User login
Personalized nutrition therapy promotes diabetes remission
LEIPZIG, GERMANY — For patients newly diagnosed with type 2 diabetes, nutrition therapy is highly effective at achieving remission. “The greater the reduction in body weight, the higher the chances that blood sugar levels will normalize,” Diana Rubin, MD, said at the fall press conference of the German Diabetes Society (DDG). Dr. Rubin is conference president and chief physician of the Center for Nutritional Medicine and Diabetology at Vivantes Humboldt Hospital and the Spandau Hospital, Berlin, Germany.
Because of the development of modern medicines, nutrition therapy has increasingly been pushed into the background over the past 50 years. However, nutrition therapy and weight reduction can effectively delay diabetes for years, said Dr. Rubin. The patients are healthy, without being healed.
Nevertheless, the remission is rarely permanent. Most of the patients develop type 2 diabetes again after 5 years.
Personalized Nutrition Therapy
It is not just developments in medicine that have pushed nutrition therapy into the background. Another contributing factor is that statutory health insurance companies do not cover personalized nutrition counseling as standard, said Dr. Rubin.
Modern research in nutrition therapy has shown that patients with diabetes should receive personalized treatment. However, this idea is not taken into consideration in current diabetes training programs, which are the only forms of nutrition therapy covered by statutory health insurance companies.
Instead, nutrition information is mostly conveyed through group training sessions. Individuals do not necessarily find each other again. What’s more, these sessions are seldom led by nutrition experts. “It is rarely helpful to use a ‘one size fits all’ approach, as is often the case with these group training sessions,” said Dr. Rubin.
The DiRECT study, in which patients reduced their weight by 15 kg and achieved remission rates of almost 90%, is an example of how nutrition therapy can be highly effective. This is especially true if the aims and methods are determined on an individual basis and if there is frequent contact with a therapist. German and international guidelines, including the DDG’s best practice guides from 2022, highlight the importance of personalized nutrition therapy.
Telemedicine Encourages Adherence
“It is very important to consider the current living situation of the person concerned,” said Dr. Rubin. “It is important to set small objectives that can also be implemented in everyday life.” This can only succeed with a professional face-to-face consultation. “Achieving this objective then also becomes realistic — i.e., losing 10% to 15% body weight and maintaining this loss,” she said. “Long-term monitoring is needed to maintain this weight.”
Weight reduction methods should generally be determined according to the preferences of the person concerned, since dietary habits and environments are personal. For example, reducing the intake of carbohydrates and fats, intermittent fasting, or using meal replacement drinks can all be considered.
New data also show that digital apps available on prescription (DiGA) can be helpful for support; this idea is reflected in the DDG’s nutrition best practice guides for patients with type 2 diabetes.
“Studies show that adherence is highly dependent on the amount of contact with therapists and the long-term nature of the treatment,” said Dr. Rubin. She referred to the need for long-term monitoring, during which the patient can be repeatedly reminded of the therapeutic objective. “In this respect, I see a lot of potential in digital apps, and also in telemedicine, to cater to the short-term contact with the person concerned.”
A 2015 meta-analysis of 92 studies revealed a significant reduction in A1c for patients with type 1 or type 2 diabetes when using telemedicine nutrition therapy. Dr. Rubin frequently prescribes DiGAs, which are approved for obesity, “simply because I can recognize it makes it easier for many patients to stick to their goals.”
Dr. Rubin also recommends connecting with sport groups and self-help groups. “Maintaining the weight is a long-term project.”
Abdominal Fat Decisive
Prediabetes is a precursor to type 2 diabetes and entails an increased risk of heart attack, kidney and eye diseases, and various kinds of cancer. To date, physicians have tried to delay the onset of type 2 diabetes by aiming to reduce the weight of patients with prediabetes. However, scientists at the German Center for Diabetes Research showed with the Prediabetes Lifestyle Intervention Study that abdominal fat plays an important role in the remission of prediabetes.
The 1-year program with a healthy diet and increased physical activity was followed by 1105 patients with prediabetes. When every subject lost at least 5% of their weight, it turned out that some achieved remission, and others did not.
People who achieved remission exhibited better insulin sensitivity and had lost more visceral abdominal fat. Visceral abdominal fat can influence insulin sensitivity, not least by an inflammatory reaction in the fatty tissue.
Reducing visceral abdominal fat is clearly crucially important in achieving prediabetes remission. Subjects who achieved remission in the study had a strongly reduced risk for type 2 diabetes for up to 2 years after the end of the program. They had improved kidney function, and their blood vessels were in better condition.
Waist Circumference
According to the new results, the chances of remission increase if body weight is reduced by 5% and waist circumference is reduced by around 4 cm in women and 7 cm in men.
“Based on the new data, remission should be the new therapeutic objective in people with prediabetes. This could potentially change clinical practice and minimize the complication rate for our patients, both male and female,” said author Reiner Jumpertz-von Schwartzenberg, MD, a researcher at the Tübingen University Hospital in Germany.
Prediabetes remission can be assumed if the fasting blood glucose falls below 100 mg/dL (5.6 mmol/L), the 2-hour glucose below 140 mg/dL (7.8 mmol/L), and the A1c value below 5.7%. From the new findings, it can be seen that the chances of remission increase the more the body weight decreases.
Dr. Jumpertz-von Schwartzenberg and his colleagues want to investigate whether this strategy is cost-effective so that the support of payers can also be ensured.
This article was translated from the Medscape German edition.
A version of this article appeared on Medscape.com.
LEIPZIG, GERMANY — For patients newly diagnosed with type 2 diabetes, nutrition therapy is highly effective at achieving remission. “The greater the reduction in body weight, the higher the chances that blood sugar levels will normalize,” Diana Rubin, MD, said at the fall press conference of the German Diabetes Society (DDG). Dr. Rubin is conference president and chief physician of the Center for Nutritional Medicine and Diabetology at Vivantes Humboldt Hospital and the Spandau Hospital, Berlin, Germany.
Because of the development of modern medicines, nutrition therapy has increasingly been pushed into the background over the past 50 years. However, nutrition therapy and weight reduction can effectively delay diabetes for years, said Dr. Rubin. The patients are healthy, without being healed.
Nevertheless, the remission is rarely permanent. Most of the patients develop type 2 diabetes again after 5 years.
Personalized Nutrition Therapy
It is not just developments in medicine that have pushed nutrition therapy into the background. Another contributing factor is that statutory health insurance companies do not cover personalized nutrition counseling as standard, said Dr. Rubin.
Modern research in nutrition therapy has shown that patients with diabetes should receive personalized treatment. However, this idea is not taken into consideration in current diabetes training programs, which are the only forms of nutrition therapy covered by statutory health insurance companies.
Instead, nutrition information is mostly conveyed through group training sessions. Individuals do not necessarily find each other again. What’s more, these sessions are seldom led by nutrition experts. “It is rarely helpful to use a ‘one size fits all’ approach, as is often the case with these group training sessions,” said Dr. Rubin.
The DiRECT study, in which patients reduced their weight by 15 kg and achieved remission rates of almost 90%, is an example of how nutrition therapy can be highly effective. This is especially true if the aims and methods are determined on an individual basis and if there is frequent contact with a therapist. German and international guidelines, including the DDG’s best practice guides from 2022, highlight the importance of personalized nutrition therapy.
Telemedicine Encourages Adherence
“It is very important to consider the current living situation of the person concerned,” said Dr. Rubin. “It is important to set small objectives that can also be implemented in everyday life.” This can only succeed with a professional face-to-face consultation. “Achieving this objective then also becomes realistic — i.e., losing 10% to 15% body weight and maintaining this loss,” she said. “Long-term monitoring is needed to maintain this weight.”
Weight reduction methods should generally be determined according to the preferences of the person concerned, since dietary habits and environments are personal. For example, reducing the intake of carbohydrates and fats, intermittent fasting, or using meal replacement drinks can all be considered.
New data also show that digital apps available on prescription (DiGA) can be helpful for support; this idea is reflected in the DDG’s nutrition best practice guides for patients with type 2 diabetes.
“Studies show that adherence is highly dependent on the amount of contact with therapists and the long-term nature of the treatment,” said Dr. Rubin. She referred to the need for long-term monitoring, during which the patient can be repeatedly reminded of the therapeutic objective. “In this respect, I see a lot of potential in digital apps, and also in telemedicine, to cater to the short-term contact with the person concerned.”
A 2015 meta-analysis of 92 studies revealed a significant reduction in A1c for patients with type 1 or type 2 diabetes when using telemedicine nutrition therapy. Dr. Rubin frequently prescribes DiGAs, which are approved for obesity, “simply because I can recognize it makes it easier for many patients to stick to their goals.”
Dr. Rubin also recommends connecting with sport groups and self-help groups. “Maintaining the weight is a long-term project.”
Abdominal Fat Decisive
Prediabetes is a precursor to type 2 diabetes and entails an increased risk of heart attack, kidney and eye diseases, and various kinds of cancer. To date, physicians have tried to delay the onset of type 2 diabetes by aiming to reduce the weight of patients with prediabetes. However, scientists at the German Center for Diabetes Research showed with the Prediabetes Lifestyle Intervention Study that abdominal fat plays an important role in the remission of prediabetes.
The 1-year program with a healthy diet and increased physical activity was followed by 1105 patients with prediabetes. When every subject lost at least 5% of their weight, it turned out that some achieved remission, and others did not.
People who achieved remission exhibited better insulin sensitivity and had lost more visceral abdominal fat. Visceral abdominal fat can influence insulin sensitivity, not least by an inflammatory reaction in the fatty tissue.
Reducing visceral abdominal fat is clearly crucially important in achieving prediabetes remission. Subjects who achieved remission in the study had a strongly reduced risk for type 2 diabetes for up to 2 years after the end of the program. They had improved kidney function, and their blood vessels were in better condition.
Waist Circumference
According to the new results, the chances of remission increase if body weight is reduced by 5% and waist circumference is reduced by around 4 cm in women and 7 cm in men.
“Based on the new data, remission should be the new therapeutic objective in people with prediabetes. This could potentially change clinical practice and minimize the complication rate for our patients, both male and female,” said author Reiner Jumpertz-von Schwartzenberg, MD, a researcher at the Tübingen University Hospital in Germany.
Prediabetes remission can be assumed if the fasting blood glucose falls below 100 mg/dL (5.6 mmol/L), the 2-hour glucose below 140 mg/dL (7.8 mmol/L), and the A1c value below 5.7%. From the new findings, it can be seen that the chances of remission increase the more the body weight decreases.
Dr. Jumpertz-von Schwartzenberg and his colleagues want to investigate whether this strategy is cost-effective so that the support of payers can also be ensured.
This article was translated from the Medscape German edition.
A version of this article appeared on Medscape.com.
LEIPZIG, GERMANY — For patients newly diagnosed with type 2 diabetes, nutrition therapy is highly effective at achieving remission. “The greater the reduction in body weight, the higher the chances that blood sugar levels will normalize,” Diana Rubin, MD, said at the fall press conference of the German Diabetes Society (DDG). Dr. Rubin is conference president and chief physician of the Center for Nutritional Medicine and Diabetology at Vivantes Humboldt Hospital and the Spandau Hospital, Berlin, Germany.
Because of the development of modern medicines, nutrition therapy has increasingly been pushed into the background over the past 50 years. However, nutrition therapy and weight reduction can effectively delay diabetes for years, said Dr. Rubin. The patients are healthy, without being healed.
Nevertheless, the remission is rarely permanent. Most of the patients develop type 2 diabetes again after 5 years.
Personalized Nutrition Therapy
It is not just developments in medicine that have pushed nutrition therapy into the background. Another contributing factor is that statutory health insurance companies do not cover personalized nutrition counseling as standard, said Dr. Rubin.
Modern research in nutrition therapy has shown that patients with diabetes should receive personalized treatment. However, this idea is not taken into consideration in current diabetes training programs, which are the only forms of nutrition therapy covered by statutory health insurance companies.
Instead, nutrition information is mostly conveyed through group training sessions. Individuals do not necessarily find each other again. What’s more, these sessions are seldom led by nutrition experts. “It is rarely helpful to use a ‘one size fits all’ approach, as is often the case with these group training sessions,” said Dr. Rubin.
The DiRECT study, in which patients reduced their weight by 15 kg and achieved remission rates of almost 90%, is an example of how nutrition therapy can be highly effective. This is especially true if the aims and methods are determined on an individual basis and if there is frequent contact with a therapist. German and international guidelines, including the DDG’s best practice guides from 2022, highlight the importance of personalized nutrition therapy.
Telemedicine Encourages Adherence
“It is very important to consider the current living situation of the person concerned,” said Dr. Rubin. “It is important to set small objectives that can also be implemented in everyday life.” This can only succeed with a professional face-to-face consultation. “Achieving this objective then also becomes realistic — i.e., losing 10% to 15% body weight and maintaining this loss,” she said. “Long-term monitoring is needed to maintain this weight.”
Weight reduction methods should generally be determined according to the preferences of the person concerned, since dietary habits and environments are personal. For example, reducing the intake of carbohydrates and fats, intermittent fasting, or using meal replacement drinks can all be considered.
New data also show that digital apps available on prescription (DiGA) can be helpful for support; this idea is reflected in the DDG’s nutrition best practice guides for patients with type 2 diabetes.
“Studies show that adherence is highly dependent on the amount of contact with therapists and the long-term nature of the treatment,” said Dr. Rubin. She referred to the need for long-term monitoring, during which the patient can be repeatedly reminded of the therapeutic objective. “In this respect, I see a lot of potential in digital apps, and also in telemedicine, to cater to the short-term contact with the person concerned.”
A 2015 meta-analysis of 92 studies revealed a significant reduction in A1c for patients with type 1 or type 2 diabetes when using telemedicine nutrition therapy. Dr. Rubin frequently prescribes DiGAs, which are approved for obesity, “simply because I can recognize it makes it easier for many patients to stick to their goals.”
Dr. Rubin also recommends connecting with sport groups and self-help groups. “Maintaining the weight is a long-term project.”
Abdominal Fat Decisive
Prediabetes is a precursor to type 2 diabetes and entails an increased risk of heart attack, kidney and eye diseases, and various kinds of cancer. To date, physicians have tried to delay the onset of type 2 diabetes by aiming to reduce the weight of patients with prediabetes. However, scientists at the German Center for Diabetes Research showed with the Prediabetes Lifestyle Intervention Study that abdominal fat plays an important role in the remission of prediabetes.
The 1-year program with a healthy diet and increased physical activity was followed by 1105 patients with prediabetes. When every subject lost at least 5% of their weight, it turned out that some achieved remission, and others did not.
People who achieved remission exhibited better insulin sensitivity and had lost more visceral abdominal fat. Visceral abdominal fat can influence insulin sensitivity, not least by an inflammatory reaction in the fatty tissue.
Reducing visceral abdominal fat is clearly crucially important in achieving prediabetes remission. Subjects who achieved remission in the study had a strongly reduced risk for type 2 diabetes for up to 2 years after the end of the program. They had improved kidney function, and their blood vessels were in better condition.
Waist Circumference
According to the new results, the chances of remission increase if body weight is reduced by 5% and waist circumference is reduced by around 4 cm in women and 7 cm in men.
“Based on the new data, remission should be the new therapeutic objective in people with prediabetes. This could potentially change clinical practice and minimize the complication rate for our patients, both male and female,” said author Reiner Jumpertz-von Schwartzenberg, MD, a researcher at the Tübingen University Hospital in Germany.
Prediabetes remission can be assumed if the fasting blood glucose falls below 100 mg/dL (5.6 mmol/L), the 2-hour glucose below 140 mg/dL (7.8 mmol/L), and the A1c value below 5.7%. From the new findings, it can be seen that the chances of remission increase the more the body weight decreases.
Dr. Jumpertz-von Schwartzenberg and his colleagues want to investigate whether this strategy is cost-effective so that the support of payers can also be ensured.
This article was translated from the Medscape German edition.
A version of this article appeared on Medscape.com.
Can AI enhance mental health treatment?
