investigators demonstrated that transcatheter arterial chemoembolization (TACE) enriched ctDNA levels in cell-free DNA in blood, and that serum ctDNA levels were increased with disease progression and reflected response to treatments.

|
| Dr. Jeremy Segal |
The diagnosis of HCC is currently based on imaging and/or biopsies. Even though there are no well-established biomarkers for early detection and monitoring of HCC at present, the data presented here indicate the potential utility of personalized ctDNA testing for individualized management of hepatocellular carcinoma patients.
Dr. Larissa V. Furtado and Dr. Jeremy P. Segal are both assistant professors and assistant directors of the division of genomic and molecular pathology in the department of pathology at the University of Chicago Medical Center. Neither has conflicts of interest.
As the oncology field advances toward implementation of personalized medicine programs, molecular and genomic analysis of circulating tumor DNA (ctDNA) represents a promising approach for diagnosis, prognosis, therapy selection, and minimal residual disease monitoring of a wide array of malignancies.

|
| Dr. Larissa Furtado |
With the purpose of assessing the utility of extracellular tumor DNA as a potential biomarker for hepatocellular carcinoma (HCC), Dr. Ono and colleagues analyzed serum ctDNA from 46 HCC patients using quantitative PCR assays for somatic rearrangements uncovered by whole-genome sequencing of their primary tumors.
For the seven patients with detectable ctDNA in preoperative serum, the incidence of recurrence and extrahepatic metastasis within 2 years following hepatectomy were significantly worse than in the ctDNA-negative group, although no significant difference in the cumulative survival rate was observed between these patients. The ctDNA positivity also was found to be an independent predictor of microscopic vascular invasion of the portal vein, and it correlated with larger tumor size and higher alpha-fetoprotein and des-gamma-carboxy prothrombin levels.
In addition, the investigators demonstrated that transcatheter arterial chemoembolization (TACE) enriched ctDNA levels in cell-free DNA in blood, and that serum ctDNA levels were increased with disease progression and reflected response to treatments.

|
| Dr. Jeremy Segal |
The diagnosis of HCC is currently based on imaging and/or biopsies. Even though there are no well-established biomarkers for early detection and monitoring of HCC at present, the data presented here indicate the potential utility of personalized ctDNA testing for individualized management of hepatocellular carcinoma patients.
Dr. Larissa V. Furtado and Dr. Jeremy P. Segal are both assistant professors and assistant directors of the division of genomic and molecular pathology in the department of pathology at the University of Chicago Medical Center. Neither has conflicts of interest.
A personalized PCR test for circulating tumor DNA identified cases of progressive hepatocellular carcinoma, investigators reported in the September issue of Cellular and Molecular Gastroenterology and Hepatology.
Patients with liver cancer who underwent resection or transplantation and were positive for ctDNA had significantly higher rates of recurrence (P <.0102) and metastasis (P <.0386), reported Dr. Atsushi Ono of Hiroshima (Japan) University and the RIKEN Center for Integrative Medical Sciences and associates. The study also found that transcatheter arterial chemoembolization [TACE] increased levels of ctDNA, compared with total cell-free DNA, making the marker easier to detect.
“Analyzing cell-free DNA after TACE in unresectable and recurrent cases as a liquid biopsy to establish cancer genome profiles might … guide selection of an individualized therapeutic regimen without requiring percutaneous biopsy,” they added.
Assays for ctDNA have shown promise for diagnosing other cancers and targeting their treatments, but HCC diagnosis relies primarily on imaging, and HCC ctDNA has not been well characterized, noted the investigators. They performed massively parallel whole-genome sequencing of DNA extracted from resected HCCs from 46 patients. They serially measured plasma ctDNA levels before and after surgery using personalized quantitative PCR assays that targeted somatic rearrangements. They also used chemiluminescent immunoassays to test for two conventional tumor markers, alpha-fetoprotein and des-gamma-carboxy prothrombin (Cell Mol Gastroenterol Hepatol. 2015 Jul 2 [doi: 10.1016/j.jcmgh.2015.06.009]).
In all, 25 somatic mutations were present in both primary tumor tissue and in cell-free DNA samples, and 83% of mutations in the primary tumor were detectable in cell-free DNA. Among seven patients who tested positive for ctDNA before surgery, six developed recurrent disease and four developed extrahepatic metastases, Dr. Ono and associates said.
Levels of ctDNA increased as disease progressed and dropped in response to treatment, and one case remained positive for ctDNA even after alpha-fetoprotein and des-gamma-carboxy prothrombin became negative or dropped below threshold after resection. “This suggests that, in some patients, ctDNA might be a better and more sensitive biomarker for HCC than the conventional tumor markers,” they said.
The assay analyzed plasma instead of serum because serum was likely to have more normal cell-free nucleic acids, which would make it harder to detect mutant alleles, the investigators noted. Testing for ctDNA could help address the problem of tumor heterogeneity because ctDNA contains the entire tumor genome, including variants from independent tumors, but the assay will need further validation, especially because its lower limits varied by primer sets, which reduced its sensitivity and meant that some cases went undetected, they added.
The study was funded by the government of Japan, the RIKEN President’s Fund, the Princess Takamatsu Cancer Research Fund, and the Takeda Science Foundation. The investigators declared no competing interests.
A personalized PCR test for circulating tumor DNA identified cases of progressive hepatocellular carcinoma, investigators reported in the September issue of Cellular and Molecular Gastroenterology and Hepatology.
Patients with liver cancer who underwent resection or transplantation and were positive for ctDNA had significantly higher rates of recurrence (P <.0102) and metastasis (P <.0386), reported Dr. Atsushi Ono of Hiroshima (Japan) University and the RIKEN Center for Integrative Medical Sciences and associates. The study also found that transcatheter arterial chemoembolization [TACE] increased levels of ctDNA, compared with total cell-free DNA, making the marker easier to detect.
“Analyzing cell-free DNA after TACE in unresectable and recurrent cases as a liquid biopsy to establish cancer genome profiles might … guide selection of an individualized therapeutic regimen without requiring percutaneous biopsy,” they added.
Assays for ctDNA have shown promise for diagnosing other cancers and targeting their treatments, but HCC diagnosis relies primarily on imaging, and HCC ctDNA has not been well characterized, noted the investigators. They performed massively parallel whole-genome sequencing of DNA extracted from resected HCCs from 46 patients. They serially measured plasma ctDNA levels before and after surgery using personalized quantitative PCR assays that targeted somatic rearrangements. They also used chemiluminescent immunoassays to test for two conventional tumor markers, alpha-fetoprotein and des-gamma-carboxy prothrombin (Cell Mol Gastroenterol Hepatol. 2015 Jul 2 [doi: 10.1016/j.jcmgh.2015.06.009]).
In all, 25 somatic mutations were present in both primary tumor tissue and in cell-free DNA samples, and 83% of mutations in the primary tumor were detectable in cell-free DNA. Among seven patients who tested positive for ctDNA before surgery, six developed recurrent disease and four developed extrahepatic metastases, Dr. Ono and associates said.
Levels of ctDNA increased as disease progressed and dropped in response to treatment, and one case remained positive for ctDNA even after alpha-fetoprotein and des-gamma-carboxy prothrombin became negative or dropped below threshold after resection. “This suggests that, in some patients, ctDNA might be a better and more sensitive biomarker for HCC than the conventional tumor markers,” they said.
The assay analyzed plasma instead of serum because serum was likely to have more normal cell-free nucleic acids, which would make it harder to detect mutant alleles, the investigators noted. Testing for ctDNA could help address the problem of tumor heterogeneity because ctDNA contains the entire tumor genome, including variants from independent tumors, but the assay will need further validation, especially because its lower limits varied by primer sets, which reduced its sensitivity and meant that some cases went undetected, they added.
The study was funded by the government of Japan, the RIKEN President’s Fund, the Princess Takamatsu Cancer Research Fund, and the Takeda Science Foundation. The investigators declared no competing interests.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: The presence of circulating tumor (ct) DNA indicated progression of hepatocellular carcinoma.
Major finding: Among seven patients who tested positive for ctDNA before undergoing surgical resection, six developed recurrent HCC and four developed extrahepatic metastases.
Data source: Real-time quantitative PCR analysis of serum samples from 46 patients with HCC who underwent hepatectomy or liver transplantation.
Disclosures: The study was funded by the government of Japan, the RIKEN President’s Fund, the Princess Takamatsu Cancer Research Fund, and the Takeda Science Foundation. The investigators declared no competing interests.
First EDition: News for and about the practice of Emergency Medicine
More bicyclists, more fatalities
BY RICHARD FRANKI
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
| The annual rate for bicyclist deaths associated with motor vehicles dropped 44% from 1975 to 2012, but the downward trend has slowed in recent years, the Centers for Disease Control and Prevention reported. |
Annual mortality among cyclists for all motor vehicle-related deaths was 0.23 per 100,000 in 2012, a decline of 44% since 1975 when the rate was 0.41 per 100,000. But the rate is up from just under 0.20 per 100,000 in 2010. In 2012, the rate topped the Healthy People 2020 goal of 0.22 for the first time since 2008, according to Jason Vargo, PhD, of the University of Wisconsin, Madison, and his associates.1
The explanation may be that the number of bicyclists has been steadily rising. “The share of total household trips taken by bicycle has doubled over the last 35 years,” with the largest share of that increase occurring in recent years. From 2000 to 2012, for example, “the number of US workers who traveled to work by bicycle increased 61%,” the researchers wrote.
The report was based on data from the Fatality Analysis Reporting System, which limits fatalities to those involving a motor vehicle on a public road.2
Surgical bolt cutters quickly cut titanium ring
BY AMY KARON
FROM EMERGENCY MEDICINE JOURNAL
| A pair of large surgical bolt cutters were used to safely and quickly cut a titanium ring from a patient’s swollen finger, according to a letter published online in the Emergency Medicine Journal. |
“Our method used simple equipment that is readily available in most hospitals at all times, took less than 30 seconds to perform, and could be performed by a sole operator without damage to the underlying finger,” wrote Dr Andrej Salibi and Dr Andrew Morritt at Sheffield (England) Teaching Hospital NHS Foundation.1
Ring constriction is a fairly common problem that can cause necrosis and loss of the digit if the ring is not removed. Basic ring cutters can sever gold and silver, but not titanium, which has become popular for rings because it is hypoallergenic, durable, lightweight, and strong—so strong that diamond-tipped saws or drills can take up to 15 minutes to cut these rings. Many facilities also lack access to such equipment, and it generates enough heat that an assistant must irrigate the surrounding skin to prevent burns.
The case report described a patient who bathed in warm water at a spa and developed a painful, swollen finger that was constricted by a titanium wedding band. Elevation and lubrication at the ED failed to remove the ring, as did finger binding, and use of a manual ring cutter.
“The fire service was called and attempted removal using specialized cutting equipment, which also failed,” the surgeons wrote. “The patient was then admitted under the plastic surgery service for hand elevation, and further attempts 8 hours later blunted two manual ring cutters.” At this point, the surgeons borrowed a large pair of bolt cutters from the operating room, and quickly severed the ring without harming the finger. Then they applied lateral traction with a pair of paper clips and removed the split ring.
The authors declared no funding sources or conflicts of interest.
Federal plan emphasizes heroin/opioid treatment over incarceration
BY WHITNEY MCKNIGHT
Frontline Medical News
| WASHINGTON—The Obama administration has announced that it will spend an additional $13.4 million fighting opioid and heroin abuse, emphasizing treatment over law enforcement. |
The increased emphasis will center on geographic areas where heroin and opioid abuse are rampant, specifically: Appalachia; New England; Philadelphia/Camden, New Jersey; metropolitan New York City, particularly northern New Jersey; and the Washington/Baltimore metropolitan region. Public safety officers and first responders will be trained in how to administer naloxone and provide other medical attention for those in the midst of a heroin or opioid overdose.
The 15 states in the targeted areas will share and leverage data to determine regional patterns of heroin and prescription painkiller-related overdose. These data are expected to delineate where the narcotics—especially those laced with other, more dangerous drugs—are being produced and distributed so that heroin response teams can disrupt the production and distribution of illegal drugs, and respond pre-emptively by expanding resources to communities hardest hit.
In a statement, Michael Botticelli, director of the White House Office of National Drug Control Policy, said the administration’s emphasis on “the national drug challenge as both a public health and public safety issue” is based on viewing drug addiction as “a chronic disease of the brain that can be successfully prevented and treated, and from which one can recover.”
The initiative also will provide additional funding for similar efforts to address opioid abuse and methamphetamine abuse in the Southwest and along the United States/Mexico border.
