User login
Pediatrician blogs generally provide accurate vaccine information
Pediatrician blogs frequently provide accurate information to parents concerning vaccines, although some blogs do provide information inconsistent with Centers for Disease Control and Prevention guidelines, a study found.
“ However, we identified two exceptions in which pediatrician blogs conveyed extremely inaccurate, antivaccine information,” wrote Mersine A. Bryan, MD, of the University of Washington, Seattle, and her colleagues. “These two extreme blogs were the only blogs that contained any information that was not consistent with CDC information. This finding is important because pediatricians are viewed by parents as a trusted source of information about vaccines.”
Ultimately, the researchers examined 31 blogs with 324 posts related to vaccine content. Most of the information addressed “specific vaccines,” which accounted for 36% of all vaccine-related blog posts. The two most discussed vaccines were MMR (41% of vaccine-specific posts) and influenza (35%). Pediatrician bloggers also commonly addressed “activism against antivaccination,” which was the second most popular topic category.
The analysis revealed that many of the blog posts (91%) on 29 pediatrician blogs provided CDCC information. Only two blogs contained inaccurate vaccine information. Vaccine safety was the most commonly refuted CDCC information, with inaccurate information such as, “We are literally poisoning unborn children with the Tdap now being given to pregnant women with no testing ever done to inject that much aluminum into pregnant animals even!”
Vaccine-scheduling CDCC information was another topic that was addressed inaccurately, with statements such as, “Routine administration of hepatitis B vaccine to 1-day-old infants, which began in 1991, is an unwarranted practice that needs to stopped as soon as possible.” Delayed vaccinations also were inaccurately discussed in 5% of blog posts from two bloggers, who recommended that hepatitis B and MMR vaccines be delayed.
The study had several limitations, including how the blogs were selected for analysis; all were identified using common search engines, which may have caused researchers to miss an unknown number of blogs. In addition, information may have been augmented by “hyperbloggers,” who account for a large proportion of blog posts about vaccines, the researchers reported in Vaccine.
“While uncommon, the presentation of inaccurate, antivaccine information on pediatrician blogs may be persuasive to parents reading vaccine information online. Parents who delay immunizations due to safety concerns are more likely to use the Internet to learn more about vaccines,” wrote Dr. Bryan and her colleagues. “While these negative pediatrician bloggers are the exception, their impact may be disproportionate as people exposed to negative vaccine information in blog format have a more negative view of vaccinations than those exposed to positive vaccine information. Half of parents do not cross-check the information they read online with their doctor.”
The authors had no relevant financial disclosures.
SOURCE: Bryan MA et al. Vaccine. 2018 Jan 29;36(5):765-70.
Facebook and Twitter are useful tools for spreading vaccine information to families, but refuting “antivaccine” information can cause pushback.
“I use social media to disseminate information to families in my practice via a practice Facebook page, as well as to a larger audience via Twitter. I also share information with personal comments on my personal Facebook page,” Deborah Greenhouse, MD, said in an interview. “I have definitely run into questions over concerns with specific vaccines, particularly HPV [human papillomavirus] vaccine and MMR vaccine. Most of these originate with anecdotal posts about vaccine adverse effects.”
When addressing vaccine fears, Dr. Greenhouse presents current, fact-based information from credible sources, stressing the fact that correlation does not equal causation. To keep the lines of communication open, she encourages her patients to call with vaccine safety related questions.
While she has had some positive experiences with refuting “antivaccine” information, it also has been unpleasant. “Sometimes my posts and tweets have led to good interactive discussion. But sometimes they have led to extremely hostile and sometimes obscenity-laden responses by antivaccine activists.”
Despite “antivaccine” concern and pushback via social media, “alternative scheduling” is not viewed as “better than nothing,” she said. The vaccine schedule is based on solid science and should be adhered to. Deviating from a recommended vaccine schedule can put a child at unnecessary, and unacceptable, risk.
Dr. Greenhouse has used social media outreach to effectively provide information to her patients, but also has noted that some pediatricians provide inaccurate information online. “They are tougher to refute than the typical layperson because their credentials make them seem credible.”
Dr. Deborah Greenhouse is a board-certified pediatrician at the Palmetto Pediatric and Adolescent Clinic in Columbia, S.C. She is also a fellow of the American Academy of Pediatrics.
Facebook and Twitter are useful tools for spreading vaccine information to families, but refuting “antivaccine” information can cause pushback.
“I use social media to disseminate information to families in my practice via a practice Facebook page, as well as to a larger audience via Twitter. I also share information with personal comments on my personal Facebook page,” Deborah Greenhouse, MD, said in an interview. “I have definitely run into questions over concerns with specific vaccines, particularly HPV [human papillomavirus] vaccine and MMR vaccine. Most of these originate with anecdotal posts about vaccine adverse effects.”
When addressing vaccine fears, Dr. Greenhouse presents current, fact-based information from credible sources, stressing the fact that correlation does not equal causation. To keep the lines of communication open, she encourages her patients to call with vaccine safety related questions.
While she has had some positive experiences with refuting “antivaccine” information, it also has been unpleasant. “Sometimes my posts and tweets have led to good interactive discussion. But sometimes they have led to extremely hostile and sometimes obscenity-laden responses by antivaccine activists.”
Despite “antivaccine” concern and pushback via social media, “alternative scheduling” is not viewed as “better than nothing,” she said. The vaccine schedule is based on solid science and should be adhered to. Deviating from a recommended vaccine schedule can put a child at unnecessary, and unacceptable, risk.
Dr. Greenhouse has used social media outreach to effectively provide information to her patients, but also has noted that some pediatricians provide inaccurate information online. “They are tougher to refute than the typical layperson because their credentials make them seem credible.”
Dr. Deborah Greenhouse is a board-certified pediatrician at the Palmetto Pediatric and Adolescent Clinic in Columbia, S.C. She is also a fellow of the American Academy of Pediatrics.
Facebook and Twitter are useful tools for spreading vaccine information to families, but refuting “antivaccine” information can cause pushback.
“I use social media to disseminate information to families in my practice via a practice Facebook page, as well as to a larger audience via Twitter. I also share information with personal comments on my personal Facebook page,” Deborah Greenhouse, MD, said in an interview. “I have definitely run into questions over concerns with specific vaccines, particularly HPV [human papillomavirus] vaccine and MMR vaccine. Most of these originate with anecdotal posts about vaccine adverse effects.”
When addressing vaccine fears, Dr. Greenhouse presents current, fact-based information from credible sources, stressing the fact that correlation does not equal causation. To keep the lines of communication open, she encourages her patients to call with vaccine safety related questions.
While she has had some positive experiences with refuting “antivaccine” information, it also has been unpleasant. “Sometimes my posts and tweets have led to good interactive discussion. But sometimes they have led to extremely hostile and sometimes obscenity-laden responses by antivaccine activists.”
Despite “antivaccine” concern and pushback via social media, “alternative scheduling” is not viewed as “better than nothing,” she said. The vaccine schedule is based on solid science and should be adhered to. Deviating from a recommended vaccine schedule can put a child at unnecessary, and unacceptable, risk.
Dr. Greenhouse has used social media outreach to effectively provide information to her patients, but also has noted that some pediatricians provide inaccurate information online. “They are tougher to refute than the typical layperson because their credentials make them seem credible.”
Dr. Deborah Greenhouse is a board-certified pediatrician at the Palmetto Pediatric and Adolescent Clinic in Columbia, S.C. She is also a fellow of the American Academy of Pediatrics.
Pediatrician blogs frequently provide accurate information to parents concerning vaccines, although some blogs do provide information inconsistent with Centers for Disease Control and Prevention guidelines, a study found.
“ However, we identified two exceptions in which pediatrician blogs conveyed extremely inaccurate, antivaccine information,” wrote Mersine A. Bryan, MD, of the University of Washington, Seattle, and her colleagues. “These two extreme blogs were the only blogs that contained any information that was not consistent with CDC information. This finding is important because pediatricians are viewed by parents as a trusted source of information about vaccines.”
Ultimately, the researchers examined 31 blogs with 324 posts related to vaccine content. Most of the information addressed “specific vaccines,” which accounted for 36% of all vaccine-related blog posts. The two most discussed vaccines were MMR (41% of vaccine-specific posts) and influenza (35%). Pediatrician bloggers also commonly addressed “activism against antivaccination,” which was the second most popular topic category.
The analysis revealed that many of the blog posts (91%) on 29 pediatrician blogs provided CDCC information. Only two blogs contained inaccurate vaccine information. Vaccine safety was the most commonly refuted CDCC information, with inaccurate information such as, “We are literally poisoning unborn children with the Tdap now being given to pregnant women with no testing ever done to inject that much aluminum into pregnant animals even!”
Vaccine-scheduling CDCC information was another topic that was addressed inaccurately, with statements such as, “Routine administration of hepatitis B vaccine to 1-day-old infants, which began in 1991, is an unwarranted practice that needs to stopped as soon as possible.” Delayed vaccinations also were inaccurately discussed in 5% of blog posts from two bloggers, who recommended that hepatitis B and MMR vaccines be delayed.
The study had several limitations, including how the blogs were selected for analysis; all were identified using common search engines, which may have caused researchers to miss an unknown number of blogs. In addition, information may have been augmented by “hyperbloggers,” who account for a large proportion of blog posts about vaccines, the researchers reported in Vaccine.
“While uncommon, the presentation of inaccurate, antivaccine information on pediatrician blogs may be persuasive to parents reading vaccine information online. Parents who delay immunizations due to safety concerns are more likely to use the Internet to learn more about vaccines,” wrote Dr. Bryan and her colleagues. “While these negative pediatrician bloggers are the exception, their impact may be disproportionate as people exposed to negative vaccine information in blog format have a more negative view of vaccinations than those exposed to positive vaccine information. Half of parents do not cross-check the information they read online with their doctor.”
The authors had no relevant financial disclosures.
SOURCE: Bryan MA et al. Vaccine. 2018 Jan 29;36(5):765-70.
Pediatrician blogs frequently provide accurate information to parents concerning vaccines, although some blogs do provide information inconsistent with Centers for Disease Control and Prevention guidelines, a study found.
“ However, we identified two exceptions in which pediatrician blogs conveyed extremely inaccurate, antivaccine information,” wrote Mersine A. Bryan, MD, of the University of Washington, Seattle, and her colleagues. “These two extreme blogs were the only blogs that contained any information that was not consistent with CDC information. This finding is important because pediatricians are viewed by parents as a trusted source of information about vaccines.”
Ultimately, the researchers examined 31 blogs with 324 posts related to vaccine content. Most of the information addressed “specific vaccines,” which accounted for 36% of all vaccine-related blog posts. The two most discussed vaccines were MMR (41% of vaccine-specific posts) and influenza (35%). Pediatrician bloggers also commonly addressed “activism against antivaccination,” which was the second most popular topic category.
The analysis revealed that many of the blog posts (91%) on 29 pediatrician blogs provided CDCC information. Only two blogs contained inaccurate vaccine information. Vaccine safety was the most commonly refuted CDCC information, with inaccurate information such as, “We are literally poisoning unborn children with the Tdap now being given to pregnant women with no testing ever done to inject that much aluminum into pregnant animals even!”
Vaccine-scheduling CDCC information was another topic that was addressed inaccurately, with statements such as, “Routine administration of hepatitis B vaccine to 1-day-old infants, which began in 1991, is an unwarranted practice that needs to stopped as soon as possible.” Delayed vaccinations also were inaccurately discussed in 5% of blog posts from two bloggers, who recommended that hepatitis B and MMR vaccines be delayed.
The study had several limitations, including how the blogs were selected for analysis; all were identified using common search engines, which may have caused researchers to miss an unknown number of blogs. In addition, information may have been augmented by “hyperbloggers,” who account for a large proportion of blog posts about vaccines, the researchers reported in Vaccine.
“While uncommon, the presentation of inaccurate, antivaccine information on pediatrician blogs may be persuasive to parents reading vaccine information online. Parents who delay immunizations due to safety concerns are more likely to use the Internet to learn more about vaccines,” wrote Dr. Bryan and her colleagues. “While these negative pediatrician bloggers are the exception, their impact may be disproportionate as people exposed to negative vaccine information in blog format have a more negative view of vaccinations than those exposed to positive vaccine information. Half of parents do not cross-check the information they read online with their doctor.”
The authors had no relevant financial disclosures.
SOURCE: Bryan MA et al. Vaccine. 2018 Jan 29;36(5):765-70.
FROM VACCINE
Key clinical point: Pediatricians usually provide accurate information via blogs.
Major finding: 91% of blog posts on 29 pediatrician blogs contained only CDC-consistent information.
Study details: A content analysis of 31 pediatrician blogs from Jan. 1, 2014, to Feb. 28, 2015.
Disclosures: The authors had no relevant financial disclosures.
Source: Bryan MA et al. Vaccine. 2018 Jan 29;36(5):765-70.
Late-breaking research presented at AAD on Saturday February 17
Dermatology News will be on site later this week at the annual meeting of the American Academy of Dermatology in San Diego. Look for the latest news and video interviews from the meeting in medical, surgical, and aesthetic dermatology at edermatologynews.com starting Friday February 16.
Coverage will include the late-breaker sessions, which will be presented on Saturday February 17.
Check out another late-breaking session – on basic science, cutaneous oncology, and pathology – which will include presentations on the growing burden of melanoma, the incidence of Merkel cell carcinoma in the United States, and the inverse genetic risk between vitiligo and cutaneous melanoma.
Find out more about these and other sessions at the official 2018 AAD Annual Meeting’s page.
Dermatology News will be on site later this week at the annual meeting of the American Academy of Dermatology in San Diego. Look for the latest news and video interviews from the meeting in medical, surgical, and aesthetic dermatology at edermatologynews.com starting Friday February 16.
Coverage will include the late-breaker sessions, which will be presented on Saturday February 17.
Check out another late-breaking session – on basic science, cutaneous oncology, and pathology – which will include presentations on the growing burden of melanoma, the incidence of Merkel cell carcinoma in the United States, and the inverse genetic risk between vitiligo and cutaneous melanoma.
Find out more about these and other sessions at the official 2018 AAD Annual Meeting’s page.
Dermatology News will be on site later this week at the annual meeting of the American Academy of Dermatology in San Diego. Look for the latest news and video interviews from the meeting in medical, surgical, and aesthetic dermatology at edermatologynews.com starting Friday February 16.
Coverage will include the late-breaker sessions, which will be presented on Saturday February 17.
Check out another late-breaking session – on basic science, cutaneous oncology, and pathology – which will include presentations on the growing burden of melanoma, the incidence of Merkel cell carcinoma in the United States, and the inverse genetic risk between vitiligo and cutaneous melanoma.
Find out more about these and other sessions at the official 2018 AAD Annual Meeting’s page.
More time with digital media impacts childhood well-being
In school-aged children, according to Stephanie Ruest, MD, of Hasbro Children’s Hospital, Providence, R.I., and her associates.
In a study surveying parents from the 2011-2012 National Survey of Children’s Health, behavior of 64,464 children aged 6-17 years was examined. Results found that 31% of children were reported to have a combined daily digital media exposure (DME) of less than 2 hours/day, 36% had 2-4 hours, 17% had 4-6 hours, and 16% had at least 6 hours/day of DME. Among the children with less than 2 hours of DME, 38% had access to media devices in their bedroom, compared with 73% in the greater than 6-hour exposure group.
Additionally, children who had 2-4 hours of DME per weekday not related to schoolwork had 22% lower odds of always/usually finishing their homework, compared with children who had less than 2 hours. Children with 4-6 hours/day had 46% lower odds and those with greater than 6 hours/day had 57% lower odds of demonstrating this marker, compared with children with less than 2 hours (P less than .001). “There was a similar decrease in odds seen with each of the remaining four flourishing markers (test for trend P less than .001 for each marker),” Dr. Ruest and her associates said.
“DME, when measured in combined daily hours, is inversely associated with behaviors and attitudes that have been identified as markers of childhood flourishing in a dose-dependent manner,” the researchers concluded. “Future studies should continue to work towards elucidating the complex relationship between total DME time in conjunction with the content of the media and how the interplay affects childhood flourishing.”
SOURCE: Ruest S et al. J Pediatr. 2018 Feb 1. doi: 10.1016/j.jpeds.2017.12.016.
In school-aged children, according to Stephanie Ruest, MD, of Hasbro Children’s Hospital, Providence, R.I., and her associates.
In a study surveying parents from the 2011-2012 National Survey of Children’s Health, behavior of 64,464 children aged 6-17 years was examined. Results found that 31% of children were reported to have a combined daily digital media exposure (DME) of less than 2 hours/day, 36% had 2-4 hours, 17% had 4-6 hours, and 16% had at least 6 hours/day of DME. Among the children with less than 2 hours of DME, 38% had access to media devices in their bedroom, compared with 73% in the greater than 6-hour exposure group.
Additionally, children who had 2-4 hours of DME per weekday not related to schoolwork had 22% lower odds of always/usually finishing their homework, compared with children who had less than 2 hours. Children with 4-6 hours/day had 46% lower odds and those with greater than 6 hours/day had 57% lower odds of demonstrating this marker, compared with children with less than 2 hours (P less than .001). “There was a similar decrease in odds seen with each of the remaining four flourishing markers (test for trend P less than .001 for each marker),” Dr. Ruest and her associates said.
“DME, when measured in combined daily hours, is inversely associated with behaviors and attitudes that have been identified as markers of childhood flourishing in a dose-dependent manner,” the researchers concluded. “Future studies should continue to work towards elucidating the complex relationship between total DME time in conjunction with the content of the media and how the interplay affects childhood flourishing.”
SOURCE: Ruest S et al. J Pediatr. 2018 Feb 1. doi: 10.1016/j.jpeds.2017.12.016.
In school-aged children, according to Stephanie Ruest, MD, of Hasbro Children’s Hospital, Providence, R.I., and her associates.
In a study surveying parents from the 2011-2012 National Survey of Children’s Health, behavior of 64,464 children aged 6-17 years was examined. Results found that 31% of children were reported to have a combined daily digital media exposure (DME) of less than 2 hours/day, 36% had 2-4 hours, 17% had 4-6 hours, and 16% had at least 6 hours/day of DME. Among the children with less than 2 hours of DME, 38% had access to media devices in their bedroom, compared with 73% in the greater than 6-hour exposure group.
Additionally, children who had 2-4 hours of DME per weekday not related to schoolwork had 22% lower odds of always/usually finishing their homework, compared with children who had less than 2 hours. Children with 4-6 hours/day had 46% lower odds and those with greater than 6 hours/day had 57% lower odds of demonstrating this marker, compared with children with less than 2 hours (P less than .001). “There was a similar decrease in odds seen with each of the remaining four flourishing markers (test for trend P less than .001 for each marker),” Dr. Ruest and her associates said.
“DME, when measured in combined daily hours, is inversely associated with behaviors and attitudes that have been identified as markers of childhood flourishing in a dose-dependent manner,” the researchers concluded. “Future studies should continue to work towards elucidating the complex relationship between total DME time in conjunction with the content of the media and how the interplay affects childhood flourishing.”
SOURCE: Ruest S et al. J Pediatr. 2018 Feb 1. doi: 10.1016/j.jpeds.2017.12.016.
FROM THE JOURNAL OF PEDIATRICS
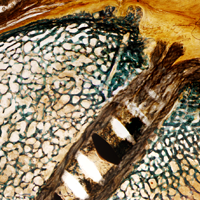
Study explores biological implications of MHC-II expression in tumor cells
SAN FRANCISCO – , and a recent analysis of MHC-II–positive tumor features provided some insight into the evolution of that response.
The analysis, which involved RNA sequencing on 58 patients with anti–programmed cell death-1 (PD-1)–treated melanoma and lung tumors and on a subset of matched pretreatment specimens at acquired resistance, also highlighted the Fc-receptor–like 6 (FCRL6) molecule as a potential novel immunotherapy target, Justin M. Balko, PharmD, PhD, of Vanderbilt University Medical Center, Nashville, Tenn., reported at the ASCO-SITC Clinical Immuno-Oncology Symposium.
MHC-II
“MHC-II functions to present class-II restricted antigens to CD4+ T cells, especially T helper cells,” he said, explaining that the expression is typically confined to the professional antigen presenting cell (pAPC) population, but has also previously been shown to be both constitutively and dynamically expressed on tumor cells.
He and his colleagues showed in a 2016 study that MHC-II expression on tumor cells had potential as a biomarker for anti-PD-1 response.
The current study was undertaken to further explore the biological implications of MHC-II expression in tumor cells.
“Importantly here, instead of using mRNA for MHC-II, which could be confounded by other cells in the stroma or microenvironment, we performed immunohistochemistry (IHC) for MHC-II specifically on the tumor compartment within these samples,” Dr. Balko said, noting that he and his colleagues were specifically looking for what was different in gene expression patterns in the MHC-II+ tumor cells.
They compared the gene sets that were enriched in HLA-DR+, or MHC-II+, tumor cells within human tumors with those from melanoma cell lines grown ex vivo in culture (which eliminated any confounding factors of RNA data from contaminating stroma or immune cells), and found substantial gene set overlap.
“These were signatures of innate autoimmunity or inflammation, including those describing allograft rejection gene sets, viral myocarditis, and asthma, suggesting there’s a tumor-intrinsic inflammation signal associated with class II expression on tumor cells,” he said. “We also previously showed in the melanoma data set that HLA-DR expression specifically on tumor cells had a strong association with CD4 infiltrate, and a slightly weaker association with the degree of CD8 infiltration within the tumors.”
Similarly, quantitative immunofluorescence of MHC-II expression in 100 triple negative breast cancer tumors showed that those tumors with HLA-DR or MHC-II expression on tumor cells had a greater degree of CD4 infiltrate than did the negative tumors. CD8 infiltrate was also increased, but enrichment was greater toward the CD4 compartment – an interesting finding given that MHC-II presents antigen to T helper cells, Dr. Balko noted.
A closer look at individual genes that were different between class II–negative and positive tumors showed that LAG-3 mRNA was more enriched in the HLA-DR+ tumors, and also in patients who experienced a significant response to anti-PD-1 therapy.
“We also had a small population of samples that were derived from relapsed specimens,” he said. “We performed IHC within a small subset where we had paired tumors from pre-PD-1 response and relapse [to look at] LAG-3+ lymphocytes in the tumor ... and saw significant enrichment of LAG-3 infiltrate in the relapsed specimens. Importantly, all of these tumors were MHC-II+.”
Findings in a mouse model
The functional significance of this was explored using an MHC-II–negative orthotopic model cell line unlikely to induce expression of MHC-II when treated with interferon-gamma in culture; MHC-class-II transactivator (CIITA), the master regulator of MHC-II, was used to transduce the cells, resulting in cells that were “constitutively 100% class II+.”