Three questions for clinicians
Artificial intelligence (AI) is already impacting the mental health care space, with several new tools available to both clinicians and patients. While this technology could be a game-changer amid a mental health crisis and clinician shortage, there are important ethical and efficacy concerns clinicians should be aware of.
Current use cases illustrate both the potential and risks of AI. On one hand, AI has the potential to improve patient care with tools that can support diagnoses and inform treatment decisions at scale. The UK’s National Health Service is using an AI-powered diagnostic tool to help clinicians diagnose mental health disorders and determine the severity of a patient’s needs. Other tools leverage AI to analyze a patient’s voice for signs of depression or anxiety.
On the other hand, there are serious potential risks involving privacy, bias, and misinformation. One chatbot tool designed to counsel patients through disordered eating was shut down after giving problematic weight-loss advice.
The number of AI tools in the healthcare space is expected to increase fivefold by 2035. Keeping up with these advances is just as important for clinicians as keeping up with the latest medication and treatment options. That means being aware of both the limitations and the potential of AI. Here are three questions clinicians can ask as they explore ways to integrate these tools into their practice while navigating the risks.
• How can AI augment, not replace, the work of my staff?
For example, documentation and the use of electronic health records have consistently been linked to clinician burnout. Using AI to cut down on documentation would leave clinicians with more time and energy to focus on patient care.
One study from the National Library of Medicine found that physicians who did not have enough time to complete documentation were nearly three times more likely to report burnout. In some cases, clinic schedules were deliberately shortened to allow time for documentation.
New tools are emerging that use audio recording, transcription services, and large language models to generate clinical summaries and other documentation support. Amazon and 3M have partnered to solve documentation challenges using AI. This is an area I’ll definitely be keeping an eye on as it develops.
• Do I have patient consent to use this tool?
Since most AI tools remain relatively new, there is a gap in the legal and regulatory framework needed to ensure patient privacy and data protection. Clinicians should draw on existing guardrails and best practices to protect patient privacy and prioritize informed consent. The bottom line: Patients need to know how their data will be used and agree to it.
In the example above regarding documentation, a clinician should obtain patient consent before using technology that records or transcribes sessions. This extends to disclosing the use of AI chat tools and other touch points that occur between sessions. One mental health nonprofit has come under fire for using ChatGPT to provide mental health counseling to thousands of patients who weren’t aware the responses were generated by AI.
Beyond disclosing the use of these tools, clinicians should sufficiently explain how they work to ensure patients understand what they’re consenting to. Some technology companies offer guidance on how informed consent applies to their products and even offer template consent forms to support clinicians. Ultimately, accountability for maintaining patient privacy rests with the clinician, not the company behind the AI tool.
• Where is there a risk of bias?
There has been much discussion around the issue of bias within large language models in particular, since these programs will inherit any bias from the data points or text used to train them. However, there is often little to no visibility into how these models are trained, the algorithms they rely on, and how efficacy is measured.
This is especially concerning within the mental health care space, where bias can contribute to lower-quality care based on a patient’s race, gender or other characteristics. One systemic review published in JAMA Network Open found that most of the AI models used for psychiatric diagnoses that have been studied had a high overall risk of bias — which can lead to outputs that are misleading or incorrect, which can be dangerous in the healthcare field.
It’s important to keep the risk of bias top-of-mind when exploring AI tools and consider whether a tool would pose any direct harm to patients. Clinicians should have active oversight with any use of AI and, ultimately, consider an AI tool’s outputs alongside their own insights, expertise, and instincts.
Clinicians have the power to shape AI’s impact
While there is plenty to be excited about as these new tools develop, clinicians should explore AI with an eye toward the risks as well as the rewards. Practitioners have a significant opportunity to help shape how this technology develops by making informed decisions about which products to invest in and holding tech companies accountable. By educating patients, prioritizing informed consent, and seeking ways to augment their work that ultimately improve quality and scale of care, clinicians can help ensure positive outcomes while minimizing unintended consequences.
Dr. Patel-Dunn is a psychiatrist and chief medical officer at Lifestance Health, Scottsdale, Ariz.
Three questions for clinicians
Three questions for clinicians
Artificial intelligence (AI) is already impacting the mental health care space, with several new tools available to both clinicians and patients. While this technology could be a game-changer amid a mental health crisis and clinician shortage, there are important ethical and efficacy concerns clinicians should be aware of.
Current use cases illustrate both the potential and risks of AI. On one hand, AI has the potential to improve patient care with tools that can support diagnoses and inform treatment decisions at scale. The UK’s National Health Service is using an AI-powered diagnostic tool to help clinicians diagnose mental health disorders and determine the severity of a patient’s needs. Other tools leverage AI to analyze a patient’s voice for signs of depression or anxiety.
On the other hand, there are serious potential risks involving privacy, bias, and misinformation. One chatbot tool designed to counsel patients through disordered eating was shut down after giving problematic weight-loss advice.
The number of AI tools in the healthcare space is expected to increase fivefold by 2035. Keeping up with these advances is just as important for clinicians as keeping up with the latest medication and treatment options. That means being aware of both the limitations and the potential of AI. Here are three questions clinicians can ask as they explore ways to integrate these tools into their practice while navigating the risks.
• How can AI augment, not replace, the work of my staff?
For example, documentation and the use of electronic health records have consistently been linked to clinician burnout. Using AI to cut down on documentation would leave clinicians with more time and energy to focus on patient care.
One study from the National Library of Medicine found that physicians who did not have enough time to complete documentation were nearly three times more likely to report burnout. In some cases, clinic schedules were deliberately shortened to allow time for documentation.
New tools are emerging that use audio recording, transcription services, and large language models to generate clinical summaries and other documentation support. Amazon and 3M have partnered to solve documentation challenges using AI. This is an area I’ll definitely be keeping an eye on as it develops.
• Do I have patient consent to use this tool?
Since most AI tools remain relatively new, there is a gap in the legal and regulatory framework needed to ensure patient privacy and data protection. Clinicians should draw on existing guardrails and best practices to protect patient privacy and prioritize informed consent. The bottom line: Patients need to know how their data will be used and agree to it.
In the example above regarding documentation, a clinician should obtain patient consent before using technology that records or transcribes sessions. This extends to disclosing the use of AI chat tools and other touch points that occur between sessions. One mental health nonprofit has come under fire for using ChatGPT to provide mental health counseling to thousands of patients who weren’t aware the responses were generated by AI.
Beyond disclosing the use of these tools, clinicians should sufficiently explain how they work to ensure patients understand what they’re consenting to. Some technology companies offer guidance on how informed consent applies to their products and even offer template consent forms to support clinicians. Ultimately, accountability for maintaining patient privacy rests with the clinician, not the company behind the AI tool.
• Where is there a risk of bias?
There has been much discussion around the issue of bias within large language models in particular, since these programs will inherit any bias from the data points or text used to train them. However, there is often little to no visibility into how these models are trained, the algorithms they rely on, and how efficacy is measured.
This is especially concerning within the mental health care space, where bias can contribute to lower-quality care based on a patient’s race, gender or other characteristics. One systemic review published in JAMA Network Open found that most of the AI models used for psychiatric diagnoses that have been studied had a high overall risk of bias — which can lead to outputs that are misleading or incorrect, which can be dangerous in the healthcare field.
It’s important to keep the risk of bias top-of-mind when exploring AI tools and consider whether a tool would pose any direct harm to patients. Clinicians should have active oversight with any use of AI and, ultimately, consider an AI tool’s outputs alongside their own insights, expertise, and instincts.
Clinicians have the power to shape AI’s impact
While there is plenty to be excited about as these new tools develop, clinicians should explore AI with an eye toward the risks as well as the rewards. Practitioners have a significant opportunity to help shape how this technology develops by making informed decisions about which products to invest in and holding tech companies accountable. By educating patients, prioritizing informed consent, and seeking ways to augment their work that ultimately improve quality and scale of care, clinicians can help ensure positive outcomes while minimizing unintended consequences.
Dr. Patel-Dunn is a psychiatrist and chief medical officer at Lifestance Health, Scottsdale, Ariz.
Artificial intelligence (AI) is already impacting the mental health care space, with several new tools available to both clinicians and patients. While this technology could be a game-changer amid a mental health crisis and clinician shortage, there are important ethical and efficacy concerns clinicians should be aware of.
Current use cases illustrate both the potential and risks of AI. On one hand, AI has the potential to improve patient care with tools that can support diagnoses and inform treatment decisions at scale. The UK’s National Health Service is using an AI-powered diagnostic tool to help clinicians diagnose mental health disorders and determine the severity of a patient’s needs. Other tools leverage AI to analyze a patient’s voice for signs of depression or anxiety.
On the other hand, there are serious potential risks involving privacy, bias, and misinformation. One chatbot tool designed to counsel patients through disordered eating was shut down after giving problematic weight-loss advice.
The number of AI tools in the healthcare space is expected to increase fivefold by 2035. Keeping up with these advances is just as important for clinicians as keeping up with the latest medication and treatment options. That means being aware of both the limitations and the potential of AI. Here are three questions clinicians can ask as they explore ways to integrate these tools into their practice while navigating the risks.
• How can AI augment, not replace, the work of my staff?
For example, documentation and the use of electronic health records have consistently been linked to clinician burnout. Using AI to cut down on documentation would leave clinicians with more time and energy to focus on patient care.
One study from the National Library of Medicine found that physicians who did not have enough time to complete documentation were nearly three times more likely to report burnout. In some cases, clinic schedules were deliberately shortened to allow time for documentation.
New tools are emerging that use audio recording, transcription services, and large language models to generate clinical summaries and other documentation support. Amazon and 3M have partnered to solve documentation challenges using AI. This is an area I’ll definitely be keeping an eye on as it develops.
• Do I have patient consent to use this tool?
Since most AI tools remain relatively new, there is a gap in the legal and regulatory framework needed to ensure patient privacy and data protection. Clinicians should draw on existing guardrails and best practices to protect patient privacy and prioritize informed consent. The bottom line: Patients need to know how their data will be used and agree to it.
In the example above regarding documentation, a clinician should obtain patient consent before using technology that records or transcribes sessions. This extends to disclosing the use of AI chat tools and other touch points that occur between sessions. One mental health nonprofit has come under fire for using ChatGPT to provide mental health counseling to thousands of patients who weren’t aware the responses were generated by AI.
Beyond disclosing the use of these tools, clinicians should sufficiently explain how they work to ensure patients understand what they’re consenting to. Some technology companies offer guidance on how informed consent applies to their products and even offer template consent forms to support clinicians. Ultimately, accountability for maintaining patient privacy rests with the clinician, not the company behind the AI tool.
• Where is there a risk of bias?
There has been much discussion around the issue of bias within large language models in particular, since these programs will inherit any bias from the data points or text used to train them. However, there is often little to no visibility into how these models are trained, the algorithms they rely on, and how efficacy is measured.
This is especially concerning within the mental health care space, where bias can contribute to lower-quality care based on a patient’s race, gender or other characteristics. One systemic review published in JAMA Network Open found that most of the AI models used for psychiatric diagnoses that have been studied had a high overall risk of bias — which can lead to outputs that are misleading or incorrect, which can be dangerous in the healthcare field.
It’s important to keep the risk of bias top-of-mind when exploring AI tools and consider whether a tool would pose any direct harm to patients. Clinicians should have active oversight with any use of AI and, ultimately, consider an AI tool’s outputs alongside their own insights, expertise, and instincts.
Clinicians have the power to shape AI’s impact
While there is plenty to be excited about as these new tools develop, clinicians should explore AI with an eye toward the risks as well as the rewards. Practitioners have a significant opportunity to help shape how this technology develops by making informed decisions about which products to invest in and holding tech companies accountable. By educating patients, prioritizing informed consent, and seeking ways to augment their work that ultimately improve quality and scale of care, clinicians can help ensure positive outcomes while minimizing unintended consequences.
Dr. Patel-Dunn is a psychiatrist and chief medical officer at Lifestance Health, Scottsdale, Ariz.
Relapsed DLBCL: With Complete Interim Response, SCT Outperforms CAR T
“In patients with relapsed DLBCL in a complete remission, treatment with auto-HCT is associated with a lower rate of relapse/progression, and a longer progression-free survival [versus CAR T therapy],” said first author Mazyar Shadman, MD, MPH, of the Division of Medical Oncology, University of Washington, Seattle.
“The data support utilization of auto-HCT in patients with relapsed LBCL achieving a complete response,” he said.
The findings were presented at the annual meeting of the American Society of Hematology in San Diego.
While approximately 60% of patients with DLBCL are successfully treated after an initial anthracycline-based and rituximab-containing chemotherapy regimen, those who do not improve have poorer outcomes, and CAR T-cell therapy has emerged as the standard of care for those patients, based on results from the ZUMA-7 and TRANSFORM clinical trials.
But with delays in accessing CAR T quite common, patients will often receive interim chemotherapy while awaiting referral to a CAR T center, and occasionally, usually unexpectedly, some will achieve a partial or complete response.
In previous research involving patients who achieved a partial remission in such interim cases, Dr. Shadman and colleagues demonstrated that auto-HCT had favorable outcomes, compared with those who received CAR T therapy.
For the new retrospective, real-world analysis, the authors compared outcomes with the treatment options among 360 patients between the ages of 18 and 75 who were enrolled in the Center for International Blood & Marrow Transplant Research registry and had received auto-HCT or CAR T therapy after achieving a complete remission following salvage chemotherapy.
Of those receiving CAR-T cell therapy, most (53.2%) received tisagenlecleucel (tisa-cel), followed by axicabtagene ciloleucel (axi-cel, 45.6%) and lisocabtagene maraleucel (liso-cel, 1.3%), between 2018 and 2021, while 281 patients were treated with auto-HCT between 2015 and 2021.
With a median follow-up of 49.7 months (range 3.0-94.4) for auto-HCT and 24.7 months (range 3.3-49.4) for CAR-T, a univariate analysis showed the rate of 2-year progression free survival was 66.2% in the auto-HCT group and 47.8% in the CAR T group (P < .001).
The results also favored auto-HCT for 2-year progression/relapse, with a cumulative incidence of 27.8% with auto-HCT versus 48% with CAR T (P < .001), and the 2-year overall survival was higher with auto-HCT (78.9% vs. 65.6%; P = .037).
After adjustment in multivariable analysis adjusting for relevant clinical variables, auto-HCT versus CAR T remained associated with a lower risk of relapse or progression (HR 2.18; P < .0001) and an improved progression-free survival (HR 1.83; P = .0011), with no significant differences in the risk of treatment-related mortality (HR 0.59; P = .36) or overall survival (HR 1.44; P = .12).
Deaths occurred among 85 patients in the auto-HCT group and 25 in the CAR T cohort, with lymphoma being the main cause of death in both groups (60% and 68%, respectively).
While 37 (13.2%) of auto-HCT patients later received subsequent CAR-T therapy, no patients receiving CAR-T had subsequent auto-HCT.
There were no differences between the CAR-T and auto-HST groups in rates of 2-year treatment-related mortality (4.1% vs. 5.9%; P = .673).
A subanalysis of those who had treatment failure at 12 months, (CAR-T = 57 and auto-HCT = 163) showed that those receiving CAR-T therapy had a higher 2-year relapse rate (46.3% vs. 25%; P < .001); an inferior 2-year progression-free survival rate (48.4% vs. 68.2%; P = .001) compared with auto-HCT, while there were no significant differences between the groups in terms of 2-year overall survival or treatment-related mortality.
After a multivariable analysis adjusting for relevant clinical factors, CAR-T therapy remained associated with higher risk of relapse (HR 2.18; P < .0001) and an inferior progression-free survival (HR 1.83; P = .0011) compared with auto-HCT, with no differences in the risk of treatment-related mortality (HR 0.59; P = .36) or overall survival (HR 1.44; P = .12).
“These results are consistent with our previously reported findings, indicating higher efficacy of auto-HCT compared with CAR T in patients with partial remission,” Dr. Shadman said.
