User login
Group creates model of arterial thrombus formation

Image by Andre E.X. Brown
A group of biophysicists have developed a mathematical model of arterial thrombus formation.
The team described the process of platelet aggregation as being similar to the video game Tetris and derived equations that allowed them to reproduce the wave process of platelet aggregate formation in a blood vessel.
Mikhail Panteleev, PhD, of Moscow State University in Russia, and his colleagues described this work in PLOS ONE.
Looking at thrombus formation in the same way as the tiles stack up in Tetris is a key aspect of the team’s model. In the game, the tiles either drop down onto a flat surface or become attached to parts sticking out from the rest of the block.
The researchers said there are only 2 differences between thrombus formation and the game.
Unlike in Tetris, when a layer of a thrombus is complete, it does not disappear. So, as time passes, a thrombus is capable of obstructing the space it is in.
And Tetris includes tiles of several different shapes. But, in a thrombus, the “falling tiles” are always the same—thrombocytes.
Having described the mathematical process of how vacant areas on the surface of a growing thrombus are filled, the researchers were able to build first a 1-dimensional model (as in Tetris) and then a 2-dimensional model (where thrombocytes are deposited in a dimensional plane).
At one point, the researchers began to consider certain thrombocytes as being dimensionless and the thrombus itself as being continuous. In other words, they went from a discrete model to a continuous model.
In a discrete model, the system under study consists of individual particles, and the behavior of each particle can be tracked individually. In a continuous model, the system under study consists of solid objects that can freely change their size or any other characteristic.
The sequential solution of the equations enabled the researchers to reproduce the dynamics of thrombus growth and study clot behavior under various conditions—in the case of damage to the vascular wall, for example.
Active media and autowaves
The researchers said the process of thrombus formation is like an autowave. And the blood, which carries platelets and proteins for coagulation, is an active medium.
The term “active medium” plays a key role in non-linear dynamics—the science of mathematical modeling of a range of systems, from mixtures of interacting chemicals and lasers to forest fires and even social networks.
One way to describe an active medium is to use the example of a forest fire. Every dry tree is not simply a passive object but a potential source of thermal energy. If there is a fire near a dry tree, it too will start to burn and provide more heat, which can then ignite other trees. The ability of elements in the system to release energy is a key feature of an active medium.
In active media, a local event (lightning striking a tree, for example) can initiate a transition process in a system from one state to another (in this case, a dry tree becomes a burning tree).
This process spreads like a wave in space, and the specific physical nature of the system is not so important. The same equation can be used to describe entirely different cases.
The term “autowave” means the wave propagation process is not passive, as in the case of seismic waves traveling from an earthquake’s epicenter, but active. At each point, the wave receives more energy.
In the case of thrombus formation, these terms apply to thrombocytes flowing in plasma. The thrombocytes can go from a free-flowing state to a deposited state.
Under normal circumstances, thrombocytes flow freely in the bloodstream, but if the vascular wall becomes damaged, they start to adhere to one another and to the vascular wall.
The blood also contains proteins required for thrombus formation. Even if there are no thrombocytes, reactions with these proteins are able to help form a clot to block a damaged vessel, and these reactions also occur in the form of autowaves.
Normally, thrombi prevent blood loss in the human body when a blood vessel has become damaged. Sometimes, however, thrombus formation occurs not as a result of an injury with damage to a blood vessel, but as a result of a reaction to a pathological process.
This type of thrombus formation can block a vessel completely and cut off the blood supply to tissues and organs. This, in turn, can lead to myocardial infarction, stroke, or gangrene of the extremities.
The researchers say their new model correctly describes arterial thrombus formation. These particular thrombi consist mainly of thrombocytes, and blood proteins play a relatively small role in the process.
“We have always had difficulty working with arterial blood clots in particular, in terms of developing and implementing computer models, because the subject involves a very difficult combination of mechanics (cell attachments), hydrodynamics with variable geometry, and biochemistry,” Dr Panteleev said.
“In our paper in PLOS ONE, we tried to use the most primitive description of a thrombus as a continuous medium, rather than discrete particles. This approximation is rough in many respects, and it limits the scope of the research, but it is able to give us some common patterns.”
“On the one hand, we plan to continue to apply it to specific tasks, as far as is possible, and on the other hand, we are developing more sophisticated and advanced models with 3-dimensional blood cells, the full mechanics of their interaction, and the proper biochemistry.” ![]()

Image by Andre E.X. Brown
A group of biophysicists have developed a mathematical model of arterial thrombus formation.
The team described the process of platelet aggregation as being similar to the video game Tetris and derived equations that allowed them to reproduce the wave process of platelet aggregate formation in a blood vessel.
Mikhail Panteleev, PhD, of Moscow State University in Russia, and his colleagues described this work in PLOS ONE.
Looking at thrombus formation in the same way as the tiles stack up in Tetris is a key aspect of the team’s model. In the game, the tiles either drop down onto a flat surface or become attached to parts sticking out from the rest of the block.
The researchers said there are only 2 differences between thrombus formation and the game.
Unlike in Tetris, when a layer of a thrombus is complete, it does not disappear. So, as time passes, a thrombus is capable of obstructing the space it is in.
And Tetris includes tiles of several different shapes. But, in a thrombus, the “falling tiles” are always the same—thrombocytes.
Having described the mathematical process of how vacant areas on the surface of a growing thrombus are filled, the researchers were able to build first a 1-dimensional model (as in Tetris) and then a 2-dimensional model (where thrombocytes are deposited in a dimensional plane).
At one point, the researchers began to consider certain thrombocytes as being dimensionless and the thrombus itself as being continuous. In other words, they went from a discrete model to a continuous model.
In a discrete model, the system under study consists of individual particles, and the behavior of each particle can be tracked individually. In a continuous model, the system under study consists of solid objects that can freely change their size or any other characteristic.
The sequential solution of the equations enabled the researchers to reproduce the dynamics of thrombus growth and study clot behavior under various conditions—in the case of damage to the vascular wall, for example.
Active media and autowaves
The researchers said the process of thrombus formation is like an autowave. And the blood, which carries platelets and proteins for coagulation, is an active medium.
The term “active medium” plays a key role in non-linear dynamics—the science of mathematical modeling of a range of systems, from mixtures of interacting chemicals and lasers to forest fires and even social networks.
One way to describe an active medium is to use the example of a forest fire. Every dry tree is not simply a passive object but a potential source of thermal energy. If there is a fire near a dry tree, it too will start to burn and provide more heat, which can then ignite other trees. The ability of elements in the system to release energy is a key feature of an active medium.
In active media, a local event (lightning striking a tree, for example) can initiate a transition process in a system from one state to another (in this case, a dry tree becomes a burning tree).
This process spreads like a wave in space, and the specific physical nature of the system is not so important. The same equation can be used to describe entirely different cases.
The term “autowave” means the wave propagation process is not passive, as in the case of seismic waves traveling from an earthquake’s epicenter, but active. At each point, the wave receives more energy.
In the case of thrombus formation, these terms apply to thrombocytes flowing in plasma. The thrombocytes can go from a free-flowing state to a deposited state.
Under normal circumstances, thrombocytes flow freely in the bloodstream, but if the vascular wall becomes damaged, they start to adhere to one another and to the vascular wall.
The blood also contains proteins required for thrombus formation. Even if there are no thrombocytes, reactions with these proteins are able to help form a clot to block a damaged vessel, and these reactions also occur in the form of autowaves.
Normally, thrombi prevent blood loss in the human body when a blood vessel has become damaged. Sometimes, however, thrombus formation occurs not as a result of an injury with damage to a blood vessel, but as a result of a reaction to a pathological process.
This type of thrombus formation can block a vessel completely and cut off the blood supply to tissues and organs. This, in turn, can lead to myocardial infarction, stroke, or gangrene of the extremities.
The researchers say their new model correctly describes arterial thrombus formation. These particular thrombi consist mainly of thrombocytes, and blood proteins play a relatively small role in the process.
“We have always had difficulty working with arterial blood clots in particular, in terms of developing and implementing computer models, because the subject involves a very difficult combination of mechanics (cell attachments), hydrodynamics with variable geometry, and biochemistry,” Dr Panteleev said.
“In our paper in PLOS ONE, we tried to use the most primitive description of a thrombus as a continuous medium, rather than discrete particles. This approximation is rough in many respects, and it limits the scope of the research, but it is able to give us some common patterns.”
“On the one hand, we plan to continue to apply it to specific tasks, as far as is possible, and on the other hand, we are developing more sophisticated and advanced models with 3-dimensional blood cells, the full mechanics of their interaction, and the proper biochemistry.” ![]()

Image by Andre E.X. Brown
A group of biophysicists have developed a mathematical model of arterial thrombus formation.
The team described the process of platelet aggregation as being similar to the video game Tetris and derived equations that allowed them to reproduce the wave process of platelet aggregate formation in a blood vessel.
Mikhail Panteleev, PhD, of Moscow State University in Russia, and his colleagues described this work in PLOS ONE.
Looking at thrombus formation in the same way as the tiles stack up in Tetris is a key aspect of the team’s model. In the game, the tiles either drop down onto a flat surface or become attached to parts sticking out from the rest of the block.
The researchers said there are only 2 differences between thrombus formation and the game.
Unlike in Tetris, when a layer of a thrombus is complete, it does not disappear. So, as time passes, a thrombus is capable of obstructing the space it is in.
And Tetris includes tiles of several different shapes. But, in a thrombus, the “falling tiles” are always the same—thrombocytes.
Having described the mathematical process of how vacant areas on the surface of a growing thrombus are filled, the researchers were able to build first a 1-dimensional model (as in Tetris) and then a 2-dimensional model (where thrombocytes are deposited in a dimensional plane).
At one point, the researchers began to consider certain thrombocytes as being dimensionless and the thrombus itself as being continuous. In other words, they went from a discrete model to a continuous model.
In a discrete model, the system under study consists of individual particles, and the behavior of each particle can be tracked individually. In a continuous model, the system under study consists of solid objects that can freely change their size or any other characteristic.
The sequential solution of the equations enabled the researchers to reproduce the dynamics of thrombus growth and study clot behavior under various conditions—in the case of damage to the vascular wall, for example.
Active media and autowaves
The researchers said the process of thrombus formation is like an autowave. And the blood, which carries platelets and proteins for coagulation, is an active medium.
The term “active medium” plays a key role in non-linear dynamics—the science of mathematical modeling of a range of systems, from mixtures of interacting chemicals and lasers to forest fires and even social networks.
One way to describe an active medium is to use the example of a forest fire. Every dry tree is not simply a passive object but a potential source of thermal energy. If there is a fire near a dry tree, it too will start to burn and provide more heat, which can then ignite other trees. The ability of elements in the system to release energy is a key feature of an active medium.
In active media, a local event (lightning striking a tree, for example) can initiate a transition process in a system from one state to another (in this case, a dry tree becomes a burning tree).
This process spreads like a wave in space, and the specific physical nature of the system is not so important. The same equation can be used to describe entirely different cases.
The term “autowave” means the wave propagation process is not passive, as in the case of seismic waves traveling from an earthquake’s epicenter, but active. At each point, the wave receives more energy.
In the case of thrombus formation, these terms apply to thrombocytes flowing in plasma. The thrombocytes can go from a free-flowing state to a deposited state.
Under normal circumstances, thrombocytes flow freely in the bloodstream, but if the vascular wall becomes damaged, they start to adhere to one another and to the vascular wall.
The blood also contains proteins required for thrombus formation. Even if there are no thrombocytes, reactions with these proteins are able to help form a clot to block a damaged vessel, and these reactions also occur in the form of autowaves.
Normally, thrombi prevent blood loss in the human body when a blood vessel has become damaged. Sometimes, however, thrombus formation occurs not as a result of an injury with damage to a blood vessel, but as a result of a reaction to a pathological process.
This type of thrombus formation can block a vessel completely and cut off the blood supply to tissues and organs. This, in turn, can lead to myocardial infarction, stroke, or gangrene of the extremities.
The researchers say their new model correctly describes arterial thrombus formation. These particular thrombi consist mainly of thrombocytes, and blood proteins play a relatively small role in the process.
“We have always had difficulty working with arterial blood clots in particular, in terms of developing and implementing computer models, because the subject involves a very difficult combination of mechanics (cell attachments), hydrodynamics with variable geometry, and biochemistry,” Dr Panteleev said.
“In our paper in PLOS ONE, we tried to use the most primitive description of a thrombus as a continuous medium, rather than discrete particles. This approximation is rough in many respects, and it limits the scope of the research, but it is able to give us some common patterns.”
“On the one hand, we plan to continue to apply it to specific tasks, as far as is possible, and on the other hand, we are developing more sophisticated and advanced models with 3-dimensional blood cells, the full mechanics of their interaction, and the proper biochemistry.” ![]()
Tools may provide better genome analysis

Photo by Darren Baker
Scientists say they have developed 2 types of data analysis software that could help genomics researchers identify genetic drivers of disease with greater efficiency and accuracy.
Details on these tools were published in PLOS Computational Biology and Scientific Reports.
The first tool, MEGENA (for Multiscale Embedded Gene Co-expression Network Analysis), projects gene expression data onto a 3-dimensional sphere.
This allows scientists to study hierarchical organizational patterns in complex networks that are characteristic of diseases such as cancer, obesity, and Alzheimer’s disease.
When tested on data from The Cancer Genome Atlas (TCGA), MEGENA identified novel regulatory targets in breast and lung cancers, outperforming other co-expression analysis methods.
The second tool, SuperExactTest, establishes the first theoretical framework for assessing the statistical significance of multi-set intersections and enables users to compare large sets of data, such as gene sets produced from genome-wide association studies (GWAS) and differential expression analysis.
Scientists ran SuperExactTest on existing TCGA and GWAS data, identifying a core set of cancer genes and detecting related patterns among complex diseases.
Both tools come from the Multiscale Network Modeling Laboratory, led by Bin Zhang, PhD, an associate professor at Icahn School of Medicine at Mount Sinai in New York, New York.
“These tools fill important and unmet needs in genomics,” Dr Zhang said. “MEGENA will help scientists flesh out novel pathways and key targets in complex diseases, while SuperExactTest will provide a clearer understanding of the genome by comparing a large number of gene signatures.”
MEGENA and SuperExactTest are available as R packages on Dr Zhang’s website and CRAN (the Comprehensive R Archive Network), a repository of open-source software. ![]()

Photo by Darren Baker
Scientists say they have developed 2 types of data analysis software that could help genomics researchers identify genetic drivers of disease with greater efficiency and accuracy.
Details on these tools were published in PLOS Computational Biology and Scientific Reports.
The first tool, MEGENA (for Multiscale Embedded Gene Co-expression Network Analysis), projects gene expression data onto a 3-dimensional sphere.
This allows scientists to study hierarchical organizational patterns in complex networks that are characteristic of diseases such as cancer, obesity, and Alzheimer’s disease.
When tested on data from The Cancer Genome Atlas (TCGA), MEGENA identified novel regulatory targets in breast and lung cancers, outperforming other co-expression analysis methods.
The second tool, SuperExactTest, establishes the first theoretical framework for assessing the statistical significance of multi-set intersections and enables users to compare large sets of data, such as gene sets produced from genome-wide association studies (GWAS) and differential expression analysis.
Scientists ran SuperExactTest on existing TCGA and GWAS data, identifying a core set of cancer genes and detecting related patterns among complex diseases.
Both tools come from the Multiscale Network Modeling Laboratory, led by Bin Zhang, PhD, an associate professor at Icahn School of Medicine at Mount Sinai in New York, New York.
“These tools fill important and unmet needs in genomics,” Dr Zhang said. “MEGENA will help scientists flesh out novel pathways and key targets in complex diseases, while SuperExactTest will provide a clearer understanding of the genome by comparing a large number of gene signatures.”
MEGENA and SuperExactTest are available as R packages on Dr Zhang’s website and CRAN (the Comprehensive R Archive Network), a repository of open-source software. ![]()

Photo by Darren Baker
Scientists say they have developed 2 types of data analysis software that could help genomics researchers identify genetic drivers of disease with greater efficiency and accuracy.
Details on these tools were published in PLOS Computational Biology and Scientific Reports.
The first tool, MEGENA (for Multiscale Embedded Gene Co-expression Network Analysis), projects gene expression data onto a 3-dimensional sphere.
This allows scientists to study hierarchical organizational patterns in complex networks that are characteristic of diseases such as cancer, obesity, and Alzheimer’s disease.
When tested on data from The Cancer Genome Atlas (TCGA), MEGENA identified novel regulatory targets in breast and lung cancers, outperforming other co-expression analysis methods.
The second tool, SuperExactTest, establishes the first theoretical framework for assessing the statistical significance of multi-set intersections and enables users to compare large sets of data, such as gene sets produced from genome-wide association studies (GWAS) and differential expression analysis.
Scientists ran SuperExactTest on existing TCGA and GWAS data, identifying a core set of cancer genes and detecting related patterns among complex diseases.
Both tools come from the Multiscale Network Modeling Laboratory, led by Bin Zhang, PhD, an associate professor at Icahn School of Medicine at Mount Sinai in New York, New York.
“These tools fill important and unmet needs in genomics,” Dr Zhang said. “MEGENA will help scientists flesh out novel pathways and key targets in complex diseases, while SuperExactTest will provide a clearer understanding of the genome by comparing a large number of gene signatures.”
MEGENA and SuperExactTest are available as R packages on Dr Zhang’s website and CRAN (the Comprehensive R Archive Network), a repository of open-source software. ![]()
Practice Transition Planning: When Is the Right Time?
If you are a solo orthopedic surgeon or practice in a small group and are 55 years or older, this article is for you. The answer to the question “When is the right time to begin planning for the transition out of practice?” is now. And planning is the most important word in that sentence.
Joining your peers who’ve quit, often rather quickly, because of Obamacare, electronic health records (EHRs), or the implementation of ICD-10 (International Classification of Diseases, Tenth Revision) may prove unsatisfying. As the saying goes, “act in haste, repent at leisure.” And as a gerontologist friend of mine liked to say, “Retiring from medicine without retiring to something is risky.” He often quipped that golf didn’t count.
Recent survey results help support his point. In the 2014 Medscape Orthopedist Compensation Report,1 respondents were asked:
What is the most rewarding part of your job?
- Gratitude/relationships with patients 43%
- Being very good at what I do/Finding answers, diagnoses 31%
- Making good money at a job that I like 10%
- Knowing that I’m making the world a better place 7%
- Being proud of being a doctor 4%
- Nothing 1%
- Let’s hope you are not part of the 1%!
In the often-quoted Deloitte 2013 Survey of U.S. Physicians,2 6 in 10 respondents predicted that many physicians will retire earlier than planned in the next 1 to 3 years. Yet even in that survey, 41% of surgical specialists said that patient relationships were the most satisfying factor about practicing medicine. Protecting and promoting individual health was second (33%), and intellectual stimulation was third (16%).2
As Steve Marsh, managing partner at The Medicus Firm, Dallas, was quoted as saying about this data, “For older doctors, being a physician is much more of a lifestyle than a job.”3 In my 40 years of working with physicians, I agree. And that’s why you, dear readers, must begin the transition planning process now, if you are 55 years or older, or soon, if you are approaching this age. Unraveling yourself from the patient relationships and the profession you have enjoyed for so long will feel like a big loss for the majority of you. There will be a grieving process. You’re not just leaving a “job,” you’re leaving your “life’s work,” and the sooner you begin planning for this shift, the less uncomfortable it will be.
Transition Planning Timeline
As the Chinese saying goes, “the longest journey begins with a single step.” The first, most challenging step in transition planning is deciding to address the issue head on—whether you see yourself practicing well into your late 60s or stepping aside 3 years from now.
Here are 7 questions to get you started. Discuss them with your spouse and a trusted advisor or mentor.
1. Have you done everything that you wanted to accomplish professionally? What’s left on your “to-do” list?
2. Are you satisfied with the legacy you are leaving to your community, partners, or employees?
3. What does your spouse think? His or her age and stage may dictate some choices. One wife said she believed in Henny Youngman’s advice: “Promise to take your wife for better or worse, but not for lunch.” Younger spouses in satisfying careers may not be ready to quit or slow down.
4. What could fill the void of, as the Medscape survey indicated, the “gratitude/patient relationships” and “being good at what you do” that you would be leaving behind? Could going on medical missions satisfy your need to keep your hands in? Or volunteering for the community clinic?
5. If you were to retire within the next 6 months, what would your routine look like? Because the first year is often filled with travel and long-postponed fun, think beyond that and describe year 3. (Assume good health and adequate finances.)
6. Are there options for part-time practice? Could you ease out instead of going basically full throttle until your retirement date?
7. Are challenges such as stress, fatigue, cognitive decline, or a feeling of burnout a reality for you? Be honest with yourself. These are real issues that not only impact your decision about when to transition, but also patient safety and care.
If you’ve reached 60 years of age and haven’t thought about questions like these, you aren’t alone. Many orthopedic surgeons delay this planning exercise for the same reasons other business owners do:
You are too busy spending all of your time putting out fires. Who has time to plan? Learning the new ICD-10 codes for local coverage determinations (LCDs), hiring a new physician assistant, firing the receptionist, and, oh by the way, taking care of a full schedule of patients, takes time and reduces the time to plan.
You think “it’s not time yet.” We often hear surgeons say, “Gosh, I don’t feel __ years old!” or “I plan to work until I’m 70.” Sound familiar?
You’re afraid to think about what life would be like without your profession. So you do nothing. Imagining a life without being needed on a daily basis can be daunting. Reread the survey results above. If you don’t have interesting and emotionally rewarding activities that will fill the void, that can cause anxiety. And the fact is, the demands on physicians, especially those in solo practice, haven’t left much time for outside interests.
Discussing personal goals and financial matters with others is messy or taboo. Transitioning out of practice is an awkward and uncomfortable topic. Plus, whom do you call for help with planning the next stage of your life?
These and others on a long list of excuses and anxieties result in fewer than 70% of all surgical specialists we talk with having a viable transition plan. Many, of course, have done a superb job of funding their retirement plans and have the assets set aside to fund a comfortable lifestyle. A lot has been written on the financial aspects of retirement. Your financial advisor, broker, or banker has formulas, tools, and advice that you’ve probably been following for decades. The 2014 Medscape Orthopedist Compensation Report shows the average salary is $413,000, with private practice doctors earning even more, $439,000 on average.1 Although such salaries should ensure the funding of retirement savings plans, undeniably, the financial crisis and stock market collapse of 2008 delayed many surgeons’ retirement. Even today, some surgeons who are considering their practice finish line are looking over their shoulder at market returns with a sense of insecurity.
Recruitment Is More Likely Than Cash Out
Thinking you can sell your practice for big bucks is a false hope. In the 1970s and early 1980s, before the onslaught of managed care, it was possible to sell your practice. A young surgeon would welcome having space, staff, and patients at the ready. This is no longer the case, since patient loyalty is now impacted by health insurance plan membership.
Pocketing a hefty sum from selling the office building may not be much of a windfall either. It depends on that all-important real estate formula: location, location, location. In addition, dividends from and investment in a surgery center rarely continue once you are no longer operating.
To maximize the profit potential that remains in this last phase of practice—which in turn can attract surgical talent as you transition—you’ve got to sharpen the sword and pay attention. One surgeon attributed a revenue decline of about 30% over the last 5 years to a combination of lesser insurance reimbursements, his taking more time off, and failing to pay attention to his staff’s write-off habits. Revenue cycle, management, coding, and practice operations must be finely tuned to optimize profitability, and failing to manage your practice effectively will make it less attractive when recruiting a younger surgeon to take your place or assume the patient base. Consider a practice evaluation regardless of where you are in your planning, which will help the practice prioritize improvements that deliver the best benefit and value within the context of your transition plan.
And if recruitment is part of that plan, be prepared to spend significant time on the search. Solo and small groups are finding it challenging to recruit just-out-of-training associates. This generation of new physicians values work-life balance and is more likely to prefer employment to entrepreneurship. Additionally, established physicians who have not invested in or adopted new technologies, such as EHR, will have a tough time attracting top talent. Having been trained using EHRs, few, if any, young doctors will find a reversion to paper records acceptable—and, in fact, most find it a turnoff. Thus, depending on your transition plan and your age and stage, updating technology may be a necessary investment.
Stepping Down But Not Out
If you’re thinking about slowing down but not ceasing practice completely just yet, 2 options are worth considering: practicing part-time and/or becoming a nonoperative orthopedist.
The 2014 Orthopaedic Practice in the United States (OPUS) report issued by the American Academy of Orthopaedic Surgeons shows that the average age of part-time surgeons is 69.14 years and that 48.6% are generalists.5 Part-time surgeons surveyed reported working an average of 23 hours per week and performing 5 procedures per month, compared with full-time surgeons who clock in at 56 hours per week and perform 31 procedures per month.5
Senior surgeons who want to pull back their hours or become nonoperative orthopedists may be quite marketable to group practices. There are several reasons for this. First, population growth will not be supported by the number of physicians graduating from Medicare-sponsored residency slots—which have not increased since 1997. Second, the physician workforce is growing older, and younger surgeons are harder to recruit. They tend to emphasize work-life balance over working the countless hours their senior counterparts did, and, thus, don’t treat as many patients as older colleagues did. And, third, a nonoperative or part-time physician may be more appealing to patients than nonphysician providers, yet accomplish the same purpose of keeping operating surgeons out of the office and in the operating room. So, that former competitor down the street may become a potential employer. You won’t be a voting partner, but that may be a low priority as you step into part-time practice.
