User login
Genetic markers may predict response to biologics in rheumatoid arthritis
WASHINGTON – Three gene expression markers appear to predict response to some of the most common and powerful rheumatoid arthritis drugs employed in clinical practice.
In the largest gene-expression study of these drugs to date, researchers from Glasgow found 23 genes that predicted response to TNF inhibitors, and 23 more that predicted response to rituximab. They also found eight genes that predicted positive response to both types of drugs.
Just as important, the team found that 10% of patients in the study had none of the markers, Duncan Porter, MD, said during a press briefing at the annual meeting of the American College of Rheumatology.
If confirmed in independent validation cohorts, the findings could revolutionize medical therapy for rheumatoid arthritis, Dr. Porter said in an interview.
“Right now, the choice of treatment is mostly a flip of the coin,” said Dr. Porter, a rheumatologist at Queen Elizabeth University Hospital in Glasgow. “We don’t have a lot of comparative data to support one drug over the other, and most head-to-head studies show noninferiority.
“So, it would be ideal to be able to identify patients who will respond to one class or the other, and give them the right medicine the first time,” he noted. “If we can do that, we have the beginnings of really meaningful personalized therapy in RA.”
Dr. Porter reported a transcriptome-wide association study of 250 patients with RA who were enrolled in the ORBIT trial (Lancet. 2016 Jul 16;388[10041]:239-47). Dr. Porter was the study’s primary investigator.
ORBIT comprised 295 patients with active, seropositive rheumatoid arthritis who had failed disease-modifying antirheumatic therapy. They were randomized to B-cell depletion with rituximab or to the TNF inhibitors adalimumab or etanercept. ORBIT concluded that clinical response was similar with all three drugs. However, while most patients did well on their assigned drug, no matter which class, 20% failed their initial assignment.
The genetic study examined RNA transcripts in whole blood samples among a subset of the ORBIT patients. Most of the samples (70%) were used to identify markers and created a prediction model; that was then verified in the remaining 30% of samples. Markers were correlated to clinical response associated with rituximab and TNF inhibition. Clinical response was defined as a 1.2-point decline in the Disease Activity Score from baseline to 3 months of therapy.
At least 1 of the 54 genetic response markers was present in 90% of the population; 50% would have responded well to either drug, or 40% to just one of them.
But 10% of the population lacked either of the response markers – a very important finding, Dr. Porter noted, because if identified early, these patients could potentially avoid ineffective medication trials.
The markers’ predictive values were uniformly high, with a sensitivity of 93% and specificity of 91%. The positive predictive value was 96%, and the negative predictive value was 86%. Patients predicted to respond at 3 months were also more likely to have a good response (43% vs. 23%) or remission (23% vs. 10%), as measured by the Disease Activity Score 28 at 12 months.
While Dr. Porter was excited about the findings, he eyed them cautiously.
“The landscape is littered with biomarkers that had great early promise but failed in later validation studies,” he said. “We must be very careful in interpreting this. However, the other response studies have been small, and have not compared two drugs. This study was large with robust results, so we are encouraged.”
Dr Porter is now designing the protocol for a large external validation cohort study, which he hopes to launch in 2017.
Roche funded aspects of the ORBIT trial and the genetic substudy. Dr. Porter has been a consultant for Roche, as well as for AbbVie and Pfizer.
[email protected]On Twitter @alz_gal
WASHINGTON – Three gene expression markers appear to predict response to some of the most common and powerful rheumatoid arthritis drugs employed in clinical practice.
In the largest gene-expression study of these drugs to date, researchers from Glasgow found 23 genes that predicted response to TNF inhibitors, and 23 more that predicted response to rituximab. They also found eight genes that predicted positive response to both types of drugs.
Just as important, the team found that 10% of patients in the study had none of the markers, Duncan Porter, MD, said during a press briefing at the annual meeting of the American College of Rheumatology.
If confirmed in independent validation cohorts, the findings could revolutionize medical therapy for rheumatoid arthritis, Dr. Porter said in an interview.
“Right now, the choice of treatment is mostly a flip of the coin,” said Dr. Porter, a rheumatologist at Queen Elizabeth University Hospital in Glasgow. “We don’t have a lot of comparative data to support one drug over the other, and most head-to-head studies show noninferiority.
“So, it would be ideal to be able to identify patients who will respond to one class or the other, and give them the right medicine the first time,” he noted. “If we can do that, we have the beginnings of really meaningful personalized therapy in RA.”
Dr. Porter reported a transcriptome-wide association study of 250 patients with RA who were enrolled in the ORBIT trial (Lancet. 2016 Jul 16;388[10041]:239-47). Dr. Porter was the study’s primary investigator.
ORBIT comprised 295 patients with active, seropositive rheumatoid arthritis who had failed disease-modifying antirheumatic therapy. They were randomized to B-cell depletion with rituximab or to the TNF inhibitors adalimumab or etanercept. ORBIT concluded that clinical response was similar with all three drugs. However, while most patients did well on their assigned drug, no matter which class, 20% failed their initial assignment.
The genetic study examined RNA transcripts in whole blood samples among a subset of the ORBIT patients. Most of the samples (70%) were used to identify markers and created a prediction model; that was then verified in the remaining 30% of samples. Markers were correlated to clinical response associated with rituximab and TNF inhibition. Clinical response was defined as a 1.2-point decline in the Disease Activity Score from baseline to 3 months of therapy.
At least 1 of the 54 genetic response markers was present in 90% of the population; 50% would have responded well to either drug, or 40% to just one of them.
But 10% of the population lacked either of the response markers – a very important finding, Dr. Porter noted, because if identified early, these patients could potentially avoid ineffective medication trials.
The markers’ predictive values were uniformly high, with a sensitivity of 93% and specificity of 91%. The positive predictive value was 96%, and the negative predictive value was 86%. Patients predicted to respond at 3 months were also more likely to have a good response (43% vs. 23%) or remission (23% vs. 10%), as measured by the Disease Activity Score 28 at 12 months.
While Dr. Porter was excited about the findings, he eyed them cautiously.
“The landscape is littered with biomarkers that had great early promise but failed in later validation studies,” he said. “We must be very careful in interpreting this. However, the other response studies have been small, and have not compared two drugs. This study was large with robust results, so we are encouraged.”
Dr Porter is now designing the protocol for a large external validation cohort study, which he hopes to launch in 2017.
Roche funded aspects of the ORBIT trial and the genetic substudy. Dr. Porter has been a consultant for Roche, as well as for AbbVie and Pfizer.
[email protected]On Twitter @alz_gal
WASHINGTON – Three gene expression markers appear to predict response to some of the most common and powerful rheumatoid arthritis drugs employed in clinical practice.
In the largest gene-expression study of these drugs to date, researchers from Glasgow found 23 genes that predicted response to TNF inhibitors, and 23 more that predicted response to rituximab. They also found eight genes that predicted positive response to both types of drugs.
Just as important, the team found that 10% of patients in the study had none of the markers, Duncan Porter, MD, said during a press briefing at the annual meeting of the American College of Rheumatology.
If confirmed in independent validation cohorts, the findings could revolutionize medical therapy for rheumatoid arthritis, Dr. Porter said in an interview.
“Right now, the choice of treatment is mostly a flip of the coin,” said Dr. Porter, a rheumatologist at Queen Elizabeth University Hospital in Glasgow. “We don’t have a lot of comparative data to support one drug over the other, and most head-to-head studies show noninferiority.
“So, it would be ideal to be able to identify patients who will respond to one class or the other, and give them the right medicine the first time,” he noted. “If we can do that, we have the beginnings of really meaningful personalized therapy in RA.”
