User login
Lenalidomide shows clinical activity in relapsed/refractory MCL
Lenalidomide alone and in combination showed “clinically significant activity” and no new safety signals in patients with mantle cell lymphoma (MCL) who had previously failed on ibrutinib, according to findings from a retrospective, observational study.
Michael Wang, MD, of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues enrolled 58 MCL patients across 11 study sites. The patients had a median age of 71 years and 88% of patients had received three or more prior therapies. Most had received ibrutinib as monotherapy and used a lenalidomide-containing therapy next.
The overall response rate was 29% (95% confidence interval, 18%-43%). The rate was similar between patients with MCL refractory to ibrutinib and patients who relapsed/progressed on or following ibrutinib use (32% versus 30%, respectively). There was a 14% complete response, though it varied by subgroup with 8% among MCL patients refractory to ibrutinib and 22% among relapsed/progressed patients. There was a 20-week median duration of response, but 82% of responders were censored so the researchers urged caution in interpreting that finding.
Among the 58 patients, more than 80% reported one or more treatment-emergent adverse events during lenalidomide treatment and 20 patients (34%) had serious events. Nine patients (16%) discontinued the drug because of adverse events.
“Lenalidomide addresses an unmet medical need and widens the therapeutic options in a difficult-to-treat patient population,” the researchers wrote.
Read the full study in the Journal of Hematology Oncology (2017 Nov 2;10[1]:171).
[email protected]
On Twitter @maryellenny
Lenalidomide alone and in combination showed “clinically significant activity” and no new safety signals in patients with mantle cell lymphoma (MCL) who had previously failed on ibrutinib, according to findings from a retrospective, observational study.
Michael Wang, MD, of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues enrolled 58 MCL patients across 11 study sites. The patients had a median age of 71 years and 88% of patients had received three or more prior therapies. Most had received ibrutinib as monotherapy and used a lenalidomide-containing therapy next.
The overall response rate was 29% (95% confidence interval, 18%-43%). The rate was similar between patients with MCL refractory to ibrutinib and patients who relapsed/progressed on or following ibrutinib use (32% versus 30%, respectively). There was a 14% complete response, though it varied by subgroup with 8% among MCL patients refractory to ibrutinib and 22% among relapsed/progressed patients. There was a 20-week median duration of response, but 82% of responders were censored so the researchers urged caution in interpreting that finding.
Among the 58 patients, more than 80% reported one or more treatment-emergent adverse events during lenalidomide treatment and 20 patients (34%) had serious events. Nine patients (16%) discontinued the drug because of adverse events.
“Lenalidomide addresses an unmet medical need and widens the therapeutic options in a difficult-to-treat patient population,” the researchers wrote.
Read the full study in the Journal of Hematology Oncology (2017 Nov 2;10[1]:171).
[email protected]
On Twitter @maryellenny
Lenalidomide alone and in combination showed “clinically significant activity” and no new safety signals in patients with mantle cell lymphoma (MCL) who had previously failed on ibrutinib, according to findings from a retrospective, observational study.
Michael Wang, MD, of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues enrolled 58 MCL patients across 11 study sites. The patients had a median age of 71 years and 88% of patients had received three or more prior therapies. Most had received ibrutinib as monotherapy and used a lenalidomide-containing therapy next.
The overall response rate was 29% (95% confidence interval, 18%-43%). The rate was similar between patients with MCL refractory to ibrutinib and patients who relapsed/progressed on or following ibrutinib use (32% versus 30%, respectively). There was a 14% complete response, though it varied by subgroup with 8% among MCL patients refractory to ibrutinib and 22% among relapsed/progressed patients. There was a 20-week median duration of response, but 82% of responders were censored so the researchers urged caution in interpreting that finding.
Among the 58 patients, more than 80% reported one or more treatment-emergent adverse events during lenalidomide treatment and 20 patients (34%) had serious events. Nine patients (16%) discontinued the drug because of adverse events.
“Lenalidomide addresses an unmet medical need and widens the therapeutic options in a difficult-to-treat patient population,” the researchers wrote.
Read the full study in the Journal of Hematology Oncology (2017 Nov 2;10[1]:171).
[email protected]
On Twitter @maryellenny
FROM THE JOURNAL OF HEMATOLOGY & ONCOLOGY
Gastrectomy mortality risk increased fivefold with same-day discharge
NATIONAL HARBOR, MD. – Laparoscopic sleeve gastrectomy has been associated with low mortality, but the mortality is even lower when it includes overnight observation, according to a national database evaluation.
Among patients discharged on the same day, 30-day mortality was 0.1%, but it fell to 0.02% among patients discharged the following day, according to Colette Inaba, MD, a surgery resident at the University of California, Irvine.*
“Surgeons who are considering same-day discharge in sleeve gastrectomy patients should have a low threshold to admit these patients for overnight observation given our findings,” Dr. Inaba reported at an annual meeting presented by the American Society for Metabolic and Bariatric Surgery and The Obesity Society.
Same-day discharge has been associated with an increased mortality risk in previously published descriptive institutional reviews, but this is the first study to evaluate this question through analysis of a national database, according to Dr. Inaba. It was based on 37,301 laparoscopic sleeve gastrectomy cases performed in 2015 and submitted to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database. All participants in this database are accredited bariatric centers.
There were baseline differences between same-day and next-day discharges, but many of these differences conferred the next-day group with higher risk. In particular, the next-day group had significantly higher rates of hypertension, diabetes mellitus, hypercholesterolemia, chronic obstructive pulmonary disease, and sleep apnea. On average, the procedure time was 13 minutes longer in the next-day versus the same-day discharge groups.
In addition to mortality, 30-day morbidity and need for revisions were compared between the two groups, but there were no significant differences between groups in the rates of these outcomes.
Overall, the baseline demographics of the patients in same-day and next-day groups were comparable, according to Dr. Inaba. She described the population as predominantly female and white with an average body mass index of 45 kg/m2. In this analysis, only primary procedures (excluding redos and revisions) were included.
Relative to the next-day discharge cases, a significantly higher percentage of same-day discharge procedures were performed with a surgical tech or another provider rather than a designated first-assist surgeon, according to Dr. Inaba. For next-day cases, a higher percentage was performed with the participation of fellows or surgical residents. There were fewer swallow studies performed before discharge in the same-day discharge group.
Very similar results were generated by a study evaluating same-day discharge after laparoscopic Roux-en-Y gastric bypass, according to John M. Morton, MD, chief of bariatric and minimally invasive surgery, Stanford (Calif.) University. Dr. Morton, first author of the study and moderator of the session in which Dr. Inaba presented the LSG data, reported that same-day discharge in that study was also associated with a trend for an increased risk of serious complications (Ann Surg. 2014;259:286-92).
“Same-day discharge is often reimbursed at a lower rate, so there is less pay and patients are at greater risk of harm,” Dr. Morton said.
The reasons that same-day discharge is associated with higher mortality cannot be derived from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database, but, Dr. Inaba said, “Our thought is it is a function of failure to rescue patients from respiratory complications.” She acknowledged that this is a speculative assessment not supported by data, but she suggested that history of sleep apnea might be a particular indication to consider next-day discharge.
Dr. Inaba reports no financial relationships relevant to this topic.
Correction, 12/4/17: An earlier version of this article misstated the 30-day mortality among patients discharged the next day.
NATIONAL HARBOR, MD. – Laparoscopic sleeve gastrectomy has been associated with low mortality, but the mortality is even lower when it includes overnight observation, according to a national database evaluation.
Among patients discharged on the same day, 30-day mortality was 0.1%, but it fell to 0.02% among patients discharged the following day, according to Colette Inaba, MD, a surgery resident at the University of California, Irvine.*
“Surgeons who are considering same-day discharge in sleeve gastrectomy patients should have a low threshold to admit these patients for overnight observation given our findings,” Dr. Inaba reported at an annual meeting presented by the American Society for Metabolic and Bariatric Surgery and The Obesity Society.
Same-day discharge has been associated with an increased mortality risk in previously published descriptive institutional reviews, but this is the first study to evaluate this question through analysis of a national database, according to Dr. Inaba. It was based on 37,301 laparoscopic sleeve gastrectomy cases performed in 2015 and submitted to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database. All participants in this database are accredited bariatric centers.
There were baseline differences between same-day and next-day discharges, but many of these differences conferred the next-day group with higher risk. In particular, the next-day group had significantly higher rates of hypertension, diabetes mellitus, hypercholesterolemia, chronic obstructive pulmonary disease, and sleep apnea. On average, the procedure time was 13 minutes longer in the next-day versus the same-day discharge groups.
In addition to mortality, 30-day morbidity and need for revisions were compared between the two groups, but there were no significant differences between groups in the rates of these outcomes.
Overall, the baseline demographics of the patients in same-day and next-day groups were comparable, according to Dr. Inaba. She described the population as predominantly female and white with an average body mass index of 45 kg/m2. In this analysis, only primary procedures (excluding redos and revisions) were included.
Relative to the next-day discharge cases, a significantly higher percentage of same-day discharge procedures were performed with a surgical tech or another provider rather than a designated first-assist surgeon, according to Dr. Inaba. For next-day cases, a higher percentage was performed with the participation of fellows or surgical residents. There were fewer swallow studies performed before discharge in the same-day discharge group.
Very similar results were generated by a study evaluating same-day discharge after laparoscopic Roux-en-Y gastric bypass, according to John M. Morton, MD, chief of bariatric and minimally invasive surgery, Stanford (Calif.) University. Dr. Morton, first author of the study and moderator of the session in which Dr. Inaba presented the LSG data, reported that same-day discharge in that study was also associated with a trend for an increased risk of serious complications (Ann Surg. 2014;259:286-92).
“Same-day discharge is often reimbursed at a lower rate, so there is less pay and patients are at greater risk of harm,” Dr. Morton said.
The reasons that same-day discharge is associated with higher mortality cannot be derived from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database, but, Dr. Inaba said, “Our thought is it is a function of failure to rescue patients from respiratory complications.” She acknowledged that this is a speculative assessment not supported by data, but she suggested that history of sleep apnea might be a particular indication to consider next-day discharge.
Dr. Inaba reports no financial relationships relevant to this topic.
Correction, 12/4/17: An earlier version of this article misstated the 30-day mortality among patients discharged the next day.
NATIONAL HARBOR, MD. – Laparoscopic sleeve gastrectomy has been associated with low mortality, but the mortality is even lower when it includes overnight observation, according to a national database evaluation.
Among patients discharged on the same day, 30-day mortality was 0.1%, but it fell to 0.02% among patients discharged the following day, according to Colette Inaba, MD, a surgery resident at the University of California, Irvine.*
“Surgeons who are considering same-day discharge in sleeve gastrectomy patients should have a low threshold to admit these patients for overnight observation given our findings,” Dr. Inaba reported at an annual meeting presented by the American Society for Metabolic and Bariatric Surgery and The Obesity Society.
Same-day discharge has been associated with an increased mortality risk in previously published descriptive institutional reviews, but this is the first study to evaluate this question through analysis of a national database, according to Dr. Inaba. It was based on 37,301 laparoscopic sleeve gastrectomy cases performed in 2015 and submitted to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database. All participants in this database are accredited bariatric centers.
There were baseline differences between same-day and next-day discharges, but many of these differences conferred the next-day group with higher risk. In particular, the next-day group had significantly higher rates of hypertension, diabetes mellitus, hypercholesterolemia, chronic obstructive pulmonary disease, and sleep apnea. On average, the procedure time was 13 minutes longer in the next-day versus the same-day discharge groups.
In addition to mortality, 30-day morbidity and need for revisions were compared between the two groups, but there were no significant differences between groups in the rates of these outcomes.
Overall, the baseline demographics of the patients in same-day and next-day groups were comparable, according to Dr. Inaba. She described the population as predominantly female and white with an average body mass index of 45 kg/m2. In this analysis, only primary procedures (excluding redos and revisions) were included.
Relative to the next-day discharge cases, a significantly higher percentage of same-day discharge procedures were performed with a surgical tech or another provider rather than a designated first-assist surgeon, according to Dr. Inaba. For next-day cases, a higher percentage was performed with the participation of fellows or surgical residents. There were fewer swallow studies performed before discharge in the same-day discharge group.
Very similar results were generated by a study evaluating same-day discharge after laparoscopic Roux-en-Y gastric bypass, according to John M. Morton, MD, chief of bariatric and minimally invasive surgery, Stanford (Calif.) University. Dr. Morton, first author of the study and moderator of the session in which Dr. Inaba presented the LSG data, reported that same-day discharge in that study was also associated with a trend for an increased risk of serious complications (Ann Surg. 2014;259:286-92).
“Same-day discharge is often reimbursed at a lower rate, so there is less pay and patients are at greater risk of harm,” Dr. Morton said.
The reasons that same-day discharge is associated with higher mortality cannot be derived from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database, but, Dr. Inaba said, “Our thought is it is a function of failure to rescue patients from respiratory complications.” She acknowledged that this is a speculative assessment not supported by data, but she suggested that history of sleep apnea might be a particular indication to consider next-day discharge.
Dr. Inaba reports no financial relationships relevant to this topic.
Correction, 12/4/17: An earlier version of this article misstated the 30-day mortality among patients discharged the next day.
AT OBESITY WEEK 2017
Key clinical point: Thirty-day mortality after laparoscopic sleeve gastrectomy is several times higher with same-day discharge relative to an overnight stay.
Major finding: In an analysis of a national database with more than 35,000 cases, the mortality odds ratio for same-day discharge was 5.7 (P = .032) relative to next-day discharge.
Data source: Retrospective database analysis.
Disclosures: Dr. Inaba reports no financial relationships relevant to this topic.
FDA approves letermovir for CMV prophylaxis
The Food and Drug Administration on Nov. 8 approved the use of letermovir (Prevymis) tablets and injections for the prevention of cytomegalovirus (CMV) infection and disease in adults exposed to the virus who have received an allogeneic hematopoietic stem cell transplant (HSCT). This is the first drug to be approved for this purpose. It had previously been granted Breakthrough Therapy and Orphan Drug designation.
CMV infection is a major risk for patients undergoing HSCT, because an estimated 65%-80% of these patients already have been exposed to the virus.
Side effects associated with the use of letermovir include nausea, diarrhea, vomiting, swelling in the arms and legs, cough, headache, tiredness, and abdominal pain. The drug is contraindicated for patients receiving pimozide and ergot alkaloids, or pitavastatin or simvastatin when coadministered with cyclosporine. Prescribing information is available at the FDA website.
The Food and Drug Administration on Nov. 8 approved the use of letermovir (Prevymis) tablets and injections for the prevention of cytomegalovirus (CMV) infection and disease in adults exposed to the virus who have received an allogeneic hematopoietic stem cell transplant (HSCT). This is the first drug to be approved for this purpose. It had previously been granted Breakthrough Therapy and Orphan Drug designation.
CMV infection is a major risk for patients undergoing HSCT, because an estimated 65%-80% of these patients already have been exposed to the virus.
Side effects associated with the use of letermovir include nausea, diarrhea, vomiting, swelling in the arms and legs, cough, headache, tiredness, and abdominal pain. The drug is contraindicated for patients receiving pimozide and ergot alkaloids, or pitavastatin or simvastatin when coadministered with cyclosporine. Prescribing information is available at the FDA website.
The Food and Drug Administration on Nov. 8 approved the use of letermovir (Prevymis) tablets and injections for the prevention of cytomegalovirus (CMV) infection and disease in adults exposed to the virus who have received an allogeneic hematopoietic stem cell transplant (HSCT). This is the first drug to be approved for this purpose. It had previously been granted Breakthrough Therapy and Orphan Drug designation.
CMV infection is a major risk for patients undergoing HSCT, because an estimated 65%-80% of these patients already have been exposed to the virus.
Side effects associated with the use of letermovir include nausea, diarrhea, vomiting, swelling in the arms and legs, cough, headache, tiredness, and abdominal pain. The drug is contraindicated for patients receiving pimozide and ergot alkaloids, or pitavastatin or simvastatin when coadministered with cyclosporine. Prescribing information is available at the FDA website.
OSA home testing less expensive than polysomnography
Home respiratory polygraphy had similar efficacy with substantially lower per-patient cost, compared with traditional polysomnography for diagnosing obstructive sleep apnea, a study showed.
Obstructive sleep apnea (OSA) is a common chronic disease associated with higher risk of cardiovascular disease and traffic accidents and a lower quality of life. Although expensive and time intensive, the polysomnography (PSG) has been the preferred test for diagnosing OSA. Home respiratory polygraphy (HRP) uses portable devices that are less complex than polysomnography and has been shown to have similar effectiveness in diagnosing OSA, compared with PSG, in patients with a high clinical suspicion of OSA. However, there is limited evidence for the cost effectiveness of HRP, compared with PSG (Am J Respir Crit Care Med. 2017 Nov 1;196[9]:1181-90).
The investigators conducted a multicenter, randomized controlled, noninferiority trial and cost-effectiveness analysis comparing PSG with HRP. Inclusion criteria included snoring or observed sleep apnea, Epworth Sleepiness Scale (ESS)of 10 or higher, and no suspicion of alternative causes for daytime sleepiness. Patients with a suspicion for OSA were randomized to polysomnography or respiratory polygraphy protocols. Both arms received counseling on proper sleep hygiene; counseling on weight loss, if overweight; and auto-CPAP titration if continuous positive airway pressure (CPAP) was clinically indicated.
Assessment of CPAP compliance or dietary and sleep hygiene compliance was assessed at months 1 and 3. ESS, quality of life measures, well-being measures, 24-hour blood pressure monitoring, auto accidents, and cardiovascular events were assessed at baseline and at month 6.
CPAP treatment was indicated in 68% of the PSG arm, compared with 53% of the HRP arm. After intention-to-treat analysis, there was no statistically significant difference between the two groups for ESS improvement (HRP mean, –4.2, vs. PSG mean, –4.9; P = .14). The groups demonstrated similar results for quality of life, blood pressure, polysomnographic assessment at 6 months, CPAP compliance, and rates of cardiovascular events and accidents at follow-up.
The cost-effective analysis demonstrated respiratory polygraphy was less expensive, saving more than 400 euros/patient. “Because the effectiveness (ESS and QALYs [quality-adjusted life-years]) was similar between arms, the HRP protocol is preferable due to its lower cost,” the authors wrote.
In all, 430 patients were randomized to HRP or PSG and consisted mostly of men (70.5%) with a mean body mass index of 30.7 kg/m2. The groups had similar rates of alcohol consumption and hypertension.
Limitations of the study included unblinded randomization to the participants and researchers and the possibility of variability in therapeutic decisions. However, the authors noted that intraobserver variability was minimized by using the Spanish Sleep Network guidelines and centralized assessment.
“[The] HRP management protocol is not inferior to PSG and presents substantially lower costs. Therefore, PSG is not necessary for most patients with suspicion of OSA. This finding could change established clinical practice, with a clear economic benefit,” the authors concluded.
Home respiratory polygraphy continues to impress
This study adds strong evidence to support the use of home respiratory polygraphy for the diagnosis of obstructive sleep apnea in patients without major comorbidities such as severe chronic restrictive or obstructive lung disease, heart failure or unstable cardiovascular disease, major psychiatric diagnoses, and neuromuscular conditions, noted Ching Li Chai-Coetzer, MBBS, PhD, and R.
Doug McEvoy, MBBS, MD, in an accompanying editorial (Am J Respir Crit Care Med. 2017 Nov 1;196[9]:1096-8). However, lower-cost methods to diagnose OSA would still not address unmet needs such as the cost of continuous positive airway pressure and scarcity of sleep physicians to assess patients with OSA, and still may be too expensive for underresourced populations, they said.
Dr. Chai-Coetzer and Dr. McEvoy are affiliated with the Adelaide Institute for Sleep Health at Flinders University and the Sleep Health Service, Southern Adelaide Local Health Network, both in South Australia.
The study was supported by Sociedad Española de Neumología, Air Liquide (Spain), Asociacion de Neumologos del Sur, and Sociedad Extremeña de Neumología. The investigators report no disclosures.
Dr. Chai-Coetzer reported grants from National Health and Medical Research Council of Australia and nonfinancial support from Biotech Pharmaceuticals. Dr. McEvoy reported grants and nonfinancial support from Philips Respironics, nonfinancial support from ResMed, and grants from Fisher & Paykel.
Home respiratory polygraphy had similar efficacy with substantially lower per-patient cost, compared with traditional polysomnography for diagnosing obstructive sleep apnea, a study showed.
Obstructive sleep apnea (OSA) is a common chronic disease associated with higher risk of cardiovascular disease and traffic accidents and a lower quality of life. Although expensive and time intensive, the polysomnography (PSG) has been the preferred test for diagnosing OSA. Home respiratory polygraphy (HRP) uses portable devices that are less complex than polysomnography and has been shown to have similar effectiveness in diagnosing OSA, compared with PSG, in patients with a high clinical suspicion of OSA. However, there is limited evidence for the cost effectiveness of HRP, compared with PSG (Am J Respir Crit Care Med. 2017 Nov 1;196[9]:1181-90).
The investigators conducted a multicenter, randomized controlled, noninferiority trial and cost-effectiveness analysis comparing PSG with HRP. Inclusion criteria included snoring or observed sleep apnea, Epworth Sleepiness Scale (ESS)of 10 or higher, and no suspicion of alternative causes for daytime sleepiness. Patients with a suspicion for OSA were randomized to polysomnography or respiratory polygraphy protocols. Both arms received counseling on proper sleep hygiene; counseling on weight loss, if overweight; and auto-CPAP titration if continuous positive airway pressure (CPAP) was clinically indicated.
Assessment of CPAP compliance or dietary and sleep hygiene compliance was assessed at months 1 and 3. ESS, quality of life measures, well-being measures, 24-hour blood pressure monitoring, auto accidents, and cardiovascular events were assessed at baseline and at month 6.
CPAP treatment was indicated in 68% of the PSG arm, compared with 53% of the HRP arm. After intention-to-treat analysis, there was no statistically significant difference between the two groups for ESS improvement (HRP mean, –4.2, vs. PSG mean, –4.9; P = .14). The groups demonstrated similar results for quality of life, blood pressure, polysomnographic assessment at 6 months, CPAP compliance, and rates of cardiovascular events and accidents at follow-up.
The cost-effective analysis demonstrated respiratory polygraphy was less expensive, saving more than 400 euros/patient. “Because the effectiveness (ESS and QALYs [quality-adjusted life-years]) was similar between arms, the HRP protocol is preferable due to its lower cost,” the authors wrote.
In all, 430 patients were randomized to HRP or PSG and consisted mostly of men (70.5%) with a mean body mass index of 30.7 kg/m2. The groups had similar rates of alcohol consumption and hypertension.
Limitations of the study included unblinded randomization to the participants and researchers and the possibility of variability in therapeutic decisions. However, the authors noted that intraobserver variability was minimized by using the Spanish Sleep Network guidelines and centralized assessment.
“[The] HRP management protocol is not inferior to PSG and presents substantially lower costs. Therefore, PSG is not necessary for most patients with suspicion of OSA. This finding could change established clinical practice, with a clear economic benefit,” the authors concluded.
Home respiratory polygraphy continues to impress
This study adds strong evidence to support the use of home respiratory polygraphy for the diagnosis of obstructive sleep apnea in patients without major comorbidities such as severe chronic restrictive or obstructive lung disease, heart failure or unstable cardiovascular disease, major psychiatric diagnoses, and neuromuscular conditions, noted Ching Li Chai-Coetzer, MBBS, PhD, and R.
Doug McEvoy, MBBS, MD, in an accompanying editorial (Am J Respir Crit Care Med. 2017 Nov 1;196[9]:1096-8). However, lower-cost methods to diagnose OSA would still not address unmet needs such as the cost of continuous positive airway pressure and scarcity of sleep physicians to assess patients with OSA, and still may be too expensive for underresourced populations, they said.
Dr. Chai-Coetzer and Dr. McEvoy are affiliated with the Adelaide Institute for Sleep Health at Flinders University and the Sleep Health Service, Southern Adelaide Local Health Network, both in South Australia.
The study was supported by Sociedad Española de Neumología, Air Liquide (Spain), Asociacion de Neumologos del Sur, and Sociedad Extremeña de Neumología. The investigators report no disclosures.
Dr. Chai-Coetzer reported grants from National Health and Medical Research Council of Australia and nonfinancial support from Biotech Pharmaceuticals. Dr. McEvoy reported grants and nonfinancial support from Philips Respironics, nonfinancial support from ResMed, and grants from Fisher & Paykel.
Home respiratory polygraphy had similar efficacy with substantially lower per-patient cost, compared with traditional polysomnography for diagnosing obstructive sleep apnea, a study showed.
Obstructive sleep apnea (OSA) is a common chronic disease associated with higher risk of cardiovascular disease and traffic accidents and a lower quality of life. Although expensive and time intensive, the polysomnography (PSG) has been the preferred test for diagnosing OSA. Home respiratory polygraphy (HRP) uses portable devices that are less complex than polysomnography and has been shown to have similar effectiveness in diagnosing OSA, compared with PSG, in patients with a high clinical suspicion of OSA. However, there is limited evidence for the cost effectiveness of HRP, compared with PSG (Am J Respir Crit Care Med. 2017 Nov 1;196[9]:1181-90).
The investigators conducted a multicenter, randomized controlled, noninferiority trial and cost-effectiveness analysis comparing PSG with HRP. Inclusion criteria included snoring or observed sleep apnea, Epworth Sleepiness Scale (ESS)of 10 or higher, and no suspicion of alternative causes for daytime sleepiness. Patients with a suspicion for OSA were randomized to polysomnography or respiratory polygraphy protocols. Both arms received counseling on proper sleep hygiene; counseling on weight loss, if overweight; and auto-CPAP titration if continuous positive airway pressure (CPAP) was clinically indicated.
Assessment of CPAP compliance or dietary and sleep hygiene compliance was assessed at months 1 and 3. ESS, quality of life measures, well-being measures, 24-hour blood pressure monitoring, auto accidents, and cardiovascular events were assessed at baseline and at month 6.
CPAP treatment was indicated in 68% of the PSG arm, compared with 53% of the HRP arm. After intention-to-treat analysis, there was no statistically significant difference between the two groups for ESS improvement (HRP mean, –4.2, vs. PSG mean, –4.9; P = .14). The groups demonstrated similar results for quality of life, blood pressure, polysomnographic assessment at 6 months, CPAP compliance, and rates of cardiovascular events and accidents at follow-up.
The cost-effective analysis demonstrated respiratory polygraphy was less expensive, saving more than 400 euros/patient. “Because the effectiveness (ESS and QALYs [quality-adjusted life-years]) was similar between arms, the HRP protocol is preferable due to its lower cost,” the authors wrote.
In all, 430 patients were randomized to HRP or PSG and consisted mostly of men (70.5%) with a mean body mass index of 30.7 kg/m2. The groups had similar rates of alcohol consumption and hypertension.