“This program demonstrates the importance of linking health to criminal justice in collaboration rather than seeing better, new drug policy as a choice between health and law enforcement,” Dr Robert L. DuPont, former director of the National Institute on Drug Abuse (NIDA) and president of the Institute for Behavior and Health, said in an interview.
Online resource is aid for preventing patient falls
BY MIKE BOCK
Frontline Medical News
| An online resource guide offers 21 targeted solutions for reducing the rate of falls in hospitals and urgent care settings,1 The Joint Commission Center for Transforming Healthcare announced in a statement. |
Developed in collaboration with seven hospitals and five health care organizations, the fall prevention methodology of the Targeted Solutions Tool could potentially reduce the number of patients injured from a fall from 117 to 45 in a typical 200-bed hospital, avoiding approximately $1 million in costs annually, the agency claims.
Some of the recommendations for reducing in-hospital falls include:
- Creating awareness among staff
- Using a validated fall risk assessment tool
- Engaging patients and their families in the fall safety program
- Hourly rounding with scheduled restroom use for patients
- Engaging all hospital staff and patients to ensure no patient walks without assistance
“Hundreds of thousands of patients fall in hospitals every year; and many of these falls result in moderate to severe injuries that can prolong hospital stays and require the patient to undergo additional treatment,” Dr Erin DuPree, vice president and chief medical officer of the Joint Commission Center for Transforming Healthcare, said in a statement.
The Joint Commission Center for Transforming Healthcare was created in 2008 as a nonprofit affiliate of The Joint Commission.
Dr Lappin is an assistant professor and an attending physician, department of emergency medicine, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
Reference - CDC More bicyclists, more fatalities
- Vargo J, Gerhardstein BG, Whitfield GP, Wendel A. Bicyclist deaths associated with motor vehicle traffic – United States, 1975-2012. MMWR Morb Mortal Wkly Rep.2015;64(31):837-841.
- National Highway Traffic Safety Administration. Fatality Analysis Reporting System (FARS). http://www.nhtsa.gov/FARS. Accessed August 20, 2015.
Reference - Surgical bolt cutters quickly cut titanium ring
- Salibi A, Morritt AN. Removing a titanium wedding ring [published online ahead of print August 13, 2015]. Emerg Med J. doi: 10.1136/emermed-2015-204962.
Reference - Online resource is aid for preventing patient falls
- Joint Commission Center for Transforming Healthcare. New! Targeted Solutions Tool for Preventing Falls. http://www.centerfortransforminghealthcare.org/tst_pfi.aspx. Accessed August 20, 2015.
More bicyclists, more fatalities
BY RICHARD FRANKI
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
| The annual rate for bicyclist deaths associated with motor vehicles dropped 44% from 1975 to 2012, but the downward trend has slowed in recent years, the Centers for Disease Control and Prevention reported. |
Annual mortality among cyclists for all motor vehicle-related deaths was 0.23 per 100,000 in 2012, a decline of 44% since 1975 when the rate was 0.41 per 100,000. But the rate is up from just under 0.20 per 100,000 in 2010. In 2012, the rate topped the Healthy People 2020 goal of 0.22 for the first time since 2008, according to Jason Vargo, PhD, of the University of Wisconsin, Madison, and his associates.1
The explanation may be that the number of bicyclists has been steadily rising. “The share of total household trips taken by bicycle has doubled over the last 35 years,” with the largest share of that increase occurring in recent years. From 2000 to 2012, for example, “the number of US workers who traveled to work by bicycle increased 61%,” the researchers wrote.
The report was based on data from the Fatality Analysis Reporting System, which limits fatalities to those involving a motor vehicle on a public road.2
Surgical bolt cutters quickly cut titanium ring
BY AMY KARON
FROM EMERGENCY MEDICINE JOURNAL
| A pair of large surgical bolt cutters were used to safely and quickly cut a titanium ring from a patient’s swollen finger, according to a letter published online in the Emergency Medicine Journal. |
“Our method used simple equipment that is readily available in most hospitals at all times, took less than 30 seconds to perform, and could be performed by a sole operator without damage to the underlying finger,” wrote Dr Andrej Salibi and Dr Andrew Morritt at Sheffield (England) Teaching Hospital NHS Foundation.1
Ring constriction is a fairly common problem that can cause necrosis and loss of the digit if the ring is not removed. Basic ring cutters can sever gold and silver, but not titanium, which has become popular for rings because it is hypoallergenic, durable, lightweight, and strong—so strong that diamond-tipped saws or drills can take up to 15 minutes to cut these rings. Many facilities also lack access to such equipment, and it generates enough heat that an assistant must irrigate the surrounding skin to prevent burns.
The case report described a patient who bathed in warm water at a spa and developed a painful, swollen finger that was constricted by a titanium wedding band. Elevation and lubrication at the ED failed to remove the ring, as did finger binding, and use of a manual ring cutter.
“The fire service was called and attempted removal using specialized cutting equipment, which also failed,” the surgeons wrote. “The patient was then admitted under the plastic surgery service for hand elevation, and further attempts 8 hours later blunted two manual ring cutters.” At this point, the surgeons borrowed a large pair of bolt cutters from the operating room, and quickly severed the ring without harming the finger. Then they applied lateral traction with a pair of paper clips and removed the split ring.
The authors declared no funding sources or conflicts of interest.
Federal plan emphasizes heroin/opioid treatment over incarceration
BY WHITNEY MCKNIGHT
Frontline Medical News
| WASHINGTON—The Obama administration has announced that it will spend an additional $13.4 million fighting opioid and heroin abuse, emphasizing treatment over law enforcement. |
The increased emphasis will center on geographic areas where heroin and opioid abuse are rampant, specifically: Appalachia; New England; Philadelphia/Camden, New Jersey; metropolitan New York City, particularly northern New Jersey; and the Washington/Baltimore metropolitan region. Public safety officers and first responders will be trained in how to administer naloxone and provide other medical attention for those in the midst of a heroin or opioid overdose.
The 15 states in the targeted areas will share and leverage data to determine regional patterns of heroin and prescription painkiller-related overdose. These data are expected to delineate where the narcotics—especially those laced with other, more dangerous drugs—are being produced and distributed so that heroin response teams can disrupt the production and distribution of illegal drugs, and respond pre-emptively by expanding resources to communities hardest hit.
In a statement, Michael Botticelli, director of the White House Office of National Drug Control Policy, said the administration’s emphasis on “the national drug challenge as both a public health and public safety issue” is based on viewing drug addiction as “a chronic disease of the brain that can be successfully prevented and treated, and from which one can recover.”
The initiative also will provide additional funding for similar efforts to address opioid abuse and methamphetamine abuse in the Southwest and along the United States/Mexico border.
“This program demonstrates the importance of linking health to criminal justice in collaboration rather than seeing better, new drug policy as a choice between health and law enforcement,” Dr Robert L. DuPont, former director of the National Institute on Drug Abuse (NIDA) and president of the Institute for Behavior and Health, said in an interview.
Online resource is aid for preventing patient falls
BY MIKE BOCK
Frontline Medical News
| An online resource guide offers 21 targeted solutions for reducing the rate of falls in hospitals and urgent care settings,1 The Joint Commission Center for Transforming Healthcare announced in a statement. |
Developed in collaboration with seven hospitals and five health care organizations, the fall prevention methodology of the Targeted Solutions Tool could potentially reduce the number of patients injured from a fall from 117 to 45 in a typical 200-bed hospital, avoiding approximately $1 million in costs annually, the agency claims.
Some of the recommendations for reducing in-hospital falls include:
- Creating awareness among staff
- Using a validated fall risk assessment tool
- Engaging patients and their families in the fall safety program
- Hourly rounding with scheduled restroom use for patients
- Engaging all hospital staff and patients to ensure no patient walks without assistance
“Hundreds of thousands of patients fall in hospitals every year; and many of these falls result in moderate to severe injuries that can prolong hospital stays and require the patient to undergo additional treatment,” Dr Erin DuPree, vice president and chief medical officer of the Joint Commission Center for Transforming Healthcare, said in a statement.
The Joint Commission Center for Transforming Healthcare was created in 2008 as a nonprofit affiliate of The Joint Commission.
Dr Lappin is an assistant professor and an attending physician, department of emergency medicine, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
More bicyclists, more fatalities
BY RICHARD FRANKI
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
| The annual rate for bicyclist deaths associated with motor vehicles dropped 44% from 1975 to 2012, but the downward trend has slowed in recent years, the Centers for Disease Control and Prevention reported. |
Annual mortality among cyclists for all motor vehicle-related deaths was 0.23 per 100,000 in 2012, a decline of 44% since 1975 when the rate was 0.41 per 100,000. But the rate is up from just under 0.20 per 100,000 in 2010. In 2012, the rate topped the Healthy People 2020 goal of 0.22 for the first time since 2008, according to Jason Vargo, PhD, of the University of Wisconsin, Madison, and his associates.1
The explanation may be that the number of bicyclists has been steadily rising. “The share of total household trips taken by bicycle has doubled over the last 35 years,” with the largest share of that increase occurring in recent years. From 2000 to 2012, for example, “the number of US workers who traveled to work by bicycle increased 61%,” the researchers wrote.
The report was based on data from the Fatality Analysis Reporting System, which limits fatalities to those involving a motor vehicle on a public road.2
Surgical bolt cutters quickly cut titanium ring
BY AMY KARON
FROM EMERGENCY MEDICINE JOURNAL
| A pair of large surgical bolt cutters were used to safely and quickly cut a titanium ring from a patient’s swollen finger, according to a letter published online in the Emergency Medicine Journal. |
“Our method used simple equipment that is readily available in most hospitals at all times, took less than 30 seconds to perform, and could be performed by a sole operator without damage to the underlying finger,” wrote Dr Andrej Salibi and Dr Andrew Morritt at Sheffield (England) Teaching Hospital NHS Foundation.1
Ring constriction is a fairly common problem that can cause necrosis and loss of the digit if the ring is not removed. Basic ring cutters can sever gold and silver, but not titanium, which has become popular for rings because it is hypoallergenic, durable, lightweight, and strong—so strong that diamond-tipped saws or drills can take up to 15 minutes to cut these rings. Many facilities also lack access to such equipment, and it generates enough heat that an assistant must irrigate the surrounding skin to prevent burns.
The case report described a patient who bathed in warm water at a spa and developed a painful, swollen finger that was constricted by a titanium wedding band. Elevation and lubrication at the ED failed to remove the ring, as did finger binding, and use of a manual ring cutter.
“The fire service was called and attempted removal using specialized cutting equipment, which also failed,” the surgeons wrote. “The patient was then admitted under the plastic surgery service for hand elevation, and further attempts 8 hours later blunted two manual ring cutters.” At this point, the surgeons borrowed a large pair of bolt cutters from the operating room, and quickly severed the ring without harming the finger. Then they applied lateral traction with a pair of paper clips and removed the split ring.
The authors declared no funding sources or conflicts of interest.
Federal plan emphasizes heroin/opioid treatment over incarceration
BY WHITNEY MCKNIGHT
Frontline Medical News
| WASHINGTON—The Obama administration has announced that it will spend an additional $13.4 million fighting opioid and heroin abuse, emphasizing treatment over law enforcement. |
The increased emphasis will center on geographic areas where heroin and opioid abuse are rampant, specifically: Appalachia; New England; Philadelphia/Camden, New Jersey; metropolitan New York City, particularly northern New Jersey; and the Washington/Baltimore metropolitan region. Public safety officers and first responders will be trained in how to administer naloxone and provide other medical attention for those in the midst of a heroin or opioid overdose.
The 15 states in the targeted areas will share and leverage data to determine regional patterns of heroin and prescription painkiller-related overdose. These data are expected to delineate where the narcotics—especially those laced with other, more dangerous drugs—are being produced and distributed so that heroin response teams can disrupt the production and distribution of illegal drugs, and respond pre-emptively by expanding resources to communities hardest hit.
In a statement, Michael Botticelli, director of the White House Office of National Drug Control Policy, said the administration’s emphasis on “the national drug challenge as both a public health and public safety issue” is based on viewing drug addiction as “a chronic disease of the brain that can be successfully prevented and treated, and from which one can recover.”
The initiative also will provide additional funding for similar efforts to address opioid abuse and methamphetamine abuse in the Southwest and along the United States/Mexico border.
“This program demonstrates the importance of linking health to criminal justice in collaboration rather than seeing better, new drug policy as a choice between health and law enforcement,” Dr Robert L. DuPont, former director of the National Institute on Drug Abuse (NIDA) and president of the Institute for Behavior and Health, said in an interview.
