User login
Antibiotic Overprescribing: Still a Major Concern

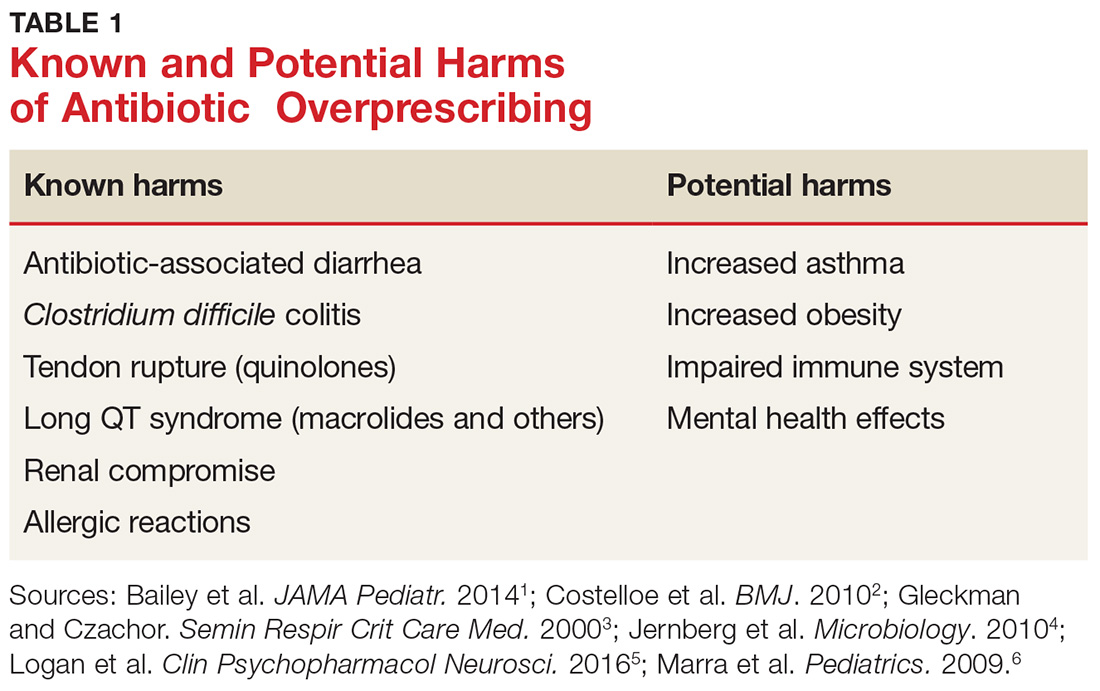
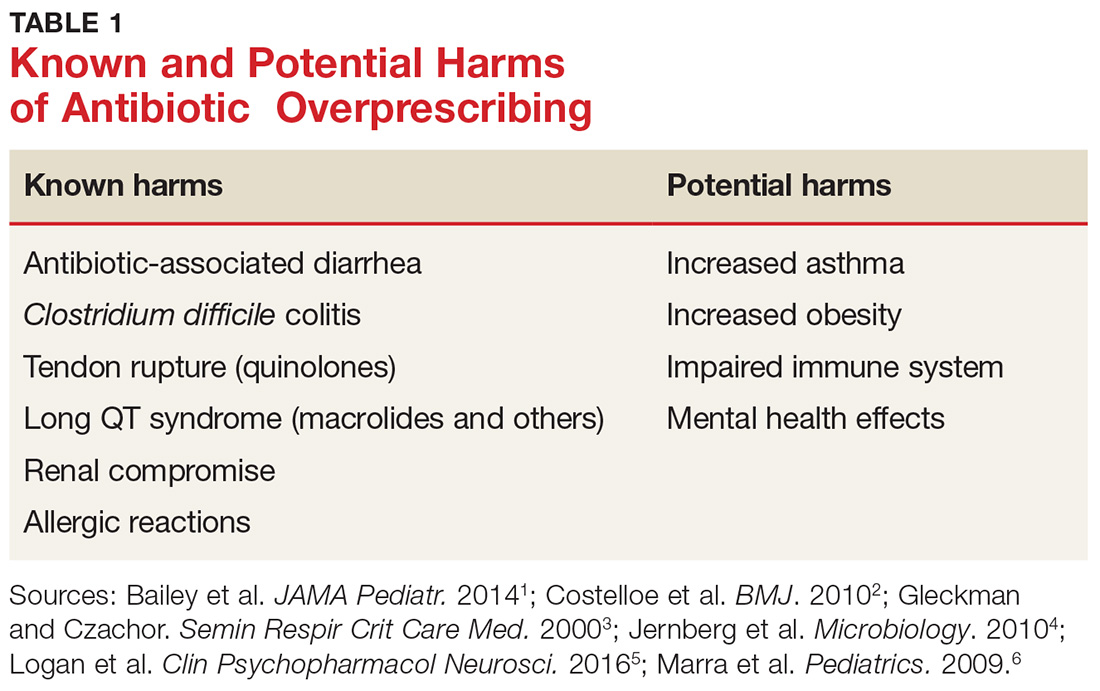
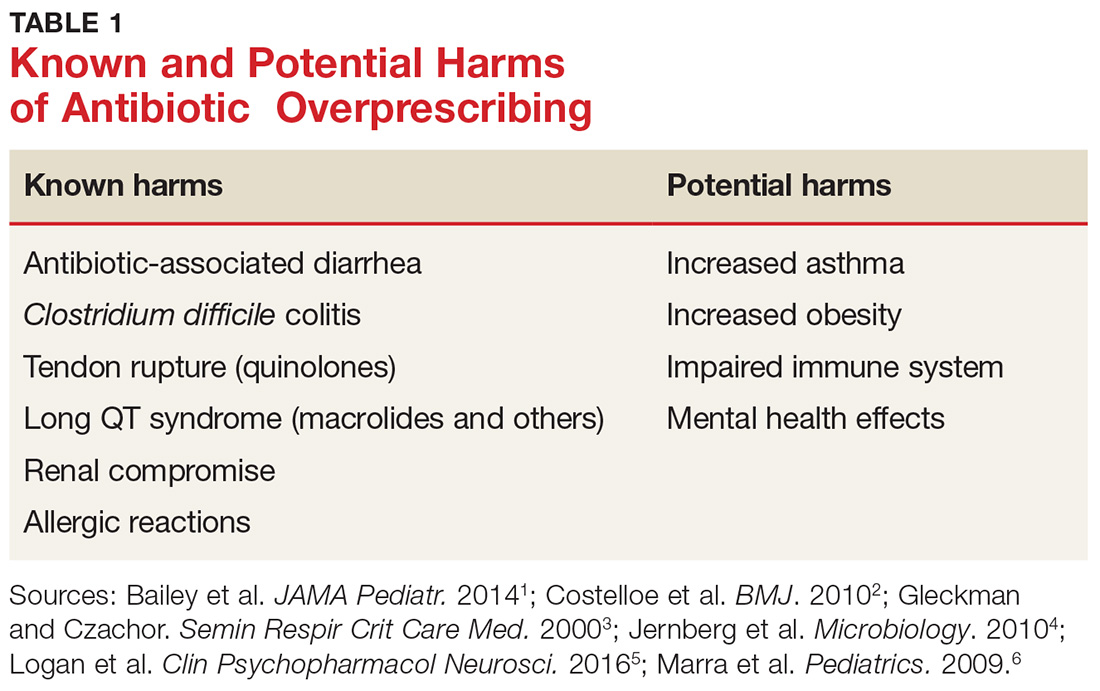
Despite universal agreement that antibiotic overprescribing is a problem, the practice continues to vex us. Antibiotic use—whether appropriate or not—has been linked to rising rates of antimicrobial resistance, disruption of the gut microbiome leading to Clostridium difficile infections (CDI), allergic reactions, and increased health care costs (see Table 1).1-6 And yet, clinicians continue to overprescribe this class of medication.
A 2016 report from the CDC estimates that at least 30% of antibiotics prescribed in US outpatient settings are unnecessary.7 Another report cites a slightly higher figure across a variety of health care settings.8 Pair these findings with the fact that there are currently few new drugs in development to target resistant bacteria, and you have the potential for a postantibiotic era in which common infections could become lethal.7
In 2003, the CDC launched its “Get Smart: Know When Antibiotics Work” program (now known as “Be Antibiotics Aware”), focused on decreasing inappropriate antibiotic use in the outpatient setting.9 In 2015, the White House released the National Action Plan for Combating Antibiotic-Resistant Bacteria, with a goal of decreasing inappropriate outpatient antibiotic use by 50% and inappropriate inpatient use by 20% by 2020.10 And, on an international level, the World Health Organization (WHO) in 2015 developed a five-year strategic framework for implementing its Global Action Plan on Antimicrobial Resistance.11
Family practitioners are on the front lines of this battle. Here’s what we can do now.
WHEN AND WHERE ARE ANTIBIOTICS MOST OFTEN INAPPROPRIATELY PRESCRIBED?
The diagnosis leading to the most frequent inappropriate prescribing of antibiotics is acute respiratory tract infection (ARTI), which includes bronchitis, otitis media, pharyngitis, sinusitis, tonsillitis, the common cold, and pneumonia. Up to 40% of antibiotic prescriptions for these conditions are unnecessary.8,12 Bronchitis is the most common ARTI diagnosis associated with inappropriate antibiotic prescriptions, while sinusitis, suppurative otitis media, and pharyngitis are the diagnoses associated with the lion’s share of all (appropriate and inappropriate) antibiotic prescriptions within the ARTI category.8,9,12,13 Refer to national clinical guidelines, which delineate when antibiotic treatment is appropriate for these conditions.14-16
With respect to setting, there are conflicting findings as to whether antibiotic prescribing differs in office-based versus emergency department (ED) settings.
- One study found a higher rate of antibiotic prescribing during ED visits than office visits (21% vs 9%), even though, between 2007 and 2009, more antibiotic prescriptions were written for adults in primary care offices than in either outpatient hospital clinics or EDs.17
- In a cross-sectional study using data from 2005 to 2010 National Ambulatory Medical Care Surveys (NAMCS) and National Hospital Ambulatory Medical Care Surveys (NHAMCS), more than half of patients with uncomplicated acute rhinosinusitis received a prescription for antibiotics, but there was no overall difference in antibiotic prescriptions between primary care and ED presentation.18
- A retrospective analysis found that between 2006 and 2010, outpatient hospital practices (56%) and community-practice offices (60%) prescribed more antibiotics for ARTIs than EDs did (51%).12
STICK TO NARROW-SPECTRUM AGENTS WHEN POSSIBLE
Using broad-spectrum antibiotics, such as quinolones or imipenem, firstline, contributes more to the problem of antibiotic resistance than does prescribing narrow-spectrum antibiotics such as amoxicillin, cephalexin, or trimethoprim-sulfamethoxazole.7 Yet between 2007 and 2009, broad-spectrum agents were prescribed for 61% of outpatient adult visits in which patients received an antibiotic prescription.17 Quinolones (25%), macrolides (20%), and aminopenicillins (12%) were most commonly prescribed, and antibiotic prescriptions were most often written for respiratory conditions, such as bronchitis, for which we now know antibiotics are rarely indicated.17
Between 2006 and 2008, pediatric patients who received antibiotic prescriptions were given broad-spectrum agents 50% of the time, of which macrolides were the class most commonly prescribed.13
More recently, researchers examined the frequency with which clinicians prescribe narrow-spectrum, firstline antibiotics for otitis media, sinusitis, and pharyngitis using 2010 to 2011 NAMCS/NHAMCS data. They found that providers used firstline agents recommended by professional guidelines 52% of the time, although it was estimated that they would have been appropriate in 80% of cases; pediatric patients were more likely to receive appropriate firstline antibiotics than adult patients.19 Macrolides, especially azithromycin, were the most common non-firstline antibiotics prescribed.19,20 The bottom line is that when antibiotics are indicated for upper respiratory infections (otitis media, sinusitis, and pharyngitis), clinicians should prescribe a narrow-spectrum antibiotic first.
ANTIBIOTIC OVERPRESCIBING AFFECTS THE GUT AND BEYOND
The human intestinal microbiome is composed of a diverse array of bacteria, viruses, and parasites.21 The main functions of the gut microbiome include interacting with the immune system and participating in biochemical reactions in the gut, such as absorption of fat-soluble vitamins and the production of vitamin K.
As we know, antibiotics decrease the diversity of gut bacteria, which, in turn, can cause less efficient nutrient extraction, as well as vulnerability to enteric infections.21 It is well known, for example, that the bacterial gut microbiome can either inhibit or promote diarrheal illnesses such as those caused by CDI. CDI is now the most common health care-related infection, accounting for about a half-million health care facility infections per year.22 It extends hospital stays an average of almost 10 days and is estimated to cost the health care system $6.3 billion annually.23
Antibiotics can also eliminate antibiotic-susceptible organisms, allowing resistant organisms to proliferate.4 They also promote the transmission of genes for antibiotic resistance between gut bacteria.4
Beyond the gut
Less well known is that gut bacteria can promote or inhibit extraintestinal infections.
Gut bacteria and HIV. In early HIV infections, for example, gut populations of Lactobacillus and Bifidobacteria are reduced, and the gut barrier becomes compromised.24 Increasing translocation of bacterial products is associated with HIV disease progression. Preservation of Lactobacillus populations in the gut is associated with markers predictive of better HIV outcomes, including a higher CD4 count, a lower viral load, and less evidence of gut microbial translocation.24 This underscores the importance of maintaining healthy gut flora in patients with HIV, using such steps as avoiding unnecessary antibiotics.
Gut bacteria and stress, depression. Antibiotics directly induce the expression of key genes that affect the stress response.25 While causative studies are lacking, there is a growing body of evidence suggesting that the gut microbiome is involved in two-way communication with the brain and can affect, and be affected by, stress and depression.21,26-30 Diseases and conditions that seem to have a putative connection to a disordered microbiome (dysbiosis) include depression, anxiety, Crohn disease, type 2 diabetes, and obesity. (For a discussion of the relationship between the gut microbiome and diabetes, see Endocrine Consult: The Gut Microbiome in Type 2 Diabetes.)
Gut bacteria and childhood obesity. Repeated use of broader-spectrum antibiotics in children younger than 24 months of age increases the risk for childhood obesity.1,6 One theory for the association is that the effects of broad-spectrum antibiotics on the intestinal flora of young children may alter long-term energy homeostasis, resulting in a higher risk for obesity.1
Gut bacteria and asthma. Studies demonstrate differences in the gut microbiomes of asthmatic and nonasthmatic patients. These differences affect the activities of helper T-cell subsets (Th1 and Th2), which in turn affect the development of immune tolerance.31
Although additional studies are needed to confirm these findings, the evidence collected thus far should make us all pause before prescribing drugs that can alter our microbiome in complex and only partially understood ways.
WHAT CAN WE DO RIGHT NOW?
The issues created by the inappropriate prescribing of antibiotics have been known for decades, and multiple attempts have been made to find solutions and implement change. Although some small successes have occurred, little overall progress has been made in reducing antibiotic prescribing in the general population. A historical review of why clinicians prescribe antibiotics inappropriately and the interventions that have successfully reduced this prescribing may prove valuable as we continue to look for new, effective answers.
Why do we overprescribe antibiotics? A 2015 systematic literature review found that patient demand, pharmaceutical company marketing activities, limited up-to-date information sources, and fear of losing patients are major reasons providers cite for prescribing antibiotics.32
In a separate study that explored antibiotic prescribing habits for acute bronchitis, clinicians cited “patient demand” as the major reason for prescribing antibiotics. Respondents also reported that “other physicians were responsible for inappropriate antibiotic prescribing.”33
Strategies that work
Some early intervention programs directed at reducing antibiotic prescribing demonstrated success (see Table 2).34-36 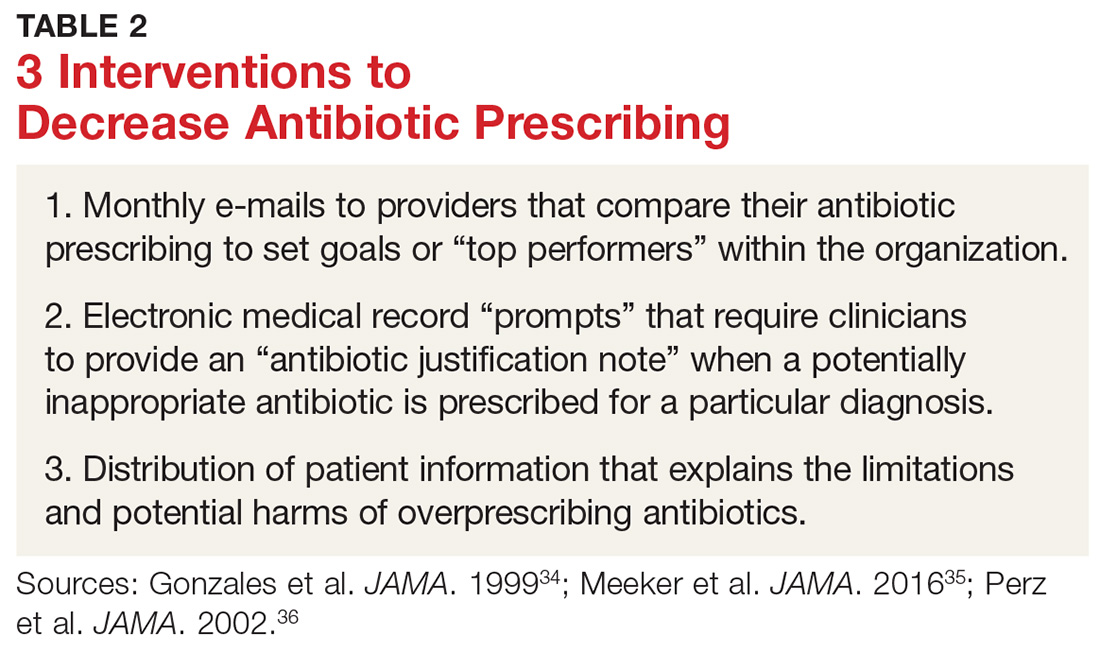
One example comes from a 1996-1998 study of four primary care practices.34 Researchers evaluated the impact of a multidimensional intervention effort targeted at clinicians and patients and aimed at lowering the use of antimicrobial agents for acute uncomplicated bronchitis in adults. It incorporated multiple elements, including office-based and household patient educational materials and a clinician intervention involving education, practice profiling, and academic detailing. Clinicians in this program reduced their rates of antibiotic prescribing for uncomplicated bronchitis from 74% to 48%.34
Employing EMRs. A more recent study focused on use of electronic medical records (EMRs) and communications to modify clinician antibiotic prescribing.35 By sending clinicians monthly emails comparing their prescribing patterns to those of peers and “typical top performers,” inappropriate antibiotic prescriptions for ARTIs went from 19.9% to 3.7%.35
In another effort, the same researchers modified providers’ EMRs to detect when potentially inappropriate antibiotics were prescribed. The system then prompted the clinician to provide an “antibiotic justification note,” which remained visible in the patient’s chart. This approach, which encouraged providers to follow prescribing guidelines by capitalizing on their concerns about their reputations, produced a 77% reduction in antibiotic prescribing.35
Focusing on the public. Studies have also examined the effectiveness of educating the public about when antibiotics are not likely to be helpful and of the harms of unnecessary antibiotics.
Studies conducted in Tennessee and Wisconsin that combined prescriber and community education about unnecessary antibiotics for children found that the intervention reduced antibiotic prescribing in both locations by about 19%, compared with about a 9% reduction in the control groups.36,37
DOES PRESCRIBING ANTIBIOTICS AFFECT PATIENT SATISFACTION?
The results are mixed as to whether prescribing antibiotics affects patient satisfaction. Two studies in the early 2000s found that both patients and parents reported higher satisfaction with clinicians who explained why antibiotics were not indicated versus those who simply prescribed them—and that such explanations do not need to take a lot of time (see Table 3 for patient care tips).37,38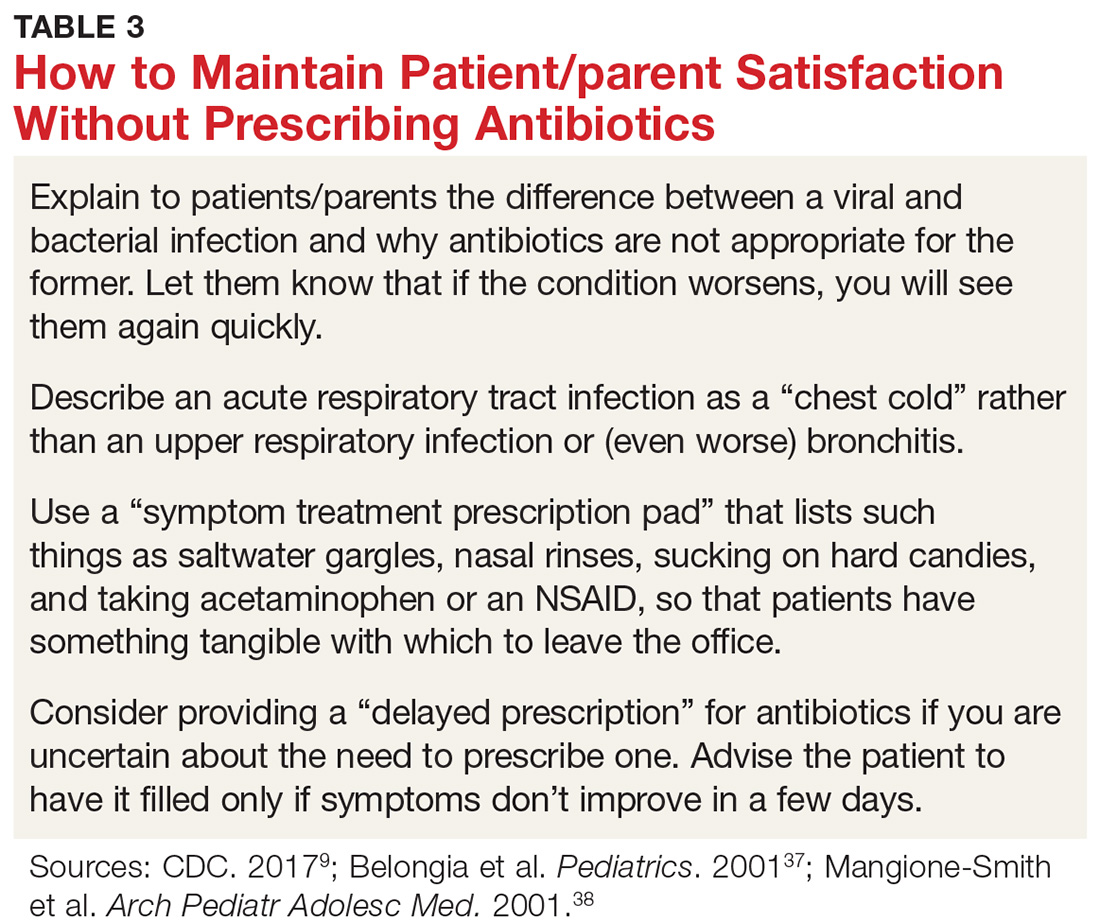
A more recent study found that higher antibiotic prescribing practices in Britain were associated with modestly higher patient satisfaction ratings.39 The authors of this study noted, however, that reduced antibiotic prescribing may be a proxy for other practice patterns that affected satisfaction ratings.
REDUCING ANTIBIOTIC PRESCRIBING REDUCES RESISTANCE
There is also strong evidence that when clinicians decrease antibiotic prescribing, antimicrobial resistance follows suit. One of the earlier landmark studies to demonstrate this was a Finnish study published in 1997.40 The authors found that a reduction of macrolide antibiotic consumption in Finland led to a reduction in streptococci macrolide resistance from 16.5% to 8.6%.40
Multiple studies have since demonstrated similar results for both respiratory and urinary tract infections.41,42 A 2017 meta-analysis of 32 studies found that antibiotic stewardship programs reduced the incidence of infections and colonization with multidrug-resistant Gram-negative bacteria (by 51%), extended-spectrum beta-lactamase–producing Gram-negative bacteria (48%), and methicillin-resistant Staphylococcus aureus (37%). There was also a reduction in the incidence of CDI (32%).43
1. Bailey LC, Forrest CB, Zhang P, et al. Association of antibiotics in infancy with early childhood obesity. JAMA Pediatr. 2014;168:1063-1069.