Limitations of the study included unblinded randomization to the participants and researchers and the possibility of variability in therapeutic decisions. However, the authors noted that intraobserver variability was minimized by using the Spanish Sleep Network guidelines and centralized assessment.
“[The] HRP management protocol is not inferior to PSG and presents substantially lower costs. Therefore, PSG is not necessary for most patients with suspicion of OSA. This finding could change established clinical practice, with a clear economic benefit,” the authors concluded.
Home respiratory polygraphy continues to impress
This study adds strong evidence to support the use of home respiratory polygraphy for the diagnosis of obstructive sleep apnea in patients without major comorbidities such as severe chronic restrictive or obstructive lung disease, heart failure or unstable cardiovascular disease, major psychiatric diagnoses, and neuromuscular conditions, noted Ching Li Chai-Coetzer, MBBS, PhD, and R.
Doug McEvoy, MBBS, MD, in an accompanying editorial (Am J Respir Crit Care Med. 2017 Nov 1;196[9]:1096-8). However, lower-cost methods to diagnose OSA would still not address unmet needs such as the cost of continuous positive airway pressure and scarcity of sleep physicians to assess patients with OSA, and still may be too expensive for underresourced populations, they said.
Dr. Chai-Coetzer and Dr. McEvoy are affiliated with the Adelaide Institute for Sleep Health at Flinders University and the Sleep Health Service, Southern Adelaide Local Health Network, both in South Australia.
The study was supported by Sociedad Española de Neumología, Air Liquide (Spain), Asociacion de Neumologos del Sur, and Sociedad Extremeña de Neumología. The investigators report no disclosures.
Dr. Chai-Coetzer reported grants from National Health and Medical Research Council of Australia and nonfinancial support from Biotech Pharmaceuticals. Dr. McEvoy reported grants and nonfinancial support from Philips Respironics, nonfinancial support from ResMed, and grants from Fisher & Paykel.
FROM THE AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
Key clinical point: Home obstructive sleep apnea testing was less costly and noninferior to polysomnography.
Major finding: Using respiratory polygraphy instead of polysomnography results in savings of more than 400 euros/patient.
Data source: A multicenter, randomized controlled, noninferiority trial and cost-effectiveness analysis of 430 patients suspected of having OSA.
Disclosures: The study was supported by Sociedad Española de Neumología, Air Liquide (Spain), Asociacion de Neumologos del Sur, and Sociedad Extremeña de Neumología. The authors report no disclosures.
ED visits after bariatric surgery may be difficult to reduce
NATIONAL HARBOR, MD. – In an evaluation of 633 emergency department visits following bariatric surgery in Michigan over a 1-year period, the vast majority were for complaints amenable to a phone call consultation or treatment in a lower-acuity setting, but few patients would have been satisfied with this type of management, according to an evaluation based on patient interviews presented at Obesity Week 2017.
“Unfortunately, 91% of the patients said that there was nothing the surgical team could have done that would have helped avoid the ED visit,” reported Haley Stevens, quality improvement coordinator at the Michigan Bariatric Surgery Collaborative, University of Michigan, Ann Arbor.
The 633 ED visits followed 7,617 bariatric surgeries for a rate of 8.3%. According to Ms. Stevens, this is consistent with the rates of 5%-11% reported previously. Based on clinically abstracted data and patient interviews conducted by trained nurses in a sample of patients involved in these ED visits, it was estimated that 62% were made without any attempt to first contact the surgical team, she reported at an annual meeting presented by the American Society for Metabolic and Bariatric Surgery and The Obesity Society.
In the interviews, a variety of reasons were offered for not first contacting the surgical team, according to Ms. Stevens. Most commonly, patients reported that a sense of urgency drove them to the ED. In 18% of cases, the complaint occurred after office hours, leading the patient to believe that the ED was the only option. Another 16% of patients reported that calling the surgeon simply did not occur to them.
“When interviewed, many patients considered the visit necessary and unavoidable even after learning subsequently that the symptoms were not serious,” Ms. Stevens reported.
The primary reasons for the ED visit were nausea, vomiting, or abdominal pain, which accounted for 50% of the visits. The next most common reasons were chest pain (8%) and concerns regarding the incision (7%). Only 30% of the ED visits ultimately resulted in a hospital admission, but 60% of the visits resulted in administration of intravenous fluids. Thirty-eight percent of ED visits resulted in oral or intravenous therapy for pain.
Based on the interviews, most patients reported that they visited the ED because they wanted an immediate evaluation of their symptoms, according to Ms. Stevens. She said that the goal in most cases was simply obtaining reassurance. While better patient education about symptoms and recovery might have circumvented patient concerns about nonurgent complaints, Ms. Stevens also suggested that visits to a lower-acuity center, such as an urgent care facility, might provide a lower-cost alternative for reassurance or simple treatments.
As this study represents the first in a series to guide a quality improvement initiative, Ms. Stevens acknowledged that the best solution to reducing unnecessary ED visits is unclear, but she did suggest that multiple strategies might be needed. Based on this and previously published studies evaluating this issue “there is no silver bullet” for reducing ED visits, Ms. Stevens said.
In an animated discussion that followed presentation of these results, others recounting efforts to reduce ED visits following bariatric surgery emphasized the importance of follow-up phone calls or home visits within 2 or 3 days of surgery. According to several of those who commented, these steps allow early identification of problems while providing the type of reassurance that can prevent unnecessary ED visits.
The average cost of an ED visit following bariatric surgery is approximately $1,300, according to Ms. Stevens. For this and other reasons, strategies to reduce ED visits are needed, but Ms. Stevens cautioned that the solutions might not be simple. Based on data from this study, the key may be providing patients with a clear route to the reassurance they need to avoid seeking care for nonurgent issues.
Ms. Stevens reports no financial relationships relevant to this topic.
NATIONAL HARBOR, MD. – In an evaluation of 633 emergency department visits following bariatric surgery in Michigan over a 1-year period, the vast majority were for complaints amenable to a phone call consultation or treatment in a lower-acuity setting, but few patients would have been satisfied with this type of management, according to an evaluation based on patient interviews presented at Obesity Week 2017.
“Unfortunately, 91% of the patients said that there was nothing the surgical team could have done that would have helped avoid the ED visit,” reported Haley Stevens, quality improvement coordinator at the Michigan Bariatric Surgery Collaborative, University of Michigan, Ann Arbor.
The 633 ED visits followed 7,617 bariatric surgeries for a rate of 8.3%. According to Ms. Stevens, this is consistent with the rates of 5%-11% reported previously. Based on clinically abstracted data and patient interviews conducted by trained nurses in a sample of patients involved in these ED visits, it was estimated that 62% were made without any attempt to first contact the surgical team, she reported at an annual meeting presented by the American Society for Metabolic and Bariatric Surgery and The Obesity Society.
In the interviews, a variety of reasons were offered for not first contacting the surgical team, according to Ms. Stevens. Most commonly, patients reported that a sense of urgency drove them to the ED. In 18% of cases, the complaint occurred after office hours, leading the patient to believe that the ED was the only option. Another 16% of patients reported that calling the surgeon simply did not occur to them.
“When interviewed, many patients considered the visit necessary and unavoidable even after learning subsequently that the symptoms were not serious,” Ms. Stevens reported.
The primary reasons for the ED visit were nausea, vomiting, or abdominal pain, which accounted for 50% of the visits. The next most common reasons were chest pain (8%) and concerns regarding the incision (7%). Only 30% of the ED visits ultimately resulted in a hospital admission, but 60% of the visits resulted in administration of intravenous fluids. Thirty-eight percent of ED visits resulted in oral or intravenous therapy for pain.
Based on the interviews, most patients reported that they visited the ED because they wanted an immediate evaluation of their symptoms, according to Ms. Stevens. She said that the goal in most cases was simply obtaining reassurance. While better patient education about symptoms and recovery might have circumvented patient concerns about nonurgent complaints, Ms. Stevens also suggested that visits to a lower-acuity center, such as an urgent care facility, might provide a lower-cost alternative for reassurance or simple treatments.
As this study represents the first in a series to guide a quality improvement initiative, Ms. Stevens acknowledged that the best solution to reducing unnecessary ED visits is unclear, but she did suggest that multiple strategies might be needed. Based on this and previously published studies evaluating this issue “there is no silver bullet” for reducing ED visits, Ms. Stevens said.
In an animated discussion that followed presentation of these results, others recounting efforts to reduce ED visits following bariatric surgery emphasized the importance of follow-up phone calls or home visits within 2 or 3 days of surgery. According to several of those who commented, these steps allow early identification of problems while providing the type of reassurance that can prevent unnecessary ED visits.
The average cost of an ED visit following bariatric surgery is approximately $1,300, according to Ms. Stevens. For this and other reasons, strategies to reduce ED visits are needed, but Ms. Stevens cautioned that the solutions might not be simple. Based on data from this study, the key may be providing patients with a clear route to the reassurance they need to avoid seeking care for nonurgent issues.
Ms. Stevens reports no financial relationships relevant to this topic.
NATIONAL HARBOR, MD. – In an evaluation of 633 emergency department visits following bariatric surgery in Michigan over a 1-year period, the vast majority were for complaints amenable to a phone call consultation or treatment in a lower-acuity setting, but few patients would have been satisfied with this type of management, according to an evaluation based on patient interviews presented at Obesity Week 2017.
“Unfortunately, 91% of the patients said that there was nothing the surgical team could have done that would have helped avoid the ED visit,” reported Haley Stevens, quality improvement coordinator at the Michigan Bariatric Surgery Collaborative, University of Michigan, Ann Arbor.
The 633 ED visits followed 7,617 bariatric surgeries for a rate of 8.3%. According to Ms. Stevens, this is consistent with the rates of 5%-11% reported previously. Based on clinically abstracted data and patient interviews conducted by trained nurses in a sample of patients involved in these ED visits, it was estimated that 62% were made without any attempt to first contact the surgical team, she reported at an annual meeting presented by the American Society for Metabolic and Bariatric Surgery and The Obesity Society.
In the interviews, a variety of reasons were offered for not first contacting the surgical team, according to Ms. Stevens. Most commonly, patients reported that a sense of urgency drove them to the ED. In 18% of cases, the complaint occurred after office hours, leading the patient to believe that the ED was the only option. Another 16% of patients reported that calling the surgeon simply did not occur to them.
“When interviewed, many patients considered the visit necessary and unavoidable even after learning subsequently that the symptoms were not serious,” Ms. Stevens reported.
The primary reasons for the ED visit were nausea, vomiting, or abdominal pain, which accounted for 50% of the visits. The next most common reasons were chest pain (8%) and concerns regarding the incision (7%). Only 30% of the ED visits ultimately resulted in a hospital admission, but 60% of the visits resulted in administration of intravenous fluids. Thirty-eight percent of ED visits resulted in oral or intravenous therapy for pain.
Based on the interviews, most patients reported that they visited the ED because they wanted an immediate evaluation of their symptoms, according to Ms. Stevens. She said that the goal in most cases was simply obtaining reassurance. While better patient education about symptoms and recovery might have circumvented patient concerns about nonurgent complaints, Ms. Stevens also suggested that visits to a lower-acuity center, such as an urgent care facility, might provide a lower-cost alternative for reassurance or simple treatments.
As this study represents the first in a series to guide a quality improvement initiative, Ms. Stevens acknowledged that the best solution to reducing unnecessary ED visits is unclear, but she did suggest that multiple strategies might be needed. Based on this and previously published studies evaluating this issue “there is no silver bullet” for reducing ED visits, Ms. Stevens said.
In an animated discussion that followed presentation of these results, others recounting efforts to reduce ED visits following bariatric surgery emphasized the importance of follow-up phone calls or home visits within 2 or 3 days of surgery. According to several of those who commented, these steps allow early identification of problems while providing the type of reassurance that can prevent unnecessary ED visits.
The average cost of an ED visit following bariatric surgery is approximately $1,300, according to Ms. Stevens. For this and other reasons, strategies to reduce ED visits are needed, but Ms. Stevens cautioned that the solutions might not be simple. Based on data from this study, the key may be providing patients with a clear route to the reassurance they need to avoid seeking care for nonurgent issues.
Ms. Stevens reports no financial relationships relevant to this topic.
AT OBESITY WEEK 2017
Key clinical point:
Major finding: In interviews after their ED visit, 91% of bariatric patients insisted the visit was needed, even when informed it was nonurgent.
Data source: Retrospective review and patient interview.
Disclosures: Ms. Stevens reports no financial relationships relevant to this topic.
Double Sequential Defibrillation for Refractory Ventricular Fibrillation and Pulseless Ventricular Tachycardia
In 1930, Kouwenhoven, an electrical engineer, invented the first external cardiac defibrillator, and the first successful defibrillation performed on a human was reported in 1947.2Defibrillation devices have since evolved from the application of paddle electrodes to self-adhesive electrodes.
With the intent of producing a life-sustaining rhythm, a large dose of an electrical current from the defibrillator is used to depolarize the heart’s entire electrical conduction system. As medicine and technology advance, we continue to strive for better and more effective ways to improve the probability of survival for patients in cardiac arrest. One area of increasing interest in potentially improving survival rates is the use of double sequential defibrillation (DSD; double simultaneous defibrillation) in patients with V-fib and ventricular tachycardia (V-tach).
Double Sequential Defibrillation
Double sequential defibrillation, also known as double simultaneous defibrillation, is the use of two defibrillators simultaneously to deliver the maximum energy that may be necessary to treat refractory V-fib. In this review, we define refractory V-fib as V-fib/pulseless V-tach that does not revert to a life-sustaining rhythm after three or more shocks from a single defibrillator plus administration of at least a single dose of intravenous (IV) epinephrine and/or amiodarone.
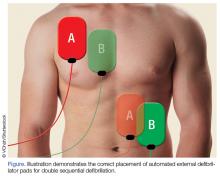
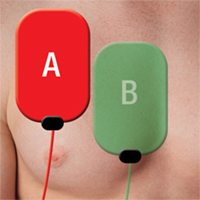
When utilizing DSD, one set of pads is placed in the anterior-posterior position and the other set of pads is placed in the anterior-lateral position as shown in the Figure.
In three retrospective cases, we describe our use of DSD for refractory V-fib in the ED, in the hopes of encouraging further exploration of this potentially life-saving treatment modality in the treatment of refractory V-fib.
Although studies to assess the benefit of DSD are still in their early stages, we believe this technique has the potential to improve the success rate in achieving return of spontaneous circulation (ROSC) when compared to the standard method of defibrillation, described in the current advanced cardiac life support (ACLS) algorithms.
Cases
Case 1
A 39-year-old man with a medical history of type 1 diabetes mellitus arrived at our ED with a 6-hour history of nausea and vomiting. Upon arrival at the ED, the patient’s vital signs were: blood pressure, 109/52 mm Hg; heart rate, 120 beats/min; and respiratory rate, 20 breaths/min. Oxygen saturation was 94% on room air. Laboratory studies included a point-of-care blood glucose test, which revealed a glucose greater than 600 mg/dL.
The patient was initially resuscitated with 3 L Ringer’s lactate solution IV; and IV ondansetron for vomiting. One hour after his arrival, the patient developed monomorphic wide-complex tachycardia at 179 beats/min and began complaining of chest pain. An IV push of adenosine 6 mg was given with no effect on rhythm. The emergency physician (EP) then administered 300 mg of IV amiodarone followed by 100 mg of IV procainamide, without termination of the tachyarrhythmia.
The patient became hypotensive with a systolic blood pressure of 86 mm Hg, and an attempt was made to apply synchronized cardioversion at 100 J for his unstable V-tach. Shortly after cardioversion, the patient went into V-fib and became unconscious. Cardiopulmonary resuscitation was initiated, and the patient was defibrillated at 200 J without success. He was then given 1 mg of IV epinephrine, 2 amp of IV sodium bicarbonate, and intubated.
The patient remained pulseless and in V-fib. A second unsuccessful defibrillation attempt at 200 J was made. Followed by CPR and a third unsuccessful attempt at defibrillation. The patient next received DSD with the two defibrillators each set at 200 J, and afterwards converted back to sinus rhythm.
After successful DSD, the patient was started on an insulin drip and was transferred to the intensive care unit (ICU). He survived to hospital discharge with a cerebral performance category (CPC) scale score of 1, defined as “good cerebral performance, neurologically intact, may lead a normal life”.3
Case 2
A 22-year-old woman with a known history of heroin abuse was brought to our ED by emergency medical services (EMS) following an unwitnessed cardiac arrest pulseless electrical activity (PEA). The patient’s parents stated that when they saw the patient approximately 5 hours earlier, she appeared normal physically and was behaving normally. Emergency medical technicians (EMTs) administered several milligrams of IV naloxone without success. The patient was intubated while en route to the hospital and CPR was performed for 35 minutes, after which ROSC was achieved.
However, en route to the hospital, the patient developed V-fib, for which she was unsuccessfully defibrillated three times at 200 J. Upon arrival at the ED, the patient was defibrillated twice more at 200 J but remained in V-fib. On the third pulse check DSD was performed, and the patient subsequently converted to a PEA rhythm; CPR was continued for two more cycles, after which the patient regained a weak pulse and an ETCO2 of 55 mm Hg. A central line was placed and the patient was started on IV epinephrine and dopamine. In the ICU she received targeted temperature management, but ultimately expired that evening.
Case 3
A 39-year-old woman with no known medical history was brought to the ED by EMS after she was discovered to be unconscious and pulseless by her husband in their home. Upon arrival, the EMTs found the patient in V-fib and performed endotracheal intubation and 30 minutes of CPR. The EMS report recorded that the patient had been defibrillated a total of five times at the scene before achieving ROSC. En route to the hospital, however, the patient’s rhythm reverted to V-fib; CPR was again initiated along with an unsuccessful attempt at defibrillation. The EMTs then administered 300 mg of IV amiodarone, 1 amp of sodium bicarbonate, and epinephrine IV every 3 to 5 minutes.
Upon arrival at the ED, the EP attempted defibrillation twice, unsuccessfully. The patient was then given IV magnesium, 1 amp of sodium bicarbonate IV, and three doses of IV epinephrine, but remained in V-fib. The EP then attempted DSD but with no success, but a second application of DSD resulted in conversion to a junctional bradycardia. After 1 hour of CPR, ROSC was achieved, and the patient was transferred to the ICU. Unfortunately, due to the burden of neurological damage from the cardiac arrest and poor predicted outcome, the patient’s family ultimately decided to have care withdrawn overnight. The patient expired shortly after being extubated.
Discussion
Out-of-hospital cardiac arrest remains a leading cause of death today; of which cardiac arrests due to V-fib are associated with the highest survival rates.4 Our three cases suggest that application of DSD may be of benefit in the ED, in the treatment of refractory V-fib and refractory pulseless V-tach. All three of the patients we described achieved ROSC after DSD and unsuccessful prior attempts with standard defibrillation, though only one of the patients was discharged home with good neurological status.
One of the earliest known studies of the applications of DSD on human subjects was described in 1994 by Hoch et al.5 The study included 2,990 patients who underwent a total of 5,450 electrophysiological studies over a period of 3 years. The researchers induced V-fib/pulseless V-tach in approximately 30% of their study population. Five of these patients, who were all men with a mean age of 55 years, experienced refractory V-fib each of whom required seven to 20 unsuccessful attempts at defibrillation. The researchers ultimately found that when they applied DSD, only one attempt was needed for successful conversion to normal sinus rhythm in all five of the patients.5The authors acknowledged that there were many limitations to their study, which will likely continue to be factors in future studies as well.
DSD exists in the form of reviews, case reports, and retrospective studies in most of the recent literature. The reason for the paucity of research is probably due to the relative rarity and random nature of refractory V-fib (0.1% of V-fib arrests),6 making it nearly impossible for researchers to conduct large-scale studies in a controlled environment. Another limitation that hinders DSD research studies is the large number of variables that can determine a patient’s chance of survival after defibrillation. These variables include age, comorbidities, risk factors, timing of arrival at the ED, application and quality of prehospital CPR, laboratory abnormalities, and other patient-specific neurological or metabolic processes.
Several case series previously reported on the use of DSD, most of which describe patients in the out-of-hospital setting. The findings from these case series appear promising—at least to the extent in which patients were converted out of V-fib through DSD.
In 2014, Cabañas et al6 reported on a retrospective case series of 10 patients treated with DSD between 2008 and 2010, and found that 70% of the patients were successfully converted by DSD out of refractory V-fib. Unfortunately, none of the patients survived to hospital discharge.
Another recent retrospective study conducted by Cortez et al7 of 12 patients with refractory V-fib treated with DSD found that nine of the 12 patients (75%) converted out of V-fib, three of whom survived to hospital discharge, with two patients (16.7%) discharged with a CPC of 1.7 Lastly, Merlin et al8 reported on a retrospective case series in 2015 of EMTs delivering DSS in the field to a total of seven patients with refractory V-fib, five of whom (71%) were successfully converted out of V-fib, with four (57%) surviving to hospital admission.8
Pharmacological Agents Post-DSD
None of the patients in the study by Hoch et al5 received any pharmacological agents between initial unsuccessful attempts at defibrillation and the final application of DSD. As previously noted, all three of the patients in our cases had the full support of ED personnel, as well as the administration of appropriate pharmacological agents.
A randomized controlled trial published in 2006 by Hohnloser et al9 reported clinically significant results in studying the effects of antiarrhythmic agents, particularly amiodarone and sotalol, on defibrillation thresholds. They found that amiodarone increased the defibrillation threshold by 1.29 J, while sotalol decreased the defibrillation threshold by 0.89 J. However, despite their findings, Hohnloser et al9 believed that such differences were highly unlikely to influence patient outcomes.
Post-DSD Effects
The short- and long-term effects of DSD on the human body are unknown. Since the mechanism responsible for the efficacy of DSD is still unclear, many professionals and researchers are concerned that doubling the energy could cause myocardial damage. Although successful return of spontaneous circulation is an important first step in a successful resuscitation, the ultimate goal is to have a patient who is neurologically intact at the time of discharge home, with the capability of maintaining a favorable quality of life.
In 2016, Ross et al10 conducted a larger study comparing CPC scores of 279 patients in refractory V-fib, who received single shock (229 patients) vs DSD (50 patients). They found no statistically significant differences in neurologically intact survival rates between the two groups. This is an important finding that should be the goal for any future studies regarding DSD.10
Limitations to Future Research
For researchers to provide DSD results considered clinically significant, more cross-sectional, randomized-controlled studies need to be performed. Such studies will require a tremendous amount of time, effort, data collection, and a substantial sample size to prove that positive DSD results are not due to chance. As previously noted, the relatively rare incidence of true refractory V-fib makes it difficult for researchers to obtain large enough sample sizes to demonstrate clinically significant study results. Additionally, since medical institutions tend to adhere to different guidelines when running a code for cardiac arrest it would involve extraordinary measures to create and impose a single, standardized procedure/protocol for research purposes that each hospital would have to unanimously agree on.
Another limitation to producing large-scale, clinically significant research is that there is no universally accepted definition of refractory V-fib/pulseless V-tach. In all three of our cases, we defined it as V-fib/pulseless V-tach does not convert after three or more standard shocks, and at least one dose of either IV epinephrine and/or amiodarone. However, other clinicians and institutions define refractory V-fib as patients remaining in cardiac arrest for which the initial rhythm was either V-fib or V-tach, despite at least three defibrillation attempts, 3 mg of epinephrine, and 300 mg of amiodarone.11,12Importantly, DSD currently is neither endorsed as a standard of care nor recommended as part of the ACLS/American Heart Association/American College of Cardiology guidelines.
Conclusion
For every minute a patient remains in V-fib, the chance of survival decreases. Although the application of DSD has not been standardized at this time, we feel that it is a reasonable treatment option for patients in V-fib and pulseless V-tach, after all conventional interventions have failed. Though studies on DSD to date, as well as the three cases presented here, all involved relatively small sample sizes and isolated case reports, the results seem to suggest that DSD does improve chance of ROSC. We believe that DSD deserves further study and may be considered in cases of refractory V-fib and pulseless V-tach.
1. Efimov IR. Naum Lazarevich Gurvich (1905–1981) and his contribution to the history of defibrillation. Cardiol J. 2009;16(2):190-193.
2. Bocka JJ. Automatic External Defibrillator. Medscape. http://emedicine.medscape.com/article/780533-overview#a1. Published May 30, 2014. Accessed September 19, 2017.
3. Ajam K, Gold LS, Beck SS, et al. Reliability of cerebral performance category to classify neurological status among survivors of ventricular fibrillation arrest: a cohort study. Scand J Trauma Resus Emerg Med. 2011;19:38. doi:10.1186/1757-7241-19-38.
4. Daya MR, Schmicker RH, Zive DM, et al; Resuscitation Outcomes Consortium Investigators. Out-of-hospital cardiac arrest survival improving over time: Results from the Resuscitation Outcomes Consortium (ROC). Resuscitation. 2015;91:108-115. doi:10.1016/j.resuscitation.2015.02.003.
5. Hoch DH, Batsford WP, Greenberg SM, et al. Double sequential external shocks for refractory ventricular fibrillation. J Am Coll Cardiol. 1994;23(5):1141-1145.
6. Cabañas JG, Myers JB, Williams JG, De Maio VJ, Bachman MW. Double sequential external defibrillation in out-of-hospital refractory ventricular fibrillation: a report of ten cases. Prehosp Emerg Care. 2015;19(1):126-130. doi:10.3109/10903127.2014.942476.
7. Cortez E, Krebs W, Davis J, Keseg DP, Panchal AR. Use of double sequential external defibrillation for refractory ventricular fibrillation during out-of-hospital cardiac arrest. Resuscitation. 2016;108:82-86. doi:10.1016/j.resuscitation.2016.08.002.
8. Merlin MA, Tagore A, Bauter R, Arshad FH. A case series of double sequence defibrillation. Prehosp Emerg Care. 2016;20(4):550-553. doi:10.3109/10903127.2015.1128026.
9. Hohnloser SH, Dorian P, Roberts R, et al. Effect of amiodarone and sotalol on ventricular defibrillation threshold: the optimal pharmacological therapy in cardioverter defibrillator patients (OPTIC) trial. Circulation. 2006;114(2):104-109. doi:10.1161/CIRCULATIONAHA.106.618421.
10. Ross EM, Redman TT, Harper SA, Mapp JG, Wampler DA, Miramontes DA. Dual defibrillation in out-of-hospital cardiac arrest: a retrospective cohort analysis. Resuscitation. 2016;106:14-17. doi:10.1016/j.resuscitation.2016.06.011.11. Driver BE, Debaty G, Plummer DW, Smith SW. Use of esmolol after failure of standard cardiopulmonary resuscitation to treat patients with refractory ventricular fibrillation. Resuscitation. 2014;85(10):1337-1341. doi:10.1016/j.resuscitation.2014.06.032.
12. Lee YH, Lee KJ, Min YH, et al. Refractory ventricular fibrillation treated with esmolol. Resuscitation. 2016;107:150-155. doi:10.1016/j.resuscitation.2016.07.243.
