User login
Simulation Training, Coaching, and Cue Cards Improve Delirium Care
Many clinicians continue to think that delirium or acute confusion is inevitable, untreatable, and harmless. However, nothing could be further from the truth.1 Delirium is a common and costly clinical syndrome that plagues a large percentage of older adults in a variety of settings. Numerous clinical studies conducted over the past 20 years have validated a high incidence of delirium in acute care hospitals.2-5 Reported rates of delirium among veteran and nonveteran populations vary widely, from 20% to 80%, but even these rates may reflect underrecognition and underreporting.6
Veterans with delirium pose a unique challenge to clinicians and health care systems because they often concurrently experience dementia, depression, posttraumatic stress disorder, and delirium. This complex syndrome caused by a myriad of environmental, physiologic, and psychological factors has been associated with profoundly poor clinical outcomes, including increased institutionalization, hospital length of stay, medication use, restraint use, falls, and mortality.3,7,8
Financial costs associated with delirium have been estimated at between $38 billion and $152 billion per year.9 In addition, this syndrome is costly in human resource expenditures, including increased burden on family members and the need for additional care providers, such as “sitters.” Families and clinicians report increased burden and stress in their interactions with these patients.10-12 Mounting evidence exists that some people with delirium never return to baseline cognitive function after even a single episode of delirium.1,8 Unfortunately, many clinicians do not recognize the seriousness of acute confusion.
Clinical practices related to routine screening for delirium vary widely. Although the Confusion Assessment Method (CAM) screening tool has high sensitivity and specificity, only 17% of hospitals consistently use this tool in clinical practice.2,6,13,14 According to a survey by Ely and colleagues, physicians reported being aware of delirium but inconsistently applying treatment protocols in clinical practice.2 Nurses noted similar difficulties in consistently screening patients and using delirium management protocols.15 Given the high incidence of delirium and its associated morbidity, including long-term cognitive impairment and human and financial costs, there is an urgent need to implement programs that enhance delirium prevention, timely recognition, and effective management to improve patient outcomes and address caregiver burden.
Over the past decade, educational strategies for improving delirium prevention, recognition, and management have included didactic education, consultation, and use of protocols.2,3,5,16 Bedside mentoring, implementation of protocols, and other interventions have been proposed as well.16,17 Several program models, including consultation by psychiatrists or psychiatric advanced practice nurses, have been implemented to increase detection and treatment of delirium.2,3,5,15 These pilot programs have been successful to varying degrees but in general have not shown independent effects beyond intervention or significantly increased recognition and management of adverse consequences for most patients. The cause of these outcomes seem to be multifactorial, but the complexity of the syndrome is part of the problem.18-20
Other possible barriers to change regarding delirium-related issues in clinical practice are lack of knowledge and skills and individual attitudes.20-22 Continuing evidence exists that clinicians feel ill-prepared to help delirious patients and frustrated enough to resort to using restraints and medication as first-line treatment.17 Yanamadala and colleagues reviewed 26 studies that identified strategies for delirium education.23 Most of the studies reported on didactic teaching methods that included information on resources. Only 1 study with nursing students reported using actors for simulation training. The programs most successful in improving knowledge, skills, attitudes, practice changes, and patient outcomes seemed to be those that used multiple educational methods, including information dissemination, use of guidelines and protocols, and peer and expert feedback.
This finding is consistent with the report that didactic learning alone, though improving competency, is less likely to change behavior or improve outcomes.24 A constellation of didactic education, mentoring, use of protocols to target high-risk patients, and a therapeutic environment has helped to reduce delirium incidence.4,25,26 Rudolph and colleagues found an association between multimodal education (risk assessment, sensory improvement, sleep promotion) and shorter hospital stays and less use of restraints.27 In clinical practice,however, implementation of evidence-based nonpharmacologic interventions, such as enhanced communication, mobility, nutrition, and meaningful activities, continues to lag despite education.28,29
Multimodal Education
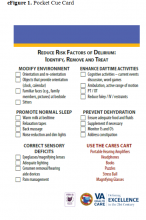
To address these gaps in knowledge and skills, a multidisciplinary delirium resource team at the Louis Stokes Cleveland VAMC in Ohio developed a multimodal educational program incorporating simulation. The team of physicians, nurses, care coordinators, and social workers met regularly and developed interventions, educational materials, cue cards (eFigure 1), sense-enhancing aids (hearing amplifiers, puzzles, books, music CDs, prism glasses), clinical protocols, and delirium resources, such as CARES (Confusion Assessment Resource Enhancement Supplies) activity carts.
The CARES carts are small, rolling wooden carts stocked with various resources that focus on comfort and entertainment. The carts hold guided imagery CDs and Playaways (small audio players that come with ear buds for individual use and preloaded with a specific guided imagery session). The carts also hold books, books on tape, magazines, portable CD players, music CDs, games, exercise bands, healthful snacks, DVDs, and a portable DVD player.
Bedside mentoring continued throughout this quality improvement (QI) project, and a CARES teaching tool kit was developed. This kit, which continues to be used, includes videos and webinars for professionals and family caregivers; delirium pocket cue cards for physicians, nurses, aides, and sitters; a list of patient diversion supplies; and a family brochure. Delirium resource team members continue to provide the health care team with education and support. Given the emphasis on clinicians and patient outcomes in intensive care units (ICUs), the teaching tool kit is a valuable guide for assessing and treating patients with delirium during rounds and consultations.
Simulation
Using a simulation center and standardized patients (SPs), teams of interdisciplinary care providers practiced communication techniques and recommended treatment strategies with the help of a delirium coach. Sessions were videotaped. This intervention, which used simulation training, was supported by VA grant T-21, to reduce institutionalization and promote patient-centered care.
In a clinical context, simulation involves activities that mimick the reality of the clinical environment, including physical symptoms, communication patterns, and critical decision making. Trained SPs have the unique advantage of providing interactive practice and immediate feedback in a safe, controlled setting.30
Standardized patient programs provide learners with real-life interactions for the development and practice of interpersonal communication and clinical skills. In a laboratory setting, SP programs use role-play scenarios that allow learners to practice complex assessment and communication skills. Standardized patients are effective in teaching clinical, interviewing, and communication skills to learners from a variety of disciplines, including medicine, nursing, dental, and law.31 Standardized patients also provide a safe, supportive environment conducive to learning and standardized assessment.
Standardized patients can serve as practice models and participate in sophisticated assessment and feedback of learners’ abilities and services. Interacting with SPs gives learners a chance to practice clinical and interpersonal skills with an emphasis on communication before meeting actual patients. After interacting with an SP, a learner receives feedback from a preceptor and/or the learner’s peers. The SP also may be asked to provide brief feedback—a component of the SP training process. Allowing time for feedback is an integral part of student learning.
For this QI project, the delirium team used the Mt. Sinai Skills and Simulation Center at Case Western Reserve University School of Medicine. The facility focuses on creative, innovative continuing learning for health care providers at all levels and is certified by the American College of Surgeons as a level 1 Comprehensive Accredited Education Institute.
After a literature review and several brainstorming sessions, the delirium team tailored case studies to veterans to simulate the intervention and train SPs for the delirium program. During training, SPs reviewed scenarios, engaged in practice sessions, and answered questions. Several SPs were familiar with the behavior of delirious patients from personal experience.
The goals of the program were to increase knowledge of delirium signs and symptoms as a medical condition that requires immediate attention; increase competency in administering CAM and in documenting its results; increase interdisciplinary communication; and increase knowledge using nonpharmacologic interventions for sensory enhancement and agitation. Enhanced interdisciplinary communication was accomplished during the simulation by assigning individuals from different disciplines to work in teams. To maximize the use of resources and limit participants’ time away from the clinical area, the administration planned and supported a daylong program that included didactic education, videos, group work sessions, and the simulation sessions with resource team members as coaches.
Methods
All participants attended an hour-long introductory didactic lecture together. Then, they were randomly assigned to 1 of 4 remaining 45-minute training sessions. Each participant attended a session that combined a video and a case study; a session of role-playing with group discussion; and 2 simulation scenario sessions. Concurrent training sessions were needed to facilitate having all 100 attendees participate within 6 hours. Attendees were multidisciplinary providers from various non-ICU medical/surgical units and outpatient geriatric clinics. They rotated among sessions to accommodate all participants.
For the simulation scenarios, 8 simulation rooms were used over 2 periods—for 16 simulation sessions total. Participants were randomly assigned to multidisciplinary groups that worked in teams to assess and recommend care and treatments for SPs who were stimulating delirium. During the simulation, delirium coaches used cue cards and verbal hints to direct teams (Simulation Exercise). After the session, participants received verbal and
Outcomes
The impact of this multimodal intervention was measured in a variety of ways—with preintervention and postintervention knowledge tests, postsimulation surveys, program surveys, and patient chart reviews. Simulation sessions had 100 attendees, including mentors (interdisciplinary resource team), champions, and nursing staff from various hospital units. Champions represented multiple disciplines and had varying levels of experience. Most of the participants were nurses (62%), followed by social workers (12%), nursing assistants (12%), psychologists (6%), and others (11%). Participants’ years of experience were < 1 year (6%), 1 to 5 years (21%), 6 to 10 years (21%), and > 10 years (52%).
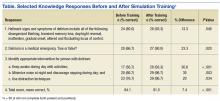
Mean knowledge survey score was 84% before training and 92% after training. Recognition of delirium as a medical emergency requiring immediate follow-up was increased (P = .02), as was knowledge about delirium management, as in increasing daytime activities (P < .001) and using distraction techniques (P = .03) (Table).
More than 94% of participants said the simulation training fulfilled their education needs. More than 80% reported using the information from the delirium workshop in their practice. In reviewing the techniques presented during the workshop, participants reported that they would approach situations differently from before the workshop by using more nonpharmacologic interventions (40%), enhanced communication (24%), and more in-depth assessment for medical causes of delirium (19%). Thirteen percent said they would not change their approach.
Thirty-five percent of respondents had positive feelings after the simulation exercise, 40% had cared for patients in similar situations, and 35% knew delirium care should start with assessment for medical causes.
The team reviewed patient charts for documentation of confusion assessment (signs and symptoms of confusion), including the standardized CAM method and nonpharmacologic interventions. Random monthly audits, 1 month before training and 5 months after, indicated an increase in confusion assessment and documentation. For veterans with delirium, nonpharmacologic interventions increased from 9% at baseline to 53% at the 5-month audit. Hospital length of stay, however, trended toward a slight increase in number of days. These findings are consistent with those reported by Rudolph and colleagues, who also piloted multimodal education and sensory enhancement.27
Discussion
Delirium assessment and management are complex skills that require well-coordinated interdisciplinary care and significant administrative support. Clinicians are becoming increasingly aware of the mounting evidence that patients with delirium feel immediate and often long-term negative effects. Strategies that support clinicians and enhance clinical care must include multimodal education and support.
In this QI project, participants supported use of simulation education, bedside coaching, and pocket cue cards to enhance delirium caregiving knowledge and skills. The majority of participants indicated that, though the simulation sessions were challenging, they also were realistic and helpful. Standardized patients provided feedback and often advised teams of needed improvement, such as spending more time in helping patients feel safe and comfortable. Coaches noted that many team members collaborated with one another but often neglected to use the pocket cue cards, family brochures, and other resources in the room. The reason is not clear. Perhaps the novelty of the resources and potential participant anxiety during the simulation were contributing factors. In future sessions, coaches must address making use of available resources.
Chart reviews indicated that nonpharmacologic management of delirium increased to 53% from < 10%. The increased use of resources in caring for patients with delirium was confirmed by the need to restock the CARES activity carts with patient diversion supplies. Given the success of this first program, another ICU education and simulation program was initiated. Findings from this QI project support using multimodal education that incorporates simulation training, bedside coaching, and pocket cue cards to enhance clinical practices for care of patients with delirium.33
Methods facilitated team collaboration, patient family communication, and synthesis of much information over a relatively short period. Didactic education alone may be insufficient to adequately enhance clinical care for delirium. The impact of a multimodal strategy—including a delirium resource consultation team that provided bedside mentoring, encouraged use of pocket cue cards, and supported evidence-based nonpharmacologic interventions—cannot be underestimated. In addition, simulation education also provided a unique opportunity for the health care teams to “practice” assessment, communication, and collaboration skills in a supportive setting with real-time feedback. These resources are being disseminated throughout the Louis Stokes Cleveland VAMC. Plans to disseminate this information to a broader national audience are under way.
Although not all facilities can access the simulation laboratory, many may be able to implement use of videos, case studies, and role-playing to enhance didactic education, to improve outcomes for patients with delirium. Enhanced clinical management of complex syndromes such as delirium may be influenced most by a combination of education, practice, and mentoring methods. Use of simulation as an adjunct teaching method is a promising strategy that may enhance care of patients with delirium. This QI project demonstrated positive educational and clinical trends in a VA setting. More studies, including randomized clinical trials, are needed in a variety of settings to further test these strategies.
Acknowledgments
The authors give special thanks to Brigid Wilson, PhD, Heather O’Leary, RN, and Patrick Kilroy, SN, for their assistance in this project. The project was developed by the Cleveland VAMC interdisciplinary delirium resource team with support of a VA T-21 grant and the VISN 10 Geriatric Research Education and Clinical Centers.
1. ICU Delirium and Cognitive Impairment Study Group, Center for Health Services Research, Vanderbilt University Medical Center. Delirium prevention and safety: starting with the ABCDEF’s. http://www.icudelirium.org/medicalprofessionals .html. Accessed November 9, 2016.
2. Ely EW, Siegel MD, Inouye SK. Delirium in the intensive care unit: an under-recognized syndrome of organ dysfunction. Semin Respir Crit Care Med. 2001;22(2):115-126.
3. Inouye SK, Bogardus ST Jr, Vitagliano G, et al. Burden of illness score for elderly persons: risk adjustment incorporating the cumulative impact of diseases, physiologic abnormalities, and functional impairments. Med Care. 2003;41(1):70-83.
4. Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49(5):516-522.
5. Foreman MD, Wakefield B, Culp K, Milisen K. Delirium in elderly patients: an overview of the state of the science. J Gerontol Nurs. 2001;27(4):12-20.
6. Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941-948.
7. Maldonado JR. Pathoetiological model of delirium: a comprehensive understanding of the neurobiology of delirium and an evidence-based approach to prevention and treatment. Crit Care Clin. 2008;24(4):789-856.
8. Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, van Gool WA. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA. 2010;304(4):443-451.
9. Leslie DL, Marcantonio ER, Zhang Y, Leo-Summers L, Inouye SK. One-year health care costs associated with delirium in the elderly population. Arch Intern Med. 2008;168(1):27-32.
10. Bruera E, Bush SH, Willey J, et al. Impact of delirium and recall on the level of distress in patients with advanced cancer and their family caregivers. Cancer. 2009;115(9):2004-2012.
11. Cohen MZ, Pace EA, Kaur G, Bruera E. Delirium in advanced cancer leading to distress in patients and family caregivers. J Palliat Care. 2009;25(3):164-171.
12. Patel RP, Gambrell M, Speroff T, et al. Delirium and sedation in the intensive care unit: survey of behaviors and attitudes of 1384 healthcare professionals. Crit Care Med. 2009;37(3):825-832.
13. Wei LA, Fearing MA, Sternberg EJ, Inouye SK. The confusion assessment method: a systematic review of current usage. J Am Geriatr Soc. 2008;56(5):823-830.
14. Neuman MD, Speck RM, Karlawish JH, Schwartz JS, Shea JA. Hospital protocols for the inpatient care of older adults: results from a statewide survey. J Am Geriatr Soc. 2010;58(10):1959-1964.
15. Idemoto BK. The assessment of delirium and depression in the intensive care unit [doctoral dissertation]. Cleveland, OH: Case Western Reserve University; 2005. No. 137.
16. Balas MC, Vasilevskis EE, Burke WJ, et al. Critical care nurses’ role in implementing the “ABCDE bundle” into practice. Crit Care Nurse. 2012;32(2):35-38, 40-47.
17. Barr J, Fraser GL, Puntillo K, et al; American College of Critical Care Medicine. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit: executive summary. Am J Health Syst Pharm. 2013;70(1):53-58.
18. Pun BT, Ely EW. The importance of diagnosing and managing ICU delirium. Chest. 2007;132(2):624-636.
19. Pisani MA, Araujo KL, Van Ness PH, Zhang Y, Ely EW, Inouye SK. A research algorithm to improve detection of delirium in the intensive care unit. Crit Care. 2006;10(4):R121.
20. Voyer P, Cole MG, McCusker J, St-Jacques S, Laplante J. Accuracy of nurse documentation of delirium symptoms in medical charts. Int J Nurs Pract. 2008;14(2):165-167.
21. Pandharipande P, Cotton BA, Shintani A, et al. Prevalence and risk factors for development of delirium in surgical and trauma intensive care unit patients. J Trauma. 2008;65(1):34-41.
22. Steis MR, Fick DM. Are nurses recognizing delirium? A systematic review. J Gerontol Nurs. 2008;34(9):40-48.
23. Yanamadala M, Wieland D, Heflin MT. Educational interventions to improve recognition of delirium: a systematic review. J Am Geriatr Soc. 2013;61(11):1983-1993.
24. Ramaswamy R, Dix EF, Drew JE, Diamond JJ, Inouye SK, Roehl BJ. Beyond grand rounds: a comprehensive and sequential intervention to improve identification of delirium. Gerontologist. 2011;51(1):122-131.
25. Lundström M, Olofsson B, Stenvall M, et al. Postoperative delirium in old patients with femoral neck fracture: a randomized intervention study. Aging Clin Exp Res. 2007;19(3):178-186.
26. Inouye SK. Predisposing and precipitating factors for delirium in hospitalized older patients. Dement Geriatr Cogn Disord. 1999;10(5):393-400.
27. Rudolph JL, Archambault E, Kelly B; VA Boston Delirium Task Force. A delirium risk modification program is associated with hospital outcomes. J Am Med Dir Assoc. 2014;15(12):957.e7-e11.
28. Hartford Institute for Geriatric Nursing. http://hartfordign.org. Accessed November 9, 2016.
29. Inouye SK. A practical program for preventing delirium in hospitalized elderly patients. Cleve Clin J Med. 2004;71(11):890-896.
30. Raurell-Torredà M, Olivet-Pujol J, Romero-Collado À, Malagon-Aguilera MC, Patiño-Masó J, Baltasar-Bagué A. Case-based learning and simulation: useful tools to enhance nurses’ education? Nonrandomized controlled trial. J Nurs Scholarsh. 2015;47(1):34-42.
31. Mast TA, Coulson LR, Meyer TC, et al. Self directed learning: wisdom from independent study programs. Res Med Educ. 1985;24:305-311.
32. Massachusetts Department of Higher Education Nursing Initiative—Simulation Scenario Library. http://www.mass.edu/nahi/Sim/Welcome.asp. Accessed November 1, 2016.
33. Vancouver Island Health Authority. Delirium in the older person: a medical emergency. Pre-Post Test. http://www.viha.ca/NR/rdonlyres/03D50FE6-AF90 -4F98-8B3B-7AE87A4B481D/0/preposttest.pdf. Reviewed August 2014. Accessed November 9, 2016.