Immunocompetent mice injected with these cells rejected tumors at a much higher rate, but IHC showed more nonregulatory CD4 cells in mice that did not reject the MHC-II+ tumors, Dr. Balko noted.
Gene expression analysis of the rejection-escaped tumors showed more mRNA for PD-1 and LAG-3, similar to what was seen in the study subjects.
“To see if the effect was truly an increase in PD-1 and LAG-3 on lymphocytes within the tumor microenvironment or in lymphoid tissues, we injected immunocompetent mice with either control or CIITA-positive tumors, and then at 7 days harvested either the contralateral lymph node, the spleen, or the proximal or tumor-draining lymph node,” he said.
This showed increased amounts of LAG-3 and PD-1-positive CD4 and CD8 cells in the tumor-draining lymph node, and more LAG-3 PD-1-positive CD8 cells within the tumor itself.
“To perform a therapeutic study, but also to eliminate any confounding factors of the rejecting mice, we waited 14 days after injection of the tumor cells and only enrolled mice with actively growing tumors. We randomized the mice to treatment with either IgG vehicle control, or anti-PD-1, or the combination of anti-PD1 plus LAG-3, and we had a very substantial [75%] complete response rate in the mice with class II–positive tumors treated with the combined PD-1 and LAG-3,” he said. “Importantly, all of the mice in this study were reinoculated with the [MHC-II–negative] cell line and had complete rejection of any subsequent injection of tumor cells.”
To assess whether any other MHC-II receptors could be expressed in the tumor microenvironment, Dr. Balko and his colleagues turned their attention to the FCRL6 molecule, which has previously been shown to be an MHC-II receptor that is expressed on cytolytic cells.
FCRL6
“[FCRL6] actually has an [immunoreceptor tyrosine-based inhibitory motif] domain in the intracellular portion of the human ortholog, which suggests that it could have some inhibitory function,” Dr. Balko said, adding that it has been shown to be expressed in a substantial proportion of natural killer cells and CD8 cells, and in a minor fraction of CD4+ T cells, which have been described as “cytotoxic CD4 cells.”
An immortalized FCRL6-negative natural killer cell line know as NK-92 was used to test for inhibitory function.
“We co-cultured it with K562 cells, which are a leukemia cell line that is both class I and class II negative; because they have a missing-self signal, the natural killer cells will naturally lyse the K562 cells, which can be measured by chromium release,” he explained.
When MHC-II was reconstituted on K562 cells, the natural killer cells still had effective lysis of the K562 cells, but when FCRL6 was also transduced on the natural killer cells, this interaction was stopped, and there was suppression of cytotoxic activity, or chromium release, in the co-cultures, suggesting that FCRL6 may have a checkpoint-like functionality, he said.
In the melanoma dataset, a look at FLCR6 mRNA in the tumor microenvironment showed that it was also much more highly expressed in HLA-DR–positive tumors and in the relapsed specimens.
In the tumors with paired specimens (three of which were MHC-II positive and three of which were MHC-II negative), IHC for FCRL6 identified greater enrichment of lymphocytes in the MHC-II–positive tumors, but the difference was not statistically significant.
In the breast cancer samples, where more LAG-3 and FCRL6 was seen in the triple-negative breast tumors, quantitative immunofluorescence showed that FCRL6-postive lymphocytes and LAG-3-positive lymphocytes had a substantial suppression of CD8-sel-positive granzyme B-positive cells within the microenvironment that was more substantial than that observed with PD-L1 expression, he noted.
“So our conclusions are that MHC-II tumors demonstrate enhanced T cell-mediated inflammation and immunity and anti-tumor immunity is circumvented through adaptive resistance by PD-1 and potentially LAG-3/MHC-II engagement in some tumors, and that ... FCRL6 may be a novel MHC-II receptor with inhibitory functionality, and could be a new immunotherapy target,” he said.
MHC-II expression could be useful for stratifying patients to combined anti-PD-1/anti-LAG-3 therapy, and eventually to combined anti-PD-1/anti-FCRL6 therapy, he added.
Combined anti-PD-1 and anti-LAG-3 therapy
The findings are of particular interest given recent findings regarding LAG-3 antibodies in development, said invited discussant Antoni Ribas, MD.
In a study reported by Ascierto et al. at ASCO 2017, for example, combined anti-PD-1 and anti-LAG-3 therapy had a 13% overall response rate in metastatic melanoma patients who progressed on anti-PD-1 therapy alone (20% and 7.1% in those with and without LAG-3 expression, respectively), said Dr. Ribas of the University of California, Los Angeles.
The 20% response rate seen in those with LAG-3 expression suggests “there could be a biomarker for this combined therapy,” he said, noting that while the overall response rate of 13% is low, “it is relevant because it is rescuing some patients who progressed on therapy, and it follows Dr. Balko’s science of why that would be the case.”
Dr. Balko has received research funding from Incyte, and holds a patent on use of HLA-DR/MHC expression to predict response to immunotherapies. Dr. Ribas owns stock in Advaxis, Arcus Ventures, Compugen, CytomX Therapeutics, Five Prime Therapeutics, FLX Bio, and Kite Pharma, and has served as a consultant or adviser for Amgen, Genentech/Roche, Merck, Novartis, and Pierre Fabre.
SOURCE: Balko J et al., ASCO-SITC abstract 180
SAN FRANCISCO – , and a recent analysis of MHC-II–positive tumor features provided some insight into the evolution of that response.
The analysis, which involved RNA sequencing on 58 patients with anti–programmed cell death-1 (PD-1)–treated melanoma and lung tumors and on a subset of matched pretreatment specimens at acquired resistance, also highlighted the Fc-receptor–like 6 (FCRL6) molecule as a potential novel immunotherapy target, Justin M. Balko, PharmD, PhD, of Vanderbilt University Medical Center, Nashville, Tenn., reported at the ASCO-SITC Clinical Immuno-Oncology Symposium.
MHC-II
“MHC-II functions to present class-II restricted antigens to CD4+ T cells, especially T helper cells,” he said, explaining that the expression is typically confined to the professional antigen presenting cell (pAPC) population, but has also previously been shown to be both constitutively and dynamically expressed on tumor cells.
He and his colleagues showed in a 2016 study that MHC-II expression on tumor cells had potential as a biomarker for anti-PD-1 response.
The current study was undertaken to further explore the biological implications of MHC-II expression in tumor cells.
“Importantly here, instead of using mRNA for MHC-II, which could be confounded by other cells in the stroma or microenvironment, we performed immunohistochemistry (IHC) for MHC-II specifically on the tumor compartment within these samples,” Dr. Balko said, noting that he and his colleagues were specifically looking for what was different in gene expression patterns in the MHC-II+ tumor cells.
They compared the gene sets that were enriched in HLA-DR+, or MHC-II+, tumor cells within human tumors with those from melanoma cell lines grown ex vivo in culture (which eliminated any confounding factors of RNA data from contaminating stroma or immune cells), and found substantial gene set overlap.
“These were signatures of innate autoimmunity or inflammation, including those describing allograft rejection gene sets, viral myocarditis, and asthma, suggesting there’s a tumor-intrinsic inflammation signal associated with class II expression on tumor cells,” he said. “We also previously showed in the melanoma data set that HLA-DR expression specifically on tumor cells had a strong association with CD4 infiltrate, and a slightly weaker association with the degree of CD8 infiltration within the tumors.”
Similarly, quantitative immunofluorescence of MHC-II expression in 100 triple negative breast cancer tumors showed that those tumors with HLA-DR or MHC-II expression on tumor cells had a greater degree of CD4 infiltrate than did the negative tumors. CD8 infiltrate was also increased, but enrichment was greater toward the CD4 compartment – an interesting finding given that MHC-II presents antigen to T helper cells, Dr. Balko noted.
A closer look at individual genes that were different between class II–negative and positive tumors showed that LAG-3 mRNA was more enriched in the HLA-DR+ tumors, and also in patients who experienced a significant response to anti-PD-1 therapy.
“We also had a small population of samples that were derived from relapsed specimens,” he said. “We performed IHC within a small subset where we had paired tumors from pre-PD-1 response and relapse [to look at] LAG-3+ lymphocytes in the tumor ... and saw significant enrichment of LAG-3 infiltrate in the relapsed specimens. Importantly, all of these tumors were MHC-II+.”
Findings in a mouse model
The functional significance of this was explored using an MHC-II–negative orthotopic model cell line unlikely to induce expression of MHC-II when treated with interferon-gamma in culture; MHC-class-II transactivator (CIITA), the master regulator of MHC-II, was used to transduce the cells, resulting in cells that were “constitutively 100% class II+.”
Immunocompetent mice injected with these cells rejected tumors at a much higher rate, but IHC showed more nonregulatory CD4 cells in mice that did not reject the MHC-II+ tumors, Dr. Balko noted.
Gene expression analysis of the rejection-escaped tumors showed more mRNA for PD-1 and LAG-3, similar to what was seen in the study subjects.
“To see if the effect was truly an increase in PD-1 and LAG-3 on lymphocytes within the tumor microenvironment or in lymphoid tissues, we injected immunocompetent mice with either control or CIITA-positive tumors, and then at 7 days harvested either the contralateral lymph node, the spleen, or the proximal or tumor-draining lymph node,” he said.
This showed increased amounts of LAG-3 and PD-1-positive CD4 and CD8 cells in the tumor-draining lymph node, and more LAG-3 PD-1-positive CD8 cells within the tumor itself.
“To perform a therapeutic study, but also to eliminate any confounding factors of the rejecting mice, we waited 14 days after injection of the tumor cells and only enrolled mice with actively growing tumors. We randomized the mice to treatment with either IgG vehicle control, or anti-PD-1, or the combination of anti-PD1 plus LAG-3, and we had a very substantial [75%] complete response rate in the mice with class II–positive tumors treated with the combined PD-1 and LAG-3,” he said. “Importantly, all of the mice in this study were reinoculated with the [MHC-II–negative] cell line and had complete rejection of any subsequent injection of tumor cells.”
To assess whether any other MHC-II receptors could be expressed in the tumor microenvironment, Dr. Balko and his colleagues turned their attention to the FCRL6 molecule, which has previously been shown to be an MHC-II receptor that is expressed on cytolytic cells.
FCRL6
“[FCRL6] actually has an [immunoreceptor tyrosine-based inhibitory motif] domain in the intracellular portion of the human ortholog, which suggests that it could have some inhibitory function,” Dr. Balko said, adding that it has been shown to be expressed in a substantial proportion of natural killer cells and CD8 cells, and in a minor fraction of CD4+ T cells, which have been described as “cytotoxic CD4 cells.”
An immortalized FCRL6-negative natural killer cell line know as NK-92 was used to test for inhibitory function.
“We co-cultured it with K562 cells, which are a leukemia cell line that is both class I and class II negative; because they have a missing-self signal, the natural killer cells will naturally lyse the K562 cells, which can be measured by chromium release,” he explained.
When MHC-II was reconstituted on K562 cells, the natural killer cells still had effective lysis of the K562 cells, but when FCRL6 was also transduced on the natural killer cells, this interaction was stopped, and there was suppression of cytotoxic activity, or chromium release, in the co-cultures, suggesting that FCRL6 may have a checkpoint-like functionality, he said.
In the melanoma dataset, a look at FLCR6 mRNA in the tumor microenvironment showed that it was also much more highly expressed in HLA-DR–positive tumors and in the relapsed specimens.
In the tumors with paired specimens (three of which were MHC-II positive and three of which were MHC-II negative), IHC for FCRL6 identified greater enrichment of lymphocytes in the MHC-II–positive tumors, but the difference was not statistically significant.
In the breast cancer samples, where more LAG-3 and FCRL6 was seen in the triple-negative breast tumors, quantitative immunofluorescence showed that FCRL6-postive lymphocytes and LAG-3-positive lymphocytes had a substantial suppression of CD8-sel-positive granzyme B-positive cells within the microenvironment that was more substantial than that observed with PD-L1 expression, he noted.
“So our conclusions are that MHC-II tumors demonstrate enhanced T cell-mediated inflammation and immunity and anti-tumor immunity is circumvented through adaptive resistance by PD-1 and potentially LAG-3/MHC-II engagement in some tumors, and that ... FCRL6 may be a novel MHC-II receptor with inhibitory functionality, and could be a new immunotherapy target,” he said.
MHC-II expression could be useful for stratifying patients to combined anti-PD-1/anti-LAG-3 therapy, and eventually to combined anti-PD-1/anti-FCRL6 therapy, he added.
Combined anti-PD-1 and anti-LAG-3 therapy
The findings are of particular interest given recent findings regarding LAG-3 antibodies in development, said invited discussant Antoni Ribas, MD.
In a study reported by Ascierto et al. at ASCO 2017, for example, combined anti-PD-1 and anti-LAG-3 therapy had a 13% overall response rate in metastatic melanoma patients who progressed on anti-PD-1 therapy alone (20% and 7.1% in those with and without LAG-3 expression, respectively), said Dr. Ribas of the University of California, Los Angeles.
The 20% response rate seen in those with LAG-3 expression suggests “there could be a biomarker for this combined therapy,” he said, noting that while the overall response rate of 13% is low, “it is relevant because it is rescuing some patients who progressed on therapy, and it follows Dr. Balko’s science of why that would be the case.”
Dr. Balko has received research funding from Incyte, and holds a patent on use of HLA-DR/MHC expression to predict response to immunotherapies. Dr. Ribas owns stock in Advaxis, Arcus Ventures, Compugen, CytomX Therapeutics, Five Prime Therapeutics, FLX Bio, and Kite Pharma, and has served as a consultant or adviser for Amgen, Genentech/Roche, Merck, Novartis, and Pierre Fabre.
SOURCE: Balko J et al., ASCO-SITC abstract 180
SAN FRANCISCO – , and a recent analysis of MHC-II–positive tumor features provided some insight into the evolution of that response.
The analysis, which involved RNA sequencing on 58 patients with anti–programmed cell death-1 (PD-1)–treated melanoma and lung tumors and on a subset of matched pretreatment specimens at acquired resistance, also highlighted the Fc-receptor–like 6 (FCRL6) molecule as a potential novel immunotherapy target, Justin M. Balko, PharmD, PhD, of Vanderbilt University Medical Center, Nashville, Tenn., reported at the ASCO-SITC Clinical Immuno-Oncology Symposium.
MHC-II
“MHC-II functions to present class-II restricted antigens to CD4+ T cells, especially T helper cells,” he said, explaining that the expression is typically confined to the professional antigen presenting cell (pAPC) population, but has also previously been shown to be both constitutively and dynamically expressed on tumor cells.
He and his colleagues showed in a 2016 study that MHC-II expression on tumor cells had potential as a biomarker for anti-PD-1 response.
The current study was undertaken to further explore the biological implications of MHC-II expression in tumor cells.
“Importantly here, instead of using mRNA for MHC-II, which could be confounded by other cells in the stroma or microenvironment, we performed immunohistochemistry (IHC) for MHC-II specifically on the tumor compartment within these samples,” Dr. Balko said, noting that he and his colleagues were specifically looking for what was different in gene expression patterns in the MHC-II+ tumor cells.
They compared the gene sets that were enriched in HLA-DR+, or MHC-II+, tumor cells within human tumors with those from melanoma cell lines grown ex vivo in culture (which eliminated any confounding factors of RNA data from contaminating stroma or immune cells), and found substantial gene set overlap.
“These were signatures of innate autoimmunity or inflammation, including those describing allograft rejection gene sets, viral myocarditis, and asthma, suggesting there’s a tumor-intrinsic inflammation signal associated with class II expression on tumor cells,” he said. “We also previously showed in the melanoma data set that HLA-DR expression specifically on tumor cells had a strong association with CD4 infiltrate, and a slightly weaker association with the degree of CD8 infiltration within the tumors.”
Similarly, quantitative immunofluorescence of MHC-II expression in 100 triple negative breast cancer tumors showed that those tumors with HLA-DR or MHC-II expression on tumor cells had a greater degree of CD4 infiltrate than did the negative tumors. CD8 infiltrate was also increased, but enrichment was greater toward the CD4 compartment – an interesting finding given that MHC-II presents antigen to T helper cells, Dr. Balko noted.
A closer look at individual genes that were different between class II–negative and positive tumors showed that LAG-3 mRNA was more enriched in the HLA-DR+ tumors, and also in patients who experienced a significant response to anti-PD-1 therapy.
“We also had a small population of samples that were derived from relapsed specimens,” he said. “We performed IHC within a small subset where we had paired tumors from pre-PD-1 response and relapse [to look at] LAG-3+ lymphocytes in the tumor ... and saw significant enrichment of LAG-3 infiltrate in the relapsed specimens. Importantly, all of these tumors were MHC-II+.”
Findings in a mouse model
The functional significance of this was explored using an MHC-II–negative orthotopic model cell line unlikely to induce expression of MHC-II when treated with interferon-gamma in culture; MHC-class-II transactivator (CIITA), the master regulator of MHC-II, was used to transduce the cells, resulting in cells that were “constitutively 100% class II+.”
Immunocompetent mice injected with these cells rejected tumors at a much higher rate, but IHC showed more nonregulatory CD4 cells in mice that did not reject the MHC-II+ tumors, Dr. Balko noted.
Gene expression analysis of the rejection-escaped tumors showed more mRNA for PD-1 and LAG-3, similar to what was seen in the study subjects.
“To see if the effect was truly an increase in PD-1 and LAG-3 on lymphocytes within the tumor microenvironment or in lymphoid tissues, we injected immunocompetent mice with either control or CIITA-positive tumors, and then at 7 days harvested either the contralateral lymph node, the spleen, or the proximal or tumor-draining lymph node,” he said.
This showed increased amounts of LAG-3 and PD-1-positive CD4 and CD8 cells in the tumor-draining lymph node, and more LAG-3 PD-1-positive CD8 cells within the tumor itself.
“To perform a therapeutic study, but also to eliminate any confounding factors of the rejecting mice, we waited 14 days after injection of the tumor cells and only enrolled mice with actively growing tumors. We randomized the mice to treatment with either IgG vehicle control, or anti-PD-1, or the combination of anti-PD1 plus LAG-3, and we had a very substantial [75%] complete response rate in the mice with class II–positive tumors treated with the combined PD-1 and LAG-3,” he said. “Importantly, all of the mice in this study were reinoculated with the [MHC-II–negative] cell line and had complete rejection of any subsequent injection of tumor cells.”
To assess whether any other MHC-II receptors could be expressed in the tumor microenvironment, Dr. Balko and his colleagues turned their attention to the FCRL6 molecule, which has previously been shown to be an MHC-II receptor that is expressed on cytolytic cells.
FCRL6
“[FCRL6] actually has an [immunoreceptor tyrosine-based inhibitory motif] domain in the intracellular portion of the human ortholog, which suggests that it could have some inhibitory function,” Dr. Balko said, adding that it has been shown to be expressed in a substantial proportion of natural killer cells and CD8 cells, and in a minor fraction of CD4+ T cells, which have been described as “cytotoxic CD4 cells.”
An immortalized FCRL6-negative natural killer cell line know as NK-92 was used to test for inhibitory function.
“We co-cultured it with K562 cells, which are a leukemia cell line that is both class I and class II negative; because they have a missing-self signal, the natural killer cells will naturally lyse the K562 cells, which can be measured by chromium release,” he explained.
When MHC-II was reconstituted on K562 cells, the natural killer cells still had effective lysis of the K562 cells, but when FCRL6 was also transduced on the natural killer cells, this interaction was stopped, and there was suppression of cytotoxic activity, or chromium release, in the co-cultures, suggesting that FCRL6 may have a checkpoint-like functionality, he said.
In the melanoma dataset, a look at FLCR6 mRNA in the tumor microenvironment showed that it was also much more highly expressed in HLA-DR–positive tumors and in the relapsed specimens.
In the tumors with paired specimens (three of which were MHC-II positive and three of which were MHC-II negative), IHC for FCRL6 identified greater enrichment of lymphocytes in the MHC-II–positive tumors, but the difference was not statistically significant.
In the breast cancer samples, where more LAG-3 and FCRL6 was seen in the triple-negative breast tumors, quantitative immunofluorescence showed that FCRL6-postive lymphocytes and LAG-3-positive lymphocytes had a substantial suppression of CD8-sel-positive granzyme B-positive cells within the microenvironment that was more substantial than that observed with PD-L1 expression, he noted.
“So our conclusions are that MHC-II tumors demonstrate enhanced T cell-mediated inflammation and immunity and anti-tumor immunity is circumvented through adaptive resistance by PD-1 and potentially LAG-3/MHC-II engagement in some tumors, and that ... FCRL6 may be a novel MHC-II receptor with inhibitory functionality, and could be a new immunotherapy target,” he said.
MHC-II expression could be useful for stratifying patients to combined anti-PD-1/anti-LAG-3 therapy, and eventually to combined anti-PD-1/anti-FCRL6 therapy, he added.
Combined anti-PD-1 and anti-LAG-3 therapy
The findings are of particular interest given recent findings regarding LAG-3 antibodies in development, said invited discussant Antoni Ribas, MD.
In a study reported by Ascierto et al. at ASCO 2017, for example, combined anti-PD-1 and anti-LAG-3 therapy had a 13% overall response rate in metastatic melanoma patients who progressed on anti-PD-1 therapy alone (20% and 7.1% in those with and without LAG-3 expression, respectively), said Dr. Ribas of the University of California, Los Angeles.
The 20% response rate seen in those with LAG-3 expression suggests “there could be a biomarker for this combined therapy,” he said, noting that while the overall response rate of 13% is low, “it is relevant because it is rescuing some patients who progressed on therapy, and it follows Dr. Balko’s science of why that would be the case.”
Dr. Balko has received research funding from Incyte, and holds a patent on use of HLA-DR/MHC expression to predict response to immunotherapies. Dr. Ribas owns stock in Advaxis, Arcus Ventures, Compugen, CytomX Therapeutics, Five Prime Therapeutics, FLX Bio, and Kite Pharma, and has served as a consultant or adviser for Amgen, Genentech/Roche, Merck, Novartis, and Pierre Fabre.
SOURCE: Balko J et al., ASCO-SITC abstract 180
REPORTING FROM THE CLINICAL IMMUNO-ONCOLOGY SYMPOSIUM
Key clinical point: MHC-II expression could be useful for stratifying patients to anti-PD-1/anti-LAG-3 and other therapies.
Major finding: The ORR was 75% for class II–positive tumors treated with combined anti-PD-1/anti-LAG-3
Study details: RNA sequencing on 58 patients with anti-PD-1-treated tumors and on matched pretreatment specimens.
