User login
New history of ACS Bulletin reflects history of the College
To celebrate the centennial of the Bulletin of the American College of Surgeons (ACS), David L. Nahrwold, MD, FACS, has written a history of the ACS member magazine, titled, “A Mirror Reflecting Surgery, Surgeons, and their College: The Bulletin of the American College of Surgeons.”
“After studying the history of the College and the content of 100 years of Bulletins,” writes Dr. Nahrwold in the book’s foreword, “I soon realized that the Bulletin has conveyed the remarkable story of how the College and its members laid the foundation for our healthcare system.”
The Bulletin began in 1916 as a series of single-subject bulletins to the Fellowship from the College’s founders. The first issue described the mission of the College, listed the requirements for admission to Fellowship, and included a packet of blank case history forms for candidates to fill out and submit with their application. Subsequent issues established hospital standards, summarized external and internal meetings and conferences, and reported on credentialing, record keeping, education, specialization, ACS finances and structure, public health issues, scientific advances, international relations, and military surgery, among other subjects.
The book covers the history of the magazine through the end of World War II, and illuminates the background, concerns, and personalities of the College’s founders and leaders as they explained and defended their actions to the members and determined what role the ACS would play in the practice of surgery.
“Given the unpredictable fates of periodicals,” Dr. Nahrwold writes, “it is remarkable – indeed astonishing – that this mirror, the Bulletin, has not only existed, but has thrived, for one hundred years. Its fortunes, of course, have been tied to those of the College, but its editors and staff have continuously adjusted the mirror to make it informative, pertinent, and interesting, and its readers have found deep within the mirror a reservoir of truthfulness, accuracy, and good taste.”
Dr. Nahrwold is Emeritus Professor of Surgery at Northwestern University Feinberg School of Medicine, Chicago, IL, where he was the Loyal and Edith Davis Professor and Chairman, department of surgery, and surgeon-in-chief, Northwestern Memorial Hospital. He served as a Regent, Chairman of the Board of Governors, First Vice-President, and Interim Director of the ACS, and in 2001 he received its highest honor – the Distinguished Service Award. He represented the College at The Joint Commission, where he was chairman of the Board of Commissioners.
He was a director and chairman of the American Board of Surgery and president of the American Board of Medical Specialties.
Dr. Nahrwold is co-author, with Peter J. Kernahan, MD, PhD, FACS, of “A Century of Surgeons and Surgery: The American College of Surgeons 1913-2012.”
“A Mirror Reflecting Surgery, Surgeons, and their College” is available for purchase for $15.95 at amazon.com.
To celebrate the centennial of the Bulletin of the American College of Surgeons (ACS), David L. Nahrwold, MD, FACS, has written a history of the ACS member magazine, titled, “A Mirror Reflecting Surgery, Surgeons, and their College: The Bulletin of the American College of Surgeons.”
“After studying the history of the College and the content of 100 years of Bulletins,” writes Dr. Nahrwold in the book’s foreword, “I soon realized that the Bulletin has conveyed the remarkable story of how the College and its members laid the foundation for our healthcare system.”
The Bulletin began in 1916 as a series of single-subject bulletins to the Fellowship from the College’s founders. The first issue described the mission of the College, listed the requirements for admission to Fellowship, and included a packet of blank case history forms for candidates to fill out and submit with their application. Subsequent issues established hospital standards, summarized external and internal meetings and conferences, and reported on credentialing, record keeping, education, specialization, ACS finances and structure, public health issues, scientific advances, international relations, and military surgery, among other subjects.
The book covers the history of the magazine through the end of World War II, and illuminates the background, concerns, and personalities of the College’s founders and leaders as they explained and defended their actions to the members and determined what role the ACS would play in the practice of surgery.
“Given the unpredictable fates of periodicals,” Dr. Nahrwold writes, “it is remarkable – indeed astonishing – that this mirror, the Bulletin, has not only existed, but has thrived, for one hundred years. Its fortunes, of course, have been tied to those of the College, but its editors and staff have continuously adjusted the mirror to make it informative, pertinent, and interesting, and its readers have found deep within the mirror a reservoir of truthfulness, accuracy, and good taste.”
Dr. Nahrwold is Emeritus Professor of Surgery at Northwestern University Feinberg School of Medicine, Chicago, IL, where he was the Loyal and Edith Davis Professor and Chairman, department of surgery, and surgeon-in-chief, Northwestern Memorial Hospital. He served as a Regent, Chairman of the Board of Governors, First Vice-President, and Interim Director of the ACS, and in 2001 he received its highest honor – the Distinguished Service Award. He represented the College at The Joint Commission, where he was chairman of the Board of Commissioners.
He was a director and chairman of the American Board of Surgery and president of the American Board of Medical Specialties.
Dr. Nahrwold is co-author, with Peter J. Kernahan, MD, PhD, FACS, of “A Century of Surgeons and Surgery: The American College of Surgeons 1913-2012.”
“A Mirror Reflecting Surgery, Surgeons, and their College” is available for purchase for $15.95 at amazon.com.
To celebrate the centennial of the Bulletin of the American College of Surgeons (ACS), David L. Nahrwold, MD, FACS, has written a history of the ACS member magazine, titled, “A Mirror Reflecting Surgery, Surgeons, and their College: The Bulletin of the American College of Surgeons.”
“After studying the history of the College and the content of 100 years of Bulletins,” writes Dr. Nahrwold in the book’s foreword, “I soon realized that the Bulletin has conveyed the remarkable story of how the College and its members laid the foundation for our healthcare system.”
The Bulletin began in 1916 as a series of single-subject bulletins to the Fellowship from the College’s founders. The first issue described the mission of the College, listed the requirements for admission to Fellowship, and included a packet of blank case history forms for candidates to fill out and submit with their application. Subsequent issues established hospital standards, summarized external and internal meetings and conferences, and reported on credentialing, record keeping, education, specialization, ACS finances and structure, public health issues, scientific advances, international relations, and military surgery, among other subjects.
The book covers the history of the magazine through the end of World War II, and illuminates the background, concerns, and personalities of the College’s founders and leaders as they explained and defended their actions to the members and determined what role the ACS would play in the practice of surgery.
“Given the unpredictable fates of periodicals,” Dr. Nahrwold writes, “it is remarkable – indeed astonishing – that this mirror, the Bulletin, has not only existed, but has thrived, for one hundred years. Its fortunes, of course, have been tied to those of the College, but its editors and staff have continuously adjusted the mirror to make it informative, pertinent, and interesting, and its readers have found deep within the mirror a reservoir of truthfulness, accuracy, and good taste.”
Dr. Nahrwold is Emeritus Professor of Surgery at Northwestern University Feinberg School of Medicine, Chicago, IL, where he was the Loyal and Edith Davis Professor and Chairman, department of surgery, and surgeon-in-chief, Northwestern Memorial Hospital. He served as a Regent, Chairman of the Board of Governors, First Vice-President, and Interim Director of the ACS, and in 2001 he received its highest honor – the Distinguished Service Award. He represented the College at The Joint Commission, where he was chairman of the Board of Commissioners.
He was a director and chairman of the American Board of Surgery and president of the American Board of Medical Specialties.
Dr. Nahrwold is co-author, with Peter J. Kernahan, MD, PhD, FACS, of “A Century of Surgeons and Surgery: The American College of Surgeons 1913-2012.”
“A Mirror Reflecting Surgery, Surgeons, and their College” is available for purchase for $15.95 at amazon.com.
Five outstanding surgeons conferred Honorary Fellowship in the ACS
Honorary Fellowship in the American College of Surgeons (ACS) was awarded to five prominent surgeons from Colombia, France, Pakistan, Japan, and Australia at the October 16 Convocation that preceded the official opening of Clinical Congress 2016 in Washington, DC. The granting of Honorary Fellowships is one of the highlights of the Clinical Congress. This year’s recipients were as follows.
Hernando Abaúnza Orjuela, MD, FACS, MACC(Hon), Bogotá, Colombia, is the founder, past-president, and current executive director of the Colombian Association of Surgery. He also is past-president of the Latin American Federation of Surgery (FELAC), which promotes research, teaching, and the practice of surgery among surgeons in Latin America. He became a Fellow of the ACS in 1970 and served on the ACS Board of Governors (1993–1999) and as President of the ACS Colombia Chapter (1990–1991). Dr. Abaúnza has written several articles on breast cancer and complex abdominal surgery problems, as well as more than 120 scientific papers and book chapters on gastric cancer, pancreaticoduodenectomy, laparoscopy, and other clinical topics. Dr. Abaúnza became professor of general surgery and chief, department of surgery, San Pedro Claver Hospital, and professor, National University of Colombia, Bogota. Dr. Abaúnza is a member of the International Society of Surgery and past-president of the Colombian Association of Gastroenterology.
Jacques Belghiti, MD, PhD, Paris, France, has made significant contributions to the fields of hepatocellular carcinoma and liver transplantation and has conducted vital studies in liver resection and hepatobiliary surgical oncology. His technical innovations include preservation of portal and caval flows during liver transplantation, the hanging maneuver to facilitate liver resection, and the use of peritoneal patch to provide an immediate and safe vascular graft. Dr. Belghiti was chief, department of hepato-bilio-pancreatic surgery and liver transplantation, Beaujon Hospital, University of Paris, for 20 years. In 2014, the department was classified as the first French surgical digestive center. French President François Hollande invited Dr. Belghiti to serve on the board of the National Health Authority in 2014; he now chairs the board’s medical devices and health technology committee for reimbursement. Dr. Belghiti is associate editor, liver surgery and biliary section, World Journal of Surgery.
S. Adibul Hasan Rizvi, MB, BS, FRCSEng, FRCSEd, Karachi, Pakistan, is the founder of the Sindh Institute of Urology and Transplantation (SIUT) and a leader of transplantation in Pakistan. He started SIUT, which has become one of the fastest-growing urological and transplant centers in the region, in 1972. SIUT offers procedures such as dialysis, lithotripsy, surgery, and transplantation. Pakistan’s first successful liver transplant was performed there in 2003, eight years after Dr. Rizvi and his team performed the first deceased renal transplant in the country. SIUT’s Dewan Farooque Medical Complex trains nurses, technical staff, and postgraduate physicians. All patient care is provided free of charge. The SIUT’s Hanifa Sulaiman Dawood Oncology Center now treats patients with post-transplant cancers and other malignancies. SIUT opened its first satellite unit in 2000, and three other dialysis centers that are part of the institute offer free dialysis to medically indigent patients in Karachi. Dr. Rizvi is a member of the World Health Organization advisory panel on organ transplantation and the Global Alliance for Transplantation.