In 1930, Kouwenhoven, an electrical engineer, invented the first external cardiac defibrillator, and the first successful defibrillation performed on a human was reported in 1947.2Defibrillation devices have since evolved from the application of paddle electrodes to self-adhesive electrodes.
With the intent of producing a life-sustaining rhythm, a large dose of an electrical current from the defibrillator is used to depolarize the heart’s entire electrical conduction system. As medicine and technology advance, we continue to strive for better and more effective ways to improve the probability of survival for patients in cardiac arrest. One area of increasing interest in potentially improving survival rates is the use of double sequential defibrillation (DSD; double simultaneous defibrillation) in patients with V-fib and ventricular tachycardia (V-tach).
Double Sequential Defibrillation
Double sequential defibrillation, also known as double simultaneous defibrillation, is the use of two defibrillators simultaneously to deliver the maximum energy that may be necessary to treat refractory V-fib. In this review, we define refractory V-fib as V-fib/pulseless V-tach that does not revert to a life-sustaining rhythm after three or more shocks from a single defibrillator plus administration of at least a single dose of intravenous (IV) epinephrine and/or amiodarone.
When utilizing DSD, one set of pads is placed in the anterior-posterior position and the other set of pads is placed in the anterior-lateral position as shown in the Figure.
In three retrospective cases, we describe our use of DSD for refractory V-fib in the ED, in the hopes of encouraging further exploration of this potentially life-saving treatment modality in the treatment of refractory V-fib.
Although studies to assess the benefit of DSD are still in their early stages, we believe this technique has the potential to improve the success rate in achieving return of spontaneous circulation (ROSC) when compared to the standard method of defibrillation, described in the current advanced cardiac life support (ACLS) algorithms.
Cases
Case 1
A 39-year-old man with a medical history of type 1 diabetes mellitus arrived at our ED with a 6-hour history of nausea and vomiting. Upon arrival at the ED, the patient’s vital signs were: blood pressure, 109/52 mm Hg; heart rate, 120 beats/min; and respiratory rate, 20 breaths/min. Oxygen saturation was 94% on room air. Laboratory studies included a point-of-care blood glucose test, which revealed a glucose greater than 600 mg/dL.
The patient was initially resuscitated with 3 L Ringer’s lactate solution IV; and IV ondansetron for vomiting. One hour after his arrival, the patient developed monomorphic wide-complex tachycardia at 179 beats/min and began complaining of chest pain. An IV push of adenosine 6 mg was given with no effect on rhythm. The emergency physician (EP) then administered 300 mg of IV amiodarone followed by 100 mg of IV procainamide, without termination of the tachyarrhythmia.
The patient became hypotensive with a systolic blood pressure of 86 mm Hg, and an attempt was made to apply synchronized cardioversion at 100 J for his unstable V-tach. Shortly after cardioversion, the patient went into V-fib and became unconscious. Cardiopulmonary resuscitation was initiated, and the patient was defibrillated at 200 J without success. He was then given 1 mg of IV epinephrine, 2 amp of IV sodium bicarbonate, and intubated.
The patient remained pulseless and in V-fib. A second unsuccessful defibrillation attempt at 200 J was made. Followed by CPR and a third unsuccessful attempt at defibrillation. The patient next received DSD with the two defibrillators each set at 200 J, and afterwards converted back to sinus rhythm.
After successful DSD, the patient was started on an insulin drip and was transferred to the intensive care unit (ICU). He survived to hospital discharge with a cerebral performance category (CPC) scale score of 1, defined as “good cerebral performance, neurologically intact, may lead a normal life”.3
Case 2
A 22-year-old woman with a known history of heroin abuse was brought to our ED by emergency medical services (EMS) following an unwitnessed cardiac arrest pulseless electrical activity (PEA). The patient’s parents stated that when they saw the patient approximately 5 hours earlier, she appeared normal physically and was behaving normally. Emergency medical technicians (EMTs) administered several milligrams of IV naloxone without success. The patient was intubated while en route to the hospital and CPR was performed for 35 minutes, after which ROSC was achieved.
However, en route to the hospital, the patient developed V-fib, for which she was unsuccessfully defibrillated three times at 200 J. Upon arrival at the ED, the patient was defibrillated twice more at 200 J but remained in V-fib. On the third pulse check DSD was performed, and the patient subsequently converted to a PEA rhythm; CPR was continued for two more cycles, after which the patient regained a weak pulse and an ETCO2 of 55 mm Hg. A central line was placed and the patient was started on IV epinephrine and dopamine. In the ICU she received targeted temperature management, but ultimately expired that evening.
Case 3
A 39-year-old woman with no known medical history was brought to the ED by EMS after she was discovered to be unconscious and pulseless by her husband in their home. Upon arrival, the EMTs found the patient in V-fib and performed endotracheal intubation and 30 minutes of CPR. The EMS report recorded that the patient had been defibrillated a total of five times at the scene before achieving ROSC. En route to the hospital, however, the patient’s rhythm reverted to V-fib; CPR was again initiated along with an unsuccessful attempt at defibrillation. The EMTs then administered 300 mg of IV amiodarone, 1 amp of sodium bicarbonate, and epinephrine IV every 3 to 5 minutes.
Upon arrival at the ED, the EP attempted defibrillation twice, unsuccessfully. The patient was then given IV magnesium, 1 amp of sodium bicarbonate IV, and three doses of IV epinephrine, but remained in V-fib. The EP then attempted DSD but with no success, but a second application of DSD resulted in conversion to a junctional bradycardia. After 1 hour of CPR, ROSC was achieved, and the patient was transferred to the ICU. Unfortunately, due to the burden of neurological damage from the cardiac arrest and poor predicted outcome, the patient’s family ultimately decided to have care withdrawn overnight. The patient expired shortly after being extubated.
Discussion
Out-of-hospital cardiac arrest remains a leading cause of death today; of which cardiac arrests due to V-fib are associated with the highest survival rates.4 Our three cases suggest that application of DSD may be of benefit in the ED, in the treatment of refractory V-fib and refractory pulseless V-tach. All three of the patients we described achieved ROSC after DSD and unsuccessful prior attempts with standard defibrillation, though only one of the patients was discharged home with good neurological status.
One of the earliest known studies of the applications of DSD on human subjects was described in 1994 by Hoch et al.5 The study included 2,990 patients who underwent a total of 5,450 electrophysiological studies over a period of 3 years. The researchers induced V-fib/pulseless V-tach in approximately 30% of their study population. Five of these patients, who were all men with a mean age of 55 years, experienced refractory V-fib each of whom required seven to 20 unsuccessful attempts at defibrillation. The researchers ultimately found that when they applied DSD, only one attempt was needed for successful conversion to normal sinus rhythm in all five of the patients.5The authors acknowledged that there were many limitations to their study, which will likely continue to be factors in future studies as well.
DSD exists in the form of reviews, case reports, and retrospective studies in most of the recent literature. The reason for the paucity of research is probably due to the relative rarity and random nature of refractory V-fib (0.1% of V-fib arrests),6 making it nearly impossible for researchers to conduct large-scale studies in a controlled environment. Another limitation that hinders DSD research studies is the large number of variables that can determine a patient’s chance of survival after defibrillation. These variables include age, comorbidities, risk factors, timing of arrival at the ED, application and quality of prehospital CPR, laboratory abnormalities, and other patient-specific neurological or metabolic processes.
Several case series previously reported on the use of DSD, most of which describe patients in the out-of-hospital setting. The findings from these case series appear promising—at least to the extent in which patients were converted out of V-fib through DSD.
In 2014, Cabañas et al6 reported on a retrospective case series of 10 patients treated with DSD between 2008 and 2010, and found that 70% of the patients were successfully converted by DSD out of refractory V-fib. Unfortunately, none of the patients survived to hospital discharge.
Another recent retrospective study conducted by Cortez et al7 of 12 patients with refractory V-fib treated with DSD found that nine of the 12 patients (75%) converted out of V-fib, three of whom survived to hospital discharge, with two patients (16.7%) discharged with a CPC of 1.7 Lastly, Merlin et al8 reported on a retrospective case series in 2015 of EMTs delivering DSS in the field to a total of seven patients with refractory V-fib, five of whom (71%) were successfully converted out of V-fib, with four (57%) surviving to hospital admission.8
Pharmacological Agents Post-DSD
None of the patients in the study by Hoch et al5 received any pharmacological agents between initial unsuccessful attempts at defibrillation and the final application of DSD. As previously noted, all three of the patients in our cases had the full support of ED personnel, as well as the administration of appropriate pharmacological agents.
A randomized controlled trial published in 2006 by Hohnloser et al9 reported clinically significant results in studying the effects of antiarrhythmic agents, particularly amiodarone and sotalol, on defibrillation thresholds. They found that amiodarone increased the defibrillation threshold by 1.29 J, while sotalol decreased the defibrillation threshold by 0.89 J. However, despite their findings, Hohnloser et al9 believed that such differences were highly unlikely to influence patient outcomes.
Post-DSD Effects
The short- and long-term effects of DSD on the human body are unknown. Since the mechanism responsible for the efficacy of DSD is still unclear, many professionals and researchers are concerned that doubling the energy could cause myocardial damage. Although successful return of spontaneous circulation is an important first step in a successful resuscitation, the ultimate goal is to have a patient who is neurologically intact at the time of discharge home, with the capability of maintaining a favorable quality of life.
In 2016, Ross et al10 conducted a larger study comparing CPC scores of 279 patients in refractory V-fib, who received single shock (229 patients) vs DSD (50 patients). They found no statistically significant differences in neurologically intact survival rates between the two groups. This is an important finding that should be the goal for any future studies regarding DSD.10
Limitations to Future Research
For researchers to provide DSD results considered clinically significant, more cross-sectional, randomized-controlled studies need to be performed. Such studies will require a tremendous amount of time, effort, data collection, and a substantial sample size to prove that positive DSD results are not due to chance. As previously noted, the relatively rare incidence of true refractory V-fib makes it difficult for researchers to obtain large enough sample sizes to demonstrate clinically significant study results. Additionally, since medical institutions tend to adhere to different guidelines when running a code for cardiac arrest it would involve extraordinary measures to create and impose a single, standardized procedure/protocol for research purposes that each hospital would have to unanimously agree on.
Another limitation to producing large-scale, clinically significant research is that there is no universally accepted definition of refractory V-fib/pulseless V-tach. In all three of our cases, we defined it as V-fib/pulseless V-tach does not convert after three or more standard shocks, and at least one dose of either IV epinephrine and/or amiodarone. However, other clinicians and institutions define refractory V-fib as patients remaining in cardiac arrest for which the initial rhythm was either V-fib or V-tach, despite at least three defibrillation attempts, 3 mg of epinephrine, and 300 mg of amiodarone.11,12Importantly, DSD currently is neither endorsed as a standard of care nor recommended as part of the ACLS/American Heart Association/American College of Cardiology guidelines.
Conclusion
For every minute a patient remains in V-fib, the chance of survival decreases. Although the application of DSD has not been standardized at this time, we feel that it is a reasonable treatment option for patients in V-fib and pulseless V-tach, after all conventional interventions have failed. Though studies on DSD to date, as well as the three cases presented here, all involved relatively small sample sizes and isolated case reports, the results seem to suggest that DSD does improve chance of ROSC. We believe that DSD deserves further study and may be considered in cases of refractory V-fib and pulseless V-tach.
In 1930, Kouwenhoven, an electrical engineer, invented the first external cardiac defibrillator, and the first successful defibrillation performed on a human was reported in 1947.2Defibrillation devices have since evolved from the application of paddle electrodes to self-adhesive electrodes.
With the intent of producing a life-sustaining rhythm, a large dose of an electrical current from the defibrillator is used to depolarize the heart’s entire electrical conduction system. As medicine and technology advance, we continue to strive for better and more effective ways to improve the probability of survival for patients in cardiac arrest. One area of increasing interest in potentially improving survival rates is the use of double sequential defibrillation (DSD; double simultaneous defibrillation) in patients with V-fib and ventricular tachycardia (V-tach).
Double Sequential Defibrillation
Double sequential defibrillation, also known as double simultaneous defibrillation, is the use of two defibrillators simultaneously to deliver the maximum energy that may be necessary to treat refractory V-fib. In this review, we define refractory V-fib as V-fib/pulseless V-tach that does not revert to a life-sustaining rhythm after three or more shocks from a single defibrillator plus administration of at least a single dose of intravenous (IV) epinephrine and/or amiodarone.
When utilizing DSD, one set of pads is placed in the anterior-posterior position and the other set of pads is placed in the anterior-lateral position as shown in the Figure.
In three retrospective cases, we describe our use of DSD for refractory V-fib in the ED, in the hopes of encouraging further exploration of this potentially life-saving treatment modality in the treatment of refractory V-fib.
Although studies to assess the benefit of DSD are still in their early stages, we believe this technique has the potential to improve the success rate in achieving return of spontaneous circulation (ROSC) when compared to the standard method of defibrillation, described in the current advanced cardiac life support (ACLS) algorithms.
Cases
Case 1
A 39-year-old man with a medical history of type 1 diabetes mellitus arrived at our ED with a 6-hour history of nausea and vomiting. Upon arrival at the ED, the patient’s vital signs were: blood pressure, 109/52 mm Hg; heart rate, 120 beats/min; and respiratory rate, 20 breaths/min. Oxygen saturation was 94% on room air. Laboratory studies included a point-of-care blood glucose test, which revealed a glucose greater than 600 mg/dL.
The patient was initially resuscitated with 3 L Ringer’s lactate solution IV; and IV ondansetron for vomiting. One hour after his arrival, the patient developed monomorphic wide-complex tachycardia at 179 beats/min and began complaining of chest pain. An IV push of adenosine 6 mg was given with no effect on rhythm. The emergency physician (EP) then administered 300 mg of IV amiodarone followed by 100 mg of IV procainamide, without termination of the tachyarrhythmia.
The patient became hypotensive with a systolic blood pressure of 86 mm Hg, and an attempt was made to apply synchronized cardioversion at 100 J for his unstable V-tach. Shortly after cardioversion, the patient went into V-fib and became unconscious. Cardiopulmonary resuscitation was initiated, and the patient was defibrillated at 200 J without success. He was then given 1 mg of IV epinephrine, 2 amp of IV sodium bicarbonate, and intubated.
The patient remained pulseless and in V-fib. A second unsuccessful defibrillation attempt at 200 J was made. Followed by CPR and a third unsuccessful attempt at defibrillation. The patient next received DSD with the two defibrillators each set at 200 J, and afterwards converted back to sinus rhythm.
After successful DSD, the patient was started on an insulin drip and was transferred to the intensive care unit (ICU). He survived to hospital discharge with a cerebral performance category (CPC) scale score of 1, defined as “good cerebral performance, neurologically intact, may lead a normal life”.3
Case 2
A 22-year-old woman with a known history of heroin abuse was brought to our ED by emergency medical services (EMS) following an unwitnessed cardiac arrest pulseless electrical activity (PEA). The patient’s parents stated that when they saw the patient approximately 5 hours earlier, she appeared normal physically and was behaving normally. Emergency medical technicians (EMTs) administered several milligrams of IV naloxone without success. The patient was intubated while en route to the hospital and CPR was performed for 35 minutes, after which ROSC was achieved.
However, en route to the hospital, the patient developed V-fib, for which she was unsuccessfully defibrillated three times at 200 J. Upon arrival at the ED, the patient was defibrillated twice more at 200 J but remained in V-fib. On the third pulse check DSD was performed, and the patient subsequently converted to a PEA rhythm; CPR was continued for two more cycles, after which the patient regained a weak pulse and an ETCO2 of 55 mm Hg. A central line was placed and the patient was started on IV epinephrine and dopamine. In the ICU she received targeted temperature management, but ultimately expired that evening.
Case 3
A 39-year-old woman with no known medical history was brought to the ED by EMS after she was discovered to be unconscious and pulseless by her husband in their home. Upon arrival, the EMTs found the patient in V-fib and performed endotracheal intubation and 30 minutes of CPR. The EMS report recorded that the patient had been defibrillated a total of five times at the scene before achieving ROSC. En route to the hospital, however, the patient’s rhythm reverted to V-fib; CPR was again initiated along with an unsuccessful attempt at defibrillation. The EMTs then administered 300 mg of IV amiodarone, 1 amp of sodium bicarbonate, and epinephrine IV every 3 to 5 minutes.
Upon arrival at the ED, the EP attempted defibrillation twice, unsuccessfully. The patient was then given IV magnesium, 1 amp of sodium bicarbonate IV, and three doses of IV epinephrine, but remained in V-fib. The EP then attempted DSD but with no success, but a second application of DSD resulted in conversion to a junctional bradycardia. After 1 hour of CPR, ROSC was achieved, and the patient was transferred to the ICU. Unfortunately, due to the burden of neurological damage from the cardiac arrest and poor predicted outcome, the patient’s family ultimately decided to have care withdrawn overnight. The patient expired shortly after being extubated.
Discussion
Out-of-hospital cardiac arrest remains a leading cause of death today; of which cardiac arrests due to V-fib are associated with the highest survival rates.4 Our three cases suggest that application of DSD may be of benefit in the ED, in the treatment of refractory V-fib and refractory pulseless V-tach. All three of the patients we described achieved ROSC after DSD and unsuccessful prior attempts with standard defibrillation, though only one of the patients was discharged home with good neurological status.
One of the earliest known studies of the applications of DSD on human subjects was described in 1994 by Hoch et al.5 The study included 2,990 patients who underwent a total of 5,450 electrophysiological studies over a period of 3 years. The researchers induced V-fib/pulseless V-tach in approximately 30% of their study population. Five of these patients, who were all men with a mean age of 55 years, experienced refractory V-fib each of whom required seven to 20 unsuccessful attempts at defibrillation. The researchers ultimately found that when they applied DSD, only one attempt was needed for successful conversion to normal sinus rhythm in all five of the patients.5The authors acknowledged that there were many limitations to their study, which will likely continue to be factors in future studies as well.
DSD exists in the form of reviews, case reports, and retrospective studies in most of the recent literature. The reason for the paucity of research is probably due to the relative rarity and random nature of refractory V-fib (0.1% of V-fib arrests),6 making it nearly impossible for researchers to conduct large-scale studies in a controlled environment. Another limitation that hinders DSD research studies is the large number of variables that can determine a patient’s chance of survival after defibrillation. These variables include age, comorbidities, risk factors, timing of arrival at the ED, application and quality of prehospital CPR, laboratory abnormalities, and other patient-specific neurological or metabolic processes.
Several case series previously reported on the use of DSD, most of which describe patients in the out-of-hospital setting. The findings from these case series appear promising—at least to the extent in which patients were converted out of V-fib through DSD.
In 2014, Cabañas et al6 reported on a retrospective case series of 10 patients treated with DSD between 2008 and 2010, and found that 70% of the patients were successfully converted by DSD out of refractory V-fib. Unfortunately, none of the patients survived to hospital discharge.
Another recent retrospective study conducted by Cortez et al7 of 12 patients with refractory V-fib treated with DSD found that nine of the 12 patients (75%) converted out of V-fib, three of whom survived to hospital discharge, with two patients (16.7%) discharged with a CPC of 1.7 Lastly, Merlin et al8 reported on a retrospective case series in 2015 of EMTs delivering DSS in the field to a total of seven patients with refractory V-fib, five of whom (71%) were successfully converted out of V-fib, with four (57%) surviving to hospital admission.8
Pharmacological Agents Post-DSD
None of the patients in the study by Hoch et al5 received any pharmacological agents between initial unsuccessful attempts at defibrillation and the final application of DSD. As previously noted, all three of the patients in our cases had the full support of ED personnel, as well as the administration of appropriate pharmacological agents.
A randomized controlled trial published in 2006 by Hohnloser et al9 reported clinically significant results in studying the effects of antiarrhythmic agents, particularly amiodarone and sotalol, on defibrillation thresholds. They found that amiodarone increased the defibrillation threshold by 1.29 J, while sotalol decreased the defibrillation threshold by 0.89 J. However, despite their findings, Hohnloser et al9 believed that such differences were highly unlikely to influence patient outcomes.
Post-DSD Effects
The short- and long-term effects of DSD on the human body are unknown. Since the mechanism responsible for the efficacy of DSD is still unclear, many professionals and researchers are concerned that doubling the energy could cause myocardial damage. Although successful return of spontaneous circulation is an important first step in a successful resuscitation, the ultimate goal is to have a patient who is neurologically intact at the time of discharge home, with the capability of maintaining a favorable quality of life.
In 2016, Ross et al10 conducted a larger study comparing CPC scores of 279 patients in refractory V-fib, who received single shock (229 patients) vs DSD (50 patients). They found no statistically significant differences in neurologically intact survival rates between the two groups. This is an important finding that should be the goal for any future studies regarding DSD.10
Limitations to Future Research
For researchers to provide DSD results considered clinically significant, more cross-sectional, randomized-controlled studies need to be performed. Such studies will require a tremendous amount of time, effort, data collection, and a substantial sample size to prove that positive DSD results are not due to chance. As previously noted, the relatively rare incidence of true refractory V-fib makes it difficult for researchers to obtain large enough sample sizes to demonstrate clinically significant study results. Additionally, since medical institutions tend to adhere to different guidelines when running a code for cardiac arrest it would involve extraordinary measures to create and impose a single, standardized procedure/protocol for research purposes that each hospital would have to unanimously agree on.
Another limitation to producing large-scale, clinically significant research is that there is no universally accepted definition of refractory V-fib/pulseless V-tach. In all three of our cases, we defined it as V-fib/pulseless V-tach does not convert after three or more standard shocks, and at least one dose of either IV epinephrine and/or amiodarone. However, other clinicians and institutions define refractory V-fib as patients remaining in cardiac arrest for which the initial rhythm was either V-fib or V-tach, despite at least three defibrillation attempts, 3 mg of epinephrine, and 300 mg of amiodarone.11,12Importantly, DSD currently is neither endorsed as a standard of care nor recommended as part of the ACLS/American Heart Association/American College of Cardiology guidelines.
Conclusion
For every minute a patient remains in V-fib, the chance of survival decreases. Although the application of DSD has not been standardized at this time, we feel that it is a reasonable treatment option for patients in V-fib and pulseless V-tach, after all conventional interventions have failed. Though studies on DSD to date, as well as the three cases presented here, all involved relatively small sample sizes and isolated case reports, the results seem to suggest that DSD does improve chance of ROSC. We believe that DSD deserves further study and may be considered in cases of refractory V-fib and pulseless V-tach.
1. Efimov IR. Naum Lazarevich Gurvich (1905–1981) and his contribution to the history of defibrillation. Cardiol J. 2009;16(2):190-193.
2. Bocka JJ. Automatic External Defibrillator. Medscape. http://emedicine.medscape.com/article/780533-overview#a1. Published May 30, 2014. Accessed September 19, 2017.
3. Ajam K, Gold LS, Beck SS, et al. Reliability of cerebral performance category to classify neurological status among survivors of ventricular fibrillation arrest: a cohort study. Scand J Trauma Resus Emerg Med. 2011;19:38. doi:10.1186/1757-7241-19-38.
4. Daya MR, Schmicker RH, Zive DM, et al; Resuscitation Outcomes Consortium Investigators. Out-of-hospital cardiac arrest survival improving over time: Results from the Resuscitation Outcomes Consortium (ROC). Resuscitation. 2015;91:108-115. doi:10.1016/j.resuscitation.2015.02.003.
5. Hoch DH, Batsford WP, Greenberg SM, et al. Double sequential external shocks for refractory ventricular fibrillation. J Am Coll Cardiol. 1994;23(5):1141-1145.
6. Cabañas JG, Myers JB, Williams JG, De Maio VJ, Bachman MW. Double sequential external defibrillation in out-of-hospital refractory ventricular fibrillation: a report of ten cases. Prehosp Emerg Care. 2015;19(1):126-130. doi:10.3109/10903127.2014.942476.
7. Cortez E, Krebs W, Davis J, Keseg DP, Panchal AR. Use of double sequential external defibrillation for refractory ventricular fibrillation during out-of-hospital cardiac arrest. Resuscitation. 2016;108:82-86. doi:10.1016/j.resuscitation.2016.08.002.
8. Merlin MA, Tagore A, Bauter R, Arshad FH. A case series of double sequence defibrillation. Prehosp Emerg Care. 2016;20(4):550-553. doi:10.3109/10903127.2015.1128026.
9. Hohnloser SH, Dorian P, Roberts R, et al. Effect of amiodarone and sotalol on ventricular defibrillation threshold: the optimal pharmacological therapy in cardioverter defibrillator patients (OPTIC) trial. Circulation. 2006;114(2):104-109. doi:10.1161/CIRCULATIONAHA.106.618421.
10. Ross EM, Redman TT, Harper SA, Mapp JG, Wampler DA, Miramontes DA. Dual defibrillation in out-of-hospital cardiac arrest: a retrospective cohort analysis. Resuscitation. 2016;106:14-17. doi:10.1016/j.resuscitation.2016.06.011.11. Driver BE, Debaty G, Plummer DW, Smith SW. Use of esmolol after failure of standard cardiopulmonary resuscitation to treat patients with refractory ventricular fibrillation. Resuscitation. 2014;85(10):1337-1341. doi:10.1016/j.resuscitation.2014.06.032.
12. Lee YH, Lee KJ, Min YH, et al. Refractory ventricular fibrillation treated with esmolol. Resuscitation. 2016;107:150-155. doi:10.1016/j.resuscitation.2016.07.243.
1. Efimov IR. Naum Lazarevich Gurvich (1905–1981) and his contribution to the history of defibrillation. Cardiol J. 2009;16(2):190-193.
2. Bocka JJ. Automatic External Defibrillator. Medscape. http://emedicine.medscape.com/article/780533-overview#a1. Published May 30, 2014. Accessed September 19, 2017.
3. Ajam K, Gold LS, Beck SS, et al. Reliability of cerebral performance category to classify neurological status among survivors of ventricular fibrillation arrest: a cohort study. Scand J Trauma Resus Emerg Med. 2011;19:38. doi:10.1186/1757-7241-19-38.
4. Daya MR, Schmicker RH, Zive DM, et al; Resuscitation Outcomes Consortium Investigators. Out-of-hospital cardiac arrest survival improving over time: Results from the Resuscitation Outcomes Consortium (ROC). Resuscitation. 2015;91:108-115. doi:10.1016/j.resuscitation.2015.02.003.
5. Hoch DH, Batsford WP, Greenberg SM, et al. Double sequential external shocks for refractory ventricular fibrillation. J Am Coll Cardiol. 1994;23(5):1141-1145.
6. Cabañas JG, Myers JB, Williams JG, De Maio VJ, Bachman MW. Double sequential external defibrillation in out-of-hospital refractory ventricular fibrillation: a report of ten cases. Prehosp Emerg Care. 2015;19(1):126-130. doi:10.3109/10903127.2014.942476.