Online resource is aid for preventing patient falls
BY MIKE BOCK
Frontline Medical News
| An online resource guide offers 21 targeted solutions for reducing the rate of falls in hospitals and urgent care settings,1 The Joint Commission Center for Transforming Healthcare announced in a statement. |
Developed in collaboration with seven hospitals and five health care organizations, the fall prevention methodology of the Targeted Solutions Tool could potentially reduce the number of patients injured from a fall from 117 to 45 in a typical 200-bed hospital, avoiding approximately $1 million in costs annually, the agency claims.
Some of the recommendations for reducing in-hospital falls include:
- Creating awareness among staff
- Using a validated fall risk assessment tool
- Engaging patients and their families in the fall safety program
- Hourly rounding with scheduled restroom use for patients
- Engaging all hospital staff and patients to ensure no patient walks without assistance
“Hundreds of thousands of patients fall in hospitals every year; and many of these falls result in moderate to severe injuries that can prolong hospital stays and require the patient to undergo additional treatment,” Dr Erin DuPree, vice president and chief medical officer of the Joint Commission Center for Transforming Healthcare, said in a statement.
The Joint Commission Center for Transforming Healthcare was created in 2008 as a nonprofit affiliate of The Joint Commission.
Dr Lappin is an assistant professor and an attending physician, department of emergency medicine, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
Reference - CDC More bicyclists, more fatalities
- Vargo J, Gerhardstein BG, Whitfield GP, Wendel A. Bicyclist deaths associated with motor vehicle traffic – United States, 1975-2012. MMWR Morb Mortal Wkly Rep.2015;64(31):837-841.
- National Highway Traffic Safety Administration. Fatality Analysis Reporting System (FARS). http://www.nhtsa.gov/FARS. Accessed August 20, 2015.
Reference - Surgical bolt cutters quickly cut titanium ring
- Salibi A, Morritt AN. Removing a titanium wedding ring [published online ahead of print August 13, 2015]. Emerg Med J. doi: 10.1136/emermed-2015-204962.
Reference - Online resource is aid for preventing patient falls
- Joint Commission Center for Transforming Healthcare. New! Targeted Solutions Tool for Preventing Falls. http://www.centerfortransforminghealthcare.org/tst_pfi.aspx. Accessed August 20, 2015.
Reference - CDC More bicyclists, more fatalities
- Vargo J, Gerhardstein BG, Whitfield GP, Wendel A. Bicyclist deaths associated with motor vehicle traffic – United States, 1975-2012. MMWR Morb Mortal Wkly Rep.2015;64(31):837-841.
- National Highway Traffic Safety Administration. Fatality Analysis Reporting System (FARS). http://www.nhtsa.gov/FARS. Accessed August 20, 2015.
Reference - Surgical bolt cutters quickly cut titanium ring
- Salibi A, Morritt AN. Removing a titanium wedding ring [published online ahead of print August 13, 2015]. Emerg Med J. doi: 10.1136/emermed-2015-204962.
Reference - Online resource is aid for preventing patient falls
- Joint Commission Center for Transforming Healthcare. New! Targeted Solutions Tool for Preventing Falls. http://www.centerfortransforminghealthcare.org/tst_pfi.aspx. Accessed August 20, 2015.
Malpractice Counsel: Missed Preeclampsia
Missed Preeclampsia
| A 24-year-old woman, gravida 1, para 1, aborta 0, presented to the ED complaining of a 1-day history of shortness of breath. Four days earlier, she had delivered a healthy baby boy via normal vaginal delivery and without complication. She denied chest pain, fever, or abdominal pain. She was otherwise in good health, stating that she was not taking any medications. She also denied smoking cigarettes. |
On physical examination, the patient’s vital signs were remarkable for the following: heart rate (HR), 86 beats/minute; blood pressure (BP), 164/94 mm Hg; respiratory rate, 18 breaths/minute; temperature, 98.6oF. Oxygen saturation was 96% on room air. The head, eye, ear, nose and throat examination was unremarkable. The lungs were clear to auscultation bilaterally, and HR and heart rhythm were normal. The abdomen was soft and nontender without guarding or rebound. The lower extremities were remarkable for 1+ pedal and pretibial edema bilaterally.
The patient presented to the same ED 2 days later, again with the chief complaint of shortness of breath. On examination, her BP was noted to be elevated and she had 1+ dependent edema bilaterally. Again, the EP was concerned for a PE and ordered a repeat CTA scan of the chest. This study, similar to the first, was read as normal, and showed no evidence of PE. The patient was diagnosed again with “shortness of breath of unknown etiology” and discharged home. The patient’s obstetrician-gynecologist (Ob/Gyn) was not consulted; however, the patient was encouraged to follow up with him.
The next day, the patient presented to the same ED via emergency medical services, this time with seizures; she had no prior history of a seizure disorder. On presentation to the ED, she was noted to be postictal, with an elevated BP and tachycardic with an HR of 104 beats/minute. On examination, the lungs were clear to auscultation and the lower extremities exhibited 1+ pedal and pretibial edema. A urinalysis revealed proteinuria. The patient was given 4 g of magnesium sulfate intravenously (IV) and her Ob/Gyn was consulted.
The patient was admitted to the hospital with a diagnosis of eclampsia. She was given an IV drip of magnesium and labetalol for the high BP. Unfortunately, the patient apparently had suffered an anoxic brain injury from the previous seizures and died on hospital day 3.
The family sued the treating EPs and the hospital for failure to diagnose preeclampsia on two separate ED presentations. They noted the patient’s Ob/Gyn was never consulted; no action was taken to treat the hypertension; and no urinalysis was ordered on either visit. The EPs and hospital settled the case prior to trial for several million dollars.
Discussion
This is an incredibly sad case, and the EPs and hospital were right to settle and not go to trial. While PE was a reasonable diagnosis to consider in this patient on her first ED visit, it should not have been the only one in the differential diagnosis. The EP became anchored to this single diagnosis and refused to consider other alternative diagnoses—even after the CTA scan of the chest ruled out PE. Moreover, it appears the EP either never considered the significance of the elevated BP and dependent edema or just ignored these findings. To repeat essentially the same exact workup on the second visit does not make sense—one should “cast a wider net, not the same net.”
The diagnosis of “shortness of breath of unknown etiology” is similarly unacceptable. While this is a common and accepted diagnosis when it pertains to abdominal pain, the same is not true for dyspnea.
Preeclampsia is characterized by hypertension (BP >140/90 mm Hg) and proteinuria; associated symptoms include edema and hyperreflexia. Postpartum preeclampsia occurs infrequently and can develop up to 4 weeks after delivery.1 In one 10-year retrospective case series, the incidence of preeclampsia in the postpartum period was 5.7%, and nearly 16% went on to develop eclampsia.2 In a retrospective study of 22 postpartum preeclamptic patients, the median time to presentation was 5 days postpartum.1 In a similar retrospective study of 152 patients, 90% of such patients presented within 7 days.3 The patient in this case initially presented on postpartum day 4.
Interestingly, in a study by Al-Safi et al,3 63% of postpartum preeclamptic patients had no antecedent diagnosis of hypertensive disease during pregnancy. These findings are consistent with the findings of others that 33% to 69% of such patients show no evidence of preeclampsia in the ante- or peripartum period.
The clinical presentation of postpartum preeclampsia is similar to preeclampsia complicating pregnancy after gestation week 20. In the study by Al-Safi et al,3 headache was the most common presenting symptom (69%), followed by shortness of breath (30%), blurry vision (21%), nausea (12.5%), and epigastric abdominal pain (5%). Similarly, Yancey et al1 found headache (82%) to be the most common presenting symptom in their series. Unfortunately, it is not known whether the patient in this case complained of headache or blurred vision as the published records note neither their presence nor absence.
The management of patients with preeclampsia includes IV magnesium to prevent seizures (ie, eclampsia) and BP control.1 A bolus of 4 to 6 g IV magnesium sulfate over 15 to 30 minutes is recommended, followed by an infusion of 2 g/h IV. Historically, IV hydralazine has been used to manage preeclamptic patients with a BP greater than 160/110 mm Hg. More recently, however, IV labetalol has become popular.5 All such patients require admission to the hospital with Ob/Gyn involvement.
Missed Subdural Hematoma
A 59-year-old man presented to the ED with a chief complaint of headache, the onset of which he stated started gradually 2 days prior. He noted the headache was worse than normal but without associated nausea, vomiting, fever, chills, or change in vision. His past medical history was significant for a lower extremity deep vein thrombosis 3 months prior, for which he was taking warfarin.
The patient’s vital signs were all normal. The physical examination, including a thorough neurological examination, was also normal. The EP ordered a prothrombin time (PT), an international normalized ratio (INR), and a noncontrast CT scan of the head. The PT/INR results were therapeutic at 22 seconds and 2.3. The CT scan was interpreted by radiology services as normal. The patient’s headache was treated with IV prochlorperazine and diphenhydramine. After treatment, the patient reported feeling better and was discharged home with instructions to follow up with his primary care physician.
Over the next several months, the patient presented to the same ED on seven different occasions, each time with the chief complaint of headache. At each of these presentations, the history and physical examination were documented as unremarkable, with no history of trauma. The thoroughness, however, of the documentation varied considerably for each ED encounter. No head CT scan was ordered on the subsequent seven visits, and at each presentation, the patient was treated symptomatically and discharged home.
Two days after his eighth visit to the same hospital ED, the patient presented to a different ED, again with a chief complaint of headache. The EP at this ED ordered a noncontrast CT of the head, which demonstrated a left subdural hematoma. The patient was admitted to the hospital, given IV vitamin K and fresh frozen plasma, and underwent evacuation of the hematoma by neurosurgery. The patient’s hospital course was unremarkable, and he was discharged home without any focal weakness.
The patient, however, claimed that he suffered cognitive impairment as a result of the missed diagnosis. He sued treating EPs at the first ED as well as the hospital for failure to timely diagnose the subdural hematoma, stating that a CT scan should have been performed at each of his ED visits since he was on warfarin. The defense claimed that a CT scan was not warranted for each visit, and that the timing of when and how the brain bleed started was uncertain. At trial, a defense verdict was returned.
Discussion
It is well known that patients receiving warfarin are at an increased risk for intracranial hemorrhage (ICH) following blunt head trauma.1 The recommendation is that all such patients have a noncontrast CT scan of the head to rule out intracranial bleeding. This is due to the fact that 60% of patients presenting with an immediate traumatic intracranial hemorrhage will have a normal mental status on examination; and 11% will have no history of loss of consciousness, a normal mental status examination, and no physical evidence of trauma above the clavicles.1 In a study by Hart et al,2 subdural hematoma accounted for 44% of all ICH in these types of patients.
More controversial is how to manage patients on warfarin who experience blunt head trauma and have a normal CT scan of the head. Because of the fear for delayed traumatic ICH, many clinicians recommend admitting such patients for neurological observation and repeat head CT scan the next morning.3 Additionally, some clinicians even recommend reversing the warfarin anticoagulation in such patients. 4 These recommendations, though, are based on expert consensus rather than on rigorous, prospective multicenter studies.1 These strategies are also problematic, since such multiple repeat CT scans would not only be incredibly expensive but also would expose the patient to high doses of radiation to the brain. Moreover, the Centers for Medicare and Medicaid Services has now made CT brain scan imaging of patients presenting to the ED with complaint of nontraumatic headache a quality measure they follow. Their goal is to decrease the number of “unnecessary” head CT scans.
The patient in this case denied any history of trauma on the subsequent seven ED visits. Unfortunately, as pointed out, even minor trauma can result in ICH, and patients may not recall the occurrence of the event.
For patients on warfarin who present with headache, a very careful history must be taken—including inquiring about minor traumatic events. Even then, as has been shown, patients may have not experienced a loss of consciousness, have a normal mental status examination, and exhibit no external evidence of head trauma. The clinician is forced to use her or his own best judgment when evaluating such patients in the ED.
Interestingly, the risk of ICH secondary to blunt head trauma in patients on warfarin is increased if they are on concomitant aspirin therapy.2 Similarly, the risk of ICH following head trauma in patients on clopidogrel is greater than for those patients taking warfarin,1 and the risk of ICH in patients taking dabigatran is less than if taking warfarin.2
Reference - Missed Preeclampsia
- Yancey LM, Withers E, Barnes K, Abbott J. Postpartum preeclampsia: emergency department presentation and management. J Emerg Med. 2011;40(4):380-384.
- Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM. Delayed postpartum preeclampsia: an experience of 151 cases. Am J Obstet Gynecol. 2004;190(5):1464-1466.