Sachiyo Suita, MD, PhD, Fukuoka, Japan, was the first woman professor to head a surgery department at a Japanese national university. Dr. Suita realized she wanted to become a surgeon during the Vietnam War, when she interned at the American Air Force Hospital, Tachikawa, Japan. A mentor at Kyushu University, Fukuoka, encouraged her interest in pediatric surgery. Dr. Suita became surgeon-in-chief at Fukuoka Children’s Hospital in 1983 and professor of pediatric surgery at Kyushu University in 1989. Her promotion to professor marked the first time a woman had been on the faculty of medicine at the university. Dr. Suita’s areas of interest include fetal surgery, neonatal surgery, pediatric oncology, clinical nutrition, liver and small bowel transplantation, and grief care. In 2004, Dr. Suita became the first woman director of Kyushu University Hospital.
John Francis Thompson, AO, MD, FACS, FRACS, FAHMS, Sydney, Australia, has provided distinguished service in the field of oncology research, particularly melanoma, in international and national professional organizations, and in medical education. Dr. Thompson has written more than 700 peer-reviewed scientific articles, which led to his appointment as an Officer of the Order of Australia in 2014. His research interests are in lymphatic mapping and regional node management of patients with melanoma and other malignancies, and local and regional therapies for recurrent and advanced limb tumors. He is executive director and research director, Melanoma Institute Australia, and professor, melanoma and surgical oncology, University of Sydney. Dr. Thompson is a member of the Melanoma Staging Committee of the American Joint Committee on Cancer and chairs the workgroup to update Australia’s clinical practice guidelines for management of cutaneous melanoma in Australia.
Presenting on behalf of the College, respectively, were Marco Patti, MD, FACS, Chicago, IL; Leslie H. Blumgart, MD, FACS, FRCS, New York, NY; Prof. Mehmet A. Haberal, MD, FACS(Hon), FICS (Hon), FASA(Hon), Ankara, Turkey; Arnold G. Coran, MD, FACS, Ann Arbor, MI; and Jeffrey E. Gershenwald, MD, FACS, Houston, TX.
Sir Rickman Godlee, president of the Royal College of Surgeons of England, was awarded the first Honorary Fellowship in the ACS during the College’s first Convocation in 1913. Since then, 458 internationally prominent surgeons, including the five chosen this year, have been named Honorary Fellows of the ACS. The citations presented at the Convocation follow.
Honorary Fellowship in the American College of Surgeons (ACS) was awarded to five prominent surgeons from Colombia, France, Pakistan, Japan, and Australia at the October 16 Convocation that preceded the official opening of Clinical Congress 2016 in Washington, DC. The granting of Honorary Fellowships is one of the highlights of the Clinical Congress. This year’s recipients were as follows.
Hernando Abaúnza Orjuela, MD, FACS, MACC(Hon), Bogotá, Colombia, is the founder, past-president, and current executive director of the Colombian Association of Surgery. He also is past-president of the Latin American Federation of Surgery (FELAC), which promotes research, teaching, and the practice of surgery among surgeons in Latin America. He became a Fellow of the ACS in 1970 and served on the ACS Board of Governors (1993–1999) and as President of the ACS Colombia Chapter (1990–1991). Dr. Abaúnza has written several articles on breast cancer and complex abdominal surgery problems, as well as more than 120 scientific papers and book chapters on gastric cancer, pancreaticoduodenectomy, laparoscopy, and other clinical topics. Dr. Abaúnza became professor of general surgery and chief, department of surgery, San Pedro Claver Hospital, and professor, National University of Colombia, Bogota. Dr. Abaúnza is a member of the International Society of Surgery and past-president of the Colombian Association of Gastroenterology.
Jacques Belghiti, MD, PhD, Paris, France, has made significant contributions to the fields of hepatocellular carcinoma and liver transplantation and has conducted vital studies in liver resection and hepatobiliary surgical oncology. His technical innovations include preservation of portal and caval flows during liver transplantation, the hanging maneuver to facilitate liver resection, and the use of peritoneal patch to provide an immediate and safe vascular graft. Dr. Belghiti was chief, department of hepato-bilio-pancreatic surgery and liver transplantation, Beaujon Hospital, University of Paris, for 20 years. In 2014, the department was classified as the first French surgical digestive center. French President François Hollande invited Dr. Belghiti to serve on the board of the National Health Authority in 2014; he now chairs the board’s medical devices and health technology committee for reimbursement. Dr. Belghiti is associate editor, liver surgery and biliary section, World Journal of Surgery.
S. Adibul Hasan Rizvi, MB, BS, FRCSEng, FRCSEd, Karachi, Pakistan, is the founder of the Sindh Institute of Urology and Transplantation (SIUT) and a leader of transplantation in Pakistan. He started SIUT, which has become one of the fastest-growing urological and transplant centers in the region, in 1972. SIUT offers procedures such as dialysis, lithotripsy, surgery, and transplantation. Pakistan’s first successful liver transplant was performed there in 2003, eight years after Dr. Rizvi and his team performed the first deceased renal transplant in the country. SIUT’s Dewan Farooque Medical Complex trains nurses, technical staff, and postgraduate physicians. All patient care is provided free of charge. The SIUT’s Hanifa Sulaiman Dawood Oncology Center now treats patients with post-transplant cancers and other malignancies. SIUT opened its first satellite unit in 2000, and three other dialysis centers that are part of the institute offer free dialysis to medically indigent patients in Karachi. Dr. Rizvi is a member of the World Health Organization advisory panel on organ transplantation and the Global Alliance for Transplantation.
Sachiyo Suita, MD, PhD, Fukuoka, Japan, was the first woman professor to head a surgery department at a Japanese national university. Dr. Suita realized she wanted to become a surgeon during the Vietnam War, when she interned at the American Air Force Hospital, Tachikawa, Japan. A mentor at Kyushu University, Fukuoka, encouraged her interest in pediatric surgery. Dr. Suita became surgeon-in-chief at Fukuoka Children’s Hospital in 1983 and professor of pediatric surgery at Kyushu University in 1989. Her promotion to professor marked the first time a woman had been on the faculty of medicine at the university. Dr. Suita’s areas of interest include fetal surgery, neonatal surgery, pediatric oncology, clinical nutrition, liver and small bowel transplantation, and grief care. In 2004, Dr. Suita became the first woman director of Kyushu University Hospital.
John Francis Thompson, AO, MD, FACS, FRACS, FAHMS, Sydney, Australia, has provided distinguished service in the field of oncology research, particularly melanoma, in international and national professional organizations, and in medical education. Dr. Thompson has written more than 700 peer-reviewed scientific articles, which led to his appointment as an Officer of the Order of Australia in 2014. His research interests are in lymphatic mapping and regional node management of patients with melanoma and other malignancies, and local and regional therapies for recurrent and advanced limb tumors. He is executive director and research director, Melanoma Institute Australia, and professor, melanoma and surgical oncology, University of Sydney. Dr. Thompson is a member of the Melanoma Staging Committee of the American Joint Committee on Cancer and chairs the workgroup to update Australia’s clinical practice guidelines for management of cutaneous melanoma in Australia.
Presenting on behalf of the College, respectively, were Marco Patti, MD, FACS, Chicago, IL; Leslie H. Blumgart, MD, FACS, FRCS, New York, NY; Prof. Mehmet A. Haberal, MD, FACS(Hon), FICS (Hon), FASA(Hon), Ankara, Turkey; Arnold G. Coran, MD, FACS, Ann Arbor, MI; and Jeffrey E. Gershenwald, MD, FACS, Houston, TX.
Sir Rickman Godlee, president of the Royal College of Surgeons of England, was awarded the first Honorary Fellowship in the ACS during the College’s first Convocation in 1913. Since then, 458 internationally prominent surgeons, including the five chosen this year, have been named Honorary Fellows of the ACS. The citations presented at the Convocation follow.
Honorary Fellowship in the American College of Surgeons (ACS) was awarded to five prominent surgeons from Colombia, France, Pakistan, Japan, and Australia at the October 16 Convocation that preceded the official opening of Clinical Congress 2016 in Washington, DC. The granting of Honorary Fellowships is one of the highlights of the Clinical Congress. This year’s recipients were as follows.
Hernando Abaúnza Orjuela, MD, FACS, MACC(Hon), Bogotá, Colombia, is the founder, past-president, and current executive director of the Colombian Association of Surgery. He also is past-president of the Latin American Federation of Surgery (FELAC), which promotes research, teaching, and the practice of surgery among surgeons in Latin America. He became a Fellow of the ACS in 1970 and served on the ACS Board of Governors (1993–1999) and as President of the ACS Colombia Chapter (1990–1991). Dr. Abaúnza has written several articles on breast cancer and complex abdominal surgery problems, as well as more than 120 scientific papers and book chapters on gastric cancer, pancreaticoduodenectomy, laparoscopy, and other clinical topics. Dr. Abaúnza became professor of general surgery and chief, department of surgery, San Pedro Claver Hospital, and professor, National University of Colombia, Bogota. Dr. Abaúnza is a member of the International Society of Surgery and past-president of the Colombian Association of Gastroenterology.
Jacques Belghiti, MD, PhD, Paris, France, has made significant contributions to the fields of hepatocellular carcinoma and liver transplantation and has conducted vital studies in liver resection and hepatobiliary surgical oncology. His technical innovations include preservation of portal and caval flows during liver transplantation, the hanging maneuver to facilitate liver resection, and the use of peritoneal patch to provide an immediate and safe vascular graft. Dr. Belghiti was chief, department of hepato-bilio-pancreatic surgery and liver transplantation, Beaujon Hospital, University of Paris, for 20 years. In 2014, the department was classified as the first French surgical digestive center. French President François Hollande invited Dr. Belghiti to serve on the board of the National Health Authority in 2014; he now chairs the board’s medical devices and health technology committee for reimbursement. Dr. Belghiti is associate editor, liver surgery and biliary section, World Journal of Surgery.
S. Adibul Hasan Rizvi, MB, BS, FRCSEng, FRCSEd, Karachi, Pakistan, is the founder of the Sindh Institute of Urology and Transplantation (SIUT) and a leader of transplantation in Pakistan. He started SIUT, which has become one of the fastest-growing urological and transplant centers in the region, in 1972. SIUT offers procedures such as dialysis, lithotripsy, surgery, and transplantation. Pakistan’s first successful liver transplant was performed there in 2003, eight years after Dr. Rizvi and his team performed the first deceased renal transplant in the country. SIUT’s Dewan Farooque Medical Complex trains nurses, technical staff, and postgraduate physicians. All patient care is provided free of charge. The SIUT’s Hanifa Sulaiman Dawood Oncology Center now treats patients with post-transplant cancers and other malignancies. SIUT opened its first satellite unit in 2000, and three other dialysis centers that are part of the institute offer free dialysis to medically indigent patients in Karachi. Dr. Rizvi is a member of the World Health Organization advisory panel on organ transplantation and the Global Alliance for Transplantation.