Dr. Porter reported a transcriptome-wide association study of 250 patients with RA who were enrolled in the ORBIT trial (Lancet. 2016 Jul 16;388[10041]:239-47). Dr. Porter was the study’s primary investigator.
ORBIT comprised 295 patients with active, seropositive rheumatoid arthritis who had failed disease-modifying antirheumatic therapy. They were randomized to B-cell depletion with rituximab or to the TNF inhibitors adalimumab or etanercept. ORBIT concluded that clinical response was similar with all three drugs. However, while most patients did well on their assigned drug, no matter which class, 20% failed their initial assignment.
The genetic study examined RNA transcripts in whole blood samples among a subset of the ORBIT patients. Most of the samples (70%) were used to identify markers and created a prediction model; that was then verified in the remaining 30% of samples. Markers were correlated to clinical response associated with rituximab and TNF inhibition. Clinical response was defined as a 1.2-point decline in the Disease Activity Score from baseline to 3 months of therapy.
At least 1 of the 54 genetic response markers was present in 90% of the population; 50% would have responded well to either drug, or 40% to just one of them.
But 10% of the population lacked either of the response markers – a very important finding, Dr. Porter noted, because if identified early, these patients could potentially avoid ineffective medication trials.
The markers’ predictive values were uniformly high, with a sensitivity of 93% and specificity of 91%. The positive predictive value was 96%, and the negative predictive value was 86%. Patients predicted to respond at 3 months were also more likely to have a good response (43% vs. 23%) or remission (23% vs. 10%), as measured by the Disease Activity Score 28 at 12 months.
While Dr. Porter was excited about the findings, he eyed them cautiously.
“The landscape is littered with biomarkers that had great early promise but failed in later validation studies,” he said. “We must be very careful in interpreting this. However, the other response studies have been small, and have not compared two drugs. This study was large with robust results, so we are encouraged.”
Dr Porter is now designing the protocol for a large external validation cohort study, which he hopes to launch in 2017.
Roche funded aspects of the ORBIT trial and the genetic substudy. Dr. Porter has been a consultant for Roche, as well as for AbbVie and Pfizer.
[email protected]On Twitter @alz_gal
Key clinical point:
Major finding: The markers’ sensitivity and specificity for clinical response exceeded 90%.
Data source: The genetic-association study comprised 250 patients.
Disclosures: Roche funded aspects of the ORBIT trial and the genetic substudy. Dr. Porter has been a consultant for Roche, as well as for AbbVie and Pfizer.
‘Skip phenomenon’ could explain fluctuating positivity for S. aureus bacteremia
NEW ORLEANS – A proportion of patients treated appropriately with antibiotics for Staphylococcus aureus bacteremia can generate a negative blood culture followed by a positive one, a new clinical entity researchers are calling the “skip phenomenon.”
“This pattern is really in cases where people have known Staph. aureus bacteremia; it seems to clear; they’re on appropriate antibiotic therapy; and despite that, we see that the blood cultures come back positive again several days later,” explained Justin A. Fiala, MD, of Mayo Clinic in Rochester, Minn.
In a video interview, Dr. Fiala outlined the findings of the first study to identify and characterize this phenomenon.
Certain patients with S. aureus bacteremia could be at higher risk for skip phenomenon, for example. The nested case-control study identified these higher-risk patients, a population that might warrant more clinical testing.
Dr. Fiala also discussed associations with patient outcomes, as well as the overall prevalence of skip phenomenon in his research, which included more than 900 patients with S. aureus bacteremia treated at Mayo Clinic.
Dr. Fiala had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – A proportion of patients treated appropriately with antibiotics for Staphylococcus aureus bacteremia can generate a negative blood culture followed by a positive one, a new clinical entity researchers are calling the “skip phenomenon.”
“This pattern is really in cases where people have known Staph. aureus bacteremia; it seems to clear; they’re on appropriate antibiotic therapy; and despite that, we see that the blood cultures come back positive again several days later,” explained Justin A. Fiala, MD, of Mayo Clinic in Rochester, Minn.
In a video interview, Dr. Fiala outlined the findings of the first study to identify and characterize this phenomenon.
Certain patients with S. aureus bacteremia could be at higher risk for skip phenomenon, for example. The nested case-control study identified these higher-risk patients, a population that might warrant more clinical testing.
Dr. Fiala also discussed associations with patient outcomes, as well as the overall prevalence of skip phenomenon in his research, which included more than 900 patients with S. aureus bacteremia treated at Mayo Clinic.
Dr. Fiala had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – A proportion of patients treated appropriately with antibiotics for Staphylococcus aureus bacteremia can generate a negative blood culture followed by a positive one, a new clinical entity researchers are calling the “skip phenomenon.”
“This pattern is really in cases where people have known Staph. aureus bacteremia; it seems to clear; they’re on appropriate antibiotic therapy; and despite that, we see that the blood cultures come back positive again several days later,” explained Justin A. Fiala, MD, of Mayo Clinic in Rochester, Minn.
In a video interview, Dr. Fiala outlined the findings of the first study to identify and characterize this phenomenon.
Certain patients with S. aureus bacteremia could be at higher risk for skip phenomenon, for example. The nested case-control study identified these higher-risk patients, a population that might warrant more clinical testing.
Dr. Fiala also discussed associations with patient outcomes, as well as the overall prevalence of skip phenomenon in his research, which included more than 900 patients with S. aureus bacteremia treated at Mayo Clinic.
Dr. Fiala had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
When school’s out, the obesity epidemic grows
NEW ORLEANS – All of the growth in the obesity epidemic in young American schoolchildren takes place during their summer vacations, Paul T. von Hippel, PhD, reported at Obesity Week 2016.
He presented an analysis from the Early Childhood Longitudinal Study, Kindergarten Class of 2010-2011 which included a nationally representative study population composed of 18,170 U.S. children in 970 schools who were followed with serial weight and height measurements from the start of kindergarten in 2010 through the end of second grade in 2013.
During the summer, the prevalence of both overweight and obesity increased by roughly 1 percentage point per month. In contrast, during the more than 9 months of each school year, the prevalence of overweight didn’t budge, while the prevalence of obesity decreased modestly, by 0.1 percentage points per month.
These data have far-reaching public health implications. The new evidence suggests that the major risk factors for obesity are located outside of schools. That helps explain why many school-based initiatives focused on improving the nutritional content of school lunches and promoting physical activity have had little impact on the pediatric obesity epidemic, said Dr. von Hippel of the University of Texas at Austin.
The data suggest it’s time to explore the potential of reshaping out-of-school behaviors by promoting summer school and summer camp, curbing food advertising directed at children, providing parental nutrition education, and other interventions, he added.
The explanation for the observed increase in body mass index during summer vacation is unclear. It’s known from other studies that children sleep less and engage in more screen time during summer, which may be relevant, according to Dr. von Hippel.
Simultaneous with Dr. von Hippel’s presentation at Obesity 2016, the study was published online in the journal Obesity (2016 Nov 2. doi: 10.1002/oby.21613).
He reported having no financial conflicts of interest regarding the study, which was funded by the Russell Sage Foundation.
NEW ORLEANS – All of the growth in the obesity epidemic in young American schoolchildren takes place during their summer vacations, Paul T. von Hippel, PhD, reported at Obesity Week 2016.
He presented an analysis from the Early Childhood Longitudinal Study, Kindergarten Class of 2010-2011 which included a nationally representative study population composed of 18,170 U.S. children in 970 schools who were followed with serial weight and height measurements from the start of kindergarten in 2010 through the end of second grade in 2013.