- Al-Safi Z, Imudia AN, Filetti LC, Hobson DT, Bahado-Singh RO, Awonuga AO. Delayed postpartum preeclampsia and eclampsia: demographics, clinical course, and complications. Obstet Gynecol. 2011;118(5):1102-1107.
- Chames MC, Livingston JC, Ivester TS, Barton JR, Sibai BM. Late postpartum eclampsia: a preventable disease? Am J Obstet Gynecol. 2002;186(6):1174-1177.
- Graeber B, Vanderwal T, Stiller RJ, Werdmann MJ. Late postpartum eclampsia as an obstetric complication seen in the ED. Am J Emerg Med. 2005;23(2):168-170.
Reference - Missed Subdural Hematoma
- Nishijima DK, Offerman SR, Ballard DW, et al; Clinical Research in Emergency Services and Treatment (CREST) Network. Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and preinjury warfarin or clopidogrel use. Ann Emerg Med. 2012;59(6):460-468.
- Hart RG, Diener HC, Yang S, Connolly SJ, Wallentin L, et al. Intracranial hemorrhage in atrial fibrillation patients during anticoagulation with warfarin or dabigatran: the RE-LY trial. Stroke. 2012;43(6): 1511-1517.
- Vos PE, Battistin L, Birbamer G, et al; European Federation of Neurological Societies. EFNS guideline on mild traumatic brain injury: report of an EFNS task force. Eur J Neurol. 2002;9(3):207-219.
- Coimbra R, Hoyt DB, Anjaria DJ, Potenza BM, Fortlage D, Hollingsworth-Fridlund P. Reversal of anticoagulation in trauma: a North-American survey on clinical practices among trauma surgeons. J Trauma. 2005;59(2):375-382.
Missed Preeclampsia
| A 24-year-old woman, gravida 1, para 1, aborta 0, presented to the ED complaining of a 1-day history of shortness of breath. Four days earlier, she had delivered a healthy baby boy via normal vaginal delivery and without complication. She denied chest pain, fever, or abdominal pain. She was otherwise in good health, stating that she was not taking any medications. She also denied smoking cigarettes. |
On physical examination, the patient’s vital signs were remarkable for the following: heart rate (HR), 86 beats/minute; blood pressure (BP), 164/94 mm Hg; respiratory rate, 18 breaths/minute; temperature, 98.6oF. Oxygen saturation was 96% on room air. The head, eye, ear, nose and throat examination was unremarkable. The lungs were clear to auscultation bilaterally, and HR and heart rhythm were normal. The abdomen was soft and nontender without guarding or rebound. The lower extremities were remarkable for 1+ pedal and pretibial edema bilaterally.
The patient presented to the same ED 2 days later, again with the chief complaint of shortness of breath. On examination, her BP was noted to be elevated and she had 1+ dependent edema bilaterally. Again, the EP was concerned for a PE and ordered a repeat CTA scan of the chest. This study, similar to the first, was read as normal, and showed no evidence of PE. The patient was diagnosed again with “shortness of breath of unknown etiology” and discharged home. The patient’s obstetrician-gynecologist (Ob/Gyn) was not consulted; however, the patient was encouraged to follow up with him.
The next day, the patient presented to the same ED via emergency medical services, this time with seizures; she had no prior history of a seizure disorder. On presentation to the ED, she was noted to be postictal, with an elevated BP and tachycardic with an HR of 104 beats/minute. On examination, the lungs were clear to auscultation and the lower extremities exhibited 1+ pedal and pretibial edema. A urinalysis revealed proteinuria. The patient was given 4 g of magnesium sulfate intravenously (IV) and her Ob/Gyn was consulted.
The patient was admitted to the hospital with a diagnosis of eclampsia. She was given an IV drip of magnesium and labetalol for the high BP. Unfortunately, the patient apparently had suffered an anoxic brain injury from the previous seizures and died on hospital day 3.
The family sued the treating EPs and the hospital for failure to diagnose preeclampsia on two separate ED presentations. They noted the patient’s Ob/Gyn was never consulted; no action was taken to treat the hypertension; and no urinalysis was ordered on either visit. The EPs and hospital settled the case prior to trial for several million dollars.
Discussion
This is an incredibly sad case, and the EPs and hospital were right to settle and not go to trial. While PE was a reasonable diagnosis to consider in this patient on her first ED visit, it should not have been the only one in the differential diagnosis. The EP became anchored to this single diagnosis and refused to consider other alternative diagnoses—even after the CTA scan of the chest ruled out PE. Moreover, it appears the EP either never considered the significance of the elevated BP and dependent edema or just ignored these findings. To repeat essentially the same exact workup on the second visit does not make sense—one should “cast a wider net, not the same net.”
The diagnosis of “shortness of breath of unknown etiology” is similarly unacceptable. While this is a common and accepted diagnosis when it pertains to abdominal pain, the same is not true for dyspnea.
Preeclampsia is characterized by hypertension (BP >140/90 mm Hg) and proteinuria; associated symptoms include edema and hyperreflexia. Postpartum preeclampsia occurs infrequently and can develop up to 4 weeks after delivery.1 In one 10-year retrospective case series, the incidence of preeclampsia in the postpartum period was 5.7%, and nearly 16% went on to develop eclampsia.2 In a retrospective study of 22 postpartum preeclamptic patients, the median time to presentation was 5 days postpartum.1 In a similar retrospective study of 152 patients, 90% of such patients presented within 7 days.3 The patient in this case initially presented on postpartum day 4.
Interestingly, in a study by Al-Safi et al,3 63% of postpartum preeclamptic patients had no antecedent diagnosis of hypertensive disease during pregnancy. These findings are consistent with the findings of others that 33% to 69% of such patients show no evidence of preeclampsia in the ante- or peripartum period.
The clinical presentation of postpartum preeclampsia is similar to preeclampsia complicating pregnancy after gestation week 20. In the study by Al-Safi et al,3 headache was the most common presenting symptom (69%), followed by shortness of breath (30%), blurry vision (21%), nausea (12.5%), and epigastric abdominal pain (5%). Similarly, Yancey et al1 found headache (82%) to be the most common presenting symptom in their series. Unfortunately, it is not known whether the patient in this case complained of headache or blurred vision as the published records note neither their presence nor absence.
The management of patients with preeclampsia includes IV magnesium to prevent seizures (ie, eclampsia) and BP control.1 A bolus of 4 to 6 g IV magnesium sulfate over 15 to 30 minutes is recommended, followed by an infusion of 2 g/h IV. Historically, IV hydralazine has been used to manage preeclamptic patients with a BP greater than 160/110 mm Hg. More recently, however, IV labetalol has become popular.5 All such patients require admission to the hospital with Ob/Gyn involvement.
Missed Subdural Hematoma
A 59-year-old man presented to the ED with a chief complaint of headache, the onset of which he stated started gradually 2 days prior. He noted the headache was worse than normal but without associated nausea, vomiting, fever, chills, or change in vision. His past medical history was significant for a lower extremity deep vein thrombosis 3 months prior, for which he was taking warfarin.
The patient’s vital signs were all normal. The physical examination, including a thorough neurological examination, was also normal. The EP ordered a prothrombin time (PT), an international normalized ratio (INR), and a noncontrast CT scan of the head. The PT/INR results were therapeutic at 22 seconds and 2.3. The CT scan was interpreted by radiology services as normal. The patient’s headache was treated with IV prochlorperazine and diphenhydramine. After treatment, the patient reported feeling better and was discharged home with instructions to follow up with his primary care physician.
Over the next several months, the patient presented to the same ED on seven different occasions, each time with the chief complaint of headache. At each of these presentations, the history and physical examination were documented as unremarkable, with no history of trauma. The thoroughness, however, of the documentation varied considerably for each ED encounter. No head CT scan was ordered on the subsequent seven visits, and at each presentation, the patient was treated symptomatically and discharged home.
Two days after his eighth visit to the same hospital ED, the patient presented to a different ED, again with a chief complaint of headache. The EP at this ED ordered a noncontrast CT of the head, which demonstrated a left subdural hematoma. The patient was admitted to the hospital, given IV vitamin K and fresh frozen plasma, and underwent evacuation of the hematoma by neurosurgery. The patient’s hospital course was unremarkable, and he was discharged home without any focal weakness.
The patient, however, claimed that he suffered cognitive impairment as a result of the missed diagnosis. He sued treating EPs at the first ED as well as the hospital for failure to timely diagnose the subdural hematoma, stating that a CT scan should have been performed at each of his ED visits since he was on warfarin. The defense claimed that a CT scan was not warranted for each visit, and that the timing of when and how the brain bleed started was uncertain. At trial, a defense verdict was returned.
Discussion
It is well known that patients receiving warfarin are at an increased risk for intracranial hemorrhage (ICH) following blunt head trauma.1 The recommendation is that all such patients have a noncontrast CT scan of the head to rule out intracranial bleeding. This is due to the fact that 60% of patients presenting with an immediate traumatic intracranial hemorrhage will have a normal mental status on examination; and 11% will have no history of loss of consciousness, a normal mental status examination, and no physical evidence of trauma above the clavicles.1 In a study by Hart et al,2 subdural hematoma accounted for 44% of all ICH in these types of patients.
More controversial is how to manage patients on warfarin who experience blunt head trauma and have a normal CT scan of the head. Because of the fear for delayed traumatic ICH, many clinicians recommend admitting such patients for neurological observation and repeat head CT scan the next morning.3 Additionally, some clinicians even recommend reversing the warfarin anticoagulation in such patients. 4 These recommendations, though, are based on expert consensus rather than on rigorous, prospective multicenter studies.1 These strategies are also problematic, since such multiple repeat CT scans would not only be incredibly expensive but also would expose the patient to high doses of radiation to the brain. Moreover, the Centers for Medicare and Medicaid Services has now made CT brain scan imaging of patients presenting to the ED with complaint of nontraumatic headache a quality measure they follow. Their goal is to decrease the number of “unnecessary” head CT scans.
The patient in this case denied any history of trauma on the subsequent seven ED visits. Unfortunately, as pointed out, even minor trauma can result in ICH, and patients may not recall the occurrence of the event.
For patients on warfarin who present with headache, a very careful history must be taken—including inquiring about minor traumatic events. Even then, as has been shown, patients may have not experienced a loss of consciousness, have a normal mental status examination, and exhibit no external evidence of head trauma. The clinician is forced to use her or his own best judgment when evaluating such patients in the ED.
Interestingly, the risk of ICH secondary to blunt head trauma in patients on warfarin is increased if they are on concomitant aspirin therapy.2 Similarly, the risk of ICH following head trauma in patients on clopidogrel is greater than for those patients taking warfarin,1 and the risk of ICH in patients taking dabigatran is less than if taking warfarin.2
Missed Preeclampsia
| A 24-year-old woman, gravida 1, para 1, aborta 0, presented to the ED complaining of a 1-day history of shortness of breath. Four days earlier, she had delivered a healthy baby boy via normal vaginal delivery and without complication. She denied chest pain, fever, or abdominal pain. She was otherwise in good health, stating that she was not taking any medications. She also denied smoking cigarettes. |
On physical examination, the patient’s vital signs were remarkable for the following: heart rate (HR), 86 beats/minute; blood pressure (BP), 164/94 mm Hg; respiratory rate, 18 breaths/minute; temperature, 98.6oF. Oxygen saturation was 96% on room air. The head, eye, ear, nose and throat examination was unremarkable. The lungs were clear to auscultation bilaterally, and HR and heart rhythm were normal. The abdomen was soft and nontender without guarding or rebound. The lower extremities were remarkable for 1+ pedal and pretibial edema bilaterally.
The patient presented to the same ED 2 days later, again with the chief complaint of shortness of breath. On examination, her BP was noted to be elevated and she had 1+ dependent edema bilaterally. Again, the EP was concerned for a PE and ordered a repeat CTA scan of the chest. This study, similar to the first, was read as normal, and showed no evidence of PE. The patient was diagnosed again with “shortness of breath of unknown etiology” and discharged home. The patient’s obstetrician-gynecologist (Ob/Gyn) was not consulted; however, the patient was encouraged to follow up with him.
The next day, the patient presented to the same ED via emergency medical services, this time with seizures; she had no prior history of a seizure disorder. On presentation to the ED, she was noted to be postictal, with an elevated BP and tachycardic with an HR of 104 beats/minute. On examination, the lungs were clear to auscultation and the lower extremities exhibited 1+ pedal and pretibial edema. A urinalysis revealed proteinuria. The patient was given 4 g of magnesium sulfate intravenously (IV) and her Ob/Gyn was consulted.
The patient was admitted to the hospital with a diagnosis of eclampsia. She was given an IV drip of magnesium and labetalol for the high BP. Unfortunately, the patient apparently had suffered an anoxic brain injury from the previous seizures and died on hospital day 3.
