User login
Pedunculated Verrucous Tumor on the Buttock
The Diagnosis: Giant Acrochordon
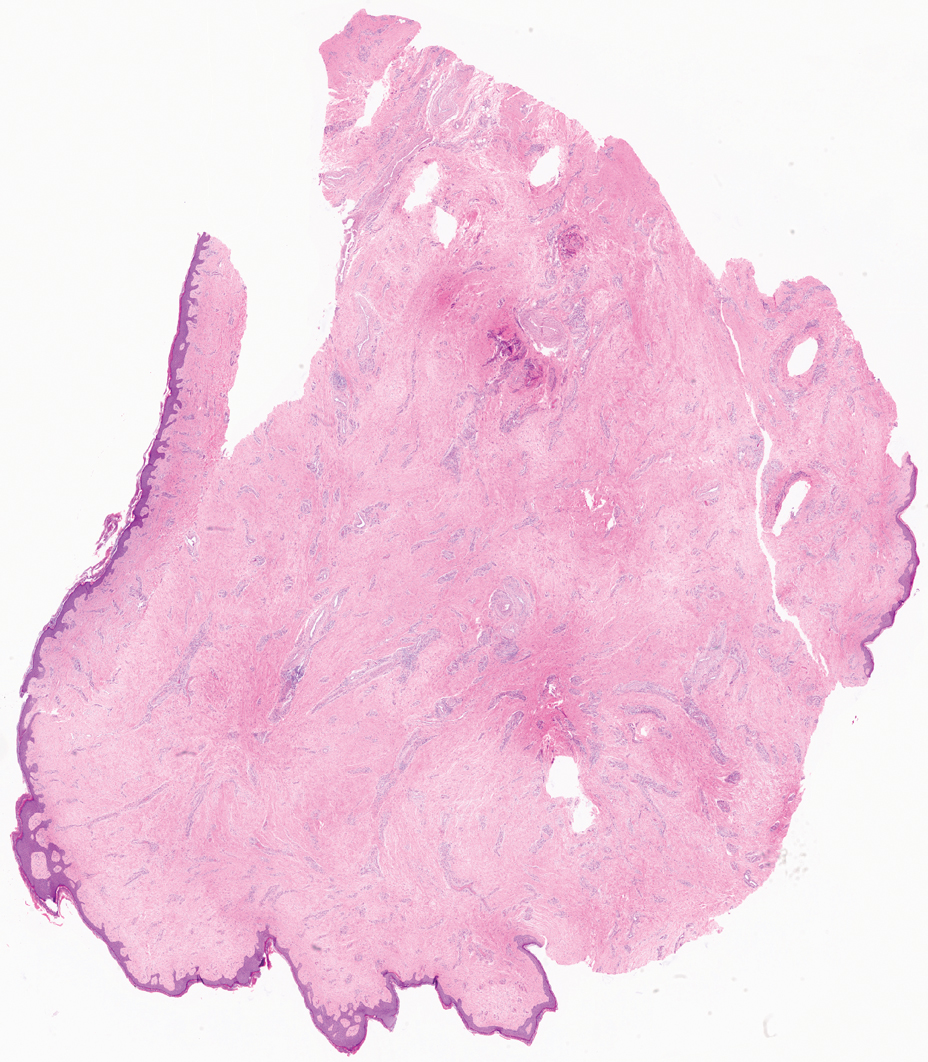
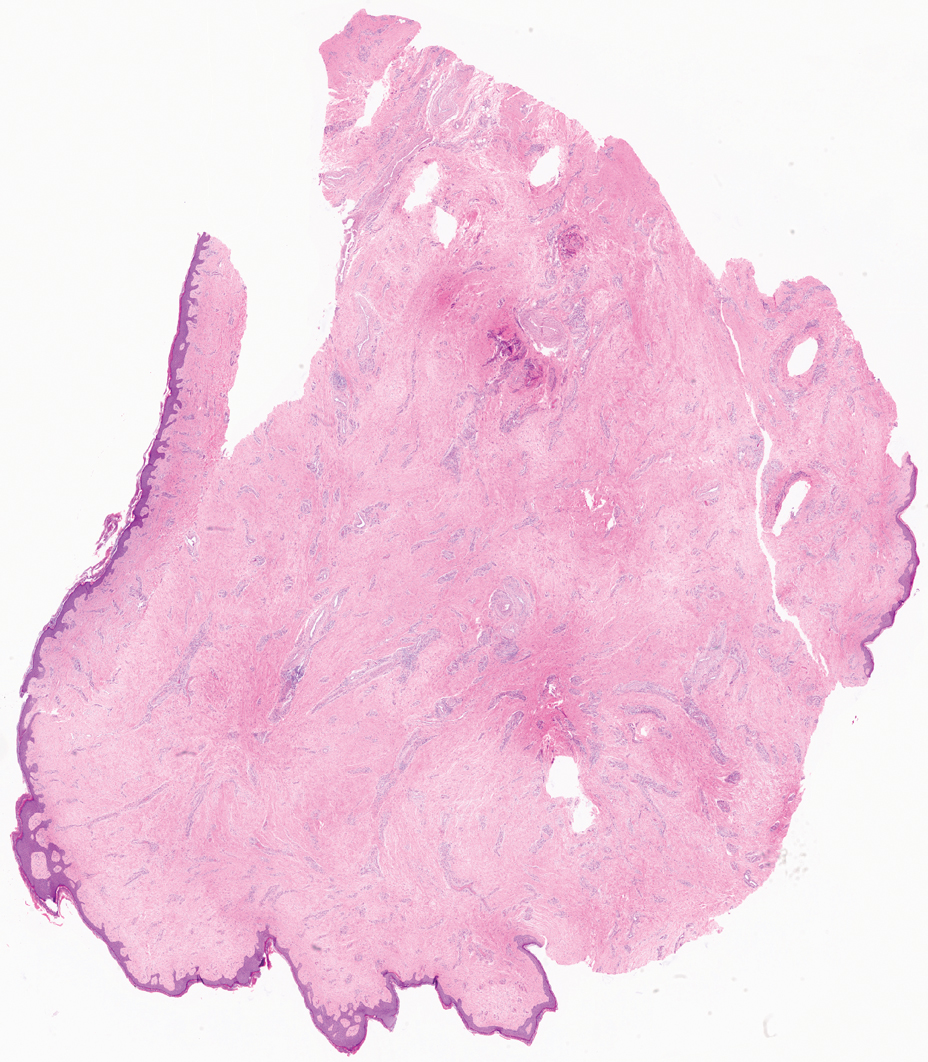
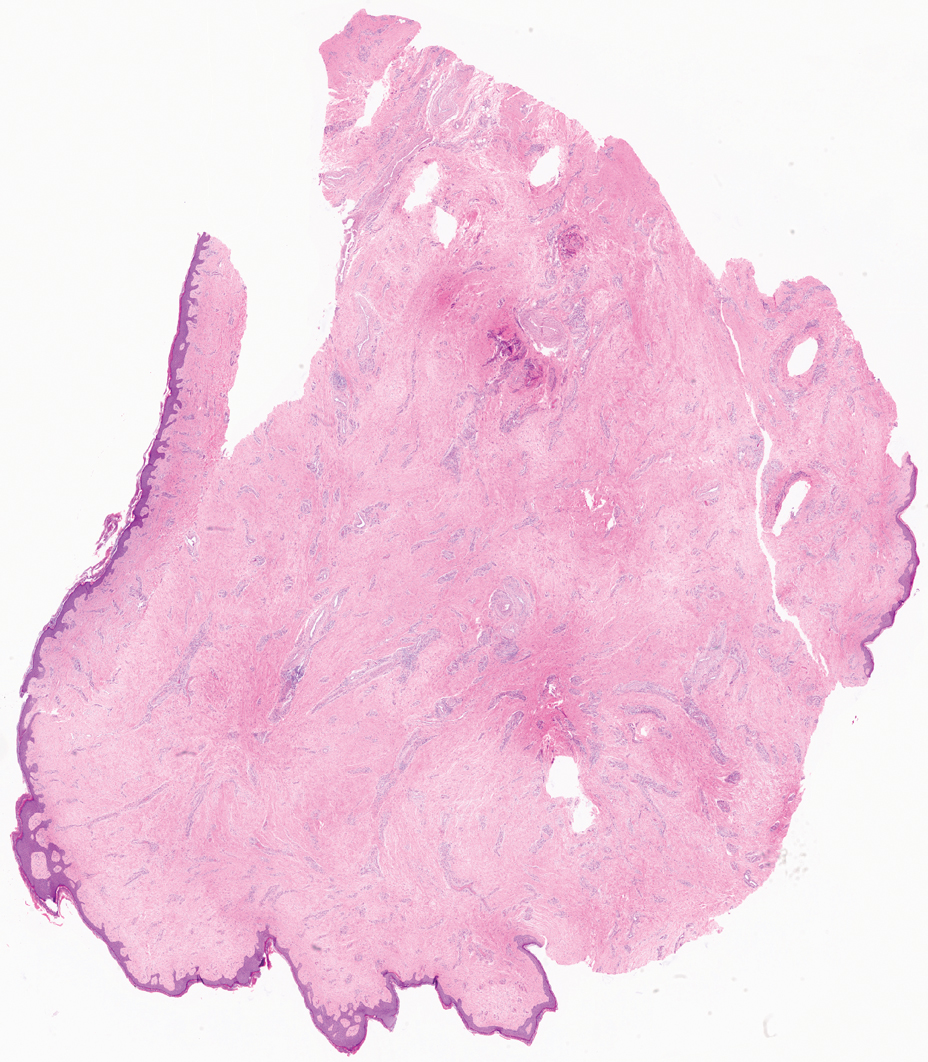
Based on the clinical and histologic findings, our patient was diagnosed with a giant acrochordon. Acrochordons (also known as fibroepithelial polyps or skin tags) are among the most commonly identified skin lesions and are believed to affect up to 46% of the general population.1,2 These benign growths typically appear after middle age in men and women alike and are believed to be of ectodermal and mesenchymal origin.3 The most common locations include the axillae, neck, and inguinal folds. They generally are small, measuring only a few millimeters, and frequently present as multiple lesions that are called giant acrochordons when their size exceeds 5 cm in length.2 Acrochordons are benign lesions with only rare reports of the presence of basal or squamous cell carcinoma within the lesion on pathology.4 In addition to being cosmetically unsightly, patients with acrochordons often report pruritus. These lesions are easily removed in an outpatient setting via snip excision, cryosurgery, or electrodesiccation. Once removed, recurrence is unlikely. Despite the prevalence of fibroepithelial polyps worldwide, reports of giant acrochordons are limited. The histopathology of giant acrochordons is similar to smaller acrochordons, with features including epidermal acanthosis and a central core of fibrovascular tissue without adnexal structures (Figure).4
The differential diagnosis of giant acrochordon includes neurofibroma, nodular melanoma, squamous cell carcinoma, and giant condylomata acuminata (Buschke-Löwenstein tumor).1 It is important to consider the clinical presentation and histopathologic findings to differentiate giant acrochordons from these other entities.
Neurofibromas typically present as multiple flesh-colored to brown nodules that invaginate into the skin when minimal external pressure is applied.5 Histopathology demonstrates a discrete, nonencapsulated, dermal collection of small nerve fibers and loosely arranged spindle cells. In contrast, giant acrochordons typically present as large, fleshcolored, pedunculated, verrucous tumors with a central stalk. Histopathology reveals epidermal acanthosis and a central core of fibrovascular tissue without adnexal structures.
Nodular melanomas usually are blue to black and grow rapidly over the course of several months.6 They have signs of hemorrhagic crust, and histopathology reveals atypical melanocytes, frequent mitoses, pleomorphic tumor cells, and irregular clumping of chromatin within the nuclei. Giant acrochordons are flesh colored, benign, and do not have these malignant features.
Squamous cell carcinoma often presents as an erythematous scaly patch or red plaque on sun-exposed areas of the skin.1 Histopathology of squamous cell carcinoma shows atypical keratinocytes with an invasive growth pattern; giant acrochordon does not show keratinocytic atypia or invasive epidermal growth.
Giant condylomata acuminata (Buschke-Löwenstein tumor) is a locally destructive verrucous plaque that typically appears on the penis but can occur elsewhere in the anogenital region.7 Histopathologic features include epidermal hyperplasia, papillomatosis, and koilocytes. In contrast, giant acrochordons typically are located on the buttocks and do not present with these epidermal changes.
Based on the clinical and histologic findings, our patient was diagnosed with a giant acrochordon, a rare variant of the common skin lesion. Excisional removal was critical for both diagnostic and treatment purposes. By considering the clinical presentation and histopathologic features of other conditions in the differential, giant acrochordons can be distinguished from other similar entities. Diagnosis and prompt surgical removal are important for management of these neoplasms and prevention of misdiagnosis.
- Alkhalili E, Prapasiri S, Russell J. Giant acrochordon of the axilla. BMJ Case Rep. 2015:bcr2015210623. doi:10.1136/bcr-2015-210623
- Banik R, Lubach D. Skin tags: localization and frequencies according to sex and age. Dermatologica. 1987;174:180-183. doi:10.1159/000249169
- Can B, Yildrim Ozluk A. Giant fibroepithelial polyps: why do they grow excessively? Med Bull Sisli Etfal Hastan Tip Bul. 2020;54:257-260. doi:10.14744/SEMB.2018.33603
- Ghosh SK, Bandyopadhyay D, Chatterjee G, et al. Giant skin tags on unusual locations. J Eur Acad Dermatol Venereol. 2009;23:233. doi:10.1111/j.1468-3083.2008.02816.x
- Messersmith L, Krauland K. Neurofibroma. StatPearls [Internet]. StatPearls Publishing; 2023.
- Saaiq M, Ashraf B, Siddiqui S. Nodular melanoma. Iran J Med Sci. 2016;41:164-165.
- Spinu D, Ra˘dulescu A, Bratu O, et al. Giant condyloma acuminatum. Buschke-Lowenstein disease: a literature review. Chirurgia (Bucur). 2014;109:445-450.
The Diagnosis: Giant Acrochordon
Based on the clinical and histologic findings, our patient was diagnosed with a giant acrochordon. Acrochordons (also known as fibroepithelial polyps or skin tags) are among the most commonly identified skin lesions and are believed to affect up to 46% of the general population.1,2 These benign growths typically appear after middle age in men and women alike and are believed to be of ectodermal and mesenchymal origin.3 The most common locations include the axillae, neck, and inguinal folds. They generally are small, measuring only a few millimeters, and frequently present as multiple lesions that are called giant acrochordons when their size exceeds 5 cm in length.2 Acrochordons are benign lesions with only rare reports of the presence of basal or squamous cell carcinoma within the lesion on pathology.4 In addition to being cosmetically unsightly, patients with acrochordons often report pruritus. These lesions are easily removed in an outpatient setting via snip excision, cryosurgery, or electrodesiccation. Once removed, recurrence is unlikely. Despite the prevalence of fibroepithelial polyps worldwide, reports of giant acrochordons are limited. The histopathology of giant acrochordons is similar to smaller acrochordons, with features including epidermal acanthosis and a central core of fibrovascular tissue without adnexal structures (Figure).4
The differential diagnosis of giant acrochordon includes neurofibroma, nodular melanoma, squamous cell carcinoma, and giant condylomata acuminata (Buschke-Löwenstein tumor).1 It is important to consider the clinical presentation and histopathologic findings to differentiate giant acrochordons from these other entities.
Neurofibromas typically present as multiple flesh-colored to brown nodules that invaginate into the skin when minimal external pressure is applied.5 Histopathology demonstrates a discrete, nonencapsulated, dermal collection of small nerve fibers and loosely arranged spindle cells. In contrast, giant acrochordons typically present as large, fleshcolored, pedunculated, verrucous tumors with a central stalk. Histopathology reveals epidermal acanthosis and a central core of fibrovascular tissue without adnexal structures.
Nodular melanomas usually are blue to black and grow rapidly over the course of several months.6 They have signs of hemorrhagic crust, and histopathology reveals atypical melanocytes, frequent mitoses, pleomorphic tumor cells, and irregular clumping of chromatin within the nuclei. Giant acrochordons are flesh colored, benign, and do not have these malignant features.
Squamous cell carcinoma often presents as an erythematous scaly patch or red plaque on sun-exposed areas of the skin.1 Histopathology of squamous cell carcinoma shows atypical keratinocytes with an invasive growth pattern; giant acrochordon does not show keratinocytic atypia or invasive epidermal growth.
Giant condylomata acuminata (Buschke-Löwenstein tumor) is a locally destructive verrucous plaque that typically appears on the penis but can occur elsewhere in the anogenital region.7 Histopathologic features include epidermal hyperplasia, papillomatosis, and koilocytes. In contrast, giant acrochordons typically are located on the buttocks and do not present with these epidermal changes.
Based on the clinical and histologic findings, our patient was diagnosed with a giant acrochordon, a rare variant of the common skin lesion. Excisional removal was critical for both diagnostic and treatment purposes. By considering the clinical presentation and histopathologic features of other conditions in the differential, giant acrochordons can be distinguished from other similar entities. Diagnosis and prompt surgical removal are important for management of these neoplasms and prevention of misdiagnosis.
The Diagnosis: Giant Acrochordon
Based on the clinical and histologic findings, our patient was diagnosed with a giant acrochordon. Acrochordons (also known as fibroepithelial polyps or skin tags) are among the most commonly identified skin lesions and are believed to affect up to 46% of the general population.1,2 These benign growths typically appear after middle age in men and women alike and are believed to be of ectodermal and mesenchymal origin.3 The most common locations include the axillae, neck, and inguinal folds. They generally are small, measuring only a few millimeters, and frequently present as multiple lesions that are called giant acrochordons when their size exceeds 5 cm in length.2 Acrochordons are benign lesions with only rare reports of the presence of basal or squamous cell carcinoma within the lesion on pathology.4 In addition to being cosmetically unsightly, patients with acrochordons often report pruritus. These lesions are easily removed in an outpatient setting via snip excision, cryosurgery, or electrodesiccation. Once removed, recurrence is unlikely. Despite the prevalence of fibroepithelial polyps worldwide, reports of giant acrochordons are limited. The histopathology of giant acrochordons is similar to smaller acrochordons, with features including epidermal acanthosis and a central core of fibrovascular tissue without adnexal structures (Figure).4
The differential diagnosis of giant acrochordon includes neurofibroma, nodular melanoma, squamous cell carcinoma, and giant condylomata acuminata (Buschke-Löwenstein tumor).1 It is important to consider the clinical presentation and histopathologic findings to differentiate giant acrochordons from these other entities.