7. Cortez E, Krebs W, Davis J, Keseg DP, Panchal AR. Use of double sequential external defibrillation for refractory ventricular fibrillation during out-of-hospital cardiac arrest. Resuscitation. 2016;108:82-86. doi:10.1016/j.resuscitation.2016.08.002.
8. Merlin MA, Tagore A, Bauter R, Arshad FH. A case series of double sequence defibrillation. Prehosp Emerg Care. 2016;20(4):550-553. doi:10.3109/10903127.2015.1128026.
9. Hohnloser SH, Dorian P, Roberts R, et al. Effect of amiodarone and sotalol on ventricular defibrillation threshold: the optimal pharmacological therapy in cardioverter defibrillator patients (OPTIC) trial. Circulation. 2006;114(2):104-109. doi:10.1161/CIRCULATIONAHA.106.618421.
10. Ross EM, Redman TT, Harper SA, Mapp JG, Wampler DA, Miramontes DA. Dual defibrillation in out-of-hospital cardiac arrest: a retrospective cohort analysis. Resuscitation. 2016;106:14-17. doi:10.1016/j.resuscitation.2016.06.011.11. Driver BE, Debaty G, Plummer DW, Smith SW. Use of esmolol after failure of standard cardiopulmonary resuscitation to treat patients with refractory ventricular fibrillation. Resuscitation. 2014;85(10):1337-1341. doi:10.1016/j.resuscitation.2014.06.032.
12. Lee YH, Lee KJ, Min YH, et al. Refractory ventricular fibrillation treated with esmolol. Resuscitation. 2016;107:150-155. doi:10.1016/j.resuscitation.2016.07.243.
Emergency Ultrasound: Pericardial Effusion and Tamponade: Making the Diagnosis at Bedside With Point-of-Care Echocardiography
Background
Pericardial effusions are usually an incidental finding on bedside echocardiogram—unless a patient shows clinical signs of tamponade physiology and obstructive shock. Echocardiogram is both sensitive and specific to detecting pericardial effusions.1 Although there are many causes of pericardial effusions, the most common causes of symptomatic effusions in the Western World are due to neoplasm, pericarditis, traumatic pathology, or idiopathic etiology. In developing countries, however, pericardial effusions are predominantly due to tuberculosis in an area where it is endemic.2,3 The size of the effusion is classified based on measurements of a fluid pocket during diastole. Mild effusion is defined as less than 10 mm; moderate effusion, 10 to 20 mm; and large effusion, greater than 20 mm.3
It is important to note that the pericardial space contains up to 50 mL of physiological fluid which may be seen on echocardiography during systole. Small effusions usually contain less than 100 mL of fluid; moderate effusions contain 100 to 500 mL of fluid; and large effusions, over 500 mL of fluid. Fluid of smaller effusions typically layer posteriorly, while the fluid of some moderate and most large effusions may be seen circumferentially.
Clinical Signs and Symptoms
Patients with large chronic effusions are often asymptomatic, and clinical symptoms usually correlate to the acuity of pericardial accumulation. Patients with symptomatic effusions present with dyspnea on exertion that is followed by orthopnea, chest pain, and sometimes dysphagia, hoarseness, or hiccups due to irritation of surrounding structures until they exhibit tamponade physiology leading to hypotension secondary to obstructive shock. The most recognized signs of tamponade physiology on bedside echocardiography are early diastolic collapse of the right atrium and right ventricle, as well as ventricular interdependence.4
Imaging Technique
Pericardial effusion and cardiac tamponade can be detected in any of the standard echocardiographic views, with fluid usually appearing as an anechoic stripe. The fluid will first appear in the dependent portion of the pericardial space, but may become circumferential as it grows (Figure 1).
After evaluating for signs of tamponade on examination, the next step is to evaluate the inferior vena cava (IVC). A simple way to identify the IVC on echocardiography is to visualize the heart in the subxiphoid view, then rotate the probe so that the marker is pointing toward the patient’s head. As demonstrated in Figure 5, the IVC should be seen entering the right atrium; if the patient is truly in obstructive shock, the IVC should be plethoric with minimal respiratory variation.
Pericardiocentesis
In the event of obstructive shock or pulseless electric activity with visualized or suspected tamponade, pericardiocentesis is considered standard of care. There are many approaches to performing a pericardiocentesis, including the classically taught blind subxiphoid approach, which is associated with high rates of morbidity and mortality.5 More recent image-guided approaches employ echocardiography-guided techniques that identify the location and distribution of fluid, and perform pericardiocentesis closest to the area largest fluid accumulation.
Most of these guided techniques involve in-plane visualization of the needle in either a subxiphoid, apical, or parasternal approach. Studies have shown that the subxiphoid approach has a higher risk of injury to the liver, heart, and IVC, with complication rates up to 20% depending on the study.6
The apical approach involves locating the cardiac apex and inserting the needle 1 cm lateral to the apex, with the point directed toward the effusion and in-line with the ultrasound probe, taking care to avoid the lingula. Studies have shown that complication rates with this approach are around 3%.7
Recent studies also suggest that in-line medial-to-lateral parasternal approaches may have minimal complications. However, when employing this approach, care must be taken to avoid the internal mammary artery, which can be identified using color-flow Doppler echocardiology.6
Conclusion
In general, bedside ultrasound is a quick and useful tool to evaluate for pericardial effusion and signs of tamponade physiology. When present, tamponade, a clinical diagnosis, is the likely cause of shock in the hemodynamically unstable patient with circumferential pericardial effusion.
While most cases of pericardial effusion are found incidentally, a stepwise approach to evaluate for tamponade is to quickly look for signs of early right-sided diastolic collapse or ventricular interdependence, as well as a plethoric IVC. For patients who have tamponade requiring pericardiocentesis, the ultrasound-guided apical or parasternal approaches have been shown to have fewer complications compared to the subxiphoid approach.
1. Imazio M, Adler Y. Management of pericardial effusion. Eur Heart J. 2013;34(16):1186-1197. doi:10.1093/eurheartj/ehs372.
2. Ben-Horin S, Bank I, Guetta V, Livneh A. Large symptomatic pericardial effusion as the presentation of unrecognized cancer: a study in 173 consecutive patients undergoing pericardiocentesis. Medicine. 2006;85(1):49-53. doi:10.1097/01.md.0000199556.69588.8e
3. Adler Y, Charron P, Imazio M, et al; European Society of Cardiology (ESC). 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2015;36(42):2921-2964. doi:10.1093/eurheartj/ehv318.
4. Nagdev A, Stone MB. Point-of-care ultrasound evaluation of pericardial effusions: does this patient have cardiac tamponade? Resuscitation. 2011;82(6):671-673. doi:10.1016/j.resuscitation.2011.02.004.
5. Kumar R, Sinha A, Lin MJ. Complications of pericardiocentesis: a clinical synopsis. Int J Crit Illn Inj Sci. 2015;5(3):206-212. doi:10.4103/2229-5151.165007.
6. Osman A, Wan Chuan T, Ab Rahman J, Via G, Tavazzi G. Ultrasound-guided pericardiocentesis: a novel parasternal approach. Eur J Emerg Med. 2017;5. doi:10.1097/MEJ.0000000000000471.
7. Ozer HO, Davutoğlu V, Cakici M. Echocardiography-guided pericardiocentesis with the apical approach. Turk Kardiyol Dern Ars. 2009;37(3):177-181.
Background
Pericardial effusions are usually an incidental finding on bedside echocardiogram—unless a patient shows clinical signs of tamponade physiology and obstructive shock. Echocardiogram is both sensitive and specific to detecting pericardial effusions.1 Although there are many causes of pericardial effusions, the most common causes of symptomatic effusions in the Western World are due to neoplasm, pericarditis, traumatic pathology, or idiopathic etiology. In developing countries, however, pericardial effusions are predominantly due to tuberculosis in an area where it is endemic.2,3 The size of the effusion is classified based on measurements of a fluid pocket during diastole. Mild effusion is defined as less than 10 mm; moderate effusion, 10 to 20 mm; and large effusion, greater than 20 mm.3
It is important to note that the pericardial space contains up to 50 mL of physiological fluid which may be seen on echocardiography during systole. Small effusions usually contain less than 100 mL of fluid; moderate effusions contain 100 to 500 mL of fluid; and large effusions, over 500 mL of fluid. Fluid of smaller effusions typically layer posteriorly, while the fluid of some moderate and most large effusions may be seen circumferentially.
Clinical Signs and Symptoms
Patients with large chronic effusions are often asymptomatic, and clinical symptoms usually correlate to the acuity of pericardial accumulation. Patients with symptomatic effusions present with dyspnea on exertion that is followed by orthopnea, chest pain, and sometimes dysphagia, hoarseness, or hiccups due to irritation of surrounding structures until they exhibit tamponade physiology leading to hypotension secondary to obstructive shock. The most recognized signs of tamponade physiology on bedside echocardiography are early diastolic collapse of the right atrium and right ventricle, as well as ventricular interdependence.4
Imaging Technique
Pericardial effusion and cardiac tamponade can be detected in any of the standard echocardiographic views, with fluid usually appearing as an anechoic stripe. The fluid will first appear in the dependent portion of the pericardial space, but may become circumferential as it grows (Figure 1).
After evaluating for signs of tamponade on examination, the next step is to evaluate the inferior vena cava (IVC). A simple way to identify the IVC on echocardiography is to visualize the heart in the subxiphoid view, then rotate the probe so that the marker is pointing toward the patient’s head. As demonstrated in Figure 5, the IVC should be seen entering the right atrium; if the patient is truly in obstructive shock, the IVC should be plethoric with minimal respiratory variation.
Pericardiocentesis
In the event of obstructive shock or pulseless electric activity with visualized or suspected tamponade, pericardiocentesis is considered standard of care. There are many approaches to performing a pericardiocentesis, including the classically taught blind subxiphoid approach, which is associated with high rates of morbidity and mortality.5 More recent image-guided approaches employ echocardiography-guided techniques that identify the location and distribution of fluid, and perform pericardiocentesis closest to the area largest fluid accumulation.
Most of these guided techniques involve in-plane visualization of the needle in either a subxiphoid, apical, or parasternal approach. Studies have shown that the subxiphoid approach has a higher risk of injury to the liver, heart, and IVC, with complication rates up to 20% depending on the study.6
The apical approach involves locating the cardiac apex and inserting the needle 1 cm lateral to the apex, with the point directed toward the effusion and in-line with the ultrasound probe, taking care to avoid the lingula. Studies have shown that complication rates with this approach are around 3%.7
Recent studies also suggest that in-line medial-to-lateral parasternal approaches may have minimal complications. However, when employing this approach, care must be taken to avoid the internal mammary artery, which can be identified using color-flow Doppler echocardiology.6
Conclusion
In general, bedside ultrasound is a quick and useful tool to evaluate for pericardial effusion and signs of tamponade physiology. When present, tamponade, a clinical diagnosis, is the likely cause of shock in the hemodynamically unstable patient with circumferential pericardial effusion.
While most cases of pericardial effusion are found incidentally, a stepwise approach to evaluate for tamponade is to quickly look for signs of early right-sided diastolic collapse or ventricular interdependence, as well as a plethoric IVC. For patients who have tamponade requiring pericardiocentesis, the ultrasound-guided apical or parasternal approaches have been shown to have fewer complications compared to the subxiphoid approach.
Background
Pericardial effusions are usually an incidental finding on bedside echocardiogram—unless a patient shows clinical signs of tamponade physiology and obstructive shock. Echocardiogram is both sensitive and specific to detecting pericardial effusions.1 Although there are many causes of pericardial effusions, the most common causes of symptomatic effusions in the Western World are due to neoplasm, pericarditis, traumatic pathology, or idiopathic etiology. In developing countries, however, pericardial effusions are predominantly due to tuberculosis in an area where it is endemic.2,3 The size of the effusion is classified based on measurements of a fluid pocket during diastole. Mild effusion is defined as less than 10 mm; moderate effusion, 10 to 20 mm; and large effusion, greater than 20 mm.3
It is important to note that the pericardial space contains up to 50 mL of physiological fluid which may be seen on echocardiography during systole. Small effusions usually contain less than 100 mL of fluid; moderate effusions contain 100 to 500 mL of fluid; and large effusions, over 500 mL of fluid. Fluid of smaller effusions typically layer posteriorly, while the fluid of some moderate and most large effusions may be seen circumferentially.
Clinical Signs and Symptoms
Patients with large chronic effusions are often asymptomatic, and clinical symptoms usually correlate to the acuity of pericardial accumulation. Patients with symptomatic effusions present with dyspnea on exertion that is followed by orthopnea, chest pain, and sometimes dysphagia, hoarseness, or hiccups due to irritation of surrounding structures until they exhibit tamponade physiology leading to hypotension secondary to obstructive shock. The most recognized signs of tamponade physiology on bedside echocardiography are early diastolic collapse of the right atrium and right ventricle, as well as ventricular interdependence.4
Imaging Technique
Pericardial effusion and cardiac tamponade can be detected in any of the standard echocardiographic views, with fluid usually appearing as an anechoic stripe. The fluid will first appear in the dependent portion of the pericardial space, but may become circumferential as it grows (Figure 1).
After evaluating for signs of tamponade on examination, the next step is to evaluate the inferior vena cava (IVC). A simple way to identify the IVC on echocardiography is to visualize the heart in the subxiphoid view, then rotate the probe so that the marker is pointing toward the patient’s head. As demonstrated in Figure 5, the IVC should be seen entering the right atrium; if the patient is truly in obstructive shock, the IVC should be plethoric with minimal respiratory variation.
Pericardiocentesis
In the event of obstructive shock or pulseless electric activity with visualized or suspected tamponade, pericardiocentesis is considered standard of care. There are many approaches to performing a pericardiocentesis, including the classically taught blind subxiphoid approach, which is associated with high rates of morbidity and mortality.5 More recent image-guided approaches employ echocardiography-guided techniques that identify the location and distribution of fluid, and perform pericardiocentesis closest to the area largest fluid accumulation.
Most of these guided techniques involve in-plane visualization of the needle in either a subxiphoid, apical, or parasternal approach. Studies have shown that the subxiphoid approach has a higher risk of injury to the liver, heart, and IVC, with complication rates up to 20% depending on the study.6
The apical approach involves locating the cardiac apex and inserting the needle 1 cm lateral to the apex, with the point directed toward the effusion and in-line with the ultrasound probe, taking care to avoid the lingula. Studies have shown that complication rates with this approach are around 3%.7
Recent studies also suggest that in-line medial-to-lateral parasternal approaches may have minimal complications. However, when employing this approach, care must be taken to avoid the internal mammary artery, which can be identified using color-flow Doppler echocardiology.6
Conclusion
In general, bedside ultrasound is a quick and useful tool to evaluate for pericardial effusion and signs of tamponade physiology. When present, tamponade, a clinical diagnosis, is the likely cause of shock in the hemodynamically unstable patient with circumferential pericardial effusion.
While most cases of pericardial effusion are found incidentally, a stepwise approach to evaluate for tamponade is to quickly look for signs of early right-sided diastolic collapse or ventricular interdependence, as well as a plethoric IVC. For patients who have tamponade requiring pericardiocentesis, the ultrasound-guided apical or parasternal approaches have been shown to have fewer complications compared to the subxiphoid approach.
1. Imazio M, Adler Y. Management of pericardial effusion. Eur Heart J. 2013;34(16):1186-1197. doi:10.1093/eurheartj/ehs372.
2. Ben-Horin S, Bank I, Guetta V, Livneh A. Large symptomatic pericardial effusion as the presentation of unrecognized cancer: a study in 173 consecutive patients undergoing pericardiocentesis. Medicine. 2006;85(1):49-53. doi:10.1097/01.md.0000199556.69588.8e
3. Adler Y, Charron P, Imazio M, et al; European Society of Cardiology (ESC). 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2015;36(42):2921-2964. doi:10.1093/eurheartj/ehv318.
4. Nagdev A, Stone MB. Point-of-care ultrasound evaluation of pericardial effusions: does this patient have cardiac tamponade? Resuscitation. 2011;82(6):671-673. doi:10.1016/j.resuscitation.2011.02.004.
5. Kumar R, Sinha A, Lin MJ. Complications of pericardiocentesis: a clinical synopsis. Int J Crit Illn Inj Sci. 2015;5(3):206-212. doi:10.4103/2229-5151.165007.
6. Osman A, Wan Chuan T, Ab Rahman J, Via G, Tavazzi G. Ultrasound-guided pericardiocentesis: a novel parasternal approach. Eur J Emerg Med. 2017;5. doi:10.1097/MEJ.0000000000000471.
7. Ozer HO, Davutoğlu V, Cakici M. Echocardiography-guided pericardiocentesis with the apical approach. Turk Kardiyol Dern Ars. 2009;37(3):177-181.
1. Imazio M, Adler Y. Management of pericardial effusion. Eur Heart J. 2013;34(16):1186-1197. doi:10.1093/eurheartj/ehs372.
2. Ben-Horin S, Bank I, Guetta V, Livneh A. Large symptomatic pericardial effusion as the presentation of unrecognized cancer: a study in 173 consecutive patients undergoing pericardiocentesis. Medicine. 2006;85(1):49-53. doi:10.1097/01.md.0000199556.69588.8e
3. Adler Y, Charron P, Imazio M, et al; European Society of Cardiology (ESC). 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2015;36(42):2921-2964. doi:10.1093/eurheartj/ehv318.
4. Nagdev A, Stone MB. Point-of-care ultrasound evaluation of pericardial effusions: does this patient have cardiac tamponade? Resuscitation. 2011;82(6):671-673. doi:10.1016/j.resuscitation.2011.02.004.
5. Kumar R, Sinha A, Lin MJ. Complications of pericardiocentesis: a clinical synopsis. Int J Crit Illn Inj Sci. 2015;5(3):206-212. doi:10.4103/2229-5151.165007.
6. Osman A, Wan Chuan T, Ab Rahman J, Via G, Tavazzi G. Ultrasound-guided pericardiocentesis: a novel parasternal approach. Eur J Emerg Med. 2017;5. doi:10.1097/MEJ.0000000000000471.
7. Ozer HO, Davutoğlu V, Cakici M. Echocardiography-guided pericardiocentesis with the apical approach. Turk Kardiyol Dern Ars. 2009;37(3):177-181.
A Case of Streptococcus pyogenes Sepsis of Possible Oral Origin
Sepsis can be the result of single or multiple factors and sources of infection. Oral sources of sepsis and systemic infection are not commonly considered as the first potential source of infection when evaluating a septic patient. Oral infections of odontogenic or periodontal origin are frequently associated with localized or diffuse cellulitis of the head and neck region. 1 The patient’s health status and complicating problems, such as an immunocompromising condition, can further reduce the immune response for controlling chronic sources of infection. This in turn can lead to acute manifestations such as cellulitis, sepsis, or necrotizing fasciitis. Necrotizing fasciitis is caused by a polymicrobial or mixed aerobic-anaerobic infection from a variety of sources, including Streptococcus pyogenes .
Case
A 57-year-old woman with a history of major depressive disorder, paroxysmal atrial fibrillation, and opioid dependence that was in remission for more than 3 years was brought to the ED by a family member after the patient developed confusion and lethargy. She was primarily experiencing right breast pain and swelling. The breast pain was associated with high fevers, nausea, vomiting, and chills.
On examination, the patient’s vital signs were: blood pressure (BP), 109/58 mm Hg; heart rate, 160 beats/min; respiratory rate, 22 breaths/min; and temperature, 104°F. Laboratory evaluation was significant for a white blood cell count (WBC) of 8.7 x 103. There was a noted skin abrasion on the patient’s right hand. She was lethargic and confused. Blood cultures were positive for S pyogenes, and a swab of the right breast was negative for bacterial growth.
The patient was admitted to the medical intensive care unit (MICU) and placed on two vasopressors for control of low BP and assistance with low urine output. After a 6-L fluid resuscitation, the patient was started on vancomycin and piperacillin/tazobactam for possible cellulitis causing sepsis. An echocardiogram was negative for endocarditis. The patient continued to decline the following day with continuing tachycardia and tachypnea with hypotension and was intubated. Pulmonology services was consulted for possible acute respiratory distress syndrome secondary to sepsis; general surgery services was consulted for possible necrotizing fasciitis of the chest wall; and cardiology services was consulted for low-cardiac output.
On hospital day 4, the patient was taken to surgery for exploration, drainage, and debridement of the right axilla and breast; cultures were taken, and lack of organism growth was noted. While in the MICU, she was followed by the infectious disease service as her WBC remained elevated and peaking at 32.6 x 103, while blood cultures were negative for bacterial growth.
The dental service was consulted on hospital day 5 to evaluate for other possible sources of infection. Upon examination, the patient’s oral condition was noted as having advanced chronic periodontal disease that required full-mouth extraction. The patient remained hemodynamically unstable with platelet counts below 50 x 109/L until hospital day 7, at which time she was taken for surgery for full mouth extraction and associated alveoloplasty. Upon extraction, the patient continued to improve and was extubated on day 11 with platelets and WBC returning to normal levels by day 13 of her hospital stay. The patient remained hospitalized for a total MICU stay of 20 days and rehabilitation stay of more than 2 weeks.
Discussion
Oral infections most often present with acute onset and noted oral-facial cellulitis or abscess. Oral source of septicemia often are considered after ruling out most other potential sources. Although it is not certain that this case is directly related to the advanced chronic periodontal disease, S pyogenes has been noted to be a pathogen in periodontal disease progression.
According to the American Dental Association in 2012, dental visits to the ED cost the US health care system $1.6 billion and an average cost of $749 per visit. There are more than 2 million ED visits each year for dental pain and infection, and 39% return due to nonresolution of the dental problem. Patients return to the ED due to lack of access and resources to routine and emergent dental care. 2 The average daily cost of an MICU stay with mechanical ventilation was $2,193 in 2002. This particular case consisted of 11 days of mechanical ventilation, 20 MICU days, and an additional 20 days of inpatient rehabilitation which resulted in costs that exceeded $50,000. 3
1. Krishnan V, Johnson JV, Helfric JF. Management of maxillofacial infections: a review of 50 cases. J Oral Maxillofac Surg. 1993;51(8):868-873; discussion 873-874.
2. Wall T, Vujicic M. Emergency department use for dental conditions continues to increase. American Dental Association: Health Policy Institute. http://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_0415_2.ashx. Published April 2015. Accessed November 6, 2017.
3. Dasta JF, McLaughlin TP, Mody SH, Piech CT. Daily cost of an intensive care unit day: the contribution of mechanical ventilation. Crit Care Med. 2005;33(6):1266-1271.
Sepsis can be the result of single or multiple factors and sources of infection. Oral sources of sepsis and systemic infection are not commonly considered as the first potential source of infection when evaluating a septic patient. Oral infections of odontogenic or periodontal origin are frequently associated with localized or diffuse cellulitis of the head and neck region. 1 The patient’s health status and complicating problems, such as an immunocompromising condition, can further reduce the immune response for controlling chronic sources of infection. This in turn can lead to acute manifestations such as cellulitis, sepsis, or necrotizing fasciitis. Necrotizing fasciitis is caused by a polymicrobial or mixed aerobic-anaerobic infection from a variety of sources, including Streptococcus pyogenes .
Case
A 57-year-old woman with a history of major depressive disorder, paroxysmal atrial fibrillation, and opioid dependence that was in remission for more than 3 years was brought to the ED by a family member after the patient developed confusion and lethargy. She was primarily experiencing right breast pain and swelling. The breast pain was associated with high fevers, nausea, vomiting, and chills.
On examination, the patient’s vital signs were: blood pressure (BP), 109/58 mm Hg; heart rate, 160 beats/min; respiratory rate, 22 breaths/min; and temperature, 104°F. Laboratory evaluation was significant for a white blood cell count (WBC) of 8.7 x 103. There was a noted skin abrasion on the patient’s right hand. She was lethargic and confused. Blood cultures were positive for S pyogenes, and a swab of the right breast was negative for bacterial growth.
The patient was admitted to the medical intensive care unit (MICU) and placed on two vasopressors for control of low BP and assistance with low urine output. After a 6-L fluid resuscitation, the patient was started on vancomycin and piperacillin/tazobactam for possible cellulitis causing sepsis. An echocardiogram was negative for endocarditis. The patient continued to decline the following day with continuing tachycardia and tachypnea with hypotension and was intubated. Pulmonology services was consulted for possible acute respiratory distress syndrome secondary to sepsis; general surgery services was consulted for possible necrotizing fasciitis of the chest wall; and cardiology services was consulted for low-cardiac output.
On hospital day 4, the patient was taken to surgery for exploration, drainage, and debridement of the right axilla and breast; cultures were taken, and lack of organism growth was noted. While in the MICU, she was followed by the infectious disease service as her WBC remained elevated and peaking at 32.6 x 103, while blood cultures were negative for bacterial growth.
The dental service was consulted on hospital day 5 to evaluate for other possible sources of infection. Upon examination, the patient’s oral condition was noted as having advanced chronic periodontal disease that required full-mouth extraction. The patient remained hemodynamically unstable with platelet counts below 50 x 109/L until hospital day 7, at which time she was taken for surgery for full mouth extraction and associated alveoloplasty. Upon extraction, the patient continued to improve and was extubated on day 11 with platelets and WBC returning to normal levels by day 13 of her hospital stay. The patient remained hospitalized for a total MICU stay of 20 days and rehabilitation stay of more than 2 weeks.
Discussion
Oral infections most often present with acute onset and noted oral-facial cellulitis or abscess. Oral source of septicemia often are considered after ruling out most other potential sources. Although it is not certain that this case is directly related to the advanced chronic periodontal disease, S pyogenes has been noted to be a pathogen in periodontal disease progression.
According to the American Dental Association in 2012, dental visits to the ED cost the US health care system $1.6 billion and an average cost of $749 per visit. There are more than 2 million ED visits each year for dental pain and infection, and 39% return due to nonresolution of the dental problem. Patients return to the ED due to lack of access and resources to routine and emergent dental care. 2 The average daily cost of an MICU stay with mechanical ventilation was $2,193 in 2002. This particular case consisted of 11 days of mechanical ventilation, 20 MICU days, and an additional 20 days of inpatient rehabilitation which resulted in costs that exceeded $50,000. 3
Sepsis can be the result of single or multiple factors and sources of infection. Oral sources of sepsis and systemic infection are not commonly considered as the first potential source of infection when evaluating a septic patient. Oral infections of odontogenic or periodontal origin are frequently associated with localized or diffuse cellulitis of the head and neck region. 1 The patient’s health status and complicating problems, such as an immunocompromising condition, can further reduce the immune response for controlling chronic sources of infection. This in turn can lead to acute manifestations such as cellulitis, sepsis, or necrotizing fasciitis. Necrotizing fasciitis is caused by a polymicrobial or mixed aerobic-anaerobic infection from a variety of sources, including Streptococcus pyogenes .