2. Costelloe C, Metcalfe C, Lovering A, et al. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 2010;340:c2096.
3. Gleckman RA, Czachor JS. Antibiotic side effects. Semin Respir Crit Care Med. 2000;21:53-60.
4. Jernberg C, Löfmark S, Edlund C, et al. Long-term impacts of antibiotic exposure on the human intestinal microbiota. Microbiology. 2010;156:3216-3223.
5. Logan AC, Jacka FN, Craig JM, et al. The microbiome and mental health: looking back, moving forward with lessons from allergic diseases. Clin Psychopharmacol Neurosci. 2016;14:131-147.
6. Marra F, Marra CA, Richardson K, et al. Antibiotic use in children is associated with increased risk of asthma. Pediatrics. 2009;123:1003-1010.
7. Harris AM, Hicks LA, Qaseem A; the High Value Care Task Force of the American College of Physicians and the CDC. Appropriate antibiotic use for acute respiratory tract infection in adults: advice for high-value care from the American College of Physicians and the Centers for Disease Control and Prevention. Ann Intern Med. 2016; 164:425-434.
8. Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010-2011. JAMA. 2016;315: 1864-1873.
9. CDC. Antibiotic prescribing and use. www.cdc.gov/antibiotic-use/index.html. Accessed January 16, 2018.
10. The White House. National action plan for combating antibiotic-resistant bacteria. March 2015:1-63. https://obamawhitehouse.archives.gov/sites/default/files/docs/national_action_plan_for_combating_antibotic-resistant_bacteria.pdf. Accessed January 16, 2018.
11. World Health Organization. Global action plan on antimicrobial resistance (2015). www.who.int/antimicrobial-resistance/global-action-plan/en/. Accessed January 16, 2018.
12. Barlam TF, Soria-Saucedo R, Cabral HJ, et al. Unnecessary antibiotics for acute respiratory tract infections: association with care setting and patient demographics. Open Forum Infect Dis. 2016;3:1-7.
13. Hersh AL, Shapiro DJ, Pavia AT, et al. Antibiotic prescribing in ambulatory pediatrics in the United States. Pediatrics. 2011;128:1053-1061.
14. Chow AW, Benninger MS, Brook I, et al. Executive summary: IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54:1041-1045.
15. Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015;152(2 suppl):S1-S39.
16. Shulman ST, Bisno AL, Clegg HW, et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis. 2012;55:1279-1282.
17. Shapiro DJ, Hicks LA, Pavia AT, et al. Antibiotic prescribing for adults in ambulatory care in the USA, 2007-09. J Antimicrob Chemother. 2014;69:234-240.
18. Bergmark RW, Sedaghat AR. Antibiotic prescription for acute rhinosinusitis: emergency departments versus primary care providers. Laryngoscope. 2016;126:2439-2444.
19. Hersh AL, Fleming-Dutra KE, Shapiro DJ, et al. Frequency of first-line antibiotic selection among US ambulatory care visits for otitis media, sinusitis, and pharyngitis. JAMA Intern Med. 2016;176:1870-1872.
20. Hicks LA, Bartoces MG, Roberts RM, et al. US outpatient antibiotic prescribing variation according to geography, patient population, and provider specialty in 2011. Clin Infect Dis. 2015;60:1308-1316.
21. Langdon A, Crook N, Dantas G. The effects of antibiotics on the microbiome throughout development and alternative approaches for therapeutic modulation. Genome Med. 2016;8:39.
22. Lessa FC, Gould CV, McDonald CL. Current status of Clostridium difficile infection epidemiology. Clin Infect Dis. 2012;55(suppl 2):S65-S70.
23. Zhang S, Palazuelos-Munoz S, Balsells EM, et al. Cost of hospital management of Clostridium difficile infection in United States—a meta-analysis and modelling study. BMC Infect Dis. 2016;16:447.
24. Pérez-Santiago J, Gianella S, Massanella M, et al. Gut lactobacillales are associated with higher CD4 and less microbial translocation during HIV infection. AIDS. 2013;27:1921-1931.
25. Maurice CF, Haiser HJ, Turnbaugh PJ. Xenobiotics shape the physiology and gene expression of the active human gut microbiome. Cell. 2013;152:39-50.
26. Bravo JA, Julio-Pieper M, Forsythe P, et al. Communication between gastrointestinal bacteria and the nervous system. Curr Opin Pharmacol. 2012;12:667-672.
27. Clemente JC, Ursell LK, Parfrey LW, et al. The impact of the gut microbiota on human health: an integrative view. Cell. 2012;148:1258-1270.
28. Dinan TG, Cryan JF. Regulation of the stress response by the gut microbiota: implications for psychoneuroendocrinology. Psychoneuroendocrinology. 2012;37:1369-1378.
29. Foster JA, McVey Neufeld KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 2013;36:305-312.
30. Wang Y, Kasper LH. The role of microbiome in central nervous system disorders. Brain Behav Immun. 2014; 38:1-12.31. Riiser A. The human microbiome, asthma, and allergy. Allergy Asthma Clin Immunol. 2015;11:35.
32. Md Rezal RS, Hassali MA, Alrasheedy AA, et al. Physicians’ knowledge, perceptions and behaviour towards antibiotic prescribing: a systematic review of the literature. Expert Rev Anti Infect Ther. 2015;13:665-680.
33. Dempsey PP, Businger AC, Whaley LE, et al. Primary care clinicians’ perceptions about antibiotic prescribing for acute bronchitis: a qualitative study. BMC Fam Pract . 2014;15:194.
34. Gonzales R, Steiner JF, Lum A, et al. Decreasing antibiotic use in ambulatory practice. JAMA . 1999;281:1512-1519.
35. Meeker D, Linder JA, Fox CR, et al. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices: a randomized clinical trial. JAMA . 2016;315:562-570.
36. Perz JF, Craig AS, Coffey CS, et al. Changes in antibiotic prescribing for children after a community-wide campaign. JAMA . 2002;287:3103-3109.
37. Belongia EA, Sullivan BJ, Chyou PH, et al. A community intervention trial to promote judicious antibiotic use and reduce penicillin-resistant Streptococcus pneumoniae carriage in children. Pediatrics . 2001;108:575-583.
38. Mangione-Smith R, McGlynn EA, Elliott MN, et al. Parent expectations for antibiotics, physician-parent communication, and satisfaction. Arch Pediatr Adolesc Med. 2001;155:800-806.
39. Ashworth M, White P, Jongsma H, et al. Antibiotic prescribing and patient satisfaction in primary care in England: cross-sectional analysis of national patient survey data and prescribing data. Br J Gen Pract . 2016;66:e40-e46.
40. Seppälä H, Klaukka T, Vuopio-Varkila J, et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in group A streptococci in Finland. N Engl J Med. 1997;337:441-446.
41. Guillemot D, Varon E, Bernède C, et al. Reduction of antibiotic use in the community reduces the rate of colonization with penicillin g–nonsusceptible Streptococcus pneumoniae . Clin Infect Dis. 2005;41:930-938.
42. Butler CC, Dunstan F, Heginbothom M, et al. Containing antibiotic resistance: decreased antibiotic-resistant coliform urinary tract infections with reduction in antibiotic prescribing by general practices. Br J Gen Pract. 2007; 57:785-792.
43. Baur D, Gladstone BP, Burkert F, et al. Effect of antibiotic stewardship on the incidence of infection and colonisation with antibiotic-resistant bacteria and Clostridium difficile infection: a systematic review and meta-analysis. Lancet Infect Dis. 2017;17:990-1001.

Despite universal agreement that antibiotic overprescribing is a problem, the practice continues to vex us. Antibiotic use—whether appropriate or not—has been linked to rising rates of antimicrobial resistance, disruption of the gut microbiome leading to Clostridium difficile infections (CDI), allergic reactions, and increased health care costs (see Table 1).1-6 And yet, clinicians continue to overprescribe this class of medication.
A 2016 report from the CDC estimates that at least 30% of antibiotics prescribed in US outpatient settings are unnecessary.7 Another report cites a slightly higher figure across a variety of health care settings.8 Pair these findings with the fact that there are currently few new drugs in development to target resistant bacteria, and you have the potential for a postantibiotic era in which common infections could become lethal.7
In 2003, the CDC launched its “Get Smart: Know When Antibiotics Work” program (now known as “Be Antibiotics Aware”), focused on decreasing inappropriate antibiotic use in the outpatient setting.9 In 2015, the White House released the National Action Plan for Combating Antibiotic-Resistant Bacteria, with a goal of decreasing inappropriate outpatient antibiotic use by 50% and inappropriate inpatient use by 20% by 2020.10 And, on an international level, the World Health Organization (WHO) in 2015 developed a five-year strategic framework for implementing its Global Action Plan on Antimicrobial Resistance.11
Family practitioners are on the front lines of this battle. Here’s what we can do now.
WHEN AND WHERE ARE ANTIBIOTICS MOST OFTEN INAPPROPRIATELY PRESCRIBED?
The diagnosis leading to the most frequent inappropriate prescribing of antibiotics is acute respiratory tract infection (ARTI), which includes bronchitis, otitis media, pharyngitis, sinusitis, tonsillitis, the common cold, and pneumonia. Up to 40% of antibiotic prescriptions for these conditions are unnecessary.8,12 Bronchitis is the most common ARTI diagnosis associated with inappropriate antibiotic prescriptions, while sinusitis, suppurative otitis media, and pharyngitis are the diagnoses associated with the lion’s share of all (appropriate and inappropriate) antibiotic prescriptions within the ARTI category.8,9,12,13 Refer to national clinical guidelines, which delineate when antibiotic treatment is appropriate for these conditions.14-16
With respect to setting, there are conflicting findings as to whether antibiotic prescribing differs in office-based versus emergency department (ED) settings.
- One study found a higher rate of antibiotic prescribing during ED visits than office visits (21% vs 9%), even though, between 2007 and 2009, more antibiotic prescriptions were written for adults in primary care offices than in either outpatient hospital clinics or EDs.17
- In a cross-sectional study using data from 2005 to 2010 National Ambulatory Medical Care Surveys (NAMCS) and National Hospital Ambulatory Medical Care Surveys (NHAMCS), more than half of patients with uncomplicated acute rhinosinusitis received a prescription for antibiotics, but there was no overall difference in antibiotic prescriptions between primary care and ED presentation.18
- A retrospective analysis found that between 2006 and 2010, outpatient hospital practices (56%) and community-practice offices (60%) prescribed more antibiotics for ARTIs than EDs did (51%).12
STICK TO NARROW-SPECTRUM AGENTS WHEN POSSIBLE
Using broad-spectrum antibiotics, such as quinolones or imipenem, firstline, contributes more to the problem of antibiotic resistance than does prescribing narrow-spectrum antibiotics such as amoxicillin, cephalexin, or trimethoprim-sulfamethoxazole.7 Yet between 2007 and 2009, broad-spectrum agents were prescribed for 61% of outpatient adult visits in which patients received an antibiotic prescription.17 Quinolones (25%), macrolides (20%), and aminopenicillins (12%) were most commonly prescribed, and antibiotic prescriptions were most often written for respiratory conditions, such as bronchitis, for which we now know antibiotics are rarely indicated.17
Between 2006 and 2008, pediatric patients who received antibiotic prescriptions were given broad-spectrum agents 50% of the time, of which macrolides were the class most commonly prescribed.13
More recently, researchers examined the frequency with which clinicians prescribe narrow-spectrum, firstline antibiotics for otitis media, sinusitis, and pharyngitis using 2010 to 2011 NAMCS/NHAMCS data. They found that providers used firstline agents recommended by professional guidelines 52% of the time, although it was estimated that they would have been appropriate in 80% of cases; pediatric patients were more likely to receive appropriate firstline antibiotics than adult patients.19 Macrolides, especially azithromycin, were the most common non-firstline antibiotics prescribed.19,20 The bottom line is that when antibiotics are indicated for upper respiratory infections (otitis media, sinusitis, and pharyngitis), clinicians should prescribe a narrow-spectrum antibiotic first.
ANTIBIOTIC OVERPRESCIBING AFFECTS THE GUT AND BEYOND
The human intestinal microbiome is composed of a diverse array of bacteria, viruses, and parasites.21 The main functions of the gut microbiome include interacting with the immune system and participating in biochemical reactions in the gut, such as absorption of fat-soluble vitamins and the production of vitamin K.
As we know, antibiotics decrease the diversity of gut bacteria, which, in turn, can cause less efficient nutrient extraction, as well as vulnerability to enteric infections.21 It is well known, for example, that the bacterial gut microbiome can either inhibit or promote diarrheal illnesses such as those caused by CDI. CDI is now the most common health care-related infection, accounting for about a half-million health care facility infections per year.22 It extends hospital stays an average of almost 10 days and is estimated to cost the health care system $6.3 billion annually.23
Antibiotics can also eliminate antibiotic-susceptible organisms, allowing resistant organisms to proliferate.4 They also promote the transmission of genes for antibiotic resistance between gut bacteria.4
Beyond the gut
Less well known is that gut bacteria can promote or inhibit extraintestinal infections.
Gut bacteria and HIV. In early HIV infections, for example, gut populations of Lactobacillus and Bifidobacteria are reduced, and the gut barrier becomes compromised.24 Increasing translocation of bacterial products is associated with HIV disease progression. Preservation of Lactobacillus populations in the gut is associated with markers predictive of better HIV outcomes, including a higher CD4 count, a lower viral load, and less evidence of gut microbial translocation.24 This underscores the importance of maintaining healthy gut flora in patients with HIV, using such steps as avoiding unnecessary antibiotics.
Gut bacteria and stress, depression. Antibiotics directly induce the expression of key genes that affect the stress response.25 While causative studies are lacking, there is a growing body of evidence suggesting that the gut microbiome is involved in two-way communication with the brain and can affect, and be affected by, stress and depression.21,26-30 Diseases and conditions that seem to have a putative connection to a disordered microbiome (dysbiosis) include depression, anxiety, Crohn disease, type 2 diabetes, and obesity. (For a discussion of the relationship between the gut microbiome and diabetes, see Endocrine Consult: The Gut Microbiome in Type 2 Diabetes.)
Gut bacteria and childhood obesity. Repeated use of broader-spectrum antibiotics in children younger than 24 months of age increases the risk for childhood obesity.1,6 One theory for the association is that the effects of broad-spectrum antibiotics on the intestinal flora of young children may alter long-term energy homeostasis, resulting in a higher risk for obesity.1
Gut bacteria and asthma. Studies demonstrate differences in the gut microbiomes of asthmatic and nonasthmatic patients. These differences affect the activities of helper T-cell subsets (Th1 and Th2), which in turn affect the development of immune tolerance.31
Although additional studies are needed to confirm these findings, the evidence collected thus far should make us all pause before prescribing drugs that can alter our microbiome in complex and only partially understood ways.
WHAT CAN WE DO RIGHT NOW?
The issues created by the inappropriate prescribing of antibiotics have been known for decades, and multiple attempts have been made to find solutions and implement change. Although some small successes have occurred, little overall progress has been made in reducing antibiotic prescribing in the general population. A historical review of why clinicians prescribe antibiotics inappropriately and the interventions that have successfully reduced this prescribing may prove valuable as we continue to look for new, effective answers.
Why do we overprescribe antibiotics? A 2015 systematic literature review found that patient demand, pharmaceutical company marketing activities, limited up-to-date information sources, and fear of losing patients are major reasons providers cite for prescribing antibiotics.32
In a separate study that explored antibiotic prescribing habits for acute bronchitis, clinicians cited “patient demand” as the major reason for prescribing antibiotics. Respondents also reported that “other physicians were responsible for inappropriate antibiotic prescribing.”33
Strategies that work
Some early intervention programs directed at reducing antibiotic prescribing demonstrated success (see Table 2).34-36 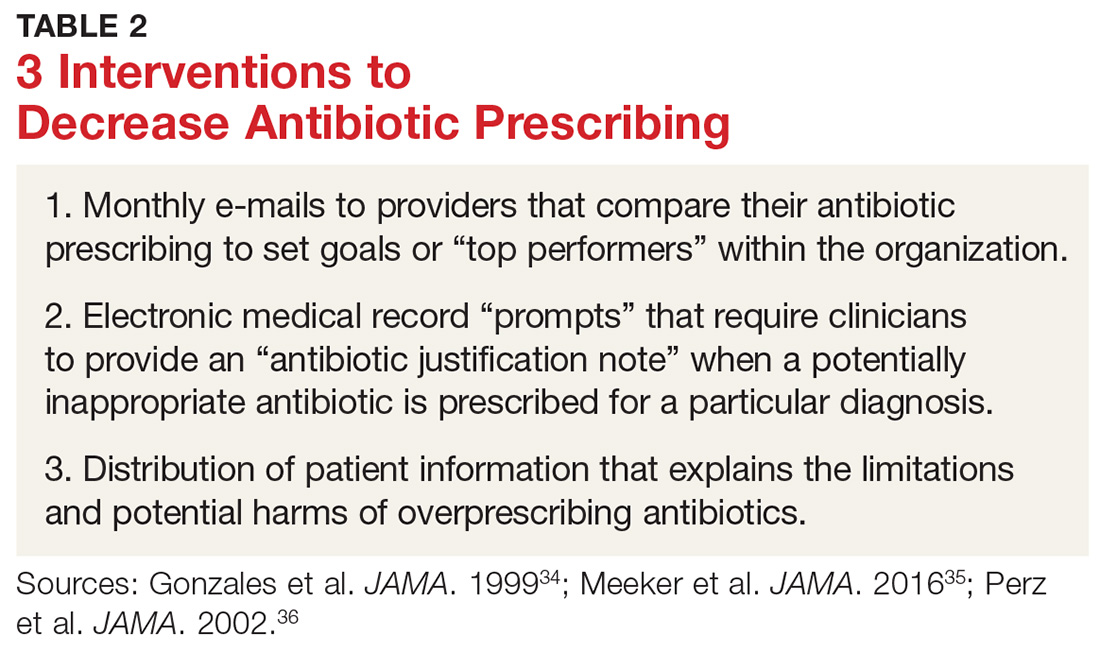
One example comes from a 1996-1998 study of four primary care practices.34 Researchers evaluated the impact of a multidimensional intervention effort targeted at clinicians and patients and aimed at lowering the use of antimicrobial agents for acute uncomplicated bronchitis in adults. It incorporated multiple elements, including office-based and household patient educational materials and a clinician intervention involving education, practice profiling, and academic detailing. Clinicians in this program reduced their rates of antibiotic prescribing for uncomplicated bronchitis from 74% to 48%.34
Employing EMRs. A more recent study focused on use of electronic medical records (EMRs) and communications to modify clinician antibiotic prescribing.35 By sending clinicians monthly emails comparing their prescribing patterns to those of peers and “typical top performers,” inappropriate antibiotic prescriptions for ARTIs went from 19.9% to 3.7%.35
In another effort, the same researchers modified providers’ EMRs to detect when potentially inappropriate antibiotics were prescribed. The system then prompted the clinician to provide an “antibiotic justification note,” which remained visible in the patient’s chart. This approach, which encouraged providers to follow prescribing guidelines by capitalizing on their concerns about their reputations, produced a 77% reduction in antibiotic prescribing.35
Focusing on the public. Studies have also examined the effectiveness of educating the public about when antibiotics are not likely to be helpful and of the harms of unnecessary antibiotics.
Studies conducted in Tennessee and Wisconsin that combined prescriber and community education about unnecessary antibiotics for children found that the intervention reduced antibiotic prescribing in both locations by about 19%, compared with about a 9% reduction in the control groups.36,37
DOES PRESCRIBING ANTIBIOTICS AFFECT PATIENT SATISFACTION?
The results are mixed as to whether prescribing antibiotics affects patient satisfaction. Two studies in the early 2000s found that both patients and parents reported higher satisfaction with clinicians who explained why antibiotics were not indicated versus those who simply prescribed them—and that such explanations do not need to take a lot of time (see Table 3 for patient care tips).37,38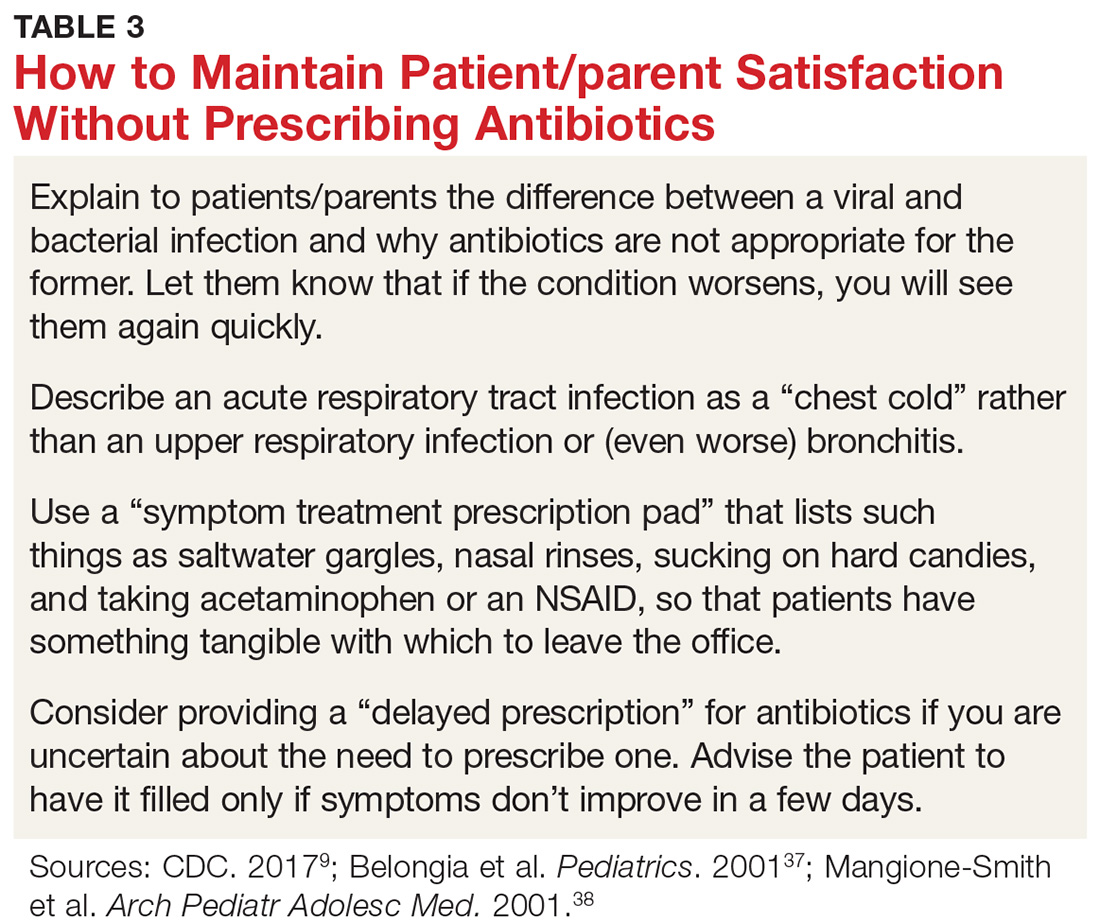
A more recent study found that higher antibiotic prescribing practices in Britain were associated with modestly higher patient satisfaction ratings.39 The authors of this study noted, however, that reduced antibiotic prescribing may be a proxy for other practice patterns that affected satisfaction ratings.
REDUCING ANTIBIOTIC PRESCRIBING REDUCES RESISTANCE
There is also strong evidence that when clinicians decrease antibiotic prescribing, antimicrobial resistance follows suit. One of the earlier landmark studies to demonstrate this was a Finnish study published in 1997.40 The authors found that a reduction of macrolide antibiotic consumption in Finland led to a reduction in streptococci macrolide resistance from 16.5% to 8.6%.40
Multiple studies have since demonstrated similar results for both respiratory and urinary tract infections.41,42 A 2017 meta-analysis of 32 studies found that antibiotic stewardship programs reduced the incidence of infections and colonization with multidrug-resistant Gram-negative bacteria (by 51%), extended-spectrum beta-lactamase–producing Gram-negative bacteria (48%), and methicillin-resistant Staphylococcus aureus (37%). There was also a reduction in the incidence of CDI (32%).43

Despite universal agreement that antibiotic overprescribing is a problem, the practice continues to vex us. Antibiotic use—whether appropriate or not—has been linked to rising rates of antimicrobial resistance, disruption of the gut microbiome leading to Clostridium difficile infections (CDI), allergic reactions, and increased health care costs (see Table 1).1-6 And yet, clinicians continue to overprescribe this class of medication.