Neurofibromas typically present as multiple flesh-colored to brown nodules that invaginate into the skin when minimal external pressure is applied.5 Histopathology demonstrates a discrete, nonencapsulated, dermal collection of small nerve fibers and loosely arranged spindle cells. In contrast, giant acrochordons typically present as large, fleshcolored, pedunculated, verrucous tumors with a central stalk. Histopathology reveals epidermal acanthosis and a central core of fibrovascular tissue without adnexal structures.
Nodular melanomas usually are blue to black and grow rapidly over the course of several months.6 They have signs of hemorrhagic crust, and histopathology reveals atypical melanocytes, frequent mitoses, pleomorphic tumor cells, and irregular clumping of chromatin within the nuclei. Giant acrochordons are flesh colored, benign, and do not have these malignant features.
Squamous cell carcinoma often presents as an erythematous scaly patch or red plaque on sun-exposed areas of the skin.1 Histopathology of squamous cell carcinoma shows atypical keratinocytes with an invasive growth pattern; giant acrochordon does not show keratinocytic atypia or invasive epidermal growth.
Giant condylomata acuminata (Buschke-Löwenstein tumor) is a locally destructive verrucous plaque that typically appears on the penis but can occur elsewhere in the anogenital region.7 Histopathologic features include epidermal hyperplasia, papillomatosis, and koilocytes. In contrast, giant acrochordons typically are located on the buttocks and do not present with these epidermal changes.
Based on the clinical and histologic findings, our patient was diagnosed with a giant acrochordon, a rare variant of the common skin lesion. Excisional removal was critical for both diagnostic and treatment purposes. By considering the clinical presentation and histopathologic features of other conditions in the differential, giant acrochordons can be distinguished from other similar entities. Diagnosis and prompt surgical removal are important for management of these neoplasms and prevention of misdiagnosis.
- Alkhalili E, Prapasiri S, Russell J. Giant acrochordon of the axilla. BMJ Case Rep. 2015:bcr2015210623. doi:10.1136/bcr-2015-210623
- Banik R, Lubach D. Skin tags: localization and frequencies according to sex and age. Dermatologica. 1987;174:180-183. doi:10.1159/000249169
- Can B, Yildrim Ozluk A. Giant fibroepithelial polyps: why do they grow excessively? Med Bull Sisli Etfal Hastan Tip Bul. 2020;54:257-260. doi:10.14744/SEMB.2018.33603
- Ghosh SK, Bandyopadhyay D, Chatterjee G, et al. Giant skin tags on unusual locations. J Eur Acad Dermatol Venereol. 2009;23:233. doi:10.1111/j.1468-3083.2008.02816.x
- Messersmith L, Krauland K. Neurofibroma. StatPearls [Internet]. StatPearls Publishing; 2023.
- Saaiq M, Ashraf B, Siddiqui S. Nodular melanoma. Iran J Med Sci. 2016;41:164-165.
- Spinu D, Ra˘dulescu A, Bratu O, et al. Giant condyloma acuminatum. Buschke-Lowenstein disease: a literature review. Chirurgia (Bucur). 2014;109:445-450.
- Alkhalili E, Prapasiri S, Russell J. Giant acrochordon of the axilla. BMJ Case Rep. 2015:bcr2015210623. doi:10.1136/bcr-2015-210623
- Banik R, Lubach D. Skin tags: localization and frequencies according to sex and age. Dermatologica. 1987;174:180-183. doi:10.1159/000249169
- Can B, Yildrim Ozluk A. Giant fibroepithelial polyps: why do they grow excessively? Med Bull Sisli Etfal Hastan Tip Bul. 2020;54:257-260. doi:10.14744/SEMB.2018.33603
- Ghosh SK, Bandyopadhyay D, Chatterjee G, et al. Giant skin tags on unusual locations. J Eur Acad Dermatol Venereol. 2009;23:233. doi:10.1111/j.1468-3083.2008.02816.x
- Messersmith L, Krauland K. Neurofibroma. StatPearls [Internet]. StatPearls Publishing; 2023.
- Saaiq M, Ashraf B, Siddiqui S. Nodular melanoma. Iran J Med Sci. 2016;41:164-165.
- Spinu D, Ra˘dulescu A, Bratu O, et al. Giant condyloma acuminatum. Buschke-Lowenstein disease: a literature review. Chirurgia (Bucur). 2014;109:445-450.
A 40-year-old man presented to our dermatology clinic with a growth on the left buttock of more than 22 years’ duration that progressively increased in size. He was otherwise in good health and reported no ongoing medical problems. Physical examination revealed a 19×12-cm, flesh-colored, pedunculated, verrucous tumor with a central stalk. The patient underwent an excisional removal, and the specimen was sent for histopathologic evaluation.

FDA approves pirtobrutinib for previously treated CLL/SLL
The agent was initially approved in January 2023 for patients with mantle cell lymphoma who had previously received a BTK inhibitor.
Like the mantle cell approval, the CLL/SLL approval was based on findings from the open-label, single-arm, phase 1/2 BRUIN study that included adults with at least two prior lines of therapy, including a BTK inhibitor and a BCL-2 inhibitor.
The trial included 108 patients with either CLL or SLL. Overall, patients demonstrated an overall response rate of 72%, all of which were partial responses, and median duration of response of 12.2 months.
Before starting pirtobrutinib, 77% of patients with CLL or SLL had discontinued their last BTK inhibitor for refractory or progressive disease.
“Once patients with CLL or SLL have progressed on covalent BTK inhibitor and BCL-2 inhibitor therapies, treatments are limited and outcomes can be poor, making the approval of Jaypirca a meaningful advance and much-needed new treatment option for these patients,” William G. Wierda, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston, said in an Eli Lilly press release.
Treatment during the study included the recommended dose of 200 mg given orally once daily until disease progression or unacceptable toxicity. Common adverse reactions that occurred in at least 20% of patients included fatigue, bruising, cough, musculoskeletal pain, COVID-19, diarrhea, pneumonia, abdominal pain, dyspnea, hemorrhage, edema, nausea, pyrexia, and headache. Grade 3 or 4 laboratory abnormalities occurring in more than 10% of patients included decreased neutrophil counts, anemia, and decreased platelet counts.
Serious infections occurred in 32% of patients, including fatal infections in 10% of patients. The prescribing information for pirtobrutinib includes warnings about infections, hemorrhage, cytopenias, cardiac arrhythmias, and secondary primary malignancies.
A version of this article first appeared on Medscape.com.
The agent was initially approved in January 2023 for patients with mantle cell lymphoma who had previously received a BTK inhibitor.
Like the mantle cell approval, the CLL/SLL approval was based on findings from the open-label, single-arm, phase 1/2 BRUIN study that included adults with at least two prior lines of therapy, including a BTK inhibitor and a BCL-2 inhibitor.
The trial included 108 patients with either CLL or SLL. Overall, patients demonstrated an overall response rate of 72%, all of which were partial responses, and median duration of response of 12.2 months.
Before starting pirtobrutinib, 77% of patients with CLL or SLL had discontinued their last BTK inhibitor for refractory or progressive disease.
“Once patients with CLL or SLL have progressed on covalent BTK inhibitor and BCL-2 inhibitor therapies, treatments are limited and outcomes can be poor, making the approval of Jaypirca a meaningful advance and much-needed new treatment option for these patients,” William G. Wierda, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston, said in an Eli Lilly press release.
Treatment during the study included the recommended dose of 200 mg given orally once daily until disease progression or unacceptable toxicity. Common adverse reactions that occurred in at least 20% of patients included fatigue, bruising, cough, musculoskeletal pain, COVID-19, diarrhea, pneumonia, abdominal pain, dyspnea, hemorrhage, edema, nausea, pyrexia, and headache. Grade 3 or 4 laboratory abnormalities occurring in more than 10% of patients included decreased neutrophil counts, anemia, and decreased platelet counts.
Serious infections occurred in 32% of patients, including fatal infections in 10% of patients. The prescribing information for pirtobrutinib includes warnings about infections, hemorrhage, cytopenias, cardiac arrhythmias, and secondary primary malignancies.
A version of this article first appeared on Medscape.com.
The agent was initially approved in January 2023 for patients with mantle cell lymphoma who had previously received a BTK inhibitor.
Like the mantle cell approval, the CLL/SLL approval was based on findings from the open-label, single-arm, phase 1/2 BRUIN study that included adults with at least two prior lines of therapy, including a BTK inhibitor and a BCL-2 inhibitor.
The trial included 108 patients with either CLL or SLL. Overall, patients demonstrated an overall response rate of 72%, all of which were partial responses, and median duration of response of 12.2 months.
Before starting pirtobrutinib, 77% of patients with CLL or SLL had discontinued their last BTK inhibitor for refractory or progressive disease.
“Once patients with CLL or SLL have progressed on covalent BTK inhibitor and BCL-2 inhibitor therapies, treatments are limited and outcomes can be poor, making the approval of Jaypirca a meaningful advance and much-needed new treatment option for these patients,” William G. Wierda, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston, said in an Eli Lilly press release.
Treatment during the study included the recommended dose of 200 mg given orally once daily until disease progression or unacceptable toxicity. Common adverse reactions that occurred in at least 20% of patients included fatigue, bruising, cough, musculoskeletal pain, COVID-19, diarrhea, pneumonia, abdominal pain, dyspnea, hemorrhage, edema, nausea, pyrexia, and headache. Grade 3 or 4 laboratory abnormalities occurring in more than 10% of patients included decreased neutrophil counts, anemia, and decreased platelet counts.
Serious infections occurred in 32% of patients, including fatal infections in 10% of patients. The prescribing information for pirtobrutinib includes warnings about infections, hemorrhage, cytopenias, cardiac arrhythmias, and secondary primary malignancies.
A version of this article first appeared on Medscape.com.
Eight wealth tips just for doctors
The average physician makes $352,000, and some earn well into the $500,000s. So, doctors don’t have to worry about money, right?
You know the answer to that.
One thing all physicians have in common about money, says James M. Dahle, MD, FACEP, founder of The White Coat Investor, is that they don’t receive any training in business, personal finance, or investing throughout their schooling or careers unless they seek it out. This leaves many unprepared to make the best investing and money-saving decisions, while others get too frustrated about their lack of knowledge to even dip their toe into the investing pool.
Exhibit A: Four out of 10 physicians have a net worth below $1 million, according to the Medscape Physician Wealth & Debt Report 2023. Elizabeth Chiang, MD, PhD, an oculoplastic surgeon and a physician money coach at Grow Your Wealthy Mindset, notes that many of those doctors are over age 65, “which means they essentially can’t retire.”
And that’s just one pain point.
Physicians have money concerns specific to their profession and background. Luckily, some fellow doctors also serve as financial and wealth advisors just for other doctors.
Blind Spot #1
The early lean years skew doctors’ money outlook. “We have an extended training period, which commonly consists of taking on a large amount of debt, followed by 3 to 8 years of being paid a modest salary, and then finally a large boost in income,” explains Dr. Chiang. This can lay a shaky foundation for the earning years to come, and as a result, a lot of doctors just don’t think about money in healthy ways. Once their incomes increase, physicians may be surprised, for example, that making a multiple six-figure salary means paying six figures in taxes.
The Fix
Treat financial health like physical health. That means money cannot be a taboo subject. “The misguided mindset is that we didn’t become physicians to make money, we did it to help people,” explains Jordan Frey, MD, creator of the blog, The Prudent Plastic Surgeon.
Dr. Frey acknowledges that the desire to help is certainly true. But the result is a false idea that “to think about our personal finances makes us a worse doctor.”
Blind Spot #2
Because doctors know a lot about one thing (medicine), they might assume they know a lot about everything (such as investing). “Totally different fields with a different language and different way to think about it,” Dahle explains. This overconfidence could lead to some negligent or risky financial decisions.
The Fix
Educate yourself. There are several books on personal finance and investing written by physicians for physicians. Dr. Chiang recommends The Physician Philosopher’s Guide to Personal Finance, by James Turner, MD; Financial Freedom Rx, by Chirag Shah, MD, and Jayanth Sridhar, MD; and The Physician’s Guide to Finance, by Nicholas Christian and Amanda Christian, MD. There are also podcasts, blogs, and courses to help educate doctors on finance, such as the Fire Your Financial Advisor course by The White Coat Investor.
Blind Spot #3
Undersaving. Retirement saving is one thing, but 24% of doctors say they don’t even put money away in a taxable savings account, according to the Wealth & Debt Report.
Cobin Soelberg, MD, JD, a board-certified anesthesiologist and founder and principal advisor with Greeley Wealth Management, is the treasurer of his anesthesiology group. “I get to see every month how much people are saving, and even on an anesthesiologist salary, where everyone’s making about $400,000 a year, a lot of people are not saving anything, which is crazy.”
Undersaving can be both a time issue and a mindset one.
Time: Doctors often start investing in their retirement accounts later than the average professional, says Dr. Chiang. “A lot of physicians will max out their 401k or 403b,” she explains. “But if you’re putting in $20,000 a year and only starting when you’re in your early 30s, that’s not enough to get you to retirement.”
Mindset: Doctors also see people of all ages who are sick, dying, and injured. “They all know someone who worked hard and saved and then dropped dead at 55,” explains Dr. Dahle. This, he says, can lead to a bit of a “you only live once” attitude that prioritizes spending over saving.
The Fix
Shoot for 20%. If you can’t save 20% of your gross now, strive to get to that point. Think of it as telling a patient they have to change their behavior or trouble will come - not if, but when. “Develop a written investing plan and then stick with it through thick and thin,” says Dr. Dahle. “Once you have a reasonable plan, all you have to do is fund it adequately by saving 20% of your gross income, and a doctor will easily retire as a multimillionaire.”
Blind Spot #4
Bad investment strategies. Thirty-six percent of doctors experience their largest financial losses from lousy investments, according to the Wealth & Debt Report. Meanwhile, 17% of PCPs and 12% of specialists say they haven’t made any investments at all. That’s a terrible mix of doing the wrong thing and doing a worse thing.
The Fix
Don’t overthink investing, but don’t underthink it either. “As high-income earners, doctors just don’t need to take this high level of risk to reach their financial goals,” Dr. Frey says. A good investment plan doesn’t require you to time the stock market or predict individual stock winners. Consider what Vanguard founder Jack Bogle once said about investing: “Be bored by the process but elated by the outcome.”
Dr. Frey suggests going super-simple: index funds. Ignore investing strategies with actively managed mutual funds or individual stocks, as well as risky alternative investments such as cryptocurrency and angel investments. Everyone assumes doctors have money to burn, and they will push sketchy investment ideas at them. Avoid.
Blind Spot #5
Not taking debt seriously enough. The average medical student debt is $250,000 and can exceed $500,000, says Dr. Soelberg. Many doctors spend the first 10 to 20 years of their careers paying this off. Today’s graduates are paying more than 7% on their loans.
And it’s not just student debt: 39% of physicians carry five or more credit cards, and 34% have mortgages larger than $300,000 (with half of those are more than than $500K), per the Wealth & Debt Report.
The Fix
Treat debt like cancer. It’s a lethal enemy you can’t get rid of right away, but a steady, aggressive, long-term attack will have the best results. Dr. Soelberg suggests allocating the most you can afford per month, whether that’s $1000 or $5000, toward debt. Raise the amount as your income grows. Do the same with your 401k or retirement plan. Whatever is left, you can spend. Five to 10 years later, you will realize, “Wow. I’m debt free.”
Blind Spot #6
Not putting in the work to improve your situation. Seventy-one percent of doctors admit they haven’t done anything to reduce major expenses, according to the Wealth & Debt Report. Are you leaving major money on the table?
The Fix
Audit yourself in major areas like housing and taxes. While the average professional may need to put 10% to 20% down on a home, physicians can qualify for physician mortgage loans and can often put down 3% or less, says Dr. Chiang. If you can afford the higher mortgage payment, excess savings earmarked for a larger down payment can be put toward debt or invested.
Another trick, if you’re able, is to seek an area that is less in demand at a higher salary. “Physicians in places like New York City or San Francisco tend to make less than physicians in the Midwest or the South,” Dr. Chiang explains. A colleague of hers moved to rural Pennsylvania, where he made a high salary and had a low cost of living for 3½ years, paid off his student debt, and then relocated to an area where he wanted to live long term.
As for taxes, become familiar with tax law. Research things like, “What is considered a business expense for doctors?” says Brett Mollard, MD, a diagnostic radiologist who provides financial advice to younger physicians. “What will your estimated total tax burden be at the end of the year? Will you need to make extra payments to prevent owing a large sum of money from underpaying or to avoid tax penalties?”
Blind Spot #7
Living like a rock star on a doctor’s income. Getting caught up in trying to live the same lifestyle as your colleagues is a classic bear trap. “Sitting in the doctor’s lounge, it’s so crazy,” Dr. Soelberg says. He describes conversations like, “‘Where did you go on your trip?’ ‘What new toys are you buying?’” There’s pressure to live up to an image of what a doctor’s life is supposed to look like before you’ve sorted the basic things like paying off debt.
The Fix
Live like a resident even if you haven’t been one for years, at least until you’re in a better financial position. “You’re already used to living a life of lower means, and you’re an expert when it comes to delaying gratification,” says Dr. Mollard. “Do it a little longer.” Live frugally and spend only on things that bring you joy. “A lot of physicians are trying to be really rich in all areas of their life instead of the ones that actually matter to them,” Dr. Soelberg says. Identify what’s important to you and only splurge on that.