Case
A 57-year-old woman with a history of major depressive disorder, paroxysmal atrial fibrillation, and opioid dependence that was in remission for more than 3 years was brought to the ED by a family member after the patient developed confusion and lethargy. She was primarily experiencing right breast pain and swelling. The breast pain was associated with high fevers, nausea, vomiting, and chills.
On examination, the patient’s vital signs were: blood pressure (BP), 109/58 mm Hg; heart rate, 160 beats/min; respiratory rate, 22 breaths/min; and temperature, 104°F. Laboratory evaluation was significant for a white blood cell count (WBC) of 8.7 x 103. There was a noted skin abrasion on the patient’s right hand. She was lethargic and confused. Blood cultures were positive for S pyogenes, and a swab of the right breast was negative for bacterial growth.
The patient was admitted to the medical intensive care unit (MICU) and placed on two vasopressors for control of low BP and assistance with low urine output. After a 6-L fluid resuscitation, the patient was started on vancomycin and piperacillin/tazobactam for possible cellulitis causing sepsis. An echocardiogram was negative for endocarditis. The patient continued to decline the following day with continuing tachycardia and tachypnea with hypotension and was intubated. Pulmonology services was consulted for possible acute respiratory distress syndrome secondary to sepsis; general surgery services was consulted for possible necrotizing fasciitis of the chest wall; and cardiology services was consulted for low-cardiac output.
On hospital day 4, the patient was taken to surgery for exploration, drainage, and debridement of the right axilla and breast; cultures were taken, and lack of organism growth was noted. While in the MICU, she was followed by the infectious disease service as her WBC remained elevated and peaking at 32.6 x 103, while blood cultures were negative for bacterial growth.
The dental service was consulted on hospital day 5 to evaluate for other possible sources of infection. Upon examination, the patient’s oral condition was noted as having advanced chronic periodontal disease that required full-mouth extraction. The patient remained hemodynamically unstable with platelet counts below 50 x 109/L until hospital day 7, at which time she was taken for surgery for full mouth extraction and associated alveoloplasty. Upon extraction, the patient continued to improve and was extubated on day 11 with platelets and WBC returning to normal levels by day 13 of her hospital stay. The patient remained hospitalized for a total MICU stay of 20 days and rehabilitation stay of more than 2 weeks.
Discussion
Oral infections most often present with acute onset and noted oral-facial cellulitis or abscess. Oral source of septicemia often are considered after ruling out most other potential sources. Although it is not certain that this case is directly related to the advanced chronic periodontal disease, S pyogenes has been noted to be a pathogen in periodontal disease progression.
According to the American Dental Association in 2012, dental visits to the ED cost the US health care system $1.6 billion and an average cost of $749 per visit. There are more than 2 million ED visits each year for dental pain and infection, and 39% return due to nonresolution of the dental problem. Patients return to the ED due to lack of access and resources to routine and emergent dental care. 2 The average daily cost of an MICU stay with mechanical ventilation was $2,193 in 2002. This particular case consisted of 11 days of mechanical ventilation, 20 MICU days, and an additional 20 days of inpatient rehabilitation which resulted in costs that exceeded $50,000. 3
1. Krishnan V, Johnson JV, Helfric JF. Management of maxillofacial infections: a review of 50 cases. J Oral Maxillofac Surg. 1993;51(8):868-873; discussion 873-874.
2. Wall T, Vujicic M. Emergency department use for dental conditions continues to increase. American Dental Association: Health Policy Institute. http://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_0415_2.ashx. Published April 2015. Accessed November 6, 2017.
3. Dasta JF, McLaughlin TP, Mody SH, Piech CT. Daily cost of an intensive care unit day: the contribution of mechanical ventilation. Crit Care Med. 2005;33(6):1266-1271.
1. Krishnan V, Johnson JV, Helfric JF. Management of maxillofacial infections: a review of 50 cases. J Oral Maxillofac Surg. 1993;51(8):868-873; discussion 873-874.
2. Wall T, Vujicic M. Emergency department use for dental conditions continues to increase. American Dental Association: Health Policy Institute. http://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_0415_2.ashx. Published April 2015. Accessed November 6, 2017.
3. Dasta JF, McLaughlin TP, Mody SH, Piech CT. Daily cost of an intensive care unit day: the contribution of mechanical ventilation. Crit Care Med. 2005;33(6):1266-1271.
Case Studies in Toxicology: DILI Dally
Case
A 50-year-old Hispanic woman with a history of rheumatoid arthritis (RA), for which she was not currently taking medication, was referred to the ED by her primary care physician (PCP) for evaluation of generalized pruritus and jaundice, and an abnormal hepatic function panel.
The patient’s recent history was significant for a positive tuberculosis test (purified protein derivative [PPD], 13 mm), for which she had been on prophylactic medication. Laboratory evaluation taken during the patient’s recent follow-up visit with her PCP revealed the following significant hepatic abnormalities: total bilirubin, 20.0 mg/dL; direct bilirubin, 16.4 mg/dL; international normalized ratio, 2.9; aspartate aminotransferase, greater than 2,000 IU/L; and alanine aminotransferase, greater than 2,000 IU/L. The patient had no history of hepatic disease, and a hepatitis panel obtained in the ED was unremarkable.
Can this be drug-induced liver injury?
Drug-induced liver injury (DILI) accounts for nearly 50% of cases of acute liver failure in the United States.1 According to the National Institutes of Health database of drugs, supplements, and herbal medications acetaminophen is the most common drug associated with hepatotoxicity in the United States, whereas amoxicillin-clavulanate is the most common implicated drug worldwide.1,2 The histological pattern of DILI varies by drug (Table).3
Who is susceptible to drug-induced liver injury?
The factors that help predict DILI include drug pharmacokinetics and metabolism, as well as patient age, sex, and comorbidities. Although some patients are at an increased risk of DILI, it is extraordinarily difficult to accurately predict which patients will develop it. In general, there is a positive correlation between age and risk of developing DILI. For example, in a large US-based tuberculosis study, the incidence of isoniazid (INH)-induced hepatotoxicity was 4.4 per 1,000 patients aged 25 to 34 years. Patients older than age 50 years had a 20.83 per 1,000 incidence of DILI, and women also appear to be at increased risk.4
Pharmacogenetic factors affecting drug metabolism such as the specific cytochrome profile and acetylator status of an individual also influence a patient’s risk of developing DILI. Although our understanding of these issues is growing rapidly, our ability to apply this knowledge to the clinical venue is limited by the available technology, regulatory requirements, and cost.
Case Continuation
A detailed, careful history-taking in the ED revealed that, 2 months prior, the patient had been started on INH, rifampin, and pyridoxine for latent tuberculosis. She had been taking methotrexate for the RA but discontinued it 3 months ago because of the positive PPD. When routine outpatient laboratory testing results demonstrated significant hepatic dysfunction, the patient’s PCP advised her to immediately discontinue her medications and referred her to the ED for further evaluation and management.
By what mechanism does INH cause DILI?
Acute INH-associated hepatitis primarily results from the direct hepatotoxic effects of INH metabolites. Isoniazid is metabolized in the liver via N-acetylation to acetylisoniazid (Figure). Oxidation of this compound in the liver leads to an accumulation of the hepatotoxic metabolites acetylhydrazine and hydrazine.5,6
Is there a role for N-acetylcysteine in INH hepatotoxicity?
No antidote is specifically designed to treat INH-induced hepatotoxicity, and management is largely supportive. Observation for progressive liver failure is indicated and evaluation for liver transplant may become necessary.
N-acetylcysteine (NAC) has a clear role in preventing hepatotoxicity from acetaminophen overdose through its ability to act as a precursor for the synthesis of glutathione—a compound that protects hepatocytes from oxidative damage. In advanced acetaminophen-toxic patients and those with non-acetaminophen toxicity, NAC has nonspecific effects that promote healing through several mechanisms, including anti-inflammatory effect and enhanced hepatic perfusion. Though there are no studies that specifically evaluate the role of NAC in patients with INH-induced hepatotoxicity, it is commonly and appropriately administered for its aforementioned nonspecific effects.8 Common side effects from NAC administration include nausea, vomiting, and diarrhea, which are generally treatable with symptomatic and supportive care.
Case Conclusion
The patient was admitted to the hepatology service for continued clinical care. Although she received NAC, hepatic function testing showed only mild improvement. Additional etiologies of liver failure were investigated, including a computed tomography scan of the abdomen/pelvis and an abdominal ultrasound with Doppler. Both studies were negative for any pathology, and autoimmune laboratory studies were likewise unremarkable.
The patient underwent a liver biopsy, which revealed inflammation and scattered eosinophils suggestive of drug-induced hepatic injury. Her clinical condition continued to deteriorate, and she was transferred to another hospital for transplant evaluation.
1. Lee WM. Drug-induced acute liver failure. Clin Liver Dis. 2013;17(4):575-586, viii. doi:10.1016/j.cld.2013.07.001.
2. National Institutes of Health Web site. LiverTox: Clinical and research information on drug-induced liver injury. https://livertox.nlm.nih.gov/. Updated February 10, 2017. Accessed October 12, 2017.
3. Ansari JA, Sayyed M, Sayeed F. Management of non alcoholic fatty liver diseases and their complications. Int J Pharmacol. 2011;7:579-588. doi:10.3923/ijp.2011.579.588.
4. Fountain FF, Tolley E, Chrisman CR, Self TH. Isoniazid hepatotoxicity associated with treatment of latent tuberculosis infection: a 7-year evaluation from a public health tuberculosis clinic. Chest. 2005;128(1):116-123. doi:10.1378/chest.128.1.116.
5. Hernon CH. Antituberculous medications. In: Hoffman RS, Howland MA, Lewin NA, Nelson LS, Goldfrank LR, eds. Goldfrank’s Toxicologic Emergencies. 10th ed. New York, NY: McGraw-Hill; 2015:787-796.
6. Teixeira RL, Morato RG, Cabello PH, et al. Genetic polymorphisms of NAT2, CYP2E1 and GST enzymes and the occurrence of antituberculosis drug-induced hepatitis in Brazilian TB patients. Mem Inst Oswaldo Cruz. 2011;106(6):716-724.
7. Mitchell JR, Thorgeirsson UP, Black M, et al. Increased incidence of isoniazid hepatitis in rapid acetylators: possible relation to hydranize metabolites. Clin Pharmacol Ther. 1975;18(1):70-79.
8. Lee WM, Hynan LS, Rossaro L, et al; Acute Liver Failure Study Group. Intravenous N-acetylcysteine improves transplant-free survival in early stage non-acetaminophen acute liver failure. Gastroenterology. 2009;137(3):856-864. doi:10.1053/j.gastro.2009.06.006.
Case
A 50-year-old Hispanic woman with a history of rheumatoid arthritis (RA), for which she was not currently taking medication, was referred to the ED by her primary care physician (PCP) for evaluation of generalized pruritus and jaundice, and an abnormal hepatic function panel.
The patient’s recent history was significant for a positive tuberculosis test (purified protein derivative [PPD], 13 mm), for which she had been on prophylactic medication. Laboratory evaluation taken during the patient’s recent follow-up visit with her PCP revealed the following significant hepatic abnormalities: total bilirubin, 20.0 mg/dL; direct bilirubin, 16.4 mg/dL; international normalized ratio, 2.9; aspartate aminotransferase, greater than 2,000 IU/L; and alanine aminotransferase, greater than 2,000 IU/L. The patient had no history of hepatic disease, and a hepatitis panel obtained in the ED was unremarkable.
Can this be drug-induced liver injury?
Drug-induced liver injury (DILI) accounts for nearly 50% of cases of acute liver failure in the United States.1 According to the National Institutes of Health database of drugs, supplements, and herbal medications acetaminophen is the most common drug associated with hepatotoxicity in the United States, whereas amoxicillin-clavulanate is the most common implicated drug worldwide.1,2 The histological pattern of DILI varies by drug (Table).3
Who is susceptible to drug-induced liver injury?
The factors that help predict DILI include drug pharmacokinetics and metabolism, as well as patient age, sex, and comorbidities. Although some patients are at an increased risk of DILI, it is extraordinarily difficult to accurately predict which patients will develop it. In general, there is a positive correlation between age and risk of developing DILI. For example, in a large US-based tuberculosis study, the incidence of isoniazid (INH)-induced hepatotoxicity was 4.4 per 1,000 patients aged 25 to 34 years. Patients older than age 50 years had a 20.83 per 1,000 incidence of DILI, and women also appear to be at increased risk.4
Pharmacogenetic factors affecting drug metabolism such as the specific cytochrome profile and acetylator status of an individual also influence a patient’s risk of developing DILI. Although our understanding of these issues is growing rapidly, our ability to apply this knowledge to the clinical venue is limited by the available technology, regulatory requirements, and cost.
Case Continuation
A detailed, careful history-taking in the ED revealed that, 2 months prior, the patient had been started on INH, rifampin, and pyridoxine for latent tuberculosis. She had been taking methotrexate for the RA but discontinued it 3 months ago because of the positive PPD. When routine outpatient laboratory testing results demonstrated significant hepatic dysfunction, the patient’s PCP advised her to immediately discontinue her medications and referred her to the ED for further evaluation and management.
By what mechanism does INH cause DILI?
Acute INH-associated hepatitis primarily results from the direct hepatotoxic effects of INH metabolites. Isoniazid is metabolized in the liver via N-acetylation to acetylisoniazid (Figure). Oxidation of this compound in the liver leads to an accumulation of the hepatotoxic metabolites acetylhydrazine and hydrazine.5,6
Is there a role for N-acetylcysteine in INH hepatotoxicity?
No antidote is specifically designed to treat INH-induced hepatotoxicity, and management is largely supportive. Observation for progressive liver failure is indicated and evaluation for liver transplant may become necessary.
N-acetylcysteine (NAC) has a clear role in preventing hepatotoxicity from acetaminophen overdose through its ability to act as a precursor for the synthesis of glutathione—a compound that protects hepatocytes from oxidative damage. In advanced acetaminophen-toxic patients and those with non-acetaminophen toxicity, NAC has nonspecific effects that promote healing through several mechanisms, including anti-inflammatory effect and enhanced hepatic perfusion. Though there are no studies that specifically evaluate the role of NAC in patients with INH-induced hepatotoxicity, it is commonly and appropriately administered for its aforementioned nonspecific effects.8 Common side effects from NAC administration include nausea, vomiting, and diarrhea, which are generally treatable with symptomatic and supportive care.
Case Conclusion
The patient was admitted to the hepatology service for continued clinical care. Although she received NAC, hepatic function testing showed only mild improvement. Additional etiologies of liver failure were investigated, including a computed tomography scan of the abdomen/pelvis and an abdominal ultrasound with Doppler. Both studies were negative for any pathology, and autoimmune laboratory studies were likewise unremarkable.
The patient underwent a liver biopsy, which revealed inflammation and scattered eosinophils suggestive of drug-induced hepatic injury. Her clinical condition continued to deteriorate, and she was transferred to another hospital for transplant evaluation.
Case
A 50-year-old Hispanic woman with a history of rheumatoid arthritis (RA), for which she was not currently taking medication, was referred to the ED by her primary care physician (PCP) for evaluation of generalized pruritus and jaundice, and an abnormal hepatic function panel.
The patient’s recent history was significant for a positive tuberculosis test (purified protein derivative [PPD], 13 mm), for which she had been on prophylactic medication. Laboratory evaluation taken during the patient’s recent follow-up visit with her PCP revealed the following significant hepatic abnormalities: total bilirubin, 20.0 mg/dL; direct bilirubin, 16.4 mg/dL; international normalized ratio, 2.9; aspartate aminotransferase, greater than 2,000 IU/L; and alanine aminotransferase, greater than 2,000 IU/L. The patient had no history of hepatic disease, and a hepatitis panel obtained in the ED was unremarkable.
Can this be drug-induced liver injury?
Drug-induced liver injury (DILI) accounts for nearly 50% of cases of acute liver failure in the United States.1 According to the National Institutes of Health database of drugs, supplements, and herbal medications acetaminophen is the most common drug associated with hepatotoxicity in the United States, whereas amoxicillin-clavulanate is the most common implicated drug worldwide.1,2 The histological pattern of DILI varies by drug (Table).3
Who is susceptible to drug-induced liver injury?
The factors that help predict DILI include drug pharmacokinetics and metabolism, as well as patient age, sex, and comorbidities. Although some patients are at an increased risk of DILI, it is extraordinarily difficult to accurately predict which patients will develop it. In general, there is a positive correlation between age and risk of developing DILI. For example, in a large US-based tuberculosis study, the incidence of isoniazid (INH)-induced hepatotoxicity was 4.4 per 1,000 patients aged 25 to 34 years. Patients older than age 50 years had a 20.83 per 1,000 incidence of DILI, and women also appear to be at increased risk.4
Pharmacogenetic factors affecting drug metabolism such as the specific cytochrome profile and acetylator status of an individual also influence a patient’s risk of developing DILI. Although our understanding of these issues is growing rapidly, our ability to apply this knowledge to the clinical venue is limited by the available technology, regulatory requirements, and cost.
Case Continuation
A detailed, careful history-taking in the ED revealed that, 2 months prior, the patient had been started on INH, rifampin, and pyridoxine for latent tuberculosis. She had been taking methotrexate for the RA but discontinued it 3 months ago because of the positive PPD. When routine outpatient laboratory testing results demonstrated significant hepatic dysfunction, the patient’s PCP advised her to immediately discontinue her medications and referred her to the ED for further evaluation and management.
By what mechanism does INH cause DILI?
Acute INH-associated hepatitis primarily results from the direct hepatotoxic effects of INH metabolites. Isoniazid is metabolized in the liver via N-acetylation to acetylisoniazid (Figure). Oxidation of this compound in the liver leads to an accumulation of the hepatotoxic metabolites acetylhydrazine and hydrazine.5,6
Is there a role for N-acetylcysteine in INH hepatotoxicity?
No antidote is specifically designed to treat INH-induced hepatotoxicity, and management is largely supportive. Observation for progressive liver failure is indicated and evaluation for liver transplant may become necessary.
N-acetylcysteine (NAC) has a clear role in preventing hepatotoxicity from acetaminophen overdose through its ability to act as a precursor for the synthesis of glutathione—a compound that protects hepatocytes from oxidative damage. In advanced acetaminophen-toxic patients and those with non-acetaminophen toxicity, NAC has nonspecific effects that promote healing through several mechanisms, including anti-inflammatory effect and enhanced hepatic perfusion. Though there are no studies that specifically evaluate the role of NAC in patients with INH-induced hepatotoxicity, it is commonly and appropriately administered for its aforementioned nonspecific effects.8 Common side effects from NAC administration include nausea, vomiting, and diarrhea, which are generally treatable with symptomatic and supportive care.
Case Conclusion
The patient was admitted to the hepatology service for continued clinical care. Although she received NAC, hepatic function testing showed only mild improvement. Additional etiologies of liver failure were investigated, including a computed tomography scan of the abdomen/pelvis and an abdominal ultrasound with Doppler. Both studies were negative for any pathology, and autoimmune laboratory studies were likewise unremarkable.
The patient underwent a liver biopsy, which revealed inflammation and scattered eosinophils suggestive of drug-induced hepatic injury. Her clinical condition continued to deteriorate, and she was transferred to another hospital for transplant evaluation.
1. Lee WM. Drug-induced acute liver failure. Clin Liver Dis. 2013;17(4):575-586, viii. doi:10.1016/j.cld.2013.07.001.
2. National Institutes of Health Web site. LiverTox: Clinical and research information on drug-induced liver injury. https://livertox.nlm.nih.gov/. Updated February 10, 2017. Accessed October 12, 2017.
3. Ansari JA, Sayyed M, Sayeed F. Management of non alcoholic fatty liver diseases and their complications. Int J Pharmacol. 2011;7:579-588. doi:10.3923/ijp.2011.579.588.
4. Fountain FF, Tolley E, Chrisman CR, Self TH. Isoniazid hepatotoxicity associated with treatment of latent tuberculosis infection: a 7-year evaluation from a public health tuberculosis clinic. Chest. 2005;128(1):116-123. doi:10.1378/chest.128.1.116.
5. Hernon CH. Antituberculous medications. In: Hoffman RS, Howland MA, Lewin NA, Nelson LS, Goldfrank LR, eds. Goldfrank’s Toxicologic Emergencies. 10th ed. New York, NY: McGraw-Hill; 2015:787-796.
6. Teixeira RL, Morato RG, Cabello PH, et al. Genetic polymorphisms of NAT2, CYP2E1 and GST enzymes and the occurrence of antituberculosis drug-induced hepatitis in Brazilian TB patients. Mem Inst Oswaldo Cruz. 2011;106(6):716-724.
7. Mitchell JR, Thorgeirsson UP, Black M, et al. Increased incidence of isoniazid hepatitis in rapid acetylators: possible relation to hydranize metabolites. Clin Pharmacol Ther. 1975;18(1):70-79.
8. Lee WM, Hynan LS, Rossaro L, et al; Acute Liver Failure Study Group. Intravenous N-acetylcysteine improves transplant-free survival in early stage non-acetaminophen acute liver failure. Gastroenterology. 2009;137(3):856-864. doi:10.1053/j.gastro.2009.06.006.
1. Lee WM. Drug-induced acute liver failure. Clin Liver Dis. 2013;17(4):575-586, viii. doi:10.1016/j.cld.2013.07.001.
2. National Institutes of Health Web site. LiverTox: Clinical and research information on drug-induced liver injury. https://livertox.nlm.nih.gov/. Updated February 10, 2017. Accessed October 12, 2017.
3. Ansari JA, Sayyed M, Sayeed F. Management of non alcoholic fatty liver diseases and their complications. Int J Pharmacol. 2011;7:579-588. doi:10.3923/ijp.2011.579.588.
4. Fountain FF, Tolley E, Chrisman CR, Self TH. Isoniazid hepatotoxicity associated with treatment of latent tuberculosis infection: a 7-year evaluation from a public health tuberculosis clinic. Chest. 2005;128(1):116-123. doi:10.1378/chest.128.1.116.
5. Hernon CH. Antituberculous medications. In: Hoffman RS, Howland MA, Lewin NA, Nelson LS, Goldfrank LR, eds. Goldfrank’s Toxicologic Emergencies. 10th ed. New York, NY: McGraw-Hill; 2015:787-796.
6. Teixeira RL, Morato RG, Cabello PH, et al. Genetic polymorphisms of NAT2, CYP2E1 and GST enzymes and the occurrence of antituberculosis drug-induced hepatitis in Brazilian TB patients. Mem Inst Oswaldo Cruz. 2011;106(6):716-724.
7. Mitchell JR, Thorgeirsson UP, Black M, et al. Increased incidence of isoniazid hepatitis in rapid acetylators: possible relation to hydranize metabolites. Clin Pharmacol Ther. 1975;18(1):70-79.
8. Lee WM, Hynan LS, Rossaro L, et al; Acute Liver Failure Study Group. Intravenous N-acetylcysteine improves transplant-free survival in early stage non-acetaminophen acute liver failure. Gastroenterology. 2009;137(3):856-864. doi:10.1053/j.gastro.2009.06.006.
Carbon Monoxide: The Other Silent Killer
Case Presentations
Case 1: Smoke Inhalation (Carbon Monoxide and Cyanide)
A 50-year-old woman was pulled from the window of a burning building and found to be in cardiac arrest with pulseless electrical activity. Standard advanced cardiac life-support was started, and infusion of intra-osseous hydroxocobalamin (OHCob) was administered at the time of intubation because of the concern for cyanide (CN) gas exposure during smoke inhalation. Return of spontaneous circulation occurred before arrival at the hospital.
Upon presentation to the ED, the patient’s vital signs were: initial blood pressure (BP), 92/47 mm Hg; heart rate (HR), 112 beats/min; respiratory rate (RR), 31 breaths/min; and temperature (T), 99.7°F. Following intubation, the patient’s oxygen saturation (SaO2) on pulse oximetry (POX) was 93%, and her fraction of inspired oxygen (FiO2) was 100%.
On physical examination, the patient’s face was covered with soot. The lung sounds were equal and clear to auscultation bilaterally. The neurological examination was significant for a Glasgow Coma Scale of 3, without administered sedation, and there were no signs of dermal burns. Initial arterial blood gas (ABG) results were: pH, 7.06; carbon dioxide partial pressure (PCO2), 58 mm Hg; partial pressure of oxygen (PO2), 152 mm Hg; bicarbonate (HCO3), 17 mm Hg; SaO2, 98% (after intubation); FiO2, 100%; carboxyhemoglobin (COHb), 30%; and lactate, 14 mmol/L.
Case 2: Household Misadventure (Carbon Monoxide)
Several days after disabling the carbon monoxide (CO) detector in his home to silence the alarm that had continued to sound, a 67-year-old man developed weakness and called his local fire department. Upon arrival at the man’s home, the fire department confirmed an ambient air CO gas concentration over 200 ppm. Emergency medical services (EMS) promptly brought the patient to the local ED for evaluation and treatment.
Shortly after arrival at the ED, the patient’s weakness had resolved. His vital signs at examination were: BP, 154/85 mm Hg; HR, 79 beats/min; RR, 15 breaths/min; and T, 98.8°F. The patient’s COHb level was 28% with administration of 100% oxygen (O2) via a nonrebreather mask (NRBM).
Carbon Monoxide Toxicity
Carbon monoxide is a toxin of considerable importance to emergency physicians (EPs). The diagnosis at times can be challenging, the interpretation of COHb can be confusing, and the role of hyperbaric oxygen (HBO) therapy in the treatment of CO poisoning remains controversial.
Natural Sources
Carbon monoxide is formed from the incomplete combustion of organic (carbonaceous) fuels, such as charcoal, wood, petroleum distillates (gasoline, kerosene, diesel fuel), and natural gas. Though the majority of atmospheric CO comes from natural sources (eg, volcanoes, forest fires, marsh gases), poisoning exposures are primarily due to man-made CO.
Man-Made Sources
Motor vehicle exhaust is the most abundant source of man-made CO, and exposures to exhaust fumes are common causes of both intentional and unintentional poisonings and death. Other frequent sources of CO poisoning include smoke inhalation from house fires; inadequate ventilation during use of kerosene space heaters; charcoal grills or hibachis; burning wood or charcoal; fuel-powered tools such as generators, fork lifts, and chain saws; or faulty (natural or bottled) gas appliances, such as stoves, furnaces, or water heaters (Table 1). Though propane is known to burn more cleanly than natural gas (ie, less harmful to the environment), it still can produce CO.
Though neither electrical appliances nor “gas leaks” are sources of CO, like CO, natural gas (mostly methane) and bottle gas (propane) are odorless, tasteless, and colorless. Utility companies add sulfur containing mercaptans to natural gas so that leaks can be detected, but CO is only formed when the fuel is burned in a gas-powered appliance.
Endogenous Carbon Monoxide
Endogenous CO production can occur from catabolism of heme or from hepatic metabolism of methylene chloride, but exposures to this solvent are unlikely to generate COHb concentrations above 10%.