Sachiyo Suita, MD, PhD, Fukuoka, Japan, was the first woman professor to head a surgery department at a Japanese national university. Dr. Suita realized she wanted to become a surgeon during the Vietnam War, when she interned at the American Air Force Hospital, Tachikawa, Japan. A mentor at Kyushu University, Fukuoka, encouraged her interest in pediatric surgery. Dr. Suita became surgeon-in-chief at Fukuoka Children’s Hospital in 1983 and professor of pediatric surgery at Kyushu University in 1989. Her promotion to professor marked the first time a woman had been on the faculty of medicine at the university. Dr. Suita’s areas of interest include fetal surgery, neonatal surgery, pediatric oncology, clinical nutrition, liver and small bowel transplantation, and grief care. In 2004, Dr. Suita became the first woman director of Kyushu University Hospital.
John Francis Thompson, AO, MD, FACS, FRACS, FAHMS, Sydney, Australia, has provided distinguished service in the field of oncology research, particularly melanoma, in international and national professional organizations, and in medical education. Dr. Thompson has written more than 700 peer-reviewed scientific articles, which led to his appointment as an Officer of the Order of Australia in 2014. His research interests are in lymphatic mapping and regional node management of patients with melanoma and other malignancies, and local and regional therapies for recurrent and advanced limb tumors. He is executive director and research director, Melanoma Institute Australia, and professor, melanoma and surgical oncology, University of Sydney. Dr. Thompson is a member of the Melanoma Staging Committee of the American Joint Committee on Cancer and chairs the workgroup to update Australia’s clinical practice guidelines for management of cutaneous melanoma in Australia.
Presenting on behalf of the College, respectively, were Marco Patti, MD, FACS, Chicago, IL; Leslie H. Blumgart, MD, FACS, FRCS, New York, NY; Prof. Mehmet A. Haberal, MD, FACS(Hon), FICS (Hon), FASA(Hon), Ankara, Turkey; Arnold G. Coran, MD, FACS, Ann Arbor, MI; and Jeffrey E. Gershenwald, MD, FACS, Houston, TX.
Sir Rickman Godlee, president of the Royal College of Surgeons of England, was awarded the first Honorary Fellowship in the ACS during the College’s first Convocation in 1913. Since then, 458 internationally prominent surgeons, including the five chosen this year, have been named Honorary Fellows of the ACS. The citations presented at the Convocation follow.
ACS leads efforts to improve quality of care for older surgical patients
The December issue of the Bulletin will feature an in-depth exploration of past, present, and future American College of Surgeons (ACS) efforts to improve the quality of surgical care for older adults. The following is a brief summary of these initiatives.
Decades of progress
Over the years, the College has been a leader in responding to the growing need for the aging American population to have access to high-quality surgical care. People older than 65 years of age represent a rapidly growing segment of the U.S. population and a disproportionate share of individuals who undergo surgical procedures. Older adults have unique physiology, which often puts them at risk for complications after surgery. At a time when the quality and value of health care are under increasing scrutiny, the need for high-quality standards to improve surgical care delivery for this vulnerable population is on the rise.
The ACS has invested in improving surgical care for older adults over several decades. The ACS has partnered with the American Geriatrics Society (AGS) and The John A. Hartford Foundation since 1995 and has had a standing Geriatric Surgery Task Force since 2004. In an interdisciplinary effort, the ACS, the AGS, and The John A. Hartford Foundation issued a set of guidelines for preoperative care of geriatric patients in 2012, with a follow-up set of guidelines for perioperative and postoperative care in 2016. Through the College’s National Surgical Quality Improvement Program (ACS NSQIP®), members of the Geriatric Surgery Task Force began collecting 14 patient-centered, geriatric-specific variables to better appreciate the unique risk factors and outcomes of older adults.
Coalition for Quality in Geriatric Surgery
Most recently, the ACS, with support from The John A. Hartford Foundation, convened a group of more than 50 stakeholders as the Coalition for Quality in Geriatric Surgery. This interdisciplinary, patient- and family-centered coalition aims to systematically improve surgical care for older adults. These improvements are intended for all geriatric surgical care programs, regardless of hospital size, location, or academic status. After an extensive standards evaluation process, the interdisciplinary panel is preparing to release the first iteration of high-quality geriatric surgery standards.
The project has garnered 74 mentions in the media as of press time, in addition to interviews on SiriusXM Doctor Radio, featuring Julia Berian, MD, ACS Clinical Scholar in Residence; Clifford Y. Ko, MD, MS, MSHS, FACS, FASCRS, Principal Investigator, and Director, ACS Division of Research and Optimal Patient Care; and Ronnie Rosenthal, MD, MS, FACS, Chair, ACS Geriatric Surgery Task Force and Co-Principal Investigator, Standards Subcommittee Co-Chair. Media outlets that have reported on the project include FOX News, Reuters, Medscape, and Surgical Products.
The December issue of the Bulletin will feature an in-depth exploration of past, present, and future American College of Surgeons (ACS) efforts to improve the quality of surgical care for older adults. The following is a brief summary of these initiatives.
Decades of progress
Over the years, the College has been a leader in responding to the growing need for the aging American population to have access to high-quality surgical care. People older than 65 years of age represent a rapidly growing segment of the U.S. population and a disproportionate share of individuals who undergo surgical procedures. Older adults have unique physiology, which often puts them at risk for complications after surgery. At a time when the quality and value of health care are under increasing scrutiny, the need for high-quality standards to improve surgical care delivery for this vulnerable population is on the rise.
The ACS has invested in improving surgical care for older adults over several decades. The ACS has partnered with the American Geriatrics Society (AGS) and The John A. Hartford Foundation since 1995 and has had a standing Geriatric Surgery Task Force since 2004. In an interdisciplinary effort, the ACS, the AGS, and The John A. Hartford Foundation issued a set of guidelines for preoperative care of geriatric patients in 2012, with a follow-up set of guidelines for perioperative and postoperative care in 2016. Through the College’s National Surgical Quality Improvement Program (ACS NSQIP®), members of the Geriatric Surgery Task Force began collecting 14 patient-centered, geriatric-specific variables to better appreciate the unique risk factors and outcomes of older adults.
Coalition for Quality in Geriatric Surgery
Most recently, the ACS, with support from The John A. Hartford Foundation, convened a group of more than 50 stakeholders as the Coalition for Quality in Geriatric Surgery. This interdisciplinary, patient- and family-centered coalition aims to systematically improve surgical care for older adults. These improvements are intended for all geriatric surgical care programs, regardless of hospital size, location, or academic status. After an extensive standards evaluation process, the interdisciplinary panel is preparing to release the first iteration of high-quality geriatric surgery standards.
The project has garnered 74 mentions in the media as of press time, in addition to interviews on SiriusXM Doctor Radio, featuring Julia Berian, MD, ACS Clinical Scholar in Residence; Clifford Y. Ko, MD, MS, MSHS, FACS, FASCRS, Principal Investigator, and Director, ACS Division of Research and Optimal Patient Care; and Ronnie Rosenthal, MD, MS, FACS, Chair, ACS Geriatric Surgery Task Force and Co-Principal Investigator, Standards Subcommittee Co-Chair. Media outlets that have reported on the project include FOX News, Reuters, Medscape, and Surgical Products.
The December issue of the Bulletin will feature an in-depth exploration of past, present, and future American College of Surgeons (ACS) efforts to improve the quality of surgical care for older adults. The following is a brief summary of these initiatives.
Decades of progress
Over the years, the College has been a leader in responding to the growing need for the aging American population to have access to high-quality surgical care. People older than 65 years of age represent a rapidly growing segment of the U.S. population and a disproportionate share of individuals who undergo surgical procedures. Older adults have unique physiology, which often puts them at risk for complications after surgery. At a time when the quality and value of health care are under increasing scrutiny, the need for high-quality standards to improve surgical care delivery for this vulnerable population is on the rise.
The ACS has invested in improving surgical care for older adults over several decades. The ACS has partnered with the American Geriatrics Society (AGS) and The John A. Hartford Foundation since 1995 and has had a standing Geriatric Surgery Task Force since 2004. In an interdisciplinary effort, the ACS, the AGS, and The John A. Hartford Foundation issued a set of guidelines for preoperative care of geriatric patients in 2012, with a follow-up set of guidelines for perioperative and postoperative care in 2016. Through the College’s National Surgical Quality Improvement Program (ACS NSQIP®), members of the Geriatric Surgery Task Force began collecting 14 patient-centered, geriatric-specific variables to better appreciate the unique risk factors and outcomes of older adults.
Coalition for Quality in Geriatric Surgery
Most recently, the ACS, with support from The John A. Hartford Foundation, convened a group of more than 50 stakeholders as the Coalition for Quality in Geriatric Surgery. This interdisciplinary, patient- and family-centered coalition aims to systematically improve surgical care for older adults. These improvements are intended for all geriatric surgical care programs, regardless of hospital size, location, or academic status. After an extensive standards evaluation process, the interdisciplinary panel is preparing to release the first iteration of high-quality geriatric surgery standards.
The project has garnered 74 mentions in the media as of press time, in addition to interviews on SiriusXM Doctor Radio, featuring Julia Berian, MD, ACS Clinical Scholar in Residence; Clifford Y. Ko, MD, MS, MSHS, FACS, FASCRS, Principal Investigator, and Director, ACS Division of Research and Optimal Patient Care; and Ronnie Rosenthal, MD, MS, FACS, Chair, ACS Geriatric Surgery Task Force and Co-Principal Investigator, Standards Subcommittee Co-Chair. Media outlets that have reported on the project include FOX News, Reuters, Medscape, and Surgical Products.
From the Washington Office: CMS says, “Pick Your Pace”
This month, we continue our discussion of the Quality Payment Program (QPP). Specifically, I write about a blog post from CMS Acting Administrator, Andy Slavitt, on Sept. 8, 2016. In that post Mr. Slavitt announced “plans for timing of reporting for the first year of the [quality payment] program” and stated that CMS “intend[s] for the Quality Payment Program to allow physicians to pick their pace of participation for the first performance period that begins Jan. 1, 2017.”