In addition to the study’s being a retrospective analysis, limitations include that more than half of patients in the CAR T cohort received tisa-cel, which could have lower efficacy compared with other approved CAR T therapies, Dr. Shadman noted.
“A repeat analysis by including more patients treated with axi-cel or liso-cel may address this issue in the future,” he said.
Discussing the results in a press briefing, Dr. Shadman underscored that “there is no question the choice of therapy for these DLBCL patients with primary refractory disease should be second-line CAR T therapy — we are not suggesting that those patients should be sent for auto-HCT,” he said.
“What we are saying is, in real-world practice ... patients may need chemotherapy treatment in the interim (awaiting CAR T treatment), and we don’t expect these patients to respond to those cycles because they have already shown us that they don’t do well with chemotherapy — however some do respond and can go into complete remission.”
The question then becomes whether patients at that point will fare better with CAR T or auto-HCT, and the results indicate that “auto-HCT gives those patients a pretty solid remission that looks better than [that with] CAR T therapy.”
Dr. Shadman noted that the results serve to inform or confirm key clinical practices, including “in patients with late relapses, after 12 months, auto-HCT should remain the standard of care.
“In patients with primary refractory disease or early relapse, CAR T should be the goal of therapy and improving access to CAR T should remain a priority.
“In the subset of patients who achieve a CR with interim treatment, a discussion about the possibility of utilizing auto-HCT seems reasonable and can provide another curative option for some patients while keeping CAR-T as a backup treatment plan in case of auto-HCT failure.”
Commenting on the study, Jonathan W. Friedberg, MD, the Samuel Durand Professor of Medicine and director of the Wilmot Cancer Institute, University of Rochester, New York, said, “these findings confirm utility of auto-HCT in patients who achieve a CR.”
However, “the problem is that only a small fraction of patients achieve CR in this situation, and we do not know who they are going to be at time of relapse,” he told this news organization.
He agreed that “given robust randomized trials showing overall survival benefit of CAR-T compared to auto-HCT in patients with high risk relapsed DLBCL, CAR-T treatment should remain the current standard.
“However, these current results help to confirm the strategy for management of low- risk (late) relapses and indicate that auto-HCT still has a place for these patients if they achieve CR with salvage therapy.”
Dr. Shadman reported relationships with ADC therapeutics, Bristol Myers Squibb, Genmab, Lilly, Vincerx, Kite (Gilead), Janssen, Fate Therapeutics, MorphoSys/Incyte, AstraZeneca, BeiGene, Pharmacyclics, Mustang Bio, AbbVie, Genentech, MEI Pharma, Regeneron, and TG Therapeutics. Dr. Friedberg had no disclosures to report.
“In patients with relapsed DLBCL in a complete remission, treatment with auto-HCT is associated with a lower rate of relapse/progression, and a longer progression-free survival [versus CAR T therapy],” said first author Mazyar Shadman, MD, MPH, of the Division of Medical Oncology, University of Washington, Seattle.
“The data support utilization of auto-HCT in patients with relapsed LBCL achieving a complete response,” he said.
The findings were presented at the annual meeting of the American Society of Hematology in San Diego.
While approximately 60% of patients with DLBCL are successfully treated after an initial anthracycline-based and rituximab-containing chemotherapy regimen, those who do not improve have poorer outcomes, and CAR T-cell therapy has emerged as the standard of care for those patients, based on results from the ZUMA-7 and TRANSFORM clinical trials.
But with delays in accessing CAR T quite common, patients will often receive interim chemotherapy while awaiting referral to a CAR T center, and occasionally, usually unexpectedly, some will achieve a partial or complete response.
In previous research involving patients who achieved a partial remission in such interim cases, Dr. Shadman and colleagues demonstrated that auto-HCT had favorable outcomes, compared with those who received CAR T therapy.
For the new retrospective, real-world analysis, the authors compared outcomes with the treatment options among 360 patients between the ages of 18 and 75 who were enrolled in the Center for International Blood & Marrow Transplant Research registry and had received auto-HCT or CAR T therapy after achieving a complete remission following salvage chemotherapy.
Of those receiving CAR-T cell therapy, most (53.2%) received tisagenlecleucel (tisa-cel), followed by axicabtagene ciloleucel (axi-cel, 45.6%) and lisocabtagene maraleucel (liso-cel, 1.3%), between 2018 and 2021, while 281 patients were treated with auto-HCT between 2015 and 2021.
With a median follow-up of 49.7 months (range 3.0-94.4) for auto-HCT and 24.7 months (range 3.3-49.4) for CAR-T, a univariate analysis showed the rate of 2-year progression free survival was 66.2% in the auto-HCT group and 47.8% in the CAR T group (P < .001).
The results also favored auto-HCT for 2-year progression/relapse, with a cumulative incidence of 27.8% with auto-HCT versus 48% with CAR T (P < .001), and the 2-year overall survival was higher with auto-HCT (78.9% vs. 65.6%; P = .037).
After adjustment in multivariable analysis adjusting for relevant clinical variables, auto-HCT versus CAR T remained associated with a lower risk of relapse or progression (HR 2.18; P < .0001) and an improved progression-free survival (HR 1.83; P = .0011), with no significant differences in the risk of treatment-related mortality (HR 0.59; P = .36) or overall survival (HR 1.44; P = .12).
Deaths occurred among 85 patients in the auto-HCT group and 25 in the CAR T cohort, with lymphoma being the main cause of death in both groups (60% and 68%, respectively).
While 37 (13.2%) of auto-HCT patients later received subsequent CAR-T therapy, no patients receiving CAR-T had subsequent auto-HCT.
There were no differences between the CAR-T and auto-HST groups in rates of 2-year treatment-related mortality (4.1% vs. 5.9%; P = .673).
A subanalysis of those who had treatment failure at 12 months, (CAR-T = 57 and auto-HCT = 163) showed that those receiving CAR-T therapy had a higher 2-year relapse rate (46.3% vs. 25%; P < .001); an inferior 2-year progression-free survival rate (48.4% vs. 68.2%; P = .001) compared with auto-HCT, while there were no significant differences between the groups in terms of 2-year overall survival or treatment-related mortality.
After a multivariable analysis adjusting for relevant clinical factors, CAR-T therapy remained associated with higher risk of relapse (HR 2.18; P < .0001) and an inferior progression-free survival (HR 1.83; P = .0011) compared with auto-HCT, with no differences in the risk of treatment-related mortality (HR 0.59; P = .36) or overall survival (HR 1.44; P = .12).
“These results are consistent with our previously reported findings, indicating higher efficacy of auto-HCT compared with CAR T in patients with partial remission,” Dr. Shadman said.
In addition to the study’s being a retrospective analysis, limitations include that more than half of patients in the CAR T cohort received tisa-cel, which could have lower efficacy compared with other approved CAR T therapies, Dr. Shadman noted.
“A repeat analysis by including more patients treated with axi-cel or liso-cel may address this issue in the future,” he said.
Discussing the results in a press briefing, Dr. Shadman underscored that “there is no question the choice of therapy for these DLBCL patients with primary refractory disease should be second-line CAR T therapy — we are not suggesting that those patients should be sent for auto-HCT,” he said.
“What we are saying is, in real-world practice ... patients may need chemotherapy treatment in the interim (awaiting CAR T treatment), and we don’t expect these patients to respond to those cycles because they have already shown us that they don’t do well with chemotherapy — however some do respond and can go into complete remission.”
The question then becomes whether patients at that point will fare better with CAR T or auto-HCT, and the results indicate that “auto-HCT gives those patients a pretty solid remission that looks better than [that with] CAR T therapy.”
Dr. Shadman noted that the results serve to inform or confirm key clinical practices, including “in patients with late relapses, after 12 months, auto-HCT should remain the standard of care.
“In patients with primary refractory disease or early relapse, CAR T should be the goal of therapy and improving access to CAR T should remain a priority.
“In the subset of patients who achieve a CR with interim treatment, a discussion about the possibility of utilizing auto-HCT seems reasonable and can provide another curative option for some patients while keeping CAR-T as a backup treatment plan in case of auto-HCT failure.”
Commenting on the study, Jonathan W. Friedberg, MD, the Samuel Durand Professor of Medicine and director of the Wilmot Cancer Institute, University of Rochester, New York, said, “these findings confirm utility of auto-HCT in patients who achieve a CR.”
However, “the problem is that only a small fraction of patients achieve CR in this situation, and we do not know who they are going to be at time of relapse,” he told this news organization.
He agreed that “given robust randomized trials showing overall survival benefit of CAR-T compared to auto-HCT in patients with high risk relapsed DLBCL, CAR-T treatment should remain the current standard.
“However, these current results help to confirm the strategy for management of low- risk (late) relapses and indicate that auto-HCT still has a place for these patients if they achieve CR with salvage therapy.”
Dr. Shadman reported relationships with ADC therapeutics, Bristol Myers Squibb, Genmab, Lilly, Vincerx, Kite (Gilead), Janssen, Fate Therapeutics, MorphoSys/Incyte, AstraZeneca, BeiGene, Pharmacyclics, Mustang Bio, AbbVie, Genentech, MEI Pharma, Regeneron, and TG Therapeutics. Dr. Friedberg had no disclosures to report.
“In patients with relapsed DLBCL in a complete remission, treatment with auto-HCT is associated with a lower rate of relapse/progression, and a longer progression-free survival [versus CAR T therapy],” said first author Mazyar Shadman, MD, MPH, of the Division of Medical Oncology, University of Washington, Seattle.
“The data support utilization of auto-HCT in patients with relapsed LBCL achieving a complete response,” he said.
The findings were presented at the annual meeting of the American Society of Hematology in San Diego.
While approximately 60% of patients with DLBCL are successfully treated after an initial anthracycline-based and rituximab-containing chemotherapy regimen, those who do not improve have poorer outcomes, and CAR T-cell therapy has emerged as the standard of care for those patients, based on results from the ZUMA-7 and TRANSFORM clinical trials.
But with delays in accessing CAR T quite common, patients will often receive interim chemotherapy while awaiting referral to a CAR T center, and occasionally, usually unexpectedly, some will achieve a partial or complete response.
In previous research involving patients who achieved a partial remission in such interim cases, Dr. Shadman and colleagues demonstrated that auto-HCT had favorable outcomes, compared with those who received CAR T therapy.
For the new retrospective, real-world analysis, the authors compared outcomes with the treatment options among 360 patients between the ages of 18 and 75 who were enrolled in the Center for International Blood & Marrow Transplant Research registry and had received auto-HCT or CAR T therapy after achieving a complete remission following salvage chemotherapy.
Of those receiving CAR-T cell therapy, most (53.2%) received tisagenlecleucel (tisa-cel), followed by axicabtagene ciloleucel (axi-cel, 45.6%) and lisocabtagene maraleucel (liso-cel, 1.3%), between 2018 and 2021, while 281 patients were treated with auto-HCT between 2015 and 2021.
With a median follow-up of 49.7 months (range 3.0-94.4) for auto-HCT and 24.7 months (range 3.3-49.4) for CAR-T, a univariate analysis showed the rate of 2-year progression free survival was 66.2% in the auto-HCT group and 47.8% in the CAR T group (P < .001).
The results also favored auto-HCT for 2-year progression/relapse, with a cumulative incidence of 27.8% with auto-HCT versus 48% with CAR T (P < .001), and the 2-year overall survival was higher with auto-HCT (78.9% vs. 65.6%; P = .037).
After adjustment in multivariable analysis adjusting for relevant clinical variables, auto-HCT versus CAR T remained associated with a lower risk of relapse or progression (HR 2.18; P < .0001) and an improved progression-free survival (HR 1.83; P = .0011), with no significant differences in the risk of treatment-related mortality (HR 0.59; P = .36) or overall survival (HR 1.44; P = .12).
Deaths occurred among 85 patients in the auto-HCT group and 25 in the CAR T cohort, with lymphoma being the main cause of death in both groups (60% and 68%, respectively).
While 37 (13.2%) of auto-HCT patients later received subsequent CAR-T therapy, no patients receiving CAR-T had subsequent auto-HCT.
There were no differences between the CAR-T and auto-HST groups in rates of 2-year treatment-related mortality (4.1% vs. 5.9%; P = .673).
A subanalysis of those who had treatment failure at 12 months, (CAR-T = 57 and auto-HCT = 163) showed that those receiving CAR-T therapy had a higher 2-year relapse rate (46.3% vs. 25%; P < .001); an inferior 2-year progression-free survival rate (48.4% vs. 68.2%; P = .001) compared with auto-HCT, while there were no significant differences between the groups in terms of 2-year overall survival or treatment-related mortality.
After a multivariable analysis adjusting for relevant clinical factors, CAR-T therapy remained associated with higher risk of relapse (HR 2.18; P < .0001) and an inferior progression-free survival (HR 1.83; P = .0011) compared with auto-HCT, with no differences in the risk of treatment-related mortality (HR 0.59; P = .36) or overall survival (HR 1.44; P = .12).
“These results are consistent with our previously reported findings, indicating higher efficacy of auto-HCT compared with CAR T in patients with partial remission,” Dr. Shadman said.
In addition to the study’s being a retrospective analysis, limitations include that more than half of patients in the CAR T cohort received tisa-cel, which could have lower efficacy compared with other approved CAR T therapies, Dr. Shadman noted.
“A repeat analysis by including more patients treated with axi-cel or liso-cel may address this issue in the future,” he said.
Discussing the results in a press briefing, Dr. Shadman underscored that “there is no question the choice of therapy for these DLBCL patients with primary refractory disease should be second-line CAR T therapy — we are not suggesting that those patients should be sent for auto-HCT,” he said.
“What we are saying is, in real-world practice ... patients may need chemotherapy treatment in the interim (awaiting CAR T treatment), and we don’t expect these patients to respond to those cycles because they have already shown us that they don’t do well with chemotherapy — however some do respond and can go into complete remission.”
The question then becomes whether patients at that point will fare better with CAR T or auto-HCT, and the results indicate that “auto-HCT gives those patients a pretty solid remission that looks better than [that with] CAR T therapy.”
Dr. Shadman noted that the results serve to inform or confirm key clinical practices, including “in patients with late relapses, after 12 months, auto-HCT should remain the standard of care.
“In patients with primary refractory disease or early relapse, CAR T should be the goal of therapy and improving access to CAR T should remain a priority.
“In the subset of patients who achieve a CR with interim treatment, a discussion about the possibility of utilizing auto-HCT seems reasonable and can provide another curative option for some patients while keeping CAR-T as a backup treatment plan in case of auto-HCT failure.”
Commenting on the study, Jonathan W. Friedberg, MD, the Samuel Durand Professor of Medicine and director of the Wilmot Cancer Institute, University of Rochester, New York, said, “these findings confirm utility of auto-HCT in patients who achieve a CR.”
However, “the problem is that only a small fraction of patients achieve CR in this situation, and we do not know who they are going to be at time of relapse,” he told this news organization.
He agreed that “given robust randomized trials showing overall survival benefit of CAR-T compared to auto-HCT in patients with high risk relapsed DLBCL, CAR-T treatment should remain the current standard.
“However, these current results help to confirm the strategy for management of low- risk (late) relapses and indicate that auto-HCT still has a place for these patients if they achieve CR with salvage therapy.”
Dr. Shadman reported relationships with ADC therapeutics, Bristol Myers Squibb, Genmab, Lilly, Vincerx, Kite (Gilead), Janssen, Fate Therapeutics, MorphoSys/Incyte, AstraZeneca, BeiGene, Pharmacyclics, Mustang Bio, AbbVie, Genentech, MEI Pharma, Regeneron, and TG Therapeutics. Dr. Friedberg had no disclosures to report.