During the summer, the prevalence of both overweight and obesity increased by roughly 1 percentage point per month. In contrast, during the more than 9 months of each school year, the prevalence of overweight didn’t budge, while the prevalence of obesity decreased modestly, by 0.1 percentage points per month.
These data have far-reaching public health implications. The new evidence suggests that the major risk factors for obesity are located outside of schools. That helps explain why many school-based initiatives focused on improving the nutritional content of school lunches and promoting physical activity have had little impact on the pediatric obesity epidemic, said Dr. von Hippel of the University of Texas at Austin.
The data suggest it’s time to explore the potential of reshaping out-of-school behaviors by promoting summer school and summer camp, curbing food advertising directed at children, providing parental nutrition education, and other interventions, he added.
The explanation for the observed increase in body mass index during summer vacation is unclear. It’s known from other studies that children sleep less and engage in more screen time during summer, which may be relevant, according to Dr. von Hippel.
Simultaneous with Dr. von Hippel’s presentation at Obesity 2016, the study was published online in the journal Obesity (2016 Nov 2. doi: 10.1002/oby.21613).
He reported having no financial conflicts of interest regarding the study, which was funded by the Russell Sage Foundation.
NEW ORLEANS – All of the growth in the obesity epidemic in young American schoolchildren takes place during their summer vacations, Paul T. von Hippel, PhD, reported at Obesity Week 2016.
He presented an analysis from the Early Childhood Longitudinal Study, Kindergarten Class of 2010-2011 which included a nationally representative study population composed of 18,170 U.S. children in 970 schools who were followed with serial weight and height measurements from the start of kindergarten in 2010 through the end of second grade in 2013.
During the summer, the prevalence of both overweight and obesity increased by roughly 1 percentage point per month. In contrast, during the more than 9 months of each school year, the prevalence of overweight didn’t budge, while the prevalence of obesity decreased modestly, by 0.1 percentage points per month.
These data have far-reaching public health implications. The new evidence suggests that the major risk factors for obesity are located outside of schools. That helps explain why many school-based initiatives focused on improving the nutritional content of school lunches and promoting physical activity have had little impact on the pediatric obesity epidemic, said Dr. von Hippel of the University of Texas at Austin.
The data suggest it’s time to explore the potential of reshaping out-of-school behaviors by promoting summer school and summer camp, curbing food advertising directed at children, providing parental nutrition education, and other interventions, he added.
The explanation for the observed increase in body mass index during summer vacation is unclear. It’s known from other studies that children sleep less and engage in more screen time during summer, which may be relevant, according to Dr. von Hippel.
Simultaneous with Dr. von Hippel’s presentation at Obesity 2016, the study was published online in the journal Obesity (2016 Nov 2. doi: 10.1002/oby.21613).
He reported having no financial conflicts of interest regarding the study, which was funded by the Russell Sage Foundation.
AT OBESITY WEEK 2016
Key clinical point:
Major finding: Between the start of kindergarten and the end of second grade, the prevalence of overweight in a large group of U.S. children grew from 23.3% to 28.7%, with all of the increase coming during their two summer vacations.
Data source: The Early Childhood Longitudinal Study, Kindergarten Class of 2010-2011 included a nationally representative study population composed of more than 18,000 children who were followed with multiple weight and height measurements from the start of kindergarten through the end of second grade.
Disclosures: The study was funded by the Russell Sage Foundation. The presenter reported having no financial conflicts of interest.
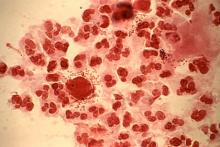
Multidose metronidazole may be better option for trichomoniasis treatment
ATLANTA – A multidose regimen of metronidazole was found to have a lower likelihood of treatment failure than a single-dose regimen in treating trichomoniasis in a meta-analysis presented at a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
In its 2015 STD treatment guidelines, the CDC recommends that women with HIV infection who receive a diagnosis of Trichomonas vaginalis infection should be treated with metronidazole 500 mg orally twice daily for 7 days, rather than with a 2-g single dose of metronidazole. However, it recommends a 2-g single dose of either metronidazole or tinidazole for other women with trichomoniasis as first-line treatment.
“[Trichomoniasis] is the most prevalent nonviral sexually transmitted infection in the U.S.; there are estimates of anywhere between 3.7 to 7 million [cases]. It eclipses gonorrhea, chlamydia, and syphilis in its prevalence, and there are about 276 million [cases] worldwide,” she said.
While single-dose therapy is inexpensive and has excellent adherence, recurrence has been a problem.
To compare the effectiveness of single- versus multidose treatment strategies, Dr. Kissinger and her coinvestigators searched Embase, Medline, and clinicaltrials.gov for any studies published before Jan. 25, 2016, that were English-language clinical trials evaluating trichomoniasis and metronidazole, and that compared single with multidose treatment regimens. Nearly 500 articles were identified and reviewed, but only six studies were included for analysis based on relevance and quality. Of those, one study included only HIV-positive women.
The primary endpoint was the pooled relative risk (RR) across all included studies of treatment failure in single- and multidose regimens.
Results showed that women who received single-dose metronidazole were 1.87 times more likely to experience treatment failure than those who received multidose therapy (95% confidence interval, 1.23-2.82; P less than .01). When the investigators excluded the one study involving HIV-positive women, the findings were similar, with those on single-dose therapy being 1.80 times more likely than those on a multidose regimen to experience treatment failure (95% CI, 1.07-3.02; P less than .03).
“Limitations [include] that the quality of the studies were not at the same level as we’d be doing in this decade,” Dr. Kissinger said. “There’s a scarcity of studies that evaluate this topic, [and] clinical trial methods have improved substantially since the 1980s, when most of these studies were done.”
Dr. Kissinger did not report information on financial disclosures.
ATLANTA – A multidose regimen of metronidazole was found to have a lower likelihood of treatment failure than a single-dose regimen in treating trichomoniasis in a meta-analysis presented at a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
In its 2015 STD treatment guidelines, the CDC recommends that women with HIV infection who receive a diagnosis of Trichomonas vaginalis infection should be treated with metronidazole 500 mg orally twice daily for 7 days, rather than with a 2-g single dose of metronidazole. However, it recommends a 2-g single dose of either metronidazole or tinidazole for other women with trichomoniasis as first-line treatment.
“[Trichomoniasis] is the most prevalent nonviral sexually transmitted infection in the U.S.; there are estimates of anywhere between 3.7 to 7 million [cases]. It eclipses gonorrhea, chlamydia, and syphilis in its prevalence, and there are about 276 million [cases] worldwide,” she said.
While single-dose therapy is inexpensive and has excellent adherence, recurrence has been a problem.
To compare the effectiveness of single- versus multidose treatment strategies, Dr. Kissinger and her coinvestigators searched Embase, Medline, and clinicaltrials.gov for any studies published before Jan. 25, 2016, that were English-language clinical trials evaluating trichomoniasis and metronidazole, and that compared single with multidose treatment regimens. Nearly 500 articles were identified and reviewed, but only six studies were included for analysis based on relevance and quality. Of those, one study included only HIV-positive women.
The primary endpoint was the pooled relative risk (RR) across all included studies of treatment failure in single- and multidose regimens.
Results showed that women who received single-dose metronidazole were 1.87 times more likely to experience treatment failure than those who received multidose therapy (95% confidence interval, 1.23-2.82; P less than .01). When the investigators excluded the one study involving HIV-positive women, the findings were similar, with those on single-dose therapy being 1.80 times more likely than those on a multidose regimen to experience treatment failure (95% CI, 1.07-3.02; P less than .03).