Though specific details are unknown at this time pending the release of the QPP final rule on or about Nov. 1, 2016, Mr. Slavitt’s post would seem to indicate that it will be possible for providers to avoid payment penalties and further that it should also be possible to receive a positive update in Medicare payment depending upon the level of one’s participation in the new program in 2017.
Options for Participation
Acting Administrator Slavitt’s post states, “During 2017, eligible physicians and other clinicians will have multiple options for participation. Choosing one of these options would ensure you do not receive a negative payment adjustment in 2019.”
Outlined below are those four options:
Option 1: Test the Quality Payment Program
With this option, one will be able to avoid a negative payment adjustment, “as long as you submit some data to the Quality Payment Program, including data from after January 1, 2017.”
This option is designed to ensure preparation for broader participation in 2018. As with all types of regulation, the “devil is in the details” and specifically, what constitutes “some data” is not defined at this time. As mentioned above, we expect such details to be described fully in the final rule, but I believe surgeons have reason to be optimistic that all should be able to avoid penalties under the first year of the QPP.
Option 2: Participate for part of the calendar year
For providers who choose to submit data for the QPP for less than a full year, i.e., “a reduced number of days,” their performance period could begin sometime after Jan. 1, 2017, and their “practice could still qualify for a small positive payment adjustment.”
For surgeons who are already participating in the current PQRS (Physician Quality Reporting System) program via the American College of Surgeons’ Surgeon Specific Registry (SSR) or other certified registry, this option presents an opportunity to be rewarded for those efforts. To reiterate, details relative to the threshold of participation required for the positive adjustment will not be known until the final rule is released. However, it is entirely possible that many surgeons will be eligible for a positive update based upon what they are already doing or could easily begin doing in 2017.
Option 3: Participate for the full calendar year
Option three is for practices that are ready to fully participate in all four components of the QPP for the entire calendar year of 2017. Those practices that submit information for the entire year on quality, the use of electronic health record technology, and their practice’s improvement activities “could qualify for a modest positive payment adjustment.”
For those practices that have invested in electronic health record technology and are already reporting PQRS data, “gearing up” to participate for the full calendar year may not be an arduous endeavor. Once the final rule is released and specific details are known, they may find that their previous efforts toward preparation for the QPP puts it well within their capability to fully participate in 2017 and receive a positive payment adjustment.
Option 4: Participate in an Advanced Alternative Payment Model (APM)
“Instead of reporting quality data and other information, the law allows you to participate in the Quality Payment Program by joining an Advanced Alternative Payment Model …” Mr. Slavitt stated.
As has been stated in previous editions of this column, for the first few years of the QPP we expect that most surgeons will participate in the QPP via the Merit-based Incentive Payment System (MIPS) pathway and not in APMs. However, the development of Advanced Alternative Payment Models widely applicable for surgeons is the object of significant and ongoing policy development efforts by the Division of Advocacy and Health Policy of the American College of Surgeons.
For those wishing to read Acting Administrator Slavitt’s post in its entirety, it may be found here: https://blog.cms.gov/2016/09/08/qualitypaymentprogram-pickyourpace.
Until next month.
Dr. Bailey is a pediatric surgeon, and Medical Director, Advocacy, for the Division of Advocacy and Health Policy in the ACS offices in Washington, D.C.
This month, we continue our discussion of the Quality Payment Program (QPP). Specifically, I write about a blog post from CMS Acting Administrator, Andy Slavitt, on Sept. 8, 2016. In that post Mr. Slavitt announced “plans for timing of reporting for the first year of the [quality payment] program” and stated that CMS “intend[s] for the Quality Payment Program to allow physicians to pick their pace of participation for the first performance period that begins Jan. 1, 2017.”
Though specific details are unknown at this time pending the release of the QPP final rule on or about Nov. 1, 2016, Mr. Slavitt’s post would seem to indicate that it will be possible for providers to avoid payment penalties and further that it should also be possible to receive a positive update in Medicare payment depending upon the level of one’s participation in the new program in 2017.
Options for Participation
Acting Administrator Slavitt’s post states, “During 2017, eligible physicians and other clinicians will have multiple options for participation. Choosing one of these options would ensure you do not receive a negative payment adjustment in 2019.”
Outlined below are those four options:
Option 1: Test the Quality Payment Program
With this option, one will be able to avoid a negative payment adjustment, “as long as you submit some data to the Quality Payment Program, including data from after January 1, 2017.”
This option is designed to ensure preparation for broader participation in 2018. As with all types of regulation, the “devil is in the details” and specifically, what constitutes “some data” is not defined at this time. As mentioned above, we expect such details to be described fully in the final rule, but I believe surgeons have reason to be optimistic that all should be able to avoid penalties under the first year of the QPP.
Option 2: Participate for part of the calendar year
For providers who choose to submit data for the QPP for less than a full year, i.e., “a reduced number of days,” their performance period could begin sometime after Jan. 1, 2017, and their “practice could still qualify for a small positive payment adjustment.”
For surgeons who are already participating in the current PQRS (Physician Quality Reporting System) program via the American College of Surgeons’ Surgeon Specific Registry (SSR) or other certified registry, this option presents an opportunity to be rewarded for those efforts. To reiterate, details relative to the threshold of participation required for the positive adjustment will not be known until the final rule is released. However, it is entirely possible that many surgeons will be eligible for a positive update based upon what they are already doing or could easily begin doing in 2017.
Option 3: Participate for the full calendar year
Option three is for practices that are ready to fully participate in all four components of the QPP for the entire calendar year of 2017. Those practices that submit information for the entire year on quality, the use of electronic health record technology, and their practice’s improvement activities “could qualify for a modest positive payment adjustment.”
For those practices that have invested in electronic health record technology and are already reporting PQRS data, “gearing up” to participate for the full calendar year may not be an arduous endeavor. Once the final rule is released and specific details are known, they may find that their previous efforts toward preparation for the QPP puts it well within their capability to fully participate in 2017 and receive a positive payment adjustment.
Option 4: Participate in an Advanced Alternative Payment Model (APM)
“Instead of reporting quality data and other information, the law allows you to participate in the Quality Payment Program by joining an Advanced Alternative Payment Model …” Mr. Slavitt stated.
As has been stated in previous editions of this column, for the first few years of the QPP we expect that most surgeons will participate in the QPP via the Merit-based Incentive Payment System (MIPS) pathway and not in APMs. However, the development of Advanced Alternative Payment Models widely applicable for surgeons is the object of significant and ongoing policy development efforts by the Division of Advocacy and Health Policy of the American College of Surgeons.
For those wishing to read Acting Administrator Slavitt’s post in its entirety, it may be found here: https://blog.cms.gov/2016/09/08/qualitypaymentprogram-pickyourpace.
Until next month.
Dr. Bailey is a pediatric surgeon, and Medical Director, Advocacy, for the Division of Advocacy and Health Policy in the ACS offices in Washington, D.C.
This month, we continue our discussion of the Quality Payment Program (QPP). Specifically, I write about a blog post from CMS Acting Administrator, Andy Slavitt, on Sept. 8, 2016. In that post Mr. Slavitt announced “plans for timing of reporting for the first year of the [quality payment] program” and stated that CMS “intend[s] for the Quality Payment Program to allow physicians to pick their pace of participation for the first performance period that begins Jan. 1, 2017.”
Though specific details are unknown at this time pending the release of the QPP final rule on or about Nov. 1, 2016, Mr. Slavitt’s post would seem to indicate that it will be possible for providers to avoid payment penalties and further that it should also be possible to receive a positive update in Medicare payment depending upon the level of one’s participation in the new program in 2017.
Options for Participation
Acting Administrator Slavitt’s post states, “During 2017, eligible physicians and other clinicians will have multiple options for participation. Choosing one of these options would ensure you do not receive a negative payment adjustment in 2019.”
Outlined below are those four options:
Option 1: Test the Quality Payment Program
With this option, one will be able to avoid a negative payment adjustment, “as long as you submit some data to the Quality Payment Program, including data from after January 1, 2017.”
This option is designed to ensure preparation for broader participation in 2018. As with all types of regulation, the “devil is in the details” and specifically, what constitutes “some data” is not defined at this time. As mentioned above, we expect such details to be described fully in the final rule, but I believe surgeons have reason to be optimistic that all should be able to avoid penalties under the first year of the QPP.
Option 2: Participate for part of the calendar year
For providers who choose to submit data for the QPP for less than a full year, i.e., “a reduced number of days,” their performance period could begin sometime after Jan. 1, 2017, and their “practice could still qualify for a small positive payment adjustment.”
For surgeons who are already participating in the current PQRS (Physician Quality Reporting System) program via the American College of Surgeons’ Surgeon Specific Registry (SSR) or other certified registry, this option presents an opportunity to be rewarded for those efforts. To reiterate, details relative to the threshold of participation required for the positive adjustment will not be known until the final rule is released. However, it is entirely possible that many surgeons will be eligible for a positive update based upon what they are already doing or could easily begin doing in 2017.
Option 3: Participate for the full calendar year
Option three is for practices that are ready to fully participate in all four components of the QPP for the entire calendar year of 2017. Those practices that submit information for the entire year on quality, the use of electronic health record technology, and their practice’s improvement activities “could qualify for a modest positive payment adjustment.”
For those practices that have invested in electronic health record technology and are already reporting PQRS data, “gearing up” to participate for the full calendar year may not be an arduous endeavor. Once the final rule is released and specific details are known, they may find that their previous efforts toward preparation for the QPP puts it well within their capability to fully participate in 2017 and receive a positive payment adjustment.
Option 4: Participate in an Advanced Alternative Payment Model (APM)
“Instead of reporting quality data and other information, the law allows you to participate in the Quality Payment Program by joining an Advanced Alternative Payment Model …” Mr. Slavitt stated.
As has been stated in previous editions of this column, for the first few years of the QPP we expect that most surgeons will participate in the QPP via the Merit-based Incentive Payment System (MIPS) pathway and not in APMs. However, the development of Advanced Alternative Payment Models widely applicable for surgeons is the object of significant and ongoing policy development efforts by the Division of Advocacy and Health Policy of the American College of Surgeons.
For those wishing to read Acting Administrator Slavitt’s post in its entirety, it may be found here: https://blog.cms.gov/2016/09/08/qualitypaymentprogram-pickyourpace.
Until next month.
Dr. Bailey is a pediatric surgeon, and Medical Director, Advocacy, for the Division of Advocacy and Health Policy in the ACS offices in Washington, D.C.
Bulletin moves online for most readers beginning with January 2017 issue
In light of production costs, American College of Surgeons (ACS) Regents and the leadership of the Board of Governors, Young Fellows Association, and Resident and Associate Society have determined that the College would be best served by transitioning readers of the Bulletin to an online publication, effective with the January 2017 issue. The Bulletin will continue to offer the same array of features, news stories, and columns online, with the added benefit of providing more timely access to the Bulletin.