We imagine an opportunity for nonoperative orthopedists similar to concierge internists, who go out of network and charge reasonable fees for longer appointments and less paperwork hassle. And this opportunity isn’t only for those practicing in groups. Solo orthopedists may see this change in practice attractive, as it offers reduced professional liability premiums, holds some clear attraction for patients not eager to go under the knife, and makes it easier to arrange time off for the doctor.
As I often tell clients about their business: “Plan your work, and work your plan.” This same maxim holds true of planning for retirement. The intangible aspects of leaving your livelihood require thought and contemplation. My hope is that you’ll put pen to paper and document the answers to the questions posed in this article, so they begin to become as important as the financial aspects of your retirement planning. Of course, the plan may be waylaid midstream owing to reimbursement challenges, an offer you can’t refuse from the hospital, or a change in your health or that of your spouse. However, taking that single step and starting your plan will give you the foundation necessary to move forward or pivot in the journey ahead.
1. Peckham C. Medscape Orthopedist Compensation Report 2014. Medscape website. http://www.medscape.com/features/slideshow/compensation/2014/orthopedics#1. Published April 15, 2014. Accessed October 29, 2015.
2. Deloitte 2013 Survey of U.S. Physicians: Physician Perspectives About Health Care Reform and the Future of the Medical Profession. Deloitte Center for Health Solutions website. http://www2.deloitte.com/content/dam/Deloitte/us/Documents/life-sciences-health-care/us-lshc-deloitte-2013-physician-survey-10012014.pdf. Accessed October 29, 2015.
3. Hyden M. Are physicians retiring early? MGMA Connection Plus. Medical Group Management Association website. http://www.mgma.com/practice-resources/mgma-connection-plus/online-only/2015/august-(1)/are-physicians-retiring-early. Published July 28, 2015. Accessed November 10, 2015.
4. The Doctor is Out: A Physician’s Guide to Closing a Practice. North Carolina Medical Board website. http://www.ncmedboard.org/images/uploads/article_images/Physicians_Guide_to_Closing_a_Practice_05_12_2014.pdf. Published May 12, 2014. Accessed October 29, 2015.
5. Oreluk H, Cherf J. Practice settings and productivity. AAOS Now. 2015;9(10). http://www.aaos.org/news/aaosnow/oct15/managing1.asp. Accessed October 29, 2015.
If you are a solo orthopedic surgeon or practice in a small group and are 55 years or older, this article is for you. The answer to the question “When is the right time to begin planning for the transition out of practice?” is now. And planning is the most important word in that sentence.
Joining your peers who’ve quit, often rather quickly, because of Obamacare, electronic health records (EHRs), or the implementation of ICD-10 (International Classification of Diseases, Tenth Revision) may prove unsatisfying. As the saying goes, “act in haste, repent at leisure.” And as a gerontologist friend of mine liked to say, “Retiring from medicine without retiring to something is risky.” He often quipped that golf didn’t count.
Recent survey results help support his point. In the 2014 Medscape Orthopedist Compensation Report,1 respondents were asked:
What is the most rewarding part of your job?
- Gratitude/relationships with patients 43%
- Being very good at what I do/Finding answers, diagnoses 31%
- Making good money at a job that I like 10%
- Knowing that I’m making the world a better place 7%
- Being proud of being a doctor 4%
- Nothing 1%
- Let’s hope you are not part of the 1%!
In the often-quoted Deloitte 2013 Survey of U.S. Physicians,2 6 in 10 respondents predicted that many physicians will retire earlier than planned in the next 1 to 3 years. Yet even in that survey, 41% of surgical specialists said that patient relationships were the most satisfying factor about practicing medicine. Protecting and promoting individual health was second (33%), and intellectual stimulation was third (16%).2
As Steve Marsh, managing partner at The Medicus Firm, Dallas, was quoted as saying about this data, “For older doctors, being a physician is much more of a lifestyle than a job.”3 In my 40 years of working with physicians, I agree. And that’s why you, dear readers, must begin the transition planning process now, if you are 55 years or older, or soon, if you are approaching this age. Unraveling yourself from the patient relationships and the profession you have enjoyed for so long will feel like a big loss for the majority of you. There will be a grieving process. You’re not just leaving a “job,” you’re leaving your “life’s work,” and the sooner you begin planning for this shift, the less uncomfortable it will be.
Transition Planning Timeline
As the Chinese saying goes, “the longest journey begins with a single step.” The first, most challenging step in transition planning is deciding to address the issue head on—whether you see yourself practicing well into your late 60s or stepping aside 3 years from now.
Here are 7 questions to get you started. Discuss them with your spouse and a trusted advisor or mentor.
1. Have you done everything that you wanted to accomplish professionally? What’s left on your “to-do” list?
2. Are you satisfied with the legacy you are leaving to your community, partners, or employees?
3. What does your spouse think? His or her age and stage may dictate some choices. One wife said she believed in Henny Youngman’s advice: “Promise to take your wife for better or worse, but not for lunch.” Younger spouses in satisfying careers may not be ready to quit or slow down.
4. What could fill the void of, as the Medscape survey indicated, the “gratitude/patient relationships” and “being good at what you do” that you would be leaving behind? Could going on medical missions satisfy your need to keep your hands in? Or volunteering for the community clinic?
5. If you were to retire within the next 6 months, what would your routine look like? Because the first year is often filled with travel and long-postponed fun, think beyond that and describe year 3. (Assume good health and adequate finances.)
6. Are there options for part-time practice? Could you ease out instead of going basically full throttle until your retirement date?
7. Are challenges such as stress, fatigue, cognitive decline, or a feeling of burnout a reality for you? Be honest with yourself. These are real issues that not only impact your decision about when to transition, but also patient safety and care.
If you’ve reached 60 years of age and haven’t thought about questions like these, you aren’t alone. Many orthopedic surgeons delay this planning exercise for the same reasons other business owners do:
You are too busy spending all of your time putting out fires. Who has time to plan? Learning the new ICD-10 codes for local coverage determinations (LCDs), hiring a new physician assistant, firing the receptionist, and, oh by the way, taking care of a full schedule of patients, takes time and reduces the time to plan.
You think “it’s not time yet.” We often hear surgeons say, “Gosh, I don’t feel __ years old!” or “I plan to work until I’m 70.” Sound familiar?
You’re afraid to think about what life would be like without your profession. So you do nothing. Imagining a life without being needed on a daily basis can be daunting. Reread the survey results above. If you don’t have interesting and emotionally rewarding activities that will fill the void, that can cause anxiety. And the fact is, the demands on physicians, especially those in solo practice, haven’t left much time for outside interests.
Discussing personal goals and financial matters with others is messy or taboo. Transitioning out of practice is an awkward and uncomfortable topic. Plus, whom do you call for help with planning the next stage of your life?
These and others on a long list of excuses and anxieties result in fewer than 70% of all surgical specialists we talk with having a viable transition plan. Many, of course, have done a superb job of funding their retirement plans and have the assets set aside to fund a comfortable lifestyle. A lot has been written on the financial aspects of retirement. Your financial advisor, broker, or banker has formulas, tools, and advice that you’ve probably been following for decades. The 2014 Medscape Orthopedist Compensation Report shows the average salary is $413,000, with private practice doctors earning even more, $439,000 on average.1 Although such salaries should ensure the funding of retirement savings plans, undeniably, the financial crisis and stock market collapse of 2008 delayed many surgeons’ retirement. Even today, some surgeons who are considering their practice finish line are looking over their shoulder at market returns with a sense of insecurity.
Recruitment Is More Likely Than Cash Out
Thinking you can sell your practice for big bucks is a false hope. In the 1970s and early 1980s, before the onslaught of managed care, it was possible to sell your practice. A young surgeon would welcome having space, staff, and patients at the ready. This is no longer the case, since patient loyalty is now impacted by health insurance plan membership.
Pocketing a hefty sum from selling the office building may not be much of a windfall either. It depends on that all-important real estate formula: location, location, location. In addition, dividends from and investment in a surgery center rarely continue once you are no longer operating.
To maximize the profit potential that remains in this last phase of practice—which in turn can attract surgical talent as you transition—you’ve got to sharpen the sword and pay attention. One surgeon attributed a revenue decline of about 30% over the last 5 years to a combination of lesser insurance reimbursements, his taking more time off, and failing to pay attention to his staff’s write-off habits. Revenue cycle, management, coding, and practice operations must be finely tuned to optimize profitability, and failing to manage your practice effectively will make it less attractive when recruiting a younger surgeon to take your place or assume the patient base. Consider a practice evaluation regardless of where you are in your planning, which will help the practice prioritize improvements that deliver the best benefit and value within the context of your transition plan.
And if recruitment is part of that plan, be prepared to spend significant time on the search. Solo and small groups are finding it challenging to recruit just-out-of-training associates. This generation of new physicians values work-life balance and is more likely to prefer employment to entrepreneurship. Additionally, established physicians who have not invested in or adopted new technologies, such as EHR, will have a tough time attracting top talent. Having been trained using EHRs, few, if any, young doctors will find a reversion to paper records acceptable—and, in fact, most find it a turnoff. Thus, depending on your transition plan and your age and stage, updating technology may be a necessary investment.
Stepping Down But Not Out
If you’re thinking about slowing down but not ceasing practice completely just yet, 2 options are worth considering: practicing part-time and/or becoming a nonoperative orthopedist.
The 2014 Orthopaedic Practice in the United States (OPUS) report issued by the American Academy of Orthopaedic Surgeons shows that the average age of part-time surgeons is 69.14 years and that 48.6% are generalists.5 Part-time surgeons surveyed reported working an average of 23 hours per week and performing 5 procedures per month, compared with full-time surgeons who clock in at 56 hours per week and perform 31 procedures per month.5
Senior surgeons who want to pull back their hours or become nonoperative orthopedists may be quite marketable to group practices. There are several reasons for this. First, population growth will not be supported by the number of physicians graduating from Medicare-sponsored residency slots—which have not increased since 1997. Second, the physician workforce is growing older, and younger surgeons are harder to recruit. They tend to emphasize work-life balance over working the countless hours their senior counterparts did, and, thus, don’t treat as many patients as older colleagues did. And, third, a nonoperative or part-time physician may be more appealing to patients than nonphysician providers, yet accomplish the same purpose of keeping operating surgeons out of the office and in the operating room. So, that former competitor down the street may become a potential employer. You won’t be a voting partner, but that may be a low priority as you step into part-time practice.
We imagine an opportunity for nonoperative orthopedists similar to concierge internists, who go out of network and charge reasonable fees for longer appointments and less paperwork hassle. And this opportunity isn’t only for those practicing in groups. Solo orthopedists may see this change in practice attractive, as it offers reduced professional liability premiums, holds some clear attraction for patients not eager to go under the knife, and makes it easier to arrange time off for the doctor.
As I often tell clients about their business: “Plan your work, and work your plan.” This same maxim holds true of planning for retirement. The intangible aspects of leaving your livelihood require thought and contemplation. My hope is that you’ll put pen to paper and document the answers to the questions posed in this article, so they begin to become as important as the financial aspects of your retirement planning. Of course, the plan may be waylaid midstream owing to reimbursement challenges, an offer you can’t refuse from the hospital, or a change in your health or that of your spouse. However, taking that single step and starting your plan will give you the foundation necessary to move forward or pivot in the journey ahead.
If you are a solo orthopedic surgeon or practice in a small group and are 55 years or older, this article is for you. The answer to the question “When is the right time to begin planning for the transition out of practice?” is now. And planning is the most important word in that sentence.
Joining your peers who’ve quit, often rather quickly, because of Obamacare, electronic health records (EHRs), or the implementation of ICD-10 (International Classification of Diseases, Tenth Revision) may prove unsatisfying. As the saying goes, “act in haste, repent at leisure.” And as a gerontologist friend of mine liked to say, “Retiring from medicine without retiring to something is risky.” He often quipped that golf didn’t count.
Recent survey results help support his point. In the 2014 Medscape Orthopedist Compensation Report,1 respondents were asked:
What is the most rewarding part of your job?
- Gratitude/relationships with patients 43%
- Being very good at what I do/Finding answers, diagnoses 31%
- Making good money at a job that I like 10%
- Knowing that I’m making the world a better place 7%
- Being proud of being a doctor 4%
- Nothing 1%
- Let’s hope you are not part of the 1%!
In the often-quoted Deloitte 2013 Survey of U.S. Physicians,2 6 in 10 respondents predicted that many physicians will retire earlier than planned in the next 1 to 3 years. Yet even in that survey, 41% of surgical specialists said that patient relationships were the most satisfying factor about practicing medicine. Protecting and promoting individual health was second (33%), and intellectual stimulation was third (16%).2
As Steve Marsh, managing partner at The Medicus Firm, Dallas, was quoted as saying about this data, “For older doctors, being a physician is much more of a lifestyle than a job.”3 In my 40 years of working with physicians, I agree. And that’s why you, dear readers, must begin the transition planning process now, if you are 55 years or older, or soon, if you are approaching this age. Unraveling yourself from the patient relationships and the profession you have enjoyed for so long will feel like a big loss for the majority of you. There will be a grieving process. You’re not just leaving a “job,” you’re leaving your “life’s work,” and the sooner you begin planning for this shift, the less uncomfortable it will be.
Transition Planning Timeline
As the Chinese saying goes, “the longest journey begins with a single step.” The first, most challenging step in transition planning is deciding to address the issue head on—whether you see yourself practicing well into your late 60s or stepping aside 3 years from now.
Here are 7 questions to get you started. Discuss them with your spouse and a trusted advisor or mentor.
1. Have you done everything that you wanted to accomplish professionally? What’s left on your “to-do” list?
2. Are you satisfied with the legacy you are leaving to your community, partners, or employees?
3. What does your spouse think? His or her age and stage may dictate some choices. One wife said she believed in Henny Youngman’s advice: “Promise to take your wife for better or worse, but not for lunch.” Younger spouses in satisfying careers may not be ready to quit or slow down.
4. What could fill the void of, as the Medscape survey indicated, the “gratitude/patient relationships” and “being good at what you do” that you would be leaving behind? Could going on medical missions satisfy your need to keep your hands in? Or volunteering for the community clinic?
5. If you were to retire within the next 6 months, what would your routine look like? Because the first year is often filled with travel and long-postponed fun, think beyond that and describe year 3. (Assume good health and adequate finances.)
6. Are there options for part-time practice? Could you ease out instead of going basically full throttle until your retirement date?
7. Are challenges such as stress, fatigue, cognitive decline, or a feeling of burnout a reality for you? Be honest with yourself. These are real issues that not only impact your decision about when to transition, but also patient safety and care.
If you’ve reached 60 years of age and haven’t thought about questions like these, you aren’t alone. Many orthopedic surgeons delay this planning exercise for the same reasons other business owners do:
You are too busy spending all of your time putting out fires. Who has time to plan? Learning the new ICD-10 codes for local coverage determinations (LCDs), hiring a new physician assistant, firing the receptionist, and, oh by the way, taking care of a full schedule of patients, takes time and reduces the time to plan.
You think “it’s not time yet.” We often hear surgeons say, “Gosh, I don’t feel __ years old!” or “I plan to work until I’m 70.” Sound familiar?
You’re afraid to think about what life would be like without your profession. So you do nothing. Imagining a life without being needed on a daily basis can be daunting. Reread the survey results above. If you don’t have interesting and emotionally rewarding activities that will fill the void, that can cause anxiety. And the fact is, the demands on physicians, especially those in solo practice, haven’t left much time for outside interests.
Discussing personal goals and financial matters with others is messy or taboo. Transitioning out of practice is an awkward and uncomfortable topic. Plus, whom do you call for help with planning the next stage of your life?
These and others on a long list of excuses and anxieties result in fewer than 70% of all surgical specialists we talk with having a viable transition plan. Many, of course, have done a superb job of funding their retirement plans and have the assets set aside to fund a comfortable lifestyle. A lot has been written on the financial aspects of retirement. Your financial advisor, broker, or banker has formulas, tools, and advice that you’ve probably been following for decades. The 2014 Medscape Orthopedist Compensation Report shows the average salary is $413,000, with private practice doctors earning even more, $439,000 on average.1 Although such salaries should ensure the funding of retirement savings plans, undeniably, the financial crisis and stock market collapse of 2008 delayed many surgeons’ retirement. Even today, some surgeons who are considering their practice finish line are looking over their shoulder at market returns with a sense of insecurity.
Recruitment Is More Likely Than Cash Out
Thinking you can sell your practice for big bucks is a false hope. In the 1970s and early 1980s, before the onslaught of managed care, it was possible to sell your practice. A young surgeon would welcome having space, staff, and patients at the ready. This is no longer the case, since patient loyalty is now impacted by health insurance plan membership.
Pocketing a hefty sum from selling the office building may not be much of a windfall either. It depends on that all-important real estate formula: location, location, location. In addition, dividends from and investment in a surgery center rarely continue once you are no longer operating.
To maximize the profit potential that remains in this last phase of practice—which in turn can attract surgical talent as you transition—you’ve got to sharpen the sword and pay attention. One surgeon attributed a revenue decline of about 30% over the last 5 years to a combination of lesser insurance reimbursements, his taking more time off, and failing to pay attention to his staff’s write-off habits. Revenue cycle, management, coding, and practice operations must be finely tuned to optimize profitability, and failing to manage your practice effectively will make it less attractive when recruiting a younger surgeon to take your place or assume the patient base. Consider a practice evaluation regardless of where you are in your planning, which will help the practice prioritize improvements that deliver the best benefit and value within the context of your transition plan.
And if recruitment is part of that plan, be prepared to spend significant time on the search. Solo and small groups are finding it challenging to recruit just-out-of-training associates. This generation of new physicians values work-life balance and is more likely to prefer employment to entrepreneurship. Additionally, established physicians who have not invested in or adopted new technologies, such as EHR, will have a tough time attracting top talent. Having been trained using EHRs, few, if any, young doctors will find a reversion to paper records acceptable—and, in fact, most find it a turnoff. Thus, depending on your transition plan and your age and stage, updating technology may be a necessary investment.
Stepping Down But Not Out
If you’re thinking about slowing down but not ceasing practice completely just yet, 2 options are worth considering: practicing part-time and/or becoming a nonoperative orthopedist.
The 2014 Orthopaedic Practice in the United States (OPUS) report issued by the American Academy of Orthopaedic Surgeons shows that the average age of part-time surgeons is 69.14 years and that 48.6% are generalists.5 Part-time surgeons surveyed reported working an average of 23 hours per week and performing 5 procedures per month, compared with full-time surgeons who clock in at 56 hours per week and perform 31 procedures per month.5
Senior surgeons who want to pull back their hours or become nonoperative orthopedists may be quite marketable to group practices. There are several reasons for this. First, population growth will not be supported by the number of physicians graduating from Medicare-sponsored residency slots—which have not increased since 1997. Second, the physician workforce is growing older, and younger surgeons are harder to recruit. They tend to emphasize work-life balance over working the countless hours their senior counterparts did, and, thus, don’t treat as many patients as older colleagues did. And, third, a nonoperative or part-time physician may be more appealing to patients than nonphysician providers, yet accomplish the same purpose of keeping operating surgeons out of the office and in the operating room. So, that former competitor down the street may become a potential employer. You won’t be a voting partner, but that may be a low priority as you step into part-time practice.
We imagine an opportunity for nonoperative orthopedists similar to concierge internists, who go out of network and charge reasonable fees for longer appointments and less paperwork hassle. And this opportunity isn’t only for those practicing in groups. Solo orthopedists may see this change in practice attractive, as it offers reduced professional liability premiums, holds some clear attraction for patients not eager to go under the knife, and makes it easier to arrange time off for the doctor.
As I often tell clients about their business: “Plan your work, and work your plan.” This same maxim holds true of planning for retirement. The intangible aspects of leaving your livelihood require thought and contemplation. My hope is that you’ll put pen to paper and document the answers to the questions posed in this article, so they begin to become as important as the financial aspects of your retirement planning. Of course, the plan may be waylaid midstream owing to reimbursement challenges, an offer you can’t refuse from the hospital, or a change in your health or that of your spouse. However, taking that single step and starting your plan will give you the foundation necessary to move forward or pivot in the journey ahead.
1. Peckham C. Medscape Orthopedist Compensation Report 2014. Medscape website. http://www.medscape.com/features/slideshow/compensation/2014/orthopedics#1. Published April 15, 2014. Accessed October 29, 2015.
2. Deloitte 2013 Survey of U.S. Physicians: Physician Perspectives About Health Care Reform and the Future of the Medical Profession. Deloitte Center for Health Solutions website. http://www2.deloitte.com/content/dam/Deloitte/us/Documents/life-sciences-health-care/us-lshc-deloitte-2013-physician-survey-10012014.pdf. Accessed October 29, 2015.
3. Hyden M. Are physicians retiring early? MGMA Connection Plus. Medical Group Management Association website. http://www.mgma.com/practice-resources/mgma-connection-plus/online-only/2015/august-(1)/are-physicians-retiring-early. Published July 28, 2015. Accessed November 10, 2015.
4. The Doctor is Out: A Physician’s Guide to Closing a Practice. North Carolina Medical Board website. http://www.ncmedboard.org/images/uploads/article_images/Physicians_Guide_to_Closing_a_Practice_05_12_2014.pdf. Published May 12, 2014. Accessed October 29, 2015.
5. Oreluk H, Cherf J. Practice settings and productivity. AAOS Now. 2015;9(10). http://www.aaos.org/news/aaosnow/oct15/managing1.asp. Accessed October 29, 2015.
1. Peckham C. Medscape Orthopedist Compensation Report 2014. Medscape website. http://www.medscape.com/features/slideshow/compensation/2014/orthopedics#1. Published April 15, 2014. Accessed October 29, 2015.
2. Deloitte 2013 Survey of U.S. Physicians: Physician Perspectives About Health Care Reform and the Future of the Medical Profession. Deloitte Center for Health Solutions website. http://www2.deloitte.com/content/dam/Deloitte/us/Documents/life-sciences-health-care/us-lshc-deloitte-2013-physician-survey-10012014.pdf. Accessed October 29, 2015.
3. Hyden M. Are physicians retiring early? MGMA Connection Plus. Medical Group Management Association website. http://www.mgma.com/practice-resources/mgma-connection-plus/online-only/2015/august-(1)/are-physicians-retiring-early. Published July 28, 2015. Accessed November 10, 2015.
4. The Doctor is Out: A Physician’s Guide to Closing a Practice. North Carolina Medical Board website. http://www.ncmedboard.org/images/uploads/article_images/Physicians_Guide_to_Closing_a_Practice_05_12_2014.pdf. Published May 12, 2014. Accessed October 29, 2015.
5. Oreluk H, Cherf J. Practice settings and productivity. AAOS Now. 2015;9(10). http://www.aaos.org/news/aaosnow/oct15/managing1.asp. Accessed October 29, 2015.
Magnetic Resonance Imaging of Complications of Anterior Cruciate Ligament Reconstruction
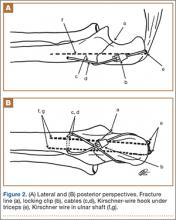
Magnetic resonance imaging (MRI) is the preferred modality in the evaluation of complications of anterior cruciate ligament reconstruction (ACL-R).1-3 ACL-R complications may be broadly characterized as those resulting in decreased range of motion (ROM), eg, arthrofibrosis and impingement, and those resulting in increased laxity, ie, graft disruption.4 Short tau inversion recovery (STIR) sequences best minimize artifact related to field inhomogeneity in the presence of metal-containing fixation devices. Patients with contraindications to MRI may undergo high-resolution computed tomographic arthrography of the knee for evaluation of postoperative graft abnormalities.1
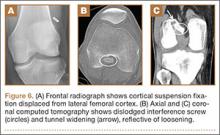
Arthrofibrosis refers to focal or diffuse synovial scar tissue, which may limit ROM. Preoperative irritation, preoperative limited ROM, and reconstruction within 4 weeks of trauma may all play a role in the development of arthrofibrosis.5,6 The focal form, cyclops lesion, named for its arthroscopic appearance, has been reported in 1% to 10% of patients with ACL-R.1 On MRI, focal arthrofibrosis may be seen as a focal or diffuse intermediate signal lesion in the anterior intercondylar notch extending linearly along the intercondylar roof1 (Figure 1).
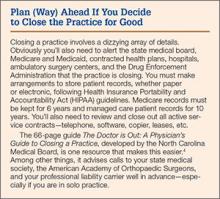
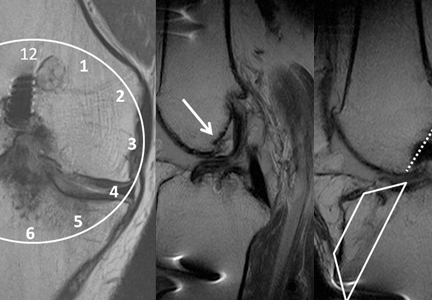
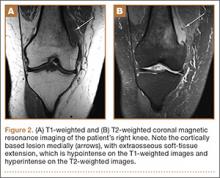
MRI can be used to accurately determine the position of the femoral and tibial tunnels. Correct femoral tunnel position results in isometry of the graft during full ROM of the knee. Graft impingement can occur when the tibial tunnel is placed too far anteriorly such that the graft contacts the roof of the intercondylar notch before the knee is able to fully extend.7 A tibial tunnel placed anterior to the intersection of the Blumensaat line and the tibia is at higher risk for impingement.1,4 Impingement may be accompanied by signal change in the graft on intermediate-weighted and fluid-sensitive sequences. The signal abnormality is usually focal and persists longer than the expected signal changes related to revascularization of immature grafts within the first year (Figure 2). If left untreated, impingement may progress to graft rupture.4
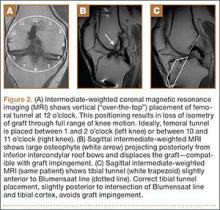
Complete graft rupture is diagnosed on the basis of discontinuity of the graft fibers. MRI findings include fluid-filled defect or absence of intact graft fibers. Other reliable signs include large joint effusion, anterior tibial translation, pivot-shift–type marrow edema pattern, and horizontal orientation, laxity, or resorption of the graft fibers.1,8,9 The diagnosis of partial graft rupture may be challenging, as there are several other causes of increased graft signal, including revascularization (within 12 months after procedure), signal heterogeneity between individual bundles of hamstring grafts, and focal signal changes related to impingment (Figures 3, 4).