Disclosures: Dr. Balko has received research funding from Incyte, and holds a patent on use of HLA-DR/MHC expression to predict response to immunotherapies. Dr. Ribas owns stock in Advaxis, Arcus Ventures, Compugen, CytomX Therapeutics, Five Prime Therapeutics, FLX Bio, and Kite Pharma, and has served as a consultant or adviser for Amgen, Genentech/Roche, Merck, Novartis, and Pierre Fabre.
Source: Balko J et al. ASCO-SITC abstract 180.
Transparency lacking in oncology clinical pathways
The use of oncology clinical pathways (OCPs) is rapidly rising as more data suggest that they can reduce cost and improve quality. But amid the advantages to pathways, there are growing concerns about hidden conflicts of interest.
“There is a lot of promise from these pathways in delivering the right care to the right patient at the right time,” said Bobby Daly, MD, an oncologist and health services researcher at Memorial Sloan Kettering Cancer Center in New York. “But oncologists and patients really want to understand how these pathways are being developed. The issue of transparency is one that patients and providers feel strongly about.”
While collaboration with industry is the key to innovation, Dr. Daly wrote that “to ensure patient and clinician trust and maintain their momentum in the value space, pathway developers will need to be transparent about [financial conflicts of interest] and how those interests are managed.”
Pathways: What’s the problem?
But as pathways have become more prevalent, concerns have emerged among physicians about who is making pathway treatment decisions and, specifically, about instances in which medications are being selected without disclosure of investments or financial relationships that could influence those decisions, said Robin Zon, MD, chair of the ASCO Task Force on Clinical Pathways.
“In addition, there have been concerns about the methodology of how treatments decisions are made with regard to efficacy, toxicity, and cost, as well as the weighting of these factors in making decisions for the pathway program,” Dr. Zon said in an interview.
Taken together, the mounting questions led to an analysis and by the ASCO task force.
“What the task force found was that standards defining high-quality pathways did not exist, so we became concerned that there could be a risk for wide variations with regards to the quality, utility, functionality, and impact of pathway programs,” Dr. Zon said.
The findings were the catalyst behind a March 2016 ASCO policy statement aimed at ensuring that clinical pathways in oncology promote – not hinder – cancer care. The task force called on pathway developers to adopt a process that was consistent and transparent to all stakeholders and to disclose potential conflicts of interest by the companies and individuals involved in pathway development.
“The criteria were developed to address the multiple issues brought to our attention by ASCO members and to be used as possible standards for pathway development, implementation, and evolution,” Dr. Zon said.
Meanwhile, the Cleveland Clinic has been utilizing pathways for more than 5 years and has published nearly 50 clinical pathways related to cancer care, Dr. Kalaycio said.
“Our care paths were designed to help physicians make clinical decisions that are in the best interest of their patients and the Cleveland Clinic,” he said in an interview. “These care paths are here for clinical reasons, not for financial reasons – we might ultimately use them to make financial decisions, but that’s not why they were developed. In contrast, the [JAMA Oncology study] is referring to pathways that are being developed by for-profit companies to control cost – big, big difference.”
The problem is that some insurers want to hide the identity of their advisors and how much they are being paid, which creates uncertainty about the validity of their pathways, he said. Dr. Kalaycio noted that the individuals selected for pathway panels and committees are often those who conducted the studies that the pathways are based upon and that those studies are frequently supported by the pharmaceutical industry.
“There is always going to be some degree of conflict of interest and as long as that’s disclosed, that’s fine,” he said. “It’s when you try to hide who’s getting paid for what that you get into trouble because you can’t say with certainty that someone’s not getting paid off.”
To address the transparency void, the California legislature in 2017 introduced the Oncology Clinical Pathways Act. The bill would have required health plans that develop and implement OCPs to provide the names, qualifications, affiliations, and conflicts of anyone involved in the research or analysis for an oncology clinical pathway if it were requested by a physician or surgeon. The bill died in committee.
Health plans push back
America’s Health Insurance Plans (AHIP) spokeswoman Cathryn Donaldson said health plans are being unfairly targeted in the drive toward more transparency. The recent efforts are an attempt to single out clinical care pathways developed by health plans as needing additional oversight standards while ignoring pathways that are developed by drug distributors, hospital systems, academic institutions, and others, Ms. Donaldson said in an interview.
ASCO’s Dr. Zon stressed that the criteria her task force created for pathways is aimed at all types of developers.
“In other words, we felt that the criteria should apply across all the pathway program developers whether they were provider or payer facing,” Dr. Zon said. “We also did not differentiate between not-for-profit and for-profit entities. Standards for high-quality criteria should apply to any pathway program being developed regardless of the source.”
Dr. Daly added that every entity that develops a pathway should have some policy around conflict of interest and how to address any transparency issues that may arise. Despite the recent debate over transparency, Dr. Daly said he believes the future of pathways is bright.
“I think the future is that pathways hold a lot of promise,” he said. “But I think we really need to ensure that the pathways that are being employed are of high quality because they influence how patients are treated.”
Dr. Daly serves as a director of Quadrant Holdings Corporation and receives compensation from this entity. This news organization is a subsidiary of Quadrant Holdings Corporation.
The use of oncology clinical pathways (OCPs) is rapidly rising as more data suggest that they can reduce cost and improve quality. But amid the advantages to pathways, there are growing concerns about hidden conflicts of interest.
“There is a lot of promise from these pathways in delivering the right care to the right patient at the right time,” said Bobby Daly, MD, an oncologist and health services researcher at Memorial Sloan Kettering Cancer Center in New York. “But oncologists and patients really want to understand how these pathways are being developed. The issue of transparency is one that patients and providers feel strongly about.”
While collaboration with industry is the key to innovation, Dr. Daly wrote that “to ensure patient and clinician trust and maintain their momentum in the value space, pathway developers will need to be transparent about [financial conflicts of interest] and how those interests are managed.”
Pathways: What’s the problem?
But as pathways have become more prevalent, concerns have emerged among physicians about who is making pathway treatment decisions and, specifically, about instances in which medications are being selected without disclosure of investments or financial relationships that could influence those decisions, said Robin Zon, MD, chair of the ASCO Task Force on Clinical Pathways.
“In addition, there have been concerns about the methodology of how treatments decisions are made with regard to efficacy, toxicity, and cost, as well as the weighting of these factors in making decisions for the pathway program,” Dr. Zon said in an interview.
Taken together, the mounting questions led to an analysis and by the ASCO task force.
“What the task force found was that standards defining high-quality pathways did not exist, so we became concerned that there could be a risk for wide variations with regards to the quality, utility, functionality, and impact of pathway programs,” Dr. Zon said.
The findings were the catalyst behind a March 2016 ASCO policy statement aimed at ensuring that clinical pathways in oncology promote – not hinder – cancer care. The task force called on pathway developers to adopt a process that was consistent and transparent to all stakeholders and to disclose potential conflicts of interest by the companies and individuals involved in pathway development.
“The criteria were developed to address the multiple issues brought to our attention by ASCO members and to be used as possible standards for pathway development, implementation, and evolution,” Dr. Zon said.
Meanwhile, the Cleveland Clinic has been utilizing pathways for more than 5 years and has published nearly 50 clinical pathways related to cancer care, Dr. Kalaycio said.
“Our care paths were designed to help physicians make clinical decisions that are in the best interest of their patients and the Cleveland Clinic,” he said in an interview. “These care paths are here for clinical reasons, not for financial reasons – we might ultimately use them to make financial decisions, but that’s not why they were developed. In contrast, the [JAMA Oncology study] is referring to pathways that are being developed by for-profit companies to control cost – big, big difference.”
The problem is that some insurers want to hide the identity of their advisors and how much they are being paid, which creates uncertainty about the validity of their pathways, he said. Dr. Kalaycio noted that the individuals selected for pathway panels and committees are often those who conducted the studies that the pathways are based upon and that those studies are frequently supported by the pharmaceutical industry.
“There is always going to be some degree of conflict of interest and as long as that’s disclosed, that’s fine,” he said. “It’s when you try to hide who’s getting paid for what that you get into trouble because you can’t say with certainty that someone’s not getting paid off.”
To address the transparency void, the California legislature in 2017 introduced the Oncology Clinical Pathways Act. The bill would have required health plans that develop and implement OCPs to provide the names, qualifications, affiliations, and conflicts of anyone involved in the research or analysis for an oncology clinical pathway if it were requested by a physician or surgeon. The bill died in committee.
Health plans push back
America’s Health Insurance Plans (AHIP) spokeswoman Cathryn Donaldson said health plans are being unfairly targeted in the drive toward more transparency. The recent efforts are an attempt to single out clinical care pathways developed by health plans as needing additional oversight standards while ignoring pathways that are developed by drug distributors, hospital systems, academic institutions, and others, Ms. Donaldson said in an interview.
ASCO’s Dr. Zon stressed that the criteria her task force created for pathways is aimed at all types of developers.
“In other words, we felt that the criteria should apply across all the pathway program developers whether they were provider or payer facing,” Dr. Zon said. “We also did not differentiate between not-for-profit and for-profit entities. Standards for high-quality criteria should apply to any pathway program being developed regardless of the source.”
Dr. Daly added that every entity that develops a pathway should have some policy around conflict of interest and how to address any transparency issues that may arise. Despite the recent debate over transparency, Dr. Daly said he believes the future of pathways is bright.
“I think the future is that pathways hold a lot of promise,” he said. “But I think we really need to ensure that the pathways that are being employed are of high quality because they influence how patients are treated.”
Dr. Daly serves as a director of Quadrant Holdings Corporation and receives compensation from this entity. This news organization is a subsidiary of Quadrant Holdings Corporation.
The use of oncology clinical pathways (OCPs) is rapidly rising as more data suggest that they can reduce cost and improve quality. But amid the advantages to pathways, there are growing concerns about hidden conflicts of interest.
“There is a lot of promise from these pathways in delivering the right care to the right patient at the right time,” said Bobby Daly, MD, an oncologist and health services researcher at Memorial Sloan Kettering Cancer Center in New York. “But oncologists and patients really want to understand how these pathways are being developed. The issue of transparency is one that patients and providers feel strongly about.”
While collaboration with industry is the key to innovation, Dr. Daly wrote that “to ensure patient and clinician trust and maintain their momentum in the value space, pathway developers will need to be transparent about [financial conflicts of interest] and how those interests are managed.”
Pathways: What’s the problem?
But as pathways have become more prevalent, concerns have emerged among physicians about who is making pathway treatment decisions and, specifically, about instances in which medications are being selected without disclosure of investments or financial relationships that could influence those decisions, said Robin Zon, MD, chair of the ASCO Task Force on Clinical Pathways.
“In addition, there have been concerns about the methodology of how treatments decisions are made with regard to efficacy, toxicity, and cost, as well as the weighting of these factors in making decisions for the pathway program,” Dr. Zon said in an interview.
Taken together, the mounting questions led to an analysis and by the ASCO task force.
“What the task force found was that standards defining high-quality pathways did not exist, so we became concerned that there could be a risk for wide variations with regards to the quality, utility, functionality, and impact of pathway programs,” Dr. Zon said.
The findings were the catalyst behind a March 2016 ASCO policy statement aimed at ensuring that clinical pathways in oncology promote – not hinder – cancer care. The task force called on pathway developers to adopt a process that was consistent and transparent to all stakeholders and to disclose potential conflicts of interest by the companies and individuals involved in pathway development.
“The criteria were developed to address the multiple issues brought to our attention by ASCO members and to be used as possible standards for pathway development, implementation, and evolution,” Dr. Zon said.
Meanwhile, the Cleveland Clinic has been utilizing pathways for more than 5 years and has published nearly 50 clinical pathways related to cancer care, Dr. Kalaycio said.
“Our care paths were designed to help physicians make clinical decisions that are in the best interest of their patients and the Cleveland Clinic,” he said in an interview. “These care paths are here for clinical reasons, not for financial reasons – we might ultimately use them to make financial decisions, but that’s not why they were developed. In contrast, the [JAMA Oncology study] is referring to pathways that are being developed by for-profit companies to control cost – big, big difference.”
The problem is that some insurers want to hide the identity of their advisors and how much they are being paid, which creates uncertainty about the validity of their pathways, he said. Dr. Kalaycio noted that the individuals selected for pathway panels and committees are often those who conducted the studies that the pathways are based upon and that those studies are frequently supported by the pharmaceutical industry.
“There is always going to be some degree of conflict of interest and as long as that’s disclosed, that’s fine,” he said. “It’s when you try to hide who’s getting paid for what that you get into trouble because you can’t say with certainty that someone’s not getting paid off.”
To address the transparency void, the California legislature in 2017 introduced the Oncology Clinical Pathways Act. The bill would have required health plans that develop and implement OCPs to provide the names, qualifications, affiliations, and conflicts of anyone involved in the research or analysis for an oncology clinical pathway if it were requested by a physician or surgeon. The bill died in committee.
Health plans push back
America’s Health Insurance Plans (AHIP) spokeswoman Cathryn Donaldson said health plans are being unfairly targeted in the drive toward more transparency. The recent efforts are an attempt to single out clinical care pathways developed by health plans as needing additional oversight standards while ignoring pathways that are developed by drug distributors, hospital systems, academic institutions, and others, Ms. Donaldson said in an interview.
ASCO’s Dr. Zon stressed that the criteria her task force created for pathways is aimed at all types of developers.
“In other words, we felt that the criteria should apply across all the pathway program developers whether they were provider or payer facing,” Dr. Zon said. “We also did not differentiate between not-for-profit and for-profit entities. Standards for high-quality criteria should apply to any pathway program being developed regardless of the source.”
Dr. Daly added that every entity that develops a pathway should have some policy around conflict of interest and how to address any transparency issues that may arise. Despite the recent debate over transparency, Dr. Daly said he believes the future of pathways is bright.
“I think the future is that pathways hold a lot of promise,” he said. “But I think we really need to ensure that the pathways that are being employed are of high quality because they influence how patients are treated.”
Dr. Daly serves as a director of Quadrant Holdings Corporation and receives compensation from this entity. This news organization is a subsidiary of Quadrant Holdings Corporation.
Abdominal CT refines treatment in refractory puerperal fever
DALLAS – Abdominal CT scans changed therapeutic management in 39% of women being unsuccessfully treated for refractory puerperal fever, a retrospective study has determined.
The scans pinpointed a definite diagnosis in the majority of the cohort, allowing clinicians to reassess their treatment, Michal Fishel-Bartal, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“This study has important clinical implications for women with refractory puerperal fever,” said Dr. Fishel-Bartal of the Chaim Sheba Medical Center, Ramat Gan, Israel. “Our department now recommends that all women with refractory puerperal fever should undergo an assessment for risk factors, including urgent cesarean section, preterm delivery, and general anesthesia, and an evaluation to see if an abdominal CT may be appropriate to investigate the possibility of septic pelvic thrombophlebitis or the need for intra-abdominal drainage.”
She and her colleagues conducted a 10-year retrospective review of refractory puerperal fever cases at Chaim Sheba Medical Center. All of the patients had a CT scan within 7 days of their delivery. A radiologist reviewed each scan, looking for potential causes of the illness, including pelvic collection (a suspected pelvic abscess or collection of 4 cm or more) or signs of septic pelvic thrombophlebitis (enlargement of an involved vein, vessel wall enhancement, or a filling defect).
The primary outcome was a treatment change due to the CT results. These included switching antibiotics, starting therapeutic low-molecular-weight heparin, or a surgical intervention (intra-abdominal drainage or laparotomy).
The cohort comprised 238 women, who were a mean age of 33 years. In comparing them with the hospital’s background population, they were significantly more likely to have delivered at less than 37 weeks (25% vs. 7%), and to have had a cesarean delivery (80% vs. 25%). Dr. Fishel-Bartal also noted that 29% of the patients had experienced general anesthesia.
Most of the scans (144; 60%) were abnormal. Findings included septic pelvic thrombophlebitis (32) and pelvic collections (112). Treatment changed in 93 women (39% of the entire cohort). Changes included adding or switching antibiotics (24), adding low-molecular-weight heparin (28), laparotomy (11), and drainage insertion (30).
The investigators also performed a multivariate analysis to identify any risk factors that significantly predicted the need to change or add treatment. General anesthesia was the only factor significantly more common among those who needed a treatment switch (70% vs. 58%). This could have been a marker for an urgent C-section – something often associated with complications, Dr. Fishel-Bartal noted.
In the discussion period, Dr. Fishel-Bartal fielded a question about whether ultrasound would be a more logical and cost-effective method of assessing these patients.
“We actually do usually start with an ultrasound evaluation in our patients with refractory puerperal fever, and 68% of this group did have one,” Dr. Fishel-Bartal replied. “Findings were positive in 37%. The ultrasound actually was very good at predicting pelvic collections, but it only identified 5 of the 32 with septic thrombophlebitis. So it’s a good modality to start with, but if the patient still has fever or there is a concern for septic pelvic thrombosis, you really still need a CT.”
She had no financial disclosures.
SOURCE: Fishel-Bartal M et al. The Pregnancy Meeting. Am J Obstet Gynecol. 2018;218:S59.
DALLAS – Abdominal CT scans changed therapeutic management in 39% of women being unsuccessfully treated for refractory puerperal fever, a retrospective study has determined.
The scans pinpointed a definite diagnosis in the majority of the cohort, allowing clinicians to reassess their treatment, Michal Fishel-Bartal, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“This study has important clinical implications for women with refractory puerperal fever,” said Dr. Fishel-Bartal of the Chaim Sheba Medical Center, Ramat Gan, Israel. “Our department now recommends that all women with refractory puerperal fever should undergo an assessment for risk factors, including urgent cesarean section, preterm delivery, and general anesthesia, and an evaluation to see if an abdominal CT may be appropriate to investigate the possibility of septic pelvic thrombophlebitis or the need for intra-abdominal drainage.”
She and her colleagues conducted a 10-year retrospective review of refractory puerperal fever cases at Chaim Sheba Medical Center. All of the patients had a CT scan within 7 days of their delivery. A radiologist reviewed each scan, looking for potential causes of the illness, including pelvic collection (a suspected pelvic abscess or collection of 4 cm or more) or signs of septic pelvic thrombophlebitis (enlargement of an involved vein, vessel wall enhancement, or a filling defect).
The primary outcome was a treatment change due to the CT results. These included switching antibiotics, starting therapeutic low-molecular-weight heparin, or a surgical intervention (intra-abdominal drainage or laparotomy).
The cohort comprised 238 women, who were a mean age of 33 years. In comparing them with the hospital’s background population, they were significantly more likely to have delivered at less than 37 weeks (25% vs. 7%), and to have had a cesarean delivery (80% vs. 25%). Dr. Fishel-Bartal also noted that 29% of the patients had experienced general anesthesia.
Most of the scans (144; 60%) were abnormal. Findings included septic pelvic thrombophlebitis (32) and pelvic collections (112). Treatment changed in 93 women (39% of the entire cohort). Changes included adding or switching antibiotics (24), adding low-molecular-weight heparin (28), laparotomy (11), and drainage insertion (30).
The investigators also performed a multivariate analysis to identify any risk factors that significantly predicted the need to change or add treatment. General anesthesia was the only factor significantly more common among those who needed a treatment switch (70% vs. 58%). This could have been a marker for an urgent C-section – something often associated with complications, Dr. Fishel-Bartal noted.
In the discussion period, Dr. Fishel-Bartal fielded a question about whether ultrasound would be a more logical and cost-effective method of assessing these patients.
“We actually do usually start with an ultrasound evaluation in our patients with refractory puerperal fever, and 68% of this group did have one,” Dr. Fishel-Bartal replied. “Findings were positive in 37%. The ultrasound actually was very good at predicting pelvic collections, but it only identified 5 of the 32 with septic thrombophlebitis. So it’s a good modality to start with, but if the patient still has fever or there is a concern for septic pelvic thrombosis, you really still need a CT.”
She had no financial disclosures.
SOURCE: Fishel-Bartal M et al. The Pregnancy Meeting. Am J Obstet Gynecol. 2018;218:S59.
DALLAS – Abdominal CT scans changed therapeutic management in 39% of women being unsuccessfully treated for refractory puerperal fever, a retrospective study has determined.
The scans pinpointed a definite diagnosis in the majority of the cohort, allowing clinicians to reassess their treatment, Michal Fishel-Bartal, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“This study has important clinical implications for women with refractory puerperal fever,” said Dr. Fishel-Bartal of the Chaim Sheba Medical Center, Ramat Gan, Israel. “Our department now recommends that all women with refractory puerperal fever should undergo an assessment for risk factors, including urgent cesarean section, preterm delivery, and general anesthesia, and an evaluation to see if an abdominal CT may be appropriate to investigate the possibility of septic pelvic thrombophlebitis or the need for intra-abdominal drainage.”
She and her colleagues conducted a 10-year retrospective review of refractory puerperal fever cases at Chaim Sheba Medical Center. All of the patients had a CT scan within 7 days of their delivery. A radiologist reviewed each scan, looking for potential causes of the illness, including pelvic collection (a suspected pelvic abscess or collection of 4 cm or more) or signs of septic pelvic thrombophlebitis (enlargement of an involved vein, vessel wall enhancement, or a filling defect).
The primary outcome was a treatment change due to the CT results. These included switching antibiotics, starting therapeutic low-molecular-weight heparin, or a surgical intervention (intra-abdominal drainage or laparotomy).
The cohort comprised 238 women, who were a mean age of 33 years. In comparing them with the hospital’s background population, they were significantly more likely to have delivered at less than 37 weeks (25% vs. 7%), and to have had a cesarean delivery (80% vs. 25%). Dr. Fishel-Bartal also noted that 29% of the patients had experienced general anesthesia.
Most of the scans (144; 60%) were abnormal. Findings included septic pelvic thrombophlebitis (32) and pelvic collections (112). Treatment changed in 93 women (39% of the entire cohort). Changes included adding or switching antibiotics (24), adding low-molecular-weight heparin (28), laparotomy (11), and drainage insertion (30).
The investigators also performed a multivariate analysis to identify any risk factors that significantly predicted the need to change or add treatment. General anesthesia was the only factor significantly more common among those who needed a treatment switch (70% vs. 58%). This could have been a marker for an urgent C-section – something often associated with complications, Dr. Fishel-Bartal noted.
In the discussion period, Dr. Fishel-Bartal fielded a question about whether ultrasound would be a more logical and cost-effective method of assessing these patients.