Members for whom we have an e-mail address will be notified each month when the new issue of the Bulletin becomes available. The e-mail notification will include a link that takes you directly to the Bulletin home page. (If your e-mail address is not on file or you need to update it, do so now via “My Profile” on the ACS website.)
From the Bulletin home page, bulletin.facs.org, you have three options: (1) start reading the current issue right there; (2) click the link on the right-hand side of the page, which will take you to a digital version that looks exactly like the print edition; or (3) download the Bulletin app, which will notify you each month when a new issue is available.
Note that, for a limited time, dues-paying members who do not have access to the Internet or who have a strong preference for print media may opt to continue receiving print copies of the Bulletin. Members who transition to non–dues-paying status will no longer receive the print edition. Dues-paying members (active Fellows, Associate Fellows, and Residents) should have received a notification from the College offering them the print option. If you do not recall receiving this notification e-mail or letter, you may request continuation of your print subscription via e-mail at [email protected] or by calling 800-621-4111. All requests should be made by December 9, 2016.
In light of production costs, American College of Surgeons (ACS) Regents and the leadership of the Board of Governors, Young Fellows Association, and Resident and Associate Society have determined that the College would be best served by transitioning readers of the Bulletin to an online publication, effective with the January 2017 issue. The Bulletin will continue to offer the same array of features, news stories, and columns online, with the added benefit of providing more timely access to the Bulletin.
Members for whom we have an e-mail address will be notified each month when the new issue of the Bulletin becomes available. The e-mail notification will include a link that takes you directly to the Bulletin home page. (If your e-mail address is not on file or you need to update it, do so now via “My Profile” on the ACS website.)
From the Bulletin home page, bulletin.facs.org, you have three options: (1) start reading the current issue right there; (2) click the link on the right-hand side of the page, which will take you to a digital version that looks exactly like the print edition; or (3) download the Bulletin app, which will notify you each month when a new issue is available.
Note that, for a limited time, dues-paying members who do not have access to the Internet or who have a strong preference for print media may opt to continue receiving print copies of the Bulletin. Members who transition to non–dues-paying status will no longer receive the print edition. Dues-paying members (active Fellows, Associate Fellows, and Residents) should have received a notification from the College offering them the print option. If you do not recall receiving this notification e-mail or letter, you may request continuation of your print subscription via e-mail at [email protected] or by calling 800-621-4111. All requests should be made by December 9, 2016.
In light of production costs, American College of Surgeons (ACS) Regents and the leadership of the Board of Governors, Young Fellows Association, and Resident and Associate Society have determined that the College would be best served by transitioning readers of the Bulletin to an online publication, effective with the January 2017 issue. The Bulletin will continue to offer the same array of features, news stories, and columns online, with the added benefit of providing more timely access to the Bulletin.
Members for whom we have an e-mail address will be notified each month when the new issue of the Bulletin becomes available. The e-mail notification will include a link that takes you directly to the Bulletin home page. (If your e-mail address is not on file or you need to update it, do so now via “My Profile” on the ACS website.)
From the Bulletin home page, bulletin.facs.org, you have three options: (1) start reading the current issue right there; (2) click the link on the right-hand side of the page, which will take you to a digital version that looks exactly like the print edition; or (3) download the Bulletin app, which will notify you each month when a new issue is available.
Note that, for a limited time, dues-paying members who do not have access to the Internet or who have a strong preference for print media may opt to continue receiving print copies of the Bulletin. Members who transition to non–dues-paying status will no longer receive the print edition. Dues-paying members (active Fellows, Associate Fellows, and Residents) should have received a notification from the College offering them the print option. If you do not recall receiving this notification e-mail or letter, you may request continuation of your print subscription via e-mail at [email protected] or by calling 800-621-4111. All requests should be made by December 9, 2016.
AJCC Releases Cancer Staging Manual, Eighth Edition
The American Joint Committee on Cancer (AJCC) has released the eighth edition of TNM Cancer Staging Manual, which reflects current understanding of cancer biology concepts and emphasizes a more individualized approach to cancer classification and treatment. This edition presents evidence-based revisions for staging cancer for a number of organ sites and includes the rationales and rules for staging; the definitions of tumor, lymph node involvement, and metastasis; stage groupings; and histologic grade.
Cancer staging provides patients and physicians with the standards for determining the best treatment approach for their disease and their prognosis. Mahul B. Amin, MD, FCAP, Editor-in-Chief of the Eighth Edition, noted that 430 experts from 184 institutions in 22 countries on six continents collaborated to produce this resource. Dr. Amin is professor and chairman emeritus, department of pathology and laboratory medicine, Cedars-Sinai Medical Center, Los Angeles, CA, and incoming chairman and endowed professor of the department of pathology and laboratory medicine at the University of Tennessee Health Sciences Center, Memphis.
Since the Seventh Edition of the manual was published in 2009, researchers and medical practitioners have learned that genomic alterations drive cancer and may vary considerably among tumors that, in the past, were thought to be in the same category, Dr. Amin said.
The American College of Surgeons Commission on Cancer will require accredited hospitals to use the Eighth Edition for all cancer cases diagnosed on or after January 1, 2017. The manual, developed in cooperation with the TNM Committee of the Union for International Cancer Control (UICC), is available for purchase online at http://www.springer.com/us/book/9783319406176.
Find additional information on licensing the content for electronic products at www.cancerstaging.org
The American Joint Committee on Cancer (AJCC) has released the eighth edition of TNM Cancer Staging Manual, which reflects current understanding of cancer biology concepts and emphasizes a more individualized approach to cancer classification and treatment. This edition presents evidence-based revisions for staging cancer for a number of organ sites and includes the rationales and rules for staging; the definitions of tumor, lymph node involvement, and metastasis; stage groupings; and histologic grade.
Cancer staging provides patients and physicians with the standards for determining the best treatment approach for their disease and their prognosis. Mahul B. Amin, MD, FCAP, Editor-in-Chief of the Eighth Edition, noted that 430 experts from 184 institutions in 22 countries on six continents collaborated to produce this resource. Dr. Amin is professor and chairman emeritus, department of pathology and laboratory medicine, Cedars-Sinai Medical Center, Los Angeles, CA, and incoming chairman and endowed professor of the department of pathology and laboratory medicine at the University of Tennessee Health Sciences Center, Memphis.
Since the Seventh Edition of the manual was published in 2009, researchers and medical practitioners have learned that genomic alterations drive cancer and may vary considerably among tumors that, in the past, were thought to be in the same category, Dr. Amin said.
The American College of Surgeons Commission on Cancer will require accredited hospitals to use the Eighth Edition for all cancer cases diagnosed on or after January 1, 2017. The manual, developed in cooperation with the TNM Committee of the Union for International Cancer Control (UICC), is available for purchase online at http://www.springer.com/us/book/9783319406176.
Find additional information on licensing the content for electronic products at www.cancerstaging.org
The American Joint Committee on Cancer (AJCC) has released the eighth edition of TNM Cancer Staging Manual, which reflects current understanding of cancer biology concepts and emphasizes a more individualized approach to cancer classification and treatment. This edition presents evidence-based revisions for staging cancer for a number of organ sites and includes the rationales and rules for staging; the definitions of tumor, lymph node involvement, and metastasis; stage groupings; and histologic grade.
Cancer staging provides patients and physicians with the standards for determining the best treatment approach for their disease and their prognosis. Mahul B. Amin, MD, FCAP, Editor-in-Chief of the Eighth Edition, noted that 430 experts from 184 institutions in 22 countries on six continents collaborated to produce this resource. Dr. Amin is professor and chairman emeritus, department of pathology and laboratory medicine, Cedars-Sinai Medical Center, Los Angeles, CA, and incoming chairman and endowed professor of the department of pathology and laboratory medicine at the University of Tennessee Health Sciences Center, Memphis.
Since the Seventh Edition of the manual was published in 2009, researchers and medical practitioners have learned that genomic alterations drive cancer and may vary considerably among tumors that, in the past, were thought to be in the same category, Dr. Amin said.
The American College of Surgeons Commission on Cancer will require accredited hospitals to use the Eighth Edition for all cancer cases diagnosed on or after January 1, 2017. The manual, developed in cooperation with the TNM Committee of the Union for International Cancer Control (UICC), is available for purchase online at http://www.springer.com/us/book/9783319406176.
Find additional information on licensing the content for electronic products at www.cancerstaging.org
20 Cancer Care facilities receive biannual CoC Outstanding Achievement Award
The Commission on Cancer (CoC) of the American College of Surgeons (ACS) has granted its mid-year 2016 Outstanding Achievement Award (OAA) to a select group of 20 accredited cancer programs throughout the U.S.
Award criteria were based on qualitative and quantitative surveys conducted January 1 through June 30, 2016. The biannual award was established in 2004 to recognize cancer programs that strive for excellence in demonstrating compliance with the CoC standards and are committed to ensuring high-quality cancer care.
A CoC-accredited cancer program is eligible to earn the OAA after completing the accreditation survey and receiving a Performance Report that indicates an accreditation award of “Three-Year with Commendation.” Specifically, the program must receive commendation ratings for the seven commendation level standards and no deficiencies for the remaining 27 standards.
View the list of this year’s first group of OAA recipients on the ACS website at https://www.facs.org/quality-programs/cancer/coc/info/outstanding/2016-part-1.
The Commission on Cancer (CoC) of the American College of Surgeons (ACS) has granted its mid-year 2016 Outstanding Achievement Award (OAA) to a select group of 20 accredited cancer programs throughout the U.S.
Award criteria were based on qualitative and quantitative surveys conducted January 1 through June 30, 2016. The biannual award was established in 2004 to recognize cancer programs that strive for excellence in demonstrating compliance with the CoC standards and are committed to ensuring high-quality cancer care.
A CoC-accredited cancer program is eligible to earn the OAA after completing the accreditation survey and receiving a Performance Report that indicates an accreditation award of “Three-Year with Commendation.” Specifically, the program must receive commendation ratings for the seven commendation level standards and no deficiencies for the remaining 27 standards.
View the list of this year’s first group of OAA recipients on the ACS website at https://www.facs.org/quality-programs/cancer/coc/info/outstanding/2016-part-1.
The Commission on Cancer (CoC) of the American College of Surgeons (ACS) has granted its mid-year 2016 Outstanding Achievement Award (OAA) to a select group of 20 accredited cancer programs throughout the U.S.
