User login
Novel AKT inhibitor active against MM cells
A novel inhibitor of AKT pathway signaling showed significant cytotoxic activity in mouse models and in human cells isolated from patients with primary or relapsed multiple myeloma (MM), investigators reported.
The experimental agent, labeled HS1793, is a derivative of the naturally occurring antioxidant compound resveratrol. In preclinical studies, HS1793 was shown to offer “great promise in eliminating MM cells and improving therapeutic responses in primary and relapsed/refractory MM patients,” according to Jin Han, MD, PhD, of Inje University in Busan, South Korea, and colleagues.
In a series of experiments, described in the journal Cancer Letters, the investigators demonstrated that HS1793 decreased AKT signaling to induce mitochondria-mediated cell death in multiple myeloma cells, and was cytotoxic and specific for myeloma cells in a mouse model of human metastatic myeloma, and in samples of human multiple myeloma cells.
When activated, AKT promotes oncogenesis by in turn activating other downstream pathways involved in proliferation or survival of malignant cells.
“AKT is frequently activated in MM cells and the incidence of AKT activation correlates positively with disease activity,” the authors noted.
They first screened 400 compounds, and narrowed in on resveratrol analogs, eventually choosing HS1793 as the most promising candidate.
This first experiment found evidence that suggested that the compound inhibits AKT activation by interfering with the interaction between AKT and its promoter HSP90.
They then showed in human MM cell lines that the antimyeloma action of HS1793 appeared to be from a dose-dependent effect that allowed for mitochondria-mediated programmed cell death.
In a separate series of experiments, they found that the inhibition by HS1793 of AKT/HSP90 interaction results in cell death by suppressing nuclear factor kappa–B (NF-KB) pathway signaling. The investigators had previously reported that a different compound, an inhibitor of spindle protein kinesin, induced MM cell death via inhibition of NF-KB signaling.
Next, the investigators showed that HS1793-induced cell death was caused by the direct inhibition of AKT that in turn suppressed NF-KB activation.
Finally, they showed in a mouse model of multiple myeloma metastatic to bone that HS1793 “dramatically decreased” lytic skull and femur lesions in treated mice, compared with mice treated with a vehicle placebo, and increased survival of the mice that received the AKT inhibitor.
They also showed that HS1793 was cytotoxic to multiple myeloma cells but not to normal plasma cells isolated from patients with MM.
“Given that HS1793 treatment specifically induced the death of primary and relapsed MM cells, HS1793 offers excellent translational potential as a novel MM therapy,” they wrote.
The study was supported by grants from the Korean government. The researchers reported having no potential conflicts of interest.
SOURCE: Song IS et al. Cancer Lett. 2018;432:205-15.
A novel inhibitor of AKT pathway signaling showed significant cytotoxic activity in mouse models and in human cells isolated from patients with primary or relapsed multiple myeloma (MM), investigators reported.
The experimental agent, labeled HS1793, is a derivative of the naturally occurring antioxidant compound resveratrol. In preclinical studies, HS1793 was shown to offer “great promise in eliminating MM cells and improving therapeutic responses in primary and relapsed/refractory MM patients,” according to Jin Han, MD, PhD, of Inje University in Busan, South Korea, and colleagues.
In a series of experiments, described in the journal Cancer Letters, the investigators demonstrated that HS1793 decreased AKT signaling to induce mitochondria-mediated cell death in multiple myeloma cells, and was cytotoxic and specific for myeloma cells in a mouse model of human metastatic myeloma, and in samples of human multiple myeloma cells.
When activated, AKT promotes oncogenesis by in turn activating other downstream pathways involved in proliferation or survival of malignant cells.
“AKT is frequently activated in MM cells and the incidence of AKT activation correlates positively with disease activity,” the authors noted.
They first screened 400 compounds, and narrowed in on resveratrol analogs, eventually choosing HS1793 as the most promising candidate.
This first experiment found evidence that suggested that the compound inhibits AKT activation by interfering with the interaction between AKT and its promoter HSP90.
They then showed in human MM cell lines that the antimyeloma action of HS1793 appeared to be from a dose-dependent effect that allowed for mitochondria-mediated programmed cell death.
In a separate series of experiments, they found that the inhibition by HS1793 of AKT/HSP90 interaction results in cell death by suppressing nuclear factor kappa–B (NF-KB) pathway signaling. The investigators had previously reported that a different compound, an inhibitor of spindle protein kinesin, induced MM cell death via inhibition of NF-KB signaling.
Next, the investigators showed that HS1793-induced cell death was caused by the direct inhibition of AKT that in turn suppressed NF-KB activation.
Finally, they showed in a mouse model of multiple myeloma metastatic to bone that HS1793 “dramatically decreased” lytic skull and femur lesions in treated mice, compared with mice treated with a vehicle placebo, and increased survival of the mice that received the AKT inhibitor.
They also showed that HS1793 was cytotoxic to multiple myeloma cells but not to normal plasma cells isolated from patients with MM.
“Given that HS1793 treatment specifically induced the death of primary and relapsed MM cells, HS1793 offers excellent translational potential as a novel MM therapy,” they wrote.
The study was supported by grants from the Korean government. The researchers reported having no potential conflicts of interest.
SOURCE: Song IS et al. Cancer Lett. 2018;432:205-15.
A novel inhibitor of AKT pathway signaling showed significant cytotoxic activity in mouse models and in human cells isolated from patients with primary or relapsed multiple myeloma (MM), investigators reported.
The experimental agent, labeled HS1793, is a derivative of the naturally occurring antioxidant compound resveratrol. In preclinical studies, HS1793 was shown to offer “great promise in eliminating MM cells and improving therapeutic responses in primary and relapsed/refractory MM patients,” according to Jin Han, MD, PhD, of Inje University in Busan, South Korea, and colleagues.
In a series of experiments, described in the journal Cancer Letters, the investigators demonstrated that HS1793 decreased AKT signaling to induce mitochondria-mediated cell death in multiple myeloma cells, and was cytotoxic and specific for myeloma cells in a mouse model of human metastatic myeloma, and in samples of human multiple myeloma cells.
When activated, AKT promotes oncogenesis by in turn activating other downstream pathways involved in proliferation or survival of malignant cells.
“AKT is frequently activated in MM cells and the incidence of AKT activation correlates positively with disease activity,” the authors noted.
They first screened 400 compounds, and narrowed in on resveratrol analogs, eventually choosing HS1793 as the most promising candidate.
This first experiment found evidence that suggested that the compound inhibits AKT activation by interfering with the interaction between AKT and its promoter HSP90.
They then showed in human MM cell lines that the antimyeloma action of HS1793 appeared to be from a dose-dependent effect that allowed for mitochondria-mediated programmed cell death.
In a separate series of experiments, they found that the inhibition by HS1793 of AKT/HSP90 interaction results in cell death by suppressing nuclear factor kappa–B (NF-KB) pathway signaling. The investigators had previously reported that a different compound, an inhibitor of spindle protein kinesin, induced MM cell death via inhibition of NF-KB signaling.
Next, the investigators showed that HS1793-induced cell death was caused by the direct inhibition of AKT that in turn suppressed NF-KB activation.
Finally, they showed in a mouse model of multiple myeloma metastatic to bone that HS1793 “dramatically decreased” lytic skull and femur lesions in treated mice, compared with mice treated with a vehicle placebo, and increased survival of the mice that received the AKT inhibitor.
They also showed that HS1793 was cytotoxic to multiple myeloma cells but not to normal plasma cells isolated from patients with MM.
“Given that HS1793 treatment specifically induced the death of primary and relapsed MM cells, HS1793 offers excellent translational potential as a novel MM therapy,” they wrote.
The study was supported by grants from the Korean government. The researchers reported having no potential conflicts of interest.
SOURCE: Song IS et al. Cancer Lett. 2018;432:205-15.
FROM CANCER LETTERS
Key clinical point:
Major finding: HS1793 showed significant multiple myeloma cytotoxicity in mouse models and in human cells isolated from patients with primary or relapsed/refractory myeloma.
Study details: Preclinical investigations in cell lines, murine models, and isolated human multiple myeloma cells.
Disclosures: The study was supported by grants from the Korean government. The researchers reported having no potential conflicts of interest.
Source: Song IS et al. Cancer Lett. 2018:432:205-15.
MDS posttransplant gene sequencing prognostic for progression
For patients with myelodysplastic syndrome, gene sequencing of bone marrow samples early after bone marrow transplant with curative intent may provide important prognostic information.
Among 86 patients with myelodysplastic syndrome (MDS), higher maximum variant allele frequency of residual disease–associated mutations at 30 days posttransplantation was significantly associated with disease progression and lower rates of progression-free survival (PFS) at 1 year, reported Eric J. Duncavage, MD, from Washington University in St. Louis, and his colleagues.
“Although this exploratory study has limitations, our results suggest that sequencing-based detection of tumor cells and measurable residual disease after allogeneic hematopoietic stem cell transplantation has prognostic significance for patients with MDS,” they wrote in the New England Journal of Medicine.
Risk of progression was significantly higher among patients who had undergone reduced-intensity conditioning prior to hematopoietic stem cell transplants (HSCT) than among patients who had undergone myeloablative conditioning regimens.
To get a better handle on the significance of molecular predictors of disease progression after HSCT, the authors used enhanced exome sequencing to evaluate paired samples of bone marrow and control DNA from normal skin, and error-corrected sequencing to identify somatic single-nucleotide variant mutations in posttransplant samples.
They detected at least one validated somatic mutation in the pretransplant samples from 86 of 90 patients. Of the 86 patients, 32 had at least one mutation with a maximum variant allele frequency of at least 0.5% detected 30 days after transplantation. The frequency is equivalent to 1 heterozygous mutant cell per 100 cells, the authors explained.
Patients who experienced disease progression had mutations with a median maximum variant allele frequency of 0.9%, compared with 0% for patients who did not have progression (P less than .001).
In all, 53.1% of patients with one or more mutations with a variant allele frequency of at least 0.5% at 30 days had disease progression within a year, compared with 13% of patients who did not have the mutations, even after adjustment for the type of conditioning regimen. The hazard ratio (HR) for disease progression in the patients with mutations was 3.86 (P less than .001).
The association between the presence of one or more mutations with a variant allele frequency of at least 0.5% with increased risk of disease progression was also seen at 100 days, even after adjustment for conditioning regimen (66.7% vs. 0%; HR, 6.52; P less than .001). In multivariable analysis controlling for prognostic scores, maximum variant allele frequency at 30 days, TP53 mutation status and conditioning regimen, the presence of a mutation with at least 0.5% variant allele frequency was associated with a more than fourfold risk of progression, including when the revised International Prognostic Scoring System score and conditioning regimen were considered as covariates. (HR, 4.48; P less than .001),
A separate multivariable analysis of PFS controlling for maximum variant allele frequency at day 30, conditioning regimen, age at transplantation, and type of MDS showed that mutations were associated with a more than twofold risk of progression or death (HR, 2.39; P = .002).
This analysis also showed that secondary acute myeloid leukemia was associated with worse PFS, compared with primary MDS (HR, 2.24; P = .001).
The investigators acknowledged that the high-coverage exome sequencing technique used for the study is not routinely available in the clinic. To control for this, they also looked at their data using a subset of genes that are usually included in gene sequencing panels for MDS and AML.
“Although we identified fewer patients with mutations with the use of this approach than with enhanced exome sequencing, the prognostic value of detection of measurable residual disease was still highly clinically significant,” they wrote.
The study was supported by grants from the Leukemia and Lymphoma Society, Edward P. Evans Foundation, National Cancer Institute, National Institutes of Health, Gabrielle’s Angel Foundation, and the Lottie Caroline Hardy Trust. Dr. Duncavage disclosed personal fees from AbbVie and Cofactor Genomics. The majority of coauthors reported nothing to disclose.
SOURCE: Duncavage EJ et al. N Engl J Med 2018;379:1028-41.
For patients with myelodysplastic syndrome, gene sequencing of bone marrow samples early after bone marrow transplant with curative intent may provide important prognostic information.
Among 86 patients with myelodysplastic syndrome (MDS), higher maximum variant allele frequency of residual disease–associated mutations at 30 days posttransplantation was significantly associated with disease progression and lower rates of progression-free survival (PFS) at 1 year, reported Eric J. Duncavage, MD, from Washington University in St. Louis, and his colleagues.
“Although this exploratory study has limitations, our results suggest that sequencing-based detection of tumor cells and measurable residual disease after allogeneic hematopoietic stem cell transplantation has prognostic significance for patients with MDS,” they wrote in the New England Journal of Medicine.
Risk of progression was significantly higher among patients who had undergone reduced-intensity conditioning prior to hematopoietic stem cell transplants (HSCT) than among patients who had undergone myeloablative conditioning regimens.
To get a better handle on the significance of molecular predictors of disease progression after HSCT, the authors used enhanced exome sequencing to evaluate paired samples of bone marrow and control DNA from normal skin, and error-corrected sequencing to identify somatic single-nucleotide variant mutations in posttransplant samples.
They detected at least one validated somatic mutation in the pretransplant samples from 86 of 90 patients. Of the 86 patients, 32 had at least one mutation with a maximum variant allele frequency of at least 0.5% detected 30 days after transplantation. The frequency is equivalent to 1 heterozygous mutant cell per 100 cells, the authors explained.
Patients who experienced disease progression had mutations with a median maximum variant allele frequency of 0.9%, compared with 0% for patients who did not have progression (P less than .001).
In all, 53.1% of patients with one or more mutations with a variant allele frequency of at least 0.5% at 30 days had disease progression within a year, compared with 13% of patients who did not have the mutations, even after adjustment for the type of conditioning regimen. The hazard ratio (HR) for disease progression in the patients with mutations was 3.86 (P less than .001).
The association between the presence of one or more mutations with a variant allele frequency of at least 0.5% with increased risk of disease progression was also seen at 100 days, even after adjustment for conditioning regimen (66.7% vs. 0%; HR, 6.52; P less than .001). In multivariable analysis controlling for prognostic scores, maximum variant allele frequency at 30 days, TP53 mutation status and conditioning regimen, the presence of a mutation with at least 0.5% variant allele frequency was associated with a more than fourfold risk of progression, including when the revised International Prognostic Scoring System score and conditioning regimen were considered as covariates. (HR, 4.48; P less than .001),
A separate multivariable analysis of PFS controlling for maximum variant allele frequency at day 30, conditioning regimen, age at transplantation, and type of MDS showed that mutations were associated with a more than twofold risk of progression or death (HR, 2.39; P = .002).
This analysis also showed that secondary acute myeloid leukemia was associated with worse PFS, compared with primary MDS (HR, 2.24; P = .001).
The investigators acknowledged that the high-coverage exome sequencing technique used for the study is not routinely available in the clinic. To control for this, they also looked at their data using a subset of genes that are usually included in gene sequencing panels for MDS and AML.
“Although we identified fewer patients with mutations with the use of this approach than with enhanced exome sequencing, the prognostic value of detection of measurable residual disease was still highly clinically significant,” they wrote.
The study was supported by grants from the Leukemia and Lymphoma Society, Edward P. Evans Foundation, National Cancer Institute, National Institutes of Health, Gabrielle’s Angel Foundation, and the Lottie Caroline Hardy Trust. Dr. Duncavage disclosed personal fees from AbbVie and Cofactor Genomics. The majority of coauthors reported nothing to disclose.
SOURCE: Duncavage EJ et al. N Engl J Med 2018;379:1028-41.
For patients with myelodysplastic syndrome, gene sequencing of bone marrow samples early after bone marrow transplant with curative intent may provide important prognostic information.
Among 86 patients with myelodysplastic syndrome (MDS), higher maximum variant allele frequency of residual disease–associated mutations at 30 days posttransplantation was significantly associated with disease progression and lower rates of progression-free survival (PFS) at 1 year, reported Eric J. Duncavage, MD, from Washington University in St. Louis, and his colleagues.
“Although this exploratory study has limitations, our results suggest that sequencing-based detection of tumor cells and measurable residual disease after allogeneic hematopoietic stem cell transplantation has prognostic significance for patients with MDS,” they wrote in the New England Journal of Medicine.
Risk of progression was significantly higher among patients who had undergone reduced-intensity conditioning prior to hematopoietic stem cell transplants (HSCT) than among patients who had undergone myeloablative conditioning regimens.
To get a better handle on the significance of molecular predictors of disease progression after HSCT, the authors used enhanced exome sequencing to evaluate paired samples of bone marrow and control DNA from normal skin, and error-corrected sequencing to identify somatic single-nucleotide variant mutations in posttransplant samples.
They detected at least one validated somatic mutation in the pretransplant samples from 86 of 90 patients. Of the 86 patients, 32 had at least one mutation with a maximum variant allele frequency of at least 0.5% detected 30 days after transplantation. The frequency is equivalent to 1 heterozygous mutant cell per 100 cells, the authors explained.
Patients who experienced disease progression had mutations with a median maximum variant allele frequency of 0.9%, compared with 0% for patients who did not have progression (P less than .001).
In all, 53.1% of patients with one or more mutations with a variant allele frequency of at least 0.5% at 30 days had disease progression within a year, compared with 13% of patients who did not have the mutations, even after adjustment for the type of conditioning regimen. The hazard ratio (HR) for disease progression in the patients with mutations was 3.86 (P less than .001).
The association between the presence of one or more mutations with a variant allele frequency of at least 0.5% with increased risk of disease progression was also seen at 100 days, even after adjustment for conditioning regimen (66.7% vs. 0%; HR, 6.52; P less than .001). In multivariable analysis controlling for prognostic scores, maximum variant allele frequency at 30 days, TP53 mutation status and conditioning regimen, the presence of a mutation with at least 0.5% variant allele frequency was associated with a more than fourfold risk of progression, including when the revised International Prognostic Scoring System score and conditioning regimen were considered as covariates. (HR, 4.48; P less than .001),
A separate multivariable analysis of PFS controlling for maximum variant allele frequency at day 30, conditioning regimen, age at transplantation, and type of MDS showed that mutations were associated with a more than twofold risk of progression or death (HR, 2.39; P = .002).
This analysis also showed that secondary acute myeloid leukemia was associated with worse PFS, compared with primary MDS (HR, 2.24; P = .001).
The investigators acknowledged that the high-coverage exome sequencing technique used for the study is not routinely available in the clinic. To control for this, they also looked at their data using a subset of genes that are usually included in gene sequencing panels for MDS and AML.
“Although we identified fewer patients with mutations with the use of this approach than with enhanced exome sequencing, the prognostic value of detection of measurable residual disease was still highly clinically significant,” they wrote.