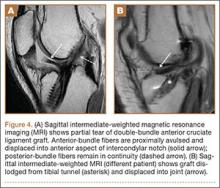
Fluid within the tunnels is a normal finding after surgery and typically resolves within the first 18 months.1 Cyst formation within the tibial tunnel is an uncommon complication of ACL-R and may be incidental to or present with clinical symptoms caused by extension into the pretibial soft tissues or expansion of the tunnel (Figure 5). Communication of cyst with joint space is important, as a noncommunicating cyst requires simple excision without need for bone grafting.7
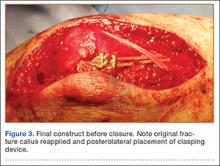
Hardware-related complications (eg, loosening of fixation devices) are uncommon but may require revision surgery (Figure 6). Septic arthritis after ACL-R has a cumulative incidence of 0.1% to 0.9% and may be difficult to diagnose clinically because of the lack of classic symptoms of a septic joint.1 Diagnosis requires joint aspiration.
MRI is reliably and accurately used to assess ACL-R complications. The clinical history helps in stratifying complications that result in decreased ROM or increased laxity.
1. Bencardino JT, Beltran J, Feldman MI, Rose DJ. MR imaging of complications of anterior cruciate ligament graft reconstruction. Radiographics. 2009;29(7):2115-2126.
2. Recht MP, Kramer J. MR imaging of the postoperative knee: a pictorial essay. Radiographics. 2002;22(4):765-774.
3. Papakonstantinou O, Chung CB, Chanchairujira K, Resnick DL. Complications of anterior cruciate ligament reconstruction: MR imaging. Eur Radiol. 2003;13(5):1106-1117.
4. Meyers AB, Haims AH, Menn K, Moukaddam H. Imaging of anterior cruciate ligament repair and its complications. AJR Am J Roentgenol. 2010;194(2):476-484.
5. Kwok CS, Harrison T, Servant C. The optimal timing for anterior cruciate ligament reconstruction with respect to the risk of postoperative stiffness. Arthroscopy. 2013;29(3):556-565.
6. Mayr HO, Weig TG, Plitz W. Arthrofibrosis following ACL reconstruction—reasons and outcome. Arch Orthop Trauma Surg. 2004;124(8):518-522.
7. Ghazikhanian V, Beltran J, Nikac V, Feldman M, Bencardino JT. Tibial tunnel and pretibial cysts following ACL graft reconstruction: MR imaging diagnosis. Skeletal Radiol. 2012;41(11):1375-1379.
8. Collins MS, Unruh KP, Bond JR, Mandrekar JN. Magnetic resonance imaging of surgically confirmed anterior cruciate ligament graft disruption. Skeletal Radiol. 2008;37(3):233-243.
9. Saupe N, White LM, Chiavaras MM, et al. Anterior cruciate ligament reconstruction grafts: MR imaging features at long-term follow-up—correlation with functional and clinical evaluation. Radiology. 2008;249(2):581-590.
Magnetic resonance imaging (MRI) is the preferred modality in the evaluation of complications of anterior cruciate ligament reconstruction (ACL-R).1-3 ACL-R complications may be broadly characterized as those resulting in decreased range of motion (ROM), eg, arthrofibrosis and impingement, and those resulting in increased laxity, ie, graft disruption.4 Short tau inversion recovery (STIR) sequences best minimize artifact related to field inhomogeneity in the presence of metal-containing fixation devices. Patients with contraindications to MRI may undergo high-resolution computed tomographic arthrography of the knee for evaluation of postoperative graft abnormalities.1
Arthrofibrosis refers to focal or diffuse synovial scar tissue, which may limit ROM. Preoperative irritation, preoperative limited ROM, and reconstruction within 4 weeks of trauma may all play a role in the development of arthrofibrosis.5,6 The focal form, cyclops lesion, named for its arthroscopic appearance, has been reported in 1% to 10% of patients with ACL-R.1 On MRI, focal arthrofibrosis may be seen as a focal or diffuse intermediate signal lesion in the anterior intercondylar notch extending linearly along the intercondylar roof1 (Figure 1).
MRI can be used to accurately determine the position of the femoral and tibial tunnels. Correct femoral tunnel position results in isometry of the graft during full ROM of the knee. Graft impingement can occur when the tibial tunnel is placed too far anteriorly such that the graft contacts the roof of the intercondylar notch before the knee is able to fully extend.7 A tibial tunnel placed anterior to the intersection of the Blumensaat line and the tibia is at higher risk for impingement.1,4 Impingement may be accompanied by signal change in the graft on intermediate-weighted and fluid-sensitive sequences. The signal abnormality is usually focal and persists longer than the expected signal changes related to revascularization of immature grafts within the first year (Figure 2). If left untreated, impingement may progress to graft rupture.4
Complete graft rupture is diagnosed on the basis of discontinuity of the graft fibers. MRI findings include fluid-filled defect or absence of intact graft fibers. Other reliable signs include large joint effusion, anterior tibial translation, pivot-shift–type marrow edema pattern, and horizontal orientation, laxity, or resorption of the graft fibers.1,8,9 The diagnosis of partial graft rupture may be challenging, as there are several other causes of increased graft signal, including revascularization (within 12 months after procedure), signal heterogeneity between individual bundles of hamstring grafts, and focal signal changes related to impingment (Figures 3, 4).
Fluid within the tunnels is a normal finding after surgery and typically resolves within the first 18 months.1 Cyst formation within the tibial tunnel is an uncommon complication of ACL-R and may be incidental to or present with clinical symptoms caused by extension into the pretibial soft tissues or expansion of the tunnel (Figure 5). Communication of cyst with joint space is important, as a noncommunicating cyst requires simple excision without need for bone grafting.7
Hardware-related complications (eg, loosening of fixation devices) are uncommon but may require revision surgery (Figure 6). Septic arthritis after ACL-R has a cumulative incidence of 0.1% to 0.9% and may be difficult to diagnose clinically because of the lack of classic symptoms of a septic joint.1 Diagnosis requires joint aspiration.
MRI is reliably and accurately used to assess ACL-R complications. The clinical history helps in stratifying complications that result in decreased ROM or increased laxity.
Magnetic resonance imaging (MRI) is the preferred modality in the evaluation of complications of anterior cruciate ligament reconstruction (ACL-R).1-3 ACL-R complications may be broadly characterized as those resulting in decreased range of motion (ROM), eg, arthrofibrosis and impingement, and those resulting in increased laxity, ie, graft disruption.4 Short tau inversion recovery (STIR) sequences best minimize artifact related to field inhomogeneity in the presence of metal-containing fixation devices. Patients with contraindications to MRI may undergo high-resolution computed tomographic arthrography of the knee for evaluation of postoperative graft abnormalities.1
Arthrofibrosis refers to focal or diffuse synovial scar tissue, which may limit ROM. Preoperative irritation, preoperative limited ROM, and reconstruction within 4 weeks of trauma may all play a role in the development of arthrofibrosis.5,6 The focal form, cyclops lesion, named for its arthroscopic appearance, has been reported in 1% to 10% of patients with ACL-R.1 On MRI, focal arthrofibrosis may be seen as a focal or diffuse intermediate signal lesion in the anterior intercondylar notch extending linearly along the intercondylar roof1 (Figure 1).
MRI can be used to accurately determine the position of the femoral and tibial tunnels. Correct femoral tunnel position results in isometry of the graft during full ROM of the knee. Graft impingement can occur when the tibial tunnel is placed too far anteriorly such that the graft contacts the roof of the intercondylar notch before the knee is able to fully extend.7 A tibial tunnel placed anterior to the intersection of the Blumensaat line and the tibia is at higher risk for impingement.1,4 Impingement may be accompanied by signal change in the graft on intermediate-weighted and fluid-sensitive sequences. The signal abnormality is usually focal and persists longer than the expected signal changes related to revascularization of immature grafts within the first year (Figure 2). If left untreated, impingement may progress to graft rupture.4
Complete graft rupture is diagnosed on the basis of discontinuity of the graft fibers. MRI findings include fluid-filled defect or absence of intact graft fibers. Other reliable signs include large joint effusion, anterior tibial translation, pivot-shift–type marrow edema pattern, and horizontal orientation, laxity, or resorption of the graft fibers.1,8,9 The diagnosis of partial graft rupture may be challenging, as there are several other causes of increased graft signal, including revascularization (within 12 months after procedure), signal heterogeneity between individual bundles of hamstring grafts, and focal signal changes related to impingment (Figures 3, 4).
Fluid within the tunnels is a normal finding after surgery and typically resolves within the first 18 months.1 Cyst formation within the tibial tunnel is an uncommon complication of ACL-R and may be incidental to or present with clinical symptoms caused by extension into the pretibial soft tissues or expansion of the tunnel (Figure 5). Communication of cyst with joint space is important, as a noncommunicating cyst requires simple excision without need for bone grafting.7
Hardware-related complications (eg, loosening of fixation devices) are uncommon but may require revision surgery (Figure 6). Septic arthritis after ACL-R has a cumulative incidence of 0.1% to 0.9% and may be difficult to diagnose clinically because of the lack of classic symptoms of a septic joint.1 Diagnosis requires joint aspiration.
MRI is reliably and accurately used to assess ACL-R complications. The clinical history helps in stratifying complications that result in decreased ROM or increased laxity.
1. Bencardino JT, Beltran J, Feldman MI, Rose DJ. MR imaging of complications of anterior cruciate ligament graft reconstruction. Radiographics. 2009;29(7):2115-2126.
2. Recht MP, Kramer J. MR imaging of the postoperative knee: a pictorial essay. Radiographics. 2002;22(4):765-774.
3. Papakonstantinou O, Chung CB, Chanchairujira K, Resnick DL. Complications of anterior cruciate ligament reconstruction: MR imaging. Eur Radiol. 2003;13(5):1106-1117.
4. Meyers AB, Haims AH, Menn K, Moukaddam H. Imaging of anterior cruciate ligament repair and its complications. AJR Am J Roentgenol. 2010;194(2):476-484.
5. Kwok CS, Harrison T, Servant C. The optimal timing for anterior cruciate ligament reconstruction with respect to the risk of postoperative stiffness. Arthroscopy. 2013;29(3):556-565.
6. Mayr HO, Weig TG, Plitz W. Arthrofibrosis following ACL reconstruction—reasons and outcome. Arch Orthop Trauma Surg. 2004;124(8):518-522.
7. Ghazikhanian V, Beltran J, Nikac V, Feldman M, Bencardino JT. Tibial tunnel and pretibial cysts following ACL graft reconstruction: MR imaging diagnosis. Skeletal Radiol. 2012;41(11):1375-1379.
8. Collins MS, Unruh KP, Bond JR, Mandrekar JN. Magnetic resonance imaging of surgically confirmed anterior cruciate ligament graft disruption. Skeletal Radiol. 2008;37(3):233-243.
9. Saupe N, White LM, Chiavaras MM, et al. Anterior cruciate ligament reconstruction grafts: MR imaging features at long-term follow-up—correlation with functional and clinical evaluation. Radiology. 2008;249(2):581-590.
1. Bencardino JT, Beltran J, Feldman MI, Rose DJ. MR imaging of complications of anterior cruciate ligament graft reconstruction. Radiographics. 2009;29(7):2115-2126.
2. Recht MP, Kramer J. MR imaging of the postoperative knee: a pictorial essay. Radiographics. 2002;22(4):765-774.
3. Papakonstantinou O, Chung CB, Chanchairujira K, Resnick DL. Complications of anterior cruciate ligament reconstruction: MR imaging. Eur Radiol. 2003;13(5):1106-1117.
4. Meyers AB, Haims AH, Menn K, Moukaddam H. Imaging of anterior cruciate ligament repair and its complications. AJR Am J Roentgenol. 2010;194(2):476-484.
5. Kwok CS, Harrison T, Servant C. The optimal timing for anterior cruciate ligament reconstruction with respect to the risk of postoperative stiffness. Arthroscopy. 2013;29(3):556-565.
6. Mayr HO, Weig TG, Plitz W. Arthrofibrosis following ACL reconstruction—reasons and outcome. Arch Orthop Trauma Surg. 2004;124(8):518-522.
7. Ghazikhanian V, Beltran J, Nikac V, Feldman M, Bencardino JT. Tibial tunnel and pretibial cysts following ACL graft reconstruction: MR imaging diagnosis. Skeletal Radiol. 2012;41(11):1375-1379.
8. Collins MS, Unruh KP, Bond JR, Mandrekar JN. Magnetic resonance imaging of surgically confirmed anterior cruciate ligament graft disruption. Skeletal Radiol. 2008;37(3):233-243.
9. Saupe N, White LM, Chiavaras MM, et al. Anterior cruciate ligament reconstruction grafts: MR imaging features at long-term follow-up—correlation with functional and clinical evaluation. Radiology. 2008;249(2):581-590.
Melia azedarach
Native to China, India, and Iran, Melia azedarach – also known as Chinaberry (Ku-lian), Pride of China, Indian lilac, Persian lilac, and white cedar – is a large nondeciduous tree now cultivated throughout the world.1-3 The leaves and fruits of this member of the Meliaceae family have been found to exhibit anthelmintic and antifeedant activity toward insects.4 The root bark or dried stem bark of the plant is used in traditional Chinese medicine to treat dermatoses and to expel and repel worms.5,6M. azedarach has also been used in Ayurveda3; it is known as Bakayn in India and Pakistan, where it has been used in traditional medicine to treat leprosy, scrofula, nausea, vomiting, thirst, and eruptive skin conditions.3,7
Traditional indications
Cropley and Hasegawa noted in 2007 that M. azedarach was used in the 19th century in the United States primarily as an anthelmintic, but also to treat tinea capitis and to eliminate lice.Further, they noted that the plant, which was widely cultivated in the South, was used, according to the literature of the 1800s, as a diuretic, as well as to promote hair growth, and treat scalp eruptions, fever, and malaria.8
A 2006 ethnopharmacologic study by Saikia et al. of medicinal plants used in Assam (Northeast India) to treat skin disorders and for cosmetic purposes revealed that M. azedarach was one of the primary plants used for medicinal purposes, including 18 skin conditions such as acne, burns, carbuncles, abscesses, measles, pediculosis, cellulitis, and prickly heat.9
Four years later, in an ethnopharmacologic study of medicinal plants used to treat cutaneous disorders and in folk cosmetics, Abbasi et al. interviewed residents in 30 remote tribal communities in the Northwest Frontier Province of Pakistan, finding that M. azedarach was one of 15 plant species identified as curative for numerous skin diseases, including boils, acne, and scabies.10
Biologic activity
Various constituents of M. azedarach have been associated with a wide range of biologic activity. The antifungal activity of the plant has been attributed to its hydroxycoumarin content; anti-inflammatory activity to its monoterpenes; bacteriostatic properties to its beta-carboline alkaloids; antiviral effects to its meliacin and meliacarpin; and insecticidal and antifeedant activity to its limonoids, which belong to the tetranortriterpenoid class of compounds.7,11 Limonoids also are reputed to confer antibacterial, antiviral, and antifungal activities.12 Recent research suggests the potential of M. azedarach to offer a correspondingly broad impact on various conditions.
Anticancer potential
Zhou et al. isolated new ring C-seco limonoids from Brazilian M. azedarach in 2004 and evaluated their cytotoxic activity, finding that two limonoids significantly inhibited HeLa S3 cancer cells.4,11
In 2009, He et al. extracted water-soluble polysaccharides from the fruit of M. azedarach and assessed their cytotoxic activity against four human cell lines in vitro. They found that the major polysaccharide component exhibited potent cytotoxic activity in the BGC-823 cell line.3 Also that year, Wu et al. isolated three new and multiple known steroids from the leaves of Chinese M. azedarach, finding that two of the newly identified steroids – (20S)-5,24(28)-ergostadiene-3-beta,7-alpha,16-beta,20-tetrol and (20S)-5-ergostene-3-beta,7-alpha,16-beta,20-tetrol – and one of the known ones exerted significant cytotoxic impact in three human cancer cell lines (A-549, H460, U251).1
Two years later, Wu et al. isolated two new triterpenoids (21,24-cycloeupha-7-ene-3-beta,16beta,21-alpha,25-tetrol and 3-beta-acetoxy-12-beta-hydroxy-eupha-7,24-dien-21,16-beta-olide) and two new steroids (29-hydroperoxy-stigmasta-7,24(28) xi-dien-3-beta-ol and 24-xi-hydroperoxy-24-vinyl-lathosterol) along with several known related substances from M. azedarach bark. Five of the known compounds demonstrated cytotoxic activity against three human cancer cell lines (A-549, H460, HGC27).6
More recently, Yuan et al. isolated two limonoids, one triterpenoid, one steroid, and one sesquiterpenoid, as well as nine known limonoids from the bark of M. azedarach. In addition, the investigators observed that seven of the limonoids exhibited significant inhibitory properties against five human tumor cell lines (HL-60, SMM-C7721, A-549, MCF-7, and SW480).5
Efficacy against head lice
In 2007, Carpinella et al. investigated in vitro the pediculicidal and ovicidal activity of an M. azedarach extract against Pediculus humanus capitis, noting the increasing resistance of head lice to synthetic drugs. A combination of 20% ripe fruit extract with 10% ripe fruit oil was found to be the most effective in eradicating adult lice (96.5%). The investigators also prepared a formulation of extract and oil at 10% combined with an emulsifier and preservatives that yielded 92.3% mortality of adult lice and complete inhibition of nymph emergence. They concluded that the use of M. azedarach formulations may be a viable and natural way to control head lice.2M. azedarach also has been the key active ingredient in an antimicrobial cream and a preparation to treat tinea pedis.7
Topical cream
Saleem et al. reported in 2008 on an herbal cream preparation using a standardized extract of M. azedarach flowers that displayed strong antibacterial activity against cellulitis, pustules, and pyogenic infections, and other conditions in clinical trials in children under the age of 10 years in four different villages in Pakistan. Subjects with bacterial infections anywhere on the body were divided into three groups, one treated with M. azedarach cream, one with placebo (negative control), and one with neomycin (positive control). Each treatment was applied twice daily for 15 days. The investigators observed that the healing effects of M. azedarach were similar to those rendered by neomycin.7
Conclusion
Not only has M. azedarach been used in several traditional medical systems, but its uses have consistently included cutaneous indications. Its most convincing modern application may be for head lice, but recent evidence and traditional uses suggest that this versatile plant may indeed warrant a more prominent role in the current dermatologic armamentarium. Future research is needed, and should provide some interesting answers.
References
1. Steroids. 2009 Sep;74(9):761-5.
2. J Am Acad Dermatol. 2007 Feb;56(2):250-6.
3. Fitoterapia. 2009 Oct;80(7):399-403.
4. Chem Pharm Bull (Tokyo). 2005 Oct;53(10):1362-5.
5. Planta Med. 2013 Jan;79(2):163-8.
6. Planta Med. 2011 Jun;77(9):922-8.
7. Phytomedicine. 2008 Apr;15(4):231-6.
8. J Am Acad Dermatol. 2007 Aug;57(2):366-7.
9. J Ethnopharmacol. 2006 Jun 30;106(2):149-57.
10. J Ethnopharmacol. 2010 Mar 24;128(2):322-35.
11. J Nat Prod. 2004 Sep;67(9):1544-7.
12. Chem Biodivers. 2010 Apr;7(4):839-59.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Native to China, India, and Iran, Melia azedarach – also known as Chinaberry (Ku-lian), Pride of China, Indian lilac, Persian lilac, and white cedar – is a large nondeciduous tree now cultivated throughout the world.1-3 The leaves and fruits of this member of the Meliaceae family have been found to exhibit anthelmintic and antifeedant activity toward insects.4 The root bark or dried stem bark of the plant is used in traditional Chinese medicine to treat dermatoses and to expel and repel worms.5,6M. azedarach has also been used in Ayurveda3; it is known as Bakayn in India and Pakistan, where it has been used in traditional medicine to treat leprosy, scrofula, nausea, vomiting, thirst, and eruptive skin conditions.3,7
Traditional indications
Cropley and Hasegawa noted in 2007 that M. azedarach was used in the 19th century in the United States primarily as an anthelmintic, but also to treat tinea capitis and to eliminate lice.Further, they noted that the plant, which was widely cultivated in the South, was used, according to the literature of the 1800s, as a diuretic, as well as to promote hair growth, and treat scalp eruptions, fever, and malaria.8
A 2006 ethnopharmacologic study by Saikia et al. of medicinal plants used in Assam (Northeast India) to treat skin disorders and for cosmetic purposes revealed that M. azedarach was one of the primary plants used for medicinal purposes, including 18 skin conditions such as acne, burns, carbuncles, abscesses, measles, pediculosis, cellulitis, and prickly heat.9
Four years later, in an ethnopharmacologic study of medicinal plants used to treat cutaneous disorders and in folk cosmetics, Abbasi et al. interviewed residents in 30 remote tribal communities in the Northwest Frontier Province of Pakistan, finding that M. azedarach was one of 15 plant species identified as curative for numerous skin diseases, including boils, acne, and scabies.10
Biologic activity
Various constituents of M. azedarach have been associated with a wide range of biologic activity. The antifungal activity of the plant has been attributed to its hydroxycoumarin content; anti-inflammatory activity to its monoterpenes; bacteriostatic properties to its beta-carboline alkaloids; antiviral effects to its meliacin and meliacarpin; and insecticidal and antifeedant activity to its limonoids, which belong to the tetranortriterpenoid class of compounds.7,11 Limonoids also are reputed to confer antibacterial, antiviral, and antifungal activities.12 Recent research suggests the potential of M. azedarach to offer a correspondingly broad impact on various conditions.
Anticancer potential
Zhou et al. isolated new ring C-seco limonoids from Brazilian M. azedarach in 2004 and evaluated their cytotoxic activity, finding that two limonoids significantly inhibited HeLa S3 cancer cells.4,11
In 2009, He et al. extracted water-soluble polysaccharides from the fruit of M. azedarach and assessed their cytotoxic activity against four human cell lines in vitro. They found that the major polysaccharide component exhibited potent cytotoxic activity in the BGC-823 cell line.3 Also that year, Wu et al. isolated three new and multiple known steroids from the leaves of Chinese M. azedarach, finding that two of the newly identified steroids – (20S)-5,24(28)-ergostadiene-3-beta,7-alpha,16-beta,20-tetrol and (20S)-5-ergostene-3-beta,7-alpha,16-beta,20-tetrol – and one of the known ones exerted significant cytotoxic impact in three human cancer cell lines (A-549, H460, U251).1
Two years later, Wu et al. isolated two new triterpenoids (21,24-cycloeupha-7-ene-3-beta,16beta,21-alpha,25-tetrol and 3-beta-acetoxy-12-beta-hydroxy-eupha-7,24-dien-21,16-beta-olide) and two new steroids (29-hydroperoxy-stigmasta-7,24(28) xi-dien-3-beta-ol and 24-xi-hydroperoxy-24-vinyl-lathosterol) along with several known related substances from M. azedarach bark. Five of the known compounds demonstrated cytotoxic activity against three human cancer cell lines (A-549, H460, HGC27).6
More recently, Yuan et al. isolated two limonoids, one triterpenoid, one steroid, and one sesquiterpenoid, as well as nine known limonoids from the bark of M. azedarach. In addition, the investigators observed that seven of the limonoids exhibited significant inhibitory properties against five human tumor cell lines (HL-60, SMM-C7721, A-549, MCF-7, and SW480).5
Efficacy against head lice
In 2007, Carpinella et al. investigated in vitro the pediculicidal and ovicidal activity of an M. azedarach extract against Pediculus humanus capitis, noting the increasing resistance of head lice to synthetic drugs. A combination of 20% ripe fruit extract with 10% ripe fruit oil was found to be the most effective in eradicating adult lice (96.5%). The investigators also prepared a formulation of extract and oil at 10% combined with an emulsifier and preservatives that yielded 92.3% mortality of adult lice and complete inhibition of nymph emergence. They concluded that the use of M. azedarach formulations may be a viable and natural way to control head lice.2M. azedarach also has been the key active ingredient in an antimicrobial cream and a preparation to treat tinea pedis.7
Topical cream
Saleem et al. reported in 2008 on an herbal cream preparation using a standardized extract of M. azedarach flowers that displayed strong antibacterial activity against cellulitis, pustules, and pyogenic infections, and other conditions in clinical trials in children under the age of 10 years in four different villages in Pakistan. Subjects with bacterial infections anywhere on the body were divided into three groups, one treated with M. azedarach cream, one with placebo (negative control), and one with neomycin (positive control). Each treatment was applied twice daily for 15 days. The investigators observed that the healing effects of M. azedarach were similar to those rendered by neomycin.7
Conclusion
Not only has M. azedarach been used in several traditional medical systems, but its uses have consistently included cutaneous indications. Its most convincing modern application may be for head lice, but recent evidence and traditional uses suggest that this versatile plant may indeed warrant a more prominent role in the current dermatologic armamentarium. Future research is needed, and should provide some interesting answers.