A 2016 report from the CDC estimates that at least 30% of antibiotics prescribed in US outpatient settings are unnecessary.7 Another report cites a slightly higher figure across a variety of health care settings.8 Pair these findings with the fact that there are currently few new drugs in development to target resistant bacteria, and you have the potential for a postantibiotic era in which common infections could become lethal.7
In 2003, the CDC launched its “Get Smart: Know When Antibiotics Work” program (now known as “Be Antibiotics Aware”), focused on decreasing inappropriate antibiotic use in the outpatient setting.9 In 2015, the White House released the National Action Plan for Combating Antibiotic-Resistant Bacteria, with a goal of decreasing inappropriate outpatient antibiotic use by 50% and inappropriate inpatient use by 20% by 2020.10 And, on an international level, the World Health Organization (WHO) in 2015 developed a five-year strategic framework for implementing its Global Action Plan on Antimicrobial Resistance.11
Family practitioners are on the front lines of this battle. Here’s what we can do now.
WHEN AND WHERE ARE ANTIBIOTICS MOST OFTEN INAPPROPRIATELY PRESCRIBED?
The diagnosis leading to the most frequent inappropriate prescribing of antibiotics is acute respiratory tract infection (ARTI), which includes bronchitis, otitis media, pharyngitis, sinusitis, tonsillitis, the common cold, and pneumonia. Up to 40% of antibiotic prescriptions for these conditions are unnecessary.8,12 Bronchitis is the most common ARTI diagnosis associated with inappropriate antibiotic prescriptions, while sinusitis, suppurative otitis media, and pharyngitis are the diagnoses associated with the lion’s share of all (appropriate and inappropriate) antibiotic prescriptions within the ARTI category.8,9,12,13 Refer to national clinical guidelines, which delineate when antibiotic treatment is appropriate for these conditions.14-16
With respect to setting, there are conflicting findings as to whether antibiotic prescribing differs in office-based versus emergency department (ED) settings.
- One study found a higher rate of antibiotic prescribing during ED visits than office visits (21% vs 9%), even though, between 2007 and 2009, more antibiotic prescriptions were written for adults in primary care offices than in either outpatient hospital clinics or EDs.17
- In a cross-sectional study using data from 2005 to 2010 National Ambulatory Medical Care Surveys (NAMCS) and National Hospital Ambulatory Medical Care Surveys (NHAMCS), more than half of patients with uncomplicated acute rhinosinusitis received a prescription for antibiotics, but there was no overall difference in antibiotic prescriptions between primary care and ED presentation.18
- A retrospective analysis found that between 2006 and 2010, outpatient hospital practices (56%) and community-practice offices (60%) prescribed more antibiotics for ARTIs than EDs did (51%).12
STICK TO NARROW-SPECTRUM AGENTS WHEN POSSIBLE
Using broad-spectrum antibiotics, such as quinolones or imipenem, firstline, contributes more to the problem of antibiotic resistance than does prescribing narrow-spectrum antibiotics such as amoxicillin, cephalexin, or trimethoprim-sulfamethoxazole.7 Yet between 2007 and 2009, broad-spectrum agents were prescribed for 61% of outpatient adult visits in which patients received an antibiotic prescription.17 Quinolones (25%), macrolides (20%), and aminopenicillins (12%) were most commonly prescribed, and antibiotic prescriptions were most often written for respiratory conditions, such as bronchitis, for which we now know antibiotics are rarely indicated.17
Between 2006 and 2008, pediatric patients who received antibiotic prescriptions were given broad-spectrum agents 50% of the time, of which macrolides were the class most commonly prescribed.13
More recently, researchers examined the frequency with which clinicians prescribe narrow-spectrum, firstline antibiotics for otitis media, sinusitis, and pharyngitis using 2010 to 2011 NAMCS/NHAMCS data. They found that providers used firstline agents recommended by professional guidelines 52% of the time, although it was estimated that they would have been appropriate in 80% of cases; pediatric patients were more likely to receive appropriate firstline antibiotics than adult patients.19 Macrolides, especially azithromycin, were the most common non-firstline antibiotics prescribed.19,20 The bottom line is that when antibiotics are indicated for upper respiratory infections (otitis media, sinusitis, and pharyngitis), clinicians should prescribe a narrow-spectrum antibiotic first.
ANTIBIOTIC OVERPRESCIBING AFFECTS THE GUT AND BEYOND
The human intestinal microbiome is composed of a diverse array of bacteria, viruses, and parasites.21 The main functions of the gut microbiome include interacting with the immune system and participating in biochemical reactions in the gut, such as absorption of fat-soluble vitamins and the production of vitamin K.
As we know, antibiotics decrease the diversity of gut bacteria, which, in turn, can cause less efficient nutrient extraction, as well as vulnerability to enteric infections.21 It is well known, for example, that the bacterial gut microbiome can either inhibit or promote diarrheal illnesses such as those caused by CDI. CDI is now the most common health care-related infection, accounting for about a half-million health care facility infections per year.22 It extends hospital stays an average of almost 10 days and is estimated to cost the health care system $6.3 billion annually.23
Antibiotics can also eliminate antibiotic-susceptible organisms, allowing resistant organisms to proliferate.4 They also promote the transmission of genes for antibiotic resistance between gut bacteria.4
Beyond the gut
Less well known is that gut bacteria can promote or inhibit extraintestinal infections.
Gut bacteria and HIV. In early HIV infections, for example, gut populations of Lactobacillus and Bifidobacteria are reduced, and the gut barrier becomes compromised.24 Increasing translocation of bacterial products is associated with HIV disease progression. Preservation of Lactobacillus populations in the gut is associated with markers predictive of better HIV outcomes, including a higher CD4 count, a lower viral load, and less evidence of gut microbial translocation.24 This underscores the importance of maintaining healthy gut flora in patients with HIV, using such steps as avoiding unnecessary antibiotics.
Gut bacteria and stress, depression. Antibiotics directly induce the expression of key genes that affect the stress response.25 While causative studies are lacking, there is a growing body of evidence suggesting that the gut microbiome is involved in two-way communication with the brain and can affect, and be affected by, stress and depression.21,26-30 Diseases and conditions that seem to have a putative connection to a disordered microbiome (dysbiosis) include depression, anxiety, Crohn disease, type 2 diabetes, and obesity. (For a discussion of the relationship between the gut microbiome and diabetes, see Endocrine Consult: The Gut Microbiome in Type 2 Diabetes.)
Gut bacteria and childhood obesity. Repeated use of broader-spectrum antibiotics in children younger than 24 months of age increases the risk for childhood obesity.1,6 One theory for the association is that the effects of broad-spectrum antibiotics on the intestinal flora of young children may alter long-term energy homeostasis, resulting in a higher risk for obesity.1
Gut bacteria and asthma. Studies demonstrate differences in the gut microbiomes of asthmatic and nonasthmatic patients. These differences affect the activities of helper T-cell subsets (Th1 and Th2), which in turn affect the development of immune tolerance.31
Although additional studies are needed to confirm these findings, the evidence collected thus far should make us all pause before prescribing drugs that can alter our microbiome in complex and only partially understood ways.
WHAT CAN WE DO RIGHT NOW?
The issues created by the inappropriate prescribing of antibiotics have been known for decades, and multiple attempts have been made to find solutions and implement change. Although some small successes have occurred, little overall progress has been made in reducing antibiotic prescribing in the general population. A historical review of why clinicians prescribe antibiotics inappropriately and the interventions that have successfully reduced this prescribing may prove valuable as we continue to look for new, effective answers.
Why do we overprescribe antibiotics? A 2015 systematic literature review found that patient demand, pharmaceutical company marketing activities, limited up-to-date information sources, and fear of losing patients are major reasons providers cite for prescribing antibiotics.32
In a separate study that explored antibiotic prescribing habits for acute bronchitis, clinicians cited “patient demand” as the major reason for prescribing antibiotics. Respondents also reported that “other physicians were responsible for inappropriate antibiotic prescribing.”33
Strategies that work
Some early intervention programs directed at reducing antibiotic prescribing demonstrated success (see Table 2).34-36 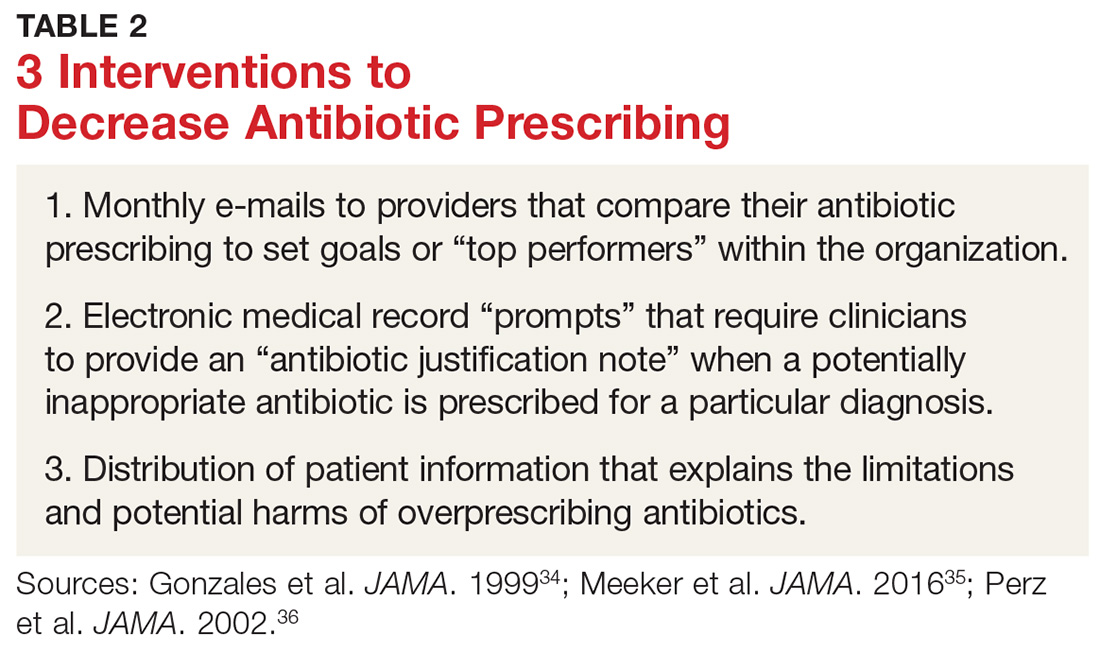
One example comes from a 1996-1998 study of four primary care practices.34 Researchers evaluated the impact of a multidimensional intervention effort targeted at clinicians and patients and aimed at lowering the use of antimicrobial agents for acute uncomplicated bronchitis in adults. It incorporated multiple elements, including office-based and household patient educational materials and a clinician intervention involving education, practice profiling, and academic detailing. Clinicians in this program reduced their rates of antibiotic prescribing for uncomplicated bronchitis from 74% to 48%.34
Employing EMRs. A more recent study focused on use of electronic medical records (EMRs) and communications to modify clinician antibiotic prescribing.35 By sending clinicians monthly emails comparing their prescribing patterns to those of peers and “typical top performers,” inappropriate antibiotic prescriptions for ARTIs went from 19.9% to 3.7%.35
In another effort, the same researchers modified providers’ EMRs to detect when potentially inappropriate antibiotics were prescribed. The system then prompted the clinician to provide an “antibiotic justification note,” which remained visible in the patient’s chart. This approach, which encouraged providers to follow prescribing guidelines by capitalizing on their concerns about their reputations, produced a 77% reduction in antibiotic prescribing.35
Focusing on the public. Studies have also examined the effectiveness of educating the public about when antibiotics are not likely to be helpful and of the harms of unnecessary antibiotics.
Studies conducted in Tennessee and Wisconsin that combined prescriber and community education about unnecessary antibiotics for children found that the intervention reduced antibiotic prescribing in both locations by about 19%, compared with about a 9% reduction in the control groups.36,37
DOES PRESCRIBING ANTIBIOTICS AFFECT PATIENT SATISFACTION?
The results are mixed as to whether prescribing antibiotics affects patient satisfaction. Two studies in the early 2000s found that both patients and parents reported higher satisfaction with clinicians who explained why antibiotics were not indicated versus those who simply prescribed them—and that such explanations do not need to take a lot of time (see Table 3 for patient care tips).37,38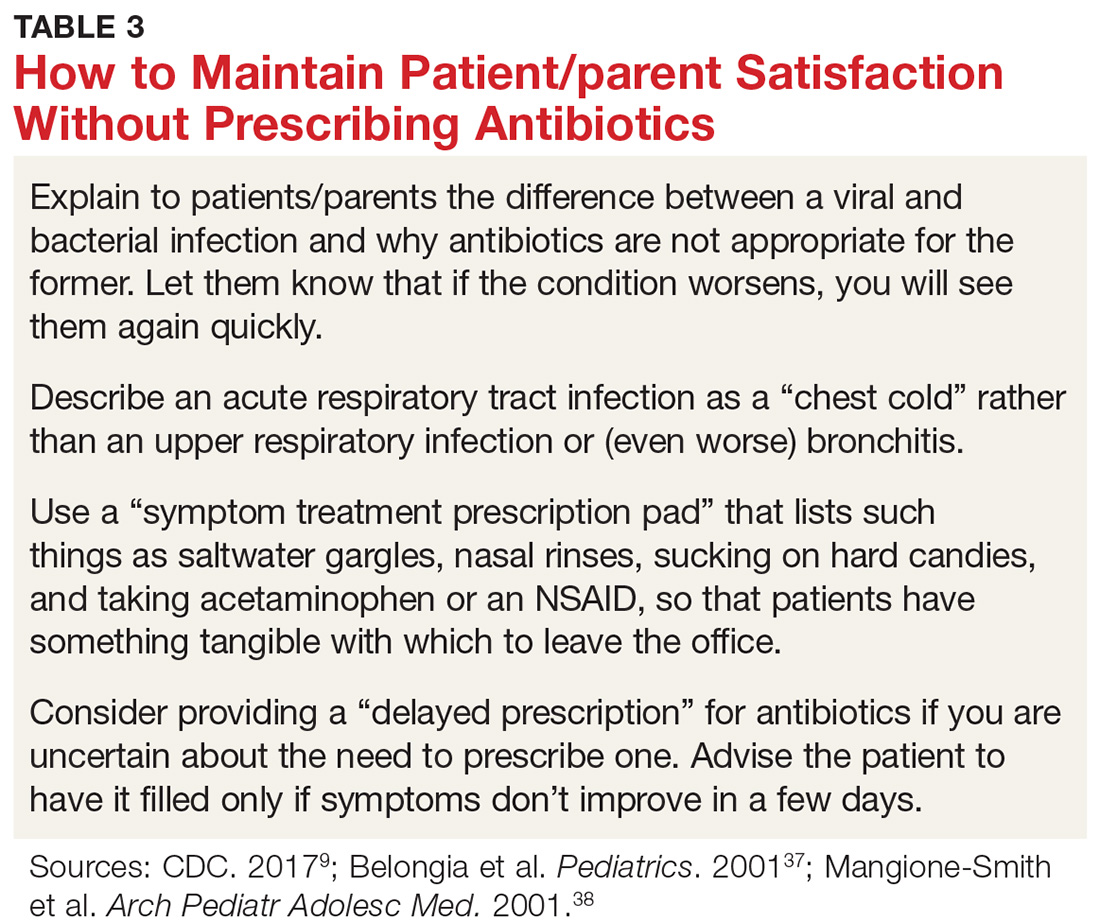
A more recent study found that higher antibiotic prescribing practices in Britain were associated with modestly higher patient satisfaction ratings.39 The authors of this study noted, however, that reduced antibiotic prescribing may be a proxy for other practice patterns that affected satisfaction ratings.
REDUCING ANTIBIOTIC PRESCRIBING REDUCES RESISTANCE
There is also strong evidence that when clinicians decrease antibiotic prescribing, antimicrobial resistance follows suit. One of the earlier landmark studies to demonstrate this was a Finnish study published in 1997.40 The authors found that a reduction of macrolide antibiotic consumption in Finland led to a reduction in streptococci macrolide resistance from 16.5% to 8.6%.40
Multiple studies have since demonstrated similar results for both respiratory and urinary tract infections.41,42 A 2017 meta-analysis of 32 studies found that antibiotic stewardship programs reduced the incidence of infections and colonization with multidrug-resistant Gram-negative bacteria (by 51%), extended-spectrum beta-lactamase–producing Gram-negative bacteria (48%), and methicillin-resistant Staphylococcus aureus (37%). There was also a reduction in the incidence of CDI (32%).43
1. Bailey LC, Forrest CB, Zhang P, et al. Association of antibiotics in infancy with early childhood obesity. JAMA Pediatr. 2014;168:1063-1069.
2. Costelloe C, Metcalfe C, Lovering A, et al. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 2010;340:c2096.
3. Gleckman RA, Czachor JS. Antibiotic side effects. Semin Respir Crit Care Med. 2000;21:53-60.
4. Jernberg C, Löfmark S, Edlund C, et al. Long-term impacts of antibiotic exposure on the human intestinal microbiota. Microbiology. 2010;156:3216-3223.
5. Logan AC, Jacka FN, Craig JM, et al. The microbiome and mental health: looking back, moving forward with lessons from allergic diseases. Clin Psychopharmacol Neurosci. 2016;14:131-147.
6. Marra F, Marra CA, Richardson K, et al. Antibiotic use in children is associated with increased risk of asthma. Pediatrics. 2009;123:1003-1010.
7. Harris AM, Hicks LA, Qaseem A; the High Value Care Task Force of the American College of Physicians and the CDC. Appropriate antibiotic use for acute respiratory tract infection in adults: advice for high-value care from the American College of Physicians and the Centers for Disease Control and Prevention. Ann Intern Med. 2016; 164:425-434.
8. Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010-2011. JAMA. 2016;315: 1864-1873.
9. CDC. Antibiotic prescribing and use. www.cdc.gov/antibiotic-use/index.html. Accessed January 16, 2018.
10. The White House. National action plan for combating antibiotic-resistant bacteria. March 2015:1-63. https://obamawhitehouse.archives.gov/sites/default/files/docs/national_action_plan_for_combating_antibotic-resistant_bacteria.pdf. Accessed January 16, 2018.
11. World Health Organization. Global action plan on antimicrobial resistance (2015). www.who.int/antimicrobial-resistance/global-action-plan/en/. Accessed January 16, 2018.
12. Barlam TF, Soria-Saucedo R, Cabral HJ, et al. Unnecessary antibiotics for acute respiratory tract infections: association with care setting and patient demographics. Open Forum Infect Dis. 2016;3:1-7.
13. Hersh AL, Shapiro DJ, Pavia AT, et al. Antibiotic prescribing in ambulatory pediatrics in the United States. Pediatrics. 2011;128:1053-1061.
14. Chow AW, Benninger MS, Brook I, et al. Executive summary: IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54:1041-1045.
15. Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015;152(2 suppl):S1-S39.
16. Shulman ST, Bisno AL, Clegg HW, et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis. 2012;55:1279-1282.
17. Shapiro DJ, Hicks LA, Pavia AT, et al. Antibiotic prescribing for adults in ambulatory care in the USA, 2007-09. J Antimicrob Chemother. 2014;69:234-240.
18. Bergmark RW, Sedaghat AR. Antibiotic prescription for acute rhinosinusitis: emergency departments versus primary care providers. Laryngoscope. 2016;126:2439-2444.
19. Hersh AL, Fleming-Dutra KE, Shapiro DJ, et al. Frequency of first-line antibiotic selection among US ambulatory care visits for otitis media, sinusitis, and pharyngitis. JAMA Intern Med. 2016;176:1870-1872.
20. Hicks LA, Bartoces MG, Roberts RM, et al. US outpatient antibiotic prescribing variation according to geography, patient population, and provider specialty in 2011. Clin Infect Dis. 2015;60:1308-1316.
21. Langdon A, Crook N, Dantas G. The effects of antibiotics on the microbiome throughout development and alternative approaches for therapeutic modulation. Genome Med. 2016;8:39.
22. Lessa FC, Gould CV, McDonald CL. Current status of Clostridium difficile infection epidemiology. Clin Infect Dis. 2012;55(suppl 2):S65-S70.
23. Zhang S, Palazuelos-Munoz S, Balsells EM, et al. Cost of hospital management of Clostridium difficile infection in United States—a meta-analysis and modelling study. BMC Infect Dis. 2016;16:447.
24. Pérez-Santiago J, Gianella S, Massanella M, et al. Gut lactobacillales are associated with higher CD4 and less microbial translocation during HIV infection. AIDS. 2013;27:1921-1931.
25. Maurice CF, Haiser HJ, Turnbaugh PJ. Xenobiotics shape the physiology and gene expression of the active human gut microbiome. Cell. 2013;152:39-50.
26. Bravo JA, Julio-Pieper M, Forsythe P, et al. Communication between gastrointestinal bacteria and the nervous system. Curr Opin Pharmacol. 2012;12:667-672.
27. Clemente JC, Ursell LK, Parfrey LW, et al. The impact of the gut microbiota on human health: an integrative view. Cell. 2012;148:1258-1270.
28. Dinan TG, Cryan JF. Regulation of the stress response by the gut microbiota: implications for psychoneuroendocrinology. Psychoneuroendocrinology. 2012;37:1369-1378.
29. Foster JA, McVey Neufeld KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 2013;36:305-312.
30. Wang Y, Kasper LH. The role of microbiome in central nervous system disorders. Brain Behav Immun. 2014; 38:1-12.31. Riiser A. The human microbiome, asthma, and allergy. Allergy Asthma Clin Immunol. 2015;11:35.
32. Md Rezal RS, Hassali MA, Alrasheedy AA, et al. Physicians’ knowledge, perceptions and behaviour towards antibiotic prescribing: a systematic review of the literature. Expert Rev Anti Infect Ther. 2015;13:665-680.
33. Dempsey PP, Businger AC, Whaley LE, et al. Primary care clinicians’ perceptions about antibiotic prescribing for acute bronchitis: a qualitative study. BMC Fam Pract . 2014;15:194.
34. Gonzales R, Steiner JF, Lum A, et al. Decreasing antibiotic use in ambulatory practice. JAMA . 1999;281:1512-1519.
35. Meeker D, Linder JA, Fox CR, et al. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices: a randomized clinical trial. JAMA . 2016;315:562-570.
36. Perz JF, Craig AS, Coffey CS, et al. Changes in antibiotic prescribing for children after a community-wide campaign. JAMA . 2002;287:3103-3109.
37. Belongia EA, Sullivan BJ, Chyou PH, et al. A community intervention trial to promote judicious antibiotic use and reduce penicillin-resistant Streptococcus pneumoniae carriage in children. Pediatrics . 2001;108:575-583.
38. Mangione-Smith R, McGlynn EA, Elliott MN, et al. Parent expectations for antibiotics, physician-parent communication, and satisfaction. Arch Pediatr Adolesc Med. 2001;155:800-806.
39. Ashworth M, White P, Jongsma H, et al. Antibiotic prescribing and patient satisfaction in primary care in England: cross-sectional analysis of national patient survey data and prescribing data. Br J Gen Pract . 2016;66:e40-e46.
40. Seppälä H, Klaukka T, Vuopio-Varkila J, et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in group A streptococci in Finland. N Engl J Med. 1997;337:441-446.
41. Guillemot D, Varon E, Bernède C, et al. Reduction of antibiotic use in the community reduces the rate of colonization with penicillin g–nonsusceptible Streptococcus pneumoniae . Clin Infect Dis. 2005;41:930-938.
42. Butler CC, Dunstan F, Heginbothom M, et al. Containing antibiotic resistance: decreased antibiotic-resistant coliform urinary tract infections with reduction in antibiotic prescribing by general practices. Br J Gen Pract. 2007; 57:785-792.