The study was supported by grants from the Leukemia and Lymphoma Society, Edward P. Evans Foundation, National Cancer Institute, National Institutes of Health, Gabrielle’s Angel Foundation, and the Lottie Caroline Hardy Trust. Dr. Duncavage disclosed personal fees from AbbVie and Cofactor Genomics. The majority of coauthors reported nothing to disclose.
SOURCE: Duncavage EJ et al. N Engl J Med 2018;379:1028-41.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Myelodysplastic syndrome (MDS)–associated mutations present 30 days after stem cell transplant may be predict disease progression and survival.
Major finding: Higher maximum variant allele frequency of residual disease–associated mutations at 30 days posttransplantation was significantly associated with disease progression and lower rates of progression-free survival at 1 year.
Study details: Exploratory study of mutations pre- and posttransplant in 90 patients with primary or therapy-related MDS or secondary acute myeloid leukemia.
Disclosures: The study was supported by grants from the Leukemia and Lymphoma Society, Edward P. Evans Foundation, National Cancer Institute, National Institutes of Health, Gabrielle’s Angel Foundation, and the Lottie Caroline Hardy Trust. Dr. Duncavage disclosed personal fees from AbbVie and Cofactor Genomics. The majority of the coauthors reported nothing to disclose.
Source: Duncavage EJ et al. N Engl J Med 2018;379:1028-41.
ICYMI: Fingolimod effective in pediatric relapsing multiple sclerosis
Fingolimod reduced the rate of relapse as well as the deposition of lesions on MRI better than interferon beta-1a did over 2 years in pediatric patients with relapsing multiple sclerosis, according to the results of the PARADIGMS trial, published online Sept. 12 in the New England Journal of Medicine (2018; 379:1017-27. doi: 10.1056/NEJMoa1800149). More serious adverse events were seen in fingolimod-treated patients.
We covered the story before it was published in the journal. Find our conference coverage at the links below.
Fingolimod reduced the rate of relapse as well as the deposition of lesions on MRI better than interferon beta-1a did over 2 years in pediatric patients with relapsing multiple sclerosis, according to the results of the PARADIGMS trial, published online Sept. 12 in the New England Journal of Medicine (2018; 379:1017-27. doi: 10.1056/NEJMoa1800149). More serious adverse events were seen in fingolimod-treated patients.
We covered the story before it was published in the journal. Find our conference coverage at the links below.
Fingolimod reduced the rate of relapse as well as the deposition of lesions on MRI better than interferon beta-1a did over 2 years in pediatric patients with relapsing multiple sclerosis, according to the results of the PARADIGMS trial, published online Sept. 12 in the New England Journal of Medicine (2018; 379:1017-27. doi: 10.1056/NEJMoa1800149). More serious adverse events were seen in fingolimod-treated patients.
We covered the story before it was published in the journal. Find our conference coverage at the links below.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Burnout may jeopardize patient care
because of depersonalization of care, according to recent research published in JAMA Internal Medicine.
“The primary conclusion of this review is that physician burnout might jeopardize patient care,” Maria Panagioti, PhD, from the National Institute for Health Research (NIHR) School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre at the University of Manchester (United Kingdom) and her colleagues wrote in their study. “Physician wellness and quality of patient care are critical [as are] complementary dimensions of health care organization efficiency.”
Dr. Panagioti and her colleagues performed a search of the MEDLINE, EMBASE, CINAHL, and PsycInfo databases and found 47 eligible studies on the topics of physician burnout and patient care, which altogether included data from a pooled cohort of 42,473 physicians. The physicians were median 38 years old, with 44.7% of studies looking at physicians in residency or early career (up to 5 years post residency) and 55.3% of studies examining experienced physicians. The meta-analysis also evaluated physicians in a hospital setting (63.8%), primary care (13.8%), and across various different health care settings (8.5%).
The researchers found physicians with burnout were significantly associated with higher rates of patient safety issues (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), reduced patient satisfaction (OR, 2.28; 95% CI, 1.42-3.68), and lower quality of care (OR, 2.31; 95% CI, 1.87-2.85). System-reported instances of patient safety issues and low professionalism were not statistically significant, but the subgroup differences did reach statistical significance (Cohen Q, 8.14; P = .007). Among residents and physicians in their early career, there was a greater association between burnout and low professionalism (OR, 3.39; 95% CI, 2.38-4.40), compared with physicians in the middle or later in their career (OR, 1.73; 95% CI, 1.46-2.01; Cohen Q, 7.27; P = .003).
“Investments in organizational strategies to jointly monitor and improve physician wellness and patient care outcomes are needed,” Dr. Panagioti and her colleagues wrote in the study. “Interventions aimed at improving the culture of health care organizations, as well as interventions focused on individual physicians but supported and funded by health care organizations, are beneficial.”
Researchers noted the study quality was low to moderate. Variation in outcomes across studies, heterogeneity among studies, potential selection bias by excluding gray literature, and the inability to establish causal links from findings because of the cross-sectional nature of the studies analyzed were potential limitations in the study, they reported.
The study was funded by the United Kingdom NIHR School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre. The authors report no relevant conflicts of interest.
SOURCE: Panagioti M et al. JAMA Intern Med. 2018 Sept 4. doi: 10.1001/jamainternmed.2018.3713.
Because of a lack of funding for research into burnout and the immediate need for change based on the effect it has on patient care seen in Pangioti et al., the question of how to address physician burnout should be answered with quality improvement programs aimed at making immediate changes in health care settings, Mark Linzer, MD, wrote in a related editorial.
“Resonating with these concepts, I propose that, for the burnout prevention and wellness field, we encourage quality improvement projects of high standards: multiple sites, concurrent control groups, longitudinal design, and blinding when feasible, with assessment of outcomes and costs,” he wrote. “These studies can point us toward what we will evaluate in larger trials and allow a place for the rapidly developing information base to be viewed and thus become part of the developing science of work conditions, burnout reduction, and the anticipated result on quality and safety.”
There are research questions that have yet to be answered on this topic, he added, such as to what extent do factors like workflow redesign, use and upkeep of electronic medical records, and chaotic workplaces affect burnout. Further, regulatory environments may play a role, and it is still not known whether reducing burnout among physicians will also reduce burnout among staff. Future studies should also look at how burnout affects trainees and female physicians, he suggested.
“The link between burnout and adverse patient outcomes is stronger, thanks to the work of Panagioti and colleagues,” Dr. Linzer said. “With close to half of U.S. physicians experiencing symptoms of burnout, more work is needed to understand how to reduce it and what we can expect from doing so.”
Dr. Linzer is from the Hennepin Healthcare Systems in Minneapolis. These comments summarize his editorial regarding the findings of Pangioti et al. He reported support for Wellness Champion training by the American College of Physicians and the Association of Chiefs and Leaders in General Internal Medicine and that he has received support for American Medical Association research projects.
Because of a lack of funding for research into burnout and the immediate need for change based on the effect it has on patient care seen in Pangioti et al., the question of how to address physician burnout should be answered with quality improvement programs aimed at making immediate changes in health care settings, Mark Linzer, MD, wrote in a related editorial.
“Resonating with these concepts, I propose that, for the burnout prevention and wellness field, we encourage quality improvement projects of high standards: multiple sites, concurrent control groups, longitudinal design, and blinding when feasible, with assessment of outcomes and costs,” he wrote. “These studies can point us toward what we will evaluate in larger trials and allow a place for the rapidly developing information base to be viewed and thus become part of the developing science of work conditions, burnout reduction, and the anticipated result on quality and safety.”
There are research questions that have yet to be answered on this topic, he added, such as to what extent do factors like workflow redesign, use and upkeep of electronic medical records, and chaotic workplaces affect burnout. Further, regulatory environments may play a role, and it is still not known whether reducing burnout among physicians will also reduce burnout among staff. Future studies should also look at how burnout affects trainees and female physicians, he suggested.
“The link between burnout and adverse patient outcomes is stronger, thanks to the work of Panagioti and colleagues,” Dr. Linzer said. “With close to half of U.S. physicians experiencing symptoms of burnout, more work is needed to understand how to reduce it and what we can expect from doing so.”
Dr. Linzer is from the Hennepin Healthcare Systems in Minneapolis. These comments summarize his editorial regarding the findings of Pangioti et al. He reported support for Wellness Champion training by the American College of Physicians and the Association of Chiefs and Leaders in General Internal Medicine and that he has received support for American Medical Association research projects.
Because of a lack of funding for research into burnout and the immediate need for change based on the effect it has on patient care seen in Pangioti et al., the question of how to address physician burnout should be answered with quality improvement programs aimed at making immediate changes in health care settings, Mark Linzer, MD, wrote in a related editorial.
“Resonating with these concepts, I propose that, for the burnout prevention and wellness field, we encourage quality improvement projects of high standards: multiple sites, concurrent control groups, longitudinal design, and blinding when feasible, with assessment of outcomes and costs,” he wrote. “These studies can point us toward what we will evaluate in larger trials and allow a place for the rapidly developing information base to be viewed and thus become part of the developing science of work conditions, burnout reduction, and the anticipated result on quality and safety.”
There are research questions that have yet to be answered on this topic, he added, such as to what extent do factors like workflow redesign, use and upkeep of electronic medical records, and chaotic workplaces affect burnout. Further, regulatory environments may play a role, and it is still not known whether reducing burnout among physicians will also reduce burnout among staff. Future studies should also look at how burnout affects trainees and female physicians, he suggested.
“The link between burnout and adverse patient outcomes is stronger, thanks to the work of Panagioti and colleagues,” Dr. Linzer said. “With close to half of U.S. physicians experiencing symptoms of burnout, more work is needed to understand how to reduce it and what we can expect from doing so.”
Dr. Linzer is from the Hennepin Healthcare Systems in Minneapolis. These comments summarize his editorial regarding the findings of Pangioti et al. He reported support for Wellness Champion training by the American College of Physicians and the Association of Chiefs and Leaders in General Internal Medicine and that he has received support for American Medical Association research projects.
because of depersonalization of care, according to recent research published in JAMA Internal Medicine.
“The primary conclusion of this review is that physician burnout might jeopardize patient care,” Maria Panagioti, PhD, from the National Institute for Health Research (NIHR) School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre at the University of Manchester (United Kingdom) and her colleagues wrote in their study. “Physician wellness and quality of patient care are critical [as are] complementary dimensions of health care organization efficiency.”
Dr. Panagioti and her colleagues performed a search of the MEDLINE, EMBASE, CINAHL, and PsycInfo databases and found 47 eligible studies on the topics of physician burnout and patient care, which altogether included data from a pooled cohort of 42,473 physicians. The physicians were median 38 years old, with 44.7% of studies looking at physicians in residency or early career (up to 5 years post residency) and 55.3% of studies examining experienced physicians. The meta-analysis also evaluated physicians in a hospital setting (63.8%), primary care (13.8%), and across various different health care settings (8.5%).
The researchers found physicians with burnout were significantly associated with higher rates of patient safety issues (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), reduced patient satisfaction (OR, 2.28; 95% CI, 1.42-3.68), and lower quality of care (OR, 2.31; 95% CI, 1.87-2.85). System-reported instances of patient safety issues and low professionalism were not statistically significant, but the subgroup differences did reach statistical significance (Cohen Q, 8.14; P = .007). Among residents and physicians in their early career, there was a greater association between burnout and low professionalism (OR, 3.39; 95% CI, 2.38-4.40), compared with physicians in the middle or later in their career (OR, 1.73; 95% CI, 1.46-2.01; Cohen Q, 7.27; P = .003).
“Investments in organizational strategies to jointly monitor and improve physician wellness and patient care outcomes are needed,” Dr. Panagioti and her colleagues wrote in the study. “Interventions aimed at improving the culture of health care organizations, as well as interventions focused on individual physicians but supported and funded by health care organizations, are beneficial.”
Researchers noted the study quality was low to moderate. Variation in outcomes across studies, heterogeneity among studies, potential selection bias by excluding gray literature, and the inability to establish causal links from findings because of the cross-sectional nature of the studies analyzed were potential limitations in the study, they reported.
The study was funded by the United Kingdom NIHR School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre. The authors report no relevant conflicts of interest.
SOURCE: Panagioti M et al. JAMA Intern Med. 2018 Sept 4. doi: 10.1001/jamainternmed.2018.3713.
because of depersonalization of care, according to recent research published in JAMA Internal Medicine.
“The primary conclusion of this review is that physician burnout might jeopardize patient care,” Maria Panagioti, PhD, from the National Institute for Health Research (NIHR) School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre at the University of Manchester (United Kingdom) and her colleagues wrote in their study. “Physician wellness and quality of patient care are critical [as are] complementary dimensions of health care organization efficiency.”
Dr. Panagioti and her colleagues performed a search of the MEDLINE, EMBASE, CINAHL, and PsycInfo databases and found 47 eligible studies on the topics of physician burnout and patient care, which altogether included data from a pooled cohort of 42,473 physicians. The physicians were median 38 years old, with 44.7% of studies looking at physicians in residency or early career (up to 5 years post residency) and 55.3% of studies examining experienced physicians. The meta-analysis also evaluated physicians in a hospital setting (63.8%), primary care (13.8%), and across various different health care settings (8.5%).
The researchers found physicians with burnout were significantly associated with higher rates of patient safety issues (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), reduced patient satisfaction (OR, 2.28; 95% CI, 1.42-3.68), and lower quality of care (OR, 2.31; 95% CI, 1.87-2.85). System-reported instances of patient safety issues and low professionalism were not statistically significant, but the subgroup differences did reach statistical significance (Cohen Q, 8.14; P = .007). Among residents and physicians in their early career, there was a greater association between burnout and low professionalism (OR, 3.39; 95% CI, 2.38-4.40), compared with physicians in the middle or later in their career (OR, 1.73; 95% CI, 1.46-2.01; Cohen Q, 7.27; P = .003).
“Investments in organizational strategies to jointly monitor and improve physician wellness and patient care outcomes are needed,” Dr. Panagioti and her colleagues wrote in the study. “Interventions aimed at improving the culture of health care organizations, as well as interventions focused on individual physicians but supported and funded by health care organizations, are beneficial.”
Researchers noted the study quality was low to moderate. Variation in outcomes across studies, heterogeneity among studies, potential selection bias by excluding gray literature, and the inability to establish causal links from findings because of the cross-sectional nature of the studies analyzed were potential limitations in the study, they reported.
The study was funded by the United Kingdom NIHR School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre. The authors report no relevant conflicts of interest.
SOURCE: Panagioti M et al. JAMA Intern Med. 2018 Sept 4. doi: 10.1001/jamainternmed.2018.3713.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Burnout among physicians was associated with lower quality of care because of unprofessionalism, reduced patient satisfaction, and an increased risk of patient safety issues.
Major finding: Physicians with burnout were significantly associated with higher rates of patient safety issues (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), reduced patient satisfaction (OR, 2.28; 95% CI, 1.42-3.68), and lower quality of care (OR, 2.31; 95% CI, 1.87-2.85).
Study details: A systematic review and meta-analysis of 42,473 physicians from 47 different studies.
Disclosures: The study was funded by the United Kingdom National Institute of Health Research (NIHR) School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre. The authors reported no relevant conflicts of interest.
Source: Panagioti M et al. JAMA Intern Med. 2018 Sept 4. doi: 10.1001/jamainternmed.2018.3713.
CDC opens Emergency Operations Center in advance of Hurricane Florence
The Centers for Disease Control and Prevention is activating its Emergency Operations Center (EOC) in advance of the landfall of Hurricane Florence, according to a CDC media statement.
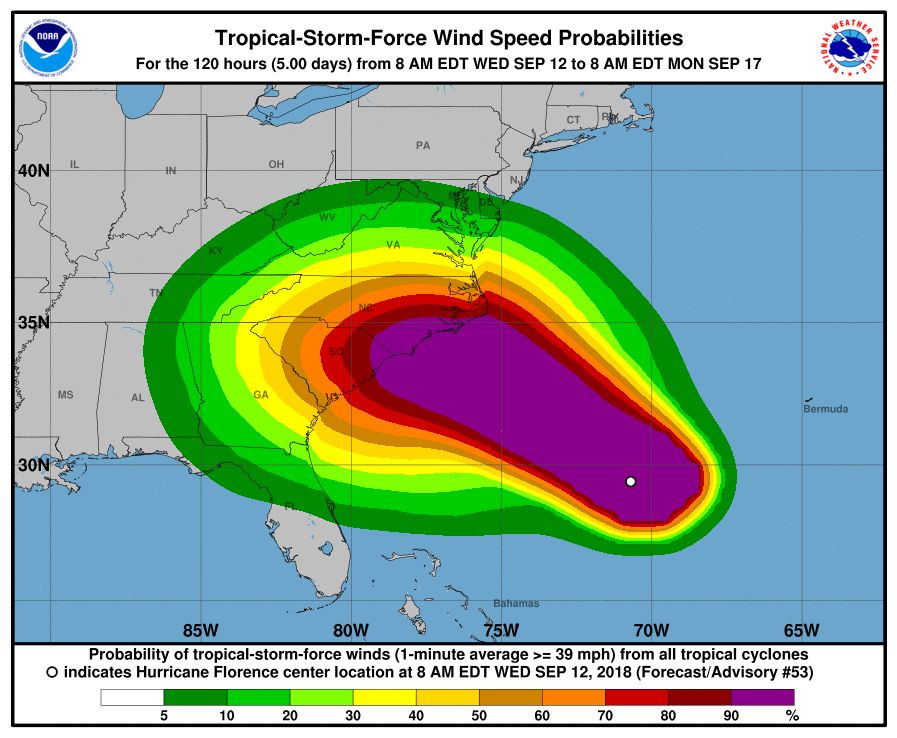
Activation of the center will allow for 24/7 management of all CDC activities before, during, and after the landfall of Hurricane Florence, including deployment of personnel and resources.
All CDC staff should be ready to provide infectious disease outbreak surveillance, public health messages, water/food safety evaluations, mold prevention and treatment, industrial contamination containment, and standing water control. The CDC is also sharing messages with the public on how to protect themselves from threats before, during, and after landfall, such as drowning and floodwater safety, carbon monoxide poisoning, downed power lines, unsafe food and water, and mold.
The EOC is the CDC’s command center for the coordination and monitoring of CDC activity with all other U.S. federal, state, and local agencies. The EOC also works with the Secretary of Health & Human Services Secretary’s Operations Center to ensure awareness and a coordinated public health and medical response, according to the statement.
Additional resources for interested parties can be found on the CDC website.