Many clinicians continue to think that delirium or acute confusion is inevitable, untreatable, and harmless. However, nothing could be further from the truth.1 Delirium is a common and costly clinical syndrome that plagues a large percentage of older adults in a variety of settings. Numerous clinical studies conducted over the past 20 years have validated a high incidence of delirium in acute care hospitals.2-5 Reported rates of delirium among veteran and nonveteran populations vary widely, from 20% to 80%, but even these rates may reflect underrecognition and underreporting.6
Veterans with delirium pose a unique challenge to clinicians and health care systems because they often concurrently experience dementia, depression, posttraumatic stress disorder, and delirium. This complex syndrome caused by a myriad of environmental, physiologic, and psychological factors has been associated with profoundly poor clinical outcomes, including increased institutionalization, hospital length of stay, medication use, restraint use, falls, and mortality.3,7,8
Financial costs associated with delirium have been estimated at between $38 billion and $152 billion per year.9 In addition, this syndrome is costly in human resource expenditures, including increased burden on family members and the need for additional care providers, such as “sitters.” Families and clinicians report increased burden and stress in their interactions with these patients.10-12 Mounting evidence exists that some people with delirium never return to baseline cognitive function after even a single episode of delirium.1,8 Unfortunately, many clinicians do not recognize the seriousness of acute confusion.
Clinical practices related to routine screening for delirium vary widely. Although the Confusion Assessment Method (CAM) screening tool has high sensitivity and specificity, only 17% of hospitals consistently use this tool in clinical practice.2,6,13,14 According to a survey by Ely and colleagues, physicians reported being aware of delirium but inconsistently applying treatment protocols in clinical practice.2 Nurses noted similar difficulties in consistently screening patients and using delirium management protocols.15 Given the high incidence of delirium and its associated morbidity, including long-term cognitive impairment and human and financial costs, there is an urgent need to implement programs that enhance delirium prevention, timely recognition, and effective management to improve patient outcomes and address caregiver burden.
Over the past decade, educational strategies for improving delirium prevention, recognition, and management have included didactic education, consultation, and use of protocols.2,3,5,16 Bedside mentoring, implementation of protocols, and other interventions have been proposed as well.16,17 Several program models, including consultation by psychiatrists or psychiatric advanced practice nurses, have been implemented to increase detection and treatment of delirium.2,3,5,15 These pilot programs have been successful to varying degrees but in general have not shown independent effects beyond intervention or significantly increased recognition and management of adverse consequences for most patients. The cause of these outcomes seem to be multifactorial, but the complexity of the syndrome is part of the problem.18-20
Other possible barriers to change regarding delirium-related issues in clinical practice are lack of knowledge and skills and individual attitudes.20-22 Continuing evidence exists that clinicians feel ill-prepared to help delirious patients and frustrated enough to resort to using restraints and medication as first-line treatment.17 Yanamadala and colleagues reviewed 26 studies that identified strategies for delirium education.23 Most of the studies reported on didactic teaching methods that included information on resources. Only 1 study with nursing students reported using actors for simulation training. The programs most successful in improving knowledge, skills, attitudes, practice changes, and patient outcomes seemed to be those that used multiple educational methods, including information dissemination, use of guidelines and protocols, and peer and expert feedback.
This finding is consistent with the report that didactic learning alone, though improving competency, is less likely to change behavior or improve outcomes.24 A constellation of didactic education, mentoring, use of protocols to target high-risk patients, and a therapeutic environment has helped to reduce delirium incidence.4,25,26 Rudolph and colleagues found an association between multimodal education (risk assessment, sensory improvement, sleep promotion) and shorter hospital stays and less use of restraints.27 In clinical practice,however, implementation of evidence-based nonpharmacologic interventions, such as enhanced communication, mobility, nutrition, and meaningful activities, continues to lag despite education.28,29
Multimodal Education
To address these gaps in knowledge and skills, a multidisciplinary delirium resource team at the Louis Stokes Cleveland VAMC in Ohio developed a multimodal educational program incorporating simulation. The team of physicians, nurses, care coordinators, and social workers met regularly and developed interventions, educational materials, cue cards (eFigure 1), sense-enhancing aids (hearing amplifiers, puzzles, books, music CDs, prism glasses), clinical protocols, and delirium resources, such as CARES (Confusion Assessment Resource Enhancement Supplies) activity carts.
The CARES carts are small, rolling wooden carts stocked with various resources that focus on comfort and entertainment. The carts hold guided imagery CDs and Playaways (small audio players that come with ear buds for individual use and preloaded with a specific guided imagery session). The carts also hold books, books on tape, magazines, portable CD players, music CDs, games, exercise bands, healthful snacks, DVDs, and a portable DVD player.
Bedside mentoring continued throughout this quality improvement (QI) project, and a CARES teaching tool kit was developed. This kit, which continues to be used, includes videos and webinars for professionals and family caregivers; delirium pocket cue cards for physicians, nurses, aides, and sitters; a list of patient diversion supplies; and a family brochure. Delirium resource team members continue to provide the health care team with education and support. Given the emphasis on clinicians and patient outcomes in intensive care units (ICUs), the teaching tool kit is a valuable guide for assessing and treating patients with delirium during rounds and consultations.
Simulation
Using a simulation center and standardized patients (SPs), teams of interdisciplinary care providers practiced communication techniques and recommended treatment strategies with the help of a delirium coach. Sessions were videotaped. This intervention, which used simulation training, was supported by VA grant T-21, to reduce institutionalization and promote patient-centered care.
In a clinical context, simulation involves activities that mimick the reality of the clinical environment, including physical symptoms, communication patterns, and critical decision making. Trained SPs have the unique advantage of providing interactive practice and immediate feedback in a safe, controlled setting.30
Standardized patient programs provide learners with real-life interactions for the development and practice of interpersonal communication and clinical skills. In a laboratory setting, SP programs use role-play scenarios that allow learners to practice complex assessment and communication skills. Standardized patients are effective in teaching clinical, interviewing, and communication skills to learners from a variety of disciplines, including medicine, nursing, dental, and law.31 Standardized patients also provide a safe, supportive environment conducive to learning and standardized assessment.
Standardized patients can serve as practice models and participate in sophisticated assessment and feedback of learners’ abilities and services. Interacting with SPs gives learners a chance to practice clinical and interpersonal skills with an emphasis on communication before meeting actual patients. After interacting with an SP, a learner receives feedback from a preceptor and/or the learner’s peers. The SP also may be asked to provide brief feedback—a component of the SP training process. Allowing time for feedback is an integral part of student learning.
For this QI project, the delirium team used the Mt. Sinai Skills and Simulation Center at Case Western Reserve University School of Medicine. The facility focuses on creative, innovative continuing learning for health care providers at all levels and is certified by the American College of Surgeons as a level 1 Comprehensive Accredited Education Institute.
After a literature review and several brainstorming sessions, the delirium team tailored case studies to veterans to simulate the intervention and train SPs for the delirium program. During training, SPs reviewed scenarios, engaged in practice sessions, and answered questions. Several SPs were familiar with the behavior of delirious patients from personal experience.
The goals of the program were to increase knowledge of delirium signs and symptoms as a medical condition that requires immediate attention; increase competency in administering CAM and in documenting its results; increase interdisciplinary communication; and increase knowledge using nonpharmacologic interventions for sensory enhancement and agitation. Enhanced interdisciplinary communication was accomplished during the simulation by assigning individuals from different disciplines to work in teams. To maximize the use of resources and limit participants’ time away from the clinical area, the administration planned and supported a daylong program that included didactic education, videos, group work sessions, and the simulation sessions with resource team members as coaches.
Methods
All participants attended an hour-long introductory didactic lecture together. Then, they were randomly assigned to 1 of 4 remaining 45-minute training sessions. Each participant attended a session that combined a video and a case study; a session of role-playing with group discussion; and 2 simulation scenario sessions. Concurrent training sessions were needed to facilitate having all 100 attendees participate within 6 hours. Attendees were multidisciplinary providers from various non-ICU medical/surgical units and outpatient geriatric clinics. They rotated among sessions to accommodate all participants.
For the simulation scenarios, 8 simulation rooms were used over 2 periods—for 16 simulation sessions total. Participants were randomly assigned to multidisciplinary groups that worked in teams to assess and recommend care and treatments for SPs who were stimulating delirium. During the simulation, delirium coaches used cue cards and verbal hints to direct teams (Simulation Exercise). After the session, participants received verbal and
Outcomes
The impact of this multimodal intervention was measured in a variety of ways—with preintervention and postintervention knowledge tests, postsimulation surveys, program surveys, and patient chart reviews. Simulation sessions had 100 attendees, including mentors (interdisciplinary resource team), champions, and nursing staff from various hospital units. Champions represented multiple disciplines and had varying levels of experience. Most of the participants were nurses (62%), followed by social workers (12%), nursing assistants (12%), psychologists (6%), and others (11%). Participants’ years of experience were < 1 year (6%), 1 to 5 years (21%), 6 to 10 years (21%), and > 10 years (52%).
Mean knowledge survey score was 84% before training and 92% after training. Recognition of delirium as a medical emergency requiring immediate follow-up was increased (P = .02), as was knowledge about delirium management, as in increasing daytime activities (P < .001) and using distraction techniques (P = .03) (Table).
More than 94% of participants said the simulation training fulfilled their education needs. More than 80% reported using the information from the delirium workshop in their practice. In reviewing the techniques presented during the workshop, participants reported that they would approach situations differently from before the workshop by using more nonpharmacologic interventions (40%), enhanced communication (24%), and more in-depth assessment for medical causes of delirium (19%). Thirteen percent said they would not change their approach.
Thirty-five percent of respondents had positive feelings after the simulation exercise, 40% had cared for patients in similar situations, and 35% knew delirium care should start with assessment for medical causes.
The team reviewed patient charts for documentation of confusion assessment (signs and symptoms of confusion), including the standardized CAM method and nonpharmacologic interventions. Random monthly audits, 1 month before training and 5 months after, indicated an increase in confusion assessment and documentation. For veterans with delirium, nonpharmacologic interventions increased from 9% at baseline to 53% at the 5-month audit. Hospital length of stay, however, trended toward a slight increase in number of days. These findings are consistent with those reported by Rudolph and colleagues, who also piloted multimodal education and sensory enhancement.27
Discussion
Delirium assessment and management are complex skills that require well-coordinated interdisciplinary care and significant administrative support. Clinicians are becoming increasingly aware of the mounting evidence that patients with delirium feel immediate and often long-term negative effects. Strategies that support clinicians and enhance clinical care must include multimodal education and support.
In this QI project, participants supported use of simulation education, bedside coaching, and pocket cue cards to enhance delirium caregiving knowledge and skills. The majority of participants indicated that, though the simulation sessions were challenging, they also were realistic and helpful. Standardized patients provided feedback and often advised teams of needed improvement, such as spending more time in helping patients feel safe and comfortable. Coaches noted that many team members collaborated with one another but often neglected to use the pocket cue cards, family brochures, and other resources in the room. The reason is not clear. Perhaps the novelty of the resources and potential participant anxiety during the simulation were contributing factors. In future sessions, coaches must address making use of available resources.
Chart reviews indicated that nonpharmacologic management of delirium increased to 53% from < 10%. The increased use of resources in caring for patients with delirium was confirmed by the need to restock the CARES activity carts with patient diversion supplies. Given the success of this first program, another ICU education and simulation program was initiated. Findings from this QI project support using multimodal education that incorporates simulation training, bedside coaching, and pocket cue cards to enhance clinical practices for care of patients with delirium.33
Methods facilitated team collaboration, patient family communication, and synthesis of much information over a relatively short period. Didactic education alone may be insufficient to adequately enhance clinical care for delirium. The impact of a multimodal strategy—including a delirium resource consultation team that provided bedside mentoring, encouraged use of pocket cue cards, and supported evidence-based nonpharmacologic interventions—cannot be underestimated. In addition, simulation education also provided a unique opportunity for the health care teams to “practice” assessment, communication, and collaboration skills in a supportive setting with real-time feedback. These resources are being disseminated throughout the Louis Stokes Cleveland VAMC. Plans to disseminate this information to a broader national audience are under way.
Although not all facilities can access the simulation laboratory, many may be able to implement use of videos, case studies, and role-playing to enhance didactic education, to improve outcomes for patients with delirium. Enhanced clinical management of complex syndromes such as delirium may be influenced most by a combination of education, practice, and mentoring methods. Use of simulation as an adjunct teaching method is a promising strategy that may enhance care of patients with delirium. This QI project demonstrated positive educational and clinical trends in a VA setting. More studies, including randomized clinical trials, are needed in a variety of settings to further test these strategies.
Acknowledgments
The authors give special thanks to Brigid Wilson, PhD, Heather O’Leary, RN, and Patrick Kilroy, SN, for their assistance in this project. The project was developed by the Cleveland VAMC interdisciplinary delirium resource team with support of a VA T-21 grant and the VISN 10 Geriatric Research Education and Clinical Centers.
Many clinicians continue to think that delirium or acute confusion is inevitable, untreatable, and harmless. However, nothing could be further from the truth.1 Delirium is a common and costly clinical syndrome that plagues a large percentage of older adults in a variety of settings. Numerous clinical studies conducted over the past 20 years have validated a high incidence of delirium in acute care hospitals.2-5 Reported rates of delirium among veteran and nonveteran populations vary widely, from 20% to 80%, but even these rates may reflect underrecognition and underreporting.6
Veterans with delirium pose a unique challenge to clinicians and health care systems because they often concurrently experience dementia, depression, posttraumatic stress disorder, and delirium. This complex syndrome caused by a myriad of environmental, physiologic, and psychological factors has been associated with profoundly poor clinical outcomes, including increased institutionalization, hospital length of stay, medication use, restraint use, falls, and mortality.3,7,8
Financial costs associated with delirium have been estimated at between $38 billion and $152 billion per year.9 In addition, this syndrome is costly in human resource expenditures, including increased burden on family members and the need for additional care providers, such as “sitters.” Families and clinicians report increased burden and stress in their interactions with these patients.10-12 Mounting evidence exists that some people with delirium never return to baseline cognitive function after even a single episode of delirium.1,8 Unfortunately, many clinicians do not recognize the seriousness of acute confusion.
Clinical practices related to routine screening for delirium vary widely. Although the Confusion Assessment Method (CAM) screening tool has high sensitivity and specificity, only 17% of hospitals consistently use this tool in clinical practice.2,6,13,14 According to a survey by Ely and colleagues, physicians reported being aware of delirium but inconsistently applying treatment protocols in clinical practice.2 Nurses noted similar difficulties in consistently screening patients and using delirium management protocols.15 Given the high incidence of delirium and its associated morbidity, including long-term cognitive impairment and human and financial costs, there is an urgent need to implement programs that enhance delirium prevention, timely recognition, and effective management to improve patient outcomes and address caregiver burden.
Over the past decade, educational strategies for improving delirium prevention, recognition, and management have included didactic education, consultation, and use of protocols.2,3,5,16 Bedside mentoring, implementation of protocols, and other interventions have been proposed as well.16,17 Several program models, including consultation by psychiatrists or psychiatric advanced practice nurses, have been implemented to increase detection and treatment of delirium.2,3,5,15 These pilot programs have been successful to varying degrees but in general have not shown independent effects beyond intervention or significantly increased recognition and management of adverse consequences for most patients. The cause of these outcomes seem to be multifactorial, but the complexity of the syndrome is part of the problem.18-20
Other possible barriers to change regarding delirium-related issues in clinical practice are lack of knowledge and skills and individual attitudes.20-22 Continuing evidence exists that clinicians feel ill-prepared to help delirious patients and frustrated enough to resort to using restraints and medication as first-line treatment.17 Yanamadala and colleagues reviewed 26 studies that identified strategies for delirium education.23 Most of the studies reported on didactic teaching methods that included information on resources. Only 1 study with nursing students reported using actors for simulation training. The programs most successful in improving knowledge, skills, attitudes, practice changes, and patient outcomes seemed to be those that used multiple educational methods, including information dissemination, use of guidelines and protocols, and peer and expert feedback.
This finding is consistent with the report that didactic learning alone, though improving competency, is less likely to change behavior or improve outcomes.24 A constellation of didactic education, mentoring, use of protocols to target high-risk patients, and a therapeutic environment has helped to reduce delirium incidence.4,25,26 Rudolph and colleagues found an association between multimodal education (risk assessment, sensory improvement, sleep promotion) and shorter hospital stays and less use of restraints.27 In clinical practice,however, implementation of evidence-based nonpharmacologic interventions, such as enhanced communication, mobility, nutrition, and meaningful activities, continues to lag despite education.28,29
Multimodal Education
To address these gaps in knowledge and skills, a multidisciplinary delirium resource team at the Louis Stokes Cleveland VAMC in Ohio developed a multimodal educational program incorporating simulation. The team of physicians, nurses, care coordinators, and social workers met regularly and developed interventions, educational materials, cue cards (eFigure 1), sense-enhancing aids (hearing amplifiers, puzzles, books, music CDs, prism glasses), clinical protocols, and delirium resources, such as CARES (Confusion Assessment Resource Enhancement Supplies) activity carts.
The CARES carts are small, rolling wooden carts stocked with various resources that focus on comfort and entertainment. The carts hold guided imagery CDs and Playaways (small audio players that come with ear buds for individual use and preloaded with a specific guided imagery session). The carts also hold books, books on tape, magazines, portable CD players, music CDs, games, exercise bands, healthful snacks, DVDs, and a portable DVD player.
Bedside mentoring continued throughout this quality improvement (QI) project, and a CARES teaching tool kit was developed. This kit, which continues to be used, includes videos and webinars for professionals and family caregivers; delirium pocket cue cards for physicians, nurses, aides, and sitters; a list of patient diversion supplies; and a family brochure. Delirium resource team members continue to provide the health care team with education and support. Given the emphasis on clinicians and patient outcomes in intensive care units (ICUs), the teaching tool kit is a valuable guide for assessing and treating patients with delirium during rounds and consultations.
Simulation
Using a simulation center and standardized patients (SPs), teams of interdisciplinary care providers practiced communication techniques and recommended treatment strategies with the help of a delirium coach. Sessions were videotaped. This intervention, which used simulation training, was supported by VA grant T-21, to reduce institutionalization and promote patient-centered care.
In a clinical context, simulation involves activities that mimick the reality of the clinical environment, including physical symptoms, communication patterns, and critical decision making. Trained SPs have the unique advantage of providing interactive practice and immediate feedback in a safe, controlled setting.30
Standardized patient programs provide learners with real-life interactions for the development and practice of interpersonal communication and clinical skills. In a laboratory setting, SP programs use role-play scenarios that allow learners to practice complex assessment and communication skills. Standardized patients are effective in teaching clinical, interviewing, and communication skills to learners from a variety of disciplines, including medicine, nursing, dental, and law.31 Standardized patients also provide a safe, supportive environment conducive to learning and standardized assessment.