References
1. Steroids. 2009 Sep;74(9):761-5.
2. J Am Acad Dermatol. 2007 Feb;56(2):250-6.
3. Fitoterapia. 2009 Oct;80(7):399-403.
4. Chem Pharm Bull (Tokyo). 2005 Oct;53(10):1362-5.
5. Planta Med. 2013 Jan;79(2):163-8.
6. Planta Med. 2011 Jun;77(9):922-8.
7. Phytomedicine. 2008 Apr;15(4):231-6.
8. J Am Acad Dermatol. 2007 Aug;57(2):366-7.
9. J Ethnopharmacol. 2006 Jun 30;106(2):149-57.
10. J Ethnopharmacol. 2010 Mar 24;128(2):322-35.
11. J Nat Prod. 2004 Sep;67(9):1544-7.
12. Chem Biodivers. 2010 Apr;7(4):839-59.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Native to China, India, and Iran, Melia azedarach – also known as Chinaberry (Ku-lian), Pride of China, Indian lilac, Persian lilac, and white cedar – is a large nondeciduous tree now cultivated throughout the world.1-3 The leaves and fruits of this member of the Meliaceae family have been found to exhibit anthelmintic and antifeedant activity toward insects.4 The root bark or dried stem bark of the plant is used in traditional Chinese medicine to treat dermatoses and to expel and repel worms.5,6M. azedarach has also been used in Ayurveda3; it is known as Bakayn in India and Pakistan, where it has been used in traditional medicine to treat leprosy, scrofula, nausea, vomiting, thirst, and eruptive skin conditions.3,7
Traditional indications
Cropley and Hasegawa noted in 2007 that M. azedarach was used in the 19th century in the United States primarily as an anthelmintic, but also to treat tinea capitis and to eliminate lice.Further, they noted that the plant, which was widely cultivated in the South, was used, according to the literature of the 1800s, as a diuretic, as well as to promote hair growth, and treat scalp eruptions, fever, and malaria.8
A 2006 ethnopharmacologic study by Saikia et al. of medicinal plants used in Assam (Northeast India) to treat skin disorders and for cosmetic purposes revealed that M. azedarach was one of the primary plants used for medicinal purposes, including 18 skin conditions such as acne, burns, carbuncles, abscesses, measles, pediculosis, cellulitis, and prickly heat.9
Four years later, in an ethnopharmacologic study of medicinal plants used to treat cutaneous disorders and in folk cosmetics, Abbasi et al. interviewed residents in 30 remote tribal communities in the Northwest Frontier Province of Pakistan, finding that M. azedarach was one of 15 plant species identified as curative for numerous skin diseases, including boils, acne, and scabies.10
Biologic activity
Various constituents of M. azedarach have been associated with a wide range of biologic activity. The antifungal activity of the plant has been attributed to its hydroxycoumarin content; anti-inflammatory activity to its monoterpenes; bacteriostatic properties to its beta-carboline alkaloids; antiviral effects to its meliacin and meliacarpin; and insecticidal and antifeedant activity to its limonoids, which belong to the tetranortriterpenoid class of compounds.7,11 Limonoids also are reputed to confer antibacterial, antiviral, and antifungal activities.12 Recent research suggests the potential of M. azedarach to offer a correspondingly broad impact on various conditions.
Anticancer potential
Zhou et al. isolated new ring C-seco limonoids from Brazilian M. azedarach in 2004 and evaluated their cytotoxic activity, finding that two limonoids significantly inhibited HeLa S3 cancer cells.4,11
In 2009, He et al. extracted water-soluble polysaccharides from the fruit of M. azedarach and assessed their cytotoxic activity against four human cell lines in vitro. They found that the major polysaccharide component exhibited potent cytotoxic activity in the BGC-823 cell line.3 Also that year, Wu et al. isolated three new and multiple known steroids from the leaves of Chinese M. azedarach, finding that two of the newly identified steroids – (20S)-5,24(28)-ergostadiene-3-beta,7-alpha,16-beta,20-tetrol and (20S)-5-ergostene-3-beta,7-alpha,16-beta,20-tetrol – and one of the known ones exerted significant cytotoxic impact in three human cancer cell lines (A-549, H460, U251).1
Two years later, Wu et al. isolated two new triterpenoids (21,24-cycloeupha-7-ene-3-beta,16beta,21-alpha,25-tetrol and 3-beta-acetoxy-12-beta-hydroxy-eupha-7,24-dien-21,16-beta-olide) and two new steroids (29-hydroperoxy-stigmasta-7,24(28) xi-dien-3-beta-ol and 24-xi-hydroperoxy-24-vinyl-lathosterol) along with several known related substances from M. azedarach bark. Five of the known compounds demonstrated cytotoxic activity against three human cancer cell lines (A-549, H460, HGC27).6
More recently, Yuan et al. isolated two limonoids, one triterpenoid, one steroid, and one sesquiterpenoid, as well as nine known limonoids from the bark of M. azedarach. In addition, the investigators observed that seven of the limonoids exhibited significant inhibitory properties against five human tumor cell lines (HL-60, SMM-C7721, A-549, MCF-7, and SW480).5
Efficacy against head lice
In 2007, Carpinella et al. investigated in vitro the pediculicidal and ovicidal activity of an M. azedarach extract against Pediculus humanus capitis, noting the increasing resistance of head lice to synthetic drugs. A combination of 20% ripe fruit extract with 10% ripe fruit oil was found to be the most effective in eradicating adult lice (96.5%). The investigators also prepared a formulation of extract and oil at 10% combined with an emulsifier and preservatives that yielded 92.3% mortality of adult lice and complete inhibition of nymph emergence. They concluded that the use of M. azedarach formulations may be a viable and natural way to control head lice.2M. azedarach also has been the key active ingredient in an antimicrobial cream and a preparation to treat tinea pedis.7
Topical cream
Saleem et al. reported in 2008 on an herbal cream preparation using a standardized extract of M. azedarach flowers that displayed strong antibacterial activity against cellulitis, pustules, and pyogenic infections, and other conditions in clinical trials in children under the age of 10 years in four different villages in Pakistan. Subjects with bacterial infections anywhere on the body were divided into three groups, one treated with M. azedarach cream, one with placebo (negative control), and one with neomycin (positive control). Each treatment was applied twice daily for 15 days. The investigators observed that the healing effects of M. azedarach were similar to those rendered by neomycin.7
Conclusion
Not only has M. azedarach been used in several traditional medical systems, but its uses have consistently included cutaneous indications. Its most convincing modern application may be for head lice, but recent evidence and traditional uses suggest that this versatile plant may indeed warrant a more prominent role in the current dermatologic armamentarium. Future research is needed, and should provide some interesting answers.
References
1. Steroids. 2009 Sep;74(9):761-5.
2. J Am Acad Dermatol. 2007 Feb;56(2):250-6.
3. Fitoterapia. 2009 Oct;80(7):399-403.
4. Chem Pharm Bull (Tokyo). 2005 Oct;53(10):1362-5.
5. Planta Med. 2013 Jan;79(2):163-8.
6. Planta Med. 2011 Jun;77(9):922-8.
7. Phytomedicine. 2008 Apr;15(4):231-6.
8. J Am Acad Dermatol. 2007 Aug;57(2):366-7.
9. J Ethnopharmacol. 2006 Jun 30;106(2):149-57.
10. J Ethnopharmacol. 2010 Mar 24;128(2):322-35.
11. J Nat Prod. 2004 Sep;67(9):1544-7.
12. Chem Biodivers. 2010 Apr;7(4):839-59.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Technique Using Isoelastic Tension Band for Treatment of Olecranon Fractures
Olecranon fractures are relatively common in adults and constitute 10% of all upper extremity injuries.1,2 An olecranon fracture may be sustained either directly (from blunt trauma or a fall onto the tip of the elbow) or indirectly (as a result of forceful hyperextension of the triceps during a fall onto an outstretched arm). Displaced olecranon fractures with extensor discontinuity require reduction and stabilization. One treatment option is tension band wiring (TBW), which is used to manage noncomminuted fractures.3 TBW, first described by Weber and Vasey4 in 1963, involves transforming the distractive forces of the triceps into dynamic compression forces across the olecranon articular surface using 2 intramedullary Kirschner wires (K-wires) and stainless steel wires looped in figure-of-8 fashion.
Various modifications of the TBW technique of Weber and Vasey4 have been proposed to reduce the frequency of complications. These modifications include substituting screws for K-wires, aiming the angle of the K-wires into the anterior coronoid cortex or loop configuration of the stainless steel wire, using double knots and twisting procedures to finalize fixation, and using alternative materials for the loop construct.5-8 In the literature and in our experience, patients often complain after surgery about prominent K-wires and the twisted knots used to tension the construct.9-12 Surgeons also must address the technical difficulties of positioning the brittle wire without kinking, and avoiding slack while tensioning.
In this article, we report on the clinical outcomes of a series of 7 patients with olecranon fracture treated with a US Food and Drug Administration–approved novel isoelastic ultrahigh-molecular-weight polyethylene (UHMWPE) cerclage cable (Iso-Elastic Cerclage System, Kinamed).
Materials and Methods
Surgical Technique
The patient is arranged in a sloppy lateral position to allow access to the posterior elbow. A nonsterile tourniquet is placed on the upper arm, and the limb is sterilely prepared and draped in standard fashion. A posterolateral incision is made around the olecranon and extended proximally 6 cm and distally 6 cm along the subcutaneous border of the ulna. The fracture is visualized and comminution identified.
To provide anchorage for a pointed reduction clamp, the surgeon drills a 2.5-mm hole in the subcutaneous border of the ulnar shaft. The fracture is reduced in extension and the clamp affixed. The elbow is then flexed and the reduction confirmed visually and by imaging. After realignment of the articular surfaces, 2 longitudinal, parallel K-wires (diameter, 1.6-2.0 mm) are passed in antegrade direction through the proximal olecranon within the medullary canal of the shaft. The proximal ends must not cross the cortex so they may fully capture the figure-of-8 wire during subsequent, final advancement, and the distal ends must not pierce the anterior cortex. A 2.5-mm transverse hole is created distal to the fracture in the dorsal aspect of the ulnar shaft from medial to lateral at 2 times the distance from the tip of the olecranon to the fracture site. This hole is expanded with a 3.5-mm drill bit, allowing both strands of the cable to be passed simultaneously medial to lateral, making the figure-of-8. The 3.5-mm hole represents about 20% of the overall width of the bone, which we have not found to create a significant stress riser in either laboratory or clinical tests of this construct. Proximally, the cables are placed on the periosteum of the olecranon but deep to the triceps tendon and adjacent to the K-wires. The locking clip is placed on the posterolateral aspect of the elbow joint in a location where it can be covered with local tissue for adequate padding. The cable is then threaded through the clamping bracket and tightened slowly and gradually with a tensioning device to low torque level (Figure 1). At this stage, tension may be released to make any necessary adjustments. Last, the locking clip is deployed, securing the tension band in the clip, and the excess cable is trimmed with a scalpel. Softening and pliability of the cable during its insertion and tensioning should be noted.
The ends of the K-wires are now curved in a hook configuration. The tines of the hooks should be parallel to accommodate the cable, and then the triceps is sharply incised to bone. If the bone is hard, an awl is used to create a pilot hole so the hook may be impaled into bone while capturing the cable. Next, the triceps is closed over the pins, minimizing the potential for pin migration and backout. The 2 K-wires are left in place to keep the fragments in proper anatomical alignment during healing and to prevent displacement with elbow motion. Figure 2 is a schematic of the final construct, and Figure 3 shows the construct in a patient.
Reduction of the olecranon fracture is assessed by imaging in full extension to check for possible implant impingement. Last, we apply the previously harvested fracture callus to the fracture site. Layered closure is performed, and bulky soft dressings are applied. Postoperative immobilization with a splint is used. Gentle range-of-motion exercises begin in about 2 weeks and progress as pain allows.
A case example with preoperative and postoperative images taken at 3-month follow-up is provided in Figure 4. The entire surgical technique can be viewed in the Video.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Clinical Cases
Between July 2007 and February 2011, 7 patients with displaced olecranon fractures underwent osteosynthesis using the isoelastic tension band (Table 1). According to the Mayo classification system, 5 of these patients had type 2A fractures, 1 had a type 2B fracture with an ipsilateral nondisplaced radial neck fracture, and 1 had a type 3B fracture. There were 4 female and 3 male patients. The injury was on the dominant side in 3 patients. All patients gave informed consent to evaluation at subsequent office visits and completed outcomes questionnaires by mail several years after surgery. Mean follow-up at which outcome measures questionnaires were obtained was 3.3 years (range, 2.1-6.8 years). Exclusion criteria were age under 18 years and inability to provide informed consent, fracture patterns with extensive articular comminution, and open fractures. Permission to conduct this research was granted by institutional review board.
At each visit, patients completed the Disabilities of the Arm, Shoulder, and Hand (DASH) functional outcome survey and were evaluated according to Broberg and Morrey’s elbow scoring system.13,14 Chart review consisted of evaluation of medical records, including radiographs and orthopedic physician notes in which preoperative examination was documented, mechanism of injury was noted, radiologic fracture pattern was evaluated, and time to bony union was recorded. Elbow motion was documented. Grip strength was measured with a calibrated Jamar dynamometer (Sammons Preston Rolyan) set at level 2, as delineated in Broberg and Morrey’s functional elbow scoring system.
Results
The 7 patients were assessed at a mean final follow-up of 19 months after surgery and received a mean Broberg and Morrey score of good (92.2/100) (Table 2). Restoration of motion and strength was excellent; compared with contralateral extremity, mean flexion arc was 96%, and mean forearm rotation was 96%. Grip was 99% of the noninjured side, perhaps the result of increased conditioning from physical therapy. Patients completed outcomes questionnaires at a mean of 3.3 years after surgery. Mean (SD) DASH score at this longest follow-up was 12.6 (17.2) (Table 2). Patients were satisfied (mean, 9.8/10; range, 9.5-10) and had little pain (mean, 0.8/10; range, 0-3). All fractures united, and there were no infections. One patient had a satisfactory union with complete restoration of motion and continued to play sports vocationally but developed pain over the locking clip 5 years after the index procedure and decided to have the implant removed. He had no radiographic evidence of K-wire or implant migration. Another patient had a minor degree of implant irritation at longest follow-up but did not request hardware removal.
Discussion
Stainless steel wire is often used in TBW because of its widespread availability, low cost, lack of immunogenicity, and relative strength.7 However, stainless steel wire has several disadvantages. It is susceptible to low-cycle fatigue failure, and fatigue strength may be seriously reduced secondary to incidental trauma to the wire on implantation.15,16 Other complications are kinking, skin irritation, implant prominence, fixation loss caused by wire loosening, and inadequate initial reduction potentially requiring revision.10,12,17-21
Isoelastic cable is a new type of cerclage cable that consists of UHMWPE strands braided over a nylon core. The particular property profile of the isoelastic tension band gives the cable intrinsic elastic and pliable qualities. In addition, unlike stainless steel, the band maintains a uniform, continuous compression force across a fracture site.22 Multifilament braided cables fatigue and fray, but the isoelastic cerclage cable showed no evidence of fraying or breakage after 1 million loading cycles.22,23 Compared with metal wire or braided metal cable, the band also has higher fatigue strength and higher ultimate tensile strength.7 Furthermore, the cable is less abrasive than stainless steel, so theoretically it is less irritating to surrounding subcutaneous tissue. Last, the pliability of the band allows the surgeon to create multiple loops of cable without the wire-failure side effects related to kinking, which is common with the metal construct.
In 2010, Ting and colleagues24 retrospectively studied implant failure complications associated with use of isoelastic cerclage cables in the treatment of periprosthetic fractures in total hip arthroplasty. They reported a breakage rate of 0% and noted that previously published breakage data for metallic cerclage devices ranged from 0% to 44%. They concluded that isoelastic cables were not associated with material failure, and there were no direct complications related to the cables. Similarly, Edwards and colleagues25 evaluated the same type of cable used in revision shoulder arthroplasty and reported excellent success and no failures. Although these data stem from use in the femur and humerus, we think the noted benefits apply to fractures of the elbow as well, as we observed a similar breakage rate (0%).
Various studies have addressed the clinical complaints and reoperation rates associated with retained metal implants after olecranon fixation. Traditional AO (Arbeitsgemeinschaft für Osteosynthesefragen) technique involves subcutaneous placement of stainless steel wires, which often results in tissue irritation. Reoperation rates as high as 80% have been reported, and a proportion of implant removals may in fact be caused by factors related to the subcutaneous placement of the metallic implants rather than K-wire migration alone.5,12,18 A nonmetallic isoelastic tension band can provide a more comfortable and less irritating implant, which could reduce the need for secondary intervention related to painful subcutaneous implant. One of our 7 patients had a symptomatic implant removed 5 years after surgery. This patient complained of pain over the area of the tension band device clip, so after fracture healing the entire fixation device was removed in the operating room. If reoperation is necessary, removal of intramedullary K-wires is relatively simple using a minimal incision; removal of stainless steel TBW may require a larger approach if the twisted knots cannot be easily retrieved.
A study of compression forces created by stainless steel wire demonstrated that a “finely tuned mechanical sense” was needed to produce optimal fixation compression when using stainless steel wire.26 It was observed that a submaximal twist created insufficient compressive force, while an ostensibly minimal increase in twisting force above optimum abruptly caused wire failure through breakage. Cerclage cables using clasping devices, such as the current isoelastic cerclage cable, were superior in ease of application. Furthermore, a clasping device allows for cable tension readjustment that is not possible with stainless steel wire. The clasping mechanism precludes the surgeon from having to bury the stainless steel knot and allows for the objective cable-tensioning not possible with stainless steel wire. Last, the tensioning device is titratable, which allows the surgeon to set the construct at a predetermined quantitative tension, which is of benefit in patients with osteopenia.
One limitation of this study is that it did not resolve the potential for K-wire migration, and we agree with previous recommendations that careful attention to surgical technique may avoid such a complication.10 In addition, the sample was small, and the study lacked a control group; a larger sample and a control group would have boosted study power. Nevertheless, the physical and functional outcomes associated with use of this technique were excellent. These results demonstrate an efficacious attempt to decrease secondary surgery rates and are therefore proof of concept that the isoelastic tension band may be used as an alternative to stainless steel in the TBW of displaced olecranon fractures with minimal or no comminution.
Conclusion
This easily reproducible technique for use of an isoelastic tension band in olecranon fracture fixation was associated with excellent physical and functional outcomes in a series of 7 patients. The rate of secondary intervention was slightly better for these patients than for patients treated with wire tension band fixation. Although more rigorous study of this device is needed, we think it is a promising alternative to wire tension band techniques.
1. Rommens PM, Küchle R, Schneider RU, Reuter M. Olecranon fractures in adults: factors influencing outcome. Injury. 2004;35(11):1149-1157.
2. Veillette CJ, Steinmann SP. Olecranon fractures. Orthop Clin North Am. 2008;39(2):229-236.
3. Newman SD, Mauffrey C, Krikler S. Olecranon fractures. Injury. 2009;40(6):575-581.
4. Weber BG, Vasey H. Osteosynthesis in olecranon fractures [in German]. Z Unfallmed Berufskr. 1963;56:90-96.
5. Netz P, Strömberg L. Non-sliding pins in traction absorbing wiring of fractures: a modified technique. Acta Orthop Scand. 1982;53(3):355-360.
6. Prayson MJ, Williams JL, Marshall MP, Scilaris TA, Lingenfelter EJ. Biomechanical comparison of fixation methods in transverse olecranon fractures: a cadaveric study. J Orthop Trauma. 1997;11(8):565-572.
7. Rothaug PG, Boston RC, Richardson DW, Nunamaker DM. A comparison of ultra-high-molecular weight polyethylene cable and stainless steel wire using two fixation techniques for repair of equine midbody sesamoid fractures: an in vitro biomechanical study. Vet Surg. 2002;31(5):445-454.
8. Harrell RM, Tong J, Weinhold PS, Dahners LE. Comparison of the mechanical properties of different tension band materials and suture techniques. J Orthop Trauma. 2003;17(2):119-122.
9. Nimura A, Nakagawa T, Wakabayashi Y, Sekiya I, Okawa A, Muneta T. Repair of olecranon fractures using FiberWire without metallic implants: report of two cases. J Orthop Surg Res. 2010;5:73.
10. Macko D, Szabo RM. Complications of tension-band wiring of olecranon fractures. J Bone Joint Surg Am. 1985;67(9):1396-1401.
11. Helm RH, Hornby R, Miller SW. The complications of surgical treatment of displaced fractures of the olecranon. Injury. 1987;18(1):48-50.
12. Romero JM, Miran A, Jensen CH. Complications and re-operation rate after tension-band wiring of olecranon fractures. J Orthop Sci. 2000;5(4):318-320.
13. Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C. Measuring the whole or the parts? Validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14(2):128-146.
14. Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68(5):669-674.
15. Bostrom MP, Asnis SE, Ernberg JJ, et al. Fatigue testing of cerclage stainless steel wire fixation. J Orthop Trauma. 1994;8(5):422-428.
16. Oh I, Sander TW, Treharne RW. The fatigue resistance of orthopaedic wire. Clin Orthop Relat Res. 1985;(192):228-236.
17. Amstutz HC, Maki S. Complications of trochanteric osteotomy in total hip replacement. J Bone Joint Surg Am. 1978;60(2):214-216.
18. Jensen CM, Olsen BB. Drawbacks of traction-absorbing wiring (TAW) in displaced fractures of the olecranon. Injury. 1986;17(3):174-175.
19. Kumar G, Mereddy PK, Hakkalamani S, Donnachie NJ. Implant removal following surgical stabilization of patella fracture. Orthopedics. 2010;33(5).
20. Hume MC, Wiss DA. Olecranon fractures. A clinical and radiographic comparison of tension band wiring and plate fixation. Clin Orthop Relat Res. 1992;(285):229-235.
21. Wolfgang G, Burke F, Bush D, et al. Surgical treatment of displaced olecranon fractures by tension band wiring technique. Clin Orthop Relat Res. 1987;(224):192-204.
22. Sarin VK, Mattchen TM, Hack B. A novel iso-elastic cerclage cable for treatment of fractures. Paper presented at: Annual Meeting of the Orthopaedic Research Society; February 20-23, 2005; Washington, DC. Paper 739.
23. Silverton CD, Jacobs JJ, Rosenberg AG, Kull L, Conley A, Galante JO. Complications of a cable grip system. J Arthroplasty. 1996;11(4):400-404.
24. Ting NT, Wera GD, Levine BR, Della Valle CJ. Early experience with a novel nonmetallic cable in reconstructive hip surgery. Clin Orthop Relat Res. 2010;468(9):2382-2386.
25. Edwards TB, Stuart KD, Trappey GJ, O’Connor DP, Sarin VK. Utility of polymer cerclage cables in revision shoulder arthroplasty. Orthopedics. 2011;34(4).
26. Shaw JA, Daubert HB. Compression capability of cerclage fixation systems. A biomechanical study. Orthopedics. 1988;11(8):1169-1174.
Olecranon fractures are relatively common in adults and constitute 10% of all upper extremity injuries.1,2 An olecranon fracture may be sustained either directly (from blunt trauma or a fall onto the tip of the elbow) or indirectly (as a result of forceful hyperextension of the triceps during a fall onto an outstretched arm). Displaced olecranon fractures with extensor discontinuity require reduction and stabilization. One treatment option is tension band wiring (TBW), which is used to manage noncomminuted fractures.3 TBW, first described by Weber and Vasey4 in 1963, involves transforming the distractive forces of the triceps into dynamic compression forces across the olecranon articular surface using 2 intramedullary Kirschner wires (K-wires) and stainless steel wires looped in figure-of-8 fashion.
Various modifications of the TBW technique of Weber and Vasey4 have been proposed to reduce the frequency of complications. These modifications include substituting screws for K-wires, aiming the angle of the K-wires into the anterior coronoid cortex or loop configuration of the stainless steel wire, using double knots and twisting procedures to finalize fixation, and using alternative materials for the loop construct.5-8 In the literature and in our experience, patients often complain after surgery about prominent K-wires and the twisted knots used to tension the construct.9-12 Surgeons also must address the technical difficulties of positioning the brittle wire without kinking, and avoiding slack while tensioning.
In this article, we report on the clinical outcomes of a series of 7 patients with olecranon fracture treated with a US Food and Drug Administration–approved novel isoelastic ultrahigh-molecular-weight polyethylene (UHMWPE) cerclage cable (Iso-Elastic Cerclage System, Kinamed).
Materials and Methods
Surgical Technique
The patient is arranged in a sloppy lateral position to allow access to the posterior elbow. A nonsterile tourniquet is placed on the upper arm, and the limb is sterilely prepared and draped in standard fashion. A posterolateral incision is made around the olecranon and extended proximally 6 cm and distally 6 cm along the subcutaneous border of the ulna. The fracture is visualized and comminution identified.