The Centers for Disease Control and Prevention is activating its Emergency Operations Center (EOC) in advance of the landfall of Hurricane Florence, according to a CDC media statement.
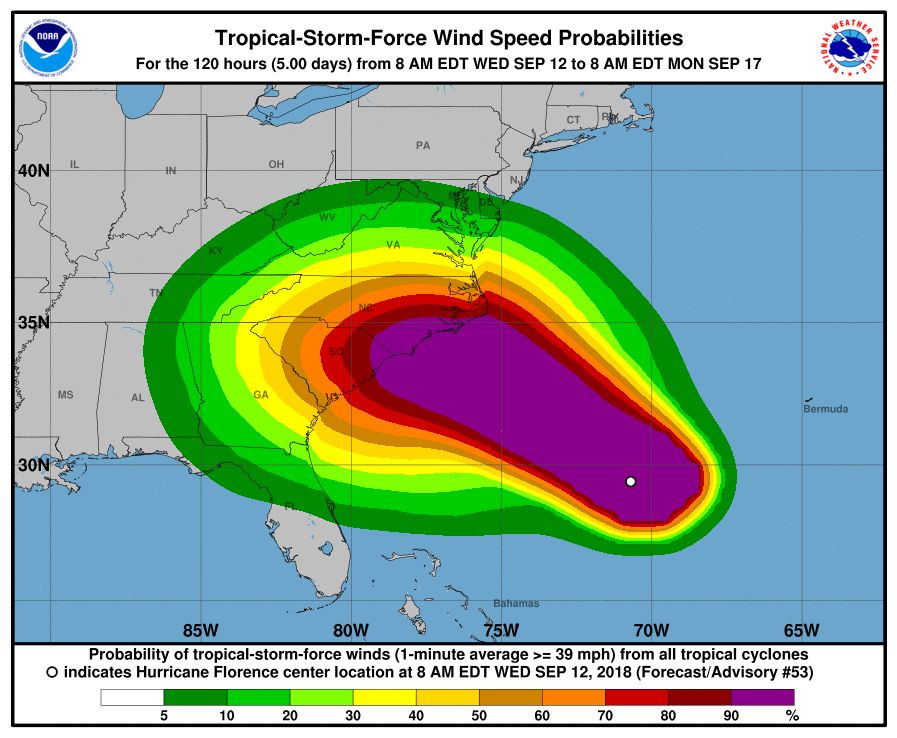
Activation of the center will allow for 24/7 management of all CDC activities before, during, and after the landfall of Hurricane Florence, including deployment of personnel and resources.
All CDC staff should be ready to provide infectious disease outbreak surveillance, public health messages, water/food safety evaluations, mold prevention and treatment, industrial contamination containment, and standing water control. The CDC is also sharing messages with the public on how to protect themselves from threats before, during, and after landfall, such as drowning and floodwater safety, carbon monoxide poisoning, downed power lines, unsafe food and water, and mold.
The EOC is the CDC’s command center for the coordination and monitoring of CDC activity with all other U.S. federal, state, and local agencies. The EOC also works with the Secretary of Health & Human Services Secretary’s Operations Center to ensure awareness and a coordinated public health and medical response, according to the statement.
Additional resources for interested parties can be found on the CDC website.
The Centers for Disease Control and Prevention is activating its Emergency Operations Center (EOC) in advance of the landfall of Hurricane Florence, according to a CDC media statement.
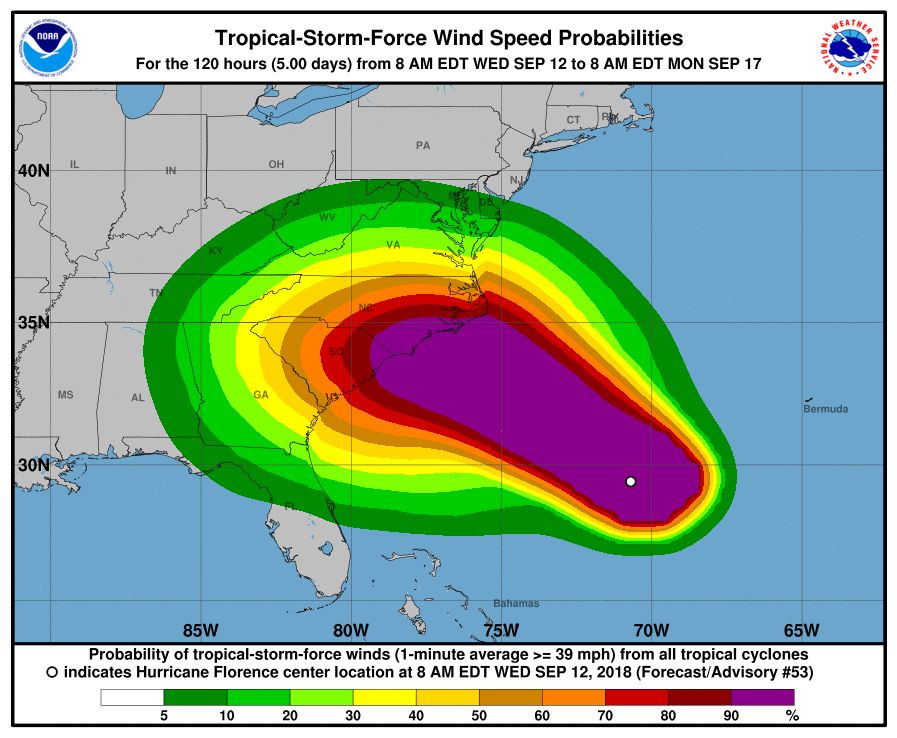
Activation of the center will allow for 24/7 management of all CDC activities before, during, and after the landfall of Hurricane Florence, including deployment of personnel and resources.
All CDC staff should be ready to provide infectious disease outbreak surveillance, public health messages, water/food safety evaluations, mold prevention and treatment, industrial contamination containment, and standing water control. The CDC is also sharing messages with the public on how to protect themselves from threats before, during, and after landfall, such as drowning and floodwater safety, carbon monoxide poisoning, downed power lines, unsafe food and water, and mold.
The EOC is the CDC’s command center for the coordination and monitoring of CDC activity with all other U.S. federal, state, and local agencies. The EOC also works with the Secretary of Health & Human Services Secretary’s Operations Center to ensure awareness and a coordinated public health and medical response, according to the statement.
Additional resources for interested parties can be found on the CDC website.
October 2018
Allergic contact dermatitis (ACD) can affect individuals regardless of age, race, or sex, but ACD accounts for 20% of all contact dermatitis reactions. ACD results in an inflammatory reaction in those who have been previously sensitized to an allergen. This type of delayed hypersensitivity reaction is known as cell-mediated hypersensitivity. Generally, no reaction is elicited upon the first exposure to the allergen. In fact, it may take years of exposure to allergens for someone to develop an allergic contact dermatitis.
Once sensitized, epidermal antigen-presenting cells (APCs) called Langerhans cells process the allergen and present it in a complex on the surface of the cell to a CD4+ T cell. Subsequently, inflammatory cytokines and mediators are released, resulting in an allergic cutaneous (eczematous) reaction. Lesions may appear to be vesicular or bullous. Occasionally, a generalized eruption may occur. With repeated exposure, reactions may be acute or chronic.
Common causes of allergic contact dermatitis include toxicodendron plants (poison ivy, oak, and sumac; cashew nut tree; and mango), metals (nickel and gold), topical antibiotics (neomycin and bacitracin), fragrance and Balsam of Peru, deodorant, preservatives (formaldehyde), and rubber (elastic and gloves).
Patch testing is the standard means of detecting which allergen is causing the sensitization in an individual. The Thin-Layer Rapid Use Epicutaneous (TRUE) test or individually prepared aluminum (Finn) chambers containing the most common allergens are applied to the patient’s upper back. The patches are removed after 48 hours and read, and then reevaluated at day 4 or 5. Positive reactions appear as eczematous or vesicular papules or plaques.
Treatment includes avoidance of the allergens. Topical corticosteroid creams are helpful. For severe or generalized reactions, oral prednisone may be used. It is important to note that patient may be allergic to topical steroids. Patch testing can be performed to elucidate such allergens.
In contrast, 80% of contact dermatitis reactions are irritant, not allergic. Irritant contact dermatitis results is a local inflammatory reaction in people who have come into contact with a substance. Previous sensitization is not required. The reaction usually occurs immediately after exposure. Common causes include alkalis (detergents, soaps), acids (often found as an industrial work exposure), metals, solvents (occupational dermatitis), hydrocarbons, and chlorinated compounds.
This case and photo were submitted by Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to [email protected].
Allergic contact dermatitis (ACD) can affect individuals regardless of age, race, or sex, but ACD accounts for 20% of all contact dermatitis reactions. ACD results in an inflammatory reaction in those who have been previously sensitized to an allergen. This type of delayed hypersensitivity reaction is known as cell-mediated hypersensitivity. Generally, no reaction is elicited upon the first exposure to the allergen. In fact, it may take years of exposure to allergens for someone to develop an allergic contact dermatitis.
Once sensitized, epidermal antigen-presenting cells (APCs) called Langerhans cells process the allergen and present it in a complex on the surface of the cell to a CD4+ T cell. Subsequently, inflammatory cytokines and mediators are released, resulting in an allergic cutaneous (eczematous) reaction. Lesions may appear to be vesicular or bullous. Occasionally, a generalized eruption may occur. With repeated exposure, reactions may be acute or chronic.
Common causes of allergic contact dermatitis include toxicodendron plants (poison ivy, oak, and sumac; cashew nut tree; and mango), metals (nickel and gold), topical antibiotics (neomycin and bacitracin), fragrance and Balsam of Peru, deodorant, preservatives (formaldehyde), and rubber (elastic and gloves).
Patch testing is the standard means of detecting which allergen is causing the sensitization in an individual. The Thin-Layer Rapid Use Epicutaneous (TRUE) test or individually prepared aluminum (Finn) chambers containing the most common allergens are applied to the patient’s upper back. The patches are removed after 48 hours and read, and then reevaluated at day 4 or 5. Positive reactions appear as eczematous or vesicular papules or plaques.
Treatment includes avoidance of the allergens. Topical corticosteroid creams are helpful. For severe or generalized reactions, oral prednisone may be used. It is important to note that patient may be allergic to topical steroids. Patch testing can be performed to elucidate such allergens.
In contrast, 80% of contact dermatitis reactions are irritant, not allergic. Irritant contact dermatitis results is a local inflammatory reaction in people who have come into contact with a substance. Previous sensitization is not required. The reaction usually occurs immediately after exposure. Common causes include alkalis (detergents, soaps), acids (often found as an industrial work exposure), metals, solvents (occupational dermatitis), hydrocarbons, and chlorinated compounds.
This case and photo were submitted by Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to [email protected].
Allergic contact dermatitis (ACD) can affect individuals regardless of age, race, or sex, but ACD accounts for 20% of all contact dermatitis reactions. ACD results in an inflammatory reaction in those who have been previously sensitized to an allergen. This type of delayed hypersensitivity reaction is known as cell-mediated hypersensitivity. Generally, no reaction is elicited upon the first exposure to the allergen. In fact, it may take years of exposure to allergens for someone to develop an allergic contact dermatitis.
Once sensitized, epidermal antigen-presenting cells (APCs) called Langerhans cells process the allergen and present it in a complex on the surface of the cell to a CD4+ T cell. Subsequently, inflammatory cytokines and mediators are released, resulting in an allergic cutaneous (eczematous) reaction. Lesions may appear to be vesicular or bullous. Occasionally, a generalized eruption may occur. With repeated exposure, reactions may be acute or chronic.
Common causes of allergic contact dermatitis include toxicodendron plants (poison ivy, oak, and sumac; cashew nut tree; and mango), metals (nickel and gold), topical antibiotics (neomycin and bacitracin), fragrance and Balsam of Peru, deodorant, preservatives (formaldehyde), and rubber (elastic and gloves).
Patch testing is the standard means of detecting which allergen is causing the sensitization in an individual. The Thin-Layer Rapid Use Epicutaneous (TRUE) test or individually prepared aluminum (Finn) chambers containing the most common allergens are applied to the patient’s upper back. The patches are removed after 48 hours and read, and then reevaluated at day 4 or 5. Positive reactions appear as eczematous or vesicular papules or plaques.
Treatment includes avoidance of the allergens. Topical corticosteroid creams are helpful. For severe or generalized reactions, oral prednisone may be used. It is important to note that patient may be allergic to topical steroids. Patch testing can be performed to elucidate such allergens.
In contrast, 80% of contact dermatitis reactions are irritant, not allergic. Irritant contact dermatitis results is a local inflammatory reaction in people who have come into contact with a substance. Previous sensitization is not required. The reaction usually occurs immediately after exposure. Common causes include alkalis (detergents, soaps), acids (often found as an industrial work exposure), metals, solvents (occupational dermatitis), hydrocarbons, and chlorinated compounds.
This case and photo were submitted by Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to [email protected].
A 30-year-old female presented with 2 days of intensely pruritic erythematous papules and vesicles on her bilateral arms and hands. The lesions began appearing 1 day after a camping trip. Her neck, chest, and upper back were clear.
Cell population appears to drive relapse in AML
Researchers believe they have identified cells that are responsible for relapse of acute myeloid leukemia (AML).
These “leukemic-regenerating cells” (LRCs), which are distinct from leukemic stem cells (LSCs), seem to arise in response to chemotherapy.
Experiments in mouse models of AML suggested that targeting LRCs could reduce the risk of relapse, and analyses of AML patient samples suggested LRCs might be used to predict relapse.
Allison Boyd, PhD, of McMaster University in Hamilton, Ont., and her colleagues reported these findings in Cancer Cell.
The researchers evaluated the leukemic populations that persist after chemotherapy by analyzing AML patient samples and xenograft AML models. The team found that LSCs were depleted by chemotherapy, and a different cell population, LRCs, appeared to arise in response to treatment.
LRCs are “molecularly distinct from therapy-naive LSCs,” the researchers said. In fact, the team identified 19 genes that are preferentially expressed by LRCs and could be treated with drugs.
One of these genes is DRD2, and the researchers found they could target LRCs using a small-molecule antagonist of DRD2.
Targeting LRCs
Dr. Boyd and her colleagues compared the effects of treatment with a DRD2 antagonist in AML xenografts populated with therapy-naive LSCs and AML xenografts that harbored LRCs following exposure to cytarabine.
The researchers said DRD2 antagonist therapy “moderately” affected AML progenitors in the LSC model but “had profound effects on regenerating LRCs.”
Treatment with the DRD2 antagonist also improved the efficacy of chemotherapy.
In xenografts derived from one AML patient, treatment with cytarabine alone left 50% of mice with residual disease. However, the addition of the DRD2 antagonist enabled 100% of the mice to achieve disease-free status.
In xenografts derived from a patient with more aggressive AML, all recipient mice had residual disease after receiving cytarabine. Treatment with the DRD2 antagonist slowed leukemic regrowth and nearly doubled the time to relapse.
Targeting LRCs also reduced disease regeneration potential in samples from other AML patients.
“This is a major clinical opportunity because this type of leukemia is very diverse and responds differently across patients,” Dr. Boyd said. “It has been a challenge in a clinical setting to find a commonality for therapeutic targeting across the wide array of patients, and these regenerative cells provide that similarity.”
Predicting relapse
Dr. Boyd and her colleagues also analyzed bone marrow samples collected from AML patients approximately 3 weeks after they completed standard induction chemotherapy.
The team found that progenitor activity was enriched among residual leukemic cells. However, patient cells lacked gene expression signatures related to therapy-naive LSCs.
“Instead, these highly regenerative AML cells preferentially expressed our LRC signature,” the researchers said.
The team also found evidence to suggest that LRC molecular profiles arise temporarily after chemotherapy. The LRC signature was not observed at diagnosis or once AML was reestablished at relapse.
“We think there are opportunities here because now we have a window where we can kick the cancer while it’s down,” Dr. Boyd said.
She and her colleagues also found the LRC signature might be useful for predicting relapse in AML patients.
The team assessed expression of SLC2A2, an LRC marker that has overlapping expression with DRD2, in seven patients who were in remission after induction.
Chemotherapy increased expression of SLC2A2 only in the four patients who had residual disease – not in the three patients who remained in disease-free remission for at least 5 years. “These results suggest that LRC populations represent reservoirs of residual disease, and LRC marker expression levels can be linked to clinical outcomes of AML relapse,” the researchers said.
This study was supported by the Canadian Cancer Society, the Canadian Institutes of Health Research, the Ontario Institute for Cancer Research, and other organizations.
SOURCE: Boyd AL et al. Cancer Cell. 2018 Sep 10. doi: 10.1016/j.ccell.2018.08.007.
Researchers believe they have identified cells that are responsible for relapse of acute myeloid leukemia (AML).
These “leukemic-regenerating cells” (LRCs), which are distinct from leukemic stem cells (LSCs), seem to arise in response to chemotherapy.
Experiments in mouse models of AML suggested that targeting LRCs could reduce the risk of relapse, and analyses of AML patient samples suggested LRCs might be used to predict relapse.
Allison Boyd, PhD, of McMaster University in Hamilton, Ont., and her colleagues reported these findings in Cancer Cell.
The researchers evaluated the leukemic populations that persist after chemotherapy by analyzing AML patient samples and xenograft AML models. The team found that LSCs were depleted by chemotherapy, and a different cell population, LRCs, appeared to arise in response to treatment.
LRCs are “molecularly distinct from therapy-naive LSCs,” the researchers said. In fact, the team identified 19 genes that are preferentially expressed by LRCs and could be treated with drugs.
One of these genes is DRD2, and the researchers found they could target LRCs using a small-molecule antagonist of DRD2.
Targeting LRCs
Dr. Boyd and her colleagues compared the effects of treatment with a DRD2 antagonist in AML xenografts populated with therapy-naive LSCs and AML xenografts that harbored LRCs following exposure to cytarabine.
The researchers said DRD2 antagonist therapy “moderately” affected AML progenitors in the LSC model but “had profound effects on regenerating LRCs.”
Treatment with the DRD2 antagonist also improved the efficacy of chemotherapy.
In xenografts derived from one AML patient, treatment with cytarabine alone left 50% of mice with residual disease. However, the addition of the DRD2 antagonist enabled 100% of the mice to achieve disease-free status.
In xenografts derived from a patient with more aggressive AML, all recipient mice had residual disease after receiving cytarabine. Treatment with the DRD2 antagonist slowed leukemic regrowth and nearly doubled the time to relapse.