Standardized patients can serve as practice models and participate in sophisticated assessment and feedback of learners’ abilities and services. Interacting with SPs gives learners a chance to practice clinical and interpersonal skills with an emphasis on communication before meeting actual patients. After interacting with an SP, a learner receives feedback from a preceptor and/or the learner’s peers. The SP also may be asked to provide brief feedback—a component of the SP training process. Allowing time for feedback is an integral part of student learning.
For this QI project, the delirium team used the Mt. Sinai Skills and Simulation Center at Case Western Reserve University School of Medicine. The facility focuses on creative, innovative continuing learning for health care providers at all levels and is certified by the American College of Surgeons as a level 1 Comprehensive Accredited Education Institute.
After a literature review and several brainstorming sessions, the delirium team tailored case studies to veterans to simulate the intervention and train SPs for the delirium program. During training, SPs reviewed scenarios, engaged in practice sessions, and answered questions. Several SPs were familiar with the behavior of delirious patients from personal experience.
The goals of the program were to increase knowledge of delirium signs and symptoms as a medical condition that requires immediate attention; increase competency in administering CAM and in documenting its results; increase interdisciplinary communication; and increase knowledge using nonpharmacologic interventions for sensory enhancement and agitation. Enhanced interdisciplinary communication was accomplished during the simulation by assigning individuals from different disciplines to work in teams. To maximize the use of resources and limit participants’ time away from the clinical area, the administration planned and supported a daylong program that included didactic education, videos, group work sessions, and the simulation sessions with resource team members as coaches.
Methods
All participants attended an hour-long introductory didactic lecture together. Then, they were randomly assigned to 1 of 4 remaining 45-minute training sessions. Each participant attended a session that combined a video and a case study; a session of role-playing with group discussion; and 2 simulation scenario sessions. Concurrent training sessions were needed to facilitate having all 100 attendees participate within 6 hours. Attendees were multidisciplinary providers from various non-ICU medical/surgical units and outpatient geriatric clinics. They rotated among sessions to accommodate all participants.
For the simulation scenarios, 8 simulation rooms were used over 2 periods—for 16 simulation sessions total. Participants were randomly assigned to multidisciplinary groups that worked in teams to assess and recommend care and treatments for SPs who were stimulating delirium. During the simulation, delirium coaches used cue cards and verbal hints to direct teams (Simulation Exercise). After the session, participants received verbal and
Outcomes
The impact of this multimodal intervention was measured in a variety of ways—with preintervention and postintervention knowledge tests, postsimulation surveys, program surveys, and patient chart reviews. Simulation sessions had 100 attendees, including mentors (interdisciplinary resource team), champions, and nursing staff from various hospital units. Champions represented multiple disciplines and had varying levels of experience. Most of the participants were nurses (62%), followed by social workers (12%), nursing assistants (12%), psychologists (6%), and others (11%). Participants’ years of experience were < 1 year (6%), 1 to 5 years (21%), 6 to 10 years (21%), and > 10 years (52%).
Mean knowledge survey score was 84% before training and 92% after training. Recognition of delirium as a medical emergency requiring immediate follow-up was increased (P = .02), as was knowledge about delirium management, as in increasing daytime activities (P < .001) and using distraction techniques (P = .03) (Table).
More than 94% of participants said the simulation training fulfilled their education needs. More than 80% reported using the information from the delirium workshop in their practice. In reviewing the techniques presented during the workshop, participants reported that they would approach situations differently from before the workshop by using more nonpharmacologic interventions (40%), enhanced communication (24%), and more in-depth assessment for medical causes of delirium (19%). Thirteen percent said they would not change their approach.
Thirty-five percent of respondents had positive feelings after the simulation exercise, 40% had cared for patients in similar situations, and 35% knew delirium care should start with assessment for medical causes.
The team reviewed patient charts for documentation of confusion assessment (signs and symptoms of confusion), including the standardized CAM method and nonpharmacologic interventions. Random monthly audits, 1 month before training and 5 months after, indicated an increase in confusion assessment and documentation. For veterans with delirium, nonpharmacologic interventions increased from 9% at baseline to 53% at the 5-month audit. Hospital length of stay, however, trended toward a slight increase in number of days. These findings are consistent with those reported by Rudolph and colleagues, who also piloted multimodal education and sensory enhancement.27
Discussion
Delirium assessment and management are complex skills that require well-coordinated interdisciplinary care and significant administrative support. Clinicians are becoming increasingly aware of the mounting evidence that patients with delirium feel immediate and often long-term negative effects. Strategies that support clinicians and enhance clinical care must include multimodal education and support.
In this QI project, participants supported use of simulation education, bedside coaching, and pocket cue cards to enhance delirium caregiving knowledge and skills. The majority of participants indicated that, though the simulation sessions were challenging, they also were realistic and helpful. Standardized patients provided feedback and often advised teams of needed improvement, such as spending more time in helping patients feel safe and comfortable. Coaches noted that many team members collaborated with one another but often neglected to use the pocket cue cards, family brochures, and other resources in the room. The reason is not clear. Perhaps the novelty of the resources and potential participant anxiety during the simulation were contributing factors. In future sessions, coaches must address making use of available resources.
Chart reviews indicated that nonpharmacologic management of delirium increased to 53% from < 10%. The increased use of resources in caring for patients with delirium was confirmed by the need to restock the CARES activity carts with patient diversion supplies. Given the success of this first program, another ICU education and simulation program was initiated. Findings from this QI project support using multimodal education that incorporates simulation training, bedside coaching, and pocket cue cards to enhance clinical practices for care of patients with delirium.33
Methods facilitated team collaboration, patient family communication, and synthesis of much information over a relatively short period. Didactic education alone may be insufficient to adequately enhance clinical care for delirium. The impact of a multimodal strategy—including a delirium resource consultation team that provided bedside mentoring, encouraged use of pocket cue cards, and supported evidence-based nonpharmacologic interventions—cannot be underestimated. In addition, simulation education also provided a unique opportunity for the health care teams to “practice” assessment, communication, and collaboration skills in a supportive setting with real-time feedback. These resources are being disseminated throughout the Louis Stokes Cleveland VAMC. Plans to disseminate this information to a broader national audience are under way.
Although not all facilities can access the simulation laboratory, many may be able to implement use of videos, case studies, and role-playing to enhance didactic education, to improve outcomes for patients with delirium. Enhanced clinical management of complex syndromes such as delirium may be influenced most by a combination of education, practice, and mentoring methods. Use of simulation as an adjunct teaching method is a promising strategy that may enhance care of patients with delirium. This QI project demonstrated positive educational and clinical trends in a VA setting. More studies, including randomized clinical trials, are needed in a variety of settings to further test these strategies.
Acknowledgments
The authors give special thanks to Brigid Wilson, PhD, Heather O’Leary, RN, and Patrick Kilroy, SN, for their assistance in this project. The project was developed by the Cleveland VAMC interdisciplinary delirium resource team with support of a VA T-21 grant and the VISN 10 Geriatric Research Education and Clinical Centers.
1. ICU Delirium and Cognitive Impairment Study Group, Center for Health Services Research, Vanderbilt University Medical Center. Delirium prevention and safety: starting with the ABCDEF’s. http://www.icudelirium.org/medicalprofessionals .html. Accessed November 9, 2016.
2. Ely EW, Siegel MD, Inouye SK. Delirium in the intensive care unit: an under-recognized syndrome of organ dysfunction. Semin Respir Crit Care Med. 2001;22(2):115-126.
3. Inouye SK, Bogardus ST Jr, Vitagliano G, et al. Burden of illness score for elderly persons: risk adjustment incorporating the cumulative impact of diseases, physiologic abnormalities, and functional impairments. Med Care. 2003;41(1):70-83.
4. Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49(5):516-522.
5. Foreman MD, Wakefield B, Culp K, Milisen K. Delirium in elderly patients: an overview of the state of the science. J Gerontol Nurs. 2001;27(4):12-20.
6. Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941-948.
7. Maldonado JR. Pathoetiological model of delirium: a comprehensive understanding of the neurobiology of delirium and an evidence-based approach to prevention and treatment. Crit Care Clin. 2008;24(4):789-856.
8. Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, van Gool WA. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA. 2010;304(4):443-451.
9. Leslie DL, Marcantonio ER, Zhang Y, Leo-Summers L, Inouye SK. One-year health care costs associated with delirium in the elderly population. Arch Intern Med. 2008;168(1):27-32.
10. Bruera E, Bush SH, Willey J, et al. Impact of delirium and recall on the level of distress in patients with advanced cancer and their family caregivers. Cancer. 2009;115(9):2004-2012.
11. Cohen MZ, Pace EA, Kaur G, Bruera E. Delirium in advanced cancer leading to distress in patients and family caregivers. J Palliat Care. 2009;25(3):164-171.
12. Patel RP, Gambrell M, Speroff T, et al. Delirium and sedation in the intensive care unit: survey of behaviors and attitudes of 1384 healthcare professionals. Crit Care Med. 2009;37(3):825-832.
13. Wei LA, Fearing MA, Sternberg EJ, Inouye SK. The confusion assessment method: a systematic review of current usage. J Am Geriatr Soc. 2008;56(5):823-830.
14. Neuman MD, Speck RM, Karlawish JH, Schwartz JS, Shea JA. Hospital protocols for the inpatient care of older adults: results from a statewide survey. J Am Geriatr Soc. 2010;58(10):1959-1964.
15. Idemoto BK. The assessment of delirium and depression in the intensive care unit [doctoral dissertation]. Cleveland, OH: Case Western Reserve University; 2005. No. 137.
16. Balas MC, Vasilevskis EE, Burke WJ, et al. Critical care nurses’ role in implementing the “ABCDE bundle” into practice. Crit Care Nurse. 2012;32(2):35-38, 40-47.
17. Barr J, Fraser GL, Puntillo K, et al; American College of Critical Care Medicine. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit: executive summary. Am J Health Syst Pharm. 2013;70(1):53-58.
18. Pun BT, Ely EW. The importance of diagnosing and managing ICU delirium. Chest. 2007;132(2):624-636.
19. Pisani MA, Araujo KL, Van Ness PH, Zhang Y, Ely EW, Inouye SK. A research algorithm to improve detection of delirium in the intensive care unit. Crit Care. 2006;10(4):R121.
20. Voyer P, Cole MG, McCusker J, St-Jacques S, Laplante J. Accuracy of nurse documentation of delirium symptoms in medical charts. Int J Nurs Pract. 2008;14(2):165-167.
21. Pandharipande P, Cotton BA, Shintani A, et al. Prevalence and risk factors for development of delirium in surgical and trauma intensive care unit patients. J Trauma. 2008;65(1):34-41.
22. Steis MR, Fick DM. Are nurses recognizing delirium? A systematic review. J Gerontol Nurs. 2008;34(9):40-48.
23. Yanamadala M, Wieland D, Heflin MT. Educational interventions to improve recognition of delirium: a systematic review. J Am Geriatr Soc. 2013;61(11):1983-1993.
24. Ramaswamy R, Dix EF, Drew JE, Diamond JJ, Inouye SK, Roehl BJ. Beyond grand rounds: a comprehensive and sequential intervention to improve identification of delirium. Gerontologist. 2011;51(1):122-131.
25. Lundström M, Olofsson B, Stenvall M, et al. Postoperative delirium in old patients with femoral neck fracture: a randomized intervention study. Aging Clin Exp Res. 2007;19(3):178-186.
26. Inouye SK. Predisposing and precipitating factors for delirium in hospitalized older patients. Dement Geriatr Cogn Disord. 1999;10(5):393-400.
27. Rudolph JL, Archambault E, Kelly B; VA Boston Delirium Task Force. A delirium risk modification program is associated with hospital outcomes. J Am Med Dir Assoc. 2014;15(12):957.e7-e11.
28. Hartford Institute for Geriatric Nursing. http://hartfordign.org. Accessed November 9, 2016.
29. Inouye SK. A practical program for preventing delirium in hospitalized elderly patients. Cleve Clin J Med. 2004;71(11):890-896.
30. Raurell-Torredà M, Olivet-Pujol J, Romero-Collado À, Malagon-Aguilera MC, Patiño-Masó J, Baltasar-Bagué A. Case-based learning and simulation: useful tools to enhance nurses’ education? Nonrandomized controlled trial. J Nurs Scholarsh. 2015;47(1):34-42.
31. Mast TA, Coulson LR, Meyer TC, et al. Self directed learning: wisdom from independent study programs. Res Med Educ. 1985;24:305-311.
32. Massachusetts Department of Higher Education Nursing Initiative—Simulation Scenario Library. http://www.mass.edu/nahi/Sim/Welcome.asp. Accessed November 1, 2016.
33. Vancouver Island Health Authority. Delirium in the older person: a medical emergency. Pre-Post Test. http://www.viha.ca/NR/rdonlyres/03D50FE6-AF90 -4F98-8B3B-7AE87A4B481D/0/preposttest.pdf. Reviewed August 2014. Accessed November 9, 2016.
1. ICU Delirium and Cognitive Impairment Study Group, Center for Health Services Research, Vanderbilt University Medical Center. Delirium prevention and safety: starting with the ABCDEF’s. http://www.icudelirium.org/medicalprofessionals .html. Accessed November 9, 2016.
2. Ely EW, Siegel MD, Inouye SK. Delirium in the intensive care unit: an under-recognized syndrome of organ dysfunction. Semin Respir Crit Care Med. 2001;22(2):115-126.
3. Inouye SK, Bogardus ST Jr, Vitagliano G, et al. Burden of illness score for elderly persons: risk adjustment incorporating the cumulative impact of diseases, physiologic abnormalities, and functional impairments. Med Care. 2003;41(1):70-83.
4. Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49(5):516-522.
5. Foreman MD, Wakefield B, Culp K, Milisen K. Delirium in elderly patients: an overview of the state of the science. J Gerontol Nurs. 2001;27(4):12-20.
6. Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941-948.
7. Maldonado JR. Pathoetiological model of delirium: a comprehensive understanding of the neurobiology of delirium and an evidence-based approach to prevention and treatment. Crit Care Clin. 2008;24(4):789-856.
8. Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, van Gool WA. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA. 2010;304(4):443-451.
9. Leslie DL, Marcantonio ER, Zhang Y, Leo-Summers L, Inouye SK. One-year health care costs associated with delirium in the elderly population. Arch Intern Med. 2008;168(1):27-32.
10. Bruera E, Bush SH, Willey J, et al. Impact of delirium and recall on the level of distress in patients with advanced cancer and their family caregivers. Cancer. 2009;115(9):2004-2012.
11. Cohen MZ, Pace EA, Kaur G, Bruera E. Delirium in advanced cancer leading to distress in patients and family caregivers. J Palliat Care. 2009;25(3):164-171.
12. Patel RP, Gambrell M, Speroff T, et al. Delirium and sedation in the intensive care unit: survey of behaviors and attitudes of 1384 healthcare professionals. Crit Care Med. 2009;37(3):825-832.
13. Wei LA, Fearing MA, Sternberg EJ, Inouye SK. The confusion assessment method: a systematic review of current usage. J Am Geriatr Soc. 2008;56(5):823-830.
14. Neuman MD, Speck RM, Karlawish JH, Schwartz JS, Shea JA. Hospital protocols for the inpatient care of older adults: results from a statewide survey. J Am Geriatr Soc. 2010;58(10):1959-1964.
15. Idemoto BK. The assessment of delirium and depression in the intensive care unit [doctoral dissertation]. Cleveland, OH: Case Western Reserve University; 2005. No. 137.
16. Balas MC, Vasilevskis EE, Burke WJ, et al. Critical care nurses’ role in implementing the “ABCDE bundle” into practice. Crit Care Nurse. 2012;32(2):35-38, 40-47.
17. Barr J, Fraser GL, Puntillo K, et al; American College of Critical Care Medicine. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit: executive summary. Am J Health Syst Pharm. 2013;70(1):53-58.
18. Pun BT, Ely EW. The importance of diagnosing and managing ICU delirium. Chest. 2007;132(2):624-636.
19. Pisani MA, Araujo KL, Van Ness PH, Zhang Y, Ely EW, Inouye SK. A research algorithm to improve detection of delirium in the intensive care unit. Crit Care. 2006;10(4):R121.
20. Voyer P, Cole MG, McCusker J, St-Jacques S, Laplante J. Accuracy of nurse documentation of delirium symptoms in medical charts. Int J Nurs Pract. 2008;14(2):165-167.
21. Pandharipande P, Cotton BA, Shintani A, et al. Prevalence and risk factors for development of delirium in surgical and trauma intensive care unit patients. J Trauma. 2008;65(1):34-41.
22. Steis MR, Fick DM. Are nurses recognizing delirium? A systematic review. J Gerontol Nurs. 2008;34(9):40-48.
23. Yanamadala M, Wieland D, Heflin MT. Educational interventions to improve recognition of delirium: a systematic review. J Am Geriatr Soc. 2013;61(11):1983-1993.
24. Ramaswamy R, Dix EF, Drew JE, Diamond JJ, Inouye SK, Roehl BJ. Beyond grand rounds: a comprehensive and sequential intervention to improve identification of delirium. Gerontologist. 2011;51(1):122-131.
25. Lundström M, Olofsson B, Stenvall M, et al. Postoperative delirium in old patients with femoral neck fracture: a randomized intervention study. Aging Clin Exp Res. 2007;19(3):178-186.
26. Inouye SK. Predisposing and precipitating factors for delirium in hospitalized older patients. Dement Geriatr Cogn Disord. 1999;10(5):393-400.
27. Rudolph JL, Archambault E, Kelly B; VA Boston Delirium Task Force. A delirium risk modification program is associated with hospital outcomes. J Am Med Dir Assoc. 2014;15(12):957.e7-e11.
28. Hartford Institute for Geriatric Nursing. http://hartfordign.org. Accessed November 9, 2016.
29. Inouye SK. A practical program for preventing delirium in hospitalized elderly patients. Cleve Clin J Med. 2004;71(11):890-896.
30. Raurell-Torredà M, Olivet-Pujol J, Romero-Collado À, Malagon-Aguilera MC, Patiño-Masó J, Baltasar-Bagué A. Case-based learning and simulation: useful tools to enhance nurses’ education? Nonrandomized controlled trial. J Nurs Scholarsh. 2015;47(1):34-42.
31. Mast TA, Coulson LR, Meyer TC, et al. Self directed learning: wisdom from independent study programs. Res Med Educ. 1985;24:305-311.
32. Massachusetts Department of Higher Education Nursing Initiative—Simulation Scenario Library. http://www.mass.edu/nahi/Sim/Welcome.asp. Accessed November 1, 2016.
33. Vancouver Island Health Authority. Delirium in the older person: a medical emergency. Pre-Post Test. http://www.viha.ca/NR/rdonlyres/03D50FE6-AF90 -4F98-8B3B-7AE87A4B481D/0/preposttest.pdf. Reviewed August 2014. Accessed November 9, 2016.