Epidemiology
The incidence of CO poisoning is likely more frequent than documented since many cases of minor exposures are unreported due to self-limiting effects and/or the vague, nonspecific nature of symptoms associated with minor exposures. In 2015, US Poison Control Centers reported over 14,000 cases of CO poisoning, only 43% of which were treated in a health care facility.1 The vast majority of exposures (97%) were unintentional and resulted in 52 deaths (0.398%).1
Data from hospitalized patients in 2007 revealed that over 200,000 ED visits and 22,000 hospitalizations were possibly associated with unintentional, non-fire-related CO exposures.2 Approximately 10% of the exposures in each of these populations were confirmed by specific International Classification of Diseases Medical E codes.2
Regardless of dataset, ED visits due to CO exposure are most common in young adults and women, occur in winter months from exposure in and around homes, and result in discharge from the ED. Elderly patients have the highest rate of hospital admission.
Carbon monoxide poisoning has long been considered a leading cause of poisoning death, though numbers appear to be declining, and CO was responsible for fewer deaths than opioids in 2017.2 The National Center for Health Statistics reported 56,133 CO-related deaths from 1979 through 1988—an average of 5,600 per year.3,4 Of these, 46% were from suicide; 28% were related to burns or house fires; and 21% (11,547) were characterized as unintentional. Motor vehicle exhaust was associated with 57% of the unintentional deaths. A more recent analysis of unintentional exposures reported 2,244 deaths during the period of 2010 to 2015—an average of 374 deaths per year (393 in 2015).5
Preventive measures are likely responsible for the significant decline in non-fire-related CO poisoning deaths from the early 1970s through the 1990s. The introduction of catalytic converters in automobiles in 1975 and O2 sensors in 1981 eventually reduced automotive CO emissions by 95% compared to pre-1975 vehicles.6 Both unintentional death and suicide rates associated with CO from motor vehicles subsequently declined by 81% and 43%, respectively. The lower decline in suicidal deaths serves as a reminder that intentional exposure to motor vehicles remains dangerous and potentially lethal.
Pathophysiology/Mechanisms of Toxicity
Carbon monoxide is a colorless, odorless gas that readily reaches the bloodstream during alveolar gas exchange. Since absorption is rapid, exposures to high CO concentrations can produce toxicity within minutes, though exposure severity is related to both inspired CO concentration and duration of exposure.
Endogenous Elimination
Carbon monoxide is eliminated from the body in expired air, with an elimination half-life dependent on FiO2 and atmospheric pressure. Accordingly, COHb decreases with a half-life (all approximate) of 4 to 6 hours when patients are breathing room air (21% O2), 60 to 90 minutes with O2 delivery at 95% to 100%, and 20 to 40 minutes under hyperbaric conditions (2.5-3.0 atmospheres absolute [ATA]).
Effect on Hemoglobin
Once absorbed, CO has an affinity for hemoglobin (Hb) that is over 200 times greater than does O2.7 The formation of COHb results in both a decreased O2-carrying capacity of Hb at the sites where O2 would have been, and because of its new configuration, COHb does not allow currently bound O2 to be offloaded. This is graphically represented by a shift of the O2-Hb dissociation curve to the left. In addition, CO continues to be bound by other intracellular heme molecules in myoglobin of skeletal and myocardial muscle, and the cytochrome oxidase system in mitochondria.8
Immunologic and Inflammatory Effects
Carbon monoxide poisoning results in a cascade of immunologic and inflammatory effects, such as generation of nitric oxide, lipid peroxidation from neutrophils, mitochondrial oxidative stress, and apoptosis. These effects result in cellular asphyxia in all organs, but the most emergent life-threatening concerns are ischemia to the brain and heart.
Severity of Toxicity and Exposure
As previously noted, the severity of CO poisoning is dose-dependent, meaning that it is related to the concentration of CO in inspired air and the duration of the exposure. Carbon monoxide is typically absent in fresh air, but levels may approach 2 to 5 ppm due to cooking, wood burning, mild air pollution, etc. The source of levels above 5 ppm should generally be investigated.
Maximum safe exposure levels for workers over an 8-hour period range from 25 to 50 ppm. Exposures to CO levels above 50 to 100 ppm are likely to elicit symptoms in most patients, depending on duration of the exposure. Carbon monoxide levels of 200 ppm may result in a mild headache after 2 to 3 hours of exposure, and a more severe headache and nausea after 1 to 2 hours of exposures to 400 ppm of CO.
Accordingly, home CO detectors use a combination of ppm and time for alarms, and they may not sound an alarm at 40 ppm until the level persists for 8 or so hours. Home CO detectors, however, will sound an alarm immediately when a level of 80 to 100 ppm is reached.
Clinical Presentation
Acute Exposure
Acute exposure to CO causes a variety of effects that are largely nonspecific, as there is no toxic syndrome (toxidrome) considered pathognomonic for CO poisoning. Ambient CO levels, duration of exposure, minute ventilation, presence of other toxic gases, and patient comorbidities can all contribute to the severity of exposure and presenting signs and symptoms. Effects associated with mild poisoning include headache, dizziness, blurred vision, fatigue or weakness, nausea, and shortness of breath. Patients with pre-existing respiratory, cardiovascular (CV), or neurological compromise are likely to present with more pronounced symptoms. In either case, these complaints may easily be confused with a viral illness, emphasizing the importance of eliciting a history of potential exposure to CO, particularly when multiple patients are involved.
As the concentration of COHb increases, more significant clinical effects can be expected, including tachycardia, chest pain, hypotension, dysrhythmias, lethargy, coma, apnea, and seizures. Hypoxia can result in myocardial injury, cerebral edema, stroke, and acute pulmonary and kidney injury.
Following acute exposure, the severity of effects correlates with the peak pretreatment COHb concentration. However, the peak concentration is usually unknown, since most patients with significant exposures will have some time period elapsed between the exposure and the determination of COHb, and the COHb will have declined at a rate depending on FiO2 and minute ventilation. In these circumstances, COHb is a poor indicator for HBO therapy and outcome.
Delayed Neurological Sequelae
Persistent, recurrent, or delayed (following period of no symptoms) neurological effects can occur in up to 40% of cases, and patients with significant exposures (eg, loss of consciousness) appear to be at greatest risk. These effects most often occur within the first 3 weeks following exposure, and have been known to persist for months to years. Such effects include headache, dizziness, impaired memory or cognition, and emotional lability. Predicting which factors in CO exposure and/or treatments can be modified to prevent neurological sequelae remains challenging.
Diagnostic Testing
Pulse Co-oximetry
Prehospital care POX typically reads COHb as oxyhemoglobin, thereby displaying a normal SaO2.9 Noninvasive CO pulse co-oximetry using a pulse oximeter (Rad-57, Masimo Corporation) provides a reading between –6 to +4 of the true COHb with a false-positive rate of 11% and false-negative rate of 46%.10 This high false-negative rate makes noninvasive CO pulse co-oximetry a poor tool to rule out a CO exposure.11 If OHCob has been administered due to concerns for CN poisoning (smoke inhalation), concentrations of COHb detected by a co-oximeter medical device may be decreased, as noted by a mean decrease of 1% in healthy volunteers exposed to OHCob only.12
Venous and Arterial Blood Gas Testing
For a patient in the hospital, exposure to CO can rapidly be determined using co-oximetry to measure COHb in a venous or arterial sample. Obtaining a venous sample may be a more practical approach, as other venous measurements will likely also be obtained. Baseline “normal” COHb levels should be less than 5%, but may be up to 8% to 10% in tobacco smokers.
Other Laboratory Studies
Other important laboratory tests that should be obtained are a complete blood count, lactate level, venous blood gas, and basic metabolic panel (to assess acid/base status). In two retrospective studies of patients exposed to CO, elevated lactate levels were associated with altered mental status.13,14 However, elevated lactate levels were not seen in a majority of patients with CO poisoning.
In addition, CN exposure should be considered when the lactate level is greater than 8 mmol/L, particularly in patients with smoke inhalation.15 Troponin I and creatinine phosphokinase tests can be used to screen for myocardial or skeletal muscle injury.
Effect of Hydroxocobalamin on Laboratory Evaluation
It is important to be cautious when interpreting the results of laboratory studies in patients who have been given OHCob due to the potential co-exposure to CN (smoke inhalation). The red discoloration of body fluids after OHCob administration makes laboratory evaluation by spectrophotometric techniques erroneous.16 Of greatest concern is the accuracy of COHb concentrations.17 In a study using rabbit models by Lee et al,17 OHCob administration was shown to falsely increase COHb concentrations.
Livshits et al18 reported conflicting effects on COHb in two human cases. In the first case, the patient’s true COHb was 93% lower (2.5% vs 34.9%) following administration of 5 g of OHCob, as measured with a rapid blood gas analyzer. In the second patient, COHb was 76% lower (10.7% vs 44%) following OHCob administration, which was also measured by a blood gas analyzer. Both of these cases illustrate lower true COHb concentrations than would be expected following the administration of only supplemental O2.
In a controlled experiment by Pace et al19 examining the effects of OHCob on measurement of COHb at both physiological (3%) and pathological (30% and 50%) concentrations in human blood samples, the degree of interference depended on the type of co-oximeter used, the degree of COHb elevation (at pathological levels only), and the concentration of OHCob added. Other studies, including an evaluation of OHCob interference by Carlsson et al20 using nine different analyzers have confirmed the interference of OHCob on photometric assays. Of particular clinical importance, a falsely increased lactate level was seen after true lactate levels were found to be below 4.8 mmol/L (but not greater) using spectrophotometric or electrochemical detection.21 This increase in the false-positive assessment of the degree of toxicity could lead unnecessary escalation of care.
These studies emphasize the need to exercise caution when interpreting laboratory test results following OHCob administration. Ideally, it would be best if blood samples were obtained prior to OHCob administration by EMS or in the ED, if the clinical scenario allows it.
Imaging Studies
For patients presenting after a closed-space fire, a chest radiograph will help assess for pulmonary injury. The classic finding of CO poisoning on head computed tomography (CT) and magnetic resonance imaging scans is evidence of ischemia in the basal ganglia. The radiographic findings may help determine the diagnosis of the altered mental status patient who presents without a history. An electrocardiogram (ECG) is also useful for detection of myocardial ischemia or dysrhythmias, when signs or symptoms of either are possible from history and physical or cardiac monitoring.
Intentional Inhalation
Intentional inhalation of fumes containing CO is a relatively common mechanism for suicide. In patients who survive, it is important for EPs and other providers to suspect additional means of self-harm. For example, at our institution, we have encountered several patients with self-inflicted trauma after remaining conscious following a medication overdose. Accordingly, patients who have intentionally inhaled CO should also be evaluated for occult medication poisoning (and trauma).
Treatment
The first step in treating a patient with CO poisoning occurs prior to arrival at the ED, when he or she is removed from continued exposure. The second step is assessing whether this is only a CO exposure, or a mixture of gases from combustion in a closed space, that might also contain CN. When CO and CN are combined OHCob is indicated to treat CN toxicity.
Additionally, if the patient is brought to the ED via EMS, O2 therapy will most likely have been initiated en route. In either case, the concentration of COHb may not accurately reflect the magnitude of exposure or prognosis, and should not be used to dictate the level of therapy or disposition. The patient’s vital signs and clinical findings of end organ toxicity should guide the appropriate supportive care.
Supplemental Oxygen Therapy
Initial administration of 100% O2 during assessment of airway, breathing, and circulation is the first step in accelerating the removal of CO from Hb. For patients suffering from smoke inhalation, assessment and establishment of a secure airway when there are signs of soot or burns in the airway must always take precedence over other actions. Continuous cardiac monitoring, POX, observation, and establishment of intravenous access are often needed for detection and management of CV instability or change in mental status in cases of moderate-to-severe CO exposures. Mild exposures with headache, nausea, and flu-like symptoms can be managed with symptomatic treatment and normobaric O2 until resolution of symptoms and improvement in COHb occur.
Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy involves the delivery of high-flow O2 (typically at 100%) under increased atmospheric pressure (2.5 -3.0 ATA). Oxygen delivered at ambient air pressure (1.0 ATA) is often referred to as normobaric oxygen. Although HBO is best known for its ability to enhance CO elimination, research points to a much more eloquent mitigation of CO toxicity on the molecular level. These mechanisms include an increased amount of dissolved O2 in blood, regeneration of cytochrome oxidase, decreased leukocyte adhesion to microvascular endothelium in the brain, decreased lipid peroxidation in the brain after loss of consciousness, and preservation of adenosine triphosphate.22
For most patients, the majority—if not all—of COHb will be eliminated by the time they present to a suitable HBO chamber. Despite the knowledge that HBO therapy has a positive toxicokinetic effect by increasing the elimination of CO, all of the major, prospective studies on the usefulness of HBO are related to prevention of neuropsychiatric sequelae mediated by immunological and inflammatory effects. The role of HBO in the treatment of CO poisoning has been debated for decades. Multiple studies that differ in methodology, patient populations, delivery of HBO treatments, and assessment of benefits fail to provide a consensus on the role of HBO therapy (Table 2).23-30
Before transferring a patient to a facility for HBO therapy, the potential risks and benefits of transport must be considered. In a 10-year retrospective study by Sloan et al31 of 297 CO-poisoned patients (mean COHb, 38%) 46% of patients had cardiopulmonary and neurological complications prior to HBO therapy at some point in the transfer pathway. During HBO therapy, 18% of patients had complications that included emesis, agitation requiring sedation, seizures, hypotension, tension pneumothorax, cardiac arrest, cardiac arrhythmias, and myocardial ischemia. It is therefore incumbent that personnel attending patients undergoing HBO therapy for CO poisoning be aware of, and able to manage, this variety of serious effects.
When an HBO chamber is at a clinical site with experts in the field and staff available 24 hours a day, the decision to utilize HBO may easily be made without obstacles. For most EPs, however, this is not the case. Locating and transferring a patient to an HBO center is typically a considerable logistical challenge. For many rural facilities, HBO is just not a timely therapeutic option. Two studies state the benefit of HBO therapy is greatest when starting within 6 hours from the end of the CO exposure.24,26
Identifying those CO-poisoned patients who meet evidence-based criteria for HBO is difficult. Patients with mild CO poisoning will do well without HBO, and critically ill patients will probably not consistently benefit from HBO. However, a pragmatic solution must be considered when efficacy studies are incongruent with conflicting results. When signs of end-organ toxicity from CO are present, but cardiac arrest has not yet occurred and the logistics are streamlined, the benefit of HBO may outweigh the risk.
Signs of end-organ toxicity include syncope, seizures, coma, ischemic changes on ECG, and pregnancy with unresolved maternal distress or fetal distress. Although a COHb level greater than 25% or 15% (pregnant) alone is commonly used as an indication for HBO, this is largely based on opinion. Conversely, HBO is unlikely to be helpful in patients who have been resuscitated after CO-related cardiac arrest.32
Treatment Guidelines
The American College of Emergency Physicians recently developed a position statement regarding the management and treatment of CO poisoning.33 The clinical policy addresses several of the controversies discussed in this review, and provides a level of evidence for each response (Table 3).
Case Conclusions
Case 1 (Smoke Inhalation Due to CO and Cyanide Poisoning)
The patient in this case suffered severe CO and CN toxicity. A head CT scan revealed diffuse edema consistent with anoxic brain injury. After conferring with the family regarding the patient’s condition and prognosis, the decision was made to withdraw life-sustaining therapy and support, and the patient died.
Case 2 (Household Misadventure)
The patient in this case was successfully treated with 100% O2 via a NRBM and was subsequently discharged home within 4 hours from presentation.
Conclusion
Exposures to CO are ubiquitous due to our heavy reliance on carbon combustion, and the manifestations of CO toxicity are protean. Therefore, CO poisoning must be considered more frequently in the differential diagnosis of indiscriminant symptoms affecting the neurological, cardiac, pulmonary, and gastrointestinal systems, especially when multiple patients have similar symptoms.
The diagnosis of CO poisoning is straightforward when a serum COHb level is obtained on a venous or arterial blood sample. Treatment starts when the patient is removed from further CO exposure and breaths normobaric oxygen at ambient levels or supplemented. Because there is no clear evidenced-based indication for HBO therapy, further treatment with HBO is naturally limited by rational constraints.
1. Mowry JB, Spyker DA, Brooks DE, Zimmerman A, Schauben JL. 2015 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 33rd Annual Report. Clin Toxicol. 2016;54(10):924-1109. doi:10.1080/15563650.2016.1245421.
2. Iqbal S, Law HZ, Clower JH, Yip FY, Elixhauser A. Hospital burden of unintentional carbon monoxide poisoning in the United States, 2007. Am J Emerg Med. 2012;30(5):657-664. doi:10.1016/j.ajem.2011.03.003.
3. Cobb N, Etzel RA. Unintentional carbon monoxide-related deaths in the United States, 1979 through 1988. JAMA. 1991;266(5):659-663.
4. Sircar K, Clower J, Shin MK, Bailey C, King M, Yip F. Carbon monoxide poisoning deaths in the United States, 1999 to 2012. Am J Emerg Med. 2015;33(9):1140-1145. doi:10.1016/j.ajem.2015.05.002.
5. Centers for Disease Control and Prevention. Environmental Public Health Tracking Network. Carbon monoxide poisoning emergency department visits. https://ephtracking.cdc.gov/showHome.action. Updated September 8, 2017. Accessed October 18, 2017.
6. Mott JA, Wolfe MI, Alverson CJ, et al. National vehicle emissions policies and practices and declining US carbon monoxide-related mortality. JAMA. 2002;288(8):988-995.
7. Buckley NA, Juurlink DN, Isbister G, Bennett MH, Lavonas EJ. Hyperbaric oxygen for carbon monoxide poisoning. Cochrane Database Syst Rev. 2011;13(4):CD002041. doi:10.1002/14651858.CD002041.pub3.
8. Hampson NB, Piantadosi CA, Thom SR, Weaver LK. Practice recommendations in the diagnosis, management, and prevention of carbon monoxide poisoning. Am J Respir Crit Care Med. 2012;186(11):1095-1101. doi:10.1164/rccm.201207-1284CI.
9. Bozeman WP, Myers RA, Barish RA. Confirmation of the pulse oximetry gap in carbon monoxide poisoning. Ann of Emerg Med. 1997;30(5):608-611.
10. Zaouter C, Zavorsky GS. The measurement of carboxyhemoglobin and methemoglobin using a non-invasive pulse CO-oximeter. Respir Physiol Neurobiol. 2012;182(2-3):88-92. doi:10.1016/j.resp.2012.05.010.
11. Shamir MY, Avramovich A, Smaka T. The current status of continuous noninvasive measurement of total, carboxy, and methemoglobin concentration. Anesth Analg. 2012;114(5);972-978. doi:10.1213/ANE.0b013e318233041a.
12. Cashin BV, Matlock AG, Kang C, Reynolds PS, Wills BK. Effect of hydroxocobalamin on surface oximetry in nonexposed humans. Prehosp Disaster Med. 2013;28(4):367-369. doi:10.1017/S1049023X13003518.
13. Moon JM, Shin MH, Chun BJ. The value of initial lactate in patients with carbon monoxide intoxication: in the emergency department. Hum Exp Toxicol. 2011;30(8):836-843. doi:10.1177/0960327110384527.
14. Doğan NÖ, Savrun A, Levent S, et al. Can initial lactate levels predict the severity of unintentional carbon monoxide poisoning? Hum Exp Toxicol. 2015;34(3):324-329. doi:10.1177/0960327114538986.
15. Baud FJ, Borron SW, Mégarbane B, et al. Value of lactic acidosis in the assessment of the severity of acute cyanide poisoning. Crit Care Med. 2002;30(9):2044-2050. doi:10.1097/01.CCM.0000026325.65944.7D.
16. Fueyo L, Robles J, Aguilar I, Yáñez AM, Socias M, Parera M. Hemolysis index to detect degree of hydroxocobalamin interference with common laboratory tests. J Clin Lab Anal. 2017;31(5):e22089. doi:10.1002/jcla.22089.
17. Lee J, Mukai D, Kreuter K, Mahon S, Tromberg B, Brenner M. Potential interference by hydroxocobalamin on cooximetry hemoglobin measurements during cyanide and smoke inhalation treatments. Ann Emerg Med. 2007;49(6):802-805. doi:10.
1016/j.annemergmed.2006.11.016.
18. Livshits Z, Lugassy DM, Shawn LK, Hoffman RS. Falsely Low Carboxyhemoglobin after Hydroxocobalamin Therapy [Letter]. N Engl J Med. 2012;367(13):1270-1271. doi:10.1056/NEJMc1114820.
19. Pace R, Bon Homme M, Hoffman RS, Lugassy D. Effects of hydroxocobalamin on carboxyhemoglobin measured under physiologic and pathologic conditions. Clin Toxicol (Phila). 2014;52(7):647-650. doi:10.3109/15563650.2014.939659.
20. Carlsson CJ, Hansen HE, Hilsted L, Malm J, Ødum L, Szecsi PB. An evaluation of the interference of hydroxycobalamin with chemistry and co-oximetry tests on nine commonly used instruments. Scand J Clin Lab Invest. 2011;71(5):378-386. doi:10.3109/00365513.2011.573573.
21. Fueyo L, Robles J, Aguilar I, Yáñez AM, Socias M, Parera M. Hemolysis index to detect degree of hydroxocobalamin interference with common laboratory tests. J Clin Lab Anal. 2017;31(5). doi:10.1002/jcla.22089.
22. Tomaszewski C. Carbon monoxide. In: Hoffman RS, Howland MA, Lewin NA, Nelson LS, Goldfrank LR, eds. Goldfrank’s Toxicologic Emergencies. 10th ed. New York, NY: McGraw-Hill; 2015:1581-1593.
23. Hampson NB, Mathieu D, Piantodosi CA et al. Carbon monoxide poisoning: interpretation of randomized clinical trials and unresolved treatment issues. Undersea Hyperb Med. 2001;28(3):157-164.
24. Raphael JC, Elkharrat D, Jars-Guincestre MC, et al. Trial of normobaric and hyperbaric oxygen for acute carbon monoxide intoxication. Lancet. 1989;2(8660):414-419.
25. Ducassé JL, Celsis P, Marc-Vergnes JP. Non-comatose patients with acute carbon monoxide poisoning: hyperbaric or normobaric oxygenation? Undersea Hyperb Med. 1995;22(1):9-15.
26. Thom SR, Taber RL, Mendiguren II, Clark JM, Hardy KR, Fisher AB. Delayed neuropsychologic sequelae after carbon monoxide poisoning: prevention by treatment with hyperbaric oxygen. Ann Emerg Med. 1995;25(4):474-480.
27. Mathieu D, Wattel F, Mathieu-Nolf M, et al. Randomized prospective study comparing the effects of HBO versus 12 hours of nbp in non comatose CO poisoned patients: results of the interim analysis. Undersea Hyperb Med. 1996;23(Suppl:7-8).
28. Scheinkestel CD, Bailey M, Myles PS, et al. Hyperbaric or normobaric oxygen for acute carbon monoxide poisoning: a randomized controlled clinical trial. Med J Aust. 1999;170(5):203-210.
29. Weaver LK, Hopkins RO, Chan KJ, et al. Hyperbaric oxygen for acute carbon monoxide poisoning. N Engl J Med. 2002;347(14):1057-1067. doi:10.1056/NEJMoa013121.
30. Annane D, Chadda K, Gajdos P, Jars-Guincestre MC, Chevret S, Raphael JC. Hyperbaric oxygen therapy for acute domestic carbon monoxide poisoning: two randomized controlled trials. Intensive Care Med. 2011;37(3):486-492. doi:10.1007/s00134-010-2093-0.
31. Sloan EP, Murphy DG, Hart R, et al. Complications and protocol considerations in carbon monoxide-poisoned patients who require hyperbaric oxygen therapy: report from a ten-year experience. Ann Emerg Med. 1989;18(6):629-634.
32. Hampson NB, Zmaeff JL. Outcome of patients experiencing cardiac arrest with carbon monoxide poisoning treated with hyperbaric oxygen. Ann Emerg Med. 2001;38(1):36-41. doi:10.1067/mem.2001.115532.
33. Wolf SJ, Maloney GE, Shih RD, Shy BD, Brown MD; American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute carbon monoxide poisoning. Ann Emerg Med. pii:S0196-0644(17)30332-3. doi:10.1016/j.annemergmed.2017.03.036.
Case Presentations
Case 1: Smoke Inhalation (Carbon Monoxide and Cyanide)
A 50-year-old woman was pulled from the window of a burning building and found to be in cardiac arrest with pulseless electrical activity. Standard advanced cardiac life-support was started, and infusion of intra-osseous hydroxocobalamin (OHCob) was administered at the time of intubation because of the concern for cyanide (CN) gas exposure during smoke inhalation. Return of spontaneous circulation occurred before arrival at the hospital.
Upon presentation to the ED, the patient’s vital signs were: initial blood pressure (BP), 92/47 mm Hg; heart rate (HR), 112 beats/min; respiratory rate (RR), 31 breaths/min; and temperature (T), 99.7°F. Following intubation, the patient’s oxygen saturation (SaO2) on pulse oximetry (POX) was 93%, and her fraction of inspired oxygen (FiO2) was 100%.
On physical examination, the patient’s face was covered with soot. The lung sounds were equal and clear to auscultation bilaterally. The neurological examination was significant for a Glasgow Coma Scale of 3, without administered sedation, and there were no signs of dermal burns. Initial arterial blood gas (ABG) results were: pH, 7.06; carbon dioxide partial pressure (PCO2), 58 mm Hg; partial pressure of oxygen (PO2), 152 mm Hg; bicarbonate (HCO3), 17 mm Hg; SaO2, 98% (after intubation); FiO2, 100%; carboxyhemoglobin (COHb), 30%; and lactate, 14 mmol/L.
Case 2: Household Misadventure (Carbon Monoxide)
Several days after disabling the carbon monoxide (CO) detector in his home to silence the alarm that had continued to sound, a 67-year-old man developed weakness and called his local fire department. Upon arrival at the man’s home, the fire department confirmed an ambient air CO gas concentration over 200 ppm. Emergency medical services (EMS) promptly brought the patient to the local ED for evaluation and treatment.
Shortly after arrival at the ED, the patient’s weakness had resolved. His vital signs at examination were: BP, 154/85 mm Hg; HR, 79 beats/min; RR, 15 breaths/min; and T, 98.8°F. The patient’s COHb level was 28% with administration of 100% oxygen (O2) via a nonrebreather mask (NRBM).
Carbon Monoxide Toxicity
Carbon monoxide is a toxin of considerable importance to emergency physicians (EPs). The diagnosis at times can be challenging, the interpretation of COHb can be confusing, and the role of hyperbaric oxygen (HBO) therapy in the treatment of CO poisoning remains controversial.
Natural Sources
Carbon monoxide is formed from the incomplete combustion of organic (carbonaceous) fuels, such as charcoal, wood, petroleum distillates (gasoline, kerosene, diesel fuel), and natural gas. Though the majority of atmospheric CO comes from natural sources (eg, volcanoes, forest fires, marsh gases), poisoning exposures are primarily due to man-made CO.