43. Baur D, Gladstone BP, Burkert F, et al. Effect of antibiotic stewardship on the incidence of infection and colonisation with antibiotic-resistant bacteria and Clostridium difficile infection: a systematic review and meta-analysis. Lancet Infect Dis. 2017;17:990-1001.
1. Bailey LC, Forrest CB, Zhang P, et al. Association of antibiotics in infancy with early childhood obesity. JAMA Pediatr. 2014;168:1063-1069.
2. Costelloe C, Metcalfe C, Lovering A, et al. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 2010;340:c2096.
3. Gleckman RA, Czachor JS. Antibiotic side effects. Semin Respir Crit Care Med. 2000;21:53-60.
4. Jernberg C, Löfmark S, Edlund C, et al. Long-term impacts of antibiotic exposure on the human intestinal microbiota. Microbiology. 2010;156:3216-3223.
5. Logan AC, Jacka FN, Craig JM, et al. The microbiome and mental health: looking back, moving forward with lessons from allergic diseases. Clin Psychopharmacol Neurosci. 2016;14:131-147.
6. Marra F, Marra CA, Richardson K, et al. Antibiotic use in children is associated with increased risk of asthma. Pediatrics. 2009;123:1003-1010.
7. Harris AM, Hicks LA, Qaseem A; the High Value Care Task Force of the American College of Physicians and the CDC. Appropriate antibiotic use for acute respiratory tract infection in adults: advice for high-value care from the American College of Physicians and the Centers for Disease Control and Prevention. Ann Intern Med. 2016; 164:425-434.
8. Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010-2011. JAMA. 2016;315: 1864-1873.
9. CDC. Antibiotic prescribing and use. www.cdc.gov/antibiotic-use/index.html. Accessed January 16, 2018.
10. The White House. National action plan for combating antibiotic-resistant bacteria. March 2015:1-63. https://obamawhitehouse.archives.gov/sites/default/files/docs/national_action_plan_for_combating_antibotic-resistant_bacteria.pdf. Accessed January 16, 2018.
11. World Health Organization. Global action plan on antimicrobial resistance (2015). www.who.int/antimicrobial-resistance/global-action-plan/en/. Accessed January 16, 2018.
12. Barlam TF, Soria-Saucedo R, Cabral HJ, et al. Unnecessary antibiotics for acute respiratory tract infections: association with care setting and patient demographics. Open Forum Infect Dis. 2016;3:1-7.
13. Hersh AL, Shapiro DJ, Pavia AT, et al. Antibiotic prescribing in ambulatory pediatrics in the United States. Pediatrics. 2011;128:1053-1061.
14. Chow AW, Benninger MS, Brook I, et al. Executive summary: IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54:1041-1045.
15. Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015;152(2 suppl):S1-S39.
16. Shulman ST, Bisno AL, Clegg HW, et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis. 2012;55:1279-1282.
17. Shapiro DJ, Hicks LA, Pavia AT, et al. Antibiotic prescribing for adults in ambulatory care in the USA, 2007-09. J Antimicrob Chemother. 2014;69:234-240.
18. Bergmark RW, Sedaghat AR. Antibiotic prescription for acute rhinosinusitis: emergency departments versus primary care providers. Laryngoscope. 2016;126:2439-2444.
19. Hersh AL, Fleming-Dutra KE, Shapiro DJ, et al. Frequency of first-line antibiotic selection among US ambulatory care visits for otitis media, sinusitis, and pharyngitis. JAMA Intern Med. 2016;176:1870-1872.
20. Hicks LA, Bartoces MG, Roberts RM, et al. US outpatient antibiotic prescribing variation according to geography, patient population, and provider specialty in 2011. Clin Infect Dis. 2015;60:1308-1316.
21. Langdon A, Crook N, Dantas G. The effects of antibiotics on the microbiome throughout development and alternative approaches for therapeutic modulation. Genome Med. 2016;8:39.
22. Lessa FC, Gould CV, McDonald CL. Current status of Clostridium difficile infection epidemiology. Clin Infect Dis. 2012;55(suppl 2):S65-S70.
23. Zhang S, Palazuelos-Munoz S, Balsells EM, et al. Cost of hospital management of Clostridium difficile infection in United States—a meta-analysis and modelling study. BMC Infect Dis. 2016;16:447.
24. Pérez-Santiago J, Gianella S, Massanella M, et al. Gut lactobacillales are associated with higher CD4 and less microbial translocation during HIV infection. AIDS. 2013;27:1921-1931.
25. Maurice CF, Haiser HJ, Turnbaugh PJ. Xenobiotics shape the physiology and gene expression of the active human gut microbiome. Cell. 2013;152:39-50.
26. Bravo JA, Julio-Pieper M, Forsythe P, et al. Communication between gastrointestinal bacteria and the nervous system. Curr Opin Pharmacol. 2012;12:667-672.
27. Clemente JC, Ursell LK, Parfrey LW, et al. The impact of the gut microbiota on human health: an integrative view. Cell. 2012;148:1258-1270.
28. Dinan TG, Cryan JF. Regulation of the stress response by the gut microbiota: implications for psychoneuroendocrinology. Psychoneuroendocrinology. 2012;37:1369-1378.
29. Foster JA, McVey Neufeld KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 2013;36:305-312.
30. Wang Y, Kasper LH. The role of microbiome in central nervous system disorders. Brain Behav Immun. 2014; 38:1-12.31. Riiser A. The human microbiome, asthma, and allergy. Allergy Asthma Clin Immunol. 2015;11:35.
32. Md Rezal RS, Hassali MA, Alrasheedy AA, et al. Physicians’ knowledge, perceptions and behaviour towards antibiotic prescribing: a systematic review of the literature. Expert Rev Anti Infect Ther. 2015;13:665-680.
33. Dempsey PP, Businger AC, Whaley LE, et al. Primary care clinicians’ perceptions about antibiotic prescribing for acute bronchitis: a qualitative study. BMC Fam Pract . 2014;15:194.
34. Gonzales R, Steiner JF, Lum A, et al. Decreasing antibiotic use in ambulatory practice. JAMA . 1999;281:1512-1519.
35. Meeker D, Linder JA, Fox CR, et al. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices: a randomized clinical trial. JAMA . 2016;315:562-570.
36. Perz JF, Craig AS, Coffey CS, et al. Changes in antibiotic prescribing for children after a community-wide campaign. JAMA . 2002;287:3103-3109.
37. Belongia EA, Sullivan BJ, Chyou PH, et al. A community intervention trial to promote judicious antibiotic use and reduce penicillin-resistant Streptococcus pneumoniae carriage in children. Pediatrics . 2001;108:575-583.
38. Mangione-Smith R, McGlynn EA, Elliott MN, et al. Parent expectations for antibiotics, physician-parent communication, and satisfaction. Arch Pediatr Adolesc Med. 2001;155:800-806.
39. Ashworth M, White P, Jongsma H, et al. Antibiotic prescribing and patient satisfaction in primary care in England: cross-sectional analysis of national patient survey data and prescribing data. Br J Gen Pract . 2016;66:e40-e46.
40. Seppälä H, Klaukka T, Vuopio-Varkila J, et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in group A streptococci in Finland. N Engl J Med. 1997;337:441-446.
41. Guillemot D, Varon E, Bernède C, et al. Reduction of antibiotic use in the community reduces the rate of colonization with penicillin g–nonsusceptible Streptococcus pneumoniae . Clin Infect Dis. 2005;41:930-938.
42. Butler CC, Dunstan F, Heginbothom M, et al. Containing antibiotic resistance: decreased antibiotic-resistant coliform urinary tract infections with reduction in antibiotic prescribing by general practices. Br J Gen Pract. 2007; 57:785-792.
43. Baur D, Gladstone BP, Burkert F, et al. Effect of antibiotic stewardship on the incidence of infection and colonisation with antibiotic-resistant bacteria and Clostridium difficile infection: a systematic review and meta-analysis. Lancet Infect Dis. 2017;17:990-1001.
Evidence-based care processes decrease mortality in Staphylococcus aureus bacteremia
Clinical questions: What are the trends in patient outcome for Staphylococcus aureus bacteremia (SAB)? Does the use of evidence-based care processes decrease mortality in SAB?
Background: SAB is associated with poor clinical outcomes. Prior research has demonstrated that several evidence-based interventions, namely appropriate antibiotics, echocardiography, and infectious disease consults, have been associated with improved outcomes. The use of these interventions in clinical practice and their large-scale impact on SAB mortality is not known.
Setting: Veterans Health Administration acute care hospitals in the continental United States from January 1, 2003, to Dec. 31, 2014.
Synopsis: This study used the Veterans Affairs Informatics and Computing Infrastructure to identify 36,868 patients across 124 acute care hospitals with a first episode of SAB. Use of evidence-based care processes (specifically appropriate antibiotic use, echocardiography, and infectious disease consults) and patient mortality were recorded.
All-cause 30-day mortality decreased 25.7% in 2003 to 16.5% in 2014. Concurrently, the rate of evidence-based care processes increased from 2003 to 2014. There was lower risk-adjusted mortality when patients received all three evidence-based care processes compared to those who received none, with an odds ratio of 0.33 (95% confidence interval, 0.30-0.37); 57.3% of the decrease in mortality was attributable to use of all three evidence-based care processes.
Given the observational nature of the study, unmeasured confounders were not considered. Generalizability of the study is limited since the patients were primarily men.
Bottom line: The use of evidence-based care processes (appropriate antibiotic use, echocardiography, and infectious disease consultation) was associated with decreased SAB mortality.
Citation: Goto M et al. Association of evidence-based care processes with mortality in Staphylococcus aureus bacteremia at Veterans Health Administration hospitals, 2003-2014. JAMA Intern Med. 2017;177(10):1489-97.
Dr. Rodriguez is a hospitalist and a clinical informatics fellow, Beth Israel Deaconess Medical Center, Boston.
Clinical questions: What are the trends in patient outcome for Staphylococcus aureus bacteremia (SAB)? Does the use of evidence-based care processes decrease mortality in SAB?
Background: SAB is associated with poor clinical outcomes. Prior research has demonstrated that several evidence-based interventions, namely appropriate antibiotics, echocardiography, and infectious disease consults, have been associated with improved outcomes. The use of these interventions in clinical practice and their large-scale impact on SAB mortality is not known.
Setting: Veterans Health Administration acute care hospitals in the continental United States from January 1, 2003, to Dec. 31, 2014.
Synopsis: This study used the Veterans Affairs Informatics and Computing Infrastructure to identify 36,868 patients across 124 acute care hospitals with a first episode of SAB. Use of evidence-based care processes (specifically appropriate antibiotic use, echocardiography, and infectious disease consults) and patient mortality were recorded.
All-cause 30-day mortality decreased 25.7% in 2003 to 16.5% in 2014. Concurrently, the rate of evidence-based care processes increased from 2003 to 2014. There was lower risk-adjusted mortality when patients received all three evidence-based care processes compared to those who received none, with an odds ratio of 0.33 (95% confidence interval, 0.30-0.37); 57.3% of the decrease in mortality was attributable to use of all three evidence-based care processes.
Given the observational nature of the study, unmeasured confounders were not considered. Generalizability of the study is limited since the patients were primarily men.
Bottom line: The use of evidence-based care processes (appropriate antibiotic use, echocardiography, and infectious disease consultation) was associated with decreased SAB mortality.
Citation: Goto M et al. Association of evidence-based care processes with mortality in Staphylococcus aureus bacteremia at Veterans Health Administration hospitals, 2003-2014. JAMA Intern Med. 2017;177(10):1489-97.
Dr. Rodriguez is a hospitalist and a clinical informatics fellow, Beth Israel Deaconess Medical Center, Boston.
Clinical questions: What are the trends in patient outcome for Staphylococcus aureus bacteremia (SAB)? Does the use of evidence-based care processes decrease mortality in SAB?
Background: SAB is associated with poor clinical outcomes. Prior research has demonstrated that several evidence-based interventions, namely appropriate antibiotics, echocardiography, and infectious disease consults, have been associated with improved outcomes. The use of these interventions in clinical practice and their large-scale impact on SAB mortality is not known.
Setting: Veterans Health Administration acute care hospitals in the continental United States from January 1, 2003, to Dec. 31, 2014.
Synopsis: This study used the Veterans Affairs Informatics and Computing Infrastructure to identify 36,868 patients across 124 acute care hospitals with a first episode of SAB. Use of evidence-based care processes (specifically appropriate antibiotic use, echocardiography, and infectious disease consults) and patient mortality were recorded.
All-cause 30-day mortality decreased 25.7% in 2003 to 16.5% in 2014. Concurrently, the rate of evidence-based care processes increased from 2003 to 2014. There was lower risk-adjusted mortality when patients received all three evidence-based care processes compared to those who received none, with an odds ratio of 0.33 (95% confidence interval, 0.30-0.37); 57.3% of the decrease in mortality was attributable to use of all three evidence-based care processes.
Given the observational nature of the study, unmeasured confounders were not considered. Generalizability of the study is limited since the patients were primarily men.
Bottom line: The use of evidence-based care processes (appropriate antibiotic use, echocardiography, and infectious disease consultation) was associated with decreased SAB mortality.
Citation: Goto M et al. Association of evidence-based care processes with mortality in Staphylococcus aureus bacteremia at Veterans Health Administration hospitals, 2003-2014. JAMA Intern Med. 2017;177(10):1489-97.
Dr. Rodriguez is a hospitalist and a clinical informatics fellow, Beth Israel Deaconess Medical Center, Boston.
Impostor syndrome
Why are you bothering to read this? What could I offer that could possibly be useful to you? In fact, I was invited to write this column simply because I happened to be at the right conference at the right time. Soon, if not already, you’ll discover I’m actually not that clever. I’m an impostor.
I’ve thought this while staring at the blank page that is to be my article for the month. Reflecting on it, I realize you’ve probably had the same feelings of fraud at one time or another. It often occurs at moments of transition, such as when you were accepted into medical school or matched into a competitive specialty. Looking at your peers, watching how your colleagues perform, you feel you just aren’t smart enough to be there; either someone made a mistake or you just got lucky.
There are potentially positive aspects of impostor syndrome: Humility can make us more effective over time and more tolerable to be around. It also, however, can be destructive. When we feel undeserving, we grow anxious and focus ever more tightly on ourselves. It can be paralyzing. When you think about how you are perceived, you fail to be present and attentive to others around you. Believing you lack innate ability, you can slip into a fixed mindset and fail to grow. Trying to keep your insecurities a secret from others, the foundation of impostor syndrome, is stressful and will stoke the fire of burnout which threatens us all. Fortunately, there is a cure.
The first step in escaping this maladaptive experience is to do what I’ve just done: Share it with others. Find colleagues or partners who care about you and who can speak frankly. By sharing how you feel with others, you banish any power that impostor syndrome might have over you. You can’t worry about being a fraud once you’ve just announced that you are a fraud; the gig is up! Choose your confidantes carefully, as not everyone is suitable to help. Avoid sharing such feelings with your patients; it can erode their confidence in you.
Reframe how you interpret situations when you feel like an impostor. Committing an error doesn’t mean you’re incompetent; moreover, you needn’t be supremely confident to be competent. Marveling at others’ abilities doesn’t mean you could not perform as well. Remember, you don’t know how much effort and time they’ve invested, and chances are you’re underestimating the work they’ve put forth.
Last, take the time to write about your success. Journaling can be a powerful tool to make your successes more salient and remind you that you are truly accomplished. Try writing in the third person, telling the story of your journey and the obstacles you’ve overcome to reach your current prestigious destination. If you still feel like a fake sometimes, there is good news. Having some self-doubt correlates with success, probably because it keeps you motivated to work hard.
Did this article resonate with you? It should. It took me lots of drafts before I got it right.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Why are you bothering to read this? What could I offer that could possibly be useful to you? In fact, I was invited to write this column simply because I happened to be at the right conference at the right time. Soon, if not already, you’ll discover I’m actually not that clever. I’m an impostor.
I’ve thought this while staring at the blank page that is to be my article for the month. Reflecting on it, I realize you’ve probably had the same feelings of fraud at one time or another. It often occurs at moments of transition, such as when you were accepted into medical school or matched into a competitive specialty. Looking at your peers, watching how your colleagues perform, you feel you just aren’t smart enough to be there; either someone made a mistake or you just got lucky.
There are potentially positive aspects of impostor syndrome: Humility can make us more effective over time and more tolerable to be around. It also, however, can be destructive. When we feel undeserving, we grow anxious and focus ever more tightly on ourselves. It can be paralyzing. When you think about how you are perceived, you fail to be present and attentive to others around you. Believing you lack innate ability, you can slip into a fixed mindset and fail to grow. Trying to keep your insecurities a secret from others, the foundation of impostor syndrome, is stressful and will stoke the fire of burnout which threatens us all. Fortunately, there is a cure.
The first step in escaping this maladaptive experience is to do what I’ve just done: Share it with others. Find colleagues or partners who care about you and who can speak frankly. By sharing how you feel with others, you banish any power that impostor syndrome might have over you. You can’t worry about being a fraud once you’ve just announced that you are a fraud; the gig is up! Choose your confidantes carefully, as not everyone is suitable to help. Avoid sharing such feelings with your patients; it can erode their confidence in you.
Reframe how you interpret situations when you feel like an impostor. Committing an error doesn’t mean you’re incompetent; moreover, you needn’t be supremely confident to be competent. Marveling at others’ abilities doesn’t mean you could not perform as well. Remember, you don’t know how much effort and time they’ve invested, and chances are you’re underestimating the work they’ve put forth.
Last, take the time to write about your success. Journaling can be a powerful tool to make your successes more salient and remind you that you are truly accomplished. Try writing in the third person, telling the story of your journey and the obstacles you’ve overcome to reach your current prestigious destination. If you still feel like a fake sometimes, there is good news. Having some self-doubt correlates with success, probably because it keeps you motivated to work hard.
Did this article resonate with you? It should. It took me lots of drafts before I got it right.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Why are you bothering to read this? What could I offer that could possibly be useful to you? In fact, I was invited to write this column simply because I happened to be at the right conference at the right time. Soon, if not already, you’ll discover I’m actually not that clever. I’m an impostor.
I’ve thought this while staring at the blank page that is to be my article for the month. Reflecting on it, I realize you’ve probably had the same feelings of fraud at one time or another. It often occurs at moments of transition, such as when you were accepted into medical school or matched into a competitive specialty. Looking at your peers, watching how your colleagues perform, you feel you just aren’t smart enough to be there; either someone made a mistake or you just got lucky.
There are potentially positive aspects of impostor syndrome: Humility can make us more effective over time and more tolerable to be around. It also, however, can be destructive. When we feel undeserving, we grow anxious and focus ever more tightly on ourselves. It can be paralyzing. When you think about how you are perceived, you fail to be present and attentive to others around you. Believing you lack innate ability, you can slip into a fixed mindset and fail to grow. Trying to keep your insecurities a secret from others, the foundation of impostor syndrome, is stressful and will stoke the fire of burnout which threatens us all. Fortunately, there is a cure.
The first step in escaping this maladaptive experience is to do what I’ve just done: Share it with others. Find colleagues or partners who care about you and who can speak frankly. By sharing how you feel with others, you banish any power that impostor syndrome might have over you. You can’t worry about being a fraud once you’ve just announced that you are a fraud; the gig is up! Choose your confidantes carefully, as not everyone is suitable to help. Avoid sharing such feelings with your patients; it can erode their confidence in you.
Reframe how you interpret situations when you feel like an impostor. Committing an error doesn’t mean you’re incompetent; moreover, you needn’t be supremely confident to be competent. Marveling at others’ abilities doesn’t mean you could not perform as well. Remember, you don’t know how much effort and time they’ve invested, and chances are you’re underestimating the work they’ve put forth.
Last, take the time to write about your success. Journaling can be a powerful tool to make your successes more salient and remind you that you are truly accomplished. Try writing in the third person, telling the story of your journey and the obstacles you’ve overcome to reach your current prestigious destination. If you still feel like a fake sometimes, there is good news. Having some self-doubt correlates with success, probably because it keeps you motivated to work hard.
Did this article resonate with you? It should. It took me lots of drafts before I got it right.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Hypopigmented Discoloration on the Thigh
The Diagnosis: Hypopigmented Mycosis Fungoides
The patient was started on clobetasol dipropionate cream 0.05% twice daily, which she did not tolerate due to a burning sensation on application. She then was started on narrowband UVB phototherapy 2 to 3 times weekly, and the hypopigmented areas began to improve. Narrowband UVB phototherapy was discontinued after 7 weeks due to the high cost to the patient, but the hypopigmented patches on the left thigh appeared to remit, and the patient did not return to the clinic for 6 months. She returned when the areas on the left thigh reappeared, along with new areas on the right buttock and right medial upper arm. Serial biopsies of the new patches also revealed a CD8+ atypical lymphocytic infiltrate consistent with hypopigmented patch-stage mycosis fungoides (MF). She was started on halobetasol ointment 0.05% twice daily to affected areas, which she tolerated well. Complete blood count and peripheral blood smear were unremarkable, and the patient continued to deny systemic symptoms. Over the next year, the patient's cutaneous findings continued to wax and wane with topical treatment, and she was referred to a regional cancer treatment center for a second opinion from a hematopathologist. Hematopathologic and dermatopathologic review of the case, including hematoxylin and eosin and immunohistochemical staining, was highly consistent with hypopigmented MF (Figures 1-3).
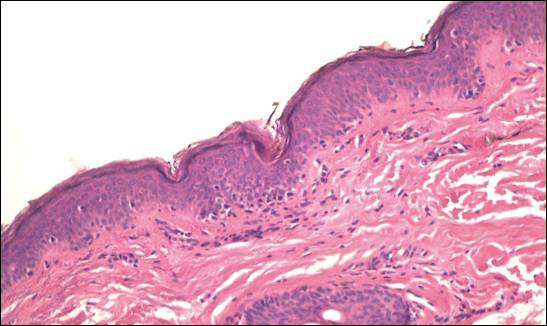
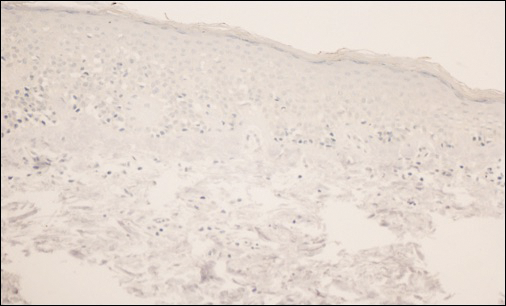
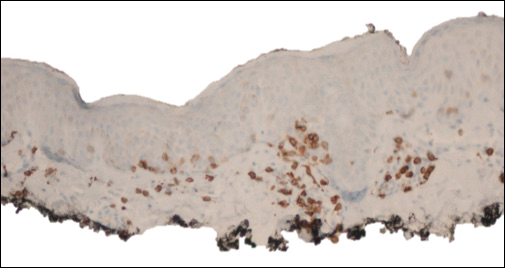
Mycosis fungoides is an uncommon disease characterized by atypical clonal T cells exhibiting epidermotropism. Most commonly, MF is characterized by a CD4+ lymphocytic infiltrate. Mycosis fungoides can be difficult to diagnose in its early stages, as it may resemble benign inflammatory conditions (eg, chronic atopic dermatitis, nummular eczema) and often requires biopsy and additional studies, such as immunohistochemistry, to secure a diagnosis. Hypopigmented MF is regarded as a subtype of MF, as it can exhibit different clinical and pathologic characteristics from classical MF. In particular, the lymphocytic phenotype in hypopigmented MF is more likely to be CD8+.
In general, the progression of MF is characterized as stage IA (patches or plaques involving less than 10% body surface area [BSA]), IB (patches or plaques involving ≥10% BSA without lymph node or visceral involvement), IIA (patches or plaques of any percentage of BSA with lymph node involvement), IIB (cutaneous tumors with or without lymph node involvement), III (erythroderma with low blood tumor burden), or IV (erythroderma with high blood tumor burden with or without visceral involvement). Hypopigmented MF generally presents in early patch stage and rarely progresses past stage IB, and thus generally has a favorable prognosis.1,2 Kim et al3 demonstrated that evolution from patch to plaque stage MF is accompanied by a shift in lymphocytes from the T helper 1 (Th1) to T helper 2 phenotype; therefore the Th1 phenotype, CD8+ T cells are associated with lower risk for disease progression. Other investigators also have hypothesized that predominance of Th1 phenotype, CD8+ T cells may have an immunoregulatory effect, thus preventing evolution of disease from patch to plaque stage and explaining why hypopigmented MF, with a predominantly CD8+ phenotype, confers better prognosis with less chance for disease progression than classical MF.4,5 The patch- or plaque-stage lesions of classical MF have a predilection for non-sun exposed areas (eg, buttocks, medial thighs, breasts),2 whereas hypopigmented MF tends to present with hypopigmented or depigmented lesions mainly distributed on the trunk, arms, and legs. These lesions may become more visible following sun exposure.1 The size of the hypopigmented lesions can vary, and patients may complain of pruritus with variable intensity.