Miguel Angel Villagra Brings Management Skills to The Hospitalist's Volunteer Editorial Advisory Board
Some have called this the “Year of the Hospitalist,” as it’s the 20th anniversary of the New England Journal of Medicine paper by Dr. Robert Wachter and Dr. Lee Goldman that first used the term “hospitalist” to describe physicians who care for hospitalized patients.
But the paper was more than just that to Miguel Angel Villagra, MD.
He saw it four years ago while training in internal medicine at Texas Tech University Health Sciences Center in El Paso, Texas.
“I was very intrigued,” Dr. Villagra says. “I asked a few of my mentors. They were very skeptical on following a hospitalist career, [but] I saw opportunities for improvement and professional growth in the field, so I decided to jump in. And after four years, I don’t regret my decision of becoming a full-time hospitalist.”
The field doesn’t regret it either. Dr. Villagra was promoted last fall to hospitalist department program medical director at White River Medical Center in Batesville, Ark. And this year, he was named one of eight new members of Team Hospitalist, The Hospitalist’s volunteer editorial advisory board.
Question: Why did you choose a career in medicine?
Answer: At age 11 and after an emergent appendectomy, I decided that I wanted to become a physician. That was one of the best decisions of my life. It is a great combination of art and science, and you get to help people in difficult moments of their life.
Q: Tell us more about your background.
A: I went to medical school in my country of origin at Universidad Autonóma de Nicaragua of Managua, and I did an internal medicine residency at Hospital Militar Escuela Dr. Alejandro Dávila Bolaños. I came to the U.S. for internal medicine residency training at Texas Tech of El Paso. I enjoy learning new skills and this power of knowledge that can help your patients in desperate moments. Most of my challenges during my training involved how to manage stress and sleep deprivation.
Q: Did you have a mentor during your training or early career? If so, who was the mentor, and what were most important lessons you learned from them?
A: Dr. Jorge Cuadra [from Hospital Militar in Nicaragua] and Dr. Manuel Rivera [from Texas Tech], both pulmonologists. They taught me that medicine is a changing field that requires everyday reading. You never end learning new things and approaches. Taking full advantage of your interaction with your patients always improves your clinical skills.
Q: What do you like most about working as a hospitalist?
A: It is an evolving field; we are still trying to “figure it out.” That creates challenges but also opportunities for growth and career development, [for example], how to tackle the readmission problem, how to improve quality at lower cost while keeping patient satisfaction, how to face the burnout challenge and improve physician engagement, just to name a few.
Q: What do you dislike most?
A: In the beginning of my career as a hospitalist, I was exposed constantly to high patient loads that were more than I should have. I also dislike the difficulties at times of electronic medical records. You have to spend excessive time sitting in front of a monitor.
Q: You note the challenges the field of HM is facing. How exciting is it to hopefully be part of the solutions?
A: I feel pumped having been part of this amazing movement of hospital medicine. I think we are leading the change from the acute-care setting front line, helping to take better care of our patients. The current healthcare changes create multiple challenges and, along with that, endless opportunities for professional growth and career development.
Q: You’ve said you see being a chief quality officer in the future. Why? What appeals about those C-suite positions?
A: I think that physicians as leaders are in a great position to drive the change within a healthcare organization toward high-value care. We are at the front line, at the bedside taking care of patients. That gives us firsthand information on what needs to be done. With appropriate training, we can be the executives the institution needs. When I started my role as medical director, initially I focused mainly on managing the group, but rapidly I was involved in several quality projects and academic activities. And soon I realized that I can have a broader impact on what I was doing, going beyond the bedside where you try to offer the best care possible for your patients to an organizational level of change.
Q: How has your journey from Nicaragua to the U.S. shaped you, and how has it shaped the way you practice medicine?
A: Certainly it shaped what I am today, coming from a country that struggles with poverty. During medical school, you lack advances in technology and depend mainly on your desire to excel and be better for the benefit of your patients. You build strong clinical skills from history to physical exam. When you move to the U.S. and have access to so many technological advances, from new diagnostic tests to top-of the-line imaging studies, you combine the best of both worlds, and [that] makes you a better physician. I am very proud of my heritage, and definitely I wouldn’t change anything on my path thus far. I believe the more you overcome difficulties and adversities, the more you appreciate what you accomplished.
Q: As a group leader, why is it important for you to continue seeing patients?
A: We lead our teams by example, and that requires treating patients. I am also a clinician, and I love my profession, so I don’t foresee myself only in an administrative role. Finding the sweet spot of clinician-administrative time is very difficult, and I am still working on it.
Q: What’s the best advice you ever received?
A: Read and learn every day, be good to people, and also dream big.
Q: What’s the worst advice you ever received?
A: Never get married. I didn’t listen.
Richard Quinn is a freelance writer in New Jersey.
Some have called this the “Year of the Hospitalist,” as it’s the 20th anniversary of the New England Journal of Medicine paper by Dr. Robert Wachter and Dr. Lee Goldman that first used the term “hospitalist” to describe physicians who care for hospitalized patients.
But the paper was more than just that to Miguel Angel Villagra, MD.
He saw it four years ago while training in internal medicine at Texas Tech University Health Sciences Center in El Paso, Texas.
“I was very intrigued,” Dr. Villagra says. “I asked a few of my mentors. They were very skeptical on following a hospitalist career, [but] I saw opportunities for improvement and professional growth in the field, so I decided to jump in. And after four years, I don’t regret my decision of becoming a full-time hospitalist.”
The field doesn’t regret it either. Dr. Villagra was promoted last fall to hospitalist department program medical director at White River Medical Center in Batesville, Ark. And this year, he was named one of eight new members of Team Hospitalist, The Hospitalist’s volunteer editorial advisory board.
Question: Why did you choose a career in medicine?
Answer: At age 11 and after an emergent appendectomy, I decided that I wanted to become a physician. That was one of the best decisions of my life. It is a great combination of art and science, and you get to help people in difficult moments of their life.
Q: Tell us more about your background.
A: I went to medical school in my country of origin at Universidad Autonóma de Nicaragua of Managua, and I did an internal medicine residency at Hospital Militar Escuela Dr. Alejandro Dávila Bolaños. I came to the U.S. for internal medicine residency training at Texas Tech of El Paso. I enjoy learning new skills and this power of knowledge that can help your patients in desperate moments. Most of my challenges during my training involved how to manage stress and sleep deprivation.
Q: Did you have a mentor during your training or early career? If so, who was the mentor, and what were most important lessons you learned from them?
A: Dr. Jorge Cuadra [from Hospital Militar in Nicaragua] and Dr. Manuel Rivera [from Texas Tech], both pulmonologists. They taught me that medicine is a changing field that requires everyday reading. You never end learning new things and approaches. Taking full advantage of your interaction with your patients always improves your clinical skills.
Q: What do you like most about working as a hospitalist?
A: It is an evolving field; we are still trying to “figure it out.” That creates challenges but also opportunities for growth and career development, [for example], how to tackle the readmission problem, how to improve quality at lower cost while keeping patient satisfaction, how to face the burnout challenge and improve physician engagement, just to name a few.
Q: What do you dislike most?
A: In the beginning of my career as a hospitalist, I was exposed constantly to high patient loads that were more than I should have. I also dislike the difficulties at times of electronic medical records. You have to spend excessive time sitting in front of a monitor.
Q: You note the challenges the field of HM is facing. How exciting is it to hopefully be part of the solutions?
A: I feel pumped having been part of this amazing movement of hospital medicine. I think we are leading the change from the acute-care setting front line, helping to take better care of our patients. The current healthcare changes create multiple challenges and, along with that, endless opportunities for professional growth and career development.
Q: You’ve said you see being a chief quality officer in the future. Why? What appeals about those C-suite positions?
A: I think that physicians as leaders are in a great position to drive the change within a healthcare organization toward high-value care. We are at the front line, at the bedside taking care of patients. That gives us firsthand information on what needs to be done. With appropriate training, we can be the executives the institution needs. When I started my role as medical director, initially I focused mainly on managing the group, but rapidly I was involved in several quality projects and academic activities. And soon I realized that I can have a broader impact on what I was doing, going beyond the bedside where you try to offer the best care possible for your patients to an organizational level of change.
Q: How has your journey from Nicaragua to the U.S. shaped you, and how has it shaped the way you practice medicine?
A: Certainly it shaped what I am today, coming from a country that struggles with poverty. During medical school, you lack advances in technology and depend mainly on your desire to excel and be better for the benefit of your patients. You build strong clinical skills from history to physical exam. When you move to the U.S. and have access to so many technological advances, from new diagnostic tests to top-of the-line imaging studies, you combine the best of both worlds, and [that] makes you a better physician. I am very proud of my heritage, and definitely I wouldn’t change anything on my path thus far. I believe the more you overcome difficulties and adversities, the more you appreciate what you accomplished.
Q: As a group leader, why is it important for you to continue seeing patients?
A: We lead our teams by example, and that requires treating patients. I am also a clinician, and I love my profession, so I don’t foresee myself only in an administrative role. Finding the sweet spot of clinician-administrative time is very difficult, and I am still working on it.
Q: What’s the best advice you ever received?
A: Read and learn every day, be good to people, and also dream big.
Q: What’s the worst advice you ever received?
A: Never get married. I didn’t listen.
Richard Quinn is a freelance writer in New Jersey.
Some have called this the “Year of the Hospitalist,” as it’s the 20th anniversary of the New England Journal of Medicine paper by Dr. Robert Wachter and Dr. Lee Goldman that first used the term “hospitalist” to describe physicians who care for hospitalized patients.
But the paper was more than just that to Miguel Angel Villagra, MD.
He saw it four years ago while training in internal medicine at Texas Tech University Health Sciences Center in El Paso, Texas.
“I was very intrigued,” Dr. Villagra says. “I asked a few of my mentors. They were very skeptical on following a hospitalist career, [but] I saw opportunities for improvement and professional growth in the field, so I decided to jump in. And after four years, I don’t regret my decision of becoming a full-time hospitalist.”
The field doesn’t regret it either. Dr. Villagra was promoted last fall to hospitalist department program medical director at White River Medical Center in Batesville, Ark. And this year, he was named one of eight new members of Team Hospitalist, The Hospitalist’s volunteer editorial advisory board.
Question: Why did you choose a career in medicine?
Answer: At age 11 and after an emergent appendectomy, I decided that I wanted to become a physician. That was one of the best decisions of my life. It is a great combination of art and science, and you get to help people in difficult moments of their life.
Q: Tell us more about your background.
A: I went to medical school in my country of origin at Universidad Autonóma de Nicaragua of Managua, and I did an internal medicine residency at Hospital Militar Escuela Dr. Alejandro Dávila Bolaños. I came to the U.S. for internal medicine residency training at Texas Tech of El Paso. I enjoy learning new skills and this power of knowledge that can help your patients in desperate moments. Most of my challenges during my training involved how to manage stress and sleep deprivation.
Q: Did you have a mentor during your training or early career? If so, who was the mentor, and what were most important lessons you learned from them?
A: Dr. Jorge Cuadra [from Hospital Militar in Nicaragua] and Dr. Manuel Rivera [from Texas Tech], both pulmonologists. They taught me that medicine is a changing field that requires everyday reading. You never end learning new things and approaches. Taking full advantage of your interaction with your patients always improves your clinical skills.
Q: What do you like most about working as a hospitalist?
A: It is an evolving field; we are still trying to “figure it out.” That creates challenges but also opportunities for growth and career development, [for example], how to tackle the readmission problem, how to improve quality at lower cost while keeping patient satisfaction, how to face the burnout challenge and improve physician engagement, just to name a few.
Q: What do you dislike most?
A: In the beginning of my career as a hospitalist, I was exposed constantly to high patient loads that were more than I should have. I also dislike the difficulties at times of electronic medical records. You have to spend excessive time sitting in front of a monitor.
Q: You note the challenges the field of HM is facing. How exciting is it to hopefully be part of the solutions?
A: I feel pumped having been part of this amazing movement of hospital medicine. I think we are leading the change from the acute-care setting front line, helping to take better care of our patients. The current healthcare changes create multiple challenges and, along with that, endless opportunities for professional growth and career development.
Q: You’ve said you see being a chief quality officer in the future. Why? What appeals about those C-suite positions?
A: I think that physicians as leaders are in a great position to drive the change within a healthcare organization toward high-value care. We are at the front line, at the bedside taking care of patients. That gives us firsthand information on what needs to be done. With appropriate training, we can be the executives the institution needs. When I started my role as medical director, initially I focused mainly on managing the group, but rapidly I was involved in several quality projects and academic activities. And soon I realized that I can have a broader impact on what I was doing, going beyond the bedside where you try to offer the best care possible for your patients to an organizational level of change.
Q: How has your journey from Nicaragua to the U.S. shaped you, and how has it shaped the way you practice medicine?
A: Certainly it shaped what I am today, coming from a country that struggles with poverty. During medical school, you lack advances in technology and depend mainly on your desire to excel and be better for the benefit of your patients. You build strong clinical skills from history to physical exam. When you move to the U.S. and have access to so many technological advances, from new diagnostic tests to top-of the-line imaging studies, you combine the best of both worlds, and [that] makes you a better physician. I am very proud of my heritage, and definitely I wouldn’t change anything on my path thus far. I believe the more you overcome difficulties and adversities, the more you appreciate what you accomplished.
Q: As a group leader, why is it important for you to continue seeing patients?
A: We lead our teams by example, and that requires treating patients. I am also a clinician, and I love my profession, so I don’t foresee myself only in an administrative role. Finding the sweet spot of clinician-administrative time is very difficult, and I am still working on it.
Q: What’s the best advice you ever received?
A: Read and learn every day, be good to people, and also dream big.
Q: What’s the worst advice you ever received?
A: Never get married. I didn’t listen.
Richard Quinn is a freelance writer in New Jersey.
How NPs and PAs Work with HM Groups
While the role of nurse practitioners (NPs) and physician assistants (PAs) in hospital medicine is far from uniform, data from the 2016 State of Hospital Medicine Report show that a majority of hospital medicine groups utilize NPs or PAs. Over the past decade, the percentage of hospital medicine groups that include NPs or PAs has grown from about 20% in 20051 to 65% in 2015.2
I suspect a large part of this growth is fueled by demand continuing to outstrip supply for hospitalist physicians and continued increases in hospitalist salaries. In academic institutions, restrictions in house staff duty hours over the past decade no doubt also contributed to the growth of NP and PA utilization.
How Should HM Groups Use NPs and PAs?
In addition to obtaining group buy-in prior to deploying NPs or PAs in a hospital medicine group, a thoughtful consideration about the role of NPs or PAs in providing care is perhaps most important. Even with careful planning, groups should expect implementation of an NP or PA model to require lead-in and training time.
The fact that NPs and PAs have been adopted by so many groups suggests that practices have found increased value; however, models vary widely. In some practices, NPs or PAs work side by side with hospitalists, assisting with documentation, meeting with patients and families, and implementing an agreed-upon management plan. In this model, NPs and PAs may also add value by helping with time-consuming discharges, freeing hospitalists to attend to other patients and thus improving productivity, bed flow, and perhaps also job sustainability.
Other groups have found niche roles for NPs or PAs, including but not limited to providing cross-coverage, performing procedures, triaging admissions, staffing observation units, and developing expertise in a specific clinical area such as consultative medicine or orthopedics.
How to Bill
Depending on the model adopted, groups must also decide whether it is advantageous for NPs or PAs to bill for services independently versus as shared services under the supervising physician’s provider number. The Centers for Medicare & Medicaid Services reimburses NPs and PAs who bill independently at 85% of the physician rate. Nonetheless, some groups may find it more cost-effective for NPs or PAs to bill independently given the substantial salary differential compared to hospitalists. Data published in the 2016 State of Hospital Medicine Report show that NPs and PAs bill independently 47.9% of the time (see Figure 1).
At the University of California, San Diego, we’ve found that our PAs added the most value when working one-on-one with a single hospitalist rather than with multiple physicians. Specifically, our PAs have added to the capacity of our non-teaching service, typically implementing a plan of care developed cooperatively with the hospitalist but also managing a select cohort of patients independently during times of excess volume. By increasing capacity, our PAs have also allowed us to avoid calling in a backup hospitalist during high census periods.
References
- Society of Hospital Medicine. 2006 State of Hospital Medicine Report.
- 2016 State of Hospital Medicine Report. Society of Hospital Medicine website. Accessed October 23, 2016.
While the role of nurse practitioners (NPs) and physician assistants (PAs) in hospital medicine is far from uniform, data from the 2016 State of Hospital Medicine Report show that a majority of hospital medicine groups utilize NPs or PAs. Over the past decade, the percentage of hospital medicine groups that include NPs or PAs has grown from about 20% in 20051 to 65% in 2015.2
I suspect a large part of this growth is fueled by demand continuing to outstrip supply for hospitalist physicians and continued increases in hospitalist salaries. In academic institutions, restrictions in house staff duty hours over the past decade no doubt also contributed to the growth of NP and PA utilization.
How Should HM Groups Use NPs and PAs?
In addition to obtaining group buy-in prior to deploying NPs or PAs in a hospital medicine group, a thoughtful consideration about the role of NPs or PAs in providing care is perhaps most important. Even with careful planning, groups should expect implementation of an NP or PA model to require lead-in and training time.
The fact that NPs and PAs have been adopted by so many groups suggests that practices have found increased value; however, models vary widely. In some practices, NPs or PAs work side by side with hospitalists, assisting with documentation, meeting with patients and families, and implementing an agreed-upon management plan. In this model, NPs and PAs may also add value by helping with time-consuming discharges, freeing hospitalists to attend to other patients and thus improving productivity, bed flow, and perhaps also job sustainability.
Other groups have found niche roles for NPs or PAs, including but not limited to providing cross-coverage, performing procedures, triaging admissions, staffing observation units, and developing expertise in a specific clinical area such as consultative medicine or orthopedics.
How to Bill
Depending on the model adopted, groups must also decide whether it is advantageous for NPs or PAs to bill for services independently versus as shared services under the supervising physician’s provider number. The Centers for Medicare & Medicaid Services reimburses NPs and PAs who bill independently at 85% of the physician rate. Nonetheless, some groups may find it more cost-effective for NPs or PAs to bill independently given the substantial salary differential compared to hospitalists. Data published in the 2016 State of Hospital Medicine Report show that NPs and PAs bill independently 47.9% of the time (see Figure 1).
At the University of California, San Diego, we’ve found that our PAs added the most value when working one-on-one with a single hospitalist rather than with multiple physicians. Specifically, our PAs have added to the capacity of our non-teaching service, typically implementing a plan of care developed cooperatively with the hospitalist but also managing a select cohort of patients independently during times of excess volume. By increasing capacity, our PAs have also allowed us to avoid calling in a backup hospitalist during high census periods.
References
- Society of Hospital Medicine. 2006 State of Hospital Medicine Report.
- 2016 State of Hospital Medicine Report. Society of Hospital Medicine website. Accessed October 23, 2016.