“Limitations [include] that the quality of the studies were not at the same level as we’d be doing in this decade,” Dr. Kissinger said. “There’s a scarcity of studies that evaluate this topic, [and] clinical trial methods have improved substantially since the 1980s, when most of these studies were done.”
Dr. Kissinger did not report information on financial disclosures.
ATLANTA – A multidose regimen of metronidazole was found to have a lower likelihood of treatment failure than a single-dose regimen in treating trichomoniasis in a meta-analysis presented at a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
In its 2015 STD treatment guidelines, the CDC recommends that women with HIV infection who receive a diagnosis of Trichomonas vaginalis infection should be treated with metronidazole 500 mg orally twice daily for 7 days, rather than with a 2-g single dose of metronidazole. However, it recommends a 2-g single dose of either metronidazole or tinidazole for other women with trichomoniasis as first-line treatment.
“[Trichomoniasis] is the most prevalent nonviral sexually transmitted infection in the U.S.; there are estimates of anywhere between 3.7 to 7 million [cases]. It eclipses gonorrhea, chlamydia, and syphilis in its prevalence, and there are about 276 million [cases] worldwide,” she said.
While single-dose therapy is inexpensive and has excellent adherence, recurrence has been a problem.
To compare the effectiveness of single- versus multidose treatment strategies, Dr. Kissinger and her coinvestigators searched Embase, Medline, and clinicaltrials.gov for any studies published before Jan. 25, 2016, that were English-language clinical trials evaluating trichomoniasis and metronidazole, and that compared single with multidose treatment regimens. Nearly 500 articles were identified and reviewed, but only six studies were included for analysis based on relevance and quality. Of those, one study included only HIV-positive women.
The primary endpoint was the pooled relative risk (RR) across all included studies of treatment failure in single- and multidose regimens.
Results showed that women who received single-dose metronidazole were 1.87 times more likely to experience treatment failure than those who received multidose therapy (95% confidence interval, 1.23-2.82; P less than .01). When the investigators excluded the one study involving HIV-positive women, the findings were similar, with those on single-dose therapy being 1.80 times more likely than those on a multidose regimen to experience treatment failure (95% CI, 1.07-3.02; P less than .03).
“Limitations [include] that the quality of the studies were not at the same level as we’d be doing in this decade,” Dr. Kissinger said. “There’s a scarcity of studies that evaluate this topic, [and] clinical trial methods have improved substantially since the 1980s, when most of these studies were done.”
Dr. Kissinger did not report information on financial disclosures.
AT THE 2016 STD PREVENTION CONFERENCE
Key clinical point:
Major finding: A single-dose regimen of metronidazole was more likely to fail, compared with a multidose regimen, with a pooled risk ratio of 1.87 (95% CI, 1.23-2.82; P less than .01).
Data source: Meta-analysis of six studies that evaluated single- and multidose metronidazole in treating T. vaginalis infections.
Disclosures: Dr. Kissinger did not report information on financial disclosures.
Hypotension ‘dose’ drives mortality in traumatic brain injury
NEW ORLEANS – The severity and duration of hypotension in traumatic brain injury patients during EMS transport to an emergency department has a tight and essentially linear relationship to their mortality rate during subsequent weeks of recovery, according to an analysis of more than 7,500 brain-injured patients.
For each doubling of the combined severity and duration of hypotension during the prehospital period, when systolic blood pressure was less than 90 mm Hg, patient mortality rose by 19%, Daniel W. Spaite, MD, reported at the American Heart Association scientific sessions.
However, the results do not address whether aggressive treatment of hypotension by EMS technicians in a patient with traumatic brain injury (TBI) leads to reduced mortality. That question is being assessed as part of the primary endpoint of the Excellence in Prehospital Injury Care-Traumatic Brain Injury (EPIC-TBI) study, which should have an answer by the end of 2017, said Dr. Spaite, professor of emergency medicine at the University of Arizona in Tuscon.
The innovation introduced by Dr. Spaite and his associates in their analysis of the EPIC-TBI data was to drill down into each patient’s hypotensive event, made possible by the 16,711 patients enrolled in EPIC-TBI.
The calculation they performed was limited to patients with EMS records of at least two blood pressure measurements during prehospital transport. These data allowed them to use both the extent to which systolic blood pressure dropped below 90 mm Hg and the amount of time pressure was below this threshold to better define the total hypotension exposure each patient received.
This meant that a TBI patient with a systolic pressure of 80 mm Hg for 10 minutes had twice the hypotension exposure of both a patient with a pressure of 85 mm Hg for 10 minutes, and a patient with a pressure of 80 mm Hg for 5 minutes.
Their analysis also adjusted the relationship of this total hypotensive dose and subsequent mortality based on several baseline demographic and clinical variables, including age, sex, injury severity, trauma type, and head-region severity score. After adjustment, the researchers found a “strikingly linear relationship” between hypotension dose and mortality, Dr. Spaite said, although a clear dose-response relationship was also evident in the unadjusted data.
EPIC-TBI enrolled TBI patients age 10 years or older during 2007-2014 through participation by dozens of EMS providers throughout Arizona. For the current analysis, the researchers identified 7,521 patients from the total group who had at least two blood pressure measurements taken during their prehospital EMS care and also met other inclusion criteria.
The best way to manage hypotension in TBI patients during the prehospital period remains unclear. Simply raising blood pressure with fluid infusion may not necessarily help, because it could exacerbate a patient’s bleeding, Dr. Spaite noted during an interview.
The primary goal of EPIC-TBI is to assess the impact of the third edition of the traumatic brain injury guidelines released in 2007 by the Brain Trauma Foundation. (The fourth edition of these guidelines came out in August 2016.) The new finding by Dr. Spaite and his associates will allow the full EPIC-TBI analysis to correlate patient outcomes with the impact that acute, prehospital treatment had on the hypotension dose received by each patient, he noted.
“What’s remarkable is that the single, prehospital parameter of hypotension for just a few minutes during transport can have such a strong impact on survival, given all the other factors that can influence outcomes” in TBI patients once they reach a hospital and during the period they remain hospitalized, Dr. Spaite said.
[email protected] On Twitter @mitchelzoler
NEW ORLEANS – The severity and duration of hypotension in traumatic brain injury patients during EMS transport to an emergency department has a tight and essentially linear relationship to their mortality rate during subsequent weeks of recovery, according to an analysis of more than 7,500 brain-injured patients.
For each doubling of the combined severity and duration of hypotension during the prehospital period, when systolic blood pressure was less than 90 mm Hg, patient mortality rose by 19%, Daniel W. Spaite, MD, reported at the American Heart Association scientific sessions.
However, the results do not address whether aggressive treatment of hypotension by EMS technicians in a patient with traumatic brain injury (TBI) leads to reduced mortality. That question is being assessed as part of the primary endpoint of the Excellence in Prehospital Injury Care-Traumatic Brain Injury (EPIC-TBI) study, which should have an answer by the end of 2017, said Dr. Spaite, professor of emergency medicine at the University of Arizona in Tuscon.
The innovation introduced by Dr. Spaite and his associates in their analysis of the EPIC-TBI data was to drill down into each patient’s hypotensive event, made possible by the 16,711 patients enrolled in EPIC-TBI.
The calculation they performed was limited to patients with EMS records of at least two blood pressure measurements during prehospital transport. These data allowed them to use both the extent to which systolic blood pressure dropped below 90 mm Hg and the amount of time pressure was below this threshold to better define the total hypotension exposure each patient received.