“We actually do usually start with an ultrasound evaluation in our patients with refractory puerperal fever, and 68% of this group did have one,” Dr. Fishel-Bartal replied. “Findings were positive in 37%. The ultrasound actually was very good at predicting pelvic collections, but it only identified 5 of the 32 with septic thrombophlebitis. So it’s a good modality to start with, but if the patient still has fever or there is a concern for septic pelvic thrombosis, you really still need a CT.”
She had no financial disclosures.
SOURCE: Fishel-Bartal M et al. The Pregnancy Meeting. Am J Obstet Gynecol. 2018;218:S59.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: An abdominal CT was the key to getting treatment right for women with refractory puerperal fever.
Major finding: After the scans, 39% of women got a change in treatment.
Study details: The retrospective review comprised 238 women.
Disclosures: Dr. Fishel-Bartal had no financial disclosures.
Source: Fishel-Bartal M et al. The Pregnancy Meeting. Am J Obstet Gynecol. 2018;218:S59.
Use of a Novel Magnesium-Based Resorbable Bone Cement for Augmenting Anchor and Tendon Fixation
ABSTRACT
The aim of this study was to assess the efficacy and safety of a novel magnesium-based resorbable bone cement (OsteoCrete, Bone Solutions Incorporated) for anchor and tendon fixation.
Cadaveric humeral testing involved straight pull-to-failure of rotator cuff suture anchors; OsteoCrete was injected through one anchor, and a second anchor served as the uninjected control. Testing was conducted 15 minutes post-injection. A canine preclinical model was used to evaluate the safety of the following parameters: Rotator cuff repair: A double-row technique was used to repair transected infraspinatus tendons; OsteoCrete was injected through both anchors in one limb, and the contralateral limb served as the uninjected control. Biceps tenodesis: The transected biceps tendon was implanted into a proximal humeral socket with a transcortical button; OsteoCrete was injected into the socket of one limb, and a screw was used for final fixation in the contralateral control limb. Nondestructive biomechanical testing and histologic assessment were performed after 12 weeks.
OsteoCrete-augmented anchors showed significantly higher load-to-failure compared to that with uninjected controls. In cadaveric humeri with reduced bone quality, OsteoCrete increased the mean load-to-failure by 99%. Within the preclinical model, there were no complications or statistically significant biomechanical/histologic differences between the techniques.
OsteoCrete has the potential for safely providing improved suture anchor and tissue fixation in patients with poor bone or tissue quality.
Continue to: Calcium phosphate bone void fillers...
Calcium phosphate bone void fillers have been commonly used in orthopedic surgery for several applications, including, but not limited to, a variety of fracture fixation or augmentation procedures.1-8 Continuing research on calcium phosphates has evidenced that the addition of magnesium phosphate to the formulation results in improved reactivity of the bone void filler. An in vitro study demonstrated enhanced attachment and proliferation of MG63 osteoblast-like cells on calcium magnesium phosphate cement (CMPC), in comparison with calcium phosphate cement (CPC), along with increased cellular alkaline phosphatase activity.9 The authors further explored the proliferation rates of MG63 cells by comparing CMPC with CPC and magnesium phosphate cement (MPC), and observed significantly increased proliferation of cells on CMPC. They also compared CMPC and CPC using a rabbit bone void model and observed substantial CMPC resorption with new bone formation at the 3-month time point and further reported that the majority of the defect had filled with new bone at 6 months, whereas CPC resulted in <10% new bone formation after 6 months.10 The authors continued to study the differences between CPC, MPC, and CMPC and identified increased proliferation of bone marrow stromal cells (bMSCs), when the cells were associated with CMPC and MPC, and when compared to that with CPC. The osteogenic differentiation of bMSCs was highest in the CMPC and CPC groups, when compared to that in the MPC group, with no significant difference between the CMPC and CPC groups. The authors also compared these 3 different formulations using a rabbit maxillary sinus floor elevation model, in which CMPC resulted in increased new bone formation and mineralization compared to that with CPC and MPC, which was further enhanced with the addition of bMSCs.11
These studies highlight the importance of having both a magnesium phosphate and a calcium phosphate component for a resorbable cement intended for use as a bone void filler. The rationale behind this strategy is related to the release of magnesium ions from the magnesium phosphate component. Magnesium has been shown to increase the proliferation of bMSCs, improve the attachment and growth of osteoblasts, stimulate the proteins involved in bone regeneration, enhance new bone formation, and boost bone mineralization.12,13
OsteoCrete (Bone Solutions Incorporation) is a novel CMPC composed of magnesium oxide, monopotassium phosphate, monosodium phosphate, hydroxyapatite, and sucrose. OsteoCrete has been demonstrated to significantly increase peak torque-to-failure of stainless-steel cortical bone screw fixation, when compared with screw fixation without augmentation and screw fixation with calcium phosphate augmentation using an in vivo equine model. In the same study, the authors showed that OsteoCrete resulted in an interface toughness that was significantly increased compared to that with no treatment, CPC augmentation, and polymethylmethacrylate (PMMA) augmentation. At 6 months after implantation, woven bone had replaced 69% of the OsteoCrete at the screw interface, compared to 44% of that with CPC.14 An equine study examined the effects of OsteoCrete on bone stability and healing using a metatarsal osteotomy model; the study reported significantly improved radiographic callus formation and a greater amount of new bone formation within the fracture gap when compared to that with CPC augmentation or no augmentation. OsteoCrete also secured the fragment significantly better than the CPC and control groups based on a decreased fracture gap over time.15 Another study using a preclinical anterior cruciate ligament (ACL) reconstruction model reported that OsteoCrete resulted in significantly better new bone formation in the tibial tunnel, a smaller amount of fibrous tissue, more cartilage formation at the tendon-bone interface, and a higher ultimate load-to-failure compared to that with standard ACL reconstruction in the contralateral limb after 6 weeks.16 OsteoCrete and PMMA were evaluated in terms of biomechanical fixation of a stemless humeral prosthesis, with data showing that both groups have higher failure loads, failure displacements, and failure cycles when compared to those with the control, nonaugmented group.17 Another preclinical model evaluated cranial bone flap augmentation with 2 resorbable cements and highlighted faster cement resorption and replacement with bone, along with superior stability within the OsteoCrete group compared to that with CPC.18 In a preclinical bone void study conducted for obtaining US Food and Drug Administration 510(k) clearance, OsteoCrete resulted in 83% greater resorption than that with CPC after 12 weeks and 35% greater resorption at 26 weeks, with 84% of OsteoCrete being resorbed and replaced with woven or lamellar mineralized bone of normal morphology at the 26-week time point (unpublished data provided by Bone Solutions Incorporated [BSI]).
These data indicate that CMPCs such as OsteoCrete appear to have potential benefits for augmenting the healing of bone implants and bone soft tissue. Therefore, the objective of this study was to assess the safety and efficacy of OsteoCrete in applications for the augmentation of anchor and tendon fixation in rotator cuff repair and biceps tenodesis procedures, respectively. Improving healing for these 2 commonly performed procedures would be of great benefit in improving the functional outcomes and mitigating the complications and morbidity.
MATERIALS AND METHODS
IN VITRO STUDY METHODS
Cadaveric humeri (N = 12, six matched pairs) of females (age, 70-75 years) were warmed to 37°C prior to testing. Two 4.75-mm vented anchors (SwiveLock, Arthrex) with FiberTape were implanted into a lateral row position (anterior and posterior anchor positioning) of a double-row rotator cuff repair within the greater tuberosity. One anchor was injected with 1 ml of OsteoCrete–after preparation according to the manufacturer’s instructions–through the cannulation channel after placement, and the other anchor served as the uninjected control for each humerus. For the six matched pairs, the OsteoCrete group and the control group were rotated with respect to anterior vs posterior location within the lateral row position. After 15 minutes of the injection, straight pull-to-failure (12 in/min) was performed. Data were compared between the groups for significant (P < .05) differences using t-tests and Pearson correlation.
Continue to: IN VIVO STUDY METHODS
IN VIVO STUDY METHODS
With Institutional Animal Care and Use Committee approval, adult (age, 2-4 years) purpose-bred dogs (N = 8) underwent aseptic surgery of both forelimbs for rotator cuff (infraspinatus) tendon repair (Figure 1) and biceps tenodesis (Figure 2). For the rotator cuff repair, two 4.75-mm vented anchors (1 medial and 1 lateral) with FiberTape were used in a modified double-row technique to repair the acutely transected infraspinatus tendon. In one limb, 1 ml of OsteoCrete was injected through both anchors; the other limb served as the uninjected control. For the biceps tenodesis procedure, the long head of the biceps tendon was transected at its origin and whip-stitched. The tendon was transposed and inserted into a 7-mm diameter socket drilled into the proximal humerus using a tension-slide technique with a transcortical button for fixation. In one limb, 1 ml of OsteoCrete was injected into the socket prior to final tensioning and tying. In the contralateral limb, a 7-mm interference screw (Bio-Tenodesis™ Screw, Arthrex) was inserted into the socket after tensioning and tying. The dogs were allowed to perform out-of-kennel monitored exercise daily for a period of 12 weeks after surgery and were then sacrificed.
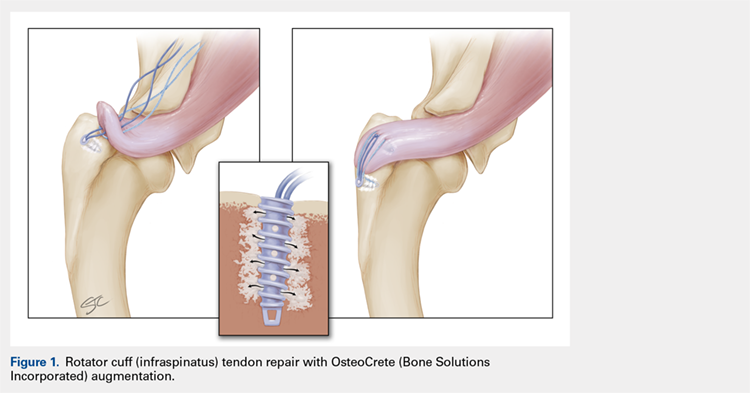
The infraspinatus and biceps bone-tendon-muscle units were excised en bloc. Custom-designed jigs were used for biomechanical testing of the bone-tendon-muscle units along the anatomical vector of muscle contraction. Optical markers were mounted at standardized anatomical locations. Elongation of the repair site was defined as the change in distance between markers and was measured to 0.01-mm resolution using an optical tracking system (Optotrak Certus, NDI), synchronized with measurement of the applied tension load. The bone-tendon-muscle units were loaded in tension to 3-mm elongation at a displacement controlled rate of 0.01 mm/s. Load at 1-mm, 2-mm, and 3-mm displacement of the tendon-bone junction was extracted from the load vs the displacement curve of each sample. Stiffness was calculated as the slope of the linear portion of the load vs the displacement curve.19,20
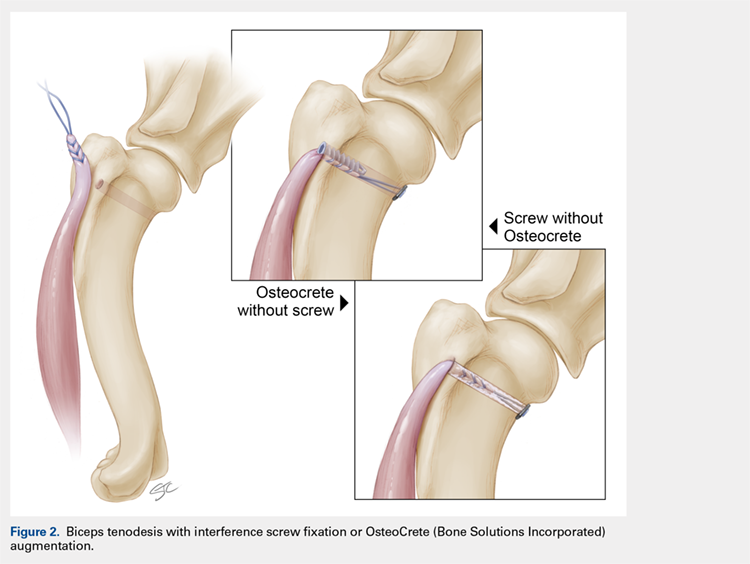
For histologic assessments, sections of each treatment site were obtained using a microsaw and alternated between decalcified and non-decalcified processing. For decalcified bone processing, formalin-fixed tissues were placed in 10% ethylenediaminetetraacetic acid with phosphate-buffered saline for 39 days and then processed routinely for the assessment of sections stained with hematoxylin and eosin (H&E), toluidine blue, and picrosirius red. For non-decalcified bone processing, the tissues were dehydrated through a series of graded ethyl alcohol solutions, embedded in PMMA, sectioned, and stained with toluidine blue and Goldner’s trichrome. Two pathologists who were blinded to the clinical application and the differences between techniques assessed the histologic sections and scored each section using the modified Bonar score that assesses cell morphology, collagen arrangement, cellularity, vascularity, and extracellular matrix using a 15-point scale, where a higher score indicates more pathology.21
Categorical data were compared for detecting statistically significant differences using the rank sum test. Continuous data were compared for identifying statistically significant differences using the t-test or one-way ANOVA. Significance was set at P < .05.
RESULTS
IN VITRO RESULTS
OsteoCrete-augmented anchors (mean = 225 N; range, 158-287 N) had significantly (P < .001) higher pull-out load-to-failure compared to that in the uninjected controls (mean = 161 N; range, 68-202 N), which translated to a 50% mean increase (range, 3%-134%) in load-to-failure (Table 1). For humeri with reduced bone quality (control anchors that failed at <160 N, 4 humeri), the mean increase in load-to-failure for OsteoCrete-augmented anchors was 99% (range, 58%-135%), with the difference between mean values being again significantly different (OsteoCrete mean = 205 N; control mean = 110 N, P < .001). When the control and OsteoCrete load-to-failure values were compared using Pearson correlation, a significantly strong positive correlation (r = 0.66, P = 0.02) was detected. When the control load-to-failure values were compared with its percent increase value when OsteoCrete was used, there was a significantly very strong negative correlation (r = −0.90, P < .001).
Table 1. Cadaveric Lateral Row Rotator Cuff Anchor Pull-To-Failure; Testing Occurred 15 Minutes Post-Injection
| Humerus No. | Control (N) | OsteoCrete (N)a | Percent Increase |
| 1-Right (PA) | 197.28 | 278.73 | 41% |
| 1-Left (AP) | 152.62 | 241.72 | 58% |
| 2-Right (PA) | 178.60 | 196.03 | 10% |
| 2-Left (AP) | 170.10 | 175.57 | 3% |
| 3-Right (PA) | 67.70 | 158.31 | 134% |
| 3-Left (AP) | 74.24 | 173.08 | 133% |
| 4-Right (PA) | 195.81 | 248.12 | 27% |
| 4-Left (AP) | 201.95 | 209.42 | 4% |
| 5-Right (PA) | 173.30 | 220.59 | 27% |
| 5-Left (AP) | 146.61 | 247.37 | 69% |
| 6-Right (PA) | 171.03 | 266.14 | 56% |
| 6-Left (AP) | 199.99 | 286.91 | 43% |
| Average | 160.77 + 45.60 | 225.17 + 43.08 | 50% + 44 |
aOsteoCrete (Bone Solutions Incorporated) resulted in significantly increased (P < 0.001) pull-to-failure. Abbreviations: AP, control anchor located in anterior position, OsteoCrete anchor located in posterior position; PA, control anchor located in posterior position, OsteoCrete anchor located in anterior position.
Continue to: IN VIVO RESULTS
IN VIVO RESULT
No intraoperative or postoperative complications were noted. All repairs were found to be intact based on the gross assessment and the completed biomechanical testing without failure. No statistically significant (P > 0.3) biomechanical differences were found between the techniques (Table 2). Histologic assessments showed low-to-mild pathology scores for all sites with no statistically significant (P > 0.3) differences between the techniques (Table 2). Both control and OsteoCrete rotator cuff repairs demonstrated tendon-to-bone integration via fibrous connective tissue attachment to bone. All anchors were in place with no evidence for loosening, tunnel expansion, or cyst formation. OsteoCrete-augmented anchor repairs were associated with cement remaining within their lumens along with a thin layer of cement interposed between the anchor and the bone interface around their entire periphery. The cement-bone interface was discrete with typical inflammatory cell infiltrate without evidence for infection, membrane or cyst formation, or other untoward pathologic responses. In the OsteoCrete biceps tenodesis group, the tendons filled the tunnels with a thin layer of cement remaining interposed between the tendon and the bone interface around the entire periphery. The tendon-cement-bone interface was discrete with typical inflammatory cell infiltrates and without evidence for infection, membrane or cyst formation, or other untoward pathologic responses. Tendon-to-bone integration was not observed in the control or OsteoCrete biceps tenodesis groups at the 12-week study endpoint. Representative histologic images of the rotator cuff tendon repairs and biceps tenodesis procedures are shown in Figures 3A, 3B and Figures 4A, 4B, respectively.
Table 2. Biomechanical Testing And Histologic Scoring Of Rotator Cuff And Biceps Tendon Repairs In A Preclinical Model
| Procedure | Force (N) at 1 mm | Force (N) at 2 mm | Force (N) at 3 mm | Stiffness (N/mm) | Histologic Score |
| Rotator Cuff - Control | 14.0 + 3.3 | 19.3 + 5.5 | 25.0 + 7.0 | 5.4 + 2.0 | 4.6 + 1.1 |
| Rotator Cuff - OsteoCrete (Bone Solutions Incorporated) | 14.8 + 3.7 | 20.4 + 6.0 | 26.4 + 8.5 | 6.3 + 2.5 | 3.9 + 1.7 |
| Biceps - Control | 23.1 + 6.2 | 35.5 + 8.5 | 52.6 + 15.0 | 17.8 + 6.4 | 3.4 + 1.2 |
| Biceps - OsteoCrete | 22.4 + 7.3 | 36.8 + 10.1 | 57.8 + 16.0 | 21.1 + 8.5 | 3.4 + 0.7 |
There were no significant differences (P < 0.05) between groups. Histologic scoring based on a 15-point scale with higher scores indicating more pathology.
DISCUSSION
The results of this study highlight the safety and efficacy of OsteoCrete in applications for the augmentation of anchor and tendon fixation in rotator cuff repair and biceps tenodesis procedures, respectively. Anchors augmented with OsteoCrete resulted in significantly increased load-to-failure pull-out strength 15 minutes after insertion. In addition, a very strong negative correlation was found between the percentage of improved load-to-failure after OsteoCrete injection and the bone quality of the humerus, which was based on the control load-to-failure values. In the validated preclinical model used in this study, OsteoCrete-based fixation was found to be noninferior to current standard-of-care techniques and was not associated with any untoward pathologic responses of humeral bone, rotator cuff tendon, or biceps tendon based on the biomechanical and histologic analyses. These data highlight the functional efficacy and biocompatibility of OsteoCrete when used for these common indications.

More than 270,000 rotator cuff procedures have been reported to be performed in the US annually (average patient age: 61 years for women, 56 years for men).22 Rotator cuff repair procedures have been associated with a 20% failure rate, with one of the causes being related to an inability for the tendon to heal, even with strong initial fixation.23 Rotator cuff repair techniques are being continuously optimized with the goal of improving patient outcomes. This goal is being realized, primarily with respect to re-tear rates.24,25 However, even with advanced techniques, there are still relatively high rates of failure reported, with increasing patient age serving as one of the primary negative prognostic factors.26 An older patient population is associated with decreased bone mass and strength, and postmenopausal females have decreased bone quality; these factors are associated with higher rotator cuff failure rates due to poor tendon healing, with anchor fixation failure also playing a role.27-29 Therefore, it is critically important to develop methods for augmenting implant and tendon fixation to bone to achieve functional healing. The results of this study suggest that OsteoCrete provides a valid method for accomplishing this goal based on the observation that proximal humeral anchor fixation was improved by 50% in load-to-failure 15 minutes post-injection with an even more profound impact on the anchors placed in poor-quality bone (99% increased load-to-failure 15 minutes post-injection). It is probable that the degree of improvement in fixation strength would be even greater 1 day after fixation, since the strength of OsteoCrete continues to increase over the first 30 hours of curing.
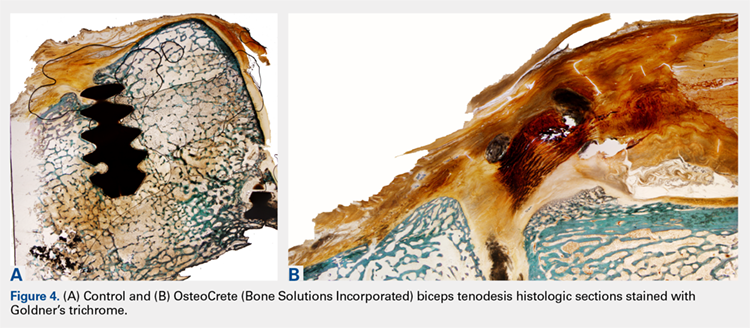
Based on the preclinical animal model data of this study, OsteoCrete augmentation of rotator cuff anchor fixation had no untoward effects on tendon healing or function and can be considered as safe for use. Previously published data also suggest that OsteoCrete may improve osseous replacement of anchors as a result of magnesium ion release, which can drive adjacent attachment and growth of osteoblasts, leading to enhanced new bone formation.9-16,18 As such, surgeons may consider this means of anchor augmentation in situations of questionable or poor-quality bone and/or when accelerated postoperative rehabilitation protocols are desired.
A very low early incidence failure rate (1.2%) has been reported when a distal biceps tendon rupture is repaired using cortical suspensory fixation in conjunction with an interference screw.30 When an early re-rupture does occur, the most common explanation for failure tends to be a lack of patient compliance, with excessive force being placed on the repair.31 This study was not meant to investigate the methods to increase the strength of a biceps tendon repair using OsteoCrete but instead to replace the interference screw with OsteoCrete in a safe and noninferior manner. Primary fixation was still dependent on cortical suspensory fixation; however, OsteoCrete was used to help aid in stabilization of the tendon without the need for interference screw fixation. Although rare, osteolysis and perianchor cyst formation have been reported adjacent to nonbiodegradable anchors (PEEK), along with several types of biodegradable anchors (PLLA, hydroxyapatite plus PLLA, β-tricalcium phosphate plus PLLA, and polyglycolic acid; the latter of the 3 resulted in the lowest incidence of perianchor cyst formation) in the shoulder and elbow.32-34 Whenever osteolysis or cyst formation occurs around an anchor, it leads to decreased bone volume and potential adjacent bone weakness, which may act as a stress riser, thus increasing the risk for fracture. This potential is probably more of a concern within the proximal radius where there is a decreased amount of bone stock around the anchor.34
Continue to: In this study...