Award criteria were based on qualitative and quantitative surveys conducted January 1 through June 30, 2016. The biannual award was established in 2004 to recognize cancer programs that strive for excellence in demonstrating compliance with the CoC standards and are committed to ensuring high-quality cancer care.
A CoC-accredited cancer program is eligible to earn the OAA after completing the accreditation survey and receiving a Performance Report that indicates an accreditation award of “Three-Year with Commendation.” Specifically, the program must receive commendation ratings for the seven commendation level standards and no deficiencies for the remaining 27 standards.
View the list of this year’s first group of OAA recipients on the ACS website at https://www.facs.org/quality-programs/cancer/coc/info/outstanding/2016-part-1.
Study eyed zinc for slowing progression of chronic liver disease
BOSTON – Oral zinc supplementation was associated with maintenance of liver function and suppression of hepatocellular carcinoma in a retrospective cohort study of 267 patients with chronic liver disease.
Additional analyses revealed stepwise inverse relationships between serum zinc levels and rates of de novo liver failure, hepatocellular carcinoma, and death, Atsushi Hosui, MD, PhD, said at the annual meeting of the American Association for the Study of Liver Diseases. No patients stopped zinc therapy because of adverse events, and there were no serious adverse events, although some patients experienced nausea, which can occur with zinc supplementation, noted Dr. Hosui of Osaka-Rosai Hospital, Japan.
To begin exploring hepatic correlates of zinc supplementation, Dr. Hosui and his associates retrospectively studied 267 patients in Japan with chronic liver diseases between 2006 and 2015. They had a median of 40 months of data for each patient. No patient had hepatocellular carcinoma at baseline. In all, 196 patients received zinc supplementation (average baseline zinc level, 51 mcg/dL), while 71 patients did not (62 mcg/dL). These two groups resembled each other in terms of etiologies of liver disease, but the zinc group was significantly older (73.2 vs. 66.4 years; P less than .0001), had a significantly higher average baseline bilirubin level (1.2 vs. 0.8 mg/dL; P less than .0001), and a significantly lower average platelet concentration and prothrombin time. (P less than .0001).
Despite having multiple indicators of worse liver disease, only 9.5% of zinc recipients developed hepatocellular carcinoma over 3 years, compared with 25% of patients in the control group (P = .005). Rates of liver failure and death were similar between the two groups, but sequential blood tests did indicate worsening liver disease among patients who did not receive zinc – their prothrombin times and branched-chain amino acid to tyrosine ratios steadily dropped over 3 years, while those in zinc recipients did not.
Next, the researchers stratified zinc recipients according to their serum zinc levels 6 months after starting supplementation. Notably, 3-year rates of mortality, liver failure, and death were significantly higher among patients whose zinc levels were lower than in patients who achieved higher serum zinc levels. For example, 3-year mortality rates were 28% among patients whose zinc level was 70-89 mcg/dL, versus 0% among patients whose zinc level was at least 90 mcg/dL (P = .02). Similarly, 3-year rates of liver failure were 3.6% among patients whose zinc level was 50-69 mcg/dL, versus 0% among patients whose serum zinc level was at least 70 mcg/dL (P = .03). Finally, over 3 years, hepatocellular carcinoma was diagnosed in 17% of patients whose zinc level was 50-69 mcg/dL, versus only 3.8% of patients whose zinc level was 70-89 mcg/dL.
“We suggest that oral zinc supplementation is effective for maintaining liver function and suppressing the development of hepatocellular carcinoma,” Dr. Hosui concluded. The data support a target serum zinc level of at least 70 mcg/dL to suppress liver-related events, including hepatocellular carcinoma, he added. The researchers are exploring clinical trials of zinc for these outcomes in Japan.
The investigators did not report funding for this study. They reported having no conflicts of interest.
BOSTON – Oral zinc supplementation was associated with maintenance of liver function and suppression of hepatocellular carcinoma in a retrospective cohort study of 267 patients with chronic liver disease.
Additional analyses revealed stepwise inverse relationships between serum zinc levels and rates of de novo liver failure, hepatocellular carcinoma, and death, Atsushi Hosui, MD, PhD, said at the annual meeting of the American Association for the Study of Liver Diseases. No patients stopped zinc therapy because of adverse events, and there were no serious adverse events, although some patients experienced nausea, which can occur with zinc supplementation, noted Dr. Hosui of Osaka-Rosai Hospital, Japan.
To begin exploring hepatic correlates of zinc supplementation, Dr. Hosui and his associates retrospectively studied 267 patients in Japan with chronic liver diseases between 2006 and 2015. They had a median of 40 months of data for each patient. No patient had hepatocellular carcinoma at baseline. In all, 196 patients received zinc supplementation (average baseline zinc level, 51 mcg/dL), while 71 patients did not (62 mcg/dL). These two groups resembled each other in terms of etiologies of liver disease, but the zinc group was significantly older (73.2 vs. 66.4 years; P less than .0001), had a significantly higher average baseline bilirubin level (1.2 vs. 0.8 mg/dL; P less than .0001), and a significantly lower average platelet concentration and prothrombin time. (P less than .0001).
Despite having multiple indicators of worse liver disease, only 9.5% of zinc recipients developed hepatocellular carcinoma over 3 years, compared with 25% of patients in the control group (P = .005). Rates of liver failure and death were similar between the two groups, but sequential blood tests did indicate worsening liver disease among patients who did not receive zinc – their prothrombin times and branched-chain amino acid to tyrosine ratios steadily dropped over 3 years, while those in zinc recipients did not.
Next, the researchers stratified zinc recipients according to their serum zinc levels 6 months after starting supplementation. Notably, 3-year rates of mortality, liver failure, and death were significantly higher among patients whose zinc levels were lower than in patients who achieved higher serum zinc levels. For example, 3-year mortality rates were 28% among patients whose zinc level was 70-89 mcg/dL, versus 0% among patients whose zinc level was at least 90 mcg/dL (P = .02). Similarly, 3-year rates of liver failure were 3.6% among patients whose zinc level was 50-69 mcg/dL, versus 0% among patients whose serum zinc level was at least 70 mcg/dL (P = .03). Finally, over 3 years, hepatocellular carcinoma was diagnosed in 17% of patients whose zinc level was 50-69 mcg/dL, versus only 3.8% of patients whose zinc level was 70-89 mcg/dL.
“We suggest that oral zinc supplementation is effective for maintaining liver function and suppressing the development of hepatocellular carcinoma,” Dr. Hosui concluded. The data support a target serum zinc level of at least 70 mcg/dL to suppress liver-related events, including hepatocellular carcinoma, he added. The researchers are exploring clinical trials of zinc for these outcomes in Japan.
The investigators did not report funding for this study. They reported having no conflicts of interest.
BOSTON – Oral zinc supplementation was associated with maintenance of liver function and suppression of hepatocellular carcinoma in a retrospective cohort study of 267 patients with chronic liver disease.
Additional analyses revealed stepwise inverse relationships between serum zinc levels and rates of de novo liver failure, hepatocellular carcinoma, and death, Atsushi Hosui, MD, PhD, said at the annual meeting of the American Association for the Study of Liver Diseases. No patients stopped zinc therapy because of adverse events, and there were no serious adverse events, although some patients experienced nausea, which can occur with zinc supplementation, noted Dr. Hosui of Osaka-Rosai Hospital, Japan.
To begin exploring hepatic correlates of zinc supplementation, Dr. Hosui and his associates retrospectively studied 267 patients in Japan with chronic liver diseases between 2006 and 2015. They had a median of 40 months of data for each patient. No patient had hepatocellular carcinoma at baseline. In all, 196 patients received zinc supplementation (average baseline zinc level, 51 mcg/dL), while 71 patients did not (62 mcg/dL). These two groups resembled each other in terms of etiologies of liver disease, but the zinc group was significantly older (73.2 vs. 66.4 years; P less than .0001), had a significantly higher average baseline bilirubin level (1.2 vs. 0.8 mg/dL; P less than .0001), and a significantly lower average platelet concentration and prothrombin time. (P less than .0001).
Despite having multiple indicators of worse liver disease, only 9.5% of zinc recipients developed hepatocellular carcinoma over 3 years, compared with 25% of patients in the control group (P = .005). Rates of liver failure and death were similar between the two groups, but sequential blood tests did indicate worsening liver disease among patients who did not receive zinc – their prothrombin times and branched-chain amino acid to tyrosine ratios steadily dropped over 3 years, while those in zinc recipients did not.
Next, the researchers stratified zinc recipients according to their serum zinc levels 6 months after starting supplementation. Notably, 3-year rates of mortality, liver failure, and death were significantly higher among patients whose zinc levels were lower than in patients who achieved higher serum zinc levels. For example, 3-year mortality rates were 28% among patients whose zinc level was 70-89 mcg/dL, versus 0% among patients whose zinc level was at least 90 mcg/dL (P = .02). Similarly, 3-year rates of liver failure were 3.6% among patients whose zinc level was 50-69 mcg/dL, versus 0% among patients whose serum zinc level was at least 70 mcg/dL (P = .03). Finally, over 3 years, hepatocellular carcinoma was diagnosed in 17% of patients whose zinc level was 50-69 mcg/dL, versus only 3.8% of patients whose zinc level was 70-89 mcg/dL.
“We suggest that oral zinc supplementation is effective for maintaining liver function and suppressing the development of hepatocellular carcinoma,” Dr. Hosui concluded. The data support a target serum zinc level of at least 70 mcg/dL to suppress liver-related events, including hepatocellular carcinoma, he added. The researchers are exploring clinical trials of zinc for these outcomes in Japan.
The investigators did not report funding for this study. They reported having no conflicts of interest.
AT THE LIVER MEETING 2016
Key clinical point: Oral zinc sulfate supplementation might help prevent the progression of chronic liver disease and associated hepatocellular carcinoma.
Major finding: Despite having multiple indicators of worse liver disease, only 9.5% of zinc recipients developed hepatocellular carcinoma over 3 years, compared with 25% of patients in the control group (P = .005).
Data source: A retrospective cohort study of 267 patients with chronic liver disease but no hepatocellular carcinoma at baseline.
Disclosures: The investigators did not report funding for this study. They reported having no conflicts of interest.