While the role of nurse practitioners (NPs) and physician assistants (PAs) in hospital medicine is far from uniform, data from the 2016 State of Hospital Medicine Report show that a majority of hospital medicine groups utilize NPs or PAs. Over the past decade, the percentage of hospital medicine groups that include NPs or PAs has grown from about 20% in 20051 to 65% in 2015.2
I suspect a large part of this growth is fueled by demand continuing to outstrip supply for hospitalist physicians and continued increases in hospitalist salaries. In academic institutions, restrictions in house staff duty hours over the past decade no doubt also contributed to the growth of NP and PA utilization.
How Should HM Groups Use NPs and PAs?
In addition to obtaining group buy-in prior to deploying NPs or PAs in a hospital medicine group, a thoughtful consideration about the role of NPs or PAs in providing care is perhaps most important. Even with careful planning, groups should expect implementation of an NP or PA model to require lead-in and training time.
The fact that NPs and PAs have been adopted by so many groups suggests that practices have found increased value; however, models vary widely. In some practices, NPs or PAs work side by side with hospitalists, assisting with documentation, meeting with patients and families, and implementing an agreed-upon management plan. In this model, NPs and PAs may also add value by helping with time-consuming discharges, freeing hospitalists to attend to other patients and thus improving productivity, bed flow, and perhaps also job sustainability.
Other groups have found niche roles for NPs or PAs, including but not limited to providing cross-coverage, performing procedures, triaging admissions, staffing observation units, and developing expertise in a specific clinical area such as consultative medicine or orthopedics.
How to Bill
Depending on the model adopted, groups must also decide whether it is advantageous for NPs or PAs to bill for services independently versus as shared services under the supervising physician’s provider number. The Centers for Medicare & Medicaid Services reimburses NPs and PAs who bill independently at 85% of the physician rate. Nonetheless, some groups may find it more cost-effective for NPs or PAs to bill independently given the substantial salary differential compared to hospitalists. Data published in the 2016 State of Hospital Medicine Report show that NPs and PAs bill independently 47.9% of the time (see Figure 1).
At the University of California, San Diego, we’ve found that our PAs added the most value when working one-on-one with a single hospitalist rather than with multiple physicians. Specifically, our PAs have added to the capacity of our non-teaching service, typically implementing a plan of care developed cooperatively with the hospitalist but also managing a select cohort of patients independently during times of excess volume. By increasing capacity, our PAs have also allowed us to avoid calling in a backup hospitalist during high census periods.
References
- Society of Hospital Medicine. 2006 State of Hospital Medicine Report.
- 2016 State of Hospital Medicine Report. Society of Hospital Medicine website. Accessed October 23, 2016.
Novel interferon appears safer than HU in PV

Photo by Zak Hubbard
SAN DIEGO—Results of the PROUD-PV trial suggest ropeginterferon alfa-2b is safer than hydroxyurea (HU) for patients with polycythemia vera (PV).
In this phase 3 trial, ropeginterferon alfa-2b demonstrated non-inferiority to HU with regard to complete hematologic response (CHR).
Ropeginterferon alfa-2b also had a significantly better overall safety profile.
Unlike the patients who received HU, none of the patients on ropeginterferon alfa-2b developed secondary malignancies.
Heinz Gisslinger, MD, of the Medical University of Vienna in Austria, presented these results at the 2016 ASH Annual Meeting (abstract 475). The PROUD-PV study was sponsored by AOP Orphan Pharmaceuticals AG.
Dr Gisslinger noted that interferons have been successful in treating PV since the 1980s, although toxicities contribute to discontinuation rates of approximately 25%. Still, interferons are the only known drugs with the potential for disease modification by specific targeting of the malignant clone.
Ropeginterferon alfa-2b is a long-acting, mono-pegylated proline interferon with improved pharmacokinetic properties that allow for administration once every 2 weeks.
The goal of PROUD-PV was to determine how this drug stacks up against HU in both treatment-naive and HU-pretreated patients with PV.
“Our results from the first and largest, prospective, controlled trial of an interferon in polycythemia vera confirm previously reported efficacy,” Dr Gisslinger said.
“The observed safety and tolerability profile of ropeginterferon appears to be superior compared to previously reported data of interferon treatment. The unique disease-modification capability of interferon and its potential to improve progression-free survival hold promise for long-term benefit for patients.”
Patients and treatment
PROUD-PV enrolled 254 patients, and they were randomized to receive ropeginterferon alfa-2b (n=127) or HU (n=127). In both arms, 100% of patients were Caucasian, slightly more than half were female, and the median age was 60 (overall range, 21-85).
The median disease duration was 1.9 months in the ropeginterferon alfa-2b arm and 3.6 months in the HU arm. Thirty-seven percent (n=47) of patients in each arm had previously received HU.
The mean hematocrit was about 50% in both arms, the median spleen length was about 13 cm, about 90% of patients had a normal/slightly enlarged spleen, and the mean JAK2V617F burden was slightly more than 40%.
The median plateau dose was 450 µg in the ropeginterferon alfa-2b arm and 1250 mg in the HU arm.
A quarter (25.2%) of patients had dose reductions due to adverse events (AEs) in the ropeginterferon alfa-2b arm, as did 51.2% of patients in the HU arm. The 12-month discontinuation rate was 16.5% in the ropeginterferon alfa-2b arm and 12.6% in the HU arm.
Response
The study’s primary objective was to demonstrate non-inferiority of ropeginterferon alfa-2b compared to HU. For this, the researchers used the 12-month CHR rate. CHR was defined as normalization of red blood cell, white blood cell, and platelet counts (without phlebotomy).
At 12 months, in the intent-to-treat population, the CHR rate was 43.1% in the ropeginterferon alfa-2b arm and 45.6% in the HU arm (P=0.0028). In the per-protocol population, the CHR rate was 44.3% and 46.5%, respectively (P=0.0036).
The researchers therefore concluded that non-inferiority was demonstrated.
The study’s pre-specified primary endpoint was actually a composite of CHR and spleen length normality. However, this was confounded by the fact that the patients’ median spleen length was almost normal at baseline and the observed change was not clinically relevant.
In the intent-to-treat-population, CHR with spleen normality occurred in 21.3% of patients in the ropeginterferon alfa-2b arm and 27.6% of patients in the HU arm (P=0.2233).
Safety
The incidence of AEs was 81.9% in the ropeginterferon alfa-2b arm and 87.4% in the HU arm. The incidence of grade 3 AEs was 16.5% and 20.5%, respectively. And the incidence of treatment-related AEs was 59.6% and 75.6%, respectively (P<0.05).
There was a significantly higher incidence (P<0.01) of the following AEs in the HU arm than the ropeginterferon alfa-2b arm: anemia (24.4% vs 6.3%), leukopenia (21.3% vs 8.7%), thrombocytopenia (28.3% vs 15.0%), and nausea (11.8% vs 2.4%).
There was no significant difference in the incidence of fatigue—13.4% in the HU arm and 12.6% in the ropeginterferon alfa-2b arm.
Patients in the ropeginterferon alfa-2b arm had a significantly higher incidence of gamma-glutamyl transferase increase—14.2% vs 0.8% in the HU arm (P<0.01).
Patients in the ropeginterferon alfa-2b arm also had a higher—but non-significant—incidence of endocrine disorders (3.1% vs 0.8%), psychiatric disorders (1.6% vs 0%), cardiac/vascular disorders (3.1% vs 1.6%), and tissue disorders (1.6% vs 0%).
None of the patients in the ropeginterferon alfa-2b arm developed secondary related malignancies. In the HU arm, however, there were 2 cases of acute leukemia, 2 cases of basal cell carcinoma, and 1 case of malignant melanoma. (This includes data from the ongoing follow-up trial CONTINUATION-PV.)
Drug development
AOP Orphan Pharmaceuticals AG said that, in the coming months, it will submit data from PROUD-PV and the ongoing follow-up trial, CONTINUATION-PV, to obtain European marketing authorization for ropeginterferon alfa-2b.
PharmaEssentia plans to submit the same data to the US Food and Drug Administration.
PharmaEssentia discovered ropeginterferon alfa-2b and has licensed the rights for development and commercialization of the drug in myeloproliferative neoplasms to AOP Orphan Pharmaceuticals AG in Europe, the Commonwealth of Independent States, and Middle Eastern markets. ![]()
*Information presented at the meeting differs from the abstract.

Photo by Zak Hubbard
SAN DIEGO—Results of the PROUD-PV trial suggest ropeginterferon alfa-2b is safer than hydroxyurea (HU) for patients with polycythemia vera (PV).
In this phase 3 trial, ropeginterferon alfa-2b demonstrated non-inferiority to HU with regard to complete hematologic response (CHR).
Ropeginterferon alfa-2b also had a significantly better overall safety profile.
Unlike the patients who received HU, none of the patients on ropeginterferon alfa-2b developed secondary malignancies.
Heinz Gisslinger, MD, of the Medical University of Vienna in Austria, presented these results at the 2016 ASH Annual Meeting (abstract 475). The PROUD-PV study was sponsored by AOP Orphan Pharmaceuticals AG.
Dr Gisslinger noted that interferons have been successful in treating PV since the 1980s, although toxicities contribute to discontinuation rates of approximately 25%. Still, interferons are the only known drugs with the potential for disease modification by specific targeting of the malignant clone.
Ropeginterferon alfa-2b is a long-acting, mono-pegylated proline interferon with improved pharmacokinetic properties that allow for administration once every 2 weeks.
The goal of PROUD-PV was to determine how this drug stacks up against HU in both treatment-naive and HU-pretreated patients with PV.
“Our results from the first and largest, prospective, controlled trial of an interferon in polycythemia vera confirm previously reported efficacy,” Dr Gisslinger said.
“The observed safety and tolerability profile of ropeginterferon appears to be superior compared to previously reported data of interferon treatment. The unique disease-modification capability of interferon and its potential to improve progression-free survival hold promise for long-term benefit for patients.”
Patients and treatment
PROUD-PV enrolled 254 patients, and they were randomized to receive ropeginterferon alfa-2b (n=127) or HU (n=127). In both arms, 100% of patients were Caucasian, slightly more than half were female, and the median age was 60 (overall range, 21-85).
The median disease duration was 1.9 months in the ropeginterferon alfa-2b arm and 3.6 months in the HU arm. Thirty-seven percent (n=47) of patients in each arm had previously received HU.
The mean hematocrit was about 50% in both arms, the median spleen length was about 13 cm, about 90% of patients had a normal/slightly enlarged spleen, and the mean JAK2V617F burden was slightly more than 40%.
The median plateau dose was 450 µg in the ropeginterferon alfa-2b arm and 1250 mg in the HU arm.
A quarter (25.2%) of patients had dose reductions due to adverse events (AEs) in the ropeginterferon alfa-2b arm, as did 51.2% of patients in the HU arm. The 12-month discontinuation rate was 16.5% in the ropeginterferon alfa-2b arm and 12.6% in the HU arm.
Response
The study’s primary objective was to demonstrate non-inferiority of ropeginterferon alfa-2b compared to HU. For this, the researchers used the 12-month CHR rate. CHR was defined as normalization of red blood cell, white blood cell, and platelet counts (without phlebotomy).
At 12 months, in the intent-to-treat population, the CHR rate was 43.1% in the ropeginterferon alfa-2b arm and 45.6% in the HU arm (P=0.0028). In the per-protocol population, the CHR rate was 44.3% and 46.5%, respectively (P=0.0036).
The researchers therefore concluded that non-inferiority was demonstrated.
The study’s pre-specified primary endpoint was actually a composite of CHR and spleen length normality. However, this was confounded by the fact that the patients’ median spleen length was almost normal at baseline and the observed change was not clinically relevant.
In the intent-to-treat-population, CHR with spleen normality occurred in 21.3% of patients in the ropeginterferon alfa-2b arm and 27.6% of patients in the HU arm (P=0.2233).
Safety
The incidence of AEs was 81.9% in the ropeginterferon alfa-2b arm and 87.4% in the HU arm. The incidence of grade 3 AEs was 16.5% and 20.5%, respectively. And the incidence of treatment-related AEs was 59.6% and 75.6%, respectively (P<0.05).
There was a significantly higher incidence (P<0.01) of the following AEs in the HU arm than the ropeginterferon alfa-2b arm: anemia (24.4% vs 6.3%), leukopenia (21.3% vs 8.7%), thrombocytopenia (28.3% vs 15.0%), and nausea (11.8% vs 2.4%).
There was no significant difference in the incidence of fatigue—13.4% in the HU arm and 12.6% in the ropeginterferon alfa-2b arm.
Patients in the ropeginterferon alfa-2b arm had a significantly higher incidence of gamma-glutamyl transferase increase—14.2% vs 0.8% in the HU arm (P<0.01).
Patients in the ropeginterferon alfa-2b arm also had a higher—but non-significant—incidence of endocrine disorders (3.1% vs 0.8%), psychiatric disorders (1.6% vs 0%), cardiac/vascular disorders (3.1% vs 1.6%), and tissue disorders (1.6% vs 0%).
None of the patients in the ropeginterferon alfa-2b arm developed secondary related malignancies. In the HU arm, however, there were 2 cases of acute leukemia, 2 cases of basal cell carcinoma, and 1 case of malignant melanoma. (This includes data from the ongoing follow-up trial CONTINUATION-PV.)
Drug development
AOP Orphan Pharmaceuticals AG said that, in the coming months, it will submit data from PROUD-PV and the ongoing follow-up trial, CONTINUATION-PV, to obtain European marketing authorization for ropeginterferon alfa-2b.
PharmaEssentia plans to submit the same data to the US Food and Drug Administration.
PharmaEssentia discovered ropeginterferon alfa-2b and has licensed the rights for development and commercialization of the drug in myeloproliferative neoplasms to AOP Orphan Pharmaceuticals AG in Europe, the Commonwealth of Independent States, and Middle Eastern markets. ![]()
*Information presented at the meeting differs from the abstract.

Photo by Zak Hubbard
SAN DIEGO—Results of the PROUD-PV trial suggest ropeginterferon alfa-2b is safer than hydroxyurea (HU) for patients with polycythemia vera (PV).
In this phase 3 trial, ropeginterferon alfa-2b demonstrated non-inferiority to HU with regard to complete hematologic response (CHR).
Ropeginterferon alfa-2b also had a significantly better overall safety profile.
Unlike the patients who received HU, none of the patients on ropeginterferon alfa-2b developed secondary malignancies.
Heinz Gisslinger, MD, of the Medical University of Vienna in Austria, presented these results at the 2016 ASH Annual Meeting (abstract 475). The PROUD-PV study was sponsored by AOP Orphan Pharmaceuticals AG.
Dr Gisslinger noted that interferons have been successful in treating PV since the 1980s, although toxicities contribute to discontinuation rates of approximately 25%. Still, interferons are the only known drugs with the potential for disease modification by specific targeting of the malignant clone.
Ropeginterferon alfa-2b is a long-acting, mono-pegylated proline interferon with improved pharmacokinetic properties that allow for administration once every 2 weeks.
The goal of PROUD-PV was to determine how this drug stacks up against HU in both treatment-naive and HU-pretreated patients with PV.
“Our results from the first and largest, prospective, controlled trial of an interferon in polycythemia vera confirm previously reported efficacy,” Dr Gisslinger said.
“The observed safety and tolerability profile of ropeginterferon appears to be superior compared to previously reported data of interferon treatment. The unique disease-modification capability of interferon and its potential to improve progression-free survival hold promise for long-term benefit for patients.”
Patients and treatment
PROUD-PV enrolled 254 patients, and they were randomized to receive ropeginterferon alfa-2b (n=127) or HU (n=127). In both arms, 100% of patients were Caucasian, slightly more than half were female, and the median age was 60 (overall range, 21-85).
The median disease duration was 1.9 months in the ropeginterferon alfa-2b arm and 3.6 months in the HU arm. Thirty-seven percent (n=47) of patients in each arm had previously received HU.
The mean hematocrit was about 50% in both arms, the median spleen length was about 13 cm, about 90% of patients had a normal/slightly enlarged spleen, and the mean JAK2V617F burden was slightly more than 40%.
The median plateau dose was 450 µg in the ropeginterferon alfa-2b arm and 1250 mg in the HU arm.
A quarter (25.2%) of patients had dose reductions due to adverse events (AEs) in the ropeginterferon alfa-2b arm, as did 51.2% of patients in the HU arm. The 12-month discontinuation rate was 16.5% in the ropeginterferon alfa-2b arm and 12.6% in the HU arm.
Response
The study’s primary objective was to demonstrate non-inferiority of ropeginterferon alfa-2b compared to HU. For this, the researchers used the 12-month CHR rate. CHR was defined as normalization of red blood cell, white blood cell, and platelet counts (without phlebotomy).
At 12 months, in the intent-to-treat population, the CHR rate was 43.1% in the ropeginterferon alfa-2b arm and 45.6% in the HU arm (P=0.0028). In the per-protocol population, the CHR rate was 44.3% and 46.5%, respectively (P=0.0036).
The researchers therefore concluded that non-inferiority was demonstrated.
The study’s pre-specified primary endpoint was actually a composite of CHR and spleen length normality. However, this was confounded by the fact that the patients’ median spleen length was almost normal at baseline and the observed change was not clinically relevant.
In the intent-to-treat-population, CHR with spleen normality occurred in 21.3% of patients in the ropeginterferon alfa-2b arm and 27.6% of patients in the HU arm (P=0.2233).
Safety
The incidence of AEs was 81.9% in the ropeginterferon alfa-2b arm and 87.4% in the HU arm. The incidence of grade 3 AEs was 16.5% and 20.5%, respectively. And the incidence of treatment-related AEs was 59.6% and 75.6%, respectively (P<0.05).
There was a significantly higher incidence (P<0.01) of the following AEs in the HU arm than the ropeginterferon alfa-2b arm: anemia (24.4% vs 6.3%), leukopenia (21.3% vs 8.7%), thrombocytopenia (28.3% vs 15.0%), and nausea (11.8% vs 2.4%).
There was no significant difference in the incidence of fatigue—13.4% in the HU arm and 12.6% in the ropeginterferon alfa-2b arm.
Patients in the ropeginterferon alfa-2b arm had a significantly higher incidence of gamma-glutamyl transferase increase—14.2% vs 0.8% in the HU arm (P<0.01).
Patients in the ropeginterferon alfa-2b arm also had a higher—but non-significant—incidence of endocrine disorders (3.1% vs 0.8%), psychiatric disorders (1.6% vs 0%), cardiac/vascular disorders (3.1% vs 1.6%), and tissue disorders (1.6% vs 0%).
None of the patients in the ropeginterferon alfa-2b arm developed secondary related malignancies. In the HU arm, however, there were 2 cases of acute leukemia, 2 cases of basal cell carcinoma, and 1 case of malignant melanoma. (This includes data from the ongoing follow-up trial CONTINUATION-PV.)
Drug development
AOP Orphan Pharmaceuticals AG said that, in the coming months, it will submit data from PROUD-PV and the ongoing follow-up trial, CONTINUATION-PV, to obtain European marketing authorization for ropeginterferon alfa-2b.
PharmaEssentia plans to submit the same data to the US Food and Drug Administration.