Hypopigmented MF presents more commonly in younger populations, in contrast to classical MF.6-8 However, like classical MF, hypopigmented MF appears to more frequently affect individuals with darker Fitzpatrick skin types.1,9,10 Although it generally is accepted that hypopigmented MF does not favor either sex, some studies suggest that hypopigmented MF has a female predominance.6,10
Classical MF is characterized by an epidermotropic infiltrate of CD4+ T helper cells,10 whereas CD8+ epidermotropism is considered hallmark in hypopigmented MF.10-12 The other typical histopathologic features of hypopigmented MF generally are identical to those of classical MF, with solitary or small groups of atypical haloed lymphocytes within the basal layer, exocytosis of lymphocytes out of proportion to spongiosis, and papillary dermal fibrosis. Immunohistochemistry generally is helpful in distinguishing between classical MF and hypopigmented MF.
The clinical differential diagnosis for hypopigmented MF includes the early (inflammatory) stage of vitiligo, postinflammatory hypopigmentation, lichen sclerosus, pityriasis alba, and leprosy.
First-line treatment for hypopigmented MF consists of phototherapy/photochemotherapy and topical steroids.9,13 Narrowband UVB phototherapy has been used with good success in pediatric patients.14 However, narrowband UVB may not be as effective in darker-skinned individuals; it has been hypothesized that this lack of efficacy could be due to the protective effects of increased melanin in the skin.1 Other topical therapies may include topical carmustine and topical nitrogen mustard.
- Furlan FC, Sanches JA. Hypopigmented mycosis fungoides: a review of its clinical features and pathophysiology. An Bras Dermatol. 2013;88:954-960.
- Girardi M, Heald PW, Wilson LD. The pathogenesis of mycosis fungoides. N Engl J Med. 2004;350:1978-1988.
- Kim EJ, Hess S, Richardson SK, et al. Immunopathogenesis and therapy of cutaneous T cell lymphoma. J Clin Invest. 2005;115:798-812.
- Stone ML, Styles AR, Cockerell CJ, et al. Hypopigmented report of 7 cases and review of the literature. Cutis. 2001;67:133-138.
- Volkenandt M, Soyer HP, Cerroni L, et al. Molecular detection of clone-specific DNA in hypopigmented lesions of a patient with early evolving mycosis fungoides. Br J Dermatol. 1993;128:423-428.
- Furlan FC, Pereira BA, Sotto MN, et al. Hypopigmented mycosis fungoides versus mycosis fungoides with concomitant hypopigmented lesions: same disease or different variants of mycosis fungoides? Dermatology. 2014;229:271-274.
- Ardigó M, Borroni G, Muscardin L, et al. Hypopigmented mycosis fungoides in Caucasian patients: a clinicopathologic study of 7 cases. J Am Acad Dermatol. 2003;49:264-270.
- Boulos S, Vaid R, Aladily TN, et al. Clinical presentation, immunopathology, and treatment of juvenile-onset mycosis fungoides: a case series of 34 patients. J Am Acad Dermatol. 2014;71:1117-1126.
- Lambroza E, Cohen SR, Phelps R, et al. Hypopigmented variant of mycosis fungoides: demography, histopathology, and treatment of seven cases. J Am Acad Dermatol. 1995;32:987-993.
- El-Shabrawi-Caelen L, Cerroni L, Medeiros LJ, et al. Hypopigmented mycosis fungoides: Frequent expression of a CD8+ T-cell phenotype. Am J Surg Pathol. 2002;26:450-457.
- Furlan FC, de Paula Pereira BA, da Silva LF, et al. Loss of melanocytes in hypopigmented mycosis fungoides: a study of 18 patients. J Cutan Pathol. 2014;41:101-107.
- Tolkachjov SN, Comfere NI. Hypopigmented mycosis fungoides: a clinical mimicker of vitiligo. J Drugs Dermatol. 2015;14:193-194.
- Duarte I, Bedrikow, R, Aoki S. Mycosis fungoides: epidemiologic study of 17 cases and evaluation of PUVA photochemotherapy. An Bras Dermatol. 2006;81:40-45.
- Onsun N, Kural Y, Su O, et al. Hypopigmented mycosis fungoides associated with atopy in two children. Pediatr Dermatol. 2006;23:493-496.
The Diagnosis: Hypopigmented Mycosis Fungoides
The patient was started on clobetasol dipropionate cream 0.05% twice daily, which she did not tolerate due to a burning sensation on application. She then was started on narrowband UVB phototherapy 2 to 3 times weekly, and the hypopigmented areas began to improve. Narrowband UVB phototherapy was discontinued after 7 weeks due to the high cost to the patient, but the hypopigmented patches on the left thigh appeared to remit, and the patient did not return to the clinic for 6 months. She returned when the areas on the left thigh reappeared, along with new areas on the right buttock and right medial upper arm. Serial biopsies of the new patches also revealed a CD8+ atypical lymphocytic infiltrate consistent with hypopigmented patch-stage mycosis fungoides (MF). She was started on halobetasol ointment 0.05% twice daily to affected areas, which she tolerated well. Complete blood count and peripheral blood smear were unremarkable, and the patient continued to deny systemic symptoms. Over the next year, the patient's cutaneous findings continued to wax and wane with topical treatment, and she was referred to a regional cancer treatment center for a second opinion from a hematopathologist. Hematopathologic and dermatopathologic review of the case, including hematoxylin and eosin and immunohistochemical staining, was highly consistent with hypopigmented MF (Figures 1-3).
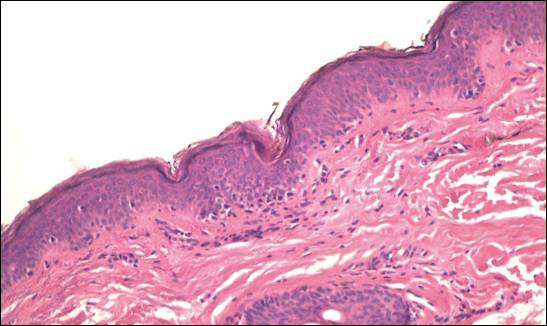
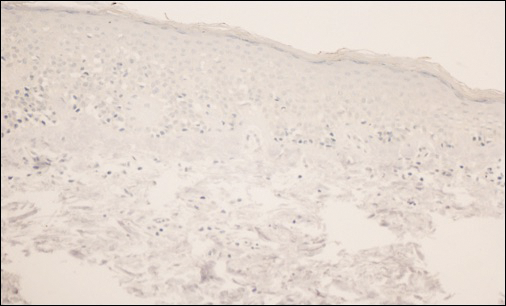
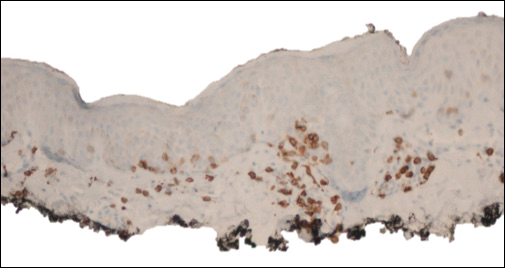
Mycosis fungoides is an uncommon disease characterized by atypical clonal T cells exhibiting epidermotropism. Most commonly, MF is characterized by a CD4+ lymphocytic infiltrate. Mycosis fungoides can be difficult to diagnose in its early stages, as it may resemble benign inflammatory conditions (eg, chronic atopic dermatitis, nummular eczema) and often requires biopsy and additional studies, such as immunohistochemistry, to secure a diagnosis. Hypopigmented MF is regarded as a subtype of MF, as it can exhibit different clinical and pathologic characteristics from classical MF. In particular, the lymphocytic phenotype in hypopigmented MF is more likely to be CD8+.
In general, the progression of MF is characterized as stage IA (patches or plaques involving less than 10% body surface area [BSA]), IB (patches or plaques involving ≥10% BSA without lymph node or visceral involvement), IIA (patches or plaques of any percentage of BSA with lymph node involvement), IIB (cutaneous tumors with or without lymph node involvement), III (erythroderma with low blood tumor burden), or IV (erythroderma with high blood tumor burden with or without visceral involvement). Hypopigmented MF generally presents in early patch stage and rarely progresses past stage IB, and thus generally has a favorable prognosis.1,2 Kim et al3 demonstrated that evolution from patch to plaque stage MF is accompanied by a shift in lymphocytes from the T helper 1 (Th1) to T helper 2 phenotype; therefore the Th1 phenotype, CD8+ T cells are associated with lower risk for disease progression. Other investigators also have hypothesized that predominance of Th1 phenotype, CD8+ T cells may have an immunoregulatory effect, thus preventing evolution of disease from patch to plaque stage and explaining why hypopigmented MF, with a predominantly CD8+ phenotype, confers better prognosis with less chance for disease progression than classical MF.4,5 The patch- or plaque-stage lesions of classical MF have a predilection for non-sun exposed areas (eg, buttocks, medial thighs, breasts),2 whereas hypopigmented MF tends to present with hypopigmented or depigmented lesions mainly distributed on the trunk, arms, and legs. These lesions may become more visible following sun exposure.1 The size of the hypopigmented lesions can vary, and patients may complain of pruritus with variable intensity.
Hypopigmented MF presents more commonly in younger populations, in contrast to classical MF.6-8 However, like classical MF, hypopigmented MF appears to more frequently affect individuals with darker Fitzpatrick skin types.1,9,10 Although it generally is accepted that hypopigmented MF does not favor either sex, some studies suggest that hypopigmented MF has a female predominance.6,10
Classical MF is characterized by an epidermotropic infiltrate of CD4+ T helper cells,10 whereas CD8+ epidermotropism is considered hallmark in hypopigmented MF.10-12 The other typical histopathologic features of hypopigmented MF generally are identical to those of classical MF, with solitary or small groups of atypical haloed lymphocytes within the basal layer, exocytosis of lymphocytes out of proportion to spongiosis, and papillary dermal fibrosis. Immunohistochemistry generally is helpful in distinguishing between classical MF and hypopigmented MF.
The clinical differential diagnosis for hypopigmented MF includes the early (inflammatory) stage of vitiligo, postinflammatory hypopigmentation, lichen sclerosus, pityriasis alba, and leprosy.
First-line treatment for hypopigmented MF consists of phototherapy/photochemotherapy and topical steroids.9,13 Narrowband UVB phototherapy has been used with good success in pediatric patients.14 However, narrowband UVB may not be as effective in darker-skinned individuals; it has been hypothesized that this lack of efficacy could be due to the protective effects of increased melanin in the skin.1 Other topical therapies may include topical carmustine and topical nitrogen mustard.
The Diagnosis: Hypopigmented Mycosis Fungoides
The patient was started on clobetasol dipropionate cream 0.05% twice daily, which she did not tolerate due to a burning sensation on application. She then was started on narrowband UVB phototherapy 2 to 3 times weekly, and the hypopigmented areas began to improve. Narrowband UVB phototherapy was discontinued after 7 weeks due to the high cost to the patient, but the hypopigmented patches on the left thigh appeared to remit, and the patient did not return to the clinic for 6 months. She returned when the areas on the left thigh reappeared, along with new areas on the right buttock and right medial upper arm. Serial biopsies of the new patches also revealed a CD8+ atypical lymphocytic infiltrate consistent with hypopigmented patch-stage mycosis fungoides (MF). She was started on halobetasol ointment 0.05% twice daily to affected areas, which she tolerated well. Complete blood count and peripheral blood smear were unremarkable, and the patient continued to deny systemic symptoms. Over the next year, the patient's cutaneous findings continued to wax and wane with topical treatment, and she was referred to a regional cancer treatment center for a second opinion from a hematopathologist. Hematopathologic and dermatopathologic review of the case, including hematoxylin and eosin and immunohistochemical staining, was highly consistent with hypopigmented MF (Figures 1-3).
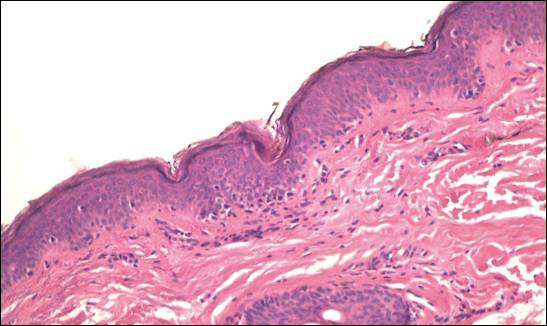
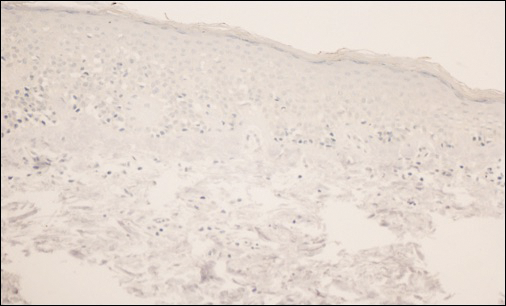
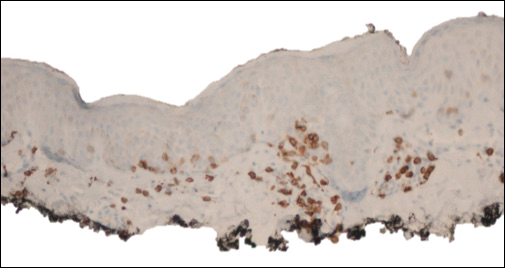
Mycosis fungoides is an uncommon disease characterized by atypical clonal T cells exhibiting epidermotropism. Most commonly, MF is characterized by a CD4+ lymphocytic infiltrate. Mycosis fungoides can be difficult to diagnose in its early stages, as it may resemble benign inflammatory conditions (eg, chronic atopic dermatitis, nummular eczema) and often requires biopsy and additional studies, such as immunohistochemistry, to secure a diagnosis. Hypopigmented MF is regarded as a subtype of MF, as it can exhibit different clinical and pathologic characteristics from classical MF. In particular, the lymphocytic phenotype in hypopigmented MF is more likely to be CD8+.
In general, the progression of MF is characterized as stage IA (patches or plaques involving less than 10% body surface area [BSA]), IB (patches or plaques involving ≥10% BSA without lymph node or visceral involvement), IIA (patches or plaques of any percentage of BSA with lymph node involvement), IIB (cutaneous tumors with or without lymph node involvement), III (erythroderma with low blood tumor burden), or IV (erythroderma with high blood tumor burden with or without visceral involvement). Hypopigmented MF generally presents in early patch stage and rarely progresses past stage IB, and thus generally has a favorable prognosis.1,2 Kim et al3 demonstrated that evolution from patch to plaque stage MF is accompanied by a shift in lymphocytes from the T helper 1 (Th1) to T helper 2 phenotype; therefore the Th1 phenotype, CD8+ T cells are associated with lower risk for disease progression. Other investigators also have hypothesized that predominance of Th1 phenotype, CD8+ T cells may have an immunoregulatory effect, thus preventing evolution of disease from patch to plaque stage and explaining why hypopigmented MF, with a predominantly CD8+ phenotype, confers better prognosis with less chance for disease progression than classical MF.4,5 The patch- or plaque-stage lesions of classical MF have a predilection for non-sun exposed areas (eg, buttocks, medial thighs, breasts),2 whereas hypopigmented MF tends to present with hypopigmented or depigmented lesions mainly distributed on the trunk, arms, and legs. These lesions may become more visible following sun exposure.1 The size of the hypopigmented lesions can vary, and patients may complain of pruritus with variable intensity.
Hypopigmented MF presents more commonly in younger populations, in contrast to classical MF.6-8 However, like classical MF, hypopigmented MF appears to more frequently affect individuals with darker Fitzpatrick skin types.1,9,10 Although it generally is accepted that hypopigmented MF does not favor either sex, some studies suggest that hypopigmented MF has a female predominance.6,10
Classical MF is characterized by an epidermotropic infiltrate of CD4+ T helper cells,10 whereas CD8+ epidermotropism is considered hallmark in hypopigmented MF.10-12 The other typical histopathologic features of hypopigmented MF generally are identical to those of classical MF, with solitary or small groups of atypical haloed lymphocytes within the basal layer, exocytosis of lymphocytes out of proportion to spongiosis, and papillary dermal fibrosis. Immunohistochemistry generally is helpful in distinguishing between classical MF and hypopigmented MF.
The clinical differential diagnosis for hypopigmented MF includes the early (inflammatory) stage of vitiligo, postinflammatory hypopigmentation, lichen sclerosus, pityriasis alba, and leprosy.
First-line treatment for hypopigmented MF consists of phototherapy/photochemotherapy and topical steroids.9,13 Narrowband UVB phototherapy has been used with good success in pediatric patients.14 However, narrowband UVB may not be as effective in darker-skinned individuals; it has been hypothesized that this lack of efficacy could be due to the protective effects of increased melanin in the skin.1 Other topical therapies may include topical carmustine and topical nitrogen mustard.
- Furlan FC, Sanches JA. Hypopigmented mycosis fungoides: a review of its clinical features and pathophysiology. An Bras Dermatol. 2013;88:954-960.
- Girardi M, Heald PW, Wilson LD. The pathogenesis of mycosis fungoides. N Engl J Med. 2004;350:1978-1988.
- Kim EJ, Hess S, Richardson SK, et al. Immunopathogenesis and therapy of cutaneous T cell lymphoma. J Clin Invest. 2005;115:798-812.
- Stone ML, Styles AR, Cockerell CJ, et al. Hypopigmented report of 7 cases and review of the literature. Cutis. 2001;67:133-138.
- Volkenandt M, Soyer HP, Cerroni L, et al. Molecular detection of clone-specific DNA in hypopigmented lesions of a patient with early evolving mycosis fungoides. Br J Dermatol. 1993;128:423-428.
- Furlan FC, Pereira BA, Sotto MN, et al. Hypopigmented mycosis fungoides versus mycosis fungoides with concomitant hypopigmented lesions: same disease or different variants of mycosis fungoides? Dermatology. 2014;229:271-274.
- Ardigó M, Borroni G, Muscardin L, et al. Hypopigmented mycosis fungoides in Caucasian patients: a clinicopathologic study of 7 cases. J Am Acad Dermatol. 2003;49:264-270.
- Boulos S, Vaid R, Aladily TN, et al. Clinical presentation, immunopathology, and treatment of juvenile-onset mycosis fungoides: a case series of 34 patients. J Am Acad Dermatol. 2014;71:1117-1126.
- Lambroza E, Cohen SR, Phelps R, et al. Hypopigmented variant of mycosis fungoides: demography, histopathology, and treatment of seven cases. J Am Acad Dermatol. 1995;32:987-993.
- El-Shabrawi-Caelen L, Cerroni L, Medeiros LJ, et al. Hypopigmented mycosis fungoides: Frequent expression of a CD8+ T-cell phenotype. Am J Surg Pathol. 2002;26:450-457.
- Furlan FC, de Paula Pereira BA, da Silva LF, et al. Loss of melanocytes in hypopigmented mycosis fungoides: a study of 18 patients. J Cutan Pathol. 2014;41:101-107.
- Tolkachjov SN, Comfere NI. Hypopigmented mycosis fungoides: a clinical mimicker of vitiligo. J Drugs Dermatol. 2015;14:193-194.
- Duarte I, Bedrikow, R, Aoki S. Mycosis fungoides: epidemiologic study of 17 cases and evaluation of PUVA photochemotherapy. An Bras Dermatol. 2006;81:40-45.
- Onsun N, Kural Y, Su O, et al. Hypopigmented mycosis fungoides associated with atopy in two children. Pediatr Dermatol. 2006;23:493-496.
- Furlan FC, Sanches JA. Hypopigmented mycosis fungoides: a review of its clinical features and pathophysiology. An Bras Dermatol. 2013;88:954-960.
- Girardi M, Heald PW, Wilson LD. The pathogenesis of mycosis fungoides. N Engl J Med. 2004;350:1978-1988.
- Kim EJ, Hess S, Richardson SK, et al. Immunopathogenesis and therapy of cutaneous T cell lymphoma. J Clin Invest. 2005;115:798-812.
- Stone ML, Styles AR, Cockerell CJ, et al. Hypopigmented report of 7 cases and review of the literature. Cutis. 2001;67:133-138.
- Volkenandt M, Soyer HP, Cerroni L, et al. Molecular detection of clone-specific DNA in hypopigmented lesions of a patient with early evolving mycosis fungoides. Br J Dermatol. 1993;128:423-428.
- Furlan FC, Pereira BA, Sotto MN, et al. Hypopigmented mycosis fungoides versus mycosis fungoides with concomitant hypopigmented lesions: same disease or different variants of mycosis fungoides? Dermatology. 2014;229:271-274.
- Ardigó M, Borroni G, Muscardin L, et al. Hypopigmented mycosis fungoides in Caucasian patients: a clinicopathologic study of 7 cases. J Am Acad Dermatol. 2003;49:264-270.
- Boulos S, Vaid R, Aladily TN, et al. Clinical presentation, immunopathology, and treatment of juvenile-onset mycosis fungoides: a case series of 34 patients. J Am Acad Dermatol. 2014;71:1117-1126.
- Lambroza E, Cohen SR, Phelps R, et al. Hypopigmented variant of mycosis fungoides: demography, histopathology, and treatment of seven cases. J Am Acad Dermatol. 1995;32:987-993.
- El-Shabrawi-Caelen L, Cerroni L, Medeiros LJ, et al. Hypopigmented mycosis fungoides: Frequent expression of a CD8+ T-cell phenotype. Am J Surg Pathol. 2002;26:450-457.
- Furlan FC, de Paula Pereira BA, da Silva LF, et al. Loss of melanocytes in hypopigmented mycosis fungoides: a study of 18 patients. J Cutan Pathol. 2014;41:101-107.
- Tolkachjov SN, Comfere NI. Hypopigmented mycosis fungoides: a clinical mimicker of vitiligo. J Drugs Dermatol. 2015;14:193-194.
- Duarte I, Bedrikow, R, Aoki S. Mycosis fungoides: epidemiologic study of 17 cases and evaluation of PUVA photochemotherapy. An Bras Dermatol. 2006;81:40-45.
- Onsun N, Kural Y, Su O, et al. Hypopigmented mycosis fungoides associated with atopy in two children. Pediatr Dermatol. 2006;23:493-496.

A 39-year-old woman presented with 2 areas of hypopigmented discoloration on the left thigh of 6 months' duration. The hypopigmentation was more visible following sun exposure because the areas did not tan. The patient had not sought prior treatment for the discoloration and denied any previous rash or trauma to the area. Her medical history was remarkable for hypothyroidism associated with mild and transient alopecia, acne, and xerosis. Her daily medications included oral contraceptive pills (norgestimate/ethinyl estradiol), oral levothyroxine/liothyronine, and sulfacetamide lotion 10%. She denied any allergies, and the remainder of her medical, surgical, social, and family history was unremarkable. A review of systems was negative for enlarged lymph nodes, fever, night sweats, and fatigue. Physical examination revealed 2 subtle hypopigmented patches with fine, atrophic, cigarette paper-like wrinkling distributed on the left medial and posterior upper thigh. Initial biopsy of the hypopigmented patches revealed a CD8+ lymphocytic infiltrate with an atypical interface.