Targeting LRCs also reduced disease regeneration potential in samples from other AML patients.
“This is a major clinical opportunity because this type of leukemia is very diverse and responds differently across patients,” Dr. Boyd said. “It has been a challenge in a clinical setting to find a commonality for therapeutic targeting across the wide array of patients, and these regenerative cells provide that similarity.”
Predicting relapse
Dr. Boyd and her colleagues also analyzed bone marrow samples collected from AML patients approximately 3 weeks after they completed standard induction chemotherapy.
The team found that progenitor activity was enriched among residual leukemic cells. However, patient cells lacked gene expression signatures related to therapy-naive LSCs.
“Instead, these highly regenerative AML cells preferentially expressed our LRC signature,” the researchers said.
The team also found evidence to suggest that LRC molecular profiles arise temporarily after chemotherapy. The LRC signature was not observed at diagnosis or once AML was reestablished at relapse.
“We think there are opportunities here because now we have a window where we can kick the cancer while it’s down,” Dr. Boyd said.
She and her colleagues also found the LRC signature might be useful for predicting relapse in AML patients.
The team assessed expression of SLC2A2, an LRC marker that has overlapping expression with DRD2, in seven patients who were in remission after induction.
Chemotherapy increased expression of SLC2A2 only in the four patients who had residual disease – not in the three patients who remained in disease-free remission for at least 5 years. “These results suggest that LRC populations represent reservoirs of residual disease, and LRC marker expression levels can be linked to clinical outcomes of AML relapse,” the researchers said.
This study was supported by the Canadian Cancer Society, the Canadian Institutes of Health Research, the Ontario Institute for Cancer Research, and other organizations.
SOURCE: Boyd AL et al. Cancer Cell. 2018 Sep 10. doi: 10.1016/j.ccell.2018.08.007.
Researchers believe they have identified cells that are responsible for relapse of acute myeloid leukemia (AML).
These “leukemic-regenerating cells” (LRCs), which are distinct from leukemic stem cells (LSCs), seem to arise in response to chemotherapy.
Experiments in mouse models of AML suggested that targeting LRCs could reduce the risk of relapse, and analyses of AML patient samples suggested LRCs might be used to predict relapse.
Allison Boyd, PhD, of McMaster University in Hamilton, Ont., and her colleagues reported these findings in Cancer Cell.
The researchers evaluated the leukemic populations that persist after chemotherapy by analyzing AML patient samples and xenograft AML models. The team found that LSCs were depleted by chemotherapy, and a different cell population, LRCs, appeared to arise in response to treatment.
LRCs are “molecularly distinct from therapy-naive LSCs,” the researchers said. In fact, the team identified 19 genes that are preferentially expressed by LRCs and could be treated with drugs.
One of these genes is DRD2, and the researchers found they could target LRCs using a small-molecule antagonist of DRD2.
Targeting LRCs
Dr. Boyd and her colleagues compared the effects of treatment with a DRD2 antagonist in AML xenografts populated with therapy-naive LSCs and AML xenografts that harbored LRCs following exposure to cytarabine.
The researchers said DRD2 antagonist therapy “moderately” affected AML progenitors in the LSC model but “had profound effects on regenerating LRCs.”
Treatment with the DRD2 antagonist also improved the efficacy of chemotherapy.
In xenografts derived from one AML patient, treatment with cytarabine alone left 50% of mice with residual disease. However, the addition of the DRD2 antagonist enabled 100% of the mice to achieve disease-free status.
In xenografts derived from a patient with more aggressive AML, all recipient mice had residual disease after receiving cytarabine. Treatment with the DRD2 antagonist slowed leukemic regrowth and nearly doubled the time to relapse.
Targeting LRCs also reduced disease regeneration potential in samples from other AML patients.
“This is a major clinical opportunity because this type of leukemia is very diverse and responds differently across patients,” Dr. Boyd said. “It has been a challenge in a clinical setting to find a commonality for therapeutic targeting across the wide array of patients, and these regenerative cells provide that similarity.”
Predicting relapse
Dr. Boyd and her colleagues also analyzed bone marrow samples collected from AML patients approximately 3 weeks after they completed standard induction chemotherapy.
The team found that progenitor activity was enriched among residual leukemic cells. However, patient cells lacked gene expression signatures related to therapy-naive LSCs.
“Instead, these highly regenerative AML cells preferentially expressed our LRC signature,” the researchers said.
The team also found evidence to suggest that LRC molecular profiles arise temporarily after chemotherapy. The LRC signature was not observed at diagnosis or once AML was reestablished at relapse.
“We think there are opportunities here because now we have a window where we can kick the cancer while it’s down,” Dr. Boyd said.
She and her colleagues also found the LRC signature might be useful for predicting relapse in AML patients.
The team assessed expression of SLC2A2, an LRC marker that has overlapping expression with DRD2, in seven patients who were in remission after induction.
Chemotherapy increased expression of SLC2A2 only in the four patients who had residual disease – not in the three patients who remained in disease-free remission for at least 5 years. “These results suggest that LRC populations represent reservoirs of residual disease, and LRC marker expression levels can be linked to clinical outcomes of AML relapse,” the researchers said.
This study was supported by the Canadian Cancer Society, the Canadian Institutes of Health Research, the Ontario Institute for Cancer Research, and other organizations.
SOURCE: Boyd AL et al. Cancer Cell. 2018 Sep 10. doi: 10.1016/j.ccell.2018.08.007.
FROM CANCER CELL
Key clinical point: “Leukemic-regenerating cells” (LRCs) may drive relapse in acute myeloid leukemia (AML).
Major finding: LRCs could be useful for predicting relapse, and targeting LRCs might reduce relapse risk.
Study details: Research in AML patient samples and xenograft AML models.
Disclosures: This study was supported by the Canadian Cancer Society and other organizations.
Source: Boyd AL et al. Cancer Cell. 2018 Sep 10. doi: 10.1016/j.ccell.2018.08.007.
Venetoclax label now includes MRD data
The Food and Drug Administration has expanded the label for venetoclax tablets (Venclexta) to include data on minimal residual disease.
The drug’s prescribing information will now include details on minimal residual disease (MRD) negativity in previously treated patients with chronic lymphocytic leukemia (CLL) who received venetoclax in combination with rituximab in the phase 3 MURANO trial.
The combination of venetoclax and rituximab was approved by the FDA in June 2018 for the treatment of patients with CLL or small lymphocytic lymphoma, with or without 17p deletion, who received at least one prior therapy.
The MURANO trial (NCT02005471), which supported the FDA approval, included 389 patients with relapsed or refractory CLL. They were randomized to receive venetoclax plus rituximab or bendamustine plus rituximab (N Engl J Med. 2018; 378:1107-20).
Researchers evaluated MRD in patients who achieved a partial response or better. MRD was assessed using allele-specific oligonucleotide polymerase chain reaction; the definition of MRD negativity was less than one CLL cell per 10,000 lymphocytes.
The researchers assessed MRD in the peripheral blood after about 9 months on therapy (3 months after the last dose of rituximab). At that time, 53% (103/194) of patients in the venetoclax-rituximab arm were MRD negative, as were 12% (23/195) of patients in the bendamustine-rituximab arm.
The researchers also assessed MRD in the peripheral blood of patients with a complete response or complete response with incomplete marrow recovery. MRD negativity was achieved by 3% (6/194) of these patients in the venetoclax-rituximab arm and 2% (3/195) in the bendamustine-rituximab arm.
Venetoclax is being developed by AbbVie and Roche. It is jointly commercialized by AbbVie and Genentech, a member of the Roche Group, in the United States and by AbbVie outside of the United States.
The Food and Drug Administration has expanded the label for venetoclax tablets (Venclexta) to include data on minimal residual disease.
The drug’s prescribing information will now include details on minimal residual disease (MRD) negativity in previously treated patients with chronic lymphocytic leukemia (CLL) who received venetoclax in combination with rituximab in the phase 3 MURANO trial.
The combination of venetoclax and rituximab was approved by the FDA in June 2018 for the treatment of patients with CLL or small lymphocytic lymphoma, with or without 17p deletion, who received at least one prior therapy.
The MURANO trial (NCT02005471), which supported the FDA approval, included 389 patients with relapsed or refractory CLL. They were randomized to receive venetoclax plus rituximab or bendamustine plus rituximab (N Engl J Med. 2018; 378:1107-20).
Researchers evaluated MRD in patients who achieved a partial response or better. MRD was assessed using allele-specific oligonucleotide polymerase chain reaction; the definition of MRD negativity was less than one CLL cell per 10,000 lymphocytes.
The researchers assessed MRD in the peripheral blood after about 9 months on therapy (3 months after the last dose of rituximab). At that time, 53% (103/194) of patients in the venetoclax-rituximab arm were MRD negative, as were 12% (23/195) of patients in the bendamustine-rituximab arm.
The researchers also assessed MRD in the peripheral blood of patients with a complete response or complete response with incomplete marrow recovery. MRD negativity was achieved by 3% (6/194) of these patients in the venetoclax-rituximab arm and 2% (3/195) in the bendamustine-rituximab arm.
Venetoclax is being developed by AbbVie and Roche. It is jointly commercialized by AbbVie and Genentech, a member of the Roche Group, in the United States and by AbbVie outside of the United States.
The Food and Drug Administration has expanded the label for venetoclax tablets (Venclexta) to include data on minimal residual disease.
The drug’s prescribing information will now include details on minimal residual disease (MRD) negativity in previously treated patients with chronic lymphocytic leukemia (CLL) who received venetoclax in combination with rituximab in the phase 3 MURANO trial.
The combination of venetoclax and rituximab was approved by the FDA in June 2018 for the treatment of patients with CLL or small lymphocytic lymphoma, with or without 17p deletion, who received at least one prior therapy.
The MURANO trial (NCT02005471), which supported the FDA approval, included 389 patients with relapsed or refractory CLL. They were randomized to receive venetoclax plus rituximab or bendamustine plus rituximab (N Engl J Med. 2018; 378:1107-20).
Researchers evaluated MRD in patients who achieved a partial response or better. MRD was assessed using allele-specific oligonucleotide polymerase chain reaction; the definition of MRD negativity was less than one CLL cell per 10,000 lymphocytes.
The researchers assessed MRD in the peripheral blood after about 9 months on therapy (3 months after the last dose of rituximab). At that time, 53% (103/194) of patients in the venetoclax-rituximab arm were MRD negative, as were 12% (23/195) of patients in the bendamustine-rituximab arm.
The researchers also assessed MRD in the peripheral blood of patients with a complete response or complete response with incomplete marrow recovery. MRD negativity was achieved by 3% (6/194) of these patients in the venetoclax-rituximab arm and 2% (3/195) in the bendamustine-rituximab arm.
Venetoclax is being developed by AbbVie and Roche. It is jointly commercialized by AbbVie and Genentech, a member of the Roche Group, in the United States and by AbbVie outside of the United States.
The Cold, Hard Facts of Cryotherapy in Orthopedics
ABSTRACT
Cryotherapy is the use of the anti-inflammatory and analgesic properties of ice to facilitate healing. Cryotherapy mediates these salutatory effects by reducing blood flow to the site of injury, down-regulating the production of inflammatory and pain-inducing prostaglandins, and diminishing the conductive ability of nerve endings. It is commonly used postoperatively in orthopedics to decrease analgesic requirements and blood loss as well as to increase range of motion, despite limited literature on its ability to produce such therapeutic effects in clinical practice. This article examines the available literature and the scientific evidence for the use and efficacy of cryotherapy in post-surgical orthopedic patients. It also reviews the potential pitfalls associated with improper use. Overall, this review seeks to provide insight into when, or whether, cryotherapy is appropriate for orthopedic patients during surgical recovery.
Continue to: Cold therapy has been a mainstay of medical treatment...
Cold therapy has been a mainstay of medical treatment since the days of Hippocrates. Initially used by ancient Egyptians to mitigate inflammation and by Hippocrates himself to treat hemorrhage, the therapeutic applications of ice evolved throughout history to become part of the treatment algorithm for a variety of health conditions.1 Ice made an ideal numbing agent for limb amputations and an anesthetic for certain cancers, but truly became ubiquitous when the first cold pack meant for medicinal use was patented in the early 1970s.1,2 Despite their armamentarium of advanced treatment modalities, physicians in the modern era continue to prescribe cryotherapy for their patients, particularly in the field of orthopedics. Most athletes know the “RICE” (Rest, Ice, Compression, Elevation) protocol and utilize it to minimize inflammation associated with soft tissue injuries.
Inflammation is a physiologic response to noxious stimuli. Cell damage results in the production of inflammatory mediators including prostaglandins, which play a crucial role in the vasodilation and pain associated with inflammation. Vasodilation and increased blood flow manifest as swelling, which can cause pain by putting pressure on nerve endings. The inflammatory prostaglandin E2 (PGE2) causes local increases in temperature and mediates pain.3,4 The application of cold therapy attenuates inflammatory microvascular and hemodynamic changes, reducing some of the deleterious effects of inflammation and minimizing pain. Animal models demonstrate that cryotherapy restores functional capillary density, reverses tumor necrosis factor-α (TNF-α)-induced microvasculature damage, and reduces the production of thrombogenic thromboxanes in injured soft tissue.5 Additionally, cold therapy after knee arthroscopy is associated with lower concentrations of PGE2 in the knee.3 Local cooling acts at the cellular level to decrease edema, reduce pain, and slow blood flow to the affected area, with the overall effect of alleviating inflammation.4,5
Cryotherapy is standard practice in postoperative orthopedic care, but there is limited literature demonstrating its efficacy in this setting. In addition, the advent of more advanced wearable cooling systems necessitates a thorough comparison of the various cryotherapy mechanisms both from healthcare and economic perspectives. The goal of this article is to examine the benefits of cryotherapy in the postoperative management of orthopedic surgical interventions and to review the effectiveness of differing types of cryotherapy. A secondary goal of this article is to review the literature on the adverse effects of cryotherapy in order to increase physician awareness of this issue and highlight the importance of patient education when utilizing cryotherapy postoperatively.
BENEFITS OF CRYOTHERAPY
Three standard types of cryotherapy are prescribed as postoperative therapy in orthopedics: compressive cryotherapy, continuous flow cryotherapy, and the application of ice. All aim to decrease the amount of inflammation of the surgical site, reduce patient pain, and aid in the recovery process. The application of ice or other cooling pack devices without compression is the most commonly used method, likely because it is the most economical and user-friendly cryotherapy option. Compressive cryotherapy is the application of ice or an ice pack secured to the site with a bandage or other device in a manner that also applies pressure to the site of injury. Finally, continuous flow cryotherapy systems are typically connected to a refrigeration control unit and apply compressive cooling through the uninterrupted flow of cold water or gas through a wrap around the injured site. Examples include the Game Ready® (CoolSystems, Inc.), Cryo/Cuff® IC Cooler (DJO Global), and Hilotherm Homecare (Hilotherm GmbH) systems, which are marketed as an improvement over traditional forms of cold therapy, as they are capable of cooling for hours at a time, allow for nighttime use, and provide the operator with temperature control.6-8
Postoperative cryotherapy is prescribed for a wide variety of orthopedic procedures, including anterior cruciate ligament (ACL) reconstruction surgery, rotator cuff surgery, and total knee arthroplasty (TKA). Current literature includes many studies monitoring postoperative outcomes in patients using cryotherapy as part of their treatment regimen, with the primary endpoints being visual analog scale (VAS) scores, analgesic consumption, and range of motion (ROM).9-16 As demonstrated by in Table 1, these studies do not provide conclusive evidence that cryotherapy significantly alters postoperative outcomes, despite its ubiquitous use by the orthopedics community. In fact, the literature reflects a seeming lack of consensus regarding the effect of cryotherapy on analgesic requirements, pain, and joint mobility following procedures. Interestingly, of the studies represented in Table 1, only half analyzed all 3 postoperative measures (analgesic consumption, pain, and ROM). Furthermore, solely Morsi13 concluded that cryotherapy resulted in significant improvements in all 3 outcome measures in a trial involving only 30 patients. Kullenberg and colleagues12 performed the largest study, but still included only 86 patients. In addition, all the studies focused on 1 joint or procedure. Thus, despite evidence that cryotherapy reduces inflammation at a molecular level, current literature does not unequivocally support the common belief that cryotherapy benefits patients in practice. More robust studies that include an analysis of analgesic consumption, VAS scores, and ROM (at minimum) and compare the relative efficacy of cryotherapy across joint types and procedures are necessary to determine whether postoperative cryotherapy in orthopedics is appropriate.
Table 1. Results from Studies that Compared Cryotherapy to Standard Care Within the First 2 Weeks Following Surgery
Author | Joint/Procedure Type | Number of Trial Participants | Cryotherapy Type | Analgesic Consumption | VAS Score | ROM |
Yu et al9 | Elbow arthrolysis | 59 | Continuous flow cryotherapy (Cryo/Cuff®; DJO Global) | No significant difference | Cryotherapy significantly decreased scores up to POD 7 (P < 0.05) | No significant difference |
Dambros et al10 | ACL reconstruction | 25 | Ice pack | Xa | No significant difference | No significant difference |
Leegwater et al11 | Hip arthroplasty | 30 | Continuous flow cryotherapy (Game Ready®; CoolSystems, Inc.) | Trend towards lower use (No significant difference) | No significant difference | Xa |
Kullenberg et al12 | Knee arthroplasty | 86 | Continuous flow cryotherapy (Cryo/Cuff®) | No significant difference | No significant difference | Significantly improved at POD 7 and POD 21 |
Morsi13 | Knee arthroplasty | 30 | Continuous flow cryotherapy | Significantly lower consumption (P < 0.01) | Cryotherapy significantly decreased scores (P < 0.001) | Significantly improved at POD 7; No significant difference 6 weeks postoperative |
Singh et al14 | Open vs arthroscopic shoulder procedures | 70 | Continuous flow cryotherapy (Breg Polar Care Glacier® Cold Therapy unit; Breg Inc.) | Xa | Cryotherapy significantly decreased scores at arthroscopic POD 14 (P = 0.043); No significant difference for open procedures | Xa |
Saito et al15 | Hip arthroplasty | 46 | Continuous flow cryotherapy (Icing System 2000; Nippon Sigmax Co., Ltd.) | Significantly lower epidural analgesic use (P < 0.001); no significant difference in adjunct analgesic consumption | Cryotherapy significantly decreased scores POD 1-4 (P < 0.05) | Xa |
Gibbons et al16 | Knee arthroplasty | 60 | Continuous flow cryotherapy (Cryo/Cuff®) | No significant difference | No significant difference | No significant difference |
Continue to: ADVANCED CRYOTHERAPY DEVICES...