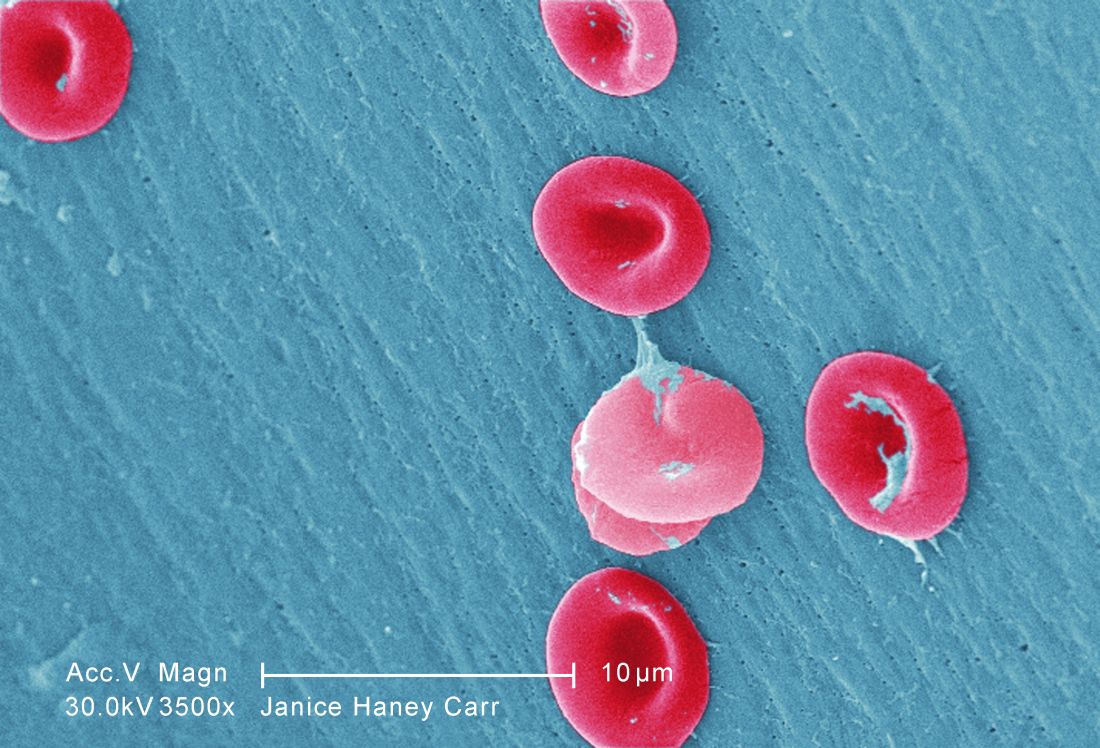
SelG1 cut pain crises in sickle cell disease
The humanized antibody SelG1 decreased the frequency of acute pain episodes in people with sickle cell disease, based on results from the multinational, randomized, double-blind, placebo-controlled SUSTAIN study that will be presented at the annual meeting of the American Society of Hematology in San Diego.
In other sickle cell disease research to be presented at the meeting, researchers will be presenting new findings from two studies conducted in Africa. One study examines a team approach to reduce mortality in pregnant women with sickle cell disease in Ghana. The other study, called SPIN, is a safety and feasibility study conducted in advance of a randomized trial in Nigerian children at risk for stroke.
After 1 year, the annual rate of sickle cell–related pain crises resulting in a visit to a medical facility was 1.6 in the group receiving the 5 mg/kg dose, compared with 3 in the placebo group. The 47% difference was statistically significant (P = .01).
Also, time to first pain crisis was a median of 4 months in those who received the 5 mg/kg dose and 1.4 months for those in the placebo group (P = .001).
Infections were not seen increased in either of the groups randomized to SelG1, and no treatment-related deaths occurred during the course of the study. The first-in-class agent “appears to be safe and well tolerated,” as well as effective in reducing pain episodes, Dr. Ataga and his colleagues wrote in their abstract.
In the Nigerian trial, led by Najibah Aliyu Galadanci, MD, MPH, of Bayero University in Kano, Nigeria, the goal was to determine whether families of children with sickle cell disease and transcranial Doppler measurements indicative of increased risk for stroke could be recruited and retained in a large clinical trial, and whether they could adhere to the medication regimen. The trial also obtained preliminary evidence for hydroxyurea’s safety in this clinical setting, where transfusion therapy is not an option for most children.
Dr. Galadanci and her colleagues approached 375 families for transcranial Doppler screening, and 90% accepted. Among families of children found to have elevated measures of risk on transcranial Doppler, 92% participated in the study and received a moderate dose of hydroxyurea (20 mg/kg) for 2 years. A comparison group included 210 children without elevated measures on transcranial Doppler. These children underwent regular monitoring but were not offered medication unless transcranial Doppler measures were found to be elevated.
Study adherence was exceptionally high: the families missed no monthly research visits, and no participants in the active treatment group dropped out voluntarily.
Also, at 2 years, the children treated with hydroxyurea did not have evidence of excessive toxicity, compared with the children who did not receive the drug. “Our results provide strong preliminary evidence supporting the current multicenter randomized controlled trial comparing hydroxyurea therapy (20 mg/kg per day vs. 10 mg/kg per day) for preventing primary strokes in children with sickle cell anemia living in Nigeria,” Dr. Galadanci and her colleagues wrote in their abstract.
In the third study, a multidisciplinary team decreased mortality in pregnant women who had sickle cell disease and lived in low and middle income settings, according to Eugenia Vicky Naa Kwarley Asare, MD, of the Ghana Institute of Clinical Genetics and the Korle-Bu Teaching Hospital in Accra.
In a prospective trial in Ghana, where maternal mortality among women with sickle cell disease is estimated to be 8,300 per 100,000 live births, compared with 690 for women without sickle cell disease, Dr. Asare and her colleagues’ multidisciplinary team included obstetricians, hematologists, pulmonologists, and nurses, and the planned intervention protocols included a number of changes to make management more consistent and intensive. A total of 154 pregnancies were evaluated before the intervention, and 91 after. Median gestational age was 24 weeks at enrollment, and median maternal age was 29 years for both pre- and post-intervention cohorts.
Maternal mortality before the intervention was 9.7% (15 of 154) and after the intervention was 1.1% (1 of 91) of total deliveries.
Dr. Ataga’s study was sponsored by Selexys Pharmaceuticals, the drug’s manufacturer, and included coinvestigators who are employees of Selexys Pharmaceuticals or who disclosed relationships with other drug manufacturers. Dr. Galadanci’s and Dr. Asare’s groups disclosed no conflicts of interest.
The humanized antibody SelG1 decreased the frequency of acute pain episodes in people with sickle cell disease, based on results from the multinational, randomized, double-blind, placebo-controlled SUSTAIN study that will be presented at the annual meeting of the American Society of Hematology in San Diego.
In other sickle cell disease research to be presented at the meeting, researchers will be presenting new findings from two studies conducted in Africa. One study examines a team approach to reduce mortality in pregnant women with sickle cell disease in Ghana. The other study, called SPIN, is a safety and feasibility study conducted in advance of a randomized trial in Nigerian children at risk for stroke.
After 1 year, the annual rate of sickle cell–related pain crises resulting in a visit to a medical facility was 1.6 in the group receiving the 5 mg/kg dose, compared with 3 in the placebo group. The 47% difference was statistically significant (P = .01).
Also, time to first pain crisis was a median of 4 months in those who received the 5 mg/kg dose and 1.4 months for those in the placebo group (P = .001).
Infections were not seen increased in either of the groups randomized to SelG1, and no treatment-related deaths occurred during the course of the study. The first-in-class agent “appears to be safe and well tolerated,” as well as effective in reducing pain episodes, Dr. Ataga and his colleagues wrote in their abstract.
In the Nigerian trial, led by Najibah Aliyu Galadanci, MD, MPH, of Bayero University in Kano, Nigeria, the goal was to determine whether families of children with sickle cell disease and transcranial Doppler measurements indicative of increased risk for stroke could be recruited and retained in a large clinical trial, and whether they could adhere to the medication regimen. The trial also obtained preliminary evidence for hydroxyurea’s safety in this clinical setting, where transfusion therapy is not an option for most children.
Dr. Galadanci and her colleagues approached 375 families for transcranial Doppler screening, and 90% accepted. Among families of children found to have elevated measures of risk on transcranial Doppler, 92% participated in the study and received a moderate dose of hydroxyurea (20 mg/kg) for 2 years. A comparison group included 210 children without elevated measures on transcranial Doppler. These children underwent regular monitoring but were not offered medication unless transcranial Doppler measures were found to be elevated.
Study adherence was exceptionally high: the families missed no monthly research visits, and no participants in the active treatment group dropped out voluntarily.
Also, at 2 years, the children treated with hydroxyurea did not have evidence of excessive toxicity, compared with the children who did not receive the drug. “Our results provide strong preliminary evidence supporting the current multicenter randomized controlled trial comparing hydroxyurea therapy (20 mg/kg per day vs. 10 mg/kg per day) for preventing primary strokes in children with sickle cell anemia living in Nigeria,” Dr. Galadanci and her colleagues wrote in their abstract.
In the third study, a multidisciplinary team decreased mortality in pregnant women who had sickle cell disease and lived in low and middle income settings, according to Eugenia Vicky Naa Kwarley Asare, MD, of the Ghana Institute of Clinical Genetics and the Korle-Bu Teaching Hospital in Accra.
In a prospective trial in Ghana, where maternal mortality among women with sickle cell disease is estimated to be 8,300 per 100,000 live births, compared with 690 for women without sickle cell disease, Dr. Asare and her colleagues’ multidisciplinary team included obstetricians, hematologists, pulmonologists, and nurses, and the planned intervention protocols included a number of changes to make management more consistent and intensive. A total of 154 pregnancies were evaluated before the intervention, and 91 after. Median gestational age was 24 weeks at enrollment, and median maternal age was 29 years for both pre- and post-intervention cohorts.
Maternal mortality before the intervention was 9.7% (15 of 154) and after the intervention was 1.1% (1 of 91) of total deliveries.
Dr. Ataga’s study was sponsored by Selexys Pharmaceuticals, the drug’s manufacturer, and included coinvestigators who are employees of Selexys Pharmaceuticals or who disclosed relationships with other drug manufacturers. Dr. Galadanci’s and Dr. Asare’s groups disclosed no conflicts of interest.
The humanized antibody SelG1 decreased the frequency of acute pain episodes in people with sickle cell disease, based on results from the multinational, randomized, double-blind, placebo-controlled SUSTAIN study that will be presented at the annual meeting of the American Society of Hematology in San Diego.
In other sickle cell disease research to be presented at the meeting, researchers will be presenting new findings from two studies conducted in Africa. One study examines a team approach to reduce mortality in pregnant women with sickle cell disease in Ghana. The other study, called SPIN, is a safety and feasibility study conducted in advance of a randomized trial in Nigerian children at risk for stroke.