Blind Spot #8
Never asking for help. The right financial planner can provide expert help. Emphasis on right. “Doctors can be very trusting of other professionals, even when they should not be,” says Dr. Dahle. He notes that in financial services, many people masquerade as knowledgeable advisors who are really just salespeople. While legitimate financial advisors strive to make their clients money, they are also ultimately out to line their pockets and love to work with physician salaries. Thus, doctors can end up working with financial planners that don’t specifically understand their situations or end up taking too much from their clients.
The Fix
Find a planner who specializes in, or at least understands, physicians. Ask them how they make money, says Dr. Chiang. If someone hesitates to tell you about their fee structure or if it sounds like a lot, shop around and ask colleagues for recommendations.
“Ultimately, the path to wealth is to create and grow the margin between what you make and what you spend,” says Dr. Frey. Throw some investing into the mix and physicians can set themselves up on a path for a stress-free financial life.
A version of this article appeared on Medscape.com.
The average physician makes $352,000, and some earn well into the $500,000s. So, doctors don’t have to worry about money, right?
You know the answer to that.
One thing all physicians have in common about money, says James M. Dahle, MD, FACEP, founder of The White Coat Investor, is that they don’t receive any training in business, personal finance, or investing throughout their schooling or careers unless they seek it out. This leaves many unprepared to make the best investing and money-saving decisions, while others get too frustrated about their lack of knowledge to even dip their toe into the investing pool.
Exhibit A: Four out of 10 physicians have a net worth below $1 million, according to the Medscape Physician Wealth & Debt Report 2023. Elizabeth Chiang, MD, PhD, an oculoplastic surgeon and a physician money coach at Grow Your Wealthy Mindset, notes that many of those doctors are over age 65, “which means they essentially can’t retire.”
And that’s just one pain point.
Physicians have money concerns specific to their profession and background. Luckily, some fellow doctors also serve as financial and wealth advisors just for other doctors.
Blind Spot #1
The early lean years skew doctors’ money outlook. “We have an extended training period, which commonly consists of taking on a large amount of debt, followed by 3 to 8 years of being paid a modest salary, and then finally a large boost in income,” explains Dr. Chiang. This can lay a shaky foundation for the earning years to come, and as a result, a lot of doctors just don’t think about money in healthy ways. Once their incomes increase, physicians may be surprised, for example, that making a multiple six-figure salary means paying six figures in taxes.
The Fix
Treat financial health like physical health. That means money cannot be a taboo subject. “The misguided mindset is that we didn’t become physicians to make money, we did it to help people,” explains Jordan Frey, MD, creator of the blog, The Prudent Plastic Surgeon.
Dr. Frey acknowledges that the desire to help is certainly true. But the result is a false idea that “to think about our personal finances makes us a worse doctor.”
Blind Spot #2
Because doctors know a lot about one thing (medicine), they might assume they know a lot about everything (such as investing). “Totally different fields with a different language and different way to think about it,” Dahle explains. This overconfidence could lead to some negligent or risky financial decisions.
The Fix
Educate yourself. There are several books on personal finance and investing written by physicians for physicians. Dr. Chiang recommends The Physician Philosopher’s Guide to Personal Finance, by James Turner, MD; Financial Freedom Rx, by Chirag Shah, MD, and Jayanth Sridhar, MD; and The Physician’s Guide to Finance, by Nicholas Christian and Amanda Christian, MD. There are also podcasts, blogs, and courses to help educate doctors on finance, such as the Fire Your Financial Advisor course by The White Coat Investor.
Blind Spot #3
Undersaving. Retirement saving is one thing, but 24% of doctors say they don’t even put money away in a taxable savings account, according to the Wealth & Debt Report.
Cobin Soelberg, MD, JD, a board-certified anesthesiologist and founder and principal advisor with Greeley Wealth Management, is the treasurer of his anesthesiology group. “I get to see every month how much people are saving, and even on an anesthesiologist salary, where everyone’s making about $400,000 a year, a lot of people are not saving anything, which is crazy.”
Undersaving can be both a time issue and a mindset one.
Time: Doctors often start investing in their retirement accounts later than the average professional, says Dr. Chiang. “A lot of physicians will max out their 401k or 403b,” she explains. “But if you’re putting in $20,000 a year and only starting when you’re in your early 30s, that’s not enough to get you to retirement.”
Mindset: Doctors also see people of all ages who are sick, dying, and injured. “They all know someone who worked hard and saved and then dropped dead at 55,” explains Dr. Dahle. This, he says, can lead to a bit of a “you only live once” attitude that prioritizes spending over saving.
The Fix
Shoot for 20%. If you can’t save 20% of your gross now, strive to get to that point. Think of it as telling a patient they have to change their behavior or trouble will come - not if, but when. “Develop a written investing plan and then stick with it through thick and thin,” says Dr. Dahle. “Once you have a reasonable plan, all you have to do is fund it adequately by saving 20% of your gross income, and a doctor will easily retire as a multimillionaire.”
Blind Spot #4
Bad investment strategies. Thirty-six percent of doctors experience their largest financial losses from lousy investments, according to the Wealth & Debt Report. Meanwhile, 17% of PCPs and 12% of specialists say they haven’t made any investments at all. That’s a terrible mix of doing the wrong thing and doing a worse thing.
The Fix
Don’t overthink investing, but don’t underthink it either. “As high-income earners, doctors just don’t need to take this high level of risk to reach their financial goals,” Dr. Frey says. A good investment plan doesn’t require you to time the stock market or predict individual stock winners. Consider what Vanguard founder Jack Bogle once said about investing: “Be bored by the process but elated by the outcome.”
Dr. Frey suggests going super-simple: index funds. Ignore investing strategies with actively managed mutual funds or individual stocks, as well as risky alternative investments such as cryptocurrency and angel investments. Everyone assumes doctors have money to burn, and they will push sketchy investment ideas at them. Avoid.
Blind Spot #5
Not taking debt seriously enough. The average medical student debt is $250,000 and can exceed $500,000, says Dr. Soelberg. Many doctors spend the first 10 to 20 years of their careers paying this off. Today’s graduates are paying more than 7% on their loans.
And it’s not just student debt: 39% of physicians carry five or more credit cards, and 34% have mortgages larger than $300,000 (with half of those are more than than $500K), per the Wealth & Debt Report.
The Fix
Treat debt like cancer. It’s a lethal enemy you can’t get rid of right away, but a steady, aggressive, long-term attack will have the best results. Dr. Soelberg suggests allocating the most you can afford per month, whether that’s $1000 or $5000, toward debt. Raise the amount as your income grows. Do the same with your 401k or retirement plan. Whatever is left, you can spend. Five to 10 years later, you will realize, “Wow. I’m debt free.”
Blind Spot #6
Not putting in the work to improve your situation. Seventy-one percent of doctors admit they haven’t done anything to reduce major expenses, according to the Wealth & Debt Report. Are you leaving major money on the table?
The Fix
Audit yourself in major areas like housing and taxes. While the average professional may need to put 10% to 20% down on a home, physicians can qualify for physician mortgage loans and can often put down 3% or less, says Dr. Chiang. If you can afford the higher mortgage payment, excess savings earmarked for a larger down payment can be put toward debt or invested.
Another trick, if you’re able, is to seek an area that is less in demand at a higher salary. “Physicians in places like New York City or San Francisco tend to make less than physicians in the Midwest or the South,” Dr. Chiang explains. A colleague of hers moved to rural Pennsylvania, where he made a high salary and had a low cost of living for 3½ years, paid off his student debt, and then relocated to an area where he wanted to live long term.
As for taxes, become familiar with tax law. Research things like, “What is considered a business expense for doctors?” says Brett Mollard, MD, a diagnostic radiologist who provides financial advice to younger physicians. “What will your estimated total tax burden be at the end of the year? Will you need to make extra payments to prevent owing a large sum of money from underpaying or to avoid tax penalties?”
Blind Spot #7
Living like a rock star on a doctor’s income. Getting caught up in trying to live the same lifestyle as your colleagues is a classic bear trap. “Sitting in the doctor’s lounge, it’s so crazy,” Dr. Soelberg says. He describes conversations like, “‘Where did you go on your trip?’ ‘What new toys are you buying?’” There’s pressure to live up to an image of what a doctor’s life is supposed to look like before you’ve sorted the basic things like paying off debt.
The Fix
Live like a resident even if you haven’t been one for years, at least until you’re in a better financial position. “You’re already used to living a life of lower means, and you’re an expert when it comes to delaying gratification,” says Dr. Mollard. “Do it a little longer.” Live frugally and spend only on things that bring you joy. “A lot of physicians are trying to be really rich in all areas of their life instead of the ones that actually matter to them,” Dr. Soelberg says. Identify what’s important to you and only splurge on that.
Blind Spot #8
Never asking for help. The right financial planner can provide expert help. Emphasis on right. “Doctors can be very trusting of other professionals, even when they should not be,” says Dr. Dahle. He notes that in financial services, many people masquerade as knowledgeable advisors who are really just salespeople. While legitimate financial advisors strive to make their clients money, they are also ultimately out to line their pockets and love to work with physician salaries. Thus, doctors can end up working with financial planners that don’t specifically understand their situations or end up taking too much from their clients.
The Fix
Find a planner who specializes in, or at least understands, physicians. Ask them how they make money, says Dr. Chiang. If someone hesitates to tell you about their fee structure or if it sounds like a lot, shop around and ask colleagues for recommendations.
“Ultimately, the path to wealth is to create and grow the margin between what you make and what you spend,” says Dr. Frey. Throw some investing into the mix and physicians can set themselves up on a path for a stress-free financial life.
A version of this article appeared on Medscape.com.
The average physician makes $352,000, and some earn well into the $500,000s. So, doctors don’t have to worry about money, right?
You know the answer to that.
One thing all physicians have in common about money, says James M. Dahle, MD, FACEP, founder of The White Coat Investor, is that they don’t receive any training in business, personal finance, or investing throughout their schooling or careers unless they seek it out. This leaves many unprepared to make the best investing and money-saving decisions, while others get too frustrated about their lack of knowledge to even dip their toe into the investing pool.
Exhibit A: Four out of 10 physicians have a net worth below $1 million, according to the Medscape Physician Wealth & Debt Report 2023. Elizabeth Chiang, MD, PhD, an oculoplastic surgeon and a physician money coach at Grow Your Wealthy Mindset, notes that many of those doctors are over age 65, “which means they essentially can’t retire.”
And that’s just one pain point.
Physicians have money concerns specific to their profession and background. Luckily, some fellow doctors also serve as financial and wealth advisors just for other doctors.
Blind Spot #1
The early lean years skew doctors’ money outlook. “We have an extended training period, which commonly consists of taking on a large amount of debt, followed by 3 to 8 years of being paid a modest salary, and then finally a large boost in income,” explains Dr. Chiang. This can lay a shaky foundation for the earning years to come, and as a result, a lot of doctors just don’t think about money in healthy ways. Once their incomes increase, physicians may be surprised, for example, that making a multiple six-figure salary means paying six figures in taxes.
The Fix
Treat financial health like physical health. That means money cannot be a taboo subject. “The misguided mindset is that we didn’t become physicians to make money, we did it to help people,” explains Jordan Frey, MD, creator of the blog, The Prudent Plastic Surgeon.
Dr. Frey acknowledges that the desire to help is certainly true. But the result is a false idea that “to think about our personal finances makes us a worse doctor.”
Blind Spot #2
Because doctors know a lot about one thing (medicine), they might assume they know a lot about everything (such as investing). “Totally different fields with a different language and different way to think about it,” Dahle explains. This overconfidence could lead to some negligent or risky financial decisions.
The Fix
Educate yourself. There are several books on personal finance and investing written by physicians for physicians. Dr. Chiang recommends The Physician Philosopher’s Guide to Personal Finance, by James Turner, MD; Financial Freedom Rx, by Chirag Shah, MD, and Jayanth Sridhar, MD; and The Physician’s Guide to Finance, by Nicholas Christian and Amanda Christian, MD. There are also podcasts, blogs, and courses to help educate doctors on finance, such as the Fire Your Financial Advisor course by The White Coat Investor.
Blind Spot #3
Undersaving. Retirement saving is one thing, but 24% of doctors say they don’t even put money away in a taxable savings account, according to the Wealth & Debt Report.
Cobin Soelberg, MD, JD, a board-certified anesthesiologist and founder and principal advisor with Greeley Wealth Management, is the treasurer of his anesthesiology group. “I get to see every month how much people are saving, and even on an anesthesiologist salary, where everyone’s making about $400,000 a year, a lot of people are not saving anything, which is crazy.”
Undersaving can be both a time issue and a mindset one.
Time: Doctors often start investing in their retirement accounts later than the average professional, says Dr. Chiang. “A lot of physicians will max out their 401k or 403b,” she explains. “But if you’re putting in $20,000 a year and only starting when you’re in your early 30s, that’s not enough to get you to retirement.”
Mindset: Doctors also see people of all ages who are sick, dying, and injured. “They all know someone who worked hard and saved and then dropped dead at 55,” explains Dr. Dahle. This, he says, can lead to a bit of a “you only live once” attitude that prioritizes spending over saving.
The Fix
Shoot for 20%. If you can’t save 20% of your gross now, strive to get to that point. Think of it as telling a patient they have to change their behavior or trouble will come - not if, but when. “Develop a written investing plan and then stick with it through thick and thin,” says Dr. Dahle. “Once you have a reasonable plan, all you have to do is fund it adequately by saving 20% of your gross income, and a doctor will easily retire as a multimillionaire.”
Blind Spot #4
Bad investment strategies. Thirty-six percent of doctors experience their largest financial losses from lousy investments, according to the Wealth & Debt Report. Meanwhile, 17% of PCPs and 12% of specialists say they haven’t made any investments at all. That’s a terrible mix of doing the wrong thing and doing a worse thing.
The Fix
Don’t overthink investing, but don’t underthink it either. “As high-income earners, doctors just don’t need to take this high level of risk to reach their financial goals,” Dr. Frey says. A good investment plan doesn’t require you to time the stock market or predict individual stock winners. Consider what Vanguard founder Jack Bogle once said about investing: “Be bored by the process but elated by the outcome.”
Dr. Frey suggests going super-simple: index funds. Ignore investing strategies with actively managed mutual funds or individual stocks, as well as risky alternative investments such as cryptocurrency and angel investments. Everyone assumes doctors have money to burn, and they will push sketchy investment ideas at them. Avoid.
Blind Spot #5
Not taking debt seriously enough. The average medical student debt is $250,000 and can exceed $500,000, says Dr. Soelberg. Many doctors spend the first 10 to 20 years of their careers paying this off. Today’s graduates are paying more than 7% on their loans.
And it’s not just student debt: 39% of physicians carry five or more credit cards, and 34% have mortgages larger than $300,000 (with half of those are more than than $500K), per the Wealth & Debt Report.
The Fix
Treat debt like cancer. It’s a lethal enemy you can’t get rid of right away, but a steady, aggressive, long-term attack will have the best results. Dr. Soelberg suggests allocating the most you can afford per month, whether that’s $1000 or $5000, toward debt. Raise the amount as your income grows. Do the same with your 401k or retirement plan. Whatever is left, you can spend. Five to 10 years later, you will realize, “Wow. I’m debt free.”
Blind Spot #6
Not putting in the work to improve your situation. Seventy-one percent of doctors admit they haven’t done anything to reduce major expenses, according to the Wealth & Debt Report. Are you leaving major money on the table?
The Fix
Audit yourself in major areas like housing and taxes. While the average professional may need to put 10% to 20% down on a home, physicians can qualify for physician mortgage loans and can often put down 3% or less, says Dr. Chiang. If you can afford the higher mortgage payment, excess savings earmarked for a larger down payment can be put toward debt or invested.
Another trick, if you’re able, is to seek an area that is less in demand at a higher salary. “Physicians in places like New York City or San Francisco tend to make less than physicians in the Midwest or the South,” Dr. Chiang explains. A colleague of hers moved to rural Pennsylvania, where he made a high salary and had a low cost of living for 3½ years, paid off his student debt, and then relocated to an area where he wanted to live long term.
As for taxes, become familiar with tax law. Research things like, “What is considered a business expense for doctors?” says Brett Mollard, MD, a diagnostic radiologist who provides financial advice to younger physicians. “What will your estimated total tax burden be at the end of the year? Will you need to make extra payments to prevent owing a large sum of money from underpaying or to avoid tax penalties?”
Blind Spot #7
Living like a rock star on a doctor’s income. Getting caught up in trying to live the same lifestyle as your colleagues is a classic bear trap. “Sitting in the doctor’s lounge, it’s so crazy,” Dr. Soelberg says. He describes conversations like, “‘Where did you go on your trip?’ ‘What new toys are you buying?’” There’s pressure to live up to an image of what a doctor’s life is supposed to look like before you’ve sorted the basic things like paying off debt.
The Fix
Live like a resident even if you haven’t been one for years, at least until you’re in a better financial position. “You’re already used to living a life of lower means, and you’re an expert when it comes to delaying gratification,” says Dr. Mollard. “Do it a little longer.” Live frugally and spend only on things that bring you joy. “A lot of physicians are trying to be really rich in all areas of their life instead of the ones that actually matter to them,” Dr. Soelberg says. Identify what’s important to you and only splurge on that.
Blind Spot #8
Never asking for help. The right financial planner can provide expert help. Emphasis on right. “Doctors can be very trusting of other professionals, even when they should not be,” says Dr. Dahle. He notes that in financial services, many people masquerade as knowledgeable advisors who are really just salespeople. While legitimate financial advisors strive to make their clients money, they are also ultimately out to line their pockets and love to work with physician salaries. Thus, doctors can end up working with financial planners that don’t specifically understand their situations or end up taking too much from their clients.