The family sued the treating EPs and the hospital for failure to diagnose preeclampsia on two separate ED presentations. They noted the patient’s Ob/Gyn was never consulted; no action was taken to treat the hypertension; and no urinalysis was ordered on either visit. The EPs and hospital settled the case prior to trial for several million dollars.
Discussion
This is an incredibly sad case, and the EPs and hospital were right to settle and not go to trial. While PE was a reasonable diagnosis to consider in this patient on her first ED visit, it should not have been the only one in the differential diagnosis. The EP became anchored to this single diagnosis and refused to consider other alternative diagnoses—even after the CTA scan of the chest ruled out PE. Moreover, it appears the EP either never considered the significance of the elevated BP and dependent edema or just ignored these findings. To repeat essentially the same exact workup on the second visit does not make sense—one should “cast a wider net, not the same net.”
The diagnosis of “shortness of breath of unknown etiology” is similarly unacceptable. While this is a common and accepted diagnosis when it pertains to abdominal pain, the same is not true for dyspnea.
Preeclampsia is characterized by hypertension (BP >140/90 mm Hg) and proteinuria; associated symptoms include edema and hyperreflexia. Postpartum preeclampsia occurs infrequently and can develop up to 4 weeks after delivery.1 In one 10-year retrospective case series, the incidence of preeclampsia in the postpartum period was 5.7%, and nearly 16% went on to develop eclampsia.2 In a retrospective study of 22 postpartum preeclamptic patients, the median time to presentation was 5 days postpartum.1 In a similar retrospective study of 152 patients, 90% of such patients presented within 7 days.3 The patient in this case initially presented on postpartum day 4.
Interestingly, in a study by Al-Safi et al,3 63% of postpartum preeclamptic patients had no antecedent diagnosis of hypertensive disease during pregnancy. These findings are consistent with the findings of others that 33% to 69% of such patients show no evidence of preeclampsia in the ante- or peripartum period.
The clinical presentation of postpartum preeclampsia is similar to preeclampsia complicating pregnancy after gestation week 20. In the study by Al-Safi et al,3 headache was the most common presenting symptom (69%), followed by shortness of breath (30%), blurry vision (21%), nausea (12.5%), and epigastric abdominal pain (5%). Similarly, Yancey et al1 found headache (82%) to be the most common presenting symptom in their series. Unfortunately, it is not known whether the patient in this case complained of headache or blurred vision as the published records note neither their presence nor absence.
The management of patients with preeclampsia includes IV magnesium to prevent seizures (ie, eclampsia) and BP control.1 A bolus of 4 to 6 g IV magnesium sulfate over 15 to 30 minutes is recommended, followed by an infusion of 2 g/h IV. Historically, IV hydralazine has been used to manage preeclamptic patients with a BP greater than 160/110 mm Hg. More recently, however, IV labetalol has become popular.5 All such patients require admission to the hospital with Ob/Gyn involvement.
Missed Subdural Hematoma
A 59-year-old man presented to the ED with a chief complaint of headache, the onset of which he stated started gradually 2 days prior. He noted the headache was worse than normal but without associated nausea, vomiting, fever, chills, or change in vision. His past medical history was significant for a lower extremity deep vein thrombosis 3 months prior, for which he was taking warfarin.
The patient’s vital signs were all normal. The physical examination, including a thorough neurological examination, was also normal. The EP ordered a prothrombin time (PT), an international normalized ratio (INR), and a noncontrast CT scan of the head. The PT/INR results were therapeutic at 22 seconds and 2.3. The CT scan was interpreted by radiology services as normal. The patient’s headache was treated with IV prochlorperazine and diphenhydramine. After treatment, the patient reported feeling better and was discharged home with instructions to follow up with his primary care physician.
Over the next several months, the patient presented to the same ED on seven different occasions, each time with the chief complaint of headache. At each of these presentations, the history and physical examination were documented as unremarkable, with no history of trauma. The thoroughness, however, of the documentation varied considerably for each ED encounter. No head CT scan was ordered on the subsequent seven visits, and at each presentation, the patient was treated symptomatically and discharged home.
Two days after his eighth visit to the same hospital ED, the patient presented to a different ED, again with a chief complaint of headache. The EP at this ED ordered a noncontrast CT of the head, which demonstrated a left subdural hematoma. The patient was admitted to the hospital, given IV vitamin K and fresh frozen plasma, and underwent evacuation of the hematoma by neurosurgery. The patient’s hospital course was unremarkable, and he was discharged home without any focal weakness.
The patient, however, claimed that he suffered cognitive impairment as a result of the missed diagnosis. He sued treating EPs at the first ED as well as the hospital for failure to timely diagnose the subdural hematoma, stating that a CT scan should have been performed at each of his ED visits since he was on warfarin. The defense claimed that a CT scan was not warranted for each visit, and that the timing of when and how the brain bleed started was uncertain. At trial, a defense verdict was returned.
Discussion
It is well known that patients receiving warfarin are at an increased risk for intracranial hemorrhage (ICH) following blunt head trauma.1 The recommendation is that all such patients have a noncontrast CT scan of the head to rule out intracranial bleeding. This is due to the fact that 60% of patients presenting with an immediate traumatic intracranial hemorrhage will have a normal mental status on examination; and 11% will have no history of loss of consciousness, a normal mental status examination, and no physical evidence of trauma above the clavicles.1 In a study by Hart et al,2 subdural hematoma accounted for 44% of all ICH in these types of patients.
More controversial is how to manage patients on warfarin who experience blunt head trauma and have a normal CT scan of the head. Because of the fear for delayed traumatic ICH, many clinicians recommend admitting such patients for neurological observation and repeat head CT scan the next morning.3 Additionally, some clinicians even recommend reversing the warfarin anticoagulation in such patients. 4 These recommendations, though, are based on expert consensus rather than on rigorous, prospective multicenter studies.1 These strategies are also problematic, since such multiple repeat CT scans would not only be incredibly expensive but also would expose the patient to high doses of radiation to the brain. Moreover, the Centers for Medicare and Medicaid Services has now made CT brain scan imaging of patients presenting to the ED with complaint of nontraumatic headache a quality measure they follow. Their goal is to decrease the number of “unnecessary” head CT scans.
The patient in this case denied any history of trauma on the subsequent seven ED visits. Unfortunately, as pointed out, even minor trauma can result in ICH, and patients may not recall the occurrence of the event.
For patients on warfarin who present with headache, a very careful history must be taken—including inquiring about minor traumatic events. Even then, as has been shown, patients may have not experienced a loss of consciousness, have a normal mental status examination, and exhibit no external evidence of head trauma. The clinician is forced to use her or his own best judgment when evaluating such patients in the ED.
Interestingly, the risk of ICH secondary to blunt head trauma in patients on warfarin is increased if they are on concomitant aspirin therapy.2 Similarly, the risk of ICH following head trauma in patients on clopidogrel is greater than for those patients taking warfarin,1 and the risk of ICH in patients taking dabigatran is less than if taking warfarin.2
Reference - Missed Preeclampsia
- Yancey LM, Withers E, Barnes K, Abbott J. Postpartum preeclampsia: emergency department presentation and management. J Emerg Med. 2011;40(4):380-384.
- Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM. Delayed postpartum preeclampsia: an experience of 151 cases. Am J Obstet Gynecol. 2004;190(5):1464-1466.
- Al-Safi Z, Imudia AN, Filetti LC, Hobson DT, Bahado-Singh RO, Awonuga AO. Delayed postpartum preeclampsia and eclampsia: demographics, clinical course, and complications. Obstet Gynecol. 2011;118(5):1102-1107.
- Chames MC, Livingston JC, Ivester TS, Barton JR, Sibai BM. Late postpartum eclampsia: a preventable disease? Am J Obstet Gynecol. 2002;186(6):1174-1177.
- Graeber B, Vanderwal T, Stiller RJ, Werdmann MJ. Late postpartum eclampsia as an obstetric complication seen in the ED. Am J Emerg Med. 2005;23(2):168-170.
Reference - Missed Subdural Hematoma
- Nishijima DK, Offerman SR, Ballard DW, et al; Clinical Research in Emergency Services and Treatment (CREST) Network. Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and preinjury warfarin or clopidogrel use. Ann Emerg Med. 2012;59(6):460-468.
- Hart RG, Diener HC, Yang S, Connolly SJ, Wallentin L, et al. Intracranial hemorrhage in atrial fibrillation patients during anticoagulation with warfarin or dabigatran: the RE-LY trial. Stroke. 2012;43(6): 1511-1517.
- Vos PE, Battistin L, Birbamer G, et al; European Federation of Neurological Societies. EFNS guideline on mild traumatic brain injury: report of an EFNS task force. Eur J Neurol. 2002;9(3):207-219.
- Coimbra R, Hoyt DB, Anjaria DJ, Potenza BM, Fortlage D, Hollingsworth-Fridlund P. Reversal of anticoagulation in trauma: a North-American survey on clinical practices among trauma surgeons. J Trauma. 2005;59(2):375-382.
Reference - Missed Preeclampsia
- Yancey LM, Withers E, Barnes K, Abbott J. Postpartum preeclampsia: emergency department presentation and management. J Emerg Med. 2011;40(4):380-384.
- Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM. Delayed postpartum preeclampsia: an experience of 151 cases. Am J Obstet Gynecol. 2004;190(5):1464-1466.
- Al-Safi Z, Imudia AN, Filetti LC, Hobson DT, Bahado-Singh RO, Awonuga AO. Delayed postpartum preeclampsia and eclampsia: demographics, clinical course, and complications. Obstet Gynecol. 2011;118(5):1102-1107.
- Chames MC, Livingston JC, Ivester TS, Barton JR, Sibai BM. Late postpartum eclampsia: a preventable disease? Am J Obstet Gynecol. 2002;186(6):1174-1177.
- Graeber B, Vanderwal T, Stiller RJ, Werdmann MJ. Late postpartum eclampsia as an obstetric complication seen in the ED. Am J Emerg Med. 2005;23(2):168-170.
Reference - Missed Subdural Hematoma
- Nishijima DK, Offerman SR, Ballard DW, et al; Clinical Research in Emergency Services and Treatment (CREST) Network. Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and preinjury warfarin or clopidogrel use. Ann Emerg Med. 2012;59(6):460-468.
- Hart RG, Diener HC, Yang S, Connolly SJ, Wallentin L, et al. Intracranial hemorrhage in atrial fibrillation patients during anticoagulation with warfarin or dabigatran: the RE-LY trial. Stroke. 2012;43(6): 1511-1517.
- Vos PE, Battistin L, Birbamer G, et al; European Federation of Neurological Societies. EFNS guideline on mild traumatic brain injury: report of an EFNS task force. Eur J Neurol. 2002;9(3):207-219.
- Coimbra R, Hoyt DB, Anjaria DJ, Potenza BM, Fortlage D, Hollingsworth-Fridlund P. Reversal of anticoagulation in trauma: a North-American survey on clinical practices among trauma surgeons. J Trauma. 2005;59(2):375-382.
Characterization of Knuckle (Garrod) Pads Using Optical Coherence Tomography In Vivo
To the Editor:
Optical coherence tomography (OCT) is a noninvasive imaging technique that uses a low-power infrared laser light for cutaneous architecture visualization up to 2 mm in depth. Both malignant and nonmalignant lesions on OCT imaging have been correlated with histopathologic analysis.1 We describe the diagnostic features of knuckle pads on OCT.
A 43-year-old-man presented with warts on the right thumb and bilateral feet of several months’ duration with noncontributory medical and social history. Physical examination revealed nontender, well-demarcated, flesh-colored, verrucous papules on the dorsal interphalangeal joints of the right thumb and several toes (Figure 1). Pinpoint vessels were absent on dermoscopy (Figure 2). Histopathologic analysis of a shave biopsy of the lesion on the left second toe revealed dense orthokeratosis with compact keratin, suggestive of reactive hyperkeratosis or a knuckle pad (Figure 3). In situ hybridization failed to demonstrate staining for human papillomavirus types 6, 11, and 16.

| 
| |
| Figure 1. Verrucous papules on the left foot.
| Figure 2. Corresponding dermoscopy of the left second toe revealed an absence of pinpoint vessels. |
Optical coherence tomography demonstrated discrete thickening of the stratum corneum with distinctive granular and coarse textural appearance of the hyperkeratotic stratum corneum compared to normal adjacent skin. This textural difference was attributed to the alteration in collagen deposition of the knuckle pads, consistent with fibrous proliferation. Finally, OCT imaging provided further characterization of the lesion demonstrating the absence of any hair follicles and acrosyringium in areas resembling glabrous skin (Figure 4).