In this study, a short-term 12-week analysis revealed no significant differences in the nondestructive biomechanical testing and histologic analysis results between the use of OsteoCrete and the use of a tenodesis anchor. These results indicate the potential for using OsteoCrete as an anchor replacement. The biceps tendon did not react negatively to the OsteoCrete material, which indicated that OsteoCrete can be used adjacent to tendons without the concern of weakening the tendon due to an inflammatory reaction. This being said, tendon-to-bone integration was not evident at this early time point. It would be helpful to further explore the potential of this technique with a longer-term study investigating tendon-to-bone integration in more detail. Ideally, a long-term study would reveal an increased amount of new bone formation within the socket when compared to that with the anchor comparison, similar to the results reported by Gulotta and colleagues16 when using a tendon for ACL reconstruction with OsteoCrete.
We do note several limitations in this study. The dogs used in this study were healthy with normal bone and tendon morphology, the tendons were transected and repaired during the course of the same surgery, and only 1 early time point was evaluated. Additional investigations continuing the characterization of these clinical applications using an osteopenic or osteoporotic preclinical model with chronic tendon pathology and longer-term evaluation are now warranted based on the positive findings of this initial work.
CONCLUSION
OsteoCrete augmentation significantly improved initial rotator cuff anchor fixation (human in vitro) and was safe and effective for anchor and tendon fixation in rotator cuff tendon repair and biceps tenodesis procedures (canine in vivo), respectively, when compared with the current standard-of-care. Of note, the significant improvements associated with OsteoCrete were the greatest in poor-quality bone. Based on these results and considering the previously discussed limitations, it can be concluded that OsteoCrete has the potential for safely providing improved suture anchor and tissue fixation in patients with poor bone or tissue quality. Further in vivo study toward potential clinical applications is warranted.
1. Russell TA, Leighton RK, Group A-BTPFS. Comparison of autogenous bone graft and endothermic calcium phosphate cement for defect augmentation in tibial plateau fractures. A multicenter, prospective, randomized study. J Bone Joint Surg Am. 2008; 90(10):2057-2061. doi:10.2106/JBJS.G.01191.
2. Egol KA, Sugi MT, Ong CC, Montero N, Davidovitch R, Zuckerman JD. Fracture site augmentation with calcium phosphate cement reduces screw penetration after open reduction-internal fixation of proximal humeral fractures. J Shoulder Elbow Surg. 2012; 21(6):741-748. doi:10.1016/j.jse.2011.09.017.
3. Cassidy C, Jupiter JB, Cohen M, et al. Norian SRS cement compared with conventional fixation in distal radial fractures. A randomized study. J Bone Joint Surg Am. 2003;85-A(11):2127-2137.
4. Mattsson P, Alberts A, Dahlberg G, Sohlman M, Hyldahl HC, Larsson S. Resorbable cement for the augmentation of internally-fixed unstable trochanteric fractures. A prospective, randomised multicentre study. J Bone Joint Surg Br. 2005;87(9):1203-1209.
5. Cohen SB, Sharkey PF. Subchondroplasty for treating bone marrow lesions. J Knee Surg. 2016;29(07):555-563. doi:10.1302/0301-620X.87B9.15792.
6. Guida P, Ragozzino R, Sorrentino B, et al. Three-in-One minimally invasive approach to surgical treatment of pediatric pathological fractures with wide bone loss through bone cysts: ESIN, curettage and packing with injectable HA bone substitute. A retrospective series of 116 cases. Injury. 2016;47(6):1222-1228. doi:10.1016/j.injury.2016.01.006.
7. Maestretti G, Sutter P, Monnard E, et al. A prospective study of percutaneous balloon kyphoplasty with calcium phosphate cement in traumatic vertebral fractures: 10-year results. Eur Spine J. 2014;23(6):1354-1360. doi:10.1007/s00586-014-3206-1.
8. Nakano M, Hirano N, Zukawa M, et al. Vertebroplasty using calcium phosphate cement for osteoporotic vertebral fractures: study of outcomes at a minimum follow-up of two years. Asian Spine J. 2012;6(1):34-42. doi:10.4184/asj.2012.6.1.34.
9. Jia J, Zhou H, Wei J, et al. Development of magnesium calcium phosphate biocement for bone regeneration. J R Soc Interface. 2010;7(49):1171-1180. doi:10.1098/rsif.2009.0559.
10. Wu F, Wei J, Guo H, Chen F, Hong H, Liu C. Self-setting bioactive calcium-magnesium phosphate cement with high strength and degradability for bone regeneration. Acta Biomater. 2008;4(6):1873-1884. doi:10.1016/j.actbio.2008.06.020.
11. Zeng D, Xia L, Zhang W, et al. Maxillary sinus floor elevation using a tissue-engineered bone with calcium-magnesium phosphate cement and bone marrow stromal cells in rabbits. Tissue Eng Part A. 2012;18(7-8):870-881. doi:10.1089/ten.TEA.2011.0379.
12. Yoshizawa S, Brown A, Barchowsky A, Sfeir C. Magnesium ion stimulation of bone marrow stromal cells enhances osteogenic activity, simulating the effect of magnesium alloy degradation. Acta Biomater. 2014;10(6):2834-2842. doi:10.1016/j.actbio.2014.02.002.
13. Liao J, Qu Y, Chu B, Zhang X, Qian Z. Biodegradable CSMA/PECA/Graphene porous hybrid scaffold for cartilage tissue engineering. Sci Rep. 2015;5:9879. doi:10.1038/srep09879.
14. Hirvinen LJ, Litsky AS, Samii VF, Weisbrode SE, Bertone AL. Influence of bone cements on bone-screw interfaces in the third metacarpal and third metatarsal bones of horses. Am J Vet Res. 2009;70(8):964-972. doi:10.2460/ajvr.70.8.964.
15. Waselau M, Samii VF, Weisbrode SE, Litsky AS, Bertone AL. Effects of a magnesium adhesive cement on bone stability and healing following a metatarsal osteotomy in horses. Am J Vet Res. 2007;68(4):370-378. doi:10.2460/ajvr.68.4.370.
16. Gulotta LV, Kovacevic D, Ying L, Ehteshami JR, Montgomery S, Rodeo SA. Augmentation of tendon-to-bone healing with a magnesium-based bone adhesive. Am J Sports Med. 2008;36(7):1290-1297. doi:10.1177/0363546508314396.
17. Kim MS, Kovacevic D, Milks RA, et al. Bone graft substitute provides metaphyseal fixation for a stemless humeral implant. Orthopedics. 2015;38(7):e597-e603. doi:10.3928/01477447-20150701-58.
18. Schendel SA, Peauroi J. Magnesium-based bone cement and bone void filler: preliminary experimental studies. J Craniofac Surg. 2009;20(2):461-464. doi:10.1097/SCS.0b013e31819b9819.
19. Pfeiffer FM, Smith MJ, Cook JL, Kuroki K. The histologic and biomechanical response of two commercially available small glenoid anchors for use in labral repairs. J Shoulder Elbow Surg. 2014;23(8):1156-1161. doi:10.1016/j.jse.2013.12.036.
20. Smith MJ, Cook JL, Kuroki K, et al. Comparison of a novel bone-tendon allograft with a human dermis-derived patch for repair of chronic large rotator cuff tears using a canine model. Arthroscopy. 2012;28(2):169-177. doi:10.1016/j.arthro.2011.08.296.
21. Fearon A, Dahlstrom JE, Twin J, Cook J, Scott A. The Bonar score revisited: region of evaluation significantly influences the standardized assessment of tendon degeneration. J Sci Med Sport. 2014;17(4):346-350. doi:10.1016/j.jsams.2013.07.008.
22. Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012;94(3):227-233. doi:10.2106/JBJS.J.00739.
23. Lädermann A, Denard PJ, Burkhart SS. Management of failed rotator cuff repair: a systematic review. J ISAKOS. 2016;1(1):32-37. doi:10.1136/jisakos-2015-000027.
24. Franceschi F, Papalia R, Franceschetti E, et al. Double-Row repair lowers the retear risk after accelerated rehabilitation. Am J Sports Med. 2016;44(4):948-956. doi:10.1177/0363546515623031.
25. Wang E, Wang L, Gao P, Li Z, Zhou X, Wang S. Single-versus double-row arthroscopic rotator cuff repair in massive tears. Med Sci Monit. 2015;21:1556-1561. doi:10.12659/MSM.893058.
26. Abtahi AM, Granger EK, Tashjian RZ. Factors affecting healing after arthroscopic rotator cuff repair. World J Orthop. 2015;6(2):211-220. doi:10.5312/wjo.v6.i2.211.
27. Chung SW, Oh JH, Gong HS, Kim JY, Kim SH. Factors affecting rotator cuff healing after arthroscopic repair: osteoporosis as one of the independent risk factors. Am J Sports Med. 2011;39(10):2099-2107. doi:10.1177/0363546511415659.
28. Tsiouri C, Mok DH. Early pullout of lateral row knotless anchor in rotator cuff repair. Int J Shoulder Surg. 2009;3(3):63-65. doi:10.4103/0973-6042.59972.
29. Boskey AL, Coleman R. Aging and bone. J Dent Res. 2010;89(12):1333-1348. doi:10.1177/0022034510377791.
30. Cusick MC, Cottrell BJ, Cain RA, Mighell MA. Low incidence of tendon rerupture after distal biceps repair by cortical button and interference screw. J Shoulder Elbow Surg. 2014;23(10):1532-1536. doi:10.1016/j.jse.2014.04.013.
31. Hinchey JW, Aronowitz JG, Sanchez-Sotelo J, Morrey BF. Re-rupture rate of primarily repaired distal biceps tendon injuries. J Shoulder Elbow Surg. 2014;23(6):850-854. doi:10.1016/j.jse.2014.02.006.
32. Shahrulazua A, Duckworth D, Bokor DJ. Perianchor radiolucency following PEEK suture anchor application associated with recurrent shoulder dislocation: a case report. Clin Ter. 2014;165(1):31-34. doi:10.7471/CT.2014.1658.
33. Kim SH, Kim dY, Kwon JE, Park JS, Oh JH. Perianchor cyst formation around biocomposite biodegradable suture anchors after rotator cuff repair. Am J Sports Med. 2015;43(12):2907-2912. doi:10.1177/0363546515608484
34. Potapov A, Laflamme YG, Gagnon S, Canet F, Rouleau DM. Progressive osteolysis of the radius after distal biceps tendon repair with the bioabsorbable screw. J Shoulder Elbow Surg. 2011;20(5):819-826. doi:10.1016/j.jse.2011.02.021.
ABSTRACT
The aim of this study was to assess the efficacy and safety of a novel magnesium-based resorbable bone cement (OsteoCrete, Bone Solutions Incorporated) for anchor and tendon fixation.
Cadaveric humeral testing involved straight pull-to-failure of rotator cuff suture anchors; OsteoCrete was injected through one anchor, and a second anchor served as the uninjected control. Testing was conducted 15 minutes post-injection. A canine preclinical model was used to evaluate the safety of the following parameters: Rotator cuff repair: A double-row technique was used to repair transected infraspinatus tendons; OsteoCrete was injected through both anchors in one limb, and the contralateral limb served as the uninjected control. Biceps tenodesis: The transected biceps tendon was implanted into a proximal humeral socket with a transcortical button; OsteoCrete was injected into the socket of one limb, and a screw was used for final fixation in the contralateral control limb. Nondestructive biomechanical testing and histologic assessment were performed after 12 weeks.
OsteoCrete-augmented anchors showed significantly higher load-to-failure compared to that with uninjected controls. In cadaveric humeri with reduced bone quality, OsteoCrete increased the mean load-to-failure by 99%. Within the preclinical model, there were no complications or statistically significant biomechanical/histologic differences between the techniques.
OsteoCrete has the potential for safely providing improved suture anchor and tissue fixation in patients with poor bone or tissue quality.
Continue to: Calcium phosphate bone void fillers...
Calcium phosphate bone void fillers have been commonly used in orthopedic surgery for several applications, including, but not limited to, a variety of fracture fixation or augmentation procedures.1-8 Continuing research on calcium phosphates has evidenced that the addition of magnesium phosphate to the formulation results in improved reactivity of the bone void filler. An in vitro study demonstrated enhanced attachment and proliferation of MG63 osteoblast-like cells on calcium magnesium phosphate cement (CMPC), in comparison with calcium phosphate cement (CPC), along with increased cellular alkaline phosphatase activity.9 The authors further explored the proliferation rates of MG63 cells by comparing CMPC with CPC and magnesium phosphate cement (MPC), and observed significantly increased proliferation of cells on CMPC. They also compared CMPC and CPC using a rabbit bone void model and observed substantial CMPC resorption with new bone formation at the 3-month time point and further reported that the majority of the defect had filled with new bone at 6 months, whereas CPC resulted in <10% new bone formation after 6 months.10 The authors continued to study the differences between CPC, MPC, and CMPC and identified increased proliferation of bone marrow stromal cells (bMSCs), when the cells were associated with CMPC and MPC, and when compared to that with CPC. The osteogenic differentiation of bMSCs was highest in the CMPC and CPC groups, when compared to that in the MPC group, with no significant difference between the CMPC and CPC groups. The authors also compared these 3 different formulations using a rabbit maxillary sinus floor elevation model, in which CMPC resulted in increased new bone formation and mineralization compared to that with CPC and MPC, which was further enhanced with the addition of bMSCs.11
These studies highlight the importance of having both a magnesium phosphate and a calcium phosphate component for a resorbable cement intended for use as a bone void filler. The rationale behind this strategy is related to the release of magnesium ions from the magnesium phosphate component. Magnesium has been shown to increase the proliferation of bMSCs, improve the attachment and growth of osteoblasts, stimulate the proteins involved in bone regeneration, enhance new bone formation, and boost bone mineralization.12,13
OsteoCrete (Bone Solutions Incorporation) is a novel CMPC composed of magnesium oxide, monopotassium phosphate, monosodium phosphate, hydroxyapatite, and sucrose. OsteoCrete has been demonstrated to significantly increase peak torque-to-failure of stainless-steel cortical bone screw fixation, when compared with screw fixation without augmentation and screw fixation with calcium phosphate augmentation using an in vivo equine model. In the same study, the authors showed that OsteoCrete resulted in an interface toughness that was significantly increased compared to that with no treatment, CPC augmentation, and polymethylmethacrylate (PMMA) augmentation. At 6 months after implantation, woven bone had replaced 69% of the OsteoCrete at the screw interface, compared to 44% of that with CPC.14 An equine study examined the effects of OsteoCrete on bone stability and healing using a metatarsal osteotomy model; the study reported significantly improved radiographic callus formation and a greater amount of new bone formation within the fracture gap when compared to that with CPC augmentation or no augmentation. OsteoCrete also secured the fragment significantly better than the CPC and control groups based on a decreased fracture gap over time.15 Another study using a preclinical anterior cruciate ligament (ACL) reconstruction model reported that OsteoCrete resulted in significantly better new bone formation in the tibial tunnel, a smaller amount of fibrous tissue, more cartilage formation at the tendon-bone interface, and a higher ultimate load-to-failure compared to that with standard ACL reconstruction in the contralateral limb after 6 weeks.16 OsteoCrete and PMMA were evaluated in terms of biomechanical fixation of a stemless humeral prosthesis, with data showing that both groups have higher failure loads, failure displacements, and failure cycles when compared to those with the control, nonaugmented group.17 Another preclinical model evaluated cranial bone flap augmentation with 2 resorbable cements and highlighted faster cement resorption and replacement with bone, along with superior stability within the OsteoCrete group compared to that with CPC.18 In a preclinical bone void study conducted for obtaining US Food and Drug Administration 510(k) clearance, OsteoCrete resulted in 83% greater resorption than that with CPC after 12 weeks and 35% greater resorption at 26 weeks, with 84% of OsteoCrete being resorbed and replaced with woven or lamellar mineralized bone of normal morphology at the 26-week time point (unpublished data provided by Bone Solutions Incorporated [BSI]).
These data indicate that CMPCs such as OsteoCrete appear to have potential benefits for augmenting the healing of bone implants and bone soft tissue. Therefore, the objective of this study was to assess the safety and efficacy of OsteoCrete in applications for the augmentation of anchor and tendon fixation in rotator cuff repair and biceps tenodesis procedures, respectively. Improving healing for these 2 commonly performed procedures would be of great benefit in improving the functional outcomes and mitigating the complications and morbidity.
MATERIALS AND METHODS
IN VITRO STUDY METHODS
Cadaveric humeri (N = 12, six matched pairs) of females (age, 70-75 years) were warmed to 37°C prior to testing. Two 4.75-mm vented anchors (SwiveLock, Arthrex) with FiberTape were implanted into a lateral row position (anterior and posterior anchor positioning) of a double-row rotator cuff repair within the greater tuberosity. One anchor was injected with 1 ml of OsteoCrete–after preparation according to the manufacturer’s instructions–through the cannulation channel after placement, and the other anchor served as the uninjected control for each humerus. For the six matched pairs, the OsteoCrete group and the control group were rotated with respect to anterior vs posterior location within the lateral row position. After 15 minutes of the injection, straight pull-to-failure (12 in/min) was performed. Data were compared between the groups for significant (P < .05) differences using t-tests and Pearson correlation.
Continue to: IN VIVO STUDY METHODS
IN VIVO STUDY METHODS
With Institutional Animal Care and Use Committee approval, adult (age, 2-4 years) purpose-bred dogs (N = 8) underwent aseptic surgery of both forelimbs for rotator cuff (infraspinatus) tendon repair (Figure 1) and biceps tenodesis (Figure 2). For the rotator cuff repair, two 4.75-mm vented anchors (1 medial and 1 lateral) with FiberTape were used in a modified double-row technique to repair the acutely transected infraspinatus tendon. In one limb, 1 ml of OsteoCrete was injected through both anchors; the other limb served as the uninjected control. For the biceps tenodesis procedure, the long head of the biceps tendon was transected at its origin and whip-stitched. The tendon was transposed and inserted into a 7-mm diameter socket drilled into the proximal humerus using a tension-slide technique with a transcortical button for fixation. In one limb, 1 ml of OsteoCrete was injected into the socket prior to final tensioning and tying. In the contralateral limb, a 7-mm interference screw (Bio-Tenodesis™ Screw, Arthrex) was inserted into the socket after tensioning and tying. The dogs were allowed to perform out-of-kennel monitored exercise daily for a period of 12 weeks after surgery and were then sacrificed.
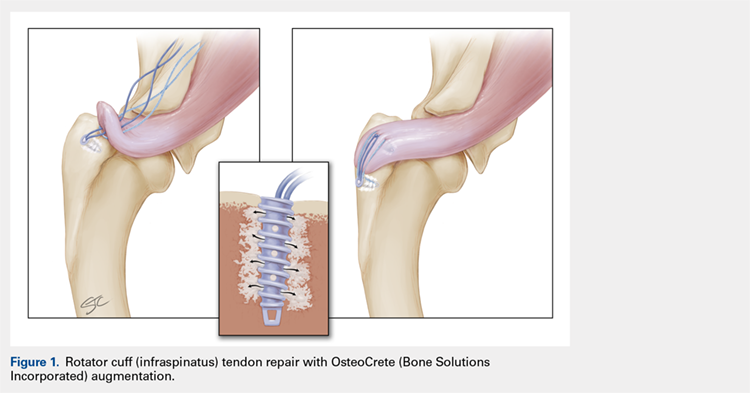
The infraspinatus and biceps bone-tendon-muscle units were excised en bloc. Custom-designed jigs were used for biomechanical testing of the bone-tendon-muscle units along the anatomical vector of muscle contraction. Optical markers were mounted at standardized anatomical locations. Elongation of the repair site was defined as the change in distance between markers and was measured to 0.01-mm resolution using an optical tracking system (Optotrak Certus, NDI), synchronized with measurement of the applied tension load. The bone-tendon-muscle units were loaded in tension to 3-mm elongation at a displacement controlled rate of 0.01 mm/s. Load at 1-mm, 2-mm, and 3-mm displacement of the tendon-bone junction was extracted from the load vs the displacement curve of each sample. Stiffness was calculated as the slope of the linear portion of the load vs the displacement curve.19,20
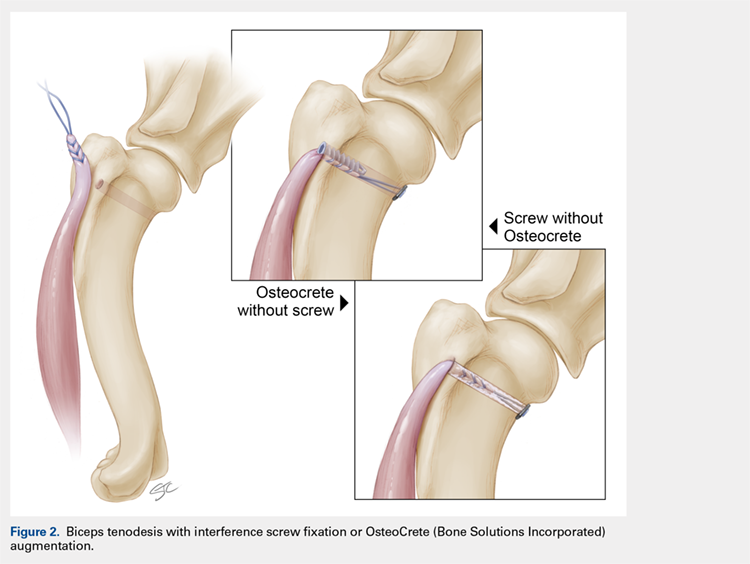
For histologic assessments, sections of each treatment site were obtained using a microsaw and alternated between decalcified and non-decalcified processing. For decalcified bone processing, formalin-fixed tissues were placed in 10% ethylenediaminetetraacetic acid with phosphate-buffered saline for 39 days and then processed routinely for the assessment of sections stained with hematoxylin and eosin (H&E), toluidine blue, and picrosirius red. For non-decalcified bone processing, the tissues were dehydrated through a series of graded ethyl alcohol solutions, embedded in PMMA, sectioned, and stained with toluidine blue and Goldner’s trichrome. Two pathologists who were blinded to the clinical application and the differences between techniques assessed the histologic sections and scored each section using the modified Bonar score that assesses cell morphology, collagen arrangement, cellularity, vascularity, and extracellular matrix using a 15-point scale, where a higher score indicates more pathology.21
Categorical data were compared for detecting statistically significant differences using the rank sum test. Continuous data were compared for identifying statistically significant differences using the t-test or one-way ANOVA. Significance was set at P < .05.