This meant that a TBI patient with a systolic pressure of 80 mm Hg for 10 minutes had twice the hypotension exposure of both a patient with a pressure of 85 mm Hg for 10 minutes, and a patient with a pressure of 80 mm Hg for 5 minutes.
Their analysis also adjusted the relationship of this total hypotensive dose and subsequent mortality based on several baseline demographic and clinical variables, including age, sex, injury severity, trauma type, and head-region severity score. After adjustment, the researchers found a “strikingly linear relationship” between hypotension dose and mortality, Dr. Spaite said, although a clear dose-response relationship was also evident in the unadjusted data.
EPIC-TBI enrolled TBI patients age 10 years or older during 2007-2014 through participation by dozens of EMS providers throughout Arizona. For the current analysis, the researchers identified 7,521 patients from the total group who had at least two blood pressure measurements taken during their prehospital EMS care and also met other inclusion criteria.
The best way to manage hypotension in TBI patients during the prehospital period remains unclear. Simply raising blood pressure with fluid infusion may not necessarily help, because it could exacerbate a patient’s bleeding, Dr. Spaite noted during an interview.
The primary goal of EPIC-TBI is to assess the impact of the third edition of the traumatic brain injury guidelines released in 2007 by the Brain Trauma Foundation. (The fourth edition of these guidelines came out in August 2016.) The new finding by Dr. Spaite and his associates will allow the full EPIC-TBI analysis to correlate patient outcomes with the impact that acute, prehospital treatment had on the hypotension dose received by each patient, he noted.
“What’s remarkable is that the single, prehospital parameter of hypotension for just a few minutes during transport can have such a strong impact on survival, given all the other factors that can influence outcomes” in TBI patients once they reach a hospital and during the period they remain hospitalized, Dr. Spaite said.
[email protected] On Twitter @mitchelzoler
NEW ORLEANS – The severity and duration of hypotension in traumatic brain injury patients during EMS transport to an emergency department has a tight and essentially linear relationship to their mortality rate during subsequent weeks of recovery, according to an analysis of more than 7,500 brain-injured patients.
For each doubling of the combined severity and duration of hypotension during the prehospital period, when systolic blood pressure was less than 90 mm Hg, patient mortality rose by 19%, Daniel W. Spaite, MD, reported at the American Heart Association scientific sessions.
However, the results do not address whether aggressive treatment of hypotension by EMS technicians in a patient with traumatic brain injury (TBI) leads to reduced mortality. That question is being assessed as part of the primary endpoint of the Excellence in Prehospital Injury Care-Traumatic Brain Injury (EPIC-TBI) study, which should have an answer by the end of 2017, said Dr. Spaite, professor of emergency medicine at the University of Arizona in Tuscon.
The innovation introduced by Dr. Spaite and his associates in their analysis of the EPIC-TBI data was to drill down into each patient’s hypotensive event, made possible by the 16,711 patients enrolled in EPIC-TBI.
The calculation they performed was limited to patients with EMS records of at least two blood pressure measurements during prehospital transport. These data allowed them to use both the extent to which systolic blood pressure dropped below 90 mm Hg and the amount of time pressure was below this threshold to better define the total hypotension exposure each patient received.
This meant that a TBI patient with a systolic pressure of 80 mm Hg for 10 minutes had twice the hypotension exposure of both a patient with a pressure of 85 mm Hg for 10 minutes, and a patient with a pressure of 80 mm Hg for 5 minutes.
Their analysis also adjusted the relationship of this total hypotensive dose and subsequent mortality based on several baseline demographic and clinical variables, including age, sex, injury severity, trauma type, and head-region severity score. After adjustment, the researchers found a “strikingly linear relationship” between hypotension dose and mortality, Dr. Spaite said, although a clear dose-response relationship was also evident in the unadjusted data.
EPIC-TBI enrolled TBI patients age 10 years or older during 2007-2014 through participation by dozens of EMS providers throughout Arizona. For the current analysis, the researchers identified 7,521 patients from the total group who had at least two blood pressure measurements taken during their prehospital EMS care and also met other inclusion criteria.
The best way to manage hypotension in TBI patients during the prehospital period remains unclear. Simply raising blood pressure with fluid infusion may not necessarily help, because it could exacerbate a patient’s bleeding, Dr. Spaite noted during an interview.
The primary goal of EPIC-TBI is to assess the impact of the third edition of the traumatic brain injury guidelines released in 2007 by the Brain Trauma Foundation. (The fourth edition of these guidelines came out in August 2016.) The new finding by Dr. Spaite and his associates will allow the full EPIC-TBI analysis to correlate patient outcomes with the impact that acute, prehospital treatment had on the hypotension dose received by each patient, he noted.
“What’s remarkable is that the single, prehospital parameter of hypotension for just a few minutes during transport can have such a strong impact on survival, given all the other factors that can influence outcomes” in TBI patients once they reach a hospital and during the period they remain hospitalized, Dr. Spaite said.
[email protected] On Twitter @mitchelzoler
Key clinical point:
Major finding: For each doubling of the dose of prehospital hypotension (a function of severity and duration), mortality rose by 19%.
Data source: EPIC-TBI, a multicenter study with 16,711 patients, including 7,521 who met inclusion criteria for the current analysis.
Disclosures: Dr. Spaite had no disclosures.
New scale bests Milan criteria in predicting posttransplant HCC recurrence
BOSTON – A new scoring system fared better than the Milan criteria in predicting risk for recurrent hepatocellular carcinoma after liver transplant.
The scoring system combines an assessment of the number and size of tumors on the explanted liver with serum alpha-fetoprotein (AFP) score and the presence of microvascular invasion to assign a numeric risk score to patients who have received liver transplant for hepatocellular carcinoma (HCC).
The risk estimation tool showed good model estimation, with a C statistic of 0.82 (95% confidence interval, 0.77-0.86), according to Neil Mehta, MD, who presented the study validating the risk estimation tool at the annual meeting of the American Association for the Study of Liver Diseases. The C statistic is a measure of goodness of fit, with values closer to 1 indicating better fit.
In a paper published simultaneously in JAMA Oncology, Dr. Mehta and his collaborators said that the tool had “superior recurrence risk classification, compared with explant Milan criteria (net reclassification index, 0.40; P = 0.001) in the study’s validation cohort” (JAMA Oncol. 2016 Nov 13. doi: 10:1001/jamaoncol2016/5116).
Under the Milan criteria, patients with HCC are eligible for liver transplant if there are no extrahepatic manifestations and no vascular invasion. One lesion must be smaller than 5 cm, and up to three lesions smaller than 3 cm are permitted.
Dr. Mehta, a gastroenterologist and transplant hepatologist at the University of California, San Francisco, worked with colleagues to narrow down a long list of factors that in previous studies had been associated with HCC recurrence. The final Risk Estimation of Tumor Recurrence After Transplant (RETREAT) score uses just three factors that multivariable analysis found were most highly predictive of HCC recurrence after liver transplant.
The three factors are microvascular invasion; AFP at the time of liver transplant; and the sum of the largest viable tumor diameter plus the number of viable tumors, assessed at the time of explant.
This last factor uses pathology examination, rather than radiology results, to assess tumor number, size, and viability. If a tumor is found to be completely necrotic, for example, it is not included when counting tumors for this component of the RETREAT score.
To develop the scoring system, Dr. Mehta and his coauthors enrolled adult patients with HCC who had liver transplant at three centers, each with a different wait time for transplant – short, medium, or long. Patients in the development cohort (n=721) had Model for End-Stage Liver Disease (MELD) score exception, and patients always met Milan criteria on imaging.