The Fix
Find a planner who specializes in, or at least understands, physicians. Ask them how they make money, says Dr. Chiang. If someone hesitates to tell you about their fee structure or if it sounds like a lot, shop around and ask colleagues for recommendations.
“Ultimately, the path to wealth is to create and grow the margin between what you make and what you spend,” says Dr. Frey. Throw some investing into the mix and physicians can set themselves up on a path for a stress-free financial life.
A version of this article appeared on Medscape.com.
PFO closure may reduce migraine days and prevent stroke
, according to a discussion at the 2023 Scottsdale Headache Symposium.
In two clinical trials evaluating whether PFO closure reduces migraine risk, the primary endpoints were not met, but a signal of benefit on secondary endpoints and the association between PFO, migraine, and stroke are among the reasons that PFO closure should be reevaluated, according to Andrew Charles MD, Director of the Goldberg Migraine Program, University of California, Los Angeles.
Other right-to-left shunt defects have also been associated with both migraine and stroke, leading Dr. Charles to suggest these defects are more a common denominator.
“Stroke during a migraine is, in fact, very uncommon,” Dr. Charles said. “This raises the possibility that it is not the migraine causing the stroke but rather there is a shared risk factor for stroke and migraine,” said Dr. Charles, referring to PFO as well as other right-to-left shunt defects, such as hereditary hemorrhaging telangiectasia in the lungs.
One Intervention, Two Potential Benefits
Fixing these defects is therefore at least theoretically attractive for preventing both migraine and stroke, but Dr. Charles said the opportunity for preventing both migraine and stroke is most attractive in migraine patients who have additional stroke risk factors.
Use of oral contraceptives, which produce a hypercoagulable state, is an example.
“Are these the people we should really be thinking about if they have PFO and migraine, particularly migraine with aura?” Dr. Charles asked.
The association between right-to-left shunts and migraine is strong. Although PFO is common, presenting in 20%-25% of the adult population, it has been found in up to 50% of individuals who have migraine with aura. In patients with migraine but no aura, the prevalence of PFO has been estimated to be approximately 35% or still somewhat elevated relative to the general population.
Primary Endpoint Missed in Clinical Trials
The question of whether risk of migraine can be reduced with repair of PFO or other right-to-left shunts remains unresolved. In two high-quality randomized trials undertaken in PFO repair, neither met its primary endpoint. In one of these, called PRIMA, which was terminated early for slow enrollment, the reduction in mean headache attacks was not significant relative to medical therapy.
In the second, called PREMIUM, device closure of PFO also failed to significantly reduce migraine attacks over sham procedure although it was associated with complete migraine remission (10% vs 1%).
A pooled analysis of these two studies that was conducted subsequently concluded that PFO closure reduces mean monthly migraine days (-3.1 vs. -1.9 days; P = -.02) and increases the likelihood of complete migraine cessation (9% vs. 0.7%; P < .001), but Dr. Charles pointed out the primary endpoint was migraine attacks not migraine days, so other analyses can only be considered hypothesis-generating.
There are several reasons to relook at the relationship between migraine and PFO but the potential to prevent both migraine and stroke with PFO closure could be one of the most important.
Several years ago, Dr. Charles and his coinvestigators from UCLA evaluated more than 700 ischemic strokes. Of these, 127 strokes were characterized as cryptogenic because of lack of another identifiable etiology. While 59% of these patients had PFO, which is several times higher than the general population, the prevalence of PFO in patients with a cryptogenic stroke and a history of migraine was 79% in this published study.
“So, in this group of patients who did not have any other clear cause for a stroke, a diagnosis of PFO was very much overrepresented,” Dr. Charles said.
Migraine Days Might Be a Better Endpoint
For patients with migraine who have risk factors for stroke, this makes PFO closure an attractive intervention, but a positive randomized trial is needed. Several are underway. Importantly, the trials now enrolling are using migraine days, which was significantly reduced in both PREMIUM and PRIMA, rather than migraine attacks as the primary endpoint.
“Migraine days is now accepted by the Food and Drug Administration as a criterion of benefit,” reported Jonathan Tobis, MD, Research Director, Interventional Cardiology, UCLA David Geffen School of Medicine, Los Angeles.
He explained that the FDA insisted on migraine attacks as the endpoint for the PREMIUM trial, but this was a far more challenging endpoint on which to show a statistical benefit. He emphasized that a new set of trials will now test efficacy on the basis of migraine days.
One of these trials, called RELIEF, which is randomizing patients to device closure of PFO or a sham procedure. Both groups are receiving clopidogrel or prasugrel based on a previous observation that patients who respond to these drugs are also more likely to respond to PFO closure.
Another trial, called COMPETE-2, is comparing PFO closure with a device to aspirin plus a sham closure. This trial is ongoing in China.
Stroke is not being evaluated as an endpoint in either trial, but Dr. Charles suggested that this does warrant attention.
“I would also just put it out there that, apart from simply migraine, this is a therapeutic approach that we might actually think about in terms of helping to prevent stroke in our migraine patients,” he said.
Senior author of a recent meta-analysis of trials evaluating PFO closure and control of migraine, Ling Liu, MD, Department of Neurology, University of Sichuan, Chengdu, China, agreed that PFO closure for the treatment of migraine deserves “a reevaluation.”
In his meta-analysis of three randomized trials, one pooled study, and eight retrospective case series with 1,165 patients, PFO closure was associated with a nearly 75% reduction (odds ratio [OR], 0.259; P = .0048) reduction in migraine days and 50% increase in resolution of migraine in patients with a history of migraine with aura (OR, 1.586; P = .227).
The incidence of stroke was not evaluated in this meta-analysis, but Dr. Liu believes that the evidence of reducing the burden of migraine with PFO closure is compelling. Given the evidence from this meta-analysis that PFO closure is safe, Dr. Liu maintained that a definitive trial is needed “especially for migraine with frequent aura.”
As an interventional cardiologist, Dr. Tobis said that when PFO closures is performed for prevention of stroke in patients with migraine, it often leads to reduced migraine activity and, in some cases, elimination of migraine. Like others, he believes new analyses should be conducted.
“Everyone involved in this field believes there is something there,” Dr. Tobis said. The missing link is a clinical trial to confirm it.
Dr. Charles and Dr. Liu report no potential conflicts of interest. Dr. Tobis reports a financial relationship with Holistick Medical.
, according to a discussion at the 2023 Scottsdale Headache Symposium.
In two clinical trials evaluating whether PFO closure reduces migraine risk, the primary endpoints were not met, but a signal of benefit on secondary endpoints and the association between PFO, migraine, and stroke are among the reasons that PFO closure should be reevaluated, according to Andrew Charles MD, Director of the Goldberg Migraine Program, University of California, Los Angeles.
Other right-to-left shunt defects have also been associated with both migraine and stroke, leading Dr. Charles to suggest these defects are more a common denominator.
“Stroke during a migraine is, in fact, very uncommon,” Dr. Charles said. “This raises the possibility that it is not the migraine causing the stroke but rather there is a shared risk factor for stroke and migraine,” said Dr. Charles, referring to PFO as well as other right-to-left shunt defects, such as hereditary hemorrhaging telangiectasia in the lungs.
One Intervention, Two Potential Benefits
Fixing these defects is therefore at least theoretically attractive for preventing both migraine and stroke, but Dr. Charles said the opportunity for preventing both migraine and stroke is most attractive in migraine patients who have additional stroke risk factors.
Use of oral contraceptives, which produce a hypercoagulable state, is an example.
“Are these the people we should really be thinking about if they have PFO and migraine, particularly migraine with aura?” Dr. Charles asked.
The association between right-to-left shunts and migraine is strong. Although PFO is common, presenting in 20%-25% of the adult population, it has been found in up to 50% of individuals who have migraine with aura. In patients with migraine but no aura, the prevalence of PFO has been estimated to be approximately 35% or still somewhat elevated relative to the general population.
Primary Endpoint Missed in Clinical Trials
The question of whether risk of migraine can be reduced with repair of PFO or other right-to-left shunts remains unresolved. In two high-quality randomized trials undertaken in PFO repair, neither met its primary endpoint. In one of these, called PRIMA, which was terminated early for slow enrollment, the reduction in mean headache attacks was not significant relative to medical therapy.
In the second, called PREMIUM, device closure of PFO also failed to significantly reduce migraine attacks over sham procedure although it was associated with complete migraine remission (10% vs 1%).
A pooled analysis of these two studies that was conducted subsequently concluded that PFO closure reduces mean monthly migraine days (-3.1 vs. -1.9 days; P = -.02) and increases the likelihood of complete migraine cessation (9% vs. 0.7%; P < .001), but Dr. Charles pointed out the primary endpoint was migraine attacks not migraine days, so other analyses can only be considered hypothesis-generating.
There are several reasons to relook at the relationship between migraine and PFO but the potential to prevent both migraine and stroke with PFO closure could be one of the most important.
Several years ago, Dr. Charles and his coinvestigators from UCLA evaluated more than 700 ischemic strokes. Of these, 127 strokes were characterized as cryptogenic because of lack of another identifiable etiology. While 59% of these patients had PFO, which is several times higher than the general population, the prevalence of PFO in patients with a cryptogenic stroke and a history of migraine was 79% in this published study.
“So, in this group of patients who did not have any other clear cause for a stroke, a diagnosis of PFO was very much overrepresented,” Dr. Charles said.
Migraine Days Might Be a Better Endpoint
For patients with migraine who have risk factors for stroke, this makes PFO closure an attractive intervention, but a positive randomized trial is needed. Several are underway. Importantly, the trials now enrolling are using migraine days, which was significantly reduced in both PREMIUM and PRIMA, rather than migraine attacks as the primary endpoint.
“Migraine days is now accepted by the Food and Drug Administration as a criterion of benefit,” reported Jonathan Tobis, MD, Research Director, Interventional Cardiology, UCLA David Geffen School of Medicine, Los Angeles.
He explained that the FDA insisted on migraine attacks as the endpoint for the PREMIUM trial, but this was a far more challenging endpoint on which to show a statistical benefit. He emphasized that a new set of trials will now test efficacy on the basis of migraine days.
One of these trials, called RELIEF, which is randomizing patients to device closure of PFO or a sham procedure. Both groups are receiving clopidogrel or prasugrel based on a previous observation that patients who respond to these drugs are also more likely to respond to PFO closure.
Another trial, called COMPETE-2, is comparing PFO closure with a device to aspirin plus a sham closure. This trial is ongoing in China.
Stroke is not being evaluated as an endpoint in either trial, but Dr. Charles suggested that this does warrant attention.
“I would also just put it out there that, apart from simply migraine, this is a therapeutic approach that we might actually think about in terms of helping to prevent stroke in our migraine patients,” he said.
Senior author of a recent meta-analysis of trials evaluating PFO closure and control of migraine, Ling Liu, MD, Department of Neurology, University of Sichuan, Chengdu, China, agreed that PFO closure for the treatment of migraine deserves “a reevaluation.”
In his meta-analysis of three randomized trials, one pooled study, and eight retrospective case series with 1,165 patients, PFO closure was associated with a nearly 75% reduction (odds ratio [OR], 0.259; P = .0048) reduction in migraine days and 50% increase in resolution of migraine in patients with a history of migraine with aura (OR, 1.586; P = .227).
The incidence of stroke was not evaluated in this meta-analysis, but Dr. Liu believes that the evidence of reducing the burden of migraine with PFO closure is compelling. Given the evidence from this meta-analysis that PFO closure is safe, Dr. Liu maintained that a definitive trial is needed “especially for migraine with frequent aura.”
As an interventional cardiologist, Dr. Tobis said that when PFO closures is performed for prevention of stroke in patients with migraine, it often leads to reduced migraine activity and, in some cases, elimination of migraine. Like others, he believes new analyses should be conducted.
“Everyone involved in this field believes there is something there,” Dr. Tobis said. The missing link is a clinical trial to confirm it.
Dr. Charles and Dr. Liu report no potential conflicts of interest. Dr. Tobis reports a financial relationship with Holistick Medical.
, according to a discussion at the 2023 Scottsdale Headache Symposium.
In two clinical trials evaluating whether PFO closure reduces migraine risk, the primary endpoints were not met, but a signal of benefit on secondary endpoints and the association between PFO, migraine, and stroke are among the reasons that PFO closure should be reevaluated, according to Andrew Charles MD, Director of the Goldberg Migraine Program, University of California, Los Angeles.
Other right-to-left shunt defects have also been associated with both migraine and stroke, leading Dr. Charles to suggest these defects are more a common denominator.
“Stroke during a migraine is, in fact, very uncommon,” Dr. Charles said. “This raises the possibility that it is not the migraine causing the stroke but rather there is a shared risk factor for stroke and migraine,” said Dr. Charles, referring to PFO as well as other right-to-left shunt defects, such as hereditary hemorrhaging telangiectasia in the lungs.
One Intervention, Two Potential Benefits
Fixing these defects is therefore at least theoretically attractive for preventing both migraine and stroke, but Dr. Charles said the opportunity for preventing both migraine and stroke is most attractive in migraine patients who have additional stroke risk factors.
Use of oral contraceptives, which produce a hypercoagulable state, is an example.
“Are these the people we should really be thinking about if they have PFO and migraine, particularly migraine with aura?” Dr. Charles asked.
The association between right-to-left shunts and migraine is strong. Although PFO is common, presenting in 20%-25% of the adult population, it has been found in up to 50% of individuals who have migraine with aura. In patients with migraine but no aura, the prevalence of PFO has been estimated to be approximately 35% or still somewhat elevated relative to the general population.
Primary Endpoint Missed in Clinical Trials
The question of whether risk of migraine can be reduced with repair of PFO or other right-to-left shunts remains unresolved. In two high-quality randomized trials undertaken in PFO repair, neither met its primary endpoint. In one of these, called PRIMA, which was terminated early for slow enrollment, the reduction in mean headache attacks was not significant relative to medical therapy.
In the second, called PREMIUM, device closure of PFO also failed to significantly reduce migraine attacks over sham procedure although it was associated with complete migraine remission (10% vs 1%).
A pooled analysis of these two studies that was conducted subsequently concluded that PFO closure reduces mean monthly migraine days (-3.1 vs. -1.9 days; P = -.02) and increases the likelihood of complete migraine cessation (9% vs. 0.7%; P < .001), but Dr. Charles pointed out the primary endpoint was migraine attacks not migraine days, so other analyses can only be considered hypothesis-generating.
There are several reasons to relook at the relationship between migraine and PFO but the potential to prevent both migraine and stroke with PFO closure could be one of the most important.
Several years ago, Dr. Charles and his coinvestigators from UCLA evaluated more than 700 ischemic strokes. Of these, 127 strokes were characterized as cryptogenic because of lack of another identifiable etiology. While 59% of these patients had PFO, which is several times higher than the general population, the prevalence of PFO in patients with a cryptogenic stroke and a history of migraine was 79% in this published study.
“So, in this group of patients who did not have any other clear cause for a stroke, a diagnosis of PFO was very much overrepresented,” Dr. Charles said.
Migraine Days Might Be a Better Endpoint
For patients with migraine who have risk factors for stroke, this makes PFO closure an attractive intervention, but a positive randomized trial is needed. Several are underway. Importantly, the trials now enrolling are using migraine days, which was significantly reduced in both PREMIUM and PRIMA, rather than migraine attacks as the primary endpoint.
“Migraine days is now accepted by the Food and Drug Administration as a criterion of benefit,” reported Jonathan Tobis, MD, Research Director, Interventional Cardiology, UCLA David Geffen School of Medicine, Los Angeles.
He explained that the FDA insisted on migraine attacks as the endpoint for the PREMIUM trial, but this was a far more challenging endpoint on which to show a statistical benefit. He emphasized that a new set of trials will now test efficacy on the basis of migraine days.
One of these trials, called RELIEF, which is randomizing patients to device closure of PFO or a sham procedure. Both groups are receiving clopidogrel or prasugrel based on a previous observation that patients who respond to these drugs are also more likely to respond to PFO closure.
Another trial, called COMPETE-2, is comparing PFO closure with a device to aspirin plus a sham closure. This trial is ongoing in China.
Stroke is not being evaluated as an endpoint in either trial, but Dr. Charles suggested that this does warrant attention.
“I would also just put it out there that, apart from simply migraine, this is a therapeutic approach that we might actually think about in terms of helping to prevent stroke in our migraine patients,” he said.
Senior author of a recent meta-analysis of trials evaluating PFO closure and control of migraine, Ling Liu, MD, Department of Neurology, University of Sichuan, Chengdu, China, agreed that PFO closure for the treatment of migraine deserves “a reevaluation.”
In his meta-analysis of three randomized trials, one pooled study, and eight retrospective case series with 1,165 patients, PFO closure was associated with a nearly 75% reduction (odds ratio [OR], 0.259; P = .0048) reduction in migraine days and 50% increase in resolution of migraine in patients with a history of migraine with aura (OR, 1.586; P = .227).
The incidence of stroke was not evaluated in this meta-analysis, but Dr. Liu believes that the evidence of reducing the burden of migraine with PFO closure is compelling. Given the evidence from this meta-analysis that PFO closure is safe, Dr. Liu maintained that a definitive trial is needed “especially for migraine with frequent aura.”
As an interventional cardiologist, Dr. Tobis said that when PFO closures is performed for prevention of stroke in patients with migraine, it often leads to reduced migraine activity and, in some cases, elimination of migraine. Like others, he believes new analyses should be conducted.
“Everyone involved in this field believes there is something there,” Dr. Tobis said. The missing link is a clinical trial to confirm it.
Dr. Charles and Dr. Liu report no potential conflicts of interest. Dr. Tobis reports a financial relationship with Holistick Medical.