RESULTS
IN VITRO RESULTS
OsteoCrete-augmented anchors (mean = 225 N; range, 158-287 N) had significantly (P < .001) higher pull-out load-to-failure compared to that in the uninjected controls (mean = 161 N; range, 68-202 N), which translated to a 50% mean increase (range, 3%-134%) in load-to-failure (Table 1). For humeri with reduced bone quality (control anchors that failed at <160 N, 4 humeri), the mean increase in load-to-failure for OsteoCrete-augmented anchors was 99% (range, 58%-135%), with the difference between mean values being again significantly different (OsteoCrete mean = 205 N; control mean = 110 N, P < .001). When the control and OsteoCrete load-to-failure values were compared using Pearson correlation, a significantly strong positive correlation (r = 0.66, P = 0.02) was detected. When the control load-to-failure values were compared with its percent increase value when OsteoCrete was used, there was a significantly very strong negative correlation (r = −0.90, P < .001).
Table 1. Cadaveric Lateral Row Rotator Cuff Anchor Pull-To-Failure; Testing Occurred 15 Minutes Post-Injection
| Humerus No. | Control (N) | OsteoCrete (N)a | Percent Increase |
| 1-Right (PA) | 197.28 | 278.73 | 41% |
| 1-Left (AP) | 152.62 | 241.72 | 58% |
| 2-Right (PA) | 178.60 | 196.03 | 10% |
| 2-Left (AP) | 170.10 | 175.57 | 3% |
| 3-Right (PA) | 67.70 | 158.31 | 134% |
| 3-Left (AP) | 74.24 | 173.08 | 133% |
| 4-Right (PA) | 195.81 | 248.12 | 27% |
| 4-Left (AP) | 201.95 | 209.42 | 4% |
| 5-Right (PA) | 173.30 | 220.59 | 27% |
| 5-Left (AP) | 146.61 | 247.37 | 69% |
| 6-Right (PA) | 171.03 | 266.14 | 56% |
| 6-Left (AP) | 199.99 | 286.91 | 43% |
| Average | 160.77 + 45.60 | 225.17 + 43.08 | 50% + 44 |
aOsteoCrete (Bone Solutions Incorporated) resulted in significantly increased (P < 0.001) pull-to-failure. Abbreviations: AP, control anchor located in anterior position, OsteoCrete anchor located in posterior position; PA, control anchor located in posterior position, OsteoCrete anchor located in anterior position.
Continue to: IN VIVO RESULTS
IN VIVO RESULT
No intraoperative or postoperative complications were noted. All repairs were found to be intact based on the gross assessment and the completed biomechanical testing without failure. No statistically significant (P > 0.3) biomechanical differences were found between the techniques (Table 2). Histologic assessments showed low-to-mild pathology scores for all sites with no statistically significant (P > 0.3) differences between the techniques (Table 2). Both control and OsteoCrete rotator cuff repairs demonstrated tendon-to-bone integration via fibrous connective tissue attachment to bone. All anchors were in place with no evidence for loosening, tunnel expansion, or cyst formation. OsteoCrete-augmented anchor repairs were associated with cement remaining within their lumens along with a thin layer of cement interposed between the anchor and the bone interface around their entire periphery. The cement-bone interface was discrete with typical inflammatory cell infiltrate without evidence for infection, membrane or cyst formation, or other untoward pathologic responses. In the OsteoCrete biceps tenodesis group, the tendons filled the tunnels with a thin layer of cement remaining interposed between the tendon and the bone interface around the entire periphery. The tendon-cement-bone interface was discrete with typical inflammatory cell infiltrates and without evidence for infection, membrane or cyst formation, or other untoward pathologic responses. Tendon-to-bone integration was not observed in the control or OsteoCrete biceps tenodesis groups at the 12-week study endpoint. Representative histologic images of the rotator cuff tendon repairs and biceps tenodesis procedures are shown in Figures 3A, 3B and Figures 4A, 4B, respectively.
Table 2. Biomechanical Testing And Histologic Scoring Of Rotator Cuff And Biceps Tendon Repairs In A Preclinical Model
| Procedure | Force (N) at 1 mm | Force (N) at 2 mm | Force (N) at 3 mm | Stiffness (N/mm) | Histologic Score |
| Rotator Cuff - Control | 14.0 + 3.3 | 19.3 + 5.5 | 25.0 + 7.0 | 5.4 + 2.0 | 4.6 + 1.1 |
| Rotator Cuff - OsteoCrete (Bone Solutions Incorporated) | 14.8 + 3.7 | 20.4 + 6.0 | 26.4 + 8.5 | 6.3 + 2.5 | 3.9 + 1.7 |
| Biceps - Control | 23.1 + 6.2 | 35.5 + 8.5 | 52.6 + 15.0 | 17.8 + 6.4 | 3.4 + 1.2 |
| Biceps - OsteoCrete | 22.4 + 7.3 | 36.8 + 10.1 | 57.8 + 16.0 | 21.1 + 8.5 | 3.4 + 0.7 |
There were no significant differences (P < 0.05) between groups. Histologic scoring based on a 15-point scale with higher scores indicating more pathology.
DISCUSSION
The results of this study highlight the safety and efficacy of OsteoCrete in applications for the augmentation of anchor and tendon fixation in rotator cuff repair and biceps tenodesis procedures, respectively. Anchors augmented with OsteoCrete resulted in significantly increased load-to-failure pull-out strength 15 minutes after insertion. In addition, a very strong negative correlation was found between the percentage of improved load-to-failure after OsteoCrete injection and the bone quality of the humerus, which was based on the control load-to-failure values. In the validated preclinical model used in this study, OsteoCrete-based fixation was found to be noninferior to current standard-of-care techniques and was not associated with any untoward pathologic responses of humeral bone, rotator cuff tendon, or biceps tendon based on the biomechanical and histologic analyses. These data highlight the functional efficacy and biocompatibility of OsteoCrete when used for these common indications.

More than 270,000 rotator cuff procedures have been reported to be performed in the US annually (average patient age: 61 years for women, 56 years for men).22 Rotator cuff repair procedures have been associated with a 20% failure rate, with one of the causes being related to an inability for the tendon to heal, even with strong initial fixation.23 Rotator cuff repair techniques are being continuously optimized with the goal of improving patient outcomes. This goal is being realized, primarily with respect to re-tear rates.24,25 However, even with advanced techniques, there are still relatively high rates of failure reported, with increasing patient age serving as one of the primary negative prognostic factors.26 An older patient population is associated with decreased bone mass and strength, and postmenopausal females have decreased bone quality; these factors are associated with higher rotator cuff failure rates due to poor tendon healing, with anchor fixation failure also playing a role.27-29 Therefore, it is critically important to develop methods for augmenting implant and tendon fixation to bone to achieve functional healing. The results of this study suggest that OsteoCrete provides a valid method for accomplishing this goal based on the observation that proximal humeral anchor fixation was improved by 50% in load-to-failure 15 minutes post-injection with an even more profound impact on the anchors placed in poor-quality bone (99% increased load-to-failure 15 minutes post-injection). It is probable that the degree of improvement in fixation strength would be even greater 1 day after fixation, since the strength of OsteoCrete continues to increase over the first 30 hours of curing.
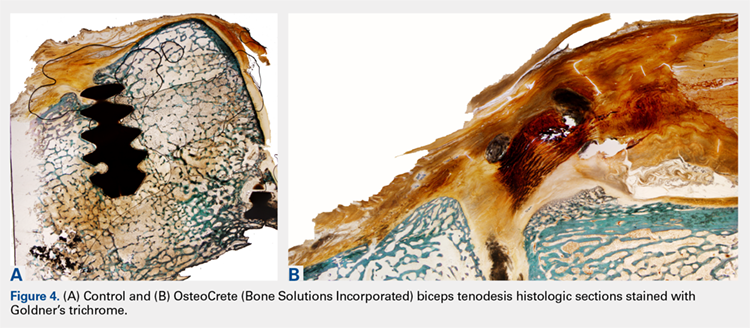
Based on the preclinical animal model data of this study, OsteoCrete augmentation of rotator cuff anchor fixation had no untoward effects on tendon healing or function and can be considered as safe for use. Previously published data also suggest that OsteoCrete may improve osseous replacement of anchors as a result of magnesium ion release, which can drive adjacent attachment and growth of osteoblasts, leading to enhanced new bone formation.9-16,18 As such, surgeons may consider this means of anchor augmentation in situations of questionable or poor-quality bone and/or when accelerated postoperative rehabilitation protocols are desired.
A very low early incidence failure rate (1.2%) has been reported when a distal biceps tendon rupture is repaired using cortical suspensory fixation in conjunction with an interference screw.30 When an early re-rupture does occur, the most common explanation for failure tends to be a lack of patient compliance, with excessive force being placed on the repair.31 This study was not meant to investigate the methods to increase the strength of a biceps tendon repair using OsteoCrete but instead to replace the interference screw with OsteoCrete in a safe and noninferior manner. Primary fixation was still dependent on cortical suspensory fixation; however, OsteoCrete was used to help aid in stabilization of the tendon without the need for interference screw fixation. Although rare, osteolysis and perianchor cyst formation have been reported adjacent to nonbiodegradable anchors (PEEK), along with several types of biodegradable anchors (PLLA, hydroxyapatite plus PLLA, β-tricalcium phosphate plus PLLA, and polyglycolic acid; the latter of the 3 resulted in the lowest incidence of perianchor cyst formation) in the shoulder and elbow.32-34 Whenever osteolysis or cyst formation occurs around an anchor, it leads to decreased bone volume and potential adjacent bone weakness, which may act as a stress riser, thus increasing the risk for fracture. This potential is probably more of a concern within the proximal radius where there is a decreased amount of bone stock around the anchor.34
Continue to: In this study...
In this study, a short-term 12-week analysis revealed no significant differences in the nondestructive biomechanical testing and histologic analysis results between the use of OsteoCrete and the use of a tenodesis anchor. These results indicate the potential for using OsteoCrete as an anchor replacement. The biceps tendon did not react negatively to the OsteoCrete material, which indicated that OsteoCrete can be used adjacent to tendons without the concern of weakening the tendon due to an inflammatory reaction. This being said, tendon-to-bone integration was not evident at this early time point. It would be helpful to further explore the potential of this technique with a longer-term study investigating tendon-to-bone integration in more detail. Ideally, a long-term study would reveal an increased amount of new bone formation within the socket when compared to that with the anchor comparison, similar to the results reported by Gulotta and colleagues16 when using a tendon for ACL reconstruction with OsteoCrete.
We do note several limitations in this study. The dogs used in this study were healthy with normal bone and tendon morphology, the tendons were transected and repaired during the course of the same surgery, and only 1 early time point was evaluated. Additional investigations continuing the characterization of these clinical applications using an osteopenic or osteoporotic preclinical model with chronic tendon pathology and longer-term evaluation are now warranted based on the positive findings of this initial work.
CONCLUSION
OsteoCrete augmentation significantly improved initial rotator cuff anchor fixation (human in vitro) and was safe and effective for anchor and tendon fixation in rotator cuff tendon repair and biceps tenodesis procedures (canine in vivo), respectively, when compared with the current standard-of-care. Of note, the significant improvements associated with OsteoCrete were the greatest in poor-quality bone. Based on these results and considering the previously discussed limitations, it can be concluded that OsteoCrete has the potential for safely providing improved suture anchor and tissue fixation in patients with poor bone or tissue quality. Further in vivo study toward potential clinical applications is warranted.
ABSTRACT
The aim of this study was to assess the efficacy and safety of a novel magnesium-based resorbable bone cement (OsteoCrete, Bone Solutions Incorporated) for anchor and tendon fixation.
Cadaveric humeral testing involved straight pull-to-failure of rotator cuff suture anchors; OsteoCrete was injected through one anchor, and a second anchor served as the uninjected control. Testing was conducted 15 minutes post-injection. A canine preclinical model was used to evaluate the safety of the following parameters: Rotator cuff repair: A double-row technique was used to repair transected infraspinatus tendons; OsteoCrete was injected through both anchors in one limb, and the contralateral limb served as the uninjected control. Biceps tenodesis: The transected biceps tendon was implanted into a proximal humeral socket with a transcortical button; OsteoCrete was injected into the socket of one limb, and a screw was used for final fixation in the contralateral control limb. Nondestructive biomechanical testing and histologic assessment were performed after 12 weeks.
OsteoCrete-augmented anchors showed significantly higher load-to-failure compared to that with uninjected controls. In cadaveric humeri with reduced bone quality, OsteoCrete increased the mean load-to-failure by 99%. Within the preclinical model, there were no complications or statistically significant biomechanical/histologic differences between the techniques.
OsteoCrete has the potential for safely providing improved suture anchor and tissue fixation in patients with poor bone or tissue quality.
Continue to: Calcium phosphate bone void fillers...
Calcium phosphate bone void fillers have been commonly used in orthopedic surgery for several applications, including, but not limited to, a variety of fracture fixation or augmentation procedures.1-8 Continuing research on calcium phosphates has evidenced that the addition of magnesium phosphate to the formulation results in improved reactivity of the bone void filler. An in vitro study demonstrated enhanced attachment and proliferation of MG63 osteoblast-like cells on calcium magnesium phosphate cement (CMPC), in comparison with calcium phosphate cement (CPC), along with increased cellular alkaline phosphatase activity.9 The authors further explored the proliferation rates of MG63 cells by comparing CMPC with CPC and magnesium phosphate cement (MPC), and observed significantly increased proliferation of cells on CMPC. They also compared CMPC and CPC using a rabbit bone void model and observed substantial CMPC resorption with new bone formation at the 3-month time point and further reported that the majority of the defect had filled with new bone at 6 months, whereas CPC resulted in <10% new bone formation after 6 months.10 The authors continued to study the differences between CPC, MPC, and CMPC and identified increased proliferation of bone marrow stromal cells (bMSCs), when the cells were associated with CMPC and MPC, and when compared to that with CPC. The osteogenic differentiation of bMSCs was highest in the CMPC and CPC groups, when compared to that in the MPC group, with no significant difference between the CMPC and CPC groups. The authors also compared these 3 different formulations using a rabbit maxillary sinus floor elevation model, in which CMPC resulted in increased new bone formation and mineralization compared to that with CPC and MPC, which was further enhanced with the addition of bMSCs.11
These studies highlight the importance of having both a magnesium phosphate and a calcium phosphate component for a resorbable cement intended for use as a bone void filler. The rationale behind this strategy is related to the release of magnesium ions from the magnesium phosphate component. Magnesium has been shown to increase the proliferation of bMSCs, improve the attachment and growth of osteoblasts, stimulate the proteins involved in bone regeneration, enhance new bone formation, and boost bone mineralization.12,13
OsteoCrete (Bone Solutions Incorporation) is a novel CMPC composed of magnesium oxide, monopotassium phosphate, monosodium phosphate, hydroxyapatite, and sucrose. OsteoCrete has been demonstrated to significantly increase peak torque-to-failure of stainless-steel cortical bone screw fixation, when compared with screw fixation without augmentation and screw fixation with calcium phosphate augmentation using an in vivo equine model. In the same study, the authors showed that OsteoCrete resulted in an interface toughness that was significantly increased compared to that with no treatment, CPC augmentation, and polymethylmethacrylate (PMMA) augmentation. At 6 months after implantation, woven bone had replaced 69% of the OsteoCrete at the screw interface, compared to 44% of that with CPC.14 An equine study examined the effects of OsteoCrete on bone stability and healing using a metatarsal osteotomy model; the study reported significantly improved radiographic callus formation and a greater amount of new bone formation within the fracture gap when compared to that with CPC augmentation or no augmentation. OsteoCrete also secured the fragment significantly better than the CPC and control groups based on a decreased fracture gap over time.15 Another study using a preclinical anterior cruciate ligament (ACL) reconstruction model reported that OsteoCrete resulted in significantly better new bone formation in the tibial tunnel, a smaller amount of fibrous tissue, more cartilage formation at the tendon-bone interface, and a higher ultimate load-to-failure compared to that with standard ACL reconstruction in the contralateral limb after 6 weeks.16 OsteoCrete and PMMA were evaluated in terms of biomechanical fixation of a stemless humeral prosthesis, with data showing that both groups have higher failure loads, failure displacements, and failure cycles when compared to those with the control, nonaugmented group.17 Another preclinical model evaluated cranial bone flap augmentation with 2 resorbable cements and highlighted faster cement resorption and replacement with bone, along with superior stability within the OsteoCrete group compared to that with CPC.18 In a preclinical bone void study conducted for obtaining US Food and Drug Administration 510(k) clearance, OsteoCrete resulted in 83% greater resorption than that with CPC after 12 weeks and 35% greater resorption at 26 weeks, with 84% of OsteoCrete being resorbed and replaced with woven or lamellar mineralized bone of normal morphology at the 26-week time point (unpublished data provided by Bone Solutions Incorporated [BSI]).
These data indicate that CMPCs such as OsteoCrete appear to have potential benefits for augmenting the healing of bone implants and bone soft tissue. Therefore, the objective of this study was to assess the safety and efficacy of OsteoCrete in applications for the augmentation of anchor and tendon fixation in rotator cuff repair and biceps tenodesis procedures, respectively. Improving healing for these 2 commonly performed procedures would be of great benefit in improving the functional outcomes and mitigating the complications and morbidity.
MATERIALS AND METHODS
IN VITRO STUDY METHODS
Cadaveric humeri (N = 12, six matched pairs) of females (age, 70-75 years) were warmed to 37°C prior to testing. Two 4.75-mm vented anchors (SwiveLock, Arthrex) with FiberTape were implanted into a lateral row position (anterior and posterior anchor positioning) of a double-row rotator cuff repair within the greater tuberosity. One anchor was injected with 1 ml of OsteoCrete–after preparation according to the manufacturer’s instructions–through the cannulation channel after placement, and the other anchor served as the uninjected control for each humerus. For the six matched pairs, the OsteoCrete group and the control group were rotated with respect to anterior vs posterior location within the lateral row position. After 15 minutes of the injection, straight pull-to-failure (12 in/min) was performed. Data were compared between the groups for significant (P < .05) differences using t-tests and Pearson correlation.
Continue to: IN VIVO STUDY METHODS
IN VIVO STUDY METHODS
With Institutional Animal Care and Use Committee approval, adult (age, 2-4 years) purpose-bred dogs (N = 8) underwent aseptic surgery of both forelimbs for rotator cuff (infraspinatus) tendon repair (Figure 1) and biceps tenodesis (Figure 2). For the rotator cuff repair, two 4.75-mm vented anchors (1 medial and 1 lateral) with FiberTape were used in a modified double-row technique to repair the acutely transected infraspinatus tendon. In one limb, 1 ml of OsteoCrete was injected through both anchors; the other limb served as the uninjected control. For the biceps tenodesis procedure, the long head of the biceps tendon was transected at its origin and whip-stitched. The tendon was transposed and inserted into a 7-mm diameter socket drilled into the proximal humerus using a tension-slide technique with a transcortical button for fixation. In one limb, 1 ml of OsteoCrete was injected into the socket prior to final tensioning and tying. In the contralateral limb, a 7-mm interference screw (Bio-Tenodesis™ Screw, Arthrex) was inserted into the socket after tensioning and tying. The dogs were allowed to perform out-of-kennel monitored exercise daily for a period of 12 weeks after surgery and were then sacrificed.
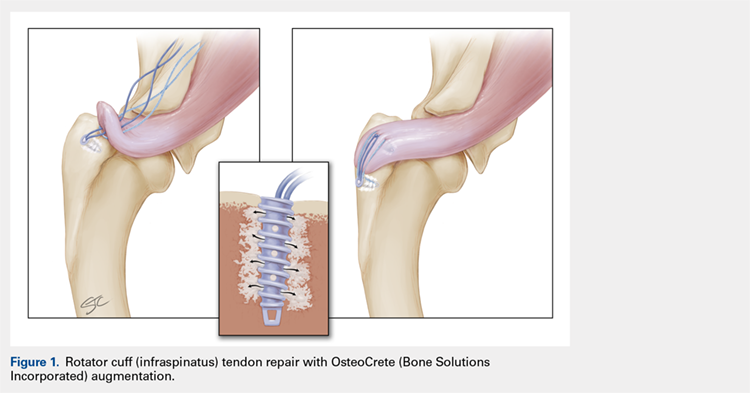
The infraspinatus and biceps bone-tendon-muscle units were excised en bloc. Custom-designed jigs were used for biomechanical testing of the bone-tendon-muscle units along the anatomical vector of muscle contraction. Optical markers were mounted at standardized anatomical locations. Elongation of the repair site was defined as the change in distance between markers and was measured to 0.01-mm resolution using an optical tracking system (Optotrak Certus, NDI), synchronized with measurement of the applied tension load. The bone-tendon-muscle units were loaded in tension to 3-mm elongation at a displacement controlled rate of 0.01 mm/s. Load at 1-mm, 2-mm, and 3-mm displacement of the tendon-bone junction was extracted from the load vs the displacement curve of each sample. Stiffness was calculated as the slope of the linear portion of the load vs the displacement curve.19,20
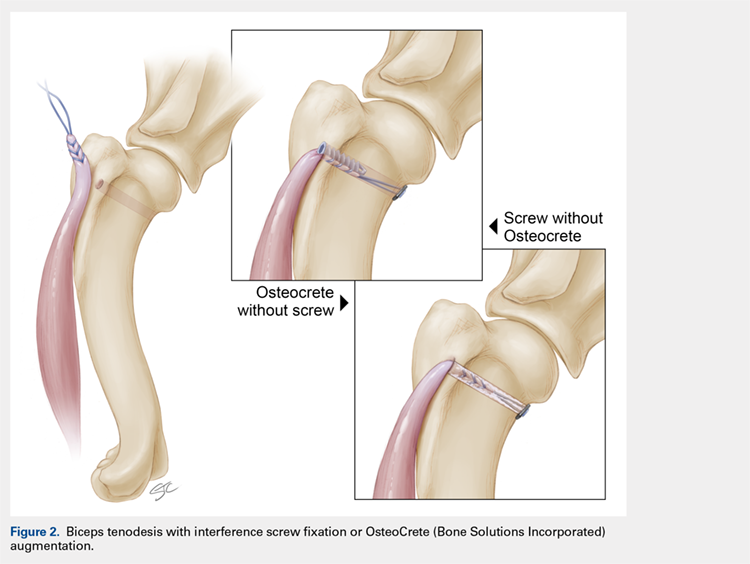
For histologic assessments, sections of each treatment site were obtained using a microsaw and alternated between decalcified and non-decalcified processing. For decalcified bone processing, formalin-fixed tissues were placed in 10% ethylenediaminetetraacetic acid with phosphate-buffered saline for 39 days and then processed routinely for the assessment of sections stained with hematoxylin and eosin (H&E), toluidine blue, and picrosirius red. For non-decalcified bone processing, the tissues were dehydrated through a series of graded ethyl alcohol solutions, embedded in PMMA, sectioned, and stained with toluidine blue and Goldner’s trichrome. Two pathologists who were blinded to the clinical application and the differences between techniques assessed the histologic sections and scored each section using the modified Bonar score that assesses cell morphology, collagen arrangement, cellularity, vascularity, and extracellular matrix using a 15-point scale, where a higher score indicates more pathology.21
Categorical data were compared for detecting statistically significant differences using the rank sum test. Continuous data were compared for identifying statistically significant differences using the t-test or one-way ANOVA. Significance was set at P < .05.