To provide anchorage for a pointed reduction clamp, the surgeon drills a 2.5-mm hole in the subcutaneous border of the ulnar shaft. The fracture is reduced in extension and the clamp affixed. The elbow is then flexed and the reduction confirmed visually and by imaging. After realignment of the articular surfaces, 2 longitudinal, parallel K-wires (diameter, 1.6-2.0 mm) are passed in antegrade direction through the proximal olecranon within the medullary canal of the shaft. The proximal ends must not cross the cortex so they may fully capture the figure-of-8 wire during subsequent, final advancement, and the distal ends must not pierce the anterior cortex. A 2.5-mm transverse hole is created distal to the fracture in the dorsal aspect of the ulnar shaft from medial to lateral at 2 times the distance from the tip of the olecranon to the fracture site. This hole is expanded with a 3.5-mm drill bit, allowing both strands of the cable to be passed simultaneously medial to lateral, making the figure-of-8. The 3.5-mm hole represents about 20% of the overall width of the bone, which we have not found to create a significant stress riser in either laboratory or clinical tests of this construct. Proximally, the cables are placed on the periosteum of the olecranon but deep to the triceps tendon and adjacent to the K-wires. The locking clip is placed on the posterolateral aspect of the elbow joint in a location where it can be covered with local tissue for adequate padding. The cable is then threaded through the clamping bracket and tightened slowly and gradually with a tensioning device to low torque level (Figure 1). At this stage, tension may be released to make any necessary adjustments. Last, the locking clip is deployed, securing the tension band in the clip, and the excess cable is trimmed with a scalpel. Softening and pliability of the cable during its insertion and tensioning should be noted.
The ends of the K-wires are now curved in a hook configuration. The tines of the hooks should be parallel to accommodate the cable, and then the triceps is sharply incised to bone. If the bone is hard, an awl is used to create a pilot hole so the hook may be impaled into bone while capturing the cable. Next, the triceps is closed over the pins, minimizing the potential for pin migration and backout. The 2 K-wires are left in place to keep the fragments in proper anatomical alignment during healing and to prevent displacement with elbow motion. Figure 2 is a schematic of the final construct, and Figure 3 shows the construct in a patient.
Reduction of the olecranon fracture is assessed by imaging in full extension to check for possible implant impingement. Last, we apply the previously harvested fracture callus to the fracture site. Layered closure is performed, and bulky soft dressings are applied. Postoperative immobilization with a splint is used. Gentle range-of-motion exercises begin in about 2 weeks and progress as pain allows.
A case example with preoperative and postoperative images taken at 3-month follow-up is provided in Figure 4. The entire surgical technique can be viewed in the Video.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Clinical Cases
Between July 2007 and February 2011, 7 patients with displaced olecranon fractures underwent osteosynthesis using the isoelastic tension band (Table 1). According to the Mayo classification system, 5 of these patients had type 2A fractures, 1 had a type 2B fracture with an ipsilateral nondisplaced radial neck fracture, and 1 had a type 3B fracture. There were 4 female and 3 male patients. The injury was on the dominant side in 3 patients. All patients gave informed consent to evaluation at subsequent office visits and completed outcomes questionnaires by mail several years after surgery. Mean follow-up at which outcome measures questionnaires were obtained was 3.3 years (range, 2.1-6.8 years). Exclusion criteria were age under 18 years and inability to provide informed consent, fracture patterns with extensive articular comminution, and open fractures. Permission to conduct this research was granted by institutional review board.
At each visit, patients completed the Disabilities of the Arm, Shoulder, and Hand (DASH) functional outcome survey and were evaluated according to Broberg and Morrey’s elbow scoring system.13,14 Chart review consisted of evaluation of medical records, including radiographs and orthopedic physician notes in which preoperative examination was documented, mechanism of injury was noted, radiologic fracture pattern was evaluated, and time to bony union was recorded. Elbow motion was documented. Grip strength was measured with a calibrated Jamar dynamometer (Sammons Preston Rolyan) set at level 2, as delineated in Broberg and Morrey’s functional elbow scoring system.
Results
The 7 patients were assessed at a mean final follow-up of 19 months after surgery and received a mean Broberg and Morrey score of good (92.2/100) (Table 2). Restoration of motion and strength was excellent; compared with contralateral extremity, mean flexion arc was 96%, and mean forearm rotation was 96%. Grip was 99% of the noninjured side, perhaps the result of increased conditioning from physical therapy. Patients completed outcomes questionnaires at a mean of 3.3 years after surgery. Mean (SD) DASH score at this longest follow-up was 12.6 (17.2) (Table 2). Patients were satisfied (mean, 9.8/10; range, 9.5-10) and had little pain (mean, 0.8/10; range, 0-3). All fractures united, and there were no infections. One patient had a satisfactory union with complete restoration of motion and continued to play sports vocationally but developed pain over the locking clip 5 years after the index procedure and decided to have the implant removed. He had no radiographic evidence of K-wire or implant migration. Another patient had a minor degree of implant irritation at longest follow-up but did not request hardware removal.
Discussion
Stainless steel wire is often used in TBW because of its widespread availability, low cost, lack of immunogenicity, and relative strength.7 However, stainless steel wire has several disadvantages. It is susceptible to low-cycle fatigue failure, and fatigue strength may be seriously reduced secondary to incidental trauma to the wire on implantation.15,16 Other complications are kinking, skin irritation, implant prominence, fixation loss caused by wire loosening, and inadequate initial reduction potentially requiring revision.10,12,17-21
Isoelastic cable is a new type of cerclage cable that consists of UHMWPE strands braided over a nylon core. The particular property profile of the isoelastic tension band gives the cable intrinsic elastic and pliable qualities. In addition, unlike stainless steel, the band maintains a uniform, continuous compression force across a fracture site.22 Multifilament braided cables fatigue and fray, but the isoelastic cerclage cable showed no evidence of fraying or breakage after 1 million loading cycles.22,23 Compared with metal wire or braided metal cable, the band also has higher fatigue strength and higher ultimate tensile strength.7 Furthermore, the cable is less abrasive than stainless steel, so theoretically it is less irritating to surrounding subcutaneous tissue. Last, the pliability of the band allows the surgeon to create multiple loops of cable without the wire-failure side effects related to kinking, which is common with the metal construct.
In 2010, Ting and colleagues24 retrospectively studied implant failure complications associated with use of isoelastic cerclage cables in the treatment of periprosthetic fractures in total hip arthroplasty. They reported a breakage rate of 0% and noted that previously published breakage data for metallic cerclage devices ranged from 0% to 44%. They concluded that isoelastic cables were not associated with material failure, and there were no direct complications related to the cables. Similarly, Edwards and colleagues25 evaluated the same type of cable used in revision shoulder arthroplasty and reported excellent success and no failures. Although these data stem from use in the femur and humerus, we think the noted benefits apply to fractures of the elbow as well, as we observed a similar breakage rate (0%).
Various studies have addressed the clinical complaints and reoperation rates associated with retained metal implants after olecranon fixation. Traditional AO (Arbeitsgemeinschaft für Osteosynthesefragen) technique involves subcutaneous placement of stainless steel wires, which often results in tissue irritation. Reoperation rates as high as 80% have been reported, and a proportion of implant removals may in fact be caused by factors related to the subcutaneous placement of the metallic implants rather than K-wire migration alone.5,12,18 A nonmetallic isoelastic tension band can provide a more comfortable and less irritating implant, which could reduce the need for secondary intervention related to painful subcutaneous implant. One of our 7 patients had a symptomatic implant removed 5 years after surgery. This patient complained of pain over the area of the tension band device clip, so after fracture healing the entire fixation device was removed in the operating room. If reoperation is necessary, removal of intramedullary K-wires is relatively simple using a minimal incision; removal of stainless steel TBW may require a larger approach if the twisted knots cannot be easily retrieved.
A study of compression forces created by stainless steel wire demonstrated that a “finely tuned mechanical sense” was needed to produce optimal fixation compression when using stainless steel wire.26 It was observed that a submaximal twist created insufficient compressive force, while an ostensibly minimal increase in twisting force above optimum abruptly caused wire failure through breakage. Cerclage cables using clasping devices, such as the current isoelastic cerclage cable, were superior in ease of application. Furthermore, a clasping device allows for cable tension readjustment that is not possible with stainless steel wire. The clasping mechanism precludes the surgeon from having to bury the stainless steel knot and allows for the objective cable-tensioning not possible with stainless steel wire. Last, the tensioning device is titratable, which allows the surgeon to set the construct at a predetermined quantitative tension, which is of benefit in patients with osteopenia.
One limitation of this study is that it did not resolve the potential for K-wire migration, and we agree with previous recommendations that careful attention to surgical technique may avoid such a complication.10 In addition, the sample was small, and the study lacked a control group; a larger sample and a control group would have boosted study power. Nevertheless, the physical and functional outcomes associated with use of this technique were excellent. These results demonstrate an efficacious attempt to decrease secondary surgery rates and are therefore proof of concept that the isoelastic tension band may be used as an alternative to stainless steel in the TBW of displaced olecranon fractures with minimal or no comminution.
Conclusion
This easily reproducible technique for use of an isoelastic tension band in olecranon fracture fixation was associated with excellent physical and functional outcomes in a series of 7 patients. The rate of secondary intervention was slightly better for these patients than for patients treated with wire tension band fixation. Although more rigorous study of this device is needed, we think it is a promising alternative to wire tension band techniques.
Olecranon fractures are relatively common in adults and constitute 10% of all upper extremity injuries.1,2 An olecranon fracture may be sustained either directly (from blunt trauma or a fall onto the tip of the elbow) or indirectly (as a result of forceful hyperextension of the triceps during a fall onto an outstretched arm). Displaced olecranon fractures with extensor discontinuity require reduction and stabilization. One treatment option is tension band wiring (TBW), which is used to manage noncomminuted fractures.3 TBW, first described by Weber and Vasey4 in 1963, involves transforming the distractive forces of the triceps into dynamic compression forces across the olecranon articular surface using 2 intramedullary Kirschner wires (K-wires) and stainless steel wires looped in figure-of-8 fashion.
Various modifications of the TBW technique of Weber and Vasey4 have been proposed to reduce the frequency of complications. These modifications include substituting screws for K-wires, aiming the angle of the K-wires into the anterior coronoid cortex or loop configuration of the stainless steel wire, using double knots and twisting procedures to finalize fixation, and using alternative materials for the loop construct.5-8 In the literature and in our experience, patients often complain after surgery about prominent K-wires and the twisted knots used to tension the construct.9-12 Surgeons also must address the technical difficulties of positioning the brittle wire without kinking, and avoiding slack while tensioning.
In this article, we report on the clinical outcomes of a series of 7 patients with olecranon fracture treated with a US Food and Drug Administration–approved novel isoelastic ultrahigh-molecular-weight polyethylene (UHMWPE) cerclage cable (Iso-Elastic Cerclage System, Kinamed).
Materials and Methods
Surgical Technique
The patient is arranged in a sloppy lateral position to allow access to the posterior elbow. A nonsterile tourniquet is placed on the upper arm, and the limb is sterilely prepared and draped in standard fashion. A posterolateral incision is made around the olecranon and extended proximally 6 cm and distally 6 cm along the subcutaneous border of the ulna. The fracture is visualized and comminution identified.
To provide anchorage for a pointed reduction clamp, the surgeon drills a 2.5-mm hole in the subcutaneous border of the ulnar shaft. The fracture is reduced in extension and the clamp affixed. The elbow is then flexed and the reduction confirmed visually and by imaging. After realignment of the articular surfaces, 2 longitudinal, parallel K-wires (diameter, 1.6-2.0 mm) are passed in antegrade direction through the proximal olecranon within the medullary canal of the shaft. The proximal ends must not cross the cortex so they may fully capture the figure-of-8 wire during subsequent, final advancement, and the distal ends must not pierce the anterior cortex. A 2.5-mm transverse hole is created distal to the fracture in the dorsal aspect of the ulnar shaft from medial to lateral at 2 times the distance from the tip of the olecranon to the fracture site. This hole is expanded with a 3.5-mm drill bit, allowing both strands of the cable to be passed simultaneously medial to lateral, making the figure-of-8. The 3.5-mm hole represents about 20% of the overall width of the bone, which we have not found to create a significant stress riser in either laboratory or clinical tests of this construct. Proximally, the cables are placed on the periosteum of the olecranon but deep to the triceps tendon and adjacent to the K-wires. The locking clip is placed on the posterolateral aspect of the elbow joint in a location where it can be covered with local tissue for adequate padding. The cable is then threaded through the clamping bracket and tightened slowly and gradually with a tensioning device to low torque level (Figure 1). At this stage, tension may be released to make any necessary adjustments. Last, the locking clip is deployed, securing the tension band in the clip, and the excess cable is trimmed with a scalpel. Softening and pliability of the cable during its insertion and tensioning should be noted.
The ends of the K-wires are now curved in a hook configuration. The tines of the hooks should be parallel to accommodate the cable, and then the triceps is sharply incised to bone. If the bone is hard, an awl is used to create a pilot hole so the hook may be impaled into bone while capturing the cable. Next, the triceps is closed over the pins, minimizing the potential for pin migration and backout. The 2 K-wires are left in place to keep the fragments in proper anatomical alignment during healing and to prevent displacement with elbow motion. Figure 2 is a schematic of the final construct, and Figure 3 shows the construct in a patient.
Reduction of the olecranon fracture is assessed by imaging in full extension to check for possible implant impingement. Last, we apply the previously harvested fracture callus to the fracture site. Layered closure is performed, and bulky soft dressings are applied. Postoperative immobilization with a splint is used. Gentle range-of-motion exercises begin in about 2 weeks and progress as pain allows.
A case example with preoperative and postoperative images taken at 3-month follow-up is provided in Figure 4. The entire surgical technique can be viewed in the Video.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Clinical Cases
Between July 2007 and February 2011, 7 patients with displaced olecranon fractures underwent osteosynthesis using the isoelastic tension band (Table 1). According to the Mayo classification system, 5 of these patients had type 2A fractures, 1 had a type 2B fracture with an ipsilateral nondisplaced radial neck fracture, and 1 had a type 3B fracture. There were 4 female and 3 male patients. The injury was on the dominant side in 3 patients. All patients gave informed consent to evaluation at subsequent office visits and completed outcomes questionnaires by mail several years after surgery. Mean follow-up at which outcome measures questionnaires were obtained was 3.3 years (range, 2.1-6.8 years). Exclusion criteria were age under 18 years and inability to provide informed consent, fracture patterns with extensive articular comminution, and open fractures. Permission to conduct this research was granted by institutional review board.
At each visit, patients completed the Disabilities of the Arm, Shoulder, and Hand (DASH) functional outcome survey and were evaluated according to Broberg and Morrey’s elbow scoring system.13,14 Chart review consisted of evaluation of medical records, including radiographs and orthopedic physician notes in which preoperative examination was documented, mechanism of injury was noted, radiologic fracture pattern was evaluated, and time to bony union was recorded. Elbow motion was documented. Grip strength was measured with a calibrated Jamar dynamometer (Sammons Preston Rolyan) set at level 2, as delineated in Broberg and Morrey’s functional elbow scoring system.
Results
The 7 patients were assessed at a mean final follow-up of 19 months after surgery and received a mean Broberg and Morrey score of good (92.2/100) (Table 2). Restoration of motion and strength was excellent; compared with contralateral extremity, mean flexion arc was 96%, and mean forearm rotation was 96%. Grip was 99% of the noninjured side, perhaps the result of increased conditioning from physical therapy. Patients completed outcomes questionnaires at a mean of 3.3 years after surgery. Mean (SD) DASH score at this longest follow-up was 12.6 (17.2) (Table 2). Patients were satisfied (mean, 9.8/10; range, 9.5-10) and had little pain (mean, 0.8/10; range, 0-3). All fractures united, and there were no infections. One patient had a satisfactory union with complete restoration of motion and continued to play sports vocationally but developed pain over the locking clip 5 years after the index procedure and decided to have the implant removed. He had no radiographic evidence of K-wire or implant migration. Another patient had a minor degree of implant irritation at longest follow-up but did not request hardware removal.
Discussion
Stainless steel wire is often used in TBW because of its widespread availability, low cost, lack of immunogenicity, and relative strength.7 However, stainless steel wire has several disadvantages. It is susceptible to low-cycle fatigue failure, and fatigue strength may be seriously reduced secondary to incidental trauma to the wire on implantation.15,16 Other complications are kinking, skin irritation, implant prominence, fixation loss caused by wire loosening, and inadequate initial reduction potentially requiring revision.10,12,17-21
Isoelastic cable is a new type of cerclage cable that consists of UHMWPE strands braided over a nylon core. The particular property profile of the isoelastic tension band gives the cable intrinsic elastic and pliable qualities. In addition, unlike stainless steel, the band maintains a uniform, continuous compression force across a fracture site.22 Multifilament braided cables fatigue and fray, but the isoelastic cerclage cable showed no evidence of fraying or breakage after 1 million loading cycles.22,23 Compared with metal wire or braided metal cable, the band also has higher fatigue strength and higher ultimate tensile strength.7 Furthermore, the cable is less abrasive than stainless steel, so theoretically it is less irritating to surrounding subcutaneous tissue. Last, the pliability of the band allows the surgeon to create multiple loops of cable without the wire-failure side effects related to kinking, which is common with the metal construct.
In 2010, Ting and colleagues24 retrospectively studied implant failure complications associated with use of isoelastic cerclage cables in the treatment of periprosthetic fractures in total hip arthroplasty. They reported a breakage rate of 0% and noted that previously published breakage data for metallic cerclage devices ranged from 0% to 44%. They concluded that isoelastic cables were not associated with material failure, and there were no direct complications related to the cables. Similarly, Edwards and colleagues25 evaluated the same type of cable used in revision shoulder arthroplasty and reported excellent success and no failures. Although these data stem from use in the femur and humerus, we think the noted benefits apply to fractures of the elbow as well, as we observed a similar breakage rate (0%).
Various studies have addressed the clinical complaints and reoperation rates associated with retained metal implants after olecranon fixation. Traditional AO (Arbeitsgemeinschaft für Osteosynthesefragen) technique involves subcutaneous placement of stainless steel wires, which often results in tissue irritation. Reoperation rates as high as 80% have been reported, and a proportion of implant removals may in fact be caused by factors related to the subcutaneous placement of the metallic implants rather than K-wire migration alone.5,12,18 A nonmetallic isoelastic tension band can provide a more comfortable and less irritating implant, which could reduce the need for secondary intervention related to painful subcutaneous implant. One of our 7 patients had a symptomatic implant removed 5 years after surgery. This patient complained of pain over the area of the tension band device clip, so after fracture healing the entire fixation device was removed in the operating room. If reoperation is necessary, removal of intramedullary K-wires is relatively simple using a minimal incision; removal of stainless steel TBW may require a larger approach if the twisted knots cannot be easily retrieved.
A study of compression forces created by stainless steel wire demonstrated that a “finely tuned mechanical sense” was needed to produce optimal fixation compression when using stainless steel wire.26 It was observed that a submaximal twist created insufficient compressive force, while an ostensibly minimal increase in twisting force above optimum abruptly caused wire failure through breakage. Cerclage cables using clasping devices, such as the current isoelastic cerclage cable, were superior in ease of application. Furthermore, a clasping device allows for cable tension readjustment that is not possible with stainless steel wire. The clasping mechanism precludes the surgeon from having to bury the stainless steel knot and allows for the objective cable-tensioning not possible with stainless steel wire. Last, the tensioning device is titratable, which allows the surgeon to set the construct at a predetermined quantitative tension, which is of benefit in patients with osteopenia.
One limitation of this study is that it did not resolve the potential for K-wire migration, and we agree with previous recommendations that careful attention to surgical technique may avoid such a complication.10 In addition, the sample was small, and the study lacked a control group; a larger sample and a control group would have boosted study power. Nevertheless, the physical and functional outcomes associated with use of this technique were excellent. These results demonstrate an efficacious attempt to decrease secondary surgery rates and are therefore proof of concept that the isoelastic tension band may be used as an alternative to stainless steel in the TBW of displaced olecranon fractures with minimal or no comminution.
Conclusion
This easily reproducible technique for use of an isoelastic tension band in olecranon fracture fixation was associated with excellent physical and functional outcomes in a series of 7 patients. The rate of secondary intervention was slightly better for these patients than for patients treated with wire tension band fixation. Although more rigorous study of this device is needed, we think it is a promising alternative to wire tension band techniques.
1. Rommens PM, Küchle R, Schneider RU, Reuter M. Olecranon fractures in adults: factors influencing outcome. Injury. 2004;35(11):1149-1157.
2. Veillette CJ, Steinmann SP. Olecranon fractures. Orthop Clin North Am. 2008;39(2):229-236.
3. Newman SD, Mauffrey C, Krikler S. Olecranon fractures. Injury. 2009;40(6):575-581.
4. Weber BG, Vasey H. Osteosynthesis in olecranon fractures [in German]. Z Unfallmed Berufskr. 1963;56:90-96.
5. Netz P, Strömberg L. Non-sliding pins in traction absorbing wiring of fractures: a modified technique. Acta Orthop Scand. 1982;53(3):355-360.
6. Prayson MJ, Williams JL, Marshall MP, Scilaris TA, Lingenfelter EJ. Biomechanical comparison of fixation methods in transverse olecranon fractures: a cadaveric study. J Orthop Trauma. 1997;11(8):565-572.
7. Rothaug PG, Boston RC, Richardson DW, Nunamaker DM. A comparison of ultra-high-molecular weight polyethylene cable and stainless steel wire using two fixation techniques for repair of equine midbody sesamoid fractures: an in vitro biomechanical study. Vet Surg. 2002;31(5):445-454.
8. Harrell RM, Tong J, Weinhold PS, Dahners LE. Comparison of the mechanical properties of different tension band materials and suture techniques. J Orthop Trauma. 2003;17(2):119-122.
9. Nimura A, Nakagawa T, Wakabayashi Y, Sekiya I, Okawa A, Muneta T. Repair of olecranon fractures using FiberWire without metallic implants: report of two cases. J Orthop Surg Res. 2010;5:73.
10. Macko D, Szabo RM. Complications of tension-band wiring of olecranon fractures. J Bone Joint Surg Am. 1985;67(9):1396-1401.
11. Helm RH, Hornby R, Miller SW. The complications of surgical treatment of displaced fractures of the olecranon. Injury. 1987;18(1):48-50.
12. Romero JM, Miran A, Jensen CH. Complications and re-operation rate after tension-band wiring of olecranon fractures. J Orthop Sci. 2000;5(4):318-320.
13. Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C. Measuring the whole or the parts? Validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14(2):128-146.
14. Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68(5):669-674.
15. Bostrom MP, Asnis SE, Ernberg JJ, et al. Fatigue testing of cerclage stainless steel wire fixation. J Orthop Trauma. 1994;8(5):422-428.
16. Oh I, Sander TW, Treharne RW. The fatigue resistance of orthopaedic wire. Clin Orthop Relat Res. 1985;(192):228-236.
17. Amstutz HC, Maki S. Complications of trochanteric osteotomy in total hip replacement. J Bone Joint Surg Am. 1978;60(2):214-216.
18. Jensen CM, Olsen BB. Drawbacks of traction-absorbing wiring (TAW) in displaced fractures of the olecranon. Injury. 1986;17(3):174-175.
19. Kumar G, Mereddy PK, Hakkalamani S, Donnachie NJ. Implant removal following surgical stabilization of patella fracture. Orthopedics. 2010;33(5).
20. Hume MC, Wiss DA. Olecranon fractures. A clinical and radiographic comparison of tension band wiring and plate fixation. Clin Orthop Relat Res. 1992;(285):229-235.
21. Wolfgang G, Burke F, Bush D, et al. Surgical treatment of displaced olecranon fractures by tension band wiring technique. Clin Orthop Relat Res. 1987;(224):192-204.
22. Sarin VK, Mattchen TM, Hack B. A novel iso-elastic cerclage cable for treatment of fractures. Paper presented at: Annual Meeting of the Orthopaedic Research Society; February 20-23, 2005; Washington, DC. Paper 739.
23. Silverton CD, Jacobs JJ, Rosenberg AG, Kull L, Conley A, Galante JO. Complications of a cable grip system. J Arthroplasty. 1996;11(4):400-404.
24. Ting NT, Wera GD, Levine BR, Della Valle CJ. Early experience with a novel nonmetallic cable in reconstructive hip surgery. Clin Orthop Relat Res. 2010;468(9):2382-2386.
25. Edwards TB, Stuart KD, Trappey GJ, O’Connor DP, Sarin VK. Utility of polymer cerclage cables in revision shoulder arthroplasty. Orthopedics. 2011;34(4).
26. Shaw JA, Daubert HB. Compression capability of cerclage fixation systems. A biomechanical study. Orthopedics. 1988;11(8):1169-1174.
1. Rommens PM, Küchle R, Schneider RU, Reuter M. Olecranon fractures in adults: factors influencing outcome. Injury. 2004;35(11):1149-1157.
2. Veillette CJ, Steinmann SP. Olecranon fractures. Orthop Clin North Am. 2008;39(2):229-236.
3. Newman SD, Mauffrey C, Krikler S. Olecranon fractures. Injury. 2009;40(6):575-581.
4. Weber BG, Vasey H. Osteosynthesis in olecranon fractures [in German]. Z Unfallmed Berufskr. 1963;56:90-96.
5. Netz P, Strömberg L. Non-sliding pins in traction absorbing wiring of fractures: a modified technique. Acta Orthop Scand. 1982;53(3):355-360.
6. Prayson MJ, Williams JL, Marshall MP, Scilaris TA, Lingenfelter EJ. Biomechanical comparison of fixation methods in transverse olecranon fractures: a cadaveric study. J Orthop Trauma. 1997;11(8):565-572.
7. Rothaug PG, Boston RC, Richardson DW, Nunamaker DM. A comparison of ultra-high-molecular weight polyethylene cable and stainless steel wire using two fixation techniques for repair of equine midbody sesamoid fractures: an in vitro biomechanical study. Vet Surg. 2002;31(5):445-454.