FROM THE 2023 SCOTTSDALE HEADACHE SYMPOSIUM
Uveitis Associated with Psoriatic Arthritis: Characteristics, Approaches, and Treatment
With the growing number of treatment options for psoriatic arthritis (PsA), therapeutic decision-making has shifted to an increasingly tailored and patient-centered approach. A number of factors contribute to the treatment decision-making process, including age, insurance restrictions, route of administration, side effect profile, comorbidities, and extra-articular manifestations of the disease. In this article, we discuss an extra-articular comorbidity, uveitis, which is frequently seen in patients with PsA. We discuss clinical characteristics of uveitis associated with PsA and describe how the presence of uveitis influences our treatment approach to PsA, based on existing data.
Uveitis refers broadly to inflammation of the uvea, the vascularized and pigmented layer of the eye composed of the iris, the ciliary body, and the choroid. While infection is a common cause of uveitis, many cases are noninfectious and are often associated with an underlying autoimmune or systemic inflammatory disorder. Uveitis is frequently reported in diseases in the spondyloarthritis (SpA) family, including axial spondyloarthritis (AxSpA) and reactive arthritis, as well as PsA. Exact estimates of the prevalence of uveitis in PsA vary widely from 7%-25%, depending on the particular cohort studied.1,2 In all forms of SpA, the anterior chamber of the uvea is the most likely to be affected.3 However, compared to patients with AxSpA, patients with PsA appear to have a higher rate of posterior involvement. In addition, patients with PsA appear to have higher frequencies of insidious, bilateral uveitis, as compared to the acute, unilateral, anterior uveitis that is most characteristic of AxSpA.4 Women with PsA may be more likely than men to experience uveitis, although this has not been a consistent finding.5
Patients with PsA who are human leukocyte antigen B27 (HLA-B27) positive may be at risk for more severe and refractory anterior uveitis compared to those who do not express the allele.5 Those who are HLA-B27 positive are also known to have higher rates of axial involvement. It has therefore been postulated that 2 phenotypes of uveitis may exist in PsA: patients who are HLA-B27 positive who have axial disease and severe, unilateral anterior uveitis reminiscent of other forms of SpA, and patients who are HLA-B27 negative, often women, with peripheral-predominant arthritis who are prone to the classic anterior uveitis but may also develop atypical bilateral, insidious, and/or posterior involvement.4 Specific characteristics of PsA may also provide information about the risk for developing uveitis. For example, dactylitis has been linked to a higher risk of developing uveitis in some, but not all, cohorts of patients with PsA, and the risk of uveitis in PsA has been found in many studies to correlate with longer duration of disease.6-8
The presence of uveitis signals a disruption in the blood-retina barrier and the subsequent entrance of inflammatory cells into the eye. An entire explanation of pathogenesis is beyond the scope of this article; however, it is worth noting that many of the inflammatory mediators of active uveitis mirror those of PsA. For instance, both the mesenchymal cells in enthesitis and the cells of the ciliary body express receptors for interleukin (IL)-23, suggesting a potential role of the signaling pathways involving this cytokine in both diseases.9 Another study found increased serum levels of IL-17, a known mediator of PsA disease, in patients with active uveitis.10 Despite these common pathogenesis links, there are limited data on the utility of certain existing PsA treatments on uveitis manifestations.
Our approach is always to manage uveitis associated with PsA in collaboration with a specialized and experienced ophthalmologist. Uncontrolled uveitis can be vision threatening and contribute to long-term morbidity associated with PsA, so timely recognition, evaluation, and appropriate treatment are important. Ocular glucocorticoid (GC) drops may be used as first-line therapy, particularly for anterior uveitis, to quickly quell inflammation. Escalation to systemic GCs for more severe or posteriorly localized disease may be considered carefully, given the known risk of worsening skin psoriasis (PsO) with GC withdrawal after a course of therapy. Use of GC-sparing therapy should be determined on a case-by-case basis. While generalized, noninfectious uveitis often resolves with GC treatment, the risk of uveitis recurrence in patients with PsA and the challenges of systemic GCs with PsO lead us to frequently consider GC-sparing therapy that addresses ocular, musculoskeletal, and cutaneous manifestations. Tumor necrosis factor inhibitors (TNF-I) are our typical first-line considerations for GC-sparing therapy in patients with PsA with inflammatory joint symptoms and uveitis, although nonbiologic therapy can be considered first-line therapy in select populations.
Data establishing the efficacy of TNF-I come largely from randomized controlled trials (RCTs) of adalimumab (ADA) compared to placebo in noninfectious uveitis.11 While these trials focused on idiopathic posterior or pan-uveitis, these data have been extrapolated to SpA-associated anterior uveitis, and large registry analyses have supported use of TNF-I in this population.12 When selecting a particular TNF-I in a patient with current or past uveitis, we frequently start with ADA, based on supportive, albeit uncontrolled, data suggesting a reduction in the risk of recurrence with this agent in patients with SpA and uveitis.12 For patients who are unable to tolerate subcutaneous injections, who fail ADA, or who we suspect will require higher, titratable dosing, we favor infliximab infusions. Other data suggest that golimumab and certolizumab are also reasonable alternatives.13,14 We do not generally use etanercept, as the limited data that are available suggest that it is less effective at reducing risk of uveitis recurrence.12 Methotrexate or leflunomide may be an appropriate first line choice for patients with peripheral-predominant PsA and uveitis, but it is important to note that these agents are not effective for axial disease.
Despite the mechanistic data implicating the role of IL-17 in uveitis associated with PsA, the IL-17A inhibitor, secukinumab, failed to show a reduction in uveitis recurrence, compared to placebo, in pooled analysis of RCTs of noninfectious uveitis.15 However, a phase 2 trial of intravenous secukinumab in noninfectious uveitis showed promise, possibly because this dosing regimen can achieve higher effective concentrations.16 It is not our current practice to use secukinumab or ixekizumab as a first-line therapy in patients with PsA and concurrent uveitis, owing to a lack of data supporting efficacy. A novel IL-17A/F inhibitor, bimekizumab (BKZ), has recently been used in several successful phase 3 trials in patients with both TNF-naïve and TNF-nonresponder SpA, including AxSpA and PsA.17 Interestingly, data from the phase 2 and 3 trials of BKZ found low incidence rates of uveitis in patients with SpA treated with BKZ compared to placebo, suggesting that BKZ might be more effective in uveitis than other IL-17 inhibitors, but these data need to be confirmed.
Successful use of Janus kinase (JAK) inhibitors in noninfectious uveitis, including cases associated with inflammatory arthritis, has been described in case reports as well as in current phase 2 trials.18 The dual IL-12/IL-23 inhibitor, ustekinumab, also showed initial promise in a small, nonrandomized, uncontrolled phase 1/2 study of the treatment of posterior uveitis, as well as success in few case reports of PsA-associated uveitis.19 However, a post-hoc analysis of extra-intestinal manifestations, including uveitis and iritis, in patients with inflammatory bowel disease treated with ustekinumab found no benefit in preventing or treating ocular disease compared to placebo.20 Given the paucity of available data, JAK inhibitors and the IL-12/IL-23 inhibitor, ustekinumab, are not part of our typical treatment algorithm for patients with PsA-associated uveitis.
In conclusion, uveitis is a frequent extra-articular comorbidity of PsA, and it may present differently than the typical acute onset, unilateral anterior uveitis seen in SpA. While uveitis may share many different immunologic threads with PsA, the most convincing data support the use of TNF-I as a GC-sparing agent in this setting, particularly ADA, infliximab, golimumab, or certolizumab. Our approach is generally to start with these agents or methotrexate when directed therapy is needed for uveitis in PsA. Further investigation into the use of the IL-17A/F inhibitor BKZ and JAK inhibitors, as well as tyrosine kinase 2 inhibitors, in PsA associated uveitis may yield additional options for our patients.21
1. De Vicente Delmas A, Sanchez-Bilbao L, Calvo-Rio V, et al. Uveitis in psoriatic arthritis: study of 406 patients in a single university center and literature review. RMD Open. 2023;9(1):e002781.
2. Rademacher J, Poddubnyy D, Pleyer U. Uveitis in spondyloarthritis. Ther Adv Musculoskelet Dis. 2020;12:1759720X20951733.
3. Zeboulon N, Dougados M, Gossec L. Prevalence and characteristics of uveitis in the spondyloarthropathies: a systematic literature review. Ann Rheum Dis. 2008;67(7):955-959.
4. Paiva ES, Macaluso DC, Edwards A, Rosenbaum JT. Characterisation of uveitis in patients with psoriatic arthritis. Ann Rheum Dis. 2000;59(1):67-70.
5. Fraga NA, Oliveira Mde F, Follador I, Rocha Bde O, Rego VR. Psoriasis and uveitis: a literature review. An Bras Dermatol. 2012;87(6):877-883.
6. Niccoli L, Nannini C, Cassara E, et al. Frequency of iridocyclitis in patients with early psoriatic arthritis: a prospective, follow up study. Int J Rheum Dis. 2012;15(4):414-418.
7. Yasar Bilge NS, Kalyoncu U, Atagunduz P, et al. Uveitis-related factors in patients with spondyloarthritis: TReasure Real-Life Results. Am J Ophthalmol. 2021;228:58-64.
8. Chia AYT, Ang GWX, Chan ASY, Chan W, Chong TKY, Leung YY. Managing psoriatic arthritis with inflammatory bowel disease and/or uveitis. Front Med (Lausanne). 2021;8:737256.
9. Reinhardt A, Yevsa T, Worbs T, et al. Interleukin-23-dependent gamma/delta T cells produce interleukin-17 and accumulate in the enthesis, aortic valve, and ciliary body in mice. Arthritis Rheumatol. 2016;68(10):2476-2486.
10. Jawad S, Liu B, Agron E, Nussenblatt RB, Sen HN. Elevated serum levels of interleukin-17A in uveitis patients. Ocul Immunol Inflamm. 2013;21(6):434-439.
11. Merrill PT, Vitale A, Zierhut M, et al. Efficacy of adalimumab in non-infectious uveitis across different etiologies: a post hoc analysis of the VISUAL I and VISUAL II Trials. Ocul Immunol Inflamm. 2021;29(7-8):1569-1575.
12. Lie E, Lindstrom U, Zverkova-Sandstrom T, et al. Tumour necrosis factor inhibitor treatment and occurrence of anterior uveitis in ankylosing spondylitis: results from the Swedish biologics register. Ann Rheum Dis. 2017;76(9):1515-1521.
13. van der Horst-Bruinsma I, van Bentum R, Verbraak FD, et al. The impact of certolizumab pegol treatment on the incidence of anterior uveitis flares in patients with axial spondyloarthritis: 48-week interim results from C-VIEW. RMD Open. 2020;6(1):e001161.
14. Calvo-Rio V, Blanco R, Santos-Gomez M, et al. Golimumab in refractory uveitis related to spondyloarthritis. Multicenter study of 15 patients. Semin Arthritis Rheum. 2016;46(1):95-101.
15. Dick AD, Tugal-Tutkun I, Foster S, et al. Secukinumab in the treatment of noninfectious uveitis: results of three randomized, controlled clinical trials. Ophthalmology. 2013;120(4):777-787.
16. Letko E, Yeh S, Foster CS, et al. Efficacy and safety of intravenous secukinumab in noninfectious uveitis requiring steroid-sparing immunosuppressive therapy. Ophthalmology. 2015;122(5):939-948.
17. van der Heijde D, Deodhar A, Baraliakos X, et al. Efficacy and safety of bimekizumab in axial spondyloarthritis: results of two parallel phase 3 randomised controlled trials. Ann Rheum Dis. 2023;82(4):515-526.
18. Dhillon S, Keam SJ. Filgotinib: first approval. Drugs. 2020;80(18):1987-1997.
19. Pepple KL, Lin P. Targeting interleukin-23 in the treatment of noninfectious uveitis. Ophthalmology. 2018;125(12):1977-1983.
20. Narula N, Aruljothy A, Wong ECL, et al. The impact of ustekinumab on extraintestinal manifestations of Crohn’s disease: a post hoc analysis of the UNITI studies. United European Gastroenterol J. 2021;9(5):581-589.
21. Rusinol L, Puig L. Tyk2 targeting in immune-mediated inflammatory diseases. Int J Mol Sci. 2023;24(4):3391.
With the growing number of treatment options for psoriatic arthritis (PsA), therapeutic decision-making has shifted to an increasingly tailored and patient-centered approach. A number of factors contribute to the treatment decision-making process, including age, insurance restrictions, route of administration, side effect profile, comorbidities, and extra-articular manifestations of the disease. In this article, we discuss an extra-articular comorbidity, uveitis, which is frequently seen in patients with PsA. We discuss clinical characteristics of uveitis associated with PsA and describe how the presence of uveitis influences our treatment approach to PsA, based on existing data.
Uveitis refers broadly to inflammation of the uvea, the vascularized and pigmented layer of the eye composed of the iris, the ciliary body, and the choroid. While infection is a common cause of uveitis, many cases are noninfectious and are often associated with an underlying autoimmune or systemic inflammatory disorder. Uveitis is frequently reported in diseases in the spondyloarthritis (SpA) family, including axial spondyloarthritis (AxSpA) and reactive arthritis, as well as PsA. Exact estimates of the prevalence of uveitis in PsA vary widely from 7%-25%, depending on the particular cohort studied.1,2 In all forms of SpA, the anterior chamber of the uvea is the most likely to be affected.3 However, compared to patients with AxSpA, patients with PsA appear to have a higher rate of posterior involvement. In addition, patients with PsA appear to have higher frequencies of insidious, bilateral uveitis, as compared to the acute, unilateral, anterior uveitis that is most characteristic of AxSpA.4 Women with PsA may be more likely than men to experience uveitis, although this has not been a consistent finding.5
Patients with PsA who are human leukocyte antigen B27 (HLA-B27) positive may be at risk for more severe and refractory anterior uveitis compared to those who do not express the allele.5 Those who are HLA-B27 positive are also known to have higher rates of axial involvement. It has therefore been postulated that 2 phenotypes of uveitis may exist in PsA: patients who are HLA-B27 positive who have axial disease and severe, unilateral anterior uveitis reminiscent of other forms of SpA, and patients who are HLA-B27 negative, often women, with peripheral-predominant arthritis who are prone to the classic anterior uveitis but may also develop atypical bilateral, insidious, and/or posterior involvement.4 Specific characteristics of PsA may also provide information about the risk for developing uveitis. For example, dactylitis has been linked to a higher risk of developing uveitis in some, but not all, cohorts of patients with PsA, and the risk of uveitis in PsA has been found in many studies to correlate with longer duration of disease.6-8
The presence of uveitis signals a disruption in the blood-retina barrier and the subsequent entrance of inflammatory cells into the eye. An entire explanation of pathogenesis is beyond the scope of this article; however, it is worth noting that many of the inflammatory mediators of active uveitis mirror those of PsA. For instance, both the mesenchymal cells in enthesitis and the cells of the ciliary body express receptors for interleukin (IL)-23, suggesting a potential role of the signaling pathways involving this cytokine in both diseases.9 Another study found increased serum levels of IL-17, a known mediator of PsA disease, in patients with active uveitis.10 Despite these common pathogenesis links, there are limited data on the utility of certain existing PsA treatments on uveitis manifestations.
Our approach is always to manage uveitis associated with PsA in collaboration with a specialized and experienced ophthalmologist. Uncontrolled uveitis can be vision threatening and contribute to long-term morbidity associated with PsA, so timely recognition, evaluation, and appropriate treatment are important. Ocular glucocorticoid (GC) drops may be used as first-line therapy, particularly for anterior uveitis, to quickly quell inflammation. Escalation to systemic GCs for more severe or posteriorly localized disease may be considered carefully, given the known risk of worsening skin psoriasis (PsO) with GC withdrawal after a course of therapy. Use of GC-sparing therapy should be determined on a case-by-case basis. While generalized, noninfectious uveitis often resolves with GC treatment, the risk of uveitis recurrence in patients with PsA and the challenges of systemic GCs with PsO lead us to frequently consider GC-sparing therapy that addresses ocular, musculoskeletal, and cutaneous manifestations. Tumor necrosis factor inhibitors (TNF-I) are our typical first-line considerations for GC-sparing therapy in patients with PsA with inflammatory joint symptoms and uveitis, although nonbiologic therapy can be considered first-line therapy in select populations.
Data establishing the efficacy of TNF-I come largely from randomized controlled trials (RCTs) of adalimumab (ADA) compared to placebo in noninfectious uveitis.11 While these trials focused on idiopathic posterior or pan-uveitis, these data have been extrapolated to SpA-associated anterior uveitis, and large registry analyses have supported use of TNF-I in this population.12 When selecting a particular TNF-I in a patient with current or past uveitis, we frequently start with ADA, based on supportive, albeit uncontrolled, data suggesting a reduction in the risk of recurrence with this agent in patients with SpA and uveitis.12 For patients who are unable to tolerate subcutaneous injections, who fail ADA, or who we suspect will require higher, titratable dosing, we favor infliximab infusions. Other data suggest that golimumab and certolizumab are also reasonable alternatives.13,14 We do not generally use etanercept, as the limited data that are available suggest that it is less effective at reducing risk of uveitis recurrence.12 Methotrexate or leflunomide may be an appropriate first line choice for patients with peripheral-predominant PsA and uveitis, but it is important to note that these agents are not effective for axial disease.
Despite the mechanistic data implicating the role of IL-17 in uveitis associated with PsA, the IL-17A inhibitor, secukinumab, failed to show a reduction in uveitis recurrence, compared to placebo, in pooled analysis of RCTs of noninfectious uveitis.15 However, a phase 2 trial of intravenous secukinumab in noninfectious uveitis showed promise, possibly because this dosing regimen can achieve higher effective concentrations.16 It is not our current practice to use secukinumab or ixekizumab as a first-line therapy in patients with PsA and concurrent uveitis, owing to a lack of data supporting efficacy. A novel IL-17A/F inhibitor, bimekizumab (BKZ), has recently been used in several successful phase 3 trials in patients with both TNF-naïve and TNF-nonresponder SpA, including AxSpA and PsA.17 Interestingly, data from the phase 2 and 3 trials of BKZ found low incidence rates of uveitis in patients with SpA treated with BKZ compared to placebo, suggesting that BKZ might be more effective in uveitis than other IL-17 inhibitors, but these data need to be confirmed.