FROM ASH 2023
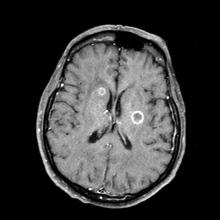
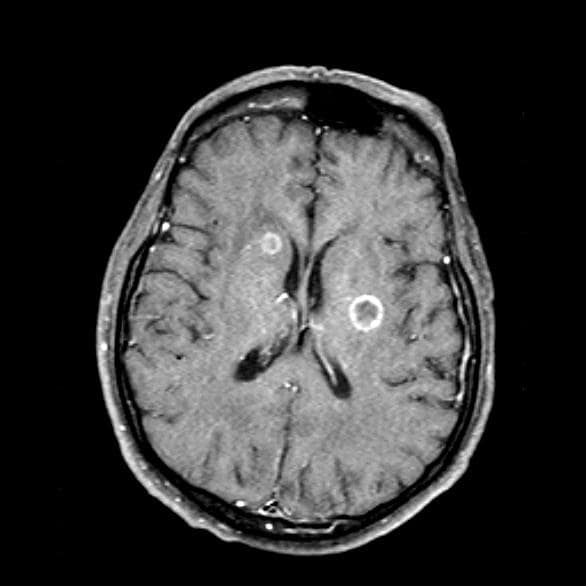
Which migraine medications are most effective?
TOPLINE:
new results from large, real-world analysis of self-reported patient data show.
METHODOLOGY:
- Researchers analyzed nearly 11 million migraine attack records extracted from Migraine Buddy, an e-diary smartphone app, over a 6-year period.
- They evaluated self-reported treatment effectiveness for 25 acute migraine medications among seven classes: acetaminophen, NSAIDs, triptans, combination analgesics, ergots, antiemetics, and opioids.
- A two-level nested multivariate logistic regression model adjusted for within-subject dependency and for concomitant medications taken within each analyzed migraine attack.
- The final analysis included nearly 5 million medication-outcome pairs from 3.1 million migraine attacks in 278,000 medication users.
TAKEAWAY:
- Using ibuprofen as the reference, triptans, ergots, and antiemetics were the top three medication classes with the highest effectiveness (mean odds ratios [OR] 4.80, 3.02, and 2.67, respectively).
- The next most effective medication classes were opioids (OR, 2.49), NSAIDs other than ibuprofen (OR, 1.94), combination analgesics acetaminophen/acetylsalicylic acid/caffeine (OR, 1.69), and others (OR, 1.49).
- Acetaminophen (OR, 0.83) was considered to be the least effective.
- The most effective individual medications were eletriptan (Relpax) (OR, 6.1); zolmitriptan (Zomig) (OR, 5.7); and sumatriptan (Imitrex) (OR, 5.2).
IN PRACTICE:
“Our findings that triptans, ergots, and antiemetics are the most effective classes of medications align with the guideline recommendations and offer generalizable insights to complement clinical practice,” the authors wrote.
SOURCE:
The study, with first author Chia-Chun Chiang, MD, Department of Neurology, Mayo Clinic, Rochester, Minnesota, was published online November 29 in Neurology.
LIMITATIONS:
The findings are based on subjective user-reported ratings of effectiveness and information on side effects, dosages, and formulations were not available. The newer migraine medication classes, gepants and ditans, were not included due to the relatively lower number of treated attacks. The regression model did not include age, gender, pain intensity, and other migraine-associated symptoms, which could potentially affect treatment effectiveness.
DISCLOSURES:
Funding for the study was provided by the Kanagawa University of Human Service research fund. A full list of author disclosures can be found with the original article.
A version of this article first appeared on Medscape.com.
TOPLINE:
new results from large, real-world analysis of self-reported patient data show.
METHODOLOGY:
- Researchers analyzed nearly 11 million migraine attack records extracted from Migraine Buddy, an e-diary smartphone app, over a 6-year period.
- They evaluated self-reported treatment effectiveness for 25 acute migraine medications among seven classes: acetaminophen, NSAIDs, triptans, combination analgesics, ergots, antiemetics, and opioids.
- A two-level nested multivariate logistic regression model adjusted for within-subject dependency and for concomitant medications taken within each analyzed migraine attack.
- The final analysis included nearly 5 million medication-outcome pairs from 3.1 million migraine attacks in 278,000 medication users.
TAKEAWAY:
- Using ibuprofen as the reference, triptans, ergots, and antiemetics were the top three medication classes with the highest effectiveness (mean odds ratios [OR] 4.80, 3.02, and 2.67, respectively).
- The next most effective medication classes were opioids (OR, 2.49), NSAIDs other than ibuprofen (OR, 1.94), combination analgesics acetaminophen/acetylsalicylic acid/caffeine (OR, 1.69), and others (OR, 1.49).
- Acetaminophen (OR, 0.83) was considered to be the least effective.
- The most effective individual medications were eletriptan (Relpax) (OR, 6.1); zolmitriptan (Zomig) (OR, 5.7); and sumatriptan (Imitrex) (OR, 5.2).
IN PRACTICE:
“Our findings that triptans, ergots, and antiemetics are the most effective classes of medications align with the guideline recommendations and offer generalizable insights to complement clinical practice,” the authors wrote.
SOURCE:
The study, with first author Chia-Chun Chiang, MD, Department of Neurology, Mayo Clinic, Rochester, Minnesota, was published online November 29 in Neurology.
LIMITATIONS:
The findings are based on subjective user-reported ratings of effectiveness and information on side effects, dosages, and formulations were not available. The newer migraine medication classes, gepants and ditans, were not included due to the relatively lower number of treated attacks. The regression model did not include age, gender, pain intensity, and other migraine-associated symptoms, which could potentially affect treatment effectiveness.
DISCLOSURES:
Funding for the study was provided by the Kanagawa University of Human Service research fund. A full list of author disclosures can be found with the original article.
A version of this article first appeared on Medscape.com.
TOPLINE:
new results from large, real-world analysis of self-reported patient data show.
METHODOLOGY:
- Researchers analyzed nearly 11 million migraine attack records extracted from Migraine Buddy, an e-diary smartphone app, over a 6-year period.
- They evaluated self-reported treatment effectiveness for 25 acute migraine medications among seven classes: acetaminophen, NSAIDs, triptans, combination analgesics, ergots, antiemetics, and opioids.
- A two-level nested multivariate logistic regression model adjusted for within-subject dependency and for concomitant medications taken within each analyzed migraine attack.
- The final analysis included nearly 5 million medication-outcome pairs from 3.1 million migraine attacks in 278,000 medication users.
TAKEAWAY:
- Using ibuprofen as the reference, triptans, ergots, and antiemetics were the top three medication classes with the highest effectiveness (mean odds ratios [OR] 4.80, 3.02, and 2.67, respectively).
- The next most effective medication classes were opioids (OR, 2.49), NSAIDs other than ibuprofen (OR, 1.94), combination analgesics acetaminophen/acetylsalicylic acid/caffeine (OR, 1.69), and others (OR, 1.49).
- Acetaminophen (OR, 0.83) was considered to be the least effective.
- The most effective individual medications were eletriptan (Relpax) (OR, 6.1); zolmitriptan (Zomig) (OR, 5.7); and sumatriptan (Imitrex) (OR, 5.2).
IN PRACTICE:
“Our findings that triptans, ergots, and antiemetics are the most effective classes of medications align with the guideline recommendations and offer generalizable insights to complement clinical practice,” the authors wrote.
SOURCE:
The study, with first author Chia-Chun Chiang, MD, Department of Neurology, Mayo Clinic, Rochester, Minnesota, was published online November 29 in Neurology.
LIMITATIONS:
The findings are based on subjective user-reported ratings of effectiveness and information on side effects, dosages, and formulations were not available. The newer migraine medication classes, gepants and ditans, were not included due to the relatively lower number of treated attacks. The regression model did not include age, gender, pain intensity, and other migraine-associated symptoms, which could potentially affect treatment effectiveness.
DISCLOSURES:
Funding for the study was provided by the Kanagawa University of Human Service research fund. A full list of author disclosures can be found with the original article.
A version of this article first appeared on Medscape.com.
Bimekizumab shows promise for palmoplantar pustular psoriasis
.
PPP is a type of pustular psoriasis that remains a treatment challenge, and available treatments for palmoplantar plaque psoriasis with pustules also “remain unsatisfactory,” according to Thierry Passeron, MD, PhD, of the dermatology service at Centre Hospitalier Universitaire de Nice (France), and colleagues. Bimekizumab, an anti-interleukin (IL)-17A and anti-IL-17F antibody therapy, has been used for psoriasis and psoriatic arthritis (PsA), but its effectiveness for PPP has not been studied, they said. In the United States, bimekizumab (Bimzelx), administered subcutaneously, was recently approved for treating moderate to severe plaque psoriasis in adults; in the European Union, it is approved for treating psoriasis, in addition to psoriatic arthritis, axial spondyloarthritis and ankylosing spondylitis.
In the case series published in JAMA Dermatology, Dr. Passeron and coinvestigators identified 11 adults with PPP and 10 with palmoplantar plaque psoriasis with pustules who were treated at one of seven tertiary dermatology centers in France from September 2022 through June 2023. PPP also has been associated with bone and joint inflammation in SAPHO (synovitis, acne, pustulosis, hyperostosis, osteitis) syndrome.
All patients received bimekizumab for at least 3 months. The patients — 19 women and 2 men — ranged in age from 24 to 68 years (mean age, 46 years). The primary outcome was complete clearance, defined as an Investigator Global Assessment (IGA) score of 0.
A total of 17 patients achieved an IGA score of zero in 1-4 months. Over 3-6 months, three patients achieved an IGA score of 1 (almost clear), and one patient achieved an IGA score of 2 (mild).
Three patients with PPP also had acrodermatitis continua of Hallopeau; in these patients, nail involvement improved by 50%-70% after 4-6 months of bimekizumab use. Two patients with SAPHO experienced complete clearance of skin lesions associated with improvement in joint pain.
Four patients developed oral and genital candidiasis during treatment, but all were treated successfully with antifungals. None of the patients discontinued bimekizumab because of adverse events. “All patients are still receiving treatment, and their psoriatic lesions remain controlled,” the authors wrote.
“The rapid and consistent improvement observed in the present case series supports the effectiveness of bimekizumab therapy in managing PPP, palmoplantar plaque psoriasis with pustules, and SAPHO syndrome,” they said in their discussion.
The study findings were limited by several factors including the small sample size and short follow-up period, and by the inclusion of only patients with severe disease; and prospective, placebo-controlled studies are needed to confirm the results, the researchers noted.
However, the results suggest that bimekizumab could be a treatment approach for PPP, palmoplantar plaque psoriasis with pustules, and SAPHO syndrome, and warrant a prospective, randomized, placebo-controlled, randomized clinical trial to confirm the findings, they concluded.
Dr. Passeron disclosed fees from AbbVie, ACM Pharma, Almirall, Boehringer Ingelheim, Bristol Myers Squibb, Calypso, Celgene, Galderma, Genzyme/Sanofi, GlaxoSmithKline, Incyte, Janssen, LEO Pharma, Eli Lilly, Novartis, Roivant Sciences, Sun Pharmaceuticals, and VYNE Therapeutics outside the current study; he is a cofounder of Yukin Therapeutics. Three authors disclosed receiving personal fees from UCB, manufacturer of bimekizumab, outside of the submitted work, another author disclosed receiving personal fees from UCB during the conduct of the study, and another reported receiving grants from UCB and several other companies, outside the submitted work.
The study findings were also presented at a meeting, Les Journées Dermatologiques de Paris 2023, on December 6, in Paris.
.
PPP is a type of pustular psoriasis that remains a treatment challenge, and available treatments for palmoplantar plaque psoriasis with pustules also “remain unsatisfactory,” according to Thierry Passeron, MD, PhD, of the dermatology service at Centre Hospitalier Universitaire de Nice (France), and colleagues. Bimekizumab, an anti-interleukin (IL)-17A and anti-IL-17F antibody therapy, has been used for psoriasis and psoriatic arthritis (PsA), but its effectiveness for PPP has not been studied, they said. In the United States, bimekizumab (Bimzelx), administered subcutaneously, was recently approved for treating moderate to severe plaque psoriasis in adults; in the European Union, it is approved for treating psoriasis, in addition to psoriatic arthritis, axial spondyloarthritis and ankylosing spondylitis.
In the case series published in JAMA Dermatology, Dr. Passeron and coinvestigators identified 11 adults with PPP and 10 with palmoplantar plaque psoriasis with pustules who were treated at one of seven tertiary dermatology centers in France from September 2022 through June 2023. PPP also has been associated with bone and joint inflammation in SAPHO (synovitis, acne, pustulosis, hyperostosis, osteitis) syndrome.
All patients received bimekizumab for at least 3 months. The patients — 19 women and 2 men — ranged in age from 24 to 68 years (mean age, 46 years). The primary outcome was complete clearance, defined as an Investigator Global Assessment (IGA) score of 0.
A total of 17 patients achieved an IGA score of zero in 1-4 months. Over 3-6 months, three patients achieved an IGA score of 1 (almost clear), and one patient achieved an IGA score of 2 (mild).
Three patients with PPP also had acrodermatitis continua of Hallopeau; in these patients, nail involvement improved by 50%-70% after 4-6 months of bimekizumab use. Two patients with SAPHO experienced complete clearance of skin lesions associated with improvement in joint pain.
Four patients developed oral and genital candidiasis during treatment, but all were treated successfully with antifungals. None of the patients discontinued bimekizumab because of adverse events. “All patients are still receiving treatment, and their psoriatic lesions remain controlled,” the authors wrote.
“The rapid and consistent improvement observed in the present case series supports the effectiveness of bimekizumab therapy in managing PPP, palmoplantar plaque psoriasis with pustules, and SAPHO syndrome,” they said in their discussion.
The study findings were limited by several factors including the small sample size and short follow-up period, and by the inclusion of only patients with severe disease; and prospective, placebo-controlled studies are needed to confirm the results, the researchers noted.
However, the results suggest that bimekizumab could be a treatment approach for PPP, palmoplantar plaque psoriasis with pustules, and SAPHO syndrome, and warrant a prospective, randomized, placebo-controlled, randomized clinical trial to confirm the findings, they concluded.
Dr. Passeron disclosed fees from AbbVie, ACM Pharma, Almirall, Boehringer Ingelheim, Bristol Myers Squibb, Calypso, Celgene, Galderma, Genzyme/Sanofi, GlaxoSmithKline, Incyte, Janssen, LEO Pharma, Eli Lilly, Novartis, Roivant Sciences, Sun Pharmaceuticals, and VYNE Therapeutics outside the current study; he is a cofounder of Yukin Therapeutics. Three authors disclosed receiving personal fees from UCB, manufacturer of bimekizumab, outside of the submitted work, another author disclosed receiving personal fees from UCB during the conduct of the study, and another reported receiving grants from UCB and several other companies, outside the submitted work.
The study findings were also presented at a meeting, Les Journées Dermatologiques de Paris 2023, on December 6, in Paris.
.
PPP is a type of pustular psoriasis that remains a treatment challenge, and available treatments for palmoplantar plaque psoriasis with pustules also “remain unsatisfactory,” according to Thierry Passeron, MD, PhD, of the dermatology service at Centre Hospitalier Universitaire de Nice (France), and colleagues. Bimekizumab, an anti-interleukin (IL)-17A and anti-IL-17F antibody therapy, has been used for psoriasis and psoriatic arthritis (PsA), but its effectiveness for PPP has not been studied, they said. In the United States, bimekizumab (Bimzelx), administered subcutaneously, was recently approved for treating moderate to severe plaque psoriasis in adults; in the European Union, it is approved for treating psoriasis, in addition to psoriatic arthritis, axial spondyloarthritis and ankylosing spondylitis.
In the case series published in JAMA Dermatology, Dr. Passeron and coinvestigators identified 11 adults with PPP and 10 with palmoplantar plaque psoriasis with pustules who were treated at one of seven tertiary dermatology centers in France from September 2022 through June 2023. PPP also has been associated with bone and joint inflammation in SAPHO (synovitis, acne, pustulosis, hyperostosis, osteitis) syndrome.
All patients received bimekizumab for at least 3 months. The patients — 19 women and 2 men — ranged in age from 24 to 68 years (mean age, 46 years). The primary outcome was complete clearance, defined as an Investigator Global Assessment (IGA) score of 0.