PharmaEssentia discovered ropeginterferon alfa-2b and has licensed the rights for development and commercialization of the drug in myeloproliferative neoplasms to AOP Orphan Pharmaceuticals AG in Europe, the Commonwealth of Independent States, and Middle Eastern markets. ![]()
*Information presented at the meeting differs from the abstract.
Company terminates study of drug for MM

multiple myeloma
BioInvent International has decided to terminate its phase 2 trial of the antibody BI-505 in patients with multiple myeloma (MM).
The decision follows a review and discussion with the US Food and Drug Administration (FDA), which put the trial on full clinical hold in November due to an adverse cardiopulmonary event.
The trial was designed to determine if BI-505 could deepen therapeutic response and thereby prevent or delay relapse in MM patients undergoing autologous stem cell transplant with high-dose melphalan.
The termination of this trial may not mean the end of BI-505. BioInvent is currently in discussions with the FDA about the potential to develop the drug for use in other patient populations.
BI-505 is a human antibody targeting ICAM-1, a protein that is elevated in MM cells. BI-505 has been shown to attack MM in 2 ways—by inducing apoptosis in MM cells and by engaging macrophages to attack and kill MM cells.
The development strategy for BI-505 has been focused on eliminating residual disease by combining the antibody with modern standard-of-care drugs used to treat MM.
BI-505 has orphan drug designation as a treatment for MM from both the FDA and the European Medicines Agency.
Results of a phase 1 trial of BI-505 in MM patients were published in Clinical Cancer Research in June 2015. ![]()

multiple myeloma
BioInvent International has decided to terminate its phase 2 trial of the antibody BI-505 in patients with multiple myeloma (MM).
The decision follows a review and discussion with the US Food and Drug Administration (FDA), which put the trial on full clinical hold in November due to an adverse cardiopulmonary event.
The trial was designed to determine if BI-505 could deepen therapeutic response and thereby prevent or delay relapse in MM patients undergoing autologous stem cell transplant with high-dose melphalan.
The termination of this trial may not mean the end of BI-505. BioInvent is currently in discussions with the FDA about the potential to develop the drug for use in other patient populations.
BI-505 is a human antibody targeting ICAM-1, a protein that is elevated in MM cells. BI-505 has been shown to attack MM in 2 ways—by inducing apoptosis in MM cells and by engaging macrophages to attack and kill MM cells.
The development strategy for BI-505 has been focused on eliminating residual disease by combining the antibody with modern standard-of-care drugs used to treat MM.
BI-505 has orphan drug designation as a treatment for MM from both the FDA and the European Medicines Agency.
Results of a phase 1 trial of BI-505 in MM patients were published in Clinical Cancer Research in June 2015. ![]()

multiple myeloma
BioInvent International has decided to terminate its phase 2 trial of the antibody BI-505 in patients with multiple myeloma (MM).
The decision follows a review and discussion with the US Food and Drug Administration (FDA), which put the trial on full clinical hold in November due to an adverse cardiopulmonary event.
The trial was designed to determine if BI-505 could deepen therapeutic response and thereby prevent or delay relapse in MM patients undergoing autologous stem cell transplant with high-dose melphalan.
The termination of this trial may not mean the end of BI-505. BioInvent is currently in discussions with the FDA about the potential to develop the drug for use in other patient populations.
BI-505 is a human antibody targeting ICAM-1, a protein that is elevated in MM cells. BI-505 has been shown to attack MM in 2 ways—by inducing apoptosis in MM cells and by engaging macrophages to attack and kill MM cells.
The development strategy for BI-505 has been focused on eliminating residual disease by combining the antibody with modern standard-of-care drugs used to treat MM.
BI-505 has orphan drug designation as a treatment for MM from both the FDA and the European Medicines Agency.
Results of a phase 1 trial of BI-505 in MM patients were published in Clinical Cancer Research in June 2015. ![]()
The Death of a Dream: Closing an NP Practice
For many nurse practitioners, having your own practice is the culmination of many years of planning and anticipation. I worked as an NP for 14 years in practices operated by others—hospitals and physicians—before I opened my own practice. During those years, I had observed which ways of doing things appeared productive and healing to me and which did not.
When the time came, having seen a need for more affordable health care that was not predicated on the assumption that every patient had health insurance, I opened a cash-only practice in the town where I resided. By eliminating the need for personnel and apparatus dedicated to insurance filing, I was able to charge about half of what other practices in the same location did for identical services. My chief goal was to be of service to the community, not to make the most money possible. I anticipated that volume would make up for the lower prices in the long run.
For about four years, our revenue grew slowly. I decided to risk all and stop teaching part-time in order to focus exclusively on my practice. This proved to be a good decision—for about one year. Then the recession hit my part of the country. Suddenly, the operation of a “cash-only” practice became an oxymoron, as many of the patients with already limited funds lost their jobs. These patients started to seek “free” care at area emergency departments, and the practice income plummeted. My revenue fell by one-half the first year and then one-half of that the next year.
In what would turn out to be my final year of practice ownership, I decided to accept a full-time position as faculty of a distance FNP program. I was practicing “on the side,” although in reality I was in my office full-time and teaching from there. I was already recognizing the difficulties of juggling my roles and responsibilities when a student in one of my classes asked what it would take for me to decide to close my practice, since I was (by this point) making no money from it.
As I pondered that question (my initial response was a quite honest “I don’t know”), I stepped onto the road toward closing my practice. From a business perspective, there was little point in keeping the practice open. However, from an emotional point of view, I had invested so much in building my dream—and, by extension, so had my family—that closing the practice seemed unthinkable.
THE DECISION
Opening a practice is a time of joy, pride, and a sense of accomplishment; closing that same practice induces a period of reflection, sadness, and even anger that circumstances did not allow continued operation. While financial considerations play a significant role in the decision to close a practice, they may not be the only, or the deciding, factor.
In my case, the financial shortfall of the practice led me to accept a teaching position in order to earn living expenses. The result of that decision was that my attention became divided: Sometimes I was in meetings or interacting with students—and for a few weeks per year, I was out of town—which meant less time devoted to seeing patients. Conversely, if I was with a patient, I of course could not be available to my students. Over time, I started to feel that I was not giving my all to either role as I shifted back and forth. Having given 100% to each of these roles at previous points in my career, I now felt that I was cheating my patients and my students.
The decision to close a practice may take months or even years before the actual process is started. I lived with my conundrum for about a year before I made the decision to close. I was exhausted—and while I was relieved to have the burden of deciding off my shoulders, it was now time to do the work of closing a practice.

NOTIFYING YOUR STAKEHOLDERS
Once the decision to close a practice is reached, the provider/owner ceases to exist in a vacuum. There are stakeholders who need to be notified—some obvious, some less so.
I started by breaking the news to my family, the people who had supported me in opening my practice (and even helped me find and refurbish furniture for my waiting room!). Although they had been aware of my internal debate, they had not lived with the decision process as I had. Having resolved at least some of my own emotions, I now had to watch others experience many of those same feelings.
Next, I had to tell my employees of the decision. Through attrition, my staff had already shrunk to two: a receptionist and a part-time licensed vocational nurse (LVN). Like my family, they had to process their own emotions about the closure. I had anticipated that the people who worked for me, concerned about their future, might choose to accept another job before we officially closed. My LVN—who had observed the practice dwindling in the preceding two years—seemed prepared for my decision. She stuck it out with me until the end and was a huge help with the influx of patients requesting records. (My MD—required by Texas law to delegate prescriptive authority to me—had already relocated his practice and was ill, so he was content with my decision.)
Of course, the biggest stakeholders in a practice are the patients. Notifying them of the impending closure is the most important action you will take (aside from making the decision to close). Although you can place notices in the local media (newspapers, TV, radio) to announce the closure of your practice to the community, you should send a notification letter directly to your patients. It should be sent at least 60 to 90 days before the closure date—and certainly not less than 30 days in any case—giving patients adequate time to find new providers and arrange for their records to be transferred.1,2 The letter should include
- A statement of gratitude for the patient’s business
- The dates of the transition period
- What is expected of the patient (eg, does he/she need to come and pick up his/her records?)
- An explanation for the closure3
I composed a letter to be sent to all patients who had been seen within the past 18 months. In it, I thanked them for being a part of the practice and gave them 60 days’ notice of the intent to close. For many patients, this was an emotional time; many understandably worried how their health care needs would be met in the future. Some responded with sadness that I had not been able to make the practice a success.
AVOIDING “ABANDONMENT”
Ideally, a provider who wants to get out of the business should seek to sell the practice—but this is not always feasible.3,4 When closure is the best (or only) option, it is important to avoid even the appearance of abandonment.
Besides giving adequate notice of practice closure, providers must have a plan for the dispersal of patients.1 Be prepared to give recommendations for new providers. Depending on the practice location (rural or urban), options may vary.
I made a concerted effort to refer patients to new providers, with the caveat that if the patient did not feel a particular provider was a good match, he/she should seek another provider of his/her choosing. Unlike in a purchased practice, where patients “go with” the practice, patients from a closed practice may be referred to one, several, or even many other providers.5
Provisions must be made to store patient records so that they are retrievable for a specified period of time. The requirements vary by state, so consultation of the state board’s rules and regulations—and/or an attorney—is in order.3 In general, the proscribed time period is seven to 10 years for adults and seven to 10 years after the patient turns 18 for pediatric patients.2 In some states, the retention time may be as short as three years for adults.1
OTHER PRACTICAL CONSIDERATIONS
While people will be your priority as you work through the process of closing, you will have “stuff” to deal with. What will you do with the furnishings and equipment? Obviously, anything that was borrowed can be returned. Beyond that, your options are to sell (to another provider or even a patient), donate, or repurpose items.
The orthopedic exam table from my practice went to a private school for their athletic training facility. Screens went to my neighbor, a chiropractor. My preschool-aged grandsons were thrilled to be given the children’s art supplies and books that had once graced my waiting area. One of my patients bought some decorative vases and a bookcase. The painting that had been carefully chosen to pull together my waiting room now hangs in my library at home.
As the closure date approaches, the practice environment may begin to look bare as furnishings are sold or moved. One item you will want to buy, however, is a fresh ink cartridge for your copier/printer. As patients request documents, you’ll use it!
RESPONSE AND AFTERMATH
The practice may be very busy immediately following the receipt of notification letters—but don’t be fooled into thinking you have made the wrong decision. The first month after the letters went out advising of the closure, my practice was busier than it had ever been! This tapered off in the second month, though.
Most patients, once they’ve heard the news, will want prescription refills and/or their records. Some may just want to know what happened to result in the closure. Remember that to the patient, this seems like a sudden decision—no matter how long you have deliberated about it.
What surprised me most, however, was that new patients continued to present to the practice, seeking care for acute issues. While I did provide this, I made them aware from the beginning that the practice was in the process of closing and that I could not assume the responsibility of being their primary provider. I made sure to provide these patients with recommendations for other providers.
Slowly the rush will settle down, as patients start to move on to other providers. A few may drop in to see you socially. On the day I closed my practice, several patients came in just to say goodbye and wish me well.
The last things I did in my practice were turn off the lights and leave a sign on the door stating that the practice was now closed.
RECOVERY
The time needed to recover from the closure of a practice will differ. Factors include how long the practice was open and how the clinician normally deals with a setback.6 For some, relief that the pressures of ownership are over may be the predominant emotion. Having a steady, stable salary in a new position goes a long way toward making the transition easier! Although if possible, take some time between closing the practice and starting a new job.
Do not be surprised if negative emotions manifest at odd times, as feelings of sadness, regret, and even a sense of failure are worked through. Life does go on—and nurse practitioners are resilient. Find a way to use the knowledge gained from your practice in your new endeavors, whatever they may be.
For me, the healing process would have started sooner if I had acknowledged how difficult giving up the dream of having my own practice was. If I had sought out others with similar experience or even talked with a counselor, my journey through this process could have been expedited. When I started to share my story, one frequently asked question was “How did you get through this?” This showed me that others could learn from my experience.
1. Tatooles JJ, Brunell A. What you need to know before leaving a medical practice: a primer for moving on. AAOS NOW. 2015;22-23.
2. Kern SI. Take these steps if selling or closing a practice. Med Econ. 2010;87(20):66.
3. Weiss GG. How to close a practice. Med Econ. 2004;81:69.
4. Zaumeyer C. How to Start an Independent Practice: The Nurse Practitioner’s Guide to Success. Philadelphia: F. A. Davis, Publishers; 2003.
5. Barrett W. The legal corner: Eleven essential steps to purchasing or selling a medical practice. J Med Pract Manage. 2014;29(5):275-277.
6. McBride JL. Personal issues to consider before leaving independent practice. Fam Pract Manag. 2013;20(4):9-12.
For many nurse practitioners, having your own practice is the culmination of many years of planning and anticipation. I worked as an NP for 14 years in practices operated by others—hospitals and physicians—before I opened my own practice. During those years, I had observed which ways of doing things appeared productive and healing to me and which did not.
When the time came, having seen a need for more affordable health care that was not predicated on the assumption that every patient had health insurance, I opened a cash-only practice in the town where I resided. By eliminating the need for personnel and apparatus dedicated to insurance filing, I was able to charge about half of what other practices in the same location did for identical services. My chief goal was to be of service to the community, not to make the most money possible. I anticipated that volume would make up for the lower prices in the long run.
For about four years, our revenue grew slowly. I decided to risk all and stop teaching part-time in order to focus exclusively on my practice. This proved to be a good decision—for about one year. Then the recession hit my part of the country. Suddenly, the operation of a “cash-only” practice became an oxymoron, as many of the patients with already limited funds lost their jobs. These patients started to seek “free” care at area emergency departments, and the practice income plummeted. My revenue fell by one-half the first year and then one-half of that the next year.
In what would turn out to be my final year of practice ownership, I decided to accept a full-time position as faculty of a distance FNP program. I was practicing “on the side,” although in reality I was in my office full-time and teaching from there. I was already recognizing the difficulties of juggling my roles and responsibilities when a student in one of my classes asked what it would take for me to decide to close my practice, since I was (by this point) making no money from it.
As I pondered that question (my initial response was a quite honest “I don’t know”), I stepped onto the road toward closing my practice. From a business perspective, there was little point in keeping the practice open. However, from an emotional point of view, I had invested so much in building my dream—and, by extension, so had my family—that closing the practice seemed unthinkable.
THE DECISION
Opening a practice is a time of joy, pride, and a sense of accomplishment; closing that same practice induces a period of reflection, sadness, and even anger that circumstances did not allow continued operation. While financial considerations play a significant role in the decision to close a practice, they may not be the only, or the deciding, factor.
In my case, the financial shortfall of the practice led me to accept a teaching position in order to earn living expenses. The result of that decision was that my attention became divided: Sometimes I was in meetings or interacting with students—and for a few weeks per year, I was out of town—which meant less time devoted to seeing patients. Conversely, if I was with a patient, I of course could not be available to my students. Over time, I started to feel that I was not giving my all to either role as I shifted back and forth. Having given 100% to each of these roles at previous points in my career, I now felt that I was cheating my patients and my students.
The decision to close a practice may take months or even years before the actual process is started. I lived with my conundrum for about a year before I made the decision to close. I was exhausted—and while I was relieved to have the burden of deciding off my shoulders, it was now time to do the work of closing a practice.

NOTIFYING YOUR STAKEHOLDERS
Once the decision to close a practice is reached, the provider/owner ceases to exist in a vacuum. There are stakeholders who need to be notified—some obvious, some less so.
I started by breaking the news to my family, the people who had supported me in opening my practice (and even helped me find and refurbish furniture for my waiting room!). Although they had been aware of my internal debate, they had not lived with the decision process as I had. Having resolved at least some of my own emotions, I now had to watch others experience many of those same feelings.
Next, I had to tell my employees of the decision. Through attrition, my staff had already shrunk to two: a receptionist and a part-time licensed vocational nurse (LVN). Like my family, they had to process their own emotions about the closure. I had anticipated that the people who worked for me, concerned about their future, might choose to accept another job before we officially closed. My LVN—who had observed the practice dwindling in the preceding two years—seemed prepared for my decision. She stuck it out with me until the end and was a huge help with the influx of patients requesting records. (My MD—required by Texas law to delegate prescriptive authority to me—had already relocated his practice and was ill, so he was content with my decision.)
Of course, the biggest stakeholders in a practice are the patients. Notifying them of the impending closure is the most important action you will take (aside from making the decision to close). Although you can place notices in the local media (newspapers, TV, radio) to announce the closure of your practice to the community, you should send a notification letter directly to your patients. It should be sent at least 60 to 90 days before the closure date—and certainly not less than 30 days in any case—giving patients adequate time to find new providers and arrange for their records to be transferred.1,2 The letter should include
- A statement of gratitude for the patient’s business
- The dates of the transition period
- What is expected of the patient (eg, does he/she need to come and pick up his/her records?)
- An explanation for the closure3
I composed a letter to be sent to all patients who had been seen within the past 18 months. In it, I thanked them for being a part of the practice and gave them 60 days’ notice of the intent to close. For many patients, this was an emotional time; many understandably worried how their health care needs would be met in the future. Some responded with sadness that I had not been able to make the practice a success.
AVOIDING “ABANDONMENT”
Ideally, a provider who wants to get out of the business should seek to sell the practice—but this is not always feasible.3,4 When closure is the best (or only) option, it is important to avoid even the appearance of abandonment.
Besides giving adequate notice of practice closure, providers must have a plan for the dispersal of patients.1 Be prepared to give recommendations for new providers. Depending on the practice location (rural or urban), options may vary.
I made a concerted effort to refer patients to new providers, with the caveat that if the patient did not feel a particular provider was a good match, he/she should seek another provider of his/her choosing. Unlike in a purchased practice, where patients “go with” the practice, patients from a closed practice may be referred to one, several, or even many other providers.5
Provisions must be made to store patient records so that they are retrievable for a specified period of time. The requirements vary by state, so consultation of the state board’s rules and regulations—and/or an attorney—is in order.3 In general, the proscribed time period is seven to 10 years for adults and seven to 10 years after the patient turns 18 for pediatric patients.2 In some states, the retention time may be as short as three years for adults.1
OTHER PRACTICAL CONSIDERATIONS
While people will be your priority as you work through the process of closing, you will have “stuff” to deal with. What will you do with the furnishings and equipment? Obviously, anything that was borrowed can be returned. Beyond that, your options are to sell (to another provider or even a patient), donate, or repurpose items.
The orthopedic exam table from my practice went to a private school for their athletic training facility. Screens went to my neighbor, a chiropractor. My preschool-aged grandsons were thrilled to be given the children’s art supplies and books that had once graced my waiting area. One of my patients bought some decorative vases and a bookcase. The painting that had been carefully chosen to pull together my waiting room now hangs in my library at home.
As the closure date approaches, the practice environment may begin to look bare as furnishings are sold or moved. One item you will want to buy, however, is a fresh ink cartridge for your copier/printer. As patients request documents, you’ll use it!
RESPONSE AND AFTERMATH
The practice may be very busy immediately following the receipt of notification letters—but don’t be fooled into thinking you have made the wrong decision. The first month after the letters went out advising of the closure, my practice was busier than it had ever been! This tapered off in the second month, though.