ADVANCED CRYOTHERAPY DEVICES
Several recent studies explored the relative postoperative benefits of advanced cryotherapeutics in lieu of the traditional ice pack.6,7,17-21 As reflected in Table 2, these studies, much like the literature comparing cryotherapy to the control, do not reveal significant benefits of continuous flow cryotherapy after surgery. In fact, the only outcome measure that was found to differ significantly in more than 1 study was ROM. Though the makers of advanced cryotherapy systems market them as a vast improvement over traditional forms of cold therapy, there is insufficient evidence to support such claims. Even the most robust study that included 280 patients failed to show significant differences in the analgesic use and ROM after surgery.20 Of note, all but 1 study compared traditional and advanced cryotherapy following procedures on the knee. Additional research exploring outcomes after surgery on other joints is necessary before any conclusions can be made regarding postoperative benefits or risks within orthopedics more generally.
Author | Joint / Procedure Type | Number of Trial Participants | Analgesic Consumption | VAS Score | ROM |
Kraeutler et al17 | Rotator cuff repair or subacromial decompression | 46 | No significant difference | No significant difference | Xa |
Thienpont18 | Knee arthroplasty | 116 | No significant difference | No significant difference | Significant reduction in active flexion with advanced cryotherapy (P = 0.02); No significant difference in other ROM tests |
Woolf et al19 | Knee arthroplasty | 53 | Decrease in night pain through POD 2 only | Xa | Xa |
Su et al20 | Knee arthroplasty | 280 | Significantly lower use with cryotherapy up to POD 14; No significant difference thereafter | Xa | No difference |
Barber21 | ACL reconstruction | 87 | Significantly lower use with cryotherapy POD 1 and 2 (P = 0.035) | Cryotherapy significantly decreased scores only POD 1 (P < 0.01) | Greater ROM with cryotherapy POD 7 (P < 0.03) |
Ruffilli et al6 | ACL reconstruction | 47 | No difference | Xa | Greater ROM with cryotherapy (P < 0.0001) |
Kuyucu et al7 | Knee arthroplasty | 60 | Xa | Cryotherapy significantly decreased scores (P < 0.05) | Greater ROM with cryotherapy (P < 0.05) |
RISKS AND ADVERSE EFFECTS OF CRYOTHERAPY
A rigorous analysis of the benefits of cryotherapy ought to incorporate other factors in addition to improvements in analgesic consumption, VAS score, and ROM. These include the financial and time investment involved in the use of continuous flow cryotherapy, which the majority of studies do not consider. Though many authors acknowledge that continuous flow cryotherapy is expensive, to our knowledge, none have yet performed a formal economic analysis of the cost of advanced cryotherapy to the patient as well as to the healthcare system at large.6,7,13,18,22-24 Dickinson and colleagues24 calculated the total cost of cryotherapy and rehabilitation following rotator cuff repair, but addressed only the up-front cost of the cold therapy system. For context, Table 3 summarizes the retail cost of the most popular cryotherapy devices on the market. Based on this information alone, it seems reasonable to conclude that these systems are associated with significantly more cost than traditional forms of cold therapy, and therefore would be an undesirable option for patients or hospital systems. Nevertheless, cost considerations are more nuanced than a simple comparison of price, necessitating more advanced economic analyses. Substantial savings may be on the table if future studies are able to prove postoperative cryotherapy shortens hospital stays, reduces medication costs, and results in fewer physical therapy sessions. Moreover, if all this is true, patients may experience quicker recovery and have overall greater post-procedure satisfaction.
Table 3. Cost of Most Popular Cryotherapy Units
System | Cost |
Cryo/Cuff® IC Cooler (DJO Global) | $125 |
DonJoy IceMan Classic (DJO Global) | $169 |
The Polar Care Kodiak (Breg, Inc.) | $180 |
Patient education required for optimal use of advanced cold therapy is another aspect of cryotherapy that is poorly represented in the literature. As Dickinson and colleagues24 point out, because it eliminates some dependency on the patient to remember to ice appropriately, continuous flow cryotherapy may have a positive impact on compliance and therefore yield improved outcomes.24 Hospital staff may be required to spend additional time with patients. However, this is necessary to ensure proper understanding on how to operate the system and avoid adverse outcomes. Patients may also find the large coolers inconvenient and may therefore be reluctant to use them, finding traditional ice more manageable. Future studies should consider gathering data on patient education, compliance, and overall reception/satisfaction to complete a more holistic investigation of the role of postoperative cryotherapy in orthopedics.
Cryotherapy is not without adverse outcomes, which have been documented primarily in the form of case study reports. Relevant case studies cited adverse outcomes including frostbite/skin loss, compartment syndrome, and perniosis as potential dangers of postoperative cryotherapy in orthopedics (Table 4).25-30 As an example, a patient recovering from patellar-tendon repair experienced bilateral frostbite and skin loss following 2 weeks of uninterrupted use of cryotherapy without any barrier between his skin and the system.29 A similar case study described 2 female patients, one recovering from a TKA and the other from a tibial revision of arthroplasty, who used cryotherapy systems without cessation and experienced frostbite and skin necrosis over the entirety of their knees.26 A third case study exploring 4 incidents of patellar frostbite and necrosis following knee arthroscopies proposed that poor patient understanding of proper cryotherapy use as well as poor recognition of the signs of frostbite contributed to these adverse outcomes. Furthermore, the cryotherapy brace used by all 4 patients included a feature designed to counteract patellar inflammation that also may have increased the likelihood of frostbite in this area due to poor tissue insulation. The authors noted that following the incidents, the makers of the brace removed patellar coverage to prevent future occurrences.30
Author | Adverse Effect | Procedure/Location |
Brown and Hahn25 | Frostbite | Bunionectomy; hallux valgus correction/feet |
Dundon et al26 | Skin necrosis | TKA/patella |
Khajavi et al27 | Compartment syndrome | Arthroscopic osteochondral autograft transfer/calf |
King et al28 | Perniosis | ACL reconstruction/knee |
Lee et al29 | Frostbite | Patellar-tendon repair/knees |
McGuire and Hendricks30 | Frostbite | Knee arthroscopy/patella |
Abbreviations: ACL, anterior cruciate ligament; TKA, total knee arthroplasty.
Frostbite linked to cryotherapy has also occurred following orthopedic procedures outside the knee. Brown and Hahn25 described 2 young females who developed skin necrosis following podiatric surgeries and constant cold therapy for roughly a week. Notably, 1 patient had cold sensitivity, which likely put her at an increased baseline risk of experiencing frostbite while using cryotherapy. Tissue necrosis is not the only danger of cold therapy discussed in this study. Surprisingly, 1 patient also developed compartment syndrome.25 Khajavi and colleagues27 also documented postoperative compartment syndrome in a patient following an arthroscopic osteochondral autograft transfer, which they attributed to reperfusion injury in the wake of first-degree frostbite. Hospital personnel also instructed this patient to use his cryotherapy system without interruption at the coldest temperature tolerable, contrary to manufacturer’s instructions.27
Continue to: King and colleagues...
King and colleagues28 described 2 cases of patients complaining of nodules, papules, and plaques soon after ACL reconstruction and the initiation of cryotherapy. A histological examination of their skin lesions demonstrated the presence of a perivascular and periadnexal superficial and deep lymphocytic infiltrate associated with perniosis. Dermatologists associated the perniosis with the cryotherapy cuff adhesive mechanisms, as their locations matched those of the lesions and symptoms subsided after cessation of cuff usage.28
Cases of adverse effects with perioperative cryotherapy have also occurred at our own institution. The authors obtained informed written consent from the patients to print and publish their images. In 2 separate incidents, patients overdid icing and experienced rather extreme side effects including burns and blisters (Figures 1 and 2). In light of these adverse events, the physicians have questioned whether RICE ought to be part of their standard perioperative recommendations. These physicians are not alone in their uncertainty. Interestingly, even Mirkin,31 who coined the RICE mnemonic, now believes that consistent icing post-injury actually inhibits the body’s natural inflammatory healing response, delaying rather than speeding recovery, and suggests that icing ought to be used for pain control only.
DISCUSSION
Though there is ample literature supporting the common belief that cryotherapy minimizes inflammation at the cellular level, whether or not it results in meaningful improvements in post-surgical orthopedic outcomes remains unclear. Table 1 reflects a dearth of evidence to support the widespread current practice of cold therapy following orthopedic procedures, but few studies could demonstrate a significant difference in the analgesic use, VAS score, or ROM between cryotherapy and control groups. It is worth noting that these studies used different cryotherapy systems. Though in theory the continuous flow cryotherapy systems are similarly designed, there are potential differences among them that have not been controlled for in this analysis. All studies had <90 participants and focused on a single joint or procedure, making it difficult to draw large scale conclusions about the utility of cold therapy in the postoperative orthopedic population at large. Furthermore, researchers measured endpoints at a range of time intervals that were inconsistent across studies. In some cases, the significance of the impact of cryotherapy on recovery within a single study differed based on the time point at which researchers measured outcomes.12-14 This raises the question as to whether cryotherapy has no benefits, or whether they are simply time-dependent. Future studies should seek to ascertain whether there is a postoperative time window in which cryotherapy could potentially expedite the recovery process.
Similarly, Table 2 shows a lack of consensus regarding the effect of advanced cryotherapy when compared to traditional ice application on pain, analgesic use, and joint mobility after surgery. However, all but 1 of these studies focused on knee procedures. Therefore, our findings may not be applicable to orthopedic surgeries on other joints. Nevertheless, the use of advanced cryotherapy in postoperative orthopedic care may wane if researchers continue to show that it is no more beneficial than its far less expensive counterpart of ice and an ace bandage.
The case studies discussed in this review serve as cautionary tales of the dangers of cryotherapy when used improperly. Though frostbite and subsequent tissue necrosis seem most common, physicians should be made aware that compartment syndrome and perniosis are also possible consequences. Orthopedic patients perhaps have an increased risk of developing these side effects due to the nature of their injuries and the large cutaneous surface area to which cryotherapy is applied. These outcomes could seemingly be avoided with improved educational initiatives targeted at both healthcare personnel and patients. Orthopedic surgeons might consider adding a short, instructive video focusing on proper usage as well as signs of adverse events to their discharge protocol to limit occurrences of these pitfalls associated with cryotherapy.
CONCLUSION
There is inadequate literature to support the of use postoperative cryotherapy of any kind in the field of orthopedics at this time. More robust, standardized studies, and a formidable economic analysis of advanced cold therapy systems are necessary before physicians prescribing cryotherapy can be confident that they are augmenting patient recovery. Nevertheless, as new developments in medicinal cryotherapy occur, it may be possible for the orthopedic community to wield its salutatory effects to limit complications and improve post-surgical outcomes.
1. Freiman N, Bouganim N. History of cryotherapy. Dermatol Online J. 2005;11(2):9.
2. Spencer JH, inventor; Nortech Lab Inc, assignee. Device for use as a hot and cold compress. US patent US3780537A. December 25, 1973.
3. Stålman A, Berglund L, Dungnerc E, Arner P, Felländer-Tsai L. Temperature-sensitive release of prostaglandin E₂ and diminished energy requirements in synovial tissue with postoperative cryotherapy: a prospective randomized study after knee arthroscopy. J Bone Joint Surg Am. 2011;93(21):1961-1968. doi:10.2106/JBJS.J.01790.
4. Kawabata A. Prostaglandin E2 and pain--an update. Biol Pharm Bull. 2011;34(8):1170-1173. doi:10.1248/bpb.34.1170.
5. Schaser KD, Stover JF, Melcher I, et al. Local cooling restores microcirculatory hemodynamics after closed soft-tissue trauma in rats. J Trauma. 2006;61(3):642-649. doi:10.1097/01.ta.0000174922.08781.2f.
6. Ruffilli A, Buda R, Castagnini F, et al. Temperature-controlled continuous cold flow device versus traditional icing regimen following anterior cruciate ligament reconstruction: a prospective randomized comparative trial. Arch Orthop Trauma Surg. 2015;135(10):1405-1410. doi:10.1007/s00402-015-2273-z.
7. Kuyucu E, Bülbül M, Kara A, Koçyiğit F, Erdil M. Is cold therapy really efficient after knee arthroplasty? Ann Med Surg. 2015;4(4):475-478. doi:10.1016/j.amsu.2015.10.019.
8. Martin SS, Spindler KP, Tarter JW, Detwiler K, Petersen HA. Cryotherapy: an effective modality for decreasing intraarticular temperature after knee arthroscopy. Am J Sports Med. 2001;29(3):288-291. doi:10.1177/03635465010290030501.
9. Yu SY, Chen S, Yan HD, Fan CY. Effect of cryotherapy after elbow arthrolysis: A prospective, single-blinded, randomized controlled study. Arch Phys Med Rehabil. 2015;96(1):1-6. doi:10.1016/j.apmr.2014.08.011.
10. Dambros C, Martimbianco ALC, Polachini LO, Lahoz GL, Chamlian TR, Cohen M. Effectiveness of cryotherapy after anterior cruciate ligament reconstruction. Acta Ortop Bras. 2012;20(5):285-290. doi:10.1590/S1413-78522012000500008.
11. Leegwater NC, Nolte PA, de Korte N, et al. The efficacy of continuous-flow cryo and cyclic compression therapy after hip fracture surgery on postoperative pain: design of a prospective, open-label, parallel, multicenter, randomized controlled, clinical trial. BMC Musculoskelet Disord. 2016;17(1):153. doi:10.1186/s12891-016-1000-4.
12. Kullenberg B, Ylipää S, Söderlund K, Resch S. Postoperative cryotherapy after total knee arthroplasty: a prospective study of 86 patients. J Arthroplasty. 2006;21(8):1175-1179. doi:10.1016/j.arth.2006.02.159.
13. Morsi E. Continuous-flow cold therapy after total knee arthroplasty. J Arthroplasty. 2002;17(6):718-722. doi:10.1054/arth.2002.33562.
14. Singh H, Osbahr DC, Holovacs TF, Cawley PW, Speer KP. The efficacy of continuous cryotherapy on the postoperative shoulder: A prospective, randomized investigation. J Shoulder Elb Surg. 2001;10(6):522-525. doi:10.1067/mse.2001.118415.
15. Saito N, Horiuchi H, Kobayashi S, Nawata M, Takaoka K. Continuous local cooling for pain relief following total hip arthroplasty. J Arthroplasty. 2004;19(3):334-337. doi:10.1016/j.arth.2003.10.011.
16. Gibbons C, Solan M, Ricketts D, Patterson M. Cryotherapy compared with Robert Jones bandage after total knee replacement: A prospective randomized trial. Int Orthop. 2001;25(4):250-252. doi:10.1007/s002640100227.
17. Kraeutler MJ, Reynolds KA, Long C, McCarty EC. Compressive cryotherapy versus ice-a prospective, randomized study on postoperative pain in patients undergoing arthroscopic rotator cuff repair or subacromial decompression. J Shoulder Elb Surg. 2015;24(6):854-859. doi:10.1016/j.jse.2015.02.004.
18. Thienpont E. Does Advanced Cryotherapy Reduce Pain and Narcotic Consumption After Knee Arthroplasty? Clin Orthop Relat Res. 2014;472(11):3417-3423. doi:10.1007/s11999-014-3810-8.
19. Woolf SK, Barfield WR, Merrill KD, McBryde AM Jr. Comparison of a continuous temperature-controlled cryotherapy device to a simple icing regimen following outpatient knee arthroscopy. J Knee Surg. 2008;21(1):15-19.
20. Su EP, Perna M, Boettner F, et al. A prospective, multi-center, randomised trial to evaluate the efficacy of a cryopneumatic device on total knee arthroplasty recovery. J Bone Joint Surg Br. 2012;94(11 Suppl A):153-156. doi:10.1302/0301-620X.94B11.30832.
21. Barber F. A comparison of crushed ice and continuous flow cold therapy. Am J Knee Surg. 2000;13(2):97-101.
22. Demoulin C, Brouwers M, Darot S, Gillet P, Crielaard JM, Vanderthommen M. Comparison of gaseous cryotherapy with more traditional forms of cryotherapy following total knee arthroplasty. Ann Phys Rehabil Med. 2012;55(4):229-240. doi:10.1016/j.rehab.2012.03.004.
23. Mumith A, Pavlou P, Barrett M, Thurston B, Garrett S. Enhancing postoperative rehabilitation following knee arthroplasty using a new cryotherapy product: a prospective study. Geriatr Orthop Surg Rehabil. 2015;6(4):316-321. doi:10.1177/2151458515609722.
24. Dickinson RN, Kuhn JE, Bergner JL, Rizzone KH. A systematic review of cost-effective treatment of postoperative rotator cuff repairs. J Shoulder Elb Surg. 2017;26(5):915-922. doi:10.1016/j.jse.2017.02.009.
25. Brown WC, Hahn DB. Frostbite of the Feet After Cryotherapy: A Report of Two Cases. J Foot Ankle Surg. 2009;48(5):577-580. doi:10.1053/j.jfas.2009.06.003.
26. Dundon JM, Rymer MC, Johnson RM. Total patellar skin loss from cryotherapy after total knee arthroplasty. J Arthroplasty. 2013;28(2):376.e5-e7. doi:10.1016/j.arth.2012.05.024.
27. Khajavi K, Pavelko T, Mishra A. Compartment syndrome arising from use of an electronic cooling pad. Am J Sports Med. 2004;32(6):1538-1541. doi:10.1177/0363546503262191.
28. King J, Plotner A, Adams B. Perniosis induced by a cold therapy system. Arch Dermatol. 2012;148(9):1101-1102.
29. Lee CK, Pardun J, Buntic R, Kiehn M, Brooks D, Buncke HJ. Severe frostbite of the knees after cryotherapy. Orthopedics. 2007;30(1):63-64.
30. McGuire DA, Hendricks SD. Incidences of frostbite in arthroscopic knee surgery postoperative cryotherapy rehabilitation. Arthroscopy. 2006;22(10):1141.e1-e6. doi:10.1016/j.arthro.2005.06.027.
31. Mirkin G. Why Ice Delays Recovery. http://www.drmirkin.com/fitness/why-ice-delays-recovery.html. Published September 16, 2015. Accessed July 17, 2017.