Knuckle pads, also known as Garrod pads, were first described by Garrod2 in 1893. They are benign, asymptomatic, fibrotic thickenings of the skin. Lesions are smooth, firm, flesh colored, and located on the dorsal aspect of the hands and feet along the metacarpophalangeal and interphalangeal joints. Knuckle pads are common, can develop at any age, and are observed more frequently in men than in women.3
Primary knuckle pads can be sporadic or associated with other conditions such as palmoplantar keratoderma, acrokeratoelastoidosis costa, fibrosing disorders, or Bart-Pumphrey syndrome.4 Secondary knuckle pads, which are more common, occur in sites of repetitive trauma or pressure. Certain occupations (eg, mechanics) or hobbies (eg, boxing) increase the risk for developing knuckle pads.3,4
The diagnosis of knuckle pads is usually made clinically, though several other conditions mimic knuckle pads, including scars, keloids, calluses, verruca vulgaris, fibromas, and rheumatoid nodules.3,5 We report a description of knuckle pads that was diagnosed with OCT imaging. Further characterization of both malignant and nonmalignant lesions on OCT imaging will contribute new insights to the role of OCT in the noninvasive diagnosis of skin diseases, pending future studies.
1. Forsea AM, Carstea EM, Ghervase L, et al. Clinical application of optical coherence tomography for the imaging of non-melanocytic cutaneous tumors: a pilot multi-modal study. J Med Life. 2010;3:381-389.
2. Garrod AE. On an unusual form of nodule upon joints of the fingers. St Bartholomew’s Hosp Rep. 1893;29:157-161.
3. Kodama BF, Gentry RH, Fitzpatrick JE. Papules and plaques over the joint spaces. knuckle pads (heloderma). Arch Dermatol. 1993;129:1044-1045, 1047.
4. Nenoff P, Woitek G. Images in clinical medicine. knuckle pads. N Engl J Med. 2011;364:2451.
5. Sehgal VN, Singh M, Saxena HM, et al. Primary knuckle pads. Clin Exp Dermatol. 1979;4:337-339.
To the Editor:
Optical coherence tomography (OCT) is a noninvasive imaging technique that uses a low-power infrared laser light for cutaneous architecture visualization up to 2 mm in depth. Both malignant and nonmalignant lesions on OCT imaging have been correlated with histopathologic analysis.1 We describe the diagnostic features of knuckle pads on OCT.
A 43-year-old-man presented with warts on the right thumb and bilateral feet of several months’ duration with noncontributory medical and social history. Physical examination revealed nontender, well-demarcated, flesh-colored, verrucous papules on the dorsal interphalangeal joints of the right thumb and several toes (Figure 1). Pinpoint vessels were absent on dermoscopy (Figure 2). Histopathologic analysis of a shave biopsy of the lesion on the left second toe revealed dense orthokeratosis with compact keratin, suggestive of reactive hyperkeratosis or a knuckle pad (Figure 3). In situ hybridization failed to demonstrate staining for human papillomavirus types 6, 11, and 16.

| 
| |
| Figure 1. Verrucous papules on the left foot.
| Figure 2. Corresponding dermoscopy of the left second toe revealed an absence of pinpoint vessels. |
Optical coherence tomography demonstrated discrete thickening of the stratum corneum with distinctive granular and coarse textural appearance of the hyperkeratotic stratum corneum compared to normal adjacent skin. This textural difference was attributed to the alteration in collagen deposition of the knuckle pads, consistent with fibrous proliferation. Finally, OCT imaging provided further characterization of the lesion demonstrating the absence of any hair follicles and acrosyringium in areas resembling glabrous skin (Figure 4).
Knuckle pads, also known as Garrod pads, were first described by Garrod2 in 1893. They are benign, asymptomatic, fibrotic thickenings of the skin. Lesions are smooth, firm, flesh colored, and located on the dorsal aspect of the hands and feet along the metacarpophalangeal and interphalangeal joints. Knuckle pads are common, can develop at any age, and are observed more frequently in men than in women.3
Primary knuckle pads can be sporadic or associated with other conditions such as palmoplantar keratoderma, acrokeratoelastoidosis costa, fibrosing disorders, or Bart-Pumphrey syndrome.4 Secondary knuckle pads, which are more common, occur in sites of repetitive trauma or pressure. Certain occupations (eg, mechanics) or hobbies (eg, boxing) increase the risk for developing knuckle pads.3,4
The diagnosis of knuckle pads is usually made clinically, though several other conditions mimic knuckle pads, including scars, keloids, calluses, verruca vulgaris, fibromas, and rheumatoid nodules.3,5 We report a description of knuckle pads that was diagnosed with OCT imaging. Further characterization of both malignant and nonmalignant lesions on OCT imaging will contribute new insights to the role of OCT in the noninvasive diagnosis of skin diseases, pending future studies.
To the Editor:
Optical coherence tomography (OCT) is a noninvasive imaging technique that uses a low-power infrared laser light for cutaneous architecture visualization up to 2 mm in depth. Both malignant and nonmalignant lesions on OCT imaging have been correlated with histopathologic analysis.1 We describe the diagnostic features of knuckle pads on OCT.
A 43-year-old-man presented with warts on the right thumb and bilateral feet of several months’ duration with noncontributory medical and social history. Physical examination revealed nontender, well-demarcated, flesh-colored, verrucous papules on the dorsal interphalangeal joints of the right thumb and several toes (Figure 1). Pinpoint vessels were absent on dermoscopy (Figure 2). Histopathologic analysis of a shave biopsy of the lesion on the left second toe revealed dense orthokeratosis with compact keratin, suggestive of reactive hyperkeratosis or a knuckle pad (Figure 3). In situ hybridization failed to demonstrate staining for human papillomavirus types 6, 11, and 16.

| 
| |
| Figure 1. Verrucous papules on the left foot.
| Figure 2. Corresponding dermoscopy of the left second toe revealed an absence of pinpoint vessels. |
Optical coherence tomography demonstrated discrete thickening of the stratum corneum with distinctive granular and coarse textural appearance of the hyperkeratotic stratum corneum compared to normal adjacent skin. This textural difference was attributed to the alteration in collagen deposition of the knuckle pads, consistent with fibrous proliferation. Finally, OCT imaging provided further characterization of the lesion demonstrating the absence of any hair follicles and acrosyringium in areas resembling glabrous skin (Figure 4).
Knuckle pads, also known as Garrod pads, were first described by Garrod2 in 1893. They are benign, asymptomatic, fibrotic thickenings of the skin. Lesions are smooth, firm, flesh colored, and located on the dorsal aspect of the hands and feet along the metacarpophalangeal and interphalangeal joints. Knuckle pads are common, can develop at any age, and are observed more frequently in men than in women.3
Primary knuckle pads can be sporadic or associated with other conditions such as palmoplantar keratoderma, acrokeratoelastoidosis costa, fibrosing disorders, or Bart-Pumphrey syndrome.4 Secondary knuckle pads, which are more common, occur in sites of repetitive trauma or pressure. Certain occupations (eg, mechanics) or hobbies (eg, boxing) increase the risk for developing knuckle pads.3,4
The diagnosis of knuckle pads is usually made clinically, though several other conditions mimic knuckle pads, including scars, keloids, calluses, verruca vulgaris, fibromas, and rheumatoid nodules.3,5 We report a description of knuckle pads that was diagnosed with OCT imaging. Further characterization of both malignant and nonmalignant lesions on OCT imaging will contribute new insights to the role of OCT in the noninvasive diagnosis of skin diseases, pending future studies.
1. Forsea AM, Carstea EM, Ghervase L, et al. Clinical application of optical coherence tomography for the imaging of non-melanocytic cutaneous tumors: a pilot multi-modal study. J Med Life. 2010;3:381-389.
2. Garrod AE. On an unusual form of nodule upon joints of the fingers. St Bartholomew’s Hosp Rep. 1893;29:157-161.
3. Kodama BF, Gentry RH, Fitzpatrick JE. Papules and plaques over the joint spaces. knuckle pads (heloderma). Arch Dermatol. 1993;129:1044-1045, 1047.
4. Nenoff P, Woitek G. Images in clinical medicine. knuckle pads. N Engl J Med. 2011;364:2451.
5. Sehgal VN, Singh M, Saxena HM, et al. Primary knuckle pads. Clin Exp Dermatol. 1979;4:337-339.
1. Forsea AM, Carstea EM, Ghervase L, et al. Clinical application of optical coherence tomography for the imaging of non-melanocytic cutaneous tumors: a pilot multi-modal study. J Med Life. 2010;3:381-389.
2. Garrod AE. On an unusual form of nodule upon joints of the fingers. St Bartholomew’s Hosp Rep. 1893;29:157-161.
3. Kodama BF, Gentry RH, Fitzpatrick JE. Papules and plaques over the joint spaces. knuckle pads (heloderma). Arch Dermatol. 1993;129:1044-1045, 1047.
4. Nenoff P, Woitek G. Images in clinical medicine. knuckle pads. N Engl J Med. 2011;364:2451.
5. Sehgal VN, Singh M, Saxena HM, et al. Primary knuckle pads. Clin Exp Dermatol. 1979;4:337-339.
Oral Lichen Planus With Malignant Transformation to Invasive Squamous Cell Carcinoma
To the Editor:
A 62-year-old woman with an extensive history of cutaneous and oral lichen planus (OLP) presented with gradual worsening of oral pain refractory to previously successful treatment regimens. The pains were described as sharp sensations originating in the right superior oral cavity, occurring almost constantly over the course of 2 months. On examination, the oral mucosa on the right side showed lacy, white, hyperkeratotic buccal lesions, as well as superficial erythematous erosion on the right upper alveolar ridge mucosa (Figure 1). On the left side, lacy, white, reticular patches were noted along the buccal mucosa. Gingival desquamation with superficial erosions were observed bilaterally, extending to the upper alveolar ridge in some locations. The skin examination revealed resolving, nonirritated, violaceous, flat-topped papules with a white-gray hue on the upper back and vulva.
The rest of the physical examination was benign, including a lack of appreciable lymphadenopathy, a cranial nerve examination without focal deficit, and the presence of fluent unaffected speech. On review of systems, the patient denied fevers, chills, weight loss, or night sweats. She had no history of skin cancer or oropharyngeal cancer. Family history revealed that her father had nonmelanoma skin cancer of the head and neck. She denied heavy alcohol use as well as history of smoking or other oral tobacco products. Laboratory tests revealed a complete blood cell count and comprehensive metabolic panel that was within reference range. Due to the refractory nature of the pain, which was out of character for OLP, the patient was referred to an oral maxillofacial surgeon who extracted right maxillary teeth adjacent to the erosion to obtain an adequate specimen for surgical biopsy of the lesion itself. Histopathology confirmed the diagnosis of chronic erosive OLP with malignant transformation to localized squamous cell carcinoma (SCC) of the right maxilla.
While awaiting treatment, she began to develop unremitting headaches and painful shooting sensations beginning in the right superior oral mucosa, radiating to the ipsilateral naris, nasolabial folds, malar cheek, and temple region. This clinical picture was consistent with neuralgia occurring along the maxillary nerve. A subsequent computed tomography scan revealed local bony destruction of the primary tumor and likely perineural involvement (Figure 2), without notable nodal involvement or metastasis (stage III: T4aN0M0). An otolaryngologist performed a wide alveolar and maxillary excision with lymph node dissection. Surgical margins were deemed as negative and there was no evidence of nodal disease. She was later seen by the oncology and radiation oncology teams and received several courses of chemoradiotherapy.

|
Figure 2. Coronal (A) and axial (B) computed tomography demonstrated right maxillary bony destruction. |
Seven months later, a new indurated ulcer was noted on the left lateral tongue. Biopsy revealed a new primary oral SCC (OSCC), which also was excised by an otolaryngologist. Recent computed tomography did not detect any recurrence or potential metastases, but the patient subsequently was lost to follow-up.