The validation cohort (n=340) had the same inclusion and exclusion criteria, but differed in several significant ways from the development cohort, with more young people, men, and individuals with hepatitis B or alcohol abuse. Individuals in the validation cohort were less likely to have received locoregional therapy (LRT) before liver transplant, but were more likely to have had a single tumor. They had more microvascular invasion, more tumors that were poorly differentiated, and more tumor staging beyond Milan criteria on explant.
The primary outcome measures for the study were overall survival and 5-year post–liver transplant HCC recurrence.
In developing the RETREAT scoring system, investigators used the final multivariable model coefficients to produce a “simplified point scale reflecting the relative impact of model covariables,” Dr. Mehta and his coauthors wrote.
RETREAT scoring ranges from 0 to 8; in the studied patients, the most common score was 1. Any microvascular invasion is assigned a point value of 2. The sum of the largest viable tumor diameter – in centimeters – plus the number of viable tumors is divided into four categories. If there are no tumors, the score is 0. For a sum of 1.1-4.9, the score is 1; a sum of 5.0-9.9 is assigned a score of 2, and a sum or 10 or greater is assigned a score of 3.
Serum AFP at the time of liver transplant (measured in ng/mL) is given a score of 0 if the value is less than 20. AFP of 20-99 is assigned a score of 1, values of 100-999 a score of 2, and 1,000 or greater a score of 3.
“Predicted risk of 1- and 5-year HCC recurrence rose with each point scored such that a patient with a RETREAT score of 5 or higher … had a predicted 1- and 5-year recurrence risk of 39.3 (95% CI, 25.5%-50.5%) and 75.2% (95% CI, 56.7%-85.8%), respectively,” the researchers wrote.
Dr. Mehta and his coauthors emphasized that the RETREAT scoring system represents an effort to strike a balance between including clinically meaningful variables to predict HCC recurrence and retaining simplicity and ease of use.
The researchers suggested guidelines for post–liver transplant HCC recurrence surveillance based on RETREAT scoring. They recommend no follow-up for a score of 0; surveillance scans and AFP monitoring every 6 months for 2 years for a score of 1-3, and every 6 months for 5 years for a score of 4. RETREAT scores of 5 or higher warrant surveillance every 3-4 months for 2 years, followed by every 6 months through year 5.
This surveillance stratification, they said, should help control costs while retaining a vigilant approach for those most at risk of recurrence. This approach is currently in use at University of California, San Francisco.
Study limitations included some missing information on AFP levels in the development cohort, and a small number of missing histologic tumor grading in both cohorts. In order to address limitations in the retrospective design of the present study, Dr. Mehta and his coauthors are planning another multicenter study to evaluate RETREAT as a surveillance tool and confirm its prognostic value.
The authors reported no conflicts of interest. The study was funded by the Biostatistics Core of the UCSF Liver Center.
[email protected]
On Twitter @karioakes
BOSTON – A new scoring system fared better than the Milan criteria in predicting risk for recurrent hepatocellular carcinoma after liver transplant.
The scoring system combines an assessment of the number and size of tumors on the explanted liver with serum alpha-fetoprotein (AFP) score and the presence of microvascular invasion to assign a numeric risk score to patients who have received liver transplant for hepatocellular carcinoma (HCC).
The risk estimation tool showed good model estimation, with a C statistic of 0.82 (95% confidence interval, 0.77-0.86), according to Neil Mehta, MD, who presented the study validating the risk estimation tool at the annual meeting of the American Association for the Study of Liver Diseases. The C statistic is a measure of goodness of fit, with values closer to 1 indicating better fit.
In a paper published simultaneously in JAMA Oncology, Dr. Mehta and his collaborators said that the tool had “superior recurrence risk classification, compared with explant Milan criteria (net reclassification index, 0.40; P = 0.001) in the study’s validation cohort” (JAMA Oncol. 2016 Nov 13. doi: 10:1001/jamaoncol2016/5116).
Under the Milan criteria, patients with HCC are eligible for liver transplant if there are no extrahepatic manifestations and no vascular invasion. One lesion must be smaller than 5 cm, and up to three lesions smaller than 3 cm are permitted.
Dr. Mehta, a gastroenterologist and transplant hepatologist at the University of California, San Francisco, worked with colleagues to narrow down a long list of factors that in previous studies had been associated with HCC recurrence. The final Risk Estimation of Tumor Recurrence After Transplant (RETREAT) score uses just three factors that multivariable analysis found were most highly predictive of HCC recurrence after liver transplant.
The three factors are microvascular invasion; AFP at the time of liver transplant; and the sum of the largest viable tumor diameter plus the number of viable tumors, assessed at the time of explant.
This last factor uses pathology examination, rather than radiology results, to assess tumor number, size, and viability. If a tumor is found to be completely necrotic, for example, it is not included when counting tumors for this component of the RETREAT score.
To develop the scoring system, Dr. Mehta and his coauthors enrolled adult patients with HCC who had liver transplant at three centers, each with a different wait time for transplant – short, medium, or long. Patients in the development cohort (n=721) had Model for End-Stage Liver Disease (MELD) score exception, and patients always met Milan criteria on imaging.
The validation cohort (n=340) had the same inclusion and exclusion criteria, but differed in several significant ways from the development cohort, with more young people, men, and individuals with hepatitis B or alcohol abuse. Individuals in the validation cohort were less likely to have received locoregional therapy (LRT) before liver transplant, but were more likely to have had a single tumor. They had more microvascular invasion, more tumors that were poorly differentiated, and more tumor staging beyond Milan criteria on explant.
The primary outcome measures for the study were overall survival and 5-year post–liver transplant HCC recurrence.
In developing the RETREAT scoring system, investigators used the final multivariable model coefficients to produce a “simplified point scale reflecting the relative impact of model covariables,” Dr. Mehta and his coauthors wrote.
RETREAT scoring ranges from 0 to 8; in the studied patients, the most common score was 1. Any microvascular invasion is assigned a point value of 2. The sum of the largest viable tumor diameter – in centimeters – plus the number of viable tumors is divided into four categories. If there are no tumors, the score is 0. For a sum of 1.1-4.9, the score is 1; a sum of 5.0-9.9 is assigned a score of 2, and a sum or 10 or greater is assigned a score of 3.
Serum AFP at the time of liver transplant (measured in ng/mL) is given a score of 0 if the value is less than 20. AFP of 20-99 is assigned a score of 1, values of 100-999 a score of 2, and 1,000 or greater a score of 3.
“Predicted risk of 1- and 5-year HCC recurrence rose with each point scored such that a patient with a RETREAT score of 5 or higher … had a predicted 1- and 5-year recurrence risk of 39.3 (95% CI, 25.5%-50.5%) and 75.2% (95% CI, 56.7%-85.8%), respectively,” the researchers wrote.
Dr. Mehta and his coauthors emphasized that the RETREAT scoring system represents an effort to strike a balance between including clinically meaningful variables to predict HCC recurrence and retaining simplicity and ease of use.
The researchers suggested guidelines for post–liver transplant HCC recurrence surveillance based on RETREAT scoring. They recommend no follow-up for a score of 0; surveillance scans and AFP monitoring every 6 months for 2 years for a score of 1-3, and every 6 months for 5 years for a score of 4. RETREAT scores of 5 or higher warrant surveillance every 3-4 months for 2 years, followed by every 6 months through year 5.
This surveillance stratification, they said, should help control costs while retaining a vigilant approach for those most at risk of recurrence. This approach is currently in use at University of California, San Francisco.