ABSTRACT
Cryotherapy is the use of the anti-inflammatory and analgesic properties of ice to facilitate healing. Cryotherapy mediates these salutatory effects by reducing blood flow to the site of injury, down-regulating the production of inflammatory and pain-inducing prostaglandins, and diminishing the conductive ability of nerve endings. It is commonly used postoperatively in orthopedics to decrease analgesic requirements and blood loss as well as to increase range of motion, despite limited literature on its ability to produce such therapeutic effects in clinical practice. This article examines the available literature and the scientific evidence for the use and efficacy of cryotherapy in post-surgical orthopedic patients. It also reviews the potential pitfalls associated with improper use. Overall, this review seeks to provide insight into when, or whether, cryotherapy is appropriate for orthopedic patients during surgical recovery.
Continue to: Cold therapy has been a mainstay of medical treatment...
Cold therapy has been a mainstay of medical treatment since the days of Hippocrates. Initially used by ancient Egyptians to mitigate inflammation and by Hippocrates himself to treat hemorrhage, the therapeutic applications of ice evolved throughout history to become part of the treatment algorithm for a variety of health conditions.1 Ice made an ideal numbing agent for limb amputations and an anesthetic for certain cancers, but truly became ubiquitous when the first cold pack meant for medicinal use was patented in the early 1970s.1,2 Despite their armamentarium of advanced treatment modalities, physicians in the modern era continue to prescribe cryotherapy for their patients, particularly in the field of orthopedics. Most athletes know the “RICE” (Rest, Ice, Compression, Elevation) protocol and utilize it to minimize inflammation associated with soft tissue injuries.
Inflammation is a physiologic response to noxious stimuli. Cell damage results in the production of inflammatory mediators including prostaglandins, which play a crucial role in the vasodilation and pain associated with inflammation. Vasodilation and increased blood flow manifest as swelling, which can cause pain by putting pressure on nerve endings. The inflammatory prostaglandin E2 (PGE2) causes local increases in temperature and mediates pain.3,4 The application of cold therapy attenuates inflammatory microvascular and hemodynamic changes, reducing some of the deleterious effects of inflammation and minimizing pain. Animal models demonstrate that cryotherapy restores functional capillary density, reverses tumor necrosis factor-α (TNF-α)-induced microvasculature damage, and reduces the production of thrombogenic thromboxanes in injured soft tissue.5 Additionally, cold therapy after knee arthroscopy is associated with lower concentrations of PGE2 in the knee.3 Local cooling acts at the cellular level to decrease edema, reduce pain, and slow blood flow to the affected area, with the overall effect of alleviating inflammation.4,5
Cryotherapy is standard practice in postoperative orthopedic care, but there is limited literature demonstrating its efficacy in this setting. In addition, the advent of more advanced wearable cooling systems necessitates a thorough comparison of the various cryotherapy mechanisms both from healthcare and economic perspectives. The goal of this article is to examine the benefits of cryotherapy in the postoperative management of orthopedic surgical interventions and to review the effectiveness of differing types of cryotherapy. A secondary goal of this article is to review the literature on the adverse effects of cryotherapy in order to increase physician awareness of this issue and highlight the importance of patient education when utilizing cryotherapy postoperatively.
BENEFITS OF CRYOTHERAPY
Three standard types of cryotherapy are prescribed as postoperative therapy in orthopedics: compressive cryotherapy, continuous flow cryotherapy, and the application of ice. All aim to decrease the amount of inflammation of the surgical site, reduce patient pain, and aid in the recovery process. The application of ice or other cooling pack devices without compression is the most commonly used method, likely because it is the most economical and user-friendly cryotherapy option. Compressive cryotherapy is the application of ice or an ice pack secured to the site with a bandage or other device in a manner that also applies pressure to the site of injury. Finally, continuous flow cryotherapy systems are typically connected to a refrigeration control unit and apply compressive cooling through the uninterrupted flow of cold water or gas through a wrap around the injured site. Examples include the Game Ready® (CoolSystems, Inc.), Cryo/Cuff® IC Cooler (DJO Global), and Hilotherm Homecare (Hilotherm GmbH) systems, which are marketed as an improvement over traditional forms of cold therapy, as they are capable of cooling for hours at a time, allow for nighttime use, and provide the operator with temperature control.6-8
Postoperative cryotherapy is prescribed for a wide variety of orthopedic procedures, including anterior cruciate ligament (ACL) reconstruction surgery, rotator cuff surgery, and total knee arthroplasty (TKA). Current literature includes many studies monitoring postoperative outcomes in patients using cryotherapy as part of their treatment regimen, with the primary endpoints being visual analog scale (VAS) scores, analgesic consumption, and range of motion (ROM).9-16 As demonstrated by in Table 1, these studies do not provide conclusive evidence that cryotherapy significantly alters postoperative outcomes, despite its ubiquitous use by the orthopedics community. In fact, the literature reflects a seeming lack of consensus regarding the effect of cryotherapy on analgesic requirements, pain, and joint mobility following procedures. Interestingly, of the studies represented in Table 1, only half analyzed all 3 postoperative measures (analgesic consumption, pain, and ROM). Furthermore, solely Morsi13 concluded that cryotherapy resulted in significant improvements in all 3 outcome measures in a trial involving only 30 patients. Kullenberg and colleagues12 performed the largest study, but still included only 86 patients. In addition, all the studies focused on 1 joint or procedure. Thus, despite evidence that cryotherapy reduces inflammation at a molecular level, current literature does not unequivocally support the common belief that cryotherapy benefits patients in practice. More robust studies that include an analysis of analgesic consumption, VAS scores, and ROM (at minimum) and compare the relative efficacy of cryotherapy across joint types and procedures are necessary to determine whether postoperative cryotherapy in orthopedics is appropriate.
Table 1. Results from Studies that Compared Cryotherapy to Standard Care Within the First 2 Weeks Following Surgery
Author | Joint/Procedure Type | Number of Trial Participants | Cryotherapy Type | Analgesic Consumption | VAS Score | ROM |
Yu et al9 | Elbow arthrolysis | 59 | Continuous flow cryotherapy (Cryo/Cuff®; DJO Global) | No significant difference | Cryotherapy significantly decreased scores up to POD 7 (P < 0.05) | No significant difference |
Dambros et al10 | ACL reconstruction | 25 | Ice pack | Xa | No significant difference | No significant difference |
Leegwater et al11 | Hip arthroplasty | 30 | Continuous flow cryotherapy (Game Ready®; CoolSystems, Inc.) | Trend towards lower use (No significant difference) | No significant difference | Xa |
Kullenberg et al12 | Knee arthroplasty | 86 | Continuous flow cryotherapy (Cryo/Cuff®) | No significant difference | No significant difference | Significantly improved at POD 7 and POD 21 |
Morsi13 | Knee arthroplasty | 30 | Continuous flow cryotherapy | Significantly lower consumption (P < 0.01) | Cryotherapy significantly decreased scores (P < 0.001) | Significantly improved at POD 7; No significant difference 6 weeks postoperative |
Singh et al14 | Open vs arthroscopic shoulder procedures | 70 | Continuous flow cryotherapy (Breg Polar Care Glacier® Cold Therapy unit; Breg Inc.) | Xa | Cryotherapy significantly decreased scores at arthroscopic POD 14 (P = 0.043); No significant difference for open procedures | Xa |
Saito et al15 | Hip arthroplasty | 46 | Continuous flow cryotherapy (Icing System 2000; Nippon Sigmax Co., Ltd.) | Significantly lower epidural analgesic use (P < 0.001); no significant difference in adjunct analgesic consumption | Cryotherapy significantly decreased scores POD 1-4 (P < 0.05) | Xa |
Gibbons et al16 | Knee arthroplasty | 60 | Continuous flow cryotherapy (Cryo/Cuff®) | No significant difference | No significant difference | No significant difference |
Continue to: ADVANCED CRYOTHERAPY DEVICES...
ADVANCED CRYOTHERAPY DEVICES
Several recent studies explored the relative postoperative benefits of advanced cryotherapeutics in lieu of the traditional ice pack.6,7,17-21 As reflected in Table 2, these studies, much like the literature comparing cryotherapy to the control, do not reveal significant benefits of continuous flow cryotherapy after surgery. In fact, the only outcome measure that was found to differ significantly in more than 1 study was ROM. Though the makers of advanced cryotherapy systems market them as a vast improvement over traditional forms of cold therapy, there is insufficient evidence to support such claims. Even the most robust study that included 280 patients failed to show significant differences in the analgesic use and ROM after surgery.20 Of note, all but 1 study compared traditional and advanced cryotherapy following procedures on the knee. Additional research exploring outcomes after surgery on other joints is necessary before any conclusions can be made regarding postoperative benefits or risks within orthopedics more generally.
Author | Joint / Procedure Type | Number of Trial Participants | Analgesic Consumption | VAS Score | ROM |
Kraeutler et al17 | Rotator cuff repair or subacromial decompression | 46 | No significant difference | No significant difference | Xa |
Thienpont18 | Knee arthroplasty | 116 | No significant difference | No significant difference | Significant reduction in active flexion with advanced cryotherapy (P = 0.02); No significant difference in other ROM tests |
Woolf et al19 | Knee arthroplasty | 53 | Decrease in night pain through POD 2 only | Xa | Xa |
Su et al20 | Knee arthroplasty | 280 | Significantly lower use with cryotherapy up to POD 14; No significant difference thereafter | Xa | No difference |
Barber21 | ACL reconstruction | 87 | Significantly lower use with cryotherapy POD 1 and 2 (P = 0.035) | Cryotherapy significantly decreased scores only POD 1 (P < 0.01) | Greater ROM with cryotherapy POD 7 (P < 0.03) |
Ruffilli et al6 | ACL reconstruction | 47 | No difference | Xa | Greater ROM with cryotherapy (P < 0.0001) |
Kuyucu et al7 | Knee arthroplasty | 60 | Xa | Cryotherapy significantly decreased scores (P < 0.05) | Greater ROM with cryotherapy (P < 0.05) |
RISKS AND ADVERSE EFFECTS OF CRYOTHERAPY
A rigorous analysis of the benefits of cryotherapy ought to incorporate other factors in addition to improvements in analgesic consumption, VAS score, and ROM. These include the financial and time investment involved in the use of continuous flow cryotherapy, which the majority of studies do not consider. Though many authors acknowledge that continuous flow cryotherapy is expensive, to our knowledge, none have yet performed a formal economic analysis of the cost of advanced cryotherapy to the patient as well as to the healthcare system at large.6,7,13,18,22-24 Dickinson and colleagues24 calculated the total cost of cryotherapy and rehabilitation following rotator cuff repair, but addressed only the up-front cost of the cold therapy system. For context, Table 3 summarizes the retail cost of the most popular cryotherapy devices on the market. Based on this information alone, it seems reasonable to conclude that these systems are associated with significantly more cost than traditional forms of cold therapy, and therefore would be an undesirable option for patients or hospital systems. Nevertheless, cost considerations are more nuanced than a simple comparison of price, necessitating more advanced economic analyses. Substantial savings may be on the table if future studies are able to prove postoperative cryotherapy shortens hospital stays, reduces medication costs, and results in fewer physical therapy sessions. Moreover, if all this is true, patients may experience quicker recovery and have overall greater post-procedure satisfaction.
Table 3. Cost of Most Popular Cryotherapy Units
System | Cost |
Cryo/Cuff® IC Cooler (DJO Global) | $125 |
DonJoy IceMan Classic (DJO Global) | $169 |
The Polar Care Kodiak (Breg, Inc.) | $180 |
Patient education required for optimal use of advanced cold therapy is another aspect of cryotherapy that is poorly represented in the literature. As Dickinson and colleagues24 point out, because it eliminates some dependency on the patient to remember to ice appropriately, continuous flow cryotherapy may have a positive impact on compliance and therefore yield improved outcomes.24 Hospital staff may be required to spend additional time with patients. However, this is necessary to ensure proper understanding on how to operate the system and avoid adverse outcomes. Patients may also find the large coolers inconvenient and may therefore be reluctant to use them, finding traditional ice more manageable. Future studies should consider gathering data on patient education, compliance, and overall reception/satisfaction to complete a more holistic investigation of the role of postoperative cryotherapy in orthopedics.
Cryotherapy is not without adverse outcomes, which have been documented primarily in the form of case study reports. Relevant case studies cited adverse outcomes including frostbite/skin loss, compartment syndrome, and perniosis as potential dangers of postoperative cryotherapy in orthopedics (Table 4).25-30 As an example, a patient recovering from patellar-tendon repair experienced bilateral frostbite and skin loss following 2 weeks of uninterrupted use of cryotherapy without any barrier between his skin and the system.29 A similar case study described 2 female patients, one recovering from a TKA and the other from a tibial revision of arthroplasty, who used cryotherapy systems without cessation and experienced frostbite and skin necrosis over the entirety of their knees.26 A third case study exploring 4 incidents of patellar frostbite and necrosis following knee arthroscopies proposed that poor patient understanding of proper cryotherapy use as well as poor recognition of the signs of frostbite contributed to these adverse outcomes. Furthermore, the cryotherapy brace used by all 4 patients included a feature designed to counteract patellar inflammation that also may have increased the likelihood of frostbite in this area due to poor tissue insulation. The authors noted that following the incidents, the makers of the brace removed patellar coverage to prevent future occurrences.30
Author | Adverse Effect | Procedure/Location |
Brown and Hahn25 | Frostbite | Bunionectomy; hallux valgus correction/feet |
Dundon et al26 | Skin necrosis | TKA/patella |
Khajavi et al27 | Compartment syndrome | Arthroscopic osteochondral autograft transfer/calf |
King et al28 | Perniosis | ACL reconstruction/knee |
Lee et al29 | Frostbite | Patellar-tendon repair/knees |
McGuire and Hendricks30 | Frostbite | Knee arthroscopy/patella |
Abbreviations: ACL, anterior cruciate ligament; TKA, total knee arthroplasty.
Frostbite linked to cryotherapy has also occurred following orthopedic procedures outside the knee. Brown and Hahn25 described 2 young females who developed skin necrosis following podiatric surgeries and constant cold therapy for roughly a week. Notably, 1 patient had cold sensitivity, which likely put her at an increased baseline risk of experiencing frostbite while using cryotherapy. Tissue necrosis is not the only danger of cold therapy discussed in this study. Surprisingly, 1 patient also developed compartment syndrome.25 Khajavi and colleagues27 also documented postoperative compartment syndrome in a patient following an arthroscopic osteochondral autograft transfer, which they attributed to reperfusion injury in the wake of first-degree frostbite. Hospital personnel also instructed this patient to use his cryotherapy system without interruption at the coldest temperature tolerable, contrary to manufacturer’s instructions.27
Continue to: King and colleagues...
King and colleagues28 described 2 cases of patients complaining of nodules, papules, and plaques soon after ACL reconstruction and the initiation of cryotherapy. A histological examination of their skin lesions demonstrated the presence of a perivascular and periadnexal superficial and deep lymphocytic infiltrate associated with perniosis. Dermatologists associated the perniosis with the cryotherapy cuff adhesive mechanisms, as their locations matched those of the lesions and symptoms subsided after cessation of cuff usage.28
Cases of adverse effects with perioperative cryotherapy have also occurred at our own institution. The authors obtained informed written consent from the patients to print and publish their images. In 2 separate incidents, patients overdid icing and experienced rather extreme side effects including burns and blisters (Figures 1 and 2). In light of these adverse events, the physicians have questioned whether RICE ought to be part of their standard perioperative recommendations. These physicians are not alone in their uncertainty. Interestingly, even Mirkin,31 who coined the RICE mnemonic, now believes that consistent icing post-injury actually inhibits the body’s natural inflammatory healing response, delaying rather than speeding recovery, and suggests that icing ought to be used for pain control only.
DISCUSSION
Though there is ample literature supporting the common belief that cryotherapy minimizes inflammation at the cellular level, whether or not it results in meaningful improvements in post-surgical orthopedic outcomes remains unclear. Table 1 reflects a dearth of evidence to support the widespread current practice of cold therapy following orthopedic procedures, but few studies could demonstrate a significant difference in the analgesic use, VAS score, or ROM between cryotherapy and control groups. It is worth noting that these studies used different cryotherapy systems. Though in theory the continuous flow cryotherapy systems are similarly designed, there are potential differences among them that have not been controlled for in this analysis. All studies had <90 participants and focused on a single joint or procedure, making it difficult to draw large scale conclusions about the utility of cold therapy in the postoperative orthopedic population at large. Furthermore, researchers measured endpoints at a range of time intervals that were inconsistent across studies. In some cases, the significance of the impact of cryotherapy on recovery within a single study differed based on the time point at which researchers measured outcomes.12-14 This raises the question as to whether cryotherapy has no benefits, or whether they are simply time-dependent. Future studies should seek to ascertain whether there is a postoperative time window in which cryotherapy could potentially expedite the recovery process.
Similarly, Table 2 shows a lack of consensus regarding the effect of advanced cryotherapy when compared to traditional ice application on pain, analgesic use, and joint mobility after surgery. However, all but 1 of these studies focused on knee procedures. Therefore, our findings may not be applicable to orthopedic surgeries on other joints. Nevertheless, the use of advanced cryotherapy in postoperative orthopedic care may wane if researchers continue to show that it is no more beneficial than its far less expensive counterpart of ice and an ace bandage.
The case studies discussed in this review serve as cautionary tales of the dangers of cryotherapy when used improperly. Though frostbite and subsequent tissue necrosis seem most common, physicians should be made aware that compartment syndrome and perniosis are also possible consequences. Orthopedic patients perhaps have an increased risk of developing these side effects due to the nature of their injuries and the large cutaneous surface area to which cryotherapy is applied. These outcomes could seemingly be avoided with improved educational initiatives targeted at both healthcare personnel and patients. Orthopedic surgeons might consider adding a short, instructive video focusing on proper usage as well as signs of adverse events to their discharge protocol to limit occurrences of these pitfalls associated with cryotherapy.
CONCLUSION
There is inadequate literature to support the of use postoperative cryotherapy of any kind in the field of orthopedics at this time. More robust, standardized studies, and a formidable economic analysis of advanced cold therapy systems are necessary before physicians prescribing cryotherapy can be confident that they are augmenting patient recovery. Nevertheless, as new developments in medicinal cryotherapy occur, it may be possible for the orthopedic community to wield its salutatory effects to limit complications and improve post-surgical outcomes.