Lichen planus is an idiopathic inflammatory disease most commonly affecting the cutaneous skin as well as the oral mucosa, genital mucosa, nails, and scalp. Oral lichen planus is a relatively common manifestation, found in approximately 1% to 2% of individuals older than 15 years.1 Epidemiologic studies revealed that OLP is uncommon in children,2,3 it affects women more frequently than men (approximately 3:1 ratio),3 and its incidence peaks between 30 and 60 years of age.4 The literature on malignant transformation of OLP is varied and controversial, with some early investigations such as Krutchkoff et al5 concluding that the reported cases often fall short of supporting OLP as a premalignant source of OSCC due to insufficient evidence in claimed case reports supporting the diagnosis of OLP histopathologically, the occurrence of OSCC in sites where OLP lesions did not previously exist, and uncertainty regarding confounding factors such as carcinogen exposure.5 In contrast, a longitudinal cohort study reported malignant transformation in 2.4% of OLP cases (N=327), with a standardized incidence ratio of 17.7 (95% confidence interval, 8.8-35.3) when compared to a control group.6 Current literature has predominantly sided with the notion that OLP, especially the erosive variant, carries the risk for malignant potential6 as well as the World Health Organization’s classification of the disorder as precancerous.3
The pathophysiology of OLP and its potential for malignant transformation are unknown. It is believed that cell-mediated immunity, specifically CD8+ lymphocytes targeting stratum basale keratinocytes for apoptosis via the caspase cascade, plays a major role in the development of OLP, beginning with Langerhans cell recognition of an unknown basal cell antigen.3 Moreover, it is postulated that antigen expression is induced by certain drugs, infections, and contact allergens such as dental amalgams, explaining their known associations with OLP initiation and exacerbation. The etiology behind OLP developing into OSCC also is poorly understood and many different hypotheses have been suggested. Modified expression of p53, a 53-kd protein, in OLP patients has been demonstrated.6 Some investigators propose that a lack of the expected keratinocyte apoptotic response to the cell-mediated attack may be etiologic in cancerous transformation.3 Given their utility in treatment of OLP, there also has been apprehension over the potential for immunosuppressant medications leading to decreased expression of antitumor regulators and development of malignant cells, though it has not been substantiated by current literature.6 Finally, some cases of OSCC are believed to have been linked to N-nitrosobenzylmethylamine, a known carcinogen produced by colonized Candida albicans, which also may play a role in OLP treated with immunosuppressants.7
Clinically, OLP lesions are known to be more chronic in nature than cutaneous lichen planus.7 There are 6 classifications of OLP: reticular (lacy white with Wickham striae), plaquelike, papular, atrophic, bullous, and erosive. The latter 3 are known to be the more symptomatic manifestations.3,7 Of note, the atrophic and erosive forms are believed to account for the vast majority of cases of malignant transformation of OLP to OSCC. Approximately 90% of patients have involvement of multiple oral sites, with the most common affected areas being the buccal mucosa (90%), gingival margin (56%), and dorsal tongue (34%).7 Symptoms include increased sensitivity to foods, intense local pain, and coarse-feeling mucosa. The nature of the disease favors an active-quiescent-active course, with flares occurring after direct irritation (ie, dental procedures, Köbner phenomenon), emotional stress, medication use, and systemic illness.7 The differential diagnosis of OLP includes bite trauma, candidiasis, pemphigus, leukoplakia, lichenoid drug reaction, pemphigoid, and graft-versus-host disease.4 Red flags of malignant transformation include induration, worsening ulceration in the setting of previously effective therapy, and presence of constitutional symptoms.
Regarding the behavior of OSCC after malignant transformation, the literature seems to suggest a tendency for well-differentiated noninvasive tumors that most often occur on the buccal mucosa (43%), tongue (33%), gingiva (19%), and palate (4.8%).8 Interestingly, one study described that only 1 (4.8%) of 21 patients with OLP and OSCC was deemed as having stage II or higher disease at time of diagnosis. Likewise, 90% of the biopsied samples revealed well-differentiated carcinomas.8 These findings clearly contrast with our case in which the patient experienced rapid conversion of localized OSCC to more invasive disease. Also of consequence in this study was the finding that a relatively high proportion of patients (29% [6/21]) developed at least one other primary OSCC lesion over the course of follow-up.8 This finding is consistent with our patient.
Last, management of OLP lesions is most commonly accomplished with topical steroids such as fluocinolone acetonide or triamcinolone acetonide.3 Treatment of gingival disease may be enhanced with the use of form-fitting trays.2 For refractory erosive disease, tacrolimus ointment has been demonstrated as a useful backup therapy but may actually be associated with the development of OSCC through alteration of MAPK and p53.3 Some investigators suggest regular 4-month follow-up of OLP patients to detect if acute worsening and or refractoriness to treatment have signified early dysplastic change. Various scoring systems also have been suggested for following up on the severity of OLP lesions.3
The management of OSCC usually is accomplished via surgery, radiation, or both. The decision is dependent on tumor stage and the patient’s individual limitations. It is highly recommended that patients with OSCC arising from OLP be closely followed after diagnosis of cancer, with some sources suggesting follow-up every 2 months for the first 6 to 9 months after diagnosis due to the relatively high rate of discovery of nodal metastases and new primary lesions in that critical time span.8 Thereafter, an examination every 4 months is suggested as sufficient for detecting future complications.
1. van der Meij EH, Schepman KP, Smeele LE, et al. A review of the recent literature regarding malignant transformation of oral lichen planus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:307-310.
2. Scattarella A, Petruzzi M, Ballini A, et al. Oral lichen planus and dental hygiene: a case report [published online ahead of print September 1, 2010]. Int J Dent Hyg. 2011;9:163-166.
3. Ismail SB, Kumar SK, Zain RB. Oral lichen planus and lichenoid reactions: etiopathogenesis, diagnosis, management and malignant transformation. J Oral Sci. 2007;49:89-106.
4. Usatine RP, Tinitigan M. Diagnosis and treatment of lichen planus. Am Fam Physician. 2011;84:53-60.
5. Krutchkoff DJ, Cutler L, Laskowski S. Oral lichen planus: the evidence regarding potential malignant transformation. J Oral Pathol. 1978;7:1-7.
6. Bombeccari GP, Guzzi G, Tettamanti M, et al. Oral lichen planus and malignant transformation: a longitudinal cohort study [published online ahead of print July 22, 2011]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:328-334.
7. Eisen D. The clinical features, malignant potential, and systemic associations of oral lichen planus: a study of 723 patients. J Am Acad Dermatol. 2002;46:207-214.
8. Mignogna MD, Lo Russo L, Fedele S, et al. Clinical behaviour of malignant transforming oral lichen planus. Eur J Surg Oncol. 2002;28:838-843.
To the Editor:
A 62-year-old woman with an extensive history of cutaneous and oral lichen planus (OLP) presented with gradual worsening of oral pain refractory to previously successful treatment regimens. The pains were described as sharp sensations originating in the right superior oral cavity, occurring almost constantly over the course of 2 months. On examination, the oral mucosa on the right side showed lacy, white, hyperkeratotic buccal lesions, as well as superficial erythematous erosion on the right upper alveolar ridge mucosa (Figure 1). On the left side, lacy, white, reticular patches were noted along the buccal mucosa. Gingival desquamation with superficial erosions were observed bilaterally, extending to the upper alveolar ridge in some locations. The skin examination revealed resolving, nonirritated, violaceous, flat-topped papules with a white-gray hue on the upper back and vulva.
The rest of the physical examination was benign, including a lack of appreciable lymphadenopathy, a cranial nerve examination without focal deficit, and the presence of fluent unaffected speech. On review of systems, the patient denied fevers, chills, weight loss, or night sweats. She had no history of skin cancer or oropharyngeal cancer. Family history revealed that her father had nonmelanoma skin cancer of the head and neck. She denied heavy alcohol use as well as history of smoking or other oral tobacco products. Laboratory tests revealed a complete blood cell count and comprehensive metabolic panel that was within reference range. Due to the refractory nature of the pain, which was out of character for OLP, the patient was referred to an oral maxillofacial surgeon who extracted right maxillary teeth adjacent to the erosion to obtain an adequate specimen for surgical biopsy of the lesion itself. Histopathology confirmed the diagnosis of chronic erosive OLP with malignant transformation to localized squamous cell carcinoma (SCC) of the right maxilla.
While awaiting treatment, she began to develop unremitting headaches and painful shooting sensations beginning in the right superior oral mucosa, radiating to the ipsilateral naris, nasolabial folds, malar cheek, and temple region. This clinical picture was consistent with neuralgia occurring along the maxillary nerve. A subsequent computed tomography scan revealed local bony destruction of the primary tumor and likely perineural involvement (Figure 2), without notable nodal involvement or metastasis (stage III: T4aN0M0). An otolaryngologist performed a wide alveolar and maxillary excision with lymph node dissection. Surgical margins were deemed as negative and there was no evidence of nodal disease. She was later seen by the oncology and radiation oncology teams and received several courses of chemoradiotherapy.

|
Figure 2. Coronal (A) and axial (B) computed tomography demonstrated right maxillary bony destruction. |
Seven months later, a new indurated ulcer was noted on the left lateral tongue. Biopsy revealed a new primary oral SCC (OSCC), which also was excised by an otolaryngologist. Recent computed tomography did not detect any recurrence or potential metastases, but the patient subsequently was lost to follow-up.
Lichen planus is an idiopathic inflammatory disease most commonly affecting the cutaneous skin as well as the oral mucosa, genital mucosa, nails, and scalp. Oral lichen planus is a relatively common manifestation, found in approximately 1% to 2% of individuals older than 15 years.1 Epidemiologic studies revealed that OLP is uncommon in children,2,3 it affects women more frequently than men (approximately 3:1 ratio),3 and its incidence peaks between 30 and 60 years of age.4 The literature on malignant transformation of OLP is varied and controversial, with some early investigations such as Krutchkoff et al5 concluding that the reported cases often fall short of supporting OLP as a premalignant source of OSCC due to insufficient evidence in claimed case reports supporting the diagnosis of OLP histopathologically, the occurrence of OSCC in sites where OLP lesions did not previously exist, and uncertainty regarding confounding factors such as carcinogen exposure.5 In contrast, a longitudinal cohort study reported malignant transformation in 2.4% of OLP cases (N=327), with a standardized incidence ratio of 17.7 (95% confidence interval, 8.8-35.3) when compared to a control group.6 Current literature has predominantly sided with the notion that OLP, especially the erosive variant, carries the risk for malignant potential6 as well as the World Health Organization’s classification of the disorder as precancerous.3
The pathophysiology of OLP and its potential for malignant transformation are unknown. It is believed that cell-mediated immunity, specifically CD8+ lymphocytes targeting stratum basale keratinocytes for apoptosis via the caspase cascade, plays a major role in the development of OLP, beginning with Langerhans cell recognition of an unknown basal cell antigen.3 Moreover, it is postulated that antigen expression is induced by certain drugs, infections, and contact allergens such as dental amalgams, explaining their known associations with OLP initiation and exacerbation. The etiology behind OLP developing into OSCC also is poorly understood and many different hypotheses have been suggested. Modified expression of p53, a 53-kd protein, in OLP patients has been demonstrated.6 Some investigators propose that a lack of the expected keratinocyte apoptotic response to the cell-mediated attack may be etiologic in cancerous transformation.3 Given their utility in treatment of OLP, there also has been apprehension over the potential for immunosuppressant medications leading to decreased expression of antitumor regulators and development of malignant cells, though it has not been substantiated by current literature.6 Finally, some cases of OSCC are believed to have been linked to N-nitrosobenzylmethylamine, a known carcinogen produced by colonized Candida albicans, which also may play a role in OLP treated with immunosuppressants.7
Clinically, OLP lesions are known to be more chronic in nature than cutaneous lichen planus.7 There are 6 classifications of OLP: reticular (lacy white with Wickham striae), plaquelike, papular, atrophic, bullous, and erosive. The latter 3 are known to be the more symptomatic manifestations.3,7 Of note, the atrophic and erosive forms are believed to account for the vast majority of cases of malignant transformation of OLP to OSCC. Approximately 90% of patients have involvement of multiple oral sites, with the most common affected areas being the buccal mucosa (90%), gingival margin (56%), and dorsal tongue (34%).7 Symptoms include increased sensitivity to foods, intense local pain, and coarse-feeling mucosa. The nature of the disease favors an active-quiescent-active course, with flares occurring after direct irritation (ie, dental procedures, Köbner phenomenon), emotional stress, medication use, and systemic illness.7 The differential diagnosis of OLP includes bite trauma, candidiasis, pemphigus, leukoplakia, lichenoid drug reaction, pemphigoid, and graft-versus-host disease.4 Red flags of malignant transformation include induration, worsening ulceration in the setting of previously effective therapy, and presence of constitutional symptoms.
Regarding the behavior of OSCC after malignant transformation, the literature seems to suggest a tendency for well-differentiated noninvasive tumors that most often occur on the buccal mucosa (43%), tongue (33%), gingiva (19%), and palate (4.8%).8 Interestingly, one study described that only 1 (4.8%) of 21 patients with OLP and OSCC was deemed as having stage II or higher disease at time of diagnosis. Likewise, 90% of the biopsied samples revealed well-differentiated carcinomas.8 These findings clearly contrast with our case in which the patient experienced rapid conversion of localized OSCC to more invasive disease. Also of consequence in this study was the finding that a relatively high proportion of patients (29% [6/21]) developed at least one other primary OSCC lesion over the course of follow-up.8 This finding is consistent with our patient.