A total of 17 patients achieved an IGA score of zero in 1-4 months. Over 3-6 months, three patients achieved an IGA score of 1 (almost clear), and one patient achieved an IGA score of 2 (mild).
Three patients with PPP also had acrodermatitis continua of Hallopeau; in these patients, nail involvement improved by 50%-70% after 4-6 months of bimekizumab use. Two patients with SAPHO experienced complete clearance of skin lesions associated with improvement in joint pain.
Four patients developed oral and genital candidiasis during treatment, but all were treated successfully with antifungals. None of the patients discontinued bimekizumab because of adverse events. “All patients are still receiving treatment, and their psoriatic lesions remain controlled,” the authors wrote.
“The rapid and consistent improvement observed in the present case series supports the effectiveness of bimekizumab therapy in managing PPP, palmoplantar plaque psoriasis with pustules, and SAPHO syndrome,” they said in their discussion.
The study findings were limited by several factors including the small sample size and short follow-up period, and by the inclusion of only patients with severe disease; and prospective, placebo-controlled studies are needed to confirm the results, the researchers noted.
However, the results suggest that bimekizumab could be a treatment approach for PPP, palmoplantar plaque psoriasis with pustules, and SAPHO syndrome, and warrant a prospective, randomized, placebo-controlled, randomized clinical trial to confirm the findings, they concluded.
Dr. Passeron disclosed fees from AbbVie, ACM Pharma, Almirall, Boehringer Ingelheim, Bristol Myers Squibb, Calypso, Celgene, Galderma, Genzyme/Sanofi, GlaxoSmithKline, Incyte, Janssen, LEO Pharma, Eli Lilly, Novartis, Roivant Sciences, Sun Pharmaceuticals, and VYNE Therapeutics outside the current study; he is a cofounder of Yukin Therapeutics. Three authors disclosed receiving personal fees from UCB, manufacturer of bimekizumab, outside of the submitted work, another author disclosed receiving personal fees from UCB during the conduct of the study, and another reported receiving grants from UCB and several other companies, outside the submitted work.
The study findings were also presented at a meeting, Les Journées Dermatologiques de Paris 2023, on December 6, in Paris.
FROM JAMA DERMATOLOGY
Tape strips detect hidradenitis suppurativa biomarkers, novel study shows
, results from a novel study showed.
“Tape strips can provide important clues to when and which drugs to use in HS in patients with both early and late disease, which can change clinical practice,” corresponding study author Emma Guttman-Yassky, MD, PhD, professor and chair of dermatology at the Icahn School of Medicine at Mount Sinai in New York City, said in an interview. “It is noninvasive and nonscarring,” she added.
Tape stripping has been validated in atopic dermatitis, psoriasis, and other dermatologic conditions in recent years. For the current study, which was published online in the Journal of the American Academy of Dermatology, and is believed to be the first of its kind, Dr. Guttman-Yassky and colleagues performed RNA sequencing from large D-Squame tape strips collected from lesional and nonlesional skin of 22 patients with HS and from 21 age- and sex-matched healthy controls. They correlated the expression of skin biomarkers between tape strips and a previously published gene-signature of HS biopsies. The mean age of patients with HS was 43 years, while the mean age of healthy controls was 35. The average International Hidradenitis Suppurativa Severity Score System (IHS4) score of the HS cohort was 36.
Consistent with published studies, the researchers found that tape strips identified an overall higher inflammatory burden in HS. Specifically, they observed an upregulation of known cytokines within the following pathways: Th1 (such as IFNG, CXCL9/10/11, and CCR5); Th17 (such as interleukin [IL]-17A/F, IL12B, IL23A, CAMP, and CCL20); Th2 (such as IL4R, IL13/IL31/IL10, CCR4, CCL7/CCL13/CCL24, TNFSF4/OX40L, and TNFRSF4/OX40); and Th22 (such as IL22 and IL32).
The researchers also found that the expression of Th17 and tumor necrosis factor (TNF)–alpha pathways were highly correlated between tape strips and biopsies and that HS clinical severity was significantly associated with expression of biomarkers, such as TNF-alpha, IL17A/F, OX40, JAK1-3, and IL4R in HS lesional and/or nonlesional skin.
“It was quite unexpected that we are able to identify, using a minimally invasive approach that samples only the upper layers of the epidermis, products and processes that are considered to be deeper-situated, such as IL-17, and other immune markers,” Dr. Guttman-Yassky said in the interview. “We were also surprised to see how well the tape-stripped–derived skin molecular profile correlated with that of biopsies, as well as how well it correlated with the clinical disease severity of HS.”
Also surprising, she added, was that the biomarkers in nonlesional tape-stripped skin, such as IL-17 and TNF alpha, “show high correlations with disease severity and provide clues to early disease.”
If using tape strips in HS is validated in larger cohort studies, the potential cost implications of using this approach in practice remain unclear, Dr. Guttman-Yassky said. “It is currently not cheap, but we are hoping that one day, we can provide a means to diagnose the disease and treat it early, and appropriately, utilizing this approach,” she commented. “We are excited about the applicability of this study to the early treatment and longitudinal follow up of HS with drugs that are targeting specific immune molecules and pathways,” she said, adding that it will also be useful for helping determine which drug should be used for which patient.
She and her co-authors acknowledged certain limitations of the study, including its small sample size and the fact that tape stripping is limited to the epidermis.
Asked to comment on the study, Jennifer L. Hsiao, MD, a dermatologist who directs the HS clinic at the University of Southern California, Los Angeles, said the findings “have important potential implications for our ability to one day personalize treatments for a patient with early HS in a minimally invasive way.”
As the study authors point out, she added, “tape strips only allow sampling of the epidermis, which is limiting in a disease like HS where much of the disruption is in the dermis with deep nodules and dermal tunnels. However, our overall goal should be to catch patients in the early stages of their disease before the occurrence of irreversible tissue damage such as dermal tunnels. Thus, the ongoing campaign for early diagnosis and early intervention by various stakeholders in the field of HS can help mitigate the impact of this inherent limitation of tape strips. It will be exciting to see larger studies that investigate tape strip results in relation to clinical phenotypes, disease progression, and therapeutic responses.”
The study was funded by an International Dermatology Outcome Measures Hidradenitis Suppurativa Grant. Dr. Guttman-Yassky disclosed that she has been a consultant to, an adviser for, and has received research grants from many pharmaceutical companies. Of the remaining authors, 2 also had multiple disclosures and 11 had no disclosures. Dr. Hsiao disclosed that she is a member of the board of directors for the Hidradenitis Suppurativa Foundation. She has also served as a consultant for AbbVie, Aclaris, Boehringer Ingelheim, Incyte, Novartis, and UCB; as a speaker for AbbVie; and as an investigator for Amgen, Boehringer Ingelheim, and Incyte.
, results from a novel study showed.
“Tape strips can provide important clues to when and which drugs to use in HS in patients with both early and late disease, which can change clinical practice,” corresponding study author Emma Guttman-Yassky, MD, PhD, professor and chair of dermatology at the Icahn School of Medicine at Mount Sinai in New York City, said in an interview. “It is noninvasive and nonscarring,” she added.
Tape stripping has been validated in atopic dermatitis, psoriasis, and other dermatologic conditions in recent years. For the current study, which was published online in the Journal of the American Academy of Dermatology, and is believed to be the first of its kind, Dr. Guttman-Yassky and colleagues performed RNA sequencing from large D-Squame tape strips collected from lesional and nonlesional skin of 22 patients with HS and from 21 age- and sex-matched healthy controls. They correlated the expression of skin biomarkers between tape strips and a previously published gene-signature of HS biopsies. The mean age of patients with HS was 43 years, while the mean age of healthy controls was 35. The average International Hidradenitis Suppurativa Severity Score System (IHS4) score of the HS cohort was 36.
Consistent with published studies, the researchers found that tape strips identified an overall higher inflammatory burden in HS. Specifically, they observed an upregulation of known cytokines within the following pathways: Th1 (such as IFNG, CXCL9/10/11, and CCR5); Th17 (such as interleukin [IL]-17A/F, IL12B, IL23A, CAMP, and CCL20); Th2 (such as IL4R, IL13/IL31/IL10, CCR4, CCL7/CCL13/CCL24, TNFSF4/OX40L, and TNFRSF4/OX40); and Th22 (such as IL22 and IL32).
The researchers also found that the expression of Th17 and tumor necrosis factor (TNF)–alpha pathways were highly correlated between tape strips and biopsies and that HS clinical severity was significantly associated with expression of biomarkers, such as TNF-alpha, IL17A/F, OX40, JAK1-3, and IL4R in HS lesional and/or nonlesional skin.
“It was quite unexpected that we are able to identify, using a minimally invasive approach that samples only the upper layers of the epidermis, products and processes that are considered to be deeper-situated, such as IL-17, and other immune markers,” Dr. Guttman-Yassky said in the interview. “We were also surprised to see how well the tape-stripped–derived skin molecular profile correlated with that of biopsies, as well as how well it correlated with the clinical disease severity of HS.”
Also surprising, she added, was that the biomarkers in nonlesional tape-stripped skin, such as IL-17 and TNF alpha, “show high correlations with disease severity and provide clues to early disease.”
If using tape strips in HS is validated in larger cohort studies, the potential cost implications of using this approach in practice remain unclear, Dr. Guttman-Yassky said. “It is currently not cheap, but we are hoping that one day, we can provide a means to diagnose the disease and treat it early, and appropriately, utilizing this approach,” she commented. “We are excited about the applicability of this study to the early treatment and longitudinal follow up of HS with drugs that are targeting specific immune molecules and pathways,” she said, adding that it will also be useful for helping determine which drug should be used for which patient.
She and her co-authors acknowledged certain limitations of the study, including its small sample size and the fact that tape stripping is limited to the epidermis.
Asked to comment on the study, Jennifer L. Hsiao, MD, a dermatologist who directs the HS clinic at the University of Southern California, Los Angeles, said the findings “have important potential implications for our ability to one day personalize treatments for a patient with early HS in a minimally invasive way.”
As the study authors point out, she added, “tape strips only allow sampling of the epidermis, which is limiting in a disease like HS where much of the disruption is in the dermis with deep nodules and dermal tunnels. However, our overall goal should be to catch patients in the early stages of their disease before the occurrence of irreversible tissue damage such as dermal tunnels. Thus, the ongoing campaign for early diagnosis and early intervention by various stakeholders in the field of HS can help mitigate the impact of this inherent limitation of tape strips. It will be exciting to see larger studies that investigate tape strip results in relation to clinical phenotypes, disease progression, and therapeutic responses.”
The study was funded by an International Dermatology Outcome Measures Hidradenitis Suppurativa Grant. Dr. Guttman-Yassky disclosed that she has been a consultant to, an adviser for, and has received research grants from many pharmaceutical companies. Of the remaining authors, 2 also had multiple disclosures and 11 had no disclosures. Dr. Hsiao disclosed that she is a member of the board of directors for the Hidradenitis Suppurativa Foundation. She has also served as a consultant for AbbVie, Aclaris, Boehringer Ingelheim, Incyte, Novartis, and UCB; as a speaker for AbbVie; and as an investigator for Amgen, Boehringer Ingelheim, and Incyte.
, results from a novel study showed.
“Tape strips can provide important clues to when and which drugs to use in HS in patients with both early and late disease, which can change clinical practice,” corresponding study author Emma Guttman-Yassky, MD, PhD, professor and chair of dermatology at the Icahn School of Medicine at Mount Sinai in New York City, said in an interview. “It is noninvasive and nonscarring,” she added.
Tape stripping has been validated in atopic dermatitis, psoriasis, and other dermatologic conditions in recent years. For the current study, which was published online in the Journal of the American Academy of Dermatology, and is believed to be the first of its kind, Dr. Guttman-Yassky and colleagues performed RNA sequencing from large D-Squame tape strips collected from lesional and nonlesional skin of 22 patients with HS and from 21 age- and sex-matched healthy controls. They correlated the expression of skin biomarkers between tape strips and a previously published gene-signature of HS biopsies. The mean age of patients with HS was 43 years, while the mean age of healthy controls was 35. The average International Hidradenitis Suppurativa Severity Score System (IHS4) score of the HS cohort was 36.
Consistent with published studies, the researchers found that tape strips identified an overall higher inflammatory burden in HS. Specifically, they observed an upregulation of known cytokines within the following pathways: Th1 (such as IFNG, CXCL9/10/11, and CCR5); Th17 (such as interleukin [IL]-17A/F, IL12B, IL23A, CAMP, and CCL20); Th2 (such as IL4R, IL13/IL31/IL10, CCR4, CCL7/CCL13/CCL24, TNFSF4/OX40L, and TNFRSF4/OX40); and Th22 (such as IL22 and IL32).
The researchers also found that the expression of Th17 and tumor necrosis factor (TNF)–alpha pathways were highly correlated between tape strips and biopsies and that HS clinical severity was significantly associated with expression of biomarkers, such as TNF-alpha, IL17A/F, OX40, JAK1-3, and IL4R in HS lesional and/or nonlesional skin.
“It was quite unexpected that we are able to identify, using a minimally invasive approach that samples only the upper layers of the epidermis, products and processes that are considered to be deeper-situated, such as IL-17, and other immune markers,” Dr. Guttman-Yassky said in the interview. “We were also surprised to see how well the tape-stripped–derived skin molecular profile correlated with that of biopsies, as well as how well it correlated with the clinical disease severity of HS.”
Also surprising, she added, was that the biomarkers in nonlesional tape-stripped skin, such as IL-17 and TNF alpha, “show high correlations with disease severity and provide clues to early disease.”
If using tape strips in HS is validated in larger cohort studies, the potential cost implications of using this approach in practice remain unclear, Dr. Guttman-Yassky said. “It is currently not cheap, but we are hoping that one day, we can provide a means to diagnose the disease and treat it early, and appropriately, utilizing this approach,” she commented. “We are excited about the applicability of this study to the early treatment and longitudinal follow up of HS with drugs that are targeting specific immune molecules and pathways,” she said, adding that it will also be useful for helping determine which drug should be used for which patient.
She and her co-authors acknowledged certain limitations of the study, including its small sample size and the fact that tape stripping is limited to the epidermis.
Asked to comment on the study, Jennifer L. Hsiao, MD, a dermatologist who directs the HS clinic at the University of Southern California, Los Angeles, said the findings “have important potential implications for our ability to one day personalize treatments for a patient with early HS in a minimally invasive way.”
As the study authors point out, she added, “tape strips only allow sampling of the epidermis, which is limiting in a disease like HS where much of the disruption is in the dermis with deep nodules and dermal tunnels. However, our overall goal should be to catch patients in the early stages of their disease before the occurrence of irreversible tissue damage such as dermal tunnels. Thus, the ongoing campaign for early diagnosis and early intervention by various stakeholders in the field of HS can help mitigate the impact of this inherent limitation of tape strips. It will be exciting to see larger studies that investigate tape strip results in relation to clinical phenotypes, disease progression, and therapeutic responses.”
The study was funded by an International Dermatology Outcome Measures Hidradenitis Suppurativa Grant. Dr. Guttman-Yassky disclosed that she has been a consultant to, an adviser for, and has received research grants from many pharmaceutical companies. Of the remaining authors, 2 also had multiple disclosures and 11 had no disclosures. Dr. Hsiao disclosed that she is a member of the board of directors for the Hidradenitis Suppurativa Foundation. She has also served as a consultant for AbbVie, Aclaris, Boehringer Ingelheim, Incyte, Novartis, and UCB; as a speaker for AbbVie; and as an investigator for Amgen, Boehringer Ingelheim, and Incyte.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
New COVID variant JN.1 could disrupt holiday plans
No one planning holiday gatherings or travel wants to hear this, but the rise of a new COVID-19 variant, JN.1, is concerning experts, who say it may threaten those good times.
The good news is recent research suggests the 2023-2024 COVID-19 vaccine appears to work against this newest variant. But so few people have gotten the latest vaccine — less than 16% of U.S. adults — that some experts suggest it’s time for the CDC to urge the public who haven’t it to do so now, so the antibodies can kick in before the festivities.