Successful use of Janus kinase (JAK) inhibitors in noninfectious uveitis, including cases associated with inflammatory arthritis, has been described in case reports as well as in current phase 2 trials.18 The dual IL-12/IL-23 inhibitor, ustekinumab, also showed initial promise in a small, nonrandomized, uncontrolled phase 1/2 study of the treatment of posterior uveitis, as well as success in few case reports of PsA-associated uveitis.19 However, a post-hoc analysis of extra-intestinal manifestations, including uveitis and iritis, in patients with inflammatory bowel disease treated with ustekinumab found no benefit in preventing or treating ocular disease compared to placebo.20 Given the paucity of available data, JAK inhibitors and the IL-12/IL-23 inhibitor, ustekinumab, are not part of our typical treatment algorithm for patients with PsA-associated uveitis.
In conclusion, uveitis is a frequent extra-articular comorbidity of PsA, and it may present differently than the typical acute onset, unilateral anterior uveitis seen in SpA. While uveitis may share many different immunologic threads with PsA, the most convincing data support the use of TNF-I as a GC-sparing agent in this setting, particularly ADA, infliximab, golimumab, or certolizumab. Our approach is generally to start with these agents or methotrexate when directed therapy is needed for uveitis in PsA. Further investigation into the use of the IL-17A/F inhibitor BKZ and JAK inhibitors, as well as tyrosine kinase 2 inhibitors, in PsA associated uveitis may yield additional options for our patients.21
With the growing number of treatment options for psoriatic arthritis (PsA), therapeutic decision-making has shifted to an increasingly tailored and patient-centered approach. A number of factors contribute to the treatment decision-making process, including age, insurance restrictions, route of administration, side effect profile, comorbidities, and extra-articular manifestations of the disease. In this article, we discuss an extra-articular comorbidity, uveitis, which is frequently seen in patients with PsA. We discuss clinical characteristics of uveitis associated with PsA and describe how the presence of uveitis influences our treatment approach to PsA, based on existing data.
Uveitis refers broadly to inflammation of the uvea, the vascularized and pigmented layer of the eye composed of the iris, the ciliary body, and the choroid. While infection is a common cause of uveitis, many cases are noninfectious and are often associated with an underlying autoimmune or systemic inflammatory disorder. Uveitis is frequently reported in diseases in the spondyloarthritis (SpA) family, including axial spondyloarthritis (AxSpA) and reactive arthritis, as well as PsA. Exact estimates of the prevalence of uveitis in PsA vary widely from 7%-25%, depending on the particular cohort studied.1,2 In all forms of SpA, the anterior chamber of the uvea is the most likely to be affected.3 However, compared to patients with AxSpA, patients with PsA appear to have a higher rate of posterior involvement. In addition, patients with PsA appear to have higher frequencies of insidious, bilateral uveitis, as compared to the acute, unilateral, anterior uveitis that is most characteristic of AxSpA.4 Women with PsA may be more likely than men to experience uveitis, although this has not been a consistent finding.5
Patients with PsA who are human leukocyte antigen B27 (HLA-B27) positive may be at risk for more severe and refractory anterior uveitis compared to those who do not express the allele.5 Those who are HLA-B27 positive are also known to have higher rates of axial involvement. It has therefore been postulated that 2 phenotypes of uveitis may exist in PsA: patients who are HLA-B27 positive who have axial disease and severe, unilateral anterior uveitis reminiscent of other forms of SpA, and patients who are HLA-B27 negative, often women, with peripheral-predominant arthritis who are prone to the classic anterior uveitis but may also develop atypical bilateral, insidious, and/or posterior involvement.4 Specific characteristics of PsA may also provide information about the risk for developing uveitis. For example, dactylitis has been linked to a higher risk of developing uveitis in some, but not all, cohorts of patients with PsA, and the risk of uveitis in PsA has been found in many studies to correlate with longer duration of disease.6-8
The presence of uveitis signals a disruption in the blood-retina barrier and the subsequent entrance of inflammatory cells into the eye. An entire explanation of pathogenesis is beyond the scope of this article; however, it is worth noting that many of the inflammatory mediators of active uveitis mirror those of PsA. For instance, both the mesenchymal cells in enthesitis and the cells of the ciliary body express receptors for interleukin (IL)-23, suggesting a potential role of the signaling pathways involving this cytokine in both diseases.9 Another study found increased serum levels of IL-17, a known mediator of PsA disease, in patients with active uveitis.10 Despite these common pathogenesis links, there are limited data on the utility of certain existing PsA treatments on uveitis manifestations.
Our approach is always to manage uveitis associated with PsA in collaboration with a specialized and experienced ophthalmologist. Uncontrolled uveitis can be vision threatening and contribute to long-term morbidity associated with PsA, so timely recognition, evaluation, and appropriate treatment are important. Ocular glucocorticoid (GC) drops may be used as first-line therapy, particularly for anterior uveitis, to quickly quell inflammation. Escalation to systemic GCs for more severe or posteriorly localized disease may be considered carefully, given the known risk of worsening skin psoriasis (PsO) with GC withdrawal after a course of therapy. Use of GC-sparing therapy should be determined on a case-by-case basis. While generalized, noninfectious uveitis often resolves with GC treatment, the risk of uveitis recurrence in patients with PsA and the challenges of systemic GCs with PsO lead us to frequently consider GC-sparing therapy that addresses ocular, musculoskeletal, and cutaneous manifestations. Tumor necrosis factor inhibitors (TNF-I) are our typical first-line considerations for GC-sparing therapy in patients with PsA with inflammatory joint symptoms and uveitis, although nonbiologic therapy can be considered first-line therapy in select populations.
Data establishing the efficacy of TNF-I come largely from randomized controlled trials (RCTs) of adalimumab (ADA) compared to placebo in noninfectious uveitis.11 While these trials focused on idiopathic posterior or pan-uveitis, these data have been extrapolated to SpA-associated anterior uveitis, and large registry analyses have supported use of TNF-I in this population.12 When selecting a particular TNF-I in a patient with current or past uveitis, we frequently start with ADA, based on supportive, albeit uncontrolled, data suggesting a reduction in the risk of recurrence with this agent in patients with SpA and uveitis.12 For patients who are unable to tolerate subcutaneous injections, who fail ADA, or who we suspect will require higher, titratable dosing, we favor infliximab infusions. Other data suggest that golimumab and certolizumab are also reasonable alternatives.13,14 We do not generally use etanercept, as the limited data that are available suggest that it is less effective at reducing risk of uveitis recurrence.12 Methotrexate or leflunomide may be an appropriate first line choice for patients with peripheral-predominant PsA and uveitis, but it is important to note that these agents are not effective for axial disease.
Despite the mechanistic data implicating the role of IL-17 in uveitis associated with PsA, the IL-17A inhibitor, secukinumab, failed to show a reduction in uveitis recurrence, compared to placebo, in pooled analysis of RCTs of noninfectious uveitis.15 However, a phase 2 trial of intravenous secukinumab in noninfectious uveitis showed promise, possibly because this dosing regimen can achieve higher effective concentrations.16 It is not our current practice to use secukinumab or ixekizumab as a first-line therapy in patients with PsA and concurrent uveitis, owing to a lack of data supporting efficacy. A novel IL-17A/F inhibitor, bimekizumab (BKZ), has recently been used in several successful phase 3 trials in patients with both TNF-naïve and TNF-nonresponder SpA, including AxSpA and PsA.17 Interestingly, data from the phase 2 and 3 trials of BKZ found low incidence rates of uveitis in patients with SpA treated with BKZ compared to placebo, suggesting that BKZ might be more effective in uveitis than other IL-17 inhibitors, but these data need to be confirmed.
Successful use of Janus kinase (JAK) inhibitors in noninfectious uveitis, including cases associated with inflammatory arthritis, has been described in case reports as well as in current phase 2 trials.18 The dual IL-12/IL-23 inhibitor, ustekinumab, also showed initial promise in a small, nonrandomized, uncontrolled phase 1/2 study of the treatment of posterior uveitis, as well as success in few case reports of PsA-associated uveitis.19 However, a post-hoc analysis of extra-intestinal manifestations, including uveitis and iritis, in patients with inflammatory bowel disease treated with ustekinumab found no benefit in preventing or treating ocular disease compared to placebo.20 Given the paucity of available data, JAK inhibitors and the IL-12/IL-23 inhibitor, ustekinumab, are not part of our typical treatment algorithm for patients with PsA-associated uveitis.
In conclusion, uveitis is a frequent extra-articular comorbidity of PsA, and it may present differently than the typical acute onset, unilateral anterior uveitis seen in SpA. While uveitis may share many different immunologic threads with PsA, the most convincing data support the use of TNF-I as a GC-sparing agent in this setting, particularly ADA, infliximab, golimumab, or certolizumab. Our approach is generally to start with these agents or methotrexate when directed therapy is needed for uveitis in PsA. Further investigation into the use of the IL-17A/F inhibitor BKZ and JAK inhibitors, as well as tyrosine kinase 2 inhibitors, in PsA associated uveitis may yield additional options for our patients.21
1. De Vicente Delmas A, Sanchez-Bilbao L, Calvo-Rio V, et al. Uveitis in psoriatic arthritis: study of 406 patients in a single university center and literature review. RMD Open. 2023;9(1):e002781.
2. Rademacher J, Poddubnyy D, Pleyer U. Uveitis in spondyloarthritis. Ther Adv Musculoskelet Dis. 2020;12:1759720X20951733.
3. Zeboulon N, Dougados M, Gossec L. Prevalence and characteristics of uveitis in the spondyloarthropathies: a systematic literature review. Ann Rheum Dis. 2008;67(7):955-959.
4. Paiva ES, Macaluso DC, Edwards A, Rosenbaum JT. Characterisation of uveitis in patients with psoriatic arthritis. Ann Rheum Dis. 2000;59(1):67-70.
5. Fraga NA, Oliveira Mde F, Follador I, Rocha Bde O, Rego VR. Psoriasis and uveitis: a literature review. An Bras Dermatol. 2012;87(6):877-883.
6. Niccoli L, Nannini C, Cassara E, et al. Frequency of iridocyclitis in patients with early psoriatic arthritis: a prospective, follow up study. Int J Rheum Dis. 2012;15(4):414-418.
7. Yasar Bilge NS, Kalyoncu U, Atagunduz P, et al. Uveitis-related factors in patients with spondyloarthritis: TReasure Real-Life Results. Am J Ophthalmol. 2021;228:58-64.
8. Chia AYT, Ang GWX, Chan ASY, Chan W, Chong TKY, Leung YY. Managing psoriatic arthritis with inflammatory bowel disease and/or uveitis. Front Med (Lausanne). 2021;8:737256.
9. Reinhardt A, Yevsa T, Worbs T, et al. Interleukin-23-dependent gamma/delta T cells produce interleukin-17 and accumulate in the enthesis, aortic valve, and ciliary body in mice. Arthritis Rheumatol. 2016;68(10):2476-2486.
10. Jawad S, Liu B, Agron E, Nussenblatt RB, Sen HN. Elevated serum levels of interleukin-17A in uveitis patients. Ocul Immunol Inflamm. 2013;21(6):434-439.
11. Merrill PT, Vitale A, Zierhut M, et al. Efficacy of adalimumab in non-infectious uveitis across different etiologies: a post hoc analysis of the VISUAL I and VISUAL II Trials. Ocul Immunol Inflamm. 2021;29(7-8):1569-1575.
12. Lie E, Lindstrom U, Zverkova-Sandstrom T, et al. Tumour necrosis factor inhibitor treatment and occurrence of anterior uveitis in ankylosing spondylitis: results from the Swedish biologics register. Ann Rheum Dis. 2017;76(9):1515-1521.
13. van der Horst-Bruinsma I, van Bentum R, Verbraak FD, et al. The impact of certolizumab pegol treatment on the incidence of anterior uveitis flares in patients with axial spondyloarthritis: 48-week interim results from C-VIEW. RMD Open. 2020;6(1):e001161.
14. Calvo-Rio V, Blanco R, Santos-Gomez M, et al. Golimumab in refractory uveitis related to spondyloarthritis. Multicenter study of 15 patients. Semin Arthritis Rheum. 2016;46(1):95-101.
15. Dick AD, Tugal-Tutkun I, Foster S, et al. Secukinumab in the treatment of noninfectious uveitis: results of three randomized, controlled clinical trials. Ophthalmology. 2013;120(4):777-787.
16. Letko E, Yeh S, Foster CS, et al. Efficacy and safety of intravenous secukinumab in noninfectious uveitis requiring steroid-sparing immunosuppressive therapy. Ophthalmology. 2015;122(5):939-948.
17. van der Heijde D, Deodhar A, Baraliakos X, et al. Efficacy and safety of bimekizumab in axial spondyloarthritis: results of two parallel phase 3 randomised controlled trials. Ann Rheum Dis. 2023;82(4):515-526.
18. Dhillon S, Keam SJ. Filgotinib: first approval. Drugs. 2020;80(18):1987-1997.
19. Pepple KL, Lin P. Targeting interleukin-23 in the treatment of noninfectious uveitis. Ophthalmology. 2018;125(12):1977-1983.
20. Narula N, Aruljothy A, Wong ECL, et al. The impact of ustekinumab on extraintestinal manifestations of Crohn’s disease: a post hoc analysis of the UNITI studies. United European Gastroenterol J. 2021;9(5):581-589.
21. Rusinol L, Puig L. Tyk2 targeting in immune-mediated inflammatory diseases. Int J Mol Sci. 2023;24(4):3391.
1. De Vicente Delmas A, Sanchez-Bilbao L, Calvo-Rio V, et al. Uveitis in psoriatic arthritis: study of 406 patients in a single university center and literature review. RMD Open. 2023;9(1):e002781.
2. Rademacher J, Poddubnyy D, Pleyer U. Uveitis in spondyloarthritis. Ther Adv Musculoskelet Dis. 2020;12:1759720X20951733.
3. Zeboulon N, Dougados M, Gossec L. Prevalence and characteristics of uveitis in the spondyloarthropathies: a systematic literature review. Ann Rheum Dis. 2008;67(7):955-959.
4. Paiva ES, Macaluso DC, Edwards A, Rosenbaum JT. Characterisation of uveitis in patients with psoriatic arthritis. Ann Rheum Dis. 2000;59(1):67-70.
5. Fraga NA, Oliveira Mde F, Follador I, Rocha Bde O, Rego VR. Psoriasis and uveitis: a literature review. An Bras Dermatol. 2012;87(6):877-883.
6. Niccoli L, Nannini C, Cassara E, et al. Frequency of iridocyclitis in patients with early psoriatic arthritis: a prospective, follow up study. Int J Rheum Dis. 2012;15(4):414-418.
7. Yasar Bilge NS, Kalyoncu U, Atagunduz P, et al. Uveitis-related factors in patients with spondyloarthritis: TReasure Real-Life Results. Am J Ophthalmol. 2021;228:58-64.
8. Chia AYT, Ang GWX, Chan ASY, Chan W, Chong TKY, Leung YY. Managing psoriatic arthritis with inflammatory bowel disease and/or uveitis. Front Med (Lausanne). 2021;8:737256.
9. Reinhardt A, Yevsa T, Worbs T, et al. Interleukin-23-dependent gamma/delta T cells produce interleukin-17 and accumulate in the enthesis, aortic valve, and ciliary body in mice. Arthritis Rheumatol. 2016;68(10):2476-2486.
10. Jawad S, Liu B, Agron E, Nussenblatt RB, Sen HN. Elevated serum levels of interleukin-17A in uveitis patients. Ocul Immunol Inflamm. 2013;21(6):434-439.
11. Merrill PT, Vitale A, Zierhut M, et al. Efficacy of adalimumab in non-infectious uveitis across different etiologies: a post hoc analysis of the VISUAL I and VISUAL II Trials. Ocul Immunol Inflamm. 2021;29(7-8):1569-1575.
12. Lie E, Lindstrom U, Zverkova-Sandstrom T, et al. Tumour necrosis factor inhibitor treatment and occurrence of anterior uveitis in ankylosing spondylitis: results from the Swedish biologics register. Ann Rheum Dis. 2017;76(9):1515-1521.
13. van der Horst-Bruinsma I, van Bentum R, Verbraak FD, et al. The impact of certolizumab pegol treatment on the incidence of anterior uveitis flares in patients with axial spondyloarthritis: 48-week interim results from C-VIEW. RMD Open. 2020;6(1):e001161.
14. Calvo-Rio V, Blanco R, Santos-Gomez M, et al. Golimumab in refractory uveitis related to spondyloarthritis. Multicenter study of 15 patients. Semin Arthritis Rheum. 2016;46(1):95-101.
15. Dick AD, Tugal-Tutkun I, Foster S, et al. Secukinumab in the treatment of noninfectious uveitis: results of three randomized, controlled clinical trials. Ophthalmology. 2013;120(4):777-787.
16. Letko E, Yeh S, Foster CS, et al. Efficacy and safety of intravenous secukinumab in noninfectious uveitis requiring steroid-sparing immunosuppressive therapy. Ophthalmology. 2015;122(5):939-948.
17. van der Heijde D, Deodhar A, Baraliakos X, et al. Efficacy and safety of bimekizumab in axial spondyloarthritis: results of two parallel phase 3 randomised controlled trials. Ann Rheum Dis. 2023;82(4):515-526.
18. Dhillon S, Keam SJ. Filgotinib: first approval. Drugs. 2020;80(18):1987-1997.
19. Pepple KL, Lin P. Targeting interleukin-23 in the treatment of noninfectious uveitis. Ophthalmology. 2018;125(12):1977-1983.
20. Narula N, Aruljothy A, Wong ECL, et al. The impact of ustekinumab on extraintestinal manifestations of Crohn’s disease: a post hoc analysis of the UNITI studies. United European Gastroenterol J. 2021;9(5):581-589.