Study limitations included some missing information on AFP levels in the development cohort, and a small number of missing histologic tumor grading in both cohorts. In order to address limitations in the retrospective design of the present study, Dr. Mehta and his coauthors are planning another multicenter study to evaluate RETREAT as a surveillance tool and confirm its prognostic value.
The authors reported no conflicts of interest. The study was funded by the Biostatistics Core of the UCSF Liver Center.
[email protected]
On Twitter @karioakes
BOSTON – A new scoring system fared better than the Milan criteria in predicting risk for recurrent hepatocellular carcinoma after liver transplant.
The scoring system combines an assessment of the number and size of tumors on the explanted liver with serum alpha-fetoprotein (AFP) score and the presence of microvascular invasion to assign a numeric risk score to patients who have received liver transplant for hepatocellular carcinoma (HCC).
The risk estimation tool showed good model estimation, with a C statistic of 0.82 (95% confidence interval, 0.77-0.86), according to Neil Mehta, MD, who presented the study validating the risk estimation tool at the annual meeting of the American Association for the Study of Liver Diseases. The C statistic is a measure of goodness of fit, with values closer to 1 indicating better fit.
In a paper published simultaneously in JAMA Oncology, Dr. Mehta and his collaborators said that the tool had “superior recurrence risk classification, compared with explant Milan criteria (net reclassification index, 0.40; P = 0.001) in the study’s validation cohort” (JAMA Oncol. 2016 Nov 13. doi: 10:1001/jamaoncol2016/5116).
Under the Milan criteria, patients with HCC are eligible for liver transplant if there are no extrahepatic manifestations and no vascular invasion. One lesion must be smaller than 5 cm, and up to three lesions smaller than 3 cm are permitted.
Dr. Mehta, a gastroenterologist and transplant hepatologist at the University of California, San Francisco, worked with colleagues to narrow down a long list of factors that in previous studies had been associated with HCC recurrence. The final Risk Estimation of Tumor Recurrence After Transplant (RETREAT) score uses just three factors that multivariable analysis found were most highly predictive of HCC recurrence after liver transplant.
The three factors are microvascular invasion; AFP at the time of liver transplant; and the sum of the largest viable tumor diameter plus the number of viable tumors, assessed at the time of explant.
This last factor uses pathology examination, rather than radiology results, to assess tumor number, size, and viability. If a tumor is found to be completely necrotic, for example, it is not included when counting tumors for this component of the RETREAT score.
To develop the scoring system, Dr. Mehta and his coauthors enrolled adult patients with HCC who had liver transplant at three centers, each with a different wait time for transplant – short, medium, or long. Patients in the development cohort (n=721) had Model for End-Stage Liver Disease (MELD) score exception, and patients always met Milan criteria on imaging.
The validation cohort (n=340) had the same inclusion and exclusion criteria, but differed in several significant ways from the development cohort, with more young people, men, and individuals with hepatitis B or alcohol abuse. Individuals in the validation cohort were less likely to have received locoregional therapy (LRT) before liver transplant, but were more likely to have had a single tumor. They had more microvascular invasion, more tumors that were poorly differentiated, and more tumor staging beyond Milan criteria on explant.
The primary outcome measures for the study were overall survival and 5-year post–liver transplant HCC recurrence.
In developing the RETREAT scoring system, investigators used the final multivariable model coefficients to produce a “simplified point scale reflecting the relative impact of model covariables,” Dr. Mehta and his coauthors wrote.
RETREAT scoring ranges from 0 to 8; in the studied patients, the most common score was 1. Any microvascular invasion is assigned a point value of 2. The sum of the largest viable tumor diameter – in centimeters – plus the number of viable tumors is divided into four categories. If there are no tumors, the score is 0. For a sum of 1.1-4.9, the score is 1; a sum of 5.0-9.9 is assigned a score of 2, and a sum or 10 or greater is assigned a score of 3.
Serum AFP at the time of liver transplant (measured in ng/mL) is given a score of 0 if the value is less than 20. AFP of 20-99 is assigned a score of 1, values of 100-999 a score of 2, and 1,000 or greater a score of 3.
“Predicted risk of 1- and 5-year HCC recurrence rose with each point scored such that a patient with a RETREAT score of 5 or higher … had a predicted 1- and 5-year recurrence risk of 39.3 (95% CI, 25.5%-50.5%) and 75.2% (95% CI, 56.7%-85.8%), respectively,” the researchers wrote.
Dr. Mehta and his coauthors emphasized that the RETREAT scoring system represents an effort to strike a balance between including clinically meaningful variables to predict HCC recurrence and retaining simplicity and ease of use.
The researchers suggested guidelines for post–liver transplant HCC recurrence surveillance based on RETREAT scoring. They recommend no follow-up for a score of 0; surveillance scans and AFP monitoring every 6 months for 2 years for a score of 1-3, and every 6 months for 5 years for a score of 4. RETREAT scores of 5 or higher warrant surveillance every 3-4 months for 2 years, followed by every 6 months through year 5.
This surveillance stratification, they said, should help control costs while retaining a vigilant approach for those most at risk of recurrence. This approach is currently in use at University of California, San Francisco.
Study limitations included some missing information on AFP levels in the development cohort, and a small number of missing histologic tumor grading in both cohorts. In order to address limitations in the retrospective design of the present study, Dr. Mehta and his coauthors are planning another multicenter study to evaluate RETREAT as a surveillance tool and confirm its prognostic value.
The authors reported no conflicts of interest. The study was funded by the Biostatistics Core of the UCSF Liver Center.
[email protected]
On Twitter @karioakes
Key clinical point:
Major finding: The RETREAT score was superior to explant Milan criteria in predicting post–liver transplant HCC recurence (P = .001)
Data source: Multivariable analysis of prognostic factors for HCC recurrence in a group of 721 patients in a development cohort and 340 in a validation cohort, all of whom had liver transplant.
Disclosures: The study investigators reported no disclosures. The study was funded by the Biostatistics Core of the University of California, San Francisco Liver Center.
Inpatient telemedicine could bridge infectious disease specialist gap
NEW ORLEANS – Telemedicine inpatient consultations are a relatively new component in health care, but they could help address the problem of infectious disease physician shortages, particularly in rural communities, according to Lewis McCurdy, MD.
Dr. McCurdy of Carolinas HealthCare System in Charlotte, N.C., shared his experience providing virtual consultations for inpatients at a rural community hospital, noting that the approach was well received by patients, and that uptake by providers doubled during the first year.
Further, the virtual consultations appeared to have important clinical benefits, because very few patients had to be transferred to higher-level acuity facilities. The consultations seemed to help providers with challenging situations that they might not have felt comfortable managing otherwise, such as bloodstream infections, he said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
In a video interview, Dr. McCurdy discussed the development of the process for using telemedicine for inpatient consultations, outcomes after about 18 months at one facility, and challenges of providing telemedicine services.
The approach could be very helpful for smaller communities without an infectious disease provider, Dr. McCurdy said.
“This allows us to sort of expand our expertise into those communities on a more efficiently scaled basis,” he explained. “So, it does provide one solution to trying to meet the demand in the community for ID expertise.”
Dr. McCurdy reported having no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – Telemedicine inpatient consultations are a relatively new component in health care, but they could help address the problem of infectious disease physician shortages, particularly in rural communities, according to Lewis McCurdy, MD.
Dr. McCurdy of Carolinas HealthCare System in Charlotte, N.C., shared his experience providing virtual consultations for inpatients at a rural community hospital, noting that the approach was well received by patients, and that uptake by providers doubled during the first year.