8. Harrell RM, Tong J, Weinhold PS, Dahners LE. Comparison of the mechanical properties of different tension band materials and suture techniques. J Orthop Trauma. 2003;17(2):119-122.
9. Nimura A, Nakagawa T, Wakabayashi Y, Sekiya I, Okawa A, Muneta T. Repair of olecranon fractures using FiberWire without metallic implants: report of two cases. J Orthop Surg Res. 2010;5:73.
10. Macko D, Szabo RM. Complications of tension-band wiring of olecranon fractures. J Bone Joint Surg Am. 1985;67(9):1396-1401.
11. Helm RH, Hornby R, Miller SW. The complications of surgical treatment of displaced fractures of the olecranon. Injury. 1987;18(1):48-50.
12. Romero JM, Miran A, Jensen CH. Complications and re-operation rate after tension-band wiring of olecranon fractures. J Orthop Sci. 2000;5(4):318-320.
13. Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C. Measuring the whole or the parts? Validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14(2):128-146.
14. Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68(5):669-674.
15. Bostrom MP, Asnis SE, Ernberg JJ, et al. Fatigue testing of cerclage stainless steel wire fixation. J Orthop Trauma. 1994;8(5):422-428.
16. Oh I, Sander TW, Treharne RW. The fatigue resistance of orthopaedic wire. Clin Orthop Relat Res. 1985;(192):228-236.
17. Amstutz HC, Maki S. Complications of trochanteric osteotomy in total hip replacement. J Bone Joint Surg Am. 1978;60(2):214-216.
18. Jensen CM, Olsen BB. Drawbacks of traction-absorbing wiring (TAW) in displaced fractures of the olecranon. Injury. 1986;17(3):174-175.
19. Kumar G, Mereddy PK, Hakkalamani S, Donnachie NJ. Implant removal following surgical stabilization of patella fracture. Orthopedics. 2010;33(5).
20. Hume MC, Wiss DA. Olecranon fractures. A clinical and radiographic comparison of tension band wiring and plate fixation. Clin Orthop Relat Res. 1992;(285):229-235.
21. Wolfgang G, Burke F, Bush D, et al. Surgical treatment of displaced olecranon fractures by tension band wiring technique. Clin Orthop Relat Res. 1987;(224):192-204.
22. Sarin VK, Mattchen TM, Hack B. A novel iso-elastic cerclage cable for treatment of fractures. Paper presented at: Annual Meeting of the Orthopaedic Research Society; February 20-23, 2005; Washington, DC. Paper 739.
23. Silverton CD, Jacobs JJ, Rosenberg AG, Kull L, Conley A, Galante JO. Complications of a cable grip system. J Arthroplasty. 1996;11(4):400-404.
24. Ting NT, Wera GD, Levine BR, Della Valle CJ. Early experience with a novel nonmetallic cable in reconstructive hip surgery. Clin Orthop Relat Res. 2010;468(9):2382-2386.
25. Edwards TB, Stuart KD, Trappey GJ, O’Connor DP, Sarin VK. Utility of polymer cerclage cables in revision shoulder arthroplasty. Orthopedics. 2011;34(4).
26. Shaw JA, Daubert HB. Compression capability of cerclage fixation systems. A biomechanical study. Orthopedics. 1988;11(8):1169-1174.
Unassigned, Undocumented Patients Take a Toll on Healthcare and Hospitalists
When a patient must remain in the acute care hospital setting—despite being well enough to transition to a lower level of care, costs continue to mount as the patient receives care at the most expensive level.
“But policymakers must understand that reducing support for essential hospitals might save dollars in the short term but ultimately threatens access to care and creates greater costs in the long run,” says Beth Feldpush, DrPH, senior vice president of policy and advocacy for America’s Essential Hospitals in Washington, D.C. The group represents more than 250 essential hospitals, which fill a safety net role and provide communitywide services, such as trauma, neonatal intensive care, and disaster response.
“Our hospitals, which already operate at a loss on average, cannot continue to sustain federal and state funding cuts,” Dr. Feldpush says. “Access to care for vulnerable patients and entire communities will suffer if we continue to chip away at crucial sources of support, such as Medicaid and Medicare disproportionate share hospital funding and payment for outpatient services.”
The Affordable Care Act (ACA) makes many changes to the healthcare system that are designed to improve the quality, value of, and access to healthcare services.
“While many are good in theory, they have faced challenges in practice,” Dr. Feldpush says.
For example, the law’s authors included deep cuts to Medicaid and Medicare disproportionate share hospital (DSH) payments, which support hospitals that provide a large volume of uncompensated care. They made these cuts with the assumption that Medicare expansion and the ACA health insurance marketplace would significantly increase coverage, lessening the need for DSH payments. The U.S. Supreme Court’s decision to give states the option of expanding Medicaid has resulted in expansion in only about half of the states, however.
“But the DSH cuts remain, meaning our hospitals are getting significantly less support for the same or more uncompensated care,” Dr. Feldpush says.
Likewise, the ACA put into place many quality incentive programs for Medicare, including those designed to reduce preventable readmissions and hospital-acquired conditions and to encourage more value-based purchasing.
“The goals are obviously good ones, but the quality measures used to calculate incentive payments or penalties fail to account for the sociodemographic challenges our patients face—and that our hospitals can’t control,” she says. “So, these programs disproportionately penalize our hospitals, which, in turn, creates a vicious circle that reduces the funding they need to make improvements.”
Access to equitable healthcare for low-income, uninsured, and other vulnerable patients is a national problem, Dr. Feldpush continues. But the severity of the problem can vary by community and region—in states that have chosen not to expand their Medicaid programs, for example, or in economically depressed areas. TH
When a patient must remain in the acute care hospital setting—despite being well enough to transition to a lower level of care, costs continue to mount as the patient receives care at the most expensive level.
“But policymakers must understand that reducing support for essential hospitals might save dollars in the short term but ultimately threatens access to care and creates greater costs in the long run,” says Beth Feldpush, DrPH, senior vice president of policy and advocacy for America’s Essential Hospitals in Washington, D.C. The group represents more than 250 essential hospitals, which fill a safety net role and provide communitywide services, such as trauma, neonatal intensive care, and disaster response.
“Our hospitals, which already operate at a loss on average, cannot continue to sustain federal and state funding cuts,” Dr. Feldpush says. “Access to care for vulnerable patients and entire communities will suffer if we continue to chip away at crucial sources of support, such as Medicaid and Medicare disproportionate share hospital funding and payment for outpatient services.”
The Affordable Care Act (ACA) makes many changes to the healthcare system that are designed to improve the quality, value of, and access to healthcare services.
“While many are good in theory, they have faced challenges in practice,” Dr. Feldpush says.
For example, the law’s authors included deep cuts to Medicaid and Medicare disproportionate share hospital (DSH) payments, which support hospitals that provide a large volume of uncompensated care. They made these cuts with the assumption that Medicare expansion and the ACA health insurance marketplace would significantly increase coverage, lessening the need for DSH payments. The U.S. Supreme Court’s decision to give states the option of expanding Medicaid has resulted in expansion in only about half of the states, however.
“But the DSH cuts remain, meaning our hospitals are getting significantly less support for the same or more uncompensated care,” Dr. Feldpush says.
Likewise, the ACA put into place many quality incentive programs for Medicare, including those designed to reduce preventable readmissions and hospital-acquired conditions and to encourage more value-based purchasing.
“The goals are obviously good ones, but the quality measures used to calculate incentive payments or penalties fail to account for the sociodemographic challenges our patients face—and that our hospitals can’t control,” she says. “So, these programs disproportionately penalize our hospitals, which, in turn, creates a vicious circle that reduces the funding they need to make improvements.”
Access to equitable healthcare for low-income, uninsured, and other vulnerable patients is a national problem, Dr. Feldpush continues. But the severity of the problem can vary by community and region—in states that have chosen not to expand their Medicaid programs, for example, or in economically depressed areas. TH
When a patient must remain in the acute care hospital setting—despite being well enough to transition to a lower level of care, costs continue to mount as the patient receives care at the most expensive level.
“But policymakers must understand that reducing support for essential hospitals might save dollars in the short term but ultimately threatens access to care and creates greater costs in the long run,” says Beth Feldpush, DrPH, senior vice president of policy and advocacy for America’s Essential Hospitals in Washington, D.C. The group represents more than 250 essential hospitals, which fill a safety net role and provide communitywide services, such as trauma, neonatal intensive care, and disaster response.
“Our hospitals, which already operate at a loss on average, cannot continue to sustain federal and state funding cuts,” Dr. Feldpush says. “Access to care for vulnerable patients and entire communities will suffer if we continue to chip away at crucial sources of support, such as Medicaid and Medicare disproportionate share hospital funding and payment for outpatient services.”
The Affordable Care Act (ACA) makes many changes to the healthcare system that are designed to improve the quality, value of, and access to healthcare services.
“While many are good in theory, they have faced challenges in practice,” Dr. Feldpush says.
For example, the law’s authors included deep cuts to Medicaid and Medicare disproportionate share hospital (DSH) payments, which support hospitals that provide a large volume of uncompensated care. They made these cuts with the assumption that Medicare expansion and the ACA health insurance marketplace would significantly increase coverage, lessening the need for DSH payments. The U.S. Supreme Court’s decision to give states the option of expanding Medicaid has resulted in expansion in only about half of the states, however.
“But the DSH cuts remain, meaning our hospitals are getting significantly less support for the same or more uncompensated care,” Dr. Feldpush says.
Likewise, the ACA put into place many quality incentive programs for Medicare, including those designed to reduce preventable readmissions and hospital-acquired conditions and to encourage more value-based purchasing.
“The goals are obviously good ones, but the quality measures used to calculate incentive payments or penalties fail to account for the sociodemographic challenges our patients face—and that our hospitals can’t control,” she says. “So, these programs disproportionately penalize our hospitals, which, in turn, creates a vicious circle that reduces the funding they need to make improvements.”
Access to equitable healthcare for low-income, uninsured, and other vulnerable patients is a national problem, Dr. Feldpush continues. But the severity of the problem can vary by community and region—in states that have chosen not to expand their Medicaid programs, for example, or in economically depressed areas. TH
SBRT may be better than RFA for large hepatocellular carcinoma lesions
A retrospective data analysis showed that stereotactic body radiotherapy (SBRT) outperformed radiofrequency ablation (RFA) on tumors larger than 2 cm in patients with hepatocellular carcinoma.
For all tumors treated with RFA, 1- and 2-year freedom from local progression (FFLP) were 83.6% and 80.2%, and for tumors treated with SBRT, rates were 97.4% and 83.8%. On tumors smaller than 2 cm, FFLP was similar for the two methods (HR, 2.50; 95% confidence interval, 0.72-8.67; P = .15) but was significantly worse for RFA treatment of larger tumors (HR, 3.35; 95% CI, 1.17-9.62, P = .025).
“These results suggest that both SBRT and RFA are excellent choices for smaller tumors but that SBRT may be preferred for larger tumors. Prospective, randomized clinical trials are needed to compare these two modalities, especially for larger tumors, although we are unaware of any such trials,” wrote Dr. Daniel R. Wahl, radiation oncologist at the University of Michigan (J Clin Oncol. 2015 Dec. 2. doi:10.1200/JCO.2015.61.4925).
The retrospective study evaluated 224 patients with nonmetastatic hepatocellular carcinoma – 161 patients (249 tumors) who underwent RFA and 63 patients (83 tumors) who underwent SBRT at the University of Michigan from 2004 to 2012. Patients treated with RFA had higher rates of cirrhosis (95% vs. 78%; P less than .001), lower AFP levels (8.8 vs. 18.6; P = .04), and fewer prior liver-directed treatments compared with patients treated with SBRT.
To investigate the impact of fiducial use for image guidance in SBRT, the researchers examined treatment failures. Of the 21 treatments that used fiducials, none had local failure, compared with six failures in 62 treatments without fiducials.
Both methods had similar low rates of late adverse events. Acute adverse events and treatment-related deaths were nonsignificantly greater with RFA, which may suggest SBRT as a better option for medically unfit patients who may not tolerate invasive procedures such as RFA.
The study included only three tumors larger than 5 cm in diameter, so rates of local control for this size tumor cannot be estimated reliably, reported Dr. Wahl and his colleagues.
The National Institutes of Health and the Taubman Institute supported the research. Dr. Wahl reported stock or other ownership in Lycera. Several of his coauthors reported ties to industry.
A retrospective data analysis showed that stereotactic body radiotherapy (SBRT) outperformed radiofrequency ablation (RFA) on tumors larger than 2 cm in patients with hepatocellular carcinoma.
For all tumors treated with RFA, 1- and 2-year freedom from local progression (FFLP) were 83.6% and 80.2%, and for tumors treated with SBRT, rates were 97.4% and 83.8%. On tumors smaller than 2 cm, FFLP was similar for the two methods (HR, 2.50; 95% confidence interval, 0.72-8.67; P = .15) but was significantly worse for RFA treatment of larger tumors (HR, 3.35; 95% CI, 1.17-9.62, P = .025).
“These results suggest that both SBRT and RFA are excellent choices for smaller tumors but that SBRT may be preferred for larger tumors. Prospective, randomized clinical trials are needed to compare these two modalities, especially for larger tumors, although we are unaware of any such trials,” wrote Dr. Daniel R. Wahl, radiation oncologist at the University of Michigan (J Clin Oncol. 2015 Dec. 2. doi:10.1200/JCO.2015.61.4925).
The retrospective study evaluated 224 patients with nonmetastatic hepatocellular carcinoma – 161 patients (249 tumors) who underwent RFA and 63 patients (83 tumors) who underwent SBRT at the University of Michigan from 2004 to 2012. Patients treated with RFA had higher rates of cirrhosis (95% vs. 78%; P less than .001), lower AFP levels (8.8 vs. 18.6; P = .04), and fewer prior liver-directed treatments compared with patients treated with SBRT.
To investigate the impact of fiducial use for image guidance in SBRT, the researchers examined treatment failures. Of the 21 treatments that used fiducials, none had local failure, compared with six failures in 62 treatments without fiducials.
Both methods had similar low rates of late adverse events. Acute adverse events and treatment-related deaths were nonsignificantly greater with RFA, which may suggest SBRT as a better option for medically unfit patients who may not tolerate invasive procedures such as RFA.
The study included only three tumors larger than 5 cm in diameter, so rates of local control for this size tumor cannot be estimated reliably, reported Dr. Wahl and his colleagues.
The National Institutes of Health and the Taubman Institute supported the research. Dr. Wahl reported stock or other ownership in Lycera. Several of his coauthors reported ties to industry.
A retrospective data analysis showed that stereotactic body radiotherapy (SBRT) outperformed radiofrequency ablation (RFA) on tumors larger than 2 cm in patients with hepatocellular carcinoma.
For all tumors treated with RFA, 1- and 2-year freedom from local progression (FFLP) were 83.6% and 80.2%, and for tumors treated with SBRT, rates were 97.4% and 83.8%. On tumors smaller than 2 cm, FFLP was similar for the two methods (HR, 2.50; 95% confidence interval, 0.72-8.67; P = .15) but was significantly worse for RFA treatment of larger tumors (HR, 3.35; 95% CI, 1.17-9.62, P = .025).
“These results suggest that both SBRT and RFA are excellent choices for smaller tumors but that SBRT may be preferred for larger tumors. Prospective, randomized clinical trials are needed to compare these two modalities, especially for larger tumors, although we are unaware of any such trials,” wrote Dr. Daniel R. Wahl, radiation oncologist at the University of Michigan (J Clin Oncol. 2015 Dec. 2. doi:10.1200/JCO.2015.61.4925).
The retrospective study evaluated 224 patients with nonmetastatic hepatocellular carcinoma – 161 patients (249 tumors) who underwent RFA and 63 patients (83 tumors) who underwent SBRT at the University of Michigan from 2004 to 2012. Patients treated with RFA had higher rates of cirrhosis (95% vs. 78%; P less than .001), lower AFP levels (8.8 vs. 18.6; P = .04), and fewer prior liver-directed treatments compared with patients treated with SBRT.
To investigate the impact of fiducial use for image guidance in SBRT, the researchers examined treatment failures. Of the 21 treatments that used fiducials, none had local failure, compared with six failures in 62 treatments without fiducials.
Both methods had similar low rates of late adverse events. Acute adverse events and treatment-related deaths were nonsignificantly greater with RFA, which may suggest SBRT as a better option for medically unfit patients who may not tolerate invasive procedures such as RFA.
The study included only three tumors larger than 5 cm in diameter, so rates of local control for this size tumor cannot be estimated reliably, reported Dr. Wahl and his colleagues.
The National Institutes of Health and the Taubman Institute supported the research. Dr. Wahl reported stock or other ownership in Lycera. Several of his coauthors reported ties to industry.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Stereotactic body radiotherapy (SBRT) and radiofrequency ablation (RFA) both achieved good local control for small hepatocellular carcinoma lesions, but for tumors larger than 2 cm, SBRT showed significantly better freedom from local progression (FFLP).
Major finding: For tumors larger than 2 cm, FFLP was worse for RFA compared with SBRT (hazard ratio, 3.35; 95% CI, 1.17-9.62, P = .025).
Data source: The retrospective study evaluated 161 patients (249 tumors) who underwent RFA and 63 patients (83 tumors) who underwent SBRT at the University of Michigan from 2004 to 2012.
Disclosures: The National Institutes of Health and the Taubman Institute supported the research. Dr. Wahl reported stock or other ownership in Lycera. Several of his coauthors reported ties to industry.
Multifocal Langerhans Cell Histiocytosis in an Adult
Eosinophilic granuloma (EG) is the most common benign form of Langerhans cell histiocytosis (LCH). Initially described by Lichtenstein in 1953, LCH encompasses a triad of proliferative granulomatous disorders primarily affecting children: EG, Hand-Schüller-Christian disease, and Letterer-Siwe disease.1 Lichtenstein first termed the disease histiocytosis X, after recognizing that the 3 syndromes had the same histology.1 The term was updated after the clonal proliferation of Langerhans cells in the pathogenesis of the disease was discovered.
As LCH is generally considered a pediatric disease, there is little in the literature regarding adult-onset LCH. The incidence of LCH in adults is reported as 1 to 2 cases per million, significantly lower than that in children.2,3 Two studies have reported the mean age at diagnosis in adults as the fourth decade of life, and have suggested a male predominance.4,5 The vast majority of adult LCH cases described are simple EG, with very few cases of multisystem disseminated disease reported.5
Adult patients with LCH typically present with solitary lesions in bone. Approximately 10% of cases have extraosseous involvement, with the lung being the most common site.6 Lesions tend to be unifocal, with fewer than 10 reports describing multifocal EG.1,7-13 The axial skeleton is most frequently involved, with the majority of lesions occurring in the skull, ribs, vertebrae, or mandible.14 While less common, the femur, humerus, and clavicle are most often involved when the appendicular skeleton is affected.5
In a literature review, a few case reports describe adult-onset EG of the skull. Only 5 case reports since the 1970s describe adult patients with EG of the femur. We present a rare case of multifocal EG in a 48-year-old woman with lesions of the femur and skull, as well as a review of the literature. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 48-year-old woman presented with progressive right knee pain that was exacerbated by weight-bearing. She denied trauma, fevers, fatigue, or weight change. Her history was significant for an EG of the skull, excised at an outside institution 2 years prior to presentation. The patient also admitted to recent onset of right-sided skull pain, near the region of her previous surgery.
Physical examination demonstrated tenderness to palpation and fullness over the right medial distal femur and a normal neurovascular examination of the right lower extremity. Radiographs of the knee showed a cortically based, lytic, destructive lesion involving the medial femoral condyle, with soft-tissue extension (Figures 1A, 1B). Magnetic resonance imaging (MRI) of the right knee showed the lesion, with extraosseous soft-tissue extension (Figures 2A, 2B). The mass was isointense to muscle on T1-weighted images and hyperintense on T2-weighted images. Technetium bone scanning showed increased uptake in the right femur and the right skull (Figures 3A, 3B). MRI of the brain confirmed a new lesion in the right diploic space, distinct from the previous EG lesion site (Figures 4A-4D). An ultrasound-guided biopsy of the femur was performed and was consistent with EG.
After reevaluation and clearance by her neurosurgeon, the patient underwent curettage and allografting of the femoral lesion, with prophylactic internal fixation using a titanium distal femoral locking plate (Figure 5). Intraoperative frozen section was consistent with EG, which was confirmed with additional immunohistochemical workup (Figures 6A-6D).
The patient recovered uneventfully and follow-up radiographs showed restoration of the bony cortex of the medial femoral condyle (Figure 7). The second skull lesion, which was also consistent with EG, was excised by her neurosurgeon.
The patient remained asymptomatic until 2 years later, when she began experiencing mild pain in her right distal thigh and knee. Radiographs showed a new lytic focus in the right distal metadiaphysis (Figure 8) which was not present on her last radiograph 6 months prior. A computed tomography (CT) scan showed a lytic lesion involving the right distal femur medullary canal with cortical thinning and destruction, most pronounced posteriorly (Figures 9A, 9B). There was also an extraosseous soft-tissue component to the lesion. Bone scan showed increased uptake in the area of the new lesion. There was no increased uptake elsewhere, including the medial distal femur at the site of the old lesion, to suggest other lesions, and no increased uptake in the skull.
Given that the location of the lesion was distinct from the prior site of curettage and bone grafting, it was thought to be consistent with a new EG lesion. The patient underwent CT-guided biopsy, with simultaneous intralesional corticosteroid injection to treat the lesion when on-site pathology confirmed the etiology. Further surgical management was deemed unnecessary because internal fixation was present and spanned the new lesion. Final analysis of the fine-needle aspirate of the new lesion was positive for numerous eosinophils and histiocytes, consistent with EG.
At 6-week follow-up after the intralesional steroid injection, the patient’s pain continued to abate, and she was ambulating with crutches. Repeat CT scan of the right distal femur showed improvement of the extraosseous soft-tissue component, while the lucency in the femur itself remained unchanged. The decision was made to proceed with a second intralesional corticosteroid injection under CT guidance. The patient’s symptoms continued to improve, and repeat imaging 1 year after her steroid injections showed substantial bony healing with reconstitution of her cortical bone (Figures 10A-10E).
The patient had had 4 distinct tumors consistent with EG and was referred to a medical oncologist for further workup. The patient began treatment with zoledronic acid to prevent development of further lesions. At most recent follow-up, the patient was 18 months out from her second intralesional corticosteroid injection and was doing very well. She reported being pain-free and was walking 3 to 4 miles per week without gait aids. There was no evidence of new disease. The medial distal femur lesion was completely healed, and the distal metaphyseal lesion was nearly healed, with very little residual evidence of lesions.
Discussion
Adult-onset multifocal EG is a rare entity. Most affected patients develop lesions in the axial skeleton, with the skull, mandible, and vertebrae most commonly involved.14 Only 5 cases of femoral EG have been reported, one of which was multifocal.11,14-17
Of these patients, 3 were between the ages of 33 and 53 years and had insidious onset of hip pain that failed conservative management.14,15,17 Further imaging and biopsy revealed unifocal EG in the proximal femur in each case. Each patient received a different form of treatment, including curettage and radiation, radiofrequency ablation, and/or physical therapy. At the time of publication, all patients had reported improvement in their clinical symptoms.14,15,17 The fourth patient was a man with human immunodeficiency virus (HIV) with 3 months of progressive thigh pain. Further evaluation found an isolated EG of the femoral diaphysis that progressed to pathologic fracture. He was treated with curettage and intramedullary nailing, and had improved symptoms and radiographic signs of healing at 30-month follow-up.16
An interesting case by Kerzl and colleagues11 reported a 63-year-old woman with a 24-year history of multiple symmetric lesions of the femora, leading to multiple pathologic fractures. Like our patient, her initial lesion was in the skull. Initial pathology specimens led to the diagnosis of EG. However, as the patient aged, she developed symptoms of diabetes insipidus and xanthelasma, which led to reevaluation of histology from 3 bony lesions. The patient was determined to have multifocal EG of the skull and femur, with simultaneous occurrence of Erdheim-Chester disease, which also causes bone lesions in addition to diabetes insipidus and xanthelasma.11
Though LCH was initially described more than 50 years ago, many aspects of LCH remain an enigma, especially in adults. The etiology of the disease is poorly understood. Controversy exists regarding whether LCH is primarily an immunoregulatory, neoplastic, or reactive disorder. The vast majority of adult cases described in the literature are EG, with very few cases of multisystem disseminated disease reported.5
The spectrum of disorders constituting LCH is heterogenous. Eosinophilic granuloma is the most common form, reportedly accounting for 60% to 70% of all cases, usually presenting as solitary bone lesions.6 Eosinophilic granuloma refers to the localized form of LCH, in which the disease is limited to bone or lung.18 This is the least aggressive form of the disease, with the most favorable prognosis. Hand- Schüller-Christian disease is a chronic, recurring form of LCH, with disseminated disease, affecting both bone and extraskeletal sites. Hand-Schüller-Christian disease is known for the classic triad of diabetes insipidus, exophthalmos, and destructive bone lesions. Patients may also present with otitis media or neurologic complaints from pathologic vertebral fractures. Letterer-Siwe disease refers to the acute, disseminated, fulminant form of LCH. This is the least common form of LCH and is predominately described in young children. Patients present with hepatosplenomegaly, lymphadenopathy, skin rash, fever, anemia, and thrombocytopenia.19 It is rapidly progressive, leading to multiorgan dysfunction and death within 1 to 2 years.18
The classification of LCH follows the Histiocyte Society guidelines developed from multicenter randomized trials in children.3 Classification is based on affected organs and is divided into 2 categories: single-system disease or multisystem disease. Single-system disease may be single site (bone, skin, or solitary lymph node) or multisite (multifocal bone disease or multiple lymph nodes). Multisystem disease is further classified into low-risk or risk groups. The low-risk group involves disseminated disease without involvement of risk organs (lungs, liver, spleen, and hematopoietic system). Involvement of 1 or more risk organs places the patient in the risk group, associated with the least favorable prognosis.3
In adults, the most common presenting symptoms are local pain from bony involvement, weight loss, and fever. Bony lesions most often occur in the skull, especially in the jaw. Long bones are less frequently involved, with lesions occurring in the long bones in approximately 17% of patients.3 The rib has also been reported as a common site of involvement in adults.5 Similar to children, diabetes insipidus remains a classic manifestation of LCH because of pituitary gland involvement. Other common symptoms of LCH in adults are cough, dyspnea, and chest pain from pulmonary involvement. Up to 20% to 30% of adult LCH patients have isolated pulmonary lesions, although pulmonary LCH may also occur as part of multisystem disease (risk group).3,4,20
Eosinophilic granuloma bone lesions have a variety of radiographic appearances but most commonly appear as lytic lesions. They often mimic aggressive lesions with permeative bone destruction, periostitis, ill-defined borders, and cortical erosion. Most lesions arise in the medullary space but can present as a destructive, cortically based lesion, as it did in our patient’s first femoral lesion. The differential diagnosis for a lytic medullary bone lesion includes benign entities, such as nonossifying fibromas, bone cysts, or osteomyelitis, but also includes malignant tumors, such as metastases, Ewing sarcoma, and lymphoma. A destructive, cortically based lesion in an adult should raise a very high suspicion for metastatic carcinoma until proven otherwise. Other diagnostic considerations for a cortically based lesion include chondromyxoid fibroma and surface bone lesions, such as surface chondroma and osteoma, or osteosarcoma (parosteal and periosteal). In the skull, lesions commonly erode the outer table more than the inner table (the typical “beveled-edge” appearance). Skull lesions also may have a small, central, dense focus within the lytic lesion (“button sequestrum”).