21. Rusinol L, Puig L. Tyk2 targeting in immune-mediated inflammatory diseases. Int J Mol Sci. 2023;24(4):3391.
COVID vaccines lower risk of serious illness in children
TOPLINE:
, according to a new study by the Centers for Disease Control and Prevention (CDC).
METHODOLOGY:
- SARS-CoV-2 infection can severely affect children who have certain chronic conditions.
- Researchers assessed the effectiveness of COVID-19 vaccines in preventing emergency ED visits and hospitalizations associated with the illness from July 2022 to September 2023.
- They drew data from the New Vaccine Surveillance Network, which conducts population-based, prospective surveillance for acute respiratory illness in children at seven pediatric medical centers.
- The period assessed was the first year vaccines were authorized for children aged 6 months to 4 years; during that period, several Omicron subvariants arose.
- Researchers used data from 7,434 infants and children; data included patients’ vaccine status and their test results for SARS-CoV-2.
TAKEAWAY:
- Of the 7,434 infants and children who had an acute respiratory illness and were hospitalized or visited the ED, 387 had COVID-19.
- Children who received two doses of a COVID-19 vaccine were 40% less likely to have a COVID-19-associated hospitalization or ED visit compared with unvaccinated youth.
- One dose of a COVID-19 vaccine reduced ED visits and hospitalizations by 31%.
IN PRACTICE:
“The findings in this report support the recommendation for COVID-19 vaccination for all children aged ≥6 months and highlight the importance of completion of a primary series for young children,” the researchers reported.
SOURCE:
The study was led by Heidi L. Moline, MD, of the CDC.
LIMITATIONS:
Because the number of children with antibodies and immunity against SARS-CoV-2 has grown, vaccine effectiveness rates in the study may no longer be as relevant. Children with preexisting chronic conditions may be more likely to be vaccinated and receive medical attention. The low rates of vaccination may have prevented researchers from conducting a more detailed analysis. The Pfizer-BioNTech vaccine requires three doses, whereas Moderna’s requires two doses; this may have skewed the estimated efficacy of the Pfizer-BioNTech vaccine.
DISCLOSURES:
The authors report a variety of potential conflicts of interest, which are detailed in the article.
A version of this article appeared on Medscape.com.
TOPLINE:
, according to a new study by the Centers for Disease Control and Prevention (CDC).
METHODOLOGY:
- SARS-CoV-2 infection can severely affect children who have certain chronic conditions.
- Researchers assessed the effectiveness of COVID-19 vaccines in preventing emergency ED visits and hospitalizations associated with the illness from July 2022 to September 2023.
- They drew data from the New Vaccine Surveillance Network, which conducts population-based, prospective surveillance for acute respiratory illness in children at seven pediatric medical centers.
- The period assessed was the first year vaccines were authorized for children aged 6 months to 4 years; during that period, several Omicron subvariants arose.
- Researchers used data from 7,434 infants and children; data included patients’ vaccine status and their test results for SARS-CoV-2.
TAKEAWAY:
- Of the 7,434 infants and children who had an acute respiratory illness and were hospitalized or visited the ED, 387 had COVID-19.
- Children who received two doses of a COVID-19 vaccine were 40% less likely to have a COVID-19-associated hospitalization or ED visit compared with unvaccinated youth.
- One dose of a COVID-19 vaccine reduced ED visits and hospitalizations by 31%.
IN PRACTICE:
“The findings in this report support the recommendation for COVID-19 vaccination for all children aged ≥6 months and highlight the importance of completion of a primary series for young children,” the researchers reported.
SOURCE:
The study was led by Heidi L. Moline, MD, of the CDC.
LIMITATIONS:
Because the number of children with antibodies and immunity against SARS-CoV-2 has grown, vaccine effectiveness rates in the study may no longer be as relevant. Children with preexisting chronic conditions may be more likely to be vaccinated and receive medical attention. The low rates of vaccination may have prevented researchers from conducting a more detailed analysis. The Pfizer-BioNTech vaccine requires three doses, whereas Moderna’s requires two doses; this may have skewed the estimated efficacy of the Pfizer-BioNTech vaccine.
DISCLOSURES:
The authors report a variety of potential conflicts of interest, which are detailed in the article.
A version of this article appeared on Medscape.com.
TOPLINE:
, according to a new study by the Centers for Disease Control and Prevention (CDC).
METHODOLOGY:
- SARS-CoV-2 infection can severely affect children who have certain chronic conditions.
- Researchers assessed the effectiveness of COVID-19 vaccines in preventing emergency ED visits and hospitalizations associated with the illness from July 2022 to September 2023.
- They drew data from the New Vaccine Surveillance Network, which conducts population-based, prospective surveillance for acute respiratory illness in children at seven pediatric medical centers.
- The period assessed was the first year vaccines were authorized for children aged 6 months to 4 years; during that period, several Omicron subvariants arose.
- Researchers used data from 7,434 infants and children; data included patients’ vaccine status and their test results for SARS-CoV-2.
TAKEAWAY:
- Of the 7,434 infants and children who had an acute respiratory illness and were hospitalized or visited the ED, 387 had COVID-19.
- Children who received two doses of a COVID-19 vaccine were 40% less likely to have a COVID-19-associated hospitalization or ED visit compared with unvaccinated youth.
- One dose of a COVID-19 vaccine reduced ED visits and hospitalizations by 31%.
IN PRACTICE:
“The findings in this report support the recommendation for COVID-19 vaccination for all children aged ≥6 months and highlight the importance of completion of a primary series for young children,” the researchers reported.
SOURCE:
The study was led by Heidi L. Moline, MD, of the CDC.
LIMITATIONS:
Because the number of children with antibodies and immunity against SARS-CoV-2 has grown, vaccine effectiveness rates in the study may no longer be as relevant. Children with preexisting chronic conditions may be more likely to be vaccinated and receive medical attention. The low rates of vaccination may have prevented researchers from conducting a more detailed analysis. The Pfizer-BioNTech vaccine requires three doses, whereas Moderna’s requires two doses; this may have skewed the estimated efficacy of the Pfizer-BioNTech vaccine.
DISCLOSURES:
The authors report a variety of potential conflicts of interest, which are detailed in the article.
A version of this article appeared on Medscape.com.
Secondhand smoke exposure linked to migraine, severe headache
TOPLINE:
, with effects of exposure varying depending on body mass index (BMI) and level of physical activity, new research shows.
METHODOLOGY:
Investigators analyzed data on 4,560 participants (median age, 43 years; 60% female; 71.5% White) from the 1999-2004 National Health and Nutrition Examination Survey.
Participants were aged 20 years or older and had never smoked.
Migraine headache status was determined by asking whether participants experienced severe headaches or migraines during the previous 3 months.
SHS exposure was categorized as unexposed (serum cotinine levels <0.05 ng/mL and no smoker in the home), low (0.05 ng/mL ≤ serum cotinine level <1 ng/mL), or heavy (1 ng/mL ≤ serum cotinine level ≤ 10 ng/mL).
TAKEAWAY:
In all, 919 (20%) participants had severe headaches or migraines.
After adjustment for demographic and lifestyle factors (including medication use), heavy SHS exposure was positively associated with severe headache or migraine (adjusted odds ratio [aOR], 2.02; 95% CI, 1.19-3.43).
No significant association was found between low SHS exposure and severe headaches or migraine (aOR, 1.15; 95% CI, 0.91-1.47).
In participants who were sedentary (P=.016) and those with a BMI <25 (P=.001), significant associations between SHS and severe headache or migraine were observed.
IN PRACTICE:
Noting a linear dose-response relationship between cotinine and severe headaches or migraine, the investigators write, “These findings underscore the need for stronger regulation of tobacco exposure, particularly in homes and public places.”
SOURCE:
Junpeng Wu, MMc, and Haitang Wang, MD, of Southern Medical University in Guangzhou, China, and their colleagues conducted the study. It was published online in Headache.
LIMITATIONS:
The study could not establish causal relationships between SHS and migraine or severe headache. In addition, the half-life of serum cotinine is 15-40 hours and thus this measure can reflect only recent SHS exposure.
DISCLOSURES:
The study was not funded. The investigators reported no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
, with effects of exposure varying depending on body mass index (BMI) and level of physical activity, new research shows.
METHODOLOGY:
Investigators analyzed data on 4,560 participants (median age, 43 years; 60% female; 71.5% White) from the 1999-2004 National Health and Nutrition Examination Survey.
Participants were aged 20 years or older and had never smoked.
Migraine headache status was determined by asking whether participants experienced severe headaches or migraines during the previous 3 months.
SHS exposure was categorized as unexposed (serum cotinine levels <0.05 ng/mL and no smoker in the home), low (0.05 ng/mL ≤ serum cotinine level <1 ng/mL), or heavy (1 ng/mL ≤ serum cotinine level ≤ 10 ng/mL).
TAKEAWAY:
In all, 919 (20%) participants had severe headaches or migraines.
After adjustment for demographic and lifestyle factors (including medication use), heavy SHS exposure was positively associated with severe headache or migraine (adjusted odds ratio [aOR], 2.02; 95% CI, 1.19-3.43).
No significant association was found between low SHS exposure and severe headaches or migraine (aOR, 1.15; 95% CI, 0.91-1.47).
In participants who were sedentary (P=.016) and those with a BMI <25 (P=.001), significant associations between SHS and severe headache or migraine were observed.
IN PRACTICE:
Noting a linear dose-response relationship between cotinine and severe headaches or migraine, the investigators write, “These findings underscore the need for stronger regulation of tobacco exposure, particularly in homes and public places.”
SOURCE:
Junpeng Wu, MMc, and Haitang Wang, MD, of Southern Medical University in Guangzhou, China, and their colleagues conducted the study. It was published online in Headache.
LIMITATIONS:
The study could not establish causal relationships between SHS and migraine or severe headache. In addition, the half-life of serum cotinine is 15-40 hours and thus this measure can reflect only recent SHS exposure.
DISCLOSURES:
The study was not funded. The investigators reported no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
, with effects of exposure varying depending on body mass index (BMI) and level of physical activity, new research shows.
METHODOLOGY:
Investigators analyzed data on 4,560 participants (median age, 43 years; 60% female; 71.5% White) from the 1999-2004 National Health and Nutrition Examination Survey.
Participants were aged 20 years or older and had never smoked.
Migraine headache status was determined by asking whether participants experienced severe headaches or migraines during the previous 3 months.
SHS exposure was categorized as unexposed (serum cotinine levels <0.05 ng/mL and no smoker in the home), low (0.05 ng/mL ≤ serum cotinine level <1 ng/mL), or heavy (1 ng/mL ≤ serum cotinine level ≤ 10 ng/mL).
TAKEAWAY:
In all, 919 (20%) participants had severe headaches or migraines.
After adjustment for demographic and lifestyle factors (including medication use), heavy SHS exposure was positively associated with severe headache or migraine (adjusted odds ratio [aOR], 2.02; 95% CI, 1.19-3.43).
No significant association was found between low SHS exposure and severe headaches or migraine (aOR, 1.15; 95% CI, 0.91-1.47).
In participants who were sedentary (P=.016) and those with a BMI <25 (P=.001), significant associations between SHS and severe headache or migraine were observed.
IN PRACTICE:
Noting a linear dose-response relationship between cotinine and severe headaches or migraine, the investigators write, “These findings underscore the need for stronger regulation of tobacco exposure, particularly in homes and public places.”
SOURCE:
Junpeng Wu, MMc, and Haitang Wang, MD, of Southern Medical University in Guangzhou, China, and their colleagues conducted the study. It was published online in Headache.
LIMITATIONS:
The study could not establish causal relationships between SHS and migraine or severe headache. In addition, the half-life of serum cotinine is 15-40 hours and thus this measure can reflect only recent SHS exposure.
DISCLOSURES:
The study was not funded. The investigators reported no disclosures.
A version of this article appeared on Medscape.com.
Autoimmune Skin Diseases Linked To Risk Of Adverse Pregnancy Outcomes
SAN DIEGO — , results from a large case-control study suggest.
Patients with systemic autoimmune conditions are known to have an increased risk for adverse pregnancy outcomes, “but we weren’t sure if that was the case for patients with autoimmune skin conditions,” presenting study author Heejo Keum, a fourth-year medical student at the University of Texas Southwestern Medical Center, Dallas, said in an interview during a poster session at the American College of Rheumatology (ACR) 2023 annual meeting. “There are case reports or nationwide population-based studies on patients with alopecia areata and vitiligo, but those were outside of the US, so we wanted to see if these outcomes could be studied in a larger population-based study in the US.”
Drawing from the TriNetX US Collaborative Network, a database of electronic medical records of 94 million patients in the United States, the researchers identified pregnant patients aged 15-44 years between January 1, 2016, and December 31, 2021. Cases were defined as patients diagnosed with at least one autoimmune skin disease (ASD) prior to the end of pregnancy, including alopecia areata, bullous pemphigoid, cicatricial pemphigoid, dermatitis herpetiformis, cutaneous lupus erythematosus, epidermolysis bullosa acquisita, morphea, pemphigus foliaceus, pemphigus vulgaris, vitiligo, and amyopathic DM. There were two control groups: healthy controls (those without ASDs, systemic lupus erythematosus or rheumatoid arthritis) and disease controls (those with SLE or RA). The researchers used ICD-10 codes to identify pregnancy endpoints, including live births, spontaneous abortion, and stillbirth. Patients with a history of hidradenitis suppurative were excluded from the analysis, as were those with common autoimmune disease such as Hashimoto’s thyroiditis, Grave’s disease, and type 1 diabetes.
The primary outcomes were adverse pregnancy outcomes defined as spontaneous abortion, gestational hypertension, preeclampsia/eclampsia, gestational diabetes, intrauterine growth restriction (IUGR), preterm premature rupture of membranes (PPROM), and preterm birth. The researchers used 1:1 propensity scoring to match patients with ASDs to controls by age, race, ethnicity, comorbidities, obesity, and substance use, and used odds ratio (OR) analysis with a 95% confidence interval (CI) to calculate each outcome.
Ms. Keum reported results from 3,654 women with ASDs, 3,654 healthy controls, 2,147 women with SLE, and 889 women with RA.
The three most common ASDs were vitiligo (30%), alopecia areata (30%), and cutaneous lupus erythematosus (27%). Compared with healthy controls, patients with ASDs were more likely to have spontaneous abortions (OR=1.5 [1.4-1.7], P<.001), and preeclampsia/eclampsia (OR=1.2 [1.0-1.3], P=.04). Compared with women with SLE, women with ASDs were less likely to have preeclampsia/eclampsia (OR=0.7 [0.6-0.9, P=.001); preterm birth (OR= 0.5 [0.4-0.7], P<.001); PPROM (OR=0.6 [0.4-0.9], P=.004), or an infant with IUGR (OR=0.6 [0.5-0.8], P<.001), but they were more likely to have a spontaneous abortion (OR=1.2 [1.1-1.3], P=.003). Overall, patients with ASDs had similar risks for adverse pregnancy outcomes as patients with RA.
“We found that patients with cutaneous lupus and vitiligo had higher rates of spontaneous abortion, which is interesting because we didn’t expect that,” Ms. Keum told this news organization. “Studies have shown that vitiligo patients might have an increased risk of pregnancy loss, so I think it’s important to have that discussion with those patients. It might benefit them to talk to a maternal-fetal medicine specialist. As for next steps, we want to look at how medication use and disease flare or disease severity play a role in APOs.”
In their poster, the researchers acknowledged limitations of the study, including the inability to verify diagnoses or assess disease severity. Also, while medication use and concomitant antiphospholipid syndrome were evaluated as risk factors for advanced pregnancy outcomes, the number of patients per group was too small for analysis.
Karl Saardi, MD, director of the inpatient dermatology service at George Washington University Hospital, Washington, who was asked to comment on the study, said that in his view, the choice of disease states included in the analysis “is a bit arbitrary.” He added that “it would have been more helpful to compare controls versus discoid lupus versus systemic lupus or controls versus amyopathic dermatomyositis versus dermatomyositis with myopathy.”
The study received funding support from the Rheumatology Research Foundation and the UT Southwestern Dean’s Research Scholar program. Neither Ms. Keum nor Dr. Saardi reported having relevant disclosures.
SAN DIEGO — , results from a large case-control study suggest.
Patients with systemic autoimmune conditions are known to have an increased risk for adverse pregnancy outcomes, “but we weren’t sure if that was the case for patients with autoimmune skin conditions,” presenting study author Heejo Keum, a fourth-year medical student at the University of Texas Southwestern Medical Center, Dallas, said in an interview during a poster session at the American College of Rheumatology (ACR) 2023 annual meeting. “There are case reports or nationwide population-based studies on patients with alopecia areata and vitiligo, but those were outside of the US, so we wanted to see if these outcomes could be studied in a larger population-based study in the US.”
Drawing from the TriNetX US Collaborative Network, a database of electronic medical records of 94 million patients in the United States, the researchers identified pregnant patients aged 15-44 years between January 1, 2016, and December 31, 2021. Cases were defined as patients diagnosed with at least one autoimmune skin disease (ASD) prior to the end of pregnancy, including alopecia areata, bullous pemphigoid, cicatricial pemphigoid, dermatitis herpetiformis, cutaneous lupus erythematosus, epidermolysis bullosa acquisita, morphea, pemphigus foliaceus, pemphigus vulgaris, vitiligo, and amyopathic DM. There were two control groups: healthy controls (those without ASDs, systemic lupus erythematosus or rheumatoid arthritis) and disease controls (those with SLE or RA). The researchers used ICD-10 codes to identify pregnancy endpoints, including live births, spontaneous abortion, and stillbirth. Patients with a history of hidradenitis suppurative were excluded from the analysis, as were those with common autoimmune disease such as Hashimoto’s thyroiditis, Grave’s disease, and type 1 diabetes.