Most patients, once they’ve heard the news, will want prescription refills and/or their records. Some may just want to know what happened to result in the closure. Remember that to the patient, this seems like a sudden decision—no matter how long you have deliberated about it.
What surprised me most, however, was that new patients continued to present to the practice, seeking care for acute issues. While I did provide this, I made them aware from the beginning that the practice was in the process of closing and that I could not assume the responsibility of being their primary provider. I made sure to provide these patients with recommendations for other providers.
Slowly the rush will settle down, as patients start to move on to other providers. A few may drop in to see you socially. On the day I closed my practice, several patients came in just to say goodbye and wish me well.
The last things I did in my practice were turn off the lights and leave a sign on the door stating that the practice was now closed.
RECOVERY
The time needed to recover from the closure of a practice will differ. Factors include how long the practice was open and how the clinician normally deals with a setback.6 For some, relief that the pressures of ownership are over may be the predominant emotion. Having a steady, stable salary in a new position goes a long way toward making the transition easier! Although if possible, take some time between closing the practice and starting a new job.
Do not be surprised if negative emotions manifest at odd times, as feelings of sadness, regret, and even a sense of failure are worked through. Life does go on—and nurse practitioners are resilient. Find a way to use the knowledge gained from your practice in your new endeavors, whatever they may be.
For me, the healing process would have started sooner if I had acknowledged how difficult giving up the dream of having my own practice was. If I had sought out others with similar experience or even talked with a counselor, my journey through this process could have been expedited. When I started to share my story, one frequently asked question was “How did you get through this?” This showed me that others could learn from my experience.
For many nurse practitioners, having your own practice is the culmination of many years of planning and anticipation. I worked as an NP for 14 years in practices operated by others—hospitals and physicians—before I opened my own practice. During those years, I had observed which ways of doing things appeared productive and healing to me and which did not.
When the time came, having seen a need for more affordable health care that was not predicated on the assumption that every patient had health insurance, I opened a cash-only practice in the town where I resided. By eliminating the need for personnel and apparatus dedicated to insurance filing, I was able to charge about half of what other practices in the same location did for identical services. My chief goal was to be of service to the community, not to make the most money possible. I anticipated that volume would make up for the lower prices in the long run.
For about four years, our revenue grew slowly. I decided to risk all and stop teaching part-time in order to focus exclusively on my practice. This proved to be a good decision—for about one year. Then the recession hit my part of the country. Suddenly, the operation of a “cash-only” practice became an oxymoron, as many of the patients with already limited funds lost their jobs. These patients started to seek “free” care at area emergency departments, and the practice income plummeted. My revenue fell by one-half the first year and then one-half of that the next year.
In what would turn out to be my final year of practice ownership, I decided to accept a full-time position as faculty of a distance FNP program. I was practicing “on the side,” although in reality I was in my office full-time and teaching from there. I was already recognizing the difficulties of juggling my roles and responsibilities when a student in one of my classes asked what it would take for me to decide to close my practice, since I was (by this point) making no money from it.
As I pondered that question (my initial response was a quite honest “I don’t know”), I stepped onto the road toward closing my practice. From a business perspective, there was little point in keeping the practice open. However, from an emotional point of view, I had invested so much in building my dream—and, by extension, so had my family—that closing the practice seemed unthinkable.
THE DECISION
Opening a practice is a time of joy, pride, and a sense of accomplishment; closing that same practice induces a period of reflection, sadness, and even anger that circumstances did not allow continued operation. While financial considerations play a significant role in the decision to close a practice, they may not be the only, or the deciding, factor.
In my case, the financial shortfall of the practice led me to accept a teaching position in order to earn living expenses. The result of that decision was that my attention became divided: Sometimes I was in meetings or interacting with students—and for a few weeks per year, I was out of town—which meant less time devoted to seeing patients. Conversely, if I was with a patient, I of course could not be available to my students. Over time, I started to feel that I was not giving my all to either role as I shifted back and forth. Having given 100% to each of these roles at previous points in my career, I now felt that I was cheating my patients and my students.
The decision to close a practice may take months or even years before the actual process is started. I lived with my conundrum for about a year before I made the decision to close. I was exhausted—and while I was relieved to have the burden of deciding off my shoulders, it was now time to do the work of closing a practice.

NOTIFYING YOUR STAKEHOLDERS
Once the decision to close a practice is reached, the provider/owner ceases to exist in a vacuum. There are stakeholders who need to be notified—some obvious, some less so.
I started by breaking the news to my family, the people who had supported me in opening my practice (and even helped me find and refurbish furniture for my waiting room!). Although they had been aware of my internal debate, they had not lived with the decision process as I had. Having resolved at least some of my own emotions, I now had to watch others experience many of those same feelings.
Next, I had to tell my employees of the decision. Through attrition, my staff had already shrunk to two: a receptionist and a part-time licensed vocational nurse (LVN). Like my family, they had to process their own emotions about the closure. I had anticipated that the people who worked for me, concerned about their future, might choose to accept another job before we officially closed. My LVN—who had observed the practice dwindling in the preceding two years—seemed prepared for my decision. She stuck it out with me until the end and was a huge help with the influx of patients requesting records. (My MD—required by Texas law to delegate prescriptive authority to me—had already relocated his practice and was ill, so he was content with my decision.)
Of course, the biggest stakeholders in a practice are the patients. Notifying them of the impending closure is the most important action you will take (aside from making the decision to close). Although you can place notices in the local media (newspapers, TV, radio) to announce the closure of your practice to the community, you should send a notification letter directly to your patients. It should be sent at least 60 to 90 days before the closure date—and certainly not less than 30 days in any case—giving patients adequate time to find new providers and arrange for their records to be transferred.1,2 The letter should include
- A statement of gratitude for the patient’s business
- The dates of the transition period
- What is expected of the patient (eg, does he/she need to come and pick up his/her records?)
- An explanation for the closure3
I composed a letter to be sent to all patients who had been seen within the past 18 months. In it, I thanked them for being a part of the practice and gave them 60 days’ notice of the intent to close. For many patients, this was an emotional time; many understandably worried how their health care needs would be met in the future. Some responded with sadness that I had not been able to make the practice a success.
AVOIDING “ABANDONMENT”
Ideally, a provider who wants to get out of the business should seek to sell the practice—but this is not always feasible.3,4 When closure is the best (or only) option, it is important to avoid even the appearance of abandonment.
Besides giving adequate notice of practice closure, providers must have a plan for the dispersal of patients.1 Be prepared to give recommendations for new providers. Depending on the practice location (rural or urban), options may vary.
I made a concerted effort to refer patients to new providers, with the caveat that if the patient did not feel a particular provider was a good match, he/she should seek another provider of his/her choosing. Unlike in a purchased practice, where patients “go with” the practice, patients from a closed practice may be referred to one, several, or even many other providers.5
Provisions must be made to store patient records so that they are retrievable for a specified period of time. The requirements vary by state, so consultation of the state board’s rules and regulations—and/or an attorney—is in order.3 In general, the proscribed time period is seven to 10 years for adults and seven to 10 years after the patient turns 18 for pediatric patients.2 In some states, the retention time may be as short as three years for adults.1
OTHER PRACTICAL CONSIDERATIONS
While people will be your priority as you work through the process of closing, you will have “stuff” to deal with. What will you do with the furnishings and equipment? Obviously, anything that was borrowed can be returned. Beyond that, your options are to sell (to another provider or even a patient), donate, or repurpose items.
The orthopedic exam table from my practice went to a private school for their athletic training facility. Screens went to my neighbor, a chiropractor. My preschool-aged grandsons were thrilled to be given the children’s art supplies and books that had once graced my waiting area. One of my patients bought some decorative vases and a bookcase. The painting that had been carefully chosen to pull together my waiting room now hangs in my library at home.
As the closure date approaches, the practice environment may begin to look bare as furnishings are sold or moved. One item you will want to buy, however, is a fresh ink cartridge for your copier/printer. As patients request documents, you’ll use it!
RESPONSE AND AFTERMATH
The practice may be very busy immediately following the receipt of notification letters—but don’t be fooled into thinking you have made the wrong decision. The first month after the letters went out advising of the closure, my practice was busier than it had ever been! This tapered off in the second month, though.
Most patients, once they’ve heard the news, will want prescription refills and/or their records. Some may just want to know what happened to result in the closure. Remember that to the patient, this seems like a sudden decision—no matter how long you have deliberated about it.
What surprised me most, however, was that new patients continued to present to the practice, seeking care for acute issues. While I did provide this, I made them aware from the beginning that the practice was in the process of closing and that I could not assume the responsibility of being their primary provider. I made sure to provide these patients with recommendations for other providers.
Slowly the rush will settle down, as patients start to move on to other providers. A few may drop in to see you socially. On the day I closed my practice, several patients came in just to say goodbye and wish me well.
The last things I did in my practice were turn off the lights and leave a sign on the door stating that the practice was now closed.
RECOVERY
The time needed to recover from the closure of a practice will differ. Factors include how long the practice was open and how the clinician normally deals with a setback.6 For some, relief that the pressures of ownership are over may be the predominant emotion. Having a steady, stable salary in a new position goes a long way toward making the transition easier! Although if possible, take some time between closing the practice and starting a new job.
Do not be surprised if negative emotions manifest at odd times, as feelings of sadness, regret, and even a sense of failure are worked through. Life does go on—and nurse practitioners are resilient. Find a way to use the knowledge gained from your practice in your new endeavors, whatever they may be.
For me, the healing process would have started sooner if I had acknowledged how difficult giving up the dream of having my own practice was. If I had sought out others with similar experience or even talked with a counselor, my journey through this process could have been expedited. When I started to share my story, one frequently asked question was “How did you get through this?” This showed me that others could learn from my experience.
1. Tatooles JJ, Brunell A. What you need to know before leaving a medical practice: a primer for moving on. AAOS NOW. 2015;22-23.
2. Kern SI. Take these steps if selling or closing a practice. Med Econ. 2010;87(20):66.
3. Weiss GG. How to close a practice. Med Econ. 2004;81:69.
4. Zaumeyer C. How to Start an Independent Practice: The Nurse Practitioner’s Guide to Success. Philadelphia: F. A. Davis, Publishers; 2003.
5. Barrett W. The legal corner: Eleven essential steps to purchasing or selling a medical practice. J Med Pract Manage. 2014;29(5):275-277.
6. McBride JL. Personal issues to consider before leaving independent practice. Fam Pract Manag. 2013;20(4):9-12.
1. Tatooles JJ, Brunell A. What you need to know before leaving a medical practice: a primer for moving on. AAOS NOW. 2015;22-23.
2. Kern SI. Take these steps if selling or closing a practice. Med Econ. 2010;87(20):66.
3. Weiss GG. How to close a practice. Med Econ. 2004;81:69.
4. Zaumeyer C. How to Start an Independent Practice: The Nurse Practitioner’s Guide to Success. Philadelphia: F. A. Davis, Publishers; 2003.
5. Barrett W. The legal corner: Eleven essential steps to purchasing or selling a medical practice. J Med Pract Manage. 2014;29(5):275-277.
6. McBride JL. Personal issues to consider before leaving independent practice. Fam Pract Manag. 2013;20(4):9-12.
Do fellowship programs help prepare general surgery residents for board exams?
WASHINGTON – Pass rates on the general surgery board exams were significantly higher for programs in which residents trained alongside surgical fellows, according to a retrospective study presented at the annual clinical congress of the American College of Surgeons.
The study adds another perspective to the ongoing debate about the impact of fellowships on general surgery residency and residency programs. Mohammed J. Al Fayyadh, MD, of the University of Texas Health Science Center at San Antonio and his associates investigated the impact of fellowships on program pass rates for general surgery boards. They reviewed American Board of Surgery exam data for the classes of 2010-2014, which included 242 programs (a total of 5,191 resident examinees), of which 148 had fellows participating (3,767 resident examinees).
The findings suggest that having fellows in a program has a positive impact on the pass rates of those taking the ABS general surgery exam. Pass rates were significantly higher for general surgery programs with fellows. This trend held for all measures studied: Qualifying (written) exam (88% vs. 86%), certifying (oral) exam (83% vs. 80%), and combined exams (74% vs. 69%). Differences between the groups were statistically significant.
The pass rates tended to be higher in programs with higher Fel:Res ratios. For example, programs with a 1.5:1 Fel:Res ratio had the highest pass rates for the qualifying, certifying, and combined exams.
The impact of subspecialty fellowships on general surgery residencies has been the subject of research and debate in recent years. Some studies have suggested that subspecialty training for fellows has meant that general surgery residents have less opportunity to operate in areas such as trauma (“Trauma operative training declining for general surgery residents,” ACS Surgery News, Oct. 4, 2016) and vascular surgery (Ann Vasc Surg. 2016;33;98-102).
Taken in this context, it is possible that the programs with more fellows simply recruit more competitive residents who tend to do better on exams. However, this could also reflect more resources in fellowship programs that are available to all trainees or better mentorship opportunities, said Dr. Al Fayyadh. He concluded that more research is needed to tease out the impact of fellowship programs on general surgery resident education.
Dr. Al Fayyadh had no disclosures.
WASHINGTON – Pass rates on the general surgery board exams were significantly higher for programs in which residents trained alongside surgical fellows, according to a retrospective study presented at the annual clinical congress of the American College of Surgeons.
The study adds another perspective to the ongoing debate about the impact of fellowships on general surgery residency and residency programs. Mohammed J. Al Fayyadh, MD, of the University of Texas Health Science Center at San Antonio and his associates investigated the impact of fellowships on program pass rates for general surgery boards. They reviewed American Board of Surgery exam data for the classes of 2010-2014, which included 242 programs (a total of 5,191 resident examinees), of which 148 had fellows participating (3,767 resident examinees).
The findings suggest that having fellows in a program has a positive impact on the pass rates of those taking the ABS general surgery exam. Pass rates were significantly higher for general surgery programs with fellows. This trend held for all measures studied: Qualifying (written) exam (88% vs. 86%), certifying (oral) exam (83% vs. 80%), and combined exams (74% vs. 69%). Differences between the groups were statistically significant.
The pass rates tended to be higher in programs with higher Fel:Res ratios. For example, programs with a 1.5:1 Fel:Res ratio had the highest pass rates for the qualifying, certifying, and combined exams.
The impact of subspecialty fellowships on general surgery residencies has been the subject of research and debate in recent years. Some studies have suggested that subspecialty training for fellows has meant that general surgery residents have less opportunity to operate in areas such as trauma (“Trauma operative training declining for general surgery residents,” ACS Surgery News, Oct. 4, 2016) and vascular surgery (Ann Vasc Surg. 2016;33;98-102).
Taken in this context, it is possible that the programs with more fellows simply recruit more competitive residents who tend to do better on exams. However, this could also reflect more resources in fellowship programs that are available to all trainees or better mentorship opportunities, said Dr. Al Fayyadh. He concluded that more research is needed to tease out the impact of fellowship programs on general surgery resident education.
Dr. Al Fayyadh had no disclosures.
WASHINGTON – Pass rates on the general surgery board exams were significantly higher for programs in which residents trained alongside surgical fellows, according to a retrospective study presented at the annual clinical congress of the American College of Surgeons.
The study adds another perspective to the ongoing debate about the impact of fellowships on general surgery residency and residency programs. Mohammed J. Al Fayyadh, MD, of the University of Texas Health Science Center at San Antonio and his associates investigated the impact of fellowships on program pass rates for general surgery boards. They reviewed American Board of Surgery exam data for the classes of 2010-2014, which included 242 programs (a total of 5,191 resident examinees), of which 148 had fellows participating (3,767 resident examinees).
The findings suggest that having fellows in a program has a positive impact on the pass rates of those taking the ABS general surgery exam. Pass rates were significantly higher for general surgery programs with fellows. This trend held for all measures studied: Qualifying (written) exam (88% vs. 86%), certifying (oral) exam (83% vs. 80%), and combined exams (74% vs. 69%). Differences between the groups were statistically significant.
The pass rates tended to be higher in programs with higher Fel:Res ratios. For example, programs with a 1.5:1 Fel:Res ratio had the highest pass rates for the qualifying, certifying, and combined exams.
The impact of subspecialty fellowships on general surgery residencies has been the subject of research and debate in recent years. Some studies have suggested that subspecialty training for fellows has meant that general surgery residents have less opportunity to operate in areas such as trauma (“Trauma operative training declining for general surgery residents,” ACS Surgery News, Oct. 4, 2016) and vascular surgery (Ann Vasc Surg. 2016;33;98-102).
Taken in this context, it is possible that the programs with more fellows simply recruit more competitive residents who tend to do better on exams. However, this could also reflect more resources in fellowship programs that are available to all trainees or better mentorship opportunities, said Dr. Al Fayyadh. He concluded that more research is needed to tease out the impact of fellowship programs on general surgery resident education.
Dr. Al Fayyadh had no disclosures.
AT THE ACS CLINICAL CONGRESS
It’s elementary: Watson aids in breast cancer decisions
SAN ANTONIO – When oncologists at Manipal Hospitals in Bangalore, India, need help with a breast cancer conundrum, they can make the electronic equivalent of the famous cry for help “Watson, come here, I want you!”
In this case, Watson is not the real-life sidekick of Alexander Graham Bell or the fictional companion of Sherlock Holmes, but Watson for Oncology (WFO), an IBM-created artificial intelligence platform being developed in the United States and used in clinical practice in India to help guide clinical decision making but not to replace clinicians’ judgment, explained S.P. Somashekhar, MBBS, MS, MCH, FRCS, chairman of the Manipal Comprehensive Cancer Center.
This is no game
WFO is the clinical cousin of the artificial intelligence platform, also named Watson, that beat all-time champion Ken Jennings on the television game show “Jeopardy!” The system was named after Thomas J. Watson, IBM’s first chief executive officer.
The version of Watson used in India was developed by physicians and investigators at Memorial Sloan Kettering Cancer Center (MSKCC) in New York and by IBM. Watson for Oncology is fed national treatment guidelines, more than 1,000 training cases, MSKCC internal guidelines, and medical literature curated by MSKCC; it then chews over the data and spits out evidence-based recommendations.
At Manipal Hospitals, the electronic medical record contains an “Ask Watson” button that allows clinicians to interrogate the artificial entity’s vast stores of medical data to offer recommendations that clinicians can then use, modify, or reject at their discretion.
The system analyzes more than 100 patient attributes and then offers options with a green label for “recommended,” amber label “for consideration,” or a red label for “not recommended.”
Concordance study
At SABCS, Dr. Somashekhar presented results of a study evaluating the concordance of treatment recommendations between WFO and the members of the Manipal Multidisciplinary Tumor Board (MTB).
They looked at data on 638 patients treated in their hospital system over the three prior years, assessing the MTBs initial, best joint decision at the time of the original treatment decision (T1), and compared it with WFO’s recommendation made in 2016 (T2) and with a blinded MTB re-review of nonconcordant cases, also made in 2016.