Man-Made Sources
Motor vehicle exhaust is the most abundant source of man-made CO, and exposures to exhaust fumes are common causes of both intentional and unintentional poisonings and death. Other frequent sources of CO poisoning include smoke inhalation from house fires; inadequate ventilation during use of kerosene space heaters; charcoal grills or hibachis; burning wood or charcoal; fuel-powered tools such as generators, fork lifts, and chain saws; or faulty (natural or bottled) gas appliances, such as stoves, furnaces, or water heaters (Table 1). Though propane is known to burn more cleanly than natural gas (ie, less harmful to the environment), it still can produce CO.
Though neither electrical appliances nor “gas leaks” are sources of CO, like CO, natural gas (mostly methane) and bottle gas (propane) are odorless, tasteless, and colorless. Utility companies add sulfur containing mercaptans to natural gas so that leaks can be detected, but CO is only formed when the fuel is burned in a gas-powered appliance.
Endogenous Carbon Monoxide
Endogenous CO production can occur from catabolism of heme or from hepatic metabolism of methylene chloride, but exposures to this solvent are unlikely to generate COHb concentrations above 10%.
Epidemiology
The incidence of CO poisoning is likely more frequent than documented since many cases of minor exposures are unreported due to self-limiting effects and/or the vague, nonspecific nature of symptoms associated with minor exposures. In 2015, US Poison Control Centers reported over 14,000 cases of CO poisoning, only 43% of which were treated in a health care facility.1 The vast majority of exposures (97%) were unintentional and resulted in 52 deaths (0.398%).1
Data from hospitalized patients in 2007 revealed that over 200,000 ED visits and 22,000 hospitalizations were possibly associated with unintentional, non-fire-related CO exposures.2 Approximately 10% of the exposures in each of these populations were confirmed by specific International Classification of Diseases Medical E codes.2
Regardless of dataset, ED visits due to CO exposure are most common in young adults and women, occur in winter months from exposure in and around homes, and result in discharge from the ED. Elderly patients have the highest rate of hospital admission.
Carbon monoxide poisoning has long been considered a leading cause of poisoning death, though numbers appear to be declining, and CO was responsible for fewer deaths than opioids in 2017.2 The National Center for Health Statistics reported 56,133 CO-related deaths from 1979 through 1988—an average of 5,600 per year.3,4 Of these, 46% were from suicide; 28% were related to burns or house fires; and 21% (11,547) were characterized as unintentional. Motor vehicle exhaust was associated with 57% of the unintentional deaths. A more recent analysis of unintentional exposures reported 2,244 deaths during the period of 2010 to 2015—an average of 374 deaths per year (393 in 2015).5
Preventive measures are likely responsible for the significant decline in non-fire-related CO poisoning deaths from the early 1970s through the 1990s. The introduction of catalytic converters in automobiles in 1975 and O2 sensors in 1981 eventually reduced automotive CO emissions by 95% compared to pre-1975 vehicles.6 Both unintentional death and suicide rates associated with CO from motor vehicles subsequently declined by 81% and 43%, respectively. The lower decline in suicidal deaths serves as a reminder that intentional exposure to motor vehicles remains dangerous and potentially lethal.
Pathophysiology/Mechanisms of Toxicity
Carbon monoxide is a colorless, odorless gas that readily reaches the bloodstream during alveolar gas exchange. Since absorption is rapid, exposures to high CO concentrations can produce toxicity within minutes, though exposure severity is related to both inspired CO concentration and duration of exposure.
Endogenous Elimination
Carbon monoxide is eliminated from the body in expired air, with an elimination half-life dependent on FiO2 and atmospheric pressure. Accordingly, COHb decreases with a half-life (all approximate) of 4 to 6 hours when patients are breathing room air (21% O2), 60 to 90 minutes with O2 delivery at 95% to 100%, and 20 to 40 minutes under hyperbaric conditions (2.5-3.0 atmospheres absolute [ATA]).
Effect on Hemoglobin
Once absorbed, CO has an affinity for hemoglobin (Hb) that is over 200 times greater than does O2.7 The formation of COHb results in both a decreased O2-carrying capacity of Hb at the sites where O2 would have been, and because of its new configuration, COHb does not allow currently bound O2 to be offloaded. This is graphically represented by a shift of the O2-Hb dissociation curve to the left. In addition, CO continues to be bound by other intracellular heme molecules in myoglobin of skeletal and myocardial muscle, and the cytochrome oxidase system in mitochondria.8
Immunologic and Inflammatory Effects
Carbon monoxide poisoning results in a cascade of immunologic and inflammatory effects, such as generation of nitric oxide, lipid peroxidation from neutrophils, mitochondrial oxidative stress, and apoptosis. These effects result in cellular asphyxia in all organs, but the most emergent life-threatening concerns are ischemia to the brain and heart.
Severity of Toxicity and Exposure
As previously noted, the severity of CO poisoning is dose-dependent, meaning that it is related to the concentration of CO in inspired air and the duration of the exposure. Carbon monoxide is typically absent in fresh air, but levels may approach 2 to 5 ppm due to cooking, wood burning, mild air pollution, etc. The source of levels above 5 ppm should generally be investigated.
Maximum safe exposure levels for workers over an 8-hour period range from 25 to 50 ppm. Exposures to CO levels above 50 to 100 ppm are likely to elicit symptoms in most patients, depending on duration of the exposure. Carbon monoxide levels of 200 ppm may result in a mild headache after 2 to 3 hours of exposure, and a more severe headache and nausea after 1 to 2 hours of exposures to 400 ppm of CO.
Accordingly, home CO detectors use a combination of ppm and time for alarms, and they may not sound an alarm at 40 ppm until the level persists for 8 or so hours. Home CO detectors, however, will sound an alarm immediately when a level of 80 to 100 ppm is reached.
Clinical Presentation
Acute Exposure
Acute exposure to CO causes a variety of effects that are largely nonspecific, as there is no toxic syndrome (toxidrome) considered pathognomonic for CO poisoning. Ambient CO levels, duration of exposure, minute ventilation, presence of other toxic gases, and patient comorbidities can all contribute to the severity of exposure and presenting signs and symptoms. Effects associated with mild poisoning include headache, dizziness, blurred vision, fatigue or weakness, nausea, and shortness of breath. Patients with pre-existing respiratory, cardiovascular (CV), or neurological compromise are likely to present with more pronounced symptoms. In either case, these complaints may easily be confused with a viral illness, emphasizing the importance of eliciting a history of potential exposure to CO, particularly when multiple patients are involved.
As the concentration of COHb increases, more significant clinical effects can be expected, including tachycardia, chest pain, hypotension, dysrhythmias, lethargy, coma, apnea, and seizures. Hypoxia can result in myocardial injury, cerebral edema, stroke, and acute pulmonary and kidney injury.
Following acute exposure, the severity of effects correlates with the peak pretreatment COHb concentration. However, the peak concentration is usually unknown, since most patients with significant exposures will have some time period elapsed between the exposure and the determination of COHb, and the COHb will have declined at a rate depending on FiO2 and minute ventilation. In these circumstances, COHb is a poor indicator for HBO therapy and outcome.
Delayed Neurological Sequelae
Persistent, recurrent, or delayed (following period of no symptoms) neurological effects can occur in up to 40% of cases, and patients with significant exposures (eg, loss of consciousness) appear to be at greatest risk. These effects most often occur within the first 3 weeks following exposure, and have been known to persist for months to years. Such effects include headache, dizziness, impaired memory or cognition, and emotional lability. Predicting which factors in CO exposure and/or treatments can be modified to prevent neurological sequelae remains challenging.
Diagnostic Testing
Pulse Co-oximetry
Prehospital care POX typically reads COHb as oxyhemoglobin, thereby displaying a normal SaO2.9 Noninvasive CO pulse co-oximetry using a pulse oximeter (Rad-57, Masimo Corporation) provides a reading between –6 to +4 of the true COHb with a false-positive rate of 11% and false-negative rate of 46%.10 This high false-negative rate makes noninvasive CO pulse co-oximetry a poor tool to rule out a CO exposure.11 If OHCob has been administered due to concerns for CN poisoning (smoke inhalation), concentrations of COHb detected by a co-oximeter medical device may be decreased, as noted by a mean decrease of 1% in healthy volunteers exposed to OHCob only.12
Venous and Arterial Blood Gas Testing
For a patient in the hospital, exposure to CO can rapidly be determined using co-oximetry to measure COHb in a venous or arterial sample. Obtaining a venous sample may be a more practical approach, as other venous measurements will likely also be obtained. Baseline “normal” COHb levels should be less than 5%, but may be up to 8% to 10% in tobacco smokers.
Other Laboratory Studies
Other important laboratory tests that should be obtained are a complete blood count, lactate level, venous blood gas, and basic metabolic panel (to assess acid/base status). In two retrospective studies of patients exposed to CO, elevated lactate levels were associated with altered mental status.13,14 However, elevated lactate levels were not seen in a majority of patients with CO poisoning.
In addition, CN exposure should be considered when the lactate level is greater than 8 mmol/L, particularly in patients with smoke inhalation.15 Troponin I and creatinine phosphokinase tests can be used to screen for myocardial or skeletal muscle injury.
Effect of Hydroxocobalamin on Laboratory Evaluation
It is important to be cautious when interpreting the results of laboratory studies in patients who have been given OHCob due to the potential co-exposure to CN (smoke inhalation). The red discoloration of body fluids after OHCob administration makes laboratory evaluation by spectrophotometric techniques erroneous.16 Of greatest concern is the accuracy of COHb concentrations.17 In a study using rabbit models by Lee et al,17 OHCob administration was shown to falsely increase COHb concentrations.
Livshits et al18 reported conflicting effects on COHb in two human cases. In the first case, the patient’s true COHb was 93% lower (2.5% vs 34.9%) following administration of 5 g of OHCob, as measured with a rapid blood gas analyzer. In the second patient, COHb was 76% lower (10.7% vs 44%) following OHCob administration, which was also measured by a blood gas analyzer. Both of these cases illustrate lower true COHb concentrations than would be expected following the administration of only supplemental O2.
In a controlled experiment by Pace et al19 examining the effects of OHCob on measurement of COHb at both physiological (3%) and pathological (30% and 50%) concentrations in human blood samples, the degree of interference depended on the type of co-oximeter used, the degree of COHb elevation (at pathological levels only), and the concentration of OHCob added. Other studies, including an evaluation of OHCob interference by Carlsson et al20 using nine different analyzers have confirmed the interference of OHCob on photometric assays. Of particular clinical importance, a falsely increased lactate level was seen after true lactate levels were found to be below 4.8 mmol/L (but not greater) using spectrophotometric or electrochemical detection.21 This increase in the false-positive assessment of the degree of toxicity could lead unnecessary escalation of care.
These studies emphasize the need to exercise caution when interpreting laboratory test results following OHCob administration. Ideally, it would be best if blood samples were obtained prior to OHCob administration by EMS or in the ED, if the clinical scenario allows it.
Imaging Studies
For patients presenting after a closed-space fire, a chest radiograph will help assess for pulmonary injury. The classic finding of CO poisoning on head computed tomography (CT) and magnetic resonance imaging scans is evidence of ischemia in the basal ganglia. The radiographic findings may help determine the diagnosis of the altered mental status patient who presents without a history. An electrocardiogram (ECG) is also useful for detection of myocardial ischemia or dysrhythmias, when signs or symptoms of either are possible from history and physical or cardiac monitoring.
Intentional Inhalation
Intentional inhalation of fumes containing CO is a relatively common mechanism for suicide. In patients who survive, it is important for EPs and other providers to suspect additional means of self-harm. For example, at our institution, we have encountered several patients with self-inflicted trauma after remaining conscious following a medication overdose. Accordingly, patients who have intentionally inhaled CO should also be evaluated for occult medication poisoning (and trauma).
Treatment
The first step in treating a patient with CO poisoning occurs prior to arrival at the ED, when he or she is removed from continued exposure. The second step is assessing whether this is only a CO exposure, or a mixture of gases from combustion in a closed space, that might also contain CN. When CO and CN are combined OHCob is indicated to treat CN toxicity.
Additionally, if the patient is brought to the ED via EMS, O2 therapy will most likely have been initiated en route. In either case, the concentration of COHb may not accurately reflect the magnitude of exposure or prognosis, and should not be used to dictate the level of therapy or disposition. The patient’s vital signs and clinical findings of end organ toxicity should guide the appropriate supportive care.
Supplemental Oxygen Therapy
Initial administration of 100% O2 during assessment of airway, breathing, and circulation is the first step in accelerating the removal of CO from Hb. For patients suffering from smoke inhalation, assessment and establishment of a secure airway when there are signs of soot or burns in the airway must always take precedence over other actions. Continuous cardiac monitoring, POX, observation, and establishment of intravenous access are often needed for detection and management of CV instability or change in mental status in cases of moderate-to-severe CO exposures. Mild exposures with headache, nausea, and flu-like symptoms can be managed with symptomatic treatment and normobaric O2 until resolution of symptoms and improvement in COHb occur.
Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy involves the delivery of high-flow O2 (typically at 100%) under increased atmospheric pressure (2.5 -3.0 ATA). Oxygen delivered at ambient air pressure (1.0 ATA) is often referred to as normobaric oxygen. Although HBO is best known for its ability to enhance CO elimination, research points to a much more eloquent mitigation of CO toxicity on the molecular level. These mechanisms include an increased amount of dissolved O2 in blood, regeneration of cytochrome oxidase, decreased leukocyte adhesion to microvascular endothelium in the brain, decreased lipid peroxidation in the brain after loss of consciousness, and preservation of adenosine triphosphate.22
For most patients, the majority—if not all—of COHb will be eliminated by the time they present to a suitable HBO chamber. Despite the knowledge that HBO therapy has a positive toxicokinetic effect by increasing the elimination of CO, all of the major, prospective studies on the usefulness of HBO are related to prevention of neuropsychiatric sequelae mediated by immunological and inflammatory effects. The role of HBO in the treatment of CO poisoning has been debated for decades. Multiple studies that differ in methodology, patient populations, delivery of HBO treatments, and assessment of benefits fail to provide a consensus on the role of HBO therapy (Table 2).23-30
Before transferring a patient to a facility for HBO therapy, the potential risks and benefits of transport must be considered. In a 10-year retrospective study by Sloan et al31 of 297 CO-poisoned patients (mean COHb, 38%) 46% of patients had cardiopulmonary and neurological complications prior to HBO therapy at some point in the transfer pathway. During HBO therapy, 18% of patients had complications that included emesis, agitation requiring sedation, seizures, hypotension, tension pneumothorax, cardiac arrest, cardiac arrhythmias, and myocardial ischemia. It is therefore incumbent that personnel attending patients undergoing HBO therapy for CO poisoning be aware of, and able to manage, this variety of serious effects.
When an HBO chamber is at a clinical site with experts in the field and staff available 24 hours a day, the decision to utilize HBO may easily be made without obstacles. For most EPs, however, this is not the case. Locating and transferring a patient to an HBO center is typically a considerable logistical challenge. For many rural facilities, HBO is just not a timely therapeutic option. Two studies state the benefit of HBO therapy is greatest when starting within 6 hours from the end of the CO exposure.24,26
Identifying those CO-poisoned patients who meet evidence-based criteria for HBO is difficult. Patients with mild CO poisoning will do well without HBO, and critically ill patients will probably not consistently benefit from HBO. However, a pragmatic solution must be considered when efficacy studies are incongruent with conflicting results. When signs of end-organ toxicity from CO are present, but cardiac arrest has not yet occurred and the logistics are streamlined, the benefit of HBO may outweigh the risk.
Signs of end-organ toxicity include syncope, seizures, coma, ischemic changes on ECG, and pregnancy with unresolved maternal distress or fetal distress. Although a COHb level greater than 25% or 15% (pregnant) alone is commonly used as an indication for HBO, this is largely based on opinion. Conversely, HBO is unlikely to be helpful in patients who have been resuscitated after CO-related cardiac arrest.32
Treatment Guidelines
The American College of Emergency Physicians recently developed a position statement regarding the management and treatment of CO poisoning.33 The clinical policy addresses several of the controversies discussed in this review, and provides a level of evidence for each response (Table 3).
Case Conclusions
Case 1 (Smoke Inhalation Due to CO and Cyanide Poisoning)
The patient in this case suffered severe CO and CN toxicity. A head CT scan revealed diffuse edema consistent with anoxic brain injury. After conferring with the family regarding the patient’s condition and prognosis, the decision was made to withdraw life-sustaining therapy and support, and the patient died.
Case 2 (Household Misadventure)
The patient in this case was successfully treated with 100% O2 via a NRBM and was subsequently discharged home within 4 hours from presentation.
Conclusion
Exposures to CO are ubiquitous due to our heavy reliance on carbon combustion, and the manifestations of CO toxicity are protean. Therefore, CO poisoning must be considered more frequently in the differential diagnosis of indiscriminant symptoms affecting the neurological, cardiac, pulmonary, and gastrointestinal systems, especially when multiple patients have similar symptoms.
The diagnosis of CO poisoning is straightforward when a serum COHb level is obtained on a venous or arterial blood sample. Treatment starts when the patient is removed from further CO exposure and breaths normobaric oxygen at ambient levels or supplemented. Because there is no clear evidenced-based indication for HBO therapy, further treatment with HBO is naturally limited by rational constraints.
Case Presentations
Case 1: Smoke Inhalation (Carbon Monoxide and Cyanide)
A 50-year-old woman was pulled from the window of a burning building and found to be in cardiac arrest with pulseless electrical activity. Standard advanced cardiac life-support was started, and infusion of intra-osseous hydroxocobalamin (OHCob) was administered at the time of intubation because of the concern for cyanide (CN) gas exposure during smoke inhalation. Return of spontaneous circulation occurred before arrival at the hospital.
Upon presentation to the ED, the patient’s vital signs were: initial blood pressure (BP), 92/47 mm Hg; heart rate (HR), 112 beats/min; respiratory rate (RR), 31 breaths/min; and temperature (T), 99.7°F. Following intubation, the patient’s oxygen saturation (SaO2) on pulse oximetry (POX) was 93%, and her fraction of inspired oxygen (FiO2) was 100%.
On physical examination, the patient’s face was covered with soot. The lung sounds were equal and clear to auscultation bilaterally. The neurological examination was significant for a Glasgow Coma Scale of 3, without administered sedation, and there were no signs of dermal burns. Initial arterial blood gas (ABG) results were: pH, 7.06; carbon dioxide partial pressure (PCO2), 58 mm Hg; partial pressure of oxygen (PO2), 152 mm Hg; bicarbonate (HCO3), 17 mm Hg; SaO2, 98% (after intubation); FiO2, 100%; carboxyhemoglobin (COHb), 30%; and lactate, 14 mmol/L.
Case 2: Household Misadventure (Carbon Monoxide)
Several days after disabling the carbon monoxide (CO) detector in his home to silence the alarm that had continued to sound, a 67-year-old man developed weakness and called his local fire department. Upon arrival at the man’s home, the fire department confirmed an ambient air CO gas concentration over 200 ppm. Emergency medical services (EMS) promptly brought the patient to the local ED for evaluation and treatment.
Shortly after arrival at the ED, the patient’s weakness had resolved. His vital signs at examination were: BP, 154/85 mm Hg; HR, 79 beats/min; RR, 15 breaths/min; and T, 98.8°F. The patient’s COHb level was 28% with administration of 100% oxygen (O2) via a nonrebreather mask (NRBM).
Carbon Monoxide Toxicity
Carbon monoxide is a toxin of considerable importance to emergency physicians (EPs). The diagnosis at times can be challenging, the interpretation of COHb can be confusing, and the role of hyperbaric oxygen (HBO) therapy in the treatment of CO poisoning remains controversial.
Natural Sources
Carbon monoxide is formed from the incomplete combustion of organic (carbonaceous) fuels, such as charcoal, wood, petroleum distillates (gasoline, kerosene, diesel fuel), and natural gas. Though the majority of atmospheric CO comes from natural sources (eg, volcanoes, forest fires, marsh gases), poisoning exposures are primarily due to man-made CO.
Man-Made Sources
Motor vehicle exhaust is the most abundant source of man-made CO, and exposures to exhaust fumes are common causes of both intentional and unintentional poisonings and death. Other frequent sources of CO poisoning include smoke inhalation from house fires; inadequate ventilation during use of kerosene space heaters; charcoal grills or hibachis; burning wood or charcoal; fuel-powered tools such as generators, fork lifts, and chain saws; or faulty (natural or bottled) gas appliances, such as stoves, furnaces, or water heaters (Table 1). Though propane is known to burn more cleanly than natural gas (ie, less harmful to the environment), it still can produce CO.
Though neither electrical appliances nor “gas leaks” are sources of CO, like CO, natural gas (mostly methane) and bottle gas (propane) are odorless, tasteless, and colorless. Utility companies add sulfur containing mercaptans to natural gas so that leaks can be detected, but CO is only formed when the fuel is burned in a gas-powered appliance.
Endogenous Carbon Monoxide
Endogenous CO production can occur from catabolism of heme or from hepatic metabolism of methylene chloride, but exposures to this solvent are unlikely to generate COHb concentrations above 10%.
Epidemiology
The incidence of CO poisoning is likely more frequent than documented since many cases of minor exposures are unreported due to self-limiting effects and/or the vague, nonspecific nature of symptoms associated with minor exposures. In 2015, US Poison Control Centers reported over 14,000 cases of CO poisoning, only 43% of which were treated in a health care facility.1 The vast majority of exposures (97%) were unintentional and resulted in 52 deaths (0.398%).1
Data from hospitalized patients in 2007 revealed that over 200,000 ED visits and 22,000 hospitalizations were possibly associated with unintentional, non-fire-related CO exposures.2 Approximately 10% of the exposures in each of these populations were confirmed by specific International Classification of Diseases Medical E codes.2
Regardless of dataset, ED visits due to CO exposure are most common in young adults and women, occur in winter months from exposure in and around homes, and result in discharge from the ED. Elderly patients have the highest rate of hospital admission.
Carbon monoxide poisoning has long been considered a leading cause of poisoning death, though numbers appear to be declining, and CO was responsible for fewer deaths than opioids in 2017.2 The National Center for Health Statistics reported 56,133 CO-related deaths from 1979 through 1988—an average of 5,600 per year.3,4 Of these, 46% were from suicide; 28% were related to burns or house fires; and 21% (11,547) were characterized as unintentional. Motor vehicle exhaust was associated with 57% of the unintentional deaths. A more recent analysis of unintentional exposures reported 2,244 deaths during the period of 2010 to 2015—an average of 374 deaths per year (393 in 2015).5
Preventive measures are likely responsible for the significant decline in non-fire-related CO poisoning deaths from the early 1970s through the 1990s. The introduction of catalytic converters in automobiles in 1975 and O2 sensors in 1981 eventually reduced automotive CO emissions by 95% compared to pre-1975 vehicles.6 Both unintentional death and suicide rates associated with CO from motor vehicles subsequently declined by 81% and 43%, respectively. The lower decline in suicidal deaths serves as a reminder that intentional exposure to motor vehicles remains dangerous and potentially lethal.
Pathophysiology/Mechanisms of Toxicity
Carbon monoxide is a colorless, odorless gas that readily reaches the bloodstream during alveolar gas exchange. Since absorption is rapid, exposures to high CO concentrations can produce toxicity within minutes, though exposure severity is related to both inspired CO concentration and duration of exposure.
Endogenous Elimination
Carbon monoxide is eliminated from the body in expired air, with an elimination half-life dependent on FiO2 and atmospheric pressure. Accordingly, COHb decreases with a half-life (all approximate) of 4 to 6 hours when patients are breathing room air (21% O2), 60 to 90 minutes with O2 delivery at 95% to 100%, and 20 to 40 minutes under hyperbaric conditions (2.5-3.0 atmospheres absolute [ATA]).
Effect on Hemoglobin
Once absorbed, CO has an affinity for hemoglobin (Hb) that is over 200 times greater than does O2.7 The formation of COHb results in both a decreased O2-carrying capacity of Hb at the sites where O2 would have been, and because of its new configuration, COHb does not allow currently bound O2 to be offloaded. This is graphically represented by a shift of the O2-Hb dissociation curve to the left. In addition, CO continues to be bound by other intracellular heme molecules in myoglobin of skeletal and myocardial muscle, and the cytochrome oxidase system in mitochondria.8
Immunologic and Inflammatory Effects
Carbon monoxide poisoning results in a cascade of immunologic and inflammatory effects, such as generation of nitric oxide, lipid peroxidation from neutrophils, mitochondrial oxidative stress, and apoptosis. These effects result in cellular asphyxia in all organs, but the most emergent life-threatening concerns are ischemia to the brain and heart.
Severity of Toxicity and Exposure
As previously noted, the severity of CO poisoning is dose-dependent, meaning that it is related to the concentration of CO in inspired air and the duration of the exposure. Carbon monoxide is typically absent in fresh air, but levels may approach 2 to 5 ppm due to cooking, wood burning, mild air pollution, etc. The source of levels above 5 ppm should generally be investigated.
Maximum safe exposure levels for workers over an 8-hour period range from 25 to 50 ppm. Exposures to CO levels above 50 to 100 ppm are likely to elicit symptoms in most patients, depending on duration of the exposure. Carbon monoxide levels of 200 ppm may result in a mild headache after 2 to 3 hours of exposure, and a more severe headache and nausea after 1 to 2 hours of exposures to 400 ppm of CO.
Accordingly, home CO detectors use a combination of ppm and time for alarms, and they may not sound an alarm at 40 ppm until the level persists for 8 or so hours. Home CO detectors, however, will sound an alarm immediately when a level of 80 to 100 ppm is reached.
Clinical Presentation
Acute Exposure
Acute exposure to CO causes a variety of effects that are largely nonspecific, as there is no toxic syndrome (toxidrome) considered pathognomonic for CO poisoning. Ambient CO levels, duration of exposure, minute ventilation, presence of other toxic gases, and patient comorbidities can all contribute to the severity of exposure and presenting signs and symptoms. Effects associated with mild poisoning include headache, dizziness, blurred vision, fatigue or weakness, nausea, and shortness of breath. Patients with pre-existing respiratory, cardiovascular (CV), or neurological compromise are likely to present with more pronounced symptoms. In either case, these complaints may easily be confused with a viral illness, emphasizing the importance of eliciting a history of potential exposure to CO, particularly when multiple patients are involved.
As the concentration of COHb increases, more significant clinical effects can be expected, including tachycardia, chest pain, hypotension, dysrhythmias, lethargy, coma, apnea, and seizures. Hypoxia can result in myocardial injury, cerebral edema, stroke, and acute pulmonary and kidney injury.