“A significant wave [of JN.1] has started here and could be blunted with a high booster rate and mitigation measures,” said Eric Topol, MD, professor and executive vice president of Scripps Research in La Jolla, CA, and editor-in-chief of Medscape, a sister site of this news organization.
COVID metrics, meanwhile, have started to climb again. Nearly 10,000 people were hospitalized for COVID in the U.S. for the week ending Nov. 25, the CDC said, a 10% increase over the previous week.
Who’s Who in the Family Tree
JN.1, an Omicron subvariant, was first detected in the U.S. in September and is termed “a notable descendent lineage” of Omicron subvariant BA.2.86 by the World Health Organization. When BA.2.86, also known as Pirola, was first identified in August, it appeared very different from other variants, the CDC said. That triggered concerns it might be more infectious than previous ones, even for people with immunity from vaccination and previous infections.
“JN.1 is Pirola’s kid,” said Rajendram Rajnarayanan, PhD, assistant dean of research and associate professor at the New York Institute of Technology at Arkansas State University, who maintains a COVID-19 variant database. The variant BA.2.86 and offspring are worrisome due to the mutations, he said.
How Widespread Is JN.1?
As of Nov. 27, the CDC says, BA.2.86 is projected to comprise 5%-15% of circulating variants in the U.S. “The expected public health risk of this variant, including its offshoot JN.1, is low,” the agency said.
Currently, JN.1 is reported more often in Europe, Dr. Rajnarayanan said, but some countries have better reporting data than others. “It has probably spread to every country tracking COVID,’’ he said, due to the mutations in the spike protein that make it easier for it to bind and infect.
Wastewater data suggest the variant’s rise is helping to fuel a wave, Dr. Topol said.
Vaccine Effectiveness Against JN.1, Other New Variants
The new XBB.1.5 monovalent vaccine, protects against XBB.1.5, another Omicron subvariant, but also JN.1 and other “emergent” viruses, a team of researchers reported Nov. 26 in a study on bioRxiv that has not yet been certified by peer review.
The updated vaccine, when given to uninfected people, boosted antibodies about 27-fold against XBB.1.5 and about 13- to 27-fold against JN.1 and other emergent viruses, the researchers reported.
While even primary doses of the COVID vaccine will likely help protect against the new JN.1 subvariant, “if you got the XBB.1.5 booster, it is going to be protecting you better against this new variant,” Dr. Rajnarayanan said.
2023-2024 Vaccine Uptake Low
In November, the CDC posted the first detailed estimates of who did. As of Nov. 18, less than 16% of U.S. adults had, with nearly 15% saying they planned to get it.
Coverage among children is lower, with just 6.3% of children up to date on the newest vaccine and 19% of parents saying they planned to get the 2023-2024 vaccine for their children.
Predictions, Mitigation
While some experts say a peak due to JN.1 is expected in the weeks ahead, Dr. Topol said it’s impossible to predict exactly how JN.1 will play out.
“It’s not going to be a repeat of November 2021,” when Omicron surfaced, Dr. Rajnarayanan predicted. Within 4 weeks of the World Health Organization declaring Omicron as a virus of concern, it spread around the world.
Mitigation measures can help, Dr. Rajnarayanan said. He suggested:
Get the new vaccine, and especially encourage vulnerable family and friends to do so.
If you are gathering inside for holiday festivities, improve circulation in the house, if possible.
Wear masks in airports and on planes and other public transportation.
A version of this article appeared on WebMD.com.
No one planning holiday gatherings or travel wants to hear this, but the rise of a new COVID-19 variant, JN.1, is concerning experts, who say it may threaten those good times.
The good news is recent research suggests the 2023-2024 COVID-19 vaccine appears to work against this newest variant. But so few people have gotten the latest vaccine — less than 16% of U.S. adults — that some experts suggest it’s time for the CDC to urge the public who haven’t it to do so now, so the antibodies can kick in before the festivities.
“A significant wave [of JN.1] has started here and could be blunted with a high booster rate and mitigation measures,” said Eric Topol, MD, professor and executive vice president of Scripps Research in La Jolla, CA, and editor-in-chief of Medscape, a sister site of this news organization.
COVID metrics, meanwhile, have started to climb again. Nearly 10,000 people were hospitalized for COVID in the U.S. for the week ending Nov. 25, the CDC said, a 10% increase over the previous week.
Who’s Who in the Family Tree
JN.1, an Omicron subvariant, was first detected in the U.S. in September and is termed “a notable descendent lineage” of Omicron subvariant BA.2.86 by the World Health Organization. When BA.2.86, also known as Pirola, was first identified in August, it appeared very different from other variants, the CDC said. That triggered concerns it might be more infectious than previous ones, even for people with immunity from vaccination and previous infections.
“JN.1 is Pirola’s kid,” said Rajendram Rajnarayanan, PhD, assistant dean of research and associate professor at the New York Institute of Technology at Arkansas State University, who maintains a COVID-19 variant database. The variant BA.2.86 and offspring are worrisome due to the mutations, he said.
How Widespread Is JN.1?
As of Nov. 27, the CDC says, BA.2.86 is projected to comprise 5%-15% of circulating variants in the U.S. “The expected public health risk of this variant, including its offshoot JN.1, is low,” the agency said.
Currently, JN.1 is reported more often in Europe, Dr. Rajnarayanan said, but some countries have better reporting data than others. “It has probably spread to every country tracking COVID,’’ he said, due to the mutations in the spike protein that make it easier for it to bind and infect.
Wastewater data suggest the variant’s rise is helping to fuel a wave, Dr. Topol said.
Vaccine Effectiveness Against JN.1, Other New Variants
The new XBB.1.5 monovalent vaccine, protects against XBB.1.5, another Omicron subvariant, but also JN.1 and other “emergent” viruses, a team of researchers reported Nov. 26 in a study on bioRxiv that has not yet been certified by peer review.
The updated vaccine, when given to uninfected people, boosted antibodies about 27-fold against XBB.1.5 and about 13- to 27-fold against JN.1 and other emergent viruses, the researchers reported.
While even primary doses of the COVID vaccine will likely help protect against the new JN.1 subvariant, “if you got the XBB.1.5 booster, it is going to be protecting you better against this new variant,” Dr. Rajnarayanan said.
2023-2024 Vaccine Uptake Low
In November, the CDC posted the first detailed estimates of who did. As of Nov. 18, less than 16% of U.S. adults had, with nearly 15% saying they planned to get it.
Coverage among children is lower, with just 6.3% of children up to date on the newest vaccine and 19% of parents saying they planned to get the 2023-2024 vaccine for their children.
Predictions, Mitigation
While some experts say a peak due to JN.1 is expected in the weeks ahead, Dr. Topol said it’s impossible to predict exactly how JN.1 will play out.
“It’s not going to be a repeat of November 2021,” when Omicron surfaced, Dr. Rajnarayanan predicted. Within 4 weeks of the World Health Organization declaring Omicron as a virus of concern, it spread around the world.
Mitigation measures can help, Dr. Rajnarayanan said. He suggested:
Get the new vaccine, and especially encourage vulnerable family and friends to do so.
If you are gathering inside for holiday festivities, improve circulation in the house, if possible.
Wear masks in airports and on planes and other public transportation.
A version of this article appeared on WebMD.com.
No one planning holiday gatherings or travel wants to hear this, but the rise of a new COVID-19 variant, JN.1, is concerning experts, who say it may threaten those good times.
The good news is recent research suggests the 2023-2024 COVID-19 vaccine appears to work against this newest variant. But so few people have gotten the latest vaccine — less than 16% of U.S. adults — that some experts suggest it’s time for the CDC to urge the public who haven’t it to do so now, so the antibodies can kick in before the festivities.
“A significant wave [of JN.1] has started here and could be blunted with a high booster rate and mitigation measures,” said Eric Topol, MD, professor and executive vice president of Scripps Research in La Jolla, CA, and editor-in-chief of Medscape, a sister site of this news organization.
COVID metrics, meanwhile, have started to climb again. Nearly 10,000 people were hospitalized for COVID in the U.S. for the week ending Nov. 25, the CDC said, a 10% increase over the previous week.
Who’s Who in the Family Tree
JN.1, an Omicron subvariant, was first detected in the U.S. in September and is termed “a notable descendent lineage” of Omicron subvariant BA.2.86 by the World Health Organization. When BA.2.86, also known as Pirola, was first identified in August, it appeared very different from other variants, the CDC said. That triggered concerns it might be more infectious than previous ones, even for people with immunity from vaccination and previous infections.
“JN.1 is Pirola’s kid,” said Rajendram Rajnarayanan, PhD, assistant dean of research and associate professor at the New York Institute of Technology at Arkansas State University, who maintains a COVID-19 variant database. The variant BA.2.86 and offspring are worrisome due to the mutations, he said.
How Widespread Is JN.1?
As of Nov. 27, the CDC says, BA.2.86 is projected to comprise 5%-15% of circulating variants in the U.S. “The expected public health risk of this variant, including its offshoot JN.1, is low,” the agency said.
Currently, JN.1 is reported more often in Europe, Dr. Rajnarayanan said, but some countries have better reporting data than others. “It has probably spread to every country tracking COVID,’’ he said, due to the mutations in the spike protein that make it easier for it to bind and infect.
Wastewater data suggest the variant’s rise is helping to fuel a wave, Dr. Topol said.
Vaccine Effectiveness Against JN.1, Other New Variants
The new XBB.1.5 monovalent vaccine, protects against XBB.1.5, another Omicron subvariant, but also JN.1 and other “emergent” viruses, a team of researchers reported Nov. 26 in a study on bioRxiv that has not yet been certified by peer review.
The updated vaccine, when given to uninfected people, boosted antibodies about 27-fold against XBB.1.5 and about 13- to 27-fold against JN.1 and other emergent viruses, the researchers reported.
While even primary doses of the COVID vaccine will likely help protect against the new JN.1 subvariant, “if you got the XBB.1.5 booster, it is going to be protecting you better against this new variant,” Dr. Rajnarayanan said.
2023-2024 Vaccine Uptake Low
In November, the CDC posted the first detailed estimates of who did. As of Nov. 18, less than 16% of U.S. adults had, with nearly 15% saying they planned to get it.
Coverage among children is lower, with just 6.3% of children up to date on the newest vaccine and 19% of parents saying they planned to get the 2023-2024 vaccine for their children.
Predictions, Mitigation
While some experts say a peak due to JN.1 is expected in the weeks ahead, Dr. Topol said it’s impossible to predict exactly how JN.1 will play out.
“It’s not going to be a repeat of November 2021,” when Omicron surfaced, Dr. Rajnarayanan predicted. Within 4 weeks of the World Health Organization declaring Omicron as a virus of concern, it spread around the world.
Mitigation measures can help, Dr. Rajnarayanan said. He suggested:
Get the new vaccine, and especially encourage vulnerable family and friends to do so.
If you are gathering inside for holiday festivities, improve circulation in the house, if possible.
Wear masks in airports and on planes and other public transportation.
A version of this article appeared on WebMD.com.
FDA approves first 2 gene-editing therapies for sickle cell
These “milestone treatments” mark the first cell-based gene therapies for this debilitating and potentially life-threatening blood disorder that affects about 100,000 people in the United States.
The two therapies are exagamglogene autotemcel, or exa-cel (Casgevy; Vertex Pharmaceuticals and Crispr Therapeutics), and lovotibeglogene autotemcel, or lovo-cel (Lyfgenia; bluebird bio).
“The approval of the first gene therapies for [sickle cell disease] represents a tremendous step forward for the [sickle cell] community, which has been historically overlooked and underfunded,” said Robert A. Brodsky, MD, of Johns Hopkins University School of Medicine, in a statement from the American Society of Hematology, following the approval.
“We are excited to advance the field, especially for individuals whose lives have been severely disrupted by the disease, by approving two cell-based gene therapies today,” Nicole Verdun, MD, of the FDA’s Center for Biologics Evaluation and Research, added in an agency press release.
Sickle cell disease involves a mutation in hemoglobin, a protein in red blood cells that provides oxygen to tissues. The mutation leads red blood cells to develop a crescent or sickle shape, which can restrict blood flow and cause severe pain and organ damage, known as vaso-occlusive events or crises.
Treatment options prior to these approvals primarily included red blood transfusions and hydroxyurea alongside pain management. The only potential curative option has been allogeneic hematopoietic stem cell transplantation, but that comes with significant risks and most patients don’t have an appropriate donor.
Exa-cel
Exa-cel uses CRISPR gene-editing technology. Before the infusion, patients undergo myeloablative conditioning, which removes cells from the bone marrow. These cells are genetically modified to produce fetal hemoglobin. Patients then receive an infusion of the edited cells, which can help restore normal hemoglobin production.
The FDA approval was based on data from the pivotal CLIMB SCD-121 trial. In an October advisory committee meeting, the FDA highlighted trial data demonstrating that 29 of 31 patients reached the trial’s primary endpoint: freedom from severe vaso-occlusive crises over a 12-month period. In addition, 28 of these patients remained free of vaso-occlusive crises for almost 2 years.
The committee noted that one of the 31 patients died about 9 months after receiving an exa-cel infusion.
The cell-based gene therapy also increased both fetal and total hemoglobin, with total hemoglobin levels increasing to > 11 g/dL by month 3 and remaining at that level afterward. No patients experienced graft failure or rejection.
The most common side effects included low platelets and white blood cell counts, mouth sores, nausea, musculoskeletal pain, vomiting, and febrile neutropenia.
Exa-cel could “provide a one-time functional cure” for patients with severe sickle cell disease, according to Franco Locatelli, MD, of Sapienza University of Rome, who presented initial findings last year.
While the current approval is for patients with infusion-dependent sickle cell disease, exa-cel is also being evaluated in patients with another blood disorder, beta-thalassemia.
Lovo-cel
Lovo-cel, a cell-based gene therapy, uses a different technology — a lentiviral vector, or gene delivery vehicle — that can also genetically modify a patient’s blood stem cells.
Like exa-cel, lovo-cel is a one-time, single-dose infusion that contains the patient’s modified cells. Before the infusion, patients undergo myeloablative conditioning. The patient’s stem cells are then genetically modified to allow them to produce the most common form of hemoglobin, HbA
This approval was based on data from a single-arm, 24-month study in patients aged 12-50 years who had sickle cell disease and a history of vaso-occlusive events.
Overall, 88% of patients (28 of 32) achieved complete resolution of vaso-occlusive events 6-18 months after the infusion.
The most common side effects included stomatitis; febrile neutropenia; and low platelet, white blood cell, and red blood cell counts.
The FDA noted that hematologic cancer has occurred in patients treated with lovo-cel, and the label includes a black-box warning about the risk.
Dr. Brodsky noted, however, that “while these new gene therapies are potentially life-changing for individuals living with [sickle cell disease], they must be accessible to be effective.”
Access is a potential concern. Exa-cel and lovo-cel could cost about $2 million.
A version of this article appeared on Medscape.com.
These “milestone treatments” mark the first cell-based gene therapies for this debilitating and potentially life-threatening blood disorder that affects about 100,000 people in the United States.
The two therapies are exagamglogene autotemcel, or exa-cel (Casgevy; Vertex Pharmaceuticals and Crispr Therapeutics), and lovotibeglogene autotemcel, or lovo-cel (Lyfgenia; bluebird bio).
“The approval of the first gene therapies for [sickle cell disease] represents a tremendous step forward for the [sickle cell] community, which has been historically overlooked and underfunded,” said Robert A. Brodsky, MD, of Johns Hopkins University School of Medicine, in a statement from the American Society of Hematology, following the approval.
“We are excited to advance the field, especially for individuals whose lives have been severely disrupted by the disease, by approving two cell-based gene therapies today,” Nicole Verdun, MD, of the FDA’s Center for Biologics Evaluation and Research, added in an agency press release.