Last, management of OLP lesions is most commonly accomplished with topical steroids such as fluocinolone acetonide or triamcinolone acetonide.3 Treatment of gingival disease may be enhanced with the use of form-fitting trays.2 For refractory erosive disease, tacrolimus ointment has been demonstrated as a useful backup therapy but may actually be associated with the development of OSCC through alteration of MAPK and p53.3 Some investigators suggest regular 4-month follow-up of OLP patients to detect if acute worsening and or refractoriness to treatment have signified early dysplastic change. Various scoring systems also have been suggested for following up on the severity of OLP lesions.3
The management of OSCC usually is accomplished via surgery, radiation, or both. The decision is dependent on tumor stage and the patient’s individual limitations. It is highly recommended that patients with OSCC arising from OLP be closely followed after diagnosis of cancer, with some sources suggesting follow-up every 2 months for the first 6 to 9 months after diagnosis due to the relatively high rate of discovery of nodal metastases and new primary lesions in that critical time span.8 Thereafter, an examination every 4 months is suggested as sufficient for detecting future complications.
To the Editor:
A 62-year-old woman with an extensive history of cutaneous and oral lichen planus (OLP) presented with gradual worsening of oral pain refractory to previously successful treatment regimens. The pains were described as sharp sensations originating in the right superior oral cavity, occurring almost constantly over the course of 2 months. On examination, the oral mucosa on the right side showed lacy, white, hyperkeratotic buccal lesions, as well as superficial erythematous erosion on the right upper alveolar ridge mucosa (Figure 1). On the left side, lacy, white, reticular patches were noted along the buccal mucosa. Gingival desquamation with superficial erosions were observed bilaterally, extending to the upper alveolar ridge in some locations. The skin examination revealed resolving, nonirritated, violaceous, flat-topped papules with a white-gray hue on the upper back and vulva.
The rest of the physical examination was benign, including a lack of appreciable lymphadenopathy, a cranial nerve examination without focal deficit, and the presence of fluent unaffected speech. On review of systems, the patient denied fevers, chills, weight loss, or night sweats. She had no history of skin cancer or oropharyngeal cancer. Family history revealed that her father had nonmelanoma skin cancer of the head and neck. She denied heavy alcohol use as well as history of smoking or other oral tobacco products. Laboratory tests revealed a complete blood cell count and comprehensive metabolic panel that was within reference range. Due to the refractory nature of the pain, which was out of character for OLP, the patient was referred to an oral maxillofacial surgeon who extracted right maxillary teeth adjacent to the erosion to obtain an adequate specimen for surgical biopsy of the lesion itself. Histopathology confirmed the diagnosis of chronic erosive OLP with malignant transformation to localized squamous cell carcinoma (SCC) of the right maxilla.
While awaiting treatment, she began to develop unremitting headaches and painful shooting sensations beginning in the right superior oral mucosa, radiating to the ipsilateral naris, nasolabial folds, malar cheek, and temple region. This clinical picture was consistent with neuralgia occurring along the maxillary nerve. A subsequent computed tomography scan revealed local bony destruction of the primary tumor and likely perineural involvement (Figure 2), without notable nodal involvement or metastasis (stage III: T4aN0M0). An otolaryngologist performed a wide alveolar and maxillary excision with lymph node dissection. Surgical margins were deemed as negative and there was no evidence of nodal disease. She was later seen by the oncology and radiation oncology teams and received several courses of chemoradiotherapy.
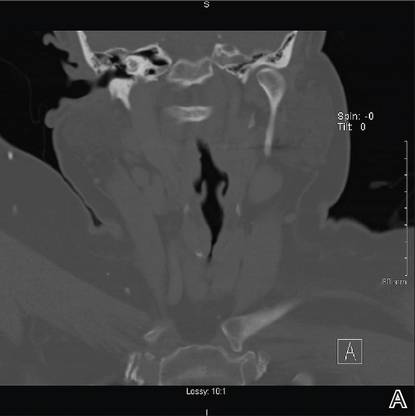

|
Figure 2. Coronal (A) and axial (B) computed tomography demonstrated right maxillary bony destruction. |
Seven months later, a new indurated ulcer was noted on the left lateral tongue. Biopsy revealed a new primary oral SCC (OSCC), which also was excised by an otolaryngologist. Recent computed tomography did not detect any recurrence or potential metastases, but the patient subsequently was lost to follow-up.
Lichen planus is an idiopathic inflammatory disease most commonly affecting the cutaneous skin as well as the oral mucosa, genital mucosa, nails, and scalp. Oral lichen planus is a relatively common manifestation, found in approximately 1% to 2% of individuals older than 15 years.1 Epidemiologic studies revealed that OLP is uncommon in children,2,3 it affects women more frequently than men (approximately 3:1 ratio),3 and its incidence peaks between 30 and 60 years of age.4 The literature on malignant transformation of OLP is varied and controversial, with some early investigations such as Krutchkoff et al5 concluding that the reported cases often fall short of supporting OLP as a premalignant source of OSCC due to insufficient evidence in claimed case reports supporting the diagnosis of OLP histopathologically, the occurrence of OSCC in sites where OLP lesions did not previously exist, and uncertainty regarding confounding factors such as carcinogen exposure.5 In contrast, a longitudinal cohort study reported malignant transformation in 2.4% of OLP cases (N=327), with a standardized incidence ratio of 17.7 (95% confidence interval, 8.8-35.3) when compared to a control group.6 Current literature has predominantly sided with the notion that OLP, especially the erosive variant, carries the risk for malignant potential6 as well as the World Health Organization’s classification of the disorder as precancerous.3
The pathophysiology of OLP and its potential for malignant transformation are unknown. It is believed that cell-mediated immunity, specifically CD8+ lymphocytes targeting stratum basale keratinocytes for apoptosis via the caspase cascade, plays a major role in the development of OLP, beginning with Langerhans cell recognition of an unknown basal cell antigen.3 Moreover, it is postulated that antigen expression is induced by certain drugs, infections, and contact allergens such as dental amalgams, explaining their known associations with OLP initiation and exacerbation. The etiology behind OLP developing into OSCC also is poorly understood and many different hypotheses have been suggested. Modified expression of p53, a 53-kd protein, in OLP patients has been demonstrated.6 Some investigators propose that a lack of the expected keratinocyte apoptotic response to the cell-mediated attack may be etiologic in cancerous transformation.3 Given their utility in treatment of OLP, there also has been apprehension over the potential for immunosuppressant medications leading to decreased expression of antitumor regulators and development of malignant cells, though it has not been substantiated by current literature.6 Finally, some cases of OSCC are believed to have been linked to N-nitrosobenzylmethylamine, a known carcinogen produced by colonized Candida albicans, which also may play a role in OLP treated with immunosuppressants.7
Clinically, OLP lesions are known to be more chronic in nature than cutaneous lichen planus.7 There are 6 classifications of OLP: reticular (lacy white with Wickham striae), plaquelike, papular, atrophic, bullous, and erosive. The latter 3 are known to be the more symptomatic manifestations.3,7 Of note, the atrophic and erosive forms are believed to account for the vast majority of cases of malignant transformation of OLP to OSCC. Approximately 90% of patients have involvement of multiple oral sites, with the most common affected areas being the buccal mucosa (90%), gingival margin (56%), and dorsal tongue (34%).7 Symptoms include increased sensitivity to foods, intense local pain, and coarse-feeling mucosa. The nature of the disease favors an active-quiescent-active course, with flares occurring after direct irritation (ie, dental procedures, Köbner phenomenon), emotional stress, medication use, and systemic illness.7 The differential diagnosis of OLP includes bite trauma, candidiasis, pemphigus, leukoplakia, lichenoid drug reaction, pemphigoid, and graft-versus-host disease.4 Red flags of malignant transformation include induration, worsening ulceration in the setting of previously effective therapy, and presence of constitutional symptoms.
Regarding the behavior of OSCC after malignant transformation, the literature seems to suggest a tendency for well-differentiated noninvasive tumors that most often occur on the buccal mucosa (43%), tongue (33%), gingiva (19%), and palate (4.8%).8 Interestingly, one study described that only 1 (4.8%) of 21 patients with OLP and OSCC was deemed as having stage II or higher disease at time of diagnosis. Likewise, 90% of the biopsied samples revealed well-differentiated carcinomas.8 These findings clearly contrast with our case in which the patient experienced rapid conversion of localized OSCC to more invasive disease. Also of consequence in this study was the finding that a relatively high proportion of patients (29% [6/21]) developed at least one other primary OSCC lesion over the course of follow-up.8 This finding is consistent with our patient.
Last, management of OLP lesions is most commonly accomplished with topical steroids such as fluocinolone acetonide or triamcinolone acetonide.3 Treatment of gingival disease may be enhanced with the use of form-fitting trays.2 For refractory erosive disease, tacrolimus ointment has been demonstrated as a useful backup therapy but may actually be associated with the development of OSCC through alteration of MAPK and p53.3 Some investigators suggest regular 4-month follow-up of OLP patients to detect if acute worsening and or refractoriness to treatment have signified early dysplastic change. Various scoring systems also have been suggested for following up on the severity of OLP lesions.3
The management of OSCC usually is accomplished via surgery, radiation, or both. The decision is dependent on tumor stage and the patient’s individual limitations. It is highly recommended that patients with OSCC arising from OLP be closely followed after diagnosis of cancer, with some sources suggesting follow-up every 2 months for the first 6 to 9 months after diagnosis due to the relatively high rate of discovery of nodal metastases and new primary lesions in that critical time span.8 Thereafter, an examination every 4 months is suggested as sufficient for detecting future complications.
1. van der Meij EH, Schepman KP, Smeele LE, et al. A review of the recent literature regarding malignant transformation of oral lichen planus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:307-310.
2. Scattarella A, Petruzzi M, Ballini A, et al. Oral lichen planus and dental hygiene: a case report [published online ahead of print September 1, 2010]. Int J Dent Hyg. 2011;9:163-166.
3. Ismail SB, Kumar SK, Zain RB. Oral lichen planus and lichenoid reactions: etiopathogenesis, diagnosis, management and malignant transformation. J Oral Sci. 2007;49:89-106.
4. Usatine RP, Tinitigan M. Diagnosis and treatment of lichen planus. Am Fam Physician. 2011;84:53-60.
5. Krutchkoff DJ, Cutler L, Laskowski S. Oral lichen planus: the evidence regarding potential malignant transformation. J Oral Pathol. 1978;7:1-7.
6. Bombeccari GP, Guzzi G, Tettamanti M, et al. Oral lichen planus and malignant transformation: a longitudinal cohort study [published online ahead of print July 22, 2011]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:328-334.
7. Eisen D. The clinical features, malignant potential, and systemic associations of oral lichen planus: a study of 723 patients. J Am Acad Dermatol. 2002;46:207-214.
8. Mignogna MD, Lo Russo L, Fedele S, et al. Clinical behaviour of malignant transforming oral lichen planus. Eur J Surg Oncol. 2002;28:838-843.
1. van der Meij EH, Schepman KP, Smeele LE, et al. A review of the recent literature regarding malignant transformation of oral lichen planus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:307-310.
2. Scattarella A, Petruzzi M, Ballini A, et al. Oral lichen planus and dental hygiene: a case report [published online ahead of print September 1, 2010]. Int J Dent Hyg. 2011;9:163-166.
3. Ismail SB, Kumar SK, Zain RB. Oral lichen planus and lichenoid reactions: etiopathogenesis, diagnosis, management and malignant transformation. J Oral Sci. 2007;49:89-106.
4. Usatine RP, Tinitigan M. Diagnosis and treatment of lichen planus. Am Fam Physician. 2011;84:53-60.
5. Krutchkoff DJ, Cutler L, Laskowski S. Oral lichen planus: the evidence regarding potential malignant transformation. J Oral Pathol. 1978;7:1-7.
6. Bombeccari GP, Guzzi G, Tettamanti M, et al. Oral lichen planus and malignant transformation: a longitudinal cohort study [published online ahead of print July 22, 2011]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:328-334.
7. Eisen D. The clinical features, malignant potential, and systemic associations of oral lichen planus: a study of 723 patients. J Am Acad Dermatol. 2002;46:207-214.
8. Mignogna MD, Lo Russo L, Fedele S, et al. Clinical behaviour of malignant transforming oral lichen planus. Eur J Surg Oncol. 2002;28:838-843.