Following acute exposure, the severity of effects correlates with the peak pretreatment COHb concentration. However, the peak concentration is usually unknown, since most patients with significant exposures will have some time period elapsed between the exposure and the determination of COHb, and the COHb will have declined at a rate depending on FiO2 and minute ventilation. In these circumstances, COHb is a poor indicator for HBO therapy and outcome.
Delayed Neurological Sequelae
Persistent, recurrent, or delayed (following period of no symptoms) neurological effects can occur in up to 40% of cases, and patients with significant exposures (eg, loss of consciousness) appear to be at greatest risk. These effects most often occur within the first 3 weeks following exposure, and have been known to persist for months to years. Such effects include headache, dizziness, impaired memory or cognition, and emotional lability. Predicting which factors in CO exposure and/or treatments can be modified to prevent neurological sequelae remains challenging.
Diagnostic Testing
Pulse Co-oximetry
Prehospital care POX typically reads COHb as oxyhemoglobin, thereby displaying a normal SaO2.9 Noninvasive CO pulse co-oximetry using a pulse oximeter (Rad-57, Masimo Corporation) provides a reading between –6 to +4 of the true COHb with a false-positive rate of 11% and false-negative rate of 46%.10 This high false-negative rate makes noninvasive CO pulse co-oximetry a poor tool to rule out a CO exposure.11 If OHCob has been administered due to concerns for CN poisoning (smoke inhalation), concentrations of COHb detected by a co-oximeter medical device may be decreased, as noted by a mean decrease of 1% in healthy volunteers exposed to OHCob only.12
Venous and Arterial Blood Gas Testing
For a patient in the hospital, exposure to CO can rapidly be determined using co-oximetry to measure COHb in a venous or arterial sample. Obtaining a venous sample may be a more practical approach, as other venous measurements will likely also be obtained. Baseline “normal” COHb levels should be less than 5%, but may be up to 8% to 10% in tobacco smokers.
Other Laboratory Studies
Other important laboratory tests that should be obtained are a complete blood count, lactate level, venous blood gas, and basic metabolic panel (to assess acid/base status). In two retrospective studies of patients exposed to CO, elevated lactate levels were associated with altered mental status.13,14 However, elevated lactate levels were not seen in a majority of patients with CO poisoning.
In addition, CN exposure should be considered when the lactate level is greater than 8 mmol/L, particularly in patients with smoke inhalation.15 Troponin I and creatinine phosphokinase tests can be used to screen for myocardial or skeletal muscle injury.
Effect of Hydroxocobalamin on Laboratory Evaluation
It is important to be cautious when interpreting the results of laboratory studies in patients who have been given OHCob due to the potential co-exposure to CN (smoke inhalation). The red discoloration of body fluids after OHCob administration makes laboratory evaluation by spectrophotometric techniques erroneous.16 Of greatest concern is the accuracy of COHb concentrations.17 In a study using rabbit models by Lee et al,17 OHCob administration was shown to falsely increase COHb concentrations.
Livshits et al18 reported conflicting effects on COHb in two human cases. In the first case, the patient’s true COHb was 93% lower (2.5% vs 34.9%) following administration of 5 g of OHCob, as measured with a rapid blood gas analyzer. In the second patient, COHb was 76% lower (10.7% vs 44%) following OHCob administration, which was also measured by a blood gas analyzer. Both of these cases illustrate lower true COHb concentrations than would be expected following the administration of only supplemental O2.
In a controlled experiment by Pace et al19 examining the effects of OHCob on measurement of COHb at both physiological (3%) and pathological (30% and 50%) concentrations in human blood samples, the degree of interference depended on the type of co-oximeter used, the degree of COHb elevation (at pathological levels only), and the concentration of OHCob added. Other studies, including an evaluation of OHCob interference by Carlsson et al20 using nine different analyzers have confirmed the interference of OHCob on photometric assays. Of particular clinical importance, a falsely increased lactate level was seen after true lactate levels were found to be below 4.8 mmol/L (but not greater) using spectrophotometric or electrochemical detection.21 This increase in the false-positive assessment of the degree of toxicity could lead unnecessary escalation of care.
These studies emphasize the need to exercise caution when interpreting laboratory test results following OHCob administration. Ideally, it would be best if blood samples were obtained prior to OHCob administration by EMS or in the ED, if the clinical scenario allows it.
Imaging Studies
For patients presenting after a closed-space fire, a chest radiograph will help assess for pulmonary injury. The classic finding of CO poisoning on head computed tomography (CT) and magnetic resonance imaging scans is evidence of ischemia in the basal ganglia. The radiographic findings may help determine the diagnosis of the altered mental status patient who presents without a history. An electrocardiogram (ECG) is also useful for detection of myocardial ischemia or dysrhythmias, when signs or symptoms of either are possible from history and physical or cardiac monitoring.
Intentional Inhalation
Intentional inhalation of fumes containing CO is a relatively common mechanism for suicide. In patients who survive, it is important for EPs and other providers to suspect additional means of self-harm. For example, at our institution, we have encountered several patients with self-inflicted trauma after remaining conscious following a medication overdose. Accordingly, patients who have intentionally inhaled CO should also be evaluated for occult medication poisoning (and trauma).
Treatment
The first step in treating a patient with CO poisoning occurs prior to arrival at the ED, when he or she is removed from continued exposure. The second step is assessing whether this is only a CO exposure, or a mixture of gases from combustion in a closed space, that might also contain CN. When CO and CN are combined OHCob is indicated to treat CN toxicity.
Additionally, if the patient is brought to the ED via EMS, O2 therapy will most likely have been initiated en route. In either case, the concentration of COHb may not accurately reflect the magnitude of exposure or prognosis, and should not be used to dictate the level of therapy or disposition. The patient’s vital signs and clinical findings of end organ toxicity should guide the appropriate supportive care.
Supplemental Oxygen Therapy
Initial administration of 100% O2 during assessment of airway, breathing, and circulation is the first step in accelerating the removal of CO from Hb. For patients suffering from smoke inhalation, assessment and establishment of a secure airway when there are signs of soot or burns in the airway must always take precedence over other actions. Continuous cardiac monitoring, POX, observation, and establishment of intravenous access are often needed for detection and management of CV instability or change in mental status in cases of moderate-to-severe CO exposures. Mild exposures with headache, nausea, and flu-like symptoms can be managed with symptomatic treatment and normobaric O2 until resolution of symptoms and improvement in COHb occur.
Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy involves the delivery of high-flow O2 (typically at 100%) under increased atmospheric pressure (2.5 -3.0 ATA). Oxygen delivered at ambient air pressure (1.0 ATA) is often referred to as normobaric oxygen. Although HBO is best known for its ability to enhance CO elimination, research points to a much more eloquent mitigation of CO toxicity on the molecular level. These mechanisms include an increased amount of dissolved O2 in blood, regeneration of cytochrome oxidase, decreased leukocyte adhesion to microvascular endothelium in the brain, decreased lipid peroxidation in the brain after loss of consciousness, and preservation of adenosine triphosphate.22
For most patients, the majority—if not all—of COHb will be eliminated by the time they present to a suitable HBO chamber. Despite the knowledge that HBO therapy has a positive toxicokinetic effect by increasing the elimination of CO, all of the major, prospective studies on the usefulness of HBO are related to prevention of neuropsychiatric sequelae mediated by immunological and inflammatory effects. The role of HBO in the treatment of CO poisoning has been debated for decades. Multiple studies that differ in methodology, patient populations, delivery of HBO treatments, and assessment of benefits fail to provide a consensus on the role of HBO therapy (Table 2).23-30
Before transferring a patient to a facility for HBO therapy, the potential risks and benefits of transport must be considered. In a 10-year retrospective study by Sloan et al31 of 297 CO-poisoned patients (mean COHb, 38%) 46% of patients had cardiopulmonary and neurological complications prior to HBO therapy at some point in the transfer pathway. During HBO therapy, 18% of patients had complications that included emesis, agitation requiring sedation, seizures, hypotension, tension pneumothorax, cardiac arrest, cardiac arrhythmias, and myocardial ischemia. It is therefore incumbent that personnel attending patients undergoing HBO therapy for CO poisoning be aware of, and able to manage, this variety of serious effects.
When an HBO chamber is at a clinical site with experts in the field and staff available 24 hours a day, the decision to utilize HBO may easily be made without obstacles. For most EPs, however, this is not the case. Locating and transferring a patient to an HBO center is typically a considerable logistical challenge. For many rural facilities, HBO is just not a timely therapeutic option. Two studies state the benefit of HBO therapy is greatest when starting within 6 hours from the end of the CO exposure.24,26
Identifying those CO-poisoned patients who meet evidence-based criteria for HBO is difficult. Patients with mild CO poisoning will do well without HBO, and critically ill patients will probably not consistently benefit from HBO. However, a pragmatic solution must be considered when efficacy studies are incongruent with conflicting results. When signs of end-organ toxicity from CO are present, but cardiac arrest has not yet occurred and the logistics are streamlined, the benefit of HBO may outweigh the risk.
Signs of end-organ toxicity include syncope, seizures, coma, ischemic changes on ECG, and pregnancy with unresolved maternal distress or fetal distress. Although a COHb level greater than 25% or 15% (pregnant) alone is commonly used as an indication for HBO, this is largely based on opinion. Conversely, HBO is unlikely to be helpful in patients who have been resuscitated after CO-related cardiac arrest.32
Treatment Guidelines
The American College of Emergency Physicians recently developed a position statement regarding the management and treatment of CO poisoning.33 The clinical policy addresses several of the controversies discussed in this review, and provides a level of evidence for each response (Table 3).
Case Conclusions
Case 1 (Smoke Inhalation Due to CO and Cyanide Poisoning)
The patient in this case suffered severe CO and CN toxicity. A head CT scan revealed diffuse edema consistent with anoxic brain injury. After conferring with the family regarding the patient’s condition and prognosis, the decision was made to withdraw life-sustaining therapy and support, and the patient died.
Case 2 (Household Misadventure)
The patient in this case was successfully treated with 100% O2 via a NRBM and was subsequently discharged home within 4 hours from presentation.
Conclusion
Exposures to CO are ubiquitous due to our heavy reliance on carbon combustion, and the manifestations of CO toxicity are protean. Therefore, CO poisoning must be considered more frequently in the differential diagnosis of indiscriminant symptoms affecting the neurological, cardiac, pulmonary, and gastrointestinal systems, especially when multiple patients have similar symptoms.
The diagnosis of CO poisoning is straightforward when a serum COHb level is obtained on a venous or arterial blood sample. Treatment starts when the patient is removed from further CO exposure and breaths normobaric oxygen at ambient levels or supplemented. Because there is no clear evidenced-based indication for HBO therapy, further treatment with HBO is naturally limited by rational constraints.
1. Mowry JB, Spyker DA, Brooks DE, Zimmerman A, Schauben JL. 2015 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 33rd Annual Report. Clin Toxicol. 2016;54(10):924-1109. doi:10.1080/15563650.2016.1245421.
2. Iqbal S, Law HZ, Clower JH, Yip FY, Elixhauser A. Hospital burden of unintentional carbon monoxide poisoning in the United States, 2007. Am J Emerg Med. 2012;30(5):657-664. doi:10.1016/j.ajem.2011.03.003.
3. Cobb N, Etzel RA. Unintentional carbon monoxide-related deaths in the United States, 1979 through 1988. JAMA. 1991;266(5):659-663.
4. Sircar K, Clower J, Shin MK, Bailey C, King M, Yip F. Carbon monoxide poisoning deaths in the United States, 1999 to 2012. Am J Emerg Med. 2015;33(9):1140-1145. doi:10.1016/j.ajem.2015.05.002.
5. Centers for Disease Control and Prevention. Environmental Public Health Tracking Network. Carbon monoxide poisoning emergency department visits. https://ephtracking.cdc.gov/showHome.action. Updated September 8, 2017. Accessed October 18, 2017.
6. Mott JA, Wolfe MI, Alverson CJ, et al. National vehicle emissions policies and practices and declining US carbon monoxide-related mortality. JAMA. 2002;288(8):988-995.
7. Buckley NA, Juurlink DN, Isbister G, Bennett MH, Lavonas EJ. Hyperbaric oxygen for carbon monoxide poisoning. Cochrane Database Syst Rev. 2011;13(4):CD002041. doi:10.1002/14651858.CD002041.pub3.
8. Hampson NB, Piantadosi CA, Thom SR, Weaver LK. Practice recommendations in the diagnosis, management, and prevention of carbon monoxide poisoning. Am J Respir Crit Care Med. 2012;186(11):1095-1101. doi:10.1164/rccm.201207-1284CI.
9. Bozeman WP, Myers RA, Barish RA. Confirmation of the pulse oximetry gap in carbon monoxide poisoning. Ann of Emerg Med. 1997;30(5):608-611.
10. Zaouter C, Zavorsky GS. The measurement of carboxyhemoglobin and methemoglobin using a non-invasive pulse CO-oximeter. Respir Physiol Neurobiol. 2012;182(2-3):88-92. doi:10.1016/j.resp.2012.05.010.
11. Shamir MY, Avramovich A, Smaka T. The current status of continuous noninvasive measurement of total, carboxy, and methemoglobin concentration. Anesth Analg. 2012;114(5);972-978. doi:10.1213/ANE.0b013e318233041a.
12. Cashin BV, Matlock AG, Kang C, Reynolds PS, Wills BK. Effect of hydroxocobalamin on surface oximetry in nonexposed humans. Prehosp Disaster Med. 2013;28(4):367-369. doi:10.1017/S1049023X13003518.
13. Moon JM, Shin MH, Chun BJ. The value of initial lactate in patients with carbon monoxide intoxication: in the emergency department. Hum Exp Toxicol. 2011;30(8):836-843. doi:10.1177/0960327110384527.
14. Doğan NÖ, Savrun A, Levent S, et al. Can initial lactate levels predict the severity of unintentional carbon monoxide poisoning? Hum Exp Toxicol. 2015;34(3):324-329. doi:10.1177/0960327114538986.
15. Baud FJ, Borron SW, Mégarbane B, et al. Value of lactic acidosis in the assessment of the severity of acute cyanide poisoning. Crit Care Med. 2002;30(9):2044-2050. doi:10.1097/01.CCM.0000026325.65944.7D.
16. Fueyo L, Robles J, Aguilar I, Yáñez AM, Socias M, Parera M. Hemolysis index to detect degree of hydroxocobalamin interference with common laboratory tests. J Clin Lab Anal. 2017;31(5):e22089. doi:10.1002/jcla.22089.
17. Lee J, Mukai D, Kreuter K, Mahon S, Tromberg B, Brenner M. Potential interference by hydroxocobalamin on cooximetry hemoglobin measurements during cyanide and smoke inhalation treatments. Ann Emerg Med. 2007;49(6):802-805. doi:10.
1016/j.annemergmed.2006.11.016.
18. Livshits Z, Lugassy DM, Shawn LK, Hoffman RS. Falsely Low Carboxyhemoglobin after Hydroxocobalamin Therapy [Letter]. N Engl J Med. 2012;367(13):1270-1271. doi:10.1056/NEJMc1114820.
19. Pace R, Bon Homme M, Hoffman RS, Lugassy D. Effects of hydroxocobalamin on carboxyhemoglobin measured under physiologic and pathologic conditions. Clin Toxicol (Phila). 2014;52(7):647-650. doi:10.3109/15563650.2014.939659.
20. Carlsson CJ, Hansen HE, Hilsted L, Malm J, Ødum L, Szecsi PB. An evaluation of the interference of hydroxycobalamin with chemistry and co-oximetry tests on nine commonly used instruments. Scand J Clin Lab Invest. 2011;71(5):378-386. doi:10.3109/00365513.2011.573573.
21. Fueyo L, Robles J, Aguilar I, Yáñez AM, Socias M, Parera M. Hemolysis index to detect degree of hydroxocobalamin interference with common laboratory tests. J Clin Lab Anal. 2017;31(5). doi:10.1002/jcla.22089.
22. Tomaszewski C. Carbon monoxide. In: Hoffman RS, Howland MA, Lewin NA, Nelson LS, Goldfrank LR, eds. Goldfrank’s Toxicologic Emergencies. 10th ed. New York, NY: McGraw-Hill; 2015:1581-1593.
23. Hampson NB, Mathieu D, Piantodosi CA et al. Carbon monoxide poisoning: interpretation of randomized clinical trials and unresolved treatment issues. Undersea Hyperb Med. 2001;28(3):157-164.
24. Raphael JC, Elkharrat D, Jars-Guincestre MC, et al. Trial of normobaric and hyperbaric oxygen for acute carbon monoxide intoxication. Lancet. 1989;2(8660):414-419.
25. Ducassé JL, Celsis P, Marc-Vergnes JP. Non-comatose patients with acute carbon monoxide poisoning: hyperbaric or normobaric oxygenation? Undersea Hyperb Med. 1995;22(1):9-15.
26. Thom SR, Taber RL, Mendiguren II, Clark JM, Hardy KR, Fisher AB. Delayed neuropsychologic sequelae after carbon monoxide poisoning: prevention by treatment with hyperbaric oxygen. Ann Emerg Med. 1995;25(4):474-480.
27. Mathieu D, Wattel F, Mathieu-Nolf M, et al. Randomized prospective study comparing the effects of HBO versus 12 hours of nbp in non comatose CO poisoned patients: results of the interim analysis. Undersea Hyperb Med. 1996;23(Suppl:7-8).
28. Scheinkestel CD, Bailey M, Myles PS, et al. Hyperbaric or normobaric oxygen for acute carbon monoxide poisoning: a randomized controlled clinical trial. Med J Aust. 1999;170(5):203-210.
29. Weaver LK, Hopkins RO, Chan KJ, et al. Hyperbaric oxygen for acute carbon monoxide poisoning. N Engl J Med. 2002;347(14):1057-1067. doi:10.1056/NEJMoa013121.
30. Annane D, Chadda K, Gajdos P, Jars-Guincestre MC, Chevret S, Raphael JC. Hyperbaric oxygen therapy for acute domestic carbon monoxide poisoning: two randomized controlled trials. Intensive Care Med. 2011;37(3):486-492. doi:10.1007/s00134-010-2093-0.
31. Sloan EP, Murphy DG, Hart R, et al. Complications and protocol considerations in carbon monoxide-poisoned patients who require hyperbaric oxygen therapy: report from a ten-year experience. Ann Emerg Med. 1989;18(6):629-634.
32. Hampson NB, Zmaeff JL. Outcome of patients experiencing cardiac arrest with carbon monoxide poisoning treated with hyperbaric oxygen. Ann Emerg Med. 2001;38(1):36-41. doi:10.1067/mem.2001.115532.
33. Wolf SJ, Maloney GE, Shih RD, Shy BD, Brown MD; American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute carbon monoxide poisoning. Ann Emerg Med. pii:S0196-0644(17)30332-3. doi:10.1016/j.annemergmed.2017.03.036.
1. Mowry JB, Spyker DA, Brooks DE, Zimmerman A, Schauben JL. 2015 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 33rd Annual Report. Clin Toxicol. 2016;54(10):924-1109. doi:10.1080/15563650.2016.1245421.
2. Iqbal S, Law HZ, Clower JH, Yip FY, Elixhauser A. Hospital burden of unintentional carbon monoxide poisoning in the United States, 2007. Am J Emerg Med. 2012;30(5):657-664. doi:10.1016/j.ajem.2011.03.003.
3. Cobb N, Etzel RA. Unintentional carbon monoxide-related deaths in the United States, 1979 through 1988. JAMA. 1991;266(5):659-663.
4. Sircar K, Clower J, Shin MK, Bailey C, King M, Yip F. Carbon monoxide poisoning deaths in the United States, 1999 to 2012. Am J Emerg Med. 2015;33(9):1140-1145. doi:10.1016/j.ajem.2015.05.002.
5. Centers for Disease Control and Prevention. Environmental Public Health Tracking Network. Carbon monoxide poisoning emergency department visits. https://ephtracking.cdc.gov/showHome.action. Updated September 8, 2017. Accessed October 18, 2017.
6. Mott JA, Wolfe MI, Alverson CJ, et al. National vehicle emissions policies and practices and declining US carbon monoxide-related mortality. JAMA. 2002;288(8):988-995.
7. Buckley NA, Juurlink DN, Isbister G, Bennett MH, Lavonas EJ. Hyperbaric oxygen for carbon monoxide poisoning. Cochrane Database Syst Rev. 2011;13(4):CD002041. doi:10.1002/14651858.CD002041.pub3.
8. Hampson NB, Piantadosi CA, Thom SR, Weaver LK. Practice recommendations in the diagnosis, management, and prevention of carbon monoxide poisoning. Am J Respir Crit Care Med. 2012;186(11):1095-1101. doi:10.1164/rccm.201207-1284CI.
9. Bozeman WP, Myers RA, Barish RA. Confirmation of the pulse oximetry gap in carbon monoxide poisoning. Ann of Emerg Med. 1997;30(5):608-611.
10. Zaouter C, Zavorsky GS. The measurement of carboxyhemoglobin and methemoglobin using a non-invasive pulse CO-oximeter. Respir Physiol Neurobiol. 2012;182(2-3):88-92. doi:10.1016/j.resp.2012.05.010.
11. Shamir MY, Avramovich A, Smaka T. The current status of continuous noninvasive measurement of total, carboxy, and methemoglobin concentration. Anesth Analg. 2012;114(5);972-978. doi:10.1213/ANE.0b013e318233041a.
12. Cashin BV, Matlock AG, Kang C, Reynolds PS, Wills BK. Effect of hydroxocobalamin on surface oximetry in nonexposed humans. Prehosp Disaster Med. 2013;28(4):367-369. doi:10.1017/S1049023X13003518.
13. Moon JM, Shin MH, Chun BJ. The value of initial lactate in patients with carbon monoxide intoxication: in the emergency department. Hum Exp Toxicol. 2011;30(8):836-843. doi:10.1177/0960327110384527.
14. Doğan NÖ, Savrun A, Levent S, et al. Can initial lactate levels predict the severity of unintentional carbon monoxide poisoning? Hum Exp Toxicol. 2015;34(3):324-329. doi:10.1177/0960327114538986.
15. Baud FJ, Borron SW, Mégarbane B, et al. Value of lactic acidosis in the assessment of the severity of acute cyanide poisoning. Crit Care Med. 2002;30(9):2044-2050. doi:10.1097/01.CCM.0000026325.65944.7D.
16. Fueyo L, Robles J, Aguilar I, Yáñez AM, Socias M, Parera M. Hemolysis index to detect degree of hydroxocobalamin interference with common laboratory tests. J Clin Lab Anal. 2017;31(5):e22089. doi:10.1002/jcla.22089.
17. Lee J, Mukai D, Kreuter K, Mahon S, Tromberg B, Brenner M. Potential interference by hydroxocobalamin on cooximetry hemoglobin measurements during cyanide and smoke inhalation treatments. Ann Emerg Med. 2007;49(6):802-805. doi:10.
1016/j.annemergmed.2006.11.016.
18. Livshits Z, Lugassy DM, Shawn LK, Hoffman RS. Falsely Low Carboxyhemoglobin after Hydroxocobalamin Therapy [Letter]. N Engl J Med. 2012;367(13):1270-1271. doi:10.1056/NEJMc1114820.
19. Pace R, Bon Homme M, Hoffman RS, Lugassy D. Effects of hydroxocobalamin on carboxyhemoglobin measured under physiologic and pathologic conditions. Clin Toxicol (Phila). 2014;52(7):647-650. doi:10.3109/15563650.2014.939659.
20. Carlsson CJ, Hansen HE, Hilsted L, Malm J, Ødum L, Szecsi PB. An evaluation of the interference of hydroxycobalamin with chemistry and co-oximetry tests on nine commonly used instruments. Scand J Clin Lab Invest. 2011;71(5):378-386. doi:10.3109/00365513.2011.573573.
21. Fueyo L, Robles J, Aguilar I, Yáñez AM, Socias M, Parera M. Hemolysis index to detect degree of hydroxocobalamin interference with common laboratory tests. J Clin Lab Anal. 2017;31(5). doi:10.1002/jcla.22089.
22. Tomaszewski C. Carbon monoxide. In: Hoffman RS, Howland MA, Lewin NA, Nelson LS, Goldfrank LR, eds. Goldfrank’s Toxicologic Emergencies. 10th ed. New York, NY: McGraw-Hill; 2015:1581-1593.
23. Hampson NB, Mathieu D, Piantodosi CA et al. Carbon monoxide poisoning: interpretation of randomized clinical trials and unresolved treatment issues. Undersea Hyperb Med. 2001;28(3):157-164.
24. Raphael JC, Elkharrat D, Jars-Guincestre MC, et al. Trial of normobaric and hyperbaric oxygen for acute carbon monoxide intoxication. Lancet. 1989;2(8660):414-419.
25. Ducassé JL, Celsis P, Marc-Vergnes JP. Non-comatose patients with acute carbon monoxide poisoning: hyperbaric or normobaric oxygenation? Undersea Hyperb Med. 1995;22(1):9-15.
26. Thom SR, Taber RL, Mendiguren II, Clark JM, Hardy KR, Fisher AB. Delayed neuropsychologic sequelae after carbon monoxide poisoning: prevention by treatment with hyperbaric oxygen. Ann Emerg Med. 1995;25(4):474-480.
27. Mathieu D, Wattel F, Mathieu-Nolf M, et al. Randomized prospective study comparing the effects of HBO versus 12 hours of nbp in non comatose CO poisoned patients: results of the interim analysis. Undersea Hyperb Med. 1996;23(Suppl:7-8).
28. Scheinkestel CD, Bailey M, Myles PS, et al. Hyperbaric or normobaric oxygen for acute carbon monoxide poisoning: a randomized controlled clinical trial. Med J Aust. 1999;170(5):203-210.
29. Weaver LK, Hopkins RO, Chan KJ, et al. Hyperbaric oxygen for acute carbon monoxide poisoning. N Engl J Med. 2002;347(14):1057-1067. doi:10.1056/NEJMoa013121.
30. Annane D, Chadda K, Gajdos P, Jars-Guincestre MC, Chevret S, Raphael JC. Hyperbaric oxygen therapy for acute domestic carbon monoxide poisoning: two randomized controlled trials. Intensive Care Med. 2011;37(3):486-492. doi:10.1007/s00134-010-2093-0.
31. Sloan EP, Murphy DG, Hart R, et al. Complications and protocol considerations in carbon monoxide-poisoned patients who require hyperbaric oxygen therapy: report from a ten-year experience. Ann Emerg Med. 1989;18(6):629-634.
32. Hampson NB, Zmaeff JL. Outcome of patients experiencing cardiac arrest with carbon monoxide poisoning treated with hyperbaric oxygen. Ann Emerg Med. 2001;38(1):36-41. doi:10.1067/mem.2001.115532.
33. Wolf SJ, Maloney GE, Shih RD, Shy BD, Brown MD; American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute carbon monoxide poisoning. Ann Emerg Med. pii:S0196-0644(17)30332-3. doi:10.1016/j.annemergmed.2017.03.036.