ABSTRACT
Cryotherapy is the use of the anti-inflammatory and analgesic properties of ice to facilitate healing. Cryotherapy mediates these salutatory effects by reducing blood flow to the site of injury, down-regulating the production of inflammatory and pain-inducing prostaglandins, and diminishing the conductive ability of nerve endings. It is commonly used postoperatively in orthopedics to decrease analgesic requirements and blood loss as well as to increase range of motion, despite limited literature on its ability to produce such therapeutic effects in clinical practice. This article examines the available literature and the scientific evidence for the use and efficacy of cryotherapy in post-surgical orthopedic patients. It also reviews the potential pitfalls associated with improper use. Overall, this review seeks to provide insight into when, or whether, cryotherapy is appropriate for orthopedic patients during surgical recovery.
Continue to: Cold therapy has been a mainstay of medical treatment...
Cold therapy has been a mainstay of medical treatment since the days of Hippocrates. Initially used by ancient Egyptians to mitigate inflammation and by Hippocrates himself to treat hemorrhage, the therapeutic applications of ice evolved throughout history to become part of the treatment algorithm for a variety of health conditions.1 Ice made an ideal numbing agent for limb amputations and an anesthetic for certain cancers, but truly became ubiquitous when the first cold pack meant for medicinal use was patented in the early 1970s.1,2 Despite their armamentarium of advanced treatment modalities, physicians in the modern era continue to prescribe cryotherapy for their patients, particularly in the field of orthopedics. Most athletes know the “RICE” (Rest, Ice, Compression, Elevation) protocol and utilize it to minimize inflammation associated with soft tissue injuries.
Inflammation is a physiologic response to noxious stimuli. Cell damage results in the production of inflammatory mediators including prostaglandins, which play a crucial role in the vasodilation and pain associated with inflammation. Vasodilation and increased blood flow manifest as swelling, which can cause pain by putting pressure on nerve endings. The inflammatory prostaglandin E2 (PGE2) causes local increases in temperature and mediates pain.3,4 The application of cold therapy attenuates inflammatory microvascular and hemodynamic changes, reducing some of the deleterious effects of inflammation and minimizing pain. Animal models demonstrate that cryotherapy restores functional capillary density, reverses tumor necrosis factor-α (TNF-α)-induced microvasculature damage, and reduces the production of thrombogenic thromboxanes in injured soft tissue.5 Additionally, cold therapy after knee arthroscopy is associated with lower concentrations of PGE2 in the knee.3 Local cooling acts at the cellular level to decrease edema, reduce pain, and slow blood flow to the affected area, with the overall effect of alleviating inflammation.4,5
Cryotherapy is standard practice in postoperative orthopedic care, but there is limited literature demonstrating its efficacy in this setting. In addition, the advent of more advanced wearable cooling systems necessitates a thorough comparison of the various cryotherapy mechanisms both from healthcare and economic perspectives. The goal of this article is to examine the benefits of cryotherapy in the postoperative management of orthopedic surgical interventions and to review the effectiveness of differing types of cryotherapy. A secondary goal of this article is to review the literature on the adverse effects of cryotherapy in order to increase physician awareness of this issue and highlight the importance of patient education when utilizing cryotherapy postoperatively.
BENEFITS OF CRYOTHERAPY
Three standard types of cryotherapy are prescribed as postoperative therapy in orthopedics: compressive cryotherapy, continuous flow cryotherapy, and the application of ice. All aim to decrease the amount of inflammation of the surgical site, reduce patient pain, and aid in the recovery process. The application of ice or other cooling pack devices without compression is the most commonly used method, likely because it is the most economical and user-friendly cryotherapy option. Compressive cryotherapy is the application of ice or an ice pack secured to the site with a bandage or other device in a manner that also applies pressure to the site of injury. Finally, continuous flow cryotherapy systems are typically connected to a refrigeration control unit and apply compressive cooling through the uninterrupted flow of cold water or gas through a wrap around the injured site. Examples include the Game Ready® (CoolSystems, Inc.), Cryo/Cuff® IC Cooler (DJO Global), and Hilotherm Homecare (Hilotherm GmbH) systems, which are marketed as an improvement over traditional forms of cold therapy, as they are capable of cooling for hours at a time, allow for nighttime use, and provide the operator with temperature control.6-8
Postoperative cryotherapy is prescribed for a wide variety of orthopedic procedures, including anterior cruciate ligament (ACL) reconstruction surgery, rotator cuff surgery, and total knee arthroplasty (TKA). Current literature includes many studies monitoring postoperative outcomes in patients using cryotherapy as part of their treatment regimen, with the primary endpoints being visual analog scale (VAS) scores, analgesic consumption, and range of motion (ROM).9-16 As demonstrated by in Table 1, these studies do not provide conclusive evidence that cryotherapy significantly alters postoperative outcomes, despite its ubiquitous use by the orthopedics community. In fact, the literature reflects a seeming lack of consensus regarding the effect of cryotherapy on analgesic requirements, pain, and joint mobility following procedures. Interestingly, of the studies represented in Table 1, only half analyzed all 3 postoperative measures (analgesic consumption, pain, and ROM). Furthermore, solely Morsi13 concluded that cryotherapy resulted in significant improvements in all 3 outcome measures in a trial involving only 30 patients. Kullenberg and colleagues12 performed the largest study, but still included only 86 patients. In addition, all the studies focused on 1 joint or procedure. Thus, despite evidence that cryotherapy reduces inflammation at a molecular level, current literature does not unequivocally support the common belief that cryotherapy benefits patients in practice. More robust studies that include an analysis of analgesic consumption, VAS scores, and ROM (at minimum) and compare the relative efficacy of cryotherapy across joint types and procedures are necessary to determine whether postoperative cryotherapy in orthopedics is appropriate.
Table 1. Results from Studies that Compared Cryotherapy to Standard Care Within the First 2 Weeks Following Surgery
Author | Joint/Procedure Type | Number of Trial Participants | Cryotherapy Type | Analgesic Consumption | VAS Score | ROM |
Yu et al9 | Elbow arthrolysis | 59 | Continuous flow cryotherapy (Cryo/Cuff®; DJO Global) | No significant difference | Cryotherapy significantly decreased scores up to POD 7 (P < 0.05) | No significant difference |
Dambros et al10 | ACL reconstruction | 25 | Ice pack | Xa | No significant difference | No significant difference |
Leegwater et al11 | Hip arthroplasty | 30 | Continuous flow cryotherapy (Game Ready®; CoolSystems, Inc.) | Trend towards lower use (No significant difference) | No significant difference | Xa |
Kullenberg et al12 | Knee arthroplasty | 86 | Continuous flow cryotherapy (Cryo/Cuff®) | No significant difference | No significant difference | Significantly improved at POD 7 and POD 21 |
Morsi13 | Knee arthroplasty | 30 | Continuous flow cryotherapy | Significantly lower consumption (P < 0.01) | Cryotherapy significantly decreased scores (P < 0.001) | Significantly improved at POD 7; No significant difference 6 weeks postoperative |
Singh et al14 | Open vs arthroscopic shoulder procedures | 70 | Continuous flow cryotherapy (Breg Polar Care Glacier® Cold Therapy unit; Breg Inc.) | Xa | Cryotherapy significantly decreased scores at arthroscopic POD 14 (P = 0.043); No significant difference for open procedures | Xa |
Saito et al15 | Hip arthroplasty | 46 | Continuous flow cryotherapy (Icing System 2000; Nippon Sigmax Co., Ltd.) | Significantly lower epidural analgesic use (P < 0.001); no significant difference in adjunct analgesic consumption | Cryotherapy significantly decreased scores POD 1-4 (P < 0.05) | Xa |
Gibbons et al16 | Knee arthroplasty | 60 | Continuous flow cryotherapy (Cryo/Cuff®) | No significant difference | No significant difference | No significant difference |
Continue to: ADVANCED CRYOTHERAPY DEVICES...
ADVANCED CRYOTHERAPY DEVICES
Several recent studies explored the relative postoperative benefits of advanced cryotherapeutics in lieu of the traditional ice pack.6,7,17-21 As reflected in Table 2, these studies, much like the literature comparing cryotherapy to the control, do not reveal significant benefits of continuous flow cryotherapy after surgery. In fact, the only outcome measure that was found to differ significantly in more than 1 study was ROM. Though the makers of advanced cryotherapy systems market them as a vast improvement over traditional forms of cold therapy, there is insufficient evidence to support such claims. Even the most robust study that included 280 patients failed to show significant differences in the analgesic use and ROM after surgery.20 Of note, all but 1 study compared traditional and advanced cryotherapy following procedures on the knee. Additional research exploring outcomes after surgery on other joints is necessary before any conclusions can be made regarding postoperative benefits or risks within orthopedics more generally.
Author | Joint / Procedure Type | Number of Trial Participants | Analgesic Consumption | VAS Score | ROM |
Kraeutler et al17 | Rotator cuff repair or subacromial decompression | 46 | No significant difference | No significant difference | Xa |
Thienpont18 | Knee arthroplasty | 116 | No significant difference | No significant difference | Significant reduction in active flexion with advanced cryotherapy (P = 0.02); No significant difference in other ROM tests |
Woolf et al19 | Knee arthroplasty | 53 | Decrease in night pain through POD 2 only | Xa | Xa |
Su et al20 | Knee arthroplasty | 280 | Significantly lower use with cryotherapy up to POD 14; No significant difference thereafter | Xa | No difference |
Barber21 | ACL reconstruction | 87 | Significantly lower use with cryotherapy POD 1 and 2 (P = 0.035) | Cryotherapy significantly decreased scores only POD 1 (P < 0.01) | Greater ROM with cryotherapy POD 7 (P < 0.03) |
Ruffilli et al6 | ACL reconstruction | 47 | No difference | Xa | Greater ROM with cryotherapy (P < 0.0001) |
Kuyucu et al7 | Knee arthroplasty | 60 | Xa | Cryotherapy significantly decreased scores (P < 0.05) | Greater ROM with cryotherapy (P < 0.05) |
RISKS AND ADVERSE EFFECTS OF CRYOTHERAPY
A rigorous analysis of the benefits of cryotherapy ought to incorporate other factors in addition to improvements in analgesic consumption, VAS score, and ROM. These include the financial and time investment involved in the use of continuous flow cryotherapy, which the majority of studies do not consider. Though many authors acknowledge that continuous flow cryotherapy is expensive, to our knowledge, none have yet performed a formal economic analysis of the cost of advanced cryotherapy to the patient as well as to the healthcare system at large.6,7,13,18,22-24 Dickinson and colleagues24 calculated the total cost of cryotherapy and rehabilitation following rotator cuff repair, but addressed only the up-front cost of the cold therapy system. For context, Table 3 summarizes the retail cost of the most popular cryotherapy devices on the market. Based on this information alone, it seems reasonable to conclude that these systems are associated with significantly more cost than traditional forms of cold therapy, and therefore would be an undesirable option for patients or hospital systems. Nevertheless, cost considerations are more nuanced than a simple comparison of price, necessitating more advanced economic analyses. Substantial savings may be on the table if future studies are able to prove postoperative cryotherapy shortens hospital stays, reduces medication costs, and results in fewer physical therapy sessions. Moreover, if all this is true, patients may experience quicker recovery and have overall greater post-procedure satisfaction.
Table 3. Cost of Most Popular Cryotherapy Units
System | Cost |
Cryo/Cuff® IC Cooler (DJO Global) | $125 |
DonJoy IceMan Classic (DJO Global) | $169 |
The Polar Care Kodiak (Breg, Inc.) | $180 |
Patient education required for optimal use of advanced cold therapy is another aspect of cryotherapy that is poorly represented in the literature. As Dickinson and colleagues24 point out, because it eliminates some dependency on the patient to remember to ice appropriately, continuous flow cryotherapy may have a positive impact on compliance and therefore yield improved outcomes.24 Hospital staff may be required to spend additional time with patients. However, this is necessary to ensure proper understanding on how to operate the system and avoid adverse outcomes. Patients may also find the large coolers inconvenient and may therefore be reluctant to use them, finding traditional ice more manageable. Future studies should consider gathering data on patient education, compliance, and overall reception/satisfaction to complete a more holistic investigation of the role of postoperative cryotherapy in orthopedics.
Cryotherapy is not without adverse outcomes, which have been documented primarily in the form of case study reports. Relevant case studies cited adverse outcomes including frostbite/skin loss, compartment syndrome, and perniosis as potential dangers of postoperative cryotherapy in orthopedics (Table 4).25-30 As an example, a patient recovering from patellar-tendon repair experienced bilateral frostbite and skin loss following 2 weeks of uninterrupted use of cryotherapy without any barrier between his skin and the system.29 A similar case study described 2 female patients, one recovering from a TKA and the other from a tibial revision of arthroplasty, who used cryotherapy systems without cessation and experienced frostbite and skin necrosis over the entirety of their knees.26 A third case study exploring 4 incidents of patellar frostbite and necrosis following knee arthroscopies proposed that poor patient understanding of proper cryotherapy use as well as poor recognition of the signs of frostbite contributed to these adverse outcomes. Furthermore, the cryotherapy brace used by all 4 patients included a feature designed to counteract patellar inflammation that also may have increased the likelihood of frostbite in this area due to poor tissue insulation. The authors noted that following the incidents, the makers of the brace removed patellar coverage to prevent future occurrences.30
Author | Adverse Effect | Procedure/Location |
Brown and Hahn25 | Frostbite | Bunionectomy; hallux valgus correction/feet |
Dundon et al26 | Skin necrosis | TKA/patella |
Khajavi et al27 | Compartment syndrome | Arthroscopic osteochondral autograft transfer/calf |
King et al28 | Perniosis | ACL reconstruction/knee |
Lee et al29 | Frostbite | Patellar-tendon repair/knees |
McGuire and Hendricks30 | Frostbite | Knee arthroscopy/patella |
Abbreviations: ACL, anterior cruciate ligament; TKA, total knee arthroplasty.
Frostbite linked to cryotherapy has also occurred following orthopedic procedures outside the knee. Brown and Hahn25 described 2 young females who developed skin necrosis following podiatric surgeries and constant cold therapy for roughly a week. Notably, 1 patient had cold sensitivity, which likely put her at an increased baseline risk of experiencing frostbite while using cryotherapy. Tissue necrosis is not the only danger of cold therapy discussed in this study. Surprisingly, 1 patient also developed compartment syndrome.25 Khajavi and colleagues27 also documented postoperative compartment syndrome in a patient following an arthroscopic osteochondral autograft transfer, which they attributed to reperfusion injury in the wake of first-degree frostbite. Hospital personnel also instructed this patient to use his cryotherapy system without interruption at the coldest temperature tolerable, contrary to manufacturer’s instructions.27
Continue to: King and colleagues...
King and colleagues28 described 2 cases of patients complaining of nodules, papules, and plaques soon after ACL reconstruction and the initiation of cryotherapy. A histological examination of their skin lesions demonstrated the presence of a perivascular and periadnexal superficial and deep lymphocytic infiltrate associated with perniosis. Dermatologists associated the perniosis with the cryotherapy cuff adhesive mechanisms, as their locations matched those of the lesions and symptoms subsided after cessation of cuff usage.28
Cases of adverse effects with perioperative cryotherapy have also occurred at our own institution. The authors obtained informed written consent from the patients to print and publish their images. In 2 separate incidents, patients overdid icing and experienced rather extreme side effects including burns and blisters (Figures 1 and 2). In light of these adverse events, the physicians have questioned whether RICE ought to be part of their standard perioperative recommendations. These physicians are not alone in their uncertainty. Interestingly, even Mirkin,31 who coined the RICE mnemonic, now believes that consistent icing post-injury actually inhibits the body’s natural inflammatory healing response, delaying rather than speeding recovery, and suggests that icing ought to be used for pain control only.
DISCUSSION
Though there is ample literature supporting the common belief that cryotherapy minimizes inflammation at the cellular level, whether or not it results in meaningful improvements in post-surgical orthopedic outcomes remains unclear. Table 1 reflects a dearth of evidence to support the widespread current practice of cold therapy following orthopedic procedures, but few studies could demonstrate a significant difference in the analgesic use, VAS score, or ROM between cryotherapy and control groups. It is worth noting that these studies used different cryotherapy systems. Though in theory the continuous flow cryotherapy systems are similarly designed, there are potential differences among them that have not been controlled for in this analysis. All studies had <90 participants and focused on a single joint or procedure, making it difficult to draw large scale conclusions about the utility of cold therapy in the postoperative orthopedic population at large. Furthermore, researchers measured endpoints at a range of time intervals that were inconsistent across studies. In some cases, the significance of the impact of cryotherapy on recovery within a single study differed based on the time point at which researchers measured outcomes.12-14 This raises the question as to whether cryotherapy has no benefits, or whether they are simply time-dependent. Future studies should seek to ascertain whether there is a postoperative time window in which cryotherapy could potentially expedite the recovery process.
Similarly, Table 2 shows a lack of consensus regarding the effect of advanced cryotherapy when compared to traditional ice application on pain, analgesic use, and joint mobility after surgery. However, all but 1 of these studies focused on knee procedures. Therefore, our findings may not be applicable to orthopedic surgeries on other joints. Nevertheless, the use of advanced cryotherapy in postoperative orthopedic care may wane if researchers continue to show that it is no more beneficial than its far less expensive counterpart of ice and an ace bandage.
The case studies discussed in this review serve as cautionary tales of the dangers of cryotherapy when used improperly. Though frostbite and subsequent tissue necrosis seem most common, physicians should be made aware that compartment syndrome and perniosis are also possible consequences. Orthopedic patients perhaps have an increased risk of developing these side effects due to the nature of their injuries and the large cutaneous surface area to which cryotherapy is applied. These outcomes could seemingly be avoided with improved educational initiatives targeted at both healthcare personnel and patients. Orthopedic surgeons might consider adding a short, instructive video focusing on proper usage as well as signs of adverse events to their discharge protocol to limit occurrences of these pitfalls associated with cryotherapy.
CONCLUSION
There is inadequate literature to support the of use postoperative cryotherapy of any kind in the field of orthopedics at this time. More robust, standardized studies, and a formidable economic analysis of advanced cold therapy systems are necessary before physicians prescribing cryotherapy can be confident that they are augmenting patient recovery. Nevertheless, as new developments in medicinal cryotherapy occur, it may be possible for the orthopedic community to wield its salutatory effects to limit complications and improve post-surgical outcomes.
1. Freiman N, Bouganim N. History of cryotherapy. Dermatol Online J. 2005;11(2):9.
2. Spencer JH, inventor; Nortech Lab Inc, assignee. Device for use as a hot and cold compress. US patent US3780537A. December 25, 1973.
3. Stålman A, Berglund L, Dungnerc E, Arner P, Felländer-Tsai L. Temperature-sensitive release of prostaglandin E₂ and diminished energy requirements in synovial tissue with postoperative cryotherapy: a prospective randomized study after knee arthroscopy. J Bone Joint Surg Am. 2011;93(21):1961-1968. doi:10.2106/JBJS.J.01790.