RESULTS
IN VITRO RESULTS
OsteoCrete-augmented anchors (mean = 225 N; range, 158-287 N) had significantly (P < .001) higher pull-out load-to-failure compared to that in the uninjected controls (mean = 161 N; range, 68-202 N), which translated to a 50% mean increase (range, 3%-134%) in load-to-failure (Table 1). For humeri with reduced bone quality (control anchors that failed at <160 N, 4 humeri), the mean increase in load-to-failure for OsteoCrete-augmented anchors was 99% (range, 58%-135%), with the difference between mean values being again significantly different (OsteoCrete mean = 205 N; control mean = 110 N, P < .001). When the control and OsteoCrete load-to-failure values were compared using Pearson correlation, a significantly strong positive correlation (r = 0.66, P = 0.02) was detected. When the control load-to-failure values were compared with its percent increase value when OsteoCrete was used, there was a significantly very strong negative correlation (r = −0.90, P < .001).
Table 1. Cadaveric Lateral Row Rotator Cuff Anchor Pull-To-Failure; Testing Occurred 15 Minutes Post-Injection
| Humerus No. | Control (N) | OsteoCrete (N)a | Percent Increase |
| 1-Right (PA) | 197.28 | 278.73 | 41% |
| 1-Left (AP) | 152.62 | 241.72 | 58% |
| 2-Right (PA) | 178.60 | 196.03 | 10% |
| 2-Left (AP) | 170.10 | 175.57 | 3% |
| 3-Right (PA) | 67.70 | 158.31 | 134% |
| 3-Left (AP) | 74.24 | 173.08 | 133% |
| 4-Right (PA) | 195.81 | 248.12 | 27% |
| 4-Left (AP) | 201.95 | 209.42 | 4% |
| 5-Right (PA) | 173.30 | 220.59 | 27% |
| 5-Left (AP) | 146.61 | 247.37 | 69% |
| 6-Right (PA) | 171.03 | 266.14 | 56% |
| 6-Left (AP) | 199.99 | 286.91 | 43% |
| Average | 160.77 + 45.60 | 225.17 + 43.08 | 50% + 44 |
aOsteoCrete (Bone Solutions Incorporated) resulted in significantly increased (P < 0.001) pull-to-failure. Abbreviations: AP, control anchor located in anterior position, OsteoCrete anchor located in posterior position; PA, control anchor located in posterior position, OsteoCrete anchor located in anterior position.
Continue to: IN VIVO RESULTS
IN VIVO RESULT
No intraoperative or postoperative complications were noted. All repairs were found to be intact based on the gross assessment and the completed biomechanical testing without failure. No statistically significant (P > 0.3) biomechanical differences were found between the techniques (Table 2). Histologic assessments showed low-to-mild pathology scores for all sites with no statistically significant (P > 0.3) differences between the techniques (Table 2). Both control and OsteoCrete rotator cuff repairs demonstrated tendon-to-bone integration via fibrous connective tissue attachment to bone. All anchors were in place with no evidence for loosening, tunnel expansion, or cyst formation. OsteoCrete-augmented anchor repairs were associated with cement remaining within their lumens along with a thin layer of cement interposed between the anchor and the bone interface around their entire periphery. The cement-bone interface was discrete with typical inflammatory cell infiltrate without evidence for infection, membrane or cyst formation, or other untoward pathologic responses. In the OsteoCrete biceps tenodesis group, the tendons filled the tunnels with a thin layer of cement remaining interposed between the tendon and the bone interface around the entire periphery. The tendon-cement-bone interface was discrete with typical inflammatory cell infiltrates and without evidence for infection, membrane or cyst formation, or other untoward pathologic responses. Tendon-to-bone integration was not observed in the control or OsteoCrete biceps tenodesis groups at the 12-week study endpoint. Representative histologic images of the rotator cuff tendon repairs and biceps tenodesis procedures are shown in Figures 3A, 3B and Figures 4A, 4B, respectively.
Table 2. Biomechanical Testing And Histologic Scoring Of Rotator Cuff And Biceps Tendon Repairs In A Preclinical Model
| Procedure | Force (N) at 1 mm | Force (N) at 2 mm | Force (N) at 3 mm | Stiffness (N/mm) | Histologic Score |
| Rotator Cuff - Control | 14.0 + 3.3 | 19.3 + 5.5 | 25.0 + 7.0 | 5.4 + 2.0 | 4.6 + 1.1 |
| Rotator Cuff - OsteoCrete (Bone Solutions Incorporated) | 14.8 + 3.7 | 20.4 + 6.0 | 26.4 + 8.5 | 6.3 + 2.5 | 3.9 + 1.7 |
| Biceps - Control | 23.1 + 6.2 | 35.5 + 8.5 | 52.6 + 15.0 | 17.8 + 6.4 | 3.4 + 1.2 |
| Biceps - OsteoCrete | 22.4 + 7.3 | 36.8 + 10.1 | 57.8 + 16.0 | 21.1 + 8.5 | 3.4 + 0.7 |
There were no significant differences (P < 0.05) between groups. Histologic scoring based on a 15-point scale with higher scores indicating more pathology.
DISCUSSION
The results of this study highlight the safety and efficacy of OsteoCrete in applications for the augmentation of anchor and tendon fixation in rotator cuff repair and biceps tenodesis procedures, respectively. Anchors augmented with OsteoCrete resulted in significantly increased load-to-failure pull-out strength 15 minutes after insertion. In addition, a very strong negative correlation was found between the percentage of improved load-to-failure after OsteoCrete injection and the bone quality of the humerus, which was based on the control load-to-failure values. In the validated preclinical model used in this study, OsteoCrete-based fixation was found to be noninferior to current standard-of-care techniques and was not associated with any untoward pathologic responses of humeral bone, rotator cuff tendon, or biceps tendon based on the biomechanical and histologic analyses. These data highlight the functional efficacy and biocompatibility of OsteoCrete when used for these common indications.

More than 270,000 rotator cuff procedures have been reported to be performed in the US annually (average patient age: 61 years for women, 56 years for men).22 Rotator cuff repair procedures have been associated with a 20% failure rate, with one of the causes being related to an inability for the tendon to heal, even with strong initial fixation.23 Rotator cuff repair techniques are being continuously optimized with the goal of improving patient outcomes. This goal is being realized, primarily with respect to re-tear rates.24,25 However, even with advanced techniques, there are still relatively high rates of failure reported, with increasing patient age serving as one of the primary negative prognostic factors.26 An older patient population is associated with decreased bone mass and strength, and postmenopausal females have decreased bone quality; these factors are associated with higher rotator cuff failure rates due to poor tendon healing, with anchor fixation failure also playing a role.27-29 Therefore, it is critically important to develop methods for augmenting implant and tendon fixation to bone to achieve functional healing. The results of this study suggest that OsteoCrete provides a valid method for accomplishing this goal based on the observation that proximal humeral anchor fixation was improved by 50% in load-to-failure 15 minutes post-injection with an even more profound impact on the anchors placed in poor-quality bone (99% increased load-to-failure 15 minutes post-injection). It is probable that the degree of improvement in fixation strength would be even greater 1 day after fixation, since the strength of OsteoCrete continues to increase over the first 30 hours of curing.
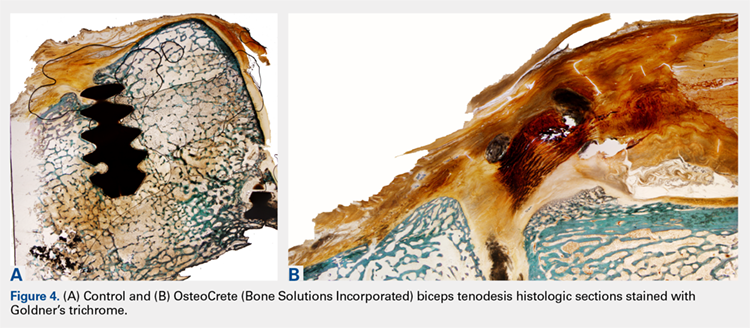
Based on the preclinical animal model data of this study, OsteoCrete augmentation of rotator cuff anchor fixation had no untoward effects on tendon healing or function and can be considered as safe for use. Previously published data also suggest that OsteoCrete may improve osseous replacement of anchors as a result of magnesium ion release, which can drive adjacent attachment and growth of osteoblasts, leading to enhanced new bone formation.9-16,18 As such, surgeons may consider this means of anchor augmentation in situations of questionable or poor-quality bone and/or when accelerated postoperative rehabilitation protocols are desired.
A very low early incidence failure rate (1.2%) has been reported when a distal biceps tendon rupture is repaired using cortical suspensory fixation in conjunction with an interference screw.30 When an early re-rupture does occur, the most common explanation for failure tends to be a lack of patient compliance, with excessive force being placed on the repair.31 This study was not meant to investigate the methods to increase the strength of a biceps tendon repair using OsteoCrete but instead to replace the interference screw with OsteoCrete in a safe and noninferior manner. Primary fixation was still dependent on cortical suspensory fixation; however, OsteoCrete was used to help aid in stabilization of the tendon without the need for interference screw fixation. Although rare, osteolysis and perianchor cyst formation have been reported adjacent to nonbiodegradable anchors (PEEK), along with several types of biodegradable anchors (PLLA, hydroxyapatite plus PLLA, β-tricalcium phosphate plus PLLA, and polyglycolic acid; the latter of the 3 resulted in the lowest incidence of perianchor cyst formation) in the shoulder and elbow.32-34 Whenever osteolysis or cyst formation occurs around an anchor, it leads to decreased bone volume and potential adjacent bone weakness, which may act as a stress riser, thus increasing the risk for fracture. This potential is probably more of a concern within the proximal radius where there is a decreased amount of bone stock around the anchor.34
Continue to: In this study...
In this study, a short-term 12-week analysis revealed no significant differences in the nondestructive biomechanical testing and histologic analysis results between the use of OsteoCrete and the use of a tenodesis anchor. These results indicate the potential for using OsteoCrete as an anchor replacement. The biceps tendon did not react negatively to the OsteoCrete material, which indicated that OsteoCrete can be used adjacent to tendons without the concern of weakening the tendon due to an inflammatory reaction. This being said, tendon-to-bone integration was not evident at this early time point. It would be helpful to further explore the potential of this technique with a longer-term study investigating tendon-to-bone integration in more detail. Ideally, a long-term study would reveal an increased amount of new bone formation within the socket when compared to that with the anchor comparison, similar to the results reported by Gulotta and colleagues16 when using a tendon for ACL reconstruction with OsteoCrete.
We do note several limitations in this study. The dogs used in this study were healthy with normal bone and tendon morphology, the tendons were transected and repaired during the course of the same surgery, and only 1 early time point was evaluated. Additional investigations continuing the characterization of these clinical applications using an osteopenic or osteoporotic preclinical model with chronic tendon pathology and longer-term evaluation are now warranted based on the positive findings of this initial work.
CONCLUSION
OsteoCrete augmentation significantly improved initial rotator cuff anchor fixation (human in vitro) and was safe and effective for anchor and tendon fixation in rotator cuff tendon repair and biceps tenodesis procedures (canine in vivo), respectively, when compared with the current standard-of-care. Of note, the significant improvements associated with OsteoCrete were the greatest in poor-quality bone. Based on these results and considering the previously discussed limitations, it can be concluded that OsteoCrete has the potential for safely providing improved suture anchor and tissue fixation in patients with poor bone or tissue quality. Further in vivo study toward potential clinical applications is warranted.
1. Russell TA, Leighton RK, Group A-BTPFS. Comparison of autogenous bone graft and endothermic calcium phosphate cement for defect augmentation in tibial plateau fractures. A multicenter, prospective, randomized study. J Bone Joint Surg Am. 2008; 90(10):2057-2061. doi:10.2106/JBJS.G.01191.
2. Egol KA, Sugi MT, Ong CC, Montero N, Davidovitch R, Zuckerman JD. Fracture site augmentation with calcium phosphate cement reduces screw penetration after open reduction-internal fixation of proximal humeral fractures. J Shoulder Elbow Surg. 2012; 21(6):741-748. doi:10.1016/j.jse.2011.09.017.
3. Cassidy C, Jupiter JB, Cohen M, et al. Norian SRS cement compared with conventional fixation in distal radial fractures. A randomized study. J Bone Joint Surg Am. 2003;85-A(11):2127-2137.
4. Mattsson P, Alberts A, Dahlberg G, Sohlman M, Hyldahl HC, Larsson S. Resorbable cement for the augmentation of internally-fixed unstable trochanteric fractures. A prospective, randomised multicentre study. J Bone Joint Surg Br. 2005;87(9):1203-1209.
5. Cohen SB, Sharkey PF. Subchondroplasty for treating bone marrow lesions. J Knee Surg. 2016;29(07):555-563. doi:10.1302/0301-620X.87B9.15792.
6. Guida P, Ragozzino R, Sorrentino B, et al. Three-in-One minimally invasive approach to surgical treatment of pediatric pathological fractures with wide bone loss through bone cysts: ESIN, curettage and packing with injectable HA bone substitute. A retrospective series of 116 cases. Injury. 2016;47(6):1222-1228. doi:10.1016/j.injury.2016.01.006.
7. Maestretti G, Sutter P, Monnard E, et al. A prospective study of percutaneous balloon kyphoplasty with calcium phosphate cement in traumatic vertebral fractures: 10-year results. Eur Spine J. 2014;23(6):1354-1360. doi:10.1007/s00586-014-3206-1.
8. Nakano M, Hirano N, Zukawa M, et al. Vertebroplasty using calcium phosphate cement for osteoporotic vertebral fractures: study of outcomes at a minimum follow-up of two years. Asian Spine J. 2012;6(1):34-42. doi:10.4184/asj.2012.6.1.34.
9. Jia J, Zhou H, Wei J, et al. Development of magnesium calcium phosphate biocement for bone regeneration. J R Soc Interface. 2010;7(49):1171-1180. doi:10.1098/rsif.2009.0559.
10. Wu F, Wei J, Guo H, Chen F, Hong H, Liu C. Self-setting bioactive calcium-magnesium phosphate cement with high strength and degradability for bone regeneration. Acta Biomater. 2008;4(6):1873-1884. doi:10.1016/j.actbio.2008.06.020.
11. Zeng D, Xia L, Zhang W, et al. Maxillary sinus floor elevation using a tissue-engineered bone with calcium-magnesium phosphate cement and bone marrow stromal cells in rabbits. Tissue Eng Part A. 2012;18(7-8):870-881. doi:10.1089/ten.TEA.2011.0379.
12. Yoshizawa S, Brown A, Barchowsky A, Sfeir C. Magnesium ion stimulation of bone marrow stromal cells enhances osteogenic activity, simulating the effect of magnesium alloy degradation. Acta Biomater. 2014;10(6):2834-2842. doi:10.1016/j.actbio.2014.02.002.
13. Liao J, Qu Y, Chu B, Zhang X, Qian Z. Biodegradable CSMA/PECA/Graphene porous hybrid scaffold for cartilage tissue engineering. Sci Rep. 2015;5:9879. doi:10.1038/srep09879.
14. Hirvinen LJ, Litsky AS, Samii VF, Weisbrode SE, Bertone AL. Influence of bone cements on bone-screw interfaces in the third metacarpal and third metatarsal bones of horses. Am J Vet Res. 2009;70(8):964-972. doi:10.2460/ajvr.70.8.964.
15. Waselau M, Samii VF, Weisbrode SE, Litsky AS, Bertone AL. Effects of a magnesium adhesive cement on bone stability and healing following a metatarsal osteotomy in horses. Am J Vet Res. 2007;68(4):370-378. doi:10.2460/ajvr.68.4.370.
16. Gulotta LV, Kovacevic D, Ying L, Ehteshami JR, Montgomery S, Rodeo SA. Augmentation of tendon-to-bone healing with a magnesium-based bone adhesive. Am J Sports Med. 2008;36(7):1290-1297. doi:10.1177/0363546508314396.
17. Kim MS, Kovacevic D, Milks RA, et al. Bone graft substitute provides metaphyseal fixation for a stemless humeral implant. Orthopedics. 2015;38(7):e597-e603. doi:10.3928/01477447-20150701-58.
18. Schendel SA, Peauroi J. Magnesium-based bone cement and bone void filler: preliminary experimental studies. J Craniofac Surg. 2009;20(2):461-464. doi:10.1097/SCS.0b013e31819b9819.
19. Pfeiffer FM, Smith MJ, Cook JL, Kuroki K. The histologic and biomechanical response of two commercially available small glenoid anchors for use in labral repairs. J Shoulder Elbow Surg. 2014;23(8):1156-1161. doi:10.1016/j.jse.2013.12.036.
20. Smith MJ, Cook JL, Kuroki K, et al. Comparison of a novel bone-tendon allograft with a human dermis-derived patch for repair of chronic large rotator cuff tears using a canine model. Arthroscopy. 2012;28(2):169-177. doi:10.1016/j.arthro.2011.08.296.
21. Fearon A, Dahlstrom JE, Twin J, Cook J, Scott A. The Bonar score revisited: region of evaluation significantly influences the standardized assessment of tendon degeneration. J Sci Med Sport. 2014;17(4):346-350. doi:10.1016/j.jsams.2013.07.008.
22. Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012;94(3):227-233. doi:10.2106/JBJS.J.00739.
23. Lädermann A, Denard PJ, Burkhart SS. Management of failed rotator cuff repair: a systematic review. J ISAKOS. 2016;1(1):32-37. doi:10.1136/jisakos-2015-000027.
24. Franceschi F, Papalia R, Franceschetti E, et al. Double-Row repair lowers the retear risk after accelerated rehabilitation. Am J Sports Med. 2016;44(4):948-956. doi:10.1177/0363546515623031.
25. Wang E, Wang L, Gao P, Li Z, Zhou X, Wang S. Single-versus double-row arthroscopic rotator cuff repair in massive tears. Med Sci Monit. 2015;21:1556-1561. doi:10.12659/MSM.893058.
26. Abtahi AM, Granger EK, Tashjian RZ. Factors affecting healing after arthroscopic rotator cuff repair. World J Orthop. 2015;6(2):211-220. doi:10.5312/wjo.v6.i2.211.
27. Chung SW, Oh JH, Gong HS, Kim JY, Kim SH. Factors affecting rotator cuff healing after arthroscopic repair: osteoporosis as one of the independent risk factors. Am J Sports Med. 2011;39(10):2099-2107. doi:10.1177/0363546511415659.
28. Tsiouri C, Mok DH. Early pullout of lateral row knotless anchor in rotator cuff repair. Int J Shoulder Surg. 2009;3(3):63-65. doi:10.4103/0973-6042.59972.
29. Boskey AL, Coleman R. Aging and bone. J Dent Res. 2010;89(12):1333-1348. doi:10.1177/0022034510377791.
30. Cusick MC, Cottrell BJ, Cain RA, Mighell MA. Low incidence of tendon rerupture after distal biceps repair by cortical button and interference screw. J Shoulder Elbow Surg. 2014;23(10):1532-1536. doi:10.1016/j.jse.2014.04.013.
31. Hinchey JW, Aronowitz JG, Sanchez-Sotelo J, Morrey BF. Re-rupture rate of primarily repaired distal biceps tendon injuries. J Shoulder Elbow Surg. 2014;23(6):850-854. doi:10.1016/j.jse.2014.02.006.
32. Shahrulazua A, Duckworth D, Bokor DJ. Perianchor radiolucency following PEEK suture anchor application associated with recurrent shoulder dislocation: a case report. Clin Ter. 2014;165(1):31-34. doi:10.7471/CT.2014.1658.
33. Kim SH, Kim dY, Kwon JE, Park JS, Oh JH. Perianchor cyst formation around biocomposite biodegradable suture anchors after rotator cuff repair. Am J Sports Med. 2015;43(12):2907-2912. doi:10.1177/0363546515608484
34. Potapov A, Laflamme YG, Gagnon S, Canet F, Rouleau DM. Progressive osteolysis of the radius after distal biceps tendon repair with the bioabsorbable screw. J Shoulder Elbow Surg. 2011;20(5):819-826. doi:10.1016/j.jse.2011.02.021.
1. Russell TA, Leighton RK, Group A-BTPFS. Comparison of autogenous bone graft and endothermic calcium phosphate cement for defect augmentation in tibial plateau fractures. A multicenter, prospective, randomized study. J Bone Joint Surg Am. 2008; 90(10):2057-2061. doi:10.2106/JBJS.G.01191.
2. Egol KA, Sugi MT, Ong CC, Montero N, Davidovitch R, Zuckerman JD. Fracture site augmentation with calcium phosphate cement reduces screw penetration after open reduction-internal fixation of proximal humeral fractures. J Shoulder Elbow Surg. 2012; 21(6):741-748. doi:10.1016/j.jse.2011.09.017.
3. Cassidy C, Jupiter JB, Cohen M, et al. Norian SRS cement compared with conventional fixation in distal radial fractures. A randomized study. J Bone Joint Surg Am. 2003;85-A(11):2127-2137.
4. Mattsson P, Alberts A, Dahlberg G, Sohlman M, Hyldahl HC, Larsson S. Resorbable cement for the augmentation of internally-fixed unstable trochanteric fractures. A prospective, randomised multicentre study. J Bone Joint Surg Br. 2005;87(9):1203-1209.
5. Cohen SB, Sharkey PF. Subchondroplasty for treating bone marrow lesions. J Knee Surg. 2016;29(07):555-563. doi:10.1302/0301-620X.87B9.15792.
6. Guida P, Ragozzino R, Sorrentino B, et al. Three-in-One minimally invasive approach to surgical treatment of pediatric pathological fractures with wide bone loss through bone cysts: ESIN, curettage and packing with injectable HA bone substitute. A retrospective series of 116 cases. Injury. 2016;47(6):1222-1228. doi:10.1016/j.injury.2016.01.006.