Bone scanning is often not as sensitive in detecting EG lesions compared with other bone tumors, although in our patient the bone scan was positive. In patients with a negative bone scan but a high index of suspicion, a radiographic skeletal survey should be obtained to rule out other lesions. MRI typically shows T2-hyperintense, T1-hypointense lesions with surrounding bone marrow edema and variable contrast enhancement, which is relatively nonspecific. The high sensitivity of MRI allows accurate delineation of the extent of the lesions and evaluates for the presence of an extraosseous soft-tissue component. Biopsy is generally necessary to establish a definitive histologic diagnosis. In our patient, despite her history of biopsy-proven EG, the aggressive appearance of a destructive, cortically based lesion made obtaining a biopsy critical to establish a definitive diagnosis in this case.
The histopathologic examination of the tissue from our patient was typical of that seen in patients with EG. It revealed tissue fragments with diffuse sheets of histiocytes displaying nuclear grooves, admixed numerous eosinophils with eosinophilic microabscesses, and scattered lymphocytes (Figures 6A, 6B). There were areas of necrosis, raising the possibility of osteomyelitis. However, the presence of classic histomorphologic features of LCH in the majority of the tissue fragments, along with CD1a- and S100-positivity in the histiocytes, confirmed the diagnosis of LCH (Figures 6C, 6D). Although not highly specific, a positive CD1a immunostain with the described histomorphologic findings in the proper clinical setting is often considered sufficient for LCH diagnosis. S100 is an important adjunct immunostain in the evaluation of histiocytic disorders. A positive S100 immunostain helps identify histiocytes, which are also CD1a-positive, because the latter immunostain can also be positive in some lymphomas and thymomas.21
After diagnosis of LCH has been confirmed, staging includes radiographs of any suspicious bone lesions, chest radiograph, bone scan, abdominal ultrasound, routine laboratory studies, and chest CT if pulmonary LCH is suspected.
The optimal treatment strategy for adult patients has not been clearly defined, and current strategies for LCH vary depending on organ involvement and extent of disease. Therapeutic options include observation, local treatment with steroids, local excision with curettage with or without bone grafting, chemotherapy, immunomodulation, irradiation, and stem cell transplantation in advanced disease. In general, patients who benefit from systemic therapy, such as chemotherapy or immunomodulation, include those with multisystem disease, refractory or recurrent lesions, and multifocal skeletal involvement.22
Patients with more limited disease, such as EG of bone, may undergo observation or local intralesional treatment. Eosinophilic granuloma of bone may resolve spontaneously and commonly does so when it is located in the pediatric spine. However, the therapeutic approach in adults with EG is controversial, given that spontaneous resolution is less likely to occur in the skeletally mature. Plasschaert and colleagues23 reported a recurrence rate of 26% in skeletally mature patients with EG of bone treated with biopsy followed by curettage with or without grafting. In the skeletally immature group, there were no clinical or radiographic signs of recurrence in the 2-year follow-up period.23 Thus, treatment in the adult population must be considered separate from the skeletally immature and in the appropriate clinical context. Depending on the location of the lesion, patients may become symptomatic or be at risk for pathologic fracture. In such circumstances, curettage with or without bone grafting and prophylactic internal fixation may be indicated. Other treatments, such as intralesional infiltration with corticosteroids, have been reported, but the role of such treatment in adults is undetermined.24,25 Radiation is typically not recommended in single-system disease unless a vital organ is threatened.26 Overall, patients with single-system disease have an excellent prognosis, and treatment should be determined on an individual basis.3
Eosinophilic granuloma represents less than 1% of all bone tumors, and adult presentation is very rare. The differential diagnosis of lytic bone lesions is broad and includes metastatic carcinoma, lymphoma/myeloma, osteomyelitis, osteoblastoma, aneurysmal bone cyst, and Ewing sarcoma. While EG is more common and easily diagnosed in children, it should be considered in the differential diagnosis in adults, so that the appropriate diagnostic workup and treatment can be performed.
1. Lahiani D, Hammami BK, Maâloul I, et al. Multifocal Langerhans cell histiocytosis of bone: late revelation in a 76-year-old woman. Rev Med Interne. 2008;29(3):249-251.
2. Baumgartner I, von Hochstetter A, Baumert B, Luetolf U, Follath F. Langerhans’-cell histiocytosis in adults. Med Pediatr Oncol. 1997;28(1):9-14.
3. Stockschlaeder M, Sucker C. Adult Langerhans cell histiocytosis. Eur J Haematol. 2006;76(5):363-368.
4. Aricò M, Girschikofsky M, Généreau T, et al. Langerhans cell histiocytosis in adults. Report from the International Registry of the Histiocyte Society. Eur J Cancer. 2003;39(16):2341-2348.
5. Islinger RB, Kuklo TR, Owens BD, et al. Langerhans’ cell histiocytosis in patients older than 21 years. Clin Orthop Relat Res. 2000;379:231-235.
6. Key SJ, O’Brien CJ, Silvester KC, Crean SJ. Eosinophilic granuloma: resolution of maxillofacial bony lesions following minimal intervention. Report of three cases and a review of the literature. J Craniomaxillofac Surg. 2004;32(3):170-175.
7. Bodner G, Kreczy A, Rachbauer F, Baechter O, Peer S. Eosinophilic granuloma of the bone: ultrasonographic imaging. Australas Radiol. 2002;46(4):418-421.
8. Boutsen Y, Esselinckx W, Delos M, Nisolle JF. Adult onset of multifocal eosinophilic granuloma of bone: a long-term follow-up with evaluation of various treatment options and spontaneous healing. Clin Rheumatol. 1999;18(1):69-73.
9. Corti F, Valicenti A, Bertolucci D, Bruno J, Gustinucci R. Multifocal Langerhans cell granulomatosis. Report of a clinical case. Minerva Med. 1994;85(7-8):413-416.
10. Demirci I. Adult eosinophilic granuloma of the lumbar spine with atypical dissemination. Case report: a long-term follow-up. Zentralbl Neurochir. 2004;65(2):84-87.
11. Kerzl R, Eyerich K, Eberlein B, et al. Parallel occurrence of Erdheim-Chester disease and eosinophilic granuloma in the same patient. J Eur Acad Dermatol Venereol. 2009;23(2):224-226.
12. Nguyen BD, Roarke MC, Chivers SF. Multifocal Langerhans cell histiocytosis with infiltrative pelvic lesions: PET/CT imaging. Clin Nucl Med. 2010;35(10): 824-826.
13. Scolozzi P, Lombardi T, Monnier P, Jaques B. Multisystem Langerhans’ cell histiocytosis (Hand-Schuller-Christian disease) in an adult: a case report and review of the literature. Eur Arch Otorhinolaryngol. 2004;261(6):326-330.
14. King JJ, Melvin JS, Iwenofu OH, Fox EJ. Thigh pain in a 53-year-old woman. Clin Orthop Relat Res. 2009;467(6):1652-1657.
15. Hair LC, Deyle GD. Eosinophilic granuloma in a patient with hip pain. J Orthop Sports Phys Ther. 2011;41(2):119.
16. Panayiotakopoulos GD, Sipsas NV, Kontos A, et al. Eosinophilic granuloma of the femur in an HIV-1 positive patient. AIDS Patient Care STDS. 2002;16(3):103-106.
17. Rodrigues RJ, Lewis HH. Eosinophilic granuloma of bone. Review of literature and case presentation. Clin Orthop Relat Res. 1971;77:183-192.
18. Stull MA, Kransdorf MJ, Devaney KO. Langerhans cell histiocytosis of bone. Radiographics. 1992;12(4):801-823.
19. Lichtenstein L. Histiocytosis X (eosinophilic granuloma of bone, Letterer-Siwe disease, and Schueller-Christian disease). Further observations of pathological and clinical importance. J Bone Joint Surg Am. 1964;46:76-90.
20. Götz G, Fichter J. Langerhans’-cell histiocytosis in 58 adults. Eur J Med Res. 2004;9(11):510-514.
21. Cheng KL, Glu PG, Weiss LM. Hematopoeitic tumors. In: Peiguo C, Weiss L, eds. Modern Immunohistochemistry. New York, NY: Cambridge University Press; 2009:503.
22. Broadbent V, Gadner H. Current therapy for Langerhans cell histiocytosis. Hematol Oncol Clin North Am. 1998;12(2):327-338.
23. Plasschaert F, Craig C, Bell R, Cole WG, Wunder JS, Alman BA. Eosinophilic granuloma. A different behaviour in children than in adults. J Bone Joint Surg Br. 2002;84(6):870-872.
24. Capanna R, Springfield DS, Ruggieri P, et al. Direct cortisone injection in osinophilic granuloma of bone: a preliminary report on 11 patients. J Pediatr Orthop. 1985;5(3):339-342.
25. Egeler RM, Thompson RC Jr, Voûte PA, Nesbit ME Jr. Intralesional infiltration of corticosteroids in localized Langerhans’ cell histiocytosis. J Pediatr Orthop. 1992;12(6):811-814.
26. Ladisch S, Gadner H. Treatment of Langerhans cell histiocytosis–evolution and current approaches. Br J Cancer Suppl. 1994;23:S41-S46.
Eosinophilic granuloma (EG) is the most common benign form of Langerhans cell histiocytosis (LCH). Initially described by Lichtenstein in 1953, LCH encompasses a triad of proliferative granulomatous disorders primarily affecting children: EG, Hand-Schüller-Christian disease, and Letterer-Siwe disease.1 Lichtenstein first termed the disease histiocytosis X, after recognizing that the 3 syndromes had the same histology.1 The term was updated after the clonal proliferation of Langerhans cells in the pathogenesis of the disease was discovered.
As LCH is generally considered a pediatric disease, there is little in the literature regarding adult-onset LCH. The incidence of LCH in adults is reported as 1 to 2 cases per million, significantly lower than that in children.2,3 Two studies have reported the mean age at diagnosis in adults as the fourth decade of life, and have suggested a male predominance.4,5 The vast majority of adult LCH cases described are simple EG, with very few cases of multisystem disseminated disease reported.5
Adult patients with LCH typically present with solitary lesions in bone. Approximately 10% of cases have extraosseous involvement, with the lung being the most common site.6 Lesions tend to be unifocal, with fewer than 10 reports describing multifocal EG.1,7-13 The axial skeleton is most frequently involved, with the majority of lesions occurring in the skull, ribs, vertebrae, or mandible.14 While less common, the femur, humerus, and clavicle are most often involved when the appendicular skeleton is affected.5
In a literature review, a few case reports describe adult-onset EG of the skull. Only 5 case reports since the 1970s describe adult patients with EG of the femur. We present a rare case of multifocal EG in a 48-year-old woman with lesions of the femur and skull, as well as a review of the literature. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 48-year-old woman presented with progressive right knee pain that was exacerbated by weight-bearing. She denied trauma, fevers, fatigue, or weight change. Her history was significant for an EG of the skull, excised at an outside institution 2 years prior to presentation. The patient also admitted to recent onset of right-sided skull pain, near the region of her previous surgery.
Physical examination demonstrated tenderness to palpation and fullness over the right medial distal femur and a normal neurovascular examination of the right lower extremity. Radiographs of the knee showed a cortically based, lytic, destructive lesion involving the medial femoral condyle, with soft-tissue extension (Figures 1A, 1B). Magnetic resonance imaging (MRI) of the right knee showed the lesion, with extraosseous soft-tissue extension (Figures 2A, 2B). The mass was isointense to muscle on T1-weighted images and hyperintense on T2-weighted images. Technetium bone scanning showed increased uptake in the right femur and the right skull (Figures 3A, 3B). MRI of the brain confirmed a new lesion in the right diploic space, distinct from the previous EG lesion site (Figures 4A-4D). An ultrasound-guided biopsy of the femur was performed and was consistent with EG.
After reevaluation and clearance by her neurosurgeon, the patient underwent curettage and allografting of the femoral lesion, with prophylactic internal fixation using a titanium distal femoral locking plate (Figure 5). Intraoperative frozen section was consistent with EG, which was confirmed with additional immunohistochemical workup (Figures 6A-6D).
The patient recovered uneventfully and follow-up radiographs showed restoration of the bony cortex of the medial femoral condyle (Figure 7). The second skull lesion, which was also consistent with EG, was excised by her neurosurgeon.
The patient remained asymptomatic until 2 years later, when she began experiencing mild pain in her right distal thigh and knee. Radiographs showed a new lytic focus in the right distal metadiaphysis (Figure 8) which was not present on her last radiograph 6 months prior. A computed tomography (CT) scan showed a lytic lesion involving the right distal femur medullary canal with cortical thinning and destruction, most pronounced posteriorly (Figures 9A, 9B). There was also an extraosseous soft-tissue component to the lesion. Bone scan showed increased uptake in the area of the new lesion. There was no increased uptake elsewhere, including the medial distal femur at the site of the old lesion, to suggest other lesions, and no increased uptake in the skull.
Given that the location of the lesion was distinct from the prior site of curettage and bone grafting, it was thought to be consistent with a new EG lesion. The patient underwent CT-guided biopsy, with simultaneous intralesional corticosteroid injection to treat the lesion when on-site pathology confirmed the etiology. Further surgical management was deemed unnecessary because internal fixation was present and spanned the new lesion. Final analysis of the fine-needle aspirate of the new lesion was positive for numerous eosinophils and histiocytes, consistent with EG.
At 6-week follow-up after the intralesional steroid injection, the patient’s pain continued to abate, and she was ambulating with crutches. Repeat CT scan of the right distal femur showed improvement of the extraosseous soft-tissue component, while the lucency in the femur itself remained unchanged. The decision was made to proceed with a second intralesional corticosteroid injection under CT guidance. The patient’s symptoms continued to improve, and repeat imaging 1 year after her steroid injections showed substantial bony healing with reconstitution of her cortical bone (Figures 10A-10E).
The patient had had 4 distinct tumors consistent with EG and was referred to a medical oncologist for further workup. The patient began treatment with zoledronic acid to prevent development of further lesions. At most recent follow-up, the patient was 18 months out from her second intralesional corticosteroid injection and was doing very well. She reported being pain-free and was walking 3 to 4 miles per week without gait aids. There was no evidence of new disease. The medial distal femur lesion was completely healed, and the distal metaphyseal lesion was nearly healed, with very little residual evidence of lesions.
Discussion
Adult-onset multifocal EG is a rare entity. Most affected patients develop lesions in the axial skeleton, with the skull, mandible, and vertebrae most commonly involved.14 Only 5 cases of femoral EG have been reported, one of which was multifocal.11,14-17
Of these patients, 3 were between the ages of 33 and 53 years and had insidious onset of hip pain that failed conservative management.14,15,17 Further imaging and biopsy revealed unifocal EG in the proximal femur in each case. Each patient received a different form of treatment, including curettage and radiation, radiofrequency ablation, and/or physical therapy. At the time of publication, all patients had reported improvement in their clinical symptoms.14,15,17 The fourth patient was a man with human immunodeficiency virus (HIV) with 3 months of progressive thigh pain. Further evaluation found an isolated EG of the femoral diaphysis that progressed to pathologic fracture. He was treated with curettage and intramedullary nailing, and had improved symptoms and radiographic signs of healing at 30-month follow-up.16
An interesting case by Kerzl and colleagues11 reported a 63-year-old woman with a 24-year history of multiple symmetric lesions of the femora, leading to multiple pathologic fractures. Like our patient, her initial lesion was in the skull. Initial pathology specimens led to the diagnosis of EG. However, as the patient aged, she developed symptoms of diabetes insipidus and xanthelasma, which led to reevaluation of histology from 3 bony lesions. The patient was determined to have multifocal EG of the skull and femur, with simultaneous occurrence of Erdheim-Chester disease, which also causes bone lesions in addition to diabetes insipidus and xanthelasma.11
Though LCH was initially described more than 50 years ago, many aspects of LCH remain an enigma, especially in adults. The etiology of the disease is poorly understood. Controversy exists regarding whether LCH is primarily an immunoregulatory, neoplastic, or reactive disorder. The vast majority of adult cases described in the literature are EG, with very few cases of multisystem disseminated disease reported.5
The spectrum of disorders constituting LCH is heterogenous. Eosinophilic granuloma is the most common form, reportedly accounting for 60% to 70% of all cases, usually presenting as solitary bone lesions.6 Eosinophilic granuloma refers to the localized form of LCH, in which the disease is limited to bone or lung.18 This is the least aggressive form of the disease, with the most favorable prognosis. Hand- Schüller-Christian disease is a chronic, recurring form of LCH, with disseminated disease, affecting both bone and extraskeletal sites. Hand-Schüller-Christian disease is known for the classic triad of diabetes insipidus, exophthalmos, and destructive bone lesions. Patients may also present with otitis media or neurologic complaints from pathologic vertebral fractures. Letterer-Siwe disease refers to the acute, disseminated, fulminant form of LCH. This is the least common form of LCH and is predominately described in young children. Patients present with hepatosplenomegaly, lymphadenopathy, skin rash, fever, anemia, and thrombocytopenia.19 It is rapidly progressive, leading to multiorgan dysfunction and death within 1 to 2 years.18
The classification of LCH follows the Histiocyte Society guidelines developed from multicenter randomized trials in children.3 Classification is based on affected organs and is divided into 2 categories: single-system disease or multisystem disease. Single-system disease may be single site (bone, skin, or solitary lymph node) or multisite (multifocal bone disease or multiple lymph nodes). Multisystem disease is further classified into low-risk or risk groups. The low-risk group involves disseminated disease without involvement of risk organs (lungs, liver, spleen, and hematopoietic system). Involvement of 1 or more risk organs places the patient in the risk group, associated with the least favorable prognosis.3
In adults, the most common presenting symptoms are local pain from bony involvement, weight loss, and fever. Bony lesions most often occur in the skull, especially in the jaw. Long bones are less frequently involved, with lesions occurring in the long bones in approximately 17% of patients.3 The rib has also been reported as a common site of involvement in adults.5 Similar to children, diabetes insipidus remains a classic manifestation of LCH because of pituitary gland involvement. Other common symptoms of LCH in adults are cough, dyspnea, and chest pain from pulmonary involvement. Up to 20% to 30% of adult LCH patients have isolated pulmonary lesions, although pulmonary LCH may also occur as part of multisystem disease (risk group).3,4,20
Eosinophilic granuloma bone lesions have a variety of radiographic appearances but most commonly appear as lytic lesions. They often mimic aggressive lesions with permeative bone destruction, periostitis, ill-defined borders, and cortical erosion. Most lesions arise in the medullary space but can present as a destructive, cortically based lesion, as it did in our patient’s first femoral lesion. The differential diagnosis for a lytic medullary bone lesion includes benign entities, such as nonossifying fibromas, bone cysts, or osteomyelitis, but also includes malignant tumors, such as metastases, Ewing sarcoma, and lymphoma. A destructive, cortically based lesion in an adult should raise a very high suspicion for metastatic carcinoma until proven otherwise. Other diagnostic considerations for a cortically based lesion include chondromyxoid fibroma and surface bone lesions, such as surface chondroma and osteoma, or osteosarcoma (parosteal and periosteal). In the skull, lesions commonly erode the outer table more than the inner table (the typical “beveled-edge” appearance). Skull lesions also may have a small, central, dense focus within the lytic lesion (“button sequestrum”).
Bone scanning is often not as sensitive in detecting EG lesions compared with other bone tumors, although in our patient the bone scan was positive. In patients with a negative bone scan but a high index of suspicion, a radiographic skeletal survey should be obtained to rule out other lesions. MRI typically shows T2-hyperintense, T1-hypointense lesions with surrounding bone marrow edema and variable contrast enhancement, which is relatively nonspecific. The high sensitivity of MRI allows accurate delineation of the extent of the lesions and evaluates for the presence of an extraosseous soft-tissue component. Biopsy is generally necessary to establish a definitive histologic diagnosis. In our patient, despite her history of biopsy-proven EG, the aggressive appearance of a destructive, cortically based lesion made obtaining a biopsy critical to establish a definitive diagnosis in this case.
The histopathologic examination of the tissue from our patient was typical of that seen in patients with EG. It revealed tissue fragments with diffuse sheets of histiocytes displaying nuclear grooves, admixed numerous eosinophils with eosinophilic microabscesses, and scattered lymphocytes (Figures 6A, 6B). There were areas of necrosis, raising the possibility of osteomyelitis. However, the presence of classic histomorphologic features of LCH in the majority of the tissue fragments, along with CD1a- and S100-positivity in the histiocytes, confirmed the diagnosis of LCH (Figures 6C, 6D). Although not highly specific, a positive CD1a immunostain with the described histomorphologic findings in the proper clinical setting is often considered sufficient for LCH diagnosis. S100 is an important adjunct immunostain in the evaluation of histiocytic disorders. A positive S100 immunostain helps identify histiocytes, which are also CD1a-positive, because the latter immunostain can also be positive in some lymphomas and thymomas.21
After diagnosis of LCH has been confirmed, staging includes radiographs of any suspicious bone lesions, chest radiograph, bone scan, abdominal ultrasound, routine laboratory studies, and chest CT if pulmonary LCH is suspected.
The optimal treatment strategy for adult patients has not been clearly defined, and current strategies for LCH vary depending on organ involvement and extent of disease. Therapeutic options include observation, local treatment with steroids, local excision with curettage with or without bone grafting, chemotherapy, immunomodulation, irradiation, and stem cell transplantation in advanced disease. In general, patients who benefit from systemic therapy, such as chemotherapy or immunomodulation, include those with multisystem disease, refractory or recurrent lesions, and multifocal skeletal involvement.22
Patients with more limited disease, such as EG of bone, may undergo observation or local intralesional treatment. Eosinophilic granuloma of bone may resolve spontaneously and commonly does so when it is located in the pediatric spine. However, the therapeutic approach in adults with EG is controversial, given that spontaneous resolution is less likely to occur in the skeletally mature. Plasschaert and colleagues23 reported a recurrence rate of 26% in skeletally mature patients with EG of bone treated with biopsy followed by curettage with or without grafting. In the skeletally immature group, there were no clinical or radiographic signs of recurrence in the 2-year follow-up period.23 Thus, treatment in the adult population must be considered separate from the skeletally immature and in the appropriate clinical context. Depending on the location of the lesion, patients may become symptomatic or be at risk for pathologic fracture. In such circumstances, curettage with or without bone grafting and prophylactic internal fixation may be indicated. Other treatments, such as intralesional infiltration with corticosteroids, have been reported, but the role of such treatment in adults is undetermined.24,25 Radiation is typically not recommended in single-system disease unless a vital organ is threatened.26 Overall, patients with single-system disease have an excellent prognosis, and treatment should be determined on an individual basis.3
Eosinophilic granuloma represents less than 1% of all bone tumors, and adult presentation is very rare. The differential diagnosis of lytic bone lesions is broad and includes metastatic carcinoma, lymphoma/myeloma, osteomyelitis, osteoblastoma, aneurysmal bone cyst, and Ewing sarcoma. While EG is more common and easily diagnosed in children, it should be considered in the differential diagnosis in adults, so that the appropriate diagnostic workup and treatment can be performed.