4. Kawabata A. Prostaglandin E2 and pain--an update. Biol Pharm Bull. 2011;34(8):1170-1173. doi:10.1248/bpb.34.1170.
5. Schaser KD, Stover JF, Melcher I, et al. Local cooling restores microcirculatory hemodynamics after closed soft-tissue trauma in rats. J Trauma. 2006;61(3):642-649. doi:10.1097/01.ta.0000174922.08781.2f.
6. Ruffilli A, Buda R, Castagnini F, et al. Temperature-controlled continuous cold flow device versus traditional icing regimen following anterior cruciate ligament reconstruction: a prospective randomized comparative trial. Arch Orthop Trauma Surg. 2015;135(10):1405-1410. doi:10.1007/s00402-015-2273-z.
7. Kuyucu E, Bülbül M, Kara A, Koçyiğit F, Erdil M. Is cold therapy really efficient after knee arthroplasty? Ann Med Surg. 2015;4(4):475-478. doi:10.1016/j.amsu.2015.10.019.
8. Martin SS, Spindler KP, Tarter JW, Detwiler K, Petersen HA. Cryotherapy: an effective modality for decreasing intraarticular temperature after knee arthroscopy. Am J Sports Med. 2001;29(3):288-291. doi:10.1177/03635465010290030501.
9. Yu SY, Chen S, Yan HD, Fan CY. Effect of cryotherapy after elbow arthrolysis: A prospective, single-blinded, randomized controlled study. Arch Phys Med Rehabil. 2015;96(1):1-6. doi:10.1016/j.apmr.2014.08.011.
10. Dambros C, Martimbianco ALC, Polachini LO, Lahoz GL, Chamlian TR, Cohen M. Effectiveness of cryotherapy after anterior cruciate ligament reconstruction. Acta Ortop Bras. 2012;20(5):285-290. doi:10.1590/S1413-78522012000500008.
11. Leegwater NC, Nolte PA, de Korte N, et al. The efficacy of continuous-flow cryo and cyclic compression therapy after hip fracture surgery on postoperative pain: design of a prospective, open-label, parallel, multicenter, randomized controlled, clinical trial. BMC Musculoskelet Disord. 2016;17(1):153. doi:10.1186/s12891-016-1000-4.
12. Kullenberg B, Ylipää S, Söderlund K, Resch S. Postoperative cryotherapy after total knee arthroplasty: a prospective study of 86 patients. J Arthroplasty. 2006;21(8):1175-1179. doi:10.1016/j.arth.2006.02.159.
13. Morsi E. Continuous-flow cold therapy after total knee arthroplasty. J Arthroplasty. 2002;17(6):718-722. doi:10.1054/arth.2002.33562.
14. Singh H, Osbahr DC, Holovacs TF, Cawley PW, Speer KP. The efficacy of continuous cryotherapy on the postoperative shoulder: A prospective, randomized investigation. J Shoulder Elb Surg. 2001;10(6):522-525. doi:10.1067/mse.2001.118415.
15. Saito N, Horiuchi H, Kobayashi S, Nawata M, Takaoka K. Continuous local cooling for pain relief following total hip arthroplasty. J Arthroplasty. 2004;19(3):334-337. doi:10.1016/j.arth.2003.10.011.
16. Gibbons C, Solan M, Ricketts D, Patterson M. Cryotherapy compared with Robert Jones bandage after total knee replacement: A prospective randomized trial. Int Orthop. 2001;25(4):250-252. doi:10.1007/s002640100227.
17. Kraeutler MJ, Reynolds KA, Long C, McCarty EC. Compressive cryotherapy versus ice-a prospective, randomized study on postoperative pain in patients undergoing arthroscopic rotator cuff repair or subacromial decompression. J Shoulder Elb Surg. 2015;24(6):854-859. doi:10.1016/j.jse.2015.02.004.
18. Thienpont E. Does Advanced Cryotherapy Reduce Pain and Narcotic Consumption After Knee Arthroplasty? Clin Orthop Relat Res. 2014;472(11):3417-3423. doi:10.1007/s11999-014-3810-8.
19. Woolf SK, Barfield WR, Merrill KD, McBryde AM Jr. Comparison of a continuous temperature-controlled cryotherapy device to a simple icing regimen following outpatient knee arthroscopy. J Knee Surg. 2008;21(1):15-19.
20. Su EP, Perna M, Boettner F, et al. A prospective, multi-center, randomised trial to evaluate the efficacy of a cryopneumatic device on total knee arthroplasty recovery. J Bone Joint Surg Br. 2012;94(11 Suppl A):153-156. doi:10.1302/0301-620X.94B11.30832.
21. Barber F. A comparison of crushed ice and continuous flow cold therapy. Am J Knee Surg. 2000;13(2):97-101.
22. Demoulin C, Brouwers M, Darot S, Gillet P, Crielaard JM, Vanderthommen M. Comparison of gaseous cryotherapy with more traditional forms of cryotherapy following total knee arthroplasty. Ann Phys Rehabil Med. 2012;55(4):229-240. doi:10.1016/j.rehab.2012.03.004.
23. Mumith A, Pavlou P, Barrett M, Thurston B, Garrett S. Enhancing postoperative rehabilitation following knee arthroplasty using a new cryotherapy product: a prospective study. Geriatr Orthop Surg Rehabil. 2015;6(4):316-321. doi:10.1177/2151458515609722.
24. Dickinson RN, Kuhn JE, Bergner JL, Rizzone KH. A systematic review of cost-effective treatment of postoperative rotator cuff repairs. J Shoulder Elb Surg. 2017;26(5):915-922. doi:10.1016/j.jse.2017.02.009.
25. Brown WC, Hahn DB. Frostbite of the Feet After Cryotherapy: A Report of Two Cases. J Foot Ankle Surg. 2009;48(5):577-580. doi:10.1053/j.jfas.2009.06.003.
26. Dundon JM, Rymer MC, Johnson RM. Total patellar skin loss from cryotherapy after total knee arthroplasty. J Arthroplasty. 2013;28(2):376.e5-e7. doi:10.1016/j.arth.2012.05.024.
27. Khajavi K, Pavelko T, Mishra A. Compartment syndrome arising from use of an electronic cooling pad. Am J Sports Med. 2004;32(6):1538-1541. doi:10.1177/0363546503262191.
28. King J, Plotner A, Adams B. Perniosis induced by a cold therapy system. Arch Dermatol. 2012;148(9):1101-1102.
29. Lee CK, Pardun J, Buntic R, Kiehn M, Brooks D, Buncke HJ. Severe frostbite of the knees after cryotherapy. Orthopedics. 2007;30(1):63-64.
30. McGuire DA, Hendricks SD. Incidences of frostbite in arthroscopic knee surgery postoperative cryotherapy rehabilitation. Arthroscopy. 2006;22(10):1141.e1-e6. doi:10.1016/j.arthro.2005.06.027.
31. Mirkin G. Why Ice Delays Recovery. http://www.drmirkin.com/fitness/why-ice-delays-recovery.html. Published September 16, 2015. Accessed July 17, 2017.
1. Freiman N, Bouganim N. History of cryotherapy. Dermatol Online J. 2005;11(2):9.
2. Spencer JH, inventor; Nortech Lab Inc, assignee. Device for use as a hot and cold compress. US patent US3780537A. December 25, 1973.
3. Stålman A, Berglund L, Dungnerc E, Arner P, Felländer-Tsai L. Temperature-sensitive release of prostaglandin E₂ and diminished energy requirements in synovial tissue with postoperative cryotherapy: a prospective randomized study after knee arthroscopy. J Bone Joint Surg Am. 2011;93(21):1961-1968. doi:10.2106/JBJS.J.01790.
4. Kawabata A. Prostaglandin E2 and pain--an update. Biol Pharm Bull. 2011;34(8):1170-1173. doi:10.1248/bpb.34.1170.
5. Schaser KD, Stover JF, Melcher I, et al. Local cooling restores microcirculatory hemodynamics after closed soft-tissue trauma in rats. J Trauma. 2006;61(3):642-649. doi:10.1097/01.ta.0000174922.08781.2f.
6. Ruffilli A, Buda R, Castagnini F, et al. Temperature-controlled continuous cold flow device versus traditional icing regimen following anterior cruciate ligament reconstruction: a prospective randomized comparative trial. Arch Orthop Trauma Surg. 2015;135(10):1405-1410. doi:10.1007/s00402-015-2273-z.
7. Kuyucu E, Bülbül M, Kara A, Koçyiğit F, Erdil M. Is cold therapy really efficient after knee arthroplasty? Ann Med Surg. 2015;4(4):475-478. doi:10.1016/j.amsu.2015.10.019.
8. Martin SS, Spindler KP, Tarter JW, Detwiler K, Petersen HA. Cryotherapy: an effective modality for decreasing intraarticular temperature after knee arthroscopy. Am J Sports Med. 2001;29(3):288-291. doi:10.1177/03635465010290030501.
9. Yu SY, Chen S, Yan HD, Fan CY. Effect of cryotherapy after elbow arthrolysis: A prospective, single-blinded, randomized controlled study. Arch Phys Med Rehabil. 2015;96(1):1-6. doi:10.1016/j.apmr.2014.08.011.
10. Dambros C, Martimbianco ALC, Polachini LO, Lahoz GL, Chamlian TR, Cohen M. Effectiveness of cryotherapy after anterior cruciate ligament reconstruction. Acta Ortop Bras. 2012;20(5):285-290. doi:10.1590/S1413-78522012000500008.
11. Leegwater NC, Nolte PA, de Korte N, et al. The efficacy of continuous-flow cryo and cyclic compression therapy after hip fracture surgery on postoperative pain: design of a prospective, open-label, parallel, multicenter, randomized controlled, clinical trial. BMC Musculoskelet Disord. 2016;17(1):153. doi:10.1186/s12891-016-1000-4.
12. Kullenberg B, Ylipää S, Söderlund K, Resch S. Postoperative cryotherapy after total knee arthroplasty: a prospective study of 86 patients. J Arthroplasty. 2006;21(8):1175-1179. doi:10.1016/j.arth.2006.02.159.
13. Morsi E. Continuous-flow cold therapy after total knee arthroplasty. J Arthroplasty. 2002;17(6):718-722. doi:10.1054/arth.2002.33562.
14. Singh H, Osbahr DC, Holovacs TF, Cawley PW, Speer KP. The efficacy of continuous cryotherapy on the postoperative shoulder: A prospective, randomized investigation. J Shoulder Elb Surg. 2001;10(6):522-525. doi:10.1067/mse.2001.118415.
15. Saito N, Horiuchi H, Kobayashi S, Nawata M, Takaoka K. Continuous local cooling for pain relief following total hip arthroplasty. J Arthroplasty. 2004;19(3):334-337. doi:10.1016/j.arth.2003.10.011.
16. Gibbons C, Solan M, Ricketts D, Patterson M. Cryotherapy compared with Robert Jones bandage after total knee replacement: A prospective randomized trial. Int Orthop. 2001;25(4):250-252. doi:10.1007/s002640100227.
17. Kraeutler MJ, Reynolds KA, Long C, McCarty EC. Compressive cryotherapy versus ice-a prospective, randomized study on postoperative pain in patients undergoing arthroscopic rotator cuff repair or subacromial decompression. J Shoulder Elb Surg. 2015;24(6):854-859. doi:10.1016/j.jse.2015.02.004.
18. Thienpont E. Does Advanced Cryotherapy Reduce Pain and Narcotic Consumption After Knee Arthroplasty? Clin Orthop Relat Res. 2014;472(11):3417-3423. doi:10.1007/s11999-014-3810-8.
19. Woolf SK, Barfield WR, Merrill KD, McBryde AM Jr. Comparison of a continuous temperature-controlled cryotherapy device to a simple icing regimen following outpatient knee arthroscopy. J Knee Surg. 2008;21(1):15-19.
20. Su EP, Perna M, Boettner F, et al. A prospective, multi-center, randomised trial to evaluate the efficacy of a cryopneumatic device on total knee arthroplasty recovery. J Bone Joint Surg Br. 2012;94(11 Suppl A):153-156. doi:10.1302/0301-620X.94B11.30832.
21. Barber F. A comparison of crushed ice and continuous flow cold therapy. Am J Knee Surg. 2000;13(2):97-101.
22. Demoulin C, Brouwers M, Darot S, Gillet P, Crielaard JM, Vanderthommen M. Comparison of gaseous cryotherapy with more traditional forms of cryotherapy following total knee arthroplasty. Ann Phys Rehabil Med. 2012;55(4):229-240. doi:10.1016/j.rehab.2012.03.004.
23. Mumith A, Pavlou P, Barrett M, Thurston B, Garrett S. Enhancing postoperative rehabilitation following knee arthroplasty using a new cryotherapy product: a prospective study. Geriatr Orthop Surg Rehabil. 2015;6(4):316-321. doi:10.1177/2151458515609722.
24. Dickinson RN, Kuhn JE, Bergner JL, Rizzone KH. A systematic review of cost-effective treatment of postoperative rotator cuff repairs. J Shoulder Elb Surg. 2017;26(5):915-922. doi:10.1016/j.jse.2017.02.009.
25. Brown WC, Hahn DB. Frostbite of the Feet After Cryotherapy: A Report of Two Cases. J Foot Ankle Surg. 2009;48(5):577-580. doi:10.1053/j.jfas.2009.06.003.
26. Dundon JM, Rymer MC, Johnson RM. Total patellar skin loss from cryotherapy after total knee arthroplasty. J Arthroplasty. 2013;28(2):376.e5-e7. doi:10.1016/j.arth.2012.05.024.
27. Khajavi K, Pavelko T, Mishra A. Compartment syndrome arising from use of an electronic cooling pad. Am J Sports Med. 2004;32(6):1538-1541. doi:10.1177/0363546503262191.
28. King J, Plotner A, Adams B. Perniosis induced by a cold therapy system. Arch Dermatol. 2012;148(9):1101-1102.
29. Lee CK, Pardun J, Buntic R, Kiehn M, Brooks D, Buncke HJ. Severe frostbite of the knees after cryotherapy. Orthopedics. 2007;30(1):63-64.
30. McGuire DA, Hendricks SD. Incidences of frostbite in arthroscopic knee surgery postoperative cryotherapy rehabilitation. Arthroscopy. 2006;22(10):1141.e1-e6. doi:10.1016/j.arthro.2005.06.027.
31. Mirkin G. Why Ice Delays Recovery. http://www.drmirkin.com/fitness/why-ice-delays-recovery.html. Published September 16, 2015. Accessed July 17, 2017.
TAKE-HOME POINTS
- Cryotherapy is often used in postoperative orthopedic care but there is limited literature demonstrating its efficacy.
- Postoperative cryotherapy has been used to reduce visual analog scale pain scores, analgesic consumption, and to increase range of motion.
- There is no consensus on the advantages of postoperative cryotherapy vs traditional ice application.
- Adverse outcomes from postoperative cryotherapy use include frostbite/skin loss, compartment syndrome, and perniosis.
- Future studies, including a formidable economic analysis of advanced cold therapy systems are necessary before physicians prescribing cryotherapy can be confident that they are augmenting patient recovery.
FDA warns kratom vendors about unproven claims
The Food and Drug Administration has issued letters of warning to – and therefore breaking federal law – according to a statement from FDA commissioner Scott Gottlieb, MD. These vendors both claimed that their kratom products could, among other things, “relieve” or “treat” opium/opioid withdrawal.
“To date, there have been no adequate and well-controlled studies involving the use of kratom as a treatment for opioid use withdrawal or other diseases in humans,” noted Dr. Gottlieb.
As Dr. Gottlieb pointed out in his statement, not only can fraudulent health claims pose direct health risks, they can also, in the case of kratom, deter or delay people who’re suffering from opioid use disorder from seeking FDA-approved treatments that have been demonstrated to be safe and effective.
Kratom, also known more formally as Mitragyna speciosa, is a plant native to Thailand, Malaysia, Indonesia, and Papua New Guinea. Some compounds in the plant are believed to be opioids, some of which may have the potential for abuse. As Dr. Gottlieb pointed out in his statement, the substance is illegal or controlled in several countries and banned in some states and municipalities in the United States.
Find out more in Dr. Gottlieb’s full statement on the FDA website.
The Food and Drug Administration has issued letters of warning to – and therefore breaking federal law – according to a statement from FDA commissioner Scott Gottlieb, MD. These vendors both claimed that their kratom products could, among other things, “relieve” or “treat” opium/opioid withdrawal.
“To date, there have been no adequate and well-controlled studies involving the use of kratom as a treatment for opioid use withdrawal or other diseases in humans,” noted Dr. Gottlieb.
As Dr. Gottlieb pointed out in his statement, not only can fraudulent health claims pose direct health risks, they can also, in the case of kratom, deter or delay people who’re suffering from opioid use disorder from seeking FDA-approved treatments that have been demonstrated to be safe and effective.
Kratom, also known more formally as Mitragyna speciosa, is a plant native to Thailand, Malaysia, Indonesia, and Papua New Guinea. Some compounds in the plant are believed to be opioids, some of which may have the potential for abuse. As Dr. Gottlieb pointed out in his statement, the substance is illegal or controlled in several countries and banned in some states and municipalities in the United States.
Find out more in Dr. Gottlieb’s full statement on the FDA website.
The Food and Drug Administration has issued letters of warning to – and therefore breaking federal law – according to a statement from FDA commissioner Scott Gottlieb, MD. These vendors both claimed that their kratom products could, among other things, “relieve” or “treat” opium/opioid withdrawal.
“To date, there have been no adequate and well-controlled studies involving the use of kratom as a treatment for opioid use withdrawal or other diseases in humans,” noted Dr. Gottlieb.
As Dr. Gottlieb pointed out in his statement, not only can fraudulent health claims pose direct health risks, they can also, in the case of kratom, deter or delay people who’re suffering from opioid use disorder from seeking FDA-approved treatments that have been demonstrated to be safe and effective.
Kratom, also known more formally as Mitragyna speciosa, is a plant native to Thailand, Malaysia, Indonesia, and Papua New Guinea. Some compounds in the plant are believed to be opioids, some of which may have the potential for abuse. As Dr. Gottlieb pointed out in his statement, the substance is illegal or controlled in several countries and banned in some states and municipalities in the United States.
Find out more in Dr. Gottlieb’s full statement on the FDA website.