7. Maestretti G, Sutter P, Monnard E, et al. A prospective study of percutaneous balloon kyphoplasty with calcium phosphate cement in traumatic vertebral fractures: 10-year results. Eur Spine J. 2014;23(6):1354-1360. doi:10.1007/s00586-014-3206-1.
8. Nakano M, Hirano N, Zukawa M, et al. Vertebroplasty using calcium phosphate cement for osteoporotic vertebral fractures: study of outcomes at a minimum follow-up of two years. Asian Spine J. 2012;6(1):34-42. doi:10.4184/asj.2012.6.1.34.
9. Jia J, Zhou H, Wei J, et al. Development of magnesium calcium phosphate biocement for bone regeneration. J R Soc Interface. 2010;7(49):1171-1180. doi:10.1098/rsif.2009.0559.
10. Wu F, Wei J, Guo H, Chen F, Hong H, Liu C. Self-setting bioactive calcium-magnesium phosphate cement with high strength and degradability for bone regeneration. Acta Biomater. 2008;4(6):1873-1884. doi:10.1016/j.actbio.2008.06.020.
11. Zeng D, Xia L, Zhang W, et al. Maxillary sinus floor elevation using a tissue-engineered bone with calcium-magnesium phosphate cement and bone marrow stromal cells in rabbits. Tissue Eng Part A. 2012;18(7-8):870-881. doi:10.1089/ten.TEA.2011.0379.
12. Yoshizawa S, Brown A, Barchowsky A, Sfeir C. Magnesium ion stimulation of bone marrow stromal cells enhances osteogenic activity, simulating the effect of magnesium alloy degradation. Acta Biomater. 2014;10(6):2834-2842. doi:10.1016/j.actbio.2014.02.002.
13. Liao J, Qu Y, Chu B, Zhang X, Qian Z. Biodegradable CSMA/PECA/Graphene porous hybrid scaffold for cartilage tissue engineering. Sci Rep. 2015;5:9879. doi:10.1038/srep09879.
14. Hirvinen LJ, Litsky AS, Samii VF, Weisbrode SE, Bertone AL. Influence of bone cements on bone-screw interfaces in the third metacarpal and third metatarsal bones of horses. Am J Vet Res. 2009;70(8):964-972. doi:10.2460/ajvr.70.8.964.
15. Waselau M, Samii VF, Weisbrode SE, Litsky AS, Bertone AL. Effects of a magnesium adhesive cement on bone stability and healing following a metatarsal osteotomy in horses. Am J Vet Res. 2007;68(4):370-378. doi:10.2460/ajvr.68.4.370.
16. Gulotta LV, Kovacevic D, Ying L, Ehteshami JR, Montgomery S, Rodeo SA. Augmentation of tendon-to-bone healing with a magnesium-based bone adhesive. Am J Sports Med. 2008;36(7):1290-1297. doi:10.1177/0363546508314396.
17. Kim MS, Kovacevic D, Milks RA, et al. Bone graft substitute provides metaphyseal fixation for a stemless humeral implant. Orthopedics. 2015;38(7):e597-e603. doi:10.3928/01477447-20150701-58.
18. Schendel SA, Peauroi J. Magnesium-based bone cement and bone void filler: preliminary experimental studies. J Craniofac Surg. 2009;20(2):461-464. doi:10.1097/SCS.0b013e31819b9819.
19. Pfeiffer FM, Smith MJ, Cook JL, Kuroki K. The histologic and biomechanical response of two commercially available small glenoid anchors for use in labral repairs. J Shoulder Elbow Surg. 2014;23(8):1156-1161. doi:10.1016/j.jse.2013.12.036.
20. Smith MJ, Cook JL, Kuroki K, et al. Comparison of a novel bone-tendon allograft with a human dermis-derived patch for repair of chronic large rotator cuff tears using a canine model. Arthroscopy. 2012;28(2):169-177. doi:10.1016/j.arthro.2011.08.296.
21. Fearon A, Dahlstrom JE, Twin J, Cook J, Scott A. The Bonar score revisited: region of evaluation significantly influences the standardized assessment of tendon degeneration. J Sci Med Sport. 2014;17(4):346-350. doi:10.1016/j.jsams.2013.07.008.
22. Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012;94(3):227-233. doi:10.2106/JBJS.J.00739.
23. Lädermann A, Denard PJ, Burkhart SS. Management of failed rotator cuff repair: a systematic review. J ISAKOS. 2016;1(1):32-37. doi:10.1136/jisakos-2015-000027.
24. Franceschi F, Papalia R, Franceschetti E, et al. Double-Row repair lowers the retear risk after accelerated rehabilitation. Am J Sports Med. 2016;44(4):948-956. doi:10.1177/0363546515623031.
25. Wang E, Wang L, Gao P, Li Z, Zhou X, Wang S. Single-versus double-row arthroscopic rotator cuff repair in massive tears. Med Sci Monit. 2015;21:1556-1561. doi:10.12659/MSM.893058.
26. Abtahi AM, Granger EK, Tashjian RZ. Factors affecting healing after arthroscopic rotator cuff repair. World J Orthop. 2015;6(2):211-220. doi:10.5312/wjo.v6.i2.211.
27. Chung SW, Oh JH, Gong HS, Kim JY, Kim SH. Factors affecting rotator cuff healing after arthroscopic repair: osteoporosis as one of the independent risk factors. Am J Sports Med. 2011;39(10):2099-2107. doi:10.1177/0363546511415659.
28. Tsiouri C, Mok DH. Early pullout of lateral row knotless anchor in rotator cuff repair. Int J Shoulder Surg. 2009;3(3):63-65. doi:10.4103/0973-6042.59972.
29. Boskey AL, Coleman R. Aging and bone. J Dent Res. 2010;89(12):1333-1348. doi:10.1177/0022034510377791.
30. Cusick MC, Cottrell BJ, Cain RA, Mighell MA. Low incidence of tendon rerupture after distal biceps repair by cortical button and interference screw. J Shoulder Elbow Surg. 2014;23(10):1532-1536. doi:10.1016/j.jse.2014.04.013.
31. Hinchey JW, Aronowitz JG, Sanchez-Sotelo J, Morrey BF. Re-rupture rate of primarily repaired distal biceps tendon injuries. J Shoulder Elbow Surg. 2014;23(6):850-854. doi:10.1016/j.jse.2014.02.006.
32. Shahrulazua A, Duckworth D, Bokor DJ. Perianchor radiolucency following PEEK suture anchor application associated with recurrent shoulder dislocation: a case report. Clin Ter. 2014;165(1):31-34. doi:10.7471/CT.2014.1658.
33. Kim SH, Kim dY, Kwon JE, Park JS, Oh JH. Perianchor cyst formation around biocomposite biodegradable suture anchors after rotator cuff repair. Am J Sports Med. 2015;43(12):2907-2912. doi:10.1177/0363546515608484
34. Potapov A, Laflamme YG, Gagnon S, Canet F, Rouleau DM. Progressive osteolysis of the radius after distal biceps tendon repair with the bioabsorbable screw. J Shoulder Elbow Surg. 2011;20(5):819-826. doi:10.1016/j.jse.2011.02.021.
TAKE-HOME POINTS
- OsteoCrete, a magnesium-based resorbable bone cement, has potential to safely and effectively augment suture anchor fixation.
- OsteoCrete increases anchor pull-out strength within 15 minutes of injection.
- OsteoCrete has a more profound impact on anchors when used within bone of decreased density and quality.
- OsteoCrete does not result in any untoward effect when placed near, or in contact with, rotator cuff or biceps tendons during fixation procedures.
- OsteoCrete can potentially be used to replace the anchor within tenodesis procedures that utilize transcortical button fixation in addition to anchor fixation.
AAD 2018: Navigating the meeting
Dermatology News editorial advisor Adam Friedman, MD, provides his recommendations for navigating the American Academy of Dermatology annual meeting at the San Diego Convention Center Feb. 16-20.
We’ve all seen the “What’s new in the tool shed/box/bucket/* insert noun here*” articles, lecture, videos ... that’s not what I am talking about. Get out of your comfort zone and check out the latest on the diagnosis and treatment of genital skin disorders in session S052 on Monday, Feb. 19, from 9 a.m. to 12 p.m. Get a taste for “Oral Diseases” with session F017 on Friday, Feb. 16, from 1 p.m. to 3 p.m. And who wouldn’t benefit from beefing up on granulomatous diseases with session F092 on Sunday, Feb. 18, from 1 p.m. to 3 p.m.? That was a rhetorical question.
Yes, be basic
Oldies but goodies
I may get older but the quality of some sessions stays the same. Nicholas Soter, MD, has been lecturing on urticaria since before I can remember – make sure to check this legend out in session U081 on Monday from 7:30 a.m. to 8:30 a.m. Joseph Jorrizo, MD, “Captain Complex Med Derm” himself, is directing the session on referral dermatology (F007) on Friday, from 9 a.m. to 11 a.m. (Yes, I know it conflicts with my session – see, no bias!). Last but not least, the ever so popular “Hot Topics” session (S048) on Monday, 9 a.m. to 12 p.m. Led by former AAD Vice President Kenneth Tomecki, MD, this session covers the gamut of what’s “so hot right now” in dermatology. Not to be missed.
Dr. Friedman is director of the residency program, director of translational research, and director of the supportive oncodermatology clinic in the department of dermatology, George Washington University, Washington.
Dermatology News editorial advisor Adam Friedman, MD, provides his recommendations for navigating the American Academy of Dermatology annual meeting at the San Diego Convention Center Feb. 16-20.
We’ve all seen the “What’s new in the tool shed/box/bucket/* insert noun here*” articles, lecture, videos ... that’s not what I am talking about. Get out of your comfort zone and check out the latest on the diagnosis and treatment of genital skin disorders in session S052 on Monday, Feb. 19, from 9 a.m. to 12 p.m. Get a taste for “Oral Diseases” with session F017 on Friday, Feb. 16, from 1 p.m. to 3 p.m. And who wouldn’t benefit from beefing up on granulomatous diseases with session F092 on Sunday, Feb. 18, from 1 p.m. to 3 p.m.? That was a rhetorical question.
Yes, be basic
Oldies but goodies
I may get older but the quality of some sessions stays the same. Nicholas Soter, MD, has been lecturing on urticaria since before I can remember – make sure to check this legend out in session U081 on Monday from 7:30 a.m. to 8:30 a.m. Joseph Jorrizo, MD, “Captain Complex Med Derm” himself, is directing the session on referral dermatology (F007) on Friday, from 9 a.m. to 11 a.m. (Yes, I know it conflicts with my session – see, no bias!). Last but not least, the ever so popular “Hot Topics” session (S048) on Monday, 9 a.m. to 12 p.m. Led by former AAD Vice President Kenneth Tomecki, MD, this session covers the gamut of what’s “so hot right now” in dermatology. Not to be missed.
Dr. Friedman is director of the residency program, director of translational research, and director of the supportive oncodermatology clinic in the department of dermatology, George Washington University, Washington.
Dermatology News editorial advisor Adam Friedman, MD, provides his recommendations for navigating the American Academy of Dermatology annual meeting at the San Diego Convention Center Feb. 16-20.
We’ve all seen the “What’s new in the tool shed/box/bucket/* insert noun here*” articles, lecture, videos ... that’s not what I am talking about. Get out of your comfort zone and check out the latest on the diagnosis and treatment of genital skin disorders in session S052 on Monday, Feb. 19, from 9 a.m. to 12 p.m. Get a taste for “Oral Diseases” with session F017 on Friday, Feb. 16, from 1 p.m. to 3 p.m. And who wouldn’t benefit from beefing up on granulomatous diseases with session F092 on Sunday, Feb. 18, from 1 p.m. to 3 p.m.? That was a rhetorical question.
Yes, be basic
Oldies but goodies
I may get older but the quality of some sessions stays the same. Nicholas Soter, MD, has been lecturing on urticaria since before I can remember – make sure to check this legend out in session U081 on Monday from 7:30 a.m. to 8:30 a.m. Joseph Jorrizo, MD, “Captain Complex Med Derm” himself, is directing the session on referral dermatology (F007) on Friday, from 9 a.m. to 11 a.m. (Yes, I know it conflicts with my session – see, no bias!). Last but not least, the ever so popular “Hot Topics” session (S048) on Monday, 9 a.m. to 12 p.m. Led by former AAD Vice President Kenneth Tomecki, MD, this session covers the gamut of what’s “so hot right now” in dermatology. Not to be missed.
Dr. Friedman is director of the residency program, director of translational research, and director of the supportive oncodermatology clinic in the department of dermatology, George Washington University, Washington.
How to avoid and manage complications when placing ports and docking



USPSTF: Routine screens for ovarian cancer not recommended
does not reduce ovarian cancer mortality and may lead to unnecessary surgery and complications, the U.S. Preventive Services Task Force concluded in a final recommendation statement.
The recommendation statement against screening, along with an evidence report, was published online in JAMA. The USPSTF had issued a recommendation categorized as a D recommendation (“not recommended”) in 2012, and the current review was undertaken to update the evidence on population-based screening.
The task force members based their decision on data from three randomized trials including 293,038 women that assessed ovarian cancer mortality and one trial of 549 women that addressed psychological outcomes.
The screening methods used in the trials included transvaginal ultrasound alone, CA-125 testing alone, and transvaginal ultrasound plus CA-125 testing.
Overall, screening by any of the three methods had no impact on reducing mortality. In addition, surgical complication rates in women without cancer ranged from 3% to 15% across the trials.
The USPSTF found insufficient evidence to comment on potential psychological harms of ovarian cancer screening but said with moderate certainty in the recommendation statement that the harms of routine screening “outweigh the benefit, and the net balance of the benefit and harms of screening is negative,” given the lack of impact on mortality.
The recommendation against screening, however, does not apply to women at increased risk for ovarian cancer because of known genetic mutations, the task force said.
The findings were limited by several factors, including the small percentage of minority women (12%) and lack of generalizability to usual care, the task force members noted. “Further research is needed to identify effective approaches for reducing ovarian cancer incidence and mortality,” they concluded.
The task force members had no financial conflicts to disclose.
SOURCE: Henderson JT et al. JAMA. 2018;319(6):595-606. doi: 10.1001/jama.2017.21421; Grossman DC et al. JAMA. 2018;319(6):588-594. doi: 10.1001/jama.2017.21926.
Abdominal surgery remains the only way to definitely confirm a positive result for ovarian cancer screening, and therefore any screening protocol must achieve a high level of accuracy to minimize the potential for unnecessary procedures in unaffected women, Charles W. Drescher, MD, and Garnet L. Anderson, PhD, wrote in an accompanying editorial in JAMA Oncology (2018 Feb 13. doi: 10.1001/jamaoncol.2018.0028).
“Screening with cancer antigen 125 (CA-125) and transvaginal sonography (TVS) appears practical, but establishing the value of screening is challenging,” they said. Data from three randomized trials failed to show a disease-specific mortality reduction, and the USPSTF recommendations against routine screening align with recent recommendations from the American College of Obstetricians and Gynecologists Committee on Gynecologic Practice and an opinion piece from the Society of Gynecologic Oncology.
Women with germline mutations that increase their risk of ovarian cancer are not included in the recommendations and may be candidates for risk reduction salpingo-oophorectomy (RRSO), which has been shown to reduce ovarian cancer risk but is not confirmed as a preventive measure, the editorialists said.
More targeted screening could improve the likelihood of overall benefit, but the USPSTF recommendations offer “sound clinical and public health recommendations against screening for average-risk, asymptomatic women,” they emphasized. In the meantime, “Potential risks and benefits of screening with CA-125 and TVS deserve to be part of the discussion with high risk women, at least for women not considering RRSO,” they said.
Dr. Drescher and Dr. Anderson are affiliated with the Fred Hutchinson Cancer Center in Seattle. They had no financial conflicts to disclose.
Abdominal surgery remains the only way to definitely confirm a positive result for ovarian cancer screening, and therefore any screening protocol must achieve a high level of accuracy to minimize the potential for unnecessary procedures in unaffected women, Charles W. Drescher, MD, and Garnet L. Anderson, PhD, wrote in an accompanying editorial in JAMA Oncology (2018 Feb 13. doi: 10.1001/jamaoncol.2018.0028).
“Screening with cancer antigen 125 (CA-125) and transvaginal sonography (TVS) appears practical, but establishing the value of screening is challenging,” they said. Data from three randomized trials failed to show a disease-specific mortality reduction, and the USPSTF recommendations against routine screening align with recent recommendations from the American College of Obstetricians and Gynecologists Committee on Gynecologic Practice and an opinion piece from the Society of Gynecologic Oncology.
Women with germline mutations that increase their risk of ovarian cancer are not included in the recommendations and may be candidates for risk reduction salpingo-oophorectomy (RRSO), which has been shown to reduce ovarian cancer risk but is not confirmed as a preventive measure, the editorialists said.
More targeted screening could improve the likelihood of overall benefit, but the USPSTF recommendations offer “sound clinical and public health recommendations against screening for average-risk, asymptomatic women,” they emphasized. In the meantime, “Potential risks and benefits of screening with CA-125 and TVS deserve to be part of the discussion with high risk women, at least for women not considering RRSO,” they said.
Dr. Drescher and Dr. Anderson are affiliated with the Fred Hutchinson Cancer Center in Seattle. They had no financial conflicts to disclose.
Abdominal surgery remains the only way to definitely confirm a positive result for ovarian cancer screening, and therefore any screening protocol must achieve a high level of accuracy to minimize the potential for unnecessary procedures in unaffected women, Charles W. Drescher, MD, and Garnet L. Anderson, PhD, wrote in an accompanying editorial in JAMA Oncology (2018 Feb 13. doi: 10.1001/jamaoncol.2018.0028).
“Screening with cancer antigen 125 (CA-125) and transvaginal sonography (TVS) appears practical, but establishing the value of screening is challenging,” they said. Data from three randomized trials failed to show a disease-specific mortality reduction, and the USPSTF recommendations against routine screening align with recent recommendations from the American College of Obstetricians and Gynecologists Committee on Gynecologic Practice and an opinion piece from the Society of Gynecologic Oncology.
Women with germline mutations that increase their risk of ovarian cancer are not included in the recommendations and may be candidates for risk reduction salpingo-oophorectomy (RRSO), which has been shown to reduce ovarian cancer risk but is not confirmed as a preventive measure, the editorialists said.
More targeted screening could improve the likelihood of overall benefit, but the USPSTF recommendations offer “sound clinical and public health recommendations against screening for average-risk, asymptomatic women,” they emphasized. In the meantime, “Potential risks and benefits of screening with CA-125 and TVS deserve to be part of the discussion with high risk women, at least for women not considering RRSO,” they said.
Dr. Drescher and Dr. Anderson are affiliated with the Fred Hutchinson Cancer Center in Seattle. They had no financial conflicts to disclose.
does not reduce ovarian cancer mortality and may lead to unnecessary surgery and complications, the U.S. Preventive Services Task Force concluded in a final recommendation statement.
The recommendation statement against screening, along with an evidence report, was published online in JAMA. The USPSTF had issued a recommendation categorized as a D recommendation (“not recommended”) in 2012, and the current review was undertaken to update the evidence on population-based screening.
The task force members based their decision on data from three randomized trials including 293,038 women that assessed ovarian cancer mortality and one trial of 549 women that addressed psychological outcomes.
The screening methods used in the trials included transvaginal ultrasound alone, CA-125 testing alone, and transvaginal ultrasound plus CA-125 testing.
Overall, screening by any of the three methods had no impact on reducing mortality. In addition, surgical complication rates in women without cancer ranged from 3% to 15% across the trials.
The USPSTF found insufficient evidence to comment on potential psychological harms of ovarian cancer screening but said with moderate certainty in the recommendation statement that the harms of routine screening “outweigh the benefit, and the net balance of the benefit and harms of screening is negative,” given the lack of impact on mortality.
The recommendation against screening, however, does not apply to women at increased risk for ovarian cancer because of known genetic mutations, the task force said.
The findings were limited by several factors, including the small percentage of minority women (12%) and lack of generalizability to usual care, the task force members noted. “Further research is needed to identify effective approaches for reducing ovarian cancer incidence and mortality,” they concluded.
The task force members had no financial conflicts to disclose.
SOURCE: Henderson JT et al. JAMA. 2018;319(6):595-606. doi: 10.1001/jama.2017.21421; Grossman DC et al. JAMA. 2018;319(6):588-594. doi: 10.1001/jama.2017.21926.
does not reduce ovarian cancer mortality and may lead to unnecessary surgery and complications, the U.S. Preventive Services Task Force concluded in a final recommendation statement.
The recommendation statement against screening, along with an evidence report, was published online in JAMA. The USPSTF had issued a recommendation categorized as a D recommendation (“not recommended”) in 2012, and the current review was undertaken to update the evidence on population-based screening.
The task force members based their decision on data from three randomized trials including 293,038 women that assessed ovarian cancer mortality and one trial of 549 women that addressed psychological outcomes.
The screening methods used in the trials included transvaginal ultrasound alone, CA-125 testing alone, and transvaginal ultrasound plus CA-125 testing.
Overall, screening by any of the three methods had no impact on reducing mortality. In addition, surgical complication rates in women without cancer ranged from 3% to 15% across the trials.
The USPSTF found insufficient evidence to comment on potential psychological harms of ovarian cancer screening but said with moderate certainty in the recommendation statement that the harms of routine screening “outweigh the benefit, and the net balance of the benefit and harms of screening is negative,” given the lack of impact on mortality.
The recommendation against screening, however, does not apply to women at increased risk for ovarian cancer because of known genetic mutations, the task force said.
The findings were limited by several factors, including the small percentage of minority women (12%) and lack of generalizability to usual care, the task force members noted. “Further research is needed to identify effective approaches for reducing ovarian cancer incidence and mortality,” they concluded.
The task force members had no financial conflicts to disclose.
SOURCE: Henderson JT et al. JAMA. 2018;319(6):595-606. doi: 10.1001/jama.2017.21421; Grossman DC et al. JAMA. 2018;319(6):588-594. doi: 10.1001/jama.2017.21926.
FROM JAMA
Key clinical point: Harms associated with ovarian cancer screening included unnecessary surgery and surgical complications.
Major finding: In three trials including 293,038 women, ovarian cancer screening had no significant impact on mortality.
Study details: The recommendations were based on data from four trials including 293,587 women.
Disclosures: The researchers had no financial conflicts to disclose.
Source: Henderson JT et al. JAMA. 2018;319(6):595-606. doi: 10.1001/jama.2017.21421; Grossman DC et al. JAMA. 2018;319(6):588-594. doi: 10.1001/jama.2017.21926.