Here comes bimekizumab, the newest IL-17 inhibitor
KAUAI, HAWAII –
And that’s not all: Much the same was true in patients with psoriatic arthritis in the parallel phase 2b BE ACTIVE study and for ankylosing spondylitis in the BE AGILE study. BE ABLE was a double-blind, 12-week, multicenter, five-arm, placebo-controlled, dose-ranging study of 250 psoriasis patients randomized to various doses of subcutaneous bimekizumab or placebo every 4 weeks. The primary outcome – the PASI 90 response rate at 12 weeks, rather than the lower-bar PASI 75 endpoint more typically used in clinical trials – was 79% at the optimal dose. The PASI 100 rate – complete clearance of disease – at 12 weeks was 60%, Craig L. Leonardi, MD, said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
lthough Dr. Leonardi is a distinguished psoriasis clinical trialist, he wasn’t involved in the BE ABLE study. Only top line results have been announced to date, although publication of the BE ABLE, BE AGILE, and BE ACTIVE results and presentations at major medical meetings are pending.
Bimekizumab is a humanized IgG1 monoclonal antibody which uniquely neutralizes both IL-17A and IL-17F. In contrast, secukinumab (Cosentyx) and ixekizumab (Taltz) specifically inhibit IL-17A, while brodalumab (Siliq) is a pan-IL-17 receptor antagonist, inhibiting the IL-17 A, A/F, E, F, and C receptors. The impressive clinical outcomes of the three BE phase 2b studies validate the notion that IL-17F is an important cytokine in tissue inflammation across a range of dermatologic and rheumatologic diseases.
A long-term extension of BE ABLE is ongoing. In addition, a phase 3 randomized trial of bimekizumab versus adalimumab (Humira) versus placebo in 450 psoriasis patients is now recruiting, as is a separate phase 3 placebo-controlled head to head comparison of bimekizumab versus ustekinumab (Stelara).
The BE ACTIVE study included 206 psoriatic arthritis patients. At the top dose of bimekizumab, the week 12 rate of at least a 50% improvement in joint symptoms, or ACR 50 response, was 46%, compared with 7% in placebo-treated controls. Patients with concomitant psoriasis over at least 3% of their body surface area demonstrated a 65% PASI 90 response rate at 12 weeks.
BE AGILE included 303 patients with ankylosing spondylitis. Forty-seven percent of those randomized to the top-performing dose of bimekizumab had at least a 40% improvement in their Ankylosing Spondylitis Activity Score, or ASAS 40, at week 12, as did 13% in the placebo arm.
Bimekizumab is being developed by UCB, which is planning additional studies advancing the biologic in all three diseases studied in the phase 2b trials.
Dr. Leonardi reported receiving research grants from well over a dozen pharmaceutical companies and serving as a consultant to UCB and others.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
KAUAI, HAWAII –
And that’s not all: Much the same was true in patients with psoriatic arthritis in the parallel phase 2b BE ACTIVE study and for ankylosing spondylitis in the BE AGILE study. BE ABLE was a double-blind, 12-week, multicenter, five-arm, placebo-controlled, dose-ranging study of 250 psoriasis patients randomized to various doses of subcutaneous bimekizumab or placebo every 4 weeks. The primary outcome – the PASI 90 response rate at 12 weeks, rather than the lower-bar PASI 75 endpoint more typically used in clinical trials – was 79% at the optimal dose. The PASI 100 rate – complete clearance of disease – at 12 weeks was 60%, Craig L. Leonardi, MD, said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
lthough Dr. Leonardi is a distinguished psoriasis clinical trialist, he wasn’t involved in the BE ABLE study. Only top line results have been announced to date, although publication of the BE ABLE, BE AGILE, and BE ACTIVE results and presentations at major medical meetings are pending.
Bimekizumab is a humanized IgG1 monoclonal antibody which uniquely neutralizes both IL-17A and IL-17F. In contrast, secukinumab (Cosentyx) and ixekizumab (Taltz) specifically inhibit IL-17A, while brodalumab (Siliq) is a pan-IL-17 receptor antagonist, inhibiting the IL-17 A, A/F, E, F, and C receptors. The impressive clinical outcomes of the three BE phase 2b studies validate the notion that IL-17F is an important cytokine in tissue inflammation across a range of dermatologic and rheumatologic diseases.
A long-term extension of BE ABLE is ongoing. In addition, a phase 3 randomized trial of bimekizumab versus adalimumab (Humira) versus placebo in 450 psoriasis patients is now recruiting, as is a separate phase 3 placebo-controlled head to head comparison of bimekizumab versus ustekinumab (Stelara).
The BE ACTIVE study included 206 psoriatic arthritis patients. At the top dose of bimekizumab, the week 12 rate of at least a 50% improvement in joint symptoms, or ACR 50 response, was 46%, compared with 7% in placebo-treated controls. Patients with concomitant psoriasis over at least 3% of their body surface area demonstrated a 65% PASI 90 response rate at 12 weeks.
BE AGILE included 303 patients with ankylosing spondylitis. Forty-seven percent of those randomized to the top-performing dose of bimekizumab had at least a 40% improvement in their Ankylosing Spondylitis Activity Score, or ASAS 40, at week 12, as did 13% in the placebo arm.
Bimekizumab is being developed by UCB, which is planning additional studies advancing the biologic in all three diseases studied in the phase 2b trials.
Dr. Leonardi reported receiving research grants from well over a dozen pharmaceutical companies and serving as a consultant to UCB and others.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
KAUAI, HAWAII –
And that’s not all: Much the same was true in patients with psoriatic arthritis in the parallel phase 2b BE ACTIVE study and for ankylosing spondylitis in the BE AGILE study. BE ABLE was a double-blind, 12-week, multicenter, five-arm, placebo-controlled, dose-ranging study of 250 psoriasis patients randomized to various doses of subcutaneous bimekizumab or placebo every 4 weeks. The primary outcome – the PASI 90 response rate at 12 weeks, rather than the lower-bar PASI 75 endpoint more typically used in clinical trials – was 79% at the optimal dose. The PASI 100 rate – complete clearance of disease – at 12 weeks was 60%, Craig L. Leonardi, MD, said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
lthough Dr. Leonardi is a distinguished psoriasis clinical trialist, he wasn’t involved in the BE ABLE study. Only top line results have been announced to date, although publication of the BE ABLE, BE AGILE, and BE ACTIVE results and presentations at major medical meetings are pending.
Bimekizumab is a humanized IgG1 monoclonal antibody which uniquely neutralizes both IL-17A and IL-17F. In contrast, secukinumab (Cosentyx) and ixekizumab (Taltz) specifically inhibit IL-17A, while brodalumab (Siliq) is a pan-IL-17 receptor antagonist, inhibiting the IL-17 A, A/F, E, F, and C receptors. The impressive clinical outcomes of the three BE phase 2b studies validate the notion that IL-17F is an important cytokine in tissue inflammation across a range of dermatologic and rheumatologic diseases.
A long-term extension of BE ABLE is ongoing. In addition, a phase 3 randomized trial of bimekizumab versus adalimumab (Humira) versus placebo in 450 psoriasis patients is now recruiting, as is a separate phase 3 placebo-controlled head to head comparison of bimekizumab versus ustekinumab (Stelara).
The BE ACTIVE study included 206 psoriatic arthritis patients. At the top dose of bimekizumab, the week 12 rate of at least a 50% improvement in joint symptoms, or ACR 50 response, was 46%, compared with 7% in placebo-treated controls. Patients with concomitant psoriasis over at least 3% of their body surface area demonstrated a 65% PASI 90 response rate at 12 weeks.
BE AGILE included 303 patients with ankylosing spondylitis. Forty-seven percent of those randomized to the top-performing dose of bimekizumab had at least a 40% improvement in their Ankylosing Spondylitis Activity Score, or ASAS 40, at week 12, as did 13% in the placebo arm.
Bimekizumab is being developed by UCB, which is planning additional studies advancing the biologic in all three diseases studied in the phase 2b trials.
Dr. Leonardi reported receiving research grants from well over a dozen pharmaceutical companies and serving as a consultant to UCB and others.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
Virtual reality–based CBT may improve social participation in psychosis
Virtual reality–based cognitive-behavioral therapy could help reduce momentary paranoia and anxiety, and improve social cognition in individuals with psychotic disorders.
Researchers reported the results of a randomized controlled trial of personalized virtual reality-based cognitive-behavioral therapy in 116 patients with a DSM IV–diagnosed psychotic disorder and paranoid ideation in an article published online Feb. 8 in Lancet Psychiatry.
Similarly, the group that received virtual reality therapy showed significantly larger decreases in momentary anxiety, compared with those in the control group. Those decreases remained significant at follow-up.
Researchers also observed a significant drop in safety behaviors – such as lack of eye contact – in the group who received the virtual reality therapy. At follow-up, this group showed less paranoid ideation in the form of lower levels of ideas of persecution and social reference.
The treatment also was associated with a small increase in time spent with others at the 6-month follow-up; a decrease was seen in the control group. Patients who underwent virtual reality therapy also showed improvements in self-stigmatization and social functioning.
The authors noted that the benefits for social functioning might take some time to emerge after therapy, as patients in symptomatic remission do not immediately start spending more time with other people.
“When patients increasingly feel more comfortable in social situations and learn that other people are less threatening than anticipated, they might try and succeed to make and maintain social contacts and find hobbies and jobs,” the authors wrote.
However, no significant differences were found between the two groups in terms of depression and anxiety, or in quality of life measurements posttreatment and at follow-up.
Virtual reality–based CBT is intended to get around some of the limitations of exposure-based therapeutic exercises for paranoid ideation. In virtual reality settings, the environment and characters can be completely controlled by the therapist, and the therapy is real time rather than retrospective and therefore not as vulnerable to patient bias.
“Finally, many patients are reluctant or unable to undergo exposure because of strong paranoid fears or negative symptoms,” the authors wrote.
The therapy took place in four virtual social environments – a street, bus, café, and supermarket. The therapist was able to control the characteristics and responses of up to 40 human avatars, enabling personalized treatment exercises for each patient.
“Patients and therapists communicated during virtual reality sessions to explore and challenge suspicious thoughts during social situations, drop safety behaviors during social situations (such as avoiding eye contact with, keeping distance from, and refraining from communication with avatars), and test harm expectancies,” they wrote.
The sessions also were designed to target safety behaviors, such as avoiding eye contact, because such behavior prevents individuals from receiving social information that can improve social cognition and reduce the chance of incorrect paranoid appraisals.
Several limitations were cited. For example, because follow-up was restricted to 6 months, it was not possible to access the long-term effects of virtual reality-based CBT. Also, some of the patients opted not to participate in the study because traveling to the therapy location proved too frightening. “Thus our sample might have been biased, because some of the most paranoid and avoidant patients could not participate,” they wrote.
The study was supported by Fonds NutsOhra and Stichting tot Steun VCVGZ. No conflicts of interest were declared.
SOURCE: Lancet Psychiatry. 2018 Feb 8. doi: 10.1016/S2215-0366(18)30053-1.
Virtual reality–based cognitive-behavioral therapy could help reduce momentary paranoia and anxiety, and improve social cognition in individuals with psychotic disorders.
Researchers reported the results of a randomized controlled trial of personalized virtual reality-based cognitive-behavioral therapy in 116 patients with a DSM IV–diagnosed psychotic disorder and paranoid ideation in an article published online Feb. 8 in Lancet Psychiatry.
Similarly, the group that received virtual reality therapy showed significantly larger decreases in momentary anxiety, compared with those in the control group. Those decreases remained significant at follow-up.
Researchers also observed a significant drop in safety behaviors – such as lack of eye contact – in the group who received the virtual reality therapy. At follow-up, this group showed less paranoid ideation in the form of lower levels of ideas of persecution and social reference.
The treatment also was associated with a small increase in time spent with others at the 6-month follow-up; a decrease was seen in the control group. Patients who underwent virtual reality therapy also showed improvements in self-stigmatization and social functioning.
The authors noted that the benefits for social functioning might take some time to emerge after therapy, as patients in symptomatic remission do not immediately start spending more time with other people.
“When patients increasingly feel more comfortable in social situations and learn that other people are less threatening than anticipated, they might try and succeed to make and maintain social contacts and find hobbies and jobs,” the authors wrote.
However, no significant differences were found between the two groups in terms of depression and anxiety, or in quality of life measurements posttreatment and at follow-up.
Virtual reality–based CBT is intended to get around some of the limitations of exposure-based therapeutic exercises for paranoid ideation. In virtual reality settings, the environment and characters can be completely controlled by the therapist, and the therapy is real time rather than retrospective and therefore not as vulnerable to patient bias.
“Finally, many patients are reluctant or unable to undergo exposure because of strong paranoid fears or negative symptoms,” the authors wrote.
The therapy took place in four virtual social environments – a street, bus, café, and supermarket. The therapist was able to control the characteristics and responses of up to 40 human avatars, enabling personalized treatment exercises for each patient.
“Patients and therapists communicated during virtual reality sessions to explore and challenge suspicious thoughts during social situations, drop safety behaviors during social situations (such as avoiding eye contact with, keeping distance from, and refraining from communication with avatars), and test harm expectancies,” they wrote.
The sessions also were designed to target safety behaviors, such as avoiding eye contact, because such behavior prevents individuals from receiving social information that can improve social cognition and reduce the chance of incorrect paranoid appraisals.
Several limitations were cited. For example, because follow-up was restricted to 6 months, it was not possible to access the long-term effects of virtual reality-based CBT. Also, some of the patients opted not to participate in the study because traveling to the therapy location proved too frightening. “Thus our sample might have been biased, because some of the most paranoid and avoidant patients could not participate,” they wrote.
The study was supported by Fonds NutsOhra and Stichting tot Steun VCVGZ. No conflicts of interest were declared.
SOURCE: Lancet Psychiatry. 2018 Feb 8. doi: 10.1016/S2215-0366(18)30053-1.
Virtual reality–based cognitive-behavioral therapy could help reduce momentary paranoia and anxiety, and improve social cognition in individuals with psychotic disorders.
Researchers reported the results of a randomized controlled trial of personalized virtual reality-based cognitive-behavioral therapy in 116 patients with a DSM IV–diagnosed psychotic disorder and paranoid ideation in an article published online Feb. 8 in Lancet Psychiatry.
Similarly, the group that received virtual reality therapy showed significantly larger decreases in momentary anxiety, compared with those in the control group. Those decreases remained significant at follow-up.
Researchers also observed a significant drop in safety behaviors – such as lack of eye contact – in the group who received the virtual reality therapy. At follow-up, this group showed less paranoid ideation in the form of lower levels of ideas of persecution and social reference.
The treatment also was associated with a small increase in time spent with others at the 6-month follow-up; a decrease was seen in the control group. Patients who underwent virtual reality therapy also showed improvements in self-stigmatization and social functioning.
The authors noted that the benefits for social functioning might take some time to emerge after therapy, as patients in symptomatic remission do not immediately start spending more time with other people.
“When patients increasingly feel more comfortable in social situations and learn that other people are less threatening than anticipated, they might try and succeed to make and maintain social contacts and find hobbies and jobs,” the authors wrote.
However, no significant differences were found between the two groups in terms of depression and anxiety, or in quality of life measurements posttreatment and at follow-up.
Virtual reality–based CBT is intended to get around some of the limitations of exposure-based therapeutic exercises for paranoid ideation. In virtual reality settings, the environment and characters can be completely controlled by the therapist, and the therapy is real time rather than retrospective and therefore not as vulnerable to patient bias.
“Finally, many patients are reluctant or unable to undergo exposure because of strong paranoid fears or negative symptoms,” the authors wrote.
The therapy took place in four virtual social environments – a street, bus, café, and supermarket. The therapist was able to control the characteristics and responses of up to 40 human avatars, enabling personalized treatment exercises for each patient.
“Patients and therapists communicated during virtual reality sessions to explore and challenge suspicious thoughts during social situations, drop safety behaviors during social situations (such as avoiding eye contact with, keeping distance from, and refraining from communication with avatars), and test harm expectancies,” they wrote.
The sessions also were designed to target safety behaviors, such as avoiding eye contact, because such behavior prevents individuals from receiving social information that can improve social cognition and reduce the chance of incorrect paranoid appraisals.
Several limitations were cited. For example, because follow-up was restricted to 6 months, it was not possible to access the long-term effects of virtual reality-based CBT. Also, some of the patients opted not to participate in the study because traveling to the therapy location proved too frightening. “Thus our sample might have been biased, because some of the most paranoid and avoidant patients could not participate,” they wrote.
The study was supported by Fonds NutsOhra and Stichting tot Steun VCVGZ. No conflicts of interest were declared.
SOURCE: Lancet Psychiatry. 2018 Feb 8. doi: 10.1016/S2215-0366(18)30053-1.
FROM LANCET PSYCHIATRY
Key clinical point:
Major finding: Patients who received virtual reality–based CBT showed significantly less momentary paranoia and momentary anxiety, and less paranoid ideation, than controls.
Data source: Randomized controlled trial in 116 patients with psychotic disorders.
Disclosures: The study was supported by Fonds NutsOhra and Stichting tot Steun VCVGZ. No conflicts of interest were declared.
Source: Pot-Kolder RMCA et al. Lancet Psychiatry. 2018 Feb 8. doi: 10.1016/S2215-0366(18)30053-1.
Expert shares tips for positioning biologics in IBD patient treatment
LAS VEGAS – In the clinical opinion of Edward V. Loftus Jr., MD, biologics for inflammatory bowel disease (IBD) patients are best positioned based on age, personal medical history, and the presence of extraintestinal manifestations.
“ and is the way to go if you’re trying to change the trajectory of illness,” Dr. Loftus said at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
In general, patients who are younger at diagnosis are going to have more severe disease than patients diagnosed older, said Dr. Loftus, professor of medicine at the Mayo Clinic, Rochester, Minn. “For CD [Crohn’s disease], the presence of fistulizing disease, especially internal fistulas, and to a lesser extent perianal fistulas, and then the presence of small-bowel disease or proximal GI disease, are all harbingers of more aggressive disease,” he said. “Multiple studies show that the time interval between diagnosis and development of intestinal complications is shorter in patients with small-bowel disease relative to colonic disease. When you add up those factors, you’re talking about 70% of CD patients, if not more. Most Crohn’s patients are going to be high-risk patients.”
For ulcerative colitis (UC), being male is a risk factor for hospitalization, surgery, and for developing colon cancer. On average, males are twice as likely as females to require surgery, and they’re twice as likely to develop colon cancer. Other predictors in UC for high-risk disease include early need for hospitalization, early need for corticosteroids, and extensive colitis at diagnosis. “You’re thinking about these things because how you’re going to treat these patients is going to differ,” he said.
According to Dr. Loftus, aminosalicylate (5-ASA) drugs are the frontline drugs of choice for low-risk UC patients with mild symptoms. “If they’re having moderate symptoms, you might initially start with a corticosteroid taper,” he noted. “That can be either prednisone or budesonide MMX. In a patient with really active symptoms, they’re going to go to IV steroids or maybe directly to anti-TNF [tumor necrosis factor] therapy.” For low-risk CD patients, consider budesonide taper then observation. “If they don’t flare again, maybe monitor that patient periodically,” he advised. “For high-risk patients, consider biologic therapy with or without thiopurine or methotrexate.”
A recent analysis of Medicare and Medicaid data from 2006 to 2013 found a significantly higher rate of mortality in IBD patients treated with prolonged corticosteroids than that seen in those treated with anti-TNF therapy (Am J Gastroenterol. Jan 16, 2018. doi: 10.1038/ajg2017.479). “That should give you pause,” Dr. Loftus said. “Don’t just put your patient on prednisone because you think it’s the easiest and safest thing to do. It’s not. It’s much more dangerous and has implications [for] the patient’s life expectancy.”
Some data are beginning to emerge about the use of biosimilars in IBD, mostly from Europe. Investigators of one randomized, controlled trial of biosimilar CT-P13 vs. originator infliximab in CD presented at the 2017 Digestive Disease Week meeting; they found in their trial that at week 6 all clinical endpoints were similar between the two agents. “If you’re forced to change your patient to this particular biosimilar, I wouldn’t be too worried about it,” Dr. Loftus said. “Of course, I’m not necessarily going to switch unless my institution or a particular third-party payer mandate it.”
In a published study funded by the Norwegian government, researchers conducted a prospective trial of switching from infliximab to CT-P13 in patients with a variety of conditions (Lancet. 2017;389:2304-16). Overall, the clinical failure rate was the same for both agents. Among CD patients, the researchers observed a nonsignificant trend toward disease worsening among those on the biosimilar, “but there was essentially no difference,” Dr. Loftus said.
He went on to discuss vedolizumab, a monoclonal antibody to alpha4beta7 integrin approved in 2014 for patients with moderate to severely active UC or CD. Phase 3 data from GEMINI I in moderate to severe UC found that relevant clinical endpoints were met by week 6 and they persisted at week 52 at both doses (N Engl J Med. 2013;369[8]:699-710). “For CD, the use of vedolizumab is a bit of a mixed picture,” Dr. Loftus said. “In GEMINI II, some of the primary endpoints were met at week 6, but at least one was missed (N Engl J Med. 2013;369[8]:711-21). The same thing was seen in GEMINI III. There’s a sense here that vedolizumab takes a little bit longer to work in CD.”
Integrated safety analyses of the GEMINI trials found no signal for increased rates of serious adverse events, and no cases of progressive multifocal leukoencephalopathy have been reported (J Crohns Colitis. 2017;11[2]:185-90). “The risk factors for serious infections were prior anti-TNF failure and opioid analgesic use in UC patients and younger age, steroid use, and opioid analgesic use in CD patients,” Dr. Loftus said.
In a trial of CD patients failing anti-TNF therapy, researchers observed a robust clinical response with ustekinumab, compared with placebo, at week 6 (N Engl J Med. 2016;375:1946-60). Even greater effects were observed in UNITI-2, a trial of ustekinumab in CD patients who hadn’t failed anti-TNFs.
Dr. Loftus cautioned that elderly and immunocompromised patients face an increased risk for infections when they’re placed on anti-TNF therapy. At the same time, researchers used a French database to determine the risk of lymphoma in IBD patients stratified by medication. For patients unexposed to such therapies, the risk of lymphoma was 1:4,000. For patients on thiopurine monotherapy, the risk was about 1:2,000; it was about 1:2,500 for those on anti-TNF monotherapy and about 1:1,000 for those on combination therapy (JAMA. 2017;318:1679-86). “One of the messages in this study is we can reassure our more risk-averse patients that the absolute risk of lymphoma is very low, even among patients on combination therapy,” he said.
Dr. Loftus called for head-to-head trials comparing the individual biologic agents and shared his recommendations on how to position currently available therapies. “I would say that for the average ‘bread and butter’ Crohn’s patient, anti-TNF therapy is the way to go,” he said. “For perianal fistulizing patients, I’m going to go with anti-TNF therapy, such as infliximab or adalimumab. For a patient with active extraintestinal manifestations, such as spondyloarthropathy, uveitis, and pyoderma, anti-TNF therapy is the way to go. However, with an elderly or immunosuppressed patient, consider vedolizumab or ustekinumab. For patients with a personal history of malignancy, an anti-TNF is very reasonable, but it may be easier to convince them to consider vedolizumab or ustekinumab.”
Recommendations for UC are largely similar, he continued. “However, I think we have enough data from GEMINI I and the integrated safety data with vedolizumab to say that, for the average ‘bread and butter’ UC patient, anti-TNF therapy or vedolizumab are appropriate. For a patient with extraintestinal manifestations I would avoid vedolizumab initially and try anti-TNF therapy. For patients with acute severe colitis, we have the bulk of evidence for efficacy resting with infliximab, so I would go with that. For the elderly or immunosuppressed patient, I would go with vedolizumab. For the person with a history of malignancy, an anti-TNF agent is reasonable, but consider vedolizumab.”
Dr. Loftus disclosed that he has consulted for AbbVie, Takeda Pharmaceutical, Janssen Pharmaceutica, UCB, Pfizer, Amgen, Eli Lilly, Celltrion Healthcare, Napo Pharmaceuticals. He has also received research support from AbbVie, Takeda Pharmaceutical, Janssen Pharmaceutica, UCB, Pfizer, Amgen, Genentech, Seres Pharmaceuticals, MedImmune, Allergan, and Robarts Clinical Trials.
*This story was updated on 3/26.
LAS VEGAS – In the clinical opinion of Edward V. Loftus Jr., MD, biologics for inflammatory bowel disease (IBD) patients are best positioned based on age, personal medical history, and the presence of extraintestinal manifestations.