Evaluating concordance by stage, they found that, for 514 cases of nonmetastatic disease, there was 79% concordance between the original MTB decisions and WFO’s recommendations for therapies in the combined “for consideration” and “recommended” categories.
For 124 cases of metastatic disease, however, Watson and its human counterparts were more frequently at odds, with only a 46% concordance.
In a subset analysis by receptor status, the investigators found that Watson was best – that is, most highly concordant – in triple-negative disease, with a 67.9% concordance in regard to MTB choices. In contrast, for patients with metastatic disease negative for the human epidermal growth factor receptor-2 (HER2), the concordance rate was a low 35%.
Dr. Somashekhar commented that part of the explanation for the discordant concordance rates by tumor subtype can be attributed to the fact that patients with triple-negative breast cancers have fewer treatment options than patients with HER2 negative–only tumors, who have a much broader array of possibilities.
One area where WFO has its two-legged colleagues beaten hands down, however, is in the time it takes to capture and analyze data: humans took a mean of 20 minutes, Watson a median of 40 seconds.
The investigators acknowledged that WFO represents a further step toward personalized medicine, but emphasized that software will never replace the doctor-patient relationship or override the treating physician’s decisions.
‘This one would actually help’
At the briefing, moderator C. Kent Osborne, MD, from Baylor College of Medicine, Houston, commented, “I guess this not going to put us out of business as physicians – at least I hope not.”
Asked whether WFO could be a useful clinical tool or just another nuisance task added to an already overcrowded clinic schedule, Dr. Osborne responded, “I think this one would actually help.”
This study was investigative and received no external funding. Dr. Somashekhar, Dr. Osborne, and Dr. Blaes reported no conflicts of interest.
SAN ANTONIO – When oncologists at Manipal Hospitals in Bangalore, India, need help with a breast cancer conundrum, they can make the electronic equivalent of the famous cry for help “Watson, come here, I want you!”
In this case, Watson is not the real-life sidekick of Alexander Graham Bell or the fictional companion of Sherlock Holmes, but Watson for Oncology (WFO), an IBM-created artificial intelligence platform being developed in the United States and used in clinical practice in India to help guide clinical decision making but not to replace clinicians’ judgment, explained S.P. Somashekhar, MBBS, MS, MCH, FRCS, chairman of the Manipal Comprehensive Cancer Center.
This is no game
WFO is the clinical cousin of the artificial intelligence platform, also named Watson, that beat all-time champion Ken Jennings on the television game show “Jeopardy!” The system was named after Thomas J. Watson, IBM’s first chief executive officer.
The version of Watson used in India was developed by physicians and investigators at Memorial Sloan Kettering Cancer Center (MSKCC) in New York and by IBM. Watson for Oncology is fed national treatment guidelines, more than 1,000 training cases, MSKCC internal guidelines, and medical literature curated by MSKCC; it then chews over the data and spits out evidence-based recommendations.
At Manipal Hospitals, the electronic medical record contains an “Ask Watson” button that allows clinicians to interrogate the artificial entity’s vast stores of medical data to offer recommendations that clinicians can then use, modify, or reject at their discretion.
The system analyzes more than 100 patient attributes and then offers options with a green label for “recommended,” amber label “for consideration,” or a red label for “not recommended.”
Concordance study
At SABCS, Dr. Somashekhar presented results of a study evaluating the concordance of treatment recommendations between WFO and the members of the Manipal Multidisciplinary Tumor Board (MTB).
They looked at data on 638 patients treated in their hospital system over the three prior years, assessing the MTBs initial, best joint decision at the time of the original treatment decision (T1), and compared it with WFO’s recommendation made in 2016 (T2) and with a blinded MTB re-review of nonconcordant cases, also made in 2016.
Evaluating concordance by stage, they found that, for 514 cases of nonmetastatic disease, there was 79% concordance between the original MTB decisions and WFO’s recommendations for therapies in the combined “for consideration” and “recommended” categories.
For 124 cases of metastatic disease, however, Watson and its human counterparts were more frequently at odds, with only a 46% concordance.
In a subset analysis by receptor status, the investigators found that Watson was best – that is, most highly concordant – in triple-negative disease, with a 67.9% concordance in regard to MTB choices. In contrast, for patients with metastatic disease negative for the human epidermal growth factor receptor-2 (HER2), the concordance rate was a low 35%.
Dr. Somashekhar commented that part of the explanation for the discordant concordance rates by tumor subtype can be attributed to the fact that patients with triple-negative breast cancers have fewer treatment options than patients with HER2 negative–only tumors, who have a much broader array of possibilities.
One area where WFO has its two-legged colleagues beaten hands down, however, is in the time it takes to capture and analyze data: humans took a mean of 20 minutes, Watson a median of 40 seconds.
The investigators acknowledged that WFO represents a further step toward personalized medicine, but emphasized that software will never replace the doctor-patient relationship or override the treating physician’s decisions.
‘This one would actually help’
At the briefing, moderator C. Kent Osborne, MD, from Baylor College of Medicine, Houston, commented, “I guess this not going to put us out of business as physicians – at least I hope not.”
Asked whether WFO could be a useful clinical tool or just another nuisance task added to an already overcrowded clinic schedule, Dr. Osborne responded, “I think this one would actually help.”
This study was investigative and received no external funding. Dr. Somashekhar, Dr. Osborne, and Dr. Blaes reported no conflicts of interest.
SAN ANTONIO – When oncologists at Manipal Hospitals in Bangalore, India, need help with a breast cancer conundrum, they can make the electronic equivalent of the famous cry for help “Watson, come here, I want you!”
In this case, Watson is not the real-life sidekick of Alexander Graham Bell or the fictional companion of Sherlock Holmes, but Watson for Oncology (WFO), an IBM-created artificial intelligence platform being developed in the United States and used in clinical practice in India to help guide clinical decision making but not to replace clinicians’ judgment, explained S.P. Somashekhar, MBBS, MS, MCH, FRCS, chairman of the Manipal Comprehensive Cancer Center.
This is no game
WFO is the clinical cousin of the artificial intelligence platform, also named Watson, that beat all-time champion Ken Jennings on the television game show “Jeopardy!” The system was named after Thomas J. Watson, IBM’s first chief executive officer.
The version of Watson used in India was developed by physicians and investigators at Memorial Sloan Kettering Cancer Center (MSKCC) in New York and by IBM. Watson for Oncology is fed national treatment guidelines, more than 1,000 training cases, MSKCC internal guidelines, and medical literature curated by MSKCC; it then chews over the data and spits out evidence-based recommendations.
At Manipal Hospitals, the electronic medical record contains an “Ask Watson” button that allows clinicians to interrogate the artificial entity’s vast stores of medical data to offer recommendations that clinicians can then use, modify, or reject at their discretion.
The system analyzes more than 100 patient attributes and then offers options with a green label for “recommended,” amber label “for consideration,” or a red label for “not recommended.”
Concordance study
At SABCS, Dr. Somashekhar presented results of a study evaluating the concordance of treatment recommendations between WFO and the members of the Manipal Multidisciplinary Tumor Board (MTB).
They looked at data on 638 patients treated in their hospital system over the three prior years, assessing the MTBs initial, best joint decision at the time of the original treatment decision (T1), and compared it with WFO’s recommendation made in 2016 (T2) and with a blinded MTB re-review of nonconcordant cases, also made in 2016.
Evaluating concordance by stage, they found that, for 514 cases of nonmetastatic disease, there was 79% concordance between the original MTB decisions and WFO’s recommendations for therapies in the combined “for consideration” and “recommended” categories.
For 124 cases of metastatic disease, however, Watson and its human counterparts were more frequently at odds, with only a 46% concordance.
In a subset analysis by receptor status, the investigators found that Watson was best – that is, most highly concordant – in triple-negative disease, with a 67.9% concordance in regard to MTB choices. In contrast, for patients with metastatic disease negative for the human epidermal growth factor receptor-2 (HER2), the concordance rate was a low 35%.
Dr. Somashekhar commented that part of the explanation for the discordant concordance rates by tumor subtype can be attributed to the fact that patients with triple-negative breast cancers have fewer treatment options than patients with HER2 negative–only tumors, who have a much broader array of possibilities.
One area where WFO has its two-legged colleagues beaten hands down, however, is in the time it takes to capture and analyze data: humans took a mean of 20 minutes, Watson a median of 40 seconds.
The investigators acknowledged that WFO represents a further step toward personalized medicine, but emphasized that software will never replace the doctor-patient relationship or override the treating physician’s decisions.
‘This one would actually help’
At the briefing, moderator C. Kent Osborne, MD, from Baylor College of Medicine, Houston, commented, “I guess this not going to put us out of business as physicians – at least I hope not.”
Asked whether WFO could be a useful clinical tool or just another nuisance task added to an already overcrowded clinic schedule, Dr. Osborne responded, “I think this one would actually help.”
This study was investigative and received no external funding. Dr. Somashekhar, Dr. Osborne, and Dr. Blaes reported no conflicts of interest.
AT SABCS 2016
Key clinical point: There was good, if imperfect, concordance in breast cancer treatment decisions between the software platform Watson for Oncology and human tumor board members.
Major finding: Concordance on treatment decisions for nonmetastatic breast cancers was 79%; concordance for metastatic cancers was 46%.
Data source: Single-institution study comparing treatment-decision concordance rates between a computerized decision tool and human reviewers.
Disclosures: This study was investigative and received no external funding. Dr. Somashekhar, Dr. Osborne, and Dr. Blaes reported no conflicts of interest.
VIDEO: Watson for Oncology offers electronic curbside consults in breast cancer
SAN ANTONIO – Watson for Oncology or WFO, is the clinical cousin of the IBM-created cognitive computing system best known as the machine that defeated all-time champions on the TV quiz show “Jeopardy!”
WFO, however, has the much more important function of providing oncologists with evidence-based support for clinical decisions. Data being presented here at the San Antonio Breast Cancer Symposium show that in Bangalore, India, where WFO is used in a large hospital system, there is good concordance between tumor board recommendations and WFO’s recommendations about the treatment of breast cancer, although much more work needs to be done. The investigators emphasize that WFO is a highly useful tool that can augment but will not replace clinical judgment, and can never replace the physician-patient relationship.
In this video interview, Andrew Norden, MD, deputy chief health officer for the IBM Watson project, based in Cambridge, Mass., describes how Watson for Oncology works, and how different versions of the Watson platform are being used in medicine throughout the world.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN ANTONIO – Watson for Oncology or WFO, is the clinical cousin of the IBM-created cognitive computing system best known as the machine that defeated all-time champions on the TV quiz show “Jeopardy!”
WFO, however, has the much more important function of providing oncologists with evidence-based support for clinical decisions. Data being presented here at the San Antonio Breast Cancer Symposium show that in Bangalore, India, where WFO is used in a large hospital system, there is good concordance between tumor board recommendations and WFO’s recommendations about the treatment of breast cancer, although much more work needs to be done. The investigators emphasize that WFO is a highly useful tool that can augment but will not replace clinical judgment, and can never replace the physician-patient relationship.
In this video interview, Andrew Norden, MD, deputy chief health officer for the IBM Watson project, based in Cambridge, Mass., describes how Watson for Oncology works, and how different versions of the Watson platform are being used in medicine throughout the world.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN ANTONIO – Watson for Oncology or WFO, is the clinical cousin of the IBM-created cognitive computing system best known as the machine that defeated all-time champions on the TV quiz show “Jeopardy!”
WFO, however, has the much more important function of providing oncologists with evidence-based support for clinical decisions. Data being presented here at the San Antonio Breast Cancer Symposium show that in Bangalore, India, where WFO is used in a large hospital system, there is good concordance between tumor board recommendations and WFO’s recommendations about the treatment of breast cancer, although much more work needs to be done. The investigators emphasize that WFO is a highly useful tool that can augment but will not replace clinical judgment, and can never replace the physician-patient relationship.
In this video interview, Andrew Norden, MD, deputy chief health officer for the IBM Watson project, based in Cambridge, Mass., describes how Watson for Oncology works, and how different versions of the Watson platform are being used in medicine throughout the world.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SABCS 2016
VIDEO: Abemaciclib reduces Ki67 expression in early HR+/HER2– breast cancer
SAN ANTONIO – Abemaciclib, both alone and in combination with anastrozole, significantly reduced Ki67 expression vs. anastrozole monotherapy after 2 weeks of treatment in the NeoMONARCH phase II neoadjuvant clinical trial of postmenopausal patients with hormone receptor–positive, HER2-negative early-stage breast cancer.
The findings, given that a change in Ki67 at 2 weeks in neoadjuvant studies appears to predict improved disease-free survival in adjuvant studies, support continued evaluation of the cyclin-dependent kinase-4 (CDK4) inhibitor for the treatment of patients with early-stage breast cancer, Sara Hurvitz, MD, reported at the San Antonio Breast Cancer Symposium.
“In hormone receptor–positive breast cancers, estrogen stimulates D-type cyclins, resulting in increased activity of CDK4 and CDK6, and then phosphorylate RB – the tumor suppressor protein retinoblastoma – which releases the E2F transcription factor,” explained Dr. Hurvitz of the University of California, Los Angeles.
This in turn ultimately leads to cell cycle progression from G1 to S.
“This increased rate of proliferation can be observed in tumor tissue samples by measuring the expression of Ki67. Blocking CDK4 and CDK6 should lead to a decrease in E2F expression, as well as a drop in the cell cycling and a drop in Ki67,” she said, adding that cell cycle arrest may induce senescence, which may also induce a phenotype that’s characterized by an immune cell infiltrate.
Indeed, in study subjects randomized to receive abemaciclib, treatment was shown to induce profound cell cycle arrest defined by decreased Ki67 and E2F targeted proliferation messenger RNAs, and reduction of expression of genes associated with senescence.
“Abemaciclib alone or in combination with anastrozole significantly reduced the Ki67 expression compared to anastrozole alone after 2 weeks of therapy, based on the geometric mean change and complete cell cycle arrest, and the study did meet its primary endpoint,” she said.
In a video interview, Dr. Hurvitz discussed the study methodology, results, and safety findings, as well as an intriguing observation regarding the effects of treatment on tumor differentiation and immune infiltrates over time.
This study was sponsored by Eli Lilly. Dr. Hurvitz has received renumeration for research and/or travel from Amgen, Bayer, BioMarin, Boehringer Ingelheim, Dignitana, Eli Lilly, Genentech, GSK, Medivation, Merrimack, Novartis, OBI Pharma, Pfizer, Puma Biotechnology, and Roche.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN ANTONIO – Abemaciclib, both alone and in combination with anastrozole, significantly reduced Ki67 expression vs. anastrozole monotherapy after 2 weeks of treatment in the NeoMONARCH phase II neoadjuvant clinical trial of postmenopausal patients with hormone receptor–positive, HER2-negative early-stage breast cancer.
The findings, given that a change in Ki67 at 2 weeks in neoadjuvant studies appears to predict improved disease-free survival in adjuvant studies, support continued evaluation of the cyclin-dependent kinase-4 (CDK4) inhibitor for the treatment of patients with early-stage breast cancer, Sara Hurvitz, MD, reported at the San Antonio Breast Cancer Symposium.
“In hormone receptor–positive breast cancers, estrogen stimulates D-type cyclins, resulting in increased activity of CDK4 and CDK6, and then phosphorylate RB – the tumor suppressor protein retinoblastoma – which releases the E2F transcription factor,” explained Dr. Hurvitz of the University of California, Los Angeles.
This in turn ultimately leads to cell cycle progression from G1 to S.
“This increased rate of proliferation can be observed in tumor tissue samples by measuring the expression of Ki67. Blocking CDK4 and CDK6 should lead to a decrease in E2F expression, as well as a drop in the cell cycling and a drop in Ki67,” she said, adding that cell cycle arrest may induce senescence, which may also induce a phenotype that’s characterized by an immune cell infiltrate.
Indeed, in study subjects randomized to receive abemaciclib, treatment was shown to induce profound cell cycle arrest defined by decreased Ki67 and E2F targeted proliferation messenger RNAs, and reduction of expression of genes associated with senescence.
“Abemaciclib alone or in combination with anastrozole significantly reduced the Ki67 expression compared to anastrozole alone after 2 weeks of therapy, based on the geometric mean change and complete cell cycle arrest, and the study did meet its primary endpoint,” she said.
In a video interview, Dr. Hurvitz discussed the study methodology, results, and safety findings, as well as an intriguing observation regarding the effects of treatment on tumor differentiation and immune infiltrates over time.
This study was sponsored by Eli Lilly. Dr. Hurvitz has received renumeration for research and/or travel from Amgen, Bayer, BioMarin, Boehringer Ingelheim, Dignitana, Eli Lilly, Genentech, GSK, Medivation, Merrimack, Novartis, OBI Pharma, Pfizer, Puma Biotechnology, and Roche.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN ANTONIO – Abemaciclib, both alone and in combination with anastrozole, significantly reduced Ki67 expression vs. anastrozole monotherapy after 2 weeks of treatment in the NeoMONARCH phase II neoadjuvant clinical trial of postmenopausal patients with hormone receptor–positive, HER2-negative early-stage breast cancer.
The findings, given that a change in Ki67 at 2 weeks in neoadjuvant studies appears to predict improved disease-free survival in adjuvant studies, support continued evaluation of the cyclin-dependent kinase-4 (CDK4) inhibitor for the treatment of patients with early-stage breast cancer, Sara Hurvitz, MD, reported at the San Antonio Breast Cancer Symposium.
“In hormone receptor–positive breast cancers, estrogen stimulates D-type cyclins, resulting in increased activity of CDK4 and CDK6, and then phosphorylate RB – the tumor suppressor protein retinoblastoma – which releases the E2F transcription factor,” explained Dr. Hurvitz of the University of California, Los Angeles.
This in turn ultimately leads to cell cycle progression from G1 to S.
“This increased rate of proliferation can be observed in tumor tissue samples by measuring the expression of Ki67. Blocking CDK4 and CDK6 should lead to a decrease in E2F expression, as well as a drop in the cell cycling and a drop in Ki67,” she said, adding that cell cycle arrest may induce senescence, which may also induce a phenotype that’s characterized by an immune cell infiltrate.
Indeed, in study subjects randomized to receive abemaciclib, treatment was shown to induce profound cell cycle arrest defined by decreased Ki67 and E2F targeted proliferation messenger RNAs, and reduction of expression of genes associated with senescence.
“Abemaciclib alone or in combination with anastrozole significantly reduced the Ki67 expression compared to anastrozole alone after 2 weeks of therapy, based on the geometric mean change and complete cell cycle arrest, and the study did meet its primary endpoint,” she said.
In a video interview, Dr. Hurvitz discussed the study methodology, results, and safety findings, as well as an intriguing observation regarding the effects of treatment on tumor differentiation and immune infiltrates over time.
This study was sponsored by Eli Lilly. Dr. Hurvitz has received renumeration for research and/or travel from Amgen, Bayer, BioMarin, Boehringer Ingelheim, Dignitana, Eli Lilly, Genentech, GSK, Medivation, Merrimack, Novartis, OBI Pharma, Pfizer, Puma Biotechnology, and Roche.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SABCS 2016