After 1 year, the annual rate of sickle cell–related pain crises resulting in a visit to a medical facility was 1.6 in the group receiving the 5 mg/kg dose, compared with 3 in the placebo group. The 47% difference was statistically significant (P = .01).
Also, time to first pain crisis was a median of 4 months in those who received the 5 mg/kg dose and 1.4 months for those in the placebo group (P = .001).
Infections were not seen increased in either of the groups randomized to SelG1, and no treatment-related deaths occurred during the course of the study. The first-in-class agent “appears to be safe and well tolerated,” as well as effective in reducing pain episodes, Dr. Ataga and his colleagues wrote in their abstract.
In the Nigerian trial, led by Najibah Aliyu Galadanci, MD, MPH, of Bayero University in Kano, Nigeria, the goal was to determine whether families of children with sickle cell disease and transcranial Doppler measurements indicative of increased risk for stroke could be recruited and retained in a large clinical trial, and whether they could adhere to the medication regimen. The trial also obtained preliminary evidence for hydroxyurea’s safety in this clinical setting, where transfusion therapy is not an option for most children.
Dr. Galadanci and her colleagues approached 375 families for transcranial Doppler screening, and 90% accepted. Among families of children found to have elevated measures of risk on transcranial Doppler, 92% participated in the study and received a moderate dose of hydroxyurea (20 mg/kg) for 2 years. A comparison group included 210 children without elevated measures on transcranial Doppler. These children underwent regular monitoring but were not offered medication unless transcranial Doppler measures were found to be elevated.
Study adherence was exceptionally high: the families missed no monthly research visits, and no participants in the active treatment group dropped out voluntarily.
Also, at 2 years, the children treated with hydroxyurea did not have evidence of excessive toxicity, compared with the children who did not receive the drug. “Our results provide strong preliminary evidence supporting the current multicenter randomized controlled trial comparing hydroxyurea therapy (20 mg/kg per day vs. 10 mg/kg per day) for preventing primary strokes in children with sickle cell anemia living in Nigeria,” Dr. Galadanci and her colleagues wrote in their abstract.
In the third study, a multidisciplinary team decreased mortality in pregnant women who had sickle cell disease and lived in low and middle income settings, according to Eugenia Vicky Naa Kwarley Asare, MD, of the Ghana Institute of Clinical Genetics and the Korle-Bu Teaching Hospital in Accra.
In a prospective trial in Ghana, where maternal mortality among women with sickle cell disease is estimated to be 8,300 per 100,000 live births, compared with 690 for women without sickle cell disease, Dr. Asare and her colleagues’ multidisciplinary team included obstetricians, hematologists, pulmonologists, and nurses, and the planned intervention protocols included a number of changes to make management more consistent and intensive. A total of 154 pregnancies were evaluated before the intervention, and 91 after. Median gestational age was 24 weeks at enrollment, and median maternal age was 29 years for both pre- and post-intervention cohorts.
Maternal mortality before the intervention was 9.7% (15 of 154) and after the intervention was 1.1% (1 of 91) of total deliveries.
Dr. Ataga’s study was sponsored by Selexys Pharmaceuticals, the drug’s manufacturer, and included coinvestigators who are employees of Selexys Pharmaceuticals or who disclosed relationships with other drug manufacturers. Dr. Galadanci’s and Dr. Asare’s groups disclosed no conflicts of interest.
FROM ASH 2016
Nivolumab’s safety profile further clarified
In patients taking nivolumab for advanced melanoma, most immunologic adverse effects are mild to moderate in intensity and resolve when existing management guidelines are followed, investigators report.
Nivolumab, a programmed death-1 (PD-1) checkpoint inhibitor antibody, is effective in several tumor types, including melanoma, but its safety profile has not been well characterized to date. Researchers pooled data from two phase I exploratory and two phase III comparative clinical trials of advanced melanoma to better examine safety outcomes, in what they described as “the largest and most comprehensive analysis to date of ... anti-PD-1 monotherapy.”
The study included 576 patients (median age, 61 years) taking nivolumab. Slightly more than half had received ipilimumab, another immune checkpoint inhibitor, previously. Twelve percent had brain metastases. The median duration of nivolumab therapy was 3.7 months, reflecting a median of nine doses of the agent per patient. Median follow-up was 7.2 months (range, 0.3-62.5 months), said Jeffrey S. Weber, MD, PhD, of Dana-Farber Cancer Institute, Boston, and his associates.
The overall rate of adverse events likely to have an immunologic etiology was 49%, and most of these were mild to moderate; severe immunologic adverse effects occurred in less than 4% of patients. Prior ipilimumab therapy did not influence the number or severity of adverse reactions to nivolumab. Most immunologic adverse effects involved the skin and GI tract, and most of them, including the few severe effects, resolved when treated according to safety management guidelines.
The types of immunologic adverse events in this study were similar to those previously reported for this class of drug. However, pneumonitis developed less frequently (less than 2% of patients) in this study population than has been reported previously and also was less severe. Rare and unusual immunologic adverse events remain a possibility with PD-1 checkpoint inhibitor antibodies. In particular, five of these study participants developed grade 3 neurologic toxicities. Further information on such effects and on optimal management is needed, the investigators wrote (J Clin Oncol. 2016 Nov 14. doi: 10.1200/JCO.66.1389).
Immune modulators – chiefly systemic, topical, or inhaled corticosteroids – were frequently used to treat immunologic adverse effects. “Although there is a theoretic concern that [this] might interfere with an anticancer immune response, the results of our analysis suggest that immune modulators do not negatively affect the rate or quality of antitumor responses [to] nivolumab therapy,” Dr. Weber and his associates said.
In patients taking nivolumab for advanced melanoma, most immunologic adverse effects are mild to moderate in intensity and resolve when existing management guidelines are followed, investigators report.
Nivolumab, a programmed death-1 (PD-1) checkpoint inhibitor antibody, is effective in several tumor types, including melanoma, but its safety profile has not been well characterized to date. Researchers pooled data from two phase I exploratory and two phase III comparative clinical trials of advanced melanoma to better examine safety outcomes, in what they described as “the largest and most comprehensive analysis to date of ... anti-PD-1 monotherapy.”
The study included 576 patients (median age, 61 years) taking nivolumab. Slightly more than half had received ipilimumab, another immune checkpoint inhibitor, previously. Twelve percent had brain metastases. The median duration of nivolumab therapy was 3.7 months, reflecting a median of nine doses of the agent per patient. Median follow-up was 7.2 months (range, 0.3-62.5 months), said Jeffrey S. Weber, MD, PhD, of Dana-Farber Cancer Institute, Boston, and his associates.
The overall rate of adverse events likely to have an immunologic etiology was 49%, and most of these were mild to moderate; severe immunologic adverse effects occurred in less than 4% of patients. Prior ipilimumab therapy did not influence the number or severity of adverse reactions to nivolumab. Most immunologic adverse effects involved the skin and GI tract, and most of them, including the few severe effects, resolved when treated according to safety management guidelines.
The types of immunologic adverse events in this study were similar to those previously reported for this class of drug. However, pneumonitis developed less frequently (less than 2% of patients) in this study population than has been reported previously and also was less severe. Rare and unusual immunologic adverse events remain a possibility with PD-1 checkpoint inhibitor antibodies. In particular, five of these study participants developed grade 3 neurologic toxicities. Further information on such effects and on optimal management is needed, the investigators wrote (J Clin Oncol. 2016 Nov 14. doi: 10.1200/JCO.66.1389).
Immune modulators – chiefly systemic, topical, or inhaled corticosteroids – were frequently used to treat immunologic adverse effects. “Although there is a theoretic concern that [this] might interfere with an anticancer immune response, the results of our analysis suggest that immune modulators do not negatively affect the rate or quality of antitumor responses [to] nivolumab therapy,” Dr. Weber and his associates said.
In patients taking nivolumab for advanced melanoma, most immunologic adverse effects are mild to moderate in intensity and resolve when existing management guidelines are followed, investigators report.
Nivolumab, a programmed death-1 (PD-1) checkpoint inhibitor antibody, is effective in several tumor types, including melanoma, but its safety profile has not been well characterized to date. Researchers pooled data from two phase I exploratory and two phase III comparative clinical trials of advanced melanoma to better examine safety outcomes, in what they described as “the largest and most comprehensive analysis to date of ... anti-PD-1 monotherapy.”
The study included 576 patients (median age, 61 years) taking nivolumab. Slightly more than half had received ipilimumab, another immune checkpoint inhibitor, previously. Twelve percent had brain metastases. The median duration of nivolumab therapy was 3.7 months, reflecting a median of nine doses of the agent per patient. Median follow-up was 7.2 months (range, 0.3-62.5 months), said Jeffrey S. Weber, MD, PhD, of Dana-Farber Cancer Institute, Boston, and his associates.
The overall rate of adverse events likely to have an immunologic etiology was 49%, and most of these were mild to moderate; severe immunologic adverse effects occurred in less than 4% of patients. Prior ipilimumab therapy did not influence the number or severity of adverse reactions to nivolumab. Most immunologic adverse effects involved the skin and GI tract, and most of them, including the few severe effects, resolved when treated according to safety management guidelines.
The types of immunologic adverse events in this study were similar to those previously reported for this class of drug. However, pneumonitis developed less frequently (less than 2% of patients) in this study population than has been reported previously and also was less severe. Rare and unusual immunologic adverse events remain a possibility with PD-1 checkpoint inhibitor antibodies. In particular, five of these study participants developed grade 3 neurologic toxicities. Further information on such effects and on optimal management is needed, the investigators wrote (J Clin Oncol. 2016 Nov 14. doi: 10.1200/JCO.66.1389).
Immune modulators – chiefly systemic, topical, or inhaled corticosteroids – were frequently used to treat immunologic adverse effects. “Although there is a theoretic concern that [this] might interfere with an anticancer immune response, the results of our analysis suggest that immune modulators do not negatively affect the rate or quality of antitumor responses [to] nivolumab therapy,” Dr. Weber and his associates said.
Key clinical point: In patients taking nivolumab for advanced melanoma, most immunologic adverse effects are mild to moderate in intensity and resolve when existing management guidelines are followed.
Major finding: The overall rate of adverse events likely to have an immunologic etiology was 49%, while the rate of severe immunologic adverse effects was less than 4%.
Data source: A pooled analysis of data from four clinical trials involving 576 patients who took nivolumab for a median of 4 months and were followed for a median of 7 months.
Disclosures: This study was supported in part by Bristol-Myers Squibb and the Royal Marsden/Institute of Cancer Research Biomedical Research Centre. Dr. Weber and his associates reported ties to numerous industry sources.