“ and is the way to go if you’re trying to change the trajectory of illness,” Dr. Loftus said at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
In general, patients who are younger at diagnosis are going to have more severe disease than patients diagnosed older, said Dr. Loftus, professor of medicine at the Mayo Clinic, Rochester, Minn. “For CD [Crohn’s disease], the presence of fistulizing disease, especially internal fistulas, and to a lesser extent perianal fistulas, and then the presence of small-bowel disease or proximal GI disease, are all harbingers of more aggressive disease,” he said. “Multiple studies show that the time interval between diagnosis and development of intestinal complications is shorter in patients with small-bowel disease relative to colonic disease. When you add up those factors, you’re talking about 70% of CD patients, if not more. Most Crohn’s patients are going to be high-risk patients.”
For ulcerative colitis (UC), being male is a risk factor for hospitalization, surgery, and for developing colon cancer. On average, males are twice as likely as females to require surgery, and they’re twice as likely to develop colon cancer. Other predictors in UC for high-risk disease include early need for hospitalization, early need for corticosteroids, and extensive colitis at diagnosis. “You’re thinking about these things because how you’re going to treat these patients is going to differ,” he said.
According to Dr. Loftus, aminosalicylate (5-ASA) drugs are the frontline drugs of choice for low-risk UC patients with mild symptoms. “If they’re having moderate symptoms, you might initially start with a corticosteroid taper,” he noted. “That can be either prednisone or budesonide MMX. In a patient with really active symptoms, they’re going to go to IV steroids or maybe directly to anti-TNF [tumor necrosis factor] therapy.” For low-risk CD patients, consider budesonide taper then observation. “If they don’t flare again, maybe monitor that patient periodically,” he advised. “For high-risk patients, consider biologic therapy with or without thiopurine or methotrexate.”
A recent analysis of Medicare and Medicaid data from 2006 to 2013 found a significantly higher rate of mortality in IBD patients treated with prolonged corticosteroids than that seen in those treated with anti-TNF therapy (Am J Gastroenterol. Jan 16, 2018. doi: 10.1038/ajg2017.479). “That should give you pause,” Dr. Loftus said. “Don’t just put your patient on prednisone because you think it’s the easiest and safest thing to do. It’s not. It’s much more dangerous and has implications [for] the patient’s life expectancy.”
Some data are beginning to emerge about the use of biosimilars in IBD, mostly from Europe. Investigators of one randomized, controlled trial of biosimilar CT-P13 vs. originator infliximab in CD presented at the 2017 Digestive Disease Week meeting; they found in their trial that at week 6 all clinical endpoints were similar between the two agents. “If you’re forced to change your patient to this particular biosimilar, I wouldn’t be too worried about it,” Dr. Loftus said. “Of course, I’m not necessarily going to switch unless my institution or a particular third-party payer mandate it.”
In a published study funded by the Norwegian government, researchers conducted a prospective trial of switching from infliximab to CT-P13 in patients with a variety of conditions (Lancet. 2017;389:2304-16). Overall, the clinical failure rate was the same for both agents. Among CD patients, the researchers observed a nonsignificant trend toward disease worsening among those on the biosimilar, “but there was essentially no difference,” Dr. Loftus said.
He went on to discuss vedolizumab, a monoclonal antibody to alpha4beta7 integrin approved in 2014 for patients with moderate to severely active UC or CD. Phase 3 data from GEMINI I in moderate to severe UC found that relevant clinical endpoints were met by week 6 and they persisted at week 52 at both doses (N Engl J Med. 2013;369[8]:699-710). “For CD, the use of vedolizumab is a bit of a mixed picture,” Dr. Loftus said. “In GEMINI II, some of the primary endpoints were met at week 6, but at least one was missed (N Engl J Med. 2013;369[8]:711-21). The same thing was seen in GEMINI III. There’s a sense here that vedolizumab takes a little bit longer to work in CD.”
Integrated safety analyses of the GEMINI trials found no signal for increased rates of serious adverse events, and no cases of progressive multifocal leukoencephalopathy have been reported (J Crohns Colitis. 2017;11[2]:185-90). “The risk factors for serious infections were prior anti-TNF failure and opioid analgesic use in UC patients and younger age, steroid use, and opioid analgesic use in CD patients,” Dr. Loftus said.
In a trial of CD patients failing anti-TNF therapy, researchers observed a robust clinical response with ustekinumab, compared with placebo, at week 6 (N Engl J Med. 2016;375:1946-60). Even greater effects were observed in UNITI-2, a trial of ustekinumab in CD patients who hadn’t failed anti-TNFs.
Dr. Loftus cautioned that elderly and immunocompromised patients face an increased risk for infections when they’re placed on anti-TNF therapy. At the same time, researchers used a French database to determine the risk of lymphoma in IBD patients stratified by medication. For patients unexposed to such therapies, the risk of lymphoma was 1:4,000. For patients on thiopurine monotherapy, the risk was about 1:2,000; it was about 1:2,500 for those on anti-TNF monotherapy and about 1:1,000 for those on combination therapy (JAMA. 2017;318:1679-86). “One of the messages in this study is we can reassure our more risk-averse patients that the absolute risk of lymphoma is very low, even among patients on combination therapy,” he said.
Dr. Loftus called for head-to-head trials comparing the individual biologic agents and shared his recommendations on how to position currently available therapies. “I would say that for the average ‘bread and butter’ Crohn’s patient, anti-TNF therapy is the way to go,” he said. “For perianal fistulizing patients, I’m going to go with anti-TNF therapy, such as infliximab or adalimumab. For a patient with active extraintestinal manifestations, such as spondyloarthropathy, uveitis, and pyoderma, anti-TNF therapy is the way to go. However, with an elderly or immunosuppressed patient, consider vedolizumab or ustekinumab. For patients with a personal history of malignancy, an anti-TNF is very reasonable, but it may be easier to convince them to consider vedolizumab or ustekinumab.”
Recommendations for UC are largely similar, he continued. “However, I think we have enough data from GEMINI I and the integrated safety data with vedolizumab to say that, for the average ‘bread and butter’ UC patient, anti-TNF therapy or vedolizumab are appropriate. For a patient with extraintestinal manifestations I would avoid vedolizumab initially and try anti-TNF therapy. For patients with acute severe colitis, we have the bulk of evidence for efficacy resting with infliximab, so I would go with that. For the elderly or immunosuppressed patient, I would go with vedolizumab. For the person with a history of malignancy, an anti-TNF agent is reasonable, but consider vedolizumab.”
Dr. Loftus disclosed that he has consulted for AbbVie, Takeda Pharmaceutical, Janssen Pharmaceutica, UCB, Pfizer, Amgen, Eli Lilly, Celltrion Healthcare, Napo Pharmaceuticals. He has also received research support from AbbVie, Takeda Pharmaceutical, Janssen Pharmaceutica, UCB, Pfizer, Amgen, Genentech, Seres Pharmaceuticals, MedImmune, Allergan, and Robarts Clinical Trials.
*This story was updated on 3/26.
LAS VEGAS – In the clinical opinion of Edward V. Loftus Jr., MD, biologics for inflammatory bowel disease (IBD) patients are best positioned based on age, personal medical history, and the presence of extraintestinal manifestations.
“ and is the way to go if you’re trying to change the trajectory of illness,” Dr. Loftus said at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
In general, patients who are younger at diagnosis are going to have more severe disease than patients diagnosed older, said Dr. Loftus, professor of medicine at the Mayo Clinic, Rochester, Minn. “For CD [Crohn’s disease], the presence of fistulizing disease, especially internal fistulas, and to a lesser extent perianal fistulas, and then the presence of small-bowel disease or proximal GI disease, are all harbingers of more aggressive disease,” he said. “Multiple studies show that the time interval between diagnosis and development of intestinal complications is shorter in patients with small-bowel disease relative to colonic disease. When you add up those factors, you’re talking about 70% of CD patients, if not more. Most Crohn’s patients are going to be high-risk patients.”
For ulcerative colitis (UC), being male is a risk factor for hospitalization, surgery, and for developing colon cancer. On average, males are twice as likely as females to require surgery, and they’re twice as likely to develop colon cancer. Other predictors in UC for high-risk disease include early need for hospitalization, early need for corticosteroids, and extensive colitis at diagnosis. “You’re thinking about these things because how you’re going to treat these patients is going to differ,” he said.
According to Dr. Loftus, aminosalicylate (5-ASA) drugs are the frontline drugs of choice for low-risk UC patients with mild symptoms. “If they’re having moderate symptoms, you might initially start with a corticosteroid taper,” he noted. “That can be either prednisone or budesonide MMX. In a patient with really active symptoms, they’re going to go to IV steroids or maybe directly to anti-TNF [tumor necrosis factor] therapy.” For low-risk CD patients, consider budesonide taper then observation. “If they don’t flare again, maybe monitor that patient periodically,” he advised. “For high-risk patients, consider biologic therapy with or without thiopurine or methotrexate.”
A recent analysis of Medicare and Medicaid data from 2006 to 2013 found a significantly higher rate of mortality in IBD patients treated with prolonged corticosteroids than that seen in those treated with anti-TNF therapy (Am J Gastroenterol. Jan 16, 2018. doi: 10.1038/ajg2017.479). “That should give you pause,” Dr. Loftus said. “Don’t just put your patient on prednisone because you think it’s the easiest and safest thing to do. It’s not. It’s much more dangerous and has implications [for] the patient’s life expectancy.”
Some data are beginning to emerge about the use of biosimilars in IBD, mostly from Europe. Investigators of one randomized, controlled trial of biosimilar CT-P13 vs. originator infliximab in CD presented at the 2017 Digestive Disease Week meeting; they found in their trial that at week 6 all clinical endpoints were similar between the two agents. “If you’re forced to change your patient to this particular biosimilar, I wouldn’t be too worried about it,” Dr. Loftus said. “Of course, I’m not necessarily going to switch unless my institution or a particular third-party payer mandate it.”
In a published study funded by the Norwegian government, researchers conducted a prospective trial of switching from infliximab to CT-P13 in patients with a variety of conditions (Lancet. 2017;389:2304-16). Overall, the clinical failure rate was the same for both agents. Among CD patients, the researchers observed a nonsignificant trend toward disease worsening among those on the biosimilar, “but there was essentially no difference,” Dr. Loftus said.
He went on to discuss vedolizumab, a monoclonal antibody to alpha4beta7 integrin approved in 2014 for patients with moderate to severely active UC or CD. Phase 3 data from GEMINI I in moderate to severe UC found that relevant clinical endpoints were met by week 6 and they persisted at week 52 at both doses (N Engl J Med. 2013;369[8]:699-710). “For CD, the use of vedolizumab is a bit of a mixed picture,” Dr. Loftus said. “In GEMINI II, some of the primary endpoints were met at week 6, but at least one was missed (N Engl J Med. 2013;369[8]:711-21). The same thing was seen in GEMINI III. There’s a sense here that vedolizumab takes a little bit longer to work in CD.”
Integrated safety analyses of the GEMINI trials found no signal for increased rates of serious adverse events, and no cases of progressive multifocal leukoencephalopathy have been reported (J Crohns Colitis. 2017;11[2]:185-90). “The risk factors for serious infections were prior anti-TNF failure and opioid analgesic use in UC patients and younger age, steroid use, and opioid analgesic use in CD patients,” Dr. Loftus said.
In a trial of CD patients failing anti-TNF therapy, researchers observed a robust clinical response with ustekinumab, compared with placebo, at week 6 (N Engl J Med. 2016;375:1946-60). Even greater effects were observed in UNITI-2, a trial of ustekinumab in CD patients who hadn’t failed anti-TNFs.
Dr. Loftus cautioned that elderly and immunocompromised patients face an increased risk for infections when they’re placed on anti-TNF therapy. At the same time, researchers used a French database to determine the risk of lymphoma in IBD patients stratified by medication. For patients unexposed to such therapies, the risk of lymphoma was 1:4,000. For patients on thiopurine monotherapy, the risk was about 1:2,000; it was about 1:2,500 for those on anti-TNF monotherapy and about 1:1,000 for those on combination therapy (JAMA. 2017;318:1679-86). “One of the messages in this study is we can reassure our more risk-averse patients that the absolute risk of lymphoma is very low, even among patients on combination therapy,” he said.
Dr. Loftus called for head-to-head trials comparing the individual biologic agents and shared his recommendations on how to position currently available therapies. “I would say that for the average ‘bread and butter’ Crohn’s patient, anti-TNF therapy is the way to go,” he said. “For perianal fistulizing patients, I’m going to go with anti-TNF therapy, such as infliximab or adalimumab. For a patient with active extraintestinal manifestations, such as spondyloarthropathy, uveitis, and pyoderma, anti-TNF therapy is the way to go. However, with an elderly or immunosuppressed patient, consider vedolizumab or ustekinumab. For patients with a personal history of malignancy, an anti-TNF is very reasonable, but it may be easier to convince them to consider vedolizumab or ustekinumab.”
Recommendations for UC are largely similar, he continued. “However, I think we have enough data from GEMINI I and the integrated safety data with vedolizumab to say that, for the average ‘bread and butter’ UC patient, anti-TNF therapy or vedolizumab are appropriate. For a patient with extraintestinal manifestations I would avoid vedolizumab initially and try anti-TNF therapy. For patients with acute severe colitis, we have the bulk of evidence for efficacy resting with infliximab, so I would go with that. For the elderly or immunosuppressed patient, I would go with vedolizumab. For the person with a history of malignancy, an anti-TNF agent is reasonable, but consider vedolizumab.”
Dr. Loftus disclosed that he has consulted for AbbVie, Takeda Pharmaceutical, Janssen Pharmaceutica, UCB, Pfizer, Amgen, Eli Lilly, Celltrion Healthcare, Napo Pharmaceuticals. He has also received research support from AbbVie, Takeda Pharmaceutical, Janssen Pharmaceutica, UCB, Pfizer, Amgen, Genentech, Seres Pharmaceuticals, MedImmune, Allergan, and Robarts Clinical Trials.
*This story was updated on 3/26.
EXPERT ANALYSIS FROM THE CROHN’S & COLITIS CONGRESS
Enzalutamide shines in nonmetastatic castration-resistant prostate cancer
SAN FRANCISCO – The androgen receptor inhibitor enzalutamide is efficacious for treating nonmetastatic castration-resistant prostate cancer accompanied by a rapidly rising prostate-specific antigen (PSA) level, according to results of the phase 3 PROSPER trial.
“Nonmetastatic castration-resistant prostate cancer is an area of unmet need with no currently approved therapies. The development of metastases is predictable in this group of patients and is associated with increasing baseline PSA and a PSA doubling time of less than 10 months,” said lead author Maha Hussain, MBChB, deputy director at the Robert H. Lurie Comprehensive Cancer Center of Northwestern University, Chicago. “Delaying time to all metastases, which is a very clinically relevant endpoint because that is the terminal phase of the disease, is important, with the potential to delay cancer-related morbidity and also prolong overall survival.”
The PROSPER investigators enrolled 1,401 men with nonmetastatic castration-resistant prostate cancer and a PSA doubling time of 10 months or less despite castrate levels of testosterone. They were randomized 2:1 to enzalutamide (Xtandi) or placebo, with continuation of androgen deprivation therapy in both groups. (At present, enzalutamide is approved by the Food and Drug Administration for untreated and docetaxel-treated metastatic castration-resistant prostate cancer).
With a median follow-up of 22 months, median metastasis-free survival (based on radiographic progression or death) was about 22 months longer with enzalutamide versus placebo, according to results reported at the 2018 Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology. The difference translated to a 71% reduction in risk of events.
Relative to peers in the placebo group, patients in the enzalutamide group also had dramatically longer time to PSA progression (93% risk reduction) and time to first use of new antineoplastic therapy (79% risk reduction). An interim analysis showed a trend toward better overall survival with the drug as well, and it was well tolerated.
Although progression on PROSPER was ascertained by conventional imaging, advent of new, more sensitive imaging modalities, such as fluciclovine and prostate-specific membrane antigen PET, are unlikely to change the calculus, according to Dr. Hussain. “These patients have micrometastatic disease. The fact that we have imaging criteria right now that are not very sensitive does not mean we don’t think the patients have micromets. With the newer technologies, certainly, a good chunk of these patients could have physical metastatic disease,” she elaborated. And cancer treatments often achieve greater benefits when moved earlier in the disease course.
Approved indications aside, oncologists will likely take a tailored approach when deciding to treat nonmetastatic castration-resistant prostate cancer with enzalutamide or a similar agent, Dr. Hussain said. “Like anything else, the issue is going to boil down to a shared decision with the patient, pros and cons, and then making a decision together.”
The findings with enzalutamide in the PROSPER trial are also noteworthy in that they largely mirror those obtained with apalutamide in the SPARTAN trial, which were reported in the same session at the symposium.
Weighing the evidence
The 2-year prolongation of metastasis-free survival with apalutamide and enzalutamide is “very impressive,” said invited discussant Philip Kantoff, MD, a medical oncologist and chair of the department of medicine, Memorial Sloan Kettering Cancer Center in New York. “These drugs are very biologically active. This potentially gives us options for men with M0 castration-resistant prostate cancer. It’s something I would like to see as a clinician, but we have to be a little bit cautious. Treating asymptomatic patients carries a certain burden of proof wherein benefit must clearly outweigh risk.”
Clinical benefit of a drug in this patient population could be shown in three ways, he said: curing disease (which is unlikely), prolonging survival (which is as yet unproven), and improving quality of life by, for example, reducing anxiety over rising PSA levels and preventing skeletal-related adverse events (which is hinted at by SPARTAN data showing that enzalutamide delayed time to symptomatic progression).
“Clinical benefit, to me, is not fully demonstrated in these two studies, and there are some untoward effects that need to be better defined,” Dr. Kantoff maintained. In particular, apalutamide was associated with higher (albeit still low) rates of grade 3 or worse falls, fractures, and rash, and enzalutamide with more deaths in the absence of radiographic progression, for unclear reasons.
“My confidence in declaring victory would be greater with further scrutiny of the toxicities and understanding how the care patterns in these studies compare with actual practice, specifically, the timing of initiation of alternative therapies in these trials as opposed to what’s going on in the community,” he said.
It is too early to determine whether one drug is superior, according to Dr. Kantoff. “These were not comparative trials, so we don’t have enough information to say one versus the other. There’s a hint of different toxicity profiles. It isn’t clear that the efficacy is different.” And when it comes to adoption by community oncology, the FDA will have a role, sifting through the data for both drugs and rendering decisions, he said.
Study details
Median metastasis-free survival in PROSPER was 36.6 months with enzalutamide and 14.7 months with placebo (hazard ratio, 0.29; P less than .0001), Dr. Hussain reported. Benefit was similar across a range of patient subgroups, including patients with PSA doubling times of less than and greater than 6 months.
Patients in the enzalutamide group had half the rate of progression events when compared with peers in the placebo group (23% vs. 49%). Among those with a metastasis-free survival event, the rate of deaths without documented radiographic progression after stopping study treatment was higher with enzalutamide (15% vs. 2%); there were somewhat more cardiovascular deaths with the drug within this subset, but no single cause was clearly predominant, she said.
Median time to PSA progression was 37.2 months with enzalutamide and merely 3.9 months with placebo (HR, 0.07; P less than .0001). Median time to first use of new antineoplastic therapy was 39.6 months and 17.7 months, respectively (HR, 0.21; P less than .0001).
Median overall survival was not yet reached in either group, but tended to be longer with enzalutamide (HR, 0.80).
“Therapy overall was well tolerated. Adverse events were generally consistent with those reported in prior clinical trials in men with castration-resistant disease,” Dr. Hussain said. The rate of grade 3 or worse events was 31% with enzalutamide and 23% with placebo. The enzalutamide group more commonly experienced grade 3 or worse hypertension (5% vs. 2%) and fatigue (3% vs. 1%).
The rate of adverse events leading to study discontinuation was 9% with enzalutamide and 6% with placebo, and that of death due to adverse events was 3% and 1%, respectively.
Dr. Hussain disclosed that she receives honoraria from OncLive; has a consulting or advisory role with Abbvie, Bayer, and Genentech/Roche; has patents, royalties, or other intellectual property pertaining to dual inhibition of MET and VEGF for the treatment of castration-resistant prostate cancer; and receives travel, accommodations, or expenses from Abbvie, Bayer, and Genentech. In addition, her institution receives research funding from AstraZeneca, Genentech, PCCTC, and Pfizer. The trial was sponsored by Pfizer, with collaboration of Astellas Pharma Inc. and Medivation LLC, a wholly owned subsidiary of Pfizer Inc.
SOURCE: Hussain M et al. Abstract 3.
SAN FRANCISCO – The androgen receptor inhibitor enzalutamide is efficacious for treating nonmetastatic castration-resistant prostate cancer accompanied by a rapidly rising prostate-specific antigen (PSA) level, according to results of the phase 3 PROSPER trial.
“Nonmetastatic castration-resistant prostate cancer is an area of unmet need with no currently approved therapies. The development of metastases is predictable in this group of patients and is associated with increasing baseline PSA and a PSA doubling time of less than 10 months,” said lead author Maha Hussain, MBChB, deputy director at the Robert H. Lurie Comprehensive Cancer Center of Northwestern University, Chicago. “Delaying time to all metastases, which is a very clinically relevant endpoint because that is the terminal phase of the disease, is important, with the potential to delay cancer-related morbidity and also prolong overall survival.”
The PROSPER investigators enrolled 1,401 men with nonmetastatic castration-resistant prostate cancer and a PSA doubling time of 10 months or less despite castrate levels of testosterone. They were randomized 2:1 to enzalutamide (Xtandi) or placebo, with continuation of androgen deprivation therapy in both groups. (At present, enzalutamide is approved by the Food and Drug Administration for untreated and docetaxel-treated metastatic castration-resistant prostate cancer).
With a median follow-up of 22 months, median metastasis-free survival (based on radiographic progression or death) was about 22 months longer with enzalutamide versus placebo, according to results reported at the 2018 Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology. The difference translated to a 71% reduction in risk of events.
Relative to peers in the placebo group, patients in the enzalutamide group also had dramatically longer time to PSA progression (93% risk reduction) and time to first use of new antineoplastic therapy (79% risk reduction). An interim analysis showed a trend toward better overall survival with the drug as well, and it was well tolerated.
Although progression on PROSPER was ascertained by conventional imaging, advent of new, more sensitive imaging modalities, such as fluciclovine and prostate-specific membrane antigen PET, are unlikely to change the calculus, according to Dr. Hussain. “These patients have micrometastatic disease. The fact that we have imaging criteria right now that are not very sensitive does not mean we don’t think the patients have micromets. With the newer technologies, certainly, a good chunk of these patients could have physical metastatic disease,” she elaborated. And cancer treatments often achieve greater benefits when moved earlier in the disease course.
Approved indications aside, oncologists will likely take a tailored approach when deciding to treat nonmetastatic castration-resistant prostate cancer with enzalutamide or a similar agent, Dr. Hussain said. “Like anything else, the issue is going to boil down to a shared decision with the patient, pros and cons, and then making a decision together.”
The findings with enzalutamide in the PROSPER trial are also noteworthy in that they largely mirror those obtained with apalutamide in the SPARTAN trial, which were reported in the same session at the symposium.
Weighing the evidence
The 2-year prolongation of metastasis-free survival with apalutamide and enzalutamide is “very impressive,” said invited discussant Philip Kantoff, MD, a medical oncologist and chair of the department of medicine, Memorial Sloan Kettering Cancer Center in New York. “These drugs are very biologically active. This potentially gives us options for men with M0 castration-resistant prostate cancer. It’s something I would like to see as a clinician, but we have to be a little bit cautious. Treating asymptomatic patients carries a certain burden of proof wherein benefit must clearly outweigh risk.”
Clinical benefit of a drug in this patient population could be shown in three ways, he said: curing disease (which is unlikely), prolonging survival (which is as yet unproven), and improving quality of life by, for example, reducing anxiety over rising PSA levels and preventing skeletal-related adverse events (which is hinted at by SPARTAN data showing that enzalutamide delayed time to symptomatic progression).
“Clinical benefit, to me, is not fully demonstrated in these two studies, and there are some untoward effects that need to be better defined,” Dr. Kantoff maintained. In particular, apalutamide was associated with higher (albeit still low) rates of grade 3 or worse falls, fractures, and rash, and enzalutamide with more deaths in the absence of radiographic progression, for unclear reasons.