Sickle cell disease involves a mutation in hemoglobin, a protein in red blood cells that provides oxygen to tissues. The mutation leads red blood cells to develop a crescent or sickle shape, which can restrict blood flow and cause severe pain and organ damage, known as vaso-occlusive events or crises.
Treatment options prior to these approvals primarily included red blood transfusions and hydroxyurea alongside pain management. The only potential curative option has been allogeneic hematopoietic stem cell transplantation, but that comes with significant risks and most patients don’t have an appropriate donor.
Exa-cel
Exa-cel uses CRISPR gene-editing technology. Before the infusion, patients undergo myeloablative conditioning, which removes cells from the bone marrow. These cells are genetically modified to produce fetal hemoglobin. Patients then receive an infusion of the edited cells, which can help restore normal hemoglobin production.
The FDA approval was based on data from the pivotal CLIMB SCD-121 trial. In an October advisory committee meeting, the FDA highlighted trial data demonstrating that 29 of 31 patients reached the trial’s primary endpoint: freedom from severe vaso-occlusive crises over a 12-month period. In addition, 28 of these patients remained free of vaso-occlusive crises for almost 2 years.
The committee noted that one of the 31 patients died about 9 months after receiving an exa-cel infusion.
The cell-based gene therapy also increased both fetal and total hemoglobin, with total hemoglobin levels increasing to > 11 g/dL by month 3 and remaining at that level afterward. No patients experienced graft failure or rejection.
The most common side effects included low platelets and white blood cell counts, mouth sores, nausea, musculoskeletal pain, vomiting, and febrile neutropenia.
Exa-cel could “provide a one-time functional cure” for patients with severe sickle cell disease, according to Franco Locatelli, MD, of Sapienza University of Rome, who presented initial findings last year.
While the current approval is for patients with infusion-dependent sickle cell disease, exa-cel is also being evaluated in patients with another blood disorder, beta-thalassemia.
Lovo-cel
Lovo-cel, a cell-based gene therapy, uses a different technology — a lentiviral vector, or gene delivery vehicle — that can also genetically modify a patient’s blood stem cells.
Like exa-cel, lovo-cel is a one-time, single-dose infusion that contains the patient’s modified cells. Before the infusion, patients undergo myeloablative conditioning. The patient’s stem cells are then genetically modified to allow them to produce the most common form of hemoglobin, HbA
This approval was based on data from a single-arm, 24-month study in patients aged 12-50 years who had sickle cell disease and a history of vaso-occlusive events.
Overall, 88% of patients (28 of 32) achieved complete resolution of vaso-occlusive events 6-18 months after the infusion.
The most common side effects included stomatitis; febrile neutropenia; and low platelet, white blood cell, and red blood cell counts.
The FDA noted that hematologic cancer has occurred in patients treated with lovo-cel, and the label includes a black-box warning about the risk.
Dr. Brodsky noted, however, that “while these new gene therapies are potentially life-changing for individuals living with [sickle cell disease], they must be accessible to be effective.”
Access is a potential concern. Exa-cel and lovo-cel could cost about $2 million.
A version of this article appeared on Medscape.com.
These “milestone treatments” mark the first cell-based gene therapies for this debilitating and potentially life-threatening blood disorder that affects about 100,000 people in the United States.
The two therapies are exagamglogene autotemcel, or exa-cel (Casgevy; Vertex Pharmaceuticals and Crispr Therapeutics), and lovotibeglogene autotemcel, or lovo-cel (Lyfgenia; bluebird bio).
“The approval of the first gene therapies for [sickle cell disease] represents a tremendous step forward for the [sickle cell] community, which has been historically overlooked and underfunded,” said Robert A. Brodsky, MD, of Johns Hopkins University School of Medicine, in a statement from the American Society of Hematology, following the approval.
“We are excited to advance the field, especially for individuals whose lives have been severely disrupted by the disease, by approving two cell-based gene therapies today,” Nicole Verdun, MD, of the FDA’s Center for Biologics Evaluation and Research, added in an agency press release.
Sickle cell disease involves a mutation in hemoglobin, a protein in red blood cells that provides oxygen to tissues. The mutation leads red blood cells to develop a crescent or sickle shape, which can restrict blood flow and cause severe pain and organ damage, known as vaso-occlusive events or crises.
Treatment options prior to these approvals primarily included red blood transfusions and hydroxyurea alongside pain management. The only potential curative option has been allogeneic hematopoietic stem cell transplantation, but that comes with significant risks and most patients don’t have an appropriate donor.
Exa-cel
Exa-cel uses CRISPR gene-editing technology. Before the infusion, patients undergo myeloablative conditioning, which removes cells from the bone marrow. These cells are genetically modified to produce fetal hemoglobin. Patients then receive an infusion of the edited cells, which can help restore normal hemoglobin production.
The FDA approval was based on data from the pivotal CLIMB SCD-121 trial. In an October advisory committee meeting, the FDA highlighted trial data demonstrating that 29 of 31 patients reached the trial’s primary endpoint: freedom from severe vaso-occlusive crises over a 12-month period. In addition, 28 of these patients remained free of vaso-occlusive crises for almost 2 years.
The committee noted that one of the 31 patients died about 9 months after receiving an exa-cel infusion.
The cell-based gene therapy also increased both fetal and total hemoglobin, with total hemoglobin levels increasing to > 11 g/dL by month 3 and remaining at that level afterward. No patients experienced graft failure or rejection.
The most common side effects included low platelets and white blood cell counts, mouth sores, nausea, musculoskeletal pain, vomiting, and febrile neutropenia.
Exa-cel could “provide a one-time functional cure” for patients with severe sickle cell disease, according to Franco Locatelli, MD, of Sapienza University of Rome, who presented initial findings last year.
While the current approval is for patients with infusion-dependent sickle cell disease, exa-cel is also being evaluated in patients with another blood disorder, beta-thalassemia.
Lovo-cel
Lovo-cel, a cell-based gene therapy, uses a different technology — a lentiviral vector, or gene delivery vehicle — that can also genetically modify a patient’s blood stem cells.
Like exa-cel, lovo-cel is a one-time, single-dose infusion that contains the patient’s modified cells. Before the infusion, patients undergo myeloablative conditioning. The patient’s stem cells are then genetically modified to allow them to produce the most common form of hemoglobin, HbA
This approval was based on data from a single-arm, 24-month study in patients aged 12-50 years who had sickle cell disease and a history of vaso-occlusive events.
Overall, 88% of patients (28 of 32) achieved complete resolution of vaso-occlusive events 6-18 months after the infusion.
The most common side effects included stomatitis; febrile neutropenia; and low platelet, white blood cell, and red blood cell counts.
The FDA noted that hematologic cancer has occurred in patients treated with lovo-cel, and the label includes a black-box warning about the risk.
Dr. Brodsky noted, however, that “while these new gene therapies are potentially life-changing for individuals living with [sickle cell disease], they must be accessible to be effective.”
Access is a potential concern. Exa-cel and lovo-cel could cost about $2 million.
A version of this article appeared on Medscape.com.
Blurred vision and shortness of breath
Given her symptomatology, imaging, and laboratory study results, this patient is diagnosed with small cell lung cancer (SCLC) and brain metastases. The pulmonologist shares the findings with the patient, and over the next several days, a multidisciplinary team, which includes oncology and radiology, forms to guide the patient through staging and treatment options.
SCLC is a neuroendocrine carcinoma, which is an aggressive form of lung cancer associated with rapid growth and early spread to distant sites and frequent association with distinct paraneoplastic syndromes. Approximately 13% of newly diagnosed lung cancers are SCLC. Clinical presentation is often advanced stage and includes shortness of breath, cough, bone pain, weight loss, fatigue, and neurologic dysfunction, including blurred vision, dizziness, and headaches that disturb sleep. Typically, symptom onset is quick, with the duration of symptoms lasting between 8 and 12 weeks before presentation.
According to CHEST guidelines, when clinical and radiographic findings suggest SCLC, diagnosis should be confirmed using the least invasive technique possible on the basis of presentation. Fine-needle aspiration or biopsy is recommended to assess a suspicious singular extrathoracic site for metastasis. If that approach is not feasible, guidelines recommend diagnosing the primary lung lesion. If there is an accessible pleural effusion, ultrasound-guided thoracentesis is recommended for diagnosis. If the result of pleural fluid cytology is negative, pleural biopsy using image-guided pleural biopsy, medical, or surgical thoracoscopy is recommended next. Common mutations associated with SCLC include RB1 and TP53 gene mutations.
Nearly all patients with SCLC (98%) have a history of tobacco use. Uranium or radon exposure has also been linked to SCLC. Pathogenesis occurs in the peribronchial region of the respiratory system and moves into the bronchial submucosa. Widespread metastases can appear early during SCLC and generally affect mediastinal lymph nodes, bones, brain, liver, and adrenal glands.
Patient education should include information about clinical trials, available treatment options, and associated adverse events. Smoking cessation is encouraged for current smokers with SCLC.
For patients with extensive-stage metastatic SCLC, the new standard of care combines the immunotherapy atezolizumab, a humanized monoclonal anti–programmed death–ligand 1 (PD-L1) antibody, with chemotherapy (cisplatin-etoposide). When used in the first-line setting, this combination has been shown to improve survival outcomes. Of course, clinical trials are ongoing; other treatments in development include additional classes of immunotherapies (programmed cell death protein1 [PD-1] inhibitor antibody, anti-PD1 antibody, and cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) inhibitor antibody) and targeted therapies (delta-like protein 3 antibody-drug conjugate).
Karl J. D'Silva, MD, Clinical Assistant Professor, Department of Medicine, Tufts University School of Medicine, Boston; Medical Director, Department of Oncology and Hematology, Lahey Hospital and Medical Center, Peabody, Massachusetts.
Karl J. D'Silva, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Given her symptomatology, imaging, and laboratory study results, this patient is diagnosed with small cell lung cancer (SCLC) and brain metastases. The pulmonologist shares the findings with the patient, and over the next several days, a multidisciplinary team, which includes oncology and radiology, forms to guide the patient through staging and treatment options.
SCLC is a neuroendocrine carcinoma, which is an aggressive form of lung cancer associated with rapid growth and early spread to distant sites and frequent association with distinct paraneoplastic syndromes. Approximately 13% of newly diagnosed lung cancers are SCLC. Clinical presentation is often advanced stage and includes shortness of breath, cough, bone pain, weight loss, fatigue, and neurologic dysfunction, including blurred vision, dizziness, and headaches that disturb sleep. Typically, symptom onset is quick, with the duration of symptoms lasting between 8 and 12 weeks before presentation.
According to CHEST guidelines, when clinical and radiographic findings suggest SCLC, diagnosis should be confirmed using the least invasive technique possible on the basis of presentation. Fine-needle aspiration or biopsy is recommended to assess a suspicious singular extrathoracic site for metastasis. If that approach is not feasible, guidelines recommend diagnosing the primary lung lesion. If there is an accessible pleural effusion, ultrasound-guided thoracentesis is recommended for diagnosis. If the result of pleural fluid cytology is negative, pleural biopsy using image-guided pleural biopsy, medical, or surgical thoracoscopy is recommended next. Common mutations associated with SCLC include RB1 and TP53 gene mutations.
Nearly all patients with SCLC (98%) have a history of tobacco use. Uranium or radon exposure has also been linked to SCLC. Pathogenesis occurs in the peribronchial region of the respiratory system and moves into the bronchial submucosa. Widespread metastases can appear early during SCLC and generally affect mediastinal lymph nodes, bones, brain, liver, and adrenal glands.
Patient education should include information about clinical trials, available treatment options, and associated adverse events. Smoking cessation is encouraged for current smokers with SCLC.
For patients with extensive-stage metastatic SCLC, the new standard of care combines the immunotherapy atezolizumab, a humanized monoclonal anti–programmed death–ligand 1 (PD-L1) antibody, with chemotherapy (cisplatin-etoposide). When used in the first-line setting, this combination has been shown to improve survival outcomes. Of course, clinical trials are ongoing; other treatments in development include additional classes of immunotherapies (programmed cell death protein1 [PD-1] inhibitor antibody, anti-PD1 antibody, and cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) inhibitor antibody) and targeted therapies (delta-like protein 3 antibody-drug conjugate).
Karl J. D'Silva, MD, Clinical Assistant Professor, Department of Medicine, Tufts University School of Medicine, Boston; Medical Director, Department of Oncology and Hematology, Lahey Hospital and Medical Center, Peabody, Massachusetts.
Karl J. D'Silva, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Given her symptomatology, imaging, and laboratory study results, this patient is diagnosed with small cell lung cancer (SCLC) and brain metastases. The pulmonologist shares the findings with the patient, and over the next several days, a multidisciplinary team, which includes oncology and radiology, forms to guide the patient through staging and treatment options.
SCLC is a neuroendocrine carcinoma, which is an aggressive form of lung cancer associated with rapid growth and early spread to distant sites and frequent association with distinct paraneoplastic syndromes. Approximately 13% of newly diagnosed lung cancers are SCLC. Clinical presentation is often advanced stage and includes shortness of breath, cough, bone pain, weight loss, fatigue, and neurologic dysfunction, including blurred vision, dizziness, and headaches that disturb sleep. Typically, symptom onset is quick, with the duration of symptoms lasting between 8 and 12 weeks before presentation.
According to CHEST guidelines, when clinical and radiographic findings suggest SCLC, diagnosis should be confirmed using the least invasive technique possible on the basis of presentation. Fine-needle aspiration or biopsy is recommended to assess a suspicious singular extrathoracic site for metastasis. If that approach is not feasible, guidelines recommend diagnosing the primary lung lesion. If there is an accessible pleural effusion, ultrasound-guided thoracentesis is recommended for diagnosis. If the result of pleural fluid cytology is negative, pleural biopsy using image-guided pleural biopsy, medical, or surgical thoracoscopy is recommended next. Common mutations associated with SCLC include RB1 and TP53 gene mutations.
Nearly all patients with SCLC (98%) have a history of tobacco use. Uranium or radon exposure has also been linked to SCLC. Pathogenesis occurs in the peribronchial region of the respiratory system and moves into the bronchial submucosa. Widespread metastases can appear early during SCLC and generally affect mediastinal lymph nodes, bones, brain, liver, and adrenal glands.
Patient education should include information about clinical trials, available treatment options, and associated adverse events. Smoking cessation is encouraged for current smokers with SCLC.
For patients with extensive-stage metastatic SCLC, the new standard of care combines the immunotherapy atezolizumab, a humanized monoclonal anti–programmed death–ligand 1 (PD-L1) antibody, with chemotherapy (cisplatin-etoposide). When used in the first-line setting, this combination has been shown to improve survival outcomes. Of course, clinical trials are ongoing; other treatments in development include additional classes of immunotherapies (programmed cell death protein1 [PD-1] inhibitor antibody, anti-PD1 antibody, and cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) inhibitor antibody) and targeted therapies (delta-like protein 3 antibody-drug conjugate).
Karl J. D'Silva, MD, Clinical Assistant Professor, Department of Medicine, Tufts University School of Medicine, Boston; Medical Director, Department of Oncology and Hematology, Lahey Hospital and Medical Center, Peabody, Massachusetts.
Karl J. D'Silva, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 66-year-old woman who is a former smoker presents to her primary care physician with a recent history of dizziness, blurred vision, shortness of breath, and headaches that wake her up in the morning. The patient reports significant weight loss, persistent cough, and fatigue over the past 2 months. The patient owns and runs a local French bakery and reports difficulty keeping up with routine productivity. In addition, she has had to skip several days of work lately and rely more on her staff, which increases business costs, because of the severity of her symptoms. Her height is 5 ft 6 in and weight is 176 lb; her BMI is 28.4.
On physical examination, her physician detects enlarged axillary lymph nodes and dullness to percussion and decreased breath sounds in the central right lung. Fundoscopy reveals increased intracranial pressure, and a neurologic exam shows abnormalities in cerebellar function. The physician orders a CT from the base of the skull to mid-thigh as well as a brain MRI. Results show tumors in the right ipsilateral hemithorax and contralateral lung and metastases in the brain. The patient is referred to pulmonology, where she undergoes a fine needle aspiration of the suspected axillary lymph nodes; cytology reveals metastatic cancer. Thereafter, the patient undergoes a bronchoscopy and transbronchial biopsy. Comprehensive genomic profiling of the tumor sample reveals TP53 and RB1 gene mutations.