The primary outcomes were adverse pregnancy outcomes defined as spontaneous abortion, gestational hypertension, preeclampsia/eclampsia, gestational diabetes, intrauterine growth restriction (IUGR), preterm premature rupture of membranes (PPROM), and preterm birth. The researchers used 1:1 propensity scoring to match patients with ASDs to controls by age, race, ethnicity, comorbidities, obesity, and substance use, and used odds ratio (OR) analysis with a 95% confidence interval (CI) to calculate each outcome.
Ms. Keum reported results from 3,654 women with ASDs, 3,654 healthy controls, 2,147 women with SLE, and 889 women with RA.
The three most common ASDs were vitiligo (30%), alopecia areata (30%), and cutaneous lupus erythematosus (27%). Compared with healthy controls, patients with ASDs were more likely to have spontaneous abortions (OR=1.5 [1.4-1.7], P<.001), and preeclampsia/eclampsia (OR=1.2 [1.0-1.3], P=.04). Compared with women with SLE, women with ASDs were less likely to have preeclampsia/eclampsia (OR=0.7 [0.6-0.9, P=.001); preterm birth (OR= 0.5 [0.4-0.7], P<.001); PPROM (OR=0.6 [0.4-0.9], P=.004), or an infant with IUGR (OR=0.6 [0.5-0.8], P<.001), but they were more likely to have a spontaneous abortion (OR=1.2 [1.1-1.3], P=.003). Overall, patients with ASDs had similar risks for adverse pregnancy outcomes as patients with RA.
“We found that patients with cutaneous lupus and vitiligo had higher rates of spontaneous abortion, which is interesting because we didn’t expect that,” Ms. Keum told this news organization. “Studies have shown that vitiligo patients might have an increased risk of pregnancy loss, so I think it’s important to have that discussion with those patients. It might benefit them to talk to a maternal-fetal medicine specialist. As for next steps, we want to look at how medication use and disease flare or disease severity play a role in APOs.”
In their poster, the researchers acknowledged limitations of the study, including the inability to verify diagnoses or assess disease severity. Also, while medication use and concomitant antiphospholipid syndrome were evaluated as risk factors for advanced pregnancy outcomes, the number of patients per group was too small for analysis.
Karl Saardi, MD, director of the inpatient dermatology service at George Washington University Hospital, Washington, who was asked to comment on the study, said that in his view, the choice of disease states included in the analysis “is a bit arbitrary.” He added that “it would have been more helpful to compare controls versus discoid lupus versus systemic lupus or controls versus amyopathic dermatomyositis versus dermatomyositis with myopathy.”
The study received funding support from the Rheumatology Research Foundation and the UT Southwestern Dean’s Research Scholar program. Neither Ms. Keum nor Dr. Saardi reported having relevant disclosures.
SAN DIEGO — , results from a large case-control study suggest.
Patients with systemic autoimmune conditions are known to have an increased risk for adverse pregnancy outcomes, “but we weren’t sure if that was the case for patients with autoimmune skin conditions,” presenting study author Heejo Keum, a fourth-year medical student at the University of Texas Southwestern Medical Center, Dallas, said in an interview during a poster session at the American College of Rheumatology (ACR) 2023 annual meeting. “There are case reports or nationwide population-based studies on patients with alopecia areata and vitiligo, but those were outside of the US, so we wanted to see if these outcomes could be studied in a larger population-based study in the US.”
Drawing from the TriNetX US Collaborative Network, a database of electronic medical records of 94 million patients in the United States, the researchers identified pregnant patients aged 15-44 years between January 1, 2016, and December 31, 2021. Cases were defined as patients diagnosed with at least one autoimmune skin disease (ASD) prior to the end of pregnancy, including alopecia areata, bullous pemphigoid, cicatricial pemphigoid, dermatitis herpetiformis, cutaneous lupus erythematosus, epidermolysis bullosa acquisita, morphea, pemphigus foliaceus, pemphigus vulgaris, vitiligo, and amyopathic DM. There were two control groups: healthy controls (those without ASDs, systemic lupus erythematosus or rheumatoid arthritis) and disease controls (those with SLE or RA). The researchers used ICD-10 codes to identify pregnancy endpoints, including live births, spontaneous abortion, and stillbirth. Patients with a history of hidradenitis suppurative were excluded from the analysis, as were those with common autoimmune disease such as Hashimoto’s thyroiditis, Grave’s disease, and type 1 diabetes.
The primary outcomes were adverse pregnancy outcomes defined as spontaneous abortion, gestational hypertension, preeclampsia/eclampsia, gestational diabetes, intrauterine growth restriction (IUGR), preterm premature rupture of membranes (PPROM), and preterm birth. The researchers used 1:1 propensity scoring to match patients with ASDs to controls by age, race, ethnicity, comorbidities, obesity, and substance use, and used odds ratio (OR) analysis with a 95% confidence interval (CI) to calculate each outcome.
Ms. Keum reported results from 3,654 women with ASDs, 3,654 healthy controls, 2,147 women with SLE, and 889 women with RA.
The three most common ASDs were vitiligo (30%), alopecia areata (30%), and cutaneous lupus erythematosus (27%). Compared with healthy controls, patients with ASDs were more likely to have spontaneous abortions (OR=1.5 [1.4-1.7], P<.001), and preeclampsia/eclampsia (OR=1.2 [1.0-1.3], P=.04). Compared with women with SLE, women with ASDs were less likely to have preeclampsia/eclampsia (OR=0.7 [0.6-0.9, P=.001); preterm birth (OR= 0.5 [0.4-0.7], P<.001); PPROM (OR=0.6 [0.4-0.9], P=.004), or an infant with IUGR (OR=0.6 [0.5-0.8], P<.001), but they were more likely to have a spontaneous abortion (OR=1.2 [1.1-1.3], P=.003). Overall, patients with ASDs had similar risks for adverse pregnancy outcomes as patients with RA.
“We found that patients with cutaneous lupus and vitiligo had higher rates of spontaneous abortion, which is interesting because we didn’t expect that,” Ms. Keum told this news organization. “Studies have shown that vitiligo patients might have an increased risk of pregnancy loss, so I think it’s important to have that discussion with those patients. It might benefit them to talk to a maternal-fetal medicine specialist. As for next steps, we want to look at how medication use and disease flare or disease severity play a role in APOs.”
In their poster, the researchers acknowledged limitations of the study, including the inability to verify diagnoses or assess disease severity. Also, while medication use and concomitant antiphospholipid syndrome were evaluated as risk factors for advanced pregnancy outcomes, the number of patients per group was too small for analysis.
Karl Saardi, MD, director of the inpatient dermatology service at George Washington University Hospital, Washington, who was asked to comment on the study, said that in his view, the choice of disease states included in the analysis “is a bit arbitrary.” He added that “it would have been more helpful to compare controls versus discoid lupus versus systemic lupus or controls versus amyopathic dermatomyositis versus dermatomyositis with myopathy.”
The study received funding support from the Rheumatology Research Foundation and the UT Southwestern Dean’s Research Scholar program. Neither Ms. Keum nor Dr. Saardi reported having relevant disclosures.
FROM ACR 2023
Optimizing Care in Metastatic Breast Cancer
AHA, AAP update neonatal resuscitation guidelines
The 2023 focused update was prompted by four systematic literature reviews by the International Liaison Committee on Resuscitation (ILCOR) Neonatal Life Support Task Force.
“Evidence evaluations by the ILCOR play a large role in the group’s process and timing of updates,” Henry Lee, MD, co-chair of the writing group, said in an interview.
He noted that updated recommendations do not change prior recommendations from the 2020 guidelines.
“However, they provide additional details to consider in neonatal resuscitation that could lead to changes in some practice in various settings,” said Dr. Lee, medical director of the University of California San Diego neonatal intensive care unit.
The focused update was simultaneously published online November 16 in Circulation and in Pediatrics.
Dr. Lee noted that effective positive-pressure ventilation (PPV) is the priority in newborn infants who need support after birth.
And while the 2020 update provided some details on devices to be used for PPV, the 2023 focused update gives guidance on use of T-piece resuscitators for providing PPV, which may be particularly helpful for preterm infants, and the use of supraglottic airways as a primary interface to deliver PPV, he explained.
Specifically, the updated guidelines state that use of a T-piece resuscitator to deliver PPV is preferred to the use of a self-inflating bag.
Because both T-piece resuscitators and flow-inflating bags require a compressed gas source to function, a self-inflating bag should be available as a backup in the event of compressed gas failure when using either of these devices.
Use of a supraglottic airway may be considered as the primary interface to administer PPV instead of a face mask for newborn infants delivered at 34 0/7 weeks’ gestation or later.
Continued Emphasis on Delayed Cord Clamping
The updated guidelines “continue to emphasize delayed cord clamping for both term and preterm newborn infants when clinically possible. There is also a new recommendation for nonvigorous infants born 35-42 weeks’ gestational age to consider umbilical cord milking,” Dr. Lee said in an interview.
Specifically, the guidelines state:
- For term and late preterm newborn infants ≥34 weeks’ gestation, and preterm newborn infants <34 weeks’ gestation, who do not require resuscitation, delayed cord clamping (≥30 seconds) can be beneficial compared with early cord clamping (<30 seconds).
- For term and late preterm newborn infants ≥34 weeks’ gestation who do not require resuscitation, intact cord milking is not known to be beneficial compared with delayed cord clamping (≥30 seconds).
- For preterm newborn infants between 28- and 34-weeks’ gestation who do not require resuscitation and in whom delayed cord clamping cannot be performed, intact cord milking may be reasonable.
- For preterm newborn infants <28 weeks’ gestation, intact cord milking is not recommended.
- For nonvigorous term and late preterm infants (35-42 weeks’ gestation), intact cord milking may be reasonable compared with early cord clamping (<30 seconds).
The guidelines also highlight the following knowledge gaps that require further research:
- Optimal management of the umbilical cord in term, late preterm, and preterm infants who require resuscitation at delivery
- Longer-term outcome data, such as anemia during infancy and neurodevelopmental outcomes, for all umbilical cord management strategies
- Cost-effectiveness of a T-piece resuscitator compared with a self-inflating bag
- The effect of a self-inflating bag with a positive end-expiratory pressure valve on outcomes in preterm newborn infants
- Comparison of either a T-piece resuscitator or a self-inflating bag with a flow-inflating bag for administering PPV
- Comparison of clinical outcomes by gestational age for any PPV device
- Comparison of supraglottic airway devices and face masks as the primary interface for PPV in high-resourced settings
- The amount and type of training required for successful supraglottic airway insertion and the potential for skill decay
- The utility of supraglottic airway devices for suctioning secretions from the airway
- The efficacy of a supraglottic airway during advanced neonatal resuscitation requiring chest compressions or the delivery of intratracheal medications
This research had no commercial funding. The authors report no relevant financial relationships.
A version of this article appeared on Medscape.com.
The 2023 focused update was prompted by four systematic literature reviews by the International Liaison Committee on Resuscitation (ILCOR) Neonatal Life Support Task Force.
“Evidence evaluations by the ILCOR play a large role in the group’s process and timing of updates,” Henry Lee, MD, co-chair of the writing group, said in an interview.
He noted that updated recommendations do not change prior recommendations from the 2020 guidelines.
“However, they provide additional details to consider in neonatal resuscitation that could lead to changes in some practice in various settings,” said Dr. Lee, medical director of the University of California San Diego neonatal intensive care unit.
The focused update was simultaneously published online November 16 in Circulation and in Pediatrics.
Dr. Lee noted that effective positive-pressure ventilation (PPV) is the priority in newborn infants who need support after birth.
And while the 2020 update provided some details on devices to be used for PPV, the 2023 focused update gives guidance on use of T-piece resuscitators for providing PPV, which may be particularly helpful for preterm infants, and the use of supraglottic airways as a primary interface to deliver PPV, he explained.
Specifically, the updated guidelines state that use of a T-piece resuscitator to deliver PPV is preferred to the use of a self-inflating bag.
Because both T-piece resuscitators and flow-inflating bags require a compressed gas source to function, a self-inflating bag should be available as a backup in the event of compressed gas failure when using either of these devices.
Use of a supraglottic airway may be considered as the primary interface to administer PPV instead of a face mask for newborn infants delivered at 34 0/7 weeks’ gestation or later.
Continued Emphasis on Delayed Cord Clamping
The updated guidelines “continue to emphasize delayed cord clamping for both term and preterm newborn infants when clinically possible. There is also a new recommendation for nonvigorous infants born 35-42 weeks’ gestational age to consider umbilical cord milking,” Dr. Lee said in an interview.
Specifically, the guidelines state:
- For term and late preterm newborn infants ≥34 weeks’ gestation, and preterm newborn infants <34 weeks’ gestation, who do not require resuscitation, delayed cord clamping (≥30 seconds) can be beneficial compared with early cord clamping (<30 seconds).
- For term and late preterm newborn infants ≥34 weeks’ gestation who do not require resuscitation, intact cord milking is not known to be beneficial compared with delayed cord clamping (≥30 seconds).
- For preterm newborn infants between 28- and 34-weeks’ gestation who do not require resuscitation and in whom delayed cord clamping cannot be performed, intact cord milking may be reasonable.
- For preterm newborn infants <28 weeks’ gestation, intact cord milking is not recommended.
- For nonvigorous term and late preterm infants (35-42 weeks’ gestation), intact cord milking may be reasonable compared with early cord clamping (<30 seconds).
The guidelines also highlight the following knowledge gaps that require further research:
- Optimal management of the umbilical cord in term, late preterm, and preterm infants who require resuscitation at delivery
- Longer-term outcome data, such as anemia during infancy and neurodevelopmental outcomes, for all umbilical cord management strategies
- Cost-effectiveness of a T-piece resuscitator compared with a self-inflating bag
- The effect of a self-inflating bag with a positive end-expiratory pressure valve on outcomes in preterm newborn infants
- Comparison of either a T-piece resuscitator or a self-inflating bag with a flow-inflating bag for administering PPV
- Comparison of clinical outcomes by gestational age for any PPV device
- Comparison of supraglottic airway devices and face masks as the primary interface for PPV in high-resourced settings
- The amount and type of training required for successful supraglottic airway insertion and the potential for skill decay
- The utility of supraglottic airway devices for suctioning secretions from the airway
- The efficacy of a supraglottic airway during advanced neonatal resuscitation requiring chest compressions or the delivery of intratracheal medications
This research had no commercial funding. The authors report no relevant financial relationships.
A version of this article appeared on Medscape.com.
The 2023 focused update was prompted by four systematic literature reviews by the International Liaison Committee on Resuscitation (ILCOR) Neonatal Life Support Task Force.
“Evidence evaluations by the ILCOR play a large role in the group’s process and timing of updates,” Henry Lee, MD, co-chair of the writing group, said in an interview.
He noted that updated recommendations do not change prior recommendations from the 2020 guidelines.
“However, they provide additional details to consider in neonatal resuscitation that could lead to changes in some practice in various settings,” said Dr. Lee, medical director of the University of California San Diego neonatal intensive care unit.
The focused update was simultaneously published online November 16 in Circulation and in Pediatrics.
Dr. Lee noted that effective positive-pressure ventilation (PPV) is the priority in newborn infants who need support after birth.
And while the 2020 update provided some details on devices to be used for PPV, the 2023 focused update gives guidance on use of T-piece resuscitators for providing PPV, which may be particularly helpful for preterm infants, and the use of supraglottic airways as a primary interface to deliver PPV, he explained.
Specifically, the updated guidelines state that use of a T-piece resuscitator to deliver PPV is preferred to the use of a self-inflating bag.
Because both T-piece resuscitators and flow-inflating bags require a compressed gas source to function, a self-inflating bag should be available as a backup in the event of compressed gas failure when using either of these devices.
Use of a supraglottic airway may be considered as the primary interface to administer PPV instead of a face mask for newborn infants delivered at 34 0/7 weeks’ gestation or later.
Continued Emphasis on Delayed Cord Clamping
The updated guidelines “continue to emphasize delayed cord clamping for both term and preterm newborn infants when clinically possible. There is also a new recommendation for nonvigorous infants born 35-42 weeks’ gestational age to consider umbilical cord milking,” Dr. Lee said in an interview.
Specifically, the guidelines state:
- For term and late preterm newborn infants ≥34 weeks’ gestation, and preterm newborn infants <34 weeks’ gestation, who do not require resuscitation, delayed cord clamping (≥30 seconds) can be beneficial compared with early cord clamping (<30 seconds).
- For term and late preterm newborn infants ≥34 weeks’ gestation who do not require resuscitation, intact cord milking is not known to be beneficial compared with delayed cord clamping (≥30 seconds).
- For preterm newborn infants between 28- and 34-weeks’ gestation who do not require resuscitation and in whom delayed cord clamping cannot be performed, intact cord milking may be reasonable.
- For preterm newborn infants <28 weeks’ gestation, intact cord milking is not recommended.
- For nonvigorous term and late preterm infants (35-42 weeks’ gestation), intact cord milking may be reasonable compared with early cord clamping (<30 seconds).
The guidelines also highlight the following knowledge gaps that require further research:
- Optimal management of the umbilical cord in term, late preterm, and preterm infants who require resuscitation at delivery
- Longer-term outcome data, such as anemia during infancy and neurodevelopmental outcomes, for all umbilical cord management strategies
- Cost-effectiveness of a T-piece resuscitator compared with a self-inflating bag
- The effect of a self-inflating bag with a positive end-expiratory pressure valve on outcomes in preterm newborn infants
- Comparison of either a T-piece resuscitator or a self-inflating bag with a flow-inflating bag for administering PPV
- Comparison of clinical outcomes by gestational age for any PPV device
- Comparison of supraglottic airway devices and face masks as the primary interface for PPV in high-resourced settings
- The amount and type of training required for successful supraglottic airway insertion and the potential for skill decay
- The utility of supraglottic airway devices for suctioning secretions from the airway
- The efficacy of a supraglottic airway during advanced neonatal resuscitation requiring chest compressions or the delivery of intratracheal medications
This research had no commercial funding. The authors report no relevant financial relationships.
A version of this article appeared on Medscape.com.