Further, the virtual consultations appeared to have important clinical benefits, because very few patients had to be transferred to higher-level acuity facilities. The consultations seemed to help providers with challenging situations that they might not have felt comfortable managing otherwise, such as bloodstream infections, he said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
In a video interview, Dr. McCurdy discussed the development of the process for using telemedicine for inpatient consultations, outcomes after about 18 months at one facility, and challenges of providing telemedicine services.
The approach could be very helpful for smaller communities without an infectious disease provider, Dr. McCurdy said.
“This allows us to sort of expand our expertise into those communities on a more efficiently scaled basis,” he explained. “So, it does provide one solution to trying to meet the demand in the community for ID expertise.”
Dr. McCurdy reported having no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – Telemedicine inpatient consultations are a relatively new component in health care, but they could help address the problem of infectious disease physician shortages, particularly in rural communities, according to Lewis McCurdy, MD.
Dr. McCurdy of Carolinas HealthCare System in Charlotte, N.C., shared his experience providing virtual consultations for inpatients at a rural community hospital, noting that the approach was well received by patients, and that uptake by providers doubled during the first year.
Further, the virtual consultations appeared to have important clinical benefits, because very few patients had to be transferred to higher-level acuity facilities. The consultations seemed to help providers with challenging situations that they might not have felt comfortable managing otherwise, such as bloodstream infections, he said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
In a video interview, Dr. McCurdy discussed the development of the process for using telemedicine for inpatient consultations, outcomes after about 18 months at one facility, and challenges of providing telemedicine services.
The approach could be very helpful for smaller communities without an infectious disease provider, Dr. McCurdy said.
“This allows us to sort of expand our expertise into those communities on a more efficiently scaled basis,” he explained. “So, it does provide one solution to trying to meet the demand in the community for ID expertise.”
Dr. McCurdy reported having no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
‘Fight the Resistance’ with Antibiotic Stewardship Mentored Implementation
In conjunction with the Centers for Disease Control & Prevention’s Get Smart about Antibiotics Week, SHM is committed to promoting improved antibiotic-prescribing behaviors among the nation’s hospitalists through its “Fight the Resistance” awareness campaign.
Display SHM’s three downloadable “Fight the Resistance” posters, available at www.fighttheresistance.org. Hang them in your break rooms, hallways, or other high-profile locations to help remind your colleagues about the dangers of antibiotic resistance. SHM will be launching a mentored implementation program on antibiotics in early 2017. To be notified when the program becomes available, visit www.hospitalmedicine.org/ABX16.
In conjunction with the Centers for Disease Control & Prevention’s Get Smart about Antibiotics Week, SHM is committed to promoting improved antibiotic-prescribing behaviors among the nation’s hospitalists through its “Fight the Resistance” awareness campaign.
Display SHM’s three downloadable “Fight the Resistance” posters, available at www.fighttheresistance.org. Hang them in your break rooms, hallways, or other high-profile locations to help remind your colleagues about the dangers of antibiotic resistance. SHM will be launching a mentored implementation program on antibiotics in early 2017. To be notified when the program becomes available, visit www.hospitalmedicine.org/ABX16.
In conjunction with the Centers for Disease Control & Prevention’s Get Smart about Antibiotics Week, SHM is committed to promoting improved antibiotic-prescribing behaviors among the nation’s hospitalists through its “Fight the Resistance” awareness campaign.
Display SHM’s three downloadable “Fight the Resistance” posters, available at www.fighttheresistance.org. Hang them in your break rooms, hallways, or other high-profile locations to help remind your colleagues about the dangers of antibiotic resistance. SHM will be launching a mentored implementation program on antibiotics in early 2017. To be notified when the program becomes available, visit www.hospitalmedicine.org/ABX16.
Track Your Hospital’s Glycemic Control Performance
There is no better time than American Diabetes Month to learn more about SHM’s Glycemic Control Program. Find out how your institution can submit point-of-care data to SHM’s Data Center, generate monthly reports, and be included in the national glucometrics benchmark report. Hospital systems are also encouraged to subscribe in order to track their individual performance as well as compare overall performance.
View a recent case study on three sites that demonstrated more rapid definitive improvements in measurable outcomes with the mentoring program, driving change through ongoing objective support, data collection, and analysis. Don’t wait: Be one of the 100 hospitals nationwide supported by SHM’s respected Glycemic Control Program. Learn more at www.hospitalmedicine.org/gc.
There is no better time than American Diabetes Month to learn more about SHM’s Glycemic Control Program. Find out how your institution can submit point-of-care data to SHM’s Data Center, generate monthly reports, and be included in the national glucometrics benchmark report. Hospital systems are also encouraged to subscribe in order to track their individual performance as well as compare overall performance.
View a recent case study on three sites that demonstrated more rapid definitive improvements in measurable outcomes with the mentoring program, driving change through ongoing objective support, data collection, and analysis. Don’t wait: Be one of the 100 hospitals nationwide supported by SHM’s respected Glycemic Control Program. Learn more at www.hospitalmedicine.org/gc.
There is no better time than American Diabetes Month to learn more about SHM’s Glycemic Control Program. Find out how your institution can submit point-of-care data to SHM’s Data Center, generate monthly reports, and be included in the national glucometrics benchmark report. Hospital systems are also encouraged to subscribe in order to track their individual performance as well as compare overall performance.
View a recent case study on three sites that demonstrated more rapid definitive improvements in measurable outcomes with the mentoring program, driving change through ongoing objective support, data collection, and analysis. Don’t wait: Be one of the 100 hospitals nationwide supported by SHM’s respected Glycemic Control Program. Learn more at www.hospitalmedicine.org/gc.
Become an SHM Ambassador for a Chance at Free Registration to HM17
Now through December 31, 2016, all active SHM members can earn 2017–2018 dues credits and special recognition for recruiting new physician, physician assistant, nurse practitioner, pharmacist, or affiliate members. Active members will be eligible for:
- A $35 credit toward 2017–2018 dues when recruiting 1 new member.
- A $50 credit toward 2017–2018 dues when recruiting 2–4 new members.
- A $75 credit toward 2017–2018 dues when recruiting 5–9 new members.
- A $125 credit toward 2017–2018 dues when recruiting 10+ new members.
For each member recruited, referrers will receive one entry into a grand-prize drawing to receive complimentary registration to Hospital Medicine 2017 in Las Vegas.
Now through December 31, 2016, all active SHM members can earn 2017–2018 dues credits and special recognition for recruiting new physician, physician assistant, nurse practitioner, pharmacist, or affiliate members. Active members will be eligible for:
- A $35 credit toward 2017–2018 dues when recruiting 1 new member.
- A $50 credit toward 2017–2018 dues when recruiting 2–4 new members.
- A $75 credit toward 2017–2018 dues when recruiting 5–9 new members.
- A $125 credit toward 2017–2018 dues when recruiting 10+ new members.
For each member recruited, referrers will receive one entry into a grand-prize drawing to receive complimentary registration to Hospital Medicine 2017 in Las Vegas.
Now through December 31, 2016, all active SHM members can earn 2017–2018 dues credits and special recognition for recruiting new physician, physician assistant, nurse practitioner, pharmacist, or affiliate members. Active members will be eligible for:
- A $35 credit toward 2017–2018 dues when recruiting 1 new member.
- A $50 credit toward 2017–2018 dues when recruiting 2–4 new members.
- A $75 credit toward 2017–2018 dues when recruiting 5–9 new members.
- A $125 credit toward 2017–2018 dues when recruiting 10+ new members.
For each member recruited, referrers will receive one entry into a grand-prize drawing to receive complimentary registration to Hospital Medicine 2017 in Las Vegas.