Trop-2 drug conjugate may trump chemo in HR+, HER2- breast cancer
SAN ANTONIO — In endocrine-resistant, HR+/HER2- metastatic breast cancer, the antibody-drug conjugate (ADC) datopotamab deruxtecan (dato-DXd, Daiichi Sankyo/AstraZeneca) has greater efficacy and a better safety profile than investigator-chosen chemotherapy, according to the latest results from the TROPION-Breast01 clinical trial.
If approved, the ADC would join sacituzumab govitecan (Trodelvy, Gilead) as agents that target trophoblast cell-surface antigen-2 (Trop-2), which is universally expressed in breast cancer, according to Aditya Bardia, MD, who presented the new results at the San Antonio Breast Cancer Symposium.
“ If this drug gets approved, we need more work in terms of biomarkers of response and resistance to understand how to select these agents and how to sequence these different agents,” Dr. Bardia said in an interview. He is associate professor of medicine at Harvard Medical School and Massachusetts General Hospital Cancer Center.
Dato-DXd has a proprietary linker technology that makes it more stable in plasma and more selective for tumor cells, where overexpressed enzymes cleave it and lead to release of the drug. This reduces off-target toxicity, said Dr. Bardia.
The primary results from TROPION-Breast01, presented at ESMO 2023, showed statistically significant improvement in progression-free survival compared to investigator’s choice of chemotherapy (hazard ratio, [HR], 0.63; P < .0001) and a higher overall response rate (36.4% versus 22.9%).
At SABCS, Dr. Bardia presented additional PFS sub-analyses and safety data.
TROPION-Breast01 included 732 patients who had failed or were ineligible for endocrine therapy, and who had received 1-2 lines of chemotherapy in the metastatic or inoperable setting. They were randomized to dato-DXd or chemotherapy.
The median PFS as determined by blinded independent central review was longer in the dato-DXd group (6.9 versus 4.5 months; P < .0001). Time to first subsequent therapy was also longer (median 8.2 versus 5.0 months; HR, 0.53; 95% CI, 0.45-0.64).
PFS benefit was similar regardless of duration of previous CDK4/6 inhibitor treatment. There was no significant difference in median PFS among patients with brain metastases at baseline (HR, 0.73; 95% CI, 0.39-1.42).
Grade 3 or higher treatment-related adverse events were less common in the dato-DXd group (21% versus 45%), as were the incidences of dose interruption (12% versus 25%), treatment-related neutropenia (11% versus 42%), grade 3 or higher treatment-related neutropenia (1% versus 31%), neutropenia-related dose interruption (0% versus 17%), and neutropenia-related dose reduction (0.3% versus 13%). G-CSF usage was lower in the dato-DXd group during treatment (3% versus 22%) and after treatment (0.3% versus 8%).
Stomatitis was more common in the dato-DXd group (50% versus 13%), including grade 3 (6% versus 3%). Dose reduction due to stomatitis was also more common (12% versus 1%), and discontinuation occurred in just 1 patient (0.3%) in the dato-DXd group.
The median time to confirmed deterioration, as measured by the Global Health Status/Quality of Life scale, was longer in the dato-DXd group (9.0 versus 4.8 months; HR, 0.76; 95% CI, 0.58-0.98).
During the Q & A period after the talk, Marc E. Lippman, MD, professor of oncology and director of the breast cancer program at Georgetown University’s Lombardi Comprehensive Cancer Center, questioned the assumption that Trop-2 is universally expressed in breast cancer, and asked if there were any data on outcomes associated with its expression. “That’s a very good question,” said Dr. Bardia. He said that the team is working on the problem, including identifying the best tool to measure Trop-2 expression, but also addressing whether expression changes over time. Finally, the team hopes to determine if treatment response might relate to levels of expression.
Trop-2 expression was studied in the ASCENT trial that examined sacituzumab govitecan in metastatic triple-negative breast cancer, and there was no apparent link. “In general, we don’t see a very strong correlation between Trop-2 expression and outcomes. In the ASCENT trial, even in patients who had low expression of Trop-2, the outcomes with Trop-2 antibody drug conjugates [were] superior to standard chemotherapy,” replied Dr. Bardia.
Ron Bose, MD, PhD, also asked if there would be broader biomarker analyses of responders versus nonresponders to dato-dxd. “I think it’s very important to know, what are the biomarkers that predict efficacy for dato-dxd. The median progression free survival improvement was only about two months, maybe a little bit more, so knowing which patients are going to get the most benefit will be very important,” Dr. Bose said in an interview. Dr. Bose is associate professor of oncology at the Washington University School of Medicine in St. Louis.
Overall, he was impressed by the results. “The median progression free survival benefit is moderate, but the safety I think is really particularly strong, and when I’m thinking about this for my patients, the fact that there is a progression free survival benefit, plus a safety benefit [compared to chemotherapy] makes it very appealing,” he said.
Dr. Bose has consulted for Genentech. Dr. Bardia has been on advisory boards for Pfizer, Novartis, Genentech, Merck, Radius Health/Menarini, Immunomedics/Gilead, Sanofi, Daiichi Pharma/AstraZeneca, Phillips, Eli Lilly, Mersana, and Foundation Medicine. He has received research grants from Genentech, Novartis, Pfizer, Merck, Sanofi, Radius Health/Menarini, Immunomedics/Gilead, Daiichi Pharma/AstraZeneca, Natera, and Eli Lilly.
SAN ANTONIO — In endocrine-resistant, HR+/HER2- metastatic breast cancer, the antibody-drug conjugate (ADC) datopotamab deruxtecan (dato-DXd, Daiichi Sankyo/AstraZeneca) has greater efficacy and a better safety profile than investigator-chosen chemotherapy, according to the latest results from the TROPION-Breast01 clinical trial.
If approved, the ADC would join sacituzumab govitecan (Trodelvy, Gilead) as agents that target trophoblast cell-surface antigen-2 (Trop-2), which is universally expressed in breast cancer, according to Aditya Bardia, MD, who presented the new results at the San Antonio Breast Cancer Symposium.
“ If this drug gets approved, we need more work in terms of biomarkers of response and resistance to understand how to select these agents and how to sequence these different agents,” Dr. Bardia said in an interview. He is associate professor of medicine at Harvard Medical School and Massachusetts General Hospital Cancer Center.
Dato-DXd has a proprietary linker technology that makes it more stable in plasma and more selective for tumor cells, where overexpressed enzymes cleave it and lead to release of the drug. This reduces off-target toxicity, said Dr. Bardia.
The primary results from TROPION-Breast01, presented at ESMO 2023, showed statistically significant improvement in progression-free survival compared to investigator’s choice of chemotherapy (hazard ratio, [HR], 0.63; P < .0001) and a higher overall response rate (36.4% versus 22.9%).
At SABCS, Dr. Bardia presented additional PFS sub-analyses and safety data.
TROPION-Breast01 included 732 patients who had failed or were ineligible for endocrine therapy, and who had received 1-2 lines of chemotherapy in the metastatic or inoperable setting. They were randomized to dato-DXd or chemotherapy.
The median PFS as determined by blinded independent central review was longer in the dato-DXd group (6.9 versus 4.5 months; P < .0001). Time to first subsequent therapy was also longer (median 8.2 versus 5.0 months; HR, 0.53; 95% CI, 0.45-0.64).
PFS benefit was similar regardless of duration of previous CDK4/6 inhibitor treatment. There was no significant difference in median PFS among patients with brain metastases at baseline (HR, 0.73; 95% CI, 0.39-1.42).
Grade 3 or higher treatment-related adverse events were less common in the dato-DXd group (21% versus 45%), as were the incidences of dose interruption (12% versus 25%), treatment-related neutropenia (11% versus 42%), grade 3 or higher treatment-related neutropenia (1% versus 31%), neutropenia-related dose interruption (0% versus 17%), and neutropenia-related dose reduction (0.3% versus 13%). G-CSF usage was lower in the dato-DXd group during treatment (3% versus 22%) and after treatment (0.3% versus 8%).
Stomatitis was more common in the dato-DXd group (50% versus 13%), including grade 3 (6% versus 3%). Dose reduction due to stomatitis was also more common (12% versus 1%), and discontinuation occurred in just 1 patient (0.3%) in the dato-DXd group.
The median time to confirmed deterioration, as measured by the Global Health Status/Quality of Life scale, was longer in the dato-DXd group (9.0 versus 4.8 months; HR, 0.76; 95% CI, 0.58-0.98).
During the Q & A period after the talk, Marc E. Lippman, MD, professor of oncology and director of the breast cancer program at Georgetown University’s Lombardi Comprehensive Cancer Center, questioned the assumption that Trop-2 is universally expressed in breast cancer, and asked if there were any data on outcomes associated with its expression. “That’s a very good question,” said Dr. Bardia. He said that the team is working on the problem, including identifying the best tool to measure Trop-2 expression, but also addressing whether expression changes over time. Finally, the team hopes to determine if treatment response might relate to levels of expression.
Trop-2 expression was studied in the ASCENT trial that examined sacituzumab govitecan in metastatic triple-negative breast cancer, and there was no apparent link. “In general, we don’t see a very strong correlation between Trop-2 expression and outcomes. In the ASCENT trial, even in patients who had low expression of Trop-2, the outcomes with Trop-2 antibody drug conjugates [were] superior to standard chemotherapy,” replied Dr. Bardia.
Ron Bose, MD, PhD, also asked if there would be broader biomarker analyses of responders versus nonresponders to dato-dxd. “I think it’s very important to know, what are the biomarkers that predict efficacy for dato-dxd. The median progression free survival improvement was only about two months, maybe a little bit more, so knowing which patients are going to get the most benefit will be very important,” Dr. Bose said in an interview. Dr. Bose is associate professor of oncology at the Washington University School of Medicine in St. Louis.
Overall, he was impressed by the results. “The median progression free survival benefit is moderate, but the safety I think is really particularly strong, and when I’m thinking about this for my patients, the fact that there is a progression free survival benefit, plus a safety benefit [compared to chemotherapy] makes it very appealing,” he said.
Dr. Bose has consulted for Genentech. Dr. Bardia has been on advisory boards for Pfizer, Novartis, Genentech, Merck, Radius Health/Menarini, Immunomedics/Gilead, Sanofi, Daiichi Pharma/AstraZeneca, Phillips, Eli Lilly, Mersana, and Foundation Medicine. He has received research grants from Genentech, Novartis, Pfizer, Merck, Sanofi, Radius Health/Menarini, Immunomedics/Gilead, Daiichi Pharma/AstraZeneca, Natera, and Eli Lilly.
SAN ANTONIO — In endocrine-resistant, HR+/HER2- metastatic breast cancer, the antibody-drug conjugate (ADC) datopotamab deruxtecan (dato-DXd, Daiichi Sankyo/AstraZeneca) has greater efficacy and a better safety profile than investigator-chosen chemotherapy, according to the latest results from the TROPION-Breast01 clinical trial.
If approved, the ADC would join sacituzumab govitecan (Trodelvy, Gilead) as agents that target trophoblast cell-surface antigen-2 (Trop-2), which is universally expressed in breast cancer, according to Aditya Bardia, MD, who presented the new results at the San Antonio Breast Cancer Symposium.
“ If this drug gets approved, we need more work in terms of biomarkers of response and resistance to understand how to select these agents and how to sequence these different agents,” Dr. Bardia said in an interview. He is associate professor of medicine at Harvard Medical School and Massachusetts General Hospital Cancer Center.
Dato-DXd has a proprietary linker technology that makes it more stable in plasma and more selective for tumor cells, where overexpressed enzymes cleave it and lead to release of the drug. This reduces off-target toxicity, said Dr. Bardia.
The primary results from TROPION-Breast01, presented at ESMO 2023, showed statistically significant improvement in progression-free survival compared to investigator’s choice of chemotherapy (hazard ratio, [HR], 0.63; P < .0001) and a higher overall response rate (36.4% versus 22.9%).
At SABCS, Dr. Bardia presented additional PFS sub-analyses and safety data.
TROPION-Breast01 included 732 patients who had failed or were ineligible for endocrine therapy, and who had received 1-2 lines of chemotherapy in the metastatic or inoperable setting. They were randomized to dato-DXd or chemotherapy.
The median PFS as determined by blinded independent central review was longer in the dato-DXd group (6.9 versus 4.5 months; P < .0001). Time to first subsequent therapy was also longer (median 8.2 versus 5.0 months; HR, 0.53; 95% CI, 0.45-0.64).
PFS benefit was similar regardless of duration of previous CDK4/6 inhibitor treatment. There was no significant difference in median PFS among patients with brain metastases at baseline (HR, 0.73; 95% CI, 0.39-1.42).
Grade 3 or higher treatment-related adverse events were less common in the dato-DXd group (21% versus 45%), as were the incidences of dose interruption (12% versus 25%), treatment-related neutropenia (11% versus 42%), grade 3 or higher treatment-related neutropenia (1% versus 31%), neutropenia-related dose interruption (0% versus 17%), and neutropenia-related dose reduction (0.3% versus 13%). G-CSF usage was lower in the dato-DXd group during treatment (3% versus 22%) and after treatment (0.3% versus 8%).
Stomatitis was more common in the dato-DXd group (50% versus 13%), including grade 3 (6% versus 3%). Dose reduction due to stomatitis was also more common (12% versus 1%), and discontinuation occurred in just 1 patient (0.3%) in the dato-DXd group.
The median time to confirmed deterioration, as measured by the Global Health Status/Quality of Life scale, was longer in the dato-DXd group (9.0 versus 4.8 months; HR, 0.76; 95% CI, 0.58-0.98).
During the Q & A period after the talk, Marc E. Lippman, MD, professor of oncology and director of the breast cancer program at Georgetown University’s Lombardi Comprehensive Cancer Center, questioned the assumption that Trop-2 is universally expressed in breast cancer, and asked if there were any data on outcomes associated with its expression. “That’s a very good question,” said Dr. Bardia. He said that the team is working on the problem, including identifying the best tool to measure Trop-2 expression, but also addressing whether expression changes over time. Finally, the team hopes to determine if treatment response might relate to levels of expression.
Trop-2 expression was studied in the ASCENT trial that examined sacituzumab govitecan in metastatic triple-negative breast cancer, and there was no apparent link. “In general, we don’t see a very strong correlation between Trop-2 expression and outcomes. In the ASCENT trial, even in patients who had low expression of Trop-2, the outcomes with Trop-2 antibody drug conjugates [were] superior to standard chemotherapy,” replied Dr. Bardia.
Ron Bose, MD, PhD, also asked if there would be broader biomarker analyses of responders versus nonresponders to dato-dxd. “I think it’s very important to know, what are the biomarkers that predict efficacy for dato-dxd. The median progression free survival improvement was only about two months, maybe a little bit more, so knowing which patients are going to get the most benefit will be very important,” Dr. Bose said in an interview. Dr. Bose is associate professor of oncology at the Washington University School of Medicine in St. Louis.
Overall, he was impressed by the results. “The median progression free survival benefit is moderate, but the safety I think is really particularly strong, and when I’m thinking about this for my patients, the fact that there is a progression free survival benefit, plus a safety benefit [compared to chemotherapy] makes it very appealing,” he said.
Dr. Bose has consulted for Genentech. Dr. Bardia has been on advisory boards for Pfizer, Novartis, Genentech, Merck, Radius Health/Menarini, Immunomedics/Gilead, Sanofi, Daiichi Pharma/AstraZeneca, Phillips, Eli Lilly, Mersana, and Foundation Medicine. He has received research grants from Genentech, Novartis, Pfizer, Merck, Sanofi, Radius Health/Menarini, Immunomedics/Gilead, Daiichi Pharma/AstraZeneca, Natera, and Eli Lilly.
AT SABCS 2023