“My confidence in declaring victory would be greater with further scrutiny of the toxicities and understanding how the care patterns in these studies compare with actual practice, specifically, the timing of initiation of alternative therapies in these trials as opposed to what’s going on in the community,” he said.
It is too early to determine whether one drug is superior, according to Dr. Kantoff. “These were not comparative trials, so we don’t have enough information to say one versus the other. There’s a hint of different toxicity profiles. It isn’t clear that the efficacy is different.” And when it comes to adoption by community oncology, the FDA will have a role, sifting through the data for both drugs and rendering decisions, he said.
Study details
Median metastasis-free survival in PROSPER was 36.6 months with enzalutamide and 14.7 months with placebo (hazard ratio, 0.29; P less than .0001), Dr. Hussain reported. Benefit was similar across a range of patient subgroups, including patients with PSA doubling times of less than and greater than 6 months.
Patients in the enzalutamide group had half the rate of progression events when compared with peers in the placebo group (23% vs. 49%). Among those with a metastasis-free survival event, the rate of deaths without documented radiographic progression after stopping study treatment was higher with enzalutamide (15% vs. 2%); there were somewhat more cardiovascular deaths with the drug within this subset, but no single cause was clearly predominant, she said.
Median time to PSA progression was 37.2 months with enzalutamide and merely 3.9 months with placebo (HR, 0.07; P less than .0001). Median time to first use of new antineoplastic therapy was 39.6 months and 17.7 months, respectively (HR, 0.21; P less than .0001).
Median overall survival was not yet reached in either group, but tended to be longer with enzalutamide (HR, 0.80).
“Therapy overall was well tolerated. Adverse events were generally consistent with those reported in prior clinical trials in men with castration-resistant disease,” Dr. Hussain said. The rate of grade 3 or worse events was 31% with enzalutamide and 23% with placebo. The enzalutamide group more commonly experienced grade 3 or worse hypertension (5% vs. 2%) and fatigue (3% vs. 1%).
The rate of adverse events leading to study discontinuation was 9% with enzalutamide and 6% with placebo, and that of death due to adverse events was 3% and 1%, respectively.
Dr. Hussain disclosed that she receives honoraria from OncLive; has a consulting or advisory role with Abbvie, Bayer, and Genentech/Roche; has patents, royalties, or other intellectual property pertaining to dual inhibition of MET and VEGF for the treatment of castration-resistant prostate cancer; and receives travel, accommodations, or expenses from Abbvie, Bayer, and Genentech. In addition, her institution receives research funding from AstraZeneca, Genentech, PCCTC, and Pfizer. The trial was sponsored by Pfizer, with collaboration of Astellas Pharma Inc. and Medivation LLC, a wholly owned subsidiary of Pfizer Inc.
SOURCE: Hussain M et al. Abstract 3.
SAN FRANCISCO – The androgen receptor inhibitor enzalutamide is efficacious for treating nonmetastatic castration-resistant prostate cancer accompanied by a rapidly rising prostate-specific antigen (PSA) level, according to results of the phase 3 PROSPER trial.
“Nonmetastatic castration-resistant prostate cancer is an area of unmet need with no currently approved therapies. The development of metastases is predictable in this group of patients and is associated with increasing baseline PSA and a PSA doubling time of less than 10 months,” said lead author Maha Hussain, MBChB, deputy director at the Robert H. Lurie Comprehensive Cancer Center of Northwestern University, Chicago. “Delaying time to all metastases, which is a very clinically relevant endpoint because that is the terminal phase of the disease, is important, with the potential to delay cancer-related morbidity and also prolong overall survival.”
The PROSPER investigators enrolled 1,401 men with nonmetastatic castration-resistant prostate cancer and a PSA doubling time of 10 months or less despite castrate levels of testosterone. They were randomized 2:1 to enzalutamide (Xtandi) or placebo, with continuation of androgen deprivation therapy in both groups. (At present, enzalutamide is approved by the Food and Drug Administration for untreated and docetaxel-treated metastatic castration-resistant prostate cancer).
With a median follow-up of 22 months, median metastasis-free survival (based on radiographic progression or death) was about 22 months longer with enzalutamide versus placebo, according to results reported at the 2018 Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology. The difference translated to a 71% reduction in risk of events.
Relative to peers in the placebo group, patients in the enzalutamide group also had dramatically longer time to PSA progression (93% risk reduction) and time to first use of new antineoplastic therapy (79% risk reduction). An interim analysis showed a trend toward better overall survival with the drug as well, and it was well tolerated.
Although progression on PROSPER was ascertained by conventional imaging, advent of new, more sensitive imaging modalities, such as fluciclovine and prostate-specific membrane antigen PET, are unlikely to change the calculus, according to Dr. Hussain. “These patients have micrometastatic disease. The fact that we have imaging criteria right now that are not very sensitive does not mean we don’t think the patients have micromets. With the newer technologies, certainly, a good chunk of these patients could have physical metastatic disease,” she elaborated. And cancer treatments often achieve greater benefits when moved earlier in the disease course.
Approved indications aside, oncologists will likely take a tailored approach when deciding to treat nonmetastatic castration-resistant prostate cancer with enzalutamide or a similar agent, Dr. Hussain said. “Like anything else, the issue is going to boil down to a shared decision with the patient, pros and cons, and then making a decision together.”
The findings with enzalutamide in the PROSPER trial are also noteworthy in that they largely mirror those obtained with apalutamide in the SPARTAN trial, which were reported in the same session at the symposium.
Weighing the evidence
The 2-year prolongation of metastasis-free survival with apalutamide and enzalutamide is “very impressive,” said invited discussant Philip Kantoff, MD, a medical oncologist and chair of the department of medicine, Memorial Sloan Kettering Cancer Center in New York. “These drugs are very biologically active. This potentially gives us options for men with M0 castration-resistant prostate cancer. It’s something I would like to see as a clinician, but we have to be a little bit cautious. Treating asymptomatic patients carries a certain burden of proof wherein benefit must clearly outweigh risk.”
Clinical benefit of a drug in this patient population could be shown in three ways, he said: curing disease (which is unlikely), prolonging survival (which is as yet unproven), and improving quality of life by, for example, reducing anxiety over rising PSA levels and preventing skeletal-related adverse events (which is hinted at by SPARTAN data showing that enzalutamide delayed time to symptomatic progression).
“Clinical benefit, to me, is not fully demonstrated in these two studies, and there are some untoward effects that need to be better defined,” Dr. Kantoff maintained. In particular, apalutamide was associated with higher (albeit still low) rates of grade 3 or worse falls, fractures, and rash, and enzalutamide with more deaths in the absence of radiographic progression, for unclear reasons.
“My confidence in declaring victory would be greater with further scrutiny of the toxicities and understanding how the care patterns in these studies compare with actual practice, specifically, the timing of initiation of alternative therapies in these trials as opposed to what’s going on in the community,” he said.
It is too early to determine whether one drug is superior, according to Dr. Kantoff. “These were not comparative trials, so we don’t have enough information to say one versus the other. There’s a hint of different toxicity profiles. It isn’t clear that the efficacy is different.” And when it comes to adoption by community oncology, the FDA will have a role, sifting through the data for both drugs and rendering decisions, he said.
Study details
Median metastasis-free survival in PROSPER was 36.6 months with enzalutamide and 14.7 months with placebo (hazard ratio, 0.29; P less than .0001), Dr. Hussain reported. Benefit was similar across a range of patient subgroups, including patients with PSA doubling times of less than and greater than 6 months.
Patients in the enzalutamide group had half the rate of progression events when compared with peers in the placebo group (23% vs. 49%). Among those with a metastasis-free survival event, the rate of deaths without documented radiographic progression after stopping study treatment was higher with enzalutamide (15% vs. 2%); there were somewhat more cardiovascular deaths with the drug within this subset, but no single cause was clearly predominant, she said.
Median time to PSA progression was 37.2 months with enzalutamide and merely 3.9 months with placebo (HR, 0.07; P less than .0001). Median time to first use of new antineoplastic therapy was 39.6 months and 17.7 months, respectively (HR, 0.21; P less than .0001).
Median overall survival was not yet reached in either group, but tended to be longer with enzalutamide (HR, 0.80).
“Therapy overall was well tolerated. Adverse events were generally consistent with those reported in prior clinical trials in men with castration-resistant disease,” Dr. Hussain said. The rate of grade 3 or worse events was 31% with enzalutamide and 23% with placebo. The enzalutamide group more commonly experienced grade 3 or worse hypertension (5% vs. 2%) and fatigue (3% vs. 1%).
The rate of adverse events leading to study discontinuation was 9% with enzalutamide and 6% with placebo, and that of death due to adverse events was 3% and 1%, respectively.
Dr. Hussain disclosed that she receives honoraria from OncLive; has a consulting or advisory role with Abbvie, Bayer, and Genentech/Roche; has patents, royalties, or other intellectual property pertaining to dual inhibition of MET and VEGF for the treatment of castration-resistant prostate cancer; and receives travel, accommodations, or expenses from Abbvie, Bayer, and Genentech. In addition, her institution receives research funding from AstraZeneca, Genentech, PCCTC, and Pfizer. The trial was sponsored by Pfizer, with collaboration of Astellas Pharma Inc. and Medivation LLC, a wholly owned subsidiary of Pfizer Inc.
SOURCE: Hussain M et al. Abstract 3.
REPORTING FROM GUCS 2018
Key clinical point:
Major finding: Metastasis-free survival was 36.6 months with enzalutamide and 14.7 months with placebo (hazard ratio, 0.29; P less than .0001).
Data source: A phase 3 randomized trial among 1,401 men with nonmetastatic castration-resistant prostate cancer and rapidly rising PSA level (PROSPER trial).
Disclosures: Dr. Hussain disclosed that she receives honoraria from OncLive; has a consulting or advisory role with Abbvie, Bayer, and Genentech/Roche; has patents, royalties, or other intellectual property pertaining to dual inhibition of MET and VEGF for the treatment of castration-resistant prostate cancer; and receives travel, accommodations, or expenses from Abbvie, Bayer, and Genentech. In addition, her institution receives research funding from AstraZeneca, Genentech, PCCTC, and Pfizer. The trial was sponsored by Pfizer, with collaboration of Astellas Pharma Inc. and Medivation LLC, a wholly owned subsidiary of Pfizer Inc.
Source: Hussain M et al. Abstract 3.
Next-day discharge after TAVR shows promise
Compared with a longer hospital stay, next-day discharge (NDD) after minimalist transcatheter aortic valve replacement (TAVR) appears safe, according to a recently reported analysis of patients treated at a single center.
The composite endpoint of mortality and readmission at 30 days was similar for NDD, compared with later discharges among patients who had a procedure that met minimalist criteria, defined in this study as transfemoral TAVR under conscious sedation and local anesthesia.
Mortality and readmission at 1 year was lower in the NDD group, mainly because of a lower risk of noncardiovascular readmissions, study authors reported in JACC: Cardiovascular Interventions. “Although superior NDD outcomes are likely attributed to selected patient characteristics, NDD in patients without in-hospital complications may be appropriate after transfemoral balloon-expandable TAVR,” wrote Norihiko Kamioka, MD, division of cardiology, Emory University, Atlanta, and associates.
The retrospective, observational analysis included 663 consecutive patients who underwent elective balloon-expandable TAVR during July 2014–July 2016. Cases with complications after the procedure were excluded.
The final analysis, which included 150 patients who had NDD and 210 discharged later, showed no difference between groups in the composite endpoint of mortality, and that 30-day readmissions were similar between groups (hazard ratio, 0.62; 95% confidence interval, 0.20-1.91).
Mortality and readmission at 1 year, the primary endpoint chosen for the study, favored the NDD group (HR, 0.47; 95% CI, 0.27-0.81), but “this finding probably reflects a healthier cohort in the NDD group,” the investigators noted. Furthermore, “although the reason for the discrepancy in the composite outcome at 1 year is mainly driven by noncardiovascular readmission, other confounding variables cannot be entirely ruled out,” Dr. Kamioka and colleagues said in the report.
Predictors of NDD included male sex, no atrial fibrillation, lower serum creatinine level, and younger age, researchers also found.
A validation cohort would be needed to confirm the findings of this study, including predictors of favorable outcomes, and to apply NDD to a wider population, study authors said.
Dr. Kamioka reported no relationships relevant to the study. Study coauthors reported disclosures related to Edwards Lifesciences, Abbott Vascular, Medtronic, Gore Vascular, and Boston Scientific.
SOURCE: JACC: Cardiovascular Interventions. 2018 Jan 22. doi: 10.1016/j.jcin.2017.10.021.
Researchers at Emory University have been leaders in promoting the so-called minimalist approach to TAVR and helping others understand how to safely reduce the length of stay without reducing the quality of care in these patients; however, the present study has significant shortcomings” that “may raise more questions than answers.
Because of these exclusions, it is difficult to know from this study if this treatment is generalizable to a larger TAVR population.
The conclusion that there was no difference in the composite outcome of death and readmission at 30 days is helpful information, offering reassurance that patient safety is not being compromised with NDD; however, the finding of superior outcomes at 1 year in the NDD group was driven by a significant reduction in noncardiovascular readmissions, which merely reemphasizes that the NDD patients in this study were lower risk rather than that they benefited by NDD.
Molly Szerlip, MD, of the Heart Hospital Baylor Plano (Tex.) made these comments in an accompanying editorial (JACC: Cardiovasc Interven. 2018 Jan 22. doi: 10.1016/j.jcin.2017.12.001). She reported disclosures related to Edwards Lifesciences and Medtronic.
Researchers at Emory University have been leaders in promoting the so-called minimalist approach to TAVR and helping others understand how to safely reduce the length of stay without reducing the quality of care in these patients; however, the present study has significant shortcomings” that “may raise more questions than answers.
Because of these exclusions, it is difficult to know from this study if this treatment is generalizable to a larger TAVR population.
The conclusion that there was no difference in the composite outcome of death and readmission at 30 days is helpful information, offering reassurance that patient safety is not being compromised with NDD; however, the finding of superior outcomes at 1 year in the NDD group was driven by a significant reduction in noncardiovascular readmissions, which merely reemphasizes that the NDD patients in this study were lower risk rather than that they benefited by NDD.
Molly Szerlip, MD, of the Heart Hospital Baylor Plano (Tex.) made these comments in an accompanying editorial (JACC: Cardiovasc Interven. 2018 Jan 22. doi: 10.1016/j.jcin.2017.12.001). She reported disclosures related to Edwards Lifesciences and Medtronic.
Researchers at Emory University have been leaders in promoting the so-called minimalist approach to TAVR and helping others understand how to safely reduce the length of stay without reducing the quality of care in these patients; however, the present study has significant shortcomings” that “may raise more questions than answers.
Because of these exclusions, it is difficult to know from this study if this treatment is generalizable to a larger TAVR population.
The conclusion that there was no difference in the composite outcome of death and readmission at 30 days is helpful information, offering reassurance that patient safety is not being compromised with NDD; however, the finding of superior outcomes at 1 year in the NDD group was driven by a significant reduction in noncardiovascular readmissions, which merely reemphasizes that the NDD patients in this study were lower risk rather than that they benefited by NDD.
Molly Szerlip, MD, of the Heart Hospital Baylor Plano (Tex.) made these comments in an accompanying editorial (JACC: Cardiovasc Interven. 2018 Jan 22. doi: 10.1016/j.jcin.2017.12.001). She reported disclosures related to Edwards Lifesciences and Medtronic.
Compared with a longer hospital stay, next-day discharge (NDD) after minimalist transcatheter aortic valve replacement (TAVR) appears safe, according to a recently reported analysis of patients treated at a single center.
The composite endpoint of mortality and readmission at 30 days was similar for NDD, compared with later discharges among patients who had a procedure that met minimalist criteria, defined in this study as transfemoral TAVR under conscious sedation and local anesthesia.
Mortality and readmission at 1 year was lower in the NDD group, mainly because of a lower risk of noncardiovascular readmissions, study authors reported in JACC: Cardiovascular Interventions. “Although superior NDD outcomes are likely attributed to selected patient characteristics, NDD in patients without in-hospital complications may be appropriate after transfemoral balloon-expandable TAVR,” wrote Norihiko Kamioka, MD, division of cardiology, Emory University, Atlanta, and associates.
The retrospective, observational analysis included 663 consecutive patients who underwent elective balloon-expandable TAVR during July 2014–July 2016. Cases with complications after the procedure were excluded.
The final analysis, which included 150 patients who had NDD and 210 discharged later, showed no difference between groups in the composite endpoint of mortality, and that 30-day readmissions were similar between groups (hazard ratio, 0.62; 95% confidence interval, 0.20-1.91).
Mortality and readmission at 1 year, the primary endpoint chosen for the study, favored the NDD group (HR, 0.47; 95% CI, 0.27-0.81), but “this finding probably reflects a healthier cohort in the NDD group,” the investigators noted. Furthermore, “although the reason for the discrepancy in the composite outcome at 1 year is mainly driven by noncardiovascular readmission, other confounding variables cannot be entirely ruled out,” Dr. Kamioka and colleagues said in the report.
Predictors of NDD included male sex, no atrial fibrillation, lower serum creatinine level, and younger age, researchers also found.
A validation cohort would be needed to confirm the findings of this study, including predictors of favorable outcomes, and to apply NDD to a wider population, study authors said.
Dr. Kamioka reported no relationships relevant to the study. Study coauthors reported disclosures related to Edwards Lifesciences, Abbott Vascular, Medtronic, Gore Vascular, and Boston Scientific.
SOURCE: JACC: Cardiovascular Interventions. 2018 Jan 22. doi: 10.1016/j.jcin.2017.10.021.
Compared with a longer hospital stay, next-day discharge (NDD) after minimalist transcatheter aortic valve replacement (TAVR) appears safe, according to a recently reported analysis of patients treated at a single center.
The composite endpoint of mortality and readmission at 30 days was similar for NDD, compared with later discharges among patients who had a procedure that met minimalist criteria, defined in this study as transfemoral TAVR under conscious sedation and local anesthesia.
Mortality and readmission at 1 year was lower in the NDD group, mainly because of a lower risk of noncardiovascular readmissions, study authors reported in JACC: Cardiovascular Interventions. “Although superior NDD outcomes are likely attributed to selected patient characteristics, NDD in patients without in-hospital complications may be appropriate after transfemoral balloon-expandable TAVR,” wrote Norihiko Kamioka, MD, division of cardiology, Emory University, Atlanta, and associates.
The retrospective, observational analysis included 663 consecutive patients who underwent elective balloon-expandable TAVR during July 2014–July 2016. Cases with complications after the procedure were excluded.
The final analysis, which included 150 patients who had NDD and 210 discharged later, showed no difference between groups in the composite endpoint of mortality, and that 30-day readmissions were similar between groups (hazard ratio, 0.62; 95% confidence interval, 0.20-1.91).
Mortality and readmission at 1 year, the primary endpoint chosen for the study, favored the NDD group (HR, 0.47; 95% CI, 0.27-0.81), but “this finding probably reflects a healthier cohort in the NDD group,” the investigators noted. Furthermore, “although the reason for the discrepancy in the composite outcome at 1 year is mainly driven by noncardiovascular readmission, other confounding variables cannot be entirely ruled out,” Dr. Kamioka and colleagues said in the report.
Predictors of NDD included male sex, no atrial fibrillation, lower serum creatinine level, and younger age, researchers also found.
A validation cohort would be needed to confirm the findings of this study, including predictors of favorable outcomes, and to apply NDD to a wider population, study authors said.
Dr. Kamioka reported no relationships relevant to the study. Study coauthors reported disclosures related to Edwards Lifesciences, Abbott Vascular, Medtronic, Gore Vascular, and Boston Scientific.
SOURCE: JACC: Cardiovascular Interventions. 2018 Jan 22. doi: 10.1016/j.jcin.2017.10.021.
FROM JACC: CARDIOVASCULAR INTERVENTIONS
Key clinical point: Next-day discharge (NDD) after minimalist TAVR appeared safe, compared with a longer hospital stay.
Major finding: The composite endpoint of mortality and readmission at 30 days was similar between groups (HR, 0.62; 95% CI, 0.20-1.91), and was lower in the NDD arm at 1 year because of fewer noncardiovascular readmissions.
Data source: A single-center, retrospective, nonrandomized observational analysis comprising 663 consecutive patients who underwent elective balloon-expandable TAVR between July 2014 and July 2016.
Disclosures: Study authors reported disclosures related to Edwards Lifesciences, Abbott Vascular, Medtronic, Gore Vascular, and Boston Scientific.
Source: JACC: Cardiovasc Interven. doi: 10.1016/j.jcin.2017.10.021.
Fetal alcohol syndrome: Context matters
Recently, there was a lot of hoopla in the popular press caused by the report by Philip A. May, PhD, and his team showing that the rates of fetal alcohol spectrum disorder (FASD) ran between 1.1 to 5.0% in first graders in four U.S. communities (JAMA. 2018;319[5]:474-82). This publication and the press it received made my heart sing because the findings made national news – meaning the issue would be in the public’s consciousness for a day or two. That is progress.
As psychiatrists, we should know that context is important. For example, I was at the Northeast Conference on Fetal Alcohol Spectrum Disorders in 2017 in Colby, Maine, and heard Larry Burd, PhD, a longstanding expert in the area of FASD, describe the drinking habits of the Native American women who had children with FASD. He described them as being alcoholics. I was floored, because engaged in social drinking during this time, but stopped cold when they realized that they were pregnant. I only saw two of 500 women that I would consider alcoholics, and one went on a 3-day binge with her girlfriends when she learned that she was pregnant. Clearly, context matters.
I continue to maintain that increasing choline in prenatal vitamins is a way out of this mess the United States is in with its hidden epidemic of FASD.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital Family Medicine Clinic in Chicago; a clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago; a former president/CEO of Community Mental Health Council; and a former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
Recently, there was a lot of hoopla in the popular press caused by the report by Philip A. May, PhD, and his team showing that the rates of fetal alcohol spectrum disorder (FASD) ran between 1.1 to 5.0% in first graders in four U.S. communities (JAMA. 2018;319[5]:474-82). This publication and the press it received made my heart sing because the findings made national news – meaning the issue would be in the public’s consciousness for a day or two. That is progress.
As psychiatrists, we should know that context is important. For example, I was at the Northeast Conference on Fetal Alcohol Spectrum Disorders in 2017 in Colby, Maine, and heard Larry Burd, PhD, a longstanding expert in the area of FASD, describe the drinking habits of the Native American women who had children with FASD. He described them as being alcoholics. I was floored, because engaged in social drinking during this time, but stopped cold when they realized that they were pregnant. I only saw two of 500 women that I would consider alcoholics, and one went on a 3-day binge with her girlfriends when she learned that she was pregnant. Clearly, context matters.
I continue to maintain that increasing choline in prenatal vitamins is a way out of this mess the United States is in with its hidden epidemic of FASD.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital Family Medicine Clinic in Chicago; a clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago; a former president/CEO of Community Mental Health Council; and a former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
Recently, there was a lot of hoopla in the popular press caused by the report by Philip A. May, PhD, and his team showing that the rates of fetal alcohol spectrum disorder (FASD) ran between 1.1 to 5.0% in first graders in four U.S. communities (JAMA. 2018;319[5]:474-82). This publication and the press it received made my heart sing because the findings made national news – meaning the issue would be in the public’s consciousness for a day or two. That is progress.
As psychiatrists, we should know that context is important. For example, I was at the Northeast Conference on Fetal Alcohol Spectrum Disorders in 2017 in Colby, Maine, and heard Larry Burd, PhD, a longstanding expert in the area of FASD, describe the drinking habits of the Native American women who had children with FASD. He described them as being alcoholics. I was floored, because engaged in social drinking during this time, but stopped cold when they realized that they were pregnant. I only saw two of 500 women that I would consider alcoholics, and one went on a 3-day binge with her girlfriends when she learned that she was pregnant. Clearly, context matters.
I continue to maintain that increasing choline in prenatal vitamins is a way out of this mess the United States is in with its hidden epidemic of FASD.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital Family Medicine Clinic in Chicago; a clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago; a former president/CEO of Community Mental Health Council; and a former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.


