Eosinophilic granuloma (EG) is the most common benign form of Langerhans cell histiocytosis (LCH). Initially described by Lichtenstein in 1953, LCH encompasses a triad of proliferative granulomatous disorders primarily affecting children: EG, Hand-Schüller-Christian disease, and Letterer-Siwe disease.1 Lichtenstein first termed the disease histiocytosis X, after recognizing that the 3 syndromes had the same histology.1 The term was updated after the clonal proliferation of Langerhans cells in the pathogenesis of the disease was discovered.
As LCH is generally considered a pediatric disease, there is little in the literature regarding adult-onset LCH. The incidence of LCH in adults is reported as 1 to 2 cases per million, significantly lower than that in children.2,3 Two studies have reported the mean age at diagnosis in adults as the fourth decade of life, and have suggested a male predominance.4,5 The vast majority of adult LCH cases described are simple EG, with very few cases of multisystem disseminated disease reported.5
Adult patients with LCH typically present with solitary lesions in bone. Approximately 10% of cases have extraosseous involvement, with the lung being the most common site.6 Lesions tend to be unifocal, with fewer than 10 reports describing multifocal EG.1,7-13 The axial skeleton is most frequently involved, with the majority of lesions occurring in the skull, ribs, vertebrae, or mandible.14 While less common, the femur, humerus, and clavicle are most often involved when the appendicular skeleton is affected.5
In a literature review, a few case reports describe adult-onset EG of the skull. Only 5 case reports since the 1970s describe adult patients with EG of the femur. We present a rare case of multifocal EG in a 48-year-old woman with lesions of the femur and skull, as well as a review of the literature. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 48-year-old woman presented with progressive right knee pain that was exacerbated by weight-bearing. She denied trauma, fevers, fatigue, or weight change. Her history was significant for an EG of the skull, excised at an outside institution 2 years prior to presentation. The patient also admitted to recent onset of right-sided skull pain, near the region of her previous surgery.
Physical examination demonstrated tenderness to palpation and fullness over the right medial distal femur and a normal neurovascular examination of the right lower extremity. Radiographs of the knee showed a cortically based, lytic, destructive lesion involving the medial femoral condyle, with soft-tissue extension (Figures 1A, 1B). Magnetic resonance imaging (MRI) of the right knee showed the lesion, with extraosseous soft-tissue extension (Figures 2A, 2B). The mass was isointense to muscle on T1-weighted images and hyperintense on T2-weighted images. Technetium bone scanning showed increased uptake in the right femur and the right skull (Figures 3A, 3B). MRI of the brain confirmed a new lesion in the right diploic space, distinct from the previous EG lesion site (Figures 4A-4D). An ultrasound-guided biopsy of the femur was performed and was consistent with EG.
After reevaluation and clearance by her neurosurgeon, the patient underwent curettage and allografting of the femoral lesion, with prophylactic internal fixation using a titanium distal femoral locking plate (Figure 5). Intraoperative frozen section was consistent with EG, which was confirmed with additional immunohistochemical workup (Figures 6A-6D).
The patient recovered uneventfully and follow-up radiographs showed restoration of the bony cortex of the medial femoral condyle (Figure 7). The second skull lesion, which was also consistent with EG, was excised by her neurosurgeon.
The patient remained asymptomatic until 2 years later, when she began experiencing mild pain in her right distal thigh and knee. Radiographs showed a new lytic focus in the right distal metadiaphysis (Figure 8) which was not present on her last radiograph 6 months prior. A computed tomography (CT) scan showed a lytic lesion involving the right distal femur medullary canal with cortical thinning and destruction, most pronounced posteriorly (Figures 9A, 9B). There was also an extraosseous soft-tissue component to the lesion. Bone scan showed increased uptake in the area of the new lesion. There was no increased uptake elsewhere, including the medial distal femur at the site of the old lesion, to suggest other lesions, and no increased uptake in the skull.
Given that the location of the lesion was distinct from the prior site of curettage and bone grafting, it was thought to be consistent with a new EG lesion. The patient underwent CT-guided biopsy, with simultaneous intralesional corticosteroid injection to treat the lesion when on-site pathology confirmed the etiology. Further surgical management was deemed unnecessary because internal fixation was present and spanned the new lesion. Final analysis of the fine-needle aspirate of the new lesion was positive for numerous eosinophils and histiocytes, consistent with EG.
At 6-week follow-up after the intralesional steroid injection, the patient’s pain continued to abate, and she was ambulating with crutches. Repeat CT scan of the right distal femur showed improvement of the extraosseous soft-tissue component, while the lucency in the femur itself remained unchanged. The decision was made to proceed with a second intralesional corticosteroid injection under CT guidance. The patient’s symptoms continued to improve, and repeat imaging 1 year after her steroid injections showed substantial bony healing with reconstitution of her cortical bone (Figures 10A-10E).
The patient had had 4 distinct tumors consistent with EG and was referred to a medical oncologist for further workup. The patient began treatment with zoledronic acid to prevent development of further lesions. At most recent follow-up, the patient was 18 months out from her second intralesional corticosteroid injection and was doing very well. She reported being pain-free and was walking 3 to 4 miles per week without gait aids. There was no evidence of new disease. The medial distal femur lesion was completely healed, and the distal metaphyseal lesion was nearly healed, with very little residual evidence of lesions.
Discussion
Adult-onset multifocal EG is a rare entity. Most affected patients develop lesions in the axial skeleton, with the skull, mandible, and vertebrae most commonly involved.14 Only 5 cases of femoral EG have been reported, one of which was multifocal.11,14-17
Of these patients, 3 were between the ages of 33 and 53 years and had insidious onset of hip pain that failed conservative management.14,15,17 Further imaging and biopsy revealed unifocal EG in the proximal femur in each case. Each patient received a different form of treatment, including curettage and radiation, radiofrequency ablation, and/or physical therapy. At the time of publication, all patients had reported improvement in their clinical symptoms.14,15,17 The fourth patient was a man with human immunodeficiency virus (HIV) with 3 months of progressive thigh pain. Further evaluation found an isolated EG of the femoral diaphysis that progressed to pathologic fracture. He was treated with curettage and intramedullary nailing, and had improved symptoms and radiographic signs of healing at 30-month follow-up.16
An interesting case by Kerzl and colleagues11 reported a 63-year-old woman with a 24-year history of multiple symmetric lesions of the femora, leading to multiple pathologic fractures. Like our patient, her initial lesion was in the skull. Initial pathology specimens led to the diagnosis of EG. However, as the patient aged, she developed symptoms of diabetes insipidus and xanthelasma, which led to reevaluation of histology from 3 bony lesions. The patient was determined to have multifocal EG of the skull and femur, with simultaneous occurrence of Erdheim-Chester disease, which also causes bone lesions in addition to diabetes insipidus and xanthelasma.11
Though LCH was initially described more than 50 years ago, many aspects of LCH remain an enigma, especially in adults. The etiology of the disease is poorly understood. Controversy exists regarding whether LCH is primarily an immunoregulatory, neoplastic, or reactive disorder. The vast majority of adult cases described in the literature are EG, with very few cases of multisystem disseminated disease reported.5
The spectrum of disorders constituting LCH is heterogenous. Eosinophilic granuloma is the most common form, reportedly accounting for 60% to 70% of all cases, usually presenting as solitary bone lesions.6 Eosinophilic granuloma refers to the localized form of LCH, in which the disease is limited to bone or lung.18 This is the least aggressive form of the disease, with the most favorable prognosis. Hand- Schüller-Christian disease is a chronic, recurring form of LCH, with disseminated disease, affecting both bone and extraskeletal sites. Hand-Schüller-Christian disease is known for the classic triad of diabetes insipidus, exophthalmos, and destructive bone lesions. Patients may also present with otitis media or neurologic complaints from pathologic vertebral fractures. Letterer-Siwe disease refers to the acute, disseminated, fulminant form of LCH. This is the least common form of LCH and is predominately described in young children. Patients present with hepatosplenomegaly, lymphadenopathy, skin rash, fever, anemia, and thrombocytopenia.19 It is rapidly progressive, leading to multiorgan dysfunction and death within 1 to 2 years.18
The classification of LCH follows the Histiocyte Society guidelines developed from multicenter randomized trials in children.3 Classification is based on affected organs and is divided into 2 categories: single-system disease or multisystem disease. Single-system disease may be single site (bone, skin, or solitary lymph node) or multisite (multifocal bone disease or multiple lymph nodes). Multisystem disease is further classified into low-risk or risk groups. The low-risk group involves disseminated disease without involvement of risk organs (lungs, liver, spleen, and hematopoietic system). Involvement of 1 or more risk organs places the patient in the risk group, associated with the least favorable prognosis.3
In adults, the most common presenting symptoms are local pain from bony involvement, weight loss, and fever. Bony lesions most often occur in the skull, especially in the jaw. Long bones are less frequently involved, with lesions occurring in the long bones in approximately 17% of patients.3 The rib has also been reported as a common site of involvement in adults.5 Similar to children, diabetes insipidus remains a classic manifestation of LCH because of pituitary gland involvement. Other common symptoms of LCH in adults are cough, dyspnea, and chest pain from pulmonary involvement. Up to 20% to 30% of adult LCH patients have isolated pulmonary lesions, although pulmonary LCH may also occur as part of multisystem disease (risk group).3,4,20
Eosinophilic granuloma bone lesions have a variety of radiographic appearances but most commonly appear as lytic lesions. They often mimic aggressive lesions with permeative bone destruction, periostitis, ill-defined borders, and cortical erosion. Most lesions arise in the medullary space but can present as a destructive, cortically based lesion, as it did in our patient’s first femoral lesion. The differential diagnosis for a lytic medullary bone lesion includes benign entities, such as nonossifying fibromas, bone cysts, or osteomyelitis, but also includes malignant tumors, such as metastases, Ewing sarcoma, and lymphoma. A destructive, cortically based lesion in an adult should raise a very high suspicion for metastatic carcinoma until proven otherwise. Other diagnostic considerations for a cortically based lesion include chondromyxoid fibroma and surface bone lesions, such as surface chondroma and osteoma, or osteosarcoma (parosteal and periosteal). In the skull, lesions commonly erode the outer table more than the inner table (the typical “beveled-edge” appearance). Skull lesions also may have a small, central, dense focus within the lytic lesion (“button sequestrum”).
Bone scanning is often not as sensitive in detecting EG lesions compared with other bone tumors, although in our patient the bone scan was positive. In patients with a negative bone scan but a high index of suspicion, a radiographic skeletal survey should be obtained to rule out other lesions. MRI typically shows T2-hyperintense, T1-hypointense lesions with surrounding bone marrow edema and variable contrast enhancement, which is relatively nonspecific. The high sensitivity of MRI allows accurate delineation of the extent of the lesions and evaluates for the presence of an extraosseous soft-tissue component. Biopsy is generally necessary to establish a definitive histologic diagnosis. In our patient, despite her history of biopsy-proven EG, the aggressive appearance of a destructive, cortically based lesion made obtaining a biopsy critical to establish a definitive diagnosis in this case.
The histopathologic examination of the tissue from our patient was typical of that seen in patients with EG. It revealed tissue fragments with diffuse sheets of histiocytes displaying nuclear grooves, admixed numerous eosinophils with eosinophilic microabscesses, and scattered lymphocytes (Figures 6A, 6B). There were areas of necrosis, raising the possibility of osteomyelitis. However, the presence of classic histomorphologic features of LCH in the majority of the tissue fragments, along with CD1a- and S100-positivity in the histiocytes, confirmed the diagnosis of LCH (Figures 6C, 6D). Although not highly specific, a positive CD1a immunostain with the described histomorphologic findings in the proper clinical setting is often considered sufficient for LCH diagnosis. S100 is an important adjunct immunostain in the evaluation of histiocytic disorders. A positive S100 immunostain helps identify histiocytes, which are also CD1a-positive, because the latter immunostain can also be positive in some lymphomas and thymomas.21
After diagnosis of LCH has been confirmed, staging includes radiographs of any suspicious bone lesions, chest radiograph, bone scan, abdominal ultrasound, routine laboratory studies, and chest CT if pulmonary LCH is suspected.
The optimal treatment strategy for adult patients has not been clearly defined, and current strategies for LCH vary depending on organ involvement and extent of disease. Therapeutic options include observation, local treatment with steroids, local excision with curettage with or without bone grafting, chemotherapy, immunomodulation, irradiation, and stem cell transplantation in advanced disease. In general, patients who benefit from systemic therapy, such as chemotherapy or immunomodulation, include those with multisystem disease, refractory or recurrent lesions, and multifocal skeletal involvement.22
Patients with more limited disease, such as EG of bone, may undergo observation or local intralesional treatment. Eosinophilic granuloma of bone may resolve spontaneously and commonly does so when it is located in the pediatric spine. However, the therapeutic approach in adults with EG is controversial, given that spontaneous resolution is less likely to occur in the skeletally mature. Plasschaert and colleagues23 reported a recurrence rate of 26% in skeletally mature patients with EG of bone treated with biopsy followed by curettage with or without grafting. In the skeletally immature group, there were no clinical or radiographic signs of recurrence in the 2-year follow-up period.23 Thus, treatment in the adult population must be considered separate from the skeletally immature and in the appropriate clinical context. Depending on the location of the lesion, patients may become symptomatic or be at risk for pathologic fracture. In such circumstances, curettage with or without bone grafting and prophylactic internal fixation may be indicated. Other treatments, such as intralesional infiltration with corticosteroids, have been reported, but the role of such treatment in adults is undetermined.24,25 Radiation is typically not recommended in single-system disease unless a vital organ is threatened.26 Overall, patients with single-system disease have an excellent prognosis, and treatment should be determined on an individual basis.3
Eosinophilic granuloma represents less than 1% of all bone tumors, and adult presentation is very rare. The differential diagnosis of lytic bone lesions is broad and includes metastatic carcinoma, lymphoma/myeloma, osteomyelitis, osteoblastoma, aneurysmal bone cyst, and Ewing sarcoma. While EG is more common and easily diagnosed in children, it should be considered in the differential diagnosis in adults, so that the appropriate diagnostic workup and treatment can be performed.
1. Lahiani D, Hammami BK, Maâloul I, et al. Multifocal Langerhans cell histiocytosis of bone: late revelation in a 76-year-old woman. Rev Med Interne. 2008;29(3):249-251.
2. Baumgartner I, von Hochstetter A, Baumert B, Luetolf U, Follath F. Langerhans’-cell histiocytosis in adults. Med Pediatr Oncol. 1997;28(1):9-14.
3. Stockschlaeder M, Sucker C. Adult Langerhans cell histiocytosis. Eur J Haematol. 2006;76(5):363-368.
4. Aricò M, Girschikofsky M, Généreau T, et al. Langerhans cell histiocytosis in adults. Report from the International Registry of the Histiocyte Society. Eur J Cancer. 2003;39(16):2341-2348.
5. Islinger RB, Kuklo TR, Owens BD, et al. Langerhans’ cell histiocytosis in patients older than 21 years. Clin Orthop Relat Res. 2000;379:231-235.
6. Key SJ, O’Brien CJ, Silvester KC, Crean SJ. Eosinophilic granuloma: resolution of maxillofacial bony lesions following minimal intervention. Report of three cases and a review of the literature. J Craniomaxillofac Surg. 2004;32(3):170-175.
7. Bodner G, Kreczy A, Rachbauer F, Baechter O, Peer S. Eosinophilic granuloma of the bone: ultrasonographic imaging. Australas Radiol. 2002;46(4):418-421.
8. Boutsen Y, Esselinckx W, Delos M, Nisolle JF. Adult onset of multifocal eosinophilic granuloma of bone: a long-term follow-up with evaluation of various treatment options and spontaneous healing. Clin Rheumatol. 1999;18(1):69-73.
9. Corti F, Valicenti A, Bertolucci D, Bruno J, Gustinucci R. Multifocal Langerhans cell granulomatosis. Report of a clinical case. Minerva Med. 1994;85(7-8):413-416.
10. Demirci I. Adult eosinophilic granuloma of the lumbar spine with atypical dissemination. Case report: a long-term follow-up. Zentralbl Neurochir. 2004;65(2):84-87.
11. Kerzl R, Eyerich K, Eberlein B, et al. Parallel occurrence of Erdheim-Chester disease and eosinophilic granuloma in the same patient. J Eur Acad Dermatol Venereol. 2009;23(2):224-226.
12. Nguyen BD, Roarke MC, Chivers SF. Multifocal Langerhans cell histiocytosis with infiltrative pelvic lesions: PET/CT imaging. Clin Nucl Med. 2010;35(10): 824-826.
13. Scolozzi P, Lombardi T, Monnier P, Jaques B. Multisystem Langerhans’ cell histiocytosis (Hand-Schuller-Christian disease) in an adult: a case report and review of the literature. Eur Arch Otorhinolaryngol. 2004;261(6):326-330.
14. King JJ, Melvin JS, Iwenofu OH, Fox EJ. Thigh pain in a 53-year-old woman. Clin Orthop Relat Res. 2009;467(6):1652-1657.
15. Hair LC, Deyle GD. Eosinophilic granuloma in a patient with hip pain. J Orthop Sports Phys Ther. 2011;41(2):119.
16. Panayiotakopoulos GD, Sipsas NV, Kontos A, et al. Eosinophilic granuloma of the femur in an HIV-1 positive patient. AIDS Patient Care STDS. 2002;16(3):103-106.
17. Rodrigues RJ, Lewis HH. Eosinophilic granuloma of bone. Review of literature and case presentation. Clin Orthop Relat Res. 1971;77:183-192.
18. Stull MA, Kransdorf MJ, Devaney KO. Langerhans cell histiocytosis of bone. Radiographics. 1992;12(4):801-823.
19. Lichtenstein L. Histiocytosis X (eosinophilic granuloma of bone, Letterer-Siwe disease, and Schueller-Christian disease). Further observations of pathological and clinical importance. J Bone Joint Surg Am. 1964;46:76-90.
20. Götz G, Fichter J. Langerhans’-cell histiocytosis in 58 adults. Eur J Med Res. 2004;9(11):510-514.
21. Cheng KL, Glu PG, Weiss LM. Hematopoeitic tumors. In: Peiguo C, Weiss L, eds. Modern Immunohistochemistry. New York, NY: Cambridge University Press; 2009:503.
22. Broadbent V, Gadner H. Current therapy for Langerhans cell histiocytosis. Hematol Oncol Clin North Am. 1998;12(2):327-338.
23. Plasschaert F, Craig C, Bell R, Cole WG, Wunder JS, Alman BA. Eosinophilic granuloma. A different behaviour in children than in adults. J Bone Joint Surg Br. 2002;84(6):870-872.
24. Capanna R, Springfield DS, Ruggieri P, et al. Direct cortisone injection in osinophilic granuloma of bone: a preliminary report on 11 patients. J Pediatr Orthop. 1985;5(3):339-342.
25. Egeler RM, Thompson RC Jr, Voûte PA, Nesbit ME Jr. Intralesional infiltration of corticosteroids in localized Langerhans’ cell histiocytosis. J Pediatr Orthop. 1992;12(6):811-814.
26. Ladisch S, Gadner H. Treatment of Langerhans cell histiocytosis–evolution and current approaches. Br J Cancer Suppl. 1994;23:S41-S46.
1. Lahiani D, Hammami BK, Maâloul I, et al. Multifocal Langerhans cell histiocytosis of bone: late revelation in a 76-year-old woman. Rev Med Interne. 2008;29(3):249-251.
2. Baumgartner I, von Hochstetter A, Baumert B, Luetolf U, Follath F. Langerhans’-cell histiocytosis in adults. Med Pediatr Oncol. 1997;28(1):9-14.
3. Stockschlaeder M, Sucker C. Adult Langerhans cell histiocytosis. Eur J Haematol. 2006;76(5):363-368.
4. Aricò M, Girschikofsky M, Généreau T, et al. Langerhans cell histiocytosis in adults. Report from the International Registry of the Histiocyte Society. Eur J Cancer. 2003;39(16):2341-2348.
5. Islinger RB, Kuklo TR, Owens BD, et al. Langerhans’ cell histiocytosis in patients older than 21 years. Clin Orthop Relat Res. 2000;379:231-235.
6. Key SJ, O’Brien CJ, Silvester KC, Crean SJ. Eosinophilic granuloma: resolution of maxillofacial bony lesions following minimal intervention. Report of three cases and a review of the literature. J Craniomaxillofac Surg. 2004;32(3):170-175.
7. Bodner G, Kreczy A, Rachbauer F, Baechter O, Peer S. Eosinophilic granuloma of the bone: ultrasonographic imaging. Australas Radiol. 2002;46(4):418-421.
8. Boutsen Y, Esselinckx W, Delos M, Nisolle JF. Adult onset of multifocal eosinophilic granuloma of bone: a long-term follow-up with evaluation of various treatment options and spontaneous healing. Clin Rheumatol. 1999;18(1):69-73.
9. Corti F, Valicenti A, Bertolucci D, Bruno J, Gustinucci R. Multifocal Langerhans cell granulomatosis. Report of a clinical case. Minerva Med. 1994;85(7-8):413-416.
10. Demirci I. Adult eosinophilic granuloma of the lumbar spine with atypical dissemination. Case report: a long-term follow-up. Zentralbl Neurochir. 2004;65(2):84-87.
11. Kerzl R, Eyerich K, Eberlein B, et al. Parallel occurrence of Erdheim-Chester disease and eosinophilic granuloma in the same patient. J Eur Acad Dermatol Venereol. 2009;23(2):224-226.
12. Nguyen BD, Roarke MC, Chivers SF. Multifocal Langerhans cell histiocytosis with infiltrative pelvic lesions: PET/CT imaging. Clin Nucl Med. 2010;35(10): 824-826.
13. Scolozzi P, Lombardi T, Monnier P, Jaques B. Multisystem Langerhans’ cell histiocytosis (Hand-Schuller-Christian disease) in an adult: a case report and review of the literature. Eur Arch Otorhinolaryngol. 2004;261(6):326-330.
14. King JJ, Melvin JS, Iwenofu OH, Fox EJ. Thigh pain in a 53-year-old woman. Clin Orthop Relat Res. 2009;467(6):1652-1657.
15. Hair LC, Deyle GD. Eosinophilic granuloma in a patient with hip pain. J Orthop Sports Phys Ther. 2011;41(2):119.
16. Panayiotakopoulos GD, Sipsas NV, Kontos A, et al. Eosinophilic granuloma of the femur in an HIV-1 positive patient. AIDS Patient Care STDS. 2002;16(3):103-106.
17. Rodrigues RJ, Lewis HH. Eosinophilic granuloma of bone. Review of literature and case presentation. Clin Orthop Relat Res. 1971;77:183-192.
18. Stull MA, Kransdorf MJ, Devaney KO. Langerhans cell histiocytosis of bone. Radiographics. 1992;12(4):801-823.
19. Lichtenstein L. Histiocytosis X (eosinophilic granuloma of bone, Letterer-Siwe disease, and Schueller-Christian disease). Further observations of pathological and clinical importance. J Bone Joint Surg Am. 1964;46:76-90.
20. Götz G, Fichter J. Langerhans’-cell histiocytosis in 58 adults. Eur J Med Res. 2004;9(11):510-514.
21. Cheng KL, Glu PG, Weiss LM. Hematopoeitic tumors. In: Peiguo C, Weiss L, eds. Modern Immunohistochemistry. New York, NY: Cambridge University Press; 2009:503.
22. Broadbent V, Gadner H. Current therapy for Langerhans cell histiocytosis. Hematol Oncol Clin North Am. 1998;12(2):327-338.
23. Plasschaert F, Craig C, Bell R, Cole WG, Wunder JS, Alman BA. Eosinophilic granuloma. A different behaviour in children than in adults. J Bone Joint Surg Br. 2002;84(6):870-872.
24. Capanna R, Springfield DS, Ruggieri P, et al. Direct cortisone injection in osinophilic granuloma of bone: a preliminary report on 11 patients. J Pediatr Orthop. 1985;5(3):339-342.
25. Egeler RM, Thompson RC Jr, Voûte PA, Nesbit ME Jr. Intralesional infiltration of corticosteroids in localized Langerhans’ cell histiocytosis. J Pediatr Orthop. 1992;12(6):811-814.
26. Ladisch S, Gadner H. Treatment of Langerhans cell histiocytosis–evolution and current approaches. Br J Cancer Suppl. 1994;23:S41-S46.
99% of Medical-Device Monitoring Alerts Not Actionable
Nearly all medical-device monitoring alerts on regular hospital units were found not to be actionable, according to a study by pediatrician and researcher Chris Bonafide, MD, MSCE, at Children’s Hospital of Philadelphia, based on reviewing hours of video from patient rooms.1
Reference
- Bonafide CP, Lin R, Zander M, et al. Association between exposure to nonactionable physiologic monitor alarms and response time in a children’s hospital. J Hosp Med. 2015; 10(6):345–351.
Nearly all medical-device monitoring alerts on regular hospital units were found not to be actionable, according to a study by pediatrician and researcher Chris Bonafide, MD, MSCE, at Children’s Hospital of Philadelphia, based on reviewing hours of video from patient rooms.1
Reference
- Bonafide CP, Lin R, Zander M, et al. Association between exposure to nonactionable physiologic monitor alarms and response time in a children’s hospital. J Hosp Med. 2015; 10(6):345–351.
Nearly all medical-device monitoring alerts on regular hospital units were found not to be actionable, according to a study by pediatrician and researcher Chris Bonafide, MD, MSCE, at Children’s Hospital of Philadelphia, based on reviewing hours of video from patient rooms.1
Reference
- Bonafide CP, Lin R, Zander M, et al. Association between exposure to nonactionable physiologic monitor alarms and response time in a children’s hospital. J Hosp Med. 2015; 10(6):345–351.